User login
How racist is your algorithm?
Every time Nathan Chomilo, MD, uses a clinical decision support tool, he tells his patients they have a choice: He can input their race or keep that field blank.
Until recently, many clinicians didn’t question the use of race as a datapoint in tools used to make decisions about diagnosis and care. But that is changing.
“I’ve almost universally had patients appreciate that someone actually told them that their kidney function was being scored differently because of the color of their skin or how they were identified in the medical chart along lines of race,” Dr. Chomilo, an adjunct assistant professor of pediatrics at the University of Minnesota Medical School, Minneapolis, said.
Dr. Chomilo is referring to the estimated glomerular filtration rate (eGFR), which combines results from a blood test with factors such as age, sex, and race to calculate kidney function.
The eGFR weighed an input of “African American” as automatically indicating a higher concentration of serum creatinine than a non African American patient on the basis of the unsubstantiated idea that Black people have more creatinine in their blood at baseline.
The calculator creates a picture of a Black patient who is not as sick as a White patient with the same levels of kidney failure. But race is based on the color of a patient’s skin, not on genetics or other clinical datapoints.
“I often use my own example of being a biracial Black man: My father’s family is from Cameroon, my mother’s family is from Norway. Are you going to assign my kidneys or my lungs to my mom’s side or my dad’s side? That’s not clear at all in the way we use race in medicine,” Dr. Chomilo, an executive committee member on the section on minority health equity and inclusion at the American Academy of Pediatrics (AAP), said.
Long before the COVID-19 pandemic so publicly exposed the depths of inequality in morbidity and mortality in the United States, health advocates had been pointing out these disparities in tools used by medical professionals. But efforts to recognize that race is a poor proxy for genetics is in its infancy.
In May, the AAP published a policy statement that kicked off its examination of clinical guidelines and policies that include race as a biological proxy. A committee for the society is combing through each guideline or calculator, evaluating the scientific basis for the use of race, and examining whether a stronger datapoint could be used instead.
The eGFR is perhaps the best example of a calculator that’s gone through the process: Health care stakeholders questioned the use of race, and investigators went back to study whether race was really a good datapoint. It wasn’t, and Dr. Chamilo’s hospital joined many others in retiring the calculator.
But the eGFR is one of countless clinical tools – from rudimentary algorithms to sophisticated machine-learning instruments – that change the course of care in part on the basis of race in the same way datapoints such as weight, age, and height are used to inform decisions about patient management. But unlike race, height, weight, and age can be objectively measured. A physician either makes a guess, or a patient enters their race on a form. And while that can be useful on a population level, race does not equal genetics or any other measurable datapoint.
In a study published in JAMA Pediatrics, researchers reviewed 414 clinical practice guidelines from sources such as PubMed and MetaLib.gov. Almost 1 in 6 guidelines included race in an inappropriate way, such as by conflating race as a biological risk factor or establishing testing or treatment thresholds using race.
Waiting for alternatives
The University of Maryland Medical System last year embarked on a project similar to the AAP initiative but within its own system. The first use of race to be eliminated was in the eGFR. The health system also recently removed the variable from a tool for diagnosing urinary tract infections (UTIs) in children younger than 2 years.
Part of that tool includes deciding to perform a catheterized urine test. If a doctor chose “White” as the race, the tool would recommend the test. If the doctor chose “Black,” the tool would recommend to not test. Joseph Wright, MD, MPH, chief health equity officer at University of Maryland Medical System, said this step in the tool is based on the unproven assumption that young Black children had a lower likelihood of UTIs than their White peers.
“We simply want folks to not by default lob race in as a decisionmaking point when we have, with a little bit more scientific diligence, the ability to include better clinical variables,” Dr. Wright, who is also an adjunct professor of health policy and management at the University of Maryland School of Public Health, College Park, said.
The developers of the UTI tool recently released a revised version that removes race in favor of two new medical datapoints: whether the patient has had a fever for over 48 hours, and whether the patient has previously had a UTI.
The process of re-examining tools, coming up with new datapoints, and implementing changes is not simple, according to Dr. Wright.
“This is just the baby step to fix the algorithms, because we’re all going to have to examine our own house, where these calculators live, whether it’s in a textbook, whether it’s in an electronic health record, and that’s the heavy lift,” he said. “All sources of clinical guidance have to be scrutinized, and it’s going to literally take years to unroot.”
Electronic medical record vendor Cerner said it generally revises its algorithms after medical societies make changes, then communicates those fixes to providers.
Rebecca C. Winokur, MD, MPH, lead physician executive and health equity service line leader at Cerner, explained that if doctors ordered an eGFR a year ago and then another today, the results might be different because of the new code that eliminates race.
“The numbers are so different, how do you know that the patient may or may not have the same function?” Dr. Winokur said.
Dr. Winokur said the company is trying to determine at which point a message should pop up in the records workflow that would inform clinicians that they may be comparing apples to cherries. The company also is reconsidering the use of race in tools that estimate the probability of a successful vaginal birth after prior cesarean delivery, a calculator that predicts the risk of urethral stones in patients with flank pain, and another that measures lung function to help diagnose pulmonary disease.
In addition to managing the logistics of removing race, health institutions also need buy-in from clinicians. At Mass General Brigham, Boston, Thomas Sequist, MD, MPH, chief medical officer, is leading a project to examine how the system uses race in calculators.
“People struggle mainly with, well, if we shouldn’t use this calculator, what should we use, because we need a calculator. And that’s a legitimate question,” Dr. Sequist said in an interview. “If we’re going to stop using this race-based calculator, I still need to know what dose of medication I give my patient. We’re not going to pull any of these calculators until we have a safe and reliable alternative.”
For each calculator, relevant specialty chiefs come to the table with Dr. Sequist and his team; current projects include examining bone density screenings and cardiac risk scores. A large part of the work is communicating the lack of science behind the inclusion of race as a variable.
“It’s hard because these tools have been in existence for decades, and people are used to using them,” Dr. Sequist said. “So this is a big-change management project.”
Some clinicians also have difficulty discerning why their health system may stratify patient outcomes by race while providers are being told that race is being removed from the calculators they use every day. The key difference is that stratifying outcomes by race illuminates systemic problems that can be targeted by a health system.
For instance, if readmission rates are higher for Black patients overall after surgery, the reason might be that nurses are not delivering the same level of care to them as they are to non-Black patients, possibly because of hidden bias. Or, perhaps Black patients at a hospital have less access to transportation for follow-up appointments after surgery. The potential reasons can be investigated, and solutions can be created.
“If you look at a population level, what you’re looking for is not for the evidence of race as a biological construct,” Dr. Chomilo said. “You’re looking for the impact of racism on populations, and that’s the difference: It’s racism, not race.”
A version of this article first appeared on Medscape.com.
Every time Nathan Chomilo, MD, uses a clinical decision support tool, he tells his patients they have a choice: He can input their race or keep that field blank.
Until recently, many clinicians didn’t question the use of race as a datapoint in tools used to make decisions about diagnosis and care. But that is changing.
“I’ve almost universally had patients appreciate that someone actually told them that their kidney function was being scored differently because of the color of their skin or how they were identified in the medical chart along lines of race,” Dr. Chomilo, an adjunct assistant professor of pediatrics at the University of Minnesota Medical School, Minneapolis, said.
Dr. Chomilo is referring to the estimated glomerular filtration rate (eGFR), which combines results from a blood test with factors such as age, sex, and race to calculate kidney function.
The eGFR weighed an input of “African American” as automatically indicating a higher concentration of serum creatinine than a non African American patient on the basis of the unsubstantiated idea that Black people have more creatinine in their blood at baseline.
The calculator creates a picture of a Black patient who is not as sick as a White patient with the same levels of kidney failure. But race is based on the color of a patient’s skin, not on genetics or other clinical datapoints.
“I often use my own example of being a biracial Black man: My father’s family is from Cameroon, my mother’s family is from Norway. Are you going to assign my kidneys or my lungs to my mom’s side or my dad’s side? That’s not clear at all in the way we use race in medicine,” Dr. Chomilo, an executive committee member on the section on minority health equity and inclusion at the American Academy of Pediatrics (AAP), said.
Long before the COVID-19 pandemic so publicly exposed the depths of inequality in morbidity and mortality in the United States, health advocates had been pointing out these disparities in tools used by medical professionals. But efforts to recognize that race is a poor proxy for genetics is in its infancy.
In May, the AAP published a policy statement that kicked off its examination of clinical guidelines and policies that include race as a biological proxy. A committee for the society is combing through each guideline or calculator, evaluating the scientific basis for the use of race, and examining whether a stronger datapoint could be used instead.
The eGFR is perhaps the best example of a calculator that’s gone through the process: Health care stakeholders questioned the use of race, and investigators went back to study whether race was really a good datapoint. It wasn’t, and Dr. Chamilo’s hospital joined many others in retiring the calculator.
But the eGFR is one of countless clinical tools – from rudimentary algorithms to sophisticated machine-learning instruments – that change the course of care in part on the basis of race in the same way datapoints such as weight, age, and height are used to inform decisions about patient management. But unlike race, height, weight, and age can be objectively measured. A physician either makes a guess, or a patient enters their race on a form. And while that can be useful on a population level, race does not equal genetics or any other measurable datapoint.
In a study published in JAMA Pediatrics, researchers reviewed 414 clinical practice guidelines from sources such as PubMed and MetaLib.gov. Almost 1 in 6 guidelines included race in an inappropriate way, such as by conflating race as a biological risk factor or establishing testing or treatment thresholds using race.
Waiting for alternatives
The University of Maryland Medical System last year embarked on a project similar to the AAP initiative but within its own system. The first use of race to be eliminated was in the eGFR. The health system also recently removed the variable from a tool for diagnosing urinary tract infections (UTIs) in children younger than 2 years.
Part of that tool includes deciding to perform a catheterized urine test. If a doctor chose “White” as the race, the tool would recommend the test. If the doctor chose “Black,” the tool would recommend to not test. Joseph Wright, MD, MPH, chief health equity officer at University of Maryland Medical System, said this step in the tool is based on the unproven assumption that young Black children had a lower likelihood of UTIs than their White peers.
“We simply want folks to not by default lob race in as a decisionmaking point when we have, with a little bit more scientific diligence, the ability to include better clinical variables,” Dr. Wright, who is also an adjunct professor of health policy and management at the University of Maryland School of Public Health, College Park, said.
The developers of the UTI tool recently released a revised version that removes race in favor of two new medical datapoints: whether the patient has had a fever for over 48 hours, and whether the patient has previously had a UTI.
The process of re-examining tools, coming up with new datapoints, and implementing changes is not simple, according to Dr. Wright.
“This is just the baby step to fix the algorithms, because we’re all going to have to examine our own house, where these calculators live, whether it’s in a textbook, whether it’s in an electronic health record, and that’s the heavy lift,” he said. “All sources of clinical guidance have to be scrutinized, and it’s going to literally take years to unroot.”
Electronic medical record vendor Cerner said it generally revises its algorithms after medical societies make changes, then communicates those fixes to providers.
Rebecca C. Winokur, MD, MPH, lead physician executive and health equity service line leader at Cerner, explained that if doctors ordered an eGFR a year ago and then another today, the results might be different because of the new code that eliminates race.
“The numbers are so different, how do you know that the patient may or may not have the same function?” Dr. Winokur said.
Dr. Winokur said the company is trying to determine at which point a message should pop up in the records workflow that would inform clinicians that they may be comparing apples to cherries. The company also is reconsidering the use of race in tools that estimate the probability of a successful vaginal birth after prior cesarean delivery, a calculator that predicts the risk of urethral stones in patients with flank pain, and another that measures lung function to help diagnose pulmonary disease.
In addition to managing the logistics of removing race, health institutions also need buy-in from clinicians. At Mass General Brigham, Boston, Thomas Sequist, MD, MPH, chief medical officer, is leading a project to examine how the system uses race in calculators.
“People struggle mainly with, well, if we shouldn’t use this calculator, what should we use, because we need a calculator. And that’s a legitimate question,” Dr. Sequist said in an interview. “If we’re going to stop using this race-based calculator, I still need to know what dose of medication I give my patient. We’re not going to pull any of these calculators until we have a safe and reliable alternative.”
For each calculator, relevant specialty chiefs come to the table with Dr. Sequist and his team; current projects include examining bone density screenings and cardiac risk scores. A large part of the work is communicating the lack of science behind the inclusion of race as a variable.
“It’s hard because these tools have been in existence for decades, and people are used to using them,” Dr. Sequist said. “So this is a big-change management project.”
Some clinicians also have difficulty discerning why their health system may stratify patient outcomes by race while providers are being told that race is being removed from the calculators they use every day. The key difference is that stratifying outcomes by race illuminates systemic problems that can be targeted by a health system.
For instance, if readmission rates are higher for Black patients overall after surgery, the reason might be that nurses are not delivering the same level of care to them as they are to non-Black patients, possibly because of hidden bias. Or, perhaps Black patients at a hospital have less access to transportation for follow-up appointments after surgery. The potential reasons can be investigated, and solutions can be created.
“If you look at a population level, what you’re looking for is not for the evidence of race as a biological construct,” Dr. Chomilo said. “You’re looking for the impact of racism on populations, and that’s the difference: It’s racism, not race.”
A version of this article first appeared on Medscape.com.
Every time Nathan Chomilo, MD, uses a clinical decision support tool, he tells his patients they have a choice: He can input their race or keep that field blank.
Until recently, many clinicians didn’t question the use of race as a datapoint in tools used to make decisions about diagnosis and care. But that is changing.
“I’ve almost universally had patients appreciate that someone actually told them that their kidney function was being scored differently because of the color of their skin or how they were identified in the medical chart along lines of race,” Dr. Chomilo, an adjunct assistant professor of pediatrics at the University of Minnesota Medical School, Minneapolis, said.
Dr. Chomilo is referring to the estimated glomerular filtration rate (eGFR), which combines results from a blood test with factors such as age, sex, and race to calculate kidney function.
The eGFR weighed an input of “African American” as automatically indicating a higher concentration of serum creatinine than a non African American patient on the basis of the unsubstantiated idea that Black people have more creatinine in their blood at baseline.
The calculator creates a picture of a Black patient who is not as sick as a White patient with the same levels of kidney failure. But race is based on the color of a patient’s skin, not on genetics or other clinical datapoints.
“I often use my own example of being a biracial Black man: My father’s family is from Cameroon, my mother’s family is from Norway. Are you going to assign my kidneys or my lungs to my mom’s side or my dad’s side? That’s not clear at all in the way we use race in medicine,” Dr. Chomilo, an executive committee member on the section on minority health equity and inclusion at the American Academy of Pediatrics (AAP), said.
Long before the COVID-19 pandemic so publicly exposed the depths of inequality in morbidity and mortality in the United States, health advocates had been pointing out these disparities in tools used by medical professionals. But efforts to recognize that race is a poor proxy for genetics is in its infancy.
In May, the AAP published a policy statement that kicked off its examination of clinical guidelines and policies that include race as a biological proxy. A committee for the society is combing through each guideline or calculator, evaluating the scientific basis for the use of race, and examining whether a stronger datapoint could be used instead.
The eGFR is perhaps the best example of a calculator that’s gone through the process: Health care stakeholders questioned the use of race, and investigators went back to study whether race was really a good datapoint. It wasn’t, and Dr. Chamilo’s hospital joined many others in retiring the calculator.
But the eGFR is one of countless clinical tools – from rudimentary algorithms to sophisticated machine-learning instruments – that change the course of care in part on the basis of race in the same way datapoints such as weight, age, and height are used to inform decisions about patient management. But unlike race, height, weight, and age can be objectively measured. A physician either makes a guess, or a patient enters their race on a form. And while that can be useful on a population level, race does not equal genetics or any other measurable datapoint.
In a study published in JAMA Pediatrics, researchers reviewed 414 clinical practice guidelines from sources such as PubMed and MetaLib.gov. Almost 1 in 6 guidelines included race in an inappropriate way, such as by conflating race as a biological risk factor or establishing testing or treatment thresholds using race.
Waiting for alternatives
The University of Maryland Medical System last year embarked on a project similar to the AAP initiative but within its own system. The first use of race to be eliminated was in the eGFR. The health system also recently removed the variable from a tool for diagnosing urinary tract infections (UTIs) in children younger than 2 years.
Part of that tool includes deciding to perform a catheterized urine test. If a doctor chose “White” as the race, the tool would recommend the test. If the doctor chose “Black,” the tool would recommend to not test. Joseph Wright, MD, MPH, chief health equity officer at University of Maryland Medical System, said this step in the tool is based on the unproven assumption that young Black children had a lower likelihood of UTIs than their White peers.
“We simply want folks to not by default lob race in as a decisionmaking point when we have, with a little bit more scientific diligence, the ability to include better clinical variables,” Dr. Wright, who is also an adjunct professor of health policy and management at the University of Maryland School of Public Health, College Park, said.
The developers of the UTI tool recently released a revised version that removes race in favor of two new medical datapoints: whether the patient has had a fever for over 48 hours, and whether the patient has previously had a UTI.
The process of re-examining tools, coming up with new datapoints, and implementing changes is not simple, according to Dr. Wright.
“This is just the baby step to fix the algorithms, because we’re all going to have to examine our own house, where these calculators live, whether it’s in a textbook, whether it’s in an electronic health record, and that’s the heavy lift,” he said. “All sources of clinical guidance have to be scrutinized, and it’s going to literally take years to unroot.”
Electronic medical record vendor Cerner said it generally revises its algorithms after medical societies make changes, then communicates those fixes to providers.
Rebecca C. Winokur, MD, MPH, lead physician executive and health equity service line leader at Cerner, explained that if doctors ordered an eGFR a year ago and then another today, the results might be different because of the new code that eliminates race.
“The numbers are so different, how do you know that the patient may or may not have the same function?” Dr. Winokur said.
Dr. Winokur said the company is trying to determine at which point a message should pop up in the records workflow that would inform clinicians that they may be comparing apples to cherries. The company also is reconsidering the use of race in tools that estimate the probability of a successful vaginal birth after prior cesarean delivery, a calculator that predicts the risk of urethral stones in patients with flank pain, and another that measures lung function to help diagnose pulmonary disease.
In addition to managing the logistics of removing race, health institutions also need buy-in from clinicians. At Mass General Brigham, Boston, Thomas Sequist, MD, MPH, chief medical officer, is leading a project to examine how the system uses race in calculators.
“People struggle mainly with, well, if we shouldn’t use this calculator, what should we use, because we need a calculator. And that’s a legitimate question,” Dr. Sequist said in an interview. “If we’re going to stop using this race-based calculator, I still need to know what dose of medication I give my patient. We’re not going to pull any of these calculators until we have a safe and reliable alternative.”
For each calculator, relevant specialty chiefs come to the table with Dr. Sequist and his team; current projects include examining bone density screenings and cardiac risk scores. A large part of the work is communicating the lack of science behind the inclusion of race as a variable.
“It’s hard because these tools have been in existence for decades, and people are used to using them,” Dr. Sequist said. “So this is a big-change management project.”
Some clinicians also have difficulty discerning why their health system may stratify patient outcomes by race while providers are being told that race is being removed from the calculators they use every day. The key difference is that stratifying outcomes by race illuminates systemic problems that can be targeted by a health system.
For instance, if readmission rates are higher for Black patients overall after surgery, the reason might be that nurses are not delivering the same level of care to them as they are to non-Black patients, possibly because of hidden bias. Or, perhaps Black patients at a hospital have less access to transportation for follow-up appointments after surgery. The potential reasons can be investigated, and solutions can be created.
“If you look at a population level, what you’re looking for is not for the evidence of race as a biological construct,” Dr. Chomilo said. “You’re looking for the impact of racism on populations, and that’s the difference: It’s racism, not race.”
A version of this article first appeared on Medscape.com.
Erythematous Pedunculated Plaque on the Dorsal Aspect of the Foot
The Diagnosis: Molluscum Contagiosum
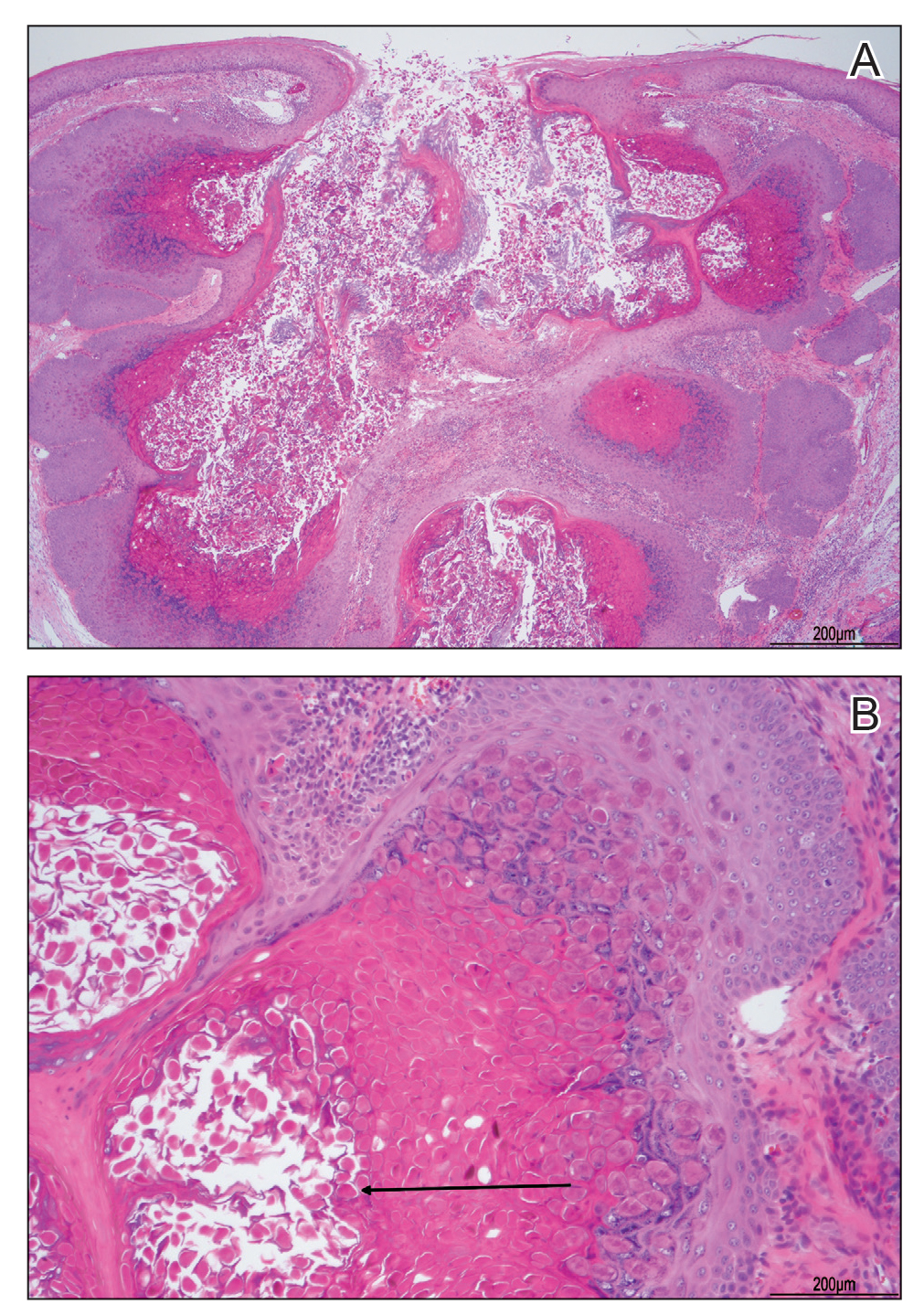
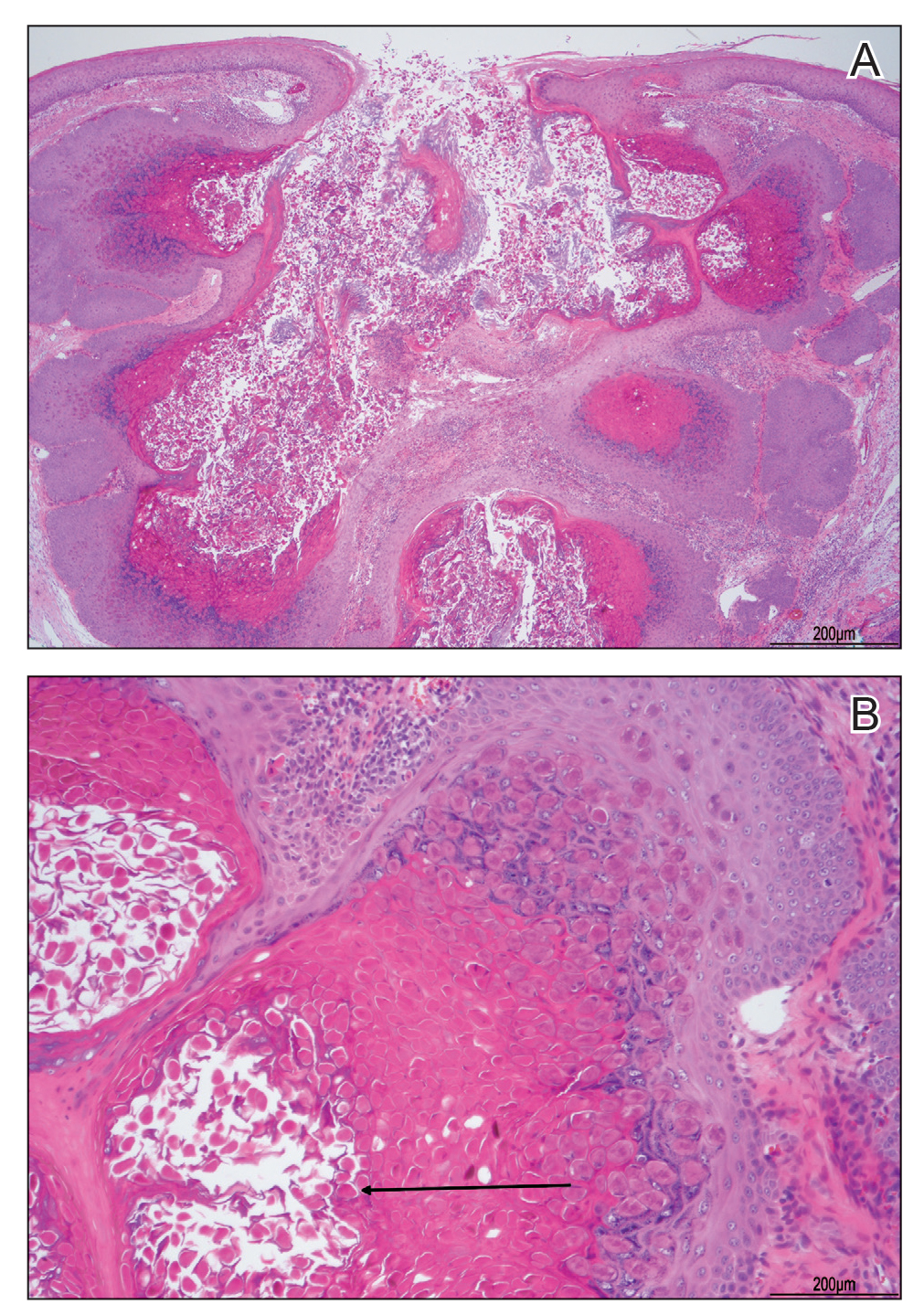
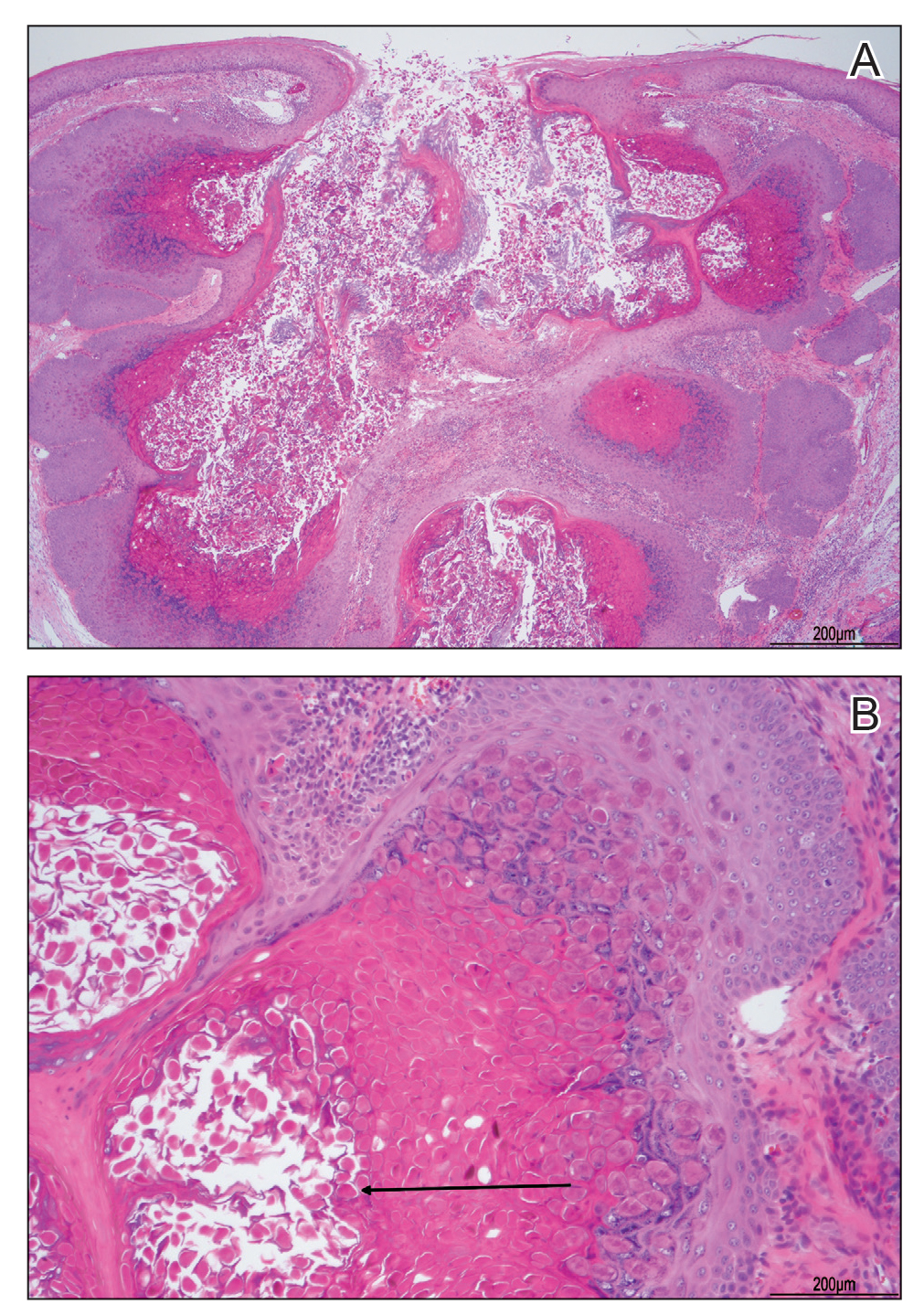
A tangential shave removal with electrocautery was performed. Histopathology demonstrated numerous eosinophilic intracytoplasmic inclusion bodies (Figure), confirming a diagnosis of molluscum contagiosum (MC).
Molluscum contagiosum is a common poxvirus infection that is transmitted through fomites, contact, or self-inoculation.1 This infection most frequently occurs in school-aged children younger than 8 years1-3; peak incidence is 6 years of age.2,3 The worldwide estimated prevalence in children is 5.1% to 11.5%.1,3 In children cohabitating with others infected by MC, approximately 40% of households experienced a spread of infection; the risk of transmission is not associated with greater number of lesions.4 In adults, infection most commonly occurs in the setting of immunodeficiency or as a sexually transmitted infection in immunocompetent patients.3 Molluscum contagiosum infection classically presents as 1- to 3-mm, flesh- or white-colored, dome-shaped, smooth papules with central umbilication.1 Lesions often occur in clusters or lines, indicating local spread. The trunk, extremities, and face are areas that frequently are involved.2,3
Atypical presentations of MC infection can occur, as demonstrated by our case. Involvement of hair follicles by the infection can result in follicular induction.1,5 Secondary infection can mimic abscess formation.1 Inflamed MC lesions demonstrating the “beginning of the end” sign often are mistaken for primary infection, which is thought to be an inflammatory immune response to the virus.6 Lesions located on the eye or eyelid can present as unilateral conjunctivitis, conjunctival or corneal nodules, eyelid abscesses, or chalazions.1 Giant MC is a nodular variant of this infection measuring larger than 1 cm in size that can present similar to epidermoid cysts, condyloma acuminatum, or verruca vulgaris.1,7 Other reported mimicked conditions include basal cell carcinoma, trichoepithelioma, appendageal tumors, keratoacanthoma, foreign body granulomas, nevus sebaceous, or ecthyma.1,3 Molluscum contagiosum also has been reported to present as large ulcerative growths.8 In immunocompromised patients, deep fungal infection is another mimicker.1 Lesions on the plantar surfaces of the feet often are misdiagnosed as plantar verruca and present with pain during ambulation.9
The diagnosis of MC is clinical, with additional diagnostic tools reserved for more challenging situations.1 In cases with atypical presentations, dermoscopy may aid diagnosis through visualization of orifices and vascular patterns including crown, radial, and punctiform vessels.10 Biopsy or fine-needle aspiration also can be utilized as a diagnostic tool. Histopathology often reveals pathognomonic intracytoplasmic inclusions or Henderson-Paterson bodies.8,10 The appearance of MC can mimic other conditions that should be included in the differential diagnosis. Pyogenic granuloma often presents as a benign red papule that may grow rapidly and become pedunculated, sometimes with bleeding and crusting, though histology reveals groups of proliferating capillaries.11 More than half of amelanotic melanomas present in the papulonodular form as vascular or ulcerated nodules, and others may appear as erythematous macules. Diagnosis of amelanotic melanoma is made through histologic examination, which reveals atypical melanocytes in nests or cords, in conjunction with immunohistochemical stains such as S-100.12 Spitz nevi often appear as round, dome-shaped papules that most commonly are red, pink, or fleshcolored. They appear histologically similar to melanoma with nests of atypical melanocytes and nuclear atypia.13
A variety of treatment modalities can be used for MC including cantharidin, curettage, and cryotherapy.14 Imiquimod no longer is recommended due to a lack of demonstrated superiority over placebo in recent studies as well as its adverse effects.3 Topical retinoids have been recommended; however, their use frequently is limited by local irritation.3,14 Cantharidin is the most frequently utilized treatment by pediatric dermatologists. Most health care providers report subjective satisfaction with its results and efficacy, though some side effects may occur including discomfort and temporary changes in pigmentation. Treatment for MC is not required, as the condition is self-limiting.14 Therapy often is reserved for those with extensive disease, complications from lesions, cosmetic or psychological concerns, or genital involvement given the potential for sexual transmission.3 Time to resolution without treatment varies and is more prolonged in immunocompromised patients. Mean time to resolution in immunocompetent hosts has been reported as 13.3 months, but most infections are noted to clear within 2 to 4 years.1,4 Although resolution without treatment occurs, transmission to others and negative impact on quality of life (QOL) can occur and support the need for treatment. Greater impact on QOL was observed in females, those with more lesions, and patients with a longer duration of symptoms. Moderate impact on QOL was reported in 28% of patients (n=301), and severe effects were reported in 11%.4
In conclusion, MC is a common, benign, treatable cutaneous viral infection that often presents as small, flesh-colored papules in children. Its appearance can mimic a variety of other conditions. In cases with abnormal presentations, definitive diagnosis with pathology can be important to differentiate MC from more dangerous etiologies that may require further treatment.
- Brown J, Janniger CK, Schwartz RA, et al. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93-99. doi:10.1111 /j.1365-4632.2006.02737.x
- Dohil MA, Lin P, Lee J, et al. The epidemiology of molluscum contagiosum in children. J Am Acad Dermatol. 2006;54:47-54. doi:10.1016/j.jaad.2005.08.035
- Robinson G, Townsend S, Jahnke MN. Molluscum contagiosum: review and update on clinical presentation, diagnosis, risk, prevention, and treatment. Curr Derm Rep. 2020;9:83-92.
- Olsen JR, Gallacher J, Finlay AY, et al. Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study. Lancet Infect Dis. 2015;15:190-195. doi:10.1016/S1473-3099(14)71053-9
- Davey J, Biswas A. Follicular induction in a case of molluscum contagiosum: possible link with secondary anetoderma-like changes? Am J Dermatopathol. 2014;36:E19-E21. doi:10.1097/DAD.0b013e31828bc7c7
- Butala N, Siegfried E, Weissler A. Molluscum BOTE sign: a predictor of imminent resolution. Pediatrics. 2013;131:E1650-E1653. doi:10.1542/peds.2012-2933
- Uzuncakmak TK, Kuru BC, Zemheri EI, et al. Isolated giant molluscum contagiosum mimicking epidermoid cyst. Dermatol Pract Concept. 2016;6:71-73. doi:10.5826/dpc.0603a15
- Singh S, Swain M, Shukla S, et al. An unusual presentation of giant molluscum contagiosum diagnosed on cytology. Diagn Cytopathol. 2018;46:794-796. doi:10.1002/dc.23964
- Cohen PR, Tschen JA. Plantar molluscum contagiosum: a case report of molluscum contagiosum occurring on the sole of the foot and a review of the world literature. Cutis. 2012;90:35-41.
- Megalla M, Bronsnick T, Noor O, et al. Dermoscopic, confocal microscopic, and histologic characteristics of an atypical presentation of molluscum contagiosum. Ann Clin Pathol. 2014;2:1038.
- Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267-276. doi:10.1111/j.1525-1470.1991.tb00931.x
- Gong H-Z, Zheng H-Y, Li J. Amelanotic melanoma. Melanoma Res. 2019;29:221-230. doi:10.1097/CMR.0000000000000571
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27(6 pt 1):901-913. doi:10.1016/0190-9622(92)70286-o
- Coloe J, Morrell DS. Cantharidin use among pediatric dermatologists in the treatment of molluscum contagiosum. Pediatr Dermatol. 2009;26:405-408.
The Diagnosis: Molluscum Contagiosum
A tangential shave removal with electrocautery was performed. Histopathology demonstrated numerous eosinophilic intracytoplasmic inclusion bodies (Figure), confirming a diagnosis of molluscum contagiosum (MC).
Molluscum contagiosum is a common poxvirus infection that is transmitted through fomites, contact, or self-inoculation.1 This infection most frequently occurs in school-aged children younger than 8 years1-3; peak incidence is 6 years of age.2,3 The worldwide estimated prevalence in children is 5.1% to 11.5%.1,3 In children cohabitating with others infected by MC, approximately 40% of households experienced a spread of infection; the risk of transmission is not associated with greater number of lesions.4 In adults, infection most commonly occurs in the setting of immunodeficiency or as a sexually transmitted infection in immunocompetent patients.3 Molluscum contagiosum infection classically presents as 1- to 3-mm, flesh- or white-colored, dome-shaped, smooth papules with central umbilication.1 Lesions often occur in clusters or lines, indicating local spread. The trunk, extremities, and face are areas that frequently are involved.2,3
Atypical presentations of MC infection can occur, as demonstrated by our case. Involvement of hair follicles by the infection can result in follicular induction.1,5 Secondary infection can mimic abscess formation.1 Inflamed MC lesions demonstrating the “beginning of the end” sign often are mistaken for primary infection, which is thought to be an inflammatory immune response to the virus.6 Lesions located on the eye or eyelid can present as unilateral conjunctivitis, conjunctival or corneal nodules, eyelid abscesses, or chalazions.1 Giant MC is a nodular variant of this infection measuring larger than 1 cm in size that can present similar to epidermoid cysts, condyloma acuminatum, or verruca vulgaris.1,7 Other reported mimicked conditions include basal cell carcinoma, trichoepithelioma, appendageal tumors, keratoacanthoma, foreign body granulomas, nevus sebaceous, or ecthyma.1,3 Molluscum contagiosum also has been reported to present as large ulcerative growths.8 In immunocompromised patients, deep fungal infection is another mimicker.1 Lesions on the plantar surfaces of the feet often are misdiagnosed as plantar verruca and present with pain during ambulation.9
The diagnosis of MC is clinical, with additional diagnostic tools reserved for more challenging situations.1 In cases with atypical presentations, dermoscopy may aid diagnosis through visualization of orifices and vascular patterns including crown, radial, and punctiform vessels.10 Biopsy or fine-needle aspiration also can be utilized as a diagnostic tool. Histopathology often reveals pathognomonic intracytoplasmic inclusions or Henderson-Paterson bodies.8,10 The appearance of MC can mimic other conditions that should be included in the differential diagnosis. Pyogenic granuloma often presents as a benign red papule that may grow rapidly and become pedunculated, sometimes with bleeding and crusting, though histology reveals groups of proliferating capillaries.11 More than half of amelanotic melanomas present in the papulonodular form as vascular or ulcerated nodules, and others may appear as erythematous macules. Diagnosis of amelanotic melanoma is made through histologic examination, which reveals atypical melanocytes in nests or cords, in conjunction with immunohistochemical stains such as S-100.12 Spitz nevi often appear as round, dome-shaped papules that most commonly are red, pink, or fleshcolored. They appear histologically similar to melanoma with nests of atypical melanocytes and nuclear atypia.13
A variety of treatment modalities can be used for MC including cantharidin, curettage, and cryotherapy.14 Imiquimod no longer is recommended due to a lack of demonstrated superiority over placebo in recent studies as well as its adverse effects.3 Topical retinoids have been recommended; however, their use frequently is limited by local irritation.3,14 Cantharidin is the most frequently utilized treatment by pediatric dermatologists. Most health care providers report subjective satisfaction with its results and efficacy, though some side effects may occur including discomfort and temporary changes in pigmentation. Treatment for MC is not required, as the condition is self-limiting.14 Therapy often is reserved for those with extensive disease, complications from lesions, cosmetic or psychological concerns, or genital involvement given the potential for sexual transmission.3 Time to resolution without treatment varies and is more prolonged in immunocompromised patients. Mean time to resolution in immunocompetent hosts has been reported as 13.3 months, but most infections are noted to clear within 2 to 4 years.1,4 Although resolution without treatment occurs, transmission to others and negative impact on quality of life (QOL) can occur and support the need for treatment. Greater impact on QOL was observed in females, those with more lesions, and patients with a longer duration of symptoms. Moderate impact on QOL was reported in 28% of patients (n=301), and severe effects were reported in 11%.4
In conclusion, MC is a common, benign, treatable cutaneous viral infection that often presents as small, flesh-colored papules in children. Its appearance can mimic a variety of other conditions. In cases with abnormal presentations, definitive diagnosis with pathology can be important to differentiate MC from more dangerous etiologies that may require further treatment.
The Diagnosis: Molluscum Contagiosum
A tangential shave removal with electrocautery was performed. Histopathology demonstrated numerous eosinophilic intracytoplasmic inclusion bodies (Figure), confirming a diagnosis of molluscum contagiosum (MC).
Molluscum contagiosum is a common poxvirus infection that is transmitted through fomites, contact, or self-inoculation.1 This infection most frequently occurs in school-aged children younger than 8 years1-3; peak incidence is 6 years of age.2,3 The worldwide estimated prevalence in children is 5.1% to 11.5%.1,3 In children cohabitating with others infected by MC, approximately 40% of households experienced a spread of infection; the risk of transmission is not associated with greater number of lesions.4 In adults, infection most commonly occurs in the setting of immunodeficiency or as a sexually transmitted infection in immunocompetent patients.3 Molluscum contagiosum infection classically presents as 1- to 3-mm, flesh- or white-colored, dome-shaped, smooth papules with central umbilication.1 Lesions often occur in clusters or lines, indicating local spread. The trunk, extremities, and face are areas that frequently are involved.2,3
Atypical presentations of MC infection can occur, as demonstrated by our case. Involvement of hair follicles by the infection can result in follicular induction.1,5 Secondary infection can mimic abscess formation.1 Inflamed MC lesions demonstrating the “beginning of the end” sign often are mistaken for primary infection, which is thought to be an inflammatory immune response to the virus.6 Lesions located on the eye or eyelid can present as unilateral conjunctivitis, conjunctival or corneal nodules, eyelid abscesses, or chalazions.1 Giant MC is a nodular variant of this infection measuring larger than 1 cm in size that can present similar to epidermoid cysts, condyloma acuminatum, or verruca vulgaris.1,7 Other reported mimicked conditions include basal cell carcinoma, trichoepithelioma, appendageal tumors, keratoacanthoma, foreign body granulomas, nevus sebaceous, or ecthyma.1,3 Molluscum contagiosum also has been reported to present as large ulcerative growths.8 In immunocompromised patients, deep fungal infection is another mimicker.1 Lesions on the plantar surfaces of the feet often are misdiagnosed as plantar verruca and present with pain during ambulation.9
The diagnosis of MC is clinical, with additional diagnostic tools reserved for more challenging situations.1 In cases with atypical presentations, dermoscopy may aid diagnosis through visualization of orifices and vascular patterns including crown, radial, and punctiform vessels.10 Biopsy or fine-needle aspiration also can be utilized as a diagnostic tool. Histopathology often reveals pathognomonic intracytoplasmic inclusions or Henderson-Paterson bodies.8,10 The appearance of MC can mimic other conditions that should be included in the differential diagnosis. Pyogenic granuloma often presents as a benign red papule that may grow rapidly and become pedunculated, sometimes with bleeding and crusting, though histology reveals groups of proliferating capillaries.11 More than half of amelanotic melanomas present in the papulonodular form as vascular or ulcerated nodules, and others may appear as erythematous macules. Diagnosis of amelanotic melanoma is made through histologic examination, which reveals atypical melanocytes in nests or cords, in conjunction with immunohistochemical stains such as S-100.12 Spitz nevi often appear as round, dome-shaped papules that most commonly are red, pink, or fleshcolored. They appear histologically similar to melanoma with nests of atypical melanocytes and nuclear atypia.13
A variety of treatment modalities can be used for MC including cantharidin, curettage, and cryotherapy.14 Imiquimod no longer is recommended due to a lack of demonstrated superiority over placebo in recent studies as well as its adverse effects.3 Topical retinoids have been recommended; however, their use frequently is limited by local irritation.3,14 Cantharidin is the most frequently utilized treatment by pediatric dermatologists. Most health care providers report subjective satisfaction with its results and efficacy, though some side effects may occur including discomfort and temporary changes in pigmentation. Treatment for MC is not required, as the condition is self-limiting.14 Therapy often is reserved for those with extensive disease, complications from lesions, cosmetic or psychological concerns, or genital involvement given the potential for sexual transmission.3 Time to resolution without treatment varies and is more prolonged in immunocompromised patients. Mean time to resolution in immunocompetent hosts has been reported as 13.3 months, but most infections are noted to clear within 2 to 4 years.1,4 Although resolution without treatment occurs, transmission to others and negative impact on quality of life (QOL) can occur and support the need for treatment. Greater impact on QOL was observed in females, those with more lesions, and patients with a longer duration of symptoms. Moderate impact on QOL was reported in 28% of patients (n=301), and severe effects were reported in 11%.4
In conclusion, MC is a common, benign, treatable cutaneous viral infection that often presents as small, flesh-colored papules in children. Its appearance can mimic a variety of other conditions. In cases with abnormal presentations, definitive diagnosis with pathology can be important to differentiate MC from more dangerous etiologies that may require further treatment.
- Brown J, Janniger CK, Schwartz RA, et al. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93-99. doi:10.1111 /j.1365-4632.2006.02737.x
- Dohil MA, Lin P, Lee J, et al. The epidemiology of molluscum contagiosum in children. J Am Acad Dermatol. 2006;54:47-54. doi:10.1016/j.jaad.2005.08.035
- Robinson G, Townsend S, Jahnke MN. Molluscum contagiosum: review and update on clinical presentation, diagnosis, risk, prevention, and treatment. Curr Derm Rep. 2020;9:83-92.
- Olsen JR, Gallacher J, Finlay AY, et al. Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study. Lancet Infect Dis. 2015;15:190-195. doi:10.1016/S1473-3099(14)71053-9
- Davey J, Biswas A. Follicular induction in a case of molluscum contagiosum: possible link with secondary anetoderma-like changes? Am J Dermatopathol. 2014;36:E19-E21. doi:10.1097/DAD.0b013e31828bc7c7
- Butala N, Siegfried E, Weissler A. Molluscum BOTE sign: a predictor of imminent resolution. Pediatrics. 2013;131:E1650-E1653. doi:10.1542/peds.2012-2933
- Uzuncakmak TK, Kuru BC, Zemheri EI, et al. Isolated giant molluscum contagiosum mimicking epidermoid cyst. Dermatol Pract Concept. 2016;6:71-73. doi:10.5826/dpc.0603a15
- Singh S, Swain M, Shukla S, et al. An unusual presentation of giant molluscum contagiosum diagnosed on cytology. Diagn Cytopathol. 2018;46:794-796. doi:10.1002/dc.23964
- Cohen PR, Tschen JA. Plantar molluscum contagiosum: a case report of molluscum contagiosum occurring on the sole of the foot and a review of the world literature. Cutis. 2012;90:35-41.
- Megalla M, Bronsnick T, Noor O, et al. Dermoscopic, confocal microscopic, and histologic characteristics of an atypical presentation of molluscum contagiosum. Ann Clin Pathol. 2014;2:1038.
- Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267-276. doi:10.1111/j.1525-1470.1991.tb00931.x
- Gong H-Z, Zheng H-Y, Li J. Amelanotic melanoma. Melanoma Res. 2019;29:221-230. doi:10.1097/CMR.0000000000000571
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27(6 pt 1):901-913. doi:10.1016/0190-9622(92)70286-o
- Coloe J, Morrell DS. Cantharidin use among pediatric dermatologists in the treatment of molluscum contagiosum. Pediatr Dermatol. 2009;26:405-408.
- Brown J, Janniger CK, Schwartz RA, et al. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93-99. doi:10.1111 /j.1365-4632.2006.02737.x
- Dohil MA, Lin P, Lee J, et al. The epidemiology of molluscum contagiosum in children. J Am Acad Dermatol. 2006;54:47-54. doi:10.1016/j.jaad.2005.08.035
- Robinson G, Townsend S, Jahnke MN. Molluscum contagiosum: review and update on clinical presentation, diagnosis, risk, prevention, and treatment. Curr Derm Rep. 2020;9:83-92.
- Olsen JR, Gallacher J, Finlay AY, et al. Time to resolution and effect on quality of life of molluscum contagiosum in children in the UK: a prospective community cohort study. Lancet Infect Dis. 2015;15:190-195. doi:10.1016/S1473-3099(14)71053-9
- Davey J, Biswas A. Follicular induction in a case of molluscum contagiosum: possible link with secondary anetoderma-like changes? Am J Dermatopathol. 2014;36:E19-E21. doi:10.1097/DAD.0b013e31828bc7c7
- Butala N, Siegfried E, Weissler A. Molluscum BOTE sign: a predictor of imminent resolution. Pediatrics. 2013;131:E1650-E1653. doi:10.1542/peds.2012-2933
- Uzuncakmak TK, Kuru BC, Zemheri EI, et al. Isolated giant molluscum contagiosum mimicking epidermoid cyst. Dermatol Pract Concept. 2016;6:71-73. doi:10.5826/dpc.0603a15
- Singh S, Swain M, Shukla S, et al. An unusual presentation of giant molluscum contagiosum diagnosed on cytology. Diagn Cytopathol. 2018;46:794-796. doi:10.1002/dc.23964
- Cohen PR, Tschen JA. Plantar molluscum contagiosum: a case report of molluscum contagiosum occurring on the sole of the foot and a review of the world literature. Cutis. 2012;90:35-41.
- Megalla M, Bronsnick T, Noor O, et al. Dermoscopic, confocal microscopic, and histologic characteristics of an atypical presentation of molluscum contagiosum. Ann Clin Pathol. 2014;2:1038.
- Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267-276. doi:10.1111/j.1525-1470.1991.tb00931.x
- Gong H-Z, Zheng H-Y, Li J. Amelanotic melanoma. Melanoma Res. 2019;29:221-230. doi:10.1097/CMR.0000000000000571
- Casso EM, Grin-Jorgensen CM, Grant-Kels JM. Spitz nevi. J Am Acad Dermatol. 1992;27(6 pt 1):901-913. doi:10.1016/0190-9622(92)70286-o
- Coloe J, Morrell DS. Cantharidin use among pediatric dermatologists in the treatment of molluscum contagiosum. Pediatr Dermatol. 2009;26:405-408.
A 13-year-old adolescent girl presented for evaluation of a lesion on the dorsal aspect of the right foot of 1 week’s duration. She had a history of acne vulgaris and seasonal allergic rhinitis. She previously had noticed a persistent, small, flesh-colored bump of unknown chronicity in the same location, which had been diagnosed as a skin tag at an outside clinic. She denied any prior treatment in this area. Approximately a week prior to presentation, the lesion became painful, larger, and darkened in color before draining yellowish fluid. Due to concern for superinfection, the patient was prescribed cephalexin by her pediatrician. Dermatologic examination revealed a 1-cm, violaceous, pedunculated plaque with hemorrhagic crust on the dorsal aspect of the right foot with surrounding erythema and tenderness.

Heart attack care not equal for women and people of color
Radiating chest pain, shortness of breath, nausea, lightheadedness. Everyone knows the telltale signs of a myocardial infarction. Yet a new study shows that despite this widespread recognition, heart attacks aren’t attended to quickly across the board. Historically, the study says, women and people of color wait longer to access emergency care for a heart attack.
Researchers from the University of California, San Francisco published these findings in the Annals of Emergency Medicine. The study used the Office of Statewide Health Planning and Development dataset to gather information on 453,136 cases of heart attack in California between 2005 and 2015. They found that over time, differences in timely treatment between the demographics narrowed, but the gap still existed.
The study defined timely treatment as receiving care for a heart attack within 3 days of admission to a hospital. Women and people of color were found to wait 3 days or more to receive care than their White male counterparts. A disparity of this sort can cause ripples of health effects across society, ripples that doctors should be aware of, says lead author Juan Carlos Montoy, MD. Dr. Montoy was “sadly surprised by our findings that disparities for women and for Black patients only decreased slightly or not at all over time.”
In the study, the team separated the dataset between the two primary types of heart attack: ST-segment elevation myocardial infarction (STEMI), caused by blood vessel blockage, and non–ST-segment elevation myocardial infarction (NSTEMI), caused by a narrowing or temporary blockage of the artery.
Regardless of the type of heart attack, the standard first step in treatment is a coronary angiogram. After finding out where blood flow is disrupted using the angiogram, a physician can proceed with treatment.
But when looking back, the team found that it took a while for many patients to receive this first step in treatment. In 2005, 50% of men and 35.7% of women with STEMI and 45% of men and 33.1% of women with NSTEMI had a timely angiography. In the same year, 46% of White patients and 31.2% of Black patients with STEMI underwent timely angiography.
By 2015, timely treatment increased across the board, but there were still discrepancies, with 76.7% of men and 66.8% of women with STEMI undergoing timely angiography and 56.3% of men and 45.9% of women with NSTEMI undergoing timely angiography. Also in 2015, 75.2% of White patients and 69.2% of Black patients underwent timely angiography for STEMI.
Although differences in care decreased between the demographics, the gap still exists. Whereas this dataset only extends to 2015, this trend may still persist today, says Robert Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, who was not involved in the study. Therefore, physicians need to consider this bias when treating patients. “The bottom line is that we continue to have much work to do to achieve equality in managing not only medical conditions but treating people who have them equally,” Dr. Glatter said.
“Raising awareness of ongoing inequality in care related to gender and ethnic disparities is critical to drive change in our institutions,” he emphasized. “We simply cannot accept the status quo.”
The study was funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Glatter and the authors declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Radiating chest pain, shortness of breath, nausea, lightheadedness. Everyone knows the telltale signs of a myocardial infarction. Yet a new study shows that despite this widespread recognition, heart attacks aren’t attended to quickly across the board. Historically, the study says, women and people of color wait longer to access emergency care for a heart attack.
Researchers from the University of California, San Francisco published these findings in the Annals of Emergency Medicine. The study used the Office of Statewide Health Planning and Development dataset to gather information on 453,136 cases of heart attack in California between 2005 and 2015. They found that over time, differences in timely treatment between the demographics narrowed, but the gap still existed.
The study defined timely treatment as receiving care for a heart attack within 3 days of admission to a hospital. Women and people of color were found to wait 3 days or more to receive care than their White male counterparts. A disparity of this sort can cause ripples of health effects across society, ripples that doctors should be aware of, says lead author Juan Carlos Montoy, MD. Dr. Montoy was “sadly surprised by our findings that disparities for women and for Black patients only decreased slightly or not at all over time.”
In the study, the team separated the dataset between the two primary types of heart attack: ST-segment elevation myocardial infarction (STEMI), caused by blood vessel blockage, and non–ST-segment elevation myocardial infarction (NSTEMI), caused by a narrowing or temporary blockage of the artery.
Regardless of the type of heart attack, the standard first step in treatment is a coronary angiogram. After finding out where blood flow is disrupted using the angiogram, a physician can proceed with treatment.
But when looking back, the team found that it took a while for many patients to receive this first step in treatment. In 2005, 50% of men and 35.7% of women with STEMI and 45% of men and 33.1% of women with NSTEMI had a timely angiography. In the same year, 46% of White patients and 31.2% of Black patients with STEMI underwent timely angiography.
By 2015, timely treatment increased across the board, but there were still discrepancies, with 76.7% of men and 66.8% of women with STEMI undergoing timely angiography and 56.3% of men and 45.9% of women with NSTEMI undergoing timely angiography. Also in 2015, 75.2% of White patients and 69.2% of Black patients underwent timely angiography for STEMI.
Although differences in care decreased between the demographics, the gap still exists. Whereas this dataset only extends to 2015, this trend may still persist today, says Robert Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, who was not involved in the study. Therefore, physicians need to consider this bias when treating patients. “The bottom line is that we continue to have much work to do to achieve equality in managing not only medical conditions but treating people who have them equally,” Dr. Glatter said.
“Raising awareness of ongoing inequality in care related to gender and ethnic disparities is critical to drive change in our institutions,” he emphasized. “We simply cannot accept the status quo.”
The study was funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Glatter and the authors declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Radiating chest pain, shortness of breath, nausea, lightheadedness. Everyone knows the telltale signs of a myocardial infarction. Yet a new study shows that despite this widespread recognition, heart attacks aren’t attended to quickly across the board. Historically, the study says, women and people of color wait longer to access emergency care for a heart attack.
Researchers from the University of California, San Francisco published these findings in the Annals of Emergency Medicine. The study used the Office of Statewide Health Planning and Development dataset to gather information on 453,136 cases of heart attack in California between 2005 and 2015. They found that over time, differences in timely treatment between the demographics narrowed, but the gap still existed.
The study defined timely treatment as receiving care for a heart attack within 3 days of admission to a hospital. Women and people of color were found to wait 3 days or more to receive care than their White male counterparts. A disparity of this sort can cause ripples of health effects across society, ripples that doctors should be aware of, says lead author Juan Carlos Montoy, MD. Dr. Montoy was “sadly surprised by our findings that disparities for women and for Black patients only decreased slightly or not at all over time.”
In the study, the team separated the dataset between the two primary types of heart attack: ST-segment elevation myocardial infarction (STEMI), caused by blood vessel blockage, and non–ST-segment elevation myocardial infarction (NSTEMI), caused by a narrowing or temporary blockage of the artery.
Regardless of the type of heart attack, the standard first step in treatment is a coronary angiogram. After finding out where blood flow is disrupted using the angiogram, a physician can proceed with treatment.
But when looking back, the team found that it took a while for many patients to receive this first step in treatment. In 2005, 50% of men and 35.7% of women with STEMI and 45% of men and 33.1% of women with NSTEMI had a timely angiography. In the same year, 46% of White patients and 31.2% of Black patients with STEMI underwent timely angiography.
By 2015, timely treatment increased across the board, but there were still discrepancies, with 76.7% of men and 66.8% of women with STEMI undergoing timely angiography and 56.3% of men and 45.9% of women with NSTEMI undergoing timely angiography. Also in 2015, 75.2% of White patients and 69.2% of Black patients underwent timely angiography for STEMI.
Although differences in care decreased between the demographics, the gap still exists. Whereas this dataset only extends to 2015, this trend may still persist today, says Robert Glatter, MD, an emergency medicine physician at Lenox Hill Hospital, New York, who was not involved in the study. Therefore, physicians need to consider this bias when treating patients. “The bottom line is that we continue to have much work to do to achieve equality in managing not only medical conditions but treating people who have them equally,” Dr. Glatter said.
“Raising awareness of ongoing inequality in care related to gender and ethnic disparities is critical to drive change in our institutions,” he emphasized. “We simply cannot accept the status quo.”
The study was funded by the National Heart, Lung, and Blood Institute of the National Institutes of Health. Dr. Glatter and the authors declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF EMERGENCY MEDICINE
Two genetic intestinal diseases linked
Two genes that have been linked separately to rare intestinal diseases appear to share a functional relationship. The genes have independently been linked to osteo-oto-hepato-enteric (O2HE) syndrome and microvillus inclusion disease (MVID), which are characterized by congenital diarrhea and, in some patients, intrahepatic cholestasis.
It appears that one gene, UNC45A, is directly responsible for the proper function of the protein encoded by the other gene, called MYO5B, according to investigators, who published their findings in Cellular and Molecular Gastroenterology and Hepatology. UNC45A is a chaperone protein that helps proteins fold properly. It has been linked to O2HE patients experiencing congenital diarrhea and intrahepatic cholestasis. The mutation has been identified in four patients from three different families with O2HE, which can also present with sensorineural hearing loss and bone fragility. Cellular analyses have shown that the mutation leads to reduction in protein expression by 70%-90%.
Intestinal symptoms similar to those in O2HE have also been described in diseases caused by mutations in genes that encode the myosin motor proteins that are involved in cellular protein trafficking. This group of disorders includes MVID. The researchers hypothesized that the UNC45A mutation in O2HE might lead to similar symptoms as MVID and others through the altered protein’s failure to assist in the folding of myosin proteins, although to date only the myosin IIa protein has been shown to be a target of UNC45A.
To investigate the possibility, they examined in more detail the relationship between UNC45A and intestinal symptoms. There are various known mutations in myosin proteins. Some have been linked to deafness, but these do not appear to contribute to intestinal symptoms since patients with myelin-related inherited deafness don’t typically have diarrhea. Bone fragility, also sometimes caused by myosin mutations, also appears to be unrelated to intestinal symptoms.
Previous experiments in yeast suggest that the related gene UNC45 may serve as a chaperone for type V myosin: Loss of a yeast version of UNC45 caused a type V myosin called MYO4P to be mislocalized in yeast. In zebrafish, reduction in intestinal levels of the UNC45A gene or the fish’s version of MYO5B interfered with development of intestinal folds.
The researchers used CRISPR-Cas9 gene editing and site-directed mutagenesis in intestinal epithelial and liver cell lines to investigate the relationships between UNC45A and MYO5B mutants. UNC45A depletion or introduction of the UNC45A mutation found in patients led to lower MYO5B expression. Within epithelial cells, loss of UNC45A led to changes in MYO5B–linked processes that are known to play a role in MVID pathogenesis. These included alteration of microvilli development and interference with the location of rat sarcoma–associated binding protein (RAB) 11A–positive recycling endosomes. When normal UNC45A was reintroduced to these cells, MYO5B expression returned. Reintroduction of either UNC45A or MYO5B repaired the alterations to recycling endosome position and microvilli development.
Loss of UNC45A did not appear to affect transcription of the MYO5B gen, which suggests a suggesting a functional interaction between the two at a protein level.
UNC45A has been shown to destabilize microtubules. Exposure of a kidney epithelial cell line to the microtubule-stabilizing drug taxol also led to displacement of RAB11A-positve recycling endosomes, though the specific changes were different than what is seen in MYO5B mutants. The researchers were unable to validate the findings in tissue derived from O2HE patients because of insufficient material, but they maintain that the cell lines used have proven to be highly predictive for the cellular characteristics of MVID.
Overall, the study suggests that reductions in MYO5B and subsequent changes to the cellular processes that depend on it may underlie the intestinal symptoms in O2HE.
The researchers noted that O2HE patients have different phenotypes. Of the four patients they studied, three had severe chronic diarrhea and required parenteral nutrition. One patient later had the diarrhea resolve and her sister did not have diarrhea at all. This heterogeneity in severity and duration of clinical symptoms may be driven by differences in the molecular effects of patient-specific mutations. The two siblings had mutations in a different region of the UNC45A gene than the other two participants.
“Taken together, this study revealed a functional relationship between UNC45A and MYO5B protein expression, thereby connecting two rare congenital diseases with overlapping intestinal symptoms at the molecular level,” the authors wrote.
The authors reported that they had no conflicts of interest.
This article was updated 7/13/22.
Congenital diarrheas and enteropathies (CoDEs) are rare monogenic disorders caused by genes important for intestinal epithelial function. The increasing availability of exome sequencing in clinical practice has accelerated the discovery of new genes associated with these disorders over the past few years. Several CoDE disorders revolve around defects in trafficking of vesicles in epithelial cells. One of these is microvillus inclusion disease which is caused by loss-of-function variants in the gene MYO5B, which encodes an important epithelial motor protein. This study by Li and colleagues reveals that a recently discovered novel CoDE gene and protein, UNC45A, is functionally linked to MYO5B and that loss of UNC45A in cells causes a very similar cellular phenotype to MYO5B-deficient cells.
Jay Thiagarajah, MD, PhD, attending in the division of gastroenterology, hepatology and nutrition and codirector of the congenital enteropathy program at Boston Children’s Hospital, as well as assistant professor in pediatrics at Harvard Medical School, also in Boston. Dr. Thiagarajah stated he had no relevant conflicts to disclose.
Congenital diarrheas and enteropathies (CoDEs) are rare monogenic disorders caused by genes important for intestinal epithelial function. The increasing availability of exome sequencing in clinical practice has accelerated the discovery of new genes associated with these disorders over the past few years. Several CoDE disorders revolve around defects in trafficking of vesicles in epithelial cells. One of these is microvillus inclusion disease which is caused by loss-of-function variants in the gene MYO5B, which encodes an important epithelial motor protein. This study by Li and colleagues reveals that a recently discovered novel CoDE gene and protein, UNC45A, is functionally linked to MYO5B and that loss of UNC45A in cells causes a very similar cellular phenotype to MYO5B-deficient cells.
Jay Thiagarajah, MD, PhD, attending in the division of gastroenterology, hepatology and nutrition and codirector of the congenital enteropathy program at Boston Children’s Hospital, as well as assistant professor in pediatrics at Harvard Medical School, also in Boston. Dr. Thiagarajah stated he had no relevant conflicts to disclose.
Congenital diarrheas and enteropathies (CoDEs) are rare monogenic disorders caused by genes important for intestinal epithelial function. The increasing availability of exome sequencing in clinical practice has accelerated the discovery of new genes associated with these disorders over the past few years. Several CoDE disorders revolve around defects in trafficking of vesicles in epithelial cells. One of these is microvillus inclusion disease which is caused by loss-of-function variants in the gene MYO5B, which encodes an important epithelial motor protein. This study by Li and colleagues reveals that a recently discovered novel CoDE gene and protein, UNC45A, is functionally linked to MYO5B and that loss of UNC45A in cells causes a very similar cellular phenotype to MYO5B-deficient cells.
Jay Thiagarajah, MD, PhD, attending in the division of gastroenterology, hepatology and nutrition and codirector of the congenital enteropathy program at Boston Children’s Hospital, as well as assistant professor in pediatrics at Harvard Medical School, also in Boston. Dr. Thiagarajah stated he had no relevant conflicts to disclose.
Two genes that have been linked separately to rare intestinal diseases appear to share a functional relationship. The genes have independently been linked to osteo-oto-hepato-enteric (O2HE) syndrome and microvillus inclusion disease (MVID), which are characterized by congenital diarrhea and, in some patients, intrahepatic cholestasis.
It appears that one gene, UNC45A, is directly responsible for the proper function of the protein encoded by the other gene, called MYO5B, according to investigators, who published their findings in Cellular and Molecular Gastroenterology and Hepatology. UNC45A is a chaperone protein that helps proteins fold properly. It has been linked to O2HE patients experiencing congenital diarrhea and intrahepatic cholestasis. The mutation has been identified in four patients from three different families with O2HE, which can also present with sensorineural hearing loss and bone fragility. Cellular analyses have shown that the mutation leads to reduction in protein expression by 70%-90%.
Intestinal symptoms similar to those in O2HE have also been described in diseases caused by mutations in genes that encode the myosin motor proteins that are involved in cellular protein trafficking. This group of disorders includes MVID. The researchers hypothesized that the UNC45A mutation in O2HE might lead to similar symptoms as MVID and others through the altered protein’s failure to assist in the folding of myosin proteins, although to date only the myosin IIa protein has been shown to be a target of UNC45A.
To investigate the possibility, they examined in more detail the relationship between UNC45A and intestinal symptoms. There are various known mutations in myosin proteins. Some have been linked to deafness, but these do not appear to contribute to intestinal symptoms since patients with myelin-related inherited deafness don’t typically have diarrhea. Bone fragility, also sometimes caused by myosin mutations, also appears to be unrelated to intestinal symptoms.
Previous experiments in yeast suggest that the related gene UNC45 may serve as a chaperone for type V myosin: Loss of a yeast version of UNC45 caused a type V myosin called MYO4P to be mislocalized in yeast. In zebrafish, reduction in intestinal levels of the UNC45A gene or the fish’s version of MYO5B interfered with development of intestinal folds.
The researchers used CRISPR-Cas9 gene editing and site-directed mutagenesis in intestinal epithelial and liver cell lines to investigate the relationships between UNC45A and MYO5B mutants. UNC45A depletion or introduction of the UNC45A mutation found in patients led to lower MYO5B expression. Within epithelial cells, loss of UNC45A led to changes in MYO5B–linked processes that are known to play a role in MVID pathogenesis. These included alteration of microvilli development and interference with the location of rat sarcoma–associated binding protein (RAB) 11A–positive recycling endosomes. When normal UNC45A was reintroduced to these cells, MYO5B expression returned. Reintroduction of either UNC45A or MYO5B repaired the alterations to recycling endosome position and microvilli development.
Loss of UNC45A did not appear to affect transcription of the MYO5B gen, which suggests a suggesting a functional interaction between the two at a protein level.
UNC45A has been shown to destabilize microtubules. Exposure of a kidney epithelial cell line to the microtubule-stabilizing drug taxol also led to displacement of RAB11A-positve recycling endosomes, though the specific changes were different than what is seen in MYO5B mutants. The researchers were unable to validate the findings in tissue derived from O2HE patients because of insufficient material, but they maintain that the cell lines used have proven to be highly predictive for the cellular characteristics of MVID.
Overall, the study suggests that reductions in MYO5B and subsequent changes to the cellular processes that depend on it may underlie the intestinal symptoms in O2HE.
The researchers noted that O2HE patients have different phenotypes. Of the four patients they studied, three had severe chronic diarrhea and required parenteral nutrition. One patient later had the diarrhea resolve and her sister did not have diarrhea at all. This heterogeneity in severity and duration of clinical symptoms may be driven by differences in the molecular effects of patient-specific mutations. The two siblings had mutations in a different region of the UNC45A gene than the other two participants.
“Taken together, this study revealed a functional relationship between UNC45A and MYO5B protein expression, thereby connecting two rare congenital diseases with overlapping intestinal symptoms at the molecular level,” the authors wrote.
The authors reported that they had no conflicts of interest.
This article was updated 7/13/22.
Two genes that have been linked separately to rare intestinal diseases appear to share a functional relationship. The genes have independently been linked to osteo-oto-hepato-enteric (O2HE) syndrome and microvillus inclusion disease (MVID), which are characterized by congenital diarrhea and, in some patients, intrahepatic cholestasis.
It appears that one gene, UNC45A, is directly responsible for the proper function of the protein encoded by the other gene, called MYO5B, according to investigators, who published their findings in Cellular and Molecular Gastroenterology and Hepatology. UNC45A is a chaperone protein that helps proteins fold properly. It has been linked to O2HE patients experiencing congenital diarrhea and intrahepatic cholestasis. The mutation has been identified in four patients from three different families with O2HE, which can also present with sensorineural hearing loss and bone fragility. Cellular analyses have shown that the mutation leads to reduction in protein expression by 70%-90%.
Intestinal symptoms similar to those in O2HE have also been described in diseases caused by mutations in genes that encode the myosin motor proteins that are involved in cellular protein trafficking. This group of disorders includes MVID. The researchers hypothesized that the UNC45A mutation in O2HE might lead to similar symptoms as MVID and others through the altered protein’s failure to assist in the folding of myosin proteins, although to date only the myosin IIa protein has been shown to be a target of UNC45A.
To investigate the possibility, they examined in more detail the relationship between UNC45A and intestinal symptoms. There are various known mutations in myosin proteins. Some have been linked to deafness, but these do not appear to contribute to intestinal symptoms since patients with myelin-related inherited deafness don’t typically have diarrhea. Bone fragility, also sometimes caused by myosin mutations, also appears to be unrelated to intestinal symptoms.
Previous experiments in yeast suggest that the related gene UNC45 may serve as a chaperone for type V myosin: Loss of a yeast version of UNC45 caused a type V myosin called MYO4P to be mislocalized in yeast. In zebrafish, reduction in intestinal levels of the UNC45A gene or the fish’s version of MYO5B interfered with development of intestinal folds.
The researchers used CRISPR-Cas9 gene editing and site-directed mutagenesis in intestinal epithelial and liver cell lines to investigate the relationships between UNC45A and MYO5B mutants. UNC45A depletion or introduction of the UNC45A mutation found in patients led to lower MYO5B expression. Within epithelial cells, loss of UNC45A led to changes in MYO5B–linked processes that are known to play a role in MVID pathogenesis. These included alteration of microvilli development and interference with the location of rat sarcoma–associated binding protein (RAB) 11A–positive recycling endosomes. When normal UNC45A was reintroduced to these cells, MYO5B expression returned. Reintroduction of either UNC45A or MYO5B repaired the alterations to recycling endosome position and microvilli development.
Loss of UNC45A did not appear to affect transcription of the MYO5B gen, which suggests a suggesting a functional interaction between the two at a protein level.
UNC45A has been shown to destabilize microtubules. Exposure of a kidney epithelial cell line to the microtubule-stabilizing drug taxol also led to displacement of RAB11A-positve recycling endosomes, though the specific changes were different than what is seen in MYO5B mutants. The researchers were unable to validate the findings in tissue derived from O2HE patients because of insufficient material, but they maintain that the cell lines used have proven to be highly predictive for the cellular characteristics of MVID.
Overall, the study suggests that reductions in MYO5B and subsequent changes to the cellular processes that depend on it may underlie the intestinal symptoms in O2HE.
The researchers noted that O2HE patients have different phenotypes. Of the four patients they studied, three had severe chronic diarrhea and required parenteral nutrition. One patient later had the diarrhea resolve and her sister did not have diarrhea at all. This heterogeneity in severity and duration of clinical symptoms may be driven by differences in the molecular effects of patient-specific mutations. The two siblings had mutations in a different region of the UNC45A gene than the other two participants.
“Taken together, this study revealed a functional relationship between UNC45A and MYO5B protein expression, thereby connecting two rare congenital diseases with overlapping intestinal symptoms at the molecular level,” the authors wrote.
The authors reported that they had no conflicts of interest.
This article was updated 7/13/22.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
The mother’s double jeopardy
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at [email protected].
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
Pediatricians’ incomes rose faster than most specialties in 2021: Survey
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”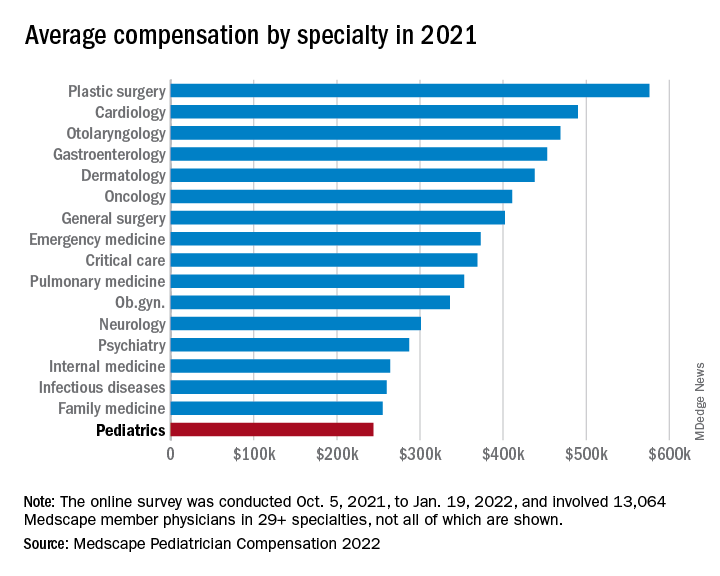
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
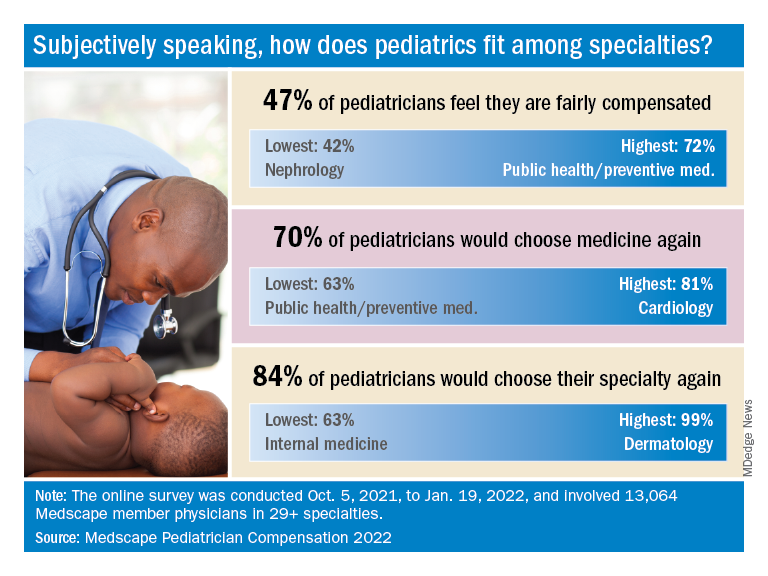
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”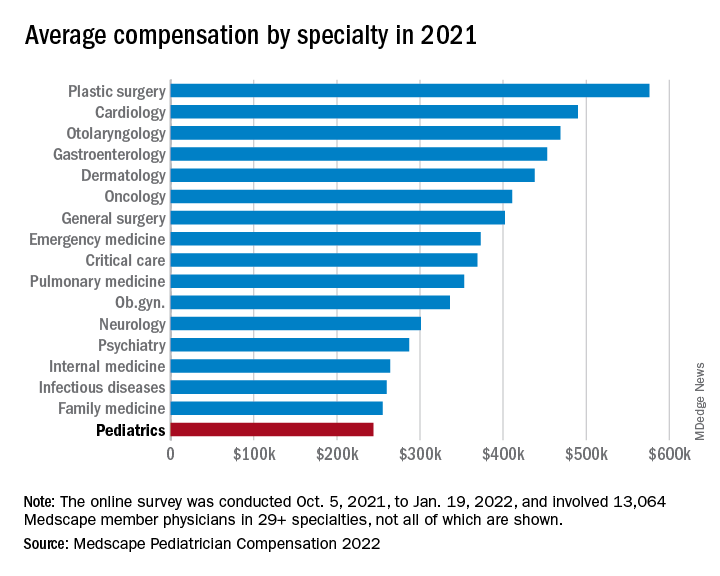
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
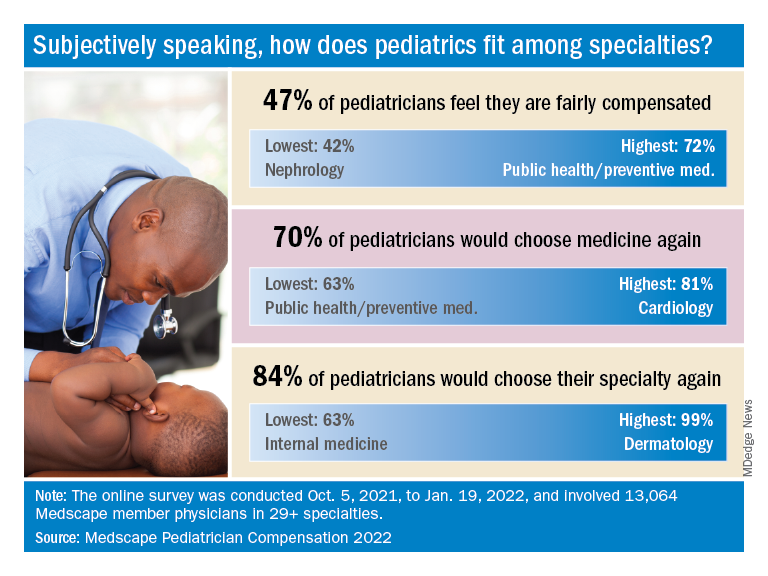
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
In an unprecedented year when income increased for all specialties, pediatricians did better than most, according to a recent survey by Medscape.
. Medscape also noted that, for the first time in the 11 years it’s been conducting these physician compensation surveys, “all specialties have seen an increase in income.”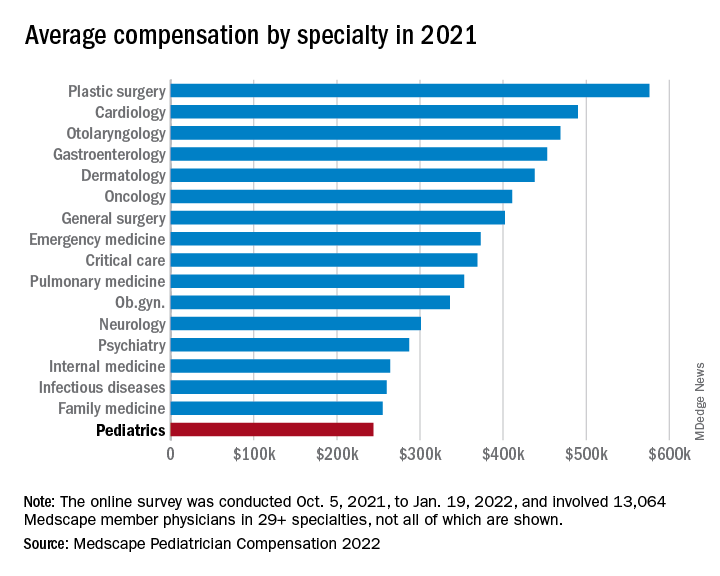
At least some of that positive news can be traced back to the reduced impact of COVID-19. “Compensation for most physicians is trending back up as demand for physicians accelerates. The market for physicians has done a complete 180 over just 7 or 8 months,” James Taylor of AMN Healthcare’s physician and leadership solutions division said in Medscape Pediatrician Compensation Report 2022.
The 10% increase in pediatricians’ income, however, was not enough to reach the average for primary care physicians, $260,000, which was up by 7.4% over 2020. It was enough, though, to move pediatricians from the bottom of the earnings-by-specialty list, where they were last year, to next-to-last this year (public health/preventive medicine, with average earnings of $243,000 in 2021, is not shown in the graph).
The gender gap in earnings left male pediatricians’ income 26% higher than their female counterparts, slightly above the gap of 25% for primary care physicians and 24% for all physicians. For specialists, the gap was 31% in favor of men, based on data from 13,064 Medscape member physicians who participated in the survey, which was conducted online from Oct. 5, 2021, to Jan. 19, 2022. For the record, 57% of the pediatricians who responded were women.
The gaps and low income averages were enough, it seems, to keep pediatricians fairly negative regarding their feelings on compensation. Only 47% think they were fairly compensated in 2021, higher only than diabetes/endocrinology and nephrology. Among the other primary care specialties, internal medicine and ob.gyn. were slightly higher at 49% and family medicine was 55% – still just middle of the pack, compared with public health/preventive medicine at 72%, Medscape said in the report.
Would you do it again?
Moving to the less-economic aspects of the survey, respondents also were asked if they would choose medicine again as a career. Once more pediatricians were low on the scale, as only 70% said that they would enter medicine again, down from 77% last year and lower than this year’s average of 73% average for all physicians.
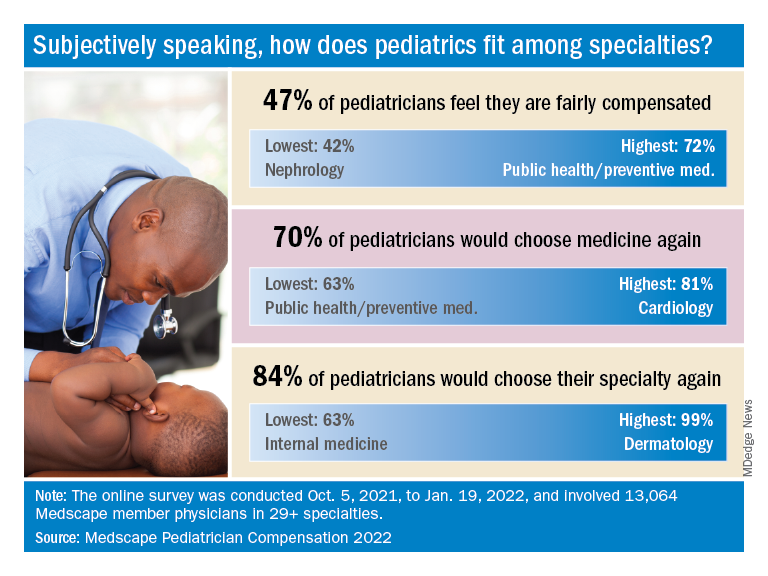
When they were asked if they would choose pediatrics again as a specialty, the response was a bit more positive: 84% said yes. That middle-of-the-pack showing was well ahead of internal medicine (63%) and family medicine (68%), but well below dermatology (99%) and orthopedics (97%), which are “among the top groups in our survey year after year,” Medscape said.
Did the administrative challenges of medical practice have an effect on those answers? Pediatrician respondents said that they spend 14.9 hours per week on paperwork and administration, close to the average of 15.5 hours for all physicians. The internists, who are least likely to choose their original specialty again, spend 18.7 hours on paperwork each week, while dermatologists, the most likely to repeat their first choice, have just 11.9 hours of paperwork per week.
The exact number of pediatricians involved in the survey was not provided, but they made up about 8% of the total cohort, which works out to somewhere between 1,000 and 1,100 individuals. All respondents had to be practicing in the United States, and compensation was analyzed for full-time physicians only. The sampling error is ±0.86% at a 95% confidence level.
Hormone therapy and breast cancer: An overview
It is projected that by 2050, 1.6 billion women in the world will have reached menopause or the postmenopausal period, a significant increase, compared with a billion women in 2020. Of all menopausal women, around 75% are affected by troublesome menopause symptoms, such as hot flashes and night sweats.
Around 84% of postmenopausal women experience genitourinary symptoms, such as vulvovaginal atrophy and incontinence.
Menopausal hormone therapy (MHT) is the most effective treatment for managing these symptoms; however, its effects on numerous aspects of female health remain uncertain, in particular with regard to breast cancer. The influence of MHT on breast cancer remains unsettled, with discordant findings from observational studies and randomized clinical trials, a factor that affects the decisions made by doctors concerning hormone therapy in menopausal women.
Background
Conjugated equine estrogens (CEEs) were introduced into clinical practice in the 1940s. For decades, MHT was the main treatment in conventional medicine for the symptoms of menopause. MHT was used in Western countries for about 600 million women starting from 1970, and it progressively increased during the 1990s. Professional organizations recommended MHT for the prevention of osteoporosis and chronic heart disease (CHD), and a third of prescriptions were for women older than 60 years.
Against this background, the National Institutes of Health launched randomized trials of MHT through the Women’s Health Initiative (WHI) to test whether the association with reduced risk for CHD found in observational studies was real and to obtain reliable information on the overall risks and benefits regarding the prevention of chronic disease for postmenopausal women aged 50-79 years.
The WHI trials tested standard-dose oral CEEs with and without standard-dose continuous medroxyprogesterone acetate (EPT). In 2002, the results of the WHI studies raised a series of concerns about the long-term safety of MHT, in particular the finding of an increased risk of breast cancer for women undergoing therapy. That risk exceeded the benefits from reductions in hip fractures and colorectal cancer.
The WHI findings received wide attention. Prescriptions for MHT dropped precipitously after 2002 and continued to decline in subsequent years. Declines were most marked for standard-dose EPT and in older women. The results of the CEE study were less negative, compared with those for EPT, as they showed no effect on CHD, a nonsignificant reduction in the risk of breast cancer, and a more favorable risk-benefit ratio for younger women, compared with older women. A decade later, it had become widely accepted that MHT should not be used for the prevention of chronic disease in older women; however, short-term use for treatment of vasomotor symptoms remains an accepted indication.
Risks and outcomes
Emerging from a series of WHI reports are complex models on the effect of hormonal therapy on the risk and outcome of breast cancer. In one study, women with an intact uterus received CEEs plus medroxyprogesterone acetate (MPA). An increase in the risk of breast cancer was observed over a median of 5.6 years of treatment, followed by a moderate reduction, with the risk increasing after 13 years of cumulative follow-up. For women treated with CEE alone, the reduction in risk observed over an average of 7.2 years of treatment was maintained for 13 years of follow-up.
Results from observational studies contrast with those from randomized controlled trials, particularly those concerning the use of estrogens only. A meta-analysis by the Collaborative Group on Hormonal Factors in Breast Cancer showed that both EPT and CEE were associated with a higher risk of breast neoplasia. Results of the Million Women Study showed a higher death rate.
Treatment methods and duration
Information from prospective studies on the effects of commencing MHT at various ages between 40 and 59 years show that for women who commenced treatment at any time within this age range, the relative risk was similar and was highly significant for all ages. Few women had started MHT treatment well after menopause at ages 60-69 years, and their excess risks during years 5-14 of current use were significant for estrogen-progestogen but not for estrogen-only MHT.
If these associations are largely causal, then for women of average weight in developed countries, 5 years of MHT, starting at age 50 years, would increase breast cancer incidence at ages 50-69 years by about 1 in every 50 users of estrogen plus daily progestogen preparations; 1 in every 70 users of estrogen plus intermittent progestogen preparations; and 1 in every 200 users of estrogen-only preparations. The corresponding excesses from 10 years of MHT would be about twice as great.
During 5-14 years of MHT use, the RRs were similarly increased if MHT use had started at ages 40-44 years, 45-49 years, 50-54 years, and 55-59 years; RRs appeared to be attenuated if MHT use had started after age 60 years. They were also attenuated by adiposity, particularly for estrogen-only MHT (which had little effect in obese women). After MHT use ceased, some excess risk of breast cancer persisted for more than a decade; this is directly correlated with the duration of treatment.
Therefore, it can be expected that the effects of MHT may vary between participants on the basis of age or time since menopause, as well as treatments (MHT type, dose, formulation, duration of use, and route of administration). Regarding formulation effects on the risk of breast cancer, new evidence shows an increased risk of 28%. Progestogens appeared to be differentially associated with breast cancer (micronized progesterone: odds ratio, 0.99; 95% confidence interval 0.55-1.79; synthetic progestin: OR, 1.28; 95% CI, 1.22-1.35). When prescribing MHT, micronized progesterone may be the safer progestogen to use.
In conclusion, MHT has a complex balance of benefits and risk on various health outcomes. Some effects differ qualitatively between ET and EPT. Regarding use of MHT, consideration should be given to the full range of effects, along with patients’ values and preferences. The overall quality of existing systematic reviews is moderate to poor. Clinicians should evaluate their scientific strength before considering applying their results in clinical practice. Regarding use of any hormone therapy regimen, consideration should be given to the full range of risk and benefits and should involve shared decisionmaking with the patient. It should be recognized that risk-benefit balance is altered by factors such as age, time from menopause, oophorectomy status, and prior hysterectomy and that some outcomes persist and there is some attenuation after stopping use.
This article was translated from Univadis Italy.
A version of the article appeared on Medscape.com.
It is projected that by 2050, 1.6 billion women in the world will have reached menopause or the postmenopausal period, a significant increase, compared with a billion women in 2020. Of all menopausal women, around 75% are affected by troublesome menopause symptoms, such as hot flashes and night sweats.
Around 84% of postmenopausal women experience genitourinary symptoms, such as vulvovaginal atrophy and incontinence.
Menopausal hormone therapy (MHT) is the most effective treatment for managing these symptoms; however, its effects on numerous aspects of female health remain uncertain, in particular with regard to breast cancer. The influence of MHT on breast cancer remains unsettled, with discordant findings from observational studies and randomized clinical trials, a factor that affects the decisions made by doctors concerning hormone therapy in menopausal women.
Background
Conjugated equine estrogens (CEEs) were introduced into clinical practice in the 1940s. For decades, MHT was the main treatment in conventional medicine for the symptoms of menopause. MHT was used in Western countries for about 600 million women starting from 1970, and it progressively increased during the 1990s. Professional organizations recommended MHT for the prevention of osteoporosis and chronic heart disease (CHD), and a third of prescriptions were for women older than 60 years.
Against this background, the National Institutes of Health launched randomized trials of MHT through the Women’s Health Initiative (WHI) to test whether the association with reduced risk for CHD found in observational studies was real and to obtain reliable information on the overall risks and benefits regarding the prevention of chronic disease for postmenopausal women aged 50-79 years.
The WHI trials tested standard-dose oral CEEs with and without standard-dose continuous medroxyprogesterone acetate (EPT). In 2002, the results of the WHI studies raised a series of concerns about the long-term safety of MHT, in particular the finding of an increased risk of breast cancer for women undergoing therapy. That risk exceeded the benefits from reductions in hip fractures and colorectal cancer.
The WHI findings received wide attention. Prescriptions for MHT dropped precipitously after 2002 and continued to decline in subsequent years. Declines were most marked for standard-dose EPT and in older women. The results of the CEE study were less negative, compared with those for EPT, as they showed no effect on CHD, a nonsignificant reduction in the risk of breast cancer, and a more favorable risk-benefit ratio for younger women, compared with older women. A decade later, it had become widely accepted that MHT should not be used for the prevention of chronic disease in older women; however, short-term use for treatment of vasomotor symptoms remains an accepted indication.
Risks and outcomes
Emerging from a series of WHI reports are complex models on the effect of hormonal therapy on the risk and outcome of breast cancer. In one study, women with an intact uterus received CEEs plus medroxyprogesterone acetate (MPA). An increase in the risk of breast cancer was observed over a median of 5.6 years of treatment, followed by a moderate reduction, with the risk increasing after 13 years of cumulative follow-up. For women treated with CEE alone, the reduction in risk observed over an average of 7.2 years of treatment was maintained for 13 years of follow-up.
Results from observational studies contrast with those from randomized controlled trials, particularly those concerning the use of estrogens only. A meta-analysis by the Collaborative Group on Hormonal Factors in Breast Cancer showed that both EPT and CEE were associated with a higher risk of breast neoplasia. Results of the Million Women Study showed a higher death rate.
Treatment methods and duration
Information from prospective studies on the effects of commencing MHT at various ages between 40 and 59 years show that for women who commenced treatment at any time within this age range, the relative risk was similar and was highly significant for all ages. Few women had started MHT treatment well after menopause at ages 60-69 years, and their excess risks during years 5-14 of current use were significant for estrogen-progestogen but not for estrogen-only MHT.
If these associations are largely causal, then for women of average weight in developed countries, 5 years of MHT, starting at age 50 years, would increase breast cancer incidence at ages 50-69 years by about 1 in every 50 users of estrogen plus daily progestogen preparations; 1 in every 70 users of estrogen plus intermittent progestogen preparations; and 1 in every 200 users of estrogen-only preparations. The corresponding excesses from 10 years of MHT would be about twice as great.
During 5-14 years of MHT use, the RRs were similarly increased if MHT use had started at ages 40-44 years, 45-49 years, 50-54 years, and 55-59 years; RRs appeared to be attenuated if MHT use had started after age 60 years. They were also attenuated by adiposity, particularly for estrogen-only MHT (which had little effect in obese women). After MHT use ceased, some excess risk of breast cancer persisted for more than a decade; this is directly correlated with the duration of treatment.
Therefore, it can be expected that the effects of MHT may vary between participants on the basis of age or time since menopause, as well as treatments (MHT type, dose, formulation, duration of use, and route of administration). Regarding formulation effects on the risk of breast cancer, new evidence shows an increased risk of 28%. Progestogens appeared to be differentially associated with breast cancer (micronized progesterone: odds ratio, 0.99; 95% confidence interval 0.55-1.79; synthetic progestin: OR, 1.28; 95% CI, 1.22-1.35). When prescribing MHT, micronized progesterone may be the safer progestogen to use.
In conclusion, MHT has a complex balance of benefits and risk on various health outcomes. Some effects differ qualitatively between ET and EPT. Regarding use of MHT, consideration should be given to the full range of effects, along with patients’ values and preferences. The overall quality of existing systematic reviews is moderate to poor. Clinicians should evaluate their scientific strength before considering applying their results in clinical practice. Regarding use of any hormone therapy regimen, consideration should be given to the full range of risk and benefits and should involve shared decisionmaking with the patient. It should be recognized that risk-benefit balance is altered by factors such as age, time from menopause, oophorectomy status, and prior hysterectomy and that some outcomes persist and there is some attenuation after stopping use.
This article was translated from Univadis Italy.
A version of the article appeared on Medscape.com.
It is projected that by 2050, 1.6 billion women in the world will have reached menopause or the postmenopausal period, a significant increase, compared with a billion women in 2020. Of all menopausal women, around 75% are affected by troublesome menopause symptoms, such as hot flashes and night sweats.
Around 84% of postmenopausal women experience genitourinary symptoms, such as vulvovaginal atrophy and incontinence.
Menopausal hormone therapy (MHT) is the most effective treatment for managing these symptoms; however, its effects on numerous aspects of female health remain uncertain, in particular with regard to breast cancer. The influence of MHT on breast cancer remains unsettled, with discordant findings from observational studies and randomized clinical trials, a factor that affects the decisions made by doctors concerning hormone therapy in menopausal women.
Background
Conjugated equine estrogens (CEEs) were introduced into clinical practice in the 1940s. For decades, MHT was the main treatment in conventional medicine for the symptoms of menopause. MHT was used in Western countries for about 600 million women starting from 1970, and it progressively increased during the 1990s. Professional organizations recommended MHT for the prevention of osteoporosis and chronic heart disease (CHD), and a third of prescriptions were for women older than 60 years.
Against this background, the National Institutes of Health launched randomized trials of MHT through the Women’s Health Initiative (WHI) to test whether the association with reduced risk for CHD found in observational studies was real and to obtain reliable information on the overall risks and benefits regarding the prevention of chronic disease for postmenopausal women aged 50-79 years.
The WHI trials tested standard-dose oral CEEs with and without standard-dose continuous medroxyprogesterone acetate (EPT). In 2002, the results of the WHI studies raised a series of concerns about the long-term safety of MHT, in particular the finding of an increased risk of breast cancer for women undergoing therapy. That risk exceeded the benefits from reductions in hip fractures and colorectal cancer.
The WHI findings received wide attention. Prescriptions for MHT dropped precipitously after 2002 and continued to decline in subsequent years. Declines were most marked for standard-dose EPT and in older women. The results of the CEE study were less negative, compared with those for EPT, as they showed no effect on CHD, a nonsignificant reduction in the risk of breast cancer, and a more favorable risk-benefit ratio for younger women, compared with older women. A decade later, it had become widely accepted that MHT should not be used for the prevention of chronic disease in older women; however, short-term use for treatment of vasomotor symptoms remains an accepted indication.
Risks and outcomes
Emerging from a series of WHI reports are complex models on the effect of hormonal therapy on the risk and outcome of breast cancer. In one study, women with an intact uterus received CEEs plus medroxyprogesterone acetate (MPA). An increase in the risk of breast cancer was observed over a median of 5.6 years of treatment, followed by a moderate reduction, with the risk increasing after 13 years of cumulative follow-up. For women treated with CEE alone, the reduction in risk observed over an average of 7.2 years of treatment was maintained for 13 years of follow-up.
Results from observational studies contrast with those from randomized controlled trials, particularly those concerning the use of estrogens only. A meta-analysis by the Collaborative Group on Hormonal Factors in Breast Cancer showed that both EPT and CEE were associated with a higher risk of breast neoplasia. Results of the Million Women Study showed a higher death rate.
Treatment methods and duration
Information from prospective studies on the effects of commencing MHT at various ages between 40 and 59 years show that for women who commenced treatment at any time within this age range, the relative risk was similar and was highly significant for all ages. Few women had started MHT treatment well after menopause at ages 60-69 years, and their excess risks during years 5-14 of current use were significant for estrogen-progestogen but not for estrogen-only MHT.
If these associations are largely causal, then for women of average weight in developed countries, 5 years of MHT, starting at age 50 years, would increase breast cancer incidence at ages 50-69 years by about 1 in every 50 users of estrogen plus daily progestogen preparations; 1 in every 70 users of estrogen plus intermittent progestogen preparations; and 1 in every 200 users of estrogen-only preparations. The corresponding excesses from 10 years of MHT would be about twice as great.
During 5-14 years of MHT use, the RRs were similarly increased if MHT use had started at ages 40-44 years, 45-49 years, 50-54 years, and 55-59 years; RRs appeared to be attenuated if MHT use had started after age 60 years. They were also attenuated by adiposity, particularly for estrogen-only MHT (which had little effect in obese women). After MHT use ceased, some excess risk of breast cancer persisted for more than a decade; this is directly correlated with the duration of treatment.
Therefore, it can be expected that the effects of MHT may vary between participants on the basis of age or time since menopause, as well as treatments (MHT type, dose, formulation, duration of use, and route of administration). Regarding formulation effects on the risk of breast cancer, new evidence shows an increased risk of 28%. Progestogens appeared to be differentially associated with breast cancer (micronized progesterone: odds ratio, 0.99; 95% confidence interval 0.55-1.79; synthetic progestin: OR, 1.28; 95% CI, 1.22-1.35). When prescribing MHT, micronized progesterone may be the safer progestogen to use.
In conclusion, MHT has a complex balance of benefits and risk on various health outcomes. Some effects differ qualitatively between ET and EPT. Regarding use of MHT, consideration should be given to the full range of effects, along with patients’ values and preferences. The overall quality of existing systematic reviews is moderate to poor. Clinicians should evaluate their scientific strength before considering applying their results in clinical practice. Regarding use of any hormone therapy regimen, consideration should be given to the full range of risk and benefits and should involve shared decisionmaking with the patient. It should be recognized that risk-benefit balance is altered by factors such as age, time from menopause, oophorectomy status, and prior hysterectomy and that some outcomes persist and there is some attenuation after stopping use.
This article was translated from Univadis Italy.
A version of the article appeared on Medscape.com.
Can dietary tweaks improve some skin diseases?
Since 1950, the terms “diet and skin” in the medical literature have markedly increased, said Vivian Shi, MD associate professor of dermatology at the University of Arkansas for Medical Sciences, Little Rock, who talked about nutritional approaches for select skin diseases at MedscapeLive’s Women’s and Pediatric Dermatology Seminar.
Myths abound, but some associations of diet with skin diseases hold water, and she said.
Acne
What’s known, Dr. Shi said, is that the prevalence of acne is substantially lower in non-Westernized countries, and that diets in those countries generally have a low glycemic load, which decreases IGF-1 insulinlike growth factor 1 (IGF-1) concentrations, an accepted risk factor for acne. The Western diet also includes the hormonal effects of cow’s milk products.
Whey protein, which is popular as a supplement, isn’t good for acne, Dr. Shi said. It takes a couple of hours to digest, while casein protein digests more slowly, over 5-7 hours. If casein protein isn’t acceptable, good alternatives to whey protein are hemp seed, plant protein blends (peas, seeds, berries), egg white, brown rice isolate, and soy isolate protein.
Dairy products increase IGF-1 levels, hormonal mediators that can make acne worse. In addition, industrial cow’s milk can contain anabolic steroids and growth factor, leading to sebogenesis, Dr. Shi said. As for the type of milk, skim milk tends to be the most acnegenic and associated with the highest blood levels of IGF-1.
Supplementing with omega-3 fatty acids and gamma-linolenic acid improved mild to moderate acne in a double-blind, controlled study. Researchers randomized 45 patients with mild to moderate acne to an omega-3 fatty acid group (2,000 mg of eicosapentaenoic acid and docosahexaenoic acid), a gamma-linolenic acid group (borage oil with 400 mg gamma-linolenic acid) or a control group. After 10 weeks in both treatment groups, there was a significant reduction in inflammatory and noninflammatory lesions.
Those with acne are more likely to be deficient in Vitamin D, research suggests. Researchers also found that among those who had vitamin D deficiency, supplementing with 1,000 IU daily for 2 months reduced inflammatory lesions by 35% after 8 weeks, compared with a 6% reduction in the control group.
Other research has found that those with a low serum zinc level had more severe acne and that 30-200 mg of zinc orally for 2-4 months reduced inflammatory acne. However, Dr. Shi cautioned that those taking zinc for more than 2 months also need a copper supplement, as zinc reduces the amount of copper absorbed by the body.
Dr. Shi’s “do’s” diet list for acne patients is a follows: Paleolithic and Mediterranean diets, omega-3 fatty acids, gamma-linolenic acids, Vitamin D, zinc, tubers, legumes, vegetables, fruits, and fish.
Unknowns, she said, include chocolate, caffeine, green tea, and high salt.
Hidradenitis suppurativa
Patents with HS who follow a Mediterranean diet most closely have less severe disease, research has found. In this study, those patients with HS with the lowest adherence had a Sartorius HS score of 59.38, while those who followed it the most closely had a score of 39 (of 80).
In another study, patients with HS reported the following foods as exacerbating HS: sweets, bread/pasta/rice, dairy, and high-fat foods. Alleviating foods included vegetables, fruit, chicken, and fish.
Dr. Shi’s dietary recommendations for patients with HS: Follow a Mediterranean diet, avoid high fat foods and highly processed foods, and focus on eating more vegetables, fresh fruit, corn-based cereal, white meat, and fish.
A retrospective study of patients with Hurley stage 1 and 2 found that oral zinc gluconate, 90 mg a day, combined with 2% topical triclosan twice a day, resulted in significantly decreased HS scores and nodules and improved quality of life after 3 months. Expect vitamin D deficiency, she added.
Lastly, Dr. Shi recommended, if necessary, “weight loss to reduce the inflammatory burden.”
Rosacea
Dietary triggers for rosacea are thought to include high-fat foods, dairy foods, spicy foods, hot drinks, cinnamon, and vanilla.
A population-based case-control study in China, which evaluated 1,347 rosacea patients and 1,290 healthy controls, found that a high intake of fatty foods positively correlated with erythematotelangiectatic rosacea (ETR) and phymatous rosacea. High-frequency dairy intake negatively correlated with ETR and papulopustular rosacea, which was a surprise, she said. And in this study, no significant correlations were found between sweets, coffee, and spicy foods. That goes against the traditional thinking, she said, but this was a Chinese cohort and their diet is probably vastly different than those in the United States.
Other rosacea triggers, Dr. Shi said, are niacin-containing foods such as turkey, chicken breast, crustaceans, dried Shiitake mushrooms, peanuts, tuna, and liver, as well as cold drinks, and formalin-containing foods (fish, squid, tofu, wet noodles).
As the field of nutrigenics – how genes affect how the body responds to food – evolves, more answers about the impact of diet on these diseases will be forthcoming, Dr. Shi said.
In an interactive panel discussion, she was asked if she talks about diet with all her patients with acne, rosacea, and HS, or just those not responding to traditional therapy.
“I think it’s an important conversation to have,” Dr. Shi responded. “When I’m done with the medication [instructions], I say: ‘There is something else you can do to augment what I just told you.’ ” That’s when she explains the dietary information. She also has a handout on diet and routinely refers patients for dietary counseling.
MedscapeLive and this news organization are owned by the same parent company. Dr. Shi disclosed consulting, investigative and research funding from several sources, but not directly related to the content of her talk.
Since 1950, the terms “diet and skin” in the medical literature have markedly increased, said Vivian Shi, MD associate professor of dermatology at the University of Arkansas for Medical Sciences, Little Rock, who talked about nutritional approaches for select skin diseases at MedscapeLive’s Women’s and Pediatric Dermatology Seminar.
Myths abound, but some associations of diet with skin diseases hold water, and she said.
Acne
What’s known, Dr. Shi said, is that the prevalence of acne is substantially lower in non-Westernized countries, and that diets in those countries generally have a low glycemic load, which decreases IGF-1 insulinlike growth factor 1 (IGF-1) concentrations, an accepted risk factor for acne. The Western diet also includes the hormonal effects of cow’s milk products.
Whey protein, which is popular as a supplement, isn’t good for acne, Dr. Shi said. It takes a couple of hours to digest, while casein protein digests more slowly, over 5-7 hours. If casein protein isn’t acceptable, good alternatives to whey protein are hemp seed, plant protein blends (peas, seeds, berries), egg white, brown rice isolate, and soy isolate protein.
Dairy products increase IGF-1 levels, hormonal mediators that can make acne worse. In addition, industrial cow’s milk can contain anabolic steroids and growth factor, leading to sebogenesis, Dr. Shi said. As for the type of milk, skim milk tends to be the most acnegenic and associated with the highest blood levels of IGF-1.
Supplementing with omega-3 fatty acids and gamma-linolenic acid improved mild to moderate acne in a double-blind, controlled study. Researchers randomized 45 patients with mild to moderate acne to an omega-3 fatty acid group (2,000 mg of eicosapentaenoic acid and docosahexaenoic acid), a gamma-linolenic acid group (borage oil with 400 mg gamma-linolenic acid) or a control group. After 10 weeks in both treatment groups, there was a significant reduction in inflammatory and noninflammatory lesions.
Those with acne are more likely to be deficient in Vitamin D, research suggests. Researchers also found that among those who had vitamin D deficiency, supplementing with 1,000 IU daily for 2 months reduced inflammatory lesions by 35% after 8 weeks, compared with a 6% reduction in the control group.
Other research has found that those with a low serum zinc level had more severe acne and that 30-200 mg of zinc orally for 2-4 months reduced inflammatory acne. However, Dr. Shi cautioned that those taking zinc for more than 2 months also need a copper supplement, as zinc reduces the amount of copper absorbed by the body.
Dr. Shi’s “do’s” diet list for acne patients is a follows: Paleolithic and Mediterranean diets, omega-3 fatty acids, gamma-linolenic acids, Vitamin D, zinc, tubers, legumes, vegetables, fruits, and fish.
Unknowns, she said, include chocolate, caffeine, green tea, and high salt.
Hidradenitis suppurativa
Patents with HS who follow a Mediterranean diet most closely have less severe disease, research has found. In this study, those patients with HS with the lowest adherence had a Sartorius HS score of 59.38, while those who followed it the most closely had a score of 39 (of 80).
In another study, patients with HS reported the following foods as exacerbating HS: sweets, bread/pasta/rice, dairy, and high-fat foods. Alleviating foods included vegetables, fruit, chicken, and fish.
Dr. Shi’s dietary recommendations for patients with HS: Follow a Mediterranean diet, avoid high fat foods and highly processed foods, and focus on eating more vegetables, fresh fruit, corn-based cereal, white meat, and fish.
A retrospective study of patients with Hurley stage 1 and 2 found that oral zinc gluconate, 90 mg a day, combined with 2% topical triclosan twice a day, resulted in significantly decreased HS scores and nodules and improved quality of life after 3 months. Expect vitamin D deficiency, she added.
Lastly, Dr. Shi recommended, if necessary, “weight loss to reduce the inflammatory burden.”
Rosacea
Dietary triggers for rosacea are thought to include high-fat foods, dairy foods, spicy foods, hot drinks, cinnamon, and vanilla.
A population-based case-control study in China, which evaluated 1,347 rosacea patients and 1,290 healthy controls, found that a high intake of fatty foods positively correlated with erythematotelangiectatic rosacea (ETR) and phymatous rosacea. High-frequency dairy intake negatively correlated with ETR and papulopustular rosacea, which was a surprise, she said. And in this study, no significant correlations were found between sweets, coffee, and spicy foods. That goes against the traditional thinking, she said, but this was a Chinese cohort and their diet is probably vastly different than those in the United States.
Other rosacea triggers, Dr. Shi said, are niacin-containing foods such as turkey, chicken breast, crustaceans, dried Shiitake mushrooms, peanuts, tuna, and liver, as well as cold drinks, and formalin-containing foods (fish, squid, tofu, wet noodles).
As the field of nutrigenics – how genes affect how the body responds to food – evolves, more answers about the impact of diet on these diseases will be forthcoming, Dr. Shi said.
In an interactive panel discussion, she was asked if she talks about diet with all her patients with acne, rosacea, and HS, or just those not responding to traditional therapy.
“I think it’s an important conversation to have,” Dr. Shi responded. “When I’m done with the medication [instructions], I say: ‘There is something else you can do to augment what I just told you.’ ” That’s when she explains the dietary information. She also has a handout on diet and routinely refers patients for dietary counseling.
MedscapeLive and this news organization are owned by the same parent company. Dr. Shi disclosed consulting, investigative and research funding from several sources, but not directly related to the content of her talk.
Since 1950, the terms “diet and skin” in the medical literature have markedly increased, said Vivian Shi, MD associate professor of dermatology at the University of Arkansas for Medical Sciences, Little Rock, who talked about nutritional approaches for select skin diseases at MedscapeLive’s Women’s and Pediatric Dermatology Seminar.
Myths abound, but some associations of diet with skin diseases hold water, and she said.
Acne
What’s known, Dr. Shi said, is that the prevalence of acne is substantially lower in non-Westernized countries, and that diets in those countries generally have a low glycemic load, which decreases IGF-1 insulinlike growth factor 1 (IGF-1) concentrations, an accepted risk factor for acne. The Western diet also includes the hormonal effects of cow’s milk products.
Whey protein, which is popular as a supplement, isn’t good for acne, Dr. Shi said. It takes a couple of hours to digest, while casein protein digests more slowly, over 5-7 hours. If casein protein isn’t acceptable, good alternatives to whey protein are hemp seed, plant protein blends (peas, seeds, berries), egg white, brown rice isolate, and soy isolate protein.
Dairy products increase IGF-1 levels, hormonal mediators that can make acne worse. In addition, industrial cow’s milk can contain anabolic steroids and growth factor, leading to sebogenesis, Dr. Shi said. As for the type of milk, skim milk tends to be the most acnegenic and associated with the highest blood levels of IGF-1.
Supplementing with omega-3 fatty acids and gamma-linolenic acid improved mild to moderate acne in a double-blind, controlled study. Researchers randomized 45 patients with mild to moderate acne to an omega-3 fatty acid group (2,000 mg of eicosapentaenoic acid and docosahexaenoic acid), a gamma-linolenic acid group (borage oil with 400 mg gamma-linolenic acid) or a control group. After 10 weeks in both treatment groups, there was a significant reduction in inflammatory and noninflammatory lesions.
Those with acne are more likely to be deficient in Vitamin D, research suggests. Researchers also found that among those who had vitamin D deficiency, supplementing with 1,000 IU daily for 2 months reduced inflammatory lesions by 35% after 8 weeks, compared with a 6% reduction in the control group.
Other research has found that those with a low serum zinc level had more severe acne and that 30-200 mg of zinc orally for 2-4 months reduced inflammatory acne. However, Dr. Shi cautioned that those taking zinc for more than 2 months also need a copper supplement, as zinc reduces the amount of copper absorbed by the body.
Dr. Shi’s “do’s” diet list for acne patients is a follows: Paleolithic and Mediterranean diets, omega-3 fatty acids, gamma-linolenic acids, Vitamin D, zinc, tubers, legumes, vegetables, fruits, and fish.
Unknowns, she said, include chocolate, caffeine, green tea, and high salt.
Hidradenitis suppurativa
Patents with HS who follow a Mediterranean diet most closely have less severe disease, research has found. In this study, those patients with HS with the lowest adherence had a Sartorius HS score of 59.38, while those who followed it the most closely had a score of 39 (of 80).
In another study, patients with HS reported the following foods as exacerbating HS: sweets, bread/pasta/rice, dairy, and high-fat foods. Alleviating foods included vegetables, fruit, chicken, and fish.
Dr. Shi’s dietary recommendations for patients with HS: Follow a Mediterranean diet, avoid high fat foods and highly processed foods, and focus on eating more vegetables, fresh fruit, corn-based cereal, white meat, and fish.
A retrospective study of patients with Hurley stage 1 and 2 found that oral zinc gluconate, 90 mg a day, combined with 2% topical triclosan twice a day, resulted in significantly decreased HS scores and nodules and improved quality of life after 3 months. Expect vitamin D deficiency, she added.
Lastly, Dr. Shi recommended, if necessary, “weight loss to reduce the inflammatory burden.”
Rosacea
Dietary triggers for rosacea are thought to include high-fat foods, dairy foods, spicy foods, hot drinks, cinnamon, and vanilla.
A population-based case-control study in China, which evaluated 1,347 rosacea patients and 1,290 healthy controls, found that a high intake of fatty foods positively correlated with erythematotelangiectatic rosacea (ETR) and phymatous rosacea. High-frequency dairy intake negatively correlated with ETR and papulopustular rosacea, which was a surprise, she said. And in this study, no significant correlations were found between sweets, coffee, and spicy foods. That goes against the traditional thinking, she said, but this was a Chinese cohort and their diet is probably vastly different than those in the United States.
Other rosacea triggers, Dr. Shi said, are niacin-containing foods such as turkey, chicken breast, crustaceans, dried Shiitake mushrooms, peanuts, tuna, and liver, as well as cold drinks, and formalin-containing foods (fish, squid, tofu, wet noodles).
As the field of nutrigenics – how genes affect how the body responds to food – evolves, more answers about the impact of diet on these diseases will be forthcoming, Dr. Shi said.
In an interactive panel discussion, she was asked if she talks about diet with all her patients with acne, rosacea, and HS, or just those not responding to traditional therapy.
“I think it’s an important conversation to have,” Dr. Shi responded. “When I’m done with the medication [instructions], I say: ‘There is something else you can do to augment what I just told you.’ ” That’s when she explains the dietary information. She also has a handout on diet and routinely refers patients for dietary counseling.
MedscapeLive and this news organization are owned by the same parent company. Dr. Shi disclosed consulting, investigative and research funding from several sources, but not directly related to the content of her talk.
FROM MEDSCAPELIVE WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
Finding HBV ‘cure’ may mean going ‘back to the drawing board’
LONDON – Achieving a functional cure for hepatitis B virus (HBV) is not going to be easily achieved with the drugs that are currently in development, according to a presentation at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
“Intriguing results have been presented at ILC 2022 that must be carefully interpreted,” said Jean-Michel Pawlotsky, MD, PhD, of Henri Mondor Hospital in Créteil, France, during the viral hepatitis highlights session on the closing day of the meeting.
“New HBV drug development looks more complicated than initially expected and its goals and strategies need to be redefined and refocused,” he added
“This is really something that came from the discussions we had during the sessions but also in the corridors,” Dr. Pawlotsky added. “We know it’s going to be difficult; we have to reset, restart – not from zero, but from not much – and revise our strategy,” he suggested.
There are many new drugs under investigation for HBV, Dr. Pawlotsky said, noting that the number of studies being presented at the meeting was reminiscent of the flurry of activity before a functional cure for hepatitis C had been found. “It’s good to see that this is happening again for HBV,” he said.
Indeed, there are many new direct-acting antiviral agents, immunomodulatory, or other approaches being tested, and some of the more advanced studies are “teaching us a few things and probably raising more questions than getting answers,” Dr. Pawlotsky said.
The B-CLEAR study
One these studies is the phase 2b B-CLEAR study presented during the late-breaker session. This study involved bepirovirsen, an antisense oligonucleotide, and tested its efficacy and safety in patients with chronic hepatitis B virus infection who were either on or off stable nucleos(t)ide analogue (NA/NUC) therapy.
A similar proportion (28% and 29%, respectively) of patients achieved an hepatitis B surface antigen (HBsAg) level below the lower limit of quantification at the end of 24 weeks treatment. However, the effect on HBsAg varied according to the treatment arm, with changes to the dosing or switching to placebo indicating that the effect might wane when the treatment is stopped or if the dose is reduced.
“Interestingly, ALT elevations were observed in association with most HBsAg declines,” Dr. Pawlotsky pointed out. “I think we still have to determine whether this is good flare/bad flare, good sign/bad sign, of what is going to happen afterward.”
The REEF studies
Another approach highlighted was the combination of the silencing or small interfering RNA (siRNA) JNJ-3989 with the capsid assembly modulator (CAM) JNJ-6379 in the phase 2 REEF-1 and REEF-2 studies.
REEF-1, conducted in patients who were either hepatitis B e antigen (HBeAg) positive or negative who were not treated with NA/NUC or were NA/NUC suppressed, showed a dose-dependent, but variable effect among individual patients as might be expected at the end of 48 weeks’ treatment. This was sustained at week 72, which was 24 weeks’ follow-up after stopping treatment.
However, pointed out Dr. Pawlotsky “I think the most important part of this is that if you add a CAM on top of the siRNA, you do not improve the effect on HBsAg levels.”
Then there is the REEF-2 study, testing the same combination but in only patients who were NA suppressed or HBeAg negative alongside standard NA/NUC therapy. As well as being the first novel combination treatment trial to report, this was essentially a stopping trial, Kosh Agarwal, BMedSci (Hons), MBBS, MD, one of the study’s investigators explained separately at a media briefing.
Patients (n = 130) were treated for 48 weeks, then all treatment – including NA/NUC – was discontinued, with 48 weeks of follow-up after discontinuation, said Dr. Agarwal, who is a consultant hepatologist based at the Institute of Liver Studies at King’s College Hospital, London. He presented data from the first 24 week period after treatment had ended.
At the end of treatment, the combination had resulted in a mean reduction in HBsAg of 1.89 log10 IU/mL versus a reduction of 0.06 for the NA/NUC-only group, which acted as the control group in this trial. But “no patient in this study lost their surface antigen, i.e., were cured of their hepatitis B in the active arm or in the control arm,” Dr. Agarwal said.
“We didn’t achieve a cure, but a significant proportion were in a ‘controlled’ viral stage,” said Dr. Agarwal. Indeed, during his presentation of the findings, he showed that HBsAg inhibition was maintained in the majority (72%) of patients after stopping the combination.
While the trial’s primary endpoint wasn’t met, “it’s a really important study,” said Dr. Agarwal. “This [study] was fulfilled and delivered in the COVID era, so a lot of patients were looked after very carefully by sites in Europe,” he observed.
Further follow-up from the trial is expected, and Dr. Agarwal said that the subsequent discussion will “take us back to the drawing board to think about whether we need better antiviral treatments or whether we need to think about different combinations, and whether actually stopping treatment with every treatment is the right strategy to take.”
Both Dr. Agarwal and Dr. Pawlotsky flagged up the case of one patient in the trial who had been in the control arm and had experienced severe HBV reactivation that required a liver transplant.
“This patient is a warning signal,” Dr. Pawlotsky suggested in his talk. “When we think about NUC stopping, we have to think about the potential benefit in terms of HbsAg loss but also the potential risks.”
While Dr. Agarwal had noted that it highlights that “careful design of retreatment criteria is important in studies assessing the NA/NUC-stopping concept”.
Monoclonal antibody shows promise
Other combinations could involve an siRNA and an immunomodulatory agent and, during the poster sessions at the meeting, Dr. Agarwal also presented data from an ongoing phase 1 study with a novel, neutralizing monoclonal antibody called VIR-3434.
This monoclonal antibody is novel because it is thought to have several modes of action, first by binding to HBV and affecting its entry into liver cells, then by presenting the virus to T cells and stimulating a ‘vaccinal’ or immune effect, and then by helping the with the clearance of HBsAg and delivery of the virus to dendritic cells.
In the study, single doses of VIR-3434 were found to be well tolerated and to produce rapid reductions in HBsAg, with the highest dose used (300 mg) producing the greatest and most durable effect up to week 8.
VIR-3434 is also being tested in combination with other drugs in the phase 2 MARCH trial. One of these combinations is VIR-3434 together with an investigational siRNA dubbed VIR-2218. Preclinical work presented at ILC 2022 suggests that this combination appears to be capable of reducing HBsAg to a greater extent than using either agent alone.
Rethinking the strategy to get to a cure
Of course, VIR-3434 is one of several immunomodulatory compounds in development. There are therapeutic vaccines, drugs targeting the innate immune response, other monoclonal antibodies, T-cell receptors, checkpoint inhibitors and PD-L1 inhibitors. Then there are other compounds such as entry inhibitors, apoptosis inducers, and farnesoid X receptor agonists.
“I finish this meeting with more questions than answers,” Dr. Pawlotsky said. “What is the right target to enhance specific anti-HBV immunity? Does in vivo induction of immune responses translate into any beneficial effect on HBV infection? Will therapeutic vaccines every work in a viral infection?”
Moreover, he asked, “how can we avoid the side effect of enhancing multiple and complex nonspecific immune responses? Are treatment-induced flares good flares or bad flares? All of these are questions that are really unanswered and that we’ll have to get answers to in the near future.”
The B-CLEAR study was sponsored by GlaxoSmithKline. The REEF-2 study was sponsored by Janssen Research & Development. The VIR-3434 studies were funded by Vir Biotechnology. Dr. Pawlotsky has received grant and research support, acted as a consultant, adviser, or speaker, and participated in advisory boards for multiple pharmaceutical and biotechnology companies. This news organization was unable to verify Dr. Agarwal’s ties to Vir Biotechnology, but he presented one of the posters on VIR-3434 at the meeting and has been involved in the phase 1 study that was reported.
LONDON – Achieving a functional cure for hepatitis B virus (HBV) is not going to be easily achieved with the drugs that are currently in development, according to a presentation at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
“Intriguing results have been presented at ILC 2022 that must be carefully interpreted,” said Jean-Michel Pawlotsky, MD, PhD, of Henri Mondor Hospital in Créteil, France, during the viral hepatitis highlights session on the closing day of the meeting.
“New HBV drug development looks more complicated than initially expected and its goals and strategies need to be redefined and refocused,” he added
“This is really something that came from the discussions we had during the sessions but also in the corridors,” Dr. Pawlotsky added. “We know it’s going to be difficult; we have to reset, restart – not from zero, but from not much – and revise our strategy,” he suggested.
There are many new drugs under investigation for HBV, Dr. Pawlotsky said, noting that the number of studies being presented at the meeting was reminiscent of the flurry of activity before a functional cure for hepatitis C had been found. “It’s good to see that this is happening again for HBV,” he said.
Indeed, there are many new direct-acting antiviral agents, immunomodulatory, or other approaches being tested, and some of the more advanced studies are “teaching us a few things and probably raising more questions than getting answers,” Dr. Pawlotsky said.
The B-CLEAR study
One these studies is the phase 2b B-CLEAR study presented during the late-breaker session. This study involved bepirovirsen, an antisense oligonucleotide, and tested its efficacy and safety in patients with chronic hepatitis B virus infection who were either on or off stable nucleos(t)ide analogue (NA/NUC) therapy.
A similar proportion (28% and 29%, respectively) of patients achieved an hepatitis B surface antigen (HBsAg) level below the lower limit of quantification at the end of 24 weeks treatment. However, the effect on HBsAg varied according to the treatment arm, with changes to the dosing or switching to placebo indicating that the effect might wane when the treatment is stopped or if the dose is reduced.
“Interestingly, ALT elevations were observed in association with most HBsAg declines,” Dr. Pawlotsky pointed out. “I think we still have to determine whether this is good flare/bad flare, good sign/bad sign, of what is going to happen afterward.”
The REEF studies
Another approach highlighted was the combination of the silencing or small interfering RNA (siRNA) JNJ-3989 with the capsid assembly modulator (CAM) JNJ-6379 in the phase 2 REEF-1 and REEF-2 studies.
REEF-1, conducted in patients who were either hepatitis B e antigen (HBeAg) positive or negative who were not treated with NA/NUC or were NA/NUC suppressed, showed a dose-dependent, but variable effect among individual patients as might be expected at the end of 48 weeks’ treatment. This was sustained at week 72, which was 24 weeks’ follow-up after stopping treatment.
However, pointed out Dr. Pawlotsky “I think the most important part of this is that if you add a CAM on top of the siRNA, you do not improve the effect on HBsAg levels.”
Then there is the REEF-2 study, testing the same combination but in only patients who were NA suppressed or HBeAg negative alongside standard NA/NUC therapy. As well as being the first novel combination treatment trial to report, this was essentially a stopping trial, Kosh Agarwal, BMedSci (Hons), MBBS, MD, one of the study’s investigators explained separately at a media briefing.
Patients (n = 130) were treated for 48 weeks, then all treatment – including NA/NUC – was discontinued, with 48 weeks of follow-up after discontinuation, said Dr. Agarwal, who is a consultant hepatologist based at the Institute of Liver Studies at King’s College Hospital, London. He presented data from the first 24 week period after treatment had ended.
At the end of treatment, the combination had resulted in a mean reduction in HBsAg of 1.89 log10 IU/mL versus a reduction of 0.06 for the NA/NUC-only group, which acted as the control group in this trial. But “no patient in this study lost their surface antigen, i.e., were cured of their hepatitis B in the active arm or in the control arm,” Dr. Agarwal said.
“We didn’t achieve a cure, but a significant proportion were in a ‘controlled’ viral stage,” said Dr. Agarwal. Indeed, during his presentation of the findings, he showed that HBsAg inhibition was maintained in the majority (72%) of patients after stopping the combination.
While the trial’s primary endpoint wasn’t met, “it’s a really important study,” said Dr. Agarwal. “This [study] was fulfilled and delivered in the COVID era, so a lot of patients were looked after very carefully by sites in Europe,” he observed.
Further follow-up from the trial is expected, and Dr. Agarwal said that the subsequent discussion will “take us back to the drawing board to think about whether we need better antiviral treatments or whether we need to think about different combinations, and whether actually stopping treatment with every treatment is the right strategy to take.”
Both Dr. Agarwal and Dr. Pawlotsky flagged up the case of one patient in the trial who had been in the control arm and had experienced severe HBV reactivation that required a liver transplant.
“This patient is a warning signal,” Dr. Pawlotsky suggested in his talk. “When we think about NUC stopping, we have to think about the potential benefit in terms of HbsAg loss but also the potential risks.”
While Dr. Agarwal had noted that it highlights that “careful design of retreatment criteria is important in studies assessing the NA/NUC-stopping concept”.
Monoclonal antibody shows promise
Other combinations could involve an siRNA and an immunomodulatory agent and, during the poster sessions at the meeting, Dr. Agarwal also presented data from an ongoing phase 1 study with a novel, neutralizing monoclonal antibody called VIR-3434.
This monoclonal antibody is novel because it is thought to have several modes of action, first by binding to HBV and affecting its entry into liver cells, then by presenting the virus to T cells and stimulating a ‘vaccinal’ or immune effect, and then by helping the with the clearance of HBsAg and delivery of the virus to dendritic cells.
In the study, single doses of VIR-3434 were found to be well tolerated and to produce rapid reductions in HBsAg, with the highest dose used (300 mg) producing the greatest and most durable effect up to week 8.
VIR-3434 is also being tested in combination with other drugs in the phase 2 MARCH trial. One of these combinations is VIR-3434 together with an investigational siRNA dubbed VIR-2218. Preclinical work presented at ILC 2022 suggests that this combination appears to be capable of reducing HBsAg to a greater extent than using either agent alone.
Rethinking the strategy to get to a cure
Of course, VIR-3434 is one of several immunomodulatory compounds in development. There are therapeutic vaccines, drugs targeting the innate immune response, other monoclonal antibodies, T-cell receptors, checkpoint inhibitors and PD-L1 inhibitors. Then there are other compounds such as entry inhibitors, apoptosis inducers, and farnesoid X receptor agonists.
“I finish this meeting with more questions than answers,” Dr. Pawlotsky said. “What is the right target to enhance specific anti-HBV immunity? Does in vivo induction of immune responses translate into any beneficial effect on HBV infection? Will therapeutic vaccines every work in a viral infection?”
Moreover, he asked, “how can we avoid the side effect of enhancing multiple and complex nonspecific immune responses? Are treatment-induced flares good flares or bad flares? All of these are questions that are really unanswered and that we’ll have to get answers to in the near future.”
The B-CLEAR study was sponsored by GlaxoSmithKline. The REEF-2 study was sponsored by Janssen Research & Development. The VIR-3434 studies were funded by Vir Biotechnology. Dr. Pawlotsky has received grant and research support, acted as a consultant, adviser, or speaker, and participated in advisory boards for multiple pharmaceutical and biotechnology companies. This news organization was unable to verify Dr. Agarwal’s ties to Vir Biotechnology, but he presented one of the posters on VIR-3434 at the meeting and has been involved in the phase 1 study that was reported.
LONDON – Achieving a functional cure for hepatitis B virus (HBV) is not going to be easily achieved with the drugs that are currently in development, according to a presentation at the annual International Liver Congress sponsored by the European Association for the Study of the Liver.
“Intriguing results have been presented at ILC 2022 that must be carefully interpreted,” said Jean-Michel Pawlotsky, MD, PhD, of Henri Mondor Hospital in Créteil, France, during the viral hepatitis highlights session on the closing day of the meeting.
“New HBV drug development looks more complicated than initially expected and its goals and strategies need to be redefined and refocused,” he added
“This is really something that came from the discussions we had during the sessions but also in the corridors,” Dr. Pawlotsky added. “We know it’s going to be difficult; we have to reset, restart – not from zero, but from not much – and revise our strategy,” he suggested.
There are many new drugs under investigation for HBV, Dr. Pawlotsky said, noting that the number of studies being presented at the meeting was reminiscent of the flurry of activity before a functional cure for hepatitis C had been found. “It’s good to see that this is happening again for HBV,” he said.
Indeed, there are many new direct-acting antiviral agents, immunomodulatory, or other approaches being tested, and some of the more advanced studies are “teaching us a few things and probably raising more questions than getting answers,” Dr. Pawlotsky said.
The B-CLEAR study
One these studies is the phase 2b B-CLEAR study presented during the late-breaker session. This study involved bepirovirsen, an antisense oligonucleotide, and tested its efficacy and safety in patients with chronic hepatitis B virus infection who were either on or off stable nucleos(t)ide analogue (NA/NUC) therapy.
A similar proportion (28% and 29%, respectively) of patients achieved an hepatitis B surface antigen (HBsAg) level below the lower limit of quantification at the end of 24 weeks treatment. However, the effect on HBsAg varied according to the treatment arm, with changes to the dosing or switching to placebo indicating that the effect might wane when the treatment is stopped or if the dose is reduced.
“Interestingly, ALT elevations were observed in association with most HBsAg declines,” Dr. Pawlotsky pointed out. “I think we still have to determine whether this is good flare/bad flare, good sign/bad sign, of what is going to happen afterward.”
The REEF studies
Another approach highlighted was the combination of the silencing or small interfering RNA (siRNA) JNJ-3989 with the capsid assembly modulator (CAM) JNJ-6379 in the phase 2 REEF-1 and REEF-2 studies.
REEF-1, conducted in patients who were either hepatitis B e antigen (HBeAg) positive or negative who were not treated with NA/NUC or were NA/NUC suppressed, showed a dose-dependent, but variable effect among individual patients as might be expected at the end of 48 weeks’ treatment. This was sustained at week 72, which was 24 weeks’ follow-up after stopping treatment.
However, pointed out Dr. Pawlotsky “I think the most important part of this is that if you add a CAM on top of the siRNA, you do not improve the effect on HBsAg levels.”
Then there is the REEF-2 study, testing the same combination but in only patients who were NA suppressed or HBeAg negative alongside standard NA/NUC therapy. As well as being the first novel combination treatment trial to report, this was essentially a stopping trial, Kosh Agarwal, BMedSci (Hons), MBBS, MD, one of the study’s investigators explained separately at a media briefing.
Patients (n = 130) were treated for 48 weeks, then all treatment – including NA/NUC – was discontinued, with 48 weeks of follow-up after discontinuation, said Dr. Agarwal, who is a consultant hepatologist based at the Institute of Liver Studies at King’s College Hospital, London. He presented data from the first 24 week period after treatment had ended.
At the end of treatment, the combination had resulted in a mean reduction in HBsAg of 1.89 log10 IU/mL versus a reduction of 0.06 for the NA/NUC-only group, which acted as the control group in this trial. But “no patient in this study lost their surface antigen, i.e., were cured of their hepatitis B in the active arm or in the control arm,” Dr. Agarwal said.
“We didn’t achieve a cure, but a significant proportion were in a ‘controlled’ viral stage,” said Dr. Agarwal. Indeed, during his presentation of the findings, he showed that HBsAg inhibition was maintained in the majority (72%) of patients after stopping the combination.
While the trial’s primary endpoint wasn’t met, “it’s a really important study,” said Dr. Agarwal. “This [study] was fulfilled and delivered in the COVID era, so a lot of patients were looked after very carefully by sites in Europe,” he observed.
Further follow-up from the trial is expected, and Dr. Agarwal said that the subsequent discussion will “take us back to the drawing board to think about whether we need better antiviral treatments or whether we need to think about different combinations, and whether actually stopping treatment with every treatment is the right strategy to take.”
Both Dr. Agarwal and Dr. Pawlotsky flagged up the case of one patient in the trial who had been in the control arm and had experienced severe HBV reactivation that required a liver transplant.
“This patient is a warning signal,” Dr. Pawlotsky suggested in his talk. “When we think about NUC stopping, we have to think about the potential benefit in terms of HbsAg loss but also the potential risks.”
While Dr. Agarwal had noted that it highlights that “careful design of retreatment criteria is important in studies assessing the NA/NUC-stopping concept”.
Monoclonal antibody shows promise
Other combinations could involve an siRNA and an immunomodulatory agent and, during the poster sessions at the meeting, Dr. Agarwal also presented data from an ongoing phase 1 study with a novel, neutralizing monoclonal antibody called VIR-3434.
This monoclonal antibody is novel because it is thought to have several modes of action, first by binding to HBV and affecting its entry into liver cells, then by presenting the virus to T cells and stimulating a ‘vaccinal’ or immune effect, and then by helping the with the clearance of HBsAg and delivery of the virus to dendritic cells.
In the study, single doses of VIR-3434 were found to be well tolerated and to produce rapid reductions in HBsAg, with the highest dose used (300 mg) producing the greatest and most durable effect up to week 8.
VIR-3434 is also being tested in combination with other drugs in the phase 2 MARCH trial. One of these combinations is VIR-3434 together with an investigational siRNA dubbed VIR-2218. Preclinical work presented at ILC 2022 suggests that this combination appears to be capable of reducing HBsAg to a greater extent than using either agent alone.
Rethinking the strategy to get to a cure
Of course, VIR-3434 is one of several immunomodulatory compounds in development. There are therapeutic vaccines, drugs targeting the innate immune response, other monoclonal antibodies, T-cell receptors, checkpoint inhibitors and PD-L1 inhibitors. Then there are other compounds such as entry inhibitors, apoptosis inducers, and farnesoid X receptor agonists.
“I finish this meeting with more questions than answers,” Dr. Pawlotsky said. “What is the right target to enhance specific anti-HBV immunity? Does in vivo induction of immune responses translate into any beneficial effect on HBV infection? Will therapeutic vaccines every work in a viral infection?”
Moreover, he asked, “how can we avoid the side effect of enhancing multiple and complex nonspecific immune responses? Are treatment-induced flares good flares or bad flares? All of these are questions that are really unanswered and that we’ll have to get answers to in the near future.”
The B-CLEAR study was sponsored by GlaxoSmithKline. The REEF-2 study was sponsored by Janssen Research & Development. The VIR-3434 studies were funded by Vir Biotechnology. Dr. Pawlotsky has received grant and research support, acted as a consultant, adviser, or speaker, and participated in advisory boards for multiple pharmaceutical and biotechnology companies. This news organization was unable to verify Dr. Agarwal’s ties to Vir Biotechnology, but he presented one of the posters on VIR-3434 at the meeting and has been involved in the phase 1 study that was reported.
AT ILC 2022









