User login
Recognizing and Treating Neuropsychiatric Symptoms in Parkinson's Disease
From the Department of Neurology, Oregon Health & Science University, Portland, OR.
Abstract
- Objective: To review the clinical characteristics, epidemiology, and management of the most common neuropsychiatric symptoms (NPS) in Parkinson’s disease (PD).
- Methods: Literature review.
- Results: PD has traditionally been considered a disease of impaired motor function. However, neuropsychiatric complications, such as fatigue, depression, anxiety, psychosis, impulse control disorders, and apathy, frequently complicate the course of the illness. Although the development of new medication options in recent years has had a positive benefit on the management of these troublesome symptoms, responses are frequently suboptimal. The development of valid instruments to measure neuropsychiatric symptoms has been vital in research efforts to bridge the gaps in our understanding. Further elucidation of neuropsychiatric pathophysiologies will help to define treatment targets and has the potential to expand our therapeutic armamentarium.
- Conclusion: While NPS affect patients with established disease, recent investigations have demonstrated risk of symptoms in those with early untreated stages of PD; therefore, better understanding of NPS should be the goal of practitioners treating the entire continuum of PD.
Parkinson’s disease (PD) has traditionally been considered a disease of impaired motor function, but increased recognition of nonmotor symptoms and in particular neuropsychiatric symptoms, such as fatigue, depression, anxiety, psychosis, impulse control disorders, and apathy, offer new opportunities for better care of patients. While neuropsychiatric symptoms affect patients with established disease, recent investigations have clearly demonstrated risk of symptoms in those with early untreated stages of PD; therefore, better understanding of neuropsychiatric symptoms should be the goal of practitioners treating the entire continuum of PD. This review will focus on the clinical characteristics, epidemiology, and management of the most common neuropsychiatric symptoms in PD.
Impulse Control Disorders
The recognition that dopaminergic drugs were successful at treating many symptoms of PD was followed by the disturbing realization that impulse control disorders could be an unfortunate side effect in a substantial minority. Impulse control disorders as defined by DSM-IV [1] are disinhibited behaviors that are maladaptive and recurrent, causing personal and relationship consequences. The impulse control disorders that became associated with PD and medication intake, particularly dopamine agonist use, included gambling, hobbyism, punding (stereotyped, seemingly purposeless behaviors), excessive sexual behavior, shopping, hoarding, and less commonly, compulsive eating. The prevalence estimates of these behavioral disturbances range from 6% to 15.5%, compared with < 2% in the general population [2,3]. The addiction-like dopamine dysregulation syndrome, whereby patients self-medicate with high doses of levodopa and short-acting dopamine agonists beyond what is needed for motor control, can lead to significant impairment of the therapeutic alliance in addition to other patient personal relations. With the advent of surgical options to treat PD and its medication complications, it was observed that stimulation of the subthalamic nucleus could be associated with the spectrum of impulse control disorders [4].
Epidemiology/Risk Factors
In a recent systematic review of the literature of impulse control disorders in PD [5], the authors determined that dopaminergic therapy caused compulsive or impulsive behaviors in approximately 10% of PD patients in the course of their treatment, with pathologic gambling and hypersexuality most frequently experienced. Multiple impulse control disorders are not uncommon and may coexist in one-quarter of patients with compulsivity. There appeared to be more disordered behavior with higher comparable doses of agonists. The authors concluded that impulse control disorder symptoms tended to occur with initiation or dose increases of direct D2/D3 agonists, such as pramipexole and ropinirole. Importantly, impulse control disorder behavior improved if not resolved with discontinuation or reduction of dosage of the agonist, even if a compensatory levodopa dosage is added or increased. Perhaps not surprisingly, it was observed that if patients had a preexisting impulse control disorder prior to PD or the initiation of treatment, there was a high likelihood of worsening of symptoms. This small subgroup is estimated at about 1% of PD subjects, which corresponds to the prevalence of impulse control disorders in the general population. Other identified potential risk factors for impulse control disorder development include male gender, young age at onset, a personal or family history of addiction, novelty or risk seeking personality, and a concurrent diagnosis of depression [3]. In a recent study of early PD patients, the risk of developing an impulse control disorder became important once treatment with dopaminergic drugs began and continued for a year or more [6].
Pathogenesis
The pathogenesis is not fully understood, however, mesolimbic dopamine alterations are strongly suspected. It has been long speculated that the high doses of dopamine needed to replete the relatively depleted dorsal striatum overdose the “intact” ventral striatum and cause this neuropsychiatric disorder [7–9]. The additional cognitive impairments in PD, which can include problems with attention, working memory, planning, forethought and decision-making, are faculties that can markedly increase susceptibility to impulse control disorder [8].
The role of serotonin deficiency in the PD brain and its part in inhibiting the patient’s ability to delay rewards adds to the complexity of impulse control disorder pathogenesis. Dorsal raphe nuclei disease in PD results in loss of serotonin innervation to substantial portions of the prefrontal and motor cortices in addition to basal ganglia substructures like the striatum, pallidum and subthalamic nucleus [10]. Together with dopamine, serotonin may work to regulate risk-sensitive decision making, response inhibition, waiting for future rewards, and overall impulse control. Its relative loss therefore also likely contributes to tipping the balance towards impulse dyscontrol [11,12]. The role of other neurotransmitters such as opiate systems involved in the process of acquisition and maintenance of addictive behaviors like dopamine dysregulation syndrome remains to be fully understood.
Treatment
The most successful strategy to address this problem is to reduce or eliminate the offending medication, usually the dopamine agonist. This may be associated with worsening apathy, anxiety or depression; however, substituting levodopa can be a successful strategy in many cases [13]. Zonisamide was described to be possibly effective in a trial of 15 subjects; however, the open label nature of this evidence must be considered as with other case reports using valproate, donepezil, and selective serotonin reuptake inhibitors (SSRIs) [14–16].
Fatigue
An easy to understand operational definition of fatigue is that it is a state of extreme tiredness, weakness, or exhaustion, either physical or mental or both. Fatigue is not uncommon in the general population [17] but is increasingly recognized to occur in numerous disease conditions and is frequently encountered in PD and multiple sclerosis. The latter is of special significance in the consideration of the neurotransmission of fatigue, as it is not thought to be a disease of dopamine deficiency. The pathophysiology remains unclear, and it may differ depending on whether the fatigue is experienced as more physical or mental, or rather motor versus nonmotor as some authors propose.
Fatigue has been conceptualized as central or peripheral in character. Peripheral fatigue is best understood as muscular fatigue caused by repetitive muscular contraction or reduced force generation [18]. Central fatigue however, is divided into mental or physical fatigue. Mental fatigue can occur after sustained attentive or emotional activity. It may alternatively be provoked after boring repetitive tasks or lack of intellectually stimulating activity. Physical fatigue is the sense of body exhaustion or energy to perform physical tasks even though the ability to carry them out exists.
Epidemiology
As recognition of the problem of fatigue increased in the last 2 decades, the realization that one-third to one-half of patients experience it at some point has improved opportunities for recognition and treatment [19]. Fatigue may be the presenting symptom in one-third of patients prior to actual motor symptom onset [20]. Half of untreated PD patients in a biomarker cohort study reported fatigue [6]. Unfortunately, it is also described by patients as one of the most disabling symptoms, causing significant impact on quality of life [19]. Fatigue in PD is associated with higher rates of depressive symptoms, but occurs with higher prevalence in nondepressed patients [21]. Poor ability to initiate and sustain activity due to fatigue is different from depression, excessive sleepiness, or impaired motor function [22,23].
Pathophysiology
The pathophysiology of fatigue remains somewhat unclear, though physical fatigue is likely a significant part of the problem and related to dopamine deficiency based on studies of time and force generation of keyboard strikes in PD subjects before and after L-dopa administration. These subjects had declines in force and increased physical fatigue which improved after L-dopa [24]. In other studies using transcranial magnetic stimulation to study changes in cortical excitability, the degree of physical fatigue correlated with abnormalities in motor evoked potentials during fatiguing exercising. These studies also support the hypothesis that fatigue is a motor symptom [25,26]. In the ELLDOPA study, fatigue worsened more in PD subjects treated with placebo [27]. Other imaging studies have suggested suggested nondopaminergic mechanisms including serotonergic pathway abnormalities [28], thus the question behind the etiology and solution for all cases of fatigue remains to be settled.
Diagnosis
The diagnosis is fatigue may be challenging as it may mask as depression or apathy. There are a number of fatigue rating scales available; however, the validated Parkinson’s Fatigue Scale (PFS) supersedes many of the problems of using a generic scale which could overlap motor questions and potentially be confounding [29,30].
Treatment
Most important is awareness and vigilance for the symptoms of fatigue, depression, and apathy and effort to distinguish between them. It may require structured interviews or assessment tools to properly diagnose the problem. Treatment is less clear in that few studies have clearly indicated the best treatment options. In placebo-controlled trials, methylphenidate did improve fatigue as did levodopa [31]. Modafinil, a hypocretin modulator and a drug first approved by the FDA for treatment of narcolepsy, has demonstrated mixed results in recent years. It may reduce physical fatigue and reduce excessive daytime sleepiness but likely does not reduce subjective symptoms of fatigue [32]. L-dopa can significantly reduce fatigue in many patients, which would argue that it often is a motor symptom [33,24]. In a post-hoc analysis of the ADAGIO delayed start study, patients taking rasagiline 1 mg/day and 2 mg/day (the latter dose exceeds the usual clinical dosing) showed significantly less worsening of symptoms on the PFS compared to placebo over time [34]. It is important to realize that once motor symptoms are optimally treated with dopaminergic medications, while many patients will feel significant relief from fatigue some patients will continue to feel symptomatic.
Apathy
The definition of apathy has become more complicated and refined, incorporating findings from the study of brain disease and behavioral analysis. Marin’s classic elaboration of apathy as lack of motivation not attributable to diminished level of consciousness, cognitive impairment, or emotional distress has been built upon by Levy and Dubois [35–37]. They suggest apathy may be better thought of as an observable behavioral syndrome characterized by a quantitative reduction of self-generated voluntary and purposeful behaviors. They suggest 3 apathetic subtypes: emotional, cognitive, and auto-activational, which reflect different disease states accounting for failure of normal goal-directed behavior.
Epidemiology
Prevalence estimates for apathy in PD vary. This is likely due to the varying recruitment criteria among studies, with some including patients with comorbid depression and dementia and others containing only “pure apathy.” Other reports may have had referral bias issues, as community-based studies report lower prevalences in general. In a group of newly diagnosed PD patients, using more restrictive criteria (apathy subscale of the neuropsychiatric inventory and the diagnostic consensus criteria for apathy validated in PD), Pedersen reported a prevalence of apathy of 14.3% [38]. In a 4-year prospective longitudinal cohort study, an annual incidence rate of 12.3% was reported, with apathy developing in 60% of the cohort by the study’s conclusion [39].
Apathy has been associated with longer disease duration, male gender [40], higher daily levodopa doses [41], more severe parkinsonism [38], and lower education status, though the latter feature remains under debate. Early cognitive deficits appear to be a risk factor for development of apathy [42]. The patterns of cognitive dysfunction and apathy remain unsettled in the literature.
Pathology
The pathology of atrophy remains unexplained and is unlikely to be reduced to a simple atrophy of one nucleus or the tone of one circuit. However, in a small neuroimaging study, severity of apathy correlated with atrophy of the bilateral nucleus accumbens [43], and it is notable that one major input to the nucleus accumbens is the amygdala. According to Braak staging, by stage 4 significant involvement of the amygdala by Lewy bodies has occurred. Others have found changes in grey matter density that could correlate with deficits of the prefrontal-basal ganglia circuitry to produce dysfunction of segregated frontal-subcortical loops. These may correlate with the “autoactivation” deficit pattern of apathy in which patients have a lack of self-initiated actions, even thoughts, though appear more normal when giving externally prompted responses [37,44].
Assessment
Clinically, the relationship between apathy and depression can be hard to disentangle, especially since many studies have found an association between them, especially with regards to apathy and anhedonia. Depression may feature negative self thoughts and sadness while apathy is notable for lack of initiation and effort. Viewed over a longer period of time, apathy tended to worsen in a linear fashion, where depression tended to fluctuate with improvements and exacerbations.
The Movement Disorders Society task force has recommended the Lille Apathy Rating Scale (LARS) for assessment of apathy; English and French versions have been validated in PD patients. It uses a semi-structured interview format assessing 4 dimensions of apathy: self awareness, intellectual curiosity, emotion, and action initiation [45–47].
The impact of apathy cannot be underestimated as this poor show of motivation or effort leads to lack of engagement in old activities or interest in new ones. Spouses may misinterpret this change in behavior as laziness or deliberate social withdrawal, or perhaps entitlement. It is not surprising that apathy routinely shows up on quality of life (QoL) questionnaires as highly impacting patients and families. In one study, apathy was the nonmotor symptom most likely to cause caregiver distress in PD [40,48–50].
Treatment
No approved drugs exist for treatment of apathy. However, clinical experience often confirms that dopaminergic modulation can be helpful in the treatment of apathy as indirect evidence suggests. A meta-analysis of controlled trials using pramipexole and Part I of the Unified Parkinson's disease rating scale (UPDRS) (secondary measure) showed the medication improved scores on this measure of motivation and mood in non-depressed subjects [51] with PD. Rare patients undergoing subthalamic deep brain stimulation have been reported to experience new and sometimes severe apathy after surgery [52]. This was posited at least in part to be the result of reduction of dopaminergic medication due to surgery.
Nondopaminergic pharmacotherapy of apathy is in its infancy. A recent controlled trial of rivastigmine in 31 French subjects with moderate to severe apathy based on LARS showed that 6 months of treatment at 9.5 mg/day improved average scores from –11.5 to –20 compared with placebo. While quality of life did not improve, caregiver burden did. The investigators found in this group of subjects that apathy was a possible herald for early dementia in PD [53].
A post-hoc analysis of the ADAGIO study (rasagiline or placebo in PD patients taking antidepressants) found that rasagiline use was associated with a nonsignificant slowing of apathy development during the trial [54].
Psychosis
Psychotic symptoms are a common occurrence in drug-treated patients, with visual hallucinations occurring in up to 30%, though over a 20-year period up to three-quarters of patients may develop visual hallucinations.After visual, the most common type of hallucination is auditory, followed by the other affected senses such as tactile, olfactory, or even taste [57]. Delusions, which tend to be paranoid in nature, occur in about 5% of patients [55–57]. The presence of psychotic symptoms is associated with poorer quality of life [58].
Symptomatology
The visual hallucinations of PD are usually quite stereotyped, and have been described as “minor” and “non-minor”[59]. Minor hallucinations refer to transient peripheral field stimuli that disappear when brought into central focus, “something flashed by,” a sense of a living being nearby, “a presence in the room,” or illusions whereby objects are transformed, eg, a bush in the yard is a deer.
Auditory hallucinations tend to be vague or indistinct sounds, like music in another room as opposed to voices speaking directly to the patient as might be experienced in a primary psychotic disorder. Tactile forms often involve insects or other animals crawling on the skin. Olfactory hallucinations may take the form of smelling perfume, toxic odors from room vents, etc.
Early in the experience, the visual hallucinations may be amusing in that they consistently remain nonthreatening, similar day to day, and sometimes oddly provide an aspect of comfort or companionship to the patient. More commonly, the hallucinations are bothersome to the patient because the experience indicates to the patient that there is something wrong with their mind. Visual hallucinations often begin in low-stimulus environments, often in the evening or other low-light conditions, but as the problem advances they can occur at any time of day. While visual hallucinations may initially occur for only seconds at a time many days apart, the frequency and duration can increase until they occur hours at a time every day and are accompanied by multiple other visual hallucinations, delusions, and confusion [60].
Delusions tend to be more distressing to patients and caregivers because they are often paranoid in nature. The patient is more likely to act out due to the anxiety the paranoia creates. For example, she may change passwords to online accounts due to a belief that unknown assailants are after her finances. He may go to great lengths trying to prove his wife is cheating.
Risk Factors
While the primary risk factor for psychotic symptom development is dementia [57], it occurs in nondemented patients. Other associations include reduced visual acuity [56], visual processing impairment [61–65], use of dopamine agonists, REM behavior disorder, duration of PD, axial rigidity subtype of disease [61,66–68]. The pathophysiology of psychosis in PD is likely complex and remains currently unexplained. The role of excess dopamine has been described above, but there is also data suggesting cholinergic deficits in the cortex may also contribute. Excess serotonin (increased 5HT2A receptor subtypes) in the temporal lobe within the visual processing pathway has been postulated to be of significance [69,70]. Hypometabolism in visual association areas of the brain in subjects with visual hallucinations has been demonstrated in PET and functional MRI studies [64,71]. This is similar to findings in patients with dementia with Lewy bodies [72].
This review focuses on the primary forms of PD-related psychosis, which occur with a clear sensorium and generally longer exposure to dopaminergic medication. It is important to distinguish 2 other common scenarios in which hallucinations or delusions may occur. In the common toxic-metabolic delirium, a clouded sensorium with attention deficits may be the only clue to the etiology of new onset confusion with visual hallucinations. It is highly likely that resolution of the underlying medical problem will lead to resolution of the new onset psychosis and encephalopathy. In a second scenario, hallucinations precede or occur very shortly after the onset of initiation of dopaminergic medication. This differs from the classic syndrome described earlier, in particular when visual hallucinations precede any initiation of medication, and likely represents the distinction between a diagnosis of Lewy body disease and PD [60].
Treatment
Management of psychosis is approachable, but often the outcome is unsatisfactory and associated with trade-offs in motor control. It is unfortunately true that psychotic symptoms are often associated with increased caregiver burden and are a cause of increased nursing home placements [73]. When considering the workup of psychotic symptoms, the differential diagnosis includes delirium, dream enactment (REM behavior disorder), or less commonly, Bonnet syndrome.
A delirium may be precipitated by a difficult to diagnose infection; new-onset confusion and psychotic symptoms may be the heralding presentation. Urinary tract or upper respiratory tract are common vulnerable sources of infection. Once infection is ruled out, the next practical step is to review the patient’s medication list and manage centrally acting drugs that could be contributing to the altered sensorium. A recent prescription of opioids for a dental treatment or a new muscle relaxant may be a culprit, though it is not that usual. A bladder anticholinergic could be suspect and is worth eliminating especially if its addition coincided with the appearance of the psychotic symptoms. Once the non-dopaminergic medications have been reduced/eliminated, then the PD medications should be considered. The general approach is to eliminate the medications that provide the least benefit while being more likely to contribute to psychotic symptoms. Anticholinergic medications, dopamine agonists, selegiline should all be uppermost in that consideration until one is left with L-dopa and COMT inhibitors (the latter function to increase levodopa availability). Then COMT inhibitors and levodopa can be reduced; however, at any point motor control can suffer with the loss of symptomatic therapies [74].
Clozapine is effective against psychotic symptoms in PD, at doses much lower than used in schizophrenia (300-600mg/day). The average dose in the US randomized controlled clinical trial was 25 mg/day, with no associated motor worsening. Patients in the United States are required by the FDA to be placed in a computer-based registry and monitored for agranulocytosis for the duration of clozapine therapy. This rare adverse event is not dose related. Orthostasis can occur at these low doses however. Fortunately the metabolic syndrome is not associated with this range of administration [75,76].
Quetiapine was not found to be effective in 3 blinded randomized controlled trials despite its rather common use for this purpose. It was not associated with motor worsening, however.
Other neuroleptic medications have not resulted in widespread use, because trials have been open label, or outcomes demonstrated motor worsening. Cholinesterase inhibitors have been the subject of a few positive case series, however results appear to be sporadic, the effect size is relatively small, and side effects of this medication class are common [77–79]. It is clear that there is an unmet need for a medication for psychotic symptoms. Clozapine is effective but onerous in its monitoring requirements. Practically speaking, there are relatively few PD patients who take advantage of it because of its feasibility challenges. Yet the problem of psychotic symptoms is a significant one that imposes important challenges to the patient and caregiver, and may limit the number of medications that the patient needs in order to optimize quality of life.
Pimavanserin, a novel medication which acts as a selective serotonin inverse agonist, is in the early application stages for FDA approval for treatment of psychotic symptoms in PD [80]. In its pivotal phase III controlled trial, the drug reduced not only positive symptoms (hallucinations/delusions) without causing motoric worsening, but also reduced caregiver burden. Pimavanserin improved certain sleep features without causing daytime sedation. If this drug meets final approval, it may present an exciting option for many patients for whom treatment was previously limited.
Depression
A study of early PD suggested that depression is often unrecognized and frequently untreated [1]. Indeed it is not unusual for depression to predate the diagnosis of PD by an average of 4 to 6 years [81]. Expanding to the larger PD population, it is generally accepted that about 30% to 50% of PD patients experience clinically significant depression, and once diagnosed may have a long term course, or may recur [82,83]. This is important as untreated depression is an important cause of poor quality of life in early PD. In addition depression can exacerbate motor disability, lead to earlier motor treatment with medication, and increase caregiver stress [83–85].
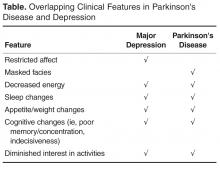
Diagnosis
A number of clinimetric rating scales for depression have been used and their advantages have been largely related to their objective nature (quantifiable); thus, they tend to be most useful in epidemiologic research studies or for larger scale screening purposes. Examples include the the Beck Depression Inventory, the Geriatric Depression Scale, and the Hamilton Depression Scale, all of which have been shown to be valid tools in PD (with the exception of the UPDRS Depression). It is important to note that they do not substitute for a diagnostic clinical interview [89].
Suicide is not common in PD, however suicidal ideation is estimated at about 11% in PD patients [90], and while there was concern initially after deep brain stimulation procedures began that suicide incidence was increased, evidence does not support this [91].
Pathophysiology
The pathophysiology of depression in PD is largely unknown however is thought to be less causally due to psychosocial factors and more etiologically driven by brainstem monoamine and serotonergic dysfunction [92]. Nonetheless, similar to other chronic conditions, PD patients can certainly develop fear of disability, guilt about impact on others, or other reactive mood changes. Overall, rates of depression are higher in PD compared with patients with similar conditions matched for disability [93].
Treatment
First, the clinician must determine if depression is a result of short-term fluctuations, chronic undertreatment of motor disease, or longer-term mood phenomenon. One important pattern to recognize are mood fluctuations, which can parallel motor OFF-ON cycling. It can be valuable to distinguish this as “subsyndromic” depression or anxiety (sometimes referred to as “OFF dysphoria”), as it can respond to improvement in antiparkinsonian medication dosing patterns that reduce fluctuations[94–96]. Similarly, elevating chronic motor undertreatment to goal therapy can result in mood normalization.
If symptoms persist despite optimization of motor/nonmotor fluctuations or chronic undertreatment and are severe enough to warrant treatment, then therapies used can range from nonpharmacologic education, support, and mental health referrals, as well as pharmacologic support in the form of medications.
A frequent but uncontrolled observation was that when undertreatment of motor disease was finally redressed, mood often improved. A multicenter randomized controlled trial of pramipexole in PD patients without motor fluctuations but with mild to moderate depressive symptoms showed the drug improved scores on the Beck Depression Inventory over a 12-week period. The improvement in mood was 6 points overall, but by 2 points over placebo, illustrating the importance of the size of the placebo effect [97]. Given the potential side effect profile of dopamine agonists, it may be useful to weigh the antidepressant effects only when their motor benefits are already being employed.
Controlled trials have demonstrated efficacy of both selective serotonin reuptake inhibitors (SSRI) and selective norepinephrine reuptake inhibitors (SNRI) antidepressants in PD. Clinical trials have demonstrated efficacy against placebo or with other antidepressant comparators. Examples of drugs with demonstrated efficacy include citalopram, paroxetine, venlafaxine, and nortriptyline. Results have attempted to illuminate the small unique differences between classes of antidepressants or dynamic properties between drugs within a class. For example, desipramine may nudge scores on a mood scale a few weeks sooner than a purer SSRI. Paroxetine (SSRI) versus venlafaxine (SNRI) improved mood scores comparably in a multicenter trial with a placebo comparator. In general, all have all been demonstrated to be effective and with a relatively low side-effect profile, comparable to the general population[98–102]. While case reports exist in the literature, the interaction of monoamine oxidase B inhibitors and SSRIs has not caused significant hypertensive crises or risk of serotonin syndrome [103,104]. Electroconvulsive therapy (ECT) can be used for severe refractory depression in PD as for non-PD patients, with case reports of very effective results. Due to the rarity of use, systematic evidence for its use is lacking [105,106].
Other novel agents and techniques such as omega-3 fatty acids [107] and repetitive transcranial magnetic stimulation [108] have been reported with promising early results. Cognitive behavioral therapy (CBT), which may involve stress management techniques, sleep hygiene, and caregiver support, additionally almost always provided improvement in measured outcomes, whether the trial was controlled or open label in design. In one RCT of CBT in PD of 14 weeks’ duration, there were significantly more treatment responders in the CBT group, with a number needed to treat of only 2 [109].
Anxiety
Anxiety is also common in PD, at least as common as depression considering that prevalence estimates suggest up to 50% of patients experience it [110–112]. Manifestations of anxiety may include panic attacks, generalized anxiety disorder, social anxiety, or other phobias [113]. Anxiety has an important negative impact on health-related quality of life and is often underrecognized by clinicians [114]. While reliable and valid scales to measure anxiety have been lacking in PD, a new effort has yielded the “Parkinson Anxiety Scale” though full clinimetric properties of the scale remain to be demonstrated (sensitivity to change) [115].
Anxiety that parallels the timing of motor OFF-ON cycling is important to recognize. This “subsyndromic” anxiety or anxiety disorder not otherwise specified (ie, the anxiety does not meet DSM-IV criteria) can respond to improvement in antiparkinsonian medication dosing patterns that reduce fluctuations [116,117]. Indeed, the presence of motor fluctuations is the principle marker of anxiety in many studies [118–120]. In an analogous manner, anxiety can predate PD by years and be part of the nonmotor amalgam of features heralding the disease [6,121].
Treatment
Systematic controlled trials of anxiolytic treatment for PD are lacking; therefore, SSRIs are prescribed for this purpose as in non-PD patients. Until SSRIs are demonstrated to be of benefit in anxiety, they are likely safer than use of benzodiazepines, which are associated with risk for falling, cognitive dysfunction, or autonomic dysregulation in PD patients when used during waking hours. Psychotherapy and other nonpharmacologic approaches are likely to be of benefit. A small study of neuromuscular (massage) therapy demonstrated improvement on the Beck Anxiety Inventory in PD [122]. A case report of ECT for severe anxiety has been published [123].
Conclusion
Neuropsychiatric symptoms are common in PD and new knowledge about clinical features, epidemiology, and treatment options has been gained in the last decade, though much remains to be discovered. The development of valid instruments to measure neuropsychiatric symptoms has been vital in these research efforts to bridge the gaps in our understanding. Further elucidation of the pathophysiologies of neuropsychiatric symptoms will help to define treatment targets and likely fuel drug development and the discovery of drugs with more potent benefit and fewer side effects.
Corresponding author: Kathryn A. Chung, MD, Department of Neurology, Oregon Health & Science University, Portland, OR, [email protected].
Financial disclosures: None.
1. American Psychiatric Association. DSM-IV. 2000.
2. Voon V, Hassan K, Zurowski M, et al. Prevalence of behaviors in Parkinson disease Neurology 2006;67;1254–7.
3. D. Weintraub D, J. Koester J, M. N. Potenza MN, et al. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol 2010;67589–95.
4. Hälbig TD, Tse W, Frisina PG, et al. Subthalamic deep brain stimulation and impulse control in Parkinson’s disease. Eur J Neuro 2009;16:493–7.
5. Callesen MB, Scheel-Krüger J, Kringelbach ML, Møller A. A systematic review of impulse control disorders in Parkinson’s disease. J Parkinsons Dis 2013;3:105–38.
6. De Riva P, Smith K, Xie SX, Weintraub D. Course of psychiatric symptoms and global cognition in early course of psychiatric symptoms and global cognition in early Parkinson disease Neurology 2014;83:1–8.
7. Cools R. Dopaminergic modulation of cognitive function-implications for L-DOPA treatment in Parkinson’s disease. Neurosci Biobehav Rev 2006;30:1–23.
8. Rowe JB, Hughes L, Ghosh BCP, et al. Parkinson’s disease and dopaminergic therapy – Differential effects on movement, reward and cognition. Brain 2008;131:2094–105.
9. Cools R, Frank MJ, Gibbs SE, et al. Striatal dopamine predicts outcome-specific reversal learning and its sensitivity to dopaminergic drug administration. J Neurosci 2009;29:1538–43.
10. Di Matteo V, Pierucci M, Esposito E, et al. Serotonin modulation of the basal ganglia circuitry: therapeutic implication for Parkinson’s disease and other motor disorders. Prog Brain Res 2008;172:423–463.
11. Campbell-Meiklejohn D, Wakeley J, Herbert V, et al. Serotonin and dopamine play complementary roles in gambling to recover losses. Neuropsychopharmacology 2011;36:402–10.
12. Macoveanu J, Rowe JB, Hornboll B, et al. Playing it safe but losing anyway-Serotonergic signaling of negative outcomes in dorsomedial prefrontal cortex in the context of risk-aversion. Eur Neuropsychopharmacol 2013;23:919–30.
13. Mamikonyan E, Siderowf AD, Duda JE, et al. NIH Public Access 2009;23:75–80.
14. Ivanco LS, Bohnen NI. Effects of donepezil on compulsive hypersexual behavior in Parkinson disease: a single case study. Am J Ther 2005;12:467–8.
15. Hicks CW, Pandya MM, Itin I, Fernandez HH. Valproate for the treatment of medication-induced impulse-control disorders in three patients with Parkinson’s disease. Parkinsonism Relat Disord 2011;5:379–81.
16. Bermejo PE, Ruiz-Huete C, Anciones B. Zonisamide in managing impulse control disorders in Parkinson’s disease. J Neurol 2010;257:1682–5.
17. Pawlikowska T, Chalder T, Hirsch SR, et al. Population based study of fatigue and psychological distress. BMJ 1994;308:763–6.
18. Lou JS, Kearns G, Oken B, et al. Exacerbated physical fatigue and mental fatigue in Parkinson’s disease. Mov Disord 2001;16:190–6.
19. Herlofson K, Larsen JP. The influence of fatigue on health-related quality of life in patients with Parkinson’s disease. Acta Neurol Scand 2003;107:1–6.
20. Hagell P, Brundin L. Towards an understanding of fatigue in Parkinson disease. J Neurol Neurosurg Psychiatry 2009;80:489–92.
21. Alves G, Wentzel-Larsen T, Larsen JP. Is fatigue an independent and persistent symptom in patients with Parkinson disease? Neurology 2004;63:1908–11.
22. Martinez-Martin P, Catalan MJ, Benito-Leon J, et al. Impact of fatigue in Parkinson’s disease: The fatigue impact scale for daily use (D-FIS). Qual Life Res 2006:15:597–606.
23. Havlikova E, Rosenberger J, Nagyova I, et al. Clinical and psychosocial factors associated with fatigue in patients with Parkinson’s disease. Parkinsonism Relat Disord 2008;14:187–92.
24. Lou JS, Kearns G, Benice T, et al. Levodopa improves physical fatigue in Parkinson’s disease: A double-blind, placebo controlled, crossover study. Mov Disord 2003;18:1108–14.
25. Khedr EM, Galal O, Said A, et al. Lack of post-exercise depression of corticospinal excitability in patients with Parkinson’s disease. Eur J Neurol 2007;14:793–6.
26. Lou JS, Benice T, Kearns G, et al. Levodopa normalizes exercise related cortico-motoneuron excitability abnormalities in Parkinson’s disease. Clin. Neurophysiol 2003;114:930–7.
27. Schifitto G, Friedman JH, Oakes D, et al. Fatigue in levodopa-naive subjects with Parkinson disease. Neurology 2008;71:481–5.
28. Pavese N, Metta V, Bose SK, et al. Fatigue in Parkinson’s disease is linked to striatal and limbic serotonergic dysfunction. Brain 2010;133:3434–43.
29. Brown RG, Dittner A, Findley L, Wessely SC. The Parkinson fatigue scale. Park Relat Disord 2005;11:49–55.
30. Grace J, Mendelsohn A, Friedman JH. A comparison of fatigue measures in Parkinson’s disease. Parkinsonism Relat Disord 2007;13:443–5.
31. Mendonça DA, Menezes K, Jog MS. Methylphenidate improves fatigue scores in Parkinson disease: a randomized controlled trial. Mov Disord 2007;22:2070–6.
32. Lou JS, Dimitrova DM, Park BS, et al. Using modafinil to treat fatigue in Parkinson disease: a double-blind, placebo-controlled pilot study. Clin Neuropharmacol 2009;32:305–10.
33. Ziv I, Avraham M, Michaelov Y, et al. Enhanced fatigue during motor performance in patients with Parkinson’s disease. Neurology 1998;51:1583–6.
34. Stocchi F. Benefits of treatment with rasagiline for fatigue symptoms in patients with early Parkinson’s disease. Eur J Neurol 2014;21:357–60.
35. Marin RS. Apathy: a neuropsychiatric syndrome. J. Neuropsychiatry Clin Neurosci 1991;3:243–4.
36. Marin RS. Apathy: concept, syndrome, neural mechanisms, and treatment. Semin Clin Neuropsychiatry 1996:1:304–14.
37. Levy R, Dubois B. Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cerebral Cortex 2006;16:916–28.
38. Pedersen KF, Larsen JP, Alves G, Aarsland D. Prevalence and clinical correlates of apathy in Parkinson’s disease: a community-based study. Parkinsonism Relat Disord 2009;15:295–9.
39. Pedersen KF, Alves G, Aarsland D, Larsen JP. Occurrence and risk factors for apathy in Parkinson disease: a 4-year prospective longitudinal study. J Neurol Neurosurg Psychiatry 2009;80:1279–82.
40. Pedersen KF, Alves G, Brønnick K, et al. Apathy in drug-naïve patients with incident Parkinson’s disease: The Norwegian ParkWest study. J Neurol 2010;257:217–23.
41. Ziropadja L, Stefanova E, Petrovic M, et al. Apathy and depression in Parkinson’s disease: The Belgrade PD study report. Parkinsonism Relat Disord 2012;18:339–42.
42. Dujardin K, Sockeel P, Devos D, et al. Characteristics of apathy in Parkinson’s disease. Mov Disord 2007;22:778–84.
43. Carriere N, Besson P, Dujardin K, et al. Apathy in Parkinson’s disease is associated with nucleus accumbens atrophy: a magnetic resonance imaging shape analysis. Mov Disord 2014;29;897–903.
44. Reijnders JSAM, Scholtissen B, Weber WEJ, et al. Neuroanatomical correlates of apathy in Parkinson’s disease: a magnetic resonance imaging study using voxel-based morphometry. Mov Disord 2010;25:2318–25.
45. Leroi I, Harbishettar V, Andrews M, et al. Carer burden in apathy and impulse control disorders in Parkinson’s disease. Int J Geriatr Psychiatry 2012;27:160–6.
46. Schiehser DM, Liu L, Lessig SL, et al. Predictors of discrepancies in Parkinson’s disease patient and caregiver ratings of apathy, disinhibition, and executive dysfunction before and after diagnosis. J Int Neuropsychol Soc 2013;19:295–304.
47. Benito-León J, Cubo E, Coronell C, et al. Impact of apathy on health-related quality of life in recently diagnosed Parkinson’s disease: The ANIMO study. Mov Disord 2012;27:211–8.
48. Sockeel P, Dujardin K, Devos D, et al. The Lille apathy rating scale (LARS), a new instrument for detecting and quantifying apathy: validation in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2006;77:579–84.
49. Zahodne LB, Young S, Kirsch-Darrow L, et al. Examination of the Lille Apathy Rating Scale in Parkinson disease. Mov Disord 2009;24:677–83.
50. Drijgers RL, Dujardin K, Reijnders JSAM, et al. Validation of diagnostic criteria for apathy in Parkinson’s disease. Parkinsonism Relat Disord 2010;16:656–60.
51. Leentjens AFG, Koester J, Fruh B, et al. The effect of pramipexole on mood and motivational symptoms in parkinson’s disease: A meta-analysis of placebo-controlled studies. Clin Ther 2009;31:89–98.
52. Thobois S, Ardouin C, Lhommée E, et al. Non-motor dopamine withdrawal syndrome after surgery for Parkinson’s disease: Predictors and underlying mesolimbic denervation. Brain 2010;133:1111–27.
53. Devos D, Moreau C, Maltête D, et al. Rivastigmine in apathetic but dementia and depression-free patients with Parkinson’s disease: a double-blind, placebo-controlled, randomised clinical trial. J Neurol Neurosurg Psychiatry 2014;85:668–74.
54. Smith KM, Eyal E, Weintraub D; ADAGIO Investigators. Combined rasagiline and antidepressant use in Parkinson disease in the ADAGIO study: effects on nonmotor symptoms and tolerability. JAMA Neurol 2015;72:88–95.
55. Forsaa EB, Larsen JP, Wentzel-Larsen T, et al. A 12-year population-based study of psychosis in Parkinson disease. Arch Neurol 2010;67:996–1001.
56. Holroyd S, Currie L, Wooten GF. Prospective study of hallucinations and delusions in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2001;70:734–8.
57. Fénelon G, Alves G. Epidemiology of psychosis in Parkinson’s disease. J Neurol Sci 2010;289:12–7.
58. Mack J, Rabins P, Anderson K, et al. Prevalence of psychotic symptoms in a community-based Parkinson disease sample. Am J Geriatr Psychiatry 2012;20:123–32.
59. Ravina B, Marder K, Fernandez HH, et al. Diagnostic criteria for psychosis in Parkinson’s disease: Report of an NINDS, NIMH Work Group. Mov Disord 2007;22:1061–8.
60. Diederich NJ, Fénelon G, Stebbins G, Goetz CG. Hallucinations in Parkinson disease. Nat Rev Neurol 2009;5:331–42.
61. Gallagher DA, Parkkinen L, O’Sullivan SS, et al. Testing an aetiological model of visual hallucinations in Parkinson’s disease. Brain 2011;134:3299–309.
62. Barnes J, Boubert L, Harris J, et al. Reality monitoring and visual hallucinations in Parkinson’s disease. Neuropsychologia 2003:41:565–74.
63. Kurita A, Murakami M, Takagi S, et al. Visual hallucinations and altered visual information processing in Parkinson disease and dementia with Lewy bodies. Mov Disord 2010;25:167–71.
64. Stebbins GT, Goetz CG, Carrillo MC, et al. Altered cortical visual processing in PD with hallucinations: an fMRI study. Neurology 2004;63:1409–16.
65. Williams DR, Lees AJ. Visual hallucinations in the diagnosis of idiopathic Parkinson’s disease: A retrospective autopsy study. Lancet Neurol 2005:4:605–10.
66. Biglan KM, Holloway RG, McDermott MP, Richard IH. Risk factors for somnolence, edema, and hallucinations in early Parkinson disease. Neurology 2007;69:187–95.
67. Kiziltan G, Ozekmekci S, Ertan S, et al. Relationship between age and subtypes of psychotic symptoms in Parkinson’s disease. J Neurol 2007;254:448–52.
68. Ecker D, Unrath A, Kassubek J, Sabolek M. Dopamine agonists and their risk to induce psychotic episodes in Parkinson’s disease: a case-control study. BMC Neurol 2009;9:23.
69. Huot P, Johnston TH, Darr T, et al. Increased 5-HT2A receptors in the temporal cortex of Parkinsonian patients with visual hallucinations. Mov Disord 2010;25:1399–408.
70. Ballanger B, Strafella AP, van Eimeren T, et al. Serotonin 2A receptors and visual hallucinations in Parkinson disease. Arch. Neurol 2010;67:416–21.
71. Boecker H, Ceballos-Baumann O, Volk D, et al. Metabolic alterations in patients with Parkinson disease and visual hallucinations. Arch Neurol 2007;64:984–8.
72. Sanchez-Castaneda C, Rene R, Ramirez-Ruiz B, et al. Frontal and associative visual areas related to visual hallucinations in dementia with Lewy bodies and Parkinson’s disease with dementia. Mov Disord 2010;25:615–22.
73. Goetz CG, Stebbins GT. Risk factors for nursing home placement in advanced Parkinson’s disease. Neurology 1993;43:2227–9.
74. Friedman JH. Parkinson disease psychosis: update. Behav.Neurol 2013;27:469–77.
75. Pollak P, Tison F, Rascol O, et al. Clozapine in drug induced psychosis in Parkinson’s disease: a randomised, placebo controlled study with open follow up. J Neurol Neurosurg Psychiatry 2004;75:689–95.
76. Parkinson Study Group. Low-dose clozapine for the treatment of drug-induced psychosis. N Engl J Med 1999;340:757–63.
77. Sobow T. Parkinson’s disease-related visual hallucinations unresponsive to atypical antipsychotics treated with cholinesterase inhibitors: a case series. Neurol Neurochir Pol 2007;41:276–9.
78. Fabbrini G, Barbanti P, Aurilia C, et al. Donepezil in the treatment of hallucinations and delusions in Parkinson’s disease. Neurol Sci 2002;23:41–3.
79. Bullock R, Cameron A, Hospital WH. Rivastigmine for the treatment of dementia and visual hallucinations associated with Parkinson’s disease: a case series. Curr Med Res Opin 2002;18,:258–64.
80. Cummings J, Isaacson S, Mills R, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet 2014;383:533–40.
81. L. Ishihara L, and C. Brayne C. A systematic review of depression and mental illness preceding Parkinson’s disease. Acta Neurol Scand 2006;113:211–20.
82. Reijnders JSAM, Ehrt U, Weber WEJ, et al. A systematic review of prevalence studies of depression in Parkinson’s disease. Mov Disord 2008;23:183–9.
83. Starkstein SE, Mayberg HS, Leiguarda R, et al. A prospective longitudinal study of depression, cognitive decline, and physical impairments in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 1992:55:377–82.
84. Müller B, Assmus J, Herlofson K, et al. Importance of motor vs. non-motor symptoms for health-related quality of life in early Parkinson’s disease. Parkinsonism Relat Disord 2013;19:1027–32.
85. Ravina B, Camicioli R, Como PG, et al. The impact of depressive symptoms in early Parkinson disease. Neurology 2007;69:342–7.
86. Marsh L, McDonald WM, Cummings J, et al. Provisional diagnostic criteria for depression in Parkinson’s disease: report of an NINDS/NIMH work group. Mov Disord 2006;21:148–58.
87. Marsh L. Depression and Parkinson’s disease: current knowledge. Curr. Neurol. Neurosci. Rep 2013; 13:409.
88. Starkstein SE, Merello M, Jorge R, et al. A validation study of depressive syndromes in Parkinson’s disease. Mov Disord 2008;23,:538–46.
89. Williams JR, Hirsch ES, Anderson K, et al. A comparison of nine scales to detect depression in Parkinson disease: which scale to use? Neurology 2012;78:998–1006.
90. Nazem S, Siderowf AD, Duda JE, et al. Suicidal and death ideation in Parkinson’s disease. Mov Disord 2008;23:1573–9.
91. Weintraub D, Duda JE, Carlson K, et al. Suicide ideation and behaviours after STN and GPi DBS surgery for Parkinson’s disease: results from a randomised, controlled trial. J Neurol Neurosurg Psychiatry 2013;84:1113–8.
92. Aarsland D, Påhlhagen S, Ballard CG, et al. Depression in Parkinson disease—epidemiology, mechanisms and management. Nat Rev Neurol 2011;8:35–47.
93. Ehmann TS, Beninger RJ, Gawel MJ, Riopelle RJ. Depressive symptoms in Parkinson’s disease: a comparison with disabled control subjects. J Geriatr Psychiatry Neurol 1990;3:3–9.
94. Witjas T, Kaphan E, Azulay JP, et al. Nonmotor fluctuations in Parkinson’s disease: frequent and disabling. Neurology 2002:59:408–13.
95. Nissenbaum H, Quinn NP, Brown RG, et al. Mood swings associated with the ‘on-off’ phenomenon in Parkinson’s disease. Psychol Med 1987;17:899–904.
96. Maricle RA, Nutt JG, Carter JH. Mood and anxiety fluctuation in Parkinson’s disease associated with levodopa infusion: preliminary findings. Mov Disord 1995;10:329–32.
97. Barone P, Poewe W, Albrecht S, et al. Pramipexole for the treatment of depressive symptoms in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 2010;9:573–80.
98. Devos D, Dujardin K, Poirot I, et al. Comparison of desipramine and citalopram treatments for depression in Parkinson’s disease: a double-blind, randomized, placebo-controlled study. Mov Disord 2008;23:850–7.
99. Richard IH, McDermott MP, Kurlan R, et al. A randomized, double-blind, placebo-controlled trial of antidepressants in Parkinson disease. Neurology 2012;78:1229–36.
100. Menza M, Dobkin RD, Marin H, et al. A controlled trial of antidepressants in patients with Parkinson disease and depression. Neurology 2009;72:886–92.
101. Seppi K, Weintraub D, Coelho M, et al. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord 2011;26 Suppl 3:S42–80.
102. Skapinakis P, Bakola E, Salanti G, et al. Efficacy and acceptability of selective serotonin reuptake inhibitors for the treatment of depression in Parkinson’s disease: a systematic review and meta-analysis of randomized controlled trials. BMC Neurol 2010;10:49.
103. Richard IH, Kurlan R, Tanner C, et al. Serotonin syndrome and the combined use of deprenyl and an antidepressant in Parkinson’s disease. Parkinson Study Group. Neurology 1997;48:1070–7.
104. Montgomery EB, Panisset M. Retrospective statistical analysis of the incidence of serotonin toxicity in patients taking rasagiline and anti-depressants in clinical trials. Mov Disord 2009;24:359.
105. Bailine S, Kremen N, Kohen I, et al. Bitemporal electroconvulsive therapy for depression in a Parkinson disease patient with a deep-brain stimulator. J ECT 2008;24:171–2.
106. Faber R, Trimble MR. Electroconvulsive therapy in Parkinson’s disease and other movement disorders. Mov Disord 1991;6:293–303.
107. da Silva TM, Munhoz RP, Alvarez C, et al. Depression in Parkinson’s disease: a double-blind, randomized, placebo-controlled pilot study of omega-3 fatty-acid supplementation. J Affect Disord 2008;111:351–9.
108. Pal E, Nagy F, Aschermann Z, et al. The impact of left prefrontal repetitive transcranial magnetic stimulation on depression in Parkinson’s disease: a randomized, double-blind, placebo-controlled study. Mov Disord 2010;25:2311–7.
109. Dobkin RD, Menza M, Allen LA, et al. Cognitive-behavioral therapy for depression in Parkinson’s disease: a randomized, controlled trial. Am J Psychiatry 2011;168:1066–74.
110. Stein MB, Heuser IJ, Juncos JL, Uhde TW. Anxiety disorders in patients with parkinson’s disease. Am J Psychiatry 1990;147:217–20.
111. Nuti A, Ceravolo R, Piccinni A, et al. Psychiatric comorbidity in a population of Parkinson’s disease patients. Eur J Neurol 2004;11:315–20.
112. Marinus J, Leentjens AFG, Visser M, et al. Evaluation of the Hospital Anxiety and Depression Scale in patients With Parkinson’s disease. Clin Neuropharmacol 2002:25:318–24.
113. Dissanayaka NNW, White E, O’Sullivan JD, et al. The clinical spectrum of anxiety in Parkinson’s disease. Mov Disord 2014;29:967–75.
114. Dissanayaka NNW, Sellbach A, Matheson S, et al. Anxiety disorders in Parkinson’s disease: prevalence and risk factors. Mov Disord 2010;25:838–45.
115. Leentjens AFG, Dujardin K, Pontone GM, et al. The Parkinson anxiety scale (PAS): Development and validation of a new anxiety scale. Mov Disord 2014;29:1035–43.
116. Maricle RA, Nutt JG, Valentine RJ, Carter JH. Dose-response relationship of levodopa with mood and anxiety in fluctuating Parkinson’s disease: a double-blind, placebo-controlled study. Neurology 1995;45:1757–60.
117. Erdal KJ. Depression and anxiety in persons with Parkinson’s disease with and without ‘on–off’ phenomena. J Clin Psychol Med Settings 2001:8:293–9.
118. Leentjens AFG, Dujardin K, Marsh L, et al. Symptomatology and markers of anxiety disorders in Parkinson’s disease: a cross-sectional study. Mov. Disord 2011;26:484–92.
119. Solla P, Cannas A, Floris GL, et al. Behavioral, neuropsychiatric and cognitive disorders in Parkinson’s disease patients with and without motor complications. Prog Neuropsychopharmacol Biol Psychiatry 2011;35:1009–13.
120. E. Stefanova E, L. Ziropadja L, M. Petrović M, et al. Screening for anxiety symptoms in Parkinson disease: a cross-sectional study. J Geriatr Psychiatry Neurol 2013;26:34–40.
121. Jacob EL, Gatto NM, Thompson A, et al. Occurrence of depression and anxiety prior to Parkinson’s disease. Parkinsonism Relat Disord 2010;16:576–81.
122. Craig LH, Svircev A, Haber M, Juncos JL. Controlled pilot study of the effects of neuromuscular therapy in patients with Parkinson’s disease. Mov Disord 2006;21:2127–33.
123. Marino L, Friedman JH. Letter to the editor: Successful use of electroconvulsive therapy for refractory anxiety in Parkinson’s disease. Int J Neurosci 2013;123:70–1.
From the Department of Neurology, Oregon Health & Science University, Portland, OR.
Abstract
- Objective: To review the clinical characteristics, epidemiology, and management of the most common neuropsychiatric symptoms (NPS) in Parkinson’s disease (PD).
- Methods: Literature review.
- Results: PD has traditionally been considered a disease of impaired motor function. However, neuropsychiatric complications, such as fatigue, depression, anxiety, psychosis, impulse control disorders, and apathy, frequently complicate the course of the illness. Although the development of new medication options in recent years has had a positive benefit on the management of these troublesome symptoms, responses are frequently suboptimal. The development of valid instruments to measure neuropsychiatric symptoms has been vital in research efforts to bridge the gaps in our understanding. Further elucidation of neuropsychiatric pathophysiologies will help to define treatment targets and has the potential to expand our therapeutic armamentarium.
- Conclusion: While NPS affect patients with established disease, recent investigations have demonstrated risk of symptoms in those with early untreated stages of PD; therefore, better understanding of NPS should be the goal of practitioners treating the entire continuum of PD.
Parkinson’s disease (PD) has traditionally been considered a disease of impaired motor function, but increased recognition of nonmotor symptoms and in particular neuropsychiatric symptoms, such as fatigue, depression, anxiety, psychosis, impulse control disorders, and apathy, offer new opportunities for better care of patients. While neuropsychiatric symptoms affect patients with established disease, recent investigations have clearly demonstrated risk of symptoms in those with early untreated stages of PD; therefore, better understanding of neuropsychiatric symptoms should be the goal of practitioners treating the entire continuum of PD. This review will focus on the clinical characteristics, epidemiology, and management of the most common neuropsychiatric symptoms in PD.
Impulse Control Disorders
The recognition that dopaminergic drugs were successful at treating many symptoms of PD was followed by the disturbing realization that impulse control disorders could be an unfortunate side effect in a substantial minority. Impulse control disorders as defined by DSM-IV [1] are disinhibited behaviors that are maladaptive and recurrent, causing personal and relationship consequences. The impulse control disorders that became associated with PD and medication intake, particularly dopamine agonist use, included gambling, hobbyism, punding (stereotyped, seemingly purposeless behaviors), excessive sexual behavior, shopping, hoarding, and less commonly, compulsive eating. The prevalence estimates of these behavioral disturbances range from 6% to 15.5%, compared with < 2% in the general population [2,3]. The addiction-like dopamine dysregulation syndrome, whereby patients self-medicate with high doses of levodopa and short-acting dopamine agonists beyond what is needed for motor control, can lead to significant impairment of the therapeutic alliance in addition to other patient personal relations. With the advent of surgical options to treat PD and its medication complications, it was observed that stimulation of the subthalamic nucleus could be associated with the spectrum of impulse control disorders [4].
Epidemiology/Risk Factors
In a recent systematic review of the literature of impulse control disorders in PD [5], the authors determined that dopaminergic therapy caused compulsive or impulsive behaviors in approximately 10% of PD patients in the course of their treatment, with pathologic gambling and hypersexuality most frequently experienced. Multiple impulse control disorders are not uncommon and may coexist in one-quarter of patients with compulsivity. There appeared to be more disordered behavior with higher comparable doses of agonists. The authors concluded that impulse control disorder symptoms tended to occur with initiation or dose increases of direct D2/D3 agonists, such as pramipexole and ropinirole. Importantly, impulse control disorder behavior improved if not resolved with discontinuation or reduction of dosage of the agonist, even if a compensatory levodopa dosage is added or increased. Perhaps not surprisingly, it was observed that if patients had a preexisting impulse control disorder prior to PD or the initiation of treatment, there was a high likelihood of worsening of symptoms. This small subgroup is estimated at about 1% of PD subjects, which corresponds to the prevalence of impulse control disorders in the general population. Other identified potential risk factors for impulse control disorder development include male gender, young age at onset, a personal or family history of addiction, novelty or risk seeking personality, and a concurrent diagnosis of depression [3]. In a recent study of early PD patients, the risk of developing an impulse control disorder became important once treatment with dopaminergic drugs began and continued for a year or more [6].
Pathogenesis
The pathogenesis is not fully understood, however, mesolimbic dopamine alterations are strongly suspected. It has been long speculated that the high doses of dopamine needed to replete the relatively depleted dorsal striatum overdose the “intact” ventral striatum and cause this neuropsychiatric disorder [7–9]. The additional cognitive impairments in PD, which can include problems with attention, working memory, planning, forethought and decision-making, are faculties that can markedly increase susceptibility to impulse control disorder [8].
The role of serotonin deficiency in the PD brain and its part in inhibiting the patient’s ability to delay rewards adds to the complexity of impulse control disorder pathogenesis. Dorsal raphe nuclei disease in PD results in loss of serotonin innervation to substantial portions of the prefrontal and motor cortices in addition to basal ganglia substructures like the striatum, pallidum and subthalamic nucleus [10]. Together with dopamine, serotonin may work to regulate risk-sensitive decision making, response inhibition, waiting for future rewards, and overall impulse control. Its relative loss therefore also likely contributes to tipping the balance towards impulse dyscontrol [11,12]. The role of other neurotransmitters such as opiate systems involved in the process of acquisition and maintenance of addictive behaviors like dopamine dysregulation syndrome remains to be fully understood.
Treatment
The most successful strategy to address this problem is to reduce or eliminate the offending medication, usually the dopamine agonist. This may be associated with worsening apathy, anxiety or depression; however, substituting levodopa can be a successful strategy in many cases [13]. Zonisamide was described to be possibly effective in a trial of 15 subjects; however, the open label nature of this evidence must be considered as with other case reports using valproate, donepezil, and selective serotonin reuptake inhibitors (SSRIs) [14–16].
Fatigue
An easy to understand operational definition of fatigue is that it is a state of extreme tiredness, weakness, or exhaustion, either physical or mental or both. Fatigue is not uncommon in the general population [17] but is increasingly recognized to occur in numerous disease conditions and is frequently encountered in PD and multiple sclerosis. The latter is of special significance in the consideration of the neurotransmission of fatigue, as it is not thought to be a disease of dopamine deficiency. The pathophysiology remains unclear, and it may differ depending on whether the fatigue is experienced as more physical or mental, or rather motor versus nonmotor as some authors propose.
Fatigue has been conceptualized as central or peripheral in character. Peripheral fatigue is best understood as muscular fatigue caused by repetitive muscular contraction or reduced force generation [18]. Central fatigue however, is divided into mental or physical fatigue. Mental fatigue can occur after sustained attentive or emotional activity. It may alternatively be provoked after boring repetitive tasks or lack of intellectually stimulating activity. Physical fatigue is the sense of body exhaustion or energy to perform physical tasks even though the ability to carry them out exists.
Epidemiology
As recognition of the problem of fatigue increased in the last 2 decades, the realization that one-third to one-half of patients experience it at some point has improved opportunities for recognition and treatment [19]. Fatigue may be the presenting symptom in one-third of patients prior to actual motor symptom onset [20]. Half of untreated PD patients in a biomarker cohort study reported fatigue [6]. Unfortunately, it is also described by patients as one of the most disabling symptoms, causing significant impact on quality of life [19]. Fatigue in PD is associated with higher rates of depressive symptoms, but occurs with higher prevalence in nondepressed patients [21]. Poor ability to initiate and sustain activity due to fatigue is different from depression, excessive sleepiness, or impaired motor function [22,23].
Pathophysiology
The pathophysiology of fatigue remains somewhat unclear, though physical fatigue is likely a significant part of the problem and related to dopamine deficiency based on studies of time and force generation of keyboard strikes in PD subjects before and after L-dopa administration. These subjects had declines in force and increased physical fatigue which improved after L-dopa [24]. In other studies using transcranial magnetic stimulation to study changes in cortical excitability, the degree of physical fatigue correlated with abnormalities in motor evoked potentials during fatiguing exercising. These studies also support the hypothesis that fatigue is a motor symptom [25,26]. In the ELLDOPA study, fatigue worsened more in PD subjects treated with placebo [27]. Other imaging studies have suggested suggested nondopaminergic mechanisms including serotonergic pathway abnormalities [28], thus the question behind the etiology and solution for all cases of fatigue remains to be settled.
Diagnosis
The diagnosis is fatigue may be challenging as it may mask as depression or apathy. There are a number of fatigue rating scales available; however, the validated Parkinson’s Fatigue Scale (PFS) supersedes many of the problems of using a generic scale which could overlap motor questions and potentially be confounding [29,30].
Treatment
Most important is awareness and vigilance for the symptoms of fatigue, depression, and apathy and effort to distinguish between them. It may require structured interviews or assessment tools to properly diagnose the problem. Treatment is less clear in that few studies have clearly indicated the best treatment options. In placebo-controlled trials, methylphenidate did improve fatigue as did levodopa [31]. Modafinil, a hypocretin modulator and a drug first approved by the FDA for treatment of narcolepsy, has demonstrated mixed results in recent years. It may reduce physical fatigue and reduce excessive daytime sleepiness but likely does not reduce subjective symptoms of fatigue [32]. L-dopa can significantly reduce fatigue in many patients, which would argue that it often is a motor symptom [33,24]. In a post-hoc analysis of the ADAGIO delayed start study, patients taking rasagiline 1 mg/day and 2 mg/day (the latter dose exceeds the usual clinical dosing) showed significantly less worsening of symptoms on the PFS compared to placebo over time [34]. It is important to realize that once motor symptoms are optimally treated with dopaminergic medications, while many patients will feel significant relief from fatigue some patients will continue to feel symptomatic.
Apathy
The definition of apathy has become more complicated and refined, incorporating findings from the study of brain disease and behavioral analysis. Marin’s classic elaboration of apathy as lack of motivation not attributable to diminished level of consciousness, cognitive impairment, or emotional distress has been built upon by Levy and Dubois [35–37]. They suggest apathy may be better thought of as an observable behavioral syndrome characterized by a quantitative reduction of self-generated voluntary and purposeful behaviors. They suggest 3 apathetic subtypes: emotional, cognitive, and auto-activational, which reflect different disease states accounting for failure of normal goal-directed behavior.
Epidemiology
Prevalence estimates for apathy in PD vary. This is likely due to the varying recruitment criteria among studies, with some including patients with comorbid depression and dementia and others containing only “pure apathy.” Other reports may have had referral bias issues, as community-based studies report lower prevalences in general. In a group of newly diagnosed PD patients, using more restrictive criteria (apathy subscale of the neuropsychiatric inventory and the diagnostic consensus criteria for apathy validated in PD), Pedersen reported a prevalence of apathy of 14.3% [38]. In a 4-year prospective longitudinal cohort study, an annual incidence rate of 12.3% was reported, with apathy developing in 60% of the cohort by the study’s conclusion [39].
Apathy has been associated with longer disease duration, male gender [40], higher daily levodopa doses [41], more severe parkinsonism [38], and lower education status, though the latter feature remains under debate. Early cognitive deficits appear to be a risk factor for development of apathy [42]. The patterns of cognitive dysfunction and apathy remain unsettled in the literature.
Pathology
The pathology of atrophy remains unexplained and is unlikely to be reduced to a simple atrophy of one nucleus or the tone of one circuit. However, in a small neuroimaging study, severity of apathy correlated with atrophy of the bilateral nucleus accumbens [43], and it is notable that one major input to the nucleus accumbens is the amygdala. According to Braak staging, by stage 4 significant involvement of the amygdala by Lewy bodies has occurred. Others have found changes in grey matter density that could correlate with deficits of the prefrontal-basal ganglia circuitry to produce dysfunction of segregated frontal-subcortical loops. These may correlate with the “autoactivation” deficit pattern of apathy in which patients have a lack of self-initiated actions, even thoughts, though appear more normal when giving externally prompted responses [37,44].
Assessment
Clinically, the relationship between apathy and depression can be hard to disentangle, especially since many studies have found an association between them, especially with regards to apathy and anhedonia. Depression may feature negative self thoughts and sadness while apathy is notable for lack of initiation and effort. Viewed over a longer period of time, apathy tended to worsen in a linear fashion, where depression tended to fluctuate with improvements and exacerbations.
The Movement Disorders Society task force has recommended the Lille Apathy Rating Scale (LARS) for assessment of apathy; English and French versions have been validated in PD patients. It uses a semi-structured interview format assessing 4 dimensions of apathy: self awareness, intellectual curiosity, emotion, and action initiation [45–47].
The impact of apathy cannot be underestimated as this poor show of motivation or effort leads to lack of engagement in old activities or interest in new ones. Spouses may misinterpret this change in behavior as laziness or deliberate social withdrawal, or perhaps entitlement. It is not surprising that apathy routinely shows up on quality of life (QoL) questionnaires as highly impacting patients and families. In one study, apathy was the nonmotor symptom most likely to cause caregiver distress in PD [40,48–50].
Treatment
No approved drugs exist for treatment of apathy. However, clinical experience often confirms that dopaminergic modulation can be helpful in the treatment of apathy as indirect evidence suggests. A meta-analysis of controlled trials using pramipexole and Part I of the Unified Parkinson's disease rating scale (UPDRS) (secondary measure) showed the medication improved scores on this measure of motivation and mood in non-depressed subjects [51] with PD. Rare patients undergoing subthalamic deep brain stimulation have been reported to experience new and sometimes severe apathy after surgery [52]. This was posited at least in part to be the result of reduction of dopaminergic medication due to surgery.
Nondopaminergic pharmacotherapy of apathy is in its infancy. A recent controlled trial of rivastigmine in 31 French subjects with moderate to severe apathy based on LARS showed that 6 months of treatment at 9.5 mg/day improved average scores from –11.5 to –20 compared with placebo. While quality of life did not improve, caregiver burden did. The investigators found in this group of subjects that apathy was a possible herald for early dementia in PD [53].
A post-hoc analysis of the ADAGIO study (rasagiline or placebo in PD patients taking antidepressants) found that rasagiline use was associated with a nonsignificant slowing of apathy development during the trial [54].
Psychosis
Psychotic symptoms are a common occurrence in drug-treated patients, with visual hallucinations occurring in up to 30%, though over a 20-year period up to three-quarters of patients may develop visual hallucinations.After visual, the most common type of hallucination is auditory, followed by the other affected senses such as tactile, olfactory, or even taste [57]. Delusions, which tend to be paranoid in nature, occur in about 5% of patients [55–57]. The presence of psychotic symptoms is associated with poorer quality of life [58].
Symptomatology
The visual hallucinations of PD are usually quite stereotyped, and have been described as “minor” and “non-minor”[59]. Minor hallucinations refer to transient peripheral field stimuli that disappear when brought into central focus, “something flashed by,” a sense of a living being nearby, “a presence in the room,” or illusions whereby objects are transformed, eg, a bush in the yard is a deer.
Auditory hallucinations tend to be vague or indistinct sounds, like music in another room as opposed to voices speaking directly to the patient as might be experienced in a primary psychotic disorder. Tactile forms often involve insects or other animals crawling on the skin. Olfactory hallucinations may take the form of smelling perfume, toxic odors from room vents, etc.
Early in the experience, the visual hallucinations may be amusing in that they consistently remain nonthreatening, similar day to day, and sometimes oddly provide an aspect of comfort or companionship to the patient. More commonly, the hallucinations are bothersome to the patient because the experience indicates to the patient that there is something wrong with their mind. Visual hallucinations often begin in low-stimulus environments, often in the evening or other low-light conditions, but as the problem advances they can occur at any time of day. While visual hallucinations may initially occur for only seconds at a time many days apart, the frequency and duration can increase until they occur hours at a time every day and are accompanied by multiple other visual hallucinations, delusions, and confusion [60].
Delusions tend to be more distressing to patients and caregivers because they are often paranoid in nature. The patient is more likely to act out due to the anxiety the paranoia creates. For example, she may change passwords to online accounts due to a belief that unknown assailants are after her finances. He may go to great lengths trying to prove his wife is cheating.
Risk Factors
While the primary risk factor for psychotic symptom development is dementia [57], it occurs in nondemented patients. Other associations include reduced visual acuity [56], visual processing impairment [61–65], use of dopamine agonists, REM behavior disorder, duration of PD, axial rigidity subtype of disease [61,66–68]. The pathophysiology of psychosis in PD is likely complex and remains currently unexplained. The role of excess dopamine has been described above, but there is also data suggesting cholinergic deficits in the cortex may also contribute. Excess serotonin (increased 5HT2A receptor subtypes) in the temporal lobe within the visual processing pathway has been postulated to be of significance [69,70]. Hypometabolism in visual association areas of the brain in subjects with visual hallucinations has been demonstrated in PET and functional MRI studies [64,71]. This is similar to findings in patients with dementia with Lewy bodies [72].
This review focuses on the primary forms of PD-related psychosis, which occur with a clear sensorium and generally longer exposure to dopaminergic medication. It is important to distinguish 2 other common scenarios in which hallucinations or delusions may occur. In the common toxic-metabolic delirium, a clouded sensorium with attention deficits may be the only clue to the etiology of new onset confusion with visual hallucinations. It is highly likely that resolution of the underlying medical problem will lead to resolution of the new onset psychosis and encephalopathy. In a second scenario, hallucinations precede or occur very shortly after the onset of initiation of dopaminergic medication. This differs from the classic syndrome described earlier, in particular when visual hallucinations precede any initiation of medication, and likely represents the distinction between a diagnosis of Lewy body disease and PD [60].
Treatment
Management of psychosis is approachable, but often the outcome is unsatisfactory and associated with trade-offs in motor control. It is unfortunately true that psychotic symptoms are often associated with increased caregiver burden and are a cause of increased nursing home placements [73]. When considering the workup of psychotic symptoms, the differential diagnosis includes delirium, dream enactment (REM behavior disorder), or less commonly, Bonnet syndrome.
A delirium may be precipitated by a difficult to diagnose infection; new-onset confusion and psychotic symptoms may be the heralding presentation. Urinary tract or upper respiratory tract are common vulnerable sources of infection. Once infection is ruled out, the next practical step is to review the patient’s medication list and manage centrally acting drugs that could be contributing to the altered sensorium. A recent prescription of opioids for a dental treatment or a new muscle relaxant may be a culprit, though it is not that usual. A bladder anticholinergic could be suspect and is worth eliminating especially if its addition coincided with the appearance of the psychotic symptoms. Once the non-dopaminergic medications have been reduced/eliminated, then the PD medications should be considered. The general approach is to eliminate the medications that provide the least benefit while being more likely to contribute to psychotic symptoms. Anticholinergic medications, dopamine agonists, selegiline should all be uppermost in that consideration until one is left with L-dopa and COMT inhibitors (the latter function to increase levodopa availability). Then COMT inhibitors and levodopa can be reduced; however, at any point motor control can suffer with the loss of symptomatic therapies [74].
Clozapine is effective against psychotic symptoms in PD, at doses much lower than used in schizophrenia (300-600mg/day). The average dose in the US randomized controlled clinical trial was 25 mg/day, with no associated motor worsening. Patients in the United States are required by the FDA to be placed in a computer-based registry and monitored for agranulocytosis for the duration of clozapine therapy. This rare adverse event is not dose related. Orthostasis can occur at these low doses however. Fortunately the metabolic syndrome is not associated with this range of administration [75,76].
Quetiapine was not found to be effective in 3 blinded randomized controlled trials despite its rather common use for this purpose. It was not associated with motor worsening, however.
Other neuroleptic medications have not resulted in widespread use, because trials have been open label, or outcomes demonstrated motor worsening. Cholinesterase inhibitors have been the subject of a few positive case series, however results appear to be sporadic, the effect size is relatively small, and side effects of this medication class are common [77–79]. It is clear that there is an unmet need for a medication for psychotic symptoms. Clozapine is effective but onerous in its monitoring requirements. Practically speaking, there are relatively few PD patients who take advantage of it because of its feasibility challenges. Yet the problem of psychotic symptoms is a significant one that imposes important challenges to the patient and caregiver, and may limit the number of medications that the patient needs in order to optimize quality of life.
Pimavanserin, a novel medication which acts as a selective serotonin inverse agonist, is in the early application stages for FDA approval for treatment of psychotic symptoms in PD [80]. In its pivotal phase III controlled trial, the drug reduced not only positive symptoms (hallucinations/delusions) without causing motoric worsening, but also reduced caregiver burden. Pimavanserin improved certain sleep features without causing daytime sedation. If this drug meets final approval, it may present an exciting option for many patients for whom treatment was previously limited.
Depression
A study of early PD suggested that depression is often unrecognized and frequently untreated [1]. Indeed it is not unusual for depression to predate the diagnosis of PD by an average of 4 to 6 years [81]. Expanding to the larger PD population, it is generally accepted that about 30% to 50% of PD patients experience clinically significant depression, and once diagnosed may have a long term course, or may recur [82,83]. This is important as untreated depression is an important cause of poor quality of life in early PD. In addition depression can exacerbate motor disability, lead to earlier motor treatment with medication, and increase caregiver stress [83–85].
Diagnosis
A number of clinimetric rating scales for depression have been used and their advantages have been largely related to their objective nature (quantifiable); thus, they tend to be most useful in epidemiologic research studies or for larger scale screening purposes. Examples include the the Beck Depression Inventory, the Geriatric Depression Scale, and the Hamilton Depression Scale, all of which have been shown to be valid tools in PD (with the exception of the UPDRS Depression). It is important to note that they do not substitute for a diagnostic clinical interview [89].
Suicide is not common in PD, however suicidal ideation is estimated at about 11% in PD patients [90], and while there was concern initially after deep brain stimulation procedures began that suicide incidence was increased, evidence does not support this [91].
Pathophysiology
The pathophysiology of depression in PD is largely unknown however is thought to be less causally due to psychosocial factors and more etiologically driven by brainstem monoamine and serotonergic dysfunction [92]. Nonetheless, similar to other chronic conditions, PD patients can certainly develop fear of disability, guilt about impact on others, or other reactive mood changes. Overall, rates of depression are higher in PD compared with patients with similar conditions matched for disability [93].
Treatment
First, the clinician must determine if depression is a result of short-term fluctuations, chronic undertreatment of motor disease, or longer-term mood phenomenon. One important pattern to recognize are mood fluctuations, which can parallel motor OFF-ON cycling. It can be valuable to distinguish this as “subsyndromic” depression or anxiety (sometimes referred to as “OFF dysphoria”), as it can respond to improvement in antiparkinsonian medication dosing patterns that reduce fluctuations[94–96]. Similarly, elevating chronic motor undertreatment to goal therapy can result in mood normalization.
If symptoms persist despite optimization of motor/nonmotor fluctuations or chronic undertreatment and are severe enough to warrant treatment, then therapies used can range from nonpharmacologic education, support, and mental health referrals, as well as pharmacologic support in the form of medications.
A frequent but uncontrolled observation was that when undertreatment of motor disease was finally redressed, mood often improved. A multicenter randomized controlled trial of pramipexole in PD patients without motor fluctuations but with mild to moderate depressive symptoms showed the drug improved scores on the Beck Depression Inventory over a 12-week period. The improvement in mood was 6 points overall, but by 2 points over placebo, illustrating the importance of the size of the placebo effect [97]. Given the potential side effect profile of dopamine agonists, it may be useful to weigh the antidepressant effects only when their motor benefits are already being employed.
Controlled trials have demonstrated efficacy of both selective serotonin reuptake inhibitors (SSRI) and selective norepinephrine reuptake inhibitors (SNRI) antidepressants in PD. Clinical trials have demonstrated efficacy against placebo or with other antidepressant comparators. Examples of drugs with demonstrated efficacy include citalopram, paroxetine, venlafaxine, and nortriptyline. Results have attempted to illuminate the small unique differences between classes of antidepressants or dynamic properties between drugs within a class. For example, desipramine may nudge scores on a mood scale a few weeks sooner than a purer SSRI. Paroxetine (SSRI) versus venlafaxine (SNRI) improved mood scores comparably in a multicenter trial with a placebo comparator. In general, all have all been demonstrated to be effective and with a relatively low side-effect profile, comparable to the general population[98–102]. While case reports exist in the literature, the interaction of monoamine oxidase B inhibitors and SSRIs has not caused significant hypertensive crises or risk of serotonin syndrome [103,104]. Electroconvulsive therapy (ECT) can be used for severe refractory depression in PD as for non-PD patients, with case reports of very effective results. Due to the rarity of use, systematic evidence for its use is lacking [105,106].
Other novel agents and techniques such as omega-3 fatty acids [107] and repetitive transcranial magnetic stimulation [108] have been reported with promising early results. Cognitive behavioral therapy (CBT), which may involve stress management techniques, sleep hygiene, and caregiver support, additionally almost always provided improvement in measured outcomes, whether the trial was controlled or open label in design. In one RCT of CBT in PD of 14 weeks’ duration, there were significantly more treatment responders in the CBT group, with a number needed to treat of only 2 [109].
Anxiety
Anxiety is also common in PD, at least as common as depression considering that prevalence estimates suggest up to 50% of patients experience it [110–112]. Manifestations of anxiety may include panic attacks, generalized anxiety disorder, social anxiety, or other phobias [113]. Anxiety has an important negative impact on health-related quality of life and is often underrecognized by clinicians [114]. While reliable and valid scales to measure anxiety have been lacking in PD, a new effort has yielded the “Parkinson Anxiety Scale” though full clinimetric properties of the scale remain to be demonstrated (sensitivity to change) [115].
Anxiety that parallels the timing of motor OFF-ON cycling is important to recognize. This “subsyndromic” anxiety or anxiety disorder not otherwise specified (ie, the anxiety does not meet DSM-IV criteria) can respond to improvement in antiparkinsonian medication dosing patterns that reduce fluctuations [116,117]. Indeed, the presence of motor fluctuations is the principle marker of anxiety in many studies [118–120]. In an analogous manner, anxiety can predate PD by years and be part of the nonmotor amalgam of features heralding the disease [6,121].
Treatment
Systematic controlled trials of anxiolytic treatment for PD are lacking; therefore, SSRIs are prescribed for this purpose as in non-PD patients. Until SSRIs are demonstrated to be of benefit in anxiety, they are likely safer than use of benzodiazepines, which are associated with risk for falling, cognitive dysfunction, or autonomic dysregulation in PD patients when used during waking hours. Psychotherapy and other nonpharmacologic approaches are likely to be of benefit. A small study of neuromuscular (massage) therapy demonstrated improvement on the Beck Anxiety Inventory in PD [122]. A case report of ECT for severe anxiety has been published [123].
Conclusion
Neuropsychiatric symptoms are common in PD and new knowledge about clinical features, epidemiology, and treatment options has been gained in the last decade, though much remains to be discovered. The development of valid instruments to measure neuropsychiatric symptoms has been vital in these research efforts to bridge the gaps in our understanding. Further elucidation of the pathophysiologies of neuropsychiatric symptoms will help to define treatment targets and likely fuel drug development and the discovery of drugs with more potent benefit and fewer side effects.
Corresponding author: Kathryn A. Chung, MD, Department of Neurology, Oregon Health & Science University, Portland, OR, [email protected].
Financial disclosures: None.
From the Department of Neurology, Oregon Health & Science University, Portland, OR.
Abstract
- Objective: To review the clinical characteristics, epidemiology, and management of the most common neuropsychiatric symptoms (NPS) in Parkinson’s disease (PD).
- Methods: Literature review.
- Results: PD has traditionally been considered a disease of impaired motor function. However, neuropsychiatric complications, such as fatigue, depression, anxiety, psychosis, impulse control disorders, and apathy, frequently complicate the course of the illness. Although the development of new medication options in recent years has had a positive benefit on the management of these troublesome symptoms, responses are frequently suboptimal. The development of valid instruments to measure neuropsychiatric symptoms has been vital in research efforts to bridge the gaps in our understanding. Further elucidation of neuropsychiatric pathophysiologies will help to define treatment targets and has the potential to expand our therapeutic armamentarium.
- Conclusion: While NPS affect patients with established disease, recent investigations have demonstrated risk of symptoms in those with early untreated stages of PD; therefore, better understanding of NPS should be the goal of practitioners treating the entire continuum of PD.
Parkinson’s disease (PD) has traditionally been considered a disease of impaired motor function, but increased recognition of nonmotor symptoms and in particular neuropsychiatric symptoms, such as fatigue, depression, anxiety, psychosis, impulse control disorders, and apathy, offer new opportunities for better care of patients. While neuropsychiatric symptoms affect patients with established disease, recent investigations have clearly demonstrated risk of symptoms in those with early untreated stages of PD; therefore, better understanding of neuropsychiatric symptoms should be the goal of practitioners treating the entire continuum of PD. This review will focus on the clinical characteristics, epidemiology, and management of the most common neuropsychiatric symptoms in PD.
Impulse Control Disorders
The recognition that dopaminergic drugs were successful at treating many symptoms of PD was followed by the disturbing realization that impulse control disorders could be an unfortunate side effect in a substantial minority. Impulse control disorders as defined by DSM-IV [1] are disinhibited behaviors that are maladaptive and recurrent, causing personal and relationship consequences. The impulse control disorders that became associated with PD and medication intake, particularly dopamine agonist use, included gambling, hobbyism, punding (stereotyped, seemingly purposeless behaviors), excessive sexual behavior, shopping, hoarding, and less commonly, compulsive eating. The prevalence estimates of these behavioral disturbances range from 6% to 15.5%, compared with < 2% in the general population [2,3]. The addiction-like dopamine dysregulation syndrome, whereby patients self-medicate with high doses of levodopa and short-acting dopamine agonists beyond what is needed for motor control, can lead to significant impairment of the therapeutic alliance in addition to other patient personal relations. With the advent of surgical options to treat PD and its medication complications, it was observed that stimulation of the subthalamic nucleus could be associated with the spectrum of impulse control disorders [4].
Epidemiology/Risk Factors
In a recent systematic review of the literature of impulse control disorders in PD [5], the authors determined that dopaminergic therapy caused compulsive or impulsive behaviors in approximately 10% of PD patients in the course of their treatment, with pathologic gambling and hypersexuality most frequently experienced. Multiple impulse control disorders are not uncommon and may coexist in one-quarter of patients with compulsivity. There appeared to be more disordered behavior with higher comparable doses of agonists. The authors concluded that impulse control disorder symptoms tended to occur with initiation or dose increases of direct D2/D3 agonists, such as pramipexole and ropinirole. Importantly, impulse control disorder behavior improved if not resolved with discontinuation or reduction of dosage of the agonist, even if a compensatory levodopa dosage is added or increased. Perhaps not surprisingly, it was observed that if patients had a preexisting impulse control disorder prior to PD or the initiation of treatment, there was a high likelihood of worsening of symptoms. This small subgroup is estimated at about 1% of PD subjects, which corresponds to the prevalence of impulse control disorders in the general population. Other identified potential risk factors for impulse control disorder development include male gender, young age at onset, a personal or family history of addiction, novelty or risk seeking personality, and a concurrent diagnosis of depression [3]. In a recent study of early PD patients, the risk of developing an impulse control disorder became important once treatment with dopaminergic drugs began and continued for a year or more [6].
Pathogenesis
The pathogenesis is not fully understood, however, mesolimbic dopamine alterations are strongly suspected. It has been long speculated that the high doses of dopamine needed to replete the relatively depleted dorsal striatum overdose the “intact” ventral striatum and cause this neuropsychiatric disorder [7–9]. The additional cognitive impairments in PD, which can include problems with attention, working memory, planning, forethought and decision-making, are faculties that can markedly increase susceptibility to impulse control disorder [8].
The role of serotonin deficiency in the PD brain and its part in inhibiting the patient’s ability to delay rewards adds to the complexity of impulse control disorder pathogenesis. Dorsal raphe nuclei disease in PD results in loss of serotonin innervation to substantial portions of the prefrontal and motor cortices in addition to basal ganglia substructures like the striatum, pallidum and subthalamic nucleus [10]. Together with dopamine, serotonin may work to regulate risk-sensitive decision making, response inhibition, waiting for future rewards, and overall impulse control. Its relative loss therefore also likely contributes to tipping the balance towards impulse dyscontrol [11,12]. The role of other neurotransmitters such as opiate systems involved in the process of acquisition and maintenance of addictive behaviors like dopamine dysregulation syndrome remains to be fully understood.
Treatment
The most successful strategy to address this problem is to reduce or eliminate the offending medication, usually the dopamine agonist. This may be associated with worsening apathy, anxiety or depression; however, substituting levodopa can be a successful strategy in many cases [13]. Zonisamide was described to be possibly effective in a trial of 15 subjects; however, the open label nature of this evidence must be considered as with other case reports using valproate, donepezil, and selective serotonin reuptake inhibitors (SSRIs) [14–16].
Fatigue
An easy to understand operational definition of fatigue is that it is a state of extreme tiredness, weakness, or exhaustion, either physical or mental or both. Fatigue is not uncommon in the general population [17] but is increasingly recognized to occur in numerous disease conditions and is frequently encountered in PD and multiple sclerosis. The latter is of special significance in the consideration of the neurotransmission of fatigue, as it is not thought to be a disease of dopamine deficiency. The pathophysiology remains unclear, and it may differ depending on whether the fatigue is experienced as more physical or mental, or rather motor versus nonmotor as some authors propose.
Fatigue has been conceptualized as central or peripheral in character. Peripheral fatigue is best understood as muscular fatigue caused by repetitive muscular contraction or reduced force generation [18]. Central fatigue however, is divided into mental or physical fatigue. Mental fatigue can occur after sustained attentive or emotional activity. It may alternatively be provoked after boring repetitive tasks or lack of intellectually stimulating activity. Physical fatigue is the sense of body exhaustion or energy to perform physical tasks even though the ability to carry them out exists.
Epidemiology
As recognition of the problem of fatigue increased in the last 2 decades, the realization that one-third to one-half of patients experience it at some point has improved opportunities for recognition and treatment [19]. Fatigue may be the presenting symptom in one-third of patients prior to actual motor symptom onset [20]. Half of untreated PD patients in a biomarker cohort study reported fatigue [6]. Unfortunately, it is also described by patients as one of the most disabling symptoms, causing significant impact on quality of life [19]. Fatigue in PD is associated with higher rates of depressive symptoms, but occurs with higher prevalence in nondepressed patients [21]. Poor ability to initiate and sustain activity due to fatigue is different from depression, excessive sleepiness, or impaired motor function [22,23].
Pathophysiology
The pathophysiology of fatigue remains somewhat unclear, though physical fatigue is likely a significant part of the problem and related to dopamine deficiency based on studies of time and force generation of keyboard strikes in PD subjects before and after L-dopa administration. These subjects had declines in force and increased physical fatigue which improved after L-dopa [24]. In other studies using transcranial magnetic stimulation to study changes in cortical excitability, the degree of physical fatigue correlated with abnormalities in motor evoked potentials during fatiguing exercising. These studies also support the hypothesis that fatigue is a motor symptom [25,26]. In the ELLDOPA study, fatigue worsened more in PD subjects treated with placebo [27]. Other imaging studies have suggested suggested nondopaminergic mechanisms including serotonergic pathway abnormalities [28], thus the question behind the etiology and solution for all cases of fatigue remains to be settled.
Diagnosis
The diagnosis is fatigue may be challenging as it may mask as depression or apathy. There are a number of fatigue rating scales available; however, the validated Parkinson’s Fatigue Scale (PFS) supersedes many of the problems of using a generic scale which could overlap motor questions and potentially be confounding [29,30].
Treatment
Most important is awareness and vigilance for the symptoms of fatigue, depression, and apathy and effort to distinguish between them. It may require structured interviews or assessment tools to properly diagnose the problem. Treatment is less clear in that few studies have clearly indicated the best treatment options. In placebo-controlled trials, methylphenidate did improve fatigue as did levodopa [31]. Modafinil, a hypocretin modulator and a drug first approved by the FDA for treatment of narcolepsy, has demonstrated mixed results in recent years. It may reduce physical fatigue and reduce excessive daytime sleepiness but likely does not reduce subjective symptoms of fatigue [32]. L-dopa can significantly reduce fatigue in many patients, which would argue that it often is a motor symptom [33,24]. In a post-hoc analysis of the ADAGIO delayed start study, patients taking rasagiline 1 mg/day and 2 mg/day (the latter dose exceeds the usual clinical dosing) showed significantly less worsening of symptoms on the PFS compared to placebo over time [34]. It is important to realize that once motor symptoms are optimally treated with dopaminergic medications, while many patients will feel significant relief from fatigue some patients will continue to feel symptomatic.
Apathy
The definition of apathy has become more complicated and refined, incorporating findings from the study of brain disease and behavioral analysis. Marin’s classic elaboration of apathy as lack of motivation not attributable to diminished level of consciousness, cognitive impairment, or emotional distress has been built upon by Levy and Dubois [35–37]. They suggest apathy may be better thought of as an observable behavioral syndrome characterized by a quantitative reduction of self-generated voluntary and purposeful behaviors. They suggest 3 apathetic subtypes: emotional, cognitive, and auto-activational, which reflect different disease states accounting for failure of normal goal-directed behavior.
Epidemiology
Prevalence estimates for apathy in PD vary. This is likely due to the varying recruitment criteria among studies, with some including patients with comorbid depression and dementia and others containing only “pure apathy.” Other reports may have had referral bias issues, as community-based studies report lower prevalences in general. In a group of newly diagnosed PD patients, using more restrictive criteria (apathy subscale of the neuropsychiatric inventory and the diagnostic consensus criteria for apathy validated in PD), Pedersen reported a prevalence of apathy of 14.3% [38]. In a 4-year prospective longitudinal cohort study, an annual incidence rate of 12.3% was reported, with apathy developing in 60% of the cohort by the study’s conclusion [39].
Apathy has been associated with longer disease duration, male gender [40], higher daily levodopa doses [41], more severe parkinsonism [38], and lower education status, though the latter feature remains under debate. Early cognitive deficits appear to be a risk factor for development of apathy [42]. The patterns of cognitive dysfunction and apathy remain unsettled in the literature.
Pathology
The pathology of atrophy remains unexplained and is unlikely to be reduced to a simple atrophy of one nucleus or the tone of one circuit. However, in a small neuroimaging study, severity of apathy correlated with atrophy of the bilateral nucleus accumbens [43], and it is notable that one major input to the nucleus accumbens is the amygdala. According to Braak staging, by stage 4 significant involvement of the amygdala by Lewy bodies has occurred. Others have found changes in grey matter density that could correlate with deficits of the prefrontal-basal ganglia circuitry to produce dysfunction of segregated frontal-subcortical loops. These may correlate with the “autoactivation” deficit pattern of apathy in which patients have a lack of self-initiated actions, even thoughts, though appear more normal when giving externally prompted responses [37,44].
Assessment
Clinically, the relationship between apathy and depression can be hard to disentangle, especially since many studies have found an association between them, especially with regards to apathy and anhedonia. Depression may feature negative self thoughts and sadness while apathy is notable for lack of initiation and effort. Viewed over a longer period of time, apathy tended to worsen in a linear fashion, where depression tended to fluctuate with improvements and exacerbations.
The Movement Disorders Society task force has recommended the Lille Apathy Rating Scale (LARS) for assessment of apathy; English and French versions have been validated in PD patients. It uses a semi-structured interview format assessing 4 dimensions of apathy: self awareness, intellectual curiosity, emotion, and action initiation [45–47].
The impact of apathy cannot be underestimated as this poor show of motivation or effort leads to lack of engagement in old activities or interest in new ones. Spouses may misinterpret this change in behavior as laziness or deliberate social withdrawal, or perhaps entitlement. It is not surprising that apathy routinely shows up on quality of life (QoL) questionnaires as highly impacting patients and families. In one study, apathy was the nonmotor symptom most likely to cause caregiver distress in PD [40,48–50].
Treatment
No approved drugs exist for treatment of apathy. However, clinical experience often confirms that dopaminergic modulation can be helpful in the treatment of apathy as indirect evidence suggests. A meta-analysis of controlled trials using pramipexole and Part I of the Unified Parkinson's disease rating scale (UPDRS) (secondary measure) showed the medication improved scores on this measure of motivation and mood in non-depressed subjects [51] with PD. Rare patients undergoing subthalamic deep brain stimulation have been reported to experience new and sometimes severe apathy after surgery [52]. This was posited at least in part to be the result of reduction of dopaminergic medication due to surgery.
Nondopaminergic pharmacotherapy of apathy is in its infancy. A recent controlled trial of rivastigmine in 31 French subjects with moderate to severe apathy based on LARS showed that 6 months of treatment at 9.5 mg/day improved average scores from –11.5 to –20 compared with placebo. While quality of life did not improve, caregiver burden did. The investigators found in this group of subjects that apathy was a possible herald for early dementia in PD [53].
A post-hoc analysis of the ADAGIO study (rasagiline or placebo in PD patients taking antidepressants) found that rasagiline use was associated with a nonsignificant slowing of apathy development during the trial [54].
Psychosis
Psychotic symptoms are a common occurrence in drug-treated patients, with visual hallucinations occurring in up to 30%, though over a 20-year period up to three-quarters of patients may develop visual hallucinations.After visual, the most common type of hallucination is auditory, followed by the other affected senses such as tactile, olfactory, or even taste [57]. Delusions, which tend to be paranoid in nature, occur in about 5% of patients [55–57]. The presence of psychotic symptoms is associated with poorer quality of life [58].
Symptomatology
The visual hallucinations of PD are usually quite stereotyped, and have been described as “minor” and “non-minor”[59]. Minor hallucinations refer to transient peripheral field stimuli that disappear when brought into central focus, “something flashed by,” a sense of a living being nearby, “a presence in the room,” or illusions whereby objects are transformed, eg, a bush in the yard is a deer.
Auditory hallucinations tend to be vague or indistinct sounds, like music in another room as opposed to voices speaking directly to the patient as might be experienced in a primary psychotic disorder. Tactile forms often involve insects or other animals crawling on the skin. Olfactory hallucinations may take the form of smelling perfume, toxic odors from room vents, etc.
Early in the experience, the visual hallucinations may be amusing in that they consistently remain nonthreatening, similar day to day, and sometimes oddly provide an aspect of comfort or companionship to the patient. More commonly, the hallucinations are bothersome to the patient because the experience indicates to the patient that there is something wrong with their mind. Visual hallucinations often begin in low-stimulus environments, often in the evening or other low-light conditions, but as the problem advances they can occur at any time of day. While visual hallucinations may initially occur for only seconds at a time many days apart, the frequency and duration can increase until they occur hours at a time every day and are accompanied by multiple other visual hallucinations, delusions, and confusion [60].
Delusions tend to be more distressing to patients and caregivers because they are often paranoid in nature. The patient is more likely to act out due to the anxiety the paranoia creates. For example, she may change passwords to online accounts due to a belief that unknown assailants are after her finances. He may go to great lengths trying to prove his wife is cheating.
Risk Factors
While the primary risk factor for psychotic symptom development is dementia [57], it occurs in nondemented patients. Other associations include reduced visual acuity [56], visual processing impairment [61–65], use of dopamine agonists, REM behavior disorder, duration of PD, axial rigidity subtype of disease [61,66–68]. The pathophysiology of psychosis in PD is likely complex and remains currently unexplained. The role of excess dopamine has been described above, but there is also data suggesting cholinergic deficits in the cortex may also contribute. Excess serotonin (increased 5HT2A receptor subtypes) in the temporal lobe within the visual processing pathway has been postulated to be of significance [69,70]. Hypometabolism in visual association areas of the brain in subjects with visual hallucinations has been demonstrated in PET and functional MRI studies [64,71]. This is similar to findings in patients with dementia with Lewy bodies [72].
This review focuses on the primary forms of PD-related psychosis, which occur with a clear sensorium and generally longer exposure to dopaminergic medication. It is important to distinguish 2 other common scenarios in which hallucinations or delusions may occur. In the common toxic-metabolic delirium, a clouded sensorium with attention deficits may be the only clue to the etiology of new onset confusion with visual hallucinations. It is highly likely that resolution of the underlying medical problem will lead to resolution of the new onset psychosis and encephalopathy. In a second scenario, hallucinations precede or occur very shortly after the onset of initiation of dopaminergic medication. This differs from the classic syndrome described earlier, in particular when visual hallucinations precede any initiation of medication, and likely represents the distinction between a diagnosis of Lewy body disease and PD [60].
Treatment
Management of psychosis is approachable, but often the outcome is unsatisfactory and associated with trade-offs in motor control. It is unfortunately true that psychotic symptoms are often associated with increased caregiver burden and are a cause of increased nursing home placements [73]. When considering the workup of psychotic symptoms, the differential diagnosis includes delirium, dream enactment (REM behavior disorder), or less commonly, Bonnet syndrome.
A delirium may be precipitated by a difficult to diagnose infection; new-onset confusion and psychotic symptoms may be the heralding presentation. Urinary tract or upper respiratory tract are common vulnerable sources of infection. Once infection is ruled out, the next practical step is to review the patient’s medication list and manage centrally acting drugs that could be contributing to the altered sensorium. A recent prescription of opioids for a dental treatment or a new muscle relaxant may be a culprit, though it is not that usual. A bladder anticholinergic could be suspect and is worth eliminating especially if its addition coincided with the appearance of the psychotic symptoms. Once the non-dopaminergic medications have been reduced/eliminated, then the PD medications should be considered. The general approach is to eliminate the medications that provide the least benefit while being more likely to contribute to psychotic symptoms. Anticholinergic medications, dopamine agonists, selegiline should all be uppermost in that consideration until one is left with L-dopa and COMT inhibitors (the latter function to increase levodopa availability). Then COMT inhibitors and levodopa can be reduced; however, at any point motor control can suffer with the loss of symptomatic therapies [74].
Clozapine is effective against psychotic symptoms in PD, at doses much lower than used in schizophrenia (300-600mg/day). The average dose in the US randomized controlled clinical trial was 25 mg/day, with no associated motor worsening. Patients in the United States are required by the FDA to be placed in a computer-based registry and monitored for agranulocytosis for the duration of clozapine therapy. This rare adverse event is not dose related. Orthostasis can occur at these low doses however. Fortunately the metabolic syndrome is not associated with this range of administration [75,76].
Quetiapine was not found to be effective in 3 blinded randomized controlled trials despite its rather common use for this purpose. It was not associated with motor worsening, however.
Other neuroleptic medications have not resulted in widespread use, because trials have been open label, or outcomes demonstrated motor worsening. Cholinesterase inhibitors have been the subject of a few positive case series, however results appear to be sporadic, the effect size is relatively small, and side effects of this medication class are common [77–79]. It is clear that there is an unmet need for a medication for psychotic symptoms. Clozapine is effective but onerous in its monitoring requirements. Practically speaking, there are relatively few PD patients who take advantage of it because of its feasibility challenges. Yet the problem of psychotic symptoms is a significant one that imposes important challenges to the patient and caregiver, and may limit the number of medications that the patient needs in order to optimize quality of life.
Pimavanserin, a novel medication which acts as a selective serotonin inverse agonist, is in the early application stages for FDA approval for treatment of psychotic symptoms in PD [80]. In its pivotal phase III controlled trial, the drug reduced not only positive symptoms (hallucinations/delusions) without causing motoric worsening, but also reduced caregiver burden. Pimavanserin improved certain sleep features without causing daytime sedation. If this drug meets final approval, it may present an exciting option for many patients for whom treatment was previously limited.
Depression
A study of early PD suggested that depression is often unrecognized and frequently untreated [1]. Indeed it is not unusual for depression to predate the diagnosis of PD by an average of 4 to 6 years [81]. Expanding to the larger PD population, it is generally accepted that about 30% to 50% of PD patients experience clinically significant depression, and once diagnosed may have a long term course, or may recur [82,83]. This is important as untreated depression is an important cause of poor quality of life in early PD. In addition depression can exacerbate motor disability, lead to earlier motor treatment with medication, and increase caregiver stress [83–85].
Diagnosis
A number of clinimetric rating scales for depression have been used and their advantages have been largely related to their objective nature (quantifiable); thus, they tend to be most useful in epidemiologic research studies or for larger scale screening purposes. Examples include the the Beck Depression Inventory, the Geriatric Depression Scale, and the Hamilton Depression Scale, all of which have been shown to be valid tools in PD (with the exception of the UPDRS Depression). It is important to note that they do not substitute for a diagnostic clinical interview [89].
Suicide is not common in PD, however suicidal ideation is estimated at about 11% in PD patients [90], and while there was concern initially after deep brain stimulation procedures began that suicide incidence was increased, evidence does not support this [91].
Pathophysiology
The pathophysiology of depression in PD is largely unknown however is thought to be less causally due to psychosocial factors and more etiologically driven by brainstem monoamine and serotonergic dysfunction [92]. Nonetheless, similar to other chronic conditions, PD patients can certainly develop fear of disability, guilt about impact on others, or other reactive mood changes. Overall, rates of depression are higher in PD compared with patients with similar conditions matched for disability [93].
Treatment
First, the clinician must determine if depression is a result of short-term fluctuations, chronic undertreatment of motor disease, or longer-term mood phenomenon. One important pattern to recognize are mood fluctuations, which can parallel motor OFF-ON cycling. It can be valuable to distinguish this as “subsyndromic” depression or anxiety (sometimes referred to as “OFF dysphoria”), as it can respond to improvement in antiparkinsonian medication dosing patterns that reduce fluctuations[94–96]. Similarly, elevating chronic motor undertreatment to goal therapy can result in mood normalization.
If symptoms persist despite optimization of motor/nonmotor fluctuations or chronic undertreatment and are severe enough to warrant treatment, then therapies used can range from nonpharmacologic education, support, and mental health referrals, as well as pharmacologic support in the form of medications.
A frequent but uncontrolled observation was that when undertreatment of motor disease was finally redressed, mood often improved. A multicenter randomized controlled trial of pramipexole in PD patients without motor fluctuations but with mild to moderate depressive symptoms showed the drug improved scores on the Beck Depression Inventory over a 12-week period. The improvement in mood was 6 points overall, but by 2 points over placebo, illustrating the importance of the size of the placebo effect [97]. Given the potential side effect profile of dopamine agonists, it may be useful to weigh the antidepressant effects only when their motor benefits are already being employed.
Controlled trials have demonstrated efficacy of both selective serotonin reuptake inhibitors (SSRI) and selective norepinephrine reuptake inhibitors (SNRI) antidepressants in PD. Clinical trials have demonstrated efficacy against placebo or with other antidepressant comparators. Examples of drugs with demonstrated efficacy include citalopram, paroxetine, venlafaxine, and nortriptyline. Results have attempted to illuminate the small unique differences between classes of antidepressants or dynamic properties between drugs within a class. For example, desipramine may nudge scores on a mood scale a few weeks sooner than a purer SSRI. Paroxetine (SSRI) versus venlafaxine (SNRI) improved mood scores comparably in a multicenter trial with a placebo comparator. In general, all have all been demonstrated to be effective and with a relatively low side-effect profile, comparable to the general population[98–102]. While case reports exist in the literature, the interaction of monoamine oxidase B inhibitors and SSRIs has not caused significant hypertensive crises or risk of serotonin syndrome [103,104]. Electroconvulsive therapy (ECT) can be used for severe refractory depression in PD as for non-PD patients, with case reports of very effective results. Due to the rarity of use, systematic evidence for its use is lacking [105,106].
Other novel agents and techniques such as omega-3 fatty acids [107] and repetitive transcranial magnetic stimulation [108] have been reported with promising early results. Cognitive behavioral therapy (CBT), which may involve stress management techniques, sleep hygiene, and caregiver support, additionally almost always provided improvement in measured outcomes, whether the trial was controlled or open label in design. In one RCT of CBT in PD of 14 weeks’ duration, there were significantly more treatment responders in the CBT group, with a number needed to treat of only 2 [109].
Anxiety
Anxiety is also common in PD, at least as common as depression considering that prevalence estimates suggest up to 50% of patients experience it [110–112]. Manifestations of anxiety may include panic attacks, generalized anxiety disorder, social anxiety, or other phobias [113]. Anxiety has an important negative impact on health-related quality of life and is often underrecognized by clinicians [114]. While reliable and valid scales to measure anxiety have been lacking in PD, a new effort has yielded the “Parkinson Anxiety Scale” though full clinimetric properties of the scale remain to be demonstrated (sensitivity to change) [115].
Anxiety that parallels the timing of motor OFF-ON cycling is important to recognize. This “subsyndromic” anxiety or anxiety disorder not otherwise specified (ie, the anxiety does not meet DSM-IV criteria) can respond to improvement in antiparkinsonian medication dosing patterns that reduce fluctuations [116,117]. Indeed, the presence of motor fluctuations is the principle marker of anxiety in many studies [118–120]. In an analogous manner, anxiety can predate PD by years and be part of the nonmotor amalgam of features heralding the disease [6,121].
Treatment
Systematic controlled trials of anxiolytic treatment for PD are lacking; therefore, SSRIs are prescribed for this purpose as in non-PD patients. Until SSRIs are demonstrated to be of benefit in anxiety, they are likely safer than use of benzodiazepines, which are associated with risk for falling, cognitive dysfunction, or autonomic dysregulation in PD patients when used during waking hours. Psychotherapy and other nonpharmacologic approaches are likely to be of benefit. A small study of neuromuscular (massage) therapy demonstrated improvement on the Beck Anxiety Inventory in PD [122]. A case report of ECT for severe anxiety has been published [123].
Conclusion
Neuropsychiatric symptoms are common in PD and new knowledge about clinical features, epidemiology, and treatment options has been gained in the last decade, though much remains to be discovered. The development of valid instruments to measure neuropsychiatric symptoms has been vital in these research efforts to bridge the gaps in our understanding. Further elucidation of the pathophysiologies of neuropsychiatric symptoms will help to define treatment targets and likely fuel drug development and the discovery of drugs with more potent benefit and fewer side effects.
Corresponding author: Kathryn A. Chung, MD, Department of Neurology, Oregon Health & Science University, Portland, OR, [email protected].
Financial disclosures: None.
1. American Psychiatric Association. DSM-IV. 2000.
2. Voon V, Hassan K, Zurowski M, et al. Prevalence of behaviors in Parkinson disease Neurology 2006;67;1254–7.
3. D. Weintraub D, J. Koester J, M. N. Potenza MN, et al. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol 2010;67589–95.
4. Hälbig TD, Tse W, Frisina PG, et al. Subthalamic deep brain stimulation and impulse control in Parkinson’s disease. Eur J Neuro 2009;16:493–7.
5. Callesen MB, Scheel-Krüger J, Kringelbach ML, Møller A. A systematic review of impulse control disorders in Parkinson’s disease. J Parkinsons Dis 2013;3:105–38.
6. De Riva P, Smith K, Xie SX, Weintraub D. Course of psychiatric symptoms and global cognition in early course of psychiatric symptoms and global cognition in early Parkinson disease Neurology 2014;83:1–8.
7. Cools R. Dopaminergic modulation of cognitive function-implications for L-DOPA treatment in Parkinson’s disease. Neurosci Biobehav Rev 2006;30:1–23.
8. Rowe JB, Hughes L, Ghosh BCP, et al. Parkinson’s disease and dopaminergic therapy – Differential effects on movement, reward and cognition. Brain 2008;131:2094–105.
9. Cools R, Frank MJ, Gibbs SE, et al. Striatal dopamine predicts outcome-specific reversal learning and its sensitivity to dopaminergic drug administration. J Neurosci 2009;29:1538–43.
10. Di Matteo V, Pierucci M, Esposito E, et al. Serotonin modulation of the basal ganglia circuitry: therapeutic implication for Parkinson’s disease and other motor disorders. Prog Brain Res 2008;172:423–463.
11. Campbell-Meiklejohn D, Wakeley J, Herbert V, et al. Serotonin and dopamine play complementary roles in gambling to recover losses. Neuropsychopharmacology 2011;36:402–10.
12. Macoveanu J, Rowe JB, Hornboll B, et al. Playing it safe but losing anyway-Serotonergic signaling of negative outcomes in dorsomedial prefrontal cortex in the context of risk-aversion. Eur Neuropsychopharmacol 2013;23:919–30.
13. Mamikonyan E, Siderowf AD, Duda JE, et al. NIH Public Access 2009;23:75–80.
14. Ivanco LS, Bohnen NI. Effects of donepezil on compulsive hypersexual behavior in Parkinson disease: a single case study. Am J Ther 2005;12:467–8.
15. Hicks CW, Pandya MM, Itin I, Fernandez HH. Valproate for the treatment of medication-induced impulse-control disorders in three patients with Parkinson’s disease. Parkinsonism Relat Disord 2011;5:379–81.
16. Bermejo PE, Ruiz-Huete C, Anciones B. Zonisamide in managing impulse control disorders in Parkinson’s disease. J Neurol 2010;257:1682–5.
17. Pawlikowska T, Chalder T, Hirsch SR, et al. Population based study of fatigue and psychological distress. BMJ 1994;308:763–6.
18. Lou JS, Kearns G, Oken B, et al. Exacerbated physical fatigue and mental fatigue in Parkinson’s disease. Mov Disord 2001;16:190–6.
19. Herlofson K, Larsen JP. The influence of fatigue on health-related quality of life in patients with Parkinson’s disease. Acta Neurol Scand 2003;107:1–6.
20. Hagell P, Brundin L. Towards an understanding of fatigue in Parkinson disease. J Neurol Neurosurg Psychiatry 2009;80:489–92.
21. Alves G, Wentzel-Larsen T, Larsen JP. Is fatigue an independent and persistent symptom in patients with Parkinson disease? Neurology 2004;63:1908–11.
22. Martinez-Martin P, Catalan MJ, Benito-Leon J, et al. Impact of fatigue in Parkinson’s disease: The fatigue impact scale for daily use (D-FIS). Qual Life Res 2006:15:597–606.
23. Havlikova E, Rosenberger J, Nagyova I, et al. Clinical and psychosocial factors associated with fatigue in patients with Parkinson’s disease. Parkinsonism Relat Disord 2008;14:187–92.
24. Lou JS, Kearns G, Benice T, et al. Levodopa improves physical fatigue in Parkinson’s disease: A double-blind, placebo controlled, crossover study. Mov Disord 2003;18:1108–14.
25. Khedr EM, Galal O, Said A, et al. Lack of post-exercise depression of corticospinal excitability in patients with Parkinson’s disease. Eur J Neurol 2007;14:793–6.
26. Lou JS, Benice T, Kearns G, et al. Levodopa normalizes exercise related cortico-motoneuron excitability abnormalities in Parkinson’s disease. Clin. Neurophysiol 2003;114:930–7.
27. Schifitto G, Friedman JH, Oakes D, et al. Fatigue in levodopa-naive subjects with Parkinson disease. Neurology 2008;71:481–5.
28. Pavese N, Metta V, Bose SK, et al. Fatigue in Parkinson’s disease is linked to striatal and limbic serotonergic dysfunction. Brain 2010;133:3434–43.
29. Brown RG, Dittner A, Findley L, Wessely SC. The Parkinson fatigue scale. Park Relat Disord 2005;11:49–55.
30. Grace J, Mendelsohn A, Friedman JH. A comparison of fatigue measures in Parkinson’s disease. Parkinsonism Relat Disord 2007;13:443–5.
31. Mendonça DA, Menezes K, Jog MS. Methylphenidate improves fatigue scores in Parkinson disease: a randomized controlled trial. Mov Disord 2007;22:2070–6.
32. Lou JS, Dimitrova DM, Park BS, et al. Using modafinil to treat fatigue in Parkinson disease: a double-blind, placebo-controlled pilot study. Clin Neuropharmacol 2009;32:305–10.
33. Ziv I, Avraham M, Michaelov Y, et al. Enhanced fatigue during motor performance in patients with Parkinson’s disease. Neurology 1998;51:1583–6.
34. Stocchi F. Benefits of treatment with rasagiline for fatigue symptoms in patients with early Parkinson’s disease. Eur J Neurol 2014;21:357–60.
35. Marin RS. Apathy: a neuropsychiatric syndrome. J. Neuropsychiatry Clin Neurosci 1991;3:243–4.
36. Marin RS. Apathy: concept, syndrome, neural mechanisms, and treatment. Semin Clin Neuropsychiatry 1996:1:304–14.
37. Levy R, Dubois B. Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cerebral Cortex 2006;16:916–28.
38. Pedersen KF, Larsen JP, Alves G, Aarsland D. Prevalence and clinical correlates of apathy in Parkinson’s disease: a community-based study. Parkinsonism Relat Disord 2009;15:295–9.
39. Pedersen KF, Alves G, Aarsland D, Larsen JP. Occurrence and risk factors for apathy in Parkinson disease: a 4-year prospective longitudinal study. J Neurol Neurosurg Psychiatry 2009;80:1279–82.
40. Pedersen KF, Alves G, Brønnick K, et al. Apathy in drug-naïve patients with incident Parkinson’s disease: The Norwegian ParkWest study. J Neurol 2010;257:217–23.
41. Ziropadja L, Stefanova E, Petrovic M, et al. Apathy and depression in Parkinson’s disease: The Belgrade PD study report. Parkinsonism Relat Disord 2012;18:339–42.
42. Dujardin K, Sockeel P, Devos D, et al. Characteristics of apathy in Parkinson’s disease. Mov Disord 2007;22:778–84.
43. Carriere N, Besson P, Dujardin K, et al. Apathy in Parkinson’s disease is associated with nucleus accumbens atrophy: a magnetic resonance imaging shape analysis. Mov Disord 2014;29;897–903.
44. Reijnders JSAM, Scholtissen B, Weber WEJ, et al. Neuroanatomical correlates of apathy in Parkinson’s disease: a magnetic resonance imaging study using voxel-based morphometry. Mov Disord 2010;25:2318–25.
45. Leroi I, Harbishettar V, Andrews M, et al. Carer burden in apathy and impulse control disorders in Parkinson’s disease. Int J Geriatr Psychiatry 2012;27:160–6.
46. Schiehser DM, Liu L, Lessig SL, et al. Predictors of discrepancies in Parkinson’s disease patient and caregiver ratings of apathy, disinhibition, and executive dysfunction before and after diagnosis. J Int Neuropsychol Soc 2013;19:295–304.
47. Benito-León J, Cubo E, Coronell C, et al. Impact of apathy on health-related quality of life in recently diagnosed Parkinson’s disease: The ANIMO study. Mov Disord 2012;27:211–8.
48. Sockeel P, Dujardin K, Devos D, et al. The Lille apathy rating scale (LARS), a new instrument for detecting and quantifying apathy: validation in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2006;77:579–84.
49. Zahodne LB, Young S, Kirsch-Darrow L, et al. Examination of the Lille Apathy Rating Scale in Parkinson disease. Mov Disord 2009;24:677–83.
50. Drijgers RL, Dujardin K, Reijnders JSAM, et al. Validation of diagnostic criteria for apathy in Parkinson’s disease. Parkinsonism Relat Disord 2010;16:656–60.
51. Leentjens AFG, Koester J, Fruh B, et al. The effect of pramipexole on mood and motivational symptoms in parkinson’s disease: A meta-analysis of placebo-controlled studies. Clin Ther 2009;31:89–98.
52. Thobois S, Ardouin C, Lhommée E, et al. Non-motor dopamine withdrawal syndrome after surgery for Parkinson’s disease: Predictors and underlying mesolimbic denervation. Brain 2010;133:1111–27.
53. Devos D, Moreau C, Maltête D, et al. Rivastigmine in apathetic but dementia and depression-free patients with Parkinson’s disease: a double-blind, placebo-controlled, randomised clinical trial. J Neurol Neurosurg Psychiatry 2014;85:668–74.
54. Smith KM, Eyal E, Weintraub D; ADAGIO Investigators. Combined rasagiline and antidepressant use in Parkinson disease in the ADAGIO study: effects on nonmotor symptoms and tolerability. JAMA Neurol 2015;72:88–95.
55. Forsaa EB, Larsen JP, Wentzel-Larsen T, et al. A 12-year population-based study of psychosis in Parkinson disease. Arch Neurol 2010;67:996–1001.
56. Holroyd S, Currie L, Wooten GF. Prospective study of hallucinations and delusions in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2001;70:734–8.
57. Fénelon G, Alves G. Epidemiology of psychosis in Parkinson’s disease. J Neurol Sci 2010;289:12–7.
58. Mack J, Rabins P, Anderson K, et al. Prevalence of psychotic symptoms in a community-based Parkinson disease sample. Am J Geriatr Psychiatry 2012;20:123–32.
59. Ravina B, Marder K, Fernandez HH, et al. Diagnostic criteria for psychosis in Parkinson’s disease: Report of an NINDS, NIMH Work Group. Mov Disord 2007;22:1061–8.
60. Diederich NJ, Fénelon G, Stebbins G, Goetz CG. Hallucinations in Parkinson disease. Nat Rev Neurol 2009;5:331–42.
61. Gallagher DA, Parkkinen L, O’Sullivan SS, et al. Testing an aetiological model of visual hallucinations in Parkinson’s disease. Brain 2011;134:3299–309.
62. Barnes J, Boubert L, Harris J, et al. Reality monitoring and visual hallucinations in Parkinson’s disease. Neuropsychologia 2003:41:565–74.
63. Kurita A, Murakami M, Takagi S, et al. Visual hallucinations and altered visual information processing in Parkinson disease and dementia with Lewy bodies. Mov Disord 2010;25:167–71.
64. Stebbins GT, Goetz CG, Carrillo MC, et al. Altered cortical visual processing in PD with hallucinations: an fMRI study. Neurology 2004;63:1409–16.
65. Williams DR, Lees AJ. Visual hallucinations in the diagnosis of idiopathic Parkinson’s disease: A retrospective autopsy study. Lancet Neurol 2005:4:605–10.
66. Biglan KM, Holloway RG, McDermott MP, Richard IH. Risk factors for somnolence, edema, and hallucinations in early Parkinson disease. Neurology 2007;69:187–95.
67. Kiziltan G, Ozekmekci S, Ertan S, et al. Relationship between age and subtypes of psychotic symptoms in Parkinson’s disease. J Neurol 2007;254:448–52.
68. Ecker D, Unrath A, Kassubek J, Sabolek M. Dopamine agonists and their risk to induce psychotic episodes in Parkinson’s disease: a case-control study. BMC Neurol 2009;9:23.
69. Huot P, Johnston TH, Darr T, et al. Increased 5-HT2A receptors in the temporal cortex of Parkinsonian patients with visual hallucinations. Mov Disord 2010;25:1399–408.
70. Ballanger B, Strafella AP, van Eimeren T, et al. Serotonin 2A receptors and visual hallucinations in Parkinson disease. Arch. Neurol 2010;67:416–21.
71. Boecker H, Ceballos-Baumann O, Volk D, et al. Metabolic alterations in patients with Parkinson disease and visual hallucinations. Arch Neurol 2007;64:984–8.
72. Sanchez-Castaneda C, Rene R, Ramirez-Ruiz B, et al. Frontal and associative visual areas related to visual hallucinations in dementia with Lewy bodies and Parkinson’s disease with dementia. Mov Disord 2010;25:615–22.
73. Goetz CG, Stebbins GT. Risk factors for nursing home placement in advanced Parkinson’s disease. Neurology 1993;43:2227–9.
74. Friedman JH. Parkinson disease psychosis: update. Behav.Neurol 2013;27:469–77.
75. Pollak P, Tison F, Rascol O, et al. Clozapine in drug induced psychosis in Parkinson’s disease: a randomised, placebo controlled study with open follow up. J Neurol Neurosurg Psychiatry 2004;75:689–95.
76. Parkinson Study Group. Low-dose clozapine for the treatment of drug-induced psychosis. N Engl J Med 1999;340:757–63.
77. Sobow T. Parkinson’s disease-related visual hallucinations unresponsive to atypical antipsychotics treated with cholinesterase inhibitors: a case series. Neurol Neurochir Pol 2007;41:276–9.
78. Fabbrini G, Barbanti P, Aurilia C, et al. Donepezil in the treatment of hallucinations and delusions in Parkinson’s disease. Neurol Sci 2002;23:41–3.
79. Bullock R, Cameron A, Hospital WH. Rivastigmine for the treatment of dementia and visual hallucinations associated with Parkinson’s disease: a case series. Curr Med Res Opin 2002;18,:258–64.
80. Cummings J, Isaacson S, Mills R, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet 2014;383:533–40.
81. L. Ishihara L, and C. Brayne C. A systematic review of depression and mental illness preceding Parkinson’s disease. Acta Neurol Scand 2006;113:211–20.
82. Reijnders JSAM, Ehrt U, Weber WEJ, et al. A systematic review of prevalence studies of depression in Parkinson’s disease. Mov Disord 2008;23:183–9.
83. Starkstein SE, Mayberg HS, Leiguarda R, et al. A prospective longitudinal study of depression, cognitive decline, and physical impairments in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 1992:55:377–82.
84. Müller B, Assmus J, Herlofson K, et al. Importance of motor vs. non-motor symptoms for health-related quality of life in early Parkinson’s disease. Parkinsonism Relat Disord 2013;19:1027–32.
85. Ravina B, Camicioli R, Como PG, et al. The impact of depressive symptoms in early Parkinson disease. Neurology 2007;69:342–7.
86. Marsh L, McDonald WM, Cummings J, et al. Provisional diagnostic criteria for depression in Parkinson’s disease: report of an NINDS/NIMH work group. Mov Disord 2006;21:148–58.
87. Marsh L. Depression and Parkinson’s disease: current knowledge. Curr. Neurol. Neurosci. Rep 2013; 13:409.
88. Starkstein SE, Merello M, Jorge R, et al. A validation study of depressive syndromes in Parkinson’s disease. Mov Disord 2008;23,:538–46.
89. Williams JR, Hirsch ES, Anderson K, et al. A comparison of nine scales to detect depression in Parkinson disease: which scale to use? Neurology 2012;78:998–1006.
90. Nazem S, Siderowf AD, Duda JE, et al. Suicidal and death ideation in Parkinson’s disease. Mov Disord 2008;23:1573–9.
91. Weintraub D, Duda JE, Carlson K, et al. Suicide ideation and behaviours after STN and GPi DBS surgery for Parkinson’s disease: results from a randomised, controlled trial. J Neurol Neurosurg Psychiatry 2013;84:1113–8.
92. Aarsland D, Påhlhagen S, Ballard CG, et al. Depression in Parkinson disease—epidemiology, mechanisms and management. Nat Rev Neurol 2011;8:35–47.
93. Ehmann TS, Beninger RJ, Gawel MJ, Riopelle RJ. Depressive symptoms in Parkinson’s disease: a comparison with disabled control subjects. J Geriatr Psychiatry Neurol 1990;3:3–9.
94. Witjas T, Kaphan E, Azulay JP, et al. Nonmotor fluctuations in Parkinson’s disease: frequent and disabling. Neurology 2002:59:408–13.
95. Nissenbaum H, Quinn NP, Brown RG, et al. Mood swings associated with the ‘on-off’ phenomenon in Parkinson’s disease. Psychol Med 1987;17:899–904.
96. Maricle RA, Nutt JG, Carter JH. Mood and anxiety fluctuation in Parkinson’s disease associated with levodopa infusion: preliminary findings. Mov Disord 1995;10:329–32.
97. Barone P, Poewe W, Albrecht S, et al. Pramipexole for the treatment of depressive symptoms in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 2010;9:573–80.
98. Devos D, Dujardin K, Poirot I, et al. Comparison of desipramine and citalopram treatments for depression in Parkinson’s disease: a double-blind, randomized, placebo-controlled study. Mov Disord 2008;23:850–7.
99. Richard IH, McDermott MP, Kurlan R, et al. A randomized, double-blind, placebo-controlled trial of antidepressants in Parkinson disease. Neurology 2012;78:1229–36.
100. Menza M, Dobkin RD, Marin H, et al. A controlled trial of antidepressants in patients with Parkinson disease and depression. Neurology 2009;72:886–92.
101. Seppi K, Weintraub D, Coelho M, et al. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord 2011;26 Suppl 3:S42–80.
102. Skapinakis P, Bakola E, Salanti G, et al. Efficacy and acceptability of selective serotonin reuptake inhibitors for the treatment of depression in Parkinson’s disease: a systematic review and meta-analysis of randomized controlled trials. BMC Neurol 2010;10:49.
103. Richard IH, Kurlan R, Tanner C, et al. Serotonin syndrome and the combined use of deprenyl and an antidepressant in Parkinson’s disease. Parkinson Study Group. Neurology 1997;48:1070–7.
104. Montgomery EB, Panisset M. Retrospective statistical analysis of the incidence of serotonin toxicity in patients taking rasagiline and anti-depressants in clinical trials. Mov Disord 2009;24:359.
105. Bailine S, Kremen N, Kohen I, et al. Bitemporal electroconvulsive therapy for depression in a Parkinson disease patient with a deep-brain stimulator. J ECT 2008;24:171–2.
106. Faber R, Trimble MR. Electroconvulsive therapy in Parkinson’s disease and other movement disorders. Mov Disord 1991;6:293–303.
107. da Silva TM, Munhoz RP, Alvarez C, et al. Depression in Parkinson’s disease: a double-blind, randomized, placebo-controlled pilot study of omega-3 fatty-acid supplementation. J Affect Disord 2008;111:351–9.
108. Pal E, Nagy F, Aschermann Z, et al. The impact of left prefrontal repetitive transcranial magnetic stimulation on depression in Parkinson’s disease: a randomized, double-blind, placebo-controlled study. Mov Disord 2010;25:2311–7.
109. Dobkin RD, Menza M, Allen LA, et al. Cognitive-behavioral therapy for depression in Parkinson’s disease: a randomized, controlled trial. Am J Psychiatry 2011;168:1066–74.
110. Stein MB, Heuser IJ, Juncos JL, Uhde TW. Anxiety disorders in patients with parkinson’s disease. Am J Psychiatry 1990;147:217–20.
111. Nuti A, Ceravolo R, Piccinni A, et al. Psychiatric comorbidity in a population of Parkinson’s disease patients. Eur J Neurol 2004;11:315–20.
112. Marinus J, Leentjens AFG, Visser M, et al. Evaluation of the Hospital Anxiety and Depression Scale in patients With Parkinson’s disease. Clin Neuropharmacol 2002:25:318–24.
113. Dissanayaka NNW, White E, O’Sullivan JD, et al. The clinical spectrum of anxiety in Parkinson’s disease. Mov Disord 2014;29:967–75.
114. Dissanayaka NNW, Sellbach A, Matheson S, et al. Anxiety disorders in Parkinson’s disease: prevalence and risk factors. Mov Disord 2010;25:838–45.
115. Leentjens AFG, Dujardin K, Pontone GM, et al. The Parkinson anxiety scale (PAS): Development and validation of a new anxiety scale. Mov Disord 2014;29:1035–43.
116. Maricle RA, Nutt JG, Valentine RJ, Carter JH. Dose-response relationship of levodopa with mood and anxiety in fluctuating Parkinson’s disease: a double-blind, placebo-controlled study. Neurology 1995;45:1757–60.
117. Erdal KJ. Depression and anxiety in persons with Parkinson’s disease with and without ‘on–off’ phenomena. J Clin Psychol Med Settings 2001:8:293–9.
118. Leentjens AFG, Dujardin K, Marsh L, et al. Symptomatology and markers of anxiety disorders in Parkinson’s disease: a cross-sectional study. Mov. Disord 2011;26:484–92.
119. Solla P, Cannas A, Floris GL, et al. Behavioral, neuropsychiatric and cognitive disorders in Parkinson’s disease patients with and without motor complications. Prog Neuropsychopharmacol Biol Psychiatry 2011;35:1009–13.
120. E. Stefanova E, L. Ziropadja L, M. Petrović M, et al. Screening for anxiety symptoms in Parkinson disease: a cross-sectional study. J Geriatr Psychiatry Neurol 2013;26:34–40.
121. Jacob EL, Gatto NM, Thompson A, et al. Occurrence of depression and anxiety prior to Parkinson’s disease. Parkinsonism Relat Disord 2010;16:576–81.
122. Craig LH, Svircev A, Haber M, Juncos JL. Controlled pilot study of the effects of neuromuscular therapy in patients with Parkinson’s disease. Mov Disord 2006;21:2127–33.
123. Marino L, Friedman JH. Letter to the editor: Successful use of electroconvulsive therapy for refractory anxiety in Parkinson’s disease. Int J Neurosci 2013;123:70–1.
1. American Psychiatric Association. DSM-IV. 2000.
2. Voon V, Hassan K, Zurowski M, et al. Prevalence of behaviors in Parkinson disease Neurology 2006;67;1254–7.
3. D. Weintraub D, J. Koester J, M. N. Potenza MN, et al. Impulse control disorders in Parkinson disease: a cross-sectional study of 3090 patients. Arch Neurol 2010;67589–95.
4. Hälbig TD, Tse W, Frisina PG, et al. Subthalamic deep brain stimulation and impulse control in Parkinson’s disease. Eur J Neuro 2009;16:493–7.
5. Callesen MB, Scheel-Krüger J, Kringelbach ML, Møller A. A systematic review of impulse control disorders in Parkinson’s disease. J Parkinsons Dis 2013;3:105–38.
6. De Riva P, Smith K, Xie SX, Weintraub D. Course of psychiatric symptoms and global cognition in early course of psychiatric symptoms and global cognition in early Parkinson disease Neurology 2014;83:1–8.
7. Cools R. Dopaminergic modulation of cognitive function-implications for L-DOPA treatment in Parkinson’s disease. Neurosci Biobehav Rev 2006;30:1–23.
8. Rowe JB, Hughes L, Ghosh BCP, et al. Parkinson’s disease and dopaminergic therapy – Differential effects on movement, reward and cognition. Brain 2008;131:2094–105.
9. Cools R, Frank MJ, Gibbs SE, et al. Striatal dopamine predicts outcome-specific reversal learning and its sensitivity to dopaminergic drug administration. J Neurosci 2009;29:1538–43.
10. Di Matteo V, Pierucci M, Esposito E, et al. Serotonin modulation of the basal ganglia circuitry: therapeutic implication for Parkinson’s disease and other motor disorders. Prog Brain Res 2008;172:423–463.
11. Campbell-Meiklejohn D, Wakeley J, Herbert V, et al. Serotonin and dopamine play complementary roles in gambling to recover losses. Neuropsychopharmacology 2011;36:402–10.
12. Macoveanu J, Rowe JB, Hornboll B, et al. Playing it safe but losing anyway-Serotonergic signaling of negative outcomes in dorsomedial prefrontal cortex in the context of risk-aversion. Eur Neuropsychopharmacol 2013;23:919–30.
13. Mamikonyan E, Siderowf AD, Duda JE, et al. NIH Public Access 2009;23:75–80.
14. Ivanco LS, Bohnen NI. Effects of donepezil on compulsive hypersexual behavior in Parkinson disease: a single case study. Am J Ther 2005;12:467–8.
15. Hicks CW, Pandya MM, Itin I, Fernandez HH. Valproate for the treatment of medication-induced impulse-control disorders in three patients with Parkinson’s disease. Parkinsonism Relat Disord 2011;5:379–81.
16. Bermejo PE, Ruiz-Huete C, Anciones B. Zonisamide in managing impulse control disorders in Parkinson’s disease. J Neurol 2010;257:1682–5.
17. Pawlikowska T, Chalder T, Hirsch SR, et al. Population based study of fatigue and psychological distress. BMJ 1994;308:763–6.
18. Lou JS, Kearns G, Oken B, et al. Exacerbated physical fatigue and mental fatigue in Parkinson’s disease. Mov Disord 2001;16:190–6.
19. Herlofson K, Larsen JP. The influence of fatigue on health-related quality of life in patients with Parkinson’s disease. Acta Neurol Scand 2003;107:1–6.
20. Hagell P, Brundin L. Towards an understanding of fatigue in Parkinson disease. J Neurol Neurosurg Psychiatry 2009;80:489–92.
21. Alves G, Wentzel-Larsen T, Larsen JP. Is fatigue an independent and persistent symptom in patients with Parkinson disease? Neurology 2004;63:1908–11.
22. Martinez-Martin P, Catalan MJ, Benito-Leon J, et al. Impact of fatigue in Parkinson’s disease: The fatigue impact scale for daily use (D-FIS). Qual Life Res 2006:15:597–606.
23. Havlikova E, Rosenberger J, Nagyova I, et al. Clinical and psychosocial factors associated with fatigue in patients with Parkinson’s disease. Parkinsonism Relat Disord 2008;14:187–92.
24. Lou JS, Kearns G, Benice T, et al. Levodopa improves physical fatigue in Parkinson’s disease: A double-blind, placebo controlled, crossover study. Mov Disord 2003;18:1108–14.
25. Khedr EM, Galal O, Said A, et al. Lack of post-exercise depression of corticospinal excitability in patients with Parkinson’s disease. Eur J Neurol 2007;14:793–6.
26. Lou JS, Benice T, Kearns G, et al. Levodopa normalizes exercise related cortico-motoneuron excitability abnormalities in Parkinson’s disease. Clin. Neurophysiol 2003;114:930–7.
27. Schifitto G, Friedman JH, Oakes D, et al. Fatigue in levodopa-naive subjects with Parkinson disease. Neurology 2008;71:481–5.
28. Pavese N, Metta V, Bose SK, et al. Fatigue in Parkinson’s disease is linked to striatal and limbic serotonergic dysfunction. Brain 2010;133:3434–43.
29. Brown RG, Dittner A, Findley L, Wessely SC. The Parkinson fatigue scale. Park Relat Disord 2005;11:49–55.
30. Grace J, Mendelsohn A, Friedman JH. A comparison of fatigue measures in Parkinson’s disease. Parkinsonism Relat Disord 2007;13:443–5.
31. Mendonça DA, Menezes K, Jog MS. Methylphenidate improves fatigue scores in Parkinson disease: a randomized controlled trial. Mov Disord 2007;22:2070–6.
32. Lou JS, Dimitrova DM, Park BS, et al. Using modafinil to treat fatigue in Parkinson disease: a double-blind, placebo-controlled pilot study. Clin Neuropharmacol 2009;32:305–10.
33. Ziv I, Avraham M, Michaelov Y, et al. Enhanced fatigue during motor performance in patients with Parkinson’s disease. Neurology 1998;51:1583–6.
34. Stocchi F. Benefits of treatment with rasagiline for fatigue symptoms in patients with early Parkinson’s disease. Eur J Neurol 2014;21:357–60.
35. Marin RS. Apathy: a neuropsychiatric syndrome. J. Neuropsychiatry Clin Neurosci 1991;3:243–4.
36. Marin RS. Apathy: concept, syndrome, neural mechanisms, and treatment. Semin Clin Neuropsychiatry 1996:1:304–14.
37. Levy R, Dubois B. Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cerebral Cortex 2006;16:916–28.
38. Pedersen KF, Larsen JP, Alves G, Aarsland D. Prevalence and clinical correlates of apathy in Parkinson’s disease: a community-based study. Parkinsonism Relat Disord 2009;15:295–9.
39. Pedersen KF, Alves G, Aarsland D, Larsen JP. Occurrence and risk factors for apathy in Parkinson disease: a 4-year prospective longitudinal study. J Neurol Neurosurg Psychiatry 2009;80:1279–82.
40. Pedersen KF, Alves G, Brønnick K, et al. Apathy in drug-naïve patients with incident Parkinson’s disease: The Norwegian ParkWest study. J Neurol 2010;257:217–23.
41. Ziropadja L, Stefanova E, Petrovic M, et al. Apathy and depression in Parkinson’s disease: The Belgrade PD study report. Parkinsonism Relat Disord 2012;18:339–42.
42. Dujardin K, Sockeel P, Devos D, et al. Characteristics of apathy in Parkinson’s disease. Mov Disord 2007;22:778–84.
43. Carriere N, Besson P, Dujardin K, et al. Apathy in Parkinson’s disease is associated with nucleus accumbens atrophy: a magnetic resonance imaging shape analysis. Mov Disord 2014;29;897–903.
44. Reijnders JSAM, Scholtissen B, Weber WEJ, et al. Neuroanatomical correlates of apathy in Parkinson’s disease: a magnetic resonance imaging study using voxel-based morphometry. Mov Disord 2010;25:2318–25.
45. Leroi I, Harbishettar V, Andrews M, et al. Carer burden in apathy and impulse control disorders in Parkinson’s disease. Int J Geriatr Psychiatry 2012;27:160–6.
46. Schiehser DM, Liu L, Lessig SL, et al. Predictors of discrepancies in Parkinson’s disease patient and caregiver ratings of apathy, disinhibition, and executive dysfunction before and after diagnosis. J Int Neuropsychol Soc 2013;19:295–304.
47. Benito-León J, Cubo E, Coronell C, et al. Impact of apathy on health-related quality of life in recently diagnosed Parkinson’s disease: The ANIMO study. Mov Disord 2012;27:211–8.
48. Sockeel P, Dujardin K, Devos D, et al. The Lille apathy rating scale (LARS), a new instrument for detecting and quantifying apathy: validation in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2006;77:579–84.
49. Zahodne LB, Young S, Kirsch-Darrow L, et al. Examination of the Lille Apathy Rating Scale in Parkinson disease. Mov Disord 2009;24:677–83.
50. Drijgers RL, Dujardin K, Reijnders JSAM, et al. Validation of diagnostic criteria for apathy in Parkinson’s disease. Parkinsonism Relat Disord 2010;16:656–60.
51. Leentjens AFG, Koester J, Fruh B, et al. The effect of pramipexole on mood and motivational symptoms in parkinson’s disease: A meta-analysis of placebo-controlled studies. Clin Ther 2009;31:89–98.
52. Thobois S, Ardouin C, Lhommée E, et al. Non-motor dopamine withdrawal syndrome after surgery for Parkinson’s disease: Predictors and underlying mesolimbic denervation. Brain 2010;133:1111–27.
53. Devos D, Moreau C, Maltête D, et al. Rivastigmine in apathetic but dementia and depression-free patients with Parkinson’s disease: a double-blind, placebo-controlled, randomised clinical trial. J Neurol Neurosurg Psychiatry 2014;85:668–74.
54. Smith KM, Eyal E, Weintraub D; ADAGIO Investigators. Combined rasagiline and antidepressant use in Parkinson disease in the ADAGIO study: effects on nonmotor symptoms and tolerability. JAMA Neurol 2015;72:88–95.
55. Forsaa EB, Larsen JP, Wentzel-Larsen T, et al. A 12-year population-based study of psychosis in Parkinson disease. Arch Neurol 2010;67:996–1001.
56. Holroyd S, Currie L, Wooten GF. Prospective study of hallucinations and delusions in Parkinson’s disease. J Neurol Neurosurg Psychiatry 2001;70:734–8.
57. Fénelon G, Alves G. Epidemiology of psychosis in Parkinson’s disease. J Neurol Sci 2010;289:12–7.
58. Mack J, Rabins P, Anderson K, et al. Prevalence of psychotic symptoms in a community-based Parkinson disease sample. Am J Geriatr Psychiatry 2012;20:123–32.
59. Ravina B, Marder K, Fernandez HH, et al. Diagnostic criteria for psychosis in Parkinson’s disease: Report of an NINDS, NIMH Work Group. Mov Disord 2007;22:1061–8.
60. Diederich NJ, Fénelon G, Stebbins G, Goetz CG. Hallucinations in Parkinson disease. Nat Rev Neurol 2009;5:331–42.
61. Gallagher DA, Parkkinen L, O’Sullivan SS, et al. Testing an aetiological model of visual hallucinations in Parkinson’s disease. Brain 2011;134:3299–309.
62. Barnes J, Boubert L, Harris J, et al. Reality monitoring and visual hallucinations in Parkinson’s disease. Neuropsychologia 2003:41:565–74.
63. Kurita A, Murakami M, Takagi S, et al. Visual hallucinations and altered visual information processing in Parkinson disease and dementia with Lewy bodies. Mov Disord 2010;25:167–71.
64. Stebbins GT, Goetz CG, Carrillo MC, et al. Altered cortical visual processing in PD with hallucinations: an fMRI study. Neurology 2004;63:1409–16.
65. Williams DR, Lees AJ. Visual hallucinations in the diagnosis of idiopathic Parkinson’s disease: A retrospective autopsy study. Lancet Neurol 2005:4:605–10.
66. Biglan KM, Holloway RG, McDermott MP, Richard IH. Risk factors for somnolence, edema, and hallucinations in early Parkinson disease. Neurology 2007;69:187–95.
67. Kiziltan G, Ozekmekci S, Ertan S, et al. Relationship between age and subtypes of psychotic symptoms in Parkinson’s disease. J Neurol 2007;254:448–52.
68. Ecker D, Unrath A, Kassubek J, Sabolek M. Dopamine agonists and their risk to induce psychotic episodes in Parkinson’s disease: a case-control study. BMC Neurol 2009;9:23.
69. Huot P, Johnston TH, Darr T, et al. Increased 5-HT2A receptors in the temporal cortex of Parkinsonian patients with visual hallucinations. Mov Disord 2010;25:1399–408.
70. Ballanger B, Strafella AP, van Eimeren T, et al. Serotonin 2A receptors and visual hallucinations in Parkinson disease. Arch. Neurol 2010;67:416–21.
71. Boecker H, Ceballos-Baumann O, Volk D, et al. Metabolic alterations in patients with Parkinson disease and visual hallucinations. Arch Neurol 2007;64:984–8.
72. Sanchez-Castaneda C, Rene R, Ramirez-Ruiz B, et al. Frontal and associative visual areas related to visual hallucinations in dementia with Lewy bodies and Parkinson’s disease with dementia. Mov Disord 2010;25:615–22.
73. Goetz CG, Stebbins GT. Risk factors for nursing home placement in advanced Parkinson’s disease. Neurology 1993;43:2227–9.
74. Friedman JH. Parkinson disease psychosis: update. Behav.Neurol 2013;27:469–77.
75. Pollak P, Tison F, Rascol O, et al. Clozapine in drug induced psychosis in Parkinson’s disease: a randomised, placebo controlled study with open follow up. J Neurol Neurosurg Psychiatry 2004;75:689–95.
76. Parkinson Study Group. Low-dose clozapine for the treatment of drug-induced psychosis. N Engl J Med 1999;340:757–63.
77. Sobow T. Parkinson’s disease-related visual hallucinations unresponsive to atypical antipsychotics treated with cholinesterase inhibitors: a case series. Neurol Neurochir Pol 2007;41:276–9.
78. Fabbrini G, Barbanti P, Aurilia C, et al. Donepezil in the treatment of hallucinations and delusions in Parkinson’s disease. Neurol Sci 2002;23:41–3.
79. Bullock R, Cameron A, Hospital WH. Rivastigmine for the treatment of dementia and visual hallucinations associated with Parkinson’s disease: a case series. Curr Med Res Opin 2002;18,:258–64.
80. Cummings J, Isaacson S, Mills R, et al. Pimavanserin for patients with Parkinson’s disease psychosis: a randomised, placebo-controlled phase 3 trial. Lancet 2014;383:533–40.
81. L. Ishihara L, and C. Brayne C. A systematic review of depression and mental illness preceding Parkinson’s disease. Acta Neurol Scand 2006;113:211–20.
82. Reijnders JSAM, Ehrt U, Weber WEJ, et al. A systematic review of prevalence studies of depression in Parkinson’s disease. Mov Disord 2008;23:183–9.
83. Starkstein SE, Mayberg HS, Leiguarda R, et al. A prospective longitudinal study of depression, cognitive decline, and physical impairments in patients with Parkinson’s disease. J Neurol Neurosurg Psychiatry 1992:55:377–82.
84. Müller B, Assmus J, Herlofson K, et al. Importance of motor vs. non-motor symptoms for health-related quality of life in early Parkinson’s disease. Parkinsonism Relat Disord 2013;19:1027–32.
85. Ravina B, Camicioli R, Como PG, et al. The impact of depressive symptoms in early Parkinson disease. Neurology 2007;69:342–7.
86. Marsh L, McDonald WM, Cummings J, et al. Provisional diagnostic criteria for depression in Parkinson’s disease: report of an NINDS/NIMH work group. Mov Disord 2006;21:148–58.
87. Marsh L. Depression and Parkinson’s disease: current knowledge. Curr. Neurol. Neurosci. Rep 2013; 13:409.
88. Starkstein SE, Merello M, Jorge R, et al. A validation study of depressive syndromes in Parkinson’s disease. Mov Disord 2008;23,:538–46.
89. Williams JR, Hirsch ES, Anderson K, et al. A comparison of nine scales to detect depression in Parkinson disease: which scale to use? Neurology 2012;78:998–1006.
90. Nazem S, Siderowf AD, Duda JE, et al. Suicidal and death ideation in Parkinson’s disease. Mov Disord 2008;23:1573–9.
91. Weintraub D, Duda JE, Carlson K, et al. Suicide ideation and behaviours after STN and GPi DBS surgery for Parkinson’s disease: results from a randomised, controlled trial. J Neurol Neurosurg Psychiatry 2013;84:1113–8.
92. Aarsland D, Påhlhagen S, Ballard CG, et al. Depression in Parkinson disease—epidemiology, mechanisms and management. Nat Rev Neurol 2011;8:35–47.
93. Ehmann TS, Beninger RJ, Gawel MJ, Riopelle RJ. Depressive symptoms in Parkinson’s disease: a comparison with disabled control subjects. J Geriatr Psychiatry Neurol 1990;3:3–9.
94. Witjas T, Kaphan E, Azulay JP, et al. Nonmotor fluctuations in Parkinson’s disease: frequent and disabling. Neurology 2002:59:408–13.
95. Nissenbaum H, Quinn NP, Brown RG, et al. Mood swings associated with the ‘on-off’ phenomenon in Parkinson’s disease. Psychol Med 1987;17:899–904.
96. Maricle RA, Nutt JG, Carter JH. Mood and anxiety fluctuation in Parkinson’s disease associated with levodopa infusion: preliminary findings. Mov Disord 1995;10:329–32.
97. Barone P, Poewe W, Albrecht S, et al. Pramipexole for the treatment of depressive symptoms in patients with Parkinson’s disease: a randomised, double-blind, placebo-controlled trial. Lancet Neurol 2010;9:573–80.
98. Devos D, Dujardin K, Poirot I, et al. Comparison of desipramine and citalopram treatments for depression in Parkinson’s disease: a double-blind, randomized, placebo-controlled study. Mov Disord 2008;23:850–7.
99. Richard IH, McDermott MP, Kurlan R, et al. A randomized, double-blind, placebo-controlled trial of antidepressants in Parkinson disease. Neurology 2012;78:1229–36.
100. Menza M, Dobkin RD, Marin H, et al. A controlled trial of antidepressants in patients with Parkinson disease and depression. Neurology 2009;72:886–92.
101. Seppi K, Weintraub D, Coelho M, et al. The Movement Disorder Society evidence-based medicine review update: treatments for the non-motor symptoms of Parkinson’s disease. Mov Disord 2011;26 Suppl 3:S42–80.
102. Skapinakis P, Bakola E, Salanti G, et al. Efficacy and acceptability of selective serotonin reuptake inhibitors for the treatment of depression in Parkinson’s disease: a systematic review and meta-analysis of randomized controlled trials. BMC Neurol 2010;10:49.
103. Richard IH, Kurlan R, Tanner C, et al. Serotonin syndrome and the combined use of deprenyl and an antidepressant in Parkinson’s disease. Parkinson Study Group. Neurology 1997;48:1070–7.
104. Montgomery EB, Panisset M. Retrospective statistical analysis of the incidence of serotonin toxicity in patients taking rasagiline and anti-depressants in clinical trials. Mov Disord 2009;24:359.
105. Bailine S, Kremen N, Kohen I, et al. Bitemporal electroconvulsive therapy for depression in a Parkinson disease patient with a deep-brain stimulator. J ECT 2008;24:171–2.
106. Faber R, Trimble MR. Electroconvulsive therapy in Parkinson’s disease and other movement disorders. Mov Disord 1991;6:293–303.
107. da Silva TM, Munhoz RP, Alvarez C, et al. Depression in Parkinson’s disease: a double-blind, randomized, placebo-controlled pilot study of omega-3 fatty-acid supplementation. J Affect Disord 2008;111:351–9.
108. Pal E, Nagy F, Aschermann Z, et al. The impact of left prefrontal repetitive transcranial magnetic stimulation on depression in Parkinson’s disease: a randomized, double-blind, placebo-controlled study. Mov Disord 2010;25:2311–7.
109. Dobkin RD, Menza M, Allen LA, et al. Cognitive-behavioral therapy for depression in Parkinson’s disease: a randomized, controlled trial. Am J Psychiatry 2011;168:1066–74.
110. Stein MB, Heuser IJ, Juncos JL, Uhde TW. Anxiety disorders in patients with parkinson’s disease. Am J Psychiatry 1990;147:217–20.
111. Nuti A, Ceravolo R, Piccinni A, et al. Psychiatric comorbidity in a population of Parkinson’s disease patients. Eur J Neurol 2004;11:315–20.
112. Marinus J, Leentjens AFG, Visser M, et al. Evaluation of the Hospital Anxiety and Depression Scale in patients With Parkinson’s disease. Clin Neuropharmacol 2002:25:318–24.
113. Dissanayaka NNW, White E, O’Sullivan JD, et al. The clinical spectrum of anxiety in Parkinson’s disease. Mov Disord 2014;29:967–75.
114. Dissanayaka NNW, Sellbach A, Matheson S, et al. Anxiety disorders in Parkinson’s disease: prevalence and risk factors. Mov Disord 2010;25:838–45.
115. Leentjens AFG, Dujardin K, Pontone GM, et al. The Parkinson anxiety scale (PAS): Development and validation of a new anxiety scale. Mov Disord 2014;29:1035–43.
116. Maricle RA, Nutt JG, Valentine RJ, Carter JH. Dose-response relationship of levodopa with mood and anxiety in fluctuating Parkinson’s disease: a double-blind, placebo-controlled study. Neurology 1995;45:1757–60.
117. Erdal KJ. Depression and anxiety in persons with Parkinson’s disease with and without ‘on–off’ phenomena. J Clin Psychol Med Settings 2001:8:293–9.
118. Leentjens AFG, Dujardin K, Marsh L, et al. Symptomatology and markers of anxiety disorders in Parkinson’s disease: a cross-sectional study. Mov. Disord 2011;26:484–92.
119. Solla P, Cannas A, Floris GL, et al. Behavioral, neuropsychiatric and cognitive disorders in Parkinson’s disease patients with and without motor complications. Prog Neuropsychopharmacol Biol Psychiatry 2011;35:1009–13.
120. E. Stefanova E, L. Ziropadja L, M. Petrović M, et al. Screening for anxiety symptoms in Parkinson disease: a cross-sectional study. J Geriatr Psychiatry Neurol 2013;26:34–40.
121. Jacob EL, Gatto NM, Thompson A, et al. Occurrence of depression and anxiety prior to Parkinson’s disease. Parkinsonism Relat Disord 2010;16:576–81.
122. Craig LH, Svircev A, Haber M, Juncos JL. Controlled pilot study of the effects of neuromuscular therapy in patients with Parkinson’s disease. Mov Disord 2006;21:2127–33.
123. Marino L, Friedman JH. Letter to the editor: Successful use of electroconvulsive therapy for refractory anxiety in Parkinson’s disease. Int J Neurosci 2013;123:70–1.
Treatments for Obstructive Sleep Apnea
From the Center for Narcolepsy, Sleep and Health Research, Department of Biobehavioral Health Science, University of Illinois at Chicago, Chicago, IL.
Abstract
- Objective: To review the efficacy of current treatment options for adults with obstructive sleep apnea (OSA).
- Methods: Review of the literature.
- Results: OSA, characterized by repetitive ≥ 10-second interruptions (apnea) or reductions (hypopnea) in airflow, is initiated by partial or complete collapse in the upper airway despite respiratory effort. When left untreated, OSA is associated with comorbid conditions, such as cardiovascular and metabolic diseases. The current “gold standard” treatment for OSA is continuous positive air pressure (CPAP), which pneumatically stabilizes the upper airways. CPAP has proven efficacy and potential cost savings via decreases in health comorbidities and/or motor-vehicle crashes. However, CPAP treatment is not well-tolerated due to various side effects, and adherence among OSA subjects can be as low as 50% in certain populations. Other treatment options for OSA include improving CPAP tolerability, increasing CPAP adherence through patient interventions, weight loss/exercise, positional therapy, nasal expiratory positive airway pressure, oral pressure therapy, oral appliances, surgery, hypoglossal nerve stimulation, drug treatment, and combining 2 or more of the aforementioned treatments. Despite the many options available to treat OSA, none of them are as efficacious as CPAP. However, many of these treatments are tolerable, and adherence rates are higher than those of the CPAP, making them a more viable treatment option for long-term use.
- Conclusion: Patients need to weigh the benefits and risks of available treatments for OSA. More large randomized controlled studies on treatments or combination of treatments for OSA are needed that measure parameters such as treatment adherence, apnea-hypopnea index, oxygen desaturation, subjective sleepiness, quality of life, and adverse events.
Obstructive sleep apnea (OSA), characterized by repetitive ≥ 10-second interruptions (apnea) or reductions (hypopnea) in airflow (measured as events/hour, called the apnea-hypopnea index [AHI]), is initiated by partial or complete collapse in the upper airway despite respiratory effort [1]. Current estimates of the prevalence of OSA (AHI ≥ 5 and Epworth Sleepiness Scale > 10) in American men and women (aged 30–70 years) are 14% and 5%, respectively, with prevalence rates increasing due to increasing rates of obesity, a risk factor for developing OSA [2]. Hypoxemia/hypercapnia, fragmented sleep, as well as exaggerated fluctuations in heart rhythm, blood pressure, and intrathoracic pressure are some of the acute physiological effects of untreated OSA [1]. These acute effects can develop into long-term sequelae, such as hypertension and other cardiovascular comorbidities [2,3], decrements in cognitive function [4,5], poor mood, reduced quality of life [6,7], and premature death [8,9]. In economic terms, health care cost estimates of OSA and its associated comorbidities rival that of diabetes [10]. Additionally, in the year 2000, more than 800,000 drivers were involved OSA-related motor-vehicle collisions, of which more than 1400 fatalities occurred [11].
Front-line treatment of OSA relies on mechanically stabilizing the upper airway with a column of air via continuous positive airway pressure (CPAP) treatment. Though CPAP is the “gold standard” treatment for OSA with proven efficacy and potential cost savings via decreases in health comorbidities and/or motor-vehicle crashes [10–12], CPAP treatment is not well-tolerated due to various side effects [13–15]. Adherence among OSA subjects can be as low as 50% in certain populations [16–18]. Improved strategies for current and innovative treatments have emerged in the last few years and are the subject of this review.
Improved CPAP Treatment
As stated previously, CPAP pneumatically splints the upper airway, thus preventing it from collapsing during sleep. However, CPAP is not well-tolerated. Modifications to standard CPAP to increase adherence have been met with disappointing results. Humidification with heated tubing delivering heated moistened air did not increase compliance compared to standard CPAP [19]. CPAP was also compared with auto-adjusting CPAP (APAP), where respiration is monitored and the minimum pressure of air is applied to splint the upper airway open. In a meta-analysis, APAP only had very small effect on compliance [20]. Lastly, reduction in pressure during expiration was investigated, and a meta-analysis showed no effect [21,22]. However, recent advances in CPAP delivery give hope to increasing compliance. The S9CPAP machine (Resmed, San Diego, CA), which combines a humidification system and an APAP, showed increased compliance compared to standard CPAP. Compliance increased by an average of 30 minutes per night, and variance of daily usage decreased (eg, patients used it more day-to-day) [23]. However, a randomized blinded study needs to be conducted to corroborate these results.
Promoting CPAP Adherence Through Patient Interventions
Educational, supportive, and behavioral interventions have been used to increase CPAP adherence and have been thoroughly reviewed via meta-analysis [24]. Briefly, 30 studies of various interventions were included and demonstrated that educational, supportive, or behavioral interventions increased CPAP usage in OSA-naive patients. Behavioral interventions increased CPAP usage by over an hour, but the evidence was of “low-quality.” Educational and supportive interventions also increased CPAP usage, with the former having “moderate-quality” evidence [24]. However, whether increased CPAP usage had an effect on symptoms and quality of life was statistically unclear, and the authors recommended further assessment [24]. Three more studies on interventions to increase CPAP usage have been conducted since the aforementioned review. In a randomized controlled study, investigators had OSA patients participate in a 30-minute group social cognitive therapy session (eg, increasing perceived self-efficacy, outcome expectations, and social support) to increase CPAP adherence. Compared to a social interaction control group, there was no increase in adherence rates [25]. In another smaller randomized controlled study that used a social cognition model of behavioral therapy, there were small increases of CPAP usage. At 3 months, the social cognitive intervention increased CPAP usage by an average of 23 minutes per night, increased the number of individuals using their CPAP machine for more than 4 hours compared to standard care group, and decreased symptom of sleepiness [26]. And lastly, a preliminary study looked at increasing adherence rates by utilizing easily accessible alternative care providers, such as nurses and respiratory therapists, for the management of OSA [27]. Though this study had no control group, it did show that good adherence and a decrease in symptoms of sleepiness could be achieved with non-physician management of OSA [27]. A randomized controlled study will be needed to validate the use of alternative care providers.
Interventions have shown some success in increasing adherence rates, but the question remains on who should receive those interventions. Predicting which OSA patients are in most need of an intervention has been studied. A recent study used a 19-question assessment tool called the Index of Nonadherence to PAP to screen for nonadherers (OSA patients who used CPAP for less than 4 hours a night, after 1 month of OSA diagnosis). The assessment tool was 87% sensitive and 63% specific at determining those OSA patients who would not adhere to CPAP treatment [28]. Another study investigated the reliability and validity of a self-rating scale measuring the side effects of CPAP and their consequences on adherence [15]. The investigators showed that the scale was able to reliably discriminate between those who adhered to CPAP treatment and those that did not [15]. Both of these scales can be used to screen OSA patients that need interventions to increase CPAP adherence. Lastly, a recent systematic review showed that a user’s CPAP experience was not defined by the user but by the user’s health care provider, who framed CPAP as “problematic” [29]. The authors argue that users of CPAP are “primed” to reflect negatively on their CPAP experience [29]. Interventions can be used to change the way OSA patients think or feel about their CPAP machines.
When OSA Patients Do Not Adhere to CPAP Treatment
With adherence rates as low as 50% [16–18], those who fail to tolerate CPAP are unlikely to be referred for additional treatment [30]. Those who do tolerate treatment dislike the side effects of CPAP and show an interest in other treatment options [14]. Other treatment options have been shown to decrease the severity of OSA.
Weight Loss and Exercise
OSA prevalence is correlated with body mass index (BMI), and the increasing rates of OSA has been attributed to the increasing rates of obesity in the United States [2]. A meta-analysis of 3 randomized controlled studies of weight loss induced by dieting or lifestyle change showed that weight loss decreased OSA severity. The effect was the greatest for OSA patients who lost more than 10 kg or had severe OSA at baseline [31]. A recent randomized controlled study involving OSA patients with type 2 diabetes investigated if either a weight loss intervention or a diabetes support and education intervention would be able to decrease OSA severity [32]. The weight loss intervention significantly decreased OSA severity, which was largely but not entirely attributed to weight loss. The participants regained 50% of their weight 4 years after the intervention and still had significantly less severe OSA compared to control intervention group. The downside to this intervention is the intensity of the regimen to which the subjects had to adapt: portion-controlled diets with liquid meals and snack bars for the first 4 months and moderate-intensity physical activity for a minimum of 3 hours a week for the first year. After that, patients were still required to follow through with the intervention for 3 years, which included one on-site visit per month and a second contact by phone, mail, or email [32]. One study looked at weight loss and sleep position (supine vs. lateral). The study showed a decrease in AHI in OSA patients that lost weight, and the biggest decrease was in AHI in the lateral sleeping position [33]. Another study looked at the more invasive procedure of bariatric surgery to decrease weight and OSA. At the 1-year follow-up, patients had significantly decreased their BMI and AHI [34]. Two more randomized controlled studies investigated if exercise or fitness level might be beneficial to OSA patients independent of weight loss. Exercise improved AHI even though there was not a significant decrease in weight between the exercise and stretching control group [35]. However, an increase in fitness level did not have any additive effect on the decrease of AHI when weight change was taken into account [36]. The difference in results might be attributed to the latter study using older type 2 diabetic patients and moderate physical activity, while the former studied incorporated moderate-intensity aerobic activity and resistance training for younger patients [35,36]. There is evidence that a sedentary lifestyle increases diurnal leg fluid volume that can shift to the neck during sleep and might play a role in pathogenesis of OSA [37]. Decreasing a sedentary lifestyle by exercising might therefore be beneficial to OSA patients. Given the increasing rates of obesity [2], implementing weight loss as a solution to OSA is viable, especially considering that OSA is not the only comorbid disease of obesity [38].
Positional Therapy
It has been known for some time that sleeping in a supine position doubles a patient’s AHI compared to sleeping in the lateral position [39]. A more recent analysis showed that 60% of patients were “supine predominant OSA;” these patients had supine AHI that was twice that of non-supine AHI [40]. Moreover, a drug-induced sleep endoscopy study showed that the upper airway collapses at multiple levels sleeping in the supine position as opposed to at a single level sleeping in the lateral position [41]. Another study showed that lateral sleeping position improved passive airway anatomy and decreased collapsibility [42]. Many studies have shown that patients who wear a device that alerts the sleeper that he or she is in a supine position (referred to as positional therapy) significantly decreases AHI, but long-term compliance is still an issue, and new and improved devices are needed [43]. Three new studies bolster the effectiveness of positional therapy [44–46]. In all 3 studies, sleeping in the supine position went down to 0% (no change in sleep efficiency [the ratio of total time spent sleeping to the total time spent in bed]), AHI decreased to less than 6, and sleep quality and daytime sleepiness increased and decreased, respectively [44–46]. Compliance was as low as 76% [44] and as high as 93% [46]. For those who cannot tolerate CPAP, positional therapy could be a substitute for decreasing severity of OSA. However, “phenotyping” OSA patients as “supine predominant OSA” would need to be implemented to guarantee efficacy of positional therapy.
Nasal Expiratory Positive Airway Pressure
Oral Pressure Therapy
Retro-palatal collapse occurs in OSA and can be prevented by applying negative pressure to the upper airway [49]. The oral pressure therapy (OPT) device applies gentle suction anteriorly and superiorly to displace the tongue and soft palate and breathing occurs via nasopharyngeal airway [12]. A recent systematic review [49] of OPT revealed that successful OPT treatment rate was 25% to 37% if using standard and stringent definitions of treatment success. Although OPT decreased AHI, residual AHI still remained high due to positional apneas and collapse of upper airway at other levels besides retro-palatal. The authors of this systematic review recommend more rigorous and controlled studies with defined “treatment success” [49]. The advantage of OPT is that adherence was good; patients used the device on average 6 hours a night. There were no severe or serious adverse events with OPT, however oral tissue discomfort or irritation, dental discomfort, and dry mouth were reported [50].
Oral Appliances
Similar to OPT, oral appliances (OAs) attempt to prevent upper airway collapse. OAs either stabilize the tongue, advance the mandible, or lift the soft palate to increase the volumes of the upper airways to avert OSA [16, 51]. The OAs, like the mandibular advancement device, for example, have the added benefit of being fitted specifically for the OSA patient. The mandible for a patient can be advanced to alleviate obstructive apneas, but can also be pulled back if the OA is too uncomfortable or painful. However, there is still dispute on how exactly to titrate these OAs [52]. A meta-analysis recently published looked at all clinical trials of OAs through September 2015. After meeting strict exclusion/inclusion criteria, 17 studies looking at OAs were included in the meta-analysis. There were robust decreases in AHI and in symptoms of sleepiness in OSA patients that used OAs compared to control groups. However, due to the strict inclusion/exclusion criteria of the meta-analysis, all the studies except one used mandibular advancement appliances; one study used a tongue-retaining appliance. The authors concluded that there is sufficient evidence for OAs to be effective in patients with mild-to-moderate OSA [51]. Since the meta-analysis, 6 new studies have been published about OAs. In 4 of the studies (all using mandibular advancement), OAs significantly decreased AHI by 50% or more in the majority of OSA patients [53–56]. The other 2 studies looked at long-term efficacy and compliance. In both studies, there were drastic decreases in AHI when OAs were applied [57, 58]. In one study, about 40% of OSA patients stopped using the OAs. When the change in AHI was stratified between users and non-users, the users group was significantly higher that the non-user group, suggesting that the non-user group were not compliant due to less of an effect of the OA on AHI [57]. In the second study, OSA patients using OAs for a median of 16.5 years were evaluated for long-term efficacy of the OAs. At the short-term follow-up, AHI decreased by more than 50% with use of an OA. However, at the long-term follow-up, the OA lost any effect on AHI. One reason for this is that the OSA patients’ AHI without the OA at the long-term follow-up nearly doubled compared to AHI without OA at the short-term follow-up. The authors conclude that OSA patients using OAs for the long-term might undergo deteriorations in treatment efficacy of OAs, and that regular follow-up appointments with sleep apnea recordings should be implemented [58].
A similarity in all these studies is that adherence was higher for OAs compared to CPAP [51]. The caveat is that most studies have relied on self-reports for adherence rates [12]. However, there were 3 studies that implemented a sensor that measured adherence and compared those results to self-reported OA adherence. All 3 studies showed a strong relationship between self-reports and sensor adherence; patients were honest about adherence to OAs [59–61]. Studies have also been conducted to predict compliance with OAs: higher therapeutic CPAP pressure, age, OSA severity [62], decreased snoring [63], and lower BMI [64, 65] predicted compliance, while dry mouth [63], oropharyngeal crowding [65], and sleeping in a supine position [66] predicted noncompliance. Though adherence rates are high, OAs do not decrease AHI as much as CPAP [67], and a recent study showed that long-term adherence rates might not be different to CPAP adherence rates [68]. OAs, due to their higher adherence rates, are a potential second choice over CPAP. However, they are less efficacious than CPAP at decreasing AHI. That may not be as important since a recent meta-analysis comparing the effects of CPAP or OAs on blood pressure showed that both treatments significantly decreased blood pressure [69]. More studies need to be conducted over long-term efficacy of OAs compared with CPAP.
Surgeries to Treat OSA
Surgery as a treatment option has been extensively reviewed and meta-analyzed [70–78]. Surgery for the treatment of OSA includes tongue suspension [70,74], maxillomandibular advancement (MMA) [72,73,78], pharyngeal surgeries (eg, uvulopharyngopalatoplasty [UPPP]) [73], laser-assisted uvulopalatoplasty (LAUP) [73], radiofrequency ablation (RFA) [73], tracheostomy [71], nasal surgery [75], and glossectomy [77], as well as multi-level and multi-phased procedures [70,74,76,77]. Most studies done on surgeries were case studies, with a minority of investigations that were randomized and controlled. Glossectomy, as part of a multi-level surgical approach, decreased AHI and symptoms of sleepiness, but glossectomy as a stand-alone surgical procedure did not improve AHI [77]. Significant improvements in AHI and sleepiness symptoms were seen in a majority of OSA patients who underwent MMA [72,73,78] and tracheostomy, although tracheostomy was performed for the morbidly obese or those who have failed other traditional surgical treatments [71]. Stand-alone tongue suspension and nasal surgery did not decrease AHI in the majority of patients, though nasal surgery did decrease subjective sleepiness [70,72,74,75]. However, tongue suspension combined with UPPP had better outcomes [70]. LAUP showed inconsistent results with the majority of studies showing no change in AHI, while UPPP and RFA seemed to improved AHI, although some studies showed no change [73]. Multi-level or multi-phase surgeries also showed improvements on OSA severity, but whether these surgeries are better than stand-alone remains to be investigated [73,76]. Morbidity and adverse events, like infection or pain, are common in all of these surgical events [70–78], but there are significant differences between the procedures. For example, MMA had fewer adverse events reported compared to UPPP [73]. More recently, glossectomy via transoral robotic surgery with UPPP [79] or epiglottoplasty [80] has been investigated; there were decreases in AHI, but response rates were between 64% to 73%. Although it seems surgical procedures to treat OSA are plausible, most studies were not rigorous enough to say this with any certainty.
Hypoglossal Nerve Stimulation
OSA subjects experience upper airway obstruction due to loss of genioglossus muscle activity during sleep. Without tongue activation, the negative pressure of breathing causes the upper airways to collapse [81]. Transcutaneous, intraoral, and intramuscular devices used to electrically activate the tongue have been developed and tested; however, although these devices decreased AHI they also induced arousals and sleep fragmentation caused by the electrical stimulus [82–86]. A new method had to be developed that would not be felt by the OSA patient.
In all trials to date, there were significant decreases in AHI as long as 3 years post implantation [87–93]. There were significant improvements in symptoms of sleepiness, mood, quality of life, and sleep quality [87,88,90–94]. When OSA patients had their neurostimulators turned off for 5 days to a week, AHI returned back to baseline levels [89,92]. However, all the trials excluded morbidly obese individuals [87–93] because investigations showed that HNS had no therapeutic effect with elevated BMI [88,90]. The drawbacks of HNS are that it is surgically invasive and minor adverse events have been reported: procedural-related events (eg, numbness/pain/swelling/infection at incision site, temporary tongue weakness) that resolved with time, pain medication, and/or antibiotic treatment, or therapy-related events (eg, tongue abrasions cause by tongue movement over teeth, discomfort associated with stimulation) that resolved after acclimation. Serious adverse events occurred infrequently, such as infection at incision site requiring device removal or subsequent surgery to reposition or replace electrode cuff or malfunctioning neurostimulator [87,88,90]. HNS durability at 18 and 36 months was still very effective, with decreased AHI and increase quality of life and sleep being sustained; adverse events were uncommon this long after implantation [91,93]. Although surgery is required and adverse events are reported, the long-term significant improvement of OSA makes this a very viable treatment option over CPAP. However, increasing prevalence rates of OSA are correlated to increasing obesity rates [2], which may limit the usefulness of HNS since a BMI of more than 40 might preclude individuals to this treatment.
Pharmacologic Treatment
There are no approved pharmacologic treatments for OSA. A recent Cochrane review and meta-analysis assessed clinical trials of various drugs treating OSA. These drugs targeted 5 strategies at alleviating OSA: increasing ventilatory drive (progestogens, theophylline, and acetazolamide), increasing upper airway tone (serotonergics and cholinergics), decreasing rapid eye movement sleep (antidepressants and clonidine), increasing arousal threshold (eszopiclone), and/or increasing the cross-sectional area or reducing the surface tension of the upper airway through topical therapy (fluticasone and lubricant). The review concluded that “some of the drugs may be helpful; however, their tolerability needs to be considered in long-term trials.” Some of these drugs had little or no effect on AHI, and if they did have an effect on AHI, side effects outweighed the benefit [95]. Since then, more investigations of other drugs targeted at the previously aforementioned strategies or via new strategies have been published.
Dronabinol (synthetic Δ9-THC), a nonselective cannabinoid type 1 and type 2 receptor agonist, significantly reduced AHI and improved subjective sleepiness and alertness in a single-blind dose-escalation (2.5, 5, or 10 mg) proof-of-concept study [96,97]. Dronabinol most likely increases upper airway tone though inhibition of vagal afferents [98,99]. There were no serious adverse events associated with dronabinol. Minor adverse events included somnolence and increased appetite. Increased appetite might lead to increased weight and contradict any beneficial effects of dronabinol; however, in the 3-week treatment period no weight gain was observed [97]. This might have been due to drug administration occurring before going to sleep with no opportunity to eat. A larger randomized controlled study will be needed to establish the safety and efficacy of dronabinol.
The sedative zopiclone was used to increase arousal threshold without effecting genioglossus activity [100]. Eszopiclone, a drug in the same class, has been used in the past with unfavorable results [95]. Zopiclone was used in a small double-blind randomized controlled cross-over study. Zopiclone significantly increased respiratory arousal threshold without effecting genioglossus activity or the upper airway’s response to negative pressure. Thus, there was a trend in the zopiclone treatment to increase sleep efficiency. However, zopiclone had no effect on AHI, and increased oxygen desaturation [100]. Similar to eszopiclone, the results for zopiclone are not promising.
A new strategy to treat OSA is to modify pharmacologically “loop gain,” a dimensionless value quantifying the stability of the ventilatory control system. A high loop gain signifies instability in the ventilatory control system and predisposes an OSA person to recurrent apneas [101–103]. Three studies used drugs that inhibit carbonic anhydrase to stabilize the ventilatory control system [104–106]. Two studies used acetazolamide, which decreased loop gain in OSA patients [104,105]. Acetazolamide only decreased AHI in non–rapid eye movement (NREM) sleep, and there was a slight correlation between decrease in loop gain and total AHI [105]. Acetazolamide also decreased ventilatory response to spontaneous arousal, thus promoting ventilatory stability [104]. In the last study, zonisamide, a carbonic anhydrase inhibitor that also causes weight loss, was investigated in OSA patients. Sleep apnea alleviation, measured in terms of absolute elimination of sleep apnea by mechanical or pharmacologic treatment, was 61% and 13% for CPAP and zonisamide, respectively, compared with placebo. In other words, zonisamide decreased AHI but not to the extent of CPAP [106]. Zonisamide also decreased arousals and marginally, but significantly, decreased weight compared to the CPAP group. Although carbonic anhydrase inhibitors have promise as an alternative treatment, long-term use is poorly tolerated [101] and further studies need to be completed.
OSA has been linked with gastroesophageal reflux disease (GERD), with studies suggesting OSA precipitates GERD [107] or GERD precipitates OSA [108]. A meta-analysis was recently published looking at studies that used proton pump inhibitors (PPI) to treat GERD and the effects it would have on OSA [109]. The meta-analysis only included 2 randomized trials and 4 prospective cohort studies. Two of the cohort studies showed a significant decrease, and one cohort showed no difference in apnea indices; and all 4 of the cohort studies showed no difference in AHI. In one trial, the frequency of apnea attacks as recorded by diaries significantly decreased. In 3 cohort studies and one trial, symptoms of sleepiness significantly decreased [109]. A study that was not included in the meta-analysis showed that 3 months of PPI treatment decreased AHI but did not alter sleep efficiency [110]. Larger randomized controlled studies need to be conducted on the effects of PPIs on OSA, especially since PPIs are well tolerated with only weak observational associations between PPI therapy and fractures, pneumonia, mortality, and nutritional deficiencies [111].
The drugs mentioned above have potential for treating OSA in patients intolerant to CPAP. The efficacy and side effects of the drugs will need to be studied for long-term use. However, development of pharmacologic treatments has been hampered by incomplete knowledge of the relevant sleep-dependent peripheral and central neural mechanisms controlling ventilatory drive and upper airway muscles. More importantly, additional basic science research needs to focus on the neurobiological and neurophysiological mechanisms underlying OSA to develop new pharmacotherapies or treatment strategies, or to modify previous treatment strategies.
Treatment Combinations and Phenotyping
It has been recently suggested that combining 2 or more of the above treatments might lead to greater decreases in AHI and greater improvements in subjective sleepiness [112,113]. In fact, one such treatment combination has occurred [114]. Both OA or positional therapy decrease AHI. However, the combination of an OA and positional therapy led to further significant decreases in AHI compared to when those treatments were used alone [114]. To correctly combine treatments, the patient will have to be “phenotyped” via polysomnography to discern the specific pathophysiology of the patient’s OSA. There are published reports of methods to phenotype patients according to their sleep positon, ventilation parameters, loop gain, arousal threshold, and upper airway gain, and if apneic events occur in REM or NREM sleep [40,115]. Defining these traits for individual OSA patients can lead to better efficacy and compliance of combination treatments for OSA. Combination treatment coupled with phenotyping are needed to try to reduce AHI to levels achieved with CPAP.
Conclusion
CPAP is the gold standard treatment because it substantially decreases the severity of OSA just by placing a mask over one’s face before going to sleep. However, it is not tolerable to continually have air forced into your upper airways, and new CPAP devices that heat and humidify the air, and auto titrate the pressure, have been developed to increase adherence rates, but with limited success. For all the treatments listed, a majority do not decrease the severity of OSA to levels achieved with CPAP. However, adherence rates are higher and therefore might, in the long-term, be a better option than CPAP. Some treatments involve invasive surgery to open or stabilize the upper airways, or to implant a stimulator, some treatments involve oral drugs with side effects, and some treatments involve placing appliances on your nose or in your mouth. And some treatments can be combined and individually tailored to the OSA patient via “phenotyping.” For all treatments, the benefits and risks need to be weighed by each patient. More importantly, more large randomized controlled studies on treatments or combination of treatments for OSA are needed using parameters such as treatment adherence, AHI, oxygen desaturation, subjective sleepiness, quality of life, and adverse events (both minor and major) to gauge treatment success in the short-term and long-term. Only then can OSA patients in partnership with their health care provider choose the best treatment option.
Corresponding author: Michael W. Calik, PhD, 845 S. Damen Ave (M/C 802), College of Nursing, Room 740, Chicago, IL 60612, [email protected].
Financial disclosures: None.
1. Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation 2008;118:1080–111.
2. Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006–14.
3. Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA 2003;290:1906–14.
4. Kim HC, Young T, Matthews CG, et al. Sleep-disordered breathing and neuropsychological deficits. A population-based study. Am J Respir Crit Care Med 1997;156:1813–9.
5. Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 2011;306:613–9.
6. Baldwin CM, Griffith KA, Nieto FJ, et al. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep 2001;24:96–105.
7. Peppard PE, Szklo-Coxe M, Hla KM, Young T. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med 2006;166:1709–15.
8. Marshall NS, Wong KK, Liu PY, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 2008;31:1079–85.
9. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 2008;31:1071–8.
10. AlGhanim N, Comondore VR, Fleetham J, et al. The economic impact of obstructive sleep apnea. Lung 2008;186:7–12.
11. Sassani A, Findley LJ, Kryger M, et al. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep 2004;27:453–8.
12. Weaver TE, Calik MW, Farabi SS, et al. Innovative treatments for adults with obstructive sleep apnea. Nat Sci Sleep 2014;6:137–47.
13. Isetta V, Negrin MA, Monasterio C, et al. A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax 2015;70:1054–61.
14. Tsuda H, Moritsuchi Y, Higuchi Y, Tsuda T. Oral health under use of continuous positive airway pressure and interest in alternative therapy in patients with obstructive sleep apnoea: a questionnaire-based survey. Gerodontology 2015 Feb 10.
15. Brostrom A, Arestedt KF, Nilsen P, et al. The side-effects to CPAP treatment inventory: the development and initial validation of a new tool for the measurement of side-effects to CPAP treatment. J Sleep Res 2010;19:603–11.
16. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 2008 Feb 15;5:173–8.
17. Hedner J, Grote L, Zou D. Pharmacological treatment of sleep apnea: current situation and future strategies. Sleep Med Rev 2008;12:33–47.
18. Smith I, Lasserson TJ, Wright J. Drug therapy for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 2006(2):CD003002.
19. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath 2011;15:479–85.
20. Xu T, Li T, Wei D, et al. Effect of automatic versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: an up-to-date meta-analysis. Sleep Breath 2012;16:1017–26.
21. Smith I, Lasserson TJ. Pressure modification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2009 (4):CD003531.
22. Dungan GC, 2nd, Marshall NS, Hoyos CM, et al. A randomized crossover trial of the effect of a novel method of pressure control (SensAwake) in automatic continuous positive airway pressure therapy to treat sleep disordered breathing. J Clin Sleep Med 2011;7:261–7.
23. Wimms AJ, Richards GN, Benjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath 2013;17:69–76.
24. Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2014;1:CD007736.
25. Bartlett D, Wong K, Richards D, et al. Increasing adherence to obstructive sleep apnea treatment with a group social cognitive therapy treatment intervention: a randomized trial. Sleep 2013;36:1647–54.
26. Deng T, Wang Y, Sun M, Chen B. Stage-matched intervention for adherence to CPAP in patients with obstructive sleep apnea: a randomized controlled trial. Sleep Breath 2013;17:791–801.
27. Pendharkar SR, Dechant A, Bischak DP, et al. An observational study of the effectiveness of alternative care providers in the management of obstructive sleep apnoea. J Sleep Res 2015 Oct 27.
28. Sawyer AM, King TS, Hanlon A, et al. Risk assessment for CPAP nonadherence in adults with newly diagnosed obstructive sleep apnea: preliminary testing of the Index for Nonadherence to PAP (I-NAP). Sleep Breath 2014;18:875–83.
29. Ward K, Hoare KJ, Gott M. What is known about the experiences of using CPAP for OSA from the users’ perspective? A systematic integrative literature review. Sleep Med Rev 2014;18:357–66.
30. Russell JO, Gales J, Bae C, Kominsky A. Referral patterns and positive airway pressure adherence upon diagnosis of obstructive sleep apnea. Otolaryngol Head Neck Surg 2015;153:881–7.
31. Hemmingsson E. Does medically induced weight loss improve obstructive sleep apnoea in the obese: review of randomized trials. Clin Obes 2011;1:26–30.
32. Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep 2013;36:641–9A.
33. Kulkas A, Leppanen T, Sahlman J, et al. Weight loss alters severity of individual nocturnal respiratory events depending on sleeping position. Physiol Meas 2014;35:2037–52.
34. Bae EK, Lee YJ, Yun CH, Heo Y. Effects of surgical weight loss for treating obstructive sleep apnea. Sleep Breath 2014;18:901–5.
35. Kline CE, Crowley EP, Ewing GB, et al. The effect of exercise training on obstructive sleep apnea and sleep quality: a randomized controlled trial. Sleep 2011;34:1631–40.
36. Kline CE, Reboussin DM, Foster GD, et al. The effect of changes in cardiorespiratory fitness and weight on obstructive sleep apnea severity in overweight adults with type 2 diabetes. Sleep 2016;39:317–25.
37. Vena D, Yadollahi A, Bradley TD. Modelling fluid accumulation in the neck using simple baseline fluid metrics: implications for sleep apnea. Conf Proc IEEE Eng Med Biol Soc 2014;2014:266–9.
38. Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083–96.
39. Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep 1984;7:110–4.
40. Joosten SA, Hamza K, Sands S, et al. Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology 2012;17:99–107.
41. Lee CH, Kim DK, Kim SY, et al. Changes in site of obstruction in obstructive sleep apnea patients according to sleep position: a DISE study. Laryngoscope 2015;125:248–54.
42. Joosten SA, Edwards BA, Wellman A, et al. The effect of body position on physiological factors that contribute to obstructive sleep apnea. Sleep 2015;38:1469–78.
43. Ravesloot MJ, van Maanen JP, Dun L, de Vries N. The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea-a review of the literature. Sleep Breath 2013;17:39–49.
44. Eijsvogel MM, Ubbink R, Dekker J, et al. Sleep position trainer versus tennis ball technique in positional obstructive sleep apnea syndrome. J Clin Sleep Med 2015;11:139–47.
45. Jackson M, Collins A, Berlowitz D, et al. Efficacy of sleep position modification to treat positional obstructive sleep apnea. Sleep Med 2015;16:545–52.
46. van Maanen JP, Meester KA, Dun LN, et al. The sleep position trainer: a new treatment for positional obstructive sleep apnoea. Sleep Breath 2013;17:771–9.
47. Morrell MJ, Arabi Y, Zahn B, Badr MS. Progressive retropalatal narrowing preceding obstructive apnea. Am J Respir Crit Care Med 1998;158:1974–81.
48. Riaz M, Certal V, Nigam G, et al. Nasal expiratory positive airway pressure devices (Provent) for OSA: a systematic review and meta-analysis. Sleep Disorders 2015;2015:15.
49. Nigam G, Pathak C, Riaz M. Effectiveness of oral pressure therapy in obstructive sleep apnea: a systematic analysis. Sleep Breath 2015 Oct 19.
50. Colrain IM, Black J, Siegel LC, et al. A multicenter evaluation of oral pressure therapy for the treatment of obstructive sleep apnea. Sleep Med 2013;14:830–7.
51. Zhu Y, Long H, Jian F, et al. The effectiveness of oral appliances for obstructive sleep apnea syndrome: A meta-analysis. J Dent 2015;43:1394–402.
52. Dieltjens M, Vanderveken OM, Heyning PH, Braem MJ. Current opinions and clinical practice in the titration of oral appliances in the treatment of sleep-disordered breathing. Sleep Med Rev 2012;16:177–85.
53. Cantore S, Ballini A, Farronato D, et al. Evaluation of an oral appliance in patients with mild to moderate obstructive sleep apnea syndrome intolerant to continuous positive airway pressure use: Preliminary results. Int J Immunopathol Pharmacol 2015 Dec 18.
54. Gjerde K, Lehmann S, Berge ME, et al. Oral appliance treatment in moderate and severe obstructive sleep apnoea patients non-adherent to CPAP. J Oral Rehabil 2015 Dec 27.
55. Jaiswal M, Srivastava GN, Pratap CB, et al. Effect of oral appliance for snoring and obstructive sleep apnea. Int J Orthod Milwaukee 2015;26:67–71.
56. Vecchierini MF, Attali V, Collet JM, et al. A custom-made mandibular repositioning device for obstructive sleep apnoea-hypopnoea syndrome: the ORCADES study. Sleep Med 2015 Jun 29.
57. Haviv Y, Bachar G, Aframian DJ, et al. A 2-year mean follow-up of oral appliance therapy for severe obstructive sleep apnea: a cohort study. Oral Dis 2015;21:386–92.
58. Marklund M. Long-term efficacy of an oral appliance in early treated patients with obstructive sleep apnea. Sleep Breath 2015 Nov 2.
59. Dieltjens M, Braem MJ, Vroegop AV, et al. Objectively measured vs self-reported compliance during oral appliance therapy for sleep-disordered breathing. Chest 2013;144:1495–502.
60. Smith YK, Verrett RG. Evaluation of a novel device for measuring patient compliance with oral appliances in the treatment of obstructive sleep apnea. J Prosthodont 2014;23:31–8.
61. Vanderveken OM, Dieltjens M, Wouters K, et al. Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax 2013;68:91–6.
62. Sutherland K, Phillips CL, Davies A, et al. CPAP pressure for prediction of oral appliance treatment response in obstructive sleep apnea. J Clin Sleep Med 2014;10:943–9.
63. Dieltjens M, Verbruggen AE, Braem MJ, et al. Determinants of objective compliance during oral appliance therapy in patients with sleep-related disordered breathing: a prospective clinical trial. JAMA Otolaryngol Head Neck Surg 2015:894–900.
64. Suzuki K, Nakata S, Tagaya M, et al. Prediction of oral appliance treatment outcome in obstructive sleep apnoea syndrome: a preliminary study. B-ENT 2014;10:185–91.
65. Tsuiki S, Ito E, Isono S, et al. Oropharyngeal crowding and obesity as predictors of oral appliance treatment response to moderate obstructive sleep apnea. Chest 2013;144:558–63.
66. Sutherland K, Takaya H, Qian J, et al. Oral appliance treatment response and polysomnographic phenotypes of obstructive sleep apnea. J Clin Sleep Med 2015;11:861–8.
67. Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 2013;187:879–87.
68. Doff MH, Hoekema A, Wijkstra PJ, et al. Oral appliance versus continuous positive airway pressure in obstructive sleep apnea syndrome: a 2-year follow-up. Sleep 2013;36:1289–96.
69. Bratton DJ, Gaisl T, Wons AM, Kohler M. CPAP vs mandibular advancement devices and blood pressure in patients with obstructive sleep apnea: a systematic review and meta-analysis. JAMA 2015;314:2280–93.
70. Bostanci A, Turhan M. A systematic review of tongue base suspension techniques as an isolated procedure or combined with uvulopalatopharyngoplasty in obstructive sleep apnea. Eur Arch Otorhinolaryngol 2015 Oct 27.
71. Camacho M, Certal V, Brietzke SE, et al. Tracheostomy as treatment for adult obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope 2014;124:803–11.
72. Camacho M, Teixeira J, Abdullatif J, et al. Maxillomandibular advancement and tracheostomy for morbidly obese obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2015;152:619–30.
73. Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep 2010;33:1396–407.
74. Handler E, Hamans E, Goldberg AN, Mickelson S. Tongue suspension: an evidence-based review and comparison to hypopharyngeal surgery for OSA. Laryngoscope 2014;124:329–36.
75. Ishii L, Roxbury C, Godoy A, et al. Does nasal surgery improve osa in patients with nasal obstruction and OSA? a meta-analysis. Otolaryngol Head Neck Surg 2015;153:326–33.
76. Lin HC, Friedman M, Chang HW, Gurpinar B. The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope 2008;118:902–8.
77. Murphey AW, Kandl JA, Nguyen SA, et al. The effect of glossectomy for obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2015;153:334–42.
78. Zaghi S, Holty JC, Certal V, et al. Maxillomandibular advancement for treatment of obstructive sleep apnea: a meta-analysis. JAMA Otolaryngol Head Neck Surg 2015 Nov 25:1–9.
79. Thaler ER, Rassekh CH, Lee JM, et al. Outcomes for multilevel surgery for sleep apnea: Obstructive sleep apnea, transoral robotic surgery, and uvulopalatopharyngoplasty. Laryngoscope 2015 Jul 7.
80. Arora A, Chaidas K, Garas G, et al. Outcome of TORS to tongue base and epiglottis in patients with OSA intolerant of conventional treatment. Sleep Breath 2015 Dec 15.
81. Remmers JE, deGroot WJ, Sauerland EK, Anch AM. Pathogenesis of upper airway occlusion during sleep. J Appl Physiol Respir Environ Exercise Physiol 1978;44:931–8.
82. Decker MJ, Haaga J, Arnold JL, et al. Functional electrical stimulation and respiration during sleep. J Appl Physiol (1985) 1993;75:1053–61.
83. Edmonds LC, Daniels BK, Stanson AW, et al. The effects of transcutaneous electrical stimulation during wakefulness and sleep in patients with obstructive sleep apnea. Am Rev Respir Dis 1992;146:1030–6.
84. Guilleminault C, Powell N, Bowman B, Stoohs R. The effect of electrical stimulation on obstructive sleep apnea syndrome. Chest 1995;107:67–73.
85. Miki H, Hida W, Chonan T, et al. Effects of submental electrical stimulation during sleep on upper airway patency in patients with obstructive sleep apnea. Am Rev Respir Dis 1989;140:1285–9.
86. Steier J, Seymour J, Rafferty GF, et al. Continuous transcutaneous submental electrical stimulation in obstructive sleep apnea: a feasibility study. Chest 2011;140:998–1007.
87. Eastwood PR, Barnes M, Walsh JH, et al. Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep 2011;34:1479–86.
88. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res 2014;23:77–83.
89. Strollo PJ, Jr., Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med 2014;370:139–49.
90. Van de Heyning PH, Badr MS, Baskin JZ, et al. Implanted upper airway stimulation device for obstructive sleep apnea. Laryngoscope 2012;122:1626–33.
91. Strollo PJ, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep 2015;38:1593–8.
92. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg 2014;151:880–7.
93. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg 2015 Nov 17.
94. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med 2016;12:43-8.
95. Mason M, Welsh EJ, Smith I. Drug therapy for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 2013;(5):CD003002.
96. Farabi SS, Prasad B, Quinn L, Carley DW. Impact of dronabinol on quantitative electroencephalogram (qEEG) measures of sleep in obstructive sleep apnea syndrome. J Clin Sleep Med 2014;10:49–56.
97. Prasad B, Radulovacki MG, Carley DW. Proof of concept trial of dronabinol in obstructive sleep apnea. Front Psychiatry 2013;4:1.
98. Calik MW, Carley DW. Cannabinoid type 1 and type 2 receptor antagonists prevent attenuation of serotonin-induced reflex apneas by dronabinol in Sprague-Dawley rats. PLoS One 2014;9:e111412.
99. Calik MW, Radulovacki M, Carley DW. Intranodose ganglion injections of dronabinol attenuate serotonin-induced apnea in Sprague-Dawley rat. Respir Physiol Neurobiol. 2014 Jan 1;190:20–4.
100. Carter SG, Berger MS, Carberry JC, et al. Zopiclone increases the arousal threshold without impairing genioglossus activity in obstructive sleep apnea. Sleep 2015 Dec 22.
101. Burgess KR. New insights from the measurement of loop gain in obstructive sleep apnoea. J Physiol 2012;590(Pt 8):1781–2.
102. Eckert DJ, White DP, Jordan AS, et al. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med 2013;188:996–1004.
103. Salloum A, Rowley JA, Mateika JH, et al. Increased propensity for central apnea in patients with obstructive sleep apnea: effect of nasal continuous positive airway pressure. Am J Respir Crit Care Med 2010;181:189–93.
104. Edwards BA, Connolly JG, Campana LM, et al. Acetazolamide attenuates the ventilatory response to arousal in patients with obstructive sleep apnea. Sleep 2013;36:281–5.
105. Edwards BA, Sands SA, Eckert DJ, et al. Acetazolamide improves loop gain but not the other physiological traits causing obstructive sleep apnoea. J Physiol 2012;590(Pt 5):1199–211.
106. Eskandari D, Zou D, Karimi M, et al. Zonisamide reduces obstructive sleep apnoea: a randomised placebo-controlled study. Eur Resp J 2014;44:140–9.
107. Yang YX, Spencer G, Schutte-Rodin S, et al. Gastroesophageal reflux and sleep events in obstructive sleep apnea. Eur J Gastroenterol Hepatol 2013;25:1017–23.
108. Gilani S, Quan SF, Pynnonen MA, Shin JJ. Obstructive sleep apnea and gastroesophageal reflux: a multivariate population-level analysis. Otolaryngol Head Neck Surg 2015 Dec 8.
109. Rassameehiran S, Klomjit S, Hosiriluck N, Nugent K. Meta-analysis of the effect of proton pump inhibitors on obstructive sleep apnea symptoms and indices in patients with gastroesophageal reflux disease. Proc (Bayl Univ Med Cent) 2016;29:3–6.
110. Ermis F, Akyuz F, Arici S, et al. Effect of proton pump inhibitor (PPI) treatment in obstructive sleep apnea syndrome: an esophageal impedance-pHmetry study. Hepatogastroenterology 2011;58:1566–73.
111. Reimer C. Safety of long-term PPI therapy. Best Pract Res 2013;27:443–54.
112. Deacon NL, Jen R, Li Y, Malhotra A. Treatment of obstructive sleep apnea. prospects for personalized combined modality therapy. Ann Am Thorac Soc 2016;13:101–8.
113. Shin W, Jen R, Li Y, Malhotra A. Tailored treatment strategies for obstructive sleep apnea. Respir Investig 2016;54:2–7.
114. Dieltjens M, Vroegop AV, Verbruggen AE, et al. A promising concept of combination therapy for positional obstructive sleep apnea. Sleep Breath 2015;19:637–44.
115. Wellman A, Edwards BA, Sands SA, et al. A simplified method for determining phenotypic traits in patients with obstructive sleep apnea. J Appl Physiol (1985) 2013;114:911–22.
From the Center for Narcolepsy, Sleep and Health Research, Department of Biobehavioral Health Science, University of Illinois at Chicago, Chicago, IL.
Abstract
- Objective: To review the efficacy of current treatment options for adults with obstructive sleep apnea (OSA).
- Methods: Review of the literature.
- Results: OSA, characterized by repetitive ≥ 10-second interruptions (apnea) or reductions (hypopnea) in airflow, is initiated by partial or complete collapse in the upper airway despite respiratory effort. When left untreated, OSA is associated with comorbid conditions, such as cardiovascular and metabolic diseases. The current “gold standard” treatment for OSA is continuous positive air pressure (CPAP), which pneumatically stabilizes the upper airways. CPAP has proven efficacy and potential cost savings via decreases in health comorbidities and/or motor-vehicle crashes. However, CPAP treatment is not well-tolerated due to various side effects, and adherence among OSA subjects can be as low as 50% in certain populations. Other treatment options for OSA include improving CPAP tolerability, increasing CPAP adherence through patient interventions, weight loss/exercise, positional therapy, nasal expiratory positive airway pressure, oral pressure therapy, oral appliances, surgery, hypoglossal nerve stimulation, drug treatment, and combining 2 or more of the aforementioned treatments. Despite the many options available to treat OSA, none of them are as efficacious as CPAP. However, many of these treatments are tolerable, and adherence rates are higher than those of the CPAP, making them a more viable treatment option for long-term use.
- Conclusion: Patients need to weigh the benefits and risks of available treatments for OSA. More large randomized controlled studies on treatments or combination of treatments for OSA are needed that measure parameters such as treatment adherence, apnea-hypopnea index, oxygen desaturation, subjective sleepiness, quality of life, and adverse events.
Obstructive sleep apnea (OSA), characterized by repetitive ≥ 10-second interruptions (apnea) or reductions (hypopnea) in airflow (measured as events/hour, called the apnea-hypopnea index [AHI]), is initiated by partial or complete collapse in the upper airway despite respiratory effort [1]. Current estimates of the prevalence of OSA (AHI ≥ 5 and Epworth Sleepiness Scale > 10) in American men and women (aged 30–70 years) are 14% and 5%, respectively, with prevalence rates increasing due to increasing rates of obesity, a risk factor for developing OSA [2]. Hypoxemia/hypercapnia, fragmented sleep, as well as exaggerated fluctuations in heart rhythm, blood pressure, and intrathoracic pressure are some of the acute physiological effects of untreated OSA [1]. These acute effects can develop into long-term sequelae, such as hypertension and other cardiovascular comorbidities [2,3], decrements in cognitive function [4,5], poor mood, reduced quality of life [6,7], and premature death [8,9]. In economic terms, health care cost estimates of OSA and its associated comorbidities rival that of diabetes [10]. Additionally, in the year 2000, more than 800,000 drivers were involved OSA-related motor-vehicle collisions, of which more than 1400 fatalities occurred [11].
Front-line treatment of OSA relies on mechanically stabilizing the upper airway with a column of air via continuous positive airway pressure (CPAP) treatment. Though CPAP is the “gold standard” treatment for OSA with proven efficacy and potential cost savings via decreases in health comorbidities and/or motor-vehicle crashes [10–12], CPAP treatment is not well-tolerated due to various side effects [13–15]. Adherence among OSA subjects can be as low as 50% in certain populations [16–18]. Improved strategies for current and innovative treatments have emerged in the last few years and are the subject of this review.
Improved CPAP Treatment
As stated previously, CPAP pneumatically splints the upper airway, thus preventing it from collapsing during sleep. However, CPAP is not well-tolerated. Modifications to standard CPAP to increase adherence have been met with disappointing results. Humidification with heated tubing delivering heated moistened air did not increase compliance compared to standard CPAP [19]. CPAP was also compared with auto-adjusting CPAP (APAP), where respiration is monitored and the minimum pressure of air is applied to splint the upper airway open. In a meta-analysis, APAP only had very small effect on compliance [20]. Lastly, reduction in pressure during expiration was investigated, and a meta-analysis showed no effect [21,22]. However, recent advances in CPAP delivery give hope to increasing compliance. The S9CPAP machine (Resmed, San Diego, CA), which combines a humidification system and an APAP, showed increased compliance compared to standard CPAP. Compliance increased by an average of 30 minutes per night, and variance of daily usage decreased (eg, patients used it more day-to-day) [23]. However, a randomized blinded study needs to be conducted to corroborate these results.
Promoting CPAP Adherence Through Patient Interventions
Educational, supportive, and behavioral interventions have been used to increase CPAP adherence and have been thoroughly reviewed via meta-analysis [24]. Briefly, 30 studies of various interventions were included and demonstrated that educational, supportive, or behavioral interventions increased CPAP usage in OSA-naive patients. Behavioral interventions increased CPAP usage by over an hour, but the evidence was of “low-quality.” Educational and supportive interventions also increased CPAP usage, with the former having “moderate-quality” evidence [24]. However, whether increased CPAP usage had an effect on symptoms and quality of life was statistically unclear, and the authors recommended further assessment [24]. Three more studies on interventions to increase CPAP usage have been conducted since the aforementioned review. In a randomized controlled study, investigators had OSA patients participate in a 30-minute group social cognitive therapy session (eg, increasing perceived self-efficacy, outcome expectations, and social support) to increase CPAP adherence. Compared to a social interaction control group, there was no increase in adherence rates [25]. In another smaller randomized controlled study that used a social cognition model of behavioral therapy, there were small increases of CPAP usage. At 3 months, the social cognitive intervention increased CPAP usage by an average of 23 minutes per night, increased the number of individuals using their CPAP machine for more than 4 hours compared to standard care group, and decreased symptom of sleepiness [26]. And lastly, a preliminary study looked at increasing adherence rates by utilizing easily accessible alternative care providers, such as nurses and respiratory therapists, for the management of OSA [27]. Though this study had no control group, it did show that good adherence and a decrease in symptoms of sleepiness could be achieved with non-physician management of OSA [27]. A randomized controlled study will be needed to validate the use of alternative care providers.
Interventions have shown some success in increasing adherence rates, but the question remains on who should receive those interventions. Predicting which OSA patients are in most need of an intervention has been studied. A recent study used a 19-question assessment tool called the Index of Nonadherence to PAP to screen for nonadherers (OSA patients who used CPAP for less than 4 hours a night, after 1 month of OSA diagnosis). The assessment tool was 87% sensitive and 63% specific at determining those OSA patients who would not adhere to CPAP treatment [28]. Another study investigated the reliability and validity of a self-rating scale measuring the side effects of CPAP and their consequences on adherence [15]. The investigators showed that the scale was able to reliably discriminate between those who adhered to CPAP treatment and those that did not [15]. Both of these scales can be used to screen OSA patients that need interventions to increase CPAP adherence. Lastly, a recent systematic review showed that a user’s CPAP experience was not defined by the user but by the user’s health care provider, who framed CPAP as “problematic” [29]. The authors argue that users of CPAP are “primed” to reflect negatively on their CPAP experience [29]. Interventions can be used to change the way OSA patients think or feel about their CPAP machines.
When OSA Patients Do Not Adhere to CPAP Treatment
With adherence rates as low as 50% [16–18], those who fail to tolerate CPAP are unlikely to be referred for additional treatment [30]. Those who do tolerate treatment dislike the side effects of CPAP and show an interest in other treatment options [14]. Other treatment options have been shown to decrease the severity of OSA.
Weight Loss and Exercise
OSA prevalence is correlated with body mass index (BMI), and the increasing rates of OSA has been attributed to the increasing rates of obesity in the United States [2]. A meta-analysis of 3 randomized controlled studies of weight loss induced by dieting or lifestyle change showed that weight loss decreased OSA severity. The effect was the greatest for OSA patients who lost more than 10 kg or had severe OSA at baseline [31]. A recent randomized controlled study involving OSA patients with type 2 diabetes investigated if either a weight loss intervention or a diabetes support and education intervention would be able to decrease OSA severity [32]. The weight loss intervention significantly decreased OSA severity, which was largely but not entirely attributed to weight loss. The participants regained 50% of their weight 4 years after the intervention and still had significantly less severe OSA compared to control intervention group. The downside to this intervention is the intensity of the regimen to which the subjects had to adapt: portion-controlled diets with liquid meals and snack bars for the first 4 months and moderate-intensity physical activity for a minimum of 3 hours a week for the first year. After that, patients were still required to follow through with the intervention for 3 years, which included one on-site visit per month and a second contact by phone, mail, or email [32]. One study looked at weight loss and sleep position (supine vs. lateral). The study showed a decrease in AHI in OSA patients that lost weight, and the biggest decrease was in AHI in the lateral sleeping position [33]. Another study looked at the more invasive procedure of bariatric surgery to decrease weight and OSA. At the 1-year follow-up, patients had significantly decreased their BMI and AHI [34]. Two more randomized controlled studies investigated if exercise or fitness level might be beneficial to OSA patients independent of weight loss. Exercise improved AHI even though there was not a significant decrease in weight between the exercise and stretching control group [35]. However, an increase in fitness level did not have any additive effect on the decrease of AHI when weight change was taken into account [36]. The difference in results might be attributed to the latter study using older type 2 diabetic patients and moderate physical activity, while the former studied incorporated moderate-intensity aerobic activity and resistance training for younger patients [35,36]. There is evidence that a sedentary lifestyle increases diurnal leg fluid volume that can shift to the neck during sleep and might play a role in pathogenesis of OSA [37]. Decreasing a sedentary lifestyle by exercising might therefore be beneficial to OSA patients. Given the increasing rates of obesity [2], implementing weight loss as a solution to OSA is viable, especially considering that OSA is not the only comorbid disease of obesity [38].
Positional Therapy
It has been known for some time that sleeping in a supine position doubles a patient’s AHI compared to sleeping in the lateral position [39]. A more recent analysis showed that 60% of patients were “supine predominant OSA;” these patients had supine AHI that was twice that of non-supine AHI [40]. Moreover, a drug-induced sleep endoscopy study showed that the upper airway collapses at multiple levels sleeping in the supine position as opposed to at a single level sleeping in the lateral position [41]. Another study showed that lateral sleeping position improved passive airway anatomy and decreased collapsibility [42]. Many studies have shown that patients who wear a device that alerts the sleeper that he or she is in a supine position (referred to as positional therapy) significantly decreases AHI, but long-term compliance is still an issue, and new and improved devices are needed [43]. Three new studies bolster the effectiveness of positional therapy [44–46]. In all 3 studies, sleeping in the supine position went down to 0% (no change in sleep efficiency [the ratio of total time spent sleeping to the total time spent in bed]), AHI decreased to less than 6, and sleep quality and daytime sleepiness increased and decreased, respectively [44–46]. Compliance was as low as 76% [44] and as high as 93% [46]. For those who cannot tolerate CPAP, positional therapy could be a substitute for decreasing severity of OSA. However, “phenotyping” OSA patients as “supine predominant OSA” would need to be implemented to guarantee efficacy of positional therapy.
Nasal Expiratory Positive Airway Pressure
Oral Pressure Therapy
Retro-palatal collapse occurs in OSA and can be prevented by applying negative pressure to the upper airway [49]. The oral pressure therapy (OPT) device applies gentle suction anteriorly and superiorly to displace the tongue and soft palate and breathing occurs via nasopharyngeal airway [12]. A recent systematic review [49] of OPT revealed that successful OPT treatment rate was 25% to 37% if using standard and stringent definitions of treatment success. Although OPT decreased AHI, residual AHI still remained high due to positional apneas and collapse of upper airway at other levels besides retro-palatal. The authors of this systematic review recommend more rigorous and controlled studies with defined “treatment success” [49]. The advantage of OPT is that adherence was good; patients used the device on average 6 hours a night. There were no severe or serious adverse events with OPT, however oral tissue discomfort or irritation, dental discomfort, and dry mouth were reported [50].
Oral Appliances
Similar to OPT, oral appliances (OAs) attempt to prevent upper airway collapse. OAs either stabilize the tongue, advance the mandible, or lift the soft palate to increase the volumes of the upper airways to avert OSA [16, 51]. The OAs, like the mandibular advancement device, for example, have the added benefit of being fitted specifically for the OSA patient. The mandible for a patient can be advanced to alleviate obstructive apneas, but can also be pulled back if the OA is too uncomfortable or painful. However, there is still dispute on how exactly to titrate these OAs [52]. A meta-analysis recently published looked at all clinical trials of OAs through September 2015. After meeting strict exclusion/inclusion criteria, 17 studies looking at OAs were included in the meta-analysis. There were robust decreases in AHI and in symptoms of sleepiness in OSA patients that used OAs compared to control groups. However, due to the strict inclusion/exclusion criteria of the meta-analysis, all the studies except one used mandibular advancement appliances; one study used a tongue-retaining appliance. The authors concluded that there is sufficient evidence for OAs to be effective in patients with mild-to-moderate OSA [51]. Since the meta-analysis, 6 new studies have been published about OAs. In 4 of the studies (all using mandibular advancement), OAs significantly decreased AHI by 50% or more in the majority of OSA patients [53–56]. The other 2 studies looked at long-term efficacy and compliance. In both studies, there were drastic decreases in AHI when OAs were applied [57, 58]. In one study, about 40% of OSA patients stopped using the OAs. When the change in AHI was stratified between users and non-users, the users group was significantly higher that the non-user group, suggesting that the non-user group were not compliant due to less of an effect of the OA on AHI [57]. In the second study, OSA patients using OAs for a median of 16.5 years were evaluated for long-term efficacy of the OAs. At the short-term follow-up, AHI decreased by more than 50% with use of an OA. However, at the long-term follow-up, the OA lost any effect on AHI. One reason for this is that the OSA patients’ AHI without the OA at the long-term follow-up nearly doubled compared to AHI without OA at the short-term follow-up. The authors conclude that OSA patients using OAs for the long-term might undergo deteriorations in treatment efficacy of OAs, and that regular follow-up appointments with sleep apnea recordings should be implemented [58].
A similarity in all these studies is that adherence was higher for OAs compared to CPAP [51]. The caveat is that most studies have relied on self-reports for adherence rates [12]. However, there were 3 studies that implemented a sensor that measured adherence and compared those results to self-reported OA adherence. All 3 studies showed a strong relationship between self-reports and sensor adherence; patients were honest about adherence to OAs [59–61]. Studies have also been conducted to predict compliance with OAs: higher therapeutic CPAP pressure, age, OSA severity [62], decreased snoring [63], and lower BMI [64, 65] predicted compliance, while dry mouth [63], oropharyngeal crowding [65], and sleeping in a supine position [66] predicted noncompliance. Though adherence rates are high, OAs do not decrease AHI as much as CPAP [67], and a recent study showed that long-term adherence rates might not be different to CPAP adherence rates [68]. OAs, due to their higher adherence rates, are a potential second choice over CPAP. However, they are less efficacious than CPAP at decreasing AHI. That may not be as important since a recent meta-analysis comparing the effects of CPAP or OAs on blood pressure showed that both treatments significantly decreased blood pressure [69]. More studies need to be conducted over long-term efficacy of OAs compared with CPAP.
Surgeries to Treat OSA
Surgery as a treatment option has been extensively reviewed and meta-analyzed [70–78]. Surgery for the treatment of OSA includes tongue suspension [70,74], maxillomandibular advancement (MMA) [72,73,78], pharyngeal surgeries (eg, uvulopharyngopalatoplasty [UPPP]) [73], laser-assisted uvulopalatoplasty (LAUP) [73], radiofrequency ablation (RFA) [73], tracheostomy [71], nasal surgery [75], and glossectomy [77], as well as multi-level and multi-phased procedures [70,74,76,77]. Most studies done on surgeries were case studies, with a minority of investigations that were randomized and controlled. Glossectomy, as part of a multi-level surgical approach, decreased AHI and symptoms of sleepiness, but glossectomy as a stand-alone surgical procedure did not improve AHI [77]. Significant improvements in AHI and sleepiness symptoms were seen in a majority of OSA patients who underwent MMA [72,73,78] and tracheostomy, although tracheostomy was performed for the morbidly obese or those who have failed other traditional surgical treatments [71]. Stand-alone tongue suspension and nasal surgery did not decrease AHI in the majority of patients, though nasal surgery did decrease subjective sleepiness [70,72,74,75]. However, tongue suspension combined with UPPP had better outcomes [70]. LAUP showed inconsistent results with the majority of studies showing no change in AHI, while UPPP and RFA seemed to improved AHI, although some studies showed no change [73]. Multi-level or multi-phase surgeries also showed improvements on OSA severity, but whether these surgeries are better than stand-alone remains to be investigated [73,76]. Morbidity and adverse events, like infection or pain, are common in all of these surgical events [70–78], but there are significant differences between the procedures. For example, MMA had fewer adverse events reported compared to UPPP [73]. More recently, glossectomy via transoral robotic surgery with UPPP [79] or epiglottoplasty [80] has been investigated; there were decreases in AHI, but response rates were between 64% to 73%. Although it seems surgical procedures to treat OSA are plausible, most studies were not rigorous enough to say this with any certainty.
Hypoglossal Nerve Stimulation
OSA subjects experience upper airway obstruction due to loss of genioglossus muscle activity during sleep. Without tongue activation, the negative pressure of breathing causes the upper airways to collapse [81]. Transcutaneous, intraoral, and intramuscular devices used to electrically activate the tongue have been developed and tested; however, although these devices decreased AHI they also induced arousals and sleep fragmentation caused by the electrical stimulus [82–86]. A new method had to be developed that would not be felt by the OSA patient.
In all trials to date, there were significant decreases in AHI as long as 3 years post implantation [87–93]. There were significant improvements in symptoms of sleepiness, mood, quality of life, and sleep quality [87,88,90–94]. When OSA patients had their neurostimulators turned off for 5 days to a week, AHI returned back to baseline levels [89,92]. However, all the trials excluded morbidly obese individuals [87–93] because investigations showed that HNS had no therapeutic effect with elevated BMI [88,90]. The drawbacks of HNS are that it is surgically invasive and minor adverse events have been reported: procedural-related events (eg, numbness/pain/swelling/infection at incision site, temporary tongue weakness) that resolved with time, pain medication, and/or antibiotic treatment, or therapy-related events (eg, tongue abrasions cause by tongue movement over teeth, discomfort associated with stimulation) that resolved after acclimation. Serious adverse events occurred infrequently, such as infection at incision site requiring device removal or subsequent surgery to reposition or replace electrode cuff or malfunctioning neurostimulator [87,88,90]. HNS durability at 18 and 36 months was still very effective, with decreased AHI and increase quality of life and sleep being sustained; adverse events were uncommon this long after implantation [91,93]. Although surgery is required and adverse events are reported, the long-term significant improvement of OSA makes this a very viable treatment option over CPAP. However, increasing prevalence rates of OSA are correlated to increasing obesity rates [2], which may limit the usefulness of HNS since a BMI of more than 40 might preclude individuals to this treatment.
Pharmacologic Treatment
There are no approved pharmacologic treatments for OSA. A recent Cochrane review and meta-analysis assessed clinical trials of various drugs treating OSA. These drugs targeted 5 strategies at alleviating OSA: increasing ventilatory drive (progestogens, theophylline, and acetazolamide), increasing upper airway tone (serotonergics and cholinergics), decreasing rapid eye movement sleep (antidepressants and clonidine), increasing arousal threshold (eszopiclone), and/or increasing the cross-sectional area or reducing the surface tension of the upper airway through topical therapy (fluticasone and lubricant). The review concluded that “some of the drugs may be helpful; however, their tolerability needs to be considered in long-term trials.” Some of these drugs had little or no effect on AHI, and if they did have an effect on AHI, side effects outweighed the benefit [95]. Since then, more investigations of other drugs targeted at the previously aforementioned strategies or via new strategies have been published.
Dronabinol (synthetic Δ9-THC), a nonselective cannabinoid type 1 and type 2 receptor agonist, significantly reduced AHI and improved subjective sleepiness and alertness in a single-blind dose-escalation (2.5, 5, or 10 mg) proof-of-concept study [96,97]. Dronabinol most likely increases upper airway tone though inhibition of vagal afferents [98,99]. There were no serious adverse events associated with dronabinol. Minor adverse events included somnolence and increased appetite. Increased appetite might lead to increased weight and contradict any beneficial effects of dronabinol; however, in the 3-week treatment period no weight gain was observed [97]. This might have been due to drug administration occurring before going to sleep with no opportunity to eat. A larger randomized controlled study will be needed to establish the safety and efficacy of dronabinol.
The sedative zopiclone was used to increase arousal threshold without effecting genioglossus activity [100]. Eszopiclone, a drug in the same class, has been used in the past with unfavorable results [95]. Zopiclone was used in a small double-blind randomized controlled cross-over study. Zopiclone significantly increased respiratory arousal threshold without effecting genioglossus activity or the upper airway’s response to negative pressure. Thus, there was a trend in the zopiclone treatment to increase sleep efficiency. However, zopiclone had no effect on AHI, and increased oxygen desaturation [100]. Similar to eszopiclone, the results for zopiclone are not promising.
A new strategy to treat OSA is to modify pharmacologically “loop gain,” a dimensionless value quantifying the stability of the ventilatory control system. A high loop gain signifies instability in the ventilatory control system and predisposes an OSA person to recurrent apneas [101–103]. Three studies used drugs that inhibit carbonic anhydrase to stabilize the ventilatory control system [104–106]. Two studies used acetazolamide, which decreased loop gain in OSA patients [104,105]. Acetazolamide only decreased AHI in non–rapid eye movement (NREM) sleep, and there was a slight correlation between decrease in loop gain and total AHI [105]. Acetazolamide also decreased ventilatory response to spontaneous arousal, thus promoting ventilatory stability [104]. In the last study, zonisamide, a carbonic anhydrase inhibitor that also causes weight loss, was investigated in OSA patients. Sleep apnea alleviation, measured in terms of absolute elimination of sleep apnea by mechanical or pharmacologic treatment, was 61% and 13% for CPAP and zonisamide, respectively, compared with placebo. In other words, zonisamide decreased AHI but not to the extent of CPAP [106]. Zonisamide also decreased arousals and marginally, but significantly, decreased weight compared to the CPAP group. Although carbonic anhydrase inhibitors have promise as an alternative treatment, long-term use is poorly tolerated [101] and further studies need to be completed.
OSA has been linked with gastroesophageal reflux disease (GERD), with studies suggesting OSA precipitates GERD [107] or GERD precipitates OSA [108]. A meta-analysis was recently published looking at studies that used proton pump inhibitors (PPI) to treat GERD and the effects it would have on OSA [109]. The meta-analysis only included 2 randomized trials and 4 prospective cohort studies. Two of the cohort studies showed a significant decrease, and one cohort showed no difference in apnea indices; and all 4 of the cohort studies showed no difference in AHI. In one trial, the frequency of apnea attacks as recorded by diaries significantly decreased. In 3 cohort studies and one trial, symptoms of sleepiness significantly decreased [109]. A study that was not included in the meta-analysis showed that 3 months of PPI treatment decreased AHI but did not alter sleep efficiency [110]. Larger randomized controlled studies need to be conducted on the effects of PPIs on OSA, especially since PPIs are well tolerated with only weak observational associations between PPI therapy and fractures, pneumonia, mortality, and nutritional deficiencies [111].
The drugs mentioned above have potential for treating OSA in patients intolerant to CPAP. The efficacy and side effects of the drugs will need to be studied for long-term use. However, development of pharmacologic treatments has been hampered by incomplete knowledge of the relevant sleep-dependent peripheral and central neural mechanisms controlling ventilatory drive and upper airway muscles. More importantly, additional basic science research needs to focus on the neurobiological and neurophysiological mechanisms underlying OSA to develop new pharmacotherapies or treatment strategies, or to modify previous treatment strategies.
Treatment Combinations and Phenotyping
It has been recently suggested that combining 2 or more of the above treatments might lead to greater decreases in AHI and greater improvements in subjective sleepiness [112,113]. In fact, one such treatment combination has occurred [114]. Both OA or positional therapy decrease AHI. However, the combination of an OA and positional therapy led to further significant decreases in AHI compared to when those treatments were used alone [114]. To correctly combine treatments, the patient will have to be “phenotyped” via polysomnography to discern the specific pathophysiology of the patient’s OSA. There are published reports of methods to phenotype patients according to their sleep positon, ventilation parameters, loop gain, arousal threshold, and upper airway gain, and if apneic events occur in REM or NREM sleep [40,115]. Defining these traits for individual OSA patients can lead to better efficacy and compliance of combination treatments for OSA. Combination treatment coupled with phenotyping are needed to try to reduce AHI to levels achieved with CPAP.
Conclusion
CPAP is the gold standard treatment because it substantially decreases the severity of OSA just by placing a mask over one’s face before going to sleep. However, it is not tolerable to continually have air forced into your upper airways, and new CPAP devices that heat and humidify the air, and auto titrate the pressure, have been developed to increase adherence rates, but with limited success. For all the treatments listed, a majority do not decrease the severity of OSA to levels achieved with CPAP. However, adherence rates are higher and therefore might, in the long-term, be a better option than CPAP. Some treatments involve invasive surgery to open or stabilize the upper airways, or to implant a stimulator, some treatments involve oral drugs with side effects, and some treatments involve placing appliances on your nose or in your mouth. And some treatments can be combined and individually tailored to the OSA patient via “phenotyping.” For all treatments, the benefits and risks need to be weighed by each patient. More importantly, more large randomized controlled studies on treatments or combination of treatments for OSA are needed using parameters such as treatment adherence, AHI, oxygen desaturation, subjective sleepiness, quality of life, and adverse events (both minor and major) to gauge treatment success in the short-term and long-term. Only then can OSA patients in partnership with their health care provider choose the best treatment option.
Corresponding author: Michael W. Calik, PhD, 845 S. Damen Ave (M/C 802), College of Nursing, Room 740, Chicago, IL 60612, [email protected].
Financial disclosures: None.
From the Center for Narcolepsy, Sleep and Health Research, Department of Biobehavioral Health Science, University of Illinois at Chicago, Chicago, IL.
Abstract
- Objective: To review the efficacy of current treatment options for adults with obstructive sleep apnea (OSA).
- Methods: Review of the literature.
- Results: OSA, characterized by repetitive ≥ 10-second interruptions (apnea) or reductions (hypopnea) in airflow, is initiated by partial or complete collapse in the upper airway despite respiratory effort. When left untreated, OSA is associated with comorbid conditions, such as cardiovascular and metabolic diseases. The current “gold standard” treatment for OSA is continuous positive air pressure (CPAP), which pneumatically stabilizes the upper airways. CPAP has proven efficacy and potential cost savings via decreases in health comorbidities and/or motor-vehicle crashes. However, CPAP treatment is not well-tolerated due to various side effects, and adherence among OSA subjects can be as low as 50% in certain populations. Other treatment options for OSA include improving CPAP tolerability, increasing CPAP adherence through patient interventions, weight loss/exercise, positional therapy, nasal expiratory positive airway pressure, oral pressure therapy, oral appliances, surgery, hypoglossal nerve stimulation, drug treatment, and combining 2 or more of the aforementioned treatments. Despite the many options available to treat OSA, none of them are as efficacious as CPAP. However, many of these treatments are tolerable, and adherence rates are higher than those of the CPAP, making them a more viable treatment option for long-term use.
- Conclusion: Patients need to weigh the benefits and risks of available treatments for OSA. More large randomized controlled studies on treatments or combination of treatments for OSA are needed that measure parameters such as treatment adherence, apnea-hypopnea index, oxygen desaturation, subjective sleepiness, quality of life, and adverse events.
Obstructive sleep apnea (OSA), characterized by repetitive ≥ 10-second interruptions (apnea) or reductions (hypopnea) in airflow (measured as events/hour, called the apnea-hypopnea index [AHI]), is initiated by partial or complete collapse in the upper airway despite respiratory effort [1]. Current estimates of the prevalence of OSA (AHI ≥ 5 and Epworth Sleepiness Scale > 10) in American men and women (aged 30–70 years) are 14% and 5%, respectively, with prevalence rates increasing due to increasing rates of obesity, a risk factor for developing OSA [2]. Hypoxemia/hypercapnia, fragmented sleep, as well as exaggerated fluctuations in heart rhythm, blood pressure, and intrathoracic pressure are some of the acute physiological effects of untreated OSA [1]. These acute effects can develop into long-term sequelae, such as hypertension and other cardiovascular comorbidities [2,3], decrements in cognitive function [4,5], poor mood, reduced quality of life [6,7], and premature death [8,9]. In economic terms, health care cost estimates of OSA and its associated comorbidities rival that of diabetes [10]. Additionally, in the year 2000, more than 800,000 drivers were involved OSA-related motor-vehicle collisions, of which more than 1400 fatalities occurred [11].
Front-line treatment of OSA relies on mechanically stabilizing the upper airway with a column of air via continuous positive airway pressure (CPAP) treatment. Though CPAP is the “gold standard” treatment for OSA with proven efficacy and potential cost savings via decreases in health comorbidities and/or motor-vehicle crashes [10–12], CPAP treatment is not well-tolerated due to various side effects [13–15]. Adherence among OSA subjects can be as low as 50% in certain populations [16–18]. Improved strategies for current and innovative treatments have emerged in the last few years and are the subject of this review.
Improved CPAP Treatment
As stated previously, CPAP pneumatically splints the upper airway, thus preventing it from collapsing during sleep. However, CPAP is not well-tolerated. Modifications to standard CPAP to increase adherence have been met with disappointing results. Humidification with heated tubing delivering heated moistened air did not increase compliance compared to standard CPAP [19]. CPAP was also compared with auto-adjusting CPAP (APAP), where respiration is monitored and the minimum pressure of air is applied to splint the upper airway open. In a meta-analysis, APAP only had very small effect on compliance [20]. Lastly, reduction in pressure during expiration was investigated, and a meta-analysis showed no effect [21,22]. However, recent advances in CPAP delivery give hope to increasing compliance. The S9CPAP machine (Resmed, San Diego, CA), which combines a humidification system and an APAP, showed increased compliance compared to standard CPAP. Compliance increased by an average of 30 minutes per night, and variance of daily usage decreased (eg, patients used it more day-to-day) [23]. However, a randomized blinded study needs to be conducted to corroborate these results.
Promoting CPAP Adherence Through Patient Interventions
Educational, supportive, and behavioral interventions have been used to increase CPAP adherence and have been thoroughly reviewed via meta-analysis [24]. Briefly, 30 studies of various interventions were included and demonstrated that educational, supportive, or behavioral interventions increased CPAP usage in OSA-naive patients. Behavioral interventions increased CPAP usage by over an hour, but the evidence was of “low-quality.” Educational and supportive interventions also increased CPAP usage, with the former having “moderate-quality” evidence [24]. However, whether increased CPAP usage had an effect on symptoms and quality of life was statistically unclear, and the authors recommended further assessment [24]. Three more studies on interventions to increase CPAP usage have been conducted since the aforementioned review. In a randomized controlled study, investigators had OSA patients participate in a 30-minute group social cognitive therapy session (eg, increasing perceived self-efficacy, outcome expectations, and social support) to increase CPAP adherence. Compared to a social interaction control group, there was no increase in adherence rates [25]. In another smaller randomized controlled study that used a social cognition model of behavioral therapy, there were small increases of CPAP usage. At 3 months, the social cognitive intervention increased CPAP usage by an average of 23 minutes per night, increased the number of individuals using their CPAP machine for more than 4 hours compared to standard care group, and decreased symptom of sleepiness [26]. And lastly, a preliminary study looked at increasing adherence rates by utilizing easily accessible alternative care providers, such as nurses and respiratory therapists, for the management of OSA [27]. Though this study had no control group, it did show that good adherence and a decrease in symptoms of sleepiness could be achieved with non-physician management of OSA [27]. A randomized controlled study will be needed to validate the use of alternative care providers.
Interventions have shown some success in increasing adherence rates, but the question remains on who should receive those interventions. Predicting which OSA patients are in most need of an intervention has been studied. A recent study used a 19-question assessment tool called the Index of Nonadherence to PAP to screen for nonadherers (OSA patients who used CPAP for less than 4 hours a night, after 1 month of OSA diagnosis). The assessment tool was 87% sensitive and 63% specific at determining those OSA patients who would not adhere to CPAP treatment [28]. Another study investigated the reliability and validity of a self-rating scale measuring the side effects of CPAP and their consequences on adherence [15]. The investigators showed that the scale was able to reliably discriminate between those who adhered to CPAP treatment and those that did not [15]. Both of these scales can be used to screen OSA patients that need interventions to increase CPAP adherence. Lastly, a recent systematic review showed that a user’s CPAP experience was not defined by the user but by the user’s health care provider, who framed CPAP as “problematic” [29]. The authors argue that users of CPAP are “primed” to reflect negatively on their CPAP experience [29]. Interventions can be used to change the way OSA patients think or feel about their CPAP machines.
When OSA Patients Do Not Adhere to CPAP Treatment
With adherence rates as low as 50% [16–18], those who fail to tolerate CPAP are unlikely to be referred for additional treatment [30]. Those who do tolerate treatment dislike the side effects of CPAP and show an interest in other treatment options [14]. Other treatment options have been shown to decrease the severity of OSA.
Weight Loss and Exercise
OSA prevalence is correlated with body mass index (BMI), and the increasing rates of OSA has been attributed to the increasing rates of obesity in the United States [2]. A meta-analysis of 3 randomized controlled studies of weight loss induced by dieting or lifestyle change showed that weight loss decreased OSA severity. The effect was the greatest for OSA patients who lost more than 10 kg or had severe OSA at baseline [31]. A recent randomized controlled study involving OSA patients with type 2 diabetes investigated if either a weight loss intervention or a diabetes support and education intervention would be able to decrease OSA severity [32]. The weight loss intervention significantly decreased OSA severity, which was largely but not entirely attributed to weight loss. The participants regained 50% of their weight 4 years after the intervention and still had significantly less severe OSA compared to control intervention group. The downside to this intervention is the intensity of the regimen to which the subjects had to adapt: portion-controlled diets with liquid meals and snack bars for the first 4 months and moderate-intensity physical activity for a minimum of 3 hours a week for the first year. After that, patients were still required to follow through with the intervention for 3 years, which included one on-site visit per month and a second contact by phone, mail, or email [32]. One study looked at weight loss and sleep position (supine vs. lateral). The study showed a decrease in AHI in OSA patients that lost weight, and the biggest decrease was in AHI in the lateral sleeping position [33]. Another study looked at the more invasive procedure of bariatric surgery to decrease weight and OSA. At the 1-year follow-up, patients had significantly decreased their BMI and AHI [34]. Two more randomized controlled studies investigated if exercise or fitness level might be beneficial to OSA patients independent of weight loss. Exercise improved AHI even though there was not a significant decrease in weight between the exercise and stretching control group [35]. However, an increase in fitness level did not have any additive effect on the decrease of AHI when weight change was taken into account [36]. The difference in results might be attributed to the latter study using older type 2 diabetic patients and moderate physical activity, while the former studied incorporated moderate-intensity aerobic activity and resistance training for younger patients [35,36]. There is evidence that a sedentary lifestyle increases diurnal leg fluid volume that can shift to the neck during sleep and might play a role in pathogenesis of OSA [37]. Decreasing a sedentary lifestyle by exercising might therefore be beneficial to OSA patients. Given the increasing rates of obesity [2], implementing weight loss as a solution to OSA is viable, especially considering that OSA is not the only comorbid disease of obesity [38].
Positional Therapy
It has been known for some time that sleeping in a supine position doubles a patient’s AHI compared to sleeping in the lateral position [39]. A more recent analysis showed that 60% of patients were “supine predominant OSA;” these patients had supine AHI that was twice that of non-supine AHI [40]. Moreover, a drug-induced sleep endoscopy study showed that the upper airway collapses at multiple levels sleeping in the supine position as opposed to at a single level sleeping in the lateral position [41]. Another study showed that lateral sleeping position improved passive airway anatomy and decreased collapsibility [42]. Many studies have shown that patients who wear a device that alerts the sleeper that he or she is in a supine position (referred to as positional therapy) significantly decreases AHI, but long-term compliance is still an issue, and new and improved devices are needed [43]. Three new studies bolster the effectiveness of positional therapy [44–46]. In all 3 studies, sleeping in the supine position went down to 0% (no change in sleep efficiency [the ratio of total time spent sleeping to the total time spent in bed]), AHI decreased to less than 6, and sleep quality and daytime sleepiness increased and decreased, respectively [44–46]. Compliance was as low as 76% [44] and as high as 93% [46]. For those who cannot tolerate CPAP, positional therapy could be a substitute for decreasing severity of OSA. However, “phenotyping” OSA patients as “supine predominant OSA” would need to be implemented to guarantee efficacy of positional therapy.
Nasal Expiratory Positive Airway Pressure
Oral Pressure Therapy
Retro-palatal collapse occurs in OSA and can be prevented by applying negative pressure to the upper airway [49]. The oral pressure therapy (OPT) device applies gentle suction anteriorly and superiorly to displace the tongue and soft palate and breathing occurs via nasopharyngeal airway [12]. A recent systematic review [49] of OPT revealed that successful OPT treatment rate was 25% to 37% if using standard and stringent definitions of treatment success. Although OPT decreased AHI, residual AHI still remained high due to positional apneas and collapse of upper airway at other levels besides retro-palatal. The authors of this systematic review recommend more rigorous and controlled studies with defined “treatment success” [49]. The advantage of OPT is that adherence was good; patients used the device on average 6 hours a night. There were no severe or serious adverse events with OPT, however oral tissue discomfort or irritation, dental discomfort, and dry mouth were reported [50].
Oral Appliances
Similar to OPT, oral appliances (OAs) attempt to prevent upper airway collapse. OAs either stabilize the tongue, advance the mandible, or lift the soft palate to increase the volumes of the upper airways to avert OSA [16, 51]. The OAs, like the mandibular advancement device, for example, have the added benefit of being fitted specifically for the OSA patient. The mandible for a patient can be advanced to alleviate obstructive apneas, but can also be pulled back if the OA is too uncomfortable or painful. However, there is still dispute on how exactly to titrate these OAs [52]. A meta-analysis recently published looked at all clinical trials of OAs through September 2015. After meeting strict exclusion/inclusion criteria, 17 studies looking at OAs were included in the meta-analysis. There were robust decreases in AHI and in symptoms of sleepiness in OSA patients that used OAs compared to control groups. However, due to the strict inclusion/exclusion criteria of the meta-analysis, all the studies except one used mandibular advancement appliances; one study used a tongue-retaining appliance. The authors concluded that there is sufficient evidence for OAs to be effective in patients with mild-to-moderate OSA [51]. Since the meta-analysis, 6 new studies have been published about OAs. In 4 of the studies (all using mandibular advancement), OAs significantly decreased AHI by 50% or more in the majority of OSA patients [53–56]. The other 2 studies looked at long-term efficacy and compliance. In both studies, there were drastic decreases in AHI when OAs were applied [57, 58]. In one study, about 40% of OSA patients stopped using the OAs. When the change in AHI was stratified between users and non-users, the users group was significantly higher that the non-user group, suggesting that the non-user group were not compliant due to less of an effect of the OA on AHI [57]. In the second study, OSA patients using OAs for a median of 16.5 years were evaluated for long-term efficacy of the OAs. At the short-term follow-up, AHI decreased by more than 50% with use of an OA. However, at the long-term follow-up, the OA lost any effect on AHI. One reason for this is that the OSA patients’ AHI without the OA at the long-term follow-up nearly doubled compared to AHI without OA at the short-term follow-up. The authors conclude that OSA patients using OAs for the long-term might undergo deteriorations in treatment efficacy of OAs, and that regular follow-up appointments with sleep apnea recordings should be implemented [58].
A similarity in all these studies is that adherence was higher for OAs compared to CPAP [51]. The caveat is that most studies have relied on self-reports for adherence rates [12]. However, there were 3 studies that implemented a sensor that measured adherence and compared those results to self-reported OA adherence. All 3 studies showed a strong relationship between self-reports and sensor adherence; patients were honest about adherence to OAs [59–61]. Studies have also been conducted to predict compliance with OAs: higher therapeutic CPAP pressure, age, OSA severity [62], decreased snoring [63], and lower BMI [64, 65] predicted compliance, while dry mouth [63], oropharyngeal crowding [65], and sleeping in a supine position [66] predicted noncompliance. Though adherence rates are high, OAs do not decrease AHI as much as CPAP [67], and a recent study showed that long-term adherence rates might not be different to CPAP adherence rates [68]. OAs, due to their higher adherence rates, are a potential second choice over CPAP. However, they are less efficacious than CPAP at decreasing AHI. That may not be as important since a recent meta-analysis comparing the effects of CPAP or OAs on blood pressure showed that both treatments significantly decreased blood pressure [69]. More studies need to be conducted over long-term efficacy of OAs compared with CPAP.
Surgeries to Treat OSA
Surgery as a treatment option has been extensively reviewed and meta-analyzed [70–78]. Surgery for the treatment of OSA includes tongue suspension [70,74], maxillomandibular advancement (MMA) [72,73,78], pharyngeal surgeries (eg, uvulopharyngopalatoplasty [UPPP]) [73], laser-assisted uvulopalatoplasty (LAUP) [73], radiofrequency ablation (RFA) [73], tracheostomy [71], nasal surgery [75], and glossectomy [77], as well as multi-level and multi-phased procedures [70,74,76,77]. Most studies done on surgeries were case studies, with a minority of investigations that were randomized and controlled. Glossectomy, as part of a multi-level surgical approach, decreased AHI and symptoms of sleepiness, but glossectomy as a stand-alone surgical procedure did not improve AHI [77]. Significant improvements in AHI and sleepiness symptoms were seen in a majority of OSA patients who underwent MMA [72,73,78] and tracheostomy, although tracheostomy was performed for the morbidly obese or those who have failed other traditional surgical treatments [71]. Stand-alone tongue suspension and nasal surgery did not decrease AHI in the majority of patients, though nasal surgery did decrease subjective sleepiness [70,72,74,75]. However, tongue suspension combined with UPPP had better outcomes [70]. LAUP showed inconsistent results with the majority of studies showing no change in AHI, while UPPP and RFA seemed to improved AHI, although some studies showed no change [73]. Multi-level or multi-phase surgeries also showed improvements on OSA severity, but whether these surgeries are better than stand-alone remains to be investigated [73,76]. Morbidity and adverse events, like infection or pain, are common in all of these surgical events [70–78], but there are significant differences between the procedures. For example, MMA had fewer adverse events reported compared to UPPP [73]. More recently, glossectomy via transoral robotic surgery with UPPP [79] or epiglottoplasty [80] has been investigated; there were decreases in AHI, but response rates were between 64% to 73%. Although it seems surgical procedures to treat OSA are plausible, most studies were not rigorous enough to say this with any certainty.
Hypoglossal Nerve Stimulation
OSA subjects experience upper airway obstruction due to loss of genioglossus muscle activity during sleep. Without tongue activation, the negative pressure of breathing causes the upper airways to collapse [81]. Transcutaneous, intraoral, and intramuscular devices used to electrically activate the tongue have been developed and tested; however, although these devices decreased AHI they also induced arousals and sleep fragmentation caused by the electrical stimulus [82–86]. A new method had to be developed that would not be felt by the OSA patient.
In all trials to date, there were significant decreases in AHI as long as 3 years post implantation [87–93]. There were significant improvements in symptoms of sleepiness, mood, quality of life, and sleep quality [87,88,90–94]. When OSA patients had their neurostimulators turned off for 5 days to a week, AHI returned back to baseline levels [89,92]. However, all the trials excluded morbidly obese individuals [87–93] because investigations showed that HNS had no therapeutic effect with elevated BMI [88,90]. The drawbacks of HNS are that it is surgically invasive and minor adverse events have been reported: procedural-related events (eg, numbness/pain/swelling/infection at incision site, temporary tongue weakness) that resolved with time, pain medication, and/or antibiotic treatment, or therapy-related events (eg, tongue abrasions cause by tongue movement over teeth, discomfort associated with stimulation) that resolved after acclimation. Serious adverse events occurred infrequently, such as infection at incision site requiring device removal or subsequent surgery to reposition or replace electrode cuff or malfunctioning neurostimulator [87,88,90]. HNS durability at 18 and 36 months was still very effective, with decreased AHI and increase quality of life and sleep being sustained; adverse events were uncommon this long after implantation [91,93]. Although surgery is required and adverse events are reported, the long-term significant improvement of OSA makes this a very viable treatment option over CPAP. However, increasing prevalence rates of OSA are correlated to increasing obesity rates [2], which may limit the usefulness of HNS since a BMI of more than 40 might preclude individuals to this treatment.
Pharmacologic Treatment
There are no approved pharmacologic treatments for OSA. A recent Cochrane review and meta-analysis assessed clinical trials of various drugs treating OSA. These drugs targeted 5 strategies at alleviating OSA: increasing ventilatory drive (progestogens, theophylline, and acetazolamide), increasing upper airway tone (serotonergics and cholinergics), decreasing rapid eye movement sleep (antidepressants and clonidine), increasing arousal threshold (eszopiclone), and/or increasing the cross-sectional area or reducing the surface tension of the upper airway through topical therapy (fluticasone and lubricant). The review concluded that “some of the drugs may be helpful; however, their tolerability needs to be considered in long-term trials.” Some of these drugs had little or no effect on AHI, and if they did have an effect on AHI, side effects outweighed the benefit [95]. Since then, more investigations of other drugs targeted at the previously aforementioned strategies or via new strategies have been published.
Dronabinol (synthetic Δ9-THC), a nonselective cannabinoid type 1 and type 2 receptor agonist, significantly reduced AHI and improved subjective sleepiness and alertness in a single-blind dose-escalation (2.5, 5, or 10 mg) proof-of-concept study [96,97]. Dronabinol most likely increases upper airway tone though inhibition of vagal afferents [98,99]. There were no serious adverse events associated with dronabinol. Minor adverse events included somnolence and increased appetite. Increased appetite might lead to increased weight and contradict any beneficial effects of dronabinol; however, in the 3-week treatment period no weight gain was observed [97]. This might have been due to drug administration occurring before going to sleep with no opportunity to eat. A larger randomized controlled study will be needed to establish the safety and efficacy of dronabinol.
The sedative zopiclone was used to increase arousal threshold without effecting genioglossus activity [100]. Eszopiclone, a drug in the same class, has been used in the past with unfavorable results [95]. Zopiclone was used in a small double-blind randomized controlled cross-over study. Zopiclone significantly increased respiratory arousal threshold without effecting genioglossus activity or the upper airway’s response to negative pressure. Thus, there was a trend in the zopiclone treatment to increase sleep efficiency. However, zopiclone had no effect on AHI, and increased oxygen desaturation [100]. Similar to eszopiclone, the results for zopiclone are not promising.
A new strategy to treat OSA is to modify pharmacologically “loop gain,” a dimensionless value quantifying the stability of the ventilatory control system. A high loop gain signifies instability in the ventilatory control system and predisposes an OSA person to recurrent apneas [101–103]. Three studies used drugs that inhibit carbonic anhydrase to stabilize the ventilatory control system [104–106]. Two studies used acetazolamide, which decreased loop gain in OSA patients [104,105]. Acetazolamide only decreased AHI in non–rapid eye movement (NREM) sleep, and there was a slight correlation between decrease in loop gain and total AHI [105]. Acetazolamide also decreased ventilatory response to spontaneous arousal, thus promoting ventilatory stability [104]. In the last study, zonisamide, a carbonic anhydrase inhibitor that also causes weight loss, was investigated in OSA patients. Sleep apnea alleviation, measured in terms of absolute elimination of sleep apnea by mechanical or pharmacologic treatment, was 61% and 13% for CPAP and zonisamide, respectively, compared with placebo. In other words, zonisamide decreased AHI but not to the extent of CPAP [106]. Zonisamide also decreased arousals and marginally, but significantly, decreased weight compared to the CPAP group. Although carbonic anhydrase inhibitors have promise as an alternative treatment, long-term use is poorly tolerated [101] and further studies need to be completed.
OSA has been linked with gastroesophageal reflux disease (GERD), with studies suggesting OSA precipitates GERD [107] or GERD precipitates OSA [108]. A meta-analysis was recently published looking at studies that used proton pump inhibitors (PPI) to treat GERD and the effects it would have on OSA [109]. The meta-analysis only included 2 randomized trials and 4 prospective cohort studies. Two of the cohort studies showed a significant decrease, and one cohort showed no difference in apnea indices; and all 4 of the cohort studies showed no difference in AHI. In one trial, the frequency of apnea attacks as recorded by diaries significantly decreased. In 3 cohort studies and one trial, symptoms of sleepiness significantly decreased [109]. A study that was not included in the meta-analysis showed that 3 months of PPI treatment decreased AHI but did not alter sleep efficiency [110]. Larger randomized controlled studies need to be conducted on the effects of PPIs on OSA, especially since PPIs are well tolerated with only weak observational associations between PPI therapy and fractures, pneumonia, mortality, and nutritional deficiencies [111].
The drugs mentioned above have potential for treating OSA in patients intolerant to CPAP. The efficacy and side effects of the drugs will need to be studied for long-term use. However, development of pharmacologic treatments has been hampered by incomplete knowledge of the relevant sleep-dependent peripheral and central neural mechanisms controlling ventilatory drive and upper airway muscles. More importantly, additional basic science research needs to focus on the neurobiological and neurophysiological mechanisms underlying OSA to develop new pharmacotherapies or treatment strategies, or to modify previous treatment strategies.
Treatment Combinations and Phenotyping
It has been recently suggested that combining 2 or more of the above treatments might lead to greater decreases in AHI and greater improvements in subjective sleepiness [112,113]. In fact, one such treatment combination has occurred [114]. Both OA or positional therapy decrease AHI. However, the combination of an OA and positional therapy led to further significant decreases in AHI compared to when those treatments were used alone [114]. To correctly combine treatments, the patient will have to be “phenotyped” via polysomnography to discern the specific pathophysiology of the patient’s OSA. There are published reports of methods to phenotype patients according to their sleep positon, ventilation parameters, loop gain, arousal threshold, and upper airway gain, and if apneic events occur in REM or NREM sleep [40,115]. Defining these traits for individual OSA patients can lead to better efficacy and compliance of combination treatments for OSA. Combination treatment coupled with phenotyping are needed to try to reduce AHI to levels achieved with CPAP.
Conclusion
CPAP is the gold standard treatment because it substantially decreases the severity of OSA just by placing a mask over one’s face before going to sleep. However, it is not tolerable to continually have air forced into your upper airways, and new CPAP devices that heat and humidify the air, and auto titrate the pressure, have been developed to increase adherence rates, but with limited success. For all the treatments listed, a majority do not decrease the severity of OSA to levels achieved with CPAP. However, adherence rates are higher and therefore might, in the long-term, be a better option than CPAP. Some treatments involve invasive surgery to open or stabilize the upper airways, or to implant a stimulator, some treatments involve oral drugs with side effects, and some treatments involve placing appliances on your nose or in your mouth. And some treatments can be combined and individually tailored to the OSA patient via “phenotyping.” For all treatments, the benefits and risks need to be weighed by each patient. More importantly, more large randomized controlled studies on treatments or combination of treatments for OSA are needed using parameters such as treatment adherence, AHI, oxygen desaturation, subjective sleepiness, quality of life, and adverse events (both minor and major) to gauge treatment success in the short-term and long-term. Only then can OSA patients in partnership with their health care provider choose the best treatment option.
Corresponding author: Michael W. Calik, PhD, 845 S. Damen Ave (M/C 802), College of Nursing, Room 740, Chicago, IL 60612, [email protected].
Financial disclosures: None.
1. Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation 2008;118:1080–111.
2. Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006–14.
3. Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA 2003;290:1906–14.
4. Kim HC, Young T, Matthews CG, et al. Sleep-disordered breathing and neuropsychological deficits. A population-based study. Am J Respir Crit Care Med 1997;156:1813–9.
5. Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 2011;306:613–9.
6. Baldwin CM, Griffith KA, Nieto FJ, et al. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep 2001;24:96–105.
7. Peppard PE, Szklo-Coxe M, Hla KM, Young T. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med 2006;166:1709–15.
8. Marshall NS, Wong KK, Liu PY, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 2008;31:1079–85.
9. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 2008;31:1071–8.
10. AlGhanim N, Comondore VR, Fleetham J, et al. The economic impact of obstructive sleep apnea. Lung 2008;186:7–12.
11. Sassani A, Findley LJ, Kryger M, et al. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep 2004;27:453–8.
12. Weaver TE, Calik MW, Farabi SS, et al. Innovative treatments for adults with obstructive sleep apnea. Nat Sci Sleep 2014;6:137–47.
13. Isetta V, Negrin MA, Monasterio C, et al. A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax 2015;70:1054–61.
14. Tsuda H, Moritsuchi Y, Higuchi Y, Tsuda T. Oral health under use of continuous positive airway pressure and interest in alternative therapy in patients with obstructive sleep apnoea: a questionnaire-based survey. Gerodontology 2015 Feb 10.
15. Brostrom A, Arestedt KF, Nilsen P, et al. The side-effects to CPAP treatment inventory: the development and initial validation of a new tool for the measurement of side-effects to CPAP treatment. J Sleep Res 2010;19:603–11.
16. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 2008 Feb 15;5:173–8.
17. Hedner J, Grote L, Zou D. Pharmacological treatment of sleep apnea: current situation and future strategies. Sleep Med Rev 2008;12:33–47.
18. Smith I, Lasserson TJ, Wright J. Drug therapy for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 2006(2):CD003002.
19. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath 2011;15:479–85.
20. Xu T, Li T, Wei D, et al. Effect of automatic versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: an up-to-date meta-analysis. Sleep Breath 2012;16:1017–26.
21. Smith I, Lasserson TJ. Pressure modification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2009 (4):CD003531.
22. Dungan GC, 2nd, Marshall NS, Hoyos CM, et al. A randomized crossover trial of the effect of a novel method of pressure control (SensAwake) in automatic continuous positive airway pressure therapy to treat sleep disordered breathing. J Clin Sleep Med 2011;7:261–7.
23. Wimms AJ, Richards GN, Benjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath 2013;17:69–76.
24. Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2014;1:CD007736.
25. Bartlett D, Wong K, Richards D, et al. Increasing adherence to obstructive sleep apnea treatment with a group social cognitive therapy treatment intervention: a randomized trial. Sleep 2013;36:1647–54.
26. Deng T, Wang Y, Sun M, Chen B. Stage-matched intervention for adherence to CPAP in patients with obstructive sleep apnea: a randomized controlled trial. Sleep Breath 2013;17:791–801.
27. Pendharkar SR, Dechant A, Bischak DP, et al. An observational study of the effectiveness of alternative care providers in the management of obstructive sleep apnoea. J Sleep Res 2015 Oct 27.
28. Sawyer AM, King TS, Hanlon A, et al. Risk assessment for CPAP nonadherence in adults with newly diagnosed obstructive sleep apnea: preliminary testing of the Index for Nonadherence to PAP (I-NAP). Sleep Breath 2014;18:875–83.
29. Ward K, Hoare KJ, Gott M. What is known about the experiences of using CPAP for OSA from the users’ perspective? A systematic integrative literature review. Sleep Med Rev 2014;18:357–66.
30. Russell JO, Gales J, Bae C, Kominsky A. Referral patterns and positive airway pressure adherence upon diagnosis of obstructive sleep apnea. Otolaryngol Head Neck Surg 2015;153:881–7.
31. Hemmingsson E. Does medically induced weight loss improve obstructive sleep apnoea in the obese: review of randomized trials. Clin Obes 2011;1:26–30.
32. Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep 2013;36:641–9A.
33. Kulkas A, Leppanen T, Sahlman J, et al. Weight loss alters severity of individual nocturnal respiratory events depending on sleeping position. Physiol Meas 2014;35:2037–52.
34. Bae EK, Lee YJ, Yun CH, Heo Y. Effects of surgical weight loss for treating obstructive sleep apnea. Sleep Breath 2014;18:901–5.
35. Kline CE, Crowley EP, Ewing GB, et al. The effect of exercise training on obstructive sleep apnea and sleep quality: a randomized controlled trial. Sleep 2011;34:1631–40.
36. Kline CE, Reboussin DM, Foster GD, et al. The effect of changes in cardiorespiratory fitness and weight on obstructive sleep apnea severity in overweight adults with type 2 diabetes. Sleep 2016;39:317–25.
37. Vena D, Yadollahi A, Bradley TD. Modelling fluid accumulation in the neck using simple baseline fluid metrics: implications for sleep apnea. Conf Proc IEEE Eng Med Biol Soc 2014;2014:266–9.
38. Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083–96.
39. Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep 1984;7:110–4.
40. Joosten SA, Hamza K, Sands S, et al. Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology 2012;17:99–107.
41. Lee CH, Kim DK, Kim SY, et al. Changes in site of obstruction in obstructive sleep apnea patients according to sleep position: a DISE study. Laryngoscope 2015;125:248–54.
42. Joosten SA, Edwards BA, Wellman A, et al. The effect of body position on physiological factors that contribute to obstructive sleep apnea. Sleep 2015;38:1469–78.
43. Ravesloot MJ, van Maanen JP, Dun L, de Vries N. The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea-a review of the literature. Sleep Breath 2013;17:39–49.
44. Eijsvogel MM, Ubbink R, Dekker J, et al. Sleep position trainer versus tennis ball technique in positional obstructive sleep apnea syndrome. J Clin Sleep Med 2015;11:139–47.
45. Jackson M, Collins A, Berlowitz D, et al. Efficacy of sleep position modification to treat positional obstructive sleep apnea. Sleep Med 2015;16:545–52.
46. van Maanen JP, Meester KA, Dun LN, et al. The sleep position trainer: a new treatment for positional obstructive sleep apnoea. Sleep Breath 2013;17:771–9.
47. Morrell MJ, Arabi Y, Zahn B, Badr MS. Progressive retropalatal narrowing preceding obstructive apnea. Am J Respir Crit Care Med 1998;158:1974–81.
48. Riaz M, Certal V, Nigam G, et al. Nasal expiratory positive airway pressure devices (Provent) for OSA: a systematic review and meta-analysis. Sleep Disorders 2015;2015:15.
49. Nigam G, Pathak C, Riaz M. Effectiveness of oral pressure therapy in obstructive sleep apnea: a systematic analysis. Sleep Breath 2015 Oct 19.
50. Colrain IM, Black J, Siegel LC, et al. A multicenter evaluation of oral pressure therapy for the treatment of obstructive sleep apnea. Sleep Med 2013;14:830–7.
51. Zhu Y, Long H, Jian F, et al. The effectiveness of oral appliances for obstructive sleep apnea syndrome: A meta-analysis. J Dent 2015;43:1394–402.
52. Dieltjens M, Vanderveken OM, Heyning PH, Braem MJ. Current opinions and clinical practice in the titration of oral appliances in the treatment of sleep-disordered breathing. Sleep Med Rev 2012;16:177–85.
53. Cantore S, Ballini A, Farronato D, et al. Evaluation of an oral appliance in patients with mild to moderate obstructive sleep apnea syndrome intolerant to continuous positive airway pressure use: Preliminary results. Int J Immunopathol Pharmacol 2015 Dec 18.
54. Gjerde K, Lehmann S, Berge ME, et al. Oral appliance treatment in moderate and severe obstructive sleep apnoea patients non-adherent to CPAP. J Oral Rehabil 2015 Dec 27.
55. Jaiswal M, Srivastava GN, Pratap CB, et al. Effect of oral appliance for snoring and obstructive sleep apnea. Int J Orthod Milwaukee 2015;26:67–71.
56. Vecchierini MF, Attali V, Collet JM, et al. A custom-made mandibular repositioning device for obstructive sleep apnoea-hypopnoea syndrome: the ORCADES study. Sleep Med 2015 Jun 29.
57. Haviv Y, Bachar G, Aframian DJ, et al. A 2-year mean follow-up of oral appliance therapy for severe obstructive sleep apnea: a cohort study. Oral Dis 2015;21:386–92.
58. Marklund M. Long-term efficacy of an oral appliance in early treated patients with obstructive sleep apnea. Sleep Breath 2015 Nov 2.
59. Dieltjens M, Braem MJ, Vroegop AV, et al. Objectively measured vs self-reported compliance during oral appliance therapy for sleep-disordered breathing. Chest 2013;144:1495–502.
60. Smith YK, Verrett RG. Evaluation of a novel device for measuring patient compliance with oral appliances in the treatment of obstructive sleep apnea. J Prosthodont 2014;23:31–8.
61. Vanderveken OM, Dieltjens M, Wouters K, et al. Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax 2013;68:91–6.
62. Sutherland K, Phillips CL, Davies A, et al. CPAP pressure for prediction of oral appliance treatment response in obstructive sleep apnea. J Clin Sleep Med 2014;10:943–9.
63. Dieltjens M, Verbruggen AE, Braem MJ, et al. Determinants of objective compliance during oral appliance therapy in patients with sleep-related disordered breathing: a prospective clinical trial. JAMA Otolaryngol Head Neck Surg 2015:894–900.
64. Suzuki K, Nakata S, Tagaya M, et al. Prediction of oral appliance treatment outcome in obstructive sleep apnoea syndrome: a preliminary study. B-ENT 2014;10:185–91.
65. Tsuiki S, Ito E, Isono S, et al. Oropharyngeal crowding and obesity as predictors of oral appliance treatment response to moderate obstructive sleep apnea. Chest 2013;144:558–63.
66. Sutherland K, Takaya H, Qian J, et al. Oral appliance treatment response and polysomnographic phenotypes of obstructive sleep apnea. J Clin Sleep Med 2015;11:861–8.
67. Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 2013;187:879–87.
68. Doff MH, Hoekema A, Wijkstra PJ, et al. Oral appliance versus continuous positive airway pressure in obstructive sleep apnea syndrome: a 2-year follow-up. Sleep 2013;36:1289–96.
69. Bratton DJ, Gaisl T, Wons AM, Kohler M. CPAP vs mandibular advancement devices and blood pressure in patients with obstructive sleep apnea: a systematic review and meta-analysis. JAMA 2015;314:2280–93.
70. Bostanci A, Turhan M. A systematic review of tongue base suspension techniques as an isolated procedure or combined with uvulopalatopharyngoplasty in obstructive sleep apnea. Eur Arch Otorhinolaryngol 2015 Oct 27.
71. Camacho M, Certal V, Brietzke SE, et al. Tracheostomy as treatment for adult obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope 2014;124:803–11.
72. Camacho M, Teixeira J, Abdullatif J, et al. Maxillomandibular advancement and tracheostomy for morbidly obese obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2015;152:619–30.
73. Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep 2010;33:1396–407.
74. Handler E, Hamans E, Goldberg AN, Mickelson S. Tongue suspension: an evidence-based review and comparison to hypopharyngeal surgery for OSA. Laryngoscope 2014;124:329–36.
75. Ishii L, Roxbury C, Godoy A, et al. Does nasal surgery improve osa in patients with nasal obstruction and OSA? a meta-analysis. Otolaryngol Head Neck Surg 2015;153:326–33.
76. Lin HC, Friedman M, Chang HW, Gurpinar B. The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope 2008;118:902–8.
77. Murphey AW, Kandl JA, Nguyen SA, et al. The effect of glossectomy for obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2015;153:334–42.
78. Zaghi S, Holty JC, Certal V, et al. Maxillomandibular advancement for treatment of obstructive sleep apnea: a meta-analysis. JAMA Otolaryngol Head Neck Surg 2015 Nov 25:1–9.
79. Thaler ER, Rassekh CH, Lee JM, et al. Outcomes for multilevel surgery for sleep apnea: Obstructive sleep apnea, transoral robotic surgery, and uvulopalatopharyngoplasty. Laryngoscope 2015 Jul 7.
80. Arora A, Chaidas K, Garas G, et al. Outcome of TORS to tongue base and epiglottis in patients with OSA intolerant of conventional treatment. Sleep Breath 2015 Dec 15.
81. Remmers JE, deGroot WJ, Sauerland EK, Anch AM. Pathogenesis of upper airway occlusion during sleep. J Appl Physiol Respir Environ Exercise Physiol 1978;44:931–8.
82. Decker MJ, Haaga J, Arnold JL, et al. Functional electrical stimulation and respiration during sleep. J Appl Physiol (1985) 1993;75:1053–61.
83. Edmonds LC, Daniels BK, Stanson AW, et al. The effects of transcutaneous electrical stimulation during wakefulness and sleep in patients with obstructive sleep apnea. Am Rev Respir Dis 1992;146:1030–6.
84. Guilleminault C, Powell N, Bowman B, Stoohs R. The effect of electrical stimulation on obstructive sleep apnea syndrome. Chest 1995;107:67–73.
85. Miki H, Hida W, Chonan T, et al. Effects of submental electrical stimulation during sleep on upper airway patency in patients with obstructive sleep apnea. Am Rev Respir Dis 1989;140:1285–9.
86. Steier J, Seymour J, Rafferty GF, et al. Continuous transcutaneous submental electrical stimulation in obstructive sleep apnea: a feasibility study. Chest 2011;140:998–1007.
87. Eastwood PR, Barnes M, Walsh JH, et al. Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep 2011;34:1479–86.
88. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res 2014;23:77–83.
89. Strollo PJ, Jr., Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med 2014;370:139–49.
90. Van de Heyning PH, Badr MS, Baskin JZ, et al. Implanted upper airway stimulation device for obstructive sleep apnea. Laryngoscope 2012;122:1626–33.
91. Strollo PJ, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep 2015;38:1593–8.
92. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg 2014;151:880–7.
93. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg 2015 Nov 17.
94. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med 2016;12:43-8.
95. Mason M, Welsh EJ, Smith I. Drug therapy for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 2013;(5):CD003002.
96. Farabi SS, Prasad B, Quinn L, Carley DW. Impact of dronabinol on quantitative electroencephalogram (qEEG) measures of sleep in obstructive sleep apnea syndrome. J Clin Sleep Med 2014;10:49–56.
97. Prasad B, Radulovacki MG, Carley DW. Proof of concept trial of dronabinol in obstructive sleep apnea. Front Psychiatry 2013;4:1.
98. Calik MW, Carley DW. Cannabinoid type 1 and type 2 receptor antagonists prevent attenuation of serotonin-induced reflex apneas by dronabinol in Sprague-Dawley rats. PLoS One 2014;9:e111412.
99. Calik MW, Radulovacki M, Carley DW. Intranodose ganglion injections of dronabinol attenuate serotonin-induced apnea in Sprague-Dawley rat. Respir Physiol Neurobiol. 2014 Jan 1;190:20–4.
100. Carter SG, Berger MS, Carberry JC, et al. Zopiclone increases the arousal threshold without impairing genioglossus activity in obstructive sleep apnea. Sleep 2015 Dec 22.
101. Burgess KR. New insights from the measurement of loop gain in obstructive sleep apnoea. J Physiol 2012;590(Pt 8):1781–2.
102. Eckert DJ, White DP, Jordan AS, et al. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med 2013;188:996–1004.
103. Salloum A, Rowley JA, Mateika JH, et al. Increased propensity for central apnea in patients with obstructive sleep apnea: effect of nasal continuous positive airway pressure. Am J Respir Crit Care Med 2010;181:189–93.
104. Edwards BA, Connolly JG, Campana LM, et al. Acetazolamide attenuates the ventilatory response to arousal in patients with obstructive sleep apnea. Sleep 2013;36:281–5.
105. Edwards BA, Sands SA, Eckert DJ, et al. Acetazolamide improves loop gain but not the other physiological traits causing obstructive sleep apnoea. J Physiol 2012;590(Pt 5):1199–211.
106. Eskandari D, Zou D, Karimi M, et al. Zonisamide reduces obstructive sleep apnoea: a randomised placebo-controlled study. Eur Resp J 2014;44:140–9.
107. Yang YX, Spencer G, Schutte-Rodin S, et al. Gastroesophageal reflux and sleep events in obstructive sleep apnea. Eur J Gastroenterol Hepatol 2013;25:1017–23.
108. Gilani S, Quan SF, Pynnonen MA, Shin JJ. Obstructive sleep apnea and gastroesophageal reflux: a multivariate population-level analysis. Otolaryngol Head Neck Surg 2015 Dec 8.
109. Rassameehiran S, Klomjit S, Hosiriluck N, Nugent K. Meta-analysis of the effect of proton pump inhibitors on obstructive sleep apnea symptoms and indices in patients with gastroesophageal reflux disease. Proc (Bayl Univ Med Cent) 2016;29:3–6.
110. Ermis F, Akyuz F, Arici S, et al. Effect of proton pump inhibitor (PPI) treatment in obstructive sleep apnea syndrome: an esophageal impedance-pHmetry study. Hepatogastroenterology 2011;58:1566–73.
111. Reimer C. Safety of long-term PPI therapy. Best Pract Res 2013;27:443–54.
112. Deacon NL, Jen R, Li Y, Malhotra A. Treatment of obstructive sleep apnea. prospects for personalized combined modality therapy. Ann Am Thorac Soc 2016;13:101–8.
113. Shin W, Jen R, Li Y, Malhotra A. Tailored treatment strategies for obstructive sleep apnea. Respir Investig 2016;54:2–7.
114. Dieltjens M, Vroegop AV, Verbruggen AE, et al. A promising concept of combination therapy for positional obstructive sleep apnea. Sleep Breath 2015;19:637–44.
115. Wellman A, Edwards BA, Sands SA, et al. A simplified method for determining phenotypic traits in patients with obstructive sleep apnea. J Appl Physiol (1985) 2013;114:911–22.
1. Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation 2008;118:1080–111.
2. Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006–14.
3. Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea: implications for cardiac and vascular disease. JAMA 2003;290:1906–14.
4. Kim HC, Young T, Matthews CG, et al. Sleep-disordered breathing and neuropsychological deficits. A population-based study. Am J Respir Crit Care Med 1997;156:1813–9.
5. Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA 2011;306:613–9.
6. Baldwin CM, Griffith KA, Nieto FJ, et al. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep 2001;24:96–105.
7. Peppard PE, Szklo-Coxe M, Hla KM, Young T. Longitudinal association of sleep-related breathing disorder and depression. Arch Intern Med 2006;166:1709–15.
8. Marshall NS, Wong KK, Liu PY, et al. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep 2008;31:1079–85.
9. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep 2008;31:1071–8.
10. AlGhanim N, Comondore VR, Fleetham J, et al. The economic impact of obstructive sleep apnea. Lung 2008;186:7–12.
11. Sassani A, Findley LJ, Kryger M, et al. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep 2004;27:453–8.
12. Weaver TE, Calik MW, Farabi SS, et al. Innovative treatments for adults with obstructive sleep apnea. Nat Sci Sleep 2014;6:137–47.
13. Isetta V, Negrin MA, Monasterio C, et al. A Bayesian cost-effectiveness analysis of a telemedicine-based strategy for the management of sleep apnoea: a multicentre randomised controlled trial. Thorax 2015;70:1054–61.
14. Tsuda H, Moritsuchi Y, Higuchi Y, Tsuda T. Oral health under use of continuous positive airway pressure and interest in alternative therapy in patients with obstructive sleep apnoea: a questionnaire-based survey. Gerodontology 2015 Feb 10.
15. Brostrom A, Arestedt KF, Nilsen P, et al. The side-effects to CPAP treatment inventory: the development and initial validation of a new tool for the measurement of side-effects to CPAP treatment. J Sleep Res 2010;19:603–11.
16. Weaver TE, Grunstein RR. Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 2008 Feb 15;5:173–8.
17. Hedner J, Grote L, Zou D. Pharmacological treatment of sleep apnea: current situation and future strategies. Sleep Med Rev 2008;12:33–47.
18. Smith I, Lasserson TJ, Wright J. Drug therapy for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 2006(2):CD003002.
19. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath 2011;15:479–85.
20. Xu T, Li T, Wei D, et al. Effect of automatic versus fixed continuous positive airway pressure for the treatment of obstructive sleep apnea: an up-to-date meta-analysis. Sleep Breath 2012;16:1017–26.
21. Smith I, Lasserson TJ. Pressure modification for improving usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2009 (4):CD003531.
22. Dungan GC, 2nd, Marshall NS, Hoyos CM, et al. A randomized crossover trial of the effect of a novel method of pressure control (SensAwake) in automatic continuous positive airway pressure therapy to treat sleep disordered breathing. J Clin Sleep Med 2011;7:261–7.
23. Wimms AJ, Richards GN, Benjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath 2013;17:69–76.
24. Wozniak DR, Lasserson TJ, Smith I. Educational, supportive and behavioural interventions to improve usage of continuous positive airway pressure machines in adults with obstructive sleep apnoea. Cochrane Database Syst Rev 2014;1:CD007736.
25. Bartlett D, Wong K, Richards D, et al. Increasing adherence to obstructive sleep apnea treatment with a group social cognitive therapy treatment intervention: a randomized trial. Sleep 2013;36:1647–54.
26. Deng T, Wang Y, Sun M, Chen B. Stage-matched intervention for adherence to CPAP in patients with obstructive sleep apnea: a randomized controlled trial. Sleep Breath 2013;17:791–801.
27. Pendharkar SR, Dechant A, Bischak DP, et al. An observational study of the effectiveness of alternative care providers in the management of obstructive sleep apnoea. J Sleep Res 2015 Oct 27.
28. Sawyer AM, King TS, Hanlon A, et al. Risk assessment for CPAP nonadherence in adults with newly diagnosed obstructive sleep apnea: preliminary testing of the Index for Nonadherence to PAP (I-NAP). Sleep Breath 2014;18:875–83.
29. Ward K, Hoare KJ, Gott M. What is known about the experiences of using CPAP for OSA from the users’ perspective? A systematic integrative literature review. Sleep Med Rev 2014;18:357–66.
30. Russell JO, Gales J, Bae C, Kominsky A. Referral patterns and positive airway pressure adherence upon diagnosis of obstructive sleep apnea. Otolaryngol Head Neck Surg 2015;153:881–7.
31. Hemmingsson E. Does medically induced weight loss improve obstructive sleep apnoea in the obese: review of randomized trials. Clin Obes 2011;1:26–30.
32. Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep 2013;36:641–9A.
33. Kulkas A, Leppanen T, Sahlman J, et al. Weight loss alters severity of individual nocturnal respiratory events depending on sleeping position. Physiol Meas 2014;35:2037–52.
34. Bae EK, Lee YJ, Yun CH, Heo Y. Effects of surgical weight loss for treating obstructive sleep apnea. Sleep Breath 2014;18:901–5.
35. Kline CE, Crowley EP, Ewing GB, et al. The effect of exercise training on obstructive sleep apnea and sleep quality: a randomized controlled trial. Sleep 2011;34:1631–40.
36. Kline CE, Reboussin DM, Foster GD, et al. The effect of changes in cardiorespiratory fitness and weight on obstructive sleep apnea severity in overweight adults with type 2 diabetes. Sleep 2016;39:317–25.
37. Vena D, Yadollahi A, Bradley TD. Modelling fluid accumulation in the neck using simple baseline fluid metrics: implications for sleep apnea. Conf Proc IEEE Eng Med Biol Soc 2014;2014:266–9.
38. Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083–96.
39. Cartwright RD. Effect of sleep position on sleep apnea severity. Sleep 1984;7:110–4.
40. Joosten SA, Hamza K, Sands S, et al. Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology 2012;17:99–107.
41. Lee CH, Kim DK, Kim SY, et al. Changes in site of obstruction in obstructive sleep apnea patients according to sleep position: a DISE study. Laryngoscope 2015;125:248–54.
42. Joosten SA, Edwards BA, Wellman A, et al. The effect of body position on physiological factors that contribute to obstructive sleep apnea. Sleep 2015;38:1469–78.
43. Ravesloot MJ, van Maanen JP, Dun L, de Vries N. The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea-a review of the literature. Sleep Breath 2013;17:39–49.
44. Eijsvogel MM, Ubbink R, Dekker J, et al. Sleep position trainer versus tennis ball technique in positional obstructive sleep apnea syndrome. J Clin Sleep Med 2015;11:139–47.
45. Jackson M, Collins A, Berlowitz D, et al. Efficacy of sleep position modification to treat positional obstructive sleep apnea. Sleep Med 2015;16:545–52.
46. van Maanen JP, Meester KA, Dun LN, et al. The sleep position trainer: a new treatment for positional obstructive sleep apnoea. Sleep Breath 2013;17:771–9.
47. Morrell MJ, Arabi Y, Zahn B, Badr MS. Progressive retropalatal narrowing preceding obstructive apnea. Am J Respir Crit Care Med 1998;158:1974–81.
48. Riaz M, Certal V, Nigam G, et al. Nasal expiratory positive airway pressure devices (Provent) for OSA: a systematic review and meta-analysis. Sleep Disorders 2015;2015:15.
49. Nigam G, Pathak C, Riaz M. Effectiveness of oral pressure therapy in obstructive sleep apnea: a systematic analysis. Sleep Breath 2015 Oct 19.
50. Colrain IM, Black J, Siegel LC, et al. A multicenter evaluation of oral pressure therapy for the treatment of obstructive sleep apnea. Sleep Med 2013;14:830–7.
51. Zhu Y, Long H, Jian F, et al. The effectiveness of oral appliances for obstructive sleep apnea syndrome: A meta-analysis. J Dent 2015;43:1394–402.
52. Dieltjens M, Vanderveken OM, Heyning PH, Braem MJ. Current opinions and clinical practice in the titration of oral appliances in the treatment of sleep-disordered breathing. Sleep Med Rev 2012;16:177–85.
53. Cantore S, Ballini A, Farronato D, et al. Evaluation of an oral appliance in patients with mild to moderate obstructive sleep apnea syndrome intolerant to continuous positive airway pressure use: Preliminary results. Int J Immunopathol Pharmacol 2015 Dec 18.
54. Gjerde K, Lehmann S, Berge ME, et al. Oral appliance treatment in moderate and severe obstructive sleep apnoea patients non-adherent to CPAP. J Oral Rehabil 2015 Dec 27.
55. Jaiswal M, Srivastava GN, Pratap CB, et al. Effect of oral appliance for snoring and obstructive sleep apnea. Int J Orthod Milwaukee 2015;26:67–71.
56. Vecchierini MF, Attali V, Collet JM, et al. A custom-made mandibular repositioning device for obstructive sleep apnoea-hypopnoea syndrome: the ORCADES study. Sleep Med 2015 Jun 29.
57. Haviv Y, Bachar G, Aframian DJ, et al. A 2-year mean follow-up of oral appliance therapy for severe obstructive sleep apnea: a cohort study. Oral Dis 2015;21:386–92.
58. Marklund M. Long-term efficacy of an oral appliance in early treated patients with obstructive sleep apnea. Sleep Breath 2015 Nov 2.
59. Dieltjens M, Braem MJ, Vroegop AV, et al. Objectively measured vs self-reported compliance during oral appliance therapy for sleep-disordered breathing. Chest 2013;144:1495–502.
60. Smith YK, Verrett RG. Evaluation of a novel device for measuring patient compliance with oral appliances in the treatment of obstructive sleep apnea. J Prosthodont 2014;23:31–8.
61. Vanderveken OM, Dieltjens M, Wouters K, et al. Objective measurement of compliance during oral appliance therapy for sleep-disordered breathing. Thorax 2013;68:91–6.
62. Sutherland K, Phillips CL, Davies A, et al. CPAP pressure for prediction of oral appliance treatment response in obstructive sleep apnea. J Clin Sleep Med 2014;10:943–9.
63. Dieltjens M, Verbruggen AE, Braem MJ, et al. Determinants of objective compliance during oral appliance therapy in patients with sleep-related disordered breathing: a prospective clinical trial. JAMA Otolaryngol Head Neck Surg 2015:894–900.
64. Suzuki K, Nakata S, Tagaya M, et al. Prediction of oral appliance treatment outcome in obstructive sleep apnoea syndrome: a preliminary study. B-ENT 2014;10:185–91.
65. Tsuiki S, Ito E, Isono S, et al. Oropharyngeal crowding and obesity as predictors of oral appliance treatment response to moderate obstructive sleep apnea. Chest 2013;144:558–63.
66. Sutherland K, Takaya H, Qian J, et al. Oral appliance treatment response and polysomnographic phenotypes of obstructive sleep apnea. J Clin Sleep Med 2015;11:861–8.
67. Phillips CL, Grunstein RR, Darendeliler MA, et al. Health outcomes of continuous positive airway pressure versus oral appliance treatment for obstructive sleep apnea: a randomized controlled trial. Am J Respir Crit Care Med 2013;187:879–87.
68. Doff MH, Hoekema A, Wijkstra PJ, et al. Oral appliance versus continuous positive airway pressure in obstructive sleep apnea syndrome: a 2-year follow-up. Sleep 2013;36:1289–96.
69. Bratton DJ, Gaisl T, Wons AM, Kohler M. CPAP vs mandibular advancement devices and blood pressure in patients with obstructive sleep apnea: a systematic review and meta-analysis. JAMA 2015;314:2280–93.
70. Bostanci A, Turhan M. A systematic review of tongue base suspension techniques as an isolated procedure or combined with uvulopalatopharyngoplasty in obstructive sleep apnea. Eur Arch Otorhinolaryngol 2015 Oct 27.
71. Camacho M, Certal V, Brietzke SE, et al. Tracheostomy as treatment for adult obstructive sleep apnea: a systematic review and meta-analysis. Laryngoscope 2014;124:803–11.
72. Camacho M, Teixeira J, Abdullatif J, et al. Maxillomandibular advancement and tracheostomy for morbidly obese obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2015;152:619–30.
73. Caples SM, Rowley JA, Prinsell JR, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep 2010;33:1396–407.
74. Handler E, Hamans E, Goldberg AN, Mickelson S. Tongue suspension: an evidence-based review and comparison to hypopharyngeal surgery for OSA. Laryngoscope 2014;124:329–36.
75. Ishii L, Roxbury C, Godoy A, et al. Does nasal surgery improve osa in patients with nasal obstruction and OSA? a meta-analysis. Otolaryngol Head Neck Surg 2015;153:326–33.
76. Lin HC, Friedman M, Chang HW, Gurpinar B. The efficacy of multilevel surgery of the upper airway in adults with obstructive sleep apnea/hypopnea syndrome. Laryngoscope 2008;118:902–8.
77. Murphey AW, Kandl JA, Nguyen SA, et al. The effect of glossectomy for obstructive sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 2015;153:334–42.
78. Zaghi S, Holty JC, Certal V, et al. Maxillomandibular advancement for treatment of obstructive sleep apnea: a meta-analysis. JAMA Otolaryngol Head Neck Surg 2015 Nov 25:1–9.
79. Thaler ER, Rassekh CH, Lee JM, et al. Outcomes for multilevel surgery for sleep apnea: Obstructive sleep apnea, transoral robotic surgery, and uvulopalatopharyngoplasty. Laryngoscope 2015 Jul 7.
80. Arora A, Chaidas K, Garas G, et al. Outcome of TORS to tongue base and epiglottis in patients with OSA intolerant of conventional treatment. Sleep Breath 2015 Dec 15.
81. Remmers JE, deGroot WJ, Sauerland EK, Anch AM. Pathogenesis of upper airway occlusion during sleep. J Appl Physiol Respir Environ Exercise Physiol 1978;44:931–8.
82. Decker MJ, Haaga J, Arnold JL, et al. Functional electrical stimulation and respiration during sleep. J Appl Physiol (1985) 1993;75:1053–61.
83. Edmonds LC, Daniels BK, Stanson AW, et al. The effects of transcutaneous electrical stimulation during wakefulness and sleep in patients with obstructive sleep apnea. Am Rev Respir Dis 1992;146:1030–6.
84. Guilleminault C, Powell N, Bowman B, Stoohs R. The effect of electrical stimulation on obstructive sleep apnea syndrome. Chest 1995;107:67–73.
85. Miki H, Hida W, Chonan T, et al. Effects of submental electrical stimulation during sleep on upper airway patency in patients with obstructive sleep apnea. Am Rev Respir Dis 1989;140:1285–9.
86. Steier J, Seymour J, Rafferty GF, et al. Continuous transcutaneous submental electrical stimulation in obstructive sleep apnea: a feasibility study. Chest 2011;140:998–1007.
87. Eastwood PR, Barnes M, Walsh JH, et al. Treating obstructive sleep apnea with hypoglossal nerve stimulation. Sleep 2011;34:1479–86.
88. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12-month outcomes. J Sleep Res 2014;23:77–83.
89. Strollo PJ, Jr., Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med 2014;370:139–49.
90. Van de Heyning PH, Badr MS, Baskin JZ, et al. Implanted upper airway stimulation device for obstructive sleep apnea. Laryngoscope 2012;122:1626–33.
91. Strollo PJ, Gillespie MB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep 2015;38:1593–8.
92. Woodson BT, Gillespie MB, Soose RJ, et al. Randomized controlled withdrawal study of upper airway stimulation on OSA: short- and long-term effect. Otolaryngol Head Neck Surg 2014;151:880–7.
93. Woodson BT, Soose RJ, Gillespie MB, et al. Three-year outcomes of cranial nerve stimulation for obstructive sleep apnea: the STAR trial. Otolaryngol Head Neck Surg 2015 Nov 17.
94. Soose RJ, Woodson BT, Gillespie MB, et al. Upper airway stimulation for obstructive sleep apnea: self-reported outcomes at 24 months. J Clin Sleep Med 2016;12:43-8.
95. Mason M, Welsh EJ, Smith I. Drug therapy for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 2013;(5):CD003002.
96. Farabi SS, Prasad B, Quinn L, Carley DW. Impact of dronabinol on quantitative electroencephalogram (qEEG) measures of sleep in obstructive sleep apnea syndrome. J Clin Sleep Med 2014;10:49–56.
97. Prasad B, Radulovacki MG, Carley DW. Proof of concept trial of dronabinol in obstructive sleep apnea. Front Psychiatry 2013;4:1.
98. Calik MW, Carley DW. Cannabinoid type 1 and type 2 receptor antagonists prevent attenuation of serotonin-induced reflex apneas by dronabinol in Sprague-Dawley rats. PLoS One 2014;9:e111412.
99. Calik MW, Radulovacki M, Carley DW. Intranodose ganglion injections of dronabinol attenuate serotonin-induced apnea in Sprague-Dawley rat. Respir Physiol Neurobiol. 2014 Jan 1;190:20–4.
100. Carter SG, Berger MS, Carberry JC, et al. Zopiclone increases the arousal threshold without impairing genioglossus activity in obstructive sleep apnea. Sleep 2015 Dec 22.
101. Burgess KR. New insights from the measurement of loop gain in obstructive sleep apnoea. J Physiol 2012;590(Pt 8):1781–2.
102. Eckert DJ, White DP, Jordan AS, et al. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am J Respir Crit Care Med 2013;188:996–1004.
103. Salloum A, Rowley JA, Mateika JH, et al. Increased propensity for central apnea in patients with obstructive sleep apnea: effect of nasal continuous positive airway pressure. Am J Respir Crit Care Med 2010;181:189–93.
104. Edwards BA, Connolly JG, Campana LM, et al. Acetazolamide attenuates the ventilatory response to arousal in patients with obstructive sleep apnea. Sleep 2013;36:281–5.
105. Edwards BA, Sands SA, Eckert DJ, et al. Acetazolamide improves loop gain but not the other physiological traits causing obstructive sleep apnoea. J Physiol 2012;590(Pt 5):1199–211.
106. Eskandari D, Zou D, Karimi M, et al. Zonisamide reduces obstructive sleep apnoea: a randomised placebo-controlled study. Eur Resp J 2014;44:140–9.
107. Yang YX, Spencer G, Schutte-Rodin S, et al. Gastroesophageal reflux and sleep events in obstructive sleep apnea. Eur J Gastroenterol Hepatol 2013;25:1017–23.
108. Gilani S, Quan SF, Pynnonen MA, Shin JJ. Obstructive sleep apnea and gastroesophageal reflux: a multivariate population-level analysis. Otolaryngol Head Neck Surg 2015 Dec 8.
109. Rassameehiran S, Klomjit S, Hosiriluck N, Nugent K. Meta-analysis of the effect of proton pump inhibitors on obstructive sleep apnea symptoms and indices in patients with gastroesophageal reflux disease. Proc (Bayl Univ Med Cent) 2016;29:3–6.
110. Ermis F, Akyuz F, Arici S, et al. Effect of proton pump inhibitor (PPI) treatment in obstructive sleep apnea syndrome: an esophageal impedance-pHmetry study. Hepatogastroenterology 2011;58:1566–73.
111. Reimer C. Safety of long-term PPI therapy. Best Pract Res 2013;27:443–54.
112. Deacon NL, Jen R, Li Y, Malhotra A. Treatment of obstructive sleep apnea. prospects for personalized combined modality therapy. Ann Am Thorac Soc 2016;13:101–8.
113. Shin W, Jen R, Li Y, Malhotra A. Tailored treatment strategies for obstructive sleep apnea. Respir Investig 2016;54:2–7.
114. Dieltjens M, Vroegop AV, Verbruggen AE, et al. A promising concept of combination therapy for positional obstructive sleep apnea. Sleep Breath 2015;19:637–44.
115. Wellman A, Edwards BA, Sands SA, et al. A simplified method for determining phenotypic traits in patients with obstructive sleep apnea. J Appl Physiol (1985) 2013;114:911–22.
2016 Update on minimally invasive gynecologic surgery
Rightly so, the topics of mechanical tissue extraction and hysterectomy approach have dominated the field of obstetrics and gynecology over the past 12 months and more. A profusion of literature has been published on these subjects. However, there are 2 important topics within the field of minimally invasive gynecologic surgery that deserve our attention as well, and I have chosen to focus on these for this Update.
First, laparoscopic treatment of ovarian endometriomas is one of the most commonly performed gynecologic procedures worldwide. Many women undergoing such surgery are of childbearing age and have the desire for future pregnancy. What are best practices for preserving ovarian function in these women? Two studies recently published in the Journal of Minimally Invasive Gynecology addressed this question.
Second, until recently, the rate of bowel injury at laparoscopic gynecologic surgery has not been well established.1 Moreover, mechanical bowel preparation is commonly employed in case intestinal injury does occur, despite the lack of evidence that outcomes of these possible injuries can be improved.2 Understanding the rate of bowel injury can shed light on the overall value of the perceived benefits of bowel preparation. Therefore, I examine 2 recent systematic reviews that analyze the incidence of bowel injury and the value of bowel prep in gynecologic laparoscopic surgery.
bipolar coagulation inferior to suturing or hemostatic sealant for preserving ovarian function
Song T, Kim WY, Lee KW, Kim KH. Effect on ovarian reserve of hemostasis by bipolar coagulation versus suture during laparoendoscopic single-site cystectomy for ovarian endometriomas. J Minim Invasive Gynecol. 2015;22(3):415−420.
Ata B, Turkgeldi E, Seyhan A, Urman B. Effect of hemostatic method on ovarian reserve following laparoscopic endometrioma excision; comparison of suture, hemostatic sealant, and bipolar dessication. A systematic review and meta-analysis. J Minim Invasive Gynecol. 2015;22(3):363−372.
The customary surgical approach for laparoscopic cystectomy is by mechanical stripping of the cyst wall (FIGURE) and the use of bipolar desiccation for hemostasis. Stripping inevitably leads to removal of healthy ovarian cortex,3 especially in inexperienced hands,4 and ovarian follicles inevitably are destroyed during electrosurgical desiccation. When compared with the use of suturing or a hemostatic agent to control bleeding in the ovarian defect, the use of bipolar electrosurgery may harm more of the ovarian cortex, resulting in a comparatively diminished follicular cohort.
Possible deleterious effects on the ovarian reserve can be determined with a blood test to measure anti-Müllerian hormone (AMH) levels postoperatively. Produced by the granulosa cells of the ovary, this hormone directly reflects the remaining ovarian egg supply. Lower levels of AMH have been shown to significantly decrease the success rate of in vitro fertilization (IVF), especially in women older than age 35.5 Moreover, AMH levels in the late reproductive years can be used as a predictive marker of menopause, with lower levels predicting significantly earlier onset.6
Data from 2 recent studies, a quasi-randomized trial by Song and colleagues and a systematic review and meta-analysis by Ata and colleagues emphasize that bipolar desiccation for hemostasis may not be best practice for protecting ovarian reserve during laparoscopic ovarian cystectomy for an endometrioma.
AMH levels decline more significantly for women undergoing bipolar desiccation
Song and colleagues conducted a prospective quasi-randomized study of 125 women whose endometriomas were laparoscopically removed via a single-site approach and managed for hemostasis with either bipolar desiccation or suturing of the ovarian defect with a 2-0 barbed suture. All surgeries were conducted by a single surgeon.
At 3 months postsurgery, mean AMH levels had declined from baseline by 42.2% (interquartile range [IR], 16.5−53.0 ng/mL) in the desiccation group and by 24.6% (IR, 11.6−37.0 ng/mL) in the suture group (P = .001). Multivariate analysis showed that the method used for hemostasis was the only determinant for reduced ovarian reserve.
In their systematic review and meta-analysis, Ata and colleagues included 10 studies--6 qualitative and 4 quantitative. All studies examined the rate of change of serum AMH levels 3 months after laparoscopic removal of an endometrioma.
In their qualitative analysis, 5 of the 6 studies reported a significantly greater decrease in ovarian reserve after bipolar desiccation (varying from 13% to 44%) or a strong trend in the same direction. In the sixth study, the desiccation group had a lower decline in absolute AMH level than in the other 5 studies. The authors note that this 2.7% decline was much lower than the values reported for the bipolar desiccation group of any other study. (Those declines ranged between 19% and 58%.)
Although not significant, in all 3 of the included randomized controlled trials (RCTs), the desiccation groups had a greater loss in AMH level than the hemostatic sealant groups, and in 2 of these RCTs, bipolar desiccation groups had a greater loss than the suturing groups.
Among the 213 study participants in the 3 RCTs and the prospective cohort study included in the quantitative meta-analysis, alternative methods to bipolar desiccation were associated with a 6.95% lower decrease in AMH-level decline (95% confidence interval [CI], −13.0% to −0.9%; P = .02).
What this EVIDENCE means for practice
Compared with the use of bipolar electrosurgery to attain hemostasis, the use of a topical biosurgical agent or suturing could be significantly better for protection of the ovarian follicles during laparoscopic ovarian cystectomy for endometrioma. These alternative methods especially could benefit those women desiring future pregnancy who are demonstrated preoperatively to have a low ovarian reserve. As needed, electrosurgery should be sparingly employed for ovarian hemostasis.
Large Study identifies incidence of bowel injury during gynecologic laproscopy
Llarena NC, Shah AB, Milad MP. Bowel injury in gynecologic laparoscopy: a systematic review. Am J Obstet Gynecol. 2015;125(6):1407−1417.
In no aspect of laparoscopic surgery are preventive strategies more cautiously employed than during peritoneal access. Regardless of the applied technique, there is an irreducible risk of injury to the underlying viscera by either adhesions between the underlying bowel and abdominal wall or during the course of pilot error. Moreover, in the best of hands, bowel injury can occur whenever normal anatomic relationships need to be restored using intra-abdominal adhesiolysis. Given the ubiquity, these risks are never out of the surgeon's mind. Gynecologists are obliged to discuss these risks during the informed consent process.
Until recently, the rate of bowel injury has not been well established. Llarena and colleagues recently have conducted the largest systematic review of the medical literature to date for incidence, presentation, mortality, cause, and location of bowel injury associated with laparoscopic surgery while not necessarily distinguishing for the type of bowel injury. Sixty retrospective and 27 prospective studies met inclusion criteria.
The risk of bowel injury overall and defined
Among 474,063 laparoscopic surgeries conducted between 1972 and 2014, 604 bowel injuries were found, for an incidence of 1 in 769, or 0.13% (95% CI, 0.12−0.14%).
The rate of bowel injury varied by procedure, year, study type, and definition of bowel injury. The incidence of injury according to:
- definition, was 1 in 416 (0.24%) for studies that clearly included serosal injuries and enterotomies versus 1 in 833 (0.12%) for studies not clearly defining the type of bowel injury (relative risk [RR], 0.47; 95% CI, 0.38−0.59; P<.001)
- study type, was 1 in 666 (0.15%) for prospective studies versus 1 in 909 (0.11%) for retrospective studies (RR, 0.78; 95% CI, 0.63−0.96; P = .02)
- procedure, was 1 in 3,333 (0.03%; 95% CI, 0.01−0.03%) for sterilization and 1 in 256 (0.39%; 95% CI, 0.35−0.45%) for hysterectomy
- year, for laparoscopic hysterectomy only, was 1 in 222 (0.45%) before the year 2000 and 1 in 294 (0.34%) after 2000 (RR, 0.75; 95% CI, 0.57−0.98; P = .03).
How were injuries caused, found, and managed?
Thirty studies described the laparoscopic instrument used during 366 reported bowel injuries. The majority of injuries (55%) occurred during initial peritoneal access, with the Veress needle or trocar causing the damage. This was followed by electrosurgery (29%), dissection (11%), and forceps or scissors (4.1%).
According to 40 studies describing 307 injuries, bowel injuries most often were managed by converting to laparotomy (80%); only 8% of injuries were managed with laparoscopy and 2% expectantly.
Surgery to repair the bowel injury was delayed in 154 (41%) of 375 cases. The median time to injury discovery was 3 days (range, 1−13 days).
In only 19 cases were the presenting signs and symptoms of bowel injury recorded. Those reported from most to least often were: peritonitis, abdominal pain, fever, abdominal distention, leukocytosis, leukopenia, and septic shock.
Mortality
Mortality as an outcome was only reported in 29 of the total 90 studies; therefore, mortality may be underreported. Overall, however, death occurred in 1 (0.8%) of 125 bowel injuries.
The overall mortality rate from bowel injury--calculated from the only 42 studies that explicitly mentioned mortality as an outcome--was 1 in 125, or 0.8% (95% CI, 0.36%-1.9%). All 5 reported deaths occurred as a result of delayed recognition of bowel injury, which made the mortality rate for unrecognized bowel injury 1 in 31, or 3.2% (95% CI, 1%-7%). No deaths occurred when the bowel injury was noted intraoperatively.
What this EVIDENCE means for practice
In this review of 474,063 laparoscopic procedures, bowel injury occurred in 1 in 769, or 0.13% of procedures. Bowel injury is more apt to occur during more complicated laparoscopic procedures (compared with laparoscopic sterilization procedures, the risk during hysterectomy was greater than 10-fold).
Most of the injuries were managed by laparotomic surgery despite the potential to repair bowel injury by laparoscopy. Validating that peritoneal access is a high risk part of laparoscopic surgery, the majority of the injuries occurred during insufflation with a Veress needle or during abdominal access by trocar insertion. Nearly one-third of the injuries were from the use of electrosurgery, which are typically associated with a delay in presentation.
In this study, 41% of the injuries were unrecognized at the time of surgery. All 5 of the reported deaths were associated with a delay in diagnosis, with an overall mortality rate of 1 of 125, or 0.8%. Since all of these deaths were associated with a delay in diagnosis, the rate of mortality in unrecognized bowel injury was 5 of 154, or 3.2%. Among women who experienced delayed diagnosis, only 19 of 154 experienced signs or symptoms diagnostic for an underlying bowel injury, particularly when the small bowel was injured.
Can mechanical bowel prep positively affect outcomes in gynecologic laparoscopy, or should it be discarded?
Arnold A, Aitchison LP, Abbott J. Preoperative mechanical bowel preparation for abdominal, laparoscopic, and vaginal surgery: a systematic review. J Minim Invasive Gynecol. 2015;22(5):737−752.
Popularized for more than 4 decades, the practice of presurgical bowel preparation is predicated on the notion that the presence of less, versus more, feces can minimize bacterial count and thereby reduce peritoneal contamination. Logically then, surgical site infections (SSIs) should be reduced with bowel preparation. Moreover, the surgical view and bowel handling during laparoscopic surgery should be improved, with surgical times consequently reduced.
Surgeons must weigh the putative benefits of mechanical bowel preparation against the unpleasant experience it causes for patients, as well as the risks of dehydration or electrolyte disturbance it may cause. To this day, a considerable percentage of gynecologists and colorectal surgeons routinely prep the bowel after weighing all of these factors, despite the paucity of evidence for the practice's efficacy to reduce SSI and improve surgical outcomes.7
The results of this recent systematic review critically question the usefulness of preoperative bowel preparation for abdominal, laparoscopic, and vaginal surgery.
Details of the analysis
The authors evaluated high-quality studies on mechanical bowel preparation to assess evidence for:
- surgeon outcomes, including the surgical field and bowel handling
- operative outcomes, including intraoperative complications and operative times
- patient outcomes, including postoperative complications, overall morbidity, and length of stay.
The authors identified RCTs and prospective or retrospective cohort studies in various surgical specialties comparing preoperative bowel preparation to no such prep. Forty-three studies met inclusion criteria: 38 compared prep to no prep, and 5 compared prep to a single rectal enema. Five high-grade studies in gynecology were included (n = 795), with 4 of them RCTs of gynecologic laparoscopy (n = 645).
Operative field and duration
Of the studies comparing bowel prep with no prep, only the 5 gynecologic ones assessed operative field. Surgical view was perceived as improved in only 1 study. In another, surgeons only could guess allocation half the time.
Sixteen studies evaluated impact of mechanical bowel preparation on duration of surgery: 1 high-quality study found a significant reduction in OR time with bowel prep, and 1 moderate-quality study found longer operative time with bowel prep.
Patient outcomes
Of all studies assessing patient outcomes, 3 high-quality studies of colorectal patients (n = 490) found increased complications from prep versus no prep, including anastomotic dehiscence (P = .05), abdominal complications (P = .028), and infectious complications (P = .05).
Length of stay was assessed in 26 studies, with 4 reporting longer hospital stay with bowel prep and the remaining finding no difference between prep and no prep.
Across all specialties, only 2 studies reported improved outcomes with mechanical bowel preparation. One was a high-quality study reporting reduced 30-day morbidity (P = .018) and infectious complication rates (P = .018), and the other was a moderate-quality study that found reduced SSI (P = .0001) and organ space infection (P = .024) in patients undergoing bowel prep.
Mechanical bowel preparation vs enema
Bowel prep was compared with a single rectal enema in 5 studies. In 2 of these, patient outcomes were worse with enema. One high-quality study of 294 patients reported increased intra-abdominal fecal soiling (P = .008) in the enema group. (The surgeons believed that bowel preparation was more likely to be inadequate in this group, 25% compared with 6%, P<.05.) Whereas there was no statistical difference in the incidence of anastomotic leak between these groups, there was higher reoperation rate in the enema-only group where leakage was diagnosed (6 [4.1%] vs 0, respectively; P = .013).
Bowel prep and preoperative and postoperative symptoms
Six high-quality studies reported on the impact of mechanical bowel preparation on patient symptoms, such as nausea, weakness, abdominal distention, and satisfaction before and after surgery. In all but 1 study patients had significantly greater discomfort with bowel preparation. In 2 of the 6 studies, patients had more diarrhea (P = .0003), a delay in the first bowel movement (P = .001), and a slower return to normal diet (P = .004).
What this EVIDENCE means for practice
The theory behind mechanical bowel preparation is not supported by the evidence. Despite the fact that the bowel is not customarily entered, up to 50% of gynecologic surgeons employ bowel preparation, with the hope of improving visualization and decreasing risk of an anastomotic leak. The colorectal studies in this review demonstrate no evidence for decreased anastomotic leak or infectious complications. By extrapolation, there is no evidence that using preoperative bowel prep bestows any benefit if bowel injury occurs inadvertently and if resection or reanastomosis is then required.
Among the 7 studies examining bowel prep in laparoscopy (4 gynecology, 3 urology, and 1 colorectal), only data from 1 demonstrated an improved surgical field (and in this case only by 1 out of 10 on a Likert scale). The impact of mechanical bowel preparation on the visual field is the same for diagnostic or complex laparoscopic surgeries. One high-quality study with deep endometriosis resection demonstrated no change in the operative field as reflected by no practical differences in OR time or complications.
Preparing the bowel for surgery is an intrusive process that reduces patient satisfaction by inducing weakness, abdominal distention, nausea, vomiting, hunger, and thirst. Whereas this systematic analysis failed to confirm any benefit of the process, it provides evidence for the potential for harm. Mechanical bowel preparation should be discarded as a routine preoperative treatment for patients undergoing minimally invasive gynecologic surgery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Rightly so, the topics of mechanical tissue extraction and hysterectomy approach have dominated the field of obstetrics and gynecology over the past 12 months and more. A profusion of literature has been published on these subjects. However, there are 2 important topics within the field of minimally invasive gynecologic surgery that deserve our attention as well, and I have chosen to focus on these for this Update.
First, laparoscopic treatment of ovarian endometriomas is one of the most commonly performed gynecologic procedures worldwide. Many women undergoing such surgery are of childbearing age and have the desire for future pregnancy. What are best practices for preserving ovarian function in these women? Two studies recently published in the Journal of Minimally Invasive Gynecology addressed this question.
Second, until recently, the rate of bowel injury at laparoscopic gynecologic surgery has not been well established.1 Moreover, mechanical bowel preparation is commonly employed in case intestinal injury does occur, despite the lack of evidence that outcomes of these possible injuries can be improved.2 Understanding the rate of bowel injury can shed light on the overall value of the perceived benefits of bowel preparation. Therefore, I examine 2 recent systematic reviews that analyze the incidence of bowel injury and the value of bowel prep in gynecologic laparoscopic surgery.
bipolar coagulation inferior to suturing or hemostatic sealant for preserving ovarian function
Song T, Kim WY, Lee KW, Kim KH. Effect on ovarian reserve of hemostasis by bipolar coagulation versus suture during laparoendoscopic single-site cystectomy for ovarian endometriomas. J Minim Invasive Gynecol. 2015;22(3):415−420.
Ata B, Turkgeldi E, Seyhan A, Urman B. Effect of hemostatic method on ovarian reserve following laparoscopic endometrioma excision; comparison of suture, hemostatic sealant, and bipolar dessication. A systematic review and meta-analysis. J Minim Invasive Gynecol. 2015;22(3):363−372.
The customary surgical approach for laparoscopic cystectomy is by mechanical stripping of the cyst wall (FIGURE) and the use of bipolar desiccation for hemostasis. Stripping inevitably leads to removal of healthy ovarian cortex,3 especially in inexperienced hands,4 and ovarian follicles inevitably are destroyed during electrosurgical desiccation. When compared with the use of suturing or a hemostatic agent to control bleeding in the ovarian defect, the use of bipolar electrosurgery may harm more of the ovarian cortex, resulting in a comparatively diminished follicular cohort.
Possible deleterious effects on the ovarian reserve can be determined with a blood test to measure anti-Müllerian hormone (AMH) levels postoperatively. Produced by the granulosa cells of the ovary, this hormone directly reflects the remaining ovarian egg supply. Lower levels of AMH have been shown to significantly decrease the success rate of in vitro fertilization (IVF), especially in women older than age 35.5 Moreover, AMH levels in the late reproductive years can be used as a predictive marker of menopause, with lower levels predicting significantly earlier onset.6
Data from 2 recent studies, a quasi-randomized trial by Song and colleagues and a systematic review and meta-analysis by Ata and colleagues emphasize that bipolar desiccation for hemostasis may not be best practice for protecting ovarian reserve during laparoscopic ovarian cystectomy for an endometrioma.
AMH levels decline more significantly for women undergoing bipolar desiccation
Song and colleagues conducted a prospective quasi-randomized study of 125 women whose endometriomas were laparoscopically removed via a single-site approach and managed for hemostasis with either bipolar desiccation or suturing of the ovarian defect with a 2-0 barbed suture. All surgeries were conducted by a single surgeon.
At 3 months postsurgery, mean AMH levels had declined from baseline by 42.2% (interquartile range [IR], 16.5−53.0 ng/mL) in the desiccation group and by 24.6% (IR, 11.6−37.0 ng/mL) in the suture group (P = .001). Multivariate analysis showed that the method used for hemostasis was the only determinant for reduced ovarian reserve.
In their systematic review and meta-analysis, Ata and colleagues included 10 studies--6 qualitative and 4 quantitative. All studies examined the rate of change of serum AMH levels 3 months after laparoscopic removal of an endometrioma.
In their qualitative analysis, 5 of the 6 studies reported a significantly greater decrease in ovarian reserve after bipolar desiccation (varying from 13% to 44%) or a strong trend in the same direction. In the sixth study, the desiccation group had a lower decline in absolute AMH level than in the other 5 studies. The authors note that this 2.7% decline was much lower than the values reported for the bipolar desiccation group of any other study. (Those declines ranged between 19% and 58%.)
Although not significant, in all 3 of the included randomized controlled trials (RCTs), the desiccation groups had a greater loss in AMH level than the hemostatic sealant groups, and in 2 of these RCTs, bipolar desiccation groups had a greater loss than the suturing groups.
Among the 213 study participants in the 3 RCTs and the prospective cohort study included in the quantitative meta-analysis, alternative methods to bipolar desiccation were associated with a 6.95% lower decrease in AMH-level decline (95% confidence interval [CI], −13.0% to −0.9%; P = .02).
What this EVIDENCE means for practice
Compared with the use of bipolar electrosurgery to attain hemostasis, the use of a topical biosurgical agent or suturing could be significantly better for protection of the ovarian follicles during laparoscopic ovarian cystectomy for endometrioma. These alternative methods especially could benefit those women desiring future pregnancy who are demonstrated preoperatively to have a low ovarian reserve. As needed, electrosurgery should be sparingly employed for ovarian hemostasis.
Large Study identifies incidence of bowel injury during gynecologic laproscopy
Llarena NC, Shah AB, Milad MP. Bowel injury in gynecologic laparoscopy: a systematic review. Am J Obstet Gynecol. 2015;125(6):1407−1417.
In no aspect of laparoscopic surgery are preventive strategies more cautiously employed than during peritoneal access. Regardless of the applied technique, there is an irreducible risk of injury to the underlying viscera by either adhesions between the underlying bowel and abdominal wall or during the course of pilot error. Moreover, in the best of hands, bowel injury can occur whenever normal anatomic relationships need to be restored using intra-abdominal adhesiolysis. Given the ubiquity, these risks are never out of the surgeon's mind. Gynecologists are obliged to discuss these risks during the informed consent process.
Until recently, the rate of bowel injury has not been well established. Llarena and colleagues recently have conducted the largest systematic review of the medical literature to date for incidence, presentation, mortality, cause, and location of bowel injury associated with laparoscopic surgery while not necessarily distinguishing for the type of bowel injury. Sixty retrospective and 27 prospective studies met inclusion criteria.
The risk of bowel injury overall and defined
Among 474,063 laparoscopic surgeries conducted between 1972 and 2014, 604 bowel injuries were found, for an incidence of 1 in 769, or 0.13% (95% CI, 0.12−0.14%).
The rate of bowel injury varied by procedure, year, study type, and definition of bowel injury. The incidence of injury according to:
- definition, was 1 in 416 (0.24%) for studies that clearly included serosal injuries and enterotomies versus 1 in 833 (0.12%) for studies not clearly defining the type of bowel injury (relative risk [RR], 0.47; 95% CI, 0.38−0.59; P<.001)
- study type, was 1 in 666 (0.15%) for prospective studies versus 1 in 909 (0.11%) for retrospective studies (RR, 0.78; 95% CI, 0.63−0.96; P = .02)
- procedure, was 1 in 3,333 (0.03%; 95% CI, 0.01−0.03%) for sterilization and 1 in 256 (0.39%; 95% CI, 0.35−0.45%) for hysterectomy
- year, for laparoscopic hysterectomy only, was 1 in 222 (0.45%) before the year 2000 and 1 in 294 (0.34%) after 2000 (RR, 0.75; 95% CI, 0.57−0.98; P = .03).
How were injuries caused, found, and managed?
Thirty studies described the laparoscopic instrument used during 366 reported bowel injuries. The majority of injuries (55%) occurred during initial peritoneal access, with the Veress needle or trocar causing the damage. This was followed by electrosurgery (29%), dissection (11%), and forceps or scissors (4.1%).
According to 40 studies describing 307 injuries, bowel injuries most often were managed by converting to laparotomy (80%); only 8% of injuries were managed with laparoscopy and 2% expectantly.
Surgery to repair the bowel injury was delayed in 154 (41%) of 375 cases. The median time to injury discovery was 3 days (range, 1−13 days).
In only 19 cases were the presenting signs and symptoms of bowel injury recorded. Those reported from most to least often were: peritonitis, abdominal pain, fever, abdominal distention, leukocytosis, leukopenia, and septic shock.
Mortality
Mortality as an outcome was only reported in 29 of the total 90 studies; therefore, mortality may be underreported. Overall, however, death occurred in 1 (0.8%) of 125 bowel injuries.
The overall mortality rate from bowel injury--calculated from the only 42 studies that explicitly mentioned mortality as an outcome--was 1 in 125, or 0.8% (95% CI, 0.36%-1.9%). All 5 reported deaths occurred as a result of delayed recognition of bowel injury, which made the mortality rate for unrecognized bowel injury 1 in 31, or 3.2% (95% CI, 1%-7%). No deaths occurred when the bowel injury was noted intraoperatively.
What this EVIDENCE means for practice
In this review of 474,063 laparoscopic procedures, bowel injury occurred in 1 in 769, or 0.13% of procedures. Bowel injury is more apt to occur during more complicated laparoscopic procedures (compared with laparoscopic sterilization procedures, the risk during hysterectomy was greater than 10-fold).
Most of the injuries were managed by laparotomic surgery despite the potential to repair bowel injury by laparoscopy. Validating that peritoneal access is a high risk part of laparoscopic surgery, the majority of the injuries occurred during insufflation with a Veress needle or during abdominal access by trocar insertion. Nearly one-third of the injuries were from the use of electrosurgery, which are typically associated with a delay in presentation.
In this study, 41% of the injuries were unrecognized at the time of surgery. All 5 of the reported deaths were associated with a delay in diagnosis, with an overall mortality rate of 1 of 125, or 0.8%. Since all of these deaths were associated with a delay in diagnosis, the rate of mortality in unrecognized bowel injury was 5 of 154, or 3.2%. Among women who experienced delayed diagnosis, only 19 of 154 experienced signs or symptoms diagnostic for an underlying bowel injury, particularly when the small bowel was injured.
Can mechanical bowel prep positively affect outcomes in gynecologic laparoscopy, or should it be discarded?
Arnold A, Aitchison LP, Abbott J. Preoperative mechanical bowel preparation for abdominal, laparoscopic, and vaginal surgery: a systematic review. J Minim Invasive Gynecol. 2015;22(5):737−752.
Popularized for more than 4 decades, the practice of presurgical bowel preparation is predicated on the notion that the presence of less, versus more, feces can minimize bacterial count and thereby reduce peritoneal contamination. Logically then, surgical site infections (SSIs) should be reduced with bowel preparation. Moreover, the surgical view and bowel handling during laparoscopic surgery should be improved, with surgical times consequently reduced.
Surgeons must weigh the putative benefits of mechanical bowel preparation against the unpleasant experience it causes for patients, as well as the risks of dehydration or electrolyte disturbance it may cause. To this day, a considerable percentage of gynecologists and colorectal surgeons routinely prep the bowel after weighing all of these factors, despite the paucity of evidence for the practice's efficacy to reduce SSI and improve surgical outcomes.7
The results of this recent systematic review critically question the usefulness of preoperative bowel preparation for abdominal, laparoscopic, and vaginal surgery.
Details of the analysis
The authors evaluated high-quality studies on mechanical bowel preparation to assess evidence for:
- surgeon outcomes, including the surgical field and bowel handling
- operative outcomes, including intraoperative complications and operative times
- patient outcomes, including postoperative complications, overall morbidity, and length of stay.
The authors identified RCTs and prospective or retrospective cohort studies in various surgical specialties comparing preoperative bowel preparation to no such prep. Forty-three studies met inclusion criteria: 38 compared prep to no prep, and 5 compared prep to a single rectal enema. Five high-grade studies in gynecology were included (n = 795), with 4 of them RCTs of gynecologic laparoscopy (n = 645).
Operative field and duration
Of the studies comparing bowel prep with no prep, only the 5 gynecologic ones assessed operative field. Surgical view was perceived as improved in only 1 study. In another, surgeons only could guess allocation half the time.
Sixteen studies evaluated impact of mechanical bowel preparation on duration of surgery: 1 high-quality study found a significant reduction in OR time with bowel prep, and 1 moderate-quality study found longer operative time with bowel prep.
Patient outcomes
Of all studies assessing patient outcomes, 3 high-quality studies of colorectal patients (n = 490) found increased complications from prep versus no prep, including anastomotic dehiscence (P = .05), abdominal complications (P = .028), and infectious complications (P = .05).
Length of stay was assessed in 26 studies, with 4 reporting longer hospital stay with bowel prep and the remaining finding no difference between prep and no prep.
Across all specialties, only 2 studies reported improved outcomes with mechanical bowel preparation. One was a high-quality study reporting reduced 30-day morbidity (P = .018) and infectious complication rates (P = .018), and the other was a moderate-quality study that found reduced SSI (P = .0001) and organ space infection (P = .024) in patients undergoing bowel prep.
Mechanical bowel preparation vs enema
Bowel prep was compared with a single rectal enema in 5 studies. In 2 of these, patient outcomes were worse with enema. One high-quality study of 294 patients reported increased intra-abdominal fecal soiling (P = .008) in the enema group. (The surgeons believed that bowel preparation was more likely to be inadequate in this group, 25% compared with 6%, P<.05.) Whereas there was no statistical difference in the incidence of anastomotic leak between these groups, there was higher reoperation rate in the enema-only group where leakage was diagnosed (6 [4.1%] vs 0, respectively; P = .013).
Bowel prep and preoperative and postoperative symptoms
Six high-quality studies reported on the impact of mechanical bowel preparation on patient symptoms, such as nausea, weakness, abdominal distention, and satisfaction before and after surgery. In all but 1 study patients had significantly greater discomfort with bowel preparation. In 2 of the 6 studies, patients had more diarrhea (P = .0003), a delay in the first bowel movement (P = .001), and a slower return to normal diet (P = .004).
What this EVIDENCE means for practice
The theory behind mechanical bowel preparation is not supported by the evidence. Despite the fact that the bowel is not customarily entered, up to 50% of gynecologic surgeons employ bowel preparation, with the hope of improving visualization and decreasing risk of an anastomotic leak. The colorectal studies in this review demonstrate no evidence for decreased anastomotic leak or infectious complications. By extrapolation, there is no evidence that using preoperative bowel prep bestows any benefit if bowel injury occurs inadvertently and if resection or reanastomosis is then required.
Among the 7 studies examining bowel prep in laparoscopy (4 gynecology, 3 urology, and 1 colorectal), only data from 1 demonstrated an improved surgical field (and in this case only by 1 out of 10 on a Likert scale). The impact of mechanical bowel preparation on the visual field is the same for diagnostic or complex laparoscopic surgeries. One high-quality study with deep endometriosis resection demonstrated no change in the operative field as reflected by no practical differences in OR time or complications.
Preparing the bowel for surgery is an intrusive process that reduces patient satisfaction by inducing weakness, abdominal distention, nausea, vomiting, hunger, and thirst. Whereas this systematic analysis failed to confirm any benefit of the process, it provides evidence for the potential for harm. Mechanical bowel preparation should be discarded as a routine preoperative treatment for patients undergoing minimally invasive gynecologic surgery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
Rightly so, the topics of mechanical tissue extraction and hysterectomy approach have dominated the field of obstetrics and gynecology over the past 12 months and more. A profusion of literature has been published on these subjects. However, there are 2 important topics within the field of minimally invasive gynecologic surgery that deserve our attention as well, and I have chosen to focus on these for this Update.
First, laparoscopic treatment of ovarian endometriomas is one of the most commonly performed gynecologic procedures worldwide. Many women undergoing such surgery are of childbearing age and have the desire for future pregnancy. What are best practices for preserving ovarian function in these women? Two studies recently published in the Journal of Minimally Invasive Gynecology addressed this question.
Second, until recently, the rate of bowel injury at laparoscopic gynecologic surgery has not been well established.1 Moreover, mechanical bowel preparation is commonly employed in case intestinal injury does occur, despite the lack of evidence that outcomes of these possible injuries can be improved.2 Understanding the rate of bowel injury can shed light on the overall value of the perceived benefits of bowel preparation. Therefore, I examine 2 recent systematic reviews that analyze the incidence of bowel injury and the value of bowel prep in gynecologic laparoscopic surgery.
bipolar coagulation inferior to suturing or hemostatic sealant for preserving ovarian function
Song T, Kim WY, Lee KW, Kim KH. Effect on ovarian reserve of hemostasis by bipolar coagulation versus suture during laparoendoscopic single-site cystectomy for ovarian endometriomas. J Minim Invasive Gynecol. 2015;22(3):415−420.
Ata B, Turkgeldi E, Seyhan A, Urman B. Effect of hemostatic method on ovarian reserve following laparoscopic endometrioma excision; comparison of suture, hemostatic sealant, and bipolar dessication. A systematic review and meta-analysis. J Minim Invasive Gynecol. 2015;22(3):363−372.
The customary surgical approach for laparoscopic cystectomy is by mechanical stripping of the cyst wall (FIGURE) and the use of bipolar desiccation for hemostasis. Stripping inevitably leads to removal of healthy ovarian cortex,3 especially in inexperienced hands,4 and ovarian follicles inevitably are destroyed during electrosurgical desiccation. When compared with the use of suturing or a hemostatic agent to control bleeding in the ovarian defect, the use of bipolar electrosurgery may harm more of the ovarian cortex, resulting in a comparatively diminished follicular cohort.
Possible deleterious effects on the ovarian reserve can be determined with a blood test to measure anti-Müllerian hormone (AMH) levels postoperatively. Produced by the granulosa cells of the ovary, this hormone directly reflects the remaining ovarian egg supply. Lower levels of AMH have been shown to significantly decrease the success rate of in vitro fertilization (IVF), especially in women older than age 35.5 Moreover, AMH levels in the late reproductive years can be used as a predictive marker of menopause, with lower levels predicting significantly earlier onset.6
Data from 2 recent studies, a quasi-randomized trial by Song and colleagues and a systematic review and meta-analysis by Ata and colleagues emphasize that bipolar desiccation for hemostasis may not be best practice for protecting ovarian reserve during laparoscopic ovarian cystectomy for an endometrioma.
AMH levels decline more significantly for women undergoing bipolar desiccation
Song and colleagues conducted a prospective quasi-randomized study of 125 women whose endometriomas were laparoscopically removed via a single-site approach and managed for hemostasis with either bipolar desiccation or suturing of the ovarian defect with a 2-0 barbed suture. All surgeries were conducted by a single surgeon.
At 3 months postsurgery, mean AMH levels had declined from baseline by 42.2% (interquartile range [IR], 16.5−53.0 ng/mL) in the desiccation group and by 24.6% (IR, 11.6−37.0 ng/mL) in the suture group (P = .001). Multivariate analysis showed that the method used for hemostasis was the only determinant for reduced ovarian reserve.
In their systematic review and meta-analysis, Ata and colleagues included 10 studies--6 qualitative and 4 quantitative. All studies examined the rate of change of serum AMH levels 3 months after laparoscopic removal of an endometrioma.
In their qualitative analysis, 5 of the 6 studies reported a significantly greater decrease in ovarian reserve after bipolar desiccation (varying from 13% to 44%) or a strong trend in the same direction. In the sixth study, the desiccation group had a lower decline in absolute AMH level than in the other 5 studies. The authors note that this 2.7% decline was much lower than the values reported for the bipolar desiccation group of any other study. (Those declines ranged between 19% and 58%.)
Although not significant, in all 3 of the included randomized controlled trials (RCTs), the desiccation groups had a greater loss in AMH level than the hemostatic sealant groups, and in 2 of these RCTs, bipolar desiccation groups had a greater loss than the suturing groups.
Among the 213 study participants in the 3 RCTs and the prospective cohort study included in the quantitative meta-analysis, alternative methods to bipolar desiccation were associated with a 6.95% lower decrease in AMH-level decline (95% confidence interval [CI], −13.0% to −0.9%; P = .02).
What this EVIDENCE means for practice
Compared with the use of bipolar electrosurgery to attain hemostasis, the use of a topical biosurgical agent or suturing could be significantly better for protection of the ovarian follicles during laparoscopic ovarian cystectomy for endometrioma. These alternative methods especially could benefit those women desiring future pregnancy who are demonstrated preoperatively to have a low ovarian reserve. As needed, electrosurgery should be sparingly employed for ovarian hemostasis.
Large Study identifies incidence of bowel injury during gynecologic laproscopy
Llarena NC, Shah AB, Milad MP. Bowel injury in gynecologic laparoscopy: a systematic review. Am J Obstet Gynecol. 2015;125(6):1407−1417.
In no aspect of laparoscopic surgery are preventive strategies more cautiously employed than during peritoneal access. Regardless of the applied technique, there is an irreducible risk of injury to the underlying viscera by either adhesions between the underlying bowel and abdominal wall or during the course of pilot error. Moreover, in the best of hands, bowel injury can occur whenever normal anatomic relationships need to be restored using intra-abdominal adhesiolysis. Given the ubiquity, these risks are never out of the surgeon's mind. Gynecologists are obliged to discuss these risks during the informed consent process.
Until recently, the rate of bowel injury has not been well established. Llarena and colleagues recently have conducted the largest systematic review of the medical literature to date for incidence, presentation, mortality, cause, and location of bowel injury associated with laparoscopic surgery while not necessarily distinguishing for the type of bowel injury. Sixty retrospective and 27 prospective studies met inclusion criteria.
The risk of bowel injury overall and defined
Among 474,063 laparoscopic surgeries conducted between 1972 and 2014, 604 bowel injuries were found, for an incidence of 1 in 769, or 0.13% (95% CI, 0.12−0.14%).
The rate of bowel injury varied by procedure, year, study type, and definition of bowel injury. The incidence of injury according to:
- definition, was 1 in 416 (0.24%) for studies that clearly included serosal injuries and enterotomies versus 1 in 833 (0.12%) for studies not clearly defining the type of bowel injury (relative risk [RR], 0.47; 95% CI, 0.38−0.59; P<.001)
- study type, was 1 in 666 (0.15%) for prospective studies versus 1 in 909 (0.11%) for retrospective studies (RR, 0.78; 95% CI, 0.63−0.96; P = .02)
- procedure, was 1 in 3,333 (0.03%; 95% CI, 0.01−0.03%) for sterilization and 1 in 256 (0.39%; 95% CI, 0.35−0.45%) for hysterectomy
- year, for laparoscopic hysterectomy only, was 1 in 222 (0.45%) before the year 2000 and 1 in 294 (0.34%) after 2000 (RR, 0.75; 95% CI, 0.57−0.98; P = .03).
How were injuries caused, found, and managed?
Thirty studies described the laparoscopic instrument used during 366 reported bowel injuries. The majority of injuries (55%) occurred during initial peritoneal access, with the Veress needle or trocar causing the damage. This was followed by electrosurgery (29%), dissection (11%), and forceps or scissors (4.1%).
According to 40 studies describing 307 injuries, bowel injuries most often were managed by converting to laparotomy (80%); only 8% of injuries were managed with laparoscopy and 2% expectantly.
Surgery to repair the bowel injury was delayed in 154 (41%) of 375 cases. The median time to injury discovery was 3 days (range, 1−13 days).
In only 19 cases were the presenting signs and symptoms of bowel injury recorded. Those reported from most to least often were: peritonitis, abdominal pain, fever, abdominal distention, leukocytosis, leukopenia, and septic shock.
Mortality
Mortality as an outcome was only reported in 29 of the total 90 studies; therefore, mortality may be underreported. Overall, however, death occurred in 1 (0.8%) of 125 bowel injuries.
The overall mortality rate from bowel injury--calculated from the only 42 studies that explicitly mentioned mortality as an outcome--was 1 in 125, or 0.8% (95% CI, 0.36%-1.9%). All 5 reported deaths occurred as a result of delayed recognition of bowel injury, which made the mortality rate for unrecognized bowel injury 1 in 31, or 3.2% (95% CI, 1%-7%). No deaths occurred when the bowel injury was noted intraoperatively.
What this EVIDENCE means for practice
In this review of 474,063 laparoscopic procedures, bowel injury occurred in 1 in 769, or 0.13% of procedures. Bowel injury is more apt to occur during more complicated laparoscopic procedures (compared with laparoscopic sterilization procedures, the risk during hysterectomy was greater than 10-fold).
Most of the injuries were managed by laparotomic surgery despite the potential to repair bowel injury by laparoscopy. Validating that peritoneal access is a high risk part of laparoscopic surgery, the majority of the injuries occurred during insufflation with a Veress needle or during abdominal access by trocar insertion. Nearly one-third of the injuries were from the use of electrosurgery, which are typically associated with a delay in presentation.
In this study, 41% of the injuries were unrecognized at the time of surgery. All 5 of the reported deaths were associated with a delay in diagnosis, with an overall mortality rate of 1 of 125, or 0.8%. Since all of these deaths were associated with a delay in diagnosis, the rate of mortality in unrecognized bowel injury was 5 of 154, or 3.2%. Among women who experienced delayed diagnosis, only 19 of 154 experienced signs or symptoms diagnostic for an underlying bowel injury, particularly when the small bowel was injured.
Can mechanical bowel prep positively affect outcomes in gynecologic laparoscopy, or should it be discarded?
Arnold A, Aitchison LP, Abbott J. Preoperative mechanical bowel preparation for abdominal, laparoscopic, and vaginal surgery: a systematic review. J Minim Invasive Gynecol. 2015;22(5):737−752.
Popularized for more than 4 decades, the practice of presurgical bowel preparation is predicated on the notion that the presence of less, versus more, feces can minimize bacterial count and thereby reduce peritoneal contamination. Logically then, surgical site infections (SSIs) should be reduced with bowel preparation. Moreover, the surgical view and bowel handling during laparoscopic surgery should be improved, with surgical times consequently reduced.
Surgeons must weigh the putative benefits of mechanical bowel preparation against the unpleasant experience it causes for patients, as well as the risks of dehydration or electrolyte disturbance it may cause. To this day, a considerable percentage of gynecologists and colorectal surgeons routinely prep the bowel after weighing all of these factors, despite the paucity of evidence for the practice's efficacy to reduce SSI and improve surgical outcomes.7
The results of this recent systematic review critically question the usefulness of preoperative bowel preparation for abdominal, laparoscopic, and vaginal surgery.
Details of the analysis
The authors evaluated high-quality studies on mechanical bowel preparation to assess evidence for:
- surgeon outcomes, including the surgical field and bowel handling
- operative outcomes, including intraoperative complications and operative times
- patient outcomes, including postoperative complications, overall morbidity, and length of stay.
The authors identified RCTs and prospective or retrospective cohort studies in various surgical specialties comparing preoperative bowel preparation to no such prep. Forty-three studies met inclusion criteria: 38 compared prep to no prep, and 5 compared prep to a single rectal enema. Five high-grade studies in gynecology were included (n = 795), with 4 of them RCTs of gynecologic laparoscopy (n = 645).
Operative field and duration
Of the studies comparing bowel prep with no prep, only the 5 gynecologic ones assessed operative field. Surgical view was perceived as improved in only 1 study. In another, surgeons only could guess allocation half the time.
Sixteen studies evaluated impact of mechanical bowel preparation on duration of surgery: 1 high-quality study found a significant reduction in OR time with bowel prep, and 1 moderate-quality study found longer operative time with bowel prep.
Patient outcomes
Of all studies assessing patient outcomes, 3 high-quality studies of colorectal patients (n = 490) found increased complications from prep versus no prep, including anastomotic dehiscence (P = .05), abdominal complications (P = .028), and infectious complications (P = .05).
Length of stay was assessed in 26 studies, with 4 reporting longer hospital stay with bowel prep and the remaining finding no difference between prep and no prep.
Across all specialties, only 2 studies reported improved outcomes with mechanical bowel preparation. One was a high-quality study reporting reduced 30-day morbidity (P = .018) and infectious complication rates (P = .018), and the other was a moderate-quality study that found reduced SSI (P = .0001) and organ space infection (P = .024) in patients undergoing bowel prep.
Mechanical bowel preparation vs enema
Bowel prep was compared with a single rectal enema in 5 studies. In 2 of these, patient outcomes were worse with enema. One high-quality study of 294 patients reported increased intra-abdominal fecal soiling (P = .008) in the enema group. (The surgeons believed that bowel preparation was more likely to be inadequate in this group, 25% compared with 6%, P<.05.) Whereas there was no statistical difference in the incidence of anastomotic leak between these groups, there was higher reoperation rate in the enema-only group where leakage was diagnosed (6 [4.1%] vs 0, respectively; P = .013).
Bowel prep and preoperative and postoperative symptoms
Six high-quality studies reported on the impact of mechanical bowel preparation on patient symptoms, such as nausea, weakness, abdominal distention, and satisfaction before and after surgery. In all but 1 study patients had significantly greater discomfort with bowel preparation. In 2 of the 6 studies, patients had more diarrhea (P = .0003), a delay in the first bowel movement (P = .001), and a slower return to normal diet (P = .004).
What this EVIDENCE means for practice
The theory behind mechanical bowel preparation is not supported by the evidence. Despite the fact that the bowel is not customarily entered, up to 50% of gynecologic surgeons employ bowel preparation, with the hope of improving visualization and decreasing risk of an anastomotic leak. The colorectal studies in this review demonstrate no evidence for decreased anastomotic leak or infectious complications. By extrapolation, there is no evidence that using preoperative bowel prep bestows any benefit if bowel injury occurs inadvertently and if resection or reanastomosis is then required.
Among the 7 studies examining bowel prep in laparoscopy (4 gynecology, 3 urology, and 1 colorectal), only data from 1 demonstrated an improved surgical field (and in this case only by 1 out of 10 on a Likert scale). The impact of mechanical bowel preparation on the visual field is the same for diagnostic or complex laparoscopic surgeries. One high-quality study with deep endometriosis resection demonstrated no change in the operative field as reflected by no practical differences in OR time or complications.
Preparing the bowel for surgery is an intrusive process that reduces patient satisfaction by inducing weakness, abdominal distention, nausea, vomiting, hunger, and thirst. Whereas this systematic analysis failed to confirm any benefit of the process, it provides evidence for the potential for harm. Mechanical bowel preparation should be discarded as a routine preoperative treatment for patients undergoing minimally invasive gynecologic surgery.
Share your thoughts! Send your Letter to the Editor to [email protected]. Please include your name and the city and state in which you practice.
In this article
- Preserving ovarian function at laparoscopic cystectomy
- Incidence of bowel injury during gyn surgery
- Usefulness and safety of mechanical bowel preparation
What’s Hot and What’s Not in Our National Organizations: An Emergency Medicine Panel, Part 1
On February 21 to 24, 2016, the Association of Academic Chairs of Emergency Medicine (AACEM) held its 8th annual retreat in Tempe, Arizona. The AACEM is comprised of full, acting, interim, and emeritus chairs and directors of departments of emergency medicine (EM) who work to improve and support academic departments of EM in the advancement of health care through high-quality education and research.
During that event, AACEM President Greg Volturo, MD, organized a panel discussion of EM leaders to provide an update on their organizations’ recent activities. This panel included representatives from seven prominent EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Emergency Medicine Residency Directors (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM).
The following is the first of a two-part article that provides highlights from that discussion, with reports from the AAEM, AAEM/RSA, ABEM, and ACEP. Part 2 will appear in the May issue and will include reports from the CORD, EMRA, and SAEM.
American Academy of Emergency Medicine
Kevin G. Rodgers, MD, FAAEM, President AAEM
Due Process. AAEM highlighted the problem of the lack of due process for many emergency physicians (EPs). By agreeing to waive their rights to due process when signing contracts with some contract management companies, EPs can unwittingly give their employers the power to terminate them without cause and without notice. AAEM is working with Centers for Medicare & Medicaid Services (CMS) and several congressmen to amend the Medicare Rules for Participation to include an “unwaivable due process guarantee.” In addition, AAEM is requesting an addition to the current Code of Federal Regulation to ensure EPs are entitled “to a fair hearing and appellate review through hospital medical staff mechanisms before any termination or restriction of their professional activity or medical staff privileges. These rights cannot be denied through a third party contract.”
AAEM Residency Visitation Program. AAEM is committed to visiting every EM residency program once every 3 to 4 years, similar to the ACEP and ABEM programs. Residency programs will have the opportunity to select from a list of well-known EM speakers; they will deliver a clinically oriented lecture, followed by a presentation on AAEM. The cost of the program is borne completely by AAEM.
AAEM Physician Group (AAEM-PG). This program was announced at the 2016 AAEM Scientific Assembly. AAEM-PG establishes and supports EM practices where physicians can operate democratically and have an equal voice. It is a practice that is run by the local physicians for the physicians. AAEM-PG will help guide new as well as established EM groups, providing for physicians’ autonomy, fair and equitable practice environments, and career and group longevity.
AAEM Resident and Student Association
Victoria Weston, MD, AAEM/RSA President
Overview. Started in 2005, AAEM/RAS now has over 3,500 members and 58 EM residency programs with 100% participation. Benefits of membership include access to EM:RAP and The Journal of Emergency Medicine, access and opportunities to contribute to an RSA peer-reviewed blog and Modern Resident, and free registration for the AAEM Annual Scientific Assembly. As part of the AAEM Scientific Assembly, AAEM/RSA coordinates a day-long education track in collaboration with the AAEM Young Physician Section, an In-Training Exam review, and a Career Fair and Social.
Congressional Elective. Members of AAEM/RSA can apply to be selected for a one-month “Congressional Elective” with Congressmen Raul Ruiz and Joe Heck, the only two EPs currently in Congress, to teach EPs the process of creating health-policy legislation on Capitol Hill. For 4 weeks, residents work directly in their congressional office and learn to work with constituents to develop relevant health-policy legislation. Residents learn to present legislative briefs, proposals, and research in a productive, succinct, and time-efficient manner. AAEM/RSA also offers an annual Advocacy Day, where residents and students have the opportunity to meet with members of Congress and/or senior congressional staff on Capitol Hill; this year it will be held on June 14, 2016 in Washington, DC.
Toxicology Mobile App. The AAEM/RSA Toxicology mobile app will soon be available for purchase, and is compatible with both iPhone and Android technology. You can search by subject, browse chapters of AAEM/RSA’s Toxicology Handbook, or contact Poison Control with a single click.
American Board of Emergency Medicine
Francis L. Counselman, MD, Immediate Past President, ABEM
Enhanced Oral (eOral) Certification Examination. ABEM has completed its second eOral examination; the third is scheduled for April 2016. Three of the examination cases are now in the new eOral format, which uses a computer monitor, patient avatar, picture archiving and communication system (PACS)-quality radiographs, and dynamic rhythm strips. Feedback from test-takers and examiners has been quite positive. ABEM will be moving more cases to the eOral format in the near future.
ABEM Director of Medical Affairs. ABEM has named its first ever Director of Medical Affairs (DMA): Melissa A. Barton, MD. Dr Barton is a former EM Residency Program Director and has been an ABEM Oral Examiner for the past 10 years. She is the recipient of several teaching and leadership awards. Dr Barton will focus on clinically oriented special projects and represent ABEM’s interests to external organizations.
Emergency Medicine Subspecialties. EM now has 13 subspecialty opportunities for EPs; that’s more than double the number from just 5 years ago. Emergency Medical Services (EMS) now has the most ABEM diplomates (445), followed by Medical Toxicology (367) and Pediatric Emergency Medicine (245).
Lifelong Learning and Self-Assessment (LLSA) Test Accessibility. To provide LLSA readings that better match a diplomate’s area of practice, the EMS and Medical Toxicology LLSA readings and tests can now be used by any diplomate to fulfill his or her Maintenance of Certification (MOC) Part II requirements. Pediatric EM LLSA readings and tests will eventually be made available to all diplomates at a later date. All LLSAs can be accessed through the ABEM Web site (https://www.abem.org).
Maintenance of Certification (MOC) Adds Value. In a survey of ABEM diplomates taking the 2014 ConCert Examination, 92.5% found value in maintaining their ABEM certification. In a follow-up survey in 2015, 90.4% stated their medical knowledge was reinforced and/or increased by preparing and taking the ConCert Examination. In addition to being relevant to our diplomates’ practice, ABEM has worked hard to control MOC costs. ABEM has not increased its fees for the last 5 years for the LLSAs; for all remaining examinations, there has been no fee increase for the past 4 years. When compared to all other boards, the expense of the ABEM MOC Program is at the median, costing EPs approximately $265 per year, or about $5 each week.
American College of Emergency Physicians
Jay A. Kaplan, MD, FACEP, ACEP President
Physician Burnout. Unfortunately, EM leads all specialties in the frequency of physician burnout. Emergency physicians must be aware of burnout, and take proactive steps to avoid it. To help EPs, ACEP has organized an “Emergency Medicine Wellness Week.” Prevention tips include eating well, getting the proper amount of sleep, regular exercise, and improving the work environment. In 2016, Wellness Week ran from January 24 to 30; there is a continuing focus on building resilience and preventing compassion fatigue.
Out of Network (OON) Balance Billing. Insurance companies know that it is solely the cost of insurance premiums that consumers pay attention to, not deductibles or exactly what the insurance covers. Those same insurance companies have been adept at portraying physicians as the cause of “surprise billing.” Emergency physicians need to change the conversation from “surprise billing” to “surprise coverage.” We need to talk about fair coverage for our patients, rather than asking for fair payment for physicians (the latter will follow the former and legislators believe that physicians are already fairly paid). ACEP is considering legal action against CMS and the Center for Consumer Information and Insurance Oversight regarding their final rule on “the greatest of three,” which establishes guidelines for how physicians are to be paid for services rendered.
Pay for Performance and Value-based Reimbursement. ACEP has created a joint task force with the Emergency Department Practice Management Association to create a toolbox for EPs to navigate the changing reimbursement landscape. This includes model legislation and best practices, and there is exploration regarding developing alternative payment models for EM.
Opioid Epidemic. ACEP is a participant in the White House working group exploring this epidemic and identifying strategies to combat this national problem. ACEP has sent a letter to CMS and Health and Human Services (HHS) requesting removal of the pain questions from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys. Emergency physicians should not be penalized on these surveys for not prescribing narcotic analgesics to patients who could be treated appropriately with nonnarcotic medications. ACEP similarly is considering sending a letter to The Joint Commission requesting removal of their emphasis on pain as the “fifth vital sign.”
Mass Casualty Incidents. ACEP has created a “New High-Threat High-Casualty Task Force” to identify best practice recommendations for provision of emergency care in high-threat environments and identify current clinical and operational knowledge gaps surrounding the issue. This in turn will help prioritize future ACEP research objectives based on these gaps. In addition, a white paper is being prepared, highlighting current national efforts and recommending clinical practice guidelines for adults and pediatric patients, as well as a future strategy for ACEP engagement as a national leader in the area of high-threat emergency care.
Diversity. There is a recognized need to increase the diversity in our current and future EM leadership. To that end, ACEP sponsored a Diversity Summit on April 14, 2016 in Dallas to explore these issues and make recommendations.
Emergency Quality Network. ACEP, along with 38 other health care organizations, received a grant in the CMS Transforming Clinical Practice Initiative to help physicians achieve large-scale health transformation. Areas of EM focus include: improving outcomes for patients with sepsis; reducing avoidable imaging in low-risk patients through implementation of ACEP’s Choosing Wisely campaign; and improving the value of ED chest pain evaluation in low-risk patients by reducing avoidable testing and admissions.
Editor’s Note: Part 2 of this article will appear in the May 2016 issue of Emergency Medicine and will feature reports from the Council of Emergency Medicine Residency Directors (CORD), the Emergency Medicine Residents’ Association (EMRA), and the Society for Academic Emergency Medicine (SAEM). Have a comment or question about this article? Let us know: [email protected].
On February 21 to 24, 2016, the Association of Academic Chairs of Emergency Medicine (AACEM) held its 8th annual retreat in Tempe, Arizona. The AACEM is comprised of full, acting, interim, and emeritus chairs and directors of departments of emergency medicine (EM) who work to improve and support academic departments of EM in the advancement of health care through high-quality education and research.
During that event, AACEM President Greg Volturo, MD, organized a panel discussion of EM leaders to provide an update on their organizations’ recent activities. This panel included representatives from seven prominent EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Emergency Medicine Residency Directors (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM).
The following is the first of a two-part article that provides highlights from that discussion, with reports from the AAEM, AAEM/RSA, ABEM, and ACEP. Part 2 will appear in the May issue and will include reports from the CORD, EMRA, and SAEM.
American Academy of Emergency Medicine
Kevin G. Rodgers, MD, FAAEM, President AAEM
Due Process. AAEM highlighted the problem of the lack of due process for many emergency physicians (EPs). By agreeing to waive their rights to due process when signing contracts with some contract management companies, EPs can unwittingly give their employers the power to terminate them without cause and without notice. AAEM is working with Centers for Medicare & Medicaid Services (CMS) and several congressmen to amend the Medicare Rules for Participation to include an “unwaivable due process guarantee.” In addition, AAEM is requesting an addition to the current Code of Federal Regulation to ensure EPs are entitled “to a fair hearing and appellate review through hospital medical staff mechanisms before any termination or restriction of their professional activity or medical staff privileges. These rights cannot be denied through a third party contract.”
AAEM Residency Visitation Program. AAEM is committed to visiting every EM residency program once every 3 to 4 years, similar to the ACEP and ABEM programs. Residency programs will have the opportunity to select from a list of well-known EM speakers; they will deliver a clinically oriented lecture, followed by a presentation on AAEM. The cost of the program is borne completely by AAEM.
AAEM Physician Group (AAEM-PG). This program was announced at the 2016 AAEM Scientific Assembly. AAEM-PG establishes and supports EM practices where physicians can operate democratically and have an equal voice. It is a practice that is run by the local physicians for the physicians. AAEM-PG will help guide new as well as established EM groups, providing for physicians’ autonomy, fair and equitable practice environments, and career and group longevity.
AAEM Resident and Student Association
Victoria Weston, MD, AAEM/RSA President
Overview. Started in 2005, AAEM/RAS now has over 3,500 members and 58 EM residency programs with 100% participation. Benefits of membership include access to EM:RAP and The Journal of Emergency Medicine, access and opportunities to contribute to an RSA peer-reviewed blog and Modern Resident, and free registration for the AAEM Annual Scientific Assembly. As part of the AAEM Scientific Assembly, AAEM/RSA coordinates a day-long education track in collaboration with the AAEM Young Physician Section, an In-Training Exam review, and a Career Fair and Social.
Congressional Elective. Members of AAEM/RSA can apply to be selected for a one-month “Congressional Elective” with Congressmen Raul Ruiz and Joe Heck, the only two EPs currently in Congress, to teach EPs the process of creating health-policy legislation on Capitol Hill. For 4 weeks, residents work directly in their congressional office and learn to work with constituents to develop relevant health-policy legislation. Residents learn to present legislative briefs, proposals, and research in a productive, succinct, and time-efficient manner. AAEM/RSA also offers an annual Advocacy Day, where residents and students have the opportunity to meet with members of Congress and/or senior congressional staff on Capitol Hill; this year it will be held on June 14, 2016 in Washington, DC.
Toxicology Mobile App. The AAEM/RSA Toxicology mobile app will soon be available for purchase, and is compatible with both iPhone and Android technology. You can search by subject, browse chapters of AAEM/RSA’s Toxicology Handbook, or contact Poison Control with a single click.
American Board of Emergency Medicine
Francis L. Counselman, MD, Immediate Past President, ABEM
Enhanced Oral (eOral) Certification Examination. ABEM has completed its second eOral examination; the third is scheduled for April 2016. Three of the examination cases are now in the new eOral format, which uses a computer monitor, patient avatar, picture archiving and communication system (PACS)-quality radiographs, and dynamic rhythm strips. Feedback from test-takers and examiners has been quite positive. ABEM will be moving more cases to the eOral format in the near future.
ABEM Director of Medical Affairs. ABEM has named its first ever Director of Medical Affairs (DMA): Melissa A. Barton, MD. Dr Barton is a former EM Residency Program Director and has been an ABEM Oral Examiner for the past 10 years. She is the recipient of several teaching and leadership awards. Dr Barton will focus on clinically oriented special projects and represent ABEM’s interests to external organizations.
Emergency Medicine Subspecialties. EM now has 13 subspecialty opportunities for EPs; that’s more than double the number from just 5 years ago. Emergency Medical Services (EMS) now has the most ABEM diplomates (445), followed by Medical Toxicology (367) and Pediatric Emergency Medicine (245).
Lifelong Learning and Self-Assessment (LLSA) Test Accessibility. To provide LLSA readings that better match a diplomate’s area of practice, the EMS and Medical Toxicology LLSA readings and tests can now be used by any diplomate to fulfill his or her Maintenance of Certification (MOC) Part II requirements. Pediatric EM LLSA readings and tests will eventually be made available to all diplomates at a later date. All LLSAs can be accessed through the ABEM Web site (https://www.abem.org).
Maintenance of Certification (MOC) Adds Value. In a survey of ABEM diplomates taking the 2014 ConCert Examination, 92.5% found value in maintaining their ABEM certification. In a follow-up survey in 2015, 90.4% stated their medical knowledge was reinforced and/or increased by preparing and taking the ConCert Examination. In addition to being relevant to our diplomates’ practice, ABEM has worked hard to control MOC costs. ABEM has not increased its fees for the last 5 years for the LLSAs; for all remaining examinations, there has been no fee increase for the past 4 years. When compared to all other boards, the expense of the ABEM MOC Program is at the median, costing EPs approximately $265 per year, or about $5 each week.
American College of Emergency Physicians
Jay A. Kaplan, MD, FACEP, ACEP President
Physician Burnout. Unfortunately, EM leads all specialties in the frequency of physician burnout. Emergency physicians must be aware of burnout, and take proactive steps to avoid it. To help EPs, ACEP has organized an “Emergency Medicine Wellness Week.” Prevention tips include eating well, getting the proper amount of sleep, regular exercise, and improving the work environment. In 2016, Wellness Week ran from January 24 to 30; there is a continuing focus on building resilience and preventing compassion fatigue.
Out of Network (OON) Balance Billing. Insurance companies know that it is solely the cost of insurance premiums that consumers pay attention to, not deductibles or exactly what the insurance covers. Those same insurance companies have been adept at portraying physicians as the cause of “surprise billing.” Emergency physicians need to change the conversation from “surprise billing” to “surprise coverage.” We need to talk about fair coverage for our patients, rather than asking for fair payment for physicians (the latter will follow the former and legislators believe that physicians are already fairly paid). ACEP is considering legal action against CMS and the Center for Consumer Information and Insurance Oversight regarding their final rule on “the greatest of three,” which establishes guidelines for how physicians are to be paid for services rendered.
Pay for Performance and Value-based Reimbursement. ACEP has created a joint task force with the Emergency Department Practice Management Association to create a toolbox for EPs to navigate the changing reimbursement landscape. This includes model legislation and best practices, and there is exploration regarding developing alternative payment models for EM.
Opioid Epidemic. ACEP is a participant in the White House working group exploring this epidemic and identifying strategies to combat this national problem. ACEP has sent a letter to CMS and Health and Human Services (HHS) requesting removal of the pain questions from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys. Emergency physicians should not be penalized on these surveys for not prescribing narcotic analgesics to patients who could be treated appropriately with nonnarcotic medications. ACEP similarly is considering sending a letter to The Joint Commission requesting removal of their emphasis on pain as the “fifth vital sign.”
Mass Casualty Incidents. ACEP has created a “New High-Threat High-Casualty Task Force” to identify best practice recommendations for provision of emergency care in high-threat environments and identify current clinical and operational knowledge gaps surrounding the issue. This in turn will help prioritize future ACEP research objectives based on these gaps. In addition, a white paper is being prepared, highlighting current national efforts and recommending clinical practice guidelines for adults and pediatric patients, as well as a future strategy for ACEP engagement as a national leader in the area of high-threat emergency care.
Diversity. There is a recognized need to increase the diversity in our current and future EM leadership. To that end, ACEP sponsored a Diversity Summit on April 14, 2016 in Dallas to explore these issues and make recommendations.
Emergency Quality Network. ACEP, along with 38 other health care organizations, received a grant in the CMS Transforming Clinical Practice Initiative to help physicians achieve large-scale health transformation. Areas of EM focus include: improving outcomes for patients with sepsis; reducing avoidable imaging in low-risk patients through implementation of ACEP’s Choosing Wisely campaign; and improving the value of ED chest pain evaluation in low-risk patients by reducing avoidable testing and admissions.
Editor’s Note: Part 2 of this article will appear in the May 2016 issue of Emergency Medicine and will feature reports from the Council of Emergency Medicine Residency Directors (CORD), the Emergency Medicine Residents’ Association (EMRA), and the Society for Academic Emergency Medicine (SAEM). Have a comment or question about this article? Let us know: [email protected].
On February 21 to 24, 2016, the Association of Academic Chairs of Emergency Medicine (AACEM) held its 8th annual retreat in Tempe, Arizona. The AACEM is comprised of full, acting, interim, and emeritus chairs and directors of departments of emergency medicine (EM) who work to improve and support academic departments of EM in the advancement of health care through high-quality education and research.
During that event, AACEM President Greg Volturo, MD, organized a panel discussion of EM leaders to provide an update on their organizations’ recent activities. This panel included representatives from seven prominent EM organizations: the American Academy of Emergency Medicine (AAEM), AAEM Resident and Student Association (AAEM/RSA), American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), Council of Emergency Medicine Residency Directors (CORD), Emergency Medicine Residents’ Association (EMRA), and Society for Academic Emergency Medicine (SAEM).
The following is the first of a two-part article that provides highlights from that discussion, with reports from the AAEM, AAEM/RSA, ABEM, and ACEP. Part 2 will appear in the May issue and will include reports from the CORD, EMRA, and SAEM.
American Academy of Emergency Medicine
Kevin G. Rodgers, MD, FAAEM, President AAEM
Due Process. AAEM highlighted the problem of the lack of due process for many emergency physicians (EPs). By agreeing to waive their rights to due process when signing contracts with some contract management companies, EPs can unwittingly give their employers the power to terminate them without cause and without notice. AAEM is working with Centers for Medicare & Medicaid Services (CMS) and several congressmen to amend the Medicare Rules for Participation to include an “unwaivable due process guarantee.” In addition, AAEM is requesting an addition to the current Code of Federal Regulation to ensure EPs are entitled “to a fair hearing and appellate review through hospital medical staff mechanisms before any termination or restriction of their professional activity or medical staff privileges. These rights cannot be denied through a third party contract.”
AAEM Residency Visitation Program. AAEM is committed to visiting every EM residency program once every 3 to 4 years, similar to the ACEP and ABEM programs. Residency programs will have the opportunity to select from a list of well-known EM speakers; they will deliver a clinically oriented lecture, followed by a presentation on AAEM. The cost of the program is borne completely by AAEM.
AAEM Physician Group (AAEM-PG). This program was announced at the 2016 AAEM Scientific Assembly. AAEM-PG establishes and supports EM practices where physicians can operate democratically and have an equal voice. It is a practice that is run by the local physicians for the physicians. AAEM-PG will help guide new as well as established EM groups, providing for physicians’ autonomy, fair and equitable practice environments, and career and group longevity.
AAEM Resident and Student Association
Victoria Weston, MD, AAEM/RSA President
Overview. Started in 2005, AAEM/RAS now has over 3,500 members and 58 EM residency programs with 100% participation. Benefits of membership include access to EM:RAP and The Journal of Emergency Medicine, access and opportunities to contribute to an RSA peer-reviewed blog and Modern Resident, and free registration for the AAEM Annual Scientific Assembly. As part of the AAEM Scientific Assembly, AAEM/RSA coordinates a day-long education track in collaboration with the AAEM Young Physician Section, an In-Training Exam review, and a Career Fair and Social.
Congressional Elective. Members of AAEM/RSA can apply to be selected for a one-month “Congressional Elective” with Congressmen Raul Ruiz and Joe Heck, the only two EPs currently in Congress, to teach EPs the process of creating health-policy legislation on Capitol Hill. For 4 weeks, residents work directly in their congressional office and learn to work with constituents to develop relevant health-policy legislation. Residents learn to present legislative briefs, proposals, and research in a productive, succinct, and time-efficient manner. AAEM/RSA also offers an annual Advocacy Day, where residents and students have the opportunity to meet with members of Congress and/or senior congressional staff on Capitol Hill; this year it will be held on June 14, 2016 in Washington, DC.
Toxicology Mobile App. The AAEM/RSA Toxicology mobile app will soon be available for purchase, and is compatible with both iPhone and Android technology. You can search by subject, browse chapters of AAEM/RSA’s Toxicology Handbook, or contact Poison Control with a single click.
American Board of Emergency Medicine
Francis L. Counselman, MD, Immediate Past President, ABEM
Enhanced Oral (eOral) Certification Examination. ABEM has completed its second eOral examination; the third is scheduled for April 2016. Three of the examination cases are now in the new eOral format, which uses a computer monitor, patient avatar, picture archiving and communication system (PACS)-quality radiographs, and dynamic rhythm strips. Feedback from test-takers and examiners has been quite positive. ABEM will be moving more cases to the eOral format in the near future.
ABEM Director of Medical Affairs. ABEM has named its first ever Director of Medical Affairs (DMA): Melissa A. Barton, MD. Dr Barton is a former EM Residency Program Director and has been an ABEM Oral Examiner for the past 10 years. She is the recipient of several teaching and leadership awards. Dr Barton will focus on clinically oriented special projects and represent ABEM’s interests to external organizations.
Emergency Medicine Subspecialties. EM now has 13 subspecialty opportunities for EPs; that’s more than double the number from just 5 years ago. Emergency Medical Services (EMS) now has the most ABEM diplomates (445), followed by Medical Toxicology (367) and Pediatric Emergency Medicine (245).
Lifelong Learning and Self-Assessment (LLSA) Test Accessibility. To provide LLSA readings that better match a diplomate’s area of practice, the EMS and Medical Toxicology LLSA readings and tests can now be used by any diplomate to fulfill his or her Maintenance of Certification (MOC) Part II requirements. Pediatric EM LLSA readings and tests will eventually be made available to all diplomates at a later date. All LLSAs can be accessed through the ABEM Web site (https://www.abem.org).
Maintenance of Certification (MOC) Adds Value. In a survey of ABEM diplomates taking the 2014 ConCert Examination, 92.5% found value in maintaining their ABEM certification. In a follow-up survey in 2015, 90.4% stated their medical knowledge was reinforced and/or increased by preparing and taking the ConCert Examination. In addition to being relevant to our diplomates’ practice, ABEM has worked hard to control MOC costs. ABEM has not increased its fees for the last 5 years for the LLSAs; for all remaining examinations, there has been no fee increase for the past 4 years. When compared to all other boards, the expense of the ABEM MOC Program is at the median, costing EPs approximately $265 per year, or about $5 each week.
American College of Emergency Physicians
Jay A. Kaplan, MD, FACEP, ACEP President
Physician Burnout. Unfortunately, EM leads all specialties in the frequency of physician burnout. Emergency physicians must be aware of burnout, and take proactive steps to avoid it. To help EPs, ACEP has organized an “Emergency Medicine Wellness Week.” Prevention tips include eating well, getting the proper amount of sleep, regular exercise, and improving the work environment. In 2016, Wellness Week ran from January 24 to 30; there is a continuing focus on building resilience and preventing compassion fatigue.
Out of Network (OON) Balance Billing. Insurance companies know that it is solely the cost of insurance premiums that consumers pay attention to, not deductibles or exactly what the insurance covers. Those same insurance companies have been adept at portraying physicians as the cause of “surprise billing.” Emergency physicians need to change the conversation from “surprise billing” to “surprise coverage.” We need to talk about fair coverage for our patients, rather than asking for fair payment for physicians (the latter will follow the former and legislators believe that physicians are already fairly paid). ACEP is considering legal action against CMS and the Center for Consumer Information and Insurance Oversight regarding their final rule on “the greatest of three,” which establishes guidelines for how physicians are to be paid for services rendered.
Pay for Performance and Value-based Reimbursement. ACEP has created a joint task force with the Emergency Department Practice Management Association to create a toolbox for EPs to navigate the changing reimbursement landscape. This includes model legislation and best practices, and there is exploration regarding developing alternative payment models for EM.
Opioid Epidemic. ACEP is a participant in the White House working group exploring this epidemic and identifying strategies to combat this national problem. ACEP has sent a letter to CMS and Health and Human Services (HHS) requesting removal of the pain questions from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys. Emergency physicians should not be penalized on these surveys for not prescribing narcotic analgesics to patients who could be treated appropriately with nonnarcotic medications. ACEP similarly is considering sending a letter to The Joint Commission requesting removal of their emphasis on pain as the “fifth vital sign.”
Mass Casualty Incidents. ACEP has created a “New High-Threat High-Casualty Task Force” to identify best practice recommendations for provision of emergency care in high-threat environments and identify current clinical and operational knowledge gaps surrounding the issue. This in turn will help prioritize future ACEP research objectives based on these gaps. In addition, a white paper is being prepared, highlighting current national efforts and recommending clinical practice guidelines for adults and pediatric patients, as well as a future strategy for ACEP engagement as a national leader in the area of high-threat emergency care.
Diversity. There is a recognized need to increase the diversity in our current and future EM leadership. To that end, ACEP sponsored a Diversity Summit on April 14, 2016 in Dallas to explore these issues and make recommendations.
Emergency Quality Network. ACEP, along with 38 other health care organizations, received a grant in the CMS Transforming Clinical Practice Initiative to help physicians achieve large-scale health transformation. Areas of EM focus include: improving outcomes for patients with sepsis; reducing avoidable imaging in low-risk patients through implementation of ACEP’s Choosing Wisely campaign; and improving the value of ED chest pain evaluation in low-risk patients by reducing avoidable testing and admissions.
Editor’s Note: Part 2 of this article will appear in the May 2016 issue of Emergency Medicine and will feature reports from the Council of Emergency Medicine Residency Directors (CORD), the Emergency Medicine Residents’ Association (EMRA), and the Society for Academic Emergency Medicine (SAEM). Have a comment or question about this article? Let us know: [email protected].
Allegations: Current Trends in Medical Malpractice, Part 2
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
Most medical malpractice cases are still resolved in a courtroom—typically after years of preparation and personal torment. Yet, overall rates of paid medical malpractice claims among all physicians have been steadily decreasing over the past two decades, with reports showing decreases of 30% to 50% in paid claims since 2000.1-3 At the same time, while median payments and insurance premiums continued to increase until the mid-2000s, they now appear to have plateaued.1
None of these changes occurred in isolation. More than 30 states now have caps on noneconomic or total damages.2 As noted in part 1, since 2000, some states have enacted comprehensive tort reform.4 However, whether these changes in malpractice patterns can be attributed directly to specific policy changes remains a hotly contested issue.
Malpractice Risk in Emergency Medicine
To what extent do the trends in medical malpractice apply to emergency medicine (EM)? While emergency physicians’ (EPs’) perception of malpractice risk ranks higher than any other medical specialty,5 in a review of a large sample of malpractice claims from 1991 through 2005, EPs ranked in the middle among specialties with respect to annual risk of a malpractice claim.6 Moreover, the annual risk of a claim for EPs is just under 8%, compared to 7.4% for all physicians. Yet, for neurosurgery and cardiothoracic surgery—the specialties with the highest overall risk of malpractice claims—the annual risk approaches 20%.6 Regarding payout statistics, less than one-fifth of the claims against EPs resulted in payment.6 In a review of a separate insurance database of closed claims, EPs were named as the primary defendant in only 19% of cases.7
Despite the discrepancies between perceived risk and absolute risk of malpractice claims among EPs, malpractice lawsuits continue to affect the practice of EM. This is evidenced in several surveys, in which the majority of EP participants admitted to practicing “defensive medicine” by ordering tests that were felt to be unnecessary and did so in response to perceived malpractice risk.8-10 Perceived risk also accounts for the significant variation in decision-making in the ED with respect to diagnostic testing and hospitalization of patients.11 One would expect that lowering malpractice risk would result in less so-called unnecessary testing, but whether or not this is truly the case remains to be seen.
Effects of Malpractice Reform
A study by Waxman et al12 on the effects of significant malpractice tort reform in ED care in Texas, Georgia, and South Carolina found no difference in rates of imaging studies, charges, or patient admissions. Furthermore, legislation reform did not increase plaintiff onus to prove proximate “gross negligence” rather than simply a breach from “reasonably skillful and careful” medicine.12 These findings suggest that perception of malpractice risk might simply be serving as a proxy for physicians’ underlying risk tolerance, and be less subject to influence by external forces.
Areas Associated With Malpractice Risk
A number of closed-claim databases attempted to identify the characteristics of patient encounters that can lead to malpractice claims, including patient conditions and sources of error. Diagnostic errors have consistently been found to be the leading cause of malpractice claims, accounting for 28% to 65% of claims, followed by inappropriate management of medical treatment and improper performance of a procedure.7,13-16 A January 2016 benchmarking system report by CRICO Strategies found that 30% of 23,658 medical malpractice claims filed between 2009 through 2013 cited failures in communication as a factor.17 The report also revealed that among these failed communications, those that occurred between health care providers are more likely to result in payout compared to miscommunications between providers and patients.17 This report further noted 70% to 80% of claims closed without payment.7,16 Closed claims were significantly more likely to involve serious injuries or death.7,18 Leading conditions that resulted in claims include myocardial infarction, nonspecific chest pain, symptoms involving the abdomen or pelvis, appendicitis, and orthopedic injuries.7,13,16
Diagnostic Errors
Errors in diagnosis have been attributed to multiple factors in the ED. The two most common factors were failure to order tests and failure to perform an adequate history and physical examination, both of which contribute to rationalization of the practice of defensive medicine under the current tort system.13 Other significant factors associated with errors in diagnosis include misinterpretation of test results or imaging studies and failure to obtain an appropriate consultation. Processes contributing to each of these potential errors include mistakes in judgment, lack of knowledge, miscommunication, and insufficient documentation (Table).15
Strategies for Reducing Malpractice Risk
In part 1, we listed several strategies EPs could adopt to help reduce malpractice risk. In this section, we will discuss in further detail how these strategies help mitigate malpractice claims.
Patient Communication
Open communication with patients is paramount in reducing the risk of a malpractice allegation. Patients are more likely to become angry or frustrated if they sense a physician is not listening to or addressing their concerns. These patients are in turn more likely to file a complaint if they are harmed or experience a bad outcome during their stay in the ED.
Situations in which patients are unable to provide pertinent information also place the EP at significant risk, as the provider must make decisions without full knowledge of the case. Communication with potential resources such as nursing home staff, the patient’s family, and emergency medical service providers to obtain additional information can help reduce risk.
Of course, when evaluating and treating patients, the EP should always take the time to listen to the patient’s concerns during the encounter to ensure his or her needs have been addressed. In the event of a patient allegation or complaint, the EP should make the effort to explore and de-escalate the situation before the patient is discharged.
Discharge Care and Instructions
According to CRICO, premature discharge as a factor in medical malpractice liability results from inadequate assessment and missed opportunities in 41% of diagnosis-related ED cases.16 The following situation illustrates a brief example of such a missed opportunity: A provider makes a diagnosis of urinary tract infection (UTI) in a patient presenting with fever and abdominal pain but whose urinalysis is suspect for contamination and in whom no pelvic examination was performed to rule out other etiologies. When the same patient later returns to the ED with worse abdominal pain, a sterile urine culture invalidates the diagnosis of UTI, and further evaluation leads to a final diagnosis of ruptured appendix.
Prior to discharging any patient, the EP should provide clear and concise at-home care instructions in a manner in which the patient can understand. Clear instructions on how the patient is to manage his or her care after discharge are vital, and failure to do so in terms the patient can understand can create problems if a harmful result occurs. This is especially important in patients with whom there is a communication barrier—eg, language barrier, hearing impairment, cognitive deficit, intoxication, or violent or irrational behavior. In these situations, the EP should always take advantage of available resources and tools such as language lines, interpreters, discharge planners, psychiatric staff, and supportive family members to help reconcile any communication barriers. These measures will in turn optimize patient outcome and reduce the risk of a later malpractice allegation.
Board Certification
All physicians should maintain their respective board certification and specialty training requirements. Efforts in this area help providers to stay up to date in current practice standards and new developments, thus reducing one’s risk of incurring a malpractice claim.
Patient Safety
All members of the care team should engender an environment that is focused on patient safety, including open communication between providers and with nursing staff and technical support teams. Although interruptions can be detrimental to patient care, simply having an understanding of this phenomenon among all staff members can alleviate some of the working stressors in the ED. Effort must be made to create an environment that allows for clarification between nursing staff and physicians without causing undue antagonism. Fostering supportive communication, having a questioning attitude, and seeking clarification can only enhance patient safety.
The importance of the supervisory role of attending physicians to trainees, physician extenders, and nursing staff must be emphasized, and appropriate guidance from the ED attending is germane in keeping patients safe in teaching environments. Additionally, in departments that suffer the burden of high numbers of admitted patient boarders in the ED, attention must be given to the transitional period between decision to admit and termination of ED care and the acquisition of care of the admitting physician. A clear plan of responsibility must be in place for these high-risk situations.
Policies and Procedures
Departmental policies and procedures should be designed to identify and address all late laboratory results data, radiological discrepancies, and culture results in a timely and uniform manner. Since unaddressed results and discrepancies can result in patient harm, patient-callback processes should be designed to reduce risk by addressing these hazards regularly, thoroughly, and in a timely fashion.
Cognitive Biases
An awareness of inherent biases in the medical decision-making process is also helpful to maintain mindfulness in the routine practice of EM and avoid medical errors. The EP should take care not to be influenced by recent events and diagnostic information that is easy to recall or common, and to ensure the differential addresses possibilities beyond the readily available diagnoses. Further, reliance on an existing opinion may be misleading if subsequent judgments are based on this “anchor,” whether it is true or false.
If the data points of the case do not line up as expected, or if there are unexplained outliers, the EP should expand the frame of reference to seek more appropriate possibilities, and avoid attempts to make the data fit a preferred or favored conclusion.
When one fails to recognize that data do not fit the diagnostic presumption, the true diagnosis can be undermined. Such confirmation bias in turn challenges diagnostic success. Hasty judgment without considering and seeking out relevant information can set up diagnostic failure and premature closure.
Remembering the Basics
Finally, providers should follow the basic principles for every patient. Vital signs are vital for a reason, and all abnormal data must be accounted for prior to patient hand off or discharge. Patient turnover is a high-risk occasion, and demands careful attention to case details between the off-going physician, the accepting physician, and the patient.
All patients presenting to the ED for care should leave the ED at their baseline functional level (ie, if they walk independently, they should still walk independently at discharge). If not, the reason should be sought out and clarified with appropriate recommendations for treatment and follow-up.
Patients and staff should always be treated with respect, which in turn will encourage effective communication. Providers should be honest with patients, document truthfully, respect privacy and confidentiality, practice within one’s competence, confirm information, and avoid assumptions. Compassion goes hand in hand with respectful and open communication. Physicians perceived as compassionate and trustworthy are less likely to be the target of a malpractice suit, even when harm has occurred.
Conclusion
Even though the number of paid medical malpractice claims has continued to decrease over the past 20 years, a discrepancy between perceived and absolute risk persists among EPs—one that perpetuates the practice of defensive medicine and continues to affect EM. Despite the current perceptions and climate, EPs can allay their risk of incurring a malpractice claim by employing the strategies outlined above.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
1. Mello MM, Studdert DM, Kachalia A. The medical liability climate and prospects for reform. JAMA. 2014;312(20):2146-2155.
2. Paik M, Black B, Hyman DA. The receding tide of medical malpractice: part 1 - national trends. J Empirical Leg Stud. 2013;10(4):612-638.
3. Bishop TF, Ryan AM, Caslino LP. Paid malpractice claims for adverse events in inpatient and outpatient settings. JAMA. 2011;305(23):2427-2431.
4. Kachalia A, Mello MM. New directions in medical liability reform. N Engl J Med. 2011;364(16):
1564-1572.
5. Carrier ER, Reschovsky JD, Mello MM, Mayrell RC, Katz D. Physicians’ fears of malpractice lawsuits are not assured by tort reforms. Health Aff. 2010;29(9):1585-1592.
6. Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011;365(7):629-636.
7. Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17(5):553-560.
8. Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617.
9. Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010;170(12):1081-1083.
10. Massachusetts Medical Society. Investigation of defensive medicine in Massachusetts. November 2008. Available at http://www.massmed.org/defensivemedicine. Accessed March 16, 2016.
11. Katz DA, Williams GC, Brown RL, et al. Emergency physicians’ fear of malpractice in evaluating patient with possible acute cardiac ischemia. Ann Emerg Med. 2005;46(6):525-533.
12. Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014;371(16):1518-1525.
13. Kachalia A, Gandhi TK, Puopolo AL, et al. Missed and delayed diagnoses in the emergency department: a study of closed malpractice claims from 4 liability insurers. Ann Emerg Med. 2007;49(2):196-205.
14. Saber Tehrani AS, Lee H, Mathews SC, et al. 25-Year summary of US malpractice claims for diagnostic errors 1986-2010: an analysis from the National Practitioner Data Bank. BMJ Qual Saf. 2013;22(8):672-680.
15. Ross J, Ranum D, Troxel DB. Emergency medicine closed claims study. The Doctors Company. Available at http://www.thedoctors.com/ecm/groups/public/@tdc/@web/@kc/@patientsafety/documents/article/con_id_004776.pdf. Accessed March 16, 2016.
16. Ruoff G, ed. 2011 Annual benchmarking report: malpractice risks in emergency medicine. CRICO strategies. 2012. Available at https://www.rmf.harvard.edu/Strategies/Home/Products-and-Services/Comparative-Data/Annual-Benchmark-Reports. Accessed March 16, 2016.
17. Failures in communication contribute to medical malpractice. January 31, 2016. https://www.rmf.harvard.edu/About-CRICO/Media/Press-Releases/News/2016/February/Failures-in-Communication-Contribute-to-Medical-Malpractice.
18. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354(19):2024-2033. Accessed March 16, 2016.
The Changing Standard of Care for Spinal Immobilization
Prehospital spinal immobilization has long been the standard of care (SOC) to prevent spinal cord injury in trauma patients, but utilizing the best data currently available, some professional societies recently released new recommendations that question this practice. Guidelines released in 2014 from the National Association of EMS Physicians (NAEMSP) and the American College of Surgeons Committee on Trauma (ACS-COT) support limited application of spinal immobilization.1 These guidelines note, “Given the rarity of unstable spinal injuries in EMS trauma patients, the number that might benefit from immobilization to prevent secondary injury is likely extremely small. For each patient who has potential benefit, hundreds to thousands of patients must undergo immobilization with no potential benefit.” Further, they advise “utilization of backboards for spinal immobilization during transport should be judicious, so that potential benefits outweigh risks.”1 Spinal immobilization should not be used at all in patients with penetrating trauma who do not present with obvious neurological injury and should be selective, based on objective findings of injury or the high potential for same.1
Questioning a Long-standing Practice
Fear of the consequences of spinal cord injury from significant vertebral fractures has dictated prehospital spinal immobilization to manage injured trauma patients for decades. For almost 50 years, it has been the SOC. However, increasing evidence that spinal immobilization is not only unnecessary, but may even cause harm has resulted in questioning this paradigm, which has lead to promoting a change in the SOC.
Spinal immobilization dates back to the mid-1960s, when Geisler et al2 reported on a cohort of patients who suffered long-term paralysis from what was believed to be improper handling and failure to discover spinal injuries. Soon after, Farrington3,4 developed and published a systematic approach to spinal immobilization during extrication following blunt force trauma, supporting the widespread acceptance of backboards and cervical collars to immobilize the spine in injured trauma patients. Logic dictated that an unstable spine fracture could be worsened, or a cord injury could result, by unnecessary movement during extrication, transport, and initial evaluation in the ED, resulting in avoidable injury. This fear of potential secondary injury grew as more papers were published examining the link between prehospital handling of blunt force trauma patients and delayed paralysis. This resulted in the use of spinal immobilization on the majority of trauma patients, regardless of mechanism of injury or presenting symptoms.5,6
One review estimated that over 50% of trauma patients with no complaint of neck or back pain were transported with full spinal immobilization.7 This immobilization on uncomfortable long backboards typically continued in the ED for prolonged periods, until the spine could be cleared by physical examination and/or imaging studies. Yet a 2001 Cochrane review found that despite increasing use of spinal immobilization, no prospective, randomized controlled trial of the appropriate use of spinal immobilization or patient outcomes had ever been conducted.8
What the Evidence Says
How much evidence exists that supports the benefits of spinal immobilization? Not much. Studies on healthy volunteers and cadavers evaluating spinal motion with immobilization have been contradictory.9 One study found there was less motion with a cervical collar in place than without,10 whereas others found that the use of a cervical collar did not effectively reduce motion in an unstable spine.11,12 Perry et al13 studied the effectiveness of different head immobilization techniques and found that none could eliminate head and neck motion during emergency medical services (EMS) transport. Still other reports, including two biomechanical studies, demonstrated increased neck motion when using conventional extrication techniques (cervical collar with backboard) versus controlled self-extrication with cervical collar only.14,15
An Abundance of Literature on the Risks
Whereas data regarding the actual benefits of spinal immobilization is lacking, an abundance of literature details the risks. One of the most frequently cited studies is also one of the most controversial. Hauswald et al16 compared the outcomes of two groups of patients with blunt force trauma who were either immobilized during transport (in New Mexico) or non-immobilized (in Malaysia) and found that the risk of disability was higher in the immobilized group (odds ratio, 2.03). Although these environments are very different, the authors noted that mechanism of injury, resources, and the size of the hospitals were similar.16
Studies of spinal immobilization in patients with penetrating trauma report even worse outcomes. In separate studies, Haut et al17 and Vanderlan et al18 demonstrated increased mortality when immobilization led to increased transport times and interference with other resuscitative measures. These and other studies have led the American College of Emergency Physicians, NAEMSP, ACS-COT, the Prehospital Trauma Life Support Executive Committee, and other national organizations to recommend no spinal immobilization in patients with penetrating neck trauma.1,19,20
Many trauma patients arrive with complaints of pain at one or more sites. Some of these complaints, particularly back pain, may be secondary to the use of the backboard itself, especially in cases of prolonged transport.21,22 In a study of healthy volunteers who were immobilized on a backboard for 30 minutes, all of them reported pain, along with headaches, most often involving the occipital and sacral regions.23 A 1996 study compared spinal immobilization utilizing a backboard versus a vacuum mattress in 37 healthy volunteers with no history of back pain or spinal disease.24 Compared to those immobilized with the vacuum mattress, patients immobilized with a backboard for 30 minutes were 3.1 times more likely to have symptoms, 7.9 times more likely to complain of occipital pain, and 4.3 times more likely to have lumbosacral pain.24
Increased pain complaints in the setting of trauma can result in increased imaging, leading to increased costs and unnecessary radiation exposure.25 Prolonged backboard times can also result in sacral pressure ulcers.26 A recent study has shown that patients who undergo computed tomography (CT) scans with automatic tube current modulation (as most modern multidetector row CT systems utilize) while on a backboard may be exposed to a significant increase in radiation dose.27
Spinal immobilization has also been linked to respiratory compromise, particularly with the use of straps across the chest, even when not applied tightly. One study found worse lung function test results in healthy immobilized volunteers.28 Other studies have shown that older patients (even when healthy) and those with lung or chest injury have an even larger degree of restriction and respiratory compromise.29,30
Risks from immobilization are not isolated to backboards. The use of cervical collars alone also carries potential risks. (See “What About Cervical Collars?”8,31-39)
Risk of Secondary Neurological Deterioration Is Low
Many EMS systems have already adopted the new standards calling for less use of spinal immobilization. Though the evidence is compelling, not all EMS systems have adopted these standards due to strongly rooted beliefs and fears of long-term patient disability and subsequent litigation. However, these fears do not appear justified.
A recent review by Oto et al40 found only 42 cases of early secondary neurological deterioration after blunt trauma in all of the indexed medical literature. They noted, “In twelve cases the authors did attribute deterioration to temporally associated precipitants, seven of which were possibly iatrogenic; these included removal of a cervical collar, placement of a halo device, patient agitation, performance of flexion/extension films, ‘unintentional manipulation,’ falling in or near the ED, and forced collar application in patients with ankylosing spondylitis.” Thirteen of these cases occurred during prehospital care, none of them sudden and movement-provoked, and all reported by a single study.” This review highlights the rarity of secondary deterioration.
When Should Immobilization Be Used?
So what’s the next step for spinal immobilization in the field? How do we appropriately protect trauma patients during transport? As always seems to be the case in medicine, more evidence is needed. Oteir et al41 recently published a review of new literature on the epidemiology and current practice of prehospital spine management. They reported that early (8-24 hours) transfer of patients with spinal injury to spinal care units, along with effective resuscitation, was the most important determinant of better neurological outcomes.41 This review reaffirms the need for more data evaluating the relationship between spinal immobilization and neurological outcomes.
Currently, recommendations call for selective spinal immobilization to decrease unnecessary application and potential harm. Use of backboards for spinal immobilization should be limited to the following types of patients:1,20
- Blunt trauma and altered level of consciousness;
- Spinal pain or tenderness;
- Neurological complaint (eg, numbness or motor weakness);
- Anatomic deformity of the spine;
- High-energy mechanism of injury and:
- Drug or alcohol intoxication;
- Inability to communicate; and/or
- Distracting injury.
Patients for whom immobilization on a backboard is not necessary include those with all of the following:
- Normal level of consciousness (GCS 15);
- No spine tenderness or anatomic abnormality;
- No neurological findings or complaints;
- No distracting injury;
- No intoxication.
Cervical collars alone are still recommended for use in patients who do not meet validated clinical rules, such as the NEXUS or Canadian C spine rules.1,20,42,43 As these rules are well validated, they can be safely used to determine who should have a cervical collar placed, with or without a backboard. In a retrospective review, selective spinal immobilization was found to be 99% sensitive in identifying patients with cervical injuries.44
Clearly, there is still work to be done. Due to the relative rarity of actual spinal cord injury with the consequences of neurological injury, prospective trials in this area are rare and very difficult to safely design. However, there is growing confidence that selective spinal protocols, together with the inclusion of validated clinical rules, can effectively limit exposure to unnecessary spinal immobilization. As the current evidence continues to mount for the potential harm in indiscriminate backboard and cervical collar use, it seems clear we should strive to decrease the overuse of prehospital and early spinal immobilization consistent with current position statements and validated clinical rules.
1. White CC, Domeier RM, Millin MG. EMS spinal precautions and the use of the long backboard - resource document to the position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18(2):306-314.
2. Geisler WO, Wynne-Jones M, Jousse AT. Early management of patients with trauma to the spinal cord. Med Serv J Can. 1966;22(7):512–523.
3. Farrington JD. Death in a ditch. Bulletin of the American College of Surgeons. 1967;52(3):121-130.
4. Farrington JD. Extrication of victims- surgical principles. J Trauma. 1968;8(4):493-512.
5. Riggins RS, Kraus JF. The risk of neurologic damage with fractures of the vertebrae. J Trauma. 1977;17(2):126-133.
6. Soderstrom CA, Brumback RJ. Early care of the patient with cervical spine injury. Orthop Clin North Am. 1986;17(1):3-13.
7. McHugh TP, Taylor JP. Unnecessary out-of-hospital use of full spinal immobilization. Acad Emerg Med. 1998;5(3):278-280.
8. Kwan I, Bunn F, Roberts I. Spinal immobilisation for trauma patients. Cochrane Database Syst Rev. 2001;(2):CD002803.
9. Sundstrøm T, Asbjørnsen H, Habiba S, Sunde GA, Wester K. Prehospital use of cervical collars in trauma patients: a critical review. J Neurotrauma. 2014;31(6):531-540.
10. Conrad BP, Rechtine G, Weight M, Clarke J, Horodyski M. Motion in the unstable cervical spine during hospital bed transfers. J Trauma. 2010;69,432-436.
11. Horodyski M, DiPaola CP, Conrad BP, Rechtine GR. Cervical collars are insufficient for immobilizing an unstable cervical spine injury. J Emerg Med. 2011;41(5):513-519.
12. Hughes SJ. How effective is the Newport/Aspen collar? A prospective radiographic evaluation in healthy adult volunteers. J Trauma. 1998;45(2):374-378.
13. Perry SD, McLellan B, McIlroy WE, Maki BE, Schwartz M, Fernie GR. The efficacy of head immobilization techniques during simulated vehicle motion. Spine (Phil Pa 1976). 1999;24(17):1839-1844.
14. Engsberg JR, Standeven JW, Shurtleff TL, Eggars JL, Shafer JS, Naunheim RS. Cervical spine motion during extrication. J Emerg Med. 2013;44(1):122-127.
15. Dixon M, O’Halloran J, Cummins NM. Biomechanical analysis of spinal immobilization during prehospital extrication—a proof of concept study. Emerg Med J. 2014;31(9):745-749.
16. Hauswald M, Ong G, Tandberg D, Omar Z. Out-of-hospital spinal immobilization: its effect on neurologic injury. Acad Emerg Med. 1998;5(3):214-219.
17. Haut ER, Kalish BT, Efron DT, et al. Spine immobilization in penetrating trauma: more harm than good? J Trauma. 2010;68(1):115-120.
18. Vanderlan WB, Tew BE, McSwain NE. Increased risk of death with cervical spine immobilization in penetrating cervical trauma. Injury. 2009;40(8):880-883.
19. Stuke LE, Pons PT, Guy JS, Chapleau WP, Butler FK, McSwain NE. Prehospital spine immobilization for penetrating trauma—review and recommendations from the Prehospital Trauma Life Support Executive Committee. J Trauma. 2011;71(3):763–769.
20. American College of Emergency Physicians. Policy Statement- EMS Management of Patients with Potential Spinal Injury. 2015. Available at: http://www.acep.org/Physician-Resources/Policies/Policy-Statements/EMS-Management-of-Patients-with-Potential-Spinal-Injury. Accessed February 9, 2016.
21. Barney RN, Cordell WH, Miller E. Pain associated with immobilization on rigid spine boards. Ann Emerg Med. 1989;18:918.
22. Cooney DR, Wallus H, Asaly M, Wojcik S. Backboard time for patients receiving spinal immobilization by emergency medical services. Int J Emerg Med. 2013;6(1):17.
23. Chan D, Goldberg R, Tascone A, Harmon S, Chan L. The effect of spinal immobilization on healthy volunteers. Ann Emerg Med. 1994;23(1):48-51.
24. Chan D, Goldberg RM, Mason J, Chan L. Backboard versus mattress splint immobilization: a comparison of symptoms generated. J Emerg Med, 1996;14(3):293-298.
25. March J, Ausband S, Brown L. Changes in physical examination caused by use of spinal immobilization. Prehosp Emerg Care. 2002;6(4):421-424.
26. Berg G, Nyberg S, Harrison P, Baumchen J, Gurss E, Hennes E. Near-infrared spectroscopy measurement of sacral tissue oxygen saturation in healthy volunteers immobilized on rigid spine boards. Prehosp Emerg Care. 2010;14(4):419-424.
27. Lee AY, Elojeimy S, Kanal KM, Gunn ML. The effect of trauma backboards on computed tomography radiation dose. Clin Radiol. 2016. Epub ahead of print.
28. Bauer D, Kowalski R. Effect of spinal immobilization devices on pulmonary function in the healthy, nonsmoking man. Ann Emerg Med. 1988;17(9):915-918.
29. Walsh M, Grant T, Mickey S. Lung function compromised by spinal immobilization. Ann Emerg Med. 1990;19(5):615-616.
30. Totten VY, Sugarman DB. Respiratory effects of spinal immobilization. Prehosp Emerg Care. 1999; 3(4):347-352.
31. Goutcher CM, Lochhead V. Reduction in mouth opening with semi-rigid cervical collars. Br J Anaesth. 2005;95(3):344-348.
32. Davies G, Deakin C, Wilson A. The effect of a rigid collar on intracranial pressure. Injury. 1996;27(9):647-649.
33. Dunham CM, Brocker BP, Collier BD, Gemmel DJ. Risks associated with magnetic resonance imaging and cervical collar in comatose, blunt trauma patients with negative comprehensive cervical spine computed tomography and no apparent spinal deficit. Crit Care. 2008;12(4):R89.
34. Mobbs RJ, Stoodley MA, Fuller J. Effect of cervical hard collar on intracranial pressure after head injury. ANZ J Surg. 2002;72(6):389-391.
35. Stone MB, Tubridy CM, Curran R. The effect of rigid cervical collars on internal jugular vein dimensions. Acad Emerg Med. 2010;17(1):100-102.
36. Ben-Galim P, Dreiangel N, Mattox KL, Reitman CA, Kalantar SB, Hipp JA. Extrication collars can result in abnormal separation between vertebrae in the presence of a dissociative injury. J Trauma. 2010;69(2):447-450.
37. Podolsky SM, Hoffman JR, Pietrafesa CA. Neurologic complications following immobilization of cervical spine fracture in a patient with ankylosing spondylitis. Ann Emerg Med. 1983;12(9):578-580.
38. Papadopoulos MC, Chakraborty A, Waldron G, Bell BA. Exacerbating cervical spine injury by applying a hard collar. BMJ. 1999;319(7203):171-172.
39. Thumbikat P, Hariharan RP, Ravichandran G, Mcclelland MR, Mathew KM. Spinal cord injury in patients with ankylosing spondylitis: a 10-year review. Spine (Phila Pa 1976). 2007;32(26):2989-2995.
40. Oto B, Corey DJ, Oswald J, Sifford D, Walsh B. Early secondary neurologic deterioration after blunt spinal trauma: a review of the literature. Acad Emerg Med. 2015;22(10):1200-1212.
41. Oteir AO, Smith K, Jennings PA, Stoelwinder JU. The prehospital management of suspected spinal cord injury: an update. Prehosp Disaster Med. 2014;29(4):399-402.
42. Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99.
43. Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841–1848.
44. Stroh G, Braude D. Can an out-of-hospital cervical spine clearance protocol identify all patients with injuries? An argument for selective immobilization. Ann Emerg Med. 2001;37(6):609-615.
Prehospital spinal immobilization has long been the standard of care (SOC) to prevent spinal cord injury in trauma patients, but utilizing the best data currently available, some professional societies recently released new recommendations that question this practice. Guidelines released in 2014 from the National Association of EMS Physicians (NAEMSP) and the American College of Surgeons Committee on Trauma (ACS-COT) support limited application of spinal immobilization.1 These guidelines note, “Given the rarity of unstable spinal injuries in EMS trauma patients, the number that might benefit from immobilization to prevent secondary injury is likely extremely small. For each patient who has potential benefit, hundreds to thousands of patients must undergo immobilization with no potential benefit.” Further, they advise “utilization of backboards for spinal immobilization during transport should be judicious, so that potential benefits outweigh risks.”1 Spinal immobilization should not be used at all in patients with penetrating trauma who do not present with obvious neurological injury and should be selective, based on objective findings of injury or the high potential for same.1
Questioning a Long-standing Practice
Fear of the consequences of spinal cord injury from significant vertebral fractures has dictated prehospital spinal immobilization to manage injured trauma patients for decades. For almost 50 years, it has been the SOC. However, increasing evidence that spinal immobilization is not only unnecessary, but may even cause harm has resulted in questioning this paradigm, which has lead to promoting a change in the SOC.
Spinal immobilization dates back to the mid-1960s, when Geisler et al2 reported on a cohort of patients who suffered long-term paralysis from what was believed to be improper handling and failure to discover spinal injuries. Soon after, Farrington3,4 developed and published a systematic approach to spinal immobilization during extrication following blunt force trauma, supporting the widespread acceptance of backboards and cervical collars to immobilize the spine in injured trauma patients. Logic dictated that an unstable spine fracture could be worsened, or a cord injury could result, by unnecessary movement during extrication, transport, and initial evaluation in the ED, resulting in avoidable injury. This fear of potential secondary injury grew as more papers were published examining the link between prehospital handling of blunt force trauma patients and delayed paralysis. This resulted in the use of spinal immobilization on the majority of trauma patients, regardless of mechanism of injury or presenting symptoms.5,6
One review estimated that over 50% of trauma patients with no complaint of neck or back pain were transported with full spinal immobilization.7 This immobilization on uncomfortable long backboards typically continued in the ED for prolonged periods, until the spine could be cleared by physical examination and/or imaging studies. Yet a 2001 Cochrane review found that despite increasing use of spinal immobilization, no prospective, randomized controlled trial of the appropriate use of spinal immobilization or patient outcomes had ever been conducted.8
What the Evidence Says
How much evidence exists that supports the benefits of spinal immobilization? Not much. Studies on healthy volunteers and cadavers evaluating spinal motion with immobilization have been contradictory.9 One study found there was less motion with a cervical collar in place than without,10 whereas others found that the use of a cervical collar did not effectively reduce motion in an unstable spine.11,12 Perry et al13 studied the effectiveness of different head immobilization techniques and found that none could eliminate head and neck motion during emergency medical services (EMS) transport. Still other reports, including two biomechanical studies, demonstrated increased neck motion when using conventional extrication techniques (cervical collar with backboard) versus controlled self-extrication with cervical collar only.14,15
An Abundance of Literature on the Risks
Whereas data regarding the actual benefits of spinal immobilization is lacking, an abundance of literature details the risks. One of the most frequently cited studies is also one of the most controversial. Hauswald et al16 compared the outcomes of two groups of patients with blunt force trauma who were either immobilized during transport (in New Mexico) or non-immobilized (in Malaysia) and found that the risk of disability was higher in the immobilized group (odds ratio, 2.03). Although these environments are very different, the authors noted that mechanism of injury, resources, and the size of the hospitals were similar.16
Studies of spinal immobilization in patients with penetrating trauma report even worse outcomes. In separate studies, Haut et al17 and Vanderlan et al18 demonstrated increased mortality when immobilization led to increased transport times and interference with other resuscitative measures. These and other studies have led the American College of Emergency Physicians, NAEMSP, ACS-COT, the Prehospital Trauma Life Support Executive Committee, and other national organizations to recommend no spinal immobilization in patients with penetrating neck trauma.1,19,20
Many trauma patients arrive with complaints of pain at one or more sites. Some of these complaints, particularly back pain, may be secondary to the use of the backboard itself, especially in cases of prolonged transport.21,22 In a study of healthy volunteers who were immobilized on a backboard for 30 minutes, all of them reported pain, along with headaches, most often involving the occipital and sacral regions.23 A 1996 study compared spinal immobilization utilizing a backboard versus a vacuum mattress in 37 healthy volunteers with no history of back pain or spinal disease.24 Compared to those immobilized with the vacuum mattress, patients immobilized with a backboard for 30 minutes were 3.1 times more likely to have symptoms, 7.9 times more likely to complain of occipital pain, and 4.3 times more likely to have lumbosacral pain.24
Increased pain complaints in the setting of trauma can result in increased imaging, leading to increased costs and unnecessary radiation exposure.25 Prolonged backboard times can also result in sacral pressure ulcers.26 A recent study has shown that patients who undergo computed tomography (CT) scans with automatic tube current modulation (as most modern multidetector row CT systems utilize) while on a backboard may be exposed to a significant increase in radiation dose.27
Spinal immobilization has also been linked to respiratory compromise, particularly with the use of straps across the chest, even when not applied tightly. One study found worse lung function test results in healthy immobilized volunteers.28 Other studies have shown that older patients (even when healthy) and those with lung or chest injury have an even larger degree of restriction and respiratory compromise.29,30
Risks from immobilization are not isolated to backboards. The use of cervical collars alone also carries potential risks. (See “What About Cervical Collars?”8,31-39)
Risk of Secondary Neurological Deterioration Is Low
Many EMS systems have already adopted the new standards calling for less use of spinal immobilization. Though the evidence is compelling, not all EMS systems have adopted these standards due to strongly rooted beliefs and fears of long-term patient disability and subsequent litigation. However, these fears do not appear justified.
A recent review by Oto et al40 found only 42 cases of early secondary neurological deterioration after blunt trauma in all of the indexed medical literature. They noted, “In twelve cases the authors did attribute deterioration to temporally associated precipitants, seven of which were possibly iatrogenic; these included removal of a cervical collar, placement of a halo device, patient agitation, performance of flexion/extension films, ‘unintentional manipulation,’ falling in or near the ED, and forced collar application in patients with ankylosing spondylitis.” Thirteen of these cases occurred during prehospital care, none of them sudden and movement-provoked, and all reported by a single study.” This review highlights the rarity of secondary deterioration.
When Should Immobilization Be Used?
So what’s the next step for spinal immobilization in the field? How do we appropriately protect trauma patients during transport? As always seems to be the case in medicine, more evidence is needed. Oteir et al41 recently published a review of new literature on the epidemiology and current practice of prehospital spine management. They reported that early (8-24 hours) transfer of patients with spinal injury to spinal care units, along with effective resuscitation, was the most important determinant of better neurological outcomes.41 This review reaffirms the need for more data evaluating the relationship between spinal immobilization and neurological outcomes.
Currently, recommendations call for selective spinal immobilization to decrease unnecessary application and potential harm. Use of backboards for spinal immobilization should be limited to the following types of patients:1,20
- Blunt trauma and altered level of consciousness;
- Spinal pain or tenderness;
- Neurological complaint (eg, numbness or motor weakness);
- Anatomic deformity of the spine;
- High-energy mechanism of injury and:
- Drug or alcohol intoxication;
- Inability to communicate; and/or
- Distracting injury.
Patients for whom immobilization on a backboard is not necessary include those with all of the following:
- Normal level of consciousness (GCS 15);
- No spine tenderness or anatomic abnormality;
- No neurological findings or complaints;
- No distracting injury;
- No intoxication.
Cervical collars alone are still recommended for use in patients who do not meet validated clinical rules, such as the NEXUS or Canadian C spine rules.1,20,42,43 As these rules are well validated, they can be safely used to determine who should have a cervical collar placed, with or without a backboard. In a retrospective review, selective spinal immobilization was found to be 99% sensitive in identifying patients with cervical injuries.44
Clearly, there is still work to be done. Due to the relative rarity of actual spinal cord injury with the consequences of neurological injury, prospective trials in this area are rare and very difficult to safely design. However, there is growing confidence that selective spinal protocols, together with the inclusion of validated clinical rules, can effectively limit exposure to unnecessary spinal immobilization. As the current evidence continues to mount for the potential harm in indiscriminate backboard and cervical collar use, it seems clear we should strive to decrease the overuse of prehospital and early spinal immobilization consistent with current position statements and validated clinical rules.
Prehospital spinal immobilization has long been the standard of care (SOC) to prevent spinal cord injury in trauma patients, but utilizing the best data currently available, some professional societies recently released new recommendations that question this practice. Guidelines released in 2014 from the National Association of EMS Physicians (NAEMSP) and the American College of Surgeons Committee on Trauma (ACS-COT) support limited application of spinal immobilization.1 These guidelines note, “Given the rarity of unstable spinal injuries in EMS trauma patients, the number that might benefit from immobilization to prevent secondary injury is likely extremely small. For each patient who has potential benefit, hundreds to thousands of patients must undergo immobilization with no potential benefit.” Further, they advise “utilization of backboards for spinal immobilization during transport should be judicious, so that potential benefits outweigh risks.”1 Spinal immobilization should not be used at all in patients with penetrating trauma who do not present with obvious neurological injury and should be selective, based on objective findings of injury or the high potential for same.1
Questioning a Long-standing Practice
Fear of the consequences of spinal cord injury from significant vertebral fractures has dictated prehospital spinal immobilization to manage injured trauma patients for decades. For almost 50 years, it has been the SOC. However, increasing evidence that spinal immobilization is not only unnecessary, but may even cause harm has resulted in questioning this paradigm, which has lead to promoting a change in the SOC.
Spinal immobilization dates back to the mid-1960s, when Geisler et al2 reported on a cohort of patients who suffered long-term paralysis from what was believed to be improper handling and failure to discover spinal injuries. Soon after, Farrington3,4 developed and published a systematic approach to spinal immobilization during extrication following blunt force trauma, supporting the widespread acceptance of backboards and cervical collars to immobilize the spine in injured trauma patients. Logic dictated that an unstable spine fracture could be worsened, or a cord injury could result, by unnecessary movement during extrication, transport, and initial evaluation in the ED, resulting in avoidable injury. This fear of potential secondary injury grew as more papers were published examining the link between prehospital handling of blunt force trauma patients and delayed paralysis. This resulted in the use of spinal immobilization on the majority of trauma patients, regardless of mechanism of injury or presenting symptoms.5,6
One review estimated that over 50% of trauma patients with no complaint of neck or back pain were transported with full spinal immobilization.7 This immobilization on uncomfortable long backboards typically continued in the ED for prolonged periods, until the spine could be cleared by physical examination and/or imaging studies. Yet a 2001 Cochrane review found that despite increasing use of spinal immobilization, no prospective, randomized controlled trial of the appropriate use of spinal immobilization or patient outcomes had ever been conducted.8
What the Evidence Says
How much evidence exists that supports the benefits of spinal immobilization? Not much. Studies on healthy volunteers and cadavers evaluating spinal motion with immobilization have been contradictory.9 One study found there was less motion with a cervical collar in place than without,10 whereas others found that the use of a cervical collar did not effectively reduce motion in an unstable spine.11,12 Perry et al13 studied the effectiveness of different head immobilization techniques and found that none could eliminate head and neck motion during emergency medical services (EMS) transport. Still other reports, including two biomechanical studies, demonstrated increased neck motion when using conventional extrication techniques (cervical collar with backboard) versus controlled self-extrication with cervical collar only.14,15
An Abundance of Literature on the Risks
Whereas data regarding the actual benefits of spinal immobilization is lacking, an abundance of literature details the risks. One of the most frequently cited studies is also one of the most controversial. Hauswald et al16 compared the outcomes of two groups of patients with blunt force trauma who were either immobilized during transport (in New Mexico) or non-immobilized (in Malaysia) and found that the risk of disability was higher in the immobilized group (odds ratio, 2.03). Although these environments are very different, the authors noted that mechanism of injury, resources, and the size of the hospitals were similar.16
Studies of spinal immobilization in patients with penetrating trauma report even worse outcomes. In separate studies, Haut et al17 and Vanderlan et al18 demonstrated increased mortality when immobilization led to increased transport times and interference with other resuscitative measures. These and other studies have led the American College of Emergency Physicians, NAEMSP, ACS-COT, the Prehospital Trauma Life Support Executive Committee, and other national organizations to recommend no spinal immobilization in patients with penetrating neck trauma.1,19,20
Many trauma patients arrive with complaints of pain at one or more sites. Some of these complaints, particularly back pain, may be secondary to the use of the backboard itself, especially in cases of prolonged transport.21,22 In a study of healthy volunteers who were immobilized on a backboard for 30 minutes, all of them reported pain, along with headaches, most often involving the occipital and sacral regions.23 A 1996 study compared spinal immobilization utilizing a backboard versus a vacuum mattress in 37 healthy volunteers with no history of back pain or spinal disease.24 Compared to those immobilized with the vacuum mattress, patients immobilized with a backboard for 30 minutes were 3.1 times more likely to have symptoms, 7.9 times more likely to complain of occipital pain, and 4.3 times more likely to have lumbosacral pain.24
Increased pain complaints in the setting of trauma can result in increased imaging, leading to increased costs and unnecessary radiation exposure.25 Prolonged backboard times can also result in sacral pressure ulcers.26 A recent study has shown that patients who undergo computed tomography (CT) scans with automatic tube current modulation (as most modern multidetector row CT systems utilize) while on a backboard may be exposed to a significant increase in radiation dose.27
Spinal immobilization has also been linked to respiratory compromise, particularly with the use of straps across the chest, even when not applied tightly. One study found worse lung function test results in healthy immobilized volunteers.28 Other studies have shown that older patients (even when healthy) and those with lung or chest injury have an even larger degree of restriction and respiratory compromise.29,30
Risks from immobilization are not isolated to backboards. The use of cervical collars alone also carries potential risks. (See “What About Cervical Collars?”8,31-39)
Risk of Secondary Neurological Deterioration Is Low
Many EMS systems have already adopted the new standards calling for less use of spinal immobilization. Though the evidence is compelling, not all EMS systems have adopted these standards due to strongly rooted beliefs and fears of long-term patient disability and subsequent litigation. However, these fears do not appear justified.
A recent review by Oto et al40 found only 42 cases of early secondary neurological deterioration after blunt trauma in all of the indexed medical literature. They noted, “In twelve cases the authors did attribute deterioration to temporally associated precipitants, seven of which were possibly iatrogenic; these included removal of a cervical collar, placement of a halo device, patient agitation, performance of flexion/extension films, ‘unintentional manipulation,’ falling in or near the ED, and forced collar application in patients with ankylosing spondylitis.” Thirteen of these cases occurred during prehospital care, none of them sudden and movement-provoked, and all reported by a single study.” This review highlights the rarity of secondary deterioration.
When Should Immobilization Be Used?
So what’s the next step for spinal immobilization in the field? How do we appropriately protect trauma patients during transport? As always seems to be the case in medicine, more evidence is needed. Oteir et al41 recently published a review of new literature on the epidemiology and current practice of prehospital spine management. They reported that early (8-24 hours) transfer of patients with spinal injury to spinal care units, along with effective resuscitation, was the most important determinant of better neurological outcomes.41 This review reaffirms the need for more data evaluating the relationship between spinal immobilization and neurological outcomes.
Currently, recommendations call for selective spinal immobilization to decrease unnecessary application and potential harm. Use of backboards for spinal immobilization should be limited to the following types of patients:1,20
- Blunt trauma and altered level of consciousness;
- Spinal pain or tenderness;
- Neurological complaint (eg, numbness or motor weakness);
- Anatomic deformity of the spine;
- High-energy mechanism of injury and:
- Drug or alcohol intoxication;
- Inability to communicate; and/or
- Distracting injury.
Patients for whom immobilization on a backboard is not necessary include those with all of the following:
- Normal level of consciousness (GCS 15);
- No spine tenderness or anatomic abnormality;
- No neurological findings or complaints;
- No distracting injury;
- No intoxication.
Cervical collars alone are still recommended for use in patients who do not meet validated clinical rules, such as the NEXUS or Canadian C spine rules.1,20,42,43 As these rules are well validated, they can be safely used to determine who should have a cervical collar placed, with or without a backboard. In a retrospective review, selective spinal immobilization was found to be 99% sensitive in identifying patients with cervical injuries.44
Clearly, there is still work to be done. Due to the relative rarity of actual spinal cord injury with the consequences of neurological injury, prospective trials in this area are rare and very difficult to safely design. However, there is growing confidence that selective spinal protocols, together with the inclusion of validated clinical rules, can effectively limit exposure to unnecessary spinal immobilization. As the current evidence continues to mount for the potential harm in indiscriminate backboard and cervical collar use, it seems clear we should strive to decrease the overuse of prehospital and early spinal immobilization consistent with current position statements and validated clinical rules.
1. White CC, Domeier RM, Millin MG. EMS spinal precautions and the use of the long backboard - resource document to the position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18(2):306-314.
2. Geisler WO, Wynne-Jones M, Jousse AT. Early management of patients with trauma to the spinal cord. Med Serv J Can. 1966;22(7):512–523.
3. Farrington JD. Death in a ditch. Bulletin of the American College of Surgeons. 1967;52(3):121-130.
4. Farrington JD. Extrication of victims- surgical principles. J Trauma. 1968;8(4):493-512.
5. Riggins RS, Kraus JF. The risk of neurologic damage with fractures of the vertebrae. J Trauma. 1977;17(2):126-133.
6. Soderstrom CA, Brumback RJ. Early care of the patient with cervical spine injury. Orthop Clin North Am. 1986;17(1):3-13.
7. McHugh TP, Taylor JP. Unnecessary out-of-hospital use of full spinal immobilization. Acad Emerg Med. 1998;5(3):278-280.
8. Kwan I, Bunn F, Roberts I. Spinal immobilisation for trauma patients. Cochrane Database Syst Rev. 2001;(2):CD002803.
9. Sundstrøm T, Asbjørnsen H, Habiba S, Sunde GA, Wester K. Prehospital use of cervical collars in trauma patients: a critical review. J Neurotrauma. 2014;31(6):531-540.
10. Conrad BP, Rechtine G, Weight M, Clarke J, Horodyski M. Motion in the unstable cervical spine during hospital bed transfers. J Trauma. 2010;69,432-436.
11. Horodyski M, DiPaola CP, Conrad BP, Rechtine GR. Cervical collars are insufficient for immobilizing an unstable cervical spine injury. J Emerg Med. 2011;41(5):513-519.
12. Hughes SJ. How effective is the Newport/Aspen collar? A prospective radiographic evaluation in healthy adult volunteers. J Trauma. 1998;45(2):374-378.
13. Perry SD, McLellan B, McIlroy WE, Maki BE, Schwartz M, Fernie GR. The efficacy of head immobilization techniques during simulated vehicle motion. Spine (Phil Pa 1976). 1999;24(17):1839-1844.
14. Engsberg JR, Standeven JW, Shurtleff TL, Eggars JL, Shafer JS, Naunheim RS. Cervical spine motion during extrication. J Emerg Med. 2013;44(1):122-127.
15. Dixon M, O’Halloran J, Cummins NM. Biomechanical analysis of spinal immobilization during prehospital extrication—a proof of concept study. Emerg Med J. 2014;31(9):745-749.
16. Hauswald M, Ong G, Tandberg D, Omar Z. Out-of-hospital spinal immobilization: its effect on neurologic injury. Acad Emerg Med. 1998;5(3):214-219.
17. Haut ER, Kalish BT, Efron DT, et al. Spine immobilization in penetrating trauma: more harm than good? J Trauma. 2010;68(1):115-120.
18. Vanderlan WB, Tew BE, McSwain NE. Increased risk of death with cervical spine immobilization in penetrating cervical trauma. Injury. 2009;40(8):880-883.
19. Stuke LE, Pons PT, Guy JS, Chapleau WP, Butler FK, McSwain NE. Prehospital spine immobilization for penetrating trauma—review and recommendations from the Prehospital Trauma Life Support Executive Committee. J Trauma. 2011;71(3):763–769.
20. American College of Emergency Physicians. Policy Statement- EMS Management of Patients with Potential Spinal Injury. 2015. Available at: http://www.acep.org/Physician-Resources/Policies/Policy-Statements/EMS-Management-of-Patients-with-Potential-Spinal-Injury. Accessed February 9, 2016.
21. Barney RN, Cordell WH, Miller E. Pain associated with immobilization on rigid spine boards. Ann Emerg Med. 1989;18:918.
22. Cooney DR, Wallus H, Asaly M, Wojcik S. Backboard time for patients receiving spinal immobilization by emergency medical services. Int J Emerg Med. 2013;6(1):17.
23. Chan D, Goldberg R, Tascone A, Harmon S, Chan L. The effect of spinal immobilization on healthy volunteers. Ann Emerg Med. 1994;23(1):48-51.
24. Chan D, Goldberg RM, Mason J, Chan L. Backboard versus mattress splint immobilization: a comparison of symptoms generated. J Emerg Med, 1996;14(3):293-298.
25. March J, Ausband S, Brown L. Changes in physical examination caused by use of spinal immobilization. Prehosp Emerg Care. 2002;6(4):421-424.
26. Berg G, Nyberg S, Harrison P, Baumchen J, Gurss E, Hennes E. Near-infrared spectroscopy measurement of sacral tissue oxygen saturation in healthy volunteers immobilized on rigid spine boards. Prehosp Emerg Care. 2010;14(4):419-424.
27. Lee AY, Elojeimy S, Kanal KM, Gunn ML. The effect of trauma backboards on computed tomography radiation dose. Clin Radiol. 2016. Epub ahead of print.
28. Bauer D, Kowalski R. Effect of spinal immobilization devices on pulmonary function in the healthy, nonsmoking man. Ann Emerg Med. 1988;17(9):915-918.
29. Walsh M, Grant T, Mickey S. Lung function compromised by spinal immobilization. Ann Emerg Med. 1990;19(5):615-616.
30. Totten VY, Sugarman DB. Respiratory effects of spinal immobilization. Prehosp Emerg Care. 1999; 3(4):347-352.
31. Goutcher CM, Lochhead V. Reduction in mouth opening with semi-rigid cervical collars. Br J Anaesth. 2005;95(3):344-348.
32. Davies G, Deakin C, Wilson A. The effect of a rigid collar on intracranial pressure. Injury. 1996;27(9):647-649.
33. Dunham CM, Brocker BP, Collier BD, Gemmel DJ. Risks associated with magnetic resonance imaging and cervical collar in comatose, blunt trauma patients with negative comprehensive cervical spine computed tomography and no apparent spinal deficit. Crit Care. 2008;12(4):R89.
34. Mobbs RJ, Stoodley MA, Fuller J. Effect of cervical hard collar on intracranial pressure after head injury. ANZ J Surg. 2002;72(6):389-391.
35. Stone MB, Tubridy CM, Curran R. The effect of rigid cervical collars on internal jugular vein dimensions. Acad Emerg Med. 2010;17(1):100-102.
36. Ben-Galim P, Dreiangel N, Mattox KL, Reitman CA, Kalantar SB, Hipp JA. Extrication collars can result in abnormal separation between vertebrae in the presence of a dissociative injury. J Trauma. 2010;69(2):447-450.
37. Podolsky SM, Hoffman JR, Pietrafesa CA. Neurologic complications following immobilization of cervical spine fracture in a patient with ankylosing spondylitis. Ann Emerg Med. 1983;12(9):578-580.
38. Papadopoulos MC, Chakraborty A, Waldron G, Bell BA. Exacerbating cervical spine injury by applying a hard collar. BMJ. 1999;319(7203):171-172.
39. Thumbikat P, Hariharan RP, Ravichandran G, Mcclelland MR, Mathew KM. Spinal cord injury in patients with ankylosing spondylitis: a 10-year review. Spine (Phila Pa 1976). 2007;32(26):2989-2995.
40. Oto B, Corey DJ, Oswald J, Sifford D, Walsh B. Early secondary neurologic deterioration after blunt spinal trauma: a review of the literature. Acad Emerg Med. 2015;22(10):1200-1212.
41. Oteir AO, Smith K, Jennings PA, Stoelwinder JU. The prehospital management of suspected spinal cord injury: an update. Prehosp Disaster Med. 2014;29(4):399-402.
42. Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99.
43. Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841–1848.
44. Stroh G, Braude D. Can an out-of-hospital cervical spine clearance protocol identify all patients with injuries? An argument for selective immobilization. Ann Emerg Med. 2001;37(6):609-615.
1. White CC, Domeier RM, Millin MG. EMS spinal precautions and the use of the long backboard - resource document to the position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18(2):306-314.
2. Geisler WO, Wynne-Jones M, Jousse AT. Early management of patients with trauma to the spinal cord. Med Serv J Can. 1966;22(7):512–523.
3. Farrington JD. Death in a ditch. Bulletin of the American College of Surgeons. 1967;52(3):121-130.
4. Farrington JD. Extrication of victims- surgical principles. J Trauma. 1968;8(4):493-512.
5. Riggins RS, Kraus JF. The risk of neurologic damage with fractures of the vertebrae. J Trauma. 1977;17(2):126-133.
6. Soderstrom CA, Brumback RJ. Early care of the patient with cervical spine injury. Orthop Clin North Am. 1986;17(1):3-13.
7. McHugh TP, Taylor JP. Unnecessary out-of-hospital use of full spinal immobilization. Acad Emerg Med. 1998;5(3):278-280.
8. Kwan I, Bunn F, Roberts I. Spinal immobilisation for trauma patients. Cochrane Database Syst Rev. 2001;(2):CD002803.
9. Sundstrøm T, Asbjørnsen H, Habiba S, Sunde GA, Wester K. Prehospital use of cervical collars in trauma patients: a critical review. J Neurotrauma. 2014;31(6):531-540.
10. Conrad BP, Rechtine G, Weight M, Clarke J, Horodyski M. Motion in the unstable cervical spine during hospital bed transfers. J Trauma. 2010;69,432-436.
11. Horodyski M, DiPaola CP, Conrad BP, Rechtine GR. Cervical collars are insufficient for immobilizing an unstable cervical spine injury. J Emerg Med. 2011;41(5):513-519.
12. Hughes SJ. How effective is the Newport/Aspen collar? A prospective radiographic evaluation in healthy adult volunteers. J Trauma. 1998;45(2):374-378.
13. Perry SD, McLellan B, McIlroy WE, Maki BE, Schwartz M, Fernie GR. The efficacy of head immobilization techniques during simulated vehicle motion. Spine (Phil Pa 1976). 1999;24(17):1839-1844.
14. Engsberg JR, Standeven JW, Shurtleff TL, Eggars JL, Shafer JS, Naunheim RS. Cervical spine motion during extrication. J Emerg Med. 2013;44(1):122-127.
15. Dixon M, O’Halloran J, Cummins NM. Biomechanical analysis of spinal immobilization during prehospital extrication—a proof of concept study. Emerg Med J. 2014;31(9):745-749.
16. Hauswald M, Ong G, Tandberg D, Omar Z. Out-of-hospital spinal immobilization: its effect on neurologic injury. Acad Emerg Med. 1998;5(3):214-219.
17. Haut ER, Kalish BT, Efron DT, et al. Spine immobilization in penetrating trauma: more harm than good? J Trauma. 2010;68(1):115-120.
18. Vanderlan WB, Tew BE, McSwain NE. Increased risk of death with cervical spine immobilization in penetrating cervical trauma. Injury. 2009;40(8):880-883.
19. Stuke LE, Pons PT, Guy JS, Chapleau WP, Butler FK, McSwain NE. Prehospital spine immobilization for penetrating trauma—review and recommendations from the Prehospital Trauma Life Support Executive Committee. J Trauma. 2011;71(3):763–769.
20. American College of Emergency Physicians. Policy Statement- EMS Management of Patients with Potential Spinal Injury. 2015. Available at: http://www.acep.org/Physician-Resources/Policies/Policy-Statements/EMS-Management-of-Patients-with-Potential-Spinal-Injury. Accessed February 9, 2016.
21. Barney RN, Cordell WH, Miller E. Pain associated with immobilization on rigid spine boards. Ann Emerg Med. 1989;18:918.
22. Cooney DR, Wallus H, Asaly M, Wojcik S. Backboard time for patients receiving spinal immobilization by emergency medical services. Int J Emerg Med. 2013;6(1):17.
23. Chan D, Goldberg R, Tascone A, Harmon S, Chan L. The effect of spinal immobilization on healthy volunteers. Ann Emerg Med. 1994;23(1):48-51.
24. Chan D, Goldberg RM, Mason J, Chan L. Backboard versus mattress splint immobilization: a comparison of symptoms generated. J Emerg Med, 1996;14(3):293-298.
25. March J, Ausband S, Brown L. Changes in physical examination caused by use of spinal immobilization. Prehosp Emerg Care. 2002;6(4):421-424.
26. Berg G, Nyberg S, Harrison P, Baumchen J, Gurss E, Hennes E. Near-infrared spectroscopy measurement of sacral tissue oxygen saturation in healthy volunteers immobilized on rigid spine boards. Prehosp Emerg Care. 2010;14(4):419-424.
27. Lee AY, Elojeimy S, Kanal KM, Gunn ML. The effect of trauma backboards on computed tomography radiation dose. Clin Radiol. 2016. Epub ahead of print.
28. Bauer D, Kowalski R. Effect of spinal immobilization devices on pulmonary function in the healthy, nonsmoking man. Ann Emerg Med. 1988;17(9):915-918.
29. Walsh M, Grant T, Mickey S. Lung function compromised by spinal immobilization. Ann Emerg Med. 1990;19(5):615-616.
30. Totten VY, Sugarman DB. Respiratory effects of spinal immobilization. Prehosp Emerg Care. 1999; 3(4):347-352.
31. Goutcher CM, Lochhead V. Reduction in mouth opening with semi-rigid cervical collars. Br J Anaesth. 2005;95(3):344-348.
32. Davies G, Deakin C, Wilson A. The effect of a rigid collar on intracranial pressure. Injury. 1996;27(9):647-649.
33. Dunham CM, Brocker BP, Collier BD, Gemmel DJ. Risks associated with magnetic resonance imaging and cervical collar in comatose, blunt trauma patients with negative comprehensive cervical spine computed tomography and no apparent spinal deficit. Crit Care. 2008;12(4):R89.
34. Mobbs RJ, Stoodley MA, Fuller J. Effect of cervical hard collar on intracranial pressure after head injury. ANZ J Surg. 2002;72(6):389-391.
35. Stone MB, Tubridy CM, Curran R. The effect of rigid cervical collars on internal jugular vein dimensions. Acad Emerg Med. 2010;17(1):100-102.
36. Ben-Galim P, Dreiangel N, Mattox KL, Reitman CA, Kalantar SB, Hipp JA. Extrication collars can result in abnormal separation between vertebrae in the presence of a dissociative injury. J Trauma. 2010;69(2):447-450.
37. Podolsky SM, Hoffman JR, Pietrafesa CA. Neurologic complications following immobilization of cervical spine fracture in a patient with ankylosing spondylitis. Ann Emerg Med. 1983;12(9):578-580.
38. Papadopoulos MC, Chakraborty A, Waldron G, Bell BA. Exacerbating cervical spine injury by applying a hard collar. BMJ. 1999;319(7203):171-172.
39. Thumbikat P, Hariharan RP, Ravichandran G, Mcclelland MR, Mathew KM. Spinal cord injury in patients with ankylosing spondylitis: a 10-year review. Spine (Phila Pa 1976). 2007;32(26):2989-2995.
40. Oto B, Corey DJ, Oswald J, Sifford D, Walsh B. Early secondary neurologic deterioration after blunt spinal trauma: a review of the literature. Acad Emerg Med. 2015;22(10):1200-1212.
41. Oteir AO, Smith K, Jennings PA, Stoelwinder JU. The prehospital management of suspected spinal cord injury: an update. Prehosp Disaster Med. 2014;29(4):399-402.
42. Hoffman JR, Mower WR, Wolfson AB, Todd KH, Zucker MI. Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. National Emergency X-Radiography Utilization Study Group. N Engl J Med. 2000;343(2):94-99.
43. Stiell IG, Wells GA, Vandemheen KL, et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841–1848.
44. Stroh G, Braude D. Can an out-of-hospital cervical spine clearance protocol identify all patients with injuries? An argument for selective immobilization. Ann Emerg Med. 2001;37(6):609-615.
A Click Is Not a Clunk: Developmental Dysplasia of the Hip in a Newborn
IN THIS ARTICLE
- Diagnosis
- Management
- Newborn hip evaluation algorithm
Developmental dysplasia of the hip (DDH), previously known as congenital dislocation of the hip, follows a spectrum of irregular anatomic hip development spanning from acetabular dysplasia to irreducible dislocation at birth. Early detection is critical to improve the overall prognosis. Prompt diagnosis requires understanding of potential risk factors, proficiency in physical examination techniques, and implementation of appropriate screening tools when indicated. Although current guidelines direct timing for physical exam screenings, imaging, and treatment, it is ultimately up to the provider to determine the best course of action on a case-by-case basis. This article provides a review of these topics and more.
CURRENT GUIDELINES
In 2000, the American Academy of Pediatrics (AAP) developed guidelines for detection of hip dysplasia, including recommendation of relevant physical exam screenings for all newborns.1 In 2007, the Pediatric Orthopaedic Society of North America (POSNA) encouraged providers to follow the AAP guidelines with a continued recommendation to perform newborn screening for hip instability and routine follow-up evaluations until the child achieves walking.2 The American Academy of Orthopaedic Surgeons (AAOS) also established clinical guidelines in 2014 that are endorsed by both AAP and POSNA.3 These guidelines support routine clinical screening; research evaluated infants up to 6 months old, however, limiting the recommendations to that age-group.
Failure to treat DDH early has been associated with serious negative sequelae that include chronic pain, degenerative arthritis, postural scoliosis, and early gait disturbances.4 Primary care providers are expected to perform thorough newborn hip exams with associated specialized tests (ie, Ortolani and Barlow, which are discussed in “Physical exam”) at each routine follow-up. Heightened clinical suspicion and risk factor awareness are key for primary care providers to promptly identify patients requiring orthopedic referral. With early diagnosis, a removable soft abduction brace can be applied as the initial treatment. When treatment is delayed, however, closed reduction under anesthesia or complex surgical intervention may be required.
EPIDEMIOLOGY
The etiology for DDH remains unknown. Hip dysplasia typically presents unilaterally but can also occur bilaterally. DDH is more likely to affect the left hip than the right.5
Reported incidence varies, ranging from 0.06 to 76.1 per 1,000 live births, and is largely affected by race and geographic location.5 Incidence is higher in countries where routine screening is required, by either physical examination or ultrasound (1.6 to 28.5 and 34.0 to 60.3 per 1,000, respectively), compared with countries not requiring routine screening (1.3 per 1,000). This may suggest that the majority of hip dysplasia cases are transient and resolve spontaneously without treatment.6,7
RISK FACTORS AND PATIENT HISTORY
Known risk factors for DDH include breech presentation (see Figure 1), positive family history, and female gender.5,8-10 Female infants are eight times more likely than males to develop DDH.10 Firstborn status is also recognized as an associated risk factor, which may be attributable to space constraints in utero. This hypothesis is further supported by the relative DDH-protective effect of prematurity and low birth weight. Other potential risk factors include advanced maternal age, birth weight that is high for gestational age, decreased hip abduction, and joint laxity. However, the majority of patients with hip dysplasia have no identifiable risk factors.3,5,9,11,12
Swaddling, which often maintains the hips in an adducted and/or extended position, has also been strongly associated with hip dysplasia.5,13 Multiple organizations, including the AAOS,AAP, POSNA, and the International Hip Dysplasia Institute, have developed or endorsed hip-healthy swaddling recommendations to minimize the risk for DDH in swaddled infants.13-15 Such practices allow the infant’s legs to bend up and out at the hips, promoting free hip movement, flexion, and abduction.13,15 Swaddling has demonstrated multiple benefits (including improved sleep and relief of excessive crying13) and continues to be recommended by many US providers; however, those caring for infants at risk for DDH should avoid traditional swaddling and/or practice hip-healthy swaddling techniques.10,13,14 Early diagnosis starts with the clinician’s knowledge of DDH risk factors and the recommended screening protocols. The presence of multiple risk factors will increase the likelihood of this condition and should lower the clinician’s threshold for ordering additional screening, regardless of hip exam findings.
PHYSICAL EXAM
Both AAP and AAOS guidelines recommend clinical screening for DDH with physical exam in all newborns.1,3 A head-to-toe musculoskeletal exam is warranted during the initial evaluation of every newborn in order to assess for any known DDH-associated conditions, which may include neuromuscular disorders, torticollis, and metatarsus adductus.5
Initial evaluation of an infant with DDH may reveal nonspecific findings, including asymmetric skin folds and limb-length inequality. The Galeazzi sign should be sought by aligning flexed knees with the child in the supine position and assessing for uneven knee heights (see Figure 2). Unilateral posterior hip dislocation or femoral shortening represents a positive Galeazzi sign.16 Joint laxity and limited hip abduction have also been associated with DDH.1,10
Barlow and Ortolani exams are more specific to DDH and should be completed at newborn screening and each subsequent well-baby exam.1 The Barlow maneuver is a provocative test with flexion, adduction, and posterior pressure through the infant’s hip (Figure 3). A palpable clunk during the Barlow maneuver indicates positive instability with posterior displacement. The Ortolani test is a reductive maneuver requiring abduction with posterior pressure to lift the greater trochanter (Figure 4). A clunk sensation with this test is positive for reduction of the hip.
The infant’s diaper should be removed during the hip evaluation. These exams are more reliable when each hip is evaluated separately with the pelvis stabilized.10 All physical exam findings must be carefully documented at each encounter.1,17
It is critical for the examiner to understand the appropriate technique and potential results when conducting each of these specialized hip exams. A true positive finding is the clunking sensation that occurs with the dislocation or relocation of the affected hip; this finding is better felt than heard. In contrast, a benign hip click with these maneuvers is a more subtle sensation—typically, a soft-tissue snapping or catching—and is not diagnostic of DDH. A click is not a clunk and is not indicative of DDH.1,3
DDH may present later in infancy or early childhood; therefore, DDH should remain within the differential diagnosis for gait asymmetry, unequal hip motion, or limb-length discrepancy. It may be beneficial to continue to evaluate for these developments during routine exams as part of a thorough pediatric musculoskeletal assessment, particularly in patients with documented risk factors for DDH.1,3,4 Delay in diagnosis of DDH, it should be noted, is a relatively common complaint in pediatric medical malpractice lawsuits; until the early 2000s, this condition represented about 75% of claims in one medical malpractice database.The decrease in claims has been attributed to better awareness and earlier diagnosis of DDH. 17
Continue for the diagnosis >>
DIAGNOSIS
A positive Ortolani or Barlow sign is diagnostic and warrants prompt orthopedic referral (Figure 5). If physical examination results are equivocal or inconclusive, follow-up at two weeks is recommended, with continued routine follow-up until walking is achieved. Patients with persistent equivocal findings at the two-week follow-up warrant ultrasound at age 3 to 4 weeks or orthopedic referral. Infants with significant risk factors, particularly breech presentation at birth, should also undergo imaging.18 AAP recommends ultrasound at age 6 weeks or radiograph after 4 months of age.1,18 AAOS recommends performing an imaging study before age 6 months when at least one of the following risk factors is present: breech presentation, positive family history of DDH, or previous clinical instability (moderate level of evidence).3
IMAGING
Ultrasound is the diagnostic test of choice for infants because radiographs have limited value until the femoral heads begin to ossify at age 4 to 6 months.18 Ultrasonography allows for visualization of the cartilaginous portion of the acetabulum and femoral head.1 Dynamic stressing is performed during ultrasound to assess the level of hip stability. A provider trained in ultrasound will measure the depth of the acetabulum and identify any potential laxity or instability of the hip joint. Accuracy of these findings is largely dependent on the experience and skill of the examiner.
Ultrasound evaluation is not recommended until after age 3 to 4 weeks. Earlier findings may include mild laxity and immature morphology of the acetabulum, which often resolve spontaneously.1,18 Use of ultrasound is currently recommended only to confirm diagnostic suspicion, based on clinical findings, or for infants with significant risk factors.18 Universal ultrasound screening in newborns is not recommended and would incur unnecessary costs.1,3,9 Plain radiographs are used after age 4 months to confirm a diagnosis of DDH or to assess for residual dysplasia.3,18
Continue for management >>
MANAGEMENT
Once hip dysplasia is suggested by physical exam or imaging study, the child’s subsequent care should be provided by an orthopedic specialist with experience in treating this condition. Treatment is preferably initiated before age 6 weeks.12 The specifics of treatment are largely based on age at diagnosis and the severity of dysplasia.
The goal of treatment is to maintain the hips in a stable position with the femoral head well covered by the acetabulum. This will improve anatomic development and function. Early clinical diagnosis is often sufficient to justify initiating conservative treatment; additionally, early detection of DDH can considerably reduce the need for surgical intervention.12 Although the potential for spontaneous resolution is high, the consequences associated with delay in care can be significant.
Preferred initial management, which can be initiated before confirmation of DDH by ultrasound, involves implementation of soft abduction support.19 The Pavlik harness is the support design of choice (Figure 6).12 This harness maintains hip flexion and abduction, creating concentric reduction of the femoral head. The brace is highly successful when its use is initiated early. Treatment in a Pavlik harness requires nearly full-time wear and close monitoring by a clinician. Unlikely potential risks associated with this treatment include avascular necrosis and femoral nerve palsy.4
Ultrasonography is used to further monitor treatment and to determine length of wear. Long-term results suggest a success rate exceeding 90%.20,21 However, this rate may be falsely elevated due to the number of hips that likely would have improved spontaneously without treatment.6,19
The Pavlik harness becomes less effective with increasing age, and a more rigid abduction brace may be considered in infants older than 6 months.20 Overall outcomes improve once the femoral head is consistently maintained in the acetabulum. Delay in treatment is associated with an increase in the long-term complications associated with residual hip dysplasia.22
Once an infant is undergoing treatment for DDH in a Pavlik harness, there is no need for primary care providers to continue to perform provocative testing, such as the Ortolani or Barlow test, at routine well-baby checks. Unnecessary stress to the hips is not beneficial, and any new results will not change the treatment being provided by the orthopedic specialist. Adjustments to the fit of the harness should be made only by the orthopedist, unless femoral nerve palsy is noted on exam. This development warrants immediate discontinuation of harness use until symptoms resolve.21
Abduction bracing may not be suitable for all cases of hip dysplasia. Newborns with irreducible hips, more advanced dysplasia, or associated neuromuscular or syndromic disorder may require closed versus open reduction and casting. More invasive surgical options may also be considered in advanced dysplasia in order to reshape the joint and improve function.20,22
Continue for patient education >>
PATIENT EDUCATION
Parents should be fully educated on the options for managing hip dysplasia. Once DDH is diagnosed, prompt referral to an orthopedic specialist is critical in order to weigh the treatment options and to develop the appropriate individualized plan for each child. Once treatment is initiated, parental compliance is essential; frequent meetings between parents and the specialist are important.
Parents of infants with known risk factors for and/or suspicion of hip dysplasia should also be educated on hip-healthy swaddling to allow for free motion of the hips and knees.10,13 Advise them that some commercial baby carriers and slings may maintain the hips in an undesirable extended position. In both swaddling and with baby carriers, care should be taken to allow for hip abduction and flexion. Caution should also be taken during diaper changes to avoid lifting the legs and thereby causing unnecessary stress to the hips.
CONCLUSION
Developmental dysplasia of the hip can be a disabling pediatric condition. Early diagnosis improves the likelihood of successful treatment during infancy and can prevent serious complications. If untreated, DDH can lead to joint degeneration and premature arthritis. Recognition and treatment within the first six weeks of life is crucial to the overall outcome.
The role of a primary care provider is to identify hip dysplasia risk factors and recognize associated physical exam findings in order to refer to an orthopedic specialist in a timely manner. Guidelines from the AAP, POSNA, and AAOS help direct this process in order to effectively identify infants at risk and in need of treatment.
REFERENCES
1. American Academy of Pediatrics. Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip. Clinical practice guideline: early detection of developmental dysplasia of the hip. Pediatrics. 2000;105(4 pt 1):896-905.
2. Schwend RM, Schoenecker P, Richards BS, et al. Screening the newborn for developmental dysplasia of the hip: now what do we do? J Pediatr Orthop. 2007;27(6):607-610.
3. Mulpuri K, Song KM, Goldberg MJ, Sevarino K. Detection and nonoperative management of pediatric developmental dysplasia of the hip in infants up to six months of age. J Am Acad Orthop Surg. 2015;23(3):202-205.
4. Thomas SRYW. A review of long-term outcomes for late presenting developmental hip dysplasia. Bone Joint J. 2015;97-B(6):729-733.
5. Loder RT, Skopelja EN. The epidemiology and demographics of hip dysplasia. ISRN Orthop. 2011;2011:238607.
6. US Preventive Services Task Force. Screening for developmental dysplasia of the hip: recommendation statement. Pediatrics. 2006;117(3):898-902.
7. Shorter D, Hong T, Osborn DA. Screening programmes for developmental dysplasia of the hip in newborn infants. Cochrane Database Syst Rev. 2011;(9):CD004595.
8. Loder RT, Shafer C. The demographics of developmental hip dysplasia in the Midwestern United States (Indiana). J Child Orthop. 2015;9(1):93-98.
9. Paton RW, Hinduja K, Thomas CD. The significance of at-risk factors in ultrasound surveillance of developmental dysplasia of the hip: a ten-year prospective study. J Bone Joint Surg Br. 2005;87(9):1264-1266.
10. Alsaleem M, Set KK, Saadeh L. Developmental dysplasia of hip: a review. Clin Pediatr (Phila). 2015;54(10):921-928.
11. Chan A, McCaul KA, Cundy PJ, et al. Perinatal risk factors for developmental dysplasia of the hip. Arch Dis Child. 1997;76(2):F94-F100.
12. Godley DR. Assessment, diagnosis, and treatment of developmental dysplasia of the hip. JAAPA. 2013;26(3):54-58.
13. Van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, et al. Swaddling: a systematic review. Pediatrics. 2007;120(4):e1097-e1106.
14. American Academy of Orthopaedic Surgeons, American Association of Orthopaedic Surgeons. Position statement: swaddling and developmental hip dysplasia. www.aaos.org/uploadedFiles/PreProduction/About/Opinion_Statements/position/1186%20Swaddling%20and%20Developmental%20Hip%20Dysplasia.pdf. Accessed January 22, 2016.
15. Clarke NM. Swaddling and hip dysplasia: an orthopaedic perspective. Arch Dis Child. 2014;99(1):5-6.
16. Storer SK, Skaggs DL. Developmental dysplasia of the hip. Am Fam Physician. 2006;74(8):1310-1316.
17. McAbee GN, Donn SM, Mendelson RA, et al. Medical diagnoses commonly associated with pediatric malpractice lawsuits in the United States. Pediatrics. 2008;122(6):e1282-e1286.
18. Imrie M, Scott V, Stearns P, et al. Is ultrasound screening for DDH in babies born breech sufficient? J Child Orthop. 2010;4(1):3-8.
19. Chen HW, Chang CH, Tsai ST, et al. Natural progression of hip dysplasia in newborns: a reflection of hip ultrasonographic screenings in newborn nurseries. J Pediatr Orthop B. 2010;19(5):418-423.
20. Gans I, Flynn JM, Sankar WN. Abduction bracing for residual acetabular dysplasia in infantile DDH. J Pediatr Orthop. 2013;33(7):714-718.
21. Murnaghan ML, Browne RH, Sucato DJ, Birch J. Femoral nerve palsy in Pavlik harness treatment for developmental dysplasia of the hip. J Bone Joint Surg Am. 2011;93(5):493-499.
22. Dezateux C, Rosendahl K. Developmental dysplasia of the hip. Lancet. 2007;369(9572):1541-1552.
IN THIS ARTICLE
- Diagnosis
- Management
- Newborn hip evaluation algorithm
Developmental dysplasia of the hip (DDH), previously known as congenital dislocation of the hip, follows a spectrum of irregular anatomic hip development spanning from acetabular dysplasia to irreducible dislocation at birth. Early detection is critical to improve the overall prognosis. Prompt diagnosis requires understanding of potential risk factors, proficiency in physical examination techniques, and implementation of appropriate screening tools when indicated. Although current guidelines direct timing for physical exam screenings, imaging, and treatment, it is ultimately up to the provider to determine the best course of action on a case-by-case basis. This article provides a review of these topics and more.
CURRENT GUIDELINES
In 2000, the American Academy of Pediatrics (AAP) developed guidelines for detection of hip dysplasia, including recommendation of relevant physical exam screenings for all newborns.1 In 2007, the Pediatric Orthopaedic Society of North America (POSNA) encouraged providers to follow the AAP guidelines with a continued recommendation to perform newborn screening for hip instability and routine follow-up evaluations until the child achieves walking.2 The American Academy of Orthopaedic Surgeons (AAOS) also established clinical guidelines in 2014 that are endorsed by both AAP and POSNA.3 These guidelines support routine clinical screening; research evaluated infants up to 6 months old, however, limiting the recommendations to that age-group.
Failure to treat DDH early has been associated with serious negative sequelae that include chronic pain, degenerative arthritis, postural scoliosis, and early gait disturbances.4 Primary care providers are expected to perform thorough newborn hip exams with associated specialized tests (ie, Ortolani and Barlow, which are discussed in “Physical exam”) at each routine follow-up. Heightened clinical suspicion and risk factor awareness are key for primary care providers to promptly identify patients requiring orthopedic referral. With early diagnosis, a removable soft abduction brace can be applied as the initial treatment. When treatment is delayed, however, closed reduction under anesthesia or complex surgical intervention may be required.
EPIDEMIOLOGY
The etiology for DDH remains unknown. Hip dysplasia typically presents unilaterally but can also occur bilaterally. DDH is more likely to affect the left hip than the right.5
Reported incidence varies, ranging from 0.06 to 76.1 per 1,000 live births, and is largely affected by race and geographic location.5 Incidence is higher in countries where routine screening is required, by either physical examination or ultrasound (1.6 to 28.5 and 34.0 to 60.3 per 1,000, respectively), compared with countries not requiring routine screening (1.3 per 1,000). This may suggest that the majority of hip dysplasia cases are transient and resolve spontaneously without treatment.6,7
RISK FACTORS AND PATIENT HISTORY
Known risk factors for DDH include breech presentation (see Figure 1), positive family history, and female gender.5,8-10 Female infants are eight times more likely than males to develop DDH.10 Firstborn status is also recognized as an associated risk factor, which may be attributable to space constraints in utero. This hypothesis is further supported by the relative DDH-protective effect of prematurity and low birth weight. Other potential risk factors include advanced maternal age, birth weight that is high for gestational age, decreased hip abduction, and joint laxity. However, the majority of patients with hip dysplasia have no identifiable risk factors.3,5,9,11,12
Swaddling, which often maintains the hips in an adducted and/or extended position, has also been strongly associated with hip dysplasia.5,13 Multiple organizations, including the AAOS,AAP, POSNA, and the International Hip Dysplasia Institute, have developed or endorsed hip-healthy swaddling recommendations to minimize the risk for DDH in swaddled infants.13-15 Such practices allow the infant’s legs to bend up and out at the hips, promoting free hip movement, flexion, and abduction.13,15 Swaddling has demonstrated multiple benefits (including improved sleep and relief of excessive crying13) and continues to be recommended by many US providers; however, those caring for infants at risk for DDH should avoid traditional swaddling and/or practice hip-healthy swaddling techniques.10,13,14 Early diagnosis starts with the clinician’s knowledge of DDH risk factors and the recommended screening protocols. The presence of multiple risk factors will increase the likelihood of this condition and should lower the clinician’s threshold for ordering additional screening, regardless of hip exam findings.
PHYSICAL EXAM
Both AAP and AAOS guidelines recommend clinical screening for DDH with physical exam in all newborns.1,3 A head-to-toe musculoskeletal exam is warranted during the initial evaluation of every newborn in order to assess for any known DDH-associated conditions, which may include neuromuscular disorders, torticollis, and metatarsus adductus.5
Initial evaluation of an infant with DDH may reveal nonspecific findings, including asymmetric skin folds and limb-length inequality. The Galeazzi sign should be sought by aligning flexed knees with the child in the supine position and assessing for uneven knee heights (see Figure 2). Unilateral posterior hip dislocation or femoral shortening represents a positive Galeazzi sign.16 Joint laxity and limited hip abduction have also been associated with DDH.1,10
Barlow and Ortolani exams are more specific to DDH and should be completed at newborn screening and each subsequent well-baby exam.1 The Barlow maneuver is a provocative test with flexion, adduction, and posterior pressure through the infant’s hip (Figure 3). A palpable clunk during the Barlow maneuver indicates positive instability with posterior displacement. The Ortolani test is a reductive maneuver requiring abduction with posterior pressure to lift the greater trochanter (Figure 4). A clunk sensation with this test is positive for reduction of the hip.
The infant’s diaper should be removed during the hip evaluation. These exams are more reliable when each hip is evaluated separately with the pelvis stabilized.10 All physical exam findings must be carefully documented at each encounter.1,17
It is critical for the examiner to understand the appropriate technique and potential results when conducting each of these specialized hip exams. A true positive finding is the clunking sensation that occurs with the dislocation or relocation of the affected hip; this finding is better felt than heard. In contrast, a benign hip click with these maneuvers is a more subtle sensation—typically, a soft-tissue snapping or catching—and is not diagnostic of DDH. A click is not a clunk and is not indicative of DDH.1,3
DDH may present later in infancy or early childhood; therefore, DDH should remain within the differential diagnosis for gait asymmetry, unequal hip motion, or limb-length discrepancy. It may be beneficial to continue to evaluate for these developments during routine exams as part of a thorough pediatric musculoskeletal assessment, particularly in patients with documented risk factors for DDH.1,3,4 Delay in diagnosis of DDH, it should be noted, is a relatively common complaint in pediatric medical malpractice lawsuits; until the early 2000s, this condition represented about 75% of claims in one medical malpractice database.The decrease in claims has been attributed to better awareness and earlier diagnosis of DDH. 17
Continue for the diagnosis >>
DIAGNOSIS
A positive Ortolani or Barlow sign is diagnostic and warrants prompt orthopedic referral (Figure 5). If physical examination results are equivocal or inconclusive, follow-up at two weeks is recommended, with continued routine follow-up until walking is achieved. Patients with persistent equivocal findings at the two-week follow-up warrant ultrasound at age 3 to 4 weeks or orthopedic referral. Infants with significant risk factors, particularly breech presentation at birth, should also undergo imaging.18 AAP recommends ultrasound at age 6 weeks or radiograph after 4 months of age.1,18 AAOS recommends performing an imaging study before age 6 months when at least one of the following risk factors is present: breech presentation, positive family history of DDH, or previous clinical instability (moderate level of evidence).3
IMAGING
Ultrasound is the diagnostic test of choice for infants because radiographs have limited value until the femoral heads begin to ossify at age 4 to 6 months.18 Ultrasonography allows for visualization of the cartilaginous portion of the acetabulum and femoral head.1 Dynamic stressing is performed during ultrasound to assess the level of hip stability. A provider trained in ultrasound will measure the depth of the acetabulum and identify any potential laxity or instability of the hip joint. Accuracy of these findings is largely dependent on the experience and skill of the examiner.
Ultrasound evaluation is not recommended until after age 3 to 4 weeks. Earlier findings may include mild laxity and immature morphology of the acetabulum, which often resolve spontaneously.1,18 Use of ultrasound is currently recommended only to confirm diagnostic suspicion, based on clinical findings, or for infants with significant risk factors.18 Universal ultrasound screening in newborns is not recommended and would incur unnecessary costs.1,3,9 Plain radiographs are used after age 4 months to confirm a diagnosis of DDH or to assess for residual dysplasia.3,18
Continue for management >>
MANAGEMENT
Once hip dysplasia is suggested by physical exam or imaging study, the child’s subsequent care should be provided by an orthopedic specialist with experience in treating this condition. Treatment is preferably initiated before age 6 weeks.12 The specifics of treatment are largely based on age at diagnosis and the severity of dysplasia.
The goal of treatment is to maintain the hips in a stable position with the femoral head well covered by the acetabulum. This will improve anatomic development and function. Early clinical diagnosis is often sufficient to justify initiating conservative treatment; additionally, early detection of DDH can considerably reduce the need for surgical intervention.12 Although the potential for spontaneous resolution is high, the consequences associated with delay in care can be significant.
Preferred initial management, which can be initiated before confirmation of DDH by ultrasound, involves implementation of soft abduction support.19 The Pavlik harness is the support design of choice (Figure 6).12 This harness maintains hip flexion and abduction, creating concentric reduction of the femoral head. The brace is highly successful when its use is initiated early. Treatment in a Pavlik harness requires nearly full-time wear and close monitoring by a clinician. Unlikely potential risks associated with this treatment include avascular necrosis and femoral nerve palsy.4
Ultrasonography is used to further monitor treatment and to determine length of wear. Long-term results suggest a success rate exceeding 90%.20,21 However, this rate may be falsely elevated due to the number of hips that likely would have improved spontaneously without treatment.6,19
The Pavlik harness becomes less effective with increasing age, and a more rigid abduction brace may be considered in infants older than 6 months.20 Overall outcomes improve once the femoral head is consistently maintained in the acetabulum. Delay in treatment is associated with an increase in the long-term complications associated with residual hip dysplasia.22
Once an infant is undergoing treatment for DDH in a Pavlik harness, there is no need for primary care providers to continue to perform provocative testing, such as the Ortolani or Barlow test, at routine well-baby checks. Unnecessary stress to the hips is not beneficial, and any new results will not change the treatment being provided by the orthopedic specialist. Adjustments to the fit of the harness should be made only by the orthopedist, unless femoral nerve palsy is noted on exam. This development warrants immediate discontinuation of harness use until symptoms resolve.21
Abduction bracing may not be suitable for all cases of hip dysplasia. Newborns with irreducible hips, more advanced dysplasia, or associated neuromuscular or syndromic disorder may require closed versus open reduction and casting. More invasive surgical options may also be considered in advanced dysplasia in order to reshape the joint and improve function.20,22
Continue for patient education >>
PATIENT EDUCATION
Parents should be fully educated on the options for managing hip dysplasia. Once DDH is diagnosed, prompt referral to an orthopedic specialist is critical in order to weigh the treatment options and to develop the appropriate individualized plan for each child. Once treatment is initiated, parental compliance is essential; frequent meetings between parents and the specialist are important.
Parents of infants with known risk factors for and/or suspicion of hip dysplasia should also be educated on hip-healthy swaddling to allow for free motion of the hips and knees.10,13 Advise them that some commercial baby carriers and slings may maintain the hips in an undesirable extended position. In both swaddling and with baby carriers, care should be taken to allow for hip abduction and flexion. Caution should also be taken during diaper changes to avoid lifting the legs and thereby causing unnecessary stress to the hips.
CONCLUSION
Developmental dysplasia of the hip can be a disabling pediatric condition. Early diagnosis improves the likelihood of successful treatment during infancy and can prevent serious complications. If untreated, DDH can lead to joint degeneration and premature arthritis. Recognition and treatment within the first six weeks of life is crucial to the overall outcome.
The role of a primary care provider is to identify hip dysplasia risk factors and recognize associated physical exam findings in order to refer to an orthopedic specialist in a timely manner. Guidelines from the AAP, POSNA, and AAOS help direct this process in order to effectively identify infants at risk and in need of treatment.
REFERENCES
1. American Academy of Pediatrics. Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip. Clinical practice guideline: early detection of developmental dysplasia of the hip. Pediatrics. 2000;105(4 pt 1):896-905.
2. Schwend RM, Schoenecker P, Richards BS, et al. Screening the newborn for developmental dysplasia of the hip: now what do we do? J Pediatr Orthop. 2007;27(6):607-610.
3. Mulpuri K, Song KM, Goldberg MJ, Sevarino K. Detection and nonoperative management of pediatric developmental dysplasia of the hip in infants up to six months of age. J Am Acad Orthop Surg. 2015;23(3):202-205.
4. Thomas SRYW. A review of long-term outcomes for late presenting developmental hip dysplasia. Bone Joint J. 2015;97-B(6):729-733.
5. Loder RT, Skopelja EN. The epidemiology and demographics of hip dysplasia. ISRN Orthop. 2011;2011:238607.
6. US Preventive Services Task Force. Screening for developmental dysplasia of the hip: recommendation statement. Pediatrics. 2006;117(3):898-902.
7. Shorter D, Hong T, Osborn DA. Screening programmes for developmental dysplasia of the hip in newborn infants. Cochrane Database Syst Rev. 2011;(9):CD004595.
8. Loder RT, Shafer C. The demographics of developmental hip dysplasia in the Midwestern United States (Indiana). J Child Orthop. 2015;9(1):93-98.
9. Paton RW, Hinduja K, Thomas CD. The significance of at-risk factors in ultrasound surveillance of developmental dysplasia of the hip: a ten-year prospective study. J Bone Joint Surg Br. 2005;87(9):1264-1266.
10. Alsaleem M, Set KK, Saadeh L. Developmental dysplasia of hip: a review. Clin Pediatr (Phila). 2015;54(10):921-928.
11. Chan A, McCaul KA, Cundy PJ, et al. Perinatal risk factors for developmental dysplasia of the hip. Arch Dis Child. 1997;76(2):F94-F100.
12. Godley DR. Assessment, diagnosis, and treatment of developmental dysplasia of the hip. JAAPA. 2013;26(3):54-58.
13. Van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, et al. Swaddling: a systematic review. Pediatrics. 2007;120(4):e1097-e1106.
14. American Academy of Orthopaedic Surgeons, American Association of Orthopaedic Surgeons. Position statement: swaddling and developmental hip dysplasia. www.aaos.org/uploadedFiles/PreProduction/About/Opinion_Statements/position/1186%20Swaddling%20and%20Developmental%20Hip%20Dysplasia.pdf. Accessed January 22, 2016.
15. Clarke NM. Swaddling and hip dysplasia: an orthopaedic perspective. Arch Dis Child. 2014;99(1):5-6.
16. Storer SK, Skaggs DL. Developmental dysplasia of the hip. Am Fam Physician. 2006;74(8):1310-1316.
17. McAbee GN, Donn SM, Mendelson RA, et al. Medical diagnoses commonly associated with pediatric malpractice lawsuits in the United States. Pediatrics. 2008;122(6):e1282-e1286.
18. Imrie M, Scott V, Stearns P, et al. Is ultrasound screening for DDH in babies born breech sufficient? J Child Orthop. 2010;4(1):3-8.
19. Chen HW, Chang CH, Tsai ST, et al. Natural progression of hip dysplasia in newborns: a reflection of hip ultrasonographic screenings in newborn nurseries. J Pediatr Orthop B. 2010;19(5):418-423.
20. Gans I, Flynn JM, Sankar WN. Abduction bracing for residual acetabular dysplasia in infantile DDH. J Pediatr Orthop. 2013;33(7):714-718.
21. Murnaghan ML, Browne RH, Sucato DJ, Birch J. Femoral nerve palsy in Pavlik harness treatment for developmental dysplasia of the hip. J Bone Joint Surg Am. 2011;93(5):493-499.
22. Dezateux C, Rosendahl K. Developmental dysplasia of the hip. Lancet. 2007;369(9572):1541-1552.
IN THIS ARTICLE
- Diagnosis
- Management
- Newborn hip evaluation algorithm
Developmental dysplasia of the hip (DDH), previously known as congenital dislocation of the hip, follows a spectrum of irregular anatomic hip development spanning from acetabular dysplasia to irreducible dislocation at birth. Early detection is critical to improve the overall prognosis. Prompt diagnosis requires understanding of potential risk factors, proficiency in physical examination techniques, and implementation of appropriate screening tools when indicated. Although current guidelines direct timing for physical exam screenings, imaging, and treatment, it is ultimately up to the provider to determine the best course of action on a case-by-case basis. This article provides a review of these topics and more.
CURRENT GUIDELINES
In 2000, the American Academy of Pediatrics (AAP) developed guidelines for detection of hip dysplasia, including recommendation of relevant physical exam screenings for all newborns.1 In 2007, the Pediatric Orthopaedic Society of North America (POSNA) encouraged providers to follow the AAP guidelines with a continued recommendation to perform newborn screening for hip instability and routine follow-up evaluations until the child achieves walking.2 The American Academy of Orthopaedic Surgeons (AAOS) also established clinical guidelines in 2014 that are endorsed by both AAP and POSNA.3 These guidelines support routine clinical screening; research evaluated infants up to 6 months old, however, limiting the recommendations to that age-group.
Failure to treat DDH early has been associated with serious negative sequelae that include chronic pain, degenerative arthritis, postural scoliosis, and early gait disturbances.4 Primary care providers are expected to perform thorough newborn hip exams with associated specialized tests (ie, Ortolani and Barlow, which are discussed in “Physical exam”) at each routine follow-up. Heightened clinical suspicion and risk factor awareness are key for primary care providers to promptly identify patients requiring orthopedic referral. With early diagnosis, a removable soft abduction brace can be applied as the initial treatment. When treatment is delayed, however, closed reduction under anesthesia or complex surgical intervention may be required.
EPIDEMIOLOGY
The etiology for DDH remains unknown. Hip dysplasia typically presents unilaterally but can also occur bilaterally. DDH is more likely to affect the left hip than the right.5
Reported incidence varies, ranging from 0.06 to 76.1 per 1,000 live births, and is largely affected by race and geographic location.5 Incidence is higher in countries where routine screening is required, by either physical examination or ultrasound (1.6 to 28.5 and 34.0 to 60.3 per 1,000, respectively), compared with countries not requiring routine screening (1.3 per 1,000). This may suggest that the majority of hip dysplasia cases are transient and resolve spontaneously without treatment.6,7
RISK FACTORS AND PATIENT HISTORY
Known risk factors for DDH include breech presentation (see Figure 1), positive family history, and female gender.5,8-10 Female infants are eight times more likely than males to develop DDH.10 Firstborn status is also recognized as an associated risk factor, which may be attributable to space constraints in utero. This hypothesis is further supported by the relative DDH-protective effect of prematurity and low birth weight. Other potential risk factors include advanced maternal age, birth weight that is high for gestational age, decreased hip abduction, and joint laxity. However, the majority of patients with hip dysplasia have no identifiable risk factors.3,5,9,11,12
Swaddling, which often maintains the hips in an adducted and/or extended position, has also been strongly associated with hip dysplasia.5,13 Multiple organizations, including the AAOS,AAP, POSNA, and the International Hip Dysplasia Institute, have developed or endorsed hip-healthy swaddling recommendations to minimize the risk for DDH in swaddled infants.13-15 Such practices allow the infant’s legs to bend up and out at the hips, promoting free hip movement, flexion, and abduction.13,15 Swaddling has demonstrated multiple benefits (including improved sleep and relief of excessive crying13) and continues to be recommended by many US providers; however, those caring for infants at risk for DDH should avoid traditional swaddling and/or practice hip-healthy swaddling techniques.10,13,14 Early diagnosis starts with the clinician’s knowledge of DDH risk factors and the recommended screening protocols. The presence of multiple risk factors will increase the likelihood of this condition and should lower the clinician’s threshold for ordering additional screening, regardless of hip exam findings.
PHYSICAL EXAM
Both AAP and AAOS guidelines recommend clinical screening for DDH with physical exam in all newborns.1,3 A head-to-toe musculoskeletal exam is warranted during the initial evaluation of every newborn in order to assess for any known DDH-associated conditions, which may include neuromuscular disorders, torticollis, and metatarsus adductus.5
Initial evaluation of an infant with DDH may reveal nonspecific findings, including asymmetric skin folds and limb-length inequality. The Galeazzi sign should be sought by aligning flexed knees with the child in the supine position and assessing for uneven knee heights (see Figure 2). Unilateral posterior hip dislocation or femoral shortening represents a positive Galeazzi sign.16 Joint laxity and limited hip abduction have also been associated with DDH.1,10
Barlow and Ortolani exams are more specific to DDH and should be completed at newborn screening and each subsequent well-baby exam.1 The Barlow maneuver is a provocative test with flexion, adduction, and posterior pressure through the infant’s hip (Figure 3). A palpable clunk during the Barlow maneuver indicates positive instability with posterior displacement. The Ortolani test is a reductive maneuver requiring abduction with posterior pressure to lift the greater trochanter (Figure 4). A clunk sensation with this test is positive for reduction of the hip.
The infant’s diaper should be removed during the hip evaluation. These exams are more reliable when each hip is evaluated separately with the pelvis stabilized.10 All physical exam findings must be carefully documented at each encounter.1,17
It is critical for the examiner to understand the appropriate technique and potential results when conducting each of these specialized hip exams. A true positive finding is the clunking sensation that occurs with the dislocation or relocation of the affected hip; this finding is better felt than heard. In contrast, a benign hip click with these maneuvers is a more subtle sensation—typically, a soft-tissue snapping or catching—and is not diagnostic of DDH. A click is not a clunk and is not indicative of DDH.1,3
DDH may present later in infancy or early childhood; therefore, DDH should remain within the differential diagnosis for gait asymmetry, unequal hip motion, or limb-length discrepancy. It may be beneficial to continue to evaluate for these developments during routine exams as part of a thorough pediatric musculoskeletal assessment, particularly in patients with documented risk factors for DDH.1,3,4 Delay in diagnosis of DDH, it should be noted, is a relatively common complaint in pediatric medical malpractice lawsuits; until the early 2000s, this condition represented about 75% of claims in one medical malpractice database.The decrease in claims has been attributed to better awareness and earlier diagnosis of DDH. 17
Continue for the diagnosis >>
DIAGNOSIS
A positive Ortolani or Barlow sign is diagnostic and warrants prompt orthopedic referral (Figure 5). If physical examination results are equivocal or inconclusive, follow-up at two weeks is recommended, with continued routine follow-up until walking is achieved. Patients with persistent equivocal findings at the two-week follow-up warrant ultrasound at age 3 to 4 weeks or orthopedic referral. Infants with significant risk factors, particularly breech presentation at birth, should also undergo imaging.18 AAP recommends ultrasound at age 6 weeks or radiograph after 4 months of age.1,18 AAOS recommends performing an imaging study before age 6 months when at least one of the following risk factors is present: breech presentation, positive family history of DDH, or previous clinical instability (moderate level of evidence).3
IMAGING
Ultrasound is the diagnostic test of choice for infants because radiographs have limited value until the femoral heads begin to ossify at age 4 to 6 months.18 Ultrasonography allows for visualization of the cartilaginous portion of the acetabulum and femoral head.1 Dynamic stressing is performed during ultrasound to assess the level of hip stability. A provider trained in ultrasound will measure the depth of the acetabulum and identify any potential laxity or instability of the hip joint. Accuracy of these findings is largely dependent on the experience and skill of the examiner.
Ultrasound evaluation is not recommended until after age 3 to 4 weeks. Earlier findings may include mild laxity and immature morphology of the acetabulum, which often resolve spontaneously.1,18 Use of ultrasound is currently recommended only to confirm diagnostic suspicion, based on clinical findings, or for infants with significant risk factors.18 Universal ultrasound screening in newborns is not recommended and would incur unnecessary costs.1,3,9 Plain radiographs are used after age 4 months to confirm a diagnosis of DDH or to assess for residual dysplasia.3,18
Continue for management >>
MANAGEMENT
Once hip dysplasia is suggested by physical exam or imaging study, the child’s subsequent care should be provided by an orthopedic specialist with experience in treating this condition. Treatment is preferably initiated before age 6 weeks.12 The specifics of treatment are largely based on age at diagnosis and the severity of dysplasia.
The goal of treatment is to maintain the hips in a stable position with the femoral head well covered by the acetabulum. This will improve anatomic development and function. Early clinical diagnosis is often sufficient to justify initiating conservative treatment; additionally, early detection of DDH can considerably reduce the need for surgical intervention.12 Although the potential for spontaneous resolution is high, the consequences associated with delay in care can be significant.
Preferred initial management, which can be initiated before confirmation of DDH by ultrasound, involves implementation of soft abduction support.19 The Pavlik harness is the support design of choice (Figure 6).12 This harness maintains hip flexion and abduction, creating concentric reduction of the femoral head. The brace is highly successful when its use is initiated early. Treatment in a Pavlik harness requires nearly full-time wear and close monitoring by a clinician. Unlikely potential risks associated with this treatment include avascular necrosis and femoral nerve palsy.4
Ultrasonography is used to further monitor treatment and to determine length of wear. Long-term results suggest a success rate exceeding 90%.20,21 However, this rate may be falsely elevated due to the number of hips that likely would have improved spontaneously without treatment.6,19
The Pavlik harness becomes less effective with increasing age, and a more rigid abduction brace may be considered in infants older than 6 months.20 Overall outcomes improve once the femoral head is consistently maintained in the acetabulum. Delay in treatment is associated with an increase in the long-term complications associated with residual hip dysplasia.22
Once an infant is undergoing treatment for DDH in a Pavlik harness, there is no need for primary care providers to continue to perform provocative testing, such as the Ortolani or Barlow test, at routine well-baby checks. Unnecessary stress to the hips is not beneficial, and any new results will not change the treatment being provided by the orthopedic specialist. Adjustments to the fit of the harness should be made only by the orthopedist, unless femoral nerve palsy is noted on exam. This development warrants immediate discontinuation of harness use until symptoms resolve.21
Abduction bracing may not be suitable for all cases of hip dysplasia. Newborns with irreducible hips, more advanced dysplasia, or associated neuromuscular or syndromic disorder may require closed versus open reduction and casting. More invasive surgical options may also be considered in advanced dysplasia in order to reshape the joint and improve function.20,22
Continue for patient education >>
PATIENT EDUCATION
Parents should be fully educated on the options for managing hip dysplasia. Once DDH is diagnosed, prompt referral to an orthopedic specialist is critical in order to weigh the treatment options and to develop the appropriate individualized plan for each child. Once treatment is initiated, parental compliance is essential; frequent meetings between parents and the specialist are important.
Parents of infants with known risk factors for and/or suspicion of hip dysplasia should also be educated on hip-healthy swaddling to allow for free motion of the hips and knees.10,13 Advise them that some commercial baby carriers and slings may maintain the hips in an undesirable extended position. In both swaddling and with baby carriers, care should be taken to allow for hip abduction and flexion. Caution should also be taken during diaper changes to avoid lifting the legs and thereby causing unnecessary stress to the hips.
CONCLUSION
Developmental dysplasia of the hip can be a disabling pediatric condition. Early diagnosis improves the likelihood of successful treatment during infancy and can prevent serious complications. If untreated, DDH can lead to joint degeneration and premature arthritis. Recognition and treatment within the first six weeks of life is crucial to the overall outcome.
The role of a primary care provider is to identify hip dysplasia risk factors and recognize associated physical exam findings in order to refer to an orthopedic specialist in a timely manner. Guidelines from the AAP, POSNA, and AAOS help direct this process in order to effectively identify infants at risk and in need of treatment.
REFERENCES
1. American Academy of Pediatrics. Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip. Clinical practice guideline: early detection of developmental dysplasia of the hip. Pediatrics. 2000;105(4 pt 1):896-905.
2. Schwend RM, Schoenecker P, Richards BS, et al. Screening the newborn for developmental dysplasia of the hip: now what do we do? J Pediatr Orthop. 2007;27(6):607-610.
3. Mulpuri K, Song KM, Goldberg MJ, Sevarino K. Detection and nonoperative management of pediatric developmental dysplasia of the hip in infants up to six months of age. J Am Acad Orthop Surg. 2015;23(3):202-205.
4. Thomas SRYW. A review of long-term outcomes for late presenting developmental hip dysplasia. Bone Joint J. 2015;97-B(6):729-733.
5. Loder RT, Skopelja EN. The epidemiology and demographics of hip dysplasia. ISRN Orthop. 2011;2011:238607.
6. US Preventive Services Task Force. Screening for developmental dysplasia of the hip: recommendation statement. Pediatrics. 2006;117(3):898-902.
7. Shorter D, Hong T, Osborn DA. Screening programmes for developmental dysplasia of the hip in newborn infants. Cochrane Database Syst Rev. 2011;(9):CD004595.
8. Loder RT, Shafer C. The demographics of developmental hip dysplasia in the Midwestern United States (Indiana). J Child Orthop. 2015;9(1):93-98.
9. Paton RW, Hinduja K, Thomas CD. The significance of at-risk factors in ultrasound surveillance of developmental dysplasia of the hip: a ten-year prospective study. J Bone Joint Surg Br. 2005;87(9):1264-1266.
10. Alsaleem M, Set KK, Saadeh L. Developmental dysplasia of hip: a review. Clin Pediatr (Phila). 2015;54(10):921-928.
11. Chan A, McCaul KA, Cundy PJ, et al. Perinatal risk factors for developmental dysplasia of the hip. Arch Dis Child. 1997;76(2):F94-F100.
12. Godley DR. Assessment, diagnosis, and treatment of developmental dysplasia of the hip. JAAPA. 2013;26(3):54-58.
13. Van Sleuwen BE, Engelberts AC, Boere-Boonekamp MM, et al. Swaddling: a systematic review. Pediatrics. 2007;120(4):e1097-e1106.
14. American Academy of Orthopaedic Surgeons, American Association of Orthopaedic Surgeons. Position statement: swaddling and developmental hip dysplasia. www.aaos.org/uploadedFiles/PreProduction/About/Opinion_Statements/position/1186%20Swaddling%20and%20Developmental%20Hip%20Dysplasia.pdf. Accessed January 22, 2016.
15. Clarke NM. Swaddling and hip dysplasia: an orthopaedic perspective. Arch Dis Child. 2014;99(1):5-6.
16. Storer SK, Skaggs DL. Developmental dysplasia of the hip. Am Fam Physician. 2006;74(8):1310-1316.
17. McAbee GN, Donn SM, Mendelson RA, et al. Medical diagnoses commonly associated with pediatric malpractice lawsuits in the United States. Pediatrics. 2008;122(6):e1282-e1286.
18. Imrie M, Scott V, Stearns P, et al. Is ultrasound screening for DDH in babies born breech sufficient? J Child Orthop. 2010;4(1):3-8.
19. Chen HW, Chang CH, Tsai ST, et al. Natural progression of hip dysplasia in newborns: a reflection of hip ultrasonographic screenings in newborn nurseries. J Pediatr Orthop B. 2010;19(5):418-423.
20. Gans I, Flynn JM, Sankar WN. Abduction bracing for residual acetabular dysplasia in infantile DDH. J Pediatr Orthop. 2013;33(7):714-718.
21. Murnaghan ML, Browne RH, Sucato DJ, Birch J. Femoral nerve palsy in Pavlik harness treatment for developmental dysplasia of the hip. J Bone Joint Surg Am. 2011;93(5):493-499.
22. Dezateux C, Rosendahl K. Developmental dysplasia of the hip. Lancet. 2007;369(9572):1541-1552.
Homelessness, HIV, and HCV
According to researchers from Columbia University in New York City, McMaster University in Hamilton, Ontario, Canada, and Ontario HIV Treatment Network, in Canada, homelessness and unstable housing situations are associated with higher rates of HIV and hepatitis C infection (HCV). They reviewed 152 studies involving 139,757 participants who had HIV or were co-infected with HCV. The researchers found “strong evidence” that the lack of stable, secure, adequate housing is a significant barrier to consistent and appropriate medical care, adherence to treatment, sustained viral suppression, and reduction of risk behaviors.
Research data showed that the worse the housing status, the less the engagement and utilization of HIV medical care. Homeless patients had more emergency department (ED) admissions; homeless males had longer hospital stays; and homeless injection-drug users were more often hospitalized than were people with HIV in high socioeconomic neighborhoods.
In another study, homelessness was significantly associated with baseline HCV-positive status. Twenty-five studies reported that homelessness or unstable housing was associated with significantly poorer outcomes on 1 or more indications of physical or mental health functioning and quality of life, mental health symptoms or diagnosis, or diagnosed physical health comorbidities, such as HCV and tuberculosis. The studies also showed the impact of having a home on both treatment and adherence to treatment. One study of co-infected patients who were on antiretroviral therapy (ART) or beginning HCV treatment found that good housing conditions reduced the risk of nonadherence to ART, regardless of the treatment of HCV. Stable housing also doubled the odds of ART use.
Data from another study also found participants with a fixed address were more likely to stop abusing drugs. Obtaining stable housing was also associated with using an outpatient setting rather than the ED as the usual source of care.
“Housing first” interventions are receiving growing attention, the researchers note, as a potential health care cost-containment strategy. As interventions for people with complex health conditions, changing housing status is “both possible and promising.”
Source:
Aidala AA, Wilson MG, Shubert V, et al. Am J Public Health. 2016;106(1):e1-e23
doi: 10.2105/AJPH.2015.302905.
According to researchers from Columbia University in New York City, McMaster University in Hamilton, Ontario, Canada, and Ontario HIV Treatment Network, in Canada, homelessness and unstable housing situations are associated with higher rates of HIV and hepatitis C infection (HCV). They reviewed 152 studies involving 139,757 participants who had HIV or were co-infected with HCV. The researchers found “strong evidence” that the lack of stable, secure, adequate housing is a significant barrier to consistent and appropriate medical care, adherence to treatment, sustained viral suppression, and reduction of risk behaviors.
Research data showed that the worse the housing status, the less the engagement and utilization of HIV medical care. Homeless patients had more emergency department (ED) admissions; homeless males had longer hospital stays; and homeless injection-drug users were more often hospitalized than were people with HIV in high socioeconomic neighborhoods.
In another study, homelessness was significantly associated with baseline HCV-positive status. Twenty-five studies reported that homelessness or unstable housing was associated with significantly poorer outcomes on 1 or more indications of physical or mental health functioning and quality of life, mental health symptoms or diagnosis, or diagnosed physical health comorbidities, such as HCV and tuberculosis. The studies also showed the impact of having a home on both treatment and adherence to treatment. One study of co-infected patients who were on antiretroviral therapy (ART) or beginning HCV treatment found that good housing conditions reduced the risk of nonadherence to ART, regardless of the treatment of HCV. Stable housing also doubled the odds of ART use.
Data from another study also found participants with a fixed address were more likely to stop abusing drugs. Obtaining stable housing was also associated with using an outpatient setting rather than the ED as the usual source of care.
“Housing first” interventions are receiving growing attention, the researchers note, as a potential health care cost-containment strategy. As interventions for people with complex health conditions, changing housing status is “both possible and promising.”
Source:
Aidala AA, Wilson MG, Shubert V, et al. Am J Public Health. 2016;106(1):e1-e23
doi: 10.2105/AJPH.2015.302905.
According to researchers from Columbia University in New York City, McMaster University in Hamilton, Ontario, Canada, and Ontario HIV Treatment Network, in Canada, homelessness and unstable housing situations are associated with higher rates of HIV and hepatitis C infection (HCV). They reviewed 152 studies involving 139,757 participants who had HIV or were co-infected with HCV. The researchers found “strong evidence” that the lack of stable, secure, adequate housing is a significant barrier to consistent and appropriate medical care, adherence to treatment, sustained viral suppression, and reduction of risk behaviors.
Research data showed that the worse the housing status, the less the engagement and utilization of HIV medical care. Homeless patients had more emergency department (ED) admissions; homeless males had longer hospital stays; and homeless injection-drug users were more often hospitalized than were people with HIV in high socioeconomic neighborhoods.
In another study, homelessness was significantly associated with baseline HCV-positive status. Twenty-five studies reported that homelessness or unstable housing was associated with significantly poorer outcomes on 1 or more indications of physical or mental health functioning and quality of life, mental health symptoms or diagnosis, or diagnosed physical health comorbidities, such as HCV and tuberculosis. The studies also showed the impact of having a home on both treatment and adherence to treatment. One study of co-infected patients who were on antiretroviral therapy (ART) or beginning HCV treatment found that good housing conditions reduced the risk of nonadherence to ART, regardless of the treatment of HCV. Stable housing also doubled the odds of ART use.
Data from another study also found participants with a fixed address were more likely to stop abusing drugs. Obtaining stable housing was also associated with using an outpatient setting rather than the ED as the usual source of care.
“Housing first” interventions are receiving growing attention, the researchers note, as a potential health care cost-containment strategy. As interventions for people with complex health conditions, changing housing status is “both possible and promising.”
Source:
Aidala AA, Wilson MG, Shubert V, et al. Am J Public Health. 2016;106(1):e1-e23
doi: 10.2105/AJPH.2015.302905.
Excessive Bleeding After Cardiac Surgery
Cardiac surgery patients have a high risk of excessive postoperative bleeding as a consequence of procoagulant blood products, vasoconstrictors, and poor organ perfusion. Researchers who conducted a study at University Hospital in São Paulo, Brazil, say that for clinicians to be prepared for timely interventions, it helps to know which patients to watch and when to identify the risk factors.
In their prospective study of 323 patients, episodes of excessive bleeding were concentrated in the first and second postoperative hours, and 21% of complications required interventions, such as vasoactive medication titration, protamine supplementation, and transfusions of blood products. During the immediate postoperative time, 105 patients developed excessive bleeding with 39 in the first hour, followed by 36 patients in the second hour, and 8 in the third hour.
The researchers found that other risk factors for excessive bleeding were chronic hypertension, greater height, body mass index (BMI) < 26.35 kg/m2, higher hematocrit, and intraoperative heparin dose > 312.5 mg without subsequent platelet transfusion. The researchers say platelet transfusions may have been protective. Certain variables, such as lower BMI and male gender, may have been explained by greater clot strength and faster rate of fibrin formation in women.
Patients at risk for excessive bleeding also had lower preoperative platelet count, although the mean value was within the normal range. But given that more than half the study group used aspirin and 11% used an adenosine diphosphate-receptor blocker, the researchers say they may have had a higher prevalence of unknown platelet dysfunctions.
Source:
Lopes CT, Brunori EFR, Cavalcante AMRZ, et al. Heart Lung. 2016;45(1):64-69.e2.
doi: 10.1016/j.hrtlng.2015.09.
Cardiac surgery patients have a high risk of excessive postoperative bleeding as a consequence of procoagulant blood products, vasoconstrictors, and poor organ perfusion. Researchers who conducted a study at University Hospital in São Paulo, Brazil, say that for clinicians to be prepared for timely interventions, it helps to know which patients to watch and when to identify the risk factors.
In their prospective study of 323 patients, episodes of excessive bleeding were concentrated in the first and second postoperative hours, and 21% of complications required interventions, such as vasoactive medication titration, protamine supplementation, and transfusions of blood products. During the immediate postoperative time, 105 patients developed excessive bleeding with 39 in the first hour, followed by 36 patients in the second hour, and 8 in the third hour.
The researchers found that other risk factors for excessive bleeding were chronic hypertension, greater height, body mass index (BMI) < 26.35 kg/m2, higher hematocrit, and intraoperative heparin dose > 312.5 mg without subsequent platelet transfusion. The researchers say platelet transfusions may have been protective. Certain variables, such as lower BMI and male gender, may have been explained by greater clot strength and faster rate of fibrin formation in women.
Patients at risk for excessive bleeding also had lower preoperative platelet count, although the mean value was within the normal range. But given that more than half the study group used aspirin and 11% used an adenosine diphosphate-receptor blocker, the researchers say they may have had a higher prevalence of unknown platelet dysfunctions.
Source:
Lopes CT, Brunori EFR, Cavalcante AMRZ, et al. Heart Lung. 2016;45(1):64-69.e2.
doi: 10.1016/j.hrtlng.2015.09.
Cardiac surgery patients have a high risk of excessive postoperative bleeding as a consequence of procoagulant blood products, vasoconstrictors, and poor organ perfusion. Researchers who conducted a study at University Hospital in São Paulo, Brazil, say that for clinicians to be prepared for timely interventions, it helps to know which patients to watch and when to identify the risk factors.
In their prospective study of 323 patients, episodes of excessive bleeding were concentrated in the first and second postoperative hours, and 21% of complications required interventions, such as vasoactive medication titration, protamine supplementation, and transfusions of blood products. During the immediate postoperative time, 105 patients developed excessive bleeding with 39 in the first hour, followed by 36 patients in the second hour, and 8 in the third hour.
The researchers found that other risk factors for excessive bleeding were chronic hypertension, greater height, body mass index (BMI) < 26.35 kg/m2, higher hematocrit, and intraoperative heparin dose > 312.5 mg without subsequent platelet transfusion. The researchers say platelet transfusions may have been protective. Certain variables, such as lower BMI and male gender, may have been explained by greater clot strength and faster rate of fibrin formation in women.
Patients at risk for excessive bleeding also had lower preoperative platelet count, although the mean value was within the normal range. But given that more than half the study group used aspirin and 11% used an adenosine diphosphate-receptor blocker, the researchers say they may have had a higher prevalence of unknown platelet dysfunctions.
Source:
Lopes CT, Brunori EFR, Cavalcante AMRZ, et al. Heart Lung. 2016;45(1):64-69.e2.
doi: 10.1016/j.hrtlng.2015.09.
How to Make Your Patient With Sleep Apnea a Super User of Positive Airway Pressure Therapy
Adherence to positive airway pressure (PAP) therapy is a difficult patient management issue. Clinicians at the John D. Dingell VA Medical Center in Detroit (VAMC Detroit) developed the O’Brien criteria and extensive patient education materials to increase patient adherence. The importance of PAP therapy and the reasons veterans should sleep with a PAP machine for 7 to 9 hours each night are stressed (many sleep only 4 to 5 hours). Several recent studies have confirmed widely varying PAP therapy adherence rates (30%-84%).1-13 A majority of patients indicated that mask discomfort is the primary reason for nonadherence.1
Adherence is affected by many factors, including heated humidity, patient education, mask type, and type of PAP machine (eg, continuous PAP [CPAP] vs bilevel PAP [BPAP]; auto-PAP vs CPAP). Other factors, such as race and economic status, also affect adherence.14 The Wisconsin Sleep Cohort Study found that patients with moderate-to-severe untreated obstructive sleep apnea (OSA) were 4 to 5 times more likely to die of a cardiovascular event and 3 times more likely to die of any cause.15 The morbidity and mortality associated with severe untreated OSA led the clinicians to intensify treatment efforts.16In this article, the authors summarize the initiative at the VAMC Detroit to enhance PAP therapy adherence in patients with sleep apnea. The goal was to motivate patients to maximize PAP machine use. This article is a guide that federal health care providers and their civilian counterparts in the private sector can use to maximize PAP machine use. Working toward that goal, a set of PAP “super user” criteria was developed and used to create a 5-point method for encouraging patients to maximize adherence to PAP therapy.
Background
Positive airway pressure is the room air pressure, measured in centimeters of H2O, which splints open the airway to prevent snoring, apneas, and hypopneas. An apnea is a 90%-plus airway obstruction that lasts longer than 10 seconds and is seen with sleep study polysomnography. A hypopnea is a 30%-plus airway obstruction that lasts longer than 10 seconds and is accompanied by a 3% drop in pulse oximetry (SpO2).
A CPAP device delivers pressure continuously through a medical air compressor or flow generator called a PAP machine. The BPAP machine has separate inspiratory pressure and expiratory pressure. Auto-PAP machines give minimum pressure and maximum pressure usually between the range of 4 cm H2O to 20 cm H2O. This machine finds the user’s median pressure (90th percentile) and maximum pressure and averages pressure over a specified period of use. The auto-PAP can then be set to CPAP mode and the pressure fixed or set to the 90th percentile.
O’Brien Criteria
The O’Brien criteria for PAP super-user status (Table 1) were developed for maximizing PAP machine use and presented at the 2013 John D. Dingell Sleep and Wake Disorders Center Symposium. There is no other published reference or criteria proposed for maximizing PAP machine adherence. A recent study on sleep time criteria suggested that a higher percentage of patients achieved normal functioning with longer duration nightly CPAP therapy, which is in line with the authors’ recommended PAP machine use duration.17
Positive airway pressure therapy is eligible for insurance reimbursement by Medicare and third-party payers for adult patients who have OSA and achieve 4 hours of nightly use for 70% of nights over 30 days. Coverage for CPAP therapy is initially limited to 12 weeks during which beneficiaries with an OSA diagnosis can be identified and any therapy benefits documented. Subsequent CPAP therapy is covered only for those OSA patients who benefit during the 12-week period.18At VAMC Detroit, the data covering the previous 30 days of use is downloaded. Medicare allows for the best 30-day period out of the 12-week window. The hospital, along with Harper Hospital and the Detroit Medical Centers in conjunction with the Wayne State University sleep program, is an Academic Center of Distinction, which follows the sleep guidelines and practice parameters for Medicare, third-party insurance companies, and the American Academy of Sleep Medicine.
The sleep clinic clinicians follow the clinical guidelines for evaluation, management, and long-term care of adults with OSA.19,20 Follow-up visits are scheduled and made on a consultation basis up to 90 days for the required download or as necessary for PAP therapy. In this initiative, practitioners offer veteran-specific patient care with PAP therapy that exceeds Medicare guidelines. The success of this process yielded a growing cohort of PAP super users at VAMC Detroit. These patients exceed the Medicare criterion of 4 hours of nightly use for 70% of nights over 30 days. Thus, 4 hours of nightly use for 100% of nights over the same period was proposed as another criterion.
The super-user criteria, which provide motivation to reach the top, stimulate many patients to achieve the Medicare criteria. All 5 criteria must be satisfied to attain super-user status, and becoming a super user is not easy. In fact, the expectation is that, if an adherence data study is conducted, it will show that only a small percentage of all users meet the criteria. Maximum adherence is expected to be the tail (3%-4%) of a bell-shaped curve.
PAP Super-User Status
At the initial evaluation, practitioners create a self-fulfilling prophecy that, as first described by Merton, sets expectations.21 A self-fulfilling prophecy is a prediction that directly or indirectly causes the prediction to become true as a result of the positive feedback between belief and behavior.21 The personnel at VAMC Detroit sleep clinic set a tone that enables patients to meet and exceed the Medicare sleep guidelines and their expectations. Patients are encouraged to make it their personal mission to achieve the goal of becoming a PAP super user. The patients receive the O’Brien criteria for PAP super-user status—guidelines thought to contribute to higher quality of life.
The Medicare criterion emphasized is the minimum required for full adherence. The goal is to reduce sleepiness and increase well-being. The literature shows that increasing duration of sleep results in lower daytime sleepiness.22 Inadequate sleep has many detrimental effects. According to a recent study, insufficient sleep contributes to weight gain.22 Desired patient outcomes are increased sleep time without arousals, increased slow-wave sleep (SWS), consolidation of memories and rapid eye movement (REM), and improvement in emotional and procedural skill memories.23 Patients are informed that using a PAP machine for 7 to 9 hours can reduce excessive daytime sleepiness and allow for more SWS and REM sleep, which help improve memory, judgment, and concentration. Many other studies have shown how 7 to 9 hours of sleep benefit adults. Thus, 7 to 9 hours became the criterion for maximizing PAP sleep time.
Initial Evaluation and Sleep Study
A primary care provider can enroll a patient into the clinic for a sleep study by requesting an evaluation. The consultation is then triaged using the STOP-BANG (Snoring, Tiredness, Observed apnea, high blood Pressure–Body mass index > 35, Age > 50, Neck circumference > 40 cm, Gender male) questionnaire. The STOP-BANG has a high sensitivity for predicting moderate-to-severe (87.0%) and severe (70.4%) sleep-disordered breathing.24 More than 3 affirmative answers indicate a high risk for sleep-disordered breathing and is cause for ordering a sleep study.
CPAP Group Class
Patients with a diagnosis of sleep apnea subsequently receive their CPAP machines when they attend a 2-hour group class taught by a respiratory therapist. Group education sessions increase the chance of issuing more machines and providing better education.25 One study found that “attendance in a group clinic designed to encourage compliance with CPAP therapy provided a simple and effective means of improving treatment of OSA.”25
In class, the respiratory therapist briefly assesses each patient’s CPAP prescription, describes the patient’s type of sleep apnea and final diagnosis, and reviews the CPAP machine’s features. Veterans are then instructed to take their CPAP machines home to use all night, every night for 4 weeks. All night is defined as a period of 7.5 to 8 hours, as population-based study results have shown that sleep of this duration is associated with lowest cardiovascular morbidity and mortality. After the initial 4-plus weeks of machine use, patients with all their CPAP equipment are seen in the sleep clinic.
First Sleep Clinic Follow-Up Visit
At first follow-up, patients are asked for a subjective evaluation of their sleep. Most state they are “better” with PAP therapy. Each patient’s mask is checked and refitted with the patient’s prescribed pressure.
Patients are informed of their PAP settings and requirements from the sleep study and told their particular “magic pressure.” Patients understand that a person’s magic pressure, determined in the laboratory, is the pressure of room air blown into the nose, mouth, or both that eliminates not only snoring, but also partial and complete airway obstructions (hypopneas, apneas). Patients are asked to remember their particular magic pressure and their AHI and told their OSA status (mild, moderate, or severe) as assessed by the laboratory study.26 Extensive education on sleep apnea and treatment are also addressed. Education and training are among the most important tenets of PAP therapy, and these are incorporated into all encounters.25,26
PAP Data Report and Leak
The CPAP data are downloaded and printed. If adherence is suboptimal, clinician and patient discuss increasing adherence and possibly becoming a super user. The patient receives a copy of the report, which can be compared with the patient’s adherence statistics and with the adherence statistics of similar patients who are super users. A few blacked-out names are posted on the board in front of the provider’s computer station. Patients can thus easily see that attaining super-user status is very difficult but possible. Some patients maximize their therapy and are designated PAP super users. These patients are proud to receive this designation, and they strive to keep it.
Data downloads are crucial for adherence. In a recent study, the American Thoracic Society stated, “Providers need to be able to interpret adherence systems.”27
The clinic provides a summary report on each patient’s adherence. A provider interpretation is added, and the report is copied into the Computer Patient Record System.
After the report is downloaded, the provider checks for correct pressure and then for a large leak. A large leak is an unintentional leak (the total amount that leaks but not including leak from the mask) > 5% of the night. A leak of > 15 minutes was added to the super-user criteria, because some software provides the average time of a large leak per day in minutes.28 Many veterans sleep only 4 to 5 hours nightly (300 minutes × 5% = 15 minutes). Therefore, the leak should not be more than 5% or 15 minutes for a veteran sleeping 5 hours.
The machine indicates a percentage of leak on the patient self-check LED screen for adherence. There is no standardized leak criterion used by all flow-generator manufacturers. Every mask has venting designed to leak intentionally so that the patient does not rebreathe air CO2. The main concern is unintentional leaks above the intentional leak or venting threshold.
The ResMed CPAP (ResMed Corp, San Diego, CA) maximum intentional leak is 24 L/min.29 Above that level is large leak. The exact leak amount varies by interface (mask) based on pressure and mask type.2,12
The larger the interface surface area, the larger the leak. Unintentional leak is higher with the full-face mask than with the nasal mask, most likely because there is more opportunity for leakage with the larger surface area of the full-face mask. Nasal pillows seem to leak less because of their smaller surface area, but more studies on mask interfaces are needed to validate this finding.
Chin Strap
Adding a chin strap improved patient adherence, nightly duration of use, residual AHI, and leak in patients with sleep apnea.30 Other investigators reported reduced OSA, confirmed by polysomnography and nasopharyngolaryngoscopy, with use of only a chin strap.31 When a nasal mask with chin strap is used, the strap should be made to fit properly over the chin, not on the throat. Properly used chin straps significantly reduce leakage and residual AHI.30
A chin strap most likely reduces large leak and dry mouth.30 Dry mouth can result from mouth leak, which is commonly caused by nasal congestion or high pressure and mouth breathing. The nasal turbinates help humidify, warm, and cool the air. Heated humidification of PAP can help prevent dry mouth.
Asking the Right Questions
The clinician should ask several key questions at the first follow-up: How is it going with your PAP machine? Do you feel PAP therapy is helping you sleep? Do you feel better with PAP therapy? To a patient who states he or she is not doing well with therapy, the clinician should ask, What type of problems are you having? In many cases, poor adherence is attributable to a large leak from a poorly fitting mask. A large leak can also increase residual AHI and cause frequent arousals.30
Some machines cannot maintain the pressure of a large leak and will shut off and trigger an alarm that wakes the patient to readjust the mask. This situation causes some patients to discontinue CPAP/BPAP use. The mask leak must be adjusted. Another common complaint is morning dry mouth. This extreme dryness—a significant clue pointing to mouth leak caused in part by the mouth dropping open during sleep with PAP—should be addressed by fitting the patient with a chin strap.30 Dry mouth also can be caused by low humidity; increasing the humidity setting usually resolves the problem. However, as one study found, use of controlled heated humidification did not improve adherence or quality of life.32 In the same study, the nasopharyngeal dryness that resulted from CPAP therapy without humidification was reduced immediately and during the first weeks of treatment.All current PAP machines feature heated humidification.
Mouth breathing can also result from nasal congestion, allergic or vasomotor rhinitis, nasal turbinate hypertrophy, obstruction from a deviated septum, polyps, or air hunger/insufficient PAP pressure. Chronic rhinosinusitis is a problem that affects up to 12.5% of the U.S. population.33
Adherence is also increased with the elimination of leak and associated arousals. Patients are shown how to use their PAP machine’s heated humidity settings to obtain desired comfort levels. The clinician explains that the nasal turbinates heat and cool the air and that they can become swollen and irritated with PAP therapy. A heated hose may be prescribed to provide optimal humidification without condensation or water dripping into the hose (rainout).
A full-face mask is used only when the patient cannot breathe out the nose adequately or when PAP becomes too high. A 2013 study found no significant differences among ResMed, Respironics, and Fisher & Paykel CPAP interfaces (Fisher & Paykel Healthcare, Irvine, CA).34 The clinician determines which mask is comfortable for a patient and tries to stay with that mask for that patient.
Adherence Report
A therapy data summary is downloaded and reviewed with the patient.28 A pattern of use report that shows daily use with times over the month is also reviewed.28 The software’s sleep therapy long-term trend report lists important statistics. The adherence data summary and the CPAP summary are also reviewed (Table 2).28 This page is printed and given to patients to reieiw their progress. For some it represents a reward for using the CPAP/BPAP machine as well as a congratulatory note.
In the Example 1 summary download (Table 2), a patient used a PAP machine 4 hours or more on 93.3% of the 30 days the machine was used.28 Residual AHI was low, 2.1, and there was no appreciable leak. The PAP of 11.2 cm H2O was in the 90th percentile. The patient was fixed to 12 cm H2O with expiratory pressure relief (EPR) of 1. The EPR is a comfort feature that reduces pressure from 1 cm H2O to 3 cm H2O to make it easier for the patient to exhale. (A flow generator that produces EPR of > 3 cm H2O is a BPAP machine.)
This patient was not a super user. Overall use was low—5 hours, 28 minutes—which could indicate behaviorally insufficient sleep syndrome. Sleep time is controversial, but the National Sleep Foundation recommends 7 to 9 hours of sleep per night.
A different patient used a PAP machine 4 hours or more on 100% (28/28) of the days when the machine was used (Table 3).29 Residual AHI was low (0.6), median use was 8 hours, 47 minutes, and there was no appreciable leak. The patient was using autoset mode with a minimum pressure of 13 cm H2O and maximum pressure of 18 cm H2O. The 95th percentile pressure was 13.6 cm H2O. The patient’s pressure was changed to 14 cm H2O with EPR of 3. This patient was a super user.
Sleep Hygiene Discussion
Providers must discuss sleep hygiene (good sleep habits) with veterans. If needed, AASM pamphlets on sleep hygiene and other educational materials can be provided. The bedroom should be cool, comfortable, quiet, and dark and should not include a television or computer. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration and tells the brain it is time to wake up.34
Patients are asked about the number of arousals they have per night. At first follow-up, providers must determine what is causing a patient to arouse while on CPAP/BPAP therapy. Some causes are air leak resulting in unresolved OSA, nocturia (may be triggered by unresolved OSA), dry mouth (indicating need for chin strap), nightmares (suggestive of unresolved OSA in REM sleep), posttraumatic stress disorder (PTSD), environmental noise, and claustrophobia. The provider should have thought-out answers to these problems in advance.
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS) is administered as part of the baseline comprehensive examination and at every sleep clinic follow-up after issuing a CPAP/BPAP machine.35 The first evaluation after the machine is issued should show a reduction in ESS. No reduction in ESS indicates that a problem needs to be addressed. The most common reason for insufficient reduction in ESS is suboptimal PAP therapy adherence, usually because of a large leak. Some cases of poor adherence may be attributable to restless legs syndrome, periodic limb movement disorder, chronic musculoskeletal pain, and sleep fragmentation caused by alcohol, smoking, caffeine, or cocaine. Excessive daytime sleepiness may persist from use of pain medications or other sedating medications. One study found a correlation between sleep duration with CPAP therapy and reduction in ESS.36 In addition to administering the ESS, patients are asked how they doing with PAP therapy, and the answer is documented. Treatment changes are made if needed to reduce excessive daytime sleepiness.
Ear-Nose-Throat Examination
A quick look into the nose with a nasal speculum is a crucial component of a thorough examination. The clinician looks for a deviated septum, swollen turbinates, obstruction, polyps, bleeding, infection, septal perforation, and discharge. In addition, the patient is checked for airflow amount, nasal congestion, and obstruction; if necessary a nasal steroid spray or a nasal saline spray is prescribed. In some cases, saline spray can be added to the steroid spray to help reduce or eliminate nasal congestion.37
Treatment of congestion requires education, as many patients improperly use these sprays. The steroid spray is not an instant vasoconstrictor; a week of regular use is needed to reduce inflammation and congestion. Saline spray and saline irrigation can be used as a treatment adjunct for symptoms of chronic rhinosinusitis.37If the steroid and saline sprays fail after a 2-month trial, consider an ear-nose-throat (ENT) consultation. A recent study found that adherence rates increased after septoplasty in patients with nasal obstruction.38 The throat is examined for macroglossia or scalloping of the tongue.39 Macroglossic Mallampati IV tongues are platterlike. They are big, long, and wide and often have impressions or scalloping along the outside from a molding of the teeth. The patient is shown a Mallampati diagram and given a Mallampati score.
Creating a Sense of Mission
The sleep physician assistant (PA)at the Detroit VAMC is a retired U.S. Army colonel who ensures that the language the physician uses aligns with the language veterans use. Behavioral techniques are used to create a common culture that helps overcome obstacles—allowing patients to understand the benefits of and need for full CPAP/BPAP therapy adherence. One technique reinforces their sense of mission accomplishment, their military pride, and their interservice rivalry to increase adherence. The mission with each patient is to “work until success is achieved...but the patient can’t quit.” The mantra given to a patient with a difficult case is, “We will not let you fail with CPAP/BPAP therapy,” which echoes a familiar military motto, “We will not leave you behind.” Also, the goal of the physician is: Never give up on the patient.
Behavioral and Psychological Principles
The behavioral and psychological principles for success with PAP super users should be studied to validate better outcomes with longer duration PAP machine use. Patients who are motivated to succeed and to participate in their care can make great strides in changing their behavior to get more and better sleep. Obese patients can get referrals to the MOVE! weight loss program. Some veterans simply follow instructions, pay attention to detail, and do what they are told regarding sleep, PAP education, and good sleep hygiene. Many veterans have poor sleep hygiene and insomnia because they watch television or play games on electronic devices right before bedtime. Many patients develop behaviorally insufficient sleep syndrome. Their behavior prevents them from going to bed at a time that will allow sufficient sleep. Some veterans smoke or drink caffeinated beverages or al cohol immediately before sleep time and then wonder why they have insomnia.
Veterans with insomnia may be referred to the insomnia clinic psychologist for cognitive behavioral therapy for insomnia.40 Referral to this psychologist can be very helpful in the treatment of insomnia after the patient’s OSA has been treated. Veterans are encouraged to follow good sleep hygiene principles and permanently discontinue detrimental sleep behaviors.
For veterans with PTSD, imagery rehearsal before sleep has been effective in resolving disturbing nightmares and excluding their violent details.41 Clinicians recommend that these veterans rehearse a pleasant dream before sleep time. Cartwright and Lamberg performed extensive research on dreams and nightmares, and their book may provide insight into reducing nightmares for veterans with severe PTSD.42 Persistent nightmares associated with PTSD also can be reduced with use of prazosin. 43
Sleep Clinic Economics
The economic impact of OSA is substantial because of increased risk of cardiovascular disease and risk of motor vehicle accidents and decreased quality of life and productivity. Results of cost-effectiveness analyses support the value of diagnosing and treating OSA. Studies have provided estimates from a payer perspective, ranging from $2,000 to $11,000 per quality-adjusted life year over 5 years for treating moderate-to-severe OSA. The Sleep Heart Health Study showed that OSA was associated with an 18% increase in predicted health care utilization based on medication use.44,45 Moreover, CPAP therapy was found to be clinically more effective than no treatment: Therapy increased life expectancy in males and females, and effective treatment of OSA was associated with lower health care and disability costs and fewer missed workdays.
The authors’ initiatives to improve PAP therapy adherence required adding a PA and a registered respiratory therapist (RT) to the staff of 2 full-time equivalent (FTE) board-certified sleep physicians. The sleep physicians trained the PA to initiate and complete all the recommendations described, and the PA attended an AASM-sponsored review course for additional training. The PA is responsible for performing comprehensive face-to-face clinical evaluations in 4 half-day clinic sessions each week, as well as providing follow-up care in 4 additional half-day clinic sessions each week.
During these sessions, the PA provides education about sleep apnea and treatment. Thirty-minute follow-up clinic appointments are reserved for downloading CPAP data, providing interpretation, and educating patients to maximize PAP therapy and become super users. The remaining clinic sessions are run by 3 sleep fellows under the supervision of the sleep physicians. During all visits, providers encourage patients to maintain good sleep hygiene. Nonadherent patients are scheduled to be seen in a separate clinic session during which the RT troubleshoots and corrects PAP machine and mask-related problems.
Setting up the CPAP group classes and follow-up clinics required adding an FTE RT at a cost of $44,000 to $48,000 per year. By recruiting an FTE PA starting at GS-12 and $75,542 instead of another board-certified sleep physician, VAMC Detroit was able to provide increased access to patient care (8 clinics) at sizable financial savings (estimate, $75,000/y). A 0.5 FTE clinical psychologist provided cognitive behavioral therapy for insomnia and PAP therapy nonadherence and helped achieve the initiative’s goals.
The sleep center projects that the overall cost-effectiveness of these initiatives in terms of admission rates, life expectancy, and productivity would not be dissimilar to that reported in the peer-reviewed literature, as noted earlier. The center’s upcoming research projects will provide more data specific to its population. Educating patients requires that only motivated providers give patients instructions during a 30-minute follow-up clinic visit—there is no additional expense. This model of intensive care can be adopted at other VAMCs.
Conclusion
Maximizing PAP machine use is a unique approach that stimulates veterans to attain the highest level of adherence. This approach is based on clinical observation and patient encounters, and treatment recommendations over 8 years.
Showing enthusiasm with patients is crucial. Enthusiasm is contagious. Clinicians who are also PAP machine users should let patients know of their PAP super-user status and add that many others have attained this status, too. The benefits of optimal treatment are reviewed with patients: increased energy, lower risk of cardiovascular disease, lower blood pressure, better insulin sensitivity, and overall reduced mortality. Some patients have difficulty using the nasal mask and chin strap and understanding and adhering to PAP therapy. These impediments can be overcome with further education and follow-up. Sleep clinic clinicians take the time to show patients how to use the machine’s self-adherence check and leak functions. Patients can then monitor their progress daily.
To motivate patients, clinicians should set expectations early, invest time in providing education at follow-up; be diligent with respect to mask fitting and download evaluation. Sleep clinic providers should also speak the veterans’ language, create a self-fulfilling prophesy for success, and schedule a follow-up sleep clinic appointment if a patient is not fulfilling the Medicare adherence criterion of 4 hours’ nightly use for 70% of nights over 30 days.
PAP therapy coaching and persistent education with provider contact and enthusiasm can improve adherence. Encouragement and praise can help patients exceed Medicare’s minimum PAP therapy criterion and improve their overall PAP experience. The sleep team should tell patients they are proud of their accomplishments with such a difficult treatment. Being genuine and caring and showing concern about their evaluation, treatment, and follow-up is important. This helps reduce their OSA-related morbidity, lessen their depression, and improves their daily well-being and quality of life.
“The variation in responses to CPAP and acceptance of CPAP suggest that focused interventions, rather than one-size-fits-all interventions, may have a greater effect on the overall outcome of CPAP adherence,” wrote Weaver and Sawyer.46
Finally, one cannot equate spending on veteran care with spending in other areas of the national budget. The real cost of not giving veterans appropriate care will be a loss of trust, given that the overarching mission is “to care for him who shall have borne the battle and for his widow and his orphan.”
1. Boyaci H, Gacar K, Baris SA, Basyigit I, Yildiz F. Positive airway pressure device compliance of patients with obstructive sleep apnea syndrome. Adv Clin Exp Med. 2013;22(6):809-815.
2. Bachour A, Vitikainen P, Virkkula P, Maasilta P. CPAP interface: satisfaction and side effects. Sleep Breath. 2013;17(2):667-672.
3. Wimms AJ, Richards GN, Genjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath. 2013;17(1):69-76.
4. Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioral interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnea. Cochrane Database Syst Rev. 2009;(2):CD007736.
5. Beecroft J, Zanon S, Lukic D, Hanly P. Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest. 2003;124(6):2200-2208.
6. Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;(4):CD005308.
7. Nilius G, Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006;130(4):1018-1024.
8. Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med. 2007;3(7):706-712.
9. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435.
10. Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53(4):290-292.
11. Haniffa M, Lasserson TJ, Smith I. Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev. 2004;(4):CD003531.
12. Kushida CA, Berry RB, Blau, A, et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titration process on efficacy, adherence, and outcomes. Sleep. 2011;34(8):1083-1092.
13. Gentina T, Fortin F, Douay B, et al. Auto bi-level with pressure relief during exhalation as a rescue therapy for optimally treated obstructive sleep apnoea patients with poor compliance to continuous positive airways pressure therapy--a pilot study. Sleep Breath. 2011;15(1):21-27.
14. Billings, ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653-1658.
15. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31(8):1071-1078.
16. Centers for Disease Control and Prevention. Effect of short sleep duration on daily activities--United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60(8):239-242.
17. Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111-119.
18. Phurrough S, Jacques L, Spencer F, Stiller J, Brechner R. Coverage decision memorandum for continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) (CAG-00093R2). Centers for Medicare & Medicaid Services Website. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204&fromdb=true. Accessed February 5, 2016.
19. Epstein LJ, Kristo D, Strollo PJ Jr, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2009;5(3):263-276.
20. Berry RB, Chediak A, Brown LK, et al; NPPV Titration Task Force of the American Academy of Sleep Medicine. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491-509.
21. Merton RK. Social Theory and Social Structure. New York, NY: Free Press; 1968.
22. Chaput JP, McNeil J, Després JP, Bouchard C, Tremblay A. Seven to eight hours of sleep a night is associated with a lower prevalence of the metabolic syndrome and reduced overall cardiometabolic risk in adults. PLoS One. 2013;8(9):e72832.
23. Born J, Wagner U. Sleep, hormones, and memory. Obstet Gynecol Clin North Am. 2009;36(4):809-829, x.
24. Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7(5):467-472.
25. Soares Pires F, Drummond M, Marinho A, et al. Effectiveness of a group education session on adherence with APAP in obstructive sleep apnea--a randomized controlled study. Sleep Breath. 2013;17(3):993-1001.
26. Berry RB, Budhiraja R, Gottlieb DJ, et al; American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597-619.
27. Schwab RJ, Badr SM, Epstein LJ, et al; ATS Subcommittee on CPAP Adherence Tracking Systems. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188(5):613-620.
28. Respironics Encore Pro and Encore Pro 2 [computer program]. Philips, Inc; May 12, 2013.
29. ResMed. Version 04.01.013. San Diego, CA.
30. Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10(4):377-383.
31. Vorona RD, Ware JC, Sinacori JT, Ford ML 3rd, Cross JP. Treatment of severe obstructive sleep apnea syndrome with a chinstrap. J Clin Sleep Med. 2007;3(7):729-730.
32. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath. 2011;15(3):479-485.
33. Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011;128(4):693-707.
34. Gooley JJ, Chamberlain K, Smith KA, et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J Clin Endocrinol Metab. 2011;96(3):E463-E472.
35. Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540-545.
36. Bednarek M, Zgierska A, Pływaczewski R, Zielinski J. The effect of CPAP treatment on excessive daytime somnolence in patients with obstructive sleep apnea [in Polish]. Pneumonol Alergol Pol. 1999;67(5-6):237-244.
37. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
38. Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2014;124(1):317-319.
39. Law JA. From the journal archives: Mallampati in two millennia: its impact then and implications now. Can J Anaesth. 2014;61(5):480-484.
40. Hood HK, Rogojanski J, Moss TG. Cognitive-behavioral therapy for chronic insomnia. Curr Treat Options Neurol. 2014;16(12):321.
41. Harb GC, Thompson R, Ross RJ, Cook JM. Combat-related PTSD nightmares and imagery rehearsal: nightmare characteristics and relation to treatment outcome. J Trauma Stress. 2012;25(5):511-518.
42. Cartwright R, Lamberg L. Crisis Dreaming: Using Your Dreams to Solve Your Problems.. New York, NY: HarperCollins;1992.
43.Writer BW, Meyer EG, Schillerstrom JE. Prazosin for military combat-related PTSD nightmares: a critical review. J Neuropsychiatry Clin Neurosci. 2014;26(1):24-33.
44. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc. 2011;86(6):549-554.
45. Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749-755.
46. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245-258.
Adherence to positive airway pressure (PAP) therapy is a difficult patient management issue. Clinicians at the John D. Dingell VA Medical Center in Detroit (VAMC Detroit) developed the O’Brien criteria and extensive patient education materials to increase patient adherence. The importance of PAP therapy and the reasons veterans should sleep with a PAP machine for 7 to 9 hours each night are stressed (many sleep only 4 to 5 hours). Several recent studies have confirmed widely varying PAP therapy adherence rates (30%-84%).1-13 A majority of patients indicated that mask discomfort is the primary reason for nonadherence.1
Adherence is affected by many factors, including heated humidity, patient education, mask type, and type of PAP machine (eg, continuous PAP [CPAP] vs bilevel PAP [BPAP]; auto-PAP vs CPAP). Other factors, such as race and economic status, also affect adherence.14 The Wisconsin Sleep Cohort Study found that patients with moderate-to-severe untreated obstructive sleep apnea (OSA) were 4 to 5 times more likely to die of a cardiovascular event and 3 times more likely to die of any cause.15 The morbidity and mortality associated with severe untreated OSA led the clinicians to intensify treatment efforts.16In this article, the authors summarize the initiative at the VAMC Detroit to enhance PAP therapy adherence in patients with sleep apnea. The goal was to motivate patients to maximize PAP machine use. This article is a guide that federal health care providers and their civilian counterparts in the private sector can use to maximize PAP machine use. Working toward that goal, a set of PAP “super user” criteria was developed and used to create a 5-point method for encouraging patients to maximize adherence to PAP therapy.
Background
Positive airway pressure is the room air pressure, measured in centimeters of H2O, which splints open the airway to prevent snoring, apneas, and hypopneas. An apnea is a 90%-plus airway obstruction that lasts longer than 10 seconds and is seen with sleep study polysomnography. A hypopnea is a 30%-plus airway obstruction that lasts longer than 10 seconds and is accompanied by a 3% drop in pulse oximetry (SpO2).
A CPAP device delivers pressure continuously through a medical air compressor or flow generator called a PAP machine. The BPAP machine has separate inspiratory pressure and expiratory pressure. Auto-PAP machines give minimum pressure and maximum pressure usually between the range of 4 cm H2O to 20 cm H2O. This machine finds the user’s median pressure (90th percentile) and maximum pressure and averages pressure over a specified period of use. The auto-PAP can then be set to CPAP mode and the pressure fixed or set to the 90th percentile.
O’Brien Criteria
The O’Brien criteria for PAP super-user status (Table 1) were developed for maximizing PAP machine use and presented at the 2013 John D. Dingell Sleep and Wake Disorders Center Symposium. There is no other published reference or criteria proposed for maximizing PAP machine adherence. A recent study on sleep time criteria suggested that a higher percentage of patients achieved normal functioning with longer duration nightly CPAP therapy, which is in line with the authors’ recommended PAP machine use duration.17
Positive airway pressure therapy is eligible for insurance reimbursement by Medicare and third-party payers for adult patients who have OSA and achieve 4 hours of nightly use for 70% of nights over 30 days. Coverage for CPAP therapy is initially limited to 12 weeks during which beneficiaries with an OSA diagnosis can be identified and any therapy benefits documented. Subsequent CPAP therapy is covered only for those OSA patients who benefit during the 12-week period.18At VAMC Detroit, the data covering the previous 30 days of use is downloaded. Medicare allows for the best 30-day period out of the 12-week window. The hospital, along with Harper Hospital and the Detroit Medical Centers in conjunction with the Wayne State University sleep program, is an Academic Center of Distinction, which follows the sleep guidelines and practice parameters for Medicare, third-party insurance companies, and the American Academy of Sleep Medicine.
The sleep clinic clinicians follow the clinical guidelines for evaluation, management, and long-term care of adults with OSA.19,20 Follow-up visits are scheduled and made on a consultation basis up to 90 days for the required download or as necessary for PAP therapy. In this initiative, practitioners offer veteran-specific patient care with PAP therapy that exceeds Medicare guidelines. The success of this process yielded a growing cohort of PAP super users at VAMC Detroit. These patients exceed the Medicare criterion of 4 hours of nightly use for 70% of nights over 30 days. Thus, 4 hours of nightly use for 100% of nights over the same period was proposed as another criterion.
The super-user criteria, which provide motivation to reach the top, stimulate many patients to achieve the Medicare criteria. All 5 criteria must be satisfied to attain super-user status, and becoming a super user is not easy. In fact, the expectation is that, if an adherence data study is conducted, it will show that only a small percentage of all users meet the criteria. Maximum adherence is expected to be the tail (3%-4%) of a bell-shaped curve.
PAP Super-User Status
At the initial evaluation, practitioners create a self-fulfilling prophecy that, as first described by Merton, sets expectations.21 A self-fulfilling prophecy is a prediction that directly or indirectly causes the prediction to become true as a result of the positive feedback between belief and behavior.21 The personnel at VAMC Detroit sleep clinic set a tone that enables patients to meet and exceed the Medicare sleep guidelines and their expectations. Patients are encouraged to make it their personal mission to achieve the goal of becoming a PAP super user. The patients receive the O’Brien criteria for PAP super-user status—guidelines thought to contribute to higher quality of life.
The Medicare criterion emphasized is the minimum required for full adherence. The goal is to reduce sleepiness and increase well-being. The literature shows that increasing duration of sleep results in lower daytime sleepiness.22 Inadequate sleep has many detrimental effects. According to a recent study, insufficient sleep contributes to weight gain.22 Desired patient outcomes are increased sleep time without arousals, increased slow-wave sleep (SWS), consolidation of memories and rapid eye movement (REM), and improvement in emotional and procedural skill memories.23 Patients are informed that using a PAP machine for 7 to 9 hours can reduce excessive daytime sleepiness and allow for more SWS and REM sleep, which help improve memory, judgment, and concentration. Many other studies have shown how 7 to 9 hours of sleep benefit adults. Thus, 7 to 9 hours became the criterion for maximizing PAP sleep time.
Initial Evaluation and Sleep Study
A primary care provider can enroll a patient into the clinic for a sleep study by requesting an evaluation. The consultation is then triaged using the STOP-BANG (Snoring, Tiredness, Observed apnea, high blood Pressure–Body mass index > 35, Age > 50, Neck circumference > 40 cm, Gender male) questionnaire. The STOP-BANG has a high sensitivity for predicting moderate-to-severe (87.0%) and severe (70.4%) sleep-disordered breathing.24 More than 3 affirmative answers indicate a high risk for sleep-disordered breathing and is cause for ordering a sleep study.
CPAP Group Class
Patients with a diagnosis of sleep apnea subsequently receive their CPAP machines when they attend a 2-hour group class taught by a respiratory therapist. Group education sessions increase the chance of issuing more machines and providing better education.25 One study found that “attendance in a group clinic designed to encourage compliance with CPAP therapy provided a simple and effective means of improving treatment of OSA.”25
In class, the respiratory therapist briefly assesses each patient’s CPAP prescription, describes the patient’s type of sleep apnea and final diagnosis, and reviews the CPAP machine’s features. Veterans are then instructed to take their CPAP machines home to use all night, every night for 4 weeks. All night is defined as a period of 7.5 to 8 hours, as population-based study results have shown that sleep of this duration is associated with lowest cardiovascular morbidity and mortality. After the initial 4-plus weeks of machine use, patients with all their CPAP equipment are seen in the sleep clinic.
First Sleep Clinic Follow-Up Visit
At first follow-up, patients are asked for a subjective evaluation of their sleep. Most state they are “better” with PAP therapy. Each patient’s mask is checked and refitted with the patient’s prescribed pressure.
Patients are informed of their PAP settings and requirements from the sleep study and told their particular “magic pressure.” Patients understand that a person’s magic pressure, determined in the laboratory, is the pressure of room air blown into the nose, mouth, or both that eliminates not only snoring, but also partial and complete airway obstructions (hypopneas, apneas). Patients are asked to remember their particular magic pressure and their AHI and told their OSA status (mild, moderate, or severe) as assessed by the laboratory study.26 Extensive education on sleep apnea and treatment are also addressed. Education and training are among the most important tenets of PAP therapy, and these are incorporated into all encounters.25,26
PAP Data Report and Leak
The CPAP data are downloaded and printed. If adherence is suboptimal, clinician and patient discuss increasing adherence and possibly becoming a super user. The patient receives a copy of the report, which can be compared with the patient’s adherence statistics and with the adherence statistics of similar patients who are super users. A few blacked-out names are posted on the board in front of the provider’s computer station. Patients can thus easily see that attaining super-user status is very difficult but possible. Some patients maximize their therapy and are designated PAP super users. These patients are proud to receive this designation, and they strive to keep it.
Data downloads are crucial for adherence. In a recent study, the American Thoracic Society stated, “Providers need to be able to interpret adherence systems.”27
The clinic provides a summary report on each patient’s adherence. A provider interpretation is added, and the report is copied into the Computer Patient Record System.
After the report is downloaded, the provider checks for correct pressure and then for a large leak. A large leak is an unintentional leak (the total amount that leaks but not including leak from the mask) > 5% of the night. A leak of > 15 minutes was added to the super-user criteria, because some software provides the average time of a large leak per day in minutes.28 Many veterans sleep only 4 to 5 hours nightly (300 minutes × 5% = 15 minutes). Therefore, the leak should not be more than 5% or 15 minutes for a veteran sleeping 5 hours.
The machine indicates a percentage of leak on the patient self-check LED screen for adherence. There is no standardized leak criterion used by all flow-generator manufacturers. Every mask has venting designed to leak intentionally so that the patient does not rebreathe air CO2. The main concern is unintentional leaks above the intentional leak or venting threshold.
The ResMed CPAP (ResMed Corp, San Diego, CA) maximum intentional leak is 24 L/min.29 Above that level is large leak. The exact leak amount varies by interface (mask) based on pressure and mask type.2,12
The larger the interface surface area, the larger the leak. Unintentional leak is higher with the full-face mask than with the nasal mask, most likely because there is more opportunity for leakage with the larger surface area of the full-face mask. Nasal pillows seem to leak less because of their smaller surface area, but more studies on mask interfaces are needed to validate this finding.
Chin Strap
Adding a chin strap improved patient adherence, nightly duration of use, residual AHI, and leak in patients with sleep apnea.30 Other investigators reported reduced OSA, confirmed by polysomnography and nasopharyngolaryngoscopy, with use of only a chin strap.31 When a nasal mask with chin strap is used, the strap should be made to fit properly over the chin, not on the throat. Properly used chin straps significantly reduce leakage and residual AHI.30
A chin strap most likely reduces large leak and dry mouth.30 Dry mouth can result from mouth leak, which is commonly caused by nasal congestion or high pressure and mouth breathing. The nasal turbinates help humidify, warm, and cool the air. Heated humidification of PAP can help prevent dry mouth.
Asking the Right Questions
The clinician should ask several key questions at the first follow-up: How is it going with your PAP machine? Do you feel PAP therapy is helping you sleep? Do you feel better with PAP therapy? To a patient who states he or she is not doing well with therapy, the clinician should ask, What type of problems are you having? In many cases, poor adherence is attributable to a large leak from a poorly fitting mask. A large leak can also increase residual AHI and cause frequent arousals.30
Some machines cannot maintain the pressure of a large leak and will shut off and trigger an alarm that wakes the patient to readjust the mask. This situation causes some patients to discontinue CPAP/BPAP use. The mask leak must be adjusted. Another common complaint is morning dry mouth. This extreme dryness—a significant clue pointing to mouth leak caused in part by the mouth dropping open during sleep with PAP—should be addressed by fitting the patient with a chin strap.30 Dry mouth also can be caused by low humidity; increasing the humidity setting usually resolves the problem. However, as one study found, use of controlled heated humidification did not improve adherence or quality of life.32 In the same study, the nasopharyngeal dryness that resulted from CPAP therapy without humidification was reduced immediately and during the first weeks of treatment.All current PAP machines feature heated humidification.
Mouth breathing can also result from nasal congestion, allergic or vasomotor rhinitis, nasal turbinate hypertrophy, obstruction from a deviated septum, polyps, or air hunger/insufficient PAP pressure. Chronic rhinosinusitis is a problem that affects up to 12.5% of the U.S. population.33
Adherence is also increased with the elimination of leak and associated arousals. Patients are shown how to use their PAP machine’s heated humidity settings to obtain desired comfort levels. The clinician explains that the nasal turbinates heat and cool the air and that they can become swollen and irritated with PAP therapy. A heated hose may be prescribed to provide optimal humidification without condensation or water dripping into the hose (rainout).
A full-face mask is used only when the patient cannot breathe out the nose adequately or when PAP becomes too high. A 2013 study found no significant differences among ResMed, Respironics, and Fisher & Paykel CPAP interfaces (Fisher & Paykel Healthcare, Irvine, CA).34 The clinician determines which mask is comfortable for a patient and tries to stay with that mask for that patient.
Adherence Report
A therapy data summary is downloaded and reviewed with the patient.28 A pattern of use report that shows daily use with times over the month is also reviewed.28 The software’s sleep therapy long-term trend report lists important statistics. The adherence data summary and the CPAP summary are also reviewed (Table 2).28 This page is printed and given to patients to reieiw their progress. For some it represents a reward for using the CPAP/BPAP machine as well as a congratulatory note.
In the Example 1 summary download (Table 2), a patient used a PAP machine 4 hours or more on 93.3% of the 30 days the machine was used.28 Residual AHI was low, 2.1, and there was no appreciable leak. The PAP of 11.2 cm H2O was in the 90th percentile. The patient was fixed to 12 cm H2O with expiratory pressure relief (EPR) of 1. The EPR is a comfort feature that reduces pressure from 1 cm H2O to 3 cm H2O to make it easier for the patient to exhale. (A flow generator that produces EPR of > 3 cm H2O is a BPAP machine.)
This patient was not a super user. Overall use was low—5 hours, 28 minutes—which could indicate behaviorally insufficient sleep syndrome. Sleep time is controversial, but the National Sleep Foundation recommends 7 to 9 hours of sleep per night.
A different patient used a PAP machine 4 hours or more on 100% (28/28) of the days when the machine was used (Table 3).29 Residual AHI was low (0.6), median use was 8 hours, 47 minutes, and there was no appreciable leak. The patient was using autoset mode with a minimum pressure of 13 cm H2O and maximum pressure of 18 cm H2O. The 95th percentile pressure was 13.6 cm H2O. The patient’s pressure was changed to 14 cm H2O with EPR of 3. This patient was a super user.
Sleep Hygiene Discussion
Providers must discuss sleep hygiene (good sleep habits) with veterans. If needed, AASM pamphlets on sleep hygiene and other educational materials can be provided. The bedroom should be cool, comfortable, quiet, and dark and should not include a television or computer. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration and tells the brain it is time to wake up.34
Patients are asked about the number of arousals they have per night. At first follow-up, providers must determine what is causing a patient to arouse while on CPAP/BPAP therapy. Some causes are air leak resulting in unresolved OSA, nocturia (may be triggered by unresolved OSA), dry mouth (indicating need for chin strap), nightmares (suggestive of unresolved OSA in REM sleep), posttraumatic stress disorder (PTSD), environmental noise, and claustrophobia. The provider should have thought-out answers to these problems in advance.
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS) is administered as part of the baseline comprehensive examination and at every sleep clinic follow-up after issuing a CPAP/BPAP machine.35 The first evaluation after the machine is issued should show a reduction in ESS. No reduction in ESS indicates that a problem needs to be addressed. The most common reason for insufficient reduction in ESS is suboptimal PAP therapy adherence, usually because of a large leak. Some cases of poor adherence may be attributable to restless legs syndrome, periodic limb movement disorder, chronic musculoskeletal pain, and sleep fragmentation caused by alcohol, smoking, caffeine, or cocaine. Excessive daytime sleepiness may persist from use of pain medications or other sedating medications. One study found a correlation between sleep duration with CPAP therapy and reduction in ESS.36 In addition to administering the ESS, patients are asked how they doing with PAP therapy, and the answer is documented. Treatment changes are made if needed to reduce excessive daytime sleepiness.
Ear-Nose-Throat Examination
A quick look into the nose with a nasal speculum is a crucial component of a thorough examination. The clinician looks for a deviated septum, swollen turbinates, obstruction, polyps, bleeding, infection, septal perforation, and discharge. In addition, the patient is checked for airflow amount, nasal congestion, and obstruction; if necessary a nasal steroid spray or a nasal saline spray is prescribed. In some cases, saline spray can be added to the steroid spray to help reduce or eliminate nasal congestion.37
Treatment of congestion requires education, as many patients improperly use these sprays. The steroid spray is not an instant vasoconstrictor; a week of regular use is needed to reduce inflammation and congestion. Saline spray and saline irrigation can be used as a treatment adjunct for symptoms of chronic rhinosinusitis.37If the steroid and saline sprays fail after a 2-month trial, consider an ear-nose-throat (ENT) consultation. A recent study found that adherence rates increased after septoplasty in patients with nasal obstruction.38 The throat is examined for macroglossia or scalloping of the tongue.39 Macroglossic Mallampati IV tongues are platterlike. They are big, long, and wide and often have impressions or scalloping along the outside from a molding of the teeth. The patient is shown a Mallampati diagram and given a Mallampati score.
Creating a Sense of Mission
The sleep physician assistant (PA)at the Detroit VAMC is a retired U.S. Army colonel who ensures that the language the physician uses aligns with the language veterans use. Behavioral techniques are used to create a common culture that helps overcome obstacles—allowing patients to understand the benefits of and need for full CPAP/BPAP therapy adherence. One technique reinforces their sense of mission accomplishment, their military pride, and their interservice rivalry to increase adherence. The mission with each patient is to “work until success is achieved...but the patient can’t quit.” The mantra given to a patient with a difficult case is, “We will not let you fail with CPAP/BPAP therapy,” which echoes a familiar military motto, “We will not leave you behind.” Also, the goal of the physician is: Never give up on the patient.
Behavioral and Psychological Principles
The behavioral and psychological principles for success with PAP super users should be studied to validate better outcomes with longer duration PAP machine use. Patients who are motivated to succeed and to participate in their care can make great strides in changing their behavior to get more and better sleep. Obese patients can get referrals to the MOVE! weight loss program. Some veterans simply follow instructions, pay attention to detail, and do what they are told regarding sleep, PAP education, and good sleep hygiene. Many veterans have poor sleep hygiene and insomnia because they watch television or play games on electronic devices right before bedtime. Many patients develop behaviorally insufficient sleep syndrome. Their behavior prevents them from going to bed at a time that will allow sufficient sleep. Some veterans smoke or drink caffeinated beverages or al cohol immediately before sleep time and then wonder why they have insomnia.
Veterans with insomnia may be referred to the insomnia clinic psychologist for cognitive behavioral therapy for insomnia.40 Referral to this psychologist can be very helpful in the treatment of insomnia after the patient’s OSA has been treated. Veterans are encouraged to follow good sleep hygiene principles and permanently discontinue detrimental sleep behaviors.
For veterans with PTSD, imagery rehearsal before sleep has been effective in resolving disturbing nightmares and excluding their violent details.41 Clinicians recommend that these veterans rehearse a pleasant dream before sleep time. Cartwright and Lamberg performed extensive research on dreams and nightmares, and their book may provide insight into reducing nightmares for veterans with severe PTSD.42 Persistent nightmares associated with PTSD also can be reduced with use of prazosin. 43
Sleep Clinic Economics
The economic impact of OSA is substantial because of increased risk of cardiovascular disease and risk of motor vehicle accidents and decreased quality of life and productivity. Results of cost-effectiveness analyses support the value of diagnosing and treating OSA. Studies have provided estimates from a payer perspective, ranging from $2,000 to $11,000 per quality-adjusted life year over 5 years for treating moderate-to-severe OSA. The Sleep Heart Health Study showed that OSA was associated with an 18% increase in predicted health care utilization based on medication use.44,45 Moreover, CPAP therapy was found to be clinically more effective than no treatment: Therapy increased life expectancy in males and females, and effective treatment of OSA was associated with lower health care and disability costs and fewer missed workdays.
The authors’ initiatives to improve PAP therapy adherence required adding a PA and a registered respiratory therapist (RT) to the staff of 2 full-time equivalent (FTE) board-certified sleep physicians. The sleep physicians trained the PA to initiate and complete all the recommendations described, and the PA attended an AASM-sponsored review course for additional training. The PA is responsible for performing comprehensive face-to-face clinical evaluations in 4 half-day clinic sessions each week, as well as providing follow-up care in 4 additional half-day clinic sessions each week.
During these sessions, the PA provides education about sleep apnea and treatment. Thirty-minute follow-up clinic appointments are reserved for downloading CPAP data, providing interpretation, and educating patients to maximize PAP therapy and become super users. The remaining clinic sessions are run by 3 sleep fellows under the supervision of the sleep physicians. During all visits, providers encourage patients to maintain good sleep hygiene. Nonadherent patients are scheduled to be seen in a separate clinic session during which the RT troubleshoots and corrects PAP machine and mask-related problems.
Setting up the CPAP group classes and follow-up clinics required adding an FTE RT at a cost of $44,000 to $48,000 per year. By recruiting an FTE PA starting at GS-12 and $75,542 instead of another board-certified sleep physician, VAMC Detroit was able to provide increased access to patient care (8 clinics) at sizable financial savings (estimate, $75,000/y). A 0.5 FTE clinical psychologist provided cognitive behavioral therapy for insomnia and PAP therapy nonadherence and helped achieve the initiative’s goals.
The sleep center projects that the overall cost-effectiveness of these initiatives in terms of admission rates, life expectancy, and productivity would not be dissimilar to that reported in the peer-reviewed literature, as noted earlier. The center’s upcoming research projects will provide more data specific to its population. Educating patients requires that only motivated providers give patients instructions during a 30-minute follow-up clinic visit—there is no additional expense. This model of intensive care can be adopted at other VAMCs.
Conclusion
Maximizing PAP machine use is a unique approach that stimulates veterans to attain the highest level of adherence. This approach is based on clinical observation and patient encounters, and treatment recommendations over 8 years.
Showing enthusiasm with patients is crucial. Enthusiasm is contagious. Clinicians who are also PAP machine users should let patients know of their PAP super-user status and add that many others have attained this status, too. The benefits of optimal treatment are reviewed with patients: increased energy, lower risk of cardiovascular disease, lower blood pressure, better insulin sensitivity, and overall reduced mortality. Some patients have difficulty using the nasal mask and chin strap and understanding and adhering to PAP therapy. These impediments can be overcome with further education and follow-up. Sleep clinic clinicians take the time to show patients how to use the machine’s self-adherence check and leak functions. Patients can then monitor their progress daily.
To motivate patients, clinicians should set expectations early, invest time in providing education at follow-up; be diligent with respect to mask fitting and download evaluation. Sleep clinic providers should also speak the veterans’ language, create a self-fulfilling prophesy for success, and schedule a follow-up sleep clinic appointment if a patient is not fulfilling the Medicare adherence criterion of 4 hours’ nightly use for 70% of nights over 30 days.
PAP therapy coaching and persistent education with provider contact and enthusiasm can improve adherence. Encouragement and praise can help patients exceed Medicare’s minimum PAP therapy criterion and improve their overall PAP experience. The sleep team should tell patients they are proud of their accomplishments with such a difficult treatment. Being genuine and caring and showing concern about their evaluation, treatment, and follow-up is important. This helps reduce their OSA-related morbidity, lessen their depression, and improves their daily well-being and quality of life.
“The variation in responses to CPAP and acceptance of CPAP suggest that focused interventions, rather than one-size-fits-all interventions, may have a greater effect on the overall outcome of CPAP adherence,” wrote Weaver and Sawyer.46
Finally, one cannot equate spending on veteran care with spending in other areas of the national budget. The real cost of not giving veterans appropriate care will be a loss of trust, given that the overarching mission is “to care for him who shall have borne the battle and for his widow and his orphan.”
Adherence to positive airway pressure (PAP) therapy is a difficult patient management issue. Clinicians at the John D. Dingell VA Medical Center in Detroit (VAMC Detroit) developed the O’Brien criteria and extensive patient education materials to increase patient adherence. The importance of PAP therapy and the reasons veterans should sleep with a PAP machine for 7 to 9 hours each night are stressed (many sleep only 4 to 5 hours). Several recent studies have confirmed widely varying PAP therapy adherence rates (30%-84%).1-13 A majority of patients indicated that mask discomfort is the primary reason for nonadherence.1
Adherence is affected by many factors, including heated humidity, patient education, mask type, and type of PAP machine (eg, continuous PAP [CPAP] vs bilevel PAP [BPAP]; auto-PAP vs CPAP). Other factors, such as race and economic status, also affect adherence.14 The Wisconsin Sleep Cohort Study found that patients with moderate-to-severe untreated obstructive sleep apnea (OSA) were 4 to 5 times more likely to die of a cardiovascular event and 3 times more likely to die of any cause.15 The morbidity and mortality associated with severe untreated OSA led the clinicians to intensify treatment efforts.16In this article, the authors summarize the initiative at the VAMC Detroit to enhance PAP therapy adherence in patients with sleep apnea. The goal was to motivate patients to maximize PAP machine use. This article is a guide that federal health care providers and their civilian counterparts in the private sector can use to maximize PAP machine use. Working toward that goal, a set of PAP “super user” criteria was developed and used to create a 5-point method for encouraging patients to maximize adherence to PAP therapy.
Background
Positive airway pressure is the room air pressure, measured in centimeters of H2O, which splints open the airway to prevent snoring, apneas, and hypopneas. An apnea is a 90%-plus airway obstruction that lasts longer than 10 seconds and is seen with sleep study polysomnography. A hypopnea is a 30%-plus airway obstruction that lasts longer than 10 seconds and is accompanied by a 3% drop in pulse oximetry (SpO2).
A CPAP device delivers pressure continuously through a medical air compressor or flow generator called a PAP machine. The BPAP machine has separate inspiratory pressure and expiratory pressure. Auto-PAP machines give minimum pressure and maximum pressure usually between the range of 4 cm H2O to 20 cm H2O. This machine finds the user’s median pressure (90th percentile) and maximum pressure and averages pressure over a specified period of use. The auto-PAP can then be set to CPAP mode and the pressure fixed or set to the 90th percentile.
O’Brien Criteria
The O’Brien criteria for PAP super-user status (Table 1) were developed for maximizing PAP machine use and presented at the 2013 John D. Dingell Sleep and Wake Disorders Center Symposium. There is no other published reference or criteria proposed for maximizing PAP machine adherence. A recent study on sleep time criteria suggested that a higher percentage of patients achieved normal functioning with longer duration nightly CPAP therapy, which is in line with the authors’ recommended PAP machine use duration.17
Positive airway pressure therapy is eligible for insurance reimbursement by Medicare and third-party payers for adult patients who have OSA and achieve 4 hours of nightly use for 70% of nights over 30 days. Coverage for CPAP therapy is initially limited to 12 weeks during which beneficiaries with an OSA diagnosis can be identified and any therapy benefits documented. Subsequent CPAP therapy is covered only for those OSA patients who benefit during the 12-week period.18At VAMC Detroit, the data covering the previous 30 days of use is downloaded. Medicare allows for the best 30-day period out of the 12-week window. The hospital, along with Harper Hospital and the Detroit Medical Centers in conjunction with the Wayne State University sleep program, is an Academic Center of Distinction, which follows the sleep guidelines and practice parameters for Medicare, third-party insurance companies, and the American Academy of Sleep Medicine.
The sleep clinic clinicians follow the clinical guidelines for evaluation, management, and long-term care of adults with OSA.19,20 Follow-up visits are scheduled and made on a consultation basis up to 90 days for the required download or as necessary for PAP therapy. In this initiative, practitioners offer veteran-specific patient care with PAP therapy that exceeds Medicare guidelines. The success of this process yielded a growing cohort of PAP super users at VAMC Detroit. These patients exceed the Medicare criterion of 4 hours of nightly use for 70% of nights over 30 days. Thus, 4 hours of nightly use for 100% of nights over the same period was proposed as another criterion.
The super-user criteria, which provide motivation to reach the top, stimulate many patients to achieve the Medicare criteria. All 5 criteria must be satisfied to attain super-user status, and becoming a super user is not easy. In fact, the expectation is that, if an adherence data study is conducted, it will show that only a small percentage of all users meet the criteria. Maximum adherence is expected to be the tail (3%-4%) of a bell-shaped curve.
PAP Super-User Status
At the initial evaluation, practitioners create a self-fulfilling prophecy that, as first described by Merton, sets expectations.21 A self-fulfilling prophecy is a prediction that directly or indirectly causes the prediction to become true as a result of the positive feedback between belief and behavior.21 The personnel at VAMC Detroit sleep clinic set a tone that enables patients to meet and exceed the Medicare sleep guidelines and their expectations. Patients are encouraged to make it their personal mission to achieve the goal of becoming a PAP super user. The patients receive the O’Brien criteria for PAP super-user status—guidelines thought to contribute to higher quality of life.
The Medicare criterion emphasized is the minimum required for full adherence. The goal is to reduce sleepiness and increase well-being. The literature shows that increasing duration of sleep results in lower daytime sleepiness.22 Inadequate sleep has many detrimental effects. According to a recent study, insufficient sleep contributes to weight gain.22 Desired patient outcomes are increased sleep time without arousals, increased slow-wave sleep (SWS), consolidation of memories and rapid eye movement (REM), and improvement in emotional and procedural skill memories.23 Patients are informed that using a PAP machine for 7 to 9 hours can reduce excessive daytime sleepiness and allow for more SWS and REM sleep, which help improve memory, judgment, and concentration. Many other studies have shown how 7 to 9 hours of sleep benefit adults. Thus, 7 to 9 hours became the criterion for maximizing PAP sleep time.
Initial Evaluation and Sleep Study
A primary care provider can enroll a patient into the clinic for a sleep study by requesting an evaluation. The consultation is then triaged using the STOP-BANG (Snoring, Tiredness, Observed apnea, high blood Pressure–Body mass index > 35, Age > 50, Neck circumference > 40 cm, Gender male) questionnaire. The STOP-BANG has a high sensitivity for predicting moderate-to-severe (87.0%) and severe (70.4%) sleep-disordered breathing.24 More than 3 affirmative answers indicate a high risk for sleep-disordered breathing and is cause for ordering a sleep study.
CPAP Group Class
Patients with a diagnosis of sleep apnea subsequently receive their CPAP machines when they attend a 2-hour group class taught by a respiratory therapist. Group education sessions increase the chance of issuing more machines and providing better education.25 One study found that “attendance in a group clinic designed to encourage compliance with CPAP therapy provided a simple and effective means of improving treatment of OSA.”25
In class, the respiratory therapist briefly assesses each patient’s CPAP prescription, describes the patient’s type of sleep apnea and final diagnosis, and reviews the CPAP machine’s features. Veterans are then instructed to take their CPAP machines home to use all night, every night for 4 weeks. All night is defined as a period of 7.5 to 8 hours, as population-based study results have shown that sleep of this duration is associated with lowest cardiovascular morbidity and mortality. After the initial 4-plus weeks of machine use, patients with all their CPAP equipment are seen in the sleep clinic.
First Sleep Clinic Follow-Up Visit
At first follow-up, patients are asked for a subjective evaluation of their sleep. Most state they are “better” with PAP therapy. Each patient’s mask is checked and refitted with the patient’s prescribed pressure.
Patients are informed of their PAP settings and requirements from the sleep study and told their particular “magic pressure.” Patients understand that a person’s magic pressure, determined in the laboratory, is the pressure of room air blown into the nose, mouth, or both that eliminates not only snoring, but also partial and complete airway obstructions (hypopneas, apneas). Patients are asked to remember their particular magic pressure and their AHI and told their OSA status (mild, moderate, or severe) as assessed by the laboratory study.26 Extensive education on sleep apnea and treatment are also addressed. Education and training are among the most important tenets of PAP therapy, and these are incorporated into all encounters.25,26
PAP Data Report and Leak
The CPAP data are downloaded and printed. If adherence is suboptimal, clinician and patient discuss increasing adherence and possibly becoming a super user. The patient receives a copy of the report, which can be compared with the patient’s adherence statistics and with the adherence statistics of similar patients who are super users. A few blacked-out names are posted on the board in front of the provider’s computer station. Patients can thus easily see that attaining super-user status is very difficult but possible. Some patients maximize their therapy and are designated PAP super users. These patients are proud to receive this designation, and they strive to keep it.
Data downloads are crucial for adherence. In a recent study, the American Thoracic Society stated, “Providers need to be able to interpret adherence systems.”27
The clinic provides a summary report on each patient’s adherence. A provider interpretation is added, and the report is copied into the Computer Patient Record System.
After the report is downloaded, the provider checks for correct pressure and then for a large leak. A large leak is an unintentional leak (the total amount that leaks but not including leak from the mask) > 5% of the night. A leak of > 15 minutes was added to the super-user criteria, because some software provides the average time of a large leak per day in minutes.28 Many veterans sleep only 4 to 5 hours nightly (300 minutes × 5% = 15 minutes). Therefore, the leak should not be more than 5% or 15 minutes for a veteran sleeping 5 hours.
The machine indicates a percentage of leak on the patient self-check LED screen for adherence. There is no standardized leak criterion used by all flow-generator manufacturers. Every mask has venting designed to leak intentionally so that the patient does not rebreathe air CO2. The main concern is unintentional leaks above the intentional leak or venting threshold.
The ResMed CPAP (ResMed Corp, San Diego, CA) maximum intentional leak is 24 L/min.29 Above that level is large leak. The exact leak amount varies by interface (mask) based on pressure and mask type.2,12
The larger the interface surface area, the larger the leak. Unintentional leak is higher with the full-face mask than with the nasal mask, most likely because there is more opportunity for leakage with the larger surface area of the full-face mask. Nasal pillows seem to leak less because of their smaller surface area, but more studies on mask interfaces are needed to validate this finding.
Chin Strap
Adding a chin strap improved patient adherence, nightly duration of use, residual AHI, and leak in patients with sleep apnea.30 Other investigators reported reduced OSA, confirmed by polysomnography and nasopharyngolaryngoscopy, with use of only a chin strap.31 When a nasal mask with chin strap is used, the strap should be made to fit properly over the chin, not on the throat. Properly used chin straps significantly reduce leakage and residual AHI.30
A chin strap most likely reduces large leak and dry mouth.30 Dry mouth can result from mouth leak, which is commonly caused by nasal congestion or high pressure and mouth breathing. The nasal turbinates help humidify, warm, and cool the air. Heated humidification of PAP can help prevent dry mouth.
Asking the Right Questions
The clinician should ask several key questions at the first follow-up: How is it going with your PAP machine? Do you feel PAP therapy is helping you sleep? Do you feel better with PAP therapy? To a patient who states he or she is not doing well with therapy, the clinician should ask, What type of problems are you having? In many cases, poor adherence is attributable to a large leak from a poorly fitting mask. A large leak can also increase residual AHI and cause frequent arousals.30
Some machines cannot maintain the pressure of a large leak and will shut off and trigger an alarm that wakes the patient to readjust the mask. This situation causes some patients to discontinue CPAP/BPAP use. The mask leak must be adjusted. Another common complaint is morning dry mouth. This extreme dryness—a significant clue pointing to mouth leak caused in part by the mouth dropping open during sleep with PAP—should be addressed by fitting the patient with a chin strap.30 Dry mouth also can be caused by low humidity; increasing the humidity setting usually resolves the problem. However, as one study found, use of controlled heated humidification did not improve adherence or quality of life.32 In the same study, the nasopharyngeal dryness that resulted from CPAP therapy without humidification was reduced immediately and during the first weeks of treatment.All current PAP machines feature heated humidification.
Mouth breathing can also result from nasal congestion, allergic or vasomotor rhinitis, nasal turbinate hypertrophy, obstruction from a deviated septum, polyps, or air hunger/insufficient PAP pressure. Chronic rhinosinusitis is a problem that affects up to 12.5% of the U.S. population.33
Adherence is also increased with the elimination of leak and associated arousals. Patients are shown how to use their PAP machine’s heated humidity settings to obtain desired comfort levels. The clinician explains that the nasal turbinates heat and cool the air and that they can become swollen and irritated with PAP therapy. A heated hose may be prescribed to provide optimal humidification without condensation or water dripping into the hose (rainout).
A full-face mask is used only when the patient cannot breathe out the nose adequately or when PAP becomes too high. A 2013 study found no significant differences among ResMed, Respironics, and Fisher & Paykel CPAP interfaces (Fisher & Paykel Healthcare, Irvine, CA).34 The clinician determines which mask is comfortable for a patient and tries to stay with that mask for that patient.
Adherence Report
A therapy data summary is downloaded and reviewed with the patient.28 A pattern of use report that shows daily use with times over the month is also reviewed.28 The software’s sleep therapy long-term trend report lists important statistics. The adherence data summary and the CPAP summary are also reviewed (Table 2).28 This page is printed and given to patients to reieiw their progress. For some it represents a reward for using the CPAP/BPAP machine as well as a congratulatory note.
In the Example 1 summary download (Table 2), a patient used a PAP machine 4 hours or more on 93.3% of the 30 days the machine was used.28 Residual AHI was low, 2.1, and there was no appreciable leak. The PAP of 11.2 cm H2O was in the 90th percentile. The patient was fixed to 12 cm H2O with expiratory pressure relief (EPR) of 1. The EPR is a comfort feature that reduces pressure from 1 cm H2O to 3 cm H2O to make it easier for the patient to exhale. (A flow generator that produces EPR of > 3 cm H2O is a BPAP machine.)
This patient was not a super user. Overall use was low—5 hours, 28 minutes—which could indicate behaviorally insufficient sleep syndrome. Sleep time is controversial, but the National Sleep Foundation recommends 7 to 9 hours of sleep per night.
A different patient used a PAP machine 4 hours or more on 100% (28/28) of the days when the machine was used (Table 3).29 Residual AHI was low (0.6), median use was 8 hours, 47 minutes, and there was no appreciable leak. The patient was using autoset mode with a minimum pressure of 13 cm H2O and maximum pressure of 18 cm H2O. The 95th percentile pressure was 13.6 cm H2O. The patient’s pressure was changed to 14 cm H2O with EPR of 3. This patient was a super user.
Sleep Hygiene Discussion
Providers must discuss sleep hygiene (good sleep habits) with veterans. If needed, AASM pamphlets on sleep hygiene and other educational materials can be provided. The bedroom should be cool, comfortable, quiet, and dark and should not include a television or computer. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration and tells the brain it is time to wake up.34
Patients are asked about the number of arousals they have per night. At first follow-up, providers must determine what is causing a patient to arouse while on CPAP/BPAP therapy. Some causes are air leak resulting in unresolved OSA, nocturia (may be triggered by unresolved OSA), dry mouth (indicating need for chin strap), nightmares (suggestive of unresolved OSA in REM sleep), posttraumatic stress disorder (PTSD), environmental noise, and claustrophobia. The provider should have thought-out answers to these problems in advance.
Epworth Sleepiness Scale
The Epworth Sleepiness Scale (ESS) is administered as part of the baseline comprehensive examination and at every sleep clinic follow-up after issuing a CPAP/BPAP machine.35 The first evaluation after the machine is issued should show a reduction in ESS. No reduction in ESS indicates that a problem needs to be addressed. The most common reason for insufficient reduction in ESS is suboptimal PAP therapy adherence, usually because of a large leak. Some cases of poor adherence may be attributable to restless legs syndrome, periodic limb movement disorder, chronic musculoskeletal pain, and sleep fragmentation caused by alcohol, smoking, caffeine, or cocaine. Excessive daytime sleepiness may persist from use of pain medications or other sedating medications. One study found a correlation between sleep duration with CPAP therapy and reduction in ESS.36 In addition to administering the ESS, patients are asked how they doing with PAP therapy, and the answer is documented. Treatment changes are made if needed to reduce excessive daytime sleepiness.
Ear-Nose-Throat Examination
A quick look into the nose with a nasal speculum is a crucial component of a thorough examination. The clinician looks for a deviated septum, swollen turbinates, obstruction, polyps, bleeding, infection, septal perforation, and discharge. In addition, the patient is checked for airflow amount, nasal congestion, and obstruction; if necessary a nasal steroid spray or a nasal saline spray is prescribed. In some cases, saline spray can be added to the steroid spray to help reduce or eliminate nasal congestion.37
Treatment of congestion requires education, as many patients improperly use these sprays. The steroid spray is not an instant vasoconstrictor; a week of regular use is needed to reduce inflammation and congestion. Saline spray and saline irrigation can be used as a treatment adjunct for symptoms of chronic rhinosinusitis.37If the steroid and saline sprays fail after a 2-month trial, consider an ear-nose-throat (ENT) consultation. A recent study found that adherence rates increased after septoplasty in patients with nasal obstruction.38 The throat is examined for macroglossia or scalloping of the tongue.39 Macroglossic Mallampati IV tongues are platterlike. They are big, long, and wide and often have impressions or scalloping along the outside from a molding of the teeth. The patient is shown a Mallampati diagram and given a Mallampati score.
Creating a Sense of Mission
The sleep physician assistant (PA)at the Detroit VAMC is a retired U.S. Army colonel who ensures that the language the physician uses aligns with the language veterans use. Behavioral techniques are used to create a common culture that helps overcome obstacles—allowing patients to understand the benefits of and need for full CPAP/BPAP therapy adherence. One technique reinforces their sense of mission accomplishment, their military pride, and their interservice rivalry to increase adherence. The mission with each patient is to “work until success is achieved...but the patient can’t quit.” The mantra given to a patient with a difficult case is, “We will not let you fail with CPAP/BPAP therapy,” which echoes a familiar military motto, “We will not leave you behind.” Also, the goal of the physician is: Never give up on the patient.
Behavioral and Psychological Principles
The behavioral and psychological principles for success with PAP super users should be studied to validate better outcomes with longer duration PAP machine use. Patients who are motivated to succeed and to participate in their care can make great strides in changing their behavior to get more and better sleep. Obese patients can get referrals to the MOVE! weight loss program. Some veterans simply follow instructions, pay attention to detail, and do what they are told regarding sleep, PAP education, and good sleep hygiene. Many veterans have poor sleep hygiene and insomnia because they watch television or play games on electronic devices right before bedtime. Many patients develop behaviorally insufficient sleep syndrome. Their behavior prevents them from going to bed at a time that will allow sufficient sleep. Some veterans smoke or drink caffeinated beverages or al cohol immediately before sleep time and then wonder why they have insomnia.
Veterans with insomnia may be referred to the insomnia clinic psychologist for cognitive behavioral therapy for insomnia.40 Referral to this psychologist can be very helpful in the treatment of insomnia after the patient’s OSA has been treated. Veterans are encouraged to follow good sleep hygiene principles and permanently discontinue detrimental sleep behaviors.
For veterans with PTSD, imagery rehearsal before sleep has been effective in resolving disturbing nightmares and excluding their violent details.41 Clinicians recommend that these veterans rehearse a pleasant dream before sleep time. Cartwright and Lamberg performed extensive research on dreams and nightmares, and their book may provide insight into reducing nightmares for veterans with severe PTSD.42 Persistent nightmares associated with PTSD also can be reduced with use of prazosin. 43
Sleep Clinic Economics
The economic impact of OSA is substantial because of increased risk of cardiovascular disease and risk of motor vehicle accidents and decreased quality of life and productivity. Results of cost-effectiveness analyses support the value of diagnosing and treating OSA. Studies have provided estimates from a payer perspective, ranging from $2,000 to $11,000 per quality-adjusted life year over 5 years for treating moderate-to-severe OSA. The Sleep Heart Health Study showed that OSA was associated with an 18% increase in predicted health care utilization based on medication use.44,45 Moreover, CPAP therapy was found to be clinically more effective than no treatment: Therapy increased life expectancy in males and females, and effective treatment of OSA was associated with lower health care and disability costs and fewer missed workdays.
The authors’ initiatives to improve PAP therapy adherence required adding a PA and a registered respiratory therapist (RT) to the staff of 2 full-time equivalent (FTE) board-certified sleep physicians. The sleep physicians trained the PA to initiate and complete all the recommendations described, and the PA attended an AASM-sponsored review course for additional training. The PA is responsible for performing comprehensive face-to-face clinical evaluations in 4 half-day clinic sessions each week, as well as providing follow-up care in 4 additional half-day clinic sessions each week.
During these sessions, the PA provides education about sleep apnea and treatment. Thirty-minute follow-up clinic appointments are reserved for downloading CPAP data, providing interpretation, and educating patients to maximize PAP therapy and become super users. The remaining clinic sessions are run by 3 sleep fellows under the supervision of the sleep physicians. During all visits, providers encourage patients to maintain good sleep hygiene. Nonadherent patients are scheduled to be seen in a separate clinic session during which the RT troubleshoots and corrects PAP machine and mask-related problems.
Setting up the CPAP group classes and follow-up clinics required adding an FTE RT at a cost of $44,000 to $48,000 per year. By recruiting an FTE PA starting at GS-12 and $75,542 instead of another board-certified sleep physician, VAMC Detroit was able to provide increased access to patient care (8 clinics) at sizable financial savings (estimate, $75,000/y). A 0.5 FTE clinical psychologist provided cognitive behavioral therapy for insomnia and PAP therapy nonadherence and helped achieve the initiative’s goals.
The sleep center projects that the overall cost-effectiveness of these initiatives in terms of admission rates, life expectancy, and productivity would not be dissimilar to that reported in the peer-reviewed literature, as noted earlier. The center’s upcoming research projects will provide more data specific to its population. Educating patients requires that only motivated providers give patients instructions during a 30-minute follow-up clinic visit—there is no additional expense. This model of intensive care can be adopted at other VAMCs.
Conclusion
Maximizing PAP machine use is a unique approach that stimulates veterans to attain the highest level of adherence. This approach is based on clinical observation and patient encounters, and treatment recommendations over 8 years.
Showing enthusiasm with patients is crucial. Enthusiasm is contagious. Clinicians who are also PAP machine users should let patients know of their PAP super-user status and add that many others have attained this status, too. The benefits of optimal treatment are reviewed with patients: increased energy, lower risk of cardiovascular disease, lower blood pressure, better insulin sensitivity, and overall reduced mortality. Some patients have difficulty using the nasal mask and chin strap and understanding and adhering to PAP therapy. These impediments can be overcome with further education and follow-up. Sleep clinic clinicians take the time to show patients how to use the machine’s self-adherence check and leak functions. Patients can then monitor their progress daily.
To motivate patients, clinicians should set expectations early, invest time in providing education at follow-up; be diligent with respect to mask fitting and download evaluation. Sleep clinic providers should also speak the veterans’ language, create a self-fulfilling prophesy for success, and schedule a follow-up sleep clinic appointment if a patient is not fulfilling the Medicare adherence criterion of 4 hours’ nightly use for 70% of nights over 30 days.
PAP therapy coaching and persistent education with provider contact and enthusiasm can improve adherence. Encouragement and praise can help patients exceed Medicare’s minimum PAP therapy criterion and improve their overall PAP experience. The sleep team should tell patients they are proud of their accomplishments with such a difficult treatment. Being genuine and caring and showing concern about their evaluation, treatment, and follow-up is important. This helps reduce their OSA-related morbidity, lessen their depression, and improves their daily well-being and quality of life.
“The variation in responses to CPAP and acceptance of CPAP suggest that focused interventions, rather than one-size-fits-all interventions, may have a greater effect on the overall outcome of CPAP adherence,” wrote Weaver and Sawyer.46
Finally, one cannot equate spending on veteran care with spending in other areas of the national budget. The real cost of not giving veterans appropriate care will be a loss of trust, given that the overarching mission is “to care for him who shall have borne the battle and for his widow and his orphan.”
1. Boyaci H, Gacar K, Baris SA, Basyigit I, Yildiz F. Positive airway pressure device compliance of patients with obstructive sleep apnea syndrome. Adv Clin Exp Med. 2013;22(6):809-815.
2. Bachour A, Vitikainen P, Virkkula P, Maasilta P. CPAP interface: satisfaction and side effects. Sleep Breath. 2013;17(2):667-672.
3. Wimms AJ, Richards GN, Genjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath. 2013;17(1):69-76.
4. Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioral interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnea. Cochrane Database Syst Rev. 2009;(2):CD007736.
5. Beecroft J, Zanon S, Lukic D, Hanly P. Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest. 2003;124(6):2200-2208.
6. Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;(4):CD005308.
7. Nilius G, Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006;130(4):1018-1024.
8. Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med. 2007;3(7):706-712.
9. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435.
10. Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53(4):290-292.
11. Haniffa M, Lasserson TJ, Smith I. Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev. 2004;(4):CD003531.
12. Kushida CA, Berry RB, Blau, A, et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titration process on efficacy, adherence, and outcomes. Sleep. 2011;34(8):1083-1092.
13. Gentina T, Fortin F, Douay B, et al. Auto bi-level with pressure relief during exhalation as a rescue therapy for optimally treated obstructive sleep apnoea patients with poor compliance to continuous positive airways pressure therapy--a pilot study. Sleep Breath. 2011;15(1):21-27.
14. Billings, ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653-1658.
15. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31(8):1071-1078.
16. Centers for Disease Control and Prevention. Effect of short sleep duration on daily activities--United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60(8):239-242.
17. Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111-119.
18. Phurrough S, Jacques L, Spencer F, Stiller J, Brechner R. Coverage decision memorandum for continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) (CAG-00093R2). Centers for Medicare & Medicaid Services Website. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204&fromdb=true. Accessed February 5, 2016.
19. Epstein LJ, Kristo D, Strollo PJ Jr, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2009;5(3):263-276.
20. Berry RB, Chediak A, Brown LK, et al; NPPV Titration Task Force of the American Academy of Sleep Medicine. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491-509.
21. Merton RK. Social Theory and Social Structure. New York, NY: Free Press; 1968.
22. Chaput JP, McNeil J, Després JP, Bouchard C, Tremblay A. Seven to eight hours of sleep a night is associated with a lower prevalence of the metabolic syndrome and reduced overall cardiometabolic risk in adults. PLoS One. 2013;8(9):e72832.
23. Born J, Wagner U. Sleep, hormones, and memory. Obstet Gynecol Clin North Am. 2009;36(4):809-829, x.
24. Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7(5):467-472.
25. Soares Pires F, Drummond M, Marinho A, et al. Effectiveness of a group education session on adherence with APAP in obstructive sleep apnea--a randomized controlled study. Sleep Breath. 2013;17(3):993-1001.
26. Berry RB, Budhiraja R, Gottlieb DJ, et al; American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597-619.
27. Schwab RJ, Badr SM, Epstein LJ, et al; ATS Subcommittee on CPAP Adherence Tracking Systems. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188(5):613-620.
28. Respironics Encore Pro and Encore Pro 2 [computer program]. Philips, Inc; May 12, 2013.
29. ResMed. Version 04.01.013. San Diego, CA.
30. Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10(4):377-383.
31. Vorona RD, Ware JC, Sinacori JT, Ford ML 3rd, Cross JP. Treatment of severe obstructive sleep apnea syndrome with a chinstrap. J Clin Sleep Med. 2007;3(7):729-730.
32. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath. 2011;15(3):479-485.
33. Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011;128(4):693-707.
34. Gooley JJ, Chamberlain K, Smith KA, et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J Clin Endocrinol Metab. 2011;96(3):E463-E472.
35. Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540-545.
36. Bednarek M, Zgierska A, Pływaczewski R, Zielinski J. The effect of CPAP treatment on excessive daytime somnolence in patients with obstructive sleep apnea [in Polish]. Pneumonol Alergol Pol. 1999;67(5-6):237-244.
37. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
38. Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2014;124(1):317-319.
39. Law JA. From the journal archives: Mallampati in two millennia: its impact then and implications now. Can J Anaesth. 2014;61(5):480-484.
40. Hood HK, Rogojanski J, Moss TG. Cognitive-behavioral therapy for chronic insomnia. Curr Treat Options Neurol. 2014;16(12):321.
41. Harb GC, Thompson R, Ross RJ, Cook JM. Combat-related PTSD nightmares and imagery rehearsal: nightmare characteristics and relation to treatment outcome. J Trauma Stress. 2012;25(5):511-518.
42. Cartwright R, Lamberg L. Crisis Dreaming: Using Your Dreams to Solve Your Problems.. New York, NY: HarperCollins;1992.
43.Writer BW, Meyer EG, Schillerstrom JE. Prazosin for military combat-related PTSD nightmares: a critical review. J Neuropsychiatry Clin Neurosci. 2014;26(1):24-33.
44. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc. 2011;86(6):549-554.
45. Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749-755.
46. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245-258.
1. Boyaci H, Gacar K, Baris SA, Basyigit I, Yildiz F. Positive airway pressure device compliance of patients with obstructive sleep apnea syndrome. Adv Clin Exp Med. 2013;22(6):809-815.
2. Bachour A, Vitikainen P, Virkkula P, Maasilta P. CPAP interface: satisfaction and side effects. Sleep Breath. 2013;17(2):667-672.
3. Wimms AJ, Richards GN, Genjafield AV. Assessment of the impact on compliance of a new CPAP system in obstructive sleep apnea. Sleep Breath. 2013;17(1):69-76.
4. Smith I, Nadig V, Lasserson TJ. Educational, supportive and behavioral interventions to improve usage of continuous positive airway pressure machines for adults with obstructive sleep apnea. Cochrane Database Syst Rev. 2009;(2):CD007736.
5. Beecroft J, Zanon S, Lukic D, Hanly P. Oral continuous positive airway pressure for sleep apnea: effectiveness, patient preference, and adherence. Chest. 2003;124(6):2200-2208.
6. Chai CL, Pathinathan A, Smith B. Continuous positive airway pressure delivery interfaces for obstructive sleep apnoea. Cochrane Database Syst Rev. 2006;(4):CD005308.
7. Nilius G, Happel A, Domanski U, Ruhle KH. Pressure-relief continuous positive airway pressure vs constant continuous positive airway pressure: a comparison of efficacy and compliance. Chest. 2006;130(4):1018-1024.
8. Ballard RD, Gay PC, Strollo PJ. Interventions to improve compliance in sleep apnea patients previously non-compliant with continuous positive airway pressure. J Clin Sleep Med. 2007;3(7):706-712.
9. Sin DD, Mayers I, Man GC, Pawluk L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea: a population-based study. Chest. 2002;121(2):430-435.
10. Mortimore IL, Whittle AT, Douglas NJ. Comparison of nose and face mask CPAP therapy for sleep apnoea. Thorax. 1998;53(4):290-292.
11. Haniffa M, Lasserson TJ, Smith I. Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea. Cochrane Database Syst Rev. 2004;(4):CD003531.
12. Kushida CA, Berry RB, Blau, A, et al. Positive airway pressure initiation: a randomized controlled trial to assess the impact of therapy mode and titration process on efficacy, adherence, and outcomes. Sleep. 2011;34(8):1083-1092.
13. Gentina T, Fortin F, Douay B, et al. Auto bi-level with pressure relief during exhalation as a rescue therapy for optimally treated obstructive sleep apnoea patients with poor compliance to continuous positive airways pressure therapy--a pilot study. Sleep Breath. 2011;15(1):21-27.
14. Billings, ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653-1658.
15. Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31(8):1071-1078.
16. Centers for Disease Control and Prevention. Effect of short sleep duration on daily activities--United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2011;60(8):239-242.
17. Antic NA, Catcheside P, Buchan C, et al. The effect of CPAP in normalizing daytime sleepiness, quality of life, and neurocognitive function in patients with moderate to severe OSA. Sleep. 2011;34(1):111-119.
18. Phurrough S, Jacques L, Spencer F, Stiller J, Brechner R. Coverage decision memorandum for continuous positive airway pressure (CPAP) therapy for obstructive sleep apnea (OSA) (CAG-00093R2). Centers for Medicare & Medicaid Services Website. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=204&fromdb=true. Accessed February 5, 2016.
19. Epstein LJ, Kristo D, Strollo PJ Jr, et al; Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2009;5(3):263-276.
20. Berry RB, Chediak A, Brown LK, et al; NPPV Titration Task Force of the American Academy of Sleep Medicine. Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med. 2010;6(5):491-509.
21. Merton RK. Social Theory and Social Structure. New York, NY: Free Press; 1968.
22. Chaput JP, McNeil J, Després JP, Bouchard C, Tremblay A. Seven to eight hours of sleep a night is associated with a lower prevalence of the metabolic syndrome and reduced overall cardiometabolic risk in adults. PLoS One. 2013;8(9):e72832.
23. Born J, Wagner U. Sleep, hormones, and memory. Obstet Gynecol Clin North Am. 2009;36(4):809-829, x.
24. Silva GE, Vana KD, Goodwin JL, Sherrill DL, Quan SF. Identification of patients with sleep disordered breathing: comparing the four-variable screening tool, STOP, STOP-Bang, and Epworth Sleepiness Scales. J Clin Sleep Med. 2011;7(5):467-472.
25. Soares Pires F, Drummond M, Marinho A, et al. Effectiveness of a group education session on adherence with APAP in obstructive sleep apnea--a randomized controlled study. Sleep Breath. 2013;17(3):993-1001.
26. Berry RB, Budhiraja R, Gottlieb DJ, et al; American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597-619.
27. Schwab RJ, Badr SM, Epstein LJ, et al; ATS Subcommittee on CPAP Adherence Tracking Systems. An official American Thoracic Society statement: continuous positive airway pressure adherence tracking systems. The optimal monitoring strategies and outcome measures in adults. Am J Respir Crit Care Med. 2013;188(5):613-620.
28. Respironics Encore Pro and Encore Pro 2 [computer program]. Philips, Inc; May 12, 2013.
29. ResMed. Version 04.01.013. San Diego, CA.
30. Knowles SR, O'Brien DT, Zhang S, Devara A, Rowley JA. Effect of addition of chin strap on PAP compliance, nightly duration of use, and other factors. J Clin Sleep Med. 2014;10(4):377-383.
31. Vorona RD, Ware JC, Sinacori JT, Ford ML 3rd, Cross JP. Treatment of severe obstructive sleep apnea syndrome with a chinstrap. J Clin Sleep Med. 2007;3(7):729-730.
32. Ruhle KH, Franke KJ, Domanski U, Nilius G. Quality of life, compliance, sleep and nasopharyngeal side effects during CPAP therapy with and without controlled heated humidification. Sleep Breath. 2011;15(3):479-485.
33. Hamilos DL. Chronic rhinosinusitis: epidemiology and medical management. J Allergy Clin Immunol. 2011;128(4):693-707.
34. Gooley JJ, Chamberlain K, Smith KA, et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J Clin Endocrinol Metab. 2011;96(3):E463-E472.
35. Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14(6):540-545.
36. Bednarek M, Zgierska A, Pływaczewski R, Zielinski J. The effect of CPAP treatment on excessive daytime somnolence in patients with obstructive sleep apnea [in Polish]. Pneumonol Alergol Pol. 1999;67(5-6):237-244.
37. Harvey R, Hannan SA, Badia L, Scadding G. Nasal saline irrigations for the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev. 2007;(3):CD006394.
38. Poirier J, George C, Rotenberg B. The effect of nasal surgery on nasal continuous positive airway pressure compliance. Laryngoscope. 2014;124(1):317-319.
39. Law JA. From the journal archives: Mallampati in two millennia: its impact then and implications now. Can J Anaesth. 2014;61(5):480-484.
40. Hood HK, Rogojanski J, Moss TG. Cognitive-behavioral therapy for chronic insomnia. Curr Treat Options Neurol. 2014;16(12):321.
41. Harb GC, Thompson R, Ross RJ, Cook JM. Combat-related PTSD nightmares and imagery rehearsal: nightmare characteristics and relation to treatment outcome. J Trauma Stress. 2012;25(5):511-518.
42. Cartwright R, Lamberg L. Crisis Dreaming: Using Your Dreams to Solve Your Problems.. New York, NY: HarperCollins;1992.
43.Writer BW, Meyer EG, Schillerstrom JE. Prazosin for military combat-related PTSD nightmares: a critical review. J Neuropsychiatry Clin Neurosci. 2014;26(1):24-33.
44. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc. 2011;86(6):549-554.
45. Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749-755.
46. Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Indian J Med Res. 2010;131:245-258.