User login
M. Alexander Otto began his reporting career early in 1999 covering the pharmaceutical industry for a national pharmacists' magazine and freelancing for the Washington Post and other newspapers. He then joined BNA, now part of Bloomberg News, covering health law and the protection of people and animals in medical research. Alex next worked for the McClatchy Company. Based on his work, Alex won a year-long Knight Science Journalism Fellowship to MIT in 2008-2009. He joined the company shortly thereafter. Alex has a newspaper journalism degree from Syracuse (N.Y.) University and a master's degree in medical science -- a physician assistant degree -- from George Washington University. Alex is based in Seattle.
Triple therapy ups response in refractory mantle cell lymphoma
A combination of ibrutinib, lenalidomide, and rituximab produced an overall response rate of 76% at 17.8 months median follow-up among 50 adults with relapsed or refractory mantle cell lymphoma, according to an open-label, single-arm, phase 2 trial.
There were complete responses in 28 patients (56%) and partial responses in 10 (20%). Median progression-free survival was 16 months and median overall survival was 22 months. Similar proportions of patients, with and without TP53 mutations, had overall and complete responses, suggesting that triple therapy might be particularly useful in patients with high-risk genetic features.
“Our results provide preliminary evidence that the triplet combination of ibrutinib, lenalidomide, and rituximab is an active regimen in patients with relapsed or refractory mantle cell lymphoma, and should be evaluated in a prospective randomized controlled trial,” wrote Mats Jerkeman, MD, of Lund University, Sweden, and colleagues. The report was published in The Lancet Haematology.
“Addition of lenalidomide to ibrutinib and rituximab might increase the proportion of patients who have complete remission ... Previous studies reported complete responses in 44% of patients on ibrutinib and rituximab, in 36% of patients on rituximab and lenalidomide, and in 19% of patients on ibrutinib alone,” they wrote.
Treatment was divided into an induction phase of 12 cycles of 28 days with all three drugs and a maintenance phase with ibrutinib and rituximab only, given until disease progression or unacceptable toxicity. All the patients had previously been treated with at least one rituximab-containing regimen.
Janssen and Celgene funded the work. Dr. Jerkeman reported ties to Janssen and Celgene, as well as AbbVie and Gilead.
SOURCE: Jerkeman M et al. Lancet Haematol. 2018 Jan 29. doi: 10.1016/S2352-3026(18)30018-8.
A combination of ibrutinib, lenalidomide, and rituximab produced an overall response rate of 76% at 17.8 months median follow-up among 50 adults with relapsed or refractory mantle cell lymphoma, according to an open-label, single-arm, phase 2 trial.
There were complete responses in 28 patients (56%) and partial responses in 10 (20%). Median progression-free survival was 16 months and median overall survival was 22 months. Similar proportions of patients, with and without TP53 mutations, had overall and complete responses, suggesting that triple therapy might be particularly useful in patients with high-risk genetic features.
“Our results provide preliminary evidence that the triplet combination of ibrutinib, lenalidomide, and rituximab is an active regimen in patients with relapsed or refractory mantle cell lymphoma, and should be evaluated in a prospective randomized controlled trial,” wrote Mats Jerkeman, MD, of Lund University, Sweden, and colleagues. The report was published in The Lancet Haematology.
“Addition of lenalidomide to ibrutinib and rituximab might increase the proportion of patients who have complete remission ... Previous studies reported complete responses in 44% of patients on ibrutinib and rituximab, in 36% of patients on rituximab and lenalidomide, and in 19% of patients on ibrutinib alone,” they wrote.
Treatment was divided into an induction phase of 12 cycles of 28 days with all three drugs and a maintenance phase with ibrutinib and rituximab only, given until disease progression or unacceptable toxicity. All the patients had previously been treated with at least one rituximab-containing regimen.
Janssen and Celgene funded the work. Dr. Jerkeman reported ties to Janssen and Celgene, as well as AbbVie and Gilead.
SOURCE: Jerkeman M et al. Lancet Haematol. 2018 Jan 29. doi: 10.1016/S2352-3026(18)30018-8.
A combination of ibrutinib, lenalidomide, and rituximab produced an overall response rate of 76% at 17.8 months median follow-up among 50 adults with relapsed or refractory mantle cell lymphoma, according to an open-label, single-arm, phase 2 trial.
There were complete responses in 28 patients (56%) and partial responses in 10 (20%). Median progression-free survival was 16 months and median overall survival was 22 months. Similar proportions of patients, with and without TP53 mutations, had overall and complete responses, suggesting that triple therapy might be particularly useful in patients with high-risk genetic features.
“Our results provide preliminary evidence that the triplet combination of ibrutinib, lenalidomide, and rituximab is an active regimen in patients with relapsed or refractory mantle cell lymphoma, and should be evaluated in a prospective randomized controlled trial,” wrote Mats Jerkeman, MD, of Lund University, Sweden, and colleagues. The report was published in The Lancet Haematology.
“Addition of lenalidomide to ibrutinib and rituximab might increase the proportion of patients who have complete remission ... Previous studies reported complete responses in 44% of patients on ibrutinib and rituximab, in 36% of patients on rituximab and lenalidomide, and in 19% of patients on ibrutinib alone,” they wrote.
Treatment was divided into an induction phase of 12 cycles of 28 days with all three drugs and a maintenance phase with ibrutinib and rituximab only, given until disease progression or unacceptable toxicity. All the patients had previously been treated with at least one rituximab-containing regimen.
Janssen and Celgene funded the work. Dr. Jerkeman reported ties to Janssen and Celgene, as well as AbbVie and Gilead.
SOURCE: Jerkeman M et al. Lancet Haematol. 2018 Jan 29. doi: 10.1016/S2352-3026(18)30018-8.
FROM THE LANCET HAEMATOLOGY
Key clinical point:
Major finding: The overall response from for the combination of the three drugs was 76% at 17.8 months median follow-up.
Study details: An open-label, single-arm, phase 2 trial of 50 adults with relapsed/refractory MCL.
Disclosures: Janssen and Celgene funded the work. Dr. Jerkeman reported ties to Janssen and Celgene, as well as AbbVie and Gilead.
Source: Jerkeman M et al. Lancet Haematol. 2018 Jan 29. doi: 10.1016/S2352-3026(18)30018-8.
Menopause accelerates RA functional decline
Rheumatoid arthritis gets worse after menopause, likely because of lower hormone levels, according to a review of 8,189 women in the National Data Bank for Rheumatic Diseases, published recently in Rheumatology.
The investigators compared scores on the Health Assessment Questionnaire (HAQ) between 2,005 premenopausal women with a mean age of 39.7 years; 611 women transitioning through menopause with a mean age of 50.7 years, and 5,573 postmenopausal women with a mean age of 62.3 years. As participants in the data bank, the women completed a questionnaire at regular intervals that included the HAQ, which is a 3-point measure of functional status, with 0 meaning no disability and 3 severe disability. They had all been diagnosed with rheumatoid arthritis prior to menopause.
“Women with RA have better functional status prior to menopause, even after controlling for covariates,” and after menopause, functional decline worsens and accelerates, said investigators led by Elizabeth Mollard, PhD, a nurse practitioner at the University of Nebraska Medical Center, Lincoln. The findings were “robust even after adjustment for other significant factors.”
The team also found that functional decline was less in women who had a longer reproductive life; had ever been pregnant; or had ever used hormone replacement therapy (HRT).
The findings support the notion that hormone exposure plays a role in RA severity, at least in women. It’s well known that RA activity trails off when women are pregnant, but increases after delivery, when hormone levels are returning to baseline. It’s also known that women who go through menopause early are at greater risk for developing RA. Longer reproductive life, pregnancy, and HRT use, meanwhile, all increase women’s hormonal exposure and were protective in the study.
“Women have changes in disease development and progression surrounding reproductive and hormonal events. ... Our results suggest further study on hormonal involvement in functional decline in women with RA,” the investigators said.
Menopausal stage was determined by survey response. Pregnant women and those with hysterectomies were excluded from the study, as were those who went through menopause before the age of 40 years, and those over the age of 55 who had not reported a menstruation cessation date.
There was no external funding for the work. Dr. Mollard had no disclosures.
SOURCE: Mollard E et. al. Rheumatology. 2018 Jan 29. doi: 10.1093/rheumatology/kex526
Rheumatoid arthritis gets worse after menopause, likely because of lower hormone levels, according to a review of 8,189 women in the National Data Bank for Rheumatic Diseases, published recently in Rheumatology.
The investigators compared scores on the Health Assessment Questionnaire (HAQ) between 2,005 premenopausal women with a mean age of 39.7 years; 611 women transitioning through menopause with a mean age of 50.7 years, and 5,573 postmenopausal women with a mean age of 62.3 years. As participants in the data bank, the women completed a questionnaire at regular intervals that included the HAQ, which is a 3-point measure of functional status, with 0 meaning no disability and 3 severe disability. They had all been diagnosed with rheumatoid arthritis prior to menopause.
“Women with RA have better functional status prior to menopause, even after controlling for covariates,” and after menopause, functional decline worsens and accelerates, said investigators led by Elizabeth Mollard, PhD, a nurse practitioner at the University of Nebraska Medical Center, Lincoln. The findings were “robust even after adjustment for other significant factors.”
The team also found that functional decline was less in women who had a longer reproductive life; had ever been pregnant; or had ever used hormone replacement therapy (HRT).
The findings support the notion that hormone exposure plays a role in RA severity, at least in women. It’s well known that RA activity trails off when women are pregnant, but increases after delivery, when hormone levels are returning to baseline. It’s also known that women who go through menopause early are at greater risk for developing RA. Longer reproductive life, pregnancy, and HRT use, meanwhile, all increase women’s hormonal exposure and were protective in the study.
“Women have changes in disease development and progression surrounding reproductive and hormonal events. ... Our results suggest further study on hormonal involvement in functional decline in women with RA,” the investigators said.
Menopausal stage was determined by survey response. Pregnant women and those with hysterectomies were excluded from the study, as were those who went through menopause before the age of 40 years, and those over the age of 55 who had not reported a menstruation cessation date.
There was no external funding for the work. Dr. Mollard had no disclosures.
SOURCE: Mollard E et. al. Rheumatology. 2018 Jan 29. doi: 10.1093/rheumatology/kex526
Rheumatoid arthritis gets worse after menopause, likely because of lower hormone levels, according to a review of 8,189 women in the National Data Bank for Rheumatic Diseases, published recently in Rheumatology.
The investigators compared scores on the Health Assessment Questionnaire (HAQ) between 2,005 premenopausal women with a mean age of 39.7 years; 611 women transitioning through menopause with a mean age of 50.7 years, and 5,573 postmenopausal women with a mean age of 62.3 years. As participants in the data bank, the women completed a questionnaire at regular intervals that included the HAQ, which is a 3-point measure of functional status, with 0 meaning no disability and 3 severe disability. They had all been diagnosed with rheumatoid arthritis prior to menopause.
“Women with RA have better functional status prior to menopause, even after controlling for covariates,” and after menopause, functional decline worsens and accelerates, said investigators led by Elizabeth Mollard, PhD, a nurse practitioner at the University of Nebraska Medical Center, Lincoln. The findings were “robust even after adjustment for other significant factors.”
The team also found that functional decline was less in women who had a longer reproductive life; had ever been pregnant; or had ever used hormone replacement therapy (HRT).
The findings support the notion that hormone exposure plays a role in RA severity, at least in women. It’s well known that RA activity trails off when women are pregnant, but increases after delivery, when hormone levels are returning to baseline. It’s also known that women who go through menopause early are at greater risk for developing RA. Longer reproductive life, pregnancy, and HRT use, meanwhile, all increase women’s hormonal exposure and were protective in the study.
“Women have changes in disease development and progression surrounding reproductive and hormonal events. ... Our results suggest further study on hormonal involvement in functional decline in women with RA,” the investigators said.
Menopausal stage was determined by survey response. Pregnant women and those with hysterectomies were excluded from the study, as were those who went through menopause before the age of 40 years, and those over the age of 55 who had not reported a menstruation cessation date.
There was no external funding for the work. Dr. Mollard had no disclosures.
SOURCE: Mollard E et. al. Rheumatology. 2018 Jan 29. doi: 10.1093/rheumatology/kex526
FROM RHEUMATOLOGY
Key clinical point:
Major finding: HAQ scores were 0.68 points higher in postmenopausal women, compared with premenopausal women of the same age.
Study details: Review of 8,189 women in the National Data Bank for Rheumatic Diseases.
Disclosures: There was no external funding for the work. The lead investigator had no disclosures.
Source: Mollard E et. al. Rheumatology. 2018 Jan 29. doi: 10.1093/rheumatology/kex526
Cold snare polypectomy works for large SSPs
Piecemeal cold snare polypectomy was effective and safe for sessile, serrated colon polyps larger than 10 mm in a series from the University of Sydney.
Endoscopic mucosal resection (EMR) is the usual choice for lesions that size, but it comes with the risks of electrocautery, including delayed bleeding in perhaps 10% of patients. The Sydney investigators took a gamble to see if cold snare polypectomy, a technique usually reserved for smaller sessile, serrated polyps (SSPs), worked as well as EMR for larger ones, but without the risks. That seemed to be the case in their pilot study; . The median lesion size was 15 mm, and ranged from 10 to 35 mm. The procedure took a median of 4.5 minutes, much quicker than EMR, and didn’t require submucosal lifting injections. There were no perforations, deep injuries to the colon wall, or intraprocedural bleeding. There were no significant adverse events at 2 weeks, including no delayed bleeding or postpolypectomy syndrome.
Most importantly, there was no evidence of recurrence in the 15 lesions that had surveillance colonoscopy by press time at a median of 6 months. “We suggest, cautiously, that this is related to the wide margin of [normal] tissue [2-3 mm] removed during the initial procedures and the meticulous examination of the defect and margin for residual tissue,” said investigators led by David Tate, MD, of the University of Sydney.
“We have demonstrated the safety and feasibility of pCSP in a tertiary referral cohort of patients referred for the removal of large SSPs. There is potential for pCSP to become the standard of care for nondysplastic SSPs. This could reduce the burden of removing SSPs on patients and health care systems, particularly by avoidance of clinically significant postendoscopic bleeding,” the investigators wrote.
“Because SSPs commonly lack high-grade histology, have a long dwell time prior to developing dysplasia, and recur less frequently than conventional adenomas, they represent comparatively indolent disease and are excellent targets for piecemeal mucosal resection,” the researchers said.
Resection was performed with a stiff thin-wire snare (TeleMed 10-mm hexagonal, TeleMed Systems). “A thin-wire snare is paramount, both to aid tissue capture and to create a crisp resection margin that can be examined for residual serrated tissue. Each progressive resection utilizes this margin to ensure snare purchase and avoid tissue islands,” the researchers said.
It took a median of three cuts to remove an SSP; complete resection was achieved in all cases.
The team used high-definition endoscopic imaging to assess the lesion and margins before the procedure, and again to assess the defect margin to ensure the absence of residual serrated tissue. “We did not use submucosal injection or a chromic dye. While we acknowledge their utility for delineation of serrated tissue, we found that high-definition imaging was sufficient for this purpose and for detecting residual serrated tissue at the resection margin,” they said.
Patients were a mean age of 69 years old; almost 80% were women. About two-thirds of the lesions were proximal to the transverse colon.
The work was supported by the Cancer Institute New South Wales. The investigators had no conflicts of interest.
[email protected]
SOURCE: Tate DJ, et al. Endoscopy. 2017 Nov 23. doi: 10.1055/s-0043-121219.
Piecemeal cold snare polypectomy was effective and safe for sessile, serrated colon polyps larger than 10 mm in a series from the University of Sydney.
Endoscopic mucosal resection (EMR) is the usual choice for lesions that size, but it comes with the risks of electrocautery, including delayed bleeding in perhaps 10% of patients. The Sydney investigators took a gamble to see if cold snare polypectomy, a technique usually reserved for smaller sessile, serrated polyps (SSPs), worked as well as EMR for larger ones, but without the risks. That seemed to be the case in their pilot study; . The median lesion size was 15 mm, and ranged from 10 to 35 mm. The procedure took a median of 4.5 minutes, much quicker than EMR, and didn’t require submucosal lifting injections. There were no perforations, deep injuries to the colon wall, or intraprocedural bleeding. There were no significant adverse events at 2 weeks, including no delayed bleeding or postpolypectomy syndrome.
Most importantly, there was no evidence of recurrence in the 15 lesions that had surveillance colonoscopy by press time at a median of 6 months. “We suggest, cautiously, that this is related to the wide margin of [normal] tissue [2-3 mm] removed during the initial procedures and the meticulous examination of the defect and margin for residual tissue,” said investigators led by David Tate, MD, of the University of Sydney.
“We have demonstrated the safety and feasibility of pCSP in a tertiary referral cohort of patients referred for the removal of large SSPs. There is potential for pCSP to become the standard of care for nondysplastic SSPs. This could reduce the burden of removing SSPs on patients and health care systems, particularly by avoidance of clinically significant postendoscopic bleeding,” the investigators wrote.
“Because SSPs commonly lack high-grade histology, have a long dwell time prior to developing dysplasia, and recur less frequently than conventional adenomas, they represent comparatively indolent disease and are excellent targets for piecemeal mucosal resection,” the researchers said.
Resection was performed with a stiff thin-wire snare (TeleMed 10-mm hexagonal, TeleMed Systems). “A thin-wire snare is paramount, both to aid tissue capture and to create a crisp resection margin that can be examined for residual serrated tissue. Each progressive resection utilizes this margin to ensure snare purchase and avoid tissue islands,” the researchers said.
It took a median of three cuts to remove an SSP; complete resection was achieved in all cases.
The team used high-definition endoscopic imaging to assess the lesion and margins before the procedure, and again to assess the defect margin to ensure the absence of residual serrated tissue. “We did not use submucosal injection or a chromic dye. While we acknowledge their utility for delineation of serrated tissue, we found that high-definition imaging was sufficient for this purpose and for detecting residual serrated tissue at the resection margin,” they said.
Patients were a mean age of 69 years old; almost 80% were women. About two-thirds of the lesions were proximal to the transverse colon.
The work was supported by the Cancer Institute New South Wales. The investigators had no conflicts of interest.
[email protected]
SOURCE: Tate DJ, et al. Endoscopy. 2017 Nov 23. doi: 10.1055/s-0043-121219.
Piecemeal cold snare polypectomy was effective and safe for sessile, serrated colon polyps larger than 10 mm in a series from the University of Sydney.
Endoscopic mucosal resection (EMR) is the usual choice for lesions that size, but it comes with the risks of electrocautery, including delayed bleeding in perhaps 10% of patients. The Sydney investigators took a gamble to see if cold snare polypectomy, a technique usually reserved for smaller sessile, serrated polyps (SSPs), worked as well as EMR for larger ones, but without the risks. That seemed to be the case in their pilot study; . The median lesion size was 15 mm, and ranged from 10 to 35 mm. The procedure took a median of 4.5 minutes, much quicker than EMR, and didn’t require submucosal lifting injections. There were no perforations, deep injuries to the colon wall, or intraprocedural bleeding. There were no significant adverse events at 2 weeks, including no delayed bleeding or postpolypectomy syndrome.
Most importantly, there was no evidence of recurrence in the 15 lesions that had surveillance colonoscopy by press time at a median of 6 months. “We suggest, cautiously, that this is related to the wide margin of [normal] tissue [2-3 mm] removed during the initial procedures and the meticulous examination of the defect and margin for residual tissue,” said investigators led by David Tate, MD, of the University of Sydney.
“We have demonstrated the safety and feasibility of pCSP in a tertiary referral cohort of patients referred for the removal of large SSPs. There is potential for pCSP to become the standard of care for nondysplastic SSPs. This could reduce the burden of removing SSPs on patients and health care systems, particularly by avoidance of clinically significant postendoscopic bleeding,” the investigators wrote.
“Because SSPs commonly lack high-grade histology, have a long dwell time prior to developing dysplasia, and recur less frequently than conventional adenomas, they represent comparatively indolent disease and are excellent targets for piecemeal mucosal resection,” the researchers said.
Resection was performed with a stiff thin-wire snare (TeleMed 10-mm hexagonal, TeleMed Systems). “A thin-wire snare is paramount, both to aid tissue capture and to create a crisp resection margin that can be examined for residual serrated tissue. Each progressive resection utilizes this margin to ensure snare purchase and avoid tissue islands,” the researchers said.
It took a median of three cuts to remove an SSP; complete resection was achieved in all cases.
The team used high-definition endoscopic imaging to assess the lesion and margins before the procedure, and again to assess the defect margin to ensure the absence of residual serrated tissue. “We did not use submucosal injection or a chromic dye. While we acknowledge their utility for delineation of serrated tissue, we found that high-definition imaging was sufficient for this purpose and for detecting residual serrated tissue at the resection margin,” they said.
Patients were a mean age of 69 years old; almost 80% were women. About two-thirds of the lesions were proximal to the transverse colon.
The work was supported by the Cancer Institute New South Wales. The investigators had no conflicts of interest.
[email protected]
SOURCE: Tate DJ, et al. Endoscopy. 2017 Nov 23. doi: 10.1055/s-0043-121219.
FROM ENDOSCOPY
Key clinical point: Piecemeal cold snare polypectomy is effective and safe for sessile, serrated colon polyps larger than 10 mm.
Major finding: There was no delayed bleeding, and no evidence of recurrence, in 15 patients who had surveillance colonoscopies at 6 months.
Study details: A case series of 34 patients.
Disclosures: The work was supported by the Cancer Institute New South Wales, Australia. The investigators had no conflicts of interest.
Source: Tate DJ et al. Endoscopy. 2017 Nov 23. doi: 10.1055/s-0043-121219
Turmeric-, frankincense-derived supplement shows OA benefit
A combination of curcumin extracted from the turmeric rhizome and boswellic acid extracted from Indian frankincense root beat placebo for reducing pain-related symptoms from knee osteoarthritis in a 12-week clinical trial from Armenia with 201 patients 40-70 years old.
The combination (Curamin) also beat a standalone curcumin preparation (CuraMed), according to a report in BMC Complementary and Alternative Medicine.
It appears that combining the two “increases the efficacy of treatment of OA presumably due to synergistic effects of curcumin and boswellic acid”; it’s also possible that boswellic acid increases curcumin bioavailability, said investigators led by Armine Haroyan, PhD, head of rheumatology at Erebuni Medical Center in Yerevan, Armenia.
The subjects were randomized evenly to the combination, curcumin alone, or placebo, all in 500-mg capsules taken three times daily. They had been diagnosed with degenerative hypertrophic OA of knee bone joints.
At the end of 12 weeks, patients on the combination outperformed those on placebo in physical performance tests and joint pain scores; curcumin outperformed placebo in only a few of the physical tests.
For instance, patients on the combination were a mean of 2.03 seconds quicker than baseline in a stair-climbing exercise by the end of the study, versus 0.22 seconds in the placebo group and 1.66 seconds in the curcumin group. Combination patients had a mean 7.38-point improvement on the Western Ontario and McMaster Universities Osteoarthritis Index, versus 2.26 points in the placebo arm and 6.34 points in the curcumin group. The differences versus placebo were statistically significant for the combination, but not for stand-alone curcumin.
The treatments were well tolerated, with only a few patients in each arm reporting nausea, gastroesophageal reflux, and similar problems.
The work was funded in part by EuroPharma USA, maker of the supplements. The authors said they had no competing interests.
SOURCE: Haroyan A et al. BMC Complement Altern Med. 2018 Jan 9;18:7. doi: 10.1186/s12906-017-2062-z
A combination of curcumin extracted from the turmeric rhizome and boswellic acid extracted from Indian frankincense root beat placebo for reducing pain-related symptoms from knee osteoarthritis in a 12-week clinical trial from Armenia with 201 patients 40-70 years old.
The combination (Curamin) also beat a standalone curcumin preparation (CuraMed), according to a report in BMC Complementary and Alternative Medicine.
It appears that combining the two “increases the efficacy of treatment of OA presumably due to synergistic effects of curcumin and boswellic acid”; it’s also possible that boswellic acid increases curcumin bioavailability, said investigators led by Armine Haroyan, PhD, head of rheumatology at Erebuni Medical Center in Yerevan, Armenia.
The subjects were randomized evenly to the combination, curcumin alone, or placebo, all in 500-mg capsules taken three times daily. They had been diagnosed with degenerative hypertrophic OA of knee bone joints.
At the end of 12 weeks, patients on the combination outperformed those on placebo in physical performance tests and joint pain scores; curcumin outperformed placebo in only a few of the physical tests.
For instance, patients on the combination were a mean of 2.03 seconds quicker than baseline in a stair-climbing exercise by the end of the study, versus 0.22 seconds in the placebo group and 1.66 seconds in the curcumin group. Combination patients had a mean 7.38-point improvement on the Western Ontario and McMaster Universities Osteoarthritis Index, versus 2.26 points in the placebo arm and 6.34 points in the curcumin group. The differences versus placebo were statistically significant for the combination, but not for stand-alone curcumin.
The treatments were well tolerated, with only a few patients in each arm reporting nausea, gastroesophageal reflux, and similar problems.
The work was funded in part by EuroPharma USA, maker of the supplements. The authors said they had no competing interests.
SOURCE: Haroyan A et al. BMC Complement Altern Med. 2018 Jan 9;18:7. doi: 10.1186/s12906-017-2062-z
A combination of curcumin extracted from the turmeric rhizome and boswellic acid extracted from Indian frankincense root beat placebo for reducing pain-related symptoms from knee osteoarthritis in a 12-week clinical trial from Armenia with 201 patients 40-70 years old.
The combination (Curamin) also beat a standalone curcumin preparation (CuraMed), according to a report in BMC Complementary and Alternative Medicine.
It appears that combining the two “increases the efficacy of treatment of OA presumably due to synergistic effects of curcumin and boswellic acid”; it’s also possible that boswellic acid increases curcumin bioavailability, said investigators led by Armine Haroyan, PhD, head of rheumatology at Erebuni Medical Center in Yerevan, Armenia.
The subjects were randomized evenly to the combination, curcumin alone, or placebo, all in 500-mg capsules taken three times daily. They had been diagnosed with degenerative hypertrophic OA of knee bone joints.
At the end of 12 weeks, patients on the combination outperformed those on placebo in physical performance tests and joint pain scores; curcumin outperformed placebo in only a few of the physical tests.
For instance, patients on the combination were a mean of 2.03 seconds quicker than baseline in a stair-climbing exercise by the end of the study, versus 0.22 seconds in the placebo group and 1.66 seconds in the curcumin group. Combination patients had a mean 7.38-point improvement on the Western Ontario and McMaster Universities Osteoarthritis Index, versus 2.26 points in the placebo arm and 6.34 points in the curcumin group. The differences versus placebo were statistically significant for the combination, but not for stand-alone curcumin.
The treatments were well tolerated, with only a few patients in each arm reporting nausea, gastroesophageal reflux, and similar problems.
The work was funded in part by EuroPharma USA, maker of the supplements. The authors said they had no competing interests.
SOURCE: Haroyan A et al. BMC Complement Altern Med. 2018 Jan 9;18:7. doi: 10.1186/s12906-017-2062-z
FROM BMC COMPLEMENTARY AND ALTERNATIVE MEDICINE
Adacel Tdap effective throughout third trimester vaccination window
, according to a prospective cohort study published in Obstetrics and Gynecology.
Timing does make a difference with the other Tdap option in pregnancy, Boostrix; pertussis protection is stronger if women receive it early in the third trimester. The investigators wanted to see if that were true as well with Adacel.
They compared pertussis antibody concentrations in maternal venous serum and umbilical cord arterial serum at the time of delivery in 52 women vaccinated from 27 to 30 6/7 weeks of gestation, and compared the results with 36 women vaccinated from 31 to 35 6/7 weeks.
Pertussis antibody concentrations did not vary by gestational age. Maternal serum pertussis toxin IgG concentrations were the same in both groups (48.6 enzyme-linked immunoassay [ELISA] units/mL), and there were no statistically significant differences in cord serum pertussis toxin IgG concentrations (92.1 ELISA units/mL in the early group, compared with 90.7 in the later group; P = .95) or cord serum pertactin IgG concentrations (798 international units/mL in the early group, versus 730 in the later group; P = .73).
Overall, cord serum pertussis toxin IgG concentrations were approximately twice maternal serum pertussis toxin IgG concentrations (91.6 vs. 48.6 ELISA units/mL; P less than .01). Cord serum pertussis toxin IgG concentrations were in the protective range (greater than 10 ELISA units/mL) in 87% of the women vaccinated from 27 to 30 6/7 weeks, and in 97% vaccinated from 31 to 35 6/7 weeks (P = .13).
Maternal vaccination in the third trimester against pertussis “was associated with a high percentage of newborns with antibody concentrations conferring protection,” said investigators led by Cynthia Abraham, MD, an ob.gyn. at Mount Sinai Hospital, New York. “We found no significant difference across the period of 27-36 weeks of gestation with respect to immunogenicity with Adacel use.”
Maternal Tdap vaccination is done to protect infants in their first 2 months of life, before they start their DTaP series. The Centers for Disease Control and Prevention recommends vaccination between 27 and 36 weeks of gestation.
It’s unclear why it doesn’t matter when within that window women receive Adacel, but protection with Boostrix if Boostrix is administered early on in the trimester.
Boostrix differs from Adacel in antigen composition and in the method of pertussis toxin detoxification. Boostrix is detoxified with formaldehyde and glutaraldehyde. Adacel is detoxified only with formaldehyde.
“Double detoxification may cause differences in immunogenicity as antigenic epitopes are further modified, perhaps providing an explanation for the difference in results between the vaccines,” the investigators said.
Women in the early group received Adacel at a mean gestational age of 29.1 weeks, versus 32.9 weeks in the later group. The women were a mean age of about 29 years; 56% were Hispanic, 23% white, and the rest were about equally split between black and Asian women.
No funding source was reported. The authors did not have any conflicts of interest.
SOURCE: Abraham C et al. Obstet Gynecol. 2018 Feb;131(2):364-9.
, according to a prospective cohort study published in Obstetrics and Gynecology.
Timing does make a difference with the other Tdap option in pregnancy, Boostrix; pertussis protection is stronger if women receive it early in the third trimester. The investigators wanted to see if that were true as well with Adacel.
They compared pertussis antibody concentrations in maternal venous serum and umbilical cord arterial serum at the time of delivery in 52 women vaccinated from 27 to 30 6/7 weeks of gestation, and compared the results with 36 women vaccinated from 31 to 35 6/7 weeks.
Pertussis antibody concentrations did not vary by gestational age. Maternal serum pertussis toxin IgG concentrations were the same in both groups (48.6 enzyme-linked immunoassay [ELISA] units/mL), and there were no statistically significant differences in cord serum pertussis toxin IgG concentrations (92.1 ELISA units/mL in the early group, compared with 90.7 in the later group; P = .95) or cord serum pertactin IgG concentrations (798 international units/mL in the early group, versus 730 in the later group; P = .73).
Overall, cord serum pertussis toxin IgG concentrations were approximately twice maternal serum pertussis toxin IgG concentrations (91.6 vs. 48.6 ELISA units/mL; P less than .01). Cord serum pertussis toxin IgG concentrations were in the protective range (greater than 10 ELISA units/mL) in 87% of the women vaccinated from 27 to 30 6/7 weeks, and in 97% vaccinated from 31 to 35 6/7 weeks (P = .13).
Maternal vaccination in the third trimester against pertussis “was associated with a high percentage of newborns with antibody concentrations conferring protection,” said investigators led by Cynthia Abraham, MD, an ob.gyn. at Mount Sinai Hospital, New York. “We found no significant difference across the period of 27-36 weeks of gestation with respect to immunogenicity with Adacel use.”
Maternal Tdap vaccination is done to protect infants in their first 2 months of life, before they start their DTaP series. The Centers for Disease Control and Prevention recommends vaccination between 27 and 36 weeks of gestation.
It’s unclear why it doesn’t matter when within that window women receive Adacel, but protection with Boostrix if Boostrix is administered early on in the trimester.
Boostrix differs from Adacel in antigen composition and in the method of pertussis toxin detoxification. Boostrix is detoxified with formaldehyde and glutaraldehyde. Adacel is detoxified only with formaldehyde.
“Double detoxification may cause differences in immunogenicity as antigenic epitopes are further modified, perhaps providing an explanation for the difference in results between the vaccines,” the investigators said.
Women in the early group received Adacel at a mean gestational age of 29.1 weeks, versus 32.9 weeks in the later group. The women were a mean age of about 29 years; 56% were Hispanic, 23% white, and the rest were about equally split between black and Asian women.
No funding source was reported. The authors did not have any conflicts of interest.
SOURCE: Abraham C et al. Obstet Gynecol. 2018 Feb;131(2):364-9.
, according to a prospective cohort study published in Obstetrics and Gynecology.
Timing does make a difference with the other Tdap option in pregnancy, Boostrix; pertussis protection is stronger if women receive it early in the third trimester. The investigators wanted to see if that were true as well with Adacel.
They compared pertussis antibody concentrations in maternal venous serum and umbilical cord arterial serum at the time of delivery in 52 women vaccinated from 27 to 30 6/7 weeks of gestation, and compared the results with 36 women vaccinated from 31 to 35 6/7 weeks.
Pertussis antibody concentrations did not vary by gestational age. Maternal serum pertussis toxin IgG concentrations were the same in both groups (48.6 enzyme-linked immunoassay [ELISA] units/mL), and there were no statistically significant differences in cord serum pertussis toxin IgG concentrations (92.1 ELISA units/mL in the early group, compared with 90.7 in the later group; P = .95) or cord serum pertactin IgG concentrations (798 international units/mL in the early group, versus 730 in the later group; P = .73).
Overall, cord serum pertussis toxin IgG concentrations were approximately twice maternal serum pertussis toxin IgG concentrations (91.6 vs. 48.6 ELISA units/mL; P less than .01). Cord serum pertussis toxin IgG concentrations were in the protective range (greater than 10 ELISA units/mL) in 87% of the women vaccinated from 27 to 30 6/7 weeks, and in 97% vaccinated from 31 to 35 6/7 weeks (P = .13).
Maternal vaccination in the third trimester against pertussis “was associated with a high percentage of newborns with antibody concentrations conferring protection,” said investigators led by Cynthia Abraham, MD, an ob.gyn. at Mount Sinai Hospital, New York. “We found no significant difference across the period of 27-36 weeks of gestation with respect to immunogenicity with Adacel use.”
Maternal Tdap vaccination is done to protect infants in their first 2 months of life, before they start their DTaP series. The Centers for Disease Control and Prevention recommends vaccination between 27 and 36 weeks of gestation.
It’s unclear why it doesn’t matter when within that window women receive Adacel, but protection with Boostrix if Boostrix is administered early on in the trimester.
Boostrix differs from Adacel in antigen composition and in the method of pertussis toxin detoxification. Boostrix is detoxified with formaldehyde and glutaraldehyde. Adacel is detoxified only with formaldehyde.
“Double detoxification may cause differences in immunogenicity as antigenic epitopes are further modified, perhaps providing an explanation for the difference in results between the vaccines,” the investigators said.
Women in the early group received Adacel at a mean gestational age of 29.1 weeks, versus 32.9 weeks in the later group. The women were a mean age of about 29 years; 56% were Hispanic, 23% white, and the rest were about equally split between black and Asian women.
No funding source was reported. The authors did not have any conflicts of interest.
SOURCE: Abraham C et al. Obstet Gynecol. 2018 Feb;131(2):364-9.
FROM OBSTETRICS AND GYNECOLOGY
Key clinical point: Unlike Boostrix, pertussis protection is the same whether pregnant women receive Adacel Tdap vaccine early in the third trimester or in the middle.
Major finding: There were no statistically significant differences in cord serum pertussis toxin IgG concentrations (92.1 ELISA units/mL in the early group, versus 90.7 in the later group, P = .95).
Study details: A prospective cohort study involving 88 women.
Disclosures: No study sponsor was reported. The authors had no disclosures.
Source: Abraham C et al. Obstet Gynecol. 2018 Feb;131(2):364-9.
APOE4 may drive tau deposition in Alzheimer’s
SAN DIEGO – The apolipoprotein E e4 allele is well known for its association with amyloid deposition in Alzheimer’s disease, but now it also appears to help drive the other key pathological process in the disease: deposition of hyperphosphorylated tau protein.
That’s according to the authors of a PET neuroimaging study presented at the annual meeting of the American Neurological Association.
The finding suggests a pathophysiologic mechanism for Alzheimer’s disease cases that predominantly affect memory.
The team then compared the results with uptake of the radiotracers in 71 cognitively normal control subjects who were a mean age of 79 years, 23 of whom (32%) were APOE4 carriers.
APOE4 was associated with higher cortical amyloid in the controls, but not tau deposition. Although AV1451 uptake in the temporal lobe was increased in e4 carriers, the effect was not statistically significant after controlling for PiB uptake.
“We saw an APOE4 effect on amyloid but not on tau in normal people,” said senior investigator Gil Rabinovici, MD, a neurologist and professor of memory and aging at the University of California, San Francisco.
All the AD patients had PiB uptake, with no difference in uptake between e4 carriers and noncarriers. However, APOE4 carriers had higher AV1451 uptake in their anterior medial temporal lobes (MTL), a difference that remained unchanged after controlling for PiB.
Carriers of the e4 allele who had AV1451 uptake in their MTLs had a harder time than other AD patients on a test in which they were asked to recall a series of words after a 10-minute break (California Verbal Learning Test), but they did not perform worse on other cognitive measures.
“In cognitively normal individuals, the effect of APOE4 on tau pathology seems to be mediated by the effect of e4 on Ab [amyloid-beta] deposition,” the investigators noted. “However, when assessing amyloid-positive symptomatic AD patients, APOE4 was associated with increased AV1451 binding in the MTL.
“This suggests that, in addition to its effect on Ab pathology, APOE4 might influence the topographical distribution of tau pathology and, potentially, the cognitive symptoms in patients,” the researchers concluded.
“We are very interested in heterogeneity in Alzheimer’s disease – age of onset, rate of progression, which brain areas are affected,” Dr. Rabinovici said. “This study is beginning to dig into some of the factors that might explain that; APOE4 is one potential modifier. It may have a direct effect on tau phosphorylation, and it changes where tau is located in the setting of Alzheimer’s disease.”
The finding of increased MTL tau in APOE4-positive Alzheimer’s patients helps explain why patients who carry the allele tend to have more memory problems, he said, while AD patients who don’t carry the allele tend to have more of a cortical-predominant presentation, with more visual-spatial and language problems.
“I think it’s very likely that APOE4-related disease may be driven by a different mechanism than APOE4-negative disease,” Dr. Rabinovici said. “In the future, APOE4-positive or APOE4-negative might be used to stratify therapy and the measurements used for disease progression. APOE4 itself may be an interesting therapeutic target because it has downstream effects on amyloid and tau.”
Meanwhile, there’s just not a lot of tau pathology in cognitively normal people, which is likely why the effect didn’t show up in the controls, noted lead investigator Renaud La Joie, PhD, a neuroimaging researcher at UCSF.
The work was funded in part by the National Institutes of Health. Avid Pharmaceuticals provided the AV1451. Dr. Rabinovici is an advisor for Genentech, Merck, and Roche, and has research support from Avid Radiopharmaceuticals and Eli Lilly, among others.
SOURCE: La Joie R, et al. Abstract M183, American Neurological Association 2017 annual meeting.
SAN DIEGO – The apolipoprotein E e4 allele is well known for its association with amyloid deposition in Alzheimer’s disease, but now it also appears to help drive the other key pathological process in the disease: deposition of hyperphosphorylated tau protein.
That’s according to the authors of a PET neuroimaging study presented at the annual meeting of the American Neurological Association.
The finding suggests a pathophysiologic mechanism for Alzheimer’s disease cases that predominantly affect memory.
The team then compared the results with uptake of the radiotracers in 71 cognitively normal control subjects who were a mean age of 79 years, 23 of whom (32%) were APOE4 carriers.
APOE4 was associated with higher cortical amyloid in the controls, but not tau deposition. Although AV1451 uptake in the temporal lobe was increased in e4 carriers, the effect was not statistically significant after controlling for PiB uptake.
“We saw an APOE4 effect on amyloid but not on tau in normal people,” said senior investigator Gil Rabinovici, MD, a neurologist and professor of memory and aging at the University of California, San Francisco.
All the AD patients had PiB uptake, with no difference in uptake between e4 carriers and noncarriers. However, APOE4 carriers had higher AV1451 uptake in their anterior medial temporal lobes (MTL), a difference that remained unchanged after controlling for PiB.
Carriers of the e4 allele who had AV1451 uptake in their MTLs had a harder time than other AD patients on a test in which they were asked to recall a series of words after a 10-minute break (California Verbal Learning Test), but they did not perform worse on other cognitive measures.
“In cognitively normal individuals, the effect of APOE4 on tau pathology seems to be mediated by the effect of e4 on Ab [amyloid-beta] deposition,” the investigators noted. “However, when assessing amyloid-positive symptomatic AD patients, APOE4 was associated with increased AV1451 binding in the MTL.
“This suggests that, in addition to its effect on Ab pathology, APOE4 might influence the topographical distribution of tau pathology and, potentially, the cognitive symptoms in patients,” the researchers concluded.
“We are very interested in heterogeneity in Alzheimer’s disease – age of onset, rate of progression, which brain areas are affected,” Dr. Rabinovici said. “This study is beginning to dig into some of the factors that might explain that; APOE4 is one potential modifier. It may have a direct effect on tau phosphorylation, and it changes where tau is located in the setting of Alzheimer’s disease.”
The finding of increased MTL tau in APOE4-positive Alzheimer’s patients helps explain why patients who carry the allele tend to have more memory problems, he said, while AD patients who don’t carry the allele tend to have more of a cortical-predominant presentation, with more visual-spatial and language problems.
“I think it’s very likely that APOE4-related disease may be driven by a different mechanism than APOE4-negative disease,” Dr. Rabinovici said. “In the future, APOE4-positive or APOE4-negative might be used to stratify therapy and the measurements used for disease progression. APOE4 itself may be an interesting therapeutic target because it has downstream effects on amyloid and tau.”
Meanwhile, there’s just not a lot of tau pathology in cognitively normal people, which is likely why the effect didn’t show up in the controls, noted lead investigator Renaud La Joie, PhD, a neuroimaging researcher at UCSF.
The work was funded in part by the National Institutes of Health. Avid Pharmaceuticals provided the AV1451. Dr. Rabinovici is an advisor for Genentech, Merck, and Roche, and has research support from Avid Radiopharmaceuticals and Eli Lilly, among others.
SOURCE: La Joie R, et al. Abstract M183, American Neurological Association 2017 annual meeting.
SAN DIEGO – The apolipoprotein E e4 allele is well known for its association with amyloid deposition in Alzheimer’s disease, but now it also appears to help drive the other key pathological process in the disease: deposition of hyperphosphorylated tau protein.
That’s according to the authors of a PET neuroimaging study presented at the annual meeting of the American Neurological Association.
The finding suggests a pathophysiologic mechanism for Alzheimer’s disease cases that predominantly affect memory.
The team then compared the results with uptake of the radiotracers in 71 cognitively normal control subjects who were a mean age of 79 years, 23 of whom (32%) were APOE4 carriers.
APOE4 was associated with higher cortical amyloid in the controls, but not tau deposition. Although AV1451 uptake in the temporal lobe was increased in e4 carriers, the effect was not statistically significant after controlling for PiB uptake.
“We saw an APOE4 effect on amyloid but not on tau in normal people,” said senior investigator Gil Rabinovici, MD, a neurologist and professor of memory and aging at the University of California, San Francisco.
All the AD patients had PiB uptake, with no difference in uptake between e4 carriers and noncarriers. However, APOE4 carriers had higher AV1451 uptake in their anterior medial temporal lobes (MTL), a difference that remained unchanged after controlling for PiB.
Carriers of the e4 allele who had AV1451 uptake in their MTLs had a harder time than other AD patients on a test in which they were asked to recall a series of words after a 10-minute break (California Verbal Learning Test), but they did not perform worse on other cognitive measures.
“In cognitively normal individuals, the effect of APOE4 on tau pathology seems to be mediated by the effect of e4 on Ab [amyloid-beta] deposition,” the investigators noted. “However, when assessing amyloid-positive symptomatic AD patients, APOE4 was associated with increased AV1451 binding in the MTL.
“This suggests that, in addition to its effect on Ab pathology, APOE4 might influence the topographical distribution of tau pathology and, potentially, the cognitive symptoms in patients,” the researchers concluded.
“We are very interested in heterogeneity in Alzheimer’s disease – age of onset, rate of progression, which brain areas are affected,” Dr. Rabinovici said. “This study is beginning to dig into some of the factors that might explain that; APOE4 is one potential modifier. It may have a direct effect on tau phosphorylation, and it changes where tau is located in the setting of Alzheimer’s disease.”
The finding of increased MTL tau in APOE4-positive Alzheimer’s patients helps explain why patients who carry the allele tend to have more memory problems, he said, while AD patients who don’t carry the allele tend to have more of a cortical-predominant presentation, with more visual-spatial and language problems.
“I think it’s very likely that APOE4-related disease may be driven by a different mechanism than APOE4-negative disease,” Dr. Rabinovici said. “In the future, APOE4-positive or APOE4-negative might be used to stratify therapy and the measurements used for disease progression. APOE4 itself may be an interesting therapeutic target because it has downstream effects on amyloid and tau.”
Meanwhile, there’s just not a lot of tau pathology in cognitively normal people, which is likely why the effect didn’t show up in the controls, noted lead investigator Renaud La Joie, PhD, a neuroimaging researcher at UCSF.
The work was funded in part by the National Institutes of Health. Avid Pharmaceuticals provided the AV1451. Dr. Rabinovici is an advisor for Genentech, Merck, and Roche, and has research support from Avid Radiopharmaceuticals and Eli Lilly, among others.
SOURCE: La Joie R, et al. Abstract M183, American Neurological Association 2017 annual meeting.
REPORTING FROM ANA 2017
Key clinical point:
Major finding: APOE4 carriers had higher AV1451-uptake in their anterior medial temporal lobes, a difference that remained unchanged after controlling for Pittsburgh compound B.
Study details: An analysis of radiotracer PET imaging in 67 Alzheimer’s disease patients and 71 controls.
Disclosures: The work was funded in part by the National Institutes of Health. Avid Pharmaceuticals provided the AV1451. The senior investigator is an advisor for Genentech, Merck, and Roche, and has research support from Avid Radiopharmaceuticals and Eli Lilly, among others.
Source: La Joie R, et al. Abstract M183, American Neurological Association 2017 annual meeting.
Medicaid expansion meant earlier presentation, better surgical outcomes
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).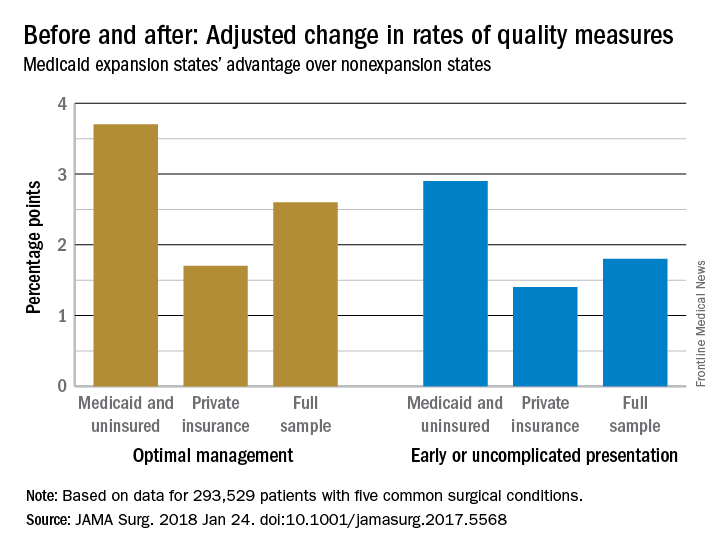
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).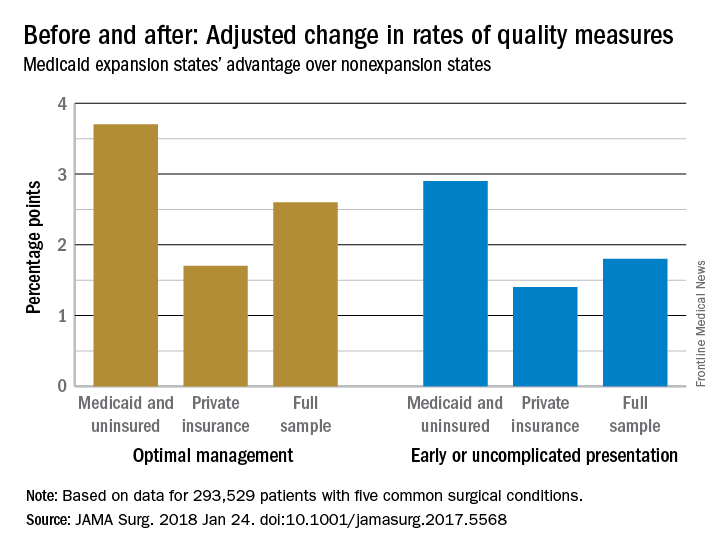
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
The for five common surgical conditions, according to a Jan. 24 report in JAMA Surgery.
“Given current debate on the ACA [Affordable Care Act] and reforms to the Medicaid program, evidence on the effects of these policies is critical ... As policy makers weigh changes to or a potential repeal of the ACA, these findings provide important new data on the early clinical effects of the law’s coverage expansion,” said investigators led by Andrew Loehrer, MD, of the department of surgical oncology at MD Anderson Cancer Center, Houston.
For a baseline, the team used hospital administrative data from the Vizient Clinical Data Base and Resource Manager to assess outcomes for appendicitis, cholecystitis, diverticulitis, peripheral artery disease, and aortic aneurysm in 42 states during 2010-2013, before the ACA took effect in 2014. They then compared outcomes during 2014-2015 in the 27 states that expanded Medicaid programs under the ACA with 15 states that did not. The study included 225,572 hospital admissions in the Medicaid expansion states and 67,957 in the nonexpansion states at more than 200 academic medical centers and affiliated hospitals.
Medicaid expansion in the 27 states was associated with a 7.5-percentage point decreased probability of patients being uninsured (95% confidence interval, –12.2 to –2.9; P = .002) and an 8.6-percentage point increased probability of having Medicaid (95% CI, 6.1-11.1; P less than .001).
Medicaid expansion was also associated with a 1.8-percentage point increase in the probability of early, uncomplicated presentation (95% CI, 0.7-2.9; P = .001) and a 2.6-percentage point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation (95% CI, 0.8-4.4; P = .006).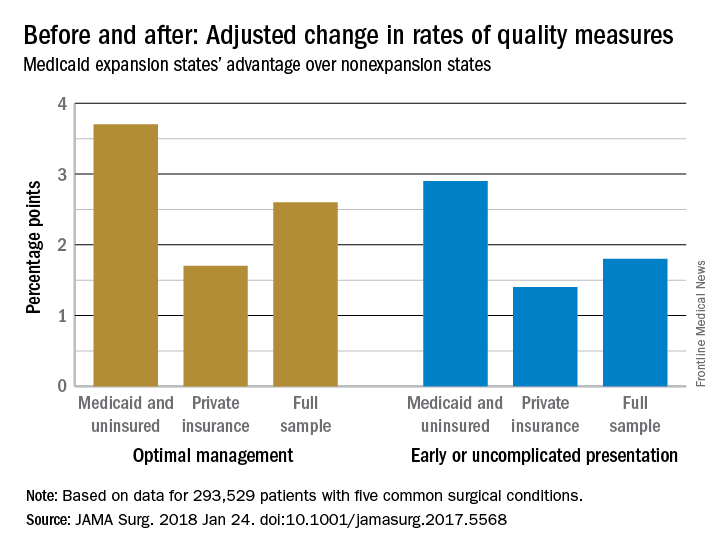
The improvements were concentrated among Medicaid and uninsured patients, who were most likely to benefit from coverage expansion, rather than those with private insurance.
The investigators acknowledged the limitations of their data for tracking changes access and quality of care for surgical patients. “We recognize that the data on improved quality of care are not as clear. Our use of composite outcomes has specific limitations,” they wrote.
“As expected for the conditions studied, our analysis found no significant change in the overall number of individuals treated but rather a change in the timeliness in which individuals received care.” Meanwhile, “our sample revealed an increase in the percentage of surgical patients who were uninsured in nonexpansion states after 2014,” which was associated with “worsening of outcomes ... whereas expansion states had stabilization or improvement,” they said. In Medicaid expansion states, the number of uninsured dropped from 14.% to 6.8%, but in the nonexpansion states, the number of uninsured actually increased slightly from 21.2% to 21.9%.
There was no funding source reported for the study. The authors had no conflicts of interest.
SOURCE: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
FROM JAMA SURGERY
Key clinical point: The Patient Protection and Affordable Care Act’s Medicaid expansion led to increased coverage of patients, earlier presentation, and improved care for five common surgical conditions.
Major finding: Medicaid expansion was associated with a 2.6 percentage-point increase in the probability of receiving optimal management after admission, most likely due to the earlier presentation.
Study details: Review of more than 200,000 patients, pre- and post-ACA
Disclosures: The authors had no disclosures.
Source: Loehrer AP et. al. JAMA Surg. 2018 Jan 24. doi: 10.1001/jamasurg.2017.5568
Junk food, energy drinks may damage teen brains
.
The latest evidence on how the teenage brain is particularly vulnerable to environmental influences, both good and bad, as it matures into adulthood is marshaled into review articles featured in a special issue of the journal Birth Defects Research entitled “The dynamic and vulnerable teenage brain” issued by the Teratology Society.
Junk food – soda, potato chips, and the like – is one of the bad influences, and not just on the waistline, according to a review by Amy Reichelt, PhD, and Michelle M. Rank, PhD, of the Royal Melbourne Institute of Technology University in Melbourne (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1173).
Under construction
“Because key neurotransmitter systems in the brain responsible for inhibition and reward signaling are still developing during the teen years, existing primarily on junk food could negatively affect decision making, increase reward-seeking behavior and influence poor eating habits throughout adulthood,” Dr. Reichelt said in a press release about the special issue.
The good news is that “the heightened neuroplasticity during adolescence ... offers a window in which diet-induced cognitive decline may be particularly amenable to intervention. This provides opportunities for nutritional intervention strategies in high-risk individuals,” she and Dr. Rank concluded in the review.
Although the literature is thinner than with junk food, there are similar concerns about the effects of energy drinks and their high levels of caffeine and taurine. Energy drinks likely are detrimental to the brain function of children and adolescents, especially when mixed with alcohol, according a second review by Christine Perdan Curran, PhD, and Cécile A. Marczinski, PhD, of Northern Kentucky University, Highland Heights. (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1177).
“We don’t know enough about the effects of high consumption of energy drinks and the ingredients found in them at this critical time in mammalian brain development,” but “our recent findings in adolescent and young adult mice exposed to high taurine levels indicate there can be adverse effects on learning and memory and increased alcohol consumption in females,” Dr. Curran said in the press release.
In short, energy drinks in adolescence raise “serious concerns about adverse effects on the brain,” the researchers concluded in their review.
It’s a happier story with exercise, according to two more reviews in the teenage brain issue.
Less couch time
“It is clear that helping adolescents dedicate more of their time to exercise, especially high intensity or aerobic activities, may not only better their physical health but also positively influence the way their brain is structured and how it functions,” said Megan Herting, PhD, and Xiaofang Chu of the University of Southern California, Los Angeles (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1178).
Aerobic exercise in the teenage years seems to improve attention, planning, problem solving, working memory, and inhibitory control. MRI studies, meanwhile, suggest that higher aerobic fitness correlates with beneficial cortical, subcortical, and white matter structural connectivity profiles in older adolescents. In a functional MRI study of 15- to 18-year-old boys, Dr. Herting and B.J. Nagel, PhD, found that the hippocampus of 17 less fit adolescents was significantly more active than that their 17 fitter peers during a word recall test, suggesting “that exercise may influence how the brain encodes new memories and that lower-fit teens may need to utilize additional brain resources to learn something new” (J Cogn Neurosci. 2013 Apr;25[4]:595-612).
Boosting the benefit
Exercise also helps with substance abuse, an effect that “appears to be attributable to more than just time occupied by the activities,” according to a review led by Nora L. Nock, PhD, of Case Western Reserve University, Cleveland (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1182).
“Substance use in adolescence has been associated with adverse structural and functional brain changes, and may further exacerbate the natural imbalance” between inhibitory and excitatory neurotransmitters, “leading to further heightened impulsive and reward-driven behaviors,” the authors said.
Exercise offsets the effects by inducing structural and functional changes in the brain, including neurogenesis and angiogenesis. “If integrated during adolescence, a window of heightened reward sensitivity and neural plasticity, exercise may help to reinforce ‘naïve’ or underdeveloped connections between neurological reward and regulatory processes ... and, in turn, help offset or dampen reward seeking from substances while concomitantly improving cardiovascular health as well as academic and social achievement,” Dr. Nock and her colleagues said.
The team is studying “assisted exercise,” which helps people peddle about 35% faster on a stationary bike than they would be able to on their own. “It may be able to provide even greater effects in suppressing reward from substance use due to potentially larger increases in neurotransmitters (e.g., dopamine) and neurotrophic factors (e.g., BDNF [brain-derived neurotrophic factor]), which may be particularly beneficial in adolescents with SUD (substance use disorder) having a dopamine deficit due to genetic variation and/or lower levels of striatal dopamine receptors ... during substance abstinence,” they said.
Given those and other findings, Dr. Nock and her colleagues proposed that exercise “be initiated during early abstinence and, potentially, started before integrating other cognitive behavioral treatment components” in adolescents with SUDs.
The authors did not report any industry disclosures.
.
The latest evidence on how the teenage brain is particularly vulnerable to environmental influences, both good and bad, as it matures into adulthood is marshaled into review articles featured in a special issue of the journal Birth Defects Research entitled “The dynamic and vulnerable teenage brain” issued by the Teratology Society.
Junk food – soda, potato chips, and the like – is one of the bad influences, and not just on the waistline, according to a review by Amy Reichelt, PhD, and Michelle M. Rank, PhD, of the Royal Melbourne Institute of Technology University in Melbourne (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1173).
Under construction
“Because key neurotransmitter systems in the brain responsible for inhibition and reward signaling are still developing during the teen years, existing primarily on junk food could negatively affect decision making, increase reward-seeking behavior and influence poor eating habits throughout adulthood,” Dr. Reichelt said in a press release about the special issue.
The good news is that “the heightened neuroplasticity during adolescence ... offers a window in which diet-induced cognitive decline may be particularly amenable to intervention. This provides opportunities for nutritional intervention strategies in high-risk individuals,” she and Dr. Rank concluded in the review.
Although the literature is thinner than with junk food, there are similar concerns about the effects of energy drinks and their high levels of caffeine and taurine. Energy drinks likely are detrimental to the brain function of children and adolescents, especially when mixed with alcohol, according a second review by Christine Perdan Curran, PhD, and Cécile A. Marczinski, PhD, of Northern Kentucky University, Highland Heights. (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1177).
“We don’t know enough about the effects of high consumption of energy drinks and the ingredients found in them at this critical time in mammalian brain development,” but “our recent findings in adolescent and young adult mice exposed to high taurine levels indicate there can be adverse effects on learning and memory and increased alcohol consumption in females,” Dr. Curran said in the press release.
In short, energy drinks in adolescence raise “serious concerns about adverse effects on the brain,” the researchers concluded in their review.
It’s a happier story with exercise, according to two more reviews in the teenage brain issue.
Less couch time
“It is clear that helping adolescents dedicate more of their time to exercise, especially high intensity or aerobic activities, may not only better their physical health but also positively influence the way their brain is structured and how it functions,” said Megan Herting, PhD, and Xiaofang Chu of the University of Southern California, Los Angeles (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1178).
Aerobic exercise in the teenage years seems to improve attention, planning, problem solving, working memory, and inhibitory control. MRI studies, meanwhile, suggest that higher aerobic fitness correlates with beneficial cortical, subcortical, and white matter structural connectivity profiles in older adolescents. In a functional MRI study of 15- to 18-year-old boys, Dr. Herting and B.J. Nagel, PhD, found that the hippocampus of 17 less fit adolescents was significantly more active than that their 17 fitter peers during a word recall test, suggesting “that exercise may influence how the brain encodes new memories and that lower-fit teens may need to utilize additional brain resources to learn something new” (J Cogn Neurosci. 2013 Apr;25[4]:595-612).
Boosting the benefit
Exercise also helps with substance abuse, an effect that “appears to be attributable to more than just time occupied by the activities,” according to a review led by Nora L. Nock, PhD, of Case Western Reserve University, Cleveland (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1182).
“Substance use in adolescence has been associated with adverse structural and functional brain changes, and may further exacerbate the natural imbalance” between inhibitory and excitatory neurotransmitters, “leading to further heightened impulsive and reward-driven behaviors,” the authors said.
Exercise offsets the effects by inducing structural and functional changes in the brain, including neurogenesis and angiogenesis. “If integrated during adolescence, a window of heightened reward sensitivity and neural plasticity, exercise may help to reinforce ‘naïve’ or underdeveloped connections between neurological reward and regulatory processes ... and, in turn, help offset or dampen reward seeking from substances while concomitantly improving cardiovascular health as well as academic and social achievement,” Dr. Nock and her colleagues said.
The team is studying “assisted exercise,” which helps people peddle about 35% faster on a stationary bike than they would be able to on their own. “It may be able to provide even greater effects in suppressing reward from substance use due to potentially larger increases in neurotransmitters (e.g., dopamine) and neurotrophic factors (e.g., BDNF [brain-derived neurotrophic factor]), which may be particularly beneficial in adolescents with SUD (substance use disorder) having a dopamine deficit due to genetic variation and/or lower levels of striatal dopamine receptors ... during substance abstinence,” they said.
Given those and other findings, Dr. Nock and her colleagues proposed that exercise “be initiated during early abstinence and, potentially, started before integrating other cognitive behavioral treatment components” in adolescents with SUDs.
The authors did not report any industry disclosures.
.
The latest evidence on how the teenage brain is particularly vulnerable to environmental influences, both good and bad, as it matures into adulthood is marshaled into review articles featured in a special issue of the journal Birth Defects Research entitled “The dynamic and vulnerable teenage brain” issued by the Teratology Society.
Junk food – soda, potato chips, and the like – is one of the bad influences, and not just on the waistline, according to a review by Amy Reichelt, PhD, and Michelle M. Rank, PhD, of the Royal Melbourne Institute of Technology University in Melbourne (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1173).
Under construction
“Because key neurotransmitter systems in the brain responsible for inhibition and reward signaling are still developing during the teen years, existing primarily on junk food could negatively affect decision making, increase reward-seeking behavior and influence poor eating habits throughout adulthood,” Dr. Reichelt said in a press release about the special issue.
The good news is that “the heightened neuroplasticity during adolescence ... offers a window in which diet-induced cognitive decline may be particularly amenable to intervention. This provides opportunities for nutritional intervention strategies in high-risk individuals,” she and Dr. Rank concluded in the review.
Although the literature is thinner than with junk food, there are similar concerns about the effects of energy drinks and their high levels of caffeine and taurine. Energy drinks likely are detrimental to the brain function of children and adolescents, especially when mixed with alcohol, according a second review by Christine Perdan Curran, PhD, and Cécile A. Marczinski, PhD, of Northern Kentucky University, Highland Heights. (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1177).
“We don’t know enough about the effects of high consumption of energy drinks and the ingredients found in them at this critical time in mammalian brain development,” but “our recent findings in adolescent and young adult mice exposed to high taurine levels indicate there can be adverse effects on learning and memory and increased alcohol consumption in females,” Dr. Curran said in the press release.
In short, energy drinks in adolescence raise “serious concerns about adverse effects on the brain,” the researchers concluded in their review.
It’s a happier story with exercise, according to two more reviews in the teenage brain issue.
Less couch time
“It is clear that helping adolescents dedicate more of their time to exercise, especially high intensity or aerobic activities, may not only better their physical health but also positively influence the way their brain is structured and how it functions,” said Megan Herting, PhD, and Xiaofang Chu of the University of Southern California, Los Angeles (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1178).
Aerobic exercise in the teenage years seems to improve attention, planning, problem solving, working memory, and inhibitory control. MRI studies, meanwhile, suggest that higher aerobic fitness correlates with beneficial cortical, subcortical, and white matter structural connectivity profiles in older adolescents. In a functional MRI study of 15- to 18-year-old boys, Dr. Herting and B.J. Nagel, PhD, found that the hippocampus of 17 less fit adolescents was significantly more active than that their 17 fitter peers during a word recall test, suggesting “that exercise may influence how the brain encodes new memories and that lower-fit teens may need to utilize additional brain resources to learn something new” (J Cogn Neurosci. 2013 Apr;25[4]:595-612).
Boosting the benefit
Exercise also helps with substance abuse, an effect that “appears to be attributable to more than just time occupied by the activities,” according to a review led by Nora L. Nock, PhD, of Case Western Reserve University, Cleveland (Birth Defects Res. 2017 Dec 1. doi: 10.1002/bdr2.1182).
“Substance use in adolescence has been associated with adverse structural and functional brain changes, and may further exacerbate the natural imbalance” between inhibitory and excitatory neurotransmitters, “leading to further heightened impulsive and reward-driven behaviors,” the authors said.
Exercise offsets the effects by inducing structural and functional changes in the brain, including neurogenesis and angiogenesis. “If integrated during adolescence, a window of heightened reward sensitivity and neural plasticity, exercise may help to reinforce ‘naïve’ or underdeveloped connections between neurological reward and regulatory processes ... and, in turn, help offset or dampen reward seeking from substances while concomitantly improving cardiovascular health as well as academic and social achievement,” Dr. Nock and her colleagues said.
The team is studying “assisted exercise,” which helps people peddle about 35% faster on a stationary bike than they would be able to on their own. “It may be able to provide even greater effects in suppressing reward from substance use due to potentially larger increases in neurotransmitters (e.g., dopamine) and neurotrophic factors (e.g., BDNF [brain-derived neurotrophic factor]), which may be particularly beneficial in adolescents with SUD (substance use disorder) having a dopamine deficit due to genetic variation and/or lower levels of striatal dopamine receptors ... during substance abstinence,” they said.
Given those and other findings, Dr. Nock and her colleagues proposed that exercise “be initiated during early abstinence and, potentially, started before integrating other cognitive behavioral treatment components” in adolescents with SUDs.
The authors did not report any industry disclosures.
FROM BIRTH DEFECTS RESEARCH
Zika-linked birth defects climbing in U.S. hot spots
The prevalence of birth defects strongly linked with congenital Zika virus infection increased 21% from the first to the second half of 2016 in areas of the United States with local, endemic transmission: Puerto Rico, south Florida, and southern Texas, according to a report in the Jan. 26 edition of Morbidity and Mortality Weekly Report.
In those areas, complications strongly associated with Zika – including microcephaly; brain and eye abnormalities; and neurogenic hip dislocation, clubfoot, hearing loss, and arthrogryposis – jumped from 2.0 to 2.4 cases per 1,000 live births, with 140 cases in the first half of the year and 169 cases in the second (P = .009). Microcephaly and brain abnormalities were the most common problems.
In places with less than one confirmed Zika case from travel per 100,000 residents, such as Hawaii and Utah, the prevalence of birth defects strongly linked to Zika actually dropped from 2.8 cases per 1,000 live births to 2.4 in 2016.
The 15 U.S. jurisdictions in the study included nearly 1 million live births, representing approximately one fourth of the total live births in the United States in 2016. The live birth rate was 92% among the 2,962 infants and fetuses with Zika-associated birth defects.
All the jurisdictions had existing birth defects surveillance systems that quickly adapted to monitor for potential Zika defects. However, although strongly associated with Zika, there’s no guarantee that the birth defects in the study were actually caused by the virus, the researchers noted.
“These data will help communities plan for needed resources to care for affected patients and families and can serve as a foundation for linking and evaluating health and developmental outcomes of affected children,” said the investigators, led by Augustina Delaney, PhD, of the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention in Atlanta.
The work was the first population-based birth defect surveillance report for Zika. The CDC follows confirmed Zika cases in pregnant women and their offspring closely, but only a small portion of women are actually tested, so there’s likely far more cases of congenital Zika infection than show up in registries. Despite its limits, birth defect surveillance likely provides a more accurate picture of the actual extent of the problem.
It’s not known why Zika-linked birth defects dropped off in areas with low or no travel-associated cases. “However ... further case ascertainment from the final quarter of 2016 is anticipated in all jurisdictions,” so the numbers could change, the authors said.
They had no conflicts of interest.
SOURCE: Delaney A, et. al. MMWR Morb Mortal Wkly Rep. 2018 Jan 26;67(3):91-6
Although these birth defects are not specific to congenital Zika virus infection, only those defects found previously to be most closely aligned with congenital Zika infection had increased prevalence.
It is critical that public health surveillance programs continue reporting the occurrence of these birth defects to monitor for trends following the Zika virus outbreak.
Brenda Fitzgerald , MD, is the director of the Centers for Disease Control and Prevention in Atlanta. Coleen A. Boyle , PhD, is the director of the CDC National Center on Birth Defects and Developmental Disabilities, and Margaret Honein , PhD, is chief of the agency’s Birth Defects Branch. They made their comments Jan. 25 in JAMA, and had no conflicts of interest (Jama. 2018 Jan 25. doi: 10.1001/jama.2018.0126).
Although these birth defects are not specific to congenital Zika virus infection, only those defects found previously to be most closely aligned with congenital Zika infection had increased prevalence.
It is critical that public health surveillance programs continue reporting the occurrence of these birth defects to monitor for trends following the Zika virus outbreak.
Brenda Fitzgerald , MD, is the director of the Centers for Disease Control and Prevention in Atlanta. Coleen A. Boyle , PhD, is the director of the CDC National Center on Birth Defects and Developmental Disabilities, and Margaret Honein , PhD, is chief of the agency’s Birth Defects Branch. They made their comments Jan. 25 in JAMA, and had no conflicts of interest (Jama. 2018 Jan 25. doi: 10.1001/jama.2018.0126).
Although these birth defects are not specific to congenital Zika virus infection, only those defects found previously to be most closely aligned with congenital Zika infection had increased prevalence.
It is critical that public health surveillance programs continue reporting the occurrence of these birth defects to monitor for trends following the Zika virus outbreak.
Brenda Fitzgerald , MD, is the director of the Centers for Disease Control and Prevention in Atlanta. Coleen A. Boyle , PhD, is the director of the CDC National Center on Birth Defects and Developmental Disabilities, and Margaret Honein , PhD, is chief of the agency’s Birth Defects Branch. They made their comments Jan. 25 in JAMA, and had no conflicts of interest (Jama. 2018 Jan 25. doi: 10.1001/jama.2018.0126).
The prevalence of birth defects strongly linked with congenital Zika virus infection increased 21% from the first to the second half of 2016 in areas of the United States with local, endemic transmission: Puerto Rico, south Florida, and southern Texas, according to a report in the Jan. 26 edition of Morbidity and Mortality Weekly Report.
In those areas, complications strongly associated with Zika – including microcephaly; brain and eye abnormalities; and neurogenic hip dislocation, clubfoot, hearing loss, and arthrogryposis – jumped from 2.0 to 2.4 cases per 1,000 live births, with 140 cases in the first half of the year and 169 cases in the second (P = .009). Microcephaly and brain abnormalities were the most common problems.
In places with less than one confirmed Zika case from travel per 100,000 residents, such as Hawaii and Utah, the prevalence of birth defects strongly linked to Zika actually dropped from 2.8 cases per 1,000 live births to 2.4 in 2016.
The 15 U.S. jurisdictions in the study included nearly 1 million live births, representing approximately one fourth of the total live births in the United States in 2016. The live birth rate was 92% among the 2,962 infants and fetuses with Zika-associated birth defects.
All the jurisdictions had existing birth defects surveillance systems that quickly adapted to monitor for potential Zika defects. However, although strongly associated with Zika, there’s no guarantee that the birth defects in the study were actually caused by the virus, the researchers noted.
“These data will help communities plan for needed resources to care for affected patients and families and can serve as a foundation for linking and evaluating health and developmental outcomes of affected children,” said the investigators, led by Augustina Delaney, PhD, of the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention in Atlanta.
The work was the first population-based birth defect surveillance report for Zika. The CDC follows confirmed Zika cases in pregnant women and their offspring closely, but only a small portion of women are actually tested, so there’s likely far more cases of congenital Zika infection than show up in registries. Despite its limits, birth defect surveillance likely provides a more accurate picture of the actual extent of the problem.
It’s not known why Zika-linked birth defects dropped off in areas with low or no travel-associated cases. “However ... further case ascertainment from the final quarter of 2016 is anticipated in all jurisdictions,” so the numbers could change, the authors said.
They had no conflicts of interest.
SOURCE: Delaney A, et. al. MMWR Morb Mortal Wkly Rep. 2018 Jan 26;67(3):91-6
The prevalence of birth defects strongly linked with congenital Zika virus infection increased 21% from the first to the second half of 2016 in areas of the United States with local, endemic transmission: Puerto Rico, south Florida, and southern Texas, according to a report in the Jan. 26 edition of Morbidity and Mortality Weekly Report.
In those areas, complications strongly associated with Zika – including microcephaly; brain and eye abnormalities; and neurogenic hip dislocation, clubfoot, hearing loss, and arthrogryposis – jumped from 2.0 to 2.4 cases per 1,000 live births, with 140 cases in the first half of the year and 169 cases in the second (P = .009). Microcephaly and brain abnormalities were the most common problems.
In places with less than one confirmed Zika case from travel per 100,000 residents, such as Hawaii and Utah, the prevalence of birth defects strongly linked to Zika actually dropped from 2.8 cases per 1,000 live births to 2.4 in 2016.
The 15 U.S. jurisdictions in the study included nearly 1 million live births, representing approximately one fourth of the total live births in the United States in 2016. The live birth rate was 92% among the 2,962 infants and fetuses with Zika-associated birth defects.
All the jurisdictions had existing birth defects surveillance systems that quickly adapted to monitor for potential Zika defects. However, although strongly associated with Zika, there’s no guarantee that the birth defects in the study were actually caused by the virus, the researchers noted.
“These data will help communities plan for needed resources to care for affected patients and families and can serve as a foundation for linking and evaluating health and developmental outcomes of affected children,” said the investigators, led by Augustina Delaney, PhD, of the National Center on Birth Defects and Developmental Disabilities at the Centers for Disease Control and Prevention in Atlanta.
The work was the first population-based birth defect surveillance report for Zika. The CDC follows confirmed Zika cases in pregnant women and their offspring closely, but only a small portion of women are actually tested, so there’s likely far more cases of congenital Zika infection than show up in registries. Despite its limits, birth defect surveillance likely provides a more accurate picture of the actual extent of the problem.
It’s not known why Zika-linked birth defects dropped off in areas with low or no travel-associated cases. “However ... further case ascertainment from the final quarter of 2016 is anticipated in all jurisdictions,” so the numbers could change, the authors said.
They had no conflicts of interest.
SOURCE: Delaney A, et. al. MMWR Morb Mortal Wkly Rep. 2018 Jan 26;67(3):91-6
FROM MMWR
Key clinical point: Although microcephaly and other birth defects strongly associated with Zika virus are holding steady or even decreasing elsewhere in the United States, there was an uptick in 2016 in areas with endemic transmission.
Major finding: The prevalence of birth defects strongly related to congenital Zika virus infection increased 21% from the first to the second half of 2016 in southern Texas, south Florida, and Puerto Rico.
Study details: Birth defects surveillance in about a quarter of the infants born in the United States in 2016.
Disclosures: The investigators had no conflicts of interest.
Source: Delaney A, et. al. MMWR Morb Mortal Wkly Rep. 2018 Jan 26;67(3):91-6
Surgical LAA occlusion tops anticoagulation for AF thromboprotection
Surgical left atrial appendage occlusion may be just as good as anticoagulation at preventing thromboembolic events in older people with atrial fibrillation, with less risk of bleeding into the brain, according to a database review of more than 10,000 patients.
Among elderly atrial fibrillation patients who underwent heart surgery with no oral follow-up oral anticoagulation, those who had the left atrial appendage surgically occluded were 74% less likely than were those who did not to be readmitted for a major thromboembolic event within 3 years, and 68% less likely to be readmitted for a hemorrhagic stroke, researchers at Duke University in Durham, N.C., found.
“The current study demonstrated that S-LAAO [surgical left atrial appendage occlusion] was associated with a significantly lower rate of thromboembolism among patients without oral anticoagulation. In the cohort of patients discharged with oral anticoagulation, S-LAAO was not associated with [reduced] thromboembolism but was associated with a lower risk for hemorrhagic stroke presumably related to eventual discontinuation of oral anticoagulation among S-LAAO patients,” reported Daniel Friedman, MD, and his coinvestigators. The study was published Jan. 23 in JAMA.
In short, the findings suggest that shutting down the left atrial appendage in older patients offers the same stroke protection as anticoagulation, but without the bleeding risk. Given the low rates of anticoagulant use, physicians have been considering that approach for a while. Even so, it’s only been a weak (IIb) recommendation so far in AF guidelines because of the lack of evidence.
That might change soon, but “additional randomized studies comparing S-LAAO without anticoagulation [versus] systemic anticoagulation alone will be needed to define the optimal use of S-LAAO,” said Dr. Friedman, a cardiothoracic surgeon at Duke, and his colleagues. Those studies are in the works.
The team found 10,524 older patients in the Society of Thoracic Surgeons Adult Cardiac Surgery Database during 2011-2012, and linked them to Medicare data so they could be followed for up to 3 years. About a third of the subjects had stand-alone coronary artery bypass grafting; the rest had mitral or aortic valve repairs with or without CABG.
The investigators compared outcomes among the 37% (3,892) who had S-LAAO with outcomes among those who did not. Participants were a median of 76 years of age, 61% were men, and they were all at high risk for AF stroke.
After a mean follow-up of 2.6 years, subjects who received S-LAAO without postoperative anticoagulation had a significantly lower risk of readmission for thromboembolism – stroke, transient ischemic attack, or systemic embolism – compared with those who received neither S-LAAO nor anticoagulation (unadjusted rate 4.2% versus 6.0%; adjusted subdistribution hazard ratio [sHR] 0.26, 95% CI, 0.17-0.40, P less than .001).
There was no extra embolic stroke protection from S-LAAO in patients who were discharged on anticoagulation (sHR 0.88, 95% CI, 0.56-1.39; P = .59), but the risk of returning with a hemorrhagic stroke was considerably less (sHR 0.32, 95% CI, 0.17-0.57, P less than .001).
The S-LAAO group more commonly had nonparoxysmal AF, a higher ejection fraction, a lower mortality risk score, and lower rates of common stroke risks, such as diabetes, hypertension, and prior stroke. The Duke team adjusted for those and a long list of other confounders, including smoking, age, preoperative warfarin, and academic hospital status.
There were important limitations. No one knows what surgeons did to close the LAA, or how well it worked, and most patients discharged on anticoagulation were sent home on warfarin, not the newer direct oral anticoagulants.
The investigators noted that “the strongest data to date for LAAO come from randomized trials comparing warfarin with percutaneous LAAO using the WATCHMAN device” from Boston Scientific.
The reduction in cardiovascular mortality in those trials appeared to be driven by a reduction in hemorrhagic stroke and occurred despite increased rates of ischemic stroke, they said.
The current study, however, showed that S-LAAO was associated with a significantly lower rate of thromboembolism in patients without oral anticoagulation, the authors said.
The work was funded, in part, by the Food and Drug Administration. Dr. Friedman reported grants from Boston Scientific and Abbott. Other authors reported financial relations with those and several other companies.
SOURCE: Friedman DJ, et. al. JAMA. 2018;319(4):365-74. doi: 10.1001/jama.2017.20125.
The implications of the study may have far-reaching consequences on the best treatment to reduce both thromboembolism and hemorrhage associated with AF treatment.
There is a strong signal that S-LAAO may be equivalent to anticoagulation prophylaxis to avoid thromboembolism in certain patients. This possibility is intriguing because it suggests that S-LAAO may be as effective as anticoagulation and could potentially avoid the bleeding risks associated with anticoagulation. A reasonable hypothesis based on the authors’ findings is that ablation procedures that occlude the left atrial appendage are adequate treatments to avoid thromboembolism and to minimize postoperative anticoagulation-related hemorrhage. This somewhat novel hypothesis, if true, could avoid a significant morbidity associated with anticoagulation while providing adequate treatment for thromboembolic complications of AF.
Importantly, the results suggest that failure to perform an S-LAAO at the time of cardiac operation in patients with nonvalvular AF is associated with significantly increased intermediate-term thromboembolic risk.
Victor M. Ferraris , MD, PhD, a cardiothoracic surgeon at the University of Kentucky, Lexington, made his comments in an accompanying editorial. He had no conflicts of interest.
The implications of the study may have far-reaching consequences on the best treatment to reduce both thromboembolism and hemorrhage associated with AF treatment.
There is a strong signal that S-LAAO may be equivalent to anticoagulation prophylaxis to avoid thromboembolism in certain patients. This possibility is intriguing because it suggests that S-LAAO may be as effective as anticoagulation and could potentially avoid the bleeding risks associated with anticoagulation. A reasonable hypothesis based on the authors’ findings is that ablation procedures that occlude the left atrial appendage are adequate treatments to avoid thromboembolism and to minimize postoperative anticoagulation-related hemorrhage. This somewhat novel hypothesis, if true, could avoid a significant morbidity associated with anticoagulation while providing adequate treatment for thromboembolic complications of AF.
Importantly, the results suggest that failure to perform an S-LAAO at the time of cardiac operation in patients with nonvalvular AF is associated with significantly increased intermediate-term thromboembolic risk.
Victor M. Ferraris , MD, PhD, a cardiothoracic surgeon at the University of Kentucky, Lexington, made his comments in an accompanying editorial. He had no conflicts of interest.
The implications of the study may have far-reaching consequences on the best treatment to reduce both thromboembolism and hemorrhage associated with AF treatment.
There is a strong signal that S-LAAO may be equivalent to anticoagulation prophylaxis to avoid thromboembolism in certain patients. This possibility is intriguing because it suggests that S-LAAO may be as effective as anticoagulation and could potentially avoid the bleeding risks associated with anticoagulation. A reasonable hypothesis based on the authors’ findings is that ablation procedures that occlude the left atrial appendage are adequate treatments to avoid thromboembolism and to minimize postoperative anticoagulation-related hemorrhage. This somewhat novel hypothesis, if true, could avoid a significant morbidity associated with anticoagulation while providing adequate treatment for thromboembolic complications of AF.
Importantly, the results suggest that failure to perform an S-LAAO at the time of cardiac operation in patients with nonvalvular AF is associated with significantly increased intermediate-term thromboembolic risk.
Victor M. Ferraris , MD, PhD, a cardiothoracic surgeon at the University of Kentucky, Lexington, made his comments in an accompanying editorial. He had no conflicts of interest.
Surgical left atrial appendage occlusion may be just as good as anticoagulation at preventing thromboembolic events in older people with atrial fibrillation, with less risk of bleeding into the brain, according to a database review of more than 10,000 patients.
Among elderly atrial fibrillation patients who underwent heart surgery with no oral follow-up oral anticoagulation, those who had the left atrial appendage surgically occluded were 74% less likely than were those who did not to be readmitted for a major thromboembolic event within 3 years, and 68% less likely to be readmitted for a hemorrhagic stroke, researchers at Duke University in Durham, N.C., found.
“The current study demonstrated that S-LAAO [surgical left atrial appendage occlusion] was associated with a significantly lower rate of thromboembolism among patients without oral anticoagulation. In the cohort of patients discharged with oral anticoagulation, S-LAAO was not associated with [reduced] thromboembolism but was associated with a lower risk for hemorrhagic stroke presumably related to eventual discontinuation of oral anticoagulation among S-LAAO patients,” reported Daniel Friedman, MD, and his coinvestigators. The study was published Jan. 23 in JAMA.
In short, the findings suggest that shutting down the left atrial appendage in older patients offers the same stroke protection as anticoagulation, but without the bleeding risk. Given the low rates of anticoagulant use, physicians have been considering that approach for a while. Even so, it’s only been a weak (IIb) recommendation so far in AF guidelines because of the lack of evidence.
That might change soon, but “additional randomized studies comparing S-LAAO without anticoagulation [versus] systemic anticoagulation alone will be needed to define the optimal use of S-LAAO,” said Dr. Friedman, a cardiothoracic surgeon at Duke, and his colleagues. Those studies are in the works.
The team found 10,524 older patients in the Society of Thoracic Surgeons Adult Cardiac Surgery Database during 2011-2012, and linked them to Medicare data so they could be followed for up to 3 years. About a third of the subjects had stand-alone coronary artery bypass grafting; the rest had mitral or aortic valve repairs with or without CABG.
The investigators compared outcomes among the 37% (3,892) who had S-LAAO with outcomes among those who did not. Participants were a median of 76 years of age, 61% were men, and they were all at high risk for AF stroke.
After a mean follow-up of 2.6 years, subjects who received S-LAAO without postoperative anticoagulation had a significantly lower risk of readmission for thromboembolism – stroke, transient ischemic attack, or systemic embolism – compared with those who received neither S-LAAO nor anticoagulation (unadjusted rate 4.2% versus 6.0%; adjusted subdistribution hazard ratio [sHR] 0.26, 95% CI, 0.17-0.40, P less than .001).
There was no extra embolic stroke protection from S-LAAO in patients who were discharged on anticoagulation (sHR 0.88, 95% CI, 0.56-1.39; P = .59), but the risk of returning with a hemorrhagic stroke was considerably less (sHR 0.32, 95% CI, 0.17-0.57, P less than .001).
The S-LAAO group more commonly had nonparoxysmal AF, a higher ejection fraction, a lower mortality risk score, and lower rates of common stroke risks, such as diabetes, hypertension, and prior stroke. The Duke team adjusted for those and a long list of other confounders, including smoking, age, preoperative warfarin, and academic hospital status.
There were important limitations. No one knows what surgeons did to close the LAA, or how well it worked, and most patients discharged on anticoagulation were sent home on warfarin, not the newer direct oral anticoagulants.
The investigators noted that “the strongest data to date for LAAO come from randomized trials comparing warfarin with percutaneous LAAO using the WATCHMAN device” from Boston Scientific.
The reduction in cardiovascular mortality in those trials appeared to be driven by a reduction in hemorrhagic stroke and occurred despite increased rates of ischemic stroke, they said.
The current study, however, showed that S-LAAO was associated with a significantly lower rate of thromboembolism in patients without oral anticoagulation, the authors said.
The work was funded, in part, by the Food and Drug Administration. Dr. Friedman reported grants from Boston Scientific and Abbott. Other authors reported financial relations with those and several other companies.
SOURCE: Friedman DJ, et. al. JAMA. 2018;319(4):365-74. doi: 10.1001/jama.2017.20125.
Surgical left atrial appendage occlusion may be just as good as anticoagulation at preventing thromboembolic events in older people with atrial fibrillation, with less risk of bleeding into the brain, according to a database review of more than 10,000 patients.
Among elderly atrial fibrillation patients who underwent heart surgery with no oral follow-up oral anticoagulation, those who had the left atrial appendage surgically occluded were 74% less likely than were those who did not to be readmitted for a major thromboembolic event within 3 years, and 68% less likely to be readmitted for a hemorrhagic stroke, researchers at Duke University in Durham, N.C., found.
“The current study demonstrated that S-LAAO [surgical left atrial appendage occlusion] was associated with a significantly lower rate of thromboembolism among patients without oral anticoagulation. In the cohort of patients discharged with oral anticoagulation, S-LAAO was not associated with [reduced] thromboembolism but was associated with a lower risk for hemorrhagic stroke presumably related to eventual discontinuation of oral anticoagulation among S-LAAO patients,” reported Daniel Friedman, MD, and his coinvestigators. The study was published Jan. 23 in JAMA.
In short, the findings suggest that shutting down the left atrial appendage in older patients offers the same stroke protection as anticoagulation, but without the bleeding risk. Given the low rates of anticoagulant use, physicians have been considering that approach for a while. Even so, it’s only been a weak (IIb) recommendation so far in AF guidelines because of the lack of evidence.
That might change soon, but “additional randomized studies comparing S-LAAO without anticoagulation [versus] systemic anticoagulation alone will be needed to define the optimal use of S-LAAO,” said Dr. Friedman, a cardiothoracic surgeon at Duke, and his colleagues. Those studies are in the works.
The team found 10,524 older patients in the Society of Thoracic Surgeons Adult Cardiac Surgery Database during 2011-2012, and linked them to Medicare data so they could be followed for up to 3 years. About a third of the subjects had stand-alone coronary artery bypass grafting; the rest had mitral or aortic valve repairs with or without CABG.
The investigators compared outcomes among the 37% (3,892) who had S-LAAO with outcomes among those who did not. Participants were a median of 76 years of age, 61% were men, and they were all at high risk for AF stroke.
After a mean follow-up of 2.6 years, subjects who received S-LAAO without postoperative anticoagulation had a significantly lower risk of readmission for thromboembolism – stroke, transient ischemic attack, or systemic embolism – compared with those who received neither S-LAAO nor anticoagulation (unadjusted rate 4.2% versus 6.0%; adjusted subdistribution hazard ratio [sHR] 0.26, 95% CI, 0.17-0.40, P less than .001).
There was no extra embolic stroke protection from S-LAAO in patients who were discharged on anticoagulation (sHR 0.88, 95% CI, 0.56-1.39; P = .59), but the risk of returning with a hemorrhagic stroke was considerably less (sHR 0.32, 95% CI, 0.17-0.57, P less than .001).
The S-LAAO group more commonly had nonparoxysmal AF, a higher ejection fraction, a lower mortality risk score, and lower rates of common stroke risks, such as diabetes, hypertension, and prior stroke. The Duke team adjusted for those and a long list of other confounders, including smoking, age, preoperative warfarin, and academic hospital status.
There were important limitations. No one knows what surgeons did to close the LAA, or how well it worked, and most patients discharged on anticoagulation were sent home on warfarin, not the newer direct oral anticoagulants.
The investigators noted that “the strongest data to date for LAAO come from randomized trials comparing warfarin with percutaneous LAAO using the WATCHMAN device” from Boston Scientific.
The reduction in cardiovascular mortality in those trials appeared to be driven by a reduction in hemorrhagic stroke and occurred despite increased rates of ischemic stroke, they said.
The current study, however, showed that S-LAAO was associated with a significantly lower rate of thromboembolism in patients without oral anticoagulation, the authors said.
The work was funded, in part, by the Food and Drug Administration. Dr. Friedman reported grants from Boston Scientific and Abbott. Other authors reported financial relations with those and several other companies.
SOURCE: Friedman DJ, et. al. JAMA. 2018;319(4):365-74. doi: 10.1001/jama.2017.20125.
FROM JAMA
Key clinical point: Surgical left atrial appendage occlusion (S-LAAO) is probably just as good as anticoagulation at preventing thromboembolic events in older people with atrial fibrillation, with less risk of bleeding into the brain.
Major finding: within 3 years, and 68% less likely to be readmitted for a hemorrhagic stroke.
Study details: Database review of more than 10,000 elderly AF patients followed for up to 3 years after cardiac surgery.
Disclosures: The work was funded, in part, by the Food and Drug Administration. The authors had financial ties to Boston Scientific, Abbott, and several other companies.
Source: Friedman DJ, et. al. JAMA. 2018;319(4):365-74. doi: 10.1001/jama.2017.20125