User login
Clinical Edge Journal Scan Commentary: Atopic Dermatitis January 2022
George Washington University School of Medicine and Health Sciences
Washington, DC
A new era of evidence-based practice for atopic dermatitis
Atopic dermatitis (AD) is one of the most common diseases of childhood and still very common in adults worldwide. AD is also a very burdensome disease with considerable patient-burden. Despite the enormous population- and patient- burden, there remain many unmet needs in the management of AD. In addition, many treatments commonly used in AD had scant or mixed evidence regarding their efficacy and safety. For example, topical corticosteroids (TCS) are the workhorse for treatment in AD and most other inflammatory skin diseases. Yet, virtually everything we know about the efficacy of TCS comes from vasoconstriction proxy assays with almost no studies formally studying the efficacy of TCS in AD. Similarly, many therapies used off-label to treat more severe AD, such as phototherapy or allergen immunotherapy have inconsistent evidence to guide their use. Well, things are finally changing and the evidence is coming in at a frenzied pace. Development of multiple novel therapeutics in AD led to renewed interest in studying the efficacy and safety of older therapies as well.
- Phototherapy is an important treatment modality in AD patients who have an inadequate response to topical therapy. Many different modalities and devices were used to treat AD over the years, including narrowband ultraviolet B (NBUVB) and ultraviolet A (UVA)-1. NBUVB is the most commonly used approach in the United States and some other regions of the world. Ben Mordehai et al. published the results of a retrospective cohort study of 390 Israeli patients with moderate-severe AD treated with NBUVB therapy between 2000-2017 with ≥3 years of follow-up. Overall, 55.4% achieved an Investigator’s Global Assessment score of clear or almost clear. Facial involvement, occurrence of adverse effects, fewer treatments, and pretreatment immunoglobulin E levels >4000 IU/ml were associated with poorer clinical response to NBUVB. Median duration of response was 12 months with more relapses in children (<18 years).
- House dust mites (HDM) were previously shown to be triggers of AD via Immunoglobulin E dependent and independent mechanisms. Unfortunately, HDM avoidance is challenging for patients and has not proven to be reliably effective in clinical trials. Previous studies examined different approaches for immunotherapy to HDM with mixed results. Langer et al. published the results of a randomized, double-blind, placebo-controlled trial of HDM sublingual immunotherapy (SLIT) or placebo for 18 months in 91 children and adults with AD and positive skin test result and/or Immunoglobulin E to Dermatophagoides pteronyssinus. After 18 months, patients treated with HDM SLIT achieved greater reductions in the SCOring AD (SCORAD) index and were more likely to achieve an Investigator’s Global Assessment score of clear or almost clear compared to placebo. Headache and abdominal pain were the most common adverse events reported by both groups. Efficacy of HDM SLIT in this study was relatively modest. Nevertheless, it appears to be a safe therapy and a reasonable adjunctive therapy in patients with AD whose disease is believed to be triggered by HDM.
- We are fortunate to have multiple non-steroidal topical therapies for atopic dermatitis, including crisaborole ointment, pimecrolimus cream and tacrolimus ointment. A number of questions remain about how these therapies compare with each other and with topical corticosteroids. Some of these questions were answered in two recent studies.
- Thom et al. compared individual data from two phase 3 studies of crisaborole ointment with previously published data for topical pimecrolimus and tacrolimus in patients ≥2 years with mild-to-moderate AD using an approach referred to as unanchored matching-adjusted indirect comparison. By week 6, the odds of achieving Investigator’s Static Global Assessment score of 0/1 was higher for crisaborole ointment vs. pimecrolimus cream and tacrolimus 0.03% ointment.
- Salava et al. followed 152 children age 1-3 years with moderate-severe AD for 36 months. They found no significant differences of topical tacrolimus 0.03% or 0.1% ointment vs. low or mid potency topical corticosteroids on AD severity (as judged by the eczema area and severity index), skin or other infections, and various cytokine levels.
While these data do not replace the need for head-to-head studies, they do provide important context about comparative efficacy and safety of the various topical agents in our toolbox.
References
- Ben Mordehai Y et al. Long-Term Narrowband UV-B Efficacy in Moderate to Severe Atopic Dermatitis. Dermatitis. 2021 (Nov 27).
- Langer SS et al. Efficacy of house dust mite sublingual immunotherapy in patients with atopic dermatitis: a randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol Pract. 2021 (Nov 9).
- Thom H et al. Matching-Adjusted Indirect Comparison of Crisaborole Ointment 2% vs. Topical Calcineurin Inhibitors in the Treatment of Patients with Mild-to-Moderate Atopic Dermatitis Dermatol Ther (Heidelb). 2021 (Dec 8).
- Salava A et al. Safety of tacrolimus 0.03% and 0.1% ointments in young children with atopic dermatitis - a 36-month follow-up study. Clin Exp Dermatol. 2021 (Nov 19).
George Washington University School of Medicine and Health Sciences
Washington, DC
A new era of evidence-based practice for atopic dermatitis
Atopic dermatitis (AD) is one of the most common diseases of childhood and still very common in adults worldwide. AD is also a very burdensome disease with considerable patient-burden. Despite the enormous population- and patient- burden, there remain many unmet needs in the management of AD. In addition, many treatments commonly used in AD had scant or mixed evidence regarding their efficacy and safety. For example, topical corticosteroids (TCS) are the workhorse for treatment in AD and most other inflammatory skin diseases. Yet, virtually everything we know about the efficacy of TCS comes from vasoconstriction proxy assays with almost no studies formally studying the efficacy of TCS in AD. Similarly, many therapies used off-label to treat more severe AD, such as phototherapy or allergen immunotherapy have inconsistent evidence to guide their use. Well, things are finally changing and the evidence is coming in at a frenzied pace. Development of multiple novel therapeutics in AD led to renewed interest in studying the efficacy and safety of older therapies as well.
- Phototherapy is an important treatment modality in AD patients who have an inadequate response to topical therapy. Many different modalities and devices were used to treat AD over the years, including narrowband ultraviolet B (NBUVB) and ultraviolet A (UVA)-1. NBUVB is the most commonly used approach in the United States and some other regions of the world. Ben Mordehai et al. published the results of a retrospective cohort study of 390 Israeli patients with moderate-severe AD treated with NBUVB therapy between 2000-2017 with ≥3 years of follow-up. Overall, 55.4% achieved an Investigator’s Global Assessment score of clear or almost clear. Facial involvement, occurrence of adverse effects, fewer treatments, and pretreatment immunoglobulin E levels >4000 IU/ml were associated with poorer clinical response to NBUVB. Median duration of response was 12 months with more relapses in children (<18 years).
- House dust mites (HDM) were previously shown to be triggers of AD via Immunoglobulin E dependent and independent mechanisms. Unfortunately, HDM avoidance is challenging for patients and has not proven to be reliably effective in clinical trials. Previous studies examined different approaches for immunotherapy to HDM with mixed results. Langer et al. published the results of a randomized, double-blind, placebo-controlled trial of HDM sublingual immunotherapy (SLIT) or placebo for 18 months in 91 children and adults with AD and positive skin test result and/or Immunoglobulin E to Dermatophagoides pteronyssinus. After 18 months, patients treated with HDM SLIT achieved greater reductions in the SCOring AD (SCORAD) index and were more likely to achieve an Investigator’s Global Assessment score of clear or almost clear compared to placebo. Headache and abdominal pain were the most common adverse events reported by both groups. Efficacy of HDM SLIT in this study was relatively modest. Nevertheless, it appears to be a safe therapy and a reasonable adjunctive therapy in patients with AD whose disease is believed to be triggered by HDM.
- We are fortunate to have multiple non-steroidal topical therapies for atopic dermatitis, including crisaborole ointment, pimecrolimus cream and tacrolimus ointment. A number of questions remain about how these therapies compare with each other and with topical corticosteroids. Some of these questions were answered in two recent studies.
- Thom et al. compared individual data from two phase 3 studies of crisaborole ointment with previously published data for topical pimecrolimus and tacrolimus in patients ≥2 years with mild-to-moderate AD using an approach referred to as unanchored matching-adjusted indirect comparison. By week 6, the odds of achieving Investigator’s Static Global Assessment score of 0/1 was higher for crisaborole ointment vs. pimecrolimus cream and tacrolimus 0.03% ointment.
- Salava et al. followed 152 children age 1-3 years with moderate-severe AD for 36 months. They found no significant differences of topical tacrolimus 0.03% or 0.1% ointment vs. low or mid potency topical corticosteroids on AD severity (as judged by the eczema area and severity index), skin or other infections, and various cytokine levels.
While these data do not replace the need for head-to-head studies, they do provide important context about comparative efficacy and safety of the various topical agents in our toolbox.
References
- Ben Mordehai Y et al. Long-Term Narrowband UV-B Efficacy in Moderate to Severe Atopic Dermatitis. Dermatitis. 2021 (Nov 27).
- Langer SS et al. Efficacy of house dust mite sublingual immunotherapy in patients with atopic dermatitis: a randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol Pract. 2021 (Nov 9).
- Thom H et al. Matching-Adjusted Indirect Comparison of Crisaborole Ointment 2% vs. Topical Calcineurin Inhibitors in the Treatment of Patients with Mild-to-Moderate Atopic Dermatitis Dermatol Ther (Heidelb). 2021 (Dec 8).
- Salava A et al. Safety of tacrolimus 0.03% and 0.1% ointments in young children with atopic dermatitis - a 36-month follow-up study. Clin Exp Dermatol. 2021 (Nov 19).
George Washington University School of Medicine and Health Sciences
Washington, DC
A new era of evidence-based practice for atopic dermatitis
Atopic dermatitis (AD) is one of the most common diseases of childhood and still very common in adults worldwide. AD is also a very burdensome disease with considerable patient-burden. Despite the enormous population- and patient- burden, there remain many unmet needs in the management of AD. In addition, many treatments commonly used in AD had scant or mixed evidence regarding their efficacy and safety. For example, topical corticosteroids (TCS) are the workhorse for treatment in AD and most other inflammatory skin diseases. Yet, virtually everything we know about the efficacy of TCS comes from vasoconstriction proxy assays with almost no studies formally studying the efficacy of TCS in AD. Similarly, many therapies used off-label to treat more severe AD, such as phototherapy or allergen immunotherapy have inconsistent evidence to guide their use. Well, things are finally changing and the evidence is coming in at a frenzied pace. Development of multiple novel therapeutics in AD led to renewed interest in studying the efficacy and safety of older therapies as well.
- Phototherapy is an important treatment modality in AD patients who have an inadequate response to topical therapy. Many different modalities and devices were used to treat AD over the years, including narrowband ultraviolet B (NBUVB) and ultraviolet A (UVA)-1. NBUVB is the most commonly used approach in the United States and some other regions of the world. Ben Mordehai et al. published the results of a retrospective cohort study of 390 Israeli patients with moderate-severe AD treated with NBUVB therapy between 2000-2017 with ≥3 years of follow-up. Overall, 55.4% achieved an Investigator’s Global Assessment score of clear or almost clear. Facial involvement, occurrence of adverse effects, fewer treatments, and pretreatment immunoglobulin E levels >4000 IU/ml were associated with poorer clinical response to NBUVB. Median duration of response was 12 months with more relapses in children (<18 years).
- House dust mites (HDM) were previously shown to be triggers of AD via Immunoglobulin E dependent and independent mechanisms. Unfortunately, HDM avoidance is challenging for patients and has not proven to be reliably effective in clinical trials. Previous studies examined different approaches for immunotherapy to HDM with mixed results. Langer et al. published the results of a randomized, double-blind, placebo-controlled trial of HDM sublingual immunotherapy (SLIT) or placebo for 18 months in 91 children and adults with AD and positive skin test result and/or Immunoglobulin E to Dermatophagoides pteronyssinus. After 18 months, patients treated with HDM SLIT achieved greater reductions in the SCOring AD (SCORAD) index and were more likely to achieve an Investigator’s Global Assessment score of clear or almost clear compared to placebo. Headache and abdominal pain were the most common adverse events reported by both groups. Efficacy of HDM SLIT in this study was relatively modest. Nevertheless, it appears to be a safe therapy and a reasonable adjunctive therapy in patients with AD whose disease is believed to be triggered by HDM.
- We are fortunate to have multiple non-steroidal topical therapies for atopic dermatitis, including crisaborole ointment, pimecrolimus cream and tacrolimus ointment. A number of questions remain about how these therapies compare with each other and with topical corticosteroids. Some of these questions were answered in two recent studies.
- Thom et al. compared individual data from two phase 3 studies of crisaborole ointment with previously published data for topical pimecrolimus and tacrolimus in patients ≥2 years with mild-to-moderate AD using an approach referred to as unanchored matching-adjusted indirect comparison. By week 6, the odds of achieving Investigator’s Static Global Assessment score of 0/1 was higher for crisaborole ointment vs. pimecrolimus cream and tacrolimus 0.03% ointment.
- Salava et al. followed 152 children age 1-3 years with moderate-severe AD for 36 months. They found no significant differences of topical tacrolimus 0.03% or 0.1% ointment vs. low or mid potency topical corticosteroids on AD severity (as judged by the eczema area and severity index), skin or other infections, and various cytokine levels.
While these data do not replace the need for head-to-head studies, they do provide important context about comparative efficacy and safety of the various topical agents in our toolbox.
References
- Ben Mordehai Y et al. Long-Term Narrowband UV-B Efficacy in Moderate to Severe Atopic Dermatitis. Dermatitis. 2021 (Nov 27).
- Langer SS et al. Efficacy of house dust mite sublingual immunotherapy in patients with atopic dermatitis: a randomized, double-blind, placebo-controlled trial. J Allergy Clin Immunol Pract. 2021 (Nov 9).
- Thom H et al. Matching-Adjusted Indirect Comparison of Crisaborole Ointment 2% vs. Topical Calcineurin Inhibitors in the Treatment of Patients with Mild-to-Moderate Atopic Dermatitis Dermatol Ther (Heidelb). 2021 (Dec 8).
- Salava A et al. Safety of tacrolimus 0.03% and 0.1% ointments in young children with atopic dermatitis - a 36-month follow-up study. Clin Exp Dermatol. 2021 (Nov 19).
Clinical Edge Journal Scan Commentary: CAP January 2022
The practitioner’s primary responsibility in managing respiratory infection is to determine which patients with community acquired pneumonia (CAP) warrant hospitalization and more aggressive management. Standard practice for mild infection dictates empiric administration of 5 days of antimicrobial agents1 particularly for the youngest, oldest and patients with underlying comorbid conditions, usually on an outpatient basis with careful follow-up.
Variables for hospitalization and for the selection of antibiotic therapy include the likelihood of a bacterial etiology, epidemiologic considerations, clinical symptoms, predisposing host factors, age, and radiographic findings. Patients who have viral processes generally have low-grade fever and are usually uncomfortable, although they may not appear toxic. However, it is not possible to distinguish between viral and bacterial pneumonia on clinical grounds alone, particularly with the emergence of COVID-19 (SARS-CoV-2), as rapid progression of an initially mild viral upper respiratory infection may become life threatening, particularly in patients with comorbid conditions, such as pulmonary disease, diabetes, and immunodeficiency. All patients with severe CAP should be tested for this viral agent. A recent study of 96 patients with chronic obstructive pulmonary disease (COPD) and COVID-19 infection showed they had higher intensive care unit (ICU) admissions, ventilation requirements, cardiovascular events, and mortality as compared to 1,129 hospitalized patients with COPD and non-COVID-19 infection.2 In addition to COVID-19, type 2 diabetes mellitus must also be considered, as such patients developing severe CAP from all causes have a higher mortality and poorer clinical outcomes than those without diabetes.3
Predicting which patients are likely to progress to severe disease from CAP is a challenging task. In the past clinicians relied on clinical assessment, along with some inflammatory lab studies such as the complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and procalcitonin. Newer tests have recently been studied for their ability to inform prognosis and likely mortality. A very simple test is the admission blood glucose level, which, if increased at hospital admission, is associated with a higher mortality.4 More recently the quick sequential organ failure assessment (qSOFA) score was shown to be better than the Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) minor criteria score in predicting mortality.5 A potential new laboratory test, serum IL-17 concentrations, demonstrated a positive correlation with CAP severity, ICU admission, longer hospital stay, mechanical ventilation, and mortality.6
Current studies have identified some potential advantages of newer antibiotics. Cefoperazone-sulbactam was shown to be equivalent to piperacillin-tazobactam (PIP-TAZO) for treating severe CAP in elderly patients, thereby avoiding the potential acute kidney injury (AKI) of the PIP-TAZO – vancomycin combination.7 This benefit of reduced AKI was supported by a retrospective cohort study that included 449,535 hospitalized adult patients with CAP.8
In a phase 3 study, lefamulin was as effective as moxifloxacin in treating bacterial CAP, including drug-resistant strains and typical, atypical, and polymicrobial infections.9 Of 1,289 study patients, a pathogen was identified in 709. Side effects were minor. This antibiotic has a unique mechanism of action through inhibition of protein synthesis, preventing the binding of transfer RNA.
Adjunctive oral dexamethasone therapy for CAP has been advocated by some experts. In a study of 354 non-ICU patients, a shorter hospital stay was seen in patients who received dexamethasone vs. placebo (4 vs. 6 days) but only in patients who had elevated neutrophil or WBC counts, or high neutrophil-lymphocyte ratios; otherwise there was no difference.10
References
- Vaughn VM et al. a statewide collaborative quality initiative to improve antibiotic duration and outcomes in patients hospitalized with uncomplicated community-acquired pneumonia. Clin Infect Dis. 2021(Nov 13):ciab950 (Nov 13).
- Sheikh D et al. Clinical outcomes in patients with COPD hospitalized with SARS-CoV-2 versus non-SARS-CoV-2 community-acquired pneumonia. Respir Med. 2021(Dec 8);191:106714.
- Huang D et al. Clinical characteristics and risk factors associated with mortality in patients with severe community-acquired pneumonia and type 2 diabetes mellitus. Crit Care. 2021(Dec 7);25:419.
- Shen Y et al. Association of admission blood glucose level with all-cause mortality according to age in patients with community acquired pneumonia. Int J Gen Med. 2021(Nov 6);14:7775-7781.
- Guo Q et al. qSOFA predicted pneumonia mortality better than minor criteria and worse than CURB-65 with robust elements and higher convergence. Am J Emerg Med. 2022(Feb);52:1-7.
- Feng CM et al. Serum interleukin-17 predicts severity and prognosis in patients with community acquired pneumonia: a prospective cohort study. BMC Pulm Med. 2021(Dec 2);21:393.
- Huang CT et al. Clinical effectiveness of cefoperazone-sulbactam versus piperacillin-tazobactam for the treatment of pneumonia in the elderly population. Int J Antimicrob Agents. 2021(Dec 4);106491.
- Le P et al. Association of antibiotic use and acute kidney injury in patients hospitalized with community-acquired pneumonia. Curr Med Res Opin. 2021 (Nov 15).
- Paukner S et al. Pooled microbiological findings and efficacy outcomes by pathogen in adults with community-acquired bacterial pneumonia from the Lefamulin Evaluation Against Pneumonia (LEAP) 1 and LEAP 2 phase 3 trials of lefamulin versus moxifloxacin. J Glob Antimicrob Resist. 2021 (Nov 14).
- Wittermans E et al. Neutrophil count, lymphocyte count and neutrophil-to-lymphocyte ratio in relation to response to adjunctive dexamethasone treatment in community-acquired pneumonia. Eur J Intern Med. 2021 (Nov 12).
The practitioner’s primary responsibility in managing respiratory infection is to determine which patients with community acquired pneumonia (CAP) warrant hospitalization and more aggressive management. Standard practice for mild infection dictates empiric administration of 5 days of antimicrobial agents1 particularly for the youngest, oldest and patients with underlying comorbid conditions, usually on an outpatient basis with careful follow-up.
Variables for hospitalization and for the selection of antibiotic therapy include the likelihood of a bacterial etiology, epidemiologic considerations, clinical symptoms, predisposing host factors, age, and radiographic findings. Patients who have viral processes generally have low-grade fever and are usually uncomfortable, although they may not appear toxic. However, it is not possible to distinguish between viral and bacterial pneumonia on clinical grounds alone, particularly with the emergence of COVID-19 (SARS-CoV-2), as rapid progression of an initially mild viral upper respiratory infection may become life threatening, particularly in patients with comorbid conditions, such as pulmonary disease, diabetes, and immunodeficiency. All patients with severe CAP should be tested for this viral agent. A recent study of 96 patients with chronic obstructive pulmonary disease (COPD) and COVID-19 infection showed they had higher intensive care unit (ICU) admissions, ventilation requirements, cardiovascular events, and mortality as compared to 1,129 hospitalized patients with COPD and non-COVID-19 infection.2 In addition to COVID-19, type 2 diabetes mellitus must also be considered, as such patients developing severe CAP from all causes have a higher mortality and poorer clinical outcomes than those without diabetes.3
Predicting which patients are likely to progress to severe disease from CAP is a challenging task. In the past clinicians relied on clinical assessment, along with some inflammatory lab studies such as the complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and procalcitonin. Newer tests have recently been studied for their ability to inform prognosis and likely mortality. A very simple test is the admission blood glucose level, which, if increased at hospital admission, is associated with a higher mortality.4 More recently the quick sequential organ failure assessment (qSOFA) score was shown to be better than the Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) minor criteria score in predicting mortality.5 A potential new laboratory test, serum IL-17 concentrations, demonstrated a positive correlation with CAP severity, ICU admission, longer hospital stay, mechanical ventilation, and mortality.6
Current studies have identified some potential advantages of newer antibiotics. Cefoperazone-sulbactam was shown to be equivalent to piperacillin-tazobactam (PIP-TAZO) for treating severe CAP in elderly patients, thereby avoiding the potential acute kidney injury (AKI) of the PIP-TAZO – vancomycin combination.7 This benefit of reduced AKI was supported by a retrospective cohort study that included 449,535 hospitalized adult patients with CAP.8
In a phase 3 study, lefamulin was as effective as moxifloxacin in treating bacterial CAP, including drug-resistant strains and typical, atypical, and polymicrobial infections.9 Of 1,289 study patients, a pathogen was identified in 709. Side effects were minor. This antibiotic has a unique mechanism of action through inhibition of protein synthesis, preventing the binding of transfer RNA.
Adjunctive oral dexamethasone therapy for CAP has been advocated by some experts. In a study of 354 non-ICU patients, a shorter hospital stay was seen in patients who received dexamethasone vs. placebo (4 vs. 6 days) but only in patients who had elevated neutrophil or WBC counts, or high neutrophil-lymphocyte ratios; otherwise there was no difference.10
References
- Vaughn VM et al. a statewide collaborative quality initiative to improve antibiotic duration and outcomes in patients hospitalized with uncomplicated community-acquired pneumonia. Clin Infect Dis. 2021(Nov 13):ciab950 (Nov 13).
- Sheikh D et al. Clinical outcomes in patients with COPD hospitalized with SARS-CoV-2 versus non-SARS-CoV-2 community-acquired pneumonia. Respir Med. 2021(Dec 8);191:106714.
- Huang D et al. Clinical characteristics and risk factors associated with mortality in patients with severe community-acquired pneumonia and type 2 diabetes mellitus. Crit Care. 2021(Dec 7);25:419.
- Shen Y et al. Association of admission blood glucose level with all-cause mortality according to age in patients with community acquired pneumonia. Int J Gen Med. 2021(Nov 6);14:7775-7781.
- Guo Q et al. qSOFA predicted pneumonia mortality better than minor criteria and worse than CURB-65 with robust elements and higher convergence. Am J Emerg Med. 2022(Feb);52:1-7.
- Feng CM et al. Serum interleukin-17 predicts severity and prognosis in patients with community acquired pneumonia: a prospective cohort study. BMC Pulm Med. 2021(Dec 2);21:393.
- Huang CT et al. Clinical effectiveness of cefoperazone-sulbactam versus piperacillin-tazobactam for the treatment of pneumonia in the elderly population. Int J Antimicrob Agents. 2021(Dec 4);106491.
- Le P et al. Association of antibiotic use and acute kidney injury in patients hospitalized with community-acquired pneumonia. Curr Med Res Opin. 2021 (Nov 15).
- Paukner S et al. Pooled microbiological findings and efficacy outcomes by pathogen in adults with community-acquired bacterial pneumonia from the Lefamulin Evaluation Against Pneumonia (LEAP) 1 and LEAP 2 phase 3 trials of lefamulin versus moxifloxacin. J Glob Antimicrob Resist. 2021 (Nov 14).
- Wittermans E et al. Neutrophil count, lymphocyte count and neutrophil-to-lymphocyte ratio in relation to response to adjunctive dexamethasone treatment in community-acquired pneumonia. Eur J Intern Med. 2021 (Nov 12).
The practitioner’s primary responsibility in managing respiratory infection is to determine which patients with community acquired pneumonia (CAP) warrant hospitalization and more aggressive management. Standard practice for mild infection dictates empiric administration of 5 days of antimicrobial agents1 particularly for the youngest, oldest and patients with underlying comorbid conditions, usually on an outpatient basis with careful follow-up.
Variables for hospitalization and for the selection of antibiotic therapy include the likelihood of a bacterial etiology, epidemiologic considerations, clinical symptoms, predisposing host factors, age, and radiographic findings. Patients who have viral processes generally have low-grade fever and are usually uncomfortable, although they may not appear toxic. However, it is not possible to distinguish between viral and bacterial pneumonia on clinical grounds alone, particularly with the emergence of COVID-19 (SARS-CoV-2), as rapid progression of an initially mild viral upper respiratory infection may become life threatening, particularly in patients with comorbid conditions, such as pulmonary disease, diabetes, and immunodeficiency. All patients with severe CAP should be tested for this viral agent. A recent study of 96 patients with chronic obstructive pulmonary disease (COPD) and COVID-19 infection showed they had higher intensive care unit (ICU) admissions, ventilation requirements, cardiovascular events, and mortality as compared to 1,129 hospitalized patients with COPD and non-COVID-19 infection.2 In addition to COVID-19, type 2 diabetes mellitus must also be considered, as such patients developing severe CAP from all causes have a higher mortality and poorer clinical outcomes than those without diabetes.3
Predicting which patients are likely to progress to severe disease from CAP is a challenging task. In the past clinicians relied on clinical assessment, along with some inflammatory lab studies such as the complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and procalcitonin. Newer tests have recently been studied for their ability to inform prognosis and likely mortality. A very simple test is the admission blood glucose level, which, if increased at hospital admission, is associated with a higher mortality.4 More recently the quick sequential organ failure assessment (qSOFA) score was shown to be better than the Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) minor criteria score in predicting mortality.5 A potential new laboratory test, serum IL-17 concentrations, demonstrated a positive correlation with CAP severity, ICU admission, longer hospital stay, mechanical ventilation, and mortality.6
Current studies have identified some potential advantages of newer antibiotics. Cefoperazone-sulbactam was shown to be equivalent to piperacillin-tazobactam (PIP-TAZO) for treating severe CAP in elderly patients, thereby avoiding the potential acute kidney injury (AKI) of the PIP-TAZO – vancomycin combination.7 This benefit of reduced AKI was supported by a retrospective cohort study that included 449,535 hospitalized adult patients with CAP.8
In a phase 3 study, lefamulin was as effective as moxifloxacin in treating bacterial CAP, including drug-resistant strains and typical, atypical, and polymicrobial infections.9 Of 1,289 study patients, a pathogen was identified in 709. Side effects were minor. This antibiotic has a unique mechanism of action through inhibition of protein synthesis, preventing the binding of transfer RNA.
Adjunctive oral dexamethasone therapy for CAP has been advocated by some experts. In a study of 354 non-ICU patients, a shorter hospital stay was seen in patients who received dexamethasone vs. placebo (4 vs. 6 days) but only in patients who had elevated neutrophil or WBC counts, or high neutrophil-lymphocyte ratios; otherwise there was no difference.10
References
- Vaughn VM et al. a statewide collaborative quality initiative to improve antibiotic duration and outcomes in patients hospitalized with uncomplicated community-acquired pneumonia. Clin Infect Dis. 2021(Nov 13):ciab950 (Nov 13).
- Sheikh D et al. Clinical outcomes in patients with COPD hospitalized with SARS-CoV-2 versus non-SARS-CoV-2 community-acquired pneumonia. Respir Med. 2021(Dec 8);191:106714.
- Huang D et al. Clinical characteristics and risk factors associated with mortality in patients with severe community-acquired pneumonia and type 2 diabetes mellitus. Crit Care. 2021(Dec 7);25:419.
- Shen Y et al. Association of admission blood glucose level with all-cause mortality according to age in patients with community acquired pneumonia. Int J Gen Med. 2021(Nov 6);14:7775-7781.
- Guo Q et al. qSOFA predicted pneumonia mortality better than minor criteria and worse than CURB-65 with robust elements and higher convergence. Am J Emerg Med. 2022(Feb);52:1-7.
- Feng CM et al. Serum interleukin-17 predicts severity and prognosis in patients with community acquired pneumonia: a prospective cohort study. BMC Pulm Med. 2021(Dec 2);21:393.
- Huang CT et al. Clinical effectiveness of cefoperazone-sulbactam versus piperacillin-tazobactam for the treatment of pneumonia in the elderly population. Int J Antimicrob Agents. 2021(Dec 4);106491.
- Le P et al. Association of antibiotic use and acute kidney injury in patients hospitalized with community-acquired pneumonia. Curr Med Res Opin. 2021 (Nov 15).
- Paukner S et al. Pooled microbiological findings and efficacy outcomes by pathogen in adults with community-acquired bacterial pneumonia from the Lefamulin Evaluation Against Pneumonia (LEAP) 1 and LEAP 2 phase 3 trials of lefamulin versus moxifloxacin. J Glob Antimicrob Resist. 2021 (Nov 14).
- Wittermans E et al. Neutrophil count, lymphocyte count and neutrophil-to-lymphocyte ratio in relation to response to adjunctive dexamethasone treatment in community-acquired pneumonia. Eur J Intern Med. 2021 (Nov 12).
Quality measurement in gastroenterology: A vision for the future
Modern efforts to monitor and improve quality in health care can trace their roots to the early 20th century. At that time, hospitals initiated mechanisms to ensure standard practices for privileging clinicians, reporting medical records and clinical data, and establishing supervised diagnostic facilities. Years later, Avedis Donabedian published “Evaluating the Quality of Medical Care,” which outlined how health care should be measured across three areas – structure, process, and outcome – and became a foundational rubric for assessing quality in medicine.
Over the ensuing decades, with the rise of professional society guidelines and increasing government involvement in the reimbursement of health care, establishing benchmarks and tracking clinical performance has become increasingly important. The passage of the Affordable Care Act subsequently established a formal, legislative mandate for assessing clinical quality tied to reimbursement. Although the context, consequences, and details for reporting have evolved, quality tracking is now firmly entrenched across clinical practice, including gastroenterology. One such mechanism for this is the Merit-Based Incentive Payment System (MIPS), which is a quality payment program (QPP) administered by the Centers for Medicare & Medicaid Services. Today, both government and private payers are assessing measurements and improvements of quality to satisfy the Quintuple Aim of achieving better health outcomes, seeking efficient cost of care, improving patient experience, improving provider experience, and enhancing equity through the reduction health inequalities.
As we transition from a fee-based to a value-based care model, several important developments relevant to the practicing gastroenterologist are likely to occur as the broader landscape of quality reporting will continue shifting. This article will outline a vision of the future in quality measurement for gastroenterology.
Gastroenterologists have relatively few specialty-specific measures on which to report. The widespread use of the adenoma detection rate for screening colonoscopy does represent a success in quality improvement because it is easily calculated, is reproducible, and has been consistently associated with clinical outcomes. But the overall measure set is limited to screening colonoscopy and the management of viral hepatitis, meaning large areas of our practice are not included in this set. Developing new metrics related to broader areas of practice will be necessary to address this current shortcoming and increase the impact of quality programs to clinicians. Indeed, a recent environmental scan performed by the Core Quality Measures Collaborative, a public-private coalition of leaders working to facilitate measure alignment, proposed future areas for development, including gastroesophageal reflux disease, nonalcoholic fatty liver disease, and medication management.
The American Gastroenterological Association, through its defined process of guideline-to-measure development, has responded by creating metrics for the management of acute pancreatitis, Lynch syndrome testing, and eradicating Helicobacter pylori in the context of gastric intestinal metaplasia; additionally, previously defined measures exist for Barrett’s esophagus and inflammatory bowel disease. Therefore, gastroenterologists can expect to report on an expanding collection of measures in the future.
However, recognizing that not all measures may be equally applicable across populations and acknowledging the importance of risk adjustment, incorporating at least an assessment for risk stratification in their future development is vital. Specifically, social risk factors will need to be accounted for during development in ways that might include risk adjustment or stratification by groups. Increasing data demonstrate that clinician performance can vary by population served and that social determinants of health (SDoH) should be incorporated into an assessment of outcomes. Risk stratification may allow clinicians or practices to report outcomes by group without jeopardy of incurring performance-based penalties. However, the ultimate goal should be reducing inequities and closing care gaps rather than inadvertently lowering the bar for clinicians who primarily treat disenfranchised populations. Eventually, any new measures aiming to be included in a QPP require formal validity testing, which can delay their inclusion in such a set. Yet including stratification in their development will provide a more robust and accurate assessment of quality of care delivered according to one’s catchment and help serve to minimize the effects of SDoH.
Another way that quality measurement may account for a more comprehensive assessment of care delivered is by bundling similarly provided services, even those across multiple specialties. Such a future model is the MIPS Value Pathways, currently under development by CMS. While the exact make-up and reporting structure remains to be determined, a group of related metrics – for example, for colonic health – would likely be grouped together. This model might include an evaluation of a practice’s performance in screening colonoscopy, Lynch testing practices, and inflammatory bowel disease management, which could also be relevant to surgeons, pathologists, and oncologists. This paradigm could serve to increase quality alignment across specialties and reinforce a commitment toward improving care delivery and fulfill a value-based mandate.
Within this framework, though, a shared challenge across specialties exists for the capture and reporting of clinical data. The financial and time costs for quality reporting are well documented, therefore any future vision of quality must address means to ease this reporting burden. Accounting for this would be especially impactful to independent as well as small- to moderate-sized practices, which must provide their own resources for collecting and reporting, with the QPP payment adjustments often insufficient to replace lost revenue or expenses. Some administrative relief has been provided by CMS during the current COVID-19 pandemic, but this focused on allowing select clinicians to avoid reporting rather than addressing the fundamental challenges presented by extracting and documenting quality measures. Moving forward, an increasing emphasis will likely be on the use of artificial intelligence (AI), such as natural language processing, combined with discrete code extraction for tracking performance. While AI has the advantage of a more hands-free approach, such a system would itself require monitoring for performance to avoid unintended consequences.
Ultimately, providing high-quality care and improving patient outcomes are universal goals, though demonstrating this aspiration by reporting on quality metrics can be challenging. Quality measurement, though, is now firmly integrated into the fabric of clinical medicine. In the future, more facets of practice will be measured, patient-level factors and cross specialty reporting will increasingly be emphasized, and administrative burdens will be reduced.
Dr. Leiman is assistant professor of medicine at Duke University, Durham, N.C., cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup, and chair of the AGA’s Quality Committee. Dr. Freedman is medical director, SE Territory, Aetna/CVS Health and cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup. Dr. Anjou is a practicing clinical gastroenterologist at Connecticut GI, Torrington, and recent member of the AGA Quality Committee. The authors reported no conflicts related to this article.
Modern efforts to monitor and improve quality in health care can trace their roots to the early 20th century. At that time, hospitals initiated mechanisms to ensure standard practices for privileging clinicians, reporting medical records and clinical data, and establishing supervised diagnostic facilities. Years later, Avedis Donabedian published “Evaluating the Quality of Medical Care,” which outlined how health care should be measured across three areas – structure, process, and outcome – and became a foundational rubric for assessing quality in medicine.
Over the ensuing decades, with the rise of professional society guidelines and increasing government involvement in the reimbursement of health care, establishing benchmarks and tracking clinical performance has become increasingly important. The passage of the Affordable Care Act subsequently established a formal, legislative mandate for assessing clinical quality tied to reimbursement. Although the context, consequences, and details for reporting have evolved, quality tracking is now firmly entrenched across clinical practice, including gastroenterology. One such mechanism for this is the Merit-Based Incentive Payment System (MIPS), which is a quality payment program (QPP) administered by the Centers for Medicare & Medicaid Services. Today, both government and private payers are assessing measurements and improvements of quality to satisfy the Quintuple Aim of achieving better health outcomes, seeking efficient cost of care, improving patient experience, improving provider experience, and enhancing equity through the reduction health inequalities.
As we transition from a fee-based to a value-based care model, several important developments relevant to the practicing gastroenterologist are likely to occur as the broader landscape of quality reporting will continue shifting. This article will outline a vision of the future in quality measurement for gastroenterology.
Gastroenterologists have relatively few specialty-specific measures on which to report. The widespread use of the adenoma detection rate for screening colonoscopy does represent a success in quality improvement because it is easily calculated, is reproducible, and has been consistently associated with clinical outcomes. But the overall measure set is limited to screening colonoscopy and the management of viral hepatitis, meaning large areas of our practice are not included in this set. Developing new metrics related to broader areas of practice will be necessary to address this current shortcoming and increase the impact of quality programs to clinicians. Indeed, a recent environmental scan performed by the Core Quality Measures Collaborative, a public-private coalition of leaders working to facilitate measure alignment, proposed future areas for development, including gastroesophageal reflux disease, nonalcoholic fatty liver disease, and medication management.
The American Gastroenterological Association, through its defined process of guideline-to-measure development, has responded by creating metrics for the management of acute pancreatitis, Lynch syndrome testing, and eradicating Helicobacter pylori in the context of gastric intestinal metaplasia; additionally, previously defined measures exist for Barrett’s esophagus and inflammatory bowel disease. Therefore, gastroenterologists can expect to report on an expanding collection of measures in the future.
However, recognizing that not all measures may be equally applicable across populations and acknowledging the importance of risk adjustment, incorporating at least an assessment for risk stratification in their future development is vital. Specifically, social risk factors will need to be accounted for during development in ways that might include risk adjustment or stratification by groups. Increasing data demonstrate that clinician performance can vary by population served and that social determinants of health (SDoH) should be incorporated into an assessment of outcomes. Risk stratification may allow clinicians or practices to report outcomes by group without jeopardy of incurring performance-based penalties. However, the ultimate goal should be reducing inequities and closing care gaps rather than inadvertently lowering the bar for clinicians who primarily treat disenfranchised populations. Eventually, any new measures aiming to be included in a QPP require formal validity testing, which can delay their inclusion in such a set. Yet including stratification in their development will provide a more robust and accurate assessment of quality of care delivered according to one’s catchment and help serve to minimize the effects of SDoH.
Another way that quality measurement may account for a more comprehensive assessment of care delivered is by bundling similarly provided services, even those across multiple specialties. Such a future model is the MIPS Value Pathways, currently under development by CMS. While the exact make-up and reporting structure remains to be determined, a group of related metrics – for example, for colonic health – would likely be grouped together. This model might include an evaluation of a practice’s performance in screening colonoscopy, Lynch testing practices, and inflammatory bowel disease management, which could also be relevant to surgeons, pathologists, and oncologists. This paradigm could serve to increase quality alignment across specialties and reinforce a commitment toward improving care delivery and fulfill a value-based mandate.
Within this framework, though, a shared challenge across specialties exists for the capture and reporting of clinical data. The financial and time costs for quality reporting are well documented, therefore any future vision of quality must address means to ease this reporting burden. Accounting for this would be especially impactful to independent as well as small- to moderate-sized practices, which must provide their own resources for collecting and reporting, with the QPP payment adjustments often insufficient to replace lost revenue or expenses. Some administrative relief has been provided by CMS during the current COVID-19 pandemic, but this focused on allowing select clinicians to avoid reporting rather than addressing the fundamental challenges presented by extracting and documenting quality measures. Moving forward, an increasing emphasis will likely be on the use of artificial intelligence (AI), such as natural language processing, combined with discrete code extraction for tracking performance. While AI has the advantage of a more hands-free approach, such a system would itself require monitoring for performance to avoid unintended consequences.
Ultimately, providing high-quality care and improving patient outcomes are universal goals, though demonstrating this aspiration by reporting on quality metrics can be challenging. Quality measurement, though, is now firmly integrated into the fabric of clinical medicine. In the future, more facets of practice will be measured, patient-level factors and cross specialty reporting will increasingly be emphasized, and administrative burdens will be reduced.
Dr. Leiman is assistant professor of medicine at Duke University, Durham, N.C., cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup, and chair of the AGA’s Quality Committee. Dr. Freedman is medical director, SE Territory, Aetna/CVS Health and cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup. Dr. Anjou is a practicing clinical gastroenterologist at Connecticut GI, Torrington, and recent member of the AGA Quality Committee. The authors reported no conflicts related to this article.
Modern efforts to monitor and improve quality in health care can trace their roots to the early 20th century. At that time, hospitals initiated mechanisms to ensure standard practices for privileging clinicians, reporting medical records and clinical data, and establishing supervised diagnostic facilities. Years later, Avedis Donabedian published “Evaluating the Quality of Medical Care,” which outlined how health care should be measured across three areas – structure, process, and outcome – and became a foundational rubric for assessing quality in medicine.
Over the ensuing decades, with the rise of professional society guidelines and increasing government involvement in the reimbursement of health care, establishing benchmarks and tracking clinical performance has become increasingly important. The passage of the Affordable Care Act subsequently established a formal, legislative mandate for assessing clinical quality tied to reimbursement. Although the context, consequences, and details for reporting have evolved, quality tracking is now firmly entrenched across clinical practice, including gastroenterology. One such mechanism for this is the Merit-Based Incentive Payment System (MIPS), which is a quality payment program (QPP) administered by the Centers for Medicare & Medicaid Services. Today, both government and private payers are assessing measurements and improvements of quality to satisfy the Quintuple Aim of achieving better health outcomes, seeking efficient cost of care, improving patient experience, improving provider experience, and enhancing equity through the reduction health inequalities.
As we transition from a fee-based to a value-based care model, several important developments relevant to the practicing gastroenterologist are likely to occur as the broader landscape of quality reporting will continue shifting. This article will outline a vision of the future in quality measurement for gastroenterology.
Gastroenterologists have relatively few specialty-specific measures on which to report. The widespread use of the adenoma detection rate for screening colonoscopy does represent a success in quality improvement because it is easily calculated, is reproducible, and has been consistently associated with clinical outcomes. But the overall measure set is limited to screening colonoscopy and the management of viral hepatitis, meaning large areas of our practice are not included in this set. Developing new metrics related to broader areas of practice will be necessary to address this current shortcoming and increase the impact of quality programs to clinicians. Indeed, a recent environmental scan performed by the Core Quality Measures Collaborative, a public-private coalition of leaders working to facilitate measure alignment, proposed future areas for development, including gastroesophageal reflux disease, nonalcoholic fatty liver disease, and medication management.
The American Gastroenterological Association, through its defined process of guideline-to-measure development, has responded by creating metrics for the management of acute pancreatitis, Lynch syndrome testing, and eradicating Helicobacter pylori in the context of gastric intestinal metaplasia; additionally, previously defined measures exist for Barrett’s esophagus and inflammatory bowel disease. Therefore, gastroenterologists can expect to report on an expanding collection of measures in the future.
However, recognizing that not all measures may be equally applicable across populations and acknowledging the importance of risk adjustment, incorporating at least an assessment for risk stratification in their future development is vital. Specifically, social risk factors will need to be accounted for during development in ways that might include risk adjustment or stratification by groups. Increasing data demonstrate that clinician performance can vary by population served and that social determinants of health (SDoH) should be incorporated into an assessment of outcomes. Risk stratification may allow clinicians or practices to report outcomes by group without jeopardy of incurring performance-based penalties. However, the ultimate goal should be reducing inequities and closing care gaps rather than inadvertently lowering the bar for clinicians who primarily treat disenfranchised populations. Eventually, any new measures aiming to be included in a QPP require formal validity testing, which can delay their inclusion in such a set. Yet including stratification in their development will provide a more robust and accurate assessment of quality of care delivered according to one’s catchment and help serve to minimize the effects of SDoH.
Another way that quality measurement may account for a more comprehensive assessment of care delivered is by bundling similarly provided services, even those across multiple specialties. Such a future model is the MIPS Value Pathways, currently under development by CMS. While the exact make-up and reporting structure remains to be determined, a group of related metrics – for example, for colonic health – would likely be grouped together. This model might include an evaluation of a practice’s performance in screening colonoscopy, Lynch testing practices, and inflammatory bowel disease management, which could also be relevant to surgeons, pathologists, and oncologists. This paradigm could serve to increase quality alignment across specialties and reinforce a commitment toward improving care delivery and fulfill a value-based mandate.
Within this framework, though, a shared challenge across specialties exists for the capture and reporting of clinical data. The financial and time costs for quality reporting are well documented, therefore any future vision of quality must address means to ease this reporting burden. Accounting for this would be especially impactful to independent as well as small- to moderate-sized practices, which must provide their own resources for collecting and reporting, with the QPP payment adjustments often insufficient to replace lost revenue or expenses. Some administrative relief has been provided by CMS during the current COVID-19 pandemic, but this focused on allowing select clinicians to avoid reporting rather than addressing the fundamental challenges presented by extracting and documenting quality measures. Moving forward, an increasing emphasis will likely be on the use of artificial intelligence (AI), such as natural language processing, combined with discrete code extraction for tracking performance. While AI has the advantage of a more hands-free approach, such a system would itself require monitoring for performance to avoid unintended consequences.
Ultimately, providing high-quality care and improving patient outcomes are universal goals, though demonstrating this aspiration by reporting on quality metrics can be challenging. Quality measurement, though, is now firmly integrated into the fabric of clinical medicine. In the future, more facets of practice will be measured, patient-level factors and cross specialty reporting will increasingly be emphasized, and administrative burdens will be reduced.
Dr. Leiman is assistant professor of medicine at Duke University, Durham, N.C., cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup, and chair of the AGA’s Quality Committee. Dr. Freedman is medical director, SE Territory, Aetna/CVS Health and cochair of the Core Quality Measure Collaborative Gastroenterology Workgroup. Dr. Anjou is a practicing clinical gastroenterologist at Connecticut GI, Torrington, and recent member of the AGA Quality Committee. The authors reported no conflicts related to this article.
The present and future of virtual care in GI
The rapid and unprecedented expansion of virtual care in response to COVID-19 is likely to leave a permanent mark on how health care is delivered. While this expansion has been critical in the near term in caring for our patients while minimizing risk of exposure during the pandemic, it is vital to be forward thinking in considering the ongoing value of virtual care in optimizing routine patient care and in reaching our high-need patients in rural and other underserved areas. We are likely to hear more in the coming months regarding the short- and long-term impacts of virtual care expansion as we transition away from COVID and begin to consider how to maximize use of virtual care in our routine practice. Many questions remain, including defining the optimal balance between virtual and in-person care, assessing whether virtual care is a substitute for in-person care or simply additive, and understanding the impacts of virtual care on outcomes. On the latter questions, a recent study from Kaiser Permanente Northern California found that primary care visits conducted virtually resulted in modestly higher rates of follow-up outpatient office visits than initial in-person visits, but no significant difference in 7-day ED visits or hospitalizations. Whether these results are generalizable to GI patient populations is unclear.
Highlights from this month’s issue of GIHN include a study evaluating the impact of a “virtual” liver transplant center on access to liver transplant listing among patients in rural areas, another suggesting lower serologic response to COVID-19 vaccines among patients with IBD, a new AGA Clinical Practice Update: Commentary offering tips regarding surveillance after endoscopic submucosal dissection for dysplasia and early-stage GI cancer, and results from a phase 3 clinical trial demonstrating the efficacy of upadacitinib for treatment of moderate to severe ulcerative colitis.
And while the winter weather here in Michigan may suggest otherwise, DDW 2022 is just around the corner – registration opens on Jan. 19, and we look forward to the GI community coming together, whether in person in sunny San Diego or virtually at home or office, for this hybrid conference.
Megan A. Adams, MD, JD, MSc
Editor in Chief
The rapid and unprecedented expansion of virtual care in response to COVID-19 is likely to leave a permanent mark on how health care is delivered. While this expansion has been critical in the near term in caring for our patients while minimizing risk of exposure during the pandemic, it is vital to be forward thinking in considering the ongoing value of virtual care in optimizing routine patient care and in reaching our high-need patients in rural and other underserved areas. We are likely to hear more in the coming months regarding the short- and long-term impacts of virtual care expansion as we transition away from COVID and begin to consider how to maximize use of virtual care in our routine practice. Many questions remain, including defining the optimal balance between virtual and in-person care, assessing whether virtual care is a substitute for in-person care or simply additive, and understanding the impacts of virtual care on outcomes. On the latter questions, a recent study from Kaiser Permanente Northern California found that primary care visits conducted virtually resulted in modestly higher rates of follow-up outpatient office visits than initial in-person visits, but no significant difference in 7-day ED visits or hospitalizations. Whether these results are generalizable to GI patient populations is unclear.
Highlights from this month’s issue of GIHN include a study evaluating the impact of a “virtual” liver transplant center on access to liver transplant listing among patients in rural areas, another suggesting lower serologic response to COVID-19 vaccines among patients with IBD, a new AGA Clinical Practice Update: Commentary offering tips regarding surveillance after endoscopic submucosal dissection for dysplasia and early-stage GI cancer, and results from a phase 3 clinical trial demonstrating the efficacy of upadacitinib for treatment of moderate to severe ulcerative colitis.
And while the winter weather here in Michigan may suggest otherwise, DDW 2022 is just around the corner – registration opens on Jan. 19, and we look forward to the GI community coming together, whether in person in sunny San Diego or virtually at home or office, for this hybrid conference.
Megan A. Adams, MD, JD, MSc
Editor in Chief
The rapid and unprecedented expansion of virtual care in response to COVID-19 is likely to leave a permanent mark on how health care is delivered. While this expansion has been critical in the near term in caring for our patients while minimizing risk of exposure during the pandemic, it is vital to be forward thinking in considering the ongoing value of virtual care in optimizing routine patient care and in reaching our high-need patients in rural and other underserved areas. We are likely to hear more in the coming months regarding the short- and long-term impacts of virtual care expansion as we transition away from COVID and begin to consider how to maximize use of virtual care in our routine practice. Many questions remain, including defining the optimal balance between virtual and in-person care, assessing whether virtual care is a substitute for in-person care or simply additive, and understanding the impacts of virtual care on outcomes. On the latter questions, a recent study from Kaiser Permanente Northern California found that primary care visits conducted virtually resulted in modestly higher rates of follow-up outpatient office visits than initial in-person visits, but no significant difference in 7-day ED visits or hospitalizations. Whether these results are generalizable to GI patient populations is unclear.
Highlights from this month’s issue of GIHN include a study evaluating the impact of a “virtual” liver transplant center on access to liver transplant listing among patients in rural areas, another suggesting lower serologic response to COVID-19 vaccines among patients with IBD, a new AGA Clinical Practice Update: Commentary offering tips regarding surveillance after endoscopic submucosal dissection for dysplasia and early-stage GI cancer, and results from a phase 3 clinical trial demonstrating the efficacy of upadacitinib for treatment of moderate to severe ulcerative colitis.
And while the winter weather here in Michigan may suggest otherwise, DDW 2022 is just around the corner – registration opens on Jan. 19, and we look forward to the GI community coming together, whether in person in sunny San Diego or virtually at home or office, for this hybrid conference.
Megan A. Adams, MD, JD, MSc
Editor in Chief
Are GI hospitalists the future of inpatient care?
Dear colleagues and friends,
After an excellent debate on the future of telemedicine in GI in our most recent Perspectives column, we continue to explore changes in the way we traditionally provide care. In this issue, we discuss the GI hospitalist service, a relatively new but growing model of providing inpatient care. Is this the new ideal, allowing for more efficient care? Or are traditional or alternative models more appropriate? As with most things, the answer often lies somewhere in the middle, driven by local needs and infrastructure. Dr. Tau and Dr. Mehendiratta explore the pros and cons of these different approaches to providing inpatient GI care. I look forward to hearing your thoughts and experiences on the AGA Community forum and by email ([email protected]).
Gyanprakash A. Ketwaroo, MD, MSc, is an assistant professor of medicine at Baylor College of Medicine, Houston. He is an associate editor for GI & Hepatology News.
The dedicated GI hospitalist: Taking ownership not ‘call’
By J. Andy Tau, MD
In my experience, a GI hospitalist provides mutual benefit to patients, employers, and consulting physicians. The patient benefits from more expedient consultations and expert endoscopic therapy, which translates to shorter hospitalizations and improved outcomes. The employer enjoys financial benefits as busy outpatient providers can stay busy without interruption. Consulting physicians enjoy having to only call a single phone number for trusted help from a familiar physician who does not rotate off service. Personally, the position provides the volume to develop valuable therapeutic endoscopy skills and techniques. With one stable physician at the helm, a sense of ownership can develop, rather than a sense of survival until “call” is over.
As a full-time GI hospitalist for a large single-specialty group, I provide inpatient GI and hepatology consultation from 7 a.m. to 5 p.m., Monday-Friday. I do not rotate off service. I cover three hospitals with a total of 1,000 beds with two advanced practice providers and one part-time physician. Except for endoscopic ultrasound, I perform all other endoscopic procedures. The census is usually 25-35 with an average of 10-15 new consults per day.
The most important benefit of a dedicated GI hospitalist is providing expedited consultation and expert endoscopy for patients. I can offer emergent (<6 hour) endoscopy for any patient. An esophageal food impaction is usually resolved within an hour of arrival to the ED during the day. I can help a surgeon intraoperatively on very short notice. As for acute GI bleeding cases, I oversee resuscitative efforts, while the endoscopy team prepares my preferred endoscopic equipment, eliminating surprises and delays before endoscopy. I have developed an expertise in hemostasis and managing esophageal perforations, along with a risk tolerance that cannot be matured in any setting other than daily emergency.
I have enacted evidence-based protocols for GI bleeding, iron-deficiency anemia, colonic pseudo-obstruction, pancreatitis, and liver decompensation, which internists have adopted over time, reducing phone calls and delays in prep or resuscitation.
While the day is unstructured and filled with interruptions, it is also very flexible. As opposed to the set time intervals of an outpatient clinic visit, I can spend an hour in a palliative care meeting or revisit high-risk patients multiple times a day to detect pending deterioration. Combined endoscopic and surgical cases are logistically easy to schedule given my flexibility. For example, patients with choledocholithiasis often can have a combined cholecystectomy and supine endoscopic retrograde cholangiopancreatography (ERCP) in the OR, shaving a day off admission.
My employer benefits financially as the outpatient doctors can stay busy without interruption from the hospital. With secure group messaging, we are able to make joint decisions and arrange close follow up. The relative value units earned from the hospital are high. Combined with proceeds from the professional service agreement with the hospital, they are more than enough to cover my compensation.
Any physician in need of a GI consult needs only to call one number for help. I make it as easy as possible to obtain a consult and never push back, as banal as any consult may seem. I stake my reputation on providing a service that is able, affable, and available. By teaching a consistent message to consulting physicians, I have now effected best evidence-based practices for GI conditions even without engaging me. The most notable examples include antibiotics for variceal bleeding, fluid resuscitation and early feeding for acute pancreatitis, risk stratification for choledocholithiasis, and last but not least, abandoning the inpatient fecal occult blood test.
I am on a first-name basis with every nurse in the hospital now. In exchange for my availability and cell phone number, they place orders for me and protect me from avoidable nuisances.
Many physician groups cover the inpatient service by rotating a week at a time. There can be at times a reluctance to take ownership over a difficult patient and instead a sense of “survival of the call”. However, in my job, “the buck stops with me” even if it is in the form of readmission. For example, I have to take some ownership of indigent patients who cannot easily follow up. Who will remove the stent I placed? How will they pay for Helicobacter pylori eradication or biologic therapy? Another example is diverticular bleeding. While 80% stop on their own, I take extraordinary efforts to endoscopically find and halt the bleeding in order to reduce the recurrence rate. I must find durable solutions because these high-risk patients are my responsibility again when they bounce back to me via the ED.
By way of volume alone, this position has allowed me to develop many therapeutic skills outside of a standard 3-year GI fellowship. While I did only 200 ERCPs in fellowship, I have become proficient in ERCP with around 400 cases per year (mostly native papilla) and have grown comfortable with the needle knife. I have learned endoscopic suturing, luminal stenting, and endoscopic vacuum-assisted therapy for perforation closure independently. Out of necessity, I developed a novel technique in optimizing the use of hemostatic powder by using a bone-wax plug. As endoscopy chief, I can purchase a wide variety of endoscopy equipment, compare brands, and understand the nuances of each.
In conclusion, the dedicated GI hospitalist indirectly improves the efficiency of an outpatient practice, while directly improving inpatient outcomes, collegiality, and even one’s own skills as an endoscopist. While it can be challenging and hectic, with the right mentality towards ownership of the service, it is also an incredibly rewarding position.
Dr. Tau practices with Austin Gastroenterology in Austin, Tex. He disclosed relationships with Cook Medical and Conmed.
Inpatient-only GI hospitalist: Not so fast
By Vaibhav Mehendiratta, MD
Over the past 2 decades, the medical hospitalist system has assumed care of hospitalized patients with the promise of reduced length of stay (LOS) and improved outcomes. Although data on LOS is promising, there have been conflicting results in terms of total medical costs and resource utilization. Inpatient care for patients with complex medical histories often requires regular communication with other subspecialties and outpatient providers to achieve better patient-centered outcomes.
Providing inpatient gastrointestinal care is complicated. Traditional models rely on physicians trying to balance outpatient obligations with inpatient rounding and procedures, which can result in delayed endoscopy and an inability to participate fully in multidisciplinary rounds and family meetings. The complexity of hospitalized patients often requires a multidisciplinary approach with coordination of care that is hard to accomplish in between seeing outpatients. GI groups, both private practice and academics, need to adopt a strategy for inpatient care that is tailored to the hospital system in which they operate.
As one of the largest private practice groups in New England, our experience can provide a framework for others to follow. We provide inpatient GI care at eight hospitals across northern Connecticut. Our inpatient service at the largest tertiary care hospital is composed of one general gastroenterologist, one advanced endoscopist, one transplant hepatologist, two advanced practitioners, and two fellows in training. Each practitioner provides coverage on a rotating basis, typically 1 week at a time every 4-8 weeks. This model also offers flexibility, such that we can typically accommodate urgent outpatient endoscopy for patients who may otherwise require inpatient care. Coverage at the other seven hospitals is tailored to local needs and ranges from half-day to whole-day coverage by general gastroenterologists and advanced practitioners. We believe that our model is financially viable and, based on our experience, inpatient relative value units generated are quite similar to a typical day in outpatient GI practice.
Inpatient GI care accounts for a substantial portion of overall inpatient care in the United States. Endoscopy delays have been the focus of many research articles looking at inpatient GI care. The delays are caused by many factors, including endoscopy unit/staff availability, anesthesia availability, and patient factors. While having a dedicated inpatient GI Hospitalist offers the potential to streamline access for hospital consultations and endoscopy, an exclusive inpatient GI hospitalist may be less familiar with a patient’s chronic GI illness and have different (and perhaps, conflicting) priorities regarding a patient’s care. Having incomplete access to outpatient records or less familiarity with the intricacies of outpatient care could also lead to duplication of work and increase the number of inpatient procedures that may have otherwise been deferred to the outpatient setting.
Additionally, with physician burnout on the rise and particularly in the inpatient setting, one must question the sustainability of an exclusively inpatient GI practice. That is, the hours and demands of inpatient care typically do not allow the quality of life that outpatient care provides. Our model provides time for dedicated inpatient care, while allowing each practitioner ample opportunity to build a robust outpatient practice.
Some health care organizations are adopting an extensivist model to provide comprehensive care to patients with multiple medical problems. Extensivists are outpatient primary care providers who take the time to coordinate with inpatient hospitalists to provide comprehensive care to their patients. Constant contact with outpatient providers during admission is expected to improve patient satisfaction, reduce hospital readmissions, and decrease inpatient resource utilization.
In conclusion, our experience highlights sustained benefits, and distinct advantages, of providing inpatient GI care without a GI hospitalist model. The pendulum in inpatient care keeps swinging and with progress arise new challenges and questions. Close collaboration between gastroenterologists and health systems to develop a program that fits local needs and allows optimal resource allocation will ensure delivery of high-quality inpatient GI care.
Dr. Mehendiratta is a gastroenterologist with Connecticut GI PC, Hartford, and assistant clinical professor in the department of medicine at the University of Connecticut, Farmington. He has no relevant conflicts of interest to disclose.
Dear colleagues and friends,
After an excellent debate on the future of telemedicine in GI in our most recent Perspectives column, we continue to explore changes in the way we traditionally provide care. In this issue, we discuss the GI hospitalist service, a relatively new but growing model of providing inpatient care. Is this the new ideal, allowing for more efficient care? Or are traditional or alternative models more appropriate? As with most things, the answer often lies somewhere in the middle, driven by local needs and infrastructure. Dr. Tau and Dr. Mehendiratta explore the pros and cons of these different approaches to providing inpatient GI care. I look forward to hearing your thoughts and experiences on the AGA Community forum and by email ([email protected]).
Gyanprakash A. Ketwaroo, MD, MSc, is an assistant professor of medicine at Baylor College of Medicine, Houston. He is an associate editor for GI & Hepatology News.
The dedicated GI hospitalist: Taking ownership not ‘call’
By J. Andy Tau, MD
In my experience, a GI hospitalist provides mutual benefit to patients, employers, and consulting physicians. The patient benefits from more expedient consultations and expert endoscopic therapy, which translates to shorter hospitalizations and improved outcomes. The employer enjoys financial benefits as busy outpatient providers can stay busy without interruption. Consulting physicians enjoy having to only call a single phone number for trusted help from a familiar physician who does not rotate off service. Personally, the position provides the volume to develop valuable therapeutic endoscopy skills and techniques. With one stable physician at the helm, a sense of ownership can develop, rather than a sense of survival until “call” is over.
As a full-time GI hospitalist for a large single-specialty group, I provide inpatient GI and hepatology consultation from 7 a.m. to 5 p.m., Monday-Friday. I do not rotate off service. I cover three hospitals with a total of 1,000 beds with two advanced practice providers and one part-time physician. Except for endoscopic ultrasound, I perform all other endoscopic procedures. The census is usually 25-35 with an average of 10-15 new consults per day.
The most important benefit of a dedicated GI hospitalist is providing expedited consultation and expert endoscopy for patients. I can offer emergent (<6 hour) endoscopy for any patient. An esophageal food impaction is usually resolved within an hour of arrival to the ED during the day. I can help a surgeon intraoperatively on very short notice. As for acute GI bleeding cases, I oversee resuscitative efforts, while the endoscopy team prepares my preferred endoscopic equipment, eliminating surprises and delays before endoscopy. I have developed an expertise in hemostasis and managing esophageal perforations, along with a risk tolerance that cannot be matured in any setting other than daily emergency.
I have enacted evidence-based protocols for GI bleeding, iron-deficiency anemia, colonic pseudo-obstruction, pancreatitis, and liver decompensation, which internists have adopted over time, reducing phone calls and delays in prep or resuscitation.
While the day is unstructured and filled with interruptions, it is also very flexible. As opposed to the set time intervals of an outpatient clinic visit, I can spend an hour in a palliative care meeting or revisit high-risk patients multiple times a day to detect pending deterioration. Combined endoscopic and surgical cases are logistically easy to schedule given my flexibility. For example, patients with choledocholithiasis often can have a combined cholecystectomy and supine endoscopic retrograde cholangiopancreatography (ERCP) in the OR, shaving a day off admission.
My employer benefits financially as the outpatient doctors can stay busy without interruption from the hospital. With secure group messaging, we are able to make joint decisions and arrange close follow up. The relative value units earned from the hospital are high. Combined with proceeds from the professional service agreement with the hospital, they are more than enough to cover my compensation.
Any physician in need of a GI consult needs only to call one number for help. I make it as easy as possible to obtain a consult and never push back, as banal as any consult may seem. I stake my reputation on providing a service that is able, affable, and available. By teaching a consistent message to consulting physicians, I have now effected best evidence-based practices for GI conditions even without engaging me. The most notable examples include antibiotics for variceal bleeding, fluid resuscitation and early feeding for acute pancreatitis, risk stratification for choledocholithiasis, and last but not least, abandoning the inpatient fecal occult blood test.
I am on a first-name basis with every nurse in the hospital now. In exchange for my availability and cell phone number, they place orders for me and protect me from avoidable nuisances.
Many physician groups cover the inpatient service by rotating a week at a time. There can be at times a reluctance to take ownership over a difficult patient and instead a sense of “survival of the call”. However, in my job, “the buck stops with me” even if it is in the form of readmission. For example, I have to take some ownership of indigent patients who cannot easily follow up. Who will remove the stent I placed? How will they pay for Helicobacter pylori eradication or biologic therapy? Another example is diverticular bleeding. While 80% stop on their own, I take extraordinary efforts to endoscopically find and halt the bleeding in order to reduce the recurrence rate. I must find durable solutions because these high-risk patients are my responsibility again when they bounce back to me via the ED.
By way of volume alone, this position has allowed me to develop many therapeutic skills outside of a standard 3-year GI fellowship. While I did only 200 ERCPs in fellowship, I have become proficient in ERCP with around 400 cases per year (mostly native papilla) and have grown comfortable with the needle knife. I have learned endoscopic suturing, luminal stenting, and endoscopic vacuum-assisted therapy for perforation closure independently. Out of necessity, I developed a novel technique in optimizing the use of hemostatic powder by using a bone-wax plug. As endoscopy chief, I can purchase a wide variety of endoscopy equipment, compare brands, and understand the nuances of each.
In conclusion, the dedicated GI hospitalist indirectly improves the efficiency of an outpatient practice, while directly improving inpatient outcomes, collegiality, and even one’s own skills as an endoscopist. While it can be challenging and hectic, with the right mentality towards ownership of the service, it is also an incredibly rewarding position.
Dr. Tau practices with Austin Gastroenterology in Austin, Tex. He disclosed relationships with Cook Medical and Conmed.
Inpatient-only GI hospitalist: Not so fast
By Vaibhav Mehendiratta, MD
Over the past 2 decades, the medical hospitalist system has assumed care of hospitalized patients with the promise of reduced length of stay (LOS) and improved outcomes. Although data on LOS is promising, there have been conflicting results in terms of total medical costs and resource utilization. Inpatient care for patients with complex medical histories often requires regular communication with other subspecialties and outpatient providers to achieve better patient-centered outcomes.
Providing inpatient gastrointestinal care is complicated. Traditional models rely on physicians trying to balance outpatient obligations with inpatient rounding and procedures, which can result in delayed endoscopy and an inability to participate fully in multidisciplinary rounds and family meetings. The complexity of hospitalized patients often requires a multidisciplinary approach with coordination of care that is hard to accomplish in between seeing outpatients. GI groups, both private practice and academics, need to adopt a strategy for inpatient care that is tailored to the hospital system in which they operate.
As one of the largest private practice groups in New England, our experience can provide a framework for others to follow. We provide inpatient GI care at eight hospitals across northern Connecticut. Our inpatient service at the largest tertiary care hospital is composed of one general gastroenterologist, one advanced endoscopist, one transplant hepatologist, two advanced practitioners, and two fellows in training. Each practitioner provides coverage on a rotating basis, typically 1 week at a time every 4-8 weeks. This model also offers flexibility, such that we can typically accommodate urgent outpatient endoscopy for patients who may otherwise require inpatient care. Coverage at the other seven hospitals is tailored to local needs and ranges from half-day to whole-day coverage by general gastroenterologists and advanced practitioners. We believe that our model is financially viable and, based on our experience, inpatient relative value units generated are quite similar to a typical day in outpatient GI practice.
Inpatient GI care accounts for a substantial portion of overall inpatient care in the United States. Endoscopy delays have been the focus of many research articles looking at inpatient GI care. The delays are caused by many factors, including endoscopy unit/staff availability, anesthesia availability, and patient factors. While having a dedicated inpatient GI Hospitalist offers the potential to streamline access for hospital consultations and endoscopy, an exclusive inpatient GI hospitalist may be less familiar with a patient’s chronic GI illness and have different (and perhaps, conflicting) priorities regarding a patient’s care. Having incomplete access to outpatient records or less familiarity with the intricacies of outpatient care could also lead to duplication of work and increase the number of inpatient procedures that may have otherwise been deferred to the outpatient setting.
Additionally, with physician burnout on the rise and particularly in the inpatient setting, one must question the sustainability of an exclusively inpatient GI practice. That is, the hours and demands of inpatient care typically do not allow the quality of life that outpatient care provides. Our model provides time for dedicated inpatient care, while allowing each practitioner ample opportunity to build a robust outpatient practice.
Some health care organizations are adopting an extensivist model to provide comprehensive care to patients with multiple medical problems. Extensivists are outpatient primary care providers who take the time to coordinate with inpatient hospitalists to provide comprehensive care to their patients. Constant contact with outpatient providers during admission is expected to improve patient satisfaction, reduce hospital readmissions, and decrease inpatient resource utilization.
In conclusion, our experience highlights sustained benefits, and distinct advantages, of providing inpatient GI care without a GI hospitalist model. The pendulum in inpatient care keeps swinging and with progress arise new challenges and questions. Close collaboration between gastroenterologists and health systems to develop a program that fits local needs and allows optimal resource allocation will ensure delivery of high-quality inpatient GI care.
Dr. Mehendiratta is a gastroenterologist with Connecticut GI PC, Hartford, and assistant clinical professor in the department of medicine at the University of Connecticut, Farmington. He has no relevant conflicts of interest to disclose.
Dear colleagues and friends,
After an excellent debate on the future of telemedicine in GI in our most recent Perspectives column, we continue to explore changes in the way we traditionally provide care. In this issue, we discuss the GI hospitalist service, a relatively new but growing model of providing inpatient care. Is this the new ideal, allowing for more efficient care? Or are traditional or alternative models more appropriate? As with most things, the answer often lies somewhere in the middle, driven by local needs and infrastructure. Dr. Tau and Dr. Mehendiratta explore the pros and cons of these different approaches to providing inpatient GI care. I look forward to hearing your thoughts and experiences on the AGA Community forum and by email ([email protected]).
Gyanprakash A. Ketwaroo, MD, MSc, is an assistant professor of medicine at Baylor College of Medicine, Houston. He is an associate editor for GI & Hepatology News.
The dedicated GI hospitalist: Taking ownership not ‘call’
By J. Andy Tau, MD
In my experience, a GI hospitalist provides mutual benefit to patients, employers, and consulting physicians. The patient benefits from more expedient consultations and expert endoscopic therapy, which translates to shorter hospitalizations and improved outcomes. The employer enjoys financial benefits as busy outpatient providers can stay busy without interruption. Consulting physicians enjoy having to only call a single phone number for trusted help from a familiar physician who does not rotate off service. Personally, the position provides the volume to develop valuable therapeutic endoscopy skills and techniques. With one stable physician at the helm, a sense of ownership can develop, rather than a sense of survival until “call” is over.
As a full-time GI hospitalist for a large single-specialty group, I provide inpatient GI and hepatology consultation from 7 a.m. to 5 p.m., Monday-Friday. I do not rotate off service. I cover three hospitals with a total of 1,000 beds with two advanced practice providers and one part-time physician. Except for endoscopic ultrasound, I perform all other endoscopic procedures. The census is usually 25-35 with an average of 10-15 new consults per day.
The most important benefit of a dedicated GI hospitalist is providing expedited consultation and expert endoscopy for patients. I can offer emergent (<6 hour) endoscopy for any patient. An esophageal food impaction is usually resolved within an hour of arrival to the ED during the day. I can help a surgeon intraoperatively on very short notice. As for acute GI bleeding cases, I oversee resuscitative efforts, while the endoscopy team prepares my preferred endoscopic equipment, eliminating surprises and delays before endoscopy. I have developed an expertise in hemostasis and managing esophageal perforations, along with a risk tolerance that cannot be matured in any setting other than daily emergency.
I have enacted evidence-based protocols for GI bleeding, iron-deficiency anemia, colonic pseudo-obstruction, pancreatitis, and liver decompensation, which internists have adopted over time, reducing phone calls and delays in prep or resuscitation.
While the day is unstructured and filled with interruptions, it is also very flexible. As opposed to the set time intervals of an outpatient clinic visit, I can spend an hour in a palliative care meeting or revisit high-risk patients multiple times a day to detect pending deterioration. Combined endoscopic and surgical cases are logistically easy to schedule given my flexibility. For example, patients with choledocholithiasis often can have a combined cholecystectomy and supine endoscopic retrograde cholangiopancreatography (ERCP) in the OR, shaving a day off admission.
My employer benefits financially as the outpatient doctors can stay busy without interruption from the hospital. With secure group messaging, we are able to make joint decisions and arrange close follow up. The relative value units earned from the hospital are high. Combined with proceeds from the professional service agreement with the hospital, they are more than enough to cover my compensation.
Any physician in need of a GI consult needs only to call one number for help. I make it as easy as possible to obtain a consult and never push back, as banal as any consult may seem. I stake my reputation on providing a service that is able, affable, and available. By teaching a consistent message to consulting physicians, I have now effected best evidence-based practices for GI conditions even without engaging me. The most notable examples include antibiotics for variceal bleeding, fluid resuscitation and early feeding for acute pancreatitis, risk stratification for choledocholithiasis, and last but not least, abandoning the inpatient fecal occult blood test.
I am on a first-name basis with every nurse in the hospital now. In exchange for my availability and cell phone number, they place orders for me and protect me from avoidable nuisances.
Many physician groups cover the inpatient service by rotating a week at a time. There can be at times a reluctance to take ownership over a difficult patient and instead a sense of “survival of the call”. However, in my job, “the buck stops with me” even if it is in the form of readmission. For example, I have to take some ownership of indigent patients who cannot easily follow up. Who will remove the stent I placed? How will they pay for Helicobacter pylori eradication or biologic therapy? Another example is diverticular bleeding. While 80% stop on their own, I take extraordinary efforts to endoscopically find and halt the bleeding in order to reduce the recurrence rate. I must find durable solutions because these high-risk patients are my responsibility again when they bounce back to me via the ED.
By way of volume alone, this position has allowed me to develop many therapeutic skills outside of a standard 3-year GI fellowship. While I did only 200 ERCPs in fellowship, I have become proficient in ERCP with around 400 cases per year (mostly native papilla) and have grown comfortable with the needle knife. I have learned endoscopic suturing, luminal stenting, and endoscopic vacuum-assisted therapy for perforation closure independently. Out of necessity, I developed a novel technique in optimizing the use of hemostatic powder by using a bone-wax plug. As endoscopy chief, I can purchase a wide variety of endoscopy equipment, compare brands, and understand the nuances of each.
In conclusion, the dedicated GI hospitalist indirectly improves the efficiency of an outpatient practice, while directly improving inpatient outcomes, collegiality, and even one’s own skills as an endoscopist. While it can be challenging and hectic, with the right mentality towards ownership of the service, it is also an incredibly rewarding position.
Dr. Tau practices with Austin Gastroenterology in Austin, Tex. He disclosed relationships with Cook Medical and Conmed.
Inpatient-only GI hospitalist: Not so fast
By Vaibhav Mehendiratta, MD
Over the past 2 decades, the medical hospitalist system has assumed care of hospitalized patients with the promise of reduced length of stay (LOS) and improved outcomes. Although data on LOS is promising, there have been conflicting results in terms of total medical costs and resource utilization. Inpatient care for patients with complex medical histories often requires regular communication with other subspecialties and outpatient providers to achieve better patient-centered outcomes.
Providing inpatient gastrointestinal care is complicated. Traditional models rely on physicians trying to balance outpatient obligations with inpatient rounding and procedures, which can result in delayed endoscopy and an inability to participate fully in multidisciplinary rounds and family meetings. The complexity of hospitalized patients often requires a multidisciplinary approach with coordination of care that is hard to accomplish in between seeing outpatients. GI groups, both private practice and academics, need to adopt a strategy for inpatient care that is tailored to the hospital system in which they operate.
As one of the largest private practice groups in New England, our experience can provide a framework for others to follow. We provide inpatient GI care at eight hospitals across northern Connecticut. Our inpatient service at the largest tertiary care hospital is composed of one general gastroenterologist, one advanced endoscopist, one transplant hepatologist, two advanced practitioners, and two fellows in training. Each practitioner provides coverage on a rotating basis, typically 1 week at a time every 4-8 weeks. This model also offers flexibility, such that we can typically accommodate urgent outpatient endoscopy for patients who may otherwise require inpatient care. Coverage at the other seven hospitals is tailored to local needs and ranges from half-day to whole-day coverage by general gastroenterologists and advanced practitioners. We believe that our model is financially viable and, based on our experience, inpatient relative value units generated are quite similar to a typical day in outpatient GI practice.
Inpatient GI care accounts for a substantial portion of overall inpatient care in the United States. Endoscopy delays have been the focus of many research articles looking at inpatient GI care. The delays are caused by many factors, including endoscopy unit/staff availability, anesthesia availability, and patient factors. While having a dedicated inpatient GI Hospitalist offers the potential to streamline access for hospital consultations and endoscopy, an exclusive inpatient GI hospitalist may be less familiar with a patient’s chronic GI illness and have different (and perhaps, conflicting) priorities regarding a patient’s care. Having incomplete access to outpatient records or less familiarity with the intricacies of outpatient care could also lead to duplication of work and increase the number of inpatient procedures that may have otherwise been deferred to the outpatient setting.
Additionally, with physician burnout on the rise and particularly in the inpatient setting, one must question the sustainability of an exclusively inpatient GI practice. That is, the hours and demands of inpatient care typically do not allow the quality of life that outpatient care provides. Our model provides time for dedicated inpatient care, while allowing each practitioner ample opportunity to build a robust outpatient practice.
Some health care organizations are adopting an extensivist model to provide comprehensive care to patients with multiple medical problems. Extensivists are outpatient primary care providers who take the time to coordinate with inpatient hospitalists to provide comprehensive care to their patients. Constant contact with outpatient providers during admission is expected to improve patient satisfaction, reduce hospital readmissions, and decrease inpatient resource utilization.
In conclusion, our experience highlights sustained benefits, and distinct advantages, of providing inpatient GI care without a GI hospitalist model. The pendulum in inpatient care keeps swinging and with progress arise new challenges and questions. Close collaboration between gastroenterologists and health systems to develop a program that fits local needs and allows optimal resource allocation will ensure delivery of high-quality inpatient GI care.
Dr. Mehendiratta is a gastroenterologist with Connecticut GI PC, Hartford, and assistant clinical professor in the department of medicine at the University of Connecticut, Farmington. He has no relevant conflicts of interest to disclose.
Top case
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Vivy Tran, MD, wrote in “Definitive diverticular hemorrhage: Diagnosis and management”:
Diverticular hemorrhage is the most common cause of colonic bleeding, accounting for 20%-65% of cases of severe lower intestinal bleeding in adults. Urgent colonoscopy after purging the colon of blood, clots, and stool is the most accurate method of diagnosing and guiding treatment of definitive diverticular hemorrhage. The diagnosis of definitive diverticular hemorrhage depends upon identification of some stigmata of recent hemorrhage in a single diverticulum, which can include active arterial bleeding, oozing, non-bleeding visible vessel, adherent clot, or flat spot. Although other approaches, such as nuclear medicine scans and angiography of various types (CT, MRI, or standard angiography), for the early diagnosis of patients with severe hematochezia are utilized in many medical centers, only active bleeding can be detected by these techniques.
Would love to hear how diverticular bleeds are managed at your institution.
See how AGA members responded and join the discussion.
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Vivy Tran, MD, wrote in “Definitive diverticular hemorrhage: Diagnosis and management”:
Diverticular hemorrhage is the most common cause of colonic bleeding, accounting for 20%-65% of cases of severe lower intestinal bleeding in adults. Urgent colonoscopy after purging the colon of blood, clots, and stool is the most accurate method of diagnosing and guiding treatment of definitive diverticular hemorrhage. The diagnosis of definitive diverticular hemorrhage depends upon identification of some stigmata of recent hemorrhage in a single diverticulum, which can include active arterial bleeding, oozing, non-bleeding visible vessel, adherent clot, or flat spot. Although other approaches, such as nuclear medicine scans and angiography of various types (CT, MRI, or standard angiography), for the early diagnosis of patients with severe hematochezia are utilized in many medical centers, only active bleeding can be detected by these techniques.
Would love to hear how diverticular bleeds are managed at your institution.
See how AGA members responded and join the discussion.
Physicians with difficult patient scenarios regularly bring their questions to the AGA Community (https://community.gastro.org) to seek advice from colleagues about therapy and disease management options, best practices, and diagnoses. Here’s a preview of a recent popular clinical discussion:
Vivy Tran, MD, wrote in “Definitive diverticular hemorrhage: Diagnosis and management”:
Diverticular hemorrhage is the most common cause of colonic bleeding, accounting for 20%-65% of cases of severe lower intestinal bleeding in adults. Urgent colonoscopy after purging the colon of blood, clots, and stool is the most accurate method of diagnosing and guiding treatment of definitive diverticular hemorrhage. The diagnosis of definitive diverticular hemorrhage depends upon identification of some stigmata of recent hemorrhage in a single diverticulum, which can include active arterial bleeding, oozing, non-bleeding visible vessel, adherent clot, or flat spot. Although other approaches, such as nuclear medicine scans and angiography of various types (CT, MRI, or standard angiography), for the early diagnosis of patients with severe hematochezia are utilized in many medical centers, only active bleeding can be detected by these techniques.
Would love to hear how diverticular bleeds are managed at your institution.
See how AGA members responded and join the discussion.
FDA to review PDE4-inhibitor roflumilast for psoriasis
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
Olanzapine-samidorphan combination for schizophrenia or bipolar I disorder
Approved by the FDA on May 28, 2021, olanzapine-samidorphan combination (OSC) (Lybalvi, manufactured and distributed by Alkermes, Inc. Waltham, MA USA) is intended to help mitigate some of the weight gain that can be anticipated with the use of olanzapine alone (Table).1-3 Olanzapine (Zyprexa, originally manufactured and distributed by Eli Lilly and Company/Lilly USA, LLC, Indianapolis, IN USA) is a second-generation antipsychotic that has been available for a quarter century.4 Although highly efficacious,5,6 olanzapine has been associated with weight gain, at times substantial, as well as disturbances in glucose and lipid metabolism.7 The addition of samidorphan, an opioid antagonist, to olanzapine in a single tablet may act to decrease the amount of long-term weight gain that can be expected for some patients taking olanzapine alone, consequently minimizing the anticipated increase in waist circumference (a proxy for the measurement of burden imposed by metabolically active adipose tissue). Approval of OSC for the treatment of schizophrenia was based on 2 pivotal randomized controlled trials and their extension studies.8-11 Approval of OSC for bipolar I disorder (acute treatment of manic/mixed episodes as a monotherapy or adjunctive to lithium or valproate, and as a monotherapy maintenance treatment) was based on legacy studies conducted with olanzapine, after establishing that samidorphan does not alter the pharmacokinetics of olanzapine, including in combination with lithium or valproate.3,12,13 OSC should be distinguished from a different combination product, olanzapine-fluoxetine combination (Symbyax, originally manufactured and distributed by Eli Lilly and Company/Lilly USA, LLC, Indianapolis, IN USA), approved for acute depressive episodes associated with bipolar I disorder and for treatment-resistant depression.14
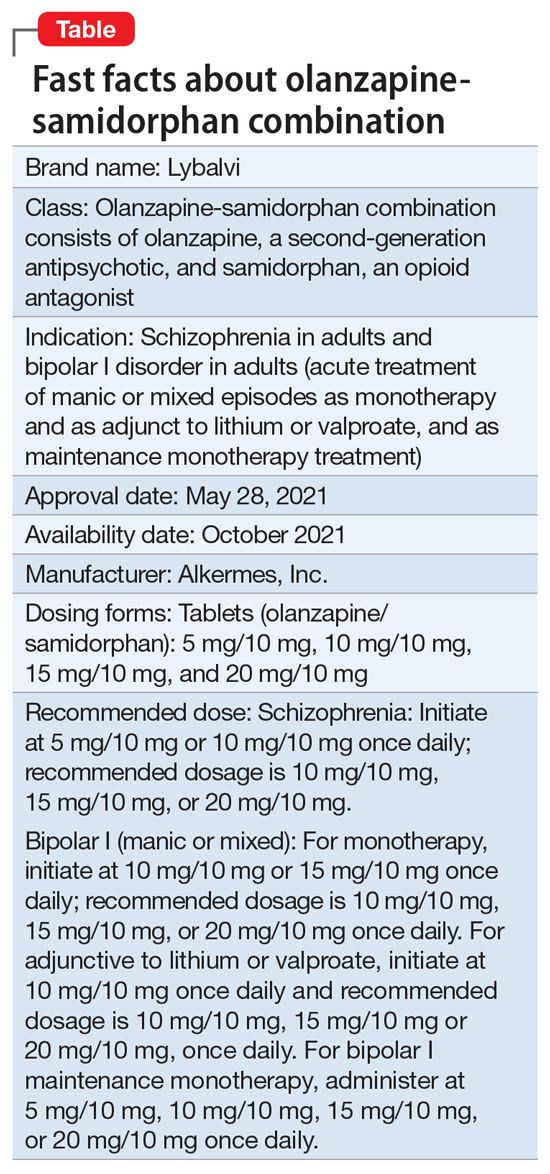
OSC offers the potential to consider olanzapine earlier in the treatment of schizophrenia or bipolar I disorder, especially among practitioners who might otherwise be hesitant to prescribe this agent because of concerns over the risk of excessive weight gain.
OSC is available in 4 dosage strengths containing 5 mg, 10 mg, 15 mg, or 20 mg of olanzapine; all tablets contain 10 mg of samidorphan.2 The recommended starting dose for OSC mirrors the language contained in the legacy olanzapine product label.4 For schizophrenia, the recommended initial dose (olanzapine/samidorphan) is 5 mg/10 mg or 10 mg/10 mg once daily. For bipolar I manic or mixed episodes, the recommended starting dose for monotherapy is 10 mg/10 mg or 15 mg/10 mg, and for use with lithium or valproate, 10 mg/10 mg. For all indications, the recommended target dose can be 10 mg/10 mg, 15 mg/10 mg, or 20 mg/10 mg, with 5 mg/10 mg as an additional potential dose for maintenance monotherapy of bipolar I disorder. The maximum dose is 20 mg/10 mg once daily. Because the amount of samidorphan in each tablet is fixed at 10 mg, combining tablets of OSC, or cutting OSC tablets in half, is not advisable.
Continue to: How it works...
How it works
Product labeling notes that olanzapine is an atypical antipsychotic, that its efficacy in schizophrenia or bipolar I disorder could be mediated through a combination of dopamine and serotonin type 2 (5HT2) antagonism, and that the mechanism of action of samidorphan could be mediated through opioid receptor antagonism.2
The pharmacodynamic profile of olanzapine is complex.2 It binds with high affinity to the following receptors: serotonin 5HT2A/2C, 5HT6 (Ki = 4, 11, and 5 nM, respectively), dopamine D1-4 (Ki = 11-31 nM), histamine H1 (Ki = 7 nM), and adrenergic alpha-1 receptors (Ki = 19 nM). Olanzapine is an antagonist with moderate affinity binding for serotonin 5HT3 (Ki = 57 nM) and muscarinic M1-5 (Ki = 73, 96, 132, 32, and 48 nM, respectively). Olanzapine binds with low affinity to gamma aminobutyric acid type A (GABA-A), benzodiazepine, and beta-adrenergic receptors (Ki >10 µM). Olanzapine’s muscarinic receptor affinity can explain why olanzapine can be associated with constipation, dry mouth, and tachycardia, all adverse reactions possibly related to cholinergic antagonism. Thus, OSC should be used with caution in patients with a current diagnosis or prior history of urinary retention, clinically significant prostatic hypertrophy, constipation, or a history of paralytic ileus or related conditions; a potential drug-drug interaction can be anticipated with concomitant use of anticholinergic medications.2 Other pharmacodynamic drug-drug interactions that can occur with the olanzapine component of OSC include the possibility that diazepam, alcohol, or other CNS-acting drugs may potentiate orthostatic hypotension, and there may be a need to reduce the dosage of concomitantly prescribed antihypertensive drugs in patients being treated for hypertension. Moreover, OSC is not recommended in patients receiving levodopa and dopamine agonists.
Samidorphan binds to the mu-, kappa-, and delta-opioid receptors (Ki = .052, .23, and 2.7 nM, respectively).2 Samidorphan is an antagonist at the mu-opioid receptors with partial agonist activity at kappa- and delta-opioid receptors. A major human metabolite of samidorphan (N-dealkylated) binds to the mu-, kappa-, and delta-opioid receptors (Ki = .26, 23, and 56 nM, respectively), and functions as a mu-opioid receptor agonist. The N-oxide major human metabolite binds to mu-, kappa-, and delta-opioid receptors (Ki = 8, 110, and 280 nM, respectively) and functions as a mu-opioid receptor antagonist. This profile differs from that of other opioid antagonists such as naltrexone.15,16
OSC is not a scheduled drug subject to the Controlled Substances Act. Because samidorphan functions as an opioid antagonist, OSC is contraindicated in patients using opioids or undergoing acute opioid withdrawal.2
Regarding cardiac electrophysiology, OSC was not observed to prolong the electrocardiogram QTc interval to any clinically relevant extent when tested at doses up to 30 mg/30 mg (1.5 times and 3 times the maximum recommended daily dosage of olanzapine and samidorphan, respectively).17
Clinical pharmacokinetics
The pharmacokinetics of both olanzapine and samidorphan are linear over the clinical dose range and there is no pharmacokinetic interaction between olanzapine and samidorphan after oral administration of OSC.2 Coadministration of OSC with lithium or valproate does not have a clinically significant effect on systemic exposure of lithium or valproate.13 OSC steady-state concentrations of olanzapine and samidorphan are reached within 7 days, with accumulation at steady state being 2-fold for olanzapine and 1.3-fold for samidorphan (at 5 days). Elimination half-life for olanzapine is 35 to 52 hours, and for samidorphan, 7 to 11 hours. Olanzapine is metabolized primarily via UGT1A4 and CYP1A2, whereas samidorphan is primarily metabolized by CYP3A4. Consequently, concomitant use of OSC with strong CYP3A4 inducers is not recommended. The recommendation regarding CYP1A2 modulators and OSC are similar to those for olanzapine2,4: consider reducing the dosage of the olanzapine component in OSC when used concomitantly with strong CYP1A2 inhibitors, and consider increasing the dosage of the olanzapine component in OSC when used concomitantly with CYP1A2 inducers. Because cigarette smoke contains polycyclic aromatic hydrocarbons that act as CYP1A2 inducers,18 olanzapine clearance is much higher in smokers than in nonsmokers.2 This translates to potentially clinically relevant differences when optimizing the dose. In a study of patients with schizophrenia, olanzapine concentrations were lower in self-reported smokers (16.5, 34.2, and 60.9 ng/mL) than in self-reported nonsmokers (25.6, 43.4, and 113.2 ng/mL) for dosages of 10, 20, and 40 mg/d, respectively.19 In contrast, samidorphan pharmacokinetics are not affected by smoking status.2
No dose adjustment of OSC is needed in patients with hepatic or renal impairment; however, OSC is not recommended for patients with end-stage renal disease because this has not been specifically studied.2
Continue to: Efficacy...
Efficacy
The efficacy of OSC in the treatment of schizophrenia in adults is supported, in part, by the extensive legacy of studies of orally administered olanzapine.2 For OSC specifically, acute efficacy was primarily demonstrated in a randomized, double-blind, phase 3, 4-week study establishing superiority vs placebo in acutely exacerbated patients with schizophrenia.8 Mitigation of weight gain was assessed separately in a randomized, double-blind, phase 3, 24-week study comparing OSC with olanzapine in non-acute outpatients with schizophrenia.10 Both of these 2 trials were accompanied by 52-week open-label extension studies.9,11
The 4-week study evaluated the antipsychotic efficacy of OSC in 401 patients experiencing an acute exacerbation or relapse of schizophrenia who required inpatient treatment.8 Patients were required to have a Positive and Negative Syndrome Scale (PANSS) total score ≥80, with a score ≥4 on at least 3 of selected positive symptoms, and a Clinical Global Impression-Severity (CGI-S) score ≥4 at baseline and screening. Patients were required to be inpatients for the first 2 weeks of the study, and were encouraged to remain as inpatients for all 4 weeks. Patients were randomized to receive OSC, olanzapine, or placebo. Dosing was once-daily and flexible based on clinical response and tolerability for the first 2 weeks of the study, and fixed thereafter. Patients assigned to OSC could receive 10 mg/10 mg or 20 mg/10 mg, and patients randomized to olanzapine could receive 10 mg or 20 mg. The study compared OSC with placebo, with olanzapine serving as an active control. Treatment with OSC resulted in significant improvements in symptoms compared with placebo at Week 4, as measured by changes in PANSS total scores from baseline. Improvement in PANSS scores with OSC relative to placebo was similar to that observed with olanzapine. The antipsychotic efficacy of OSC relative to placebo was also supported by improvements in CGI-S scores. Thus, the inclusion of samidorphan in OSC did not negatively impact the antipsychotic efficacy of olanzapine.
In the 24-week study, 561 patients were randomized to OSC or olanzapine.10 There was no placebo control. Patients were treated with doses of OSC 10 mg/10 mg or 20 mg/10 mg, or with doses of olanzapine 10 mg or 20 mg. Dosing was flexible for the first 4 weeks of the study and fixed thereafter. Eligible patients were age 18 to 55 years (younger than the 4-week study, where the maximum age was 70 years), with a body mass index of 18 to 30 kg/m2 (lower than the upper limit of 40 kg/m2 used in the 4-week study). In contrast to the acutely exacerbated patients in the 4-week study, patients were required to have a PANSS total score of 50 to 90, CGI-S score ≤4, and symptoms suitable for outpatient treatment. The co-primary endpoints were percent change from baseline in body weight and proportion of patients who gained ≥10% body weight at Week 24. Treatment with OSC or olanzapine resulted in similar improvements in PANSS total and CGI-S scores, but treatment with OSC was associated with statistically significantly less weight gain than treatment with olanzapine, and with a smaller proportion of patients who gained ≥10% body weight. The least squares mean percent weight change from baseline to the end of treatment was 4.2% with OSC vs 6.6% with olanzapine. Although patients treated with OSC or olanzapine had similar weight gain for the first 4 weeks of treatment, OSC weight gain stabilized after approximately the 6th week, whereas patients who received olanzapine continued to gain weight throughout the remainder of the treatment period. The risk of gaining ≥10% body weight from baseline was reduced by 50% with OSC compared with olanzapine. Moreover, the odds of gaining ≥7% body weight from baseline at Week 24 were also reduced by 50% for OSC compared with olanzapine. OSC was also associated with smaller increases in waist circumference compared with olanzapine, which was observable as early as Week 1. The risk of experiencing a 5-cm increase in waist circumference was 50% lower for patients treated with OSC vs olanzapine, a relevant threshold in assessing risk of all-cause mortality and cardiovascular disease.20 However, changes in metabolic laboratory parameters in patients treated with OSC or olanzapine were generally small and were similar between groups. In addition, there were little differences between the 2 treatment groups in metabolic parameter changes considered to be of potential clinical significance, based on commonly used thresholds.
Patients on stable, chronic olanzapine therapy were not specifically studied, so the weight effect of switching from olanzapine to OSC is unknown.For bipolar I manic or mixed episodes, the use of OSC as monotherapy or in combination with lithium or valproate, as well as for maintenance monotherapy, was approved based on legacy clinical trials with olanzapine, as described in product labeling,2,4 as well as pharmacokinetic data evidencing that OSC did not have a clinically significant effect on the pharmacokinetics of lithium or valproate.13 A study is in progress to evaluate the effect of OSC compared with olanzapine on body weight in young adults with schizophrenia, schizophreniform, or bipolar I disorder who are early in their illness (ClinicalTrials.gov identifier: NCT03187769).
Overall tolerability and safety
The systemic safety and tolerability profile for OSC would be expected to be similar to that for olanzapine, unless there are adverse events that are specifically related to the samidorphan component. In the 4-week acute study described above,8 adverse events that occurred at least twice the rate of placebo with OSC included increased weight (18.7%, 14.3%, 3.0%, for OSC, olanzapine, and placebo, respectively), somnolence (9.0%, 9.8%, 2.2%), dry mouth (7.5%, 5.3%, 0.7%), and headache (6.0%, 5.3%, 3.0%). In the 24-week study,10 which did not have a placebo control, the most commonly reported adverse events (≥10% of patients) were increased weight (24.8% vs 36.2% for OSC vs olanzapine), somnolence (21.2% vs 18.1%), dry mouth (12.8% vs 8.0%), and increased appetite (10.9% vs 12.3%). In both studies, rates of discontinuation due to adverse events were low and similar between groups (in the 4-week study, 1.5% for OSC, 2.3% for olanzapine, and 5.2% for placebo; in the 24-week study, 12.0% for OSC and 9.8% for olanzapine).
In the 2 open-label, phase 3, 52-week extension studies,9,11 long-term tolerability was evidenced by low rates discontinuation due to adverse events (≤6%). Neither extension study reported any clinically meaningful changes over time in hematology, biochemistry, vital signs, or electrocardiogram parameters.3 In addition to durability of antipsychotic response as evidenced by sustained improvements in PANSS and CGI-S scores over time, waist circumference and weight remained stable, and the observed long-term changes in weight were consistent with weight changes observed with other second-generation antipsychotics.3 Long-term changes in metabolic laboratory parameter values were small and remained stable, and there was little change in glycosylated hemoglobin (hemoglobin A1c) values, which suggests that glycemic control was maintained with long-term OSC treatment.3 Caveats to consider are that the extension studies were open label without comparators, and they may have selected for patients who responded favorably to OSC treatment in the preceding studies.3Warnings and precautions in OSC product labeling are generally similar to those for other second-generation antipsychotics,21 other than warnings and precautions specifically related to samidorphan being an opioid antagonist, and special mention of “Drug Reaction with Eosinophilia and Systemic Symptoms” and “Anticholinergic (Antimuscarinic) Effects” warnings, which also are contained in the olanzapine legacy label.2,4
Summary
Olanzapine has a plethora of evidence supporting its robust efficacy profile5,6; however, its use is stymied by an unfavorable weight and metabolic profile.7 OSC may help mitigate at least some of the weight gain that would be expected with the use of olanzapine alone in the long-term treatment of patients with schizophrenia or bipolar I disorder. The addition of samidorphan does not deleteriously affect the efficacy of olanzapine, but decreases the risk of gaining ≥10% or ≥7% of baseline body weight by approximately 50% compared with olanzapine alone. Increase in waist circumference, a proxy for how much metabolically active fat one has, is lower with OSC than it is with olanzapine. Because samidorphan is an opioid receptor antagonist, OSC is contraindicated in patients using opioids and in those undergoing acute opioid withdrawal. Dosage strengths available for OSC parallel those for olanzapine, and all strengths including the same fixed dose of samidorphan—10 mg—so advise patients not to double up on the tablets, and to not split them.
Related Resource
• Olanzapine and samidorphan (Lybalvi) prescribing information. https://www.lybalvi.com/lybalvi-prescribing-information.pdf
Drug Brand Names
Diazepam • Valium
Lithium • Eskalith, Lithobid
Olanzapine • Zyprexa
Olanzapine-fluoxetine combination • Symbyax
Olanzapine-samidorphan combination • Lybalvi
Valproate • Depakote, Depakene
Bottom Line
Olanzapine-samidorphan combination (OSC) is intended to mitigate some of the weight gain anticipated when using olanzapine alone. For clinicians who have prescribed olanzapine and have seen its therapeutic benefits, OSC will be a welcome addition to the therapeutic armamentarium. For practitioners who may have avoided olanzapine entirely, OSC can provide another means of offering this therapeutic option and counter “olanzapine hesitancy.”
1. US Food and Drug Administration. NDA 213378 approval letter. May 28, 2021. Accessed November 24, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/213378Orig1Orig2s000Approv.pdf
2. Alkermes, Inc. LYBALVI™ (olanzapine and samidorphan) tablets, for oral use. Prescribing information. May 2021. Accessed November 24, 2021. https://www.lybalvi.com/lybalvi-prescribing-information.pdf
3. Citrome L, Graham C, Simmons A, et al. An evidence-based review of OLZ/SAM for treatment of adults with schizophrenia or bipolar I disorder. Neuropsychiatr Dis Treat. 2021;17:2885-2904.
4. Eli Lilly and Company. ZYPREXA (olanzapine) tablet for oral use; ZYPREXA ZYDIS (olanzapine) tablet, orally disintegrating for oral use; ZYPREXA intramuscular (olanzapine) injection, powder, for solution for intramuscular use. Prescribing information. February 2021. Accessed November 24, 2021. https://pi.lilly.com/us/zyprexa-pi.pdf
5. Citrome L, McEvoy JP, Todtenkopf MS, et al. A commentary on the efficacy of olanzapine for the treatment of schizophrenia: the past, present, and future. Neuropsychiatr Dis Treat. 2019;15:2559-2569.
6. Meftah AM, Deckler E, Citrome L, et al. New discoveries for an old drug: a review of recent olanzapine research. Postgrad Med. 2020;132(1):80-90.
7. Citrome L, Holt RI, Walker DJ, et al. Weight gain and changes in metabolic variables following olanzapine treatment in schizophrenia and bipolar disorder. Clin Drug Investig. 2011;31(7):455-482.
8. Potkin SG, Kunovac J, Silverman BL, et al. Efficacy and safety of a combination of olanzapine and samidorphan in adult patients with an acute exacerbation of schizophrenia: outcomes from the randomized, phase 3 ENLIGHTEN-1 study. J Clin Psychiatry. 2020;81(2):19m12769.
9. Yagoda S, Graham C, Simmons A, et al. Long-term safety and durability of effect with a combination of olanzapine and samidorphan in patients with schizophrenia: results from a 1-year open-label extension study. CNS Spectr. 2021;26(4):383-392.
10. Correll CU, Newcomer JW, Silverman B, et al. Effects of olanzapine combined with samidorphan on weight gain in schizophrenia: a 24-week phase 3 study. Am J Psychiatry. 2020;177(12):1168-1178.
11. Kahn RS, Silverman BL, DiPetrillo L, et al. A phase 3, multicenter study to assess the 1-year safety and tolerability of a combination of olanzapine and samidorphan in patients with schizophrenia: results from the ENLIGHTEN-2 long-term extension. Schizophr Res. 2021;232:45-53.
12. US Food and Drug Administration. Drug approval package: Lybalvi. June 26, 2021. Accessed November 24, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/213378Orig1Orig2s000TOC.cfm
13. Sun L, Yagoda S, Yao B, et al. Combination of olanzapine and samidorphan has no clinically significant effect on the pharmacokinetics of lithium or valproate. Clin Drug Investig. 2020;40(1):55-64.
14. Eli Lilly and Company. SYMBYAX (olanzapine and fluoxetine) capsules for oral use. Prescribing information. September 2021. Accessed November 24, 2021. https://pi.lilly.com/us/symbyax-pi.pdf
15. Wentland MP, Lu Q, Lou R, et al. Synthesis and opioid receptor binding properties of a highly potent 4-hydroxy analogue of naltrexone. Bioorg Med Chem Lett. 2005;15(8):2107-2110.
16. Lee MW, Fujioka K. Naltrexone for the treatment of obesity: review and update. Expert Opin Pharmacother. 2009;10(11):1841-1845.
17. Sun L, Yagoda S, Xue H, et al. Combination of olanzapine and samidorphan has no clinically relevant effects on ECG parameters, including the QTc interval: results from a phase 1 QT/QTc study. Prog Neuropsychopharmacol Biol Psychiatry. 2020;100:109881.
18. Zhou SF, Yang LP, Zhou ZW, et al. Insights into the substrate specificity, inhibitors, regulation, and polymorphisms and the clinical impact of human cytochrome P450 1A2. AAPS J. 2009;11(3):481-494.
19. Citrome L, Stauffer VL, Chen L, et al. Olanzapine plasma concentrations after treatment with 10, 20, and 40 mg/d in patients with schizophrenia: an analysis of correlations with efficacy, weight gain, and prolactin concentration. J Clin Psychopharmacol. 2009;29(3):278-283.
20. Cerhan JR, Moore SC, Jacobs EJ, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin Proc. 2014;89(3):335-345.
21. Citrome L, Nasrallah HA. On-label on the table: what the package insert informs us about the tolerability profile of oral atypical antipsychotics, and what it does not. Expert Opin Pharmacother. 2012;13(11):1599-1613.
Approved by the FDA on May 28, 2021, olanzapine-samidorphan combination (OSC) (Lybalvi, manufactured and distributed by Alkermes, Inc. Waltham, MA USA) is intended to help mitigate some of the weight gain that can be anticipated with the use of olanzapine alone (Table).1-3 Olanzapine (Zyprexa, originally manufactured and distributed by Eli Lilly and Company/Lilly USA, LLC, Indianapolis, IN USA) is a second-generation antipsychotic that has been available for a quarter century.4 Although highly efficacious,5,6 olanzapine has been associated with weight gain, at times substantial, as well as disturbances in glucose and lipid metabolism.7 The addition of samidorphan, an opioid antagonist, to olanzapine in a single tablet may act to decrease the amount of long-term weight gain that can be expected for some patients taking olanzapine alone, consequently minimizing the anticipated increase in waist circumference (a proxy for the measurement of burden imposed by metabolically active adipose tissue). Approval of OSC for the treatment of schizophrenia was based on 2 pivotal randomized controlled trials and their extension studies.8-11 Approval of OSC for bipolar I disorder (acute treatment of manic/mixed episodes as a monotherapy or adjunctive to lithium or valproate, and as a monotherapy maintenance treatment) was based on legacy studies conducted with olanzapine, after establishing that samidorphan does not alter the pharmacokinetics of olanzapine, including in combination with lithium or valproate.3,12,13 OSC should be distinguished from a different combination product, olanzapine-fluoxetine combination (Symbyax, originally manufactured and distributed by Eli Lilly and Company/Lilly USA, LLC, Indianapolis, IN USA), approved for acute depressive episodes associated with bipolar I disorder and for treatment-resistant depression.14
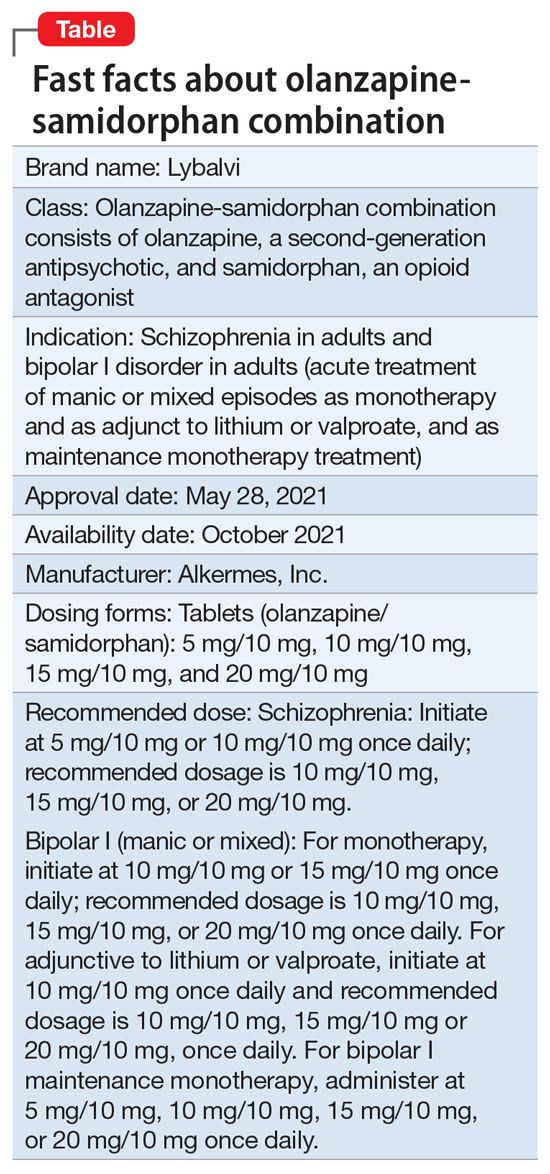
OSC offers the potential to consider olanzapine earlier in the treatment of schizophrenia or bipolar I disorder, especially among practitioners who might otherwise be hesitant to prescribe this agent because of concerns over the risk of excessive weight gain.
OSC is available in 4 dosage strengths containing 5 mg, 10 mg, 15 mg, or 20 mg of olanzapine; all tablets contain 10 mg of samidorphan.2 The recommended starting dose for OSC mirrors the language contained in the legacy olanzapine product label.4 For schizophrenia, the recommended initial dose (olanzapine/samidorphan) is 5 mg/10 mg or 10 mg/10 mg once daily. For bipolar I manic or mixed episodes, the recommended starting dose for monotherapy is 10 mg/10 mg or 15 mg/10 mg, and for use with lithium or valproate, 10 mg/10 mg. For all indications, the recommended target dose can be 10 mg/10 mg, 15 mg/10 mg, or 20 mg/10 mg, with 5 mg/10 mg as an additional potential dose for maintenance monotherapy of bipolar I disorder. The maximum dose is 20 mg/10 mg once daily. Because the amount of samidorphan in each tablet is fixed at 10 mg, combining tablets of OSC, or cutting OSC tablets in half, is not advisable.
Continue to: How it works...
How it works
Product labeling notes that olanzapine is an atypical antipsychotic, that its efficacy in schizophrenia or bipolar I disorder could be mediated through a combination of dopamine and serotonin type 2 (5HT2) antagonism, and that the mechanism of action of samidorphan could be mediated through opioid receptor antagonism.2
The pharmacodynamic profile of olanzapine is complex.2 It binds with high affinity to the following receptors: serotonin 5HT2A/2C, 5HT6 (Ki = 4, 11, and 5 nM, respectively), dopamine D1-4 (Ki = 11-31 nM), histamine H1 (Ki = 7 nM), and adrenergic alpha-1 receptors (Ki = 19 nM). Olanzapine is an antagonist with moderate affinity binding for serotonin 5HT3 (Ki = 57 nM) and muscarinic M1-5 (Ki = 73, 96, 132, 32, and 48 nM, respectively). Olanzapine binds with low affinity to gamma aminobutyric acid type A (GABA-A), benzodiazepine, and beta-adrenergic receptors (Ki >10 µM). Olanzapine’s muscarinic receptor affinity can explain why olanzapine can be associated with constipation, dry mouth, and tachycardia, all adverse reactions possibly related to cholinergic antagonism. Thus, OSC should be used with caution in patients with a current diagnosis or prior history of urinary retention, clinically significant prostatic hypertrophy, constipation, or a history of paralytic ileus or related conditions; a potential drug-drug interaction can be anticipated with concomitant use of anticholinergic medications.2 Other pharmacodynamic drug-drug interactions that can occur with the olanzapine component of OSC include the possibility that diazepam, alcohol, or other CNS-acting drugs may potentiate orthostatic hypotension, and there may be a need to reduce the dosage of concomitantly prescribed antihypertensive drugs in patients being treated for hypertension. Moreover, OSC is not recommended in patients receiving levodopa and dopamine agonists.
Samidorphan binds to the mu-, kappa-, and delta-opioid receptors (Ki = .052, .23, and 2.7 nM, respectively).2 Samidorphan is an antagonist at the mu-opioid receptors with partial agonist activity at kappa- and delta-opioid receptors. A major human metabolite of samidorphan (N-dealkylated) binds to the mu-, kappa-, and delta-opioid receptors (Ki = .26, 23, and 56 nM, respectively), and functions as a mu-opioid receptor agonist. The N-oxide major human metabolite binds to mu-, kappa-, and delta-opioid receptors (Ki = 8, 110, and 280 nM, respectively) and functions as a mu-opioid receptor antagonist. This profile differs from that of other opioid antagonists such as naltrexone.15,16
OSC is not a scheduled drug subject to the Controlled Substances Act. Because samidorphan functions as an opioid antagonist, OSC is contraindicated in patients using opioids or undergoing acute opioid withdrawal.2
Regarding cardiac electrophysiology, OSC was not observed to prolong the electrocardiogram QTc interval to any clinically relevant extent when tested at doses up to 30 mg/30 mg (1.5 times and 3 times the maximum recommended daily dosage of olanzapine and samidorphan, respectively).17
Clinical pharmacokinetics
The pharmacokinetics of both olanzapine and samidorphan are linear over the clinical dose range and there is no pharmacokinetic interaction between olanzapine and samidorphan after oral administration of OSC.2 Coadministration of OSC with lithium or valproate does not have a clinically significant effect on systemic exposure of lithium or valproate.13 OSC steady-state concentrations of olanzapine and samidorphan are reached within 7 days, with accumulation at steady state being 2-fold for olanzapine and 1.3-fold for samidorphan (at 5 days). Elimination half-life for olanzapine is 35 to 52 hours, and for samidorphan, 7 to 11 hours. Olanzapine is metabolized primarily via UGT1A4 and CYP1A2, whereas samidorphan is primarily metabolized by CYP3A4. Consequently, concomitant use of OSC with strong CYP3A4 inducers is not recommended. The recommendation regarding CYP1A2 modulators and OSC are similar to those for olanzapine2,4: consider reducing the dosage of the olanzapine component in OSC when used concomitantly with strong CYP1A2 inhibitors, and consider increasing the dosage of the olanzapine component in OSC when used concomitantly with CYP1A2 inducers. Because cigarette smoke contains polycyclic aromatic hydrocarbons that act as CYP1A2 inducers,18 olanzapine clearance is much higher in smokers than in nonsmokers.2 This translates to potentially clinically relevant differences when optimizing the dose. In a study of patients with schizophrenia, olanzapine concentrations were lower in self-reported smokers (16.5, 34.2, and 60.9 ng/mL) than in self-reported nonsmokers (25.6, 43.4, and 113.2 ng/mL) for dosages of 10, 20, and 40 mg/d, respectively.19 In contrast, samidorphan pharmacokinetics are not affected by smoking status.2
No dose adjustment of OSC is needed in patients with hepatic or renal impairment; however, OSC is not recommended for patients with end-stage renal disease because this has not been specifically studied.2
Continue to: Efficacy...
Efficacy
The efficacy of OSC in the treatment of schizophrenia in adults is supported, in part, by the extensive legacy of studies of orally administered olanzapine.2 For OSC specifically, acute efficacy was primarily demonstrated in a randomized, double-blind, phase 3, 4-week study establishing superiority vs placebo in acutely exacerbated patients with schizophrenia.8 Mitigation of weight gain was assessed separately in a randomized, double-blind, phase 3, 24-week study comparing OSC with olanzapine in non-acute outpatients with schizophrenia.10 Both of these 2 trials were accompanied by 52-week open-label extension studies.9,11
The 4-week study evaluated the antipsychotic efficacy of OSC in 401 patients experiencing an acute exacerbation or relapse of schizophrenia who required inpatient treatment.8 Patients were required to have a Positive and Negative Syndrome Scale (PANSS) total score ≥80, with a score ≥4 on at least 3 of selected positive symptoms, and a Clinical Global Impression-Severity (CGI-S) score ≥4 at baseline and screening. Patients were required to be inpatients for the first 2 weeks of the study, and were encouraged to remain as inpatients for all 4 weeks. Patients were randomized to receive OSC, olanzapine, or placebo. Dosing was once-daily and flexible based on clinical response and tolerability for the first 2 weeks of the study, and fixed thereafter. Patients assigned to OSC could receive 10 mg/10 mg or 20 mg/10 mg, and patients randomized to olanzapine could receive 10 mg or 20 mg. The study compared OSC with placebo, with olanzapine serving as an active control. Treatment with OSC resulted in significant improvements in symptoms compared with placebo at Week 4, as measured by changes in PANSS total scores from baseline. Improvement in PANSS scores with OSC relative to placebo was similar to that observed with olanzapine. The antipsychotic efficacy of OSC relative to placebo was also supported by improvements in CGI-S scores. Thus, the inclusion of samidorphan in OSC did not negatively impact the antipsychotic efficacy of olanzapine.
In the 24-week study, 561 patients were randomized to OSC or olanzapine.10 There was no placebo control. Patients were treated with doses of OSC 10 mg/10 mg or 20 mg/10 mg, or with doses of olanzapine 10 mg or 20 mg. Dosing was flexible for the first 4 weeks of the study and fixed thereafter. Eligible patients were age 18 to 55 years (younger than the 4-week study, where the maximum age was 70 years), with a body mass index of 18 to 30 kg/m2 (lower than the upper limit of 40 kg/m2 used in the 4-week study). In contrast to the acutely exacerbated patients in the 4-week study, patients were required to have a PANSS total score of 50 to 90, CGI-S score ≤4, and symptoms suitable for outpatient treatment. The co-primary endpoints were percent change from baseline in body weight and proportion of patients who gained ≥10% body weight at Week 24. Treatment with OSC or olanzapine resulted in similar improvements in PANSS total and CGI-S scores, but treatment with OSC was associated with statistically significantly less weight gain than treatment with olanzapine, and with a smaller proportion of patients who gained ≥10% body weight. The least squares mean percent weight change from baseline to the end of treatment was 4.2% with OSC vs 6.6% with olanzapine. Although patients treated with OSC or olanzapine had similar weight gain for the first 4 weeks of treatment, OSC weight gain stabilized after approximately the 6th week, whereas patients who received olanzapine continued to gain weight throughout the remainder of the treatment period. The risk of gaining ≥10% body weight from baseline was reduced by 50% with OSC compared with olanzapine. Moreover, the odds of gaining ≥7% body weight from baseline at Week 24 were also reduced by 50% for OSC compared with olanzapine. OSC was also associated with smaller increases in waist circumference compared with olanzapine, which was observable as early as Week 1. The risk of experiencing a 5-cm increase in waist circumference was 50% lower for patients treated with OSC vs olanzapine, a relevant threshold in assessing risk of all-cause mortality and cardiovascular disease.20 However, changes in metabolic laboratory parameters in patients treated with OSC or olanzapine were generally small and were similar between groups. In addition, there were little differences between the 2 treatment groups in metabolic parameter changes considered to be of potential clinical significance, based on commonly used thresholds.
Patients on stable, chronic olanzapine therapy were not specifically studied, so the weight effect of switching from olanzapine to OSC is unknown.For bipolar I manic or mixed episodes, the use of OSC as monotherapy or in combination with lithium or valproate, as well as for maintenance monotherapy, was approved based on legacy clinical trials with olanzapine, as described in product labeling,2,4 as well as pharmacokinetic data evidencing that OSC did not have a clinically significant effect on the pharmacokinetics of lithium or valproate.13 A study is in progress to evaluate the effect of OSC compared with olanzapine on body weight in young adults with schizophrenia, schizophreniform, or bipolar I disorder who are early in their illness (ClinicalTrials.gov identifier: NCT03187769).
Overall tolerability and safety
The systemic safety and tolerability profile for OSC would be expected to be similar to that for olanzapine, unless there are adverse events that are specifically related to the samidorphan component. In the 4-week acute study described above,8 adverse events that occurred at least twice the rate of placebo with OSC included increased weight (18.7%, 14.3%, 3.0%, for OSC, olanzapine, and placebo, respectively), somnolence (9.0%, 9.8%, 2.2%), dry mouth (7.5%, 5.3%, 0.7%), and headache (6.0%, 5.3%, 3.0%). In the 24-week study,10 which did not have a placebo control, the most commonly reported adverse events (≥10% of patients) were increased weight (24.8% vs 36.2% for OSC vs olanzapine), somnolence (21.2% vs 18.1%), dry mouth (12.8% vs 8.0%), and increased appetite (10.9% vs 12.3%). In both studies, rates of discontinuation due to adverse events were low and similar between groups (in the 4-week study, 1.5% for OSC, 2.3% for olanzapine, and 5.2% for placebo; in the 24-week study, 12.0% for OSC and 9.8% for olanzapine).
In the 2 open-label, phase 3, 52-week extension studies,9,11 long-term tolerability was evidenced by low rates discontinuation due to adverse events (≤6%). Neither extension study reported any clinically meaningful changes over time in hematology, biochemistry, vital signs, or electrocardiogram parameters.3 In addition to durability of antipsychotic response as evidenced by sustained improvements in PANSS and CGI-S scores over time, waist circumference and weight remained stable, and the observed long-term changes in weight were consistent with weight changes observed with other second-generation antipsychotics.3 Long-term changes in metabolic laboratory parameter values were small and remained stable, and there was little change in glycosylated hemoglobin (hemoglobin A1c) values, which suggests that glycemic control was maintained with long-term OSC treatment.3 Caveats to consider are that the extension studies were open label without comparators, and they may have selected for patients who responded favorably to OSC treatment in the preceding studies.3Warnings and precautions in OSC product labeling are generally similar to those for other second-generation antipsychotics,21 other than warnings and precautions specifically related to samidorphan being an opioid antagonist, and special mention of “Drug Reaction with Eosinophilia and Systemic Symptoms” and “Anticholinergic (Antimuscarinic) Effects” warnings, which also are contained in the olanzapine legacy label.2,4
Summary
Olanzapine has a plethora of evidence supporting its robust efficacy profile5,6; however, its use is stymied by an unfavorable weight and metabolic profile.7 OSC may help mitigate at least some of the weight gain that would be expected with the use of olanzapine alone in the long-term treatment of patients with schizophrenia or bipolar I disorder. The addition of samidorphan does not deleteriously affect the efficacy of olanzapine, but decreases the risk of gaining ≥10% or ≥7% of baseline body weight by approximately 50% compared with olanzapine alone. Increase in waist circumference, a proxy for how much metabolically active fat one has, is lower with OSC than it is with olanzapine. Because samidorphan is an opioid receptor antagonist, OSC is contraindicated in patients using opioids and in those undergoing acute opioid withdrawal. Dosage strengths available for OSC parallel those for olanzapine, and all strengths including the same fixed dose of samidorphan—10 mg—so advise patients not to double up on the tablets, and to not split them.
Related Resource
• Olanzapine and samidorphan (Lybalvi) prescribing information. https://www.lybalvi.com/lybalvi-prescribing-information.pdf
Drug Brand Names
Diazepam • Valium
Lithium • Eskalith, Lithobid
Olanzapine • Zyprexa
Olanzapine-fluoxetine combination • Symbyax
Olanzapine-samidorphan combination • Lybalvi
Valproate • Depakote, Depakene
Bottom Line
Olanzapine-samidorphan combination (OSC) is intended to mitigate some of the weight gain anticipated when using olanzapine alone. For clinicians who have prescribed olanzapine and have seen its therapeutic benefits, OSC will be a welcome addition to the therapeutic armamentarium. For practitioners who may have avoided olanzapine entirely, OSC can provide another means of offering this therapeutic option and counter “olanzapine hesitancy.”
Approved by the FDA on May 28, 2021, olanzapine-samidorphan combination (OSC) (Lybalvi, manufactured and distributed by Alkermes, Inc. Waltham, MA USA) is intended to help mitigate some of the weight gain that can be anticipated with the use of olanzapine alone (Table).1-3 Olanzapine (Zyprexa, originally manufactured and distributed by Eli Lilly and Company/Lilly USA, LLC, Indianapolis, IN USA) is a second-generation antipsychotic that has been available for a quarter century.4 Although highly efficacious,5,6 olanzapine has been associated with weight gain, at times substantial, as well as disturbances in glucose and lipid metabolism.7 The addition of samidorphan, an opioid antagonist, to olanzapine in a single tablet may act to decrease the amount of long-term weight gain that can be expected for some patients taking olanzapine alone, consequently minimizing the anticipated increase in waist circumference (a proxy for the measurement of burden imposed by metabolically active adipose tissue). Approval of OSC for the treatment of schizophrenia was based on 2 pivotal randomized controlled trials and their extension studies.8-11 Approval of OSC for bipolar I disorder (acute treatment of manic/mixed episodes as a monotherapy or adjunctive to lithium or valproate, and as a monotherapy maintenance treatment) was based on legacy studies conducted with olanzapine, after establishing that samidorphan does not alter the pharmacokinetics of olanzapine, including in combination with lithium or valproate.3,12,13 OSC should be distinguished from a different combination product, olanzapine-fluoxetine combination (Symbyax, originally manufactured and distributed by Eli Lilly and Company/Lilly USA, LLC, Indianapolis, IN USA), approved for acute depressive episodes associated with bipolar I disorder and for treatment-resistant depression.14
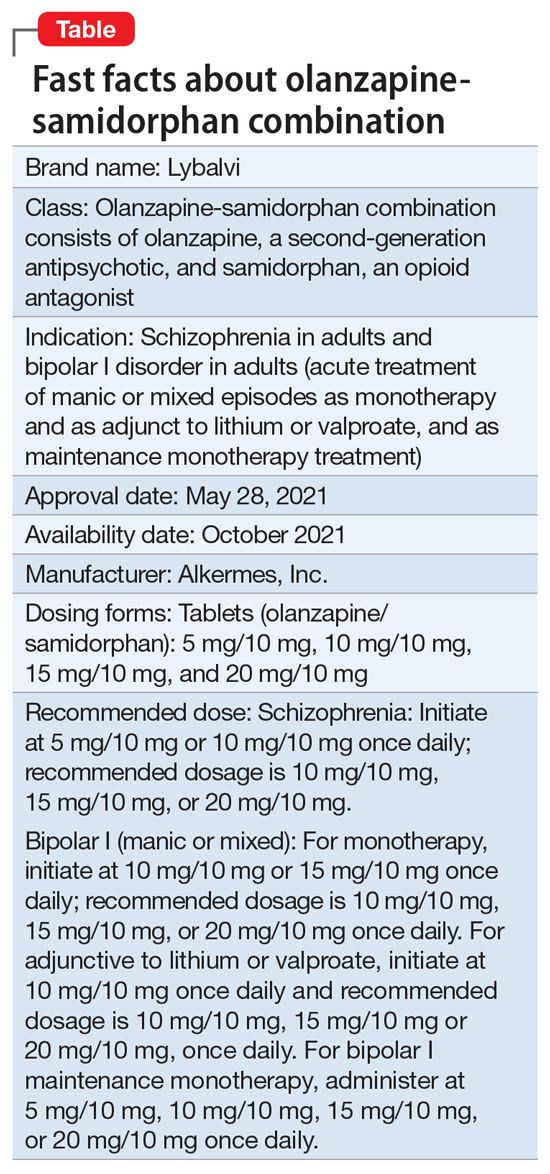
OSC offers the potential to consider olanzapine earlier in the treatment of schizophrenia or bipolar I disorder, especially among practitioners who might otherwise be hesitant to prescribe this agent because of concerns over the risk of excessive weight gain.
OSC is available in 4 dosage strengths containing 5 mg, 10 mg, 15 mg, or 20 mg of olanzapine; all tablets contain 10 mg of samidorphan.2 The recommended starting dose for OSC mirrors the language contained in the legacy olanzapine product label.4 For schizophrenia, the recommended initial dose (olanzapine/samidorphan) is 5 mg/10 mg or 10 mg/10 mg once daily. For bipolar I manic or mixed episodes, the recommended starting dose for monotherapy is 10 mg/10 mg or 15 mg/10 mg, and for use with lithium or valproate, 10 mg/10 mg. For all indications, the recommended target dose can be 10 mg/10 mg, 15 mg/10 mg, or 20 mg/10 mg, with 5 mg/10 mg as an additional potential dose for maintenance monotherapy of bipolar I disorder. The maximum dose is 20 mg/10 mg once daily. Because the amount of samidorphan in each tablet is fixed at 10 mg, combining tablets of OSC, or cutting OSC tablets in half, is not advisable.
Continue to: How it works...
How it works
Product labeling notes that olanzapine is an atypical antipsychotic, that its efficacy in schizophrenia or bipolar I disorder could be mediated through a combination of dopamine and serotonin type 2 (5HT2) antagonism, and that the mechanism of action of samidorphan could be mediated through opioid receptor antagonism.2
The pharmacodynamic profile of olanzapine is complex.2 It binds with high affinity to the following receptors: serotonin 5HT2A/2C, 5HT6 (Ki = 4, 11, and 5 nM, respectively), dopamine D1-4 (Ki = 11-31 nM), histamine H1 (Ki = 7 nM), and adrenergic alpha-1 receptors (Ki = 19 nM). Olanzapine is an antagonist with moderate affinity binding for serotonin 5HT3 (Ki = 57 nM) and muscarinic M1-5 (Ki = 73, 96, 132, 32, and 48 nM, respectively). Olanzapine binds with low affinity to gamma aminobutyric acid type A (GABA-A), benzodiazepine, and beta-adrenergic receptors (Ki >10 µM). Olanzapine’s muscarinic receptor affinity can explain why olanzapine can be associated with constipation, dry mouth, and tachycardia, all adverse reactions possibly related to cholinergic antagonism. Thus, OSC should be used with caution in patients with a current diagnosis or prior history of urinary retention, clinically significant prostatic hypertrophy, constipation, or a history of paralytic ileus or related conditions; a potential drug-drug interaction can be anticipated with concomitant use of anticholinergic medications.2 Other pharmacodynamic drug-drug interactions that can occur with the olanzapine component of OSC include the possibility that diazepam, alcohol, or other CNS-acting drugs may potentiate orthostatic hypotension, and there may be a need to reduce the dosage of concomitantly prescribed antihypertensive drugs in patients being treated for hypertension. Moreover, OSC is not recommended in patients receiving levodopa and dopamine agonists.
Samidorphan binds to the mu-, kappa-, and delta-opioid receptors (Ki = .052, .23, and 2.7 nM, respectively).2 Samidorphan is an antagonist at the mu-opioid receptors with partial agonist activity at kappa- and delta-opioid receptors. A major human metabolite of samidorphan (N-dealkylated) binds to the mu-, kappa-, and delta-opioid receptors (Ki = .26, 23, and 56 nM, respectively), and functions as a mu-opioid receptor agonist. The N-oxide major human metabolite binds to mu-, kappa-, and delta-opioid receptors (Ki = 8, 110, and 280 nM, respectively) and functions as a mu-opioid receptor antagonist. This profile differs from that of other opioid antagonists such as naltrexone.15,16
OSC is not a scheduled drug subject to the Controlled Substances Act. Because samidorphan functions as an opioid antagonist, OSC is contraindicated in patients using opioids or undergoing acute opioid withdrawal.2
Regarding cardiac electrophysiology, OSC was not observed to prolong the electrocardiogram QTc interval to any clinically relevant extent when tested at doses up to 30 mg/30 mg (1.5 times and 3 times the maximum recommended daily dosage of olanzapine and samidorphan, respectively).17
Clinical pharmacokinetics
The pharmacokinetics of both olanzapine and samidorphan are linear over the clinical dose range and there is no pharmacokinetic interaction between olanzapine and samidorphan after oral administration of OSC.2 Coadministration of OSC with lithium or valproate does not have a clinically significant effect on systemic exposure of lithium or valproate.13 OSC steady-state concentrations of olanzapine and samidorphan are reached within 7 days, with accumulation at steady state being 2-fold for olanzapine and 1.3-fold for samidorphan (at 5 days). Elimination half-life for olanzapine is 35 to 52 hours, and for samidorphan, 7 to 11 hours. Olanzapine is metabolized primarily via UGT1A4 and CYP1A2, whereas samidorphan is primarily metabolized by CYP3A4. Consequently, concomitant use of OSC with strong CYP3A4 inducers is not recommended. The recommendation regarding CYP1A2 modulators and OSC are similar to those for olanzapine2,4: consider reducing the dosage of the olanzapine component in OSC when used concomitantly with strong CYP1A2 inhibitors, and consider increasing the dosage of the olanzapine component in OSC when used concomitantly with CYP1A2 inducers. Because cigarette smoke contains polycyclic aromatic hydrocarbons that act as CYP1A2 inducers,18 olanzapine clearance is much higher in smokers than in nonsmokers.2 This translates to potentially clinically relevant differences when optimizing the dose. In a study of patients with schizophrenia, olanzapine concentrations were lower in self-reported smokers (16.5, 34.2, and 60.9 ng/mL) than in self-reported nonsmokers (25.6, 43.4, and 113.2 ng/mL) for dosages of 10, 20, and 40 mg/d, respectively.19 In contrast, samidorphan pharmacokinetics are not affected by smoking status.2
No dose adjustment of OSC is needed in patients with hepatic or renal impairment; however, OSC is not recommended for patients with end-stage renal disease because this has not been specifically studied.2
Continue to: Efficacy...
Efficacy
The efficacy of OSC in the treatment of schizophrenia in adults is supported, in part, by the extensive legacy of studies of orally administered olanzapine.2 For OSC specifically, acute efficacy was primarily demonstrated in a randomized, double-blind, phase 3, 4-week study establishing superiority vs placebo in acutely exacerbated patients with schizophrenia.8 Mitigation of weight gain was assessed separately in a randomized, double-blind, phase 3, 24-week study comparing OSC with olanzapine in non-acute outpatients with schizophrenia.10 Both of these 2 trials were accompanied by 52-week open-label extension studies.9,11
The 4-week study evaluated the antipsychotic efficacy of OSC in 401 patients experiencing an acute exacerbation or relapse of schizophrenia who required inpatient treatment.8 Patients were required to have a Positive and Negative Syndrome Scale (PANSS) total score ≥80, with a score ≥4 on at least 3 of selected positive symptoms, and a Clinical Global Impression-Severity (CGI-S) score ≥4 at baseline and screening. Patients were required to be inpatients for the first 2 weeks of the study, and were encouraged to remain as inpatients for all 4 weeks. Patients were randomized to receive OSC, olanzapine, or placebo. Dosing was once-daily and flexible based on clinical response and tolerability for the first 2 weeks of the study, and fixed thereafter. Patients assigned to OSC could receive 10 mg/10 mg or 20 mg/10 mg, and patients randomized to olanzapine could receive 10 mg or 20 mg. The study compared OSC with placebo, with olanzapine serving as an active control. Treatment with OSC resulted in significant improvements in symptoms compared with placebo at Week 4, as measured by changes in PANSS total scores from baseline. Improvement in PANSS scores with OSC relative to placebo was similar to that observed with olanzapine. The antipsychotic efficacy of OSC relative to placebo was also supported by improvements in CGI-S scores. Thus, the inclusion of samidorphan in OSC did not negatively impact the antipsychotic efficacy of olanzapine.
In the 24-week study, 561 patients were randomized to OSC or olanzapine.10 There was no placebo control. Patients were treated with doses of OSC 10 mg/10 mg or 20 mg/10 mg, or with doses of olanzapine 10 mg or 20 mg. Dosing was flexible for the first 4 weeks of the study and fixed thereafter. Eligible patients were age 18 to 55 years (younger than the 4-week study, where the maximum age was 70 years), with a body mass index of 18 to 30 kg/m2 (lower than the upper limit of 40 kg/m2 used in the 4-week study). In contrast to the acutely exacerbated patients in the 4-week study, patients were required to have a PANSS total score of 50 to 90, CGI-S score ≤4, and symptoms suitable for outpatient treatment. The co-primary endpoints were percent change from baseline in body weight and proportion of patients who gained ≥10% body weight at Week 24. Treatment with OSC or olanzapine resulted in similar improvements in PANSS total and CGI-S scores, but treatment with OSC was associated with statistically significantly less weight gain than treatment with olanzapine, and with a smaller proportion of patients who gained ≥10% body weight. The least squares mean percent weight change from baseline to the end of treatment was 4.2% with OSC vs 6.6% with olanzapine. Although patients treated with OSC or olanzapine had similar weight gain for the first 4 weeks of treatment, OSC weight gain stabilized after approximately the 6th week, whereas patients who received olanzapine continued to gain weight throughout the remainder of the treatment period. The risk of gaining ≥10% body weight from baseline was reduced by 50% with OSC compared with olanzapine. Moreover, the odds of gaining ≥7% body weight from baseline at Week 24 were also reduced by 50% for OSC compared with olanzapine. OSC was also associated with smaller increases in waist circumference compared with olanzapine, which was observable as early as Week 1. The risk of experiencing a 5-cm increase in waist circumference was 50% lower for patients treated with OSC vs olanzapine, a relevant threshold in assessing risk of all-cause mortality and cardiovascular disease.20 However, changes in metabolic laboratory parameters in patients treated with OSC or olanzapine were generally small and were similar between groups. In addition, there were little differences between the 2 treatment groups in metabolic parameter changes considered to be of potential clinical significance, based on commonly used thresholds.
Patients on stable, chronic olanzapine therapy were not specifically studied, so the weight effect of switching from olanzapine to OSC is unknown.For bipolar I manic or mixed episodes, the use of OSC as monotherapy or in combination with lithium or valproate, as well as for maintenance monotherapy, was approved based on legacy clinical trials with olanzapine, as described in product labeling,2,4 as well as pharmacokinetic data evidencing that OSC did not have a clinically significant effect on the pharmacokinetics of lithium or valproate.13 A study is in progress to evaluate the effect of OSC compared with olanzapine on body weight in young adults with schizophrenia, schizophreniform, or bipolar I disorder who are early in their illness (ClinicalTrials.gov identifier: NCT03187769).
Overall tolerability and safety
The systemic safety and tolerability profile for OSC would be expected to be similar to that for olanzapine, unless there are adverse events that are specifically related to the samidorphan component. In the 4-week acute study described above,8 adverse events that occurred at least twice the rate of placebo with OSC included increased weight (18.7%, 14.3%, 3.0%, for OSC, olanzapine, and placebo, respectively), somnolence (9.0%, 9.8%, 2.2%), dry mouth (7.5%, 5.3%, 0.7%), and headache (6.0%, 5.3%, 3.0%). In the 24-week study,10 which did not have a placebo control, the most commonly reported adverse events (≥10% of patients) were increased weight (24.8% vs 36.2% for OSC vs olanzapine), somnolence (21.2% vs 18.1%), dry mouth (12.8% vs 8.0%), and increased appetite (10.9% vs 12.3%). In both studies, rates of discontinuation due to adverse events were low and similar between groups (in the 4-week study, 1.5% for OSC, 2.3% for olanzapine, and 5.2% for placebo; in the 24-week study, 12.0% for OSC and 9.8% for olanzapine).
In the 2 open-label, phase 3, 52-week extension studies,9,11 long-term tolerability was evidenced by low rates discontinuation due to adverse events (≤6%). Neither extension study reported any clinically meaningful changes over time in hematology, biochemistry, vital signs, or electrocardiogram parameters.3 In addition to durability of antipsychotic response as evidenced by sustained improvements in PANSS and CGI-S scores over time, waist circumference and weight remained stable, and the observed long-term changes in weight were consistent with weight changes observed with other second-generation antipsychotics.3 Long-term changes in metabolic laboratory parameter values were small and remained stable, and there was little change in glycosylated hemoglobin (hemoglobin A1c) values, which suggests that glycemic control was maintained with long-term OSC treatment.3 Caveats to consider are that the extension studies were open label without comparators, and they may have selected for patients who responded favorably to OSC treatment in the preceding studies.3Warnings and precautions in OSC product labeling are generally similar to those for other second-generation antipsychotics,21 other than warnings and precautions specifically related to samidorphan being an opioid antagonist, and special mention of “Drug Reaction with Eosinophilia and Systemic Symptoms” and “Anticholinergic (Antimuscarinic) Effects” warnings, which also are contained in the olanzapine legacy label.2,4
Summary
Olanzapine has a plethora of evidence supporting its robust efficacy profile5,6; however, its use is stymied by an unfavorable weight and metabolic profile.7 OSC may help mitigate at least some of the weight gain that would be expected with the use of olanzapine alone in the long-term treatment of patients with schizophrenia or bipolar I disorder. The addition of samidorphan does not deleteriously affect the efficacy of olanzapine, but decreases the risk of gaining ≥10% or ≥7% of baseline body weight by approximately 50% compared with olanzapine alone. Increase in waist circumference, a proxy for how much metabolically active fat one has, is lower with OSC than it is with olanzapine. Because samidorphan is an opioid receptor antagonist, OSC is contraindicated in patients using opioids and in those undergoing acute opioid withdrawal. Dosage strengths available for OSC parallel those for olanzapine, and all strengths including the same fixed dose of samidorphan—10 mg—so advise patients not to double up on the tablets, and to not split them.
Related Resource
• Olanzapine and samidorphan (Lybalvi) prescribing information. https://www.lybalvi.com/lybalvi-prescribing-information.pdf
Drug Brand Names
Diazepam • Valium
Lithium • Eskalith, Lithobid
Olanzapine • Zyprexa
Olanzapine-fluoxetine combination • Symbyax
Olanzapine-samidorphan combination • Lybalvi
Valproate • Depakote, Depakene
Bottom Line
Olanzapine-samidorphan combination (OSC) is intended to mitigate some of the weight gain anticipated when using olanzapine alone. For clinicians who have prescribed olanzapine and have seen its therapeutic benefits, OSC will be a welcome addition to the therapeutic armamentarium. For practitioners who may have avoided olanzapine entirely, OSC can provide another means of offering this therapeutic option and counter “olanzapine hesitancy.”
1. US Food and Drug Administration. NDA 213378 approval letter. May 28, 2021. Accessed November 24, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/213378Orig1Orig2s000Approv.pdf
2. Alkermes, Inc. LYBALVI™ (olanzapine and samidorphan) tablets, for oral use. Prescribing information. May 2021. Accessed November 24, 2021. https://www.lybalvi.com/lybalvi-prescribing-information.pdf
3. Citrome L, Graham C, Simmons A, et al. An evidence-based review of OLZ/SAM for treatment of adults with schizophrenia or bipolar I disorder. Neuropsychiatr Dis Treat. 2021;17:2885-2904.
4. Eli Lilly and Company. ZYPREXA (olanzapine) tablet for oral use; ZYPREXA ZYDIS (olanzapine) tablet, orally disintegrating for oral use; ZYPREXA intramuscular (olanzapine) injection, powder, for solution for intramuscular use. Prescribing information. February 2021. Accessed November 24, 2021. https://pi.lilly.com/us/zyprexa-pi.pdf
5. Citrome L, McEvoy JP, Todtenkopf MS, et al. A commentary on the efficacy of olanzapine for the treatment of schizophrenia: the past, present, and future. Neuropsychiatr Dis Treat. 2019;15:2559-2569.
6. Meftah AM, Deckler E, Citrome L, et al. New discoveries for an old drug: a review of recent olanzapine research. Postgrad Med. 2020;132(1):80-90.
7. Citrome L, Holt RI, Walker DJ, et al. Weight gain and changes in metabolic variables following olanzapine treatment in schizophrenia and bipolar disorder. Clin Drug Investig. 2011;31(7):455-482.
8. Potkin SG, Kunovac J, Silverman BL, et al. Efficacy and safety of a combination of olanzapine and samidorphan in adult patients with an acute exacerbation of schizophrenia: outcomes from the randomized, phase 3 ENLIGHTEN-1 study. J Clin Psychiatry. 2020;81(2):19m12769.
9. Yagoda S, Graham C, Simmons A, et al. Long-term safety and durability of effect with a combination of olanzapine and samidorphan in patients with schizophrenia: results from a 1-year open-label extension study. CNS Spectr. 2021;26(4):383-392.
10. Correll CU, Newcomer JW, Silverman B, et al. Effects of olanzapine combined with samidorphan on weight gain in schizophrenia: a 24-week phase 3 study. Am J Psychiatry. 2020;177(12):1168-1178.
11. Kahn RS, Silverman BL, DiPetrillo L, et al. A phase 3, multicenter study to assess the 1-year safety and tolerability of a combination of olanzapine and samidorphan in patients with schizophrenia: results from the ENLIGHTEN-2 long-term extension. Schizophr Res. 2021;232:45-53.
12. US Food and Drug Administration. Drug approval package: Lybalvi. June 26, 2021. Accessed November 24, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/213378Orig1Orig2s000TOC.cfm
13. Sun L, Yagoda S, Yao B, et al. Combination of olanzapine and samidorphan has no clinically significant effect on the pharmacokinetics of lithium or valproate. Clin Drug Investig. 2020;40(1):55-64.
14. Eli Lilly and Company. SYMBYAX (olanzapine and fluoxetine) capsules for oral use. Prescribing information. September 2021. Accessed November 24, 2021. https://pi.lilly.com/us/symbyax-pi.pdf
15. Wentland MP, Lu Q, Lou R, et al. Synthesis and opioid receptor binding properties of a highly potent 4-hydroxy analogue of naltrexone. Bioorg Med Chem Lett. 2005;15(8):2107-2110.
16. Lee MW, Fujioka K. Naltrexone for the treatment of obesity: review and update. Expert Opin Pharmacother. 2009;10(11):1841-1845.
17. Sun L, Yagoda S, Xue H, et al. Combination of olanzapine and samidorphan has no clinically relevant effects on ECG parameters, including the QTc interval: results from a phase 1 QT/QTc study. Prog Neuropsychopharmacol Biol Psychiatry. 2020;100:109881.
18. Zhou SF, Yang LP, Zhou ZW, et al. Insights into the substrate specificity, inhibitors, regulation, and polymorphisms and the clinical impact of human cytochrome P450 1A2. AAPS J. 2009;11(3):481-494.
19. Citrome L, Stauffer VL, Chen L, et al. Olanzapine plasma concentrations after treatment with 10, 20, and 40 mg/d in patients with schizophrenia: an analysis of correlations with efficacy, weight gain, and prolactin concentration. J Clin Psychopharmacol. 2009;29(3):278-283.
20. Cerhan JR, Moore SC, Jacobs EJ, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin Proc. 2014;89(3):335-345.
21. Citrome L, Nasrallah HA. On-label on the table: what the package insert informs us about the tolerability profile of oral atypical antipsychotics, and what it does not. Expert Opin Pharmacother. 2012;13(11):1599-1613.
1. US Food and Drug Administration. NDA 213378 approval letter. May 28, 2021. Accessed November 24, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/213378Orig1Orig2s000Approv.pdf
2. Alkermes, Inc. LYBALVI™ (olanzapine and samidorphan) tablets, for oral use. Prescribing information. May 2021. Accessed November 24, 2021. https://www.lybalvi.com/lybalvi-prescribing-information.pdf
3. Citrome L, Graham C, Simmons A, et al. An evidence-based review of OLZ/SAM for treatment of adults with schizophrenia or bipolar I disorder. Neuropsychiatr Dis Treat. 2021;17:2885-2904.
4. Eli Lilly and Company. ZYPREXA (olanzapine) tablet for oral use; ZYPREXA ZYDIS (olanzapine) tablet, orally disintegrating for oral use; ZYPREXA intramuscular (olanzapine) injection, powder, for solution for intramuscular use. Prescribing information. February 2021. Accessed November 24, 2021. https://pi.lilly.com/us/zyprexa-pi.pdf
5. Citrome L, McEvoy JP, Todtenkopf MS, et al. A commentary on the efficacy of olanzapine for the treatment of schizophrenia: the past, present, and future. Neuropsychiatr Dis Treat. 2019;15:2559-2569.
6. Meftah AM, Deckler E, Citrome L, et al. New discoveries for an old drug: a review of recent olanzapine research. Postgrad Med. 2020;132(1):80-90.
7. Citrome L, Holt RI, Walker DJ, et al. Weight gain and changes in metabolic variables following olanzapine treatment in schizophrenia and bipolar disorder. Clin Drug Investig. 2011;31(7):455-482.
8. Potkin SG, Kunovac J, Silverman BL, et al. Efficacy and safety of a combination of olanzapine and samidorphan in adult patients with an acute exacerbation of schizophrenia: outcomes from the randomized, phase 3 ENLIGHTEN-1 study. J Clin Psychiatry. 2020;81(2):19m12769.
9. Yagoda S, Graham C, Simmons A, et al. Long-term safety and durability of effect with a combination of olanzapine and samidorphan in patients with schizophrenia: results from a 1-year open-label extension study. CNS Spectr. 2021;26(4):383-392.
10. Correll CU, Newcomer JW, Silverman B, et al. Effects of olanzapine combined with samidorphan on weight gain in schizophrenia: a 24-week phase 3 study. Am J Psychiatry. 2020;177(12):1168-1178.
11. Kahn RS, Silverman BL, DiPetrillo L, et al. A phase 3, multicenter study to assess the 1-year safety and tolerability of a combination of olanzapine and samidorphan in patients with schizophrenia: results from the ENLIGHTEN-2 long-term extension. Schizophr Res. 2021;232:45-53.
12. US Food and Drug Administration. Drug approval package: Lybalvi. June 26, 2021. Accessed November 24, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2021/213378Orig1Orig2s000TOC.cfm
13. Sun L, Yagoda S, Yao B, et al. Combination of olanzapine and samidorphan has no clinically significant effect on the pharmacokinetics of lithium or valproate. Clin Drug Investig. 2020;40(1):55-64.
14. Eli Lilly and Company. SYMBYAX (olanzapine and fluoxetine) capsules for oral use. Prescribing information. September 2021. Accessed November 24, 2021. https://pi.lilly.com/us/symbyax-pi.pdf
15. Wentland MP, Lu Q, Lou R, et al. Synthesis and opioid receptor binding properties of a highly potent 4-hydroxy analogue of naltrexone. Bioorg Med Chem Lett. 2005;15(8):2107-2110.
16. Lee MW, Fujioka K. Naltrexone for the treatment of obesity: review and update. Expert Opin Pharmacother. 2009;10(11):1841-1845.
17. Sun L, Yagoda S, Xue H, et al. Combination of olanzapine and samidorphan has no clinically relevant effects on ECG parameters, including the QTc interval: results from a phase 1 QT/QTc study. Prog Neuropsychopharmacol Biol Psychiatry. 2020;100:109881.
18. Zhou SF, Yang LP, Zhou ZW, et al. Insights into the substrate specificity, inhibitors, regulation, and polymorphisms and the clinical impact of human cytochrome P450 1A2. AAPS J. 2009;11(3):481-494.
19. Citrome L, Stauffer VL, Chen L, et al. Olanzapine plasma concentrations after treatment with 10, 20, and 40 mg/d in patients with schizophrenia: an analysis of correlations with efficacy, weight gain, and prolactin concentration. J Clin Psychopharmacol. 2009;29(3):278-283.
20. Cerhan JR, Moore SC, Jacobs EJ, et al. A pooled analysis of waist circumference and mortality in 650,000 adults. Mayo Clin Proc. 2014;89(3):335-345.
21. Citrome L, Nasrallah HA. On-label on the table: what the package insert informs us about the tolerability profile of oral atypical antipsychotics, and what it does not. Expert Opin Pharmacother. 2012;13(11):1599-1613.
New understanding of suicide attempts emerges
even in the absence of a psychiatric disorder.
This finding suggests the genetic underpinnings of suicide attempts are partially shared and partially distinct from those of related psychiatric disorders, the investigators note.
“This study brings us a step closer to understanding the neurobiology of suicidality, with the ultimate goal of developing new treatments and prevention strategies,” Niamh Mullins, PhD, department of psychiatry, department of genetics and genomic sciences, Icahn School of Medicine at Mount Sinai in New York, said in an interview.
The study was published online in Biological Psychiatry.
Largest study to date
In the largest genetic association study of suicide attempt published to date, the researchers conducted a genome-wide association study (GWAS) of 29,782 suicide attempt cases and 519,961 controls in the International Suicide Genetics Consortium (ISGC).
Two loci reached genome-wide significance for suicide attempt – the major histocompatibility complex and an intergenic locus on chromosome 7, the latter of which remained associated with suicide attempt after conditioning on psychiatric disorders and was replicated in an independent cohort of over 14,000 veterans in the Million Veteran Program.
“This is the first replicated genetic locus that contributes more to suicide attempt than related psychiatric disorders,” Dr. Mullins said.
“The study found overlap in the genetic basis of suicide attempt and that of related psychiatric disorders, particularly major depression, but also with that of nonpsychiatric risk factors such as smoking, pain, risk-taking behavior, sleep disturbances, and poorer general health,” Dr. Mullins said.
“These genetic relationships between suicide attempt and nonpsychiatric risk factors were not a by-product of comorbid psychiatric illness, suggesting that there is some shared biological basis between suicide attempt and nonpsychiatric risk factors,” she added.
Dr. Mullins cautioned that the findings do not have any immediate impact on patient care.
“The ultimate goal of this research is to gain insight into the underlying biological pathways involved in suicide attempts or suicidal thoughts, providing potential avenues to treatments and prevention strategies,” she said.
“The study findings also point to the importance of studying the potential direct causal paths between these risk factors and suicide attempt in patients with and without psychiatric illness,” Douglas Ruderfer, PhD, of Vanderbilt University Medical Center, Nashville, Tenn., cofounder and cochair of the consortium and senior author of the paper, added in a news release.
A version of this article first appeared on Medscape.com.
even in the absence of a psychiatric disorder.
This finding suggests the genetic underpinnings of suicide attempts are partially shared and partially distinct from those of related psychiatric disorders, the investigators note.
“This study brings us a step closer to understanding the neurobiology of suicidality, with the ultimate goal of developing new treatments and prevention strategies,” Niamh Mullins, PhD, department of psychiatry, department of genetics and genomic sciences, Icahn School of Medicine at Mount Sinai in New York, said in an interview.
The study was published online in Biological Psychiatry.
Largest study to date
In the largest genetic association study of suicide attempt published to date, the researchers conducted a genome-wide association study (GWAS) of 29,782 suicide attempt cases and 519,961 controls in the International Suicide Genetics Consortium (ISGC).
Two loci reached genome-wide significance for suicide attempt – the major histocompatibility complex and an intergenic locus on chromosome 7, the latter of which remained associated with suicide attempt after conditioning on psychiatric disorders and was replicated in an independent cohort of over 14,000 veterans in the Million Veteran Program.
“This is the first replicated genetic locus that contributes more to suicide attempt than related psychiatric disorders,” Dr. Mullins said.
“The study found overlap in the genetic basis of suicide attempt and that of related psychiatric disorders, particularly major depression, but also with that of nonpsychiatric risk factors such as smoking, pain, risk-taking behavior, sleep disturbances, and poorer general health,” Dr. Mullins said.
“These genetic relationships between suicide attempt and nonpsychiatric risk factors were not a by-product of comorbid psychiatric illness, suggesting that there is some shared biological basis between suicide attempt and nonpsychiatric risk factors,” she added.
Dr. Mullins cautioned that the findings do not have any immediate impact on patient care.
“The ultimate goal of this research is to gain insight into the underlying biological pathways involved in suicide attempts or suicidal thoughts, providing potential avenues to treatments and prevention strategies,” she said.
“The study findings also point to the importance of studying the potential direct causal paths between these risk factors and suicide attempt in patients with and without psychiatric illness,” Douglas Ruderfer, PhD, of Vanderbilt University Medical Center, Nashville, Tenn., cofounder and cochair of the consortium and senior author of the paper, added in a news release.
A version of this article first appeared on Medscape.com.
even in the absence of a psychiatric disorder.
This finding suggests the genetic underpinnings of suicide attempts are partially shared and partially distinct from those of related psychiatric disorders, the investigators note.
“This study brings us a step closer to understanding the neurobiology of suicidality, with the ultimate goal of developing new treatments and prevention strategies,” Niamh Mullins, PhD, department of psychiatry, department of genetics and genomic sciences, Icahn School of Medicine at Mount Sinai in New York, said in an interview.
The study was published online in Biological Psychiatry.
Largest study to date
In the largest genetic association study of suicide attempt published to date, the researchers conducted a genome-wide association study (GWAS) of 29,782 suicide attempt cases and 519,961 controls in the International Suicide Genetics Consortium (ISGC).
Two loci reached genome-wide significance for suicide attempt – the major histocompatibility complex and an intergenic locus on chromosome 7, the latter of which remained associated with suicide attempt after conditioning on psychiatric disorders and was replicated in an independent cohort of over 14,000 veterans in the Million Veteran Program.
“This is the first replicated genetic locus that contributes more to suicide attempt than related psychiatric disorders,” Dr. Mullins said.
“The study found overlap in the genetic basis of suicide attempt and that of related psychiatric disorders, particularly major depression, but also with that of nonpsychiatric risk factors such as smoking, pain, risk-taking behavior, sleep disturbances, and poorer general health,” Dr. Mullins said.
“These genetic relationships between suicide attempt and nonpsychiatric risk factors were not a by-product of comorbid psychiatric illness, suggesting that there is some shared biological basis between suicide attempt and nonpsychiatric risk factors,” she added.
Dr. Mullins cautioned that the findings do not have any immediate impact on patient care.
“The ultimate goal of this research is to gain insight into the underlying biological pathways involved in suicide attempts or suicidal thoughts, providing potential avenues to treatments and prevention strategies,” she said.
“The study findings also point to the importance of studying the potential direct causal paths between these risk factors and suicide attempt in patients with and without psychiatric illness,” Douglas Ruderfer, PhD, of Vanderbilt University Medical Center, Nashville, Tenn., cofounder and cochair of the consortium and senior author of the paper, added in a news release.
A version of this article first appeared on Medscape.com.
FROM BIOLOGICAL PSYCHIATRY
Alan F. Schatzberg, MD, on the state of psychiatry
For this Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Alan F. Schatzberg, MD. Dr. Schatzberg is the Kenneth T. Norris, Jr., Professor of Psychiatry and Behavioral Sciences at Stanford University. He served as the Chair of the Department at Stanford until 2010 and currently directs the Stanford Mood Disorders Center. He was the 136th president of the American Psychiatric Association (APA) (2009-2010). He has been an active investigator in the biology and psychopharmacology of depressive disorders, and has authored more than 700 publications and abstracts, including Schatzberg’s Manual of Clinical Psychopharmacology. Dr. Schatzberg is also the coeditor of the Textbook of Psychopharmacology with Charles B. Nemeroff, MD, PhD. He is a Past President of the American College of Neuropsychopharmacology (ACNP) and the Society of Biological Psychiatry, and was also the Secretary-General of the International Society of Psychoneuroendocrinology (ISPNE). In 2003, he was elected to the Institute of Medicine of the National Academy of Sciences (National Academy of Medicine). He has received numerous prestigious awards, including the 2005 Distinguished Service in Psychiatry Award from the American College of Psychiatrists, the 2005 Falcone Award from the National Alliance for Research in Schizophrenia and Affective Disorders, the 2014 Kraepelin Gold Medal from the Max Planck Institute of Psychiatry, the 2015 Gold Medal from the Society of Biological Psychiatry, the 2015 Lifetime Achievement Award of the ISPNE, the 2017 Julius Axelrod Mentorship Award from the ACNP, the 2018 Donald Klein, MD, Lifetime Achievement Award from the American Society of Clinical Psychopharmacology, and the 2018 Jules Marmor, MD, Award for Biopsychosocial Research from the APA.
Dr. Aftab: You have devoted much of your career to the development of psychopharmacology. What is your perspective on where the field of psychopharmacology stands at present, especially amid the widespread recognition of “treatment resistance” as a pervasive phenomenon and the scarcity of validated neurobiologic etiological models for psychiatric disorders?
Dr. Schatzberg: We have made considerable progress in the development of new classes of agents for major depression, but as we develop new agents, we still see a large percentage of patients who do not seem to demonstrate adequate responses, particularly in major depressive disorder. This has driven us to look for agents that work differently than previous ones. Although we have some new agents with seeming efficacy and newer mechanisms of action, eg, esketamine, these have largely been derived from clinical, often serendipitous, observations of antidepressant effects rather than from prospective development based on a known pharmacological effect or a biological construct of the disorder. Another intriguing and possibly effective anxiolytic and antidepressive agent is psilocybin, whose potential use is largely derived from clinicians who found it helpful in their practices in combination with psychotherapy. These 2 demonstrate how as we branch out into new territory, we find ourselves moving more and more toward drugs of known clinical risk; eg, mind-altering agents or drugs of abuse. These agents may offer risk-benefit ratios that can ultimately prove to be less attractive than what we might have wanted when we ventured on the journey. Unfortunately, there has been little dialogue about the limitations of several of these agents.
In the case of esketamine, the notion has been that the drug is a blocker of the N-methyl-
One approach that has been applied recently is target validation that purports to use functional MRI to assess behavioral and cognitive effects of drugs to allow inferences regarding efficacy in specific disorders. As we have discussed in a recent paper published in the American Journal of Psychiatry,4 this can be quite misleading and may provide both false positive and negative information. From my perspective, these tests do not appear sensitive enough to screen for patients having a disorder, nor for assessing possible drug effects in those patients. Thus, it is unclear if they can provide answers today that we can be confident in.
Continue to: Dr. Aftab...
Dr. Aftab: What do you see as some of the strengths of psychiatry as a profession?
Dr. Schatzberg: Psychiatry as a specialty combines 2 major perspectives—psychological processes and psychobiology—to develop methods for treating patients who suffer from disorders of the mind/brain. It is the most challenging of our specialties because we cannot study the brain directly. We cannot do procedures as we do in cardiology and pulmonology because they may prove dangerously invasive. That hands-off approach limits us, but for the curious it provides an opportunity to begin to unravel the processes that underlie brain functioning. Fortunately, we have therapies—both psychosocial and somatic—that can provide great relief to patients. These can be shown to be effective in sufficient numbers of patients to help many.
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Schatzberg: We need to train our residents in a host of approaches, and not just medications and psychotherapy. They need to understand the basis of brain stimulation approaches (such as repetitive transcranial magnetic stimulation) as well as know how to apply them. We need to train residents more in substance abuse problems and the biology of addiction if they are to better understand the risks of certain new classes of medication. Lastly, we need to train residents in the application of genomics, proteomics, and brain imaging to somatic treatment development.
Dr. Aftab: What is your perception of the threats that psychiatry faces or is likely to face in the future?
Dr. Schatzberg: The biggest threats come from ourselves. We need to do better with our classification approaches, such as the Diagnostic and Statistical Manual of Mental Disorders or the Research Domain Criteria. They need to become more rapidly adaptive to research in the field. We need to be more open to looking at what is a potentially dangerous trend in developing drugs of abuse and mind-altering drugs as therapeutics. We need to be able to demonstrate that telepsychiatry can be as effective as face-to-face treatment and should be reimbursed. Lastly, we need to develop better models for taking care of the psychiatric patient. We have too many patients and not enough psychiatrists.
Dr. Aftab: What do you envision for the future of psychiatry? What sort of opportunities lie ahead for us?
Dr. Schatzberg: I see the future as bright. Over the past 10 years, led by efforts at the APA, some while I was President, reimbursement has increased dramatically. Over the past 10 years, we have done well developing some new drugs and somatic therapies, and these will continue. Less than a decade ago, large pharmaceutical had abandoned psychiatric drug development and investment into biotech start-ups had waned to near zero. However, the last year few years have seen a dramatic surge in investment, and these should yield novel agents and ones that may be combined with innovative biomarkers as companions.
1. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215. doi:10.1176/appi.ajp.2018.18020138
2. Williams NR, Heifets BD, Bentzley BS, et al. Attenuation of antidepressant and antisuicidal effects of ketamine by opioid receptor antagonism. Mol Psychiatry. 2019;24(12):1779-1786. doi:10.1038/s41380-019-0503-4
3. Bonaventura J, Lam S, Carlton M, et al. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry. 2021;10.1038/s41380-021-01093-2. doi:10.1038/s41380-021-01093-2
4. Schatzberg AF. Can target engagement studies miss their targets and mislead drug development? Am J Psychiatry. 2021;178(5):372-374. doi:10.1176/appi.ajp.2020.21030247
For this Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Alan F. Schatzberg, MD. Dr. Schatzberg is the Kenneth T. Norris, Jr., Professor of Psychiatry and Behavioral Sciences at Stanford University. He served as the Chair of the Department at Stanford until 2010 and currently directs the Stanford Mood Disorders Center. He was the 136th president of the American Psychiatric Association (APA) (2009-2010). He has been an active investigator in the biology and psychopharmacology of depressive disorders, and has authored more than 700 publications and abstracts, including Schatzberg’s Manual of Clinical Psychopharmacology. Dr. Schatzberg is also the coeditor of the Textbook of Psychopharmacology with Charles B. Nemeroff, MD, PhD. He is a Past President of the American College of Neuropsychopharmacology (ACNP) and the Society of Biological Psychiatry, and was also the Secretary-General of the International Society of Psychoneuroendocrinology (ISPNE). In 2003, he was elected to the Institute of Medicine of the National Academy of Sciences (National Academy of Medicine). He has received numerous prestigious awards, including the 2005 Distinguished Service in Psychiatry Award from the American College of Psychiatrists, the 2005 Falcone Award from the National Alliance for Research in Schizophrenia and Affective Disorders, the 2014 Kraepelin Gold Medal from the Max Planck Institute of Psychiatry, the 2015 Gold Medal from the Society of Biological Psychiatry, the 2015 Lifetime Achievement Award of the ISPNE, the 2017 Julius Axelrod Mentorship Award from the ACNP, the 2018 Donald Klein, MD, Lifetime Achievement Award from the American Society of Clinical Psychopharmacology, and the 2018 Jules Marmor, MD, Award for Biopsychosocial Research from the APA.
Dr. Aftab: You have devoted much of your career to the development of psychopharmacology. What is your perspective on where the field of psychopharmacology stands at present, especially amid the widespread recognition of “treatment resistance” as a pervasive phenomenon and the scarcity of validated neurobiologic etiological models for psychiatric disorders?
Dr. Schatzberg: We have made considerable progress in the development of new classes of agents for major depression, but as we develop new agents, we still see a large percentage of patients who do not seem to demonstrate adequate responses, particularly in major depressive disorder. This has driven us to look for agents that work differently than previous ones. Although we have some new agents with seeming efficacy and newer mechanisms of action, eg, esketamine, these have largely been derived from clinical, often serendipitous, observations of antidepressant effects rather than from prospective development based on a known pharmacological effect or a biological construct of the disorder. Another intriguing and possibly effective anxiolytic and antidepressive agent is psilocybin, whose potential use is largely derived from clinicians who found it helpful in their practices in combination with psychotherapy. These 2 demonstrate how as we branch out into new territory, we find ourselves moving more and more toward drugs of known clinical risk; eg, mind-altering agents or drugs of abuse. These agents may offer risk-benefit ratios that can ultimately prove to be less attractive than what we might have wanted when we ventured on the journey. Unfortunately, there has been little dialogue about the limitations of several of these agents.
In the case of esketamine, the notion has been that the drug is a blocker of the N-methyl-
One approach that has been applied recently is target validation that purports to use functional MRI to assess behavioral and cognitive effects of drugs to allow inferences regarding efficacy in specific disorders. As we have discussed in a recent paper published in the American Journal of Psychiatry,4 this can be quite misleading and may provide both false positive and negative information. From my perspective, these tests do not appear sensitive enough to screen for patients having a disorder, nor for assessing possible drug effects in those patients. Thus, it is unclear if they can provide answers today that we can be confident in.
Continue to: Dr. Aftab...
Dr. Aftab: What do you see as some of the strengths of psychiatry as a profession?
Dr. Schatzberg: Psychiatry as a specialty combines 2 major perspectives—psychological processes and psychobiology—to develop methods for treating patients who suffer from disorders of the mind/brain. It is the most challenging of our specialties because we cannot study the brain directly. We cannot do procedures as we do in cardiology and pulmonology because they may prove dangerously invasive. That hands-off approach limits us, but for the curious it provides an opportunity to begin to unravel the processes that underlie brain functioning. Fortunately, we have therapies—both psychosocial and somatic—that can provide great relief to patients. These can be shown to be effective in sufficient numbers of patients to help many.
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Schatzberg: We need to train our residents in a host of approaches, and not just medications and psychotherapy. They need to understand the basis of brain stimulation approaches (such as repetitive transcranial magnetic stimulation) as well as know how to apply them. We need to train residents more in substance abuse problems and the biology of addiction if they are to better understand the risks of certain new classes of medication. Lastly, we need to train residents in the application of genomics, proteomics, and brain imaging to somatic treatment development.
Dr. Aftab: What is your perception of the threats that psychiatry faces or is likely to face in the future?
Dr. Schatzberg: The biggest threats come from ourselves. We need to do better with our classification approaches, such as the Diagnostic and Statistical Manual of Mental Disorders or the Research Domain Criteria. They need to become more rapidly adaptive to research in the field. We need to be more open to looking at what is a potentially dangerous trend in developing drugs of abuse and mind-altering drugs as therapeutics. We need to be able to demonstrate that telepsychiatry can be as effective as face-to-face treatment and should be reimbursed. Lastly, we need to develop better models for taking care of the psychiatric patient. We have too many patients and not enough psychiatrists.
Dr. Aftab: What do you envision for the future of psychiatry? What sort of opportunities lie ahead for us?
Dr. Schatzberg: I see the future as bright. Over the past 10 years, led by efforts at the APA, some while I was President, reimbursement has increased dramatically. Over the past 10 years, we have done well developing some new drugs and somatic therapies, and these will continue. Less than a decade ago, large pharmaceutical had abandoned psychiatric drug development and investment into biotech start-ups had waned to near zero. However, the last year few years have seen a dramatic surge in investment, and these should yield novel agents and ones that may be combined with innovative biomarkers as companions.
For this Psychiatry Leaders’ Perspectives, Awais Aftab, MD, interviewed Alan F. Schatzberg, MD. Dr. Schatzberg is the Kenneth T. Norris, Jr., Professor of Psychiatry and Behavioral Sciences at Stanford University. He served as the Chair of the Department at Stanford until 2010 and currently directs the Stanford Mood Disorders Center. He was the 136th president of the American Psychiatric Association (APA) (2009-2010). He has been an active investigator in the biology and psychopharmacology of depressive disorders, and has authored more than 700 publications and abstracts, including Schatzberg’s Manual of Clinical Psychopharmacology. Dr. Schatzberg is also the coeditor of the Textbook of Psychopharmacology with Charles B. Nemeroff, MD, PhD. He is a Past President of the American College of Neuropsychopharmacology (ACNP) and the Society of Biological Psychiatry, and was also the Secretary-General of the International Society of Psychoneuroendocrinology (ISPNE). In 2003, he was elected to the Institute of Medicine of the National Academy of Sciences (National Academy of Medicine). He has received numerous prestigious awards, including the 2005 Distinguished Service in Psychiatry Award from the American College of Psychiatrists, the 2005 Falcone Award from the National Alliance for Research in Schizophrenia and Affective Disorders, the 2014 Kraepelin Gold Medal from the Max Planck Institute of Psychiatry, the 2015 Gold Medal from the Society of Biological Psychiatry, the 2015 Lifetime Achievement Award of the ISPNE, the 2017 Julius Axelrod Mentorship Award from the ACNP, the 2018 Donald Klein, MD, Lifetime Achievement Award from the American Society of Clinical Psychopharmacology, and the 2018 Jules Marmor, MD, Award for Biopsychosocial Research from the APA.
Dr. Aftab: You have devoted much of your career to the development of psychopharmacology. What is your perspective on where the field of psychopharmacology stands at present, especially amid the widespread recognition of “treatment resistance” as a pervasive phenomenon and the scarcity of validated neurobiologic etiological models for psychiatric disorders?
Dr. Schatzberg: We have made considerable progress in the development of new classes of agents for major depression, but as we develop new agents, we still see a large percentage of patients who do not seem to demonstrate adequate responses, particularly in major depressive disorder. This has driven us to look for agents that work differently than previous ones. Although we have some new agents with seeming efficacy and newer mechanisms of action, eg, esketamine, these have largely been derived from clinical, often serendipitous, observations of antidepressant effects rather than from prospective development based on a known pharmacological effect or a biological construct of the disorder. Another intriguing and possibly effective anxiolytic and antidepressive agent is psilocybin, whose potential use is largely derived from clinicians who found it helpful in their practices in combination with psychotherapy. These 2 demonstrate how as we branch out into new territory, we find ourselves moving more and more toward drugs of known clinical risk; eg, mind-altering agents or drugs of abuse. These agents may offer risk-benefit ratios that can ultimately prove to be less attractive than what we might have wanted when we ventured on the journey. Unfortunately, there has been little dialogue about the limitations of several of these agents.
In the case of esketamine, the notion has been that the drug is a blocker of the N-methyl-
One approach that has been applied recently is target validation that purports to use functional MRI to assess behavioral and cognitive effects of drugs to allow inferences regarding efficacy in specific disorders. As we have discussed in a recent paper published in the American Journal of Psychiatry,4 this can be quite misleading and may provide both false positive and negative information. From my perspective, these tests do not appear sensitive enough to screen for patients having a disorder, nor for assessing possible drug effects in those patients. Thus, it is unclear if they can provide answers today that we can be confident in.
Continue to: Dr. Aftab...
Dr. Aftab: What do you see as some of the strengths of psychiatry as a profession?
Dr. Schatzberg: Psychiatry as a specialty combines 2 major perspectives—psychological processes and psychobiology—to develop methods for treating patients who suffer from disorders of the mind/brain. It is the most challenging of our specialties because we cannot study the brain directly. We cannot do procedures as we do in cardiology and pulmonology because they may prove dangerously invasive. That hands-off approach limits us, but for the curious it provides an opportunity to begin to unravel the processes that underlie brain functioning. Fortunately, we have therapies—both psychosocial and somatic—that can provide great relief to patients. These can be shown to be effective in sufficient numbers of patients to help many.
Dr. Aftab: Are there ways in which the status quo in psychiatry falls short of the ideal? What are our areas of relative weakness?
Dr. Schatzberg: We need to train our residents in a host of approaches, and not just medications and psychotherapy. They need to understand the basis of brain stimulation approaches (such as repetitive transcranial magnetic stimulation) as well as know how to apply them. We need to train residents more in substance abuse problems and the biology of addiction if they are to better understand the risks of certain new classes of medication. Lastly, we need to train residents in the application of genomics, proteomics, and brain imaging to somatic treatment development.
Dr. Aftab: What is your perception of the threats that psychiatry faces or is likely to face in the future?
Dr. Schatzberg: The biggest threats come from ourselves. We need to do better with our classification approaches, such as the Diagnostic and Statistical Manual of Mental Disorders or the Research Domain Criteria. They need to become more rapidly adaptive to research in the field. We need to be more open to looking at what is a potentially dangerous trend in developing drugs of abuse and mind-altering drugs as therapeutics. We need to be able to demonstrate that telepsychiatry can be as effective as face-to-face treatment and should be reimbursed. Lastly, we need to develop better models for taking care of the psychiatric patient. We have too many patients and not enough psychiatrists.
Dr. Aftab: What do you envision for the future of psychiatry? What sort of opportunities lie ahead for us?
Dr. Schatzberg: I see the future as bright. Over the past 10 years, led by efforts at the APA, some while I was President, reimbursement has increased dramatically. Over the past 10 years, we have done well developing some new drugs and somatic therapies, and these will continue. Less than a decade ago, large pharmaceutical had abandoned psychiatric drug development and investment into biotech start-ups had waned to near zero. However, the last year few years have seen a dramatic surge in investment, and these should yield novel agents and ones that may be combined with innovative biomarkers as companions.
1. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215. doi:10.1176/appi.ajp.2018.18020138
2. Williams NR, Heifets BD, Bentzley BS, et al. Attenuation of antidepressant and antisuicidal effects of ketamine by opioid receptor antagonism. Mol Psychiatry. 2019;24(12):1779-1786. doi:10.1038/s41380-019-0503-4
3. Bonaventura J, Lam S, Carlton M, et al. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry. 2021;10.1038/s41380-021-01093-2. doi:10.1038/s41380-021-01093-2
4. Schatzberg AF. Can target engagement studies miss their targets and mislead drug development? Am J Psychiatry. 2021;178(5):372-374. doi:10.1176/appi.ajp.2020.21030247
1. Williams NR, Heifets BD, Blasey C, et al. Attenuation of antidepressant effects of ketamine by opioid receptor antagonism. Am J Psychiatry. 2018;175(12):1205-1215. doi:10.1176/appi.ajp.2018.18020138
2. Williams NR, Heifets BD, Bentzley BS, et al. Attenuation of antidepressant and antisuicidal effects of ketamine by opioid receptor antagonism. Mol Psychiatry. 2019;24(12):1779-1786. doi:10.1038/s41380-019-0503-4
3. Bonaventura J, Lam S, Carlton M, et al. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry. 2021;10.1038/s41380-021-01093-2. doi:10.1038/s41380-021-01093-2
4. Schatzberg AF. Can target engagement studies miss their targets and mislead drug development? Am J Psychiatry. 2021;178(5):372-374. doi:10.1176/appi.ajp.2020.21030247