User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
U.S. health system ranks last among 11 high-income countries
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.
The U.S. health care system ranked last overall among 11 high-income countries in an analysis by the nonprofit Commonwealth Fund, according to a report released on Aug. 4.
The report is the seventh international comparison of countries’ health systems by the Commonwealth Fund since 2004, and the United States has ranked last in every edition, David Blumenthal, MD, president of the Commonwealth Fund, told reporters during a press briefing.
Researchers analyzed survey answers from tens of thousands of patients and physicians in 11 countries. They analyzed performance on 71 measures across five categories – access to care, care process, administrative efficiency, equity, and health care outcomes. Administrative data were gathered from the Organisation for Economic Cooperation and Development and the World Health Organization.
Among contributors to the poor showing by the United States is that half (50%) of lower-income U.S. adults and 27% of higher-income U.S. adults say costs keep them from getting needed health care.
“In no other country does income inequality so profoundly limit access to care,” Dr. Blumenthal said.
In the United Kingdom, only 12% with lower incomes and 7% with higher incomes said costs kept them from care.
In a stark comparison, the researchers found that “a high-income person in the U.S. was more likely to report financial barriers than a low-income person in nearly all the other countries surveyed: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, and the U.K.”
Norway, the Netherlands, and Australia were ranked at the top overall in that order. Rounding out the 11 in overall ranking were the U.K., Germany, New Zealand, Sweden, France, Switzerland, Canada, and the United States.
“What this report tells us is that our health care system is not working for Americans, particularly those with lower incomes, who are at a severe disadvantage compared to citizens of other countries. And they are paying the price with their health and their lives,” Dr. Blumenthal said in a press release.
“To catch up with other high-income countries, the administration and Congress would have to expand access to health care, equitably, to all Americans, act aggressively to control costs, and invest in the social services we know can lead to a healthier population.”
High infant mortality, low life expectancy in U.S.
Several factors contributed to the U.S. ranking at the bottom of the outcomes category. Among them are that the United States has the highest infant mortality rate (5.7 deaths per 1,000 live births) and lowest life expectancy at age 60 (living on average 23.1 years after age 60), compared with the other countries surveyed. The U.S. rate of preventable mortality (177 deaths per 100,000 population) is more than double that of the best-performing country, Switzerland.
Lead author Eric Schneider, MD, senior vice president for policy and research at the Commonwealth Fund, pointed out that, in terms of the change in avoidable mortality over a decade, not only did the United States have the highest rate, compared with the other countries surveyed, “it also experienced the smallest decline in avoidable mortality over that 10-year period.”
The U.S. maternal mortality rate of 17.4 deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births).
U.S. excelled in only one category
The only category in which the United States did not rank last was in “care process,” where it ranked second behind only New Zealand.
The care process category combines preventive care, safe care, coordinated care, and patient engagement and preferences. The category includes indicators such as mammography screening and influenza vaccination for older adults as well as the percentage of adults counseled by a health care provider about nutrition, smoking, or alcohol use.
The United States and Germany performed best on engagement and patient preferences, although U.S. adults have the lowest rates of continuity with the same doctor.
New Zealand and the United States ranked highest in the safe care category, with higher reported use of computerized alerts and routine review of medications.
‘Too little, too late’: Key recommendations for U.S. to improve
Reginald Williams, vice president of International Health Policy and Practice Innovations at the Commonwealth Fund, pointed out that the U.S. shortcomings in health care come despite spending more than twice as much of its GDP (17% in 2019) as the average OECD country.
“It appears that the US delivers too little of the care that is most needed and often delivers that care too late, especially for people with chronic illnesses,” he said.
He then summarized the team’s recommendations on how the United States can change course.
First is expanding insurance coverage, he said, noting that the United States is the only one of the 11 countries that lacks universal coverage and nearly 30 million people remain uninsured.
Top-performing countries in the survey have universal coverage, annual out-of-pocket caps on covered benefits, and full coverage for primary care and treatment for chronic conditions, he said.
The United States must also improve access to care, he said.
“Top-ranking countries like the Netherlands and Norway ensure timely availability to care by telephone on nights and weekends, and in-person follow-up at home, if needed,” he said.
Mr. Williams said reducing administrative burdens is also critical to free up resources for improving health. He gave an example: “Norway determines patient copayments or physician fees on a regional basis, applying standardized copayments to all physicians within a specialty in a geographic area.”
Reducing income-related barriers is important as well, he said.
The fear of unpredictably high bills and other issues prevent people in the United States from getting the care they ultimately need, he said, adding that top-performing countries invest more in social services to reduce health risks.
That could have implications for the COVID-19 response.
Responding effectively to COVID-19 requires that patients can access affordable health care services, Mr. Williams noted.
“We know from our research that more than two-thirds of U.S. adults say their potential out-of-pocket costs would figure prominently in their decisions to get care if they had coronavirus symptoms,” he said.
Dr. Schneider summed up in the press release: “This study makes clear that higher U.S. spending on health care is not producing better health especially as the U.S. continues on a path of deepening inequality. A country that spends as much as we do should have the best health system in the world. We should adapt what works in other high-income countries to build a better health care system that provides affordable, high-quality health care for everyone.”
Dr. Blumenthal, Dr. Schneider, and Mr. Williams reported no relevant financial relationships outside their employment with the Commonwealth Fund.
A version of this article first appeared on Medscape.com.
Will the Delta variant peak and then burn out?
When the Delta variant of the coronavirus was first identified in India in December 2020, the threat may have seemed too remote to trigger worry in the United States, although the horror of it ripping through the country was soon hard to ignore.
Within months, the Delta variant had spread to more than 98 countries, including Scotland, the United Kingdom, Israel, and now, of course, the United States. The CDC said this week the Delta variant now accounts for 93% of all COVID cases.
Fueled by Delta, COVID-19 cases, hospitalizations, and deaths are increasing in nearly all states, according to the latest CDC data. After the 7-day average number of cases dipped by June 22 to about 11,000, it rose by Aug. 3 to more than 85,000.
Some experts are heartened by the recent decrease in COVID-19 cases in the United Kingdom and India, both hard-hit with the Delta variant. COVID-19 cases in India peaked at more than 400,000 a day in May; by Aug. 2, that had dropped to about 30,500 daily.
Andy Slavitt, former Biden White House senior adviser for COVID-19 response, tweeted July 26 that, if the Delta variant acted the same in the United Kingdom as in India, it would have a quick rise and a quick drop.
The prediction seems to have come true. As of Aug. 3, U.K. cases have dropped to 7,467, compared with more than 46,800 July 19.
So the question of the summer has become: “When will Delta burn out here?”
Like other pandemic predictions, these are all over the board. Here are five predictions about when COVID cases will peak, then fall. They range from less than 2 weeks to more than 2 months:
- Mid-August: Among the most optimistic predictions of when the Delta-driven COVID-19 cases will decline is from Scott Gottlieb, MD, former FDA director. He told CNBC on July 28 that he would expect cases to decline in 2-3 weeks – so by August 11.
- Mid-August to mid-September: Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said that, “right now for the U.S. as a country, cases will peak mid-August” and then decline. He is citing projections by the university’s Institute for Health Metrics and Evaluation. In its “most likely” scenario, it predicts COVID deaths will peak at about 1,000 daily by mid-September, then decline. (As of Aug. 3, daily deaths averaged 371.)
- September: “I am hoping we get over this Delta hump [by then],” says Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape. “But sometimes, I am too much of an optimist.”
- Mid-October: Experts at the COVID-19 Scenario Modeling Hub, a consortium of researchers from leading institutions who consult with the CDC, said the Delta-fueled pandemic will steadily increase through summer and fall, with a mid-October peak.
- Unclear: Because cases are underestimated, “I think it is unclear when we will see a peak of Delta,” says Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore. He predicts a decline in cases as “more people get infected and develop natural immunity.”
The predictions are based on different scenarios, such as most likely or worst case. Factors such as personal behaviors, public mandates, and vaccination rates could all alter the projections.
What a difference vaccination may make
An uptick in vaccinations could change all the models and predictions, experts agree. As of Aug. 3, almost half (49.7%) of the total U.S. population was fully vaccinated, the CDC said. (And 80.1% of those 65 and over were.)
But that’s a long way from the 70% or 80% figure often cited to reach herd immunity. Recently, Ricardo Franco, MD, of the University of Alabama at Birmingham, said at a briefing by the Infectious Diseases Society of America that the infectiousness of the Delta variant may mean the herd immunity threshold is actually closer to 90%.
Dr. Mokdad estimates that by Nov. 1, based on the current rate of infections, 64% of people in the United States will be immune to a variant like Delta, taking into account those already infected and those vaccinated against COVID-19.
Justin Lessler, PhD, a University of North Carolina at Chapel Hill epidemiologist involved in the modeling hub, says if enough people get vaccinated, it could stop the Delta variant in its tracks. But that percentage is high.
“I am relatively confident that if we could get 90% or more of the eligible population vaccinated that we would see the epidemic begin to recede,” he says.
It’s a huge leap from 50%, or even 64%, to 90%. Could the Delta surge really motivate that many people to head to a vaccination site?
That’s hard to predict, Dr. Topol said. Some unvaccinated people may feel like soldiers in a foxhole, especially if they are in hard-hit states like Louisiana, and rush to get the vaccine as soon as possible. Others, hearing about the “breakthrough” cases in the vaccinated, may dig in their heels and ask: “Why bother?” as they mistakenly conclude that the vaccine has not done its job.
Roles of public policy, individual behavior
Besides an increase in vaccinations, individual behaviors and mandates can change the scenario. Doctors can remind even vaccinated patients that behaviors such as social distancing and masks still matter, experts said.
“Don’t ‘stress test’ your vaccine, “ Dr. Topol said.
The vaccines against COVID are good but not perfect and, he notes, they offer less protection if many months have passed since the vaccines were given.
The best advice now, Dr. Topol said, is: “Don’t be inside without a mask.”
Even if outdoors, depending on how close others are and the level of the conversation, a mask might be wise, he says.
Dr. Mokdad finds that “when cases go up, people put on their best behavior,” such as going back to masks and social distancing.
“Unfortunately, we have two countries,” he said, referring to the way public health measures and mandates vary from state to state.
Once the Delta variant subsides, what’s next?
It’s not a matter of if there is another variant on the heels of Delta, but when, Dr. Topol and other experts said. A new variant, Lambda, was first identified in Peru in August 2020 but now makes up about 90% of the country’s infections.
There’s also Delta-plus, just found in two people in South Korea.
Future variants could be even more transmissible than Delta, “which would be a horror show,” Dr. Topol said. “This [Delta] is by far the worst version. The virus is going to keep evolving. It is not done with us.”
On the horizon: Variant-proof vaccines
What’s needed to tackle the next variant is another approach to vaccine development, according to Dr. Topol and his colleague, Dennis R. Burton, a professor of immunology and microbiology at Scripps Research Institute.
Writing a commentary in Nature published in 2021, the two propose using a special class of protective antibodies, known as broadly neutralizing antibodies, to develop these vaccines. The success of the current COVID-19 vaccines is likely because of the vaccine’s ability to prompt the body to make protective neutralizing antibodies. These proteins bind to the viruses and prevent them from infecting the body’s cells.
The broadly neutralizing antibodies, however, can act against many different strains of related viruses, Dr. Topol and Mr. Burton wrote. Using this approach, which is already under study, scientists could make vaccines that would be effective against a family of viruses. The goal: to stop future outbreaks from becoming epidemics and then pandemics.
A version of this article first appeared on WebMD.com.
When the Delta variant of the coronavirus was first identified in India in December 2020, the threat may have seemed too remote to trigger worry in the United States, although the horror of it ripping through the country was soon hard to ignore.
Within months, the Delta variant had spread to more than 98 countries, including Scotland, the United Kingdom, Israel, and now, of course, the United States. The CDC said this week the Delta variant now accounts for 93% of all COVID cases.
Fueled by Delta, COVID-19 cases, hospitalizations, and deaths are increasing in nearly all states, according to the latest CDC data. After the 7-day average number of cases dipped by June 22 to about 11,000, it rose by Aug. 3 to more than 85,000.
Some experts are heartened by the recent decrease in COVID-19 cases in the United Kingdom and India, both hard-hit with the Delta variant. COVID-19 cases in India peaked at more than 400,000 a day in May; by Aug. 2, that had dropped to about 30,500 daily.
Andy Slavitt, former Biden White House senior adviser for COVID-19 response, tweeted July 26 that, if the Delta variant acted the same in the United Kingdom as in India, it would have a quick rise and a quick drop.
The prediction seems to have come true. As of Aug. 3, U.K. cases have dropped to 7,467, compared with more than 46,800 July 19.
So the question of the summer has become: “When will Delta burn out here?”
Like other pandemic predictions, these are all over the board. Here are five predictions about when COVID cases will peak, then fall. They range from less than 2 weeks to more than 2 months:
- Mid-August: Among the most optimistic predictions of when the Delta-driven COVID-19 cases will decline is from Scott Gottlieb, MD, former FDA director. He told CNBC on July 28 that he would expect cases to decline in 2-3 weeks – so by August 11.
- Mid-August to mid-September: Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said that, “right now for the U.S. as a country, cases will peak mid-August” and then decline. He is citing projections by the university’s Institute for Health Metrics and Evaluation. In its “most likely” scenario, it predicts COVID deaths will peak at about 1,000 daily by mid-September, then decline. (As of Aug. 3, daily deaths averaged 371.)
- September: “I am hoping we get over this Delta hump [by then],” says Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape. “But sometimes, I am too much of an optimist.”
- Mid-October: Experts at the COVID-19 Scenario Modeling Hub, a consortium of researchers from leading institutions who consult with the CDC, said the Delta-fueled pandemic will steadily increase through summer and fall, with a mid-October peak.
- Unclear: Because cases are underestimated, “I think it is unclear when we will see a peak of Delta,” says Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore. He predicts a decline in cases as “more people get infected and develop natural immunity.”
The predictions are based on different scenarios, such as most likely or worst case. Factors such as personal behaviors, public mandates, and vaccination rates could all alter the projections.
What a difference vaccination may make
An uptick in vaccinations could change all the models and predictions, experts agree. As of Aug. 3, almost half (49.7%) of the total U.S. population was fully vaccinated, the CDC said. (And 80.1% of those 65 and over were.)
But that’s a long way from the 70% or 80% figure often cited to reach herd immunity. Recently, Ricardo Franco, MD, of the University of Alabama at Birmingham, said at a briefing by the Infectious Diseases Society of America that the infectiousness of the Delta variant may mean the herd immunity threshold is actually closer to 90%.
Dr. Mokdad estimates that by Nov. 1, based on the current rate of infections, 64% of people in the United States will be immune to a variant like Delta, taking into account those already infected and those vaccinated against COVID-19.
Justin Lessler, PhD, a University of North Carolina at Chapel Hill epidemiologist involved in the modeling hub, says if enough people get vaccinated, it could stop the Delta variant in its tracks. But that percentage is high.
“I am relatively confident that if we could get 90% or more of the eligible population vaccinated that we would see the epidemic begin to recede,” he says.
It’s a huge leap from 50%, or even 64%, to 90%. Could the Delta surge really motivate that many people to head to a vaccination site?
That’s hard to predict, Dr. Topol said. Some unvaccinated people may feel like soldiers in a foxhole, especially if they are in hard-hit states like Louisiana, and rush to get the vaccine as soon as possible. Others, hearing about the “breakthrough” cases in the vaccinated, may dig in their heels and ask: “Why bother?” as they mistakenly conclude that the vaccine has not done its job.
Roles of public policy, individual behavior
Besides an increase in vaccinations, individual behaviors and mandates can change the scenario. Doctors can remind even vaccinated patients that behaviors such as social distancing and masks still matter, experts said.
“Don’t ‘stress test’ your vaccine, “ Dr. Topol said.
The vaccines against COVID are good but not perfect and, he notes, they offer less protection if many months have passed since the vaccines were given.
The best advice now, Dr. Topol said, is: “Don’t be inside without a mask.”
Even if outdoors, depending on how close others are and the level of the conversation, a mask might be wise, he says.
Dr. Mokdad finds that “when cases go up, people put on their best behavior,” such as going back to masks and social distancing.
“Unfortunately, we have two countries,” he said, referring to the way public health measures and mandates vary from state to state.
Once the Delta variant subsides, what’s next?
It’s not a matter of if there is another variant on the heels of Delta, but when, Dr. Topol and other experts said. A new variant, Lambda, was first identified in Peru in August 2020 but now makes up about 90% of the country’s infections.
There’s also Delta-plus, just found in two people in South Korea.
Future variants could be even more transmissible than Delta, “which would be a horror show,” Dr. Topol said. “This [Delta] is by far the worst version. The virus is going to keep evolving. It is not done with us.”
On the horizon: Variant-proof vaccines
What’s needed to tackle the next variant is another approach to vaccine development, according to Dr. Topol and his colleague, Dennis R. Burton, a professor of immunology and microbiology at Scripps Research Institute.
Writing a commentary in Nature published in 2021, the two propose using a special class of protective antibodies, known as broadly neutralizing antibodies, to develop these vaccines. The success of the current COVID-19 vaccines is likely because of the vaccine’s ability to prompt the body to make protective neutralizing antibodies. These proteins bind to the viruses and prevent them from infecting the body’s cells.
The broadly neutralizing antibodies, however, can act against many different strains of related viruses, Dr. Topol and Mr. Burton wrote. Using this approach, which is already under study, scientists could make vaccines that would be effective against a family of viruses. The goal: to stop future outbreaks from becoming epidemics and then pandemics.
A version of this article first appeared on WebMD.com.
When the Delta variant of the coronavirus was first identified in India in December 2020, the threat may have seemed too remote to trigger worry in the United States, although the horror of it ripping through the country was soon hard to ignore.
Within months, the Delta variant had spread to more than 98 countries, including Scotland, the United Kingdom, Israel, and now, of course, the United States. The CDC said this week the Delta variant now accounts for 93% of all COVID cases.
Fueled by Delta, COVID-19 cases, hospitalizations, and deaths are increasing in nearly all states, according to the latest CDC data. After the 7-day average number of cases dipped by June 22 to about 11,000, it rose by Aug. 3 to more than 85,000.
Some experts are heartened by the recent decrease in COVID-19 cases in the United Kingdom and India, both hard-hit with the Delta variant. COVID-19 cases in India peaked at more than 400,000 a day in May; by Aug. 2, that had dropped to about 30,500 daily.
Andy Slavitt, former Biden White House senior adviser for COVID-19 response, tweeted July 26 that, if the Delta variant acted the same in the United Kingdom as in India, it would have a quick rise and a quick drop.
The prediction seems to have come true. As of Aug. 3, U.K. cases have dropped to 7,467, compared with more than 46,800 July 19.
So the question of the summer has become: “When will Delta burn out here?”
Like other pandemic predictions, these are all over the board. Here are five predictions about when COVID cases will peak, then fall. They range from less than 2 weeks to more than 2 months:
- Mid-August: Among the most optimistic predictions of when the Delta-driven COVID-19 cases will decline is from Scott Gottlieb, MD, former FDA director. He told CNBC on July 28 that he would expect cases to decline in 2-3 weeks – so by August 11.
- Mid-August to mid-September: Ali Mokdad, PhD, chief strategy officer for population health at the University of Washington, Seattle, said that, “right now for the U.S. as a country, cases will peak mid-August” and then decline. He is citing projections by the university’s Institute for Health Metrics and Evaluation. In its “most likely” scenario, it predicts COVID deaths will peak at about 1,000 daily by mid-September, then decline. (As of Aug. 3, daily deaths averaged 371.)
- September: “I am hoping we get over this Delta hump [by then],” says Eric Topol, MD, founder and director of the Scripps Research Translational Institute in La Jolla, Calif., and editor-in-chief of Medscape. “But sometimes, I am too much of an optimist.”
- Mid-October: Experts at the COVID-19 Scenario Modeling Hub, a consortium of researchers from leading institutions who consult with the CDC, said the Delta-fueled pandemic will steadily increase through summer and fall, with a mid-October peak.
- Unclear: Because cases are underestimated, “I think it is unclear when we will see a peak of Delta,” says Amesh Adalja, MD, a senior scholar at the Johns Hopkins Center for Health Security, Baltimore. He predicts a decline in cases as “more people get infected and develop natural immunity.”
The predictions are based on different scenarios, such as most likely or worst case. Factors such as personal behaviors, public mandates, and vaccination rates could all alter the projections.
What a difference vaccination may make
An uptick in vaccinations could change all the models and predictions, experts agree. As of Aug. 3, almost half (49.7%) of the total U.S. population was fully vaccinated, the CDC said. (And 80.1% of those 65 and over were.)
But that’s a long way from the 70% or 80% figure often cited to reach herd immunity. Recently, Ricardo Franco, MD, of the University of Alabama at Birmingham, said at a briefing by the Infectious Diseases Society of America that the infectiousness of the Delta variant may mean the herd immunity threshold is actually closer to 90%.
Dr. Mokdad estimates that by Nov. 1, based on the current rate of infections, 64% of people in the United States will be immune to a variant like Delta, taking into account those already infected and those vaccinated against COVID-19.
Justin Lessler, PhD, a University of North Carolina at Chapel Hill epidemiologist involved in the modeling hub, says if enough people get vaccinated, it could stop the Delta variant in its tracks. But that percentage is high.
“I am relatively confident that if we could get 90% or more of the eligible population vaccinated that we would see the epidemic begin to recede,” he says.
It’s a huge leap from 50%, or even 64%, to 90%. Could the Delta surge really motivate that many people to head to a vaccination site?
That’s hard to predict, Dr. Topol said. Some unvaccinated people may feel like soldiers in a foxhole, especially if they are in hard-hit states like Louisiana, and rush to get the vaccine as soon as possible. Others, hearing about the “breakthrough” cases in the vaccinated, may dig in their heels and ask: “Why bother?” as they mistakenly conclude that the vaccine has not done its job.
Roles of public policy, individual behavior
Besides an increase in vaccinations, individual behaviors and mandates can change the scenario. Doctors can remind even vaccinated patients that behaviors such as social distancing and masks still matter, experts said.
“Don’t ‘stress test’ your vaccine, “ Dr. Topol said.
The vaccines against COVID are good but not perfect and, he notes, they offer less protection if many months have passed since the vaccines were given.
The best advice now, Dr. Topol said, is: “Don’t be inside without a mask.”
Even if outdoors, depending on how close others are and the level of the conversation, a mask might be wise, he says.
Dr. Mokdad finds that “when cases go up, people put on their best behavior,” such as going back to masks and social distancing.
“Unfortunately, we have two countries,” he said, referring to the way public health measures and mandates vary from state to state.
Once the Delta variant subsides, what’s next?
It’s not a matter of if there is another variant on the heels of Delta, but when, Dr. Topol and other experts said. A new variant, Lambda, was first identified in Peru in August 2020 but now makes up about 90% of the country’s infections.
There’s also Delta-plus, just found in two people in South Korea.
Future variants could be even more transmissible than Delta, “which would be a horror show,” Dr. Topol said. “This [Delta] is by far the worst version. The virus is going to keep evolving. It is not done with us.”
On the horizon: Variant-proof vaccines
What’s needed to tackle the next variant is another approach to vaccine development, according to Dr. Topol and his colleague, Dennis R. Burton, a professor of immunology and microbiology at Scripps Research Institute.
Writing a commentary in Nature published in 2021, the two propose using a special class of protective antibodies, known as broadly neutralizing antibodies, to develop these vaccines. The success of the current COVID-19 vaccines is likely because of the vaccine’s ability to prompt the body to make protective neutralizing antibodies. These proteins bind to the viruses and prevent them from infecting the body’s cells.
The broadly neutralizing antibodies, however, can act against many different strains of related viruses, Dr. Topol and Mr. Burton wrote. Using this approach, which is already under study, scientists could make vaccines that would be effective against a family of viruses. The goal: to stop future outbreaks from becoming epidemics and then pandemics.
A version of this article first appeared on WebMD.com.
Androgenetic alopecia fuels negative emotions and poor quality of life
and meta-analysis of 41 studies.
“Hair loss affects self-image, causes trichodynia, and plays a role in emotions and social activity, which may be associated with psychiatric problems and impaired health-related quality of life,” wrote Chun-Hsien Huang, MD, of Chang Gung Memorial Hospital, Linkou, Taiwan, and colleagues. However, systematic reviews of the associations between androgenetic alopecia (AGA) and health-related quality of life (HRQOL) are lacking, they said.
In a study published in JAMA Dermatology, the researchers reviewed data from a total of 7,995 AGA patients in 41 studies. The studies included 11 tools for HRQOL assessment and 29 tools for psychological assessment. Of these, the Dermatology Life Quality Index (DLQI) and the Hair-Specific Skindex-29 were used to assess quality of life, and the Center for Epidemiologic Studies Depression Scale (CES-D) was used for psychological assessment in the meta-analysis.
Overall, 27 studies identified 18 factors associated with HRQOL; those with an inverse effect were higher self-rated hair loss severity, lower VAS score, and higher educational level. Of note, neither physician-rated hair loss severity nor treatment response were factors in HRQOL, the researchers said.
The pooled DLQI score across studies was 8.16, and subgroup analysis showed no differences in HRQOL between men and women or between patients from European vs. Asian countries. However, five studies showed significant differences in HRQOL between men and women when different assessment tools were used, which emphasized the need for more studies to examine the association of AGA with HRQOL by sex, the researchers said.
The meta-analysis of the Hair-Specific Skindex-29 scores showed pooled averages of 21.95 for symptom dimension, 18.52 in function dimension, and 29.22 in emotion dimension. Of these, the emotion dimension scores indicated moderate emotional impairment.
The average pooled score on the CES-D in the meta-analysis was 14.98, indicating no association between AGA and depression, the researchers said. However, “depression accounts for only a part of the emotion dimension,” they said. “Therefore, emotion dimension could be impaired even if no depressive symptoms were noted.”
The pooled DLQI scores for AGA (8.16) were higher than scores for other skin conditions including alopecia areata (6.3), contact dermatitis (7.35), and acne vulgaris (7.45), but lower than the pooled scores for vitiligo (9.11), urticaria (9.8), psoriasis (10.53), and atopic dermatitis (11.2), the researchers noted. “However, additional head-to-head studies are needed for direct comparisons of HRQOL in patients with various dermatoses,” they said.
The study findings were limited by the cross-sectional design of many of the included studies, and the limited number of assessment tools included in the analysis, the researchers noted. Other limitations were the lack of specific domain scores and the inclusion of only three studies from China, they said.
However, the results are consistent with findings from previous studies, and suggest that patients with AGA may benefit from psychological and psychosocial support, the researchers said.
Quality of life issues deserve attention
“Studies of the quality-of-life impact of various conditions are becoming more common in the medical literature,” Jamie B. MacKelfresh, MD, associate professor of dermatology, Emory University, Atlanta, said in an interview.
“Androgenetic alopecia is the most common type of hair loss in men and women,” she noted. “Hair loss can be labeled as a cosmetic concern, so it is important that providers understand the significant quality-of-life impact androgenetic alopecia has on the many people with this diagnosis,” she emphasized.
Dr. MacKelfresh, who was asked to comment on the study, said she was surprised that the subgroup analysis of the DLQI showed no significant difference between men and women. “This surprised me because a number of past studies have highlighted the relatively greater quality-of-life impact of hair loss on women compared to men,” she noted.
However, she added, “I was not surprised to see that androgenetic alopecia has a significant quality-of-life impact on many patients, and that physician objective assessments of the hair loss do not always correlate with the amount of quality-of-life impact,” said Dr. MacKelfresh. “In the patients I see, I find hair loss very often has a significant quality-of-life impact on patients, regardless of gender, and the amount of quality-of-life impact definitely does not always correlate with the objective amount of hair loss,” she noted.
A takeaway message for clinicians is to be aware that androgenetic alopecia frequently has a significant impact on patients, “particularly in the emotional dimension,” and can affect both men and women, Dr. MacKelfresh said. “Objective assessments of hair loss severity by providers may not accurately predict the degree of quality-of-life impact a patient may experience; therefore providers should include quality-of-life questions as part of their standard evaluation of patients with androgenetic alopecia,” she said. In addition to treating the hair loss, providers can help these patients by guiding them to psychological support resources, she emphasized.
More research is needed to assess the impact of androgenetic alopecia on “men, women, and the non-binary gender population,” as well as the relationship between self-esteem and hair loss, she said. “Finally, it would be helpful to understand what interventions can best help improve androgenetic alopecia patients’ quality of life,” she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. MacKelfresh had no financial conflicts to disclose.
and meta-analysis of 41 studies.
“Hair loss affects self-image, causes trichodynia, and plays a role in emotions and social activity, which may be associated with psychiatric problems and impaired health-related quality of life,” wrote Chun-Hsien Huang, MD, of Chang Gung Memorial Hospital, Linkou, Taiwan, and colleagues. However, systematic reviews of the associations between androgenetic alopecia (AGA) and health-related quality of life (HRQOL) are lacking, they said.
In a study published in JAMA Dermatology, the researchers reviewed data from a total of 7,995 AGA patients in 41 studies. The studies included 11 tools for HRQOL assessment and 29 tools for psychological assessment. Of these, the Dermatology Life Quality Index (DLQI) and the Hair-Specific Skindex-29 were used to assess quality of life, and the Center for Epidemiologic Studies Depression Scale (CES-D) was used for psychological assessment in the meta-analysis.
Overall, 27 studies identified 18 factors associated with HRQOL; those with an inverse effect were higher self-rated hair loss severity, lower VAS score, and higher educational level. Of note, neither physician-rated hair loss severity nor treatment response were factors in HRQOL, the researchers said.
The pooled DLQI score across studies was 8.16, and subgroup analysis showed no differences in HRQOL between men and women or between patients from European vs. Asian countries. However, five studies showed significant differences in HRQOL between men and women when different assessment tools were used, which emphasized the need for more studies to examine the association of AGA with HRQOL by sex, the researchers said.
The meta-analysis of the Hair-Specific Skindex-29 scores showed pooled averages of 21.95 for symptom dimension, 18.52 in function dimension, and 29.22 in emotion dimension. Of these, the emotion dimension scores indicated moderate emotional impairment.
The average pooled score on the CES-D in the meta-analysis was 14.98, indicating no association between AGA and depression, the researchers said. However, “depression accounts for only a part of the emotion dimension,” they said. “Therefore, emotion dimension could be impaired even if no depressive symptoms were noted.”
The pooled DLQI scores for AGA (8.16) were higher than scores for other skin conditions including alopecia areata (6.3), contact dermatitis (7.35), and acne vulgaris (7.45), but lower than the pooled scores for vitiligo (9.11), urticaria (9.8), psoriasis (10.53), and atopic dermatitis (11.2), the researchers noted. “However, additional head-to-head studies are needed for direct comparisons of HRQOL in patients with various dermatoses,” they said.
The study findings were limited by the cross-sectional design of many of the included studies, and the limited number of assessment tools included in the analysis, the researchers noted. Other limitations were the lack of specific domain scores and the inclusion of only three studies from China, they said.
However, the results are consistent with findings from previous studies, and suggest that patients with AGA may benefit from psychological and psychosocial support, the researchers said.
Quality of life issues deserve attention
“Studies of the quality-of-life impact of various conditions are becoming more common in the medical literature,” Jamie B. MacKelfresh, MD, associate professor of dermatology, Emory University, Atlanta, said in an interview.
“Androgenetic alopecia is the most common type of hair loss in men and women,” she noted. “Hair loss can be labeled as a cosmetic concern, so it is important that providers understand the significant quality-of-life impact androgenetic alopecia has on the many people with this diagnosis,” she emphasized.
Dr. MacKelfresh, who was asked to comment on the study, said she was surprised that the subgroup analysis of the DLQI showed no significant difference between men and women. “This surprised me because a number of past studies have highlighted the relatively greater quality-of-life impact of hair loss on women compared to men,” she noted.
However, she added, “I was not surprised to see that androgenetic alopecia has a significant quality-of-life impact on many patients, and that physician objective assessments of the hair loss do not always correlate with the amount of quality-of-life impact,” said Dr. MacKelfresh. “In the patients I see, I find hair loss very often has a significant quality-of-life impact on patients, regardless of gender, and the amount of quality-of-life impact definitely does not always correlate with the objective amount of hair loss,” she noted.
A takeaway message for clinicians is to be aware that androgenetic alopecia frequently has a significant impact on patients, “particularly in the emotional dimension,” and can affect both men and women, Dr. MacKelfresh said. “Objective assessments of hair loss severity by providers may not accurately predict the degree of quality-of-life impact a patient may experience; therefore providers should include quality-of-life questions as part of their standard evaluation of patients with androgenetic alopecia,” she said. In addition to treating the hair loss, providers can help these patients by guiding them to psychological support resources, she emphasized.
More research is needed to assess the impact of androgenetic alopecia on “men, women, and the non-binary gender population,” as well as the relationship between self-esteem and hair loss, she said. “Finally, it would be helpful to understand what interventions can best help improve androgenetic alopecia patients’ quality of life,” she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. MacKelfresh had no financial conflicts to disclose.
and meta-analysis of 41 studies.
“Hair loss affects self-image, causes trichodynia, and plays a role in emotions and social activity, which may be associated with psychiatric problems and impaired health-related quality of life,” wrote Chun-Hsien Huang, MD, of Chang Gung Memorial Hospital, Linkou, Taiwan, and colleagues. However, systematic reviews of the associations between androgenetic alopecia (AGA) and health-related quality of life (HRQOL) are lacking, they said.
In a study published in JAMA Dermatology, the researchers reviewed data from a total of 7,995 AGA patients in 41 studies. The studies included 11 tools for HRQOL assessment and 29 tools for psychological assessment. Of these, the Dermatology Life Quality Index (DLQI) and the Hair-Specific Skindex-29 were used to assess quality of life, and the Center for Epidemiologic Studies Depression Scale (CES-D) was used for psychological assessment in the meta-analysis.
Overall, 27 studies identified 18 factors associated with HRQOL; those with an inverse effect were higher self-rated hair loss severity, lower VAS score, and higher educational level. Of note, neither physician-rated hair loss severity nor treatment response were factors in HRQOL, the researchers said.
The pooled DLQI score across studies was 8.16, and subgroup analysis showed no differences in HRQOL between men and women or between patients from European vs. Asian countries. However, five studies showed significant differences in HRQOL between men and women when different assessment tools were used, which emphasized the need for more studies to examine the association of AGA with HRQOL by sex, the researchers said.
The meta-analysis of the Hair-Specific Skindex-29 scores showed pooled averages of 21.95 for symptom dimension, 18.52 in function dimension, and 29.22 in emotion dimension. Of these, the emotion dimension scores indicated moderate emotional impairment.
The average pooled score on the CES-D in the meta-analysis was 14.98, indicating no association between AGA and depression, the researchers said. However, “depression accounts for only a part of the emotion dimension,” they said. “Therefore, emotion dimension could be impaired even if no depressive symptoms were noted.”
The pooled DLQI scores for AGA (8.16) were higher than scores for other skin conditions including alopecia areata (6.3), contact dermatitis (7.35), and acne vulgaris (7.45), but lower than the pooled scores for vitiligo (9.11), urticaria (9.8), psoriasis (10.53), and atopic dermatitis (11.2), the researchers noted. “However, additional head-to-head studies are needed for direct comparisons of HRQOL in patients with various dermatoses,” they said.
The study findings were limited by the cross-sectional design of many of the included studies, and the limited number of assessment tools included in the analysis, the researchers noted. Other limitations were the lack of specific domain scores and the inclusion of only three studies from China, they said.
However, the results are consistent with findings from previous studies, and suggest that patients with AGA may benefit from psychological and psychosocial support, the researchers said.
Quality of life issues deserve attention
“Studies of the quality-of-life impact of various conditions are becoming more common in the medical literature,” Jamie B. MacKelfresh, MD, associate professor of dermatology, Emory University, Atlanta, said in an interview.
“Androgenetic alopecia is the most common type of hair loss in men and women,” she noted. “Hair loss can be labeled as a cosmetic concern, so it is important that providers understand the significant quality-of-life impact androgenetic alopecia has on the many people with this diagnosis,” she emphasized.
Dr. MacKelfresh, who was asked to comment on the study, said she was surprised that the subgroup analysis of the DLQI showed no significant difference between men and women. “This surprised me because a number of past studies have highlighted the relatively greater quality-of-life impact of hair loss on women compared to men,” she noted.
However, she added, “I was not surprised to see that androgenetic alopecia has a significant quality-of-life impact on many patients, and that physician objective assessments of the hair loss do not always correlate with the amount of quality-of-life impact,” said Dr. MacKelfresh. “In the patients I see, I find hair loss very often has a significant quality-of-life impact on patients, regardless of gender, and the amount of quality-of-life impact definitely does not always correlate with the objective amount of hair loss,” she noted.
A takeaway message for clinicians is to be aware that androgenetic alopecia frequently has a significant impact on patients, “particularly in the emotional dimension,” and can affect both men and women, Dr. MacKelfresh said. “Objective assessments of hair loss severity by providers may not accurately predict the degree of quality-of-life impact a patient may experience; therefore providers should include quality-of-life questions as part of their standard evaluation of patients with androgenetic alopecia,” she said. In addition to treating the hair loss, providers can help these patients by guiding them to psychological support resources, she emphasized.
More research is needed to assess the impact of androgenetic alopecia on “men, women, and the non-binary gender population,” as well as the relationship between self-esteem and hair loss, she said. “Finally, it would be helpful to understand what interventions can best help improve androgenetic alopecia patients’ quality of life,” she noted.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. MacKelfresh had no financial conflicts to disclose.
FROM JAMA DERMATOLOGY
Graying of hair: Could it be reversed?
as hair pigment goes through its natural progression of senescence.
However, the recent publication that is a collaboration between the department of psychiatry at Columbia University, New York; and the departments of dermatology at the University College Dublin, University of Miami, and the University of Manchester (England); and the Monasterium Laboratory in Münster, Germany, demonstrates a quantitative mapping of human hair graying – and its reversal – in relation to stress.
In the study, hair color of single strands of hair from seven healthy females and seven healthy males, whose mean age was 35 years (range, 9-65 years), were analyzed. In addition to hair pigment analysis, study subjects documented the stress they were experiencing each week in diaries. Using either high resolution image scanners, electron microscopy, and/or hair shaft proteomics, the investigators were able to evaluate loss of pigment within fragments small enough to have grown over one hour.
When changes in hair color were noted, variations in up to 300 proteins were documented, including an up-regulation of the fatty acid synthesis and metabolism machinery in graying. Recent studies also corroborate that fatty acid synthesis by fatty acid synthase and “transport by CPT1A ... are sufficient drivers of cell senescence, and that fatty acid metabolism regulates melanocyte aging biology” the authors wrote.
Molecularly, the investigators found that gray hairs up-regulate proteins associated with energy metabolism, mitochondria, and antioxidant defenses. The graying correlated with stress was also reversible, “at least temporarily,” based on their retrospective analysis and analysis over the 2.5-year recruitment period, the investigators wrote. Specifically, they found that graying hair “may be acutely triggered by stressful life experiences, the removal of which can trigger reversal.” From the data, they also developed a mathematical model to predict what might happen to human hair over time.
Through this study, proof-of-concept evidence is provided indicating that biobehavioral factors are linked to human hair graying dynamics. Future analysis with larger sample sizes and incorporating neuroendocrine markers may further support these correlations. This is an interesting study that elucidates the mechanisms responsible for how stress and other life exposures manifest in human biology, and, if we as human beings effectively manage that stress, how it may both reverse the negative impact and outcomes affecting our body and health.
The study was supported by the Wharton Fund and grants from the National Institutes of Health.
Dr. Wesley and Dr. Lily Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They have no relevant disclosures.
as hair pigment goes through its natural progression of senescence.
However, the recent publication that is a collaboration between the department of psychiatry at Columbia University, New York; and the departments of dermatology at the University College Dublin, University of Miami, and the University of Manchester (England); and the Monasterium Laboratory in Münster, Germany, demonstrates a quantitative mapping of human hair graying – and its reversal – in relation to stress.
In the study, hair color of single strands of hair from seven healthy females and seven healthy males, whose mean age was 35 years (range, 9-65 years), were analyzed. In addition to hair pigment analysis, study subjects documented the stress they were experiencing each week in diaries. Using either high resolution image scanners, electron microscopy, and/or hair shaft proteomics, the investigators were able to evaluate loss of pigment within fragments small enough to have grown over one hour.
When changes in hair color were noted, variations in up to 300 proteins were documented, including an up-regulation of the fatty acid synthesis and metabolism machinery in graying. Recent studies also corroborate that fatty acid synthesis by fatty acid synthase and “transport by CPT1A ... are sufficient drivers of cell senescence, and that fatty acid metabolism regulates melanocyte aging biology” the authors wrote.
Molecularly, the investigators found that gray hairs up-regulate proteins associated with energy metabolism, mitochondria, and antioxidant defenses. The graying correlated with stress was also reversible, “at least temporarily,” based on their retrospective analysis and analysis over the 2.5-year recruitment period, the investigators wrote. Specifically, they found that graying hair “may be acutely triggered by stressful life experiences, the removal of which can trigger reversal.” From the data, they also developed a mathematical model to predict what might happen to human hair over time.
Through this study, proof-of-concept evidence is provided indicating that biobehavioral factors are linked to human hair graying dynamics. Future analysis with larger sample sizes and incorporating neuroendocrine markers may further support these correlations. This is an interesting study that elucidates the mechanisms responsible for how stress and other life exposures manifest in human biology, and, if we as human beings effectively manage that stress, how it may both reverse the negative impact and outcomes affecting our body and health.
The study was supported by the Wharton Fund and grants from the National Institutes of Health.
Dr. Wesley and Dr. Lily Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They have no relevant disclosures.
as hair pigment goes through its natural progression of senescence.
However, the recent publication that is a collaboration between the department of psychiatry at Columbia University, New York; and the departments of dermatology at the University College Dublin, University of Miami, and the University of Manchester (England); and the Monasterium Laboratory in Münster, Germany, demonstrates a quantitative mapping of human hair graying – and its reversal – in relation to stress.
In the study, hair color of single strands of hair from seven healthy females and seven healthy males, whose mean age was 35 years (range, 9-65 years), were analyzed. In addition to hair pigment analysis, study subjects documented the stress they were experiencing each week in diaries. Using either high resolution image scanners, electron microscopy, and/or hair shaft proteomics, the investigators were able to evaluate loss of pigment within fragments small enough to have grown over one hour.
When changes in hair color were noted, variations in up to 300 proteins were documented, including an up-regulation of the fatty acid synthesis and metabolism machinery in graying. Recent studies also corroborate that fatty acid synthesis by fatty acid synthase and “transport by CPT1A ... are sufficient drivers of cell senescence, and that fatty acid metabolism regulates melanocyte aging biology” the authors wrote.
Molecularly, the investigators found that gray hairs up-regulate proteins associated with energy metabolism, mitochondria, and antioxidant defenses. The graying correlated with stress was also reversible, “at least temporarily,” based on their retrospective analysis and analysis over the 2.5-year recruitment period, the investigators wrote. Specifically, they found that graying hair “may be acutely triggered by stressful life experiences, the removal of which can trigger reversal.” From the data, they also developed a mathematical model to predict what might happen to human hair over time.
Through this study, proof-of-concept evidence is provided indicating that biobehavioral factors are linked to human hair graying dynamics. Future analysis with larger sample sizes and incorporating neuroendocrine markers may further support these correlations. This is an interesting study that elucidates the mechanisms responsible for how stress and other life exposures manifest in human biology, and, if we as human beings effectively manage that stress, how it may both reverse the negative impact and outcomes affecting our body and health.
The study was supported by the Wharton Fund and grants from the National Institutes of Health.
Dr. Wesley and Dr. Lily Talakoub are cocontributors to this column. Dr. Wesley practices dermatology in Beverly Hills, Calif. Dr. Talakoub is in private practice in McLean, Va. This month’s column is by Dr. Wesley. Write to them at [email protected]. They have no relevant disclosures.
Isolated Scrotal Granular Parakeratosis: An Atypical Clinical Presentation
To the Editor:
Granular parakeratosis is a rare condition with an unclear etiology that results from a myriad of factors, including exposure to irritants, friction, moisture, and heat. The diagnosis is made based on a distinct histologic reaction pattern that may be protective against the triggers. We present a case of isolated scrotal granular parakeratosis in a patient with compensatory hyperhidrosis after endoscopic thoracic sympathectomy.
A 52-year-old man presented with a 5-year history of a recurrent rash affecting the scrotum. He experienced monthly flares that were exacerbated by inguinal hyperhidrosis. His symptoms included a burning sensation and pruritus followed by superficial desquamation, with gradual yet temporary improvement. His medical history was remarkable for primary axillary and palmoplantar hyperhidrosis, with compensatory inguinal hyperhidrosis after endoscopic thoracic sympathectomy 8 years prior to presentation.
Physical examination revealed a well-demarcated, scaly, erythematous plaque affecting the scrotal skin with sparing of the median raphe, penis, and inguinal folds (Figure 1). There were no other lesions noted in the axillary region or other skin folds.

Prior treatments prescribed by other providers included topical pimecrolimus, antifungal creams, topical corticosteroids, zinc oxide ointment, and daily application of an over-the-counter medicated powder with no resolution.
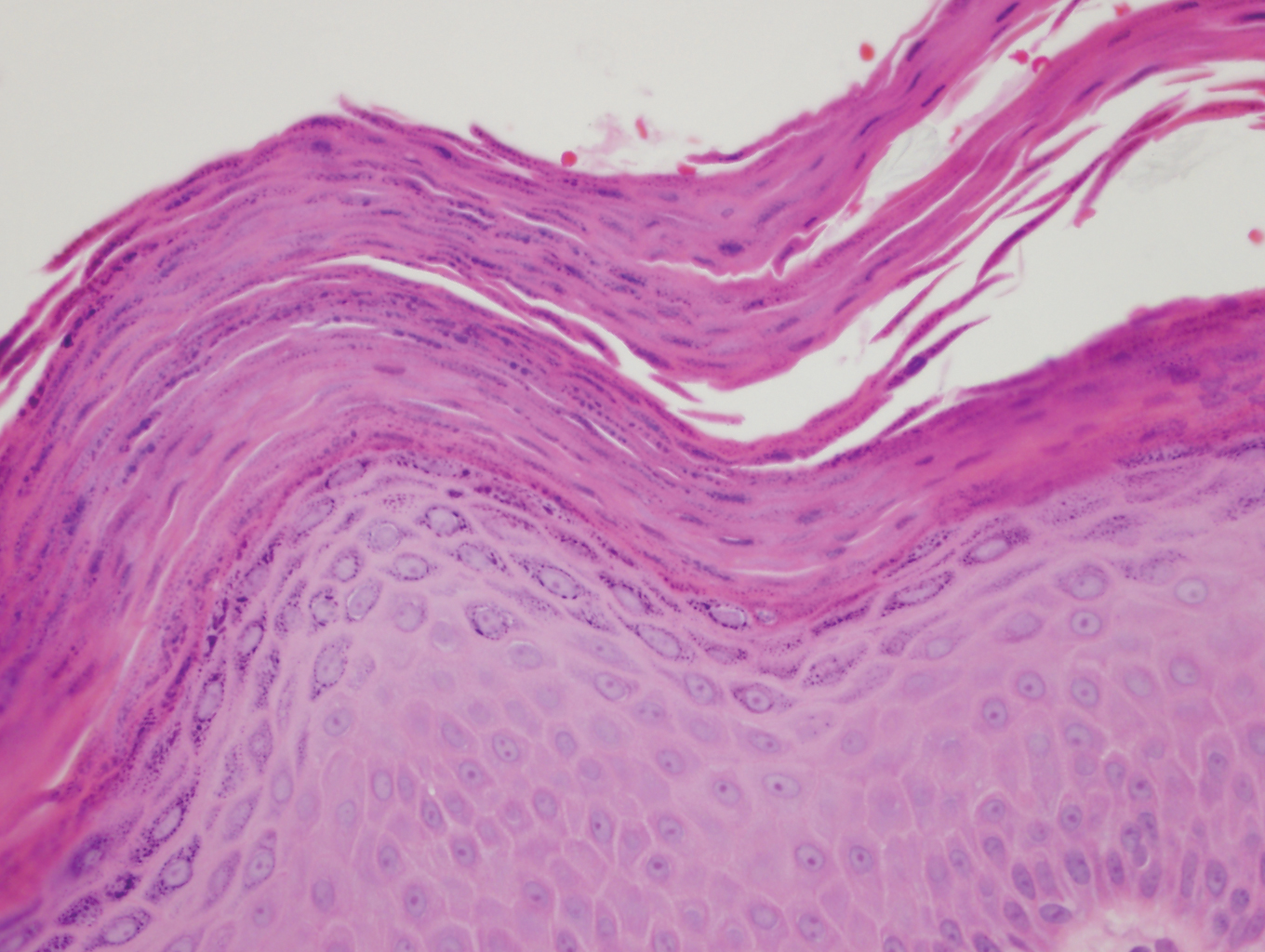
A punch biopsy performed at the current presentation showed psoriasiform hyperplasia of the epidermis with only a focally diminished granular layer. There was overlying thick parakeratosis and retention of keratohyalin granules (Figure 2). Grocott-Gomori methenamine- silver staining was negative for fungal elements in the sections examined. Clinical history, morphology of the eruption, and histologic features were consistent with granular parakeratosis.
Since the first reported incident of granular parakeratosis of the axilla in 1991,1 granular parakeratosis has been reported in other intertriginous areas, including the inframammary folds, inguinal folds, genitalia, perianal skin, and beneath the abdominal pannus.2 One case study in 1998 reported a patient with isolated involvement of the inguinal region3; however, this presentation is rare.4 This condition has been reported in both sexes and all age groups, including children.5
Granular parakeratosis classically presents as erythematous to brown hyperkeratotic papules that coalesce into plaques.6 It is thought to be a reactive inflammatory condition secondary to aggravating factors such as exposure to heat,7 moisture, and friction; skin occlusion; repeated washing; irritation from external agents; antiperspirants; and use of depilatory creams.8 Histopathology is characteristic and consists of retained nuclei and keratohyalin granules within the stratum corneum, beneath which there is a retained stratum granulosum. Epidermal changes may be varied and include atrophy or hyperplasia.
Murine models have postulated that granular parakeratosis may result from a deficiency in caspase 14, a protease vital to the formation of a well-functioning skin barrier.9 A cornified envelope often is noted in granular parakeratotic cells with no defects in desmosomes and cell membranes, suggesting that the pathogenesis lies within processing of profilaggrin to filaggrin, resulting in a failure to degrade keratohyalin granules and aggregation of keratin filaments.10 Granular parakeratosis is not known to be associated with other medical conditions, but it has been observed in patients receiving chemotherapy for breast11 and ovarian12 carcinomas. In infants with atopic dermatitis, granular parakeratosis was reported in 5 out of 7 cases.6 In our patient with secondary inguinal hyperhidrosis after thoracic sympathectomy, granular parakeratosis may be reactive to excess sweating and friction in the scrotal area.
Granular parakeratosis follows a waxing and waning pattern that may spontaneously resolve without any treatment; it also can follow a protracted course, as in a case with associated facial papules that persisted for 20 years.13 Topical corticosteroids alone or in combination with topical antifungal agents have been used for the treatment of granular parakeratosis with the goal of accelerating resolution.2,14 However, the efficacy of these therapeutic interventions is limited, and no controlled trials are underway. Topical vitamin D analogues15,16 and topical retinoids17 also have been reported with successful outcomes. Spontaneous resolution also has been observed in 2 different cases after previously being unresponsive to topical treatment.18,19 Treatment with Clostridium botulinum toxin A resulted in complete remission of the disease observed at 6-month follow-up. The pharmacologic action of the neurotoxin disrupts the stimulation of eccrine sweat glands, resulting in decreased sweating, a known exacerbating factor of granular parakeratosis.20
In summary, our case represents a unique clinical presentation of granular parakeratosis with classic histopathologic features. A high index of suspicion and a biopsy are vital to arriving at the correct diagnosis.
- Northcutt AD, Nelson DM, Tschen JA. Axillary granular parakeratosis. J Am Acad Dermatol. 1991;24:541-544.
- Burford C. Granular parakeratosis of multiple intertriginous areas. Australas J Dermatol. 2008;49:35-38.
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496.
- Leclerc-Mercier S, Prost-Squarcioni C, Hamel-Teillac D, et al. A case of congenital granular parakeratosis. Am J Dermatopathol. 2011;33:531-533.
- Scheinfeld NS, Mones J. Granular parakeratosis: pathologic and clinical correlation of 18 cases of granular parakeratosis. J Am Acad Dermatol. 2005;52:863-867.
- Akkaya AD, Oram Y, Aydin O. Infantile granular parakeratosis: cytologic examination of superficial scrapings as an aid to diagnosis. Pediatr Dermatol. 2015;32:392-396.
- Rodríguez G. Axillary granular parakeratosis [in Spanish]. Biomedica. 2002;22:519-523.
- Samrao A, Reis M, Niedt G, et al. Granular parakeratosis: response to calcipotriene and brief review of current therapeutic options. Skinmed. 2010;8:357-359.
- Hoste E, Denecker G, Gilbert B, et al. Caspase-14-deficient mice are more prone to the development of parakeratosis. J Invest Dermatol. 2013;133:742-750.
- Metze D, Rutten A. Granular parakeratosis—a unique acquired disorder of keratinization. J Cutan Pathol. 1999;26:339-352.
- Wallace CA, Pichardo RO, Yosipovitch G, et al. Granular parakeratosis: a case report and literature review. J Cutan Pathol. 2003;30:332-335.
- Jaconelli L, Doebelin B, Kanitakis J, et al. Granular parakeratosis in a patient treated with liposomal doxorubicin for ovarian carcinoma. J Am Acad Dermatol. 2008;58(5 suppl 1):S84-S87.
- Reddy IS, Swarnalata G, Mody T. Intertriginous granular parakeratosis persisting for 20 years. Indian J Dermatol Venereol Leprol. 2008;74:405-407.
- Dearden C, al-Nakib W, Andries K, et al. Drug resistant rhinoviruses from the nose of experimentally treated volunteers. Arch Virol. 1989;109:71-81.
- Patel U, Patel T, Skinner RB Jr. Resolution of granular parakeratosis with topical calcitriol. Arch Dermatol. 2011;147:997-998.
- Contreras ME, Gottfried LC, Bang RH, et al. Axillary intertriginous granular parakeratosis responsive to topical calcipotriene and ammonium lactate. Int J Dermatol. 2003;42:382-383.
- Brown SK, Heilman ER. Granular parakeratosis: resolution with topical tretinoin. J Am Acad Dermatol. 2002;47(5 suppl):S279-S280.
- Compton AK, Jackson JM. Isotretinoin as a treatment for axillary granular parakeratosis. Cutis. 2007;80:55-56.
- Webster CG, Resnik KS, Webster GF. Axillary granular parakeratosis: response to isotretinoin. J Am Acad Dermatol. 1997; 37:789-790.
- Ravitskiy L, Heymann WR. Botulinum toxin-induced resolution of axillary granular parakeratosis. Skinmed. 2005;4:118-120.
To the Editor:
Granular parakeratosis is a rare condition with an unclear etiology that results from a myriad of factors, including exposure to irritants, friction, moisture, and heat. The diagnosis is made based on a distinct histologic reaction pattern that may be protective against the triggers. We present a case of isolated scrotal granular parakeratosis in a patient with compensatory hyperhidrosis after endoscopic thoracic sympathectomy.
A 52-year-old man presented with a 5-year history of a recurrent rash affecting the scrotum. He experienced monthly flares that were exacerbated by inguinal hyperhidrosis. His symptoms included a burning sensation and pruritus followed by superficial desquamation, with gradual yet temporary improvement. His medical history was remarkable for primary axillary and palmoplantar hyperhidrosis, with compensatory inguinal hyperhidrosis after endoscopic thoracic sympathectomy 8 years prior to presentation.
Physical examination revealed a well-demarcated, scaly, erythematous plaque affecting the scrotal skin with sparing of the median raphe, penis, and inguinal folds (Figure 1). There were no other lesions noted in the axillary region or other skin folds.

Prior treatments prescribed by other providers included topical pimecrolimus, antifungal creams, topical corticosteroids, zinc oxide ointment, and daily application of an over-the-counter medicated powder with no resolution.
A punch biopsy performed at the current presentation showed psoriasiform hyperplasia of the epidermis with only a focally diminished granular layer. There was overlying thick parakeratosis and retention of keratohyalin granules (Figure 2). Grocott-Gomori methenamine- silver staining was negative for fungal elements in the sections examined. Clinical history, morphology of the eruption, and histologic features were consistent with granular parakeratosis.
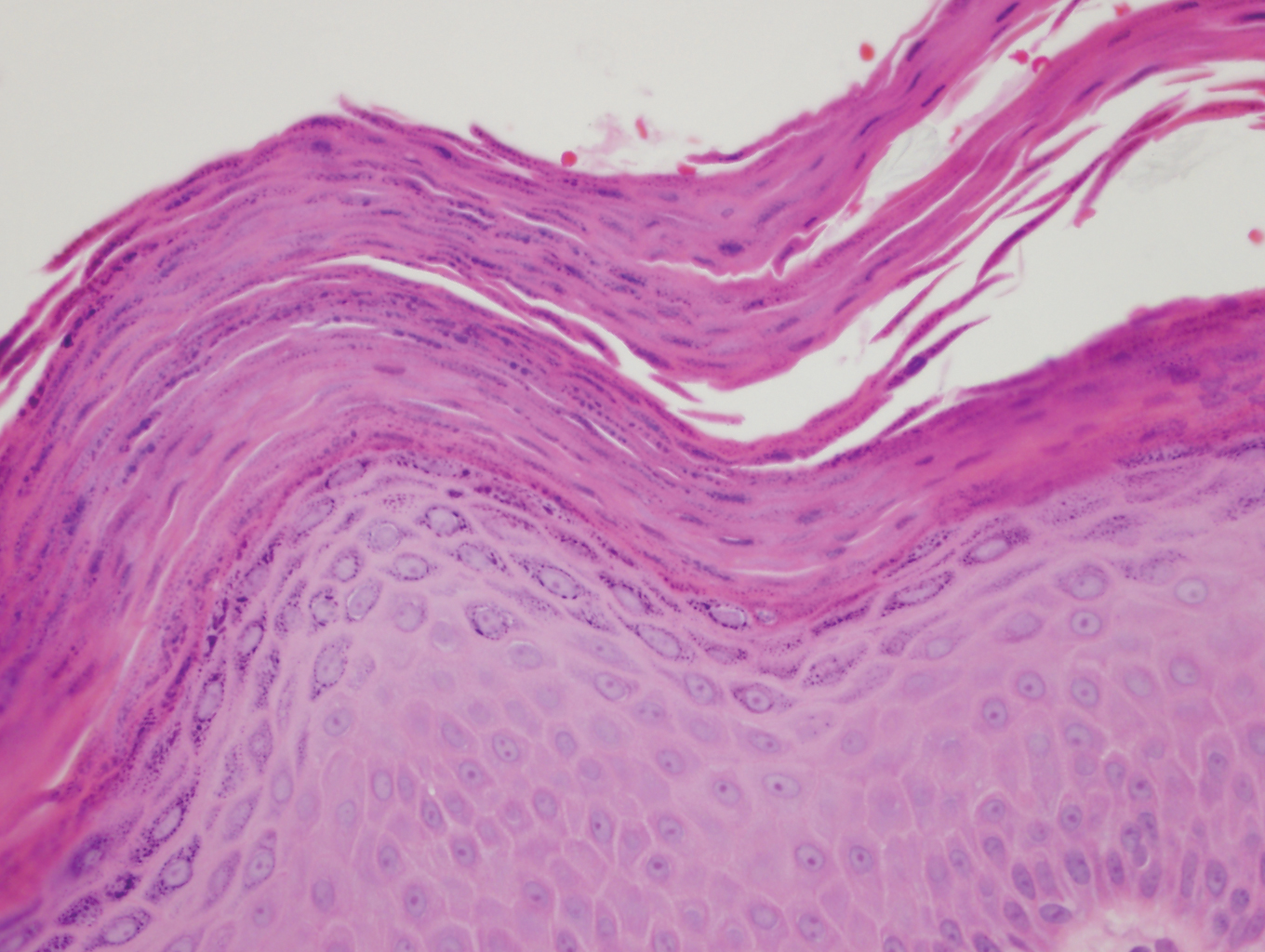
Since the first reported incident of granular parakeratosis of the axilla in 1991,1 granular parakeratosis has been reported in other intertriginous areas, including the inframammary folds, inguinal folds, genitalia, perianal skin, and beneath the abdominal pannus.2 One case study in 1998 reported a patient with isolated involvement of the inguinal region3; however, this presentation is rare.4 This condition has been reported in both sexes and all age groups, including children.5
Granular parakeratosis classically presents as erythematous to brown hyperkeratotic papules that coalesce into plaques.6 It is thought to be a reactive inflammatory condition secondary to aggravating factors such as exposure to heat,7 moisture, and friction; skin occlusion; repeated washing; irritation from external agents; antiperspirants; and use of depilatory creams.8 Histopathology is characteristic and consists of retained nuclei and keratohyalin granules within the stratum corneum, beneath which there is a retained stratum granulosum. Epidermal changes may be varied and include atrophy or hyperplasia.
Murine models have postulated that granular parakeratosis may result from a deficiency in caspase 14, a protease vital to the formation of a well-functioning skin barrier.9 A cornified envelope often is noted in granular parakeratotic cells with no defects in desmosomes and cell membranes, suggesting that the pathogenesis lies within processing of profilaggrin to filaggrin, resulting in a failure to degrade keratohyalin granules and aggregation of keratin filaments.10 Granular parakeratosis is not known to be associated with other medical conditions, but it has been observed in patients receiving chemotherapy for breast11 and ovarian12 carcinomas. In infants with atopic dermatitis, granular parakeratosis was reported in 5 out of 7 cases.6 In our patient with secondary inguinal hyperhidrosis after thoracic sympathectomy, granular parakeratosis may be reactive to excess sweating and friction in the scrotal area.
Granular parakeratosis follows a waxing and waning pattern that may spontaneously resolve without any treatment; it also can follow a protracted course, as in a case with associated facial papules that persisted for 20 years.13 Topical corticosteroids alone or in combination with topical antifungal agents have been used for the treatment of granular parakeratosis with the goal of accelerating resolution.2,14 However, the efficacy of these therapeutic interventions is limited, and no controlled trials are underway. Topical vitamin D analogues15,16 and topical retinoids17 also have been reported with successful outcomes. Spontaneous resolution also has been observed in 2 different cases after previously being unresponsive to topical treatment.18,19 Treatment with Clostridium botulinum toxin A resulted in complete remission of the disease observed at 6-month follow-up. The pharmacologic action of the neurotoxin disrupts the stimulation of eccrine sweat glands, resulting in decreased sweating, a known exacerbating factor of granular parakeratosis.20
In summary, our case represents a unique clinical presentation of granular parakeratosis with classic histopathologic features. A high index of suspicion and a biopsy are vital to arriving at the correct diagnosis.
To the Editor:
Granular parakeratosis is a rare condition with an unclear etiology that results from a myriad of factors, including exposure to irritants, friction, moisture, and heat. The diagnosis is made based on a distinct histologic reaction pattern that may be protective against the triggers. We present a case of isolated scrotal granular parakeratosis in a patient with compensatory hyperhidrosis after endoscopic thoracic sympathectomy.
A 52-year-old man presented with a 5-year history of a recurrent rash affecting the scrotum. He experienced monthly flares that were exacerbated by inguinal hyperhidrosis. His symptoms included a burning sensation and pruritus followed by superficial desquamation, with gradual yet temporary improvement. His medical history was remarkable for primary axillary and palmoplantar hyperhidrosis, with compensatory inguinal hyperhidrosis after endoscopic thoracic sympathectomy 8 years prior to presentation.
Physical examination revealed a well-demarcated, scaly, erythematous plaque affecting the scrotal skin with sparing of the median raphe, penis, and inguinal folds (Figure 1). There were no other lesions noted in the axillary region or other skin folds.

Prior treatments prescribed by other providers included topical pimecrolimus, antifungal creams, topical corticosteroids, zinc oxide ointment, and daily application of an over-the-counter medicated powder with no resolution.
A punch biopsy performed at the current presentation showed psoriasiform hyperplasia of the epidermis with only a focally diminished granular layer. There was overlying thick parakeratosis and retention of keratohyalin granules (Figure 2). Grocott-Gomori methenamine- silver staining was negative for fungal elements in the sections examined. Clinical history, morphology of the eruption, and histologic features were consistent with granular parakeratosis.
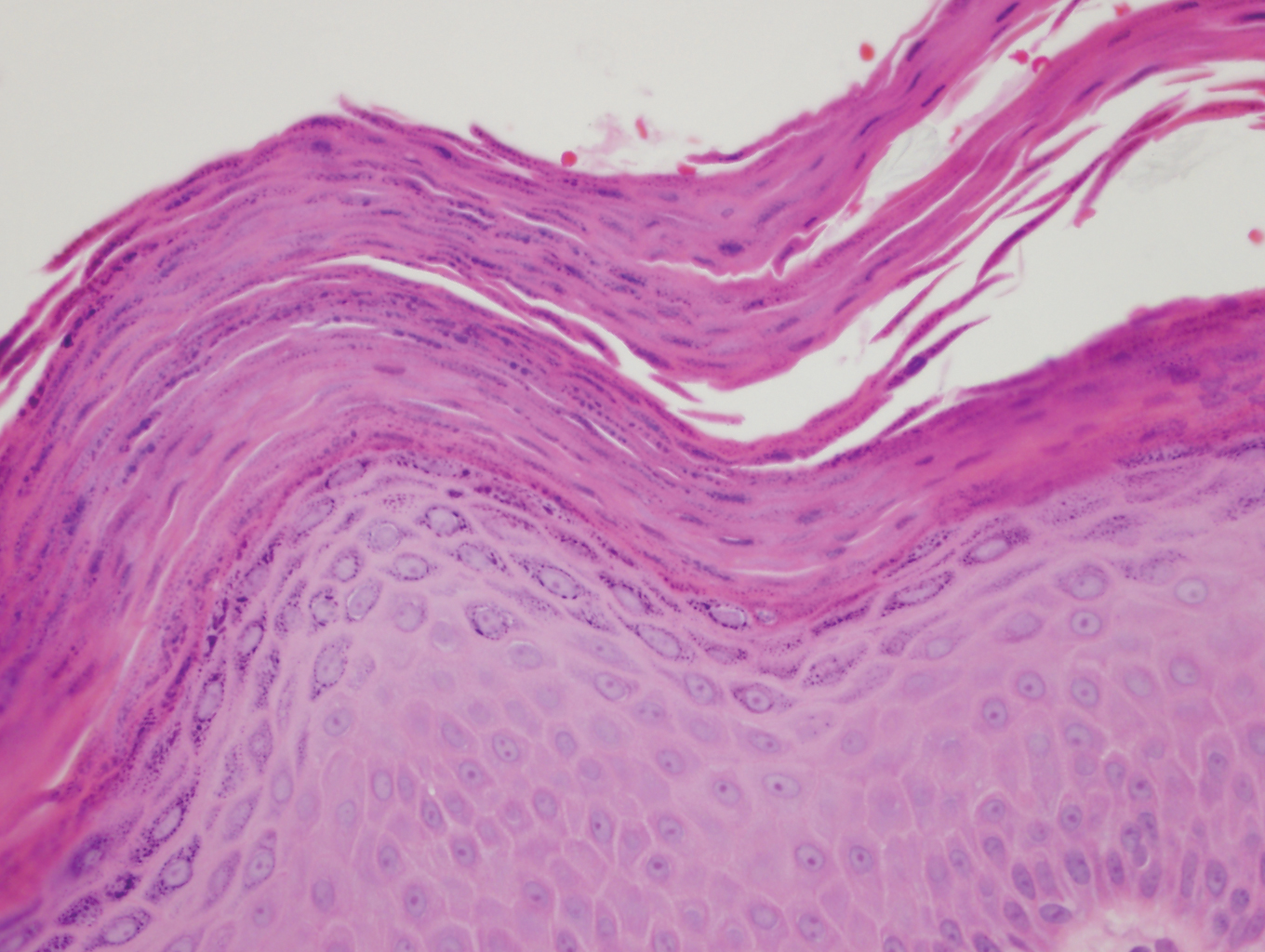
Since the first reported incident of granular parakeratosis of the axilla in 1991,1 granular parakeratosis has been reported in other intertriginous areas, including the inframammary folds, inguinal folds, genitalia, perianal skin, and beneath the abdominal pannus.2 One case study in 1998 reported a patient with isolated involvement of the inguinal region3; however, this presentation is rare.4 This condition has been reported in both sexes and all age groups, including children.5
Granular parakeratosis classically presents as erythematous to brown hyperkeratotic papules that coalesce into plaques.6 It is thought to be a reactive inflammatory condition secondary to aggravating factors such as exposure to heat,7 moisture, and friction; skin occlusion; repeated washing; irritation from external agents; antiperspirants; and use of depilatory creams.8 Histopathology is characteristic and consists of retained nuclei and keratohyalin granules within the stratum corneum, beneath which there is a retained stratum granulosum. Epidermal changes may be varied and include atrophy or hyperplasia.
Murine models have postulated that granular parakeratosis may result from a deficiency in caspase 14, a protease vital to the formation of a well-functioning skin barrier.9 A cornified envelope often is noted in granular parakeratotic cells with no defects in desmosomes and cell membranes, suggesting that the pathogenesis lies within processing of profilaggrin to filaggrin, resulting in a failure to degrade keratohyalin granules and aggregation of keratin filaments.10 Granular parakeratosis is not known to be associated with other medical conditions, but it has been observed in patients receiving chemotherapy for breast11 and ovarian12 carcinomas. In infants with atopic dermatitis, granular parakeratosis was reported in 5 out of 7 cases.6 In our patient with secondary inguinal hyperhidrosis after thoracic sympathectomy, granular parakeratosis may be reactive to excess sweating and friction in the scrotal area.
Granular parakeratosis follows a waxing and waning pattern that may spontaneously resolve without any treatment; it also can follow a protracted course, as in a case with associated facial papules that persisted for 20 years.13 Topical corticosteroids alone or in combination with topical antifungal agents have been used for the treatment of granular parakeratosis with the goal of accelerating resolution.2,14 However, the efficacy of these therapeutic interventions is limited, and no controlled trials are underway. Topical vitamin D analogues15,16 and topical retinoids17 also have been reported with successful outcomes. Spontaneous resolution also has been observed in 2 different cases after previously being unresponsive to topical treatment.18,19 Treatment with Clostridium botulinum toxin A resulted in complete remission of the disease observed at 6-month follow-up. The pharmacologic action of the neurotoxin disrupts the stimulation of eccrine sweat glands, resulting in decreased sweating, a known exacerbating factor of granular parakeratosis.20
In summary, our case represents a unique clinical presentation of granular parakeratosis with classic histopathologic features. A high index of suspicion and a biopsy are vital to arriving at the correct diagnosis.
- Northcutt AD, Nelson DM, Tschen JA. Axillary granular parakeratosis. J Am Acad Dermatol. 1991;24:541-544.
- Burford C. Granular parakeratosis of multiple intertriginous areas. Australas J Dermatol. 2008;49:35-38.
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496.
- Leclerc-Mercier S, Prost-Squarcioni C, Hamel-Teillac D, et al. A case of congenital granular parakeratosis. Am J Dermatopathol. 2011;33:531-533.
- Scheinfeld NS, Mones J. Granular parakeratosis: pathologic and clinical correlation of 18 cases of granular parakeratosis. J Am Acad Dermatol. 2005;52:863-867.
- Akkaya AD, Oram Y, Aydin O. Infantile granular parakeratosis: cytologic examination of superficial scrapings as an aid to diagnosis. Pediatr Dermatol. 2015;32:392-396.
- Rodríguez G. Axillary granular parakeratosis [in Spanish]. Biomedica. 2002;22:519-523.
- Samrao A, Reis M, Niedt G, et al. Granular parakeratosis: response to calcipotriene and brief review of current therapeutic options. Skinmed. 2010;8:357-359.
- Hoste E, Denecker G, Gilbert B, et al. Caspase-14-deficient mice are more prone to the development of parakeratosis. J Invest Dermatol. 2013;133:742-750.
- Metze D, Rutten A. Granular parakeratosis—a unique acquired disorder of keratinization. J Cutan Pathol. 1999;26:339-352.
- Wallace CA, Pichardo RO, Yosipovitch G, et al. Granular parakeratosis: a case report and literature review. J Cutan Pathol. 2003;30:332-335.
- Jaconelli L, Doebelin B, Kanitakis J, et al. Granular parakeratosis in a patient treated with liposomal doxorubicin for ovarian carcinoma. J Am Acad Dermatol. 2008;58(5 suppl 1):S84-S87.
- Reddy IS, Swarnalata G, Mody T. Intertriginous granular parakeratosis persisting for 20 years. Indian J Dermatol Venereol Leprol. 2008;74:405-407.
- Dearden C, al-Nakib W, Andries K, et al. Drug resistant rhinoviruses from the nose of experimentally treated volunteers. Arch Virol. 1989;109:71-81.
- Patel U, Patel T, Skinner RB Jr. Resolution of granular parakeratosis with topical calcitriol. Arch Dermatol. 2011;147:997-998.
- Contreras ME, Gottfried LC, Bang RH, et al. Axillary intertriginous granular parakeratosis responsive to topical calcipotriene and ammonium lactate. Int J Dermatol. 2003;42:382-383.
- Brown SK, Heilman ER. Granular parakeratosis: resolution with topical tretinoin. J Am Acad Dermatol. 2002;47(5 suppl):S279-S280.
- Compton AK, Jackson JM. Isotretinoin as a treatment for axillary granular parakeratosis. Cutis. 2007;80:55-56.
- Webster CG, Resnik KS, Webster GF. Axillary granular parakeratosis: response to isotretinoin. J Am Acad Dermatol. 1997; 37:789-790.
- Ravitskiy L, Heymann WR. Botulinum toxin-induced resolution of axillary granular parakeratosis. Skinmed. 2005;4:118-120.
- Northcutt AD, Nelson DM, Tschen JA. Axillary granular parakeratosis. J Am Acad Dermatol. 1991;24:541-544.
- Burford C. Granular parakeratosis of multiple intertriginous areas. Australas J Dermatol. 2008;49:35-38.
- Mehregan DA, Thomas JE, Mehregan DR. Intertriginous granular parakeratosis. J Am Acad Dermatol. 1998;39:495-496.
- Leclerc-Mercier S, Prost-Squarcioni C, Hamel-Teillac D, et al. A case of congenital granular parakeratosis. Am J Dermatopathol. 2011;33:531-533.
- Scheinfeld NS, Mones J. Granular parakeratosis: pathologic and clinical correlation of 18 cases of granular parakeratosis. J Am Acad Dermatol. 2005;52:863-867.
- Akkaya AD, Oram Y, Aydin O. Infantile granular parakeratosis: cytologic examination of superficial scrapings as an aid to diagnosis. Pediatr Dermatol. 2015;32:392-396.
- Rodríguez G. Axillary granular parakeratosis [in Spanish]. Biomedica. 2002;22:519-523.
- Samrao A, Reis M, Niedt G, et al. Granular parakeratosis: response to calcipotriene and brief review of current therapeutic options. Skinmed. 2010;8:357-359.
- Hoste E, Denecker G, Gilbert B, et al. Caspase-14-deficient mice are more prone to the development of parakeratosis. J Invest Dermatol. 2013;133:742-750.
- Metze D, Rutten A. Granular parakeratosis—a unique acquired disorder of keratinization. J Cutan Pathol. 1999;26:339-352.
- Wallace CA, Pichardo RO, Yosipovitch G, et al. Granular parakeratosis: a case report and literature review. J Cutan Pathol. 2003;30:332-335.
- Jaconelli L, Doebelin B, Kanitakis J, et al. Granular parakeratosis in a patient treated with liposomal doxorubicin for ovarian carcinoma. J Am Acad Dermatol. 2008;58(5 suppl 1):S84-S87.
- Reddy IS, Swarnalata G, Mody T. Intertriginous granular parakeratosis persisting for 20 years. Indian J Dermatol Venereol Leprol. 2008;74:405-407.
- Dearden C, al-Nakib W, Andries K, et al. Drug resistant rhinoviruses from the nose of experimentally treated volunteers. Arch Virol. 1989;109:71-81.
- Patel U, Patel T, Skinner RB Jr. Resolution of granular parakeratosis with topical calcitriol. Arch Dermatol. 2011;147:997-998.
- Contreras ME, Gottfried LC, Bang RH, et al. Axillary intertriginous granular parakeratosis responsive to topical calcipotriene and ammonium lactate. Int J Dermatol. 2003;42:382-383.
- Brown SK, Heilman ER. Granular parakeratosis: resolution with topical tretinoin. J Am Acad Dermatol. 2002;47(5 suppl):S279-S280.
- Compton AK, Jackson JM. Isotretinoin as a treatment for axillary granular parakeratosis. Cutis. 2007;80:55-56.
- Webster CG, Resnik KS, Webster GF. Axillary granular parakeratosis: response to isotretinoin. J Am Acad Dermatol. 1997; 37:789-790.
- Ravitskiy L, Heymann WR. Botulinum toxin-induced resolution of axillary granular parakeratosis. Skinmed. 2005;4:118-120.
Practice Points
- Granular parakeratosis can occur in response to triggers such as irritants, friction, hyperhidrosis, and heat.
- Granular parakeratosis can have an atypical presentation; therefore, a high index of suspicion and punch biopsy are vital to arrive at the correct diagnosis.
- Classic histopathology demonstrates retained nuclei and keratohyalin granules within the stratum corneum beneath which there is a retained stratum granulosum.
Please interrupt me, but don't heat your fish
Bother me, I’m working
Although some of us have been comfortably functioning in a virtual work environment, others are now trickling back into the office. And you know what that means? People come to your desk to show you pictures of their cat or tell you about their kid’s birthday party. You may sneer at the interruption, but a study shows you actually like it.
A team of researchers at the University of Cincinnati surveyed 111 full-time employees twice a day for 3 weeks about their work experience. They asked about mental exhaustion, workplace interruptions, sense of belonging, and overall job satisfaction. They found that employees had a higher sense of belonging and job satisfaction when interrupted with a social versus work interruption.
“Interruptions can actually benefit individuals from an interpersonal perspective – people feel like they belong when others come and talk to them or ask them questions, even while being distracted from their tasks,” said Heather C. Vough, senior investigator and a former university faculty member.
Chitchatting at work is often seen as a distraction, but this study suggests that it’s not like heating up fish in the breakroom microwave.
So the next time someone hits you with the “Hey, do you have a sec?,” do yourself a favor and enjoy the interruption.
A smorgasbord of science
It’s probably difficult to recruit patients for some medical trials. Try this new drug and potentially get all sorts of interesting and unpleasant side effects. Pass. We suggest the approach a group of researchers from the University of Kansas took for a recent study into weight gain: Invite a bunch of 20-something adults to an all-you-can-eat buffet. They’ll be beating down your door in no time.
Their study, published in Appetite, focused on hyperpalatable food – the sort of food you can keep eating – and compared it with high-energy-dense food and ultra processed food. The test patients had their body composition measured, were let loose on the buffet, and were measured again a year later.
The patients who favored salty/carbohydrate-filled hyperpalatable food (such as pretzels or popcorn) were much more likely to gain weight, compared with those who focused on salty/fat-filled food of any variety. As a matter of fact, those who stuck to fatty food during the buffet had no change in weight over the 1-year study period. The researchers noted that those who ate the carb-filled food tended more toward hedonic eating, or the act of eating simply for pleasure.
The study is no doubt helpful in the long battle against obesity and overeating, but it’s also a very helpful guide to getting the most bang for your buck at the buffet. Stay away from the cheap salty snack food. Go for the steak and seafood. Get your money’s worth. In the long run you won’t even gain any weight. No promises about tomorrow though.
There’s a cheat code for that
For a large percentage of kids and young adults, and maybe even older adults (we don’t judge), a storm warning means a cozy night in playing video games. Staying inside is probably the safest bet when there’s a storm, and the weatherman never says to avoid playing video games when there’s lightning.
Maybe he should, though, since a man from Tennessee reportedly got struck by lightning through his game controller. Emergency crews determined that lightning either hit the man’s house or struck near it and went through the controller. The type of console was not revealed, even though some people may want to know the specifics before playing during the next storm.
Luckily, the man was not seriously hurt and did not need to go to the hospital. This is apparently not unheard of, as a professional gamer was shocked through a wired controller last year, causing burns on her hands and a broken controller.
This might be our cue to do less electrical types of activities during thunderstorms, like knitting or reading by candlelight.
Freeze, squeeze, and enjoy … cramping
As you were ingesting last week’s installment of the never-ending buffet that is LOTME, you probably wondered: What’s going on? Where’s the latest bodily insult being perpetuated by the gang over at TikTok?
Have no fear, good readers. We would never make you go 2 straight weeks without serving up some hyperpalatable TikTok tidbits.
Our bodily insult du jour is frozen honey, and it’s exploding all over TikTok … and a few other places. “The hashtag ‘#FrozenHoney’ has been viewed nearly 600 million times, and the hashtag ‘#FrozenHoneyChallenge’ has been viewed more than 80 million times,” NBC News recently reported.
After a few hours in the freezer, honey can be squeezed out of a plastic bottle as a semisolid, toothpastelike goo – it’s stiff enough to rise out of a container that’s pointed straight up – and bitten off in large chunks. And therein lies the problem.
Some people are overdoing it. “Honey is great, but having it in small amounts to sweeten is really a healthy relationship with food, and using it to get a lot of followers and a lot of attention and having it in excess amounts is crazy,” Kristin Kirkpatrick, a registered dietitian at the Cleveland Clinic, told NBC.
Besides the possible weight gain from eating massive amounts of sugar, experts warned that “gobbling up bottles of frozen honey” could lead to stomach cramping, bloating, and diarrhea. Some TikTokers, NBC noted, said that they “were running for the bathroom.”
As we said, it’s a trend that is exploding.
Be sure to tune in next week, when we learn how TikTokers use ground meat as a skin moisturizer.
Bother me, I’m working
Although some of us have been comfortably functioning in a virtual work environment, others are now trickling back into the office. And you know what that means? People come to your desk to show you pictures of their cat or tell you about their kid’s birthday party. You may sneer at the interruption, but a study shows you actually like it.
A team of researchers at the University of Cincinnati surveyed 111 full-time employees twice a day for 3 weeks about their work experience. They asked about mental exhaustion, workplace interruptions, sense of belonging, and overall job satisfaction. They found that employees had a higher sense of belonging and job satisfaction when interrupted with a social versus work interruption.
“Interruptions can actually benefit individuals from an interpersonal perspective – people feel like they belong when others come and talk to them or ask them questions, even while being distracted from their tasks,” said Heather C. Vough, senior investigator and a former university faculty member.
Chitchatting at work is often seen as a distraction, but this study suggests that it’s not like heating up fish in the breakroom microwave.
So the next time someone hits you with the “Hey, do you have a sec?,” do yourself a favor and enjoy the interruption.
A smorgasbord of science
It’s probably difficult to recruit patients for some medical trials. Try this new drug and potentially get all sorts of interesting and unpleasant side effects. Pass. We suggest the approach a group of researchers from the University of Kansas took for a recent study into weight gain: Invite a bunch of 20-something adults to an all-you-can-eat buffet. They’ll be beating down your door in no time.
Their study, published in Appetite, focused on hyperpalatable food – the sort of food you can keep eating – and compared it with high-energy-dense food and ultra processed food. The test patients had their body composition measured, were let loose on the buffet, and were measured again a year later.
The patients who favored salty/carbohydrate-filled hyperpalatable food (such as pretzels or popcorn) were much more likely to gain weight, compared with those who focused on salty/fat-filled food of any variety. As a matter of fact, those who stuck to fatty food during the buffet had no change in weight over the 1-year study period. The researchers noted that those who ate the carb-filled food tended more toward hedonic eating, or the act of eating simply for pleasure.
The study is no doubt helpful in the long battle against obesity and overeating, but it’s also a very helpful guide to getting the most bang for your buck at the buffet. Stay away from the cheap salty snack food. Go for the steak and seafood. Get your money’s worth. In the long run you won’t even gain any weight. No promises about tomorrow though.
There’s a cheat code for that
For a large percentage of kids and young adults, and maybe even older adults (we don’t judge), a storm warning means a cozy night in playing video games. Staying inside is probably the safest bet when there’s a storm, and the weatherman never says to avoid playing video games when there’s lightning.
Maybe he should, though, since a man from Tennessee reportedly got struck by lightning through his game controller. Emergency crews determined that lightning either hit the man’s house or struck near it and went through the controller. The type of console was not revealed, even though some people may want to know the specifics before playing during the next storm.
Luckily, the man was not seriously hurt and did not need to go to the hospital. This is apparently not unheard of, as a professional gamer was shocked through a wired controller last year, causing burns on her hands and a broken controller.
This might be our cue to do less electrical types of activities during thunderstorms, like knitting or reading by candlelight.
Freeze, squeeze, and enjoy … cramping
As you were ingesting last week’s installment of the never-ending buffet that is LOTME, you probably wondered: What’s going on? Where’s the latest bodily insult being perpetuated by the gang over at TikTok?
Have no fear, good readers. We would never make you go 2 straight weeks without serving up some hyperpalatable TikTok tidbits.
Our bodily insult du jour is frozen honey, and it’s exploding all over TikTok … and a few other places. “The hashtag ‘#FrozenHoney’ has been viewed nearly 600 million times, and the hashtag ‘#FrozenHoneyChallenge’ has been viewed more than 80 million times,” NBC News recently reported.
After a few hours in the freezer, honey can be squeezed out of a plastic bottle as a semisolid, toothpastelike goo – it’s stiff enough to rise out of a container that’s pointed straight up – and bitten off in large chunks. And therein lies the problem.
Some people are overdoing it. “Honey is great, but having it in small amounts to sweeten is really a healthy relationship with food, and using it to get a lot of followers and a lot of attention and having it in excess amounts is crazy,” Kristin Kirkpatrick, a registered dietitian at the Cleveland Clinic, told NBC.
Besides the possible weight gain from eating massive amounts of sugar, experts warned that “gobbling up bottles of frozen honey” could lead to stomach cramping, bloating, and diarrhea. Some TikTokers, NBC noted, said that they “were running for the bathroom.”
As we said, it’s a trend that is exploding.
Be sure to tune in next week, when we learn how TikTokers use ground meat as a skin moisturizer.
Bother me, I’m working
Although some of us have been comfortably functioning in a virtual work environment, others are now trickling back into the office. And you know what that means? People come to your desk to show you pictures of their cat or tell you about their kid’s birthday party. You may sneer at the interruption, but a study shows you actually like it.
A team of researchers at the University of Cincinnati surveyed 111 full-time employees twice a day for 3 weeks about their work experience. They asked about mental exhaustion, workplace interruptions, sense of belonging, and overall job satisfaction. They found that employees had a higher sense of belonging and job satisfaction when interrupted with a social versus work interruption.
“Interruptions can actually benefit individuals from an interpersonal perspective – people feel like they belong when others come and talk to them or ask them questions, even while being distracted from their tasks,” said Heather C. Vough, senior investigator and a former university faculty member.
Chitchatting at work is often seen as a distraction, but this study suggests that it’s not like heating up fish in the breakroom microwave.
So the next time someone hits you with the “Hey, do you have a sec?,” do yourself a favor and enjoy the interruption.
A smorgasbord of science
It’s probably difficult to recruit patients for some medical trials. Try this new drug and potentially get all sorts of interesting and unpleasant side effects. Pass. We suggest the approach a group of researchers from the University of Kansas took for a recent study into weight gain: Invite a bunch of 20-something adults to an all-you-can-eat buffet. They’ll be beating down your door in no time.
Their study, published in Appetite, focused on hyperpalatable food – the sort of food you can keep eating – and compared it with high-energy-dense food and ultra processed food. The test patients had their body composition measured, were let loose on the buffet, and were measured again a year later.
The patients who favored salty/carbohydrate-filled hyperpalatable food (such as pretzels or popcorn) were much more likely to gain weight, compared with those who focused on salty/fat-filled food of any variety. As a matter of fact, those who stuck to fatty food during the buffet had no change in weight over the 1-year study period. The researchers noted that those who ate the carb-filled food tended more toward hedonic eating, or the act of eating simply for pleasure.
The study is no doubt helpful in the long battle against obesity and overeating, but it’s also a very helpful guide to getting the most bang for your buck at the buffet. Stay away from the cheap salty snack food. Go for the steak and seafood. Get your money’s worth. In the long run you won’t even gain any weight. No promises about tomorrow though.
There’s a cheat code for that
For a large percentage of kids and young adults, and maybe even older adults (we don’t judge), a storm warning means a cozy night in playing video games. Staying inside is probably the safest bet when there’s a storm, and the weatherman never says to avoid playing video games when there’s lightning.
Maybe he should, though, since a man from Tennessee reportedly got struck by lightning through his game controller. Emergency crews determined that lightning either hit the man’s house or struck near it and went through the controller. The type of console was not revealed, even though some people may want to know the specifics before playing during the next storm.
Luckily, the man was not seriously hurt and did not need to go to the hospital. This is apparently not unheard of, as a professional gamer was shocked through a wired controller last year, causing burns on her hands and a broken controller.
This might be our cue to do less electrical types of activities during thunderstorms, like knitting or reading by candlelight.
Freeze, squeeze, and enjoy … cramping
As you were ingesting last week’s installment of the never-ending buffet that is LOTME, you probably wondered: What’s going on? Where’s the latest bodily insult being perpetuated by the gang over at TikTok?
Have no fear, good readers. We would never make you go 2 straight weeks without serving up some hyperpalatable TikTok tidbits.
Our bodily insult du jour is frozen honey, and it’s exploding all over TikTok … and a few other places. “The hashtag ‘#FrozenHoney’ has been viewed nearly 600 million times, and the hashtag ‘#FrozenHoneyChallenge’ has been viewed more than 80 million times,” NBC News recently reported.
After a few hours in the freezer, honey can be squeezed out of a plastic bottle as a semisolid, toothpastelike goo – it’s stiff enough to rise out of a container that’s pointed straight up – and bitten off in large chunks. And therein lies the problem.
Some people are overdoing it. “Honey is great, but having it in small amounts to sweeten is really a healthy relationship with food, and using it to get a lot of followers and a lot of attention and having it in excess amounts is crazy,” Kristin Kirkpatrick, a registered dietitian at the Cleveland Clinic, told NBC.
Besides the possible weight gain from eating massive amounts of sugar, experts warned that “gobbling up bottles of frozen honey” could lead to stomach cramping, bloating, and diarrhea. Some TikTokers, NBC noted, said that they “were running for the bathroom.”
As we said, it’s a trend that is exploding.
Be sure to tune in next week, when we learn how TikTokers use ground meat as a skin moisturizer.
Fulminant Hemorrhagic Bullae of the Upper Extremities Arising in the Setting of IV Placement During Severe COVID-19 Infection: Observations From a Major Consultative Practice
To the Editor:
A range of dermatologic manifestations of COVID-19 have been reported, including nonspecific maculopapular exanthems, urticaria, and varicellalike eruptions.1 Additionally, there have been sporadic accounts of cutaneous vasculopathic signs such as perniolike lesions, acro-ischemia, livedo reticularis, and retiform purpura.2 We describe exuberant hemorrhagic bullae occurring on the extremities of 2 critically ill patients with COVID-19. We hypothesized that the bullae were vasculopathic in nature and possibly exacerbated by peripheral intravenous (IV)–related injury.
A 62-year-old woman with a history of diabetes mellitus and chronic obstructive pulmonary disease was admitted to the intensive care unit for acute hypoxemic respiratory failure secondary to COVID-19 infection. Dermatology was consulted for evaluation of blisters on the right arm. A new peripheral IV line was inserted into the patient’s right forearm for treatment of secondary methicillin-resistant Staphylococcus aureus pneumonia. The peripheral IV was inserted into the right proximal forearm for 2 days prior to development of ecchymosis and blisters. Intravenous medications included vancomycin, cefepime, methylprednisolone, and famotidine, as well as maintenance fluids (normal saline). Physical examination revealed extensive confluent ecchymoses with overlying tense bullae (Figure 1). Notable laboratory findings included an elevated D-dimer (peak of 8.67 μg/mL fibrinogen-equivalent units [FEUs], reference range <0.5 μg/mL FEU) and fibrinogen (789 mg/dL, reference range 200–400 mg/dL) levels. Three days later she developed worsening edema of the right arm, accompanied by more extensive bullae formation (Figure 2). Computed tomography of the right arm showed extensive subcutaneous stranding and subcutaneous edema. An orthopedic consultation determined that there was no compartment syndrome, and surgical intervention was not recommended. The patient’s course was complicated by multiorgan failure, and she died 18 days after admission.


A 67-year-old man with coronary artery disease, diabetes mellitus, and hemiparesis secondary to stroke was admitted to the intensive care unit due to hypoxemia secondary to COVID-19 pneumonia. Dermatology was consulted for the evaluation of blisters on both arms. The right forearm peripheral IV line was used for 4 days prior to the development of cutaneous symptoms. Intravenous medications included cefepime, famotidine, and methylprednisolone. The left forearm peripheral IV line was in place for 1 day prior to the development of blisters and was used for the infusion of maintenance fluids (lactated Ringer’s solution). On the first day of the eruption, small bullae were noted at sites of prior peripheral IV lines (Figure 3). On day 3 of admission, the eruption progressed to larger and more confluent tense bullae with ecchymosis (Figure 4). Additionally, laboratory test results were notable for an elevated D-dimer (peak of >20.00 ug/mL FEU) and fibrinogen (748 mg/dL) levels. Computed tomography of the arms showed extensive subcutaneous stranding and fluid along the fascial planes of the arms, with no gas or abscess formation. Surgical intervention was not recommended following an orthopedic consultation. The patient’s course was complicated by acute kidney injury and rhabdomyolysis; he was later discharged to a skilled nursing facility in stable condition.


Reports from China indicate that approximately 50% of COVID-19 patients have elevated D-dimer levels and are at risk for thrombosis.3 We hypothesize that the exuberant hemorrhagic bullous eruptions in our 2 cases may be mediated in part by a hypercoagulable state secondary to COVID-19 infection combined with IV-related trauma or extravasation injury. However, a direct cytotoxic effect of the virus cannot be entirely excluded as a potential inciting factor. Other entities considered in the differential for localized bullae included trauma-induced bullous pemphigoid as well as bullous cellulitis. Both patients were treated with high-dose steroids as well as broad-spectrum antibiotics, which were expected to lead to improvement in symptoms of bullous pemphigoid and cellulitis, respectively; however, they did not lead to symptom improvement.
Extravasation injury results from unintentional administration of potentially vesicant substances into tissues surrounding the intended vascular channel.4 The mechanism of action of these injuries is postulated to arise from direct tissue injury from cytotoxic substances, elevated osmotic pressure, and reduced blood supply if vasoconstrictive substances are infused.5 In our patients, these injuries also may have promoted vascular occlusion leading to the brisk reaction observed. Although ecchymoses typically are associated with hypocoagulable states, both of our patients were noted to have normal platelet levels throughout hospitalization. Additionally, findings of elevated D-dimer and fibrinogen levels point to a hypercoagulable state. However, there is a possibility of platelet dysfunction leading to the observed cutaneous findings of ecchymoses. Thrombocytopenia is a common finding in patients with COVID-19 and is found to be associated with increased in-hospital mortality.6 Additional study of these reactions is needed given the propensity for multiorgan failure and death in patients with COVID-19 from suspected diffuse microvascular damage.3
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective [published online March 26, 2020]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.16387
- Zhang Y, Cao W, Xiao M, et al. Clinical and coagulation characteristics of 7 patients with critical COVID-19 pneumonia and acro-ischemia [in Chinese][published online March 28, 2020]. Zhonghua Xue Ye Xue Za Zhi. 2020;41:E006.
- Mei H, Hu Y. Characteristics, causes, diagnosis and treatment of coagulation dysfunction in patients with COVID-19 [in Chinese][published online March 14, 2020]. Zhonghua Xue Ye Xue Za Zhi. 2020;41:E002.
- Sauerland C, Engelking C, Wickham R, et al. Vesicant extravasation part I: mechanisms, pathogenesis, and nursing care to reduce risk. Oncol Nurs Forum. 2006;33:1134-1141.
- Reynolds PM, MacLaren R, Mueller SW, et al. Management of extravasation injuries: a focused evaluation of noncytotoxic medications. Pharmacotherapy. 2014;34:617-632.
- Yang X, Yang Q, Wang Y, et al. Thrombocytopenia and its association with mortality in patients with COVID-19. J Thromb Haemost. 2020;18:1469‐1472.
To the Editor:
A range of dermatologic manifestations of COVID-19 have been reported, including nonspecific maculopapular exanthems, urticaria, and varicellalike eruptions.1 Additionally, there have been sporadic accounts of cutaneous vasculopathic signs such as perniolike lesions, acro-ischemia, livedo reticularis, and retiform purpura.2 We describe exuberant hemorrhagic bullae occurring on the extremities of 2 critically ill patients with COVID-19. We hypothesized that the bullae were vasculopathic in nature and possibly exacerbated by peripheral intravenous (IV)–related injury.
A 62-year-old woman with a history of diabetes mellitus and chronic obstructive pulmonary disease was admitted to the intensive care unit for acute hypoxemic respiratory failure secondary to COVID-19 infection. Dermatology was consulted for evaluation of blisters on the right arm. A new peripheral IV line was inserted into the patient’s right forearm for treatment of secondary methicillin-resistant Staphylococcus aureus pneumonia. The peripheral IV was inserted into the right proximal forearm for 2 days prior to development of ecchymosis and blisters. Intravenous medications included vancomycin, cefepime, methylprednisolone, and famotidine, as well as maintenance fluids (normal saline). Physical examination revealed extensive confluent ecchymoses with overlying tense bullae (Figure 1). Notable laboratory findings included an elevated D-dimer (peak of 8.67 μg/mL fibrinogen-equivalent units [FEUs], reference range <0.5 μg/mL FEU) and fibrinogen (789 mg/dL, reference range 200–400 mg/dL) levels. Three days later she developed worsening edema of the right arm, accompanied by more extensive bullae formation (Figure 2). Computed tomography of the right arm showed extensive subcutaneous stranding and subcutaneous edema. An orthopedic consultation determined that there was no compartment syndrome, and surgical intervention was not recommended. The patient’s course was complicated by multiorgan failure, and she died 18 days after admission.


A 67-year-old man with coronary artery disease, diabetes mellitus, and hemiparesis secondary to stroke was admitted to the intensive care unit due to hypoxemia secondary to COVID-19 pneumonia. Dermatology was consulted for the evaluation of blisters on both arms. The right forearm peripheral IV line was used for 4 days prior to the development of cutaneous symptoms. Intravenous medications included cefepime, famotidine, and methylprednisolone. The left forearm peripheral IV line was in place for 1 day prior to the development of blisters and was used for the infusion of maintenance fluids (lactated Ringer’s solution). On the first day of the eruption, small bullae were noted at sites of prior peripheral IV lines (Figure 3). On day 3 of admission, the eruption progressed to larger and more confluent tense bullae with ecchymosis (Figure 4). Additionally, laboratory test results were notable for an elevated D-dimer (peak of >20.00 ug/mL FEU) and fibrinogen (748 mg/dL) levels. Computed tomography of the arms showed extensive subcutaneous stranding and fluid along the fascial planes of the arms, with no gas or abscess formation. Surgical intervention was not recommended following an orthopedic consultation. The patient’s course was complicated by acute kidney injury and rhabdomyolysis; he was later discharged to a skilled nursing facility in stable condition.


Reports from China indicate that approximately 50% of COVID-19 patients have elevated D-dimer levels and are at risk for thrombosis.3 We hypothesize that the exuberant hemorrhagic bullous eruptions in our 2 cases may be mediated in part by a hypercoagulable state secondary to COVID-19 infection combined with IV-related trauma or extravasation injury. However, a direct cytotoxic effect of the virus cannot be entirely excluded as a potential inciting factor. Other entities considered in the differential for localized bullae included trauma-induced bullous pemphigoid as well as bullous cellulitis. Both patients were treated with high-dose steroids as well as broad-spectrum antibiotics, which were expected to lead to improvement in symptoms of bullous pemphigoid and cellulitis, respectively; however, they did not lead to symptom improvement.
Extravasation injury results from unintentional administration of potentially vesicant substances into tissues surrounding the intended vascular channel.4 The mechanism of action of these injuries is postulated to arise from direct tissue injury from cytotoxic substances, elevated osmotic pressure, and reduced blood supply if vasoconstrictive substances are infused.5 In our patients, these injuries also may have promoted vascular occlusion leading to the brisk reaction observed. Although ecchymoses typically are associated with hypocoagulable states, both of our patients were noted to have normal platelet levels throughout hospitalization. Additionally, findings of elevated D-dimer and fibrinogen levels point to a hypercoagulable state. However, there is a possibility of platelet dysfunction leading to the observed cutaneous findings of ecchymoses. Thrombocytopenia is a common finding in patients with COVID-19 and is found to be associated with increased in-hospital mortality.6 Additional study of these reactions is needed given the propensity for multiorgan failure and death in patients with COVID-19 from suspected diffuse microvascular damage.3
To the Editor:
A range of dermatologic manifestations of COVID-19 have been reported, including nonspecific maculopapular exanthems, urticaria, and varicellalike eruptions.1 Additionally, there have been sporadic accounts of cutaneous vasculopathic signs such as perniolike lesions, acro-ischemia, livedo reticularis, and retiform purpura.2 We describe exuberant hemorrhagic bullae occurring on the extremities of 2 critically ill patients with COVID-19. We hypothesized that the bullae were vasculopathic in nature and possibly exacerbated by peripheral intravenous (IV)–related injury.
A 62-year-old woman with a history of diabetes mellitus and chronic obstructive pulmonary disease was admitted to the intensive care unit for acute hypoxemic respiratory failure secondary to COVID-19 infection. Dermatology was consulted for evaluation of blisters on the right arm. A new peripheral IV line was inserted into the patient’s right forearm for treatment of secondary methicillin-resistant Staphylococcus aureus pneumonia. The peripheral IV was inserted into the right proximal forearm for 2 days prior to development of ecchymosis and blisters. Intravenous medications included vancomycin, cefepime, methylprednisolone, and famotidine, as well as maintenance fluids (normal saline). Physical examination revealed extensive confluent ecchymoses with overlying tense bullae (Figure 1). Notable laboratory findings included an elevated D-dimer (peak of 8.67 μg/mL fibrinogen-equivalent units [FEUs], reference range <0.5 μg/mL FEU) and fibrinogen (789 mg/dL, reference range 200–400 mg/dL) levels. Three days later she developed worsening edema of the right arm, accompanied by more extensive bullae formation (Figure 2). Computed tomography of the right arm showed extensive subcutaneous stranding and subcutaneous edema. An orthopedic consultation determined that there was no compartment syndrome, and surgical intervention was not recommended. The patient’s course was complicated by multiorgan failure, and she died 18 days after admission.


A 67-year-old man with coronary artery disease, diabetes mellitus, and hemiparesis secondary to stroke was admitted to the intensive care unit due to hypoxemia secondary to COVID-19 pneumonia. Dermatology was consulted for the evaluation of blisters on both arms. The right forearm peripheral IV line was used for 4 days prior to the development of cutaneous symptoms. Intravenous medications included cefepime, famotidine, and methylprednisolone. The left forearm peripheral IV line was in place for 1 day prior to the development of blisters and was used for the infusion of maintenance fluids (lactated Ringer’s solution). On the first day of the eruption, small bullae were noted at sites of prior peripheral IV lines (Figure 3). On day 3 of admission, the eruption progressed to larger and more confluent tense bullae with ecchymosis (Figure 4). Additionally, laboratory test results were notable for an elevated D-dimer (peak of >20.00 ug/mL FEU) and fibrinogen (748 mg/dL) levels. Computed tomography of the arms showed extensive subcutaneous stranding and fluid along the fascial planes of the arms, with no gas or abscess formation. Surgical intervention was not recommended following an orthopedic consultation. The patient’s course was complicated by acute kidney injury and rhabdomyolysis; he was later discharged to a skilled nursing facility in stable condition.


Reports from China indicate that approximately 50% of COVID-19 patients have elevated D-dimer levels and are at risk for thrombosis.3 We hypothesize that the exuberant hemorrhagic bullous eruptions in our 2 cases may be mediated in part by a hypercoagulable state secondary to COVID-19 infection combined with IV-related trauma or extravasation injury. However, a direct cytotoxic effect of the virus cannot be entirely excluded as a potential inciting factor. Other entities considered in the differential for localized bullae included trauma-induced bullous pemphigoid as well as bullous cellulitis. Both patients were treated with high-dose steroids as well as broad-spectrum antibiotics, which were expected to lead to improvement in symptoms of bullous pemphigoid and cellulitis, respectively; however, they did not lead to symptom improvement.
Extravasation injury results from unintentional administration of potentially vesicant substances into tissues surrounding the intended vascular channel.4 The mechanism of action of these injuries is postulated to arise from direct tissue injury from cytotoxic substances, elevated osmotic pressure, and reduced blood supply if vasoconstrictive substances are infused.5 In our patients, these injuries also may have promoted vascular occlusion leading to the brisk reaction observed. Although ecchymoses typically are associated with hypocoagulable states, both of our patients were noted to have normal platelet levels throughout hospitalization. Additionally, findings of elevated D-dimer and fibrinogen levels point to a hypercoagulable state. However, there is a possibility of platelet dysfunction leading to the observed cutaneous findings of ecchymoses. Thrombocytopenia is a common finding in patients with COVID-19 and is found to be associated with increased in-hospital mortality.6 Additional study of these reactions is needed given the propensity for multiorgan failure and death in patients with COVID-19 from suspected diffuse microvascular damage.3
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective [published online March 26, 2020]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.16387
- Zhang Y, Cao W, Xiao M, et al. Clinical and coagulation characteristics of 7 patients with critical COVID-19 pneumonia and acro-ischemia [in Chinese][published online March 28, 2020]. Zhonghua Xue Ye Xue Za Zhi. 2020;41:E006.
- Mei H, Hu Y. Characteristics, causes, diagnosis and treatment of coagulation dysfunction in patients with COVID-19 [in Chinese][published online March 14, 2020]. Zhonghua Xue Ye Xue Za Zhi. 2020;41:E002.
- Sauerland C, Engelking C, Wickham R, et al. Vesicant extravasation part I: mechanisms, pathogenesis, and nursing care to reduce risk. Oncol Nurs Forum. 2006;33:1134-1141.
- Reynolds PM, MacLaren R, Mueller SW, et al. Management of extravasation injuries: a focused evaluation of noncytotoxic medications. Pharmacotherapy. 2014;34:617-632.
- Yang X, Yang Q, Wang Y, et al. Thrombocytopenia and its association with mortality in patients with COVID-19. J Thromb Haemost. 2020;18:1469‐1472.
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective [published online March 26, 2020]. J Eur Acad Dermatol Venereol. doi:10.1111/jdv.16387
- Zhang Y, Cao W, Xiao M, et al. Clinical and coagulation characteristics of 7 patients with critical COVID-19 pneumonia and acro-ischemia [in Chinese][published online March 28, 2020]. Zhonghua Xue Ye Xue Za Zhi. 2020;41:E006.
- Mei H, Hu Y. Characteristics, causes, diagnosis and treatment of coagulation dysfunction in patients with COVID-19 [in Chinese][published online March 14, 2020]. Zhonghua Xue Ye Xue Za Zhi. 2020;41:E002.
- Sauerland C, Engelking C, Wickham R, et al. Vesicant extravasation part I: mechanisms, pathogenesis, and nursing care to reduce risk. Oncol Nurs Forum. 2006;33:1134-1141.
- Reynolds PM, MacLaren R, Mueller SW, et al. Management of extravasation injuries: a focused evaluation of noncytotoxic medications. Pharmacotherapy. 2014;34:617-632.
- Yang X, Yang Q, Wang Y, et al. Thrombocytopenia and its association with mortality in patients with COVID-19. J Thromb Haemost. 2020;18:1469‐1472.
Practice Points
- Hemorrhagic bullae are an uncommon cutaneous manifestation of COVID-19 infection in hospitalized individuals.
- Although there is no reported treatment for COVID-19–associated hemorrhagic bullae, we recommend supportive care and management of underlying etiology.
Delta variant could drive herd immunity threshold over 80%
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Because the Delta variant of SARS-CoV-2 spreads more easily than the original virus, the proportion of the population that needs to be vaccinated to reach herd immunity could be upward of 80% or more, experts say.
Also, it could be time to consider wearing an N95 mask in public indoor spaces regardless of vaccination status, according to a media briefing on Aug. 3 sponsored by the Infectious Diseases Society of America.
Furthermore, giving booster shots to the fully vaccinated is not the top public health priority now. Instead, third vaccinations should be reserved for more vulnerable populations – and efforts should focus on getting first vaccinations to unvaccinated people in the United States and around the world.
“The problem here is that the Delta variant is ... more transmissible than the original virus. That pushes the overall population herd immunity threshold much higher,” Ricardo Franco, MD, assistant professor of medicine at the University of Alabama at Birmingham, said during the briefing.
“For Delta, those threshold estimates go well over 80% and may be approaching 90%,” he said.
To put that figure in context, the original SARS-CoV-2 virus required an estimated 67% of the population to be vaccinated to achieve herd immunity. Also, measles has one of the highest herd immunity thresholds at 95%, Dr. Franco added.
Herd immunity is the point at which enough people are immunized that the entire population gains protection. And it’s already happening. “Unvaccinated people are actually benefiting from greater herd immunity protection in high-vaccination counties compared to low-vaccination ones,” he said.
Maximize mask protection
Unlike early in the COVID-19 pandemic with widespread shortages of personal protective equipment, face masks are now readily available. This includes N95 masks, which offer enhanced protection against SARS-CoV-2, Ezekiel J. Emanuel, MD, PhD, said during the briefing.
Following the July 27 CDC recommendation that most Americans wear masks indoors when in public places, “I do think we need to upgrade our masks,” said Dr. Emanuel, who is Diane v.S. Levy & Robert M. Levy professor at the University of Pennsylvania, Philadelphia.
“It’s not just any mask,” he added. “Good masks make a big difference and are very important.”
Mask protection is about blocking 0.3-mcm particles, “and I think we need to make sure that people have masks that can filter that out,” he said. Although surgical masks are very good, he added, “they’re not quite as good as N95s.” As their name implies, N95s filter out 95% of these particles.
Dr. Emanuel acknowledged that people are tired of COVID-19 and complying with public health measures but urged perseverance. “We’ve sacrificed a lot. We should not throw it away in just a few months because we are tired. We’re all tired, but we do have to do the little bit extra getting vaccinated, wearing masks indoors, and protecting ourselves, our families, and our communities.”
Dealing with a disconnect
In response to a reporter’s question about the possibility that the large crowd at the Lollapalooza music festival in Chicago could become a superspreader event, Dr. Emanuel said, “it is worrisome.”
“I would say that, if you’re going to go to a gathering like that, wearing an N95 mask is wise, and not spending too long at any one place is also wise,” he said.
On the plus side, the event was held outdoors with lots of air circulation, Dr. Emanuel said.
However, “this is the kind of thing where we’ve got a sort of disconnect between people’s desire to get back to normal ... and the fact that we’re in the middle of this upsurge.”
Another potential problem is the event brought people together from many different locations, so when they travel home, they could be “potentially seeding lots of other communities.”
Boosters for some, for now
Even though not officially recommended, some fully vaccinated Americans are seeking a third or booster vaccination on their own.
Asked for his opinion, Dr. Emanuel said: “We’re probably going to have to be giving boosters to immunocompromised people and people who are susceptible. That’s where we are going to start.”
More research is needed regarding booster shots, he said. “There are very small studies – and the ‘very small’ should be emphasized – given that we’ve given shots to over 160 million people.”
“But it does appear that the boosters increase the antibodies and protection,” he said.
Instead of boosters, it is more important for people who haven’t been vaccinated to get fully vaccinated.
“We need to put our priorities in the right places,” he said.
Emanuel noted that, except for people in rural areas that might have to travel long distances, access to vaccines is no longer an issue. “It’s very hard not to find a vaccine if you want it.”
A remaining hurdle is “battling a major disinformation initiative. I don’t think this is misinformation. I think there’s very clear evidence that it is disinformation – false facts about the vaccines being spread,” Dr. Emanuel said.
The breakthrough infection dilemma
Breakthrough cases “remain the vast minority of infections at this time ... that is reassuring,” Dr. Franco said.
Also, tracking symptomatic breakthrough infections remains easier than studying fully vaccinated people who become infected with SARS-CoV-2 but remain symptom free.
“We really don’t have a good handle on the frequency of asymptomatic cases,” Dr. Emanuel said. “If you’re missing breakthrough infections, a lot of them, you may be missing some [virus] evolution that would be very important for us to follow.” This missing information could include the emergence of new variants.
The asymptomatic breakthrough cases are the most worrisome group,” Dr. Emanuel said. “You get infected, you’re feeling fine. Maybe you’ve got a little sneeze or cough, but nothing unusual. And then you’re still able to transmit the Delta variant.”
The big picture
The upsurge in cases, hospitalizations, and deaths is a major challenge, Dr. Emanuel said. “We need to address that by getting many more people vaccinated right now with what are very good vaccines.”
“But it also means that we have to stop being U.S. focused alone.” He pointed out that Delta and other variants originated overseas, “so getting the world vaccinated ... has to be a top priority.”
“We are obviously all facing a challenge as we move into the fall,” Dr. Emanuel said. “With schools opening and employers bringing their employees back together, even if these groups are vaccinated, there are going to be major challenges for all of us.”
A version of this article first appeared on Medscape.com.
Pink, Scaly, Annular Plaques in Concentric Rings Localized to Vitiliginous Patches
The Diagnosis: Tinea Pseudoimbricata
Tinea pseudoimbricata and tinea indecisiva are synonyms describing cases of tinea corporis that manifest in scaly plaques in concentric rings evocative of those present in tinea imbricata. However, in contrast to tinea imbricata, cases of tinea pseudoimbricata are caused by dermatophytes other than Trichophyton concentricum. 1 Tinea pseudoimbricata usually presents in association with immunosuppression, either systemic or local, and can be produced by application of topical medications such as corticosteroids.2 Mask-Bull et al3 reported the case of a 21-year-old man in the United States with no history of immunosuppressive conditions who presented with scaly erythematous annular plaques on the lateral neck that resolved with 2 pulsed doses of terbinafine. Potassium hydroxide preparation and fungal culture were both consistent with Trichophyton tonsurans.3
Trichophyton concentricum is an anthropophilic species of dermatophyte endemic to areas within the South Pacific, Southeast Asia, and Central and South America. Infection with T concentricum produces tinea imbricata, which presents with concentric, scaly, annular rings. Cutaneous lesions of tinea imbricata caused by T concentricum have a more generalized distribution and more densely grouped, concentric circles than the cutaneous findings seen in patients with tinea pseudoimbricata.4 Affected patients typically demonstrate negative delayed-type hypersensitivity to T concentricum cytoplasmic antigen and T-lymphocyte hyporeactivity, which may contribute to the development of sequential waves of scaling observed in tinea imbricata.5
Trichophyton rubrum, the most common cause of tinea corporis, has been reported to cause some cases of tinea pseudoimbricata (indecisiva).1,2 It utilizes keratinases such as subtilisins (Sub3 and Sub4), leucine aminopeptidases (Lap1 and Lap2), and dipeptidyl peptidases (DppIV and DppV) to invade the skin. Once inside, mannans, glycoprotein constituents of the cell wall, are released and bind to the cell surface of mononuclear phagocytes, subsequently moving into the cell by phagocytosis, thereafter interfering with RNA synthesis that is necessary for presentation of antigens to appropriate T cells and allowing for initiation of chronic infection.6,7 The cytotoxic response to superficial dermatophyte infection is triggered by major histocompatibility complex class I molecule activation of CD8+ cells.6,8
Our case is of interest given the localization of the superficial dermatophyte infection to only vitiliginous skin. This distribution and appearance while undergoing narrowband UVB (NB-UVB) treatment is rare. We postulate that our patient likely represents a case of locus minoris resistentiae, a phenomenon in which an area of skin exhibits a compromised immune microenvironment that predisposes it to disease.9
In vitiligo, NB-UVB modulates the immune response by increasing IL-10, thereby promoting regulatory T-cell differentiation with suppression of autoreactive T cells and induction of direct T-lymphocyte apoptosis.10,11 Although the mechanism accounting for our patient’s presentation is unknown, we suspect NB-UVB–induced immunosuppression enabled persistence of the dermatophyte infection. The localization of the infection to the vitiliginous patches may result from the greater penetration of the UV light relative to the surrounding, normally pigmented skin. This relative difference in UV penetration would be expected to result in increased immunosuppression in the vitiliginous lesions and enhanced susceptibility to the fungal organisms.
Erythema annulare centrifugum is characterized by annular lesions with a trailing scale instead of the concentric rings seen in tinea pseudoimbricata. Erythema marginatum is seen in acute rheumatic fever and presents with a transient nonpruritic rash, usually on the trunk or extremities. Erythema migrans presents with fewer lesions that are less circinate in shape, and the patient often has a history of a tick bite. Tinea imbricata is caused by T concentricum, while tinea pseudoimbricata is caused by T tonsurans and other dermatophytes.
With the increasing use of immunosuppressant drugs, the prevalence of tinea pseudoimbricata is hypothesized to increase.1 The presence of tinea pseudoimbricata should alert dermatologists to the possible overuse of topical corticosteroids, and other forms of immunosuppression also should be considered.
- Lim SP, Smith AG. “Tinea pseudoimbricata”: tinea corporis in a renal transplant recipient mimicking the concentric rings of tinea imbricata. Clin Exp Dermatol. 2003;28:332-333.
- Batta K, Ramlogan D, Smith AG, et al. ‘Tinea indecisiva’ may mimic the concentric rings of tinea imbricata. Br J Dermatol. 2002;147:384.
- Mask-Bull L, Patel R, Tarbox MB. America’s first case of tinea pseudoimbricata. Am J Dermatol Venereol. 2015;4:15-17.
- Meena M, Mittal A. Tinea pseudo-imbricata. J Assoc Physicians India. 2018;66:79.
- Hay RJ, Reid S, Talwat E, et al. Immune responses of patients with tinea imbricata. Br J Dermatol. 1983;108:581-586.
- Dahl MV. Suppression of immunity and inflammation by products produced by dermatophytes. J Am Acad Dermatol. 1993;28(5 pt 1):S19-S23.
- Blutfield MS, Lohre JM, Pawich DA, et al. The immunologic response to Trichophyton rubrum in lower extremity fungal infections. J Fungi (Basel). 2015;1:130-137.
- De Hoog S, Monod M, Dawson T, et al. Skin fungi from colonization to infection [published online July 2017]. Microbiol Spectr. doi:10.1128/ microbiolspec.FUNK-0049-2016
- Lo Schiavo A, Ruocco E, Russo T, et al. Locus minoris resistentiae: an old but still valid way of thinking in medicine. Clin Dermatol. 2014;32:553-556.
- Ponsonby AL, Lucas RM, van der Mei IA. UVR, vitamin D and three autoimmune diseases—multiple sclerosis, type 1 diabetes, rheumatoid arthritis. Photochem Photobiol. 2005;81:1267-1275.
- Yazdani Abyaneh M, Griffith RD, Falto-Aizpurua L, et al. Narrowband ultraviolet B phototherapy in combination with other therapies for vitiligo: mechanisms and efficacies. J Eur Acad Dermatol Venereol. 2014;28:1610-1622.
The Diagnosis: Tinea Pseudoimbricata
Tinea pseudoimbricata and tinea indecisiva are synonyms describing cases of tinea corporis that manifest in scaly plaques in concentric rings evocative of those present in tinea imbricata. However, in contrast to tinea imbricata, cases of tinea pseudoimbricata are caused by dermatophytes other than Trichophyton concentricum. 1 Tinea pseudoimbricata usually presents in association with immunosuppression, either systemic or local, and can be produced by application of topical medications such as corticosteroids.2 Mask-Bull et al3 reported the case of a 21-year-old man in the United States with no history of immunosuppressive conditions who presented with scaly erythematous annular plaques on the lateral neck that resolved with 2 pulsed doses of terbinafine. Potassium hydroxide preparation and fungal culture were both consistent with Trichophyton tonsurans.3
Trichophyton concentricum is an anthropophilic species of dermatophyte endemic to areas within the South Pacific, Southeast Asia, and Central and South America. Infection with T concentricum produces tinea imbricata, which presents with concentric, scaly, annular rings. Cutaneous lesions of tinea imbricata caused by T concentricum have a more generalized distribution and more densely grouped, concentric circles than the cutaneous findings seen in patients with tinea pseudoimbricata.4 Affected patients typically demonstrate negative delayed-type hypersensitivity to T concentricum cytoplasmic antigen and T-lymphocyte hyporeactivity, which may contribute to the development of sequential waves of scaling observed in tinea imbricata.5
Trichophyton rubrum, the most common cause of tinea corporis, has been reported to cause some cases of tinea pseudoimbricata (indecisiva).1,2 It utilizes keratinases such as subtilisins (Sub3 and Sub4), leucine aminopeptidases (Lap1 and Lap2), and dipeptidyl peptidases (DppIV and DppV) to invade the skin. Once inside, mannans, glycoprotein constituents of the cell wall, are released and bind to the cell surface of mononuclear phagocytes, subsequently moving into the cell by phagocytosis, thereafter interfering with RNA synthesis that is necessary for presentation of antigens to appropriate T cells and allowing for initiation of chronic infection.6,7 The cytotoxic response to superficial dermatophyte infection is triggered by major histocompatibility complex class I molecule activation of CD8+ cells.6,8
Our case is of interest given the localization of the superficial dermatophyte infection to only vitiliginous skin. This distribution and appearance while undergoing narrowband UVB (NB-UVB) treatment is rare. We postulate that our patient likely represents a case of locus minoris resistentiae, a phenomenon in which an area of skin exhibits a compromised immune microenvironment that predisposes it to disease.9
In vitiligo, NB-UVB modulates the immune response by increasing IL-10, thereby promoting regulatory T-cell differentiation with suppression of autoreactive T cells and induction of direct T-lymphocyte apoptosis.10,11 Although the mechanism accounting for our patient’s presentation is unknown, we suspect NB-UVB–induced immunosuppression enabled persistence of the dermatophyte infection. The localization of the infection to the vitiliginous patches may result from the greater penetration of the UV light relative to the surrounding, normally pigmented skin. This relative difference in UV penetration would be expected to result in increased immunosuppression in the vitiliginous lesions and enhanced susceptibility to the fungal organisms.
Erythema annulare centrifugum is characterized by annular lesions with a trailing scale instead of the concentric rings seen in tinea pseudoimbricata. Erythema marginatum is seen in acute rheumatic fever and presents with a transient nonpruritic rash, usually on the trunk or extremities. Erythema migrans presents with fewer lesions that are less circinate in shape, and the patient often has a history of a tick bite. Tinea imbricata is caused by T concentricum, while tinea pseudoimbricata is caused by T tonsurans and other dermatophytes.
With the increasing use of immunosuppressant drugs, the prevalence of tinea pseudoimbricata is hypothesized to increase.1 The presence of tinea pseudoimbricata should alert dermatologists to the possible overuse of topical corticosteroids, and other forms of immunosuppression also should be considered.
The Diagnosis: Tinea Pseudoimbricata
Tinea pseudoimbricata and tinea indecisiva are synonyms describing cases of tinea corporis that manifest in scaly plaques in concentric rings evocative of those present in tinea imbricata. However, in contrast to tinea imbricata, cases of tinea pseudoimbricata are caused by dermatophytes other than Trichophyton concentricum. 1 Tinea pseudoimbricata usually presents in association with immunosuppression, either systemic or local, and can be produced by application of topical medications such as corticosteroids.2 Mask-Bull et al3 reported the case of a 21-year-old man in the United States with no history of immunosuppressive conditions who presented with scaly erythematous annular plaques on the lateral neck that resolved with 2 pulsed doses of terbinafine. Potassium hydroxide preparation and fungal culture were both consistent with Trichophyton tonsurans.3
Trichophyton concentricum is an anthropophilic species of dermatophyte endemic to areas within the South Pacific, Southeast Asia, and Central and South America. Infection with T concentricum produces tinea imbricata, which presents with concentric, scaly, annular rings. Cutaneous lesions of tinea imbricata caused by T concentricum have a more generalized distribution and more densely grouped, concentric circles than the cutaneous findings seen in patients with tinea pseudoimbricata.4 Affected patients typically demonstrate negative delayed-type hypersensitivity to T concentricum cytoplasmic antigen and T-lymphocyte hyporeactivity, which may contribute to the development of sequential waves of scaling observed in tinea imbricata.5
Trichophyton rubrum, the most common cause of tinea corporis, has been reported to cause some cases of tinea pseudoimbricata (indecisiva).1,2 It utilizes keratinases such as subtilisins (Sub3 and Sub4), leucine aminopeptidases (Lap1 and Lap2), and dipeptidyl peptidases (DppIV and DppV) to invade the skin. Once inside, mannans, glycoprotein constituents of the cell wall, are released and bind to the cell surface of mononuclear phagocytes, subsequently moving into the cell by phagocytosis, thereafter interfering with RNA synthesis that is necessary for presentation of antigens to appropriate T cells and allowing for initiation of chronic infection.6,7 The cytotoxic response to superficial dermatophyte infection is triggered by major histocompatibility complex class I molecule activation of CD8+ cells.6,8
Our case is of interest given the localization of the superficial dermatophyte infection to only vitiliginous skin. This distribution and appearance while undergoing narrowband UVB (NB-UVB) treatment is rare. We postulate that our patient likely represents a case of locus minoris resistentiae, a phenomenon in which an area of skin exhibits a compromised immune microenvironment that predisposes it to disease.9
In vitiligo, NB-UVB modulates the immune response by increasing IL-10, thereby promoting regulatory T-cell differentiation with suppression of autoreactive T cells and induction of direct T-lymphocyte apoptosis.10,11 Although the mechanism accounting for our patient’s presentation is unknown, we suspect NB-UVB–induced immunosuppression enabled persistence of the dermatophyte infection. The localization of the infection to the vitiliginous patches may result from the greater penetration of the UV light relative to the surrounding, normally pigmented skin. This relative difference in UV penetration would be expected to result in increased immunosuppression in the vitiliginous lesions and enhanced susceptibility to the fungal organisms.
Erythema annulare centrifugum is characterized by annular lesions with a trailing scale instead of the concentric rings seen in tinea pseudoimbricata. Erythema marginatum is seen in acute rheumatic fever and presents with a transient nonpruritic rash, usually on the trunk or extremities. Erythema migrans presents with fewer lesions that are less circinate in shape, and the patient often has a history of a tick bite. Tinea imbricata is caused by T concentricum, while tinea pseudoimbricata is caused by T tonsurans and other dermatophytes.
With the increasing use of immunosuppressant drugs, the prevalence of tinea pseudoimbricata is hypothesized to increase.1 The presence of tinea pseudoimbricata should alert dermatologists to the possible overuse of topical corticosteroids, and other forms of immunosuppression also should be considered.
- Lim SP, Smith AG. “Tinea pseudoimbricata”: tinea corporis in a renal transplant recipient mimicking the concentric rings of tinea imbricata. Clin Exp Dermatol. 2003;28:332-333.
- Batta K, Ramlogan D, Smith AG, et al. ‘Tinea indecisiva’ may mimic the concentric rings of tinea imbricata. Br J Dermatol. 2002;147:384.
- Mask-Bull L, Patel R, Tarbox MB. America’s first case of tinea pseudoimbricata. Am J Dermatol Venereol. 2015;4:15-17.
- Meena M, Mittal A. Tinea pseudo-imbricata. J Assoc Physicians India. 2018;66:79.
- Hay RJ, Reid S, Talwat E, et al. Immune responses of patients with tinea imbricata. Br J Dermatol. 1983;108:581-586.
- Dahl MV. Suppression of immunity and inflammation by products produced by dermatophytes. J Am Acad Dermatol. 1993;28(5 pt 1):S19-S23.
- Blutfield MS, Lohre JM, Pawich DA, et al. The immunologic response to Trichophyton rubrum in lower extremity fungal infections. J Fungi (Basel). 2015;1:130-137.
- De Hoog S, Monod M, Dawson T, et al. Skin fungi from colonization to infection [published online July 2017]. Microbiol Spectr. doi:10.1128/ microbiolspec.FUNK-0049-2016
- Lo Schiavo A, Ruocco E, Russo T, et al. Locus minoris resistentiae: an old but still valid way of thinking in medicine. Clin Dermatol. 2014;32:553-556.
- Ponsonby AL, Lucas RM, van der Mei IA. UVR, vitamin D and three autoimmune diseases—multiple sclerosis, type 1 diabetes, rheumatoid arthritis. Photochem Photobiol. 2005;81:1267-1275.
- Yazdani Abyaneh M, Griffith RD, Falto-Aizpurua L, et al. Narrowband ultraviolet B phototherapy in combination with other therapies for vitiligo: mechanisms and efficacies. J Eur Acad Dermatol Venereol. 2014;28:1610-1622.
- Lim SP, Smith AG. “Tinea pseudoimbricata”: tinea corporis in a renal transplant recipient mimicking the concentric rings of tinea imbricata. Clin Exp Dermatol. 2003;28:332-333.
- Batta K, Ramlogan D, Smith AG, et al. ‘Tinea indecisiva’ may mimic the concentric rings of tinea imbricata. Br J Dermatol. 2002;147:384.
- Mask-Bull L, Patel R, Tarbox MB. America’s first case of tinea pseudoimbricata. Am J Dermatol Venereol. 2015;4:15-17.
- Meena M, Mittal A. Tinea pseudo-imbricata. J Assoc Physicians India. 2018;66:79.
- Hay RJ, Reid S, Talwat E, et al. Immune responses of patients with tinea imbricata. Br J Dermatol. 1983;108:581-586.
- Dahl MV. Suppression of immunity and inflammation by products produced by dermatophytes. J Am Acad Dermatol. 1993;28(5 pt 1):S19-S23.
- Blutfield MS, Lohre JM, Pawich DA, et al. The immunologic response to Trichophyton rubrum in lower extremity fungal infections. J Fungi (Basel). 2015;1:130-137.
- De Hoog S, Monod M, Dawson T, et al. Skin fungi from colonization to infection [published online July 2017]. Microbiol Spectr. doi:10.1128/ microbiolspec.FUNK-0049-2016
- Lo Schiavo A, Ruocco E, Russo T, et al. Locus minoris resistentiae: an old but still valid way of thinking in medicine. Clin Dermatol. 2014;32:553-556.
- Ponsonby AL, Lucas RM, van der Mei IA. UVR, vitamin D and three autoimmune diseases—multiple sclerosis, type 1 diabetes, rheumatoid arthritis. Photochem Photobiol. 2005;81:1267-1275.
- Yazdani Abyaneh M, Griffith RD, Falto-Aizpurua L, et al. Narrowband ultraviolet B phototherapy in combination with other therapies for vitiligo: mechanisms and efficacies. J Eur Acad Dermatol Venereol. 2014;28:1610-1622.
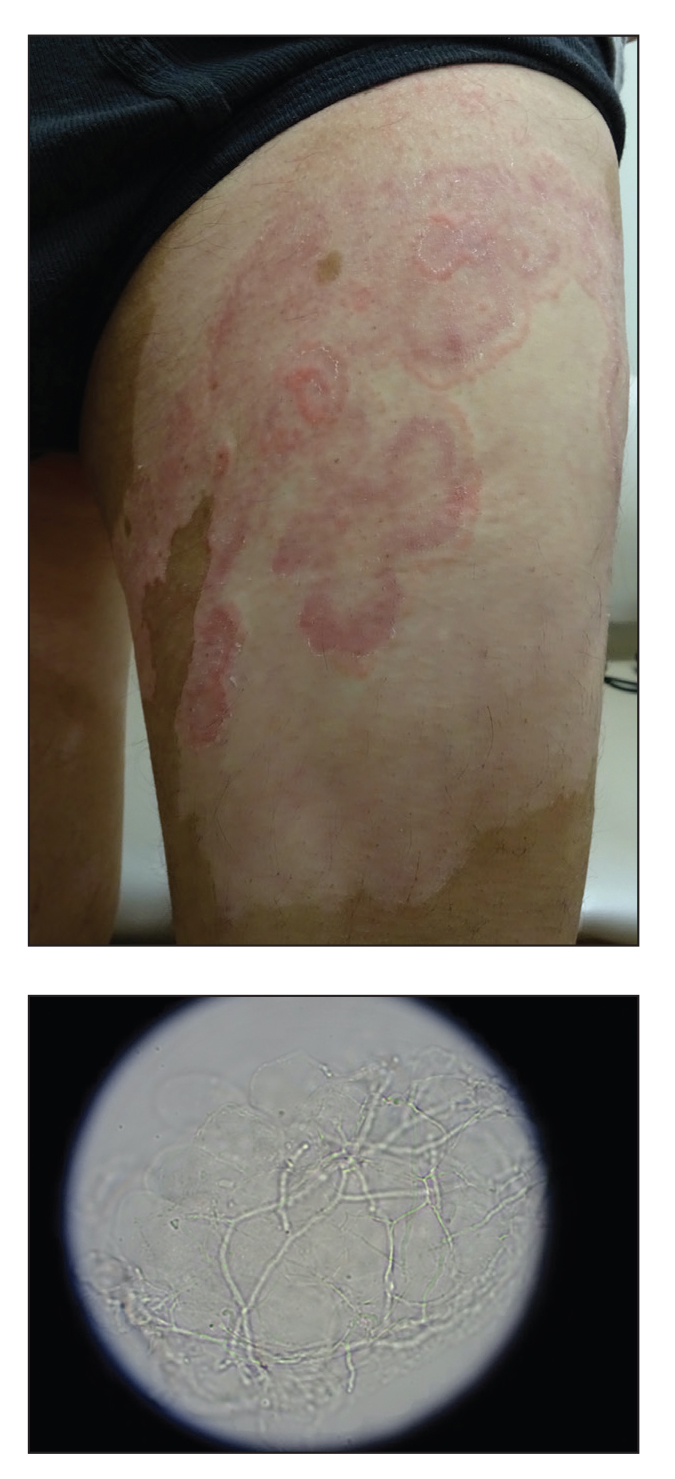
A 64-year-old man presented with generalized vitiligo. In addition to extensive depigmented macules, physical examination revealed the presence of onychomycosis and tinea corporis confirmed by microscopic examination of potassium hydroxide–treated superficial skin scrapings. Vitiligo treatment was postponed, and a 3-month course of oral terbinafine and naftifine cream was undertaken for the dermatophyte infections. Subsequent examination revealed that the patient’s tinea corporis had improved, though there were localized areas of persistence. Given the patient’s eagerness to treat his vitiligo, narrowband UVB phototherapy was started along with tolnaftate cream 1% for treatment of the residual tinea corporis. After 2 months of narrowband UVB, partial repigmentation of the vitiligo was observed; however, he had developed extensive pink, scaly, annular plaques in concentric rings within residual vitiliginous patches on the lower extremities (top). Repeat examination of potassium hydroxide–treated skin scrapings revealed numerous hyphae (bottom). A fungal culture identified Trichophyton rubrum.
Untreatable, drug-resistant fungus found in Texas and Washington, D.C.
The CDC has reported two clusters of Candida auris infections resistant to all antifungal medications in long-term care facilities in 2021. Because these panresistant infections occurred without any exposure to antifungal drugs, the cases are even more worrisome. These clusters are the first time such nosocomial transmission has been detected.
In the District of Columbia, three panresistant isolates were discovered through screening for skin colonization with resistant organisms at a long-term acute care facility (LTAC) that cares for patients who are seriously ill, often on mechanical ventilation.
In Texas, the resistant organisms were found both by screening and in specimens from ill patients at an LTAC and a short-term acute care hospital that share patients. Two were panresistant, and five others were resistant to fluconazole and echinocandins.
These clusters occurred simultaneously and independently of each other; there were no links between the two institutions.
Colonization of skin with C. auris can lead to invasive infections in 5%-10% of affected patients. Routine skin surveillance cultures are not commonly done for Candida, although perirectal cultures for vancomycin-resistant enterococci and nasal swabs for MRSA have been done for years. Some areas, like Los Angeles, have recommended screening for C. auris in high-risk patients – defined as those who were on a ventilator or had a tracheostomy admitted from an LTAC or skilled nursing facility in Los Angeles County, New York, New Jersey, or Illinois.
In the past, about 85% of C. auris isolates in the United States have been resistant to azoles (for example, fluconazole), 33% to amphotericin B, and 1% to echinocandins. Because of generally strong susceptibility, an echinocandin such as micafungin or caspofungin has been the drug of choice for an invasive Candida infection.
C. auris is particularly difficult to deal with for several reasons. First, it can continue to live in the environment, on both dry or moist surfaces, for up to 2 weeks. Outbreaks have occurred both from hand (person-to-person) transmission or via inanimate surfaces that have become contaminated. Equally troublesome is that people become colonized with the yeast indefinitely.
Meghan Lyman, MD, of the fungal diseases branch of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, said in an interview that facilities might be slow in recognizing the problem and in identifying the organism. “We encounter problems in noninvasive specimens, especially urine,” Dr. Lyman added.
“Sometimes ... they consider Candida [to represent] colonization so they will often not speciate it.” She emphasized the need for facilities that care for ventilated patients to consider screening. “Higher priority ... are places in areas where there’s a lot of C. auris transmission or in nearby areas that are likely to get introductions.” Even those that do speciate may have difficulty identifying C. auris.
Further, Dr. Lyman stressed “the importance of antifungal susceptibility testing and testing for resistance. Because that’s also something that’s not widely available at all hospitals and clinical labs ... you can send it to the [CDC’s] antimicrobial resistance lab network” for testing.
COVID-19 has brought particular challenges. Rodney E. Rohde, PhD, MS, professor and chair, clinical lab science program, Texas State University, San Marcos, said in an interview that he is worried about all the steroids and broad-spectrum antibiotics patients receive.
They’re “being given medical interventions, whether it’s ventilators or [extracorporeal membrane oxygenation] or IVs or central lines or catheters for UTIs and you’re creating highways, right for something that may be right there,” said Dr. Rohde, who was not involved in the CDC study. “It’s a perfect storm, not just for C. auris, but I worry about bacterial resistance agents, too, like MRSA and so forth, having kind of a spike in those types of infections with COVID. So, it’s kind of a doubly dangerous time, I think.”
Multiresistant bacteria are a major health problem, causing illnesses in 2.8 million people annually in the United States, and causing about 35,000 deaths.
Dr. Rohde raised another, rarely mentioned concern. “We’re in crisis mode. People are leaving our field more than they ever had before. The medical laboratory is being decimated because people have burned out after these past 14 months. And so I worry just about competent medical laboratory professionals that are on board to deal with these types of other crises that are popping up within hospitals and long-term care facilities. It kind of keeps me awake.”
Dr. Rohde and Dr. Lyman shared their concern that COVID caused a decrease in screening for other infections and drug-resistant organisms. Bare-bones staffing and shortages of personal protective equipment have likely fueled the spread of these infections as well.
In an outbreak of C. auris in a Florida hospital’s COVID unit in 2020, 35 of 67 patients became colonized, and 6 became ill. The epidemiologists investigating thought that contaminated gowns or gloves, computers, and other equipment were likely sources of transmission.
Low pay, especially in nursing homes, is another problem Dr. Rohde mentioned. It’s an additional problem in both acute and long-term care that “some of the lowest-paid people are the environmental services people, and so the turnover is crazy.” Yet, we rely on them to keep everyone safe. He added that, in addition to pay, he “tries to give them the appreciation and the recognition that they really deserve.”
There are a few specific measures that can be taken to protect patients. Dr. Lyman concluded. “The best way is identifying cases and really ensuring good infection control to prevent the spread.” It’s back to basics – limiting broad-spectrum antibiotics and invasive medical devices, and especially good handwashing and thorough cleaning.
Dr. Lyman and Dr. Rohde have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The CDC has reported two clusters of Candida auris infections resistant to all antifungal medications in long-term care facilities in 2021. Because these panresistant infections occurred without any exposure to antifungal drugs, the cases are even more worrisome. These clusters are the first time such nosocomial transmission has been detected.
In the District of Columbia, three panresistant isolates were discovered through screening for skin colonization with resistant organisms at a long-term acute care facility (LTAC) that cares for patients who are seriously ill, often on mechanical ventilation.
In Texas, the resistant organisms were found both by screening and in specimens from ill patients at an LTAC and a short-term acute care hospital that share patients. Two were panresistant, and five others were resistant to fluconazole and echinocandins.
These clusters occurred simultaneously and independently of each other; there were no links between the two institutions.
Colonization of skin with C. auris can lead to invasive infections in 5%-10% of affected patients. Routine skin surveillance cultures are not commonly done for Candida, although perirectal cultures for vancomycin-resistant enterococci and nasal swabs for MRSA have been done for years. Some areas, like Los Angeles, have recommended screening for C. auris in high-risk patients – defined as those who were on a ventilator or had a tracheostomy admitted from an LTAC or skilled nursing facility in Los Angeles County, New York, New Jersey, or Illinois.
In the past, about 85% of C. auris isolates in the United States have been resistant to azoles (for example, fluconazole), 33% to amphotericin B, and 1% to echinocandins. Because of generally strong susceptibility, an echinocandin such as micafungin or caspofungin has been the drug of choice for an invasive Candida infection.
C. auris is particularly difficult to deal with for several reasons. First, it can continue to live in the environment, on both dry or moist surfaces, for up to 2 weeks. Outbreaks have occurred both from hand (person-to-person) transmission or via inanimate surfaces that have become contaminated. Equally troublesome is that people become colonized with the yeast indefinitely.
Meghan Lyman, MD, of the fungal diseases branch of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, said in an interview that facilities might be slow in recognizing the problem and in identifying the organism. “We encounter problems in noninvasive specimens, especially urine,” Dr. Lyman added.
“Sometimes ... they consider Candida [to represent] colonization so they will often not speciate it.” She emphasized the need for facilities that care for ventilated patients to consider screening. “Higher priority ... are places in areas where there’s a lot of C. auris transmission or in nearby areas that are likely to get introductions.” Even those that do speciate may have difficulty identifying C. auris.
Further, Dr. Lyman stressed “the importance of antifungal susceptibility testing and testing for resistance. Because that’s also something that’s not widely available at all hospitals and clinical labs ... you can send it to the [CDC’s] antimicrobial resistance lab network” for testing.
COVID-19 has brought particular challenges. Rodney E. Rohde, PhD, MS, professor and chair, clinical lab science program, Texas State University, San Marcos, said in an interview that he is worried about all the steroids and broad-spectrum antibiotics patients receive.
They’re “being given medical interventions, whether it’s ventilators or [extracorporeal membrane oxygenation] or IVs or central lines or catheters for UTIs and you’re creating highways, right for something that may be right there,” said Dr. Rohde, who was not involved in the CDC study. “It’s a perfect storm, not just for C. auris, but I worry about bacterial resistance agents, too, like MRSA and so forth, having kind of a spike in those types of infections with COVID. So, it’s kind of a doubly dangerous time, I think.”
Multiresistant bacteria are a major health problem, causing illnesses in 2.8 million people annually in the United States, and causing about 35,000 deaths.
Dr. Rohde raised another, rarely mentioned concern. “We’re in crisis mode. People are leaving our field more than they ever had before. The medical laboratory is being decimated because people have burned out after these past 14 months. And so I worry just about competent medical laboratory professionals that are on board to deal with these types of other crises that are popping up within hospitals and long-term care facilities. It kind of keeps me awake.”
Dr. Rohde and Dr. Lyman shared their concern that COVID caused a decrease in screening for other infections and drug-resistant organisms. Bare-bones staffing and shortages of personal protective equipment have likely fueled the spread of these infections as well.
In an outbreak of C. auris in a Florida hospital’s COVID unit in 2020, 35 of 67 patients became colonized, and 6 became ill. The epidemiologists investigating thought that contaminated gowns or gloves, computers, and other equipment were likely sources of transmission.
Low pay, especially in nursing homes, is another problem Dr. Rohde mentioned. It’s an additional problem in both acute and long-term care that “some of the lowest-paid people are the environmental services people, and so the turnover is crazy.” Yet, we rely on them to keep everyone safe. He added that, in addition to pay, he “tries to give them the appreciation and the recognition that they really deserve.”
There are a few specific measures that can be taken to protect patients. Dr. Lyman concluded. “The best way is identifying cases and really ensuring good infection control to prevent the spread.” It’s back to basics – limiting broad-spectrum antibiotics and invasive medical devices, and especially good handwashing and thorough cleaning.
Dr. Lyman and Dr. Rohde have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The CDC has reported two clusters of Candida auris infections resistant to all antifungal medications in long-term care facilities in 2021. Because these panresistant infections occurred without any exposure to antifungal drugs, the cases are even more worrisome. These clusters are the first time such nosocomial transmission has been detected.
In the District of Columbia, three panresistant isolates were discovered through screening for skin colonization with resistant organisms at a long-term acute care facility (LTAC) that cares for patients who are seriously ill, often on mechanical ventilation.
In Texas, the resistant organisms were found both by screening and in specimens from ill patients at an LTAC and a short-term acute care hospital that share patients. Two were panresistant, and five others were resistant to fluconazole and echinocandins.
These clusters occurred simultaneously and independently of each other; there were no links between the two institutions.
Colonization of skin with C. auris can lead to invasive infections in 5%-10% of affected patients. Routine skin surveillance cultures are not commonly done for Candida, although perirectal cultures for vancomycin-resistant enterococci and nasal swabs for MRSA have been done for years. Some areas, like Los Angeles, have recommended screening for C. auris in high-risk patients – defined as those who were on a ventilator or had a tracheostomy admitted from an LTAC or skilled nursing facility in Los Angeles County, New York, New Jersey, or Illinois.
In the past, about 85% of C. auris isolates in the United States have been resistant to azoles (for example, fluconazole), 33% to amphotericin B, and 1% to echinocandins. Because of generally strong susceptibility, an echinocandin such as micafungin or caspofungin has been the drug of choice for an invasive Candida infection.
C. auris is particularly difficult to deal with for several reasons. First, it can continue to live in the environment, on both dry or moist surfaces, for up to 2 weeks. Outbreaks have occurred both from hand (person-to-person) transmission or via inanimate surfaces that have become contaminated. Equally troublesome is that people become colonized with the yeast indefinitely.
Meghan Lyman, MD, of the fungal diseases branch of the CDC’s National Center for Emerging and Zoonotic Infectious Diseases, said in an interview that facilities might be slow in recognizing the problem and in identifying the organism. “We encounter problems in noninvasive specimens, especially urine,” Dr. Lyman added.
“Sometimes ... they consider Candida [to represent] colonization so they will often not speciate it.” She emphasized the need for facilities that care for ventilated patients to consider screening. “Higher priority ... are places in areas where there’s a lot of C. auris transmission or in nearby areas that are likely to get introductions.” Even those that do speciate may have difficulty identifying C. auris.
Further, Dr. Lyman stressed “the importance of antifungal susceptibility testing and testing for resistance. Because that’s also something that’s not widely available at all hospitals and clinical labs ... you can send it to the [CDC’s] antimicrobial resistance lab network” for testing.
COVID-19 has brought particular challenges. Rodney E. Rohde, PhD, MS, professor and chair, clinical lab science program, Texas State University, San Marcos, said in an interview that he is worried about all the steroids and broad-spectrum antibiotics patients receive.
They’re “being given medical interventions, whether it’s ventilators or [extracorporeal membrane oxygenation] or IVs or central lines or catheters for UTIs and you’re creating highways, right for something that may be right there,” said Dr. Rohde, who was not involved in the CDC study. “It’s a perfect storm, not just for C. auris, but I worry about bacterial resistance agents, too, like MRSA and so forth, having kind of a spike in those types of infections with COVID. So, it’s kind of a doubly dangerous time, I think.”
Multiresistant bacteria are a major health problem, causing illnesses in 2.8 million people annually in the United States, and causing about 35,000 deaths.
Dr. Rohde raised another, rarely mentioned concern. “We’re in crisis mode. People are leaving our field more than they ever had before. The medical laboratory is being decimated because people have burned out after these past 14 months. And so I worry just about competent medical laboratory professionals that are on board to deal with these types of other crises that are popping up within hospitals and long-term care facilities. It kind of keeps me awake.”
Dr. Rohde and Dr. Lyman shared their concern that COVID caused a decrease in screening for other infections and drug-resistant organisms. Bare-bones staffing and shortages of personal protective equipment have likely fueled the spread of these infections as well.
In an outbreak of C. auris in a Florida hospital’s COVID unit in 2020, 35 of 67 patients became colonized, and 6 became ill. The epidemiologists investigating thought that contaminated gowns or gloves, computers, and other equipment were likely sources of transmission.
Low pay, especially in nursing homes, is another problem Dr. Rohde mentioned. It’s an additional problem in both acute and long-term care that “some of the lowest-paid people are the environmental services people, and so the turnover is crazy.” Yet, we rely on them to keep everyone safe. He added that, in addition to pay, he “tries to give them the appreciation and the recognition that they really deserve.”
There are a few specific measures that can be taken to protect patients. Dr. Lyman concluded. “The best way is identifying cases and really ensuring good infection control to prevent the spread.” It’s back to basics – limiting broad-spectrum antibiotics and invasive medical devices, and especially good handwashing and thorough cleaning.
Dr. Lyman and Dr. Rohde have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.