User login
Simple Intraoperative Technique to Improve Wound Edge Approximation for Residents
Practice Gap
Dermatology residents can struggle with surgical closure early in their training years. Although experienced dermatologic surgeons may intuitively be able to align edges for maximal cosmesis, doing so can prove challenging in the context of learning basic surgical techniques for early residents.
Furthermore, local anesthesia can distort cutaneous anatomy and surgical landmarks, requiring the surgeon to reexamine their closure technique. Patients may require position changes or may make involuntary movements, both of which require dynamic thinking and planning on the part of the dermatologic surgeon to achieve optimal outcomes.
The Technique
We propose the use of sutures to intraoperatively guide placement of the dermal needle. This technique can be used for various closure types; here, we demonstrate its use in a standard elliptical excision.
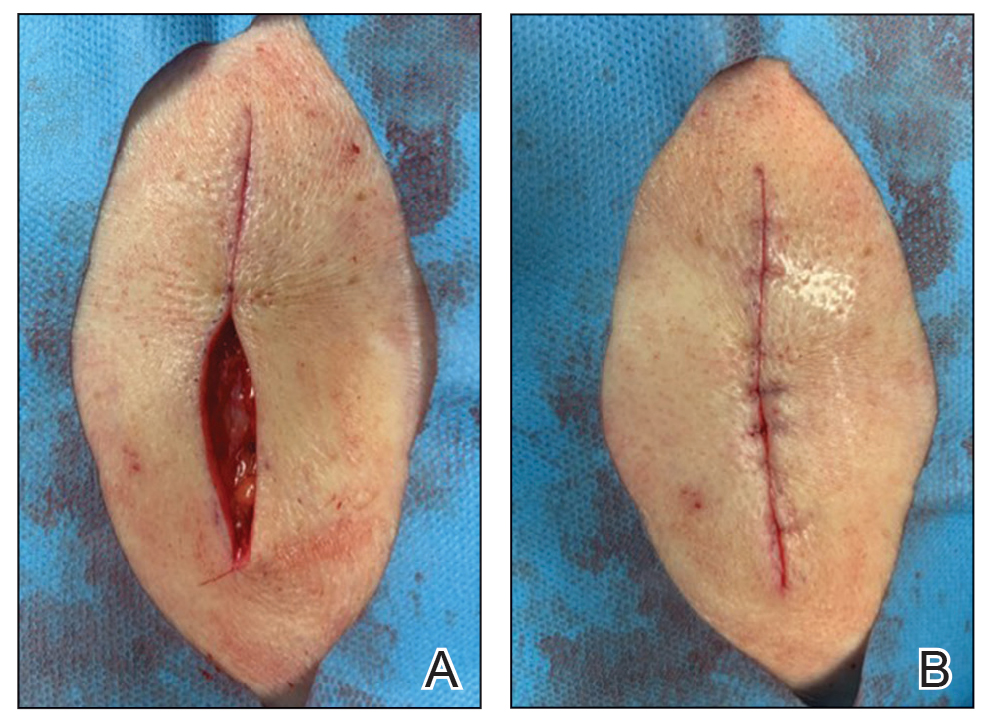
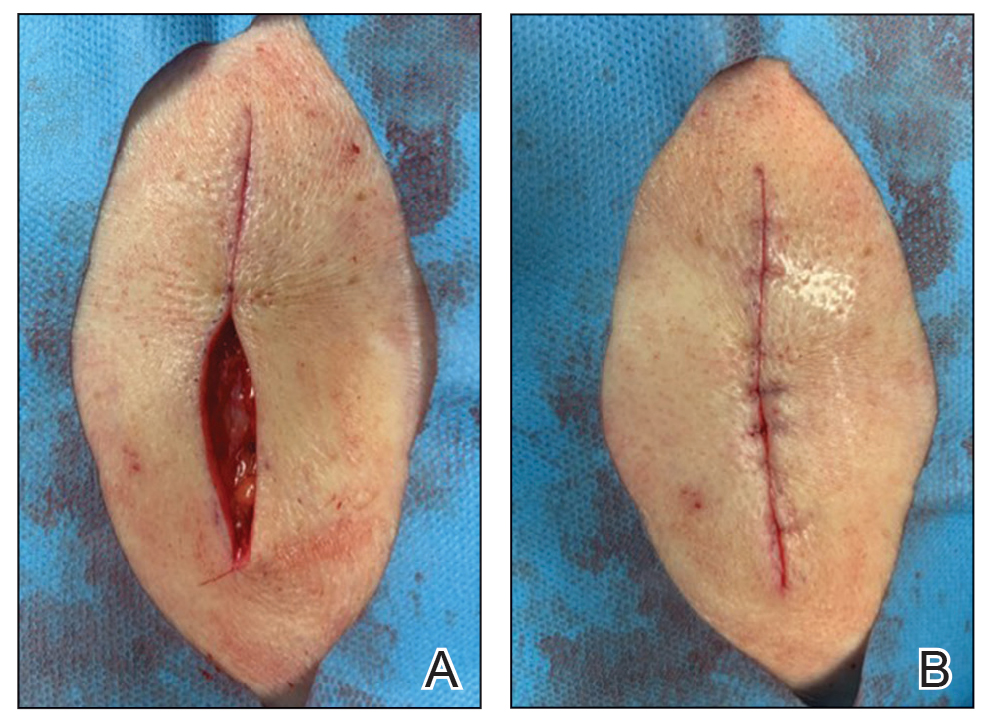
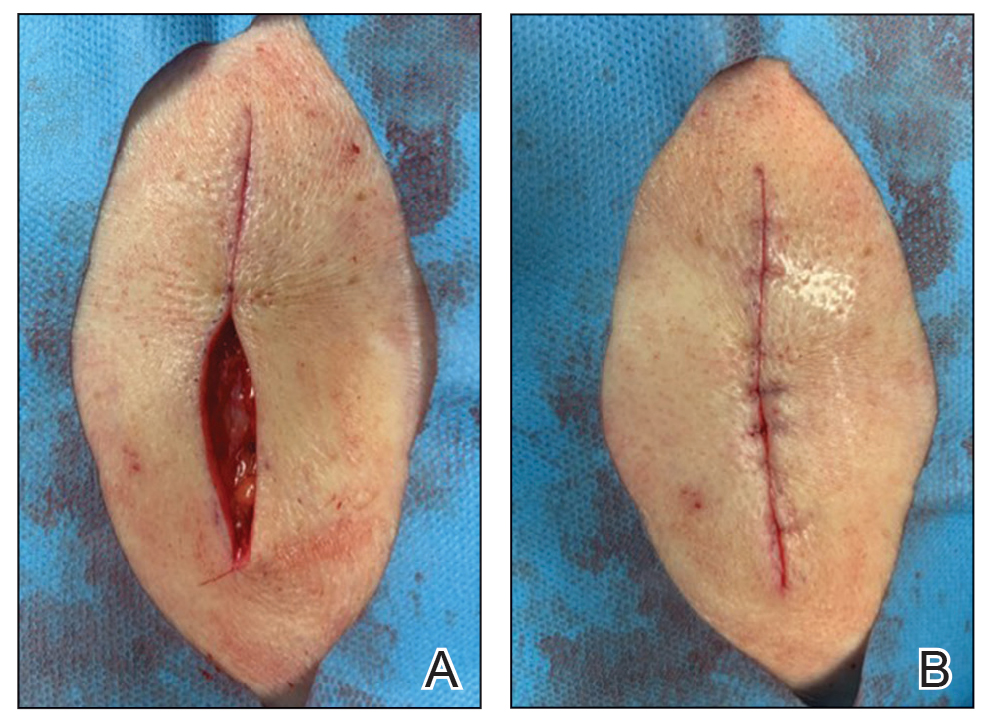
To begin, a standard length to width ellipse ratio of 3:1 is drawn with appropriate margins around a neoplasm.1 After excision and appropriate undermining of the ellipse, we typically use deep sutures to close the deep space. The first pass of the needle through tissue can be performed in a place of the surgeon’s preference but typically abides by the rule of halves or the zipper method (Figure 1A). To determine optimal placement of the second needle pass through tissue, we recommend applying gentle opposing traction forces to the wound apices to approximate the linear outcome of the wound edges. The surgeon can use a skin hook to guide placement of the needle to the contralateral wound edge in an unassisted method of this technique (Figure 1B). The surgeon’s assistant also can aid in applying cutaneous traction along the length of the excision if the surgeon wishes to free their hands (Figure 1C). Because the risk of needlestick injury at this step is small, it is prudent for the surgeon to advise the assistant to avoid needlestick injury by keeping their hands away from the needle path in the surgical site.
Although traction is being applied to the wound apices, the deep suture should extend across the wound with just enough pressure to leave a serosanguineous notched mark in the contralateral tissue edge (Figure 1D). After releasing traction on the wound edges, the surgeon can effortlessly visualize the target for needle placement and make a throw through the tissue accordingly.

This process can be continued until wound closure is complete (Figure 2). Top sutures or adhesive strips can be placed afterward for completing approximation of the wound edges superficially.
Practice Implications
By using this technique to align wound edges intraoperatively, the surgeon can have a functional guide for needle placement. The technique allows improvement of function and cosmesis of surgical wounds, while also accounting for topographical variations in the patient’s surgical site. Approximation of the wound edges is particularly important at the beginning of closure, as the wound edges align and approximate more with each subsequent stitch, with decreasing tension.2
In addition, when operating on a curvilinear or challenging topographical surface of the body, this technique can provide a clear template for guiding suture placement for approximating wound edges. Furthermore, local biodynamic anatomy might become distorted after excision of the tissue specimen due to release of centripetal tangential forces that were present in the pre-excised skin.1 Local change in biodynamic forces may be difficult to plan for preoperatively using other techniques.3
Although this technique can be utilized for all suture placements in closure, it is of greatest value when placing the first few sutures and when operating on nonplanar surfaces that might become distorted after excision. To ensure the best outcome, it is important to be certain that the area has been properly cleaned prior to surgery and a sterile technique is used.
- Paul SP. Biodynamic excisional skin tension lines for excisional surgery of the lower limb and the technique of using parallel relaxing incisions to further reduce wound tension. Plast Reconstr Surg Glob Open. 2017;5:E1614. doi:10.1097/GOX.0000000000001614
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
- Parikh SA, Sloan B. Clinical pearl: a simple and effective technique for improving surgical closures for the early-learning resident. Cutis. 2017;100:338-339.
Practice Gap
Dermatology residents can struggle with surgical closure early in their training years. Although experienced dermatologic surgeons may intuitively be able to align edges for maximal cosmesis, doing so can prove challenging in the context of learning basic surgical techniques for early residents.
Furthermore, local anesthesia can distort cutaneous anatomy and surgical landmarks, requiring the surgeon to reexamine their closure technique. Patients may require position changes or may make involuntary movements, both of which require dynamic thinking and planning on the part of the dermatologic surgeon to achieve optimal outcomes.
The Technique
We propose the use of sutures to intraoperatively guide placement of the dermal needle. This technique can be used for various closure types; here, we demonstrate its use in a standard elliptical excision.
To begin, a standard length to width ellipse ratio of 3:1 is drawn with appropriate margins around a neoplasm.1 After excision and appropriate undermining of the ellipse, we typically use deep sutures to close the deep space. The first pass of the needle through tissue can be performed in a place of the surgeon’s preference but typically abides by the rule of halves or the zipper method (Figure 1A). To determine optimal placement of the second needle pass through tissue, we recommend applying gentle opposing traction forces to the wound apices to approximate the linear outcome of the wound edges. The surgeon can use a skin hook to guide placement of the needle to the contralateral wound edge in an unassisted method of this technique (Figure 1B). The surgeon’s assistant also can aid in applying cutaneous traction along the length of the excision if the surgeon wishes to free their hands (Figure 1C). Because the risk of needlestick injury at this step is small, it is prudent for the surgeon to advise the assistant to avoid needlestick injury by keeping their hands away from the needle path in the surgical site.
Although traction is being applied to the wound apices, the deep suture should extend across the wound with just enough pressure to leave a serosanguineous notched mark in the contralateral tissue edge (Figure 1D). After releasing traction on the wound edges, the surgeon can effortlessly visualize the target for needle placement and make a throw through the tissue accordingly.

This process can be continued until wound closure is complete (Figure 2). Top sutures or adhesive strips can be placed afterward for completing approximation of the wound edges superficially.
Practice Implications
By using this technique to align wound edges intraoperatively, the surgeon can have a functional guide for needle placement. The technique allows improvement of function and cosmesis of surgical wounds, while also accounting for topographical variations in the patient’s surgical site. Approximation of the wound edges is particularly important at the beginning of closure, as the wound edges align and approximate more with each subsequent stitch, with decreasing tension.2
In addition, when operating on a curvilinear or challenging topographical surface of the body, this technique can provide a clear template for guiding suture placement for approximating wound edges. Furthermore, local biodynamic anatomy might become distorted after excision of the tissue specimen due to release of centripetal tangential forces that were present in the pre-excised skin.1 Local change in biodynamic forces may be difficult to plan for preoperatively using other techniques.3
Although this technique can be utilized for all suture placements in closure, it is of greatest value when placing the first few sutures and when operating on nonplanar surfaces that might become distorted after excision. To ensure the best outcome, it is important to be certain that the area has been properly cleaned prior to surgery and a sterile technique is used.
Practice Gap
Dermatology residents can struggle with surgical closure early in their training years. Although experienced dermatologic surgeons may intuitively be able to align edges for maximal cosmesis, doing so can prove challenging in the context of learning basic surgical techniques for early residents.
Furthermore, local anesthesia can distort cutaneous anatomy and surgical landmarks, requiring the surgeon to reexamine their closure technique. Patients may require position changes or may make involuntary movements, both of which require dynamic thinking and planning on the part of the dermatologic surgeon to achieve optimal outcomes.
The Technique
We propose the use of sutures to intraoperatively guide placement of the dermal needle. This technique can be used for various closure types; here, we demonstrate its use in a standard elliptical excision.
To begin, a standard length to width ellipse ratio of 3:1 is drawn with appropriate margins around a neoplasm.1 After excision and appropriate undermining of the ellipse, we typically use deep sutures to close the deep space. The first pass of the needle through tissue can be performed in a place of the surgeon’s preference but typically abides by the rule of halves or the zipper method (Figure 1A). To determine optimal placement of the second needle pass through tissue, we recommend applying gentle opposing traction forces to the wound apices to approximate the linear outcome of the wound edges. The surgeon can use a skin hook to guide placement of the needle to the contralateral wound edge in an unassisted method of this technique (Figure 1B). The surgeon’s assistant also can aid in applying cutaneous traction along the length of the excision if the surgeon wishes to free their hands (Figure 1C). Because the risk of needlestick injury at this step is small, it is prudent for the surgeon to advise the assistant to avoid needlestick injury by keeping their hands away from the needle path in the surgical site.
Although traction is being applied to the wound apices, the deep suture should extend across the wound with just enough pressure to leave a serosanguineous notched mark in the contralateral tissue edge (Figure 1D). After releasing traction on the wound edges, the surgeon can effortlessly visualize the target for needle placement and make a throw through the tissue accordingly.

This process can be continued until wound closure is complete (Figure 2). Top sutures or adhesive strips can be placed afterward for completing approximation of the wound edges superficially.
Practice Implications
By using this technique to align wound edges intraoperatively, the surgeon can have a functional guide for needle placement. The technique allows improvement of function and cosmesis of surgical wounds, while also accounting for topographical variations in the patient’s surgical site. Approximation of the wound edges is particularly important at the beginning of closure, as the wound edges align and approximate more with each subsequent stitch, with decreasing tension.2
In addition, when operating on a curvilinear or challenging topographical surface of the body, this technique can provide a clear template for guiding suture placement for approximating wound edges. Furthermore, local biodynamic anatomy might become distorted after excision of the tissue specimen due to release of centripetal tangential forces that were present in the pre-excised skin.1 Local change in biodynamic forces may be difficult to plan for preoperatively using other techniques.3
Although this technique can be utilized for all suture placements in closure, it is of greatest value when placing the first few sutures and when operating on nonplanar surfaces that might become distorted after excision. To ensure the best outcome, it is important to be certain that the area has been properly cleaned prior to surgery and a sterile technique is used.
- Paul SP. Biodynamic excisional skin tension lines for excisional surgery of the lower limb and the technique of using parallel relaxing incisions to further reduce wound tension. Plast Reconstr Surg Glob Open. 2017;5:E1614. doi:10.1097/GOX.0000000000001614
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
- Parikh SA, Sloan B. Clinical pearl: a simple and effective technique for improving surgical closures for the early-learning resident. Cutis. 2017;100:338-339.
- Paul SP. Biodynamic excisional skin tension lines for excisional surgery of the lower limb and the technique of using parallel relaxing incisions to further reduce wound tension. Plast Reconstr Surg Glob Open. 2017;5:E1614. doi:10.1097/GOX.0000000000001614
- Miller CJ, Antunes MB, Sobanko JF. Surgical technique for optimal outcomes: part II. repairing tissue: suturing. J Am Acad Dermatol. 2015;72:389-402. doi:10.1016/j.jaad.2014.08.006
- Parikh SA, Sloan B. Clinical pearl: a simple and effective technique for improving surgical closures for the early-learning resident. Cutis. 2017;100:338-339.
Itchy Vesicular Rash
The Diagnosis: Tinea Corporis Bullosa
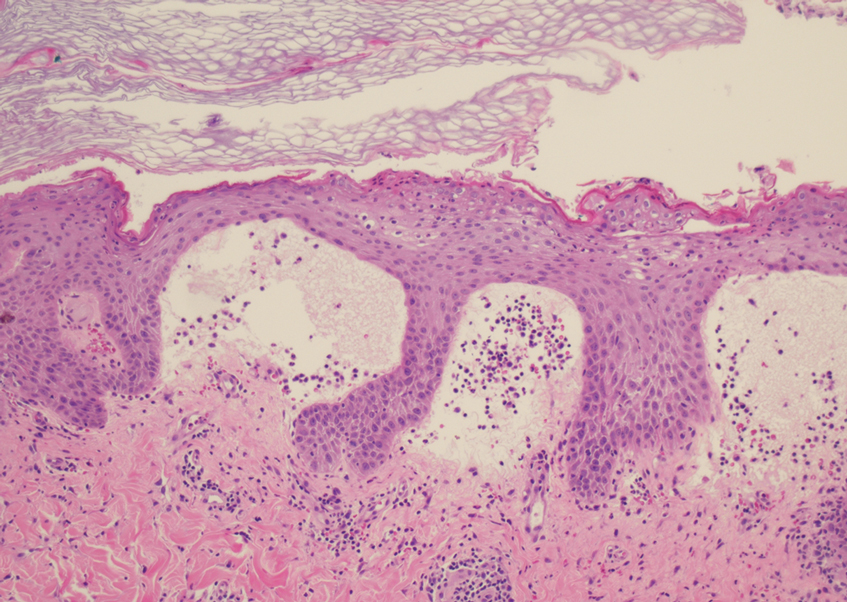
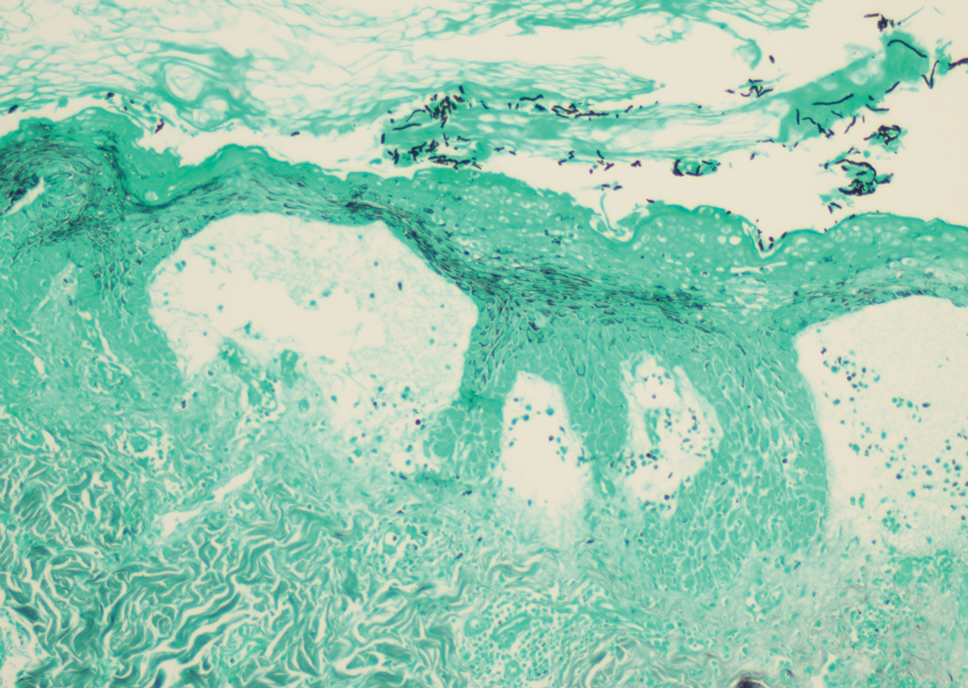
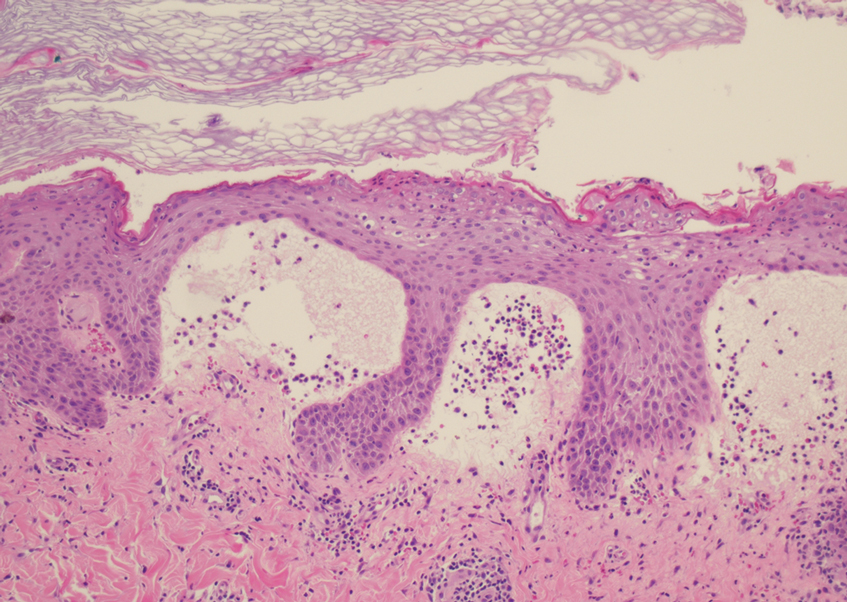
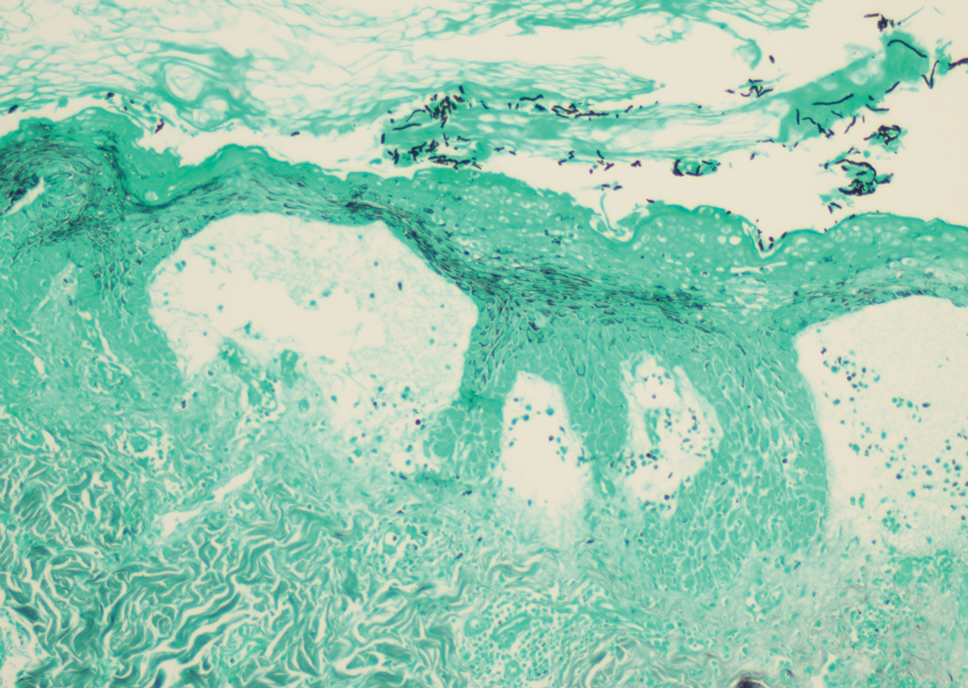
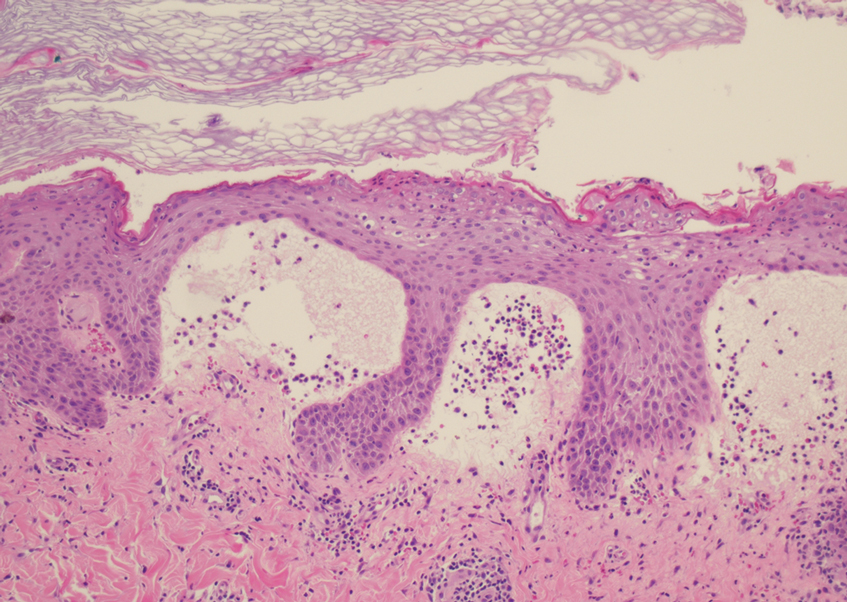
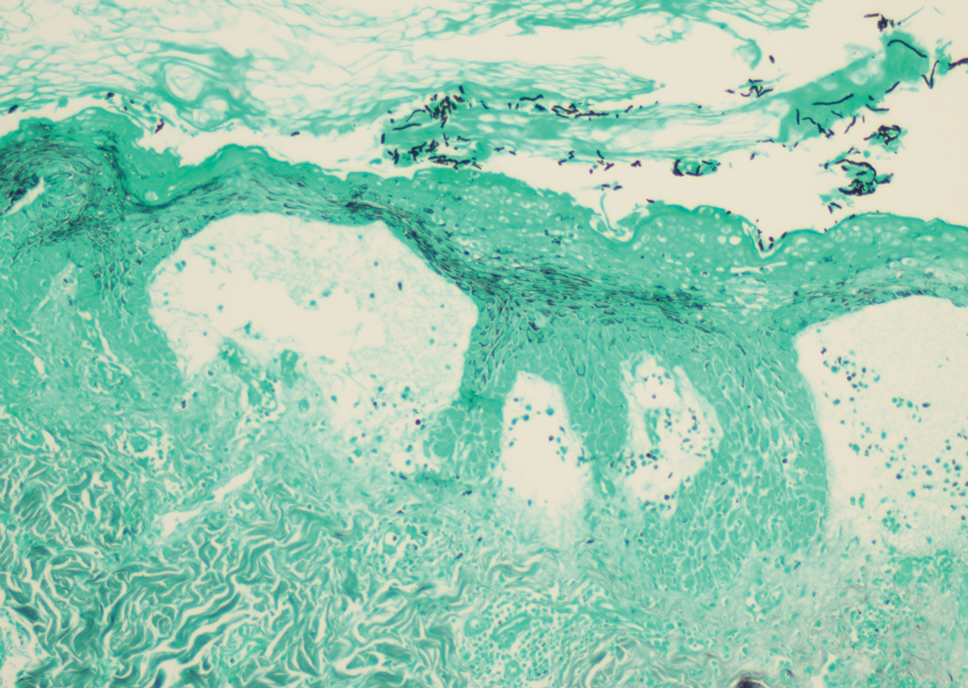
At the time of presentation, a potassium hydroxide (KOH) preparation, fungal culture, and punch biopsy of the right ventral wrist was performed. The KOH preparation was positive for fungal hyphae characteristic of dermatophyte infections. Histologically, the biopsy showed intraepidermal and subepidermal blisters with neutrophil- and lymphocyte-rich contents (Figure 1). Fungal hyphae and spores were present within the stratum corneum and superficial epidermis (Figure 2), and fungal cultures grew Microsporum canis. The extent of the rash (upper and lower extremities, chest, and back), positive fungal culture, and KOH preparation all supported the diagnosis of tinea corporis bullosa, which was confirmed with biopsy. Oral prednisone use was discouraged and triamcinolone ointment was discontinued given that inappropriate treatment with steroids in the setting of fungal infection suppresses an inflammatory response and alters clinical appearance, obviating the persistent underlying infection.
Tinea corporis bullosa is a rare superficial dermatophyte fungal infection that often is acquired by close personto- person contact or contact with domestic animals. The infection begins as a circular pruritic plaque, generally with raised borders, which may be erythematous or hyperpigmented. By definition, tinea corporis occurs in sites other than the face, feet, hands, or groin area. Bullae formation is thought to be secondary to a delayed hypersensitivity reaction provoked by the presence of a dermatophyte antigen.1
Linear IgA bullous dermatosis is an immunemediated disease characterized by IgA deposition at the dermoepidermal junction. Linear IgA bullous dermatosis classically presents as widespread tense vesicles in an arciform or annular pattern. Mucosal involvement is common and typically presents with erosions, ulcerations, and scarring.2 Given the absence of mucosal involvement in our patient and a positive KOH preparation, linear IgA bullous dermatosis was an unlikely diagnosis.
Benign inoculation lymphoreticulosis, more commonly known as cat scratch disease (CSD), is a Bartonella henselae infection that results from a cat scratch or bite. Cat scratch disease can present as localized cutaneous and nodal involvement (lymphadenopathy) near the site of inoculation, or it may present as disseminated disease. Cutaneous lesions generally progress through vesicular, erythematous, and papular phases. Regional lymphadenopathy proximal to the inoculation site is the hallmark of CSD.3 Given the absence of lymphadenopathy in our patient as well as the sporadic distribution of lesions, CSD was an unlikely diagnosis.
Dermatitis herpetiformis (DH) is an autoimmune disorder with cutaneous manifestations of gluten sensitivity. Dermatitis herpetiformis presents as extremely pruritic papules and vesicles arranged in groups on areas such as the elbows, dorsal aspects of the forearms, knees, scalp, back, and buttocks. Most patients with DH have celiac disease or small bowel disease related to gluten sensitivity.4 Given our patient’s acute presentation in adulthood and lack of gluten sensitivity, DH was an unlikely diagnosis.
Bullous fixed drug reaction is a cutaneous eruption that typically presents in the setting of exposure to an offending drug/agent. Drug reactions can have various cutaneous presentations, with the most common being pigmented macules that progress into plaques.5 Given the isolated nature of our patient’s episode and apparent lack of association with medication, bullous fixed drug reaction was an unlikely diagnosis.
Tinea corporis bullosa is a rare clinical variant of tinea corporis that has only been reported in patients with a history of contact with different animals. There are many causative organisms related to tinea corporis; Trichophyton rubrum is the most common etiology of tinea corporis, while tinea corporis due to close contact with domesticated animals often is caused by M canis.6 The immunoinhibitory properties of the mannans in the fungal cell wall allow the organisms to adhere to the skin prior to invasion. Cutaneous invasion into dead cornified layers of the skin is credited to the proteases, subtilisinlike proteases (subtilases), and keratinases produced by the fungus.1 There are many different clinical presentations of tinea corporis due to the variability of causative organisms. An annular (ring-shaped) lesion with a central plaque and advancing border is the most typical presentation. Tinea corporis bullosa is characterized by the presence of bullae or vesicles in the borders of the scaly plaque. Rupture of the bullae subsequently leads to erosions and crusts over the plaque.
The diagnosis of tinea corporis bullosa often is clinical if the lesion is typical and can be confirmed using KOH preparation and fungal culture. Once the diagnosis is confirmed, topical antifungals are the standard treatment approach for localized superficial tinea corporis. Systemic antifungal treatment can be initiated if the lesion is extensive, recurrent, chronic, or unresponsive to topical treatment.1 Given our patient’s characteristic presentation, she was managed with an over-the-counter topical antifungal (terbinafine). The patient’s lesions dramatically improved, rendering oral therapy unnecessary. At 1-month follow-up, the rash had nearly resolved.
- Leung AK, Lam JM, Leong KF, et al. Tinea corporis: an updated review [published online July 20, 2020]. Drugs Context. doi:10.7573/dic.2020-5-6
- Guide SV, Marinkovich MP. Linear IgA bullous dermatosis. Clin Dermatol. 2001;19:719-727.
- Lamps LW, Scott MA. Cat-scratch disease: historic, clinical, and pathologic perspectives. Pathology Patterns Reviews. 2004;121(suppl):S71-S80.
- Caproni M, Antiga E, Melani L, et al. Guidelines for the diagnosis and treatment of dermatitis herpetiformis. J Eur Acad Dermatol Venereol. 2009;23:633-638.
- Patel S, John AM, Handler MZ, et al. Fixed drug eruptions: an update, emphasizing the potentially lethal generalized bullous fixed drug eruption. Am J Clin Dermatol. 2020;21:393-399.
- Ziemer M, Seyfarth F, Elsner P, et al. Atypical manifestations of tinea corporis. Mycoses. 2007;50:31-35.
The Diagnosis: Tinea Corporis Bullosa
At the time of presentation, a potassium hydroxide (KOH) preparation, fungal culture, and punch biopsy of the right ventral wrist was performed. The KOH preparation was positive for fungal hyphae characteristic of dermatophyte infections. Histologically, the biopsy showed intraepidermal and subepidermal blisters with neutrophil- and lymphocyte-rich contents (Figure 1). Fungal hyphae and spores were present within the stratum corneum and superficial epidermis (Figure 2), and fungal cultures grew Microsporum canis. The extent of the rash (upper and lower extremities, chest, and back), positive fungal culture, and KOH preparation all supported the diagnosis of tinea corporis bullosa, which was confirmed with biopsy. Oral prednisone use was discouraged and triamcinolone ointment was discontinued given that inappropriate treatment with steroids in the setting of fungal infection suppresses an inflammatory response and alters clinical appearance, obviating the persistent underlying infection.
Tinea corporis bullosa is a rare superficial dermatophyte fungal infection that often is acquired by close personto- person contact or contact with domestic animals. The infection begins as a circular pruritic plaque, generally with raised borders, which may be erythematous or hyperpigmented. By definition, tinea corporis occurs in sites other than the face, feet, hands, or groin area. Bullae formation is thought to be secondary to a delayed hypersensitivity reaction provoked by the presence of a dermatophyte antigen.1
Linear IgA bullous dermatosis is an immunemediated disease characterized by IgA deposition at the dermoepidermal junction. Linear IgA bullous dermatosis classically presents as widespread tense vesicles in an arciform or annular pattern. Mucosal involvement is common and typically presents with erosions, ulcerations, and scarring.2 Given the absence of mucosal involvement in our patient and a positive KOH preparation, linear IgA bullous dermatosis was an unlikely diagnosis.
Benign inoculation lymphoreticulosis, more commonly known as cat scratch disease (CSD), is a Bartonella henselae infection that results from a cat scratch or bite. Cat scratch disease can present as localized cutaneous and nodal involvement (lymphadenopathy) near the site of inoculation, or it may present as disseminated disease. Cutaneous lesions generally progress through vesicular, erythematous, and papular phases. Regional lymphadenopathy proximal to the inoculation site is the hallmark of CSD.3 Given the absence of lymphadenopathy in our patient as well as the sporadic distribution of lesions, CSD was an unlikely diagnosis.
Dermatitis herpetiformis (DH) is an autoimmune disorder with cutaneous manifestations of gluten sensitivity. Dermatitis herpetiformis presents as extremely pruritic papules and vesicles arranged in groups on areas such as the elbows, dorsal aspects of the forearms, knees, scalp, back, and buttocks. Most patients with DH have celiac disease or small bowel disease related to gluten sensitivity.4 Given our patient’s acute presentation in adulthood and lack of gluten sensitivity, DH was an unlikely diagnosis.
Bullous fixed drug reaction is a cutaneous eruption that typically presents in the setting of exposure to an offending drug/agent. Drug reactions can have various cutaneous presentations, with the most common being pigmented macules that progress into plaques.5 Given the isolated nature of our patient’s episode and apparent lack of association with medication, bullous fixed drug reaction was an unlikely diagnosis.
Tinea corporis bullosa is a rare clinical variant of tinea corporis that has only been reported in patients with a history of contact with different animals. There are many causative organisms related to tinea corporis; Trichophyton rubrum is the most common etiology of tinea corporis, while tinea corporis due to close contact with domesticated animals often is caused by M canis.6 The immunoinhibitory properties of the mannans in the fungal cell wall allow the organisms to adhere to the skin prior to invasion. Cutaneous invasion into dead cornified layers of the skin is credited to the proteases, subtilisinlike proteases (subtilases), and keratinases produced by the fungus.1 There are many different clinical presentations of tinea corporis due to the variability of causative organisms. An annular (ring-shaped) lesion with a central plaque and advancing border is the most typical presentation. Tinea corporis bullosa is characterized by the presence of bullae or vesicles in the borders of the scaly plaque. Rupture of the bullae subsequently leads to erosions and crusts over the plaque.
The diagnosis of tinea corporis bullosa often is clinical if the lesion is typical and can be confirmed using KOH preparation and fungal culture. Once the diagnosis is confirmed, topical antifungals are the standard treatment approach for localized superficial tinea corporis. Systemic antifungal treatment can be initiated if the lesion is extensive, recurrent, chronic, or unresponsive to topical treatment.1 Given our patient’s characteristic presentation, she was managed with an over-the-counter topical antifungal (terbinafine). The patient’s lesions dramatically improved, rendering oral therapy unnecessary. At 1-month follow-up, the rash had nearly resolved.
The Diagnosis: Tinea Corporis Bullosa
At the time of presentation, a potassium hydroxide (KOH) preparation, fungal culture, and punch biopsy of the right ventral wrist was performed. The KOH preparation was positive for fungal hyphae characteristic of dermatophyte infections. Histologically, the biopsy showed intraepidermal and subepidermal blisters with neutrophil- and lymphocyte-rich contents (Figure 1). Fungal hyphae and spores were present within the stratum corneum and superficial epidermis (Figure 2), and fungal cultures grew Microsporum canis. The extent of the rash (upper and lower extremities, chest, and back), positive fungal culture, and KOH preparation all supported the diagnosis of tinea corporis bullosa, which was confirmed with biopsy. Oral prednisone use was discouraged and triamcinolone ointment was discontinued given that inappropriate treatment with steroids in the setting of fungal infection suppresses an inflammatory response and alters clinical appearance, obviating the persistent underlying infection.
Tinea corporis bullosa is a rare superficial dermatophyte fungal infection that often is acquired by close personto- person contact or contact with domestic animals. The infection begins as a circular pruritic plaque, generally with raised borders, which may be erythematous or hyperpigmented. By definition, tinea corporis occurs in sites other than the face, feet, hands, or groin area. Bullae formation is thought to be secondary to a delayed hypersensitivity reaction provoked by the presence of a dermatophyte antigen.1
Linear IgA bullous dermatosis is an immunemediated disease characterized by IgA deposition at the dermoepidermal junction. Linear IgA bullous dermatosis classically presents as widespread tense vesicles in an arciform or annular pattern. Mucosal involvement is common and typically presents with erosions, ulcerations, and scarring.2 Given the absence of mucosal involvement in our patient and a positive KOH preparation, linear IgA bullous dermatosis was an unlikely diagnosis.
Benign inoculation lymphoreticulosis, more commonly known as cat scratch disease (CSD), is a Bartonella henselae infection that results from a cat scratch or bite. Cat scratch disease can present as localized cutaneous and nodal involvement (lymphadenopathy) near the site of inoculation, or it may present as disseminated disease. Cutaneous lesions generally progress through vesicular, erythematous, and papular phases. Regional lymphadenopathy proximal to the inoculation site is the hallmark of CSD.3 Given the absence of lymphadenopathy in our patient as well as the sporadic distribution of lesions, CSD was an unlikely diagnosis.
Dermatitis herpetiformis (DH) is an autoimmune disorder with cutaneous manifestations of gluten sensitivity. Dermatitis herpetiformis presents as extremely pruritic papules and vesicles arranged in groups on areas such as the elbows, dorsal aspects of the forearms, knees, scalp, back, and buttocks. Most patients with DH have celiac disease or small bowel disease related to gluten sensitivity.4 Given our patient’s acute presentation in adulthood and lack of gluten sensitivity, DH was an unlikely diagnosis.
Bullous fixed drug reaction is a cutaneous eruption that typically presents in the setting of exposure to an offending drug/agent. Drug reactions can have various cutaneous presentations, with the most common being pigmented macules that progress into plaques.5 Given the isolated nature of our patient’s episode and apparent lack of association with medication, bullous fixed drug reaction was an unlikely diagnosis.
Tinea corporis bullosa is a rare clinical variant of tinea corporis that has only been reported in patients with a history of contact with different animals. There are many causative organisms related to tinea corporis; Trichophyton rubrum is the most common etiology of tinea corporis, while tinea corporis due to close contact with domesticated animals often is caused by M canis.6 The immunoinhibitory properties of the mannans in the fungal cell wall allow the organisms to adhere to the skin prior to invasion. Cutaneous invasion into dead cornified layers of the skin is credited to the proteases, subtilisinlike proteases (subtilases), and keratinases produced by the fungus.1 There are many different clinical presentations of tinea corporis due to the variability of causative organisms. An annular (ring-shaped) lesion with a central plaque and advancing border is the most typical presentation. Tinea corporis bullosa is characterized by the presence of bullae or vesicles in the borders of the scaly plaque. Rupture of the bullae subsequently leads to erosions and crusts over the plaque.
The diagnosis of tinea corporis bullosa often is clinical if the lesion is typical and can be confirmed using KOH preparation and fungal culture. Once the diagnosis is confirmed, topical antifungals are the standard treatment approach for localized superficial tinea corporis. Systemic antifungal treatment can be initiated if the lesion is extensive, recurrent, chronic, or unresponsive to topical treatment.1 Given our patient’s characteristic presentation, she was managed with an over-the-counter topical antifungal (terbinafine). The patient’s lesions dramatically improved, rendering oral therapy unnecessary. At 1-month follow-up, the rash had nearly resolved.
- Leung AK, Lam JM, Leong KF, et al. Tinea corporis: an updated review [published online July 20, 2020]. Drugs Context. doi:10.7573/dic.2020-5-6
- Guide SV, Marinkovich MP. Linear IgA bullous dermatosis. Clin Dermatol. 2001;19:719-727.
- Lamps LW, Scott MA. Cat-scratch disease: historic, clinical, and pathologic perspectives. Pathology Patterns Reviews. 2004;121(suppl):S71-S80.
- Caproni M, Antiga E, Melani L, et al. Guidelines for the diagnosis and treatment of dermatitis herpetiformis. J Eur Acad Dermatol Venereol. 2009;23:633-638.
- Patel S, John AM, Handler MZ, et al. Fixed drug eruptions: an update, emphasizing the potentially lethal generalized bullous fixed drug eruption. Am J Clin Dermatol. 2020;21:393-399.
- Ziemer M, Seyfarth F, Elsner P, et al. Atypical manifestations of tinea corporis. Mycoses. 2007;50:31-35.
- Leung AK, Lam JM, Leong KF, et al. Tinea corporis: an updated review [published online July 20, 2020]. Drugs Context. doi:10.7573/dic.2020-5-6
- Guide SV, Marinkovich MP. Linear IgA bullous dermatosis. Clin Dermatol. 2001;19:719-727.
- Lamps LW, Scott MA. Cat-scratch disease: historic, clinical, and pathologic perspectives. Pathology Patterns Reviews. 2004;121(suppl):S71-S80.
- Caproni M, Antiga E, Melani L, et al. Guidelines for the diagnosis and treatment of dermatitis herpetiformis. J Eur Acad Dermatol Venereol. 2009;23:633-638.
- Patel S, John AM, Handler MZ, et al. Fixed drug eruptions: an update, emphasizing the potentially lethal generalized bullous fixed drug eruption. Am J Clin Dermatol. 2020;21:393-399.
- Ziemer M, Seyfarth F, Elsner P, et al. Atypical manifestations of tinea corporis. Mycoses. 2007;50:31-35.
A 38-year-old woman presented with a rash of 5 days’ duration that initially appeared on the wrists after playing with her kitten, with subsequent involvement of the chest, back, abdomen, and upper and lower extremities. Physical examination revealed multiple annular plaques with raised erythematous borders, rare peripheral vesicles, and superficial central scaling. Extreme pruritus accompanied the plaques, both of which developed after playing with her kitten. The patient noted that all lesions on the upper extremities evolved in areas subject to deep puncture while more superficially excoriated areas were unaffected. She denied any other prior skin conditions and had received a 5-day course of azithromycin without improvement prior to presentation; triamcinolone ointment 0.1% had provided only temporary relief. Primary care providers prescribed a short course of oral prednisone; however, she did not start it prior to presentation.

Frequent asthma deteriorations? Check for bronchiectasis
, according to the authors of a retrospective study in the Journal of Allergy and Clinical Immunology: In Practice. While bronchiectasis is known to worsen the clinical and functional outcomes in patients with asthma, data regarding the long-term effects of bronchiectasis on the clinical course of asthma have been limited, stated corresponding author Jung-Kyu Lee, MD, division of pulmonary and critical care medicine, Seoul (Republic of Korea) Metropolitan Government – Seoul National University.
Moderate to severe acute clinical deterioration risks were increased among the 251 patients (mean age 66.6 years, 77.2% men) with bronchiectasis out of 667 asthma patients included in the study. All studied patients underwent chest computed tomography and pulmonary function tests from 2013 to 2019 at two tertiary hospitals in Seoul. The primary outcome, annual incidence of moderate to severe acute exacerbations requiring additional treatment (systemic steroids, antibiotics, or both), was significantly higher in patients with bronchiectasis after a mean follow-up period of 3.96 years. Compared with patients who did not exhibit bronchiectasis, the annual rates of severe exacerbations (0.15 ± 0.43 vs. 0.08 ± 0.27; P = .010), moderate to severe (0.47 ± 0.79 vs. 0.34 ± 0.63; P = .018), and acute exacerbations during the follow-up period (49.8% vs. 39.4%; P = .009) were all significantly higher. There was no difference in the proportion of frequent exacerbators between the two groups, however. Severe acute exacerbations leading to hospitalizations, also, were more frequent in the group with bronchiectasis.
Risk factors explored
Significant factors conferring greater risk of severe and moderate to severe acute exacerbations in multivariable analysis included low body mass index, low baseline forced expiratory volume in 1 second (FEV1), high use of inhaled corticosteroids, high medication possession, and high neutrophil/lymphocyte ratios. The existence of bronchiectasis remained an independent risk factor for severe and moderate to severe acute exacerbations despite adjustment for all other factors. While bronchiectasis score showed no association with annual rate of acute exacerbation, progression of bronchiectasis confirmed on follow-up CT was associated with increased risks of severe and moderate to severe acute exacerbation.
Included patients had a diagnosis of asthma confirmed by variable expiratory airflow limitation with pulmonary function tests (that is, positive bronchodilator response, positive bronchial provocation test, or excessive variation in lung function between visits). Past histories of tuberculosis and nontuberculous mycobacterial lung disease, lower absolute and predicted values of both baseline FEV1 and forced vital capacity were more common among patients with bronchiectasis.
Dividing the study population into a group that had at least one moderate to severe acute exacerbation during the follow-up period and a group that did not, the researchers identified characteristics shared by exacerbators: a greater proportion were women, they had lower forced vital capacity and lung-diffusing capacity for carbon monoxide, higher blood FVC and blood neutrophil/lymphocyte ratio, and more medication use (inhaled corticosteroids, long-acting antimuscarinic agent, leukotriene-receptor antagonist, and methylxanthine), compared with the nonexacerbators. More bronchiectasis, more severe bronchiectasis (higher bronchiectasis score), and more progression of bronchiectasis were common among the exacerbators.
Higher acute exacerbation risks accompanied bronchiectasis, at 1.47-fold for moderate, 1.72-fold for severe, and 1.50-fold for moderate to severe exacerbations. Higher risk for severe and moderate to severe exacerbations was conferred by bronchiectasis progression, also.
The researchers pointed to contradictory effects of inhaled corticosteroid use, noting both corticosteroids’ essential role in controlling airway inflammation and hyperresponsiveness, exacerbations, and lung-function decline in asthma patients and that longer or greater inhaled corticosteroid use is associated with both clinical deterioration in asthma and bronchiectasis, and exacerbation history. For bronchiectasis, however, inhaled corticosteroid use offers no benefit while increasing susceptibility to infection and its risks through partial immunosuppression.
“Considering these contradictory effects of inhaled corticosteroid use, further research is needed regarding its risks and benefits in asthma patients with bronchiectasis, including differences in the benefit of inhaled corticosteroid use according to patient phenotype,” Dr. Kim and his colleagues concluded.
The role of corticosteroids
“One of the more important points discussed in this observational cohort study is the role of inhaled corticosteroid use in bronchiectasis,” said Mary Jo Farmer, MD, PhD, director of pulmonary hypertension services, Baystate Health, and assistant professor of medicine, University of Massachusetts – Baystate, both in Springfield, in an interview with this news organization. She cited a review finding no significant benefit versus placebo in spirometry, exacerbation rate, or sputum volume in the Cochrane Database of Systematic Reviews and another suggesting that quality of life was improved with inhaled corticosteroid use in individuals with blood eosinophils greater than 3%, compared with those not using inhaled corticosteroids or having lower eosinophil counts in the European Respiratory Journal. She cited also higher percentages (48% versus 23%) of adrenal insufficiency in bronchiectasis patients among those taking inhaled corticosteroids versus those not taking them.
Dr. Farmer added, “According to the 2018 Cochrane review of inhaled corticosteroid treatment for non–cystic fibrosis bronchiectasis, results from most randomized, placebo-controlled trials have been disappointing in terms of effects on most endpoints such as pulmonary function and exacerbation frequency. As such, the European Respiratory Society guidelines for the management of adult bronchiectasis advise against prescribing inhaled corticosteroids to patients with bronchiectasis, unless otherwise indicated by either an asthma or chronic obstructive pulmonary disease diagnosis. Also, inhaled corticosteroid treatment in asthma and COPD is associated with common side effects such as oral candidiasis, dysphonia and, in some cases, systemic corticosteroid effects. The rate of adverse events from inhaled corticosteroid treatment of bronchiectasis, however, is largely unknown.Dr. Lee and Dr. Farmer reported no relevant financial relationships. The study was independently supported.
, according to the authors of a retrospective study in the Journal of Allergy and Clinical Immunology: In Practice. While bronchiectasis is known to worsen the clinical and functional outcomes in patients with asthma, data regarding the long-term effects of bronchiectasis on the clinical course of asthma have been limited, stated corresponding author Jung-Kyu Lee, MD, division of pulmonary and critical care medicine, Seoul (Republic of Korea) Metropolitan Government – Seoul National University.
Moderate to severe acute clinical deterioration risks were increased among the 251 patients (mean age 66.6 years, 77.2% men) with bronchiectasis out of 667 asthma patients included in the study. All studied patients underwent chest computed tomography and pulmonary function tests from 2013 to 2019 at two tertiary hospitals in Seoul. The primary outcome, annual incidence of moderate to severe acute exacerbations requiring additional treatment (systemic steroids, antibiotics, or both), was significantly higher in patients with bronchiectasis after a mean follow-up period of 3.96 years. Compared with patients who did not exhibit bronchiectasis, the annual rates of severe exacerbations (0.15 ± 0.43 vs. 0.08 ± 0.27; P = .010), moderate to severe (0.47 ± 0.79 vs. 0.34 ± 0.63; P = .018), and acute exacerbations during the follow-up period (49.8% vs. 39.4%; P = .009) were all significantly higher. There was no difference in the proportion of frequent exacerbators between the two groups, however. Severe acute exacerbations leading to hospitalizations, also, were more frequent in the group with bronchiectasis.
Risk factors explored
Significant factors conferring greater risk of severe and moderate to severe acute exacerbations in multivariable analysis included low body mass index, low baseline forced expiratory volume in 1 second (FEV1), high use of inhaled corticosteroids, high medication possession, and high neutrophil/lymphocyte ratios. The existence of bronchiectasis remained an independent risk factor for severe and moderate to severe acute exacerbations despite adjustment for all other factors. While bronchiectasis score showed no association with annual rate of acute exacerbation, progression of bronchiectasis confirmed on follow-up CT was associated with increased risks of severe and moderate to severe acute exacerbation.
Included patients had a diagnosis of asthma confirmed by variable expiratory airflow limitation with pulmonary function tests (that is, positive bronchodilator response, positive bronchial provocation test, or excessive variation in lung function between visits). Past histories of tuberculosis and nontuberculous mycobacterial lung disease, lower absolute and predicted values of both baseline FEV1 and forced vital capacity were more common among patients with bronchiectasis.
Dividing the study population into a group that had at least one moderate to severe acute exacerbation during the follow-up period and a group that did not, the researchers identified characteristics shared by exacerbators: a greater proportion were women, they had lower forced vital capacity and lung-diffusing capacity for carbon monoxide, higher blood FVC and blood neutrophil/lymphocyte ratio, and more medication use (inhaled corticosteroids, long-acting antimuscarinic agent, leukotriene-receptor antagonist, and methylxanthine), compared with the nonexacerbators. More bronchiectasis, more severe bronchiectasis (higher bronchiectasis score), and more progression of bronchiectasis were common among the exacerbators.
Higher acute exacerbation risks accompanied bronchiectasis, at 1.47-fold for moderate, 1.72-fold for severe, and 1.50-fold for moderate to severe exacerbations. Higher risk for severe and moderate to severe exacerbations was conferred by bronchiectasis progression, also.
The researchers pointed to contradictory effects of inhaled corticosteroid use, noting both corticosteroids’ essential role in controlling airway inflammation and hyperresponsiveness, exacerbations, and lung-function decline in asthma patients and that longer or greater inhaled corticosteroid use is associated with both clinical deterioration in asthma and bronchiectasis, and exacerbation history. For bronchiectasis, however, inhaled corticosteroid use offers no benefit while increasing susceptibility to infection and its risks through partial immunosuppression.
“Considering these contradictory effects of inhaled corticosteroid use, further research is needed regarding its risks and benefits in asthma patients with bronchiectasis, including differences in the benefit of inhaled corticosteroid use according to patient phenotype,” Dr. Kim and his colleagues concluded.
The role of corticosteroids
“One of the more important points discussed in this observational cohort study is the role of inhaled corticosteroid use in bronchiectasis,” said Mary Jo Farmer, MD, PhD, director of pulmonary hypertension services, Baystate Health, and assistant professor of medicine, University of Massachusetts – Baystate, both in Springfield, in an interview with this news organization. She cited a review finding no significant benefit versus placebo in spirometry, exacerbation rate, or sputum volume in the Cochrane Database of Systematic Reviews and another suggesting that quality of life was improved with inhaled corticosteroid use in individuals with blood eosinophils greater than 3%, compared with those not using inhaled corticosteroids or having lower eosinophil counts in the European Respiratory Journal. She cited also higher percentages (48% versus 23%) of adrenal insufficiency in bronchiectasis patients among those taking inhaled corticosteroids versus those not taking them.
Dr. Farmer added, “According to the 2018 Cochrane review of inhaled corticosteroid treatment for non–cystic fibrosis bronchiectasis, results from most randomized, placebo-controlled trials have been disappointing in terms of effects on most endpoints such as pulmonary function and exacerbation frequency. As such, the European Respiratory Society guidelines for the management of adult bronchiectasis advise against prescribing inhaled corticosteroids to patients with bronchiectasis, unless otherwise indicated by either an asthma or chronic obstructive pulmonary disease diagnosis. Also, inhaled corticosteroid treatment in asthma and COPD is associated with common side effects such as oral candidiasis, dysphonia and, in some cases, systemic corticosteroid effects. The rate of adverse events from inhaled corticosteroid treatment of bronchiectasis, however, is largely unknown.Dr. Lee and Dr. Farmer reported no relevant financial relationships. The study was independently supported.
, according to the authors of a retrospective study in the Journal of Allergy and Clinical Immunology: In Practice. While bronchiectasis is known to worsen the clinical and functional outcomes in patients with asthma, data regarding the long-term effects of bronchiectasis on the clinical course of asthma have been limited, stated corresponding author Jung-Kyu Lee, MD, division of pulmonary and critical care medicine, Seoul (Republic of Korea) Metropolitan Government – Seoul National University.
Moderate to severe acute clinical deterioration risks were increased among the 251 patients (mean age 66.6 years, 77.2% men) with bronchiectasis out of 667 asthma patients included in the study. All studied patients underwent chest computed tomography and pulmonary function tests from 2013 to 2019 at two tertiary hospitals in Seoul. The primary outcome, annual incidence of moderate to severe acute exacerbations requiring additional treatment (systemic steroids, antibiotics, or both), was significantly higher in patients with bronchiectasis after a mean follow-up period of 3.96 years. Compared with patients who did not exhibit bronchiectasis, the annual rates of severe exacerbations (0.15 ± 0.43 vs. 0.08 ± 0.27; P = .010), moderate to severe (0.47 ± 0.79 vs. 0.34 ± 0.63; P = .018), and acute exacerbations during the follow-up period (49.8% vs. 39.4%; P = .009) were all significantly higher. There was no difference in the proportion of frequent exacerbators between the two groups, however. Severe acute exacerbations leading to hospitalizations, also, were more frequent in the group with bronchiectasis.
Risk factors explored
Significant factors conferring greater risk of severe and moderate to severe acute exacerbations in multivariable analysis included low body mass index, low baseline forced expiratory volume in 1 second (FEV1), high use of inhaled corticosteroids, high medication possession, and high neutrophil/lymphocyte ratios. The existence of bronchiectasis remained an independent risk factor for severe and moderate to severe acute exacerbations despite adjustment for all other factors. While bronchiectasis score showed no association with annual rate of acute exacerbation, progression of bronchiectasis confirmed on follow-up CT was associated with increased risks of severe and moderate to severe acute exacerbation.
Included patients had a diagnosis of asthma confirmed by variable expiratory airflow limitation with pulmonary function tests (that is, positive bronchodilator response, positive bronchial provocation test, or excessive variation in lung function between visits). Past histories of tuberculosis and nontuberculous mycobacterial lung disease, lower absolute and predicted values of both baseline FEV1 and forced vital capacity were more common among patients with bronchiectasis.
Dividing the study population into a group that had at least one moderate to severe acute exacerbation during the follow-up period and a group that did not, the researchers identified characteristics shared by exacerbators: a greater proportion were women, they had lower forced vital capacity and lung-diffusing capacity for carbon monoxide, higher blood FVC and blood neutrophil/lymphocyte ratio, and more medication use (inhaled corticosteroids, long-acting antimuscarinic agent, leukotriene-receptor antagonist, and methylxanthine), compared with the nonexacerbators. More bronchiectasis, more severe bronchiectasis (higher bronchiectasis score), and more progression of bronchiectasis were common among the exacerbators.
Higher acute exacerbation risks accompanied bronchiectasis, at 1.47-fold for moderate, 1.72-fold for severe, and 1.50-fold for moderate to severe exacerbations. Higher risk for severe and moderate to severe exacerbations was conferred by bronchiectasis progression, also.
The researchers pointed to contradictory effects of inhaled corticosteroid use, noting both corticosteroids’ essential role in controlling airway inflammation and hyperresponsiveness, exacerbations, and lung-function decline in asthma patients and that longer or greater inhaled corticosteroid use is associated with both clinical deterioration in asthma and bronchiectasis, and exacerbation history. For bronchiectasis, however, inhaled corticosteroid use offers no benefit while increasing susceptibility to infection and its risks through partial immunosuppression.
“Considering these contradictory effects of inhaled corticosteroid use, further research is needed regarding its risks and benefits in asthma patients with bronchiectasis, including differences in the benefit of inhaled corticosteroid use according to patient phenotype,” Dr. Kim and his colleagues concluded.
The role of corticosteroids
“One of the more important points discussed in this observational cohort study is the role of inhaled corticosteroid use in bronchiectasis,” said Mary Jo Farmer, MD, PhD, director of pulmonary hypertension services, Baystate Health, and assistant professor of medicine, University of Massachusetts – Baystate, both in Springfield, in an interview with this news organization. She cited a review finding no significant benefit versus placebo in spirometry, exacerbation rate, or sputum volume in the Cochrane Database of Systematic Reviews and another suggesting that quality of life was improved with inhaled corticosteroid use in individuals with blood eosinophils greater than 3%, compared with those not using inhaled corticosteroids or having lower eosinophil counts in the European Respiratory Journal. She cited also higher percentages (48% versus 23%) of adrenal insufficiency in bronchiectasis patients among those taking inhaled corticosteroids versus those not taking them.
Dr. Farmer added, “According to the 2018 Cochrane review of inhaled corticosteroid treatment for non–cystic fibrosis bronchiectasis, results from most randomized, placebo-controlled trials have been disappointing in terms of effects on most endpoints such as pulmonary function and exacerbation frequency. As such, the European Respiratory Society guidelines for the management of adult bronchiectasis advise against prescribing inhaled corticosteroids to patients with bronchiectasis, unless otherwise indicated by either an asthma or chronic obstructive pulmonary disease diagnosis. Also, inhaled corticosteroid treatment in asthma and COPD is associated with common side effects such as oral candidiasis, dysphonia and, in some cases, systemic corticosteroid effects. The rate of adverse events from inhaled corticosteroid treatment of bronchiectasis, however, is largely unknown.Dr. Lee and Dr. Farmer reported no relevant financial relationships. The study was independently supported.
FROM JOURNAL OF ALLERGY AND CLINICAL IMMUNOLOGY: IN PRACTICE
Doctors still overprescribing fluoroquinolones despite risks
When Amy Moser had a simple urinary tract infection in her late 20s, her doctor prescribed Cipro, a powerful antibiotic used to treat anthrax and some of the most fearsome bacterial infections.
Nearly 2 weeks after she finished her treatment, her left kneecap dislocated while she was trying on a swimsuit at a retail store. Shortly afterward, she had painful ligament ruptures in her wrists, then her shoulder dislocated, followed by three Achilles tendon tears.
“That’s when I fell apart,” says Ms. Moser, a Phoenix health blogger and book author. “From that moment on, for almost the next 2.5 years consistently, I had new tendon tears every few weeks.”
Ms. Moser’s doctors had no answer for what was causing her injuries, all of which required surgical fixes. A married mother of three, she was otherwise healthy and fit. So, after her third Achilles tear, she turned to the FDA’s website for answers. There, she found many warnings about side effects of Cipro, Levaquin, and other so-called fluoroquinolones, including risks for tendon and ligament injuries.
“When all the ruptures started to happen, my doctor kept asking me if I’d ever taken Levaquin, and every time I was like, ‘No.’ So I did what all doctors don’t want you to do: I Googled ‘Levaquin,’ ” she recalls.
Her search led to FDA warnings and articles about the possibility of tendon and ligament ruptures with fluroquinolones.
“That was the first time I’d ever even heard that word ‘fluroquinolones,’ and I found Cipro on that list ... and I realized that I’d just been prescribed that before everything started,” she says.
That was 12 years ago. Since then, the FDA has issued more warnings about fluoroquinolone risks. In that time, Ms. Moser, now 40, has had more than 30 surgeries to correct tendon ruptures and injuries, including a double-knee replacement this year.
“I am in chronic pain all the time,” she says. “I am chronically injured. I have a lot of tears that I’ve not fixed because they’re very complicated, and I don’t know if the rest of my body can handle the strain of recovering from those surgeries.”
Ms. Moser’s is hardly an isolated case. Since the 1980s, more than 60,000 patients have reported hundreds of thousands of serious events linked to fluoroquinolones to the FDA, including 6,575 reports of deaths.
The most common side effects were tendon rupture, as well as neurological and psychiatric symptoms. But experts estimate only 1%-10% of such events are reported to the FDA. That suggests that fluoroquinolones might have harmed hundreds of thousands of people in the United States alone, says Charles Bennett, MD, a hematologist at the University of South Carolina’s College of Pharmacy, Columbia.
Yet despite the many patient reports and FDA warnings on dangerous side effects, better treated with less risky antibiotics.
“There probably is overprescription by primary care doctors for urinary tract infections and respiratory infections, when there could be alternatives that are safer to use,” says Amesh Adalja, MD, an infectious disease specialist and senior scholar with the Johns Hopkins Center for Health Security.
“I would say that’s probably the case in the outpatient setting, not necessarily in the hospital setting or among infectious disease doctors ... but I think it’s important to say there are still some judicious uses of fluoroquinolones,” he says. “However, there probably is a lot of injudicious use of fluoroquinolones along with many other antibiotics in the primary care setting.”
FDA warnings on fluoroquinolones
Fluoroquinolones are a class of broad-spectrum antibiotics used for decades to treat certain bacterial infections.
FDA-approved fluoroquinolones include ciprofloxacin (Cipro), ciprofloxacin extended-release tablets, delafloxacin (Baxdela), gemifloxacin (Factive) levofloxacin (Levaquin), moxifloxacin (Avelox), and ofloxacin (Floxin). More than 60 generic versions of these brand-name medicines are also on the market, making them among the most prescribed antibiotics in the U.S.
Over the past 2 decades, a wide range of physical and mental health side effects have been tied to fluoroquinolones. As a result of these “adverse event reports” and research published in medical literature, the FDA has required an escalating series of warnings and safety labeling changes for doctors who prescribe these drugs.
- In 2008, the FDA first added a “black box” warning to fluoroquinolones, citing an increased risk of tendinitis and tendon rupture in patients prescribed these meds.
- In 2011, the agency required the warning label to include risks of worsening symptoms for those with myasthenia gravis, a chronic autoimmune disease that causes muscle weakness, vision problems, and speech problems.
- In 2013, regulators required updated labels noting the potential for irreversible peripheral neuropathy (serious nerve damage).
- In 2016, the FDA issued its strongest warning against the use of such antibiotics for simple bacterial infections – such as uncomplicated urinary tract infections (UTIs), acute sinusitis, and acute bronchitis – saying the “association of fluoroquinolones with disabling and potentially permanent side effects involving tendons, muscles, joints, nerves and the central nervous system ... outweighs the benefits for patients.”
- And in 2018, regulators required safety labeling changes to include warnings about the risks of aortic aneurysm – a life-threatening enlargement of the main vessel that delivers blood to the body – as well as mental health side effects and serious blood sugar disturbances.
But FDA regulators have stopped short of barring fluoroquinolone use in the treatment of bacterial infections, citing the benefits for certain conditions.
“For some patients, the benefits of fluoroquinolones may continue to outweigh the risks for treatment of serious bacterial infections, such as pneumonia or intra-abdominal infections,” said former FDA Commissioner Scott Gottlieb, MD, “but there are other serious, known risks associated with these strong antibiotics that must be carefully weighed when considering their use.”
In December 2021, a study published in the journal JAMA Network Open found the FDA’s warnings may have helped lower prescribing of the drugs in Medicare patients. But not all doctors have been responsive to those warnings, researchers found.
“An overall decline in change over time and an immediate change in fluoroquinolone prescribing was observed after the 2016 FDA warning,” the authors concluded. “Certain physicians, such as primary care physicians, were more responsive to FDA warnings than others. ... Findings of this study suggest that identifying the association of physician and organizational characteristics with fluoroquinolone prescribing practices could help in developing mechanisms for improving de-adoption.”
Some critics say the FDA should do more to spotlight the dangers of fluoroquinolones and require doctors and patients to sign checklist consent forms to show they are aware of the potential side effects of these drugs.
Rachel Brummert, a patient advocate who sits on an FDA consumer advisory board, believes the FDA needs to improve its communication to doctors on fluoroquinolone risks and get tougher with those who continue to inappropriately prescribe the drugs.
“I think there needs to be a system in place, where if something comes down from the FDA about a drug, the physician has to sign off on it, the patient has to sign off on it and mark that they understand that there are these ‘black box’ warnings,” says Ms. Brummert, 52, a representative on the FDA’s Medical Devices Advisory Committee.
As an example, she points to Australia’s medical laws requiring doctors and patients to sign a checklist before any fluoroquinolone prescription is approved.
“When a physician prescribes a fluoroquinolone antibiotic, there’s a checklist – does the patient have an infection, is it a simple infection, do they have allergies?” she notes. “And you can’t even get the prescription out – it won’t even print out, it won’t go into the system – unless you check all of the boxes. But we don’t do that here. We don’t have that type of system right now.”
Ms. Brummert says such a system might have prevented the harm from taking Levaquin her doctor prescribed for a suspected sinus infection in 2006.
Soon after she began taking the antibiotic, she ruptured her Achilles tendon, requiring surgery. By 2009, she’d had three ruptures, each needing surgical fixes. To date, she’s had more than 30 surgeries to correct tendon ruptures. She’s also had seizures, blood pressure issues, depression, chronic pain, and memory problems she attributes to taking Levaquin.
As it turns out, her doctor misdiagnosed her condition – a misstep that would have been averted with a system like Australia’s, which requires doctors to verify the presence of a bacterial infection through a simple test before prescribing a fluoroquinolone.
“When I got the Levaquin, it was for a suspected sinus infection that it turned out I didn’t even have in the first place,” she notes. “So, I took the Levaquin basically for nothing. But what I would have asked my doctor had I known is: ‘Why should I take something so strong for so simple an infection?’
“It seems common sense to me now that you don’t prescribe something that can kill anthrax for a simple sinus infection. It’s like an atom bomb killing a mosquito. I agree that there are uses for these drugs, but they are being overprescribed. And so, here I am 16 years later – I’m still rupturing, I’m still having surgery, and I’m still in pain – all for something I didn’t even need medicine for in the first place.”
Should guidelines be stronger?
So, why are so many doctors continuing to prescribe fluoroquinolones for simple infections? Dr. Adalja and other experts say several things are at work.
For one thing, Dr. Adalja notes, fluoroquinolones are broad-spectrum antibiotics that are effective against dangerous germs, including “gram-negative” bacterial infections, and are “100% bioavailable.” That means they are as effective when given in pill form as they are if put directly into a vein. So they can be used in an outpatient setting or to allow a patient to be discharged from a hospital sooner because they don’t need an IV to receive treatment.
“There are still some uses for these drugs because they are so bioavailable, and I think that drives some of the use, and those are legitimate uses, knowing that there are risks when you do it,” he says. “But no drug is without risks, and you have to weigh risks and benefits – that’s what medicine is about: deciding what the best drug is for a patient.”
But Dr. Adalja says the overprescription of fluoroquinolones is part of the larger trend of antibiotic overuse. That is driving up antibiotic resistance, which in turn is another thing leading doctors to turn to Cipro and other fluoroquinolones after other drugs have proven ineffective.
“You can’t separate this from the fact that 80% of antibiotic prescriptions in the outpatient setting are probably illegitimate or not warranted,” he notes. “And because fluoroquinolones are highly effective drugs against certain pathogens, they are the go-to [drug] for many people who are prescribing antibiotics.”
That’s why patients should be wary whenever a doctor prescribes a fluoroquinolone, or any drug to treat a suspected infection, he says.
“Any time a patient is getting prescribed an antibiotic by a physician, they should ask: ‘Do I really need this antibiotic?’ That should be the first question they ask,” he advises. “And if they’re getting a fluoroquinolone, they may want to ask: ‘Is this the best antibiotic for me?’ ”
What you can do
Ms. Brummert and Ms. Moser say they are sharing their stories to raise awareness of the dangers of fluoroquinolones.
Ms. Moser has published a book on her experiences, “The Magnificent Story of a Lame Author,” and provides a wealth of consumer resources on her blog: Mountains and Mustard Seeds.
“As much as I hate what has happened to me, it has put me in a place where I am glad that I can inform other patients,” she says.
Ms. Brummert supplements her advocacy work as an FDA adviser with useful materials she provides on her website: Drugwatch.com.
“Pain into purpose – that’s what I call it,” she says. “I can’t change what happened to me, but I can warn others.”
The upshot for patients?
- the FDA’s Drug Safety Communication on Fluoroquinolones online to learn more about the risks and benefits of these powerful antibiotics.
- If you believe you’ve been harmed by fluoroquinolones, MedWatch website to report your experiences.
Ms. Brummert also advises patients to ask 12 critical questions of any doctor who wants to prescribe a fluoroquinolone, including the following listed on her website:
- For what condition is this medication prescribed, and is there another drug specific to my condition?
- What are the risks associated with this medication, and do the benefits outweigh them?
- Will this medication interact with my other drugs and/or other health conditions?
- What are the “boxed” warnings for this medication, and where can I report adverse events?
“I would also do my own research,” she says. “I wouldn’t just take a prescription from a physician and just say, ‘OK, doctor knows best.’ ”
Ms. Moser agrees that you have to be your own patient advocate and not simply take a doctor’s advice on any medical issue without having a deeper conversation.
“I’ve had arguments with doctors who legitimately did not believe me when I told them what happened to me,” she says. “And I actually told them, ‘Go get your Physicians’ Desk Reference [for prescription drugs]’ and they opened the book in front of me and read the warnings. Obviously, they had not been keeping up with the added warnings. So, I do think that doctors do need to be better informed.”
“So, yes, it’s the FDA’s responsibility, but it is also the doctors’ responsibility to make sure that they’re watching out for the side effects and they’re reporting them when their patients come up with them and making those connections.”
A version of this article first appeared on WebMD.com.
When Amy Moser had a simple urinary tract infection in her late 20s, her doctor prescribed Cipro, a powerful antibiotic used to treat anthrax and some of the most fearsome bacterial infections.
Nearly 2 weeks after she finished her treatment, her left kneecap dislocated while she was trying on a swimsuit at a retail store. Shortly afterward, she had painful ligament ruptures in her wrists, then her shoulder dislocated, followed by three Achilles tendon tears.
“That’s when I fell apart,” says Ms. Moser, a Phoenix health blogger and book author. “From that moment on, for almost the next 2.5 years consistently, I had new tendon tears every few weeks.”
Ms. Moser’s doctors had no answer for what was causing her injuries, all of which required surgical fixes. A married mother of three, she was otherwise healthy and fit. So, after her third Achilles tear, she turned to the FDA’s website for answers. There, she found many warnings about side effects of Cipro, Levaquin, and other so-called fluoroquinolones, including risks for tendon and ligament injuries.
“When all the ruptures started to happen, my doctor kept asking me if I’d ever taken Levaquin, and every time I was like, ‘No.’ So I did what all doctors don’t want you to do: I Googled ‘Levaquin,’ ” she recalls.
Her search led to FDA warnings and articles about the possibility of tendon and ligament ruptures with fluroquinolones.
“That was the first time I’d ever even heard that word ‘fluroquinolones,’ and I found Cipro on that list ... and I realized that I’d just been prescribed that before everything started,” she says.
That was 12 years ago. Since then, the FDA has issued more warnings about fluoroquinolone risks. In that time, Ms. Moser, now 40, has had more than 30 surgeries to correct tendon ruptures and injuries, including a double-knee replacement this year.
“I am in chronic pain all the time,” she says. “I am chronically injured. I have a lot of tears that I’ve not fixed because they’re very complicated, and I don’t know if the rest of my body can handle the strain of recovering from those surgeries.”
Ms. Moser’s is hardly an isolated case. Since the 1980s, more than 60,000 patients have reported hundreds of thousands of serious events linked to fluoroquinolones to the FDA, including 6,575 reports of deaths.
The most common side effects were tendon rupture, as well as neurological and psychiatric symptoms. But experts estimate only 1%-10% of such events are reported to the FDA. That suggests that fluoroquinolones might have harmed hundreds of thousands of people in the United States alone, says Charles Bennett, MD, a hematologist at the University of South Carolina’s College of Pharmacy, Columbia.
Yet despite the many patient reports and FDA warnings on dangerous side effects, better treated with less risky antibiotics.
“There probably is overprescription by primary care doctors for urinary tract infections and respiratory infections, when there could be alternatives that are safer to use,” says Amesh Adalja, MD, an infectious disease specialist and senior scholar with the Johns Hopkins Center for Health Security.
“I would say that’s probably the case in the outpatient setting, not necessarily in the hospital setting or among infectious disease doctors ... but I think it’s important to say there are still some judicious uses of fluoroquinolones,” he says. “However, there probably is a lot of injudicious use of fluoroquinolones along with many other antibiotics in the primary care setting.”
FDA warnings on fluoroquinolones
Fluoroquinolones are a class of broad-spectrum antibiotics used for decades to treat certain bacterial infections.
FDA-approved fluoroquinolones include ciprofloxacin (Cipro), ciprofloxacin extended-release tablets, delafloxacin (Baxdela), gemifloxacin (Factive) levofloxacin (Levaquin), moxifloxacin (Avelox), and ofloxacin (Floxin). More than 60 generic versions of these brand-name medicines are also on the market, making them among the most prescribed antibiotics in the U.S.
Over the past 2 decades, a wide range of physical and mental health side effects have been tied to fluoroquinolones. As a result of these “adverse event reports” and research published in medical literature, the FDA has required an escalating series of warnings and safety labeling changes for doctors who prescribe these drugs.
- In 2008, the FDA first added a “black box” warning to fluoroquinolones, citing an increased risk of tendinitis and tendon rupture in patients prescribed these meds.
- In 2011, the agency required the warning label to include risks of worsening symptoms for those with myasthenia gravis, a chronic autoimmune disease that causes muscle weakness, vision problems, and speech problems.
- In 2013, regulators required updated labels noting the potential for irreversible peripheral neuropathy (serious nerve damage).
- In 2016, the FDA issued its strongest warning against the use of such antibiotics for simple bacterial infections – such as uncomplicated urinary tract infections (UTIs), acute sinusitis, and acute bronchitis – saying the “association of fluoroquinolones with disabling and potentially permanent side effects involving tendons, muscles, joints, nerves and the central nervous system ... outweighs the benefits for patients.”
- And in 2018, regulators required safety labeling changes to include warnings about the risks of aortic aneurysm – a life-threatening enlargement of the main vessel that delivers blood to the body – as well as mental health side effects and serious blood sugar disturbances.
But FDA regulators have stopped short of barring fluoroquinolone use in the treatment of bacterial infections, citing the benefits for certain conditions.
“For some patients, the benefits of fluoroquinolones may continue to outweigh the risks for treatment of serious bacterial infections, such as pneumonia or intra-abdominal infections,” said former FDA Commissioner Scott Gottlieb, MD, “but there are other serious, known risks associated with these strong antibiotics that must be carefully weighed when considering their use.”
In December 2021, a study published in the journal JAMA Network Open found the FDA’s warnings may have helped lower prescribing of the drugs in Medicare patients. But not all doctors have been responsive to those warnings, researchers found.
“An overall decline in change over time and an immediate change in fluoroquinolone prescribing was observed after the 2016 FDA warning,” the authors concluded. “Certain physicians, such as primary care physicians, were more responsive to FDA warnings than others. ... Findings of this study suggest that identifying the association of physician and organizational characteristics with fluoroquinolone prescribing practices could help in developing mechanisms for improving de-adoption.”
Some critics say the FDA should do more to spotlight the dangers of fluoroquinolones and require doctors and patients to sign checklist consent forms to show they are aware of the potential side effects of these drugs.
Rachel Brummert, a patient advocate who sits on an FDA consumer advisory board, believes the FDA needs to improve its communication to doctors on fluoroquinolone risks and get tougher with those who continue to inappropriately prescribe the drugs.
“I think there needs to be a system in place, where if something comes down from the FDA about a drug, the physician has to sign off on it, the patient has to sign off on it and mark that they understand that there are these ‘black box’ warnings,” says Ms. Brummert, 52, a representative on the FDA’s Medical Devices Advisory Committee.
As an example, she points to Australia’s medical laws requiring doctors and patients to sign a checklist before any fluoroquinolone prescription is approved.
“When a physician prescribes a fluoroquinolone antibiotic, there’s a checklist – does the patient have an infection, is it a simple infection, do they have allergies?” she notes. “And you can’t even get the prescription out – it won’t even print out, it won’t go into the system – unless you check all of the boxes. But we don’t do that here. We don’t have that type of system right now.”
Ms. Brummert says such a system might have prevented the harm from taking Levaquin her doctor prescribed for a suspected sinus infection in 2006.
Soon after she began taking the antibiotic, she ruptured her Achilles tendon, requiring surgery. By 2009, she’d had three ruptures, each needing surgical fixes. To date, she’s had more than 30 surgeries to correct tendon ruptures. She’s also had seizures, blood pressure issues, depression, chronic pain, and memory problems she attributes to taking Levaquin.
As it turns out, her doctor misdiagnosed her condition – a misstep that would have been averted with a system like Australia’s, which requires doctors to verify the presence of a bacterial infection through a simple test before prescribing a fluoroquinolone.
“When I got the Levaquin, it was for a suspected sinus infection that it turned out I didn’t even have in the first place,” she notes. “So, I took the Levaquin basically for nothing. But what I would have asked my doctor had I known is: ‘Why should I take something so strong for so simple an infection?’
“It seems common sense to me now that you don’t prescribe something that can kill anthrax for a simple sinus infection. It’s like an atom bomb killing a mosquito. I agree that there are uses for these drugs, but they are being overprescribed. And so, here I am 16 years later – I’m still rupturing, I’m still having surgery, and I’m still in pain – all for something I didn’t even need medicine for in the first place.”
Should guidelines be stronger?
So, why are so many doctors continuing to prescribe fluoroquinolones for simple infections? Dr. Adalja and other experts say several things are at work.
For one thing, Dr. Adalja notes, fluoroquinolones are broad-spectrum antibiotics that are effective against dangerous germs, including “gram-negative” bacterial infections, and are “100% bioavailable.” That means they are as effective when given in pill form as they are if put directly into a vein. So they can be used in an outpatient setting or to allow a patient to be discharged from a hospital sooner because they don’t need an IV to receive treatment.
“There are still some uses for these drugs because they are so bioavailable, and I think that drives some of the use, and those are legitimate uses, knowing that there are risks when you do it,” he says. “But no drug is without risks, and you have to weigh risks and benefits – that’s what medicine is about: deciding what the best drug is for a patient.”
But Dr. Adalja says the overprescription of fluoroquinolones is part of the larger trend of antibiotic overuse. That is driving up antibiotic resistance, which in turn is another thing leading doctors to turn to Cipro and other fluoroquinolones after other drugs have proven ineffective.
“You can’t separate this from the fact that 80% of antibiotic prescriptions in the outpatient setting are probably illegitimate or not warranted,” he notes. “And because fluoroquinolones are highly effective drugs against certain pathogens, they are the go-to [drug] for many people who are prescribing antibiotics.”
That’s why patients should be wary whenever a doctor prescribes a fluoroquinolone, or any drug to treat a suspected infection, he says.
“Any time a patient is getting prescribed an antibiotic by a physician, they should ask: ‘Do I really need this antibiotic?’ That should be the first question they ask,” he advises. “And if they’re getting a fluoroquinolone, they may want to ask: ‘Is this the best antibiotic for me?’ ”
What you can do
Ms. Brummert and Ms. Moser say they are sharing their stories to raise awareness of the dangers of fluoroquinolones.
Ms. Moser has published a book on her experiences, “The Magnificent Story of a Lame Author,” and provides a wealth of consumer resources on her blog: Mountains and Mustard Seeds.
“As much as I hate what has happened to me, it has put me in a place where I am glad that I can inform other patients,” she says.
Ms. Brummert supplements her advocacy work as an FDA adviser with useful materials she provides on her website: Drugwatch.com.
“Pain into purpose – that’s what I call it,” she says. “I can’t change what happened to me, but I can warn others.”
The upshot for patients?
- the FDA’s Drug Safety Communication on Fluoroquinolones online to learn more about the risks and benefits of these powerful antibiotics.
- If you believe you’ve been harmed by fluoroquinolones, MedWatch website to report your experiences.
Ms. Brummert also advises patients to ask 12 critical questions of any doctor who wants to prescribe a fluoroquinolone, including the following listed on her website:
- For what condition is this medication prescribed, and is there another drug specific to my condition?
- What are the risks associated with this medication, and do the benefits outweigh them?
- Will this medication interact with my other drugs and/or other health conditions?
- What are the “boxed” warnings for this medication, and where can I report adverse events?
“I would also do my own research,” she says. “I wouldn’t just take a prescription from a physician and just say, ‘OK, doctor knows best.’ ”
Ms. Moser agrees that you have to be your own patient advocate and not simply take a doctor’s advice on any medical issue without having a deeper conversation.
“I’ve had arguments with doctors who legitimately did not believe me when I told them what happened to me,” she says. “And I actually told them, ‘Go get your Physicians’ Desk Reference [for prescription drugs]’ and they opened the book in front of me and read the warnings. Obviously, they had not been keeping up with the added warnings. So, I do think that doctors do need to be better informed.”
“So, yes, it’s the FDA’s responsibility, but it is also the doctors’ responsibility to make sure that they’re watching out for the side effects and they’re reporting them when their patients come up with them and making those connections.”
A version of this article first appeared on WebMD.com.
When Amy Moser had a simple urinary tract infection in her late 20s, her doctor prescribed Cipro, a powerful antibiotic used to treat anthrax and some of the most fearsome bacterial infections.
Nearly 2 weeks after she finished her treatment, her left kneecap dislocated while she was trying on a swimsuit at a retail store. Shortly afterward, she had painful ligament ruptures in her wrists, then her shoulder dislocated, followed by three Achilles tendon tears.
“That’s when I fell apart,” says Ms. Moser, a Phoenix health blogger and book author. “From that moment on, for almost the next 2.5 years consistently, I had new tendon tears every few weeks.”
Ms. Moser’s doctors had no answer for what was causing her injuries, all of which required surgical fixes. A married mother of three, she was otherwise healthy and fit. So, after her third Achilles tear, she turned to the FDA’s website for answers. There, she found many warnings about side effects of Cipro, Levaquin, and other so-called fluoroquinolones, including risks for tendon and ligament injuries.
“When all the ruptures started to happen, my doctor kept asking me if I’d ever taken Levaquin, and every time I was like, ‘No.’ So I did what all doctors don’t want you to do: I Googled ‘Levaquin,’ ” she recalls.
Her search led to FDA warnings and articles about the possibility of tendon and ligament ruptures with fluroquinolones.
“That was the first time I’d ever even heard that word ‘fluroquinolones,’ and I found Cipro on that list ... and I realized that I’d just been prescribed that before everything started,” she says.
That was 12 years ago. Since then, the FDA has issued more warnings about fluoroquinolone risks. In that time, Ms. Moser, now 40, has had more than 30 surgeries to correct tendon ruptures and injuries, including a double-knee replacement this year.
“I am in chronic pain all the time,” she says. “I am chronically injured. I have a lot of tears that I’ve not fixed because they’re very complicated, and I don’t know if the rest of my body can handle the strain of recovering from those surgeries.”
Ms. Moser’s is hardly an isolated case. Since the 1980s, more than 60,000 patients have reported hundreds of thousands of serious events linked to fluoroquinolones to the FDA, including 6,575 reports of deaths.
The most common side effects were tendon rupture, as well as neurological and psychiatric symptoms. But experts estimate only 1%-10% of such events are reported to the FDA. That suggests that fluoroquinolones might have harmed hundreds of thousands of people in the United States alone, says Charles Bennett, MD, a hematologist at the University of South Carolina’s College of Pharmacy, Columbia.
Yet despite the many patient reports and FDA warnings on dangerous side effects, better treated with less risky antibiotics.
“There probably is overprescription by primary care doctors for urinary tract infections and respiratory infections, when there could be alternatives that are safer to use,” says Amesh Adalja, MD, an infectious disease specialist and senior scholar with the Johns Hopkins Center for Health Security.
“I would say that’s probably the case in the outpatient setting, not necessarily in the hospital setting or among infectious disease doctors ... but I think it’s important to say there are still some judicious uses of fluoroquinolones,” he says. “However, there probably is a lot of injudicious use of fluoroquinolones along with many other antibiotics in the primary care setting.”
FDA warnings on fluoroquinolones
Fluoroquinolones are a class of broad-spectrum antibiotics used for decades to treat certain bacterial infections.
FDA-approved fluoroquinolones include ciprofloxacin (Cipro), ciprofloxacin extended-release tablets, delafloxacin (Baxdela), gemifloxacin (Factive) levofloxacin (Levaquin), moxifloxacin (Avelox), and ofloxacin (Floxin). More than 60 generic versions of these brand-name medicines are also on the market, making them among the most prescribed antibiotics in the U.S.
Over the past 2 decades, a wide range of physical and mental health side effects have been tied to fluoroquinolones. As a result of these “adverse event reports” and research published in medical literature, the FDA has required an escalating series of warnings and safety labeling changes for doctors who prescribe these drugs.
- In 2008, the FDA first added a “black box” warning to fluoroquinolones, citing an increased risk of tendinitis and tendon rupture in patients prescribed these meds.
- In 2011, the agency required the warning label to include risks of worsening symptoms for those with myasthenia gravis, a chronic autoimmune disease that causes muscle weakness, vision problems, and speech problems.
- In 2013, regulators required updated labels noting the potential for irreversible peripheral neuropathy (serious nerve damage).
- In 2016, the FDA issued its strongest warning against the use of such antibiotics for simple bacterial infections – such as uncomplicated urinary tract infections (UTIs), acute sinusitis, and acute bronchitis – saying the “association of fluoroquinolones with disabling and potentially permanent side effects involving tendons, muscles, joints, nerves and the central nervous system ... outweighs the benefits for patients.”
- And in 2018, regulators required safety labeling changes to include warnings about the risks of aortic aneurysm – a life-threatening enlargement of the main vessel that delivers blood to the body – as well as mental health side effects and serious blood sugar disturbances.
But FDA regulators have stopped short of barring fluoroquinolone use in the treatment of bacterial infections, citing the benefits for certain conditions.
“For some patients, the benefits of fluoroquinolones may continue to outweigh the risks for treatment of serious bacterial infections, such as pneumonia or intra-abdominal infections,” said former FDA Commissioner Scott Gottlieb, MD, “but there are other serious, known risks associated with these strong antibiotics that must be carefully weighed when considering their use.”
In December 2021, a study published in the journal JAMA Network Open found the FDA’s warnings may have helped lower prescribing of the drugs in Medicare patients. But not all doctors have been responsive to those warnings, researchers found.
“An overall decline in change over time and an immediate change in fluoroquinolone prescribing was observed after the 2016 FDA warning,” the authors concluded. “Certain physicians, such as primary care physicians, were more responsive to FDA warnings than others. ... Findings of this study suggest that identifying the association of physician and organizational characteristics with fluoroquinolone prescribing practices could help in developing mechanisms for improving de-adoption.”
Some critics say the FDA should do more to spotlight the dangers of fluoroquinolones and require doctors and patients to sign checklist consent forms to show they are aware of the potential side effects of these drugs.
Rachel Brummert, a patient advocate who sits on an FDA consumer advisory board, believes the FDA needs to improve its communication to doctors on fluoroquinolone risks and get tougher with those who continue to inappropriately prescribe the drugs.
“I think there needs to be a system in place, where if something comes down from the FDA about a drug, the physician has to sign off on it, the patient has to sign off on it and mark that they understand that there are these ‘black box’ warnings,” says Ms. Brummert, 52, a representative on the FDA’s Medical Devices Advisory Committee.
As an example, she points to Australia’s medical laws requiring doctors and patients to sign a checklist before any fluoroquinolone prescription is approved.
“When a physician prescribes a fluoroquinolone antibiotic, there’s a checklist – does the patient have an infection, is it a simple infection, do they have allergies?” she notes. “And you can’t even get the prescription out – it won’t even print out, it won’t go into the system – unless you check all of the boxes. But we don’t do that here. We don’t have that type of system right now.”
Ms. Brummert says such a system might have prevented the harm from taking Levaquin her doctor prescribed for a suspected sinus infection in 2006.
Soon after she began taking the antibiotic, she ruptured her Achilles tendon, requiring surgery. By 2009, she’d had three ruptures, each needing surgical fixes. To date, she’s had more than 30 surgeries to correct tendon ruptures. She’s also had seizures, blood pressure issues, depression, chronic pain, and memory problems she attributes to taking Levaquin.
As it turns out, her doctor misdiagnosed her condition – a misstep that would have been averted with a system like Australia’s, which requires doctors to verify the presence of a bacterial infection through a simple test before prescribing a fluoroquinolone.
“When I got the Levaquin, it was for a suspected sinus infection that it turned out I didn’t even have in the first place,” she notes. “So, I took the Levaquin basically for nothing. But what I would have asked my doctor had I known is: ‘Why should I take something so strong for so simple an infection?’
“It seems common sense to me now that you don’t prescribe something that can kill anthrax for a simple sinus infection. It’s like an atom bomb killing a mosquito. I agree that there are uses for these drugs, but they are being overprescribed. And so, here I am 16 years later – I’m still rupturing, I’m still having surgery, and I’m still in pain – all for something I didn’t even need medicine for in the first place.”
Should guidelines be stronger?
So, why are so many doctors continuing to prescribe fluoroquinolones for simple infections? Dr. Adalja and other experts say several things are at work.
For one thing, Dr. Adalja notes, fluoroquinolones are broad-spectrum antibiotics that are effective against dangerous germs, including “gram-negative” bacterial infections, and are “100% bioavailable.” That means they are as effective when given in pill form as they are if put directly into a vein. So they can be used in an outpatient setting or to allow a patient to be discharged from a hospital sooner because they don’t need an IV to receive treatment.
“There are still some uses for these drugs because they are so bioavailable, and I think that drives some of the use, and those are legitimate uses, knowing that there are risks when you do it,” he says. “But no drug is without risks, and you have to weigh risks and benefits – that’s what medicine is about: deciding what the best drug is for a patient.”
But Dr. Adalja says the overprescription of fluoroquinolones is part of the larger trend of antibiotic overuse. That is driving up antibiotic resistance, which in turn is another thing leading doctors to turn to Cipro and other fluoroquinolones after other drugs have proven ineffective.
“You can’t separate this from the fact that 80% of antibiotic prescriptions in the outpatient setting are probably illegitimate or not warranted,” he notes. “And because fluoroquinolones are highly effective drugs against certain pathogens, they are the go-to [drug] for many people who are prescribing antibiotics.”
That’s why patients should be wary whenever a doctor prescribes a fluoroquinolone, or any drug to treat a suspected infection, he says.
“Any time a patient is getting prescribed an antibiotic by a physician, they should ask: ‘Do I really need this antibiotic?’ That should be the first question they ask,” he advises. “And if they’re getting a fluoroquinolone, they may want to ask: ‘Is this the best antibiotic for me?’ ”
What you can do
Ms. Brummert and Ms. Moser say they are sharing their stories to raise awareness of the dangers of fluoroquinolones.
Ms. Moser has published a book on her experiences, “The Magnificent Story of a Lame Author,” and provides a wealth of consumer resources on her blog: Mountains and Mustard Seeds.
“As much as I hate what has happened to me, it has put me in a place where I am glad that I can inform other patients,” she says.
Ms. Brummert supplements her advocacy work as an FDA adviser with useful materials she provides on her website: Drugwatch.com.
“Pain into purpose – that’s what I call it,” she says. “I can’t change what happened to me, but I can warn others.”
The upshot for patients?
- the FDA’s Drug Safety Communication on Fluoroquinolones online to learn more about the risks and benefits of these powerful antibiotics.
- If you believe you’ve been harmed by fluoroquinolones, MedWatch website to report your experiences.
Ms. Brummert also advises patients to ask 12 critical questions of any doctor who wants to prescribe a fluoroquinolone, including the following listed on her website:
- For what condition is this medication prescribed, and is there another drug specific to my condition?
- What are the risks associated with this medication, and do the benefits outweigh them?
- Will this medication interact with my other drugs and/or other health conditions?
- What are the “boxed” warnings for this medication, and where can I report adverse events?
“I would also do my own research,” she says. “I wouldn’t just take a prescription from a physician and just say, ‘OK, doctor knows best.’ ”
Ms. Moser agrees that you have to be your own patient advocate and not simply take a doctor’s advice on any medical issue without having a deeper conversation.
“I’ve had arguments with doctors who legitimately did not believe me when I told them what happened to me,” she says. “And I actually told them, ‘Go get your Physicians’ Desk Reference [for prescription drugs]’ and they opened the book in front of me and read the warnings. Obviously, they had not been keeping up with the added warnings. So, I do think that doctors do need to be better informed.”
“So, yes, it’s the FDA’s responsibility, but it is also the doctors’ responsibility to make sure that they’re watching out for the side effects and they’re reporting them when their patients come up with them and making those connections.”
A version of this article first appeared on WebMD.com.
Scientists find brain mechanism behind age-related memory loss
Scientists at Johns Hopkins University have identified a mechanism in the brain behind age-related memory loss, expanding our knowledge of the inner workings of the aging brain and possibly opening the door to new Alzheimer’s treatments.
The researchers looked at the hippocampus, a part of the brain thought to store long-term memories.
Neurons there are responsible for a pair of memory functions – called pattern separation and pattern completion – that work together in young, healthy brains. These functions can swing out of balance with age, impacting memory.
The Johns Hopkins team may have discovered what causes this imbalance. Their findings – reported in a paper in the journal Current Biology – may not only help us improve dementia treatments, but even prevent or delay a loss of thinking skills in the first place, the researchers say.
Pattern separation vs. pattern completion
To understand how the hippocampus changes with age, the researchers looked at rats’ brains. In rats and in humans, pattern separation and pattern completion are present, controlled by neurons in the hippocampus.
As the name suggests, pattern completion is when you take a few details or fragments of information – a few notes of music, or the start of a famous movie quote – and your brain retrieves the full memory. Pattern separation, on the other hand, is being able to tell similar observations or experiences apart (like two visits to the same restaurant) to be stored as separate memories.
These functions occur along a gradient across a tiny region called CA3. That gradient, the study found, disappears with aging, said lead study author Hey-Kyoung Lee, PhD, an assistant research scientist at the university’s Zanvyl Krieger Mind/Brain Institute. “The main consequence of the loss,” Dr. Lee said, “is that pattern completion becomes more dominant in rats as they age.”
What’s happening in the brain
Neurons responsible for pattern completion occupy the “distal” end of CA3, while those in charge of pattern separation reside at the “proximal” end. Dr. Lee said prior studies had not examined the proximal and distal regions separately, as she and her team did in this study.
What was surprising, said Dr. Lee, “was that hyperactivity in aging was observed toward the proximal CA3 region, not the expected distal region.” Contrary to their expectations, that hyperactivity did not enhance function in that area but rather dampened it. Hence: “There is diminished pattern separation and augmented pattern completion,” she said.
– they may recall a certain restaurant they’d been to but not be able to separate what happened during one visit versus another.
Why do some older adults stay sharp?
That memory impairment does not happen to everyone, and it doesn’t happen to all rats either. In fact, the researchers found that some older rats performed spatial-learning tasks as well as young rats did – even though their brains were already beginning to favor pattern completion.
If we can better understand why this happens, we may uncover new therapies for age-related memory loss, Dr. Lee said.
Coauthor Michela Gallagher’s team previously demonstrated that the anti-epilepsy drug levetiracetam improves memory performance by reducing hyperactivity in the hippocampus.
The extra detail this study adds may allow scientists to better aim such drugs in the future, Dr. Lee speculated. “It would give us better control of where we could possibly target the deficits we see.”
A version of this article first appeared on WebMD.com.
Scientists at Johns Hopkins University have identified a mechanism in the brain behind age-related memory loss, expanding our knowledge of the inner workings of the aging brain and possibly opening the door to new Alzheimer’s treatments.
The researchers looked at the hippocampus, a part of the brain thought to store long-term memories.
Neurons there are responsible for a pair of memory functions – called pattern separation and pattern completion – that work together in young, healthy brains. These functions can swing out of balance with age, impacting memory.
The Johns Hopkins team may have discovered what causes this imbalance. Their findings – reported in a paper in the journal Current Biology – may not only help us improve dementia treatments, but even prevent or delay a loss of thinking skills in the first place, the researchers say.
Pattern separation vs. pattern completion
To understand how the hippocampus changes with age, the researchers looked at rats’ brains. In rats and in humans, pattern separation and pattern completion are present, controlled by neurons in the hippocampus.
As the name suggests, pattern completion is when you take a few details or fragments of information – a few notes of music, or the start of a famous movie quote – and your brain retrieves the full memory. Pattern separation, on the other hand, is being able to tell similar observations or experiences apart (like two visits to the same restaurant) to be stored as separate memories.
These functions occur along a gradient across a tiny region called CA3. That gradient, the study found, disappears with aging, said lead study author Hey-Kyoung Lee, PhD, an assistant research scientist at the university’s Zanvyl Krieger Mind/Brain Institute. “The main consequence of the loss,” Dr. Lee said, “is that pattern completion becomes more dominant in rats as they age.”
What’s happening in the brain
Neurons responsible for pattern completion occupy the “distal” end of CA3, while those in charge of pattern separation reside at the “proximal” end. Dr. Lee said prior studies had not examined the proximal and distal regions separately, as she and her team did in this study.
What was surprising, said Dr. Lee, “was that hyperactivity in aging was observed toward the proximal CA3 region, not the expected distal region.” Contrary to their expectations, that hyperactivity did not enhance function in that area but rather dampened it. Hence: “There is diminished pattern separation and augmented pattern completion,” she said.
– they may recall a certain restaurant they’d been to but not be able to separate what happened during one visit versus another.
Why do some older adults stay sharp?
That memory impairment does not happen to everyone, and it doesn’t happen to all rats either. In fact, the researchers found that some older rats performed spatial-learning tasks as well as young rats did – even though their brains were already beginning to favor pattern completion.
If we can better understand why this happens, we may uncover new therapies for age-related memory loss, Dr. Lee said.
Coauthor Michela Gallagher’s team previously demonstrated that the anti-epilepsy drug levetiracetam improves memory performance by reducing hyperactivity in the hippocampus.
The extra detail this study adds may allow scientists to better aim such drugs in the future, Dr. Lee speculated. “It would give us better control of where we could possibly target the deficits we see.”
A version of this article first appeared on WebMD.com.
Scientists at Johns Hopkins University have identified a mechanism in the brain behind age-related memory loss, expanding our knowledge of the inner workings of the aging brain and possibly opening the door to new Alzheimer’s treatments.
The researchers looked at the hippocampus, a part of the brain thought to store long-term memories.
Neurons there are responsible for a pair of memory functions – called pattern separation and pattern completion – that work together in young, healthy brains. These functions can swing out of balance with age, impacting memory.
The Johns Hopkins team may have discovered what causes this imbalance. Their findings – reported in a paper in the journal Current Biology – may not only help us improve dementia treatments, but even prevent or delay a loss of thinking skills in the first place, the researchers say.
Pattern separation vs. pattern completion
To understand how the hippocampus changes with age, the researchers looked at rats’ brains. In rats and in humans, pattern separation and pattern completion are present, controlled by neurons in the hippocampus.
As the name suggests, pattern completion is when you take a few details or fragments of information – a few notes of music, or the start of a famous movie quote – and your brain retrieves the full memory. Pattern separation, on the other hand, is being able to tell similar observations or experiences apart (like two visits to the same restaurant) to be stored as separate memories.
These functions occur along a gradient across a tiny region called CA3. That gradient, the study found, disappears with aging, said lead study author Hey-Kyoung Lee, PhD, an assistant research scientist at the university’s Zanvyl Krieger Mind/Brain Institute. “The main consequence of the loss,” Dr. Lee said, “is that pattern completion becomes more dominant in rats as they age.”
What’s happening in the brain
Neurons responsible for pattern completion occupy the “distal” end of CA3, while those in charge of pattern separation reside at the “proximal” end. Dr. Lee said prior studies had not examined the proximal and distal regions separately, as she and her team did in this study.
What was surprising, said Dr. Lee, “was that hyperactivity in aging was observed toward the proximal CA3 region, not the expected distal region.” Contrary to their expectations, that hyperactivity did not enhance function in that area but rather dampened it. Hence: “There is diminished pattern separation and augmented pattern completion,” she said.
– they may recall a certain restaurant they’d been to but not be able to separate what happened during one visit versus another.
Why do some older adults stay sharp?
That memory impairment does not happen to everyone, and it doesn’t happen to all rats either. In fact, the researchers found that some older rats performed spatial-learning tasks as well as young rats did – even though their brains were already beginning to favor pattern completion.
If we can better understand why this happens, we may uncover new therapies for age-related memory loss, Dr. Lee said.
Coauthor Michela Gallagher’s team previously demonstrated that the anti-epilepsy drug levetiracetam improves memory performance by reducing hyperactivity in the hippocampus.
The extra detail this study adds may allow scientists to better aim such drugs in the future, Dr. Lee speculated. “It would give us better control of where we could possibly target the deficits we see.”
A version of this article first appeared on WebMD.com.
FROM CURRENT BIOLOGY
What is palliative care and what’s new in practicing this type of medicine?
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
The World Health Organization defines palliative care as “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual.”1
The common misperception is that palliative care is only for those at end of life or only in the advanced stages of their illness. However, palliative care is ideally most helpful following individuals from diagnosis through their illness trajectory. Another misperception is that palliative care and hospice are the same thing. Though all hospice is palliative care, all palliative care is not hospice. Both palliative care and hospice provide care for individuals facing a serious illness and focus on the same philosophy of care, but palliative care can be initiated at any stage of illness, even if the goal is to pursue curative and life-prolonging therapies/interventions.
In contrast, hospice is considered for those who are at the end of life and are usually not pursuing life-prolonging therapies or interventions, instead focusing on comfort, symptom management, and optimization of quality of life.
Though there is a growing need for palliative care, there is a shortage of specialist palliative care providers. Much of the palliative care needs can be met by all providers who can offer basic symptom management, identification surrounding goals of care and discussions of advance care planning, and understanding of illness/prognosis and treatment options, which is called primary palliative care.2 In fact, two-thirds of patients with a serious illness other than cancer prefer discussion of end-of-life care or advance care planning with their primary care providers.3
Referral to specialty palliative care should be considered when there are more complexities to symptom/pain management and goals of care/end of life, transition to hospice, or complex communication dynamics.4
Though specialty palliative care was shown to be more comprehensive, both primary palliative care and specialty palliative care have led to improvements in the quality of life in individuals living with serious illness.5 Early integration of palliative care into routine care has been shown to improve symptom burden, mood, quality of life, survival, and health care costs.6
Updates in alternative and complementary therapies to palliative care
There are several alternative and complementary therapies to palliative care, including cannabis and psychedelics. These therapies are becoming or may become a familiar part of medical therapies that are listed in a patient’s history as part of their medical regimen, especially as more states continue to legalize and/or decriminalize the use of these alternative therapies for recreational or medicinal use.
Both cannabis and psychedelics have a longstanding history of therapeutic and holistic use. Cannabis has been used to manage symptoms such as pain since the 16th and 17th century.7 In palliative care, more patients may turn to various forms of cannabis as a source of relief from symptoms and suffering as their focus shifts more to quality of life.
Even with the increasing popularity of the use of cannabis among seriously ill patients, there is still a lack of evidence of the benefits of medical cannabis use in palliative care, and there is a lack of standardization of type of cannabis used and state regulations regarding their use.7
A recent systematic review found that despite the reported positive treatment effects of cannabis in palliative care, the results of the studies were conflicting. This highlights the need for further high-quality research to determine whether cannabis products are an effective treatment in palliative care patients.8
One limitation to note is that the majority of the included studies focused on cannabis use in patients with cancer for cancer-related symptoms. Few studies included patients with other serious conditions.
Psychedelics
There is evidence that psychedelic assisted therapy (PAT) is a safe and effective treatment for individuals with refractory depression, posttraumatic stress disorder, and substance use disorder.9 Plus, there have been ample studies providing support that PAT improves symptoms such as refractory anxiety/depression, demoralization, and existential distress in seriously ill patients, thus improving their quality of life and overall well-being.9
Nine U.S. cities and the State of Oregon have decriminalized or legalized the psychedelic psilocybin, based on the medical benefits patients have experienced evidenced from using it.10
In light of the increasing interest in PAT, Dr. Ira Byock provided the following points on what “all clinicians should know as they enter this uncharted territory”:
- Psychedelics have been around for a long time.
- Psychedelic-assisted therapies’ therapeutic effects are experiential.
- There are a variety of terms for specific categories of psychedelic compounds.
- Some palliative care teams are already caring for patients who undergo psychedelic experiences.
- Use of psychedelics should be well-observed by a skilled clinician with expertise.
I am hoping this provides a general refresher on palliative care and an overview of updates to alternative and complementary therapies for patients living with serious illness.9
Dr. Kang is a geriatrician and palliative care provider at the University of Washington, Seattle in the division of geriatrics and gerontology. She has no conflicts related to the content of this piece.
References
1. World Health Organization. Palliative care. 2020 Aug 5..
2. Weissman DE and Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting a consensus report from the center to advance palliative care. J Palliat Med. 2011;14(1):17-23.
3. Sherry D et al. Is primary care physician involvement associated with earlier advance care planning? A study of patients in an academic primary care setting. J Palliat Med. 2022;25(1):75-80.
4. Quill TE and Abernethy AP. Generalist plus specialist palliative care-creating a more sustainable model. N Engl J Med. 2013;368:1173-75.
5. Ernecoff NC et al. Comparing specialty and primary palliative care interventions: Analysis of a systematic review. J Palliat Med. 2020;23(3):389-96.
6. Temmel JS et al. Early palliative care for patients with metastatic non–small-cell lung cancer. N Engl J Med. 2011;363:733-42.
7. Kogan M and Sexton M. Medical cannabis: A new old tool for palliative care. J Altern Complement Med . 2020 Sep;26(9):776-8.
8. Doppen M et al. Cannabis in palliative care: A systematic review of the current evidence. J Pain Symptom Manage. 2022 Jun 12;S0885-3924(22)00760-6.
9. Byock I. Psychedelics for serious illness: Five things clinicians need to know. The Center to Advance Palliative Care. Psychedelics for Serious Illness, Palliative in Practice, Center to Advance Palliative Care (capc.org). June 13, 2022.
10. Marks M. A strategy for rescheduling psilocybin. Scientific American. Oct. 11, 2021.
Physicians react: Compensation isn’t worth the hassles. What’s the solution?
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
Can bone density scans help predict dementia risk?
, new research suggests.
In an analysis of more than 900 study participants, women in their 70s with more advanced abdominal aortic calcification (AAC) seen on lateral spine images during dual-energy x-ray absorptiometry (DXA) had a two- to fourfold higher risk for late-life dementia than those with low AAC.
This finding was independent of cardiovascular risk factors and apolipoprotein E (APOE ) genotype.
“While these results are exciting, we now need to undertake further large screening studies in older men and women using this approach to show that the findings are generalizable to older men and can identify people with greater cognitive decline,” coinvestigator Marc Sim, PhD, Edith Cowan University, Joondalup, Australia, said in an interview.
“This will hopefully open the door to studies of early disease-modifying interventions,” Sim said.
The findings were published online in The Lancet Regional Health – Western Pacific.
AAC and cognition
Late-life dementia occurring after age 80 is increasingly common because of both vascular and nonvascular risk factors.
Two recent studies in middle-aged and older men and women showed that AAC identified on bone densitometry was associated with poorer cognition, suggesting it may be related to cognitive decline and increased dementia risk.
This provided the rationale for the current study, Dr. Sim noted.
The researchers assessed AAC using DXA lateral spine images captured in the late 1990s in a prospective cohort of 958 older women who were participating in an osteoporosis study.
AAC was classified into established low, moderate, and extensive categories. At baseline, all women were aged 70 and older, and 45% had low AAC, 36% had moderate AAC, and 19% had extensive AAC.
Over 14.5 years, 150 women (15.7%) had a late-life hospitalization and/or died.
Improved risk prediction
Results showed that, compared with women who had low AAC, women with moderate and extensive AAC were more likely to experience late-life dementia hospitalization (9.3% low, 15.5% moderate, and 18.3% extensive) and death (2.8%, 8.3%, and 9.4%, respectively).
After multivariable adjustment, women with moderate AAC had a two- and threefold increased relative risk for late-life dementia hospitalization or death, compared with their peers who had low AAC.
Women with extensive AAC had a two- and fourfold increase in the adjusted relative risk for late-life dementia hospitalization or death.
“To our knowledge this is the first time it has been shown that AAC from these scans is related to late-life dementia,” Dr. Sim said.
“We demonstrated that AAC improved risk prediction in addition to cardiovascular risk factors and APOE genotype, a genetic risk factor for Alzheimer’s disease, the major form of dementia,” he added.
Dr. Sim noted “these additional lateral spine images” can be taken at the same time that hip and spine bone density tests are done.
“This provides an opportunity to identify AAC in large numbers of people,” he said.
He cautioned, however, that further studies with detailed dementia-related phenotypes, brain imaging, and measures of cognition are needed to confirm whether AAC will add value to dementia risk prediction.
‘Not surprising’
Commenting on the findings for this article, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, Chicago, noted that AAC is a marker of atherosclerosis and is associated with vascular health outcomes.
Therefore, it is “not surprising it would be associated with dementia too. There’s been previous research linking atherosclerosis and Alzheimer’s disease,” Dr. Sexton said.
“What’s novel about this research is that it’s looking at AAC specifically, which can be identified through a relatively simple test that is already in widespread use,” she added.
Dr. Sexton noted that “much more research” is now needed in larger, more diverse populations in order to better understand the link between AAC and dementia – and whether bone density testing may be an appropriate dementia-screening tool.
“The good news is vascular conditions like atherosclerosis can be managed through lifestyle changes like eating a healthy diet and getting regular exercise. And research tells us what’s good for the heart is good for the brain,” Dr. Sexton said.
The study was funded by Kidney Health Australia, Healthway Health Promotion Foundation of Western Australia, Sir Charles Gairdner Hospital Research Advisory Committee Grant, and the National Health and Medical Research Council of Australia. Dr. Sim and Dr. Sexton have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In an analysis of more than 900 study participants, women in their 70s with more advanced abdominal aortic calcification (AAC) seen on lateral spine images during dual-energy x-ray absorptiometry (DXA) had a two- to fourfold higher risk for late-life dementia than those with low AAC.
This finding was independent of cardiovascular risk factors and apolipoprotein E (APOE ) genotype.
“While these results are exciting, we now need to undertake further large screening studies in older men and women using this approach to show that the findings are generalizable to older men and can identify people with greater cognitive decline,” coinvestigator Marc Sim, PhD, Edith Cowan University, Joondalup, Australia, said in an interview.
“This will hopefully open the door to studies of early disease-modifying interventions,” Sim said.
The findings were published online in The Lancet Regional Health – Western Pacific.
AAC and cognition
Late-life dementia occurring after age 80 is increasingly common because of both vascular and nonvascular risk factors.
Two recent studies in middle-aged and older men and women showed that AAC identified on bone densitometry was associated with poorer cognition, suggesting it may be related to cognitive decline and increased dementia risk.
This provided the rationale for the current study, Dr. Sim noted.
The researchers assessed AAC using DXA lateral spine images captured in the late 1990s in a prospective cohort of 958 older women who were participating in an osteoporosis study.
AAC was classified into established low, moderate, and extensive categories. At baseline, all women were aged 70 and older, and 45% had low AAC, 36% had moderate AAC, and 19% had extensive AAC.
Over 14.5 years, 150 women (15.7%) had a late-life hospitalization and/or died.
Improved risk prediction
Results showed that, compared with women who had low AAC, women with moderate and extensive AAC were more likely to experience late-life dementia hospitalization (9.3% low, 15.5% moderate, and 18.3% extensive) and death (2.8%, 8.3%, and 9.4%, respectively).
After multivariable adjustment, women with moderate AAC had a two- and threefold increased relative risk for late-life dementia hospitalization or death, compared with their peers who had low AAC.
Women with extensive AAC had a two- and fourfold increase in the adjusted relative risk for late-life dementia hospitalization or death.
“To our knowledge this is the first time it has been shown that AAC from these scans is related to late-life dementia,” Dr. Sim said.
“We demonstrated that AAC improved risk prediction in addition to cardiovascular risk factors and APOE genotype, a genetic risk factor for Alzheimer’s disease, the major form of dementia,” he added.
Dr. Sim noted “these additional lateral spine images” can be taken at the same time that hip and spine bone density tests are done.
“This provides an opportunity to identify AAC in large numbers of people,” he said.
He cautioned, however, that further studies with detailed dementia-related phenotypes, brain imaging, and measures of cognition are needed to confirm whether AAC will add value to dementia risk prediction.
‘Not surprising’
Commenting on the findings for this article, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, Chicago, noted that AAC is a marker of atherosclerosis and is associated with vascular health outcomes.
Therefore, it is “not surprising it would be associated with dementia too. There’s been previous research linking atherosclerosis and Alzheimer’s disease,” Dr. Sexton said.
“What’s novel about this research is that it’s looking at AAC specifically, which can be identified through a relatively simple test that is already in widespread use,” she added.
Dr. Sexton noted that “much more research” is now needed in larger, more diverse populations in order to better understand the link between AAC and dementia – and whether bone density testing may be an appropriate dementia-screening tool.
“The good news is vascular conditions like atherosclerosis can be managed through lifestyle changes like eating a healthy diet and getting regular exercise. And research tells us what’s good for the heart is good for the brain,” Dr. Sexton said.
The study was funded by Kidney Health Australia, Healthway Health Promotion Foundation of Western Australia, Sir Charles Gairdner Hospital Research Advisory Committee Grant, and the National Health and Medical Research Council of Australia. Dr. Sim and Dr. Sexton have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In an analysis of more than 900 study participants, women in their 70s with more advanced abdominal aortic calcification (AAC) seen on lateral spine images during dual-energy x-ray absorptiometry (DXA) had a two- to fourfold higher risk for late-life dementia than those with low AAC.
This finding was independent of cardiovascular risk factors and apolipoprotein E (APOE ) genotype.
“While these results are exciting, we now need to undertake further large screening studies in older men and women using this approach to show that the findings are generalizable to older men and can identify people with greater cognitive decline,” coinvestigator Marc Sim, PhD, Edith Cowan University, Joondalup, Australia, said in an interview.
“This will hopefully open the door to studies of early disease-modifying interventions,” Sim said.
The findings were published online in The Lancet Regional Health – Western Pacific.
AAC and cognition
Late-life dementia occurring after age 80 is increasingly common because of both vascular and nonvascular risk factors.
Two recent studies in middle-aged and older men and women showed that AAC identified on bone densitometry was associated with poorer cognition, suggesting it may be related to cognitive decline and increased dementia risk.
This provided the rationale for the current study, Dr. Sim noted.
The researchers assessed AAC using DXA lateral spine images captured in the late 1990s in a prospective cohort of 958 older women who were participating in an osteoporosis study.
AAC was classified into established low, moderate, and extensive categories. At baseline, all women were aged 70 and older, and 45% had low AAC, 36% had moderate AAC, and 19% had extensive AAC.
Over 14.5 years, 150 women (15.7%) had a late-life hospitalization and/or died.
Improved risk prediction
Results showed that, compared with women who had low AAC, women with moderate and extensive AAC were more likely to experience late-life dementia hospitalization (9.3% low, 15.5% moderate, and 18.3% extensive) and death (2.8%, 8.3%, and 9.4%, respectively).
After multivariable adjustment, women with moderate AAC had a two- and threefold increased relative risk for late-life dementia hospitalization or death, compared with their peers who had low AAC.
Women with extensive AAC had a two- and fourfold increase in the adjusted relative risk for late-life dementia hospitalization or death.
“To our knowledge this is the first time it has been shown that AAC from these scans is related to late-life dementia,” Dr. Sim said.
“We demonstrated that AAC improved risk prediction in addition to cardiovascular risk factors and APOE genotype, a genetic risk factor for Alzheimer’s disease, the major form of dementia,” he added.
Dr. Sim noted “these additional lateral spine images” can be taken at the same time that hip and spine bone density tests are done.
“This provides an opportunity to identify AAC in large numbers of people,” he said.
He cautioned, however, that further studies with detailed dementia-related phenotypes, brain imaging, and measures of cognition are needed to confirm whether AAC will add value to dementia risk prediction.
‘Not surprising’
Commenting on the findings for this article, Claire Sexton, DPhil, senior director of scientific programs and outreach at the Alzheimer’s Association, Chicago, noted that AAC is a marker of atherosclerosis and is associated with vascular health outcomes.
Therefore, it is “not surprising it would be associated with dementia too. There’s been previous research linking atherosclerosis and Alzheimer’s disease,” Dr. Sexton said.
“What’s novel about this research is that it’s looking at AAC specifically, which can be identified through a relatively simple test that is already in widespread use,” she added.
Dr. Sexton noted that “much more research” is now needed in larger, more diverse populations in order to better understand the link between AAC and dementia – and whether bone density testing may be an appropriate dementia-screening tool.
“The good news is vascular conditions like atherosclerosis can be managed through lifestyle changes like eating a healthy diet and getting regular exercise. And research tells us what’s good for the heart is good for the brain,” Dr. Sexton said.
The study was funded by Kidney Health Australia, Healthway Health Promotion Foundation of Western Australia, Sir Charles Gairdner Hospital Research Advisory Committee Grant, and the National Health and Medical Research Council of Australia. Dr. Sim and Dr. Sexton have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET REGIONAL HEALTH – WESTERN PACIFIC
Monkeypox: What FPs need to know, now
The Centers for Disease Control and Prevention (CDC) and the World Health Organization are investigating an outbreak of monkeypox cases that have occurred around the world in countries that do not have endemic monkeypox virus.1,2 As of July 5, there have been 6924 cases documented in 52 countries, including 560 cases that have occurred in the United States.2 In the United States, as well as globally, a large proportion of cases have been in men who have sex with men.
First, what is monkeypox? Monkeypox is an orthopox virus that is closely related to variola (smallpox) and vaccinia (the virus used in the smallpox vaccine). It is endemic in western and central Africa and is contracted by contact with an infected mammal (including humans). Transmission can occur through direct contact with infected body fluids or lesions, via infectious fomites, or through respiratory secretions (although this usually requires prolonged exposure).
What is the disease course? The incubation period is 4 to 17 days. The initial symptoms include fever, malaise, headache, sore throat, and lymphadenopathy. A rash erupts 1 to 4 days after the prodrome and progresses synchronously from macules to papules to vesicles and then to pustules, which eventually scab over and fall off. In some cases reported in the United States, the rash started in the groin and genital area.
Don’t be fooled by other exanthems. Monkeypox can be confused with chickenpox and molluscum contagiosum (MC). However, the lesions in chickenpox appear asynchronously (all 4 stages present at the same time) and the papules of MC contain a central pit.
Can monkeypox be prevented? There are currently 2 vaccines against orthopox viruses: ACAM2000 and Jynneos. Currently, these vaccines are routinely recommended only for those at occupational risk of orthopox exposure.3
What you should know—and do. Be alert for any patient who presents with a suspicious rash; if there is a possibility of monkeypox, the local public health department should be contacted. They will investigate and collect samples for laboratory testing and will elicit contact names and locations. If monkeypox is confirmed, they may offer close contacts 1 of the 2 vaccines, which if administered within 4 days of exposure can prevent infection.
Advise all patients confirmed to have monkeypox to self-isolate until all skin lesions have healed. Good infection control practices in the clinical setting will prevent spread to staff and other patients.
More information about monkeypox, including images of typical lesions—as well as an update on the current investigation in the United States and worldwide—can be found on the CDC website.4
1. Minhaj FS, Ogale YP, Whitehill F, et al. Monkeypox outbreak—nine states, May 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:764-769. doi: http://dx.doi.org/10.15585/mmwr.mm7123e1
2. CDC. US monkeypox outbreak 2022: situation summary. Updated June 29, 2022. Accessed July 5, 2022.
3. Rao AK, Petersen BW, Whitehill F, et al. Use of JYNNEOS (smallpox and monkeypox vaccine, live, nonreplicating) for preexposure vaccination of persons at risk for occupational exposure to orthopoxviruses: recommendations of the Advisory Committee on Immunization Practices—United States, 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:734-742. doi: http://dx.doi.org/10.15585/mmwr.mm7122e1
4. CDC. 2022 monkeypox: information for healthcare professionals. Updated June 23, 2022. Accessed July 5, 2022.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization are investigating an outbreak of monkeypox cases that have occurred around the world in countries that do not have endemic monkeypox virus.1,2 As of July 5, there have been 6924 cases documented in 52 countries, including 560 cases that have occurred in the United States.2 In the United States, as well as globally, a large proportion of cases have been in men who have sex with men.
First, what is monkeypox? Monkeypox is an orthopox virus that is closely related to variola (smallpox) and vaccinia (the virus used in the smallpox vaccine). It is endemic in western and central Africa and is contracted by contact with an infected mammal (including humans). Transmission can occur through direct contact with infected body fluids or lesions, via infectious fomites, or through respiratory secretions (although this usually requires prolonged exposure).
What is the disease course? The incubation period is 4 to 17 days. The initial symptoms include fever, malaise, headache, sore throat, and lymphadenopathy. A rash erupts 1 to 4 days after the prodrome and progresses synchronously from macules to papules to vesicles and then to pustules, which eventually scab over and fall off. In some cases reported in the United States, the rash started in the groin and genital area.
Don’t be fooled by other exanthems. Monkeypox can be confused with chickenpox and molluscum contagiosum (MC). However, the lesions in chickenpox appear asynchronously (all 4 stages present at the same time) and the papules of MC contain a central pit.
Can monkeypox be prevented? There are currently 2 vaccines against orthopox viruses: ACAM2000 and Jynneos. Currently, these vaccines are routinely recommended only for those at occupational risk of orthopox exposure.3
What you should know—and do. Be alert for any patient who presents with a suspicious rash; if there is a possibility of monkeypox, the local public health department should be contacted. They will investigate and collect samples for laboratory testing and will elicit contact names and locations. If monkeypox is confirmed, they may offer close contacts 1 of the 2 vaccines, which if administered within 4 days of exposure can prevent infection.
Advise all patients confirmed to have monkeypox to self-isolate until all skin lesions have healed. Good infection control practices in the clinical setting will prevent spread to staff and other patients.
More information about monkeypox, including images of typical lesions—as well as an update on the current investigation in the United States and worldwide—can be found on the CDC website.4
The Centers for Disease Control and Prevention (CDC) and the World Health Organization are investigating an outbreak of monkeypox cases that have occurred around the world in countries that do not have endemic monkeypox virus.1,2 As of July 5, there have been 6924 cases documented in 52 countries, including 560 cases that have occurred in the United States.2 In the United States, as well as globally, a large proportion of cases have been in men who have sex with men.
First, what is monkeypox? Monkeypox is an orthopox virus that is closely related to variola (smallpox) and vaccinia (the virus used in the smallpox vaccine). It is endemic in western and central Africa and is contracted by contact with an infected mammal (including humans). Transmission can occur through direct contact with infected body fluids or lesions, via infectious fomites, or through respiratory secretions (although this usually requires prolonged exposure).
What is the disease course? The incubation period is 4 to 17 days. The initial symptoms include fever, malaise, headache, sore throat, and lymphadenopathy. A rash erupts 1 to 4 days after the prodrome and progresses synchronously from macules to papules to vesicles and then to pustules, which eventually scab over and fall off. In some cases reported in the United States, the rash started in the groin and genital area.
Don’t be fooled by other exanthems. Monkeypox can be confused with chickenpox and molluscum contagiosum (MC). However, the lesions in chickenpox appear asynchronously (all 4 stages present at the same time) and the papules of MC contain a central pit.
Can monkeypox be prevented? There are currently 2 vaccines against orthopox viruses: ACAM2000 and Jynneos. Currently, these vaccines are routinely recommended only for those at occupational risk of orthopox exposure.3
What you should know—and do. Be alert for any patient who presents with a suspicious rash; if there is a possibility of monkeypox, the local public health department should be contacted. They will investigate and collect samples for laboratory testing and will elicit contact names and locations. If monkeypox is confirmed, they may offer close contacts 1 of the 2 vaccines, which if administered within 4 days of exposure can prevent infection.
Advise all patients confirmed to have monkeypox to self-isolate until all skin lesions have healed. Good infection control practices in the clinical setting will prevent spread to staff and other patients.
More information about monkeypox, including images of typical lesions—as well as an update on the current investigation in the United States and worldwide—can be found on the CDC website.4
1. Minhaj FS, Ogale YP, Whitehill F, et al. Monkeypox outbreak—nine states, May 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:764-769. doi: http://dx.doi.org/10.15585/mmwr.mm7123e1
2. CDC. US monkeypox outbreak 2022: situation summary. Updated June 29, 2022. Accessed July 5, 2022.
3. Rao AK, Petersen BW, Whitehill F, et al. Use of JYNNEOS (smallpox and monkeypox vaccine, live, nonreplicating) for preexposure vaccination of persons at risk for occupational exposure to orthopoxviruses: recommendations of the Advisory Committee on Immunization Practices—United States, 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:734-742. doi: http://dx.doi.org/10.15585/mmwr.mm7122e1
4. CDC. 2022 monkeypox: information for healthcare professionals. Updated June 23, 2022. Accessed July 5, 2022.
1. Minhaj FS, Ogale YP, Whitehill F, et al. Monkeypox outbreak—nine states, May 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:764-769. doi: http://dx.doi.org/10.15585/mmwr.mm7123e1
2. CDC. US monkeypox outbreak 2022: situation summary. Updated June 29, 2022. Accessed July 5, 2022.
3. Rao AK, Petersen BW, Whitehill F, et al. Use of JYNNEOS (smallpox and monkeypox vaccine, live, nonreplicating) for preexposure vaccination of persons at risk for occupational exposure to orthopoxviruses: recommendations of the Advisory Committee on Immunization Practices—United States, 2022. MMWR Morbid Mortal Wkly Rep. 2022;71:734-742. doi: http://dx.doi.org/10.15585/mmwr.mm7122e1
4. CDC. 2022 monkeypox: information for healthcare professionals. Updated June 23, 2022. Accessed July 5, 2022.
Caring for the young elite athlete
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Concerns about the potential harm resulting from overzealous training regimens and performance schedules for young elite athletes seems to come in cycles much like the Olympics. But, more recently, the media attention has become more intense fueled by the very visible psychological vulnerabilities of some young gymnasts, tennis players, and figure skaters. Accusations of physical and psychological abuse by team physicians and coaches continue to surface with troubling regularity.
A recent article in the Wall St. Journal explores a variety of initiatives aimed at redefining the relationship between youth sports and the physical and mental health of its elite athletes. (Louise Radnofsky, The Wall Street Journal, June 9, 2022).
An example of the new awareness is the recent invitation of Peter Donnelly, PhD, an emeritus professor at the University of Toronto and long-time advocate for regulatory protections for youth athletes, to deliver a paper at a global conference in South Africa devoted to the elimination of child labor. Referring to youth sports, Dr. Donnelly observes “What if McDonalds had the same accident rate? ... There would be huge commissions of inquiry, regulations, and policies.” He suggests that the United Nations Convention on the Rights of the Child might be a mechanism to address the problem.
Writing in the Marquette University Sports Law Review in 2015, Kristin Hoffman, a law student at the time, suggested that the federal Fair Labor Standards Act or state child labor laws could be used to restructure sports like gymnastics or figure skating with tarnished histories. California law prohibits child actors from working more than 5 hours a day on school days and 7 hours on nonschool days but says little about child athletes. On paper, the National Collegiate Athletic Association limits college athletes to 20 hours participation per week but teenagers on club teams are not limited and may sometimes practice 30 hours or more.
Regulation in any form is a tough sell in this country. Coaches, parents, and athletes caught up in the myth that more repetitions and more touches on the ball are always the ticket to success will argue that most elite athletes are self-motivated and don’t view the long hours as a hardship.
Exactly how many are self-driven and how many are being pushed by parents and coaches is unknown. Across the street from us lived a young girl who, despite not having the obvious physical gifts, was clearly committed to excel in sports. She begged her parents to set up lights to allow her to practice well into the evening. She went on to have a good college career as a player and a very successful career as a Division I coach. Now in retirement, she is very open about her mental health history that in large part explains her inner drive and her subsequent troubles.
We need to be realistic in our hope for regulating the current state of youth sports out of its current situation. State laws that put reasonable limits on the hourly commitment to sports much like the California child actor laws feel like a reasonable goal. However, as physicians for these young athletes we must take each child – and we must remind ourselves that they are still children – as an individual.
When faced with patients who are clearly on the elite sport pathway, our goal is to protect their health – both physical and mental. If they are having symptoms of overuse we need to help them find alternative activities that will rest their injuries but still allow them to satisfy their competitive zeal. However, we must be ever alert to the risk that what appears to be unusual self-motivation may be instead a warning that pathologic obsession and compulsion lurk below the surface.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].