User login
Treating Digestive Disease Across the Lifespan
Pediatric gastroenterologists are a vital, yet often overlooked segment of the GI workforce and an important part of AGA’s diverse membership. Per the American Board of Pediatrics, 2,232 pediatricians have been board certified in pediatric gastroenterology since formal certification was first offered in 1990, and AGA Institute Council’s Pediatric Gastroenterology and Developmental Biology Section has nearly 1,900 members.
According to a recently published study in the journal Pediatrics, the pediatric GI workforce is expected to double by 2040, growing at a rate faster than that of most other pediatric subspecialties. This is largely due to the increased scope and complexity of the field driven by scientific advances and the increasing prevalence of digestive and liver diseases in children, including inflammatory bowel and other diseases.
In this month’s Member Spotlight, we highlight Dr. Yoyo Zhang, a pediatric gastroenterologist at Stanford Children’s Health specializing in intestinal and liver transplantation. Her passion for her profession and for improving the lives of her patients shines brightly, and her interview provides fascinating insights into the complexities and rewards of the rapidly expanding field of pediatric gastroenterology.
Also in our November issue, we update you on the FDA’s recent approval of the “next-gen” Cologuard test and query a panel of primary care and GI experts on their thoughts regarding the role that newly FDA-approved (but not yet guideline-recommended) Guardant blood-based CRC screening test should play in CRC screening moving forward.
In our Perspectives feature, we offer expert insights on how to appropriately screen patients for certain rare malignancies. Is it worthwhile screening for pancreatic cancer, and if so, how should it be done? Likewise, diagnosing cholangiocarcinoma is challenging; how best should one evaluate for this in higher-risk populations?
We hope you enjoy all the content in our November issue – as always, thanks for reading!
Megan A. Adams, MD, JD, MSc
Editor in Chief
Pediatric gastroenterologists are a vital, yet often overlooked segment of the GI workforce and an important part of AGA’s diverse membership. Per the American Board of Pediatrics, 2,232 pediatricians have been board certified in pediatric gastroenterology since formal certification was first offered in 1990, and AGA Institute Council’s Pediatric Gastroenterology and Developmental Biology Section has nearly 1,900 members.
According to a recently published study in the journal Pediatrics, the pediatric GI workforce is expected to double by 2040, growing at a rate faster than that of most other pediatric subspecialties. This is largely due to the increased scope and complexity of the field driven by scientific advances and the increasing prevalence of digestive and liver diseases in children, including inflammatory bowel and other diseases.
In this month’s Member Spotlight, we highlight Dr. Yoyo Zhang, a pediatric gastroenterologist at Stanford Children’s Health specializing in intestinal and liver transplantation. Her passion for her profession and for improving the lives of her patients shines brightly, and her interview provides fascinating insights into the complexities and rewards of the rapidly expanding field of pediatric gastroenterology.
Also in our November issue, we update you on the FDA’s recent approval of the “next-gen” Cologuard test and query a panel of primary care and GI experts on their thoughts regarding the role that newly FDA-approved (but not yet guideline-recommended) Guardant blood-based CRC screening test should play in CRC screening moving forward.
In our Perspectives feature, we offer expert insights on how to appropriately screen patients for certain rare malignancies. Is it worthwhile screening for pancreatic cancer, and if so, how should it be done? Likewise, diagnosing cholangiocarcinoma is challenging; how best should one evaluate for this in higher-risk populations?
We hope you enjoy all the content in our November issue – as always, thanks for reading!
Megan A. Adams, MD, JD, MSc
Editor in Chief
Pediatric gastroenterologists are a vital, yet often overlooked segment of the GI workforce and an important part of AGA’s diverse membership. Per the American Board of Pediatrics, 2,232 pediatricians have been board certified in pediatric gastroenterology since formal certification was first offered in 1990, and AGA Institute Council’s Pediatric Gastroenterology and Developmental Biology Section has nearly 1,900 members.
According to a recently published study in the journal Pediatrics, the pediatric GI workforce is expected to double by 2040, growing at a rate faster than that of most other pediatric subspecialties. This is largely due to the increased scope and complexity of the field driven by scientific advances and the increasing prevalence of digestive and liver diseases in children, including inflammatory bowel and other diseases.
In this month’s Member Spotlight, we highlight Dr. Yoyo Zhang, a pediatric gastroenterologist at Stanford Children’s Health specializing in intestinal and liver transplantation. Her passion for her profession and for improving the lives of her patients shines brightly, and her interview provides fascinating insights into the complexities and rewards of the rapidly expanding field of pediatric gastroenterology.
Also in our November issue, we update you on the FDA’s recent approval of the “next-gen” Cologuard test and query a panel of primary care and GI experts on their thoughts regarding the role that newly FDA-approved (but not yet guideline-recommended) Guardant blood-based CRC screening test should play in CRC screening moving forward.
In our Perspectives feature, we offer expert insights on how to appropriately screen patients for certain rare malignancies. Is it worthwhile screening for pancreatic cancer, and if so, how should it be done? Likewise, diagnosing cholangiocarcinoma is challenging; how best should one evaluate for this in higher-risk populations?
We hope you enjoy all the content in our November issue – as always, thanks for reading!
Megan A. Adams, MD, JD, MSc
Editor in Chief
Managing Age-Related Muscle Loss in Primary Care
Scene 1: Exercise Medicine Clinic, Rio de Janeiro, Brazil I just finished one evaluation on physical fitness and health and looked at my schedule. My next patient would be a 65-year-old man. How fit will he be? Will he have evident age-related muscle loss? I gave myself a short break and my mind went to the late 1970s.
Once upon a time, the practice of medicine was based primarily on the skill of your physical examination, previous experiences, and your ability to reason logically and make solid deductions. In 1979, the stethoscope was part of my dress code. After one elective semester as a research fellow at the Ambrose Cardiorespiratory Unit at McMaster University Medical Centre, in Hamilton, Canada, where I was honored to witness the dawn of evidence-based medicine, I graduated from Federal University of Rio de Janeiro. I still remember being introduced to some promising novelties in cardiology, such as M-mode echocardiograms and myocardial scintigraphy. Radiology was primarily centered on x-rays, and lab testing was basic and poorly automatized.
Over the following decades, medical practice changed dramatically with the incorporation of new technologies. Recent advances in diagnostic tools, genetics, artificial intelligence, and sophisticated statistical analyses, along with well-collected scientific data, have molded how clinicians should think and work.
At the same time, clinical profiles also changed. Internists and primary care physicians are regularly managing patients who are, on average, older and have or are on the way to having potentially life-threatening chronic diseases, accompanied by poor lifestyle habits, and, highly important, often some degree of disability, frailty, and loss of independence. Many of them exhibit age-related muscle loss.
Scene 2: Exercise Medicine Clinic, Rio de Janeiro, Brazil
Conscious of the benefits of interrupting my sitting time with activity, I left my office and walked to meet my patient in the waiting room. I called his name and introduced myself. I watched how he listened and reacted to my speech, and how easy or hard it was for him to rise from the chair — readiness, velocity, and number of supports required: none, one, or two hands. I offered my own hand to him, and when we shook, I gauged the strength of his grip.
I invited him into my office and took note of his somatotype and body composition, and whether he had any central obesity. Of course, and I should by no means miss this chance, I carefully observed how he walked in — his gait, speed, balance, posture — how he pulled up the chair, and how he managed to lower himself into his seat. Before I even sat in my own chair, I asked him if he remembered what his body weight was 5 years ago and what it was today. Before we got started in earnest, I had already managed to collect several pieces of relevant information.
Exercise Physiology: Changing Landscape
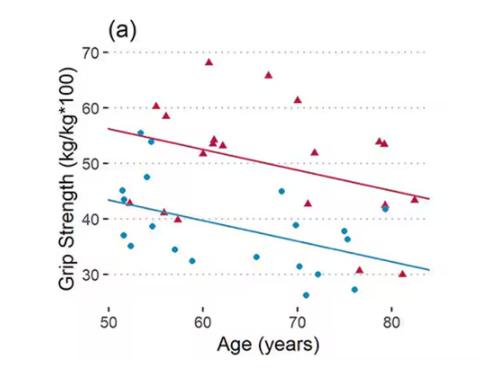
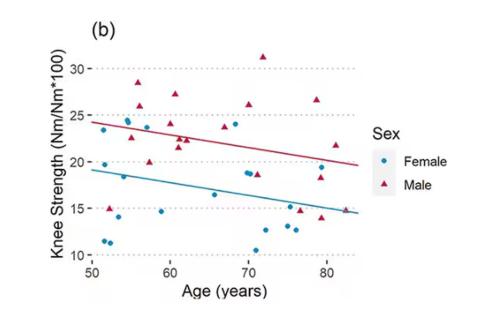
Muscle activity depends on muscle mass and function, and peaks somewhere between ages 25 and 35 before declining. The drop is slow in the early stages but accelerates rapidly after age 60 or 65.
Two of the most relevant variables in muscle function are strength and power. As a product of force and velocity, muscle power could be a more crucial factor than strength for many daily activities that demand movement against gravity or inertia, such as placing carry-on baggage in the overhead bin of an airplane or rising from the floor or chair.
The association between muscle mass and muscle strength or power is moderate, and physiologic data have indicated that the decline of muscle power with aging is faster and larger than that of muscle strength.
The term “sarcopenia” has become definitively incorporated into the medical glossary. From the Greek (“sark” and “penia”), sarcopenia was defined as reduced muscle mass, but more recently it has encompassed muscle strength in its definition. However, a recent consensus paper from the Global Leadership Initiative in Sarcopenia, using a Delphi approach, rejected the inclusion of muscle power in the concept of sarcopenia. On the other hand, a long time ago, some authors coined and advocated the use the term “dynapenia” to more precisely reflect the reduced levels of muscle strength and power that often accompany aging.
The best available intervention to counteract age-related deterioration of muscle activity is resistance exercise. The types of resistance exercises vary widely — by number of sets and repetitions, intervals between sets, speed of execution of movement, and percentage of maximal weight/load.
We recently proposed that, after an evaluation to identify the main muscle variable requiring attention, the resistance exercise program should be individually tailored and prescribed according to the objective to counteract sarcopenia or dynapenia.
What is more important for autonomy and better daily living conditions in old and very old individuals: muscle mass, muscle strength, or muscle power? More likely the response is muscle power — in practical terms, dynapenia rather than sarcopenia. This short video presents practical tips for obtaining optimal results in fighting dynapenia. The first choice should be power training or high velocity–based training, emphasizing two to three sets of six to eight repetitions performed as fast as possible (on the concentric or shortening phase of muscle contraction) with relatively high loads.
Internists and primary care physicians are most likely satisfied with the information they obtain by simple observation, and already can superficially grade the magnitude of a patient’s age-related muscle loss and its consequences to daily living.
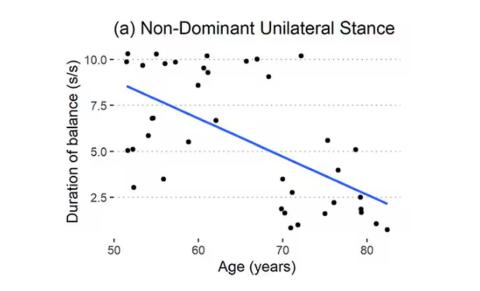
However, those who want more objective information on nonaerobic physical fitness can add one to three simple tests to their consultation: the sitting-rising test (SRT); the 10-second one-legged test (10sOLS test); and the Flexitest. Poor performance on each of these — and particularly all three — is strongly associated with an increased risk for premature death in middle-aged and older individuals. These tests require no extra equipment and can be performed rapidly, and interpreting the results takes only a few moments using published reference values.
Age-related muscle loss profoundly affects our ability to sit and rise from the floor, so if time is limited, the SRT is the best assessment, as it measures all nonaerobic components of physical fitness. For a quick interpretation, consider that SRT scores vary from 0 to 10, do not substantially differ by sex, and that a composite score equal to or greater than 8 will reflect a minimum age-adjusted percentile of 61, most likely indicating relevant age-related muscle loss is not yet occurring.
Dr. Araújo is Professor and Dean of Research and Education, Exercise Medicine Clinic (CLINIMEX), Rio de Janeiro, Brazil. He reported conflicts of interest with INBRAMED.
A version of this article first appeared on Medscape.com.
Scene 1: Exercise Medicine Clinic, Rio de Janeiro, Brazil I just finished one evaluation on physical fitness and health and looked at my schedule. My next patient would be a 65-year-old man. How fit will he be? Will he have evident age-related muscle loss? I gave myself a short break and my mind went to the late 1970s.
Once upon a time, the practice of medicine was based primarily on the skill of your physical examination, previous experiences, and your ability to reason logically and make solid deductions. In 1979, the stethoscope was part of my dress code. After one elective semester as a research fellow at the Ambrose Cardiorespiratory Unit at McMaster University Medical Centre, in Hamilton, Canada, where I was honored to witness the dawn of evidence-based medicine, I graduated from Federal University of Rio de Janeiro. I still remember being introduced to some promising novelties in cardiology, such as M-mode echocardiograms and myocardial scintigraphy. Radiology was primarily centered on x-rays, and lab testing was basic and poorly automatized.
Over the following decades, medical practice changed dramatically with the incorporation of new technologies. Recent advances in diagnostic tools, genetics, artificial intelligence, and sophisticated statistical analyses, along with well-collected scientific data, have molded how clinicians should think and work.
At the same time, clinical profiles also changed. Internists and primary care physicians are regularly managing patients who are, on average, older and have or are on the way to having potentially life-threatening chronic diseases, accompanied by poor lifestyle habits, and, highly important, often some degree of disability, frailty, and loss of independence. Many of them exhibit age-related muscle loss.
Scene 2: Exercise Medicine Clinic, Rio de Janeiro, Brazil
Conscious of the benefits of interrupting my sitting time with activity, I left my office and walked to meet my patient in the waiting room. I called his name and introduced myself. I watched how he listened and reacted to my speech, and how easy or hard it was for him to rise from the chair — readiness, velocity, and number of supports required: none, one, or two hands. I offered my own hand to him, and when we shook, I gauged the strength of his grip.
I invited him into my office and took note of his somatotype and body composition, and whether he had any central obesity. Of course, and I should by no means miss this chance, I carefully observed how he walked in — his gait, speed, balance, posture — how he pulled up the chair, and how he managed to lower himself into his seat. Before I even sat in my own chair, I asked him if he remembered what his body weight was 5 years ago and what it was today. Before we got started in earnest, I had already managed to collect several pieces of relevant information.
Exercise Physiology: Changing Landscape
Muscle activity depends on muscle mass and function, and peaks somewhere between ages 25 and 35 before declining. The drop is slow in the early stages but accelerates rapidly after age 60 or 65.
Two of the most relevant variables in muscle function are strength and power. As a product of force and velocity, muscle power could be a more crucial factor than strength for many daily activities that demand movement against gravity or inertia, such as placing carry-on baggage in the overhead bin of an airplane or rising from the floor or chair.
The association between muscle mass and muscle strength or power is moderate, and physiologic data have indicated that the decline of muscle power with aging is faster and larger than that of muscle strength.
The term “sarcopenia” has become definitively incorporated into the medical glossary. From the Greek (“sark” and “penia”), sarcopenia was defined as reduced muscle mass, but more recently it has encompassed muscle strength in its definition. However, a recent consensus paper from the Global Leadership Initiative in Sarcopenia, using a Delphi approach, rejected the inclusion of muscle power in the concept of sarcopenia. On the other hand, a long time ago, some authors coined and advocated the use the term “dynapenia” to more precisely reflect the reduced levels of muscle strength and power that often accompany aging.
The best available intervention to counteract age-related deterioration of muscle activity is resistance exercise. The types of resistance exercises vary widely — by number of sets and repetitions, intervals between sets, speed of execution of movement, and percentage of maximal weight/load.
We recently proposed that, after an evaluation to identify the main muscle variable requiring attention, the resistance exercise program should be individually tailored and prescribed according to the objective to counteract sarcopenia or dynapenia.
What is more important for autonomy and better daily living conditions in old and very old individuals: muscle mass, muscle strength, or muscle power? More likely the response is muscle power — in practical terms, dynapenia rather than sarcopenia. This short video presents practical tips for obtaining optimal results in fighting dynapenia. The first choice should be power training or high velocity–based training, emphasizing two to three sets of six to eight repetitions performed as fast as possible (on the concentric or shortening phase of muscle contraction) with relatively high loads.
Internists and primary care physicians are most likely satisfied with the information they obtain by simple observation, and already can superficially grade the magnitude of a patient’s age-related muscle loss and its consequences to daily living.
However, those who want more objective information on nonaerobic physical fitness can add one to three simple tests to their consultation: the sitting-rising test (SRT); the 10-second one-legged test (10sOLS test); and the Flexitest. Poor performance on each of these — and particularly all three — is strongly associated with an increased risk for premature death in middle-aged and older individuals. These tests require no extra equipment and can be performed rapidly, and interpreting the results takes only a few moments using published reference values.
Age-related muscle loss profoundly affects our ability to sit and rise from the floor, so if time is limited, the SRT is the best assessment, as it measures all nonaerobic components of physical fitness. For a quick interpretation, consider that SRT scores vary from 0 to 10, do not substantially differ by sex, and that a composite score equal to or greater than 8 will reflect a minimum age-adjusted percentile of 61, most likely indicating relevant age-related muscle loss is not yet occurring.
Dr. Araújo is Professor and Dean of Research and Education, Exercise Medicine Clinic (CLINIMEX), Rio de Janeiro, Brazil. He reported conflicts of interest with INBRAMED.
A version of this article first appeared on Medscape.com.
Scene 1: Exercise Medicine Clinic, Rio de Janeiro, Brazil I just finished one evaluation on physical fitness and health and looked at my schedule. My next patient would be a 65-year-old man. How fit will he be? Will he have evident age-related muscle loss? I gave myself a short break and my mind went to the late 1970s.
Once upon a time, the practice of medicine was based primarily on the skill of your physical examination, previous experiences, and your ability to reason logically and make solid deductions. In 1979, the stethoscope was part of my dress code. After one elective semester as a research fellow at the Ambrose Cardiorespiratory Unit at McMaster University Medical Centre, in Hamilton, Canada, where I was honored to witness the dawn of evidence-based medicine, I graduated from Federal University of Rio de Janeiro. I still remember being introduced to some promising novelties in cardiology, such as M-mode echocardiograms and myocardial scintigraphy. Radiology was primarily centered on x-rays, and lab testing was basic and poorly automatized.
Over the following decades, medical practice changed dramatically with the incorporation of new technologies. Recent advances in diagnostic tools, genetics, artificial intelligence, and sophisticated statistical analyses, along with well-collected scientific data, have molded how clinicians should think and work.
At the same time, clinical profiles also changed. Internists and primary care physicians are regularly managing patients who are, on average, older and have or are on the way to having potentially life-threatening chronic diseases, accompanied by poor lifestyle habits, and, highly important, often some degree of disability, frailty, and loss of independence. Many of them exhibit age-related muscle loss.
Scene 2: Exercise Medicine Clinic, Rio de Janeiro, Brazil
Conscious of the benefits of interrupting my sitting time with activity, I left my office and walked to meet my patient in the waiting room. I called his name and introduced myself. I watched how he listened and reacted to my speech, and how easy or hard it was for him to rise from the chair — readiness, velocity, and number of supports required: none, one, or two hands. I offered my own hand to him, and when we shook, I gauged the strength of his grip.
I invited him into my office and took note of his somatotype and body composition, and whether he had any central obesity. Of course, and I should by no means miss this chance, I carefully observed how he walked in — his gait, speed, balance, posture — how he pulled up the chair, and how he managed to lower himself into his seat. Before I even sat in my own chair, I asked him if he remembered what his body weight was 5 years ago and what it was today. Before we got started in earnest, I had already managed to collect several pieces of relevant information.
Exercise Physiology: Changing Landscape
Muscle activity depends on muscle mass and function, and peaks somewhere between ages 25 and 35 before declining. The drop is slow in the early stages but accelerates rapidly after age 60 or 65.
Two of the most relevant variables in muscle function are strength and power. As a product of force and velocity, muscle power could be a more crucial factor than strength for many daily activities that demand movement against gravity or inertia, such as placing carry-on baggage in the overhead bin of an airplane or rising from the floor or chair.
The association between muscle mass and muscle strength or power is moderate, and physiologic data have indicated that the decline of muscle power with aging is faster and larger than that of muscle strength.
The term “sarcopenia” has become definitively incorporated into the medical glossary. From the Greek (“sark” and “penia”), sarcopenia was defined as reduced muscle mass, but more recently it has encompassed muscle strength in its definition. However, a recent consensus paper from the Global Leadership Initiative in Sarcopenia, using a Delphi approach, rejected the inclusion of muscle power in the concept of sarcopenia. On the other hand, a long time ago, some authors coined and advocated the use the term “dynapenia” to more precisely reflect the reduced levels of muscle strength and power that often accompany aging.
The best available intervention to counteract age-related deterioration of muscle activity is resistance exercise. The types of resistance exercises vary widely — by number of sets and repetitions, intervals between sets, speed of execution of movement, and percentage of maximal weight/load.
We recently proposed that, after an evaluation to identify the main muscle variable requiring attention, the resistance exercise program should be individually tailored and prescribed according to the objective to counteract sarcopenia or dynapenia.
What is more important for autonomy and better daily living conditions in old and very old individuals: muscle mass, muscle strength, or muscle power? More likely the response is muscle power — in practical terms, dynapenia rather than sarcopenia. This short video presents practical tips for obtaining optimal results in fighting dynapenia. The first choice should be power training or high velocity–based training, emphasizing two to three sets of six to eight repetitions performed as fast as possible (on the concentric or shortening phase of muscle contraction) with relatively high loads.
Internists and primary care physicians are most likely satisfied with the information they obtain by simple observation, and already can superficially grade the magnitude of a patient’s age-related muscle loss and its consequences to daily living.
However, those who want more objective information on nonaerobic physical fitness can add one to three simple tests to their consultation: the sitting-rising test (SRT); the 10-second one-legged test (10sOLS test); and the Flexitest. Poor performance on each of these — and particularly all three — is strongly associated with an increased risk for premature death in middle-aged and older individuals. These tests require no extra equipment and can be performed rapidly, and interpreting the results takes only a few moments using published reference values.
Age-related muscle loss profoundly affects our ability to sit and rise from the floor, so if time is limited, the SRT is the best assessment, as it measures all nonaerobic components of physical fitness. For a quick interpretation, consider that SRT scores vary from 0 to 10, do not substantially differ by sex, and that a composite score equal to or greater than 8 will reflect a minimum age-adjusted percentile of 61, most likely indicating relevant age-related muscle loss is not yet occurring.
Dr. Araújo is Professor and Dean of Research and Education, Exercise Medicine Clinic (CLINIMEX), Rio de Janeiro, Brazil. He reported conflicts of interest with INBRAMED.
A version of this article first appeared on Medscape.com.
Obesity: A Social Vulnerability
Sometime in the last year or 2 I wrote that, despite my considerable reservations, I had finally come to the conclusion that the American Medical Association’s decision to designate obesity as a disease was appropriate. My rationalization was that the disease label would open more opportunities for funding obesity treatments. However, the explosive growth and popularity of glucagon-like peptide 1 (GLP-1) agonists over the last year has had me rethinking my decision to suppress my long-held reservations about the disease designation.
So, if it’s not a disease, then what should we call it? How do we explain its surge in high-income countries that began in the 1980s? While there are still some folks who see obesity as a character flaw, I think you and I as healthcare providers have difficulty explaining the increase prevalence of obesity as either global breakdown of willpower or a widespread genetic shift as the result of burst of radiation from solar flares.
However, if we want to continue our search and finger-pointing we need to have a better definition of exactly what obesity is. If we’re going to continue calling it a disease we have done a pretty sloppy job of creating diagnostic criteria. To be honest, we aren’t doing such a hot job with “long COVID” either.
A recent article in the New York Times makes it clear that I’m not the only physician who is feeling uncomfortable with this lack of diagnostic specificity.
We know that using body mass index (BMI) as a criteria is imprecise. There are healthy individuals with elevated BMIs and there are others who are carrying an unhealthy amount of fat who have normal BMIs. And, there are individuals who have what might appear to be an excess amount of fat who are fit and healthy by other criteria.
Some investigators feel that a set of measurements that includes a waist and/or hip measurement may be a more accurate way of determining visceral adipose tissue. However, this body roundness index (BRI) currently relies on a tape measurement. Until the technique can be preformed by an inexpensive and readily available scanner, the BRI cannot be considered a practical tool for determining obesity.
Dr. Francisco Rubino, the chair of metabolic and bariatric surgery at Kings College in London, England, has been quoted as saying that, “if one defines a disease inaccurately, everything that stems from that – from diagnosis to treatment to policies – will be distorted and biased.”
Denmark has been forced to relabel obesity as a risk factor because the disease designation was stressing the financial viability of their healthcare system as more and more patients were being prescribe GLP-1 agonists, sometimes off label. A rationing strategy was resulting in suboptimal treatment of a significant portion of the obese population.
Spearheaded by Dr. Rubino, a Lancet Commission composed of physicians has tasked itself to define an “evidence-based diagnosis for obesity. Instead of relying on a single metric such as the BMI or BRI, diagnosing “clinical obesity” would involve a broad array of observations including a history, physical examination, standard laboratory and additional testing, “naming signs and symptoms, organ by organ, tissue by tissue, with plausible mechanisms for each one.” In other words, treating each patient as an individual using evidence-based criteria to make a diagnosis. While likely to be time consuming, this strategy feels like a more scientific approach. I suspect once clinical obesity is more rigorously defined it could be divided into several subtypes. For example, there would be a few conditions that were genetic; Prader-Willi syndrome being the best known.
However, I think the Lancet Commission’s strategy will find that the majority of individuals who make up this half-century global surge have become clinically obese because they have been unable to adapt to the obeseogenic forces in our society, which include diet, autocentricity, and attractive sedentary forms of entertainment, to name just three.
In some cases these unfortunate individuals are more vulnerable because there were born into an economically disadvantaged situation. In other scenarios a lack of foresight and/or political will may have left individuals with no other choice but to rely on automobiles to get around. Still others may find themselves living in a nutritional desert because all of the grocery stores have closed.
I recently encountered a descriptor in a story about the Federal Emergency Management Agency which could easily be adapted to describe this large and growing subtype of individuals with clinical obesity. “Social vulnerability” is measure of how well a community can withstand external stressors that impact human health. For example, the emergency management folks are thinking in terms of natural disaster such as hurricanes, floods, and tornadoes and are asking how well a given community can meet the challenges one would create.
But, the term social vulnerability can easily be applied to individuals living in a society in which unhealthy food is abundant, an infrastructure that discourages or outright prevents non-motorized travel, and the temptation of sedentary entertainment options is unavoidable. Fortunately, not every citizen living in an obesogenic society becomes obese. What factors have protected the non-obese individuals from these obeseogenic stressors? What are the characteristics of the unfortunate “vulnerables” living in the same society who end up being obese?
It is time to shift our focus away from a poorly defined disease model to one in which we begin looking at our society to find out why we have so many socially vulnerable individuals. The toll of obesity as it is currently defined is many order of magnitudes greater than any natural disaster. We have become communities that can no longer withstand the its obesogenic stressors many of which we have created and/or allowed to accumulate over the last century.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Sometime in the last year or 2 I wrote that, despite my considerable reservations, I had finally come to the conclusion that the American Medical Association’s decision to designate obesity as a disease was appropriate. My rationalization was that the disease label would open more opportunities for funding obesity treatments. However, the explosive growth and popularity of glucagon-like peptide 1 (GLP-1) agonists over the last year has had me rethinking my decision to suppress my long-held reservations about the disease designation.
So, if it’s not a disease, then what should we call it? How do we explain its surge in high-income countries that began in the 1980s? While there are still some folks who see obesity as a character flaw, I think you and I as healthcare providers have difficulty explaining the increase prevalence of obesity as either global breakdown of willpower or a widespread genetic shift as the result of burst of radiation from solar flares.
However, if we want to continue our search and finger-pointing we need to have a better definition of exactly what obesity is. If we’re going to continue calling it a disease we have done a pretty sloppy job of creating diagnostic criteria. To be honest, we aren’t doing such a hot job with “long COVID” either.
A recent article in the New York Times makes it clear that I’m not the only physician who is feeling uncomfortable with this lack of diagnostic specificity.
We know that using body mass index (BMI) as a criteria is imprecise. There are healthy individuals with elevated BMIs and there are others who are carrying an unhealthy amount of fat who have normal BMIs. And, there are individuals who have what might appear to be an excess amount of fat who are fit and healthy by other criteria.
Some investigators feel that a set of measurements that includes a waist and/or hip measurement may be a more accurate way of determining visceral adipose tissue. However, this body roundness index (BRI) currently relies on a tape measurement. Until the technique can be preformed by an inexpensive and readily available scanner, the BRI cannot be considered a practical tool for determining obesity.
Dr. Francisco Rubino, the chair of metabolic and bariatric surgery at Kings College in London, England, has been quoted as saying that, “if one defines a disease inaccurately, everything that stems from that – from diagnosis to treatment to policies – will be distorted and biased.”
Denmark has been forced to relabel obesity as a risk factor because the disease designation was stressing the financial viability of their healthcare system as more and more patients were being prescribe GLP-1 agonists, sometimes off label. A rationing strategy was resulting in suboptimal treatment of a significant portion of the obese population.
Spearheaded by Dr. Rubino, a Lancet Commission composed of physicians has tasked itself to define an “evidence-based diagnosis for obesity. Instead of relying on a single metric such as the BMI or BRI, diagnosing “clinical obesity” would involve a broad array of observations including a history, physical examination, standard laboratory and additional testing, “naming signs and symptoms, organ by organ, tissue by tissue, with plausible mechanisms for each one.” In other words, treating each patient as an individual using evidence-based criteria to make a diagnosis. While likely to be time consuming, this strategy feels like a more scientific approach. I suspect once clinical obesity is more rigorously defined it could be divided into several subtypes. For example, there would be a few conditions that were genetic; Prader-Willi syndrome being the best known.
However, I think the Lancet Commission’s strategy will find that the majority of individuals who make up this half-century global surge have become clinically obese because they have been unable to adapt to the obeseogenic forces in our society, which include diet, autocentricity, and attractive sedentary forms of entertainment, to name just three.
In some cases these unfortunate individuals are more vulnerable because there were born into an economically disadvantaged situation. In other scenarios a lack of foresight and/or political will may have left individuals with no other choice but to rely on automobiles to get around. Still others may find themselves living in a nutritional desert because all of the grocery stores have closed.
I recently encountered a descriptor in a story about the Federal Emergency Management Agency which could easily be adapted to describe this large and growing subtype of individuals with clinical obesity. “Social vulnerability” is measure of how well a community can withstand external stressors that impact human health. For example, the emergency management folks are thinking in terms of natural disaster such as hurricanes, floods, and tornadoes and are asking how well a given community can meet the challenges one would create.
But, the term social vulnerability can easily be applied to individuals living in a society in which unhealthy food is abundant, an infrastructure that discourages or outright prevents non-motorized travel, and the temptation of sedentary entertainment options is unavoidable. Fortunately, not every citizen living in an obesogenic society becomes obese. What factors have protected the non-obese individuals from these obeseogenic stressors? What are the characteristics of the unfortunate “vulnerables” living in the same society who end up being obese?
It is time to shift our focus away from a poorly defined disease model to one in which we begin looking at our society to find out why we have so many socially vulnerable individuals. The toll of obesity as it is currently defined is many order of magnitudes greater than any natural disaster. We have become communities that can no longer withstand the its obesogenic stressors many of which we have created and/or allowed to accumulate over the last century.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Sometime in the last year or 2 I wrote that, despite my considerable reservations, I had finally come to the conclusion that the American Medical Association’s decision to designate obesity as a disease was appropriate. My rationalization was that the disease label would open more opportunities for funding obesity treatments. However, the explosive growth and popularity of glucagon-like peptide 1 (GLP-1) agonists over the last year has had me rethinking my decision to suppress my long-held reservations about the disease designation.
So, if it’s not a disease, then what should we call it? How do we explain its surge in high-income countries that began in the 1980s? While there are still some folks who see obesity as a character flaw, I think you and I as healthcare providers have difficulty explaining the increase prevalence of obesity as either global breakdown of willpower or a widespread genetic shift as the result of burst of radiation from solar flares.
However, if we want to continue our search and finger-pointing we need to have a better definition of exactly what obesity is. If we’re going to continue calling it a disease we have done a pretty sloppy job of creating diagnostic criteria. To be honest, we aren’t doing such a hot job with “long COVID” either.
A recent article in the New York Times makes it clear that I’m not the only physician who is feeling uncomfortable with this lack of diagnostic specificity.
We know that using body mass index (BMI) as a criteria is imprecise. There are healthy individuals with elevated BMIs and there are others who are carrying an unhealthy amount of fat who have normal BMIs. And, there are individuals who have what might appear to be an excess amount of fat who are fit and healthy by other criteria.
Some investigators feel that a set of measurements that includes a waist and/or hip measurement may be a more accurate way of determining visceral adipose tissue. However, this body roundness index (BRI) currently relies on a tape measurement. Until the technique can be preformed by an inexpensive and readily available scanner, the BRI cannot be considered a practical tool for determining obesity.
Dr. Francisco Rubino, the chair of metabolic and bariatric surgery at Kings College in London, England, has been quoted as saying that, “if one defines a disease inaccurately, everything that stems from that – from diagnosis to treatment to policies – will be distorted and biased.”
Denmark has been forced to relabel obesity as a risk factor because the disease designation was stressing the financial viability of their healthcare system as more and more patients were being prescribe GLP-1 agonists, sometimes off label. A rationing strategy was resulting in suboptimal treatment of a significant portion of the obese population.
Spearheaded by Dr. Rubino, a Lancet Commission composed of physicians has tasked itself to define an “evidence-based diagnosis for obesity. Instead of relying on a single metric such as the BMI or BRI, diagnosing “clinical obesity” would involve a broad array of observations including a history, physical examination, standard laboratory and additional testing, “naming signs and symptoms, organ by organ, tissue by tissue, with plausible mechanisms for each one.” In other words, treating each patient as an individual using evidence-based criteria to make a diagnosis. While likely to be time consuming, this strategy feels like a more scientific approach. I suspect once clinical obesity is more rigorously defined it could be divided into several subtypes. For example, there would be a few conditions that were genetic; Prader-Willi syndrome being the best known.
However, I think the Lancet Commission’s strategy will find that the majority of individuals who make up this half-century global surge have become clinically obese because they have been unable to adapt to the obeseogenic forces in our society, which include diet, autocentricity, and attractive sedentary forms of entertainment, to name just three.
In some cases these unfortunate individuals are more vulnerable because there were born into an economically disadvantaged situation. In other scenarios a lack of foresight and/or political will may have left individuals with no other choice but to rely on automobiles to get around. Still others may find themselves living in a nutritional desert because all of the grocery stores have closed.
I recently encountered a descriptor in a story about the Federal Emergency Management Agency which could easily be adapted to describe this large and growing subtype of individuals with clinical obesity. “Social vulnerability” is measure of how well a community can withstand external stressors that impact human health. For example, the emergency management folks are thinking in terms of natural disaster such as hurricanes, floods, and tornadoes and are asking how well a given community can meet the challenges one would create.
But, the term social vulnerability can easily be applied to individuals living in a society in which unhealthy food is abundant, an infrastructure that discourages or outright prevents non-motorized travel, and the temptation of sedentary entertainment options is unavoidable. Fortunately, not every citizen living in an obesogenic society becomes obese. What factors have protected the non-obese individuals from these obeseogenic stressors? What are the characteristics of the unfortunate “vulnerables” living in the same society who end up being obese?
It is time to shift our focus away from a poorly defined disease model to one in which we begin looking at our society to find out why we have so many socially vulnerable individuals. The toll of obesity as it is currently defined is many order of magnitudes greater than any natural disaster. We have become communities that can no longer withstand the its obesogenic stressors many of which we have created and/or allowed to accumulate over the last century.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Preventing Pediatric Migraine
I suspect you all have some experience with childhood migraine. It can mean a painful several hours for the patient, arriving often without warning, with recurrences spaced months or sometimes even years apart. It may be accompanied by vomiting, which in some cases overshadows the severity of the headache. It can result in lost days from school and ruin family activities. It can occur so infrequently that the family can’t recall accurately when the last episode happened. In some ways it is a different animal than the adult version.
Most of the pediatric patients with migraine I have seen have experienced attacks that were occurring so infrequently that the families and I seldom discussed medication as an option. Back then imipramine was the only choice. However, currently there are more than a half dozen medications and combinations that have been tried. Recently a review of 45 clinical trials of these medications was published in JAMA Network Open.
I will let you review for yourself the details of these Iranian investigators’ network meta-analysis, but the bottom line is that some medications were associated with a reduction in migraine frequency. Others were associated with headache intensity. “However, no treatments were associated with significant improvements in quality of life or reduction of the duration of migraine attacks.”
Obviously, this paper illustrates clearly that we have not yet discovered the medicinal magic bullet for pediatric migraine prophylaxis. This doesn’t surprise me. After listening to scores of families tell their migraine stories, it became apparent to me that there was often a pattern in which the child’s headache had arrived after a period of acute sleep deprivation. For example, a trip to an amusement park in which travel or excitement may have resulted in the child going to bed later and/or getting up earlier. By afternoon the child’s reserves of something (currently unknown) were depleted to a point that the headache and/or vomiting struck.
Because these episodes were often so infrequent, separated by months, that taking a history demonstrating a recurring pattern could take considerable patience on the part of the family and the provider, even for a physician like myself who believes that better sleep is the answer for everything. However, once I could convince a family of the connection between the sleep deprivation and the headaches, they could often recall other episodes in the past that substantiated my explanation.
In some cases there was no obvious history of acute sleep deprivation, or at least it was so subtle that even a history taker with a sleep obsession couldn’t detect it. However, in these cases I could usually elicit a history of chronic sleep deprivation. For example, falling asleep instantly on automobile rides, difficulty with waking in the morning, or unhealthy bedtime routines. With this underlying vulnerability of chronic sleep deprivation, a slightly more exciting or vigorous day was all that was necessary to trigger the headache.
For those of you who don’t share my contention that childhood migraine is usually the result of sleep deprivation, consider the similarity between an epileptic seizure, which can be triggered by fatigue. Both events are usually followed by a deep sleep from which the child wakes refreshed and symptom free.
I think it is interesting that this recent meta-analysis could find no benefit in the quality of life for any of the medications. The explanation may be that the child with migraine already had a somewhat diminished quality of life as a result of the sleep deprivation, either acute or chronic.
When speaking with parents of migraine sufferers, I would tell them that once the headache had started there was little I had to offer to forestall the inevitable pain and vomiting. Certainly not in the form of an oral medication. While many adults will have an aura that warns them of the headache onset, I have found that most children don’t describe an aura. It may be they simply lack the ability to express it. Occasionally an observant parent may detect pallor or a behavior change that indicates a migraine is beginning. On rare occasions a parent may be able to abort the attack by quickly getting the child to a quiet, dark, and calm environment.
Although this recent meta-analysis review of treatment options is discouraging, it may be providing a clue to effective prophylaxis. Some of the medications that decrease the frequency of the attacks may be doing so because they improve the patient’s sleep patterns. Those that decrease the intensity of the pain are probably working on pain pathway that is not specific to migraine.
Continuing a search for a prophylactic medication is a worthy goal, particularly for those patients in which their migraines are debilitating. However, based on my experience, enhanced by my bias, the safest and most effective prophylaxis results from increasing the family’s awareness of the role that sleep deprivation plays in the illness. Even when the family buys into the message and attempts to avoid situations that will tax their vulnerable children, parents will need to accept that sometimes stuff happens even though siblings and peers may be able to tolerate the situation. Spontaneous activities can converge on a day when for whatever reason the migraine-prone child is overtired and the headache and vomiting will erupt.
A lifestyle change is always preferable to a pharmacological intervention. However, that doesn’t mean it is always easy to achieve.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I suspect you all have some experience with childhood migraine. It can mean a painful several hours for the patient, arriving often without warning, with recurrences spaced months or sometimes even years apart. It may be accompanied by vomiting, which in some cases overshadows the severity of the headache. It can result in lost days from school and ruin family activities. It can occur so infrequently that the family can’t recall accurately when the last episode happened. In some ways it is a different animal than the adult version.
Most of the pediatric patients with migraine I have seen have experienced attacks that were occurring so infrequently that the families and I seldom discussed medication as an option. Back then imipramine was the only choice. However, currently there are more than a half dozen medications and combinations that have been tried. Recently a review of 45 clinical trials of these medications was published in JAMA Network Open.
I will let you review for yourself the details of these Iranian investigators’ network meta-analysis, but the bottom line is that some medications were associated with a reduction in migraine frequency. Others were associated with headache intensity. “However, no treatments were associated with significant improvements in quality of life or reduction of the duration of migraine attacks.”
Obviously, this paper illustrates clearly that we have not yet discovered the medicinal magic bullet for pediatric migraine prophylaxis. This doesn’t surprise me. After listening to scores of families tell their migraine stories, it became apparent to me that there was often a pattern in which the child’s headache had arrived after a period of acute sleep deprivation. For example, a trip to an amusement park in which travel or excitement may have resulted in the child going to bed later and/or getting up earlier. By afternoon the child’s reserves of something (currently unknown) were depleted to a point that the headache and/or vomiting struck.
Because these episodes were often so infrequent, separated by months, that taking a history demonstrating a recurring pattern could take considerable patience on the part of the family and the provider, even for a physician like myself who believes that better sleep is the answer for everything. However, once I could convince a family of the connection between the sleep deprivation and the headaches, they could often recall other episodes in the past that substantiated my explanation.
In some cases there was no obvious history of acute sleep deprivation, or at least it was so subtle that even a history taker with a sleep obsession couldn’t detect it. However, in these cases I could usually elicit a history of chronic sleep deprivation. For example, falling asleep instantly on automobile rides, difficulty with waking in the morning, or unhealthy bedtime routines. With this underlying vulnerability of chronic sleep deprivation, a slightly more exciting or vigorous day was all that was necessary to trigger the headache.
For those of you who don’t share my contention that childhood migraine is usually the result of sleep deprivation, consider the similarity between an epileptic seizure, which can be triggered by fatigue. Both events are usually followed by a deep sleep from which the child wakes refreshed and symptom free.
I think it is interesting that this recent meta-analysis could find no benefit in the quality of life for any of the medications. The explanation may be that the child with migraine already had a somewhat diminished quality of life as a result of the sleep deprivation, either acute or chronic.
When speaking with parents of migraine sufferers, I would tell them that once the headache had started there was little I had to offer to forestall the inevitable pain and vomiting. Certainly not in the form of an oral medication. While many adults will have an aura that warns them of the headache onset, I have found that most children don’t describe an aura. It may be they simply lack the ability to express it. Occasionally an observant parent may detect pallor or a behavior change that indicates a migraine is beginning. On rare occasions a parent may be able to abort the attack by quickly getting the child to a quiet, dark, and calm environment.
Although this recent meta-analysis review of treatment options is discouraging, it may be providing a clue to effective prophylaxis. Some of the medications that decrease the frequency of the attacks may be doing so because they improve the patient’s sleep patterns. Those that decrease the intensity of the pain are probably working on pain pathway that is not specific to migraine.
Continuing a search for a prophylactic medication is a worthy goal, particularly for those patients in which their migraines are debilitating. However, based on my experience, enhanced by my bias, the safest and most effective prophylaxis results from increasing the family’s awareness of the role that sleep deprivation plays in the illness. Even when the family buys into the message and attempts to avoid situations that will tax their vulnerable children, parents will need to accept that sometimes stuff happens even though siblings and peers may be able to tolerate the situation. Spontaneous activities can converge on a day when for whatever reason the migraine-prone child is overtired and the headache and vomiting will erupt.
A lifestyle change is always preferable to a pharmacological intervention. However, that doesn’t mean it is always easy to achieve.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
I suspect you all have some experience with childhood migraine. It can mean a painful several hours for the patient, arriving often without warning, with recurrences spaced months or sometimes even years apart. It may be accompanied by vomiting, which in some cases overshadows the severity of the headache. It can result in lost days from school and ruin family activities. It can occur so infrequently that the family can’t recall accurately when the last episode happened. In some ways it is a different animal than the adult version.
Most of the pediatric patients with migraine I have seen have experienced attacks that were occurring so infrequently that the families and I seldom discussed medication as an option. Back then imipramine was the only choice. However, currently there are more than a half dozen medications and combinations that have been tried. Recently a review of 45 clinical trials of these medications was published in JAMA Network Open.
I will let you review for yourself the details of these Iranian investigators’ network meta-analysis, but the bottom line is that some medications were associated with a reduction in migraine frequency. Others were associated with headache intensity. “However, no treatments were associated with significant improvements in quality of life or reduction of the duration of migraine attacks.”
Obviously, this paper illustrates clearly that we have not yet discovered the medicinal magic bullet for pediatric migraine prophylaxis. This doesn’t surprise me. After listening to scores of families tell their migraine stories, it became apparent to me that there was often a pattern in which the child’s headache had arrived after a period of acute sleep deprivation. For example, a trip to an amusement park in which travel or excitement may have resulted in the child going to bed later and/or getting up earlier. By afternoon the child’s reserves of something (currently unknown) were depleted to a point that the headache and/or vomiting struck.
Because these episodes were often so infrequent, separated by months, that taking a history demonstrating a recurring pattern could take considerable patience on the part of the family and the provider, even for a physician like myself who believes that better sleep is the answer for everything. However, once I could convince a family of the connection between the sleep deprivation and the headaches, they could often recall other episodes in the past that substantiated my explanation.
In some cases there was no obvious history of acute sleep deprivation, or at least it was so subtle that even a history taker with a sleep obsession couldn’t detect it. However, in these cases I could usually elicit a history of chronic sleep deprivation. For example, falling asleep instantly on automobile rides, difficulty with waking in the morning, or unhealthy bedtime routines. With this underlying vulnerability of chronic sleep deprivation, a slightly more exciting or vigorous day was all that was necessary to trigger the headache.
For those of you who don’t share my contention that childhood migraine is usually the result of sleep deprivation, consider the similarity between an epileptic seizure, which can be triggered by fatigue. Both events are usually followed by a deep sleep from which the child wakes refreshed and symptom free.
I think it is interesting that this recent meta-analysis could find no benefit in the quality of life for any of the medications. The explanation may be that the child with migraine already had a somewhat diminished quality of life as a result of the sleep deprivation, either acute or chronic.
When speaking with parents of migraine sufferers, I would tell them that once the headache had started there was little I had to offer to forestall the inevitable pain and vomiting. Certainly not in the form of an oral medication. While many adults will have an aura that warns them of the headache onset, I have found that most children don’t describe an aura. It may be they simply lack the ability to express it. Occasionally an observant parent may detect pallor or a behavior change that indicates a migraine is beginning. On rare occasions a parent may be able to abort the attack by quickly getting the child to a quiet, dark, and calm environment.
Although this recent meta-analysis review of treatment options is discouraging, it may be providing a clue to effective prophylaxis. Some of the medications that decrease the frequency of the attacks may be doing so because they improve the patient’s sleep patterns. Those that decrease the intensity of the pain are probably working on pain pathway that is not specific to migraine.
Continuing a search for a prophylactic medication is a worthy goal, particularly for those patients in which their migraines are debilitating. However, based on my experience, enhanced by my bias, the safest and most effective prophylaxis results from increasing the family’s awareness of the role that sleep deprivation plays in the illness. Even when the family buys into the message and attempts to avoid situations that will tax their vulnerable children, parents will need to accept that sometimes stuff happens even though siblings and peers may be able to tolerate the situation. Spontaneous activities can converge on a day when for whatever reason the migraine-prone child is overtired and the headache and vomiting will erupt.
A lifestyle change is always preferable to a pharmacological intervention. However, that doesn’t mean it is always easy to achieve.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Is Being ‘Manly’ a Threat to a Man’s Health?
When my normally adorable cat Biscuit bit my ankle in a playful stalking exercise gone wrong, I washed it with soap and some rubbing alcohol, slapped on a Band-Aid, and went about my day.
The next morning, when it was swollen, I told myself it was probably just a hematoma and went about my day.
The next day, when the swelling had increased and red lines started creeping up my leg, I called my doctor. Long story short, I ended up hospitalized for intravenous antibiotics.
This is all to say that, yes, I’m sort of an idiot, but also to introduce the idea that maybe I minimized my very obvious lymphangitis because I am a man.
This week, we have empirical evidence that men downplay their medical symptoms — and that manlier men downplay them even more.
I’m going to talk about a study that links manliness (or, scientifically speaking, “male gender expressivity”) to medical diagnoses that are based on hard evidence and medical diagnoses that are based on self-report. You see where this is going but I want to walk you through the methods here because they are fairly interesting.
This study used data from the US National Longitudinal Study of Adolescent to Adult Health. This study enrolled 20,000 adolescents who were in grades 7-12 in the 1994-1995 school year and has been following them ever since — about 30 years so far.
The authors wanted to link early gender roles to long-term outcomes, so they cut that 20,000 number down to the 4230 males in the group who had complete follow-up.
Now comes the first interesting question. How do you quantify the “male gender expressivity” of boys in 7th-12th grade? There was no survey item that asked them how masculine or manly they felt. What the authors did was look at the surveys that were administered and identify the questions on those surveys where boys and girls gave the most disparate answers. I have some examples here. 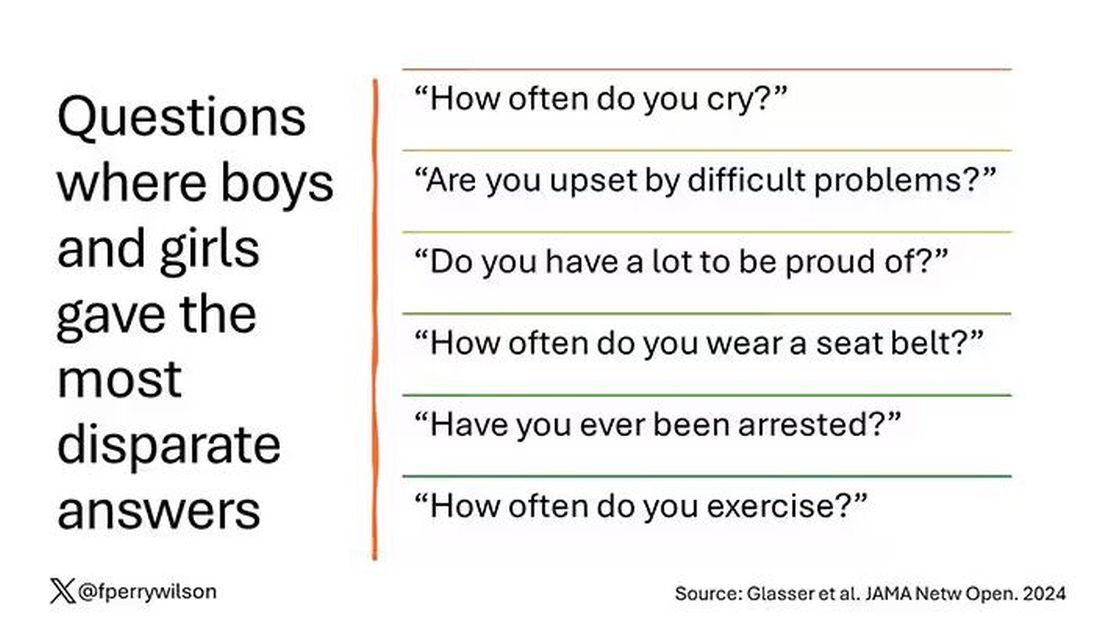
Some of these questions make sense when it comes to gender expressivity: “How often do you cry?” for example, has a lot of validity for the social construct that is gender. But some questions where boys and girls gave very different answers — like “How often do you exercise?” — don’t quite fit that mold. Regardless, this structure allowed the researchers to take individual kids’ responses to these questions and combine them into what amounts to a manliness score — how much their answers aligned with the typical male answer.
The score was established in adolescence — which is interesting because I’m sure some of this stuff may change over time — but notable because adolescence is where many gender roles develop.
Now we can fast-forward 30 years and see how these manliness scores link to various outcomes. The authors were interested in fairly common diseases: diabetes, hypertension, and hyperlipidemia.
Let’s start simply. Are males with higher gender expressivity in adolescence more or less likely to have these diseases in the future?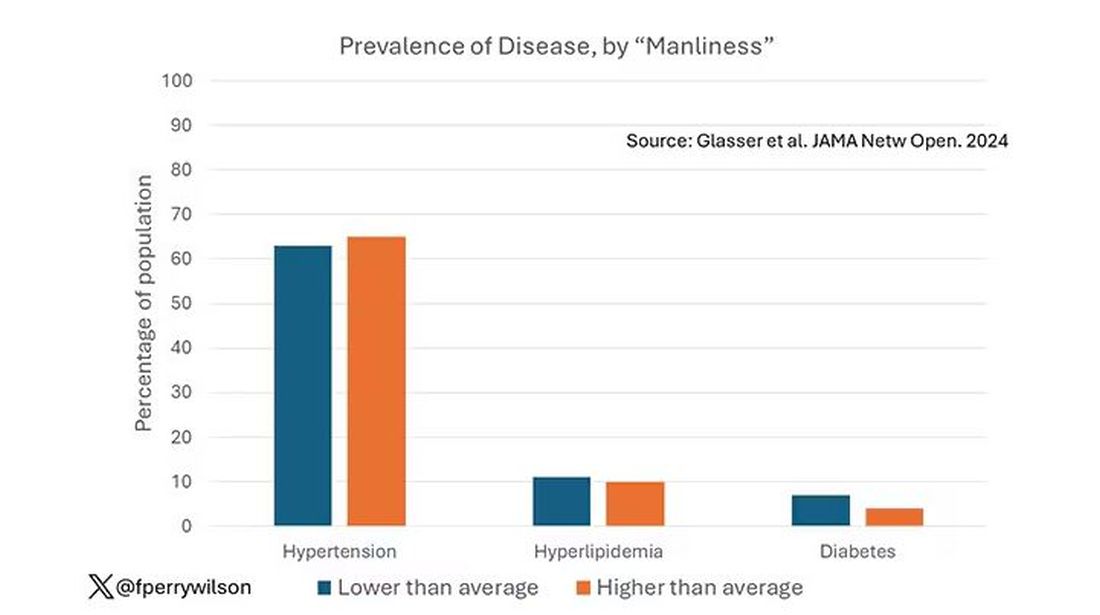
Not really. Those above the average in male gender expressivity had similar rates of hypertension and hyperlipidemia as those below the median. They were actually a bit less likely to have diabetes.
But that’s not what’s really interesting here.
I told you that there was no difference in the rate of hypertension among those with high vs low male gender expressivity. But there was a significant difference in their answer to the question “Do you have hypertension?” The same was seen for hyperlipidemia. In other words, those with higher manliness scores are less likely to admit (or perhaps know) that they have a particular disease.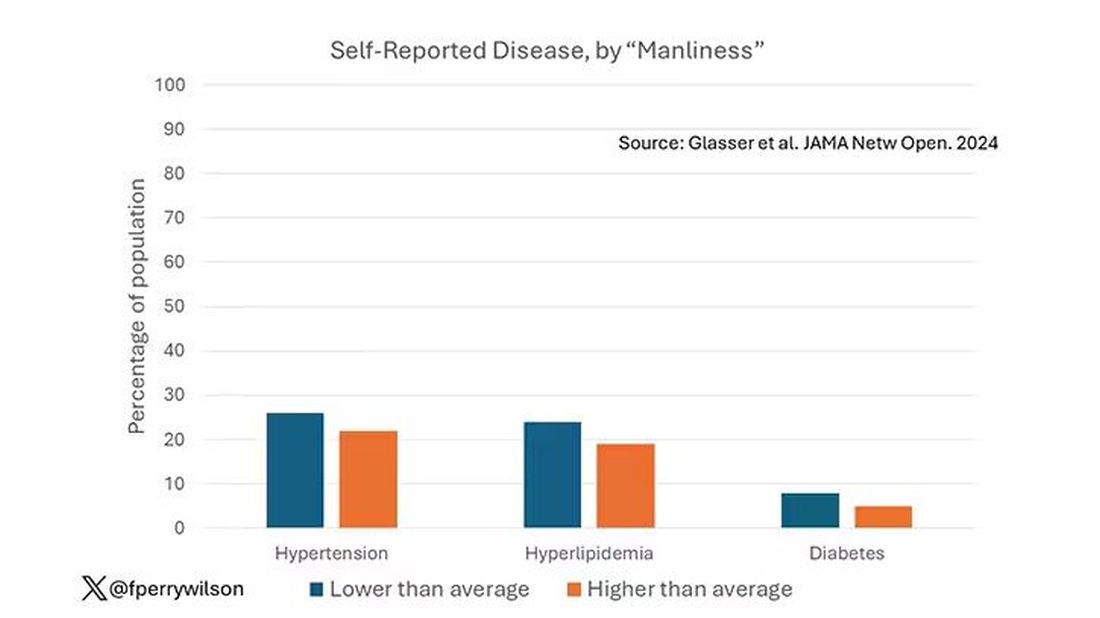
You can see the relationship across the manliness spectrum here in a series of adjusted models. The x-axis is the male gender expressivity score, and the y-axis is the percentage of people who report having the disease that we know they have based on the actual laboratory tests or vital sign measurements. As manliness increases, the self-report of a given disease decreases.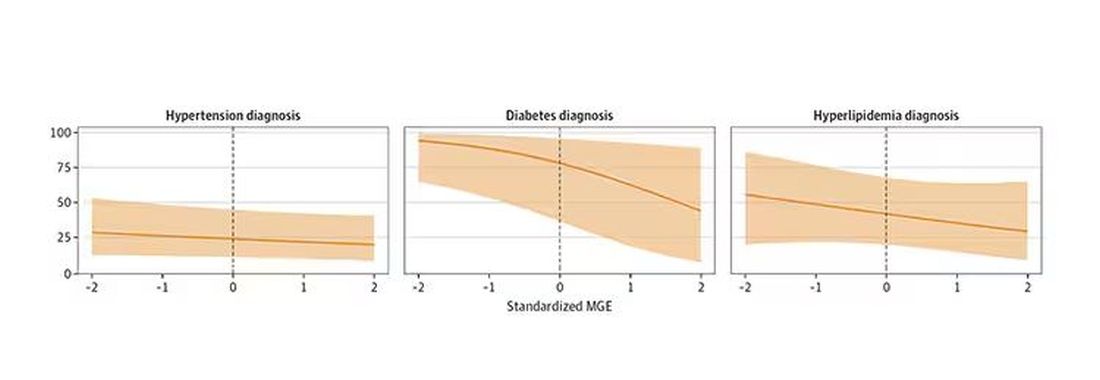
There are some important consequences of this systematic denial. Specifically, men with the diseases of interest who have higher male gender expressivity are less likely to get treatment. And, as we all know, the lack of treatment of something like hypertension puts people at risk for bad downstream outcomes.
Putting this all together, I’m not that surprised. Society trains boys from a young age to behave in certain ways: to hide emotions, to eschew vulnerability, to not complain when we are hurt. And those lessons can persist into later life. Whether the disease that strikes is hypertension or Pasteurella multocida from a slightly psychotic house cat, men are more likely to ignore it, to their detriment.
So, gents, be brave. Get your blood tests and check your blood pressure. If there’s something wrong, admit it, and fix it. After all, fixing problems — that’s a manly thing, right?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
When my normally adorable cat Biscuit bit my ankle in a playful stalking exercise gone wrong, I washed it with soap and some rubbing alcohol, slapped on a Band-Aid, and went about my day.
The next morning, when it was swollen, I told myself it was probably just a hematoma and went about my day.
The next day, when the swelling had increased and red lines started creeping up my leg, I called my doctor. Long story short, I ended up hospitalized for intravenous antibiotics.
This is all to say that, yes, I’m sort of an idiot, but also to introduce the idea that maybe I minimized my very obvious lymphangitis because I am a man.
This week, we have empirical evidence that men downplay their medical symptoms — and that manlier men downplay them even more.
I’m going to talk about a study that links manliness (or, scientifically speaking, “male gender expressivity”) to medical diagnoses that are based on hard evidence and medical diagnoses that are based on self-report. You see where this is going but I want to walk you through the methods here because they are fairly interesting.
This study used data from the US National Longitudinal Study of Adolescent to Adult Health. This study enrolled 20,000 adolescents who were in grades 7-12 in the 1994-1995 school year and has been following them ever since — about 30 years so far.
The authors wanted to link early gender roles to long-term outcomes, so they cut that 20,000 number down to the 4230 males in the group who had complete follow-up.
Now comes the first interesting question. How do you quantify the “male gender expressivity” of boys in 7th-12th grade? There was no survey item that asked them how masculine or manly they felt. What the authors did was look at the surveys that were administered and identify the questions on those surveys where boys and girls gave the most disparate answers. I have some examples here. 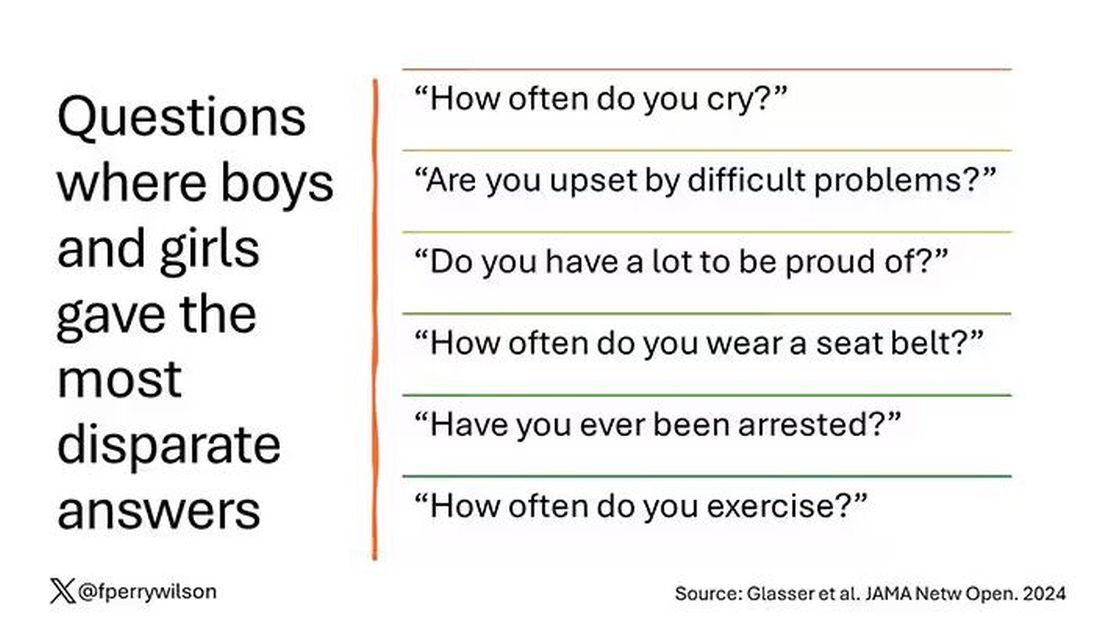
Some of these questions make sense when it comes to gender expressivity: “How often do you cry?” for example, has a lot of validity for the social construct that is gender. But some questions where boys and girls gave very different answers — like “How often do you exercise?” — don’t quite fit that mold. Regardless, this structure allowed the researchers to take individual kids’ responses to these questions and combine them into what amounts to a manliness score — how much their answers aligned with the typical male answer.
The score was established in adolescence — which is interesting because I’m sure some of this stuff may change over time — but notable because adolescence is where many gender roles develop.
Now we can fast-forward 30 years and see how these manliness scores link to various outcomes. The authors were interested in fairly common diseases: diabetes, hypertension, and hyperlipidemia.
Let’s start simply. Are males with higher gender expressivity in adolescence more or less likely to have these diseases in the future?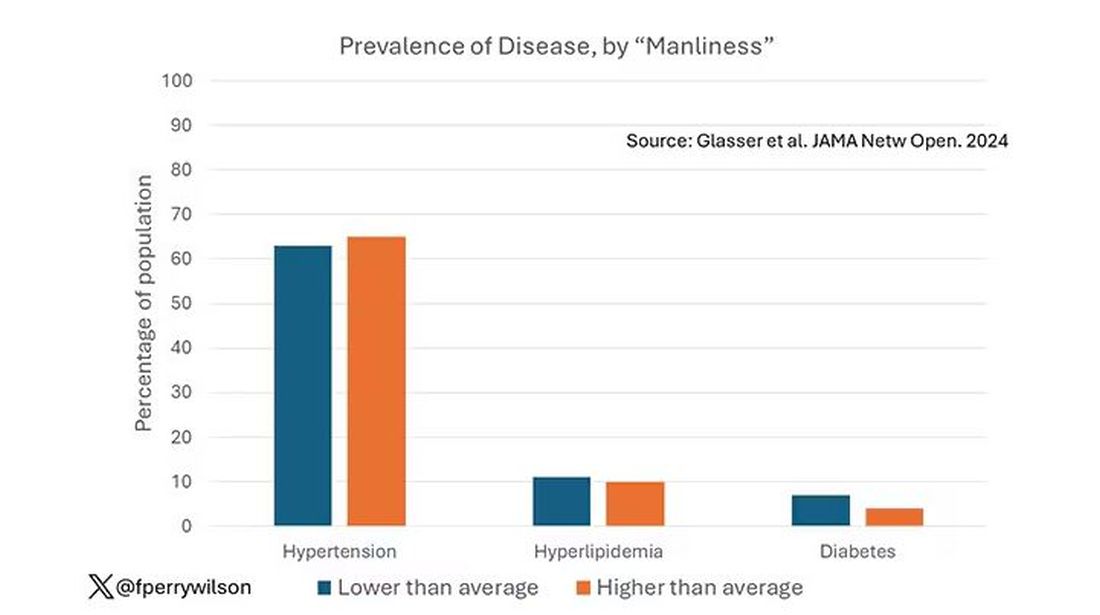
Not really. Those above the average in male gender expressivity had similar rates of hypertension and hyperlipidemia as those below the median. They were actually a bit less likely to have diabetes.
But that’s not what’s really interesting here.
I told you that there was no difference in the rate of hypertension among those with high vs low male gender expressivity. But there was a significant difference in their answer to the question “Do you have hypertension?” The same was seen for hyperlipidemia. In other words, those with higher manliness scores are less likely to admit (or perhaps know) that they have a particular disease.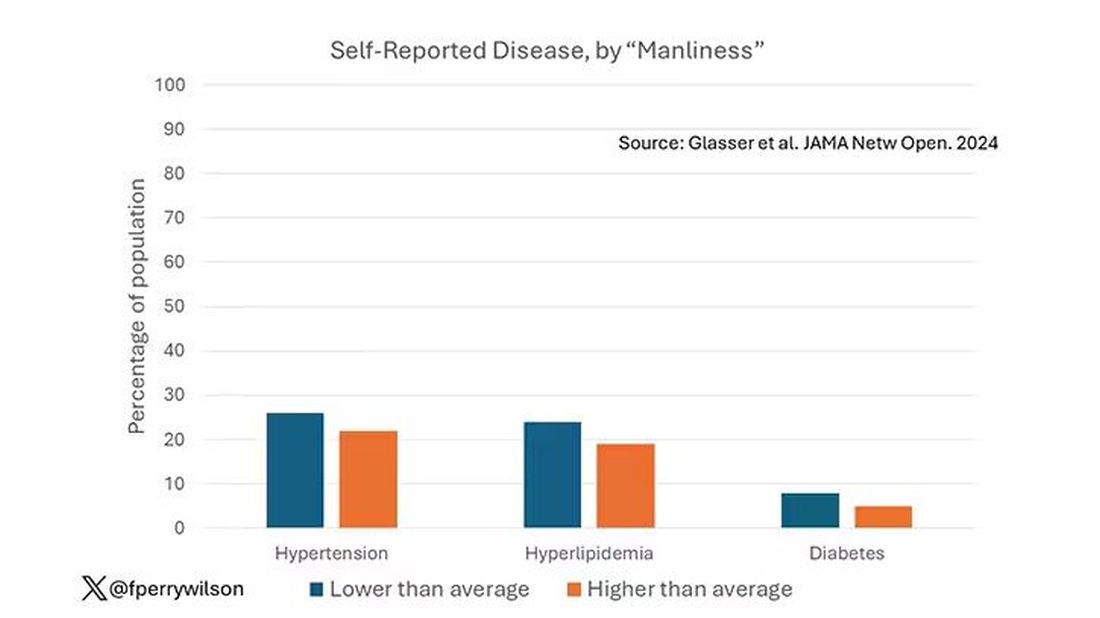
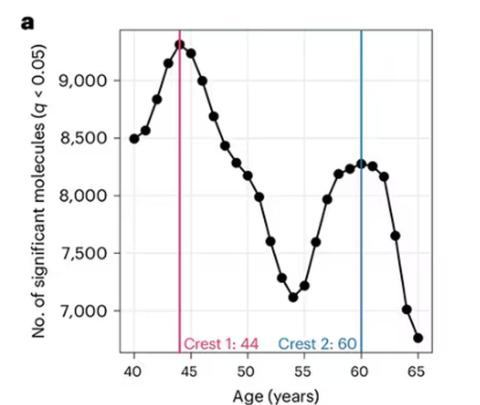
You can see the relationship across the manliness spectrum here in a series of adjusted models. The x-axis is the male gender expressivity score, and the y-axis is the percentage of people who report having the disease that we know they have based on the actual laboratory tests or vital sign measurements. As manliness increases, the self-report of a given disease decreases.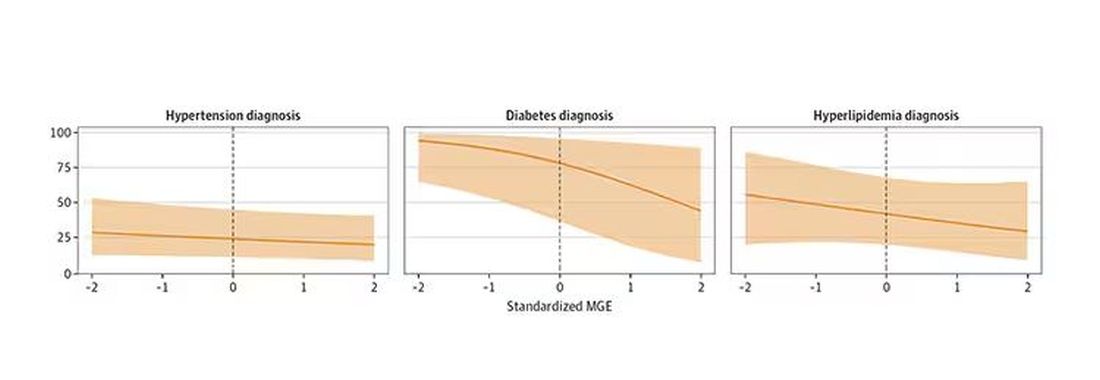
There are some important consequences of this systematic denial. Specifically, men with the diseases of interest who have higher male gender expressivity are less likely to get treatment. And, as we all know, the lack of treatment of something like hypertension puts people at risk for bad downstream outcomes.
Putting this all together, I’m not that surprised. Society trains boys from a young age to behave in certain ways: to hide emotions, to eschew vulnerability, to not complain when we are hurt. And those lessons can persist into later life. Whether the disease that strikes is hypertension or Pasteurella multocida from a slightly psychotic house cat, men are more likely to ignore it, to their detriment.
So, gents, be brave. Get your blood tests and check your blood pressure. If there’s something wrong, admit it, and fix it. After all, fixing problems — that’s a manly thing, right?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
When my normally adorable cat Biscuit bit my ankle in a playful stalking exercise gone wrong, I washed it with soap and some rubbing alcohol, slapped on a Band-Aid, and went about my day.
The next morning, when it was swollen, I told myself it was probably just a hematoma and went about my day.
The next day, when the swelling had increased and red lines started creeping up my leg, I called my doctor. Long story short, I ended up hospitalized for intravenous antibiotics.
This is all to say that, yes, I’m sort of an idiot, but also to introduce the idea that maybe I minimized my very obvious lymphangitis because I am a man.
This week, we have empirical evidence that men downplay their medical symptoms — and that manlier men downplay them even more.
I’m going to talk about a study that links manliness (or, scientifically speaking, “male gender expressivity”) to medical diagnoses that are based on hard evidence and medical diagnoses that are based on self-report. You see where this is going but I want to walk you through the methods here because they are fairly interesting.
This study used data from the US National Longitudinal Study of Adolescent to Adult Health. This study enrolled 20,000 adolescents who were in grades 7-12 in the 1994-1995 school year and has been following them ever since — about 30 years so far.
The authors wanted to link early gender roles to long-term outcomes, so they cut that 20,000 number down to the 4230 males in the group who had complete follow-up.
Now comes the first interesting question. How do you quantify the “male gender expressivity” of boys in 7th-12th grade? There was no survey item that asked them how masculine or manly they felt. What the authors did was look at the surveys that were administered and identify the questions on those surveys where boys and girls gave the most disparate answers. I have some examples here. 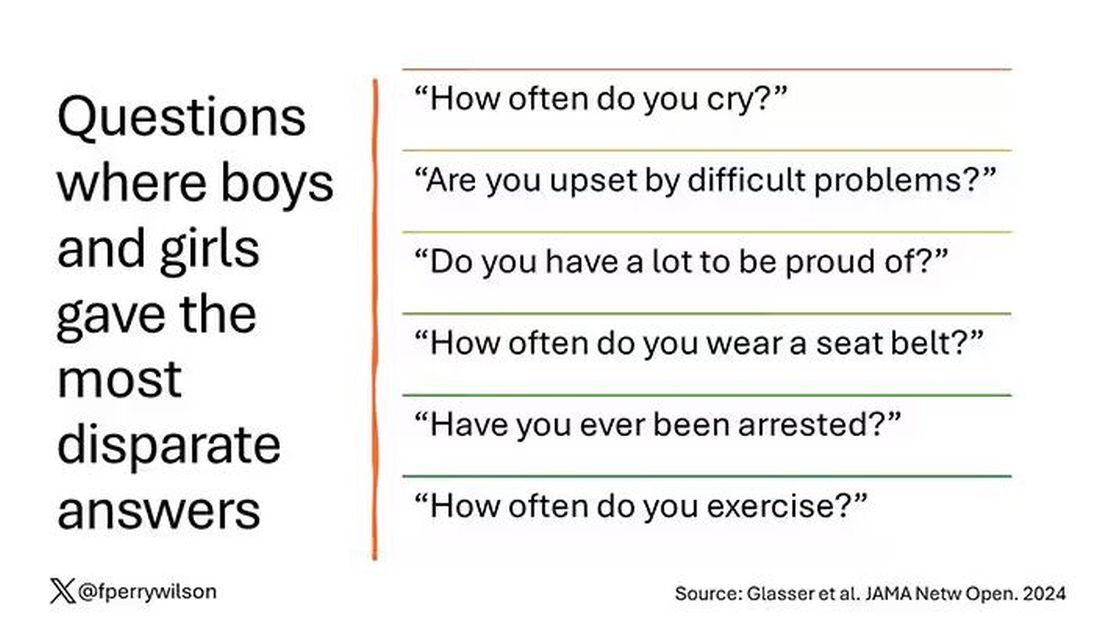
Some of these questions make sense when it comes to gender expressivity: “How often do you cry?” for example, has a lot of validity for the social construct that is gender. But some questions where boys and girls gave very different answers — like “How often do you exercise?” — don’t quite fit that mold. Regardless, this structure allowed the researchers to take individual kids’ responses to these questions and combine them into what amounts to a manliness score — how much their answers aligned with the typical male answer.
The score was established in adolescence — which is interesting because I’m sure some of this stuff may change over time — but notable because adolescence is where many gender roles develop.
Now we can fast-forward 30 years and see how these manliness scores link to various outcomes. The authors were interested in fairly common diseases: diabetes, hypertension, and hyperlipidemia.
Let’s start simply. Are males with higher gender expressivity in adolescence more or less likely to have these diseases in the future?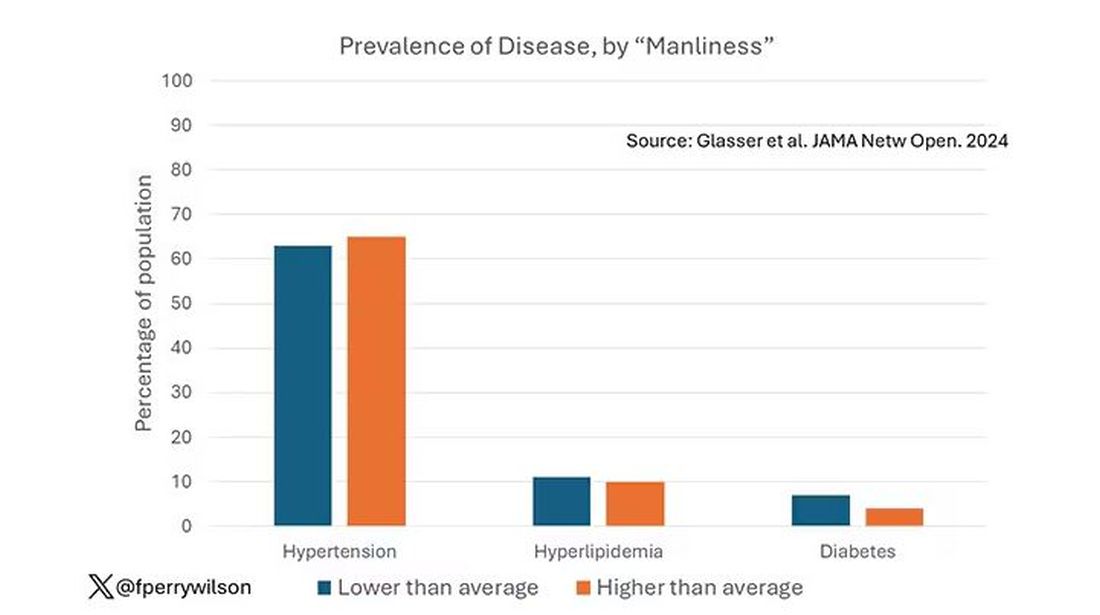
Not really. Those above the average in male gender expressivity had similar rates of hypertension and hyperlipidemia as those below the median. They were actually a bit less likely to have diabetes.
But that’s not what’s really interesting here.
I told you that there was no difference in the rate of hypertension among those with high vs low male gender expressivity. But there was a significant difference in their answer to the question “Do you have hypertension?” The same was seen for hyperlipidemia. In other words, those with higher manliness scores are less likely to admit (or perhaps know) that they have a particular disease.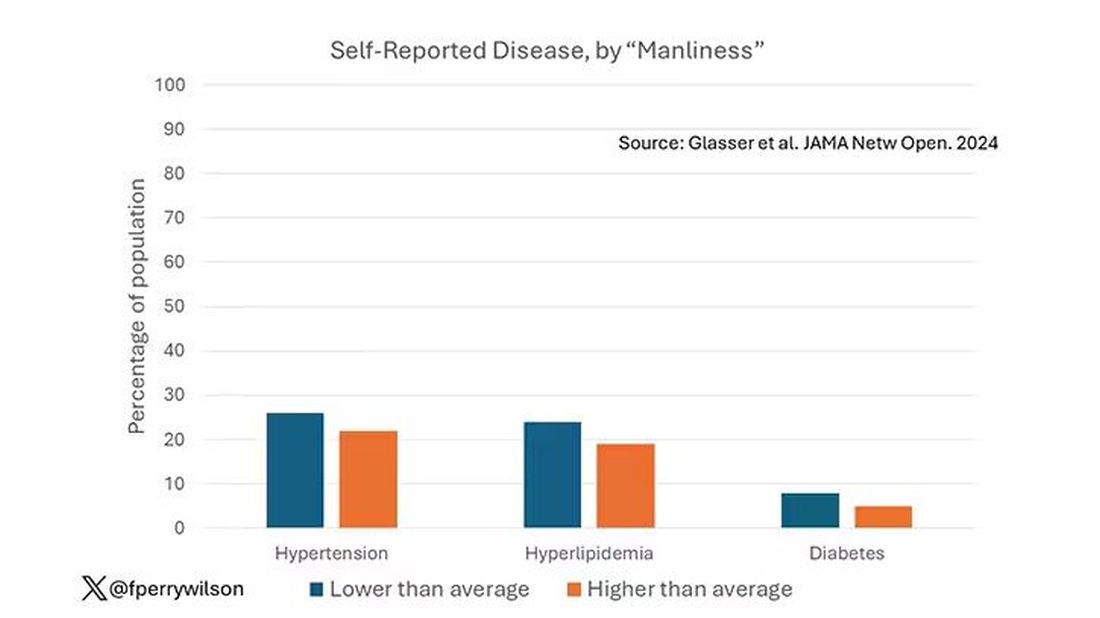
You can see the relationship across the manliness spectrum here in a series of adjusted models. The x-axis is the male gender expressivity score, and the y-axis is the percentage of people who report having the disease that we know they have based on the actual laboratory tests or vital sign measurements. As manliness increases, the self-report of a given disease decreases.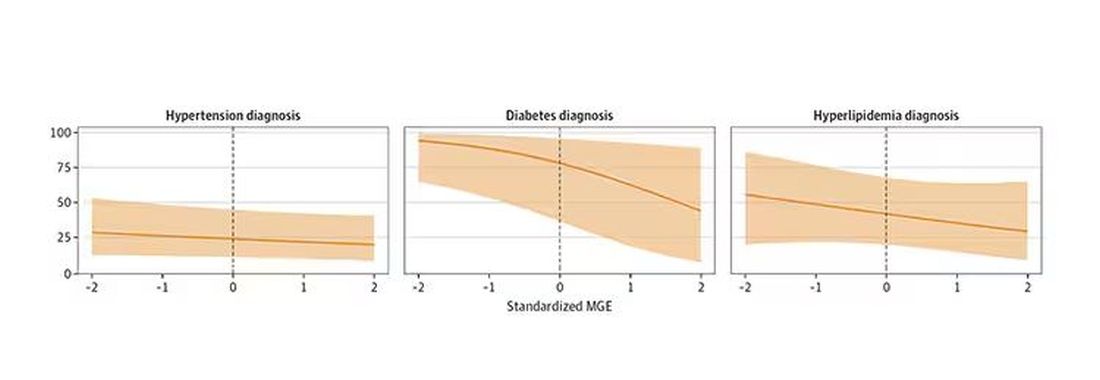
There are some important consequences of this systematic denial. Specifically, men with the diseases of interest who have higher male gender expressivity are less likely to get treatment. And, as we all know, the lack of treatment of something like hypertension puts people at risk for bad downstream outcomes.
Putting this all together, I’m not that surprised. Society trains boys from a young age to behave in certain ways: to hide emotions, to eschew vulnerability, to not complain when we are hurt. And those lessons can persist into later life. Whether the disease that strikes is hypertension or Pasteurella multocida from a slightly psychotic house cat, men are more likely to ignore it, to their detriment.
So, gents, be brave. Get your blood tests and check your blood pressure. If there’s something wrong, admit it, and fix it. After all, fixing problems — that’s a manly thing, right?
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Myth of the Month: Are Thickened Liquids Helpful in Dysphagia Patients?
Case: An 80-year-old man with advanced Alzheimer’s disease is admitted to the hospital after a fall. He is noted to have coughing spells after drinking liquids. He has a swallowing study done which shows severe slowing of motility in the esophagus.
What do you recommend?
A. Feeding tube
B. Thickened liquids
C. Continue current diet
The correct answer for this patient is to allow them to continue their current diet. They do not need thickened liquids. A feeding tube would not be recommended.1
So are there any data supporting the widespread use of thickened liquid diets for patients with dysphagia and aspiration?
Multiple clinical guidelines for stroke recommend the use of thickened liquids despite minimal to no evidence of efficacy.2 It is a common practice to give patients with advanced dementia thickened liquids, especially in the hospital setting. Does this help?
Makhnevich and colleagues published a cohort study of Alzheimer’s disease patients with dysphagia admitted to the hospital over a 5-year period.3 Almost half of the cohort received a thickened liquid diet; these patients were matched with patients who received a thin liquid diet. There was no significant difference in hospital mortality between the groups that received thick liquids and thin liquids (hazard ratio, 0.92; P = .46). Patients receiving thickened liquids were less likely to be intubated but were more likely to have pulmonary infections.
A 2018 Cochrane review concluded that there was no consensus on immediate and long-term effects of modifying the consistency of fluid for swallowing difficulties in dementia because too few studies have been completed.4 So why is this important information or lack of information?
What is so bad about a thickened liquid diet?
Eric Widera, MD, shared in JAMA Internal Medicine his experience along with his hospice and palliative care team of drinking thickened liquids.5 He drank only thickened liquids for a 12-hour period. “The challenge was eye-opening. It was the first time I experienced the terrible taste and texture of thickened liquids,” he wrote. He shared some of the risks of thickened liquids: dehydration, poor oral intake, and decreased quality of life.
The bottom line is that there is scant evidence for the benefit of thickened liquids, especially for patients with advanced dementia and dysphagia, and giving thickened liquids is not a benign intervention, because of poor tolerability of the diet.
References
1. American Geriatrics Society Ethics Committee and Clinical Practice and Models of Care Committee. J Am Geriatr Soc. 2014;62(8):1590-3.
2. McCurtin A et al. J Eval Clin Pract. 2020;26:1744-60.
3. Makhnevich A et al. JAMA Intern Med. 2024 Jul 1;184(7):778-85.
4. Flynn E et al. Cochrane Database Syst Rev. 2018 Sep 24;9(9):CD011077.
5. Widera E. JAMA Intern Med. 2024 Jul 1;184(7):786-7.
Case: An 80-year-old man with advanced Alzheimer’s disease is admitted to the hospital after a fall. He is noted to have coughing spells after drinking liquids. He has a swallowing study done which shows severe slowing of motility in the esophagus.
What do you recommend?
A. Feeding tube
B. Thickened liquids
C. Continue current diet
The correct answer for this patient is to allow them to continue their current diet. They do not need thickened liquids. A feeding tube would not be recommended.1
So are there any data supporting the widespread use of thickened liquid diets for patients with dysphagia and aspiration?
Multiple clinical guidelines for stroke recommend the use of thickened liquids despite minimal to no evidence of efficacy.2 It is a common practice to give patients with advanced dementia thickened liquids, especially in the hospital setting. Does this help?
Makhnevich and colleagues published a cohort study of Alzheimer’s disease patients with dysphagia admitted to the hospital over a 5-year period.3 Almost half of the cohort received a thickened liquid diet; these patients were matched with patients who received a thin liquid diet. There was no significant difference in hospital mortality between the groups that received thick liquids and thin liquids (hazard ratio, 0.92; P = .46). Patients receiving thickened liquids were less likely to be intubated but were more likely to have pulmonary infections.
A 2018 Cochrane review concluded that there was no consensus on immediate and long-term effects of modifying the consistency of fluid for swallowing difficulties in dementia because too few studies have been completed.4 So why is this important information or lack of information?
What is so bad about a thickened liquid diet?
Eric Widera, MD, shared in JAMA Internal Medicine his experience along with his hospice and palliative care team of drinking thickened liquids.5 He drank only thickened liquids for a 12-hour period. “The challenge was eye-opening. It was the first time I experienced the terrible taste and texture of thickened liquids,” he wrote. He shared some of the risks of thickened liquids: dehydration, poor oral intake, and decreased quality of life.
The bottom line is that there is scant evidence for the benefit of thickened liquids, especially for patients with advanced dementia and dysphagia, and giving thickened liquids is not a benign intervention, because of poor tolerability of the diet.
References
1. American Geriatrics Society Ethics Committee and Clinical Practice and Models of Care Committee. J Am Geriatr Soc. 2014;62(8):1590-3.
2. McCurtin A et al. J Eval Clin Pract. 2020;26:1744-60.
3. Makhnevich A et al. JAMA Intern Med. 2024 Jul 1;184(7):778-85.
4. Flynn E et al. Cochrane Database Syst Rev. 2018 Sep 24;9(9):CD011077.
5. Widera E. JAMA Intern Med. 2024 Jul 1;184(7):786-7.
Case: An 80-year-old man with advanced Alzheimer’s disease is admitted to the hospital after a fall. He is noted to have coughing spells after drinking liquids. He has a swallowing study done which shows severe slowing of motility in the esophagus.
What do you recommend?
A. Feeding tube
B. Thickened liquids
C. Continue current diet
The correct answer for this patient is to allow them to continue their current diet. They do not need thickened liquids. A feeding tube would not be recommended.1
So are there any data supporting the widespread use of thickened liquid diets for patients with dysphagia and aspiration?
Multiple clinical guidelines for stroke recommend the use of thickened liquids despite minimal to no evidence of efficacy.2 It is a common practice to give patients with advanced dementia thickened liquids, especially in the hospital setting. Does this help?
Makhnevich and colleagues published a cohort study of Alzheimer’s disease patients with dysphagia admitted to the hospital over a 5-year period.3 Almost half of the cohort received a thickened liquid diet; these patients were matched with patients who received a thin liquid diet. There was no significant difference in hospital mortality between the groups that received thick liquids and thin liquids (hazard ratio, 0.92; P = .46). Patients receiving thickened liquids were less likely to be intubated but were more likely to have pulmonary infections.
A 2018 Cochrane review concluded that there was no consensus on immediate and long-term effects of modifying the consistency of fluid for swallowing difficulties in dementia because too few studies have been completed.4 So why is this important information or lack of information?
What is so bad about a thickened liquid diet?
Eric Widera, MD, shared in JAMA Internal Medicine his experience along with his hospice and palliative care team of drinking thickened liquids.5 He drank only thickened liquids for a 12-hour period. “The challenge was eye-opening. It was the first time I experienced the terrible taste and texture of thickened liquids,” he wrote. He shared some of the risks of thickened liquids: dehydration, poor oral intake, and decreased quality of life.
The bottom line is that there is scant evidence for the benefit of thickened liquids, especially for patients with advanced dementia and dysphagia, and giving thickened liquids is not a benign intervention, because of poor tolerability of the diet.
References
1. American Geriatrics Society Ethics Committee and Clinical Practice and Models of Care Committee. J Am Geriatr Soc. 2014;62(8):1590-3.
2. McCurtin A et al. J Eval Clin Pract. 2020;26:1744-60.
3. Makhnevich A et al. JAMA Intern Med. 2024 Jul 1;184(7):778-85.
4. Flynn E et al. Cochrane Database Syst Rev. 2018 Sep 24;9(9):CD011077.
5. Widera E. JAMA Intern Med. 2024 Jul 1;184(7):786-7.
Just Call It ‘Chronic Rhinitis’ and Reach for These Treatments
This transcript has been edited for clarity.
Matthew F. Watto, MD: I’m here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams. Paul, are you ready to talk about rhinitis?
Paul N. Williams, MD: I’m excited. It’s always the season to talk about rhinitis.
Watto: We had a great guest for this podcast, Rhinitis and Environmental Allergies with Dr. Olajumoke Fadugba from Penn Medicine. She’s an allergist and immunologist. One of her pet peeves is when people just call everything “allergic rhinitis” because we should be calling it “chronic rhinitis,” if it’s chronic. That’s an umbrella term, and there are many buckets underneath it that people could fall into.
When you’re taking a history, you have to figure out whether it’s perennial (meaning it happens year round) because certain things can cause that. Cat dander is around all the time, so people with cats might have sinus symptoms all year. Dust mites are another one, and it’s pretty hard to avoid those. Those are some perennial allergens.
Then there is allergic vs nonallergic rhinitis, which is something I hadn’t really put too much thought into.
Williams: I didn’t realize exactly how nuanced it got. Nonallergic rhinitis can still be seasonal because changes in temperature and humidity can trigger the rhinitis. And it matters what medications you use for what.
Watto: Here are some ways you can try to figure out if rhinitis is allergic or nonallergic. Ask the patient if they have itchy eyes and are sneezing a lot. That can be more of an allergic rhinitis, but both allergic and nonallergic rhinitis have the congestion, the rhinorrhea, so you can’t figure it out based on that alone.
Dr. Fadugba said that one clue that it might be nonallergic rhinitis is the age of onset. If the symptoms are later in onset (older age), then 30%-40% of rhinitis is nonallergic. If the patient has never had allergies and now all of a sudden they have new chronic sinus symptoms, it’s probably nonallergic rhinitis. It’s a diagnosis of exclusion.
I guess they need allergy testing?
Williams: If you want to make a definitive diagnosis, you need to rule it out. I suspect that you might be able to get away with some empirical treatment. If they get better, you can feel like a winner because getting booked in for allergy testing can be a little bit of a challenge.
Watto: The main treatment difference is that the oral antihistamines do not really seem to work for nonallergic rhinitis, but they can help with allergic rhinitis. Weirdly, the nasal antihistamines and nasal steroids do seem to work for both allergic and nonallergic rhinitis.
I don’t understand the mechanism there, but if you think someone might have nonallergic rhinitis, I wouldn’t go with the oral antihistamines as your first-line treatment. I would go with a nasal spray; you pretty much can’t go wrong with either an antihistamine or a steroid nasal spray.
Williams: We typically start with the nasal sprays. That’s kind of first-line for almost everybody, allergic or nonallergic. You’re probably going to start with an intranasal steroid, and then it’s kind of dealer’s choice what the patient can tolerate and afford. Sometimes you can get them covered by insurance, at least in my experience.
I will say that this is one of the medications — like nicotine patches and other things — where we as doctors don’t really counsel patients on how to use it appropriately. So with our expert, we revisited the idea of the patient pointing the nasal spray laterally, toward their ear basically, and not spraying toward their brain. There should not be a slurping sound afterward, because “if you taste it, you waste it,” as the allergists and immunologists say. It’s supposed to sit up there and not be swallowed immediately.
If your patient is sensitive to the floral flavor of some of the fluticasones (which I don’t mind so much as a user myself), then you can try mometasone or the other formulations. They are all roughly equivalent.
Speaking of medications, which medications can cause rhinitis? Any meds we commonly use in primary care?
Williams: Apparently the combined hormonal oral contraceptives can do it. Also the phosphodiesterase 5 (PDE-5) inhibitors. Drugs that cause vasodilation can also do it. Some of the antihypertensives. I’ve seen beta-blockers and angiotensin-converting enzyme (ACE) inhibitors listed specifically, and some of the medications for benign prostatic hyperplasia (BPH). So there are a couple of medications that you can think about as a potential cause of rhinitis, although my suspicion is not going to be as high as for some of the other causes.
Watto: We mentioned medication treatments for patients who are really bothered by rhinorrhea, and maybe they are already on a steroid or an antihistamine.
You can try nasal ipratropium for people that have really prominent rhinorrhea. Dr. Fadugba said that can work well, and it’s usually taken three or four times a day. I’ve had good success prescribing it for my patients. Another one that I have never prescribed, but that Dr. Fadugba said is available over the counter, is intranasal cromolyn — a mast cell stabilizer. She said it can be beneficial.
Let’s say I had a cat allergy and I was going to visit Paul. I could use the intranasal cromolyn ahead of time to reduce rhinitis when I’m around the cats.
Paul, what about montelukast? I never know what to do with that one.
Williams: I’ve seen it prescribed as a last-ditch attempt to fix chronic rhinitis. Dr. Fadugba said she only ever prescribes it for patients who have rhinitis symptoms and asthma and never just for chronic rhinitis because it doesn’t work. And also, there have been some new black-box warnings from the US Food and Drug Administration (FDA). So unless there’s a solid indication for it, montelukast is not something you should just prescribe to try to see if it will work. That’s probably not the right approach for this.
But if the patient has challenging control asthma, and as a component, challenging nasal symptoms as well, it might be a reasonable medication to try.
Watto: And finally, Paul, how does climate change possibly have anything to do with rhinitis?
Williams: I feel like I’m just seeing more and more of the stuff every year. I don’t know if I’m more sensitive to it or because I’m having more symptoms myself, but it turns out the prevalence actually is going up.
We’re seeing more of it in part because it’s getting hotter outside, which is in turn worsening the production of allergens and increasing the allergen exposure and the severity of the symptoms that go along with it. More people are having more severe disease because the world is changing as a result of the stuff that we do. So fix that. But also be mindful and expect to see even more of these problems as you move forward in your careers.
Watto: Dr. Fadugba gave us so many great tips. You can listen to the full podcast episode here.
Dr. Watto, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, has disclosed no relevant financial relationships. Dr. Williams, Associate Professor of Clinical Medicine, Department of General Internal Medicine, Lewis Katz School of Medicine; Staff Physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, disclosed ties with The Curbsiders.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Matthew F. Watto, MD: I’m here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams. Paul, are you ready to talk about rhinitis?
Paul N. Williams, MD: I’m excited. It’s always the season to talk about rhinitis.
Watto: We had a great guest for this podcast, Rhinitis and Environmental Allergies with Dr. Olajumoke Fadugba from Penn Medicine. She’s an allergist and immunologist. One of her pet peeves is when people just call everything “allergic rhinitis” because we should be calling it “chronic rhinitis,” if it’s chronic. That’s an umbrella term, and there are many buckets underneath it that people could fall into.
When you’re taking a history, you have to figure out whether it’s perennial (meaning it happens year round) because certain things can cause that. Cat dander is around all the time, so people with cats might have sinus symptoms all year. Dust mites are another one, and it’s pretty hard to avoid those. Those are some perennial allergens.
Then there is allergic vs nonallergic rhinitis, which is something I hadn’t really put too much thought into.
Williams: I didn’t realize exactly how nuanced it got. Nonallergic rhinitis can still be seasonal because changes in temperature and humidity can trigger the rhinitis. And it matters what medications you use for what.
Watto: Here are some ways you can try to figure out if rhinitis is allergic or nonallergic. Ask the patient if they have itchy eyes and are sneezing a lot. That can be more of an allergic rhinitis, but both allergic and nonallergic rhinitis have the congestion, the rhinorrhea, so you can’t figure it out based on that alone.
Dr. Fadugba said that one clue that it might be nonallergic rhinitis is the age of onset. If the symptoms are later in onset (older age), then 30%-40% of rhinitis is nonallergic. If the patient has never had allergies and now all of a sudden they have new chronic sinus symptoms, it’s probably nonallergic rhinitis. It’s a diagnosis of exclusion.
I guess they need allergy testing?
Williams: If you want to make a definitive diagnosis, you need to rule it out. I suspect that you might be able to get away with some empirical treatment. If they get better, you can feel like a winner because getting booked in for allergy testing can be a little bit of a challenge.
Watto: The main treatment difference is that the oral antihistamines do not really seem to work for nonallergic rhinitis, but they can help with allergic rhinitis. Weirdly, the nasal antihistamines and nasal steroids do seem to work for both allergic and nonallergic rhinitis.
I don’t understand the mechanism there, but if you think someone might have nonallergic rhinitis, I wouldn’t go with the oral antihistamines as your first-line treatment. I would go with a nasal spray; you pretty much can’t go wrong with either an antihistamine or a steroid nasal spray.
Williams: We typically start with the nasal sprays. That’s kind of first-line for almost everybody, allergic or nonallergic. You’re probably going to start with an intranasal steroid, and then it’s kind of dealer’s choice what the patient can tolerate and afford. Sometimes you can get them covered by insurance, at least in my experience.
I will say that this is one of the medications — like nicotine patches and other things — where we as doctors don’t really counsel patients on how to use it appropriately. So with our expert, we revisited the idea of the patient pointing the nasal spray laterally, toward their ear basically, and not spraying toward their brain. There should not be a slurping sound afterward, because “if you taste it, you waste it,” as the allergists and immunologists say. It’s supposed to sit up there and not be swallowed immediately.
If your patient is sensitive to the floral flavor of some of the fluticasones (which I don’t mind so much as a user myself), then you can try mometasone or the other formulations. They are all roughly equivalent.
Speaking of medications, which medications can cause rhinitis? Any meds we commonly use in primary care?
Williams: Apparently the combined hormonal oral contraceptives can do it. Also the phosphodiesterase 5 (PDE-5) inhibitors. Drugs that cause vasodilation can also do it. Some of the antihypertensives. I’ve seen beta-blockers and angiotensin-converting enzyme (ACE) inhibitors listed specifically, and some of the medications for benign prostatic hyperplasia (BPH). So there are a couple of medications that you can think about as a potential cause of rhinitis, although my suspicion is not going to be as high as for some of the other causes.
Watto: We mentioned medication treatments for patients who are really bothered by rhinorrhea, and maybe they are already on a steroid or an antihistamine.
You can try nasal ipratropium for people that have really prominent rhinorrhea. Dr. Fadugba said that can work well, and it’s usually taken three or four times a day. I’ve had good success prescribing it for my patients. Another one that I have never prescribed, but that Dr. Fadugba said is available over the counter, is intranasal cromolyn — a mast cell stabilizer. She said it can be beneficial.
Let’s say I had a cat allergy and I was going to visit Paul. I could use the intranasal cromolyn ahead of time to reduce rhinitis when I’m around the cats.
Paul, what about montelukast? I never know what to do with that one.
Williams: I’ve seen it prescribed as a last-ditch attempt to fix chronic rhinitis. Dr. Fadugba said she only ever prescribes it for patients who have rhinitis symptoms and asthma and never just for chronic rhinitis because it doesn’t work. And also, there have been some new black-box warnings from the US Food and Drug Administration (FDA). So unless there’s a solid indication for it, montelukast is not something you should just prescribe to try to see if it will work. That’s probably not the right approach for this.
But if the patient has challenging control asthma, and as a component, challenging nasal symptoms as well, it might be a reasonable medication to try.
Watto: And finally, Paul, how does climate change possibly have anything to do with rhinitis?
Williams: I feel like I’m just seeing more and more of the stuff every year. I don’t know if I’m more sensitive to it or because I’m having more symptoms myself, but it turns out the prevalence actually is going up.
We’re seeing more of it in part because it’s getting hotter outside, which is in turn worsening the production of allergens and increasing the allergen exposure and the severity of the symptoms that go along with it. More people are having more severe disease because the world is changing as a result of the stuff that we do. So fix that. But also be mindful and expect to see even more of these problems as you move forward in your careers.
Watto: Dr. Fadugba gave us so many great tips. You can listen to the full podcast episode here.
Dr. Watto, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, has disclosed no relevant financial relationships. Dr. Williams, Associate Professor of Clinical Medicine, Department of General Internal Medicine, Lewis Katz School of Medicine; Staff Physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, disclosed ties with The Curbsiders.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Matthew F. Watto, MD: I’m here with my great friend and America’s primary care physician, Dr. Paul Nelson Williams. Paul, are you ready to talk about rhinitis?
Paul N. Williams, MD: I’m excited. It’s always the season to talk about rhinitis.
Watto: We had a great guest for this podcast, Rhinitis and Environmental Allergies with Dr. Olajumoke Fadugba from Penn Medicine. She’s an allergist and immunologist. One of her pet peeves is when people just call everything “allergic rhinitis” because we should be calling it “chronic rhinitis,” if it’s chronic. That’s an umbrella term, and there are many buckets underneath it that people could fall into.
When you’re taking a history, you have to figure out whether it’s perennial (meaning it happens year round) because certain things can cause that. Cat dander is around all the time, so people with cats might have sinus symptoms all year. Dust mites are another one, and it’s pretty hard to avoid those. Those are some perennial allergens.
Then there is allergic vs nonallergic rhinitis, which is something I hadn’t really put too much thought into.
Williams: I didn’t realize exactly how nuanced it got. Nonallergic rhinitis can still be seasonal because changes in temperature and humidity can trigger the rhinitis. And it matters what medications you use for what.
Watto: Here are some ways you can try to figure out if rhinitis is allergic or nonallergic. Ask the patient if they have itchy eyes and are sneezing a lot. That can be more of an allergic rhinitis, but both allergic and nonallergic rhinitis have the congestion, the rhinorrhea, so you can’t figure it out based on that alone.
Dr. Fadugba said that one clue that it might be nonallergic rhinitis is the age of onset. If the symptoms are later in onset (older age), then 30%-40% of rhinitis is nonallergic. If the patient has never had allergies and now all of a sudden they have new chronic sinus symptoms, it’s probably nonallergic rhinitis. It’s a diagnosis of exclusion.
I guess they need allergy testing?
Williams: If you want to make a definitive diagnosis, you need to rule it out. I suspect that you might be able to get away with some empirical treatment. If they get better, you can feel like a winner because getting booked in for allergy testing can be a little bit of a challenge.
Watto: The main treatment difference is that the oral antihistamines do not really seem to work for nonallergic rhinitis, but they can help with allergic rhinitis. Weirdly, the nasal antihistamines and nasal steroids do seem to work for both allergic and nonallergic rhinitis.
I don’t understand the mechanism there, but if you think someone might have nonallergic rhinitis, I wouldn’t go with the oral antihistamines as your first-line treatment. I would go with a nasal spray; you pretty much can’t go wrong with either an antihistamine or a steroid nasal spray.
Williams: We typically start with the nasal sprays. That’s kind of first-line for almost everybody, allergic or nonallergic. You’re probably going to start with an intranasal steroid, and then it’s kind of dealer’s choice what the patient can tolerate and afford. Sometimes you can get them covered by insurance, at least in my experience.
I will say that this is one of the medications — like nicotine patches and other things — where we as doctors don’t really counsel patients on how to use it appropriately. So with our expert, we revisited the idea of the patient pointing the nasal spray laterally, toward their ear basically, and not spraying toward their brain. There should not be a slurping sound afterward, because “if you taste it, you waste it,” as the allergists and immunologists say. It’s supposed to sit up there and not be swallowed immediately.
If your patient is sensitive to the floral flavor of some of the fluticasones (which I don’t mind so much as a user myself), then you can try mometasone or the other formulations. They are all roughly equivalent.
Speaking of medications, which medications can cause rhinitis? Any meds we commonly use in primary care?
Williams: Apparently the combined hormonal oral contraceptives can do it. Also the phosphodiesterase 5 (PDE-5) inhibitors. Drugs that cause vasodilation can also do it. Some of the antihypertensives. I’ve seen beta-blockers and angiotensin-converting enzyme (ACE) inhibitors listed specifically, and some of the medications for benign prostatic hyperplasia (BPH). So there are a couple of medications that you can think about as a potential cause of rhinitis, although my suspicion is not going to be as high as for some of the other causes.
Watto: We mentioned medication treatments for patients who are really bothered by rhinorrhea, and maybe they are already on a steroid or an antihistamine.
You can try nasal ipratropium for people that have really prominent rhinorrhea. Dr. Fadugba said that can work well, and it’s usually taken three or four times a day. I’ve had good success prescribing it for my patients. Another one that I have never prescribed, but that Dr. Fadugba said is available over the counter, is intranasal cromolyn — a mast cell stabilizer. She said it can be beneficial.
Let’s say I had a cat allergy and I was going to visit Paul. I could use the intranasal cromolyn ahead of time to reduce rhinitis when I’m around the cats.
Paul, what about montelukast? I never know what to do with that one.
Williams: I’ve seen it prescribed as a last-ditch attempt to fix chronic rhinitis. Dr. Fadugba said she only ever prescribes it for patients who have rhinitis symptoms and asthma and never just for chronic rhinitis because it doesn’t work. And also, there have been some new black-box warnings from the US Food and Drug Administration (FDA). So unless there’s a solid indication for it, montelukast is not something you should just prescribe to try to see if it will work. That’s probably not the right approach for this.
But if the patient has challenging control asthma, and as a component, challenging nasal symptoms as well, it might be a reasonable medication to try.
Watto: And finally, Paul, how does climate change possibly have anything to do with rhinitis?
Williams: I feel like I’m just seeing more and more of the stuff every year. I don’t know if I’m more sensitive to it or because I’m having more symptoms myself, but it turns out the prevalence actually is going up.
We’re seeing more of it in part because it’s getting hotter outside, which is in turn worsening the production of allergens and increasing the allergen exposure and the severity of the symptoms that go along with it. More people are having more severe disease because the world is changing as a result of the stuff that we do. So fix that. But also be mindful and expect to see even more of these problems as you move forward in your careers.
Watto: Dr. Fadugba gave us so many great tips. You can listen to the full podcast episode here.
Dr. Watto, Clinical Assistant Professor, Department of Medicine, Perelman School of Medicine at University of Pennsylvania; Internist, Department of Medicine, Hospital Medicine Section, Pennsylvania Hospital, Philadelphia, has disclosed no relevant financial relationships. Dr. Williams, Associate Professor of Clinical Medicine, Department of General Internal Medicine, Lewis Katz School of Medicine; Staff Physician, Department of General Internal Medicine, Temple Internal Medicine Associates, Philadelphia, disclosed ties with The Curbsiders.
A version of this article first appeared on Medscape.com.
Cardiovascular Disease 2050: No, GLP-1s Won’t Save the Day
This transcript has been edited for clarity .
Robert A. Harrington, MD: I’m here in London at the European Society of Cardiology meetings, at theheart.org | Medscape Cardiology booth, using the meetings as an opportunity to meet with colleagues to talk about recent things that they’ve been writing about.
Today I’m joined by a good friend and colleague, Dr. Dhruv Kazi from Beth Israel Deaconess in Boston. Thanks for joining us.
Dhruv S. Kazi, MD, MS: Thank you for having me.
Harrington: Dr. Kazi is an associate professor of medicine at Harvard Medical School. He’s also the associate director of the Smith Center, which is an outcomes research center at the Beth Israel Deaconess. Thanks for joining us.
Kazi: Excited to be here.
Harrington: The topic I think you know that I want to discuss is a really important paper. There are two papers. They’re part of the American Heart Association’s 100th anniversary celebration, if you will. Many of the papers looked back at where science taken us.
With your coauthor, Karen Joynt Maddox, your papers are looking forward. They’re about the burden of cardiovascular disease in 2050. One paper really focused on what I would call the clinical and public health issues. Yours is focused on the economics. Is that a good description?
Kazi: Perfect.
Harrington: Tell us what you, Karen, and the other writers set out to do. What were you asked to do?
Kazi: As you know, the American Heart Association is entering its second century. Part of this was an exercise to say, where will the country be in 2050, which is a long enough time horizon for us to start planning for the future.
We looked back and said, if prior trends remain the same, where will we be in 2050, accounting for changes in demographics, changes in the composition of the population, and knowing that some of the cardiovascular risk factors are getting worse?
Harrington: For me, what was really striking is that, when I first saw the title and read “2050,” I thought, Oh, that’s a long way away. Then as I started reading it, I realized that this is not so far away.
Kazi: Absolutely.
Harrington: If we’re going to make a difference, it might take us 25 years.
Kazi: Especially if we set ourselves ambitious goals, we›re going to have to dig deep. Business-as-usual is not going to get us there.
Harrington: No. What I think has happened is we›ve spent so much time taking care of acute illness. Case fatality rates are fantastic. I was actually making the comment yesterday to a colleague that when I was an intern, the 30-day death rate from acute myocardial infarction was about 20%.
Kazi: Oh, wow.
Harrington: Now it’s 5%. That’s a big difference in a career.
Trends in the Wrong Direction
Kazi: There are fundamental trends. The decline in case fatalities is a really positive development, and I would hope that, going forward, that would continue. Those are risk-adjusted death rates and what is happening is that risk is going up. This is a function of the fact that the US population is aging; 2030 will be the first year that all the baby boomers will be over the age of 65.
By the mid-2030s, we’ll have more adults over the age of 65 than kids. That aging of the population is going to increase risk. The second is — and this is a positive development — we are a more diverse population, but the populations that are minoritized have higher cardiovascular risk, for a variety of reasons.
As the population of Asian Americans increases and doubles, in fact, as the population of Hispanic Americans doubles, we’re going to see an increase in risk related to cardiovascular disease. The third is that, over the past decade, there are some risk factors that are going in the wrong direction.
Harrington: Let’s talk about that because that’s humbling. I’m involved, as you know, with the American Heart Association, as are you. Despite all the work on Life’s Simple 7 and now Life’s Essential 8, we still have some issues.
Kazi: The big ones that come to mind are hypertension, diabetes, and obesity, all of which are trending in the wrong direction. Hypertension, we were gaining traction; and then over the past decade, we’ve slipped again. As you know, national blood pressure control rates have declined in many populations.
Harrington: Rather substantially.
Kazi: Substantially so, which has implications, in particular, for stroke rates in the future and stroke rates in young adults in the future. Obesity is a problem that we have very little control over. We’re already at 40% on average, which means that some populations are already in the 60% range.
Harrington: We also have obesity in kids — the burden, I’ll call it, of obesity. It’s not that you become obese in your thirties or your forties; you›re becoming obese as a teenager or even younger.
Kazi: Exactly. Since the 1990s, obesity in US adults has doubled, but obesity in US children has quadrupled. It’s starting from a lower base, but it’s very much an escalating problem.
Harrington: Diabetes is tightly linked to it but not totally explained.
Kazi: Exactly. The increase in diabetes is largely driven by obesity, but it›s probably also driven by changes in diet and lifestyle that don›t go through obesity.
Harrington: Yeah, it’s interesting. I think I have this figure correctly. It used to be rare that you saw a child with type 2 diabetes or what we call type 2 diabetes.
Kazi: Yeah.
Harrington: Now, the vast majority of kids with diabetes have type 2 diabetes.
Kazi: In the adolescents/young adults age group, most of it is type 2.
Harrington: Diabetes going up, obesity up, hypertension not well controlled, smoking combustible cigarettes way down.
Kazi: Yeah.
Harrington: Cholesterol levels. I was surprised. Cholesterol looked better. You said — because I was at a meeting where somebody asked you — that’s not explained by treatment.
Kazi: No, it’s not, at least going back to the ‘70s, but likely even sooner. I think that can only be attributed to substantial dietary changes. We are consuming less fat and less trans-fat. It’s possible that those collectively are improving our cholesterol levels, possibly at the expense of our glucose levels, because we basically substituted fats in our diet with more carbs at a population level.
Cigarettes and Vaping
Harrington: Some things certainly trend in the right direction but others in a really difficult direction. It’s going to lead to pretty large changes in risk for coronary disease, atrial fibrillation, and heart failure.
Kazi: I want to go back to the tobacco point. There are definitely marked declines in tobacco, still tightly related to income in the country. You see much higher prevalence of tobacco use in lower-income populations, but it’s unclear to me where it’s going in kids. We know that combustible tobacco use is going down but e-cigarettes went up. What that leads to over the next 30 years is unclear to me.
Harrington: That is a really important comment that’s worth sidebarring. The vaping use has been a terrible epidemic among our high schoolers. What is that going to lead to? Is it going to lead to the use of combustible cigarettes and we’re going to see that go back up? It remains to be seen.
Kazi: Yes, it remains to be seen. Going back to your point about this change in risk factors and this change in demographics, both aging and becoming a more diverse population means that we have large increases in some healthcare conditions.
Coronary heart disease goes up some, there›s a big jump in stroke — nearly a doubling in stroke — which is related to hypertension, obesity, an aging population, and a more diverse population. There are changes in stroke in the young, and atrial fibrillation related to, again, hypertension. We’re seeing these projections, and with them come these pretty large projections in changes in healthcare spending.
Healthcare Spending Not Sustainable
Harrington: Big. I mean, it’s not sustainable. Give the audience the number — it’s pretty frightening.
Kazi: We’re talking about a quadrupling of healthcare costs related to cardiovascular disease over 25 years. We’ve gotten used to the narrative that healthcare in the US is expensive and drugs are expensive, but this is an enormous problem — an unsustainable problem, like you called it.
It’s a doubling as a proportion of the economy. I was looking this up this morning. If the US healthcare economy were its own economy, it would be the fourth largest economy in the world.
Harrington: Healthcare as it is today, is it 21% of our economy?
Kazi: It’s 17% now. If it were its own economy, it would be the fourth largest in the world. We are spending more on healthcare than all but two other countries’ total economies. It’s kind of crazy.
Harrington: We’re talking about a quadrupling.
Kazi: Within that, the cardiovascular piece is a big piece, and we›re talking about a quadrupling.
Harrington: That’s both direct and indirect costs.
Kazi: The quadrupling of costs is just the direct costs. Indirect costs, for the listeners, refer to costs unrelated to healthcare but changes in productivity, either because people are disabled and unable to participate fully in the workforce or they die early.
The productivity costs are also increased substantially as a result. If you look at both healthcare and productivity, that goes up threefold. These are very large changes.
Harrington: Let’s now get to what we can do about it. I made the comment to you when I first read the papers that I was very depressed. Then, after I went through my Kübler-Ross stages of depression, death, and dying, I came to acceptance.
What are we going to do about it? This is a focus on policy, but also a focus on how we deliver healthcare, how we think about healthcare, and how we develop drugs and devices.
The drug question is going to be the one the audience is thinking about. They say, well, what about GLP-1 agonists? Aren’t those going to save the day?
Kazi: Yes and no. I’ll say that, early in my career, I used to be very attracted to simple solutions to complex problems. I’ve come to realize that simple solutions are elegant, attractive, and wrong. We›re dealing with a very complex issue and I think we’re going to need a multipronged approach.
The way I think about it is that there was a group of people who are at very high risk today. How do we help those individuals? Then how do we help the future generation so that they’re not dealing with the projections that we’re talking about.
My colleague, Karen Joynt Maddox, who led one of the papers, as you mentioned, has an elegant line in the paper where she says projections are not destiny. These are things we can change.
Harrington: If nothing changes, this is what it’s going to look like.
Kazi: This is where we’re headed.
Harrington: We can change. We’ve got some time to change, but we don’t have forever.
Kazi: Yes, exactly. We picked the 25-year timeline instead of a “let’s plan for the next century” timeline because we want something concrete and actionable. It’s close enough to be meaningful but far enough to give us the runway we need to act.
Harrington: Give me two things from the policy perspective, because it’s mostly policy.
Kazi: There are policy and clinical interventions. From the policy perspective, if I had to list two things, one is expansion of access to care. As we talk about this big increase in the burden of disease and risk factors, if you have a large proportion of your population that has hypertension or diabetes, you’re going to have to expand access to care to ensure that people get treated so they can get access to this care before they develop the complications that we worry about, like stroke and heart disease, that are very expensive to treat downstream.
The second, more broadly related to access to care, is the access to medications that are effective. You bring up GLP-1s. I think we need a real strategy for how we can give people access to GLP-1s at a price that is affordable to individuals but also affordable to the health system, and to help them stay on the drugs.
GLP-1s are transformative in what they do for weight loss and for diabetes, but more than 50% of people who start one are off it at 12 months. There’s something fundamentally wrong about how we’re delivering GLP-1s today. It’s not just about the cost of the drugs but the support system people need to stay on.
Harrington: I’ve made the comment, in many forms now, that we know the drugs work. We have to figure out how to use them.
Kazi: Exactly, yes.
Harrington: Using them includes chronicity. This is a chronic condition. Some people can come off the drugs, but many can’t. We’re going to have to figure this out, and maybe the newer generations of drugs will help us address what people call the off-ramping. How are we going to do that? I think you’re spot-on. Those are critically important questions.
Kazi: As we looked at this modeling, I’ll tell you — I had a come-to-Jesus moment where I was like, there is no way to fix cardiovascular disease in the US without going through obesity and diabetes. We have to address obesity in the US. We can’t just treat our way out of it. Obesity is fundamentally a food problem and we’ve got to engage again with food policy in a meaningful way.
Harrington: As you know, with the American Heart Association, we›re doing a large amount of work now on food as medicine and food is medicine. We are trying to figure out what the levers are that we can pull to actually help people eat healthier diets.
Kazi: Yes. Rather than framing it as an individual choice that people are eating poorly, it’s, how do we make healthy diets the default in the environment?
Harrington: This is where you get to the children as well.
Kazi: Exactly.
Harrington: I could talk about this all day. I’ve had the benefit of reading the papers now a few times and talking to you on several occasions. Thank you for joining us.
Kazi: Thank you.
Dr. Harrington, Stephen and Suzanne Weiss Dean, Weill Cornell Medicine; Provost for Medical Affairs, Cornell University, New York, NY, disclosed ties with Baim Institute (DSMB); CSL (RCT Executive Committee); Janssen (RCT Char), NHLBI (RCT Executive Committee, DSMB Chair); PCORI (RCT Co-Chair); DCRI, Atropos Health; Bitterroot Bio; Bristol Myers Squibb; BridgeBio; Element Science; Edwards Lifesciences; Foresite Labs; Medscape/WebMD Board of Directors for: American Heart Association; College of the Holy Cross; and Cytokinetics. Dr. Kazi, Associate Director, Smith Center for Outcomes Research, Associate Professor, Department of Medicine (Cardiology), Harvard Medical School, Director, Department of Cardiac Critical Care Unit, Beth Israel Deaconess Medical Center, Boston, Massachusetts, has disclosed receiving a research grant from Boston Scientific (grant to examine the economics of stroke prevention).
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity .
Robert A. Harrington, MD: I’m here in London at the European Society of Cardiology meetings, at theheart.org | Medscape Cardiology booth, using the meetings as an opportunity to meet with colleagues to talk about recent things that they’ve been writing about.
Today I’m joined by a good friend and colleague, Dr. Dhruv Kazi from Beth Israel Deaconess in Boston. Thanks for joining us.
Dhruv S. Kazi, MD, MS: Thank you for having me.
Harrington: Dr. Kazi is an associate professor of medicine at Harvard Medical School. He’s also the associate director of the Smith Center, which is an outcomes research center at the Beth Israel Deaconess. Thanks for joining us.
Kazi: Excited to be here.
Harrington: The topic I think you know that I want to discuss is a really important paper. There are two papers. They’re part of the American Heart Association’s 100th anniversary celebration, if you will. Many of the papers looked back at where science taken us.
With your coauthor, Karen Joynt Maddox, your papers are looking forward. They’re about the burden of cardiovascular disease in 2050. One paper really focused on what I would call the clinical and public health issues. Yours is focused on the economics. Is that a good description?
Kazi: Perfect.
Harrington: Tell us what you, Karen, and the other writers set out to do. What were you asked to do?
Kazi: As you know, the American Heart Association is entering its second century. Part of this was an exercise to say, where will the country be in 2050, which is a long enough time horizon for us to start planning for the future.
We looked back and said, if prior trends remain the same, where will we be in 2050, accounting for changes in demographics, changes in the composition of the population, and knowing that some of the cardiovascular risk factors are getting worse?
Harrington: For me, what was really striking is that, when I first saw the title and read “2050,” I thought, Oh, that’s a long way away. Then as I started reading it, I realized that this is not so far away.
Kazi: Absolutely.
Harrington: If we’re going to make a difference, it might take us 25 years.
Kazi: Especially if we set ourselves ambitious goals, we›re going to have to dig deep. Business-as-usual is not going to get us there.
Harrington: No. What I think has happened is we›ve spent so much time taking care of acute illness. Case fatality rates are fantastic. I was actually making the comment yesterday to a colleague that when I was an intern, the 30-day death rate from acute myocardial infarction was about 20%.
Kazi: Oh, wow.
Harrington: Now it’s 5%. That’s a big difference in a career.
Trends in the Wrong Direction
Kazi: There are fundamental trends. The decline in case fatalities is a really positive development, and I would hope that, going forward, that would continue. Those are risk-adjusted death rates and what is happening is that risk is going up. This is a function of the fact that the US population is aging; 2030 will be the first year that all the baby boomers will be over the age of 65.
By the mid-2030s, we’ll have more adults over the age of 65 than kids. That aging of the population is going to increase risk. The second is — and this is a positive development — we are a more diverse population, but the populations that are minoritized have higher cardiovascular risk, for a variety of reasons.
As the population of Asian Americans increases and doubles, in fact, as the population of Hispanic Americans doubles, we’re going to see an increase in risk related to cardiovascular disease. The third is that, over the past decade, there are some risk factors that are going in the wrong direction.
Harrington: Let’s talk about that because that’s humbling. I’m involved, as you know, with the American Heart Association, as are you. Despite all the work on Life’s Simple 7 and now Life’s Essential 8, we still have some issues.
Kazi: The big ones that come to mind are hypertension, diabetes, and obesity, all of which are trending in the wrong direction. Hypertension, we were gaining traction; and then over the past decade, we’ve slipped again. As you know, national blood pressure control rates have declined in many populations.
Harrington: Rather substantially.
Kazi: Substantially so, which has implications, in particular, for stroke rates in the future and stroke rates in young adults in the future. Obesity is a problem that we have very little control over. We’re already at 40% on average, which means that some populations are already in the 60% range.
Harrington: We also have obesity in kids — the burden, I’ll call it, of obesity. It’s not that you become obese in your thirties or your forties; you›re becoming obese as a teenager or even younger.
Kazi: Exactly. Since the 1990s, obesity in US adults has doubled, but obesity in US children has quadrupled. It’s starting from a lower base, but it’s very much an escalating problem.
Harrington: Diabetes is tightly linked to it but not totally explained.
Kazi: Exactly. The increase in diabetes is largely driven by obesity, but it›s probably also driven by changes in diet and lifestyle that don›t go through obesity.
Harrington: Yeah, it’s interesting. I think I have this figure correctly. It used to be rare that you saw a child with type 2 diabetes or what we call type 2 diabetes.
Kazi: Yeah.
Harrington: Now, the vast majority of kids with diabetes have type 2 diabetes.
Kazi: In the adolescents/young adults age group, most of it is type 2.
Harrington: Diabetes going up, obesity up, hypertension not well controlled, smoking combustible cigarettes way down.
Kazi: Yeah.
Harrington: Cholesterol levels. I was surprised. Cholesterol looked better. You said — because I was at a meeting where somebody asked you — that’s not explained by treatment.
Kazi: No, it’s not, at least going back to the ‘70s, but likely even sooner. I think that can only be attributed to substantial dietary changes. We are consuming less fat and less trans-fat. It’s possible that those collectively are improving our cholesterol levels, possibly at the expense of our glucose levels, because we basically substituted fats in our diet with more carbs at a population level.
Cigarettes and Vaping
Harrington: Some things certainly trend in the right direction but others in a really difficult direction. It’s going to lead to pretty large changes in risk for coronary disease, atrial fibrillation, and heart failure.
Kazi: I want to go back to the tobacco point. There are definitely marked declines in tobacco, still tightly related to income in the country. You see much higher prevalence of tobacco use in lower-income populations, but it’s unclear to me where it’s going in kids. We know that combustible tobacco use is going down but e-cigarettes went up. What that leads to over the next 30 years is unclear to me.
Harrington: That is a really important comment that’s worth sidebarring. The vaping use has been a terrible epidemic among our high schoolers. What is that going to lead to? Is it going to lead to the use of combustible cigarettes and we’re going to see that go back up? It remains to be seen.
Kazi: Yes, it remains to be seen. Going back to your point about this change in risk factors and this change in demographics, both aging and becoming a more diverse population means that we have large increases in some healthcare conditions.
Coronary heart disease goes up some, there›s a big jump in stroke — nearly a doubling in stroke — which is related to hypertension, obesity, an aging population, and a more diverse population. There are changes in stroke in the young, and atrial fibrillation related to, again, hypertension. We’re seeing these projections, and with them come these pretty large projections in changes in healthcare spending.
Healthcare Spending Not Sustainable
Harrington: Big. I mean, it’s not sustainable. Give the audience the number — it’s pretty frightening.
Kazi: We’re talking about a quadrupling of healthcare costs related to cardiovascular disease over 25 years. We’ve gotten used to the narrative that healthcare in the US is expensive and drugs are expensive, but this is an enormous problem — an unsustainable problem, like you called it.
It’s a doubling as a proportion of the economy. I was looking this up this morning. If the US healthcare economy were its own economy, it would be the fourth largest economy in the world.
Harrington: Healthcare as it is today, is it 21% of our economy?
Kazi: It’s 17% now. If it were its own economy, it would be the fourth largest in the world. We are spending more on healthcare than all but two other countries’ total economies. It’s kind of crazy.
Harrington: We’re talking about a quadrupling.
Kazi: Within that, the cardiovascular piece is a big piece, and we›re talking about a quadrupling.
Harrington: That’s both direct and indirect costs.
Kazi: The quadrupling of costs is just the direct costs. Indirect costs, for the listeners, refer to costs unrelated to healthcare but changes in productivity, either because people are disabled and unable to participate fully in the workforce or they die early.
The productivity costs are also increased substantially as a result. If you look at both healthcare and productivity, that goes up threefold. These are very large changes.
Harrington: Let’s now get to what we can do about it. I made the comment to you when I first read the papers that I was very depressed. Then, after I went through my Kübler-Ross stages of depression, death, and dying, I came to acceptance.
What are we going to do about it? This is a focus on policy, but also a focus on how we deliver healthcare, how we think about healthcare, and how we develop drugs and devices.
The drug question is going to be the one the audience is thinking about. They say, well, what about GLP-1 agonists? Aren’t those going to save the day?
Kazi: Yes and no. I’ll say that, early in my career, I used to be very attracted to simple solutions to complex problems. I’ve come to realize that simple solutions are elegant, attractive, and wrong. We›re dealing with a very complex issue and I think we’re going to need a multipronged approach.
The way I think about it is that there was a group of people who are at very high risk today. How do we help those individuals? Then how do we help the future generation so that they’re not dealing with the projections that we’re talking about.
My colleague, Karen Joynt Maddox, who led one of the papers, as you mentioned, has an elegant line in the paper where she says projections are not destiny. These are things we can change.
Harrington: If nothing changes, this is what it’s going to look like.
Kazi: This is where we’re headed.
Harrington: We can change. We’ve got some time to change, but we don’t have forever.
Kazi: Yes, exactly. We picked the 25-year timeline instead of a “let’s plan for the next century” timeline because we want something concrete and actionable. It’s close enough to be meaningful but far enough to give us the runway we need to act.
Harrington: Give me two things from the policy perspective, because it’s mostly policy.
Kazi: There are policy and clinical interventions. From the policy perspective, if I had to list two things, one is expansion of access to care. As we talk about this big increase in the burden of disease and risk factors, if you have a large proportion of your population that has hypertension or diabetes, you’re going to have to expand access to care to ensure that people get treated so they can get access to this care before they develop the complications that we worry about, like stroke and heart disease, that are very expensive to treat downstream.
The second, more broadly related to access to care, is the access to medications that are effective. You bring up GLP-1s. I think we need a real strategy for how we can give people access to GLP-1s at a price that is affordable to individuals but also affordable to the health system, and to help them stay on the drugs.
GLP-1s are transformative in what they do for weight loss and for diabetes, but more than 50% of people who start one are off it at 12 months. There’s something fundamentally wrong about how we’re delivering GLP-1s today. It’s not just about the cost of the drugs but the support system people need to stay on.
Harrington: I’ve made the comment, in many forms now, that we know the drugs work. We have to figure out how to use them.
Kazi: Exactly, yes.
Harrington: Using them includes chronicity. This is a chronic condition. Some people can come off the drugs, but many can’t. We’re going to have to figure this out, and maybe the newer generations of drugs will help us address what people call the off-ramping. How are we going to do that? I think you’re spot-on. Those are critically important questions.
Kazi: As we looked at this modeling, I’ll tell you — I had a come-to-Jesus moment where I was like, there is no way to fix cardiovascular disease in the US without going through obesity and diabetes. We have to address obesity in the US. We can’t just treat our way out of it. Obesity is fundamentally a food problem and we’ve got to engage again with food policy in a meaningful way.
Harrington: As you know, with the American Heart Association, we›re doing a large amount of work now on food as medicine and food is medicine. We are trying to figure out what the levers are that we can pull to actually help people eat healthier diets.
Kazi: Yes. Rather than framing it as an individual choice that people are eating poorly, it’s, how do we make healthy diets the default in the environment?
Harrington: This is where you get to the children as well.
Kazi: Exactly.
Harrington: I could talk about this all day. I’ve had the benefit of reading the papers now a few times and talking to you on several occasions. Thank you for joining us.
Kazi: Thank you.
Dr. Harrington, Stephen and Suzanne Weiss Dean, Weill Cornell Medicine; Provost for Medical Affairs, Cornell University, New York, NY, disclosed ties with Baim Institute (DSMB); CSL (RCT Executive Committee); Janssen (RCT Char), NHLBI (RCT Executive Committee, DSMB Chair); PCORI (RCT Co-Chair); DCRI, Atropos Health; Bitterroot Bio; Bristol Myers Squibb; BridgeBio; Element Science; Edwards Lifesciences; Foresite Labs; Medscape/WebMD Board of Directors for: American Heart Association; College of the Holy Cross; and Cytokinetics. Dr. Kazi, Associate Director, Smith Center for Outcomes Research, Associate Professor, Department of Medicine (Cardiology), Harvard Medical School, Director, Department of Cardiac Critical Care Unit, Beth Israel Deaconess Medical Center, Boston, Massachusetts, has disclosed receiving a research grant from Boston Scientific (grant to examine the economics of stroke prevention).
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity .
Robert A. Harrington, MD: I’m here in London at the European Society of Cardiology meetings, at theheart.org | Medscape Cardiology booth, using the meetings as an opportunity to meet with colleagues to talk about recent things that they’ve been writing about.
Today I’m joined by a good friend and colleague, Dr. Dhruv Kazi from Beth Israel Deaconess in Boston. Thanks for joining us.
Dhruv S. Kazi, MD, MS: Thank you for having me.
Harrington: Dr. Kazi is an associate professor of medicine at Harvard Medical School. He’s also the associate director of the Smith Center, which is an outcomes research center at the Beth Israel Deaconess. Thanks for joining us.
Kazi: Excited to be here.
Harrington: The topic I think you know that I want to discuss is a really important paper. There are two papers. They’re part of the American Heart Association’s 100th anniversary celebration, if you will. Many of the papers looked back at where science taken us.
With your coauthor, Karen Joynt Maddox, your papers are looking forward. They’re about the burden of cardiovascular disease in 2050. One paper really focused on what I would call the clinical and public health issues. Yours is focused on the economics. Is that a good description?
Kazi: Perfect.
Harrington: Tell us what you, Karen, and the other writers set out to do. What were you asked to do?
Kazi: As you know, the American Heart Association is entering its second century. Part of this was an exercise to say, where will the country be in 2050, which is a long enough time horizon for us to start planning for the future.
We looked back and said, if prior trends remain the same, where will we be in 2050, accounting for changes in demographics, changes in the composition of the population, and knowing that some of the cardiovascular risk factors are getting worse?
Harrington: For me, what was really striking is that, when I first saw the title and read “2050,” I thought, Oh, that’s a long way away. Then as I started reading it, I realized that this is not so far away.
Kazi: Absolutely.
Harrington: If we’re going to make a difference, it might take us 25 years.
Kazi: Especially if we set ourselves ambitious goals, we›re going to have to dig deep. Business-as-usual is not going to get us there.
Harrington: No. What I think has happened is we›ve spent so much time taking care of acute illness. Case fatality rates are fantastic. I was actually making the comment yesterday to a colleague that when I was an intern, the 30-day death rate from acute myocardial infarction was about 20%.
Kazi: Oh, wow.
Harrington: Now it’s 5%. That’s a big difference in a career.
Trends in the Wrong Direction
Kazi: There are fundamental trends. The decline in case fatalities is a really positive development, and I would hope that, going forward, that would continue. Those are risk-adjusted death rates and what is happening is that risk is going up. This is a function of the fact that the US population is aging; 2030 will be the first year that all the baby boomers will be over the age of 65.
By the mid-2030s, we’ll have more adults over the age of 65 than kids. That aging of the population is going to increase risk. The second is — and this is a positive development — we are a more diverse population, but the populations that are minoritized have higher cardiovascular risk, for a variety of reasons.
As the population of Asian Americans increases and doubles, in fact, as the population of Hispanic Americans doubles, we’re going to see an increase in risk related to cardiovascular disease. The third is that, over the past decade, there are some risk factors that are going in the wrong direction.
Harrington: Let’s talk about that because that’s humbling. I’m involved, as you know, with the American Heart Association, as are you. Despite all the work on Life’s Simple 7 and now Life’s Essential 8, we still have some issues.
Kazi: The big ones that come to mind are hypertension, diabetes, and obesity, all of which are trending in the wrong direction. Hypertension, we were gaining traction; and then over the past decade, we’ve slipped again. As you know, national blood pressure control rates have declined in many populations.
Harrington: Rather substantially.
Kazi: Substantially so, which has implications, in particular, for stroke rates in the future and stroke rates in young adults in the future. Obesity is a problem that we have very little control over. We’re already at 40% on average, which means that some populations are already in the 60% range.
Harrington: We also have obesity in kids — the burden, I’ll call it, of obesity. It’s not that you become obese in your thirties or your forties; you›re becoming obese as a teenager or even younger.
Kazi: Exactly. Since the 1990s, obesity in US adults has doubled, but obesity in US children has quadrupled. It’s starting from a lower base, but it’s very much an escalating problem.
Harrington: Diabetes is tightly linked to it but not totally explained.
Kazi: Exactly. The increase in diabetes is largely driven by obesity, but it›s probably also driven by changes in diet and lifestyle that don›t go through obesity.
Harrington: Yeah, it’s interesting. I think I have this figure correctly. It used to be rare that you saw a child with type 2 diabetes or what we call type 2 diabetes.
Kazi: Yeah.
Harrington: Now, the vast majority of kids with diabetes have type 2 diabetes.
Kazi: In the adolescents/young adults age group, most of it is type 2.
Harrington: Diabetes going up, obesity up, hypertension not well controlled, smoking combustible cigarettes way down.
Kazi: Yeah.
Harrington: Cholesterol levels. I was surprised. Cholesterol looked better. You said — because I was at a meeting where somebody asked you — that’s not explained by treatment.
Kazi: No, it’s not, at least going back to the ‘70s, but likely even sooner. I think that can only be attributed to substantial dietary changes. We are consuming less fat and less trans-fat. It’s possible that those collectively are improving our cholesterol levels, possibly at the expense of our glucose levels, because we basically substituted fats in our diet with more carbs at a population level.
Cigarettes and Vaping
Harrington: Some things certainly trend in the right direction but others in a really difficult direction. It’s going to lead to pretty large changes in risk for coronary disease, atrial fibrillation, and heart failure.
Kazi: I want to go back to the tobacco point. There are definitely marked declines in tobacco, still tightly related to income in the country. You see much higher prevalence of tobacco use in lower-income populations, but it’s unclear to me where it’s going in kids. We know that combustible tobacco use is going down but e-cigarettes went up. What that leads to over the next 30 years is unclear to me.
Harrington: That is a really important comment that’s worth sidebarring. The vaping use has been a terrible epidemic among our high schoolers. What is that going to lead to? Is it going to lead to the use of combustible cigarettes and we’re going to see that go back up? It remains to be seen.
Kazi: Yes, it remains to be seen. Going back to your point about this change in risk factors and this change in demographics, both aging and becoming a more diverse population means that we have large increases in some healthcare conditions.
Coronary heart disease goes up some, there›s a big jump in stroke — nearly a doubling in stroke — which is related to hypertension, obesity, an aging population, and a more diverse population. There are changes in stroke in the young, and atrial fibrillation related to, again, hypertension. We’re seeing these projections, and with them come these pretty large projections in changes in healthcare spending.
Healthcare Spending Not Sustainable
Harrington: Big. I mean, it’s not sustainable. Give the audience the number — it’s pretty frightening.
Kazi: We’re talking about a quadrupling of healthcare costs related to cardiovascular disease over 25 years. We’ve gotten used to the narrative that healthcare in the US is expensive and drugs are expensive, but this is an enormous problem — an unsustainable problem, like you called it.
It’s a doubling as a proportion of the economy. I was looking this up this morning. If the US healthcare economy were its own economy, it would be the fourth largest economy in the world.
Harrington: Healthcare as it is today, is it 21% of our economy?
Kazi: It’s 17% now. If it were its own economy, it would be the fourth largest in the world. We are spending more on healthcare than all but two other countries’ total economies. It’s kind of crazy.
Harrington: We’re talking about a quadrupling.
Kazi: Within that, the cardiovascular piece is a big piece, and we›re talking about a quadrupling.
Harrington: That’s both direct and indirect costs.
Kazi: The quadrupling of costs is just the direct costs. Indirect costs, for the listeners, refer to costs unrelated to healthcare but changes in productivity, either because people are disabled and unable to participate fully in the workforce or they die early.
The productivity costs are also increased substantially as a result. If you look at both healthcare and productivity, that goes up threefold. These are very large changes.
Harrington: Let’s now get to what we can do about it. I made the comment to you when I first read the papers that I was very depressed. Then, after I went through my Kübler-Ross stages of depression, death, and dying, I came to acceptance.
What are we going to do about it? This is a focus on policy, but also a focus on how we deliver healthcare, how we think about healthcare, and how we develop drugs and devices.
The drug question is going to be the one the audience is thinking about. They say, well, what about GLP-1 agonists? Aren’t those going to save the day?
Kazi: Yes and no. I’ll say that, early in my career, I used to be very attracted to simple solutions to complex problems. I’ve come to realize that simple solutions are elegant, attractive, and wrong. We›re dealing with a very complex issue and I think we’re going to need a multipronged approach.
The way I think about it is that there was a group of people who are at very high risk today. How do we help those individuals? Then how do we help the future generation so that they’re not dealing with the projections that we’re talking about.
My colleague, Karen Joynt Maddox, who led one of the papers, as you mentioned, has an elegant line in the paper where she says projections are not destiny. These are things we can change.
Harrington: If nothing changes, this is what it’s going to look like.
Kazi: This is where we’re headed.
Harrington: We can change. We’ve got some time to change, but we don’t have forever.
Kazi: Yes, exactly. We picked the 25-year timeline instead of a “let’s plan for the next century” timeline because we want something concrete and actionable. It’s close enough to be meaningful but far enough to give us the runway we need to act.
Harrington: Give me two things from the policy perspective, because it’s mostly policy.
Kazi: There are policy and clinical interventions. From the policy perspective, if I had to list two things, one is expansion of access to care. As we talk about this big increase in the burden of disease and risk factors, if you have a large proportion of your population that has hypertension or diabetes, you’re going to have to expand access to care to ensure that people get treated so they can get access to this care before they develop the complications that we worry about, like stroke and heart disease, that are very expensive to treat downstream.
The second, more broadly related to access to care, is the access to medications that are effective. You bring up GLP-1s. I think we need a real strategy for how we can give people access to GLP-1s at a price that is affordable to individuals but also affordable to the health system, and to help them stay on the drugs.
GLP-1s are transformative in what they do for weight loss and for diabetes, but more than 50% of people who start one are off it at 12 months. There’s something fundamentally wrong about how we’re delivering GLP-1s today. It’s not just about the cost of the drugs but the support system people need to stay on.
Harrington: I’ve made the comment, in many forms now, that we know the drugs work. We have to figure out how to use them.
Kazi: Exactly, yes.
Harrington: Using them includes chronicity. This is a chronic condition. Some people can come off the drugs, but many can’t. We’re going to have to figure this out, and maybe the newer generations of drugs will help us address what people call the off-ramping. How are we going to do that? I think you’re spot-on. Those are critically important questions.
Kazi: As we looked at this modeling, I’ll tell you — I had a come-to-Jesus moment where I was like, there is no way to fix cardiovascular disease in the US without going through obesity and diabetes. We have to address obesity in the US. We can’t just treat our way out of it. Obesity is fundamentally a food problem and we’ve got to engage again with food policy in a meaningful way.
Harrington: As you know, with the American Heart Association, we›re doing a large amount of work now on food as medicine and food is medicine. We are trying to figure out what the levers are that we can pull to actually help people eat healthier diets.
Kazi: Yes. Rather than framing it as an individual choice that people are eating poorly, it’s, how do we make healthy diets the default in the environment?
Harrington: This is where you get to the children as well.
Kazi: Exactly.
Harrington: I could talk about this all day. I’ve had the benefit of reading the papers now a few times and talking to you on several occasions. Thank you for joining us.
Kazi: Thank you.
Dr. Harrington, Stephen and Suzanne Weiss Dean, Weill Cornell Medicine; Provost for Medical Affairs, Cornell University, New York, NY, disclosed ties with Baim Institute (DSMB); CSL (RCT Executive Committee); Janssen (RCT Char), NHLBI (RCT Executive Committee, DSMB Chair); PCORI (RCT Co-Chair); DCRI, Atropos Health; Bitterroot Bio; Bristol Myers Squibb; BridgeBio; Element Science; Edwards Lifesciences; Foresite Labs; Medscape/WebMD Board of Directors for: American Heart Association; College of the Holy Cross; and Cytokinetics. Dr. Kazi, Associate Director, Smith Center for Outcomes Research, Associate Professor, Department of Medicine (Cardiology), Harvard Medical School, Director, Department of Cardiac Critical Care Unit, Beth Israel Deaconess Medical Center, Boston, Massachusetts, has disclosed receiving a research grant from Boston Scientific (grant to examine the economics of stroke prevention).
A version of this article appeared on Medscape.com.
A 51-year-old woman presented for a routine full body skin exam after vacationing in Hawaii.
Primary adrenal insufficiency (Addison’s disease) results from a dysfunction of the adrenal glands, which may be secondary to autoimmune diseases, genetic conditions, infections, and vasculopathies,or may be drug-induced (e.g. checkpoint inhibitors), among others . In contrast, secondary adrenal insufficiency results from pituitary dysfunction of low adrenocorticotropic hormone (ACTH). The most common cause of primary adrenal insufficiency in developed countries is autoimmune adrenalitis, which accounts for upwards of 90% of cases. Typically, 21-hydroxylase autoantibodies are identified and account for destruction of the adrenal cortex through cell-mediated and humoral immune responses.
Palmar creases, subungual surfaces, sites of trauma, and joint spaces (including the knees, spine, elbows, and shoulders) are commonly affected. Hair depletes in the pubic area and axillary vaults. Nevi may also appear darker. In patients with autoimmune adrenalitis, vitiligo may be seen secondary to autoimmune destruction of melanocytes.
Diagnosis may be difficult in the early stages, but historical findings of fatigue and clinical findings of hyperpigmentation in classic areas may prompt appropriate lab screening workup. It is essential to determine whether adrenal insufficiency is primary or secondary. Evaluation of decreased cortisol production, determination of whether production is ACTH-dependent or -independent, and evaluation for the underlying causes of adrenal dysfunction are important. Lab screening includes morning serum cortisol, morning ACTH (cosyntropin) stimulation test, fasting CBC with differential, and CMP to evaluate for normocytic normochromic anemia, hyponatremia, hyperkalemia, hypoglycemia, plasma renin/aldosterone ratio, and 21-hydroxylase autoantibodies.
Management strategies of primary adrenal insufficiency require corticosteroid supplementation and multidisciplinary collaboration with endocrinology. If untreated, primary adrenal insufficiency can be fatal. Adrenal crisis is a critical condition following a precipitating event, such as GI infection, fever, acute stress, and/or untreated adrenal or pituitary disorders. Clinical findings include acute shock with hypotension, nausea, vomiting, abdominal pain, back or leg pain, and a change in mental status. In this scenario, increasing the dose of corticosteroid supplementation is essential for reducing mortality.
Upon examining this patient’s new skin findings of hyperpigmentation and discussing her fatigue, primary adrenal insufficiency was suspected. With further prompting, the patient reported an ICU hospitalization several months prior because of sepsis originating from a peritonsillar abscess. With these clinical and historical findings, preliminary workup was conducted by dermatology, which included morning cortisol level, ACTH, CBC with differential, CMP, plasma renin-aldosterone ratio, and 21-hydroxylase autoantibodies. Work up demonstrated a low morning cortisol level of 1.3 mcg/dL, an elevated ACTH of 2,739 pg/mL, and positive 21-hydroxylase autoantibodies. The patient was urgently referred to endocrinology and started on oral hydrocortisone. Her fatigue immediately improved, and at 1-year follow-up with dermatology, her mucocutaneous hyperpigmentation had subsided dramatically.
Dermatologists can play a major role in the early diagnosis of primary adrenal insufficiency, which is essential for reducing patient morbidity and mortality. Skin findings on full body skin exams can clue in dermatologists for ordering preliminary workup to expedite care for these patients.
The case and photos were submitted by Dr. Akhiyat, Scripps Clinic Medical Group, La Jolla, California. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
J Am Acad Dermatol. 2014 May;70(5):Supplement 1AB118. doi: 10.1016/j.jaad.2014.01.491.
Michels A, Michels N. Am Fam Physician. 2014 Apr 1;89(7):563-568.
Kauzman A et al. J Can Dent Assoc. 2004 Nov;70(10):682-683.
Primary adrenal insufficiency (Addison’s disease) results from a dysfunction of the adrenal glands, which may be secondary to autoimmune diseases, genetic conditions, infections, and vasculopathies,or may be drug-induced (e.g. checkpoint inhibitors), among others . In contrast, secondary adrenal insufficiency results from pituitary dysfunction of low adrenocorticotropic hormone (ACTH). The most common cause of primary adrenal insufficiency in developed countries is autoimmune adrenalitis, which accounts for upwards of 90% of cases. Typically, 21-hydroxylase autoantibodies are identified and account for destruction of the adrenal cortex through cell-mediated and humoral immune responses.
Palmar creases, subungual surfaces, sites of trauma, and joint spaces (including the knees, spine, elbows, and shoulders) are commonly affected. Hair depletes in the pubic area and axillary vaults. Nevi may also appear darker. In patients with autoimmune adrenalitis, vitiligo may be seen secondary to autoimmune destruction of melanocytes.
Diagnosis may be difficult in the early stages, but historical findings of fatigue and clinical findings of hyperpigmentation in classic areas may prompt appropriate lab screening workup. It is essential to determine whether adrenal insufficiency is primary or secondary. Evaluation of decreased cortisol production, determination of whether production is ACTH-dependent or -independent, and evaluation for the underlying causes of adrenal dysfunction are important. Lab screening includes morning serum cortisol, morning ACTH (cosyntropin) stimulation test, fasting CBC with differential, and CMP to evaluate for normocytic normochromic anemia, hyponatremia, hyperkalemia, hypoglycemia, plasma renin/aldosterone ratio, and 21-hydroxylase autoantibodies.
Management strategies of primary adrenal insufficiency require corticosteroid supplementation and multidisciplinary collaboration with endocrinology. If untreated, primary adrenal insufficiency can be fatal. Adrenal crisis is a critical condition following a precipitating event, such as GI infection, fever, acute stress, and/or untreated adrenal or pituitary disorders. Clinical findings include acute shock with hypotension, nausea, vomiting, abdominal pain, back or leg pain, and a change in mental status. In this scenario, increasing the dose of corticosteroid supplementation is essential for reducing mortality.
Upon examining this patient’s new skin findings of hyperpigmentation and discussing her fatigue, primary adrenal insufficiency was suspected. With further prompting, the patient reported an ICU hospitalization several months prior because of sepsis originating from a peritonsillar abscess. With these clinical and historical findings, preliminary workup was conducted by dermatology, which included morning cortisol level, ACTH, CBC with differential, CMP, plasma renin-aldosterone ratio, and 21-hydroxylase autoantibodies. Work up demonstrated a low morning cortisol level of 1.3 mcg/dL, an elevated ACTH of 2,739 pg/mL, and positive 21-hydroxylase autoantibodies. The patient was urgently referred to endocrinology and started on oral hydrocortisone. Her fatigue immediately improved, and at 1-year follow-up with dermatology, her mucocutaneous hyperpigmentation had subsided dramatically.
Dermatologists can play a major role in the early diagnosis of primary adrenal insufficiency, which is essential for reducing patient morbidity and mortality. Skin findings on full body skin exams can clue in dermatologists for ordering preliminary workup to expedite care for these patients.
The case and photos were submitted by Dr. Akhiyat, Scripps Clinic Medical Group, La Jolla, California. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
J Am Acad Dermatol. 2014 May;70(5):Supplement 1AB118. doi: 10.1016/j.jaad.2014.01.491.
Michels A, Michels N. Am Fam Physician. 2014 Apr 1;89(7):563-568.
Kauzman A et al. J Can Dent Assoc. 2004 Nov;70(10):682-683.
Primary adrenal insufficiency (Addison’s disease) results from a dysfunction of the adrenal glands, which may be secondary to autoimmune diseases, genetic conditions, infections, and vasculopathies,or may be drug-induced (e.g. checkpoint inhibitors), among others . In contrast, secondary adrenal insufficiency results from pituitary dysfunction of low adrenocorticotropic hormone (ACTH). The most common cause of primary adrenal insufficiency in developed countries is autoimmune adrenalitis, which accounts for upwards of 90% of cases. Typically, 21-hydroxylase autoantibodies are identified and account for destruction of the adrenal cortex through cell-mediated and humoral immune responses.
Palmar creases, subungual surfaces, sites of trauma, and joint spaces (including the knees, spine, elbows, and shoulders) are commonly affected. Hair depletes in the pubic area and axillary vaults. Nevi may also appear darker. In patients with autoimmune adrenalitis, vitiligo may be seen secondary to autoimmune destruction of melanocytes.
Diagnosis may be difficult in the early stages, but historical findings of fatigue and clinical findings of hyperpigmentation in classic areas may prompt appropriate lab screening workup. It is essential to determine whether adrenal insufficiency is primary or secondary. Evaluation of decreased cortisol production, determination of whether production is ACTH-dependent or -independent, and evaluation for the underlying causes of adrenal dysfunction are important. Lab screening includes morning serum cortisol, morning ACTH (cosyntropin) stimulation test, fasting CBC with differential, and CMP to evaluate for normocytic normochromic anemia, hyponatremia, hyperkalemia, hypoglycemia, plasma renin/aldosterone ratio, and 21-hydroxylase autoantibodies.
Management strategies of primary adrenal insufficiency require corticosteroid supplementation and multidisciplinary collaboration with endocrinology. If untreated, primary adrenal insufficiency can be fatal. Adrenal crisis is a critical condition following a precipitating event, such as GI infection, fever, acute stress, and/or untreated adrenal or pituitary disorders. Clinical findings include acute shock with hypotension, nausea, vomiting, abdominal pain, back or leg pain, and a change in mental status. In this scenario, increasing the dose of corticosteroid supplementation is essential for reducing mortality.
Upon examining this patient’s new skin findings of hyperpigmentation and discussing her fatigue, primary adrenal insufficiency was suspected. With further prompting, the patient reported an ICU hospitalization several months prior because of sepsis originating from a peritonsillar abscess. With these clinical and historical findings, preliminary workup was conducted by dermatology, which included morning cortisol level, ACTH, CBC with differential, CMP, plasma renin-aldosterone ratio, and 21-hydroxylase autoantibodies. Work up demonstrated a low morning cortisol level of 1.3 mcg/dL, an elevated ACTH of 2,739 pg/mL, and positive 21-hydroxylase autoantibodies. The patient was urgently referred to endocrinology and started on oral hydrocortisone. Her fatigue immediately improved, and at 1-year follow-up with dermatology, her mucocutaneous hyperpigmentation had subsided dramatically.
Dermatologists can play a major role in the early diagnosis of primary adrenal insufficiency, which is essential for reducing patient morbidity and mortality. Skin findings on full body skin exams can clue in dermatologists for ordering preliminary workup to expedite care for these patients.
The case and photos were submitted by Dr. Akhiyat, Scripps Clinic Medical Group, La Jolla, California. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to [email protected].
References
J Am Acad Dermatol. 2014 May;70(5):Supplement 1AB118. doi: 10.1016/j.jaad.2014.01.491.
Michels A, Michels N. Am Fam Physician. 2014 Apr 1;89(7):563-568.
Kauzman A et al. J Can Dent Assoc. 2004 Nov;70(10):682-683.
How Old Are You? Stand on One Leg and I’ll Tell You
This transcript has been edited for clarity.
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
So I was lying in bed the other night, trying to read my phone, and started complaining to my wife about how my vision keeps getting worse, and then how stiff I feel when I wake up in the morning, and how a recent injury is taking too long to heal, and she said, “Well, yeah. You’re 44. That’s when things start to head downhill.”
And I was like, “Forty-four? That seems very specific. I thought 50 was what people complain about.” And she said, “No, it’s a thing — 44 years old and 60 years old. There’s a drop-off there.”
And you know what? She was right.
A study, “Nonlinear dynamics of multi-omics profiles during human aging,” published in Nature Aging in August 2024, analyzed a ton of proteins and metabolites in people of various ages and found, when you put it all together, that I should know better than to doubt my brilliant spouse.
But deep down, I believe the cliché that age is just a number. I don’t particularly care about being 44, or turning 50 or 60. I care about how my body and brain are aging. If I can be a happy, healthy, 80-year-old in full command of my faculties, I would consider that a major win no matter what the calendar says.
So I’m always interested in ways to quantify how my body is aging, independent of how many birthdays I have passed. And, according to a new study, there’s actually a really easy way to do this: Just stand on one leg.
The surprising results come from “Age-related changes in gait, balance, and strength parameters: A cross-sectional study,” appearing in PLOS One, which analyzed 40 individuals — half under age 65 and half over age 65 — across a variety of domains of strength, balance, and gait. The conceit of the study? We all know that things like strength and balance worsen over time, but what worsens fastest? What might be the best metric to tell us how our bodies are aging?
To that end, you have a variety of correlations between various metrics and calendar age.
As age increases, grip strength goes down. Men (inexplicably in pink) have higher grip strength overall, and women (confusingly in blue) lower. Somewhat less strong correlations were seen for knee strength.
What about balance?
To assess this, the researchers had the participants stand on a pressure plate. In one scenario, they did this with eyes open, and the next with eyes closed. They then measured how much the pressure varied around the center of the individual on the plate — basically, how much the person swayed while they were standing there.
Sway increased as age increased. Sway increased a bit more with eyes closed than with eyes open.
But the strongest correlation between any of these metrics and age was a simple one: How long can you stand on one leg?
Particularly for the nondominant leg, what you see here is a pretty dramatic drop-off in balance time around age 65, with younger people able to do 10 seconds with ease and some older people barely being able to make it to 2.
Of course, I had to try this for myself. And as I was standing around on one leg, it became clear to me exactly why this might be a good metric. It really integrates balance and strength in a way that the other tests don’t: balance, clearly, since you have to stay vertical over a relatively small base; but strength as well, because, well, one leg is holding up all the rest of you. You do feel it after a while.
So this metric passes the smell test to me, at least as a potential proxy for age-related physical decline.
But I should be careful to note that this was a cross-sectional study; the researchers looked at various people who were all different ages, not the same people over time to watch how these things change as they aged.
Also, the use of the correlation coefficient in graphs like this implies a certain linear relationship between age and standing-on-one-foot time. The raw data — the points on this graph — don’t appear that linear to me. As I mentioned above, it seems like there might be a bit of a sharp drop-off somewhere in the mid-60s. That means that we may not be able to use this as a sensitive test for aging that slowly changes as your body gets older. It might be that you’re able to essentially stand on one leg as long as you want until, one day, you can’t. That gives us less warning and less to act on.
And finally, we don’t know that changing this metric will change your health for the better. I’m sure a good physiatrist or physical therapist could design some exercises to increase any of our standing-on-one leg times. And no doubt, with practice, you could get your numbers way up. But that doesn’t necessarily mean you’re healthier. It’s like “teaching to the test”; you might score better on the standardized exam but you didn’t really learn the material.
So I am not adding one-leg standing to my daily exercise routine. But I won’t lie and tell you that, from time to time, and certainly on my 60th birthday, you may find me standing like a flamingo with a stopwatch in my hand.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.