User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Moving beyond the hospital ward
SHM is entering an exciting new chapter in its history because we will soon see Dr. Eric Howell take the reins from Dr. Larry Wellikson as CEO, as we watch Dr. Danielle Scheurer assume the role of president from Dr. Chris Frost, and as a side note, I will try to fill Dr. Scheurer’s shoes as physician editor of The Hospitalist.
This changing of the guard of SHM’s leadership will take place amid the backdrop of an acrimonious presidential election and the emergence of a novel coronavirus that threatens to upend the typical routines of our social and professional lives.
Without a doubt, our leaders, whether national, regional, or local, will be at the helm during one of the most uncertain times in the history of modern health care. Will we see a U.S. President who is a proponent of supporting the Affordable Care Act? Will we see further erosion of Obamacare under a second term of President Trump? Will we see rural hospitals continue to close or shrink1 as their margins get squeezed by skyrocketing denials for inpatient status in favor of observation or outpatient status?2
Forces that seem beyond our control threaten to drastically alter our professions and even our livelihoods. In the space of the few weeks during which I began and finished this piece, every day brought a whole new world of changes in my hospital, town, state, and country. No leader can predict the future with any semblance of certitude.
In the face of these swirling winds of uncertainty, what is clear is that maintaining our commitment as hospitalists to providing evidence-based, high-quality care to our patients while providing support to our colleagues in the health care industry will greatly benefit from collaborating effectively under the “big tent” philosophy of SHM. Over my career, I have benefited from great role models and colleagues as my career took me from primary care med-peds to the “new” field of hospital medicine as a med-peds hospitalist, to a leadership role in pediatric hospital medicine. I have also benefited from “learning opportunities,” as I have made my fair share of mistakes in efforts to improve systems of care. Nearly all of these mistakes share a common thread – not collaborating effectively with critical stakeholders, both within and outside of my institution.3 As this pandemic progresses, I am (and likely you are) witnessing your leaders succeed or fail based on their ability to collaborate across the institution.
As a field, we risk making similar errors by being too narrowly focused as we strive to improve the care of our patients. Recently, Dr. Russell Buhr and his colleagues at the University of California, Los Angeles, demonstrated that a majority of 30-day readmissions for chronic obstructive pulmonary disease (COPD) are due to non-COPD diagnoses.4 As we discharge our COPD patients, we may be satisfied that we’ve “tuned up” our patient’s COPD, but have we adequately arranged for appropriate ongoing care of their other medical problems? This requires an activity undertaken less and less these days in medicine – a conversation between hospitalists and outpatient medical providers. The coronavirus disease 2019 (COVID-19) pandemic has made this more challenging, but I can assure you that you can neither transmit nor catch the coronavirus from a phone call.
Perhaps we can learn from our hospitalist colleagues trained in family medicine. A recent study found that hospitalists in a team made up of family medicine–trained physicians in an academic health center achieved a 33% shorter length of stay for patients from the family medicine clinic, after adjustment for disease, demographics, and disease severity.5 The conclusion of the authors was that this was likely caused by greater familiarity with outpatient resources. I would conjecture that family medicine hospitalists were also more likely to have a conversation with a patient’s outpatient primary care provider (PCP).
Of course, I am the first to admit that chatting with a PCP is not as easy as it used to be – when we could bump into each other in the doctor’s lounge drinking coffee or in radiology while pulling x-ray films (remember those?) – and in the age of COVID-19, these interactions are even less likely. It can take considerable time and effort to get PCP colleagues on the phone unless you’re chummy enough to have their cell phone numbers. And time is a resource in short supply because most hospital medicine groups are understaffed – in the 2018 SHM State of Hospital Medicine (SoHM) Report, 66.4% of responding groups had open positions, with a median of 12% understaffing reported. The 2020 SoHM report is being compiled as we speak, but I suspect this situation will not have improved, and as the pandemic strikes, staffing models have been completely blown up.
To dig ourselves out of this staffing hole and still stay under (or not too over) budget, bringing more advanced practice providers (APP) into our groups/divisions will be needed. We must recognize, however, that APPs can’t just be hired rapidly and thrown into the schedule. As Tracy Cardin, ACNP-BC, SFHM, stated in her December 2019 blog post on the Hospital Leader website, leaders need to implement consistent onboarding, training, and support of APPs, just as they would for any other hospitalist in their group.6 Physician hospitalists need to develop and maintain proven competency in effectively interacting with APPs practicing at the top of their skills and productivity. No time has ever proven the need to allow APPs to practice at the top of their skills than the age of COVID-19.7
But if your “field” doesn’t even recognize you at all? That is the fate of many providers left behind by the field of pediatric hospital medicine. Over the past year, we have seen PHM attain a great achievement in its recognition as a board-certified subspecialty established by the American Board of Pediatrics (ABP), only to have the process beset by allegations of gender and maternal bias. While a groundswell of opposition from pediatric hospitalists triggered by the exclusion of applicants to the Practice Pathway to board certification led the ABP to remove the practice interruption criteria, other potential sources of gender and maternal bias remain.8
This does not even address pediatric hospitalists trained in family medicine who cannot be eligible for PHM board certification through experience or fellowship, med-peds trained pediatric hospitalists who cannot quality because of insufficient time spent on pediatric inpatient care, newborn hospitalists (who do not qualify), and APPs specialized in pediatric inpatient care. While it is completely understandable that the ABP cannot provide a certification pathway for all of these groups, this still leaves a gap for these providers when it comes to being in a professional community that supports their professional development, ongoing education, and training. Fortunately, leaders of the three societies that have significant numbers of pediatric hospitalists – SHM, American Academy of Pediatrics, and Academic Pediatric Association – are working to develop a PHM designation outside of the ABP board certification pathway that will extend the professional community to those left out of board certification.
As we move bravely into this new era of SHM, our clarion call is to collaborate whenever and wherever we can, with our practice administrators, APPs, outpatient providers, subspecialist providers, and patient/family advocates – pandemic or no pandemic. In fact, what this pandemic has shown us is that rapid cycle, fully 360-degree collaboration is the only way hospitalists and hospital leaders will weather the storms of changing reimbursement, pandemics, or politics. This will be our challenge for the next decade, to ensure that SHM collaboratively moves beyond the confines of the hospital ward.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. Frakt A. A Sense of Alarm as Rural Hospitals Keep Closing. The New York Times. 2018. https://www.nytimes.com/2018/10/29/upshot/a-sense-of-alarm-as-rural-hospitals-keep-closing.html. Accessed February 28, 2020.
2. Poonacha TK, Chamoun F. The burden of prior authorizations and denials in health care. Medpage Today’s KevinMD. 2019. https://www.kevinmd.com/blog/2019/12/the-burden-of-prior-authorizations-and-denials-in-health-care.html. Accessed February 28, 2020.
3. 10 reasons healthcare leaders fail and how to prevent them. Becker’s Hospital Review. 2015. https://www.beckershospitalreview.com/hospital-management-administration/10-reasons-healthcare-leaders-fail-and-how-to-prevent-them.html. Accessed March 15, 2020
4. Buhr RG et al. Comorbidity and thirty-day hospital readmission odds in chronic obstructive pulmonary disease: a comparison of the Charlson and Elixhauser comorbidity indices. BMC Health Serv Res. 2019;19:701.
5. Garrison GM et al. Family medicine patients have shorter length of stay when cared for on a family medicine inpatient service. J Prim Care Community Health. 2019. doi: 10.1177/2150132719840517.
6. Cardin T. Work the Program for NP/PAs, and the Program Will Work. The Hospital Leader: Official Blog of SHM. 2019. https://thehospitalleader.org/work-the-program-for-np-pas-and-the-program-will-work/
7. Mittman DE. More physician assistants are ready to help with COVID-19 – now governors must empower them. The Hill. 2020. https://thehill.com/opinion/healthcare/489985-more-physician-assistants-are-ready-to-help-with-covid-19-now-governors. Accessed March 31, 2020.
8. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019;14:630-2.
SHM is entering an exciting new chapter in its history because we will soon see Dr. Eric Howell take the reins from Dr. Larry Wellikson as CEO, as we watch Dr. Danielle Scheurer assume the role of president from Dr. Chris Frost, and as a side note, I will try to fill Dr. Scheurer’s shoes as physician editor of The Hospitalist.
This changing of the guard of SHM’s leadership will take place amid the backdrop of an acrimonious presidential election and the emergence of a novel coronavirus that threatens to upend the typical routines of our social and professional lives.
Without a doubt, our leaders, whether national, regional, or local, will be at the helm during one of the most uncertain times in the history of modern health care. Will we see a U.S. President who is a proponent of supporting the Affordable Care Act? Will we see further erosion of Obamacare under a second term of President Trump? Will we see rural hospitals continue to close or shrink1 as their margins get squeezed by skyrocketing denials for inpatient status in favor of observation or outpatient status?2
Forces that seem beyond our control threaten to drastically alter our professions and even our livelihoods. In the space of the few weeks during which I began and finished this piece, every day brought a whole new world of changes in my hospital, town, state, and country. No leader can predict the future with any semblance of certitude.
In the face of these swirling winds of uncertainty, what is clear is that maintaining our commitment as hospitalists to providing evidence-based, high-quality care to our patients while providing support to our colleagues in the health care industry will greatly benefit from collaborating effectively under the “big tent” philosophy of SHM. Over my career, I have benefited from great role models and colleagues as my career took me from primary care med-peds to the “new” field of hospital medicine as a med-peds hospitalist, to a leadership role in pediatric hospital medicine. I have also benefited from “learning opportunities,” as I have made my fair share of mistakes in efforts to improve systems of care. Nearly all of these mistakes share a common thread – not collaborating effectively with critical stakeholders, both within and outside of my institution.3 As this pandemic progresses, I am (and likely you are) witnessing your leaders succeed or fail based on their ability to collaborate across the institution.
As a field, we risk making similar errors by being too narrowly focused as we strive to improve the care of our patients. Recently, Dr. Russell Buhr and his colleagues at the University of California, Los Angeles, demonstrated that a majority of 30-day readmissions for chronic obstructive pulmonary disease (COPD) are due to non-COPD diagnoses.4 As we discharge our COPD patients, we may be satisfied that we’ve “tuned up” our patient’s COPD, but have we adequately arranged for appropriate ongoing care of their other medical problems? This requires an activity undertaken less and less these days in medicine – a conversation between hospitalists and outpatient medical providers. The coronavirus disease 2019 (COVID-19) pandemic has made this more challenging, but I can assure you that you can neither transmit nor catch the coronavirus from a phone call.
Perhaps we can learn from our hospitalist colleagues trained in family medicine. A recent study found that hospitalists in a team made up of family medicine–trained physicians in an academic health center achieved a 33% shorter length of stay for patients from the family medicine clinic, after adjustment for disease, demographics, and disease severity.5 The conclusion of the authors was that this was likely caused by greater familiarity with outpatient resources. I would conjecture that family medicine hospitalists were also more likely to have a conversation with a patient’s outpatient primary care provider (PCP).
Of course, I am the first to admit that chatting with a PCP is not as easy as it used to be – when we could bump into each other in the doctor’s lounge drinking coffee or in radiology while pulling x-ray films (remember those?) – and in the age of COVID-19, these interactions are even less likely. It can take considerable time and effort to get PCP colleagues on the phone unless you’re chummy enough to have their cell phone numbers. And time is a resource in short supply because most hospital medicine groups are understaffed – in the 2018 SHM State of Hospital Medicine (SoHM) Report, 66.4% of responding groups had open positions, with a median of 12% understaffing reported. The 2020 SoHM report is being compiled as we speak, but I suspect this situation will not have improved, and as the pandemic strikes, staffing models have been completely blown up.
To dig ourselves out of this staffing hole and still stay under (or not too over) budget, bringing more advanced practice providers (APP) into our groups/divisions will be needed. We must recognize, however, that APPs can’t just be hired rapidly and thrown into the schedule. As Tracy Cardin, ACNP-BC, SFHM, stated in her December 2019 blog post on the Hospital Leader website, leaders need to implement consistent onboarding, training, and support of APPs, just as they would for any other hospitalist in their group.6 Physician hospitalists need to develop and maintain proven competency in effectively interacting with APPs practicing at the top of their skills and productivity. No time has ever proven the need to allow APPs to practice at the top of their skills than the age of COVID-19.7
But if your “field” doesn’t even recognize you at all? That is the fate of many providers left behind by the field of pediatric hospital medicine. Over the past year, we have seen PHM attain a great achievement in its recognition as a board-certified subspecialty established by the American Board of Pediatrics (ABP), only to have the process beset by allegations of gender and maternal bias. While a groundswell of opposition from pediatric hospitalists triggered by the exclusion of applicants to the Practice Pathway to board certification led the ABP to remove the practice interruption criteria, other potential sources of gender and maternal bias remain.8
This does not even address pediatric hospitalists trained in family medicine who cannot be eligible for PHM board certification through experience or fellowship, med-peds trained pediatric hospitalists who cannot quality because of insufficient time spent on pediatric inpatient care, newborn hospitalists (who do not qualify), and APPs specialized in pediatric inpatient care. While it is completely understandable that the ABP cannot provide a certification pathway for all of these groups, this still leaves a gap for these providers when it comes to being in a professional community that supports their professional development, ongoing education, and training. Fortunately, leaders of the three societies that have significant numbers of pediatric hospitalists – SHM, American Academy of Pediatrics, and Academic Pediatric Association – are working to develop a PHM designation outside of the ABP board certification pathway that will extend the professional community to those left out of board certification.
As we move bravely into this new era of SHM, our clarion call is to collaborate whenever and wherever we can, with our practice administrators, APPs, outpatient providers, subspecialist providers, and patient/family advocates – pandemic or no pandemic. In fact, what this pandemic has shown us is that rapid cycle, fully 360-degree collaboration is the only way hospitalists and hospital leaders will weather the storms of changing reimbursement, pandemics, or politics. This will be our challenge for the next decade, to ensure that SHM collaboratively moves beyond the confines of the hospital ward.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. Frakt A. A Sense of Alarm as Rural Hospitals Keep Closing. The New York Times. 2018. https://www.nytimes.com/2018/10/29/upshot/a-sense-of-alarm-as-rural-hospitals-keep-closing.html. Accessed February 28, 2020.
2. Poonacha TK, Chamoun F. The burden of prior authorizations and denials in health care. Medpage Today’s KevinMD. 2019. https://www.kevinmd.com/blog/2019/12/the-burden-of-prior-authorizations-and-denials-in-health-care.html. Accessed February 28, 2020.
3. 10 reasons healthcare leaders fail and how to prevent them. Becker’s Hospital Review. 2015. https://www.beckershospitalreview.com/hospital-management-administration/10-reasons-healthcare-leaders-fail-and-how-to-prevent-them.html. Accessed March 15, 2020
4. Buhr RG et al. Comorbidity and thirty-day hospital readmission odds in chronic obstructive pulmonary disease: a comparison of the Charlson and Elixhauser comorbidity indices. BMC Health Serv Res. 2019;19:701.
5. Garrison GM et al. Family medicine patients have shorter length of stay when cared for on a family medicine inpatient service. J Prim Care Community Health. 2019. doi: 10.1177/2150132719840517.
6. Cardin T. Work the Program for NP/PAs, and the Program Will Work. The Hospital Leader: Official Blog of SHM. 2019. https://thehospitalleader.org/work-the-program-for-np-pas-and-the-program-will-work/
7. Mittman DE. More physician assistants are ready to help with COVID-19 – now governors must empower them. The Hill. 2020. https://thehill.com/opinion/healthcare/489985-more-physician-assistants-are-ready-to-help-with-covid-19-now-governors. Accessed March 31, 2020.
8. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019;14:630-2.
SHM is entering an exciting new chapter in its history because we will soon see Dr. Eric Howell take the reins from Dr. Larry Wellikson as CEO, as we watch Dr. Danielle Scheurer assume the role of president from Dr. Chris Frost, and as a side note, I will try to fill Dr. Scheurer’s shoes as physician editor of The Hospitalist.
This changing of the guard of SHM’s leadership will take place amid the backdrop of an acrimonious presidential election and the emergence of a novel coronavirus that threatens to upend the typical routines of our social and professional lives.
Without a doubt, our leaders, whether national, regional, or local, will be at the helm during one of the most uncertain times in the history of modern health care. Will we see a U.S. President who is a proponent of supporting the Affordable Care Act? Will we see further erosion of Obamacare under a second term of President Trump? Will we see rural hospitals continue to close or shrink1 as their margins get squeezed by skyrocketing denials for inpatient status in favor of observation or outpatient status?2
Forces that seem beyond our control threaten to drastically alter our professions and even our livelihoods. In the space of the few weeks during which I began and finished this piece, every day brought a whole new world of changes in my hospital, town, state, and country. No leader can predict the future with any semblance of certitude.
In the face of these swirling winds of uncertainty, what is clear is that maintaining our commitment as hospitalists to providing evidence-based, high-quality care to our patients while providing support to our colleagues in the health care industry will greatly benefit from collaborating effectively under the “big tent” philosophy of SHM. Over my career, I have benefited from great role models and colleagues as my career took me from primary care med-peds to the “new” field of hospital medicine as a med-peds hospitalist, to a leadership role in pediatric hospital medicine. I have also benefited from “learning opportunities,” as I have made my fair share of mistakes in efforts to improve systems of care. Nearly all of these mistakes share a common thread – not collaborating effectively with critical stakeholders, both within and outside of my institution.3 As this pandemic progresses, I am (and likely you are) witnessing your leaders succeed or fail based on their ability to collaborate across the institution.
As a field, we risk making similar errors by being too narrowly focused as we strive to improve the care of our patients. Recently, Dr. Russell Buhr and his colleagues at the University of California, Los Angeles, demonstrated that a majority of 30-day readmissions for chronic obstructive pulmonary disease (COPD) are due to non-COPD diagnoses.4 As we discharge our COPD patients, we may be satisfied that we’ve “tuned up” our patient’s COPD, but have we adequately arranged for appropriate ongoing care of their other medical problems? This requires an activity undertaken less and less these days in medicine – a conversation between hospitalists and outpatient medical providers. The coronavirus disease 2019 (COVID-19) pandemic has made this more challenging, but I can assure you that you can neither transmit nor catch the coronavirus from a phone call.
Perhaps we can learn from our hospitalist colleagues trained in family medicine. A recent study found that hospitalists in a team made up of family medicine–trained physicians in an academic health center achieved a 33% shorter length of stay for patients from the family medicine clinic, after adjustment for disease, demographics, and disease severity.5 The conclusion of the authors was that this was likely caused by greater familiarity with outpatient resources. I would conjecture that family medicine hospitalists were also more likely to have a conversation with a patient’s outpatient primary care provider (PCP).
Of course, I am the first to admit that chatting with a PCP is not as easy as it used to be – when we could bump into each other in the doctor’s lounge drinking coffee or in radiology while pulling x-ray films (remember those?) – and in the age of COVID-19, these interactions are even less likely. It can take considerable time and effort to get PCP colleagues on the phone unless you’re chummy enough to have their cell phone numbers. And time is a resource in short supply because most hospital medicine groups are understaffed – in the 2018 SHM State of Hospital Medicine (SoHM) Report, 66.4% of responding groups had open positions, with a median of 12% understaffing reported. The 2020 SoHM report is being compiled as we speak, but I suspect this situation will not have improved, and as the pandemic strikes, staffing models have been completely blown up.
To dig ourselves out of this staffing hole and still stay under (or not too over) budget, bringing more advanced practice providers (APP) into our groups/divisions will be needed. We must recognize, however, that APPs can’t just be hired rapidly and thrown into the schedule. As Tracy Cardin, ACNP-BC, SFHM, stated in her December 2019 blog post on the Hospital Leader website, leaders need to implement consistent onboarding, training, and support of APPs, just as they would for any other hospitalist in their group.6 Physician hospitalists need to develop and maintain proven competency in effectively interacting with APPs practicing at the top of their skills and productivity. No time has ever proven the need to allow APPs to practice at the top of their skills than the age of COVID-19.7
But if your “field” doesn’t even recognize you at all? That is the fate of many providers left behind by the field of pediatric hospital medicine. Over the past year, we have seen PHM attain a great achievement in its recognition as a board-certified subspecialty established by the American Board of Pediatrics (ABP), only to have the process beset by allegations of gender and maternal bias. While a groundswell of opposition from pediatric hospitalists triggered by the exclusion of applicants to the Practice Pathway to board certification led the ABP to remove the practice interruption criteria, other potential sources of gender and maternal bias remain.8
This does not even address pediatric hospitalists trained in family medicine who cannot be eligible for PHM board certification through experience or fellowship, med-peds trained pediatric hospitalists who cannot quality because of insufficient time spent on pediatric inpatient care, newborn hospitalists (who do not qualify), and APPs specialized in pediatric inpatient care. While it is completely understandable that the ABP cannot provide a certification pathway for all of these groups, this still leaves a gap for these providers when it comes to being in a professional community that supports their professional development, ongoing education, and training. Fortunately, leaders of the three societies that have significant numbers of pediatric hospitalists – SHM, American Academy of Pediatrics, and Academic Pediatric Association – are working to develop a PHM designation outside of the ABP board certification pathway that will extend the professional community to those left out of board certification.
As we move bravely into this new era of SHM, our clarion call is to collaborate whenever and wherever we can, with our practice administrators, APPs, outpatient providers, subspecialist providers, and patient/family advocates – pandemic or no pandemic. In fact, what this pandemic has shown us is that rapid cycle, fully 360-degree collaboration is the only way hospitalists and hospital leaders will weather the storms of changing reimbursement, pandemics, or politics. This will be our challenge for the next decade, to ensure that SHM collaboratively moves beyond the confines of the hospital ward.
Dr. Chang is chief of pediatric hospital medicine at Baystate Children’s Hospital in Springfield, Mass., and associate professor of pediatrics at the University of Massachusetts, also in Springfield.
References
1. Frakt A. A Sense of Alarm as Rural Hospitals Keep Closing. The New York Times. 2018. https://www.nytimes.com/2018/10/29/upshot/a-sense-of-alarm-as-rural-hospitals-keep-closing.html. Accessed February 28, 2020.
2. Poonacha TK, Chamoun F. The burden of prior authorizations and denials in health care. Medpage Today’s KevinMD. 2019. https://www.kevinmd.com/blog/2019/12/the-burden-of-prior-authorizations-and-denials-in-health-care.html. Accessed February 28, 2020.
3. 10 reasons healthcare leaders fail and how to prevent them. Becker’s Hospital Review. 2015. https://www.beckershospitalreview.com/hospital-management-administration/10-reasons-healthcare-leaders-fail-and-how-to-prevent-them.html. Accessed March 15, 2020
4. Buhr RG et al. Comorbidity and thirty-day hospital readmission odds in chronic obstructive pulmonary disease: a comparison of the Charlson and Elixhauser comorbidity indices. BMC Health Serv Res. 2019;19:701.
5. Garrison GM et al. Family medicine patients have shorter length of stay when cared for on a family medicine inpatient service. J Prim Care Community Health. 2019. doi: 10.1177/2150132719840517.
6. Cardin T. Work the Program for NP/PAs, and the Program Will Work. The Hospital Leader: Official Blog of SHM. 2019. https://thehospitalleader.org/work-the-program-for-np-pas-and-the-program-will-work/
7. Mittman DE. More physician assistants are ready to help with COVID-19 – now governors must empower them. The Hill. 2020. https://thehill.com/opinion/healthcare/489985-more-physician-assistants-are-ready-to-help-with-covid-19-now-governors. Accessed March 31, 2020.
8. Gold JM et al. Collective action and effective dialogue to address gender bias in medicine. J Hosp Med. 2019;14:630-2.
Multisociety roadmap eyes restarting elective cardiac cases
As COVID-19 case levels plateau in some regions, 16 North American cardiovascular societies have released a framework for reintroducing cardiovascular services disrupted by the pandemic.
The consensus document outlines a phased approach to restarting invasive cardiovascular (CV) procedures and diagnostic tests that aims to reduce patient and health care provider exposure to the coronavirus and still provide essential care. It also emphasizes some of the ethical considerations in patient selection and the need for a collaborative approach.
“The key message in our document is we need a new unprecedented collaboration with public health officials so that we can carefully monitor the situation and we’re aware of what’s happening with the penetrance of the pandemic in the community, but they’re aware of the morbidity and mortality that’s occurring on our ever-growing waiting list,” lead author David A. Wood, MD, told theheart.org | Medscape Cardiology.
The recommendations were jointly published May 4 in the Canadian Journal of Cardiology , the Journal of the American College of Cardiology, and The Annals of Thoracic Surgery, and are endorsed by, among others, the American Heart Association, American College of Cardiology (ACC), and Canadian Cardiovascular Society.
The guidance comes as hospitals are facing revenue shortfalls because of canceled elective procedures and resource-intensive COVID-19 cases, prompting some healthcare systems to furlough, lay off, or even fire staff.
“It’s obvious that volumes are down between 40% and 60%,” said Wood, director of the cardiac catheterization laboratory at Vancouver General Hospital and professor of medicine at the University of British Columbia, Canada. “Part of that is that some areas have restricted case volumes totally appropriately and it’s partly because patients are very afraid of coming to the hospital and, unfortunately, are having bad events at home. And some are dying.”
The new report features a detailed table outlining three different response levels: reintroduction of some services (level 2); reintroduction of most services (level 1); and regular services (level 0). It covers a range of services from transthoracic echocardiography and exercise testing with imaging to care for acute coronary syndrome and ST-segment elevation myocardial infarction.
“We’ve learned that we can very quickly turn off the tap and go to doing only 10% of our normal volumes, whether that’s surgery, cath lab, EP, diagnostic tests,” Wood said. “It’s much more difficult to thoughtfully turn the tap part way back on or restart the engine … you don’t just go from 0 to 100 [mph]. You go from 0 to 30 to 60 then maybe to 80 [mph].”
The document also includes eight guiding principles such as:
- The expectation that response levels will be different between regions, and even within a given region.
- A “transparent collaborative plan” for COVID-19 testing and personal protective equipment (PPE) must be in place before restarting cases.
- A less invasive test or alternate imaging modality should be considered, if both tests have similar efficacy.
- In general, a minimally invasive procedure with a shorter length of stay is preferable, if both strategies have similar efficacy and safety.
Although previous reports on cath lab considerations during the pandemic or restarting elective surgeries peg various actions to specific thresholds or time intervals, the language here is noticeably and intentionally broad.
Instead of stating when cardiovascular services should resume, for example, the experts say it’s appropriate to put the guidance document into place if there’s a “sustained reduction” in the rate of new COVID-19 admissions and deaths in the relevant geographic region for a “prespecified time interval.”
As for when or how frequently patients and healthcare providers should be tested for COVID-19, the document encourages “routine screening of all patients prior to any cardiovascular procedure or test.”
Overly prescriptive language in previous documents wasn’t felt to be that helpful, whereas language like “selective” cases and “some” or “most” cardiovascular procedures gives clinicians, health systems, and policy makers flexibility when moving between response levels, Wood explained.
“Different regions might be at different levels based on principles of public health as far as the penetrance of the pandemic in that community, as well as how can you actually do the physical distancing in your hospital or ambulatory clinic. Because, I tell you, that is the Achilles heel,” he said. “Our run rates are going to be determined by testing, the availability of PPE, but also how we’re going to use our existing infrastructure and maintain physical distancing.”
That may mean using telehealth for initial visits, having clinics open earlier in the morning or on weekends, or doing partial volumes for surgery or in the cath lab so patients can be staggered and recover at different times and in different areas of the hospital. “These are very granular, specific infrastructure things that we’ve never really had to consider before,” Wood observed.
The document also had to be flexible and nimble enough to respond to a potential rebound of COVID-19 cases, which in newly released models are projected to rise sharply to 200,000 cases a day and be accompanied by some 3,000 deaths each day by June 1.
“This is my own personal opinion but I think it’s foolish to think that we are going to be able to come back to 100% of the cases we were doing before, even with testing, PPE, and all of that until we have a vaccine,” he said.
Similar to decisions made in preparation for the initial COVID-19 surge, the consensus document outlines the need for ethical considerations when turning the tap back on. This means prioritizing procedures and tests that are likely to benefit more people and to a greater degree, and ensuring that patients are treated fairly and consistently, regardless of their ethnicity, perceived social worth, or ability to pay, said coauthor and ACC President Athena Poppas, MD, Brown University School of Medicine, Providence, Rhode Island.
“It’s an ethical tenet that exists in a lot of places but it’s usually not overtly called out,” Poppas told theheart.org | Medscape Cardiology. “It’s not rationing care; I think people jump to that but it’s actually the opposite of rationing care. It’s about being thoughtful about prioritizing patients.”
“There’s a variety of data that should help in the prioritization, not only how much hospital resources are utilized, that’s on one side, but there’s also the patient risk of delaying or doing a procedure, and then the societal risk,” she said.
Susheel Kodali, MD, of New York–Presbyterian Hospital/Columbia University Irving Medical Center, who recently published recommendations on restructuring structural heart disease practice during the pandemic, said the document is timely as centers, including his own, are trying to restart some outpatient visits, as early as next week.
“They made a point about talking about cohesive partnerships with regional public health officials and I think that’s great. The question is how does that happen,” he told theheart.org | Medscape Cardiology. “In New York, we’re not allowed to do elective cases but what’s considered elective is not so clearly defined. An AS [aortic stenosis] patient that had a syncopal episode 2 weeks ago, is that considered elective or is that semi-urgent? I think that’s one of the challenges and that’s where these partnerships would be useful.”
Other challenges include the need for regional partnerships to better align hospitals, which in the New York area means half a dozen large healthcare systems, and to coordinate care between hospital departments – all of which will be scheduling imaging and OR time for their own backlog of hernia, knee, or hip surgeries.
Finally, there’s the need for a lot of conversation with the patient and their family about returning to a hospital amid a deadly pandemic.
“I had a patient today and the daughter was very concerned about bringing her in,” Kodali said. “She’s in class IV heart failure but her [daughter’s] big concern was: who is she going to be exposed to when she gets the echo? What kind of protection is there for her? Is the tech wearing a mask?
“It’s not just the health care providers that have to have the comfort, but it’s the patients and their families who have to feel comfortable bringing their loved ones here for treatment,” he said. “Because everyone is concerned about the environment.”
Wood reports receiving unrestricted grant support from Edwards Lifesciences and Abbott Vascular and serving as a consultant for Edwards Lifesciences, Medtronic, Abbott Vascular, and Boston Scientific. Poppas reports no relevant conflicts of interest. Kodali reports consultant (honoraria) from Admedus, Meril Life Sciences, JenaValve, and Abbott Vascular; SAB (equity) from Dura Biotech, MicroInterventional Devices, Thubrikar Aortic Valve, Supira, and Admedus; and institutional funding from Edwards Lifesciences, Medtronic, Abbott Vascular, Boston Scientific, and JenaValve.
This article first appeared on Medscape.com.
As COVID-19 case levels plateau in some regions, 16 North American cardiovascular societies have released a framework for reintroducing cardiovascular services disrupted by the pandemic.
The consensus document outlines a phased approach to restarting invasive cardiovascular (CV) procedures and diagnostic tests that aims to reduce patient and health care provider exposure to the coronavirus and still provide essential care. It also emphasizes some of the ethical considerations in patient selection and the need for a collaborative approach.
“The key message in our document is we need a new unprecedented collaboration with public health officials so that we can carefully monitor the situation and we’re aware of what’s happening with the penetrance of the pandemic in the community, but they’re aware of the morbidity and mortality that’s occurring on our ever-growing waiting list,” lead author David A. Wood, MD, told theheart.org | Medscape Cardiology.
The recommendations were jointly published May 4 in the Canadian Journal of Cardiology , the Journal of the American College of Cardiology, and The Annals of Thoracic Surgery, and are endorsed by, among others, the American Heart Association, American College of Cardiology (ACC), and Canadian Cardiovascular Society.
The guidance comes as hospitals are facing revenue shortfalls because of canceled elective procedures and resource-intensive COVID-19 cases, prompting some healthcare systems to furlough, lay off, or even fire staff.
“It’s obvious that volumes are down between 40% and 60%,” said Wood, director of the cardiac catheterization laboratory at Vancouver General Hospital and professor of medicine at the University of British Columbia, Canada. “Part of that is that some areas have restricted case volumes totally appropriately and it’s partly because patients are very afraid of coming to the hospital and, unfortunately, are having bad events at home. And some are dying.”
The new report features a detailed table outlining three different response levels: reintroduction of some services (level 2); reintroduction of most services (level 1); and regular services (level 0). It covers a range of services from transthoracic echocardiography and exercise testing with imaging to care for acute coronary syndrome and ST-segment elevation myocardial infarction.
“We’ve learned that we can very quickly turn off the tap and go to doing only 10% of our normal volumes, whether that’s surgery, cath lab, EP, diagnostic tests,” Wood said. “It’s much more difficult to thoughtfully turn the tap part way back on or restart the engine … you don’t just go from 0 to 100 [mph]. You go from 0 to 30 to 60 then maybe to 80 [mph].”
The document also includes eight guiding principles such as:
- The expectation that response levels will be different between regions, and even within a given region.
- A “transparent collaborative plan” for COVID-19 testing and personal protective equipment (PPE) must be in place before restarting cases.
- A less invasive test or alternate imaging modality should be considered, if both tests have similar efficacy.
- In general, a minimally invasive procedure with a shorter length of stay is preferable, if both strategies have similar efficacy and safety.
Although previous reports on cath lab considerations during the pandemic or restarting elective surgeries peg various actions to specific thresholds or time intervals, the language here is noticeably and intentionally broad.
Instead of stating when cardiovascular services should resume, for example, the experts say it’s appropriate to put the guidance document into place if there’s a “sustained reduction” in the rate of new COVID-19 admissions and deaths in the relevant geographic region for a “prespecified time interval.”
As for when or how frequently patients and healthcare providers should be tested for COVID-19, the document encourages “routine screening of all patients prior to any cardiovascular procedure or test.”
Overly prescriptive language in previous documents wasn’t felt to be that helpful, whereas language like “selective” cases and “some” or “most” cardiovascular procedures gives clinicians, health systems, and policy makers flexibility when moving between response levels, Wood explained.
“Different regions might be at different levels based on principles of public health as far as the penetrance of the pandemic in that community, as well as how can you actually do the physical distancing in your hospital or ambulatory clinic. Because, I tell you, that is the Achilles heel,” he said. “Our run rates are going to be determined by testing, the availability of PPE, but also how we’re going to use our existing infrastructure and maintain physical distancing.”
That may mean using telehealth for initial visits, having clinics open earlier in the morning or on weekends, or doing partial volumes for surgery or in the cath lab so patients can be staggered and recover at different times and in different areas of the hospital. “These are very granular, specific infrastructure things that we’ve never really had to consider before,” Wood observed.
The document also had to be flexible and nimble enough to respond to a potential rebound of COVID-19 cases, which in newly released models are projected to rise sharply to 200,000 cases a day and be accompanied by some 3,000 deaths each day by June 1.
“This is my own personal opinion but I think it’s foolish to think that we are going to be able to come back to 100% of the cases we were doing before, even with testing, PPE, and all of that until we have a vaccine,” he said.
Similar to decisions made in preparation for the initial COVID-19 surge, the consensus document outlines the need for ethical considerations when turning the tap back on. This means prioritizing procedures and tests that are likely to benefit more people and to a greater degree, and ensuring that patients are treated fairly and consistently, regardless of their ethnicity, perceived social worth, or ability to pay, said coauthor and ACC President Athena Poppas, MD, Brown University School of Medicine, Providence, Rhode Island.
“It’s an ethical tenet that exists in a lot of places but it’s usually not overtly called out,” Poppas told theheart.org | Medscape Cardiology. “It’s not rationing care; I think people jump to that but it’s actually the opposite of rationing care. It’s about being thoughtful about prioritizing patients.”
“There’s a variety of data that should help in the prioritization, not only how much hospital resources are utilized, that’s on one side, but there’s also the patient risk of delaying or doing a procedure, and then the societal risk,” she said.
Susheel Kodali, MD, of New York–Presbyterian Hospital/Columbia University Irving Medical Center, who recently published recommendations on restructuring structural heart disease practice during the pandemic, said the document is timely as centers, including his own, are trying to restart some outpatient visits, as early as next week.
“They made a point about talking about cohesive partnerships with regional public health officials and I think that’s great. The question is how does that happen,” he told theheart.org | Medscape Cardiology. “In New York, we’re not allowed to do elective cases but what’s considered elective is not so clearly defined. An AS [aortic stenosis] patient that had a syncopal episode 2 weeks ago, is that considered elective or is that semi-urgent? I think that’s one of the challenges and that’s where these partnerships would be useful.”
Other challenges include the need for regional partnerships to better align hospitals, which in the New York area means half a dozen large healthcare systems, and to coordinate care between hospital departments – all of which will be scheduling imaging and OR time for their own backlog of hernia, knee, or hip surgeries.
Finally, there’s the need for a lot of conversation with the patient and their family about returning to a hospital amid a deadly pandemic.
“I had a patient today and the daughter was very concerned about bringing her in,” Kodali said. “She’s in class IV heart failure but her [daughter’s] big concern was: who is she going to be exposed to when she gets the echo? What kind of protection is there for her? Is the tech wearing a mask?
“It’s not just the health care providers that have to have the comfort, but it’s the patients and their families who have to feel comfortable bringing their loved ones here for treatment,” he said. “Because everyone is concerned about the environment.”
Wood reports receiving unrestricted grant support from Edwards Lifesciences and Abbott Vascular and serving as a consultant for Edwards Lifesciences, Medtronic, Abbott Vascular, and Boston Scientific. Poppas reports no relevant conflicts of interest. Kodali reports consultant (honoraria) from Admedus, Meril Life Sciences, JenaValve, and Abbott Vascular; SAB (equity) from Dura Biotech, MicroInterventional Devices, Thubrikar Aortic Valve, Supira, and Admedus; and institutional funding from Edwards Lifesciences, Medtronic, Abbott Vascular, Boston Scientific, and JenaValve.
This article first appeared on Medscape.com.
As COVID-19 case levels plateau in some regions, 16 North American cardiovascular societies have released a framework for reintroducing cardiovascular services disrupted by the pandemic.
The consensus document outlines a phased approach to restarting invasive cardiovascular (CV) procedures and diagnostic tests that aims to reduce patient and health care provider exposure to the coronavirus and still provide essential care. It also emphasizes some of the ethical considerations in patient selection and the need for a collaborative approach.
“The key message in our document is we need a new unprecedented collaboration with public health officials so that we can carefully monitor the situation and we’re aware of what’s happening with the penetrance of the pandemic in the community, but they’re aware of the morbidity and mortality that’s occurring on our ever-growing waiting list,” lead author David A. Wood, MD, told theheart.org | Medscape Cardiology.
The recommendations were jointly published May 4 in the Canadian Journal of Cardiology , the Journal of the American College of Cardiology, and The Annals of Thoracic Surgery, and are endorsed by, among others, the American Heart Association, American College of Cardiology (ACC), and Canadian Cardiovascular Society.
The guidance comes as hospitals are facing revenue shortfalls because of canceled elective procedures and resource-intensive COVID-19 cases, prompting some healthcare systems to furlough, lay off, or even fire staff.
“It’s obvious that volumes are down between 40% and 60%,” said Wood, director of the cardiac catheterization laboratory at Vancouver General Hospital and professor of medicine at the University of British Columbia, Canada. “Part of that is that some areas have restricted case volumes totally appropriately and it’s partly because patients are very afraid of coming to the hospital and, unfortunately, are having bad events at home. And some are dying.”
The new report features a detailed table outlining three different response levels: reintroduction of some services (level 2); reintroduction of most services (level 1); and regular services (level 0). It covers a range of services from transthoracic echocardiography and exercise testing with imaging to care for acute coronary syndrome and ST-segment elevation myocardial infarction.
“We’ve learned that we can very quickly turn off the tap and go to doing only 10% of our normal volumes, whether that’s surgery, cath lab, EP, diagnostic tests,” Wood said. “It’s much more difficult to thoughtfully turn the tap part way back on or restart the engine … you don’t just go from 0 to 100 [mph]. You go from 0 to 30 to 60 then maybe to 80 [mph].”
The document also includes eight guiding principles such as:
- The expectation that response levels will be different between regions, and even within a given region.
- A “transparent collaborative plan” for COVID-19 testing and personal protective equipment (PPE) must be in place before restarting cases.
- A less invasive test or alternate imaging modality should be considered, if both tests have similar efficacy.
- In general, a minimally invasive procedure with a shorter length of stay is preferable, if both strategies have similar efficacy and safety.
Although previous reports on cath lab considerations during the pandemic or restarting elective surgeries peg various actions to specific thresholds or time intervals, the language here is noticeably and intentionally broad.
Instead of stating when cardiovascular services should resume, for example, the experts say it’s appropriate to put the guidance document into place if there’s a “sustained reduction” in the rate of new COVID-19 admissions and deaths in the relevant geographic region for a “prespecified time interval.”
As for when or how frequently patients and healthcare providers should be tested for COVID-19, the document encourages “routine screening of all patients prior to any cardiovascular procedure or test.”
Overly prescriptive language in previous documents wasn’t felt to be that helpful, whereas language like “selective” cases and “some” or “most” cardiovascular procedures gives clinicians, health systems, and policy makers flexibility when moving between response levels, Wood explained.
“Different regions might be at different levels based on principles of public health as far as the penetrance of the pandemic in that community, as well as how can you actually do the physical distancing in your hospital or ambulatory clinic. Because, I tell you, that is the Achilles heel,” he said. “Our run rates are going to be determined by testing, the availability of PPE, but also how we’re going to use our existing infrastructure and maintain physical distancing.”
That may mean using telehealth for initial visits, having clinics open earlier in the morning or on weekends, or doing partial volumes for surgery or in the cath lab so patients can be staggered and recover at different times and in different areas of the hospital. “These are very granular, specific infrastructure things that we’ve never really had to consider before,” Wood observed.
The document also had to be flexible and nimble enough to respond to a potential rebound of COVID-19 cases, which in newly released models are projected to rise sharply to 200,000 cases a day and be accompanied by some 3,000 deaths each day by June 1.
“This is my own personal opinion but I think it’s foolish to think that we are going to be able to come back to 100% of the cases we were doing before, even with testing, PPE, and all of that until we have a vaccine,” he said.
Similar to decisions made in preparation for the initial COVID-19 surge, the consensus document outlines the need for ethical considerations when turning the tap back on. This means prioritizing procedures and tests that are likely to benefit more people and to a greater degree, and ensuring that patients are treated fairly and consistently, regardless of their ethnicity, perceived social worth, or ability to pay, said coauthor and ACC President Athena Poppas, MD, Brown University School of Medicine, Providence, Rhode Island.
“It’s an ethical tenet that exists in a lot of places but it’s usually not overtly called out,” Poppas told theheart.org | Medscape Cardiology. “It’s not rationing care; I think people jump to that but it’s actually the opposite of rationing care. It’s about being thoughtful about prioritizing patients.”
“There’s a variety of data that should help in the prioritization, not only how much hospital resources are utilized, that’s on one side, but there’s also the patient risk of delaying or doing a procedure, and then the societal risk,” she said.
Susheel Kodali, MD, of New York–Presbyterian Hospital/Columbia University Irving Medical Center, who recently published recommendations on restructuring structural heart disease practice during the pandemic, said the document is timely as centers, including his own, are trying to restart some outpatient visits, as early as next week.
“They made a point about talking about cohesive partnerships with regional public health officials and I think that’s great. The question is how does that happen,” he told theheart.org | Medscape Cardiology. “In New York, we’re not allowed to do elective cases but what’s considered elective is not so clearly defined. An AS [aortic stenosis] patient that had a syncopal episode 2 weeks ago, is that considered elective or is that semi-urgent? I think that’s one of the challenges and that’s where these partnerships would be useful.”
Other challenges include the need for regional partnerships to better align hospitals, which in the New York area means half a dozen large healthcare systems, and to coordinate care between hospital departments – all of which will be scheduling imaging and OR time for their own backlog of hernia, knee, or hip surgeries.
Finally, there’s the need for a lot of conversation with the patient and their family about returning to a hospital amid a deadly pandemic.
“I had a patient today and the daughter was very concerned about bringing her in,” Kodali said. “She’s in class IV heart failure but her [daughter’s] big concern was: who is she going to be exposed to when she gets the echo? What kind of protection is there for her? Is the tech wearing a mask?
“It’s not just the health care providers that have to have the comfort, but it’s the patients and their families who have to feel comfortable bringing their loved ones here for treatment,” he said. “Because everyone is concerned about the environment.”
Wood reports receiving unrestricted grant support from Edwards Lifesciences and Abbott Vascular and serving as a consultant for Edwards Lifesciences, Medtronic, Abbott Vascular, and Boston Scientific. Poppas reports no relevant conflicts of interest. Kodali reports consultant (honoraria) from Admedus, Meril Life Sciences, JenaValve, and Abbott Vascular; SAB (equity) from Dura Biotech, MicroInterventional Devices, Thubrikar Aortic Valve, Supira, and Admedus; and institutional funding from Edwards Lifesciences, Medtronic, Abbott Vascular, Boston Scientific, and JenaValve.
This article first appeared on Medscape.com.
Triage, L&D, postpartum care during the COVID-19 pandemic
The meteoric rise in the number of test-positive and clinical cases of COVID-19 because of infection with the SARS coronavirus (SARS-CoV-2) in states and cities across the United States has added urgency to the efforts to develop protocols for hospital triage, admission, labor and delivery management, and other aspects of obstetrical care.
Emerging data suggest that, while SARS-CoV-2 is less lethal overall than the severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) proved to be, it is significantly more contagious. Although a severe disease, the limited worldwide data so far available (as of early May) do not indicate that pregnant women are at greater risk of severe disease, compared with the general population. However, there remains a critical need for data on maternal and perinatal outcomes in women infected with SARS-CoV-2.
Multiple physiological changes in pregnancy, from reduced cell-based immune competence to changes in respiratory tract and pulmonary function – e.g., edema of the respiratory tract, increases in secretions and oxygen consumption, elevation of the diaphragm, and decrease in functional residual capacity – have historically contributed to worse obstetric outcomes in pregnant women who have had viral pneumonias. Furthermore, limited published experience with COVID-19 in China suggests worse perinatal outcomes in some affected pregnancies, including prematurity and perinatal death.
With evolution of the pandemic and accumulation of experience, it is expected that data-driven guidelines on assessment and management of infected pregnant women will contribute to improved maternal and perinatal outcomes. What is clear now, however, is that,
Here are my recommendations, based on a currently limited body of literature on COVID-19 and other communicable viral respiratory disorders, as well my experience in the greater Detroit area, a COVID-19 hot spot.
Preparing for hospital evaluation and admission
The obstetric triage or labor and delivery (L&D) unit should be notified prior to the arrival of a patient suspected of or known to be infected with the virus. This will minimize staff exposure and allow sufficient time to prepare appropriate accommodations, equipment, and supplies for the patient’s care. Hospital infection control should be promptly notified by L&D of the expected arrival of such a patient. Placement ideally should be in a negative-pressure room, which allows outside air to flow into the room but prevents contaminated air from escaping. In the absence of a negative-pressure room, an infection isolation area should be utilized.
The patient and one accompanying support individual should wear either medical-grade masks brought from home or supplied upon entry to the hospital or homemade masks or bandanas. This will reduce the risk of viral transmission to hospital workers and other individuals encountered in the hospital prior to arriving in L&D. An ideal setup is to have separate entry areas, access corridors, and elevators for patients known or suspected to have COVID-19 infection. The patient and visitor should be expeditiously escorted to the prepared area for evaluation. Patients who are not known or suspected to be infected ideally should be tested.
Screening of patients & support individuals
Proper screening of patients and support individuals is critical to protecting both patients and staff in the L&D unit. This should include an expanded questionnaire that asks about disturbances of smell and taste and GI symptoms like loss of appetite – not only the more commonly queried symptoms of fever, shortness of breath, coughing, and exposure to someone who may have been ill.
Recent studies regarding presenting symptoms cast significant doubt, in fact, on the validity of patients with “asymptomatic COVID-19.” Over 15% of patients with confirmed infection in one published case series had solely GI symptoms and almost all had some digestive symptoms, for example, and almost 90% in another study had absent or reduced sense of smell and/or taste.1,2 In fact, the use of the term “paucisymptomatic” rather than “asymptomatic” may be most appropriate.
Support individuals also should undergo temperature screening, ideally with laser noncontact thermometers on entry to the hospital or triage.
Visitor policy
The number of visitors/support individuals should be kept to a minimum to reduce transmission risk. The actual number will be determined by hospital or state policy, but up to one visitor in the labor room appears reasonable. Very strong individual justification should be required to exceed this threshold! The visitor should not only be screened for an expanded list of symptoms, but they also should be queried for underlying illnesses (e.g., diabetes, cardiovascular disease, significant lung disease, undergoing cancer therapy) as well as for age over 65 years, each of which increase the chances of severe COVID-19 disease should infection occur. The visitor should be informed of such risks and, especially when accompanying a patient with known or suspected COVID-19, provided the option of voluntarily revoking their visitor status. A visitor with known or suspected COVID-19 infection based on testing or screening should not be allowed into the L&D unit.
In addition, institutions may be considered to have obligations to the visitor/support person beyond screening. These include instructions in proper mask usage, hand washing, and limiting the touching of surfaces to lower infection risk.
“Visitor relays” where one visitor replaces another should be strongly discouraged. Visitors should similarly not be allowed to wander around the hospital (to use phones, for instance); transiting back and forth to obtain food and coffee should be kept to a strict minimum. For visitors accompanying COVID-19–-infected women, “visitor’s plates” provided by the hospital at reasonable cost is a much-preferred arrangement for obtaining meals during the course of the hospital stay. In addition, visitors should be sent out of the room during the performance of aerosolizing procedures.
Labor and delivery management
The successful management of patients with COVID-19 requires a rigorous infection control protocol informed by guidelines from national entities, such as the Centers for Disease Control and Prevention, the Society for Maternal-Fetal Medicine, and the American College of Obstetricians and Gynecologists, and by state health departments when available.
Strict limits on the number of obstetricians and other health care workers (HCWs) entering the patient’s room should be enforced and documented to minimize risk to the HCWs attending to patients who have a positive diagnosis or who are under investigation. Only in cases of demonstrable clinical benefit should repeat visits by the same or additional HCWs be permitted. Conventional and electronic tablets present an excellent opportunity for patient follow-up visits without room entry. In our institution, this has been successfully piloted in nonpregnant patients. Obstetricians and others caring for obstetrical patients – especially those who are infected or under investigation for infection – should always wear a properly fitted N95 mask.
Because patients with COVID-19 may have or go on to develop a constellation of organ abnormalities (e.g., cardiovascular, renal, pulmonary), it is vital that a standardized panel of baseline laboratory studies be developed for pregnant patients. This will minimize the need for repeated blood draws and other testing which may increase HCW exposure.
A negative screen based on nonreport of symptoms, lack of temperature elevation, and reported nonexposure to individuals with COVID-19 symptoms still has limitations in terms of disease detection. A recent report from a tertiary care hospital in New York City found that close to one-third of pregnant patients with confirmed COVID-19 admitted over a 2-week period had no viral symptoms or instructive history on initial admission.3 This is consistent with our clinical experience. Most importantly, therefore, routine quantitative reverse transcription polymerase chain reaction testing should be performed on all patients admitted to the L&D unit.
Given the reported variability in the accuracy of polymerase chain reaction testing induced by variable effectiveness of sampling techniques, stage of infection, and inherent test accuracy issues, symptomatic patients with a negative test should first obtain clearance from infectious disease specialists before isolation precautions are discontinued. Repeat testing in 24 hours, including testing of multiple sites, may subsequently yield a positive result in persistently symptomatic patients.
Intrapartum management
As much as possible, standard obstetric indications should guide the timing and route of delivery. In the case of a COVID-19–positive patient or a patient under investigation, nonobstetric factors may bear heavily on decision making, and management flexibility is of great value. For example, in cases of severe or critical disease status, evidence suggests that early delivery regardless of gestational age can improve maternal oxygenation; this supports the liberal use of C-sections in these circumstances. In addition, shortening labor length as well as duration of hospitalization may be expected to reduce the risk of transmission to HCWs, other staff, and other patients.
High rates of cesarean delivery unsurprisingly have been reported thus far: One review of 108 case reports and series of test-positive COVID-19 pregnancies found a 92% C-section rate, and another review and meta-analysis of studies of SARS, MERS, and COVID-19 during pregnancy similarly found that the majority of patients – 84% across all coronavirus infections and 91% in COVID-19 pregnancies – were delivered by C-section.4,5 Given these high rates of cesarean deliveries, the early placement of neuraxial anesthesia while the patient is stable appears to be prudent and obviates the need for intubation, the latter of which is associated with increased aerosol generation and increased virus transmission risk.
Strict protocols for the optimal protection of staff should be observed, including proper personal protective equipment (PPE) protection. Protocols have been detailed in various guidelines and publications; they include the wearing of shoe covers, gowns, N95 masks, goggles, face shields, and two layers of gloves.
For institutions that currently do not offer routine COVID-19 testing to pregnant patients – especially those in areas of outbreaks – N95 masks and eye protection should still be provided to all HCWs involved in the intrapartum management of untested asymptomatic patients, particularly those in the active phase of labor. This protection is justified given the limitations of symptom- and history-based screening and the not-uncommon experience of the patient with a negative screen who subsequently develops the clinical syndrome.
Obstetric management of labor requires close patient contact that potentially elevates the risk of contamination and infection. During the active stage of labor, patient shouting, rapid mouth breathing, and other behaviors inherent to labor all increase the risk of aerosolization of oronasal secretions. In addition, nasal-prong oxygen administration is believed to independently increase the risk of aerosolization of secretions. The casual practice of nasal oxygen application should thus be discontinued and, where felt to be absolutely necessary, a mask should be worn on top of the prongs.
Regarding operative delivery, each participating obstetric surgeon should observe guidelines and recommendations of governing national organizations and professional groups – including the American College of Surgeons – regarding the safe conduct of operations on patients with COVID-19. Written guidelines should be tailored as needed to the performance of C-sections and readily available in L&D. Drills and simulations are generally valuable, and expertise and support should always be available in the labor room to assist with donning and doffing of PPE.
Postpartum care
Expeditious separation of the COVID-19–positive mother from her infant is recommended, including avoidance of delayed cord clamping because of insufficient evidence of benefit to the infant. Insufficient evidence exists to support vertical transmission, but the possibility of maternal-infant transmission is clinically accepted based on small case reports of infection in a neonate at 30 hours of life and in infants of mothers with suspected or confirmed COVID-19.6,7 Accordingly, it is recommended that the benefit of early infant separation should be discussed with the mother. If approved, the infant should be kept in a separate isolation area and observed.
There is no evidence of breast milk transmission of the virus. For those electing to breastfeed, the patient should be provided with a breast pump to express and store the milk for subsequent bottle feeding. For mothers who elect to room in with the infant, a separation distance of 6 feet is recommended with an intervening barrier curtain. For COVID-19–positive mothers who elect breastfeeding, meticulous hand and face washing, continuous wearing of a mask, and cleansing of the breast prior to feeding needs to be maintained.
Restrictive visiting policies of no more than one visitor should be maintained. For severely or critically ill patients with COVID-19, it has been suggested that no visitors be allowed. As with other hospitalizations of COVID-19 patients, the HCW contact should be kept at a justifiable minimum to reduce the risk of transmission.
Protecting the obstetrician and other HCWs
Protecting the health of obstetricians and other HCWs is central to any successful strategy to fight the COVID-19 epidemic. For the individual obstetrician, careful attention to national and local hospital guidelines is required as these are rapidly evolving.
Physicians and their leadership must maintain an ongoing dialogue with hospital leadership to continually upgrade and optimize infection prevention and control measures, and to uphold best practices. The experience in Wuhan, China, illustrates the effectiveness of the proper use of PPE along with population control measures to reduce infections in HCWs. Prior to understanding the mechanism of virus transmission and using protective equipment, infection rates of 3%-29% were reported among HCWs. With the meticulous utilization of mitigation strategies and population control measures – including consistent use of PPE – the rate of infection of HCWs reportedly fell to zero.
In outpatient offices, all staff and HCWs should wear masks at all times and engage in social distancing and in frequent hand sanitization. Patients should be strongly encouraged to wear masks during office visits and on all other occasions when they will be in physical proximity to other individuals outside of the home.
Reports from epidemic areas describe transmission from household sources as a significant cause of HCW infection. The information emphasizes the need for ongoing vigilance and attention to sanitization measures even when at home with one’s family. An additional benefit is reduced risk of transmission from HCWs to family members.
Dr. Bahado-Singh is professor and chair of obstetrics and gynecology at Oakland University, Rochester, Mich., and health system chair for obstetrics and gynecology at Beaumont Health System.
References
1. Luo S et al. Clin Gastroenterol Hepatol. 2020 Mar 20. doi: 10.1016/j.cgh.2020.03.043.
2. Lechien JR et al. Eur Arch Otorhinolaryngol. 2020 Apr 6. doi: 10.1007/s00405-020-05965-1.
3. Breslin N et al. Am J Obstet Gynecol MFM. 2020 Apr 9. doi: 10.1016/j.ajogmf.2020.100118.
4. Zaigham M, Andersson O. Acta Obstet Gynecol Scand. 2020 Apr 7. doi: 10.1111/aogs.13867.
5. Di Mascio D et al. Am J Obstet Gynecol MFM. 2020 Mar 25. doi: 10.1016/j.ajogmf.2020.100107.
6. Ital J. Pediatr 2020;46(1) doi: 10.1186/s13052-020-0820-x.
7. Int J Gynaecol Obstet. 2020;149(2):130-6.
*This article was updated 5/6/2020.
The meteoric rise in the number of test-positive and clinical cases of COVID-19 because of infection with the SARS coronavirus (SARS-CoV-2) in states and cities across the United States has added urgency to the efforts to develop protocols for hospital triage, admission, labor and delivery management, and other aspects of obstetrical care.
Emerging data suggest that, while SARS-CoV-2 is less lethal overall than the severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) proved to be, it is significantly more contagious. Although a severe disease, the limited worldwide data so far available (as of early May) do not indicate that pregnant women are at greater risk of severe disease, compared with the general population. However, there remains a critical need for data on maternal and perinatal outcomes in women infected with SARS-CoV-2.
Multiple physiological changes in pregnancy, from reduced cell-based immune competence to changes in respiratory tract and pulmonary function – e.g., edema of the respiratory tract, increases in secretions and oxygen consumption, elevation of the diaphragm, and decrease in functional residual capacity – have historically contributed to worse obstetric outcomes in pregnant women who have had viral pneumonias. Furthermore, limited published experience with COVID-19 in China suggests worse perinatal outcomes in some affected pregnancies, including prematurity and perinatal death.
With evolution of the pandemic and accumulation of experience, it is expected that data-driven guidelines on assessment and management of infected pregnant women will contribute to improved maternal and perinatal outcomes. What is clear now, however, is that,
Here are my recommendations, based on a currently limited body of literature on COVID-19 and other communicable viral respiratory disorders, as well my experience in the greater Detroit area, a COVID-19 hot spot.
Preparing for hospital evaluation and admission
The obstetric triage or labor and delivery (L&D) unit should be notified prior to the arrival of a patient suspected of or known to be infected with the virus. This will minimize staff exposure and allow sufficient time to prepare appropriate accommodations, equipment, and supplies for the patient’s care. Hospital infection control should be promptly notified by L&D of the expected arrival of such a patient. Placement ideally should be in a negative-pressure room, which allows outside air to flow into the room but prevents contaminated air from escaping. In the absence of a negative-pressure room, an infection isolation area should be utilized.
The patient and one accompanying support individual should wear either medical-grade masks brought from home or supplied upon entry to the hospital or homemade masks or bandanas. This will reduce the risk of viral transmission to hospital workers and other individuals encountered in the hospital prior to arriving in L&D. An ideal setup is to have separate entry areas, access corridors, and elevators for patients known or suspected to have COVID-19 infection. The patient and visitor should be expeditiously escorted to the prepared area for evaluation. Patients who are not known or suspected to be infected ideally should be tested.
Screening of patients & support individuals
Proper screening of patients and support individuals is critical to protecting both patients and staff in the L&D unit. This should include an expanded questionnaire that asks about disturbances of smell and taste and GI symptoms like loss of appetite – not only the more commonly queried symptoms of fever, shortness of breath, coughing, and exposure to someone who may have been ill.
Recent studies regarding presenting symptoms cast significant doubt, in fact, on the validity of patients with “asymptomatic COVID-19.” Over 15% of patients with confirmed infection in one published case series had solely GI symptoms and almost all had some digestive symptoms, for example, and almost 90% in another study had absent or reduced sense of smell and/or taste.1,2 In fact, the use of the term “paucisymptomatic” rather than “asymptomatic” may be most appropriate.
Support individuals also should undergo temperature screening, ideally with laser noncontact thermometers on entry to the hospital or triage.
Visitor policy
The number of visitors/support individuals should be kept to a minimum to reduce transmission risk. The actual number will be determined by hospital or state policy, but up to one visitor in the labor room appears reasonable. Very strong individual justification should be required to exceed this threshold! The visitor should not only be screened for an expanded list of symptoms, but they also should be queried for underlying illnesses (e.g., diabetes, cardiovascular disease, significant lung disease, undergoing cancer therapy) as well as for age over 65 years, each of which increase the chances of severe COVID-19 disease should infection occur. The visitor should be informed of such risks and, especially when accompanying a patient with known or suspected COVID-19, provided the option of voluntarily revoking their visitor status. A visitor with known or suspected COVID-19 infection based on testing or screening should not be allowed into the L&D unit.
In addition, institutions may be considered to have obligations to the visitor/support person beyond screening. These include instructions in proper mask usage, hand washing, and limiting the touching of surfaces to lower infection risk.
“Visitor relays” where one visitor replaces another should be strongly discouraged. Visitors should similarly not be allowed to wander around the hospital (to use phones, for instance); transiting back and forth to obtain food and coffee should be kept to a strict minimum. For visitors accompanying COVID-19–-infected women, “visitor’s plates” provided by the hospital at reasonable cost is a much-preferred arrangement for obtaining meals during the course of the hospital stay. In addition, visitors should be sent out of the room during the performance of aerosolizing procedures.
Labor and delivery management
The successful management of patients with COVID-19 requires a rigorous infection control protocol informed by guidelines from national entities, such as the Centers for Disease Control and Prevention, the Society for Maternal-Fetal Medicine, and the American College of Obstetricians and Gynecologists, and by state health departments when available.
Strict limits on the number of obstetricians and other health care workers (HCWs) entering the patient’s room should be enforced and documented to minimize risk to the HCWs attending to patients who have a positive diagnosis or who are under investigation. Only in cases of demonstrable clinical benefit should repeat visits by the same or additional HCWs be permitted. Conventional and electronic tablets present an excellent opportunity for patient follow-up visits without room entry. In our institution, this has been successfully piloted in nonpregnant patients. Obstetricians and others caring for obstetrical patients – especially those who are infected or under investigation for infection – should always wear a properly fitted N95 mask.
Because patients with COVID-19 may have or go on to develop a constellation of organ abnormalities (e.g., cardiovascular, renal, pulmonary), it is vital that a standardized panel of baseline laboratory studies be developed for pregnant patients. This will minimize the need for repeated blood draws and other testing which may increase HCW exposure.
A negative screen based on nonreport of symptoms, lack of temperature elevation, and reported nonexposure to individuals with COVID-19 symptoms still has limitations in terms of disease detection. A recent report from a tertiary care hospital in New York City found that close to one-third of pregnant patients with confirmed COVID-19 admitted over a 2-week period had no viral symptoms or instructive history on initial admission.3 This is consistent with our clinical experience. Most importantly, therefore, routine quantitative reverse transcription polymerase chain reaction testing should be performed on all patients admitted to the L&D unit.
Given the reported variability in the accuracy of polymerase chain reaction testing induced by variable effectiveness of sampling techniques, stage of infection, and inherent test accuracy issues, symptomatic patients with a negative test should first obtain clearance from infectious disease specialists before isolation precautions are discontinued. Repeat testing in 24 hours, including testing of multiple sites, may subsequently yield a positive result in persistently symptomatic patients.
Intrapartum management
As much as possible, standard obstetric indications should guide the timing and route of delivery. In the case of a COVID-19–positive patient or a patient under investigation, nonobstetric factors may bear heavily on decision making, and management flexibility is of great value. For example, in cases of severe or critical disease status, evidence suggests that early delivery regardless of gestational age can improve maternal oxygenation; this supports the liberal use of C-sections in these circumstances. In addition, shortening labor length as well as duration of hospitalization may be expected to reduce the risk of transmission to HCWs, other staff, and other patients.
High rates of cesarean delivery unsurprisingly have been reported thus far: One review of 108 case reports and series of test-positive COVID-19 pregnancies found a 92% C-section rate, and another review and meta-analysis of studies of SARS, MERS, and COVID-19 during pregnancy similarly found that the majority of patients – 84% across all coronavirus infections and 91% in COVID-19 pregnancies – were delivered by C-section.4,5 Given these high rates of cesarean deliveries, the early placement of neuraxial anesthesia while the patient is stable appears to be prudent and obviates the need for intubation, the latter of which is associated with increased aerosol generation and increased virus transmission risk.
Strict protocols for the optimal protection of staff should be observed, including proper personal protective equipment (PPE) protection. Protocols have been detailed in various guidelines and publications; they include the wearing of shoe covers, gowns, N95 masks, goggles, face shields, and two layers of gloves.
For institutions that currently do not offer routine COVID-19 testing to pregnant patients – especially those in areas of outbreaks – N95 masks and eye protection should still be provided to all HCWs involved in the intrapartum management of untested asymptomatic patients, particularly those in the active phase of labor. This protection is justified given the limitations of symptom- and history-based screening and the not-uncommon experience of the patient with a negative screen who subsequently develops the clinical syndrome.
Obstetric management of labor requires close patient contact that potentially elevates the risk of contamination and infection. During the active stage of labor, patient shouting, rapid mouth breathing, and other behaviors inherent to labor all increase the risk of aerosolization of oronasal secretions. In addition, nasal-prong oxygen administration is believed to independently increase the risk of aerosolization of secretions. The casual practice of nasal oxygen application should thus be discontinued and, where felt to be absolutely necessary, a mask should be worn on top of the prongs.
Regarding operative delivery, each participating obstetric surgeon should observe guidelines and recommendations of governing national organizations and professional groups – including the American College of Surgeons – regarding the safe conduct of operations on patients with COVID-19. Written guidelines should be tailored as needed to the performance of C-sections and readily available in L&D. Drills and simulations are generally valuable, and expertise and support should always be available in the labor room to assist with donning and doffing of PPE.
Postpartum care
Expeditious separation of the COVID-19–positive mother from her infant is recommended, including avoidance of delayed cord clamping because of insufficient evidence of benefit to the infant. Insufficient evidence exists to support vertical transmission, but the possibility of maternal-infant transmission is clinically accepted based on small case reports of infection in a neonate at 30 hours of life and in infants of mothers with suspected or confirmed COVID-19.6,7 Accordingly, it is recommended that the benefit of early infant separation should be discussed with the mother. If approved, the infant should be kept in a separate isolation area and observed.
There is no evidence of breast milk transmission of the virus. For those electing to breastfeed, the patient should be provided with a breast pump to express and store the milk for subsequent bottle feeding. For mothers who elect to room in with the infant, a separation distance of 6 feet is recommended with an intervening barrier curtain. For COVID-19–positive mothers who elect breastfeeding, meticulous hand and face washing, continuous wearing of a mask, and cleansing of the breast prior to feeding needs to be maintained.
Restrictive visiting policies of no more than one visitor should be maintained. For severely or critically ill patients with COVID-19, it has been suggested that no visitors be allowed. As with other hospitalizations of COVID-19 patients, the HCW contact should be kept at a justifiable minimum to reduce the risk of transmission.
Protecting the obstetrician and other HCWs
Protecting the health of obstetricians and other HCWs is central to any successful strategy to fight the COVID-19 epidemic. For the individual obstetrician, careful attention to national and local hospital guidelines is required as these are rapidly evolving.
Physicians and their leadership must maintain an ongoing dialogue with hospital leadership to continually upgrade and optimize infection prevention and control measures, and to uphold best practices. The experience in Wuhan, China, illustrates the effectiveness of the proper use of PPE along with population control measures to reduce infections in HCWs. Prior to understanding the mechanism of virus transmission and using protective equipment, infection rates of 3%-29% were reported among HCWs. With the meticulous utilization of mitigation strategies and population control measures – including consistent use of PPE – the rate of infection of HCWs reportedly fell to zero.
In outpatient offices, all staff and HCWs should wear masks at all times and engage in social distancing and in frequent hand sanitization. Patients should be strongly encouraged to wear masks during office visits and on all other occasions when they will be in physical proximity to other individuals outside of the home.
Reports from epidemic areas describe transmission from household sources as a significant cause of HCW infection. The information emphasizes the need for ongoing vigilance and attention to sanitization measures even when at home with one’s family. An additional benefit is reduced risk of transmission from HCWs to family members.
Dr. Bahado-Singh is professor and chair of obstetrics and gynecology at Oakland University, Rochester, Mich., and health system chair for obstetrics and gynecology at Beaumont Health System.
References
1. Luo S et al. Clin Gastroenterol Hepatol. 2020 Mar 20. doi: 10.1016/j.cgh.2020.03.043.
2. Lechien JR et al. Eur Arch Otorhinolaryngol. 2020 Apr 6. doi: 10.1007/s00405-020-05965-1.
3. Breslin N et al. Am J Obstet Gynecol MFM. 2020 Apr 9. doi: 10.1016/j.ajogmf.2020.100118.
4. Zaigham M, Andersson O. Acta Obstet Gynecol Scand. 2020 Apr 7. doi: 10.1111/aogs.13867.
5. Di Mascio D et al. Am J Obstet Gynecol MFM. 2020 Mar 25. doi: 10.1016/j.ajogmf.2020.100107.
6. Ital J. Pediatr 2020;46(1) doi: 10.1186/s13052-020-0820-x.
7. Int J Gynaecol Obstet. 2020;149(2):130-6.
*This article was updated 5/6/2020.
The meteoric rise in the number of test-positive and clinical cases of COVID-19 because of infection with the SARS coronavirus (SARS-CoV-2) in states and cities across the United States has added urgency to the efforts to develop protocols for hospital triage, admission, labor and delivery management, and other aspects of obstetrical care.
Emerging data suggest that, while SARS-CoV-2 is less lethal overall than the severe acute respiratory syndrome coronavirus (SARS-CoV) and Middle East respiratory syndrome coronavirus (MERS-CoV) proved to be, it is significantly more contagious. Although a severe disease, the limited worldwide data so far available (as of early May) do not indicate that pregnant women are at greater risk of severe disease, compared with the general population. However, there remains a critical need for data on maternal and perinatal outcomes in women infected with SARS-CoV-2.
Multiple physiological changes in pregnancy, from reduced cell-based immune competence to changes in respiratory tract and pulmonary function – e.g., edema of the respiratory tract, increases in secretions and oxygen consumption, elevation of the diaphragm, and decrease in functional residual capacity – have historically contributed to worse obstetric outcomes in pregnant women who have had viral pneumonias. Furthermore, limited published experience with COVID-19 in China suggests worse perinatal outcomes in some affected pregnancies, including prematurity and perinatal death.
With evolution of the pandemic and accumulation of experience, it is expected that data-driven guidelines on assessment and management of infected pregnant women will contribute to improved maternal and perinatal outcomes. What is clear now, however, is that,
Here are my recommendations, based on a currently limited body of literature on COVID-19 and other communicable viral respiratory disorders, as well my experience in the greater Detroit area, a COVID-19 hot spot.
Preparing for hospital evaluation and admission
The obstetric triage or labor and delivery (L&D) unit should be notified prior to the arrival of a patient suspected of or known to be infected with the virus. This will minimize staff exposure and allow sufficient time to prepare appropriate accommodations, equipment, and supplies for the patient’s care. Hospital infection control should be promptly notified by L&D of the expected arrival of such a patient. Placement ideally should be in a negative-pressure room, which allows outside air to flow into the room but prevents contaminated air from escaping. In the absence of a negative-pressure room, an infection isolation area should be utilized.
The patient and one accompanying support individual should wear either medical-grade masks brought from home or supplied upon entry to the hospital or homemade masks or bandanas. This will reduce the risk of viral transmission to hospital workers and other individuals encountered in the hospital prior to arriving in L&D. An ideal setup is to have separate entry areas, access corridors, and elevators for patients known or suspected to have COVID-19 infection. The patient and visitor should be expeditiously escorted to the prepared area for evaluation. Patients who are not known or suspected to be infected ideally should be tested.
Screening of patients & support individuals
Proper screening of patients and support individuals is critical to protecting both patients and staff in the L&D unit. This should include an expanded questionnaire that asks about disturbances of smell and taste and GI symptoms like loss of appetite – not only the more commonly queried symptoms of fever, shortness of breath, coughing, and exposure to someone who may have been ill.
Recent studies regarding presenting symptoms cast significant doubt, in fact, on the validity of patients with “asymptomatic COVID-19.” Over 15% of patients with confirmed infection in one published case series had solely GI symptoms and almost all had some digestive symptoms, for example, and almost 90% in another study had absent or reduced sense of smell and/or taste.1,2 In fact, the use of the term “paucisymptomatic” rather than “asymptomatic” may be most appropriate.
Support individuals also should undergo temperature screening, ideally with laser noncontact thermometers on entry to the hospital or triage.
Visitor policy
The number of visitors/support individuals should be kept to a minimum to reduce transmission risk. The actual number will be determined by hospital or state policy, but up to one visitor in the labor room appears reasonable. Very strong individual justification should be required to exceed this threshold! The visitor should not only be screened for an expanded list of symptoms, but they also should be queried for underlying illnesses (e.g., diabetes, cardiovascular disease, significant lung disease, undergoing cancer therapy) as well as for age over 65 years, each of which increase the chances of severe COVID-19 disease should infection occur. The visitor should be informed of such risks and, especially when accompanying a patient with known or suspected COVID-19, provided the option of voluntarily revoking their visitor status. A visitor with known or suspected COVID-19 infection based on testing or screening should not be allowed into the L&D unit.
In addition, institutions may be considered to have obligations to the visitor/support person beyond screening. These include instructions in proper mask usage, hand washing, and limiting the touching of surfaces to lower infection risk.
“Visitor relays” where one visitor replaces another should be strongly discouraged. Visitors should similarly not be allowed to wander around the hospital (to use phones, for instance); transiting back and forth to obtain food and coffee should be kept to a strict minimum. For visitors accompanying COVID-19–-infected women, “visitor’s plates” provided by the hospital at reasonable cost is a much-preferred arrangement for obtaining meals during the course of the hospital stay. In addition, visitors should be sent out of the room during the performance of aerosolizing procedures.
Labor and delivery management
The successful management of patients with COVID-19 requires a rigorous infection control protocol informed by guidelines from national entities, such as the Centers for Disease Control and Prevention, the Society for Maternal-Fetal Medicine, and the American College of Obstetricians and Gynecologists, and by state health departments when available.
Strict limits on the number of obstetricians and other health care workers (HCWs) entering the patient’s room should be enforced and documented to minimize risk to the HCWs attending to patients who have a positive diagnosis or who are under investigation. Only in cases of demonstrable clinical benefit should repeat visits by the same or additional HCWs be permitted. Conventional and electronic tablets present an excellent opportunity for patient follow-up visits without room entry. In our institution, this has been successfully piloted in nonpregnant patients. Obstetricians and others caring for obstetrical patients – especially those who are infected or under investigation for infection – should always wear a properly fitted N95 mask.
Because patients with COVID-19 may have or go on to develop a constellation of organ abnormalities (e.g., cardiovascular, renal, pulmonary), it is vital that a standardized panel of baseline laboratory studies be developed for pregnant patients. This will minimize the need for repeated blood draws and other testing which may increase HCW exposure.
A negative screen based on nonreport of symptoms, lack of temperature elevation, and reported nonexposure to individuals with COVID-19 symptoms still has limitations in terms of disease detection. A recent report from a tertiary care hospital in New York City found that close to one-third of pregnant patients with confirmed COVID-19 admitted over a 2-week period had no viral symptoms or instructive history on initial admission.3 This is consistent with our clinical experience. Most importantly, therefore, routine quantitative reverse transcription polymerase chain reaction testing should be performed on all patients admitted to the L&D unit.
Given the reported variability in the accuracy of polymerase chain reaction testing induced by variable effectiveness of sampling techniques, stage of infection, and inherent test accuracy issues, symptomatic patients with a negative test should first obtain clearance from infectious disease specialists before isolation precautions are discontinued. Repeat testing in 24 hours, including testing of multiple sites, may subsequently yield a positive result in persistently symptomatic patients.
Intrapartum management
As much as possible, standard obstetric indications should guide the timing and route of delivery. In the case of a COVID-19–positive patient or a patient under investigation, nonobstetric factors may bear heavily on decision making, and management flexibility is of great value. For example, in cases of severe or critical disease status, evidence suggests that early delivery regardless of gestational age can improve maternal oxygenation; this supports the liberal use of C-sections in these circumstances. In addition, shortening labor length as well as duration of hospitalization may be expected to reduce the risk of transmission to HCWs, other staff, and other patients.
High rates of cesarean delivery unsurprisingly have been reported thus far: One review of 108 case reports and series of test-positive COVID-19 pregnancies found a 92% C-section rate, and another review and meta-analysis of studies of SARS, MERS, and COVID-19 during pregnancy similarly found that the majority of patients – 84% across all coronavirus infections and 91% in COVID-19 pregnancies – were delivered by C-section.4,5 Given these high rates of cesarean deliveries, the early placement of neuraxial anesthesia while the patient is stable appears to be prudent and obviates the need for intubation, the latter of which is associated with increased aerosol generation and increased virus transmission risk.
Strict protocols for the optimal protection of staff should be observed, including proper personal protective equipment (PPE) protection. Protocols have been detailed in various guidelines and publications; they include the wearing of shoe covers, gowns, N95 masks, goggles, face shields, and two layers of gloves.
For institutions that currently do not offer routine COVID-19 testing to pregnant patients – especially those in areas of outbreaks – N95 masks and eye protection should still be provided to all HCWs involved in the intrapartum management of untested asymptomatic patients, particularly those in the active phase of labor. This protection is justified given the limitations of symptom- and history-based screening and the not-uncommon experience of the patient with a negative screen who subsequently develops the clinical syndrome.
Obstetric management of labor requires close patient contact that potentially elevates the risk of contamination and infection. During the active stage of labor, patient shouting, rapid mouth breathing, and other behaviors inherent to labor all increase the risk of aerosolization of oronasal secretions. In addition, nasal-prong oxygen administration is believed to independently increase the risk of aerosolization of secretions. The casual practice of nasal oxygen application should thus be discontinued and, where felt to be absolutely necessary, a mask should be worn on top of the prongs.
Regarding operative delivery, each participating obstetric surgeon should observe guidelines and recommendations of governing national organizations and professional groups – including the American College of Surgeons – regarding the safe conduct of operations on patients with COVID-19. Written guidelines should be tailored as needed to the performance of C-sections and readily available in L&D. Drills and simulations are generally valuable, and expertise and support should always be available in the labor room to assist with donning and doffing of PPE.
Postpartum care
Expeditious separation of the COVID-19–positive mother from her infant is recommended, including avoidance of delayed cord clamping because of insufficient evidence of benefit to the infant. Insufficient evidence exists to support vertical transmission, but the possibility of maternal-infant transmission is clinically accepted based on small case reports of infection in a neonate at 30 hours of life and in infants of mothers with suspected or confirmed COVID-19.6,7 Accordingly, it is recommended that the benefit of early infant separation should be discussed with the mother. If approved, the infant should be kept in a separate isolation area and observed.
There is no evidence of breast milk transmission of the virus. For those electing to breastfeed, the patient should be provided with a breast pump to express and store the milk for subsequent bottle feeding. For mothers who elect to room in with the infant, a separation distance of 6 feet is recommended with an intervening barrier curtain. For COVID-19–positive mothers who elect breastfeeding, meticulous hand and face washing, continuous wearing of a mask, and cleansing of the breast prior to feeding needs to be maintained.
Restrictive visiting policies of no more than one visitor should be maintained. For severely or critically ill patients with COVID-19, it has been suggested that no visitors be allowed. As with other hospitalizations of COVID-19 patients, the HCW contact should be kept at a justifiable minimum to reduce the risk of transmission.
Protecting the obstetrician and other HCWs
Protecting the health of obstetricians and other HCWs is central to any successful strategy to fight the COVID-19 epidemic. For the individual obstetrician, careful attention to national and local hospital guidelines is required as these are rapidly evolving.
Physicians and their leadership must maintain an ongoing dialogue with hospital leadership to continually upgrade and optimize infection prevention and control measures, and to uphold best practices. The experience in Wuhan, China, illustrates the effectiveness of the proper use of PPE along with population control measures to reduce infections in HCWs. Prior to understanding the mechanism of virus transmission and using protective equipment, infection rates of 3%-29% were reported among HCWs. With the meticulous utilization of mitigation strategies and population control measures – including consistent use of PPE – the rate of infection of HCWs reportedly fell to zero.
In outpatient offices, all staff and HCWs should wear masks at all times and engage in social distancing and in frequent hand sanitization. Patients should be strongly encouraged to wear masks during office visits and on all other occasions when they will be in physical proximity to other individuals outside of the home.
Reports from epidemic areas describe transmission from household sources as a significant cause of HCW infection. The information emphasizes the need for ongoing vigilance and attention to sanitization measures even when at home with one’s family. An additional benefit is reduced risk of transmission from HCWs to family members.
Dr. Bahado-Singh is professor and chair of obstetrics and gynecology at Oakland University, Rochester, Mich., and health system chair for obstetrics and gynecology at Beaumont Health System.
References
1. Luo S et al. Clin Gastroenterol Hepatol. 2020 Mar 20. doi: 10.1016/j.cgh.2020.03.043.
2. Lechien JR et al. Eur Arch Otorhinolaryngol. 2020 Apr 6. doi: 10.1007/s00405-020-05965-1.
3. Breslin N et al. Am J Obstet Gynecol MFM. 2020 Apr 9. doi: 10.1016/j.ajogmf.2020.100118.
4. Zaigham M, Andersson O. Acta Obstet Gynecol Scand. 2020 Apr 7. doi: 10.1111/aogs.13867.
5. Di Mascio D et al. Am J Obstet Gynecol MFM. 2020 Mar 25. doi: 10.1016/j.ajogmf.2020.100107.
6. Ital J. Pediatr 2020;46(1) doi: 10.1186/s13052-020-0820-x.
7. Int J Gynaecol Obstet. 2020;149(2):130-6.
*This article was updated 5/6/2020.
Obstetrics during the COVID-19 pandemic
The identification of the SARS coronavirus (SARS-CoV-2) and emergence of the associated infectious respiratory disease, COVID-19, in late 2019 catapulted the citizens of the world, especially those in the health care professions, into an era of considerable uncertainty. At this moment in human history, calm reassurance – founded in fact and evidence – seems its greatest need. Much of the focus within the biomedical community has been on containment, prevention, and treatment of this highly contagious and, for some, extremely virulent disease.
However, for ob.gyns on the front lines of the COVID-19 fight, there is the additional challenge of caring for at least two patients simultaneously: the mother and her unborn baby. Studies in mother-baby dyads, while being published at an incredible pace, are still quite scarce. In addition, published reports are limited by the small sample size of the patient population (many are single-case reports), lack of uniformity in the timing and types of clinical samples collected, testing delays, and varying isolation protocols in cases where the mother has confirmed SARS-CoV-2.
Five months into a pandemic that has swept the world, we still know very little about COVID-19 infection in the general population, let alone the obstetric one. We do not know if having and resolving COVID-19 infection provides any long-term protection against future disease. We do not know if vertical transmission of SARS-CoV-2 occurs. We do not know if maternal infection confers any immunologic benefit to the neonate. The list goes on.
What we do know is that taking extra precautions works. Use of personal protective equipment saves health care practitioner and patient lives. Prohibiting or restricting visitors to only one person in hospitals reduces risk of transmission to vulnerable patients.
Additionally, we know that leading with compassion is vital to easing patient – and practitioner – anxiety and stress. Most importantly, we know that people are extraordinarily resilient, especially when it comes to safeguarding the health of their families.
To address some of the major concerns that many ob.gyns. have regarding their risk of coronavirus exposure when caring for patients, we have invited Ray Bahado-Singh, MD, professor and chair of obstetrics and gynecology at Oakland University, Rochester, Mich., and health system chair for obstetrics and gynecology at Beaumont Health System, who works in a suburb of Detroit, one of our nation’s COVID-19 hot spots.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
The identification of the SARS coronavirus (SARS-CoV-2) and emergence of the associated infectious respiratory disease, COVID-19, in late 2019 catapulted the citizens of the world, especially those in the health care professions, into an era of considerable uncertainty. At this moment in human history, calm reassurance – founded in fact and evidence – seems its greatest need. Much of the focus within the biomedical community has been on containment, prevention, and treatment of this highly contagious and, for some, extremely virulent disease.
However, for ob.gyns on the front lines of the COVID-19 fight, there is the additional challenge of caring for at least two patients simultaneously: the mother and her unborn baby. Studies in mother-baby dyads, while being published at an incredible pace, are still quite scarce. In addition, published reports are limited by the small sample size of the patient population (many are single-case reports), lack of uniformity in the timing and types of clinical samples collected, testing delays, and varying isolation protocols in cases where the mother has confirmed SARS-CoV-2.
Five months into a pandemic that has swept the world, we still know very little about COVID-19 infection in the general population, let alone the obstetric one. We do not know if having and resolving COVID-19 infection provides any long-term protection against future disease. We do not know if vertical transmission of SARS-CoV-2 occurs. We do not know if maternal infection confers any immunologic benefit to the neonate. The list goes on.
What we do know is that taking extra precautions works. Use of personal protective equipment saves health care practitioner and patient lives. Prohibiting or restricting visitors to only one person in hospitals reduces risk of transmission to vulnerable patients.
Additionally, we know that leading with compassion is vital to easing patient – and practitioner – anxiety and stress. Most importantly, we know that people are extraordinarily resilient, especially when it comes to safeguarding the health of their families.
To address some of the major concerns that many ob.gyns. have regarding their risk of coronavirus exposure when caring for patients, we have invited Ray Bahado-Singh, MD, professor and chair of obstetrics and gynecology at Oakland University, Rochester, Mich., and health system chair for obstetrics and gynecology at Beaumont Health System, who works in a suburb of Detroit, one of our nation’s COVID-19 hot spots.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
The identification of the SARS coronavirus (SARS-CoV-2) and emergence of the associated infectious respiratory disease, COVID-19, in late 2019 catapulted the citizens of the world, especially those in the health care professions, into an era of considerable uncertainty. At this moment in human history, calm reassurance – founded in fact and evidence – seems its greatest need. Much of the focus within the biomedical community has been on containment, prevention, and treatment of this highly contagious and, for some, extremely virulent disease.
However, for ob.gyns on the front lines of the COVID-19 fight, there is the additional challenge of caring for at least two patients simultaneously: the mother and her unborn baby. Studies in mother-baby dyads, while being published at an incredible pace, are still quite scarce. In addition, published reports are limited by the small sample size of the patient population (many are single-case reports), lack of uniformity in the timing and types of clinical samples collected, testing delays, and varying isolation protocols in cases where the mother has confirmed SARS-CoV-2.
Five months into a pandemic that has swept the world, we still know very little about COVID-19 infection in the general population, let alone the obstetric one. We do not know if having and resolving COVID-19 infection provides any long-term protection against future disease. We do not know if vertical transmission of SARS-CoV-2 occurs. We do not know if maternal infection confers any immunologic benefit to the neonate. The list goes on.
What we do know is that taking extra precautions works. Use of personal protective equipment saves health care practitioner and patient lives. Prohibiting or restricting visitors to only one person in hospitals reduces risk of transmission to vulnerable patients.
Additionally, we know that leading with compassion is vital to easing patient – and practitioner – anxiety and stress. Most importantly, we know that people are extraordinarily resilient, especially when it comes to safeguarding the health of their families.
To address some of the major concerns that many ob.gyns. have regarding their risk of coronavirus exposure when caring for patients, we have invited Ray Bahado-Singh, MD, professor and chair of obstetrics and gynecology at Oakland University, Rochester, Mich., and health system chair for obstetrics and gynecology at Beaumont Health System, who works in a suburb of Detroit, one of our nation’s COVID-19 hot spots.
Dr. Reece, who specializes in maternal-fetal medicine, is executive vice president for medical affairs at the University of Maryland School of Medicine as well as the John Z. and Akiko K. Bowers Distinguished Professor and dean of the school of medicine. He is the medical editor of this column. He said he had no relevant financial disclosures. Contact him at [email protected].
FMT may improve outcomes without clearing multidrug-resistant organisms
For seriously ill patients with multidrug-resistant organisms (MDROs) in their gastrointestinal tract, performing a fecal microbiota transplant (FMT) may result in fewer and less severe infections, as well as shorter hospital stays, according to investigators.
Significant clinical improvements were observed across the group even though 59% of patients did not clear MDROs, which suggests that complete decolonization of resistant organisms may be unnecessary for patients to benefit from FMT, reported lead author Julian Marchesi, PhD, of Cardiff (Wales) University and Imperial College London (England).
“We see the quality of life for these patients is hugely improved even when we don’t get rid of the organism totally,” Dr. Marchesi said in a virtual press conference.
Although previous studies have suggested that FMT may be used to decolonize MDROs, little research has addressed other clinical outcomes, the investigators wrote in an abstract released as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
The present study involved 20 patients with MDROs, including extended-spectrum beta-lactamase Enterobacteriaceae (ESBL), carbapenemase-producing Enterobacteriaceae (CPE), or vancomycin-resistant enterococci (VRE). Approximately half of the population (n = 11) had chronic hematological disease. The other half (n = 9) had recurrent urinary tract infections with ESBL, including patients who had undergone renal transplant or had recurrent Clostridioides difficile infection.
For each transplant, 200-300 mL of fecal slurry was delivered via nasogastric tube into the small intestine. Fecal donors underwent a strict screening process that included blood, fecal, and behavioral testing.
Multiple clinical outcomes were evaluated in the 6 months leading up to FMT, then compared with outcomes in the 6 months following fecal transplant. Out of 20 patients, 17 completed the 6-month follow-up. Although only 7 of these patients (41%) were decolonized of MDROs, multiple significant clinical improvements were observed across the group, including reductions in MDRO bloodstream infections (P = .047), all bloodstream infections (P = .03), length of stay in hospital (P = .0002), and duration of carbapenem use (P = .0005). Eight out of 11 patients with hematologic disease improved enough to undergo stem cell transplantation within 6 months of FMT, and in the subgroup of patients who had undergone renal transplant, the rate of urinary tract infections was significantly improved (P = .008).
No serious adverse events were encountered during the trial, which led the investigators to conclude that FMT was safe and well tolerated, even in patients with bloodstream infections and those who were highly immunosuppressed.
Beyond clinical implications, Dr. Marchesi suggested that the study findings should influence FMT trial methodology.
“We’ve got to start thinking a little bit differently in terms of how we measure the impact of FMT,” he said. “It’s not all about ... getting rid of these opportunistic pathogens. There are other quality-of-life factors that we need to measure, because they’re also important for the patient.”
Dr. Marchesi said that more research is needed to confirm findings and gain a mechanistic understanding of why patients may improve despite a lack of decolonization.
“We think we’re on a strong foundation here to take this into a clinical trial,” he said.
The research was funded by the National Institute for Health Research and the Medical Research Council. The investigators reported no conflicts of interest.
For seriously ill patients with multidrug-resistant organisms (MDROs) in their gastrointestinal tract, performing a fecal microbiota transplant (FMT) may result in fewer and less severe infections, as well as shorter hospital stays, according to investigators.
Significant clinical improvements were observed across the group even though 59% of patients did not clear MDROs, which suggests that complete decolonization of resistant organisms may be unnecessary for patients to benefit from FMT, reported lead author Julian Marchesi, PhD, of Cardiff (Wales) University and Imperial College London (England).
“We see the quality of life for these patients is hugely improved even when we don’t get rid of the organism totally,” Dr. Marchesi said in a virtual press conference.
Although previous studies have suggested that FMT may be used to decolonize MDROs, little research has addressed other clinical outcomes, the investigators wrote in an abstract released as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
The present study involved 20 patients with MDROs, including extended-spectrum beta-lactamase Enterobacteriaceae (ESBL), carbapenemase-producing Enterobacteriaceae (CPE), or vancomycin-resistant enterococci (VRE). Approximately half of the population (n = 11) had chronic hematological disease. The other half (n = 9) had recurrent urinary tract infections with ESBL, including patients who had undergone renal transplant or had recurrent Clostridioides difficile infection.
For each transplant, 200-300 mL of fecal slurry was delivered via nasogastric tube into the small intestine. Fecal donors underwent a strict screening process that included blood, fecal, and behavioral testing.
Multiple clinical outcomes were evaluated in the 6 months leading up to FMT, then compared with outcomes in the 6 months following fecal transplant. Out of 20 patients, 17 completed the 6-month follow-up. Although only 7 of these patients (41%) were decolonized of MDROs, multiple significant clinical improvements were observed across the group, including reductions in MDRO bloodstream infections (P = .047), all bloodstream infections (P = .03), length of stay in hospital (P = .0002), and duration of carbapenem use (P = .0005). Eight out of 11 patients with hematologic disease improved enough to undergo stem cell transplantation within 6 months of FMT, and in the subgroup of patients who had undergone renal transplant, the rate of urinary tract infections was significantly improved (P = .008).
No serious adverse events were encountered during the trial, which led the investigators to conclude that FMT was safe and well tolerated, even in patients with bloodstream infections and those who were highly immunosuppressed.
Beyond clinical implications, Dr. Marchesi suggested that the study findings should influence FMT trial methodology.
“We’ve got to start thinking a little bit differently in terms of how we measure the impact of FMT,” he said. “It’s not all about ... getting rid of these opportunistic pathogens. There are other quality-of-life factors that we need to measure, because they’re also important for the patient.”
Dr. Marchesi said that more research is needed to confirm findings and gain a mechanistic understanding of why patients may improve despite a lack of decolonization.
“We think we’re on a strong foundation here to take this into a clinical trial,” he said.
The research was funded by the National Institute for Health Research and the Medical Research Council. The investigators reported no conflicts of interest.
For seriously ill patients with multidrug-resistant organisms (MDROs) in their gastrointestinal tract, performing a fecal microbiota transplant (FMT) may result in fewer and less severe infections, as well as shorter hospital stays, according to investigators.
Significant clinical improvements were observed across the group even though 59% of patients did not clear MDROs, which suggests that complete decolonization of resistant organisms may be unnecessary for patients to benefit from FMT, reported lead author Julian Marchesi, PhD, of Cardiff (Wales) University and Imperial College London (England).
“We see the quality of life for these patients is hugely improved even when we don’t get rid of the organism totally,” Dr. Marchesi said in a virtual press conference.
Although previous studies have suggested that FMT may be used to decolonize MDROs, little research has addressed other clinical outcomes, the investigators wrote in an abstract released as part of the annual Digestive Disease Week®, which was canceled because of COVID-19.
The present study involved 20 patients with MDROs, including extended-spectrum beta-lactamase Enterobacteriaceae (ESBL), carbapenemase-producing Enterobacteriaceae (CPE), or vancomycin-resistant enterococci (VRE). Approximately half of the population (n = 11) had chronic hematological disease. The other half (n = 9) had recurrent urinary tract infections with ESBL, including patients who had undergone renal transplant or had recurrent Clostridioides difficile infection.
For each transplant, 200-300 mL of fecal slurry was delivered via nasogastric tube into the small intestine. Fecal donors underwent a strict screening process that included blood, fecal, and behavioral testing.
Multiple clinical outcomes were evaluated in the 6 months leading up to FMT, then compared with outcomes in the 6 months following fecal transplant. Out of 20 patients, 17 completed the 6-month follow-up. Although only 7 of these patients (41%) were decolonized of MDROs, multiple significant clinical improvements were observed across the group, including reductions in MDRO bloodstream infections (P = .047), all bloodstream infections (P = .03), length of stay in hospital (P = .0002), and duration of carbapenem use (P = .0005). Eight out of 11 patients with hematologic disease improved enough to undergo stem cell transplantation within 6 months of FMT, and in the subgroup of patients who had undergone renal transplant, the rate of urinary tract infections was significantly improved (P = .008).
No serious adverse events were encountered during the trial, which led the investigators to conclude that FMT was safe and well tolerated, even in patients with bloodstream infections and those who were highly immunosuppressed.
Beyond clinical implications, Dr. Marchesi suggested that the study findings should influence FMT trial methodology.
“We’ve got to start thinking a little bit differently in terms of how we measure the impact of FMT,” he said. “It’s not all about ... getting rid of these opportunistic pathogens. There are other quality-of-life factors that we need to measure, because they’re also important for the patient.”
Dr. Marchesi said that more research is needed to confirm findings and gain a mechanistic understanding of why patients may improve despite a lack of decolonization.
“We think we’re on a strong foundation here to take this into a clinical trial,” he said.
The research was funded by the National Institute for Health Research and the Medical Research Council. The investigators reported no conflicts of interest.
FROM DDW 2020
Pandemic effect: All other health care visits can wait
according to survey conducted at the end of April.
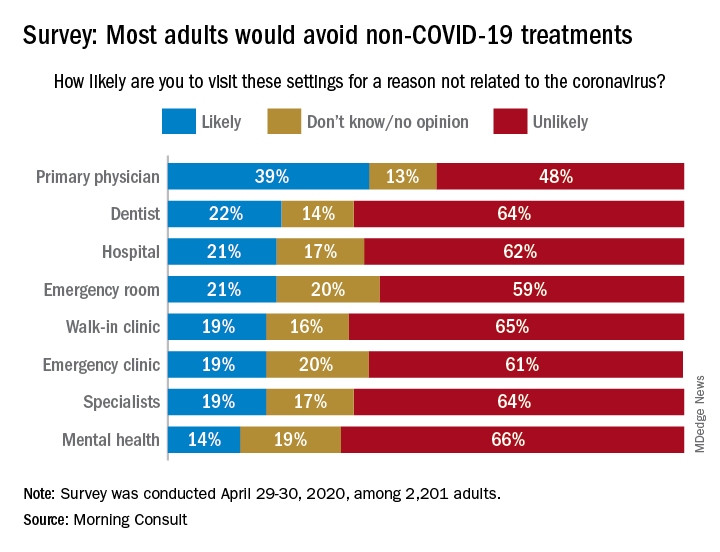
When asked how likely they were to visit a variety of health care settings for treatment not related to the coronavirus, 62% of respondents said it was unlikely that they would go to a hospital, 64% wouldn’t go to a specialist, and 65% would avoid walk-in clinics, digital media company Morning Consult reported May 4.
The only setting with less than a majority on the unlikely-to-visit side was primary physicians, who managed to combine a 39% likely vote with a 13% undecided/no-opinion tally, Morning Consult said after surveying 2,201 adults on April 29-30 (margin of error, ±2 percentage points).
As to when they might feel comfortable making such an in-person visit with their primary physician, 24% of respondents said they would willing to go in the next month, 14% said 2 months, 18% said 3 months, 13% said 6 months, and 10% said more than 6 months, the Morning Consult data show.
“Hospitals, despite being overburdened in recent weeks in coronavirus hot spots such as New York City, have reported dips in revenue as a result of potential patients opting against receiving elective surgeries out of fear of contracting COVID-19,” Morning Consult wrote, and these poll results suggest that “health care companies could continue to feel the pinch as long as the coronavirus lingers.”
according to survey conducted at the end of April.
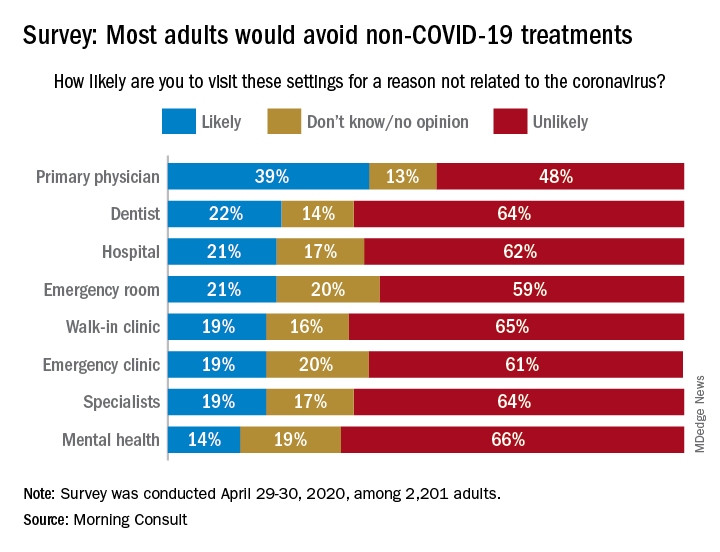
When asked how likely they were to visit a variety of health care settings for treatment not related to the coronavirus, 62% of respondents said it was unlikely that they would go to a hospital, 64% wouldn’t go to a specialist, and 65% would avoid walk-in clinics, digital media company Morning Consult reported May 4.
The only setting with less than a majority on the unlikely-to-visit side was primary physicians, who managed to combine a 39% likely vote with a 13% undecided/no-opinion tally, Morning Consult said after surveying 2,201 adults on April 29-30 (margin of error, ±2 percentage points).
As to when they might feel comfortable making such an in-person visit with their primary physician, 24% of respondents said they would willing to go in the next month, 14% said 2 months, 18% said 3 months, 13% said 6 months, and 10% said more than 6 months, the Morning Consult data show.
“Hospitals, despite being overburdened in recent weeks in coronavirus hot spots such as New York City, have reported dips in revenue as a result of potential patients opting against receiving elective surgeries out of fear of contracting COVID-19,” Morning Consult wrote, and these poll results suggest that “health care companies could continue to feel the pinch as long as the coronavirus lingers.”
according to survey conducted at the end of April.
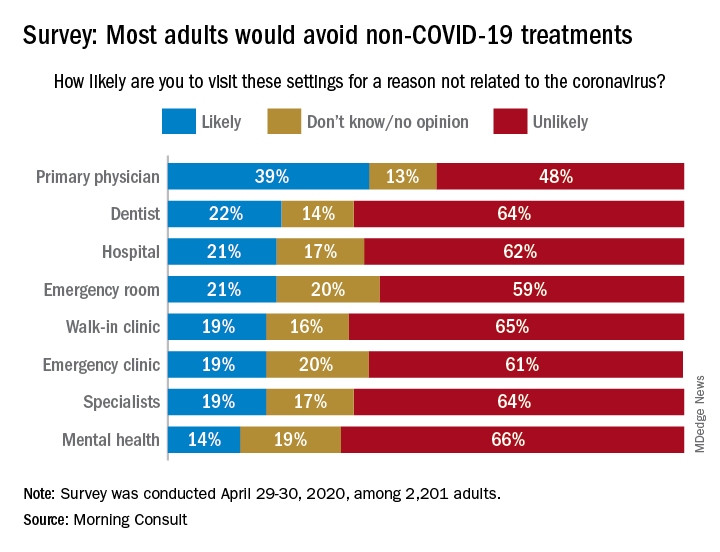
When asked how likely they were to visit a variety of health care settings for treatment not related to the coronavirus, 62% of respondents said it was unlikely that they would go to a hospital, 64% wouldn’t go to a specialist, and 65% would avoid walk-in clinics, digital media company Morning Consult reported May 4.
The only setting with less than a majority on the unlikely-to-visit side was primary physicians, who managed to combine a 39% likely vote with a 13% undecided/no-opinion tally, Morning Consult said after surveying 2,201 adults on April 29-30 (margin of error, ±2 percentage points).
As to when they might feel comfortable making such an in-person visit with their primary physician, 24% of respondents said they would willing to go in the next month, 14% said 2 months, 18% said 3 months, 13% said 6 months, and 10% said more than 6 months, the Morning Consult data show.
“Hospitals, despite being overburdened in recent weeks in coronavirus hot spots such as New York City, have reported dips in revenue as a result of potential patients opting against receiving elective surgeries out of fear of contracting COVID-19,” Morning Consult wrote, and these poll results suggest that “health care companies could continue to feel the pinch as long as the coronavirus lingers.”
FDA grants EUA to muscle stimulator to reduce mechanical ventilator usage
The Food and Drug Administration has issued an Emergency Use Authorization (EUA) for the VentFree Respiratory Muscle Stimulator in order to potentially reduce the number of days adult patients, including those with COVID-19, require mechanical ventilation, according to a press release from Liberate Medical.
In comparison with mechanical ventilation, which is invasive and commonly weakens the breathing muscles, the VentFree system uses noninvasive neuromuscular electrical stimulation to contract the abdominal wall muscles in synchrony with exhalation during mechanical ventilation, according to the press release. This allows patients to begin treatment during the early stages of ventilation while they are sedated and to continue until they are weaned off of ventilation.
A pair of pilot randomized, controlled studies, completed in Europe and Australia, showed that VentFree helped to reduce ventilation duration and ICU length of stay, compared with placebo stimulation. The FDA granted VentFree Breakthrough Device status in 2019.
“We are grateful to the FDA for recognizing the potential of VentFree and feel privileged to have the opportunity to help patients on mechanical ventilation during the COVID-19 pandemic,” Angus McLachlan PhD, cofounder and CEO of Liberate Medical, said in the press release.
VentFree has been authorized for use only for the duration of the current COVID-19 emergency, as it has not yet been approved or cleared for usage by primary care providers.
The Food and Drug Administration has issued an Emergency Use Authorization (EUA) for the VentFree Respiratory Muscle Stimulator in order to potentially reduce the number of days adult patients, including those with COVID-19, require mechanical ventilation, according to a press release from Liberate Medical.
In comparison with mechanical ventilation, which is invasive and commonly weakens the breathing muscles, the VentFree system uses noninvasive neuromuscular electrical stimulation to contract the abdominal wall muscles in synchrony with exhalation during mechanical ventilation, according to the press release. This allows patients to begin treatment during the early stages of ventilation while they are sedated and to continue until they are weaned off of ventilation.
A pair of pilot randomized, controlled studies, completed in Europe and Australia, showed that VentFree helped to reduce ventilation duration and ICU length of stay, compared with placebo stimulation. The FDA granted VentFree Breakthrough Device status in 2019.
“We are grateful to the FDA for recognizing the potential of VentFree and feel privileged to have the opportunity to help patients on mechanical ventilation during the COVID-19 pandemic,” Angus McLachlan PhD, cofounder and CEO of Liberate Medical, said in the press release.
VentFree has been authorized for use only for the duration of the current COVID-19 emergency, as it has not yet been approved or cleared for usage by primary care providers.
The Food and Drug Administration has issued an Emergency Use Authorization (EUA) for the VentFree Respiratory Muscle Stimulator in order to potentially reduce the number of days adult patients, including those with COVID-19, require mechanical ventilation, according to a press release from Liberate Medical.
In comparison with mechanical ventilation, which is invasive and commonly weakens the breathing muscles, the VentFree system uses noninvasive neuromuscular electrical stimulation to contract the abdominal wall muscles in synchrony with exhalation during mechanical ventilation, according to the press release. This allows patients to begin treatment during the early stages of ventilation while they are sedated and to continue until they are weaned off of ventilation.
A pair of pilot randomized, controlled studies, completed in Europe and Australia, showed that VentFree helped to reduce ventilation duration and ICU length of stay, compared with placebo stimulation. The FDA granted VentFree Breakthrough Device status in 2019.
“We are grateful to the FDA for recognizing the potential of VentFree and feel privileged to have the opportunity to help patients on mechanical ventilation during the COVID-19 pandemic,” Angus McLachlan PhD, cofounder and CEO of Liberate Medical, said in the press release.
VentFree has been authorized for use only for the duration of the current COVID-19 emergency, as it has not yet been approved or cleared for usage by primary care providers.
COVID-19 death rate was twice as high in cancer patients in NYC study
COVID-19 patients with cancer had double the fatality rate of COVID-19 patients without cancer treated in an urban New York hospital system, according to data from a retrospective study.
with COVID-19 treated during the same time period in the same hospital system.
Vikas Mehta, MD, of Montefiore Medical Center, New York, and colleagues reported these results in Cancer Discovery.
“As New York has emerged as the current epicenter of the pandemic, we sought to investigate the risk posed by COVID-19 to our cancer population,” the authors wrote.
They identified 218 cancer patients treated for COVID-19 in the Montefiore Health System between March 18 and April 8, 2020. Three-quarters of patients had solid tumors, and 25% had hematologic malignancies. Most patients were adults (98.6%), their median age was 69 years (range, 10-92 years), and 58% were men.
In all, 28% of the cancer patients (61/218) died from COVID-19, including 25% (41/164) of those with solid tumors and 37% (20/54) of those with hematologic malignancies.
Deaths by cancer type
Among the 164 patients with solid tumors, case fatality rates were as follows:
- Pancreatic – 67% (2/3)
- Lung – 55% (6/11)
- Colorectal – 38% (8/21)
- Upper gastrointestinal – 38% (3/8)
- Gynecologic – 38% (5/13)
- Skin – 33% (1/3)
- Hepatobiliary – 29% (2/7)
- Bone/soft tissue – 20% (1/5)
- Genitourinary – 15% (7/46)
- Breast – 14% (4/28)
- Neurologic – 13% (1/8)
- Head and neck – 13% (1/8).
None of the three patients with neuroendocrine tumors died.
Among the 54 patients with hematologic malignancies, case fatality rates were as follows:
- Chronic myeloid leukemia – 100% (1/1)
- Hodgkin lymphoma – 60% (3/5)
- Myelodysplastic syndromes – 60% (3/5)
- Multiple myeloma – 38% (5/13)
- Non-Hodgkin lymphoma – 33% (5/15)
- Chronic lymphocytic leukemia – 33% (1/3)
- Myeloproliferative neoplasms – 29% (2/7).
None of the four patients with acute lymphoblastic leukemia died, and there was one patient with acute myeloid leukemia who did not die.
Factors associated with increased mortality
The researchers compared the 218 cancer patients with COVID-19 with 1,090 age- and sex-matched noncancer patients with COVID-19 treated in the Montefiore Health System between March 18 and April 8, 2020.
Case fatality rates in cancer patients with COVID-19 were significantly increased in all age groups, but older age was associated with higher mortality.
“We observed case fatality rates were elevated in all age cohorts in cancer patients and achieved statistical significance in the age groups 45-64 and in patients older than 75 years of age,” the authors reported.
Other factors significantly associated with higher mortality in a multivariable analysis included the presence of multiple comorbidities; the need for ICU support; and increased levels of d-dimer, lactate, and lactate dehydrogenase.
Additional factors, such as socioeconomic and health disparities, may also be significant predictors of mortality, according to the authors. They noted that this cohort largely consisted of patients from a socioeconomically underprivileged community where mortality because of COVID-19 is reportedly higher.
Proactive strategies moving forward
“We have been addressing the significant burden of the COVID-19 pandemic on our vulnerable cancer patients through a variety of ways,” said study author Balazs Halmos, MD, of Montefiore Medical Center.
The center set up a separate infusion unit exclusively for COVID-positive patients and established separate inpatient areas. Dr. Halmos and colleagues are also providing telemedicine, virtual supportive care services, telephonic counseling, and bilingual peer-support programs.
“Many questions remain as we continue to establish new practices for our cancer patients,” Dr. Halmos said. “We will find answers to these questions as we continue to focus on adaptation and not acceptance in response to the COVID crisis. Our patients deserve nothing less.”
The Albert Einstein Cancer Center supported this study. The authors reported having no conflicts of interest.
SOURCE: Mehta V et al. Cancer Discov. 2020 May 1. doi: 10.1158/2159-8290.CD-20-0516.
COVID-19 patients with cancer had double the fatality rate of COVID-19 patients without cancer treated in an urban New York hospital system, according to data from a retrospective study.
with COVID-19 treated during the same time period in the same hospital system.
Vikas Mehta, MD, of Montefiore Medical Center, New York, and colleagues reported these results in Cancer Discovery.
“As New York has emerged as the current epicenter of the pandemic, we sought to investigate the risk posed by COVID-19 to our cancer population,” the authors wrote.
They identified 218 cancer patients treated for COVID-19 in the Montefiore Health System between March 18 and April 8, 2020. Three-quarters of patients had solid tumors, and 25% had hematologic malignancies. Most patients were adults (98.6%), their median age was 69 years (range, 10-92 years), and 58% were men.
In all, 28% of the cancer patients (61/218) died from COVID-19, including 25% (41/164) of those with solid tumors and 37% (20/54) of those with hematologic malignancies.
Deaths by cancer type
Among the 164 patients with solid tumors, case fatality rates were as follows:
- Pancreatic – 67% (2/3)
- Lung – 55% (6/11)
- Colorectal – 38% (8/21)
- Upper gastrointestinal – 38% (3/8)
- Gynecologic – 38% (5/13)
- Skin – 33% (1/3)
- Hepatobiliary – 29% (2/7)
- Bone/soft tissue – 20% (1/5)
- Genitourinary – 15% (7/46)
- Breast – 14% (4/28)
- Neurologic – 13% (1/8)
- Head and neck – 13% (1/8).
None of the three patients with neuroendocrine tumors died.
Among the 54 patients with hematologic malignancies, case fatality rates were as follows:
- Chronic myeloid leukemia – 100% (1/1)
- Hodgkin lymphoma – 60% (3/5)
- Myelodysplastic syndromes – 60% (3/5)
- Multiple myeloma – 38% (5/13)
- Non-Hodgkin lymphoma – 33% (5/15)
- Chronic lymphocytic leukemia – 33% (1/3)
- Myeloproliferative neoplasms – 29% (2/7).
None of the four patients with acute lymphoblastic leukemia died, and there was one patient with acute myeloid leukemia who did not die.
Factors associated with increased mortality
The researchers compared the 218 cancer patients with COVID-19 with 1,090 age- and sex-matched noncancer patients with COVID-19 treated in the Montefiore Health System between March 18 and April 8, 2020.
Case fatality rates in cancer patients with COVID-19 were significantly increased in all age groups, but older age was associated with higher mortality.
“We observed case fatality rates were elevated in all age cohorts in cancer patients and achieved statistical significance in the age groups 45-64 and in patients older than 75 years of age,” the authors reported.
Other factors significantly associated with higher mortality in a multivariable analysis included the presence of multiple comorbidities; the need for ICU support; and increased levels of d-dimer, lactate, and lactate dehydrogenase.
Additional factors, such as socioeconomic and health disparities, may also be significant predictors of mortality, according to the authors. They noted that this cohort largely consisted of patients from a socioeconomically underprivileged community where mortality because of COVID-19 is reportedly higher.
Proactive strategies moving forward
“We have been addressing the significant burden of the COVID-19 pandemic on our vulnerable cancer patients through a variety of ways,” said study author Balazs Halmos, MD, of Montefiore Medical Center.
The center set up a separate infusion unit exclusively for COVID-positive patients and established separate inpatient areas. Dr. Halmos and colleagues are also providing telemedicine, virtual supportive care services, telephonic counseling, and bilingual peer-support programs.
“Many questions remain as we continue to establish new practices for our cancer patients,” Dr. Halmos said. “We will find answers to these questions as we continue to focus on adaptation and not acceptance in response to the COVID crisis. Our patients deserve nothing less.”
The Albert Einstein Cancer Center supported this study. The authors reported having no conflicts of interest.
SOURCE: Mehta V et al. Cancer Discov. 2020 May 1. doi: 10.1158/2159-8290.CD-20-0516.
COVID-19 patients with cancer had double the fatality rate of COVID-19 patients without cancer treated in an urban New York hospital system, according to data from a retrospective study.
with COVID-19 treated during the same time period in the same hospital system.
Vikas Mehta, MD, of Montefiore Medical Center, New York, and colleagues reported these results in Cancer Discovery.
“As New York has emerged as the current epicenter of the pandemic, we sought to investigate the risk posed by COVID-19 to our cancer population,” the authors wrote.
They identified 218 cancer patients treated for COVID-19 in the Montefiore Health System between March 18 and April 8, 2020. Three-quarters of patients had solid tumors, and 25% had hematologic malignancies. Most patients were adults (98.6%), their median age was 69 years (range, 10-92 years), and 58% were men.
In all, 28% of the cancer patients (61/218) died from COVID-19, including 25% (41/164) of those with solid tumors and 37% (20/54) of those with hematologic malignancies.
Deaths by cancer type
Among the 164 patients with solid tumors, case fatality rates were as follows:
- Pancreatic – 67% (2/3)
- Lung – 55% (6/11)
- Colorectal – 38% (8/21)
- Upper gastrointestinal – 38% (3/8)
- Gynecologic – 38% (5/13)
- Skin – 33% (1/3)
- Hepatobiliary – 29% (2/7)
- Bone/soft tissue – 20% (1/5)
- Genitourinary – 15% (7/46)
- Breast – 14% (4/28)
- Neurologic – 13% (1/8)
- Head and neck – 13% (1/8).
None of the three patients with neuroendocrine tumors died.
Among the 54 patients with hematologic malignancies, case fatality rates were as follows:
- Chronic myeloid leukemia – 100% (1/1)
- Hodgkin lymphoma – 60% (3/5)
- Myelodysplastic syndromes – 60% (3/5)
- Multiple myeloma – 38% (5/13)
- Non-Hodgkin lymphoma – 33% (5/15)
- Chronic lymphocytic leukemia – 33% (1/3)
- Myeloproliferative neoplasms – 29% (2/7).
None of the four patients with acute lymphoblastic leukemia died, and there was one patient with acute myeloid leukemia who did not die.
Factors associated with increased mortality
The researchers compared the 218 cancer patients with COVID-19 with 1,090 age- and sex-matched noncancer patients with COVID-19 treated in the Montefiore Health System between March 18 and April 8, 2020.
Case fatality rates in cancer patients with COVID-19 were significantly increased in all age groups, but older age was associated with higher mortality.
“We observed case fatality rates were elevated in all age cohorts in cancer patients and achieved statistical significance in the age groups 45-64 and in patients older than 75 years of age,” the authors reported.
Other factors significantly associated with higher mortality in a multivariable analysis included the presence of multiple comorbidities; the need for ICU support; and increased levels of d-dimer, lactate, and lactate dehydrogenase.
Additional factors, such as socioeconomic and health disparities, may also be significant predictors of mortality, according to the authors. They noted that this cohort largely consisted of patients from a socioeconomically underprivileged community where mortality because of COVID-19 is reportedly higher.
Proactive strategies moving forward
“We have been addressing the significant burden of the COVID-19 pandemic on our vulnerable cancer patients through a variety of ways,” said study author Balazs Halmos, MD, of Montefiore Medical Center.
The center set up a separate infusion unit exclusively for COVID-positive patients and established separate inpatient areas. Dr. Halmos and colleagues are also providing telemedicine, virtual supportive care services, telephonic counseling, and bilingual peer-support programs.
“Many questions remain as we continue to establish new practices for our cancer patients,” Dr. Halmos said. “We will find answers to these questions as we continue to focus on adaptation and not acceptance in response to the COVID crisis. Our patients deserve nothing less.”
The Albert Einstein Cancer Center supported this study. The authors reported having no conflicts of interest.
SOURCE: Mehta V et al. Cancer Discov. 2020 May 1. doi: 10.1158/2159-8290.CD-20-0516.
FROM CANCER DISCOVERY
Sepsis patients with hypothermia face greater mortality risk
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.
Background: Fevers (like other vital sign abnormalities) often trigger interventions from providers. However, hypothermia (temperature under 36° C) may also be associated with higher mortality.
Study design: Retrospective subanalysis of a previous study (Focused Outcome Research on Emergency Care for Acute respiratory distress syndrome, Sepsis and Trauma [FORECAST]).
Setting: Adult patients with severe sepsis based on Sepsis-2 in 59 ICUs in Japan.
Synopsis: The study involved 1,143 patients admitted to ICUs with severe sepsis (62.6% with septic shock). The median age was 73 years with a median APACHE II and SOFA scores of 22 and 9, respectively. Core temperatures were measured on admission to ICU with patients categorized into three arms: temperature under 36° C (hypothermic), temperature 36°-38° C, and febrile patients with temperature greater than 38° C. Of studied patients, 11.1% were hypothermic on presentation. These patients were older, sicker (higher APACHE/SOFA scores), had lower body mass indexes, and had higher prevalence of septic shock than did the febrile patients. Hypothermic patients fared worse in every clinical outcome measured – in-hospital mortality, 28-day mortality, ventilator-free days, ICU-free days, length of hospital stay, and likelihood of discharge home. The odds ratio of in-hospital mortality for hypothermic patients, compared with reference febrile patients, was 1.76 (95% CI, 1.14-2.73). Patients with hypothermia were also significantly less likely to receive the entire 3-hour resuscitation bundle, including broad-spectrum antibiotics (56.3%) versus 60.8% of patients with temperature 36-38° C and 71.1% for febrile group (P = .003).
Bottom line: Hypothermia in patients with severe sepsis is associated with a significantly higher disease severity, mortality risk, and lower implementation of sepsis bundles. More emphasis on earlier identification and treatment of this specific patient population appears needed.
Citation: Kushimoto S et al. Impact of body temperature abnormalities on the implementation of sepsis bundles and outcomes in patients with severe sepsis: A retrospective sub-analysis of the focused outcome of research of emergency care for acute respiratory distress syndrome, sepsis and trauma study. Crit Care Med. 2019 May;47(5):691-9.
Dr. Sekaran is a hospitalist at Massachusetts General Hospital.
Fountains of Wayne, and a hospitalist’s first day, remembered
Like many in the health care field, I have found it hard to watch the news over these past couple of months when it seems that almost every story is about COVID-19 or its repercussions. Luckily, I have two young daughters who “encourage” me to listen to the Frozen 2 soundtrack instead of putting on the evening news when I get home from work. Still, news manages to seep through my defenses. As I scrolled through some headlines recently, I learned of the death of musician Adam Schlesinger from COVID-19. He wasn’t a household name, but his death still hit me in unexpected ways.
I started internship in late June 2005, in a city (Portland, Ore.) about as different from my previous home (Dallas) as any two places can possibly be. I think the day before internship started still ranks as the most nervous of my life. I’m not sure how I slept at all that night, but somehow I did and arrived at the Portland Veterans Affairs Hospital the following morning to start my new career.
And then … nothing happened. Early on that first day, the electronic medical records crashed, and no patients were admitted during our time on “short call.” My upper level resident took care of the one or two established patients on the team (both discharged), so I ended the day with records that would not be broken during the remainder of my residency: 0 notes written, 0 patients seen. Perhaps the most successful first day that any intern, anywhere has ever had, although it prepared me quite poorly for all the subsequent days.
Since I had some time on my hands, I made the 20-minute walk to one of my new hometown’s record stores where Fountains of Wayne (FOW) was playing an acoustic in-store set. Their album from a few years prior, “Welcome Interstate Managers,” was in heavy rotation when I made the drive from Dallas to Portland. It was (and is) a great album for long drives – melodic, catchy, and (mostly) up-tempo. Adam and the band’s singer, Chris Collingwood, played several songs that night on the store’s stage. Then they headed out to the next city, and I headed back home and on to many far-busier days of residency.
We would cross paths again a decade later. I moved back to Texas and became a hospitalist. It turns out that, if you have enough hospitalists of a certain age and if enough of those hospitalists have unearned confidence in their musical ability, then a covers band will undoubtedly be formed. And so, it happened here in San Antonio. We were not selective in our song choices – we played songs from every decade of the last 50 years, bands as popular as the Beatles and as indie as the Rentals. And we played some FOW.
Our band (which will go nameless here so that our YouTube recordings are more difficult to find) played a grand total of one gig during our years of intermittent practicing. That one gig was my wedding rehearsal dinner and the penultimate song we played was “Stacy’s Mom,” which is notable for being both FOW’s biggest hit and a completely inappropriate song to play at a wedding rehearsal dinner. The crowd was probably around the same size as the one that had seen Adam and Chris play in Portland 10 years prior. I don’t think the applause we received was quite as genuine or deserved, though.
After Adam and Chris played their gig, there was an autograph session and I took home a signed poster. Last year, I decided to take it out of storage and hang it in my office. The date of the show and the first day of my physician career, a date now nearly 15 years ago, is written in psychedelic typography at the bottom. The store that I went to that day is no longer there, a victim of progress like so many other record stores across the country. Another location of the same store is still open in Portland. I hope that it and all the other small book and music stores across the country can survive this current crisis, but I know that many will not.
So, here’s to you Adam, and to all the others who have lost their lives to this terrible illness. As a small token of remembrance, I’ll be playing some Fountains of Wayne on the drive home tonight. It’s not quite the same as playing it on a cross-country drive, but hopefully, we will all be able to do that again soon.
Dr. Sehgal is a clinical associate professor of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. He is a member of the editorial advisory board for The Hospitalist.
Like many in the health care field, I have found it hard to watch the news over these past couple of months when it seems that almost every story is about COVID-19 or its repercussions. Luckily, I have two young daughters who “encourage” me to listen to the Frozen 2 soundtrack instead of putting on the evening news when I get home from work. Still, news manages to seep through my defenses. As I scrolled through some headlines recently, I learned of the death of musician Adam Schlesinger from COVID-19. He wasn’t a household name, but his death still hit me in unexpected ways.
I started internship in late June 2005, in a city (Portland, Ore.) about as different from my previous home (Dallas) as any two places can possibly be. I think the day before internship started still ranks as the most nervous of my life. I’m not sure how I slept at all that night, but somehow I did and arrived at the Portland Veterans Affairs Hospital the following morning to start my new career.
And then … nothing happened. Early on that first day, the electronic medical records crashed, and no patients were admitted during our time on “short call.” My upper level resident took care of the one or two established patients on the team (both discharged), so I ended the day with records that would not be broken during the remainder of my residency: 0 notes written, 0 patients seen. Perhaps the most successful first day that any intern, anywhere has ever had, although it prepared me quite poorly for all the subsequent days.
Since I had some time on my hands, I made the 20-minute walk to one of my new hometown’s record stores where Fountains of Wayne (FOW) was playing an acoustic in-store set. Their album from a few years prior, “Welcome Interstate Managers,” was in heavy rotation when I made the drive from Dallas to Portland. It was (and is) a great album for long drives – melodic, catchy, and (mostly) up-tempo. Adam and the band’s singer, Chris Collingwood, played several songs that night on the store’s stage. Then they headed out to the next city, and I headed back home and on to many far-busier days of residency.
We would cross paths again a decade later. I moved back to Texas and became a hospitalist. It turns out that, if you have enough hospitalists of a certain age and if enough of those hospitalists have unearned confidence in their musical ability, then a covers band will undoubtedly be formed. And so, it happened here in San Antonio. We were not selective in our song choices – we played songs from every decade of the last 50 years, bands as popular as the Beatles and as indie as the Rentals. And we played some FOW.
Our band (which will go nameless here so that our YouTube recordings are more difficult to find) played a grand total of one gig during our years of intermittent practicing. That one gig was my wedding rehearsal dinner and the penultimate song we played was “Stacy’s Mom,” which is notable for being both FOW’s biggest hit and a completely inappropriate song to play at a wedding rehearsal dinner. The crowd was probably around the same size as the one that had seen Adam and Chris play in Portland 10 years prior. I don’t think the applause we received was quite as genuine or deserved, though.
After Adam and Chris played their gig, there was an autograph session and I took home a signed poster. Last year, I decided to take it out of storage and hang it in my office. The date of the show and the first day of my physician career, a date now nearly 15 years ago, is written in psychedelic typography at the bottom. The store that I went to that day is no longer there, a victim of progress like so many other record stores across the country. Another location of the same store is still open in Portland. I hope that it and all the other small book and music stores across the country can survive this current crisis, but I know that many will not.
So, here’s to you Adam, and to all the others who have lost their lives to this terrible illness. As a small token of remembrance, I’ll be playing some Fountains of Wayne on the drive home tonight. It’s not quite the same as playing it on a cross-country drive, but hopefully, we will all be able to do that again soon.
Dr. Sehgal is a clinical associate professor of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. He is a member of the editorial advisory board for The Hospitalist.
Like many in the health care field, I have found it hard to watch the news over these past couple of months when it seems that almost every story is about COVID-19 or its repercussions. Luckily, I have two young daughters who “encourage” me to listen to the Frozen 2 soundtrack instead of putting on the evening news when I get home from work. Still, news manages to seep through my defenses. As I scrolled through some headlines recently, I learned of the death of musician Adam Schlesinger from COVID-19. He wasn’t a household name, but his death still hit me in unexpected ways.
I started internship in late June 2005, in a city (Portland, Ore.) about as different from my previous home (Dallas) as any two places can possibly be. I think the day before internship started still ranks as the most nervous of my life. I’m not sure how I slept at all that night, but somehow I did and arrived at the Portland Veterans Affairs Hospital the following morning to start my new career.
And then … nothing happened. Early on that first day, the electronic medical records crashed, and no patients were admitted during our time on “short call.” My upper level resident took care of the one or two established patients on the team (both discharged), so I ended the day with records that would not be broken during the remainder of my residency: 0 notes written, 0 patients seen. Perhaps the most successful first day that any intern, anywhere has ever had, although it prepared me quite poorly for all the subsequent days.
Since I had some time on my hands, I made the 20-minute walk to one of my new hometown’s record stores where Fountains of Wayne (FOW) was playing an acoustic in-store set. Their album from a few years prior, “Welcome Interstate Managers,” was in heavy rotation when I made the drive from Dallas to Portland. It was (and is) a great album for long drives – melodic, catchy, and (mostly) up-tempo. Adam and the band’s singer, Chris Collingwood, played several songs that night on the store’s stage. Then they headed out to the next city, and I headed back home and on to many far-busier days of residency.
We would cross paths again a decade later. I moved back to Texas and became a hospitalist. It turns out that, if you have enough hospitalists of a certain age and if enough of those hospitalists have unearned confidence in their musical ability, then a covers band will undoubtedly be formed. And so, it happened here in San Antonio. We were not selective in our song choices – we played songs from every decade of the last 50 years, bands as popular as the Beatles and as indie as the Rentals. And we played some FOW.
Our band (which will go nameless here so that our YouTube recordings are more difficult to find) played a grand total of one gig during our years of intermittent practicing. That one gig was my wedding rehearsal dinner and the penultimate song we played was “Stacy’s Mom,” which is notable for being both FOW’s biggest hit and a completely inappropriate song to play at a wedding rehearsal dinner. The crowd was probably around the same size as the one that had seen Adam and Chris play in Portland 10 years prior. I don’t think the applause we received was quite as genuine or deserved, though.
After Adam and Chris played their gig, there was an autograph session and I took home a signed poster. Last year, I decided to take it out of storage and hang it in my office. The date of the show and the first day of my physician career, a date now nearly 15 years ago, is written in psychedelic typography at the bottom. The store that I went to that day is no longer there, a victim of progress like so many other record stores across the country. Another location of the same store is still open in Portland. I hope that it and all the other small book and music stores across the country can survive this current crisis, but I know that many will not.
So, here’s to you Adam, and to all the others who have lost their lives to this terrible illness. As a small token of remembrance, I’ll be playing some Fountains of Wayne on the drive home tonight. It’s not quite the same as playing it on a cross-country drive, but hopefully, we will all be able to do that again soon.
Dr. Sehgal is a clinical associate professor of medicine in the division of general and hospital medicine at the South Texas Veterans Health Care System and UT-Health San Antonio. He is a member of the editorial advisory board for The Hospitalist.