User login
Hypothesis: Milk and beef ‘causally linked’ to colorectal cancer
Bovine meat and milk factors (BMMF), the recently discovered pathogenic agents found in milk products and beef, could play a role in the development of colorectal cancer, say German scientists.
The team was headed by Harald zur Hausen, MD, PhD, division of episomal-persistent DNA in cancer and chronic diseases, German Cancer Research Center, Heidelberg, who received the Nobel Prize in Physiology or Medicine in 2008 for his discovery of the role of human papillomaviruses in the development of cervical cancer.
The team has been researching the link between BMMF and colorectal cancer for some years, and the latest study was published in the Proceedings of the National Academy of Sciences.
“The results support our hypothesis that the consumption of milk and beef is causally linked to the development of colon cancer,” Dr. Hausen said in a related press statement.
Pathogenic agents, found in vicinity of tumors
BMMF are infectious agents that occur as circular single strands of DNA and have a notable similarity to the sequences of some bacterial plasmids.
A few years ago, Dr. Hausen and colleagues found these pathogenic agents in colon cancer patients, in the immediate vicinity of tumors.
They therefore put forward the hypothesis that BMMF could trigger chronic local inflammation, which in turn could cause genetic mutations via oxidative stress and lead to the development of cancer over the long term.
The German researchers were also able to show in in vitro models that BMMF multiply in human cells where the H1MSB.1 Rep protein, which is required for their replication, is synthesized.
In their latest study, the scientists analyzed tissue samples from colorectal cancer patients and from individuals without the disease.
The team found that BMMF could trigger chronic inflammation in the intestinal tissue of cancer patients, as demonstrated via the presence of proinflammatory macrophages.
The researchers also used anti-Rep antibodies to show that the Rep protein was present around and inside the macrophages. In cancer patients, 7.3% of all the intestinal cells in the tumor environment were positive for Rep versus just 1.7% of those in the control group.
In addition, the researchers reported increased levels of reactive oxygen species close to Rep-positive cells.
“These oxygen radicals promote the development of genetic changes,” Dr. Hausen said.
The inflammation was particularly localized to the immediate vicinity of the intestinal crypts, where the intestinal stem cells, which are responsible for the constant regeneration of the intestinal mucosa, are found.
“We therefore think of the BMMF as indirect carcinogens, some of which will probably have an impact on dividing cells in the intestinal mucosa for decades,” Dr. Hausen explained.
He assumes that infection with BMMF typically occurs early in life. This “opens up the possibility of early intervention,” he suggested.
The early detection of BMMF could allow the identification of individuals particularly at risk, and for these patients to be offered timely colon cancer screening.
The researchers stressed, however, that further study will be required to confirm the results.
They nevertheless believed that BMMF could help explain the link between the consumption of red meat and dairy products and other cancers and diseases, in particular breast, prostate, and lung cancers.
Finally, the pathogenic agents could partially explain the preventive effect of anti-inflammatory dugs such as aspirin and ibuprofen on the incidence of colon cancer and other cancers via the reduction of chronic inflammation.
This work was supported by an unrestricted grant from ORYX Alpha. One coauthor was supported by the EOS Foundation, the SFBTR-179 and 209, and a European Research Council consolidator grant. The other coauthors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bovine meat and milk factors (BMMF), the recently discovered pathogenic agents found in milk products and beef, could play a role in the development of colorectal cancer, say German scientists.
The team was headed by Harald zur Hausen, MD, PhD, division of episomal-persistent DNA in cancer and chronic diseases, German Cancer Research Center, Heidelberg, who received the Nobel Prize in Physiology or Medicine in 2008 for his discovery of the role of human papillomaviruses in the development of cervical cancer.
The team has been researching the link between BMMF and colorectal cancer for some years, and the latest study was published in the Proceedings of the National Academy of Sciences.
“The results support our hypothesis that the consumption of milk and beef is causally linked to the development of colon cancer,” Dr. Hausen said in a related press statement.
Pathogenic agents, found in vicinity of tumors
BMMF are infectious agents that occur as circular single strands of DNA and have a notable similarity to the sequences of some bacterial plasmids.
A few years ago, Dr. Hausen and colleagues found these pathogenic agents in colon cancer patients, in the immediate vicinity of tumors.
They therefore put forward the hypothesis that BMMF could trigger chronic local inflammation, which in turn could cause genetic mutations via oxidative stress and lead to the development of cancer over the long term.
The German researchers were also able to show in in vitro models that BMMF multiply in human cells where the H1MSB.1 Rep protein, which is required for their replication, is synthesized.
In their latest study, the scientists analyzed tissue samples from colorectal cancer patients and from individuals without the disease.
The team found that BMMF could trigger chronic inflammation in the intestinal tissue of cancer patients, as demonstrated via the presence of proinflammatory macrophages.
The researchers also used anti-Rep antibodies to show that the Rep protein was present around and inside the macrophages. In cancer patients, 7.3% of all the intestinal cells in the tumor environment were positive for Rep versus just 1.7% of those in the control group.
In addition, the researchers reported increased levels of reactive oxygen species close to Rep-positive cells.
“These oxygen radicals promote the development of genetic changes,” Dr. Hausen said.
The inflammation was particularly localized to the immediate vicinity of the intestinal crypts, where the intestinal stem cells, which are responsible for the constant regeneration of the intestinal mucosa, are found.
“We therefore think of the BMMF as indirect carcinogens, some of which will probably have an impact on dividing cells in the intestinal mucosa for decades,” Dr. Hausen explained.
He assumes that infection with BMMF typically occurs early in life. This “opens up the possibility of early intervention,” he suggested.
The early detection of BMMF could allow the identification of individuals particularly at risk, and for these patients to be offered timely colon cancer screening.
The researchers stressed, however, that further study will be required to confirm the results.
They nevertheless believed that BMMF could help explain the link between the consumption of red meat and dairy products and other cancers and diseases, in particular breast, prostate, and lung cancers.
Finally, the pathogenic agents could partially explain the preventive effect of anti-inflammatory dugs such as aspirin and ibuprofen on the incidence of colon cancer and other cancers via the reduction of chronic inflammation.
This work was supported by an unrestricted grant from ORYX Alpha. One coauthor was supported by the EOS Foundation, the SFBTR-179 and 209, and a European Research Council consolidator grant. The other coauthors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bovine meat and milk factors (BMMF), the recently discovered pathogenic agents found in milk products and beef, could play a role in the development of colorectal cancer, say German scientists.
The team was headed by Harald zur Hausen, MD, PhD, division of episomal-persistent DNA in cancer and chronic diseases, German Cancer Research Center, Heidelberg, who received the Nobel Prize in Physiology or Medicine in 2008 for his discovery of the role of human papillomaviruses in the development of cervical cancer.
The team has been researching the link between BMMF and colorectal cancer for some years, and the latest study was published in the Proceedings of the National Academy of Sciences.
“The results support our hypothesis that the consumption of milk and beef is causally linked to the development of colon cancer,” Dr. Hausen said in a related press statement.
Pathogenic agents, found in vicinity of tumors
BMMF are infectious agents that occur as circular single strands of DNA and have a notable similarity to the sequences of some bacterial plasmids.
A few years ago, Dr. Hausen and colleagues found these pathogenic agents in colon cancer patients, in the immediate vicinity of tumors.
They therefore put forward the hypothesis that BMMF could trigger chronic local inflammation, which in turn could cause genetic mutations via oxidative stress and lead to the development of cancer over the long term.
The German researchers were also able to show in in vitro models that BMMF multiply in human cells where the H1MSB.1 Rep protein, which is required for their replication, is synthesized.
In their latest study, the scientists analyzed tissue samples from colorectal cancer patients and from individuals without the disease.
The team found that BMMF could trigger chronic inflammation in the intestinal tissue of cancer patients, as demonstrated via the presence of proinflammatory macrophages.
The researchers also used anti-Rep antibodies to show that the Rep protein was present around and inside the macrophages. In cancer patients, 7.3% of all the intestinal cells in the tumor environment were positive for Rep versus just 1.7% of those in the control group.
In addition, the researchers reported increased levels of reactive oxygen species close to Rep-positive cells.
“These oxygen radicals promote the development of genetic changes,” Dr. Hausen said.
The inflammation was particularly localized to the immediate vicinity of the intestinal crypts, where the intestinal stem cells, which are responsible for the constant regeneration of the intestinal mucosa, are found.
“We therefore think of the BMMF as indirect carcinogens, some of which will probably have an impact on dividing cells in the intestinal mucosa for decades,” Dr. Hausen explained.
He assumes that infection with BMMF typically occurs early in life. This “opens up the possibility of early intervention,” he suggested.
The early detection of BMMF could allow the identification of individuals particularly at risk, and for these patients to be offered timely colon cancer screening.
The researchers stressed, however, that further study will be required to confirm the results.
They nevertheless believed that BMMF could help explain the link between the consumption of red meat and dairy products and other cancers and diseases, in particular breast, prostate, and lung cancers.
Finally, the pathogenic agents could partially explain the preventive effect of anti-inflammatory dugs such as aspirin and ibuprofen on the incidence of colon cancer and other cancers via the reduction of chronic inflammation.
This work was supported by an unrestricted grant from ORYX Alpha. One coauthor was supported by the EOS Foundation, the SFBTR-179 and 209, and a European Research Council consolidator grant. The other coauthors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Study: Spanking may change children’s brains
Rare is the parent who has never so much as thought about spanking an unruly child. But a new study provides another reason to avoid corporal punishment: Spanking may cause changes in the same areas of a child’s brain that are affected by more severe physical and sexual abuse.
Previous research has consistently found links between spanking and behavioral problems, aggression, depression, and anxiety, says Jorge Cuartas, a doctoral candidate at the Harvard Graduate School of Education and first author of the study. “We wanted to look at one potential mechanism, brain development, that might explain how corporal punishment can impact children’s behavior and cognitive development.”
The study, published in Child Development, used functional MRIs to map brain changes in 147 tweens who’d never experienced physical or sexual abuse. Researchers tracked which parts of the children’s brains activated in response to neutral or fearful facial expressions. When shown pictures of someone looking fearful, kids who reported having been spanked had a larger response in certain parts of the brain than kids who hadn’t been. Those areas drive the response to environmental cues, recognizing threats and reacting to them. If a child’s brain overreacts, behavioral challenges can result.
“We saw those changes in the same areas as more severe forms of abuse or domestic violence. It suggests the difference is of degree rather than type,” Mr. Cuartas says. As far as a child’s brain is concerned, “It’s all violence.”
It’s a significant finding because many parents don’t think of spanking as being violent, says Vincent J. Palusci, MD, a pediatrician and editor-in-chief of the journal Child Maltreatment. “We want to raise kids who are happy and healthy, and many parents who use spanking are doing it with that goal.”
Spanking in the U.S.
Around the world, 62 states and countries have outlawed corporal punishment. While the U.S. has no such protections, both the American Academy of Pediatrics and the American Psychological Association have condemned the practice. Acceptance of spanking seems to be shrinking: The percentage of parents in this country who say they spank their children is trending downward. In 1993, 50% of parents surveyed said they did, but by 2017 that number had fallen to 35%. Still far too many, Mr. Cuartas and Dr. Palusci say, but a promising trend.
“While we wouldn’t as parents want to hurt our kids,” Dr. Palusci says, “we need to understand that spanking can be just as bad as things we’d never do.”
Discipline vs. punishment
For some parents, it may require a shift in thinking, differentiating between discipline and punishment. “Discipline changes behavior – it teaches positive behavior, empathy, essential social skills. But that’s different from punishment,” Mr. Cuartas says. “That makes somebody feel pain or shame. We have to start thinking about spanking as punishment.”
That can be difficult, especially for adults who’ve been spanked themselves. They may believe that since they turned out fine, spanking must be fine, too. But the study doesn’t suggest that every child who’s spanked will have these difficulties – it just shows they happen, Mr. Cuartas says. “Compare this to smoking. We all know someone who smokes who’s healthy, but that doesn’t mean smoking is good,” he says. “Individual cases aren’t enough to understand whether certain experiences are good or bad.”
Dr. Palusci draws parallels to the advice pregnant women receive about taking medications: If it hasn’t been tested in pregnancy specifically, no amount can be considered safe. “We don’t have the studies to say how much spanking is dangerous, so we have to think that any amount has this potential.”
A version of this article first appeared on Medscape.com.
Rare is the parent who has never so much as thought about spanking an unruly child. But a new study provides another reason to avoid corporal punishment: Spanking may cause changes in the same areas of a child’s brain that are affected by more severe physical and sexual abuse.
Previous research has consistently found links between spanking and behavioral problems, aggression, depression, and anxiety, says Jorge Cuartas, a doctoral candidate at the Harvard Graduate School of Education and first author of the study. “We wanted to look at one potential mechanism, brain development, that might explain how corporal punishment can impact children’s behavior and cognitive development.”
The study, published in Child Development, used functional MRIs to map brain changes in 147 tweens who’d never experienced physical or sexual abuse. Researchers tracked which parts of the children’s brains activated in response to neutral or fearful facial expressions. When shown pictures of someone looking fearful, kids who reported having been spanked had a larger response in certain parts of the brain than kids who hadn’t been. Those areas drive the response to environmental cues, recognizing threats and reacting to them. If a child’s brain overreacts, behavioral challenges can result.
“We saw those changes in the same areas as more severe forms of abuse or domestic violence. It suggests the difference is of degree rather than type,” Mr. Cuartas says. As far as a child’s brain is concerned, “It’s all violence.”
It’s a significant finding because many parents don’t think of spanking as being violent, says Vincent J. Palusci, MD, a pediatrician and editor-in-chief of the journal Child Maltreatment. “We want to raise kids who are happy and healthy, and many parents who use spanking are doing it with that goal.”
Spanking in the U.S.
Around the world, 62 states and countries have outlawed corporal punishment. While the U.S. has no such protections, both the American Academy of Pediatrics and the American Psychological Association have condemned the practice. Acceptance of spanking seems to be shrinking: The percentage of parents in this country who say they spank their children is trending downward. In 1993, 50% of parents surveyed said they did, but by 2017 that number had fallen to 35%. Still far too many, Mr. Cuartas and Dr. Palusci say, but a promising trend.
“While we wouldn’t as parents want to hurt our kids,” Dr. Palusci says, “we need to understand that spanking can be just as bad as things we’d never do.”
Discipline vs. punishment
For some parents, it may require a shift in thinking, differentiating between discipline and punishment. “Discipline changes behavior – it teaches positive behavior, empathy, essential social skills. But that’s different from punishment,” Mr. Cuartas says. “That makes somebody feel pain or shame. We have to start thinking about spanking as punishment.”
That can be difficult, especially for adults who’ve been spanked themselves. They may believe that since they turned out fine, spanking must be fine, too. But the study doesn’t suggest that every child who’s spanked will have these difficulties – it just shows they happen, Mr. Cuartas says. “Compare this to smoking. We all know someone who smokes who’s healthy, but that doesn’t mean smoking is good,” he says. “Individual cases aren’t enough to understand whether certain experiences are good or bad.”
Dr. Palusci draws parallels to the advice pregnant women receive about taking medications: If it hasn’t been tested in pregnancy specifically, no amount can be considered safe. “We don’t have the studies to say how much spanking is dangerous, so we have to think that any amount has this potential.”
A version of this article first appeared on Medscape.com.
Rare is the parent who has never so much as thought about spanking an unruly child. But a new study provides another reason to avoid corporal punishment: Spanking may cause changes in the same areas of a child’s brain that are affected by more severe physical and sexual abuse.
Previous research has consistently found links between spanking and behavioral problems, aggression, depression, and anxiety, says Jorge Cuartas, a doctoral candidate at the Harvard Graduate School of Education and first author of the study. “We wanted to look at one potential mechanism, brain development, that might explain how corporal punishment can impact children’s behavior and cognitive development.”
The study, published in Child Development, used functional MRIs to map brain changes in 147 tweens who’d never experienced physical or sexual abuse. Researchers tracked which parts of the children’s brains activated in response to neutral or fearful facial expressions. When shown pictures of someone looking fearful, kids who reported having been spanked had a larger response in certain parts of the brain than kids who hadn’t been. Those areas drive the response to environmental cues, recognizing threats and reacting to them. If a child’s brain overreacts, behavioral challenges can result.
“We saw those changes in the same areas as more severe forms of abuse or domestic violence. It suggests the difference is of degree rather than type,” Mr. Cuartas says. As far as a child’s brain is concerned, “It’s all violence.”
It’s a significant finding because many parents don’t think of spanking as being violent, says Vincent J. Palusci, MD, a pediatrician and editor-in-chief of the journal Child Maltreatment. “We want to raise kids who are happy and healthy, and many parents who use spanking are doing it with that goal.”
Spanking in the U.S.
Around the world, 62 states and countries have outlawed corporal punishment. While the U.S. has no such protections, both the American Academy of Pediatrics and the American Psychological Association have condemned the practice. Acceptance of spanking seems to be shrinking: The percentage of parents in this country who say they spank their children is trending downward. In 1993, 50% of parents surveyed said they did, but by 2017 that number had fallen to 35%. Still far too many, Mr. Cuartas and Dr. Palusci say, but a promising trend.
“While we wouldn’t as parents want to hurt our kids,” Dr. Palusci says, “we need to understand that spanking can be just as bad as things we’d never do.”
Discipline vs. punishment
For some parents, it may require a shift in thinking, differentiating between discipline and punishment. “Discipline changes behavior – it teaches positive behavior, empathy, essential social skills. But that’s different from punishment,” Mr. Cuartas says. “That makes somebody feel pain or shame. We have to start thinking about spanking as punishment.”
That can be difficult, especially for adults who’ve been spanked themselves. They may believe that since they turned out fine, spanking must be fine, too. But the study doesn’t suggest that every child who’s spanked will have these difficulties – it just shows they happen, Mr. Cuartas says. “Compare this to smoking. We all know someone who smokes who’s healthy, but that doesn’t mean smoking is good,” he says. “Individual cases aren’t enough to understand whether certain experiences are good or bad.”
Dr. Palusci draws parallels to the advice pregnant women receive about taking medications: If it hasn’t been tested in pregnancy specifically, no amount can be considered safe. “We don’t have the studies to say how much spanking is dangerous, so we have to think that any amount has this potential.”
A version of this article first appeared on Medscape.com.
First AI device for colonoscopy: Extra set of expert ‘eyes’
The GI Genius module is the first and only commercially available computer-aided detection system that uses AI to identify colorectal polyps during routine colonoscopy.
The technology is compatible with most standard video endoscopy systems and has been “trained” to identify colonic lesions that are possibly cancerous, according to Medtronic, the distributor of the device.
“I think that anything we can do within a reasonable cost that enhances quality and patient outcomes during colonoscopy warrants very close consideration,” David Johnson, MD, professor of medicine and chief of gastroenterology, Eastern Virginia Medical School, Norfolk, said in an interview.
He was not involved with the development of the GI Genius system but has worked with a similar AI device that is used in conjunction with colonoscopy.
“The whole development of the technology for AI is done by inputting repetitive images into the computer, where it develops what is called the ‘neural network,’ ” he explained.
The computer then draws upon the “education” of this neural network to identify different types of colonic lesions, “and the more inputs that are put into the computer to enhance the neural network, the more capable the program becomes in the identification of variants and lesion size and characteristics,” Dr. Johnson added.
During routine colonoscopy, the GI Genius system generates visual markers – essentially, small green squares – and a low-volume sound whenever the software detects a region of interest.
These squares are superimposed on the video generated by the endoscope camera to alert the colonoscopist to regions that may require closer assessment, either visually, by tissue sampling, or by removal of the lesion itself.
“Colonoscopy is a durable screening and surveillance strategy, but it’s not perfect [because] it depends on a physician’s skill and their ability to pick up polyps in the colon,” Jeremy Glissen Brown, MD, of Beth Israel Deaconess Medical Center, Boston, said in an interview. He has also worked with an AI device.
Studies of adenoma detection during “all-comer” colonoscopies show that the rate of missed lesions ranges from a low of 6% to 40%, “so polyps are still missed during colonoscopy, and any technology that can solve parts of that problem is welcome,” Dr. Glissen Brown commented.
Clinical trial data that led to approval
The recent FDA approval of the GI Genius device was based on a prospective, randomized trial that was published in Gastroenterology in 2020. That trial involved 700 patients who were being screened or followed with colonoscopy every 3 years or longer. Participants underwent either white-light standard colonoscopy with the assistance of the GI Genius technology or standard white-light colonoscopy alone.
Results showed that the combination of standard colonoscopy and the GI Genius module identified laboratory-confirmed adenomas or carcinomas in 54.8% of patients, compared with 40.4% of patients who underwent colonoscopy alone.
In the Gastroenterology article, the authors wrote that the “14% absolute increase in adenoma detection rate obtained by computer-aided detection (CADe) in our study indicates that failure in polyp recognition is a clinically relevant cause of miss rate. Of note, the efficacy of CADe in reversing such miss rate also indicates that the same operator who missed the lesion in the first place was able to correctly diagnose it when the lesion was presented by the CADe. This underlines that the main cognitive challenge in polyp recognition is the discrimination between the candidate lesion and the surrounding healthy mucosa, whereas its correct characterization as neoplastic tissue that occurs after CADe detection is apparently a much easier task.”
The authors also noted that they did “not assess the actual number of false-positive activations by the system, as this would have altered the routine setting of our study,” but they refer to a study published in Gut in 2020 in which false-positive frames were seen in fewer than 1% of frames from the whole colonoscopy.
Because the new device improves on the ability of colonoscopy to detect lesions overall, it may reduce the risk of interval cancers between colonoscopies, Medtronic suggests.
Previous research has shown that every 1% increase in the adenoma detection rate results in a 3% decrease in the risk for colorectal cancer.
“More than 19 million screening colonoscopies are performed in the United State each year. ... Detection of adenomas during colonoscopy is an important quality metric,” James Weber, MD, a gastroenterologist affiliated with Texas Digestive Disease Consultants, Southlake, commented in a Medtronic press release.
“The addition of AI can increase the quality of colonoscopies, potentially improving diagnosis and outcomes for colon cancer patients,” he added.
Dr. Weber is also the CEO of GI Alliance, a physician-led national health care platform of independent GI practices in six states in the United States.
Computer-aided detection
Unlike other computer-aided detection technologies, GI Genius does not characterize or “diagnose” a lesion, nor does it replace laboratory sampling as a means of confirming a cancer diagnosis.
The technology acts essentially as an extra set of expert “eyes” to detect suspicious lesions during colonoscopy, which should prove helpful, Dr. Johnson and Dr. Glissen Brown both commented.
“When a gastroenterologist looks at the video image, typically, our eyes are focused in the center of that image – that’s where our 20/20 vision is,” Dr. Johnson explained.
The computer has 20/20 vision over the whole image, including the periphery, “so the technology really gives an extremely expanded acuity of vision and highlights areas that we may need to investigate further,” he added.
Dr. Glissen Brown was involved in a trial of another AI device – the real-time automatic polyp detection system (Shanghai Wision AI). That study showed an increase in colonoscopic polyp and adenoma detection rates, but this was mainly because of a higher number of diminutive adenomas detected by the automatic detection system, Dr. Gliseen Brown said. There was no important difference in the number of larger adenomas detected with the device and the number detected without it.
However, there was a significant increase in the detection of hyperplastic polyps when the automatic detection system was used. “We definitely want to look at the false positive rate – both the false positive rate under the camera when we are doing colonoscopy and under the microscope when we do biopsies,” Dr. Glissen Brown acknowledged.
In numerous prospective studies of various computer-aided detection technologies such as the GI Genius system, the false positive rate resulting in the performance of biopsy of insignificant lesions is relatively low, he said.
“Ultimately, the decision to remove or biopsy a lesion is with the physician, because the GI Genius technology just points the provider to the area of concern, and then it’s up to them to look at it and decide whether it needs to be biopsied or not,” Dr. Glissen Brown said.
“So the technology serves more as a digital safety net and points the physician in the right direction, so it shouldn’t lead to much in the way of histologic false positives,” he noted.
The only potential disadvantage to using an AI system such as the GI Genius module is the time it might take for endoscopists to learn how to use it and how much the technology might increase the time required to perform the procedure, he added.
For about 18 months, Dr. Johnson has been running a clinical trial with a similar type of AI technology during colonoscopy. He has found that the learning curve for using these systems is “inordinately short.” Dr. Glissen Brown agreed and suggested that, if physicians are already performing colonoscopies regularly, they could probably learn to use an AI system such as GI Genius in about a week.
In his experience, Dr. Johnson has found that the delay caused by use of an AI system during colonoscopy is “minimal.”
If there is any delay at all, “we know that time in the colon on withdrawal increases the detection of polyps, so more time during withdrawal may be a good thing,” he added. It should be noted that endoscopy societies recommend a withdrawal time of at least 6 minutes, which is one of the metrics used to ensure the quality of a colonoscopy, Dr. Glissen Brown explained.
Indeed, the pivotal study upon which the FDA approved the GI Genius module required a minimum withdrawal time of 6 minutes. Participants said they did not find that using the GI Genius increased withdrawal time, he added.
“I think there is enough prospective evidence at this point to suggest that this technology may really be of benefit to clinicians with a lot of different skill levels, so I would be eager to know how clinicians interact with it in the clinical setting,” Dr. Glissen Brown commented.
Dr. Johnson agreed, noting that “even the good can get better.”
Dr. Johnson disclosed relationships with this news organization, CRH Medical, the American College of Gastroenterology Research Institute, and HyGIeaCare. Dr. Glissen Brown disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Article updated April 21, 2021.
The GI Genius module is the first and only commercially available computer-aided detection system that uses AI to identify colorectal polyps during routine colonoscopy.
The technology is compatible with most standard video endoscopy systems and has been “trained” to identify colonic lesions that are possibly cancerous, according to Medtronic, the distributor of the device.
“I think that anything we can do within a reasonable cost that enhances quality and patient outcomes during colonoscopy warrants very close consideration,” David Johnson, MD, professor of medicine and chief of gastroenterology, Eastern Virginia Medical School, Norfolk, said in an interview.
He was not involved with the development of the GI Genius system but has worked with a similar AI device that is used in conjunction with colonoscopy.
“The whole development of the technology for AI is done by inputting repetitive images into the computer, where it develops what is called the ‘neural network,’ ” he explained.
The computer then draws upon the “education” of this neural network to identify different types of colonic lesions, “and the more inputs that are put into the computer to enhance the neural network, the more capable the program becomes in the identification of variants and lesion size and characteristics,” Dr. Johnson added.
During routine colonoscopy, the GI Genius system generates visual markers – essentially, small green squares – and a low-volume sound whenever the software detects a region of interest.
These squares are superimposed on the video generated by the endoscope camera to alert the colonoscopist to regions that may require closer assessment, either visually, by tissue sampling, or by removal of the lesion itself.
“Colonoscopy is a durable screening and surveillance strategy, but it’s not perfect [because] it depends on a physician’s skill and their ability to pick up polyps in the colon,” Jeremy Glissen Brown, MD, of Beth Israel Deaconess Medical Center, Boston, said in an interview. He has also worked with an AI device.
Studies of adenoma detection during “all-comer” colonoscopies show that the rate of missed lesions ranges from a low of 6% to 40%, “so polyps are still missed during colonoscopy, and any technology that can solve parts of that problem is welcome,” Dr. Glissen Brown commented.
Clinical trial data that led to approval
The recent FDA approval of the GI Genius device was based on a prospective, randomized trial that was published in Gastroenterology in 2020. That trial involved 700 patients who were being screened or followed with colonoscopy every 3 years or longer. Participants underwent either white-light standard colonoscopy with the assistance of the GI Genius technology or standard white-light colonoscopy alone.
Results showed that the combination of standard colonoscopy and the GI Genius module identified laboratory-confirmed adenomas or carcinomas in 54.8% of patients, compared with 40.4% of patients who underwent colonoscopy alone.
In the Gastroenterology article, the authors wrote that the “14% absolute increase in adenoma detection rate obtained by computer-aided detection (CADe) in our study indicates that failure in polyp recognition is a clinically relevant cause of miss rate. Of note, the efficacy of CADe in reversing such miss rate also indicates that the same operator who missed the lesion in the first place was able to correctly diagnose it when the lesion was presented by the CADe. This underlines that the main cognitive challenge in polyp recognition is the discrimination between the candidate lesion and the surrounding healthy mucosa, whereas its correct characterization as neoplastic tissue that occurs after CADe detection is apparently a much easier task.”
The authors also noted that they did “not assess the actual number of false-positive activations by the system, as this would have altered the routine setting of our study,” but they refer to a study published in Gut in 2020 in which false-positive frames were seen in fewer than 1% of frames from the whole colonoscopy.
Because the new device improves on the ability of colonoscopy to detect lesions overall, it may reduce the risk of interval cancers between colonoscopies, Medtronic suggests.
Previous research has shown that every 1% increase in the adenoma detection rate results in a 3% decrease in the risk for colorectal cancer.
“More than 19 million screening colonoscopies are performed in the United State each year. ... Detection of adenomas during colonoscopy is an important quality metric,” James Weber, MD, a gastroenterologist affiliated with Texas Digestive Disease Consultants, Southlake, commented in a Medtronic press release.
“The addition of AI can increase the quality of colonoscopies, potentially improving diagnosis and outcomes for colon cancer patients,” he added.
Dr. Weber is also the CEO of GI Alliance, a physician-led national health care platform of independent GI practices in six states in the United States.
Computer-aided detection
Unlike other computer-aided detection technologies, GI Genius does not characterize or “diagnose” a lesion, nor does it replace laboratory sampling as a means of confirming a cancer diagnosis.
The technology acts essentially as an extra set of expert “eyes” to detect suspicious lesions during colonoscopy, which should prove helpful, Dr. Johnson and Dr. Glissen Brown both commented.
“When a gastroenterologist looks at the video image, typically, our eyes are focused in the center of that image – that’s where our 20/20 vision is,” Dr. Johnson explained.
The computer has 20/20 vision over the whole image, including the periphery, “so the technology really gives an extremely expanded acuity of vision and highlights areas that we may need to investigate further,” he added.
Dr. Glissen Brown was involved in a trial of another AI device – the real-time automatic polyp detection system (Shanghai Wision AI). That study showed an increase in colonoscopic polyp and adenoma detection rates, but this was mainly because of a higher number of diminutive adenomas detected by the automatic detection system, Dr. Gliseen Brown said. There was no important difference in the number of larger adenomas detected with the device and the number detected without it.
However, there was a significant increase in the detection of hyperplastic polyps when the automatic detection system was used. “We definitely want to look at the false positive rate – both the false positive rate under the camera when we are doing colonoscopy and under the microscope when we do biopsies,” Dr. Glissen Brown acknowledged.
In numerous prospective studies of various computer-aided detection technologies such as the GI Genius system, the false positive rate resulting in the performance of biopsy of insignificant lesions is relatively low, he said.
“Ultimately, the decision to remove or biopsy a lesion is with the physician, because the GI Genius technology just points the provider to the area of concern, and then it’s up to them to look at it and decide whether it needs to be biopsied or not,” Dr. Glissen Brown said.
“So the technology serves more as a digital safety net and points the physician in the right direction, so it shouldn’t lead to much in the way of histologic false positives,” he noted.
The only potential disadvantage to using an AI system such as the GI Genius module is the time it might take for endoscopists to learn how to use it and how much the technology might increase the time required to perform the procedure, he added.
For about 18 months, Dr. Johnson has been running a clinical trial with a similar type of AI technology during colonoscopy. He has found that the learning curve for using these systems is “inordinately short.” Dr. Glissen Brown agreed and suggested that, if physicians are already performing colonoscopies regularly, they could probably learn to use an AI system such as GI Genius in about a week.
In his experience, Dr. Johnson has found that the delay caused by use of an AI system during colonoscopy is “minimal.”
If there is any delay at all, “we know that time in the colon on withdrawal increases the detection of polyps, so more time during withdrawal may be a good thing,” he added. It should be noted that endoscopy societies recommend a withdrawal time of at least 6 minutes, which is one of the metrics used to ensure the quality of a colonoscopy, Dr. Glissen Brown explained.
Indeed, the pivotal study upon which the FDA approved the GI Genius module required a minimum withdrawal time of 6 minutes. Participants said they did not find that using the GI Genius increased withdrawal time, he added.
“I think there is enough prospective evidence at this point to suggest that this technology may really be of benefit to clinicians with a lot of different skill levels, so I would be eager to know how clinicians interact with it in the clinical setting,” Dr. Glissen Brown commented.
Dr. Johnson agreed, noting that “even the good can get better.”
Dr. Johnson disclosed relationships with this news organization, CRH Medical, the American College of Gastroenterology Research Institute, and HyGIeaCare. Dr. Glissen Brown disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Article updated April 21, 2021.
The GI Genius module is the first and only commercially available computer-aided detection system that uses AI to identify colorectal polyps during routine colonoscopy.
The technology is compatible with most standard video endoscopy systems and has been “trained” to identify colonic lesions that are possibly cancerous, according to Medtronic, the distributor of the device.
“I think that anything we can do within a reasonable cost that enhances quality and patient outcomes during colonoscopy warrants very close consideration,” David Johnson, MD, professor of medicine and chief of gastroenterology, Eastern Virginia Medical School, Norfolk, said in an interview.
He was not involved with the development of the GI Genius system but has worked with a similar AI device that is used in conjunction with colonoscopy.
“The whole development of the technology for AI is done by inputting repetitive images into the computer, where it develops what is called the ‘neural network,’ ” he explained.
The computer then draws upon the “education” of this neural network to identify different types of colonic lesions, “and the more inputs that are put into the computer to enhance the neural network, the more capable the program becomes in the identification of variants and lesion size and characteristics,” Dr. Johnson added.
During routine colonoscopy, the GI Genius system generates visual markers – essentially, small green squares – and a low-volume sound whenever the software detects a region of interest.
These squares are superimposed on the video generated by the endoscope camera to alert the colonoscopist to regions that may require closer assessment, either visually, by tissue sampling, or by removal of the lesion itself.
“Colonoscopy is a durable screening and surveillance strategy, but it’s not perfect [because] it depends on a physician’s skill and their ability to pick up polyps in the colon,” Jeremy Glissen Brown, MD, of Beth Israel Deaconess Medical Center, Boston, said in an interview. He has also worked with an AI device.
Studies of adenoma detection during “all-comer” colonoscopies show that the rate of missed lesions ranges from a low of 6% to 40%, “so polyps are still missed during colonoscopy, and any technology that can solve parts of that problem is welcome,” Dr. Glissen Brown commented.
Clinical trial data that led to approval
The recent FDA approval of the GI Genius device was based on a prospective, randomized trial that was published in Gastroenterology in 2020. That trial involved 700 patients who were being screened or followed with colonoscopy every 3 years or longer. Participants underwent either white-light standard colonoscopy with the assistance of the GI Genius technology or standard white-light colonoscopy alone.
Results showed that the combination of standard colonoscopy and the GI Genius module identified laboratory-confirmed adenomas or carcinomas in 54.8% of patients, compared with 40.4% of patients who underwent colonoscopy alone.
In the Gastroenterology article, the authors wrote that the “14% absolute increase in adenoma detection rate obtained by computer-aided detection (CADe) in our study indicates that failure in polyp recognition is a clinically relevant cause of miss rate. Of note, the efficacy of CADe in reversing such miss rate also indicates that the same operator who missed the lesion in the first place was able to correctly diagnose it when the lesion was presented by the CADe. This underlines that the main cognitive challenge in polyp recognition is the discrimination between the candidate lesion and the surrounding healthy mucosa, whereas its correct characterization as neoplastic tissue that occurs after CADe detection is apparently a much easier task.”
The authors also noted that they did “not assess the actual number of false-positive activations by the system, as this would have altered the routine setting of our study,” but they refer to a study published in Gut in 2020 in which false-positive frames were seen in fewer than 1% of frames from the whole colonoscopy.
Because the new device improves on the ability of colonoscopy to detect lesions overall, it may reduce the risk of interval cancers between colonoscopies, Medtronic suggests.
Previous research has shown that every 1% increase in the adenoma detection rate results in a 3% decrease in the risk for colorectal cancer.
“More than 19 million screening colonoscopies are performed in the United State each year. ... Detection of adenomas during colonoscopy is an important quality metric,” James Weber, MD, a gastroenterologist affiliated with Texas Digestive Disease Consultants, Southlake, commented in a Medtronic press release.
“The addition of AI can increase the quality of colonoscopies, potentially improving diagnosis and outcomes for colon cancer patients,” he added.
Dr. Weber is also the CEO of GI Alliance, a physician-led national health care platform of independent GI practices in six states in the United States.
Computer-aided detection
Unlike other computer-aided detection technologies, GI Genius does not characterize or “diagnose” a lesion, nor does it replace laboratory sampling as a means of confirming a cancer diagnosis.
The technology acts essentially as an extra set of expert “eyes” to detect suspicious lesions during colonoscopy, which should prove helpful, Dr. Johnson and Dr. Glissen Brown both commented.
“When a gastroenterologist looks at the video image, typically, our eyes are focused in the center of that image – that’s where our 20/20 vision is,” Dr. Johnson explained.
The computer has 20/20 vision over the whole image, including the periphery, “so the technology really gives an extremely expanded acuity of vision and highlights areas that we may need to investigate further,” he added.
Dr. Glissen Brown was involved in a trial of another AI device – the real-time automatic polyp detection system (Shanghai Wision AI). That study showed an increase in colonoscopic polyp and adenoma detection rates, but this was mainly because of a higher number of diminutive adenomas detected by the automatic detection system, Dr. Gliseen Brown said. There was no important difference in the number of larger adenomas detected with the device and the number detected without it.
However, there was a significant increase in the detection of hyperplastic polyps when the automatic detection system was used. “We definitely want to look at the false positive rate – both the false positive rate under the camera when we are doing colonoscopy and under the microscope when we do biopsies,” Dr. Glissen Brown acknowledged.
In numerous prospective studies of various computer-aided detection technologies such as the GI Genius system, the false positive rate resulting in the performance of biopsy of insignificant lesions is relatively low, he said.
“Ultimately, the decision to remove or biopsy a lesion is with the physician, because the GI Genius technology just points the provider to the area of concern, and then it’s up to them to look at it and decide whether it needs to be biopsied or not,” Dr. Glissen Brown said.
“So the technology serves more as a digital safety net and points the physician in the right direction, so it shouldn’t lead to much in the way of histologic false positives,” he noted.
The only potential disadvantage to using an AI system such as the GI Genius module is the time it might take for endoscopists to learn how to use it and how much the technology might increase the time required to perform the procedure, he added.
For about 18 months, Dr. Johnson has been running a clinical trial with a similar type of AI technology during colonoscopy. He has found that the learning curve for using these systems is “inordinately short.” Dr. Glissen Brown agreed and suggested that, if physicians are already performing colonoscopies regularly, they could probably learn to use an AI system such as GI Genius in about a week.
In his experience, Dr. Johnson has found that the delay caused by use of an AI system during colonoscopy is “minimal.”
If there is any delay at all, “we know that time in the colon on withdrawal increases the detection of polyps, so more time during withdrawal may be a good thing,” he added. It should be noted that endoscopy societies recommend a withdrawal time of at least 6 minutes, which is one of the metrics used to ensure the quality of a colonoscopy, Dr. Glissen Brown explained.
Indeed, the pivotal study upon which the FDA approved the GI Genius module required a minimum withdrawal time of 6 minutes. Participants said they did not find that using the GI Genius increased withdrawal time, he added.
“I think there is enough prospective evidence at this point to suggest that this technology may really be of benefit to clinicians with a lot of different skill levels, so I would be eager to know how clinicians interact with it in the clinical setting,” Dr. Glissen Brown commented.
Dr. Johnson agreed, noting that “even the good can get better.”
Dr. Johnson disclosed relationships with this news organization, CRH Medical, the American College of Gastroenterology Research Institute, and HyGIeaCare. Dr. Glissen Brown disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Article updated April 21, 2021.
Stroke is ‘not a common complication’ in COVID-19
One study showed a stroke rate of 2.2% among patients with COVID-19 admitted to intensive care in 52 different countries. Another found a stroke rate of 1.48% in patients hospitalized with COVID-19 from 70 different countries. These researchers also found a reduction in stroke presentations and stroke care during the pandemic.
Both studies will be presented at the American Academy of Neurology’s 2021 annual meeting.
“Stroke has been a known serious complication of COVID-19, with some studies reporting a higher-than-expected occurrence, especially in young people,” said coauthor of the intensive care study, Jonathon Fanning, MBBS, PhD, University of Queensland, Brisbane, Australia.
“However, among the sickest of COVID patients – those admitted to an ICU – our research found that stroke was not a common complication and that ischemic stroke did not increase the risk of death,” he added.
Hemorrhagic stroke more common?
In this study, researchers analyzed a database of 2,699 patients who were admitted to the intensive care unit with COVID-19 in 52 countries and found that 59 of these patients (2.2%) subsequently sustained a stroke.
Most of the strokes identified in this cohort were hemorrhagic (46%), with 32% being ischemic and 22% unspecified. Hemorrhagic stroke was associated with a fivefold increased risk for death compared with patients who did not have a stroke. Of those with a hemorrhagic stroke, 72% died, but only 15% died of the stroke. Rather, multiorgan failure was the leading cause of death.
There was no association between ischemic stroke and mortality.
“There is scarce research on new-onset stroke complicating ICU admissions, and many of the limitations of assessing stroke in ICU populations confound the true values and result in variability in reported incidence anywhere from a 1%-4% incidence,” Dr. Fanning said.
He noted that a large Korean study had shown a 1.2% rate of stroke in patients without COVID admitted to non-neurologic ICUs. “In light of this, I think this 2% is higher than we would expect in a general ICU population, but in the context of earlier reports of COVID-19–associated risk for stroke, this figure is actually somewhat reassuring,” Dr. Fanning said.
Asked how this study compared with the large American Heart Association study recently reported that showed an overall rate of ischemic stroke of 0.75%, Dr. Fanning said the two studies reported on different populations, which makes them difficult to compare.
“Our study specifically reports on new-onset stroke complicating ICU admission,” he noted. “The AHA study is a large study of all patients admitted to hospital, but both studies identified less than previous estimates of COVID-related stroke.”
Largest sample to date
The other study, which includes 119,967 COVID-19 hospitalizations and represents the largest sample reporting the concomitant diagnoses of stroke and SARS-CoV-2 infection to date, was presented at the AAN meeting by Thanh N. Nguyen, MD, a professor at Boston University.
This study has also been published online in Neurology, with first author Raul G. Nogueira, MD, Emory University, Atlanta.
In this international observational, retrospective study across 6 continents, 70 countries, and 457 stroke centers, there was a 1.48% stroke rate across 119,967 COVID-19 hospitalizations. SARS-CoV-2 infection was noted in 3.3% (1,722) of all stroke admissions, which numbered 52,026.
The researchers identified stroke diagnoses by the International Classification of Diseases, 10th revision, codes and/or classifications in stroke center databases, and rates of stroke hospitalizations and numbers of patients receiving thrombolysis were compared between the first 4 months of the pandemic (March to June 2020) compared with two control 4-month periods.
Global decline in stroke care during pandemic
Results showed a global decline in the number of stroke patients admitted to the hospital as well as acute stroke treatments, such as thrombolysis, during the first wave of the COVID-19 pandemic. The researchers found that there were 91,373 stroke admissions in the 4 months immediately before the pandemic, compared with 80,894 admissions during the first 4 pandemic months, representing an 11.5% decline.
They also report that 13,334 stroke patients received intravenous thrombolysis in the 4 months preceding the pandemic, compared with 11,570 during the first 4 pandemic months, representing a 13.2% drop.
Interhospital transfers after thrombolysis for a higher level of stroke care decreased from 1,337 before the pandemic to 1,178 during the pandemic, a reduction of 11.9%.
There were greater declines in primary compared with comprehensive stroke centers for stroke hospitalizations (change, –17.3% vs. –10.3%) and for the number of patients receiving thrombolysis (change, –15.5% vs. –12.6%).
The volume of stroke hospitalizations increased by 9.5% in the two later pandemic months (May, June) versus the two earlier months (March, April), with greater recovery in hospitals with lower COVID-19 hospitalization volume, high-volume stroke centers, and comprehensive stroke centers.
Dr. Nguyen suggested that reasons for the reductions in these stroke numbers at the beginning of the pandemic could include a reduction in stroke risk due to a reduction of exposure to other viral infections or patients not presenting to the hospital for fear of contracting the coronavirus.
The higher recovery of stroke volume in high-volume stroke centers and comprehensive stroke centers may represent patients with higher needs – those having more severe strokes – seeking care more frequently than those with milder symptoms, she noted.
“Preserving access to stroke care and emergency stroke care amidst a pandemic is as important as educating patients on the importance of presenting to the hospital in the event of stroke-like symptoms,” Dr. Nguyen concluded.
“We continue to advocate that if a patient has stroke-like symptoms, such as loss of speech, strength, vision, or balance, it is important for the patient to seek medical care as an emergency, as there are treatments that can improve a patient’s ability to recover from disabling stroke in earlier rather than later time windows,” she added.
In the publication, the authors wrote, “Our results concur with other recent reports on the collateral effects of the COVID-19 pandemic on stroke systems of care,” but added that “this is among the first descriptions of the change at a global level, including primary and comprehensive stroke centers.”
They said that hospital access related to high COVID-19 burden was unlikely a factor because the decline was seen in centers with a few or no patients with COVID-19. They suggested that patient fear of contracting coronavirus may have played a role, along with a decrease in presentation of transient ischemic attacks, mild strokes, or moderate strokes, and physical distancing measures may have prevented the timely witnessing of a stroke.
A version of this article first appeared on Medscape.com.
One study showed a stroke rate of 2.2% among patients with COVID-19 admitted to intensive care in 52 different countries. Another found a stroke rate of 1.48% in patients hospitalized with COVID-19 from 70 different countries. These researchers also found a reduction in stroke presentations and stroke care during the pandemic.
Both studies will be presented at the American Academy of Neurology’s 2021 annual meeting.
“Stroke has been a known serious complication of COVID-19, with some studies reporting a higher-than-expected occurrence, especially in young people,” said coauthor of the intensive care study, Jonathon Fanning, MBBS, PhD, University of Queensland, Brisbane, Australia.
“However, among the sickest of COVID patients – those admitted to an ICU – our research found that stroke was not a common complication and that ischemic stroke did not increase the risk of death,” he added.
Hemorrhagic stroke more common?
In this study, researchers analyzed a database of 2,699 patients who were admitted to the intensive care unit with COVID-19 in 52 countries and found that 59 of these patients (2.2%) subsequently sustained a stroke.
Most of the strokes identified in this cohort were hemorrhagic (46%), with 32% being ischemic and 22% unspecified. Hemorrhagic stroke was associated with a fivefold increased risk for death compared with patients who did not have a stroke. Of those with a hemorrhagic stroke, 72% died, but only 15% died of the stroke. Rather, multiorgan failure was the leading cause of death.
There was no association between ischemic stroke and mortality.
“There is scarce research on new-onset stroke complicating ICU admissions, and many of the limitations of assessing stroke in ICU populations confound the true values and result in variability in reported incidence anywhere from a 1%-4% incidence,” Dr. Fanning said.
He noted that a large Korean study had shown a 1.2% rate of stroke in patients without COVID admitted to non-neurologic ICUs. “In light of this, I think this 2% is higher than we would expect in a general ICU population, but in the context of earlier reports of COVID-19–associated risk for stroke, this figure is actually somewhat reassuring,” Dr. Fanning said.
Asked how this study compared with the large American Heart Association study recently reported that showed an overall rate of ischemic stroke of 0.75%, Dr. Fanning said the two studies reported on different populations, which makes them difficult to compare.
“Our study specifically reports on new-onset stroke complicating ICU admission,” he noted. “The AHA study is a large study of all patients admitted to hospital, but both studies identified less than previous estimates of COVID-related stroke.”
Largest sample to date
The other study, which includes 119,967 COVID-19 hospitalizations and represents the largest sample reporting the concomitant diagnoses of stroke and SARS-CoV-2 infection to date, was presented at the AAN meeting by Thanh N. Nguyen, MD, a professor at Boston University.
This study has also been published online in Neurology, with first author Raul G. Nogueira, MD, Emory University, Atlanta.
In this international observational, retrospective study across 6 continents, 70 countries, and 457 stroke centers, there was a 1.48% stroke rate across 119,967 COVID-19 hospitalizations. SARS-CoV-2 infection was noted in 3.3% (1,722) of all stroke admissions, which numbered 52,026.
The researchers identified stroke diagnoses by the International Classification of Diseases, 10th revision, codes and/or classifications in stroke center databases, and rates of stroke hospitalizations and numbers of patients receiving thrombolysis were compared between the first 4 months of the pandemic (March to June 2020) compared with two control 4-month periods.
Global decline in stroke care during pandemic
Results showed a global decline in the number of stroke patients admitted to the hospital as well as acute stroke treatments, such as thrombolysis, during the first wave of the COVID-19 pandemic. The researchers found that there were 91,373 stroke admissions in the 4 months immediately before the pandemic, compared with 80,894 admissions during the first 4 pandemic months, representing an 11.5% decline.
They also report that 13,334 stroke patients received intravenous thrombolysis in the 4 months preceding the pandemic, compared with 11,570 during the first 4 pandemic months, representing a 13.2% drop.
Interhospital transfers after thrombolysis for a higher level of stroke care decreased from 1,337 before the pandemic to 1,178 during the pandemic, a reduction of 11.9%.
There were greater declines in primary compared with comprehensive stroke centers for stroke hospitalizations (change, –17.3% vs. –10.3%) and for the number of patients receiving thrombolysis (change, –15.5% vs. –12.6%).
The volume of stroke hospitalizations increased by 9.5% in the two later pandemic months (May, June) versus the two earlier months (March, April), with greater recovery in hospitals with lower COVID-19 hospitalization volume, high-volume stroke centers, and comprehensive stroke centers.
Dr. Nguyen suggested that reasons for the reductions in these stroke numbers at the beginning of the pandemic could include a reduction in stroke risk due to a reduction of exposure to other viral infections or patients not presenting to the hospital for fear of contracting the coronavirus.
The higher recovery of stroke volume in high-volume stroke centers and comprehensive stroke centers may represent patients with higher needs – those having more severe strokes – seeking care more frequently than those with milder symptoms, she noted.
“Preserving access to stroke care and emergency stroke care amidst a pandemic is as important as educating patients on the importance of presenting to the hospital in the event of stroke-like symptoms,” Dr. Nguyen concluded.
“We continue to advocate that if a patient has stroke-like symptoms, such as loss of speech, strength, vision, or balance, it is important for the patient to seek medical care as an emergency, as there are treatments that can improve a patient’s ability to recover from disabling stroke in earlier rather than later time windows,” she added.
In the publication, the authors wrote, “Our results concur with other recent reports on the collateral effects of the COVID-19 pandemic on stroke systems of care,” but added that “this is among the first descriptions of the change at a global level, including primary and comprehensive stroke centers.”
They said that hospital access related to high COVID-19 burden was unlikely a factor because the decline was seen in centers with a few or no patients with COVID-19. They suggested that patient fear of contracting coronavirus may have played a role, along with a decrease in presentation of transient ischemic attacks, mild strokes, or moderate strokes, and physical distancing measures may have prevented the timely witnessing of a stroke.
A version of this article first appeared on Medscape.com.
One study showed a stroke rate of 2.2% among patients with COVID-19 admitted to intensive care in 52 different countries. Another found a stroke rate of 1.48% in patients hospitalized with COVID-19 from 70 different countries. These researchers also found a reduction in stroke presentations and stroke care during the pandemic.
Both studies will be presented at the American Academy of Neurology’s 2021 annual meeting.
“Stroke has been a known serious complication of COVID-19, with some studies reporting a higher-than-expected occurrence, especially in young people,” said coauthor of the intensive care study, Jonathon Fanning, MBBS, PhD, University of Queensland, Brisbane, Australia.
“However, among the sickest of COVID patients – those admitted to an ICU – our research found that stroke was not a common complication and that ischemic stroke did not increase the risk of death,” he added.
Hemorrhagic stroke more common?
In this study, researchers analyzed a database of 2,699 patients who were admitted to the intensive care unit with COVID-19 in 52 countries and found that 59 of these patients (2.2%) subsequently sustained a stroke.
Most of the strokes identified in this cohort were hemorrhagic (46%), with 32% being ischemic and 22% unspecified. Hemorrhagic stroke was associated with a fivefold increased risk for death compared with patients who did not have a stroke. Of those with a hemorrhagic stroke, 72% died, but only 15% died of the stroke. Rather, multiorgan failure was the leading cause of death.
There was no association between ischemic stroke and mortality.
“There is scarce research on new-onset stroke complicating ICU admissions, and many of the limitations of assessing stroke in ICU populations confound the true values and result in variability in reported incidence anywhere from a 1%-4% incidence,” Dr. Fanning said.
He noted that a large Korean study had shown a 1.2% rate of stroke in patients without COVID admitted to non-neurologic ICUs. “In light of this, I think this 2% is higher than we would expect in a general ICU population, but in the context of earlier reports of COVID-19–associated risk for stroke, this figure is actually somewhat reassuring,” Dr. Fanning said.
Asked how this study compared with the large American Heart Association study recently reported that showed an overall rate of ischemic stroke of 0.75%, Dr. Fanning said the two studies reported on different populations, which makes them difficult to compare.
“Our study specifically reports on new-onset stroke complicating ICU admission,” he noted. “The AHA study is a large study of all patients admitted to hospital, but both studies identified less than previous estimates of COVID-related stroke.”
Largest sample to date
The other study, which includes 119,967 COVID-19 hospitalizations and represents the largest sample reporting the concomitant diagnoses of stroke and SARS-CoV-2 infection to date, was presented at the AAN meeting by Thanh N. Nguyen, MD, a professor at Boston University.
This study has also been published online in Neurology, with first author Raul G. Nogueira, MD, Emory University, Atlanta.
In this international observational, retrospective study across 6 continents, 70 countries, and 457 stroke centers, there was a 1.48% stroke rate across 119,967 COVID-19 hospitalizations. SARS-CoV-2 infection was noted in 3.3% (1,722) of all stroke admissions, which numbered 52,026.
The researchers identified stroke diagnoses by the International Classification of Diseases, 10th revision, codes and/or classifications in stroke center databases, and rates of stroke hospitalizations and numbers of patients receiving thrombolysis were compared between the first 4 months of the pandemic (March to June 2020) compared with two control 4-month periods.
Global decline in stroke care during pandemic
Results showed a global decline in the number of stroke patients admitted to the hospital as well as acute stroke treatments, such as thrombolysis, during the first wave of the COVID-19 pandemic. The researchers found that there were 91,373 stroke admissions in the 4 months immediately before the pandemic, compared with 80,894 admissions during the first 4 pandemic months, representing an 11.5% decline.
They also report that 13,334 stroke patients received intravenous thrombolysis in the 4 months preceding the pandemic, compared with 11,570 during the first 4 pandemic months, representing a 13.2% drop.
Interhospital transfers after thrombolysis for a higher level of stroke care decreased from 1,337 before the pandemic to 1,178 during the pandemic, a reduction of 11.9%.
There were greater declines in primary compared with comprehensive stroke centers for stroke hospitalizations (change, –17.3% vs. –10.3%) and for the number of patients receiving thrombolysis (change, –15.5% vs. –12.6%).
The volume of stroke hospitalizations increased by 9.5% in the two later pandemic months (May, June) versus the two earlier months (March, April), with greater recovery in hospitals with lower COVID-19 hospitalization volume, high-volume stroke centers, and comprehensive stroke centers.
Dr. Nguyen suggested that reasons for the reductions in these stroke numbers at the beginning of the pandemic could include a reduction in stroke risk due to a reduction of exposure to other viral infections or patients not presenting to the hospital for fear of contracting the coronavirus.
The higher recovery of stroke volume in high-volume stroke centers and comprehensive stroke centers may represent patients with higher needs – those having more severe strokes – seeking care more frequently than those with milder symptoms, she noted.
“Preserving access to stroke care and emergency stroke care amidst a pandemic is as important as educating patients on the importance of presenting to the hospital in the event of stroke-like symptoms,” Dr. Nguyen concluded.
“We continue to advocate that if a patient has stroke-like symptoms, such as loss of speech, strength, vision, or balance, it is important for the patient to seek medical care as an emergency, as there are treatments that can improve a patient’s ability to recover from disabling stroke in earlier rather than later time windows,” she added.
In the publication, the authors wrote, “Our results concur with other recent reports on the collateral effects of the COVID-19 pandemic on stroke systems of care,” but added that “this is among the first descriptions of the change at a global level, including primary and comprehensive stroke centers.”
They said that hospital access related to high COVID-19 burden was unlikely a factor because the decline was seen in centers with a few or no patients with COVID-19. They suggested that patient fear of contracting coronavirus may have played a role, along with a decrease in presentation of transient ischemic attacks, mild strokes, or moderate strokes, and physical distancing measures may have prevented the timely witnessing of a stroke.
A version of this article first appeared on Medscape.com.
From AAN 2021
Ten reasons airborne transmission of SARS-CoV-2 appears airtight
The scientific evidence for airborne transmission of the SARS-CoV-2 virus from different researchers all point in the same direction – that infectious aerosols are the principal means of person-to-person transmission, according to experts.
Not that it’s without controversy.
The science backing aerosol transmission “is clear-cut, but it is not accepted in many circles,” Trisha Greenhalgh, PhD, said in an interview.
“In particular, some in the evidence-based medicine movement and some infectious diseases clinicians are remarkably resistant to the evidence,” added Dr. Greenhalgh, professor of primary care health sciences at the University of Oxford (England).
“It’s very hard to see why, since the evidence all stacks up,” Dr. Greenhalgh said.
“The scientific evidence on spread from both near-field and far-field aerosols has been clear since early on in the pandemic, but there was resistance to acknowledging this in some circles, including the medical journals,” Joseph G. Allen, DSc, MPH, told this news organization when asked to comment.
“This is the week the dam broke. Three new commentaries came out … in top medical journals – BMJ, The Lancet, JAMA – all making the same point that aerosols are the dominant mode of transmission,” added Dr. Allen, associate professor of exposure assessment science at the Harvard T.H. Chan School of Public Health in Boston.
Dr. Greenhalgh and colleagues point to an increase in COVID-19 cases in the aftermath of so-called “super-spreader” events, spread of SARS-CoV-2 to people across different hotel rooms, and the relatively lower transmission detected after outdoor events.
Top 10 reasons
They outlined 10 scientific reasons backing airborne transmission in a commentary published online April 15 in The Lancet:
- The dominance of airborne transmission is supported by long-range transmission observed at super-spreader events.
- Long-range transmission has been reported among rooms at COVID-19 quarantine hotels, settings where infected people never spent time in the same room.
- Asymptomatic individuals account for an estimated 33%-59% of SARS-CoV-2 transmission, and could be spreading the virus through speaking, which produces thousands of aerosol particles and few large droplets.
- Transmission outdoors and in well-ventilated indoor spaces is lower than in enclosed spaces.
- Nosocomial infections are reported in health care settings where protective measures address large droplets but not aerosols.
- Viable SARS-CoV-2 has been detected in the air of hospital rooms and in the car of an infected person.
- Investigators found SARS-CoV-2 in hospital air filters and building ducts.
- It’s not just humans – infected animals can infect animals in other cages connected only through an air duct.
- No strong evidence refutes airborne transmission, and contact tracing supports secondary transmission in crowded, poorly ventilated indoor spaces.
- Only limited evidence supports other means of SARS-CoV-2 transmission, including through fomites or large droplets.
“We thought we’d summarize [the evidence] to clarify the arguments for and against. We looked hard for evidence against but found none,” Dr. Greenhalgh said.
“Although other routes can contribute, we believe that the airborne route is likely to be dominant,” the authors note.
The evidence on airborne transmission was there very early on but the Centers for Disease Control and Prevention, World Health Organization, and others repeated the message that the primary concern was droplets and fomites.
Response to a review
The top 10 list is also part rebuttal of a systematic review funded by the WHO and published last month that points to inconclusive evidence for airborne transmission. The researchers involved with that review state that “the lack of recoverable viral culture samples of SARS-CoV-2 prevents firm conclusions to be drawn about airborne transmission.”
However, Dr. Greenhalgh and colleagues note that “this conclusion, and the wide circulation of the review’s findings, is concerning because of the public health implications.”
The current authors also argue that enough evidence already exists on airborne transmission. “Policy should change. We don’t need more research on this topic; we need different policy,” Dr. Greenhalgh said. “We need ventilation front and center, air filtration when necessary, and better-fitting masks worn whenever indoors.”
Dr. Allen agreed that guidance hasn’t always kept pace with the science. “With all of the new evidence accumulated on airborne transmission since last winter, there is still widespread confusion in the public about modes of transmission,” he said. Dr. Allen also serves as commissioner of The Lancet COVID-19 Commission and is chair of the commission’s Task Force on Safe Work, Safe Schools, and Safe Travel.
“It was only just last week that CDC pulled back on guidance on ‘deep cleaning’ and in its place correctly said that the risk from touching surfaces is low,” he added. “The science has been clear on this for over a year, but official guidance was only recently updated.”
As a result, many companies and organizations continued to focus on “hygiene theatre,” Dr. Allen said, “wasting resources on overcleaning surfaces. Unbelievably, many schools still close for an entire day each week for deep cleaning and some still quarantine library books. The message that shared air is the problem, not shared surfaces, is a message that still needs to be reinforced.”
The National Institute for Health Research, Economic and Social Research Council, and Wellcome support Dr. Greenhalgh’s research. Dr. Greenhalgh and Dr. Allen had no relevant financial relationships to disclose.
A version of this article first appeared on Medscape.com.
The scientific evidence for airborne transmission of the SARS-CoV-2 virus from different researchers all point in the same direction – that infectious aerosols are the principal means of person-to-person transmission, according to experts.
Not that it’s without controversy.
The science backing aerosol transmission “is clear-cut, but it is not accepted in many circles,” Trisha Greenhalgh, PhD, said in an interview.
“In particular, some in the evidence-based medicine movement and some infectious diseases clinicians are remarkably resistant to the evidence,” added Dr. Greenhalgh, professor of primary care health sciences at the University of Oxford (England).
“It’s very hard to see why, since the evidence all stacks up,” Dr. Greenhalgh said.
“The scientific evidence on spread from both near-field and far-field aerosols has been clear since early on in the pandemic, but there was resistance to acknowledging this in some circles, including the medical journals,” Joseph G. Allen, DSc, MPH, told this news organization when asked to comment.
“This is the week the dam broke. Three new commentaries came out … in top medical journals – BMJ, The Lancet, JAMA – all making the same point that aerosols are the dominant mode of transmission,” added Dr. Allen, associate professor of exposure assessment science at the Harvard T.H. Chan School of Public Health in Boston.
Dr. Greenhalgh and colleagues point to an increase in COVID-19 cases in the aftermath of so-called “super-spreader” events, spread of SARS-CoV-2 to people across different hotel rooms, and the relatively lower transmission detected after outdoor events.
Top 10 reasons
They outlined 10 scientific reasons backing airborne transmission in a commentary published online April 15 in The Lancet:
- The dominance of airborne transmission is supported by long-range transmission observed at super-spreader events.
- Long-range transmission has been reported among rooms at COVID-19 quarantine hotels, settings where infected people never spent time in the same room.
- Asymptomatic individuals account for an estimated 33%-59% of SARS-CoV-2 transmission, and could be spreading the virus through speaking, which produces thousands of aerosol particles and few large droplets.
- Transmission outdoors and in well-ventilated indoor spaces is lower than in enclosed spaces.
- Nosocomial infections are reported in health care settings where protective measures address large droplets but not aerosols.
- Viable SARS-CoV-2 has been detected in the air of hospital rooms and in the car of an infected person.
- Investigators found SARS-CoV-2 in hospital air filters and building ducts.
- It’s not just humans – infected animals can infect animals in other cages connected only through an air duct.
- No strong evidence refutes airborne transmission, and contact tracing supports secondary transmission in crowded, poorly ventilated indoor spaces.
- Only limited evidence supports other means of SARS-CoV-2 transmission, including through fomites or large droplets.
“We thought we’d summarize [the evidence] to clarify the arguments for and against. We looked hard for evidence against but found none,” Dr. Greenhalgh said.
“Although other routes can contribute, we believe that the airborne route is likely to be dominant,” the authors note.
The evidence on airborne transmission was there very early on but the Centers for Disease Control and Prevention, World Health Organization, and others repeated the message that the primary concern was droplets and fomites.
Response to a review
The top 10 list is also part rebuttal of a systematic review funded by the WHO and published last month that points to inconclusive evidence for airborne transmission. The researchers involved with that review state that “the lack of recoverable viral culture samples of SARS-CoV-2 prevents firm conclusions to be drawn about airborne transmission.”
However, Dr. Greenhalgh and colleagues note that “this conclusion, and the wide circulation of the review’s findings, is concerning because of the public health implications.”
The current authors also argue that enough evidence already exists on airborne transmission. “Policy should change. We don’t need more research on this topic; we need different policy,” Dr. Greenhalgh said. “We need ventilation front and center, air filtration when necessary, and better-fitting masks worn whenever indoors.”
Dr. Allen agreed that guidance hasn’t always kept pace with the science. “With all of the new evidence accumulated on airborne transmission since last winter, there is still widespread confusion in the public about modes of transmission,” he said. Dr. Allen also serves as commissioner of The Lancet COVID-19 Commission and is chair of the commission’s Task Force on Safe Work, Safe Schools, and Safe Travel.
“It was only just last week that CDC pulled back on guidance on ‘deep cleaning’ and in its place correctly said that the risk from touching surfaces is low,” he added. “The science has been clear on this for over a year, but official guidance was only recently updated.”
As a result, many companies and organizations continued to focus on “hygiene theatre,” Dr. Allen said, “wasting resources on overcleaning surfaces. Unbelievably, many schools still close for an entire day each week for deep cleaning and some still quarantine library books. The message that shared air is the problem, not shared surfaces, is a message that still needs to be reinforced.”
The National Institute for Health Research, Economic and Social Research Council, and Wellcome support Dr. Greenhalgh’s research. Dr. Greenhalgh and Dr. Allen had no relevant financial relationships to disclose.
A version of this article first appeared on Medscape.com.
The scientific evidence for airborne transmission of the SARS-CoV-2 virus from different researchers all point in the same direction – that infectious aerosols are the principal means of person-to-person transmission, according to experts.
Not that it’s without controversy.
The science backing aerosol transmission “is clear-cut, but it is not accepted in many circles,” Trisha Greenhalgh, PhD, said in an interview.
“In particular, some in the evidence-based medicine movement and some infectious diseases clinicians are remarkably resistant to the evidence,” added Dr. Greenhalgh, professor of primary care health sciences at the University of Oxford (England).
“It’s very hard to see why, since the evidence all stacks up,” Dr. Greenhalgh said.
“The scientific evidence on spread from both near-field and far-field aerosols has been clear since early on in the pandemic, but there was resistance to acknowledging this in some circles, including the medical journals,” Joseph G. Allen, DSc, MPH, told this news organization when asked to comment.
“This is the week the dam broke. Three new commentaries came out … in top medical journals – BMJ, The Lancet, JAMA – all making the same point that aerosols are the dominant mode of transmission,” added Dr. Allen, associate professor of exposure assessment science at the Harvard T.H. Chan School of Public Health in Boston.
Dr. Greenhalgh and colleagues point to an increase in COVID-19 cases in the aftermath of so-called “super-spreader” events, spread of SARS-CoV-2 to people across different hotel rooms, and the relatively lower transmission detected after outdoor events.
Top 10 reasons
They outlined 10 scientific reasons backing airborne transmission in a commentary published online April 15 in The Lancet:
- The dominance of airborne transmission is supported by long-range transmission observed at super-spreader events.
- Long-range transmission has been reported among rooms at COVID-19 quarantine hotels, settings where infected people never spent time in the same room.
- Asymptomatic individuals account for an estimated 33%-59% of SARS-CoV-2 transmission, and could be spreading the virus through speaking, which produces thousands of aerosol particles and few large droplets.
- Transmission outdoors and in well-ventilated indoor spaces is lower than in enclosed spaces.
- Nosocomial infections are reported in health care settings where protective measures address large droplets but not aerosols.
- Viable SARS-CoV-2 has been detected in the air of hospital rooms and in the car of an infected person.
- Investigators found SARS-CoV-2 in hospital air filters and building ducts.
- It’s not just humans – infected animals can infect animals in other cages connected only through an air duct.
- No strong evidence refutes airborne transmission, and contact tracing supports secondary transmission in crowded, poorly ventilated indoor spaces.
- Only limited evidence supports other means of SARS-CoV-2 transmission, including through fomites or large droplets.
“We thought we’d summarize [the evidence] to clarify the arguments for and against. We looked hard for evidence against but found none,” Dr. Greenhalgh said.
“Although other routes can contribute, we believe that the airborne route is likely to be dominant,” the authors note.
The evidence on airborne transmission was there very early on but the Centers for Disease Control and Prevention, World Health Organization, and others repeated the message that the primary concern was droplets and fomites.
Response to a review
The top 10 list is also part rebuttal of a systematic review funded by the WHO and published last month that points to inconclusive evidence for airborne transmission. The researchers involved with that review state that “the lack of recoverable viral culture samples of SARS-CoV-2 prevents firm conclusions to be drawn about airborne transmission.”
However, Dr. Greenhalgh and colleagues note that “this conclusion, and the wide circulation of the review’s findings, is concerning because of the public health implications.”
The current authors also argue that enough evidence already exists on airborne transmission. “Policy should change. We don’t need more research on this topic; we need different policy,” Dr. Greenhalgh said. “We need ventilation front and center, air filtration when necessary, and better-fitting masks worn whenever indoors.”
Dr. Allen agreed that guidance hasn’t always kept pace with the science. “With all of the new evidence accumulated on airborne transmission since last winter, there is still widespread confusion in the public about modes of transmission,” he said. Dr. Allen also serves as commissioner of The Lancet COVID-19 Commission and is chair of the commission’s Task Force on Safe Work, Safe Schools, and Safe Travel.
“It was only just last week that CDC pulled back on guidance on ‘deep cleaning’ and in its place correctly said that the risk from touching surfaces is low,” he added. “The science has been clear on this for over a year, but official guidance was only recently updated.”
As a result, many companies and organizations continued to focus on “hygiene theatre,” Dr. Allen said, “wasting resources on overcleaning surfaces. Unbelievably, many schools still close for an entire day each week for deep cleaning and some still quarantine library books. The message that shared air is the problem, not shared surfaces, is a message that still needs to be reinforced.”
The National Institute for Health Research, Economic and Social Research Council, and Wellcome support Dr. Greenhalgh’s research. Dr. Greenhalgh and Dr. Allen had no relevant financial relationships to disclose.
A version of this article first appeared on Medscape.com.
Correlating hospitalist work schedules with patient outcomes
Background: Studies show better outcomes, decreased length of stay, increased patient satisfaction, improved quality, and decreased readmission rates when hospitalist services are used. This study looks at how hospitalist schedules affect these outcomes.
Study design: Retrospective cohort study.
Setting: 229 hospitals in Texas.
Synopsis: This cohort study used 3 years of Medicare data from 229 hospitals in Texas. It included 114,777 medical admissions of patients with a 3- to 6-day length of stay. The study used the percentage of hospitalist working days that were blocks of 7 days or longer. ICU stays and patients requiring two or more E&M codes were excluded since they are associated with greater illness severity.
The primary outcome was mortality within 30 days of discharge and secondary outcomes were 30-day readmission rates, discharge destination, and 30-day postdischarge costs.
Patients receiving care from hospitalists working several days in a row had better outcomes. It is postulated that continuity of care by one hospitalist is important for several reasons. Most importantly, the development of rapport with patient and family is key to deciding the plan of care and destination post discharge as it is quite challenging to effectively transfer all important information during verbal or written handoffs.
Bottom line: Care provided by hospitalists working more days in a row improved patient outcomes. A variety of hospitalist schedules are being practiced currently; however, these findings must be taken into account as schedules are designed.
Citation: Goodwin JS et al. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020;180(2):215-22. doi: 10.1001/jamainternmed.2019.5193.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Background: Studies show better outcomes, decreased length of stay, increased patient satisfaction, improved quality, and decreased readmission rates when hospitalist services are used. This study looks at how hospitalist schedules affect these outcomes.
Study design: Retrospective cohort study.
Setting: 229 hospitals in Texas.
Synopsis: This cohort study used 3 years of Medicare data from 229 hospitals in Texas. It included 114,777 medical admissions of patients with a 3- to 6-day length of stay. The study used the percentage of hospitalist working days that were blocks of 7 days or longer. ICU stays and patients requiring two or more E&M codes were excluded since they are associated with greater illness severity.
The primary outcome was mortality within 30 days of discharge and secondary outcomes were 30-day readmission rates, discharge destination, and 30-day postdischarge costs.
Patients receiving care from hospitalists working several days in a row had better outcomes. It is postulated that continuity of care by one hospitalist is important for several reasons. Most importantly, the development of rapport with patient and family is key to deciding the plan of care and destination post discharge as it is quite challenging to effectively transfer all important information during verbal or written handoffs.
Bottom line: Care provided by hospitalists working more days in a row improved patient outcomes. A variety of hospitalist schedules are being practiced currently; however, these findings must be taken into account as schedules are designed.
Citation: Goodwin JS et al. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020;180(2):215-22. doi: 10.1001/jamainternmed.2019.5193.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Background: Studies show better outcomes, decreased length of stay, increased patient satisfaction, improved quality, and decreased readmission rates when hospitalist services are used. This study looks at how hospitalist schedules affect these outcomes.
Study design: Retrospective cohort study.
Setting: 229 hospitals in Texas.
Synopsis: This cohort study used 3 years of Medicare data from 229 hospitals in Texas. It included 114,777 medical admissions of patients with a 3- to 6-day length of stay. The study used the percentage of hospitalist working days that were blocks of 7 days or longer. ICU stays and patients requiring two or more E&M codes were excluded since they are associated with greater illness severity.
The primary outcome was mortality within 30 days of discharge and secondary outcomes were 30-day readmission rates, discharge destination, and 30-day postdischarge costs.
Patients receiving care from hospitalists working several days in a row had better outcomes. It is postulated that continuity of care by one hospitalist is important for several reasons. Most importantly, the development of rapport with patient and family is key to deciding the plan of care and destination post discharge as it is quite challenging to effectively transfer all important information during verbal or written handoffs.
Bottom line: Care provided by hospitalists working more days in a row improved patient outcomes. A variety of hospitalist schedules are being practiced currently; however, these findings must be taken into account as schedules are designed.
Citation: Goodwin JS et al. Association of the work schedules of hospitalists with patient outcomes of hospitalization. JAMA Intern Med. 2020;180(2):215-22. doi: 10.1001/jamainternmed.2019.5193.
Dr. Ahmed is assistant professor in the division of hospital medicine, Loyola University Medical Center, Maywood, Ill.
Children’s share of COVID-19 burden has never been higher
For the first time since the pandemic began, children’s share of weekly COVID-19 cases topped 20% in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
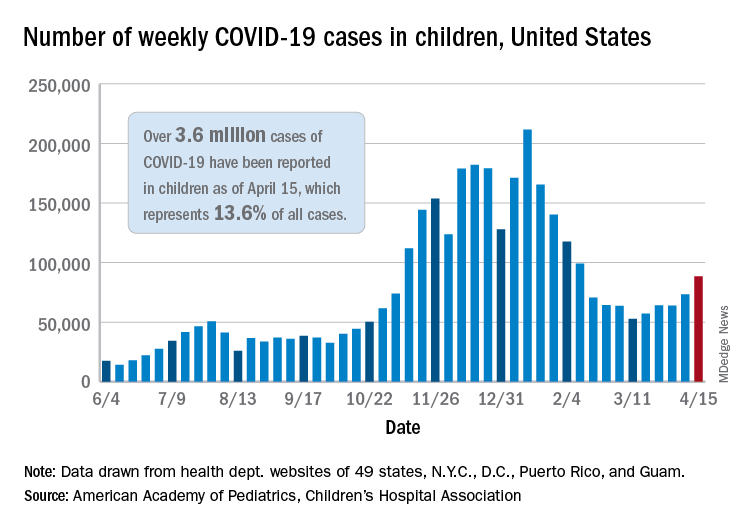
That represented 20.6% of all new cases for the week, eclipsing the previous high of 19.1% recorded just 3 weeks ago, based on data collected by the AAP and CHA from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Cumulative cases of COVID-19 in children exceed 3.6 million in those jurisdictions, which is 13.6% of the total reported among all ages, and the overall rate of coronavirus infection is 4,824 cases per 100,000 children in the population, the AAP and CHA said in their weekly COVID-19 report.
Among the 53 reporting jurisdictions, North Dakota has the highest cumulative rate, 9,167 per 100,000 children, followed by Tennessee (8,580), South Carolina (7,948), South Dakota (7,938), and Connecticut (7,707). Children’s share of cumulative cases is highest in Vermont, at 21.9%, with Alaska next at 20.0% and Wyoming at 19.2%, the AAP and CHA said.
Since the beginning of April, the largest local increases in cases reported came in Michigan (21.6%), Vermont (15.9%), and Maine (15.6%). Nationally, the increase over those same 2 weeks is just under 5%, the two organizations noted.
There were 5 deaths among children during the week of April 9-15, bringing the total to 297, but the recent increases in cases have not affected the long-term trends for serious illness. The death rate for children with COVID-19 has been 0.01% since early November – 43 states, New York City, Puerto Rico, and Guam are reporting such data – and the hospitalization rate has been 0.8% since mid-January in 24 states and New York City, the AAP/CHA data show.
For the first time since the pandemic began, children’s share of weekly COVID-19 cases topped 20% in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
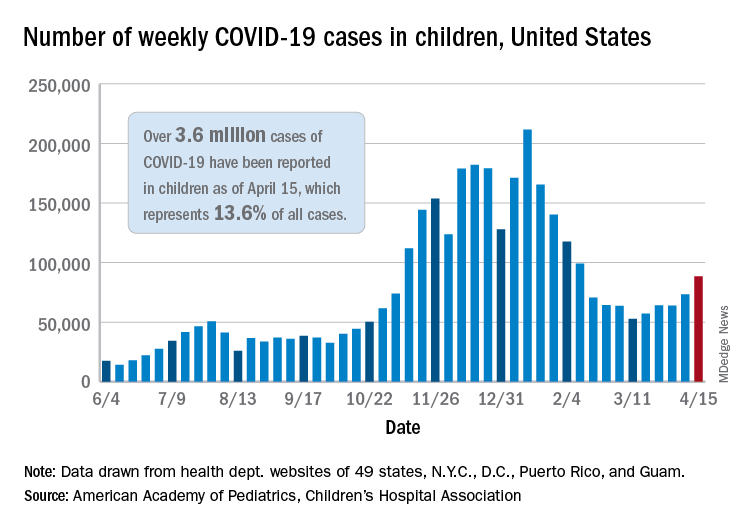
That represented 20.6% of all new cases for the week, eclipsing the previous high of 19.1% recorded just 3 weeks ago, based on data collected by the AAP and CHA from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Cumulative cases of COVID-19 in children exceed 3.6 million in those jurisdictions, which is 13.6% of the total reported among all ages, and the overall rate of coronavirus infection is 4,824 cases per 100,000 children in the population, the AAP and CHA said in their weekly COVID-19 report.
Among the 53 reporting jurisdictions, North Dakota has the highest cumulative rate, 9,167 per 100,000 children, followed by Tennessee (8,580), South Carolina (7,948), South Dakota (7,938), and Connecticut (7,707). Children’s share of cumulative cases is highest in Vermont, at 21.9%, with Alaska next at 20.0% and Wyoming at 19.2%, the AAP and CHA said.
Since the beginning of April, the largest local increases in cases reported came in Michigan (21.6%), Vermont (15.9%), and Maine (15.6%). Nationally, the increase over those same 2 weeks is just under 5%, the two organizations noted.
There were 5 deaths among children during the week of April 9-15, bringing the total to 297, but the recent increases in cases have not affected the long-term trends for serious illness. The death rate for children with COVID-19 has been 0.01% since early November – 43 states, New York City, Puerto Rico, and Guam are reporting such data – and the hospitalization rate has been 0.8% since mid-January in 24 states and New York City, the AAP/CHA data show.
For the first time since the pandemic began, children’s share of weekly COVID-19 cases topped 20% in the United States, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
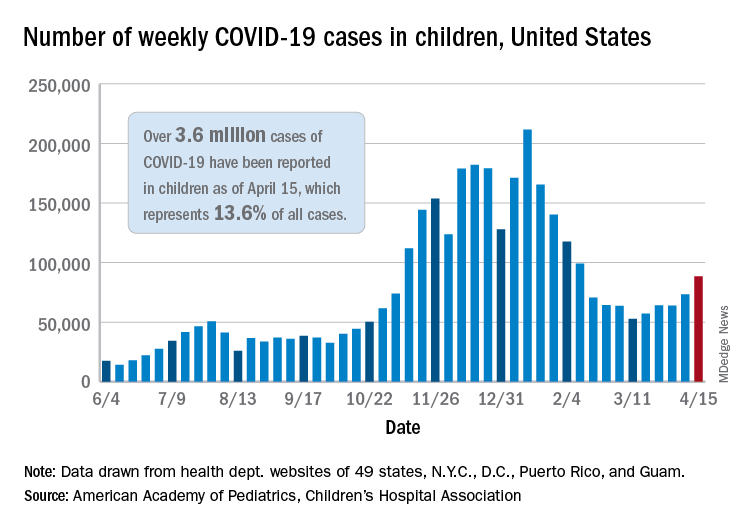
That represented 20.6% of all new cases for the week, eclipsing the previous high of 19.1% recorded just 3 weeks ago, based on data collected by the AAP and CHA from 49 states, the District of Columbia, New York City, Puerto Rico, and Guam.
Cumulative cases of COVID-19 in children exceed 3.6 million in those jurisdictions, which is 13.6% of the total reported among all ages, and the overall rate of coronavirus infection is 4,824 cases per 100,000 children in the population, the AAP and CHA said in their weekly COVID-19 report.
Among the 53 reporting jurisdictions, North Dakota has the highest cumulative rate, 9,167 per 100,000 children, followed by Tennessee (8,580), South Carolina (7,948), South Dakota (7,938), and Connecticut (7,707). Children’s share of cumulative cases is highest in Vermont, at 21.9%, with Alaska next at 20.0% and Wyoming at 19.2%, the AAP and CHA said.
Since the beginning of April, the largest local increases in cases reported came in Michigan (21.6%), Vermont (15.9%), and Maine (15.6%). Nationally, the increase over those same 2 weeks is just under 5%, the two organizations noted.
There were 5 deaths among children during the week of April 9-15, bringing the total to 297, but the recent increases in cases have not affected the long-term trends for serious illness. The death rate for children with COVID-19 has been 0.01% since early November – 43 states, New York City, Puerto Rico, and Guam are reporting such data – and the hospitalization rate has been 0.8% since mid-January in 24 states and New York City, the AAP/CHA data show.
VEXAS syndrome: Implications for dermatologists
When I was a medical student, I always found it gratifying when there was a unifying mechanism that explained the symptoms of a disease. Part of the reason I chose dermatology as a specialty was how frequently we are able to “see” these mechanisms in the skin, both clinically and histologically. What’s even more interesting is that this condition is caused by a postzygotic somatic mutation, an apparently underrecognized cause of disease that we are just now beginning to understand. An example of a postzygotic somatic mutation causing a disease that we all learned about in medical school is paroxysmal nocturnal hemoglobinuria.
Using a “bottom-up” approach, researchers at the National Institutes of Health and in the United Kingdom identified 25 patients with somatic UBA1 mutations and noticed that they had strikingly similar autoinflammatory syndromes. UBA1 encodes ubiquitin E1, which is part of the pathway the breaks down proteins as part of the normal cellular machine. It is localized to the X chromosome, so all 25 affected patients were males, and most were aged between 40 and 70 years. These patients had an autoinflammatory syndrome characterized by fever, chondritis (similar to relapsing polychondritis), vasculitis, and neutrophilic dermatoses. Many patients also had features of myelodysplastic syndrome and plasma cell dyscrasia. The inflammatory pattern in this condition seems to show elevations in tumor necrosis factor, interleukin-6, and interferon-gamma.
So why is this syndrome relevant to dermatology? We are often asked to evaluate patients for neutrophilic dermatosis and vasculitis, and many affected patients had clinical and histologic findings compatible with polyarteritis nodosa and Sweet syndrome. When confronted with a neutrophilic dermatosis, we’ve all been taught to evaluate for myelodysplastic syndrome, which many of these patients appeared to have, at least on the surface. When bone marrow biopsies were done, the myeloid cell precursors that give rise to neutrophils were noted to have prominent cytoplasmic vacuoles, hence the “V” in VEXAS.
In reading the article describing 25 patients with this syndrome, which was published in the New England Journal of Medicine, I was struck by how refractory they were to treatment. Most patients had been treated with systemic steroids, multiple biologics, and several nonbiologic medications that are mainstays of treatment for neutrophilic dermatosis like dapsone and colchicine. I was fortunate enough to speak to Amanda Ombrello, MD, of the National Human Genome Research Institute, one of the lead authors of the paper, who drew my attention to the supplementary appendix, which showed the marked injection-site reactions some patients had to anakinra – yet another reason why a patient might end up in a dermatology clinic. In my mind, all of these features could be a clue to a diagnosis of VEXAS syndrome.
Many patients seemed to fare poorly, with 40% of patients dying before the completion of the study. When it comes to extremely rare diseases, it seems that the more physicians who are aware of the existence of a particular syndrome, the more likely it is a patient will come under our care and be correctly diagnosed.
Dr. Saardi is a dermatologist and internist, and is director of the inpatient dermatology service at the George Washington University Hospital, Washington. He has no disclosures.
When I was a medical student, I always found it gratifying when there was a unifying mechanism that explained the symptoms of a disease. Part of the reason I chose dermatology as a specialty was how frequently we are able to “see” these mechanisms in the skin, both clinically and histologically. What’s even more interesting is that this condition is caused by a postzygotic somatic mutation, an apparently underrecognized cause of disease that we are just now beginning to understand. An example of a postzygotic somatic mutation causing a disease that we all learned about in medical school is paroxysmal nocturnal hemoglobinuria.
Using a “bottom-up” approach, researchers at the National Institutes of Health and in the United Kingdom identified 25 patients with somatic UBA1 mutations and noticed that they had strikingly similar autoinflammatory syndromes. UBA1 encodes ubiquitin E1, which is part of the pathway the breaks down proteins as part of the normal cellular machine. It is localized to the X chromosome, so all 25 affected patients were males, and most were aged between 40 and 70 years. These patients had an autoinflammatory syndrome characterized by fever, chondritis (similar to relapsing polychondritis), vasculitis, and neutrophilic dermatoses. Many patients also had features of myelodysplastic syndrome and plasma cell dyscrasia. The inflammatory pattern in this condition seems to show elevations in tumor necrosis factor, interleukin-6, and interferon-gamma.
So why is this syndrome relevant to dermatology? We are often asked to evaluate patients for neutrophilic dermatosis and vasculitis, and many affected patients had clinical and histologic findings compatible with polyarteritis nodosa and Sweet syndrome. When confronted with a neutrophilic dermatosis, we’ve all been taught to evaluate for myelodysplastic syndrome, which many of these patients appeared to have, at least on the surface. When bone marrow biopsies were done, the myeloid cell precursors that give rise to neutrophils were noted to have prominent cytoplasmic vacuoles, hence the “V” in VEXAS.
In reading the article describing 25 patients with this syndrome, which was published in the New England Journal of Medicine, I was struck by how refractory they were to treatment. Most patients had been treated with systemic steroids, multiple biologics, and several nonbiologic medications that are mainstays of treatment for neutrophilic dermatosis like dapsone and colchicine. I was fortunate enough to speak to Amanda Ombrello, MD, of the National Human Genome Research Institute, one of the lead authors of the paper, who drew my attention to the supplementary appendix, which showed the marked injection-site reactions some patients had to anakinra – yet another reason why a patient might end up in a dermatology clinic. In my mind, all of these features could be a clue to a diagnosis of VEXAS syndrome.
Many patients seemed to fare poorly, with 40% of patients dying before the completion of the study. When it comes to extremely rare diseases, it seems that the more physicians who are aware of the existence of a particular syndrome, the more likely it is a patient will come under our care and be correctly diagnosed.
Dr. Saardi is a dermatologist and internist, and is director of the inpatient dermatology service at the George Washington University Hospital, Washington. He has no disclosures.
When I was a medical student, I always found it gratifying when there was a unifying mechanism that explained the symptoms of a disease. Part of the reason I chose dermatology as a specialty was how frequently we are able to “see” these mechanisms in the skin, both clinically and histologically. What’s even more interesting is that this condition is caused by a postzygotic somatic mutation, an apparently underrecognized cause of disease that we are just now beginning to understand. An example of a postzygotic somatic mutation causing a disease that we all learned about in medical school is paroxysmal nocturnal hemoglobinuria.
Using a “bottom-up” approach, researchers at the National Institutes of Health and in the United Kingdom identified 25 patients with somatic UBA1 mutations and noticed that they had strikingly similar autoinflammatory syndromes. UBA1 encodes ubiquitin E1, which is part of the pathway the breaks down proteins as part of the normal cellular machine. It is localized to the X chromosome, so all 25 affected patients were males, and most were aged between 40 and 70 years. These patients had an autoinflammatory syndrome characterized by fever, chondritis (similar to relapsing polychondritis), vasculitis, and neutrophilic dermatoses. Many patients also had features of myelodysplastic syndrome and plasma cell dyscrasia. The inflammatory pattern in this condition seems to show elevations in tumor necrosis factor, interleukin-6, and interferon-gamma.
So why is this syndrome relevant to dermatology? We are often asked to evaluate patients for neutrophilic dermatosis and vasculitis, and many affected patients had clinical and histologic findings compatible with polyarteritis nodosa and Sweet syndrome. When confronted with a neutrophilic dermatosis, we’ve all been taught to evaluate for myelodysplastic syndrome, which many of these patients appeared to have, at least on the surface. When bone marrow biopsies were done, the myeloid cell precursors that give rise to neutrophils were noted to have prominent cytoplasmic vacuoles, hence the “V” in VEXAS.
In reading the article describing 25 patients with this syndrome, which was published in the New England Journal of Medicine, I was struck by how refractory they were to treatment. Most patients had been treated with systemic steroids, multiple biologics, and several nonbiologic medications that are mainstays of treatment for neutrophilic dermatosis like dapsone and colchicine. I was fortunate enough to speak to Amanda Ombrello, MD, of the National Human Genome Research Institute, one of the lead authors of the paper, who drew my attention to the supplementary appendix, which showed the marked injection-site reactions some patients had to anakinra – yet another reason why a patient might end up in a dermatology clinic. In my mind, all of these features could be a clue to a diagnosis of VEXAS syndrome.
Many patients seemed to fare poorly, with 40% of patients dying before the completion of the study. When it comes to extremely rare diseases, it seems that the more physicians who are aware of the existence of a particular syndrome, the more likely it is a patient will come under our care and be correctly diagnosed.
Dr. Saardi is a dermatologist and internist, and is director of the inpatient dermatology service at the George Washington University Hospital, Washington. He has no disclosures.
Study shows potential of remote Parkinson’s disease genotyping
according to a pilot study sponsored by the Parkinson’s Foundation.
“Overall we found high levels of participant satisfaction with Parkinson’s testing and genetic counseling and no significant difference in outcomes concerning satisfaction, knowledge, and impact of genetic testing between disclosure of results and genetic counseling in-person by either a neurologist or a genetic counselor or via telephone by a remove genetic counselor at a centralized center,” said Jennifer L. Verbrugge, MS, a genetic counselor at Indiana University, Indianapolis, in reporting results of the PD GENEration pilot study, presented at the 2021 annual meeting of the American Academy of Neurology.
COVID complication
The study launched in the summer of 2019 with the goal of enrolling 600 participants. However, because of the COVID-19 pandemic, enrollment was truncated. The pilot study eventually enrolled 289 patients, 205 of whom returned their postgenetic counseling surveys, Ms. Verbrugge said. The pilot study goal was to evaluate the feasibility and impact of in-person versus remote genetic testing and counseling for people with Parkinson’s disease.
“The study hopes to reach its ultimate goal, which is to deliver Parkinson’s disease–related genetic testing and counseling to upward of 15,000 people with Parkinson’s,” Ms. Verbrugge said. The program is also planning to expand to include Spanish speakers.
In the pilot study, genetic results were positive in 17% of patients, with 15% (n = 42) having positive heterozygous variants and 8% having variants of uncertain significance. “We did not see significant differences in these outcomes when we compared the mode and genetic counselors involved,” Ms. Verbrugge said.
The study did find that in-person testing and counseling “was associated with increased participant feelings that they were partners in care,” Ms. Verbrugge added. “This is something we are going to continue to evaluate as time goes on.”
However, as the COVID-19 pandemic pushed clinicians to develop virtual platforms, it resulted in a function through which participants can complete all genetic study activities remotely, she said. The study organizers anticipate that as pandemic restrictions ease, they will be able to reach their original goal of 600 participants along with those recruited in an expansion phase.
“As restrictions related to the pandemic ease, we anticipate that more Parkinson’s disease gene-targeted clinical trials will emerge, with aims to recruit people who carry certain gene variants,” Ms. Verbrugge said in an interview. “Many people with Parkinson’s disease may therefore benefit from genetic testing and learning if they carry a Parkinson’s disease related gene variant from participation in the PD GENEration study.”
Increasing patient access
To scale up to the 15,000-population goal for the program, PD GENEration has launched a new protocol designed to increase patient access at new study sites, Ms. Verbrugge said. “This protocol includes an abbreviate version of the clinical data collected, while it maintains the critical component of genetic counseling in the testing process.”
Going forward, the PD GENEration study will focus on improving access to genetic testing and counseling in underrepresented and rural populations, Ms. Verbrugge said. “These efforts will also generate valuable genomic data, allowing researchers to learn more about the causes of Parkinson’s disease in diverse and underrepresented populations. The study will be expanding research efforts concerning the genomic data to gain insights about the seven key genes studied as well as new genes linked to Parkinson’s disease.”
The work of the PD GENEration study is timely, said David K. Simon, MD, PhD, of Harvard Medical School and director of the Parkinson’s Disease & Movement Disorders Center at Beth Israel Deaconess Medical Center, both in Boston. “This is very important to identify such patients now, as clinical trials targeting people with specific genetic mutations or variants are coming soon, and in some cases already are underway. The feasibility and speed of enrollment for those trials will be greatly facilitate if we know in advance who are the people with Parkinson’s disease who have mutations that would make them eligible for the particular trials.”
The fact that the study provides free genetic testing to people with Parkinson’s disease isn’t to be overlooked. “This was an important study to address the question of whether or not remote genetic counseling was feasible and effective, and the results are meaningful given the randomized prospective design,” Dr. Simon said.
Ms. Verbrugge has no relevant relationships to disclose. Dr. Simon reports receiving research funding from the Parkinson’s Foundation.
according to a pilot study sponsored by the Parkinson’s Foundation.
“Overall we found high levels of participant satisfaction with Parkinson’s testing and genetic counseling and no significant difference in outcomes concerning satisfaction, knowledge, and impact of genetic testing between disclosure of results and genetic counseling in-person by either a neurologist or a genetic counselor or via telephone by a remove genetic counselor at a centralized center,” said Jennifer L. Verbrugge, MS, a genetic counselor at Indiana University, Indianapolis, in reporting results of the PD GENEration pilot study, presented at the 2021 annual meeting of the American Academy of Neurology.
COVID complication
The study launched in the summer of 2019 with the goal of enrolling 600 participants. However, because of the COVID-19 pandemic, enrollment was truncated. The pilot study eventually enrolled 289 patients, 205 of whom returned their postgenetic counseling surveys, Ms. Verbrugge said. The pilot study goal was to evaluate the feasibility and impact of in-person versus remote genetic testing and counseling for people with Parkinson’s disease.
“The study hopes to reach its ultimate goal, which is to deliver Parkinson’s disease–related genetic testing and counseling to upward of 15,000 people with Parkinson’s,” Ms. Verbrugge said. The program is also planning to expand to include Spanish speakers.
In the pilot study, genetic results were positive in 17% of patients, with 15% (n = 42) having positive heterozygous variants and 8% having variants of uncertain significance. “We did not see significant differences in these outcomes when we compared the mode and genetic counselors involved,” Ms. Verbrugge said.
The study did find that in-person testing and counseling “was associated with increased participant feelings that they were partners in care,” Ms. Verbrugge added. “This is something we are going to continue to evaluate as time goes on.”
However, as the COVID-19 pandemic pushed clinicians to develop virtual platforms, it resulted in a function through which participants can complete all genetic study activities remotely, she said. The study organizers anticipate that as pandemic restrictions ease, they will be able to reach their original goal of 600 participants along with those recruited in an expansion phase.
“As restrictions related to the pandemic ease, we anticipate that more Parkinson’s disease gene-targeted clinical trials will emerge, with aims to recruit people who carry certain gene variants,” Ms. Verbrugge said in an interview. “Many people with Parkinson’s disease may therefore benefit from genetic testing and learning if they carry a Parkinson’s disease related gene variant from participation in the PD GENEration study.”
Increasing patient access
To scale up to the 15,000-population goal for the program, PD GENEration has launched a new protocol designed to increase patient access at new study sites, Ms. Verbrugge said. “This protocol includes an abbreviate version of the clinical data collected, while it maintains the critical component of genetic counseling in the testing process.”
Going forward, the PD GENEration study will focus on improving access to genetic testing and counseling in underrepresented and rural populations, Ms. Verbrugge said. “These efforts will also generate valuable genomic data, allowing researchers to learn more about the causes of Parkinson’s disease in diverse and underrepresented populations. The study will be expanding research efforts concerning the genomic data to gain insights about the seven key genes studied as well as new genes linked to Parkinson’s disease.”
The work of the PD GENEration study is timely, said David K. Simon, MD, PhD, of Harvard Medical School and director of the Parkinson’s Disease & Movement Disorders Center at Beth Israel Deaconess Medical Center, both in Boston. “This is very important to identify such patients now, as clinical trials targeting people with specific genetic mutations or variants are coming soon, and in some cases already are underway. The feasibility and speed of enrollment for those trials will be greatly facilitate if we know in advance who are the people with Parkinson’s disease who have mutations that would make them eligible for the particular trials.”
The fact that the study provides free genetic testing to people with Parkinson’s disease isn’t to be overlooked. “This was an important study to address the question of whether or not remote genetic counseling was feasible and effective, and the results are meaningful given the randomized prospective design,” Dr. Simon said.
Ms. Verbrugge has no relevant relationships to disclose. Dr. Simon reports receiving research funding from the Parkinson’s Foundation.
according to a pilot study sponsored by the Parkinson’s Foundation.
“Overall we found high levels of participant satisfaction with Parkinson’s testing and genetic counseling and no significant difference in outcomes concerning satisfaction, knowledge, and impact of genetic testing between disclosure of results and genetic counseling in-person by either a neurologist or a genetic counselor or via telephone by a remove genetic counselor at a centralized center,” said Jennifer L. Verbrugge, MS, a genetic counselor at Indiana University, Indianapolis, in reporting results of the PD GENEration pilot study, presented at the 2021 annual meeting of the American Academy of Neurology.
COVID complication
The study launched in the summer of 2019 with the goal of enrolling 600 participants. However, because of the COVID-19 pandemic, enrollment was truncated. The pilot study eventually enrolled 289 patients, 205 of whom returned their postgenetic counseling surveys, Ms. Verbrugge said. The pilot study goal was to evaluate the feasibility and impact of in-person versus remote genetic testing and counseling for people with Parkinson’s disease.
“The study hopes to reach its ultimate goal, which is to deliver Parkinson’s disease–related genetic testing and counseling to upward of 15,000 people with Parkinson’s,” Ms. Verbrugge said. The program is also planning to expand to include Spanish speakers.
In the pilot study, genetic results were positive in 17% of patients, with 15% (n = 42) having positive heterozygous variants and 8% having variants of uncertain significance. “We did not see significant differences in these outcomes when we compared the mode and genetic counselors involved,” Ms. Verbrugge said.
The study did find that in-person testing and counseling “was associated with increased participant feelings that they were partners in care,” Ms. Verbrugge added. “This is something we are going to continue to evaluate as time goes on.”
However, as the COVID-19 pandemic pushed clinicians to develop virtual platforms, it resulted in a function through which participants can complete all genetic study activities remotely, she said. The study organizers anticipate that as pandemic restrictions ease, they will be able to reach their original goal of 600 participants along with those recruited in an expansion phase.
“As restrictions related to the pandemic ease, we anticipate that more Parkinson’s disease gene-targeted clinical trials will emerge, with aims to recruit people who carry certain gene variants,” Ms. Verbrugge said in an interview. “Many people with Parkinson’s disease may therefore benefit from genetic testing and learning if they carry a Parkinson’s disease related gene variant from participation in the PD GENEration study.”
Increasing patient access
To scale up to the 15,000-population goal for the program, PD GENEration has launched a new protocol designed to increase patient access at new study sites, Ms. Verbrugge said. “This protocol includes an abbreviate version of the clinical data collected, while it maintains the critical component of genetic counseling in the testing process.”
Going forward, the PD GENEration study will focus on improving access to genetic testing and counseling in underrepresented and rural populations, Ms. Verbrugge said. “These efforts will also generate valuable genomic data, allowing researchers to learn more about the causes of Parkinson’s disease in diverse and underrepresented populations. The study will be expanding research efforts concerning the genomic data to gain insights about the seven key genes studied as well as new genes linked to Parkinson’s disease.”
The work of the PD GENEration study is timely, said David K. Simon, MD, PhD, of Harvard Medical School and director of the Parkinson’s Disease & Movement Disorders Center at Beth Israel Deaconess Medical Center, both in Boston. “This is very important to identify such patients now, as clinical trials targeting people with specific genetic mutations or variants are coming soon, and in some cases already are underway. The feasibility and speed of enrollment for those trials will be greatly facilitate if we know in advance who are the people with Parkinson’s disease who have mutations that would make them eligible for the particular trials.”
The fact that the study provides free genetic testing to people with Parkinson’s disease isn’t to be overlooked. “This was an important study to address the question of whether or not remote genetic counseling was feasible and effective, and the results are meaningful given the randomized prospective design,” Dr. Simon said.
Ms. Verbrugge has no relevant relationships to disclose. Dr. Simon reports receiving research funding from the Parkinson’s Foundation.
FROM AAN 2021
The ripple effect
“I want my life to mean something.”
She was young, energetic, and idealistic. She was seeing me for her migraines, but our conversation had turned to her applying for medical school.
“I want my life to mean something.”
I reflected on that later. I once said similar things, but now found myself wondering, two-thirds of the way through my career, did it?
The world certainly isn’t safer, geopolitically or environmentally, now than it was when I left medical school. Hell, the idea that there’d actually be another worldwide pandemic was pretty much beyond me then. That seemed so 1918.
I can’t even say I’ve made a huge difference in medicine. I’m not on the front line of research, inventing cures and tests that will change what we do.
I’m certainly far removed from the front lines of the pandemic.
But realistically, none of those things were ever really my goal, either.
“I want my life to mean something.”
Sometimes it’s hard to think I’ve made a difference. Day in and day out I’m at my office, quietly sitting behind a desk and trying to look smart. For all good intentions ... at some point it’s just a job.
Then I realized that the job isn’t about me. It’s about her, and the many other people who come to me for help. The real meaning is the impact on their lives.
Anytime we see a patient and make their lives better, either through treatment or compassion, it creates a ripple effect. It helps their family, friends, and coworkers. Whether we’re actually giving help or just understanding.
It might even inspire one of them to go into medicine, because my generation will be drifting toward retirement in the next 10 years.
Our care may set off a chain reaction we can’t see. Perhaps the patient you help will return to work and initiate some action that will bring a marked benefit to us all. Or someone in their circle, freed or inspired by their improvement, will bring about such a change.
And that’s meaning enough for me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I want my life to mean something.”
She was young, energetic, and idealistic. She was seeing me for her migraines, but our conversation had turned to her applying for medical school.
“I want my life to mean something.”
I reflected on that later. I once said similar things, but now found myself wondering, two-thirds of the way through my career, did it?
The world certainly isn’t safer, geopolitically or environmentally, now than it was when I left medical school. Hell, the idea that there’d actually be another worldwide pandemic was pretty much beyond me then. That seemed so 1918.
I can’t even say I’ve made a huge difference in medicine. I’m not on the front line of research, inventing cures and tests that will change what we do.
I’m certainly far removed from the front lines of the pandemic.
But realistically, none of those things were ever really my goal, either.
“I want my life to mean something.”
Sometimes it’s hard to think I’ve made a difference. Day in and day out I’m at my office, quietly sitting behind a desk and trying to look smart. For all good intentions ... at some point it’s just a job.
Then I realized that the job isn’t about me. It’s about her, and the many other people who come to me for help. The real meaning is the impact on their lives.
Anytime we see a patient and make their lives better, either through treatment or compassion, it creates a ripple effect. It helps their family, friends, and coworkers. Whether we’re actually giving help or just understanding.
It might even inspire one of them to go into medicine, because my generation will be drifting toward retirement in the next 10 years.
Our care may set off a chain reaction we can’t see. Perhaps the patient you help will return to work and initiate some action that will bring a marked benefit to us all. Or someone in their circle, freed or inspired by their improvement, will bring about such a change.
And that’s meaning enough for me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
“I want my life to mean something.”
She was young, energetic, and idealistic. She was seeing me for her migraines, but our conversation had turned to her applying for medical school.
“I want my life to mean something.”
I reflected on that later. I once said similar things, but now found myself wondering, two-thirds of the way through my career, did it?
The world certainly isn’t safer, geopolitically or environmentally, now than it was when I left medical school. Hell, the idea that there’d actually be another worldwide pandemic was pretty much beyond me then. That seemed so 1918.
I can’t even say I’ve made a huge difference in medicine. I’m not on the front line of research, inventing cures and tests that will change what we do.
I’m certainly far removed from the front lines of the pandemic.
But realistically, none of those things were ever really my goal, either.
“I want my life to mean something.”
Sometimes it’s hard to think I’ve made a difference. Day in and day out I’m at my office, quietly sitting behind a desk and trying to look smart. For all good intentions ... at some point it’s just a job.
Then I realized that the job isn’t about me. It’s about her, and the many other people who come to me for help. The real meaning is the impact on their lives.
Anytime we see a patient and make their lives better, either through treatment or compassion, it creates a ripple effect. It helps their family, friends, and coworkers. Whether we’re actually giving help or just understanding.
It might even inspire one of them to go into medicine, because my generation will be drifting toward retirement in the next 10 years.
Our care may set off a chain reaction we can’t see. Perhaps the patient you help will return to work and initiate some action that will bring a marked benefit to us all. Or someone in their circle, freed or inspired by their improvement, will bring about such a change.
And that’s meaning enough for me.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.