User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Center-based childcare associated with healthier body weight
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
The findings of the prospective Canadian study suggest that professional childcare centers that engage in standard practices are having a positive and lasting impact on children’s health, reported lead author Michaela Kucab, RD, MHSc, of the University of Toronto and colleagues.
“Attending center-based childcare in early childhood may influence important health behaviors including nutrition, physical activity, and routines related to child growth and weight status,” the investigators wrote in their abstract, which Ms. Kucab presented at the virtual conference sponsored by the American Society for Nutrition.
Their study involved 3,503 children who attended childcare in Canada during early childhood (mean age at baseline was 2.7 years) with follow-up from ages 4-10.
Overweight/obesity risk reduced
Children who received full-time, center-based care had a 22% lower risk of overweight/obesity and a mean body mass index z score (zBMI) that was 0.11 points lower at age 4 and 7 years than those who received non–center-based care. The benefits of center-based care were even more pronounced among children from lower-income families, who, at age 10, had a 48% lower risk of overweight/obesity and a mean zBMI that was 0.32 points lower with center-based versus non–center-based care.
In a written comment, Ms. Kucab and principal author Jonathon Maguire, MD, MSc, of the University of Toronto, explained that the former difference in zBMI translates to approximately half a pound of bodyweight in an average child, whereas the larger difference in zBMI among children from lower-income families would amount to approximately three pounds. They emphasized that these are rough estimations.
Ms. Kucab and Dr. Maguire noted that body weight differences correlated with the amount of time spent in center-based care.
“There was an observed trend, whereby the estimated mean difference [in zBMI] became slightly larger (or stronger) with a higher intensity of center-based childcare compared to non–center-based childcare,” they said.
To learn more about the earliest impacts of center-based care, the investigators are conducting a clinical trial, The Nutrition Recommendation Intervention Trials in Children’s Health Care (NuRISH), which will involve 600 children aged younger than 2 years.
Center-based childcare may reduce disadvantages of low-income children
“Although more research is needed, our findings suggest that center-based childcare may help” reduce disadvantages children from low-income families experience related to their heath,” Ms. Kucab said in a press release.
Laurent Legault, MD, an associate professor specializing in endocrinology in the department of pediatrics at McGill University, Montreal, highlighted the “quite significant” sample size of more than 3,000 participants, noting that “it’s quite tough to have numerous children” involved in a study, especially with several years of follow-up.
Dr. Legault also praised the investigators for considering socioeconomic status, “which is absolutely paramount, because, unfortunately, it’s not necessarily an even playing field for these families.”
He said the findings deserve to be promoted, as they highlight the benefits of center-based care, including ones with room for physical activity, opportunities for social interaction with other children, and a structured routine.
Still, Dr. Legault said it’s “very difficult to pinpoint specifically” what led to healthier body weights. “The problem, of course, is that obesity is very multifactorial in nature,” although “early intervention is more likely to be efficient.”
Center-based care appears to be one such intervention, he said, which should “push people to make centered care more affordable and easy to access for everyone.”The investigators and Dr. Legault reported no conflicts of interest.
FROM NUTRITION 2022
Interventional Radiology Treatment for Uterine Fibroids
Interventional approaches are being used as a standard of care more and more to provide image-guided techniques to perform minimally invasive procedures. With this being said, what are some indications and best practices used with interventional radiology for the treatment of uterine fibroids?
Dr. Boone: Interventional radiologists offer minimally invasive non-surgical treatment options for the management of symptomatic uterine fibroids. These approaches include uterine artery embolization or UAE. It may also be called uterine fibroid embolization or UFE. In this procedure, the uterine arteries are embolized with permanent embolic particles to block blood flow to the fibroids.
The goal of this treatment is to shrink the fibroids. It usually leads to a gradual shrinkage of fibroids and can also be particularly effective for reducing bleeding from fibroids. This procedure has been around for more than 20 years and has a lot of data describing its safety and efficacy.
Another treatment, which is non-invasive, but some interventional radiologists offer, is magnetic resonance-guided focused ultrasound. This might also be called high intensity focused ultrasound or HIFU. In this treatment, MRI is used to direct high intensity ultrasound waves onto the fibroid. This focused application of these high intensity ultrasound waves generates heat and leads to coagulative necrosis of the fibroid.
This procedure is newer than uterine artery embolization, but it has some benefits of avoiding ionizing radiation. Although, it can have longer procedure times. For both procedures, the indications are symptomatic uterine fibroids.
The symptoms we're concerned about include menorrhagia, which can result in anemia. There are also “bulk” symptoms, related to the actual bulk of the fibroids, which can cause bladder or bowel dysfunction. Some patients also have protrusion of their abdomen, dysmenorrhea, and infertility.
The goal is to help reduce those symptoms. The Society for Interventional Radiology has published best practices. For expected outcomes, with the uterine artery embolization, it is 50% to 60% reduction in the size of fibroid of the fibroids themselves, 40% to 50% reduction in the size of the uterus, 88% to 92% of reduction of the bulk symptoms.
Every consultation should discuss the range of treatment options—the medical, surgical, and non-surgical or interventional. I wanted to point out that there is a real need for this. The Society for Interventional Radiology commissioned a poll in 2017 of patients–women who had been diagnosed with uterine fibroids—and found that 44% of patients noted never hearing of uterine artery embolization. Eleven percent of these patients believed that hysterectomy was their only treatment option. Further, a recent article from NPR noted concerns about disparities in which women of color, particularly Black women, were not offered or made aware of more minimally invasive options during consultations. Very broad patient education about the range of treatment options is important.
In addition, we want to consider other differential diagnoses that patients may have, such as adenomyosis or rare malignancies. Leiomyosarcoma can present with similar symptoms to uterine fibroids or can even coexist with uterine fibroids. In the case of leiomyosarcoma, the treatment pathway may be completely different, and we don't want to undertreat or delay diagnosis. Other considerations that can have bearing on the selection of treatment can be the number and the size of the fibroids.
To help with the decision-making process, these patients need a complete workup. We want to get lab tests. We want to also make sure they have a complete gynecologic evaluation, which includes an ultrasound and an MRI. Particularly, contrast-enhanced MRI has great accuracy for evaluating fibroid location because we’re imaging the entire pelvis. We can see where everything is and map out our target fibroids.
We can also see the enhancement characteristics of the fibroids. Some fibroids are not just supplied by uterine arteries but ovarian arteries, which can affect the efficacy of the treatment and even some of the risks of the treatment.
What is your role and particularly what is the role of the Nurse Practitioner when thinking about diagnosis and treatment and how do you and the nurse practitioner work together?
Dr. Boone: I would say the specific roles for the physicians and nurse practitioners on an interventional radiology team can vary with a lot of different factors. It could depend on the practice setting, such as, whether you're in a busy academic center or in a small private practice. It can depend on the types of cases we're doing. Even some of the local regulations of the institution and state can come into play. The roles tend to be laid out and specified by the supervising physician based on this context.
For example, ideally, all of that work up and planning is happening in that clinic setting before the patient even comes down to the suite for the procedure. In this setting, nurse practitioners can provide a significant role in obtaining the data that we need. They'll perform the history and physical exam, which helps the team learn about the patients. It helps answer relevant questions: What symptoms is the patient having? What are their wishes for the procedure? What are the things they're hoping to avoid or hoping to get from having the procedure done? They review for those relevant labs and imaging, and in order to recognize the information we don’t have.
The next step is developing the assessment and plan which is usually done in conjunction with the interventional radiologist. This is especially important with new patients. Once that assessment and plan are determined, the nurse practitioner can be helpful in explaining the process in depth to the patient and their family or caregivers while they're in the clinic.
Another important role for nurse practitioners in this setting is the consent. I can talk a little bit more about that later, but informed consent is critical. It can be a pretty extensive discussion, especially if we want to talk about this wide range of treatment options. So that is substantial value added by the nurse practitioner.
The other important role is the follow up visits, which may be almost completely independently by a nurse practitioner. They see patients post-procedure, evaluating how they’re doing and what's changed. This is critical because we need to determine: 1. Have we gotten the result that we want? 2. Do we want to give more time to see changes? and; 3. Do we need to do another procedure? We also want to follow these patients and their response to treatment to look out for something concerning that might raise concern for malignancy, such as the fibroid continuing to grow rapidly. Those follow up visits are also a critical role for NPs.
In the inpatient setting, the attending and senior interventional radiology residents may actually determine the roles and tasks the other team members are going to perform to help the IR service run smoothly. And typically, nurse practitioners and also physician assistants will share many of those responsibilities of running that interventional radiology service outside of the procedure room.
There are also cases where nurse practitioners and physician assistants can have a dedicated role in performing certain procedures. Personally, I've seen physician assistants in these cases, where they were our dedicated bone marrow biopsy providers. Throughout the day, they would do all the bone marrow biopsy cases. Another example I saw was placement of vascular access catheters, whether for ports or dialysis. NPs see many patients throughout the day and perform these procedures. This is helpful because these are very popular procedures and are needed. While those are being done, it frees up time for the other members of the team to do other, more time-consuming, procedures as well.
In all cases, we work closely together. We're sharing this responsibility of patient care. We communicate frequently and it's a valuable team dynamic. NPs are fantastic team members
Dr. Boone, you talked about the treatments and how you work together with NPs. Can you touch on the interventional procedures and the value or benefit over conservative treatments and drugs, particularly, where you receive support or recommendations from nurse practitioners at this stage?
Dr. Boone: Regarding more conservative treatment, there’s expectant management where the patients may not want to undergo an intervention at that time. You’re following the patient and watching for possible worsening of symptoms that may lead to a change in management.
There’s also medical management, which generally gets broken down into hormonal or non-hormonal medications. Among these, there's a lot of different drugs that are available. Among the more frequently used hormonal therapies would be gonadotropin-releasing hormone agonists.
The non-hormonal therapies such as, NSAIDs, or procoagulation medications, like tranexamic acid, are more targeted at symptom control. Particularly, these target the abnormal uterine bleeding and the pain.
For these therapies, the limitations can be side-effect profiles. Sometimes these side effects are just not acceptable to patients. Hormonal therapies like the gonadotropin-releasing hormone agonists create this hypoestrogenic state. Patients may not like having the menopause-like symptoms.
Additionally, medications are more short-term in their benefit. For example, with the cessation of gonadotropin-releasing hormone agonists, the fibroids actually can show rapid rebound growth. Some of the non-surgical interventions can provide longer term benefit, even if they may require re-intervention more frequently compared to surgical interventions.
For interventional radiology, we primarily focus on the procedures. We don't typically manage the medical therapy. These treatment approaches are cultivated more by gynecology or other clinicians.
When it comes to interventional radiology treatment for uterine fibroids in your day-to-day practices, which you've talked a lot about today, what has been your experience in working with Nurse Practitioners overall and where do they, should they or could they potentially add even more value?
Dr. Boone: Nurse practitioners play an integral role on the team and, I think, they provide a lot of value. They have an important role in teaching settings, were they provide continuity of care. They can also greatly impact with teaching of trainees.
In teaching settings, there's a substantial turnover of trainees because -- and this includes residents, medical students, in some cases fellows -- they're rotating between different hospitals every few weeks. Even at the end of the year, the most senior residents, the most experience trainees, leave to go to new jobs. Nurse practitioners on the IR team are a critical source of continuity and consistency for patients and for the rest of the team because they spend the most time on the service and they know the team members well. They also know how to get things done efficiently and really know the system.
They've also honed the skills that trainees, particularly junior residents, are learning. In my experience, I first learned to place and remove tunneled catheters and bone marrow biopsies by spending the day with a physician assistant and a nurse practitioner. Both from the educational standpoint and also consistent, efficient care standpoint, having NPs and PAs on our team is hugely valuable.
Emphasizing that role in teaching is highly valuable. I would encourage nurse practitioners on an IR team with trainees to take ownership of teaching a particular skill or a certain topic, because they're going to bring a different perspective and that's extremely valuable.
Another arena where there's a lot of value, is in the informed consent and patient education portion of patient care. Interventional radiology is not the most familiar medical field for a lot of people. Interventional radiologists also perform a wide array of procedures and they can be very different. Even treatments for the same problem, uterine artery embolization and MRI-guided focused ultrasound, are very different procedures in terms of how they're actually performed.
For example, if you mentioned surgery to most people, there is some idea of what that entails and who performs it. But if you say embolization to most people, they may not entirely understand all those components. For a patient to sufficiently be informed and able to consent, they do need to understand not only their disease and the treatment being offered, but also the risks, the benefits, and the alternatives. They need to understand what to expect from the procedure.
Doing this well can take a substantial amount of time, but it is important. From a physician standpoint, that entails balancing. Along with performing the procedures and reviewing patient imaging as well as other clinical duties this is very challenging. Nurse practitioners can really leverage their expertise in patient communication and education to fill in those knowledge gaps and best serve the patient while also helping the IR service. These are just two of many areas in which NPs can be highly valuable to an IR practice.
1. Kröncke T, David M. MR-Guided Focused Ultrasound in Fibroid Treatment – Results of the 4th Radiological-Gynecological Expert Meeting. Fortschr Röntgenstr. 2019;191(07):626-629. doi:10.1055/a-0884-3143
2. Sridhar D, Kohi M. Updates on MR-Guided Focused Ultrasound for Symptomatic Uterine Fibroids. Semin intervent Radiol. 2018;35(01):017-022. doi:10.1055/s-0038-1636516
3. Kohi MP, Spies JB. Updates on Uterine Artery Embolization. Semin intervent Radiol. 2018;35(1):48-55. doi:10.1055/s-0038-1636521
4. Dariushnia SR, Nikolic B, Stokes LS, Spies JB. Quality Improvement Guidelines for Uterine Artery Embolization for Symptomatic Leiomyomata. Journal of Vascular and Interventional Radiology. 2014;25(11):1737-1747. doi:10.1016/j.jvir.2014.08.029
5. Wise A. Facing invasive treatments for uterine fibroids, Black women advocate for better care. NPR. https://www.npr.org/sections/health-shots/2022/04/10/1087483675/facing-invasive-treatments-for-uterine-fibroids-black-women-advocate-for-better-. Published April 10, 2022. Accessed June 9, 2022.
6. http://fyra.io. SIR Survey Shows Public Awareness Shortcomings for UFE as Treatment Option for Uterine Fibroids. Endovascular Today. Accessed June 9, 2022. https://evtoday.com/news/sir-survey-shows-public-awareness-shortcomings-for-ufe-as-treatment-option-for-uterine-fibroids
Interventional approaches are being used as a standard of care more and more to provide image-guided techniques to perform minimally invasive procedures. With this being said, what are some indications and best practices used with interventional radiology for the treatment of uterine fibroids?
Dr. Boone: Interventional radiologists offer minimally invasive non-surgical treatment options for the management of symptomatic uterine fibroids. These approaches include uterine artery embolization or UAE. It may also be called uterine fibroid embolization or UFE. In this procedure, the uterine arteries are embolized with permanent embolic particles to block blood flow to the fibroids.
The goal of this treatment is to shrink the fibroids. It usually leads to a gradual shrinkage of fibroids and can also be particularly effective for reducing bleeding from fibroids. This procedure has been around for more than 20 years and has a lot of data describing its safety and efficacy.
Another treatment, which is non-invasive, but some interventional radiologists offer, is magnetic resonance-guided focused ultrasound. This might also be called high intensity focused ultrasound or HIFU. In this treatment, MRI is used to direct high intensity ultrasound waves onto the fibroid. This focused application of these high intensity ultrasound waves generates heat and leads to coagulative necrosis of the fibroid.
This procedure is newer than uterine artery embolization, but it has some benefits of avoiding ionizing radiation. Although, it can have longer procedure times. For both procedures, the indications are symptomatic uterine fibroids.
The symptoms we're concerned about include menorrhagia, which can result in anemia. There are also “bulk” symptoms, related to the actual bulk of the fibroids, which can cause bladder or bowel dysfunction. Some patients also have protrusion of their abdomen, dysmenorrhea, and infertility.
The goal is to help reduce those symptoms. The Society for Interventional Radiology has published best practices. For expected outcomes, with the uterine artery embolization, it is 50% to 60% reduction in the size of fibroid of the fibroids themselves, 40% to 50% reduction in the size of the uterus, 88% to 92% of reduction of the bulk symptoms.
Every consultation should discuss the range of treatment options—the medical, surgical, and non-surgical or interventional. I wanted to point out that there is a real need for this. The Society for Interventional Radiology commissioned a poll in 2017 of patients–women who had been diagnosed with uterine fibroids—and found that 44% of patients noted never hearing of uterine artery embolization. Eleven percent of these patients believed that hysterectomy was their only treatment option. Further, a recent article from NPR noted concerns about disparities in which women of color, particularly Black women, were not offered or made aware of more minimally invasive options during consultations. Very broad patient education about the range of treatment options is important.
In addition, we want to consider other differential diagnoses that patients may have, such as adenomyosis or rare malignancies. Leiomyosarcoma can present with similar symptoms to uterine fibroids or can even coexist with uterine fibroids. In the case of leiomyosarcoma, the treatment pathway may be completely different, and we don't want to undertreat or delay diagnosis. Other considerations that can have bearing on the selection of treatment can be the number and the size of the fibroids.
To help with the decision-making process, these patients need a complete workup. We want to get lab tests. We want to also make sure they have a complete gynecologic evaluation, which includes an ultrasound and an MRI. Particularly, contrast-enhanced MRI has great accuracy for evaluating fibroid location because we’re imaging the entire pelvis. We can see where everything is and map out our target fibroids.
We can also see the enhancement characteristics of the fibroids. Some fibroids are not just supplied by uterine arteries but ovarian arteries, which can affect the efficacy of the treatment and even some of the risks of the treatment.
What is your role and particularly what is the role of the Nurse Practitioner when thinking about diagnosis and treatment and how do you and the nurse practitioner work together?
Dr. Boone: I would say the specific roles for the physicians and nurse practitioners on an interventional radiology team can vary with a lot of different factors. It could depend on the practice setting, such as, whether you're in a busy academic center or in a small private practice. It can depend on the types of cases we're doing. Even some of the local regulations of the institution and state can come into play. The roles tend to be laid out and specified by the supervising physician based on this context.
For example, ideally, all of that work up and planning is happening in that clinic setting before the patient even comes down to the suite for the procedure. In this setting, nurse practitioners can provide a significant role in obtaining the data that we need. They'll perform the history and physical exam, which helps the team learn about the patients. It helps answer relevant questions: What symptoms is the patient having? What are their wishes for the procedure? What are the things they're hoping to avoid or hoping to get from having the procedure done? They review for those relevant labs and imaging, and in order to recognize the information we don’t have.
The next step is developing the assessment and plan which is usually done in conjunction with the interventional radiologist. This is especially important with new patients. Once that assessment and plan are determined, the nurse practitioner can be helpful in explaining the process in depth to the patient and their family or caregivers while they're in the clinic.
Another important role for nurse practitioners in this setting is the consent. I can talk a little bit more about that later, but informed consent is critical. It can be a pretty extensive discussion, especially if we want to talk about this wide range of treatment options. So that is substantial value added by the nurse practitioner.
The other important role is the follow up visits, which may be almost completely independently by a nurse practitioner. They see patients post-procedure, evaluating how they’re doing and what's changed. This is critical because we need to determine: 1. Have we gotten the result that we want? 2. Do we want to give more time to see changes? and; 3. Do we need to do another procedure? We also want to follow these patients and their response to treatment to look out for something concerning that might raise concern for malignancy, such as the fibroid continuing to grow rapidly. Those follow up visits are also a critical role for NPs.
In the inpatient setting, the attending and senior interventional radiology residents may actually determine the roles and tasks the other team members are going to perform to help the IR service run smoothly. And typically, nurse practitioners and also physician assistants will share many of those responsibilities of running that interventional radiology service outside of the procedure room.
There are also cases where nurse practitioners and physician assistants can have a dedicated role in performing certain procedures. Personally, I've seen physician assistants in these cases, where they were our dedicated bone marrow biopsy providers. Throughout the day, they would do all the bone marrow biopsy cases. Another example I saw was placement of vascular access catheters, whether for ports or dialysis. NPs see many patients throughout the day and perform these procedures. This is helpful because these are very popular procedures and are needed. While those are being done, it frees up time for the other members of the team to do other, more time-consuming, procedures as well.
In all cases, we work closely together. We're sharing this responsibility of patient care. We communicate frequently and it's a valuable team dynamic. NPs are fantastic team members
Dr. Boone, you talked about the treatments and how you work together with NPs. Can you touch on the interventional procedures and the value or benefit over conservative treatments and drugs, particularly, where you receive support or recommendations from nurse practitioners at this stage?
Dr. Boone: Regarding more conservative treatment, there’s expectant management where the patients may not want to undergo an intervention at that time. You’re following the patient and watching for possible worsening of symptoms that may lead to a change in management.
There’s also medical management, which generally gets broken down into hormonal or non-hormonal medications. Among these, there's a lot of different drugs that are available. Among the more frequently used hormonal therapies would be gonadotropin-releasing hormone agonists.
The non-hormonal therapies such as, NSAIDs, or procoagulation medications, like tranexamic acid, are more targeted at symptom control. Particularly, these target the abnormal uterine bleeding and the pain.
For these therapies, the limitations can be side-effect profiles. Sometimes these side effects are just not acceptable to patients. Hormonal therapies like the gonadotropin-releasing hormone agonists create this hypoestrogenic state. Patients may not like having the menopause-like symptoms.
Additionally, medications are more short-term in their benefit. For example, with the cessation of gonadotropin-releasing hormone agonists, the fibroids actually can show rapid rebound growth. Some of the non-surgical interventions can provide longer term benefit, even if they may require re-intervention more frequently compared to surgical interventions.
For interventional radiology, we primarily focus on the procedures. We don't typically manage the medical therapy. These treatment approaches are cultivated more by gynecology or other clinicians.
When it comes to interventional radiology treatment for uterine fibroids in your day-to-day practices, which you've talked a lot about today, what has been your experience in working with Nurse Practitioners overall and where do they, should they or could they potentially add even more value?
Dr. Boone: Nurse practitioners play an integral role on the team and, I think, they provide a lot of value. They have an important role in teaching settings, were they provide continuity of care. They can also greatly impact with teaching of trainees.
In teaching settings, there's a substantial turnover of trainees because -- and this includes residents, medical students, in some cases fellows -- they're rotating between different hospitals every few weeks. Even at the end of the year, the most senior residents, the most experience trainees, leave to go to new jobs. Nurse practitioners on the IR team are a critical source of continuity and consistency for patients and for the rest of the team because they spend the most time on the service and they know the team members well. They also know how to get things done efficiently and really know the system.
They've also honed the skills that trainees, particularly junior residents, are learning. In my experience, I first learned to place and remove tunneled catheters and bone marrow biopsies by spending the day with a physician assistant and a nurse practitioner. Both from the educational standpoint and also consistent, efficient care standpoint, having NPs and PAs on our team is hugely valuable.
Emphasizing that role in teaching is highly valuable. I would encourage nurse practitioners on an IR team with trainees to take ownership of teaching a particular skill or a certain topic, because they're going to bring a different perspective and that's extremely valuable.
Another arena where there's a lot of value, is in the informed consent and patient education portion of patient care. Interventional radiology is not the most familiar medical field for a lot of people. Interventional radiologists also perform a wide array of procedures and they can be very different. Even treatments for the same problem, uterine artery embolization and MRI-guided focused ultrasound, are very different procedures in terms of how they're actually performed.
For example, if you mentioned surgery to most people, there is some idea of what that entails and who performs it. But if you say embolization to most people, they may not entirely understand all those components. For a patient to sufficiently be informed and able to consent, they do need to understand not only their disease and the treatment being offered, but also the risks, the benefits, and the alternatives. They need to understand what to expect from the procedure.
Doing this well can take a substantial amount of time, but it is important. From a physician standpoint, that entails balancing. Along with performing the procedures and reviewing patient imaging as well as other clinical duties this is very challenging. Nurse practitioners can really leverage their expertise in patient communication and education to fill in those knowledge gaps and best serve the patient while also helping the IR service. These are just two of many areas in which NPs can be highly valuable to an IR practice.
Interventional approaches are being used as a standard of care more and more to provide image-guided techniques to perform minimally invasive procedures. With this being said, what are some indications and best practices used with interventional radiology for the treatment of uterine fibroids?
Dr. Boone: Interventional radiologists offer minimally invasive non-surgical treatment options for the management of symptomatic uterine fibroids. These approaches include uterine artery embolization or UAE. It may also be called uterine fibroid embolization or UFE. In this procedure, the uterine arteries are embolized with permanent embolic particles to block blood flow to the fibroids.
The goal of this treatment is to shrink the fibroids. It usually leads to a gradual shrinkage of fibroids and can also be particularly effective for reducing bleeding from fibroids. This procedure has been around for more than 20 years and has a lot of data describing its safety and efficacy.
Another treatment, which is non-invasive, but some interventional radiologists offer, is magnetic resonance-guided focused ultrasound. This might also be called high intensity focused ultrasound or HIFU. In this treatment, MRI is used to direct high intensity ultrasound waves onto the fibroid. This focused application of these high intensity ultrasound waves generates heat and leads to coagulative necrosis of the fibroid.
This procedure is newer than uterine artery embolization, but it has some benefits of avoiding ionizing radiation. Although, it can have longer procedure times. For both procedures, the indications are symptomatic uterine fibroids.
The symptoms we're concerned about include menorrhagia, which can result in anemia. There are also “bulk” symptoms, related to the actual bulk of the fibroids, which can cause bladder or bowel dysfunction. Some patients also have protrusion of their abdomen, dysmenorrhea, and infertility.
The goal is to help reduce those symptoms. The Society for Interventional Radiology has published best practices. For expected outcomes, with the uterine artery embolization, it is 50% to 60% reduction in the size of fibroid of the fibroids themselves, 40% to 50% reduction in the size of the uterus, 88% to 92% of reduction of the bulk symptoms.
Every consultation should discuss the range of treatment options—the medical, surgical, and non-surgical or interventional. I wanted to point out that there is a real need for this. The Society for Interventional Radiology commissioned a poll in 2017 of patients–women who had been diagnosed with uterine fibroids—and found that 44% of patients noted never hearing of uterine artery embolization. Eleven percent of these patients believed that hysterectomy was their only treatment option. Further, a recent article from NPR noted concerns about disparities in which women of color, particularly Black women, were not offered or made aware of more minimally invasive options during consultations. Very broad patient education about the range of treatment options is important.
In addition, we want to consider other differential diagnoses that patients may have, such as adenomyosis or rare malignancies. Leiomyosarcoma can present with similar symptoms to uterine fibroids or can even coexist with uterine fibroids. In the case of leiomyosarcoma, the treatment pathway may be completely different, and we don't want to undertreat or delay diagnosis. Other considerations that can have bearing on the selection of treatment can be the number and the size of the fibroids.
To help with the decision-making process, these patients need a complete workup. We want to get lab tests. We want to also make sure they have a complete gynecologic evaluation, which includes an ultrasound and an MRI. Particularly, contrast-enhanced MRI has great accuracy for evaluating fibroid location because we’re imaging the entire pelvis. We can see where everything is and map out our target fibroids.
We can also see the enhancement characteristics of the fibroids. Some fibroids are not just supplied by uterine arteries but ovarian arteries, which can affect the efficacy of the treatment and even some of the risks of the treatment.
What is your role and particularly what is the role of the Nurse Practitioner when thinking about diagnosis and treatment and how do you and the nurse practitioner work together?
Dr. Boone: I would say the specific roles for the physicians and nurse practitioners on an interventional radiology team can vary with a lot of different factors. It could depend on the practice setting, such as, whether you're in a busy academic center or in a small private practice. It can depend on the types of cases we're doing. Even some of the local regulations of the institution and state can come into play. The roles tend to be laid out and specified by the supervising physician based on this context.
For example, ideally, all of that work up and planning is happening in that clinic setting before the patient even comes down to the suite for the procedure. In this setting, nurse practitioners can provide a significant role in obtaining the data that we need. They'll perform the history and physical exam, which helps the team learn about the patients. It helps answer relevant questions: What symptoms is the patient having? What are their wishes for the procedure? What are the things they're hoping to avoid or hoping to get from having the procedure done? They review for those relevant labs and imaging, and in order to recognize the information we don’t have.
The next step is developing the assessment and plan which is usually done in conjunction with the interventional radiologist. This is especially important with new patients. Once that assessment and plan are determined, the nurse practitioner can be helpful in explaining the process in depth to the patient and their family or caregivers while they're in the clinic.
Another important role for nurse practitioners in this setting is the consent. I can talk a little bit more about that later, but informed consent is critical. It can be a pretty extensive discussion, especially if we want to talk about this wide range of treatment options. So that is substantial value added by the nurse practitioner.
The other important role is the follow up visits, which may be almost completely independently by a nurse practitioner. They see patients post-procedure, evaluating how they’re doing and what's changed. This is critical because we need to determine: 1. Have we gotten the result that we want? 2. Do we want to give more time to see changes? and; 3. Do we need to do another procedure? We also want to follow these patients and their response to treatment to look out for something concerning that might raise concern for malignancy, such as the fibroid continuing to grow rapidly. Those follow up visits are also a critical role for NPs.
In the inpatient setting, the attending and senior interventional radiology residents may actually determine the roles and tasks the other team members are going to perform to help the IR service run smoothly. And typically, nurse practitioners and also physician assistants will share many of those responsibilities of running that interventional radiology service outside of the procedure room.
There are also cases where nurse practitioners and physician assistants can have a dedicated role in performing certain procedures. Personally, I've seen physician assistants in these cases, where they were our dedicated bone marrow biopsy providers. Throughout the day, they would do all the bone marrow biopsy cases. Another example I saw was placement of vascular access catheters, whether for ports or dialysis. NPs see many patients throughout the day and perform these procedures. This is helpful because these are very popular procedures and are needed. While those are being done, it frees up time for the other members of the team to do other, more time-consuming, procedures as well.
In all cases, we work closely together. We're sharing this responsibility of patient care. We communicate frequently and it's a valuable team dynamic. NPs are fantastic team members
Dr. Boone, you talked about the treatments and how you work together with NPs. Can you touch on the interventional procedures and the value or benefit over conservative treatments and drugs, particularly, where you receive support or recommendations from nurse practitioners at this stage?
Dr. Boone: Regarding more conservative treatment, there’s expectant management where the patients may not want to undergo an intervention at that time. You’re following the patient and watching for possible worsening of symptoms that may lead to a change in management.
There’s also medical management, which generally gets broken down into hormonal or non-hormonal medications. Among these, there's a lot of different drugs that are available. Among the more frequently used hormonal therapies would be gonadotropin-releasing hormone agonists.
The non-hormonal therapies such as, NSAIDs, or procoagulation medications, like tranexamic acid, are more targeted at symptom control. Particularly, these target the abnormal uterine bleeding and the pain.
For these therapies, the limitations can be side-effect profiles. Sometimes these side effects are just not acceptable to patients. Hormonal therapies like the gonadotropin-releasing hormone agonists create this hypoestrogenic state. Patients may not like having the menopause-like symptoms.
Additionally, medications are more short-term in their benefit. For example, with the cessation of gonadotropin-releasing hormone agonists, the fibroids actually can show rapid rebound growth. Some of the non-surgical interventions can provide longer term benefit, even if they may require re-intervention more frequently compared to surgical interventions.
For interventional radiology, we primarily focus on the procedures. We don't typically manage the medical therapy. These treatment approaches are cultivated more by gynecology or other clinicians.
When it comes to interventional radiology treatment for uterine fibroids in your day-to-day practices, which you've talked a lot about today, what has been your experience in working with Nurse Practitioners overall and where do they, should they or could they potentially add even more value?
Dr. Boone: Nurse practitioners play an integral role on the team and, I think, they provide a lot of value. They have an important role in teaching settings, were they provide continuity of care. They can also greatly impact with teaching of trainees.
In teaching settings, there's a substantial turnover of trainees because -- and this includes residents, medical students, in some cases fellows -- they're rotating between different hospitals every few weeks. Even at the end of the year, the most senior residents, the most experience trainees, leave to go to new jobs. Nurse practitioners on the IR team are a critical source of continuity and consistency for patients and for the rest of the team because they spend the most time on the service and they know the team members well. They also know how to get things done efficiently and really know the system.
They've also honed the skills that trainees, particularly junior residents, are learning. In my experience, I first learned to place and remove tunneled catheters and bone marrow biopsies by spending the day with a physician assistant and a nurse practitioner. Both from the educational standpoint and also consistent, efficient care standpoint, having NPs and PAs on our team is hugely valuable.
Emphasizing that role in teaching is highly valuable. I would encourage nurse practitioners on an IR team with trainees to take ownership of teaching a particular skill or a certain topic, because they're going to bring a different perspective and that's extremely valuable.
Another arena where there's a lot of value, is in the informed consent and patient education portion of patient care. Interventional radiology is not the most familiar medical field for a lot of people. Interventional radiologists also perform a wide array of procedures and they can be very different. Even treatments for the same problem, uterine artery embolization and MRI-guided focused ultrasound, are very different procedures in terms of how they're actually performed.
For example, if you mentioned surgery to most people, there is some idea of what that entails and who performs it. But if you say embolization to most people, they may not entirely understand all those components. For a patient to sufficiently be informed and able to consent, they do need to understand not only their disease and the treatment being offered, but also the risks, the benefits, and the alternatives. They need to understand what to expect from the procedure.
Doing this well can take a substantial amount of time, but it is important. From a physician standpoint, that entails balancing. Along with performing the procedures and reviewing patient imaging as well as other clinical duties this is very challenging. Nurse practitioners can really leverage their expertise in patient communication and education to fill in those knowledge gaps and best serve the patient while also helping the IR service. These are just two of many areas in which NPs can be highly valuable to an IR practice.
1. Kröncke T, David M. MR-Guided Focused Ultrasound in Fibroid Treatment – Results of the 4th Radiological-Gynecological Expert Meeting. Fortschr Röntgenstr. 2019;191(07):626-629. doi:10.1055/a-0884-3143
2. Sridhar D, Kohi M. Updates on MR-Guided Focused Ultrasound for Symptomatic Uterine Fibroids. Semin intervent Radiol. 2018;35(01):017-022. doi:10.1055/s-0038-1636516
3. Kohi MP, Spies JB. Updates on Uterine Artery Embolization. Semin intervent Radiol. 2018;35(1):48-55. doi:10.1055/s-0038-1636521
4. Dariushnia SR, Nikolic B, Stokes LS, Spies JB. Quality Improvement Guidelines for Uterine Artery Embolization for Symptomatic Leiomyomata. Journal of Vascular and Interventional Radiology. 2014;25(11):1737-1747. doi:10.1016/j.jvir.2014.08.029
5. Wise A. Facing invasive treatments for uterine fibroids, Black women advocate for better care. NPR. https://www.npr.org/sections/health-shots/2022/04/10/1087483675/facing-invasive-treatments-for-uterine-fibroids-black-women-advocate-for-better-. Published April 10, 2022. Accessed June 9, 2022.
6. http://fyra.io. SIR Survey Shows Public Awareness Shortcomings for UFE as Treatment Option for Uterine Fibroids. Endovascular Today. Accessed June 9, 2022. https://evtoday.com/news/sir-survey-shows-public-awareness-shortcomings-for-ufe-as-treatment-option-for-uterine-fibroids
1. Kröncke T, David M. MR-Guided Focused Ultrasound in Fibroid Treatment – Results of the 4th Radiological-Gynecological Expert Meeting. Fortschr Röntgenstr. 2019;191(07):626-629. doi:10.1055/a-0884-3143
2. Sridhar D, Kohi M. Updates on MR-Guided Focused Ultrasound for Symptomatic Uterine Fibroids. Semin intervent Radiol. 2018;35(01):017-022. doi:10.1055/s-0038-1636516
3. Kohi MP, Spies JB. Updates on Uterine Artery Embolization. Semin intervent Radiol. 2018;35(1):48-55. doi:10.1055/s-0038-1636521
4. Dariushnia SR, Nikolic B, Stokes LS, Spies JB. Quality Improvement Guidelines for Uterine Artery Embolization for Symptomatic Leiomyomata. Journal of Vascular and Interventional Radiology. 2014;25(11):1737-1747. doi:10.1016/j.jvir.2014.08.029
5. Wise A. Facing invasive treatments for uterine fibroids, Black women advocate for better care. NPR. https://www.npr.org/sections/health-shots/2022/04/10/1087483675/facing-invasive-treatments-for-uterine-fibroids-black-women-advocate-for-better-. Published April 10, 2022. Accessed June 9, 2022.
6. http://fyra.io. SIR Survey Shows Public Awareness Shortcomings for UFE as Treatment Option for Uterine Fibroids. Endovascular Today. Accessed June 9, 2022. https://evtoday.com/news/sir-survey-shows-public-awareness-shortcomings-for-ufe-as-treatment-option-for-uterine-fibroids
Tampon shortage linked to supply chain, inflation issues
Social media users have posted about bare shelves and higher costs for months, marking the latest products to face stress under global supply chain concerns after baby formula, cars, and appliances.
Other menstrual products have increased in price as well because of inflation, according to Bloomberg News. The average price for a package of menstrual pads has increased about 8% this year, and the price of a box of tampons has increased about 10%.
Andre Schulten, the chief financial officer for Procter & Gamble, which makes and sells 4.5 billion boxes of Tampax each year, said on a recent earnings call that it has been “costly and highly volatile” to acquire the raw materials needed for production.
Raw materials such as cotton, rayon, and plastic, for instance, have been used to produce personal protective gear during the pandemic, which has led to shortages. The cost of transportation for consumer goods has also nearly tripled, and pandemic policies at ports have led to shipping delays.
Edgewell Personal Care, which makes the brands Playtex and o.b., has had a severe staff shortage at its Delaware facility where tampons are made, according to Time. The FDA has classified tampons as class II medical devices, which require certain quality-control regulations and qualified workers on the assembly line, the news outlet reported.
Representatives for CVS and Walgreens confirmed that they’ve had shortages in recent weeks, according to The Washington Post. Procter & Gamble said it is working with retail partners to make feminine care products more available.
“We understand it is frustrating for consumers when they can’t find what they need,” the company told the newspaper. “We can assure you this is a temporary situation.”
Kimberly-Clark, which makes U by Kotex tampons, told the Post that it “has not experienced a product or supply shortage” in the United States, saying it is “working closely with our retail partners to keep shelves stocked.”
But the shortage may grow worse as the year goes on and the peak season for shipping approaches, the newspaper reported.
“Capacity is only going to get tighter as we move toward the end of the year,” Vaughn Moore, chief executive of AIT Worldwide Logistics, told the Post.
While the situation is being straightened out, gynecologists have recommended against extending supply at home by wearing tampons for longer stretches of time, according to The New York Times. Toxic shock syndrome is a rare but potentially fatal condition that can occur when tampons are worn for more than 8 hours.
There are other options, such as reusable menstrual pads, period underwear, and menstrual cups and discs, the Times reported. But some of these may be less appealing to use, or they may cost too much.
A version of this article first appeared on WebMD.com.
Social media users have posted about bare shelves and higher costs for months, marking the latest products to face stress under global supply chain concerns after baby formula, cars, and appliances.
Other menstrual products have increased in price as well because of inflation, according to Bloomberg News. The average price for a package of menstrual pads has increased about 8% this year, and the price of a box of tampons has increased about 10%.
Andre Schulten, the chief financial officer for Procter & Gamble, which makes and sells 4.5 billion boxes of Tampax each year, said on a recent earnings call that it has been “costly and highly volatile” to acquire the raw materials needed for production.
Raw materials such as cotton, rayon, and plastic, for instance, have been used to produce personal protective gear during the pandemic, which has led to shortages. The cost of transportation for consumer goods has also nearly tripled, and pandemic policies at ports have led to shipping delays.
Edgewell Personal Care, which makes the brands Playtex and o.b., has had a severe staff shortage at its Delaware facility where tampons are made, according to Time. The FDA has classified tampons as class II medical devices, which require certain quality-control regulations and qualified workers on the assembly line, the news outlet reported.
Representatives for CVS and Walgreens confirmed that they’ve had shortages in recent weeks, according to The Washington Post. Procter & Gamble said it is working with retail partners to make feminine care products more available.
“We understand it is frustrating for consumers when they can’t find what they need,” the company told the newspaper. “We can assure you this is a temporary situation.”
Kimberly-Clark, which makes U by Kotex tampons, told the Post that it “has not experienced a product or supply shortage” in the United States, saying it is “working closely with our retail partners to keep shelves stocked.”
But the shortage may grow worse as the year goes on and the peak season for shipping approaches, the newspaper reported.
“Capacity is only going to get tighter as we move toward the end of the year,” Vaughn Moore, chief executive of AIT Worldwide Logistics, told the Post.
While the situation is being straightened out, gynecologists have recommended against extending supply at home by wearing tampons for longer stretches of time, according to The New York Times. Toxic shock syndrome is a rare but potentially fatal condition that can occur when tampons are worn for more than 8 hours.
There are other options, such as reusable menstrual pads, period underwear, and menstrual cups and discs, the Times reported. But some of these may be less appealing to use, or they may cost too much.
A version of this article first appeared on WebMD.com.
Social media users have posted about bare shelves and higher costs for months, marking the latest products to face stress under global supply chain concerns after baby formula, cars, and appliances.
Other menstrual products have increased in price as well because of inflation, according to Bloomberg News. The average price for a package of menstrual pads has increased about 8% this year, and the price of a box of tampons has increased about 10%.
Andre Schulten, the chief financial officer for Procter & Gamble, which makes and sells 4.5 billion boxes of Tampax each year, said on a recent earnings call that it has been “costly and highly volatile” to acquire the raw materials needed for production.
Raw materials such as cotton, rayon, and plastic, for instance, have been used to produce personal protective gear during the pandemic, which has led to shortages. The cost of transportation for consumer goods has also nearly tripled, and pandemic policies at ports have led to shipping delays.
Edgewell Personal Care, which makes the brands Playtex and o.b., has had a severe staff shortage at its Delaware facility where tampons are made, according to Time. The FDA has classified tampons as class II medical devices, which require certain quality-control regulations and qualified workers on the assembly line, the news outlet reported.
Representatives for CVS and Walgreens confirmed that they’ve had shortages in recent weeks, according to The Washington Post. Procter & Gamble said it is working with retail partners to make feminine care products more available.
“We understand it is frustrating for consumers when they can’t find what they need,” the company told the newspaper. “We can assure you this is a temporary situation.”
Kimberly-Clark, which makes U by Kotex tampons, told the Post that it “has not experienced a product or supply shortage” in the United States, saying it is “working closely with our retail partners to keep shelves stocked.”
But the shortage may grow worse as the year goes on and the peak season for shipping approaches, the newspaper reported.
“Capacity is only going to get tighter as we move toward the end of the year,” Vaughn Moore, chief executive of AIT Worldwide Logistics, told the Post.
While the situation is being straightened out, gynecologists have recommended against extending supply at home by wearing tampons for longer stretches of time, according to The New York Times. Toxic shock syndrome is a rare but potentially fatal condition that can occur when tampons are worn for more than 8 hours.
There are other options, such as reusable menstrual pads, period underwear, and menstrual cups and discs, the Times reported. But some of these may be less appealing to use, or they may cost too much.
A version of this article first appeared on WebMD.com.
‘DIY’ artificial pancreas systems found to be safe, effective: CREATE trial
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW ORLEANS – Open-source automated insulin delivery systems appear to be both effective and safe in adults and children, new research finds.
Automated insulin delivery (AID) system, also known as closed-loop systems or an artificial pancreas, link an insulin pump and a continuous glucose monitor (CGM) with an algorithm that automatically adjusts insulin delivery to optimize glycemic control.
Prior to the availability of commercial AID systems, Dana Lewis, a patient with type 1 diabetes, and her partner codeveloped an algorithm that could link older versions of an insulin pump and CGM.
In 2015, they made the code and all related materials open-source, so that anyone who wanted to create their own AID system could do so. Today thousands of people worldwide with type 1 diabetes are using the systems, which are sometimes called “do-it-yourself (DIY)” AID systems although the approach has been community based.
AID systems are not approved by any regulatory body, and despite several nonrandomized studies demonstrating their effectiveness and safety, there is still concern among some health professionals about their safety. In 2019, the U.S. Food and Drug Administration warned against the use of any nonapproved devices or algorithms. (Now, though, at least one open-source AID system algorithm is under FDA review.)
Aimed at addressing those concerns, CREATE (Community Derived Automated Insulin Delivery) is the first randomized controlled clinical trial to compare an open-source AID system to insulin pump therapy and CGM (without any communication between the two) in patients with type 1 diabetes, most of whom were naive to AID systems.
Doctors uncomfortable with open source; study provides reassurance
The findings were presented at the American Diabetes Association scientific sessions by Martin I. de Bock, PhD, a pediatric endocrinologist and senior lecturer at the University of Otago, Christchurch, New Zealand.
The study compared the most commonly used open-source AID system (using the OpenAPS algorithm from a version of AndroidAPS implemented in a smartphone with the DANA-i insulin pump and Dexcom G6 CGM) to any insulin pump plus CGM as a comparator group.
The open-source AID system led to a significant reduction in hemoglobin A1c with no major safety issues.
“The acceptance [among clinicians] of open-source systems is diverse and complicated, [with varying] personal comfort levels of seeing someone using an AID system that has no regulatory approval,” Dr. de Bock told this news organization.
“This is one of the reasons that it was so important to conduct the CREATE trial for the many thousands of open-source AID users. Given that the trial demonstrated safety and efficacy using the most robust scientific methodology available – a long-term randomized controlled trial – it may go some way to provide assurance for providers when they are seeing people using an open-source automated system,” he said.
Asked for comment, session moderator Diana Isaacs, PharmD, CDCES, an endocrine clinical pharmacist at the Cleveland Clinic, told this news organization: “There has been concern that these systems aren’t safe, so showing the safety is important. I think people deserve choice. As long as they’re safe, patients should be able to use what they want to use, and we should support them.”
Dr. Isaacs pointed out that an advantage of open-source systems over current commercial AIDs for patients is the ability to customize glucose targets, but in CREATE, those targets were established in the protocol by the investigators.
“I think it’s nice having the data, although in the trial they had specific requirements. They had a target range and active insulin time that they were recommending. So it’s a little different than true DIY where you don’t really have those guidelines you have to follow. It is exciting, it’s very interesting, but I wouldn’t say it’s a true mirror of the real world.”
Open-source systems improved time-in-range, no safety issues
For the CREATE study, 100 participants were enrolled, including 50 children aged 7-15 years and 50 adults aged 16-70 years. All participants had been using insulin pumps for at least 6 months. Most of the children and about two-thirds of the adults were also using CGMs, but just 6% of the children and 18% of the adults had prior experience with AID systems.
Baseline A1c in children was 7.5% and in adults was 7.7%.
After a 4-week run-in, all patients were randomized to the open-source AID or insulin pump plus CGM for 6 months.
The final group analyzed consisted of 42 patients in the open-source AID group and 53 patients in the comparator group.
The primary outcome, the adjusted mean difference in percent time-in-range (glucose of 70-180 mg/dL) during the final 2 weeks of the 6-month trial, showed a significant difference of 14% (P < .001) with open-source AID compared with pump plus CGM only.
Time-in-range in the open-source AID group rose from 61.2% to 71.2%, while it actually dropped slightly in the comparator group, from 57.7% to 54.5%.
The proportion of patients achieving time-in-range greater than 70% with open-source AID was 60% versus just 15% with pump plus CGM.
Glycemic improvements with open-source AID were significant for adults and children and were greater for those with higher baseline A1c levels. The effect was immediate and sustained throughout the study period, “which is super-pleasing, because there was a worry that the technical burden of open source might be [leading to] dropout, but we didn’t see that. It was sustained right through to the end of the trial,” Dr. de Bock commented.
Hypoglycemic rates didn’t differ between groups, and there were no episodes of severe hypoglycemia or diabetic ketoacidosis.
No more waiting: What is the future of open-source AID?
When the open-source APS was first developed, users coined the motto: “We are not waiting.” But now that the “wait” is over and several commercial AIDs have been approved by regulatory bodies, with others still in the pipeline, will people still use open-source systems?
There are no current data on people moving from DIY to commercial systems. However, Dr. de Bock said, “For most who undertook an open-source option, the precision of the settings that they can use and enjoy would mean that most would likely stick to their open source.”
Dr. Isaacs agrees: “I actually don’t think it’s going to go away in the near future, because the FDA has very specific criteria for where these [formally approved] devices can be in terms of their target ranges and requirements versus with open source you can really customize. So I still think there’s going to be a subset of people who want that customization, who want the lower targets.”
Dana Lewis, the originator of the DIY system and a CREATE coauthor, told this news organization: “I don’t believe there has been a fall-off, and in fact, I think open-source AID has continued to have ongoing uptake as awareness increases about options and as more pumps and CGMs become interoperable with various open-source AID choices.”
“I think uptake increasing is also influenced by the fact that in places like Europe, Asia, and Australia there are in-warranty on-the-market pumps that are compatible and interoperable with open-source AID. I think awareness of AID overall increases uptake of commercial and open source alike,” she said.
“Clinicians, as emphasized in recent position statements, must maintain support of the person with diabetes, irrespective of the mode of treatment they are on. ... Health care providers should be encouraged to learn from the experiences of the people who have stuck with open-source AID or switched, so that they can inform themselves of the relative strengths and benefits of each system,” Dr. de Bock advised.
Ms. Lewis noted: “We are seeing increasing awareness and comfort in endocrinologists from the community perspective, and we do hope that this study helps increase conversation and awareness of the safety and efficacy of open-source AID systems as an option for people with diabetes.”
In fact, the team published an article specifically about clinicians’ experience in CREATE. “The learning curve is similar across AID technology,” she observed.
Findings of a 6-month continuation phase of CREATE, in which all participants used the open-source AID, are scheduled to be presented in September at the European Association for the Study of Diabetes annual meeting.
The study was funded by the Health Research Council of New Zealand, with hardware support from SOOIL Developments, South Korea; Dexcom; and Vodafone New Zealand. Dr. de Bock has reported receiving honoraria and/or research funding from Novo Nordisk, Sanofi, Pfizer, Medtronic, Lilly, Ypsomed, and Dexcom. Dr. Isaacs has reported serving as a consultant for LifeScan, Lilly, and Insulet, and as a speaker for Dexcom, Medtronic, Abbott, and Novo Nordisk. Ms. Lewis has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT ADA 2022
Nonhealing Violaceous Plaque of the Hand Following a Splinter Injury
The Diagnosis: Chromoblastomycosis
This case highlights the importance of routine skin biopsy and tissue culture when clinical suspicion for mycotic infection is high. Despite nonspecific biopsy results (Figure), a diagnosis of chromoblastomycosis (CBM) was reached based on tissue culture. Surgical excision was not possible in our patient due to the size and location of the lesion. The patient was referred to infectious disease, with the plan to start long-term itraconazole for at least 6 to 12 months.
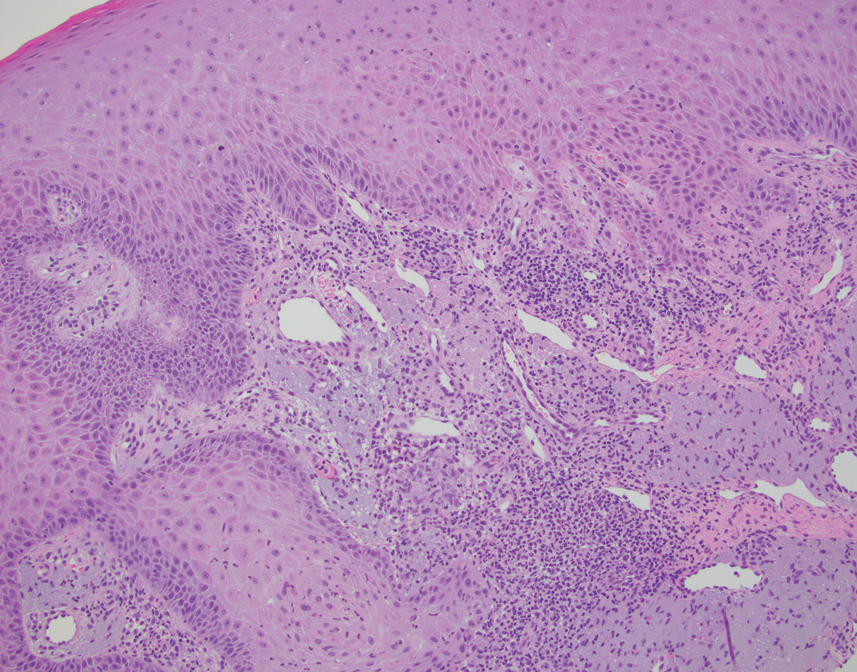
Cases of CBM were first documented in 1914 and distinguished by the appearance of spherical, brown, muriform cells on skin biopsy—features that now serve as the hallmark of CBM diagnoses.1,2 The implantation mycosis commonly is caused by agents such as Fonsecaea pedrosoi and Fonsecaea monophora of the bantiana-clade, as classified according to molecular phylogeny2; these agents have been isolated from soil, plants, and wood sources in tropical and subtropical regions and are strongly associated with agricultural activities.3
Chromoblastomycosis lesions tend to be asymptomatic with a variable amount of time between inoculation and lesion presentation, delaying medical care by months to years.3 The fungus causes a granulomatous reaction after skin damage, with noticeable pseudoepitheliomatous hyperplasia of the epidermis and granulomas formed by epithelioid and Langerhans cells in the dermis.4 Typically, CBM initially presents as an erythematous macular skin lesion, which then progresses to become more pink, papular, and sometimes pruritic.2 Muriform (sclerotic) bodies, which reflect fungal components, extrude transepidermally and appear as black dots on the lesion’s surface.4 Chromoblastomycosis is limited to the subcutaneous tissue and has been classified into 5 types of lesions: nodular, tumoral, verrucous, scarring, and plaque.2 Diagnosis is established using fungal tests such as potassium hydroxide direct microscopy, which exposes muriform bodies often in combination with dematiaceous hyphae, while fungal culture of F pedrosoi in Sabouraud agar produces velvety dark colonies.3 Although an immune response to CBM infection remains unclear, it has been demonstrated that the response differs based on the severity of the infection. The severe form of CBM produces high levels of IL-10, low levels of IFN-γ, and inefficient T-cell proliferation, while milder forms of CBM display low levels of IL-10, high levels of IFN-γ, and efficient T-cell proliferation.5 Complications of CBM include chronic lymphedema, ankylosis, and secondary bacterial infections, which largely are observed in advanced cases; malignant transformation to squamous cell carcinoma, though rare, also has been observed.6
Several therapeutic methods have been implemented in the treatment of CBM, but lesions often remain refractory, especially in advanced cases.6 Approaches to treatment can be divided into antifungal and physical methods. Commonly employed antifungal agents include itraconazole and terbinafine, which must be taken daily for a period ranging from 6 months to 1 year or longer; flucytosine with or without amphotericin also has been employed.4 Among the physical methods, surgical excision is not suggested due to possible dissemination of disease; other options include cryotherapy, thermotherapy, and laser vaporization.6 The prognosis has improved since the use of extended-spectrum triazoles, but high rates of refractory disease remain unchanged.2
The differential diagnosis includes other infections. Nocardiosis is a bacterial infection in which cutaneous disease can result in actinomycetoma, which presents with grains that are small, round, and stain blue on hematoxylin and eosin with eosinophilic rays at the periphery.7 Although the clinical features and pseudoepitheliomatous hyperplasia seen in CBM can mimic squamous cell carcinoma, the latter would show variable degrees of differentiation, keratinization, nuclear atypia, and architectural atypia with a negative tissue culture.8 Eumycetoma is a fungal infection that typically is not caused by F pedrosoi but rather most commonly Madurella mycetomatis.9 Leishmaniasis is a parasitic infection in which a biopsy of cutaneous lesions often displays parasite-filled histiocytes.10
- Rudolph M. Über die brasilianische “figueira” (vorläufige mitteilung). Arch Schiffs Trop Hyg. 1914;18:498-499.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276. doi:10.1128/CMR.00032-16
- Brito AC, Bittencourt MJS. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol. 2018;93:495-506. doi:10.1590/abd1806-4841.20187321
- Kurien G, Sugumar K, Chandran V. Chromoblastomycosis. StatPearls. StatPearls Publishing; 2021. Accessed June 4, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470253/
- Mazo Fávero Gimenes V, Da Glória de Souza M, Ferreira KS, et al. Cytokines and lymphocyte proliferation in patients with different clinical forms of chromoblastomycosis. Microbes Infect. 2005;7:708-713. doi:10.1016/j.micinf.2005.01.006
- Krzys´ciak PM, Pindycka-Piaszczyn´ska M, Piaszczyn´ski M. Chromoblastomycosis. Postepy Dermatol Alergol. 2014;31:310-321. doi:10.5114/pdia.2014.40949
- Siddig EE, van de Sande WWJ, Fahal AH. Actinomycetoma laboratory-based diagnosis: a mini-review. Trans R Soc Trop Med Hyg. 2021;115:355-363.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525. doi:10.1016/j.cll .2017.06.003
- Nenoff P, van de Sande WWJ, Fahal AH, et al. Eumycetoma and actinomycetoma—an update on causative agents, epidemiology, pathogenesis, diagnostics and therapy. J Eur Acad Dermatol Venereol. 2015;29:1873-1883. doi:10.1111/jdv.13008
- Saliba M, Shalhoub A, Taraif S, et al. Cutaneous leishmaniasis: an evolving disease with ancient roots. Int J Dermatol. 2019;58:834-843. doi:10.1111/ijd.14451
The Diagnosis: Chromoblastomycosis
This case highlights the importance of routine skin biopsy and tissue culture when clinical suspicion for mycotic infection is high. Despite nonspecific biopsy results (Figure), a diagnosis of chromoblastomycosis (CBM) was reached based on tissue culture. Surgical excision was not possible in our patient due to the size and location of the lesion. The patient was referred to infectious disease, with the plan to start long-term itraconazole for at least 6 to 12 months.
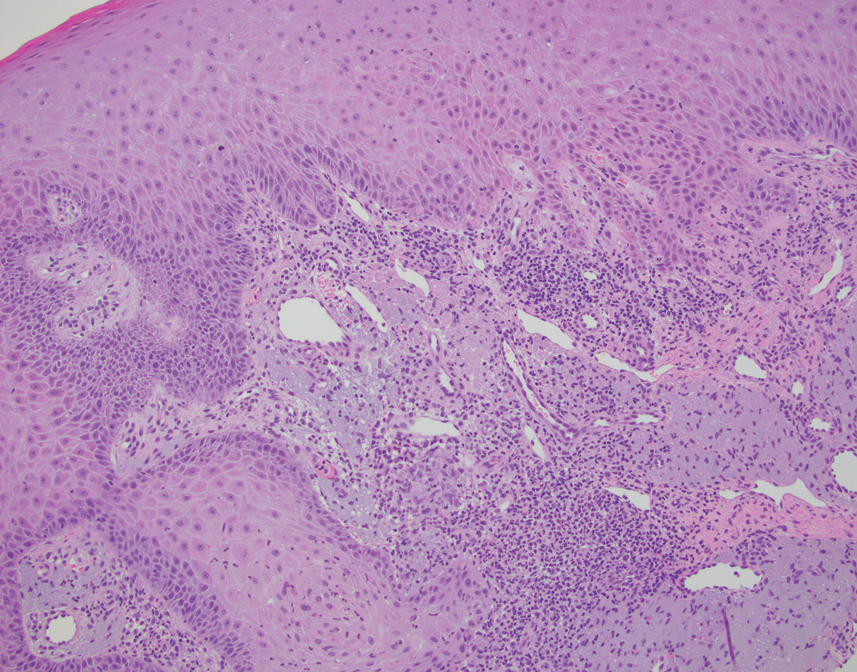
Cases of CBM were first documented in 1914 and distinguished by the appearance of spherical, brown, muriform cells on skin biopsy—features that now serve as the hallmark of CBM diagnoses.1,2 The implantation mycosis commonly is caused by agents such as Fonsecaea pedrosoi and Fonsecaea monophora of the bantiana-clade, as classified according to molecular phylogeny2; these agents have been isolated from soil, plants, and wood sources in tropical and subtropical regions and are strongly associated with agricultural activities.3
Chromoblastomycosis lesions tend to be asymptomatic with a variable amount of time between inoculation and lesion presentation, delaying medical care by months to years.3 The fungus causes a granulomatous reaction after skin damage, with noticeable pseudoepitheliomatous hyperplasia of the epidermis and granulomas formed by epithelioid and Langerhans cells in the dermis.4 Typically, CBM initially presents as an erythematous macular skin lesion, which then progresses to become more pink, papular, and sometimes pruritic.2 Muriform (sclerotic) bodies, which reflect fungal components, extrude transepidermally and appear as black dots on the lesion’s surface.4 Chromoblastomycosis is limited to the subcutaneous tissue and has been classified into 5 types of lesions: nodular, tumoral, verrucous, scarring, and plaque.2 Diagnosis is established using fungal tests such as potassium hydroxide direct microscopy, which exposes muriform bodies often in combination with dematiaceous hyphae, while fungal culture of F pedrosoi in Sabouraud agar produces velvety dark colonies.3 Although an immune response to CBM infection remains unclear, it has been demonstrated that the response differs based on the severity of the infection. The severe form of CBM produces high levels of IL-10, low levels of IFN-γ, and inefficient T-cell proliferation, while milder forms of CBM display low levels of IL-10, high levels of IFN-γ, and efficient T-cell proliferation.5 Complications of CBM include chronic lymphedema, ankylosis, and secondary bacterial infections, which largely are observed in advanced cases; malignant transformation to squamous cell carcinoma, though rare, also has been observed.6
Several therapeutic methods have been implemented in the treatment of CBM, but lesions often remain refractory, especially in advanced cases.6 Approaches to treatment can be divided into antifungal and physical methods. Commonly employed antifungal agents include itraconazole and terbinafine, which must be taken daily for a period ranging from 6 months to 1 year or longer; flucytosine with or without amphotericin also has been employed.4 Among the physical methods, surgical excision is not suggested due to possible dissemination of disease; other options include cryotherapy, thermotherapy, and laser vaporization.6 The prognosis has improved since the use of extended-spectrum triazoles, but high rates of refractory disease remain unchanged.2
The differential diagnosis includes other infections. Nocardiosis is a bacterial infection in which cutaneous disease can result in actinomycetoma, which presents with grains that are small, round, and stain blue on hematoxylin and eosin with eosinophilic rays at the periphery.7 Although the clinical features and pseudoepitheliomatous hyperplasia seen in CBM can mimic squamous cell carcinoma, the latter would show variable degrees of differentiation, keratinization, nuclear atypia, and architectural atypia with a negative tissue culture.8 Eumycetoma is a fungal infection that typically is not caused by F pedrosoi but rather most commonly Madurella mycetomatis.9 Leishmaniasis is a parasitic infection in which a biopsy of cutaneous lesions often displays parasite-filled histiocytes.10
The Diagnosis: Chromoblastomycosis
This case highlights the importance of routine skin biopsy and tissue culture when clinical suspicion for mycotic infection is high. Despite nonspecific biopsy results (Figure), a diagnosis of chromoblastomycosis (CBM) was reached based on tissue culture. Surgical excision was not possible in our patient due to the size and location of the lesion. The patient was referred to infectious disease, with the plan to start long-term itraconazole for at least 6 to 12 months.
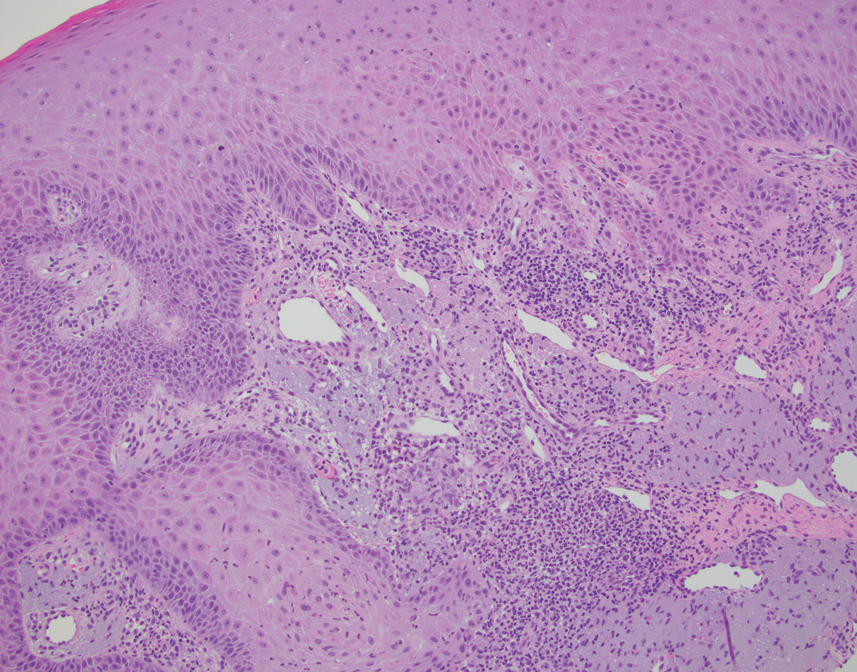
Cases of CBM were first documented in 1914 and distinguished by the appearance of spherical, brown, muriform cells on skin biopsy—features that now serve as the hallmark of CBM diagnoses.1,2 The implantation mycosis commonly is caused by agents such as Fonsecaea pedrosoi and Fonsecaea monophora of the bantiana-clade, as classified according to molecular phylogeny2; these agents have been isolated from soil, plants, and wood sources in tropical and subtropical regions and are strongly associated with agricultural activities.3
Chromoblastomycosis lesions tend to be asymptomatic with a variable amount of time between inoculation and lesion presentation, delaying medical care by months to years.3 The fungus causes a granulomatous reaction after skin damage, with noticeable pseudoepitheliomatous hyperplasia of the epidermis and granulomas formed by epithelioid and Langerhans cells in the dermis.4 Typically, CBM initially presents as an erythematous macular skin lesion, which then progresses to become more pink, papular, and sometimes pruritic.2 Muriform (sclerotic) bodies, which reflect fungal components, extrude transepidermally and appear as black dots on the lesion’s surface.4 Chromoblastomycosis is limited to the subcutaneous tissue and has been classified into 5 types of lesions: nodular, tumoral, verrucous, scarring, and plaque.2 Diagnosis is established using fungal tests such as potassium hydroxide direct microscopy, which exposes muriform bodies often in combination with dematiaceous hyphae, while fungal culture of F pedrosoi in Sabouraud agar produces velvety dark colonies.3 Although an immune response to CBM infection remains unclear, it has been demonstrated that the response differs based on the severity of the infection. The severe form of CBM produces high levels of IL-10, low levels of IFN-γ, and inefficient T-cell proliferation, while milder forms of CBM display low levels of IL-10, high levels of IFN-γ, and efficient T-cell proliferation.5 Complications of CBM include chronic lymphedema, ankylosis, and secondary bacterial infections, which largely are observed in advanced cases; malignant transformation to squamous cell carcinoma, though rare, also has been observed.6
Several therapeutic methods have been implemented in the treatment of CBM, but lesions often remain refractory, especially in advanced cases.6 Approaches to treatment can be divided into antifungal and physical methods. Commonly employed antifungal agents include itraconazole and terbinafine, which must be taken daily for a period ranging from 6 months to 1 year or longer; flucytosine with or without amphotericin also has been employed.4 Among the physical methods, surgical excision is not suggested due to possible dissemination of disease; other options include cryotherapy, thermotherapy, and laser vaporization.6 The prognosis has improved since the use of extended-spectrum triazoles, but high rates of refractory disease remain unchanged.2
The differential diagnosis includes other infections. Nocardiosis is a bacterial infection in which cutaneous disease can result in actinomycetoma, which presents with grains that are small, round, and stain blue on hematoxylin and eosin with eosinophilic rays at the periphery.7 Although the clinical features and pseudoepitheliomatous hyperplasia seen in CBM can mimic squamous cell carcinoma, the latter would show variable degrees of differentiation, keratinization, nuclear atypia, and architectural atypia with a negative tissue culture.8 Eumycetoma is a fungal infection that typically is not caused by F pedrosoi but rather most commonly Madurella mycetomatis.9 Leishmaniasis is a parasitic infection in which a biopsy of cutaneous lesions often displays parasite-filled histiocytes.10
- Rudolph M. Über die brasilianische “figueira” (vorläufige mitteilung). Arch Schiffs Trop Hyg. 1914;18:498-499.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276. doi:10.1128/CMR.00032-16
- Brito AC, Bittencourt MJS. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol. 2018;93:495-506. doi:10.1590/abd1806-4841.20187321
- Kurien G, Sugumar K, Chandran V. Chromoblastomycosis. StatPearls. StatPearls Publishing; 2021. Accessed June 4, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470253/
- Mazo Fávero Gimenes V, Da Glória de Souza M, Ferreira KS, et al. Cytokines and lymphocyte proliferation in patients with different clinical forms of chromoblastomycosis. Microbes Infect. 2005;7:708-713. doi:10.1016/j.micinf.2005.01.006
- Krzys´ciak PM, Pindycka-Piaszczyn´ska M, Piaszczyn´ski M. Chromoblastomycosis. Postepy Dermatol Alergol. 2014;31:310-321. doi:10.5114/pdia.2014.40949
- Siddig EE, van de Sande WWJ, Fahal AH. Actinomycetoma laboratory-based diagnosis: a mini-review. Trans R Soc Trop Med Hyg. 2021;115:355-363.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525. doi:10.1016/j.cll .2017.06.003
- Nenoff P, van de Sande WWJ, Fahal AH, et al. Eumycetoma and actinomycetoma—an update on causative agents, epidemiology, pathogenesis, diagnostics and therapy. J Eur Acad Dermatol Venereol. 2015;29:1873-1883. doi:10.1111/jdv.13008
- Saliba M, Shalhoub A, Taraif S, et al. Cutaneous leishmaniasis: an evolving disease with ancient roots. Int J Dermatol. 2019;58:834-843. doi:10.1111/ijd.14451
- Rudolph M. Über die brasilianische “figueira” (vorläufige mitteilung). Arch Schiffs Trop Hyg. 1914;18:498-499.
- Queiroz-Telles F, de Hoog S, Santos DW, et al. Chromoblastomycosis. Clin Microbiol Rev. 2017;30:233-276. doi:10.1128/CMR.00032-16
- Brito AC, Bittencourt MJS. Chromoblastomycosis: an etiological, epidemiological, clinical, diagnostic, and treatment update. An Bras Dermatol. 2018;93:495-506. doi:10.1590/abd1806-4841.20187321
- Kurien G, Sugumar K, Chandran V. Chromoblastomycosis. StatPearls. StatPearls Publishing; 2021. Accessed June 4, 2022. https://www.ncbi.nlm.nih.gov/books/NBK470253/
- Mazo Fávero Gimenes V, Da Glória de Souza M, Ferreira KS, et al. Cytokines and lymphocyte proliferation in patients with different clinical forms of chromoblastomycosis. Microbes Infect. 2005;7:708-713. doi:10.1016/j.micinf.2005.01.006
- Krzys´ciak PM, Pindycka-Piaszczyn´ska M, Piaszczyn´ski M. Chromoblastomycosis. Postepy Dermatol Alergol. 2014;31:310-321. doi:10.5114/pdia.2014.40949
- Siddig EE, van de Sande WWJ, Fahal AH. Actinomycetoma laboratory-based diagnosis: a mini-review. Trans R Soc Trop Med Hyg. 2021;115:355-363.
- Parekh V, Seykora JT. Cutaneous squamous cell carcinoma. Clin Lab Med. 2017;37:503-525. doi:10.1016/j.cll .2017.06.003
- Nenoff P, van de Sande WWJ, Fahal AH, et al. Eumycetoma and actinomycetoma—an update on causative agents, epidemiology, pathogenesis, diagnostics and therapy. J Eur Acad Dermatol Venereol. 2015;29:1873-1883. doi:10.1111/jdv.13008
- Saliba M, Shalhoub A, Taraif S, et al. Cutaneous leishmaniasis: an evolving disease with ancient roots. Int J Dermatol. 2019;58:834-843. doi:10.1111/ijd.14451
A 70-year-old immunocompetent man presented to the dermatology department with a progressive asymptomatic hand wound of 2 years’ duration following a splinter injury in Belize. Prior treatment included oral antibiotics without improvement. Physical examination revealed a 5.1×3.0 cm, pink to violaceous, nonpurulent plaque with a cobblestonelike appearance on the dorsal aspect of the right hand. Both the initial and a repeat skin biopsy revealed nonspecific changes, including hyperkeratosis, hypergranulosis, acute and chronic inflammation, and vascular ectasia. Grocott-Gomori methenamine-silver staining was negative for fungal organisms. One month after the repeat biopsy, a tissue culture returned positive for the rare Fonsecaea pedrosoi.

Children and COVID: New cases hold steady in nonholiday week
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
The new-case count for the most recent reporting week – 87,644 for June 3-9 – did go up from the previous week, but by only 270 cases, the American Academy of Pediatrics and Children’s Hospital Association said in their weekly COVID report. That’s just 0.31% higher than a week ago and probably is affected by reduced testing and reporting because of Memorial Day, as the AAP and CHA noted earlier.
That hint of a continued decline accompanies the latest trend for new cases for all age groups: They have leveled out over the last month, with the moving 7-day daily average hovering around 100,000-110,000 since mid-May, data from the Centers for Disease Control and Prevention show.
The Food and Drug Administration, meanwhile, is in the news this week as two of its advisory panels take the next steps toward pediatric approvals of vaccines from Pfizer/BioNTtech and Moderna. The panels could advance the approvals of the Pfizer vaccine for children under the age of 5 years and the Moderna vaccine for children aged 6 months to 17 years.
Matthew Harris, MD, medical director of the COVID-19 vaccination program for Northwell Health in New Hyde Park, N.Y., emphasized the importance of vaccinations, as well as the continued challenge of convincing parents to get the shots for eligible children. “We still have a long way to go for primary vaccines and boosters for children 5 years and above,” he said in an interview.
The vaccination effort against COVID-19 has stalled somewhat as interest has waned since the Omicron surge. Weekly initial vaccinations for children aged 5-11 years, which topped 100,000 as recently as mid-March, have been about 43,000 a week for the last 3 weeks, while 12- to 17-year-olds had around 27,000 or 28,000 initial vaccinations per week over that span, the AAP said in a separate report.
The latest data available from the CDC show that overall vaccine coverage levels for the younger group are only about half those of the 12- to 17-year-olds, both in terms of initial doses and completions. The 5- to 11-year-olds are not eligible for boosters yet, but 26.5% of the older children had received one as of June 13, according to the CDC’s COVID Data Tracker.
Surgery during a pandemic? COVID vaccination status matters – or not
An online survey captured mixed information about people’s willingness to undergo surgery during a viral pandemic in relation to the vaccine status of the patient and staff. The findings showcase opportunities for public education and “skillful messaging,” researchers report.
In survey scenarios that asked people to imagine their vaccination status, people were more willing to undergo surgery if it was lifesaving, rather than elective, especially if vaccinated. The prospect of no hospital stay tipped the scales further toward surgery. The vaccination status of hospital staff played only a minor role in decision making, according to the study, which was published in Vaccine.
But as a post hoc analysis revealed, it was participants who were not vaccinated against COVID-19 in real life who were more willing to undergo surgery, compared with those who had one or two shots.
In either case, too many people were unwilling to undergo lifesaving surgery, even though the risk of hospital-acquired COVID-19 is low. “Making this choice for an actual health problem would result in an unacceptably high rate of potential morbidity attributable to pandemic-related fears, the authors wrote.
In an unusual approach, the researchers used Amazon’s Mechanical Turk to electronically recruit 2,006 adults. The participants answered a 26-item survey about a hypothetical surgery in an unnamed pandemic with different combinations of vaccine status for patient and staff.
Coauthor and anesthesiologist Keith J. Ruskin, MD, of the University of Chicago, told this news organization that they “wanted to make this timeless” and independent of COVID “so that when the next thing came about, the paper would still be relevant.”
The researchers were surprised by the findings at the extreme ends of attitudes toward surgery. Some were still willing to have elective surgery with (hypothetically) unvaccinated patients and staff.
“And people at the other end, even though they are vaccinated, the hospital staff is vaccinated, and the surgery is lifesaving, they absolutely won’t have surgery,” Dr. Ruskin said.
He viewed these two groups as opportunities for education. “You can present information in the most positive light to get them to do the right thing with what’s best for themselves,” he said.
As an example, Dr. Ruskin pointed to an ad in Illinois. “It’s not only people saying I’m getting vaccinated for myself and my family, but there are people who said I got vaccinated and I still got COVID, but it could have been much worse. Please, if you’re on the fence, just get vaccinated,” he said.
Coauthor Anna Clebone Ruskin, MD, an anesthesiologist at the University of Chicago, said, “Humans are programmed to see things in extremes. With surgery, people tend to think of surgery as a monolith – surgery is all good, or surgery is all bad, where there is a huge in between. So we saw those extremes. ... Seeing that dichotomy with people on either end was pretty surprising.
“Getting surgery is not always good. Getting surgery is not always bad. It’s a risk-versus-benefit analysis and educating the public to consider the risks and benefits of medical decisions, in general, would be enormously beneficial,” she said.
A post hoc analysis found that “participants who were not actually vaccinated against COVID-19 were generally more willing to undergo surgery compared to those who had one vaccination or two vaccinations,” the authors wrote.
In a second post hoc finding, participants who reported high wariness of vaccines were generally more likely to be willing to undergo surgery. Notably, 15% of participants “were unwilling to undergo lifesaving surgery during a pandemic even when they and the health care staff were vaccinated,” the authors wrote.
Dr. Keith J. Ruskin hypothesized about this result, saying, “What we think is that potentially actually getting vaccinated against COVID-19 may indicate that you have a lower risk tolerance. So you may be less likely to do anything you perceive to be risky if you’re vaccinated against COVID-19.”
The authors stated that “the risk of hospital-acquired COVID-19 even prior to vaccination is vanishingly small.” The risk of nosocomial COVID varies among different studies. An EPIC-based study between April 2020 and October 2021 found the risk to be 1.8%; EPIC describes the fears of a patient catching COVID at a hospital as “likely unfounded.”
In the United Kingdom, the risk was as high as 24% earlier in the pandemic and then declined to approximately 5% a year ago. Omicron also brought more infections. Rates varied significantly among hospitals – and, notably, the risk of death from a nosocomial COVID infection was 21% in April-September 2020.
Emily Landon, MD, an epidemiologist and executive medical director for infection prevention and control at the University of Chicago Medicine, told this news organization that the study’s data were collected during Delta, a “time when we thought that this was a pandemic of the unvaccinated. But there was serious politicization of the vaccine.”
Dr. Landon said one of the study’s strengths was the large number of participants. A limitation was, “You’re going to have less participants who are generally poor and indigent, and fewer old participants, probably because they’re less likely to respond to an online survey.
“But the most interesting results are that people who were wary of vaccines or who hadn’t been vaccinated, were much more willing to undergo surgical procedures in the time of a pandemic, regardless of status, which reflects the fact that not being vaccinated correlates with not worrying much about COVID. Vaccinated individuals had a lot more wariness about undergoing surgical procedures during a pandemic.”
It appeared “individuals who were vaccinated in real life [were] worried about staff vaccination,” Dr. Landon noted. She concluded, “I think it supports the need for mandatory vaccinations in health care workers.”
The study has implications for hospital vaccination policies and practices. In Cumberland, Md., when COVID was high and vaccines first became available, the Maryland Hospital Association said that all health care staff should be vaccinated. The local hospital, UPMC–Western Maryland Hospital, refused.
Two months later, the local news reporter, Teresa McMinn, wrote, “While Maryland’s largest hospital systems have ‘led by example by mandating vaccines for all of their hospital staff,’ other facilities – including UPMC Western Maryland and Garrett Regional Medical Center – have taken no such action even though it’s been 8 months since vaccines were made available to health care workers.”
The hospital would not tell patients whether staff were vaccinated, either. An ongoing concern for members of the community is the lack of communication with UPMC, which erodes trust in the health system – the only hospital available in this rural community.
This vaccine study supports that the vaccination status of the staff may influence some patients’ decision on whether to have surgery.
The Ruskins and Dr. Landon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An online survey captured mixed information about people’s willingness to undergo surgery during a viral pandemic in relation to the vaccine status of the patient and staff. The findings showcase opportunities for public education and “skillful messaging,” researchers report.
In survey scenarios that asked people to imagine their vaccination status, people were more willing to undergo surgery if it was lifesaving, rather than elective, especially if vaccinated. The prospect of no hospital stay tipped the scales further toward surgery. The vaccination status of hospital staff played only a minor role in decision making, according to the study, which was published in Vaccine.
But as a post hoc analysis revealed, it was participants who were not vaccinated against COVID-19 in real life who were more willing to undergo surgery, compared with those who had one or two shots.
In either case, too many people were unwilling to undergo lifesaving surgery, even though the risk of hospital-acquired COVID-19 is low. “Making this choice for an actual health problem would result in an unacceptably high rate of potential morbidity attributable to pandemic-related fears, the authors wrote.
In an unusual approach, the researchers used Amazon’s Mechanical Turk to electronically recruit 2,006 adults. The participants answered a 26-item survey about a hypothetical surgery in an unnamed pandemic with different combinations of vaccine status for patient and staff.
Coauthor and anesthesiologist Keith J. Ruskin, MD, of the University of Chicago, told this news organization that they “wanted to make this timeless” and independent of COVID “so that when the next thing came about, the paper would still be relevant.”
The researchers were surprised by the findings at the extreme ends of attitudes toward surgery. Some were still willing to have elective surgery with (hypothetically) unvaccinated patients and staff.
“And people at the other end, even though they are vaccinated, the hospital staff is vaccinated, and the surgery is lifesaving, they absolutely won’t have surgery,” Dr. Ruskin said.
He viewed these two groups as opportunities for education. “You can present information in the most positive light to get them to do the right thing with what’s best for themselves,” he said.
As an example, Dr. Ruskin pointed to an ad in Illinois. “It’s not only people saying I’m getting vaccinated for myself and my family, but there are people who said I got vaccinated and I still got COVID, but it could have been much worse. Please, if you’re on the fence, just get vaccinated,” he said.
Coauthor Anna Clebone Ruskin, MD, an anesthesiologist at the University of Chicago, said, “Humans are programmed to see things in extremes. With surgery, people tend to think of surgery as a monolith – surgery is all good, or surgery is all bad, where there is a huge in between. So we saw those extremes. ... Seeing that dichotomy with people on either end was pretty surprising.
“Getting surgery is not always good. Getting surgery is not always bad. It’s a risk-versus-benefit analysis and educating the public to consider the risks and benefits of medical decisions, in general, would be enormously beneficial,” she said.
A post hoc analysis found that “participants who were not actually vaccinated against COVID-19 were generally more willing to undergo surgery compared to those who had one vaccination or two vaccinations,” the authors wrote.
In a second post hoc finding, participants who reported high wariness of vaccines were generally more likely to be willing to undergo surgery. Notably, 15% of participants “were unwilling to undergo lifesaving surgery during a pandemic even when they and the health care staff were vaccinated,” the authors wrote.
Dr. Keith J. Ruskin hypothesized about this result, saying, “What we think is that potentially actually getting vaccinated against COVID-19 may indicate that you have a lower risk tolerance. So you may be less likely to do anything you perceive to be risky if you’re vaccinated against COVID-19.”
The authors stated that “the risk of hospital-acquired COVID-19 even prior to vaccination is vanishingly small.” The risk of nosocomial COVID varies among different studies. An EPIC-based study between April 2020 and October 2021 found the risk to be 1.8%; EPIC describes the fears of a patient catching COVID at a hospital as “likely unfounded.”
In the United Kingdom, the risk was as high as 24% earlier in the pandemic and then declined to approximately 5% a year ago. Omicron also brought more infections. Rates varied significantly among hospitals – and, notably, the risk of death from a nosocomial COVID infection was 21% in April-September 2020.
Emily Landon, MD, an epidemiologist and executive medical director for infection prevention and control at the University of Chicago Medicine, told this news organization that the study’s data were collected during Delta, a “time when we thought that this was a pandemic of the unvaccinated. But there was serious politicization of the vaccine.”
Dr. Landon said one of the study’s strengths was the large number of participants. A limitation was, “You’re going to have less participants who are generally poor and indigent, and fewer old participants, probably because they’re less likely to respond to an online survey.
“But the most interesting results are that people who were wary of vaccines or who hadn’t been vaccinated, were much more willing to undergo surgical procedures in the time of a pandemic, regardless of status, which reflects the fact that not being vaccinated correlates with not worrying much about COVID. Vaccinated individuals had a lot more wariness about undergoing surgical procedures during a pandemic.”
It appeared “individuals who were vaccinated in real life [were] worried about staff vaccination,” Dr. Landon noted. She concluded, “I think it supports the need for mandatory vaccinations in health care workers.”
The study has implications for hospital vaccination policies and practices. In Cumberland, Md., when COVID was high and vaccines first became available, the Maryland Hospital Association said that all health care staff should be vaccinated. The local hospital, UPMC–Western Maryland Hospital, refused.
Two months later, the local news reporter, Teresa McMinn, wrote, “While Maryland’s largest hospital systems have ‘led by example by mandating vaccines for all of their hospital staff,’ other facilities – including UPMC Western Maryland and Garrett Regional Medical Center – have taken no such action even though it’s been 8 months since vaccines were made available to health care workers.”
The hospital would not tell patients whether staff were vaccinated, either. An ongoing concern for members of the community is the lack of communication with UPMC, which erodes trust in the health system – the only hospital available in this rural community.
This vaccine study supports that the vaccination status of the staff may influence some patients’ decision on whether to have surgery.
The Ruskins and Dr. Landon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
An online survey captured mixed information about people’s willingness to undergo surgery during a viral pandemic in relation to the vaccine status of the patient and staff. The findings showcase opportunities for public education and “skillful messaging,” researchers report.
In survey scenarios that asked people to imagine their vaccination status, people were more willing to undergo surgery if it was lifesaving, rather than elective, especially if vaccinated. The prospect of no hospital stay tipped the scales further toward surgery. The vaccination status of hospital staff played only a minor role in decision making, according to the study, which was published in Vaccine.
But as a post hoc analysis revealed, it was participants who were not vaccinated against COVID-19 in real life who were more willing to undergo surgery, compared with those who had one or two shots.
In either case, too many people were unwilling to undergo lifesaving surgery, even though the risk of hospital-acquired COVID-19 is low. “Making this choice for an actual health problem would result in an unacceptably high rate of potential morbidity attributable to pandemic-related fears, the authors wrote.
In an unusual approach, the researchers used Amazon’s Mechanical Turk to electronically recruit 2,006 adults. The participants answered a 26-item survey about a hypothetical surgery in an unnamed pandemic with different combinations of vaccine status for patient and staff.
Coauthor and anesthesiologist Keith J. Ruskin, MD, of the University of Chicago, told this news organization that they “wanted to make this timeless” and independent of COVID “so that when the next thing came about, the paper would still be relevant.”
The researchers were surprised by the findings at the extreme ends of attitudes toward surgery. Some were still willing to have elective surgery with (hypothetically) unvaccinated patients and staff.
“And people at the other end, even though they are vaccinated, the hospital staff is vaccinated, and the surgery is lifesaving, they absolutely won’t have surgery,” Dr. Ruskin said.
He viewed these two groups as opportunities for education. “You can present information in the most positive light to get them to do the right thing with what’s best for themselves,” he said.
As an example, Dr. Ruskin pointed to an ad in Illinois. “It’s not only people saying I’m getting vaccinated for myself and my family, but there are people who said I got vaccinated and I still got COVID, but it could have been much worse. Please, if you’re on the fence, just get vaccinated,” he said.
Coauthor Anna Clebone Ruskin, MD, an anesthesiologist at the University of Chicago, said, “Humans are programmed to see things in extremes. With surgery, people tend to think of surgery as a monolith – surgery is all good, or surgery is all bad, where there is a huge in between. So we saw those extremes. ... Seeing that dichotomy with people on either end was pretty surprising.
“Getting surgery is not always good. Getting surgery is not always bad. It’s a risk-versus-benefit analysis and educating the public to consider the risks and benefits of medical decisions, in general, would be enormously beneficial,” she said.
A post hoc analysis found that “participants who were not actually vaccinated against COVID-19 were generally more willing to undergo surgery compared to those who had one vaccination or two vaccinations,” the authors wrote.
In a second post hoc finding, participants who reported high wariness of vaccines were generally more likely to be willing to undergo surgery. Notably, 15% of participants “were unwilling to undergo lifesaving surgery during a pandemic even when they and the health care staff were vaccinated,” the authors wrote.
Dr. Keith J. Ruskin hypothesized about this result, saying, “What we think is that potentially actually getting vaccinated against COVID-19 may indicate that you have a lower risk tolerance. So you may be less likely to do anything you perceive to be risky if you’re vaccinated against COVID-19.”
The authors stated that “the risk of hospital-acquired COVID-19 even prior to vaccination is vanishingly small.” The risk of nosocomial COVID varies among different studies. An EPIC-based study between April 2020 and October 2021 found the risk to be 1.8%; EPIC describes the fears of a patient catching COVID at a hospital as “likely unfounded.”
In the United Kingdom, the risk was as high as 24% earlier in the pandemic and then declined to approximately 5% a year ago. Omicron also brought more infections. Rates varied significantly among hospitals – and, notably, the risk of death from a nosocomial COVID infection was 21% in April-September 2020.
Emily Landon, MD, an epidemiologist and executive medical director for infection prevention and control at the University of Chicago Medicine, told this news organization that the study’s data were collected during Delta, a “time when we thought that this was a pandemic of the unvaccinated. But there was serious politicization of the vaccine.”
Dr. Landon said one of the study’s strengths was the large number of participants. A limitation was, “You’re going to have less participants who are generally poor and indigent, and fewer old participants, probably because they’re less likely to respond to an online survey.
“But the most interesting results are that people who were wary of vaccines or who hadn’t been vaccinated, were much more willing to undergo surgical procedures in the time of a pandemic, regardless of status, which reflects the fact that not being vaccinated correlates with not worrying much about COVID. Vaccinated individuals had a lot more wariness about undergoing surgical procedures during a pandemic.”
It appeared “individuals who were vaccinated in real life [were] worried about staff vaccination,” Dr. Landon noted. She concluded, “I think it supports the need for mandatory vaccinations in health care workers.”
The study has implications for hospital vaccination policies and practices. In Cumberland, Md., when COVID was high and vaccines first became available, the Maryland Hospital Association said that all health care staff should be vaccinated. The local hospital, UPMC–Western Maryland Hospital, refused.
Two months later, the local news reporter, Teresa McMinn, wrote, “While Maryland’s largest hospital systems have ‘led by example by mandating vaccines for all of their hospital staff,’ other facilities – including UPMC Western Maryland and Garrett Regional Medical Center – have taken no such action even though it’s been 8 months since vaccines were made available to health care workers.”
The hospital would not tell patients whether staff were vaccinated, either. An ongoing concern for members of the community is the lack of communication with UPMC, which erodes trust in the health system – the only hospital available in this rural community.
This vaccine study supports that the vaccination status of the staff may influence some patients’ decision on whether to have surgery.
The Ruskins and Dr. Landon have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hormonal contraceptives protective against suicide?
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
Contrary to previous analyses, new research suggests.
In a study of more than 800 women younger than age 50 who attempted suicide and more than 3,000 age-matched peers, results showed those who took hormonal contraceptives had a 27% reduced risk for attempted suicide.
Further analysis showed this was confined to women without a history of psychiatric illness and the reduction in risk rose to 43% among those who took combined hormonal contraceptives rather than progestin-only versions.
The protective effect against attempted suicide increased further to 46% if ethinyl estradiol (EE)–containing preparations were used. Moreover, the beneficial effect of contraceptive use increased over time.
The main message is the “current use of hormonal contraceptives is not associated with an increased risk of attempted suicide in our population,” study presenter Elena Toffol, MD, PhD, department of public health, University of Helsinki, told meeting attendees at the European Psychiatric Association 2022 Congress.
Age range differences
Dr. Toffol said there could be “several reasons” why the results are different from those in previous studies, including that the researchers included a “larger age range.” She noted it is known that “older women have a lower rate of attempted suicide and use different types of contraceptives.”
Dr. Toffol said in an interview that, although it’s “hard to estimate any causality” because this is an observational study, it is “tempting to speculate, and it is plausible, that hormones partly play a role with some, but not all, women being more sensitive to hormonal influences.”
However, the results “may also reflect life choices or a protective life status; for example, more stable relationships or more conscious and health-focused behaviors,” she said.
“It may also be that the underlying characteristics of women who are prescribed or opt for certain types of contraceptives are somehow related to their suicidal risk,” she added.
In 2019, the global age-standardized suicide rate was 9.0 per 100,000, which translates into more than 700,000 deaths every year, Dr. Toffol noted.
However, she emphasized the World Health Organization has calculated that, for every adult who dies by suicide, more than 20 people attempt suicide. In addition, data from the U.S. Centers for Disease Control and Prevention indicate that attempted suicides are three times more common among young women than in men.
“What are the reasons for this gender gap?” Dr. Toffol asked during her presentation.
“It is known that the major risk factor for suicidal behavior is a psychiatric disorder, and in particular depression and mood disorders. And depression and mood disorders are more common in women than in men,” she said.
However, there is also “growing interest into the role of biological factors” in the risk for suicide, including hormones and hormonal contraception. Some studies have also suggested that there is an increased risk for depression and “both completed and attempted suicide” after starting hormonal contraception.
Dr. Toffol added that about 70% of European women use some form of contraception and, among Finnish women, 40% choose a hormonal contraceptive.
Nested analysis
The researchers conducted a nested case-control analysis combining 2017 national prescription data on 587,823 women aged 15-49 years with information from general and primary healthcare registers for the years 2018 to 2019.
They were able to identify 818 cases of attempted suicide among the women. These were matched 4:1 with 3,272 age-matched healthy women who acted as the control group. Use of hormonal contraceptives in the previous 180 days was determined for the whole cohort.
Among users of hormonal contraceptives, there were 344 attempted suicides in 2017, at an incidence rate of 0.59 per 1,000 person-years. This compared with 474 attempted suicides among nonusers, at an incidence rate of 0.81 per 1000 person-years.
Kaplan-Meier analysis showed there was a significant difference in rates for attempted suicide among hormonal contraceptive users versus nonusers, at an incidence rate ratio of 0.73 (P < .0001) – and the difference increased over time.
In addition, the incidence of attempted suicide decreased with increasing age, with the highest incidence rate in women aged 15-19 years (1.62 per 1,000 person-years).
Conditional logistic regression analysis that controlled for education, marital status, chronic disease, recent psychiatric hospitalization, and current use of psychotropic medication showed hormonal contraceptive use was not linked to an increased risk of attempted suicide overall, at an odds ratio of 0.79 (95% confidence interval, 0.56-1.11).
However, when they looked specifically at women without a history of psychiatric illness, the association became significant, at an OR of 0.73 for attempted suicide among hormonal contraceptive users (95% CI, 0.58-0.91), while the relationship remained nonsignificant in women with a history of psychiatric disorders.
Further analysis suggested the significant association was confined to women taking combined hormonal contraceptives, at an OR of 0.57 for suicide attempt versus nonusers (95% CI, 0.44-0.75), and those use EE-containing preparations (OR, 0.54; 95% CI, 0.40-0.73).
There was a suggestion in the data that hormonal contraceptives containing desogestrel or drospirenone alongside EE may offer the greatest reduction in attempted suicide risk, but that did not survive multivariate analysis.
Dr. Toffol also noted that they were not able to capture data on use of intrauterine devices in their analysis.
“There is a growing number of municipalities in Finland that are providing free-of-charge contraception to young women” that is often an intrauterine device, she said. The researchers hope to include these women in a future analysis.
‘Age matters’
Commenting on the findings, Alexis C. Edwards, PhD, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said the current study’s findings “made a lot of sense.” Dr. Edwards wasn’t involved with this study but conducted a previous study of 216,702 Swedish women aged 15-22 years that showed use of combination or progestin-only oral contraceptives was associated with an increased risk for suicidal behavior.
She agreed with Dr. Toffol that the “much larger age range” in the new study may have played a role in showing the opposite result.
“The trajectory that we saw if we had been able to continue following the women for longer – which we couldn’t, due to limitations of the registries – [was that] using hormonal contraceptives was going to end up being protective, so I do think that it matters what age you’re looking at,” she said.
Dr. Edwards noted the takeaway from both studies “is that, even if there is a slight increase in risk from using hormonal contraceptives, it’s short lived and it’s probably specific to young women, which is important.”
She suggested the hormonal benefit from extended contraceptive use could come from the regulation of mood, as it offers a “more stable hormonal course than what their body might be putting them through in the absence of using the pill.”
Overall, it is “really lovely to see very well-executed studies on this, providing more empirical evidence on this question, because it is something that’s relevant to anyone who’s potentially going to be using hormonal contraception,” Dr. Edwards said.
Clinical implications?
Andrea Fiorillo, MD, PhD, department of psychiatry, University of Campania “Luigi Vanvitelli,” Naples, Italy, said in a press release that the “striking” findings of the current study need “careful evaluation.”
They also need to be replicated in “different cohorts of women and controlled for the impact of several psychosocial stressors, such as economic upheavals, social insecurity, and uncertainty due to the COVID pandemic,” said Dr. Fiorillo, who was not involved with the research.
Nevertheless, she believes the “clinical implications of the study are obvious and may help to destigmatize the use of hormonal contraceptives.”
The study was funded by the Jane and Aatos Erkko Foundation, the Avohoidon Tsukimis äätiö (Foundation for Primary Care Research), the Yrj ö Jahnsson Foundation, and the Finnish Cultural Foundation. No relevant financial relationships were reported.
A version of this article first appeared on Medscape.com.
FROM EPA 2022
A fish tale? More on that seafood, melanoma study
A recent study linking the consumption of fish to melanoma had sushi eaters looking up the number of the nearest dermatologist. But experts said the findings had several important limitations and that no one should change their diet based on the results.
“It wouldn’t impact my fish consumption at all,” said Sancy Leachman, MD, PhD, who directs the melanoma program at Oregon Health & Science University’s Knight Cancer Institute in Portland. “Fish are part of a healthy diet,” particularly if it replaces less healthy proteins such as beef.
Even the authors of the study advised caution when interpreting the findings.
“I wouldn’t encourage anyone to change their fish consumption habits just because of this paper,” said study leader Eunyoung Cho, ScD, an epidemiologist at Brown University, Providence, R.I. “Fish is cardioprotective and is related to reduced risk of developing certain cancers too.”
Solid findings or fishing expedition?
The study quickly generated headlines and was the most viewed article of the journal Cancer Causes & Control within a day of its publication.
Dr. Cho, who is on the editorial board of the journal, analyzed the results of a study funded by the National Institutes of Health and the Association for the Advancement of Retired Persons that began in the 1990s and explored possible links between fish consumption and developing different forms of cancer.
Previous research from this project had shown eating fish was associated with an increased risk of melanoma – but no other type of cancer.
Dr. Cho speculated that the risk is due to contaminants, such as mercury and arsenic, in fish. But she was curious to see if she could find a connection between the amount of fish consumed and the risk of developing skin cancer.
At the beginning of the study people reported how much fish they had consumed over the previous year, which varied widely by person. Then researchers tracked participants for 15 years, recording who developed cancer and who did not.
Dietary recall can be difficult; people often say they can’t remember what they ate yesterday, much less 1 year ago. Still, dietitian Clare Collins, PhD, of the University of Newcastle (Australia), noted that previous research showed that the dietary recall tool for this study is reliable.
NIH researchers never checked to see how their diet changed over time, as this was a study meant to observe changes in health status starting from a baseline point. The researchers assumed that the level of fish intake recorded at the beginning of the study remained steady.
Of 491,000 people tracked in the study, 5,000 developed malignant melanoma and another 3,300 developed melanoma cells on the skin surface. People who ate the most fish – an average of almost 43 g, or about 1.5 ounces, per day – were 23% more likely to develop melanoma than the lightest fish eaters, who averaged 3 g per day.
That risk is modest, Dr. Leachman said, especially for people with red hair who, she said, are 400% more likely to get melanoma than others. “A 23% increase, in the whole scheme of things, is not nearly as important as not getting sunburned if you’re a redhead,” Dr. Leachman said.
And what about the sun? Sun exposure is the principal risk factor for developing melanoma, and the researchers didn’t account for that factor. People who developed melanoma during the study may simply have spent more time in tanning beds or on the beach – or perhaps fishing and then eating their catch.
Dr. Cho and colleagues tried to consider the effects of solar radiation by looking at average sun exposure times in the places where the participants in the study were living when the research began. Using that framework, variation in sun exposure made no difference to melanoma risk, but Dr. Leachman said the technique isn’t foolproof.
“They assumed that they were going to get a certain amount of ultraviolet light just based on where they lived. We don’t know how long they lived there or if they really had ultraviolet exposure or not,” Dr. Leachman said. Someone in presumably less sunny Pennsylvania could get more sun than someone in sun-drenched Arizona depending on their lifestyle and habits.
The kind of study Dr. Cho published cannot account for individual behaviors related to sun exposure, a limitation her team readily acknowledges. Nor does it include information about moles or hair color – important considerations for skin cancers. It may be that redheads with moles who barely ate any fish developed melanoma at higher rates than anyone else, but the data don’t allow for that kind of analysis.
Dr. Cho’s group found that canned tuna and any type of fish that wasn’t fried were associated with a higher risk of developing melanoma, as people reported eating more of those products. However, people who said they ate greater quantities of fried fish had a lower risk of melanoma, a counterintuitive finding that she said warrants further research.
Given that the study showed only a modest chance of developing melanoma regardless of fish intake, and left so many questions unanswered, what was the point?
Other journals declined to publish this paper, Dr. Cho acknowledged, but she defended the article as a step toward better understanding the health impact of environmental contaminants in fish.
Dr. Leachman agreed. “These kinds of studies are very important to do. They have large data sets, where you can start to see trends that may be important,” she said. “They can help you identify things that might be related. These experiments are hypothesis generating.”
“I already published an article showing that total mercury level is related to skin cancer, and we know very well that in the U.S. fish consumption is the major source of mercury contamination,” Dr. Cho said. “So, I naturally thought that fish consumption may be associated with increased risk of skin cancer too.” Dr. Cho said she believed the findings confirm that hypothesis.
Dr. Cho said the next step would be to measure blood levels of different contaminants such as mercury and arsenic in people with melanoma, to determine which toxin is the biggest driver of melanoma. She said she plans to seek funding for that research.
Meanwhile, pass the salmon – but go light on the salt.
Dr. Cho and Dr. Leachman reported no relevant financial relationships. Dr. Cho is on the editorial board of Cancer Causes & Control.
A version of this article first appeared on Medscape.com.
A recent study linking the consumption of fish to melanoma had sushi eaters looking up the number of the nearest dermatologist. But experts said the findings had several important limitations and that no one should change their diet based on the results.
“It wouldn’t impact my fish consumption at all,” said Sancy Leachman, MD, PhD, who directs the melanoma program at Oregon Health & Science University’s Knight Cancer Institute in Portland. “Fish are part of a healthy diet,” particularly if it replaces less healthy proteins such as beef.
Even the authors of the study advised caution when interpreting the findings.
“I wouldn’t encourage anyone to change their fish consumption habits just because of this paper,” said study leader Eunyoung Cho, ScD, an epidemiologist at Brown University, Providence, R.I. “Fish is cardioprotective and is related to reduced risk of developing certain cancers too.”
Solid findings or fishing expedition?
The study quickly generated headlines and was the most viewed article of the journal Cancer Causes & Control within a day of its publication.
Dr. Cho, who is on the editorial board of the journal, analyzed the results of a study funded by the National Institutes of Health and the Association for the Advancement of Retired Persons that began in the 1990s and explored possible links between fish consumption and developing different forms of cancer.
Previous research from this project had shown eating fish was associated with an increased risk of melanoma – but no other type of cancer.
Dr. Cho speculated that the risk is due to contaminants, such as mercury and arsenic, in fish. But she was curious to see if she could find a connection between the amount of fish consumed and the risk of developing skin cancer.
At the beginning of the study people reported how much fish they had consumed over the previous year, which varied widely by person. Then researchers tracked participants for 15 years, recording who developed cancer and who did not.
Dietary recall can be difficult; people often say they can’t remember what they ate yesterday, much less 1 year ago. Still, dietitian Clare Collins, PhD, of the University of Newcastle (Australia), noted that previous research showed that the dietary recall tool for this study is reliable.
NIH researchers never checked to see how their diet changed over time, as this was a study meant to observe changes in health status starting from a baseline point. The researchers assumed that the level of fish intake recorded at the beginning of the study remained steady.
Of 491,000 people tracked in the study, 5,000 developed malignant melanoma and another 3,300 developed melanoma cells on the skin surface. People who ate the most fish – an average of almost 43 g, or about 1.5 ounces, per day – were 23% more likely to develop melanoma than the lightest fish eaters, who averaged 3 g per day.
That risk is modest, Dr. Leachman said, especially for people with red hair who, she said, are 400% more likely to get melanoma than others. “A 23% increase, in the whole scheme of things, is not nearly as important as not getting sunburned if you’re a redhead,” Dr. Leachman said.
And what about the sun? Sun exposure is the principal risk factor for developing melanoma, and the researchers didn’t account for that factor. People who developed melanoma during the study may simply have spent more time in tanning beds or on the beach – or perhaps fishing and then eating their catch.
Dr. Cho and colleagues tried to consider the effects of solar radiation by looking at average sun exposure times in the places where the participants in the study were living when the research began. Using that framework, variation in sun exposure made no difference to melanoma risk, but Dr. Leachman said the technique isn’t foolproof.
“They assumed that they were going to get a certain amount of ultraviolet light just based on where they lived. We don’t know how long they lived there or if they really had ultraviolet exposure or not,” Dr. Leachman said. Someone in presumably less sunny Pennsylvania could get more sun than someone in sun-drenched Arizona depending on their lifestyle and habits.
The kind of study Dr. Cho published cannot account for individual behaviors related to sun exposure, a limitation her team readily acknowledges. Nor does it include information about moles or hair color – important considerations for skin cancers. It may be that redheads with moles who barely ate any fish developed melanoma at higher rates than anyone else, but the data don’t allow for that kind of analysis.
Dr. Cho’s group found that canned tuna and any type of fish that wasn’t fried were associated with a higher risk of developing melanoma, as people reported eating more of those products. However, people who said they ate greater quantities of fried fish had a lower risk of melanoma, a counterintuitive finding that she said warrants further research.
Given that the study showed only a modest chance of developing melanoma regardless of fish intake, and left so many questions unanswered, what was the point?
Other journals declined to publish this paper, Dr. Cho acknowledged, but she defended the article as a step toward better understanding the health impact of environmental contaminants in fish.
Dr. Leachman agreed. “These kinds of studies are very important to do. They have large data sets, where you can start to see trends that may be important,” she said. “They can help you identify things that might be related. These experiments are hypothesis generating.”
“I already published an article showing that total mercury level is related to skin cancer, and we know very well that in the U.S. fish consumption is the major source of mercury contamination,” Dr. Cho said. “So, I naturally thought that fish consumption may be associated with increased risk of skin cancer too.” Dr. Cho said she believed the findings confirm that hypothesis.
Dr. Cho said the next step would be to measure blood levels of different contaminants such as mercury and arsenic in people with melanoma, to determine which toxin is the biggest driver of melanoma. She said she plans to seek funding for that research.
Meanwhile, pass the salmon – but go light on the salt.
Dr. Cho and Dr. Leachman reported no relevant financial relationships. Dr. Cho is on the editorial board of Cancer Causes & Control.
A version of this article first appeared on Medscape.com.
A recent study linking the consumption of fish to melanoma had sushi eaters looking up the number of the nearest dermatologist. But experts said the findings had several important limitations and that no one should change their diet based on the results.
“It wouldn’t impact my fish consumption at all,” said Sancy Leachman, MD, PhD, who directs the melanoma program at Oregon Health & Science University’s Knight Cancer Institute in Portland. “Fish are part of a healthy diet,” particularly if it replaces less healthy proteins such as beef.
Even the authors of the study advised caution when interpreting the findings.
“I wouldn’t encourage anyone to change their fish consumption habits just because of this paper,” said study leader Eunyoung Cho, ScD, an epidemiologist at Brown University, Providence, R.I. “Fish is cardioprotective and is related to reduced risk of developing certain cancers too.”
Solid findings or fishing expedition?
The study quickly generated headlines and was the most viewed article of the journal Cancer Causes & Control within a day of its publication.
Dr. Cho, who is on the editorial board of the journal, analyzed the results of a study funded by the National Institutes of Health and the Association for the Advancement of Retired Persons that began in the 1990s and explored possible links between fish consumption and developing different forms of cancer.
Previous research from this project had shown eating fish was associated with an increased risk of melanoma – but no other type of cancer.
Dr. Cho speculated that the risk is due to contaminants, such as mercury and arsenic, in fish. But she was curious to see if she could find a connection between the amount of fish consumed and the risk of developing skin cancer.
At the beginning of the study people reported how much fish they had consumed over the previous year, which varied widely by person. Then researchers tracked participants for 15 years, recording who developed cancer and who did not.
Dietary recall can be difficult; people often say they can’t remember what they ate yesterday, much less 1 year ago. Still, dietitian Clare Collins, PhD, of the University of Newcastle (Australia), noted that previous research showed that the dietary recall tool for this study is reliable.
NIH researchers never checked to see how their diet changed over time, as this was a study meant to observe changes in health status starting from a baseline point. The researchers assumed that the level of fish intake recorded at the beginning of the study remained steady.
Of 491,000 people tracked in the study, 5,000 developed malignant melanoma and another 3,300 developed melanoma cells on the skin surface. People who ate the most fish – an average of almost 43 g, or about 1.5 ounces, per day – were 23% more likely to develop melanoma than the lightest fish eaters, who averaged 3 g per day.
That risk is modest, Dr. Leachman said, especially for people with red hair who, she said, are 400% more likely to get melanoma than others. “A 23% increase, in the whole scheme of things, is not nearly as important as not getting sunburned if you’re a redhead,” Dr. Leachman said.
And what about the sun? Sun exposure is the principal risk factor for developing melanoma, and the researchers didn’t account for that factor. People who developed melanoma during the study may simply have spent more time in tanning beds or on the beach – or perhaps fishing and then eating their catch.
Dr. Cho and colleagues tried to consider the effects of solar radiation by looking at average sun exposure times in the places where the participants in the study were living when the research began. Using that framework, variation in sun exposure made no difference to melanoma risk, but Dr. Leachman said the technique isn’t foolproof.
“They assumed that they were going to get a certain amount of ultraviolet light just based on where they lived. We don’t know how long they lived there or if they really had ultraviolet exposure or not,” Dr. Leachman said. Someone in presumably less sunny Pennsylvania could get more sun than someone in sun-drenched Arizona depending on their lifestyle and habits.
The kind of study Dr. Cho published cannot account for individual behaviors related to sun exposure, a limitation her team readily acknowledges. Nor does it include information about moles or hair color – important considerations for skin cancers. It may be that redheads with moles who barely ate any fish developed melanoma at higher rates than anyone else, but the data don’t allow for that kind of analysis.
Dr. Cho’s group found that canned tuna and any type of fish that wasn’t fried were associated with a higher risk of developing melanoma, as people reported eating more of those products. However, people who said they ate greater quantities of fried fish had a lower risk of melanoma, a counterintuitive finding that she said warrants further research.
Given that the study showed only a modest chance of developing melanoma regardless of fish intake, and left so many questions unanswered, what was the point?
Other journals declined to publish this paper, Dr. Cho acknowledged, but she defended the article as a step toward better understanding the health impact of environmental contaminants in fish.
Dr. Leachman agreed. “These kinds of studies are very important to do. They have large data sets, where you can start to see trends that may be important,” she said. “They can help you identify things that might be related. These experiments are hypothesis generating.”
“I already published an article showing that total mercury level is related to skin cancer, and we know very well that in the U.S. fish consumption is the major source of mercury contamination,” Dr. Cho said. “So, I naturally thought that fish consumption may be associated with increased risk of skin cancer too.” Dr. Cho said she believed the findings confirm that hypothesis.
Dr. Cho said the next step would be to measure blood levels of different contaminants such as mercury and arsenic in people with melanoma, to determine which toxin is the biggest driver of melanoma. She said she plans to seek funding for that research.
Meanwhile, pass the salmon – but go light on the salt.
Dr. Cho and Dr. Leachman reported no relevant financial relationships. Dr. Cho is on the editorial board of Cancer Causes & Control.
A version of this article first appeared on Medscape.com.
Prediabetes is linked independently to myocardial infarction
Prediabetes is not only a predictor of diabetes and the cardiovascular complications that ensue, but it is also a risk factor by itself for myocardial infarction, according to data drawn from almost 1.8 million patients hospitalized for MI.
“Our study serves as a wakeup call for clinicians and patients to shift the focus to preventing prediabetes, and not just diabetes, said Geethika Thota, MD, at the annual meeting of the Endocrine Society.
There are plenty of data suggesting that prediabetes places patients on a trajectory toward cardiovascular disease. In a meta-analysis of 129 studies published 2 years ago, prediabetes was not only associated with a statistically significant 16% increase in coronary heart disease, but also a 13% increased risk of all-cause mortality relative to those with normoglycemia.
Data drawn from 1.8 million patients
In this study, 1,794,149 weighted patient hospitalizations for MI were drawn from the National Inpatient Sample database. Excluding patients who eventually developed diabetes, roughly 1% of these patients had a history of prediabetes in the past, according to a search of ICD-10 codes.
Before adjustment for other risk factors, prediabetes was linked to a greater than 40% increased odds of MI (odds ratio, 1.41; P < .01). After adjustment for a large array of known MI risk factors – including prior history of MI, dyslipidemia, hypertension, nicotine dependence, and obesity – prediabetes remained an independent risk factor, corresponding with a 25% increased risk of MI (OR, 1.25; P < .01).
A history of prediabetes was also an independent risk factor for percutaneous intervention and coronary artery bypass grafting, with increased risk of 45% and 95%, respectively.
As a retrospective study looking at prediabetes as a risk factor in those who already had a MI, it is possible that not all patients with prediabetes were properly coded, but Dr. Thota said that was unlikely to have been an issue of sufficient magnitude to have affected the major conclusions.
Relevance seen for community care
Although the study was drawn from hospitalized patients, its relevance is for the community setting, where screening and intervention for prediabetes has the potential to alter the risk, according to Dr. Thota.
Most clinicians are likely aware of the value of screening for prediabetes, which was defined in this study as a hemoglobin A1c of 5.7%-6.4%, but Dr. Thota suggested that many might not fully grasp the full scope of goals. Early detection and prevention will prevent diabetes and, by extension, cardiovascular disease, but her data suggest that control of prediabetes with lower cardiovascular risk by a more direct route.
“Despite mounting evidence, many clinicians are unaware that prediabetes is also a major risk factor for atherosclerotic cardiovascular disease,” said Dr. Thota, an internal medicine resident at Saint Peter’s University Hospital, New Brunswick, N.J.
Like diabetes, the prevalence of prediabetes is growing rapidly, according to data from the Centers for Disease Control that Dr. Thota cited. In 2020, the Centers for Disease Control and Prevention estimated that 38% of the adult population have prediabetes. By 2030, one model predicts a further 25% growth.
Screening for hyperglycemia is part of routine patient evaluations at Dr. Thota’s center. In an interview, she said that once a diagnosis of prediabetes is entered in the electronic medical record, the history is carried forward so that changes in status are continually monitored.
Worsening prediabetes should be addressed
“Prediabetes is not treated with medication, at least initially,” Dr. Thota explained. Rather, patients are educated about important lifestyle changes, such as diet and physical activity, that can reverse the diagnosis. However, patients who remain on a path of worsening hyperglycemia are candidates for more intensive lifestyle intervention and might be considered selectively for metformin.
“Early recognition of prediabetes through screening is important,” Dr. Thota emphasized. The benefit for preventing patients from progressing to diabetes is well recognized, but these data provide the basis for incentivizing lifestyle changes in patients with prediabetes by telling them that it can reduce their risk for MI.
These data have an important message, but they are not surprising, according to Deepak L. Bhatt, MD, executive director, interventional cardiovascular programs, Brigham and Women’s Hospital Heart & Vascular Center, Boston.
“In fact, in daily practice we see a substantial percentage of patients with MI who have prediabetes that had not been previously recognized or formally diagnosed,” Dr. Bhatt said in an interview.
“Identifying these patients – preferably prior to coming in with cardiovascular complications – is important both to reduce cardiovascular risk but also to try and prevent progression at diabetes,” he added.
Dr. Bhatt went on to say that this large analysis, confirming that prediabetes is independently associated with MI, should prompt clinicians to screen patients rigorously for this condition.
“At a minimum, such patients would be candidates for intensive lifestyle modification aimed at weight loss and treatment of frequent coexistent conditions, such as hypertension and dyslipidemia,” Dr. Bhatt said.
Dr. Thota reports no potential conflicts of interest. Dr. Bhatt has financial relationships with more than 30 pharmaceutical companies, many of which make products relevant to the management of diabetes and cardiovascular disease.
Prediabetes is not only a predictor of diabetes and the cardiovascular complications that ensue, but it is also a risk factor by itself for myocardial infarction, according to data drawn from almost 1.8 million patients hospitalized for MI.
“Our study serves as a wakeup call for clinicians and patients to shift the focus to preventing prediabetes, and not just diabetes, said Geethika Thota, MD, at the annual meeting of the Endocrine Society.
There are plenty of data suggesting that prediabetes places patients on a trajectory toward cardiovascular disease. In a meta-analysis of 129 studies published 2 years ago, prediabetes was not only associated with a statistically significant 16% increase in coronary heart disease, but also a 13% increased risk of all-cause mortality relative to those with normoglycemia.
Data drawn from 1.8 million patients
In this study, 1,794,149 weighted patient hospitalizations for MI were drawn from the National Inpatient Sample database. Excluding patients who eventually developed diabetes, roughly 1% of these patients had a history of prediabetes in the past, according to a search of ICD-10 codes.
Before adjustment for other risk factors, prediabetes was linked to a greater than 40% increased odds of MI (odds ratio, 1.41; P < .01). After adjustment for a large array of known MI risk factors – including prior history of MI, dyslipidemia, hypertension, nicotine dependence, and obesity – prediabetes remained an independent risk factor, corresponding with a 25% increased risk of MI (OR, 1.25; P < .01).
A history of prediabetes was also an independent risk factor for percutaneous intervention and coronary artery bypass grafting, with increased risk of 45% and 95%, respectively.
As a retrospective study looking at prediabetes as a risk factor in those who already had a MI, it is possible that not all patients with prediabetes were properly coded, but Dr. Thota said that was unlikely to have been an issue of sufficient magnitude to have affected the major conclusions.
Relevance seen for community care
Although the study was drawn from hospitalized patients, its relevance is for the community setting, where screening and intervention for prediabetes has the potential to alter the risk, according to Dr. Thota.
Most clinicians are likely aware of the value of screening for prediabetes, which was defined in this study as a hemoglobin A1c of 5.7%-6.4%, but Dr. Thota suggested that many might not fully grasp the full scope of goals. Early detection and prevention will prevent diabetes and, by extension, cardiovascular disease, but her data suggest that control of prediabetes with lower cardiovascular risk by a more direct route.
“Despite mounting evidence, many clinicians are unaware that prediabetes is also a major risk factor for atherosclerotic cardiovascular disease,” said Dr. Thota, an internal medicine resident at Saint Peter’s University Hospital, New Brunswick, N.J.
Like diabetes, the prevalence of prediabetes is growing rapidly, according to data from the Centers for Disease Control that Dr. Thota cited. In 2020, the Centers for Disease Control and Prevention estimated that 38% of the adult population have prediabetes. By 2030, one model predicts a further 25% growth.
Screening for hyperglycemia is part of routine patient evaluations at Dr. Thota’s center. In an interview, she said that once a diagnosis of prediabetes is entered in the electronic medical record, the history is carried forward so that changes in status are continually monitored.
Worsening prediabetes should be addressed
“Prediabetes is not treated with medication, at least initially,” Dr. Thota explained. Rather, patients are educated about important lifestyle changes, such as diet and physical activity, that can reverse the diagnosis. However, patients who remain on a path of worsening hyperglycemia are candidates for more intensive lifestyle intervention and might be considered selectively for metformin.
“Early recognition of prediabetes through screening is important,” Dr. Thota emphasized. The benefit for preventing patients from progressing to diabetes is well recognized, but these data provide the basis for incentivizing lifestyle changes in patients with prediabetes by telling them that it can reduce their risk for MI.
These data have an important message, but they are not surprising, according to Deepak L. Bhatt, MD, executive director, interventional cardiovascular programs, Brigham and Women’s Hospital Heart & Vascular Center, Boston.
“In fact, in daily practice we see a substantial percentage of patients with MI who have prediabetes that had not been previously recognized or formally diagnosed,” Dr. Bhatt said in an interview.
“Identifying these patients – preferably prior to coming in with cardiovascular complications – is important both to reduce cardiovascular risk but also to try and prevent progression at diabetes,” he added.
Dr. Bhatt went on to say that this large analysis, confirming that prediabetes is independently associated with MI, should prompt clinicians to screen patients rigorously for this condition.
“At a minimum, such patients would be candidates for intensive lifestyle modification aimed at weight loss and treatment of frequent coexistent conditions, such as hypertension and dyslipidemia,” Dr. Bhatt said.
Dr. Thota reports no potential conflicts of interest. Dr. Bhatt has financial relationships with more than 30 pharmaceutical companies, many of which make products relevant to the management of diabetes and cardiovascular disease.
Prediabetes is not only a predictor of diabetes and the cardiovascular complications that ensue, but it is also a risk factor by itself for myocardial infarction, according to data drawn from almost 1.8 million patients hospitalized for MI.
“Our study serves as a wakeup call for clinicians and patients to shift the focus to preventing prediabetes, and not just diabetes, said Geethika Thota, MD, at the annual meeting of the Endocrine Society.
There are plenty of data suggesting that prediabetes places patients on a trajectory toward cardiovascular disease. In a meta-analysis of 129 studies published 2 years ago, prediabetes was not only associated with a statistically significant 16% increase in coronary heart disease, but also a 13% increased risk of all-cause mortality relative to those with normoglycemia.
Data drawn from 1.8 million patients
In this study, 1,794,149 weighted patient hospitalizations for MI were drawn from the National Inpatient Sample database. Excluding patients who eventually developed diabetes, roughly 1% of these patients had a history of prediabetes in the past, according to a search of ICD-10 codes.
Before adjustment for other risk factors, prediabetes was linked to a greater than 40% increased odds of MI (odds ratio, 1.41; P < .01). After adjustment for a large array of known MI risk factors – including prior history of MI, dyslipidemia, hypertension, nicotine dependence, and obesity – prediabetes remained an independent risk factor, corresponding with a 25% increased risk of MI (OR, 1.25; P < .01).
A history of prediabetes was also an independent risk factor for percutaneous intervention and coronary artery bypass grafting, with increased risk of 45% and 95%, respectively.
As a retrospective study looking at prediabetes as a risk factor in those who already had a MI, it is possible that not all patients with prediabetes were properly coded, but Dr. Thota said that was unlikely to have been an issue of sufficient magnitude to have affected the major conclusions.
Relevance seen for community care
Although the study was drawn from hospitalized patients, its relevance is for the community setting, where screening and intervention for prediabetes has the potential to alter the risk, according to Dr. Thota.
Most clinicians are likely aware of the value of screening for prediabetes, which was defined in this study as a hemoglobin A1c of 5.7%-6.4%, but Dr. Thota suggested that many might not fully grasp the full scope of goals. Early detection and prevention will prevent diabetes and, by extension, cardiovascular disease, but her data suggest that control of prediabetes with lower cardiovascular risk by a more direct route.
“Despite mounting evidence, many clinicians are unaware that prediabetes is also a major risk factor for atherosclerotic cardiovascular disease,” said Dr. Thota, an internal medicine resident at Saint Peter’s University Hospital, New Brunswick, N.J.
Like diabetes, the prevalence of prediabetes is growing rapidly, according to data from the Centers for Disease Control that Dr. Thota cited. In 2020, the Centers for Disease Control and Prevention estimated that 38% of the adult population have prediabetes. By 2030, one model predicts a further 25% growth.
Screening for hyperglycemia is part of routine patient evaluations at Dr. Thota’s center. In an interview, she said that once a diagnosis of prediabetes is entered in the electronic medical record, the history is carried forward so that changes in status are continually monitored.
Worsening prediabetes should be addressed
“Prediabetes is not treated with medication, at least initially,” Dr. Thota explained. Rather, patients are educated about important lifestyle changes, such as diet and physical activity, that can reverse the diagnosis. However, patients who remain on a path of worsening hyperglycemia are candidates for more intensive lifestyle intervention and might be considered selectively for metformin.
“Early recognition of prediabetes through screening is important,” Dr. Thota emphasized. The benefit for preventing patients from progressing to diabetes is well recognized, but these data provide the basis for incentivizing lifestyle changes in patients with prediabetes by telling them that it can reduce their risk for MI.
These data have an important message, but they are not surprising, according to Deepak L. Bhatt, MD, executive director, interventional cardiovascular programs, Brigham and Women’s Hospital Heart & Vascular Center, Boston.
“In fact, in daily practice we see a substantial percentage of patients with MI who have prediabetes that had not been previously recognized or formally diagnosed,” Dr. Bhatt said in an interview.
“Identifying these patients – preferably prior to coming in with cardiovascular complications – is important both to reduce cardiovascular risk but also to try and prevent progression at diabetes,” he added.
Dr. Bhatt went on to say that this large analysis, confirming that prediabetes is independently associated with MI, should prompt clinicians to screen patients rigorously for this condition.
“At a minimum, such patients would be candidates for intensive lifestyle modification aimed at weight loss and treatment of frequent coexistent conditions, such as hypertension and dyslipidemia,” Dr. Bhatt said.
Dr. Thota reports no potential conflicts of interest. Dr. Bhatt has financial relationships with more than 30 pharmaceutical companies, many of which make products relevant to the management of diabetes and cardiovascular disease.
FROM ENDO 2022








