User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Maternal Lifestyle Interventions Boost Babies’ Heart Health
Infants born to women with obesity showed improved measures of cardiovascular health when their mothers adopted healthier lifestyles before and during pregnancy, based on data from a systematic review presented at the annual meeting of the Society for Reproductive Investigation.
Previous research has shown that children born to mothers with a high body mass index (BMI) are more likely to die from cardiovascular disease in later life, said presenting author Samuel J. Burden, PhD, in an interview.
“Surprisingly, early signs of these heart issues can start before birth and continue into childhood,” said Dr. Burden, a research associate in the Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom.
To examine the effect of interventions such as a healthy diet and exercise in pregnant women with obesity on the heart health of their infants, Dr. Burden and colleagues reviewed data from eight randomized, controlled trials involving diet and exercise for pregnant women with obesity. Of these, two used antenatal exercise, two used diet and physical activity, and one used preconception diet and physical activity. The studies ranged in size from 18 to 404 participants. Two studies included infants younger than 2 months of age, and four studies included children aged 3-7 years.
Overall, lifestyle interventions before conception and before birth were associated with significant changes in cardiac remodeling, specifically reduced interventricular septal wall thickness.
In addition, one of three studies of cardiac diastolic function and four of five studies of systolic function showed significant improvements. The five studies of cardiac systolic function and three studies of diastolic function also showed improvement in systolic and diastolic blood pressure in infants of mothers who took part in the interventions. The studies were limited mainly by large attrition rates, the researchers wrote in their presentation. However, more studies in larger populations that also include older children could confirm the findings and inform public health strategies to promote healthy lifestyles for pregnant women, they noted.
Encourage Healthy Lifestyle Before and During Pregnancy
The evidence supports the findings from animal studies showing that an offspring’s health is influenced by maternal lifestyle before and during pregnancy, Dr. Burden said in an interview. The data suggest that healthcare providers should encourage women with a high BMI who want to become pregnant to eat healthfully and become more active as a way to enhance the future cardiovascular health of their children, he said.
The full results of the current study are soon to be published, but more work is needed, said Dr. Burden. “While we observed a protective effect from these lifestyle programs, there is a need for more extensive studies involving a larger number of women (and their children) who were part of the initial research,” he said. “Additionally, it will be crucial to track these children into adulthood to determine whether these antenatal lifestyle interventions persist in lowering the risk of future cardiovascular disease.”
Beginning healthy lifestyle programs prior to pregnancy might yield the best results for promoting infant cardiovascular health, and more prepregnancy interventions for women with obesity are needed, Dr. Burden added.
The current study adds to the growing body of evidence that the in utero environment can have lifelong effects on offspring, Joseph R. Biggio Jr, MD, system chair of maternal fetal medicine at Ochsner Health, New Orleans, Louisiana, said in an interview.
“Several studies have previously shown that the children of mothers with diabetes, hypertension, or obesity are at increased risk for developing signs of metabolic syndrome and cardiovascular changes during childhood or adolescence,” said Dr. Biggio.
The data from this systematic review support the potential value of interventions aimed at improving maternal weight gain and cardiovascular performance before and during pregnancy that may result in reduced cardiovascular remodeling and myocardial thickening in infants, he said.
The study was supported by a British Heart Foundation Special Project Grant. The researchers had no financial conflicts to disclose. Dr. Biggio had no financial conflicts to disclose.
Infants born to women with obesity showed improved measures of cardiovascular health when their mothers adopted healthier lifestyles before and during pregnancy, based on data from a systematic review presented at the annual meeting of the Society for Reproductive Investigation.
Previous research has shown that children born to mothers with a high body mass index (BMI) are more likely to die from cardiovascular disease in later life, said presenting author Samuel J. Burden, PhD, in an interview.
“Surprisingly, early signs of these heart issues can start before birth and continue into childhood,” said Dr. Burden, a research associate in the Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom.
To examine the effect of interventions such as a healthy diet and exercise in pregnant women with obesity on the heart health of their infants, Dr. Burden and colleagues reviewed data from eight randomized, controlled trials involving diet and exercise for pregnant women with obesity. Of these, two used antenatal exercise, two used diet and physical activity, and one used preconception diet and physical activity. The studies ranged in size from 18 to 404 participants. Two studies included infants younger than 2 months of age, and four studies included children aged 3-7 years.
Overall, lifestyle interventions before conception and before birth were associated with significant changes in cardiac remodeling, specifically reduced interventricular septal wall thickness.
In addition, one of three studies of cardiac diastolic function and four of five studies of systolic function showed significant improvements. The five studies of cardiac systolic function and three studies of diastolic function also showed improvement in systolic and diastolic blood pressure in infants of mothers who took part in the interventions. The studies were limited mainly by large attrition rates, the researchers wrote in their presentation. However, more studies in larger populations that also include older children could confirm the findings and inform public health strategies to promote healthy lifestyles for pregnant women, they noted.
Encourage Healthy Lifestyle Before and During Pregnancy
The evidence supports the findings from animal studies showing that an offspring’s health is influenced by maternal lifestyle before and during pregnancy, Dr. Burden said in an interview. The data suggest that healthcare providers should encourage women with a high BMI who want to become pregnant to eat healthfully and become more active as a way to enhance the future cardiovascular health of their children, he said.
The full results of the current study are soon to be published, but more work is needed, said Dr. Burden. “While we observed a protective effect from these lifestyle programs, there is a need for more extensive studies involving a larger number of women (and their children) who were part of the initial research,” he said. “Additionally, it will be crucial to track these children into adulthood to determine whether these antenatal lifestyle interventions persist in lowering the risk of future cardiovascular disease.”
Beginning healthy lifestyle programs prior to pregnancy might yield the best results for promoting infant cardiovascular health, and more prepregnancy interventions for women with obesity are needed, Dr. Burden added.
The current study adds to the growing body of evidence that the in utero environment can have lifelong effects on offspring, Joseph R. Biggio Jr, MD, system chair of maternal fetal medicine at Ochsner Health, New Orleans, Louisiana, said in an interview.
“Several studies have previously shown that the children of mothers with diabetes, hypertension, or obesity are at increased risk for developing signs of metabolic syndrome and cardiovascular changes during childhood or adolescence,” said Dr. Biggio.
The data from this systematic review support the potential value of interventions aimed at improving maternal weight gain and cardiovascular performance before and during pregnancy that may result in reduced cardiovascular remodeling and myocardial thickening in infants, he said.
The study was supported by a British Heart Foundation Special Project Grant. The researchers had no financial conflicts to disclose. Dr. Biggio had no financial conflicts to disclose.
Infants born to women with obesity showed improved measures of cardiovascular health when their mothers adopted healthier lifestyles before and during pregnancy, based on data from a systematic review presented at the annual meeting of the Society for Reproductive Investigation.
Previous research has shown that children born to mothers with a high body mass index (BMI) are more likely to die from cardiovascular disease in later life, said presenting author Samuel J. Burden, PhD, in an interview.
“Surprisingly, early signs of these heart issues can start before birth and continue into childhood,” said Dr. Burden, a research associate in the Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom.
To examine the effect of interventions such as a healthy diet and exercise in pregnant women with obesity on the heart health of their infants, Dr. Burden and colleagues reviewed data from eight randomized, controlled trials involving diet and exercise for pregnant women with obesity. Of these, two used antenatal exercise, two used diet and physical activity, and one used preconception diet and physical activity. The studies ranged in size from 18 to 404 participants. Two studies included infants younger than 2 months of age, and four studies included children aged 3-7 years.
Overall, lifestyle interventions before conception and before birth were associated with significant changes in cardiac remodeling, specifically reduced interventricular septal wall thickness.
In addition, one of three studies of cardiac diastolic function and four of five studies of systolic function showed significant improvements. The five studies of cardiac systolic function and three studies of diastolic function also showed improvement in systolic and diastolic blood pressure in infants of mothers who took part in the interventions. The studies were limited mainly by large attrition rates, the researchers wrote in their presentation. However, more studies in larger populations that also include older children could confirm the findings and inform public health strategies to promote healthy lifestyles for pregnant women, they noted.
Encourage Healthy Lifestyle Before and During Pregnancy
The evidence supports the findings from animal studies showing that an offspring’s health is influenced by maternal lifestyle before and during pregnancy, Dr. Burden said in an interview. The data suggest that healthcare providers should encourage women with a high BMI who want to become pregnant to eat healthfully and become more active as a way to enhance the future cardiovascular health of their children, he said.
The full results of the current study are soon to be published, but more work is needed, said Dr. Burden. “While we observed a protective effect from these lifestyle programs, there is a need for more extensive studies involving a larger number of women (and their children) who were part of the initial research,” he said. “Additionally, it will be crucial to track these children into adulthood to determine whether these antenatal lifestyle interventions persist in lowering the risk of future cardiovascular disease.”
Beginning healthy lifestyle programs prior to pregnancy might yield the best results for promoting infant cardiovascular health, and more prepregnancy interventions for women with obesity are needed, Dr. Burden added.
The current study adds to the growing body of evidence that the in utero environment can have lifelong effects on offspring, Joseph R. Biggio Jr, MD, system chair of maternal fetal medicine at Ochsner Health, New Orleans, Louisiana, said in an interview.
“Several studies have previously shown that the children of mothers with diabetes, hypertension, or obesity are at increased risk for developing signs of metabolic syndrome and cardiovascular changes during childhood or adolescence,” said Dr. Biggio.
The data from this systematic review support the potential value of interventions aimed at improving maternal weight gain and cardiovascular performance before and during pregnancy that may result in reduced cardiovascular remodeling and myocardial thickening in infants, he said.
The study was supported by a British Heart Foundation Special Project Grant. The researchers had no financial conflicts to disclose. Dr. Biggio had no financial conflicts to disclose.
Delaying Embryo Transfers May Benefit Patients With Endometrial Polyps
A longer time between hysteroscopic polypectomy and frozen embryo transfer may improve the odds of successful pregnancy, based on data from a new analysis presented at the annual meeting of the Society for Reproductive Investigation.
Although uterine polyps have a negative effect on pregnancy rates, data supporting a specific time interval between hysteroscopic polypectomy (HP) and frozen embryo transfer (FET) are limited, according to Audrey Messelt, MD, of Baylor College of Medicine, Houston, Texas, and colleagues.
“Hysteroscopic polypectomy is a common procedure performed before embryo transfer to optimize the receptivity of the endometrium. Currently, there is no ideal recovery time lapse between surgery and an embryo transfer,” said senior author Laura Detti, MD, professor of obstetrics and gynecology at Baylor, in an interview. “This is often the last step prior to embryo transfer, and identifying a recovery time that allows the best outcome is important.”
In a retrospective analysis, the researchers examined the effect of the time between HP and FET on pregnancy outcomes. They identified 65 patients with uterine pathology based on saline-infusion sonogram who underwent hysteroscopy and FET between June 1, 2022, and September 30, 2023.
The endometrial preparation for FET included sequential administration of oral or transdermal estradiol and intramuscular progesterone.
Overall, 46 patients were diagnosed with endometrial polyps at the time of surgery; three had endometritis, one had a uterine septum that was resected, 15 had no abnormal pathology or had normal endometrium at the time of examination. No cases of hyperplasia or malignancy were identified.
A total of 58 patients underwent FET with a single euploid embryo, four with a single untested embryo, one with a low-mosaic embryo, and two with a double-embryo transfer (one euploid and one low mosaic).
After FET, 50 patients conceived and 15 did not. Patients with ongoing pregnancies who had a history of endometrial polyps had significantly more days from surgery to FET, compared to patients with a history of polyps who failed to conceive (median 70 days vs 45 days, P = .01).
By contrast, the time between hysteroscopy and FET was similar among patients with no endometrial pathology who did and did not have ongoing pregnancies (median 45 vs 52.5 days, P = .95).
The findings were limited by the relatively small sample size and exclusion of patients with pathologies other than polyps, as well as a lack of data on age group breakdowns. However, the results suggest that patients with uterine polyps may benefit from more time between HP and FET, while patients with normal surgical findings could undergo FET sooner, the researchers concluded.
Postpolypectomy Timing May Affect Pregnancy Outcomes
“We used to think that having had the first menses from surgery would be enough recovery time for the uterine cavity, even if it was just 2 weeks,” Dr. Detti said in an interview. “This still holds true when no endometrial polyps are diagnosed in the pathological specimen; however, we learned that if endometrial polyps are removed at the time of hysteroscopy, the ideal recovery time prior to an embryo transfer should be longer,” she said.
The current study is important because approximately 15% of women are diagnosed with endometrial polyps during their reproductive years, said Mark P. Trolice, MD, professor at the University of Central Florida, Orlando, and founder/medical director of the IVF Center of Central Florida in Winter Park, in an interview.
“Abnormalities of the uterine cavity have been shown to reduce embryo implantation and increase the risk of miscarriage,” said Dr. Trolice. Although the impact of small endometrial polyps on fertility and pregnancy are uncertain, most infertility specialists recommend removal of endometrial polyps via hysteroscopic polypectomy in general and prior to IVF embryo transfer in particular, he said.
Although infertility patients are anxious to undergo embryo transfer, the current study suggests a benefit in delaying the procedure following the removal of any polyps identified during the pretransfer evaluation, Dr. Trolice said in an interview. As for additional research, “it would be helpful to know the age group breakdown of patients and if the results were consistent among all categories,” he said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Trolice had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
A longer time between hysteroscopic polypectomy and frozen embryo transfer may improve the odds of successful pregnancy, based on data from a new analysis presented at the annual meeting of the Society for Reproductive Investigation.
Although uterine polyps have a negative effect on pregnancy rates, data supporting a specific time interval between hysteroscopic polypectomy (HP) and frozen embryo transfer (FET) are limited, according to Audrey Messelt, MD, of Baylor College of Medicine, Houston, Texas, and colleagues.
“Hysteroscopic polypectomy is a common procedure performed before embryo transfer to optimize the receptivity of the endometrium. Currently, there is no ideal recovery time lapse between surgery and an embryo transfer,” said senior author Laura Detti, MD, professor of obstetrics and gynecology at Baylor, in an interview. “This is often the last step prior to embryo transfer, and identifying a recovery time that allows the best outcome is important.”
In a retrospective analysis, the researchers examined the effect of the time between HP and FET on pregnancy outcomes. They identified 65 patients with uterine pathology based on saline-infusion sonogram who underwent hysteroscopy and FET between June 1, 2022, and September 30, 2023.
The endometrial preparation for FET included sequential administration of oral or transdermal estradiol and intramuscular progesterone.
Overall, 46 patients were diagnosed with endometrial polyps at the time of surgery; three had endometritis, one had a uterine septum that was resected, 15 had no abnormal pathology or had normal endometrium at the time of examination. No cases of hyperplasia or malignancy were identified.
A total of 58 patients underwent FET with a single euploid embryo, four with a single untested embryo, one with a low-mosaic embryo, and two with a double-embryo transfer (one euploid and one low mosaic).
After FET, 50 patients conceived and 15 did not. Patients with ongoing pregnancies who had a history of endometrial polyps had significantly more days from surgery to FET, compared to patients with a history of polyps who failed to conceive (median 70 days vs 45 days, P = .01).
By contrast, the time between hysteroscopy and FET was similar among patients with no endometrial pathology who did and did not have ongoing pregnancies (median 45 vs 52.5 days, P = .95).
The findings were limited by the relatively small sample size and exclusion of patients with pathologies other than polyps, as well as a lack of data on age group breakdowns. However, the results suggest that patients with uterine polyps may benefit from more time between HP and FET, while patients with normal surgical findings could undergo FET sooner, the researchers concluded.
Postpolypectomy Timing May Affect Pregnancy Outcomes
“We used to think that having had the first menses from surgery would be enough recovery time for the uterine cavity, even if it was just 2 weeks,” Dr. Detti said in an interview. “This still holds true when no endometrial polyps are diagnosed in the pathological specimen; however, we learned that if endometrial polyps are removed at the time of hysteroscopy, the ideal recovery time prior to an embryo transfer should be longer,” she said.
The current study is important because approximately 15% of women are diagnosed with endometrial polyps during their reproductive years, said Mark P. Trolice, MD, professor at the University of Central Florida, Orlando, and founder/medical director of the IVF Center of Central Florida in Winter Park, in an interview.
“Abnormalities of the uterine cavity have been shown to reduce embryo implantation and increase the risk of miscarriage,” said Dr. Trolice. Although the impact of small endometrial polyps on fertility and pregnancy are uncertain, most infertility specialists recommend removal of endometrial polyps via hysteroscopic polypectomy in general and prior to IVF embryo transfer in particular, he said.
Although infertility patients are anxious to undergo embryo transfer, the current study suggests a benefit in delaying the procedure following the removal of any polyps identified during the pretransfer evaluation, Dr. Trolice said in an interview. As for additional research, “it would be helpful to know the age group breakdown of patients and if the results were consistent among all categories,” he said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Trolice had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
A longer time between hysteroscopic polypectomy and frozen embryo transfer may improve the odds of successful pregnancy, based on data from a new analysis presented at the annual meeting of the Society for Reproductive Investigation.
Although uterine polyps have a negative effect on pregnancy rates, data supporting a specific time interval between hysteroscopic polypectomy (HP) and frozen embryo transfer (FET) are limited, according to Audrey Messelt, MD, of Baylor College of Medicine, Houston, Texas, and colleagues.
“Hysteroscopic polypectomy is a common procedure performed before embryo transfer to optimize the receptivity of the endometrium. Currently, there is no ideal recovery time lapse between surgery and an embryo transfer,” said senior author Laura Detti, MD, professor of obstetrics and gynecology at Baylor, in an interview. “This is often the last step prior to embryo transfer, and identifying a recovery time that allows the best outcome is important.”
In a retrospective analysis, the researchers examined the effect of the time between HP and FET on pregnancy outcomes. They identified 65 patients with uterine pathology based on saline-infusion sonogram who underwent hysteroscopy and FET between June 1, 2022, and September 30, 2023.
The endometrial preparation for FET included sequential administration of oral or transdermal estradiol and intramuscular progesterone.
Overall, 46 patients were diagnosed with endometrial polyps at the time of surgery; three had endometritis, one had a uterine septum that was resected, 15 had no abnormal pathology or had normal endometrium at the time of examination. No cases of hyperplasia or malignancy were identified.
A total of 58 patients underwent FET with a single euploid embryo, four with a single untested embryo, one with a low-mosaic embryo, and two with a double-embryo transfer (one euploid and one low mosaic).
After FET, 50 patients conceived and 15 did not. Patients with ongoing pregnancies who had a history of endometrial polyps had significantly more days from surgery to FET, compared to patients with a history of polyps who failed to conceive (median 70 days vs 45 days, P = .01).
By contrast, the time between hysteroscopy and FET was similar among patients with no endometrial pathology who did and did not have ongoing pregnancies (median 45 vs 52.5 days, P = .95).
The findings were limited by the relatively small sample size and exclusion of patients with pathologies other than polyps, as well as a lack of data on age group breakdowns. However, the results suggest that patients with uterine polyps may benefit from more time between HP and FET, while patients with normal surgical findings could undergo FET sooner, the researchers concluded.
Postpolypectomy Timing May Affect Pregnancy Outcomes
“We used to think that having had the first menses from surgery would be enough recovery time for the uterine cavity, even if it was just 2 weeks,” Dr. Detti said in an interview. “This still holds true when no endometrial polyps are diagnosed in the pathological specimen; however, we learned that if endometrial polyps are removed at the time of hysteroscopy, the ideal recovery time prior to an embryo transfer should be longer,” she said.
The current study is important because approximately 15% of women are diagnosed with endometrial polyps during their reproductive years, said Mark P. Trolice, MD, professor at the University of Central Florida, Orlando, and founder/medical director of the IVF Center of Central Florida in Winter Park, in an interview.
“Abnormalities of the uterine cavity have been shown to reduce embryo implantation and increase the risk of miscarriage,” said Dr. Trolice. Although the impact of small endometrial polyps on fertility and pregnancy are uncertain, most infertility specialists recommend removal of endometrial polyps via hysteroscopic polypectomy in general and prior to IVF embryo transfer in particular, he said.
Although infertility patients are anxious to undergo embryo transfer, the current study suggests a benefit in delaying the procedure following the removal of any polyps identified during the pretransfer evaluation, Dr. Trolice said in an interview. As for additional research, “it would be helpful to know the age group breakdown of patients and if the results were consistent among all categories,” he said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Trolice had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
Teen Pregnancy Linked With Risk for Premature Death
Teen pregnancy is associated with a higher risk for premature mortality, both among those who carry the pregnancies to term and those who miscarry, according to a new study.
Among 2.2 million female teenagers in Ontario, Canada, the risk for premature death by age 31 years was 1.5 times higher among those who had one teen pregnancy and 2.1 times higher among those with two or more teen pregnancies.
“No person should die during childhood or early adulthood. Such deaths, unexpected and tragic, are often from preventable causes, including intentional injury,” lead author Joel Ray, MD, an obstetric medicine specialist and epidemiologist at St. Michael’s Hospital in Toronto, told this news organization.
“Women who experience teen pregnancy appear more vulnerable, often having experienced a history of adverse experiences in childhood, including abuse and economic challenges,” he said.
The study was published online in JAMA Network Open.
Analyzing Pregnancy Associations
The investigators conducted a population-based cohort study of all girls who were alive at age 12 years from April 1991 to March 2021 in Ontario. They evaluated the risk for all-cause mortality from age 12 years onward in association with the number of teen pregnancies between ages 12 and 19 years and the age at first pregnancy. The investigators adjusted the hazard ratios for year of birth, comorbidities at ages 9-11 years, area-level education, income level, and rural status.
Among more than 2.2 million teens, 163,124 (7.3%) had a pregnancy at a median age of 18 years, including 121,276 (74.3%) who had one pregnancy and 41,848 (25.6%) who had two or more. These teens were more likely to live in the lowest neighborhood income quintile and in an area with a lower rate of high school completion. They also had a higher prevalence of self-harm history between ages 12 and 19 years but not a higher prevalence of physical or mental comorbidities.
Among all teens who had a pregnancy, 60,037 (36.8%) ended in a birth, including 59,485 (99.1%) live births. A further 106,135 (65.1%) ended in induced abortion, and 17,945 (11%) ended in miscarriage or ectopic pregnancy.
Overall, there were 6030 premature deaths among those without a teen pregnancy, or 1.9 per 10,000 person-years. There were 701 deaths among those with one teen pregnancy (4.1 per 10,000 person-years) and 345 deaths among those with two or more teen pregnancies (6.1 per 10,000 person-years).
The adjusted hazard ratios (AHRs) for mortality were 1.51 for those with one pregnancy and 2.14 for those with two or more pregnancies. Compared with no teen pregnancy, the AHRs for premature death were 1.41 if the first teen pregnancy ended in an induced abortion and 2.10 if it ended in a miscarriage or birth.
Comparing those with a teen pregnancy and those without, the AHRs for premature death were 1.25 from noninjury, 2.06 from unintentional injury, and 2.02 from intentional injury. Among patients with teen pregnancy, noninjury-related premature mortality was more common, at 2.0 per 10,000 person-years, than unintentional and intentional injuries, at 1.0 per 10,000 person-years and 0.4 per 10,000 person-years, respectively.
A teen pregnancy before age 16 years entailed the highest associated risk for premature death, with an AHR of 2.00.
Next Research Steps
“We were not surprised by our findings, but it was new to us to see that the risk for premature death was higher for women who had an induced abortion in their teen years,” said Dr. Ray. “It was even higher in those whose pregnancy ended in a birth or miscarriage.”
The investigators plan to evaluate whether the future risk for premature death after teen pregnancy differs by the type of induced abortion, such as procedural or pharmaceutical, or by whether the pregnancy ended in a live birth, stillbirth, or miscarriage. Among those with a live birth, the researchers will also analyze the risk for premature death in relation to whether the newborn was taken into custody by child protection services in Canada.
Other factors associated with teen pregnancy and overall mortality, particularly adverse childhood experiences, may point to the reasons for premature mortality and should be studied further, the authors wrote. Structural and systems-related factors should be considered as well.
Stigmatization and Isolation
“Some teens choose to become pregnant, but most teen pregnancies are unintended, which exposes shortcomings in the systems that exist to educate, guide, and support young people,” said Elizabeth Cook, a research scientist at Child Trends in Rockville, Maryland.
Dr. Cook, who wasn’t involved with this study, wrote an accompanying editorial in JAMA Network Open. She conducts studies of sexual and reproductive health for Child Trends.
“Teens who become pregnant often experience stigmatization and isolation that can make it more difficult to thrive in adulthood, especially if they lack the necessary support to navigate such a significant decision,” she said. “Fortunately, the systems that youths encounter, such as healthcare, education, and child welfare, are taking on a larger role in prevention efforts than they have in the past.”
These systems are shifting the burden of unintended teen pregnancy from the teens themselves and their behaviors to the health and education systems, Dr. Cook noted, though more work is needed around local policies and lack of access to healthcare facilities.
“Teen pregnancy may offer an opportunity to intervene in the lives of people at higher risk for premature death, but knowing how best to offer support requires an understanding of the context of their lives,” she said. “As a starting point, we must celebrate and listen to all pregnant young people so they can tell us what they need to live long, fulfilled lives.”
The study was funded by grants from the PSI Foundation and the Canadian Institutes of Health Research, as well as ICES, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Ray and Dr. Cook reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Teen pregnancy is associated with a higher risk for premature mortality, both among those who carry the pregnancies to term and those who miscarry, according to a new study.
Among 2.2 million female teenagers in Ontario, Canada, the risk for premature death by age 31 years was 1.5 times higher among those who had one teen pregnancy and 2.1 times higher among those with two or more teen pregnancies.
“No person should die during childhood or early adulthood. Such deaths, unexpected and tragic, are often from preventable causes, including intentional injury,” lead author Joel Ray, MD, an obstetric medicine specialist and epidemiologist at St. Michael’s Hospital in Toronto, told this news organization.
“Women who experience teen pregnancy appear more vulnerable, often having experienced a history of adverse experiences in childhood, including abuse and economic challenges,” he said.
The study was published online in JAMA Network Open.
Analyzing Pregnancy Associations
The investigators conducted a population-based cohort study of all girls who were alive at age 12 years from April 1991 to March 2021 in Ontario. They evaluated the risk for all-cause mortality from age 12 years onward in association with the number of teen pregnancies between ages 12 and 19 years and the age at first pregnancy. The investigators adjusted the hazard ratios for year of birth, comorbidities at ages 9-11 years, area-level education, income level, and rural status.
Among more than 2.2 million teens, 163,124 (7.3%) had a pregnancy at a median age of 18 years, including 121,276 (74.3%) who had one pregnancy and 41,848 (25.6%) who had two or more. These teens were more likely to live in the lowest neighborhood income quintile and in an area with a lower rate of high school completion. They also had a higher prevalence of self-harm history between ages 12 and 19 years but not a higher prevalence of physical or mental comorbidities.
Among all teens who had a pregnancy, 60,037 (36.8%) ended in a birth, including 59,485 (99.1%) live births. A further 106,135 (65.1%) ended in induced abortion, and 17,945 (11%) ended in miscarriage or ectopic pregnancy.
Overall, there were 6030 premature deaths among those without a teen pregnancy, or 1.9 per 10,000 person-years. There were 701 deaths among those with one teen pregnancy (4.1 per 10,000 person-years) and 345 deaths among those with two or more teen pregnancies (6.1 per 10,000 person-years).
The adjusted hazard ratios (AHRs) for mortality were 1.51 for those with one pregnancy and 2.14 for those with two or more pregnancies. Compared with no teen pregnancy, the AHRs for premature death were 1.41 if the first teen pregnancy ended in an induced abortion and 2.10 if it ended in a miscarriage or birth.
Comparing those with a teen pregnancy and those without, the AHRs for premature death were 1.25 from noninjury, 2.06 from unintentional injury, and 2.02 from intentional injury. Among patients with teen pregnancy, noninjury-related premature mortality was more common, at 2.0 per 10,000 person-years, than unintentional and intentional injuries, at 1.0 per 10,000 person-years and 0.4 per 10,000 person-years, respectively.
A teen pregnancy before age 16 years entailed the highest associated risk for premature death, with an AHR of 2.00.
Next Research Steps
“We were not surprised by our findings, but it was new to us to see that the risk for premature death was higher for women who had an induced abortion in their teen years,” said Dr. Ray. “It was even higher in those whose pregnancy ended in a birth or miscarriage.”
The investigators plan to evaluate whether the future risk for premature death after teen pregnancy differs by the type of induced abortion, such as procedural or pharmaceutical, or by whether the pregnancy ended in a live birth, stillbirth, or miscarriage. Among those with a live birth, the researchers will also analyze the risk for premature death in relation to whether the newborn was taken into custody by child protection services in Canada.
Other factors associated with teen pregnancy and overall mortality, particularly adverse childhood experiences, may point to the reasons for premature mortality and should be studied further, the authors wrote. Structural and systems-related factors should be considered as well.
Stigmatization and Isolation
“Some teens choose to become pregnant, but most teen pregnancies are unintended, which exposes shortcomings in the systems that exist to educate, guide, and support young people,” said Elizabeth Cook, a research scientist at Child Trends in Rockville, Maryland.
Dr. Cook, who wasn’t involved with this study, wrote an accompanying editorial in JAMA Network Open. She conducts studies of sexual and reproductive health for Child Trends.
“Teens who become pregnant often experience stigmatization and isolation that can make it more difficult to thrive in adulthood, especially if they lack the necessary support to navigate such a significant decision,” she said. “Fortunately, the systems that youths encounter, such as healthcare, education, and child welfare, are taking on a larger role in prevention efforts than they have in the past.”
These systems are shifting the burden of unintended teen pregnancy from the teens themselves and their behaviors to the health and education systems, Dr. Cook noted, though more work is needed around local policies and lack of access to healthcare facilities.
“Teen pregnancy may offer an opportunity to intervene in the lives of people at higher risk for premature death, but knowing how best to offer support requires an understanding of the context of their lives,” she said. “As a starting point, we must celebrate and listen to all pregnant young people so they can tell us what they need to live long, fulfilled lives.”
The study was funded by grants from the PSI Foundation and the Canadian Institutes of Health Research, as well as ICES, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Ray and Dr. Cook reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Teen pregnancy is associated with a higher risk for premature mortality, both among those who carry the pregnancies to term and those who miscarry, according to a new study.
Among 2.2 million female teenagers in Ontario, Canada, the risk for premature death by age 31 years was 1.5 times higher among those who had one teen pregnancy and 2.1 times higher among those with two or more teen pregnancies.
“No person should die during childhood or early adulthood. Such deaths, unexpected and tragic, are often from preventable causes, including intentional injury,” lead author Joel Ray, MD, an obstetric medicine specialist and epidemiologist at St. Michael’s Hospital in Toronto, told this news organization.
“Women who experience teen pregnancy appear more vulnerable, often having experienced a history of adverse experiences in childhood, including abuse and economic challenges,” he said.
The study was published online in JAMA Network Open.
Analyzing Pregnancy Associations
The investigators conducted a population-based cohort study of all girls who were alive at age 12 years from April 1991 to March 2021 in Ontario. They evaluated the risk for all-cause mortality from age 12 years onward in association with the number of teen pregnancies between ages 12 and 19 years and the age at first pregnancy. The investigators adjusted the hazard ratios for year of birth, comorbidities at ages 9-11 years, area-level education, income level, and rural status.
Among more than 2.2 million teens, 163,124 (7.3%) had a pregnancy at a median age of 18 years, including 121,276 (74.3%) who had one pregnancy and 41,848 (25.6%) who had two or more. These teens were more likely to live in the lowest neighborhood income quintile and in an area with a lower rate of high school completion. They also had a higher prevalence of self-harm history between ages 12 and 19 years but not a higher prevalence of physical or mental comorbidities.
Among all teens who had a pregnancy, 60,037 (36.8%) ended in a birth, including 59,485 (99.1%) live births. A further 106,135 (65.1%) ended in induced abortion, and 17,945 (11%) ended in miscarriage or ectopic pregnancy.
Overall, there were 6030 premature deaths among those without a teen pregnancy, or 1.9 per 10,000 person-years. There were 701 deaths among those with one teen pregnancy (4.1 per 10,000 person-years) and 345 deaths among those with two or more teen pregnancies (6.1 per 10,000 person-years).
The adjusted hazard ratios (AHRs) for mortality were 1.51 for those with one pregnancy and 2.14 for those with two or more pregnancies. Compared with no teen pregnancy, the AHRs for premature death were 1.41 if the first teen pregnancy ended in an induced abortion and 2.10 if it ended in a miscarriage or birth.
Comparing those with a teen pregnancy and those without, the AHRs for premature death were 1.25 from noninjury, 2.06 from unintentional injury, and 2.02 from intentional injury. Among patients with teen pregnancy, noninjury-related premature mortality was more common, at 2.0 per 10,000 person-years, than unintentional and intentional injuries, at 1.0 per 10,000 person-years and 0.4 per 10,000 person-years, respectively.
A teen pregnancy before age 16 years entailed the highest associated risk for premature death, with an AHR of 2.00.
Next Research Steps
“We were not surprised by our findings, but it was new to us to see that the risk for premature death was higher for women who had an induced abortion in their teen years,” said Dr. Ray. “It was even higher in those whose pregnancy ended in a birth or miscarriage.”
The investigators plan to evaluate whether the future risk for premature death after teen pregnancy differs by the type of induced abortion, such as procedural or pharmaceutical, or by whether the pregnancy ended in a live birth, stillbirth, or miscarriage. Among those with a live birth, the researchers will also analyze the risk for premature death in relation to whether the newborn was taken into custody by child protection services in Canada.
Other factors associated with teen pregnancy and overall mortality, particularly adverse childhood experiences, may point to the reasons for premature mortality and should be studied further, the authors wrote. Structural and systems-related factors should be considered as well.
Stigmatization and Isolation
“Some teens choose to become pregnant, but most teen pregnancies are unintended, which exposes shortcomings in the systems that exist to educate, guide, and support young people,” said Elizabeth Cook, a research scientist at Child Trends in Rockville, Maryland.
Dr. Cook, who wasn’t involved with this study, wrote an accompanying editorial in JAMA Network Open. She conducts studies of sexual and reproductive health for Child Trends.
“Teens who become pregnant often experience stigmatization and isolation that can make it more difficult to thrive in adulthood, especially if they lack the necessary support to navigate such a significant decision,” she said. “Fortunately, the systems that youths encounter, such as healthcare, education, and child welfare, are taking on a larger role in prevention efforts than they have in the past.”
These systems are shifting the burden of unintended teen pregnancy from the teens themselves and their behaviors to the health and education systems, Dr. Cook noted, though more work is needed around local policies and lack of access to healthcare facilities.
“Teen pregnancy may offer an opportunity to intervene in the lives of people at higher risk for premature death, but knowing how best to offer support requires an understanding of the context of their lives,” she said. “As a starting point, we must celebrate and listen to all pregnant young people so they can tell us what they need to live long, fulfilled lives.”
The study was funded by grants from the PSI Foundation and the Canadian Institutes of Health Research, as well as ICES, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Ray and Dr. Cook reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Time Is Money: Should Physicians Be Compensated for EHR Engagement?
Electronic health records (EHRs) make providing coordinated, efficient care easier and reduce medical errors and test duplications; research has also correlated EHR adoption with higher patient satisfaction and outcomes. However, for physicians, the benefits come at a cost.
Physicians spend significantly more time in healthcare portals, making notes, entering orders, reviewing clinical reports, and responding to patient messages.
“I spend at least the same amount of time in the portal that I do in scheduled clinical time with patients,” said Eve Rittenberg, MD, primary care physician at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, Boston. “So, if I have a 4-hour session of seeing patients, I spend at least another 4 or more hours in the patient portal.”
The latest data showed that primary care physicians logged a median of 36.2 minutes in the healthcare portal per patient visit, spending 58.9% more time on orders, 24.4% more time reading and responding to messages, and 13% more time on chart review compared with prepandemic portal use.
“EHRs can be very powerful tools,” said Ralph DeBiasi, MD, a clinical cardiac electrophysiologist at Yale New Haven Health in Connecticut. “We’re still working on how to best harness that power to make us better doctors and better care teams and to take better care of our patients because their use can take up a lot of time.”
Portal Time Isn’t Paid Time
Sharp increases in the amount of time spent in the EHR responding to messages or dispensing medical advice via the portal often aren’t linked to increases in compensation; most portal time is unpaid.
“There isn’t specific time allocated to working in the portal; it’s either done in the office while a patient is sitting in an exam room or in the mornings and evenings outside of traditional working hours,” Dr. DeBiasi told this news organization. “I think it’s reasonable to consider it being reimbursed because we’re taking our time and effort and making decisions to help the patient.”
Compensation for portal time affects all physicians, but the degree of impact depends on their specialties. Primary care physicians spent significantly more daily and after-hours time in the EHR, entering notes and orders, and doing clinical reviews compared to surgical and medical specialties.
In addition to the outsized impact on primary care, physician compensation for portal time is also an equity issue.
Dr. Rittenberg researched the issue and found a higher volume of communication from both patients and staff to female physicians than male physicians. As a result, female physicians spend 41.4 minutes more on the EHR than their male counterparts, which equates to more unpaid time. It’s likely no coincidence then that burnout rates are also higher among female physicians, who also leave the clinical workforce in higher numbers, especially in primary care.
“Finding ways to fairly compensate physicians for their work also will address some of the equity issues in workload and the consequences,” Dr. Rittenberg said.
Addressing the Issue
Some health systems have started charging patients who seek medical advice via patient portals, equating the communication to asynchronous acute care or an additional care touch point and billing based on the length and complexity of the messages. Patient fees for seeking medical advice via portals vary widely depending on their health system and insurance.
At University of California San Francisco Health, billing patients for EHR communication led to a sharp decrease in patient messages, which eased physician workload. At Cleveland Clinic, physicians receive “productivity credits” for the time spent in the EHR that can be used to reduce their clinic hours (but have no impact on their compensation).
Changes to the Medicare Physician Fee Schedule also allow physicians to bill for “digital evaluation and management” based on the time spent in an EHR responding to patient-initiated questions and requests.
However, more efforts are needed to ease burnout and reverse the number of physicians who are seeing fewer patients or leaving medical practice altogether as a direct result of spending increasing amounts of unpaid time in the EHR. Dr. Rittenberg, who spends an estimated 50% of her working hours in the portal, had to reduce her clinical workload by 25% due to such heavy portal requirements.
“The workload has become unsustainable,” she said. “The work has undergone a dramatic change over the past decade, and the compensation system has not kept up with that change.”
Prioritizing Patient and Physician Experiences
The ever-expanding use of EHRs is a result of their value as a healthcare tool. Data showed that the electronic exchange of information between patients and physicians improves diagnostics, reduces medical errors, enhances communication, and leads to more patient-centered care — and physicians want their patients to use the portal to maximize their healthcare.
“[The EHR] is good for patients,” said Dr. DeBiasi. “Sometimes, patients have access issues with healthcare, whether that’s not knowing what number to call or getting the right message to the right person at the right office. If [the portal] is good for them and helps them get access to care, we should embrace that and figure out a way to work it into our day-to-day schedules.”
But maximizing the patient experience shouldn’t come at the physicians’ expense. Dr. Rittenberg advocates a model that compensates physicians for the time spent in the EHR and prioritizes a team approach to rebalance the EHR workload to ensure that physicians aren’t devoting too much time to administrative tasks and can, instead, focus their time on clinical tasks.
“The way in which we provide healthcare has fundamentally shifted, and compensation models need to reflect that new reality,” Dr. Rittenberg added.
A version of this article first appeared on Medscape.com.
Electronic health records (EHRs) make providing coordinated, efficient care easier and reduce medical errors and test duplications; research has also correlated EHR adoption with higher patient satisfaction and outcomes. However, for physicians, the benefits come at a cost.
Physicians spend significantly more time in healthcare portals, making notes, entering orders, reviewing clinical reports, and responding to patient messages.
“I spend at least the same amount of time in the portal that I do in scheduled clinical time with patients,” said Eve Rittenberg, MD, primary care physician at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, Boston. “So, if I have a 4-hour session of seeing patients, I spend at least another 4 or more hours in the patient portal.”
The latest data showed that primary care physicians logged a median of 36.2 minutes in the healthcare portal per patient visit, spending 58.9% more time on orders, 24.4% more time reading and responding to messages, and 13% more time on chart review compared with prepandemic portal use.
“EHRs can be very powerful tools,” said Ralph DeBiasi, MD, a clinical cardiac electrophysiologist at Yale New Haven Health in Connecticut. “We’re still working on how to best harness that power to make us better doctors and better care teams and to take better care of our patients because their use can take up a lot of time.”
Portal Time Isn’t Paid Time
Sharp increases in the amount of time spent in the EHR responding to messages or dispensing medical advice via the portal often aren’t linked to increases in compensation; most portal time is unpaid.
“There isn’t specific time allocated to working in the portal; it’s either done in the office while a patient is sitting in an exam room or in the mornings and evenings outside of traditional working hours,” Dr. DeBiasi told this news organization. “I think it’s reasonable to consider it being reimbursed because we’re taking our time and effort and making decisions to help the patient.”
Compensation for portal time affects all physicians, but the degree of impact depends on their specialties. Primary care physicians spent significantly more daily and after-hours time in the EHR, entering notes and orders, and doing clinical reviews compared to surgical and medical specialties.
In addition to the outsized impact on primary care, physician compensation for portal time is also an equity issue.
Dr. Rittenberg researched the issue and found a higher volume of communication from both patients and staff to female physicians than male physicians. As a result, female physicians spend 41.4 minutes more on the EHR than their male counterparts, which equates to more unpaid time. It’s likely no coincidence then that burnout rates are also higher among female physicians, who also leave the clinical workforce in higher numbers, especially in primary care.
“Finding ways to fairly compensate physicians for their work also will address some of the equity issues in workload and the consequences,” Dr. Rittenberg said.
Addressing the Issue
Some health systems have started charging patients who seek medical advice via patient portals, equating the communication to asynchronous acute care or an additional care touch point and billing based on the length and complexity of the messages. Patient fees for seeking medical advice via portals vary widely depending on their health system and insurance.
At University of California San Francisco Health, billing patients for EHR communication led to a sharp decrease in patient messages, which eased physician workload. At Cleveland Clinic, physicians receive “productivity credits” for the time spent in the EHR that can be used to reduce their clinic hours (but have no impact on their compensation).
Changes to the Medicare Physician Fee Schedule also allow physicians to bill for “digital evaluation and management” based on the time spent in an EHR responding to patient-initiated questions and requests.
However, more efforts are needed to ease burnout and reverse the number of physicians who are seeing fewer patients or leaving medical practice altogether as a direct result of spending increasing amounts of unpaid time in the EHR. Dr. Rittenberg, who spends an estimated 50% of her working hours in the portal, had to reduce her clinical workload by 25% due to such heavy portal requirements.
“The workload has become unsustainable,” she said. “The work has undergone a dramatic change over the past decade, and the compensation system has not kept up with that change.”
Prioritizing Patient and Physician Experiences
The ever-expanding use of EHRs is a result of their value as a healthcare tool. Data showed that the electronic exchange of information between patients and physicians improves diagnostics, reduces medical errors, enhances communication, and leads to more patient-centered care — and physicians want their patients to use the portal to maximize their healthcare.
“[The EHR] is good for patients,” said Dr. DeBiasi. “Sometimes, patients have access issues with healthcare, whether that’s not knowing what number to call or getting the right message to the right person at the right office. If [the portal] is good for them and helps them get access to care, we should embrace that and figure out a way to work it into our day-to-day schedules.”
But maximizing the patient experience shouldn’t come at the physicians’ expense. Dr. Rittenberg advocates a model that compensates physicians for the time spent in the EHR and prioritizes a team approach to rebalance the EHR workload to ensure that physicians aren’t devoting too much time to administrative tasks and can, instead, focus their time on clinical tasks.
“The way in which we provide healthcare has fundamentally shifted, and compensation models need to reflect that new reality,” Dr. Rittenberg added.
A version of this article first appeared on Medscape.com.
Electronic health records (EHRs) make providing coordinated, efficient care easier and reduce medical errors and test duplications; research has also correlated EHR adoption with higher patient satisfaction and outcomes. However, for physicians, the benefits come at a cost.
Physicians spend significantly more time in healthcare portals, making notes, entering orders, reviewing clinical reports, and responding to patient messages.
“I spend at least the same amount of time in the portal that I do in scheduled clinical time with patients,” said Eve Rittenberg, MD, primary care physician at Brigham and Women’s Hospital and assistant professor at Harvard Medical School, Boston. “So, if I have a 4-hour session of seeing patients, I spend at least another 4 or more hours in the patient portal.”
The latest data showed that primary care physicians logged a median of 36.2 minutes in the healthcare portal per patient visit, spending 58.9% more time on orders, 24.4% more time reading and responding to messages, and 13% more time on chart review compared with prepandemic portal use.
“EHRs can be very powerful tools,” said Ralph DeBiasi, MD, a clinical cardiac electrophysiologist at Yale New Haven Health in Connecticut. “We’re still working on how to best harness that power to make us better doctors and better care teams and to take better care of our patients because their use can take up a lot of time.”
Portal Time Isn’t Paid Time
Sharp increases in the amount of time spent in the EHR responding to messages or dispensing medical advice via the portal often aren’t linked to increases in compensation; most portal time is unpaid.
“There isn’t specific time allocated to working in the portal; it’s either done in the office while a patient is sitting in an exam room or in the mornings and evenings outside of traditional working hours,” Dr. DeBiasi told this news organization. “I think it’s reasonable to consider it being reimbursed because we’re taking our time and effort and making decisions to help the patient.”
Compensation for portal time affects all physicians, but the degree of impact depends on their specialties. Primary care physicians spent significantly more daily and after-hours time in the EHR, entering notes and orders, and doing clinical reviews compared to surgical and medical specialties.
In addition to the outsized impact on primary care, physician compensation for portal time is also an equity issue.
Dr. Rittenberg researched the issue and found a higher volume of communication from both patients and staff to female physicians than male physicians. As a result, female physicians spend 41.4 minutes more on the EHR than their male counterparts, which equates to more unpaid time. It’s likely no coincidence then that burnout rates are also higher among female physicians, who also leave the clinical workforce in higher numbers, especially in primary care.
“Finding ways to fairly compensate physicians for their work also will address some of the equity issues in workload and the consequences,” Dr. Rittenberg said.
Addressing the Issue
Some health systems have started charging patients who seek medical advice via patient portals, equating the communication to asynchronous acute care or an additional care touch point and billing based on the length and complexity of the messages. Patient fees for seeking medical advice via portals vary widely depending on their health system and insurance.
At University of California San Francisco Health, billing patients for EHR communication led to a sharp decrease in patient messages, which eased physician workload. At Cleveland Clinic, physicians receive “productivity credits” for the time spent in the EHR that can be used to reduce their clinic hours (but have no impact on their compensation).
Changes to the Medicare Physician Fee Schedule also allow physicians to bill for “digital evaluation and management” based on the time spent in an EHR responding to patient-initiated questions and requests.
However, more efforts are needed to ease burnout and reverse the number of physicians who are seeing fewer patients or leaving medical practice altogether as a direct result of spending increasing amounts of unpaid time in the EHR. Dr. Rittenberg, who spends an estimated 50% of her working hours in the portal, had to reduce her clinical workload by 25% due to such heavy portal requirements.
“The workload has become unsustainable,” she said. “The work has undergone a dramatic change over the past decade, and the compensation system has not kept up with that change.”
Prioritizing Patient and Physician Experiences
The ever-expanding use of EHRs is a result of their value as a healthcare tool. Data showed that the electronic exchange of information between patients and physicians improves diagnostics, reduces medical errors, enhances communication, and leads to more patient-centered care — and physicians want their patients to use the portal to maximize their healthcare.
“[The EHR] is good for patients,” said Dr. DeBiasi. “Sometimes, patients have access issues with healthcare, whether that’s not knowing what number to call or getting the right message to the right person at the right office. If [the portal] is good for them and helps them get access to care, we should embrace that and figure out a way to work it into our day-to-day schedules.”
But maximizing the patient experience shouldn’t come at the physicians’ expense. Dr. Rittenberg advocates a model that compensates physicians for the time spent in the EHR and prioritizes a team approach to rebalance the EHR workload to ensure that physicians aren’t devoting too much time to administrative tasks and can, instead, focus their time on clinical tasks.
“The way in which we provide healthcare has fundamentally shifted, and compensation models need to reflect that new reality,” Dr. Rittenberg added.
A version of this article first appeared on Medscape.com.
Active Surveillance for Cancer Doesn’t Increase Malpractice Risk
TOPLINE:
METHODOLOGY:
- Although practice guidelines from the National Comprehensive Cancer Network consider active surveillance an effective strategy for managing low-risk cancers, some physicians have been hesitant to incorporate it into their practice because of concerns about potential litigation.
- Researchers used Westlaw Edge and LexisNexis Advance databases to identify malpractice trends involving active surveillance related to thyroid, prostate, kidney, and or from 1990 to 2022.
- Data included unpublished cases, trial orders, jury verdicts, and administrative decisions.
- Researchers identified 201 malpractice cases across all low-risk cancers in the initial screening. Out of these, only five cases, all , involved active surveillance as the point of allegation.
TAKEAWAY:
- Out of the five prostate cancer cases, two involved incarcerated patients with Gleason 6 very-low-risk prostate adenocarcinoma that was managed with active surveillance by their urologists.
- In these two cases, the patients claimed that active surveillance violated their 8th Amendment right to be free from cruel or unusual punishment. In both cases, there was no metastasis or spread detected and the court determined active surveillance management was performed under national standards.
- The other three cases involved litigation claiming that active surveillance was not explicitly recommended as a treatment option for patients who all had very-low-risk prostate adenocarcinoma and had reported negligence from an intervention ( or cryoablation). However, all cases had documented informed consent for active surveillance.
- No relevant cases were found relating to active surveillance in any other type of cancer, whether in an initial diagnosis or recurrence.
IN PRACTICE:
“This data should bolster physicians’ confidence in recommending active surveillance for their patients when it is an appropriate option,” study coauthor Timothy Daskivich, MD, assistant professor of surgery at Cedars-Sinai Medical Center, Los Angeles, said in a statement . “Active surveillance maximizes quality of life and avoids unnecessary overtreatment, and it does not increase medicolegal liability to physicians, as detailed in the case dismissals identified in this study.”
SOURCE:
This study, led by Samuel Chang, JD, with Athene Law LLP, San Francisco, was recently published in Annals of Surgery.
LIMITATIONS:
The Westlaw and Lexis databases may not contain all cases or decisions issued by a state regulatory agency, like a medical board. Federal and state decisions from lower courts may not be published and available. Also, settlements outside of court or suits filed and not pursued were not included in the data.
DISCLOSURES:
The researchers did not provide any disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Although practice guidelines from the National Comprehensive Cancer Network consider active surveillance an effective strategy for managing low-risk cancers, some physicians have been hesitant to incorporate it into their practice because of concerns about potential litigation.
- Researchers used Westlaw Edge and LexisNexis Advance databases to identify malpractice trends involving active surveillance related to thyroid, prostate, kidney, and or from 1990 to 2022.
- Data included unpublished cases, trial orders, jury verdicts, and administrative decisions.
- Researchers identified 201 malpractice cases across all low-risk cancers in the initial screening. Out of these, only five cases, all , involved active surveillance as the point of allegation.
TAKEAWAY:
- Out of the five prostate cancer cases, two involved incarcerated patients with Gleason 6 very-low-risk prostate adenocarcinoma that was managed with active surveillance by their urologists.
- In these two cases, the patients claimed that active surveillance violated their 8th Amendment right to be free from cruel or unusual punishment. In both cases, there was no metastasis or spread detected and the court determined active surveillance management was performed under national standards.
- The other three cases involved litigation claiming that active surveillance was not explicitly recommended as a treatment option for patients who all had very-low-risk prostate adenocarcinoma and had reported negligence from an intervention ( or cryoablation). However, all cases had documented informed consent for active surveillance.
- No relevant cases were found relating to active surveillance in any other type of cancer, whether in an initial diagnosis or recurrence.
IN PRACTICE:
“This data should bolster physicians’ confidence in recommending active surveillance for their patients when it is an appropriate option,” study coauthor Timothy Daskivich, MD, assistant professor of surgery at Cedars-Sinai Medical Center, Los Angeles, said in a statement . “Active surveillance maximizes quality of life and avoids unnecessary overtreatment, and it does not increase medicolegal liability to physicians, as detailed in the case dismissals identified in this study.”
SOURCE:
This study, led by Samuel Chang, JD, with Athene Law LLP, San Francisco, was recently published in Annals of Surgery.
LIMITATIONS:
The Westlaw and Lexis databases may not contain all cases or decisions issued by a state regulatory agency, like a medical board. Federal and state decisions from lower courts may not be published and available. Also, settlements outside of court or suits filed and not pursued were not included in the data.
DISCLOSURES:
The researchers did not provide any disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Although practice guidelines from the National Comprehensive Cancer Network consider active surveillance an effective strategy for managing low-risk cancers, some physicians have been hesitant to incorporate it into their practice because of concerns about potential litigation.
- Researchers used Westlaw Edge and LexisNexis Advance databases to identify malpractice trends involving active surveillance related to thyroid, prostate, kidney, and or from 1990 to 2022.
- Data included unpublished cases, trial orders, jury verdicts, and administrative decisions.
- Researchers identified 201 malpractice cases across all low-risk cancers in the initial screening. Out of these, only five cases, all , involved active surveillance as the point of allegation.
TAKEAWAY:
- Out of the five prostate cancer cases, two involved incarcerated patients with Gleason 6 very-low-risk prostate adenocarcinoma that was managed with active surveillance by their urologists.
- In these two cases, the patients claimed that active surveillance violated their 8th Amendment right to be free from cruel or unusual punishment. In both cases, there was no metastasis or spread detected and the court determined active surveillance management was performed under national standards.
- The other three cases involved litigation claiming that active surveillance was not explicitly recommended as a treatment option for patients who all had very-low-risk prostate adenocarcinoma and had reported negligence from an intervention ( or cryoablation). However, all cases had documented informed consent for active surveillance.
- No relevant cases were found relating to active surveillance in any other type of cancer, whether in an initial diagnosis or recurrence.
IN PRACTICE:
“This data should bolster physicians’ confidence in recommending active surveillance for their patients when it is an appropriate option,” study coauthor Timothy Daskivich, MD, assistant professor of surgery at Cedars-Sinai Medical Center, Los Angeles, said in a statement . “Active surveillance maximizes quality of life and avoids unnecessary overtreatment, and it does not increase medicolegal liability to physicians, as detailed in the case dismissals identified in this study.”
SOURCE:
This study, led by Samuel Chang, JD, with Athene Law LLP, San Francisco, was recently published in Annals of Surgery.
LIMITATIONS:
The Westlaw and Lexis databases may not contain all cases or decisions issued by a state regulatory agency, like a medical board. Federal and state decisions from lower courts may not be published and available. Also, settlements outside of court or suits filed and not pursued were not included in the data.
DISCLOSURES:
The researchers did not provide any disclosures.
A version of this article appeared on Medscape.com.
Women’s Cancers: Clinicians Research, Advise on Sexual Dysfunction
Decreased sexual function is a side effect of many types of cancer, notably uterine, cervical, ovarian, and breast cancer, that often goes unaddressed, according to the authors of several studies presented at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
Patients want to talk about sex, but not necessarily at the start of their diagnosis or treatment, suggest the findings of a study presented at the meeting. Jesse T. Brewer of Weill Cornell Medicine in New York City and colleagues enrolled 63 patients who underwent surgery with documented hereditary breast cancer, ovarian cancer, or Lynch syndrome in a cross-sectional survey.
Overall, 86% said that sexuality and intimacy were very or somewhat important, and 78% said that the healthcare team addressing the issue was very or somewhat important, the researchers found. However, only 40% of the respondents said that they wanted to discuss sexuality at the time of diagnosis because the idea was too overwhelming.
Oncologists are more aware of sexual side effects and the potential for sexual issues that persist long after treatment, but many patients may not have opportunities to talk about sexual concerns, said Don S. Dizon, MD, an oncologist specializing in women’s cancers at Brown University, Providence, Rhode Island, in an interview.
“It is important that we [oncologists] be the ones to open the door to these conversations; people with cancer will not bring it up spontaneously, for fear of making their provider uncomfortable, especially if they’ve never been asked about it before,” Dr. Dizon said in an interview.
He advised clinicians to find a network within their health systems so they can refer patients to specialized services, such as sex therapy, couples counseling, pelvic rehabilitation, or menopausal experts as needed.
In another study presented at the meeting, Naaman Mehta, MD, of NYU Langone Health, and colleagues reviewed data from 166 healthcare providers who completed a 23-item survey about evaluating and managing sexual health concerns of their patients. Most of the respondents were gynecologic oncologists (93.4%), but one radiation oncologist and 10 other healthcare providers also completed the survey.
Overall, approximately 60% of the respondents routinely asked about the sexual health concerns of their patients, and 98% of these said they believed that sexual health discussions should be held with a gynecologic oncologist. Just over half (54%) also said that the patient should be the one to initiate a discussion of sexual health concerns.
Female providers were significantly more likely to discuss sexual health with patients, compared with male providers, after controlling for the hospital setting and training level, the researchers noted (odds ratio, 1.4;P < .01).
The results suggest a need for more ways to integrate sexual health screening into gynecologic oncologic clinics, the researchers concluded.
The provider survey findings are similar to the results of a survey conducted by Dr. Dizon and colleagues in 2007. In that study, less than half of respondents took a sexual history, but 80% felt there was insufficient time to explore sexual issues.
“It is critical to understand that people with cancer do not expect their oncologists to be sexual health experts, but as with all other side effects caused by treatment and the diagnosis, we can be the ones who recognize it,” Dr. Dizon noted, in an interview.
Common Complaints and Causes
In Dr. Dizon’s experience, local symptoms including vaginal dryness, pain with penetration, and vaginal thinning, are common sexual complaints in women with cancer, as are systemic issues such as lack of interest and menopause-type symptoms.
“For those undergoing radiation, the vaginal tunnel can actually develop adhesions, and if not treated proactively this can lead to vaginal stenosis,” said Dr. Dizon, who was not involved in the studies presented at the meeting.
Comorbidities such as diabetes, cardiovascular disease, and musculoskeletal conditions can contribute to sexual issues in women with cancer, according to Nora Lersch, DNP, FNP-BC, AOCNP, and Nicole Dreibelbis, CRNP, the authors of other research presented at the meeting.
Culture, religion, fitness level, history of sexual violence, and gender spectrum health also play a role, as do anxiety and depression, dementia, and substance abuse disorders, the authors wrote in their presentation, “Prioritizing Sexual Health in Gynecological Oncology Care.”
Low libido is a frequent complaint across all cancer types, Ms. Dreibelbis, a nurse practitioner specializing in gynecologic oncology at the UPMC Hillman Cancer Center, Pittsburgh, Pennsylvania, said in an interview.
“Breast cancer patients, especially those on [aromatase inhibitor] therapy, often experience vaginal dryness and therefore dyspareunia,” she added.
The pelvic floor muscles, with their important role in sexual response, can be weakened by cancer treatment or surgery, and the pudendal nerves, which are the primary nerves responsible for sexual response in women, can be affected as well, Dr. Lersch and Ms. Dreibelbis wrote.
Taking Sex Seriously
Researchers are exploring the impact of different cancer prevention treatments for women to mitigate sexual side effects, as illustrated by another study presented at the meeting.
Dr. Barbara Norquist, MD, a gynecologic oncologist at the University of Washington, Seattle, and colleagues compared the sexual function and menopausal symptoms of patients at high risk of ovarian carcinoma who underwent either interval salpingectomy/delayed oophorectomy (ISDO) or risk-reducing salpingo-oophorectomy (RRSO).
“For patients at high risk for ovarian cancer, surgical removal of the tubes and ovaries is the mainstay of prevention, as screening is not effective at reducing death from ovarian cancer. As a result of surgery, many patients become suddenly postmenopausal from losing their ovaries,” Dr. Norquist said in an interview.
Some patients delay surgery out of concern for health and quality of life, including sexual function, she said.
In the study (known as the WISP trial) the researchers compared data from 166 patients who underwent immediate removal of the fallopian tubes and ovaries and 171 who underwent fallopian tube removal and delayed oophorectomy. All patients completed questionnaires about sexual function. The primary outcome was change in sexual function based on the sexual function index (FSFI) from baseline to 6 months after surgery.
Overall, changes in sexual function were significantly greater in the immediate oophorectomy group, compared with the delayed oophorectomy group at 6 months (33% vs 17%) and also at 12 months (43% vs 20%).
A further review of patients using hormone therapy showed that those in the immediate oophorectomy group still had greater decreases in sexual function, compared with the delayed group, though the difference between groups of patients using hormone therapy was less dramatic.
“I was surprised that, even with hormone replacement therapy, patients undergoing removal of the ovaries still had significant detrimental changes to sexual function when compared to those having the tubes removed, although this was even worse in those who could not take HRT,” Dr. Norquist said, in an interview. “I was reassured that menopausal symptoms in general were well managed with HRT, as these patients did not score differently on menopause symptoms, compared with those having their tubes removed,” she said.
Patients deserve accurate information about predicted changes in menopausal symptoms and sexual function as a result of ovary removal, and HRT should be provided when there is no contraindication, Dr. Norquist told this news organization.
Dr. Norquist and colleagues are awaiting the results of clinical trials investigating the safety of salpingectomy with delayed oophorectomy in terms of ovarian cancer prevention, but more research is needed to identify optimal management of the menopausal and sexual side effects associated with surgical menopause, she noted.
“Findings from the WISP study show the importance of hormones in women undergoing prophylactic surgery,” Dr. Dizon said. The findings indicate that salpingectomy has less of a negative influence on sexual function compared to removal of the ovaries, and the impact of hormone therapy and the relatively young age of the patients who took hormones reinforces current knowledge about hormones and sex, he added.
Barriers and Solutions
Barriers to asking women with cancer about sexual issues reported by providers include limited time, lack of training in sexual health, a desire to avoid offending the patient or making them uncomfortable, and uncertainty about how to answer the questions, Dr. Lersch and Ms. Dreibelbis wrote in their presentation.
Barriers to asking healthcare providers about their sexual issues reported by patients include the beliefs that the clinician should initiate the discussion, that sexual function will not be taken seriously, and that they might make the provider uncomfortable.
“Fortunately, more information and research has been done on sexual health and gynecological cancer in recent years, so oncologists are becoming more aware of the issues women may have,” said Dr. Lersch who is an oncology nurse practitioner at Providence Franz Cancer Institute in Portland, Oregon, in an interview.
Telling patients early in their cancer treatment about potential sexual side effects and opportunities for help is essential, she added.
Although oncologists have become more aware of the importance of sexual health and well-being for their patients, “I think there has historically been a disconnect in including sexual health education in medical training,” Ms. Dreibelbis said in an interview.
Dr. Lersch and Ms. Dreibelbis advised a multidimensional approach to managing sexual problems in cancer patients that includes consideration of biological and psychological symptoms, but also social, cultural, and interpersonal factors, in their presentation.
Their suggestions include discussing dyspareunia with their patients, asking for details such as whether the pain is internal or external, whether it occurs with activities outside of sex including masturbation, and whether bleeding is present.
Oncology therapies and surgeries can decrease or eliminate an individual’s ability to produce their own lubricant; for example, removal of the cervix eliminates cervical mucous, which helps with internal lubrication, they wrote in their presentation.
For patients with dyspareunia, Dr. Lersch and Ms. Dreibelbis recommend a vaginal moisturizer especially formulated for vaginal tissue that can be absorbed by the mucosal tissue of the vagina. Use of this type of product can increase the effectiveness of lubricants and help restore integrity of the vaginal tissue. Such moisturizers are available as gels, creams, or suppositories over the counter, and do not contain hormones.
Vaginal estrogen can be helpful for burning, itching, irritation, tissue fragility, and pain with sex, according to Dr. Lersch and Ms. Dreibelbis. Adequate estrogen therapy can promote normalization of vaginal pH and microflora, as well increase vaginal secretion and reduce pain and dryness with intercourse, the presenters stated in their presentation. In addition, dilator therapy can be used to help prevent vaginal stenosis, and penetration bumpers can help relieve discomfort during intercourse, they wrote.
Looking ahead, more research is needed to serve a wider patient population, Ms. Dreibelbis said, in an interview.
“LGBTQIA [individuals] have not been included in sexual health research and there are more people than ever who identify within this group of people. I know there has also been some very early work on shielding the clitoris from the impacts of radiation, and I believe this is extremely important up-and-coming research,” she said.
Dr. Lersch, Ms. Dreibelbi, Dr. Dizon, Dr. Norquist, Ms. Brewer, and Dr. Mehta had no financial conflicts to disclose.
Decreased sexual function is a side effect of many types of cancer, notably uterine, cervical, ovarian, and breast cancer, that often goes unaddressed, according to the authors of several studies presented at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
Patients want to talk about sex, but not necessarily at the start of their diagnosis or treatment, suggest the findings of a study presented at the meeting. Jesse T. Brewer of Weill Cornell Medicine in New York City and colleagues enrolled 63 patients who underwent surgery with documented hereditary breast cancer, ovarian cancer, or Lynch syndrome in a cross-sectional survey.
Overall, 86% said that sexuality and intimacy were very or somewhat important, and 78% said that the healthcare team addressing the issue was very or somewhat important, the researchers found. However, only 40% of the respondents said that they wanted to discuss sexuality at the time of diagnosis because the idea was too overwhelming.
Oncologists are more aware of sexual side effects and the potential for sexual issues that persist long after treatment, but many patients may not have opportunities to talk about sexual concerns, said Don S. Dizon, MD, an oncologist specializing in women’s cancers at Brown University, Providence, Rhode Island, in an interview.
“It is important that we [oncologists] be the ones to open the door to these conversations; people with cancer will not bring it up spontaneously, for fear of making their provider uncomfortable, especially if they’ve never been asked about it before,” Dr. Dizon said in an interview.
He advised clinicians to find a network within their health systems so they can refer patients to specialized services, such as sex therapy, couples counseling, pelvic rehabilitation, or menopausal experts as needed.
In another study presented at the meeting, Naaman Mehta, MD, of NYU Langone Health, and colleagues reviewed data from 166 healthcare providers who completed a 23-item survey about evaluating and managing sexual health concerns of their patients. Most of the respondents were gynecologic oncologists (93.4%), but one radiation oncologist and 10 other healthcare providers also completed the survey.
Overall, approximately 60% of the respondents routinely asked about the sexual health concerns of their patients, and 98% of these said they believed that sexual health discussions should be held with a gynecologic oncologist. Just over half (54%) also said that the patient should be the one to initiate a discussion of sexual health concerns.
Female providers were significantly more likely to discuss sexual health with patients, compared with male providers, after controlling for the hospital setting and training level, the researchers noted (odds ratio, 1.4;P < .01).
The results suggest a need for more ways to integrate sexual health screening into gynecologic oncologic clinics, the researchers concluded.
The provider survey findings are similar to the results of a survey conducted by Dr. Dizon and colleagues in 2007. In that study, less than half of respondents took a sexual history, but 80% felt there was insufficient time to explore sexual issues.
“It is critical to understand that people with cancer do not expect their oncologists to be sexual health experts, but as with all other side effects caused by treatment and the diagnosis, we can be the ones who recognize it,” Dr. Dizon noted, in an interview.
Common Complaints and Causes
In Dr. Dizon’s experience, local symptoms including vaginal dryness, pain with penetration, and vaginal thinning, are common sexual complaints in women with cancer, as are systemic issues such as lack of interest and menopause-type symptoms.
“For those undergoing radiation, the vaginal tunnel can actually develop adhesions, and if not treated proactively this can lead to vaginal stenosis,” said Dr. Dizon, who was not involved in the studies presented at the meeting.
Comorbidities such as diabetes, cardiovascular disease, and musculoskeletal conditions can contribute to sexual issues in women with cancer, according to Nora Lersch, DNP, FNP-BC, AOCNP, and Nicole Dreibelbis, CRNP, the authors of other research presented at the meeting.
Culture, religion, fitness level, history of sexual violence, and gender spectrum health also play a role, as do anxiety and depression, dementia, and substance abuse disorders, the authors wrote in their presentation, “Prioritizing Sexual Health in Gynecological Oncology Care.”
Low libido is a frequent complaint across all cancer types, Ms. Dreibelbis, a nurse practitioner specializing in gynecologic oncology at the UPMC Hillman Cancer Center, Pittsburgh, Pennsylvania, said in an interview.
“Breast cancer patients, especially those on [aromatase inhibitor] therapy, often experience vaginal dryness and therefore dyspareunia,” she added.
The pelvic floor muscles, with their important role in sexual response, can be weakened by cancer treatment or surgery, and the pudendal nerves, which are the primary nerves responsible for sexual response in women, can be affected as well, Dr. Lersch and Ms. Dreibelbis wrote.
Taking Sex Seriously
Researchers are exploring the impact of different cancer prevention treatments for women to mitigate sexual side effects, as illustrated by another study presented at the meeting.
Dr. Barbara Norquist, MD, a gynecologic oncologist at the University of Washington, Seattle, and colleagues compared the sexual function and menopausal symptoms of patients at high risk of ovarian carcinoma who underwent either interval salpingectomy/delayed oophorectomy (ISDO) or risk-reducing salpingo-oophorectomy (RRSO).
“For patients at high risk for ovarian cancer, surgical removal of the tubes and ovaries is the mainstay of prevention, as screening is not effective at reducing death from ovarian cancer. As a result of surgery, many patients become suddenly postmenopausal from losing their ovaries,” Dr. Norquist said in an interview.
Some patients delay surgery out of concern for health and quality of life, including sexual function, she said.
In the study (known as the WISP trial) the researchers compared data from 166 patients who underwent immediate removal of the fallopian tubes and ovaries and 171 who underwent fallopian tube removal and delayed oophorectomy. All patients completed questionnaires about sexual function. The primary outcome was change in sexual function based on the sexual function index (FSFI) from baseline to 6 months after surgery.
Overall, changes in sexual function were significantly greater in the immediate oophorectomy group, compared with the delayed oophorectomy group at 6 months (33% vs 17%) and also at 12 months (43% vs 20%).
A further review of patients using hormone therapy showed that those in the immediate oophorectomy group still had greater decreases in sexual function, compared with the delayed group, though the difference between groups of patients using hormone therapy was less dramatic.
“I was surprised that, even with hormone replacement therapy, patients undergoing removal of the ovaries still had significant detrimental changes to sexual function when compared to those having the tubes removed, although this was even worse in those who could not take HRT,” Dr. Norquist said, in an interview. “I was reassured that menopausal symptoms in general were well managed with HRT, as these patients did not score differently on menopause symptoms, compared with those having their tubes removed,” she said.
Patients deserve accurate information about predicted changes in menopausal symptoms and sexual function as a result of ovary removal, and HRT should be provided when there is no contraindication, Dr. Norquist told this news organization.
Dr. Norquist and colleagues are awaiting the results of clinical trials investigating the safety of salpingectomy with delayed oophorectomy in terms of ovarian cancer prevention, but more research is needed to identify optimal management of the menopausal and sexual side effects associated with surgical menopause, she noted.
“Findings from the WISP study show the importance of hormones in women undergoing prophylactic surgery,” Dr. Dizon said. The findings indicate that salpingectomy has less of a negative influence on sexual function compared to removal of the ovaries, and the impact of hormone therapy and the relatively young age of the patients who took hormones reinforces current knowledge about hormones and sex, he added.
Barriers and Solutions
Barriers to asking women with cancer about sexual issues reported by providers include limited time, lack of training in sexual health, a desire to avoid offending the patient or making them uncomfortable, and uncertainty about how to answer the questions, Dr. Lersch and Ms. Dreibelbis wrote in their presentation.
Barriers to asking healthcare providers about their sexual issues reported by patients include the beliefs that the clinician should initiate the discussion, that sexual function will not be taken seriously, and that they might make the provider uncomfortable.
“Fortunately, more information and research has been done on sexual health and gynecological cancer in recent years, so oncologists are becoming more aware of the issues women may have,” said Dr. Lersch who is an oncology nurse practitioner at Providence Franz Cancer Institute in Portland, Oregon, in an interview.
Telling patients early in their cancer treatment about potential sexual side effects and opportunities for help is essential, she added.
Although oncologists have become more aware of the importance of sexual health and well-being for their patients, “I think there has historically been a disconnect in including sexual health education in medical training,” Ms. Dreibelbis said in an interview.
Dr. Lersch and Ms. Dreibelbis advised a multidimensional approach to managing sexual problems in cancer patients that includes consideration of biological and psychological symptoms, but also social, cultural, and interpersonal factors, in their presentation.
Their suggestions include discussing dyspareunia with their patients, asking for details such as whether the pain is internal or external, whether it occurs with activities outside of sex including masturbation, and whether bleeding is present.
Oncology therapies and surgeries can decrease or eliminate an individual’s ability to produce their own lubricant; for example, removal of the cervix eliminates cervical mucous, which helps with internal lubrication, they wrote in their presentation.
For patients with dyspareunia, Dr. Lersch and Ms. Dreibelbis recommend a vaginal moisturizer especially formulated for vaginal tissue that can be absorbed by the mucosal tissue of the vagina. Use of this type of product can increase the effectiveness of lubricants and help restore integrity of the vaginal tissue. Such moisturizers are available as gels, creams, or suppositories over the counter, and do not contain hormones.
Vaginal estrogen can be helpful for burning, itching, irritation, tissue fragility, and pain with sex, according to Dr. Lersch and Ms. Dreibelbis. Adequate estrogen therapy can promote normalization of vaginal pH and microflora, as well increase vaginal secretion and reduce pain and dryness with intercourse, the presenters stated in their presentation. In addition, dilator therapy can be used to help prevent vaginal stenosis, and penetration bumpers can help relieve discomfort during intercourse, they wrote.
Looking ahead, more research is needed to serve a wider patient population, Ms. Dreibelbis said, in an interview.
“LGBTQIA [individuals] have not been included in sexual health research and there are more people than ever who identify within this group of people. I know there has also been some very early work on shielding the clitoris from the impacts of radiation, and I believe this is extremely important up-and-coming research,” she said.
Dr. Lersch, Ms. Dreibelbi, Dr. Dizon, Dr. Norquist, Ms. Brewer, and Dr. Mehta had no financial conflicts to disclose.
Decreased sexual function is a side effect of many types of cancer, notably uterine, cervical, ovarian, and breast cancer, that often goes unaddressed, according to the authors of several studies presented at the Society of Gynecologic Oncology (SGO)’s Annual Meeting on Women’s Cancer.
Patients want to talk about sex, but not necessarily at the start of their diagnosis or treatment, suggest the findings of a study presented at the meeting. Jesse T. Brewer of Weill Cornell Medicine in New York City and colleagues enrolled 63 patients who underwent surgery with documented hereditary breast cancer, ovarian cancer, or Lynch syndrome in a cross-sectional survey.
Overall, 86% said that sexuality and intimacy were very or somewhat important, and 78% said that the healthcare team addressing the issue was very or somewhat important, the researchers found. However, only 40% of the respondents said that they wanted to discuss sexuality at the time of diagnosis because the idea was too overwhelming.
Oncologists are more aware of sexual side effects and the potential for sexual issues that persist long after treatment, but many patients may not have opportunities to talk about sexual concerns, said Don S. Dizon, MD, an oncologist specializing in women’s cancers at Brown University, Providence, Rhode Island, in an interview.
“It is important that we [oncologists] be the ones to open the door to these conversations; people with cancer will not bring it up spontaneously, for fear of making their provider uncomfortable, especially if they’ve never been asked about it before,” Dr. Dizon said in an interview.
He advised clinicians to find a network within their health systems so they can refer patients to specialized services, such as sex therapy, couples counseling, pelvic rehabilitation, or menopausal experts as needed.
In another study presented at the meeting, Naaman Mehta, MD, of NYU Langone Health, and colleagues reviewed data from 166 healthcare providers who completed a 23-item survey about evaluating and managing sexual health concerns of their patients. Most of the respondents were gynecologic oncologists (93.4%), but one radiation oncologist and 10 other healthcare providers also completed the survey.
Overall, approximately 60% of the respondents routinely asked about the sexual health concerns of their patients, and 98% of these said they believed that sexual health discussions should be held with a gynecologic oncologist. Just over half (54%) also said that the patient should be the one to initiate a discussion of sexual health concerns.
Female providers were significantly more likely to discuss sexual health with patients, compared with male providers, after controlling for the hospital setting and training level, the researchers noted (odds ratio, 1.4;P < .01).
The results suggest a need for more ways to integrate sexual health screening into gynecologic oncologic clinics, the researchers concluded.
The provider survey findings are similar to the results of a survey conducted by Dr. Dizon and colleagues in 2007. In that study, less than half of respondents took a sexual history, but 80% felt there was insufficient time to explore sexual issues.
“It is critical to understand that people with cancer do not expect their oncologists to be sexual health experts, but as with all other side effects caused by treatment and the diagnosis, we can be the ones who recognize it,” Dr. Dizon noted, in an interview.
Common Complaints and Causes
In Dr. Dizon’s experience, local symptoms including vaginal dryness, pain with penetration, and vaginal thinning, are common sexual complaints in women with cancer, as are systemic issues such as lack of interest and menopause-type symptoms.
“For those undergoing radiation, the vaginal tunnel can actually develop adhesions, and if not treated proactively this can lead to vaginal stenosis,” said Dr. Dizon, who was not involved in the studies presented at the meeting.
Comorbidities such as diabetes, cardiovascular disease, and musculoskeletal conditions can contribute to sexual issues in women with cancer, according to Nora Lersch, DNP, FNP-BC, AOCNP, and Nicole Dreibelbis, CRNP, the authors of other research presented at the meeting.
Culture, religion, fitness level, history of sexual violence, and gender spectrum health also play a role, as do anxiety and depression, dementia, and substance abuse disorders, the authors wrote in their presentation, “Prioritizing Sexual Health in Gynecological Oncology Care.”
Low libido is a frequent complaint across all cancer types, Ms. Dreibelbis, a nurse practitioner specializing in gynecologic oncology at the UPMC Hillman Cancer Center, Pittsburgh, Pennsylvania, said in an interview.
“Breast cancer patients, especially those on [aromatase inhibitor] therapy, often experience vaginal dryness and therefore dyspareunia,” she added.
The pelvic floor muscles, with their important role in sexual response, can be weakened by cancer treatment or surgery, and the pudendal nerves, which are the primary nerves responsible for sexual response in women, can be affected as well, Dr. Lersch and Ms. Dreibelbis wrote.
Taking Sex Seriously
Researchers are exploring the impact of different cancer prevention treatments for women to mitigate sexual side effects, as illustrated by another study presented at the meeting.
Dr. Barbara Norquist, MD, a gynecologic oncologist at the University of Washington, Seattle, and colleagues compared the sexual function and menopausal symptoms of patients at high risk of ovarian carcinoma who underwent either interval salpingectomy/delayed oophorectomy (ISDO) or risk-reducing salpingo-oophorectomy (RRSO).
“For patients at high risk for ovarian cancer, surgical removal of the tubes and ovaries is the mainstay of prevention, as screening is not effective at reducing death from ovarian cancer. As a result of surgery, many patients become suddenly postmenopausal from losing their ovaries,” Dr. Norquist said in an interview.
Some patients delay surgery out of concern for health and quality of life, including sexual function, she said.
In the study (known as the WISP trial) the researchers compared data from 166 patients who underwent immediate removal of the fallopian tubes and ovaries and 171 who underwent fallopian tube removal and delayed oophorectomy. All patients completed questionnaires about sexual function. The primary outcome was change in sexual function based on the sexual function index (FSFI) from baseline to 6 months after surgery.
Overall, changes in sexual function were significantly greater in the immediate oophorectomy group, compared with the delayed oophorectomy group at 6 months (33% vs 17%) and also at 12 months (43% vs 20%).
A further review of patients using hormone therapy showed that those in the immediate oophorectomy group still had greater decreases in sexual function, compared with the delayed group, though the difference between groups of patients using hormone therapy was less dramatic.
“I was surprised that, even with hormone replacement therapy, patients undergoing removal of the ovaries still had significant detrimental changes to sexual function when compared to those having the tubes removed, although this was even worse in those who could not take HRT,” Dr. Norquist said, in an interview. “I was reassured that menopausal symptoms in general were well managed with HRT, as these patients did not score differently on menopause symptoms, compared with those having their tubes removed,” she said.
Patients deserve accurate information about predicted changes in menopausal symptoms and sexual function as a result of ovary removal, and HRT should be provided when there is no contraindication, Dr. Norquist told this news organization.
Dr. Norquist and colleagues are awaiting the results of clinical trials investigating the safety of salpingectomy with delayed oophorectomy in terms of ovarian cancer prevention, but more research is needed to identify optimal management of the menopausal and sexual side effects associated with surgical menopause, she noted.
“Findings from the WISP study show the importance of hormones in women undergoing prophylactic surgery,” Dr. Dizon said. The findings indicate that salpingectomy has less of a negative influence on sexual function compared to removal of the ovaries, and the impact of hormone therapy and the relatively young age of the patients who took hormones reinforces current knowledge about hormones and sex, he added.
Barriers and Solutions
Barriers to asking women with cancer about sexual issues reported by providers include limited time, lack of training in sexual health, a desire to avoid offending the patient or making them uncomfortable, and uncertainty about how to answer the questions, Dr. Lersch and Ms. Dreibelbis wrote in their presentation.
Barriers to asking healthcare providers about their sexual issues reported by patients include the beliefs that the clinician should initiate the discussion, that sexual function will not be taken seriously, and that they might make the provider uncomfortable.
“Fortunately, more information and research has been done on sexual health and gynecological cancer in recent years, so oncologists are becoming more aware of the issues women may have,” said Dr. Lersch who is an oncology nurse practitioner at Providence Franz Cancer Institute in Portland, Oregon, in an interview.
Telling patients early in their cancer treatment about potential sexual side effects and opportunities for help is essential, she added.
Although oncologists have become more aware of the importance of sexual health and well-being for their patients, “I think there has historically been a disconnect in including sexual health education in medical training,” Ms. Dreibelbis said in an interview.
Dr. Lersch and Ms. Dreibelbis advised a multidimensional approach to managing sexual problems in cancer patients that includes consideration of biological and psychological symptoms, but also social, cultural, and interpersonal factors, in their presentation.
Their suggestions include discussing dyspareunia with their patients, asking for details such as whether the pain is internal or external, whether it occurs with activities outside of sex including masturbation, and whether bleeding is present.
Oncology therapies and surgeries can decrease or eliminate an individual’s ability to produce their own lubricant; for example, removal of the cervix eliminates cervical mucous, which helps with internal lubrication, they wrote in their presentation.
For patients with dyspareunia, Dr. Lersch and Ms. Dreibelbis recommend a vaginal moisturizer especially formulated for vaginal tissue that can be absorbed by the mucosal tissue of the vagina. Use of this type of product can increase the effectiveness of lubricants and help restore integrity of the vaginal tissue. Such moisturizers are available as gels, creams, or suppositories over the counter, and do not contain hormones.
Vaginal estrogen can be helpful for burning, itching, irritation, tissue fragility, and pain with sex, according to Dr. Lersch and Ms. Dreibelbis. Adequate estrogen therapy can promote normalization of vaginal pH and microflora, as well increase vaginal secretion and reduce pain and dryness with intercourse, the presenters stated in their presentation. In addition, dilator therapy can be used to help prevent vaginal stenosis, and penetration bumpers can help relieve discomfort during intercourse, they wrote.
Looking ahead, more research is needed to serve a wider patient population, Ms. Dreibelbis said, in an interview.
“LGBTQIA [individuals] have not been included in sexual health research and there are more people than ever who identify within this group of people. I know there has also been some very early work on shielding the clitoris from the impacts of radiation, and I believe this is extremely important up-and-coming research,” she said.
Dr. Lersch, Ms. Dreibelbi, Dr. Dizon, Dr. Norquist, Ms. Brewer, and Dr. Mehta had no financial conflicts to disclose.
FROM SGO 2024
Ultrasound and Its Role In Diagnosing and Managing Endometriosis
Introduction: Imaging for Endometriosis — A Necessary Prerequisite
While the gold standard in the diagnosis of endometriosis remains laparoscopy, it is now recognized that thorough evaluation via ultrasound offers an acceptable, less expensive, and less invasive alternative. It is especially useful for the diagnosis of deep infiltrative disease, which penetrates more than 5 mm into the peritoneum, ovarian endometrioma, and when anatomic distortion occurs, such as to the path of the ureter.
Besides establishing the diagnosis, ultrasound imaging has become, along with MRI, the most important aid for proper preoperative planning. Not only does imaging provide the surgeon and patient with knowledge regarding the extent of the upcoming procedure, but it also allows the minimally invasive gynecologic (MIG) surgeon to involve colleagues, such as colorectal surgeons or urologists. For example, deep infiltrative endometriosis penetrating into the bowel mucosa will require a discoid or segmental bowel resection.
While many endometriosis experts rely on MRI, many MIG surgeons are dependent on ultrasound. I would not consider taking a patient with signs and symptoms suggestive of endometriosis to surgery without 2D/3D transvaginal ultrasound. If the patient possesses a uterus, a saline-infused sonogram is performed to potentially diagnose adenomyosis.
It is a pleasure and honor to welcome Professor Caterina Exacoustos MD, PhD, associate professor of ob.gyn. at the University of Rome “Tor Vergata,” to this edition of the Master Class in Gynecologic Surgery to discuss “Ultrasound and Its Role in the Diagnosis of and Management of Endometriosis, Including DIE.”
Prof. Exacoustos’ main areas of interest are endometriosis and benign diseases including uterine pathology and infertility. Her extensive body of work comprises over 120 scientific publications and numerous book chapters both in English and in Italian.
Prof. Exacoustos continues to be one of the most well respected lecturers speaking about ultrasound throughout the world.
Dr. Miller is professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago. Dr. Miller has no conflicts of interest to report.
Ultrasound and Its Role In Diagnosing and Managing Endometriosis
Endometriosis affects approximately 10%-20% of premenopausal women worldwide. It is the leading cause of chronic pelvic pain, is often associated with infertility, and has a significant impact on quality of life. Although the natural history of endometriosis remains unknown, emerging evidence suggests that the pathophysiological steps of initiation and development of endometriosis must occur earlier in the lifespan. Most notably, the onset of endometriosis-associated pain symptoms is often reported during adolescence and young adulthood.1
While many patients with endometriosis are referred with dysmenorrhea at a young age, at age ≤ 25 years,2 symptoms are often highly underestimated and considered to be normal and transient.3,4 Clinical and pelvic exams are often negative in young women, and delays in endometriosis diagnosis are well known.
The presentation of primary dysmenorrhea with no anatomical cause embodies the paradigm that dysmenorrhea in adolescents is most often an insignificant disorder. This perspective is probably a root cause of delayed endometriosis diagnosis in young patients. However, another issue behind delayed diagnosis is the reluctance of the physician to perform a diagnostic laparoscopy — historically the gold standard for diagnosing endometriosis — for seemingly common symptoms such as dysmenorrhea in young patients.
Today we know that there are typical aspects of ultrasound imaging that identify endometriosis in the pelvis, and notably, the 2022 European Society for Human Reproduction and Embryology (ESHRE) endometriosis guideline5 recognizes imaging (ultrasound or MRI) as the standard for endometriosis diagnosis without requiring laparoscopic or histological confirmation.
An early and noninvasive method of diagnosis aids in timely diagnosis and provides for the timely initiation of medical management to improve quality of life and prevent progression of disease (Figure 1).
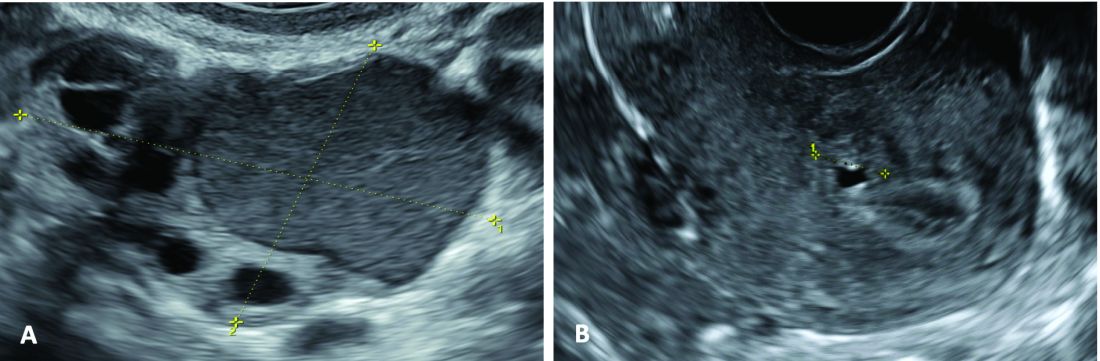
(A. Transvaginal ultrasound appearance of a small ovarian endometrioma in a 16-year-old girl. Note the unilocular cyst with ground glass echogenicity surrounded by multifollicular ovarian tissue. B. Ultrasound image of a retroverted uterus of an 18-year-old girl with focal adenomyosis of the posterior wall. Note the round cystic anechoic areas in the inner myometrium or junctional zone. The small intra-myometrial cyst is surrounded by a hyperechoic ring).
Indeed, the typical appearance of endometriotic pelvic lesions on transvaginal sonography, such as endometriomas and rectal deep infiltrating endometriosis (DIE) — as well as adenomyosis – can be medically treated without histologic confirmation .
When surgery is advisable, ultrasound findings also play a valuable role in presurgical staging, planning, and counseling for patients of all ages. Determining the extent and location of DIE preoperatively, for instance, facilitates the engagement of the appropriate surgical specialists so that multiple surgeries can be avoided. It also enables patients to be optimally informed before surgery of possible outcomes and complications.
Moreover, in the context of infertility, ultrasound can be a valuable tool for understanding uterine pathology and assessing for adenomyosis so that affected patients may be treated surgically or medically before turning to assisted reproductive technology.
Uniformity, Standardization in the Sonographic Assessment
In Europe, as in the United States, transvaginal sonography (TVS) is the first-line imaging tool for the diagnosis and management of endometriosis. In Europe, many ob.gyns. perform ultrasound themselves, as do treating surgeons. When diagnostic findings are negative but clinical suspicion is high, MRI is often utilized. Laparoscopy may then be considered in patients with negative imaging results.
Efforts to standardize terms, definitions, measurements, and sonographic features of different types of endometriosis have been made to make it easier for physicians to share data and communicate with each other. A lack of uniformity has contributed to variability in the reported diagnostic accuracy of TVS.
About 10 years ago, in one such effort, we assessed the accuracy of TVS for DIE by comparing TVS results with laparoscopic/histologic findings, and developed an ultrasound mapping system to accurately record the location, size and depth of lesions visualized by TVS. The accuracy of TVS ranged from 76% for the diagnosis of vaginal endometriosis to 97% for the diagnosis of bladder lesions and posterior cul-de-sac obliteration. Accuracy was 93% and 91% for detecting ureteral involvement (right and left); 87% for uterosacral ligament endometriotic lesions; and 87% for parametrial involvement.6
Shortly after, with a focus on DIE, expert sonographers and physician-sonographers from across Europe — as well as some experts from Australia, Japan, Brazil, Chile, and the United States (Y. Osuga from Brigham and Women’s Hospital and Harvard Medical School) — came together to agree on a uniform approach to the sonographic evaluation for suspected endometriosis and a standardization of terminology.
The consensus opinion from the International Deep Endometriosis Analysis (IDEA) group details four steps for examining women with suspected DIE: 1) Evaluation of the uterus and adnexa, 2) evaluation of transvaginal sonographic “soft markers” (ie. site-specific tenderness and ovarian mobility), 3) assessment of the status of the posterior cul-de-sac using real-time ultrasound-based “sliding sign,” and 4) assessment for DIE nodules in the anterior and posterior compartments.7
Our paper describing a mapping system and the IDEA paper describe how to detect deep endometriosis in the pelvis by utilizing an ultrasound view of normal anatomy and pelvic organ structure to provide landmarks for accurately defining the site of DIE lesions (Figure 2).
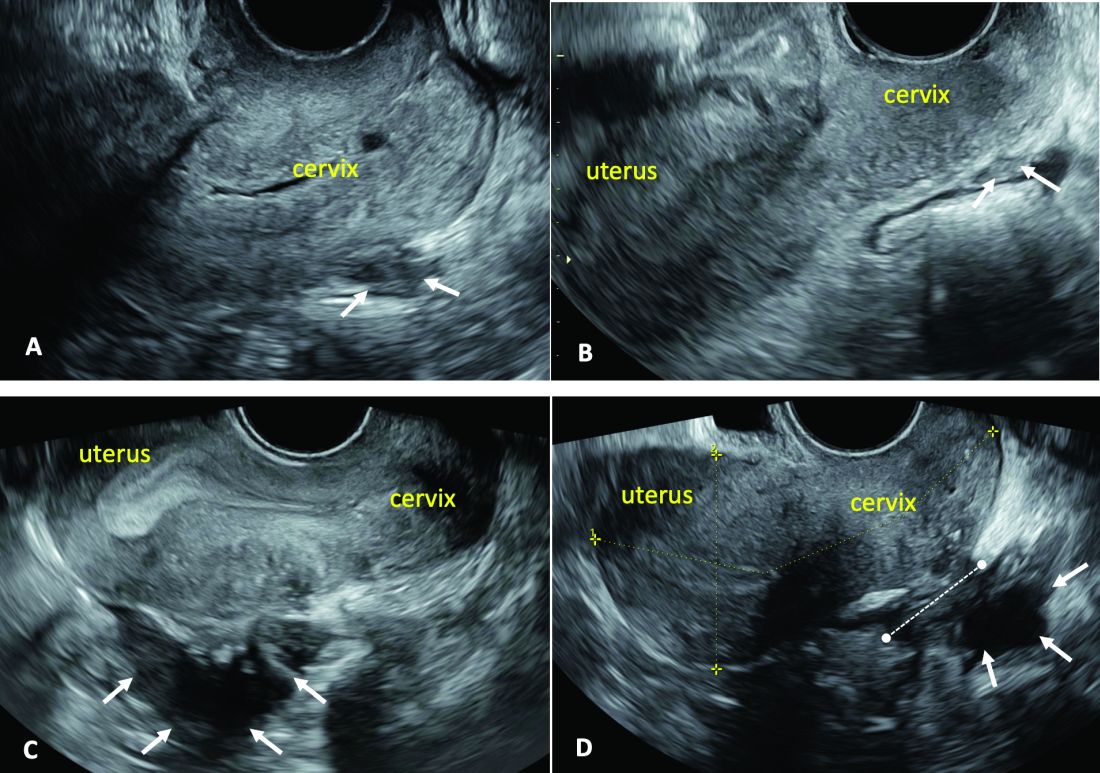
(A. Ultrasound appearance of a small DIE lesion of the retrocervical area [white arrows], which involved the torus uterinum and the right uterosacral ligament [USL]. The lesion appears as hypoechoic tissue with irregular margins caused by the fibrosis induced by the DIE. B. TVS appearance of small nodules of DIE of the left USL. Note the small retrocervical DIE lesion [white arrows], which appears hypoechoic due to the infiltration of the hyperechoic USL. C) Ultrasound appearance of a DIE nodule of the recto-sigmoid wall. Note the hypoechoic thickening of the muscular layers of the bowel wall attached to the corpus of the uterus and the adenomyosis of the posterior wall. The retrocervical area is free. D. TVS appearance of nodules of DIE of the lower rectal wall. Note the hypoechoic lesion [white arrows] of the rectum is attached to a retrocervical DIE fibrosis of the torus and USL [white dotted line]).
So-called rectovaginal endometriosis can be well assessed, for instance, since the involvement of the rectum, sigmoid colon, vaginal wall, rectovaginal septum, and posterior cul-de-sac uterosacral ligament can be seen by ultrasound as a single structure, making the location, size, and depth of any lesions discernible.
Again, this evaluation of the extent of disease is important for presurgical assessment so the surgeon can organize the right team and time of surgery and so the patient can be counseled on the advantages and possible complications of the treatment.
Notably, an accurate ultrasound description of pelvic endometriosis is helpful for accurate classification of disease. Endometriosis classification systems such as that of the American Association of Gynecologic Laparoscopists (AAGL)8 and the American Society of Reproductive Medicine (ASRM),9 as well as the #Enzian surgical description system,10 have been adapted to cover findings from ultrasound as well as MRI imaging.
A Systematic Evaluation
In keeping with the IDEA consensus opinion and based on our years of experience at the University of Rome, I advise that patients with typical pain symptoms of endometriosis or infertility undergo an accurate sonographic assessment of the pelvis with particular evaluation not only of the uterus and ovaries but of all pelvic retroperitoneal spaces.
The TVS examination should start with a slightly filled bladder, which permits a better evaluation of the bladder walls and the presence of endometriotic nodules. These nodules appear as hyperechoic linear or spherical lesions bulging toward the lumen and involving the serosa, muscularis, or (sub)mucosa of the bladder.
Then, an accurate evaluation of the uterus in 2D and 3D permits the diagnosis of adenomyosis. 3D sonographic evaluation of the myometrium and of the junctional zone are important; alteration and infiltration of the junctional zone and the presence of small adenomyotic cysts in the inner or outer myometrium are direct, specific signs of adenomyosis and should be ruled out in patients with dysmenorrhea, heavy menstrual bleeding, infertility, and pregnancy complications.
Endometriomas of the ovaries can be easily detected as having the typical appearance of a cyst with ground glass content. Adhesions of the ovaries and the uterus also should be evaluated with a dynamic ultrasound approach that utilizes the sliding sign and mobilization by palpation of the organs during the TVS scan.
Finally, the posterior and lateral retroperitoneal compartments should be carefully evaluated, with symptoms guiding the TVS examination whenever possible. Deep endometriotic nodules of the rectum appear as hypoechoic lesions or linear or nodular retroperitoneal thickening with irregular borders, penetrating into the intestinal wall and distorting its normal structure. In young patients, it seems very important to assess for small lesions below the peritoneum between the vagina and rectum, and in the parametria and around the ureter and nerves — lesions that, notably, would not be seen by diagnostic laparoscopy.
The Evaluation of Young Patients
In adolescent and young patients, endometriosis and adenomyosis are often present with small lesions and shallow tissue invasion, making a very careful and experienced approach to ultrasound essential for detection. Endometriomas are often of small diameter, and DIE is not always easily diagnosed because retroperitoneal lesions are similarly very small.
In a series of 270 adolescents (ages 12-20) who were referred to our outpatient gynecologic ultrasound unit over a 5-year period for various indications, at least one ultrasound feature of endometriosis was observed in 13.3%. In those with dysmenorrhea, the detection of endometriosis increased to 21%. Endometrioma was the most common type of endometriosis we found in the study, but DIE and adenomyosis were found in 4%-11%.
Although endometriotic lesions typically are small in young patients, they are often associated with severe pain symptoms, including chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, and dyschezia, all of which can have a serious effect on the quality of life of these young women. These symptoms keep them away from school during menstruation, away from sports, and cause painful intercourse and infertility. In young patients, an accurate TVS can provide a lot of information, and the ability to detect retroperitoneal endometriotic lesions and adenomyosis is probably better than with purely diagnostic laparoscopy, which would evaluate only superficial lesions.
TVS or, when needed, transrectal ultrasound, can enable adequate treatment and follow-up of the disease and its symptoms. There are no guidelines recommending adequate follow-up times to evaluate the effectiveness of medical therapy in patients with ultrasound signs of endometriosis. (Likewise, there are no indications for follow-up in patients with severe dysmenorrhea without ultrasound signs of endometriosis.) Certainly, our studies suggest careful evaluation over time of young patients with severe dysmenorrhea by serial ultrasound scans. With such follow-up, disease progress can be monitored and the medical or surgical treatment approach modified if needed.
The diagnosis of endometriosis at a young age has significant benefits not only in avoiding or reducing progression of the disease, but also in improving quality of life and aiding women in their desire for pregnancy.
Dr. Exacoustos is associate professor of ob.gyn. at the University of Rome “Tor Vergata.” She has no conflicts of interest to report.
References
1. Zondervan KT et al. N Engl J Med. 2020;382:1244-56.
2. Greene R et al. Fertil Steril. 2009;91:32-9.
3. Chapron C et al. J Pediatr Adolesc Gynecol. 2011;24:S7-12.
4. Randhawa AE et al. J Pediatr Adolesc Gynecol. 2021;34:643-8.
5. Becker CM et al. Hum Reprod Open. 2022(2):hoac009.
6. Exacoustos C et al. Fertil Steril. 2014;102:143-9. 7. Guerriero S et al. Ultrasound Obstet Gynecol. 2016;48(3):318-32.
8. Abrao MS et al. J Minim Invasive Gynecol. 2021;28:1941-50.9. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67:817-21. 10. Keckstein J et al. Acta Obstet Gynecol Scand. 2021;100:1165-75.
11. Martire FG et al. Fertil Steril. 2020;114(5):1049-57.
Introduction: Imaging for Endometriosis — A Necessary Prerequisite
While the gold standard in the diagnosis of endometriosis remains laparoscopy, it is now recognized that thorough evaluation via ultrasound offers an acceptable, less expensive, and less invasive alternative. It is especially useful for the diagnosis of deep infiltrative disease, which penetrates more than 5 mm into the peritoneum, ovarian endometrioma, and when anatomic distortion occurs, such as to the path of the ureter.
Besides establishing the diagnosis, ultrasound imaging has become, along with MRI, the most important aid for proper preoperative planning. Not only does imaging provide the surgeon and patient with knowledge regarding the extent of the upcoming procedure, but it also allows the minimally invasive gynecologic (MIG) surgeon to involve colleagues, such as colorectal surgeons or urologists. For example, deep infiltrative endometriosis penetrating into the bowel mucosa will require a discoid or segmental bowel resection.
While many endometriosis experts rely on MRI, many MIG surgeons are dependent on ultrasound. I would not consider taking a patient with signs and symptoms suggestive of endometriosis to surgery without 2D/3D transvaginal ultrasound. If the patient possesses a uterus, a saline-infused sonogram is performed to potentially diagnose adenomyosis.
It is a pleasure and honor to welcome Professor Caterina Exacoustos MD, PhD, associate professor of ob.gyn. at the University of Rome “Tor Vergata,” to this edition of the Master Class in Gynecologic Surgery to discuss “Ultrasound and Its Role in the Diagnosis of and Management of Endometriosis, Including DIE.”
Prof. Exacoustos’ main areas of interest are endometriosis and benign diseases including uterine pathology and infertility. Her extensive body of work comprises over 120 scientific publications and numerous book chapters both in English and in Italian.
Prof. Exacoustos continues to be one of the most well respected lecturers speaking about ultrasound throughout the world.
Dr. Miller is professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago. Dr. Miller has no conflicts of interest to report.
Ultrasound and Its Role In Diagnosing and Managing Endometriosis
Endometriosis affects approximately 10%-20% of premenopausal women worldwide. It is the leading cause of chronic pelvic pain, is often associated with infertility, and has a significant impact on quality of life. Although the natural history of endometriosis remains unknown, emerging evidence suggests that the pathophysiological steps of initiation and development of endometriosis must occur earlier in the lifespan. Most notably, the onset of endometriosis-associated pain symptoms is often reported during adolescence and young adulthood.1
While many patients with endometriosis are referred with dysmenorrhea at a young age, at age ≤ 25 years,2 symptoms are often highly underestimated and considered to be normal and transient.3,4 Clinical and pelvic exams are often negative in young women, and delays in endometriosis diagnosis are well known.
The presentation of primary dysmenorrhea with no anatomical cause embodies the paradigm that dysmenorrhea in adolescents is most often an insignificant disorder. This perspective is probably a root cause of delayed endometriosis diagnosis in young patients. However, another issue behind delayed diagnosis is the reluctance of the physician to perform a diagnostic laparoscopy — historically the gold standard for diagnosing endometriosis — for seemingly common symptoms such as dysmenorrhea in young patients.
Today we know that there are typical aspects of ultrasound imaging that identify endometriosis in the pelvis, and notably, the 2022 European Society for Human Reproduction and Embryology (ESHRE) endometriosis guideline5 recognizes imaging (ultrasound or MRI) as the standard for endometriosis diagnosis without requiring laparoscopic or histological confirmation.
An early and noninvasive method of diagnosis aids in timely diagnosis and provides for the timely initiation of medical management to improve quality of life and prevent progression of disease (Figure 1).
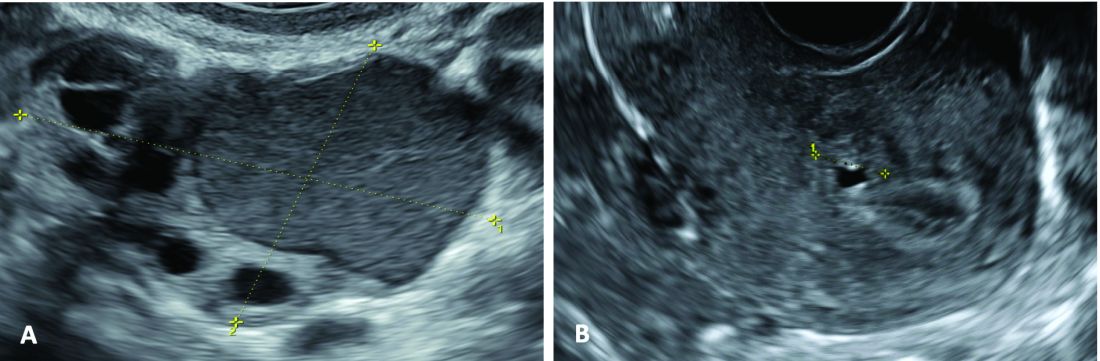
(A. Transvaginal ultrasound appearance of a small ovarian endometrioma in a 16-year-old girl. Note the unilocular cyst with ground glass echogenicity surrounded by multifollicular ovarian tissue. B. Ultrasound image of a retroverted uterus of an 18-year-old girl with focal adenomyosis of the posterior wall. Note the round cystic anechoic areas in the inner myometrium or junctional zone. The small intra-myometrial cyst is surrounded by a hyperechoic ring).
Indeed, the typical appearance of endometriotic pelvic lesions on transvaginal sonography, such as endometriomas and rectal deep infiltrating endometriosis (DIE) — as well as adenomyosis – can be medically treated without histologic confirmation .
When surgery is advisable, ultrasound findings also play a valuable role in presurgical staging, planning, and counseling for patients of all ages. Determining the extent and location of DIE preoperatively, for instance, facilitates the engagement of the appropriate surgical specialists so that multiple surgeries can be avoided. It also enables patients to be optimally informed before surgery of possible outcomes and complications.
Moreover, in the context of infertility, ultrasound can be a valuable tool for understanding uterine pathology and assessing for adenomyosis so that affected patients may be treated surgically or medically before turning to assisted reproductive technology.
Uniformity, Standardization in the Sonographic Assessment
In Europe, as in the United States, transvaginal sonography (TVS) is the first-line imaging tool for the diagnosis and management of endometriosis. In Europe, many ob.gyns. perform ultrasound themselves, as do treating surgeons. When diagnostic findings are negative but clinical suspicion is high, MRI is often utilized. Laparoscopy may then be considered in patients with negative imaging results.
Efforts to standardize terms, definitions, measurements, and sonographic features of different types of endometriosis have been made to make it easier for physicians to share data and communicate with each other. A lack of uniformity has contributed to variability in the reported diagnostic accuracy of TVS.
About 10 years ago, in one such effort, we assessed the accuracy of TVS for DIE by comparing TVS results with laparoscopic/histologic findings, and developed an ultrasound mapping system to accurately record the location, size and depth of lesions visualized by TVS. The accuracy of TVS ranged from 76% for the diagnosis of vaginal endometriosis to 97% for the diagnosis of bladder lesions and posterior cul-de-sac obliteration. Accuracy was 93% and 91% for detecting ureteral involvement (right and left); 87% for uterosacral ligament endometriotic lesions; and 87% for parametrial involvement.6
Shortly after, with a focus on DIE, expert sonographers and physician-sonographers from across Europe — as well as some experts from Australia, Japan, Brazil, Chile, and the United States (Y. Osuga from Brigham and Women’s Hospital and Harvard Medical School) — came together to agree on a uniform approach to the sonographic evaluation for suspected endometriosis and a standardization of terminology.
The consensus opinion from the International Deep Endometriosis Analysis (IDEA) group details four steps for examining women with suspected DIE: 1) Evaluation of the uterus and adnexa, 2) evaluation of transvaginal sonographic “soft markers” (ie. site-specific tenderness and ovarian mobility), 3) assessment of the status of the posterior cul-de-sac using real-time ultrasound-based “sliding sign,” and 4) assessment for DIE nodules in the anterior and posterior compartments.7
Our paper describing a mapping system and the IDEA paper describe how to detect deep endometriosis in the pelvis by utilizing an ultrasound view of normal anatomy and pelvic organ structure to provide landmarks for accurately defining the site of DIE lesions (Figure 2).
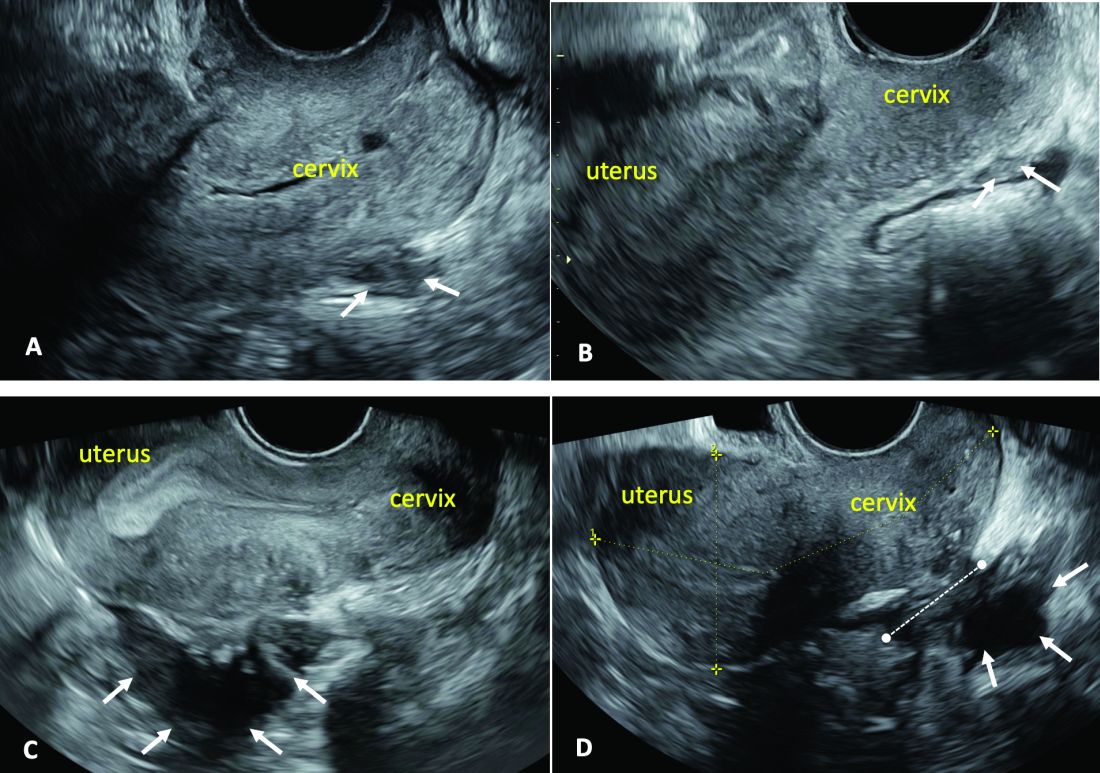
(A. Ultrasound appearance of a small DIE lesion of the retrocervical area [white arrows], which involved the torus uterinum and the right uterosacral ligament [USL]. The lesion appears as hypoechoic tissue with irregular margins caused by the fibrosis induced by the DIE. B. TVS appearance of small nodules of DIE of the left USL. Note the small retrocervical DIE lesion [white arrows], which appears hypoechoic due to the infiltration of the hyperechoic USL. C) Ultrasound appearance of a DIE nodule of the recto-sigmoid wall. Note the hypoechoic thickening of the muscular layers of the bowel wall attached to the corpus of the uterus and the adenomyosis of the posterior wall. The retrocervical area is free. D. TVS appearance of nodules of DIE of the lower rectal wall. Note the hypoechoic lesion [white arrows] of the rectum is attached to a retrocervical DIE fibrosis of the torus and USL [white dotted line]).
So-called rectovaginal endometriosis can be well assessed, for instance, since the involvement of the rectum, sigmoid colon, vaginal wall, rectovaginal septum, and posterior cul-de-sac uterosacral ligament can be seen by ultrasound as a single structure, making the location, size, and depth of any lesions discernible.
Again, this evaluation of the extent of disease is important for presurgical assessment so the surgeon can organize the right team and time of surgery and so the patient can be counseled on the advantages and possible complications of the treatment.
Notably, an accurate ultrasound description of pelvic endometriosis is helpful for accurate classification of disease. Endometriosis classification systems such as that of the American Association of Gynecologic Laparoscopists (AAGL)8 and the American Society of Reproductive Medicine (ASRM),9 as well as the #Enzian surgical description system,10 have been adapted to cover findings from ultrasound as well as MRI imaging.
A Systematic Evaluation
In keeping with the IDEA consensus opinion and based on our years of experience at the University of Rome, I advise that patients with typical pain symptoms of endometriosis or infertility undergo an accurate sonographic assessment of the pelvis with particular evaluation not only of the uterus and ovaries but of all pelvic retroperitoneal spaces.
The TVS examination should start with a slightly filled bladder, which permits a better evaluation of the bladder walls and the presence of endometriotic nodules. These nodules appear as hyperechoic linear or spherical lesions bulging toward the lumen and involving the serosa, muscularis, or (sub)mucosa of the bladder.
Then, an accurate evaluation of the uterus in 2D and 3D permits the diagnosis of adenomyosis. 3D sonographic evaluation of the myometrium and of the junctional zone are important; alteration and infiltration of the junctional zone and the presence of small adenomyotic cysts in the inner or outer myometrium are direct, specific signs of adenomyosis and should be ruled out in patients with dysmenorrhea, heavy menstrual bleeding, infertility, and pregnancy complications.
Endometriomas of the ovaries can be easily detected as having the typical appearance of a cyst with ground glass content. Adhesions of the ovaries and the uterus also should be evaluated with a dynamic ultrasound approach that utilizes the sliding sign and mobilization by palpation of the organs during the TVS scan.
Finally, the posterior and lateral retroperitoneal compartments should be carefully evaluated, with symptoms guiding the TVS examination whenever possible. Deep endometriotic nodules of the rectum appear as hypoechoic lesions or linear or nodular retroperitoneal thickening with irregular borders, penetrating into the intestinal wall and distorting its normal structure. In young patients, it seems very important to assess for small lesions below the peritoneum between the vagina and rectum, and in the parametria and around the ureter and nerves — lesions that, notably, would not be seen by diagnostic laparoscopy.
The Evaluation of Young Patients
In adolescent and young patients, endometriosis and adenomyosis are often present with small lesions and shallow tissue invasion, making a very careful and experienced approach to ultrasound essential for detection. Endometriomas are often of small diameter, and DIE is not always easily diagnosed because retroperitoneal lesions are similarly very small.
In a series of 270 adolescents (ages 12-20) who were referred to our outpatient gynecologic ultrasound unit over a 5-year period for various indications, at least one ultrasound feature of endometriosis was observed in 13.3%. In those with dysmenorrhea, the detection of endometriosis increased to 21%. Endometrioma was the most common type of endometriosis we found in the study, but DIE and adenomyosis were found in 4%-11%.
Although endometriotic lesions typically are small in young patients, they are often associated with severe pain symptoms, including chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, and dyschezia, all of which can have a serious effect on the quality of life of these young women. These symptoms keep them away from school during menstruation, away from sports, and cause painful intercourse and infertility. In young patients, an accurate TVS can provide a lot of information, and the ability to detect retroperitoneal endometriotic lesions and adenomyosis is probably better than with purely diagnostic laparoscopy, which would evaluate only superficial lesions.
TVS or, when needed, transrectal ultrasound, can enable adequate treatment and follow-up of the disease and its symptoms. There are no guidelines recommending adequate follow-up times to evaluate the effectiveness of medical therapy in patients with ultrasound signs of endometriosis. (Likewise, there are no indications for follow-up in patients with severe dysmenorrhea without ultrasound signs of endometriosis.) Certainly, our studies suggest careful evaluation over time of young patients with severe dysmenorrhea by serial ultrasound scans. With such follow-up, disease progress can be monitored and the medical or surgical treatment approach modified if needed.
The diagnosis of endometriosis at a young age has significant benefits not only in avoiding or reducing progression of the disease, but also in improving quality of life and aiding women in their desire for pregnancy.
Dr. Exacoustos is associate professor of ob.gyn. at the University of Rome “Tor Vergata.” She has no conflicts of interest to report.
References
1. Zondervan KT et al. N Engl J Med. 2020;382:1244-56.
2. Greene R et al. Fertil Steril. 2009;91:32-9.
3. Chapron C et al. J Pediatr Adolesc Gynecol. 2011;24:S7-12.
4. Randhawa AE et al. J Pediatr Adolesc Gynecol. 2021;34:643-8.
5. Becker CM et al. Hum Reprod Open. 2022(2):hoac009.
6. Exacoustos C et al. Fertil Steril. 2014;102:143-9. 7. Guerriero S et al. Ultrasound Obstet Gynecol. 2016;48(3):318-32.
8. Abrao MS et al. J Minim Invasive Gynecol. 2021;28:1941-50.9. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67:817-21. 10. Keckstein J et al. Acta Obstet Gynecol Scand. 2021;100:1165-75.
11. Martire FG et al. Fertil Steril. 2020;114(5):1049-57.
Introduction: Imaging for Endometriosis — A Necessary Prerequisite
While the gold standard in the diagnosis of endometriosis remains laparoscopy, it is now recognized that thorough evaluation via ultrasound offers an acceptable, less expensive, and less invasive alternative. It is especially useful for the diagnosis of deep infiltrative disease, which penetrates more than 5 mm into the peritoneum, ovarian endometrioma, and when anatomic distortion occurs, such as to the path of the ureter.
Besides establishing the diagnosis, ultrasound imaging has become, along with MRI, the most important aid for proper preoperative planning. Not only does imaging provide the surgeon and patient with knowledge regarding the extent of the upcoming procedure, but it also allows the minimally invasive gynecologic (MIG) surgeon to involve colleagues, such as colorectal surgeons or urologists. For example, deep infiltrative endometriosis penetrating into the bowel mucosa will require a discoid or segmental bowel resection.
While many endometriosis experts rely on MRI, many MIG surgeons are dependent on ultrasound. I would not consider taking a patient with signs and symptoms suggestive of endometriosis to surgery without 2D/3D transvaginal ultrasound. If the patient possesses a uterus, a saline-infused sonogram is performed to potentially diagnose adenomyosis.
It is a pleasure and honor to welcome Professor Caterina Exacoustos MD, PhD, associate professor of ob.gyn. at the University of Rome “Tor Vergata,” to this edition of the Master Class in Gynecologic Surgery to discuss “Ultrasound and Its Role in the Diagnosis of and Management of Endometriosis, Including DIE.”
Prof. Exacoustos’ main areas of interest are endometriosis and benign diseases including uterine pathology and infertility. Her extensive body of work comprises over 120 scientific publications and numerous book chapters both in English and in Italian.
Prof. Exacoustos continues to be one of the most well respected lecturers speaking about ultrasound throughout the world.
Dr. Miller is professor of obstetrics and gynecology, department of clinical sciences, Rosalind Franklin University of Medicine and Science, North Chicago. Dr. Miller has no conflicts of interest to report.
Ultrasound and Its Role In Diagnosing and Managing Endometriosis
Endometriosis affects approximately 10%-20% of premenopausal women worldwide. It is the leading cause of chronic pelvic pain, is often associated with infertility, and has a significant impact on quality of life. Although the natural history of endometriosis remains unknown, emerging evidence suggests that the pathophysiological steps of initiation and development of endometriosis must occur earlier in the lifespan. Most notably, the onset of endometriosis-associated pain symptoms is often reported during adolescence and young adulthood.1
While many patients with endometriosis are referred with dysmenorrhea at a young age, at age ≤ 25 years,2 symptoms are often highly underestimated and considered to be normal and transient.3,4 Clinical and pelvic exams are often negative in young women, and delays in endometriosis diagnosis are well known.
The presentation of primary dysmenorrhea with no anatomical cause embodies the paradigm that dysmenorrhea in adolescents is most often an insignificant disorder. This perspective is probably a root cause of delayed endometriosis diagnosis in young patients. However, another issue behind delayed diagnosis is the reluctance of the physician to perform a diagnostic laparoscopy — historically the gold standard for diagnosing endometriosis — for seemingly common symptoms such as dysmenorrhea in young patients.
Today we know that there are typical aspects of ultrasound imaging that identify endometriosis in the pelvis, and notably, the 2022 European Society for Human Reproduction and Embryology (ESHRE) endometriosis guideline5 recognizes imaging (ultrasound or MRI) as the standard for endometriosis diagnosis without requiring laparoscopic or histological confirmation.
An early and noninvasive method of diagnosis aids in timely diagnosis and provides for the timely initiation of medical management to improve quality of life and prevent progression of disease (Figure 1).
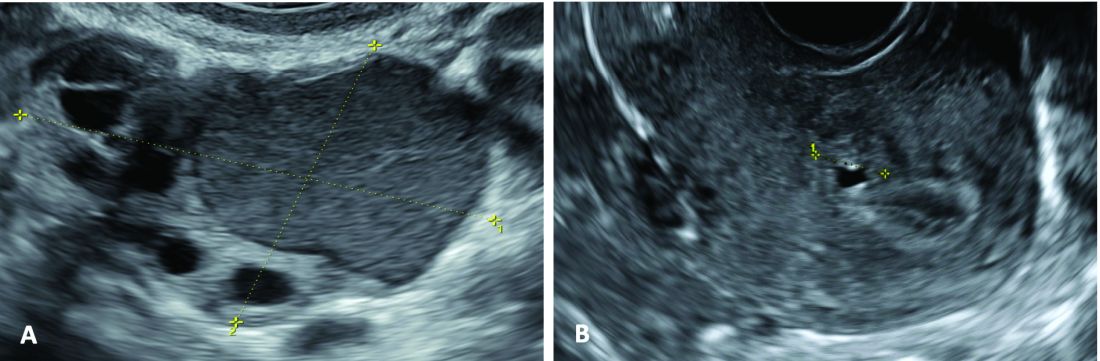
(A. Transvaginal ultrasound appearance of a small ovarian endometrioma in a 16-year-old girl. Note the unilocular cyst with ground glass echogenicity surrounded by multifollicular ovarian tissue. B. Ultrasound image of a retroverted uterus of an 18-year-old girl with focal adenomyosis of the posterior wall. Note the round cystic anechoic areas in the inner myometrium or junctional zone. The small intra-myometrial cyst is surrounded by a hyperechoic ring).
Indeed, the typical appearance of endometriotic pelvic lesions on transvaginal sonography, such as endometriomas and rectal deep infiltrating endometriosis (DIE) — as well as adenomyosis – can be medically treated without histologic confirmation .
When surgery is advisable, ultrasound findings also play a valuable role in presurgical staging, planning, and counseling for patients of all ages. Determining the extent and location of DIE preoperatively, for instance, facilitates the engagement of the appropriate surgical specialists so that multiple surgeries can be avoided. It also enables patients to be optimally informed before surgery of possible outcomes and complications.
Moreover, in the context of infertility, ultrasound can be a valuable tool for understanding uterine pathology and assessing for adenomyosis so that affected patients may be treated surgically or medically before turning to assisted reproductive technology.
Uniformity, Standardization in the Sonographic Assessment
In Europe, as in the United States, transvaginal sonography (TVS) is the first-line imaging tool for the diagnosis and management of endometriosis. In Europe, many ob.gyns. perform ultrasound themselves, as do treating surgeons. When diagnostic findings are negative but clinical suspicion is high, MRI is often utilized. Laparoscopy may then be considered in patients with negative imaging results.
Efforts to standardize terms, definitions, measurements, and sonographic features of different types of endometriosis have been made to make it easier for physicians to share data and communicate with each other. A lack of uniformity has contributed to variability in the reported diagnostic accuracy of TVS.
About 10 years ago, in one such effort, we assessed the accuracy of TVS for DIE by comparing TVS results with laparoscopic/histologic findings, and developed an ultrasound mapping system to accurately record the location, size and depth of lesions visualized by TVS. The accuracy of TVS ranged from 76% for the diagnosis of vaginal endometriosis to 97% for the diagnosis of bladder lesions and posterior cul-de-sac obliteration. Accuracy was 93% and 91% for detecting ureteral involvement (right and left); 87% for uterosacral ligament endometriotic lesions; and 87% for parametrial involvement.6
Shortly after, with a focus on DIE, expert sonographers and physician-sonographers from across Europe — as well as some experts from Australia, Japan, Brazil, Chile, and the United States (Y. Osuga from Brigham and Women’s Hospital and Harvard Medical School) — came together to agree on a uniform approach to the sonographic evaluation for suspected endometriosis and a standardization of terminology.
The consensus opinion from the International Deep Endometriosis Analysis (IDEA) group details four steps for examining women with suspected DIE: 1) Evaluation of the uterus and adnexa, 2) evaluation of transvaginal sonographic “soft markers” (ie. site-specific tenderness and ovarian mobility), 3) assessment of the status of the posterior cul-de-sac using real-time ultrasound-based “sliding sign,” and 4) assessment for DIE nodules in the anterior and posterior compartments.7
Our paper describing a mapping system and the IDEA paper describe how to detect deep endometriosis in the pelvis by utilizing an ultrasound view of normal anatomy and pelvic organ structure to provide landmarks for accurately defining the site of DIE lesions (Figure 2).
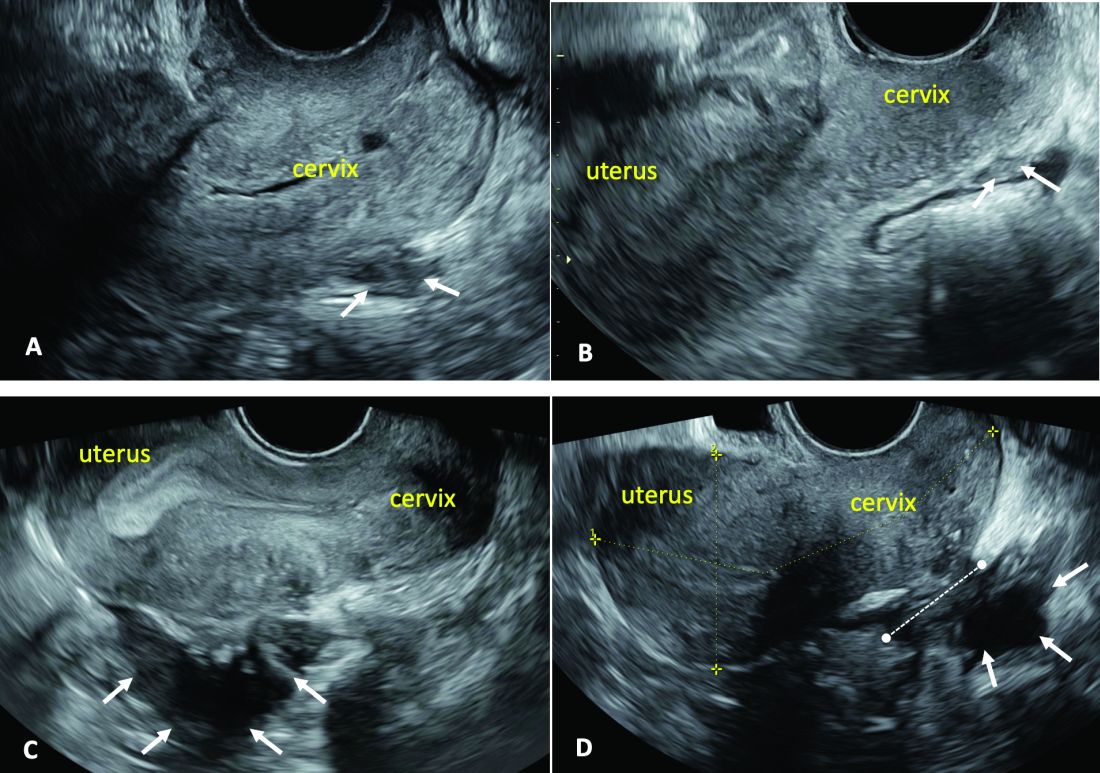
(A. Ultrasound appearance of a small DIE lesion of the retrocervical area [white arrows], which involved the torus uterinum and the right uterosacral ligament [USL]. The lesion appears as hypoechoic tissue with irregular margins caused by the fibrosis induced by the DIE. B. TVS appearance of small nodules of DIE of the left USL. Note the small retrocervical DIE lesion [white arrows], which appears hypoechoic due to the infiltration of the hyperechoic USL. C) Ultrasound appearance of a DIE nodule of the recto-sigmoid wall. Note the hypoechoic thickening of the muscular layers of the bowel wall attached to the corpus of the uterus and the adenomyosis of the posterior wall. The retrocervical area is free. D. TVS appearance of nodules of DIE of the lower rectal wall. Note the hypoechoic lesion [white arrows] of the rectum is attached to a retrocervical DIE fibrosis of the torus and USL [white dotted line]).
So-called rectovaginal endometriosis can be well assessed, for instance, since the involvement of the rectum, sigmoid colon, vaginal wall, rectovaginal septum, and posterior cul-de-sac uterosacral ligament can be seen by ultrasound as a single structure, making the location, size, and depth of any lesions discernible.
Again, this evaluation of the extent of disease is important for presurgical assessment so the surgeon can organize the right team and time of surgery and so the patient can be counseled on the advantages and possible complications of the treatment.
Notably, an accurate ultrasound description of pelvic endometriosis is helpful for accurate classification of disease. Endometriosis classification systems such as that of the American Association of Gynecologic Laparoscopists (AAGL)8 and the American Society of Reproductive Medicine (ASRM),9 as well as the #Enzian surgical description system,10 have been adapted to cover findings from ultrasound as well as MRI imaging.
A Systematic Evaluation
In keeping with the IDEA consensus opinion and based on our years of experience at the University of Rome, I advise that patients with typical pain symptoms of endometriosis or infertility undergo an accurate sonographic assessment of the pelvis with particular evaluation not only of the uterus and ovaries but of all pelvic retroperitoneal spaces.
The TVS examination should start with a slightly filled bladder, which permits a better evaluation of the bladder walls and the presence of endometriotic nodules. These nodules appear as hyperechoic linear or spherical lesions bulging toward the lumen and involving the serosa, muscularis, or (sub)mucosa of the bladder.
Then, an accurate evaluation of the uterus in 2D and 3D permits the diagnosis of adenomyosis. 3D sonographic evaluation of the myometrium and of the junctional zone are important; alteration and infiltration of the junctional zone and the presence of small adenomyotic cysts in the inner or outer myometrium are direct, specific signs of adenomyosis and should be ruled out in patients with dysmenorrhea, heavy menstrual bleeding, infertility, and pregnancy complications.
Endometriomas of the ovaries can be easily detected as having the typical appearance of a cyst with ground glass content. Adhesions of the ovaries and the uterus also should be evaluated with a dynamic ultrasound approach that utilizes the sliding sign and mobilization by palpation of the organs during the TVS scan.
Finally, the posterior and lateral retroperitoneal compartments should be carefully evaluated, with symptoms guiding the TVS examination whenever possible. Deep endometriotic nodules of the rectum appear as hypoechoic lesions or linear or nodular retroperitoneal thickening with irregular borders, penetrating into the intestinal wall and distorting its normal structure. In young patients, it seems very important to assess for small lesions below the peritoneum between the vagina and rectum, and in the parametria and around the ureter and nerves — lesions that, notably, would not be seen by diagnostic laparoscopy.
The Evaluation of Young Patients
In adolescent and young patients, endometriosis and adenomyosis are often present with small lesions and shallow tissue invasion, making a very careful and experienced approach to ultrasound essential for detection. Endometriomas are often of small diameter, and DIE is not always easily diagnosed because retroperitoneal lesions are similarly very small.
In a series of 270 adolescents (ages 12-20) who were referred to our outpatient gynecologic ultrasound unit over a 5-year period for various indications, at least one ultrasound feature of endometriosis was observed in 13.3%. In those with dysmenorrhea, the detection of endometriosis increased to 21%. Endometrioma was the most common type of endometriosis we found in the study, but DIE and adenomyosis were found in 4%-11%.
Although endometriotic lesions typically are small in young patients, they are often associated with severe pain symptoms, including chronic pelvic pain, dysmenorrhea, dyspareunia, dysuria, and dyschezia, all of which can have a serious effect on the quality of life of these young women. These symptoms keep them away from school during menstruation, away from sports, and cause painful intercourse and infertility. In young patients, an accurate TVS can provide a lot of information, and the ability to detect retroperitoneal endometriotic lesions and adenomyosis is probably better than with purely diagnostic laparoscopy, which would evaluate only superficial lesions.
TVS or, when needed, transrectal ultrasound, can enable adequate treatment and follow-up of the disease and its symptoms. There are no guidelines recommending adequate follow-up times to evaluate the effectiveness of medical therapy in patients with ultrasound signs of endometriosis. (Likewise, there are no indications for follow-up in patients with severe dysmenorrhea without ultrasound signs of endometriosis.) Certainly, our studies suggest careful evaluation over time of young patients with severe dysmenorrhea by serial ultrasound scans. With such follow-up, disease progress can be monitored and the medical or surgical treatment approach modified if needed.
The diagnosis of endometriosis at a young age has significant benefits not only in avoiding or reducing progression of the disease, but also in improving quality of life and aiding women in their desire for pregnancy.
Dr. Exacoustos is associate professor of ob.gyn. at the University of Rome “Tor Vergata.” She has no conflicts of interest to report.
References
1. Zondervan KT et al. N Engl J Med. 2020;382:1244-56.
2. Greene R et al. Fertil Steril. 2009;91:32-9.
3. Chapron C et al. J Pediatr Adolesc Gynecol. 2011;24:S7-12.
4. Randhawa AE et al. J Pediatr Adolesc Gynecol. 2021;34:643-8.
5. Becker CM et al. Hum Reprod Open. 2022(2):hoac009.
6. Exacoustos C et al. Fertil Steril. 2014;102:143-9. 7. Guerriero S et al. Ultrasound Obstet Gynecol. 2016;48(3):318-32.
8. Abrao MS et al. J Minim Invasive Gynecol. 2021;28:1941-50.9. Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67:817-21. 10. Keckstein J et al. Acta Obstet Gynecol Scand. 2021;100:1165-75.
11. Martire FG et al. Fertil Steril. 2020;114(5):1049-57.
Meditating in the Mundane
I don’t recommend ice baths. Perhaps I should. On my podcast-filled commute, I am reminded for miles of the mental and physical benefits of this revolutionary wellness routine: Cold exposure causes a spike in adrenaline and raises your baseline dopamine, thereby giving you superhuman focus and energy. Goodbye procrastination! Eliminate your ADHD in one icy step! I’m trying to be the fashionable mustached-columnist here so maybe I should get on board.
In fact, a heavyset, similarly-mustached 32-year-old patient just asked if I do ice baths. It was meant as a compliment, I believe. Displaying poise wearing my Chief of Dermatology embroidered white coat in my toddler-art-adorned office, I could hear him thinking: “This doc is legit. On fleek.” (Note, this is an approximation and the patient’s actual thoughts may have varied). We were talking podcasts and he was curious about my daily routine.
Now, ice baths probably do have the benefits that Andrew Huberman, Joe Rogan, and the others have described, I don’t argue. And the experience is oft described as invigorating with a runner’s high-like euphoria that follows a good dunk. I’ve tried it. I would describe it as “very uncomfortable.” To boot, following icy-cold morning showers, I wasn’t any better able to stave off opening my New York Times app on a newsy day. No, cold water isn’t my jams. But then again, I don’t journal like Marcus Aurelius or sleep on a mattress that keeps my body a chill 97 degrees like an inverse sous vide. If I were asked by Huberman in an interview what I do to be mentally strong, I’d answer, “I clean the pool.”
“Here’s how I do it, Dr. Huberman,” I’d say. “First, open the pool cover. Then with a cup with pool water from about 12 inches down, fill these little beakers with water and add a few drops of chemical reagents. Then calculate the ounces of calcium hypochlorite, muriatic acid, and other chemicals to make your pools sparkle. After skimming, take your pool brush and brush the bottom and sides of your pool. Rack your equipment when done and close the cover back up. This exercise takes about 15 minutes.” It’s a mundane task, but ah, there’s the point. Like folding the laundry, weeding the garden, emptying the dishwasher, they can be oh, so gratifying. Each of these has a crisp beginning and end and offer a lovely spot to be present. Let the thoughts flow with each stroke of the brush. Watch the water ripple the surface as you slowly pull the long pole out, dripping 7.4 pH water as you glide it in for the next pass. This is the Benabio secret to success.
I hope I’ve not disappointed you with this advice. Much as I’d like to think I’m on trend, I don’t believe self-improvement in the mundane will catch fire like taking magnesium or Wim Hof breathing. I wish it would. A distinction between gardening or pool cleaning or doing laundry and taking ice-baths is that the former aren’t just about you. I’ve got rows of spinach and Swiss chard that depend on me. My self-help is to water them. Feed them. Weed them. Because of me, they are growing deep green and beautiful. Although no one is swimming in our cool pool yet, they will soon. And the water will be sparkly clean, thanks to me. A stack of bright white towels is resting on our bathroom shelf waiting for someone to step out of the shower and need one. I did that.
Speaking of Huberman and the podcast gurus, Arnold Schwarzenegger is making the rounds lately hawking his book, “Be Useful.” It has the usual common sense ideas as most self-help books for the last 100 years.That’s the advice I passed along to my hirsute coming-of-manhood patient. I don’t do ice-baths, but each day I drop in deep on taking care of my patients, providing for my family, refilling the bird feeder in our yard. Why the heck would I sit in a currently 63-degree hot tub when I could be cleaning it? Then everyone is just a little better off, not just me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
I don’t recommend ice baths. Perhaps I should. On my podcast-filled commute, I am reminded for miles of the mental and physical benefits of this revolutionary wellness routine: Cold exposure causes a spike in adrenaline and raises your baseline dopamine, thereby giving you superhuman focus and energy. Goodbye procrastination! Eliminate your ADHD in one icy step! I’m trying to be the fashionable mustached-columnist here so maybe I should get on board.
In fact, a heavyset, similarly-mustached 32-year-old patient just asked if I do ice baths. It was meant as a compliment, I believe. Displaying poise wearing my Chief of Dermatology embroidered white coat in my toddler-art-adorned office, I could hear him thinking: “This doc is legit. On fleek.” (Note, this is an approximation and the patient’s actual thoughts may have varied). We were talking podcasts and he was curious about my daily routine.
Now, ice baths probably do have the benefits that Andrew Huberman, Joe Rogan, and the others have described, I don’t argue. And the experience is oft described as invigorating with a runner’s high-like euphoria that follows a good dunk. I’ve tried it. I would describe it as “very uncomfortable.” To boot, following icy-cold morning showers, I wasn’t any better able to stave off opening my New York Times app on a newsy day. No, cold water isn’t my jams. But then again, I don’t journal like Marcus Aurelius or sleep on a mattress that keeps my body a chill 97 degrees like an inverse sous vide. If I were asked by Huberman in an interview what I do to be mentally strong, I’d answer, “I clean the pool.”
“Here’s how I do it, Dr. Huberman,” I’d say. “First, open the pool cover. Then with a cup with pool water from about 12 inches down, fill these little beakers with water and add a few drops of chemical reagents. Then calculate the ounces of calcium hypochlorite, muriatic acid, and other chemicals to make your pools sparkle. After skimming, take your pool brush and brush the bottom and sides of your pool. Rack your equipment when done and close the cover back up. This exercise takes about 15 minutes.” It’s a mundane task, but ah, there’s the point. Like folding the laundry, weeding the garden, emptying the dishwasher, they can be oh, so gratifying. Each of these has a crisp beginning and end and offer a lovely spot to be present. Let the thoughts flow with each stroke of the brush. Watch the water ripple the surface as you slowly pull the long pole out, dripping 7.4 pH water as you glide it in for the next pass. This is the Benabio secret to success.
I hope I’ve not disappointed you with this advice. Much as I’d like to think I’m on trend, I don’t believe self-improvement in the mundane will catch fire like taking magnesium or Wim Hof breathing. I wish it would. A distinction between gardening or pool cleaning or doing laundry and taking ice-baths is that the former aren’t just about you. I’ve got rows of spinach and Swiss chard that depend on me. My self-help is to water them. Feed them. Weed them. Because of me, they are growing deep green and beautiful. Although no one is swimming in our cool pool yet, they will soon. And the water will be sparkly clean, thanks to me. A stack of bright white towels is resting on our bathroom shelf waiting for someone to step out of the shower and need one. I did that.
Speaking of Huberman and the podcast gurus, Arnold Schwarzenegger is making the rounds lately hawking his book, “Be Useful.” It has the usual common sense ideas as most self-help books for the last 100 years.That’s the advice I passed along to my hirsute coming-of-manhood patient. I don’t do ice-baths, but each day I drop in deep on taking care of my patients, providing for my family, refilling the bird feeder in our yard. Why the heck would I sit in a currently 63-degree hot tub when I could be cleaning it? Then everyone is just a little better off, not just me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
I don’t recommend ice baths. Perhaps I should. On my podcast-filled commute, I am reminded for miles of the mental and physical benefits of this revolutionary wellness routine: Cold exposure causes a spike in adrenaline and raises your baseline dopamine, thereby giving you superhuman focus and energy. Goodbye procrastination! Eliminate your ADHD in one icy step! I’m trying to be the fashionable mustached-columnist here so maybe I should get on board.
In fact, a heavyset, similarly-mustached 32-year-old patient just asked if I do ice baths. It was meant as a compliment, I believe. Displaying poise wearing my Chief of Dermatology embroidered white coat in my toddler-art-adorned office, I could hear him thinking: “This doc is legit. On fleek.” (Note, this is an approximation and the patient’s actual thoughts may have varied). We were talking podcasts and he was curious about my daily routine.
Now, ice baths probably do have the benefits that Andrew Huberman, Joe Rogan, and the others have described, I don’t argue. And the experience is oft described as invigorating with a runner’s high-like euphoria that follows a good dunk. I’ve tried it. I would describe it as “very uncomfortable.” To boot, following icy-cold morning showers, I wasn’t any better able to stave off opening my New York Times app on a newsy day. No, cold water isn’t my jams. But then again, I don’t journal like Marcus Aurelius or sleep on a mattress that keeps my body a chill 97 degrees like an inverse sous vide. If I were asked by Huberman in an interview what I do to be mentally strong, I’d answer, “I clean the pool.”
“Here’s how I do it, Dr. Huberman,” I’d say. “First, open the pool cover. Then with a cup with pool water from about 12 inches down, fill these little beakers with water and add a few drops of chemical reagents. Then calculate the ounces of calcium hypochlorite, muriatic acid, and other chemicals to make your pools sparkle. After skimming, take your pool brush and brush the bottom and sides of your pool. Rack your equipment when done and close the cover back up. This exercise takes about 15 minutes.” It’s a mundane task, but ah, there’s the point. Like folding the laundry, weeding the garden, emptying the dishwasher, they can be oh, so gratifying. Each of these has a crisp beginning and end and offer a lovely spot to be present. Let the thoughts flow with each stroke of the brush. Watch the water ripple the surface as you slowly pull the long pole out, dripping 7.4 pH water as you glide it in for the next pass. This is the Benabio secret to success.
I hope I’ve not disappointed you with this advice. Much as I’d like to think I’m on trend, I don’t believe self-improvement in the mundane will catch fire like taking magnesium or Wim Hof breathing. I wish it would. A distinction between gardening or pool cleaning or doing laundry and taking ice-baths is that the former aren’t just about you. I’ve got rows of spinach and Swiss chard that depend on me. My self-help is to water them. Feed them. Weed them. Because of me, they are growing deep green and beautiful. Although no one is swimming in our cool pool yet, they will soon. And the water will be sparkly clean, thanks to me. A stack of bright white towels is resting on our bathroom shelf waiting for someone to step out of the shower and need one. I did that.
Speaking of Huberman and the podcast gurus, Arnold Schwarzenegger is making the rounds lately hawking his book, “Be Useful.” It has the usual common sense ideas as most self-help books for the last 100 years.That’s the advice I passed along to my hirsute coming-of-manhood patient. I don’t do ice-baths, but each day I drop in deep on taking care of my patients, providing for my family, refilling the bird feeder in our yard. Why the heck would I sit in a currently 63-degree hot tub when I could be cleaning it? Then everyone is just a little better off, not just me.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on X. Write to him at [email protected].
You Can’t Spell ‘Medicine’ Without D, E, and I
Please note that this is a commentary, an opinion piece: my opinion. The statements here do not necessarily represent those of this news organization or any of the myriad people or institutions that comprise this corner of the human universe.
Some days, speaking as a long-time physician and editor, I wish that there were no such things as race or ethnicity or even geographic origin for that matter. We can’t get away from sex, gender, disability, age, or culture. I’m not sure about religion. I wish people were just people.
But race is deeply embedded in the American experience — an almost invisible but inevitable presence in all of our thoughts and expressions about human activities.
In medical education (for eons it seems) the student has been taught to mention race in the first sentence of a given patient presentation, along with age and sex. In human epidemiologic research, race is almost always a studied variable. In clinical and basic medical research, looking at the impact of race on this, that, or the other is commonplace. “Mixed race not otherwise specified” is ubiquitous in the United States yet blithely ignored by most who tally these statistics. Race is rarely gene-specific. It is more of a social and cultural construct but with plainly visible overt phenotypic markers — an almost infinite mix of daily reality.
Our country, and much of Western civilization in 2024, is based on the principle that all men are created equal, although the originators of that notion were unaware of their own “equity-challenged” situation.
Many organizations, in and out of government, are now understanding, developing, and implementing programs (and thought/language patterns) to socialize diversity, equity, and inclusion (known as DEI) into their culture. It should not be surprising that many who prefer the status quo are not happy with the pressure from this movement and are using whatever methods are available to them to prevent full DEI. Such it always is.
The trusty Copilot from Bing provides these definitions:
- Diversity refers to the presence of variety within the organizational workforce. This includes aspects such as gender, culture, ethnicity, religion, disability, age, and opinion.
- Equity encompasses concepts of fairness and justice. It involves fair compensation, substantive equality, and addressing societal disparities. Equity also considers unique circumstances and adjusts treatment to achieve equal outcomes.
- Inclusion focuses on creating an organizational culture where all employees feel heard, fostering a sense of belonging and integration.
I am more than proud that my old domain of peer-reviewed, primary source, medical (and science) journals is taking a leading role in this noble, necessary, and long overdue movement for medicine.
As the central repository and transmitter of new medical information, including scientific studies, clinical medicine reports, ethics measures, and education, medical journals (including those deemed prestigious) have historically been among the worst offenders in perpetuating non-DEI objectives in their leadership, staffing, focus, instructions for authors, style manuals, and published materials.
This issue came to a head in March 2021 when a JAMA podcast about racism in American medicine was followed by this promotional tweet: “No physician is racist, so how can there be structural racism in health care?”
Reactions and actions were rapid, strong, and decisive. After an interregnum at JAMA, a new editor in chief, Kirsten Bibbins-Domingo, PhD, MD, MAS, was named. She and her large staff of editors and editorial board members from the multijournal JAMA Network joined a worldwide movement of (currently) 56 publishing organizations representing 15,000 journals called the Joint Commitment for Action on Inclusion and Diversity in Publishing.
A recent JAMA editorial with 29 authors describes the entire commitment initiative of publishers-editors. It reports JAMA Network data from 2023 and 2024 from surveys of 455 editors (a 91% response rate) about their own gender (five choices), ethnic origins or geographic ancestry (13 choices), and race (eight choices), demonstrating considerable progress toward DEI goals. The survey’s complex multinational classifications may not jibe with the categorizations used in some countries (too bad that “mixed” is not “mixed in” — a missed opportunity).
This encouraging movement will not fix it all. But when people of certain groups are represented at the table, that point of view is far more likely to make it into the lexicon, language, and omnipresent work products, potentially changing cultural norms. Even the measurement of movement related to disparity in healthcare is marred by frequent variations of data accuracy. More consistency in what to measure can help a lot, and the medical literature can be very influential.
A personal anecdote: When I was a professor at UC Davis in 1978, Allan Bakke, MD, was my student. Some of you will remember the saga of affirmative action on admissions, which was just revisited in the light of a recent decision by the US Supreme Court.
Back in 1978, the dean at UC Davis told me that he kept two file folders on the admission processes in different desk drawers. One categorized all applicants and enrollees by race, and the other did not. Depending on who came to visit and ask questions, he would choose one or the other file to share once he figured out what they were looking for (this is not a joke).
The strength of the current active political pushback against the entire DEI movement has deep roots and should not be underestimated. There will be a lot of to-ing and fro-ing.
French writer Victor Hugo is credited with stating, “There is nothing as powerful as an idea whose time has come.” A majority of Americans, physicians, and other healthcare professionals believe in basic fairness. The time for DEI in all aspects of medicine is now.
Dr. Lundberg, editor in chief of Cancer Commons, disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
Please note that this is a commentary, an opinion piece: my opinion. The statements here do not necessarily represent those of this news organization or any of the myriad people or institutions that comprise this corner of the human universe.
Some days, speaking as a long-time physician and editor, I wish that there were no such things as race or ethnicity or even geographic origin for that matter. We can’t get away from sex, gender, disability, age, or culture. I’m not sure about religion. I wish people were just people.
But race is deeply embedded in the American experience — an almost invisible but inevitable presence in all of our thoughts and expressions about human activities.
In medical education (for eons it seems) the student has been taught to mention race in the first sentence of a given patient presentation, along with age and sex. In human epidemiologic research, race is almost always a studied variable. In clinical and basic medical research, looking at the impact of race on this, that, or the other is commonplace. “Mixed race not otherwise specified” is ubiquitous in the United States yet blithely ignored by most who tally these statistics. Race is rarely gene-specific. It is more of a social and cultural construct but with plainly visible overt phenotypic markers — an almost infinite mix of daily reality.
Our country, and much of Western civilization in 2024, is based on the principle that all men are created equal, although the originators of that notion were unaware of their own “equity-challenged” situation.
Many organizations, in and out of government, are now understanding, developing, and implementing programs (and thought/language patterns) to socialize diversity, equity, and inclusion (known as DEI) into their culture. It should not be surprising that many who prefer the status quo are not happy with the pressure from this movement and are using whatever methods are available to them to prevent full DEI. Such it always is.
The trusty Copilot from Bing provides these definitions:
- Diversity refers to the presence of variety within the organizational workforce. This includes aspects such as gender, culture, ethnicity, religion, disability, age, and opinion.
- Equity encompasses concepts of fairness and justice. It involves fair compensation, substantive equality, and addressing societal disparities. Equity also considers unique circumstances and adjusts treatment to achieve equal outcomes.
- Inclusion focuses on creating an organizational culture where all employees feel heard, fostering a sense of belonging and integration.
I am more than proud that my old domain of peer-reviewed, primary source, medical (and science) journals is taking a leading role in this noble, necessary, and long overdue movement for medicine.
As the central repository and transmitter of new medical information, including scientific studies, clinical medicine reports, ethics measures, and education, medical journals (including those deemed prestigious) have historically been among the worst offenders in perpetuating non-DEI objectives in their leadership, staffing, focus, instructions for authors, style manuals, and published materials.
This issue came to a head in March 2021 when a JAMA podcast about racism in American medicine was followed by this promotional tweet: “No physician is racist, so how can there be structural racism in health care?”
Reactions and actions were rapid, strong, and decisive. After an interregnum at JAMA, a new editor in chief, Kirsten Bibbins-Domingo, PhD, MD, MAS, was named. She and her large staff of editors and editorial board members from the multijournal JAMA Network joined a worldwide movement of (currently) 56 publishing organizations representing 15,000 journals called the Joint Commitment for Action on Inclusion and Diversity in Publishing.
A recent JAMA editorial with 29 authors describes the entire commitment initiative of publishers-editors. It reports JAMA Network data from 2023 and 2024 from surveys of 455 editors (a 91% response rate) about their own gender (five choices), ethnic origins or geographic ancestry (13 choices), and race (eight choices), demonstrating considerable progress toward DEI goals. The survey’s complex multinational classifications may not jibe with the categorizations used in some countries (too bad that “mixed” is not “mixed in” — a missed opportunity).
This encouraging movement will not fix it all. But when people of certain groups are represented at the table, that point of view is far more likely to make it into the lexicon, language, and omnipresent work products, potentially changing cultural norms. Even the measurement of movement related to disparity in healthcare is marred by frequent variations of data accuracy. More consistency in what to measure can help a lot, and the medical literature can be very influential.
A personal anecdote: When I was a professor at UC Davis in 1978, Allan Bakke, MD, was my student. Some of you will remember the saga of affirmative action on admissions, which was just revisited in the light of a recent decision by the US Supreme Court.
Back in 1978, the dean at UC Davis told me that he kept two file folders on the admission processes in different desk drawers. One categorized all applicants and enrollees by race, and the other did not. Depending on who came to visit and ask questions, he would choose one or the other file to share once he figured out what they were looking for (this is not a joke).
The strength of the current active political pushback against the entire DEI movement has deep roots and should not be underestimated. There will be a lot of to-ing and fro-ing.
French writer Victor Hugo is credited with stating, “There is nothing as powerful as an idea whose time has come.” A majority of Americans, physicians, and other healthcare professionals believe in basic fairness. The time for DEI in all aspects of medicine is now.
Dr. Lundberg, editor in chief of Cancer Commons, disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
Please note that this is a commentary, an opinion piece: my opinion. The statements here do not necessarily represent those of this news organization or any of the myriad people or institutions that comprise this corner of the human universe.
Some days, speaking as a long-time physician and editor, I wish that there were no such things as race or ethnicity or even geographic origin for that matter. We can’t get away from sex, gender, disability, age, or culture. I’m not sure about religion. I wish people were just people.
But race is deeply embedded in the American experience — an almost invisible but inevitable presence in all of our thoughts and expressions about human activities.
In medical education (for eons it seems) the student has been taught to mention race in the first sentence of a given patient presentation, along with age and sex. In human epidemiologic research, race is almost always a studied variable. In clinical and basic medical research, looking at the impact of race on this, that, or the other is commonplace. “Mixed race not otherwise specified” is ubiquitous in the United States yet blithely ignored by most who tally these statistics. Race is rarely gene-specific. It is more of a social and cultural construct but with plainly visible overt phenotypic markers — an almost infinite mix of daily reality.
Our country, and much of Western civilization in 2024, is based on the principle that all men are created equal, although the originators of that notion were unaware of their own “equity-challenged” situation.
Many organizations, in and out of government, are now understanding, developing, and implementing programs (and thought/language patterns) to socialize diversity, equity, and inclusion (known as DEI) into their culture. It should not be surprising that many who prefer the status quo are not happy with the pressure from this movement and are using whatever methods are available to them to prevent full DEI. Such it always is.
The trusty Copilot from Bing provides these definitions:
- Diversity refers to the presence of variety within the organizational workforce. This includes aspects such as gender, culture, ethnicity, religion, disability, age, and opinion.
- Equity encompasses concepts of fairness and justice. It involves fair compensation, substantive equality, and addressing societal disparities. Equity also considers unique circumstances and adjusts treatment to achieve equal outcomes.
- Inclusion focuses on creating an organizational culture where all employees feel heard, fostering a sense of belonging and integration.
I am more than proud that my old domain of peer-reviewed, primary source, medical (and science) journals is taking a leading role in this noble, necessary, and long overdue movement for medicine.
As the central repository and transmitter of new medical information, including scientific studies, clinical medicine reports, ethics measures, and education, medical journals (including those deemed prestigious) have historically been among the worst offenders in perpetuating non-DEI objectives in their leadership, staffing, focus, instructions for authors, style manuals, and published materials.
This issue came to a head in March 2021 when a JAMA podcast about racism in American medicine was followed by this promotional tweet: “No physician is racist, so how can there be structural racism in health care?”
Reactions and actions were rapid, strong, and decisive. After an interregnum at JAMA, a new editor in chief, Kirsten Bibbins-Domingo, PhD, MD, MAS, was named. She and her large staff of editors and editorial board members from the multijournal JAMA Network joined a worldwide movement of (currently) 56 publishing organizations representing 15,000 journals called the Joint Commitment for Action on Inclusion and Diversity in Publishing.
A recent JAMA editorial with 29 authors describes the entire commitment initiative of publishers-editors. It reports JAMA Network data from 2023 and 2024 from surveys of 455 editors (a 91% response rate) about their own gender (five choices), ethnic origins or geographic ancestry (13 choices), and race (eight choices), demonstrating considerable progress toward DEI goals. The survey’s complex multinational classifications may not jibe with the categorizations used in some countries (too bad that “mixed” is not “mixed in” — a missed opportunity).
This encouraging movement will not fix it all. But when people of certain groups are represented at the table, that point of view is far more likely to make it into the lexicon, language, and omnipresent work products, potentially changing cultural norms. Even the measurement of movement related to disparity in healthcare is marred by frequent variations of data accuracy. More consistency in what to measure can help a lot, and the medical literature can be very influential.
A personal anecdote: When I was a professor at UC Davis in 1978, Allan Bakke, MD, was my student. Some of you will remember the saga of affirmative action on admissions, which was just revisited in the light of a recent decision by the US Supreme Court.
Back in 1978, the dean at UC Davis told me that he kept two file folders on the admission processes in different desk drawers. One categorized all applicants and enrollees by race, and the other did not. Depending on who came to visit and ask questions, he would choose one or the other file to share once he figured out what they were looking for (this is not a joke).
The strength of the current active political pushback against the entire DEI movement has deep roots and should not be underestimated. There will be a lot of to-ing and fro-ing.
French writer Victor Hugo is credited with stating, “There is nothing as powerful as an idea whose time has come.” A majority of Americans, physicians, and other healthcare professionals believe in basic fairness. The time for DEI in all aspects of medicine is now.
Dr. Lundberg, editor in chief of Cancer Commons, disclosed having no relevant financial relationships.
A version of this article appeared on Medscape.com.
New Data: Black Women More Likely to Die From Common Endometrial Cancer Subtype
A recent analysis identified significant disparities in survival outcomes as well as clinical and genetic features between Black and White women with a common subtype of endometrial cancer.
In addition to observing differences in clinical and molecular characteristics, the analysis of real-world registries and clinical trials revealed that Black patients with endometrioid endometrial carcinoma had about a twofold higher risk for cancer-related deaths than White patients.
“Even with propensity-score matching, Black patients had a significantly increased risk of death,” Zachary Kopelman, DO, with Walter Reed National Military Medical Center, Bethesda, Maryland, noted in a presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Importantly, Dr. Kopelman added, the analysis also confirmed “dramatic” underrepresentation of Black patients with endometrioid endometrial carcinoma in clinical trials.
Endometrial cancer is one of the most common cancers among women in the United States, with data showing rising incidence and mortality rates. “Worryingly, endometrial cancer is estimated to overtake ovarian cancer as the deadliest gynecologic malignancy this year,” Dr. Kopelman told attendees.
Previous studies have shown that Black patients with endometrial cancer consistently are more likely to have aggressive histologic subtypes, high-grade tumors, and advanced-stage disease and are twice as likely to die from the disease as White patients, he noted.
Within endometrial cancer, the most common histologic subtype is endometrioid, comprising 65%-75% of cases. In other studies examining racial disparities, the endometrioid histology is often combined with other subtypes, such as aggressive uterine serous carcinoma, which may influence study outcomes, Dr. Kopelman explained.
Dr. Kopelman and colleagues focused their analyses on Black and White women with endometrioid endometrial carcinoma, with the goal of identifying disparities in cancer-related and non-cancer deaths, as well as clinical and molecular features in this patient population.
All women included in the analysis had undergone hysterectomy with or without adjuvant treatment. The researchers used a four-pronged approach incorporating data from the SEER program (2004-2016), the National Cancer Database (2004-2017), eight National Cancer Institute-sponsored randomized phase 3 clinical trials, and the Genomics Evidence Neoplasia Information Exchange project.
Dr. Kopelman and colleagues then performed propensity score matching in the National Cancer Database and exact matching in the randomized controlled trials.
When comparing 47,959 White patients with 4397 Black patients in the SEER dataset, Dr. Kopelman and colleagues found that Black patients had more than two times the risk of dying from their cancer (hazard ratio [HR], 2.04) and a 22% greater risk for a non-cancer death compared with White patients (HR, 1.22).
In the overall National Cancer Database cohort comparing 155,706 White and 13,468 Black patients, Black patients had a 52% greater risk of dying from any cause (HR, 1.52). In the propensity score-matched cohort of 13,468 White and 13,468 Black patients, survival among Black patients remained significantly worse, with a 29% greater risk of dying from any cause (HR, 1.29).
When looking at clinical trial data, Black patients were more likely than White patients to have worse performance status and a higher grade or recurrent disease, Dr. Kopelman noted.
Black patients in the clinical trials also had significantly worse progression-free survival in both the original cohort (HR, 2.05) and the matched cohort (adjusted HR [aHR], 1.22), which matched patients for grade, stage, and treatment arm within each trial and balanced age and performance status. Black patients also had worse overall survival in the original cohort (HR, 2.19) and matched cohort (aHR, 1.32).
Looking at molecular features, Black patients had significantly fewer mutations in a handful of cancer-related gene pathways, including PTEN, PIK3R1, FBXW7, NF1, mTOR, CCND1, and PI3K pathways.
One caveat, said Dr. Kopelman, is that mutations in PTEN are still present in a high percentage of both Black (62%) and White (72%), which «offers a potential attractive therapeutic opportunity.»
The analysis also revealed a major gap in the number of Black vs White patients enrolled in randomized clinical trials, which is a major “problem,” said Dr. Kopelman.
The study confirms “ongoing disparities in enrollment and underrepresentation of minorities in gynecologic cancer clinical trials, as well as poor outcomes, and should really promote us to enhance research in these areas,” said study discussant Mariam AlHilli, MD, with Cleveland Clinic Lerner College of Medicine and Case Western Reserve University, Cleveland, Ohio.
David M. O’Malley, MD, who gave a separate talk during the same session on practical considerations for implication of clinical trials, encouraged clinicians to “just ask.”
“Just ask the patient in front of you — no matter what their ethnicity, their race, or where they’re coming from — are they interested in participating in a clinical trial?” Or better yet, “I have a clinical trial now which I’m excited about for you,” said Dr. O’Malley, with The Ohio State University, James Comprehensive Cancer Center, Columbus, Ohio.The study had no commercial funding. Dr. Kopelman, Dr. O’Malley, and Dr. AlHilli had no relevant disclosures.
A version of this article appeared on Medscape.com .
A recent analysis identified significant disparities in survival outcomes as well as clinical and genetic features between Black and White women with a common subtype of endometrial cancer.
In addition to observing differences in clinical and molecular characteristics, the analysis of real-world registries and clinical trials revealed that Black patients with endometrioid endometrial carcinoma had about a twofold higher risk for cancer-related deaths than White patients.
“Even with propensity-score matching, Black patients had a significantly increased risk of death,” Zachary Kopelman, DO, with Walter Reed National Military Medical Center, Bethesda, Maryland, noted in a presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Importantly, Dr. Kopelman added, the analysis also confirmed “dramatic” underrepresentation of Black patients with endometrioid endometrial carcinoma in clinical trials.
Endometrial cancer is one of the most common cancers among women in the United States, with data showing rising incidence and mortality rates. “Worryingly, endometrial cancer is estimated to overtake ovarian cancer as the deadliest gynecologic malignancy this year,” Dr. Kopelman told attendees.
Previous studies have shown that Black patients with endometrial cancer consistently are more likely to have aggressive histologic subtypes, high-grade tumors, and advanced-stage disease and are twice as likely to die from the disease as White patients, he noted.
Within endometrial cancer, the most common histologic subtype is endometrioid, comprising 65%-75% of cases. In other studies examining racial disparities, the endometrioid histology is often combined with other subtypes, such as aggressive uterine serous carcinoma, which may influence study outcomes, Dr. Kopelman explained.
Dr. Kopelman and colleagues focused their analyses on Black and White women with endometrioid endometrial carcinoma, with the goal of identifying disparities in cancer-related and non-cancer deaths, as well as clinical and molecular features in this patient population.
All women included in the analysis had undergone hysterectomy with or without adjuvant treatment. The researchers used a four-pronged approach incorporating data from the SEER program (2004-2016), the National Cancer Database (2004-2017), eight National Cancer Institute-sponsored randomized phase 3 clinical trials, and the Genomics Evidence Neoplasia Information Exchange project.
Dr. Kopelman and colleagues then performed propensity score matching in the National Cancer Database and exact matching in the randomized controlled trials.
When comparing 47,959 White patients with 4397 Black patients in the SEER dataset, Dr. Kopelman and colleagues found that Black patients had more than two times the risk of dying from their cancer (hazard ratio [HR], 2.04) and a 22% greater risk for a non-cancer death compared with White patients (HR, 1.22).
In the overall National Cancer Database cohort comparing 155,706 White and 13,468 Black patients, Black patients had a 52% greater risk of dying from any cause (HR, 1.52). In the propensity score-matched cohort of 13,468 White and 13,468 Black patients, survival among Black patients remained significantly worse, with a 29% greater risk of dying from any cause (HR, 1.29).
When looking at clinical trial data, Black patients were more likely than White patients to have worse performance status and a higher grade or recurrent disease, Dr. Kopelman noted.
Black patients in the clinical trials also had significantly worse progression-free survival in both the original cohort (HR, 2.05) and the matched cohort (adjusted HR [aHR], 1.22), which matched patients for grade, stage, and treatment arm within each trial and balanced age and performance status. Black patients also had worse overall survival in the original cohort (HR, 2.19) and matched cohort (aHR, 1.32).
Looking at molecular features, Black patients had significantly fewer mutations in a handful of cancer-related gene pathways, including PTEN, PIK3R1, FBXW7, NF1, mTOR, CCND1, and PI3K pathways.
One caveat, said Dr. Kopelman, is that mutations in PTEN are still present in a high percentage of both Black (62%) and White (72%), which «offers a potential attractive therapeutic opportunity.»
The analysis also revealed a major gap in the number of Black vs White patients enrolled in randomized clinical trials, which is a major “problem,” said Dr. Kopelman.
The study confirms “ongoing disparities in enrollment and underrepresentation of minorities in gynecologic cancer clinical trials, as well as poor outcomes, and should really promote us to enhance research in these areas,” said study discussant Mariam AlHilli, MD, with Cleveland Clinic Lerner College of Medicine and Case Western Reserve University, Cleveland, Ohio.
David M. O’Malley, MD, who gave a separate talk during the same session on practical considerations for implication of clinical trials, encouraged clinicians to “just ask.”
“Just ask the patient in front of you — no matter what their ethnicity, their race, or where they’re coming from — are they interested in participating in a clinical trial?” Or better yet, “I have a clinical trial now which I’m excited about for you,” said Dr. O’Malley, with The Ohio State University, James Comprehensive Cancer Center, Columbus, Ohio.The study had no commercial funding. Dr. Kopelman, Dr. O’Malley, and Dr. AlHilli had no relevant disclosures.
A version of this article appeared on Medscape.com .
A recent analysis identified significant disparities in survival outcomes as well as clinical and genetic features between Black and White women with a common subtype of endometrial cancer.
In addition to observing differences in clinical and molecular characteristics, the analysis of real-world registries and clinical trials revealed that Black patients with endometrioid endometrial carcinoma had about a twofold higher risk for cancer-related deaths than White patients.
“Even with propensity-score matching, Black patients had a significantly increased risk of death,” Zachary Kopelman, DO, with Walter Reed National Military Medical Center, Bethesda, Maryland, noted in a presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer.
Importantly, Dr. Kopelman added, the analysis also confirmed “dramatic” underrepresentation of Black patients with endometrioid endometrial carcinoma in clinical trials.
Endometrial cancer is one of the most common cancers among women in the United States, with data showing rising incidence and mortality rates. “Worryingly, endometrial cancer is estimated to overtake ovarian cancer as the deadliest gynecologic malignancy this year,” Dr. Kopelman told attendees.
Previous studies have shown that Black patients with endometrial cancer consistently are more likely to have aggressive histologic subtypes, high-grade tumors, and advanced-stage disease and are twice as likely to die from the disease as White patients, he noted.
Within endometrial cancer, the most common histologic subtype is endometrioid, comprising 65%-75% of cases. In other studies examining racial disparities, the endometrioid histology is often combined with other subtypes, such as aggressive uterine serous carcinoma, which may influence study outcomes, Dr. Kopelman explained.
Dr. Kopelman and colleagues focused their analyses on Black and White women with endometrioid endometrial carcinoma, with the goal of identifying disparities in cancer-related and non-cancer deaths, as well as clinical and molecular features in this patient population.
All women included in the analysis had undergone hysterectomy with or without adjuvant treatment. The researchers used a four-pronged approach incorporating data from the SEER program (2004-2016), the National Cancer Database (2004-2017), eight National Cancer Institute-sponsored randomized phase 3 clinical trials, and the Genomics Evidence Neoplasia Information Exchange project.
Dr. Kopelman and colleagues then performed propensity score matching in the National Cancer Database and exact matching in the randomized controlled trials.
When comparing 47,959 White patients with 4397 Black patients in the SEER dataset, Dr. Kopelman and colleagues found that Black patients had more than two times the risk of dying from their cancer (hazard ratio [HR], 2.04) and a 22% greater risk for a non-cancer death compared with White patients (HR, 1.22).
In the overall National Cancer Database cohort comparing 155,706 White and 13,468 Black patients, Black patients had a 52% greater risk of dying from any cause (HR, 1.52). In the propensity score-matched cohort of 13,468 White and 13,468 Black patients, survival among Black patients remained significantly worse, with a 29% greater risk of dying from any cause (HR, 1.29).
When looking at clinical trial data, Black patients were more likely than White patients to have worse performance status and a higher grade or recurrent disease, Dr. Kopelman noted.
Black patients in the clinical trials also had significantly worse progression-free survival in both the original cohort (HR, 2.05) and the matched cohort (adjusted HR [aHR], 1.22), which matched patients for grade, stage, and treatment arm within each trial and balanced age and performance status. Black patients also had worse overall survival in the original cohort (HR, 2.19) and matched cohort (aHR, 1.32).
Looking at molecular features, Black patients had significantly fewer mutations in a handful of cancer-related gene pathways, including PTEN, PIK3R1, FBXW7, NF1, mTOR, CCND1, and PI3K pathways.
One caveat, said Dr. Kopelman, is that mutations in PTEN are still present in a high percentage of both Black (62%) and White (72%), which «offers a potential attractive therapeutic opportunity.»
The analysis also revealed a major gap in the number of Black vs White patients enrolled in randomized clinical trials, which is a major “problem,” said Dr. Kopelman.
The study confirms “ongoing disparities in enrollment and underrepresentation of minorities in gynecologic cancer clinical trials, as well as poor outcomes, and should really promote us to enhance research in these areas,” said study discussant Mariam AlHilli, MD, with Cleveland Clinic Lerner College of Medicine and Case Western Reserve University, Cleveland, Ohio.
David M. O’Malley, MD, who gave a separate talk during the same session on practical considerations for implication of clinical trials, encouraged clinicians to “just ask.”
“Just ask the patient in front of you — no matter what their ethnicity, their race, or where they’re coming from — are they interested in participating in a clinical trial?” Or better yet, “I have a clinical trial now which I’m excited about for you,” said Dr. O’Malley, with The Ohio State University, James Comprehensive Cancer Center, Columbus, Ohio.The study had no commercial funding. Dr. Kopelman, Dr. O’Malley, and Dr. AlHilli had no relevant disclosures.
A version of this article appeared on Medscape.com .
FROM SGO 2024









