User login
Consider the stresses experienced by LGBTQ people of color
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
Given that Pride month is coinciding with so much upheaval in our community around racism and oppression, it is important to discuss the overlap in the experiences of both LGBTQ and people of color (POC).
The year 2020 will go down in history books. We will always remember the issues faced during this critical year. At least I hope so, because as we have seen, history repeats itself. How do these issues that we are currently facing relate to LGBTQ youth? The histories are linked. One cannot look at the history of LGBTQ rights without looking at other civil rights movements, particularly those for black people. The timing of these social movements often intertwined, both being inspired by and inspiring each other. For example, Bayard Rustin worked with Dr. Martin Luther King Jr. as an organizer for the March on Washington for Jobs and Freedom in addition to being a public advocate for gay rights later on in his life. Similarly, the Stonewall Uprising that is known by many to be one of the first acts of the gay liberation movement, prominently featured Marsha P. Johnson (a black, transgender, self-identified drag queen) and Sylvia Rivera (a Latina American transgender rights activist). As we reflect on these histories, it is important to think about the effect of minority stress and intersectionality and how this impacts LGBTQ-POC and their health disparities.
Minority stress shows that . One example of such stressors is microaggressions – brief interactions that one might not realize are discriminatory or hurtful, but to the person on the receiving end of such comments, they are harmful and they add up. A suspicious look from a store owner as one browses the aisles of a local convenience store, a comment about how one “doesn’t’ seem gay” or “doesn’t sound black” all are examples of microaggressions.
Overt discrimination, expectation of rejection, and hate crimes also contribute to minority stress. LGBTQ individuals often also have to hide their identity whereas POC might not be able to hide their identity. Experiencing constant bombardment of discrimination from the outside world can lead one to internalize these thoughts of homophobia, transphobia, or racism.
Minority stress becomes even more complicated when you apply the theoretical framework of intersectionality – overlapping identities that compound one’s minority stress. Lesbian, gay, bisexual, transgender, and queer people of color (LGBTQ-POC) are a classic example of intersecting identities. They may experience racism from the LGBT community or homophobia/transphobia from their own racial or ethnic community in addition to the discrimination they already face from the majority population for both identities. Some LGBTQ people of color may feel the need to choose between these two identities, forcing them to compartmentalize one aspect of their identity from the other. Imagine how stressful that must be! In addition, LGBTQ-POC are less likely to come out to family members.
Most of us are aware that health disparities exist, both for the LGBTQ community as well as for racial and ethnic minorities; couple these together and the effect can be additive, placing LGBTQ-POC at higher risk for adverse health outcomes. In the late 1990s, racial and ethnic minority men having sex with men made up 48% of all HIV infection cases, a number that is clearly disproportionate to their representation in our overall society. Given both LGBTQ and POC have issues accessing care, one can only imagine that this would make it hard to get diagnosed or treated regularly for these issues.
Transgender POC also are particularly vulnerable to health disparities. The 2015 U.S. Transgender Survey looked at the experiences of over 28,000 transgender people in the United States, but the survey also broke down the experiences for transgender people of color. Black transgender individuals were more likely than their black cisgender counterparts to experience unemployment (20% vs. 10%) and poverty (38% vs. 24%). They were more likely to experience homelessness compared with the overall transgender sample (42% vs. 30%) and more likely to have been sexually assaulted in their lives (53% vs. 47%). Understandably, 67% of black transgender respondents said they would feel somewhat or very uncomfortable asking the police for help.
The findings were similar for Latinx transgender respondents: 21% were unemployed compared with the overall rate of unemployment for Latinx in the United States at 7%, and 43% were living in poverty compared with 18% of their cisgender peers.
Perhaps the most striking result among American Indian and Alaska Native respondents was that 57% had experienced homelessness – nearly twice the rate of the survey sample overall (30%). For the transgender Asian and Native Hawaiian/Pacific Islander respondents, 32% were living in poverty and 39% had experienced serious psychological distress in the month before completing the survey.
So please, check in on your patients, friends, and family that identify as both LGBTQ and POC. Imagine how scary this must be for LGBTQ youth of color. They can be targeted for both their race and their sexuality and/or gender identity.
Dr. Lawlis is assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, Oklahoma City, and an adolescent medicine specialist at OU Children’s. She has no relevant financial disclosures. Email her at [email protected].
Perfect storm of SARS-CoV-2 during flu season
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
COVID-19 now. The urban phase of the U.S. pandemic is leveling somewhat, while the rural phase is accelerating – in part because of food processing and handling industries. The pediatric burden has been surprisingly small, with the multisystem inflammatory disease (MIS-c) in children noted in several hundred cases now being seen across the country.

Next wave? Given ongoing COVID-19 disease, controversy rages about when and how to re-open the country. Regardless how more reopening occurs over the next months, we should expect a next or ongoing COVID-19 wave, particularly given loss of social distancing during social justice protests. A sawtooth disease prevalence pattern is predicted by many experts: a drop in prevalence leading to reopening, leading to scattered prevalence increases and regional if not local restriction tightening, followed by another drop in prevalence. Then “rinse and repeat” until 70% of the population is immune either by disease experience or vaccine-induced immunity, likely sometime in 2021.
Influenza too. A COVID-19 up-cycle is likely during influenza season, although influenza season’s onset could be altered because of whatever social distancing rules are in place in November and December. That said, we need to consider the worst. We have seen what happens if we fail to prepare and then react only after a prevalent respiratory infection has surged into the overall population. Best estimates are that at most 20% of the U.S. population is currently immune to SARS-CoV-2. Given that at least some of that 20% of individuals currently immune to SARS-CoV-2 will lose their neutralizing antibody over the next 4-6 months, we can still expect 70%-80% of the U.S. population to be susceptible to SARS-CoV-2 infection in the fall of 2020.
Pediatric preparedness. As pediatric providers, we have struggled with lower patient loads and dramatic income losses/declines. Many clinics/offices’ attendance remain less than 50% of pre–COVID-19 levels, with necessary furloughs of personnel and spotty office hours. But influenza is coming, and SARS-CoV-2 will not be gone yet. How do we prepare for concurrent influenza and COVID-19?
The annual purchase/administration of influenza vaccine in summer/fall is expensive, time consuming, and logistically difficult even in the best times. Given the loss of income, likely reluctance of patients to come to clinics/offices if COVID-19 is still circulating, and likely need for some form of social distancing during late summer and early fall, how will providers, health departments, and hospitals implement influenza vaccine administration this year?
Minimize double whammy infections. It is easy to understand why we should maximize influenza protection in SARS-CoV-2 vulnerables (elderly or persons with existing comorbidities). But is it as critical for otherwise healthy children? My answer is yes.
Children are not currently known as SARS-CoV-2 vectors, but children are excellent influenza vectors, shedding higher titers for longer than other age groups. As with SARS-CoV-2, influenza exposure is cumulative, i.e., the more intense and more frequently a person is exposed, the more likely that infection/disease will result. So, the fewer who get and can transmit influenza during the COVID-19 pandemic, the fewer people are likely to get a double whammy of SARS-CoV-2 concurrent or in tandem with influenza. Double whammy infections likely would further increase the medical care burden and return us to March-April crisis mode.
One alarming new question is whether recent influenza could make children vulnerable to SARS-CoV-2 and trigger hospitalizations. A surge in pediatric plus adult COVID-19 disease plus a surge in all-ages influenza disease would likely break the medical care system, at least in some areas.
Staggering COVID-19 burden. As of June 8, we have had approximately 2 million SARS-CoV-2 cases with 500,000 hospitalizations and 120,000 deaths. Over the past 10 years, total annual U.S. influenza hospitalizations ranged from 180,000 (2011-2012) to 825,000 (2017-2018). The interquartile range for hospitalization length of stay for influenza is 4-6 days1 vs. 15-23 days2 for SARS-CoV-2. One COVID-19 hospitalization uses hospital resources roughly equal to four influenza hospitalizations. To date COVID-19 hospitalizations have used resources equal to an estimated 1.9 million influenza hospitalizations – over twice the worst influenza season in this century – and we are still on the rise. We are likely not even halfway to truly controlling the U.S. pandemic, so expect another 500,000 hospitalizations – equal to another 1.9 million influenza hospitalizations. Further, pneumonia deaths have skyrocketed this year when COVID-19 was superimposed on the last third of influenza season. One hope is that widespread use of antivirals (for example, new antivirals, convalescent plasma, or other interventions) can reduce length of stay by 30% for COVID-19 hospitalizations, yet even with that the numbers remain grim.
Less influenza disease can free up medical resources. Planning ahead could prevent a bad influenza season (for example, up to 850,000 hospitalizations just for influenza). Can we preemptively use vaccine to reduce influenza hospitalizations below 2011-2012 levels – less than 150,000 hospitalizations? Perhaps, if we start by reducing pediatric influenza.
1. Aim to exceed 75% influenza vaccine uptake in your patients.
a. It is ambitious, but if there was ever a year that needed influenza herd immunity, it is 2020-2021.
2. Review practice/group/institution plans for vaccine purchase and ensure adequate personnel to administer vaccine.
3. Plan safe and efficient processes to vaccinate large numbers in August through November.
a. Consider that routine and influenza vaccines can be given concurrently with the annual uptick in school and sports physical examinations.
b. What social distancing and masking rules will be needed?
i. Will patients need to bring their own masks, or will you supply them?
c. What extra supplies and efforts are needed, e.g. hand sanitizer, new signage, 6-foot interval markings on floors or sidewalks, families calling from parking lot to announce their arrivals, etc.?
d. Remember younger patients need two doses before Dec 1, 2020.
e. Be creative, for example, are parking-lot tents for influenza vaccination feasible?
f. Can we partner with other providers to implement influenza vaccine–specific mass clinics?
Ramping up to give seasonal influenza vaccine in 2020 is daunting. But if we do not prepare, it will be even more difficult. Let’s make this the mildest influenza season in memory by vaccinating more than any time in memory – and by doing so, we can hope to blunt medical care burdens despite ongoing COVID-19 disease.
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Kansas City (Mo.). Children’s Mercy receives funding from GlaxoSmithKline, Merck, and Pfizer for vaccine research studies on which Dr. Harrison is an investigator. Email him at [email protected].
References
1.. HCUP Statistical Brief #253. 2019 Oct.
2. medrxiv. 2020 Apr 10. doi: 10.1101/2020.04.07.20057299.
Addressing suicide prevention among South Asian Americans
Multifaceted strategies are needed to address unique cultural factors
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
Multifaceted strategies are needed to address unique cultural factors
Multifaceted strategies are needed to address unique cultural factors
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
On first glance, the age-adjusted rate of suicide for Asian and Pacific Islander populations living in the United States looks comparatively low.
Over the past 2 decades in the United States, for example, the overall rate increased by 35%, from, 10.5 to 14.2 per 100,000 individuals. That compares with a rate of 7.0 per 100,000 among Asian and Pacific Islander communities.1
However, because of the aggregate nature (national suicide mortality data combine people of Asian, Native Hawaiian, and other Pacific Islander descent into a single group) in which these data are reported, a significant amount of salient information on subgroups of Asian Americans is lost.2 There is a growing body of research on the mental health of Asian Americans, but the dearth of information and research on suicide in South Asians is striking.3 In fact, a review of literature finds fewer than 10 articles on the topic that have been published in peer-reviewed journals in the last decade. to provide effective, culturally sensitive care.
Diverse group
There are 3.4 million individuals of South Asian descent in the United States. Geographically, South Asians may have familial and cultural/historical roots in Bangladesh, Bhutan, India, Maldives, Nepal, and Pakistan.4 They enjoy a rich diversity in terms of cultural and religious beliefs, language, socioeconomic status, modes of acculturation, and immigration patterns. Asian Indians are the largest group of South Asians in the United States. They are highly educated, with a larger proportion of them pursuing an undergraduate and/or graduate level education than the general population. The median household income of Asian Indians is also higher than the national average.5
In general, suicide, like all mental health issues, is a stigmatized and taboo topic in the South Asian community.6 Also, South Asian Americans are hesitant to seek mental health care because of a perceived inability of Western health care professionals to understand their cultural views. Extrapolation from data on South Asians in the United Kingdom, aggregate statistics for Asian Americans and Pacific Islanders, and studies on South Asians in the United States highlight two South Asian subgroups that are particularly vulnerable to suicide. These are young adults (aged 18-24 years) and women.7
Suicide is the second-leading cause of death for young Asian American men in the United States. Rates of lifetime suicidal ideation and attempts are higher among younger Asian Americans (aged 18-24 years) than among older Asian American adults. Young Asian American adults have been found to have higher levels of suicidal ideation than their white counterparts.8,9 Acculturation or assimilating into a different culture, familial violence as a child, hopelessness or a thought pattern with a pessimistic outlook, depression, and childhood sexual abuse have all been found to be positively correlated with suicidal ideation and attempted suicide in South Asian Americans. One study that conducted0 in-group analysis on undergraduate university students of South Asian descent living in New York found higher levels of hopelessness and depression in Asian Indians relative to Bangladeshi or Pakistani Americans.10
In addition, higher levels of suicidal ideation are reported in Asian Indians relative to Bangladeshi or Pakistani Americans. These results resemble findings from similar studies in the United Kingdom. A posited reason for these findings is a difference in religious beliefs. Pakistani and Bangladeshi Americans are predominantly Muslim, have stronger moral beliefs against suicide, and consider it a sin as defined by Islamic beliefs. Asian Indians, in contrast, are majority Hindu and believe in reincarnation – a context that might make suicide seem more permissible.11
South Asian women are particularly vulnerable to domestic violence, childhood sexual abuse, intimate partner violence, and/or familial violence. Cultural gender norms, traditional norms, and patriarchal ideology in the South Asian community make quantifying the level of childhood sexual abuse and familial violence a challenge. Furthermore, culturally, South Asian women are often considered subordinate relative to men, and discussion around family violence and childhood sexual abuse is avoided. Studies from the United Kingdom find a lack of knowledge around, disclosure of, and fear of reporting childhood sexual abuse in South Asian women. A study of a sample of representative South Asian American women found that 25.2% had experienced some form of childhood sexual abuse.12
Research also suggests that South Asians in the United States have some of the highest rates of intimate partner violence. Another study in the United States found that two out of five South Asian women have experienced physical and/or sexual intimate partner violence. This is much higher than the rate found in representative general U.S. population samples.
Literature suggests that exposure to these factors increases womens’ risk for suicidal ideation and attempted suicide. In the United Kingdom, research on South Asian women (aged 18-24 years) has found rates of attempted suicide to be three times higher than those of their white counterparts. Research from the United Kingdom and the United States suggests that younger married South Asian women are exposed to emotional and/or physical abuse from their spouse or in-laws, which is often a mediating factor in their increased risk for suicide.
Attempts to address suicide in the South Asian American community have to be multifaceted. An ideal approach would consist of educating, and connecting with, the community through ethnic media and trusted community sources, such as primary care doctors, caregivers, and social workers. In line with established American Psychological Association guidelines on caring for individuals of immigrant origin, health care professionals should document the patient’s number of generations in the country, number of years in the country, language fluency, family and community support, educational level, social status changes related to immigration, intimate relationships with people of different backgrounds, and stress related to acculturation. Special attention should be paid to South Asian women. Health care professionals should screen South Asian women for past and current intimate partner violence, provide culturally appropriate intimate partner violence resources, and be prepared to refer them to legal counseling services. Also, South Asian women should be screened for a history of exposure to familial violence and childhood sexual abuse.1
To adequately serve this population, there is a need to build capacity in the provision of culturally appropriate mental health services. Access to mental health care professionals through settings such as shelters for abused women, South Asian community–based organizations, youth centers, college counseling, and senior centers would encourage individuals to seek care without the threat of being stigmatized.
References
1. Hedegaard H et al. Suicide mortality in the United States, 1999–2017. NCHS Data Brief, No. 330. 2018 Nov.
2. Ahmad-Stout DJ and Nath SR. J College Stud Psychother. 2013 Jan 10;27(1):43-61.
3. Li H and Keshavan M. Asian J Psychiatry. 2011;4(1):1.
4. Nagaraj NC et al. J Immigr Minor Health. 2019 Oct;21(5):978-1003.
5. Nagaraj NC et al. J Comm Health. 2018;43(3):543-51.
6. Cao KO. Generations. 2014;30(4):82-5.
7. Hurwitz EJ et al. J Immigr Minor Health. 2006;8(3):251-61.
8. Polanco-Roman L et al. Cultur Divers Ethnic Minor Psychol. 2019 Dec 23. doi: 10.1037/cpd0000313.
9. Erausquin JT et al. J Youth Adolesc. 2019 Sep;48(9):1796-1805.
10. Lane R et al. Asian Am J Psychol. 2016;7(2):120-8.
11. Nath SR et al. Asian Am J Psychol. 2018;9(4):334-343.
12. Robertson HA et al. J Immigr Minor Health. 2016 Jul 31;18(4):921-7.
Mr. Kaleka is a medical student in the class of 2021 at Central Michigan University (CMU) College of Medicine, Mt. Pleasant. He has no disclosures. Mr. Kaleka would like to thank his mentor, Furhut Janssen, DO, for her continued guidance and support in research on mental health in immigrant populations.
If you reopen it, will they come?
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
On April 16, the White House released federal guidelines for reopening American businesses – followed 3 days later by specific recommendations from the Centers for Medicare and Medicaid Services for .
Depending on where you live, you may have already reopened (or even never closed), or you may be awaiting the relaxation of restrictions in your state. (As I write this on June 10, the stay-at-home order in my state, New Jersey, is being rescinded.)
The big question, of course, is whether patients can be convinced that it is safe to leave their homes and come to your office. The answer may depend on how well you time your reopening and adhere to the appropriate federal, state, and independent guidelines.
The federal guidelines have three sections: criteria, which outline conditions each region or state should satisfy before reopening; preparedness, which lists how states should prepare for reopening; and phase guidelines, which detail responsibilities of individuals and employers during distinct reopening phases.
You should pay the most attention to the “criteria” section. The key question to ask: “Has my state or region satisfied the basic criteria for reopening?”
Those criteria are as follows:
- Symptoms reported within a 14-day period should be on a downward trajectory.
- Cases documented (or positive tests as a percentage of total tests) within a 14-day period should also be on a downward trajectory.
- Hospitals should be treating all patients without crisis care. They should also have a robust testing program in place for at-risk health care workers.
If your area meets these criteria, you can proceed to the CMS recommendations. They cover general advice related to personal protective equipment (PPE), workforce availability, facility considerations, sanitation protocols, supplies, and testing capacity.
The key takeaway: As long as your area has the resources to quickly respond to a surge of COVID-19 cases, you can start offering care to non-COVID patients. Keep seeing patients via telehealth as often as possible, and prioritize surgical/procedural care and high-complexity chronic disease management before moving on to preventive and cosmetic services.
The American Medical Association has issued its own checklist of criteria for reopening your practice to supplement the federal guidelines. Highlights include the following:
- Sit down with a calendar and pick an expected reopening day. Ideally, this should include a “soft reopening.” Make a plan to stock necessary PPE and write down plans for cleaning and staffing if an employee or patient is diagnosed with COVID-19 after visiting your office.
- Take a stepwise approach so you can identify challenges early and address them. It’s important to figure out which visits can continue via telehealth, and begin with just a few in-person visits each day. Plan out a schedule and clearly communicate it to patients, clinicians, and staff.
- Patient safety is your top concern. Encourage patients to visit without companions whenever possible, and of course, all individuals who visit the office should wear a cloth face covering.
- Screen employees for fevers and other symptoms of COVID-19; remember that those records are subject to HIPAA rules and must be kept confidential. Minimize contact between employees as much as possible.
- Do your best to screen patients before in-person visits, to verify they don’t have symptoms of COVID-19. Consider creating a script that office staff can use to contact patients 24 hours before they come in. Use this as a chance to ask about symptoms, and explain any reopening logistics they should know about.
- Contact your malpractice insurance carrier to discuss whether you need to make any changes to your coverage.
This would also be a great time to review your confidentiality, privacy, and data security protocols. COVID-19 presents new challenges for data privacy – for example, if you must inform coworkers or patients that they have come into contact with someone who tested positive. Make a plan that follows HIPAA guidelines during COVID-19. Also, make sure you have a plan for handling issues like paid sick leave or reporting COVID-19 cases to your local health department.
Another useful resource is the Medical Group Management Association’s COVID-19 Medical Practice Reopening Checklist. You can use it to confirm that you are addressing all the important items, and that you haven’t missed anything.
As for me, I am advising patients who are reluctant to seek treatment that many medical problems pose more risk than COVID-19, faster treatment means better outcomes, and because we maintain strict disinfection protocols, they are far less likely to be infected with COVID-19 in my office than, say, at a grocery store.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Surge in colonoscopies postponed by COVID-19 expected
An expected surge in the number of people seeking colonoscopy after the peak of the COVID-19 pandemic passes could cause physicians to rethink patient prioritization, could create a strain on endoscopy capacity, and might raise the specter of detecting colorectal cancer in more patients at a later stage of disease.

Furthermore, months of delay in diagnosis of colorectal cancer (CRC) could shorten survival, although more data is needed, according to expert analysis from a gastroenterologist, a medical oncologist, and a colorectal surgeon.
“It has been a big decrease in the number of colonoscopies performed at our hospital in Alicante, Spain,” Rodrigo Jover Martinez, MD, PhD, said during a COVID-19 and Digestive Health webinar presented by United European Gastroenterology (UEG). He estimated colonoscopy procedures are down 60%-90%, and the number of CRC surgeries has dropped by 60%. “As you know, the COVID-19 pandemic is hitting Europe hard.”
When patients do return, “the backlog will be huge ... in already exhausted endoscopy units,” predicted Dr. Martinez, a gastroenterologist at Hospital General Universitario in Alicante.
Multiple risks
Not knowing which patients with CRC will develop severe COVID-19 infection is another challenge, Bartomeu Massuti, MD, of the medical oncology service at the Hospital General Universitario de Alicante, said during the webinar.
Caution is warranted because “we know cancer patients have an increased risk of infection.” However, he added, most evidence supports an elevated risk for bacterial infections, not viral infections.
Therefore, physicians must continue to balance the risks associated with potential COVID-19 exposure against the risks associated with postponed treatment, Dr. Massuti said. “The goal of oncology care is to try to maintain the preplanned treatment and follow-up. We need mainly to avoid stopping or delaying treatment ... because we will lose efficacy in oncology disease outcomes.”
Imran Aslam, MD, PhD, a colorectal surgeon who moderated and presented during the webinar, agreed: “By delaying the treatment, we might do harm to our patients.”
Dr. Aslam cited data about clinical costs of delaying CRC surgery. A 2019 population-based study in PLOS ONE evaluated different times from diagnosis to treatment. The researchers found a delay of more than 150 days “significantly reduced survival, even during stage I, II, and III disease,” he said. The stage I hazard ratio was 2.66, compared with a reference HR of 1.00 for 90 days or fewer. They also reported elevated risk for people with stage II CRC (HR, 2.80), stage III CRC (HR, 2.70), and stage IV CRC (HR, 1.36).
“This could become more and more abysmal if the pandemic continues,” added Dr. Aslam, consultant colorectal surgeon at University Hospitals of Coventry and Warwickshire, England.
Prioritizing patients
Restarting endoscopy with prioritization strategies and increasing patient capacity are possible solutions. Dr. Martinez suggested a four-quadrant matrix in which physicians place patients into “now,” “next,” “delayed,” or “never” categories based on clinical indicators. The priority 1 “now” patients, for example, will be those with suspected CRC based on physical examination, imaging results, and/or an abnormal fecal immunochemical test result.
He suggested, furthermore, that more widespread CRC screening can resume once “endoscopy units have been alleviated of priority 1, symptomatic patients.”
Dr. Massuti concurred with Dr. Martinez’s call to prioritize patients carefully. He suggested a green, yellow, and red classification system based on treatment priority recommendations from the European Society for Medical Oncology. The green group, for example, should receive priority for intervention based on a condition that is immediately clinically unstable or life threatening.
“The main goal is to preserve the continuum of care,” he added.
Another concern – although data are limited – is that treatment might also increase risk of mortality among cancer patients with COVID-19, according to a cohort study of nearly 1,000 such patients reported May 2020 in The Lancet. Dr. Massuti, who was not affiliated with the research, noted that 12% of the patients had GI tumors. In addition to increased risk associated with male sex (odds ratio, 1.63), cytotoxic cancer treatment in the prior 4 weeks increased risk (OR, 1.47), as did surgery in the same time frame (OR, 1.52).
“This means patients on treatment have an increased risk of mortality,” Dr. Massuti said.
Moving forward
Implementing telehealth information and communication technologies will continue to grow in importance, Dr. Massuti said. Dr. Aslam noted that video consultation with patients before surgery is already replacing face-to-face interaction, and most follow-up care at his hospital is now done by telephone.
Postoperative care is just as essential in the COVID-19 era, if not more so. “We need to be very vigilant to manage postoperative complications – any symptoms of pyrexia or sepsis, or any sign of COVID,” Dr. Aslam said, including postoperative fever. “If there is any doubt, do a chest CT scan.”
Dr. Aslam predicted the time to perform endoscopy or surgery for each patient will be longer, “so the number of patients done in 1 day will be less than 4 months ago.” In addition, elective surgery patients at his institution undergo COVID-19 testing twice, 3 days apart, prior to intervention.
“This disease will continue in the community for a while, so we have to continue what we’ve done well, like social distancing,” Dr. Aslam said. “We’ve gone through a storm and we are awaiting a tsunami. That tsunami of patients will overwhelm us in the coming months.”
Dr. Martinez, Dr. Massuti, and Dr. Aslam had no relevant disclosures.
An expected surge in the number of people seeking colonoscopy after the peak of the COVID-19 pandemic passes could cause physicians to rethink patient prioritization, could create a strain on endoscopy capacity, and might raise the specter of detecting colorectal cancer in more patients at a later stage of disease.

Furthermore, months of delay in diagnosis of colorectal cancer (CRC) could shorten survival, although more data is needed, according to expert analysis from a gastroenterologist, a medical oncologist, and a colorectal surgeon.
“It has been a big decrease in the number of colonoscopies performed at our hospital in Alicante, Spain,” Rodrigo Jover Martinez, MD, PhD, said during a COVID-19 and Digestive Health webinar presented by United European Gastroenterology (UEG). He estimated colonoscopy procedures are down 60%-90%, and the number of CRC surgeries has dropped by 60%. “As you know, the COVID-19 pandemic is hitting Europe hard.”
When patients do return, “the backlog will be huge ... in already exhausted endoscopy units,” predicted Dr. Martinez, a gastroenterologist at Hospital General Universitario in Alicante.
Multiple risks
Not knowing which patients with CRC will develop severe COVID-19 infection is another challenge, Bartomeu Massuti, MD, of the medical oncology service at the Hospital General Universitario de Alicante, said during the webinar.
Caution is warranted because “we know cancer patients have an increased risk of infection.” However, he added, most evidence supports an elevated risk for bacterial infections, not viral infections.
Therefore, physicians must continue to balance the risks associated with potential COVID-19 exposure against the risks associated with postponed treatment, Dr. Massuti said. “The goal of oncology care is to try to maintain the preplanned treatment and follow-up. We need mainly to avoid stopping or delaying treatment ... because we will lose efficacy in oncology disease outcomes.”
Imran Aslam, MD, PhD, a colorectal surgeon who moderated and presented during the webinar, agreed: “By delaying the treatment, we might do harm to our patients.”
Dr. Aslam cited data about clinical costs of delaying CRC surgery. A 2019 population-based study in PLOS ONE evaluated different times from diagnosis to treatment. The researchers found a delay of more than 150 days “significantly reduced survival, even during stage I, II, and III disease,” he said. The stage I hazard ratio was 2.66, compared with a reference HR of 1.00 for 90 days or fewer. They also reported elevated risk for people with stage II CRC (HR, 2.80), stage III CRC (HR, 2.70), and stage IV CRC (HR, 1.36).
“This could become more and more abysmal if the pandemic continues,” added Dr. Aslam, consultant colorectal surgeon at University Hospitals of Coventry and Warwickshire, England.
Prioritizing patients
Restarting endoscopy with prioritization strategies and increasing patient capacity are possible solutions. Dr. Martinez suggested a four-quadrant matrix in which physicians place patients into “now,” “next,” “delayed,” or “never” categories based on clinical indicators. The priority 1 “now” patients, for example, will be those with suspected CRC based on physical examination, imaging results, and/or an abnormal fecal immunochemical test result.
He suggested, furthermore, that more widespread CRC screening can resume once “endoscopy units have been alleviated of priority 1, symptomatic patients.”
Dr. Massuti concurred with Dr. Martinez’s call to prioritize patients carefully. He suggested a green, yellow, and red classification system based on treatment priority recommendations from the European Society for Medical Oncology. The green group, for example, should receive priority for intervention based on a condition that is immediately clinically unstable or life threatening.
“The main goal is to preserve the continuum of care,” he added.
Another concern – although data are limited – is that treatment might also increase risk of mortality among cancer patients with COVID-19, according to a cohort study of nearly 1,000 such patients reported May 2020 in The Lancet. Dr. Massuti, who was not affiliated with the research, noted that 12% of the patients had GI tumors. In addition to increased risk associated with male sex (odds ratio, 1.63), cytotoxic cancer treatment in the prior 4 weeks increased risk (OR, 1.47), as did surgery in the same time frame (OR, 1.52).
“This means patients on treatment have an increased risk of mortality,” Dr. Massuti said.
Moving forward
Implementing telehealth information and communication technologies will continue to grow in importance, Dr. Massuti said. Dr. Aslam noted that video consultation with patients before surgery is already replacing face-to-face interaction, and most follow-up care at his hospital is now done by telephone.
Postoperative care is just as essential in the COVID-19 era, if not more so. “We need to be very vigilant to manage postoperative complications – any symptoms of pyrexia or sepsis, or any sign of COVID,” Dr. Aslam said, including postoperative fever. “If there is any doubt, do a chest CT scan.”
Dr. Aslam predicted the time to perform endoscopy or surgery for each patient will be longer, “so the number of patients done in 1 day will be less than 4 months ago.” In addition, elective surgery patients at his institution undergo COVID-19 testing twice, 3 days apart, prior to intervention.
“This disease will continue in the community for a while, so we have to continue what we’ve done well, like social distancing,” Dr. Aslam said. “We’ve gone through a storm and we are awaiting a tsunami. That tsunami of patients will overwhelm us in the coming months.”
Dr. Martinez, Dr. Massuti, and Dr. Aslam had no relevant disclosures.
An expected surge in the number of people seeking colonoscopy after the peak of the COVID-19 pandemic passes could cause physicians to rethink patient prioritization, could create a strain on endoscopy capacity, and might raise the specter of detecting colorectal cancer in more patients at a later stage of disease.

Furthermore, months of delay in diagnosis of colorectal cancer (CRC) could shorten survival, although more data is needed, according to expert analysis from a gastroenterologist, a medical oncologist, and a colorectal surgeon.
“It has been a big decrease in the number of colonoscopies performed at our hospital in Alicante, Spain,” Rodrigo Jover Martinez, MD, PhD, said during a COVID-19 and Digestive Health webinar presented by United European Gastroenterology (UEG). He estimated colonoscopy procedures are down 60%-90%, and the number of CRC surgeries has dropped by 60%. “As you know, the COVID-19 pandemic is hitting Europe hard.”
When patients do return, “the backlog will be huge ... in already exhausted endoscopy units,” predicted Dr. Martinez, a gastroenterologist at Hospital General Universitario in Alicante.
Multiple risks
Not knowing which patients with CRC will develop severe COVID-19 infection is another challenge, Bartomeu Massuti, MD, of the medical oncology service at the Hospital General Universitario de Alicante, said during the webinar.
Caution is warranted because “we know cancer patients have an increased risk of infection.” However, he added, most evidence supports an elevated risk for bacterial infections, not viral infections.
Therefore, physicians must continue to balance the risks associated with potential COVID-19 exposure against the risks associated with postponed treatment, Dr. Massuti said. “The goal of oncology care is to try to maintain the preplanned treatment and follow-up. We need mainly to avoid stopping or delaying treatment ... because we will lose efficacy in oncology disease outcomes.”
Imran Aslam, MD, PhD, a colorectal surgeon who moderated and presented during the webinar, agreed: “By delaying the treatment, we might do harm to our patients.”
Dr. Aslam cited data about clinical costs of delaying CRC surgery. A 2019 population-based study in PLOS ONE evaluated different times from diagnosis to treatment. The researchers found a delay of more than 150 days “significantly reduced survival, even during stage I, II, and III disease,” he said. The stage I hazard ratio was 2.66, compared with a reference HR of 1.00 for 90 days or fewer. They also reported elevated risk for people with stage II CRC (HR, 2.80), stage III CRC (HR, 2.70), and stage IV CRC (HR, 1.36).
“This could become more and more abysmal if the pandemic continues,” added Dr. Aslam, consultant colorectal surgeon at University Hospitals of Coventry and Warwickshire, England.
Prioritizing patients
Restarting endoscopy with prioritization strategies and increasing patient capacity are possible solutions. Dr. Martinez suggested a four-quadrant matrix in which physicians place patients into “now,” “next,” “delayed,” or “never” categories based on clinical indicators. The priority 1 “now” patients, for example, will be those with suspected CRC based on physical examination, imaging results, and/or an abnormal fecal immunochemical test result.
He suggested, furthermore, that more widespread CRC screening can resume once “endoscopy units have been alleviated of priority 1, symptomatic patients.”
Dr. Massuti concurred with Dr. Martinez’s call to prioritize patients carefully. He suggested a green, yellow, and red classification system based on treatment priority recommendations from the European Society for Medical Oncology. The green group, for example, should receive priority for intervention based on a condition that is immediately clinically unstable or life threatening.
“The main goal is to preserve the continuum of care,” he added.
Another concern – although data are limited – is that treatment might also increase risk of mortality among cancer patients with COVID-19, according to a cohort study of nearly 1,000 such patients reported May 2020 in The Lancet. Dr. Massuti, who was not affiliated with the research, noted that 12% of the patients had GI tumors. In addition to increased risk associated with male sex (odds ratio, 1.63), cytotoxic cancer treatment in the prior 4 weeks increased risk (OR, 1.47), as did surgery in the same time frame (OR, 1.52).
“This means patients on treatment have an increased risk of mortality,” Dr. Massuti said.
Moving forward
Implementing telehealth information and communication technologies will continue to grow in importance, Dr. Massuti said. Dr. Aslam noted that video consultation with patients before surgery is already replacing face-to-face interaction, and most follow-up care at his hospital is now done by telephone.
Postoperative care is just as essential in the COVID-19 era, if not more so. “We need to be very vigilant to manage postoperative complications – any symptoms of pyrexia or sepsis, or any sign of COVID,” Dr. Aslam said, including postoperative fever. “If there is any doubt, do a chest CT scan.”
Dr. Aslam predicted the time to perform endoscopy or surgery for each patient will be longer, “so the number of patients done in 1 day will be less than 4 months ago.” In addition, elective surgery patients at his institution undergo COVID-19 testing twice, 3 days apart, prior to intervention.
“This disease will continue in the community for a while, so we have to continue what we’ve done well, like social distancing,” Dr. Aslam said. “We’ve gone through a storm and we are awaiting a tsunami. That tsunami of patients will overwhelm us in the coming months.”
Dr. Martinez, Dr. Massuti, and Dr. Aslam had no relevant disclosures.
Time for grit and resilience
Grandma Exie used to tell a story about her grandmother on her father’s side, who lived in northeastern Arkansas. Towards the end of the Civil War, Northern and Southern troops were expected to “live off the land,” and both sides had torn through her poor dirt farm and carried off all the livestock and crops. The only thing they didn’t take was her bull mastiff, who was a pretty fair hunting and guard dog. Starving, she had no other option than to pack up and head east for Tennessee, where her husband was stationed with Joseph Hooker’s army. Many thousands of destitute women and children, most of whom were related to one of the troops, followed the army, where some of the army’s rations could be shared with them.
She headed out on foot and all went well until day 3 or so, when a panther attacked them, but she, armed with a branch, and her loyal dog were able to drive it off. The panther followed them for 3 days while she hid in a tree at night with her dog at the foot of a tree. Eventually, the panther gave up and she made it to Tennessee to safety.
Grandma Exie said her grandmother had “grit” and used this story whenever any of us would complain about how hard times were or how we were mistreated.
It is time for all of us to buck up and show a little grit in the face of a viral pandemic and social unrest. The answers are not easy or clear, but our health care system and our nation have faced much greater challenges. The 1918 flu pandemic was much more devastating, killing millions worldwide, and recall, 620,000 died in the Civil War, more than all other American wars combined. There is a deep seam of grit and resilience in Americans. We don’t always get it right immediately, but we usually do in the end.
The protests are justifiable outrage over police brutality, fueled by a high unemployment rate, both of which are a cause for frustration. The looting and destruction appears to be opportunistic thievery and some organized vandalization in my opinion. Most of the damage caused by riots and looting is not covered by insurance, and this will be a death blow to many small businesses already facing major financial setbacks as customers have stayed home for months and laying off staff has become necessary.
As for the impact on our practices, most physicians have been lucky and not been looted or burned out. In most of the country, the disease incidence has become lower, and the risk of not seeing the doctor is now greater than catching COVID-19.
So show grit, be careful, be vigilant, and practice your profession. Support your local small businesses, particularly if they have been the victims of senseless violence. We will work our way through these times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. He had no disclosures related to this column. Write to him at [email protected].
Grandma Exie used to tell a story about her grandmother on her father’s side, who lived in northeastern Arkansas. Towards the end of the Civil War, Northern and Southern troops were expected to “live off the land,” and both sides had torn through her poor dirt farm and carried off all the livestock and crops. The only thing they didn’t take was her bull mastiff, who was a pretty fair hunting and guard dog. Starving, she had no other option than to pack up and head east for Tennessee, where her husband was stationed with Joseph Hooker’s army. Many thousands of destitute women and children, most of whom were related to one of the troops, followed the army, where some of the army’s rations could be shared with them.
She headed out on foot and all went well until day 3 or so, when a panther attacked them, but she, armed with a branch, and her loyal dog were able to drive it off. The panther followed them for 3 days while she hid in a tree at night with her dog at the foot of a tree. Eventually, the panther gave up and she made it to Tennessee to safety.
Grandma Exie said her grandmother had “grit” and used this story whenever any of us would complain about how hard times were or how we were mistreated.
It is time for all of us to buck up and show a little grit in the face of a viral pandemic and social unrest. The answers are not easy or clear, but our health care system and our nation have faced much greater challenges. The 1918 flu pandemic was much more devastating, killing millions worldwide, and recall, 620,000 died in the Civil War, more than all other American wars combined. There is a deep seam of grit and resilience in Americans. We don’t always get it right immediately, but we usually do in the end.
The protests are justifiable outrage over police brutality, fueled by a high unemployment rate, both of which are a cause for frustration. The looting and destruction appears to be opportunistic thievery and some organized vandalization in my opinion. Most of the damage caused by riots and looting is not covered by insurance, and this will be a death blow to many small businesses already facing major financial setbacks as customers have stayed home for months and laying off staff has become necessary.
As for the impact on our practices, most physicians have been lucky and not been looted or burned out. In most of the country, the disease incidence has become lower, and the risk of not seeing the doctor is now greater than catching COVID-19.
So show grit, be careful, be vigilant, and practice your profession. Support your local small businesses, particularly if they have been the victims of senseless violence. We will work our way through these times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. He had no disclosures related to this column. Write to him at [email protected].
Grandma Exie used to tell a story about her grandmother on her father’s side, who lived in northeastern Arkansas. Towards the end of the Civil War, Northern and Southern troops were expected to “live off the land,” and both sides had torn through her poor dirt farm and carried off all the livestock and crops. The only thing they didn’t take was her bull mastiff, who was a pretty fair hunting and guard dog. Starving, she had no other option than to pack up and head east for Tennessee, where her husband was stationed with Joseph Hooker’s army. Many thousands of destitute women and children, most of whom were related to one of the troops, followed the army, where some of the army’s rations could be shared with them.
She headed out on foot and all went well until day 3 or so, when a panther attacked them, but she, armed with a branch, and her loyal dog were able to drive it off. The panther followed them for 3 days while she hid in a tree at night with her dog at the foot of a tree. Eventually, the panther gave up and she made it to Tennessee to safety.
Grandma Exie said her grandmother had “grit” and used this story whenever any of us would complain about how hard times were or how we were mistreated.
It is time for all of us to buck up and show a little grit in the face of a viral pandemic and social unrest. The answers are not easy or clear, but our health care system and our nation have faced much greater challenges. The 1918 flu pandemic was much more devastating, killing millions worldwide, and recall, 620,000 died in the Civil War, more than all other American wars combined. There is a deep seam of grit and resilience in Americans. We don’t always get it right immediately, but we usually do in the end.
The protests are justifiable outrage over police brutality, fueled by a high unemployment rate, both of which are a cause for frustration. The looting and destruction appears to be opportunistic thievery and some organized vandalization in my opinion. Most of the damage caused by riots and looting is not covered by insurance, and this will be a death blow to many small businesses already facing major financial setbacks as customers have stayed home for months and laying off staff has become necessary.
As for the impact on our practices, most physicians have been lucky and not been looted or burned out. In most of the country, the disease incidence has become lower, and the risk of not seeing the doctor is now greater than catching COVID-19.
So show grit, be careful, be vigilant, and practice your profession. Support your local small businesses, particularly if they have been the victims of senseless violence. We will work our way through these times.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. He had no disclosures related to this column. Write to him at [email protected].
The future of psychiatric diagnosis
Melissa R. Arbuckle, MD: Hi. I’m Dr. Melissa Arbuckle, vice chair for education and training in the Department of Psychiatry at Columbia University. I’m reporting on behalf of Medscape and our Columbia Psychiatry partnership. Today we’ll be discussing biomarkers with Dr. Jeffrey Lieberman. Welcome.
Jeffrey A. Lieberman, MD: Thanks, Melissa. Great to be here to talk about a subject that is near and dear to my heart.
Dr. Arbuckle: Dr. Lieberman is chair of the Department of Psychiatry at Columbia and is also director of the New York State Psychiatric Institute. Tell us about biomarkers and psychiatry, Dr Lieberman.
Dr. Lieberman: It would be nice if we had some! But first let me tell you what a biomarker is and what it would do for us. A biomarker is a biologic measure, a biologic feature, whether it’s blood pressure, pulse rate, an analyte in blood or cerebrospinal fluid, or a feature of an MRI or PET scan image of the brain that has diagnostic, prognostic, or theragnostic significance. A biomarker identifies an individual with symptoms of a specific disorder, indicates that they have this disorder, and can suggest a particular prognosis – less severe, more severe – or specify which treatment a person would likely respond to. For the entire history of our discipline, as long as physicians have studied mental illness, we have not had a diagnostic test for it. It’s a clinical diagnosis.
All illnesses in medicine began with clinical diagnosis: seizure disorder, epilepsy, was falling sickness; congestive heart failure was dropsy; for diabetes you tasted the urine to see if it was sweet or watery. But when we began to measure glucose and hemoglobin A1c, or when we developed the electrocardiogram to measure heart rhythms, and the electroencephalogram to measure brain activity, those were diagnostic tests based on biomarkers. We just don’t have them yet in psychiatry. The day we do have our first diagnostic tests, courtesy of a validated biomarker, will be a real milestone in the history of our profession.
Dr. Arbuckle: How far off might that be for psychiatry?
Dr. Lieberman: I’ve been in this profession for more than 30 years, and I’ve been saying for a while that it is coming soon. But we’re still waiting. Let me just add a cautionary note. Ever since psychiatry became scientifically minded and used scientific methodology and technology to understand the underpinnings of mental illness, there’s been an effort to identify biomarkers. It began in the 1960s with a series of false leads. There was something called the pink spot, as well as other metabolites, which were indicators on chromatographs linked to schizophrenia. This turned out to be wrong.
There was also the dexamethasone suppression test, to identify people who hypersecreted cortisol, which was believed to be diagnostic of depression. That turned out to be inadequate also.
There was the identification of genes beginning in the late 1980s. But the specific genes that indicated manic depressive illness and schizophrenia were not replicated. And now we know that the genetics of these disorders is polygenic and very complex.
So we cannot overpromise. I don’t want to say exactly when, but I will say that this is an area of intense research. There are a variety of different technologies that could yield this holy grail of diagnostic measures, including imaging measures such as MRI, PET, and nuclear medicine imaging, the use of genetics to create a polygenic risk score, and serologic analyses of blood to develop a panel of measures that may predict a specific condition or specific subtype of a condition.
It’s very likely, though, that we’ll not have a single pathognomonic test. I suspect that we’ll have several measures that, in combination, will be diagnostic or prognostic, in the same way that with cancer you have nomograms that give a prognosis. Or in the case of cardiovascular disease, where you have a lipid panel that takes into account a variety of lipid analytes to give you a risk score. I do believe that certainly within my professional lifetime, and hopefully sooner rather than later, we will see a diagnostic test.
Dr. Arbuckle: Given the different tests that did not pan out, what guidance can we offer clinicians as data come out and new potential biomarkers hit the media? How can we sift through what may or may not hold real promise?
Dr. Lieberman: I can tell practicing clinicians what not to do. Do not do what some of the charlatans in our field do. There are self-promoting psychiatrists out there who use SPECT scans to get a picture of the brain that is little more than pseudo color phrenology, and then they tell patients, “See this? This indicates that you have (this condition or that condition).” You can’t do that. Nothing we have now has that kind of validity or specificity.
However, even though a standard workup for an illness like schizophrenia does not require specific diagnostic tests, other than to rule out other conditions, imaging procedures can be useful additional information. For example, if you have an individual who presents with symptoms that meet criteria for schizophrenia and you obtain an MRI to rule out other possibilities, and the patient turns out to have dilated lateral ventricles or specific reductions in the size or distortions in the shape of certain temporal cortical structures, particularly in the hippocampus, that adds substance to your clinical diagnosis. So those kinds of things are useful. Similarly, with genetic testing, some institutions are now doing exome sequencing or whole genome sequencing that can provide a risk score. It adds something beyond a family history. These are not diagnostic, but they can add to your understanding.
Finally, with respect to schizophrenia and MRI in particular, if it does show structural abnormalities that are among the ones that have been reported for schizophrenia, this can be informative prognostically; such an individual may have a greater likelihood of having a chronic course with progression of the illness. And if that were my patient, I would be thinking that greater effort needs to be taken to ensure that the patient remains on treatment and does not suffer relapse.
Dr. Arbuckle: How do we prepare our trainees for a future of psychiatry with more biomarkers?
Dr. Lieberman: In medical school and postgraduate training, apart from understanding the method of diagnosis and the criteria for diagnoses, it’s important to understand the ancillary measures that are used in clinical medicine: blood testing, electrophysiologic measures, imaging procedures, neurocognitive testing, etc. This is a standard in terms of general medical training.
In terms of then applying it to mental illness and psychiatry, it’s a matter of knowing that these will be relevant at some point, staying apprised of the research literature that is generating data that pertain to the use of these measures for diagnostic, prognostic, or treatment-specific purposes, and then gauging how useful these will be. Right now, these measures are not required for diagnosis. They’re not validated sufficiently so that third-party payers will uniformly reimburse for them, but at some point they will be. Even before that time occurs, there are some measures that can be informative and enhance confidence in the diagnosis or add information about treatment response and outcome.
Dr. Arbuckle: We’re hearing about biotypes and how biotypes may not map to our current diagnostic systems. What are your thoughts about that?
Dr. Lieberman: You know, psychiatry has always been kind of the stepchild of medicine. And related to that, the Diagnostic and Statistical Manual of Mental Disorders (DSM) is the punching bag of the critics of psychiatry and the purported reason it hasn’t progressed faster. Sitting here at Columbia, the home of Robert Spitzer, who was the pioneer of the modern method of nosology that we still use in the DSM, it’s disappointing that we continue to lob tomatoes at this system, which is the best. It took psychiatry out of what was a dark age of clinical methodology and put it on solid scientific footing. That was in the late 1970s with [the development of] DSM-III.
And as much as we would like to have further progress, which would allow for not using a list of criteria in a menu-driven fashion to establish diagnoses, we’d like to have it be like a glucose tolerance test or an angiogram.
We’d like to do that, but we can’t yet. So there’s this aspirational desire to have something better, and this is permeating and motivating a lot of the research, which is good. But to claim that these don’t map to the current DSM and therefore invalidate the DSM-defined diagnoses is wrong and self-defeating. So if they don’t map to the current DSM diagnosis, is the diagnosis wrong or are the biotypes wrong? I believe it’s wishful thinking; individuals are trying to project their desires onto clinical practice, and it’s not desirable to do that. If there was anything that was an improvement on the DSM, it would have been incorporated into our practice.
The question about the limitations of DSM and the improved methods of neuroscientifically informed diagnostic systems was an issue that brought me into a confrontation with our former director of the National Institute of Mental Health (NIMH) in 2013.
After 5 years of the DSM task force laboring to revise the fifth edition of the DSM, as it was about to be launched, our former director, Tom Insel, disavowed it and proposed as a preferable alternative the research domains criteria (RDoC) system that was in development at the NIMH, which I believe epitomized this kind of sour grapes at what psychiatry didn’t have – an aspiration to have a more neuroscientifically informed diagnostic system. And as soon as he made the statement publicly, he had to walk it back because the RDoC system or any other system was not ready for prime time. It would have been a catastrophe if it would have been the one that informed clinical psychiatry. There was nothing that was superior to the DSM to be used at the time. This shows how frustration sometimes impels people to make rash statements.
We’re on the right track. Our field is progressing enormously, and one has to remember that everything that’s relevant in terms of being scientifically based and validated through empirical research in clinical psychiatry and mental illness has happened since the last half of the 20th century.
It is a very short period of time. We’ve made tremendous progress, and we’re continuing to make progress toward the milestone we’re all hoping for, where we have diagnostic tests. But we shouldn’t shortchange ourselves or underestimate the progress we have made in the meantime.
Dr. Arbuckle: This has been a great conversation. Signing off for Medscape and Columbia Psychiatry. Thank you.
Dr. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association. Dr. Arbuckle is vice chair for education and director of resident education in the Department of Psychiatry at Columbia University. She is particularly interested in the role of medical education in translating research into the practice of psychiatry.
This article first appeared on Medscape.com.
Melissa R. Arbuckle, MD: Hi. I’m Dr. Melissa Arbuckle, vice chair for education and training in the Department of Psychiatry at Columbia University. I’m reporting on behalf of Medscape and our Columbia Psychiatry partnership. Today we’ll be discussing biomarkers with Dr. Jeffrey Lieberman. Welcome.
Jeffrey A. Lieberman, MD: Thanks, Melissa. Great to be here to talk about a subject that is near and dear to my heart.
Dr. Arbuckle: Dr. Lieberman is chair of the Department of Psychiatry at Columbia and is also director of the New York State Psychiatric Institute. Tell us about biomarkers and psychiatry, Dr Lieberman.
Dr. Lieberman: It would be nice if we had some! But first let me tell you what a biomarker is and what it would do for us. A biomarker is a biologic measure, a biologic feature, whether it’s blood pressure, pulse rate, an analyte in blood or cerebrospinal fluid, or a feature of an MRI or PET scan image of the brain that has diagnostic, prognostic, or theragnostic significance. A biomarker identifies an individual with symptoms of a specific disorder, indicates that they have this disorder, and can suggest a particular prognosis – less severe, more severe – or specify which treatment a person would likely respond to. For the entire history of our discipline, as long as physicians have studied mental illness, we have not had a diagnostic test for it. It’s a clinical diagnosis.
All illnesses in medicine began with clinical diagnosis: seizure disorder, epilepsy, was falling sickness; congestive heart failure was dropsy; for diabetes you tasted the urine to see if it was sweet or watery. But when we began to measure glucose and hemoglobin A1c, or when we developed the electrocardiogram to measure heart rhythms, and the electroencephalogram to measure brain activity, those were diagnostic tests based on biomarkers. We just don’t have them yet in psychiatry. The day we do have our first diagnostic tests, courtesy of a validated biomarker, will be a real milestone in the history of our profession.
Dr. Arbuckle: How far off might that be for psychiatry?
Dr. Lieberman: I’ve been in this profession for more than 30 years, and I’ve been saying for a while that it is coming soon. But we’re still waiting. Let me just add a cautionary note. Ever since psychiatry became scientifically minded and used scientific methodology and technology to understand the underpinnings of mental illness, there’s been an effort to identify biomarkers. It began in the 1960s with a series of false leads. There was something called the pink spot, as well as other metabolites, which were indicators on chromatographs linked to schizophrenia. This turned out to be wrong.
There was also the dexamethasone suppression test, to identify people who hypersecreted cortisol, which was believed to be diagnostic of depression. That turned out to be inadequate also.
There was the identification of genes beginning in the late 1980s. But the specific genes that indicated manic depressive illness and schizophrenia were not replicated. And now we know that the genetics of these disorders is polygenic and very complex.
So we cannot overpromise. I don’t want to say exactly when, but I will say that this is an area of intense research. There are a variety of different technologies that could yield this holy grail of diagnostic measures, including imaging measures such as MRI, PET, and nuclear medicine imaging, the use of genetics to create a polygenic risk score, and serologic analyses of blood to develop a panel of measures that may predict a specific condition or specific subtype of a condition.
It’s very likely, though, that we’ll not have a single pathognomonic test. I suspect that we’ll have several measures that, in combination, will be diagnostic or prognostic, in the same way that with cancer you have nomograms that give a prognosis. Or in the case of cardiovascular disease, where you have a lipid panel that takes into account a variety of lipid analytes to give you a risk score. I do believe that certainly within my professional lifetime, and hopefully sooner rather than later, we will see a diagnostic test.
Dr. Arbuckle: Given the different tests that did not pan out, what guidance can we offer clinicians as data come out and new potential biomarkers hit the media? How can we sift through what may or may not hold real promise?
Dr. Lieberman: I can tell practicing clinicians what not to do. Do not do what some of the charlatans in our field do. There are self-promoting psychiatrists out there who use SPECT scans to get a picture of the brain that is little more than pseudo color phrenology, and then they tell patients, “See this? This indicates that you have (this condition or that condition).” You can’t do that. Nothing we have now has that kind of validity or specificity.
However, even though a standard workup for an illness like schizophrenia does not require specific diagnostic tests, other than to rule out other conditions, imaging procedures can be useful additional information. For example, if you have an individual who presents with symptoms that meet criteria for schizophrenia and you obtain an MRI to rule out other possibilities, and the patient turns out to have dilated lateral ventricles or specific reductions in the size or distortions in the shape of certain temporal cortical structures, particularly in the hippocampus, that adds substance to your clinical diagnosis. So those kinds of things are useful. Similarly, with genetic testing, some institutions are now doing exome sequencing or whole genome sequencing that can provide a risk score. It adds something beyond a family history. These are not diagnostic, but they can add to your understanding.
Finally, with respect to schizophrenia and MRI in particular, if it does show structural abnormalities that are among the ones that have been reported for schizophrenia, this can be informative prognostically; such an individual may have a greater likelihood of having a chronic course with progression of the illness. And if that were my patient, I would be thinking that greater effort needs to be taken to ensure that the patient remains on treatment and does not suffer relapse.
Dr. Arbuckle: How do we prepare our trainees for a future of psychiatry with more biomarkers?
Dr. Lieberman: In medical school and postgraduate training, apart from understanding the method of diagnosis and the criteria for diagnoses, it’s important to understand the ancillary measures that are used in clinical medicine: blood testing, electrophysiologic measures, imaging procedures, neurocognitive testing, etc. This is a standard in terms of general medical training.
In terms of then applying it to mental illness and psychiatry, it’s a matter of knowing that these will be relevant at some point, staying apprised of the research literature that is generating data that pertain to the use of these measures for diagnostic, prognostic, or treatment-specific purposes, and then gauging how useful these will be. Right now, these measures are not required for diagnosis. They’re not validated sufficiently so that third-party payers will uniformly reimburse for them, but at some point they will be. Even before that time occurs, there are some measures that can be informative and enhance confidence in the diagnosis or add information about treatment response and outcome.
Dr. Arbuckle: We’re hearing about biotypes and how biotypes may not map to our current diagnostic systems. What are your thoughts about that?
Dr. Lieberman: You know, psychiatry has always been kind of the stepchild of medicine. And related to that, the Diagnostic and Statistical Manual of Mental Disorders (DSM) is the punching bag of the critics of psychiatry and the purported reason it hasn’t progressed faster. Sitting here at Columbia, the home of Robert Spitzer, who was the pioneer of the modern method of nosology that we still use in the DSM, it’s disappointing that we continue to lob tomatoes at this system, which is the best. It took psychiatry out of what was a dark age of clinical methodology and put it on solid scientific footing. That was in the late 1970s with [the development of] DSM-III.
And as much as we would like to have further progress, which would allow for not using a list of criteria in a menu-driven fashion to establish diagnoses, we’d like to have it be like a glucose tolerance test or an angiogram.
We’d like to do that, but we can’t yet. So there’s this aspirational desire to have something better, and this is permeating and motivating a lot of the research, which is good. But to claim that these don’t map to the current DSM and therefore invalidate the DSM-defined diagnoses is wrong and self-defeating. So if they don’t map to the current DSM diagnosis, is the diagnosis wrong or are the biotypes wrong? I believe it’s wishful thinking; individuals are trying to project their desires onto clinical practice, and it’s not desirable to do that. If there was anything that was an improvement on the DSM, it would have been incorporated into our practice.
The question about the limitations of DSM and the improved methods of neuroscientifically informed diagnostic systems was an issue that brought me into a confrontation with our former director of the National Institute of Mental Health (NIMH) in 2013.
After 5 years of the DSM task force laboring to revise the fifth edition of the DSM, as it was about to be launched, our former director, Tom Insel, disavowed it and proposed as a preferable alternative the research domains criteria (RDoC) system that was in development at the NIMH, which I believe epitomized this kind of sour grapes at what psychiatry didn’t have – an aspiration to have a more neuroscientifically informed diagnostic system. And as soon as he made the statement publicly, he had to walk it back because the RDoC system or any other system was not ready for prime time. It would have been a catastrophe if it would have been the one that informed clinical psychiatry. There was nothing that was superior to the DSM to be used at the time. This shows how frustration sometimes impels people to make rash statements.
We’re on the right track. Our field is progressing enormously, and one has to remember that everything that’s relevant in terms of being scientifically based and validated through empirical research in clinical psychiatry and mental illness has happened since the last half of the 20th century.
It is a very short period of time. We’ve made tremendous progress, and we’re continuing to make progress toward the milestone we’re all hoping for, where we have diagnostic tests. But we shouldn’t shortchange ourselves or underestimate the progress we have made in the meantime.
Dr. Arbuckle: This has been a great conversation. Signing off for Medscape and Columbia Psychiatry. Thank you.
Dr. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association. Dr. Arbuckle is vice chair for education and director of resident education in the Department of Psychiatry at Columbia University. She is particularly interested in the role of medical education in translating research into the practice of psychiatry.
This article first appeared on Medscape.com.
Melissa R. Arbuckle, MD: Hi. I’m Dr. Melissa Arbuckle, vice chair for education and training in the Department of Psychiatry at Columbia University. I’m reporting on behalf of Medscape and our Columbia Psychiatry partnership. Today we’ll be discussing biomarkers with Dr. Jeffrey Lieberman. Welcome.
Jeffrey A. Lieberman, MD: Thanks, Melissa. Great to be here to talk about a subject that is near and dear to my heart.
Dr. Arbuckle: Dr. Lieberman is chair of the Department of Psychiatry at Columbia and is also director of the New York State Psychiatric Institute. Tell us about biomarkers and psychiatry, Dr Lieberman.
Dr. Lieberman: It would be nice if we had some! But first let me tell you what a biomarker is and what it would do for us. A biomarker is a biologic measure, a biologic feature, whether it’s blood pressure, pulse rate, an analyte in blood or cerebrospinal fluid, or a feature of an MRI or PET scan image of the brain that has diagnostic, prognostic, or theragnostic significance. A biomarker identifies an individual with symptoms of a specific disorder, indicates that they have this disorder, and can suggest a particular prognosis – less severe, more severe – or specify which treatment a person would likely respond to. For the entire history of our discipline, as long as physicians have studied mental illness, we have not had a diagnostic test for it. It’s a clinical diagnosis.
All illnesses in medicine began with clinical diagnosis: seizure disorder, epilepsy, was falling sickness; congestive heart failure was dropsy; for diabetes you tasted the urine to see if it was sweet or watery. But when we began to measure glucose and hemoglobin A1c, or when we developed the electrocardiogram to measure heart rhythms, and the electroencephalogram to measure brain activity, those were diagnostic tests based on biomarkers. We just don’t have them yet in psychiatry. The day we do have our first diagnostic tests, courtesy of a validated biomarker, will be a real milestone in the history of our profession.
Dr. Arbuckle: How far off might that be for psychiatry?
Dr. Lieberman: I’ve been in this profession for more than 30 years, and I’ve been saying for a while that it is coming soon. But we’re still waiting. Let me just add a cautionary note. Ever since psychiatry became scientifically minded and used scientific methodology and technology to understand the underpinnings of mental illness, there’s been an effort to identify biomarkers. It began in the 1960s with a series of false leads. There was something called the pink spot, as well as other metabolites, which were indicators on chromatographs linked to schizophrenia. This turned out to be wrong.
There was also the dexamethasone suppression test, to identify people who hypersecreted cortisol, which was believed to be diagnostic of depression. That turned out to be inadequate also.
There was the identification of genes beginning in the late 1980s. But the specific genes that indicated manic depressive illness and schizophrenia were not replicated. And now we know that the genetics of these disorders is polygenic and very complex.
So we cannot overpromise. I don’t want to say exactly when, but I will say that this is an area of intense research. There are a variety of different technologies that could yield this holy grail of diagnostic measures, including imaging measures such as MRI, PET, and nuclear medicine imaging, the use of genetics to create a polygenic risk score, and serologic analyses of blood to develop a panel of measures that may predict a specific condition or specific subtype of a condition.
It’s very likely, though, that we’ll not have a single pathognomonic test. I suspect that we’ll have several measures that, in combination, will be diagnostic or prognostic, in the same way that with cancer you have nomograms that give a prognosis. Or in the case of cardiovascular disease, where you have a lipid panel that takes into account a variety of lipid analytes to give you a risk score. I do believe that certainly within my professional lifetime, and hopefully sooner rather than later, we will see a diagnostic test.
Dr. Arbuckle: Given the different tests that did not pan out, what guidance can we offer clinicians as data come out and new potential biomarkers hit the media? How can we sift through what may or may not hold real promise?
Dr. Lieberman: I can tell practicing clinicians what not to do. Do not do what some of the charlatans in our field do. There are self-promoting psychiatrists out there who use SPECT scans to get a picture of the brain that is little more than pseudo color phrenology, and then they tell patients, “See this? This indicates that you have (this condition or that condition).” You can’t do that. Nothing we have now has that kind of validity or specificity.
However, even though a standard workup for an illness like schizophrenia does not require specific diagnostic tests, other than to rule out other conditions, imaging procedures can be useful additional information. For example, if you have an individual who presents with symptoms that meet criteria for schizophrenia and you obtain an MRI to rule out other possibilities, and the patient turns out to have dilated lateral ventricles or specific reductions in the size or distortions in the shape of certain temporal cortical structures, particularly in the hippocampus, that adds substance to your clinical diagnosis. So those kinds of things are useful. Similarly, with genetic testing, some institutions are now doing exome sequencing or whole genome sequencing that can provide a risk score. It adds something beyond a family history. These are not diagnostic, but they can add to your understanding.
Finally, with respect to schizophrenia and MRI in particular, if it does show structural abnormalities that are among the ones that have been reported for schizophrenia, this can be informative prognostically; such an individual may have a greater likelihood of having a chronic course with progression of the illness. And if that were my patient, I would be thinking that greater effort needs to be taken to ensure that the patient remains on treatment and does not suffer relapse.
Dr. Arbuckle: How do we prepare our trainees for a future of psychiatry with more biomarkers?
Dr. Lieberman: In medical school and postgraduate training, apart from understanding the method of diagnosis and the criteria for diagnoses, it’s important to understand the ancillary measures that are used in clinical medicine: blood testing, electrophysiologic measures, imaging procedures, neurocognitive testing, etc. This is a standard in terms of general medical training.
In terms of then applying it to mental illness and psychiatry, it’s a matter of knowing that these will be relevant at some point, staying apprised of the research literature that is generating data that pertain to the use of these measures for diagnostic, prognostic, or treatment-specific purposes, and then gauging how useful these will be. Right now, these measures are not required for diagnosis. They’re not validated sufficiently so that third-party payers will uniformly reimburse for them, but at some point they will be. Even before that time occurs, there are some measures that can be informative and enhance confidence in the diagnosis or add information about treatment response and outcome.
Dr. Arbuckle: We’re hearing about biotypes and how biotypes may not map to our current diagnostic systems. What are your thoughts about that?
Dr. Lieberman: You know, psychiatry has always been kind of the stepchild of medicine. And related to that, the Diagnostic and Statistical Manual of Mental Disorders (DSM) is the punching bag of the critics of psychiatry and the purported reason it hasn’t progressed faster. Sitting here at Columbia, the home of Robert Spitzer, who was the pioneer of the modern method of nosology that we still use in the DSM, it’s disappointing that we continue to lob tomatoes at this system, which is the best. It took psychiatry out of what was a dark age of clinical methodology and put it on solid scientific footing. That was in the late 1970s with [the development of] DSM-III.
And as much as we would like to have further progress, which would allow for not using a list of criteria in a menu-driven fashion to establish diagnoses, we’d like to have it be like a glucose tolerance test or an angiogram.
We’d like to do that, but we can’t yet. So there’s this aspirational desire to have something better, and this is permeating and motivating a lot of the research, which is good. But to claim that these don’t map to the current DSM and therefore invalidate the DSM-defined diagnoses is wrong and self-defeating. So if they don’t map to the current DSM diagnosis, is the diagnosis wrong or are the biotypes wrong? I believe it’s wishful thinking; individuals are trying to project their desires onto clinical practice, and it’s not desirable to do that. If there was anything that was an improvement on the DSM, it would have been incorporated into our practice.
The question about the limitations of DSM and the improved methods of neuroscientifically informed diagnostic systems was an issue that brought me into a confrontation with our former director of the National Institute of Mental Health (NIMH) in 2013.
After 5 years of the DSM task force laboring to revise the fifth edition of the DSM, as it was about to be launched, our former director, Tom Insel, disavowed it and proposed as a preferable alternative the research domains criteria (RDoC) system that was in development at the NIMH, which I believe epitomized this kind of sour grapes at what psychiatry didn’t have – an aspiration to have a more neuroscientifically informed diagnostic system. And as soon as he made the statement publicly, he had to walk it back because the RDoC system or any other system was not ready for prime time. It would have been a catastrophe if it would have been the one that informed clinical psychiatry. There was nothing that was superior to the DSM to be used at the time. This shows how frustration sometimes impels people to make rash statements.
We’re on the right track. Our field is progressing enormously, and one has to remember that everything that’s relevant in terms of being scientifically based and validated through empirical research in clinical psychiatry and mental illness has happened since the last half of the 20th century.
It is a very short period of time. We’ve made tremendous progress, and we’re continuing to make progress toward the milestone we’re all hoping for, where we have diagnostic tests. But we shouldn’t shortchange ourselves or underestimate the progress we have made in the meantime.
Dr. Arbuckle: This has been a great conversation. Signing off for Medscape and Columbia Psychiatry. Thank you.
Dr. Lieberman is chairman of the Department of Psychiatry at Columbia University. He is a former president of the American Psychiatric Association. Dr. Arbuckle is vice chair for education and director of resident education in the Department of Psychiatry at Columbia University. She is particularly interested in the role of medical education in translating research into the practice of psychiatry.
This article first appeared on Medscape.com.
Medical ethics in the time of COVID-19
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
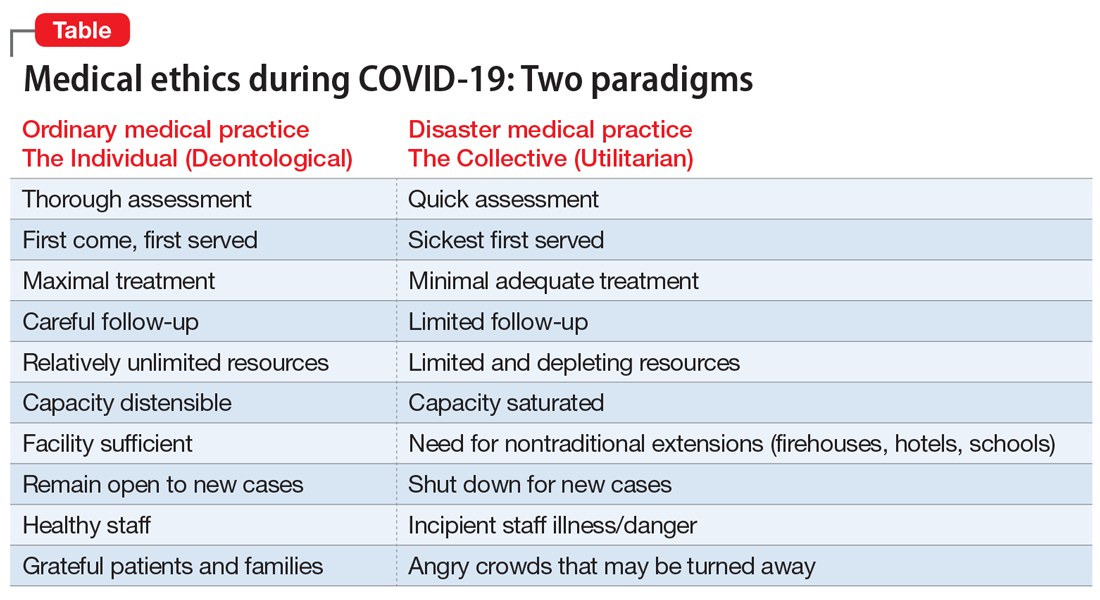
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
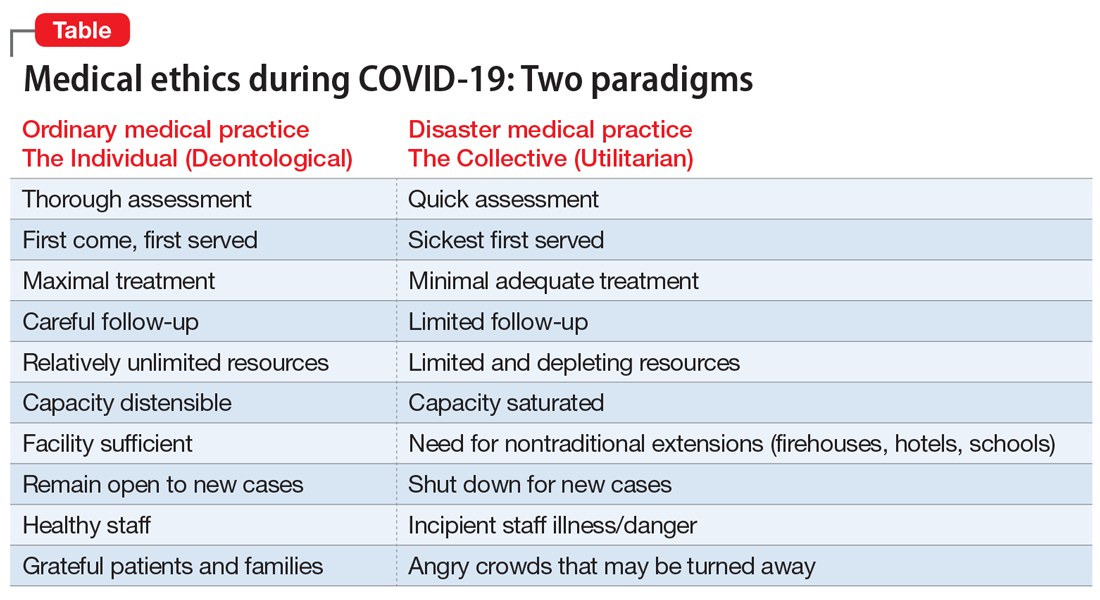
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
It is clear that the coronavirus 2019 disease (COVID-19) pandemic is one of the most extraordinary epochs of our professional and personal lives. Besides the challenges to the techniques and technologies of care for this illness, we are seeing challenges to the fundamentals of health care, both to the systems whereby it is delivered, and to the ethical principles that guide that delivery. There is unprecedented relevance of certain ethical issues in the practice of medicine, many of which have previously been discussed in classrooms and textbooks, but now are at play in daily practice, particularly at the frontlines of the war against COVID-19.1 In this article, I highlight several ethical dilemmas that are salient to these unique times. Some of the most compelling issues can be sorted into 2 clearly overlapping domains: triage ethics and equity ethics.
Triage ethics
In the areas most greatly affected by the COVID-19 pandemic, scarcity of treatment resources, such as ventilators, is a legitimate concern. French surgeon Dominique Jean Larry was the first to establish medical sorting protocols in the context of the battles of the Napoleonic wars, for which he used the French word triage, meaning “sorting.”2 He articulated 3 prognostic categories: 1) those who would die even with treatment, 2) those who would live without treatment, and 3) those who would die unless treated. Triage decisions arise in the context of insufficient resources, particularly space, staff, and supplies. Although usually identified with disasters, these decisions can arise in other contexts where personnel or technological resources are inadequate. Indeed, one of the first modern incarnations of triage ethics in American civilian life was in the early days of hemodialysis, when so-called “God committees” made complex decisions about which patients would be able to use this new, rare technology.3
Two fundamental moral constructs undergird medical ethics: deontological and utilitarian. The former, in which most clinicians traffic in ordinary practice, is driven by principles or moral rules such as the sanctity of life, the rule of fairness, and the principle of autonomy.4 They apply primarily in the context of treating an individual patient. The utilitarian way of reasoning is not as familiar to clinicians. It is focused on the broader context, the common good, the health of the group. It asks to calculate “the greatest good for the greatest number” as a means of navigating ethical dilemmas.5 The utilitarian perspective is far more familiar to policymakers, health care administrators, and public health professionals. It tends to be anathema to clinicians. However, disasters such as the COVID-19 pandemic ask some clinicians, particularly inpatient physicians, to shift from their usual deontological perspective to a utilitarian one, because triage ethics fundamentally draw on utilitarian reasoning. This can be quite anguishing to clinicians who typically work with individual patients in settings of more adequate, if not abundant, resources. What may feel wrong in a deontological mode can be seen as ethically right in a utilitarian framework.
The Table compares and contrasts these 2 paradigms and how they manifest in the clinical trenches, in a protracted health care crisis with limited resources.
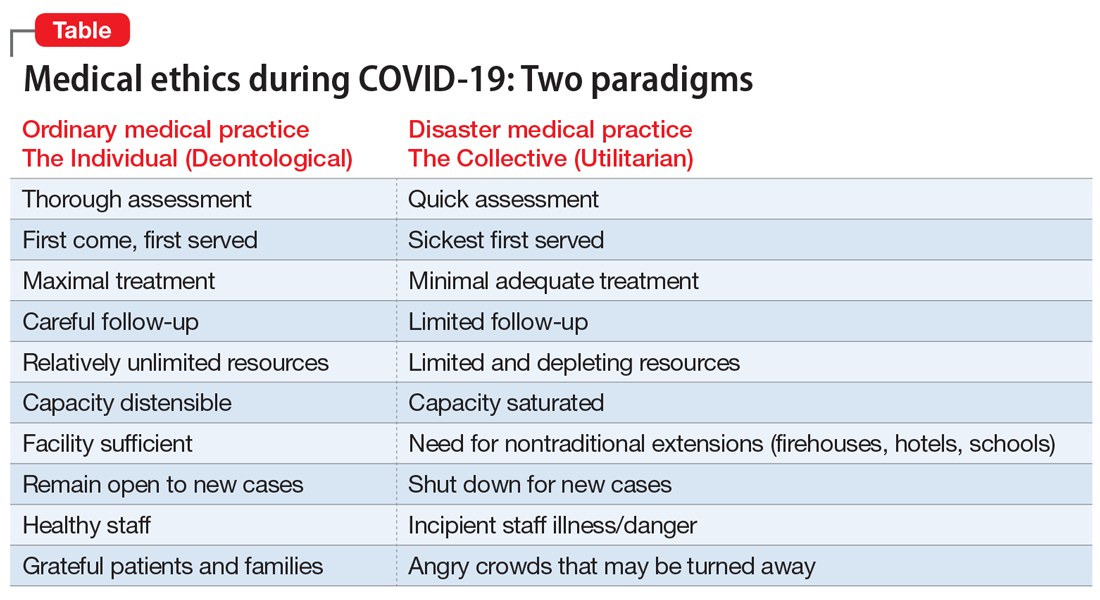
The COVID-19 crisis has produced an unprecedented and extended exposure of clinicians to triage situations in the face of limited resources such as ventilators, personnel, personal protective equipment, etc.6 Numerous possible approaches to deploying limited supplies are being considered. On what basis should such decisions be made? How can fairness be optimally manifest? Some possibilities include:
- first come, first served
- youngest first
- lottery
- short-term survivability
- long-term prognosis for quality of life
- value of a patient to the lives of others (eg, parents, health care workers, vaccine researchers).
One particularly interesting exploration of these questions was done in Maryland and reported in the “Maryland Framework for the Allocation of Scarce Life-sustaining Medical Resources in a Catastrophic Public Health Emergency.”7 This was the product of a multi-year consultation, ending in 2017, with several constituencies, including clinicians, politicians, hospital administrators, and members of the public brainstorming about approaches to allocating a hypothetical scarcity of ventilators. Interestingly, there was one broad consensus among these groups: a ventilator should not be withdrawn from a patient already using it to give to a “better” candidate who comes along later.
Some institutions have developed a method of making triage decisions that takes such decisions out of the hands of individual clinicians and instead assigns them to specialized “triage teams” made up of ethicists and clinicians experienced in critical care, to develop more distance from the emotions at the bedside. To minimize bias, such teams are often insulated from getting personal information about the patient, and receive only acute clinical information.8
Continue to: The pros and cons of these approaches...
The pros and cons of these approaches and the underlying ethical reasoning is beyond the scope of this overview. Policy documents from different states, regions, nations, and institutions have various approaches to making these choices. Presently, there is no coherent national or international agreement on triage ethics.9 It is important, however, that there be transparency in whatever approach an institution adopts for triage decisions.
Equity ethics
Though the equitable distribution of health care delivery has long been a concern, this problem has become magnified by the COVID-19 crisis. Race, sex, age, socioeconomic class, and type of illness have all been perennial sources of division between those who have better or worse access to health care and its outcomes. All of these distinctions have created differentials in rates of cases, hospitalizations, and deaths in the COVID-19 pandemic.10
The shifting of acute health care facilities to mostly COVID-19–related treatment, and postponing less critical and more “elective” care, creates a divide based on illness type. Many facilities have stopped taking admissions for other kinds of cases. This is particularly relevant to psychiatric units, many of which have had to decrease their bed capacities to make all rooms private, and limit their usual treatments offered to inpatients.11 Many long-term units, such as at state hospitals, are closing to new admissions. Many day hospitals and intensive outpatient programs remain closed, not even shifting to telehealth. In areas most affected by COVID-19, some institutions have closed psychiatric wards and reallocated psychiatrists to cover some of the medical units. So the availability of the more intensive, institutionally-based levels of care is significantly reduced, particularly for psychiatric patients.12 These patients already are a disadvantaged population in the distribution of health care resources, and the care of individuals with serious mental illness is more likely to be seen as “nonessential” in this time of suddenly scarcer institutional resources.
One of the cherished ethical values in health care is autonomy, and in a deontological triage environment, honoring patient autonomy is carefully and tenderly administered. However, in a utilitarian-driven triage environment, considerations of the common good can trump autonomy, even in subtle ways that create inequities. Clinicians have been advised to have more frank conversations with patients, particularly those with chronic illnesses, stepping up initiatives to make advanced directives during this crisis, explicitly reminding patients that there may not be enough ventilators for all who need one.13 Some have argued that such physician-initiated conversations can be inherently coercive, making these decisions not as autonomous as it may appear, similar to physicians suggesting medical euthanasia as an option.14 Interestingly, some jurisdictions that offer euthanasia have been suspending such services during the COVID-19 crisis.15 Some hospitals have even wrestled with the possibility that all COVID-19 admissions should be considered “do not resuscitate,” especially because cardiopulmonary resuscitation significantly elevates the risks of viral exposure for the treatment team.16,17 A more explicit example of how current standards protecting patient autonomy may be challenged is patients who are admitted involuntarily to a psychiatric unit. These are patients whose presumptively impaired autonomy is already being overridden by the involuntary nature of the admission. If a psychiatric unit requires admissions to be COVID-19–negative, and if patients refuse COVID-19 testing, should the testing be forced upon them to protect the entire milieu?
Many ethicists are highlighting the embedded equity bias known as “ableism” inherent in triage decisions—implicitly disfavoring resources for patients with COVID-19 who are already physically or intellectually disabled, chronically ill, aged, homeless, psychosocially low functioning, etc.18 Without explicit protections for individuals who are chronically disabled, triage decisions unguided by policy safeguards may reflexively favor the more “abled.” This bias towards the more abled is often inherent in how difficult it is to access health care. It can also be manifested in bedside triage decisions made in the moment by individual clinicians. Many disability rights advocates have been sounding this alarm during the COVID-19 crisis.19
Continue to: A special circumstance of equity...
A special circumstance of equity is arising during this ongoing pandemic—the possibility of treating health care workers as a privileged class. Unlike typical disasters, where health care workers come in afterwards, and therefore are in relatively less danger, pandemics create particularly high risks of danger for such individuals, with repeated exposure to the virus. They are both responders and potential victims. Should they have higher priority for ventilators, vaccines, funding, etc?6 This is a more robust degree of compensatory justice than merely giving appreciation. Giving health care workers such advantages may seem intuitively appealing, but perhaps professionalism and the self-obligation of duty mitigates such claims.20
A unique opportunity
The magnitude and pervasiveness of this pandemic crisis is unique in our lifetimes, as both professionals and as citizens. In the crucible of this extraordinary time, these and other medical ethics dilemmas burn hotter than ever before. Different societies and institutions may come up with different answers, based on their cultures and values. It is important, however, that the venerable ethos of medical ethics, which has evolved through the millennia, codified in oaths, codes, and scholarship, can be a compass at the bedside and in the meetings of legislatures, leaders, and policymakers. Perhaps we can emerge from this time with more clarity about how to balance the preciousness of individual rights with the needs of the common good.
Bottom Line
The coronavirus disease 2019 (COVID-19) pandemic has brought increased attention to triage ethics and equity ethics. There is no coherent national or international agreement on how to best deploy limited supplies such as ventilators and personal protective equipment. Although the equitable distribution of health care delivery has long been a concern, this problem has become magnified by COVID-19. Clinicians may be asked to view health care through the less familiar lens of the common good, as opposed to focusing strictly on an individual patient.
Related Resources
- Johns Hopkins Berman Institute of Bioethics. Coronavirus ethics and policy insights and resources. https://bioethics.jhu.edu/research-and-outreach/covid-19-bioethics-expert-insights/.
- Daugherty-Biddison L, Gwon H, Regenberg A, et al. Maryland framework for the allocation of scarce lifesustaining medical resources in a catastrophic public health emergency. www.law.umaryland.edu/media/SOL/pdfs/Programs/Health-Law/MHECN/ASR%20Framework_Final.pdf.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.
1. AMA Journal of Ethics. COVID-19 ethics resource center. https://journalofethics.ama-assn.org/COVID-19-ethics-resource-center. Updated May 2020. Accessed May 26, 2020.
2. Skandakalis PN, Lainas P, Zoras O, et al. “To afford the wounded speedy assistance”: Dominique Jean Larrey and Napoleon. World J Surg. 2006;30(8):1392-1399.
3. Ross W. God panels and the history of hemodialysis in America: a cautionary tale. Virtual Mentor. 2012;14(11):890-896.
4. Alexander L, Moore M. Deontological ethics. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/ethics-deontological/. Revised October 17, 2016. Accessed May 26, 2020.
5. Driver J. The history of utilitarianism. In: Zalta EN, ed. Stanford encyclopedia of philosophy. https://plato.stanford.edu/entries/utilitarianism-history/. Revised September 22, 2014. Accessed May 26, 2020.
6. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020;382(21):2049-2055.
7. Daugherty-Biddison EL, Faden R, Gwon HW, et al. Too many patients…a framework to guide statewide allocation of scarce mechanical ventilation during disasters. Chest. 2019;155(4):848-854.
8. Dudzinski D, Campelia G, Brazg T. Pandemic resources including COVID-19 materials. Department of Bioethics and Humanities, University of Washington Medicine. http://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/detail/245. Published April 6, 2020. Accessed May 26, 2020.
9. Antommaria AHM, Gibb TS, McGuire AL, et al; Task Force of the Association of Bioethics Program Directors. Ventilator triage policies during the COVID-19 pandemic at U.S. hospitals associated with members of the Association of Bioethics Program Directors [published online April 24, 2020]. Ann Intern Med. 2020;M20-1738. doi: 10.7326/M20-1738.
10. Cooney E. Who gets hospitalized for COVID-19? Report shows differences by race and sex. STAT. https://www.statnews.com/2020/04/09/hospitalized-COVID-19-patients-differences-by-race-and-sex/. Published April 9, 2020. Accessed May 26, 2020.
11. Gessen M. Why psychiatric wards are uniquely vulnerable to the coronavirus. The New Yorker. https://www.newyorker.com/news/news-desk/why-psychiatric-wards-are-uniquely-vulnerable-to-the-coronavirus. Published April 21, 2020. Accessed May 26, 2020.
12. American Psychiatric Association Ethics Committee. COVID-19 related opinions of the APA Ethics Committee. American Psychiatric Association. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/Ethics/APA-COVID-19-Ethics-Opinions.pdf. Published May 5, 2020. Accessed May 26, 2020.
13. Wee M. Coronavirus and the misuse of ‘do not resuscitate’ orders. The Spectator. https://www.spectator.co.uk/article/coronavirus-and-the-misuse-of-do-not-resuscitate-orders. Published May 6, 2020. Accessed May 26, 2020.
14. Prokopetz JZ, Lehmann LS. Redefining physicians’ role in assisted dying. N Engl J Med. 2012;367(20):97-99.
15. Yuill K, Boer T. What COVID-19 has revealed about euthanasia. spiked. https://www.spiked-online.com/2020/04/14/COVID-19-has-revealed-the-ugliness-of-euthanasia/. Published April 14, 2020. Accessed May 26, 2020.
16. Plunkett AJ. COVID-19: hospitals should consider CoP carefully before deciding on DNR policy. PSQH. https://www.psqh.com/news/COVID-19-hospitals-should-consider-cop-carefully-before-deciding-on-dnr-policy/. Published March 26, 2020. Accessed May 26, 2020.
17. Kramer DB, Lo B, Dickert NW. CPR in the COVID-19 era: an ethical framework [published online May 6, 2020]. N Engl J Med. doi: 10.1056/NEJMp2010758.
18. Mykitiuk R, Lemmens T. Assessing the value of a life: COVID-19 triage orders mustn’t work against those with disabilities. CBC News. https://www.cbc.ca/news/opinion/opinion-disabled-COVID-19-triage-orders-1.5532137. Published April 19, 2020. Accessed May 26, 2020.
19. Solomon MZ, Wynia MK, Gostin LO. COVID-19 crisis triage—optimizing health outcomes and disability rights [published online May 19, 2020]. N Engl J Med. doi: 10.1056/NEJMp2008300.
20. Appel JM. Ethics consult: who’s first to get COVID-19 Vax? MD/JD bangs gavel. MedPage Today. https://www.medpagetoday.com/infectiousdisease/COVID19/86260. Published May 1, 2020. Accessed May 26, 2020.
Kids with food allergies the newest victims of COVID-19?
Food insecurity is not knowing how you will get your next meal. This pandemic has led to a lot of it, especially as a result of massive unemployment. Now imagine being in that situation with a food-allergic child. It would be frightening.
There is always a level of anxiety for parents of food-allergic children, but the Food and Drug Administration–mandated labeling of food allergens has helped to allay some of those concerns. Shopping can feel safer, even if it’s not foolproof.
Now, that fear for the safety of food-allergic children is going to be compounded by the FDA’s latest announcement, made at the behest of the food industry.
Disruptions in the food supply chain caused by the COVID-19 pandemic have created some problems for the food industry. The industry sought – and received – relief from the FDA; they are now allowing some ingredient substitutions without mandating a change in labeling. These changes were made without opportunity for public comment, according to the FDA, because of the exigency of the situation. Furthermore, the changes may stay in effect for an indeterminate period of time after the pandemic is deemed under control.
Labeling of gluten and the major eight allergens (peanuts, tree nuts, milk, eggs, soy, wheat, fish, and crustacean shellfish) cannot change under the new guidelines. The FDA also advised “consideration” of major food allergens recognized in other countries (sesame, celery, lupin, buckwheat, molluscan shellfish, and mustard). Of these, lupin is known to cross-react with peanut, and sesame seed allergy is increasingly prevalent. In fact, the FDA has considered adding it to the list of major allergens.
Meanwhile, according to this temporary FDA policy, substitutions should be limited to no more than 2% of the weight of the final product unless it is a variety of the same ingredient. The example provided is substitution of one type of mushroom for another, but even that could be an issue for the rare patient. And what if this is misinterpreted – as will surely happen somewhere – and one seed is substituted for another?
A friend of mine is a pediatrician and mother of a child who is allergic to sesame, peanuts, tree nuts, and garbanzo beans. Naturally, she had grave concerns about these changes. She also wondered what the liability would be for the food manufacturing company in the current situation despite the FDA notice, which seems like a valid point. It is worth noting that, at the very top of this FDA notice, are the words “contains nonbinding recommendations,” so manufacturers may want to think twice about how they approach this. A minority of companies have pledged to relabel foods if necessary. Meanwhile, without any alert in advance, it is now up to patients and their physicians to sort out the attendant risks.
The FDA should have advised or mandated that food manufacturers give notice to online and physical retailers of ingredient changes. A simple sign in front of a display or alert online would be a very reasonable solution and pose no burden to those involved. It should be self-evident that mistakes always happen, especially under duress, and that the loosening of these regulations will have unintended consequences. To the severe problem of food insecurity, we can add one more concern for the parents of allergic children: food-allergen insecurity.
A version of this article originally appeared on Medscape.com.
Food insecurity is not knowing how you will get your next meal. This pandemic has led to a lot of it, especially as a result of massive unemployment. Now imagine being in that situation with a food-allergic child. It would be frightening.
There is always a level of anxiety for parents of food-allergic children, but the Food and Drug Administration–mandated labeling of food allergens has helped to allay some of those concerns. Shopping can feel safer, even if it’s not foolproof.
Now, that fear for the safety of food-allergic children is going to be compounded by the FDA’s latest announcement, made at the behest of the food industry.
Disruptions in the food supply chain caused by the COVID-19 pandemic have created some problems for the food industry. The industry sought – and received – relief from the FDA; they are now allowing some ingredient substitutions without mandating a change in labeling. These changes were made without opportunity for public comment, according to the FDA, because of the exigency of the situation. Furthermore, the changes may stay in effect for an indeterminate period of time after the pandemic is deemed under control.
Labeling of gluten and the major eight allergens (peanuts, tree nuts, milk, eggs, soy, wheat, fish, and crustacean shellfish) cannot change under the new guidelines. The FDA also advised “consideration” of major food allergens recognized in other countries (sesame, celery, lupin, buckwheat, molluscan shellfish, and mustard). Of these, lupin is known to cross-react with peanut, and sesame seed allergy is increasingly prevalent. In fact, the FDA has considered adding it to the list of major allergens.
Meanwhile, according to this temporary FDA policy, substitutions should be limited to no more than 2% of the weight of the final product unless it is a variety of the same ingredient. The example provided is substitution of one type of mushroom for another, but even that could be an issue for the rare patient. And what if this is misinterpreted – as will surely happen somewhere – and one seed is substituted for another?
A friend of mine is a pediatrician and mother of a child who is allergic to sesame, peanuts, tree nuts, and garbanzo beans. Naturally, she had grave concerns about these changes. She also wondered what the liability would be for the food manufacturing company in the current situation despite the FDA notice, which seems like a valid point. It is worth noting that, at the very top of this FDA notice, are the words “contains nonbinding recommendations,” so manufacturers may want to think twice about how they approach this. A minority of companies have pledged to relabel foods if necessary. Meanwhile, without any alert in advance, it is now up to patients and their physicians to sort out the attendant risks.
The FDA should have advised or mandated that food manufacturers give notice to online and physical retailers of ingredient changes. A simple sign in front of a display or alert online would be a very reasonable solution and pose no burden to those involved. It should be self-evident that mistakes always happen, especially under duress, and that the loosening of these regulations will have unintended consequences. To the severe problem of food insecurity, we can add one more concern for the parents of allergic children: food-allergen insecurity.
A version of this article originally appeared on Medscape.com.
Food insecurity is not knowing how you will get your next meal. This pandemic has led to a lot of it, especially as a result of massive unemployment. Now imagine being in that situation with a food-allergic child. It would be frightening.
There is always a level of anxiety for parents of food-allergic children, but the Food and Drug Administration–mandated labeling of food allergens has helped to allay some of those concerns. Shopping can feel safer, even if it’s not foolproof.
Now, that fear for the safety of food-allergic children is going to be compounded by the FDA’s latest announcement, made at the behest of the food industry.
Disruptions in the food supply chain caused by the COVID-19 pandemic have created some problems for the food industry. The industry sought – and received – relief from the FDA; they are now allowing some ingredient substitutions without mandating a change in labeling. These changes were made without opportunity for public comment, according to the FDA, because of the exigency of the situation. Furthermore, the changes may stay in effect for an indeterminate period of time after the pandemic is deemed under control.
Labeling of gluten and the major eight allergens (peanuts, tree nuts, milk, eggs, soy, wheat, fish, and crustacean shellfish) cannot change under the new guidelines. The FDA also advised “consideration” of major food allergens recognized in other countries (sesame, celery, lupin, buckwheat, molluscan shellfish, and mustard). Of these, lupin is known to cross-react with peanut, and sesame seed allergy is increasingly prevalent. In fact, the FDA has considered adding it to the list of major allergens.
Meanwhile, according to this temporary FDA policy, substitutions should be limited to no more than 2% of the weight of the final product unless it is a variety of the same ingredient. The example provided is substitution of one type of mushroom for another, but even that could be an issue for the rare patient. And what if this is misinterpreted – as will surely happen somewhere – and one seed is substituted for another?
A friend of mine is a pediatrician and mother of a child who is allergic to sesame, peanuts, tree nuts, and garbanzo beans. Naturally, she had grave concerns about these changes. She also wondered what the liability would be for the food manufacturing company in the current situation despite the FDA notice, which seems like a valid point. It is worth noting that, at the very top of this FDA notice, are the words “contains nonbinding recommendations,” so manufacturers may want to think twice about how they approach this. A minority of companies have pledged to relabel foods if necessary. Meanwhile, without any alert in advance, it is now up to patients and their physicians to sort out the attendant risks.
The FDA should have advised or mandated that food manufacturers give notice to online and physical retailers of ingredient changes. A simple sign in front of a display or alert online would be a very reasonable solution and pose no burden to those involved. It should be self-evident that mistakes always happen, especially under duress, and that the loosening of these regulations will have unintended consequences. To the severe problem of food insecurity, we can add one more concern for the parents of allergic children: food-allergen insecurity.
A version of this article originally appeared on Medscape.com.
Human sitters in the COVID era
Data collection needed for care of suicidal hospitalized patients
I am writing this commentary to bring to readers’ attention a medical and ethical complexity related to human sitters for presumably suicidal, COVID-19–positive hospitalized patients.
To shape and bundle the ethics issues addressed here into a single question, I offer the following: Should policies and practices requiring that patients in presumed need of a sitter because of assessed suicidality change when the patient is COVID-19–positive? Although the analysis might be similar when a sitter is monitoring a Patient Under Investigation (PUI), here I focus only on COVID-19–positive patients. Similarly, there are other reasons for sitters, of course, such as to prevent elopement, or, if a patient is in restraints, to prevent the patient from pulling out lines or tubes. Again, discussion of some of these ethical complications is beyond the scope of this piece. Just considering the matter of potential suicidality and sitters is complex enough. And so, to start, I sought out existing sources for guidance.
In looking for such sources, I first turned to the Centers for Medicare and Medicaid Services before COVID-19. CMS has required that there be a sitter for a patient who is suicidal and that the sitter remain in the room so that the sitter can intervene expeditiously if the patient tries to hurt himself or herself. There has been no change in this guidance since the COVID-19 pandemic in the United States. To the best of my knowledge, there is no substantive guidance for protecting sitters from contagion other than PPE. Given this, it begs the question:
In my hospital, I already have begun discussing the potential risks of harm and potential benefits to our suicidal patients of having a sitter directly outside the patient’s room. I also have considered whether to have one sitter watching several room cameras at once, commonly referred to as “telehealth strategies.”
To be sure, sitting for hours in the room of a COVID-19–positive patient is onerous. The sitter is required to be in full PPE (N-95 mask, gown, and gloves), which is hot and uncomfortable. Current practice is resource intensive in other ways. It requires changing out the sitter every 2 hours, which uses substantial amounts of PPE and multiple sitters.
Regardless, however, there are really no data upon which to base any sound ethics judgment about what should or should not be tried. We just have no information on how to attempt to balance potential risks and prospects for the benefit of whom and when. And, given that good clinical ethics always begin with the facts, I write this piece to see whether readers have thought about these issues before – and whether any of clinicians have started collecting the valuable data needed to begin making sound ethical judgments about how to care for our presumably suicidal COVID-19–positive patients and the sitters who watch over them.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
This column is an outcome of a discussion that occurred during Psych/Ethics rounds on June 5, and does not represent any official statements of Medstar Washington Hospital Center or any entity of the MedStar Corp. Dr. Ritchie would like to thank Evan G. DeRenzo, PhD, of the John J. Lynch Center for Ethics, for her thoughtful review of a previous draft of this commentary.
Data collection needed for care of suicidal hospitalized patients
Data collection needed for care of suicidal hospitalized patients
I am writing this commentary to bring to readers’ attention a medical and ethical complexity related to human sitters for presumably suicidal, COVID-19–positive hospitalized patients.
To shape and bundle the ethics issues addressed here into a single question, I offer the following: Should policies and practices requiring that patients in presumed need of a sitter because of assessed suicidality change when the patient is COVID-19–positive? Although the analysis might be similar when a sitter is monitoring a Patient Under Investigation (PUI), here I focus only on COVID-19–positive patients. Similarly, there are other reasons for sitters, of course, such as to prevent elopement, or, if a patient is in restraints, to prevent the patient from pulling out lines or tubes. Again, discussion of some of these ethical complications is beyond the scope of this piece. Just considering the matter of potential suicidality and sitters is complex enough. And so, to start, I sought out existing sources for guidance.
In looking for such sources, I first turned to the Centers for Medicare and Medicaid Services before COVID-19. CMS has required that there be a sitter for a patient who is suicidal and that the sitter remain in the room so that the sitter can intervene expeditiously if the patient tries to hurt himself or herself. There has been no change in this guidance since the COVID-19 pandemic in the United States. To the best of my knowledge, there is no substantive guidance for protecting sitters from contagion other than PPE. Given this, it begs the question:
In my hospital, I already have begun discussing the potential risks of harm and potential benefits to our suicidal patients of having a sitter directly outside the patient’s room. I also have considered whether to have one sitter watching several room cameras at once, commonly referred to as “telehealth strategies.”
To be sure, sitting for hours in the room of a COVID-19–positive patient is onerous. The sitter is required to be in full PPE (N-95 mask, gown, and gloves), which is hot and uncomfortable. Current practice is resource intensive in other ways. It requires changing out the sitter every 2 hours, which uses substantial amounts of PPE and multiple sitters.
Regardless, however, there are really no data upon which to base any sound ethics judgment about what should or should not be tried. We just have no information on how to attempt to balance potential risks and prospects for the benefit of whom and when. And, given that good clinical ethics always begin with the facts, I write this piece to see whether readers have thought about these issues before – and whether any of clinicians have started collecting the valuable data needed to begin making sound ethical judgments about how to care for our presumably suicidal COVID-19–positive patients and the sitters who watch over them.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
This column is an outcome of a discussion that occurred during Psych/Ethics rounds on June 5, and does not represent any official statements of Medstar Washington Hospital Center or any entity of the MedStar Corp. Dr. Ritchie would like to thank Evan G. DeRenzo, PhD, of the John J. Lynch Center for Ethics, for her thoughtful review of a previous draft of this commentary.
I am writing this commentary to bring to readers’ attention a medical and ethical complexity related to human sitters for presumably suicidal, COVID-19–positive hospitalized patients.
To shape and bundle the ethics issues addressed here into a single question, I offer the following: Should policies and practices requiring that patients in presumed need of a sitter because of assessed suicidality change when the patient is COVID-19–positive? Although the analysis might be similar when a sitter is monitoring a Patient Under Investigation (PUI), here I focus only on COVID-19–positive patients. Similarly, there are other reasons for sitters, of course, such as to prevent elopement, or, if a patient is in restraints, to prevent the patient from pulling out lines or tubes. Again, discussion of some of these ethical complications is beyond the scope of this piece. Just considering the matter of potential suicidality and sitters is complex enough. And so, to start, I sought out existing sources for guidance.
In looking for such sources, I first turned to the Centers for Medicare and Medicaid Services before COVID-19. CMS has required that there be a sitter for a patient who is suicidal and that the sitter remain in the room so that the sitter can intervene expeditiously if the patient tries to hurt himself or herself. There has been no change in this guidance since the COVID-19 pandemic in the United States. To the best of my knowledge, there is no substantive guidance for protecting sitters from contagion other than PPE. Given this, it begs the question:
In my hospital, I already have begun discussing the potential risks of harm and potential benefits to our suicidal patients of having a sitter directly outside the patient’s room. I also have considered whether to have one sitter watching several room cameras at once, commonly referred to as “telehealth strategies.”
To be sure, sitting for hours in the room of a COVID-19–positive patient is onerous. The sitter is required to be in full PPE (N-95 mask, gown, and gloves), which is hot and uncomfortable. Current practice is resource intensive in other ways. It requires changing out the sitter every 2 hours, which uses substantial amounts of PPE and multiple sitters.
Regardless, however, there are really no data upon which to base any sound ethics judgment about what should or should not be tried. We just have no information on how to attempt to balance potential risks and prospects for the benefit of whom and when. And, given that good clinical ethics always begin with the facts, I write this piece to see whether readers have thought about these issues before – and whether any of clinicians have started collecting the valuable data needed to begin making sound ethical judgments about how to care for our presumably suicidal COVID-19–positive patients and the sitters who watch over them.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
This column is an outcome of a discussion that occurred during Psych/Ethics rounds on June 5, and does not represent any official statements of Medstar Washington Hospital Center or any entity of the MedStar Corp. Dr. Ritchie would like to thank Evan G. DeRenzo, PhD, of the John J. Lynch Center for Ethics, for her thoughtful review of a previous draft of this commentary.











