User login
FLIP panometry tops HRM for esophageal motility measurement
Functional luminal imaging probe (FLIP) panometry proved superior to high-resolution manometry (HRM) for evaluation of esophageal motility, according to a new study based on data from 329 adults.
HRM is generally considered the primary method for evaluating esophageal motility, but current recommendations include the use of a FLIP or timed barium esophogram (TBE) if HRM yields inconclusive results, Dustin A. Carlson, MD, of Northwestern University, Chicago, and colleagues wrote in the recent study. FLIP has several potential advantages over HRM, including that “the test is performed on a sedated patient at the time of endoscopy, as opposed to the awake transnasal catheter used for HRM”; however, comparisons of the two methods for predicting esophageal retention are lacking.
In the study published in the American Journal of Gastroenterology, the researchers reviewed data from 329 consecutive patients aged 18-89 years who completed FLIP, HRM, and TBE for evaluation of primary esophageal motility. They excluded patients with previous foregut surgery. The researchers compared the ability of FLIP and HRM to predict esophageal retention based on abnormal TBE findings, which was defined as a 1-minute column height greater than 5 cm or as impaction of a 12.5-mm barium tablet.
For HRM, the integrated relaxation pressure (IRP) was assessed in the supine and upright patient positions to predict abnormal TBE findings. For FLIP, esophagogastric junction (EGJ) opening was assessed with a 16-cm FLIP performed during sedated endoscopy, and the presence of abnormal TBE findings was determined using the EGJ–distensibility index and maximum EGJ diameter.
The area under the ROC curve for identifying abnormal TBE findings was 0.79 (95% confidence interval, 0.75-0.84) for supine, 0.79 (95% CI, 0.76-0.86) for upright IRP, 0.84 (95% CI, 0.79-0.88) for the EGJ–distensibility index, and 0.88 (95% CI, 0.85-0.92) for the maximum EGJ diameter.
In a logistic regression analysis, the odds ratios for predicting abnormal TBE findings were 1.8 (95% confidence interval, 0.84-3.7; P < .133) for consistent elevation of IRP in HRM, compared with normal IRP, and 39.7 (95% CI, 16.4-96.2; P < .001) for reduced EGJ opening on FLIP panometry, compared with normal EGJ opening.
“Both the IRP on HRM and FLIP panometry metrics of EGJ opening (EGJ–[distensibility index] and maximum EGJ diameter) demonstrated capabilities to differentiate between abnormal and normal esophageal retention, which supports confidence in both tools,” the authors explained. “However, FLIP panometry parameters did so more accurately and with greater predictive capability as reflected by ROC and regression analysis.”
A total of 40 patients (12%) showed discordance between their HRM and FLIP panometry measures, and among these, FLIP showed stronger detection of esophageal retention. FLIP panometry was consistent with TBE in 78% of cases, while HRM-IRP was consistent with TBE in 23%. “Discordant results between HRM and FLIP panometry were observed in previous studies and again in this study, a scenario with unclear clinical significance,” the authors noted, which was why they used TBE as “an objective measure of esophageal retention that was independent of both HRM and FLIP to compare the two modalities.”
The study findings were limited by several factors including ones related to the use of TBE as the primary outcome, as well as the lack of longitudinal outcomes, the researchers noted. There is also the potential for referral bias and selection bias with an overrepresentation of patients with achalasia and EGJ outflow obstruction. However, the results were strengthened by the large sample size of patients who completed evaluations with HRM, FLIP, and TBE.
The study “provides additional support for the use of FLIP panometry to evaluate esophageal motility because it accurately identifies normal and abnormal retention, but also identifies patients who should undergo further complementary diagnostic testing,” they noted. Longitudinal studies are needed to explore best practices for managing esophageal motor disorders. In the meantime, evaluation with FLIP panometry, TBE, and HRM likely remains necessary for some patients, “particularly those with equivocal findings on a single test,” to better characterize disease and guide treatment, the researchers concluded.
Findings support potential of FLIP
“The endoscopic FLIP is an exciting clinical tool that utilizes distension of a catheter-mounted balloon to different volumes to acquire esophageal dimensions and pressures,” Amit Patel, MD, of Duke University, Durham, N.C., said in an interview.
“Accumulating data on FLIP inspired [recently published guidelines] to suggest the use of FLIP to complement high-resolution manometry in the setting of obstructive esophageal symptoms and borderline HRM findings, for patients in whom an HRM study cannot be completed, and for intraprocedural use during interventions for achalasia,” Dr. Patel said. “However, the comparative utility of FLIP, particularly among foundational esophageal diagnostics such as HRM and TBE, is less well developed at this point.”
Dr. Patel said he was surprised by some of the findings. “The characteristics of FLIP metrics (specifically, EGJ–distensibility index <2 mm2/mm Hg and/or maximum EGJ diameter <12 mm) were numerically superior to those for traditional IRP metrics from HRM in predicting retention on TBE on AUROC, regression analyses, and discordant cases in this study,” said Dr. Patel. “Although this study also corroborated the value of IRP on HRM, these findings were somewhat surprising for HRM, given its well-earned reputation as the gold standard for the diagnosis of esophageal motor disorders, its widespread use, and the record of strong data supporting its important role in clinical practice.”
Overall, this study suggests these metrics from FLIP (namely, EGJ–distensibility index and EGJ diameter) may have “diagnostic value beyond traditional IRP metrics from HRM to identify objective retention on TBE,” said Dr. Patel, who also said these exciting findings “support the growth of the complementary role of FLIP ... particularly in cases where HRM may be inconclusive or not tolerated by patients.”
However, more research is needed. “Taking into account other HRM metrics beyond IRP, such as intrabolus pressures or evaluation of bolus transit on impedance, and provocative maneuvers on HRM, such as rapid drink challenges or solid swallows, may be appropriate for further evaluation, as will improved arbitration of ‘borderline’ metrics or less clear cases,” Dr. Patel emphasized. Future studies should also incorporate management interventions and assessments of outcomes.
The study was supported by a grant from the Public Health service to a coinvestigator, and by the American College of Gastroenterology Junior Faculty Development Award to lead author Dr. Carlson. Dr. Carlson also disclosed speaking and consulting relationships with Medtronic, which manufactures FLIP panometry systems. Northwestern University and several coauthors also disclosed intellectual property rights and ownership surrounding FLIP panometry systems, methods, and apparatus with Medtronic. Dr. Patel had no financial conflicts to disclose.
This article was updated Oct. 13, 2021.
Functional luminal imaging probe (FLIP) panometry proved superior to high-resolution manometry (HRM) for evaluation of esophageal motility, according to a new study based on data from 329 adults.
HRM is generally considered the primary method for evaluating esophageal motility, but current recommendations include the use of a FLIP or timed barium esophogram (TBE) if HRM yields inconclusive results, Dustin A. Carlson, MD, of Northwestern University, Chicago, and colleagues wrote in the recent study. FLIP has several potential advantages over HRM, including that “the test is performed on a sedated patient at the time of endoscopy, as opposed to the awake transnasal catheter used for HRM”; however, comparisons of the two methods for predicting esophageal retention are lacking.
In the study published in the American Journal of Gastroenterology, the researchers reviewed data from 329 consecutive patients aged 18-89 years who completed FLIP, HRM, and TBE for evaluation of primary esophageal motility. They excluded patients with previous foregut surgery. The researchers compared the ability of FLIP and HRM to predict esophageal retention based on abnormal TBE findings, which was defined as a 1-minute column height greater than 5 cm or as impaction of a 12.5-mm barium tablet.
For HRM, the integrated relaxation pressure (IRP) was assessed in the supine and upright patient positions to predict abnormal TBE findings. For FLIP, esophagogastric junction (EGJ) opening was assessed with a 16-cm FLIP performed during sedated endoscopy, and the presence of abnormal TBE findings was determined using the EGJ–distensibility index and maximum EGJ diameter.
The area under the ROC curve for identifying abnormal TBE findings was 0.79 (95% confidence interval, 0.75-0.84) for supine, 0.79 (95% CI, 0.76-0.86) for upright IRP, 0.84 (95% CI, 0.79-0.88) for the EGJ–distensibility index, and 0.88 (95% CI, 0.85-0.92) for the maximum EGJ diameter.
In a logistic regression analysis, the odds ratios for predicting abnormal TBE findings were 1.8 (95% confidence interval, 0.84-3.7; P < .133) for consistent elevation of IRP in HRM, compared with normal IRP, and 39.7 (95% CI, 16.4-96.2; P < .001) for reduced EGJ opening on FLIP panometry, compared with normal EGJ opening.
“Both the IRP on HRM and FLIP panometry metrics of EGJ opening (EGJ–[distensibility index] and maximum EGJ diameter) demonstrated capabilities to differentiate between abnormal and normal esophageal retention, which supports confidence in both tools,” the authors explained. “However, FLIP panometry parameters did so more accurately and with greater predictive capability as reflected by ROC and regression analysis.”
A total of 40 patients (12%) showed discordance between their HRM and FLIP panometry measures, and among these, FLIP showed stronger detection of esophageal retention. FLIP panometry was consistent with TBE in 78% of cases, while HRM-IRP was consistent with TBE in 23%. “Discordant results between HRM and FLIP panometry were observed in previous studies and again in this study, a scenario with unclear clinical significance,” the authors noted, which was why they used TBE as “an objective measure of esophageal retention that was independent of both HRM and FLIP to compare the two modalities.”
The study findings were limited by several factors including ones related to the use of TBE as the primary outcome, as well as the lack of longitudinal outcomes, the researchers noted. There is also the potential for referral bias and selection bias with an overrepresentation of patients with achalasia and EGJ outflow obstruction. However, the results were strengthened by the large sample size of patients who completed evaluations with HRM, FLIP, and TBE.
The study “provides additional support for the use of FLIP panometry to evaluate esophageal motility because it accurately identifies normal and abnormal retention, but also identifies patients who should undergo further complementary diagnostic testing,” they noted. Longitudinal studies are needed to explore best practices for managing esophageal motor disorders. In the meantime, evaluation with FLIP panometry, TBE, and HRM likely remains necessary for some patients, “particularly those with equivocal findings on a single test,” to better characterize disease and guide treatment, the researchers concluded.
Findings support potential of FLIP
“The endoscopic FLIP is an exciting clinical tool that utilizes distension of a catheter-mounted balloon to different volumes to acquire esophageal dimensions and pressures,” Amit Patel, MD, of Duke University, Durham, N.C., said in an interview.
“Accumulating data on FLIP inspired [recently published guidelines] to suggest the use of FLIP to complement high-resolution manometry in the setting of obstructive esophageal symptoms and borderline HRM findings, for patients in whom an HRM study cannot be completed, and for intraprocedural use during interventions for achalasia,” Dr. Patel said. “However, the comparative utility of FLIP, particularly among foundational esophageal diagnostics such as HRM and TBE, is less well developed at this point.”
Dr. Patel said he was surprised by some of the findings. “The characteristics of FLIP metrics (specifically, EGJ–distensibility index <2 mm2/mm Hg and/or maximum EGJ diameter <12 mm) were numerically superior to those for traditional IRP metrics from HRM in predicting retention on TBE on AUROC, regression analyses, and discordant cases in this study,” said Dr. Patel. “Although this study also corroborated the value of IRP on HRM, these findings were somewhat surprising for HRM, given its well-earned reputation as the gold standard for the diagnosis of esophageal motor disorders, its widespread use, and the record of strong data supporting its important role in clinical practice.”
Overall, this study suggests these metrics from FLIP (namely, EGJ–distensibility index and EGJ diameter) may have “diagnostic value beyond traditional IRP metrics from HRM to identify objective retention on TBE,” said Dr. Patel, who also said these exciting findings “support the growth of the complementary role of FLIP ... particularly in cases where HRM may be inconclusive or not tolerated by patients.”
However, more research is needed. “Taking into account other HRM metrics beyond IRP, such as intrabolus pressures or evaluation of bolus transit on impedance, and provocative maneuvers on HRM, such as rapid drink challenges or solid swallows, may be appropriate for further evaluation, as will improved arbitration of ‘borderline’ metrics or less clear cases,” Dr. Patel emphasized. Future studies should also incorporate management interventions and assessments of outcomes.
The study was supported by a grant from the Public Health service to a coinvestigator, and by the American College of Gastroenterology Junior Faculty Development Award to lead author Dr. Carlson. Dr. Carlson also disclosed speaking and consulting relationships with Medtronic, which manufactures FLIP panometry systems. Northwestern University and several coauthors also disclosed intellectual property rights and ownership surrounding FLIP panometry systems, methods, and apparatus with Medtronic. Dr. Patel had no financial conflicts to disclose.
This article was updated Oct. 13, 2021.
Functional luminal imaging probe (FLIP) panometry proved superior to high-resolution manometry (HRM) for evaluation of esophageal motility, according to a new study based on data from 329 adults.
HRM is generally considered the primary method for evaluating esophageal motility, but current recommendations include the use of a FLIP or timed barium esophogram (TBE) if HRM yields inconclusive results, Dustin A. Carlson, MD, of Northwestern University, Chicago, and colleagues wrote in the recent study. FLIP has several potential advantages over HRM, including that “the test is performed on a sedated patient at the time of endoscopy, as opposed to the awake transnasal catheter used for HRM”; however, comparisons of the two methods for predicting esophageal retention are lacking.
In the study published in the American Journal of Gastroenterology, the researchers reviewed data from 329 consecutive patients aged 18-89 years who completed FLIP, HRM, and TBE for evaluation of primary esophageal motility. They excluded patients with previous foregut surgery. The researchers compared the ability of FLIP and HRM to predict esophageal retention based on abnormal TBE findings, which was defined as a 1-minute column height greater than 5 cm or as impaction of a 12.5-mm barium tablet.
For HRM, the integrated relaxation pressure (IRP) was assessed in the supine and upright patient positions to predict abnormal TBE findings. For FLIP, esophagogastric junction (EGJ) opening was assessed with a 16-cm FLIP performed during sedated endoscopy, and the presence of abnormal TBE findings was determined using the EGJ–distensibility index and maximum EGJ diameter.
The area under the ROC curve for identifying abnormal TBE findings was 0.79 (95% confidence interval, 0.75-0.84) for supine, 0.79 (95% CI, 0.76-0.86) for upright IRP, 0.84 (95% CI, 0.79-0.88) for the EGJ–distensibility index, and 0.88 (95% CI, 0.85-0.92) for the maximum EGJ diameter.
In a logistic regression analysis, the odds ratios for predicting abnormal TBE findings were 1.8 (95% confidence interval, 0.84-3.7; P < .133) for consistent elevation of IRP in HRM, compared with normal IRP, and 39.7 (95% CI, 16.4-96.2; P < .001) for reduced EGJ opening on FLIP panometry, compared with normal EGJ opening.
“Both the IRP on HRM and FLIP panometry metrics of EGJ opening (EGJ–[distensibility index] and maximum EGJ diameter) demonstrated capabilities to differentiate between abnormal and normal esophageal retention, which supports confidence in both tools,” the authors explained. “However, FLIP panometry parameters did so more accurately and with greater predictive capability as reflected by ROC and regression analysis.”
A total of 40 patients (12%) showed discordance between their HRM and FLIP panometry measures, and among these, FLIP showed stronger detection of esophageal retention. FLIP panometry was consistent with TBE in 78% of cases, while HRM-IRP was consistent with TBE in 23%. “Discordant results between HRM and FLIP panometry were observed in previous studies and again in this study, a scenario with unclear clinical significance,” the authors noted, which was why they used TBE as “an objective measure of esophageal retention that was independent of both HRM and FLIP to compare the two modalities.”
The study findings were limited by several factors including ones related to the use of TBE as the primary outcome, as well as the lack of longitudinal outcomes, the researchers noted. There is also the potential for referral bias and selection bias with an overrepresentation of patients with achalasia and EGJ outflow obstruction. However, the results were strengthened by the large sample size of patients who completed evaluations with HRM, FLIP, and TBE.
The study “provides additional support for the use of FLIP panometry to evaluate esophageal motility because it accurately identifies normal and abnormal retention, but also identifies patients who should undergo further complementary diagnostic testing,” they noted. Longitudinal studies are needed to explore best practices for managing esophageal motor disorders. In the meantime, evaluation with FLIP panometry, TBE, and HRM likely remains necessary for some patients, “particularly those with equivocal findings on a single test,” to better characterize disease and guide treatment, the researchers concluded.
Findings support potential of FLIP
“The endoscopic FLIP is an exciting clinical tool that utilizes distension of a catheter-mounted balloon to different volumes to acquire esophageal dimensions and pressures,” Amit Patel, MD, of Duke University, Durham, N.C., said in an interview.
“Accumulating data on FLIP inspired [recently published guidelines] to suggest the use of FLIP to complement high-resolution manometry in the setting of obstructive esophageal symptoms and borderline HRM findings, for patients in whom an HRM study cannot be completed, and for intraprocedural use during interventions for achalasia,” Dr. Patel said. “However, the comparative utility of FLIP, particularly among foundational esophageal diagnostics such as HRM and TBE, is less well developed at this point.”
Dr. Patel said he was surprised by some of the findings. “The characteristics of FLIP metrics (specifically, EGJ–distensibility index <2 mm2/mm Hg and/or maximum EGJ diameter <12 mm) were numerically superior to those for traditional IRP metrics from HRM in predicting retention on TBE on AUROC, regression analyses, and discordant cases in this study,” said Dr. Patel. “Although this study also corroborated the value of IRP on HRM, these findings were somewhat surprising for HRM, given its well-earned reputation as the gold standard for the diagnosis of esophageal motor disorders, its widespread use, and the record of strong data supporting its important role in clinical practice.”
Overall, this study suggests these metrics from FLIP (namely, EGJ–distensibility index and EGJ diameter) may have “diagnostic value beyond traditional IRP metrics from HRM to identify objective retention on TBE,” said Dr. Patel, who also said these exciting findings “support the growth of the complementary role of FLIP ... particularly in cases where HRM may be inconclusive or not tolerated by patients.”
However, more research is needed. “Taking into account other HRM metrics beyond IRP, such as intrabolus pressures or evaluation of bolus transit on impedance, and provocative maneuvers on HRM, such as rapid drink challenges or solid swallows, may be appropriate for further evaluation, as will improved arbitration of ‘borderline’ metrics or less clear cases,” Dr. Patel emphasized. Future studies should also incorporate management interventions and assessments of outcomes.
The study was supported by a grant from the Public Health service to a coinvestigator, and by the American College of Gastroenterology Junior Faculty Development Award to lead author Dr. Carlson. Dr. Carlson also disclosed speaking and consulting relationships with Medtronic, which manufactures FLIP panometry systems. Northwestern University and several coauthors also disclosed intellectual property rights and ownership surrounding FLIP panometry systems, methods, and apparatus with Medtronic. Dr. Patel had no financial conflicts to disclose.
This article was updated Oct. 13, 2021.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
PHM 2021: Leading through adversity
PHM 2021 session
Leading through adversity
Presenter
Ilan Alhadeff, MD, MBA, SFHM, CLHM
Session summary
As the VP of hospitalist services and a practicing hospitalist in Boca Raton, Fla., Dr. Alhadeff shared an emotional journey where the impact of lives lost has led to organizational innovation and advocacy. He started this journey on the date of the Parkland High School shooting, Feb. 14, 2018. On this day, he lost his 14 year-old daughter Alyssa and described subsequent emotions of anger, sadness, hopelessness, and feeling the pressure to be the protector of his family. Despite receiving an outpouring of support through memorials, texts, letters, and social media posts, he was immersed in “survival mode.” He likens this to the experience many of us may be having during the pandemic. He described caring for patients with limited empathy and the impact this likely had on patient care. During this challenging time, the strongest supports became those that stated they couldn’t imagine how this event could have impacted Dr. Alhadeff’s life but offered support in any way needed – true empathic communication.
“It ain’t about how hard you hit. It’s about how hard you can get hit and keep moving forward.” – Rocky Balboa (2006)
Despite the above, he and his wife founded Make Our Schools Safe (MOSS), a student-forward organization that promotes a culture of safety where all involved are counseled, “If you see something, say something.” Students are encouraged to use social media as an anonymous reporting tool. Likewise, this organization supports efforts for silent safety alerts in schools and fencing around schools to allow for 1-point entry. Lessons Dr. Alhadeff learned that might impact any pediatric hospitalist include the knowledge that mental health concerns aren’t going away; for example, after a school shooting any student affected should be provided counseling services as needed, the need to prevent triggering events, and turning grief into action can help.
“Life is like riding a bicycle. To keep your balance, you must keep moving.” – Albert Einstein (1930)
Dr. Alhadeff then described the process of “moving on” for him and his family. For his children, this initially meant “busying” their lives. They then gradually eased into therapy, and ultimately adopted a support dog. He experienced recurrent loss with his father passing away in March 2019, and he persevered in legislative advocacy in New Jersey and Florida and personal/professional development with work toward his MBA degree. Through this work, he collaborated with many legislators and two presidents. He describes resiliency as the ability to bounce back from adversity, with components including self-awareness, mindfulness, self-care, positive relationships, and purpose. While many of us have not had the great personal losses and challenge experienced by Dr. Alhadeff, we all are experiencing an once-in-a-lifetime transformation of health care with political and social interference. It is up to each of us to determine our role and how we can use our influence for positive change.
As noted by Dr. Alhadeff, “We are not all in the same boat. We ARE in the same storm.”
Key takeaways
- How PHM can promote MOSS: Allow children to be part of the work to keep schools safe. Advocate for local MOSS chapters. Support legislative advocacy for school safety.
- Despite adversity, we have the ability to demonstrate resilience. We do so through development of self-awareness, mindfulness, engagement in self-care, nurturing positive relationships, and continuing to pursue our greater purpose.
Dr. King is a pediatric hospitalist at Children’s MN and the director of medical education, an associate program director for the Pediatrics Residency program at the University of Minnesota. She received her medical degree from Wright State University Boonshoft School of Medicine and completed pediatric residency and chief residency at the University of Minnesota.
PHM 2021 session
Leading through adversity
Presenter
Ilan Alhadeff, MD, MBA, SFHM, CLHM
Session summary
As the VP of hospitalist services and a practicing hospitalist in Boca Raton, Fla., Dr. Alhadeff shared an emotional journey where the impact of lives lost has led to organizational innovation and advocacy. He started this journey on the date of the Parkland High School shooting, Feb. 14, 2018. On this day, he lost his 14 year-old daughter Alyssa and described subsequent emotions of anger, sadness, hopelessness, and feeling the pressure to be the protector of his family. Despite receiving an outpouring of support through memorials, texts, letters, and social media posts, he was immersed in “survival mode.” He likens this to the experience many of us may be having during the pandemic. He described caring for patients with limited empathy and the impact this likely had on patient care. During this challenging time, the strongest supports became those that stated they couldn’t imagine how this event could have impacted Dr. Alhadeff’s life but offered support in any way needed – true empathic communication.
“It ain’t about how hard you hit. It’s about how hard you can get hit and keep moving forward.” – Rocky Balboa (2006)
Despite the above, he and his wife founded Make Our Schools Safe (MOSS), a student-forward organization that promotes a culture of safety where all involved are counseled, “If you see something, say something.” Students are encouraged to use social media as an anonymous reporting tool. Likewise, this organization supports efforts for silent safety alerts in schools and fencing around schools to allow for 1-point entry. Lessons Dr. Alhadeff learned that might impact any pediatric hospitalist include the knowledge that mental health concerns aren’t going away; for example, after a school shooting any student affected should be provided counseling services as needed, the need to prevent triggering events, and turning grief into action can help.
“Life is like riding a bicycle. To keep your balance, you must keep moving.” – Albert Einstein (1930)
Dr. Alhadeff then described the process of “moving on” for him and his family. For his children, this initially meant “busying” their lives. They then gradually eased into therapy, and ultimately adopted a support dog. He experienced recurrent loss with his father passing away in March 2019, and he persevered in legislative advocacy in New Jersey and Florida and personal/professional development with work toward his MBA degree. Through this work, he collaborated with many legislators and two presidents. He describes resiliency as the ability to bounce back from adversity, with components including self-awareness, mindfulness, self-care, positive relationships, and purpose. While many of us have not had the great personal losses and challenge experienced by Dr. Alhadeff, we all are experiencing an once-in-a-lifetime transformation of health care with political and social interference. It is up to each of us to determine our role and how we can use our influence for positive change.
As noted by Dr. Alhadeff, “We are not all in the same boat. We ARE in the same storm.”
Key takeaways
- How PHM can promote MOSS: Allow children to be part of the work to keep schools safe. Advocate for local MOSS chapters. Support legislative advocacy for school safety.
- Despite adversity, we have the ability to demonstrate resilience. We do so through development of self-awareness, mindfulness, engagement in self-care, nurturing positive relationships, and continuing to pursue our greater purpose.
Dr. King is a pediatric hospitalist at Children’s MN and the director of medical education, an associate program director for the Pediatrics Residency program at the University of Minnesota. She received her medical degree from Wright State University Boonshoft School of Medicine and completed pediatric residency and chief residency at the University of Minnesota.
PHM 2021 session
Leading through adversity
Presenter
Ilan Alhadeff, MD, MBA, SFHM, CLHM
Session summary
As the VP of hospitalist services and a practicing hospitalist in Boca Raton, Fla., Dr. Alhadeff shared an emotional journey where the impact of lives lost has led to organizational innovation and advocacy. He started this journey on the date of the Parkland High School shooting, Feb. 14, 2018. On this day, he lost his 14 year-old daughter Alyssa and described subsequent emotions of anger, sadness, hopelessness, and feeling the pressure to be the protector of his family. Despite receiving an outpouring of support through memorials, texts, letters, and social media posts, he was immersed in “survival mode.” He likens this to the experience many of us may be having during the pandemic. He described caring for patients with limited empathy and the impact this likely had on patient care. During this challenging time, the strongest supports became those that stated they couldn’t imagine how this event could have impacted Dr. Alhadeff’s life but offered support in any way needed – true empathic communication.
“It ain’t about how hard you hit. It’s about how hard you can get hit and keep moving forward.” – Rocky Balboa (2006)
Despite the above, he and his wife founded Make Our Schools Safe (MOSS), a student-forward organization that promotes a culture of safety where all involved are counseled, “If you see something, say something.” Students are encouraged to use social media as an anonymous reporting tool. Likewise, this organization supports efforts for silent safety alerts in schools and fencing around schools to allow for 1-point entry. Lessons Dr. Alhadeff learned that might impact any pediatric hospitalist include the knowledge that mental health concerns aren’t going away; for example, after a school shooting any student affected should be provided counseling services as needed, the need to prevent triggering events, and turning grief into action can help.
“Life is like riding a bicycle. To keep your balance, you must keep moving.” – Albert Einstein (1930)
Dr. Alhadeff then described the process of “moving on” for him and his family. For his children, this initially meant “busying” their lives. They then gradually eased into therapy, and ultimately adopted a support dog. He experienced recurrent loss with his father passing away in March 2019, and he persevered in legislative advocacy in New Jersey and Florida and personal/professional development with work toward his MBA degree. Through this work, he collaborated with many legislators and two presidents. He describes resiliency as the ability to bounce back from adversity, with components including self-awareness, mindfulness, self-care, positive relationships, and purpose. While many of us have not had the great personal losses and challenge experienced by Dr. Alhadeff, we all are experiencing an once-in-a-lifetime transformation of health care with political and social interference. It is up to each of us to determine our role and how we can use our influence for positive change.
As noted by Dr. Alhadeff, “We are not all in the same boat. We ARE in the same storm.”
Key takeaways
- How PHM can promote MOSS: Allow children to be part of the work to keep schools safe. Advocate for local MOSS chapters. Support legislative advocacy for school safety.
- Despite adversity, we have the ability to demonstrate resilience. We do so through development of self-awareness, mindfulness, engagement in self-care, nurturing positive relationships, and continuing to pursue our greater purpose.
Dr. King is a pediatric hospitalist at Children’s MN and the director of medical education, an associate program director for the Pediatrics Residency program at the University of Minnesota. She received her medical degree from Wright State University Boonshoft School of Medicine and completed pediatric residency and chief residency at the University of Minnesota.
Want to see what COVID strain you have? The government says no
Every day, more than 140,000 people in the United States are diagnosed with COVID-19. But no matter how curious they are about which variant they are fighting, none of them will find out.
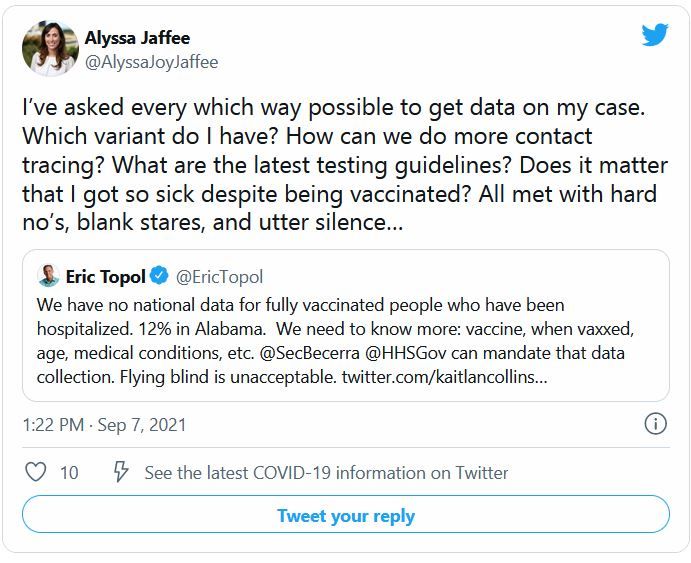
The country is dotted with labs that sequence the genomes of COVID-19 cases, and the Centers for Disease Control and Prevention tracks those results. But federal rules say those results are not allowed to make their way back to patients or doctors.
According to public health and infectious disease experts, this is unlikely to change any time soon.
“I know people want to know – I’ve had a lot of friends or family who’ve asked me how they can find out,” says Aubree Gordon, PhD, an epidemiology specialist at the University of Michigan, Ann Arbor. “I think it’s an interesting thing to find out, for sure. And it would certainly be nice to know. But because it probably isn’t necessary, there is little motivation to change the rules.”
Because the tests that are used have not been approved as diagnostic tools under the Clinical Laboratory Improvement Amendments program, which is overseen by the Centers for Medicare & Medicaid Services, they can only be used for research purposes.
In fact, the scientists doing the sequencing rarely have any patient information, Dr. Gordon says. For example, the Lauring Lab at University of Michigan – run by Adam Lauring, MD – focuses on viral evolution and currently tests for variants. But this is not done for the sake of the patient or the doctors treating the patient.
“The samples come in ... and they’ve been de-identified,”Dr. Gordon says. “This is just for research purposes. Not much patient information is shared with the researchers.”
But as of now, aside from sheer curiosity, there is not a reason to change this, says Timothy Brewer, MD, a professor of medicine and epidemiology at University of California, Los Angeles.
Although there are emerging variants – including the new Mu variant, also known as B.1.621 and recently classified as a “variant of interest” – the Delta variant accounts for about 99% of U.S. cases.
In addition, Dr. Brewer says, treatments are the same for all COVID-19 patients, regardless of the variant.
“There would have to be some clinical significance for there to be a good reason to give this information,” he says. “That would mean we would be doing something different treatment-wise depending on the variant. As of now, that is not the case.”
There is a loophole that allows labs to release variant information: They can develop their own tests. But they then must go through a lengthy validation process that proves their tests are as effective as the gold standard, says Mark Pandori, PhD, director of the Nevada State Public Health Laboratory.
But even with validation, it is too time-consuming and costly to sequence large numbers of cases, he says.
“The reason we’re not doing it routinely is there’s no way to do the genomic analysis on all the positives,” Dr. Pandori says. “It is about $110 dollars to do a sequence. It’s not like a standard PCR test.”
There is a hypothetical situation that may warrant the release of these results, Dr. Brewer says: If a variant emerges that evades vaccines.
“That would be a real public health issue,” he says. “You want to make sure there aren’t variants emerging somewhere that are escaping immunity.”
A version of this article first appeared on WebMD.com.
Every day, more than 140,000 people in the United States are diagnosed with COVID-19. But no matter how curious they are about which variant they are fighting, none of them will find out.
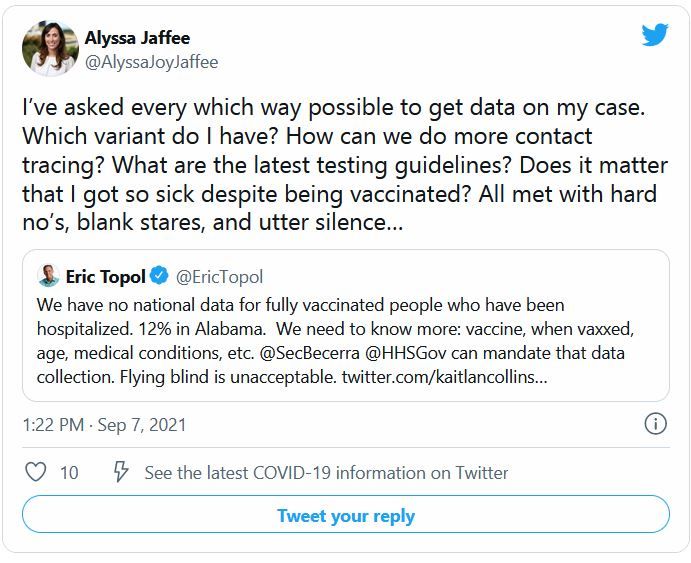
The country is dotted with labs that sequence the genomes of COVID-19 cases, and the Centers for Disease Control and Prevention tracks those results. But federal rules say those results are not allowed to make their way back to patients or doctors.
According to public health and infectious disease experts, this is unlikely to change any time soon.
“I know people want to know – I’ve had a lot of friends or family who’ve asked me how they can find out,” says Aubree Gordon, PhD, an epidemiology specialist at the University of Michigan, Ann Arbor. “I think it’s an interesting thing to find out, for sure. And it would certainly be nice to know. But because it probably isn’t necessary, there is little motivation to change the rules.”
Because the tests that are used have not been approved as diagnostic tools under the Clinical Laboratory Improvement Amendments program, which is overseen by the Centers for Medicare & Medicaid Services, they can only be used for research purposes.
In fact, the scientists doing the sequencing rarely have any patient information, Dr. Gordon says. For example, the Lauring Lab at University of Michigan – run by Adam Lauring, MD – focuses on viral evolution and currently tests for variants. But this is not done for the sake of the patient or the doctors treating the patient.
“The samples come in ... and they’ve been de-identified,”Dr. Gordon says. “This is just for research purposes. Not much patient information is shared with the researchers.”
But as of now, aside from sheer curiosity, there is not a reason to change this, says Timothy Brewer, MD, a professor of medicine and epidemiology at University of California, Los Angeles.
Although there are emerging variants – including the new Mu variant, also known as B.1.621 and recently classified as a “variant of interest” – the Delta variant accounts for about 99% of U.S. cases.
In addition, Dr. Brewer says, treatments are the same for all COVID-19 patients, regardless of the variant.
“There would have to be some clinical significance for there to be a good reason to give this information,” he says. “That would mean we would be doing something different treatment-wise depending on the variant. As of now, that is not the case.”
There is a loophole that allows labs to release variant information: They can develop their own tests. But they then must go through a lengthy validation process that proves their tests are as effective as the gold standard, says Mark Pandori, PhD, director of the Nevada State Public Health Laboratory.
But even with validation, it is too time-consuming and costly to sequence large numbers of cases, he says.
“The reason we’re not doing it routinely is there’s no way to do the genomic analysis on all the positives,” Dr. Pandori says. “It is about $110 dollars to do a sequence. It’s not like a standard PCR test.”
There is a hypothetical situation that may warrant the release of these results, Dr. Brewer says: If a variant emerges that evades vaccines.
“That would be a real public health issue,” he says. “You want to make sure there aren’t variants emerging somewhere that are escaping immunity.”
A version of this article first appeared on WebMD.com.
Every day, more than 140,000 people in the United States are diagnosed with COVID-19. But no matter how curious they are about which variant they are fighting, none of them will find out.
The country is dotted with labs that sequence the genomes of COVID-19 cases, and the Centers for Disease Control and Prevention tracks those results. But federal rules say those results are not allowed to make their way back to patients or doctors.
According to public health and infectious disease experts, this is unlikely to change any time soon.
“I know people want to know – I’ve had a lot of friends or family who’ve asked me how they can find out,” says Aubree Gordon, PhD, an epidemiology specialist at the University of Michigan, Ann Arbor. “I think it’s an interesting thing to find out, for sure. And it would certainly be nice to know. But because it probably isn’t necessary, there is little motivation to change the rules.”
Because the tests that are used have not been approved as diagnostic tools under the Clinical Laboratory Improvement Amendments program, which is overseen by the Centers for Medicare & Medicaid Services, they can only be used for research purposes.
In fact, the scientists doing the sequencing rarely have any patient information, Dr. Gordon says. For example, the Lauring Lab at University of Michigan – run by Adam Lauring, MD – focuses on viral evolution and currently tests for variants. But this is not done for the sake of the patient or the doctors treating the patient.
“The samples come in ... and they’ve been de-identified,”Dr. Gordon says. “This is just for research purposes. Not much patient information is shared with the researchers.”
But as of now, aside from sheer curiosity, there is not a reason to change this, says Timothy Brewer, MD, a professor of medicine and epidemiology at University of California, Los Angeles.
Although there are emerging variants – including the new Mu variant, also known as B.1.621 and recently classified as a “variant of interest” – the Delta variant accounts for about 99% of U.S. cases.
In addition, Dr. Brewer says, treatments are the same for all COVID-19 patients, regardless of the variant.
“There would have to be some clinical significance for there to be a good reason to give this information,” he says. “That would mean we would be doing something different treatment-wise depending on the variant. As of now, that is not the case.”
There is a loophole that allows labs to release variant information: They can develop their own tests. But they then must go through a lengthy validation process that proves their tests are as effective as the gold standard, says Mark Pandori, PhD, director of the Nevada State Public Health Laboratory.
But even with validation, it is too time-consuming and costly to sequence large numbers of cases, he says.
“The reason we’re not doing it routinely is there’s no way to do the genomic analysis on all the positives,” Dr. Pandori says. “It is about $110 dollars to do a sequence. It’s not like a standard PCR test.”
There is a hypothetical situation that may warrant the release of these results, Dr. Brewer says: If a variant emerges that evades vaccines.
“That would be a real public health issue,” he says. “You want to make sure there aren’t variants emerging somewhere that are escaping immunity.”
A version of this article first appeared on WebMD.com.
Lipid levels tied to ALS risk
, new research shows.
The study also linked a higher ratio of total cholesterol to HDL with an increased risk for ALS. These findings, investigators noted, point to potential future biomarkers in screening for ALS and perhaps an approach to reduce risk or delay onset of ALS in the longer term.
“They may help build a biochemical picture of what’s going on and who might be at risk of developing ALS in the near future, particularly in people with a genetic predisposition to ALS,” study investigator Alexander G. Thompson, DPhil, Medical Research Council clinician scientist, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom, said in an interview.
He emphasized that although the current observational study cannot show cause and effect, such a relationship may exist.
The study was published online September 13 in the Journal of Neurology, Neurosurgery and Psychiatry.
Registry data
ALS is a disorder of progressive degeneration of upper and lower motor neurons. Genetic variants account for fewer than 15% of cases. The factors that are associated with the greatest risk are unclear.
To investigate, the researchers used data from the UK Biobank, a prospective cohort study of persons aged 39-72 years. Participants underwent an initial assessment between March 2006 and October 2010 and were followed for a median of 11.9 years.
In addition to providing demographic and health information, participants provided blood samples for biochemical analysis. This included measurements of total cholesterol, HDL, low-density lipoprotein (LDL) cholesterol, triglycerides, apoA1, apolipoprotein B (apoB), A1c, and creatinine.
Researchers used diagnostic codes in inpatient health records and death certificate information to verify ALS diagnoses.
The analysis included data from 502,409 participants. The mean age of the participants was 58 years, and 54.4% were women. During follow-up, 343 participants were diagnosed with ALS, yielding a crude incidence of 5.85 per 100,000 per year (95% confidence interval, 5.25-6.51).
After controlling for sex and age, results showed that higher HDL (hazard ratio, 0.84; 95% CI, 0.73-0.96; P = .010) and higher apoA1 (HR, 0.83; 95% CI, 0.72-0.94, P = .005) were associated with a reduced risk for subsequent ALS.
A higher ratio of total cholesterol to HDL was associated with increased ALS risk.
A rise in neurofilaments and other markers of neuronal loss typically occur within about a year of ALS symptom onset. To ensure that they were capturing participants whose blood samples were taken before the onset of neurodegeneration, the researchers performed a secondary analysis that excluded ALS diagnoses within 5 years of the baseline study visit.
Results of the analysis were largely consistent with models incorporating all participants with regard to magnitude and direction of associations. In addition, the findings persisted in models that controlled for statin use, smoking, and vascular disease.
Mechanism unclear
To more closely examine lipid status prior to ALS diagnosis, the researchers performed a nested case-control analysis that involved matching each participant who developed ALS with 20 participants of similar age, sex, and time of enrollment who did not develop the disease.
Linear models showed that levels of LDL and apoB, which are closely correlated, decrease over time in those who developed ALS. This was not the case for HDL and apoA1. “This suggests LDL levels are going down, and we think it’s happening quite some time before symptoms start, even before neurodegeneration starts,” said Dr. Thompson.
How blood lipid levels correlate with ALS risk is unclear. Dr. Thompson noted that LDL is an oxidative stressor and can provoke inflammation, whereas HDL is an antioxidant that is involved in healing. However, given that LDL and HDL don’t cross into the brain in great amounts, “the lipid changes may be a reflection of something else going on that contributes to the risk of ALS,” he said.
More evidence of a causal relationship is needed before any clinical implications can be drawn, including the potential manipulation of lipid levels to prevent ALS, said Dr. Thompson. In addition, even were such a relationship to be established, altering lipid levels in a healthy individual who has no family history of ALS would be unlikely to alter risk.
Dr. Thompson added that among those with a genetic predisposition, lipid changes “may be a marker or clue that something’s going wrong in the nervous system and that ALS might be about to start. That would be the ideal time to treat people at risk of ALS with gene therapy.”
Metabolism gone awry
Commenting on the findings, Stephen Goutman, MD, director, Pranger ALS Clinic, associate professor of neurology, Neuromuscular Program, University of Michigan, Ann Arbor, called the study “very interesting.” Of particular note was a trend of decreasing LDL and apoB levels prior to an ALS diagnosis, said Dr. Goutman.
The results are in agreement with several studies that show an alteration in metabolism in individuals with ALS, he said. “These altered metabolic pathways may provide some signal that something has gone awry,” he commented.
He agreed that an “ultimate goal” is to identify factors or biomarkers that can be used to predict whether individuals will develop ALS and to enable intervention to decrease the risk.
This new research highlights the value of population-based registries and large prospective cohorts, said Dr. Goutman. “These help to better define the genetic, environmental, and metabolic factors that increase and predict ALS risk,” he said.
But more work is needed, said Dr. Goutman. He noted that in the study, only 192 participants were diagnosed with ALS more than 5 years after enrollment. “This means additional large cohort studies are needed, especially those that reflect the diversity of the population, for us to solve the mystery of ALS and to prevent it,” he said.
Dr. Thompson and Dr. Goutman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows.
The study also linked a higher ratio of total cholesterol to HDL with an increased risk for ALS. These findings, investigators noted, point to potential future biomarkers in screening for ALS and perhaps an approach to reduce risk or delay onset of ALS in the longer term.
“They may help build a biochemical picture of what’s going on and who might be at risk of developing ALS in the near future, particularly in people with a genetic predisposition to ALS,” study investigator Alexander G. Thompson, DPhil, Medical Research Council clinician scientist, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom, said in an interview.
He emphasized that although the current observational study cannot show cause and effect, such a relationship may exist.
The study was published online September 13 in the Journal of Neurology, Neurosurgery and Psychiatry.
Registry data
ALS is a disorder of progressive degeneration of upper and lower motor neurons. Genetic variants account for fewer than 15% of cases. The factors that are associated with the greatest risk are unclear.
To investigate, the researchers used data from the UK Biobank, a prospective cohort study of persons aged 39-72 years. Participants underwent an initial assessment between March 2006 and October 2010 and were followed for a median of 11.9 years.
In addition to providing demographic and health information, participants provided blood samples for biochemical analysis. This included measurements of total cholesterol, HDL, low-density lipoprotein (LDL) cholesterol, triglycerides, apoA1, apolipoprotein B (apoB), A1c, and creatinine.
Researchers used diagnostic codes in inpatient health records and death certificate information to verify ALS diagnoses.
The analysis included data from 502,409 participants. The mean age of the participants was 58 years, and 54.4% were women. During follow-up, 343 participants were diagnosed with ALS, yielding a crude incidence of 5.85 per 100,000 per year (95% confidence interval, 5.25-6.51).
After controlling for sex and age, results showed that higher HDL (hazard ratio, 0.84; 95% CI, 0.73-0.96; P = .010) and higher apoA1 (HR, 0.83; 95% CI, 0.72-0.94, P = .005) were associated with a reduced risk for subsequent ALS.
A higher ratio of total cholesterol to HDL was associated with increased ALS risk.
A rise in neurofilaments and other markers of neuronal loss typically occur within about a year of ALS symptom onset. To ensure that they were capturing participants whose blood samples were taken before the onset of neurodegeneration, the researchers performed a secondary analysis that excluded ALS diagnoses within 5 years of the baseline study visit.
Results of the analysis were largely consistent with models incorporating all participants with regard to magnitude and direction of associations. In addition, the findings persisted in models that controlled for statin use, smoking, and vascular disease.
Mechanism unclear
To more closely examine lipid status prior to ALS diagnosis, the researchers performed a nested case-control analysis that involved matching each participant who developed ALS with 20 participants of similar age, sex, and time of enrollment who did not develop the disease.
Linear models showed that levels of LDL and apoB, which are closely correlated, decrease over time in those who developed ALS. This was not the case for HDL and apoA1. “This suggests LDL levels are going down, and we think it’s happening quite some time before symptoms start, even before neurodegeneration starts,” said Dr. Thompson.
How blood lipid levels correlate with ALS risk is unclear. Dr. Thompson noted that LDL is an oxidative stressor and can provoke inflammation, whereas HDL is an antioxidant that is involved in healing. However, given that LDL and HDL don’t cross into the brain in great amounts, “the lipid changes may be a reflection of something else going on that contributes to the risk of ALS,” he said.
More evidence of a causal relationship is needed before any clinical implications can be drawn, including the potential manipulation of lipid levels to prevent ALS, said Dr. Thompson. In addition, even were such a relationship to be established, altering lipid levels in a healthy individual who has no family history of ALS would be unlikely to alter risk.
Dr. Thompson added that among those with a genetic predisposition, lipid changes “may be a marker or clue that something’s going wrong in the nervous system and that ALS might be about to start. That would be the ideal time to treat people at risk of ALS with gene therapy.”
Metabolism gone awry
Commenting on the findings, Stephen Goutman, MD, director, Pranger ALS Clinic, associate professor of neurology, Neuromuscular Program, University of Michigan, Ann Arbor, called the study “very interesting.” Of particular note was a trend of decreasing LDL and apoB levels prior to an ALS diagnosis, said Dr. Goutman.
The results are in agreement with several studies that show an alteration in metabolism in individuals with ALS, he said. “These altered metabolic pathways may provide some signal that something has gone awry,” he commented.
He agreed that an “ultimate goal” is to identify factors or biomarkers that can be used to predict whether individuals will develop ALS and to enable intervention to decrease the risk.
This new research highlights the value of population-based registries and large prospective cohorts, said Dr. Goutman. “These help to better define the genetic, environmental, and metabolic factors that increase and predict ALS risk,” he said.
But more work is needed, said Dr. Goutman. He noted that in the study, only 192 participants were diagnosed with ALS more than 5 years after enrollment. “This means additional large cohort studies are needed, especially those that reflect the diversity of the population, for us to solve the mystery of ALS and to prevent it,” he said.
Dr. Thompson and Dr. Goutman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows.
The study also linked a higher ratio of total cholesterol to HDL with an increased risk for ALS. These findings, investigators noted, point to potential future biomarkers in screening for ALS and perhaps an approach to reduce risk or delay onset of ALS in the longer term.
“They may help build a biochemical picture of what’s going on and who might be at risk of developing ALS in the near future, particularly in people with a genetic predisposition to ALS,” study investigator Alexander G. Thompson, DPhil, Medical Research Council clinician scientist, Nuffield Department of Clinical Neurosciences, University of Oxford, United Kingdom, said in an interview.
He emphasized that although the current observational study cannot show cause and effect, such a relationship may exist.
The study was published online September 13 in the Journal of Neurology, Neurosurgery and Psychiatry.
Registry data
ALS is a disorder of progressive degeneration of upper and lower motor neurons. Genetic variants account for fewer than 15% of cases. The factors that are associated with the greatest risk are unclear.
To investigate, the researchers used data from the UK Biobank, a prospective cohort study of persons aged 39-72 years. Participants underwent an initial assessment between March 2006 and October 2010 and were followed for a median of 11.9 years.
In addition to providing demographic and health information, participants provided blood samples for biochemical analysis. This included measurements of total cholesterol, HDL, low-density lipoprotein (LDL) cholesterol, triglycerides, apoA1, apolipoprotein B (apoB), A1c, and creatinine.
Researchers used diagnostic codes in inpatient health records and death certificate information to verify ALS diagnoses.
The analysis included data from 502,409 participants. The mean age of the participants was 58 years, and 54.4% were women. During follow-up, 343 participants were diagnosed with ALS, yielding a crude incidence of 5.85 per 100,000 per year (95% confidence interval, 5.25-6.51).
After controlling for sex and age, results showed that higher HDL (hazard ratio, 0.84; 95% CI, 0.73-0.96; P = .010) and higher apoA1 (HR, 0.83; 95% CI, 0.72-0.94, P = .005) were associated with a reduced risk for subsequent ALS.
A higher ratio of total cholesterol to HDL was associated with increased ALS risk.
A rise in neurofilaments and other markers of neuronal loss typically occur within about a year of ALS symptom onset. To ensure that they were capturing participants whose blood samples were taken before the onset of neurodegeneration, the researchers performed a secondary analysis that excluded ALS diagnoses within 5 years of the baseline study visit.
Results of the analysis were largely consistent with models incorporating all participants with regard to magnitude and direction of associations. In addition, the findings persisted in models that controlled for statin use, smoking, and vascular disease.
Mechanism unclear
To more closely examine lipid status prior to ALS diagnosis, the researchers performed a nested case-control analysis that involved matching each participant who developed ALS with 20 participants of similar age, sex, and time of enrollment who did not develop the disease.
Linear models showed that levels of LDL and apoB, which are closely correlated, decrease over time in those who developed ALS. This was not the case for HDL and apoA1. “This suggests LDL levels are going down, and we think it’s happening quite some time before symptoms start, even before neurodegeneration starts,” said Dr. Thompson.
How blood lipid levels correlate with ALS risk is unclear. Dr. Thompson noted that LDL is an oxidative stressor and can provoke inflammation, whereas HDL is an antioxidant that is involved in healing. However, given that LDL and HDL don’t cross into the brain in great amounts, “the lipid changes may be a reflection of something else going on that contributes to the risk of ALS,” he said.
More evidence of a causal relationship is needed before any clinical implications can be drawn, including the potential manipulation of lipid levels to prevent ALS, said Dr. Thompson. In addition, even were such a relationship to be established, altering lipid levels in a healthy individual who has no family history of ALS would be unlikely to alter risk.
Dr. Thompson added that among those with a genetic predisposition, lipid changes “may be a marker or clue that something’s going wrong in the nervous system and that ALS might be about to start. That would be the ideal time to treat people at risk of ALS with gene therapy.”
Metabolism gone awry
Commenting on the findings, Stephen Goutman, MD, director, Pranger ALS Clinic, associate professor of neurology, Neuromuscular Program, University of Michigan, Ann Arbor, called the study “very interesting.” Of particular note was a trend of decreasing LDL and apoB levels prior to an ALS diagnosis, said Dr. Goutman.
The results are in agreement with several studies that show an alteration in metabolism in individuals with ALS, he said. “These altered metabolic pathways may provide some signal that something has gone awry,” he commented.
He agreed that an “ultimate goal” is to identify factors or biomarkers that can be used to predict whether individuals will develop ALS and to enable intervention to decrease the risk.
This new research highlights the value of population-based registries and large prospective cohorts, said Dr. Goutman. “These help to better define the genetic, environmental, and metabolic factors that increase and predict ALS risk,” he said.
But more work is needed, said Dr. Goutman. He noted that in the study, only 192 participants were diagnosed with ALS more than 5 years after enrollment. “This means additional large cohort studies are needed, especially those that reflect the diversity of the population, for us to solve the mystery of ALS and to prevent it,” he said.
Dr. Thompson and Dr. Goutman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From Journal of Neurology, Neurosurgery, and Psychiatry
Office clutter linked to work, life burnout
As people begin to return to offices after working remotely, a new study suggests that clutter on the job is more than just an annoyance to neatniks. It might also be an indicator that employees are unhappy at work, especially if they have upper-level positions.
Researchers surveyed 202 office workers and linked higher perceived levels of clutter to less satisfaction/pleasure from work and more work-related burnout/tension. While the findings don’t confirm which came first – clutter or unhappiness on the job – they do suggest that the office work environment is more than an matter of appearances.
Study lead author Joseph R. Ferrari, PhD, a professor of psychology at DePaul University, Chicago, goes even further and suggests that clutter might undermine well-being. “If someone comes into [a therapist’s office] with lots of clutter, they probably have it at home and work, and it’s hindering their life,” Dr. Ferrari said in an interview. “Having a lot of clutter piles is really not a good thing. It makes you less effective.”
Dr. Ferrari has conducted several studies into clutter. He and colleagues launched the new study, published in the International Journal of Psychological Research and Reviews, to explore the impact of clutter at the office.
“The impact of clutter on employee well-being may affect profit, staff motivation, the buildup of slack/extraneous resources, interpersonal conflict, attitudes about work, and employee behavior,” Dr. Ferrari and colleagues wrote.
The researchers surveyed participants in 290 workers in 2019 and focused on 209 who worked in offices (60% were men, 87% were 45 years old or younger, 65% held a college or advanced degree, and 79% were White). Most were lower-level employees rather than higher-level employees with management responsibilities.
Both upper-and lower-level employees mentioned the same types of clutter most often – paper, office equipment, and trash, such as used coffee cups. The upper-level workers reported more problems with clutter, although this might be because they are more sensitive to it than lower-level workers, Dr. Ferrari said.
The researchers found that “office clutter was significantly negatively related to ... satisfaction/pleasure from work and significantly positively related to a risk for burnout/tension from work.” They also reported that “upper-level workers were significantly more likely to report clutter and being at risk for burnout/tension than lower-level workers.”
Specifically, a technique known as exploratory factor analysis determined that “63% of office clutter behavior can be explained by either satisfaction/pleasure with one’s work or risk for burnout,” Dr. Ferrari said. The findings suggest that clutter leads to negative feelings about work, not the other way around, he said.
The new study does not address whether clutter has positive attributes, as suggested by a 2013 report published in Psychological Science.
Darby Saxbe, PhD, an associate professor of psychology at the University of Southern California, Los Angeles, who studies work stress, said in an interview that it can be difficult to figure out the direction of causality in a study like this. “Someone who’s overwhelmed might generate more clutter and not have the bandwidth to put things away. If the space is really cluttered, you won’t be able to find things as effectively, or keep track of projects as well, and that will feed more feelings of stress and burnout.”
David Spiegel, MD, Willson Professor of psychiatry and behavioral sciences at Stanford (Calif.) University, agreed.
“The idea of clutter in the environment having a negative effect on mood is interesting, but it is equally likely that clutter reflects burnout, inability to complete tasks and dispose of their remnants,” he said in an interview. “There may be a relationship, and they may interact, but the direction is not clear,” said Dr. Spiegel, who is also director of Stanford’s Center on Stress and Health.
Still, he said, “in these days of Zoom therapy, observing clutter in a patient’s room or office may provide a hint about potential burnout and depression.”
No funding is reported. Dr. Ferrari, Dr. Saxbe, and Dr. Spiegel reported no disclosures.
As people begin to return to offices after working remotely, a new study suggests that clutter on the job is more than just an annoyance to neatniks. It might also be an indicator that employees are unhappy at work, especially if they have upper-level positions.
Researchers surveyed 202 office workers and linked higher perceived levels of clutter to less satisfaction/pleasure from work and more work-related burnout/tension. While the findings don’t confirm which came first – clutter or unhappiness on the job – they do suggest that the office work environment is more than an matter of appearances.
Study lead author Joseph R. Ferrari, PhD, a professor of psychology at DePaul University, Chicago, goes even further and suggests that clutter might undermine well-being. “If someone comes into [a therapist’s office] with lots of clutter, they probably have it at home and work, and it’s hindering their life,” Dr. Ferrari said in an interview. “Having a lot of clutter piles is really not a good thing. It makes you less effective.”
Dr. Ferrari has conducted several studies into clutter. He and colleagues launched the new study, published in the International Journal of Psychological Research and Reviews, to explore the impact of clutter at the office.
“The impact of clutter on employee well-being may affect profit, staff motivation, the buildup of slack/extraneous resources, interpersonal conflict, attitudes about work, and employee behavior,” Dr. Ferrari and colleagues wrote.
The researchers surveyed participants in 290 workers in 2019 and focused on 209 who worked in offices (60% were men, 87% were 45 years old or younger, 65% held a college or advanced degree, and 79% were White). Most were lower-level employees rather than higher-level employees with management responsibilities.
Both upper-and lower-level employees mentioned the same types of clutter most often – paper, office equipment, and trash, such as used coffee cups. The upper-level workers reported more problems with clutter, although this might be because they are more sensitive to it than lower-level workers, Dr. Ferrari said.
The researchers found that “office clutter was significantly negatively related to ... satisfaction/pleasure from work and significantly positively related to a risk for burnout/tension from work.” They also reported that “upper-level workers were significantly more likely to report clutter and being at risk for burnout/tension than lower-level workers.”
Specifically, a technique known as exploratory factor analysis determined that “63% of office clutter behavior can be explained by either satisfaction/pleasure with one’s work or risk for burnout,” Dr. Ferrari said. The findings suggest that clutter leads to negative feelings about work, not the other way around, he said.
The new study does not address whether clutter has positive attributes, as suggested by a 2013 report published in Psychological Science.
Darby Saxbe, PhD, an associate professor of psychology at the University of Southern California, Los Angeles, who studies work stress, said in an interview that it can be difficult to figure out the direction of causality in a study like this. “Someone who’s overwhelmed might generate more clutter and not have the bandwidth to put things away. If the space is really cluttered, you won’t be able to find things as effectively, or keep track of projects as well, and that will feed more feelings of stress and burnout.”
David Spiegel, MD, Willson Professor of psychiatry and behavioral sciences at Stanford (Calif.) University, agreed.
“The idea of clutter in the environment having a negative effect on mood is interesting, but it is equally likely that clutter reflects burnout, inability to complete tasks and dispose of their remnants,” he said in an interview. “There may be a relationship, and they may interact, but the direction is not clear,” said Dr. Spiegel, who is also director of Stanford’s Center on Stress and Health.
Still, he said, “in these days of Zoom therapy, observing clutter in a patient’s room or office may provide a hint about potential burnout and depression.”
No funding is reported. Dr. Ferrari, Dr. Saxbe, and Dr. Spiegel reported no disclosures.
As people begin to return to offices after working remotely, a new study suggests that clutter on the job is more than just an annoyance to neatniks. It might also be an indicator that employees are unhappy at work, especially if they have upper-level positions.
Researchers surveyed 202 office workers and linked higher perceived levels of clutter to less satisfaction/pleasure from work and more work-related burnout/tension. While the findings don’t confirm which came first – clutter or unhappiness on the job – they do suggest that the office work environment is more than an matter of appearances.
Study lead author Joseph R. Ferrari, PhD, a professor of psychology at DePaul University, Chicago, goes even further and suggests that clutter might undermine well-being. “If someone comes into [a therapist’s office] with lots of clutter, they probably have it at home and work, and it’s hindering their life,” Dr. Ferrari said in an interview. “Having a lot of clutter piles is really not a good thing. It makes you less effective.”
Dr. Ferrari has conducted several studies into clutter. He and colleagues launched the new study, published in the International Journal of Psychological Research and Reviews, to explore the impact of clutter at the office.
“The impact of clutter on employee well-being may affect profit, staff motivation, the buildup of slack/extraneous resources, interpersonal conflict, attitudes about work, and employee behavior,” Dr. Ferrari and colleagues wrote.
The researchers surveyed participants in 290 workers in 2019 and focused on 209 who worked in offices (60% were men, 87% were 45 years old or younger, 65% held a college or advanced degree, and 79% were White). Most were lower-level employees rather than higher-level employees with management responsibilities.
Both upper-and lower-level employees mentioned the same types of clutter most often – paper, office equipment, and trash, such as used coffee cups. The upper-level workers reported more problems with clutter, although this might be because they are more sensitive to it than lower-level workers, Dr. Ferrari said.
The researchers found that “office clutter was significantly negatively related to ... satisfaction/pleasure from work and significantly positively related to a risk for burnout/tension from work.” They also reported that “upper-level workers were significantly more likely to report clutter and being at risk for burnout/tension than lower-level workers.”
Specifically, a technique known as exploratory factor analysis determined that “63% of office clutter behavior can be explained by either satisfaction/pleasure with one’s work or risk for burnout,” Dr. Ferrari said. The findings suggest that clutter leads to negative feelings about work, not the other way around, he said.
The new study does not address whether clutter has positive attributes, as suggested by a 2013 report published in Psychological Science.
Darby Saxbe, PhD, an associate professor of psychology at the University of Southern California, Los Angeles, who studies work stress, said in an interview that it can be difficult to figure out the direction of causality in a study like this. “Someone who’s overwhelmed might generate more clutter and not have the bandwidth to put things away. If the space is really cluttered, you won’t be able to find things as effectively, or keep track of projects as well, and that will feed more feelings of stress and burnout.”
David Spiegel, MD, Willson Professor of psychiatry and behavioral sciences at Stanford (Calif.) University, agreed.
“The idea of clutter in the environment having a negative effect on mood is interesting, but it is equally likely that clutter reflects burnout, inability to complete tasks and dispose of their remnants,” he said in an interview. “There may be a relationship, and they may interact, but the direction is not clear,” said Dr. Spiegel, who is also director of Stanford’s Center on Stress and Health.
Still, he said, “in these days of Zoom therapy, observing clutter in a patient’s room or office may provide a hint about potential burnout and depression.”
No funding is reported. Dr. Ferrari, Dr. Saxbe, and Dr. Spiegel reported no disclosures.
FROM THE INTERNATIONAL JOURNAL OF PSYCHOLOGICAL RESEARCH AND REVIEWS
Medicare patients’ cost burden for specialty psoriasis, PsA drugs remains high
High out-of-pocket costs for medications remain a barrier for patients with psoriasis or psoriatic arthritis on Medicare, according to findings from a cross-sectional analysis of the Centers for Medicare & Medicaid Services Prescription Drug Plan Formulary Data from the fourth quarter of 2020.
Although biologics have demonstrated safety and effectiveness for psoriasis and psoriatic arthritis, their costs have risen, which has led patients to switch or discontinue biologics and consequently incur greater health care costs, wrote Sarah P. Pourali and colleagues at Vanderbilt University, Nashville, Tenn.
The authors also noted that Medicare patients in particular experience a financial burden if they have no limits on out-of-pocket spending, and while patient assistance programs may offset some out-of-pocket spending for specialty drugs, not all patients are aware of or qualify for them. Ineligibility for low-income subsidies also serves as a barrier and is associated with lower adherence to treatment.
In a study published in JAMA Dermatology, the researchers identified 5,011 formularies using the CMS data. The medications were etanercept, adalimumab, golimumab, ustekinumab, certolizumab pegol, apremilast, secukinumab, abatacept, ixekizumab, brodalumab, tofacitinib, tofacitinib XR, guselkumab, tildrakizumab, and risankizumab.
Overall, coverage for those 15 specialty medications ranged from 10.0% to 99.8% across products and Part D plans. The most commonly covered medications were adalimumab and ustekinumab (99.8% for both) and the least covered were brodalumab and tildrakizumab (10.9% and 10.0%, respectively).
Prior authorization was required by 90.5%-100% of the plans when medications were covered, and plans with limits on the quantity of medications covered ranged from 1.0% of plans (for guselkumab) to 78% of plans (for tofacitinib).
Copays were relatively rare; 2.4%-5.5% of the plans offered copays on any of the 15 medications.
The standard Medicare benefit for 2021 included a $445 deductible, 25% coinsurance for initial drug spending, and 5% coinsurance for drug spending in the catastrophic phase of coverage, the researchers noted. Overall, apremilast had the lowest estimated out-of-pocket costs for initial fills, under the catastrophic coverage phase, and annual cost, and ustekinumab had the highest. The estimated out-of-pocket costs for an initial fill ranged from $1,234 for apremilast to $3,426 for ustekinumab. Out-of-pocket costs for medications under the catastrophic phase ranged from $181 for apremilast to $1,175 for ustekinumab. Estimated out-of-pocket costs for a year of treatment ranged from $4,423 for apremilast to $6,950 for ustekinumab.
Median point-of-sale prices per fill – meaning pricing with no rebates or discounts – were lowest for apremilast ($3,620.40) and reached $23,492.93 per fill for ustekinumab, the researchers wrote. Other medications with point-of-sale prices above $10,000 were guselkumab ($11,511.52), tildrakizumab ($14,112.13), and risankizumab ($16,248.90).
The study was supported by grants from the Commonwealth Fund and the Leukemia & Lymphoma Society. One author disclosed receiving grants from Arnold Ventures, the Commonwealth Fund, and the Robert Wood Johnson Foundation for unrelated work, as well as honoraria from West Health and the Institute for Clinical and Economic Review.
High out-of-pocket costs for medications remain a barrier for patients with psoriasis or psoriatic arthritis on Medicare, according to findings from a cross-sectional analysis of the Centers for Medicare & Medicaid Services Prescription Drug Plan Formulary Data from the fourth quarter of 2020.
Although biologics have demonstrated safety and effectiveness for psoriasis and psoriatic arthritis, their costs have risen, which has led patients to switch or discontinue biologics and consequently incur greater health care costs, wrote Sarah P. Pourali and colleagues at Vanderbilt University, Nashville, Tenn.
The authors also noted that Medicare patients in particular experience a financial burden if they have no limits on out-of-pocket spending, and while patient assistance programs may offset some out-of-pocket spending for specialty drugs, not all patients are aware of or qualify for them. Ineligibility for low-income subsidies also serves as a barrier and is associated with lower adherence to treatment.
In a study published in JAMA Dermatology, the researchers identified 5,011 formularies using the CMS data. The medications were etanercept, adalimumab, golimumab, ustekinumab, certolizumab pegol, apremilast, secukinumab, abatacept, ixekizumab, brodalumab, tofacitinib, tofacitinib XR, guselkumab, tildrakizumab, and risankizumab.
Overall, coverage for those 15 specialty medications ranged from 10.0% to 99.8% across products and Part D plans. The most commonly covered medications were adalimumab and ustekinumab (99.8% for both) and the least covered were brodalumab and tildrakizumab (10.9% and 10.0%, respectively).
Prior authorization was required by 90.5%-100% of the plans when medications were covered, and plans with limits on the quantity of medications covered ranged from 1.0% of plans (for guselkumab) to 78% of plans (for tofacitinib).
Copays were relatively rare; 2.4%-5.5% of the plans offered copays on any of the 15 medications.
The standard Medicare benefit for 2021 included a $445 deductible, 25% coinsurance for initial drug spending, and 5% coinsurance for drug spending in the catastrophic phase of coverage, the researchers noted. Overall, apremilast had the lowest estimated out-of-pocket costs for initial fills, under the catastrophic coverage phase, and annual cost, and ustekinumab had the highest. The estimated out-of-pocket costs for an initial fill ranged from $1,234 for apremilast to $3,426 for ustekinumab. Out-of-pocket costs for medications under the catastrophic phase ranged from $181 for apremilast to $1,175 for ustekinumab. Estimated out-of-pocket costs for a year of treatment ranged from $4,423 for apremilast to $6,950 for ustekinumab.
Median point-of-sale prices per fill – meaning pricing with no rebates or discounts – were lowest for apremilast ($3,620.40) and reached $23,492.93 per fill for ustekinumab, the researchers wrote. Other medications with point-of-sale prices above $10,000 were guselkumab ($11,511.52), tildrakizumab ($14,112.13), and risankizumab ($16,248.90).
The study was supported by grants from the Commonwealth Fund and the Leukemia & Lymphoma Society. One author disclosed receiving grants from Arnold Ventures, the Commonwealth Fund, and the Robert Wood Johnson Foundation for unrelated work, as well as honoraria from West Health and the Institute for Clinical and Economic Review.
High out-of-pocket costs for medications remain a barrier for patients with psoriasis or psoriatic arthritis on Medicare, according to findings from a cross-sectional analysis of the Centers for Medicare & Medicaid Services Prescription Drug Plan Formulary Data from the fourth quarter of 2020.
Although biologics have demonstrated safety and effectiveness for psoriasis and psoriatic arthritis, their costs have risen, which has led patients to switch or discontinue biologics and consequently incur greater health care costs, wrote Sarah P. Pourali and colleagues at Vanderbilt University, Nashville, Tenn.
The authors also noted that Medicare patients in particular experience a financial burden if they have no limits on out-of-pocket spending, and while patient assistance programs may offset some out-of-pocket spending for specialty drugs, not all patients are aware of or qualify for them. Ineligibility for low-income subsidies also serves as a barrier and is associated with lower adherence to treatment.
In a study published in JAMA Dermatology, the researchers identified 5,011 formularies using the CMS data. The medications were etanercept, adalimumab, golimumab, ustekinumab, certolizumab pegol, apremilast, secukinumab, abatacept, ixekizumab, brodalumab, tofacitinib, tofacitinib XR, guselkumab, tildrakizumab, and risankizumab.
Overall, coverage for those 15 specialty medications ranged from 10.0% to 99.8% across products and Part D plans. The most commonly covered medications were adalimumab and ustekinumab (99.8% for both) and the least covered were brodalumab and tildrakizumab (10.9% and 10.0%, respectively).
Prior authorization was required by 90.5%-100% of the plans when medications were covered, and plans with limits on the quantity of medications covered ranged from 1.0% of plans (for guselkumab) to 78% of plans (for tofacitinib).
Copays were relatively rare; 2.4%-5.5% of the plans offered copays on any of the 15 medications.
The standard Medicare benefit for 2021 included a $445 deductible, 25% coinsurance for initial drug spending, and 5% coinsurance for drug spending in the catastrophic phase of coverage, the researchers noted. Overall, apremilast had the lowest estimated out-of-pocket costs for initial fills, under the catastrophic coverage phase, and annual cost, and ustekinumab had the highest. The estimated out-of-pocket costs for an initial fill ranged from $1,234 for apremilast to $3,426 for ustekinumab. Out-of-pocket costs for medications under the catastrophic phase ranged from $181 for apremilast to $1,175 for ustekinumab. Estimated out-of-pocket costs for a year of treatment ranged from $4,423 for apremilast to $6,950 for ustekinumab.
Median point-of-sale prices per fill – meaning pricing with no rebates or discounts – were lowest for apremilast ($3,620.40) and reached $23,492.93 per fill for ustekinumab, the researchers wrote. Other medications with point-of-sale prices above $10,000 were guselkumab ($11,511.52), tildrakizumab ($14,112.13), and risankizumab ($16,248.90).
The study was supported by grants from the Commonwealth Fund and the Leukemia & Lymphoma Society. One author disclosed receiving grants from Arnold Ventures, the Commonwealth Fund, and the Robert Wood Johnson Foundation for unrelated work, as well as honoraria from West Health and the Institute for Clinical and Economic Review.
FROM JAMA DERMATOLOGY
POSEIDON: Two ICIs plus chemo up survival in mNSCLC
The study involved over 1,000 patients with stage IV NSCLC. Participants were randomly assigned to receive either two ICIs (tremelimumab and durvalumab [Imfinzi]) plus chemotherapy, or one immunotherapy (durvalumab) plus chemotherapy, or chemotherapy alone.
Adding durvalumab to chemotherapy significantly improved PFS by 26% but did not significantly improve OS, the researchers reported. However, adding both tremelimumab and durvalumab significantly increased both PFS (by 28%) and OS (by 23%). Median OS was 14.0 months versus 11.7 months for chemotherapy.
The results were presented on Sept. 9 at a presidential symposium of the World Conference on Lung Cancer 2021.
The two immunotherapies act at different immune checkpoints – tremelimumab acts at CTLA-4, and durvalumab acts at programmed death–1/PD–ligand 1 (PD-L1). Both drugs are from AstraZeneca, which sponsored the POSEIDON trial.
With no new safety signals identified, the triple therapy combination “represents a potential new frontline treatment option for metastatic non–small cell lung cancer,” said lead researcher Melissa L. Johnson, MD, from the Sarah Cannon Research Institute, Nashville, Tenn.
Reacting to the new results in a discussion of the paper, Julie R. Brahmer, MD, from Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins Medicine, Baltimore, said that, with so many first-line treatment choices now available for advanced NSCLC, she feels like “a kid in the candy store.”
POSEIDON may give her “another choice,” but she pointed out that there are some aspects of the study to consider.
The study required patients to undergo four cycles of chemotherapy along with immunotherapy, “which certainly is standard in many of our practices.”
However, only two cycles of chemotherapy were given in the CheckMate 9LA trial, in which nivolumab (Opdivo) and ipilimumab (Yervoy) were added to chemotherapy for the treatment of stage IV NSCLC. This combination of immunotherapies, which block CTLA-4 and PD-1, is similar to the combination that was studied in the current trial, and it is already approved for use in some patients with lung cancer.
“Also key to point out,” said Dr. Brahmer, is that, in the POSEIDON trial, “there was a trend toward more poor prognostic factors in the chemotherapy arm, where these patients had more liver or central nervous system metastases.”
Despite these differences, the survival outcomes were similar in the two trials, and in both trials, the tails of the curves indicate that “we need to see long-term data” to determine whether the benefit is ongoing.
Which patients for which combos?
Considering all the data from key trials in advanced NSCLC, Dr. Brahmer said that she believes that, for patients with high PD-L1 expression, treatment with a single immunotherapy directed against PD-1 or PD-L1 “is appropriate” and that she didn’t see that adding a CTLA-4 inhibitor to the PD-L1 inhibitor and chemotherapy would give any advantage.
“But for PD-L1–negative disease, I do think CTLA-4 antibodies seem to provide a benefit, specifically seen in the CheckMate studies,” particularly for patients with squamous disease, although she noted that in POSEIDON, histology and PD-L1 status have not been analyzed.
Dr. Brahmer concluded that, although the triple therapy improved survival outcomes in the current study, several key questions remain.
These include determining what CTLA-4 inhibition adds to PD-L1 blockade and asking whether the “slightly increased toxicity” is “worth the slightly increased long-term duration of response” and improved survival outcomes.
Furthermore, it needs to be determined “which populations truly need” the combined approach; “to get to this, we need to find the biomarker for CTLA-4 benefit,” Dr. Brahmer said.
She also noted “a practical question: Is there room in the clinic for another CTLA-4 antibody in addition to the nivolumab/ipilimumab combinations?”
This last point was appreciated on social media. Jill Feldman, a lung cancer patient and advocate, described it on Twitter as a “great question.”
She said that, for her, “options equal hope,” but that it is “critical” to give the “best treatment first. ... So as a patient, I would ask: How do I know/you know which treatment would be best for me?”
With “so many options in the first-line setting,” subsets of patients who may benefit from quadruplet therapy versus monotherapy need to be defined, commented Charu Aggarwal, MD, MPH, Leslye M. Heisler Associate Professor for Lung Cancer Excellence, Penn Medicine, Philadelphia. He added that “PD-L1 may be one biomarker, but we need more.”
More details of the POSEIDON trial
In the POSEIDON trial, investigators had the choice of different chemotherapy regimens: platinum/gemcitabine for patients with squamous disease, platinum/pemetrexed for patients with nonsquamous disease, and nab-paclitaxel/carboplatin for patients with disease of either histology, Dr. Johnson reported.
It is noteworthy that the majority of patients were from Eastern Europe and Asia, “and the proportion of squamous patients enrolled was higher than is typically seen in mixed histology lung cancer studies,” she added.
The patients were stratified by PD-L1 expression at a cutoff of 50%, disease stage, and tumor histology.
Overall, 1,013 patients were enrolled. The three treatment arms were relatively well balanced in terms of baseline characteristics.
Dr. Johnson noted that there were “a few minor imbalances” in the durvalumab plus tremelimumab arm, with “fewer females, fewer Asians, and fewer never-smokers relative to the other two arms.”
The primary endpoint analysis after a median follow-up of 10.3 months demonstrated that PFS was significantly improved with durvalumab plus chemotherapy over chemotherapy alone, at a median of 5.5 months versus 4.8 months (hazard ratio, 0.74; P = .00093).
Although OS improved numerically with the addition of durvalumab to chemotherapy, it did not reach significance (13.3 months vs. 11.7 months with chemotherapy alone; HR, 0.86; P = .07581).
The positive PFS benefit with durvalumab plus chemotherapy triggered a secondary endpoint analysis, which showed that adding tremelimumab to durvalumab plus chemotherapy improved both survival outcomes.
Median PFS with the triple combination therapy was 6.2 months, significantly longer than the 4.8 months seen with chemotherapy alone (HR, 0.72; P = .00031).
At 12 months, 26.6% of patients who underwent treatment with durvalumab plus tremelimumab plus chemotherapy had not experienced disease progression, compared with 13.1% in the chemotherapy-alone arm.
OS was also significantly improved, at 14.0 months among patients in the triple therapy arm versus 11.7 in the chemotherapy-alone arm (HR, 0.77; P = .00304).
The results also showed that at 24 months, 32.9% of triple therapy patients were still alive versus 22.1% in the chemotherapy-alone arm.
Analysis indicated that “most subgroups favored the addition of immunotherapy to chemotherapy.” There was a “trend toward improved survival for all patients treated with durvalumab plus tremelimumab plus chemotherapy,” Dr. Johnson said.
This was seen “in particular for the nonsquamous patients” and for those with tumor PD-L1 expression of less than 1%, he added.
It is notable that for a large proportion of combination-therapy patients, response had continued at 12 months. This was the case for 38.9% of those who underwent treatment with durvalumab plus chemotherapy and for 49.7% of those given triple therapy versus 21.4% in the chemotherapy-alone arm.
As was seen across the whole cohort, among patients with nonsquamous disease, PFS and OS improved with the addition of immunotherapy. Of those patients with nonsquamous disease, 95.5% received pemetrexed plus platinum chemotherapy.
However, among patients with squamous tumors, of whom 88.3% received gemcitabine plus platinum chemotherapy, PFS and OS were “poor ... across all treatment arms,” Dr. Johnson reported, “with little separation of the curves.”
She highlighted the fact that the proportion of patients who experienced grade 3/4 adverse events, whether of any cause or treatment related, was only slightly higher in the two immunotherapy arms, indicating that “most events were driven by the chemotherapy.”
The rates of treatment discontinuation and adverse events leading to death were also similar across the three treatment arms, albeit they were slightly higher with the addition of immunotherapy.
Dr. Johnson also noted that, although there were more immune-mediated adverse events with durvalumab plus tremelimumab plus chemotherapy, compared with durvalumab plus chemotherapy, the “majority were grade 1/2 and were manageable.”
The most common immune-mediated events in the two immunotherapy arms were hypothyroid and hepatic events, pneumonitis, dermatitis, and rash.
The study was sponsored by AstraZeneca. Dr. Johnson reported numerous relationships with pharmaceutical companies. Dr. Brahmer reported relationships with Amgen, AstratZeneca, BMA, Genentech/Roche, Eli Lilly, Eisai, GlaxoSmithKline, Janssen, Merck, RAPT Therapeutics, Regeneron, Revolution Medicine, and Sanofi.
A version of this article first appeared on Medscape.com.
The study involved over 1,000 patients with stage IV NSCLC. Participants were randomly assigned to receive either two ICIs (tremelimumab and durvalumab [Imfinzi]) plus chemotherapy, or one immunotherapy (durvalumab) plus chemotherapy, or chemotherapy alone.
Adding durvalumab to chemotherapy significantly improved PFS by 26% but did not significantly improve OS, the researchers reported. However, adding both tremelimumab and durvalumab significantly increased both PFS (by 28%) and OS (by 23%). Median OS was 14.0 months versus 11.7 months for chemotherapy.
The results were presented on Sept. 9 at a presidential symposium of the World Conference on Lung Cancer 2021.
The two immunotherapies act at different immune checkpoints – tremelimumab acts at CTLA-4, and durvalumab acts at programmed death–1/PD–ligand 1 (PD-L1). Both drugs are from AstraZeneca, which sponsored the POSEIDON trial.
With no new safety signals identified, the triple therapy combination “represents a potential new frontline treatment option for metastatic non–small cell lung cancer,” said lead researcher Melissa L. Johnson, MD, from the Sarah Cannon Research Institute, Nashville, Tenn.
Reacting to the new results in a discussion of the paper, Julie R. Brahmer, MD, from Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins Medicine, Baltimore, said that, with so many first-line treatment choices now available for advanced NSCLC, she feels like “a kid in the candy store.”
POSEIDON may give her “another choice,” but she pointed out that there are some aspects of the study to consider.
The study required patients to undergo four cycles of chemotherapy along with immunotherapy, “which certainly is standard in many of our practices.”
However, only two cycles of chemotherapy were given in the CheckMate 9LA trial, in which nivolumab (Opdivo) and ipilimumab (Yervoy) were added to chemotherapy for the treatment of stage IV NSCLC. This combination of immunotherapies, which block CTLA-4 and PD-1, is similar to the combination that was studied in the current trial, and it is already approved for use in some patients with lung cancer.
“Also key to point out,” said Dr. Brahmer, is that, in the POSEIDON trial, “there was a trend toward more poor prognostic factors in the chemotherapy arm, where these patients had more liver or central nervous system metastases.”
Despite these differences, the survival outcomes were similar in the two trials, and in both trials, the tails of the curves indicate that “we need to see long-term data” to determine whether the benefit is ongoing.
Which patients for which combos?
Considering all the data from key trials in advanced NSCLC, Dr. Brahmer said that she believes that, for patients with high PD-L1 expression, treatment with a single immunotherapy directed against PD-1 or PD-L1 “is appropriate” and that she didn’t see that adding a CTLA-4 inhibitor to the PD-L1 inhibitor and chemotherapy would give any advantage.
“But for PD-L1–negative disease, I do think CTLA-4 antibodies seem to provide a benefit, specifically seen in the CheckMate studies,” particularly for patients with squamous disease, although she noted that in POSEIDON, histology and PD-L1 status have not been analyzed.
Dr. Brahmer concluded that, although the triple therapy improved survival outcomes in the current study, several key questions remain.
These include determining what CTLA-4 inhibition adds to PD-L1 blockade and asking whether the “slightly increased toxicity” is “worth the slightly increased long-term duration of response” and improved survival outcomes.
Furthermore, it needs to be determined “which populations truly need” the combined approach; “to get to this, we need to find the biomarker for CTLA-4 benefit,” Dr. Brahmer said.
She also noted “a practical question: Is there room in the clinic for another CTLA-4 antibody in addition to the nivolumab/ipilimumab combinations?”
This last point was appreciated on social media. Jill Feldman, a lung cancer patient and advocate, described it on Twitter as a “great question.”
She said that, for her, “options equal hope,” but that it is “critical” to give the “best treatment first. ... So as a patient, I would ask: How do I know/you know which treatment would be best for me?”
With “so many options in the first-line setting,” subsets of patients who may benefit from quadruplet therapy versus monotherapy need to be defined, commented Charu Aggarwal, MD, MPH, Leslye M. Heisler Associate Professor for Lung Cancer Excellence, Penn Medicine, Philadelphia. He added that “PD-L1 may be one biomarker, but we need more.”
More details of the POSEIDON trial
In the POSEIDON trial, investigators had the choice of different chemotherapy regimens: platinum/gemcitabine for patients with squamous disease, platinum/pemetrexed for patients with nonsquamous disease, and nab-paclitaxel/carboplatin for patients with disease of either histology, Dr. Johnson reported.
It is noteworthy that the majority of patients were from Eastern Europe and Asia, “and the proportion of squamous patients enrolled was higher than is typically seen in mixed histology lung cancer studies,” she added.
The patients were stratified by PD-L1 expression at a cutoff of 50%, disease stage, and tumor histology.
Overall, 1,013 patients were enrolled. The three treatment arms were relatively well balanced in terms of baseline characteristics.
Dr. Johnson noted that there were “a few minor imbalances” in the durvalumab plus tremelimumab arm, with “fewer females, fewer Asians, and fewer never-smokers relative to the other two arms.”
The primary endpoint analysis after a median follow-up of 10.3 months demonstrated that PFS was significantly improved with durvalumab plus chemotherapy over chemotherapy alone, at a median of 5.5 months versus 4.8 months (hazard ratio, 0.74; P = .00093).
Although OS improved numerically with the addition of durvalumab to chemotherapy, it did not reach significance (13.3 months vs. 11.7 months with chemotherapy alone; HR, 0.86; P = .07581).
The positive PFS benefit with durvalumab plus chemotherapy triggered a secondary endpoint analysis, which showed that adding tremelimumab to durvalumab plus chemotherapy improved both survival outcomes.
Median PFS with the triple combination therapy was 6.2 months, significantly longer than the 4.8 months seen with chemotherapy alone (HR, 0.72; P = .00031).
At 12 months, 26.6% of patients who underwent treatment with durvalumab plus tremelimumab plus chemotherapy had not experienced disease progression, compared with 13.1% in the chemotherapy-alone arm.
OS was also significantly improved, at 14.0 months among patients in the triple therapy arm versus 11.7 in the chemotherapy-alone arm (HR, 0.77; P = .00304).
The results also showed that at 24 months, 32.9% of triple therapy patients were still alive versus 22.1% in the chemotherapy-alone arm.
Analysis indicated that “most subgroups favored the addition of immunotherapy to chemotherapy.” There was a “trend toward improved survival for all patients treated with durvalumab plus tremelimumab plus chemotherapy,” Dr. Johnson said.
This was seen “in particular for the nonsquamous patients” and for those with tumor PD-L1 expression of less than 1%, he added.
It is notable that for a large proportion of combination-therapy patients, response had continued at 12 months. This was the case for 38.9% of those who underwent treatment with durvalumab plus chemotherapy and for 49.7% of those given triple therapy versus 21.4% in the chemotherapy-alone arm.
As was seen across the whole cohort, among patients with nonsquamous disease, PFS and OS improved with the addition of immunotherapy. Of those patients with nonsquamous disease, 95.5% received pemetrexed plus platinum chemotherapy.
However, among patients with squamous tumors, of whom 88.3% received gemcitabine plus platinum chemotherapy, PFS and OS were “poor ... across all treatment arms,” Dr. Johnson reported, “with little separation of the curves.”
She highlighted the fact that the proportion of patients who experienced grade 3/4 adverse events, whether of any cause or treatment related, was only slightly higher in the two immunotherapy arms, indicating that “most events were driven by the chemotherapy.”
The rates of treatment discontinuation and adverse events leading to death were also similar across the three treatment arms, albeit they were slightly higher with the addition of immunotherapy.
Dr. Johnson also noted that, although there were more immune-mediated adverse events with durvalumab plus tremelimumab plus chemotherapy, compared with durvalumab plus chemotherapy, the “majority were grade 1/2 and were manageable.”
The most common immune-mediated events in the two immunotherapy arms were hypothyroid and hepatic events, pneumonitis, dermatitis, and rash.
The study was sponsored by AstraZeneca. Dr. Johnson reported numerous relationships with pharmaceutical companies. Dr. Brahmer reported relationships with Amgen, AstratZeneca, BMA, Genentech/Roche, Eli Lilly, Eisai, GlaxoSmithKline, Janssen, Merck, RAPT Therapeutics, Regeneron, Revolution Medicine, and Sanofi.
A version of this article first appeared on Medscape.com.
The study involved over 1,000 patients with stage IV NSCLC. Participants were randomly assigned to receive either two ICIs (tremelimumab and durvalumab [Imfinzi]) plus chemotherapy, or one immunotherapy (durvalumab) plus chemotherapy, or chemotherapy alone.
Adding durvalumab to chemotherapy significantly improved PFS by 26% but did not significantly improve OS, the researchers reported. However, adding both tremelimumab and durvalumab significantly increased both PFS (by 28%) and OS (by 23%). Median OS was 14.0 months versus 11.7 months for chemotherapy.
The results were presented on Sept. 9 at a presidential symposium of the World Conference on Lung Cancer 2021.
The two immunotherapies act at different immune checkpoints – tremelimumab acts at CTLA-4, and durvalumab acts at programmed death–1/PD–ligand 1 (PD-L1). Both drugs are from AstraZeneca, which sponsored the POSEIDON trial.
With no new safety signals identified, the triple therapy combination “represents a potential new frontline treatment option for metastatic non–small cell lung cancer,” said lead researcher Melissa L. Johnson, MD, from the Sarah Cannon Research Institute, Nashville, Tenn.
Reacting to the new results in a discussion of the paper, Julie R. Brahmer, MD, from Sidney Kimmel Comprehensive Cancer Center, Johns Hopkins Medicine, Baltimore, said that, with so many first-line treatment choices now available for advanced NSCLC, she feels like “a kid in the candy store.”
POSEIDON may give her “another choice,” but she pointed out that there are some aspects of the study to consider.
The study required patients to undergo four cycles of chemotherapy along with immunotherapy, “which certainly is standard in many of our practices.”
However, only two cycles of chemotherapy were given in the CheckMate 9LA trial, in which nivolumab (Opdivo) and ipilimumab (Yervoy) were added to chemotherapy for the treatment of stage IV NSCLC. This combination of immunotherapies, which block CTLA-4 and PD-1, is similar to the combination that was studied in the current trial, and it is already approved for use in some patients with lung cancer.
“Also key to point out,” said Dr. Brahmer, is that, in the POSEIDON trial, “there was a trend toward more poor prognostic factors in the chemotherapy arm, where these patients had more liver or central nervous system metastases.”
Despite these differences, the survival outcomes were similar in the two trials, and in both trials, the tails of the curves indicate that “we need to see long-term data” to determine whether the benefit is ongoing.
Which patients for which combos?
Considering all the data from key trials in advanced NSCLC, Dr. Brahmer said that she believes that, for patients with high PD-L1 expression, treatment with a single immunotherapy directed against PD-1 or PD-L1 “is appropriate” and that she didn’t see that adding a CTLA-4 inhibitor to the PD-L1 inhibitor and chemotherapy would give any advantage.
“But for PD-L1–negative disease, I do think CTLA-4 antibodies seem to provide a benefit, specifically seen in the CheckMate studies,” particularly for patients with squamous disease, although she noted that in POSEIDON, histology and PD-L1 status have not been analyzed.
Dr. Brahmer concluded that, although the triple therapy improved survival outcomes in the current study, several key questions remain.
These include determining what CTLA-4 inhibition adds to PD-L1 blockade and asking whether the “slightly increased toxicity” is “worth the slightly increased long-term duration of response” and improved survival outcomes.
Furthermore, it needs to be determined “which populations truly need” the combined approach; “to get to this, we need to find the biomarker for CTLA-4 benefit,” Dr. Brahmer said.
She also noted “a practical question: Is there room in the clinic for another CTLA-4 antibody in addition to the nivolumab/ipilimumab combinations?”
This last point was appreciated on social media. Jill Feldman, a lung cancer patient and advocate, described it on Twitter as a “great question.”
She said that, for her, “options equal hope,” but that it is “critical” to give the “best treatment first. ... So as a patient, I would ask: How do I know/you know which treatment would be best for me?”
With “so many options in the first-line setting,” subsets of patients who may benefit from quadruplet therapy versus monotherapy need to be defined, commented Charu Aggarwal, MD, MPH, Leslye M. Heisler Associate Professor for Lung Cancer Excellence, Penn Medicine, Philadelphia. He added that “PD-L1 may be one biomarker, but we need more.”
More details of the POSEIDON trial
In the POSEIDON trial, investigators had the choice of different chemotherapy regimens: platinum/gemcitabine for patients with squamous disease, platinum/pemetrexed for patients with nonsquamous disease, and nab-paclitaxel/carboplatin for patients with disease of either histology, Dr. Johnson reported.
It is noteworthy that the majority of patients were from Eastern Europe and Asia, “and the proportion of squamous patients enrolled was higher than is typically seen in mixed histology lung cancer studies,” she added.
The patients were stratified by PD-L1 expression at a cutoff of 50%, disease stage, and tumor histology.
Overall, 1,013 patients were enrolled. The three treatment arms were relatively well balanced in terms of baseline characteristics.
Dr. Johnson noted that there were “a few minor imbalances” in the durvalumab plus tremelimumab arm, with “fewer females, fewer Asians, and fewer never-smokers relative to the other two arms.”
The primary endpoint analysis after a median follow-up of 10.3 months demonstrated that PFS was significantly improved with durvalumab plus chemotherapy over chemotherapy alone, at a median of 5.5 months versus 4.8 months (hazard ratio, 0.74; P = .00093).
Although OS improved numerically with the addition of durvalumab to chemotherapy, it did not reach significance (13.3 months vs. 11.7 months with chemotherapy alone; HR, 0.86; P = .07581).
The positive PFS benefit with durvalumab plus chemotherapy triggered a secondary endpoint analysis, which showed that adding tremelimumab to durvalumab plus chemotherapy improved both survival outcomes.
Median PFS with the triple combination therapy was 6.2 months, significantly longer than the 4.8 months seen with chemotherapy alone (HR, 0.72; P = .00031).
At 12 months, 26.6% of patients who underwent treatment with durvalumab plus tremelimumab plus chemotherapy had not experienced disease progression, compared with 13.1% in the chemotherapy-alone arm.
OS was also significantly improved, at 14.0 months among patients in the triple therapy arm versus 11.7 in the chemotherapy-alone arm (HR, 0.77; P = .00304).
The results also showed that at 24 months, 32.9% of triple therapy patients were still alive versus 22.1% in the chemotherapy-alone arm.
Analysis indicated that “most subgroups favored the addition of immunotherapy to chemotherapy.” There was a “trend toward improved survival for all patients treated with durvalumab plus tremelimumab plus chemotherapy,” Dr. Johnson said.
This was seen “in particular for the nonsquamous patients” and for those with tumor PD-L1 expression of less than 1%, he added.
It is notable that for a large proportion of combination-therapy patients, response had continued at 12 months. This was the case for 38.9% of those who underwent treatment with durvalumab plus chemotherapy and for 49.7% of those given triple therapy versus 21.4% in the chemotherapy-alone arm.
As was seen across the whole cohort, among patients with nonsquamous disease, PFS and OS improved with the addition of immunotherapy. Of those patients with nonsquamous disease, 95.5% received pemetrexed plus platinum chemotherapy.
However, among patients with squamous tumors, of whom 88.3% received gemcitabine plus platinum chemotherapy, PFS and OS were “poor ... across all treatment arms,” Dr. Johnson reported, “with little separation of the curves.”
She highlighted the fact that the proportion of patients who experienced grade 3/4 adverse events, whether of any cause or treatment related, was only slightly higher in the two immunotherapy arms, indicating that “most events were driven by the chemotherapy.”
The rates of treatment discontinuation and adverse events leading to death were also similar across the three treatment arms, albeit they were slightly higher with the addition of immunotherapy.
Dr. Johnson also noted that, although there were more immune-mediated adverse events with durvalumab plus tremelimumab plus chemotherapy, compared with durvalumab plus chemotherapy, the “majority were grade 1/2 and were manageable.”
The most common immune-mediated events in the two immunotherapy arms were hypothyroid and hepatic events, pneumonitis, dermatitis, and rash.
The study was sponsored by AstraZeneca. Dr. Johnson reported numerous relationships with pharmaceutical companies. Dr. Brahmer reported relationships with Amgen, AstratZeneca, BMA, Genentech/Roche, Eli Lilly, Eisai, GlaxoSmithKline, Janssen, Merck, RAPT Therapeutics, Regeneron, Revolution Medicine, and Sanofi.
A version of this article first appeared on Medscape.com.
Weight-loss surgery linked to fewer cardiovascular events, more so with RYGB
Those are the key findings of a retrospective analysis of a large group of patients who received care at the Cleveland Clinic between 1998 and 2017. MACE is defined as first occurrence of coronary artery events, cerebrovascular events, heart failure, nephropathy, atrial fibrillation, and all-cause mortality.
“I think what it tells us is that, in making these choices and in counseling patients about the potential advantages of undergoing bariatric surgery for their obesity and diabetes, that they should know that they’re more likely to be protected by a Roux-en-Y gastric bypass, although certainly sleeve gastrectomy is effective,” said study coauthor Steven E. Nissen, MD, who is the chief academic officer of the Heart and Vascular Institute at the Cleveland Clinic.
Previous studies have shown a benefit to metabolic surgery in patients with type 2 diabetes and obesity, improving diabetes control and altering cardiometabolic risk factors. Others have shown a link between surgery and reduced mortality. Most studies examined the impact of RYGB. SG is a newer procedure, but its relative simplicity and lower complication rate have helped it become the most commonly performed metabolic surgery in the world.
“There was no study to compare gastric bypass and sleeve gastrectomy head to head in terms of reduction in risk of cardiovascular disease. There are studies comparing these two procedures for diabetes control and weight loss, but not specifically in terms of effects on their risk of developing cardiovascular disease. That’s the unique feature of this study,” said lead author Ali Aminian, MD, who is director of the Bariatric and Metabolic Institute at the Cleveland Clinic.
The researchers included 2,287 adults with type 2 diabetes and a body mass index of at least 30 kg/m2, with no history of solid organ transplant, severe heart failure, or active cancer. 1,362 underwent RYGB, and 693 SG. Outcomes were compared with 11,435 matched nonsurgical patients.
At 5 years, 13.7% of the RYGB group experienced a MACE (95% confidence interval, 11.4-15.9), compared with 24.7% of the SG group for a relative reduction of 33% (95% CI, 19.0-30.0; adjusted hazard ratio, 0.77; P = .035). The nonsurgical group had a 5-year MACE incidence of 30.4% (95% CI, 29.4-31.5). Compared with usual care, the risk of MACE was lower in both the RYGB group (HR, 0.53; P < .001) and the SG group (HR, 0.69; P < .001). The researchers also analyzed the cumulative incidence of all-cause mortality, myocardial infarction, and ischemic stroke (three-component MACE) at 5 years. The cumulative incidence of three-component MACE at 5 years was 15.5% in the usual care group, 6.4% in the RYGB group (HR, 0.53 versus usual care; P < .001) and 11.8% in the SG group (HR vs. usual care, 0.65; P = .006).
The RYGB group had less nephropathy at 5 years (2.8% vs. 8.3%; HR, 0.47; P = .005), and experienced a greater reduction in weight, glycated hemoglobin, and diabetes and cardiovascular medication use. At 5 years, RYGB was associated with a higher frequency of upper endoscopy (45.8% vs. 35.6%, P < .001) and abdominal surgical procedures (10.8% vs. 5.4%, P = .001), compared with SG.
“Both procedures are extremely safe and extremely effective,” said Dr. Aminian. He pointed out the need to consider multiple factors when choosing between the procedures, including overall health, weight, comorbidities, and the patient’s values and goals.
A few factors may be contraindicated for one procedure or another. The sleeve may worsen severe reflux disease, while the gastric bypass may interfere more with absorption of psychiatric medications. Some patients may have multiple comorbidities that could point to a less risky procedure. “Decision-making should not be solely based on findings of this study. All these conditions need to be considered when patients and surgeons make a final decision about the most appropriate procedure,” said Dr. Aminian.
Dr. Nissen noted that the associations were wide ranging, including classic outcomes like death, stroke, and heart failure, but also extending to heart failure, coronary events, cerebral vascular events, nephropathy, and atrial fibrillation. “I found the nephropathy results to be amongst the most striking, that Roux-en-Y really dramatically reduced the risk of neuropathy,” he added. That’s a particularly important point because end-stage renal disease is a common cause of diabetes mortality.
Dr. Nissen acknowledged the limitations of the retrospective nature of the study, though he feels confident that the relationships are causal. “Bariatric surgery desperately needs a randomized, controlled trial, where both groups get intensive dietary and lifestyle counseling, but one group gets metabolic surgery and the other doesn’t. Given the dramatic effects in diabetic patients of reducing their hemoglobin A1c in a sustained way, reducing their body weight. We think these are very strong data to suggest that we have a major reduction in all the endpoints. If we’re right about this, the randomized controlled trial will show that dramatic effect, and will convince even the skeptics that metabolic surgery is the best way to go.”
Those are the key findings of a retrospective analysis of a large group of patients who received care at the Cleveland Clinic between 1998 and 2017. MACE is defined as first occurrence of coronary artery events, cerebrovascular events, heart failure, nephropathy, atrial fibrillation, and all-cause mortality.
“I think what it tells us is that, in making these choices and in counseling patients about the potential advantages of undergoing bariatric surgery for their obesity and diabetes, that they should know that they’re more likely to be protected by a Roux-en-Y gastric bypass, although certainly sleeve gastrectomy is effective,” said study coauthor Steven E. Nissen, MD, who is the chief academic officer of the Heart and Vascular Institute at the Cleveland Clinic.
Previous studies have shown a benefit to metabolic surgery in patients with type 2 diabetes and obesity, improving diabetes control and altering cardiometabolic risk factors. Others have shown a link between surgery and reduced mortality. Most studies examined the impact of RYGB. SG is a newer procedure, but its relative simplicity and lower complication rate have helped it become the most commonly performed metabolic surgery in the world.
“There was no study to compare gastric bypass and sleeve gastrectomy head to head in terms of reduction in risk of cardiovascular disease. There are studies comparing these two procedures for diabetes control and weight loss, but not specifically in terms of effects on their risk of developing cardiovascular disease. That’s the unique feature of this study,” said lead author Ali Aminian, MD, who is director of the Bariatric and Metabolic Institute at the Cleveland Clinic.
The researchers included 2,287 adults with type 2 diabetes and a body mass index of at least 30 kg/m2, with no history of solid organ transplant, severe heart failure, or active cancer. 1,362 underwent RYGB, and 693 SG. Outcomes were compared with 11,435 matched nonsurgical patients.
At 5 years, 13.7% of the RYGB group experienced a MACE (95% confidence interval, 11.4-15.9), compared with 24.7% of the SG group for a relative reduction of 33% (95% CI, 19.0-30.0; adjusted hazard ratio, 0.77; P = .035). The nonsurgical group had a 5-year MACE incidence of 30.4% (95% CI, 29.4-31.5). Compared with usual care, the risk of MACE was lower in both the RYGB group (HR, 0.53; P < .001) and the SG group (HR, 0.69; P < .001). The researchers also analyzed the cumulative incidence of all-cause mortality, myocardial infarction, and ischemic stroke (three-component MACE) at 5 years. The cumulative incidence of three-component MACE at 5 years was 15.5% in the usual care group, 6.4% in the RYGB group (HR, 0.53 versus usual care; P < .001) and 11.8% in the SG group (HR vs. usual care, 0.65; P = .006).
The RYGB group had less nephropathy at 5 years (2.8% vs. 8.3%; HR, 0.47; P = .005), and experienced a greater reduction in weight, glycated hemoglobin, and diabetes and cardiovascular medication use. At 5 years, RYGB was associated with a higher frequency of upper endoscopy (45.8% vs. 35.6%, P < .001) and abdominal surgical procedures (10.8% vs. 5.4%, P = .001), compared with SG.
“Both procedures are extremely safe and extremely effective,” said Dr. Aminian. He pointed out the need to consider multiple factors when choosing between the procedures, including overall health, weight, comorbidities, and the patient’s values and goals.
A few factors may be contraindicated for one procedure or another. The sleeve may worsen severe reflux disease, while the gastric bypass may interfere more with absorption of psychiatric medications. Some patients may have multiple comorbidities that could point to a less risky procedure. “Decision-making should not be solely based on findings of this study. All these conditions need to be considered when patients and surgeons make a final decision about the most appropriate procedure,” said Dr. Aminian.
Dr. Nissen noted that the associations were wide ranging, including classic outcomes like death, stroke, and heart failure, but also extending to heart failure, coronary events, cerebral vascular events, nephropathy, and atrial fibrillation. “I found the nephropathy results to be amongst the most striking, that Roux-en-Y really dramatically reduced the risk of neuropathy,” he added. That’s a particularly important point because end-stage renal disease is a common cause of diabetes mortality.
Dr. Nissen acknowledged the limitations of the retrospective nature of the study, though he feels confident that the relationships are causal. “Bariatric surgery desperately needs a randomized, controlled trial, where both groups get intensive dietary and lifestyle counseling, but one group gets metabolic surgery and the other doesn’t. Given the dramatic effects in diabetic patients of reducing their hemoglobin A1c in a sustained way, reducing their body weight. We think these are very strong data to suggest that we have a major reduction in all the endpoints. If we’re right about this, the randomized controlled trial will show that dramatic effect, and will convince even the skeptics that metabolic surgery is the best way to go.”
Those are the key findings of a retrospective analysis of a large group of patients who received care at the Cleveland Clinic between 1998 and 2017. MACE is defined as first occurrence of coronary artery events, cerebrovascular events, heart failure, nephropathy, atrial fibrillation, and all-cause mortality.
“I think what it tells us is that, in making these choices and in counseling patients about the potential advantages of undergoing bariatric surgery for their obesity and diabetes, that they should know that they’re more likely to be protected by a Roux-en-Y gastric bypass, although certainly sleeve gastrectomy is effective,” said study coauthor Steven E. Nissen, MD, who is the chief academic officer of the Heart and Vascular Institute at the Cleveland Clinic.
Previous studies have shown a benefit to metabolic surgery in patients with type 2 diabetes and obesity, improving diabetes control and altering cardiometabolic risk factors. Others have shown a link between surgery and reduced mortality. Most studies examined the impact of RYGB. SG is a newer procedure, but its relative simplicity and lower complication rate have helped it become the most commonly performed metabolic surgery in the world.
“There was no study to compare gastric bypass and sleeve gastrectomy head to head in terms of reduction in risk of cardiovascular disease. There are studies comparing these two procedures for diabetes control and weight loss, but not specifically in terms of effects on their risk of developing cardiovascular disease. That’s the unique feature of this study,” said lead author Ali Aminian, MD, who is director of the Bariatric and Metabolic Institute at the Cleveland Clinic.
The researchers included 2,287 adults with type 2 diabetes and a body mass index of at least 30 kg/m2, with no history of solid organ transplant, severe heart failure, or active cancer. 1,362 underwent RYGB, and 693 SG. Outcomes were compared with 11,435 matched nonsurgical patients.
At 5 years, 13.7% of the RYGB group experienced a MACE (95% confidence interval, 11.4-15.9), compared with 24.7% of the SG group for a relative reduction of 33% (95% CI, 19.0-30.0; adjusted hazard ratio, 0.77; P = .035). The nonsurgical group had a 5-year MACE incidence of 30.4% (95% CI, 29.4-31.5). Compared with usual care, the risk of MACE was lower in both the RYGB group (HR, 0.53; P < .001) and the SG group (HR, 0.69; P < .001). The researchers also analyzed the cumulative incidence of all-cause mortality, myocardial infarction, and ischemic stroke (three-component MACE) at 5 years. The cumulative incidence of three-component MACE at 5 years was 15.5% in the usual care group, 6.4% in the RYGB group (HR, 0.53 versus usual care; P < .001) and 11.8% in the SG group (HR vs. usual care, 0.65; P = .006).
The RYGB group had less nephropathy at 5 years (2.8% vs. 8.3%; HR, 0.47; P = .005), and experienced a greater reduction in weight, glycated hemoglobin, and diabetes and cardiovascular medication use. At 5 years, RYGB was associated with a higher frequency of upper endoscopy (45.8% vs. 35.6%, P < .001) and abdominal surgical procedures (10.8% vs. 5.4%, P = .001), compared with SG.
“Both procedures are extremely safe and extremely effective,” said Dr. Aminian. He pointed out the need to consider multiple factors when choosing between the procedures, including overall health, weight, comorbidities, and the patient’s values and goals.
A few factors may be contraindicated for one procedure or another. The sleeve may worsen severe reflux disease, while the gastric bypass may interfere more with absorption of psychiatric medications. Some patients may have multiple comorbidities that could point to a less risky procedure. “Decision-making should not be solely based on findings of this study. All these conditions need to be considered when patients and surgeons make a final decision about the most appropriate procedure,” said Dr. Aminian.
Dr. Nissen noted that the associations were wide ranging, including classic outcomes like death, stroke, and heart failure, but also extending to heart failure, coronary events, cerebral vascular events, nephropathy, and atrial fibrillation. “I found the nephropathy results to be amongst the most striking, that Roux-en-Y really dramatically reduced the risk of neuropathy,” he added. That’s a particularly important point because end-stage renal disease is a common cause of diabetes mortality.
Dr. Nissen acknowledged the limitations of the retrospective nature of the study, though he feels confident that the relationships are causal. “Bariatric surgery desperately needs a randomized, controlled trial, where both groups get intensive dietary and lifestyle counseling, but one group gets metabolic surgery and the other doesn’t. Given the dramatic effects in diabetic patients of reducing their hemoglobin A1c in a sustained way, reducing their body weight. We think these are very strong data to suggest that we have a major reduction in all the endpoints. If we’re right about this, the randomized controlled trial will show that dramatic effect, and will convince even the skeptics that metabolic surgery is the best way to go.”
FROM DIABETES CARE
Cannabidiol found no better than placebo for hand arthritis pain
Use of cannabidiol (CBD) as an add-on pain management technique in patients with either hand osteoarthritis (OA) or psoriatic arthritis (PsA) did not significantly decrease pain intensity when compared with a placebo in a randomized, double-blind trial described as the first of its kind to investigate the effect of pure CBD as an add-on analgesic therapy in patients with joint disease.
Although data on the use of medical cannabis as a modulator of joint pain are limited, some studies suggest an effect from CBD without the addition of delta-9-tetrahydrocannabinol (THC), wrote Jonathan Vela, MD, of Aalborg (Denmark) University Hospital, and colleagues.
CBD is being used for pain conditions despite a lack of data on safety and effectiveness, the researchers emphasized. Notably, in a 2018 online survey, 62% of respondents reported using CBD for medical conditions, primarily for chronic pain and arthritis or joint pain, they wrote.
In a study published in the journal Pain, the researchers randomized 59 adults with PsA and 77 adults with hand OA to 20-30 mg of synthetic CBD or a placebo daily for 12 weeks in addition to conventional pain management. Patients initially received either oral CBD 10 mg or a placebo tablet once daily, increasing to 10 mg twice daily after 2 weeks, and once again up to 10 mg three times daily at 4 weeks if the patient did not experience more than 20-mm improvement on the visual analog scale (VAS).
The primary outcome in the trial was patient-reported pain intensity during the last 24 hours as assessed on a paper-based 100-mm VAS with the text, “How much pain have you experienced in the most symptomatic joint during the last 24 hours?” with 0 representing no pain and 100 representing the worst pain imaginable.
Overall, both CBD and placebo groups achieved significant reductions in pain intensity of 11-12 mm at 12 weeks. The mean between-group difference on the VAS was 0.23 mm (P = .96). Twenty-two percent of patients who received CBD and 21% who received placebo demonstrated a pain intensity reduction greater than 30 mm on the VAS. Pain reduction greater than 50% was reported by 17 patients (25%) in the CBD group and 16 (27%) in the placebo group. CBD had a similar effect in patients with either PsA or hand OA.
Four serious adverse events occurred during the 12-week study period, but none of these were deemed adverse drug reactions. Serious adverse events in the CBD patients included one case of ductal carcinoma and one case of lipotymia; serious adverse events in the placebo group included one case of acute shoulder fracture and one case of malignant hypertension. Fifty-nine patients reported adverse events during the study. The CBD group reported more ear-nose-throat adverse events, compared with the placebo group (8 vs. 0).
The researchers assessed the impact of CBD vs. placebo on sleep quality, depression, anxiety, or pain catastrophizing scores using the Pittsburgh Sleep Quality Index, Hospital Anxiety and Depression Scale, Pain Catastrophizing Scale, and Health Assessment Questionnaire but found no differences in patients taking CBD vs. placebo.
The study findings were limited by several factors, including the potentially insufficient dose level to evoke a pain relief response, and a lack of data on additional daily use of analgesics or of the study drug beyond the prescribed dosage, the researchers noted.
The results were strengthened by the randomized, double-blind trial design and its relatively large sample size, they wrote. However, the researchers also cautioned that their study focused on CBD as a single ingredient, and the results might not generalize to other CBD formulations. They also noted that more research is needed to examine both higher doses of CBD and different types of pain disorders.
The study was supported by the Danish Psoriasis Foundation Grant and the Danish Rheumatism Foundation. The researchers had no financial conflicts to disclose.
Use of cannabidiol (CBD) as an add-on pain management technique in patients with either hand osteoarthritis (OA) or psoriatic arthritis (PsA) did not significantly decrease pain intensity when compared with a placebo in a randomized, double-blind trial described as the first of its kind to investigate the effect of pure CBD as an add-on analgesic therapy in patients with joint disease.
Although data on the use of medical cannabis as a modulator of joint pain are limited, some studies suggest an effect from CBD without the addition of delta-9-tetrahydrocannabinol (THC), wrote Jonathan Vela, MD, of Aalborg (Denmark) University Hospital, and colleagues.
CBD is being used for pain conditions despite a lack of data on safety and effectiveness, the researchers emphasized. Notably, in a 2018 online survey, 62% of respondents reported using CBD for medical conditions, primarily for chronic pain and arthritis or joint pain, they wrote.
In a study published in the journal Pain, the researchers randomized 59 adults with PsA and 77 adults with hand OA to 20-30 mg of synthetic CBD or a placebo daily for 12 weeks in addition to conventional pain management. Patients initially received either oral CBD 10 mg or a placebo tablet once daily, increasing to 10 mg twice daily after 2 weeks, and once again up to 10 mg three times daily at 4 weeks if the patient did not experience more than 20-mm improvement on the visual analog scale (VAS).
The primary outcome in the trial was patient-reported pain intensity during the last 24 hours as assessed on a paper-based 100-mm VAS with the text, “How much pain have you experienced in the most symptomatic joint during the last 24 hours?” with 0 representing no pain and 100 representing the worst pain imaginable.
Overall, both CBD and placebo groups achieved significant reductions in pain intensity of 11-12 mm at 12 weeks. The mean between-group difference on the VAS was 0.23 mm (P = .96). Twenty-two percent of patients who received CBD and 21% who received placebo demonstrated a pain intensity reduction greater than 30 mm on the VAS. Pain reduction greater than 50% was reported by 17 patients (25%) in the CBD group and 16 (27%) in the placebo group. CBD had a similar effect in patients with either PsA or hand OA.
Four serious adverse events occurred during the 12-week study period, but none of these were deemed adverse drug reactions. Serious adverse events in the CBD patients included one case of ductal carcinoma and one case of lipotymia; serious adverse events in the placebo group included one case of acute shoulder fracture and one case of malignant hypertension. Fifty-nine patients reported adverse events during the study. The CBD group reported more ear-nose-throat adverse events, compared with the placebo group (8 vs. 0).
The researchers assessed the impact of CBD vs. placebo on sleep quality, depression, anxiety, or pain catastrophizing scores using the Pittsburgh Sleep Quality Index, Hospital Anxiety and Depression Scale, Pain Catastrophizing Scale, and Health Assessment Questionnaire but found no differences in patients taking CBD vs. placebo.
The study findings were limited by several factors, including the potentially insufficient dose level to evoke a pain relief response, and a lack of data on additional daily use of analgesics or of the study drug beyond the prescribed dosage, the researchers noted.
The results were strengthened by the randomized, double-blind trial design and its relatively large sample size, they wrote. However, the researchers also cautioned that their study focused on CBD as a single ingredient, and the results might not generalize to other CBD formulations. They also noted that more research is needed to examine both higher doses of CBD and different types of pain disorders.
The study was supported by the Danish Psoriasis Foundation Grant and the Danish Rheumatism Foundation. The researchers had no financial conflicts to disclose.
Use of cannabidiol (CBD) as an add-on pain management technique in patients with either hand osteoarthritis (OA) or psoriatic arthritis (PsA) did not significantly decrease pain intensity when compared with a placebo in a randomized, double-blind trial described as the first of its kind to investigate the effect of pure CBD as an add-on analgesic therapy in patients with joint disease.
Although data on the use of medical cannabis as a modulator of joint pain are limited, some studies suggest an effect from CBD without the addition of delta-9-tetrahydrocannabinol (THC), wrote Jonathan Vela, MD, of Aalborg (Denmark) University Hospital, and colleagues.
CBD is being used for pain conditions despite a lack of data on safety and effectiveness, the researchers emphasized. Notably, in a 2018 online survey, 62% of respondents reported using CBD for medical conditions, primarily for chronic pain and arthritis or joint pain, they wrote.
In a study published in the journal Pain, the researchers randomized 59 adults with PsA and 77 adults with hand OA to 20-30 mg of synthetic CBD or a placebo daily for 12 weeks in addition to conventional pain management. Patients initially received either oral CBD 10 mg or a placebo tablet once daily, increasing to 10 mg twice daily after 2 weeks, and once again up to 10 mg three times daily at 4 weeks if the patient did not experience more than 20-mm improvement on the visual analog scale (VAS).
The primary outcome in the trial was patient-reported pain intensity during the last 24 hours as assessed on a paper-based 100-mm VAS with the text, “How much pain have you experienced in the most symptomatic joint during the last 24 hours?” with 0 representing no pain and 100 representing the worst pain imaginable.
Overall, both CBD and placebo groups achieved significant reductions in pain intensity of 11-12 mm at 12 weeks. The mean between-group difference on the VAS was 0.23 mm (P = .96). Twenty-two percent of patients who received CBD and 21% who received placebo demonstrated a pain intensity reduction greater than 30 mm on the VAS. Pain reduction greater than 50% was reported by 17 patients (25%) in the CBD group and 16 (27%) in the placebo group. CBD had a similar effect in patients with either PsA or hand OA.
Four serious adverse events occurred during the 12-week study period, but none of these were deemed adverse drug reactions. Serious adverse events in the CBD patients included one case of ductal carcinoma and one case of lipotymia; serious adverse events in the placebo group included one case of acute shoulder fracture and one case of malignant hypertension. Fifty-nine patients reported adverse events during the study. The CBD group reported more ear-nose-throat adverse events, compared with the placebo group (8 vs. 0).
The researchers assessed the impact of CBD vs. placebo on sleep quality, depression, anxiety, or pain catastrophizing scores using the Pittsburgh Sleep Quality Index, Hospital Anxiety and Depression Scale, Pain Catastrophizing Scale, and Health Assessment Questionnaire but found no differences in patients taking CBD vs. placebo.
The study findings were limited by several factors, including the potentially insufficient dose level to evoke a pain relief response, and a lack of data on additional daily use of analgesics or of the study drug beyond the prescribed dosage, the researchers noted.
The results were strengthened by the randomized, double-blind trial design and its relatively large sample size, they wrote. However, the researchers also cautioned that their study focused on CBD as a single ingredient, and the results might not generalize to other CBD formulations. They also noted that more research is needed to examine both higher doses of CBD and different types of pain disorders.
The study was supported by the Danish Psoriasis Foundation Grant and the Danish Rheumatism Foundation. The researchers had no financial conflicts to disclose.
FROM PAIN
75-year-old man • fatigue • unintentional weight loss • anemia • Dx?
THE CASE
A 75-year-old man with a history of osteoarthritis presented to our clinic with worsening weakness over the previous month. His signs and symptoms included profound fatigue, subjective fevers, a 10-pound weight loss, ankle swelling, myalgias in his legs and back, shortness of breath, and a persistent cough. The patient was otherwise previously healthy.
The patient’s heart and lung exams were normal. Initial outpatient labs showed significantly elevated inflammatory markers, with an erythrocyte sedimentation rate (ESR) of 102 mm/h (normal range for men ≥ 50 years, 0-20 mm/h) and a C-reactive protein (CRP) level of 11.1 mg/L (normal range, < 3 mg/L). The patient also had an elevated white blood cell count of 12,000/mcL (normal range, 4500-11,000/mcL). His hemoglobin was low (11 g/dL; normal range, 13.5-17.5 g/dL) and so was his albumin level (2.9 g/dL; normal range, 3.4-5.4 g/dL). The results of his prostate-specific antigen and brain natriuretic peptide tests were both normal. The results of a computed tomography scan of his thorax, abdomen, and pelvis were negative for malignancy.
The patient returned to our clinic 3 days later with severe weakness, which inhibited him from walking. He complained of a severe spasmodic pain between his shoulder blades. He denied joint stiffness, headaches, vision changes, or jaw claudication. The patient’s son had noted an overall increase in his father’s baseline heart rate, with readings increasing from the 50 beats/min range to the 70 beats/min range; this raised concern for a catecholamine-secreting tumor. There was also concern for occult infection and malignancy, or an autoimmune process, such as polymyalgia rheumatica. Due to his extreme weakness, the patient was directly admitted to the hospital for further work-up.
THE DIAGNOSIS
Concern for a smoldering infection prompted an order for a transthoracic echocardiogram. Images revealed a large mass on the mitral valve (FIGURE 1). Blood cultures quickly grew Streptococcus sanguinis. Additional work-up with a transesophageal echocardiogram (TEE) showed a “windsock” deformity (thinning and ballooning of the mitral valve), a known sequela of infective endocarditis (FIGURE 2).1 Further history obtained after the TEE revealed the patient had had a routine dental cleaning the month before his symptoms began. A murmur was then also detected.
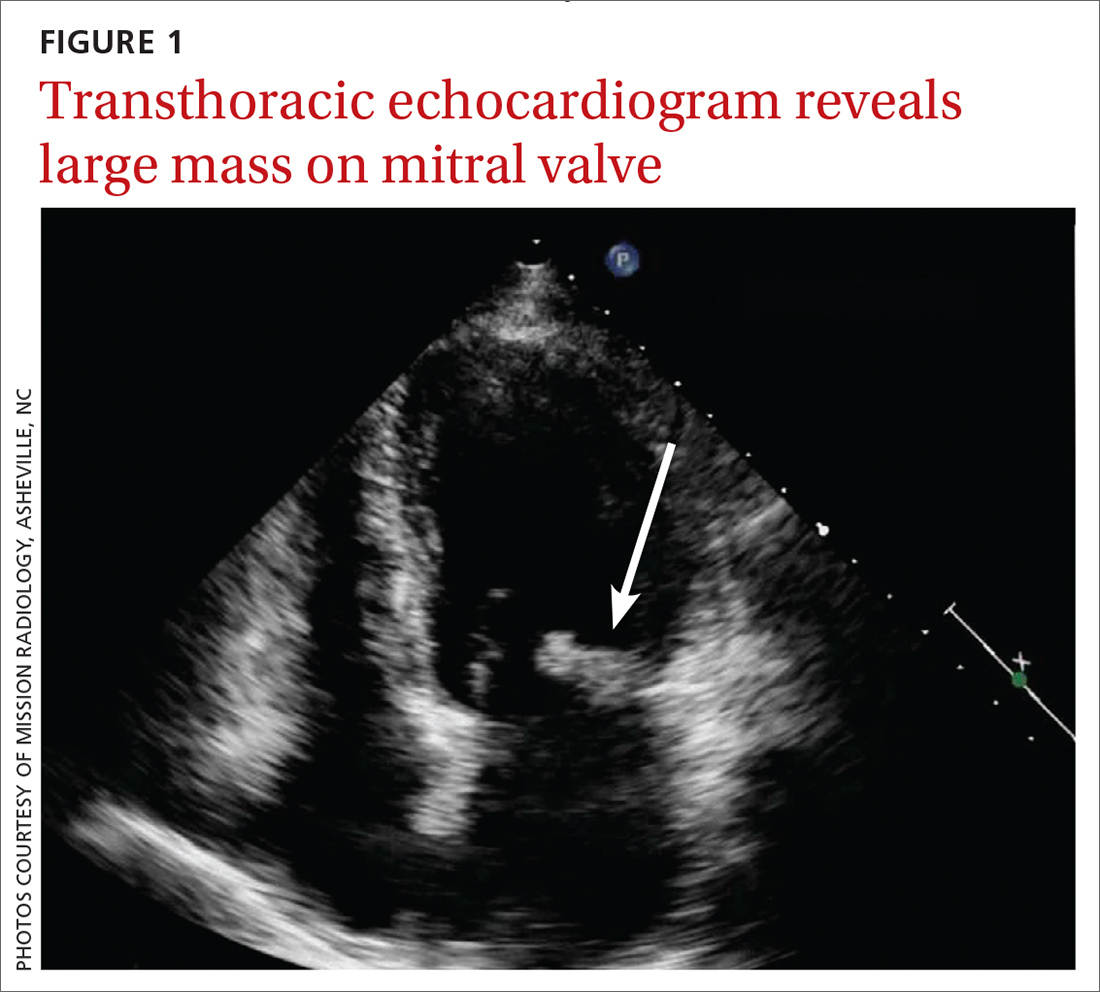
DISCUSSION
Infective endocarditis (IE) is uncommon and difficult to diagnose; it has a high early-mortality rate of 30%.2 TEE is the recommended imaging study for IE, because it is more sensitive than a transthoracic echocardiogram for identifying vegetations on the valves and it is more cost effective.3
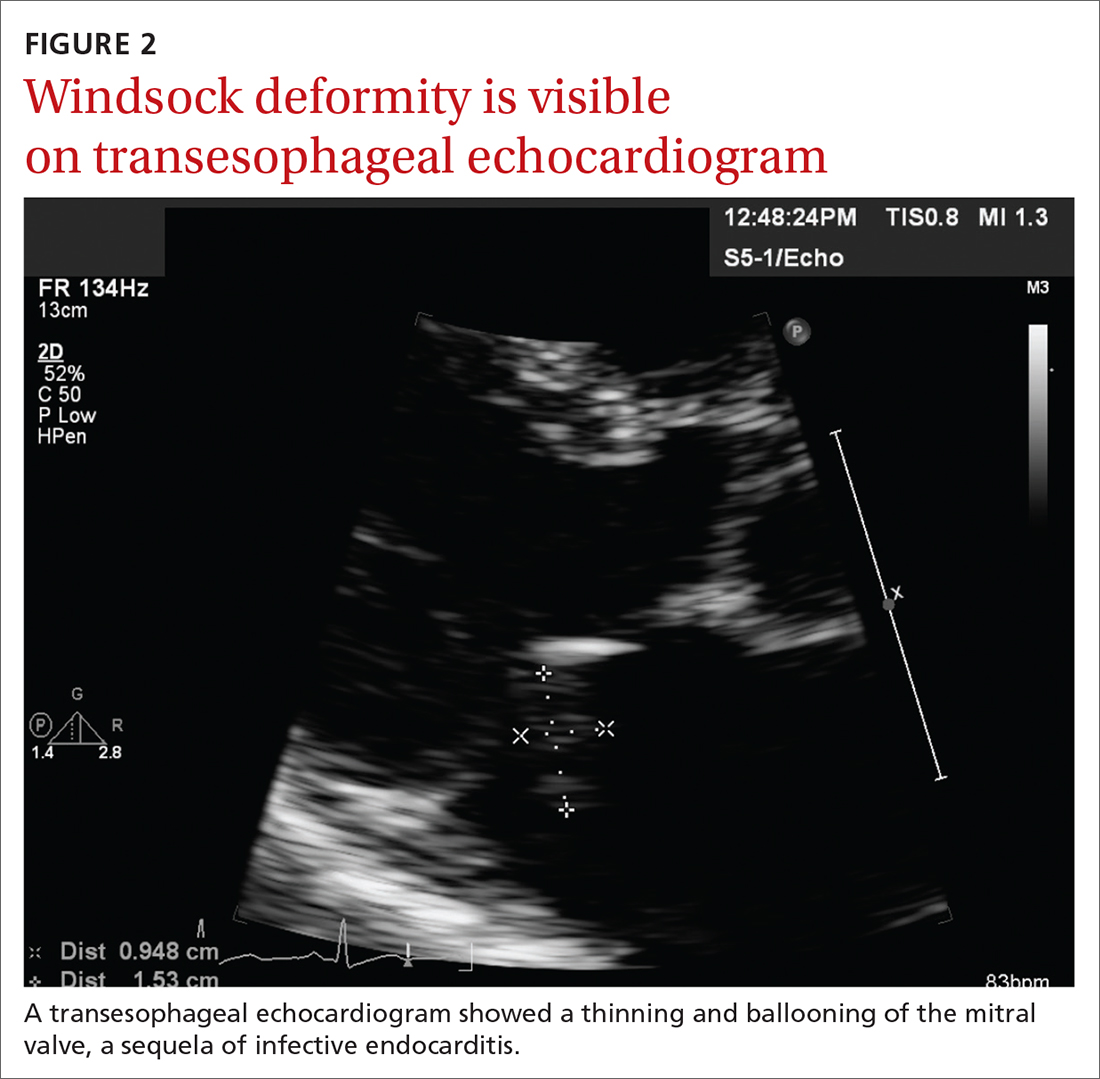
The modified Duke Criteria provide guidance for diagnosis of endocarditis. Major criteria focus on positive blood cultures and evidence of endocardial involvement. Minor criteria include predisposing heart conditions, intravenous drug use (IVDU), fever, and vascular and immunologic phenomena. As many as 90% of patients have a fever and often experience weight loss.4 Murmurs are auscultated in up to 85% of patients, and embolic features are present in up to 25% of patients at the time of diagnosis.4 In the developed world, Janeway lesions, Osler nodes, and splinter hemorrhages are increasingly rare, as patients usually present earlier in the disease course.4 While ESR and CRP are generally elevated in cases of IE, they are not part of the Duke Criteria.4
A closer look at risk factors
In 2007, guidelines for the prevention, treatment, and management of endocarditis were given significant categorical revision by the American Heart Association for the first time in 50 years.5 Recommendations for antibiotic prophylaxis prior to dental procedures became more restrictive, to include only 4 groups of high-risk patients: those with prosthetic cardiac valves, those with a history of IE, those with congenital heart disease, and cardiac transplant recipients.4 The rationale for these restrictions included the small risk for anaphylaxis and potential increase in risk for bacterial resistance associated with antibiotic prophylaxis.4 A review published in 2021 noted no increase in the frequency of, nor the morbidity and mortality from, viridans group streptococcal IE since the guideline updates.5
Continue to: There is an emerging consensus...
There is an emerging consensus that poor oral hygiene and gingival bleeding after tooth brushing promote a chronic low-grade bacteremia that may be more strongly associated with IE than an isolated dental extraction.6 Poor dental hygiene, defined as dental plaque and calculus, is especially common in the elderly, who are known to let their dental hygiene lapse.6 In our patient’s case, his generally poor oral hygiene was more likely the cause of his IE than his routine dental cleaning.
Other risk factors include IV drug use. At our tertiary care hospital in western North Carolina, 48% of patients with endocarditis had an additional diagnosis of opiate or narcotic dependence (Ryan Tilton, PharmD, email communication, June 7, 2018). Interestingly, though, only 16% of patients in North America with endocarditis were found to be currently using IV drugs.7
Our patient was treated with IV antibiotics for 4 weeks and underwent rehabilitation at a skilled nursing facility. Four weeks after diagnosis, he underwent an endoscopic porcine mitral valve replacement. Two months after that, he returned to his previously active lifestyle and began riding his stationary bike. The patient also began taking a daily aspirin. Consistent with current guidelines, he now gets antibiotic prophylaxis prior to dental procedures.
THE TAKEAWAY
This patient, without any history of IVDU or cardiac valvular abnormalities, presented with symptoms classic for a developing malignancy or possible rheumatologic condition. Subacute IE may manifest similarly, with vague symptoms such as myalgias, fatigue, chills, and/or anemia. In non-drug users, suspicion for endocarditis should be highest in men older than age 60. Also, it’s important to auscultate for a new heart murmur. In our patient’s case, no murmur was auscultated until after his TEE. JFP
CORRESPONDENCE
Ginger Poulton, MD, 123 Hendersonville Road, Asheville, NC 28803; [email protected]
1. Paruchuru PK, Adluri K, Patel RL. Windsock deformity of the mitral valve—a late presentation of endocarditis. Eur J Cardiothorac Surg. 2002;21:88. doi: 10.1016/s1010-7940(01)01038-7
2. Toyoda N, Chikwe J, Itagaki S, et al. Trends in infective endocarditis in California and New York State, 1998-2013. JAMA. 2017;317:1652-1660. doi: 10.1001/jama.2017.4287
3. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435-1486. doi: 10.1161/CIR.0000000000000296
4. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-3128. doi: 10.1093/eurheartj/ehv319
5. Wilson, WR, Gewitz, M, Lockhart PB et al. Prevention of Viridans Group Streptococcal Infective Endocarditis. A Scientific Statement from the American Heart Association. Circulation. 2021; 143e963-e978.
6. Lockhart PB, Brennan MT, Thornhill M, et al. Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc. 2009;140:1238-1244. doi: 10.14219/jada.archive.2009.0046
7. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463-473. doi: 10.1001/archinternmed.2008.603
THE CASE
A 75-year-old man with a history of osteoarthritis presented to our clinic with worsening weakness over the previous month. His signs and symptoms included profound fatigue, subjective fevers, a 10-pound weight loss, ankle swelling, myalgias in his legs and back, shortness of breath, and a persistent cough. The patient was otherwise previously healthy.
The patient’s heart and lung exams were normal. Initial outpatient labs showed significantly elevated inflammatory markers, with an erythrocyte sedimentation rate (ESR) of 102 mm/h (normal range for men ≥ 50 years, 0-20 mm/h) and a C-reactive protein (CRP) level of 11.1 mg/L (normal range, < 3 mg/L). The patient also had an elevated white blood cell count of 12,000/mcL (normal range, 4500-11,000/mcL). His hemoglobin was low (11 g/dL; normal range, 13.5-17.5 g/dL) and so was his albumin level (2.9 g/dL; normal range, 3.4-5.4 g/dL). The results of his prostate-specific antigen and brain natriuretic peptide tests were both normal. The results of a computed tomography scan of his thorax, abdomen, and pelvis were negative for malignancy.
The patient returned to our clinic 3 days later with severe weakness, which inhibited him from walking. He complained of a severe spasmodic pain between his shoulder blades. He denied joint stiffness, headaches, vision changes, or jaw claudication. The patient’s son had noted an overall increase in his father’s baseline heart rate, with readings increasing from the 50 beats/min range to the 70 beats/min range; this raised concern for a catecholamine-secreting tumor. There was also concern for occult infection and malignancy, or an autoimmune process, such as polymyalgia rheumatica. Due to his extreme weakness, the patient was directly admitted to the hospital for further work-up.
THE DIAGNOSIS
Concern for a smoldering infection prompted an order for a transthoracic echocardiogram. Images revealed a large mass on the mitral valve (FIGURE 1). Blood cultures quickly grew Streptococcus sanguinis. Additional work-up with a transesophageal echocardiogram (TEE) showed a “windsock” deformity (thinning and ballooning of the mitral valve), a known sequela of infective endocarditis (FIGURE 2).1 Further history obtained after the TEE revealed the patient had had a routine dental cleaning the month before his symptoms began. A murmur was then also detected.
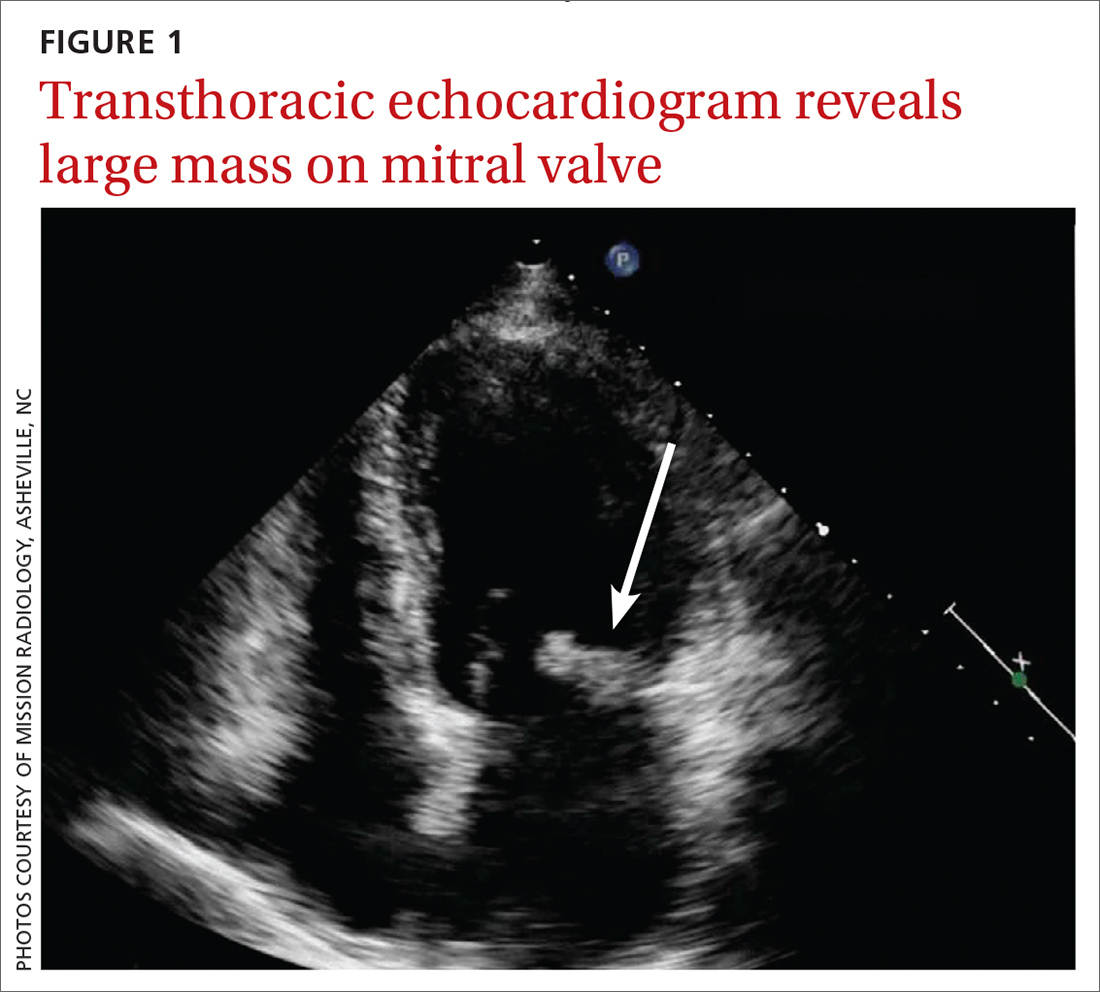
DISCUSSION
Infective endocarditis (IE) is uncommon and difficult to diagnose; it has a high early-mortality rate of 30%.2 TEE is the recommended imaging study for IE, because it is more sensitive than a transthoracic echocardiogram for identifying vegetations on the valves and it is more cost effective.3
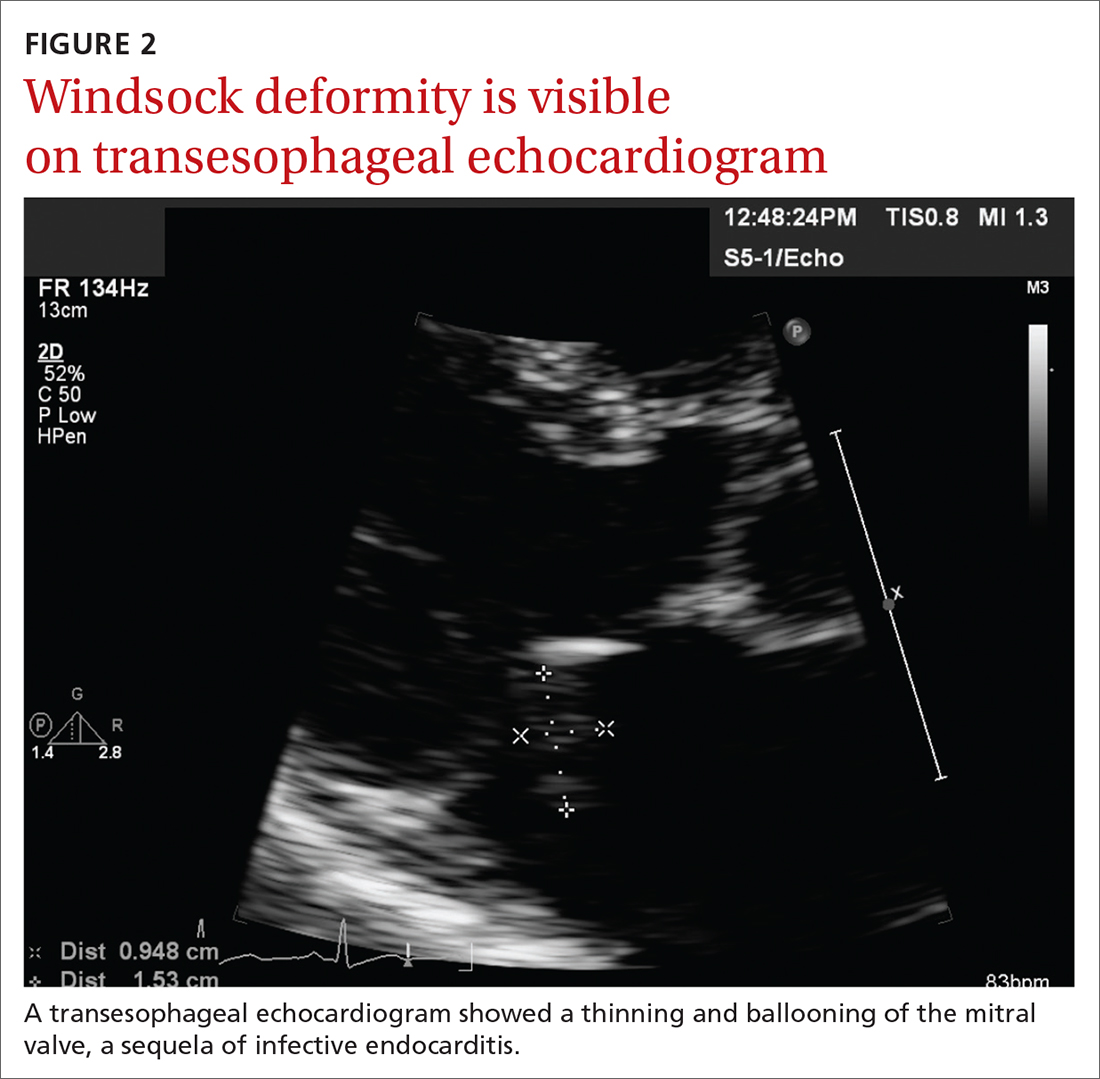
The modified Duke Criteria provide guidance for diagnosis of endocarditis. Major criteria focus on positive blood cultures and evidence of endocardial involvement. Minor criteria include predisposing heart conditions, intravenous drug use (IVDU), fever, and vascular and immunologic phenomena. As many as 90% of patients have a fever and often experience weight loss.4 Murmurs are auscultated in up to 85% of patients, and embolic features are present in up to 25% of patients at the time of diagnosis.4 In the developed world, Janeway lesions, Osler nodes, and splinter hemorrhages are increasingly rare, as patients usually present earlier in the disease course.4 While ESR and CRP are generally elevated in cases of IE, they are not part of the Duke Criteria.4
A closer look at risk factors
In 2007, guidelines for the prevention, treatment, and management of endocarditis were given significant categorical revision by the American Heart Association for the first time in 50 years.5 Recommendations for antibiotic prophylaxis prior to dental procedures became more restrictive, to include only 4 groups of high-risk patients: those with prosthetic cardiac valves, those with a history of IE, those with congenital heart disease, and cardiac transplant recipients.4 The rationale for these restrictions included the small risk for anaphylaxis and potential increase in risk for bacterial resistance associated with antibiotic prophylaxis.4 A review published in 2021 noted no increase in the frequency of, nor the morbidity and mortality from, viridans group streptococcal IE since the guideline updates.5
Continue to: There is an emerging consensus...
There is an emerging consensus that poor oral hygiene and gingival bleeding after tooth brushing promote a chronic low-grade bacteremia that may be more strongly associated with IE than an isolated dental extraction.6 Poor dental hygiene, defined as dental plaque and calculus, is especially common in the elderly, who are known to let their dental hygiene lapse.6 In our patient’s case, his generally poor oral hygiene was more likely the cause of his IE than his routine dental cleaning.
Other risk factors include IV drug use. At our tertiary care hospital in western North Carolina, 48% of patients with endocarditis had an additional diagnosis of opiate or narcotic dependence (Ryan Tilton, PharmD, email communication, June 7, 2018). Interestingly, though, only 16% of patients in North America with endocarditis were found to be currently using IV drugs.7
Our patient was treated with IV antibiotics for 4 weeks and underwent rehabilitation at a skilled nursing facility. Four weeks after diagnosis, he underwent an endoscopic porcine mitral valve replacement. Two months after that, he returned to his previously active lifestyle and began riding his stationary bike. The patient also began taking a daily aspirin. Consistent with current guidelines, he now gets antibiotic prophylaxis prior to dental procedures.
THE TAKEAWAY
This patient, without any history of IVDU or cardiac valvular abnormalities, presented with symptoms classic for a developing malignancy or possible rheumatologic condition. Subacute IE may manifest similarly, with vague symptoms such as myalgias, fatigue, chills, and/or anemia. In non-drug users, suspicion for endocarditis should be highest in men older than age 60. Also, it’s important to auscultate for a new heart murmur. In our patient’s case, no murmur was auscultated until after his TEE. JFP
CORRESPONDENCE
Ginger Poulton, MD, 123 Hendersonville Road, Asheville, NC 28803; [email protected]
THE CASE
A 75-year-old man with a history of osteoarthritis presented to our clinic with worsening weakness over the previous month. His signs and symptoms included profound fatigue, subjective fevers, a 10-pound weight loss, ankle swelling, myalgias in his legs and back, shortness of breath, and a persistent cough. The patient was otherwise previously healthy.
The patient’s heart and lung exams were normal. Initial outpatient labs showed significantly elevated inflammatory markers, with an erythrocyte sedimentation rate (ESR) of 102 mm/h (normal range for men ≥ 50 years, 0-20 mm/h) and a C-reactive protein (CRP) level of 11.1 mg/L (normal range, < 3 mg/L). The patient also had an elevated white blood cell count of 12,000/mcL (normal range, 4500-11,000/mcL). His hemoglobin was low (11 g/dL; normal range, 13.5-17.5 g/dL) and so was his albumin level (2.9 g/dL; normal range, 3.4-5.4 g/dL). The results of his prostate-specific antigen and brain natriuretic peptide tests were both normal. The results of a computed tomography scan of his thorax, abdomen, and pelvis were negative for malignancy.
The patient returned to our clinic 3 days later with severe weakness, which inhibited him from walking. He complained of a severe spasmodic pain between his shoulder blades. He denied joint stiffness, headaches, vision changes, or jaw claudication. The patient’s son had noted an overall increase in his father’s baseline heart rate, with readings increasing from the 50 beats/min range to the 70 beats/min range; this raised concern for a catecholamine-secreting tumor. There was also concern for occult infection and malignancy, or an autoimmune process, such as polymyalgia rheumatica. Due to his extreme weakness, the patient was directly admitted to the hospital for further work-up.
THE DIAGNOSIS
Concern for a smoldering infection prompted an order for a transthoracic echocardiogram. Images revealed a large mass on the mitral valve (FIGURE 1). Blood cultures quickly grew Streptococcus sanguinis. Additional work-up with a transesophageal echocardiogram (TEE) showed a “windsock” deformity (thinning and ballooning of the mitral valve), a known sequela of infective endocarditis (FIGURE 2).1 Further history obtained after the TEE revealed the patient had had a routine dental cleaning the month before his symptoms began. A murmur was then also detected.
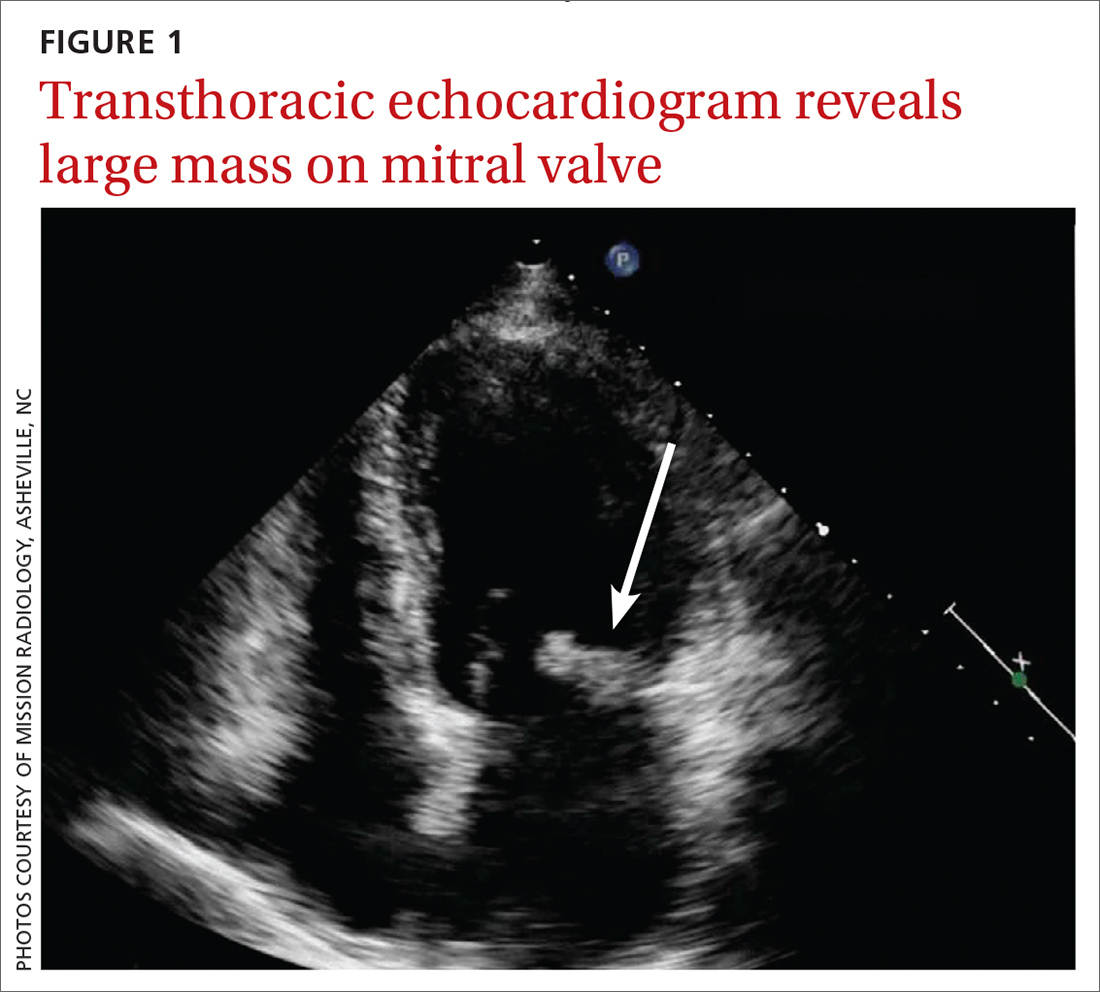
DISCUSSION
Infective endocarditis (IE) is uncommon and difficult to diagnose; it has a high early-mortality rate of 30%.2 TEE is the recommended imaging study for IE, because it is more sensitive than a transthoracic echocardiogram for identifying vegetations on the valves and it is more cost effective.3
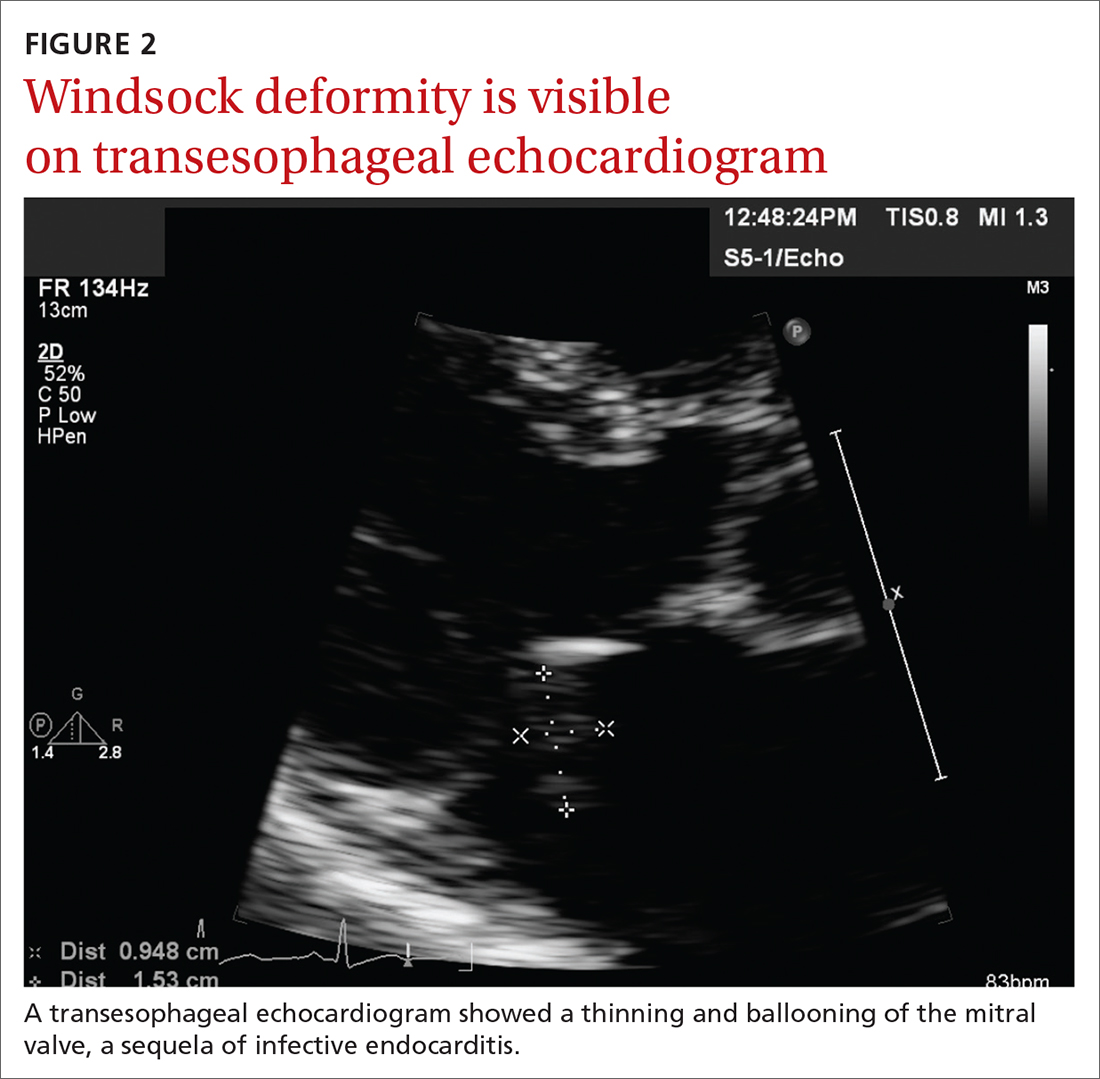
The modified Duke Criteria provide guidance for diagnosis of endocarditis. Major criteria focus on positive blood cultures and evidence of endocardial involvement. Minor criteria include predisposing heart conditions, intravenous drug use (IVDU), fever, and vascular and immunologic phenomena. As many as 90% of patients have a fever and often experience weight loss.4 Murmurs are auscultated in up to 85% of patients, and embolic features are present in up to 25% of patients at the time of diagnosis.4 In the developed world, Janeway lesions, Osler nodes, and splinter hemorrhages are increasingly rare, as patients usually present earlier in the disease course.4 While ESR and CRP are generally elevated in cases of IE, they are not part of the Duke Criteria.4
A closer look at risk factors
In 2007, guidelines for the prevention, treatment, and management of endocarditis were given significant categorical revision by the American Heart Association for the first time in 50 years.5 Recommendations for antibiotic prophylaxis prior to dental procedures became more restrictive, to include only 4 groups of high-risk patients: those with prosthetic cardiac valves, those with a history of IE, those with congenital heart disease, and cardiac transplant recipients.4 The rationale for these restrictions included the small risk for anaphylaxis and potential increase in risk for bacterial resistance associated with antibiotic prophylaxis.4 A review published in 2021 noted no increase in the frequency of, nor the morbidity and mortality from, viridans group streptococcal IE since the guideline updates.5
Continue to: There is an emerging consensus...
There is an emerging consensus that poor oral hygiene and gingival bleeding after tooth brushing promote a chronic low-grade bacteremia that may be more strongly associated with IE than an isolated dental extraction.6 Poor dental hygiene, defined as dental plaque and calculus, is especially common in the elderly, who are known to let their dental hygiene lapse.6 In our patient’s case, his generally poor oral hygiene was more likely the cause of his IE than his routine dental cleaning.
Other risk factors include IV drug use. At our tertiary care hospital in western North Carolina, 48% of patients with endocarditis had an additional diagnosis of opiate or narcotic dependence (Ryan Tilton, PharmD, email communication, June 7, 2018). Interestingly, though, only 16% of patients in North America with endocarditis were found to be currently using IV drugs.7
Our patient was treated with IV antibiotics for 4 weeks and underwent rehabilitation at a skilled nursing facility. Four weeks after diagnosis, he underwent an endoscopic porcine mitral valve replacement. Two months after that, he returned to his previously active lifestyle and began riding his stationary bike. The patient also began taking a daily aspirin. Consistent with current guidelines, he now gets antibiotic prophylaxis prior to dental procedures.
THE TAKEAWAY
This patient, without any history of IVDU or cardiac valvular abnormalities, presented with symptoms classic for a developing malignancy or possible rheumatologic condition. Subacute IE may manifest similarly, with vague symptoms such as myalgias, fatigue, chills, and/or anemia. In non-drug users, suspicion for endocarditis should be highest in men older than age 60. Also, it’s important to auscultate for a new heart murmur. In our patient’s case, no murmur was auscultated until after his TEE. JFP
CORRESPONDENCE
Ginger Poulton, MD, 123 Hendersonville Road, Asheville, NC 28803; [email protected]
1. Paruchuru PK, Adluri K, Patel RL. Windsock deformity of the mitral valve—a late presentation of endocarditis. Eur J Cardiothorac Surg. 2002;21:88. doi: 10.1016/s1010-7940(01)01038-7
2. Toyoda N, Chikwe J, Itagaki S, et al. Trends in infective endocarditis in California and New York State, 1998-2013. JAMA. 2017;317:1652-1660. doi: 10.1001/jama.2017.4287
3. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435-1486. doi: 10.1161/CIR.0000000000000296
4. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-3128. doi: 10.1093/eurheartj/ehv319
5. Wilson, WR, Gewitz, M, Lockhart PB et al. Prevention of Viridans Group Streptococcal Infective Endocarditis. A Scientific Statement from the American Heart Association. Circulation. 2021; 143e963-e978.
6. Lockhart PB, Brennan MT, Thornhill M, et al. Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc. 2009;140:1238-1244. doi: 10.14219/jada.archive.2009.0046
7. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463-473. doi: 10.1001/archinternmed.2008.603
1. Paruchuru PK, Adluri K, Patel RL. Windsock deformity of the mitral valve—a late presentation of endocarditis. Eur J Cardiothorac Surg. 2002;21:88. doi: 10.1016/s1010-7940(01)01038-7
2. Toyoda N, Chikwe J, Itagaki S, et al. Trends in infective endocarditis in California and New York State, 1998-2013. JAMA. 2017;317:1652-1660. doi: 10.1001/jama.2017.4287
3. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132:1435-1486. doi: 10.1161/CIR.0000000000000296
4. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-3128. doi: 10.1093/eurheartj/ehv319
5. Wilson, WR, Gewitz, M, Lockhart PB et al. Prevention of Viridans Group Streptococcal Infective Endocarditis. A Scientific Statement from the American Heart Association. Circulation. 2021; 143e963-e978.
6. Lockhart PB, Brennan MT, Thornhill M, et al. Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc. 2009;140:1238-1244. doi: 10.14219/jada.archive.2009.0046
7. Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169:463-473. doi: 10.1001/archinternmed.2008.603