User login
MD jailed for road rage, career spirals downhill
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
It was a 95° F day in July 2015, and emergency physician Martin Maag, MD, was driving down Bee Ridge Road, a busy seven-lane thoroughfare in Sarasota, Fla., on his way home from a family dinner. To distance himself from a truck blowing black smoke, Dr. Maag says he had just passed some vehicles, when a motorcycle flew past him in the turning lane and the passenger flipped him off.
“I started laughing because I knew we were coming up to a red light,” said Dr. Maag. “When we pulled up to the light, I put my window down and said: ‘Hey, you ought to be a little more careful about who you’re flipping off! You never know who it might be and what they might do.’ ”
The female passenger cursed at Dr. Maag, and the two traded profanities. The male driver then told Dr. Maag: “Get out of the car, old man,” according to Dr. Maag. Fuming, Dr. Maag got out of his black Tesla, and the two men met in the middle of the street.
“As soon as I got close enough to see him, I could tell he really looked young,” Dr. Maag recalls. “I said: ‘You’re like 12 years old. I’m going to end up beating your ass and then I’m going to go to jail. Go get on your bike, and ride home to your mom.’ I don’t remember what he said to me, but I spun around and said: ‘If you want to act like a man, meet me up the street in a parking lot and let’s have at it like men.’ ”
The motorcyclist got back on his white Suzuki and sped off, and Dr. Maag followed. Both vehicles went racing down the road, swerving between cars, and reaching speeds of 100 miles per hour, Dr. Maag said. At one point, Dr. Maag says he drove in front of the motorcyclist to slow him down, and the motorcycle clipped the back of his car. No one was seriously hurt, but soon Dr. Maag was in the back of a police cruiser headed to jail.
Dr. Maag wishes he could take back his actions that summer day 6 years ago. Those few minutes of fury have had lasting effects on the doctor’s life. The incident resulted in criminal charges, a jail sentence, thousands of dollars in legal fees, and a 3-year departure from emergency medicine. Although Dr. Maag did not lose his medical license as a result of the incident, the physician’s Medicare billing privileges were suspended because of a federal provision that ties some felonies to enrollment revocations.
“Every doctor, every health professional needs to know that there are a lot of consequences that go with our actions outside of work,” he said. “In my situation, what happened had nothing to do with medicine, it had nothing to do with patients, it had nothing to do my professional demeanor. But yet it affected my entire career, and I lost the ability to practice emergency medicine for 3 years. Three years for any doctor is a long time. Three years for emergency medicine is a lifetime.”
The physician ends up in jail
After the collision, Dr. Maag pulled over in a parking lot and dialed 911. Several passing motorists did the same. It appeared the biker was trying to get away, and Dr. Maag was concerned about the damage to his Tesla, he said.
When police arrived, they heard very different accounts of what happened. The motorcyclist and his girlfriend claimed Dr. Maag was the aggressor during the altercation, and that he deliberately tried to hit them with his vehicle. Two witnesses at the scene said they had watched Dr. Maag pursue the motorcycle in his vehicle, and that they believed he crossed into their lane intentionally to strike the motorcycle, according to police reports.
“[The motorcyclist] stated that the vehicle struck his right foot when it hit the motorcycle and that he was able to keep his balance and not lay the bike down,” Sarasota County Deputy C. Moore wrote in his report. “The motorcycle was damaged on the right side near [his] foot, verifying his story. Both victims were adamant that the defendant actually and intentionally struck the motorcycle with his car due to the previous altercation.”
Dr. Maag told officers the motorcyclist had initiated the confrontation. He acknowledged racing after the biker, but said it was the motorcyclist who hit his vehicle. In an interview, Dr. Maag disputed the witnesses’ accounts, saying that one of the witnesses was without a car and made claims to police that were impossible from her distance.
In the end, the officer believed the motorcyclist, writing in his report that the damage to the Tesla was consistent with the biker’s version of events. Dr. Maag was handcuffed and taken to the Sarasota County Jail.
“I was in shock,” he said. “When we got to the jail, they got me booked in and fingerprinted. I sat down and said [to an officer]: ‘So, when do I get to bond out?’ The guy started laughing and said: ‘You’re not going anywhere. You’re spending the night in jail, my friend.’ He said: ‘Your charge is one step below murder.’”
‘I like to drive fast’
Aside from speeding tickets, Dr. Maag said he had never been in serious trouble with the law before.
The husband and father of two has practiced emergency medicine for more 15 years, and his license has remained in good standing. Florida Department of Health records show Dr. Maag’s medical license as clear and active with no discipline cases or public complaints on file.
“I did my best for every patient that came through that door,” he said. “There were a lot of people who didn’t like my personality. I’ve said many times: ‘I’m not here to be liked. I’m here to take care of people and provide the best care possible.’ ”
Sarasota County records show that Dr. Maag has received traffic citations in the past for careless driving, unlawful speed, and failure to stop at a red light, among others. He admits to having a “lead foot,” but says he had never before been involved in a road rage incident.
“I’m not going to lie, I like to drive fast,” he said. “I like that feeling. It just seems to slow everything down for me, the faster I’m going.”
After being booked into jail that July evening in 2015, Dr. Maag called his wife to explain what happened.
“She said, ‘I can’t believe you’ve done this. I’ve told you a million times, don’t worry about how other people drive. Keep your mouth shut,’” he recalled. “I asked her to call my work and let them know I wouldn’t be coming in the next day. Until that happened, I had never missed a day of work since becoming a physician.”
After an anxious night in his jail cell, Dr. Maag lined up with the other inmates the next morning for his bond hearing. His charges included felony, aggravated battery, and felony aggravated assault with a deadly weapon. A prosecutor recommended Dr. Maag’s bond be set at $1 million, which a judge lowered to $500,000.
Michael Fayard, a criminal defense attorney who represented Dr. Maag in the case, said even with the reduction, $500,000 was an outrageous bond for such a case.
“The prosecutor’s arguments to the judge were that he was a physician driving a Tesla,” Mr. Fayard said. “That was his exact argument for charging him a higher bond. It shouldn’t have been that high. I argued he was not a flight risk. He didn’t even have a passport.”
The Florida State Attorney’s Office did not return messages seeking comment about the case.
Dr. Maag spent 2 more nights in jail while he and his wife came up with $50,000 in cash, in accordance with the 10% bond rule. In the meantime, the government put a lien on their house. A circuit court judge later agreed the bond was excessive, according to Mr. Fayard, but by that time, the $50,000 was paid and Dr. Maag was released.
New evidence lowers charges
Dr. Maag ultimately accepted a plea deal from the prosecutor’s office and pled no contest to one count of felony criminal mischief and one count of misdemeanor reckless driving. In return, the state dropped the two more serious felonies. A no-contest plea is not considered an admission of guilt.
Mr. Fayard said his investigation into the road rage victim unearthed evidence that poked holes in the motorcyclist’s credibility, and that contributed to the plea offer.
“We found tons of evidence about the kid being a hot-rodding rider on his motorcycle, videos of him traveling 140 miles an hour, popping wheelies, and darting in and out of traffic,” he said. “There was a lot of mitigation that came up during the course of the investigation.”
The plea deal was a favorable result for Dr. Maag considering his original charges, Mr. Fayard said. He added that the criminal case could have ended much differently.
“Given the facts of this case and given the fact that there were no serious injuries, we supported the state’s decision to accept our mitigation and come out with the sentence that they did,” Mr. Fayard said. “If there would have been injuries, the outcome would have likely been much worse for Dr. Maag.”
With the plea agreement reached, Dr. Maag faced his next consequence – jail time. He was sentenced to 60 days in jail, a $1,000 fine, 12 months of probation, and 8 months of house arrest. Unlike his first jail stay, Dr. Maag said the second, longer stint behind bars was more relaxing.
“It was the first time since I had become an emergency physician that I remember my dreams,” he recalled. “I had nothing to worry about, nothing to do. All I had to do was get up and eat. Every now and then, I would mop the floors because I’m kind of a clean freak, and I would talk to guys and that was it. It wasn’t bad at all.”
Dr. Maag told no one that he was a doctor because he didn’t want to be treated differently. The anonymity led to interesting tidbits from other inmates about the best pill mills in the area for example, how to make crack cocaine, and selling items for drugs. On his last day in jail, the other inmates learned from his discharge paperwork that Dr. Maag was a physician.
“One of the corrections officers said: ‘You’re a doctor? We’ve never had a doctor in here before!’” Dr. Maag remembers. “He said: ‘What did a doctor do to get into jail?’ I said: ‘Do you really want to know?’ ”
About the time that Dr. Maag was released from jail, the Florida Board of Medicine learned of his charges and began reviewing his case. Mr. Fayard presented the same facts to the board and argued for Dr. Maag to keep his license, emphasizing the offenses in which he was convicted were significantly less severe than the original felonies charged. The board agreed to dismiss the case.
“The probable cause panel for the board of medicine considered the complaint that has been filed against your client in the above referenced case,” Peter Delia, then-assistant general counsel for the Florida Department of Health, wrote in a letter dated April 27, 2016. “After careful review of all information and evidence obtained in this case, the panel determined that probable cause of a violation does not exist and directed this case to be closed.”
A short-lived celebration
Once home, Dr. Maag was on house arrest, but he was granted permission to travel for work. He continued to practice emergency medicine. After several months, authorities dropped the house arrest, and a judge canceled his probation early. It appeared the road rage incident was finally behind him.
But a year later, in 2018, the doctor received a letter from the Centers for Medicare & Medicaid Services informing him that because of his charges, his Medicare number had been revoked in November 2015.
“It took them 3 years to find me and tell me, even though I never moved,” he said. “Medicare said because I never reported this, they were hitting me up with falsification of documentation because I had signed other Medicare paperwork saying I had never been barred from Medicare, because I didn’t know that I was.”
Dr. Maag hired a different attorney to help him fight the 3-year enrollment ban. He requested reconsideration from CMS, but a hearing officer in October 2017 upheld the revocation. Because his privileges had been revoked in 2015, Dr. Maag’s practice group had to return all money billed by Dr. Maag to Medicare over the 3-year period, which totaled about $190,000.
A CMS spokeswoman declined to comment about Dr. Maag’s case, referring a reporter for this news organization to an administrative law judge’s decision that summarizes the agency’s findings.
According to the summary, in separate reconsidered determinations, the CMS hearing officer concluded that the revocation was proper under section 424.535(a)(3). The regulation, enacted in 2011, allows CMS to revoke billing privileges if a provider was convicted of a federal or state felony within the preceding 10 years that the agency determines is detrimental to the Medicare program and its beneficiaries.
The hearing officer reasoned that Dr. Maag “had been convicted of a felony that is akin to assault and, even if it were not, his actions showed a reckless disregard for the safety of others.” She concluded also that CMS could appropriately revoke Dr. Maag’s Medicare enrollment because he did not report his felony conviction within 30 days as required.
Dr. Maag went through several phases of fighting the revocation, including an appeal to the Department of Health & Human Services Departmental Appeals Board. He argued that his plea was a no-contest plea, which is not considered an admission of guilt. Dr. Maag and his attorney provided CMS a 15-page paper about his background, education, career accomplishments, and patient care history. They emphasized that Dr. Maag had never harmed or threatened a patient, and that his offense had nothing to do with his practice.
In February 2021, Judge Carolyn Cozad Hughes, an administrative law judge with CMS, upheld the 3-year revocation. In her decision, she wrote that for purposes of revocation under CMS law, “convicted” means that a judgment of conviction has been entered by a federal, state, or local court regardless of whether the judgment of conviction has been expunged or otherwise removed. She disagreed with Dr. Maag’s contention that his was a crime against property and, therefore, not akin to any of the felony offenses enumerated under the revocation section, which are crimes against persons.
“Even disregarding the allegations contained in the probable cause affidavit, Petitioner cannot escape the undisputed fact, established by his conviction and his own admissions, that the ‘property’ he so ‘willfully and maliciously’ damaged was a motorcycle traveling at a high rate of speed, and, that two young people were sitting atop that motorcycle,” Judge Hughes wrote. “Moreover, as part of the same conduct, he was charged – and convicted – of misdemeanor reckless driving with ‘willful and wanton disregard for the safety of persons or property.’ Thus, even accepting Petitioner’s description of the events, he unquestionably showed no regard for the safety of the young people on that motorcycle.”
Judge Hughes noted that, although Dr. Maag’s crimes may not be among those specified in the regulation, CMS has broad authority to determine which felonies are detrimental to the best interests of the program and its beneficiaries.
A new career path
Unable to practice emergency medicine and beset with debt, Dr. Maag spiraled into a dark depression. His family had to start using retirement money that he was saving for the future care of his son, who has autism.
“I was suicidal,” he said. “There were two times that I came very close to going out to the woods by my house and hanging myself. All I wanted was to have everything go away. My wife saved my life.”
Slowly, Dr. Maag climbed out of the despondency and began considering new career options. After working and training briefly in hair restoration, Dr. Maag became a hair transplant specialist and opened his own hair restoration practice. It was a way to practice and help patients without having to accept Medicare. Today, he is the founder of Honest Hair Restoration in Bradenton, Fla.
Hair restoration is not the type of medicine that he “was designed to do,” Dr. Maag said, but he has embraced its advantages, such as learning about the business aspects of medicine and having a slower-paced work life. The business, which opened in 2019, is doing well and growing steadily.
Earlier this month, Dr. Maag learned CMS had reinstated his Medicare billing privileges. If an opportunity arises to go back into emergency medicine or urgent care, he is open to the possibilities, he said, but he plans to continue hair restoration for now. He hopes the lessons learned from his road rage incident may help others in similar circumstances.
“If I could go back to that very moment, I would’ve just kept my window up and I wouldn’t have said anything,” Dr. Maag said. “I would’ve kept my mouth shut and gone on about my day. Would I have loved it to have never happened? Yeah, and I’d probably be starting my retirement now. Am I stronger now? Well, I’m probably a hell of a lot wiser. But when all is said and done, I don’t want anybody feeling sorry for me. It was all my doing and I have to live with the consequences.”
Mr. Fayard, the attorney, says the case is a cautionary tale for doctors.
“No one is really above the law,” he said. “There aren’t two legal systems. You can’t just pay a little money and be done. At every level, serious charges have serious ramifications for everyone involved. Law enforcement and judges are not going to care of you’re a physician and you commit a crime. But physicians have a lot more on the line than many others. They can lose their ability to practice.”
A version of this article first appeared on Medscape.com.
Patient-facing mobile apps: Are ObGyns uniquely positioned to integrate them into practice?
Incorporating mobile apps into patient care programs can add immense value. Mobile apps enable data collection when a patient is beyond the walls of a doctor’s office and equip clinicians with new and relevant patient data. Patient engagement apps also provide a mechanism to “nudge” patients to encourage adherence to their care programs. These additional data and increased patient adherence can enable more personalized care,1 and ultimately can lead to improved outcomes. For example, a meta-analysis of 1,657 patients with diabetes showed a 5% reduction in hemoglobin A1c (HbA1c) values for those who used a diabetes-related app.2 The literature also shows positive results for heart failure, weight management, smoking reduction, and lifestyle improvement.3-5 Given their value, why aren’t patient engagement apps more routinely integrated into patient care programs?
From a software development perspective, mobile apps are fairly easy to create. However, from a user retention standpoint, creating an app with a large, sustainable userbase is challenging.5 User retention is measured in monthly active users. We are familiar with unused apps collecting digital dust on our smartphone home screens. A 2019 study showed that 25% of people typically use an application only once,6 and health care apps are not an exception. There are hundreds of thousands of mobile health apps on the market, but only 7% of these applications have more than 50,000 monthly active users. Further, 62% of digital health apps have less than 1,000 monthly active users.7
Using a new app daily or several times weekly requires new habit formation. Anyone who has tried to incorporate a new routine into their daily life knows how difficult habit formation can be. However, ObGyn patients may be particularly well suited to incorporate ObGyn-related apps into their care, given how many women already use mobile applications to track their menstrual cycles. A recent survey found that across all age groups, 47% of women use a mobile phone app to track their menstrual cycle,8 compared with 8% of US adults who regularly use an app to measure general health metrics.7 This removes one of the largest obstacles of market penetration since the habit of using an app for ObGyn purposes has already been established. As such, it presents an exciting opportunity to capitalize on the userbase already leveraging mobile apps to track their cycles and expand the patient engagement footprint into additional features that can broaden care to create a seamless, holistic patient application for ObGyn patient care.
One can envision a future in which a patient is “prescribed” an ObGyn app during their ObGyn appointment. Within the app, the patient can track their health data, engage with health providers, and gain access to educational materials. The clinician would be able to access data captured in the patient app at an aggregate level to analyze trends over time.
Current, patient-facing ObGyn mobile apps available for download on smartphones are for targeted aspects of ObGyn health. For example, there are separate apps for menstrual cycle tracking, contraception education, and medication adherence tracking. In the future, it would be ideal for clinicians and patients to have access to a single, holistic ObGyn mobile app that supports the end-to-end ObGyn patient journey, one in which clinicians could turn modules on or off given specific patient concerns. The technology for this type of holistic patient engagement platform exists, but unfortunately it is not as simple as downloading a mobile app. Standing up an end-to-end patient engagement platform requires enterprise-wide buy-in, tailoring user workflows, and building out integrations (eg, integrating provider dashboards into the existing electronic health record system). Full-scale solutions are powerful, but they can be expensive and time consuming to stand up. Until there is a more streamlined, outside-the-box ObGyn-tailored solution, there are patientfacing mobile apps available to support your patients for specific concerns.
Continue to: The top 3 recommended menstrual cycle tracking apps...
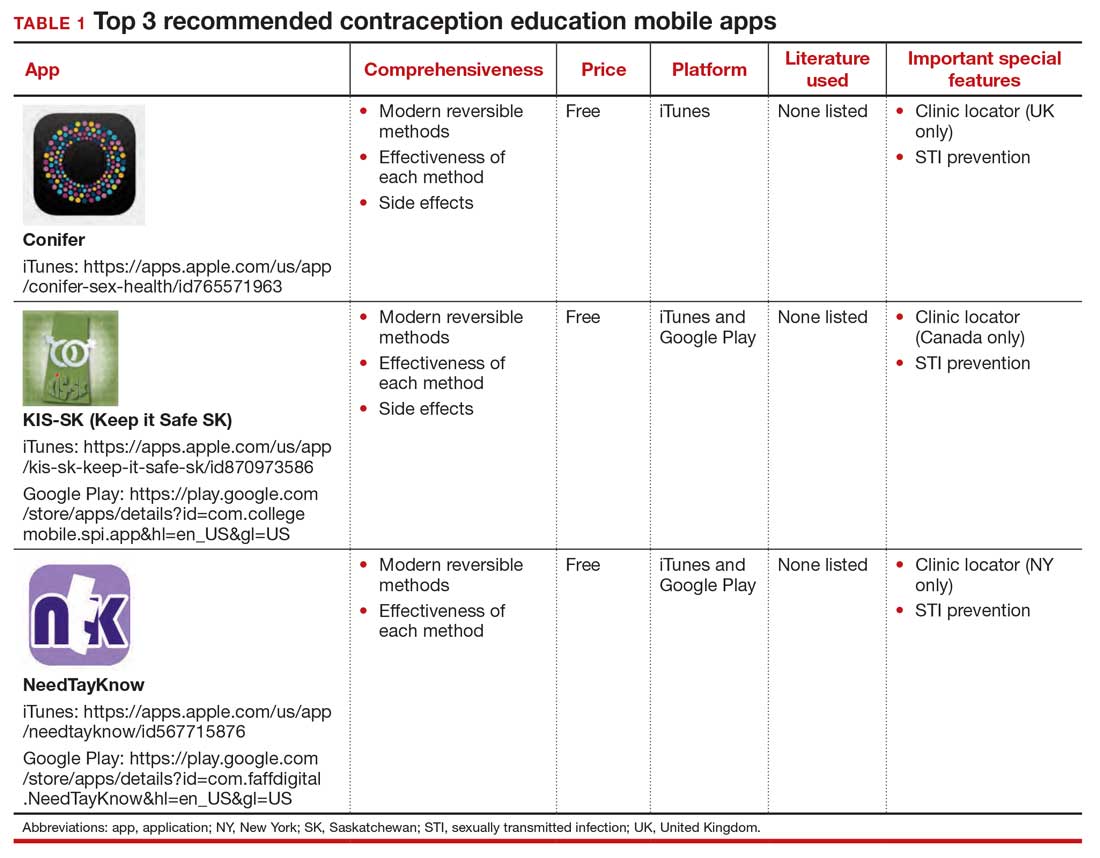
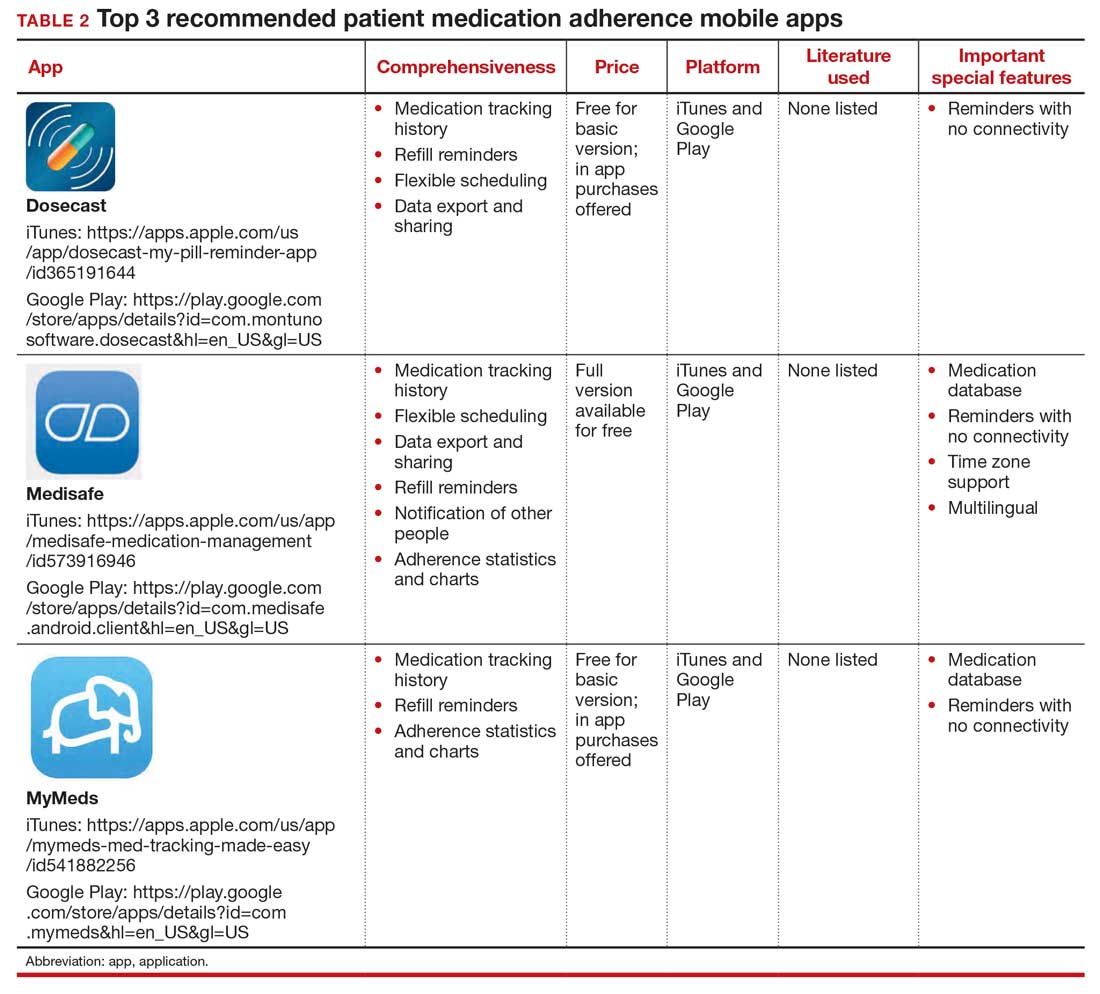
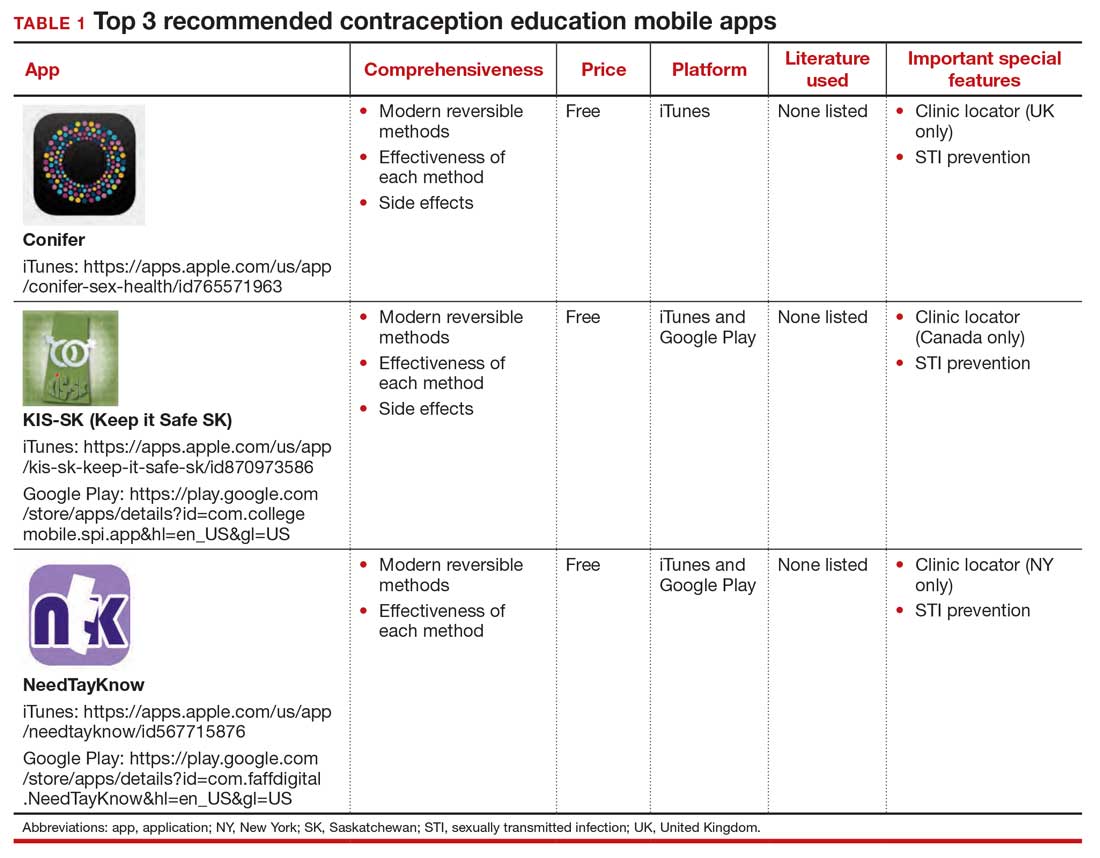
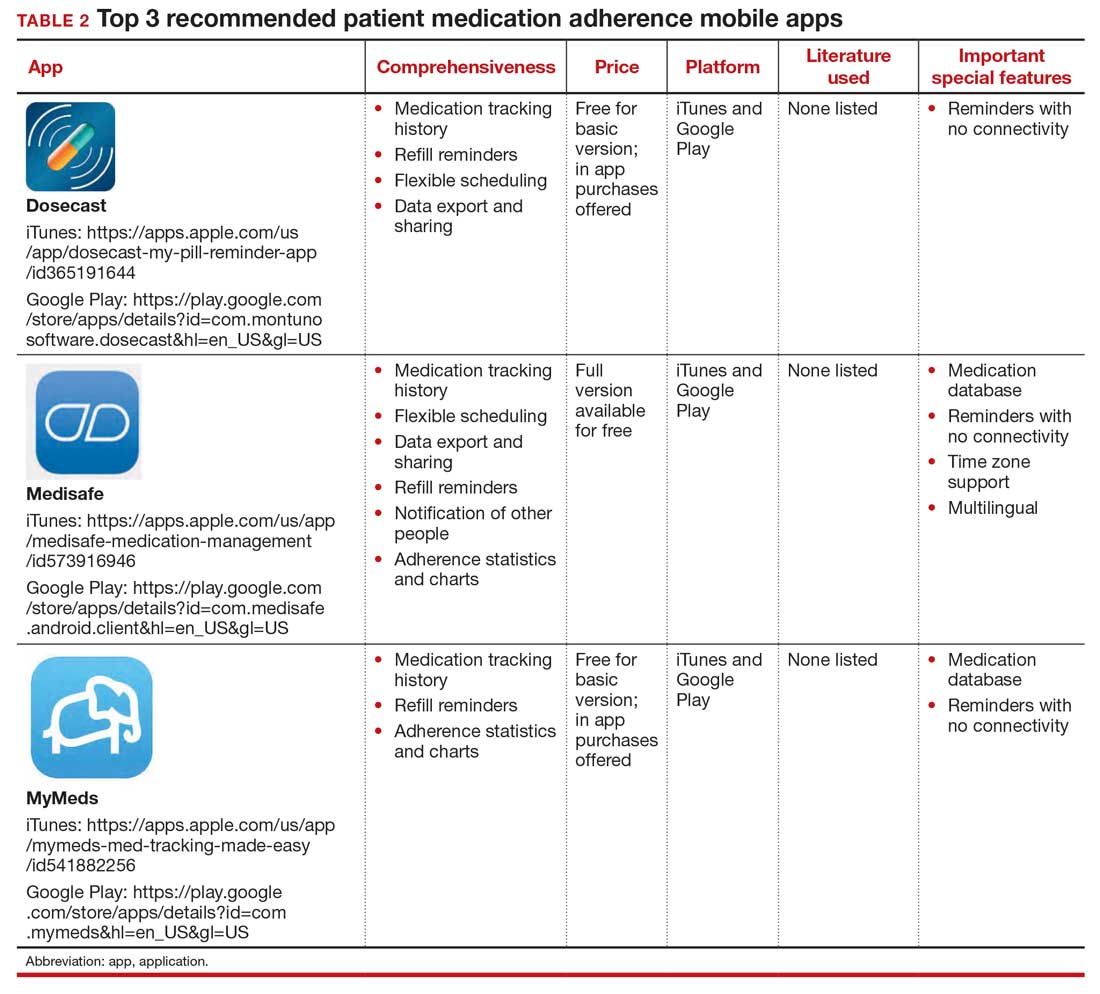
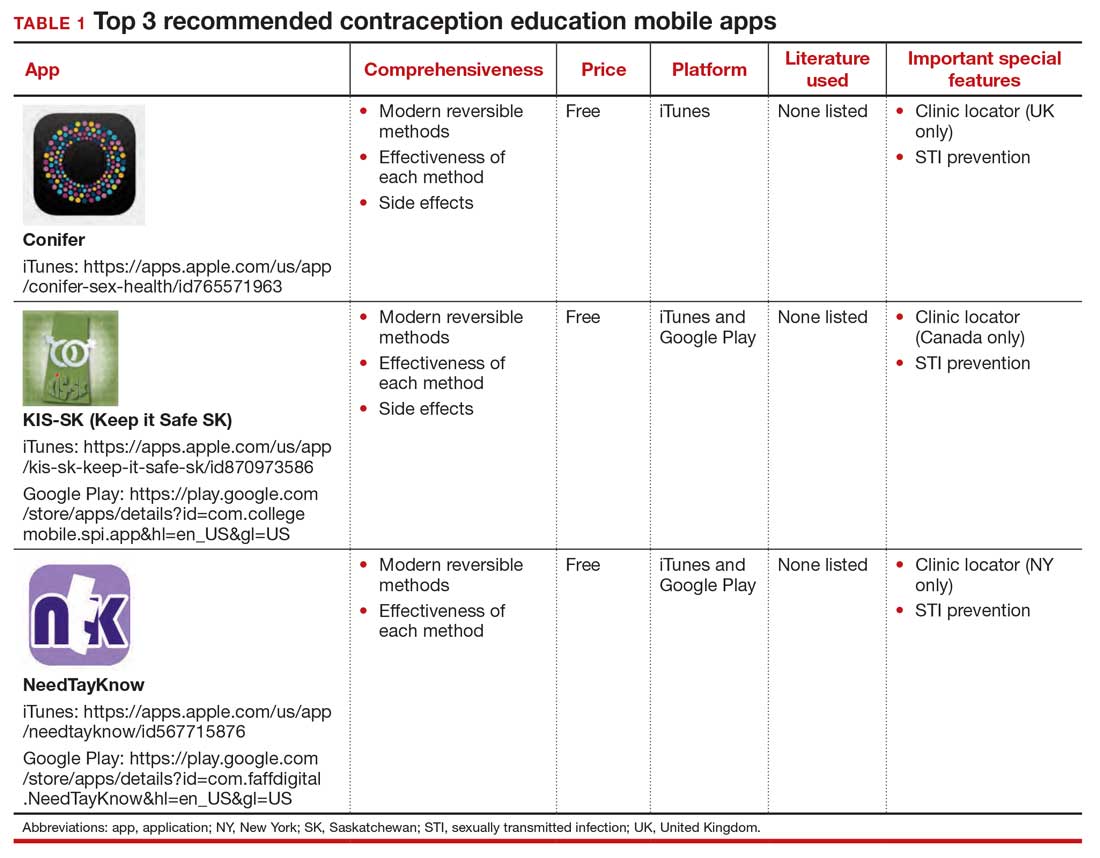
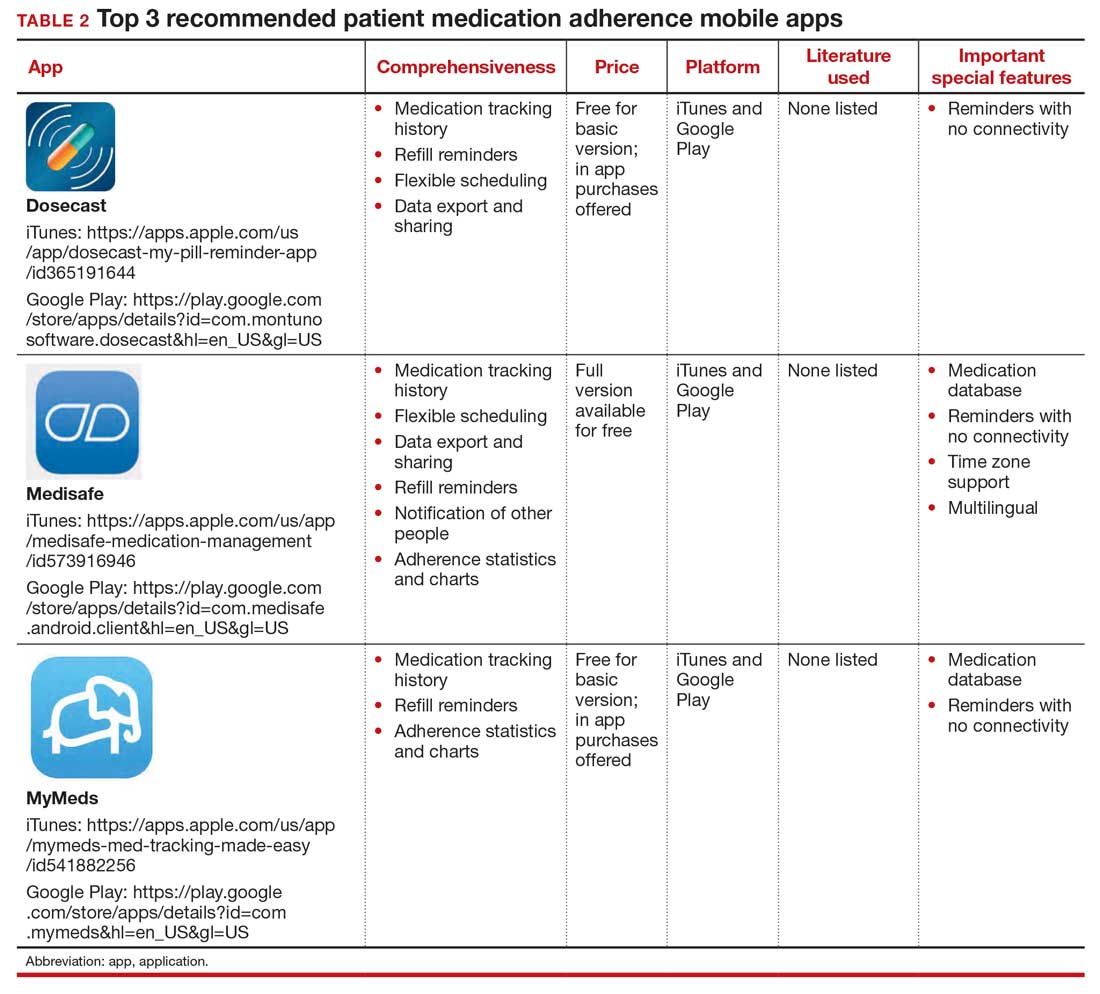
The top 3 recommended menstrual cycle tracking apps from Moglia and colleagues9 are listed in Dr. Chen’s article, “Top free menstrual cycle tracking apps for your patients.”10 The top 3 recommended contraception education mobile apps from Lunde and colleagues11 are listed in TABLE 1 and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, important special features).12 The top 3 recommended patient medication adherence mobile apps from the study by Santo and colleagues13 are listed in TABLE 2. The apps in the Stoyanov et al14 study were evaluated using the 23-item Mobile App Rating System scale. ●
- van Dijk MR, Koster MPH, et al. Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod BioMed Online. 2017;35:453-460. doi:10.1016/j. rbmo.2017.06.014.
- Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a metaanalysis. Diabet Med. 2011;28:455-463. doi:10.1111/j.1464- 5491.2010.03180.x.
- Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients. Ann Intern Med. 2014;161(10 suppl):S5-S12. doi:10.7326/m13-3005.
- Dennison L, Morrison L, Conway G, et al. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J Med Internet Res. 2013;15:E86. doi:10.2196/jmir.2583.
- Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13:127. doi:10.1186/s12966- 016-0454-y.
- 25% of users abandon apps after one use. Upland Software website. Accessed May 6, 2021. https://uplandsoftware.com /localytics/resources/blog/25-of-users-abandon-apps-afterone-use/.
- mHealth economics 2017/2018 – connectivity in digital health. Published March 5, 2019. Accessed May 6, 2021. https:// research2guidance.com/product/connectivity-in-digitalhealth/.
- Epstein DA, Lee NB, Kang JH, et al. Examining menstrual tracking to inform the design of personal informatics tools. Proc SIGCHI Conf Hum Factor Comput Syst. 2017;2017:6876- 6888. doi:10.1145/3025453.3025635.
- Moglia M, Nguyen H, Chyjek K, et al. Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICATIONS scoring system. Obstet Gynecol. 2016;127:1153-1160. doi:10.1097/AOG.0000000000001444.
- Chen KT. Top free menstrual cycle tracking apps for your patients. OBG Manag. 2017;27:44-45.
- Lunde B, Perry R, Sridhar A, et al. An evaluation of contraception education and health promotion applications for patients. Womens Health Issues. 2017;27:29-35. doi:10.1016/j.whi.2016.09.012.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483. doi:10.1097 /AOG.0000000000000842.
- Santo K, Richtering SS, Chalmers J, et al. Mobile phone apps to improve medication adherence: a systematic stepwise process to identify high-quality apps. JMIR Mhealth Uhealth. 2016;4:E132. doi:10.2196/mhealth.6742.
- Stoyanov SR, Hides L, Kavanagh DJ, et al. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015;3:E27. doi:10.2196 /mhealth.3422.
Incorporating mobile apps into patient care programs can add immense value. Mobile apps enable data collection when a patient is beyond the walls of a doctor’s office and equip clinicians with new and relevant patient data. Patient engagement apps also provide a mechanism to “nudge” patients to encourage adherence to their care programs. These additional data and increased patient adherence can enable more personalized care,1 and ultimately can lead to improved outcomes. For example, a meta-analysis of 1,657 patients with diabetes showed a 5% reduction in hemoglobin A1c (HbA1c) values for those who used a diabetes-related app.2 The literature also shows positive results for heart failure, weight management, smoking reduction, and lifestyle improvement.3-5 Given their value, why aren’t patient engagement apps more routinely integrated into patient care programs?
From a software development perspective, mobile apps are fairly easy to create. However, from a user retention standpoint, creating an app with a large, sustainable userbase is challenging.5 User retention is measured in monthly active users. We are familiar with unused apps collecting digital dust on our smartphone home screens. A 2019 study showed that 25% of people typically use an application only once,6 and health care apps are not an exception. There are hundreds of thousands of mobile health apps on the market, but only 7% of these applications have more than 50,000 monthly active users. Further, 62% of digital health apps have less than 1,000 monthly active users.7
Using a new app daily or several times weekly requires new habit formation. Anyone who has tried to incorporate a new routine into their daily life knows how difficult habit formation can be. However, ObGyn patients may be particularly well suited to incorporate ObGyn-related apps into their care, given how many women already use mobile applications to track their menstrual cycles. A recent survey found that across all age groups, 47% of women use a mobile phone app to track their menstrual cycle,8 compared with 8% of US adults who regularly use an app to measure general health metrics.7 This removes one of the largest obstacles of market penetration since the habit of using an app for ObGyn purposes has already been established. As such, it presents an exciting opportunity to capitalize on the userbase already leveraging mobile apps to track their cycles and expand the patient engagement footprint into additional features that can broaden care to create a seamless, holistic patient application for ObGyn patient care.
One can envision a future in which a patient is “prescribed” an ObGyn app during their ObGyn appointment. Within the app, the patient can track their health data, engage with health providers, and gain access to educational materials. The clinician would be able to access data captured in the patient app at an aggregate level to analyze trends over time.
Current, patient-facing ObGyn mobile apps available for download on smartphones are for targeted aspects of ObGyn health. For example, there are separate apps for menstrual cycle tracking, contraception education, and medication adherence tracking. In the future, it would be ideal for clinicians and patients to have access to a single, holistic ObGyn mobile app that supports the end-to-end ObGyn patient journey, one in which clinicians could turn modules on or off given specific patient concerns. The technology for this type of holistic patient engagement platform exists, but unfortunately it is not as simple as downloading a mobile app. Standing up an end-to-end patient engagement platform requires enterprise-wide buy-in, tailoring user workflows, and building out integrations (eg, integrating provider dashboards into the existing electronic health record system). Full-scale solutions are powerful, but they can be expensive and time consuming to stand up. Until there is a more streamlined, outside-the-box ObGyn-tailored solution, there are patientfacing mobile apps available to support your patients for specific concerns.
Continue to: The top 3 recommended menstrual cycle tracking apps...
The top 3 recommended menstrual cycle tracking apps from Moglia and colleagues9 are listed in Dr. Chen’s article, “Top free menstrual cycle tracking apps for your patients.”10 The top 3 recommended contraception education mobile apps from Lunde and colleagues11 are listed in TABLE 1 and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, important special features).12 The top 3 recommended patient medication adherence mobile apps from the study by Santo and colleagues13 are listed in TABLE 2. The apps in the Stoyanov et al14 study were evaluated using the 23-item Mobile App Rating System scale. ●
Incorporating mobile apps into patient care programs can add immense value. Mobile apps enable data collection when a patient is beyond the walls of a doctor’s office and equip clinicians with new and relevant patient data. Patient engagement apps also provide a mechanism to “nudge” patients to encourage adherence to their care programs. These additional data and increased patient adherence can enable more personalized care,1 and ultimately can lead to improved outcomes. For example, a meta-analysis of 1,657 patients with diabetes showed a 5% reduction in hemoglobin A1c (HbA1c) values for those who used a diabetes-related app.2 The literature also shows positive results for heart failure, weight management, smoking reduction, and lifestyle improvement.3-5 Given their value, why aren’t patient engagement apps more routinely integrated into patient care programs?
From a software development perspective, mobile apps are fairly easy to create. However, from a user retention standpoint, creating an app with a large, sustainable userbase is challenging.5 User retention is measured in monthly active users. We are familiar with unused apps collecting digital dust on our smartphone home screens. A 2019 study showed that 25% of people typically use an application only once,6 and health care apps are not an exception. There are hundreds of thousands of mobile health apps on the market, but only 7% of these applications have more than 50,000 monthly active users. Further, 62% of digital health apps have less than 1,000 monthly active users.7
Using a new app daily or several times weekly requires new habit formation. Anyone who has tried to incorporate a new routine into their daily life knows how difficult habit formation can be. However, ObGyn patients may be particularly well suited to incorporate ObGyn-related apps into their care, given how many women already use mobile applications to track their menstrual cycles. A recent survey found that across all age groups, 47% of women use a mobile phone app to track their menstrual cycle,8 compared with 8% of US adults who regularly use an app to measure general health metrics.7 This removes one of the largest obstacles of market penetration since the habit of using an app for ObGyn purposes has already been established. As such, it presents an exciting opportunity to capitalize on the userbase already leveraging mobile apps to track their cycles and expand the patient engagement footprint into additional features that can broaden care to create a seamless, holistic patient application for ObGyn patient care.
One can envision a future in which a patient is “prescribed” an ObGyn app during their ObGyn appointment. Within the app, the patient can track their health data, engage with health providers, and gain access to educational materials. The clinician would be able to access data captured in the patient app at an aggregate level to analyze trends over time.
Current, patient-facing ObGyn mobile apps available for download on smartphones are for targeted aspects of ObGyn health. For example, there are separate apps for menstrual cycle tracking, contraception education, and medication adherence tracking. In the future, it would be ideal for clinicians and patients to have access to a single, holistic ObGyn mobile app that supports the end-to-end ObGyn patient journey, one in which clinicians could turn modules on or off given specific patient concerns. The technology for this type of holistic patient engagement platform exists, but unfortunately it is not as simple as downloading a mobile app. Standing up an end-to-end patient engagement platform requires enterprise-wide buy-in, tailoring user workflows, and building out integrations (eg, integrating provider dashboards into the existing electronic health record system). Full-scale solutions are powerful, but they can be expensive and time consuming to stand up. Until there is a more streamlined, outside-the-box ObGyn-tailored solution, there are patientfacing mobile apps available to support your patients for specific concerns.
Continue to: The top 3 recommended menstrual cycle tracking apps...
The top 3 recommended menstrual cycle tracking apps from Moglia and colleagues9 are listed in Dr. Chen’s article, “Top free menstrual cycle tracking apps for your patients.”10 The top 3 recommended contraception education mobile apps from Lunde and colleagues11 are listed in TABLE 1 and are detailed with a shortened version of the APPLICATIONS scoring system, APPLI (app comprehensiveness, price, platform, literature use, important special features).12 The top 3 recommended patient medication adherence mobile apps from the study by Santo and colleagues13 are listed in TABLE 2. The apps in the Stoyanov et al14 study were evaluated using the 23-item Mobile App Rating System scale. ●
- van Dijk MR, Koster MPH, et al. Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod BioMed Online. 2017;35:453-460. doi:10.1016/j. rbmo.2017.06.014.
- Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a metaanalysis. Diabet Med. 2011;28:455-463. doi:10.1111/j.1464- 5491.2010.03180.x.
- Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients. Ann Intern Med. 2014;161(10 suppl):S5-S12. doi:10.7326/m13-3005.
- Dennison L, Morrison L, Conway G, et al. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J Med Internet Res. 2013;15:E86. doi:10.2196/jmir.2583.
- Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13:127. doi:10.1186/s12966- 016-0454-y.
- 25% of users abandon apps after one use. Upland Software website. Accessed May 6, 2021. https://uplandsoftware.com /localytics/resources/blog/25-of-users-abandon-apps-afterone-use/.
- mHealth economics 2017/2018 – connectivity in digital health. Published March 5, 2019. Accessed May 6, 2021. https:// research2guidance.com/product/connectivity-in-digitalhealth/.
- Epstein DA, Lee NB, Kang JH, et al. Examining menstrual tracking to inform the design of personal informatics tools. Proc SIGCHI Conf Hum Factor Comput Syst. 2017;2017:6876- 6888. doi:10.1145/3025453.3025635.
- Moglia M, Nguyen H, Chyjek K, et al. Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICATIONS scoring system. Obstet Gynecol. 2016;127:1153-1160. doi:10.1097/AOG.0000000000001444.
- Chen KT. Top free menstrual cycle tracking apps for your patients. OBG Manag. 2017;27:44-45.
- Lunde B, Perry R, Sridhar A, et al. An evaluation of contraception education and health promotion applications for patients. Womens Health Issues. 2017;27:29-35. doi:10.1016/j.whi.2016.09.012.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483. doi:10.1097 /AOG.0000000000000842.
- Santo K, Richtering SS, Chalmers J, et al. Mobile phone apps to improve medication adherence: a systematic stepwise process to identify high-quality apps. JMIR Mhealth Uhealth. 2016;4:E132. doi:10.2196/mhealth.6742.
- Stoyanov SR, Hides L, Kavanagh DJ, et al. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015;3:E27. doi:10.2196 /mhealth.3422.
- van Dijk MR, Koster MPH, et al. Healthy preconception nutrition and lifestyle using personalized mobile health coaching is associated with enhanced pregnancy chance. Reprod BioMed Online. 2017;35:453-460. doi:10.1016/j. rbmo.2017.06.014.
- Liang X, Wang Q, Yang X, et al. Effect of mobile phone intervention for diabetes on glycaemic control: a metaanalysis. Diabet Med. 2011;28:455-463. doi:10.1111/j.1464- 5491.2010.03180.x.
- Laing BY, Mangione CM, Tseng C-H, et al. Effectiveness of a smartphone application for weight loss compared with usual care in overweight primary care patients. Ann Intern Med. 2014;161(10 suppl):S5-S12. doi:10.7326/m13-3005.
- Dennison L, Morrison L, Conway G, et al. Opportunities and challenges for smartphone applications in supporting health behavior change: qualitative study. J Med Internet Res. 2013;15:E86. doi:10.2196/jmir.2583.
- Schoeppe S, Alley S, Van Lippevelde W, et al. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act. 2016;13:127. doi:10.1186/s12966- 016-0454-y.
- 25% of users abandon apps after one use. Upland Software website. Accessed May 6, 2021. https://uplandsoftware.com /localytics/resources/blog/25-of-users-abandon-apps-afterone-use/.
- mHealth economics 2017/2018 – connectivity in digital health. Published March 5, 2019. Accessed May 6, 2021. https:// research2guidance.com/product/connectivity-in-digitalhealth/.
- Epstein DA, Lee NB, Kang JH, et al. Examining menstrual tracking to inform the design of personal informatics tools. Proc SIGCHI Conf Hum Factor Comput Syst. 2017;2017:6876- 6888. doi:10.1145/3025453.3025635.
- Moglia M, Nguyen H, Chyjek K, et al. Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICATIONS scoring system. Obstet Gynecol. 2016;127:1153-1160. doi:10.1097/AOG.0000000000001444.
- Chen KT. Top free menstrual cycle tracking apps for your patients. OBG Manag. 2017;27:44-45.
- Lunde B, Perry R, Sridhar A, et al. An evaluation of contraception education and health promotion applications for patients. Womens Health Issues. 2017;27:29-35. doi:10.1016/j.whi.2016.09.012.
- Chyjek K, Farag S, Chen KT. Rating pregnancy wheel applications using the APPLICATIONS scoring system. Obstet Gynecol. 2015;125:1478-1483. doi:10.1097 /AOG.0000000000000842.
- Santo K, Richtering SS, Chalmers J, et al. Mobile phone apps to improve medication adherence: a systematic stepwise process to identify high-quality apps. JMIR Mhealth Uhealth. 2016;4:E132. doi:10.2196/mhealth.6742.
- Stoyanov SR, Hides L, Kavanagh DJ, et al. Mobile app rating scale: a new tool for assessing the quality of health mobile apps. JMIR Mhealth Uhealth. 2015;3:E27. doi:10.2196 /mhealth.3422.
Dermatoethics for Dermatology Residents
As dermatology residents, we have a lot on our plates. With so many diagnoses to learn and treatments to understand, the sheer volume of knowledge we are expected to be familiar with sometimes can be overwhelming. The thought of adding yet another thing to the list of many things we already need to know—least of all a topic such as dermatoethics—may be unappealing. This article will discuss the importance of ethics training in dermatology residency as well as provide helpful resources for how this training can be achieved.
Professionalism as a Core Competency
The Accreditation Council for Graduate Medical Education (ACGME) considers professionalism as 1 of its 6 core competencies.1 These competencies provide a conceptual framework detailing the domains physicians should be proficient in before they can enter autonomous practice. When it comes to professionalism, residents are expected to demonstrate compassion, integrity, and respect for others; honesty with patients; respect for patient confidentiality and autonomy; appropriate relationships with patients; accountability to patients, society, and the profession; and a sensitivity and responsiveness to diverse patient population.1
The ACGME milestones are intended to assess resident development within the 6 competencies with more specific parameters for evaluation.2 Those pertaining to professionalism evaluate a resident’s ability to demonstrate professional behavior, an understanding of ethical principles, accountability, and conscientiousness, as well as self-awareness and the ability to seek help for personal or professional well-being. The crux of the kinds of activities that constitute acquisition of these professional skills are specialty specific. The ACGME ultimately believes that having a working knowledge of professionalism and ethical principles prepares residents for practicing medicine in the real world. Because of these requirements, residency programs are expected to provide resources for residents to explore ethical problems faced by dermatologists.
Beyond “Passing” Residency
The reality is that learning about medical ethics and practicing professional behavior is not just about ticking boxes to get ACGME accreditation or to “pass” residency. The data suggest that having a strong foundation in these principles is good for overall personal well-being, job satisfaction, and patient care. Studies have shown that unprofessional behavior in medical school is correlated to disciplinary action by state licensing boards against practicing physicians.3,4 In fact, a study found that in one cohort of physicians (N=68), 95% of disciplinary actions were for lapses in professionalism, which included activities such as sexual misconduct and inappropriate prescribing.4 Behaving appropriately protects your license to practice medicine.
Thinking through these problematic ethical scenarios also goes beyond coming up with the right answer. Exploring ethical conundrums is thought to develop analytical skills that can help one navigate future tricky situations that can be morally distressing and can lead to burnout. Introspection and self-awareness coupled with these skills ideally will help physicians think through sensitive and difficult situations with the courage to hold true to their convictions and ultimately uphold the professionalism of the specialty.5
Self-awareness has the additional bonus of empowering physicians to acknowledge personal and professional limitations with the goal of seeking help when it is needed before it is too late. It comes as no surprise that how we feel as physicians directly impacts how we treat our patients. One study found that depressed residents were more than 6 times more likely to make medication errors compared to nondepressed colleagues.6 Regularly taking stock of our professional and personal reserves can go a long way to improving overall well-being.
Resources for Dermatoethics Training
The best starting point for developing a robust dermatoethics curriculum is the material provided by the American Board of Dermatology, which is available online.7 An ad hoc subcommittee of the American Board of Dermatology composed of experts in dermatoethics and resident education reviewed relevant ethics literature and identified 6 core domains considered fundamental to dermatology resident education in ethics and professionalism.8 This team also provided a thorough list of relevant background readings for each topic. To cover pertinent material, the subcommittee recommended a 60-minute teaching session every other month with the intent of covering all the material over a 3-year period. If your program directors are not aware of this great resource and you feel your own ethics training may be lacking, bringing this up as a template might be helpful. A detailed description of an innovative dermatoethics curriculum organized at the Department of Dermatology at the Warren Alpert Medical School of Brown University (Providence, Rhode Island) in 2001 also may serve as a guide for programs hoping to design their own approach.5
For those interested in self-study, there is an excellent text dedicated to dermatoethics, which is aptly entitled Dermatoethics: Contemporary Ethics and Professionalism in Dermatology.9 This book offers superb case-based discussions on a wide range of ethical quandaries that dermatologists may face, ranging from unsolicited dermatologic advice (eg, Is it wrong to tell the person next to you in the grocery store that they might have a melanoma?) to research and publication ethics. This text provides a toolkit for handling tough situations in the clinic and beyond. The Journal of the American Academy of Dermatology publishes an Ethics Journal Club for which contributors can submit real-life practical ethical dilemmas, and the journal solicits a resolution or response from a dermatoethicist.
Additionally, a pilot curriculum project out of the University of Utah (Salt Lake City, Utah), of which I am a team member, currently is designing and testing several dermatoethics PowerPoint modules with the intention of making this material widely available through medical education portals.
The Hidden Curriculum
A formal curriculum can only provide so much when it comes to ethics training. In truth, much of what we learn as ethically minded dermatologists comes from our day-to-day practice.10 Paying attention to the more informal curriculum that we are immersed in during routine as well as unusual encounters also is important for achieving milestones. Teaching moments for thinking through ethical dilemmas abound, and this approach easily can be incorporated into routine workflow.11 Next time you encounter an ethical situation that gives you pause (eg, Can I biopsy an intubated patient without getting appropriate consent?), talk it through with your supervisor. Gems of autonomous practice often can be mined from these off-the-cuff conversations.
Can Professionalism Be Taught?
Finally, it is worth mentioning that while the number of resources available to dermatology residents for honing their ethics skills is increasing, ways of measuring the impact of this additional training in vivo are not.12 There are no good tools available to determine how ethics training influences resident behaviors. Similarly, there is no good evidence for what constitutes the most effective method for teaching medical ethics to trainees. It is a growing field with lots of room for more robust research. For now, the overall goal of a dermatoethics curriculum is to provide a mix of curriculum opportunities, ranging from formal lectures and readings to more informal conversations, with the hope of providing residents a toolbox for dealing with ethical dilemmas and a working knowledge of professionalism.
Final Thoughts
There are several resources available for dermatology programs to provide quality dermatoethics training to their residents. These can be mixed and matched to create a tailored formal curriculum alongside the more informal ethics training that happens in the clinic and on the wards. Providing this education is about more than just fulfilling accreditation requirements. Understanding ethical principles and how they can be applied to navigate sensitive situations is ultimately good for both professional and personal well-being.
- Accreditation Council for Graduate Medical Education. ACGME common program requirements (residency). ACGME website. Accessed June 10, 2021. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2020.pdf
- Edgar L, McLean S, Hogan SO, et al. The milestones guidebook. Accreditation Council for Graduate Medical Education website. Accessed June 10, 2021. acgme.org/portals/0/MilestonesGuidebook.pdf
- Papadakis MA, Teherani A, Banach MA, et al. Disciplinary action by medical boards and prior behavior in medical school. N Engl J Med. 2005;353:2673-2682.
- Papadakis MA, Hodgson CS, Teherani A, et al. Unprofessional behavior in medical school is associated with subsequent disciplinary action by a state medical board. Acad Med. 2004;79:244-249.
- Bercovitch L, Long TP. Dermatoethics: a curriculum in bioethics and professionalism for dermatology residents at Brown Medical School. J Am Acad Dermatol. 2007;56:679-682.
- Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488-491.
- Recommended topics for 3-year dermatoethics curricular cycle. American Board of Dermatology website. Accessed June 10, 2021. https://www.abderm.org/residents-and-fellows/dermatoethics.aspx
- Stoff BK, Grant-Kels JM, Brodell RT, et al. Introducing a curriculum in ethics and professionalism for dermatology residencies. J Am Acad Dermatol. 2018;78:1032-1034.
- Bercovitch L, Perlis C, Stoff BK, et al, eds. Dermatoethics: Contemporary Ethics and Professionalism in Dermatology. 2nd ed. Springer International Publishing; 2021.
- Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med. 1994;69:861-871.
- Aldrich N, Mostow E. Incorporating teaching dermatoethics in a busy outpatient clinic. J Am Acad Dermatol. 2011;65:423-424.
- de la Garza S, Phuoc V, Throneberry S, et al. Teaching medical ethics in graduate and undergraduate medical education: a systematic review of effectiveness. Acad Psychiatry. 2017;41:520-525.
As dermatology residents, we have a lot on our plates. With so many diagnoses to learn and treatments to understand, the sheer volume of knowledge we are expected to be familiar with sometimes can be overwhelming. The thought of adding yet another thing to the list of many things we already need to know—least of all a topic such as dermatoethics—may be unappealing. This article will discuss the importance of ethics training in dermatology residency as well as provide helpful resources for how this training can be achieved.
Professionalism as a Core Competency
The Accreditation Council for Graduate Medical Education (ACGME) considers professionalism as 1 of its 6 core competencies.1 These competencies provide a conceptual framework detailing the domains physicians should be proficient in before they can enter autonomous practice. When it comes to professionalism, residents are expected to demonstrate compassion, integrity, and respect for others; honesty with patients; respect for patient confidentiality and autonomy; appropriate relationships with patients; accountability to patients, society, and the profession; and a sensitivity and responsiveness to diverse patient population.1
The ACGME milestones are intended to assess resident development within the 6 competencies with more specific parameters for evaluation.2 Those pertaining to professionalism evaluate a resident’s ability to demonstrate professional behavior, an understanding of ethical principles, accountability, and conscientiousness, as well as self-awareness and the ability to seek help for personal or professional well-being. The crux of the kinds of activities that constitute acquisition of these professional skills are specialty specific. The ACGME ultimately believes that having a working knowledge of professionalism and ethical principles prepares residents for practicing medicine in the real world. Because of these requirements, residency programs are expected to provide resources for residents to explore ethical problems faced by dermatologists.
Beyond “Passing” Residency
The reality is that learning about medical ethics and practicing professional behavior is not just about ticking boxes to get ACGME accreditation or to “pass” residency. The data suggest that having a strong foundation in these principles is good for overall personal well-being, job satisfaction, and patient care. Studies have shown that unprofessional behavior in medical school is correlated to disciplinary action by state licensing boards against practicing physicians.3,4 In fact, a study found that in one cohort of physicians (N=68), 95% of disciplinary actions were for lapses in professionalism, which included activities such as sexual misconduct and inappropriate prescribing.4 Behaving appropriately protects your license to practice medicine.
Thinking through these problematic ethical scenarios also goes beyond coming up with the right answer. Exploring ethical conundrums is thought to develop analytical skills that can help one navigate future tricky situations that can be morally distressing and can lead to burnout. Introspection and self-awareness coupled with these skills ideally will help physicians think through sensitive and difficult situations with the courage to hold true to their convictions and ultimately uphold the professionalism of the specialty.5
Self-awareness has the additional bonus of empowering physicians to acknowledge personal and professional limitations with the goal of seeking help when it is needed before it is too late. It comes as no surprise that how we feel as physicians directly impacts how we treat our patients. One study found that depressed residents were more than 6 times more likely to make medication errors compared to nondepressed colleagues.6 Regularly taking stock of our professional and personal reserves can go a long way to improving overall well-being.
Resources for Dermatoethics Training
The best starting point for developing a robust dermatoethics curriculum is the material provided by the American Board of Dermatology, which is available online.7 An ad hoc subcommittee of the American Board of Dermatology composed of experts in dermatoethics and resident education reviewed relevant ethics literature and identified 6 core domains considered fundamental to dermatology resident education in ethics and professionalism.8 This team also provided a thorough list of relevant background readings for each topic. To cover pertinent material, the subcommittee recommended a 60-minute teaching session every other month with the intent of covering all the material over a 3-year period. If your program directors are not aware of this great resource and you feel your own ethics training may be lacking, bringing this up as a template might be helpful. A detailed description of an innovative dermatoethics curriculum organized at the Department of Dermatology at the Warren Alpert Medical School of Brown University (Providence, Rhode Island) in 2001 also may serve as a guide for programs hoping to design their own approach.5
For those interested in self-study, there is an excellent text dedicated to dermatoethics, which is aptly entitled Dermatoethics: Contemporary Ethics and Professionalism in Dermatology.9 This book offers superb case-based discussions on a wide range of ethical quandaries that dermatologists may face, ranging from unsolicited dermatologic advice (eg, Is it wrong to tell the person next to you in the grocery store that they might have a melanoma?) to research and publication ethics. This text provides a toolkit for handling tough situations in the clinic and beyond. The Journal of the American Academy of Dermatology publishes an Ethics Journal Club for which contributors can submit real-life practical ethical dilemmas, and the journal solicits a resolution or response from a dermatoethicist.
Additionally, a pilot curriculum project out of the University of Utah (Salt Lake City, Utah), of which I am a team member, currently is designing and testing several dermatoethics PowerPoint modules with the intention of making this material widely available through medical education portals.
The Hidden Curriculum
A formal curriculum can only provide so much when it comes to ethics training. In truth, much of what we learn as ethically minded dermatologists comes from our day-to-day practice.10 Paying attention to the more informal curriculum that we are immersed in during routine as well as unusual encounters also is important for achieving milestones. Teaching moments for thinking through ethical dilemmas abound, and this approach easily can be incorporated into routine workflow.11 Next time you encounter an ethical situation that gives you pause (eg, Can I biopsy an intubated patient without getting appropriate consent?), talk it through with your supervisor. Gems of autonomous practice often can be mined from these off-the-cuff conversations.
Can Professionalism Be Taught?
Finally, it is worth mentioning that while the number of resources available to dermatology residents for honing their ethics skills is increasing, ways of measuring the impact of this additional training in vivo are not.12 There are no good tools available to determine how ethics training influences resident behaviors. Similarly, there is no good evidence for what constitutes the most effective method for teaching medical ethics to trainees. It is a growing field with lots of room for more robust research. For now, the overall goal of a dermatoethics curriculum is to provide a mix of curriculum opportunities, ranging from formal lectures and readings to more informal conversations, with the hope of providing residents a toolbox for dealing with ethical dilemmas and a working knowledge of professionalism.
Final Thoughts
There are several resources available for dermatology programs to provide quality dermatoethics training to their residents. These can be mixed and matched to create a tailored formal curriculum alongside the more informal ethics training that happens in the clinic and on the wards. Providing this education is about more than just fulfilling accreditation requirements. Understanding ethical principles and how they can be applied to navigate sensitive situations is ultimately good for both professional and personal well-being.
As dermatology residents, we have a lot on our plates. With so many diagnoses to learn and treatments to understand, the sheer volume of knowledge we are expected to be familiar with sometimes can be overwhelming. The thought of adding yet another thing to the list of many things we already need to know—least of all a topic such as dermatoethics—may be unappealing. This article will discuss the importance of ethics training in dermatology residency as well as provide helpful resources for how this training can be achieved.
Professionalism as a Core Competency
The Accreditation Council for Graduate Medical Education (ACGME) considers professionalism as 1 of its 6 core competencies.1 These competencies provide a conceptual framework detailing the domains physicians should be proficient in before they can enter autonomous practice. When it comes to professionalism, residents are expected to demonstrate compassion, integrity, and respect for others; honesty with patients; respect for patient confidentiality and autonomy; appropriate relationships with patients; accountability to patients, society, and the profession; and a sensitivity and responsiveness to diverse patient population.1
The ACGME milestones are intended to assess resident development within the 6 competencies with more specific parameters for evaluation.2 Those pertaining to professionalism evaluate a resident’s ability to demonstrate professional behavior, an understanding of ethical principles, accountability, and conscientiousness, as well as self-awareness and the ability to seek help for personal or professional well-being. The crux of the kinds of activities that constitute acquisition of these professional skills are specialty specific. The ACGME ultimately believes that having a working knowledge of professionalism and ethical principles prepares residents for practicing medicine in the real world. Because of these requirements, residency programs are expected to provide resources for residents to explore ethical problems faced by dermatologists.
Beyond “Passing” Residency
The reality is that learning about medical ethics and practicing professional behavior is not just about ticking boxes to get ACGME accreditation or to “pass” residency. The data suggest that having a strong foundation in these principles is good for overall personal well-being, job satisfaction, and patient care. Studies have shown that unprofessional behavior in medical school is correlated to disciplinary action by state licensing boards against practicing physicians.3,4 In fact, a study found that in one cohort of physicians (N=68), 95% of disciplinary actions were for lapses in professionalism, which included activities such as sexual misconduct and inappropriate prescribing.4 Behaving appropriately protects your license to practice medicine.
Thinking through these problematic ethical scenarios also goes beyond coming up with the right answer. Exploring ethical conundrums is thought to develop analytical skills that can help one navigate future tricky situations that can be morally distressing and can lead to burnout. Introspection and self-awareness coupled with these skills ideally will help physicians think through sensitive and difficult situations with the courage to hold true to their convictions and ultimately uphold the professionalism of the specialty.5
Self-awareness has the additional bonus of empowering physicians to acknowledge personal and professional limitations with the goal of seeking help when it is needed before it is too late. It comes as no surprise that how we feel as physicians directly impacts how we treat our patients. One study found that depressed residents were more than 6 times more likely to make medication errors compared to nondepressed colleagues.6 Regularly taking stock of our professional and personal reserves can go a long way to improving overall well-being.
Resources for Dermatoethics Training
The best starting point for developing a robust dermatoethics curriculum is the material provided by the American Board of Dermatology, which is available online.7 An ad hoc subcommittee of the American Board of Dermatology composed of experts in dermatoethics and resident education reviewed relevant ethics literature and identified 6 core domains considered fundamental to dermatology resident education in ethics and professionalism.8 This team also provided a thorough list of relevant background readings for each topic. To cover pertinent material, the subcommittee recommended a 60-minute teaching session every other month with the intent of covering all the material over a 3-year period. If your program directors are not aware of this great resource and you feel your own ethics training may be lacking, bringing this up as a template might be helpful. A detailed description of an innovative dermatoethics curriculum organized at the Department of Dermatology at the Warren Alpert Medical School of Brown University (Providence, Rhode Island) in 2001 also may serve as a guide for programs hoping to design their own approach.5
For those interested in self-study, there is an excellent text dedicated to dermatoethics, which is aptly entitled Dermatoethics: Contemporary Ethics and Professionalism in Dermatology.9 This book offers superb case-based discussions on a wide range of ethical quandaries that dermatologists may face, ranging from unsolicited dermatologic advice (eg, Is it wrong to tell the person next to you in the grocery store that they might have a melanoma?) to research and publication ethics. This text provides a toolkit for handling tough situations in the clinic and beyond. The Journal of the American Academy of Dermatology publishes an Ethics Journal Club for which contributors can submit real-life practical ethical dilemmas, and the journal solicits a resolution or response from a dermatoethicist.
Additionally, a pilot curriculum project out of the University of Utah (Salt Lake City, Utah), of which I am a team member, currently is designing and testing several dermatoethics PowerPoint modules with the intention of making this material widely available through medical education portals.
The Hidden Curriculum
A formal curriculum can only provide so much when it comes to ethics training. In truth, much of what we learn as ethically minded dermatologists comes from our day-to-day practice.10 Paying attention to the more informal curriculum that we are immersed in during routine as well as unusual encounters also is important for achieving milestones. Teaching moments for thinking through ethical dilemmas abound, and this approach easily can be incorporated into routine workflow.11 Next time you encounter an ethical situation that gives you pause (eg, Can I biopsy an intubated patient without getting appropriate consent?), talk it through with your supervisor. Gems of autonomous practice often can be mined from these off-the-cuff conversations.
Can Professionalism Be Taught?
Finally, it is worth mentioning that while the number of resources available to dermatology residents for honing their ethics skills is increasing, ways of measuring the impact of this additional training in vivo are not.12 There are no good tools available to determine how ethics training influences resident behaviors. Similarly, there is no good evidence for what constitutes the most effective method for teaching medical ethics to trainees. It is a growing field with lots of room for more robust research. For now, the overall goal of a dermatoethics curriculum is to provide a mix of curriculum opportunities, ranging from formal lectures and readings to more informal conversations, with the hope of providing residents a toolbox for dealing with ethical dilemmas and a working knowledge of professionalism.
Final Thoughts
There are several resources available for dermatology programs to provide quality dermatoethics training to their residents. These can be mixed and matched to create a tailored formal curriculum alongside the more informal ethics training that happens in the clinic and on the wards. Providing this education is about more than just fulfilling accreditation requirements. Understanding ethical principles and how they can be applied to navigate sensitive situations is ultimately good for both professional and personal well-being.
- Accreditation Council for Graduate Medical Education. ACGME common program requirements (residency). ACGME website. Accessed June 10, 2021. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2020.pdf
- Edgar L, McLean S, Hogan SO, et al. The milestones guidebook. Accreditation Council for Graduate Medical Education website. Accessed June 10, 2021. acgme.org/portals/0/MilestonesGuidebook.pdf
- Papadakis MA, Teherani A, Banach MA, et al. Disciplinary action by medical boards and prior behavior in medical school. N Engl J Med. 2005;353:2673-2682.
- Papadakis MA, Hodgson CS, Teherani A, et al. Unprofessional behavior in medical school is associated with subsequent disciplinary action by a state medical board. Acad Med. 2004;79:244-249.
- Bercovitch L, Long TP. Dermatoethics: a curriculum in bioethics and professionalism for dermatology residents at Brown Medical School. J Am Acad Dermatol. 2007;56:679-682.
- Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488-491.
- Recommended topics for 3-year dermatoethics curricular cycle. American Board of Dermatology website. Accessed June 10, 2021. https://www.abderm.org/residents-and-fellows/dermatoethics.aspx
- Stoff BK, Grant-Kels JM, Brodell RT, et al. Introducing a curriculum in ethics and professionalism for dermatology residencies. J Am Acad Dermatol. 2018;78:1032-1034.
- Bercovitch L, Perlis C, Stoff BK, et al, eds. Dermatoethics: Contemporary Ethics and Professionalism in Dermatology. 2nd ed. Springer International Publishing; 2021.
- Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med. 1994;69:861-871.
- Aldrich N, Mostow E. Incorporating teaching dermatoethics in a busy outpatient clinic. J Am Acad Dermatol. 2011;65:423-424.
- de la Garza S, Phuoc V, Throneberry S, et al. Teaching medical ethics in graduate and undergraduate medical education: a systematic review of effectiveness. Acad Psychiatry. 2017;41:520-525.
- Accreditation Council for Graduate Medical Education. ACGME common program requirements (residency). ACGME website. Accessed June 10, 2021. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2020.pdf
- Edgar L, McLean S, Hogan SO, et al. The milestones guidebook. Accreditation Council for Graduate Medical Education website. Accessed June 10, 2021. acgme.org/portals/0/MilestonesGuidebook.pdf
- Papadakis MA, Teherani A, Banach MA, et al. Disciplinary action by medical boards and prior behavior in medical school. N Engl J Med. 2005;353:2673-2682.
- Papadakis MA, Hodgson CS, Teherani A, et al. Unprofessional behavior in medical school is associated with subsequent disciplinary action by a state medical board. Acad Med. 2004;79:244-249.
- Bercovitch L, Long TP. Dermatoethics: a curriculum in bioethics and professionalism for dermatology residents at Brown Medical School. J Am Acad Dermatol. 2007;56:679-682.
- Fahrenkopf AM, Sectish TC, Barger LK, et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488-491.
- Recommended topics for 3-year dermatoethics curricular cycle. American Board of Dermatology website. Accessed June 10, 2021. https://www.abderm.org/residents-and-fellows/dermatoethics.aspx
- Stoff BK, Grant-Kels JM, Brodell RT, et al. Introducing a curriculum in ethics and professionalism for dermatology residencies. J Am Acad Dermatol. 2018;78:1032-1034.
- Bercovitch L, Perlis C, Stoff BK, et al, eds. Dermatoethics: Contemporary Ethics and Professionalism in Dermatology. 2nd ed. Springer International Publishing; 2021.
- Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med. 1994;69:861-871.
- Aldrich N, Mostow E. Incorporating teaching dermatoethics in a busy outpatient clinic. J Am Acad Dermatol. 2011;65:423-424.
- de la Garza S, Phuoc V, Throneberry S, et al. Teaching medical ethics in graduate and undergraduate medical education: a systematic review of effectiveness. Acad Psychiatry. 2017;41:520-525.
Resident Pearls
- Professionalism is one of the 6 core competencies used by the Accreditation Council for Graduate Medical Education (ACGME) to evaluate physician preparedness for autonomous practice. Dermatology residency programs are expected to provide resources for achieving this competency.
- Several resources for exploring ethical issues in dermatology are available and can be utilized to create a formal curriculum alongside the more tacit learning that takes place in daily practice.
- Learning about ethical principles and their application can ultimately help practicing physicians avoid disciplinary action and improve overall well-being.
Difficult patient, or something else? A review of personality disorders
Specific behaviors or expressed thoughts may signal a need for screening. Take into account an individual’s strengths and limitations when designing a Tx approach.
THE CASES
Winston S* is a 23-year-old man referred by a psychiatrist colleague for primary care. He works delivering papers in the early morning hours and spends his day alone in his apartment mainly eating frozen pizza. He has worked solitary jobs his entire life and says he prefers it that way. His answers to questions lack emotion. He doesn’t seem to have any friends or regular contact with family. He follows the medical advice he receives but can’t seem to get out of the house to exercise or socialize. His psychiatrist was treating him with a selective serotonin reuptake inhibitor for depression when he was referred.
Denise L* is a 37-year-old woman who transferred to your practice because she says the previous practice’s office manager was disrespectful and the doctor did not listen to her. She has been “very appreciative” of you and your “well-run office.” You have addressed her fibromyalgia and she has shared several personal details about her life. In the following weeks, you receive several phone calls and messages from her. At a follow-up visit, she asks questions about your family and seems agitated when you hesitate to answer. She questions whether you remember details of her history. She pushes, “Did you remember that, doctor?” She also mentions that your front desk staff seems rude to her.
Ruth B* is an 82-year-old woman whose blood pressure measured in your office is 176/94 mm Hg. When you recommend starting a medication and getting blood tests, she responds with a litany of fearful questions. She seems immobilized by worries about treatment and equally so about the risks of nontreatment. You can’t seem to get past the anxiety to decide on a satisfactory plan. She has to write everything down on a notepad and worries if she does not get every detail.
●
* This patient’s name has been changed to protect his identity. The other 2 patients are an amalgam of patients for whom the authors have provided care.
According to a survey of practicing primary care physicians, as many as 15% of patient encounters can be difficult.1 Demanding, intrusive, or angry patients who reject health care interventions are often-cited sources of these difficulties.2,3 While it is true that patient, physician, and environmental factors may contribute to challenging interactions, some patients who are “difficult” may actually have a personality disorder that requires a distinctive approach to care. Recognizing these patients can help empower physicians to provide compassionate and effective care, reduce team angst, and minimize burnout.
❚ What qualifies as a personality disorder? A personality disorder is an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is unchanging over time, and leads to distress or impairment in social or occupational functioning.4 The prevalence of any personality disorder seems to have increased over the past decade from 9.1%4 to 12.16%.5 The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classifies personality disorders in 3 clusters—A, B, and C (TABLE4)—with prevalence rates at 7.23%, 5.53%, and 6.7%, respectively.5 The review below will focus on the distinct personality disorders exhibited by the patients described in the opening cases.
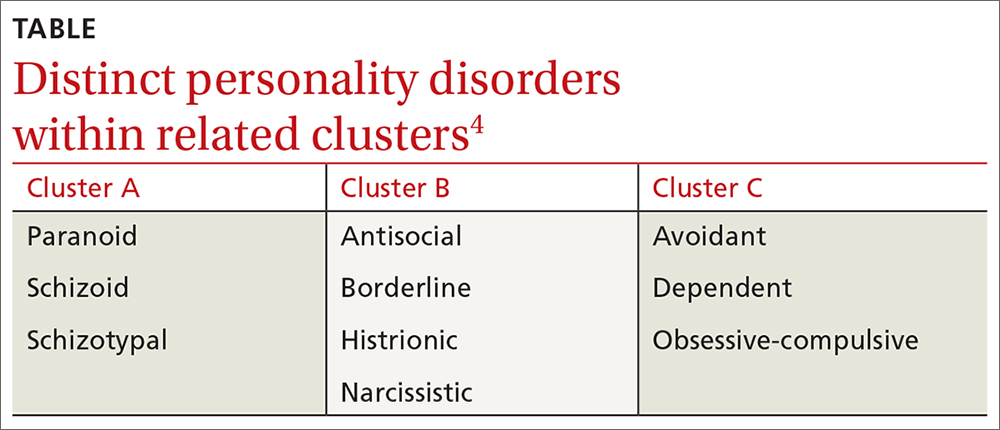
Continue to: A closer look at the clusters...
A closer look at the clusters
Cluster A disorders
Paranoid, schizoid, and schizotypal disorders are part of this cluster. These patients exhibit odd or eccentric thinking and behavior. Individuals with schizoid personality disorder, for instance, usually lack relationships and lack the desire to acquire and maintain relationships.4 They often organize their lives to remain isolated and will choose occupations that require little social interaction. They sometimes view themselves as observers rather than participants in their own lives.6
Cluster B disorders
Dramatic, overly emotional, or unpredictable thinking and behavior are characteristic of individuals who have antisocial, borderline, histrionic, or narcissistic disorders. Patients with borderline personality disorder (BPD), for example, demonstrate a longstanding pattern of instability in affect, self-image, and relationships.4 Patients with BPD often display extreme interpersonal hypersensitivity and make frantic efforts to avoid real or imagined abandonment. Identity disturbance, feelings of emptiness, and efforts to avoid abandonment have all been associated with increased suicide risk.7
In a primary care setting, such a patient may display extremely strong reactions to minor disappointments. When the physician is unavailable for a last-minute appointment or to authorize an unscheduled medication refill or to receive an after-hours phone call, the patient may become irate. The physician, who previously was idealized by the patient as “the only person who understands me,” is now devalued as “the worst doctor I’ve ever had.”8
Cluster C disorders
With these individuals, anxious or fearful thinking and behavior predominate. Avoidant, dependent, and obsessive-compulsive disorders are included in this cluster.
Dependent personality disorder (DPD) is characterized by a pervasive and extreme need to be taken care of. Submissive and clingy behavior and fear of separation are excessive. This patient may have difficulty making everyday decisions, being assertive, or expressing disagreement with others.4
Obsessive-compulsive personality disorder falls in this cluster and is typified by a pervasive preoccupation with orderliness, perfectionism, and control, at the price of flexibility and efficiency. This individual may be reluctant to get rid of sentimental objects, have rigid moral beliefs, and have significant difficulty working with others who do not follow their rules.4
Continue to: These clues may suggest...
These clues may suggest a personality disorder
If you find that encounters with a particular patient are growing increasingly difficult, consider whether the following behaviors, attitudes, and patterns of thinking are coming into play. If they are, you may want to consider using a screening tool, which we’ll discuss in a moment.
❚ Clues to cluster A disorders
- The patient has no peer relationships outside immediate family.
- The patient almost always chooses solitary activities for work and personal enjoyment.
❚ Cluster B clues
- Hypersensitivity to treatment disagreements or cancelled appointments are common (and likely experienced as rejection).
- Mood changes occur very quickly, even during a single visit.
- There is a history of many failed relationships with providers and others.
- The patient will describe an individual as both “wonderful” and “terrible” (ie, splitting) and may do so during the course of one visit.
- The patient may also split groups (eg, medical staff) by affective extremes (eg, adoration and hatred).
- The patient may hint at suicide or acts of self-harm.7
❚ Cluster C clues
- There is an excessive dependency on family, friends, or providers.
- Significant anxiety is experienced when the patient has to make an independent decision.
- There is a fear of relationship loss and resultant vulnerability to exploitation or abuse.
- Pervasive perfectionism makes treatment planning or course changes difficult.
- Anxiety and fear are unrelieved despite support and ample information.
Consider these screening tools
Several screening tools for personality disorders can be used to follow up on your initial clinical impressions. We also highly recommend you consider concurrent screening for substance abuse, as addiction is a common comorbidity with personality disorders.
❚
❚ A sampling of screening tools. The Standardised Assessment of Personality Abbreviated Scale (SAPAS)9 is an 8-item measure that correlates well with disorders in clusters A and C.
BPD (cluster B) has many brief scale options, including the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD).10 This 10-item questionnaire demonstrates sensitivity and specificity for BPD.
The International Personality Disorder Examination (IPDE) includes a 15-minute screening tool to help identify patients who may have any personality disorder, regardless of cluster.11
Improve patient encounters with these Tx pearls
In the family medicine clinic, a collaborative primary care and behavioral health team can be extremely helpful in the diagnosis and management of patients with personality disorders.12 First-line treatment of these disorders is psychotherapy, whereas medications are mainly used for symptom management. See Black and colleagues’ work for a thorough discussion on psychopharmacology considerations with personality disorders. 13
The following tips can help you to improve your interactions with patients who have personality disorders.
❚ Cluster A approaches
- Recommend treatment that respects the patient’s need for relative isolation.14
- Don’t be personally offended by your patient’s flat or disinterested affect or concrete thinking; don’t let it diminish the emotional support you provide.6
- Consult with a health psychologist (who has expertise in physical health conditions, brief treatments, and the medical system) to connect the patient with a long-term therapist. It is better to focus on fundamental changes, rather than employing brief behavioral techniques, for symptom relief. Patients with personality disorders tend to have better outcomes with long-term psychological care.15
❚ Cluster B approaches
- Set boundaries—eg, specific time limits for visits—and keep them.8
- Schedule brief, more frequent, appointments to reduce perceived feelings of abandonment.
- Coordinate plans with the entire clinic team to avoid splitting and blaming.16
- Avoid providing patients with personal information, as it may provide fodder for splitting behavior. 8
- Do not take things personally. Let patients “own” their own distress. These patients often take an emotional toll on the provider.16
- Engage the help of a health psychologist to reduce burnout and for more long-term continuity of care. A health psychologist who specializes in dialectical behavioral therapy to work on emotion regulation, distress tolerance, and interpersonal effectiveness would be ideal.17
Continue to: Cluster C approaches...
❚
❚ Cluster C approaches
- Engage the help of family and other trusted individuals in supporting treatment plans.18,19
- Try to provide just 2 treatment choices to the patient and reinforce his or her responsibility to help make the decision collaboratively. This step is important since it is difficult to enhance autonomy in these patients.20
- Engage the help of a cognitive behavioral therapist who can work on assertiveness and problem-solving skills.19
- Be empathetic with the patient and patiently build a trusting relationship, rather than “arguing” with the patient about each specific worry.20
- Make only one change at a time. Give small assignments to the patient, such as monitoring symptoms or reading up on their condition. These can help the patient feel more in control.21
- Present information in brief, clear terms. Avoid “grey areas” to reduce anxiety.21
- Engage a behavioral health provider to reduce rigid expectations and ideally increase feelings of self-esteem; this has been shown to predict better treatment outcomes.22
CASES
Mr. S displays cluster-A characteristics of schizoid personality disorder in addition to the depression he is being treated for. His physician was not put off by his flat affect and respected his limitations with social activities. Use of a stationary bike was recommended for exercise rather than walks outdoors. He also preferred phone calls to in-person encounters, so his follow-up visits were conducted by phone.
Ms. L exhibits cluster-B characteristics of BPD. You begin the tricky dance of setting limits, keeping communication clear, and not blaming yourself or others on your team for Ms. L’s feelings. You schedule regular visits with explicit time limits and discuss with your entire team how to avoid splitting. You involve a psychologist, familiar with treating BPD, who helps the patient learn positive interpersonal coping skills.
Ms. B displays cluster-C characteristics of dependent and obsessive-compulsive personality disorders. At her follow-up visit, you provide a great deal of empathy and try not to argue her out of each worry that she brings up. You make one change at a time and enlist the help of her daughter in giving her pills at home and offering reassurance. You collaborate with a cognitive behavioral therapist who works on exposing her to moderately anxiety-provoking situations/decisions.
1. Hull SK, Broquet K. How to manage difficult patient encounters. Fam Pract Manag. 2007;14:30-34.
2. Groves JE. Taking care of the hateful patient. N Engl J Med.1978;298: 883-887.
3. O’Dowd TC. Five years of heartsink patients in primary care. BMJ. 1988;297:528-530.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition (DSM-5). American Psychiatric Publishing; 2013.
5. Volkert J, Gablonski TC, Rabung S. Prevalence of personality disorders in the general adult population in Western countries: systematic review and meta-analysis. Br J Psychiatry. 2018;213:709-715.
6. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32:515-528.
7. Yen S, Peters JR, Nishar S, et al. Association of borderline personality disorder criteria with suicide attempts: findings from the collaborative longitudinal study of personality disorders over 10 years of follow-up. JAMA Psychiatry. 2021;78:187-194.
8. Dubovsky AN, Kiefer MM. Borderline personality disorder in the primary care setting. Med Clin North Am. 2014;98:1049-1064.
9. Hesse M, Moran P. (2010). Screening for personality disorder with the Standardised Assessment of Personality: Abbreviated Scale (SAPAS): further evidence of concurrent validity. BMC Psychiatry. 2010;10:10.
10. Zanarini MC, Vujanovic AA, Parachini EA, et al. A screening measure for BPD: the McLean screening instrument for borderline personality disorder (MSI-BPD). J Pers Disord. 2003;17:568-573.
11. Loranger AW, Sartorius N, Andreoli A, et al. The International Personality Disorder Examination. The World Health Organization/Alcohol, Drug Abuse, and Mental Health Administration international pilot study of personality disorders. Arch Gen Psychiatry. 1994;51:215-224.12. Nelson KJ, Skodol A, Friedman M. Pharmacotherapy for personality disorders. UpToDate. Accessed April 22, 2021. www.uptodate.com/contents/pharmacotherapy-for-personality-disorders
13. Black D, Paris J, Schulz C. Evidence-based integrated biopsychosocial treatment of borderline personality disorder. In: Muse M (ed). Cognitive Behavioral Psychopharmacology: the Clinical Practice of Evidence-Based Biopsychosocial Integration. Wiley; 2017:137-166.
14. Beck AT, Davis DD, Freeman A. Cognitive Therapy of Personality Disorders. 3rd ed. The Guilford Press; 2015.
15. Thylstrup B, Hesse M. “I am not complaining”–ambivalence construct in schizoid personality disorder. Am J Psychother. 2009;63:147-167.
16. Ricke AK, Lee MJ, Chambers JE. The difficult patient: borderline personality disorder in the obstetrical and gynecological patient. Obstet Gynecol Surv. 2012;67:495-502.
17. Seow LLY, Page AC, Hooke GR. Severity of borderline personality disorder symptoms as a moderator of the association between the use of dialectical behaviour therapy skills and treatment outcomes. Psychother Res. 2020;30:920-933.
18. Nichols WC. Integrative marital and family treatment of dependent personality disorders. In: MacFarlane MM (Ed.) Family Treatment of Personality Disorders: Advances in Clinical Practice. Haworth Clinical Practice Press; 2004:173-204.
19. Disney KL. Dependent personality disorder: a critical review. Clin Psychol Rev. 2013;33:1184-1196.
20. Bender DS. The therapeutic alliance in the treatment of personality disorders. J Psychiatr Pract. 2005;11:73-87.
21. Ward RK. Assessment and management of personality disorders. Am Fam Physician. 2004;70:1505-1512.
22. Cummings JA, Hayes AM, Cardaciotto L, et al. The dynamics of self-esteem in cognitive therapy for avoidant and obsessive-compulsive personality disorders: an adaptive role of self-esteem variability? Cognit Ther Res. 2012;36:272-281.
Specific behaviors or expressed thoughts may signal a need for screening. Take into account an individual’s strengths and limitations when designing a Tx approach.
Specific behaviors or expressed thoughts may signal a need for screening. Take into account an individual’s strengths and limitations when designing a Tx approach.
THE CASES
Winston S* is a 23-year-old man referred by a psychiatrist colleague for primary care. He works delivering papers in the early morning hours and spends his day alone in his apartment mainly eating frozen pizza. He has worked solitary jobs his entire life and says he prefers it that way. His answers to questions lack emotion. He doesn’t seem to have any friends or regular contact with family. He follows the medical advice he receives but can’t seem to get out of the house to exercise or socialize. His psychiatrist was treating him with a selective serotonin reuptake inhibitor for depression when he was referred.
Denise L* is a 37-year-old woman who transferred to your practice because she says the previous practice’s office manager was disrespectful and the doctor did not listen to her. She has been “very appreciative” of you and your “well-run office.” You have addressed her fibromyalgia and she has shared several personal details about her life. In the following weeks, you receive several phone calls and messages from her. At a follow-up visit, she asks questions about your family and seems agitated when you hesitate to answer. She questions whether you remember details of her history. She pushes, “Did you remember that, doctor?” She also mentions that your front desk staff seems rude to her.
Ruth B* is an 82-year-old woman whose blood pressure measured in your office is 176/94 mm Hg. When you recommend starting a medication and getting blood tests, she responds with a litany of fearful questions. She seems immobilized by worries about treatment and equally so about the risks of nontreatment. You can’t seem to get past the anxiety to decide on a satisfactory plan. She has to write everything down on a notepad and worries if she does not get every detail.
●
* This patient’s name has been changed to protect his identity. The other 2 patients are an amalgam of patients for whom the authors have provided care.
According to a survey of practicing primary care physicians, as many as 15% of patient encounters can be difficult.1 Demanding, intrusive, or angry patients who reject health care interventions are often-cited sources of these difficulties.2,3 While it is true that patient, physician, and environmental factors may contribute to challenging interactions, some patients who are “difficult” may actually have a personality disorder that requires a distinctive approach to care. Recognizing these patients can help empower physicians to provide compassionate and effective care, reduce team angst, and minimize burnout.
❚ What qualifies as a personality disorder? A personality disorder is an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is unchanging over time, and leads to distress or impairment in social or occupational functioning.4 The prevalence of any personality disorder seems to have increased over the past decade from 9.1%4 to 12.16%.5 The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classifies personality disorders in 3 clusters—A, B, and C (TABLE4)—with prevalence rates at 7.23%, 5.53%, and 6.7%, respectively.5 The review below will focus on the distinct personality disorders exhibited by the patients described in the opening cases.
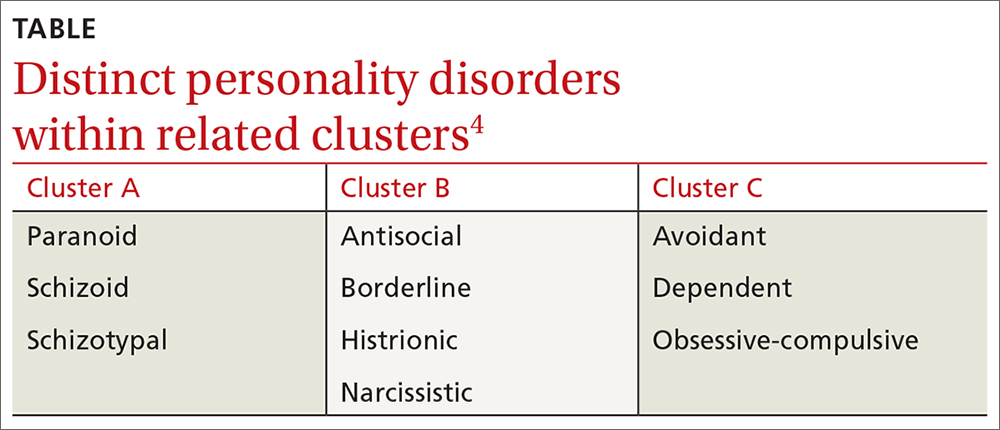
Continue to: A closer look at the clusters...
A closer look at the clusters
Cluster A disorders
Paranoid, schizoid, and schizotypal disorders are part of this cluster. These patients exhibit odd or eccentric thinking and behavior. Individuals with schizoid personality disorder, for instance, usually lack relationships and lack the desire to acquire and maintain relationships.4 They often organize their lives to remain isolated and will choose occupations that require little social interaction. They sometimes view themselves as observers rather than participants in their own lives.6
Cluster B disorders
Dramatic, overly emotional, or unpredictable thinking and behavior are characteristic of individuals who have antisocial, borderline, histrionic, or narcissistic disorders. Patients with borderline personality disorder (BPD), for example, demonstrate a longstanding pattern of instability in affect, self-image, and relationships.4 Patients with BPD often display extreme interpersonal hypersensitivity and make frantic efforts to avoid real or imagined abandonment. Identity disturbance, feelings of emptiness, and efforts to avoid abandonment have all been associated with increased suicide risk.7
In a primary care setting, such a patient may display extremely strong reactions to minor disappointments. When the physician is unavailable for a last-minute appointment or to authorize an unscheduled medication refill or to receive an after-hours phone call, the patient may become irate. The physician, who previously was idealized by the patient as “the only person who understands me,” is now devalued as “the worst doctor I’ve ever had.”8
Cluster C disorders
With these individuals, anxious or fearful thinking and behavior predominate. Avoidant, dependent, and obsessive-compulsive disorders are included in this cluster.
Dependent personality disorder (DPD) is characterized by a pervasive and extreme need to be taken care of. Submissive and clingy behavior and fear of separation are excessive. This patient may have difficulty making everyday decisions, being assertive, or expressing disagreement with others.4
Obsessive-compulsive personality disorder falls in this cluster and is typified by a pervasive preoccupation with orderliness, perfectionism, and control, at the price of flexibility and efficiency. This individual may be reluctant to get rid of sentimental objects, have rigid moral beliefs, and have significant difficulty working with others who do not follow their rules.4
Continue to: These clues may suggest...
These clues may suggest a personality disorder
If you find that encounters with a particular patient are growing increasingly difficult, consider whether the following behaviors, attitudes, and patterns of thinking are coming into play. If they are, you may want to consider using a screening tool, which we’ll discuss in a moment.
❚ Clues to cluster A disorders
- The patient has no peer relationships outside immediate family.
- The patient almost always chooses solitary activities for work and personal enjoyment.
❚ Cluster B clues
- Hypersensitivity to treatment disagreements or cancelled appointments are common (and likely experienced as rejection).
- Mood changes occur very quickly, even during a single visit.
- There is a history of many failed relationships with providers and others.
- The patient will describe an individual as both “wonderful” and “terrible” (ie, splitting) and may do so during the course of one visit.
- The patient may also split groups (eg, medical staff) by affective extremes (eg, adoration and hatred).
- The patient may hint at suicide or acts of self-harm.7
❚ Cluster C clues
- There is an excessive dependency on family, friends, or providers.
- Significant anxiety is experienced when the patient has to make an independent decision.
- There is a fear of relationship loss and resultant vulnerability to exploitation or abuse.
- Pervasive perfectionism makes treatment planning or course changes difficult.
- Anxiety and fear are unrelieved despite support and ample information.
Consider these screening tools
Several screening tools for personality disorders can be used to follow up on your initial clinical impressions. We also highly recommend you consider concurrent screening for substance abuse, as addiction is a common comorbidity with personality disorders.
❚
❚ A sampling of screening tools. The Standardised Assessment of Personality Abbreviated Scale (SAPAS)9 is an 8-item measure that correlates well with disorders in clusters A and C.
BPD (cluster B) has many brief scale options, including the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD).10 This 10-item questionnaire demonstrates sensitivity and specificity for BPD.
The International Personality Disorder Examination (IPDE) includes a 15-minute screening tool to help identify patients who may have any personality disorder, regardless of cluster.11
Improve patient encounters with these Tx pearls
In the family medicine clinic, a collaborative primary care and behavioral health team can be extremely helpful in the diagnosis and management of patients with personality disorders.12 First-line treatment of these disorders is psychotherapy, whereas medications are mainly used for symptom management. See Black and colleagues’ work for a thorough discussion on psychopharmacology considerations with personality disorders. 13
The following tips can help you to improve your interactions with patients who have personality disorders.
❚ Cluster A approaches
- Recommend treatment that respects the patient’s need for relative isolation.14
- Don’t be personally offended by your patient’s flat or disinterested affect or concrete thinking; don’t let it diminish the emotional support you provide.6
- Consult with a health psychologist (who has expertise in physical health conditions, brief treatments, and the medical system) to connect the patient with a long-term therapist. It is better to focus on fundamental changes, rather than employing brief behavioral techniques, for symptom relief. Patients with personality disorders tend to have better outcomes with long-term psychological care.15
❚ Cluster B approaches
- Set boundaries—eg, specific time limits for visits—and keep them.8
- Schedule brief, more frequent, appointments to reduce perceived feelings of abandonment.
- Coordinate plans with the entire clinic team to avoid splitting and blaming.16
- Avoid providing patients with personal information, as it may provide fodder for splitting behavior. 8
- Do not take things personally. Let patients “own” their own distress. These patients often take an emotional toll on the provider.16
- Engage the help of a health psychologist to reduce burnout and for more long-term continuity of care. A health psychologist who specializes in dialectical behavioral therapy to work on emotion regulation, distress tolerance, and interpersonal effectiveness would be ideal.17
Continue to: Cluster C approaches...
❚
❚ Cluster C approaches
- Engage the help of family and other trusted individuals in supporting treatment plans.18,19
- Try to provide just 2 treatment choices to the patient and reinforce his or her responsibility to help make the decision collaboratively. This step is important since it is difficult to enhance autonomy in these patients.20
- Engage the help of a cognitive behavioral therapist who can work on assertiveness and problem-solving skills.19
- Be empathetic with the patient and patiently build a trusting relationship, rather than “arguing” with the patient about each specific worry.20
- Make only one change at a time. Give small assignments to the patient, such as monitoring symptoms or reading up on their condition. These can help the patient feel more in control.21
- Present information in brief, clear terms. Avoid “grey areas” to reduce anxiety.21
- Engage a behavioral health provider to reduce rigid expectations and ideally increase feelings of self-esteem; this has been shown to predict better treatment outcomes.22
CASES
Mr. S displays cluster-A characteristics of schizoid personality disorder in addition to the depression he is being treated for. His physician was not put off by his flat affect and respected his limitations with social activities. Use of a stationary bike was recommended for exercise rather than walks outdoors. He also preferred phone calls to in-person encounters, so his follow-up visits were conducted by phone.
Ms. L exhibits cluster-B characteristics of BPD. You begin the tricky dance of setting limits, keeping communication clear, and not blaming yourself or others on your team for Ms. L’s feelings. You schedule regular visits with explicit time limits and discuss with your entire team how to avoid splitting. You involve a psychologist, familiar with treating BPD, who helps the patient learn positive interpersonal coping skills.
Ms. B displays cluster-C characteristics of dependent and obsessive-compulsive personality disorders. At her follow-up visit, you provide a great deal of empathy and try not to argue her out of each worry that she brings up. You make one change at a time and enlist the help of her daughter in giving her pills at home and offering reassurance. You collaborate with a cognitive behavioral therapist who works on exposing her to moderately anxiety-provoking situations/decisions.
THE CASES
Winston S* is a 23-year-old man referred by a psychiatrist colleague for primary care. He works delivering papers in the early morning hours and spends his day alone in his apartment mainly eating frozen pizza. He has worked solitary jobs his entire life and says he prefers it that way. His answers to questions lack emotion. He doesn’t seem to have any friends or regular contact with family. He follows the medical advice he receives but can’t seem to get out of the house to exercise or socialize. His psychiatrist was treating him with a selective serotonin reuptake inhibitor for depression when he was referred.
Denise L* is a 37-year-old woman who transferred to your practice because she says the previous practice’s office manager was disrespectful and the doctor did not listen to her. She has been “very appreciative” of you and your “well-run office.” You have addressed her fibromyalgia and she has shared several personal details about her life. In the following weeks, you receive several phone calls and messages from her. At a follow-up visit, she asks questions about your family and seems agitated when you hesitate to answer. She questions whether you remember details of her history. She pushes, “Did you remember that, doctor?” She also mentions that your front desk staff seems rude to her.
Ruth B* is an 82-year-old woman whose blood pressure measured in your office is 176/94 mm Hg. When you recommend starting a medication and getting blood tests, she responds with a litany of fearful questions. She seems immobilized by worries about treatment and equally so about the risks of nontreatment. You can’t seem to get past the anxiety to decide on a satisfactory plan. She has to write everything down on a notepad and worries if she does not get every detail.
●
* This patient’s name has been changed to protect his identity. The other 2 patients are an amalgam of patients for whom the authors have provided care.
According to a survey of practicing primary care physicians, as many as 15% of patient encounters can be difficult.1 Demanding, intrusive, or angry patients who reject health care interventions are often-cited sources of these difficulties.2,3 While it is true that patient, physician, and environmental factors may contribute to challenging interactions, some patients who are “difficult” may actually have a personality disorder that requires a distinctive approach to care. Recognizing these patients can help empower physicians to provide compassionate and effective care, reduce team angst, and minimize burnout.
❚ What qualifies as a personality disorder? A personality disorder is an enduring pattern of inner experience and behavior that deviates markedly from the expectations of the individual’s culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is unchanging over time, and leads to distress or impairment in social or occupational functioning.4 The prevalence of any personality disorder seems to have increased over the past decade from 9.1%4 to 12.16%.5 The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classifies personality disorders in 3 clusters—A, B, and C (TABLE4)—with prevalence rates at 7.23%, 5.53%, and 6.7%, respectively.5 The review below will focus on the distinct personality disorders exhibited by the patients described in the opening cases.
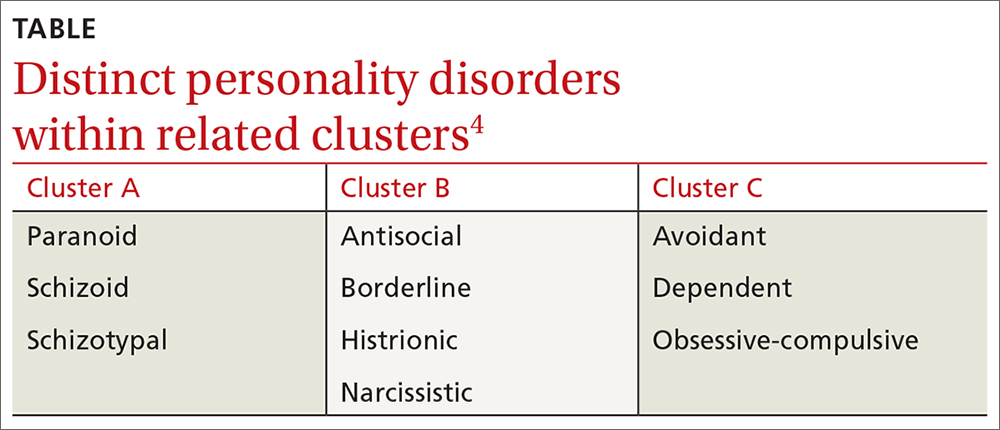
Continue to: A closer look at the clusters...
A closer look at the clusters
Cluster A disorders
Paranoid, schizoid, and schizotypal disorders are part of this cluster. These patients exhibit odd or eccentric thinking and behavior. Individuals with schizoid personality disorder, for instance, usually lack relationships and lack the desire to acquire and maintain relationships.4 They often organize their lives to remain isolated and will choose occupations that require little social interaction. They sometimes view themselves as observers rather than participants in their own lives.6
Cluster B disorders
Dramatic, overly emotional, or unpredictable thinking and behavior are characteristic of individuals who have antisocial, borderline, histrionic, or narcissistic disorders. Patients with borderline personality disorder (BPD), for example, demonstrate a longstanding pattern of instability in affect, self-image, and relationships.4 Patients with BPD often display extreme interpersonal hypersensitivity and make frantic efforts to avoid real or imagined abandonment. Identity disturbance, feelings of emptiness, and efforts to avoid abandonment have all been associated with increased suicide risk.7
In a primary care setting, such a patient may display extremely strong reactions to minor disappointments. When the physician is unavailable for a last-minute appointment or to authorize an unscheduled medication refill or to receive an after-hours phone call, the patient may become irate. The physician, who previously was idealized by the patient as “the only person who understands me,” is now devalued as “the worst doctor I’ve ever had.”8
Cluster C disorders
With these individuals, anxious or fearful thinking and behavior predominate. Avoidant, dependent, and obsessive-compulsive disorders are included in this cluster.
Dependent personality disorder (DPD) is characterized by a pervasive and extreme need to be taken care of. Submissive and clingy behavior and fear of separation are excessive. This patient may have difficulty making everyday decisions, being assertive, or expressing disagreement with others.4
Obsessive-compulsive personality disorder falls in this cluster and is typified by a pervasive preoccupation with orderliness, perfectionism, and control, at the price of flexibility and efficiency. This individual may be reluctant to get rid of sentimental objects, have rigid moral beliefs, and have significant difficulty working with others who do not follow their rules.4
Continue to: These clues may suggest...
These clues may suggest a personality disorder
If you find that encounters with a particular patient are growing increasingly difficult, consider whether the following behaviors, attitudes, and patterns of thinking are coming into play. If they are, you may want to consider using a screening tool, which we’ll discuss in a moment.
❚ Clues to cluster A disorders
- The patient has no peer relationships outside immediate family.
- The patient almost always chooses solitary activities for work and personal enjoyment.
❚ Cluster B clues
- Hypersensitivity to treatment disagreements or cancelled appointments are common (and likely experienced as rejection).
- Mood changes occur very quickly, even during a single visit.
- There is a history of many failed relationships with providers and others.
- The patient will describe an individual as both “wonderful” and “terrible” (ie, splitting) and may do so during the course of one visit.
- The patient may also split groups (eg, medical staff) by affective extremes (eg, adoration and hatred).
- The patient may hint at suicide or acts of self-harm.7
❚ Cluster C clues
- There is an excessive dependency on family, friends, or providers.
- Significant anxiety is experienced when the patient has to make an independent decision.
- There is a fear of relationship loss and resultant vulnerability to exploitation or abuse.
- Pervasive perfectionism makes treatment planning or course changes difficult.
- Anxiety and fear are unrelieved despite support and ample information.
Consider these screening tools
Several screening tools for personality disorders can be used to follow up on your initial clinical impressions. We also highly recommend you consider concurrent screening for substance abuse, as addiction is a common comorbidity with personality disorders.
❚
❚ A sampling of screening tools. The Standardised Assessment of Personality Abbreviated Scale (SAPAS)9 is an 8-item measure that correlates well with disorders in clusters A and C.
BPD (cluster B) has many brief scale options, including the McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD).10 This 10-item questionnaire demonstrates sensitivity and specificity for BPD.
The International Personality Disorder Examination (IPDE) includes a 15-minute screening tool to help identify patients who may have any personality disorder, regardless of cluster.11
Improve patient encounters with these Tx pearls
In the family medicine clinic, a collaborative primary care and behavioral health team can be extremely helpful in the diagnosis and management of patients with personality disorders.12 First-line treatment of these disorders is psychotherapy, whereas medications are mainly used for symptom management. See Black and colleagues’ work for a thorough discussion on psychopharmacology considerations with personality disorders. 13
The following tips can help you to improve your interactions with patients who have personality disorders.
❚ Cluster A approaches
- Recommend treatment that respects the patient’s need for relative isolation.14
- Don’t be personally offended by your patient’s flat or disinterested affect or concrete thinking; don’t let it diminish the emotional support you provide.6
- Consult with a health psychologist (who has expertise in physical health conditions, brief treatments, and the medical system) to connect the patient with a long-term therapist. It is better to focus on fundamental changes, rather than employing brief behavioral techniques, for symptom relief. Patients with personality disorders tend to have better outcomes with long-term psychological care.15
❚ Cluster B approaches
- Set boundaries—eg, specific time limits for visits—and keep them.8
- Schedule brief, more frequent, appointments to reduce perceived feelings of abandonment.
- Coordinate plans with the entire clinic team to avoid splitting and blaming.16
- Avoid providing patients with personal information, as it may provide fodder for splitting behavior. 8
- Do not take things personally. Let patients “own” their own distress. These patients often take an emotional toll on the provider.16
- Engage the help of a health psychologist to reduce burnout and for more long-term continuity of care. A health psychologist who specializes in dialectical behavioral therapy to work on emotion regulation, distress tolerance, and interpersonal effectiveness would be ideal.17
Continue to: Cluster C approaches...
❚
❚ Cluster C approaches
- Engage the help of family and other trusted individuals in supporting treatment plans.18,19
- Try to provide just 2 treatment choices to the patient and reinforce his or her responsibility to help make the decision collaboratively. This step is important since it is difficult to enhance autonomy in these patients.20
- Engage the help of a cognitive behavioral therapist who can work on assertiveness and problem-solving skills.19
- Be empathetic with the patient and patiently build a trusting relationship, rather than “arguing” with the patient about each specific worry.20
- Make only one change at a time. Give small assignments to the patient, such as monitoring symptoms or reading up on their condition. These can help the patient feel more in control.21
- Present information in brief, clear terms. Avoid “grey areas” to reduce anxiety.21
- Engage a behavioral health provider to reduce rigid expectations and ideally increase feelings of self-esteem; this has been shown to predict better treatment outcomes.22
CASES
Mr. S displays cluster-A characteristics of schizoid personality disorder in addition to the depression he is being treated for. His physician was not put off by his flat affect and respected his limitations with social activities. Use of a stationary bike was recommended for exercise rather than walks outdoors. He also preferred phone calls to in-person encounters, so his follow-up visits were conducted by phone.
Ms. L exhibits cluster-B characteristics of BPD. You begin the tricky dance of setting limits, keeping communication clear, and not blaming yourself or others on your team for Ms. L’s feelings. You schedule regular visits with explicit time limits and discuss with your entire team how to avoid splitting. You involve a psychologist, familiar with treating BPD, who helps the patient learn positive interpersonal coping skills.
Ms. B displays cluster-C characteristics of dependent and obsessive-compulsive personality disorders. At her follow-up visit, you provide a great deal of empathy and try not to argue her out of each worry that she brings up. You make one change at a time and enlist the help of her daughter in giving her pills at home and offering reassurance. You collaborate with a cognitive behavioral therapist who works on exposing her to moderately anxiety-provoking situations/decisions.
1. Hull SK, Broquet K. How to manage difficult patient encounters. Fam Pract Manag. 2007;14:30-34.
2. Groves JE. Taking care of the hateful patient. N Engl J Med.1978;298: 883-887.
3. O’Dowd TC. Five years of heartsink patients in primary care. BMJ. 1988;297:528-530.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition (DSM-5). American Psychiatric Publishing; 2013.
5. Volkert J, Gablonski TC, Rabung S. Prevalence of personality disorders in the general adult population in Western countries: systematic review and meta-analysis. Br J Psychiatry. 2018;213:709-715.
6. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32:515-528.
7. Yen S, Peters JR, Nishar S, et al. Association of borderline personality disorder criteria with suicide attempts: findings from the collaborative longitudinal study of personality disorders over 10 years of follow-up. JAMA Psychiatry. 2021;78:187-194.
8. Dubovsky AN, Kiefer MM. Borderline personality disorder in the primary care setting. Med Clin North Am. 2014;98:1049-1064.
9. Hesse M, Moran P. (2010). Screening for personality disorder with the Standardised Assessment of Personality: Abbreviated Scale (SAPAS): further evidence of concurrent validity. BMC Psychiatry. 2010;10:10.
10. Zanarini MC, Vujanovic AA, Parachini EA, et al. A screening measure for BPD: the McLean screening instrument for borderline personality disorder (MSI-BPD). J Pers Disord. 2003;17:568-573.
11. Loranger AW, Sartorius N, Andreoli A, et al. The International Personality Disorder Examination. The World Health Organization/Alcohol, Drug Abuse, and Mental Health Administration international pilot study of personality disorders. Arch Gen Psychiatry. 1994;51:215-224.12. Nelson KJ, Skodol A, Friedman M. Pharmacotherapy for personality disorders. UpToDate. Accessed April 22, 2021. www.uptodate.com/contents/pharmacotherapy-for-personality-disorders
13. Black D, Paris J, Schulz C. Evidence-based integrated biopsychosocial treatment of borderline personality disorder. In: Muse M (ed). Cognitive Behavioral Psychopharmacology: the Clinical Practice of Evidence-Based Biopsychosocial Integration. Wiley; 2017:137-166.
14. Beck AT, Davis DD, Freeman A. Cognitive Therapy of Personality Disorders. 3rd ed. The Guilford Press; 2015.
15. Thylstrup B, Hesse M. “I am not complaining”–ambivalence construct in schizoid personality disorder. Am J Psychother. 2009;63:147-167.
16. Ricke AK, Lee MJ, Chambers JE. The difficult patient: borderline personality disorder in the obstetrical and gynecological patient. Obstet Gynecol Surv. 2012;67:495-502.
17. Seow LLY, Page AC, Hooke GR. Severity of borderline personality disorder symptoms as a moderator of the association between the use of dialectical behaviour therapy skills and treatment outcomes. Psychother Res. 2020;30:920-933.
18. Nichols WC. Integrative marital and family treatment of dependent personality disorders. In: MacFarlane MM (Ed.) Family Treatment of Personality Disorders: Advances in Clinical Practice. Haworth Clinical Practice Press; 2004:173-204.
19. Disney KL. Dependent personality disorder: a critical review. Clin Psychol Rev. 2013;33:1184-1196.
20. Bender DS. The therapeutic alliance in the treatment of personality disorders. J Psychiatr Pract. 2005;11:73-87.
21. Ward RK. Assessment and management of personality disorders. Am Fam Physician. 2004;70:1505-1512.
22. Cummings JA, Hayes AM, Cardaciotto L, et al. The dynamics of self-esteem in cognitive therapy for avoidant and obsessive-compulsive personality disorders: an adaptive role of self-esteem variability? Cognit Ther Res. 2012;36:272-281.
1. Hull SK, Broquet K. How to manage difficult patient encounters. Fam Pract Manag. 2007;14:30-34.
2. Groves JE. Taking care of the hateful patient. N Engl J Med.1978;298: 883-887.
3. O’Dowd TC. Five years of heartsink patients in primary care. BMJ. 1988;297:528-530.
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition (DSM-5). American Psychiatric Publishing; 2013.
5. Volkert J, Gablonski TC, Rabung S. Prevalence of personality disorders in the general adult population in Western countries: systematic review and meta-analysis. Br J Psychiatry. 2018;213:709-715.
6. Esterberg ML, Goulding SM, Walker EF. Cluster A personality disorders: schizotypal, schizoid and paranoid personality disorders in childhood and adolescence. J Psychopathol Behav Assess. 2010;32:515-528.
7. Yen S, Peters JR, Nishar S, et al. Association of borderline personality disorder criteria with suicide attempts: findings from the collaborative longitudinal study of personality disorders over 10 years of follow-up. JAMA Psychiatry. 2021;78:187-194.
8. Dubovsky AN, Kiefer MM. Borderline personality disorder in the primary care setting. Med Clin North Am. 2014;98:1049-1064.
9. Hesse M, Moran P. (2010). Screening for personality disorder with the Standardised Assessment of Personality: Abbreviated Scale (SAPAS): further evidence of concurrent validity. BMC Psychiatry. 2010;10:10.
10. Zanarini MC, Vujanovic AA, Parachini EA, et al. A screening measure for BPD: the McLean screening instrument for borderline personality disorder (MSI-BPD). J Pers Disord. 2003;17:568-573.
11. Loranger AW, Sartorius N, Andreoli A, et al. The International Personality Disorder Examination. The World Health Organization/Alcohol, Drug Abuse, and Mental Health Administration international pilot study of personality disorders. Arch Gen Psychiatry. 1994;51:215-224.12. Nelson KJ, Skodol A, Friedman M. Pharmacotherapy for personality disorders. UpToDate. Accessed April 22, 2021. www.uptodate.com/contents/pharmacotherapy-for-personality-disorders
13. Black D, Paris J, Schulz C. Evidence-based integrated biopsychosocial treatment of borderline personality disorder. In: Muse M (ed). Cognitive Behavioral Psychopharmacology: the Clinical Practice of Evidence-Based Biopsychosocial Integration. Wiley; 2017:137-166.
14. Beck AT, Davis DD, Freeman A. Cognitive Therapy of Personality Disorders. 3rd ed. The Guilford Press; 2015.
15. Thylstrup B, Hesse M. “I am not complaining”–ambivalence construct in schizoid personality disorder. Am J Psychother. 2009;63:147-167.
16. Ricke AK, Lee MJ, Chambers JE. The difficult patient: borderline personality disorder in the obstetrical and gynecological patient. Obstet Gynecol Surv. 2012;67:495-502.
17. Seow LLY, Page AC, Hooke GR. Severity of borderline personality disorder symptoms as a moderator of the association between the use of dialectical behaviour therapy skills and treatment outcomes. Psychother Res. 2020;30:920-933.
18. Nichols WC. Integrative marital and family treatment of dependent personality disorders. In: MacFarlane MM (Ed.) Family Treatment of Personality Disorders: Advances in Clinical Practice. Haworth Clinical Practice Press; 2004:173-204.
19. Disney KL. Dependent personality disorder: a critical review. Clin Psychol Rev. 2013;33:1184-1196.
20. Bender DS. The therapeutic alliance in the treatment of personality disorders. J Psychiatr Pract. 2005;11:73-87.
21. Ward RK. Assessment and management of personality disorders. Am Fam Physician. 2004;70:1505-1512.
22. Cummings JA, Hayes AM, Cardaciotto L, et al. The dynamics of self-esteem in cognitive therapy for avoidant and obsessive-compulsive personality disorders: an adaptive role of self-esteem variability? Cognit Ther Res. 2012;36:272-281.
High rates of work-related trauma, PTSD in intern physicians
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”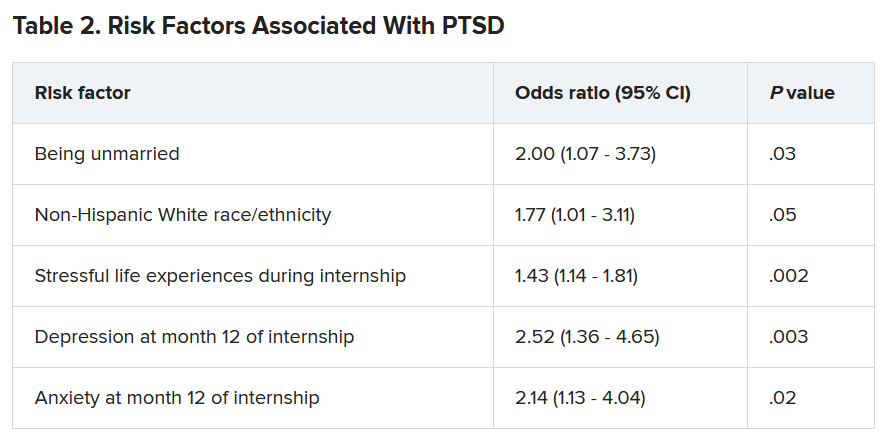
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”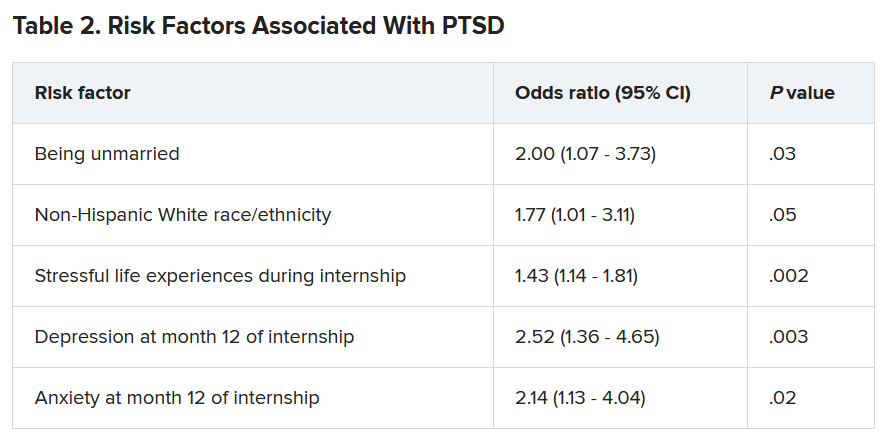
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Work-related posttraumatic stress disorder is three times higher in interns than the general population, new research shows.
Investigators assessed PTSD in more than 1,100 physicians at the end of their internship year and found that a little over half reported work-related trauma exposure, and of these, 20% screened positive for PTSD.
Overall, 10% of participants screened positive for PTSD by the end of the internship year, compared with a 12-month PTSD prevalence of 3.6% in the general population.
“Work-related trauma exposure and PTSD are common and underdiscussed phenomena among intern physicians,” lead author Mary Vance, MD, assistant professor of psychiatry, Uniformed Services University of the Health Sciences, Bethesda, Md., said in an interview.
“I urge medical educators and policy makers to include this topic in their discussions about physician well-being and to implement effective interventions to mitigate the impact of work-related trauma and PTSD among physician trainees,” she said.
The study was published online June 8 in JAMA Network Open.
Burnout, depression, suicide
“Burnout, depression, and suicide are increasingly recognized as occupational mental health hazards among health care professionals, including physicians,” Dr. Vance said.
“However, in my professional experience as a physician and educator, despite observing anecdotal evidence among my peers and trainees that this is also an issue,” she added.
This gap prompted her “to investigate rates of work-related trauma exposure and PTSD among physicians.”
The researchers sent emails to 4,350 individuals during academic year 2018-2019, 2 months prior to starting internships. Of these, 2,129 agreed to participate and 1,134 (58.6% female, 61.6% non-Hispanic White; mean age, 27.52) completed the study.
Prior to beginning internship, participants completed a baseline survey that assessed demographic characteristics as well as medical education and psychological and psychosocial factors.
Participants completed follow-up surveys sent by email at 3, 6, 9, and 12 months of the internship year. The surveys assessed stressful life events, concern over perceived medical errors in the past 3 months, and number of hours worked over the past week.
At month 12, current PTSD and symptoms of depression and anxiety were also assessed using the Primary Care PTSD Screen for DSM-5, the 9-item Patient Health Questionnaire, and the Generalized Anxiety Disorder 7-item scale, respectively.
Participants were asked to self-report whether they ever had an episode of depression and to complete the Risky Families Questionnaire to assess if they had experienced childhood abuse, neglect, and family conflict. Additionally, they completed an 11-item scale developed specifically for the study regarding recent stressful events.
‘Crucible’ year
A total of 56.4% of respondents reported work-related trauma exposure, and among these, 19.0% screened positive for PTSD. One-tenth (10.8%) of the entire sample screened positive for PTSD by the end of internship year, which is three times higher than the 12-month prevalence of PTSD in the general population (3.6%), the authors noted.
Trauma exposure differed by specialty, ranging from 43.1% in anesthesiology to 72.4% in emergency medicine. Of the respondents in internal medicine, surgery, and medicine/pediatrics, 56.6%, 63.3%, and 71%, respectively, reported work-related trauma exposure.
Work-related PTSD also differed by specialty, ranging from 7.5% in ob.gyn. to 30.0% in pediatrics. Of respondents in internal medicine and family practice, 23.9% and 25.9%, respectively, reported work-related PTSD.
Dr. Vance called the intern year “a crucible, during which newly minted doctors receive intensive on-the-job training at the front lines of patient care [and] work long hours in rapidly shifting environments, often caring for critically ill patients.”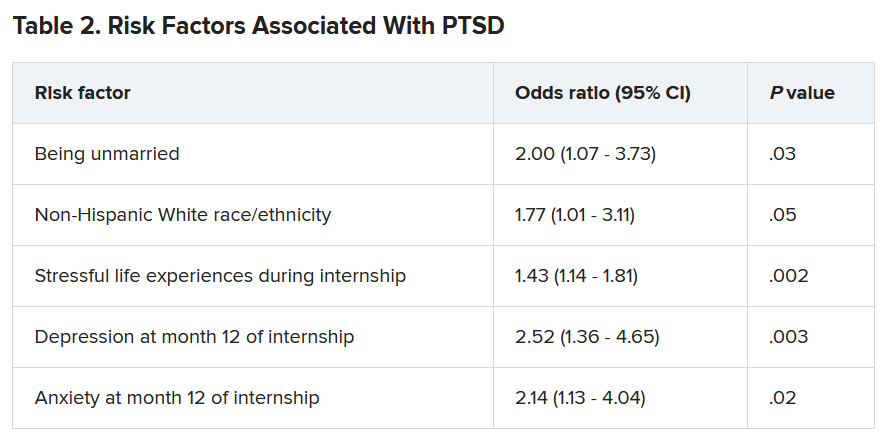
Work-related trauma exposure “is more likely to occur during this high-stress internship year than during the same year in the general population,” she said.
She noted that the “issue of workplace trauma and PTSD among health care workers became even more salient during the height of COVID,” adding that she expects it “to remain a pressure issue for healthcare workers in the post-COVID era.”
Call to action
Commenting on the study David A. Marcus, MD, chair, GME Physician Well-Being Committee, Northwell Health, New Hyde Park, N.Y., noted the study’s “relatively low response rate” is a “significant limitation” of the study.
An additional limitation is the lack of a baseline PTSD assessment, said Dr. Marcus, an assistant professor at Hofstra University, Hempstead, N.Y., who was not involved in the research.
Nevertheless, the “overall prevalence [of work-related PTSD] should serve as a call to action for physician leaders and for leaders in academic medicine,” he said.
Additionally, the study “reminds us that trauma-informed care should be an essential part of mental health support services provided to trainees and to physicians in general,” Dr. Marcus stated.
Also commenting on the study, Lotte N. Dyrbye, MD, professor of medicine and medical education, Mayo Clinic, Rochester, Minn., agreed.
“Organizational strategies should include system-level interventions to reduce the risk of frightening, horrible, or traumatic events from occurring in the workplace in the first place, as well as faculty development efforts to upskill teaching faculty in their ability to support trainees when such events do occur,” she said.
These approaches “should coincide with organizational efforts to support individual trainees by providing adequate time off after traumatic events, ensuring trainees can access affordable mental healthcare, and reducing other barriers to appropriate help-seeking, such as stigma, and efforts to build a culture of well-being,” suggested Dr. Dyrbye, who is codirector of the Mayo Clinic Program on Physician Wellbeing and was not involved in the study.
The study was supported by grants from the Blue Cross Blue Shield Foundation of Michigan and National Institutes of Health. Dr. Vance and coauthors, Dr. Marcus, and Dr. Dyrbye reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ten killer steps to writing a great medical thriller
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
For many physicians and other professionals, aspirations of crafting a work of fiction are not uncommon — and with good reason. We are, after all, a generally well-disciplined bunch capable of completing complex tasks, and there is certainly no shortage of excitement and drama in medicine and surgery — ample fodder for thrilling stories. Nonetheless, writing a novel is a major commitment, and it requires persistence, patience, and dedicated time, especially for one with a busy medical career.
Getting started is not easy. Writing workshops are helpful, and in my case, I tried to mentor with some of the best. Before writing my novel, I attended workshops for aspiring novelists, given by noted physician authors Tess Gerritsen (Body Double, The Surgeon) and the late Michael Palmer (The Society, The Fifth Vial).
Writers are often advised to “write about what you know.” In my case, I combined my knowledge of medicine and my experience with the thoroughbred racing world to craft a thriller that one reviewer described as “Dick Francis meets Robin Cook.” For those who have never read the Dick Francis series, he was a renowned crime writer whose novels centered on horse racing in England. Having been an avid reader of both authors, that comparison was the ultimate compliment.
So against that backdrop, the novel Shedrow, along with some shared wisdom from a few legendary writers.
1. Start with the big “what if.” Any great story starts with that simple “what if” question. What if a series of high-profile executives in the managed care industry are serially murdered (Michael Palmer’s The Society)? What if a multimillion-dollar stallion dies suddenly under very mysterious circumstances on a supposedly secure farm in Kentucky (Dean DeLuke’s Shedrow)?
2. Put a MacGuffin to work in your story. Popularized by Alfred Hitchcock, the MacGuffin is that essential plot element that drives virtually all characters in the story, although it may be rather vague and meaningless to the story itself. In the iconic movie Pulp Fiction, the MacGuffin is the briefcase — everyone wants it, and we never do find out what’s in it.
3. Pacing is critical. Plot out the timeline of emotional highs and lows in a story. It should look like a rolling pattern of highs and lows that crescendo upward to the ultimate crisis. Take advantage of the fact that following any of those emotional peaks, you probably have the reader’s undivided attention. That would be a good time to provide backstory or fill in needed information for the reader – information that may be critical but perhaps not as exciting as what just transpired.
4. Torture your protagonists. Just when the reader thinks that the hero is finally home free, throw in another obstacle. Readers will empathize with the character and be drawn in by the unexpected hurdle.
5. Be original and surprise your readers. Create twists and turns that are totally unexpected, yet believable. This is easier said than done but will go a long way toward making your novel original, gripping, and unpredictable.
6. As a general rule, consider short sentences and short chapters. This is strictly a personal preference, but who can argue with James Patterson’s short chapters or with Robert Parker’s short and engaging sentences? Sentence length can be varied for effect, too, with shorter sentences serving to heighten action or increase tension.
7. Avoid the passive voice. Your readers want action. This is an important rule in almost any type of writing.
8. Keep descriptions brief. Long, drawn-out descriptions of the way characters look, or even setting descriptions, are easily overdone in a thriller. The thriller genre is very different from literary fiction in this regard. Stephen King advises writers to “just say what they see, then get on with the story.”
9. Sustain the reader’s interest throughout. Assess each chapter ending and determine whether the reader has been given enough reason to want to continue reading. Pose a question, end with a minor cliffhanger, or at least ensure that there is enough accumulated tension in the story.
10. Edit aggressively and cut out the fluff. Ernest Hemingway once confided to F. Scott Fitzgerald, “I write one page of masterpiece to 91 pages of shit. I try to put the shit in the wastebasket.”
Dr. DeLuke is professor emeritus of oral and facial surgery at Virginia Commonwealth University and author of the novel Shedrow.
A version of this article first appeared on Medscape.com.
Telemedicine is poised to drive new models of care
Telemedicine has been proposed as a solution for an array of health care access problems over decades of gradual growth. The vast ramping up of , according to an update at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
“The cat is out of the bag,” said Jaspal Singh, MD, professor of medicine, Atrium Health, Charlotte, N.C. Due to changes in access and reimbursement to telemedicine driven by the pandemic, he said, “we now have permission to explore new models of care.”
Prior to February 2020, telemedicine was crawling forward at a leisurely pace, according to Dr. Singh. After March 2020, it broke into a run due to enormous demand and was met by a rapid response from the U.S. Congress. The first of four legislative bills that directly or indirectly supported telemedicine was passed on March 6, 2020.
The Centers for Medicare and Medicaid Services responded in kind, making modifications in a number of rules that removed obstacles to telehealth. One modification on April 6, 2020, for example, removed the requirement for a preexisting relationship between the clinician and patient, Dr. Singh said. The CMS also subsequently modified reimbursement policies in order to make telemedicine more tenable for physicians.
Given the risk of contagion from face-to-face encounters, telemedicine in the early days of the pandemic was not just attractive but the only practical and safe approach to medical care in many circumstances. Physicians and patients were anxious for health care that did not require in-office visits even though many critical issues for telemedicine, including its relative effectiveness, had not yet been fully evaluated.
Much has been learned regarding the feasibility and acceptability of telemedicine during the pandemic, but Dr. Singh noted that quality of care relative to in-person visits remains weakly supported for most indications. Indeed, he outlined sizable list of incompletely resolved issues, including optimal payment models, management of privacy concerns, and how to balance advantages to disadvantages.
For patients and physicians, the strengths of telemedicine include greater convenience made possible by the elimination of travel and waiting rooms. For the health care system, it can include less infrastructure and overhead. For many physicians, telemedicine might be perceived as more efficient.
On the other hand, some patients might feel that a clinical encounter is incomplete without a physical examination even when the physician does not feel the physical examination is needed, according to Dr. Singh. He cited a survey suggesting nearly half of patients expressed concern about a lack of connection to health care providers following a virtual visit.
In the same 2020 National Poll on Healthy Aging 2020 survey conducted by the University of Michigan 67% of respondents reported that the quality of care was not as good as that provided by in-patient visits, and 24% expressed concern about privacy. However, at the time the poll was taken in May 2020, experience with telemedicine among many of the respondents may have been limited. As telemedicine is integrated into routine care, perceptions might change as experience increases.
A distinction between telemedicine in routine care and telemedicine as a strategy to respond to a pandemic is important, Dr. Singh indicated. Dr. Singh was the lead author for a position paper on telemedicine for the diagnosis and treatment of sleep disorders from the American Academy of Sleep Medicine 5 years ago, but he acknowledged that models of care might differ when responding to abnormal surges in health care demand.
The surge in demand for COVID-19–related care engendered numerous innovative solutions. As examples, Dr. Singh recounted how a virtual hospital was created at his own institution. In a published study, 1,477 patients diagnosed with COVID-19 over a 6-week period remained at home and received care in a virtual observation unit (VCU) or a virtual acute care unit (VACU) . Only a small percentage required eventual hospital admission. In the VACU, patients were able to receive advanced care including IV fluids and some form of respiratory support .
It is unclear how the COVID-19 pandemic will change telemedicine. Now, with declining cases of the infection, telemedicine is back to a walk after the sprint required during the height of the pandemic, according to Dr. Singh. However, Dr. Singh thinks many physicians and patients will have a different perception of telemedicine after the widespread exposure to this type of care.
In terms of the relative role of in-patient and virtual visits across indications, “we do not know how this will play out, but we will probably end up toggling between the two,” Dr. Singh said.
This is an area that is being followed closely by the CHEST Health Policy and Advocacy Committee, according to Kathleen Sarmiento, MD, director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System. A member of that committee and moderator of the session in which Dr. Singh spoke,
Dr. Sarmiento called the effort to bring permanent coverage of telehealth services “the shared responsibility of every medical society engaged in advocacy.”
However, she cautioned that there might be intended and unintended consequences from telehealth that require analysis to develop policies that are in the best interests of effective care. She said, the “ACCP, along with its sister societies, does have a role in supporting the evaluation of the impact of these changes on both patients and providers in the fields of pulmonary medicine, critical care, and sleep medicine.”
Dr. Singh reports a financial relationship with AstraZeneca. Dr. Sarmiento reports no relevant financial relationship with AstraZeneca.
Telemedicine has been proposed as a solution for an array of health care access problems over decades of gradual growth. The vast ramping up of , according to an update at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
“The cat is out of the bag,” said Jaspal Singh, MD, professor of medicine, Atrium Health, Charlotte, N.C. Due to changes in access and reimbursement to telemedicine driven by the pandemic, he said, “we now have permission to explore new models of care.”
Prior to February 2020, telemedicine was crawling forward at a leisurely pace, according to Dr. Singh. After March 2020, it broke into a run due to enormous demand and was met by a rapid response from the U.S. Congress. The first of four legislative bills that directly or indirectly supported telemedicine was passed on March 6, 2020.
The Centers for Medicare and Medicaid Services responded in kind, making modifications in a number of rules that removed obstacles to telehealth. One modification on April 6, 2020, for example, removed the requirement for a preexisting relationship between the clinician and patient, Dr. Singh said. The CMS also subsequently modified reimbursement policies in order to make telemedicine more tenable for physicians.
Given the risk of contagion from face-to-face encounters, telemedicine in the early days of the pandemic was not just attractive but the only practical and safe approach to medical care in many circumstances. Physicians and patients were anxious for health care that did not require in-office visits even though many critical issues for telemedicine, including its relative effectiveness, had not yet been fully evaluated.
Much has been learned regarding the feasibility and acceptability of telemedicine during the pandemic, but Dr. Singh noted that quality of care relative to in-person visits remains weakly supported for most indications. Indeed, he outlined sizable list of incompletely resolved issues, including optimal payment models, management of privacy concerns, and how to balance advantages to disadvantages.
For patients and physicians, the strengths of telemedicine include greater convenience made possible by the elimination of travel and waiting rooms. For the health care system, it can include less infrastructure and overhead. For many physicians, telemedicine might be perceived as more efficient.
On the other hand, some patients might feel that a clinical encounter is incomplete without a physical examination even when the physician does not feel the physical examination is needed, according to Dr. Singh. He cited a survey suggesting nearly half of patients expressed concern about a lack of connection to health care providers following a virtual visit.
In the same 2020 National Poll on Healthy Aging 2020 survey conducted by the University of Michigan 67% of respondents reported that the quality of care was not as good as that provided by in-patient visits, and 24% expressed concern about privacy. However, at the time the poll was taken in May 2020, experience with telemedicine among many of the respondents may have been limited. As telemedicine is integrated into routine care, perceptions might change as experience increases.
A distinction between telemedicine in routine care and telemedicine as a strategy to respond to a pandemic is important, Dr. Singh indicated. Dr. Singh was the lead author for a position paper on telemedicine for the diagnosis and treatment of sleep disorders from the American Academy of Sleep Medicine 5 years ago, but he acknowledged that models of care might differ when responding to abnormal surges in health care demand.
The surge in demand for COVID-19–related care engendered numerous innovative solutions. As examples, Dr. Singh recounted how a virtual hospital was created at his own institution. In a published study, 1,477 patients diagnosed with COVID-19 over a 6-week period remained at home and received care in a virtual observation unit (VCU) or a virtual acute care unit (VACU) . Only a small percentage required eventual hospital admission. In the VACU, patients were able to receive advanced care including IV fluids and some form of respiratory support .
It is unclear how the COVID-19 pandemic will change telemedicine. Now, with declining cases of the infection, telemedicine is back to a walk after the sprint required during the height of the pandemic, according to Dr. Singh. However, Dr. Singh thinks many physicians and patients will have a different perception of telemedicine after the widespread exposure to this type of care.
In terms of the relative role of in-patient and virtual visits across indications, “we do not know how this will play out, but we will probably end up toggling between the two,” Dr. Singh said.
This is an area that is being followed closely by the CHEST Health Policy and Advocacy Committee, according to Kathleen Sarmiento, MD, director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System. A member of that committee and moderator of the session in which Dr. Singh spoke,
Dr. Sarmiento called the effort to bring permanent coverage of telehealth services “the shared responsibility of every medical society engaged in advocacy.”
However, she cautioned that there might be intended and unintended consequences from telehealth that require analysis to develop policies that are in the best interests of effective care. She said, the “ACCP, along with its sister societies, does have a role in supporting the evaluation of the impact of these changes on both patients and providers in the fields of pulmonary medicine, critical care, and sleep medicine.”
Dr. Singh reports a financial relationship with AstraZeneca. Dr. Sarmiento reports no relevant financial relationship with AstraZeneca.
Telemedicine has been proposed as a solution for an array of health care access problems over decades of gradual growth. The vast ramping up of , according to an update at the annual health policy and advocacy conference sponsored by the American College of Chest Physicians.
“The cat is out of the bag,” said Jaspal Singh, MD, professor of medicine, Atrium Health, Charlotte, N.C. Due to changes in access and reimbursement to telemedicine driven by the pandemic, he said, “we now have permission to explore new models of care.”
Prior to February 2020, telemedicine was crawling forward at a leisurely pace, according to Dr. Singh. After March 2020, it broke into a run due to enormous demand and was met by a rapid response from the U.S. Congress. The first of four legislative bills that directly or indirectly supported telemedicine was passed on March 6, 2020.
The Centers for Medicare and Medicaid Services responded in kind, making modifications in a number of rules that removed obstacles to telehealth. One modification on April 6, 2020, for example, removed the requirement for a preexisting relationship between the clinician and patient, Dr. Singh said. The CMS also subsequently modified reimbursement policies in order to make telemedicine more tenable for physicians.
Given the risk of contagion from face-to-face encounters, telemedicine in the early days of the pandemic was not just attractive but the only practical and safe approach to medical care in many circumstances. Physicians and patients were anxious for health care that did not require in-office visits even though many critical issues for telemedicine, including its relative effectiveness, had not yet been fully evaluated.
Much has been learned regarding the feasibility and acceptability of telemedicine during the pandemic, but Dr. Singh noted that quality of care relative to in-person visits remains weakly supported for most indications. Indeed, he outlined sizable list of incompletely resolved issues, including optimal payment models, management of privacy concerns, and how to balance advantages to disadvantages.
For patients and physicians, the strengths of telemedicine include greater convenience made possible by the elimination of travel and waiting rooms. For the health care system, it can include less infrastructure and overhead. For many physicians, telemedicine might be perceived as more efficient.
On the other hand, some patients might feel that a clinical encounter is incomplete without a physical examination even when the physician does not feel the physical examination is needed, according to Dr. Singh. He cited a survey suggesting nearly half of patients expressed concern about a lack of connection to health care providers following a virtual visit.
In the same 2020 National Poll on Healthy Aging 2020 survey conducted by the University of Michigan 67% of respondents reported that the quality of care was not as good as that provided by in-patient visits, and 24% expressed concern about privacy. However, at the time the poll was taken in May 2020, experience with telemedicine among many of the respondents may have been limited. As telemedicine is integrated into routine care, perceptions might change as experience increases.
A distinction between telemedicine in routine care and telemedicine as a strategy to respond to a pandemic is important, Dr. Singh indicated. Dr. Singh was the lead author for a position paper on telemedicine for the diagnosis and treatment of sleep disorders from the American Academy of Sleep Medicine 5 years ago, but he acknowledged that models of care might differ when responding to abnormal surges in health care demand.
The surge in demand for COVID-19–related care engendered numerous innovative solutions. As examples, Dr. Singh recounted how a virtual hospital was created at his own institution. In a published study, 1,477 patients diagnosed with COVID-19 over a 6-week period remained at home and received care in a virtual observation unit (VCU) or a virtual acute care unit (VACU) . Only a small percentage required eventual hospital admission. In the VACU, patients were able to receive advanced care including IV fluids and some form of respiratory support .
It is unclear how the COVID-19 pandemic will change telemedicine. Now, with declining cases of the infection, telemedicine is back to a walk after the sprint required during the height of the pandemic, according to Dr. Singh. However, Dr. Singh thinks many physicians and patients will have a different perception of telemedicine after the widespread exposure to this type of care.
In terms of the relative role of in-patient and virtual visits across indications, “we do not know how this will play out, but we will probably end up toggling between the two,” Dr. Singh said.
This is an area that is being followed closely by the CHEST Health Policy and Advocacy Committee, according to Kathleen Sarmiento, MD, director, VISN 21 Sleep Clinical Resource Hub for the San Francisco VA Health Care System. A member of that committee and moderator of the session in which Dr. Singh spoke,
Dr. Sarmiento called the effort to bring permanent coverage of telehealth services “the shared responsibility of every medical society engaged in advocacy.”
However, she cautioned that there might be intended and unintended consequences from telehealth that require analysis to develop policies that are in the best interests of effective care. She said, the “ACCP, along with its sister societies, does have a role in supporting the evaluation of the impact of these changes on both patients and providers in the fields of pulmonary medicine, critical care, and sleep medicine.”
Dr. Singh reports a financial relationship with AstraZeneca. Dr. Sarmiento reports no relevant financial relationship with AstraZeneca.
FROM A HEALTH POLICY AND ADVOCACY CONFERENCE
Complying with the Americans With Disabilities Act
. And 7 years ago, the government raised the penalties for failing to do so. So it might be time to re-educate yourself on what the ADA requires.
ADA compliance is not an issue that we talk about or provide training for in medical schools or with our professional organizations. Since fines for small businesses are now $75,000 for a first offense and $150,000 for each subsequent violation, this could be an expensive oversight that malpractice and other liability policies will not cover.
A 2019 study in Boston examined physicians’ knowledge of legal obligations when caring for patients with disabilities. Researchers concluded that most physicians interviewed “exhibited a superficial or incorrect understanding of their legal responsibilities to patients with a disability.” If you feel you’re in that boat, you might want to consult federal guidance with information and common questions physicians ask about their ADA obligations.
The ADA defines a person with a disability as someone with “a physical or mental impairment that substantially limits one or more life activities”; someone with a record of such an impairment; or someone who is “regarded as having such an impairment.” Among the ADA standards required for accessible exam rooms, according to the guidance:
- The entry door to the exam room should be a minimum width of 32 inches when the door is opened at a 90-degree angle.
- There should be a minimum of 30 by 48 inches of clear floor space next to the exam table.
- An accessible exam table should be able to be lowered to the height of the patient’s wheelchair seat, 17 to 19 inches from the floor.
This does not mean that all of your exam rooms must meet these standards, of course; but if you see any patients with disabilities – and who doesn’t? – you need at least one room that meets the criteria.
Federal guidance also includes requirements on removal of architectural barriers, accessible parking, and entrance and maneuvering spaces – which apply to both for-profit and nonprofit organizations. Among them:
- Designated accessible parking spaces must be included among any parking the business provides for the public “if doing so is readily achievable.” Those parking spaces should be the closest to the accessible entrance, on level ground. The spaces should be at least eight feet wide, with an access aisle on either side.
- For accessible spaces for cars, the adjacent access aisle must be at least five feet wide; for van spaces, eight feet wide.
- “If achievable,” an accessible service counter must have a maximum height of 36 inches, with a clear floor space of 30 by 48 inches to permit the use of a wheelchair.
A common misconception is that only new construction and alterations need to be accessible, and that older facilities are “grandfathered,” but that’s not true. Because the ADA is a civil rights law and not a building code, ADA rules apply equally to all facilities, young and old. This is particularly important to remember in light of the long-standing cottage industry of attorneys who sue small businesses for alleged ADA violations.
Another common mistake made by physicians who lease their office space is to assume that their landlord is responsible for meeting all ADA obligations. In fact, The ADA places the legal obligation on both the landlord and the tenant. The landlord and the tenant may decide among themselves who will actually make the changes and provide the aids and services, but both remain legally responsible.
Another aspect that you might not have thought of is access to your website. While ADA applicability to online services remains vague, lawsuits have been filed, and are likely to increase. Online accessibility issues that have been identified include:
- Ability to find and process information on a website (e.g., providing audio descriptions for video content, for the sight-impaired).
- Ability to navigate and use a website (e.g., ensuring that all site functions are easily accessible with only a keyboard).
- Ability to comprehend all information (including clearly understandable error messages).
Hearing-impaired patients present their own considerations for delivering adequate care, which I will discuss in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
. And 7 years ago, the government raised the penalties for failing to do so. So it might be time to re-educate yourself on what the ADA requires.
ADA compliance is not an issue that we talk about or provide training for in medical schools or with our professional organizations. Since fines for small businesses are now $75,000 for a first offense and $150,000 for each subsequent violation, this could be an expensive oversight that malpractice and other liability policies will not cover.
A 2019 study in Boston examined physicians’ knowledge of legal obligations when caring for patients with disabilities. Researchers concluded that most physicians interviewed “exhibited a superficial or incorrect understanding of their legal responsibilities to patients with a disability.” If you feel you’re in that boat, you might want to consult federal guidance with information and common questions physicians ask about their ADA obligations.
The ADA defines a person with a disability as someone with “a physical or mental impairment that substantially limits one or more life activities”; someone with a record of such an impairment; or someone who is “regarded as having such an impairment.” Among the ADA standards required for accessible exam rooms, according to the guidance:
- The entry door to the exam room should be a minimum width of 32 inches when the door is opened at a 90-degree angle.
- There should be a minimum of 30 by 48 inches of clear floor space next to the exam table.
- An accessible exam table should be able to be lowered to the height of the patient’s wheelchair seat, 17 to 19 inches from the floor.
This does not mean that all of your exam rooms must meet these standards, of course; but if you see any patients with disabilities – and who doesn’t? – you need at least one room that meets the criteria.
Federal guidance also includes requirements on removal of architectural barriers, accessible parking, and entrance and maneuvering spaces – which apply to both for-profit and nonprofit organizations. Among them:
- Designated accessible parking spaces must be included among any parking the business provides for the public “if doing so is readily achievable.” Those parking spaces should be the closest to the accessible entrance, on level ground. The spaces should be at least eight feet wide, with an access aisle on either side.
- For accessible spaces for cars, the adjacent access aisle must be at least five feet wide; for van spaces, eight feet wide.
- “If achievable,” an accessible service counter must have a maximum height of 36 inches, with a clear floor space of 30 by 48 inches to permit the use of a wheelchair.
A common misconception is that only new construction and alterations need to be accessible, and that older facilities are “grandfathered,” but that’s not true. Because the ADA is a civil rights law and not a building code, ADA rules apply equally to all facilities, young and old. This is particularly important to remember in light of the long-standing cottage industry of attorneys who sue small businesses for alleged ADA violations.
Another common mistake made by physicians who lease their office space is to assume that their landlord is responsible for meeting all ADA obligations. In fact, The ADA places the legal obligation on both the landlord and the tenant. The landlord and the tenant may decide among themselves who will actually make the changes and provide the aids and services, but both remain legally responsible.
Another aspect that you might not have thought of is access to your website. While ADA applicability to online services remains vague, lawsuits have been filed, and are likely to increase. Online accessibility issues that have been identified include:
- Ability to find and process information on a website (e.g., providing audio descriptions for video content, for the sight-impaired).
- Ability to navigate and use a website (e.g., ensuring that all site functions are easily accessible with only a keyboard).
- Ability to comprehend all information (including clearly understandable error messages).
Hearing-impaired patients present their own considerations for delivering adequate care, which I will discuss in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
. And 7 years ago, the government raised the penalties for failing to do so. So it might be time to re-educate yourself on what the ADA requires.
ADA compliance is not an issue that we talk about or provide training for in medical schools or with our professional organizations. Since fines for small businesses are now $75,000 for a first offense and $150,000 for each subsequent violation, this could be an expensive oversight that malpractice and other liability policies will not cover.
A 2019 study in Boston examined physicians’ knowledge of legal obligations when caring for patients with disabilities. Researchers concluded that most physicians interviewed “exhibited a superficial or incorrect understanding of their legal responsibilities to patients with a disability.” If you feel you’re in that boat, you might want to consult federal guidance with information and common questions physicians ask about their ADA obligations.
The ADA defines a person with a disability as someone with “a physical or mental impairment that substantially limits one or more life activities”; someone with a record of such an impairment; or someone who is “regarded as having such an impairment.” Among the ADA standards required for accessible exam rooms, according to the guidance:
- The entry door to the exam room should be a minimum width of 32 inches when the door is opened at a 90-degree angle.
- There should be a minimum of 30 by 48 inches of clear floor space next to the exam table.
- An accessible exam table should be able to be lowered to the height of the patient’s wheelchair seat, 17 to 19 inches from the floor.
This does not mean that all of your exam rooms must meet these standards, of course; but if you see any patients with disabilities – and who doesn’t? – you need at least one room that meets the criteria.
Federal guidance also includes requirements on removal of architectural barriers, accessible parking, and entrance and maneuvering spaces – which apply to both for-profit and nonprofit organizations. Among them:
- Designated accessible parking spaces must be included among any parking the business provides for the public “if doing so is readily achievable.” Those parking spaces should be the closest to the accessible entrance, on level ground. The spaces should be at least eight feet wide, with an access aisle on either side.
- For accessible spaces for cars, the adjacent access aisle must be at least five feet wide; for van spaces, eight feet wide.
- “If achievable,” an accessible service counter must have a maximum height of 36 inches, with a clear floor space of 30 by 48 inches to permit the use of a wheelchair.
A common misconception is that only new construction and alterations need to be accessible, and that older facilities are “grandfathered,” but that’s not true. Because the ADA is a civil rights law and not a building code, ADA rules apply equally to all facilities, young and old. This is particularly important to remember in light of the long-standing cottage industry of attorneys who sue small businesses for alleged ADA violations.
Another common mistake made by physicians who lease their office space is to assume that their landlord is responsible for meeting all ADA obligations. In fact, The ADA places the legal obligation on both the landlord and the tenant. The landlord and the tenant may decide among themselves who will actually make the changes and provide the aids and services, but both remain legally responsible.
Another aspect that you might not have thought of is access to your website. While ADA applicability to online services remains vague, lawsuits have been filed, and are likely to increase. Online accessibility issues that have been identified include:
- Ability to find and process information on a website (e.g., providing audio descriptions for video content, for the sight-impaired).
- Ability to navigate and use a website (e.g., ensuring that all site functions are easily accessible with only a keyboard).
- Ability to comprehend all information (including clearly understandable error messages).
Hearing-impaired patients present their own considerations for delivering adequate care, which I will discuss in my next column.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
AMA acknowledges medical education racism of past, vows better future
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
The report received overwhelming support at the House of Delegates, the AMA’s legislative policy making body, during an online meeting held June 13.
The Council on Medical Education’s report recommends that the AMA acknowledge the harm caused by the Flexner Report, which was issued in 1910 and has since shaped medical education. The Flexner Report caused harm not only to historically Black medical schools, but also to physician workforce diversity and to the clinical outcomes of minority and marginalized patients, according to the medical education advisory body.
The council also recommended conducting a study on medical education with a focus on health equity and racial justice, improving diversity among healthcare workers, and fixing inequitable outcomes from minorities and marginalized patient populations.
The report comes on the heels of the resignation of JAMA editor-in-chief Howard Bauchner, MD, and another high-ranking editor following a February podcast on systemic racism in medicine. The AMA has since released a strategic plan addressing racism and health inequity that has divided membership.
Flexner Report’s effect on physician diversity
The Council on Medical Education’s report observed that as a result of the Flexner Report’s recommendations, 89 medical schools, including 5 of the 7 existing medical schools training Black physicians, were closed because they didn’t meet the report’s standards. In addition, the report created a limited role for Black physicians while “hint[ing] that Black physicians possessed less potential and ability than their White counterparts,” read the Council’s report.
In addition to consigning the role of the Black physician to “educating the [Black] race to know and to practice fundamental hygienic principles,” the Flexner Report also observed that “a well-taught negro sanitarian will be immensely useful,” per the Council’s report.
The impact of the closure of medical schools training Black physicians was dramatic. According to the Council’s report, in 1964, 93% of medical students in the United States were men and 97% of those students were non-Hispanic White.
Today, 56% of physicians identify as White, 17% as Asian, 6% as Hispanic, and 5% as Black or African American, per the Association of American Medical Colleges; nearly 14% of active physicians didn’t report their race in the survey. By means of contrast, the U.S. population in 2019 was 60% White, 19% Latino/Hispanic, 13% Black or African American, and 6% Asian American, according to the Brookings Institute.
Abraham Flexner, who wrote the Flexner Report, is often referred to as the “father of modern medical education,” according to the AAMC. In November, the AAMC observed that the Flexner Report contained racist and sexist ideas and that his work contributed to the closure of historically Black medical schools. Both statements were included in AAMC’s announcement about the removal of Flexner’s name from its most prestigious award. As of January, the award is now called the AAMC Award for Excellence in Medical Education.
Pathway programs can increase diversity
Pathway programs, which leverage targeted milestones along the journey to becoming a physician in order to increase diversity, were an area of focus in the council’s report. These programs “can exert a meaningful, positive effect on student outcomes and increase diversity across various levels of educational settings,” according to its report.
Centers of Excellence, which provides grants for mentorship and training programs, is one of many pathway programs. During the 2018-2019 academic year, Centers of Excellence supported more than 1,300 trainees – 99% of them were underrepresented minorities and 64% came from financially or educationally disadvantaged backgrounds. In 2006, federal funding was cut to these programs and the number of Centers of Excellence fell.
Still, the report cites the passage of federal funding in 2020 of $50 million for public institutions of higher education that train physicians; educational institutions in states with a projected primary care shortage in 2025 are given priority in the grant-funding process.
AMA council’s report garners support from delegates
Delegates voiced overwhelming support of the council’s report during the June 13 meeting. Lou Edje, MD, a Perrysburgh, Ohio–based family physician, voiced strong support for the council’s report, in particular its recommendations that recognize the harm caused by the Flexner Report. Dr. Edje observed that the Flexner Report, with its elimination of five of seven Black medical schools, “[set] back admissions of Black students into medicine by 50 years.”
“Empathy is what we are called to have as physicians. I implore you to simply substitute your ethnicity into these quotes to help understand the historic need for health equity in medicine today. This CME report is part of the antidote to Flexner. We support [it] fully,” concluded Dr. Edje, who spoke for the Great Lakes States Coalition of the AMA.
Rohan Khazanchi, a medical student at the University of Nebraska, Omaha, and a member of the council, said, “Our broad attempt with this report was twofold: to fill gaps in AMA policy with evidence-based recommendations which could improve diversity in our health workforce and, second, to enhance our organization’s vision for truth, reconciliation, and healing to redress the historic marginalization of minoritized physicians in medicine.”
According to an AMA spokesperson, the House of Delegates will vote on this and other policies this week, after which the policies are considered final.
A version of this article first appeared on Medscape.com.
Minnesota named best place to practice in 2021
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.

In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.

In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.
For physicians who are just starting out or thinking about moving, the “Land of 10,000 Lakes” could be the land of opportunity, according to a recent Medscape analysis.

In a ranking of the 50 states, Minnesota “claimed top marks for livability, low incidence of adverse actions against doctors, and the performance of its health system,” Shelly Reese wrote in Medscape’s “Best & Worst Places to Practice 2021.”
Minnesota is below average where it’s good to be below average – share of physicians reporting burnout and/or depression – but above average in the share of physicians who say they’re “very happy” outside of work, Medscape said in the annual report.
and adverse actions and a high level of livability. Third place went to Washington (called the most livable state in the country by U.S. News and World Report), fourth to Colorado (physicians happy at and outside of work, high retention rate for residents), and fifth to Utah (low crime rate, high quality of life), Medscape said.
At the bottom of the list for 2021 is West Virginia, where physicians “may confront a bevy of challenges” in the form of low livability, a high rate of adverse actions, and relatively high malpractice payouts, Ms. Reese noted in the report.
State number 49 is Louisiana, where livability is low, malpractice payouts are high, and more than half of physicians say that they’re burned out and/or depressed. New Mexico is 48th (very high rate of adverse actions, poor resident retention), Nevada is 47th (low marks for avoidable hospital use and disparity in care), and Rhode Island is 46th (high malpractice payouts, low physician compensation), Medscape said.
Continuing with the group-of-five theme, America’s three most populous states finished in the top half of the ranking – California 16th, Texas 11th, and Florida 21st – but New York and Pennsylvania, numbers four and five by population size, did not.
The rankings are based on states’ performance in 10 different measures, three of which were sourced from Medscape surveys – happiness at work, happiness outside of work, and burnout/depression – and seven from other organizations: adverse actions against physicians, malpractice payouts, compensation (adjusted for cost of living), overall health, health system performance, overall livability, resident retention.