User login
Expert dispels myths about hair care in patients with skin of color
HONOLULU –
“This is false,” Dr. Heath, director of pediatric dermatology at Temple University, Philadelphia, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! With little manipulation, length may be retained, since tightly coiled hair has a higher likelihood of breakage, she said. “But washing the scalp and hair is recommended for tightly coiled hair weekly or every other week. Exclusively co-washing – a technique where hair conditioner is used instead of shampooing – is also not advised due to scalp build-up.”
Other myths she addressed include the following:
“I have a weak spot (or stress spot) on the top of my scalp.” These terms may be used to describe hair on a spot that goes through cycles of breaking off and re-growing. This is false. “If someone were to say that, and we see short hairs on the top of a patient’s scalp, with or without tenderness, pruritus, or pain, we want to recognize that as possibly an early sign of central centrifugal cicatricial alopecia [CCCA],” she said. “We want to pick up cases of CCCA forme fruste [central hair breakage] early.”
Medicated shampoos are helpful for all patients with seborrheic dermatitis. This notion is more complicated. “In theory, medicated shampoos like ketoconazole should be helpful, but if the shampoos are too drying for the hair and they cause further hair breakage, that’s going to be a problem as well,” explained Dr. Heath, who was the senior author of an article on how to address common conditions affecting pediatric and adolescent patients with skin of color. For patients with tightly coiled hair, she recommends applying antifungal shampoos to the scalp only, waiting 5-10 minutes, rinsing, and shampooing the scalp and hair with a moisturizing shampoo and rinsing. They can then condition with a moisturizing conditioner and style their hair as desired.
Don’t touch a Black woman’s hair. That unwritten rule may apply to a woman you pass on the street, she said, but not during clinical exams in cases where clinicians and patients seeking hair loss treatment have different hair types. “Touch the hair; don’t do a lean-in exam,” emphasized Dr. Heath, who is the inaugural faculty scholar at Temple University Lewis Katz School of Medicine’s Office of Health Equity Diversity, and Inclusion. “You want to perform the scalp and hair exam with cultural humility.” Understanding the patient’s hair care goals and perspective allows dermatologists to take a more individualized approach to their concerns, especially in race-discordant patient-physician interactions.
Going natural (chemical-free) will solve scarring hair loss problems. This is false. “Genetic defects in the hair shaft have been described as the cause of some CCCA cases, so we need to stop solely blaming the patient for that condition,” she said. Dr. Heath noted that the transition point between natural hair and relaxed hair is highly prone to breakage. She suggests low or lower tension options such as knotless braids, and crochet hairstyles, and when patients have locs, they should be shoulder length or higher to reduce tension.
Dr. Heath disclosed that she has served as a consultant or adviser for Arcutis, CeraVe, Janssen Pharmaceuticals, Johnson & Johnson Pharmaceutical Research & Development, Leo, Lilly, Pfizer, and Regeneron Pharmaceuticals.
Medscape and this news organization are owned by the same parent company.
HONOLULU –
“This is false,” Dr. Heath, director of pediatric dermatology at Temple University, Philadelphia, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! With little manipulation, length may be retained, since tightly coiled hair has a higher likelihood of breakage, she said. “But washing the scalp and hair is recommended for tightly coiled hair weekly or every other week. Exclusively co-washing – a technique where hair conditioner is used instead of shampooing – is also not advised due to scalp build-up.”
Other myths she addressed include the following:
“I have a weak spot (or stress spot) on the top of my scalp.” These terms may be used to describe hair on a spot that goes through cycles of breaking off and re-growing. This is false. “If someone were to say that, and we see short hairs on the top of a patient’s scalp, with or without tenderness, pruritus, or pain, we want to recognize that as possibly an early sign of central centrifugal cicatricial alopecia [CCCA],” she said. “We want to pick up cases of CCCA forme fruste [central hair breakage] early.”
Medicated shampoos are helpful for all patients with seborrheic dermatitis. This notion is more complicated. “In theory, medicated shampoos like ketoconazole should be helpful, but if the shampoos are too drying for the hair and they cause further hair breakage, that’s going to be a problem as well,” explained Dr. Heath, who was the senior author of an article on how to address common conditions affecting pediatric and adolescent patients with skin of color. For patients with tightly coiled hair, she recommends applying antifungal shampoos to the scalp only, waiting 5-10 minutes, rinsing, and shampooing the scalp and hair with a moisturizing shampoo and rinsing. They can then condition with a moisturizing conditioner and style their hair as desired.
Don’t touch a Black woman’s hair. That unwritten rule may apply to a woman you pass on the street, she said, but not during clinical exams in cases where clinicians and patients seeking hair loss treatment have different hair types. “Touch the hair; don’t do a lean-in exam,” emphasized Dr. Heath, who is the inaugural faculty scholar at Temple University Lewis Katz School of Medicine’s Office of Health Equity Diversity, and Inclusion. “You want to perform the scalp and hair exam with cultural humility.” Understanding the patient’s hair care goals and perspective allows dermatologists to take a more individualized approach to their concerns, especially in race-discordant patient-physician interactions.
Going natural (chemical-free) will solve scarring hair loss problems. This is false. “Genetic defects in the hair shaft have been described as the cause of some CCCA cases, so we need to stop solely blaming the patient for that condition,” she said. Dr. Heath noted that the transition point between natural hair and relaxed hair is highly prone to breakage. She suggests low or lower tension options such as knotless braids, and crochet hairstyles, and when patients have locs, they should be shoulder length or higher to reduce tension.
Dr. Heath disclosed that she has served as a consultant or adviser for Arcutis, CeraVe, Janssen Pharmaceuticals, Johnson & Johnson Pharmaceutical Research & Development, Leo, Lilly, Pfizer, and Regeneron Pharmaceuticals.
Medscape and this news organization are owned by the same parent company.
HONOLULU –
“This is false,” Dr. Heath, director of pediatric dermatology at Temple University, Philadelphia, said at the Hawaii Dermatology Seminar provided by MedscapeLIVE! With little manipulation, length may be retained, since tightly coiled hair has a higher likelihood of breakage, she said. “But washing the scalp and hair is recommended for tightly coiled hair weekly or every other week. Exclusively co-washing – a technique where hair conditioner is used instead of shampooing – is also not advised due to scalp build-up.”
Other myths she addressed include the following:
“I have a weak spot (or stress spot) on the top of my scalp.” These terms may be used to describe hair on a spot that goes through cycles of breaking off and re-growing. This is false. “If someone were to say that, and we see short hairs on the top of a patient’s scalp, with or without tenderness, pruritus, or pain, we want to recognize that as possibly an early sign of central centrifugal cicatricial alopecia [CCCA],” she said. “We want to pick up cases of CCCA forme fruste [central hair breakage] early.”
Medicated shampoos are helpful for all patients with seborrheic dermatitis. This notion is more complicated. “In theory, medicated shampoos like ketoconazole should be helpful, but if the shampoos are too drying for the hair and they cause further hair breakage, that’s going to be a problem as well,” explained Dr. Heath, who was the senior author of an article on how to address common conditions affecting pediatric and adolescent patients with skin of color. For patients with tightly coiled hair, she recommends applying antifungal shampoos to the scalp only, waiting 5-10 minutes, rinsing, and shampooing the scalp and hair with a moisturizing shampoo and rinsing. They can then condition with a moisturizing conditioner and style their hair as desired.
Don’t touch a Black woman’s hair. That unwritten rule may apply to a woman you pass on the street, she said, but not during clinical exams in cases where clinicians and patients seeking hair loss treatment have different hair types. “Touch the hair; don’t do a lean-in exam,” emphasized Dr. Heath, who is the inaugural faculty scholar at Temple University Lewis Katz School of Medicine’s Office of Health Equity Diversity, and Inclusion. “You want to perform the scalp and hair exam with cultural humility.” Understanding the patient’s hair care goals and perspective allows dermatologists to take a more individualized approach to their concerns, especially in race-discordant patient-physician interactions.
Going natural (chemical-free) will solve scarring hair loss problems. This is false. “Genetic defects in the hair shaft have been described as the cause of some CCCA cases, so we need to stop solely blaming the patient for that condition,” she said. Dr. Heath noted that the transition point between natural hair and relaxed hair is highly prone to breakage. She suggests low or lower tension options such as knotless braids, and crochet hairstyles, and when patients have locs, they should be shoulder length or higher to reduce tension.
Dr. Heath disclosed that she has served as a consultant or adviser for Arcutis, CeraVe, Janssen Pharmaceuticals, Johnson & Johnson Pharmaceutical Research & Development, Leo, Lilly, Pfizer, and Regeneron Pharmaceuticals.
Medscape and this news organization are owned by the same parent company.
AT THE MEDSCAPE LIVE! HAWAII DERMATOLOGY SEMINAR
Who’s at higher risk for breast cancer recurrence?
New research shows that patients with ER-negative disease have a higher risk of a second breast cancer within a 5-year window post diagnosis, compared with patients with ER-positive disease.
“Our findings suggest that primary breast cancer ER status could be used to identify women at highest risk of second breast cancer events during the early post-treatment period and should be a consideration for guidelines and decision-making regarding surveillance imaging regimens for breast cancer survivors,” the study authors, led by Kathryn P. Lowry, MD, of Fred Hutchinson Cancer Center in Seattle, concluded.
The study was published online in Cancer.
Breast cancer survivors are at risk for a second breast cancer, making ongoing surveillance essential. Surveillance could be informed by better understanding an individual’s recurrence risk, but whether differences exist for women with ER‐positive vs. ER‐negative cancers remains unclear.
Dr. Lowry and colleagues analyzed women diagnosed with stage I-III breast cancer between 2000 and 2017, drawing from six Breast Cancer Surveillance Consortium registries. The team collected information on patients’ ER status as well as second breast cancer events detectable by surveillance imaging. Second breast cancer rates were assessed 1-5 years and 6-10 years after diagnosis. The final study cohort included 23,139 women with ER-positive disease and 4,605 with ER-negative disease.
The researchers found that, at the 5-year mark, the cumulative breast cancer incidence was 7.1% for ER‐negative disease and 3.6% for ER‐positive disease. At the 10-year mark, the cumulative breast cancer incidence was still higher for women with ER-negative disease – 11.8% vs. 7.5% among those with ER-positive disease.
Patients with ER-negative disease also had higher rates of second breast cancers within the first 5 years of follow-ups – 16.0 per 1,000 person‐years vs. 7.8 per 1,000 person‐years for those with ER‐positive breast cancer – though after 5 years, the rates by ER status were similar among the two groups (12.1 per 1,000 vs. 9.3 per 1,000 person‐years, respectively).
Overall, the findings indicate that the “ER status of the primary invasive cancer was an important prognostic factor for both the magnitude and the timing of second breast cancer events,” the authors concluded.
The team noted several limitations to their study, including that information on the presence of pathogenic variants, such as BRCA1 and BRCA2, were not available. Given that these variants tend to be more common among women with ER-negative breast cancers, this could represent a confounder.
Marisa C. Weiss, MD, chief medical officer and founder of Breastcancer.org, who was not involved in the research, highlighted two important details to keep in mind.
“We do know that triple negative breast cancers are associated with a higher risk of having an inherited genetic abnormality like BRCA1, which predicts a higher risk of second malignancies,” said Dr. Weiss, a breast oncologist at Lankenau Medical Center in Wynnewood, Pa. “Also, it should be noted that patients with HR-positive breast cancer have a higher incidence of local recurrence spread out over 10-plus years.”
What might these results mean for practice and following patients over the long term?
According to the researchers, “further study is needed to evaluate whether women with ER‐negative primary cancers may potentially benefit from more intensive surveillance in the early postdiagnosis period.”
Dr. Weiss noted as well that “each person’s situation is unique,” and it is “very important to develop a customized survivorship care plan with close surveillance,” which includes genetic testing.
Dr. Lowry reported grants from the American Cancer Society and personal fees from the Radiological Society of North America outside the submitted work. Several coauthors also reported disclosures. Dr. Weiss reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New research shows that patients with ER-negative disease have a higher risk of a second breast cancer within a 5-year window post diagnosis, compared with patients with ER-positive disease.
“Our findings suggest that primary breast cancer ER status could be used to identify women at highest risk of second breast cancer events during the early post-treatment period and should be a consideration for guidelines and decision-making regarding surveillance imaging regimens for breast cancer survivors,” the study authors, led by Kathryn P. Lowry, MD, of Fred Hutchinson Cancer Center in Seattle, concluded.
The study was published online in Cancer.
Breast cancer survivors are at risk for a second breast cancer, making ongoing surveillance essential. Surveillance could be informed by better understanding an individual’s recurrence risk, but whether differences exist for women with ER‐positive vs. ER‐negative cancers remains unclear.
Dr. Lowry and colleagues analyzed women diagnosed with stage I-III breast cancer between 2000 and 2017, drawing from six Breast Cancer Surveillance Consortium registries. The team collected information on patients’ ER status as well as second breast cancer events detectable by surveillance imaging. Second breast cancer rates were assessed 1-5 years and 6-10 years after diagnosis. The final study cohort included 23,139 women with ER-positive disease and 4,605 with ER-negative disease.
The researchers found that, at the 5-year mark, the cumulative breast cancer incidence was 7.1% for ER‐negative disease and 3.6% for ER‐positive disease. At the 10-year mark, the cumulative breast cancer incidence was still higher for women with ER-negative disease – 11.8% vs. 7.5% among those with ER-positive disease.
Patients with ER-negative disease also had higher rates of second breast cancers within the first 5 years of follow-ups – 16.0 per 1,000 person‐years vs. 7.8 per 1,000 person‐years for those with ER‐positive breast cancer – though after 5 years, the rates by ER status were similar among the two groups (12.1 per 1,000 vs. 9.3 per 1,000 person‐years, respectively).
Overall, the findings indicate that the “ER status of the primary invasive cancer was an important prognostic factor for both the magnitude and the timing of second breast cancer events,” the authors concluded.
The team noted several limitations to their study, including that information on the presence of pathogenic variants, such as BRCA1 and BRCA2, were not available. Given that these variants tend to be more common among women with ER-negative breast cancers, this could represent a confounder.
Marisa C. Weiss, MD, chief medical officer and founder of Breastcancer.org, who was not involved in the research, highlighted two important details to keep in mind.
“We do know that triple negative breast cancers are associated with a higher risk of having an inherited genetic abnormality like BRCA1, which predicts a higher risk of second malignancies,” said Dr. Weiss, a breast oncologist at Lankenau Medical Center in Wynnewood, Pa. “Also, it should be noted that patients with HR-positive breast cancer have a higher incidence of local recurrence spread out over 10-plus years.”
What might these results mean for practice and following patients over the long term?
According to the researchers, “further study is needed to evaluate whether women with ER‐negative primary cancers may potentially benefit from more intensive surveillance in the early postdiagnosis period.”
Dr. Weiss noted as well that “each person’s situation is unique,” and it is “very important to develop a customized survivorship care plan with close surveillance,” which includes genetic testing.
Dr. Lowry reported grants from the American Cancer Society and personal fees from the Radiological Society of North America outside the submitted work. Several coauthors also reported disclosures. Dr. Weiss reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New research shows that patients with ER-negative disease have a higher risk of a second breast cancer within a 5-year window post diagnosis, compared with patients with ER-positive disease.
“Our findings suggest that primary breast cancer ER status could be used to identify women at highest risk of second breast cancer events during the early post-treatment period and should be a consideration for guidelines and decision-making regarding surveillance imaging regimens for breast cancer survivors,” the study authors, led by Kathryn P. Lowry, MD, of Fred Hutchinson Cancer Center in Seattle, concluded.
The study was published online in Cancer.
Breast cancer survivors are at risk for a second breast cancer, making ongoing surveillance essential. Surveillance could be informed by better understanding an individual’s recurrence risk, but whether differences exist for women with ER‐positive vs. ER‐negative cancers remains unclear.
Dr. Lowry and colleagues analyzed women diagnosed with stage I-III breast cancer between 2000 and 2017, drawing from six Breast Cancer Surveillance Consortium registries. The team collected information on patients’ ER status as well as second breast cancer events detectable by surveillance imaging. Second breast cancer rates were assessed 1-5 years and 6-10 years after diagnosis. The final study cohort included 23,139 women with ER-positive disease and 4,605 with ER-negative disease.
The researchers found that, at the 5-year mark, the cumulative breast cancer incidence was 7.1% for ER‐negative disease and 3.6% for ER‐positive disease. At the 10-year mark, the cumulative breast cancer incidence was still higher for women with ER-negative disease – 11.8% vs. 7.5% among those with ER-positive disease.
Patients with ER-negative disease also had higher rates of second breast cancers within the first 5 years of follow-ups – 16.0 per 1,000 person‐years vs. 7.8 per 1,000 person‐years for those with ER‐positive breast cancer – though after 5 years, the rates by ER status were similar among the two groups (12.1 per 1,000 vs. 9.3 per 1,000 person‐years, respectively).
Overall, the findings indicate that the “ER status of the primary invasive cancer was an important prognostic factor for both the magnitude and the timing of second breast cancer events,” the authors concluded.
The team noted several limitations to their study, including that information on the presence of pathogenic variants, such as BRCA1 and BRCA2, were not available. Given that these variants tend to be more common among women with ER-negative breast cancers, this could represent a confounder.
Marisa C. Weiss, MD, chief medical officer and founder of Breastcancer.org, who was not involved in the research, highlighted two important details to keep in mind.
“We do know that triple negative breast cancers are associated with a higher risk of having an inherited genetic abnormality like BRCA1, which predicts a higher risk of second malignancies,” said Dr. Weiss, a breast oncologist at Lankenau Medical Center in Wynnewood, Pa. “Also, it should be noted that patients with HR-positive breast cancer have a higher incidence of local recurrence spread out over 10-plus years.”
What might these results mean for practice and following patients over the long term?
According to the researchers, “further study is needed to evaluate whether women with ER‐negative primary cancers may potentially benefit from more intensive surveillance in the early postdiagnosis period.”
Dr. Weiss noted as well that “each person’s situation is unique,” and it is “very important to develop a customized survivorship care plan with close surveillance,” which includes genetic testing.
Dr. Lowry reported grants from the American Cancer Society and personal fees from the Radiological Society of North America outside the submitted work. Several coauthors also reported disclosures. Dr. Weiss reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANCER
Commentary: Sorting out useful atopic dermatitis research from filler, March 2023
Another study caught my attention this month for having presented a lot of information with no clinically important conclusions. In "Mode of Delivery and Offspring Atopic Dermatitis in a Swedish Nationwide Study," Mubanga and colleagues studied 1.4 million children! With that many participants, they were almost certain to find associations that were statistically significant and clinically irrelevant. They reported that children born by instrumental vaginal delivery, emergency caesarean section, and elective caesarean section were at a higher risk for AD compared with those born by uncomplicated vaginal delivery. They failed to report the absolute magnitude of the associations, which were undoubtedly so small as to be clinically meaningless. Even if the observed association were not due to some hidden bias, the association is not anything that would change treatment in any way.
On the other hand, the small, open label registry analysis, "Experiences From Daily Practice of Upadacitinib Treatment on Atopic Dermatitis With a Focus on Hand Eczema: Results From the BioDay Registry," published by Kamphuis and colleagues, is of much greater value, reporting the effectiveness and safety of upadacitinib on hand eczema. Not surprisingly, there were large improvements in the investigators' assessments of the dermatitis and in patients' quality of life. This small study is informative about efficacy; it is too small, though, to evaluate how frequently rare severe adverse events occur.
The use of probiotics to safely improve skin disease is such an appealing concept, yet it sounds a lot like hocus-pocus to me. Feíto-Rodríguez and colleagues report in the journal Clinical and Experimental Dermatology that a probiotic mixture of Bifidobacterium lactis, Bifidobacterium longum, and Lactobacillus casei improved atopic dermatitis more than did placebo. The findings are not compelling. Differences were small. Rates of being clear or almost clear weren't reported. We can get atopic dermatitis to clear up in a few days with topical triamcinolone (if we can get patients to use it); so far, the effects of probiotics on the presumed gut-immune system-skin axis seem very much underwhelming.
Another study caught my attention this month for having presented a lot of information with no clinically important conclusions. In "Mode of Delivery and Offspring Atopic Dermatitis in a Swedish Nationwide Study," Mubanga and colleagues studied 1.4 million children! With that many participants, they were almost certain to find associations that were statistically significant and clinically irrelevant. They reported that children born by instrumental vaginal delivery, emergency caesarean section, and elective caesarean section were at a higher risk for AD compared with those born by uncomplicated vaginal delivery. They failed to report the absolute magnitude of the associations, which were undoubtedly so small as to be clinically meaningless. Even if the observed association were not due to some hidden bias, the association is not anything that would change treatment in any way.
On the other hand, the small, open label registry analysis, "Experiences From Daily Practice of Upadacitinib Treatment on Atopic Dermatitis With a Focus on Hand Eczema: Results From the BioDay Registry," published by Kamphuis and colleagues, is of much greater value, reporting the effectiveness and safety of upadacitinib on hand eczema. Not surprisingly, there were large improvements in the investigators' assessments of the dermatitis and in patients' quality of life. This small study is informative about efficacy; it is too small, though, to evaluate how frequently rare severe adverse events occur.
The use of probiotics to safely improve skin disease is such an appealing concept, yet it sounds a lot like hocus-pocus to me. Feíto-Rodríguez and colleagues report in the journal Clinical and Experimental Dermatology that a probiotic mixture of Bifidobacterium lactis, Bifidobacterium longum, and Lactobacillus casei improved atopic dermatitis more than did placebo. The findings are not compelling. Differences were small. Rates of being clear or almost clear weren't reported. We can get atopic dermatitis to clear up in a few days with topical triamcinolone (if we can get patients to use it); so far, the effects of probiotics on the presumed gut-immune system-skin axis seem very much underwhelming.
Another study caught my attention this month for having presented a lot of information with no clinically important conclusions. In "Mode of Delivery and Offspring Atopic Dermatitis in a Swedish Nationwide Study," Mubanga and colleagues studied 1.4 million children! With that many participants, they were almost certain to find associations that were statistically significant and clinically irrelevant. They reported that children born by instrumental vaginal delivery, emergency caesarean section, and elective caesarean section were at a higher risk for AD compared with those born by uncomplicated vaginal delivery. They failed to report the absolute magnitude of the associations, which were undoubtedly so small as to be clinically meaningless. Even if the observed association were not due to some hidden bias, the association is not anything that would change treatment in any way.
On the other hand, the small, open label registry analysis, "Experiences From Daily Practice of Upadacitinib Treatment on Atopic Dermatitis With a Focus on Hand Eczema: Results From the BioDay Registry," published by Kamphuis and colleagues, is of much greater value, reporting the effectiveness and safety of upadacitinib on hand eczema. Not surprisingly, there were large improvements in the investigators' assessments of the dermatitis and in patients' quality of life. This small study is informative about efficacy; it is too small, though, to evaluate how frequently rare severe adverse events occur.
The use of probiotics to safely improve skin disease is such an appealing concept, yet it sounds a lot like hocus-pocus to me. Feíto-Rodríguez and colleagues report in the journal Clinical and Experimental Dermatology that a probiotic mixture of Bifidobacterium lactis, Bifidobacterium longum, and Lactobacillus casei improved atopic dermatitis more than did placebo. The findings are not compelling. Differences were small. Rates of being clear or almost clear weren't reported. We can get atopic dermatitis to clear up in a few days with topical triamcinolone (if we can get patients to use it); so far, the effects of probiotics on the presumed gut-immune system-skin axis seem very much underwhelming.
Back pain: Red flags and when to image
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. On tonight’s episode, we are going to be talking about back pain. I’ll use one of my famous teaching techniques: If the patient has any kind of back pain, they should just not move. Right?
Paul N. Williams, MD: That’s right, Matt – we should recommend bedrest until they get better for anyone who has any back pain? No. For back pain, early activity and exercise are great. Patients are often concerned that physical therapy will make their pain worse, so they don’t exercise. This misunderstanding is not surprising. They believe that if they are experiencing pain, it’s facilitating more damage, which is not necessarily the case. It will get better, and a little bit of anticipatory guidance goes a long way in terms of managing patient expectations related to early mobilization, early exercise, and physical therapy.
Dr. Watto: Absolutely. One of the goals of treatment is symptom relief to the extent that we’re able to achieve. We’re not expecting the pain to go to zero. That just doesn’t happen, especially if someone’s on a medication long term. Another goal is return to function. We want them sleeping. We want them to be able to tolerate movement.
We have medications – NSAIDs and muscle relaxants, which are actually tranquilizers. But most therapy for back pain doesn’t involve medications. It involves active movement, so we have to find movement that the patient enjoys doing. Passive treatments, things being done to patients, just don’t work as well.
Dr. Williams: We should be clear – we’re talking primarily about chronic back pain here. For acute back pain, we actually have some decent medications, but acute back pain tends to improve no matter what you do. We don’t have much to offer pharmacologically for chronic low back pain. The best modalities usually involve physical activity of some kind.
Dr. Watto: Let’s discuss the evaluation of back pain. Something that always comes up: Should we order imaging, and is there a right time to get it? Dr. Baraki was very clear about when to do imaging. Two big buckets of patients might need imaging.
First, a patient who has a serious underlying condition and you’re using imaging to try to diagnose it; or in a chronic setting, a patient who needs surgery, and imaging is part of the presurgical evaluation. We talked about red flags.
The red flags are major trauma, where we have reason to believe there might be something going on – if we strongly suspect infection, or the patient is injecting drugs. If the patient has a history of cancer, we would be worried that they might have a recurrence. Those are some of the main red flags. With a patient who has osteoporosis or is on chronic steroids, you might even be able to get by with plain films instead of an MRI to look for fracture.
The other thing I wanted to ask you about is, when should we get imaging? Are there any pitfalls we need to worry about?
Dr. Williams: I always like podcasts I’m not on because I enjoy listening to them much more. Dr. Baraki talked about the very specific language that is used in radiology reports, such as spondylitis, spondylolysis, and multilevel degenerative disease. They sound bad, but if they are just reframed as age-related degenerative changes, that sounds so much more benign. When discussing with patients, we should avoid medical jargon and say that we saw some changes that we would expect for someone of your age. That sounds so much better than saying we saw multilevel degenerative disease, which sounds like an alarming pathology if you’re not a physician. Without being inaccurate, we should frame the discussion such that we aren’t providing a very specific diagnosis, because that is rarely the case with chronic low back pain. Typically, many things are going on and you may never identify a single unifying diagnosis, which doesn’t tend to help anyway.
Dr. Watto: There’s evidence showing that if the radiology report uses clinical terminology that both clinician and patient think of as less serious, they are less likely to proceed to more invasive treatments. Calling an episode of back pain a “lumbar strain” helps the patient understand that this is a pretty common thing. Almost everyone is going to have an episode of back pain at some point in their life, and almost all of them will get better. Most of the time there’s no serious underlying condition.
This was a great discussion with Dr. Baraki. Click on Back Pain Update with Dr Austin Baraki to hear the full discussion. Until next time, I’ve been Dr. Matthew Frank Watto.
Dr. Williams: And I’m Dr. Paul Nelson Williams.
Dr. Watto is Clinical Assistant Professor, Department of Medicine, University of Pennsylvania, Philadelphia. Dr. Williams is Associate Professor of Clinical Medicine, Department of General Internal Medicine, Temple University, Philadelphia. Neither reported any conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. On tonight’s episode, we are going to be talking about back pain. I’ll use one of my famous teaching techniques: If the patient has any kind of back pain, they should just not move. Right?
Paul N. Williams, MD: That’s right, Matt – we should recommend bedrest until they get better for anyone who has any back pain? No. For back pain, early activity and exercise are great. Patients are often concerned that physical therapy will make their pain worse, so they don’t exercise. This misunderstanding is not surprising. They believe that if they are experiencing pain, it’s facilitating more damage, which is not necessarily the case. It will get better, and a little bit of anticipatory guidance goes a long way in terms of managing patient expectations related to early mobilization, early exercise, and physical therapy.
Dr. Watto: Absolutely. One of the goals of treatment is symptom relief to the extent that we’re able to achieve. We’re not expecting the pain to go to zero. That just doesn’t happen, especially if someone’s on a medication long term. Another goal is return to function. We want them sleeping. We want them to be able to tolerate movement.
We have medications – NSAIDs and muscle relaxants, which are actually tranquilizers. But most therapy for back pain doesn’t involve medications. It involves active movement, so we have to find movement that the patient enjoys doing. Passive treatments, things being done to patients, just don’t work as well.
Dr. Williams: We should be clear – we’re talking primarily about chronic back pain here. For acute back pain, we actually have some decent medications, but acute back pain tends to improve no matter what you do. We don’t have much to offer pharmacologically for chronic low back pain. The best modalities usually involve physical activity of some kind.
Dr. Watto: Let’s discuss the evaluation of back pain. Something that always comes up: Should we order imaging, and is there a right time to get it? Dr. Baraki was very clear about when to do imaging. Two big buckets of patients might need imaging.
First, a patient who has a serious underlying condition and you’re using imaging to try to diagnose it; or in a chronic setting, a patient who needs surgery, and imaging is part of the presurgical evaluation. We talked about red flags.
The red flags are major trauma, where we have reason to believe there might be something going on – if we strongly suspect infection, or the patient is injecting drugs. If the patient has a history of cancer, we would be worried that they might have a recurrence. Those are some of the main red flags. With a patient who has osteoporosis or is on chronic steroids, you might even be able to get by with plain films instead of an MRI to look for fracture.
The other thing I wanted to ask you about is, when should we get imaging? Are there any pitfalls we need to worry about?
Dr. Williams: I always like podcasts I’m not on because I enjoy listening to them much more. Dr. Baraki talked about the very specific language that is used in radiology reports, such as spondylitis, spondylolysis, and multilevel degenerative disease. They sound bad, but if they are just reframed as age-related degenerative changes, that sounds so much more benign. When discussing with patients, we should avoid medical jargon and say that we saw some changes that we would expect for someone of your age. That sounds so much better than saying we saw multilevel degenerative disease, which sounds like an alarming pathology if you’re not a physician. Without being inaccurate, we should frame the discussion such that we aren’t providing a very specific diagnosis, because that is rarely the case with chronic low back pain. Typically, many things are going on and you may never identify a single unifying diagnosis, which doesn’t tend to help anyway.
Dr. Watto: There’s evidence showing that if the radiology report uses clinical terminology that both clinician and patient think of as less serious, they are less likely to proceed to more invasive treatments. Calling an episode of back pain a “lumbar strain” helps the patient understand that this is a pretty common thing. Almost everyone is going to have an episode of back pain at some point in their life, and almost all of them will get better. Most of the time there’s no serious underlying condition.
This was a great discussion with Dr. Baraki. Click on Back Pain Update with Dr Austin Baraki to hear the full discussion. Until next time, I’ve been Dr. Matthew Frank Watto.
Dr. Williams: And I’m Dr. Paul Nelson Williams.
Dr. Watto is Clinical Assistant Professor, Department of Medicine, University of Pennsylvania, Philadelphia. Dr. Williams is Associate Professor of Clinical Medicine, Department of General Internal Medicine, Temple University, Philadelphia. Neither reported any conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Matthew F. Watto, MD: Welcome back to The Curbsiders. On tonight’s episode, we are going to be talking about back pain. I’ll use one of my famous teaching techniques: If the patient has any kind of back pain, they should just not move. Right?
Paul N. Williams, MD: That’s right, Matt – we should recommend bedrest until they get better for anyone who has any back pain? No. For back pain, early activity and exercise are great. Patients are often concerned that physical therapy will make their pain worse, so they don’t exercise. This misunderstanding is not surprising. They believe that if they are experiencing pain, it’s facilitating more damage, which is not necessarily the case. It will get better, and a little bit of anticipatory guidance goes a long way in terms of managing patient expectations related to early mobilization, early exercise, and physical therapy.
Dr. Watto: Absolutely. One of the goals of treatment is symptom relief to the extent that we’re able to achieve. We’re not expecting the pain to go to zero. That just doesn’t happen, especially if someone’s on a medication long term. Another goal is return to function. We want them sleeping. We want them to be able to tolerate movement.
We have medications – NSAIDs and muscle relaxants, which are actually tranquilizers. But most therapy for back pain doesn’t involve medications. It involves active movement, so we have to find movement that the patient enjoys doing. Passive treatments, things being done to patients, just don’t work as well.
Dr. Williams: We should be clear – we’re talking primarily about chronic back pain here. For acute back pain, we actually have some decent medications, but acute back pain tends to improve no matter what you do. We don’t have much to offer pharmacologically for chronic low back pain. The best modalities usually involve physical activity of some kind.
Dr. Watto: Let’s discuss the evaluation of back pain. Something that always comes up: Should we order imaging, and is there a right time to get it? Dr. Baraki was very clear about when to do imaging. Two big buckets of patients might need imaging.
First, a patient who has a serious underlying condition and you’re using imaging to try to diagnose it; or in a chronic setting, a patient who needs surgery, and imaging is part of the presurgical evaluation. We talked about red flags.
The red flags are major trauma, where we have reason to believe there might be something going on – if we strongly suspect infection, or the patient is injecting drugs. If the patient has a history of cancer, we would be worried that they might have a recurrence. Those are some of the main red flags. With a patient who has osteoporosis or is on chronic steroids, you might even be able to get by with plain films instead of an MRI to look for fracture.
The other thing I wanted to ask you about is, when should we get imaging? Are there any pitfalls we need to worry about?
Dr. Williams: I always like podcasts I’m not on because I enjoy listening to them much more. Dr. Baraki talked about the very specific language that is used in radiology reports, such as spondylitis, spondylolysis, and multilevel degenerative disease. They sound bad, but if they are just reframed as age-related degenerative changes, that sounds so much more benign. When discussing with patients, we should avoid medical jargon and say that we saw some changes that we would expect for someone of your age. That sounds so much better than saying we saw multilevel degenerative disease, which sounds like an alarming pathology if you’re not a physician. Without being inaccurate, we should frame the discussion such that we aren’t providing a very specific diagnosis, because that is rarely the case with chronic low back pain. Typically, many things are going on and you may never identify a single unifying diagnosis, which doesn’t tend to help anyway.
Dr. Watto: There’s evidence showing that if the radiology report uses clinical terminology that both clinician and patient think of as less serious, they are less likely to proceed to more invasive treatments. Calling an episode of back pain a “lumbar strain” helps the patient understand that this is a pretty common thing. Almost everyone is going to have an episode of back pain at some point in their life, and almost all of them will get better. Most of the time there’s no serious underlying condition.
This was a great discussion with Dr. Baraki. Click on Back Pain Update with Dr Austin Baraki to hear the full discussion. Until next time, I’ve been Dr. Matthew Frank Watto.
Dr. Williams: And I’m Dr. Paul Nelson Williams.
Dr. Watto is Clinical Assistant Professor, Department of Medicine, University of Pennsylvania, Philadelphia. Dr. Williams is Associate Professor of Clinical Medicine, Department of General Internal Medicine, Temple University, Philadelphia. Neither reported any conflicts of interest.
A version of this article first appeared on Medscape.com.
Commentary: Concerning PsA treatments and comorbidities, March 2023
With regard to advanced targeted therapies, there is concern about the side effects of Janus kinase (JAK) inhibitors, especially in patients with comorbidities. To address safety concerns with upadacitinib, a selective JAK1 inhibitor, Burmester and colleagues conducted an integrated safety analysis of 12 phase 3 trials that included 6991 patients (PsA n = 907; rheumatoid arthritis [RA] n = 3209; ankylosing spondylitis n = 182; and atopic dermatitis n = 2693) who received upadacitinib (15 or 30 mg once daily). Some trials included active comparators; therefore, safety among 1008 patients (RA n = 579; PsA n = 429) who received 40-mg adalimumab every other week and 314 patients with RA who received methotrexate were compared with those treated with upadacitinib. Overall, patients with PsA receiving 15-mg upadacitinib once daily had acceptable rates of treatment-emergent adverse events (TEAE; 244.8/100 patient-years [PY]), serious TEAE (11.1/100 PY), TEAE leading to discontinuation (5.4/100 PY), and death (0.8/100 PY). Patients with PsA treated with upadacitinib had higher rates of herpes zoster, nonmelanoma skin cancer, and elevations in creatine phosphokinase when compared with patients treated with adalimumab. Although these results are reassuring to clinicians treating PsA, continued surveillance regarding the risks for venous thrombosis, cardiovascular events, and cancer are required.
In a post hoc analysis of 10 clinical trials that included patients with PsA (n = 783) and psoriasis (n = 3663) who received tofacitinib, Kristensen and colleagues reported that the risk for major adverse cardiac events was higher among patients with PsA and a high 10-year atherosclerotic cardiovascular disease (ASCVD) risk vs patients with a low ASCVD risk. The incidence of cancer was highest in patients with PsA and an intermediate 10-year ASCVD risk. Although these studies are reassuring, the assessment and risk stratification of adverse events with JAK inhibitors and therapies in PsA will require longer-term comparative clinical trials as well as an evaluation of observational data from disease registries.
Comorbidities also have an impact on treatment persistence in PsA. Tillett and colleagues conducted a retrospective study including 9057 patients with plaque psoriasis alone or with concomitant PsA who received either ustekinumab or conventional systemic disease-modifying antirheumatic drugs. They demonstrated that among patients receiving ustekinumab, those with concomitant PsA had a higher comorbidity burden, including diabetes, hypertension, and obesity, and a shorter time to ustekinumab discontinuation when compared with those with psoriasis alone. Secondary failure of advanced therapies is increasingly noted in the management of psoriatic disease. Female sex, depression, previous exposure to biologics, and the presence of comorbidities are important risk factors. Comprehensive management of psoriatic disease should include appropriate management of comorbidities for better long-term treatment persistence and outcomes.
With regard to advanced targeted therapies, there is concern about the side effects of Janus kinase (JAK) inhibitors, especially in patients with comorbidities. To address safety concerns with upadacitinib, a selective JAK1 inhibitor, Burmester and colleagues conducted an integrated safety analysis of 12 phase 3 trials that included 6991 patients (PsA n = 907; rheumatoid arthritis [RA] n = 3209; ankylosing spondylitis n = 182; and atopic dermatitis n = 2693) who received upadacitinib (15 or 30 mg once daily). Some trials included active comparators; therefore, safety among 1008 patients (RA n = 579; PsA n = 429) who received 40-mg adalimumab every other week and 314 patients with RA who received methotrexate were compared with those treated with upadacitinib. Overall, patients with PsA receiving 15-mg upadacitinib once daily had acceptable rates of treatment-emergent adverse events (TEAE; 244.8/100 patient-years [PY]), serious TEAE (11.1/100 PY), TEAE leading to discontinuation (5.4/100 PY), and death (0.8/100 PY). Patients with PsA treated with upadacitinib had higher rates of herpes zoster, nonmelanoma skin cancer, and elevations in creatine phosphokinase when compared with patients treated with adalimumab. Although these results are reassuring to clinicians treating PsA, continued surveillance regarding the risks for venous thrombosis, cardiovascular events, and cancer are required.
In a post hoc analysis of 10 clinical trials that included patients with PsA (n = 783) and psoriasis (n = 3663) who received tofacitinib, Kristensen and colleagues reported that the risk for major adverse cardiac events was higher among patients with PsA and a high 10-year atherosclerotic cardiovascular disease (ASCVD) risk vs patients with a low ASCVD risk. The incidence of cancer was highest in patients with PsA and an intermediate 10-year ASCVD risk. Although these studies are reassuring, the assessment and risk stratification of adverse events with JAK inhibitors and therapies in PsA will require longer-term comparative clinical trials as well as an evaluation of observational data from disease registries.
Comorbidities also have an impact on treatment persistence in PsA. Tillett and colleagues conducted a retrospective study including 9057 patients with plaque psoriasis alone or with concomitant PsA who received either ustekinumab or conventional systemic disease-modifying antirheumatic drugs. They demonstrated that among patients receiving ustekinumab, those with concomitant PsA had a higher comorbidity burden, including diabetes, hypertension, and obesity, and a shorter time to ustekinumab discontinuation when compared with those with psoriasis alone. Secondary failure of advanced therapies is increasingly noted in the management of psoriatic disease. Female sex, depression, previous exposure to biologics, and the presence of comorbidities are important risk factors. Comprehensive management of psoriatic disease should include appropriate management of comorbidities for better long-term treatment persistence and outcomes.
With regard to advanced targeted therapies, there is concern about the side effects of Janus kinase (JAK) inhibitors, especially in patients with comorbidities. To address safety concerns with upadacitinib, a selective JAK1 inhibitor, Burmester and colleagues conducted an integrated safety analysis of 12 phase 3 trials that included 6991 patients (PsA n = 907; rheumatoid arthritis [RA] n = 3209; ankylosing spondylitis n = 182; and atopic dermatitis n = 2693) who received upadacitinib (15 or 30 mg once daily). Some trials included active comparators; therefore, safety among 1008 patients (RA n = 579; PsA n = 429) who received 40-mg adalimumab every other week and 314 patients with RA who received methotrexate were compared with those treated with upadacitinib. Overall, patients with PsA receiving 15-mg upadacitinib once daily had acceptable rates of treatment-emergent adverse events (TEAE; 244.8/100 patient-years [PY]), serious TEAE (11.1/100 PY), TEAE leading to discontinuation (5.4/100 PY), and death (0.8/100 PY). Patients with PsA treated with upadacitinib had higher rates of herpes zoster, nonmelanoma skin cancer, and elevations in creatine phosphokinase when compared with patients treated with adalimumab. Although these results are reassuring to clinicians treating PsA, continued surveillance regarding the risks for venous thrombosis, cardiovascular events, and cancer are required.
In a post hoc analysis of 10 clinical trials that included patients with PsA (n = 783) and psoriasis (n = 3663) who received tofacitinib, Kristensen and colleagues reported that the risk for major adverse cardiac events was higher among patients with PsA and a high 10-year atherosclerotic cardiovascular disease (ASCVD) risk vs patients with a low ASCVD risk. The incidence of cancer was highest in patients with PsA and an intermediate 10-year ASCVD risk. Although these studies are reassuring, the assessment and risk stratification of adverse events with JAK inhibitors and therapies in PsA will require longer-term comparative clinical trials as well as an evaluation of observational data from disease registries.
Comorbidities also have an impact on treatment persistence in PsA. Tillett and colleagues conducted a retrospective study including 9057 patients with plaque psoriasis alone or with concomitant PsA who received either ustekinumab or conventional systemic disease-modifying antirheumatic drugs. They demonstrated that among patients receiving ustekinumab, those with concomitant PsA had a higher comorbidity burden, including diabetes, hypertension, and obesity, and a shorter time to ustekinumab discontinuation when compared with those with psoriasis alone. Secondary failure of advanced therapies is increasingly noted in the management of psoriatic disease. Female sex, depression, previous exposure to biologics, and the presence of comorbidities are important risk factors. Comprehensive management of psoriatic disease should include appropriate management of comorbidities for better long-term treatment persistence and outcomes.
ESMO guidelines provide ‘clear blueprint’ for managing immunotherapy toxicities
This transcript has been edited for clarity.
I’m David Kerr, professor of cancer medicine at the University of Oxford. I’d like to talk to you today about something specific and generic around guidelines.
It’s around the management of toxicities from immunotherapy, and it’s the ESMO Clinical Practice Guideline for diagnosis, treatment, and follow-up, delivered by Dr. Haanen and, of course, a number of colleagues on behalf of the wider committee.
Have a look at it. I’m not going to talk about the details of it. It’s very well written. It’s very clear and evidence based, of course. There are many helpful hints and a very clear blueprint as to how we should better manage the myriad of potential side effects from immunotherapy.
It tells us a little about the basis of the science, some of the mechanistic work that’s going on in allowing us to understand why some people react in such different ways, almost as if the immune systems are primed to overreact. It gives a very helpful, stepwise look at how we best diagnose, manage, and, in the longer term, follow up patients who have problems with these very important drugs.
All of us recognize the extraordinary impact they’ve made across a wide range of different tumor types, and therefore, as practicing oncologists and health care professionals in the field, all of us need to understand better the details as to how we better care for our patients on these drugs.
Have a look at it. It’s well written and useful, and I think it’s a document that I’ll turn to when I’m looking for a refresher or advice in the future.
The generic focus is about guidelines. Many years ago, I was one of the architects of the British National Cancer Plan, and for me, there were four simple principles at that stage in our development of how we would improve the delivery of cancer control in the United Kingdom. It was around site specialization, particularly of our surgical colleagues who embraced this with vigor. God bless them.
It was using guidelines to help level up the quality of treatment that we were giving, of course underpinned by research, and using – one would hope – modern IT and telecommunications to improve the networking that we use to deliver multidisciplinary cancer care, one of the key elements. Guidelines were embedded in that.
A couple of years ago, we did a survey of cancer physicians around the world. Almost 30 different countries were represented, and we asked which guidelines were most used. It was a very interesting set of responses. The three dominant guidelines – this will surprise no one – are the NCCN (National Comprehensive Cancer Network) guidelines, the ESMO guidelines, and the ASCO (American Society of Clinical Oncology) guidelines.
Rather than selecting one and one being completely dominant, what seemed to be the case is that our colleagues around the world dipped in and used all three. They may prefer NCCN for some particular tumor type or some particular aspect of how they’re structured, but at the same time, we would dip into the ESMO guidelines for specific bits of help, as well as the ASCO guidelines.
I find this fascinating. I assume that in different regions, depending on how they were affiliated in terms of additional training or links to Europe or links to the United States, that one or other of these guideline groups would predominate, but no. In each country, in each region, given the large data bank that we have of guidelines now, it’s a sort of pick-and-mix situation.
I was initially surprised but then took comfort from it. There’s nothing I hate more than the wasted energy of reduplication and saying, well come on, if there is one guideline set that does truly command the attention of the world, then the other should stop. It’s wasted energy, which is something that none of us can afford.
The fact that each of these trusted, evidence-based, beautifully presented guidelines is used in different ways was important. A message to the guideline groups from me is: “Thank you for your professionalism, for the hard work of hundreds of cancer specialists from all different specialties, and for their contribution to developing these guidelines.”
It’s worth it, it’s working, people are using them, and they’re making a difference. It’s all about leveling up the quality of cancer care that we deliver.
Specifically, have a look at the ESMO immune guidelines. They are great. I hope you find them helpful. Generically, thanks to all of you who are contributing and working so hard to make these data available to improve the quality of cancer care around the world.
Thanks for listening, as always. I’m interested in any comments that you might have, but for the time being, Medscapers, ahoy.
David J. Kerr, CBE, MD, DSc, is a professor of cancer medicine at the University of Oxford. He reported conflicts of interest with Celleron Therapeutics, Oxford Cancer Biomarkers, Afrox, GlaxoSmithKline, Bayer, Genomic Health, and Merck Serono.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m David Kerr, professor of cancer medicine at the University of Oxford. I’d like to talk to you today about something specific and generic around guidelines.
It’s around the management of toxicities from immunotherapy, and it’s the ESMO Clinical Practice Guideline for diagnosis, treatment, and follow-up, delivered by Dr. Haanen and, of course, a number of colleagues on behalf of the wider committee.
Have a look at it. I’m not going to talk about the details of it. It’s very well written. It’s very clear and evidence based, of course. There are many helpful hints and a very clear blueprint as to how we should better manage the myriad of potential side effects from immunotherapy.
It tells us a little about the basis of the science, some of the mechanistic work that’s going on in allowing us to understand why some people react in such different ways, almost as if the immune systems are primed to overreact. It gives a very helpful, stepwise look at how we best diagnose, manage, and, in the longer term, follow up patients who have problems with these very important drugs.
All of us recognize the extraordinary impact they’ve made across a wide range of different tumor types, and therefore, as practicing oncologists and health care professionals in the field, all of us need to understand better the details as to how we better care for our patients on these drugs.
Have a look at it. It’s well written and useful, and I think it’s a document that I’ll turn to when I’m looking for a refresher or advice in the future.
The generic focus is about guidelines. Many years ago, I was one of the architects of the British National Cancer Plan, and for me, there were four simple principles at that stage in our development of how we would improve the delivery of cancer control in the United Kingdom. It was around site specialization, particularly of our surgical colleagues who embraced this with vigor. God bless them.
It was using guidelines to help level up the quality of treatment that we were giving, of course underpinned by research, and using – one would hope – modern IT and telecommunications to improve the networking that we use to deliver multidisciplinary cancer care, one of the key elements. Guidelines were embedded in that.
A couple of years ago, we did a survey of cancer physicians around the world. Almost 30 different countries were represented, and we asked which guidelines were most used. It was a very interesting set of responses. The three dominant guidelines – this will surprise no one – are the NCCN (National Comprehensive Cancer Network) guidelines, the ESMO guidelines, and the ASCO (American Society of Clinical Oncology) guidelines.
Rather than selecting one and one being completely dominant, what seemed to be the case is that our colleagues around the world dipped in and used all three. They may prefer NCCN for some particular tumor type or some particular aspect of how they’re structured, but at the same time, we would dip into the ESMO guidelines for specific bits of help, as well as the ASCO guidelines.
I find this fascinating. I assume that in different regions, depending on how they were affiliated in terms of additional training or links to Europe or links to the United States, that one or other of these guideline groups would predominate, but no. In each country, in each region, given the large data bank that we have of guidelines now, it’s a sort of pick-and-mix situation.
I was initially surprised but then took comfort from it. There’s nothing I hate more than the wasted energy of reduplication and saying, well come on, if there is one guideline set that does truly command the attention of the world, then the other should stop. It’s wasted energy, which is something that none of us can afford.
The fact that each of these trusted, evidence-based, beautifully presented guidelines is used in different ways was important. A message to the guideline groups from me is: “Thank you for your professionalism, for the hard work of hundreds of cancer specialists from all different specialties, and for their contribution to developing these guidelines.”
It’s worth it, it’s working, people are using them, and they’re making a difference. It’s all about leveling up the quality of cancer care that we deliver.
Specifically, have a look at the ESMO immune guidelines. They are great. I hope you find them helpful. Generically, thanks to all of you who are contributing and working so hard to make these data available to improve the quality of cancer care around the world.
Thanks for listening, as always. I’m interested in any comments that you might have, but for the time being, Medscapers, ahoy.
David J. Kerr, CBE, MD, DSc, is a professor of cancer medicine at the University of Oxford. He reported conflicts of interest with Celleron Therapeutics, Oxford Cancer Biomarkers, Afrox, GlaxoSmithKline, Bayer, Genomic Health, and Merck Serono.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I’m David Kerr, professor of cancer medicine at the University of Oxford. I’d like to talk to you today about something specific and generic around guidelines.
It’s around the management of toxicities from immunotherapy, and it’s the ESMO Clinical Practice Guideline for diagnosis, treatment, and follow-up, delivered by Dr. Haanen and, of course, a number of colleagues on behalf of the wider committee.
Have a look at it. I’m not going to talk about the details of it. It’s very well written. It’s very clear and evidence based, of course. There are many helpful hints and a very clear blueprint as to how we should better manage the myriad of potential side effects from immunotherapy.
It tells us a little about the basis of the science, some of the mechanistic work that’s going on in allowing us to understand why some people react in such different ways, almost as if the immune systems are primed to overreact. It gives a very helpful, stepwise look at how we best diagnose, manage, and, in the longer term, follow up patients who have problems with these very important drugs.
All of us recognize the extraordinary impact they’ve made across a wide range of different tumor types, and therefore, as practicing oncologists and health care professionals in the field, all of us need to understand better the details as to how we better care for our patients on these drugs.
Have a look at it. It’s well written and useful, and I think it’s a document that I’ll turn to when I’m looking for a refresher or advice in the future.
The generic focus is about guidelines. Many years ago, I was one of the architects of the British National Cancer Plan, and for me, there were four simple principles at that stage in our development of how we would improve the delivery of cancer control in the United Kingdom. It was around site specialization, particularly of our surgical colleagues who embraced this with vigor. God bless them.
It was using guidelines to help level up the quality of treatment that we were giving, of course underpinned by research, and using – one would hope – modern IT and telecommunications to improve the networking that we use to deliver multidisciplinary cancer care, one of the key elements. Guidelines were embedded in that.
A couple of years ago, we did a survey of cancer physicians around the world. Almost 30 different countries were represented, and we asked which guidelines were most used. It was a very interesting set of responses. The three dominant guidelines – this will surprise no one – are the NCCN (National Comprehensive Cancer Network) guidelines, the ESMO guidelines, and the ASCO (American Society of Clinical Oncology) guidelines.
Rather than selecting one and one being completely dominant, what seemed to be the case is that our colleagues around the world dipped in and used all three. They may prefer NCCN for some particular tumor type or some particular aspect of how they’re structured, but at the same time, we would dip into the ESMO guidelines for specific bits of help, as well as the ASCO guidelines.
I find this fascinating. I assume that in different regions, depending on how they were affiliated in terms of additional training or links to Europe or links to the United States, that one or other of these guideline groups would predominate, but no. In each country, in each region, given the large data bank that we have of guidelines now, it’s a sort of pick-and-mix situation.
I was initially surprised but then took comfort from it. There’s nothing I hate more than the wasted energy of reduplication and saying, well come on, if there is one guideline set that does truly command the attention of the world, then the other should stop. It’s wasted energy, which is something that none of us can afford.
The fact that each of these trusted, evidence-based, beautifully presented guidelines is used in different ways was important. A message to the guideline groups from me is: “Thank you for your professionalism, for the hard work of hundreds of cancer specialists from all different specialties, and for their contribution to developing these guidelines.”
It’s worth it, it’s working, people are using them, and they’re making a difference. It’s all about leveling up the quality of cancer care that we deliver.
Specifically, have a look at the ESMO immune guidelines. They are great. I hope you find them helpful. Generically, thanks to all of you who are contributing and working so hard to make these data available to improve the quality of cancer care around the world.
Thanks for listening, as always. I’m interested in any comments that you might have, but for the time being, Medscapers, ahoy.
David J. Kerr, CBE, MD, DSc, is a professor of cancer medicine at the University of Oxford. He reported conflicts of interest with Celleron Therapeutics, Oxford Cancer Biomarkers, Afrox, GlaxoSmithKline, Bayer, Genomic Health, and Merck Serono.
A version of this article first appeared on Medscape.com.
Human and nonhuman milk products have similar effect on preemies’ gut microbiota
No significant differences emerged in gut microbial diversity in preterm infants who exclusively received human milk products, compared with those receiving bovine milk formula or fortifiers, a randomized controlled trial found. Nor were any differences noted in the secondary endpoint of clinical outcomes in the U.K. study, published online in JAMA Network Open.
The finding was unanticipated, according to lead author Nicholas D. Embleton, MBBS, MD, a professor of neonatal medicine at Newcastle University in England. “Over the last 10 years we’ve focused particularly on the role of the microbiome to better understand causal mechanisms of necrotizing enterocolitis, or NEC,” he said in an interview. “We anticipated that an exclusive human milk diet would have measurable impacts on microbiome diversity as a potential mechanism [in] disease modulation as part of the mechanism by which exclusive human milk diets benefit preterm infants.”
Shortfalls in a mother’s own milk supply often necessitate the use of bovine formula or pasteurized human milk from donor milk banks or commercial suppliers.
The effect of an exclusive human milk diet versus one containing bovine products on vulnerable preterm infants is unclear, but some studies have shown lower rates of key neonatal morbidities, possibly mediated by the gut microbiome. In two randomized controlled trials, for example, one showed a lower rate of NEC with donated human milk while the other showed no difference.
Neither, however, was powered to detect a clinically important difference in surgical NEC.
Milk and the microbiome
The current study’s primary endpoint was the effect of an exclusive human milk diet on gut bacterial richness and diversity, as well as the proportions of specific microbial taxa in preterm infants from enrollment to 34 weeks’ postmenstrual age.
Conducted at four neonatal intensive care units in the United Kingdom from 2017 to 2020, the study recruited 126 infants born at less than 30 weeks’ gestation and fed exclusively with their own mother’s milk before 72 hours of age. With a median gestational age of 27 weeks and a median birth weight of just over 900 grams, the babies were randomized 1:1 either to their own mother’s milk plus a pasteurized ready-to-feed human milk product or to their mother’s milk plus a standard preterm formula (controls). Stool samples were collected to analyze intestinal microbiota.
In terms of clinical outcomes, four infants died in the standard-care control group and eight in the intervention group at a median postnatal age of 25 days and 15 days, respectively, but none died primarily of NEC. Formula and ready-to-feed human milk both represented less than 1% of all fluid intake, respectively.
Although there were no effects on overall measures of gut bacterial diversity, there were some insignificant effects on specific bacterial taxa previously associated with human milk feeding. “These findings suggest that the clinical impact of human milk-derived products is not modulated via microbiomic mechanisms,” the authors wrote.
Human milk could benefit, however, via components such as specific oligosaccharides, which act largely by modulating the growth of friendly Bifidobacteria and other species, Dr. Embleton said. “However, it’s possible these oligosaccharides might also directly interact via the gut epithelium as a signaling molecule. And, of course, there are many other components that might also act directly on the gut without changing the microbiome.”
*Commenting on the study but not involved in it, Brenda L. Poindexter, MD, MS, chief of the division of neonatology at Children’s Healthcare of Atlanta and Emory University, called it “incredibly important,” especially in the context of the claims of superiority made by the manufacturers of human-milk-based fortifiers. “These findings convincingly debunk the notion that the use of bovine-derived fortifiers increases risk of morbidities such as NEC through the mechanism of alterations in the microbiome, Dr. Poindexter said.
“They refute that claim as there was no difference in NEC between the groups and, interestingly, no impact on the microbiome. One of the hypothesized mechanisms for those who purport that bovine fortifiers are ‘bad’ is that they alter the microbiome, which increases risk of NEC,” she said. “The only limitation is that the study was not powered to detect a difference in NEC, but it is incredibly important nonetheless.”
The current findings differ somewhat from those of a similar trial from 2022 showing lower microbial diversity and higher relative abundances of Enterobacteriaceae and lower abundances of Clostridium sensu stricto in preterm infants receiving an exclusive human milk diet. “These results highlight how nutrient fortifiers impact the microbiota of very-low-birth-weight infants during a critical developmental window,” the authors wrote.
Dr. Embleton conceded that his group’s study set the bar deliberately high to avoid finding too many differences purely due to chance, and it therefore might have missed bacterial changes present in low proportions. “Also, the technique we used, 16s rRNA, doesn’t explore the microbiome at the strain level, so there may have been changes we didn’t detect.”
He added that the study populations also had a relatively high usage of mother’s own milk and findings may differ in other populations and settings where the use of mother’s own milk is much lower. Furthermore, the differences reported by individual hospitals in the babies’ gut microbiomes were more significant than most feeding interventions.
So can mothers needing to use nonhuman supplements be reassured by the results? “It is difficult to know how parents may interpret our findings. We need more studies powered to detect differences in functional outcomes before we can draw conclusions and share those findings in a way parents can understand,” Dr. Embleton said. “At present, there is perhaps a too simplistic message that cow milk formula is ‘harmful.’ ”
Most babies exposed to cow’s milk fortifier or formula do not develop NEC, and many with NEC have only ever received their own mother’s milk or donor milk, he added. “It could be that with advances in pasteurization or other similar techniques the quality and therefore the functional benefits of human milk can be better preserved.”
More research is needed on the mechanisms of preterm feeding interventions, including donor human milk, fortifiers, and probiotics, Dr. Embleton said. “The gut microbiome in preterm infants is complex and very different from that in term infants.”
The study was sponsored by Newcastle Hospitals NHS Foundation Trust and funded by Prolacta Biosciences, which provided human milk formula and fortifier. Dr. Embleton reported financial ties to Danone Early Life Nutrition, Nestlé Nutrition Institute Lecture, Astarte Lecture, and NeoKare outside of the submitted work. Several coauthors reported similar ties to multiple private companies and various research funding bodies. Dr. Poindexter has no conflicts of interest.
*This story was updated on March 3, 2023.
No significant differences emerged in gut microbial diversity in preterm infants who exclusively received human milk products, compared with those receiving bovine milk formula or fortifiers, a randomized controlled trial found. Nor were any differences noted in the secondary endpoint of clinical outcomes in the U.K. study, published online in JAMA Network Open.
The finding was unanticipated, according to lead author Nicholas D. Embleton, MBBS, MD, a professor of neonatal medicine at Newcastle University in England. “Over the last 10 years we’ve focused particularly on the role of the microbiome to better understand causal mechanisms of necrotizing enterocolitis, or NEC,” he said in an interview. “We anticipated that an exclusive human milk diet would have measurable impacts on microbiome diversity as a potential mechanism [in] disease modulation as part of the mechanism by which exclusive human milk diets benefit preterm infants.”
Shortfalls in a mother’s own milk supply often necessitate the use of bovine formula or pasteurized human milk from donor milk banks or commercial suppliers.
The effect of an exclusive human milk diet versus one containing bovine products on vulnerable preterm infants is unclear, but some studies have shown lower rates of key neonatal morbidities, possibly mediated by the gut microbiome. In two randomized controlled trials, for example, one showed a lower rate of NEC with donated human milk while the other showed no difference.
Neither, however, was powered to detect a clinically important difference in surgical NEC.
Milk and the microbiome
The current study’s primary endpoint was the effect of an exclusive human milk diet on gut bacterial richness and diversity, as well as the proportions of specific microbial taxa in preterm infants from enrollment to 34 weeks’ postmenstrual age.
Conducted at four neonatal intensive care units in the United Kingdom from 2017 to 2020, the study recruited 126 infants born at less than 30 weeks’ gestation and fed exclusively with their own mother’s milk before 72 hours of age. With a median gestational age of 27 weeks and a median birth weight of just over 900 grams, the babies were randomized 1:1 either to their own mother’s milk plus a pasteurized ready-to-feed human milk product or to their mother’s milk plus a standard preterm formula (controls). Stool samples were collected to analyze intestinal microbiota.
In terms of clinical outcomes, four infants died in the standard-care control group and eight in the intervention group at a median postnatal age of 25 days and 15 days, respectively, but none died primarily of NEC. Formula and ready-to-feed human milk both represented less than 1% of all fluid intake, respectively.
Although there were no effects on overall measures of gut bacterial diversity, there were some insignificant effects on specific bacterial taxa previously associated with human milk feeding. “These findings suggest that the clinical impact of human milk-derived products is not modulated via microbiomic mechanisms,” the authors wrote.
Human milk could benefit, however, via components such as specific oligosaccharides, which act largely by modulating the growth of friendly Bifidobacteria and other species, Dr. Embleton said. “However, it’s possible these oligosaccharides might also directly interact via the gut epithelium as a signaling molecule. And, of course, there are many other components that might also act directly on the gut without changing the microbiome.”
*Commenting on the study but not involved in it, Brenda L. Poindexter, MD, MS, chief of the division of neonatology at Children’s Healthcare of Atlanta and Emory University, called it “incredibly important,” especially in the context of the claims of superiority made by the manufacturers of human-milk-based fortifiers. “These findings convincingly debunk the notion that the use of bovine-derived fortifiers increases risk of morbidities such as NEC through the mechanism of alterations in the microbiome, Dr. Poindexter said.
“They refute that claim as there was no difference in NEC between the groups and, interestingly, no impact on the microbiome. One of the hypothesized mechanisms for those who purport that bovine fortifiers are ‘bad’ is that they alter the microbiome, which increases risk of NEC,” she said. “The only limitation is that the study was not powered to detect a difference in NEC, but it is incredibly important nonetheless.”
The current findings differ somewhat from those of a similar trial from 2022 showing lower microbial diversity and higher relative abundances of Enterobacteriaceae and lower abundances of Clostridium sensu stricto in preterm infants receiving an exclusive human milk diet. “These results highlight how nutrient fortifiers impact the microbiota of very-low-birth-weight infants during a critical developmental window,” the authors wrote.
Dr. Embleton conceded that his group’s study set the bar deliberately high to avoid finding too many differences purely due to chance, and it therefore might have missed bacterial changes present in low proportions. “Also, the technique we used, 16s rRNA, doesn’t explore the microbiome at the strain level, so there may have been changes we didn’t detect.”
He added that the study populations also had a relatively high usage of mother’s own milk and findings may differ in other populations and settings where the use of mother’s own milk is much lower. Furthermore, the differences reported by individual hospitals in the babies’ gut microbiomes were more significant than most feeding interventions.
So can mothers needing to use nonhuman supplements be reassured by the results? “It is difficult to know how parents may interpret our findings. We need more studies powered to detect differences in functional outcomes before we can draw conclusions and share those findings in a way parents can understand,” Dr. Embleton said. “At present, there is perhaps a too simplistic message that cow milk formula is ‘harmful.’ ”
Most babies exposed to cow’s milk fortifier or formula do not develop NEC, and many with NEC have only ever received their own mother’s milk or donor milk, he added. “It could be that with advances in pasteurization or other similar techniques the quality and therefore the functional benefits of human milk can be better preserved.”
More research is needed on the mechanisms of preterm feeding interventions, including donor human milk, fortifiers, and probiotics, Dr. Embleton said. “The gut microbiome in preterm infants is complex and very different from that in term infants.”
The study was sponsored by Newcastle Hospitals NHS Foundation Trust and funded by Prolacta Biosciences, which provided human milk formula and fortifier. Dr. Embleton reported financial ties to Danone Early Life Nutrition, Nestlé Nutrition Institute Lecture, Astarte Lecture, and NeoKare outside of the submitted work. Several coauthors reported similar ties to multiple private companies and various research funding bodies. Dr. Poindexter has no conflicts of interest.
*This story was updated on March 3, 2023.
No significant differences emerged in gut microbial diversity in preterm infants who exclusively received human milk products, compared with those receiving bovine milk formula or fortifiers, a randomized controlled trial found. Nor were any differences noted in the secondary endpoint of clinical outcomes in the U.K. study, published online in JAMA Network Open.
The finding was unanticipated, according to lead author Nicholas D. Embleton, MBBS, MD, a professor of neonatal medicine at Newcastle University in England. “Over the last 10 years we’ve focused particularly on the role of the microbiome to better understand causal mechanisms of necrotizing enterocolitis, or NEC,” he said in an interview. “We anticipated that an exclusive human milk diet would have measurable impacts on microbiome diversity as a potential mechanism [in] disease modulation as part of the mechanism by which exclusive human milk diets benefit preterm infants.”
Shortfalls in a mother’s own milk supply often necessitate the use of bovine formula or pasteurized human milk from donor milk banks or commercial suppliers.
The effect of an exclusive human milk diet versus one containing bovine products on vulnerable preterm infants is unclear, but some studies have shown lower rates of key neonatal morbidities, possibly mediated by the gut microbiome. In two randomized controlled trials, for example, one showed a lower rate of NEC with donated human milk while the other showed no difference.
Neither, however, was powered to detect a clinically important difference in surgical NEC.
Milk and the microbiome
The current study’s primary endpoint was the effect of an exclusive human milk diet on gut bacterial richness and diversity, as well as the proportions of specific microbial taxa in preterm infants from enrollment to 34 weeks’ postmenstrual age.
Conducted at four neonatal intensive care units in the United Kingdom from 2017 to 2020, the study recruited 126 infants born at less than 30 weeks’ gestation and fed exclusively with their own mother’s milk before 72 hours of age. With a median gestational age of 27 weeks and a median birth weight of just over 900 grams, the babies were randomized 1:1 either to their own mother’s milk plus a pasteurized ready-to-feed human milk product or to their mother’s milk plus a standard preterm formula (controls). Stool samples were collected to analyze intestinal microbiota.
In terms of clinical outcomes, four infants died in the standard-care control group and eight in the intervention group at a median postnatal age of 25 days and 15 days, respectively, but none died primarily of NEC. Formula and ready-to-feed human milk both represented less than 1% of all fluid intake, respectively.
Although there were no effects on overall measures of gut bacterial diversity, there were some insignificant effects on specific bacterial taxa previously associated with human milk feeding. “These findings suggest that the clinical impact of human milk-derived products is not modulated via microbiomic mechanisms,” the authors wrote.
Human milk could benefit, however, via components such as specific oligosaccharides, which act largely by modulating the growth of friendly Bifidobacteria and other species, Dr. Embleton said. “However, it’s possible these oligosaccharides might also directly interact via the gut epithelium as a signaling molecule. And, of course, there are many other components that might also act directly on the gut without changing the microbiome.”
*Commenting on the study but not involved in it, Brenda L. Poindexter, MD, MS, chief of the division of neonatology at Children’s Healthcare of Atlanta and Emory University, called it “incredibly important,” especially in the context of the claims of superiority made by the manufacturers of human-milk-based fortifiers. “These findings convincingly debunk the notion that the use of bovine-derived fortifiers increases risk of morbidities such as NEC through the mechanism of alterations in the microbiome, Dr. Poindexter said.
“They refute that claim as there was no difference in NEC between the groups and, interestingly, no impact on the microbiome. One of the hypothesized mechanisms for those who purport that bovine fortifiers are ‘bad’ is that they alter the microbiome, which increases risk of NEC,” she said. “The only limitation is that the study was not powered to detect a difference in NEC, but it is incredibly important nonetheless.”
The current findings differ somewhat from those of a similar trial from 2022 showing lower microbial diversity and higher relative abundances of Enterobacteriaceae and lower abundances of Clostridium sensu stricto in preterm infants receiving an exclusive human milk diet. “These results highlight how nutrient fortifiers impact the microbiota of very-low-birth-weight infants during a critical developmental window,” the authors wrote.
Dr. Embleton conceded that his group’s study set the bar deliberately high to avoid finding too many differences purely due to chance, and it therefore might have missed bacterial changes present in low proportions. “Also, the technique we used, 16s rRNA, doesn’t explore the microbiome at the strain level, so there may have been changes we didn’t detect.”
He added that the study populations also had a relatively high usage of mother’s own milk and findings may differ in other populations and settings where the use of mother’s own milk is much lower. Furthermore, the differences reported by individual hospitals in the babies’ gut microbiomes were more significant than most feeding interventions.
So can mothers needing to use nonhuman supplements be reassured by the results? “It is difficult to know how parents may interpret our findings. We need more studies powered to detect differences in functional outcomes before we can draw conclusions and share those findings in a way parents can understand,” Dr. Embleton said. “At present, there is perhaps a too simplistic message that cow milk formula is ‘harmful.’ ”
Most babies exposed to cow’s milk fortifier or formula do not develop NEC, and many with NEC have only ever received their own mother’s milk or donor milk, he added. “It could be that with advances in pasteurization or other similar techniques the quality and therefore the functional benefits of human milk can be better preserved.”
More research is needed on the mechanisms of preterm feeding interventions, including donor human milk, fortifiers, and probiotics, Dr. Embleton said. “The gut microbiome in preterm infants is complex and very different from that in term infants.”
The study was sponsored by Newcastle Hospitals NHS Foundation Trust and funded by Prolacta Biosciences, which provided human milk formula and fortifier. Dr. Embleton reported financial ties to Danone Early Life Nutrition, Nestlé Nutrition Institute Lecture, Astarte Lecture, and NeoKare outside of the submitted work. Several coauthors reported similar ties to multiple private companies and various research funding bodies. Dr. Poindexter has no conflicts of interest.
*This story was updated on March 3, 2023.
FROM JAMA NETWORK OPEN
Non-Surgical Treatment of Heavy Menstrual Bleeding From Fibroids: A New Paradigm
GnRH antagonists with estrogen/progesterone are promising new uterine-sparing options for treating uterine fibroids. Two experts review data from two recent clinical trials to bring you up to speed on the benefits and risks of this treatment approach.
After reading this short article, you have an opportunity to earn 1.0 CME credits.
GnRH antagonists with estrogen/progesterone are promising new uterine-sparing options for treating uterine fibroids. Two experts review data from two recent clinical trials to bring you up to speed on the benefits and risks of this treatment approach.
After reading this short article, you have an opportunity to earn 1.0 CME credits.
GnRH antagonists with estrogen/progesterone are promising new uterine-sparing options for treating uterine fibroids. Two experts review data from two recent clinical trials to bring you up to speed on the benefits and risks of this treatment approach.
After reading this short article, you have an opportunity to earn 1.0 CME credits.
The Cognition Self-Assessment Rating Scale for patients with schizophrenia
Cognition represents the most important function of the human brain and the essence of the mind. Cognitive functions such as memory, learning, comprehension, processing speed, attention, planning, and problem-solving are the best indicators of the status of brain health.
Many psychiatric brain disorders are associated with cognitive impairments. Decades of extensive research have documented that the most severe cognitive deficits occur in schizophrenia. No wonder Emil Kraepelin coined the term “dementia praecox,” which means premature dementia (in youth)1 for this neuropsychiatric brain disorder. This condition was later renamed schizophrenia by Eugen Bleuler,2 who regarded it primarily as a thought disorder, with splitting of associations (not split personality, as misinterpreted by many in the public). Interestingly, a century ago both of those early masters of psychiatry de-emphasized psychotic symptoms (delusions and hallucinations), regarding them as “supplemental symptoms.”3 Yet for the next 100 years, clinicians overemphasized psychotic symptoms in schizophrenia and overlooked the more disabling cognitive impairment and negative symptoms, referred to as Bleuler’s 4 A’s—Associations disruption, Ambivalence, Affect pathology, and Avolition—symptoms that persist even after the psychotic symptoms are successfully treated.3
Most contemporary researchers regard cognitive impairment as the “core” feature of schizophrenia.4 The justification of this view is that cognitive deficits are detected in childhood and early adolescence (by age 13),5 long before the appearance of psychotic symptoms, and many studies have confirmed that cognitive deficits are the primary cause of functional disability and unemployment of patients with schizophrenia. Cognitive dysfunction is also found in milder forms in the parents and siblings of patients with schizophrenia,6 and is thus considered an “endophenotype” of the illness.
Because of its centrality, cognition has emerged as a major focus of schizophrenia research over the past 20 years. Multiple stakeholders (academic investigators, the National Institute of Mental Health, and the FDA) have collaborated to develop a standard measurement for cognition in schizophrenia. The project culminated in what was labeled MATRICS (Measurement and Treatment Research to Improve Cognition in Schizophrenia).7 The MATRICS settled on a battery of 7 major cognitive functions that are often impaired in individuals with schizophrenia (Table 18). Most contemporary researchers have adopted MATRICS in their studies, which facilitates replication to confirm research findings.
Measuring cognition in patients with schizophrenia is extremely important, as critical as measuring fasting glucose in patients with diabetes or blood pressure in patients with hypertension. Measuring the extent of impairment or nonimpairment across various cognitive tests can help with vocational rehabilitation, to place a patient in a job consistent with their level of cognitive functioning. In addition, once medications are developed and approved for cognitive impairments in schizophrenia, measuring cognition will be necessary to gauge the degree of improvement.
Currently, few psychiatric practitioners measure cognition in their patients. This is perplexing because cognitive measurement is important for confirming the diagnosis of schizophrenia in first-episode psychosis, or distinguishing it from other psychotic disorders (such as drug-induced psychosis, brief reactive psychosis, or delusional disorders) that do not have severe cognitive deficits.
The scores of various cognitive functions in individuals with schizophrenia range from .75 to 2.0 SD below the performance of the general population (matched for age and gender).9 This translates to dismally low percentiles of 2% and 24%. It is essential that all clinicians measure cognition in every patient with psychotic symptoms. It can be argued that cognition should even be measured in other psychiatric patients because cognitive deficits have been well documented in bipolar disorder, major depressive disorder, attention-deficit/hyperactivity disorder, and other disorders, albeit not as severe as in schizophrenia, and these deficits usually correlate with the patient’s vocational and social functioning.
Continue to: So how is cognition measured...
So how is cognition measured, and can clinicians incorporate cognitive batteries in their practices? The most logical answer is to refer the patient to a board-certified neuropsychologist. These specialists are well-trained in assessing cognitive functions, and their evaluations generally are covered by health insurance. They use various validated cognitive batteries. Table 210-18 lists the currently recognized cognitive assessments and how much time they require. Psychiatrists can have nurses or medical assistants administer a brief cognitive test.
C-SARS: A self-rated cognition scale
Patient self-rating can provide psychiatric clinicians with valuable information, and is a time-saver. The widely used Patient Health Questionaire-9 (PHQ-9)19 is an excellent example of a self-rating scale for depression that enables patients to recognize and rate their depressive symptoms. It immediately informs the clinician how depressed their patient is and whether the severity of the depression has improved from the previous visit, which can indicate whether the prescribed medication is working. Based on the PHQ-9, which I regularly use—and recognizing that there is no cognition counterpart and that almost all clinicians could use a practical method of measuring their patients’ cognitive function—I developed an instrument called the Cognition Self-Assessment Rating Scale (C-SARS) (Table 3). The C-SARS can be completed online at https://curesz.org/csars/ and patients will be emailed the results within a minute. The C-SARS can be completed by the patient (with the help of their family or caregiver, if necessary, who observe the patient’s daily functioning, which corresponds to their cognition). The main purpose of the C-SARS is to inform the clinician about serious cognitive dysfunction in their patients, which should instigate a referral for formal neurocognitive assessment by a neuropsychology expert.
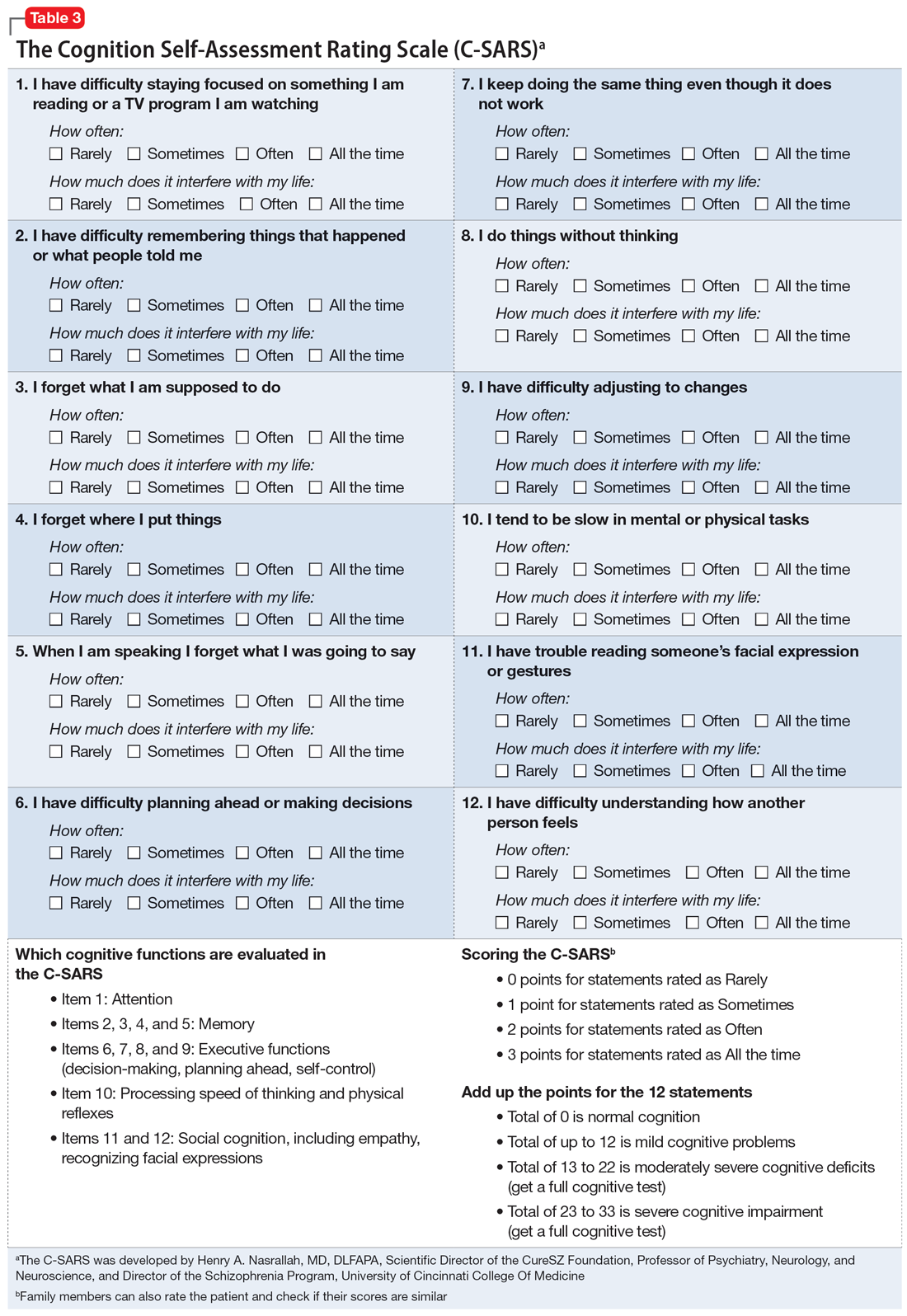
The items on the C-SARS reflect how well the patient is performing routine daily functions, each of which correlates with one of the cognitive domains of the MATRICS battery. Table 3 shows the 12 items in the C-SARS, their scoring, and their clinical implications (ie, when the results require referral for formal neurocognitive testing). In the future, when the FDA approves medications for addressing cognitive impairment (and several molecules are currently undergoing clinical trials), clinicians will be able to gauge a patient’s response to such treatments using the C-SARS and formal testing as needed. It may take several weeks to detect a significant reversal of cognitive deficits, but doing so would address a major unmet need in schizophrenia and may speed up vocational rehabilitation. The C-SARS also contains 2 items related to social cognition (items 11 and 12), which is also impaired in schizophrenia.20 Future medications that improve social cognition in addition to neurocognition may also lead to improved social functioning among patients with schizophrenia.
In conclusion, the C-SARS, which needs to be validated in controlled studies, is the first cognition self-rating scale for schizophrenia and may be useful for other major psychiatric disorders. It will be a substantial time-saver for clinicians and will facilitate the routine incorporation of the cognitive assessment of patients with psychotic symptoms to help with the differential diagnosis of schizophrenia vs other psychotic disorders. Measuring cognitive functions is a vital step towards the valid diagnosis and treatment of this major clinical challenge in schizophrenia and improving patient outcomes in this serious psychiatric brain syndrome, in which up to 98% of patients have cognitive impairment across several domains.21
1. Kraepelin E. Dementia Praecox and Paraphrenia. Barth; 1904.
2. Bleuler E. Dementia Praecox or the Group of Schizophrenias. International Universities Press; 1950.
3. Nasrallah HA, Smeltzer DJ. Contemporary Diagnosis and Management of the Patient with Schizophrenia. Handbooks in Health Care Company; 2011.
4. Kahn RS, Keefe RSE. Schizophrenia is a cognitive illness: time for a change in focus. JAMA Psychiatry. 2013;70(10):1107-1112.
5. van Oel CJ, Sitskoorn MM, Cremer MPM, et al. School performance as a premorbid marker for schizophrenia: a twin study. Schizophr Bull. 2002;28(3):401-414.
6. Jameson KG, Nasrallah HA, Northern TG, et al. Executive function in first-degree relatives of persons with schizophrenia: a meta-analysis of controlled studies. Asian J Psychiatry 2011;4(2):96-99.
7. Marder SR, Fenton W. Measurement and Treatment Research to Improve Cognition in Schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res. 2004;72(1):5-9.
8. Neuchterlein KH, Barch DM, Gold JM, et al. Identification of separable cognitive factors in schizophrenia. Schizophr Res. 2004;72(1):29-39.
9. Heinrich RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12(3):426-445.
10. Nuechterlein KH, Green MF. MATRICS Consensus Cognitive Battery (MCCB). 3rd ed. MATRICS Assessment Inc.; 2016.
11. Robins TW, James M, Owen AM, et al. Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia. 1994;5(5):266-281.
12. Pietrzak RH, Olver J, Norman T, et al. A comparison of the CogState Schizophrenia Battery and the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) battery in assessing cognitive impairment in chronic schizophrenia. J Clin Exp Neuropsychol. 2009;31(7):848-859.
13. Keefe RSE, Goldberg TE, Harvey PD, et al. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68(2-3):283-297.
14. Randolph C, Tierney MC, Mohr E, et al. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol. 1998;20(3):310-319.
15. Velligan DI, DiCocco M, Bow-Thomas CC, et al. A brief cognitive assessment for use with schizophrenia patients in community clinics. Schizophr Res. 2004;71(2-3):272-283.
16. Huford IM, Marder SR, Keefe RSE, et al. A brief cognitive assessment tool for schizophrenia: construction of a tool for clinicians. Schizophr Bull. 2011;37(3):538-545.
17. Ventura J, Reise SP, Keefe RSE, et al. The Cognitive Assessment Interview (CAI): reliability and validity of a brief interview-based measure of cognition. Schizophr Bull. 2013;39(3):583-591.
18. Keefe RSE, Poe M, Walker TM, et al. The Schizophrenia Cognition Rating Scale: an interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity. Am J Psychiatry. 2006;163(3):426-432.
19. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J. Gen Intern Med. 2001;16(9):606-613.
20. Green MF, Horan WP, Lee J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry. 2019;18(2):146-161.
21. Keefe RS, Eesley CE, Poe MP. Defining a cognitive function decrement in schizophrenia. Biol Psychiatry. 2005;57(6):688-691.
Cognition represents the most important function of the human brain and the essence of the mind. Cognitive functions such as memory, learning, comprehension, processing speed, attention, planning, and problem-solving are the best indicators of the status of brain health.
Many psychiatric brain disorders are associated with cognitive impairments. Decades of extensive research have documented that the most severe cognitive deficits occur in schizophrenia. No wonder Emil Kraepelin coined the term “dementia praecox,” which means premature dementia (in youth)1 for this neuropsychiatric brain disorder. This condition was later renamed schizophrenia by Eugen Bleuler,2 who regarded it primarily as a thought disorder, with splitting of associations (not split personality, as misinterpreted by many in the public). Interestingly, a century ago both of those early masters of psychiatry de-emphasized psychotic symptoms (delusions and hallucinations), regarding them as “supplemental symptoms.”3 Yet for the next 100 years, clinicians overemphasized psychotic symptoms in schizophrenia and overlooked the more disabling cognitive impairment and negative symptoms, referred to as Bleuler’s 4 A’s—Associations disruption, Ambivalence, Affect pathology, and Avolition—symptoms that persist even after the psychotic symptoms are successfully treated.3
Most contemporary researchers regard cognitive impairment as the “core” feature of schizophrenia.4 The justification of this view is that cognitive deficits are detected in childhood and early adolescence (by age 13),5 long before the appearance of psychotic symptoms, and many studies have confirmed that cognitive deficits are the primary cause of functional disability and unemployment of patients with schizophrenia. Cognitive dysfunction is also found in milder forms in the parents and siblings of patients with schizophrenia,6 and is thus considered an “endophenotype” of the illness.
Because of its centrality, cognition has emerged as a major focus of schizophrenia research over the past 20 years. Multiple stakeholders (academic investigators, the National Institute of Mental Health, and the FDA) have collaborated to develop a standard measurement for cognition in schizophrenia. The project culminated in what was labeled MATRICS (Measurement and Treatment Research to Improve Cognition in Schizophrenia).7 The MATRICS settled on a battery of 7 major cognitive functions that are often impaired in individuals with schizophrenia (Table 18). Most contemporary researchers have adopted MATRICS in their studies, which facilitates replication to confirm research findings.
Measuring cognition in patients with schizophrenia is extremely important, as critical as measuring fasting glucose in patients with diabetes or blood pressure in patients with hypertension. Measuring the extent of impairment or nonimpairment across various cognitive tests can help with vocational rehabilitation, to place a patient in a job consistent with their level of cognitive functioning. In addition, once medications are developed and approved for cognitive impairments in schizophrenia, measuring cognition will be necessary to gauge the degree of improvement.
Currently, few psychiatric practitioners measure cognition in their patients. This is perplexing because cognitive measurement is important for confirming the diagnosis of schizophrenia in first-episode psychosis, or distinguishing it from other psychotic disorders (such as drug-induced psychosis, brief reactive psychosis, or delusional disorders) that do not have severe cognitive deficits.
The scores of various cognitive functions in individuals with schizophrenia range from .75 to 2.0 SD below the performance of the general population (matched for age and gender).9 This translates to dismally low percentiles of 2% and 24%. It is essential that all clinicians measure cognition in every patient with psychotic symptoms. It can be argued that cognition should even be measured in other psychiatric patients because cognitive deficits have been well documented in bipolar disorder, major depressive disorder, attention-deficit/hyperactivity disorder, and other disorders, albeit not as severe as in schizophrenia, and these deficits usually correlate with the patient’s vocational and social functioning.
Continue to: So how is cognition measured...
So how is cognition measured, and can clinicians incorporate cognitive batteries in their practices? The most logical answer is to refer the patient to a board-certified neuropsychologist. These specialists are well-trained in assessing cognitive functions, and their evaluations generally are covered by health insurance. They use various validated cognitive batteries. Table 210-18 lists the currently recognized cognitive assessments and how much time they require. Psychiatrists can have nurses or medical assistants administer a brief cognitive test.
C-SARS: A self-rated cognition scale
Patient self-rating can provide psychiatric clinicians with valuable information, and is a time-saver. The widely used Patient Health Questionaire-9 (PHQ-9)19 is an excellent example of a self-rating scale for depression that enables patients to recognize and rate their depressive symptoms. It immediately informs the clinician how depressed their patient is and whether the severity of the depression has improved from the previous visit, which can indicate whether the prescribed medication is working. Based on the PHQ-9, which I regularly use—and recognizing that there is no cognition counterpart and that almost all clinicians could use a practical method of measuring their patients’ cognitive function—I developed an instrument called the Cognition Self-Assessment Rating Scale (C-SARS) (Table 3). The C-SARS can be completed online at https://curesz.org/csars/ and patients will be emailed the results within a minute. The C-SARS can be completed by the patient (with the help of their family or caregiver, if necessary, who observe the patient’s daily functioning, which corresponds to their cognition). The main purpose of the C-SARS is to inform the clinician about serious cognitive dysfunction in their patients, which should instigate a referral for formal neurocognitive assessment by a neuropsychology expert.
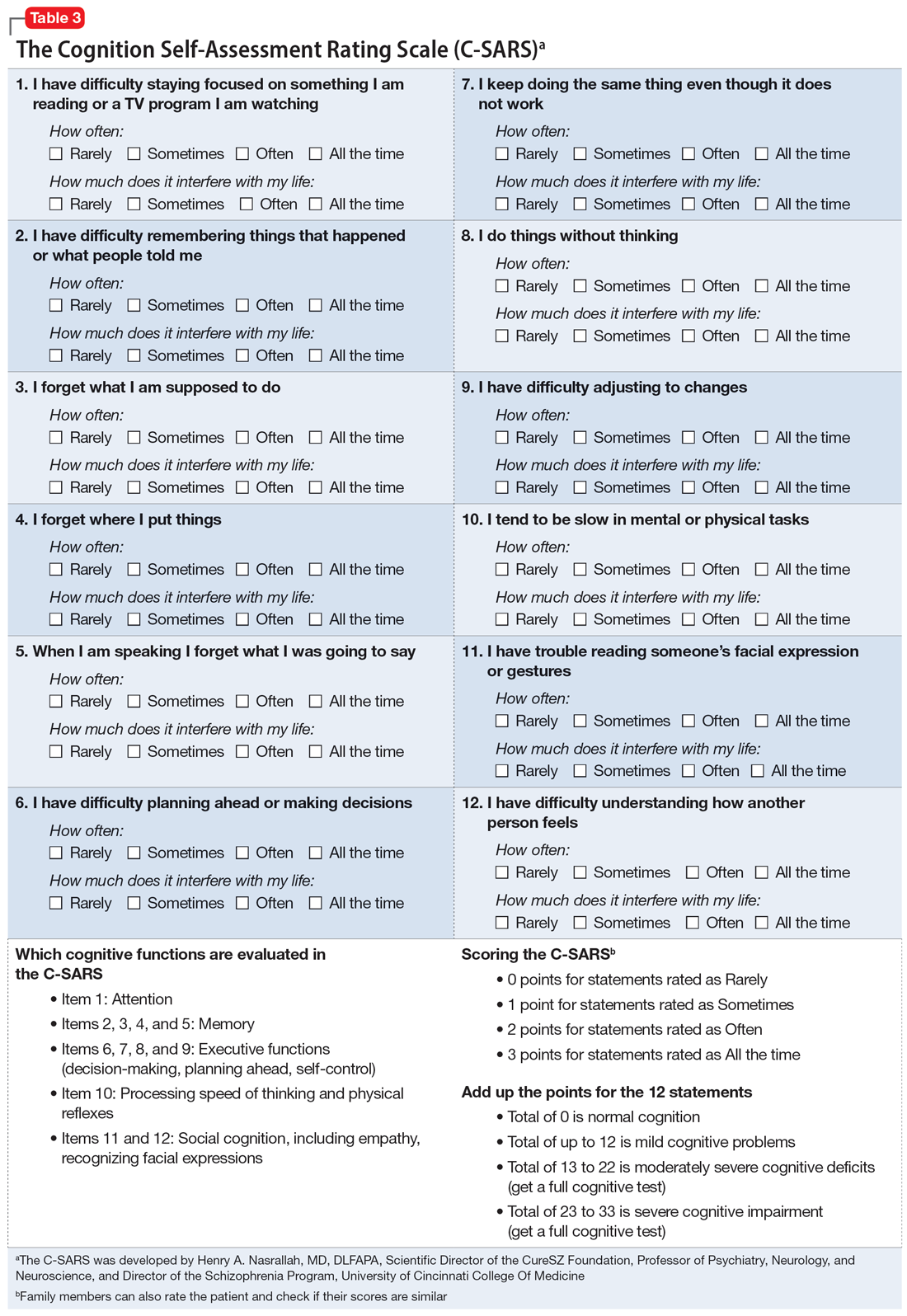
The items on the C-SARS reflect how well the patient is performing routine daily functions, each of which correlates with one of the cognitive domains of the MATRICS battery. Table 3 shows the 12 items in the C-SARS, their scoring, and their clinical implications (ie, when the results require referral for formal neurocognitive testing). In the future, when the FDA approves medications for addressing cognitive impairment (and several molecules are currently undergoing clinical trials), clinicians will be able to gauge a patient’s response to such treatments using the C-SARS and formal testing as needed. It may take several weeks to detect a significant reversal of cognitive deficits, but doing so would address a major unmet need in schizophrenia and may speed up vocational rehabilitation. The C-SARS also contains 2 items related to social cognition (items 11 and 12), which is also impaired in schizophrenia.20 Future medications that improve social cognition in addition to neurocognition may also lead to improved social functioning among patients with schizophrenia.
In conclusion, the C-SARS, which needs to be validated in controlled studies, is the first cognition self-rating scale for schizophrenia and may be useful for other major psychiatric disorders. It will be a substantial time-saver for clinicians and will facilitate the routine incorporation of the cognitive assessment of patients with psychotic symptoms to help with the differential diagnosis of schizophrenia vs other psychotic disorders. Measuring cognitive functions is a vital step towards the valid diagnosis and treatment of this major clinical challenge in schizophrenia and improving patient outcomes in this serious psychiatric brain syndrome, in which up to 98% of patients have cognitive impairment across several domains.21
Cognition represents the most important function of the human brain and the essence of the mind. Cognitive functions such as memory, learning, comprehension, processing speed, attention, planning, and problem-solving are the best indicators of the status of brain health.
Many psychiatric brain disorders are associated with cognitive impairments. Decades of extensive research have documented that the most severe cognitive deficits occur in schizophrenia. No wonder Emil Kraepelin coined the term “dementia praecox,” which means premature dementia (in youth)1 for this neuropsychiatric brain disorder. This condition was later renamed schizophrenia by Eugen Bleuler,2 who regarded it primarily as a thought disorder, with splitting of associations (not split personality, as misinterpreted by many in the public). Interestingly, a century ago both of those early masters of psychiatry de-emphasized psychotic symptoms (delusions and hallucinations), regarding them as “supplemental symptoms.”3 Yet for the next 100 years, clinicians overemphasized psychotic symptoms in schizophrenia and overlooked the more disabling cognitive impairment and negative symptoms, referred to as Bleuler’s 4 A’s—Associations disruption, Ambivalence, Affect pathology, and Avolition—symptoms that persist even after the psychotic symptoms are successfully treated.3
Most contemporary researchers regard cognitive impairment as the “core” feature of schizophrenia.4 The justification of this view is that cognitive deficits are detected in childhood and early adolescence (by age 13),5 long before the appearance of psychotic symptoms, and many studies have confirmed that cognitive deficits are the primary cause of functional disability and unemployment of patients with schizophrenia. Cognitive dysfunction is also found in milder forms in the parents and siblings of patients with schizophrenia,6 and is thus considered an “endophenotype” of the illness.
Because of its centrality, cognition has emerged as a major focus of schizophrenia research over the past 20 years. Multiple stakeholders (academic investigators, the National Institute of Mental Health, and the FDA) have collaborated to develop a standard measurement for cognition in schizophrenia. The project culminated in what was labeled MATRICS (Measurement and Treatment Research to Improve Cognition in Schizophrenia).7 The MATRICS settled on a battery of 7 major cognitive functions that are often impaired in individuals with schizophrenia (Table 18). Most contemporary researchers have adopted MATRICS in their studies, which facilitates replication to confirm research findings.
Measuring cognition in patients with schizophrenia is extremely important, as critical as measuring fasting glucose in patients with diabetes or blood pressure in patients with hypertension. Measuring the extent of impairment or nonimpairment across various cognitive tests can help with vocational rehabilitation, to place a patient in a job consistent with their level of cognitive functioning. In addition, once medications are developed and approved for cognitive impairments in schizophrenia, measuring cognition will be necessary to gauge the degree of improvement.
Currently, few psychiatric practitioners measure cognition in their patients. This is perplexing because cognitive measurement is important for confirming the diagnosis of schizophrenia in first-episode psychosis, or distinguishing it from other psychotic disorders (such as drug-induced psychosis, brief reactive psychosis, or delusional disorders) that do not have severe cognitive deficits.
The scores of various cognitive functions in individuals with schizophrenia range from .75 to 2.0 SD below the performance of the general population (matched for age and gender).9 This translates to dismally low percentiles of 2% and 24%. It is essential that all clinicians measure cognition in every patient with psychotic symptoms. It can be argued that cognition should even be measured in other psychiatric patients because cognitive deficits have been well documented in bipolar disorder, major depressive disorder, attention-deficit/hyperactivity disorder, and other disorders, albeit not as severe as in schizophrenia, and these deficits usually correlate with the patient’s vocational and social functioning.
Continue to: So how is cognition measured...
So how is cognition measured, and can clinicians incorporate cognitive batteries in their practices? The most logical answer is to refer the patient to a board-certified neuropsychologist. These specialists are well-trained in assessing cognitive functions, and their evaluations generally are covered by health insurance. They use various validated cognitive batteries. Table 210-18 lists the currently recognized cognitive assessments and how much time they require. Psychiatrists can have nurses or medical assistants administer a brief cognitive test.
C-SARS: A self-rated cognition scale
Patient self-rating can provide psychiatric clinicians with valuable information, and is a time-saver. The widely used Patient Health Questionaire-9 (PHQ-9)19 is an excellent example of a self-rating scale for depression that enables patients to recognize and rate their depressive symptoms. It immediately informs the clinician how depressed their patient is and whether the severity of the depression has improved from the previous visit, which can indicate whether the prescribed medication is working. Based on the PHQ-9, which I regularly use—and recognizing that there is no cognition counterpart and that almost all clinicians could use a practical method of measuring their patients’ cognitive function—I developed an instrument called the Cognition Self-Assessment Rating Scale (C-SARS) (Table 3). The C-SARS can be completed online at https://curesz.org/csars/ and patients will be emailed the results within a minute. The C-SARS can be completed by the patient (with the help of their family or caregiver, if necessary, who observe the patient’s daily functioning, which corresponds to their cognition). The main purpose of the C-SARS is to inform the clinician about serious cognitive dysfunction in their patients, which should instigate a referral for formal neurocognitive assessment by a neuropsychology expert.
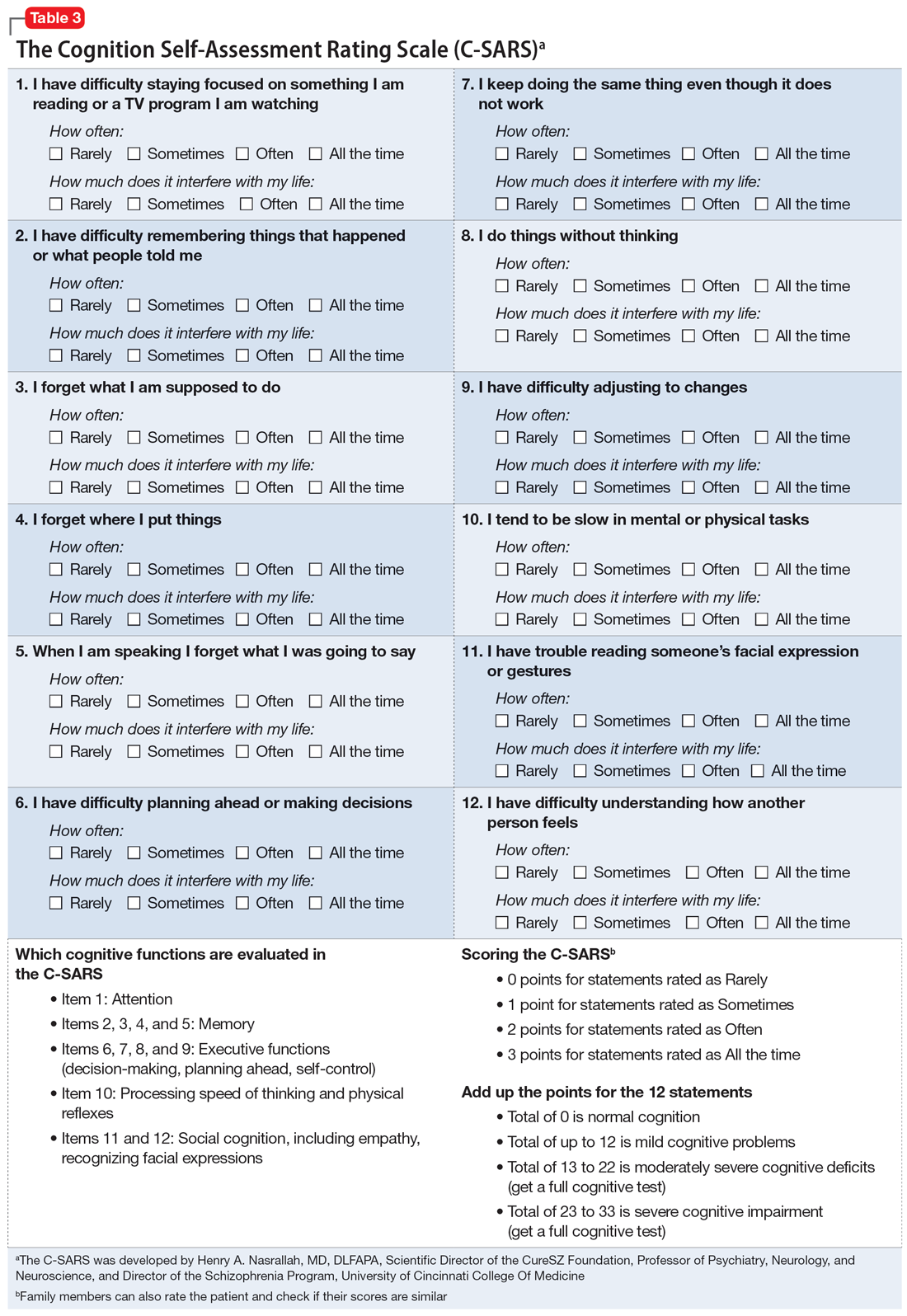
The items on the C-SARS reflect how well the patient is performing routine daily functions, each of which correlates with one of the cognitive domains of the MATRICS battery. Table 3 shows the 12 items in the C-SARS, their scoring, and their clinical implications (ie, when the results require referral for formal neurocognitive testing). In the future, when the FDA approves medications for addressing cognitive impairment (and several molecules are currently undergoing clinical trials), clinicians will be able to gauge a patient’s response to such treatments using the C-SARS and formal testing as needed. It may take several weeks to detect a significant reversal of cognitive deficits, but doing so would address a major unmet need in schizophrenia and may speed up vocational rehabilitation. The C-SARS also contains 2 items related to social cognition (items 11 and 12), which is also impaired in schizophrenia.20 Future medications that improve social cognition in addition to neurocognition may also lead to improved social functioning among patients with schizophrenia.
In conclusion, the C-SARS, which needs to be validated in controlled studies, is the first cognition self-rating scale for schizophrenia and may be useful for other major psychiatric disorders. It will be a substantial time-saver for clinicians and will facilitate the routine incorporation of the cognitive assessment of patients with psychotic symptoms to help with the differential diagnosis of schizophrenia vs other psychotic disorders. Measuring cognitive functions is a vital step towards the valid diagnosis and treatment of this major clinical challenge in schizophrenia and improving patient outcomes in this serious psychiatric brain syndrome, in which up to 98% of patients have cognitive impairment across several domains.21
1. Kraepelin E. Dementia Praecox and Paraphrenia. Barth; 1904.
2. Bleuler E. Dementia Praecox or the Group of Schizophrenias. International Universities Press; 1950.
3. Nasrallah HA, Smeltzer DJ. Contemporary Diagnosis and Management of the Patient with Schizophrenia. Handbooks in Health Care Company; 2011.
4. Kahn RS, Keefe RSE. Schizophrenia is a cognitive illness: time for a change in focus. JAMA Psychiatry. 2013;70(10):1107-1112.
5. van Oel CJ, Sitskoorn MM, Cremer MPM, et al. School performance as a premorbid marker for schizophrenia: a twin study. Schizophr Bull. 2002;28(3):401-414.
6. Jameson KG, Nasrallah HA, Northern TG, et al. Executive function in first-degree relatives of persons with schizophrenia: a meta-analysis of controlled studies. Asian J Psychiatry 2011;4(2):96-99.
7. Marder SR, Fenton W. Measurement and Treatment Research to Improve Cognition in Schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res. 2004;72(1):5-9.
8. Neuchterlein KH, Barch DM, Gold JM, et al. Identification of separable cognitive factors in schizophrenia. Schizophr Res. 2004;72(1):29-39.
9. Heinrich RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12(3):426-445.
10. Nuechterlein KH, Green MF. MATRICS Consensus Cognitive Battery (MCCB). 3rd ed. MATRICS Assessment Inc.; 2016.
11. Robins TW, James M, Owen AM, et al. Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia. 1994;5(5):266-281.
12. Pietrzak RH, Olver J, Norman T, et al. A comparison of the CogState Schizophrenia Battery and the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) battery in assessing cognitive impairment in chronic schizophrenia. J Clin Exp Neuropsychol. 2009;31(7):848-859.
13. Keefe RSE, Goldberg TE, Harvey PD, et al. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68(2-3):283-297.
14. Randolph C, Tierney MC, Mohr E, et al. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol. 1998;20(3):310-319.
15. Velligan DI, DiCocco M, Bow-Thomas CC, et al. A brief cognitive assessment for use with schizophrenia patients in community clinics. Schizophr Res. 2004;71(2-3):272-283.
16. Huford IM, Marder SR, Keefe RSE, et al. A brief cognitive assessment tool for schizophrenia: construction of a tool for clinicians. Schizophr Bull. 2011;37(3):538-545.
17. Ventura J, Reise SP, Keefe RSE, et al. The Cognitive Assessment Interview (CAI): reliability and validity of a brief interview-based measure of cognition. Schizophr Bull. 2013;39(3):583-591.
18. Keefe RSE, Poe M, Walker TM, et al. The Schizophrenia Cognition Rating Scale: an interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity. Am J Psychiatry. 2006;163(3):426-432.
19. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J. Gen Intern Med. 2001;16(9):606-613.
20. Green MF, Horan WP, Lee J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry. 2019;18(2):146-161.
21. Keefe RS, Eesley CE, Poe MP. Defining a cognitive function decrement in schizophrenia. Biol Psychiatry. 2005;57(6):688-691.
1. Kraepelin E. Dementia Praecox and Paraphrenia. Barth; 1904.
2. Bleuler E. Dementia Praecox or the Group of Schizophrenias. International Universities Press; 1950.
3. Nasrallah HA, Smeltzer DJ. Contemporary Diagnosis and Management of the Patient with Schizophrenia. Handbooks in Health Care Company; 2011.
4. Kahn RS, Keefe RSE. Schizophrenia is a cognitive illness: time for a change in focus. JAMA Psychiatry. 2013;70(10):1107-1112.
5. van Oel CJ, Sitskoorn MM, Cremer MPM, et al. School performance as a premorbid marker for schizophrenia: a twin study. Schizophr Bull. 2002;28(3):401-414.
6. Jameson KG, Nasrallah HA, Northern TG, et al. Executive function in first-degree relatives of persons with schizophrenia: a meta-analysis of controlled studies. Asian J Psychiatry 2011;4(2):96-99.
7. Marder SR, Fenton W. Measurement and Treatment Research to Improve Cognition in Schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res. 2004;72(1):5-9.
8. Neuchterlein KH, Barch DM, Gold JM, et al. Identification of separable cognitive factors in schizophrenia. Schizophr Res. 2004;72(1):29-39.
9. Heinrich RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology. 1998;12(3):426-445.
10. Nuechterlein KH, Green MF. MATRICS Consensus Cognitive Battery (MCCB). 3rd ed. MATRICS Assessment Inc.; 2016.
11. Robins TW, James M, Owen AM, et al. Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia. 1994;5(5):266-281.
12. Pietrzak RH, Olver J, Norman T, et al. A comparison of the CogState Schizophrenia Battery and the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) battery in assessing cognitive impairment in chronic schizophrenia. J Clin Exp Neuropsychol. 2009;31(7):848-859.
13. Keefe RSE, Goldberg TE, Harvey PD, et al. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68(2-3):283-297.
14. Randolph C, Tierney MC, Mohr E, et al. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol. 1998;20(3):310-319.
15. Velligan DI, DiCocco M, Bow-Thomas CC, et al. A brief cognitive assessment for use with schizophrenia patients in community clinics. Schizophr Res. 2004;71(2-3):272-283.
16. Huford IM, Marder SR, Keefe RSE, et al. A brief cognitive assessment tool for schizophrenia: construction of a tool for clinicians. Schizophr Bull. 2011;37(3):538-545.
17. Ventura J, Reise SP, Keefe RSE, et al. The Cognitive Assessment Interview (CAI): reliability and validity of a brief interview-based measure of cognition. Schizophr Bull. 2013;39(3):583-591.
18. Keefe RSE, Poe M, Walker TM, et al. The Schizophrenia Cognition Rating Scale: an interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity. Am J Psychiatry. 2006;163(3):426-432.
19. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J. Gen Intern Med. 2001;16(9):606-613.
20. Green MF, Horan WP, Lee J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry. 2019;18(2):146-161.
21. Keefe RS, Eesley CE, Poe MP. Defining a cognitive function decrement in schizophrenia. Biol Psychiatry. 2005;57(6):688-691.
Digital therapeutics could help patients with IBS
, according to a new review of available products.
These tools aren’t widely used by gastroenterologists yet, but the market is expected to grow broadly during the next decade.
“Digital therapeutics make so much sense and solve so many access issues,” coauthor William Chey, MD, chief of gastroenterology at the University of Michigan, Ann Arbor, said in an interview. “Because of this, their promise could easily outstrip their substance. We need to hold digital therapeutics companies accountable for proper evidence of benefit, so patients and doctors don’t end up chasing the latest shiny object.”
The review was published online in The American Journal of Gastroenterology.
Understanding the apps
IBS is most effectively treated with a combination of medications, diet changes, and behavioral interventions that are specific to the patient, the authors write. Cognitive behavioral therapy (CBT) and gut-directed hypnotherapy (GDH) have been effective at modifying behaviors and thought patterns, they add.
However, many gastroenterologists and their patients with IBS don’t have easy access to the mental health services component of integrated gastrointestinal (GI) care. DTx may offer a solution.
The review by Dr. Chey and colleagues is intended to serve as a primer for gastroenterologists about the current generation of DTx that provide virtual behavioral health interventions. For each product, they include a description of its services, evidence supporting its use, and other key information.
Mahana IBS, made by Mahana Therapeutics, is an FDA-approved, prescription-only CBT program for adults with IBS. The maximum out-of-pocket cost is $90. The product includes 10 sessions over 12 weeks.
Available as a mobile app or Web-based platform, Mahana IBS was validated in a randomized comparative effectiveness trial in a group of 558 patients, divided into three groups who received Web-based CBT, phone-based CBT, or treatment as usual. Before treatment, the mean IBS Symptom Severity Score for the entire group was 265.
At 12 weeks, the control group had an average reduction of 52.9 points, while the phone-based therapy group had a reduction of 133.3 points, and the Web-based therapy group had a reduction of 101.2 points. The average Work and Social Adjustment Scale (WSAS) decreased by an additional 3.5 points in the phone-based group and 3 points in the Web-based group, compared with the control group.
Zemedy, made by Bold Health, is a mobile app that provides virtual CBT through a chat bot for patients with IBS. It costs $19.49 per month or $154.99 per year. The app isn’t FDA-approved and doesn’t require a prescription.
The program includes six weekly psychoeducational modules with information about IBS and CBT, followed by CBT training modules. Users can chat with an automated system that provides computer-generated responses for support. A “flare module” supports patients when symptoms worsen.
Zemedy was evaluated in a crossover randomized controlled trial with 62 people in an active treatment group and 59 people in a wait-list control group. The app improved several measures, including self-reported IBS-quality of life, GI symptoms on the IBS rating scale, the Fear of Food Questionnaire, the Visceral Sensitivity Index, and the Depression Anxiety Stress Scale.
A larger clinical trial to validate the results is ongoing.
Regulora, made by metaMe Health, is an FDA-approved, prescription-only GDH program aimed at addressing abdominal pain related to IBS. The maximum out-of-pocket cost is $75. The protocols were developed by GI behavioral health researchers at the University of North Carolina at Chapel Hill. Available on a Web-based platform or as a mobile app, the program includes seven sessions of 30 minutes each over 12 weeks.
Regulora was evaluated in a randomized comparative effectiveness trial of 362 patients who used either this program or an app focused on muscle relaxation. The primary endpoint was the proportion of patients with a 30% or more reduction in abdominal pain intensity, and although the researchers found no significant difference between them, there was some relief. In the GDH group, 31% of participants reported a 30% or greater reduction in abdominal pain intensity, and 45% experienced a 30% or greater improvement in the proportion of stools with normal consistency.
The complete results of the trial still need to receive formal peer review and publication in a scientific journal.
Nerva, made by Mindset Health, is a GDH program delivered by mobile app or Web browser that costs $79.99 for 3 months. It isn’t FDA-approved and doesn’t require a prescription. The protocols were developed in collaboration with researchers from Monash University in Melbourne. The program features 6 weeks of daily sessions, psychoeducation readings, and breathing techniques.
Nerva was evaluated in an observational cohort study of 190 patients who completed all 42 sessions, typically within 2 months. About 64% responded to the program, with a 20 mm or greater symptom reduction on the Visual Analog Scale and median improvement of 33 mm. Participants also reported improvements in abdominal pain, bloating, dissatisfaction with stool consistency, flatulence, and nausea.
Results were reported as an abstract, and full findings from a formal randomized controlled trial aren’t yet available.
Patient and provider benefits
Although DTx tools are still in the early stages of development and validation, they can improve patient care and add value to a gastroenterologist’s practice, the authors write.
The products should undergo the same level of scientific rigor as pharmaceutical therapies, including randomized controlled trials in diverse patient groups, and patient data handling must be secure and transparent, the authors write. Cost analyses will be an important factor in clinical integration and adoption, they add.
“Change is inevitable, and the right change will bring benefits to providers and their patients,” Dr. Chey said. “Don’t be afraid of it, but do your due diligence before you embrace it. Our primer is intended to help providers conduct that due diligence.”
While behavioral health care is essential for many patients with IBS, there aren’t enough therapists with GI knowledge to meet the demand, Melissa Hunt, PhD, associate director of clinical training in psychology at the University of Pennsylvania, Philadelphia, said in an interview. The population prevalence of IBS is 6%, which means about 18 million people in the United States need guidance, she said.
Dr. Hunt, who wasn’t involved with this paper, has evaluated DTx options for patients with IBS, including the randomized controlled trial of Zemedy. Her research suggests that about 50% of IBS patients could benefit from self-help DTx.
“I get two to three new patient referrals a week and have a 6-month wait-list for my private practice,” Dr. Hunt said. “DTx is a cutting edge, evidence-based way to address the gaps in service and meet the needs of this population.”
The study didn’t receive any funding. The authors disclosed research, consultant, and leadership relationships with several companies not related to this report. Dr. Hunt declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, according to a new review of available products.
These tools aren’t widely used by gastroenterologists yet, but the market is expected to grow broadly during the next decade.
“Digital therapeutics make so much sense and solve so many access issues,” coauthor William Chey, MD, chief of gastroenterology at the University of Michigan, Ann Arbor, said in an interview. “Because of this, their promise could easily outstrip their substance. We need to hold digital therapeutics companies accountable for proper evidence of benefit, so patients and doctors don’t end up chasing the latest shiny object.”
The review was published online in The American Journal of Gastroenterology.
Understanding the apps
IBS is most effectively treated with a combination of medications, diet changes, and behavioral interventions that are specific to the patient, the authors write. Cognitive behavioral therapy (CBT) and gut-directed hypnotherapy (GDH) have been effective at modifying behaviors and thought patterns, they add.
However, many gastroenterologists and their patients with IBS don’t have easy access to the mental health services component of integrated gastrointestinal (GI) care. DTx may offer a solution.
The review by Dr. Chey and colleagues is intended to serve as a primer for gastroenterologists about the current generation of DTx that provide virtual behavioral health interventions. For each product, they include a description of its services, evidence supporting its use, and other key information.
Mahana IBS, made by Mahana Therapeutics, is an FDA-approved, prescription-only CBT program for adults with IBS. The maximum out-of-pocket cost is $90. The product includes 10 sessions over 12 weeks.
Available as a mobile app or Web-based platform, Mahana IBS was validated in a randomized comparative effectiveness trial in a group of 558 patients, divided into three groups who received Web-based CBT, phone-based CBT, or treatment as usual. Before treatment, the mean IBS Symptom Severity Score for the entire group was 265.
At 12 weeks, the control group had an average reduction of 52.9 points, while the phone-based therapy group had a reduction of 133.3 points, and the Web-based therapy group had a reduction of 101.2 points. The average Work and Social Adjustment Scale (WSAS) decreased by an additional 3.5 points in the phone-based group and 3 points in the Web-based group, compared with the control group.
Zemedy, made by Bold Health, is a mobile app that provides virtual CBT through a chat bot for patients with IBS. It costs $19.49 per month or $154.99 per year. The app isn’t FDA-approved and doesn’t require a prescription.
The program includes six weekly psychoeducational modules with information about IBS and CBT, followed by CBT training modules. Users can chat with an automated system that provides computer-generated responses for support. A “flare module” supports patients when symptoms worsen.
Zemedy was evaluated in a crossover randomized controlled trial with 62 people in an active treatment group and 59 people in a wait-list control group. The app improved several measures, including self-reported IBS-quality of life, GI symptoms on the IBS rating scale, the Fear of Food Questionnaire, the Visceral Sensitivity Index, and the Depression Anxiety Stress Scale.
A larger clinical trial to validate the results is ongoing.
Regulora, made by metaMe Health, is an FDA-approved, prescription-only GDH program aimed at addressing abdominal pain related to IBS. The maximum out-of-pocket cost is $75. The protocols were developed by GI behavioral health researchers at the University of North Carolina at Chapel Hill. Available on a Web-based platform or as a mobile app, the program includes seven sessions of 30 minutes each over 12 weeks.
Regulora was evaluated in a randomized comparative effectiveness trial of 362 patients who used either this program or an app focused on muscle relaxation. The primary endpoint was the proportion of patients with a 30% or more reduction in abdominal pain intensity, and although the researchers found no significant difference between them, there was some relief. In the GDH group, 31% of participants reported a 30% or greater reduction in abdominal pain intensity, and 45% experienced a 30% or greater improvement in the proportion of stools with normal consistency.
The complete results of the trial still need to receive formal peer review and publication in a scientific journal.
Nerva, made by Mindset Health, is a GDH program delivered by mobile app or Web browser that costs $79.99 for 3 months. It isn’t FDA-approved and doesn’t require a prescription. The protocols were developed in collaboration with researchers from Monash University in Melbourne. The program features 6 weeks of daily sessions, psychoeducation readings, and breathing techniques.
Nerva was evaluated in an observational cohort study of 190 patients who completed all 42 sessions, typically within 2 months. About 64% responded to the program, with a 20 mm or greater symptom reduction on the Visual Analog Scale and median improvement of 33 mm. Participants also reported improvements in abdominal pain, bloating, dissatisfaction with stool consistency, flatulence, and nausea.
Results were reported as an abstract, and full findings from a formal randomized controlled trial aren’t yet available.
Patient and provider benefits
Although DTx tools are still in the early stages of development and validation, they can improve patient care and add value to a gastroenterologist’s practice, the authors write.
The products should undergo the same level of scientific rigor as pharmaceutical therapies, including randomized controlled trials in diverse patient groups, and patient data handling must be secure and transparent, the authors write. Cost analyses will be an important factor in clinical integration and adoption, they add.
“Change is inevitable, and the right change will bring benefits to providers and their patients,” Dr. Chey said. “Don’t be afraid of it, but do your due diligence before you embrace it. Our primer is intended to help providers conduct that due diligence.”
While behavioral health care is essential for many patients with IBS, there aren’t enough therapists with GI knowledge to meet the demand, Melissa Hunt, PhD, associate director of clinical training in psychology at the University of Pennsylvania, Philadelphia, said in an interview. The population prevalence of IBS is 6%, which means about 18 million people in the United States need guidance, she said.
Dr. Hunt, who wasn’t involved with this paper, has evaluated DTx options for patients with IBS, including the randomized controlled trial of Zemedy. Her research suggests that about 50% of IBS patients could benefit from self-help DTx.
“I get two to three new patient referrals a week and have a 6-month wait-list for my private practice,” Dr. Hunt said. “DTx is a cutting edge, evidence-based way to address the gaps in service and meet the needs of this population.”
The study didn’t receive any funding. The authors disclosed research, consultant, and leadership relationships with several companies not related to this report. Dr. Hunt declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
, according to a new review of available products.
These tools aren’t widely used by gastroenterologists yet, but the market is expected to grow broadly during the next decade.
“Digital therapeutics make so much sense and solve so many access issues,” coauthor William Chey, MD, chief of gastroenterology at the University of Michigan, Ann Arbor, said in an interview. “Because of this, their promise could easily outstrip their substance. We need to hold digital therapeutics companies accountable for proper evidence of benefit, so patients and doctors don’t end up chasing the latest shiny object.”
The review was published online in The American Journal of Gastroenterology.
Understanding the apps
IBS is most effectively treated with a combination of medications, diet changes, and behavioral interventions that are specific to the patient, the authors write. Cognitive behavioral therapy (CBT) and gut-directed hypnotherapy (GDH) have been effective at modifying behaviors and thought patterns, they add.
However, many gastroenterologists and their patients with IBS don’t have easy access to the mental health services component of integrated gastrointestinal (GI) care. DTx may offer a solution.
The review by Dr. Chey and colleagues is intended to serve as a primer for gastroenterologists about the current generation of DTx that provide virtual behavioral health interventions. For each product, they include a description of its services, evidence supporting its use, and other key information.
Mahana IBS, made by Mahana Therapeutics, is an FDA-approved, prescription-only CBT program for adults with IBS. The maximum out-of-pocket cost is $90. The product includes 10 sessions over 12 weeks.
Available as a mobile app or Web-based platform, Mahana IBS was validated in a randomized comparative effectiveness trial in a group of 558 patients, divided into three groups who received Web-based CBT, phone-based CBT, or treatment as usual. Before treatment, the mean IBS Symptom Severity Score for the entire group was 265.
At 12 weeks, the control group had an average reduction of 52.9 points, while the phone-based therapy group had a reduction of 133.3 points, and the Web-based therapy group had a reduction of 101.2 points. The average Work and Social Adjustment Scale (WSAS) decreased by an additional 3.5 points in the phone-based group and 3 points in the Web-based group, compared with the control group.
Zemedy, made by Bold Health, is a mobile app that provides virtual CBT through a chat bot for patients with IBS. It costs $19.49 per month or $154.99 per year. The app isn’t FDA-approved and doesn’t require a prescription.
The program includes six weekly psychoeducational modules with information about IBS and CBT, followed by CBT training modules. Users can chat with an automated system that provides computer-generated responses for support. A “flare module” supports patients when symptoms worsen.
Zemedy was evaluated in a crossover randomized controlled trial with 62 people in an active treatment group and 59 people in a wait-list control group. The app improved several measures, including self-reported IBS-quality of life, GI symptoms on the IBS rating scale, the Fear of Food Questionnaire, the Visceral Sensitivity Index, and the Depression Anxiety Stress Scale.
A larger clinical trial to validate the results is ongoing.
Regulora, made by metaMe Health, is an FDA-approved, prescription-only GDH program aimed at addressing abdominal pain related to IBS. The maximum out-of-pocket cost is $75. The protocols were developed by GI behavioral health researchers at the University of North Carolina at Chapel Hill. Available on a Web-based platform or as a mobile app, the program includes seven sessions of 30 minutes each over 12 weeks.
Regulora was evaluated in a randomized comparative effectiveness trial of 362 patients who used either this program or an app focused on muscle relaxation. The primary endpoint was the proportion of patients with a 30% or more reduction in abdominal pain intensity, and although the researchers found no significant difference between them, there was some relief. In the GDH group, 31% of participants reported a 30% or greater reduction in abdominal pain intensity, and 45% experienced a 30% or greater improvement in the proportion of stools with normal consistency.
The complete results of the trial still need to receive formal peer review and publication in a scientific journal.
Nerva, made by Mindset Health, is a GDH program delivered by mobile app or Web browser that costs $79.99 for 3 months. It isn’t FDA-approved and doesn’t require a prescription. The protocols were developed in collaboration with researchers from Monash University in Melbourne. The program features 6 weeks of daily sessions, psychoeducation readings, and breathing techniques.
Nerva was evaluated in an observational cohort study of 190 patients who completed all 42 sessions, typically within 2 months. About 64% responded to the program, with a 20 mm or greater symptom reduction on the Visual Analog Scale and median improvement of 33 mm. Participants also reported improvements in abdominal pain, bloating, dissatisfaction with stool consistency, flatulence, and nausea.
Results were reported as an abstract, and full findings from a formal randomized controlled trial aren’t yet available.
Patient and provider benefits
Although DTx tools are still in the early stages of development and validation, they can improve patient care and add value to a gastroenterologist’s practice, the authors write.
The products should undergo the same level of scientific rigor as pharmaceutical therapies, including randomized controlled trials in diverse patient groups, and patient data handling must be secure and transparent, the authors write. Cost analyses will be an important factor in clinical integration and adoption, they add.
“Change is inevitable, and the right change will bring benefits to providers and their patients,” Dr. Chey said. “Don’t be afraid of it, but do your due diligence before you embrace it. Our primer is intended to help providers conduct that due diligence.”
While behavioral health care is essential for many patients with IBS, there aren’t enough therapists with GI knowledge to meet the demand, Melissa Hunt, PhD, associate director of clinical training in psychology at the University of Pennsylvania, Philadelphia, said in an interview. The population prevalence of IBS is 6%, which means about 18 million people in the United States need guidance, she said.
Dr. Hunt, who wasn’t involved with this paper, has evaluated DTx options for patients with IBS, including the randomized controlled trial of Zemedy. Her research suggests that about 50% of IBS patients could benefit from self-help DTx.
“I get two to three new patient referrals a week and have a 6-month wait-list for my private practice,” Dr. Hunt said. “DTx is a cutting edge, evidence-based way to address the gaps in service and meet the needs of this population.”
The study didn’t receive any funding. The authors disclosed research, consultant, and leadership relationships with several companies not related to this report. Dr. Hunt declared no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY