User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
New update focuses on NAFLD in lean people
Ongoing follow-up and lifestyle interventions are needed in lean patients with nonalcoholic fatty liver disease (NAFLD), suggests a panel of experts in a recent review.
They also urge screening for NAFLD in individuals who are older than 40 years with type 2 diabetes, even if they are not overweight.
NAFLD is a leading cause of chronic liver disease that affects more than 25% of the United States and worldwide populations, note lead author Michelle T. Long, MD, Boston Medical Center, Boston University, and colleagues.
They add that around one-quarter of those affected have nonalcoholic steatohepatitis, which is associated with significant morbidity and mortality due to complications of liver cirrhosis, hepatic decompensation, and hepatocellular carcinoma.
Although NAFLD occurs primarily in individuals with obesity or type 2 diabetes, between 7%-20% have a lean body habitus, they write.
There are differences in rates of disease progression, associated conditions, and diagnostic and management approaches between lean and non-lean patients, the authors note, but there is limited guidance on the appropriate clinical evaluation of the former group.
The American Gastroenterological Association therefore commissioned an expert review to provide best practice advice on key clinical issues relating to the diagnosis, risk stratification, and treatment of NAFLD in lean individuals.
Their review was published online in Gastroenterology.
Evidence-based approaches
The 15 best practice advice statements covered a wide range of clinical areas, first defining lean as a body mass index (BMI) less than 25 in non-Asian persons and less than 23 in Asian persons.
The authors go on to stipulate, for example, that lean individuals in the general population should not be screened for NAFLD but that screening should be considered for individuals older than 40 years with type 2 diabetes.
More broadly, they write that the condition should be considered in lean individuals with metabolic diseases, such as type 2 diabetes, dyslipidemia, and hypertension, as well as elevated values on liver biochemical tests or incidentally noted hepatic steatosis.
After other causes of liver diseases are ruled out, the authors note that clinicians should consider liver biopsy as the reference test if uncertainties remain about liver injury causes and/or liver fibrosis staging.
They also write that the NAFLD fibrosis score and Fibrosis-4 score, along with imaging techniques, may be used as alternatives to biopsy for staging and during follow-up.
The authors, who provide a diagnosis and management algorithm to aid clinicians, suggest that lean patients with NAFLD follow lifestyle interventions, such as exercise, diet modification, and avoidance of fructose- and sugar-sweetened drinks, to achieve weight loss of 3%-5%.
Vitamin E may be considered, they continue, in patients with biopsy-confirmed nonalcoholic steatohepatitis but without type 2 diabetes or cirrhosis. Additionally, oral pioglitazone may be considered in lean persons with biopsy-confirmed nonalcoholic steatohepatitis without cirrhosis.
In contrast, they write that the role of glucagonlike peptide 1 agonists and sodium-glucose cotransporter 2 inhibitors requires further investigation.
The advice also says that lean patients with NAFLD should be routinely evaluated for comorbid conditions, such as type 2 diabetes, dyslipidemia, and hypertension, and risk-stratified for hepatic fibrosis to identify those with advanced fibrosis or cirrhosis.
For lean patients with NAFLD and clinical markers compatible with liver cirrhosis, twice-yearly surveillance for hepatocellular carcinoma is also advised.
Fatty liver disease in lean people with metabolic conditions
Approached for comment, Liyun Yuan, MD, PhD, assistant professor of clinical medicine, University of Southern California, Los Angeles, said it is very important to have uniform guidelines for general practitioners and other specialties on NAFLD in lean individuals.
Dr. Yuan, who was not involved in the review, told this news organization that it is crucial to raise awareness of NAFLD, just like awareness of breast cancer screening among women of a certain age was increased, so that individuals are screened for metabolic conditions regardless of whether they have obesity or overweight.
Zobair Younossi, MD, MPH, professor of medicine, Virginia Commonwealth University, Inova Campus, Falls Church, Va., added that there is a lack of awareness that NAFLD occurs in lean individuals, especially in those who have diabetes.
He said in an interview that although it is accurate to define individuals as being lean in terms of their BMI, the best way is to look not only at BMI but also at waist circumference.
Dr. Younossi said that he and his colleagues have shown that when BMI is combined with waist circumference, the prediction of mortality risk in NAFLD is affected, such that lean individuals with an obese waist circumference have a higher risk for all-cause mortality.
Dr. Long is supported in part by the National Institute of Diabetes and Digestive and Kidney Diseases, Doris Duke Charitable Foundation, Gilead Sciences Research Scholars Award, Boston University School of Medicine Department of Medicine Career Investment Award, and Boston University Clinical Translational Science Institute. Dr. Long declares relationships with Novo Nordisk, Echosens Corporation, and Gilead Sciences. Dr. Yuan declares relationships with Genfit, Intercept, and Gilead Sciences. Dr. Younossi declares no relevant relationships.
A version of this article first appeared on Medscape.com.
*This article was updated on July 27, 2022.
Ongoing follow-up and lifestyle interventions are needed in lean patients with nonalcoholic fatty liver disease (NAFLD), suggests a panel of experts in a recent review.
They also urge screening for NAFLD in individuals who are older than 40 years with type 2 diabetes, even if they are not overweight.
NAFLD is a leading cause of chronic liver disease that affects more than 25% of the United States and worldwide populations, note lead author Michelle T. Long, MD, Boston Medical Center, Boston University, and colleagues.
They add that around one-quarter of those affected have nonalcoholic steatohepatitis, which is associated with significant morbidity and mortality due to complications of liver cirrhosis, hepatic decompensation, and hepatocellular carcinoma.
Although NAFLD occurs primarily in individuals with obesity or type 2 diabetes, between 7%-20% have a lean body habitus, they write.
There are differences in rates of disease progression, associated conditions, and diagnostic and management approaches between lean and non-lean patients, the authors note, but there is limited guidance on the appropriate clinical evaluation of the former group.
The American Gastroenterological Association therefore commissioned an expert review to provide best practice advice on key clinical issues relating to the diagnosis, risk stratification, and treatment of NAFLD in lean individuals.
Their review was published online in Gastroenterology.
Evidence-based approaches
The 15 best practice advice statements covered a wide range of clinical areas, first defining lean as a body mass index (BMI) less than 25 in non-Asian persons and less than 23 in Asian persons.
The authors go on to stipulate, for example, that lean individuals in the general population should not be screened for NAFLD but that screening should be considered for individuals older than 40 years with type 2 diabetes.
More broadly, they write that the condition should be considered in lean individuals with metabolic diseases, such as type 2 diabetes, dyslipidemia, and hypertension, as well as elevated values on liver biochemical tests or incidentally noted hepatic steatosis.
After other causes of liver diseases are ruled out, the authors note that clinicians should consider liver biopsy as the reference test if uncertainties remain about liver injury causes and/or liver fibrosis staging.
They also write that the NAFLD fibrosis score and Fibrosis-4 score, along with imaging techniques, may be used as alternatives to biopsy for staging and during follow-up.
The authors, who provide a diagnosis and management algorithm to aid clinicians, suggest that lean patients with NAFLD follow lifestyle interventions, such as exercise, diet modification, and avoidance of fructose- and sugar-sweetened drinks, to achieve weight loss of 3%-5%.
Vitamin E may be considered, they continue, in patients with biopsy-confirmed nonalcoholic steatohepatitis but without type 2 diabetes or cirrhosis. Additionally, oral pioglitazone may be considered in lean persons with biopsy-confirmed nonalcoholic steatohepatitis without cirrhosis.
In contrast, they write that the role of glucagonlike peptide 1 agonists and sodium-glucose cotransporter 2 inhibitors requires further investigation.
The advice also says that lean patients with NAFLD should be routinely evaluated for comorbid conditions, such as type 2 diabetes, dyslipidemia, and hypertension, and risk-stratified for hepatic fibrosis to identify those with advanced fibrosis or cirrhosis.
For lean patients with NAFLD and clinical markers compatible with liver cirrhosis, twice-yearly surveillance for hepatocellular carcinoma is also advised.
Fatty liver disease in lean people with metabolic conditions
Approached for comment, Liyun Yuan, MD, PhD, assistant professor of clinical medicine, University of Southern California, Los Angeles, said it is very important to have uniform guidelines for general practitioners and other specialties on NAFLD in lean individuals.
Dr. Yuan, who was not involved in the review, told this news organization that it is crucial to raise awareness of NAFLD, just like awareness of breast cancer screening among women of a certain age was increased, so that individuals are screened for metabolic conditions regardless of whether they have obesity or overweight.
Zobair Younossi, MD, MPH, professor of medicine, Virginia Commonwealth University, Inova Campus, Falls Church, Va., added that there is a lack of awareness that NAFLD occurs in lean individuals, especially in those who have diabetes.
He said in an interview that although it is accurate to define individuals as being lean in terms of their BMI, the best way is to look not only at BMI but also at waist circumference.
Dr. Younossi said that he and his colleagues have shown that when BMI is combined with waist circumference, the prediction of mortality risk in NAFLD is affected, such that lean individuals with an obese waist circumference have a higher risk for all-cause mortality.
Dr. Long is supported in part by the National Institute of Diabetes and Digestive and Kidney Diseases, Doris Duke Charitable Foundation, Gilead Sciences Research Scholars Award, Boston University School of Medicine Department of Medicine Career Investment Award, and Boston University Clinical Translational Science Institute. Dr. Long declares relationships with Novo Nordisk, Echosens Corporation, and Gilead Sciences. Dr. Yuan declares relationships with Genfit, Intercept, and Gilead Sciences. Dr. Younossi declares no relevant relationships.
A version of this article first appeared on Medscape.com.
*This article was updated on July 27, 2022.
Ongoing follow-up and lifestyle interventions are needed in lean patients with nonalcoholic fatty liver disease (NAFLD), suggests a panel of experts in a recent review.
They also urge screening for NAFLD in individuals who are older than 40 years with type 2 diabetes, even if they are not overweight.
NAFLD is a leading cause of chronic liver disease that affects more than 25% of the United States and worldwide populations, note lead author Michelle T. Long, MD, Boston Medical Center, Boston University, and colleagues.
They add that around one-quarter of those affected have nonalcoholic steatohepatitis, which is associated with significant morbidity and mortality due to complications of liver cirrhosis, hepatic decompensation, and hepatocellular carcinoma.
Although NAFLD occurs primarily in individuals with obesity or type 2 diabetes, between 7%-20% have a lean body habitus, they write.
There are differences in rates of disease progression, associated conditions, and diagnostic and management approaches between lean and non-lean patients, the authors note, but there is limited guidance on the appropriate clinical evaluation of the former group.
The American Gastroenterological Association therefore commissioned an expert review to provide best practice advice on key clinical issues relating to the diagnosis, risk stratification, and treatment of NAFLD in lean individuals.
Their review was published online in Gastroenterology.
Evidence-based approaches
The 15 best practice advice statements covered a wide range of clinical areas, first defining lean as a body mass index (BMI) less than 25 in non-Asian persons and less than 23 in Asian persons.
The authors go on to stipulate, for example, that lean individuals in the general population should not be screened for NAFLD but that screening should be considered for individuals older than 40 years with type 2 diabetes.
More broadly, they write that the condition should be considered in lean individuals with metabolic diseases, such as type 2 diabetes, dyslipidemia, and hypertension, as well as elevated values on liver biochemical tests or incidentally noted hepatic steatosis.
After other causes of liver diseases are ruled out, the authors note that clinicians should consider liver biopsy as the reference test if uncertainties remain about liver injury causes and/or liver fibrosis staging.
They also write that the NAFLD fibrosis score and Fibrosis-4 score, along with imaging techniques, may be used as alternatives to biopsy for staging and during follow-up.
The authors, who provide a diagnosis and management algorithm to aid clinicians, suggest that lean patients with NAFLD follow lifestyle interventions, such as exercise, diet modification, and avoidance of fructose- and sugar-sweetened drinks, to achieve weight loss of 3%-5%.
Vitamin E may be considered, they continue, in patients with biopsy-confirmed nonalcoholic steatohepatitis but without type 2 diabetes or cirrhosis. Additionally, oral pioglitazone may be considered in lean persons with biopsy-confirmed nonalcoholic steatohepatitis without cirrhosis.
In contrast, they write that the role of glucagonlike peptide 1 agonists and sodium-glucose cotransporter 2 inhibitors requires further investigation.
The advice also says that lean patients with NAFLD should be routinely evaluated for comorbid conditions, such as type 2 diabetes, dyslipidemia, and hypertension, and risk-stratified for hepatic fibrosis to identify those with advanced fibrosis or cirrhosis.
For lean patients with NAFLD and clinical markers compatible with liver cirrhosis, twice-yearly surveillance for hepatocellular carcinoma is also advised.
Fatty liver disease in lean people with metabolic conditions
Approached for comment, Liyun Yuan, MD, PhD, assistant professor of clinical medicine, University of Southern California, Los Angeles, said it is very important to have uniform guidelines for general practitioners and other specialties on NAFLD in lean individuals.
Dr. Yuan, who was not involved in the review, told this news organization that it is crucial to raise awareness of NAFLD, just like awareness of breast cancer screening among women of a certain age was increased, so that individuals are screened for metabolic conditions regardless of whether they have obesity or overweight.
Zobair Younossi, MD, MPH, professor of medicine, Virginia Commonwealth University, Inova Campus, Falls Church, Va., added that there is a lack of awareness that NAFLD occurs in lean individuals, especially in those who have diabetes.
He said in an interview that although it is accurate to define individuals as being lean in terms of their BMI, the best way is to look not only at BMI but also at waist circumference.
Dr. Younossi said that he and his colleagues have shown that when BMI is combined with waist circumference, the prediction of mortality risk in NAFLD is affected, such that lean individuals with an obese waist circumference have a higher risk for all-cause mortality.
Dr. Long is supported in part by the National Institute of Diabetes and Digestive and Kidney Diseases, Doris Duke Charitable Foundation, Gilead Sciences Research Scholars Award, Boston University School of Medicine Department of Medicine Career Investment Award, and Boston University Clinical Translational Science Institute. Dr. Long declares relationships with Novo Nordisk, Echosens Corporation, and Gilead Sciences. Dr. Yuan declares relationships with Genfit, Intercept, and Gilead Sciences. Dr. Younossi declares no relevant relationships.
A version of this article first appeared on Medscape.com.
*This article was updated on July 27, 2022.
FROM GASTROENTEROLOGY
Children and COVID: Many parents see vaccine as the greater risk
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.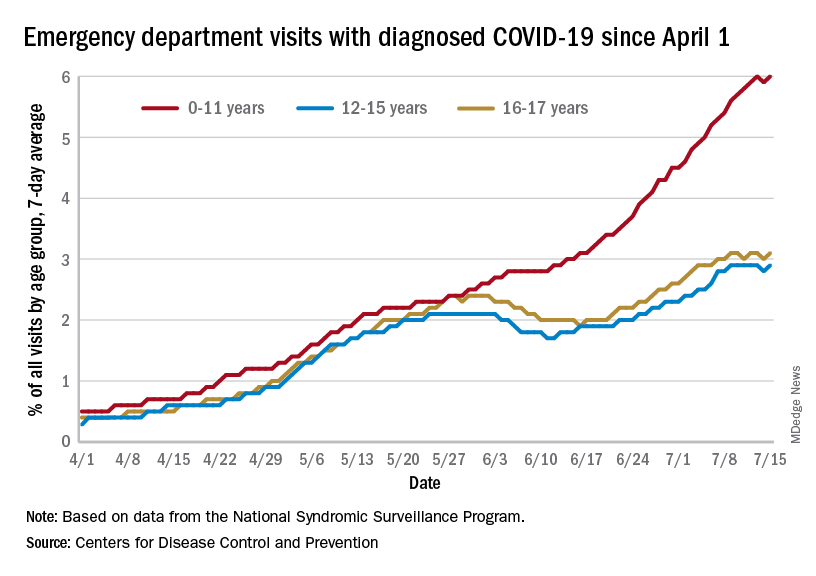
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.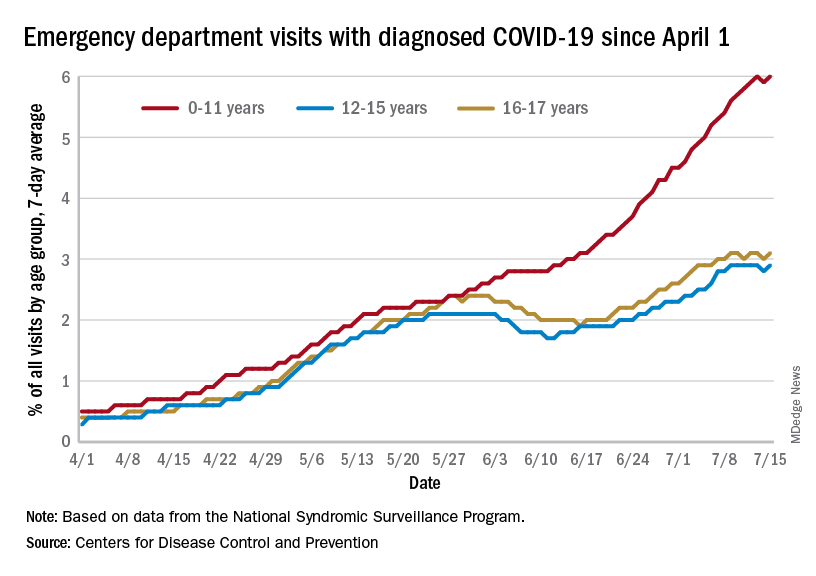
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
New COVID-19 cases rose for the second week in a row as cumulative cases among U.S. children passed the 14-million mark, but a recent survey shows that more than half of parents believe that the vaccine is a greater risk to children under age 5 years than the virus.
In a Kaiser Family Foundation survey conducted July 7-17, 53% of parents with children aged 6 months to 5 years said that the vaccine is “a bigger risk to their child’s health than getting infected with COVID-19, compared to 44% who say getting infected is the bigger risk,” KFF reported July 26.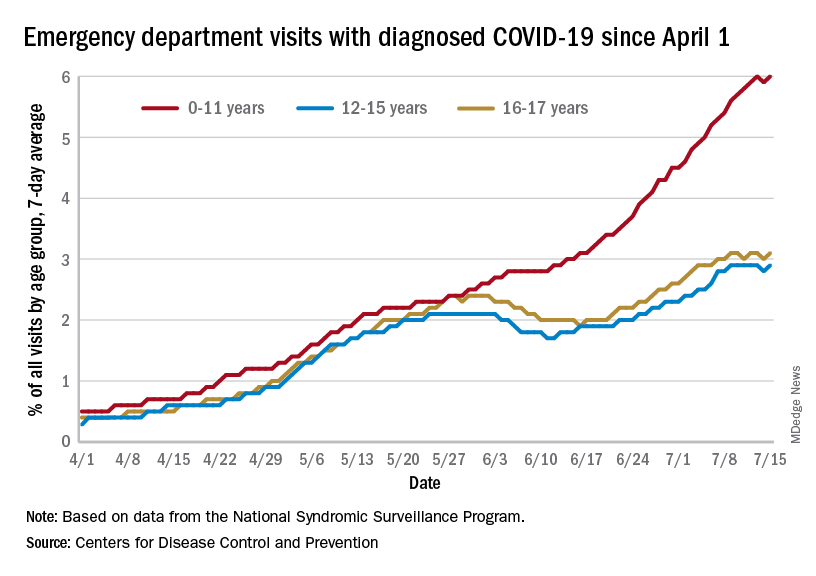
More than 4 out of 10 of respondents (43%) said that they will “definitely not” get their eligible children vaccinated, while only 7% said that their children had already received it and 10% said their children would get it as soon as possible, according to the KFF survey, which had an overall sample size of 1,847 adults, including an oversample of 471 parents of children under age 5.
Vaccine initiation has been slow in the first month since it was approved for the youngest children. Just 2.8% of all eligible children under age 5 had received an initial dose as of July 19, compared with first-month uptake figures of more than 18% for the 5- to 11-year-olds and 27% for those aged 12-15, based on data from the Centers for Disease Control and Prevention.
The current rates for vaccination in those aged 5 and older look like this: 70.2% of 12- to 17-year-olds have received at least one dose, versus 37.1% of those aged 5-11. Just over 60% of the older children were fully vaccinated as of July 19, as were 30.2% of the 5- to 11-year-olds, the CDC reported on its COVID Data Tracker.
Number of new cases hits 2-month high
Despite the vaccine, SARS-CoV-2 and its various mutations have continued with their summer travels. With 92,000 newly infected children added for the week of July 15-21, there have now been a total of 14,003,497 pediatric cases reported since the start of the pandemic, which works out to 18.6% of cases in all ages, the American Academy of Pediatrics and the Children’s Hospital Association said in their weekly COVID-19 report.
The 92,000 new cases represent an increase of almost 22% over the previous week and mark the highest 1-week count since May, when the total passed 100,000 for 2 consecutive weeks. More recently the trend had seemed more stable as weekly cases dropped twice and rose twice as the total hovered around 70,000, based on the data collected by the AAP and CHA from state and territorial health departments.
A different scenario has played out for emergency department visits and hospital admissions, which have risen steadily since the beginning of April. The admission rate for children aged 0-17, which was just 0.13 new patients per 100,000 population on April 11, was up to 0.44 per 100,000 on July 21. By comparison, the highest rate reached last year during the Delta surge was 0.47 per 100,000, based on CDC data.
The 7-day average of emergency dept. visits among the youngest age group, 0-11 years, shows the same general increase as hospital admissions, but the older children have diverged form that path (see graph). For those aged 12-15 and 16-17, hospitalizations started dropping in late May and into mid-June before climbing again, although more slowly than for the youngest group, the CDC data show.
The ED visit rate with diagnosed COVID among those aged 0-11, measured at 6.1% of all visits on July 19, is, in fact, considerably higher than at any time during the Delta surge last year, when it never passed 4.0%, although much lower than peak Omicron (14.1%). That 6.1% was also higher than any other age group on that day, adults included, the CDC said.
Boosting hypertension screening, treatment would cut global mortality 7%
If 80% of individuals with hypertension were screened, 80% received treatment, and 80% then reached guideline-specified targets, up to 200 million cases of cardiovascular disease (CVD) and 130 million deaths could be averted by 2050, a modeling study suggests.
Achievement of the 80-80-80 target “could be one of the single most important global public health accomplishments of the coming decades,” according to the authors.
“We need to reprioritize hypertension care in our practices,” principal investigator David A. Watkins, MD, MPH, University of Washington, Seattle, told this news organization. “Only about one in five persons with hypertension around the world has their blood pressure well controlled. Oftentimes, clinicians are focused on addressing patients’ other health needs, many of which can be pressing in the short term, and we forget to talk about blood pressure, which has more than earned its reputation as ‘the silent killer.’ ”
The modeling study was published online in Nature Medicine, with lead author Sarah J. Pickersgill, MPH, also from the University of Washington.
Two interventions, three scenarios
Dr. Watkins and colleagues based their analysis on two approaches to blood pressure (BP) control shown to be beneficial: drug treatment to a systolic BP of either 130 mm Hg or 140 mm Hg or less, depending on local guidelines, and dietary sodium reduction, as recommended by the World Health Organization.
The team modeled the impacts of these interventions in 182 countries according to three scenarios:
- Business as usual (control): allowing hypertension to increase at historic rates of change and mean sodium intake to remain at current levels
- Progress: matching historically high-performing countries (for example, accelerating hypertension control by about 3% per year at intermediate levels of intervention coverage) while lowering mean sodium intake by 15% by 2030
- Aspirational: hypertension control achieved faster than historically high-performing countries (about 4% per year) and mean sodium intake decreased by 30% by 2027
The analysis suggests that in the progressive scenario, all countries could achieve 80-80-80 targets by 2050 and most countries by 2040; the aspirational scenario would have all countries meeting them by 2040. That would result in reductions in all-cause mortality of 4%-7% (76 million to 130 million deaths averted) with progressive and aspirational interventions, respectively, compared with the control scenario.
There would also be a slower rise in expected CVD from population growth and aging (110 million to 200 million cases averted). That is, the probability of dying from any CVD cause between the ages of 30 and 80 years would be reduced by 16% in the progressive scenario and 26% in the aspirational scenario.
Of note, about 83%-85% of the potential mortality reductions would result from scaling up hypertension treatment in the progressive and aspirational scenarios, respectively, with the remaining 15%-17% coming from sodium reduction, the researchers state.
Further, they propose, scaling up BP interventions could reduce CVD inequalities across countries, with low-income and lower-middle-income countries likely experiencing the largest reductions in disease rates and mortality.
Implementation barriers
“Health systems in many low- and middle-income countries have not traditionally been set up to succeed in chronic disease management in primary care,” Dr. Watkins noted. For interventions to be successful, he said, “several barriers need to be addressed, including: low population awareness of chronic diseases like hypertension and diabetes, which leads to low rates of screening and treatment; high out-of-pocket cost and low availability of medicines for chronic diseases; and need for adherence support and provider incentives for improving quality of chronic disease care in primary care settings.”
“Based on the analysis, achieving the 80-80-80 seems feasible, though actually getting there may be much more complicated. I wonder whether countries have the resources to implement the needed policies,” Rodrigo M. Carrillo-Larco, MD, researcher, department of epidemiology and biostatistics, School of Public Health, Imperial College London, told this news organization.
“It may be challenging, particularly after COVID-19, which revealed deficiencies in many health care systems, and care for hypertension may have been disturbed,” said Dr. Carrillo-Larco, who is not connected with the analysis.
That said, simplified BP screening approaches could help maximize the number of people screened overall, potentially identifying those with hypertension and raising awareness, he proposed. His team’s recent study showed that such approaches vary from country to country but are generally reliable and can be used effectively for population screening.
In addition, Dr. Carrillo-Larco said, any efforts by clinicians to improve adherence and help patients achieve BP control “would also have positive effects at the population level.”
The study was supported by a grant from the Bill & Melinda Gates Foundation, with additional funding by a grant to Dr. Watkins from Resolve to Save Lives. No conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
If 80% of individuals with hypertension were screened, 80% received treatment, and 80% then reached guideline-specified targets, up to 200 million cases of cardiovascular disease (CVD) and 130 million deaths could be averted by 2050, a modeling study suggests.
Achievement of the 80-80-80 target “could be one of the single most important global public health accomplishments of the coming decades,” according to the authors.
“We need to reprioritize hypertension care in our practices,” principal investigator David A. Watkins, MD, MPH, University of Washington, Seattle, told this news organization. “Only about one in five persons with hypertension around the world has their blood pressure well controlled. Oftentimes, clinicians are focused on addressing patients’ other health needs, many of which can be pressing in the short term, and we forget to talk about blood pressure, which has more than earned its reputation as ‘the silent killer.’ ”
The modeling study was published online in Nature Medicine, with lead author Sarah J. Pickersgill, MPH, also from the University of Washington.
Two interventions, three scenarios
Dr. Watkins and colleagues based their analysis on two approaches to blood pressure (BP) control shown to be beneficial: drug treatment to a systolic BP of either 130 mm Hg or 140 mm Hg or less, depending on local guidelines, and dietary sodium reduction, as recommended by the World Health Organization.
The team modeled the impacts of these interventions in 182 countries according to three scenarios:
- Business as usual (control): allowing hypertension to increase at historic rates of change and mean sodium intake to remain at current levels
- Progress: matching historically high-performing countries (for example, accelerating hypertension control by about 3% per year at intermediate levels of intervention coverage) while lowering mean sodium intake by 15% by 2030
- Aspirational: hypertension control achieved faster than historically high-performing countries (about 4% per year) and mean sodium intake decreased by 30% by 2027
The analysis suggests that in the progressive scenario, all countries could achieve 80-80-80 targets by 2050 and most countries by 2040; the aspirational scenario would have all countries meeting them by 2040. That would result in reductions in all-cause mortality of 4%-7% (76 million to 130 million deaths averted) with progressive and aspirational interventions, respectively, compared with the control scenario.
There would also be a slower rise in expected CVD from population growth and aging (110 million to 200 million cases averted). That is, the probability of dying from any CVD cause between the ages of 30 and 80 years would be reduced by 16% in the progressive scenario and 26% in the aspirational scenario.
Of note, about 83%-85% of the potential mortality reductions would result from scaling up hypertension treatment in the progressive and aspirational scenarios, respectively, with the remaining 15%-17% coming from sodium reduction, the researchers state.
Further, they propose, scaling up BP interventions could reduce CVD inequalities across countries, with low-income and lower-middle-income countries likely experiencing the largest reductions in disease rates and mortality.
Implementation barriers
“Health systems in many low- and middle-income countries have not traditionally been set up to succeed in chronic disease management in primary care,” Dr. Watkins noted. For interventions to be successful, he said, “several barriers need to be addressed, including: low population awareness of chronic diseases like hypertension and diabetes, which leads to low rates of screening and treatment; high out-of-pocket cost and low availability of medicines for chronic diseases; and need for adherence support and provider incentives for improving quality of chronic disease care in primary care settings.”
“Based on the analysis, achieving the 80-80-80 seems feasible, though actually getting there may be much more complicated. I wonder whether countries have the resources to implement the needed policies,” Rodrigo M. Carrillo-Larco, MD, researcher, department of epidemiology and biostatistics, School of Public Health, Imperial College London, told this news organization.
“It may be challenging, particularly after COVID-19, which revealed deficiencies in many health care systems, and care for hypertension may have been disturbed,” said Dr. Carrillo-Larco, who is not connected with the analysis.
That said, simplified BP screening approaches could help maximize the number of people screened overall, potentially identifying those with hypertension and raising awareness, he proposed. His team’s recent study showed that such approaches vary from country to country but are generally reliable and can be used effectively for population screening.
In addition, Dr. Carrillo-Larco said, any efforts by clinicians to improve adherence and help patients achieve BP control “would also have positive effects at the population level.”
The study was supported by a grant from the Bill & Melinda Gates Foundation, with additional funding by a grant to Dr. Watkins from Resolve to Save Lives. No conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
If 80% of individuals with hypertension were screened, 80% received treatment, and 80% then reached guideline-specified targets, up to 200 million cases of cardiovascular disease (CVD) and 130 million deaths could be averted by 2050, a modeling study suggests.
Achievement of the 80-80-80 target “could be one of the single most important global public health accomplishments of the coming decades,” according to the authors.
“We need to reprioritize hypertension care in our practices,” principal investigator David A. Watkins, MD, MPH, University of Washington, Seattle, told this news organization. “Only about one in five persons with hypertension around the world has their blood pressure well controlled. Oftentimes, clinicians are focused on addressing patients’ other health needs, many of which can be pressing in the short term, and we forget to talk about blood pressure, which has more than earned its reputation as ‘the silent killer.’ ”
The modeling study was published online in Nature Medicine, with lead author Sarah J. Pickersgill, MPH, also from the University of Washington.
Two interventions, three scenarios
Dr. Watkins and colleagues based their analysis on two approaches to blood pressure (BP) control shown to be beneficial: drug treatment to a systolic BP of either 130 mm Hg or 140 mm Hg or less, depending on local guidelines, and dietary sodium reduction, as recommended by the World Health Organization.
The team modeled the impacts of these interventions in 182 countries according to three scenarios:
- Business as usual (control): allowing hypertension to increase at historic rates of change and mean sodium intake to remain at current levels
- Progress: matching historically high-performing countries (for example, accelerating hypertension control by about 3% per year at intermediate levels of intervention coverage) while lowering mean sodium intake by 15% by 2030
- Aspirational: hypertension control achieved faster than historically high-performing countries (about 4% per year) and mean sodium intake decreased by 30% by 2027
The analysis suggests that in the progressive scenario, all countries could achieve 80-80-80 targets by 2050 and most countries by 2040; the aspirational scenario would have all countries meeting them by 2040. That would result in reductions in all-cause mortality of 4%-7% (76 million to 130 million deaths averted) with progressive and aspirational interventions, respectively, compared with the control scenario.
There would also be a slower rise in expected CVD from population growth and aging (110 million to 200 million cases averted). That is, the probability of dying from any CVD cause between the ages of 30 and 80 years would be reduced by 16% in the progressive scenario and 26% in the aspirational scenario.
Of note, about 83%-85% of the potential mortality reductions would result from scaling up hypertension treatment in the progressive and aspirational scenarios, respectively, with the remaining 15%-17% coming from sodium reduction, the researchers state.
Further, they propose, scaling up BP interventions could reduce CVD inequalities across countries, with low-income and lower-middle-income countries likely experiencing the largest reductions in disease rates and mortality.
Implementation barriers
“Health systems in many low- and middle-income countries have not traditionally been set up to succeed in chronic disease management in primary care,” Dr. Watkins noted. For interventions to be successful, he said, “several barriers need to be addressed, including: low population awareness of chronic diseases like hypertension and diabetes, which leads to low rates of screening and treatment; high out-of-pocket cost and low availability of medicines for chronic diseases; and need for adherence support and provider incentives for improving quality of chronic disease care in primary care settings.”
“Based on the analysis, achieving the 80-80-80 seems feasible, though actually getting there may be much more complicated. I wonder whether countries have the resources to implement the needed policies,” Rodrigo M. Carrillo-Larco, MD, researcher, department of epidemiology and biostatistics, School of Public Health, Imperial College London, told this news organization.
“It may be challenging, particularly after COVID-19, which revealed deficiencies in many health care systems, and care for hypertension may have been disturbed,” said Dr. Carrillo-Larco, who is not connected with the analysis.
That said, simplified BP screening approaches could help maximize the number of people screened overall, potentially identifying those with hypertension and raising awareness, he proposed. His team’s recent study showed that such approaches vary from country to country but are generally reliable and can be used effectively for population screening.
In addition, Dr. Carrillo-Larco said, any efforts by clinicians to improve adherence and help patients achieve BP control “would also have positive effects at the population level.”
The study was supported by a grant from the Bill & Melinda Gates Foundation, with additional funding by a grant to Dr. Watkins from Resolve to Save Lives. No conflicts of interest were declared.
A version of this article first appeared on Medscape.com.
Multiple Fingerlike Projections on the Leg
The Diagnosis: Elephantiasis Nostras Verrucosa
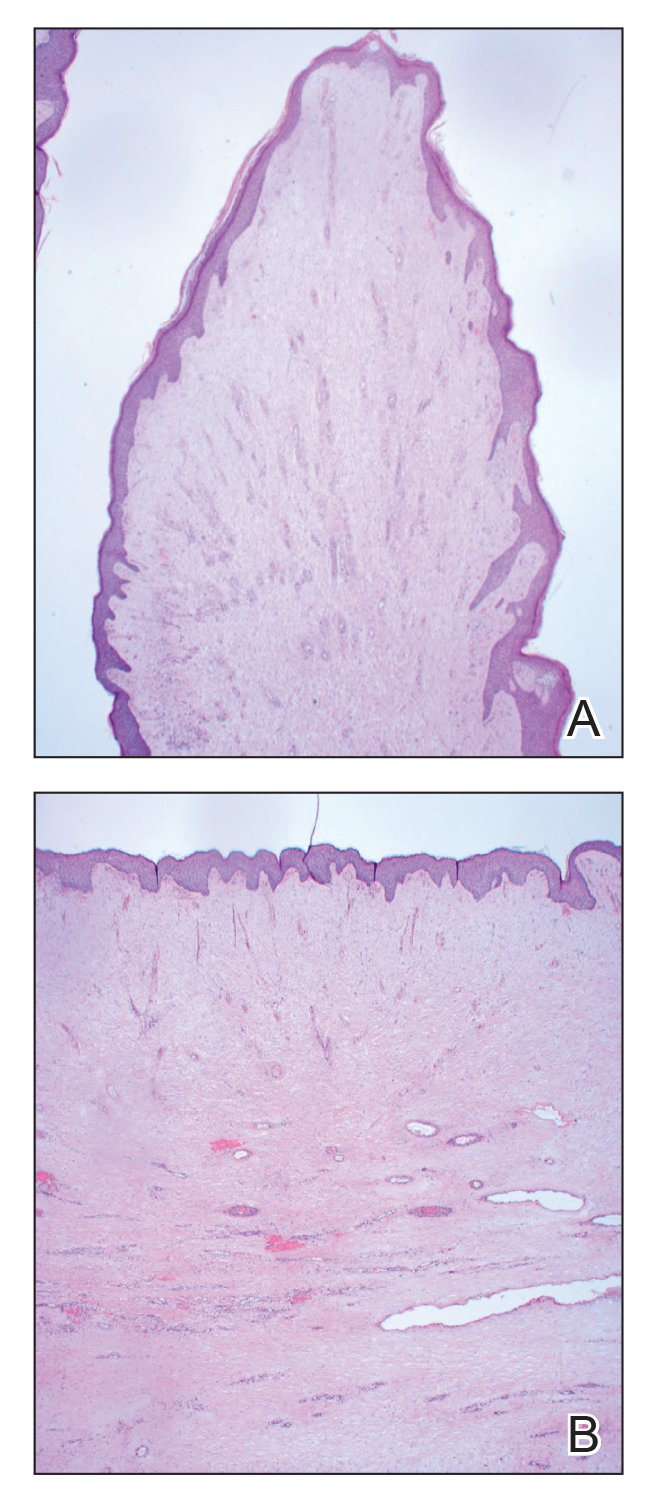
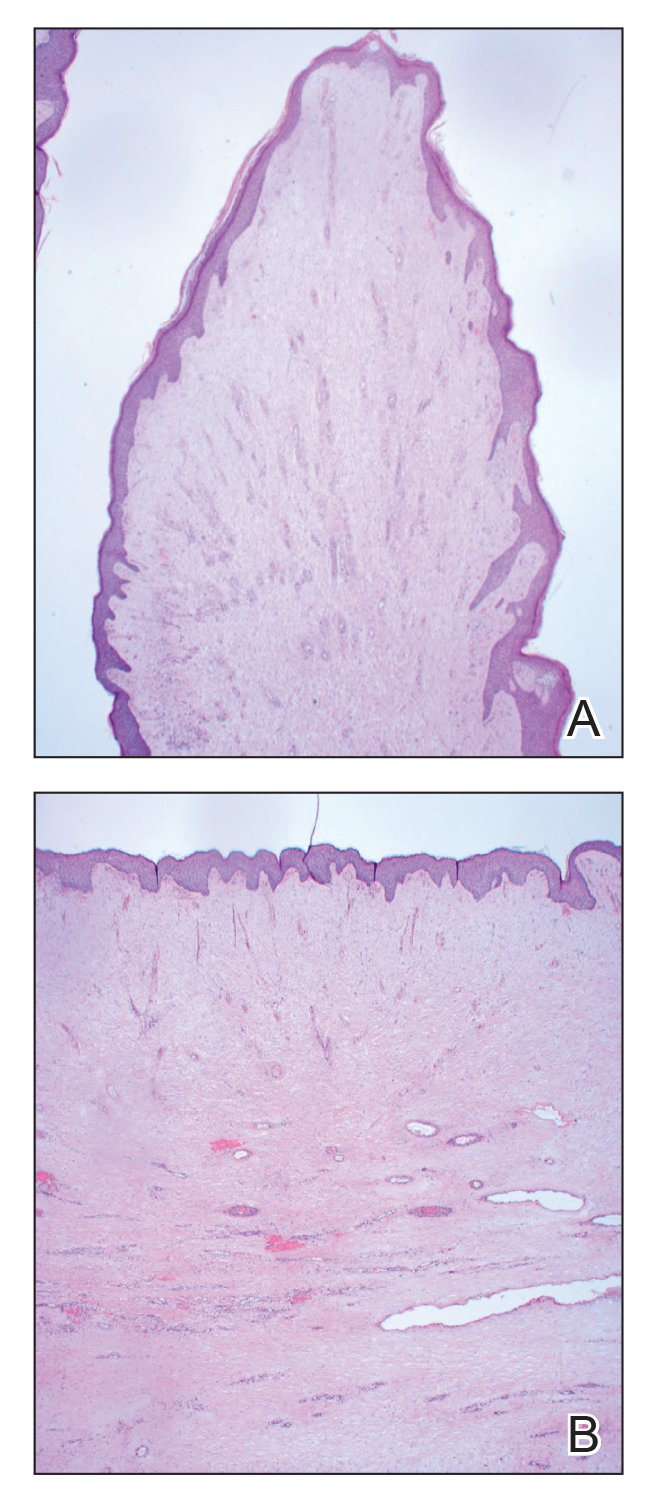
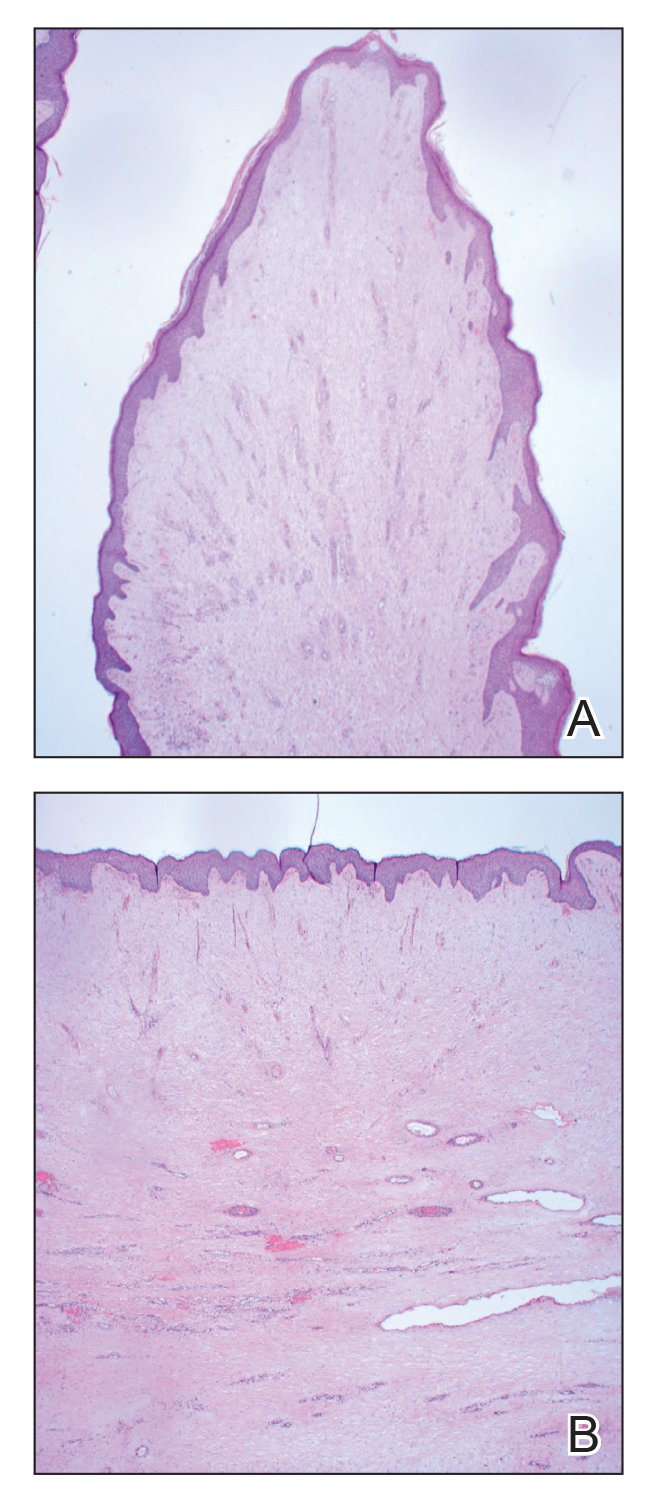
Histopathology revealed a benign fibroepithelial polyp demonstrating areas of hyperkeratosis, acanthosis, and focal papillomatosis (Figure, A). Increased superficial vessels with dilated lymphatics, stellate fibroblasts, edematous stroma, and plasmolymphocytosis also were noted (Figure, B). Clinical and histopathological findings led to a diagnosis of lymphedema papules in the setting of elephantiasis nostra verrucosa (ENV).
Elephantiasis nostras verrucosa is a complication of long-standing nonfilarial obstruction of lymphatic drainage leading to grotesque enlargement of the affected areas. Common cutaneous manifestations of ENV include nonpitting edema, dermal fibrosis, and extensive hyperkeratosis with verrucous and papillomatous lesions.1 In the beginning stages of ENV, the skin has a cobblestonelike appearance. As the disease progresses, the verrucous lesions continue to enlarge, giving the affected area a mossy appearance. Although less common, groupings of large papillomas similar to our patient’s presentation also can form.2 Ulcer formation is more likely to occur in advanced disease states, increasing the risk for bacterial and fungal colonization. Elephantiasis nostras verrucosa classically affects the legs; however, this condition can develop in any area with chronic lymphedema. Cases of ENV involving the arms, abdomen, scrotum, and ear have been documented.3-5
The pathogenesis of ENV involves the proliferation of fibroblasts and fibrosis secondary to lymphostasis and inflammation.6 When interstitial fluid builds up in the affected region, the protein-rich fluid is believed to trigger fibrogenesis and increase macrophage, keratinocyte, and adipocyte activity.7 Because of this inflammatory process, dilation and fibrosis of the lymphatic channels develop. Lymphatic obstruction can have several etiologies, most notably infection and malignancy. Staphylococcal lymphangitis and erysipelas create fibrosis of the lymphatic system and are the main infectious causes of ENV.6 Large tumors or lymphomas are insidious causes of lymphatic obstruction and should be ruled out when investigating for ENV. Other risk factors include obesity, chronic venous insufficiency, surgery, trauma, radiation, and uncontrolled congestive heart failure.1,6,8
An ENV diagnosis is clinicopathologic, involving a comprehensive metabolic panel and complete blood cell count with differential. A biopsy is needed for pathologic confirmation and to rule out malignancy. Histologically, ENV is characterized by pseudoepitheliomatous hyperplasia, dermal fibrosis, hyperkeratosis of the epidermis, and dilated lymphatic vessels.6,8 Additional studies for diagnosis include wound and lymph node culture, Wood lamp examination, and lymphoscintigraphy.
Given the chronic and progressive nature of the disease, ENV is difficult to treat. There currently is no standard of treatment, but the mainstay of management involves reducing peripheral edema. Lifestyle changes including weight loss, extremity elevation, and increased ambulation are helpful first-line therapies.3 Compression of the affected extremity using stockings or intermittent pneumatic compression devices has proven to be beneficial with long-term use.7 Patients should be followed for wound care to prevent the infection of ulcers.2 Pharmacologic treatments include systemic retinoids, which have been shown to reduce the appearance of hyperkeratosis, verrucous lesions, and papillomatous nodules.6 Prophylactic antibiotics are reserved for advanced stages of disease or in patients with recurrent infections.2,7 In severe cases of ENV that are unresponsive to medical management, surgical intervention such as lymphatic anastomosis and debulking may be considered.9,10
Other diagnoses to consider for ENV include pretibial myxedema, lymphatic filariasis, Stewart-Treves syndrome, and papillomatosis cutis carcinoides. Pretibial myxedema is an uncommon dermatologic manifestation of Graves disease. It is a local autoimmune reaction in the cutaneous tissue characterized by hyperpigmentation, nonpitting edema, and nodules on the anterior leg. Histopathology shows increased hyaluronic acid and chondroitin as well as compression of dermal lymphatics.11
Filariasis is a parasitic infection caused by Wuchereria bancrofti, Brugia malayi or Brugia timori, and Onchocerca volvulus.6 This condition presents with elephantiasis of the affected extremities but should be considered in areas endemic for filarial parasites such as tropical and subtropical countries.12 Eosinophilia and identification of microfilaria in a peripheral blood smear would indicate parasitic infection. Stewart-Treves syndrome is a rare angiosarcoma that arises in areas of chronic lymphedema. This condition classically is seen on the upper extremities following a mastectomy with lymphadenectomy, lymph node irradiation, or both.
Stewart-Treves syndrome presents with coalescing purpuric macules and nodules that eventually coalesce into cutaneous masses. Histopathology reveals proliferating vascular channels that split apart dermal collagen with hyperchromatism and pleomorphism in the tumor endothelial cells that line these channels.13
Papillomatosis cutis carcinoides is a low-grade squamous cell carcinoma that occurs secondary to human papillomavirus commonly affecting the mouth, anogenital area, and the plantar surfaces of the feet. It presents with exophytic growths and ulcerated tumors that are unilateral and asymmetrical. The presence of blunt-shaped tumor projections extending deep into the dermis to form sinuses and keratin-filled cysts is characteristic of papillomatosis cutis carcinoides.14
- Dean SM, Zirwas MJ, Horst AV. Elephantiasis nostras verrucosa: an institutional analysis of 21 cases. J Am Acad Dermatol. 2011;64: 1104-1110. doi:10.1016/j.jaad.2010.04.047
- Fife CE, Farrow W, Hebert AA, et al. Skin and wound care in lymphedema patients: a taxonomy, primer, and literature review. Adv Skin Wound Care. 2017;30:305-318. doi:10.1097/01.ASW.0000520501.23702.82
- Boyd J, Sloan S, Meffert J. Elephantiasis nostrum verrucosa of the abdomen: clinical results with tazarotene. J Drugs Dermatol. 2004; 3:446-448.
- Nakai K, Taoka R, Sugimoto M, et al. Genital elephantiasis possibly caused by chronic inguinal eczema with streptococcal infection. J Dermatol. 2019;46:E196-E198. doi:10.1111/1346-8138.14746
- Carlson JA, Mazza J, Kircher K, et al. Otophyma: a case report and review of the literature of lymphedema (elephantiasis) of the ear. Am J Dermatopathol. 2008;30:67-72. doi:10.1097/DAD.0b013e31815cd937
- Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146. doi:10.2165/00128071-200809030-00001
- Yoho RM, Budny AM, Pea AS. Elephantiasis nostras verrucosa. J Am Podiatr Med Assoc. 2006;96:442-444. doi:10.7547/0960442
- Yosipovitch G, DeVore A, Dawn A. Obesity and the skin: skin physiology and skin manifestations of obesity. J Am Acad Dermatol. 2007;56:901-920. doi:10.1016/j.jaad.2006.12.004
- Iwao F, Sato-Matsumura KC, Sawamura D, et al. Elephantiasis nostras verrucosa successfully treated by surgical debridement. Dermatol Surg. 2004;30:939-941. doi:10.1111/j.1524-4725.2004.30267.x
- Tiwari A, Cheng KS, Button M, et al. Differential diagnosis, investigation, and current treatment of lower limb lymphedema. Arch Surg. 2003;138:152-161. doi:10.1001/archsurg.138.2.152
- Fatourechi V. Pretibial myxedema: pathophysiology and treatment options. Am J Clin Dermatol. 2005;6:295-309. doi:10.2165 /00128071-200506050-00003
- Addiss DG, Brady MA. Morbidity management in the Global Programme to Eliminate Lymphatic Filariasis: a review of the scientific literature. Filaria J. 2007;6:2. doi:10.1186/1475-2883-6-2
- Bernia E, Rios-Viñuela E, Requena C. Stewart-Treves syndrome. JAMA Dermatol. 2021;157:721. doi:10.1001/jamadermatol.2021.0341
- Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-24. doi:10.1016/0190-9622(95)90177-9
The Diagnosis: Elephantiasis Nostras Verrucosa
Histopathology revealed a benign fibroepithelial polyp demonstrating areas of hyperkeratosis, acanthosis, and focal papillomatosis (Figure, A). Increased superficial vessels with dilated lymphatics, stellate fibroblasts, edematous stroma, and plasmolymphocytosis also were noted (Figure, B). Clinical and histopathological findings led to a diagnosis of lymphedema papules in the setting of elephantiasis nostra verrucosa (ENV).
Elephantiasis nostras verrucosa is a complication of long-standing nonfilarial obstruction of lymphatic drainage leading to grotesque enlargement of the affected areas. Common cutaneous manifestations of ENV include nonpitting edema, dermal fibrosis, and extensive hyperkeratosis with verrucous and papillomatous lesions.1 In the beginning stages of ENV, the skin has a cobblestonelike appearance. As the disease progresses, the verrucous lesions continue to enlarge, giving the affected area a mossy appearance. Although less common, groupings of large papillomas similar to our patient’s presentation also can form.2 Ulcer formation is more likely to occur in advanced disease states, increasing the risk for bacterial and fungal colonization. Elephantiasis nostras verrucosa classically affects the legs; however, this condition can develop in any area with chronic lymphedema. Cases of ENV involving the arms, abdomen, scrotum, and ear have been documented.3-5
The pathogenesis of ENV involves the proliferation of fibroblasts and fibrosis secondary to lymphostasis and inflammation.6 When interstitial fluid builds up in the affected region, the protein-rich fluid is believed to trigger fibrogenesis and increase macrophage, keratinocyte, and adipocyte activity.7 Because of this inflammatory process, dilation and fibrosis of the lymphatic channels develop. Lymphatic obstruction can have several etiologies, most notably infection and malignancy. Staphylococcal lymphangitis and erysipelas create fibrosis of the lymphatic system and are the main infectious causes of ENV.6 Large tumors or lymphomas are insidious causes of lymphatic obstruction and should be ruled out when investigating for ENV. Other risk factors include obesity, chronic venous insufficiency, surgery, trauma, radiation, and uncontrolled congestive heart failure.1,6,8
An ENV diagnosis is clinicopathologic, involving a comprehensive metabolic panel and complete blood cell count with differential. A biopsy is needed for pathologic confirmation and to rule out malignancy. Histologically, ENV is characterized by pseudoepitheliomatous hyperplasia, dermal fibrosis, hyperkeratosis of the epidermis, and dilated lymphatic vessels.6,8 Additional studies for diagnosis include wound and lymph node culture, Wood lamp examination, and lymphoscintigraphy.
Given the chronic and progressive nature of the disease, ENV is difficult to treat. There currently is no standard of treatment, but the mainstay of management involves reducing peripheral edema. Lifestyle changes including weight loss, extremity elevation, and increased ambulation are helpful first-line therapies.3 Compression of the affected extremity using stockings or intermittent pneumatic compression devices has proven to be beneficial with long-term use.7 Patients should be followed for wound care to prevent the infection of ulcers.2 Pharmacologic treatments include systemic retinoids, which have been shown to reduce the appearance of hyperkeratosis, verrucous lesions, and papillomatous nodules.6 Prophylactic antibiotics are reserved for advanced stages of disease or in patients with recurrent infections.2,7 In severe cases of ENV that are unresponsive to medical management, surgical intervention such as lymphatic anastomosis and debulking may be considered.9,10
Other diagnoses to consider for ENV include pretibial myxedema, lymphatic filariasis, Stewart-Treves syndrome, and papillomatosis cutis carcinoides. Pretibial myxedema is an uncommon dermatologic manifestation of Graves disease. It is a local autoimmune reaction in the cutaneous tissue characterized by hyperpigmentation, nonpitting edema, and nodules on the anterior leg. Histopathology shows increased hyaluronic acid and chondroitin as well as compression of dermal lymphatics.11
Filariasis is a parasitic infection caused by Wuchereria bancrofti, Brugia malayi or Brugia timori, and Onchocerca volvulus.6 This condition presents with elephantiasis of the affected extremities but should be considered in areas endemic for filarial parasites such as tropical and subtropical countries.12 Eosinophilia and identification of microfilaria in a peripheral blood smear would indicate parasitic infection. Stewart-Treves syndrome is a rare angiosarcoma that arises in areas of chronic lymphedema. This condition classically is seen on the upper extremities following a mastectomy with lymphadenectomy, lymph node irradiation, or both.
Stewart-Treves syndrome presents with coalescing purpuric macules and nodules that eventually coalesce into cutaneous masses. Histopathology reveals proliferating vascular channels that split apart dermal collagen with hyperchromatism and pleomorphism in the tumor endothelial cells that line these channels.13
Papillomatosis cutis carcinoides is a low-grade squamous cell carcinoma that occurs secondary to human papillomavirus commonly affecting the mouth, anogenital area, and the plantar surfaces of the feet. It presents with exophytic growths and ulcerated tumors that are unilateral and asymmetrical. The presence of blunt-shaped tumor projections extending deep into the dermis to form sinuses and keratin-filled cysts is characteristic of papillomatosis cutis carcinoides.14
The Diagnosis: Elephantiasis Nostras Verrucosa
Histopathology revealed a benign fibroepithelial polyp demonstrating areas of hyperkeratosis, acanthosis, and focal papillomatosis (Figure, A). Increased superficial vessels with dilated lymphatics, stellate fibroblasts, edematous stroma, and plasmolymphocytosis also were noted (Figure, B). Clinical and histopathological findings led to a diagnosis of lymphedema papules in the setting of elephantiasis nostra verrucosa (ENV).
Elephantiasis nostras verrucosa is a complication of long-standing nonfilarial obstruction of lymphatic drainage leading to grotesque enlargement of the affected areas. Common cutaneous manifestations of ENV include nonpitting edema, dermal fibrosis, and extensive hyperkeratosis with verrucous and papillomatous lesions.1 In the beginning stages of ENV, the skin has a cobblestonelike appearance. As the disease progresses, the verrucous lesions continue to enlarge, giving the affected area a mossy appearance. Although less common, groupings of large papillomas similar to our patient’s presentation also can form.2 Ulcer formation is more likely to occur in advanced disease states, increasing the risk for bacterial and fungal colonization. Elephantiasis nostras verrucosa classically affects the legs; however, this condition can develop in any area with chronic lymphedema. Cases of ENV involving the arms, abdomen, scrotum, and ear have been documented.3-5
The pathogenesis of ENV involves the proliferation of fibroblasts and fibrosis secondary to lymphostasis and inflammation.6 When interstitial fluid builds up in the affected region, the protein-rich fluid is believed to trigger fibrogenesis and increase macrophage, keratinocyte, and adipocyte activity.7 Because of this inflammatory process, dilation and fibrosis of the lymphatic channels develop. Lymphatic obstruction can have several etiologies, most notably infection and malignancy. Staphylococcal lymphangitis and erysipelas create fibrosis of the lymphatic system and are the main infectious causes of ENV.6 Large tumors or lymphomas are insidious causes of lymphatic obstruction and should be ruled out when investigating for ENV. Other risk factors include obesity, chronic venous insufficiency, surgery, trauma, radiation, and uncontrolled congestive heart failure.1,6,8
An ENV diagnosis is clinicopathologic, involving a comprehensive metabolic panel and complete blood cell count with differential. A biopsy is needed for pathologic confirmation and to rule out malignancy. Histologically, ENV is characterized by pseudoepitheliomatous hyperplasia, dermal fibrosis, hyperkeratosis of the epidermis, and dilated lymphatic vessels.6,8 Additional studies for diagnosis include wound and lymph node culture, Wood lamp examination, and lymphoscintigraphy.
Given the chronic and progressive nature of the disease, ENV is difficult to treat. There currently is no standard of treatment, but the mainstay of management involves reducing peripheral edema. Lifestyle changes including weight loss, extremity elevation, and increased ambulation are helpful first-line therapies.3 Compression of the affected extremity using stockings or intermittent pneumatic compression devices has proven to be beneficial with long-term use.7 Patients should be followed for wound care to prevent the infection of ulcers.2 Pharmacologic treatments include systemic retinoids, which have been shown to reduce the appearance of hyperkeratosis, verrucous lesions, and papillomatous nodules.6 Prophylactic antibiotics are reserved for advanced stages of disease or in patients with recurrent infections.2,7 In severe cases of ENV that are unresponsive to medical management, surgical intervention such as lymphatic anastomosis and debulking may be considered.9,10
Other diagnoses to consider for ENV include pretibial myxedema, lymphatic filariasis, Stewart-Treves syndrome, and papillomatosis cutis carcinoides. Pretibial myxedema is an uncommon dermatologic manifestation of Graves disease. It is a local autoimmune reaction in the cutaneous tissue characterized by hyperpigmentation, nonpitting edema, and nodules on the anterior leg. Histopathology shows increased hyaluronic acid and chondroitin as well as compression of dermal lymphatics.11
Filariasis is a parasitic infection caused by Wuchereria bancrofti, Brugia malayi or Brugia timori, and Onchocerca volvulus.6 This condition presents with elephantiasis of the affected extremities but should be considered in areas endemic for filarial parasites such as tropical and subtropical countries.12 Eosinophilia and identification of microfilaria in a peripheral blood smear would indicate parasitic infection. Stewart-Treves syndrome is a rare angiosarcoma that arises in areas of chronic lymphedema. This condition classically is seen on the upper extremities following a mastectomy with lymphadenectomy, lymph node irradiation, or both.
Stewart-Treves syndrome presents with coalescing purpuric macules and nodules that eventually coalesce into cutaneous masses. Histopathology reveals proliferating vascular channels that split apart dermal collagen with hyperchromatism and pleomorphism in the tumor endothelial cells that line these channels.13
Papillomatosis cutis carcinoides is a low-grade squamous cell carcinoma that occurs secondary to human papillomavirus commonly affecting the mouth, anogenital area, and the plantar surfaces of the feet. It presents with exophytic growths and ulcerated tumors that are unilateral and asymmetrical. The presence of blunt-shaped tumor projections extending deep into the dermis to form sinuses and keratin-filled cysts is characteristic of papillomatosis cutis carcinoides.14
- Dean SM, Zirwas MJ, Horst AV. Elephantiasis nostras verrucosa: an institutional analysis of 21 cases. J Am Acad Dermatol. 2011;64: 1104-1110. doi:10.1016/j.jaad.2010.04.047
- Fife CE, Farrow W, Hebert AA, et al. Skin and wound care in lymphedema patients: a taxonomy, primer, and literature review. Adv Skin Wound Care. 2017;30:305-318. doi:10.1097/01.ASW.0000520501.23702.82
- Boyd J, Sloan S, Meffert J. Elephantiasis nostrum verrucosa of the abdomen: clinical results with tazarotene. J Drugs Dermatol. 2004; 3:446-448.
- Nakai K, Taoka R, Sugimoto M, et al. Genital elephantiasis possibly caused by chronic inguinal eczema with streptococcal infection. J Dermatol. 2019;46:E196-E198. doi:10.1111/1346-8138.14746
- Carlson JA, Mazza J, Kircher K, et al. Otophyma: a case report and review of the literature of lymphedema (elephantiasis) of the ear. Am J Dermatopathol. 2008;30:67-72. doi:10.1097/DAD.0b013e31815cd937
- Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146. doi:10.2165/00128071-200809030-00001
- Yoho RM, Budny AM, Pea AS. Elephantiasis nostras verrucosa. J Am Podiatr Med Assoc. 2006;96:442-444. doi:10.7547/0960442
- Yosipovitch G, DeVore A, Dawn A. Obesity and the skin: skin physiology and skin manifestations of obesity. J Am Acad Dermatol. 2007;56:901-920. doi:10.1016/j.jaad.2006.12.004
- Iwao F, Sato-Matsumura KC, Sawamura D, et al. Elephantiasis nostras verrucosa successfully treated by surgical debridement. Dermatol Surg. 2004;30:939-941. doi:10.1111/j.1524-4725.2004.30267.x
- Tiwari A, Cheng KS, Button M, et al. Differential diagnosis, investigation, and current treatment of lower limb lymphedema. Arch Surg. 2003;138:152-161. doi:10.1001/archsurg.138.2.152
- Fatourechi V. Pretibial myxedema: pathophysiology and treatment options. Am J Clin Dermatol. 2005;6:295-309. doi:10.2165 /00128071-200506050-00003
- Addiss DG, Brady MA. Morbidity management in the Global Programme to Eliminate Lymphatic Filariasis: a review of the scientific literature. Filaria J. 2007;6:2. doi:10.1186/1475-2883-6-2
- Bernia E, Rios-Viñuela E, Requena C. Stewart-Treves syndrome. JAMA Dermatol. 2021;157:721. doi:10.1001/jamadermatol.2021.0341
- Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-24. doi:10.1016/0190-9622(95)90177-9
- Dean SM, Zirwas MJ, Horst AV. Elephantiasis nostras verrucosa: an institutional analysis of 21 cases. J Am Acad Dermatol. 2011;64: 1104-1110. doi:10.1016/j.jaad.2010.04.047
- Fife CE, Farrow W, Hebert AA, et al. Skin and wound care in lymphedema patients: a taxonomy, primer, and literature review. Adv Skin Wound Care. 2017;30:305-318. doi:10.1097/01.ASW.0000520501.23702.82
- Boyd J, Sloan S, Meffert J. Elephantiasis nostrum verrucosa of the abdomen: clinical results with tazarotene. J Drugs Dermatol. 2004; 3:446-448.
- Nakai K, Taoka R, Sugimoto M, et al. Genital elephantiasis possibly caused by chronic inguinal eczema with streptococcal infection. J Dermatol. 2019;46:E196-E198. doi:10.1111/1346-8138.14746
- Carlson JA, Mazza J, Kircher K, et al. Otophyma: a case report and review of the literature of lymphedema (elephantiasis) of the ear. Am J Dermatopathol. 2008;30:67-72. doi:10.1097/DAD.0b013e31815cd937
- Sisto K, Khachemoune A. Elephantiasis nostras verrucosa: a review. Am J Clin Dermatol. 2008;9:141-146. doi:10.2165/00128071-200809030-00001
- Yoho RM, Budny AM, Pea AS. Elephantiasis nostras verrucosa. J Am Podiatr Med Assoc. 2006;96:442-444. doi:10.7547/0960442
- Yosipovitch G, DeVore A, Dawn A. Obesity and the skin: skin physiology and skin manifestations of obesity. J Am Acad Dermatol. 2007;56:901-920. doi:10.1016/j.jaad.2006.12.004
- Iwao F, Sato-Matsumura KC, Sawamura D, et al. Elephantiasis nostras verrucosa successfully treated by surgical debridement. Dermatol Surg. 2004;30:939-941. doi:10.1111/j.1524-4725.2004.30267.x
- Tiwari A, Cheng KS, Button M, et al. Differential diagnosis, investigation, and current treatment of lower limb lymphedema. Arch Surg. 2003;138:152-161. doi:10.1001/archsurg.138.2.152
- Fatourechi V. Pretibial myxedema: pathophysiology and treatment options. Am J Clin Dermatol. 2005;6:295-309. doi:10.2165 /00128071-200506050-00003
- Addiss DG, Brady MA. Morbidity management in the Global Programme to Eliminate Lymphatic Filariasis: a review of the scientific literature. Filaria J. 2007;6:2. doi:10.1186/1475-2883-6-2
- Bernia E, Rios-Viñuela E, Requena C. Stewart-Treves syndrome. JAMA Dermatol. 2021;157:721. doi:10.1001/jamadermatol.2021.0341
- Schwartz RA. Verrucous carcinoma of the skin and mucosa. J Am Acad Dermatol. 1995;32:1-24. doi:10.1016/0190-9622(95)90177-9
A 61-year-old man presented with painful skin growths on the right pretibial region of several months’ duration. The patient reported pain due to friction between the lesions and underlying skin, leading to erosions. His medical history was remarkable for morbid obesity (body mass index of 62), chronic venous stasis, and chronic lymphedema. The patient was followed for wound care of venous stasis ulcers. Dermatologic examination revealed multiple 5- to 30-mm, flesh-colored, fingerlike projections on the right tibial region. A biopsy was obtained and submitted for histopathologic analysis.

The next blood pressure breakthrough: temporary tattoos
As scientists work on wearable technology that promises to revolutionize health care, researchers from the University of Texas at Austin and Texas A&M University, College Station, are reporting a big win in the pursuit of one highly popular target: a noninvasive solution for continuous blood pressure monitoring at home.
Not only that, but this development comes in the surprising form of a temporary tattoo. That’s right: Just like the kind that children like to wear.
the researchers report in their new study.
“With this new technology, we are going to have an opportunity to understand how our blood pressure fluctuates during the day. We will be able to quantify how stress is impacting us,” says Roozbeh Jafari, PhD, a professor of biomedical engineering, electrical engineering, and computer science at Texas A&M, College Station, and a coauthor of the study.
Revealing the whole picture, not just dots
At-home blood pressure monitors have been around for many years now. They work just like the blood pressure machines doctors use at their office: You place your arm inside a cuff, press a button, feel a squeeze on your arm, and get a reading.
While results from this method are accurate, they are also just a moment in time. Our blood pressure can vary greatly throughout the day – especially among people who have labile hypertension, where blood pressure changes from one extreme to the other. So, looking at point-in-time readings is a bit like focusing on a few dots inside of a pointillism painting – one might miss the bigger picture.
Doctors may also find continuous monitoring useful for getting rid of false readings from “white coat syndrome.” Basically, this means a person’s blood pressure rises due to the anxiety of being in a doctor’s office but is not true hypertension.
Bottom line: The ability to monitor a person’s blood pressure continuously for hours or even days can provide clearer, and more accurate, insights into a person’s health.
How do health monitoring tattoos work?
Electronic tattoos for health monitoring are not completely new. John A. Rogers, PhD, of Northwestern University, Chicago, first put forth the idea of monitoring through temporary tattoos 12 years ago. Some concepts, such as UV monitoring tattoos, had already been adopted by scientists and put on the market. But the existing models weren’t suitable for monitoring blood pressure, according to Deji Akinwande, PhD, a professor of electrical and computer engineering at the University of Texas at Austin and another coauthor of the study.
“[UV monitoring tattoos] are very thick,” he says. “They create too much movement when used to measure blood pressure because they slide around.”
So, the Texas-based research team worked to develop an option that was slimmer and more stable.
“The key ingredient within e-tattoos is graphene,” says Dr. Akinwande.
Graphene is carbon that’s similar to what’s inside your graphite pencil. The material is conductive, meaning it can conduct small electrical currents through the skin. For blood pressure monitoring, graphene promotes bioelectrical impedance analysis (BIA), which is like the technology used in smart scales that measure body fat.
With e-tattoos, the thin layers of graphene stick to the skin and do not slide around, getting rid of “artifacts,” or bad data. The graphene e-tattoos can be worn on the skin for about a week – or roughly as long as the temporary tattoos kids love.
Once the graphene captures the raw data, a machine learning algorithm interprets the information and provides results in units used for measuring blood pressure: millimeters of mercury (mmHg), commonly referred to as blood pressure “points.”
How accurate are the results? The tests measured blood pressure within 0.2 ± 5.8 mmHg (systolic), 0.2 ± 4.5 mmHg (diastolic), and 0.1 ± 5.3 mmHg (mean arterial pressure). In other words: If this were a basketball player shooting baskets, the great majority of shots taken would be swishes and occasionally a few would hit the rim. That means good accuracy.
When will e-tattoos be available?
The teams of Dr. Jafari and Dr. Akinwande are working on a second generation of their e-tattoo that they expect to be available in the next 5 years.
The upgrade they envision will be smaller and compatible with smartwatches and phones that use Bluetooth technology and near-field communication (NFC) to transfer data and give it power. With these updates, e-tattoos for continuous blood pressure monitoring will be ready for clinical trials and mainstream use soon after.
“Everyone can benefit from knowing their blood pressure recordings,” Dr. Akinwande says. “It is not just for people at risk for hypertension but for others to proactively monitor their health, for stress and other factors.”
A version of this article first appeared on WebMD.com.
As scientists work on wearable technology that promises to revolutionize health care, researchers from the University of Texas at Austin and Texas A&M University, College Station, are reporting a big win in the pursuit of one highly popular target: a noninvasive solution for continuous blood pressure monitoring at home.
Not only that, but this development comes in the surprising form of a temporary tattoo. That’s right: Just like the kind that children like to wear.
the researchers report in their new study.
“With this new technology, we are going to have an opportunity to understand how our blood pressure fluctuates during the day. We will be able to quantify how stress is impacting us,” says Roozbeh Jafari, PhD, a professor of biomedical engineering, electrical engineering, and computer science at Texas A&M, College Station, and a coauthor of the study.
Revealing the whole picture, not just dots
At-home blood pressure monitors have been around for many years now. They work just like the blood pressure machines doctors use at their office: You place your arm inside a cuff, press a button, feel a squeeze on your arm, and get a reading.
While results from this method are accurate, they are also just a moment in time. Our blood pressure can vary greatly throughout the day – especially among people who have labile hypertension, where blood pressure changes from one extreme to the other. So, looking at point-in-time readings is a bit like focusing on a few dots inside of a pointillism painting – one might miss the bigger picture.
Doctors may also find continuous monitoring useful for getting rid of false readings from “white coat syndrome.” Basically, this means a person’s blood pressure rises due to the anxiety of being in a doctor’s office but is not true hypertension.
Bottom line: The ability to monitor a person’s blood pressure continuously for hours or even days can provide clearer, and more accurate, insights into a person’s health.
How do health monitoring tattoos work?
Electronic tattoos for health monitoring are not completely new. John A. Rogers, PhD, of Northwestern University, Chicago, first put forth the idea of monitoring through temporary tattoos 12 years ago. Some concepts, such as UV monitoring tattoos, had already been adopted by scientists and put on the market. But the existing models weren’t suitable for monitoring blood pressure, according to Deji Akinwande, PhD, a professor of electrical and computer engineering at the University of Texas at Austin and another coauthor of the study.
“[UV monitoring tattoos] are very thick,” he says. “They create too much movement when used to measure blood pressure because they slide around.”
So, the Texas-based research team worked to develop an option that was slimmer and more stable.
“The key ingredient within e-tattoos is graphene,” says Dr. Akinwande.
Graphene is carbon that’s similar to what’s inside your graphite pencil. The material is conductive, meaning it can conduct small electrical currents through the skin. For blood pressure monitoring, graphene promotes bioelectrical impedance analysis (BIA), which is like the technology used in smart scales that measure body fat.
With e-tattoos, the thin layers of graphene stick to the skin and do not slide around, getting rid of “artifacts,” or bad data. The graphene e-tattoos can be worn on the skin for about a week – or roughly as long as the temporary tattoos kids love.
Once the graphene captures the raw data, a machine learning algorithm interprets the information and provides results in units used for measuring blood pressure: millimeters of mercury (mmHg), commonly referred to as blood pressure “points.”
How accurate are the results? The tests measured blood pressure within 0.2 ± 5.8 mmHg (systolic), 0.2 ± 4.5 mmHg (diastolic), and 0.1 ± 5.3 mmHg (mean arterial pressure). In other words: If this were a basketball player shooting baskets, the great majority of shots taken would be swishes and occasionally a few would hit the rim. That means good accuracy.
When will e-tattoos be available?
The teams of Dr. Jafari and Dr. Akinwande are working on a second generation of their e-tattoo that they expect to be available in the next 5 years.
The upgrade they envision will be smaller and compatible with smartwatches and phones that use Bluetooth technology and near-field communication (NFC) to transfer data and give it power. With these updates, e-tattoos for continuous blood pressure monitoring will be ready for clinical trials and mainstream use soon after.
“Everyone can benefit from knowing their blood pressure recordings,” Dr. Akinwande says. “It is not just for people at risk for hypertension but for others to proactively monitor their health, for stress and other factors.”
A version of this article first appeared on WebMD.com.
As scientists work on wearable technology that promises to revolutionize health care, researchers from the University of Texas at Austin and Texas A&M University, College Station, are reporting a big win in the pursuit of one highly popular target: a noninvasive solution for continuous blood pressure monitoring at home.
Not only that, but this development comes in the surprising form of a temporary tattoo. That’s right: Just like the kind that children like to wear.
the researchers report in their new study.
“With this new technology, we are going to have an opportunity to understand how our blood pressure fluctuates during the day. We will be able to quantify how stress is impacting us,” says Roozbeh Jafari, PhD, a professor of biomedical engineering, electrical engineering, and computer science at Texas A&M, College Station, and a coauthor of the study.
Revealing the whole picture, not just dots
At-home blood pressure monitors have been around for many years now. They work just like the blood pressure machines doctors use at their office: You place your arm inside a cuff, press a button, feel a squeeze on your arm, and get a reading.
While results from this method are accurate, they are also just a moment in time. Our blood pressure can vary greatly throughout the day – especially among people who have labile hypertension, where blood pressure changes from one extreme to the other. So, looking at point-in-time readings is a bit like focusing on a few dots inside of a pointillism painting – one might miss the bigger picture.
Doctors may also find continuous monitoring useful for getting rid of false readings from “white coat syndrome.” Basically, this means a person’s blood pressure rises due to the anxiety of being in a doctor’s office but is not true hypertension.
Bottom line: The ability to monitor a person’s blood pressure continuously for hours or even days can provide clearer, and more accurate, insights into a person’s health.
How do health monitoring tattoos work?
Electronic tattoos for health monitoring are not completely new. John A. Rogers, PhD, of Northwestern University, Chicago, first put forth the idea of monitoring through temporary tattoos 12 years ago. Some concepts, such as UV monitoring tattoos, had already been adopted by scientists and put on the market. But the existing models weren’t suitable for monitoring blood pressure, according to Deji Akinwande, PhD, a professor of electrical and computer engineering at the University of Texas at Austin and another coauthor of the study.
“[UV monitoring tattoos] are very thick,” he says. “They create too much movement when used to measure blood pressure because they slide around.”
So, the Texas-based research team worked to develop an option that was slimmer and more stable.
“The key ingredient within e-tattoos is graphene,” says Dr. Akinwande.
Graphene is carbon that’s similar to what’s inside your graphite pencil. The material is conductive, meaning it can conduct small electrical currents through the skin. For blood pressure monitoring, graphene promotes bioelectrical impedance analysis (BIA), which is like the technology used in smart scales that measure body fat.
With e-tattoos, the thin layers of graphene stick to the skin and do not slide around, getting rid of “artifacts,” or bad data. The graphene e-tattoos can be worn on the skin for about a week – or roughly as long as the temporary tattoos kids love.
Once the graphene captures the raw data, a machine learning algorithm interprets the information and provides results in units used for measuring blood pressure: millimeters of mercury (mmHg), commonly referred to as blood pressure “points.”
How accurate are the results? The tests measured blood pressure within 0.2 ± 5.8 mmHg (systolic), 0.2 ± 4.5 mmHg (diastolic), and 0.1 ± 5.3 mmHg (mean arterial pressure). In other words: If this were a basketball player shooting baskets, the great majority of shots taken would be swishes and occasionally a few would hit the rim. That means good accuracy.
When will e-tattoos be available?
The teams of Dr. Jafari and Dr. Akinwande are working on a second generation of their e-tattoo that they expect to be available in the next 5 years.
The upgrade they envision will be smaller and compatible with smartwatches and phones that use Bluetooth technology and near-field communication (NFC) to transfer data and give it power. With these updates, e-tattoos for continuous blood pressure monitoring will be ready for clinical trials and mainstream use soon after.
“Everyone can benefit from knowing their blood pressure recordings,” Dr. Akinwande says. “It is not just for people at risk for hypertension but for others to proactively monitor their health, for stress and other factors.”
A version of this article first appeared on WebMD.com.
Two distinct phenotypes of COVID-related myocarditis emerge
Researchers from France have identified two distinct phenotypes of fulminant COVID-19–related myocarditis in adults, with different clinical presentations, immunologic profiles, and outcomes.
Differentiation between the two bioclinical entities is important to understand for patient management and further pathophysiological studies, they said.
The first phenotype occurs early (within a few days) in acute SARS-CoV-2 infection, with active viral replication (polymerase chain reaction positive) in adults who meet criteria for multisystem inflammatory syndrome (MIS-A+).
In this early phenotype, there is “limited systemic inflammation without skin and mucosal involvement, but myocardial dysfunction is fulminant and frequently associated with large pericardial effusions. These cases more often require extracorporeal membrane oxygenation [ECMO],” Guy Gorochov, MD, PhD, Sorbonne University, Paris, said in an interview.
The second is a delayed, postinfectious, immune-driven phenotype that occurs in adults who fail to meet the criteria for MIS-A (MIS-A–).
This phenotype occurs weeks after SARS-CoV-2 infection, usually beyond detectable active viral replication (PCR–) in the context of specific immune response and severe systemic inflammation with skin and mucosal involvement. Myocardial dysfunction is more progressive and rarely associated with large pericardial effusions, Dr. Gorochov explained.
The study was published in the Journal of the American College of Cardiology.
Evolving understanding
The findings are based on a retrospective analysis of 38 patients without a history of COVID-19 vaccination who were admitted to the intensive care unit from March 2020 to June 2021 for suspected fulminant COVID-19 myocarditis.
Patients were confirmed to have SARS-CoV-2 infection by PCR and/or by serologic testing. As noted in other studies, the patients were predominantly young men (66%; median age, 27.5 years). Twenty-five (66%) patients were MIS-A+ and 13 (34%) were MIS-A–.
In general, the MIS-A– patients were sicker and had worse outcomes.
Specifically, compared with the MIS-A+ patients, MIS-A– patients had a shorter time between the onset of COVID-19 symptoms and the development of myocarditis, a shorter time to ICU admission, and more severe presentations assessed using lower left ventricular ejection fraction and sequential organ failure assessment scores.
MIS-A– patients also had higher lactate levels, were more likely to need venoarterial ECMO (92% vs 16%), had higher ICU mortality (31% vs. 4%), and a had lower probability of survival at 3 months (68% vs. 96%), compared with their MIS-A+ peers.
Immunologic differences
The immunologic profiles of these two distinct clinical phenotypes also differed.
In MIS-A– early-type COVID-19 myocarditis, RNA polymerase III autoantibodies are frequently positive and serum levels of antiviral interferon-alpha and granulocyte-attracting interleukin-8 are elevated.
In contrast, in MIS-A+ delayed-type COVID-19 myocarditis, RNA polymerase III autoantibodies are negative and serum levels of IL-17 and IL-22 are highly elevated.
“We suggest that IL-17 and IL-22 are novel criteria that should help to assess in adults the recently recognized MIS-A,” Dr. Gorochov told this news organization. “It should be tested whether IL-17 and IL-22 are also elevated in children with MIS-C.”
The researchers also observed “extremely” high serum IL-10 levels in both patient groups. This has been previously associated with severe myocardial injury and an increase in the risk for death in severe COVID-19 patients.
The researchers said the phenotypic clustering of patients with fulminant COVID-19–related myocarditis “seems relevant” for their management.
MIS-A– cases, owing to the high risk for evolution toward refractory cardiogenic shock, should be “urgently” referred to a center with venoarterial ECMO and closely monitored to prevent a “too-late” cannulation, especially under cardiopulmonary resuscitation, known to be associated with poor outcomes, they advised.
They noted that the five patients who died in their series had late venoarterial ECMO implantation, while undergoing multiple organ failures or resuscitation.
Conversely, the risk for evolution to refractory cardiogenic shock is lower in MIS-A+ cases. However, identifying MIS-A+ cases is “all the more important given that numerous data support the efficacy of corticosteroids and/or intravenous immunoglobulins in MIS-C,” Dr. Gorochov and colleagues wrote.
The authors of a linked editorial said the French team should be “commended on their work in furthering our understanding of fulminant myocarditis related to COVID-19 infection.”
Ajith Nair, MD, Baylor College of Medicine, and Anita Deswal, MD, MPH, University of Texas M.D. Anderson Cancer Center, both in Houston, noted that fulminant myocarditis is rare and can result from either of two mechanisms: viral tropism or an immune-mediated mechanism.
“It remains to be seen whether using antiviral therapy versus immunomodulatory therapy on the basis of clinical and cytokine profiles will yield benefits,” they wrote.
“Fulminant myocarditis invariably requires hemodynamic support and carries a high mortality risk if it is recognized late. However, the long-term prognosis in patients who survive the critical period is favorable, with recovery of myocardial function,” they added.
“This study highlights the ever-shifting understanding of the pathophysiology and therapeutic approaches to fulminant myocarditis,” Dr. Nair and Dr. Deswal concluded.
This research was supported in part by the Foundation of France, French National Research Agency, Sorbonne University, and Clinical Research Hospital. The researchers have filed a patent application based on these results. Dr. Nair and Dr. Deswal have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Researchers from France have identified two distinct phenotypes of fulminant COVID-19–related myocarditis in adults, with different clinical presentations, immunologic profiles, and outcomes.
Differentiation between the two bioclinical entities is important to understand for patient management and further pathophysiological studies, they said.
The first phenotype occurs early (within a few days) in acute SARS-CoV-2 infection, with active viral replication (polymerase chain reaction positive) in adults who meet criteria for multisystem inflammatory syndrome (MIS-A+).
In this early phenotype, there is “limited systemic inflammation without skin and mucosal involvement, but myocardial dysfunction is fulminant and frequently associated with large pericardial effusions. These cases more often require extracorporeal membrane oxygenation [ECMO],” Guy Gorochov, MD, PhD, Sorbonne University, Paris, said in an interview.
The second is a delayed, postinfectious, immune-driven phenotype that occurs in adults who fail to meet the criteria for MIS-A (MIS-A–).
This phenotype occurs weeks after SARS-CoV-2 infection, usually beyond detectable active viral replication (PCR–) in the context of specific immune response and severe systemic inflammation with skin and mucosal involvement. Myocardial dysfunction is more progressive and rarely associated with large pericardial effusions, Dr. Gorochov explained.
The study was published in the Journal of the American College of Cardiology.
Evolving understanding
The findings are based on a retrospective analysis of 38 patients without a history of COVID-19 vaccination who were admitted to the intensive care unit from March 2020 to June 2021 for suspected fulminant COVID-19 myocarditis.
Patients were confirmed to have SARS-CoV-2 infection by PCR and/or by serologic testing. As noted in other studies, the patients were predominantly young men (66%; median age, 27.5 years). Twenty-five (66%) patients were MIS-A+ and 13 (34%) were MIS-A–.
In general, the MIS-A– patients were sicker and had worse outcomes.
Specifically, compared with the MIS-A+ patients, MIS-A– patients had a shorter time between the onset of COVID-19 symptoms and the development of myocarditis, a shorter time to ICU admission, and more severe presentations assessed using lower left ventricular ejection fraction and sequential organ failure assessment scores.
MIS-A– patients also had higher lactate levels, were more likely to need venoarterial ECMO (92% vs 16%), had higher ICU mortality (31% vs. 4%), and a had lower probability of survival at 3 months (68% vs. 96%), compared with their MIS-A+ peers.
Immunologic differences
The immunologic profiles of these two distinct clinical phenotypes also differed.
In MIS-A– early-type COVID-19 myocarditis, RNA polymerase III autoantibodies are frequently positive and serum levels of antiviral interferon-alpha and granulocyte-attracting interleukin-8 are elevated.
In contrast, in MIS-A+ delayed-type COVID-19 myocarditis, RNA polymerase III autoantibodies are negative and serum levels of IL-17 and IL-22 are highly elevated.
“We suggest that IL-17 and IL-22 are novel criteria that should help to assess in adults the recently recognized MIS-A,” Dr. Gorochov told this news organization. “It should be tested whether IL-17 and IL-22 are also elevated in children with MIS-C.”
The researchers also observed “extremely” high serum IL-10 levels in both patient groups. This has been previously associated with severe myocardial injury and an increase in the risk for death in severe COVID-19 patients.
The researchers said the phenotypic clustering of patients with fulminant COVID-19–related myocarditis “seems relevant” for their management.
MIS-A– cases, owing to the high risk for evolution toward refractory cardiogenic shock, should be “urgently” referred to a center with venoarterial ECMO and closely monitored to prevent a “too-late” cannulation, especially under cardiopulmonary resuscitation, known to be associated with poor outcomes, they advised.
They noted that the five patients who died in their series had late venoarterial ECMO implantation, while undergoing multiple organ failures or resuscitation.
Conversely, the risk for evolution to refractory cardiogenic shock is lower in MIS-A+ cases. However, identifying MIS-A+ cases is “all the more important given that numerous data support the efficacy of corticosteroids and/or intravenous immunoglobulins in MIS-C,” Dr. Gorochov and colleagues wrote.
The authors of a linked editorial said the French team should be “commended on their work in furthering our understanding of fulminant myocarditis related to COVID-19 infection.”
Ajith Nair, MD, Baylor College of Medicine, and Anita Deswal, MD, MPH, University of Texas M.D. Anderson Cancer Center, both in Houston, noted that fulminant myocarditis is rare and can result from either of two mechanisms: viral tropism or an immune-mediated mechanism.
“It remains to be seen whether using antiviral therapy versus immunomodulatory therapy on the basis of clinical and cytokine profiles will yield benefits,” they wrote.
“Fulminant myocarditis invariably requires hemodynamic support and carries a high mortality risk if it is recognized late. However, the long-term prognosis in patients who survive the critical period is favorable, with recovery of myocardial function,” they added.
“This study highlights the ever-shifting understanding of the pathophysiology and therapeutic approaches to fulminant myocarditis,” Dr. Nair and Dr. Deswal concluded.
This research was supported in part by the Foundation of France, French National Research Agency, Sorbonne University, and Clinical Research Hospital. The researchers have filed a patent application based on these results. Dr. Nair and Dr. Deswal have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Researchers from France have identified two distinct phenotypes of fulminant COVID-19–related myocarditis in adults, with different clinical presentations, immunologic profiles, and outcomes.
Differentiation between the two bioclinical entities is important to understand for patient management and further pathophysiological studies, they said.
The first phenotype occurs early (within a few days) in acute SARS-CoV-2 infection, with active viral replication (polymerase chain reaction positive) in adults who meet criteria for multisystem inflammatory syndrome (MIS-A+).
In this early phenotype, there is “limited systemic inflammation without skin and mucosal involvement, but myocardial dysfunction is fulminant and frequently associated with large pericardial effusions. These cases more often require extracorporeal membrane oxygenation [ECMO],” Guy Gorochov, MD, PhD, Sorbonne University, Paris, said in an interview.
The second is a delayed, postinfectious, immune-driven phenotype that occurs in adults who fail to meet the criteria for MIS-A (MIS-A–).
This phenotype occurs weeks after SARS-CoV-2 infection, usually beyond detectable active viral replication (PCR–) in the context of specific immune response and severe systemic inflammation with skin and mucosal involvement. Myocardial dysfunction is more progressive and rarely associated with large pericardial effusions, Dr. Gorochov explained.
The study was published in the Journal of the American College of Cardiology.
Evolving understanding
The findings are based on a retrospective analysis of 38 patients without a history of COVID-19 vaccination who were admitted to the intensive care unit from March 2020 to June 2021 for suspected fulminant COVID-19 myocarditis.
Patients were confirmed to have SARS-CoV-2 infection by PCR and/or by serologic testing. As noted in other studies, the patients were predominantly young men (66%; median age, 27.5 years). Twenty-five (66%) patients were MIS-A+ and 13 (34%) were MIS-A–.
In general, the MIS-A– patients were sicker and had worse outcomes.
Specifically, compared with the MIS-A+ patients, MIS-A– patients had a shorter time between the onset of COVID-19 symptoms and the development of myocarditis, a shorter time to ICU admission, and more severe presentations assessed using lower left ventricular ejection fraction and sequential organ failure assessment scores.
MIS-A– patients also had higher lactate levels, were more likely to need venoarterial ECMO (92% vs 16%), had higher ICU mortality (31% vs. 4%), and a had lower probability of survival at 3 months (68% vs. 96%), compared with their MIS-A+ peers.
Immunologic differences
The immunologic profiles of these two distinct clinical phenotypes also differed.
In MIS-A– early-type COVID-19 myocarditis, RNA polymerase III autoantibodies are frequently positive and serum levels of antiviral interferon-alpha and granulocyte-attracting interleukin-8 are elevated.
In contrast, in MIS-A+ delayed-type COVID-19 myocarditis, RNA polymerase III autoantibodies are negative and serum levels of IL-17 and IL-22 are highly elevated.
“We suggest that IL-17 and IL-22 are novel criteria that should help to assess in adults the recently recognized MIS-A,” Dr. Gorochov told this news organization. “It should be tested whether IL-17 and IL-22 are also elevated in children with MIS-C.”
The researchers also observed “extremely” high serum IL-10 levels in both patient groups. This has been previously associated with severe myocardial injury and an increase in the risk for death in severe COVID-19 patients.
The researchers said the phenotypic clustering of patients with fulminant COVID-19–related myocarditis “seems relevant” for their management.
MIS-A– cases, owing to the high risk for evolution toward refractory cardiogenic shock, should be “urgently” referred to a center with venoarterial ECMO and closely monitored to prevent a “too-late” cannulation, especially under cardiopulmonary resuscitation, known to be associated with poor outcomes, they advised.
They noted that the five patients who died in their series had late venoarterial ECMO implantation, while undergoing multiple organ failures or resuscitation.
Conversely, the risk for evolution to refractory cardiogenic shock is lower in MIS-A+ cases. However, identifying MIS-A+ cases is “all the more important given that numerous data support the efficacy of corticosteroids and/or intravenous immunoglobulins in MIS-C,” Dr. Gorochov and colleagues wrote.
The authors of a linked editorial said the French team should be “commended on their work in furthering our understanding of fulminant myocarditis related to COVID-19 infection.”
Ajith Nair, MD, Baylor College of Medicine, and Anita Deswal, MD, MPH, University of Texas M.D. Anderson Cancer Center, both in Houston, noted that fulminant myocarditis is rare and can result from either of two mechanisms: viral tropism or an immune-mediated mechanism.
“It remains to be seen whether using antiviral therapy versus immunomodulatory therapy on the basis of clinical and cytokine profiles will yield benefits,” they wrote.
“Fulminant myocarditis invariably requires hemodynamic support and carries a high mortality risk if it is recognized late. However, the long-term prognosis in patients who survive the critical period is favorable, with recovery of myocardial function,” they added.
“This study highlights the ever-shifting understanding of the pathophysiology and therapeutic approaches to fulminant myocarditis,” Dr. Nair and Dr. Deswal concluded.
This research was supported in part by the Foundation of France, French National Research Agency, Sorbonne University, and Clinical Research Hospital. The researchers have filed a patent application based on these results. Dr. Nair and Dr. Deswal have no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Questionnaire for patients with psoriasis might identify risk of axial involvement
Preliminary findings are encouraging
NEW YORK – A questionnaire-based screening tool appears to accelerate the time to diagnosis of axial involvement in patients presenting with psoriasis but no clinical signs of joint pain, according to a study called ATTRACT that was presented at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
The risk of a delayed diagnosis of an axial component in patients with psoriasis, meaning a delay in the underlying diagnosis of psoriatic arthritis (PsA), is substantial, according to Devis Benfaremo, MD, of the department of clinical and molecular science at Marche Polytechnic University, Ancona, Italy.
There is “no consensus for the best strategy to achieve early detection of joint disease” in patients presenting with psoriasis, but Dr. Benfaremo pointed out that missing axial involvement is a particular problem because it is far more likely than swollen joints to be missed on clinical examination.
While about one in three patients with psoriasis have or will develop psoriatic arthritis, according to the National Psoriasis Foundation, delays in diagnosis are common, according to Dr. Benfaremo. In patients with undiagnosed PsA characterized by axial involvement alone, subtle symptoms can be overlooked or attributed to other causes.
There are several screening questionnaires to detect joint symptoms in patients presenting with psoriasis, such as the five-question Psoriasis Epidemiology Screening Tool, but the questionnaire tested in the ATTRACT trial is focused on detecting axial involvement specifically. It was characterized as the first to do so.
In the ongoing ATTRACT study, 253 patients with psoriasis but no history of PsA or axial disease have been enrolled so far. In the study, patients are screened for PsA based on a patient-completed yes-or-no questionnaire, which takes only a few minutes to complete.
“It is a validated questionnaire for axial [spondyloarthritis], but we have adopted it for detection of psoriasis patients with PsA,” Dr. Benfaremo explained.
The questionnaire for axial spondyloarthritis (axSpA) was initially evaluated and validated by Fabian Proft, MD, head of the clinical trials unit at Charité Hospital, Berlin. In addition to a patient self-completed questionnaire, Dr. Proft and coinvestigators have also created a related questionnaire to be administered by physicians.
In the ATTRACT study, patients completed the questionnaire on an electronic device in the waiting room. Positive answers to specific questions about symptoms, which addressed back pain and joint function as well as joint symptoms, divided patients into three groups:
- Group A patients did not respond positively to any of the symptom questions that would prompt suspicion of axial disease. These represented about one-third of those screened so far.
- Group B patients were those who answered positively to at least two questions that related to a high suspicion of axial involvement. These represented 45% of patients.
- The remaining patients were placed in Group C, a category of intermediate risk based on positive responses to some, but not all, questions relating to axial symptoms.
Those in group B are being referred to rheumatology. Patients in group C are given “conditional” eligibility based on the presence of additional risk factors.
AxSpA screening tool ‘makes sense’ for potential use in PsA
The primary outcome of the ATTRACT trial is early identification of axial PsA. Correctly identifying patients with or without peripheral joint involvement is one of several secondary outcomes. The identification of patients who fulfill Assessment Spondyloarthritis International Society (ASAS) criteria for axSpA is another secondary outcome.
Of the 114 patients placed in group B and analyzed so far, 87 have completed an assessment by a rheumatologist with laboratory analyses and imaging, as well as a clinical examination.
Of those 87 assessed by a rheumatologist, 17 did not have either axial or peripheral inflammation. Another 19 were diagnosed with axial disease, including 14 who met ASAS criteria. A total of 10 were classified as having PsA with peripheral inflammation, according to Classification for Psoriatic Arthritis criteria, and 41 are still being considered for a diagnosis of axial or peripheral PsA on the basis of further workup.
“Among the patients with axial PsA, only 10% had elevated C-reactive protein levels,” according to Dr. Benfaremo, echoing previous evidence that inflammatory biomarkers by themselves have limited value for identifying psoriasis patients at high risk of joint involvement.
The findings are preliminary, but Dr. Benfaremo reported that the questionnaire is showing promise for the routine stratification of patients who should be considered for a rheumatology consultation.
If further analyses validate the clinical utility of these stratifications, there is the potential for a substantial acceleration to the diagnosis of PsA.
When contacted to comment about this work, Dr. Proft said that there is an important need for new strategies reduce delay in the diagnosis of PsA among patients presenting with psoriasis. He thinks the screening tool he developed for axSpA “makes sense” as a potential tool in PsA.
“If validated, this could be a very useful for earlier identification of PsA,” Dr. Proft said. He reiterated the importance of focusing on axial involvement.
“Previous screening tools have focused on symptoms of PsA more generally, but inflammation in the peripheral joints is something that you can easily see in most patients,” he said.
In addition to the patient-completed questionnaire and the physician-administered questionnaire, Dr. Proft has also evaluated an online self-referral tool for patients.
“If we can diagnose PsA earlier in the course of disease, we can start treatment earlier, prevent or delay joint damage, and potentially improve outcomes for patients,” Dr. Proft said. He considers this an important direction of research.
Dr. Benfaremo and Dr. Proft reported no potential conflicts of interest.
Preliminary findings are encouraging
Preliminary findings are encouraging
NEW YORK – A questionnaire-based screening tool appears to accelerate the time to diagnosis of axial involvement in patients presenting with psoriasis but no clinical signs of joint pain, according to a study called ATTRACT that was presented at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
The risk of a delayed diagnosis of an axial component in patients with psoriasis, meaning a delay in the underlying diagnosis of psoriatic arthritis (PsA), is substantial, according to Devis Benfaremo, MD, of the department of clinical and molecular science at Marche Polytechnic University, Ancona, Italy.
There is “no consensus for the best strategy to achieve early detection of joint disease” in patients presenting with psoriasis, but Dr. Benfaremo pointed out that missing axial involvement is a particular problem because it is far more likely than swollen joints to be missed on clinical examination.
While about one in three patients with psoriasis have or will develop psoriatic arthritis, according to the National Psoriasis Foundation, delays in diagnosis are common, according to Dr. Benfaremo. In patients with undiagnosed PsA characterized by axial involvement alone, subtle symptoms can be overlooked or attributed to other causes.
There are several screening questionnaires to detect joint symptoms in patients presenting with psoriasis, such as the five-question Psoriasis Epidemiology Screening Tool, but the questionnaire tested in the ATTRACT trial is focused on detecting axial involvement specifically. It was characterized as the first to do so.
In the ongoing ATTRACT study, 253 patients with psoriasis but no history of PsA or axial disease have been enrolled so far. In the study, patients are screened for PsA based on a patient-completed yes-or-no questionnaire, which takes only a few minutes to complete.
“It is a validated questionnaire for axial [spondyloarthritis], but we have adopted it for detection of psoriasis patients with PsA,” Dr. Benfaremo explained.
The questionnaire for axial spondyloarthritis (axSpA) was initially evaluated and validated by Fabian Proft, MD, head of the clinical trials unit at Charité Hospital, Berlin. In addition to a patient self-completed questionnaire, Dr. Proft and coinvestigators have also created a related questionnaire to be administered by physicians.
In the ATTRACT study, patients completed the questionnaire on an electronic device in the waiting room. Positive answers to specific questions about symptoms, which addressed back pain and joint function as well as joint symptoms, divided patients into three groups:
- Group A patients did not respond positively to any of the symptom questions that would prompt suspicion of axial disease. These represented about one-third of those screened so far.
- Group B patients were those who answered positively to at least two questions that related to a high suspicion of axial involvement. These represented 45% of patients.
- The remaining patients were placed in Group C, a category of intermediate risk based on positive responses to some, but not all, questions relating to axial symptoms.
Those in group B are being referred to rheumatology. Patients in group C are given “conditional” eligibility based on the presence of additional risk factors.
AxSpA screening tool ‘makes sense’ for potential use in PsA
The primary outcome of the ATTRACT trial is early identification of axial PsA. Correctly identifying patients with or without peripheral joint involvement is one of several secondary outcomes. The identification of patients who fulfill Assessment Spondyloarthritis International Society (ASAS) criteria for axSpA is another secondary outcome.
Of the 114 patients placed in group B and analyzed so far, 87 have completed an assessment by a rheumatologist with laboratory analyses and imaging, as well as a clinical examination.
Of those 87 assessed by a rheumatologist, 17 did not have either axial or peripheral inflammation. Another 19 were diagnosed with axial disease, including 14 who met ASAS criteria. A total of 10 were classified as having PsA with peripheral inflammation, according to Classification for Psoriatic Arthritis criteria, and 41 are still being considered for a diagnosis of axial or peripheral PsA on the basis of further workup.
“Among the patients with axial PsA, only 10% had elevated C-reactive protein levels,” according to Dr. Benfaremo, echoing previous evidence that inflammatory biomarkers by themselves have limited value for identifying psoriasis patients at high risk of joint involvement.
The findings are preliminary, but Dr. Benfaremo reported that the questionnaire is showing promise for the routine stratification of patients who should be considered for a rheumatology consultation.
If further analyses validate the clinical utility of these stratifications, there is the potential for a substantial acceleration to the diagnosis of PsA.
When contacted to comment about this work, Dr. Proft said that there is an important need for new strategies reduce delay in the diagnosis of PsA among patients presenting with psoriasis. He thinks the screening tool he developed for axSpA “makes sense” as a potential tool in PsA.
“If validated, this could be a very useful for earlier identification of PsA,” Dr. Proft said. He reiterated the importance of focusing on axial involvement.
“Previous screening tools have focused on symptoms of PsA more generally, but inflammation in the peripheral joints is something that you can easily see in most patients,” he said.
In addition to the patient-completed questionnaire and the physician-administered questionnaire, Dr. Proft has also evaluated an online self-referral tool for patients.
“If we can diagnose PsA earlier in the course of disease, we can start treatment earlier, prevent or delay joint damage, and potentially improve outcomes for patients,” Dr. Proft said. He considers this an important direction of research.
Dr. Benfaremo and Dr. Proft reported no potential conflicts of interest.
NEW YORK – A questionnaire-based screening tool appears to accelerate the time to diagnosis of axial involvement in patients presenting with psoriasis but no clinical signs of joint pain, according to a study called ATTRACT that was presented at the annual meeting of the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
The risk of a delayed diagnosis of an axial component in patients with psoriasis, meaning a delay in the underlying diagnosis of psoriatic arthritis (PsA), is substantial, according to Devis Benfaremo, MD, of the department of clinical and molecular science at Marche Polytechnic University, Ancona, Italy.
There is “no consensus for the best strategy to achieve early detection of joint disease” in patients presenting with psoriasis, but Dr. Benfaremo pointed out that missing axial involvement is a particular problem because it is far more likely than swollen joints to be missed on clinical examination.
While about one in three patients with psoriasis have or will develop psoriatic arthritis, according to the National Psoriasis Foundation, delays in diagnosis are common, according to Dr. Benfaremo. In patients with undiagnosed PsA characterized by axial involvement alone, subtle symptoms can be overlooked or attributed to other causes.
There are several screening questionnaires to detect joint symptoms in patients presenting with psoriasis, such as the five-question Psoriasis Epidemiology Screening Tool, but the questionnaire tested in the ATTRACT trial is focused on detecting axial involvement specifically. It was characterized as the first to do so.
In the ongoing ATTRACT study, 253 patients with psoriasis but no history of PsA or axial disease have been enrolled so far. In the study, patients are screened for PsA based on a patient-completed yes-or-no questionnaire, which takes only a few minutes to complete.
“It is a validated questionnaire for axial [spondyloarthritis], but we have adopted it for detection of psoriasis patients with PsA,” Dr. Benfaremo explained.
The questionnaire for axial spondyloarthritis (axSpA) was initially evaluated and validated by Fabian Proft, MD, head of the clinical trials unit at Charité Hospital, Berlin. In addition to a patient self-completed questionnaire, Dr. Proft and coinvestigators have also created a related questionnaire to be administered by physicians.
In the ATTRACT study, patients completed the questionnaire on an electronic device in the waiting room. Positive answers to specific questions about symptoms, which addressed back pain and joint function as well as joint symptoms, divided patients into three groups:
- Group A patients did not respond positively to any of the symptom questions that would prompt suspicion of axial disease. These represented about one-third of those screened so far.
- Group B patients were those who answered positively to at least two questions that related to a high suspicion of axial involvement. These represented 45% of patients.
- The remaining patients were placed in Group C, a category of intermediate risk based on positive responses to some, but not all, questions relating to axial symptoms.
Those in group B are being referred to rheumatology. Patients in group C are given “conditional” eligibility based on the presence of additional risk factors.
AxSpA screening tool ‘makes sense’ for potential use in PsA
The primary outcome of the ATTRACT trial is early identification of axial PsA. Correctly identifying patients with or without peripheral joint involvement is one of several secondary outcomes. The identification of patients who fulfill Assessment Spondyloarthritis International Society (ASAS) criteria for axSpA is another secondary outcome.
Of the 114 patients placed in group B and analyzed so far, 87 have completed an assessment by a rheumatologist with laboratory analyses and imaging, as well as a clinical examination.
Of those 87 assessed by a rheumatologist, 17 did not have either axial or peripheral inflammation. Another 19 were diagnosed with axial disease, including 14 who met ASAS criteria. A total of 10 were classified as having PsA with peripheral inflammation, according to Classification for Psoriatic Arthritis criteria, and 41 are still being considered for a diagnosis of axial or peripheral PsA on the basis of further workup.
“Among the patients with axial PsA, only 10% had elevated C-reactive protein levels,” according to Dr. Benfaremo, echoing previous evidence that inflammatory biomarkers by themselves have limited value for identifying psoriasis patients at high risk of joint involvement.
The findings are preliminary, but Dr. Benfaremo reported that the questionnaire is showing promise for the routine stratification of patients who should be considered for a rheumatology consultation.
If further analyses validate the clinical utility of these stratifications, there is the potential for a substantial acceleration to the diagnosis of PsA.
When contacted to comment about this work, Dr. Proft said that there is an important need for new strategies reduce delay in the diagnosis of PsA among patients presenting with psoriasis. He thinks the screening tool he developed for axSpA “makes sense” as a potential tool in PsA.
“If validated, this could be a very useful for earlier identification of PsA,” Dr. Proft said. He reiterated the importance of focusing on axial involvement.
“Previous screening tools have focused on symptoms of PsA more generally, but inflammation in the peripheral joints is something that you can easily see in most patients,” he said.
In addition to the patient-completed questionnaire and the physician-administered questionnaire, Dr. Proft has also evaluated an online self-referral tool for patients.
“If we can diagnose PsA earlier in the course of disease, we can start treatment earlier, prevent or delay joint damage, and potentially improve outcomes for patients,” Dr. Proft said. He considers this an important direction of research.
Dr. Benfaremo and Dr. Proft reported no potential conflicts of interest.
AT GRAPPA 2022
Hypertension heightens risk for severe COVID-19, even in the fully vaxxed
Adults with hypertension who were vaccinated for COVID-19 with at least one booster were more than twice as likely as vaccinated and boosted individuals without hypertension to be hospitalized for severe COVID-19, according to data from more than 900 individuals.
“We were surprised to learn that many people who were hospitalized with COVID-19 had hypertension and no other risk factors,” said Susan Cheng, MD, MPH, director of the Institute for Research on Healthy Aging in the department of cardiology at the Smidt Heart Institute, Los Angeles, and a senior author of the study. “This is concerning when you consider that almost half of American adults have high blood pressure.”
COVID-19 vaccines demonstrated ability to reduce death and some of the most severe side effects from the infection in the early stages of the pandemic. Although the Omicron surge prompted recommendations for a third mRNA vaccine dose, “a proportion of individuals who received three mRNA vaccine doses still required hospitalization for COVID-19 during the Omicron surge,” and the characteristics associated with severe illness in vaccinated and boosted patients have not been explored, Joseph Ebinger, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote.
Previous research has shown an association between high blood pressure an increased risk for developing severe COVID-19 compared to several other chronic health conditions, including kidney disease, type 2 diabetes, chronic obstructive pulmonary disease, and heart failure, the researchers noted.
In a study published in Hypertension, the researchers identified 912 adults who received at least three doses of mRNA COVID-19 vaccine and were later diagnosed with COVID-19 during the surge in infections from the Omicron variant between December 2021 and April 2022.
A total of 145 of the individuals were hospitalized (16%); of these, 125 (86%) had hypertension.
Patients with hypertension were the most likely to be hospitalized, with an odds ratio of 2.9. In addition to high blood pressure, factors including older age (OR, 1.3), chronic kidney disease (OR, 2.2), prior myocardial infarction or heart failure (OR, 2.2), and longer time since the last vaccination and COVID-19 infection were associated with increased risk of hospitalization in a multivariate analysis.
However, the increased risk of severe illness and hospitalization associated with high blood pressure persisted, with an OR of 2.6, in the absence of comorbid conditions such as type 2 diabetes, kidney disease, and heart failure, the researchers emphasized.
“Although the mechanism for hypertension-associated COVID-19 risk remains unclear, prior studies have identified delayed SARS-CoV-2 viral clearance and prolonged inflammatory response among hypertensive patients, which may contribute to greater disease severity,” they wrote.
The findings were limited by several factors, including the use of data from a single center and lack of information on which Omicron variants and subvariants were behind the infections, the researchers noted.
However, the results highlight the need for more research on how to reduce the risks of severe COVID-19 in vulnerable populations, and on the mechanism for a potential connection between high blood pressure and severe COVID-19, they said.
Given the high prevalence of hypertension worldwide, increased understanding of the hypertension-specific risks and identification of individual and population-level risk reduction strategies will be important to the transition of COVID-19 from pandemic to endemic, they concluded.
Omicron changes the game
“When the pandemic initially started, many conditions were seen to increase risk for more severe COVID illness, and hypertension was one of those factors – and then things changed,” lead author Dr. Ebinger said in an interview. “First, vaccines arrived on the scene and substantially reduced risk of severe COVID for everyone who received them. Second, Omicron arrived and, while more transmissible, this variant has been less likely to cause severe COVID. On the one hand, we have vaccines and boosters that we want to think of as ‘the great equalizer’ when it comes to preexisting conditions. On the other hand, we have a dominant set of SARS-CoV-2 subvariants that seem less virulent in most people.
“Taken together, we have been hoping and even assuming that we have been doing pretty well with minimizing risks. Unfortunately, our study results indicate this is not exactly the case,” he said.
“Although vaccines and boosters appear to have equalized or minimized the risks of severe COVID for some people, this has not happened for others – even in the setting of the milder Omicron variant. Of individuals who were fully vaccinated and boosted, having hypertension increased the odds of needing to be hospitalized after getting infected with Omicron by 2.6-fold, even when accounting for or in the absence of having any major chronic disease that might otherwise predispose to more severe COVID-19 illness,” Dr. Ebinger added.
“So, while the originally seen risks of having obesity or diabetes seem to have been minimized during this current era of pandemic, the risk of having hypertension has persisted. We found this both surprising and concerning, because hypertension is very common and present in over half of people over age 50.”
Surprisingly, “we found that a fair number of people, even after being fully vaccinated plus a having gotten a booster, will not only catch Omicron but get sick enough to need hospital care,” Dr. Ebinger emphasized. “Moreover, it is not just older adults with major comorbid conditions who are vulnerable. Our data show that this can happen to an adult of any age and especially if a person has only hypertension and otherwise no major chronic disease.”
The first takeaway message for clinicians at this time is to raise awareness, Dr. Ebinger stressed in the interview. “We need to raise understanding around the fact that receiving three doses of vaccine may not prevent severe COVID-19 illness in everyone, even when the circulating viral variant is presumed to be causing only mild disease in most people. Moreover, the people who are most at risk are not whom we might think they are. They are not the sickest of the sick. They include people who might not have major conditions such as heart disease or kidney disease, but they do have hypertension.”
Second, “we need more research to understand out why there is this link between hypertension and excess risk for the more severe forms of COVID-19, despite it arising from a supposedly milder variant,” said Dr. Ebinger.
“Third, we need to determine how to reduce these risks, whether through more tailored vaccine regimens or novel therapeutics or a combination approach,” he said.
Looking ahead, “the biological mechanism underpinning the association between hypertension and severe COVID-19 remains underexplored. Future work should focus on understanding the factors linking hypertension to severe COVID-19, as this may elucidate both information on how SARS-CoV-2 effects the body and potential targets for intervention,” Dr. Ebinger added.
The study was supported in part by Cedars-Sinai Medical Center, the Erika J. Glazer Family Foundation and the National Institutes of Health. The researchers had no financial conflicts to disclose.
Adults with hypertension who were vaccinated for COVID-19 with at least one booster were more than twice as likely as vaccinated and boosted individuals without hypertension to be hospitalized for severe COVID-19, according to data from more than 900 individuals.
“We were surprised to learn that many people who were hospitalized with COVID-19 had hypertension and no other risk factors,” said Susan Cheng, MD, MPH, director of the Institute for Research on Healthy Aging in the department of cardiology at the Smidt Heart Institute, Los Angeles, and a senior author of the study. “This is concerning when you consider that almost half of American adults have high blood pressure.”
COVID-19 vaccines demonstrated ability to reduce death and some of the most severe side effects from the infection in the early stages of the pandemic. Although the Omicron surge prompted recommendations for a third mRNA vaccine dose, “a proportion of individuals who received three mRNA vaccine doses still required hospitalization for COVID-19 during the Omicron surge,” and the characteristics associated with severe illness in vaccinated and boosted patients have not been explored, Joseph Ebinger, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote.
Previous research has shown an association between high blood pressure an increased risk for developing severe COVID-19 compared to several other chronic health conditions, including kidney disease, type 2 diabetes, chronic obstructive pulmonary disease, and heart failure, the researchers noted.
In a study published in Hypertension, the researchers identified 912 adults who received at least three doses of mRNA COVID-19 vaccine and were later diagnosed with COVID-19 during the surge in infections from the Omicron variant between December 2021 and April 2022.
A total of 145 of the individuals were hospitalized (16%); of these, 125 (86%) had hypertension.
Patients with hypertension were the most likely to be hospitalized, with an odds ratio of 2.9. In addition to high blood pressure, factors including older age (OR, 1.3), chronic kidney disease (OR, 2.2), prior myocardial infarction or heart failure (OR, 2.2), and longer time since the last vaccination and COVID-19 infection were associated with increased risk of hospitalization in a multivariate analysis.
However, the increased risk of severe illness and hospitalization associated with high blood pressure persisted, with an OR of 2.6, in the absence of comorbid conditions such as type 2 diabetes, kidney disease, and heart failure, the researchers emphasized.
“Although the mechanism for hypertension-associated COVID-19 risk remains unclear, prior studies have identified delayed SARS-CoV-2 viral clearance and prolonged inflammatory response among hypertensive patients, which may contribute to greater disease severity,” they wrote.
The findings were limited by several factors, including the use of data from a single center and lack of information on which Omicron variants and subvariants were behind the infections, the researchers noted.
However, the results highlight the need for more research on how to reduce the risks of severe COVID-19 in vulnerable populations, and on the mechanism for a potential connection between high blood pressure and severe COVID-19, they said.
Given the high prevalence of hypertension worldwide, increased understanding of the hypertension-specific risks and identification of individual and population-level risk reduction strategies will be important to the transition of COVID-19 from pandemic to endemic, they concluded.
Omicron changes the game
“When the pandemic initially started, many conditions were seen to increase risk for more severe COVID illness, and hypertension was one of those factors – and then things changed,” lead author Dr. Ebinger said in an interview. “First, vaccines arrived on the scene and substantially reduced risk of severe COVID for everyone who received them. Second, Omicron arrived and, while more transmissible, this variant has been less likely to cause severe COVID. On the one hand, we have vaccines and boosters that we want to think of as ‘the great equalizer’ when it comes to preexisting conditions. On the other hand, we have a dominant set of SARS-CoV-2 subvariants that seem less virulent in most people.
“Taken together, we have been hoping and even assuming that we have been doing pretty well with minimizing risks. Unfortunately, our study results indicate this is not exactly the case,” he said.
“Although vaccines and boosters appear to have equalized or minimized the risks of severe COVID for some people, this has not happened for others – even in the setting of the milder Omicron variant. Of individuals who were fully vaccinated and boosted, having hypertension increased the odds of needing to be hospitalized after getting infected with Omicron by 2.6-fold, even when accounting for or in the absence of having any major chronic disease that might otherwise predispose to more severe COVID-19 illness,” Dr. Ebinger added.
“So, while the originally seen risks of having obesity or diabetes seem to have been minimized during this current era of pandemic, the risk of having hypertension has persisted. We found this both surprising and concerning, because hypertension is very common and present in over half of people over age 50.”
Surprisingly, “we found that a fair number of people, even after being fully vaccinated plus a having gotten a booster, will not only catch Omicron but get sick enough to need hospital care,” Dr. Ebinger emphasized. “Moreover, it is not just older adults with major comorbid conditions who are vulnerable. Our data show that this can happen to an adult of any age and especially if a person has only hypertension and otherwise no major chronic disease.”
The first takeaway message for clinicians at this time is to raise awareness, Dr. Ebinger stressed in the interview. “We need to raise understanding around the fact that receiving three doses of vaccine may not prevent severe COVID-19 illness in everyone, even when the circulating viral variant is presumed to be causing only mild disease in most people. Moreover, the people who are most at risk are not whom we might think they are. They are not the sickest of the sick. They include people who might not have major conditions such as heart disease or kidney disease, but they do have hypertension.”
Second, “we need more research to understand out why there is this link between hypertension and excess risk for the more severe forms of COVID-19, despite it arising from a supposedly milder variant,” said Dr. Ebinger.
“Third, we need to determine how to reduce these risks, whether through more tailored vaccine regimens or novel therapeutics or a combination approach,” he said.
Looking ahead, “the biological mechanism underpinning the association between hypertension and severe COVID-19 remains underexplored. Future work should focus on understanding the factors linking hypertension to severe COVID-19, as this may elucidate both information on how SARS-CoV-2 effects the body and potential targets for intervention,” Dr. Ebinger added.
The study was supported in part by Cedars-Sinai Medical Center, the Erika J. Glazer Family Foundation and the National Institutes of Health. The researchers had no financial conflicts to disclose.
Adults with hypertension who were vaccinated for COVID-19 with at least one booster were more than twice as likely as vaccinated and boosted individuals without hypertension to be hospitalized for severe COVID-19, according to data from more than 900 individuals.
“We were surprised to learn that many people who were hospitalized with COVID-19 had hypertension and no other risk factors,” said Susan Cheng, MD, MPH, director of the Institute for Research on Healthy Aging in the department of cardiology at the Smidt Heart Institute, Los Angeles, and a senior author of the study. “This is concerning when you consider that almost half of American adults have high blood pressure.”
COVID-19 vaccines demonstrated ability to reduce death and some of the most severe side effects from the infection in the early stages of the pandemic. Although the Omicron surge prompted recommendations for a third mRNA vaccine dose, “a proportion of individuals who received three mRNA vaccine doses still required hospitalization for COVID-19 during the Omicron surge,” and the characteristics associated with severe illness in vaccinated and boosted patients have not been explored, Joseph Ebinger, MD, of Cedars-Sinai Medical Center, Los Angeles, and colleagues wrote.
Previous research has shown an association between high blood pressure an increased risk for developing severe COVID-19 compared to several other chronic health conditions, including kidney disease, type 2 diabetes, chronic obstructive pulmonary disease, and heart failure, the researchers noted.
In a study published in Hypertension, the researchers identified 912 adults who received at least three doses of mRNA COVID-19 vaccine and were later diagnosed with COVID-19 during the surge in infections from the Omicron variant between December 2021 and April 2022.
A total of 145 of the individuals were hospitalized (16%); of these, 125 (86%) had hypertension.
Patients with hypertension were the most likely to be hospitalized, with an odds ratio of 2.9. In addition to high blood pressure, factors including older age (OR, 1.3), chronic kidney disease (OR, 2.2), prior myocardial infarction or heart failure (OR, 2.2), and longer time since the last vaccination and COVID-19 infection were associated with increased risk of hospitalization in a multivariate analysis.
However, the increased risk of severe illness and hospitalization associated with high blood pressure persisted, with an OR of 2.6, in the absence of comorbid conditions such as type 2 diabetes, kidney disease, and heart failure, the researchers emphasized.
“Although the mechanism for hypertension-associated COVID-19 risk remains unclear, prior studies have identified delayed SARS-CoV-2 viral clearance and prolonged inflammatory response among hypertensive patients, which may contribute to greater disease severity,” they wrote.
The findings were limited by several factors, including the use of data from a single center and lack of information on which Omicron variants and subvariants were behind the infections, the researchers noted.
However, the results highlight the need for more research on how to reduce the risks of severe COVID-19 in vulnerable populations, and on the mechanism for a potential connection between high blood pressure and severe COVID-19, they said.
Given the high prevalence of hypertension worldwide, increased understanding of the hypertension-specific risks and identification of individual and population-level risk reduction strategies will be important to the transition of COVID-19 from pandemic to endemic, they concluded.
Omicron changes the game
“When the pandemic initially started, many conditions were seen to increase risk for more severe COVID illness, and hypertension was one of those factors – and then things changed,” lead author Dr. Ebinger said in an interview. “First, vaccines arrived on the scene and substantially reduced risk of severe COVID for everyone who received them. Second, Omicron arrived and, while more transmissible, this variant has been less likely to cause severe COVID. On the one hand, we have vaccines and boosters that we want to think of as ‘the great equalizer’ when it comes to preexisting conditions. On the other hand, we have a dominant set of SARS-CoV-2 subvariants that seem less virulent in most people.
“Taken together, we have been hoping and even assuming that we have been doing pretty well with minimizing risks. Unfortunately, our study results indicate this is not exactly the case,” he said.
“Although vaccines and boosters appear to have equalized or minimized the risks of severe COVID for some people, this has not happened for others – even in the setting of the milder Omicron variant. Of individuals who were fully vaccinated and boosted, having hypertension increased the odds of needing to be hospitalized after getting infected with Omicron by 2.6-fold, even when accounting for or in the absence of having any major chronic disease that might otherwise predispose to more severe COVID-19 illness,” Dr. Ebinger added.
“So, while the originally seen risks of having obesity or diabetes seem to have been minimized during this current era of pandemic, the risk of having hypertension has persisted. We found this both surprising and concerning, because hypertension is very common and present in over half of people over age 50.”
Surprisingly, “we found that a fair number of people, even after being fully vaccinated plus a having gotten a booster, will not only catch Omicron but get sick enough to need hospital care,” Dr. Ebinger emphasized. “Moreover, it is not just older adults with major comorbid conditions who are vulnerable. Our data show that this can happen to an adult of any age and especially if a person has only hypertension and otherwise no major chronic disease.”
The first takeaway message for clinicians at this time is to raise awareness, Dr. Ebinger stressed in the interview. “We need to raise understanding around the fact that receiving three doses of vaccine may not prevent severe COVID-19 illness in everyone, even when the circulating viral variant is presumed to be causing only mild disease in most people. Moreover, the people who are most at risk are not whom we might think they are. They are not the sickest of the sick. They include people who might not have major conditions such as heart disease or kidney disease, but they do have hypertension.”
Second, “we need more research to understand out why there is this link between hypertension and excess risk for the more severe forms of COVID-19, despite it arising from a supposedly milder variant,” said Dr. Ebinger.
“Third, we need to determine how to reduce these risks, whether through more tailored vaccine regimens or novel therapeutics or a combination approach,” he said.
Looking ahead, “the biological mechanism underpinning the association between hypertension and severe COVID-19 remains underexplored. Future work should focus on understanding the factors linking hypertension to severe COVID-19, as this may elucidate both information on how SARS-CoV-2 effects the body and potential targets for intervention,” Dr. Ebinger added.
The study was supported in part by Cedars-Sinai Medical Center, the Erika J. Glazer Family Foundation and the National Institutes of Health. The researchers had no financial conflicts to disclose.
FROM HYPERTENSION
Science lags behind for kids with long COVID
Emma Sherman, a 13-year-old girl in Ascot, England, woke up to a dizzying aura of blind spots and flashing lights in her field of vision. It was May 2020, and she also had crippling nausea and headaches. By August, her dizziness was so overwhelming, she couldn’t hold her head up, lying in her mother’s lap for hours, too fatigued to attend school.
The former competitive gymnast, who had hoped to try out for the cheerleading squad, now used a wheelchair and was a shadow of her former self. She had been diagnosed with COVID-induced postural orthostatic tachycardia syndrome, a condition often caused by an infection that results in a higher heart rate, extreme nausea, dizziness, and fatigue.
“I was so into sports before I got long COVID, and afterwards I could barely walk,” Emma said.
Even minor movements sent her heart rate sky-high. Her long chestnut hair turned gray and fell out in clumps. In the hospital, she was pricked and prodded, her blood tested for numerous conditions.
“They ran every scan known to man and took an MRI of her brain,” said Emma’s mother, Marie Sherman. “All was clear.”
Emma’s pediatrician determined that the teen had long COVID after having had a mild case of the virus in March, about 2 months before her puzzling symptoms began. But beyond a positive antibody test, doctors have found little evidence of what was causing Emma’s symptoms.
For Emma and others with long COVID, there are no medications shown to directly target the condition. Instead, caregivers target their symptoms, which include nausea, dizziness, fatigue, headaches, and a racing heart, said Laura Malone, MD, codirector of the Johns Hopkins Kennedy Krieger Pediatric Post–COVID-19 Rehabilitation Clinic in Baltimore.
“Right now, it’s a rehabilitation-based approach focused on improving symptoms and functioning so that kids can go back to their usual activities as much as possible,” she says.
Depression and anxiety are common, although doctors are struggling to figure out whether COVID is changing the brain or whether mental health symptoms result from all the life disruptions. There’s little research to show how may kids have depression because of long COVID. Dr. Malone said about half of her patients at the Kennedy Krieger Institute›s long COVID clinic are also dealing with mental health issues.
Patients with headaches, dizziness, and nausea are given pain and nausea medications and recommendations for a healthy diet with added fruits and vegetables, monounsaturated fats, lower sodium, unprocessed foods, and whole grains. Kids with irregular or racing heart rates are referred to cardiologists and potentially prescribed beta-blockers to treat their heart arrhythmias, while children with breathing problems may be referred to pulmonologists and those with depression to a psychiatrist.
Still, many patients like Emma go to their doctors with phantom symptoms that don’t show up on scans or blood tests.
“We’re not seeing any evidence of structural damage to the brain, for example,” said Dr. Malone. “When we do MRIs, they often come out normal.”
It’s possible that the virus lingers in some patients, said Rajeev Fernando, MD, an infectious disease specialist and a fellow at Harvard Medical School, Boston. Kids’ strong immune systems often fend off problems that can be noticed. But on the inside, dead fragments of the virus persist, floating in hidden parts of the body and activating the immune system long after the threat has passed.
The virus can be in the gut and in the brain, which may help explain why symptoms like brain fog and nausea can linger in children.
“The immune system doesn’t recognize whether fragments of the virus are dead or alive. It continues to think it’s fighting active COVID,” said Dr. Fernando.
There is little data on how long symptoms last, Dr. Fernando said, as well as how many kids get them and why some are more vulnerable than others. Some research has found that about 5%-15% of children with COVID may get long COVID, but the statistics vary globally.
“Children with long COVID have largely been ignored. And while we’re talking about it now, we’ve got some work to do,” said Dr. Fernando.
As for Emma, she recovered in January of 2021, heading back to school and her friends, although her cardiologist advised her to skip gym classes.
“For the first time in months, I was feeling like myself again,” she said.
But the coronavirus found its way to Emma again. Although she was fully vaccinated in the fall of 2021, when the Omicron variant swept the world late that year, she was infected again.
“When the wave of Omicron descended, Emma was like a sitting duck,” her mother said.
She was bedridden with a high fever and cough. The cold-like symptoms eventually went away, but the issues in her gut stuck around. Since then, Emma has had extreme nausea, losing most of the weight she had gained back.
For her part, Ms. Sherman has found solace in a group called Long COVID Kids, a nonprofit in Europe and the United States. The group is raising awareness about the condition in kids to increase funding, boost understanding, and improve treatment and outcomes.
“There’s nothing worse than watching your child suffer and not being able to do anything about it,” she said. “I tell Emma all the time: If I could just crawl in your body and take it, I would do it in a second.”
Emma is hoping for a fresh start with her family’s move in the coming weeks to Sotogrande in southern Spain.
“I miss the simplest things like going for a run, going to the fair with my friends, and just feeling well,” she said. “I have a long list of things I’ll do once this is all done.”
A version of this article first appeared on WebMD.com.
Emma Sherman, a 13-year-old girl in Ascot, England, woke up to a dizzying aura of blind spots and flashing lights in her field of vision. It was May 2020, and she also had crippling nausea and headaches. By August, her dizziness was so overwhelming, she couldn’t hold her head up, lying in her mother’s lap for hours, too fatigued to attend school.
The former competitive gymnast, who had hoped to try out for the cheerleading squad, now used a wheelchair and was a shadow of her former self. She had been diagnosed with COVID-induced postural orthostatic tachycardia syndrome, a condition often caused by an infection that results in a higher heart rate, extreme nausea, dizziness, and fatigue.
“I was so into sports before I got long COVID, and afterwards I could barely walk,” Emma said.
Even minor movements sent her heart rate sky-high. Her long chestnut hair turned gray and fell out in clumps. In the hospital, she was pricked and prodded, her blood tested for numerous conditions.
“They ran every scan known to man and took an MRI of her brain,” said Emma’s mother, Marie Sherman. “All was clear.”
Emma’s pediatrician determined that the teen had long COVID after having had a mild case of the virus in March, about 2 months before her puzzling symptoms began. But beyond a positive antibody test, doctors have found little evidence of what was causing Emma’s symptoms.
For Emma and others with long COVID, there are no medications shown to directly target the condition. Instead, caregivers target their symptoms, which include nausea, dizziness, fatigue, headaches, and a racing heart, said Laura Malone, MD, codirector of the Johns Hopkins Kennedy Krieger Pediatric Post–COVID-19 Rehabilitation Clinic in Baltimore.
“Right now, it’s a rehabilitation-based approach focused on improving symptoms and functioning so that kids can go back to their usual activities as much as possible,” she says.
Depression and anxiety are common, although doctors are struggling to figure out whether COVID is changing the brain or whether mental health symptoms result from all the life disruptions. There’s little research to show how may kids have depression because of long COVID. Dr. Malone said about half of her patients at the Kennedy Krieger Institute›s long COVID clinic are also dealing with mental health issues.
Patients with headaches, dizziness, and nausea are given pain and nausea medications and recommendations for a healthy diet with added fruits and vegetables, monounsaturated fats, lower sodium, unprocessed foods, and whole grains. Kids with irregular or racing heart rates are referred to cardiologists and potentially prescribed beta-blockers to treat their heart arrhythmias, while children with breathing problems may be referred to pulmonologists and those with depression to a psychiatrist.
Still, many patients like Emma go to their doctors with phantom symptoms that don’t show up on scans or blood tests.
“We’re not seeing any evidence of structural damage to the brain, for example,” said Dr. Malone. “When we do MRIs, they often come out normal.”
It’s possible that the virus lingers in some patients, said Rajeev Fernando, MD, an infectious disease specialist and a fellow at Harvard Medical School, Boston. Kids’ strong immune systems often fend off problems that can be noticed. But on the inside, dead fragments of the virus persist, floating in hidden parts of the body and activating the immune system long after the threat has passed.
The virus can be in the gut and in the brain, which may help explain why symptoms like brain fog and nausea can linger in children.
“The immune system doesn’t recognize whether fragments of the virus are dead or alive. It continues to think it’s fighting active COVID,” said Dr. Fernando.
There is little data on how long symptoms last, Dr. Fernando said, as well as how many kids get them and why some are more vulnerable than others. Some research has found that about 5%-15% of children with COVID may get long COVID, but the statistics vary globally.
“Children with long COVID have largely been ignored. And while we’re talking about it now, we’ve got some work to do,” said Dr. Fernando.
As for Emma, she recovered in January of 2021, heading back to school and her friends, although her cardiologist advised her to skip gym classes.
“For the first time in months, I was feeling like myself again,” she said.
But the coronavirus found its way to Emma again. Although she was fully vaccinated in the fall of 2021, when the Omicron variant swept the world late that year, she was infected again.
“When the wave of Omicron descended, Emma was like a sitting duck,” her mother said.
She was bedridden with a high fever and cough. The cold-like symptoms eventually went away, but the issues in her gut stuck around. Since then, Emma has had extreme nausea, losing most of the weight she had gained back.
For her part, Ms. Sherman has found solace in a group called Long COVID Kids, a nonprofit in Europe and the United States. The group is raising awareness about the condition in kids to increase funding, boost understanding, and improve treatment and outcomes.
“There’s nothing worse than watching your child suffer and not being able to do anything about it,” she said. “I tell Emma all the time: If I could just crawl in your body and take it, I would do it in a second.”
Emma is hoping for a fresh start with her family’s move in the coming weeks to Sotogrande in southern Spain.
“I miss the simplest things like going for a run, going to the fair with my friends, and just feeling well,” she said. “I have a long list of things I’ll do once this is all done.”
A version of this article first appeared on WebMD.com.
Emma Sherman, a 13-year-old girl in Ascot, England, woke up to a dizzying aura of blind spots and flashing lights in her field of vision. It was May 2020, and she also had crippling nausea and headaches. By August, her dizziness was so overwhelming, she couldn’t hold her head up, lying in her mother’s lap for hours, too fatigued to attend school.
The former competitive gymnast, who had hoped to try out for the cheerleading squad, now used a wheelchair and was a shadow of her former self. She had been diagnosed with COVID-induced postural orthostatic tachycardia syndrome, a condition often caused by an infection that results in a higher heart rate, extreme nausea, dizziness, and fatigue.
“I was so into sports before I got long COVID, and afterwards I could barely walk,” Emma said.
Even minor movements sent her heart rate sky-high. Her long chestnut hair turned gray and fell out in clumps. In the hospital, she was pricked and prodded, her blood tested for numerous conditions.
“They ran every scan known to man and took an MRI of her brain,” said Emma’s mother, Marie Sherman. “All was clear.”
Emma’s pediatrician determined that the teen had long COVID after having had a mild case of the virus in March, about 2 months before her puzzling symptoms began. But beyond a positive antibody test, doctors have found little evidence of what was causing Emma’s symptoms.
For Emma and others with long COVID, there are no medications shown to directly target the condition. Instead, caregivers target their symptoms, which include nausea, dizziness, fatigue, headaches, and a racing heart, said Laura Malone, MD, codirector of the Johns Hopkins Kennedy Krieger Pediatric Post–COVID-19 Rehabilitation Clinic in Baltimore.
“Right now, it’s a rehabilitation-based approach focused on improving symptoms and functioning so that kids can go back to their usual activities as much as possible,” she says.
Depression and anxiety are common, although doctors are struggling to figure out whether COVID is changing the brain or whether mental health symptoms result from all the life disruptions. There’s little research to show how may kids have depression because of long COVID. Dr. Malone said about half of her patients at the Kennedy Krieger Institute›s long COVID clinic are also dealing with mental health issues.
Patients with headaches, dizziness, and nausea are given pain and nausea medications and recommendations for a healthy diet with added fruits and vegetables, monounsaturated fats, lower sodium, unprocessed foods, and whole grains. Kids with irregular or racing heart rates are referred to cardiologists and potentially prescribed beta-blockers to treat their heart arrhythmias, while children with breathing problems may be referred to pulmonologists and those with depression to a psychiatrist.
Still, many patients like Emma go to their doctors with phantom symptoms that don’t show up on scans or blood tests.
“We’re not seeing any evidence of structural damage to the brain, for example,” said Dr. Malone. “When we do MRIs, they often come out normal.”
It’s possible that the virus lingers in some patients, said Rajeev Fernando, MD, an infectious disease specialist and a fellow at Harvard Medical School, Boston. Kids’ strong immune systems often fend off problems that can be noticed. But on the inside, dead fragments of the virus persist, floating in hidden parts of the body and activating the immune system long after the threat has passed.
The virus can be in the gut and in the brain, which may help explain why symptoms like brain fog and nausea can linger in children.
“The immune system doesn’t recognize whether fragments of the virus are dead or alive. It continues to think it’s fighting active COVID,” said Dr. Fernando.
There is little data on how long symptoms last, Dr. Fernando said, as well as how many kids get them and why some are more vulnerable than others. Some research has found that about 5%-15% of children with COVID may get long COVID, but the statistics vary globally.
“Children with long COVID have largely been ignored. And while we’re talking about it now, we’ve got some work to do,” said Dr. Fernando.
As for Emma, she recovered in January of 2021, heading back to school and her friends, although her cardiologist advised her to skip gym classes.
“For the first time in months, I was feeling like myself again,” she said.
But the coronavirus found its way to Emma again. Although she was fully vaccinated in the fall of 2021, when the Omicron variant swept the world late that year, she was infected again.
“When the wave of Omicron descended, Emma was like a sitting duck,” her mother said.
She was bedridden with a high fever and cough. The cold-like symptoms eventually went away, but the issues in her gut stuck around. Since then, Emma has had extreme nausea, losing most of the weight she had gained back.
For her part, Ms. Sherman has found solace in a group called Long COVID Kids, a nonprofit in Europe and the United States. The group is raising awareness about the condition in kids to increase funding, boost understanding, and improve treatment and outcomes.
“There’s nothing worse than watching your child suffer and not being able to do anything about it,” she said. “I tell Emma all the time: If I could just crawl in your body and take it, I would do it in a second.”
Emma is hoping for a fresh start with her family’s move in the coming weeks to Sotogrande in southern Spain.
“I miss the simplest things like going for a run, going to the fair with my friends, and just feeling well,” she said. “I have a long list of things I’ll do once this is all done.”
A version of this article first appeared on WebMD.com.
Body-brain neuroinflammation loop may cause chronic ME/CFS, long COVID symptoms
ME/CFS has been established as resulting from infections, environmental exposures, stressors, and surgery. Similarities have been drawn during the COVID-19 pandemic between ME/CFS and a large subgroup of patients with post-acute sequelae of SARS-CoV-2 infection – also known as post-COVID conditions, or long COVID – who continue to have viral fatigue and other lingering symptoms after their infection resolves.
What has been less clearly understood, the researchers said, is the reason behind why ME/CFS and other postviral fatigue tends to be chronic and can sometime develop into a lifelong condition.
“These diseases are very closely related, and it is clear the biological basis of long COVID is unequivocally connected to the original COVID infection – so there should no longer be any debate and doubt about the fact that postviral fatigue syndromes like ME/CFS are biologically based and involve much disturbed physiology,” Warren Tate, MSc, PhD, emeritus professor in the department of biochemistry at the University of Otago in Dunedin, New Zealand, stated in a press release.
Their hypothesis, set forth in a study published in Frontiers of Neurology, proposes that the systemic immune/inflammatory response that occurs after an infection or stressful event does not revolve, which results in a “fluctuating chronic neuroinflammation that sustains and controls the complex neurological symptoms of ME/CFS and long COVID and facilitates frequent more serious relapses in response to life stress, as evidenced from a comprehensive disruption to the cellular molecular biology and body’s physiological pathways.”
Dr. Tate and colleagues said that it is still unclear how the neuroinflammation occurs, why it’s persistent in ME/CFS, and how it causes symptoms associated with ME/CFS. In their hypothesis, “abnormal signaling or transport of molecules/cells occurs through one or both of neurovascular pathways and/or a dysfunctional blood brain barrier,” they said, noting “the normally separate and contained brain/CNS compartment in the healthy person becomes more porous.” The neurological symptoms associated with ME/CFS occur due to strong signals sent because of persistent “inflammatory signals or immune cells/molecules migrating into the brain,” they explained.
This results in a continuous loop where the central nervous system sends signals back to the body through the hypothalamus/paraventricular nucleus and the brain stem. “The resulting symptoms and the neurologically driven ‘sickness response’ for the ME/CFS patient would persist, preventing healing and a return to the preinfectious/stress-related state,” Dr. Tate and colleagues said.
Lingering inflammation may be the culprit
Commenting on the study, Achillefs Ntranos, MD, a board-certified neurologist in private practice in Scarsdale, N.Y., who was not involved with the research, said previous studies have shown that long COVID is linked to chronic activation of microglia in the brain, which has also been seen to activate in patients with ME/CFS.
“The hypothesis that lingering inflammation in the brain is the culprit behind the neurological symptoms of long COVID and ME/CFS is valid,” he said. “If these cells remain activated in the brain, they can cause a state of increased and lingering inflammation, which can interfere with the function of neurons, thus producing neurological symptoms. Since the neurological symptoms are similar between these entities, the mechanisms that produce them might also be similar.”
While the exact cause of ME/CFS is still unclear, it is often tied to the aftereffects of a flu-like illness, Dr. Ntranos said. “This has led researchers to propose that it arises after a viral infection, with many different types of viruses being associated with it. Other ways researchers think ME/CFS is being brought on after a viral illness is via changes in the immune system, such as chronic production of cytokines, neuroinflammation, and disruption of the hypothalamic-pituitary-adrenal axis, which regulates the body’s response to stress,” he explained.
While a newer condition, long COVID is not all that different from ME/CFS, Dr. Ntranos noted, sharing the catalyst of a viral infection and core neurological symptoms such as fatigue, postexertional malaise, a “brain fog” that makes thinking or concentrating difficult, sleep problems, and lightheadedness, but there are differences that set it apart from ME/CFS.
“Long COVID is unique in having additional symptoms that are specific to the SARS-CoV-2 virus, such as respiratory and cardiovascular symptoms and loss of smell and taste. However most central nervous system effects are the same between these two entities,” he said.
Dr. Ntranos said long COVID’s neurological symptoms are similar to that of multiple sclerosis (MS), such as “brain fog” and postexertional malaise. “Since MS only affects the brain and spinal cord, there are no symptoms from other organ systems, such as the lungs, heart, or digestive system, contrary to long COVID. Furthermore, MS rarely affects smell and taste, making these symptoms unique to COVID,” he said.
However, he pointed out that brain fog and fatigue symptoms on their own can be nonspecific and attributed to many different conditions, such as obstructive sleep apnea, migraines, depression, anxiety, thyroid problems, vitamin deficiencies, dehydration, sleep disorders, and side effects of medications.
“More research needs to be done to understand how these cells are being activated, how they interfere with neuronal function, and why they remain in that state in some people, who then go on to develop fatigue and brain fog,” he said.
This study was funded by the Healthcare Otago Charitable Trust, the Associated New Zealand Myalgic Encephalomyelitis Society, and donations from families of patients with ME/CFS. The authors and Dr. Ntranos report no relevant financial disclosures.
ME/CFS has been established as resulting from infections, environmental exposures, stressors, and surgery. Similarities have been drawn during the COVID-19 pandemic between ME/CFS and a large subgroup of patients with post-acute sequelae of SARS-CoV-2 infection – also known as post-COVID conditions, or long COVID – who continue to have viral fatigue and other lingering symptoms after their infection resolves.
What has been less clearly understood, the researchers said, is the reason behind why ME/CFS and other postviral fatigue tends to be chronic and can sometime develop into a lifelong condition.
“These diseases are very closely related, and it is clear the biological basis of long COVID is unequivocally connected to the original COVID infection – so there should no longer be any debate and doubt about the fact that postviral fatigue syndromes like ME/CFS are biologically based and involve much disturbed physiology,” Warren Tate, MSc, PhD, emeritus professor in the department of biochemistry at the University of Otago in Dunedin, New Zealand, stated in a press release.
Their hypothesis, set forth in a study published in Frontiers of Neurology, proposes that the systemic immune/inflammatory response that occurs after an infection or stressful event does not revolve, which results in a “fluctuating chronic neuroinflammation that sustains and controls the complex neurological symptoms of ME/CFS and long COVID and facilitates frequent more serious relapses in response to life stress, as evidenced from a comprehensive disruption to the cellular molecular biology and body’s physiological pathways.”
Dr. Tate and colleagues said that it is still unclear how the neuroinflammation occurs, why it’s persistent in ME/CFS, and how it causes symptoms associated with ME/CFS. In their hypothesis, “abnormal signaling or transport of molecules/cells occurs through one or both of neurovascular pathways and/or a dysfunctional blood brain barrier,” they said, noting “the normally separate and contained brain/CNS compartment in the healthy person becomes more porous.” The neurological symptoms associated with ME/CFS occur due to strong signals sent because of persistent “inflammatory signals or immune cells/molecules migrating into the brain,” they explained.
This results in a continuous loop where the central nervous system sends signals back to the body through the hypothalamus/paraventricular nucleus and the brain stem. “The resulting symptoms and the neurologically driven ‘sickness response’ for the ME/CFS patient would persist, preventing healing and a return to the preinfectious/stress-related state,” Dr. Tate and colleagues said.
Lingering inflammation may be the culprit
Commenting on the study, Achillefs Ntranos, MD, a board-certified neurologist in private practice in Scarsdale, N.Y., who was not involved with the research, said previous studies have shown that long COVID is linked to chronic activation of microglia in the brain, which has also been seen to activate in patients with ME/CFS.
“The hypothesis that lingering inflammation in the brain is the culprit behind the neurological symptoms of long COVID and ME/CFS is valid,” he said. “If these cells remain activated in the brain, they can cause a state of increased and lingering inflammation, which can interfere with the function of neurons, thus producing neurological symptoms. Since the neurological symptoms are similar between these entities, the mechanisms that produce them might also be similar.”
While the exact cause of ME/CFS is still unclear, it is often tied to the aftereffects of a flu-like illness, Dr. Ntranos said. “This has led researchers to propose that it arises after a viral infection, with many different types of viruses being associated with it. Other ways researchers think ME/CFS is being brought on after a viral illness is via changes in the immune system, such as chronic production of cytokines, neuroinflammation, and disruption of the hypothalamic-pituitary-adrenal axis, which regulates the body’s response to stress,” he explained.
While a newer condition, long COVID is not all that different from ME/CFS, Dr. Ntranos noted, sharing the catalyst of a viral infection and core neurological symptoms such as fatigue, postexertional malaise, a “brain fog” that makes thinking or concentrating difficult, sleep problems, and lightheadedness, but there are differences that set it apart from ME/CFS.
“Long COVID is unique in having additional symptoms that are specific to the SARS-CoV-2 virus, such as respiratory and cardiovascular symptoms and loss of smell and taste. However most central nervous system effects are the same between these two entities,” he said.
Dr. Ntranos said long COVID’s neurological symptoms are similar to that of multiple sclerosis (MS), such as “brain fog” and postexertional malaise. “Since MS only affects the brain and spinal cord, there are no symptoms from other organ systems, such as the lungs, heart, or digestive system, contrary to long COVID. Furthermore, MS rarely affects smell and taste, making these symptoms unique to COVID,” he said.
However, he pointed out that brain fog and fatigue symptoms on their own can be nonspecific and attributed to many different conditions, such as obstructive sleep apnea, migraines, depression, anxiety, thyroid problems, vitamin deficiencies, dehydration, sleep disorders, and side effects of medications.
“More research needs to be done to understand how these cells are being activated, how they interfere with neuronal function, and why they remain in that state in some people, who then go on to develop fatigue and brain fog,” he said.
This study was funded by the Healthcare Otago Charitable Trust, the Associated New Zealand Myalgic Encephalomyelitis Society, and donations from families of patients with ME/CFS. The authors and Dr. Ntranos report no relevant financial disclosures.
ME/CFS has been established as resulting from infections, environmental exposures, stressors, and surgery. Similarities have been drawn during the COVID-19 pandemic between ME/CFS and a large subgroup of patients with post-acute sequelae of SARS-CoV-2 infection – also known as post-COVID conditions, or long COVID – who continue to have viral fatigue and other lingering symptoms after their infection resolves.
What has been less clearly understood, the researchers said, is the reason behind why ME/CFS and other postviral fatigue tends to be chronic and can sometime develop into a lifelong condition.
“These diseases are very closely related, and it is clear the biological basis of long COVID is unequivocally connected to the original COVID infection – so there should no longer be any debate and doubt about the fact that postviral fatigue syndromes like ME/CFS are biologically based and involve much disturbed physiology,” Warren Tate, MSc, PhD, emeritus professor in the department of biochemistry at the University of Otago in Dunedin, New Zealand, stated in a press release.
Their hypothesis, set forth in a study published in Frontiers of Neurology, proposes that the systemic immune/inflammatory response that occurs after an infection or stressful event does not revolve, which results in a “fluctuating chronic neuroinflammation that sustains and controls the complex neurological symptoms of ME/CFS and long COVID and facilitates frequent more serious relapses in response to life stress, as evidenced from a comprehensive disruption to the cellular molecular biology and body’s physiological pathways.”
Dr. Tate and colleagues said that it is still unclear how the neuroinflammation occurs, why it’s persistent in ME/CFS, and how it causes symptoms associated with ME/CFS. In their hypothesis, “abnormal signaling or transport of molecules/cells occurs through one or both of neurovascular pathways and/or a dysfunctional blood brain barrier,” they said, noting “the normally separate and contained brain/CNS compartment in the healthy person becomes more porous.” The neurological symptoms associated with ME/CFS occur due to strong signals sent because of persistent “inflammatory signals or immune cells/molecules migrating into the brain,” they explained.
This results in a continuous loop where the central nervous system sends signals back to the body through the hypothalamus/paraventricular nucleus and the brain stem. “The resulting symptoms and the neurologically driven ‘sickness response’ for the ME/CFS patient would persist, preventing healing and a return to the preinfectious/stress-related state,” Dr. Tate and colleagues said.
Lingering inflammation may be the culprit
Commenting on the study, Achillefs Ntranos, MD, a board-certified neurologist in private practice in Scarsdale, N.Y., who was not involved with the research, said previous studies have shown that long COVID is linked to chronic activation of microglia in the brain, which has also been seen to activate in patients with ME/CFS.
“The hypothesis that lingering inflammation in the brain is the culprit behind the neurological symptoms of long COVID and ME/CFS is valid,” he said. “If these cells remain activated in the brain, they can cause a state of increased and lingering inflammation, which can interfere with the function of neurons, thus producing neurological symptoms. Since the neurological symptoms are similar between these entities, the mechanisms that produce them might also be similar.”
While the exact cause of ME/CFS is still unclear, it is often tied to the aftereffects of a flu-like illness, Dr. Ntranos said. “This has led researchers to propose that it arises after a viral infection, with many different types of viruses being associated with it. Other ways researchers think ME/CFS is being brought on after a viral illness is via changes in the immune system, such as chronic production of cytokines, neuroinflammation, and disruption of the hypothalamic-pituitary-adrenal axis, which regulates the body’s response to stress,” he explained.
While a newer condition, long COVID is not all that different from ME/CFS, Dr. Ntranos noted, sharing the catalyst of a viral infection and core neurological symptoms such as fatigue, postexertional malaise, a “brain fog” that makes thinking or concentrating difficult, sleep problems, and lightheadedness, but there are differences that set it apart from ME/CFS.
“Long COVID is unique in having additional symptoms that are specific to the SARS-CoV-2 virus, such as respiratory and cardiovascular symptoms and loss of smell and taste. However most central nervous system effects are the same between these two entities,” he said.
Dr. Ntranos said long COVID’s neurological symptoms are similar to that of multiple sclerosis (MS), such as “brain fog” and postexertional malaise. “Since MS only affects the brain and spinal cord, there are no symptoms from other organ systems, such as the lungs, heart, or digestive system, contrary to long COVID. Furthermore, MS rarely affects smell and taste, making these symptoms unique to COVID,” he said.
However, he pointed out that brain fog and fatigue symptoms on their own can be nonspecific and attributed to many different conditions, such as obstructive sleep apnea, migraines, depression, anxiety, thyroid problems, vitamin deficiencies, dehydration, sleep disorders, and side effects of medications.
“More research needs to be done to understand how these cells are being activated, how they interfere with neuronal function, and why they remain in that state in some people, who then go on to develop fatigue and brain fog,” he said.
This study was funded by the Healthcare Otago Charitable Trust, the Associated New Zealand Myalgic Encephalomyelitis Society, and donations from families of patients with ME/CFS. The authors and Dr. Ntranos report no relevant financial disclosures.
FROM FRONTIERS IN NEUROLOGY









