User login
Stethoscope and Doppler may outperform newer intrapartum fetal monitoring techniques
For intrapartum fetal surveillance, the old way may be the best way, according to a meta-analysis involving more than 118,000 patients.
Intermittent auscultation with a Pinard stethoscope and handheld Doppler was associated with a significantly lower risk of emergency cesarean deliveries than newer monitoring techniques without jeopardizing maternal or neonatal outcomes, reported lead author Bassel H. Al Wattar, MD, PhD, of University of Warwick, Coventry, England, and University College London Hospitals, and colleagues.
“Over the last 50 years, several newer surveillance methods have been evaluated, with varied uptake in practice,” the investigators wrote in the Canadian Medical Association Journal, noting that cardiotocography (CTG) is the most common method for high-risk pregnancies, typically coupled with at least one other modality, such as fetal scalp pH analysis (FBS), fetal pulse oximetry (FPO), or fetal heart electrocardiogram (STAN).
“Despite extensive investment in clinical research, the overall effectiveness of such methods in improving maternal and neonatal outcomes remains debatable as stillbirth rates have plateaued worldwide, while cesarean delivery rates continue to rise,” the investigators wrote. Previous meta-analyses have relied upon head-to-head comparisons of monitoring techniques and did not take into account effects on maternal and neonatal outcomes.
To address this knowledge gap, Dr. Al Wattar and colleagues conducted the present systematic review and meta-analysis, ultimately including 33 trials with 118,863 women who underwent intrapartum fetal surveillance, dating back to 1976. Ten surveillance types were evaluated, including intermittent auscultation with Pinard stethoscope and handheld Doppler, CTG with or without computer-aided decision models (cCTG), and CTG or cCTG combined with one or two other techniques, such as FBS, FPO, and STAN.
This revealed that intermittent auscultation outperformed all other techniques in terms of emergency cesarean deliveries and emergency cesarean deliveries because of fetal distress.
Specifically, intermittent auscultation significantly reduced risk of emergency cesarean deliveries, compared with CTG (relative risk, 0.83; 95% confidence interval, 0.72-0.97), CTG-FBS (RR, 0.71; 95% CI, 0.63-0.80), CTG-lactate (RR, 0.77; 95% CI, 0.64-0.92), and FPO-CTG-FBS (RR, 0.81; 95% CI, 0.67-0.99). Conversely, compared with IA, STAN-CTG-FBS and cCTG-FBS raised risk of emergency cesarean deliveries by 17% and 21%, respectively.
Compared with other modalities, the superiority of intermittent auscultation was even more pronounced in terms of emergency cesarean deliveries because of fetal distress. Intermittent auscultation reduced risk by 43%, compared with CTG, 66% compared with CTG-FBS, 58%, compared with FPO-CTG, and 17%, compared with FPO-CTG-FBS. Conversely, compared with intermittent auscultation, STAN-CTG and cCTG-FBS increased risk of emergency cesarean deliveries because of fetal distress by 39% and 80%, respectively.
Further analysis showed that all types of surveillance had similar effects on neonatal outcomes, such as admission to neonatal unit and neonatal acidemia. Although a combination of STAN or FPO with CTG-FBS “seemed to improve the likelihood of reducing adverse neonatal outcomes,” the investigators noted that these differences were not significant in network meta-analysis.
“New fetal surveillance methods did not improve neonatal outcomes or reduce unnecessary maternal interventions,” Dr. Al Wattar and colleagues concluded. “Further evidence is needed to evaluate the effects of fetal pulse oximetry and fetal heart electrocardiography in labor.”
Courtney Rhoades, DO, MBA, FACOG, medical director of labor and delivery and assistant professor of obstetrics and gynecology at the University of Florida, Jacksonville, suggested that the meta-analysis supports the safety of intermittent auscultation, but the results may not be entirely applicable to real-world practice.
“It is hard, in practice, to draw the same conclusion that they do in the study that the newer methods may cause too many emergency C-sections because our fetal monitoring equipment, methodology for interpretation, ability to do emergency C-sections and maternal risk factors have changed in the last 50 years,” Dr. Rhoades said. “Continuous fetal monitoring gives more data points during labor, and with more data points, there are more opportunities to interpret and act – either correctly or incorrectly. As they state in the study, the decision to do a C-section is multifactorial.”
Dr. Rhoades, who recently authored a textbook chapter on intrapartum monitoring and fetal assessment, recommended that intermittent auscultation be reserved for low-risk patients.
“The American College of Obstetricians and Gynecologists has endorsed intermittent auscultation for low-risk pregnancies and this study affirms their support,” Dr. Rhoades said. “Women with a low-risk pregnancy can benefit from intermittent auscultation because it allows them more autonomy and movement during labor so it should be offered to our low-risk patients.”
Dr. Al Wattar reported a personal Academic Clinical Lectureship from the U.K. National Health Institute of Research. Dr. Khan disclosed funding from the Beatriz Galindo Program Grant given to the University of Granada by the Ministry of Science, Innovation, and Universities of the Spanish Government.
For intrapartum fetal surveillance, the old way may be the best way, according to a meta-analysis involving more than 118,000 patients.
Intermittent auscultation with a Pinard stethoscope and handheld Doppler was associated with a significantly lower risk of emergency cesarean deliveries than newer monitoring techniques without jeopardizing maternal or neonatal outcomes, reported lead author Bassel H. Al Wattar, MD, PhD, of University of Warwick, Coventry, England, and University College London Hospitals, and colleagues.
“Over the last 50 years, several newer surveillance methods have been evaluated, with varied uptake in practice,” the investigators wrote in the Canadian Medical Association Journal, noting that cardiotocography (CTG) is the most common method for high-risk pregnancies, typically coupled with at least one other modality, such as fetal scalp pH analysis (FBS), fetal pulse oximetry (FPO), or fetal heart electrocardiogram (STAN).
“Despite extensive investment in clinical research, the overall effectiveness of such methods in improving maternal and neonatal outcomes remains debatable as stillbirth rates have plateaued worldwide, while cesarean delivery rates continue to rise,” the investigators wrote. Previous meta-analyses have relied upon head-to-head comparisons of monitoring techniques and did not take into account effects on maternal and neonatal outcomes.
To address this knowledge gap, Dr. Al Wattar and colleagues conducted the present systematic review and meta-analysis, ultimately including 33 trials with 118,863 women who underwent intrapartum fetal surveillance, dating back to 1976. Ten surveillance types were evaluated, including intermittent auscultation with Pinard stethoscope and handheld Doppler, CTG with or without computer-aided decision models (cCTG), and CTG or cCTG combined with one or two other techniques, such as FBS, FPO, and STAN.
This revealed that intermittent auscultation outperformed all other techniques in terms of emergency cesarean deliveries and emergency cesarean deliveries because of fetal distress.
Specifically, intermittent auscultation significantly reduced risk of emergency cesarean deliveries, compared with CTG (relative risk, 0.83; 95% confidence interval, 0.72-0.97), CTG-FBS (RR, 0.71; 95% CI, 0.63-0.80), CTG-lactate (RR, 0.77; 95% CI, 0.64-0.92), and FPO-CTG-FBS (RR, 0.81; 95% CI, 0.67-0.99). Conversely, compared with IA, STAN-CTG-FBS and cCTG-FBS raised risk of emergency cesarean deliveries by 17% and 21%, respectively.
Compared with other modalities, the superiority of intermittent auscultation was even more pronounced in terms of emergency cesarean deliveries because of fetal distress. Intermittent auscultation reduced risk by 43%, compared with CTG, 66% compared with CTG-FBS, 58%, compared with FPO-CTG, and 17%, compared with FPO-CTG-FBS. Conversely, compared with intermittent auscultation, STAN-CTG and cCTG-FBS increased risk of emergency cesarean deliveries because of fetal distress by 39% and 80%, respectively.
Further analysis showed that all types of surveillance had similar effects on neonatal outcomes, such as admission to neonatal unit and neonatal acidemia. Although a combination of STAN or FPO with CTG-FBS “seemed to improve the likelihood of reducing adverse neonatal outcomes,” the investigators noted that these differences were not significant in network meta-analysis.
“New fetal surveillance methods did not improve neonatal outcomes or reduce unnecessary maternal interventions,” Dr. Al Wattar and colleagues concluded. “Further evidence is needed to evaluate the effects of fetal pulse oximetry and fetal heart electrocardiography in labor.”
Courtney Rhoades, DO, MBA, FACOG, medical director of labor and delivery and assistant professor of obstetrics and gynecology at the University of Florida, Jacksonville, suggested that the meta-analysis supports the safety of intermittent auscultation, but the results may not be entirely applicable to real-world practice.
“It is hard, in practice, to draw the same conclusion that they do in the study that the newer methods may cause too many emergency C-sections because our fetal monitoring equipment, methodology for interpretation, ability to do emergency C-sections and maternal risk factors have changed in the last 50 years,” Dr. Rhoades said. “Continuous fetal monitoring gives more data points during labor, and with more data points, there are more opportunities to interpret and act – either correctly or incorrectly. As they state in the study, the decision to do a C-section is multifactorial.”
Dr. Rhoades, who recently authored a textbook chapter on intrapartum monitoring and fetal assessment, recommended that intermittent auscultation be reserved for low-risk patients.
“The American College of Obstetricians and Gynecologists has endorsed intermittent auscultation for low-risk pregnancies and this study affirms their support,” Dr. Rhoades said. “Women with a low-risk pregnancy can benefit from intermittent auscultation because it allows them more autonomy and movement during labor so it should be offered to our low-risk patients.”
Dr. Al Wattar reported a personal Academic Clinical Lectureship from the U.K. National Health Institute of Research. Dr. Khan disclosed funding from the Beatriz Galindo Program Grant given to the University of Granada by the Ministry of Science, Innovation, and Universities of the Spanish Government.
For intrapartum fetal surveillance, the old way may be the best way, according to a meta-analysis involving more than 118,000 patients.
Intermittent auscultation with a Pinard stethoscope and handheld Doppler was associated with a significantly lower risk of emergency cesarean deliveries than newer monitoring techniques without jeopardizing maternal or neonatal outcomes, reported lead author Bassel H. Al Wattar, MD, PhD, of University of Warwick, Coventry, England, and University College London Hospitals, and colleagues.
“Over the last 50 years, several newer surveillance methods have been evaluated, with varied uptake in practice,” the investigators wrote in the Canadian Medical Association Journal, noting that cardiotocography (CTG) is the most common method for high-risk pregnancies, typically coupled with at least one other modality, such as fetal scalp pH analysis (FBS), fetal pulse oximetry (FPO), or fetal heart electrocardiogram (STAN).
“Despite extensive investment in clinical research, the overall effectiveness of such methods in improving maternal and neonatal outcomes remains debatable as stillbirth rates have plateaued worldwide, while cesarean delivery rates continue to rise,” the investigators wrote. Previous meta-analyses have relied upon head-to-head comparisons of monitoring techniques and did not take into account effects on maternal and neonatal outcomes.
To address this knowledge gap, Dr. Al Wattar and colleagues conducted the present systematic review and meta-analysis, ultimately including 33 trials with 118,863 women who underwent intrapartum fetal surveillance, dating back to 1976. Ten surveillance types were evaluated, including intermittent auscultation with Pinard stethoscope and handheld Doppler, CTG with or without computer-aided decision models (cCTG), and CTG or cCTG combined with one or two other techniques, such as FBS, FPO, and STAN.
This revealed that intermittent auscultation outperformed all other techniques in terms of emergency cesarean deliveries and emergency cesarean deliveries because of fetal distress.
Specifically, intermittent auscultation significantly reduced risk of emergency cesarean deliveries, compared with CTG (relative risk, 0.83; 95% confidence interval, 0.72-0.97), CTG-FBS (RR, 0.71; 95% CI, 0.63-0.80), CTG-lactate (RR, 0.77; 95% CI, 0.64-0.92), and FPO-CTG-FBS (RR, 0.81; 95% CI, 0.67-0.99). Conversely, compared with IA, STAN-CTG-FBS and cCTG-FBS raised risk of emergency cesarean deliveries by 17% and 21%, respectively.
Compared with other modalities, the superiority of intermittent auscultation was even more pronounced in terms of emergency cesarean deliveries because of fetal distress. Intermittent auscultation reduced risk by 43%, compared with CTG, 66% compared with CTG-FBS, 58%, compared with FPO-CTG, and 17%, compared with FPO-CTG-FBS. Conversely, compared with intermittent auscultation, STAN-CTG and cCTG-FBS increased risk of emergency cesarean deliveries because of fetal distress by 39% and 80%, respectively.
Further analysis showed that all types of surveillance had similar effects on neonatal outcomes, such as admission to neonatal unit and neonatal acidemia. Although a combination of STAN or FPO with CTG-FBS “seemed to improve the likelihood of reducing adverse neonatal outcomes,” the investigators noted that these differences were not significant in network meta-analysis.
“New fetal surveillance methods did not improve neonatal outcomes or reduce unnecessary maternal interventions,” Dr. Al Wattar and colleagues concluded. “Further evidence is needed to evaluate the effects of fetal pulse oximetry and fetal heart electrocardiography in labor.”
Courtney Rhoades, DO, MBA, FACOG, medical director of labor and delivery and assistant professor of obstetrics and gynecology at the University of Florida, Jacksonville, suggested that the meta-analysis supports the safety of intermittent auscultation, but the results may not be entirely applicable to real-world practice.
“It is hard, in practice, to draw the same conclusion that they do in the study that the newer methods may cause too many emergency C-sections because our fetal monitoring equipment, methodology for interpretation, ability to do emergency C-sections and maternal risk factors have changed in the last 50 years,” Dr. Rhoades said. “Continuous fetal monitoring gives more data points during labor, and with more data points, there are more opportunities to interpret and act – either correctly or incorrectly. As they state in the study, the decision to do a C-section is multifactorial.”
Dr. Rhoades, who recently authored a textbook chapter on intrapartum monitoring and fetal assessment, recommended that intermittent auscultation be reserved for low-risk patients.
“The American College of Obstetricians and Gynecologists has endorsed intermittent auscultation for low-risk pregnancies and this study affirms their support,” Dr. Rhoades said. “Women with a low-risk pregnancy can benefit from intermittent auscultation because it allows them more autonomy and movement during labor so it should be offered to our low-risk patients.”
Dr. Al Wattar reported a personal Academic Clinical Lectureship from the U.K. National Health Institute of Research. Dr. Khan disclosed funding from the Beatriz Galindo Program Grant given to the University of Granada by the Ministry of Science, Innovation, and Universities of the Spanish Government.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
New combo shows benefit even in patients with high-risk HCC
Updated data continue to show significant clinical benefits for patients with unresectable hepatocellular carcinoma (HCC) with the combination of the immune checkpoint inhibitor atezolizumab and the angiogenesis inhibitor bevacizumab.
The new analysis shows benefit even in patients with high-risk disease.
The findings come from the practice-changing IMBRave150 trial, and the new data are from a median follow-up of 15.6 months. They show that median overall survival in the intention-to-treat (ITT) population, which included both high-risk and non–high-risk patients, was 19.2 months for patients randomized to atezolizumab-bevacizumab vs. 13.4 months for patients on sorafenib (P = .0009).
Jennifer J. Knox, MD, of Princess Margaret Cancer Centre at the University of Toronto, said that the updated data confirm her first impressions of the atezolizumab-bevacizumab combination.
“As a clinician who treats HCC, I can’t tell you how exciting it was to see these [survival] curves, now published in The New England Journal of Medicine, where you can see the superiority of the atezolizumab-bevacizumab combination over sorafenib, with early separation of the curves that last in both overall survival and progression-free survival,” she said.
Dr. Knox was acting as a discussant for the presentation, where the new data were reported by Richard S. Finn, MD, of Jonsson Comprehensive Cancer Center at the University of California, Los Angeles, at the American Association for Cancer Research Annual Meeting 2021: Week 1 (Abstract CT009).
Benefit seen also in high-risk group
At the meeting, Dr. Finn reported results from a subgroup of 101 patients who had high-risk disease (from 501 patients in the ITT population).
High-risk disease included tumor invasion of the main trunk of the portal vein of the liver and/or the portal vein branch contralateral to the primarily involved lobe (Vp4), and/or bile duct invasion, and/or tumor occupancy of at least 50% of the liver. Many of these patients would have been excluded from contemporary trials in HCC, Dr. Finn noted.
In this subgroup of patients with high-risk disease, the median overall survival with atezolizumab-bevacizumab was 7.6 months, compared with 5.5 months with sorafenib. This difference translated into a hazard ratio (HR) for death of 0.62 for the combination, although the upper limit of the 95% confidence was 1.00, and therefore statistically not significant.
The overall survival benefit for high-risk patients was similar to that in the non–high-risk population of 400 patients (HR, 0.68; 95% CI 0.51 - 0.91), Dr. Finn said.
Median progression-free survival (PFS) among high-risk patients was 5.4 months vs. 2.8 months with sorafenib, although this difference too was not significant, possibly because of the relatively small sample size.
“The data in this high-risk group is generally consistent with what we saw in the intent-to-treat population, and that is to say that atezo-bev has improved overall survival and PFS as compared to sorafenib, and a very similar objective response rate in this high-risk group as in the intent-to-treat population,” he said.
However, there were five fatal upper gastrointestinal bleeding events among high-risk patients treated with the combination, compared with none in the sorafenib arm. None of the deaths were considered by investigators to be treatment related, Dr. Finn said. All five patients who died had microvascular invasion, suggesting that patients with these features are at especially elevated risk for adverse events, he noted.
Overall, there were 23 on-study deaths among patients who received the combination (10 high-risk and 13 non–high-risk patients), compared with 9 patients treated with sorafenib (3 high-risk and 6 non–high-risk). Six of the deaths in the combination arm were attributed to treatment vs. one in the sorafenib arm.
Treatment-related adverse events of any grade, and grade 3 or 4 adverse events, occurred more frequently with sorafenib than with the combination in both high-risk and non–high-risk patients.
In both treatment groups, however, the incidence of serious adverse events was higher with the combination. Dr. Finn noted that the duration of therapy was longer with atezolizumab-bevacizumab than with sorafenib, which could account for the higher incidence of serious adverse events with the combination.
What’s next?
In her discussion, Dr. Knox noted that several other combinations are currently being explored for first-line treatment of HCC, including two trials with dual checkpoint inhibitors, and two comparing a tyrosine kinase inhibitor plus checkpoint inhibitor with tyrosine kinase inhibitors alone.
“There’s a lot of excitement about seeing these results, and I think when they read out in the next year or two, there will be a lot of cross-trial comparisons with patient groups and outcomes with the IMBRave150 data, which will be informative in choosing treatments for our patients,” she said.
“This abstract has shown that there is real benefit across both the high- and the lower-risk patients, and that clinicians need to be careful about the risk of hemorrhage in portal vein thrombosis,” Dr. Knox summarized.
The IMBRave150 trial is sponsored by F. Hoffmann–La Roche. Dr. Finn disclosed consulting activities for F. Hoffmann–La Roche, and institutional grant/research support from Roche and others. Dr. Knox disclosed grant/research support from F. Hoffmann–La Roche and others, and consulting for Merck, Pfizer, and Esai.
A version of this article first appeared on Medscape.com.
Updated data continue to show significant clinical benefits for patients with unresectable hepatocellular carcinoma (HCC) with the combination of the immune checkpoint inhibitor atezolizumab and the angiogenesis inhibitor bevacizumab.
The new analysis shows benefit even in patients with high-risk disease.
The findings come from the practice-changing IMBRave150 trial, and the new data are from a median follow-up of 15.6 months. They show that median overall survival in the intention-to-treat (ITT) population, which included both high-risk and non–high-risk patients, was 19.2 months for patients randomized to atezolizumab-bevacizumab vs. 13.4 months for patients on sorafenib (P = .0009).
Jennifer J. Knox, MD, of Princess Margaret Cancer Centre at the University of Toronto, said that the updated data confirm her first impressions of the atezolizumab-bevacizumab combination.
“As a clinician who treats HCC, I can’t tell you how exciting it was to see these [survival] curves, now published in The New England Journal of Medicine, where you can see the superiority of the atezolizumab-bevacizumab combination over sorafenib, with early separation of the curves that last in both overall survival and progression-free survival,” she said.
Dr. Knox was acting as a discussant for the presentation, where the new data were reported by Richard S. Finn, MD, of Jonsson Comprehensive Cancer Center at the University of California, Los Angeles, at the American Association for Cancer Research Annual Meeting 2021: Week 1 (Abstract CT009).
Benefit seen also in high-risk group
At the meeting, Dr. Finn reported results from a subgroup of 101 patients who had high-risk disease (from 501 patients in the ITT population).
High-risk disease included tumor invasion of the main trunk of the portal vein of the liver and/or the portal vein branch contralateral to the primarily involved lobe (Vp4), and/or bile duct invasion, and/or tumor occupancy of at least 50% of the liver. Many of these patients would have been excluded from contemporary trials in HCC, Dr. Finn noted.
In this subgroup of patients with high-risk disease, the median overall survival with atezolizumab-bevacizumab was 7.6 months, compared with 5.5 months with sorafenib. This difference translated into a hazard ratio (HR) for death of 0.62 for the combination, although the upper limit of the 95% confidence was 1.00, and therefore statistically not significant.
The overall survival benefit for high-risk patients was similar to that in the non–high-risk population of 400 patients (HR, 0.68; 95% CI 0.51 - 0.91), Dr. Finn said.
Median progression-free survival (PFS) among high-risk patients was 5.4 months vs. 2.8 months with sorafenib, although this difference too was not significant, possibly because of the relatively small sample size.
“The data in this high-risk group is generally consistent with what we saw in the intent-to-treat population, and that is to say that atezo-bev has improved overall survival and PFS as compared to sorafenib, and a very similar objective response rate in this high-risk group as in the intent-to-treat population,” he said.
However, there were five fatal upper gastrointestinal bleeding events among high-risk patients treated with the combination, compared with none in the sorafenib arm. None of the deaths were considered by investigators to be treatment related, Dr. Finn said. All five patients who died had microvascular invasion, suggesting that patients with these features are at especially elevated risk for adverse events, he noted.
Overall, there were 23 on-study deaths among patients who received the combination (10 high-risk and 13 non–high-risk patients), compared with 9 patients treated with sorafenib (3 high-risk and 6 non–high-risk). Six of the deaths in the combination arm were attributed to treatment vs. one in the sorafenib arm.
Treatment-related adverse events of any grade, and grade 3 or 4 adverse events, occurred more frequently with sorafenib than with the combination in both high-risk and non–high-risk patients.
In both treatment groups, however, the incidence of serious adverse events was higher with the combination. Dr. Finn noted that the duration of therapy was longer with atezolizumab-bevacizumab than with sorafenib, which could account for the higher incidence of serious adverse events with the combination.
What’s next?
In her discussion, Dr. Knox noted that several other combinations are currently being explored for first-line treatment of HCC, including two trials with dual checkpoint inhibitors, and two comparing a tyrosine kinase inhibitor plus checkpoint inhibitor with tyrosine kinase inhibitors alone.
“There’s a lot of excitement about seeing these results, and I think when they read out in the next year or two, there will be a lot of cross-trial comparisons with patient groups and outcomes with the IMBRave150 data, which will be informative in choosing treatments for our patients,” she said.
“This abstract has shown that there is real benefit across both the high- and the lower-risk patients, and that clinicians need to be careful about the risk of hemorrhage in portal vein thrombosis,” Dr. Knox summarized.
The IMBRave150 trial is sponsored by F. Hoffmann–La Roche. Dr. Finn disclosed consulting activities for F. Hoffmann–La Roche, and institutional grant/research support from Roche and others. Dr. Knox disclosed grant/research support from F. Hoffmann–La Roche and others, and consulting for Merck, Pfizer, and Esai.
A version of this article first appeared on Medscape.com.
Updated data continue to show significant clinical benefits for patients with unresectable hepatocellular carcinoma (HCC) with the combination of the immune checkpoint inhibitor atezolizumab and the angiogenesis inhibitor bevacizumab.
The new analysis shows benefit even in patients with high-risk disease.
The findings come from the practice-changing IMBRave150 trial, and the new data are from a median follow-up of 15.6 months. They show that median overall survival in the intention-to-treat (ITT) population, which included both high-risk and non–high-risk patients, was 19.2 months for patients randomized to atezolizumab-bevacizumab vs. 13.4 months for patients on sorafenib (P = .0009).
Jennifer J. Knox, MD, of Princess Margaret Cancer Centre at the University of Toronto, said that the updated data confirm her first impressions of the atezolizumab-bevacizumab combination.
“As a clinician who treats HCC, I can’t tell you how exciting it was to see these [survival] curves, now published in The New England Journal of Medicine, where you can see the superiority of the atezolizumab-bevacizumab combination over sorafenib, with early separation of the curves that last in both overall survival and progression-free survival,” she said.
Dr. Knox was acting as a discussant for the presentation, where the new data were reported by Richard S. Finn, MD, of Jonsson Comprehensive Cancer Center at the University of California, Los Angeles, at the American Association for Cancer Research Annual Meeting 2021: Week 1 (Abstract CT009).
Benefit seen also in high-risk group
At the meeting, Dr. Finn reported results from a subgroup of 101 patients who had high-risk disease (from 501 patients in the ITT population).
High-risk disease included tumor invasion of the main trunk of the portal vein of the liver and/or the portal vein branch contralateral to the primarily involved lobe (Vp4), and/or bile duct invasion, and/or tumor occupancy of at least 50% of the liver. Many of these patients would have been excluded from contemporary trials in HCC, Dr. Finn noted.
In this subgroup of patients with high-risk disease, the median overall survival with atezolizumab-bevacizumab was 7.6 months, compared with 5.5 months with sorafenib. This difference translated into a hazard ratio (HR) for death of 0.62 for the combination, although the upper limit of the 95% confidence was 1.00, and therefore statistically not significant.
The overall survival benefit for high-risk patients was similar to that in the non–high-risk population of 400 patients (HR, 0.68; 95% CI 0.51 - 0.91), Dr. Finn said.
Median progression-free survival (PFS) among high-risk patients was 5.4 months vs. 2.8 months with sorafenib, although this difference too was not significant, possibly because of the relatively small sample size.
“The data in this high-risk group is generally consistent with what we saw in the intent-to-treat population, and that is to say that atezo-bev has improved overall survival and PFS as compared to sorafenib, and a very similar objective response rate in this high-risk group as in the intent-to-treat population,” he said.
However, there were five fatal upper gastrointestinal bleeding events among high-risk patients treated with the combination, compared with none in the sorafenib arm. None of the deaths were considered by investigators to be treatment related, Dr. Finn said. All five patients who died had microvascular invasion, suggesting that patients with these features are at especially elevated risk for adverse events, he noted.
Overall, there were 23 on-study deaths among patients who received the combination (10 high-risk and 13 non–high-risk patients), compared with 9 patients treated with sorafenib (3 high-risk and 6 non–high-risk). Six of the deaths in the combination arm were attributed to treatment vs. one in the sorafenib arm.
Treatment-related adverse events of any grade, and grade 3 or 4 adverse events, occurred more frequently with sorafenib than with the combination in both high-risk and non–high-risk patients.
In both treatment groups, however, the incidence of serious adverse events was higher with the combination. Dr. Finn noted that the duration of therapy was longer with atezolizumab-bevacizumab than with sorafenib, which could account for the higher incidence of serious adverse events with the combination.
What’s next?
In her discussion, Dr. Knox noted that several other combinations are currently being explored for first-line treatment of HCC, including two trials with dual checkpoint inhibitors, and two comparing a tyrosine kinase inhibitor plus checkpoint inhibitor with tyrosine kinase inhibitors alone.
“There’s a lot of excitement about seeing these results, and I think when they read out in the next year or two, there will be a lot of cross-trial comparisons with patient groups and outcomes with the IMBRave150 data, which will be informative in choosing treatments for our patients,” she said.
“This abstract has shown that there is real benefit across both the high- and the lower-risk patients, and that clinicians need to be careful about the risk of hemorrhage in portal vein thrombosis,” Dr. Knox summarized.
The IMBRave150 trial is sponsored by F. Hoffmann–La Roche. Dr. Finn disclosed consulting activities for F. Hoffmann–La Roche, and institutional grant/research support from Roche and others. Dr. Knox disclosed grant/research support from F. Hoffmann–La Roche and others, and consulting for Merck, Pfizer, and Esai.
A version of this article first appeared on Medscape.com.
FROM AACR 2021
Navigating challenges in COVID-19 care
Early strategies for adapting to a moving target
During the early months of the COVID-19 pandemic, hospital groups and systems scrambled to create protocols and models to respond to the novel coronavirus. In the pre-pandemic world, hospital groups have traditionally focused on standardizing clinical protocols and care models that rely on evidence-based medical practices or extended experience.
During COVID-19, however, our team at Dell Medical School needed to rapidly and iteratively standardize care based on evolving science, effectively communicate that approach across rotating hospital medicine physicians and residents, and update care models, workflows, and technology every few days. In this article, we review our initial experiences, describe the strategies we employed to respond to these challenges, and reflect on the lessons learned and our proposed strategy moving forward.
Early pandemic challenges
Our initial inpatient strategies focused on containment, infection prevention, and bracing ourselves rather than creating a COVID Center of Excellence (COE). In fact, our hospital network’s initial strategy was to have COVID-19 patients transferred to a different hospital within our network. However, as March progressed, we became the designated COVID-19 hospital in our area’s network because of the increasing volume of patients we saw.
Patients from the surrounding regional hospitals were transferring their COVID-19 patients to us and we quickly saw the wide spectrum of illness, ranging from mild pneumonia to severe disease requiring mechanical ventilation upon admission. All frontline providers felt the stress of needing to find treatment options quickly for our sickest patients. We realized that to provide safe, effective, and high-quality care to COVID-19 patients, we needed to create a sustainable and standardized interdisciplinary approach.
COVID-19 testing was a major challenge when the pandemic hit as testing kits and personal protective equipment were in limited supply. How would we choose who to test or empirically place in COVID-19 isolation? In addition, we faced questions surrounding safe discharge practices, especially for patients who could not self-isolate in their home (if they even had one).
In March, emergency use authorization (EUA) for hydroxychloroquine was granted by the U.S. FDA despite limited data. This resulted in pressure from the public to use this drug in our patients. At the same time, we saw that some patients quickly got better on their own with supportive care. As clinicians striving to practice evidence-based medicine, we certainly did not want to give patients an unproven therapy that could do more harm than good. We also felt the need to respond with statements about what we could do that worked – rather than negotiate about withholding certain treatments featured in the news. Clearly, a “one-size-fits-all” approach to therapeutics was not going to work in treating patients with COVID-19.
We realized we were going to have to learn and adapt together – quickly. It became apparent that we needed to create structures to rapidly adjudicate and integrate emerging science into standardized clinical care delivery.
Solutions in the form of better structures
In response to these challenges, we created early morning meetings or “huddles” among COVID-19 care teams and hospital administration. A designated “COVID ID” physician from Infectious Diseases would meet with hospitalist and critical care teams each morning in our daily huddles to review all newly admitted patients, current hospitalized patients, and patients with pending COVID-19 tests or suspected initial false-negative tests.
Together, and via the newly developed Therapeutics and Informatics Committee, we created early treatment recommendations based upon available evidence, treatment availability, and the patient’s severity of illness. Within the first ten days of admitting our first patient, it had become standard practice to review eligible patients soon after admission for therapies such as convalescent plasma, and, later, remdesivir and steroids.
We codified these consensus recommendations and processes in our Dell Med COVID Manual, a living document that was frequently updated and disseminated to our group. It created a single ‘true north’ of standardized workflows for triage, diagnosis, management, discharge coordination, and end-of-life care. The document allowed for continuous and asynchronous multi-person collaboration and extremely rapid cycles of improvement. Between March and December 2020, this 100-page handbook went through more than 130 iterations.
Strategy for the future
This approach – communicating frequently, adapting on a daily to weekly basis, and continuously scanning the science for opportunities to improve our care delivery – became the foundation of our approach and the Therapeutics and Informatics Committee. Just as importantly, this created a culture of engagement, collaboration, and shared problem-solving that helped us stay organized, keep up to date with the latest science, and innovate rather than panic when faced with ongoing unpredictability and chaos in the early days of the pandemic.
As the pandemic enters into its 13th month, we carry this foundation and our strategies forward. The infrastructure and systems of communication that we have set in place will allow us to be nimble in our response as COVID-19 numbers surge in our region.
Dr. Gandhi is an assistant professor in the department of internal medicine at Dell Medical School, University of Texas, Austin. Dr. Mondy is chief of the division of infectious disease and associate professor in the department of internal medicine at Dell Medical School. Dr. Busch and Dr. Brode are assistant professors in the department of internal medicine at Dell Medical School. This article is part of a series originally published in The Hospital Leader, the official blog of SHM.
Early strategies for adapting to a moving target
Early strategies for adapting to a moving target
During the early months of the COVID-19 pandemic, hospital groups and systems scrambled to create protocols and models to respond to the novel coronavirus. In the pre-pandemic world, hospital groups have traditionally focused on standardizing clinical protocols and care models that rely on evidence-based medical practices or extended experience.
During COVID-19, however, our team at Dell Medical School needed to rapidly and iteratively standardize care based on evolving science, effectively communicate that approach across rotating hospital medicine physicians and residents, and update care models, workflows, and technology every few days. In this article, we review our initial experiences, describe the strategies we employed to respond to these challenges, and reflect on the lessons learned and our proposed strategy moving forward.
Early pandemic challenges
Our initial inpatient strategies focused on containment, infection prevention, and bracing ourselves rather than creating a COVID Center of Excellence (COE). In fact, our hospital network’s initial strategy was to have COVID-19 patients transferred to a different hospital within our network. However, as March progressed, we became the designated COVID-19 hospital in our area’s network because of the increasing volume of patients we saw.
Patients from the surrounding regional hospitals were transferring their COVID-19 patients to us and we quickly saw the wide spectrum of illness, ranging from mild pneumonia to severe disease requiring mechanical ventilation upon admission. All frontline providers felt the stress of needing to find treatment options quickly for our sickest patients. We realized that to provide safe, effective, and high-quality care to COVID-19 patients, we needed to create a sustainable and standardized interdisciplinary approach.
COVID-19 testing was a major challenge when the pandemic hit as testing kits and personal protective equipment were in limited supply. How would we choose who to test or empirically place in COVID-19 isolation? In addition, we faced questions surrounding safe discharge practices, especially for patients who could not self-isolate in their home (if they even had one).
In March, emergency use authorization (EUA) for hydroxychloroquine was granted by the U.S. FDA despite limited data. This resulted in pressure from the public to use this drug in our patients. At the same time, we saw that some patients quickly got better on their own with supportive care. As clinicians striving to practice evidence-based medicine, we certainly did not want to give patients an unproven therapy that could do more harm than good. We also felt the need to respond with statements about what we could do that worked – rather than negotiate about withholding certain treatments featured in the news. Clearly, a “one-size-fits-all” approach to therapeutics was not going to work in treating patients with COVID-19.
We realized we were going to have to learn and adapt together – quickly. It became apparent that we needed to create structures to rapidly adjudicate and integrate emerging science into standardized clinical care delivery.
Solutions in the form of better structures
In response to these challenges, we created early morning meetings or “huddles” among COVID-19 care teams and hospital administration. A designated “COVID ID” physician from Infectious Diseases would meet with hospitalist and critical care teams each morning in our daily huddles to review all newly admitted patients, current hospitalized patients, and patients with pending COVID-19 tests or suspected initial false-negative tests.
Together, and via the newly developed Therapeutics and Informatics Committee, we created early treatment recommendations based upon available evidence, treatment availability, and the patient’s severity of illness. Within the first ten days of admitting our first patient, it had become standard practice to review eligible patients soon after admission for therapies such as convalescent plasma, and, later, remdesivir and steroids.
We codified these consensus recommendations and processes in our Dell Med COVID Manual, a living document that was frequently updated and disseminated to our group. It created a single ‘true north’ of standardized workflows for triage, diagnosis, management, discharge coordination, and end-of-life care. The document allowed for continuous and asynchronous multi-person collaboration and extremely rapid cycles of improvement. Between March and December 2020, this 100-page handbook went through more than 130 iterations.
Strategy for the future
This approach – communicating frequently, adapting on a daily to weekly basis, and continuously scanning the science for opportunities to improve our care delivery – became the foundation of our approach and the Therapeutics and Informatics Committee. Just as importantly, this created a culture of engagement, collaboration, and shared problem-solving that helped us stay organized, keep up to date with the latest science, and innovate rather than panic when faced with ongoing unpredictability and chaos in the early days of the pandemic.
As the pandemic enters into its 13th month, we carry this foundation and our strategies forward. The infrastructure and systems of communication that we have set in place will allow us to be nimble in our response as COVID-19 numbers surge in our region.
Dr. Gandhi is an assistant professor in the department of internal medicine at Dell Medical School, University of Texas, Austin. Dr. Mondy is chief of the division of infectious disease and associate professor in the department of internal medicine at Dell Medical School. Dr. Busch and Dr. Brode are assistant professors in the department of internal medicine at Dell Medical School. This article is part of a series originally published in The Hospital Leader, the official blog of SHM.
During the early months of the COVID-19 pandemic, hospital groups and systems scrambled to create protocols and models to respond to the novel coronavirus. In the pre-pandemic world, hospital groups have traditionally focused on standardizing clinical protocols and care models that rely on evidence-based medical practices or extended experience.
During COVID-19, however, our team at Dell Medical School needed to rapidly and iteratively standardize care based on evolving science, effectively communicate that approach across rotating hospital medicine physicians and residents, and update care models, workflows, and technology every few days. In this article, we review our initial experiences, describe the strategies we employed to respond to these challenges, and reflect on the lessons learned and our proposed strategy moving forward.
Early pandemic challenges
Our initial inpatient strategies focused on containment, infection prevention, and bracing ourselves rather than creating a COVID Center of Excellence (COE). In fact, our hospital network’s initial strategy was to have COVID-19 patients transferred to a different hospital within our network. However, as March progressed, we became the designated COVID-19 hospital in our area’s network because of the increasing volume of patients we saw.
Patients from the surrounding regional hospitals were transferring their COVID-19 patients to us and we quickly saw the wide spectrum of illness, ranging from mild pneumonia to severe disease requiring mechanical ventilation upon admission. All frontline providers felt the stress of needing to find treatment options quickly for our sickest patients. We realized that to provide safe, effective, and high-quality care to COVID-19 patients, we needed to create a sustainable and standardized interdisciplinary approach.
COVID-19 testing was a major challenge when the pandemic hit as testing kits and personal protective equipment were in limited supply. How would we choose who to test or empirically place in COVID-19 isolation? In addition, we faced questions surrounding safe discharge practices, especially for patients who could not self-isolate in their home (if they even had one).
In March, emergency use authorization (EUA) for hydroxychloroquine was granted by the U.S. FDA despite limited data. This resulted in pressure from the public to use this drug in our patients. At the same time, we saw that some patients quickly got better on their own with supportive care. As clinicians striving to practice evidence-based medicine, we certainly did not want to give patients an unproven therapy that could do more harm than good. We also felt the need to respond with statements about what we could do that worked – rather than negotiate about withholding certain treatments featured in the news. Clearly, a “one-size-fits-all” approach to therapeutics was not going to work in treating patients with COVID-19.
We realized we were going to have to learn and adapt together – quickly. It became apparent that we needed to create structures to rapidly adjudicate and integrate emerging science into standardized clinical care delivery.
Solutions in the form of better structures
In response to these challenges, we created early morning meetings or “huddles” among COVID-19 care teams and hospital administration. A designated “COVID ID” physician from Infectious Diseases would meet with hospitalist and critical care teams each morning in our daily huddles to review all newly admitted patients, current hospitalized patients, and patients with pending COVID-19 tests or suspected initial false-negative tests.
Together, and via the newly developed Therapeutics and Informatics Committee, we created early treatment recommendations based upon available evidence, treatment availability, and the patient’s severity of illness. Within the first ten days of admitting our first patient, it had become standard practice to review eligible patients soon after admission for therapies such as convalescent plasma, and, later, remdesivir and steroids.
We codified these consensus recommendations and processes in our Dell Med COVID Manual, a living document that was frequently updated and disseminated to our group. It created a single ‘true north’ of standardized workflows for triage, diagnosis, management, discharge coordination, and end-of-life care. The document allowed for continuous and asynchronous multi-person collaboration and extremely rapid cycles of improvement. Between March and December 2020, this 100-page handbook went through more than 130 iterations.
Strategy for the future
This approach – communicating frequently, adapting on a daily to weekly basis, and continuously scanning the science for opportunities to improve our care delivery – became the foundation of our approach and the Therapeutics and Informatics Committee. Just as importantly, this created a culture of engagement, collaboration, and shared problem-solving that helped us stay organized, keep up to date with the latest science, and innovate rather than panic when faced with ongoing unpredictability and chaos in the early days of the pandemic.
As the pandemic enters into its 13th month, we carry this foundation and our strategies forward. The infrastructure and systems of communication that we have set in place will allow us to be nimble in our response as COVID-19 numbers surge in our region.
Dr. Gandhi is an assistant professor in the department of internal medicine at Dell Medical School, University of Texas, Austin. Dr. Mondy is chief of the division of infectious disease and associate professor in the department of internal medicine at Dell Medical School. Dr. Busch and Dr. Brode are assistant professors in the department of internal medicine at Dell Medical School. This article is part of a series originally published in The Hospital Leader, the official blog of SHM.
COVID vaccine ‘side effect’ or functional neurologic disorder?
The development of unusual movements after COVID-19 vaccination may be a result of functional neurologic disorder rather than being a direct adverse effect of the vaccine, it has been suggested.
Writing in an article published online in JAMA Neurology on April 9, 2021, two neurologists and a psychiatrist report the recent circulation of videos on social media about major neurologic adverse events, including continuous movements of the trunk and limbs or walking difficulties after administration of the COVID-19 vaccine. Some of these videos have been viewed millions of times by the public, they noted.
While these videos may be unsubstantiated, and it is not definitively known if the COVID-19 vaccine was administered in these cases, it was reported in the news that at least one patient was told by their physician that the diagnosis was conversion disorder, also known as functional neurological disorder (FND), the authors noted.
In addition, the Functional Neurological Disorder Society released a statement in January 2021 pointing out that the conditions described in these videos are seemingly consistent with FND, they added.
“We thought it would be useful to explain more about what functional neurological disorder is, as many people are not familiar with it,” lead author David Kim, MD, said in an interview. “We wanted to provide some contextual information about the condition, as these reports may not necessarily mean the vaccine is unsafe.”
Dr. Kim, who is part of the division of cognitive behavioral neurology at Massachusetts General Hospital, Boston, explained that, in FND, physical symptoms can be brought about after events such as head injury, surgery, vaccination, other medical procedures, or life events such as loss of employment.
“Many different factors can bring these symptoms on, and while there are definitely cases associated with stressful events, it is not necessarily stress induced,” he said. “However, the event itself does not cause the condition, rather it is the reaction of the patient to the event.”
FND is now viewed as a true brain-based disorder, Dr. Kim noted. “While in the past it has been described as psychosomatic, we are now moving away from that terminology, toward the idea of a neurological disorder that affects function. It is a neuropsychiatric disorder on the borderline between neurology and psychiatry.”
The authors believed that some of these cases of unusual movements reported after COVID vaccination are likely to be FND.
“In these cases, it is not the substance in the vaccine that is causing the condition, but the common side effects that can occur after vaccination such as aches and chills bring the attention of the patient to their bodily functions and this reaction can become maladaptive, triggering FND,” Dr. Kim said.
“We believe that health care professionals should be more aware of FND at the current time. They need to know that the general public are aware that some people are experiencing movement disorders after COVID vaccination, and that this conversation is happening on social media,” he commented. “If they see patients with these symptoms, they could consider FND to be one possibility.”
The authors emphasized that, because they have not seen the individual patients, they cannot comment on any specific cases.
“But as some of these videos circulating can be consistent with the condition being FND, and especially with news reports indicating that at least one patient was given that diagnosis, we wanted to raise awareness of this condition among health professionals,” Dr. Kim added.
He explained that, in the past, FND has been a diagnosis of exclusion but now it is diagnosed with a clinical history and physical examination, looking for appropriate rule-in signs. Ancillary testing such as neuroimaging, electrophysiological studies, and blood tests are often used to rule out other conditions.
“Neurologists have a lot of training in this condition, as it is the second most common reason for a patient to visit a neurologist after headache,” Dr. Kim noted.
It is managed with education, counseling, physical rehabilitation and cognitive behavioral therapy. “A key part of the therapeutic process is working with the patient to explain the diagnosis. If they understand the condition, they do better. Patients can learn distraction techniques to allow more fluid movements,” he reported.
“As neurologists, and health care professionals more broadly, we must explain transparently and nonjudgmentally the nature of FND, including that these symptoms are real but not the direct result of toxic vaccine effects,” the authors wrote.
“Transparency and effective communication are needed in our society more than ever, and a condition as prevalent and potentially debilitating as FND can no longer remain marginalized and in the shadows. Effective communication will help educate the public and reduce fears so that patients can make informed decisions for themselves on receiving the vaccine to reduce the risk of COVID-19,” they concluded.
A version of this article first appeared on Medscape.com.
The development of unusual movements after COVID-19 vaccination may be a result of functional neurologic disorder rather than being a direct adverse effect of the vaccine, it has been suggested.
Writing in an article published online in JAMA Neurology on April 9, 2021, two neurologists and a psychiatrist report the recent circulation of videos on social media about major neurologic adverse events, including continuous movements of the trunk and limbs or walking difficulties after administration of the COVID-19 vaccine. Some of these videos have been viewed millions of times by the public, they noted.
While these videos may be unsubstantiated, and it is not definitively known if the COVID-19 vaccine was administered in these cases, it was reported in the news that at least one patient was told by their physician that the diagnosis was conversion disorder, also known as functional neurological disorder (FND), the authors noted.
In addition, the Functional Neurological Disorder Society released a statement in January 2021 pointing out that the conditions described in these videos are seemingly consistent with FND, they added.
“We thought it would be useful to explain more about what functional neurological disorder is, as many people are not familiar with it,” lead author David Kim, MD, said in an interview. “We wanted to provide some contextual information about the condition, as these reports may not necessarily mean the vaccine is unsafe.”
Dr. Kim, who is part of the division of cognitive behavioral neurology at Massachusetts General Hospital, Boston, explained that, in FND, physical symptoms can be brought about after events such as head injury, surgery, vaccination, other medical procedures, or life events such as loss of employment.
“Many different factors can bring these symptoms on, and while there are definitely cases associated with stressful events, it is not necessarily stress induced,” he said. “However, the event itself does not cause the condition, rather it is the reaction of the patient to the event.”
FND is now viewed as a true brain-based disorder, Dr. Kim noted. “While in the past it has been described as psychosomatic, we are now moving away from that terminology, toward the idea of a neurological disorder that affects function. It is a neuropsychiatric disorder on the borderline between neurology and psychiatry.”
The authors believed that some of these cases of unusual movements reported after COVID vaccination are likely to be FND.
“In these cases, it is not the substance in the vaccine that is causing the condition, but the common side effects that can occur after vaccination such as aches and chills bring the attention of the patient to their bodily functions and this reaction can become maladaptive, triggering FND,” Dr. Kim said.
“We believe that health care professionals should be more aware of FND at the current time. They need to know that the general public are aware that some people are experiencing movement disorders after COVID vaccination, and that this conversation is happening on social media,” he commented. “If they see patients with these symptoms, they could consider FND to be one possibility.”
The authors emphasized that, because they have not seen the individual patients, they cannot comment on any specific cases.
“But as some of these videos circulating can be consistent with the condition being FND, and especially with news reports indicating that at least one patient was given that diagnosis, we wanted to raise awareness of this condition among health professionals,” Dr. Kim added.
He explained that, in the past, FND has been a diagnosis of exclusion but now it is diagnosed with a clinical history and physical examination, looking for appropriate rule-in signs. Ancillary testing such as neuroimaging, electrophysiological studies, and blood tests are often used to rule out other conditions.
“Neurologists have a lot of training in this condition, as it is the second most common reason for a patient to visit a neurologist after headache,” Dr. Kim noted.
It is managed with education, counseling, physical rehabilitation and cognitive behavioral therapy. “A key part of the therapeutic process is working with the patient to explain the diagnosis. If they understand the condition, they do better. Patients can learn distraction techniques to allow more fluid movements,” he reported.
“As neurologists, and health care professionals more broadly, we must explain transparently and nonjudgmentally the nature of FND, including that these symptoms are real but not the direct result of toxic vaccine effects,” the authors wrote.
“Transparency and effective communication are needed in our society more than ever, and a condition as prevalent and potentially debilitating as FND can no longer remain marginalized and in the shadows. Effective communication will help educate the public and reduce fears so that patients can make informed decisions for themselves on receiving the vaccine to reduce the risk of COVID-19,” they concluded.
A version of this article first appeared on Medscape.com.
The development of unusual movements after COVID-19 vaccination may be a result of functional neurologic disorder rather than being a direct adverse effect of the vaccine, it has been suggested.
Writing in an article published online in JAMA Neurology on April 9, 2021, two neurologists and a psychiatrist report the recent circulation of videos on social media about major neurologic adverse events, including continuous movements of the trunk and limbs or walking difficulties after administration of the COVID-19 vaccine. Some of these videos have been viewed millions of times by the public, they noted.
While these videos may be unsubstantiated, and it is not definitively known if the COVID-19 vaccine was administered in these cases, it was reported in the news that at least one patient was told by their physician that the diagnosis was conversion disorder, also known as functional neurological disorder (FND), the authors noted.
In addition, the Functional Neurological Disorder Society released a statement in January 2021 pointing out that the conditions described in these videos are seemingly consistent with FND, they added.
“We thought it would be useful to explain more about what functional neurological disorder is, as many people are not familiar with it,” lead author David Kim, MD, said in an interview. “We wanted to provide some contextual information about the condition, as these reports may not necessarily mean the vaccine is unsafe.”
Dr. Kim, who is part of the division of cognitive behavioral neurology at Massachusetts General Hospital, Boston, explained that, in FND, physical symptoms can be brought about after events such as head injury, surgery, vaccination, other medical procedures, or life events such as loss of employment.
“Many different factors can bring these symptoms on, and while there are definitely cases associated with stressful events, it is not necessarily stress induced,” he said. “However, the event itself does not cause the condition, rather it is the reaction of the patient to the event.”
FND is now viewed as a true brain-based disorder, Dr. Kim noted. “While in the past it has been described as psychosomatic, we are now moving away from that terminology, toward the idea of a neurological disorder that affects function. It is a neuropsychiatric disorder on the borderline between neurology and psychiatry.”
The authors believed that some of these cases of unusual movements reported after COVID vaccination are likely to be FND.
“In these cases, it is not the substance in the vaccine that is causing the condition, but the common side effects that can occur after vaccination such as aches and chills bring the attention of the patient to their bodily functions and this reaction can become maladaptive, triggering FND,” Dr. Kim said.
“We believe that health care professionals should be more aware of FND at the current time. They need to know that the general public are aware that some people are experiencing movement disorders after COVID vaccination, and that this conversation is happening on social media,” he commented. “If they see patients with these symptoms, they could consider FND to be one possibility.”
The authors emphasized that, because they have not seen the individual patients, they cannot comment on any specific cases.
“But as some of these videos circulating can be consistent with the condition being FND, and especially with news reports indicating that at least one patient was given that diagnosis, we wanted to raise awareness of this condition among health professionals,” Dr. Kim added.
He explained that, in the past, FND has been a diagnosis of exclusion but now it is diagnosed with a clinical history and physical examination, looking for appropriate rule-in signs. Ancillary testing such as neuroimaging, electrophysiological studies, and blood tests are often used to rule out other conditions.
“Neurologists have a lot of training in this condition, as it is the second most common reason for a patient to visit a neurologist after headache,” Dr. Kim noted.
It is managed with education, counseling, physical rehabilitation and cognitive behavioral therapy. “A key part of the therapeutic process is working with the patient to explain the diagnosis. If they understand the condition, they do better. Patients can learn distraction techniques to allow more fluid movements,” he reported.
“As neurologists, and health care professionals more broadly, we must explain transparently and nonjudgmentally the nature of FND, including that these symptoms are real but not the direct result of toxic vaccine effects,” the authors wrote.
“Transparency and effective communication are needed in our society more than ever, and a condition as prevalent and potentially debilitating as FND can no longer remain marginalized and in the shadows. Effective communication will help educate the public and reduce fears so that patients can make informed decisions for themselves on receiving the vaccine to reduce the risk of COVID-19,” they concluded.
A version of this article first appeared on Medscape.com.
Blacks and Hispanics have higher inpatient use for mycosis fungoides
according to an analysis of the 2012-2017 National Inpatient Sample (NIS).
The findings are consistent with prior studies implicating earlier and more severe disease in Black and Hispanic patients, and reinforce the importance of accurate diagnosis and early treatment.
Dermatologists should maintain “a higher index of suspicion for MF in patients with skin of color, as early diagnosis may help mitigate the downstream costs of management,” Justin Choi, BA, a medical student at the University of Illinois at Chicago, said at the annual Skin of Color Society symposium.
Mr. Choi and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified hospital admissions for MF in the NIS for 10,790 White patients, 4,020 Black patients, and 1,615 Hispanic patients over the 5-year period. The inpatient prevalence of MF – the most common variant of primary cutaneous T-cell lymphoma – was highest in these groups.
Black and Hispanic patients who were hospitalized for MF were significantly younger than White patients, with a mean age of 51.7 years and 48.5 years, respectively, compared with 59.9 years (P < .001 in each case). They also had longer lengths of stay: 8.34 days on average for Black patients and 8.88 for Hispanic patients, compared with 6.66 days for White patients (P < .001 and P = .001, respectively).
Hispanic patients accrued the highest costs of care (a mean of $107,242 vs. $64,049, P =.003) and underwent more procedures (a mean of 2.43 vs. 1.93, P = .004) than White patients. Black patients similarly had higher costs associated with their hospital stay (a mean of $75,053 vs. $64,049, P =.042).
In a multivariate linear regression adjusted for age, sex and insurance type, Black race remained significantly associated with a longer LOS than White race, and Hispanic ethnicity with a longer LOS, increased costs, and more procedures than White race.
The NIS is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Choi is a dermatology research fellow working under the guidance of Dr. Kwatra.
according to an analysis of the 2012-2017 National Inpatient Sample (NIS).
The findings are consistent with prior studies implicating earlier and more severe disease in Black and Hispanic patients, and reinforce the importance of accurate diagnosis and early treatment.
Dermatologists should maintain “a higher index of suspicion for MF in patients with skin of color, as early diagnosis may help mitigate the downstream costs of management,” Justin Choi, BA, a medical student at the University of Illinois at Chicago, said at the annual Skin of Color Society symposium.
Mr. Choi and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified hospital admissions for MF in the NIS for 10,790 White patients, 4,020 Black patients, and 1,615 Hispanic patients over the 5-year period. The inpatient prevalence of MF – the most common variant of primary cutaneous T-cell lymphoma – was highest in these groups.
Black and Hispanic patients who were hospitalized for MF were significantly younger than White patients, with a mean age of 51.7 years and 48.5 years, respectively, compared with 59.9 years (P < .001 in each case). They also had longer lengths of stay: 8.34 days on average for Black patients and 8.88 for Hispanic patients, compared with 6.66 days for White patients (P < .001 and P = .001, respectively).
Hispanic patients accrued the highest costs of care (a mean of $107,242 vs. $64,049, P =.003) and underwent more procedures (a mean of 2.43 vs. 1.93, P = .004) than White patients. Black patients similarly had higher costs associated with their hospital stay (a mean of $75,053 vs. $64,049, P =.042).
In a multivariate linear regression adjusted for age, sex and insurance type, Black race remained significantly associated with a longer LOS than White race, and Hispanic ethnicity with a longer LOS, increased costs, and more procedures than White race.
The NIS is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Choi is a dermatology research fellow working under the guidance of Dr. Kwatra.
according to an analysis of the 2012-2017 National Inpatient Sample (NIS).
The findings are consistent with prior studies implicating earlier and more severe disease in Black and Hispanic patients, and reinforce the importance of accurate diagnosis and early treatment.
Dermatologists should maintain “a higher index of suspicion for MF in patients with skin of color, as early diagnosis may help mitigate the downstream costs of management,” Justin Choi, BA, a medical student at the University of Illinois at Chicago, said at the annual Skin of Color Society symposium.
Mr. Choi and coinvestigators, led by Shawn Kwatra, MD, of Johns Hopkins University, Baltimore, identified hospital admissions for MF in the NIS for 10,790 White patients, 4,020 Black patients, and 1,615 Hispanic patients over the 5-year period. The inpatient prevalence of MF – the most common variant of primary cutaneous T-cell lymphoma – was highest in these groups.
Black and Hispanic patients who were hospitalized for MF were significantly younger than White patients, with a mean age of 51.7 years and 48.5 years, respectively, compared with 59.9 years (P < .001 in each case). They also had longer lengths of stay: 8.34 days on average for Black patients and 8.88 for Hispanic patients, compared with 6.66 days for White patients (P < .001 and P = .001, respectively).
Hispanic patients accrued the highest costs of care (a mean of $107,242 vs. $64,049, P =.003) and underwent more procedures (a mean of 2.43 vs. 1.93, P = .004) than White patients. Black patients similarly had higher costs associated with their hospital stay (a mean of $75,053 vs. $64,049, P =.042).
In a multivariate linear regression adjusted for age, sex and insurance type, Black race remained significantly associated with a longer LOS than White race, and Hispanic ethnicity with a longer LOS, increased costs, and more procedures than White race.
The NIS is a publicly available, all-payer inpatient care database developed for the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project.
Mr. Choi is a dermatology research fellow working under the guidance of Dr. Kwatra.
FROM SOC SOCIETY 2021
HDL anti-inflammatory effects show prognostic potential
The high-density lipoprotein particle’s complexity as a mediator of cardiovascular risk was on display in a case-control study that, the researchers say, points to its anti-inflammatory capacity as potentially a worthy addition to standard CV risk assessments.
A measure of HDL anti-inflammatory capacity in a prospective community cohort was inversely related to future CV risk independent of HDL’s role in cholesterol transport, total cholesterol, and other established biomarkers, as well as any lipid-modifying therapy.
The current analysis “identified an impaired HDL anti-inflammatory capacity as a functional metric prospectively associated with increased cardiovascular risk in the general population,” observed the authors of the study, published April 12, 2021, in Circulation, led by Congzhuo Jia, MD, University of Groningen (the Netherlands).
“In contrast with the cholesterol efflux function of HDL that tracks moderately with HDL cholesterol levels,” they wrote, HDL anti-inflammatory capacity was not significantly correlated with actual levels of the lipoprotein or a major constituent, apolipoprotein A1 (apoA1). Nor was it correlated with levels of a more generalized inflammatory biomarker, C-reactive protein by high-sensitivity assay (hsCRP).
In a test of its independence as a prognosticator, HDL anti-inflammatory capacity significantly and meaningfully improved prediction of CV events in the study after it was added to the familiar Framingham risk equations.
Measurement of HDL anti-inflammatory properties, therefore, has the potential to improve current CV risk assessments in people without clinical heart disease, the authors proposed.
The study “adds to our understanding of the potential cardioprotective role of HDL,” Michael Miller, MD, University of Maryland, Baltimore, said in an interview.
“We’ve known for some time that HDL has anti-inflammatory properties in vitro, and my understanding is this is the first study to assess these anti-inflammatory properties in a clinical trial,” said Dr. Miller, who studies lipid metabolism and directs the Center for Preventive Cardiology at his center but isn’t an author of the report.
The study is part of a long line of research aiming to “untangle the complexities of HDL and try to get a better handle as to the properties that make it cardioprotective,” he said. For example, “high levels are not always associated with cardioprotection, and low levels don’t always imply increased risk.”
The current findings highlight a quality of HDL that might be prognostic but also independent of its concentrations, apoA1 content, or cholesterol efflux capacity, Dr. Miller noted. That makes HDL anti-inflammatory capacity a “promising feature” of HDL that, if confirmed in further studies, could potentially be brought into the mainstream for CV risk prediction. “But it’s too premature at this time.”
The study of participants in the population-based PREVEND cohort study compared 340 patients with a first CV event – CV death, ischemic heart disease, nonfatal MI, or coronary revascularization – over a median of about 10 years with the same number of participants without such events. The two cohorts of people from the same city in the Netherlands had been matched according to sex, smoking status, age, and HDL cholesterol levels at baseline.
No measured clinical or laboratory value, the group wrote, was significantly correlated with HDL anti-inflammatory capacity, defined here as ability to suppress vascular cell adhesion molecule-1 (VCAM-1) mRNA expression as induced by tumor necrosis factor–alpha in endothelial cells in vitro.
HDL anti-inflammatory capacity was significantly lower in the case cohort, compared with the control cohort (P < .001), and was inversely related to new CV events, at an odds ratio per 1 standard deviation of 0.74 (95% confidence interval, 0.61-0.90; P = .002). Covariate adjustments included body mass index; alcohol intake; diabetes and hypertension status; use of lipid-lowering medicine; levels of total cholesterol, apoA1, triglyceride, and hsCRP; and measures of renal function.
No significant association was seen between HDL anti-inflammatory capacity and cholesterol efflux capacity (coefficient of correlation, −0.02; P > .05). But both metrics were independently associated with CV disease events. The OR per 1 standard deviation was 0.74 (95% CI, 0.61-0.90; P = .002) for cholesterol efflux capacity and 0.66 (95% CI, 0.54-0.81; P < .001) for HDL anti-inflammatory capacity.
Adding HDL anti-inflammatory capacity to the Framingham risk score significantly improved its predictive power; its likelihood-ratio statistic rose from 10.50 to 20.40 (P = .002), the group wrote. The addition of cholesterol efflux capacity further elevated the risk score’s likelihood-ratio statistic to 32.84 (P = .0005).
The analysis has all the limitations of a case-control study, Dr. Miller said, but it does “show a potential reasonable association” between anti-inflammatory capacity and CV risk “that needs to be taken to the next level.”
For example, it could be explored in a controlled trial that tracks anti-inflammatory capacity in individuals who receive an intervention that is likely to improve the biomarker – such as weight loss, he proposed – and follows them for clinical outcomes.
“If you want to elevate the stature of the anti-inflammatory index,” Dr. Miller said, “you will need to show that it’s clinically meaningful.”
Dr. Jia reported no conflicts. Dr. Miller has no relevant disclosures.
A version of this article first appeared on Medscape.com.
The high-density lipoprotein particle’s complexity as a mediator of cardiovascular risk was on display in a case-control study that, the researchers say, points to its anti-inflammatory capacity as potentially a worthy addition to standard CV risk assessments.
A measure of HDL anti-inflammatory capacity in a prospective community cohort was inversely related to future CV risk independent of HDL’s role in cholesterol transport, total cholesterol, and other established biomarkers, as well as any lipid-modifying therapy.
The current analysis “identified an impaired HDL anti-inflammatory capacity as a functional metric prospectively associated with increased cardiovascular risk in the general population,” observed the authors of the study, published April 12, 2021, in Circulation, led by Congzhuo Jia, MD, University of Groningen (the Netherlands).
“In contrast with the cholesterol efflux function of HDL that tracks moderately with HDL cholesterol levels,” they wrote, HDL anti-inflammatory capacity was not significantly correlated with actual levels of the lipoprotein or a major constituent, apolipoprotein A1 (apoA1). Nor was it correlated with levels of a more generalized inflammatory biomarker, C-reactive protein by high-sensitivity assay (hsCRP).
In a test of its independence as a prognosticator, HDL anti-inflammatory capacity significantly and meaningfully improved prediction of CV events in the study after it was added to the familiar Framingham risk equations.
Measurement of HDL anti-inflammatory properties, therefore, has the potential to improve current CV risk assessments in people without clinical heart disease, the authors proposed.
The study “adds to our understanding of the potential cardioprotective role of HDL,” Michael Miller, MD, University of Maryland, Baltimore, said in an interview.
“We’ve known for some time that HDL has anti-inflammatory properties in vitro, and my understanding is this is the first study to assess these anti-inflammatory properties in a clinical trial,” said Dr. Miller, who studies lipid metabolism and directs the Center for Preventive Cardiology at his center but isn’t an author of the report.
The study is part of a long line of research aiming to “untangle the complexities of HDL and try to get a better handle as to the properties that make it cardioprotective,” he said. For example, “high levels are not always associated with cardioprotection, and low levels don’t always imply increased risk.”
The current findings highlight a quality of HDL that might be prognostic but also independent of its concentrations, apoA1 content, or cholesterol efflux capacity, Dr. Miller noted. That makes HDL anti-inflammatory capacity a “promising feature” of HDL that, if confirmed in further studies, could potentially be brought into the mainstream for CV risk prediction. “But it’s too premature at this time.”
The study of participants in the population-based PREVEND cohort study compared 340 patients with a first CV event – CV death, ischemic heart disease, nonfatal MI, or coronary revascularization – over a median of about 10 years with the same number of participants without such events. The two cohorts of people from the same city in the Netherlands had been matched according to sex, smoking status, age, and HDL cholesterol levels at baseline.
No measured clinical or laboratory value, the group wrote, was significantly correlated with HDL anti-inflammatory capacity, defined here as ability to suppress vascular cell adhesion molecule-1 (VCAM-1) mRNA expression as induced by tumor necrosis factor–alpha in endothelial cells in vitro.
HDL anti-inflammatory capacity was significantly lower in the case cohort, compared with the control cohort (P < .001), and was inversely related to new CV events, at an odds ratio per 1 standard deviation of 0.74 (95% confidence interval, 0.61-0.90; P = .002). Covariate adjustments included body mass index; alcohol intake; diabetes and hypertension status; use of lipid-lowering medicine; levels of total cholesterol, apoA1, triglyceride, and hsCRP; and measures of renal function.
No significant association was seen between HDL anti-inflammatory capacity and cholesterol efflux capacity (coefficient of correlation, −0.02; P > .05). But both metrics were independently associated with CV disease events. The OR per 1 standard deviation was 0.74 (95% CI, 0.61-0.90; P = .002) for cholesterol efflux capacity and 0.66 (95% CI, 0.54-0.81; P < .001) for HDL anti-inflammatory capacity.
Adding HDL anti-inflammatory capacity to the Framingham risk score significantly improved its predictive power; its likelihood-ratio statistic rose from 10.50 to 20.40 (P = .002), the group wrote. The addition of cholesterol efflux capacity further elevated the risk score’s likelihood-ratio statistic to 32.84 (P = .0005).
The analysis has all the limitations of a case-control study, Dr. Miller said, but it does “show a potential reasonable association” between anti-inflammatory capacity and CV risk “that needs to be taken to the next level.”
For example, it could be explored in a controlled trial that tracks anti-inflammatory capacity in individuals who receive an intervention that is likely to improve the biomarker – such as weight loss, he proposed – and follows them for clinical outcomes.
“If you want to elevate the stature of the anti-inflammatory index,” Dr. Miller said, “you will need to show that it’s clinically meaningful.”
Dr. Jia reported no conflicts. Dr. Miller has no relevant disclosures.
A version of this article first appeared on Medscape.com.
The high-density lipoprotein particle’s complexity as a mediator of cardiovascular risk was on display in a case-control study that, the researchers say, points to its anti-inflammatory capacity as potentially a worthy addition to standard CV risk assessments.
A measure of HDL anti-inflammatory capacity in a prospective community cohort was inversely related to future CV risk independent of HDL’s role in cholesterol transport, total cholesterol, and other established biomarkers, as well as any lipid-modifying therapy.
The current analysis “identified an impaired HDL anti-inflammatory capacity as a functional metric prospectively associated with increased cardiovascular risk in the general population,” observed the authors of the study, published April 12, 2021, in Circulation, led by Congzhuo Jia, MD, University of Groningen (the Netherlands).
“In contrast with the cholesterol efflux function of HDL that tracks moderately with HDL cholesterol levels,” they wrote, HDL anti-inflammatory capacity was not significantly correlated with actual levels of the lipoprotein or a major constituent, apolipoprotein A1 (apoA1). Nor was it correlated with levels of a more generalized inflammatory biomarker, C-reactive protein by high-sensitivity assay (hsCRP).
In a test of its independence as a prognosticator, HDL anti-inflammatory capacity significantly and meaningfully improved prediction of CV events in the study after it was added to the familiar Framingham risk equations.
Measurement of HDL anti-inflammatory properties, therefore, has the potential to improve current CV risk assessments in people without clinical heart disease, the authors proposed.
The study “adds to our understanding of the potential cardioprotective role of HDL,” Michael Miller, MD, University of Maryland, Baltimore, said in an interview.
“We’ve known for some time that HDL has anti-inflammatory properties in vitro, and my understanding is this is the first study to assess these anti-inflammatory properties in a clinical trial,” said Dr. Miller, who studies lipid metabolism and directs the Center for Preventive Cardiology at his center but isn’t an author of the report.
The study is part of a long line of research aiming to “untangle the complexities of HDL and try to get a better handle as to the properties that make it cardioprotective,” he said. For example, “high levels are not always associated with cardioprotection, and low levels don’t always imply increased risk.”
The current findings highlight a quality of HDL that might be prognostic but also independent of its concentrations, apoA1 content, or cholesterol efflux capacity, Dr. Miller noted. That makes HDL anti-inflammatory capacity a “promising feature” of HDL that, if confirmed in further studies, could potentially be brought into the mainstream for CV risk prediction. “But it’s too premature at this time.”
The study of participants in the population-based PREVEND cohort study compared 340 patients with a first CV event – CV death, ischemic heart disease, nonfatal MI, or coronary revascularization – over a median of about 10 years with the same number of participants without such events. The two cohorts of people from the same city in the Netherlands had been matched according to sex, smoking status, age, and HDL cholesterol levels at baseline.
No measured clinical or laboratory value, the group wrote, was significantly correlated with HDL anti-inflammatory capacity, defined here as ability to suppress vascular cell adhesion molecule-1 (VCAM-1) mRNA expression as induced by tumor necrosis factor–alpha in endothelial cells in vitro.
HDL anti-inflammatory capacity was significantly lower in the case cohort, compared with the control cohort (P < .001), and was inversely related to new CV events, at an odds ratio per 1 standard deviation of 0.74 (95% confidence interval, 0.61-0.90; P = .002). Covariate adjustments included body mass index; alcohol intake; diabetes and hypertension status; use of lipid-lowering medicine; levels of total cholesterol, apoA1, triglyceride, and hsCRP; and measures of renal function.
No significant association was seen between HDL anti-inflammatory capacity and cholesterol efflux capacity (coefficient of correlation, −0.02; P > .05). But both metrics were independently associated with CV disease events. The OR per 1 standard deviation was 0.74 (95% CI, 0.61-0.90; P = .002) for cholesterol efflux capacity and 0.66 (95% CI, 0.54-0.81; P < .001) for HDL anti-inflammatory capacity.
Adding HDL anti-inflammatory capacity to the Framingham risk score significantly improved its predictive power; its likelihood-ratio statistic rose from 10.50 to 20.40 (P = .002), the group wrote. The addition of cholesterol efflux capacity further elevated the risk score’s likelihood-ratio statistic to 32.84 (P = .0005).
The analysis has all the limitations of a case-control study, Dr. Miller said, but it does “show a potential reasonable association” between anti-inflammatory capacity and CV risk “that needs to be taken to the next level.”
For example, it could be explored in a controlled trial that tracks anti-inflammatory capacity in individuals who receive an intervention that is likely to improve the biomarker – such as weight loss, he proposed – and follows them for clinical outcomes.
“If you want to elevate the stature of the anti-inflammatory index,” Dr. Miller said, “you will need to show that it’s clinically meaningful.”
Dr. Jia reported no conflicts. Dr. Miller has no relevant disclosures.
A version of this article first appeared on Medscape.com.
Adverse reactions to immunotherapy can appear after a year
Clinicians should be on the lookout for immune-related adverse events (irAEs) even after patients have been receiving anti-PD-1 immunotherapy for a year or longer, according to team of international investigators.
They reported that, among melanoma patients, the incidence of new-onset reactions that occurred 1 year or longer after anti-PD-1 treatment was 5.3%.
In a review of 118 patients, the investigators found that irAEs are often “high grade, difficult to manage, and can lead to death.”
Reactions are more likely to occur in those for whom treatment with an anti-PD-1 checkpoint inhibitor – primarily pembrolizumab and nivolumab – continued for longer than a year, and patients can present “long after stopping” the treatment, the investigators noted.
The findings were published online in Annals of Oncology.
“We do not yet understand why some patients have no side effects for months or years, then develop toxicities so late in their course,” said one of the coauthors, Douglas Johnson, MD, assistant professor of hematology/oncology at Vanderbilt University, Nashville, Tenn.
“Physicians should continue to monitor patients for side effects, even if they have been on anti-PD-1 therapy for some time, since delayed side effects may cause morbidity and even death,” Dr. Johnson said.
Patients and clinicians need “to be aware of these risks when making decisions regarding therapy continuation” and need “to consider irAE as a possible diagnosis in any presentation where there is a history of checkpoint inhibitor treatment, regardless of the time frame, to enable early recognition and appropriate treatment,” Dr. Johnson and colleagues concluded.
Largest series to document delayed reactions
Immunotherapies have revolutionized cancer treatment of many types of tumors, but they carry a well known risk for autoimmune toxicity, which typically occurs within the first 4-6 months, the authors wrote.
Delayed reactions have been reported but are not as well described. The new study is the largest to date on this question, and Dr. Johnson said the findings likely apply across indications, not simply in regard to melanoma patients.
An expert not involved in the study agrees.
“We are definitely seeing delayed reactions to immunotherapy in our practice” in several organ systems, including the skin, said Jennifer Choi, MD, chief of oncodermatology at Northwestern University’s Comprehensive Cancer Center, Chicago.
“Some of these side effects can take months to resolve and may require systemic treatment, such as steroids, nonsteroidal immunosuppressants, or biologics. Clinicians must be on high alert of any possible side effect for a patient on immunotherapy throughout their entire course, and even after they have completed treatment,” Dr. Choi said in an interview.
Anti-PD-1 therapy doesn’t “follow the typical drug hypersensitivity laws and rules with respect to timing,” said Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington.
Median onset was 16 months
The investigators reported in detail on 118 patients. A total of 140 delayed irAEs that occurred 1 year or longer after treatment were identified in 20 centers around the world.
The median onset of delayed irAE was 16 months after start of treatment. Most occurred in conjunction with stand-alone anti-PD-1 therapy, but in the case of 20 patients, a combination of an anti-PD-1 drug and the anti-CTLA-4 drug ipilimumab was used.
In 39% of patients (n = 55), the adverse reaction was of grade 3 or worse. These included two deaths: one case of fatal encephalitis with concurrent anti-PD-1 use, and a death from immune-related multiple organ failure 11 months after anti-PD-1 discontinuation.
Most of the patients (n = 87; 74%) were receiving anti-PD-1 therapy at the time of onset of the adverse reaction; 15 patients (12%) were within 3 months of their last dose, and 16 (14%) were 3 months past their last dose.
Among the subgroup who developed an irAE after discontinuation of treatment was a patient with grade 4 colitis that required colectomy 26 months afterward, although Dr. Johnson noted it’s difficult to be sure that the colitis was related to the immunotherapy, because it occurred so long after treatment had ended.
An early warning system
The most common reactions were colitis, pneumonitis, and rash.
The reactions were often tough to manage, the authors reported. Eighty patients (68%) required steroids, and 27 (23%) required steroids plus additional immunosuppressives, such as tumor necrosis factor blockers, particularly for colitis and renal, rheumatologic, and neurologic complications. Rheumatologic events required a median corticosteroid course of 15 months plus additional immunosuppression in half of cases and often left patients with ongoing morbidity.
“Often, the skin is one of the first and most easily visible immune-related adverse event that develops,” said Bernice Kwong, MD, director of the supportive dermato-oncology program at Stanford (Calif.) University, who was not involved in the study and was approached for comment.
Presentations can range from small itchy plaques to total body dermatitis. It is something to be aware of, because the skin can act as an early warning system to catch internal organ damage earlier, she said.
On a positive note, the investigators found no indication that the effect of immunotherapy was diminished by delayed reactions and their treatment.
Managing events “gets a little complicated” when anti-PD-1 drugs are still being administered, but “we have successfully utilized systemic steroid pulses for several weeks without impeding the efficacy of the therapy. For the lichenoid and psoriasiform dermatitis, topical steroids and oral retinoids have been useful and can be used concurrently with immunotherapy,” Dr. Friedman said.
Question on treatment duration
No obvious factors were predictive of delayed events, including previous autoimmune disease or earlier reactions, which usually affected different organs, the authors said.
The findings raise a question about the appropriate duration of anti-PD-1 therapy, at least for melanoma.
The standard duration of adjuvant therapy was empirically determined to be 1 year for melanoma, and trials support anti-PD-1 therapy for up to 2 years for metastatic disease.
However, the authors suggest that “shorter treatment duration may reduce the risk of delayed irAE” and may be sufficient for patients who have a complete response.
“This should be considered when making decisions regarding therapy continuation in responding patients,” they wrote.
Ongoing clinical trials are investigating the optimal duration of therapy, they wrote.
No outside funding was reported. Dr. Johnson has been an adviser for Array Biopharma, BMS, Iovance, Jansen, Merck, and Novartis and has received research funding from BMS and Incyte. Other investigators reported similar ties. Dr. Choi, Dr. Kwong, and Dr. Friedman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Clinicians should be on the lookout for immune-related adverse events (irAEs) even after patients have been receiving anti-PD-1 immunotherapy for a year or longer, according to team of international investigators.
They reported that, among melanoma patients, the incidence of new-onset reactions that occurred 1 year or longer after anti-PD-1 treatment was 5.3%.
In a review of 118 patients, the investigators found that irAEs are often “high grade, difficult to manage, and can lead to death.”
Reactions are more likely to occur in those for whom treatment with an anti-PD-1 checkpoint inhibitor – primarily pembrolizumab and nivolumab – continued for longer than a year, and patients can present “long after stopping” the treatment, the investigators noted.
The findings were published online in Annals of Oncology.
“We do not yet understand why some patients have no side effects for months or years, then develop toxicities so late in their course,” said one of the coauthors, Douglas Johnson, MD, assistant professor of hematology/oncology at Vanderbilt University, Nashville, Tenn.
“Physicians should continue to monitor patients for side effects, even if they have been on anti-PD-1 therapy for some time, since delayed side effects may cause morbidity and even death,” Dr. Johnson said.
Patients and clinicians need “to be aware of these risks when making decisions regarding therapy continuation” and need “to consider irAE as a possible diagnosis in any presentation where there is a history of checkpoint inhibitor treatment, regardless of the time frame, to enable early recognition and appropriate treatment,” Dr. Johnson and colleagues concluded.
Largest series to document delayed reactions
Immunotherapies have revolutionized cancer treatment of many types of tumors, but they carry a well known risk for autoimmune toxicity, which typically occurs within the first 4-6 months, the authors wrote.
Delayed reactions have been reported but are not as well described. The new study is the largest to date on this question, and Dr. Johnson said the findings likely apply across indications, not simply in regard to melanoma patients.
An expert not involved in the study agrees.
“We are definitely seeing delayed reactions to immunotherapy in our practice” in several organ systems, including the skin, said Jennifer Choi, MD, chief of oncodermatology at Northwestern University’s Comprehensive Cancer Center, Chicago.
“Some of these side effects can take months to resolve and may require systemic treatment, such as steroids, nonsteroidal immunosuppressants, or biologics. Clinicians must be on high alert of any possible side effect for a patient on immunotherapy throughout their entire course, and even after they have completed treatment,” Dr. Choi said in an interview.
Anti-PD-1 therapy doesn’t “follow the typical drug hypersensitivity laws and rules with respect to timing,” said Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington.
Median onset was 16 months
The investigators reported in detail on 118 patients. A total of 140 delayed irAEs that occurred 1 year or longer after treatment were identified in 20 centers around the world.
The median onset of delayed irAE was 16 months after start of treatment. Most occurred in conjunction with stand-alone anti-PD-1 therapy, but in the case of 20 patients, a combination of an anti-PD-1 drug and the anti-CTLA-4 drug ipilimumab was used.
In 39% of patients (n = 55), the adverse reaction was of grade 3 or worse. These included two deaths: one case of fatal encephalitis with concurrent anti-PD-1 use, and a death from immune-related multiple organ failure 11 months after anti-PD-1 discontinuation.
Most of the patients (n = 87; 74%) were receiving anti-PD-1 therapy at the time of onset of the adverse reaction; 15 patients (12%) were within 3 months of their last dose, and 16 (14%) were 3 months past their last dose.
Among the subgroup who developed an irAE after discontinuation of treatment was a patient with grade 4 colitis that required colectomy 26 months afterward, although Dr. Johnson noted it’s difficult to be sure that the colitis was related to the immunotherapy, because it occurred so long after treatment had ended.
An early warning system
The most common reactions were colitis, pneumonitis, and rash.
The reactions were often tough to manage, the authors reported. Eighty patients (68%) required steroids, and 27 (23%) required steroids plus additional immunosuppressives, such as tumor necrosis factor blockers, particularly for colitis and renal, rheumatologic, and neurologic complications. Rheumatologic events required a median corticosteroid course of 15 months plus additional immunosuppression in half of cases and often left patients with ongoing morbidity.
“Often, the skin is one of the first and most easily visible immune-related adverse event that develops,” said Bernice Kwong, MD, director of the supportive dermato-oncology program at Stanford (Calif.) University, who was not involved in the study and was approached for comment.
Presentations can range from small itchy plaques to total body dermatitis. It is something to be aware of, because the skin can act as an early warning system to catch internal organ damage earlier, she said.
On a positive note, the investigators found no indication that the effect of immunotherapy was diminished by delayed reactions and their treatment.
Managing events “gets a little complicated” when anti-PD-1 drugs are still being administered, but “we have successfully utilized systemic steroid pulses for several weeks without impeding the efficacy of the therapy. For the lichenoid and psoriasiform dermatitis, topical steroids and oral retinoids have been useful and can be used concurrently with immunotherapy,” Dr. Friedman said.
Question on treatment duration
No obvious factors were predictive of delayed events, including previous autoimmune disease or earlier reactions, which usually affected different organs, the authors said.
The findings raise a question about the appropriate duration of anti-PD-1 therapy, at least for melanoma.
The standard duration of adjuvant therapy was empirically determined to be 1 year for melanoma, and trials support anti-PD-1 therapy for up to 2 years for metastatic disease.
However, the authors suggest that “shorter treatment duration may reduce the risk of delayed irAE” and may be sufficient for patients who have a complete response.
“This should be considered when making decisions regarding therapy continuation in responding patients,” they wrote.
Ongoing clinical trials are investigating the optimal duration of therapy, they wrote.
No outside funding was reported. Dr. Johnson has been an adviser for Array Biopharma, BMS, Iovance, Jansen, Merck, and Novartis and has received research funding from BMS and Incyte. Other investigators reported similar ties. Dr. Choi, Dr. Kwong, and Dr. Friedman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Clinicians should be on the lookout for immune-related adverse events (irAEs) even after patients have been receiving anti-PD-1 immunotherapy for a year or longer, according to team of international investigators.
They reported that, among melanoma patients, the incidence of new-onset reactions that occurred 1 year or longer after anti-PD-1 treatment was 5.3%.
In a review of 118 patients, the investigators found that irAEs are often “high grade, difficult to manage, and can lead to death.”
Reactions are more likely to occur in those for whom treatment with an anti-PD-1 checkpoint inhibitor – primarily pembrolizumab and nivolumab – continued for longer than a year, and patients can present “long after stopping” the treatment, the investigators noted.
The findings were published online in Annals of Oncology.
“We do not yet understand why some patients have no side effects for months or years, then develop toxicities so late in their course,” said one of the coauthors, Douglas Johnson, MD, assistant professor of hematology/oncology at Vanderbilt University, Nashville, Tenn.
“Physicians should continue to monitor patients for side effects, even if they have been on anti-PD-1 therapy for some time, since delayed side effects may cause morbidity and even death,” Dr. Johnson said.
Patients and clinicians need “to be aware of these risks when making decisions regarding therapy continuation” and need “to consider irAE as a possible diagnosis in any presentation where there is a history of checkpoint inhibitor treatment, regardless of the time frame, to enable early recognition and appropriate treatment,” Dr. Johnson and colleagues concluded.
Largest series to document delayed reactions
Immunotherapies have revolutionized cancer treatment of many types of tumors, but they carry a well known risk for autoimmune toxicity, which typically occurs within the first 4-6 months, the authors wrote.
Delayed reactions have been reported but are not as well described. The new study is the largest to date on this question, and Dr. Johnson said the findings likely apply across indications, not simply in regard to melanoma patients.
An expert not involved in the study agrees.
“We are definitely seeing delayed reactions to immunotherapy in our practice” in several organ systems, including the skin, said Jennifer Choi, MD, chief of oncodermatology at Northwestern University’s Comprehensive Cancer Center, Chicago.
“Some of these side effects can take months to resolve and may require systemic treatment, such as steroids, nonsteroidal immunosuppressants, or biologics. Clinicians must be on high alert of any possible side effect for a patient on immunotherapy throughout their entire course, and even after they have completed treatment,” Dr. Choi said in an interview.
Anti-PD-1 therapy doesn’t “follow the typical drug hypersensitivity laws and rules with respect to timing,” said Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington.
Median onset was 16 months
The investigators reported in detail on 118 patients. A total of 140 delayed irAEs that occurred 1 year or longer after treatment were identified in 20 centers around the world.
The median onset of delayed irAE was 16 months after start of treatment. Most occurred in conjunction with stand-alone anti-PD-1 therapy, but in the case of 20 patients, a combination of an anti-PD-1 drug and the anti-CTLA-4 drug ipilimumab was used.
In 39% of patients (n = 55), the adverse reaction was of grade 3 or worse. These included two deaths: one case of fatal encephalitis with concurrent anti-PD-1 use, and a death from immune-related multiple organ failure 11 months after anti-PD-1 discontinuation.
Most of the patients (n = 87; 74%) were receiving anti-PD-1 therapy at the time of onset of the adverse reaction; 15 patients (12%) were within 3 months of their last dose, and 16 (14%) were 3 months past their last dose.
Among the subgroup who developed an irAE after discontinuation of treatment was a patient with grade 4 colitis that required colectomy 26 months afterward, although Dr. Johnson noted it’s difficult to be sure that the colitis was related to the immunotherapy, because it occurred so long after treatment had ended.
An early warning system
The most common reactions were colitis, pneumonitis, and rash.
The reactions were often tough to manage, the authors reported. Eighty patients (68%) required steroids, and 27 (23%) required steroids plus additional immunosuppressives, such as tumor necrosis factor blockers, particularly for colitis and renal, rheumatologic, and neurologic complications. Rheumatologic events required a median corticosteroid course of 15 months plus additional immunosuppression in half of cases and often left patients with ongoing morbidity.
“Often, the skin is one of the first and most easily visible immune-related adverse event that develops,” said Bernice Kwong, MD, director of the supportive dermato-oncology program at Stanford (Calif.) University, who was not involved in the study and was approached for comment.
Presentations can range from small itchy plaques to total body dermatitis. It is something to be aware of, because the skin can act as an early warning system to catch internal organ damage earlier, she said.
On a positive note, the investigators found no indication that the effect of immunotherapy was diminished by delayed reactions and their treatment.
Managing events “gets a little complicated” when anti-PD-1 drugs are still being administered, but “we have successfully utilized systemic steroid pulses for several weeks without impeding the efficacy of the therapy. For the lichenoid and psoriasiform dermatitis, topical steroids and oral retinoids have been useful and can be used concurrently with immunotherapy,” Dr. Friedman said.
Question on treatment duration
No obvious factors were predictive of delayed events, including previous autoimmune disease or earlier reactions, which usually affected different organs, the authors said.
The findings raise a question about the appropriate duration of anti-PD-1 therapy, at least for melanoma.
The standard duration of adjuvant therapy was empirically determined to be 1 year for melanoma, and trials support anti-PD-1 therapy for up to 2 years for metastatic disease.
However, the authors suggest that “shorter treatment duration may reduce the risk of delayed irAE” and may be sufficient for patients who have a complete response.
“This should be considered when making decisions regarding therapy continuation in responding patients,” they wrote.
Ongoing clinical trials are investigating the optimal duration of therapy, they wrote.
No outside funding was reported. Dr. Johnson has been an adviser for Array Biopharma, BMS, Iovance, Jansen, Merck, and Novartis and has received research funding from BMS and Incyte. Other investigators reported similar ties. Dr. Choi, Dr. Kwong, and Dr. Friedman have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Goodbye, OTC hydroquinone
In 1972, an over-the-counter drug review process was established by the Food and Drug Administration to regulate the safety and efficacy of over-the-counter (OTC) drugs. This created a book or “monograph” for each medication category that describes the active ingredients, indications, doses, route of administration, testing, and labeling. If a drug meets the criteria in its therapeutic category, it does not have to undergo an FDA review before being marketed to consumers.
As part of this process, drugs are classified into one of three categories: category I: generally recognized as safe and effective (GRASE) and not misbranded; category II: not GRASE; category III: lacking sufficient data on safety and efficacy to permit classification. This methodology was outdated and made it difficult under the old guidelines to make changes to medications in the evolving world of drug development. Some categories of OTC drugs, including hand sanitizers, hydroquinone, and sunscreens, have been marketed for years without a final monograph.
The signing of the “Coronavirus Aid, Relief, and Economic Security” (CARES) Act in March 2020 included reforms in the FDA monograph process for OTC medications. Under this proceeding, a final monograph determination was made for all OTC categories. While drugs in category I and some in category III may remain on the market, if certain specifications are met, category II drugs had to be removed within 180 days of the enactment of the CARES Act.
Hydroquinone was one of those that fell victim to the ban. This ban is similar to hydroquinone bans in other places, including Europe. However, for manufacturers, this issue was under the radar and packaged in a seemingly irrelevant piece of legislation.
Among dermatologists, there is no consensus as to whether 2% hydroquinone is safe or not. However, the unmonitored use and overuse that is common for this type of medication has led to heightened safety concerns. Common side effects of hydroquinone include irritant and allergic contact dermatitis; the most difficult to treat side effect with long-term use is ochronosis. But there are no reported cancer data in humans with the use of topical hydroquinone as previously thought. Hydroquinone used short term is a very safe and effective treatment for hard to treat hyperpigmentation and is often necessary when other topicals are ineffective, particularly in our patients with skin of color.
The bigger problem however is the legislative process involved, as exemplified by this ban, which only came to light because of the CARES act.
Dr. Talakoub and Naissan O. Wesley, MD, are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
In 1972, an over-the-counter drug review process was established by the Food and Drug Administration to regulate the safety and efficacy of over-the-counter (OTC) drugs. This created a book or “monograph” for each medication category that describes the active ingredients, indications, doses, route of administration, testing, and labeling. If a drug meets the criteria in its therapeutic category, it does not have to undergo an FDA review before being marketed to consumers.
As part of this process, drugs are classified into one of three categories: category I: generally recognized as safe and effective (GRASE) and not misbranded; category II: not GRASE; category III: lacking sufficient data on safety and efficacy to permit classification. This methodology was outdated and made it difficult under the old guidelines to make changes to medications in the evolving world of drug development. Some categories of OTC drugs, including hand sanitizers, hydroquinone, and sunscreens, have been marketed for years without a final monograph.
The signing of the “Coronavirus Aid, Relief, and Economic Security” (CARES) Act in March 2020 included reforms in the FDA monograph process for OTC medications. Under this proceeding, a final monograph determination was made for all OTC categories. While drugs in category I and some in category III may remain on the market, if certain specifications are met, category II drugs had to be removed within 180 days of the enactment of the CARES Act.
Hydroquinone was one of those that fell victim to the ban. This ban is similar to hydroquinone bans in other places, including Europe. However, for manufacturers, this issue was under the radar and packaged in a seemingly irrelevant piece of legislation.
Among dermatologists, there is no consensus as to whether 2% hydroquinone is safe or not. However, the unmonitored use and overuse that is common for this type of medication has led to heightened safety concerns. Common side effects of hydroquinone include irritant and allergic contact dermatitis; the most difficult to treat side effect with long-term use is ochronosis. But there are no reported cancer data in humans with the use of topical hydroquinone as previously thought. Hydroquinone used short term is a very safe and effective treatment for hard to treat hyperpigmentation and is often necessary when other topicals are ineffective, particularly in our patients with skin of color.
The bigger problem however is the legislative process involved, as exemplified by this ban, which only came to light because of the CARES act.
Dr. Talakoub and Naissan O. Wesley, MD, are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
In 1972, an over-the-counter drug review process was established by the Food and Drug Administration to regulate the safety and efficacy of over-the-counter (OTC) drugs. This created a book or “monograph” for each medication category that describes the active ingredients, indications, doses, route of administration, testing, and labeling. If a drug meets the criteria in its therapeutic category, it does not have to undergo an FDA review before being marketed to consumers.
As part of this process, drugs are classified into one of three categories: category I: generally recognized as safe and effective (GRASE) and not misbranded; category II: not GRASE; category III: lacking sufficient data on safety and efficacy to permit classification. This methodology was outdated and made it difficult under the old guidelines to make changes to medications in the evolving world of drug development. Some categories of OTC drugs, including hand sanitizers, hydroquinone, and sunscreens, have been marketed for years without a final monograph.
The signing of the “Coronavirus Aid, Relief, and Economic Security” (CARES) Act in March 2020 included reforms in the FDA monograph process for OTC medications. Under this proceeding, a final monograph determination was made for all OTC categories. While drugs in category I and some in category III may remain on the market, if certain specifications are met, category II drugs had to be removed within 180 days of the enactment of the CARES Act.
Hydroquinone was one of those that fell victim to the ban. This ban is similar to hydroquinone bans in other places, including Europe. However, for manufacturers, this issue was under the radar and packaged in a seemingly irrelevant piece of legislation.
Among dermatologists, there is no consensus as to whether 2% hydroquinone is safe or not. However, the unmonitored use and overuse that is common for this type of medication has led to heightened safety concerns. Common side effects of hydroquinone include irritant and allergic contact dermatitis; the most difficult to treat side effect with long-term use is ochronosis. But there are no reported cancer data in humans with the use of topical hydroquinone as previously thought. Hydroquinone used short term is a very safe and effective treatment for hard to treat hyperpigmentation and is often necessary when other topicals are ineffective, particularly in our patients with skin of color.
The bigger problem however is the legislative process involved, as exemplified by this ban, which only came to light because of the CARES act.
Dr. Talakoub and Naissan O. Wesley, MD, are cocontributors to this column. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub. Write to them at [email protected]. They had no relevant disclosures.
Tick talk for families and pediatricians
Spring 2021 has arrived with summer quickly approaching. It is our second spring and summer during the pandemic. Travel restrictions have minimally eased for vaccinated adults. However, neither domestic nor international leisure travel is encouraged for anyone. Ironically, air travel is increasing. For many families, it is time to make decisions regarding summer activities. Outdoor activities have been encouraged throughout the pandemic, which makes it a good time to review tick-borne diseases. Depending on your location, your patients may only have to travel as far as their backyard to sustain a tick bite.
Ticks are a group of obligate, bloodsucking arthropods that feed on mammals, birds, and reptiles. There are three families of ticks. Two families, Ixodidae (hard-bodied ticks) and Argasidae (soft-bodied ticks) are responsible for transmitting the most diseases to humans in the United States. Once a tick is infected with a pathogen it usually survives and transmits it to its next host. Ticks efficiently transmit bacteria, spirochetes, protozoa, rickettsiae, nematodes, and toxins to humans during feeding when the site is exposed to infected salivary gland secretions or regurgitated midgut contents. Pathogen transmission can also occur when the feeding site is contaminated by feces or coxal fluid. Sometimes a tick can transmit multiple pathogens. Not all pathogens are infectious (e.g., tick paralysis, which occurs after exposure to a neurotoxin and red meat allergy because of alpha-gal). Ticks require a blood meal to transform to their next stage of development (larva to nymph to adult). Life cycles of hard and soft ticks differ with most hard ticks undergoing a 2-year life cycle and feeding slowly over many days. In contrast, soft ticks feed multiple times often for less than 1 hour and are capable of transmitting diseases in less than 1 minute.
Rocky Mountain spotted fever was the first recognized tick-borne disease (TBD) in humans. Since then, 18 additional pathogens transmitted by ticks have been identified with 40% being described since 1980. The increased discovery of tickborne pathogens has been attributed to physician awareness of TBD and improved diagnostics. The number of cases of TBD has risen yearly. Ticks are responsible for most vector-transmitted diseases in the United States with Lyme disease most frequently reported.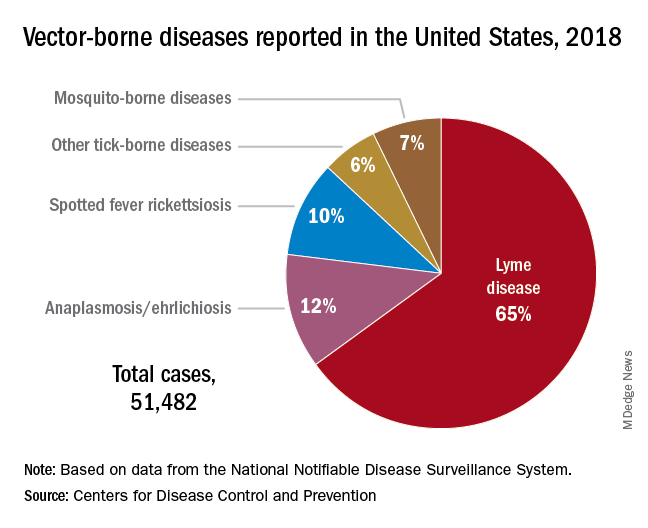
Mosquito transmission accounts for only 7% of vector-borne diseases. Three species of ticks are responsible for most human disease: Ixodes scapularis (Black-legged tick), Amblyomma americanum (Lone Star tick), and Dermacentor variabilis (American dog tick). Each is capable of transmitting agents that cause multiple diseases.
Risk for acquisition of a specific disease is dependent upon the type of tick, its geographic location, the season, and duration of the exposure.
Humans are usually incidental hosts. Tick exposure can occur year-round, but tick activity is greatest between April and September. Ticks are generally found near the ground, in brushy or wooded areas. They can climb tall grasses or shrubs and wait for a potential host to brush against them. When this occurs, they seek a site for attachment.
In the absence of a vaccine, prevention of TBD is totally dependent upon your patients/parents understanding of when and where they are at risk for exposure and for us as physicians to know which pathogens can potentially be transmitted by ticks. Data regarding potential exposure risks are based on where a TBD was diagnosed, not necessarily where it was acquired. National maps that illustrate the distribution of medically significant ticks and presence or prevalence of tick-borne pathogens in specific areas within a region previously may have been incomplete or outdated. The Centers for Disease Control and Prevention initiated a national tick surveillance program in 2017; five universities were established as regional centers of excellence to help prevent and rapidly respond to emerging vector-borne diseases across the United States. One goal is to standardize tick surveillance activities at the state level. For state-specific activity go to https://www.cdc.gov/ncezid/dvbd/vital-signs/index.html.
Prevention: Here are a few environmental interventions you can recommend to your patients
- Remove leaf litter, clear tall brush, and grass around the home and at edge of lawns. Mow the lawn frequently.
- Keep playground equipment, decks, and patios away from yard edges and trees.
- Live near a wooded area? Place a 3-ft.-wide barrier of gravel or wood chips between the areas.
- Put up a fence to keep unwanted animals out.
- Keep the yard free of potential hiding place for ticks (e.g., mattresses or furniture).
- Stack wood neatly and in a dry area.
- Use pesticides, but do not rely on them solely to prevent ticks exposure.
Personal interventions for patients when outdoors
- Use Environmental Protection Agency–registered insect repellents. Note: Oil of lemon-, eucalyptus-, and para-menthane-diol–containing products should not be used in children aged3 years or less.
- Treat clothing and gear with products containing 0.5% permethrin to repel mosquitoes and ticks.
- Check cloths for ticks. Drying clothes on high heat for 10 minutes will kill ticks. If washing is needed use hot water. Lower temperatures will not kill ticks.
- Do daily body checks for ticks after coming indoors.
- Check pets for ticks.
Tick removal
- Take tweezers, grasp the tick as close to the skin’s surface as possible.
- Pull upward. Do not twist or jerk the tick. Place in a container. Ideally submit for species identification.
- After removal, clean the bite area with alcohol or soap and water.
- Never crush a tick with your fingers.
When should you include TBD in your differential for a sick child?
Headache, fever, arthralgia, and rash are symptoms for several infectious diseases. Obtaining a history of recent activities, tick bite, or travel to areas where these diseases are more prevalent is important. You must have a high index of suspicion. Clinical and laboratory clues may help.
Delay in treatment is more detrimental. If you suspect rickettsia, ehrlichiosis, or anaplasmosis, doxycycline should be started promptly regardless of age. Consultation with an infectious disease specialist is recommended.
The United States recognizes it is not adequately prepared to address the continuing rise of vector-borne diseases. In response, on Jan. 20, 2021, the CDC’s division of vector-borne diseases with input from five federal departments and the EPA developed a joint National Public Health Framework for the Prevention and Control of Vector-Borne Diseases in Humans to tackle issues including risk, detection, diagnosis, treatment, prevention and control of TBD. Stay tuned.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Spring 2021 has arrived with summer quickly approaching. It is our second spring and summer during the pandemic. Travel restrictions have minimally eased for vaccinated adults. However, neither domestic nor international leisure travel is encouraged for anyone. Ironically, air travel is increasing. For many families, it is time to make decisions regarding summer activities. Outdoor activities have been encouraged throughout the pandemic, which makes it a good time to review tick-borne diseases. Depending on your location, your patients may only have to travel as far as their backyard to sustain a tick bite.
Ticks are a group of obligate, bloodsucking arthropods that feed on mammals, birds, and reptiles. There are three families of ticks. Two families, Ixodidae (hard-bodied ticks) and Argasidae (soft-bodied ticks) are responsible for transmitting the most diseases to humans in the United States. Once a tick is infected with a pathogen it usually survives and transmits it to its next host. Ticks efficiently transmit bacteria, spirochetes, protozoa, rickettsiae, nematodes, and toxins to humans during feeding when the site is exposed to infected salivary gland secretions or regurgitated midgut contents. Pathogen transmission can also occur when the feeding site is contaminated by feces or coxal fluid. Sometimes a tick can transmit multiple pathogens. Not all pathogens are infectious (e.g., tick paralysis, which occurs after exposure to a neurotoxin and red meat allergy because of alpha-gal). Ticks require a blood meal to transform to their next stage of development (larva to nymph to adult). Life cycles of hard and soft ticks differ with most hard ticks undergoing a 2-year life cycle and feeding slowly over many days. In contrast, soft ticks feed multiple times often for less than 1 hour and are capable of transmitting diseases in less than 1 minute.
Rocky Mountain spotted fever was the first recognized tick-borne disease (TBD) in humans. Since then, 18 additional pathogens transmitted by ticks have been identified with 40% being described since 1980. The increased discovery of tickborne pathogens has been attributed to physician awareness of TBD and improved diagnostics. The number of cases of TBD has risen yearly. Ticks are responsible for most vector-transmitted diseases in the United States with Lyme disease most frequently reported.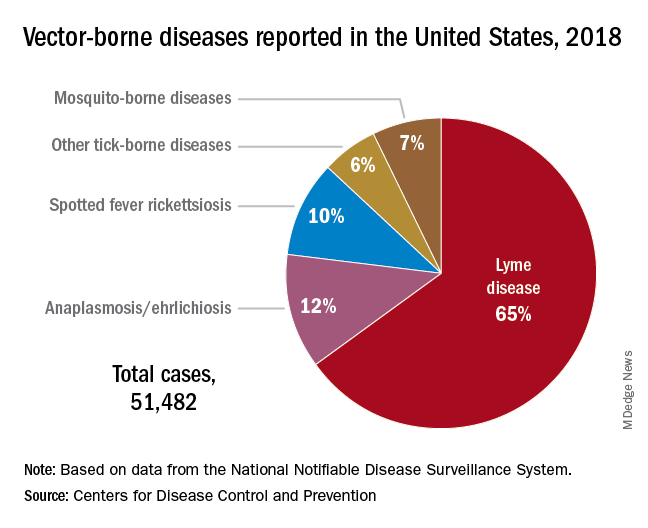
Mosquito transmission accounts for only 7% of vector-borne diseases. Three species of ticks are responsible for most human disease: Ixodes scapularis (Black-legged tick), Amblyomma americanum (Lone Star tick), and Dermacentor variabilis (American dog tick). Each is capable of transmitting agents that cause multiple diseases.
Risk for acquisition of a specific disease is dependent upon the type of tick, its geographic location, the season, and duration of the exposure.
Humans are usually incidental hosts. Tick exposure can occur year-round, but tick activity is greatest between April and September. Ticks are generally found near the ground, in brushy or wooded areas. They can climb tall grasses or shrubs and wait for a potential host to brush against them. When this occurs, they seek a site for attachment.
In the absence of a vaccine, prevention of TBD is totally dependent upon your patients/parents understanding of when and where they are at risk for exposure and for us as physicians to know which pathogens can potentially be transmitted by ticks. Data regarding potential exposure risks are based on where a TBD was diagnosed, not necessarily where it was acquired. National maps that illustrate the distribution of medically significant ticks and presence or prevalence of tick-borne pathogens in specific areas within a region previously may have been incomplete or outdated. The Centers for Disease Control and Prevention initiated a national tick surveillance program in 2017; five universities were established as regional centers of excellence to help prevent and rapidly respond to emerging vector-borne diseases across the United States. One goal is to standardize tick surveillance activities at the state level. For state-specific activity go to https://www.cdc.gov/ncezid/dvbd/vital-signs/index.html.
Prevention: Here are a few environmental interventions you can recommend to your patients
- Remove leaf litter, clear tall brush, and grass around the home and at edge of lawns. Mow the lawn frequently.
- Keep playground equipment, decks, and patios away from yard edges and trees.
- Live near a wooded area? Place a 3-ft.-wide barrier of gravel or wood chips between the areas.
- Put up a fence to keep unwanted animals out.
- Keep the yard free of potential hiding place for ticks (e.g., mattresses or furniture).
- Stack wood neatly and in a dry area.
- Use pesticides, but do not rely on them solely to prevent ticks exposure.
Personal interventions for patients when outdoors
- Use Environmental Protection Agency–registered insect repellents. Note: Oil of lemon-, eucalyptus-, and para-menthane-diol–containing products should not be used in children aged3 years or less.
- Treat clothing and gear with products containing 0.5% permethrin to repel mosquitoes and ticks.
- Check cloths for ticks. Drying clothes on high heat for 10 minutes will kill ticks. If washing is needed use hot water. Lower temperatures will not kill ticks.
- Do daily body checks for ticks after coming indoors.
- Check pets for ticks.
Tick removal
- Take tweezers, grasp the tick as close to the skin’s surface as possible.
- Pull upward. Do not twist or jerk the tick. Place in a container. Ideally submit for species identification.
- After removal, clean the bite area with alcohol or soap and water.
- Never crush a tick with your fingers.
When should you include TBD in your differential for a sick child?
Headache, fever, arthralgia, and rash are symptoms for several infectious diseases. Obtaining a history of recent activities, tick bite, or travel to areas where these diseases are more prevalent is important. You must have a high index of suspicion. Clinical and laboratory clues may help.
Delay in treatment is more detrimental. If you suspect rickettsia, ehrlichiosis, or anaplasmosis, doxycycline should be started promptly regardless of age. Consultation with an infectious disease specialist is recommended.
The United States recognizes it is not adequately prepared to address the continuing rise of vector-borne diseases. In response, on Jan. 20, 2021, the CDC’s division of vector-borne diseases with input from five federal departments and the EPA developed a joint National Public Health Framework for the Prevention and Control of Vector-Borne Diseases in Humans to tackle issues including risk, detection, diagnosis, treatment, prevention and control of TBD. Stay tuned.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Spring 2021 has arrived with summer quickly approaching. It is our second spring and summer during the pandemic. Travel restrictions have minimally eased for vaccinated adults. However, neither domestic nor international leisure travel is encouraged for anyone. Ironically, air travel is increasing. For many families, it is time to make decisions regarding summer activities. Outdoor activities have been encouraged throughout the pandemic, which makes it a good time to review tick-borne diseases. Depending on your location, your patients may only have to travel as far as their backyard to sustain a tick bite.
Ticks are a group of obligate, bloodsucking arthropods that feed on mammals, birds, and reptiles. There are three families of ticks. Two families, Ixodidae (hard-bodied ticks) and Argasidae (soft-bodied ticks) are responsible for transmitting the most diseases to humans in the United States. Once a tick is infected with a pathogen it usually survives and transmits it to its next host. Ticks efficiently transmit bacteria, spirochetes, protozoa, rickettsiae, nematodes, and toxins to humans during feeding when the site is exposed to infected salivary gland secretions or regurgitated midgut contents. Pathogen transmission can also occur when the feeding site is contaminated by feces or coxal fluid. Sometimes a tick can transmit multiple pathogens. Not all pathogens are infectious (e.g., tick paralysis, which occurs after exposure to a neurotoxin and red meat allergy because of alpha-gal). Ticks require a blood meal to transform to their next stage of development (larva to nymph to adult). Life cycles of hard and soft ticks differ with most hard ticks undergoing a 2-year life cycle and feeding slowly over many days. In contrast, soft ticks feed multiple times often for less than 1 hour and are capable of transmitting diseases in less than 1 minute.
Rocky Mountain spotted fever was the first recognized tick-borne disease (TBD) in humans. Since then, 18 additional pathogens transmitted by ticks have been identified with 40% being described since 1980. The increased discovery of tickborne pathogens has been attributed to physician awareness of TBD and improved diagnostics. The number of cases of TBD has risen yearly. Ticks are responsible for most vector-transmitted diseases in the United States with Lyme disease most frequently reported.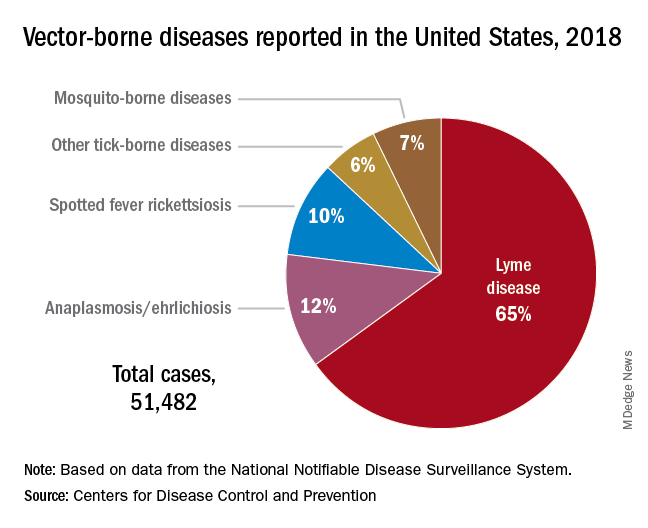
Mosquito transmission accounts for only 7% of vector-borne diseases. Three species of ticks are responsible for most human disease: Ixodes scapularis (Black-legged tick), Amblyomma americanum (Lone Star tick), and Dermacentor variabilis (American dog tick). Each is capable of transmitting agents that cause multiple diseases.
Risk for acquisition of a specific disease is dependent upon the type of tick, its geographic location, the season, and duration of the exposure.
Humans are usually incidental hosts. Tick exposure can occur year-round, but tick activity is greatest between April and September. Ticks are generally found near the ground, in brushy or wooded areas. They can climb tall grasses or shrubs and wait for a potential host to brush against them. When this occurs, they seek a site for attachment.
In the absence of a vaccine, prevention of TBD is totally dependent upon your patients/parents understanding of when and where they are at risk for exposure and for us as physicians to know which pathogens can potentially be transmitted by ticks. Data regarding potential exposure risks are based on where a TBD was diagnosed, not necessarily where it was acquired. National maps that illustrate the distribution of medically significant ticks and presence or prevalence of tick-borne pathogens in specific areas within a region previously may have been incomplete or outdated. The Centers for Disease Control and Prevention initiated a national tick surveillance program in 2017; five universities were established as regional centers of excellence to help prevent and rapidly respond to emerging vector-borne diseases across the United States. One goal is to standardize tick surveillance activities at the state level. For state-specific activity go to https://www.cdc.gov/ncezid/dvbd/vital-signs/index.html.
Prevention: Here are a few environmental interventions you can recommend to your patients
- Remove leaf litter, clear tall brush, and grass around the home and at edge of lawns. Mow the lawn frequently.
- Keep playground equipment, decks, and patios away from yard edges and trees.
- Live near a wooded area? Place a 3-ft.-wide barrier of gravel or wood chips between the areas.
- Put up a fence to keep unwanted animals out.
- Keep the yard free of potential hiding place for ticks (e.g., mattresses or furniture).
- Stack wood neatly and in a dry area.
- Use pesticides, but do not rely on them solely to prevent ticks exposure.
Personal interventions for patients when outdoors
- Use Environmental Protection Agency–registered insect repellents. Note: Oil of lemon-, eucalyptus-, and para-menthane-diol–containing products should not be used in children aged3 years or less.
- Treat clothing and gear with products containing 0.5% permethrin to repel mosquitoes and ticks.
- Check cloths for ticks. Drying clothes on high heat for 10 minutes will kill ticks. If washing is needed use hot water. Lower temperatures will not kill ticks.
- Do daily body checks for ticks after coming indoors.
- Check pets for ticks.
Tick removal
- Take tweezers, grasp the tick as close to the skin’s surface as possible.
- Pull upward. Do not twist or jerk the tick. Place in a container. Ideally submit for species identification.
- After removal, clean the bite area with alcohol or soap and water.
- Never crush a tick with your fingers.
When should you include TBD in your differential for a sick child?
Headache, fever, arthralgia, and rash are symptoms for several infectious diseases. Obtaining a history of recent activities, tick bite, or travel to areas where these diseases are more prevalent is important. You must have a high index of suspicion. Clinical and laboratory clues may help.
Delay in treatment is more detrimental. If you suspect rickettsia, ehrlichiosis, or anaplasmosis, doxycycline should be started promptly regardless of age. Consultation with an infectious disease specialist is recommended.
The United States recognizes it is not adequately prepared to address the continuing rise of vector-borne diseases. In response, on Jan. 20, 2021, the CDC’s division of vector-borne diseases with input from five federal departments and the EPA developed a joint National Public Health Framework for the Prevention and Control of Vector-Borne Diseases in Humans to tackle issues including risk, detection, diagnosis, treatment, prevention and control of TBD. Stay tuned.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Adolescent substance use and the COVID-19 pandemic
During the past year, adolescents, families, educators, and health care providers have had to press forward through myriad challenges and stressors with flexibility and adaptability. With appropriate concern, we ask ourselves how children and youth are coping emotionally with the unprecedented changes of the past year.
Adolescent substance use represents an important area of concern. What has happened during the pandemic? Has youth substance use increased or decreased? Has access to substances increased or decreased, has monitoring and support for at-risk youth increased or decreased?
The answers to these questions are mixed. If anything, the pandemic has highlighted the heterogeneity of adolescent substance use. Now is a key time for assessment, support, and conversation with teens and families.
Monitoring the Future (MTF), a nationally representative annual survey, has provided a broad perspective on trends of adolescent substance use for decades.1 The MTF data is usually collected from February to May and was cut short in 2020 because of school closures associated with the pandemic. The sample size, though still nationally representative, was about a quarter of the typical volume. Some of the data are encouraging, including a flattening out of previous years’ stark increase in vaping of both nicotine and cannabis products (though overall numbers remain alarmingly high). Other data are more concerning including a continued increase in misuse of cough medicine, amphetamines, and inhalants among the youngest cohort surveyed (eighth graders). However, these data were largely representative of prepandemic circumstances.
The COVID-19 pandemic has significantly affected risk and protective factors for teen drug and alcohol use. Most notably, it has had a widely observed negative impact on adolescent mental health, across multiple disease categories.2 In addition, the cancellation of in-person academic and extracurricular activities such as arts and athletics markedly increased unstructured time, a known associated factor for higher-risk activities including substance use. This has also led to decreased contact with many supportive adults such as teachers and coaches. On the other hand, some adolescents now have more time with supportive parents and caregivers, more meals together, and more supervision, all of which are associated with decreased likelihood of substance use disorders.
The highly variable reasons for substance use affect highly variable pandemic-related changes in use. Understanding the impetus for use is a good place to start conversation and can help providers assess risk of escalation during the pandemic. Some teens primarily use for social enhancement while others use as a means of coping with stress or to mask or escape negative emotions. Still others continue use because of physiological dependence, craving, and other symptoms consistent with use disorders.
Highlighting the heterogeneity of this issue, one study assessing use early in the pandemic showed a decrease in the percentage of teens who use substances but an increase in frequency of use for those who are using.3 Though expected, an increase in frequency of use by oneself as compared with peers was also notable. Using substances alone is associated with more severe use disorders, carries greater risk of overdose, and can increase shame and secrecy, further fueling use disorders.
The pandemic has thus represented a protective pause for some experimental or socially motivated substance-using teens who have experienced a period of abstinence even if not fully by choice. For others, it has represented an acute amplification of risk factors and use has accelerated. This latter group includes those whose use represents an effort to cope with depression, anxiety, and loneliness or for whom isolation at home represents less monitoring, increased access, and greater exposure to substances.
Over the past year, in the treatment of adolescents struggling with substance use, many clinicians have observed a sifting effect during these unprecedented social changes. Many youth, who no longer have access to substances, have found they can “take it or leave it”. Other youth have been observed engaging in additional risk or going to greater lengths to access substances and continue their use. For both groups and everyone in between, this is an important time for screening, clinical assessment, and support.
While anticipating further research and data regarding broad substance use trends, including MTF data from 2021, recognizing that the impact of the COVID-19 pandemic is individual, with marked differences from adolescent to adolescent, will help us continue to act now to assess this important area of adolescent health. The first step for primary care providers is unchanged: to routinely screen for and discuss substance use in clinical settings.
Two brief, validated, easily accessible screening tools are available for primary care settings. They can both be self-administered and take less than 2 minutes to complete. Screening, Brief Intervention and Referral to Treatment and the Brief Screener for Tobacco, Alcohol and other Drugs can both be used for youth aged 12-17 years.4,5 Both screens are available online at drugabuse.gov.6
Routine screening will normalize conversations about substance use and healthy choices, provide opportunities for positive reinforcement, identify adolescents at risk, increase comfort and competence in providing brief intervention, and expedite referrals for additional support and treatment.
A false assumption that a particular adolescent isn’t using substances creates a missed opportunity to offer guidance and treatment. An oft-overlooked opportunity is that of providing positive reinforcement for an adolescent who isn’t using any substances or experimenting at all. Positive reinforcement is a strong component of reinforcing health maintenance.
Parent guidance and family assessment will also be critical tools. Parents and caregivers play a primary role in substance use treatment for teens and have a contributory impact on risk through both genes and environment. Of note, research suggests a moderate overall increase in adult substance use during the pandemic, particularly substances that are widely available such as alcohol. Adolescents may thus have greater access and exposure to substance use. A remarkably high percentage, 42%, of substance-using teens surveyed early in the pandemic indicated that they were using substances with their parents.3 Parents, who have equally been challenged by the pandemic, may need guidance in balancing compassion and support for struggling youth, while setting appropriate limits and maintaining expectations of healthy activities.
Unprecedented change and uncertainty provide an opportunity to reassess risks and openly discuss substance use with youth and families. Even with much on our minds during the COVID-19 pandemic, we can maintain focus on this significant risk to adolescent health and wellness. Our efforts now, from screening to treatment for adolescent substance use should be reinforced rather than delayed.
Dr. Jackson is assistant professor of psychiatry at the University of Vermont, Burlington.
References
1. Monitoringthefuture.org
2. Jones EAK et al. Int J Environ Res Public Health, 2021;18(5):2470.
3. Dumas TM et al. J Adolesc Health, 2020;67(3):354-61.
4. Levy S et al. JAMA Pediatr. 2014;168(9):822-8.
5. Kelly SM et al. Pediatrics. 2014;133(5):819-26.
6. National Institute on Drug Abuse. Adolescent Substance Use Screening Tools. 2016 Apr 27. https://www.drugabuse.gov/nidamed-medical-health-professionals/screening-tools-prevention/screening-tools-adolescent-substance-use/adolescent-substance-use-screening-tools
During the past year, adolescents, families, educators, and health care providers have had to press forward through myriad challenges and stressors with flexibility and adaptability. With appropriate concern, we ask ourselves how children and youth are coping emotionally with the unprecedented changes of the past year.
Adolescent substance use represents an important area of concern. What has happened during the pandemic? Has youth substance use increased or decreased? Has access to substances increased or decreased, has monitoring and support for at-risk youth increased or decreased?
The answers to these questions are mixed. If anything, the pandemic has highlighted the heterogeneity of adolescent substance use. Now is a key time for assessment, support, and conversation with teens and families.
Monitoring the Future (MTF), a nationally representative annual survey, has provided a broad perspective on trends of adolescent substance use for decades.1 The MTF data is usually collected from February to May and was cut short in 2020 because of school closures associated with the pandemic. The sample size, though still nationally representative, was about a quarter of the typical volume. Some of the data are encouraging, including a flattening out of previous years’ stark increase in vaping of both nicotine and cannabis products (though overall numbers remain alarmingly high). Other data are more concerning including a continued increase in misuse of cough medicine, amphetamines, and inhalants among the youngest cohort surveyed (eighth graders). However, these data were largely representative of prepandemic circumstances.
The COVID-19 pandemic has significantly affected risk and protective factors for teen drug and alcohol use. Most notably, it has had a widely observed negative impact on adolescent mental health, across multiple disease categories.2 In addition, the cancellation of in-person academic and extracurricular activities such as arts and athletics markedly increased unstructured time, a known associated factor for higher-risk activities including substance use. This has also led to decreased contact with many supportive adults such as teachers and coaches. On the other hand, some adolescents now have more time with supportive parents and caregivers, more meals together, and more supervision, all of which are associated with decreased likelihood of substance use disorders.
The highly variable reasons for substance use affect highly variable pandemic-related changes in use. Understanding the impetus for use is a good place to start conversation and can help providers assess risk of escalation during the pandemic. Some teens primarily use for social enhancement while others use as a means of coping with stress or to mask or escape negative emotions. Still others continue use because of physiological dependence, craving, and other symptoms consistent with use disorders.
Highlighting the heterogeneity of this issue, one study assessing use early in the pandemic showed a decrease in the percentage of teens who use substances but an increase in frequency of use for those who are using.3 Though expected, an increase in frequency of use by oneself as compared with peers was also notable. Using substances alone is associated with more severe use disorders, carries greater risk of overdose, and can increase shame and secrecy, further fueling use disorders.
The pandemic has thus represented a protective pause for some experimental or socially motivated substance-using teens who have experienced a period of abstinence even if not fully by choice. For others, it has represented an acute amplification of risk factors and use has accelerated. This latter group includes those whose use represents an effort to cope with depression, anxiety, and loneliness or for whom isolation at home represents less monitoring, increased access, and greater exposure to substances.
Over the past year, in the treatment of adolescents struggling with substance use, many clinicians have observed a sifting effect during these unprecedented social changes. Many youth, who no longer have access to substances, have found they can “take it or leave it”. Other youth have been observed engaging in additional risk or going to greater lengths to access substances and continue their use. For both groups and everyone in between, this is an important time for screening, clinical assessment, and support.
While anticipating further research and data regarding broad substance use trends, including MTF data from 2021, recognizing that the impact of the COVID-19 pandemic is individual, with marked differences from adolescent to adolescent, will help us continue to act now to assess this important area of adolescent health. The first step for primary care providers is unchanged: to routinely screen for and discuss substance use in clinical settings.
Two brief, validated, easily accessible screening tools are available for primary care settings. They can both be self-administered and take less than 2 minutes to complete. Screening, Brief Intervention and Referral to Treatment and the Brief Screener for Tobacco, Alcohol and other Drugs can both be used for youth aged 12-17 years.4,5 Both screens are available online at drugabuse.gov.6
Routine screening will normalize conversations about substance use and healthy choices, provide opportunities for positive reinforcement, identify adolescents at risk, increase comfort and competence in providing brief intervention, and expedite referrals for additional support and treatment.
A false assumption that a particular adolescent isn’t using substances creates a missed opportunity to offer guidance and treatment. An oft-overlooked opportunity is that of providing positive reinforcement for an adolescent who isn’t using any substances or experimenting at all. Positive reinforcement is a strong component of reinforcing health maintenance.
Parent guidance and family assessment will also be critical tools. Parents and caregivers play a primary role in substance use treatment for teens and have a contributory impact on risk through both genes and environment. Of note, research suggests a moderate overall increase in adult substance use during the pandemic, particularly substances that are widely available such as alcohol. Adolescents may thus have greater access and exposure to substance use. A remarkably high percentage, 42%, of substance-using teens surveyed early in the pandemic indicated that they were using substances with their parents.3 Parents, who have equally been challenged by the pandemic, may need guidance in balancing compassion and support for struggling youth, while setting appropriate limits and maintaining expectations of healthy activities.
Unprecedented change and uncertainty provide an opportunity to reassess risks and openly discuss substance use with youth and families. Even with much on our minds during the COVID-19 pandemic, we can maintain focus on this significant risk to adolescent health and wellness. Our efforts now, from screening to treatment for adolescent substance use should be reinforced rather than delayed.
Dr. Jackson is assistant professor of psychiatry at the University of Vermont, Burlington.
References
1. Monitoringthefuture.org
2. Jones EAK et al. Int J Environ Res Public Health, 2021;18(5):2470.
3. Dumas TM et al. J Adolesc Health, 2020;67(3):354-61.
4. Levy S et al. JAMA Pediatr. 2014;168(9):822-8.
5. Kelly SM et al. Pediatrics. 2014;133(5):819-26.
6. National Institute on Drug Abuse. Adolescent Substance Use Screening Tools. 2016 Apr 27. https://www.drugabuse.gov/nidamed-medical-health-professionals/screening-tools-prevention/screening-tools-adolescent-substance-use/adolescent-substance-use-screening-tools
During the past year, adolescents, families, educators, and health care providers have had to press forward through myriad challenges and stressors with flexibility and adaptability. With appropriate concern, we ask ourselves how children and youth are coping emotionally with the unprecedented changes of the past year.
Adolescent substance use represents an important area of concern. What has happened during the pandemic? Has youth substance use increased or decreased? Has access to substances increased or decreased, has monitoring and support for at-risk youth increased or decreased?
The answers to these questions are mixed. If anything, the pandemic has highlighted the heterogeneity of adolescent substance use. Now is a key time for assessment, support, and conversation with teens and families.
Monitoring the Future (MTF), a nationally representative annual survey, has provided a broad perspective on trends of adolescent substance use for decades.1 The MTF data is usually collected from February to May and was cut short in 2020 because of school closures associated with the pandemic. The sample size, though still nationally representative, was about a quarter of the typical volume. Some of the data are encouraging, including a flattening out of previous years’ stark increase in vaping of both nicotine and cannabis products (though overall numbers remain alarmingly high). Other data are more concerning including a continued increase in misuse of cough medicine, amphetamines, and inhalants among the youngest cohort surveyed (eighth graders). However, these data were largely representative of prepandemic circumstances.
The COVID-19 pandemic has significantly affected risk and protective factors for teen drug and alcohol use. Most notably, it has had a widely observed negative impact on adolescent mental health, across multiple disease categories.2 In addition, the cancellation of in-person academic and extracurricular activities such as arts and athletics markedly increased unstructured time, a known associated factor for higher-risk activities including substance use. This has also led to decreased contact with many supportive adults such as teachers and coaches. On the other hand, some adolescents now have more time with supportive parents and caregivers, more meals together, and more supervision, all of which are associated with decreased likelihood of substance use disorders.
The highly variable reasons for substance use affect highly variable pandemic-related changes in use. Understanding the impetus for use is a good place to start conversation and can help providers assess risk of escalation during the pandemic. Some teens primarily use for social enhancement while others use as a means of coping with stress or to mask or escape negative emotions. Still others continue use because of physiological dependence, craving, and other symptoms consistent with use disorders.
Highlighting the heterogeneity of this issue, one study assessing use early in the pandemic showed a decrease in the percentage of teens who use substances but an increase in frequency of use for those who are using.3 Though expected, an increase in frequency of use by oneself as compared with peers was also notable. Using substances alone is associated with more severe use disorders, carries greater risk of overdose, and can increase shame and secrecy, further fueling use disorders.
The pandemic has thus represented a protective pause for some experimental or socially motivated substance-using teens who have experienced a period of abstinence even if not fully by choice. For others, it has represented an acute amplification of risk factors and use has accelerated. This latter group includes those whose use represents an effort to cope with depression, anxiety, and loneliness or for whom isolation at home represents less monitoring, increased access, and greater exposure to substances.
Over the past year, in the treatment of adolescents struggling with substance use, many clinicians have observed a sifting effect during these unprecedented social changes. Many youth, who no longer have access to substances, have found they can “take it or leave it”. Other youth have been observed engaging in additional risk or going to greater lengths to access substances and continue their use. For both groups and everyone in between, this is an important time for screening, clinical assessment, and support.
While anticipating further research and data regarding broad substance use trends, including MTF data from 2021, recognizing that the impact of the COVID-19 pandemic is individual, with marked differences from adolescent to adolescent, will help us continue to act now to assess this important area of adolescent health. The first step for primary care providers is unchanged: to routinely screen for and discuss substance use in clinical settings.
Two brief, validated, easily accessible screening tools are available for primary care settings. They can both be self-administered and take less than 2 minutes to complete. Screening, Brief Intervention and Referral to Treatment and the Brief Screener for Tobacco, Alcohol and other Drugs can both be used for youth aged 12-17 years.4,5 Both screens are available online at drugabuse.gov.6
Routine screening will normalize conversations about substance use and healthy choices, provide opportunities for positive reinforcement, identify adolescents at risk, increase comfort and competence in providing brief intervention, and expedite referrals for additional support and treatment.
A false assumption that a particular adolescent isn’t using substances creates a missed opportunity to offer guidance and treatment. An oft-overlooked opportunity is that of providing positive reinforcement for an adolescent who isn’t using any substances or experimenting at all. Positive reinforcement is a strong component of reinforcing health maintenance.
Parent guidance and family assessment will also be critical tools. Parents and caregivers play a primary role in substance use treatment for teens and have a contributory impact on risk through both genes and environment. Of note, research suggests a moderate overall increase in adult substance use during the pandemic, particularly substances that are widely available such as alcohol. Adolescents may thus have greater access and exposure to substance use. A remarkably high percentage, 42%, of substance-using teens surveyed early in the pandemic indicated that they were using substances with their parents.3 Parents, who have equally been challenged by the pandemic, may need guidance in balancing compassion and support for struggling youth, while setting appropriate limits and maintaining expectations of healthy activities.
Unprecedented change and uncertainty provide an opportunity to reassess risks and openly discuss substance use with youth and families. Even with much on our minds during the COVID-19 pandemic, we can maintain focus on this significant risk to adolescent health and wellness. Our efforts now, from screening to treatment for adolescent substance use should be reinforced rather than delayed.
Dr. Jackson is assistant professor of psychiatry at the University of Vermont, Burlington.
References
1. Monitoringthefuture.org
2. Jones EAK et al. Int J Environ Res Public Health, 2021;18(5):2470.
3. Dumas TM et al. J Adolesc Health, 2020;67(3):354-61.
4. Levy S et al. JAMA Pediatr. 2014;168(9):822-8.
5. Kelly SM et al. Pediatrics. 2014;133(5):819-26.
6. National Institute on Drug Abuse. Adolescent Substance Use Screening Tools. 2016 Apr 27. https://www.drugabuse.gov/nidamed-medical-health-professionals/screening-tools-prevention/screening-tools-adolescent-substance-use/adolescent-substance-use-screening-tools