User login
We all benefit from this powerful pairing
In this issue of JFP, Rajesh and colleagues present a scholarly review that details why it makes sense to integrate behavioral health into primary care. There is strong evidence that the presence of behavioral health care managers in primary care practices improves outcomes for patients with anxiety and depression. The mental health–trained care manager serves as a link between the primary care physician and mental health professional and can provide psychotherapy, as well.
A more integrated model, however, includes a full range of behavioral health services on site. Although not as well studied, co-location is a powerful pairing of physical and mental health treatment. Primary care physicians benefit because referral and feedback are immediate and seamless through warm hand-offs and easy access to medical and mental health notes in a common medical record. Patients benefit because they are more likely to engage with treatment when the physician introduces them to the mental health professional and expresses confidence in his or her abilities.
We know that trust improves treatment outcomes. What better way to encourage trust than with a warm smile and handshake when a patient is most vulnerable? In addition, integrating behavioral health into primary care helps patients avoid the stigma of going to a “mental health clinic.”
Integrating medical and mental health professionals into one practice is hardly a new idea and is spreading quickly in some parts of the country. It is perhaps no coincidence that Rajesh refers to a study of behavioral health integration in Colorado family practice offices. Recently, I (JH) presented a CME program to family physicians in Colorado, and, after reviewing recent studies of anxiety and depression, I asked how many participants had mental health professionals working in their practices. A full third raised their hands.
I (JH) had an excellent psychologist in my practice as far back as 1980, and he was an integral member of the care team. It seems that behavioral health integration has been a long time coming, and as a health care community we would be wise to spread this model of whole-person care to all primary care practices.
In this issue of JFP, Rajesh and colleagues present a scholarly review that details why it makes sense to integrate behavioral health into primary care. There is strong evidence that the presence of behavioral health care managers in primary care practices improves outcomes for patients with anxiety and depression. The mental health–trained care manager serves as a link between the primary care physician and mental health professional and can provide psychotherapy, as well.
A more integrated model, however, includes a full range of behavioral health services on site. Although not as well studied, co-location is a powerful pairing of physical and mental health treatment. Primary care physicians benefit because referral and feedback are immediate and seamless through warm hand-offs and easy access to medical and mental health notes in a common medical record. Patients benefit because they are more likely to engage with treatment when the physician introduces them to the mental health professional and expresses confidence in his or her abilities.
We know that trust improves treatment outcomes. What better way to encourage trust than with a warm smile and handshake when a patient is most vulnerable? In addition, integrating behavioral health into primary care helps patients avoid the stigma of going to a “mental health clinic.”
Integrating medical and mental health professionals into one practice is hardly a new idea and is spreading quickly in some parts of the country. It is perhaps no coincidence that Rajesh refers to a study of behavioral health integration in Colorado family practice offices. Recently, I (JH) presented a CME program to family physicians in Colorado, and, after reviewing recent studies of anxiety and depression, I asked how many participants had mental health professionals working in their practices. A full third raised their hands.
I (JH) had an excellent psychologist in my practice as far back as 1980, and he was an integral member of the care team. It seems that behavioral health integration has been a long time coming, and as a health care community we would be wise to spread this model of whole-person care to all primary care practices.
In this issue of JFP, Rajesh and colleagues present a scholarly review that details why it makes sense to integrate behavioral health into primary care. There is strong evidence that the presence of behavioral health care managers in primary care practices improves outcomes for patients with anxiety and depression. The mental health–trained care manager serves as a link between the primary care physician and mental health professional and can provide psychotherapy, as well.
A more integrated model, however, includes a full range of behavioral health services on site. Although not as well studied, co-location is a powerful pairing of physical and mental health treatment. Primary care physicians benefit because referral and feedback are immediate and seamless through warm hand-offs and easy access to medical and mental health notes in a common medical record. Patients benefit because they are more likely to engage with treatment when the physician introduces them to the mental health professional and expresses confidence in his or her abilities.
We know that trust improves treatment outcomes. What better way to encourage trust than with a warm smile and handshake when a patient is most vulnerable? In addition, integrating behavioral health into primary care helps patients avoid the stigma of going to a “mental health clinic.”
Integrating medical and mental health professionals into one practice is hardly a new idea and is spreading quickly in some parts of the country. It is perhaps no coincidence that Rajesh refers to a study of behavioral health integration in Colorado family practice offices. Recently, I (JH) presented a CME program to family physicians in Colorado, and, after reviewing recent studies of anxiety and depression, I asked how many participants had mental health professionals working in their practices. A full third raised their hands.
I (JH) had an excellent psychologist in my practice as far back as 1980, and he was an integral member of the care team. It seems that behavioral health integration has been a long time coming, and as a health care community we would be wise to spread this model of whole-person care to all primary care practices.
Phototherapy: Is It Still Important?
Phototherapy has been used to treat skin diseases for millennia. From the Incas to the ancient Greeks and Egyptians, nearly every major civilization has attempted to harness the sun, with some even worshipping it for its healing powers.1 Today, phototherapy remains as important as ever. Despite the technological advances that have brought about biologic medications, small molecule inhibitors, and elegant vehicle delivery systems, phototherapy continues to be a valuable tool in the dermatologist’s armamentarium.
Patient Access to Phototherapy
An important step in successfully managing any disease is access to treatment. In today’s health care landscape, therapeutic decisions frequently are dictated by a patient’s financial situation as well as by the discretion of payers. Costly medications such as biologics often are not accessible to patients on government insurance who fall into the Medicare “donut hole” and may be denied by insurance companies for a myriad of reasons. Luckily, phototherapy typically is well covered and is even a first-line treatment option for some conditions, such as mycosis fungoides.
Nevertheless, phototherapy also has its own unique accessibility hurdles. The time-consuming nature of office-based phototherapy treatment is the main barrier, and many patients find it difficult to incorporate treatments into their daily lives. Additionally, office-based phototherapy units often are clustered in major cities, making access more difficult for rural patients. Because light-responsive conditions often are chronic and may require a lifetime of treatment, home phototherapy units are now being recognized as cost-effective treatment options and are increasingly covered by insurance. In fact, one study comparing psoriasis patients treated with home narrowband UVB (NB-UVB) vs outpatient NB-UVB found that in-home treatment was equally as effective as office-based treatment at a similar cost.2 Because studies comparing the effectiveness of office-based vs home-based phototherapy treatment are underway for various other diseases, hopefully more patients will be able to receive home units, thus increasing access to safe and effective treatment.
Wide Range of Treatment Indications
Another merit of phototherapy is its ability to be used in almost all patient populations. It is one of the few modalities whose indications span the entire length of the human lifetime—from pediatric atopic dermatitis to chronic pruritus in elderly patients. Phototherapy also is one of the few treatment options that is safe to use in patients with an active malignancy or in patients who have multiple other medical conditions. Comorbidities including congestive heart failure, chronic infections, and demyelinating disorders often prevent the use of oral and injectable medications for immune-mediated disorders such as psoriasis or atopic dermatitis. In patients with multiple comorbidities whose disease remains uncontrolled despite an adequate topical regimen, phototherapy is one of the few effective treatment options that remain. Additionally, there is a considerable number of patients who prefer external treatments for cutaneous diseases. For these patients, phototherapy offers the opportunity to control skin conditions without the use of an internal medication.
Favorable Safety Profile
Phototherapy is a largely benign intervention with an excellent safety profile. Its main potential adverse events include erythema, pruritus, xerosis, recurrence of herpes simplex virus infection, and premature skin aging. The effects of phototherapy on skin carcinogenesis have long been controversial; however, data suggest a clear distinction in risk between treatment with NB-UVB and psoralen plus UVA (PUVA). A systematic review of psoriasis patients treated with phototherapy found no evidence to suggest an increased risk of melanoma or nonmelanoma skin cancer with NB-UVB treatment.3 The same cannot be said for psoriasis patients treated with PUVA, who were noted to have a higher incidence of nonmelanoma skin cancer than the general population. This increased risk was more substantial in American cohorts than in European cohorts, likely due to multiple factors including variable skin types and treatment regimens. Increased rates of melanoma also were noted in American PUVA cohorts, with no similar increase seen in their European counterparts.3
Broad vs Targeted Therapies
Targeted therapies have dominated the health care landscape over the last few years, with the majority of new medications being highly focused and only efficacious in a few conditions. One of phototherapy’s greatest strengths is its lack of specificity. Because the field of dermatology is filled with rare, overlapping, and often poorly understood diseases, nonspecific treatment options are needed to fill the gaps. Many generalized skin conditions may lack treatment options indicated by the US Food and Drug Administration. Phototherapy is the ultimate untargeted intervention and may be broadly used for a wide range of cutaneous conditions. Although classically utilized for atopic dermatitis and psoriasis, NB-UVB also can effectively treat generalized pruritus, vitiligo, urticaria, and seborrheic dermatitis.4 Not to be outdone, PUVA has shown success in treating more than 50 different dermatologic conditions including lichen planus, alopecia areata, and mycosis fungoides.
Final Thoughts
Phototherapy is a safe, accessible, and widely applicable treatment for a range of cutaneous disorders. Although more precisely engineered internal therapies have begun to replace UV light in psoriasis and atopic dermatitis, phototherapy likely will always remain an ideal treatment for a wide cohort of patients. Between increased access to home units and the continued validation of its excellent safety record, the future of phototherapy is looking bright.
- Grzybowski A, Sak J, Pawlikowski J. A brief report on the history of phototherapy. Clin Dermatol. 2016;34:532-537.
- Koek MB, Sigurdsson V, van Weelden H, et al. Cost effectiveness of home ultraviolet B phototherapy for psoriasis: economic evaluation of a randomised controlled trial (PLUTO study). BMJ. 2010;340:c1490.
- Archier E, Devaux S, Castela E, et al. Carcinogenic risks of psoralen UV-A therapy and narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012;26(suppl 3):22-31.
- Gambichler T, Breuckmann F, Boms S, et al. Narrowband UVB phototherapy in skin conditions beyond psoriasis. J Am Acad Dermatol. 2005;52:660-670.
- Ledo E, Ledo A. Phototherapy, photochemotherapy, and photodynamic therapy: unapproved uses or indications. Clin Dermatol. 2000;18:77-86.
Phototherapy has been used to treat skin diseases for millennia. From the Incas to the ancient Greeks and Egyptians, nearly every major civilization has attempted to harness the sun, with some even worshipping it for its healing powers.1 Today, phototherapy remains as important as ever. Despite the technological advances that have brought about biologic medications, small molecule inhibitors, and elegant vehicle delivery systems, phototherapy continues to be a valuable tool in the dermatologist’s armamentarium.
Patient Access to Phototherapy
An important step in successfully managing any disease is access to treatment. In today’s health care landscape, therapeutic decisions frequently are dictated by a patient’s financial situation as well as by the discretion of payers. Costly medications such as biologics often are not accessible to patients on government insurance who fall into the Medicare “donut hole” and may be denied by insurance companies for a myriad of reasons. Luckily, phototherapy typically is well covered and is even a first-line treatment option for some conditions, such as mycosis fungoides.
Nevertheless, phototherapy also has its own unique accessibility hurdles. The time-consuming nature of office-based phototherapy treatment is the main barrier, and many patients find it difficult to incorporate treatments into their daily lives. Additionally, office-based phototherapy units often are clustered in major cities, making access more difficult for rural patients. Because light-responsive conditions often are chronic and may require a lifetime of treatment, home phototherapy units are now being recognized as cost-effective treatment options and are increasingly covered by insurance. In fact, one study comparing psoriasis patients treated with home narrowband UVB (NB-UVB) vs outpatient NB-UVB found that in-home treatment was equally as effective as office-based treatment at a similar cost.2 Because studies comparing the effectiveness of office-based vs home-based phototherapy treatment are underway for various other diseases, hopefully more patients will be able to receive home units, thus increasing access to safe and effective treatment.
Wide Range of Treatment Indications
Another merit of phototherapy is its ability to be used in almost all patient populations. It is one of the few modalities whose indications span the entire length of the human lifetime—from pediatric atopic dermatitis to chronic pruritus in elderly patients. Phototherapy also is one of the few treatment options that is safe to use in patients with an active malignancy or in patients who have multiple other medical conditions. Comorbidities including congestive heart failure, chronic infections, and demyelinating disorders often prevent the use of oral and injectable medications for immune-mediated disorders such as psoriasis or atopic dermatitis. In patients with multiple comorbidities whose disease remains uncontrolled despite an adequate topical regimen, phototherapy is one of the few effective treatment options that remain. Additionally, there is a considerable number of patients who prefer external treatments for cutaneous diseases. For these patients, phototherapy offers the opportunity to control skin conditions without the use of an internal medication.
Favorable Safety Profile
Phototherapy is a largely benign intervention with an excellent safety profile. Its main potential adverse events include erythema, pruritus, xerosis, recurrence of herpes simplex virus infection, and premature skin aging. The effects of phototherapy on skin carcinogenesis have long been controversial; however, data suggest a clear distinction in risk between treatment with NB-UVB and psoralen plus UVA (PUVA). A systematic review of psoriasis patients treated with phototherapy found no evidence to suggest an increased risk of melanoma or nonmelanoma skin cancer with NB-UVB treatment.3 The same cannot be said for psoriasis patients treated with PUVA, who were noted to have a higher incidence of nonmelanoma skin cancer than the general population. This increased risk was more substantial in American cohorts than in European cohorts, likely due to multiple factors including variable skin types and treatment regimens. Increased rates of melanoma also were noted in American PUVA cohorts, with no similar increase seen in their European counterparts.3
Broad vs Targeted Therapies
Targeted therapies have dominated the health care landscape over the last few years, with the majority of new medications being highly focused and only efficacious in a few conditions. One of phototherapy’s greatest strengths is its lack of specificity. Because the field of dermatology is filled with rare, overlapping, and often poorly understood diseases, nonspecific treatment options are needed to fill the gaps. Many generalized skin conditions may lack treatment options indicated by the US Food and Drug Administration. Phototherapy is the ultimate untargeted intervention and may be broadly used for a wide range of cutaneous conditions. Although classically utilized for atopic dermatitis and psoriasis, NB-UVB also can effectively treat generalized pruritus, vitiligo, urticaria, and seborrheic dermatitis.4 Not to be outdone, PUVA has shown success in treating more than 50 different dermatologic conditions including lichen planus, alopecia areata, and mycosis fungoides.
Final Thoughts
Phototherapy is a safe, accessible, and widely applicable treatment for a range of cutaneous disorders. Although more precisely engineered internal therapies have begun to replace UV light in psoriasis and atopic dermatitis, phototherapy likely will always remain an ideal treatment for a wide cohort of patients. Between increased access to home units and the continued validation of its excellent safety record, the future of phototherapy is looking bright.
Phototherapy has been used to treat skin diseases for millennia. From the Incas to the ancient Greeks and Egyptians, nearly every major civilization has attempted to harness the sun, with some even worshipping it for its healing powers.1 Today, phototherapy remains as important as ever. Despite the technological advances that have brought about biologic medications, small molecule inhibitors, and elegant vehicle delivery systems, phototherapy continues to be a valuable tool in the dermatologist’s armamentarium.
Patient Access to Phototherapy
An important step in successfully managing any disease is access to treatment. In today’s health care landscape, therapeutic decisions frequently are dictated by a patient’s financial situation as well as by the discretion of payers. Costly medications such as biologics often are not accessible to patients on government insurance who fall into the Medicare “donut hole” and may be denied by insurance companies for a myriad of reasons. Luckily, phototherapy typically is well covered and is even a first-line treatment option for some conditions, such as mycosis fungoides.
Nevertheless, phototherapy also has its own unique accessibility hurdles. The time-consuming nature of office-based phototherapy treatment is the main barrier, and many patients find it difficult to incorporate treatments into their daily lives. Additionally, office-based phototherapy units often are clustered in major cities, making access more difficult for rural patients. Because light-responsive conditions often are chronic and may require a lifetime of treatment, home phototherapy units are now being recognized as cost-effective treatment options and are increasingly covered by insurance. In fact, one study comparing psoriasis patients treated with home narrowband UVB (NB-UVB) vs outpatient NB-UVB found that in-home treatment was equally as effective as office-based treatment at a similar cost.2 Because studies comparing the effectiveness of office-based vs home-based phototherapy treatment are underway for various other diseases, hopefully more patients will be able to receive home units, thus increasing access to safe and effective treatment.
Wide Range of Treatment Indications
Another merit of phototherapy is its ability to be used in almost all patient populations. It is one of the few modalities whose indications span the entire length of the human lifetime—from pediatric atopic dermatitis to chronic pruritus in elderly patients. Phototherapy also is one of the few treatment options that is safe to use in patients with an active malignancy or in patients who have multiple other medical conditions. Comorbidities including congestive heart failure, chronic infections, and demyelinating disorders often prevent the use of oral and injectable medications for immune-mediated disorders such as psoriasis or atopic dermatitis. In patients with multiple comorbidities whose disease remains uncontrolled despite an adequate topical regimen, phototherapy is one of the few effective treatment options that remain. Additionally, there is a considerable number of patients who prefer external treatments for cutaneous diseases. For these patients, phototherapy offers the opportunity to control skin conditions without the use of an internal medication.
Favorable Safety Profile
Phototherapy is a largely benign intervention with an excellent safety profile. Its main potential adverse events include erythema, pruritus, xerosis, recurrence of herpes simplex virus infection, and premature skin aging. The effects of phototherapy on skin carcinogenesis have long been controversial; however, data suggest a clear distinction in risk between treatment with NB-UVB and psoralen plus UVA (PUVA). A systematic review of psoriasis patients treated with phototherapy found no evidence to suggest an increased risk of melanoma or nonmelanoma skin cancer with NB-UVB treatment.3 The same cannot be said for psoriasis patients treated with PUVA, who were noted to have a higher incidence of nonmelanoma skin cancer than the general population. This increased risk was more substantial in American cohorts than in European cohorts, likely due to multiple factors including variable skin types and treatment regimens. Increased rates of melanoma also were noted in American PUVA cohorts, with no similar increase seen in their European counterparts.3
Broad vs Targeted Therapies
Targeted therapies have dominated the health care landscape over the last few years, with the majority of new medications being highly focused and only efficacious in a few conditions. One of phototherapy’s greatest strengths is its lack of specificity. Because the field of dermatology is filled with rare, overlapping, and often poorly understood diseases, nonspecific treatment options are needed to fill the gaps. Many generalized skin conditions may lack treatment options indicated by the US Food and Drug Administration. Phototherapy is the ultimate untargeted intervention and may be broadly used for a wide range of cutaneous conditions. Although classically utilized for atopic dermatitis and psoriasis, NB-UVB also can effectively treat generalized pruritus, vitiligo, urticaria, and seborrheic dermatitis.4 Not to be outdone, PUVA has shown success in treating more than 50 different dermatologic conditions including lichen planus, alopecia areata, and mycosis fungoides.
Final Thoughts
Phototherapy is a safe, accessible, and widely applicable treatment for a range of cutaneous disorders. Although more precisely engineered internal therapies have begun to replace UV light in psoriasis and atopic dermatitis, phototherapy likely will always remain an ideal treatment for a wide cohort of patients. Between increased access to home units and the continued validation of its excellent safety record, the future of phototherapy is looking bright.
- Grzybowski A, Sak J, Pawlikowski J. A brief report on the history of phototherapy. Clin Dermatol. 2016;34:532-537.
- Koek MB, Sigurdsson V, van Weelden H, et al. Cost effectiveness of home ultraviolet B phototherapy for psoriasis: economic evaluation of a randomised controlled trial (PLUTO study). BMJ. 2010;340:c1490.
- Archier E, Devaux S, Castela E, et al. Carcinogenic risks of psoralen UV-A therapy and narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012;26(suppl 3):22-31.
- Gambichler T, Breuckmann F, Boms S, et al. Narrowband UVB phototherapy in skin conditions beyond psoriasis. J Am Acad Dermatol. 2005;52:660-670.
- Ledo E, Ledo A. Phototherapy, photochemotherapy, and photodynamic therapy: unapproved uses or indications. Clin Dermatol. 2000;18:77-86.
- Grzybowski A, Sak J, Pawlikowski J. A brief report on the history of phototherapy. Clin Dermatol. 2016;34:532-537.
- Koek MB, Sigurdsson V, van Weelden H, et al. Cost effectiveness of home ultraviolet B phototherapy for psoriasis: economic evaluation of a randomised controlled trial (PLUTO study). BMJ. 2010;340:c1490.
- Archier E, Devaux S, Castela E, et al. Carcinogenic risks of psoralen UV-A therapy and narrowband UV-B therapy in chronic plaque psoriasis: a systematic literature review. J Eur Acad Dermatol Venereol. 2012;26(suppl 3):22-31.
- Gambichler T, Breuckmann F, Boms S, et al. Narrowband UVB phototherapy in skin conditions beyond psoriasis. J Am Acad Dermatol. 2005;52:660-670.
- Ledo E, Ledo A. Phototherapy, photochemotherapy, and photodynamic therapy: unapproved uses or indications. Clin Dermatol. 2000;18:77-86.
Addressing Health Literacy for Miscommunication in Dermatology
To the Editor:
We read with interest the Cutis Resident Corner column by Tracey1 on miscommunication with dermatology patients in which the author highlighted how seemingly straightforward language can deceivingly complicate effective communication between dermatologists and their patients. The examples she provided, including subtleties in describing what constitutes the “affected area” for proper application of a topical treatment or the inconsistent use of trade names for medications, underscore how misperceptions of verbal instruction can lead to poor treatment adherence and unintended health outcomes.1
In addition to how dermatologists deliver treatment information to their patients, a broader aspect of physician-patient communication is health literacy, which is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”2 Health literacy involves reading, listening, numeracy, decision-making, and health knowledge; patients who are potentially at risk for having limited skills in these areas include the elderly, those with poor English language proficiency, and those of lower socioeconomic status.3
In 2003, the National Assessment of Adult Literacy found that only 12% of individuals older than 16 years had a proficient level of health literacy.4 In an effort to address gaps in communication between health care providers and patients, the American Medical Association, National Institutes of Health, and the US Department of Health & Human Services recommend that educational materials be written at no higher than a 6th grade reading level.5,6 Currently, only 2% of dermatology educational materials meet this recommendation; the average reading level of patient dermatology materials is at a 12th grade level, despite the average American adult reading at an 8th grade level.7
It is imperative that dermatologists seek to improve both their verbal and nonverbal communication skills to effectively reach a broader patient population. Visual cues, such as pamphlets to illustrate what is meant by a “pea-sized” amount of adapalene or a photograph demonstrating “border asymmetry” in a melanoma, may be more effective than verbal or written communication alone. In addition, when certain drugs or treatments may be called by various names or when different drug names sound similar
The visual nature of dermatology creates unique psychosocial scenarios that may inherently motivate patients to understand their cutaneous disease; for example, providing photographs that depict acne improvement at different time points throughout isotretinoin treatment allows for more realistic expectations during therapy. Therefore, it is only fitting that instructive imagery would serve to benefit patient education.
In conclusion, communication between dermatologists and their patients involves multiple variables that can contribute to successful patient instruction for the management of dermatologic disease. Indeed, successful interaction not only includes mutual awareness of words or phrases that can otherwise be misconstrued but also attention to the readability of written materials and the benefits of visual instruction in the clinic setting. Integrating these aspects of health literacy can optimize rapport, treatment adherence, and health outcomes.
- Tracey E. Miscommunication with dermatology patients: are we speaking the same language? Cutis. 2018;102:E27-E28.
- Selden CR, Zorn M, Ratzan SC, et al, eds. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services; 2000.
- Institute of Medicine (US) Committee on Health Literacy; Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
- Kutner M, Greenberg E, Baer J. A First Look at the Literacy of America’s Adults in the 21st Century. Jessup, MD: National Center for Education Statistics, US Department of Education, Institute of Education Sciences; 2006. http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006470. Published December 15, 2005. Accessed May 21, 2019.
- Weiss BD. Health Literacy: A Manual for Clinicians. Chicago, IL: American Medical Association Foundation and American Medical Association; 2003.
- How to write easy-to-read health materials. National Library of Medicine website. http://www.nlm.nih.gov/medlineplus/etr.html. Accessed May 21, 2019.
- Prabhu AV, Gupta R, Kim C, et al. Patient education materials in dermatology: addressing the health literacy needs of patients. JAMA Dermatol. 2016;152:946-947.
To the Editor:
We read with interest the Cutis Resident Corner column by Tracey1 on miscommunication with dermatology patients in which the author highlighted how seemingly straightforward language can deceivingly complicate effective communication between dermatologists and their patients. The examples she provided, including subtleties in describing what constitutes the “affected area” for proper application of a topical treatment or the inconsistent use of trade names for medications, underscore how misperceptions of verbal instruction can lead to poor treatment adherence and unintended health outcomes.1
In addition to how dermatologists deliver treatment information to their patients, a broader aspect of physician-patient communication is health literacy, which is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”2 Health literacy involves reading, listening, numeracy, decision-making, and health knowledge; patients who are potentially at risk for having limited skills in these areas include the elderly, those with poor English language proficiency, and those of lower socioeconomic status.3
In 2003, the National Assessment of Adult Literacy found that only 12% of individuals older than 16 years had a proficient level of health literacy.4 In an effort to address gaps in communication between health care providers and patients, the American Medical Association, National Institutes of Health, and the US Department of Health & Human Services recommend that educational materials be written at no higher than a 6th grade reading level.5,6 Currently, only 2% of dermatology educational materials meet this recommendation; the average reading level of patient dermatology materials is at a 12th grade level, despite the average American adult reading at an 8th grade level.7
It is imperative that dermatologists seek to improve both their verbal and nonverbal communication skills to effectively reach a broader patient population. Visual cues, such as pamphlets to illustrate what is meant by a “pea-sized” amount of adapalene or a photograph demonstrating “border asymmetry” in a melanoma, may be more effective than verbal or written communication alone. In addition, when certain drugs or treatments may be called by various names or when different drug names sound similar
The visual nature of dermatology creates unique psychosocial scenarios that may inherently motivate patients to understand their cutaneous disease; for example, providing photographs that depict acne improvement at different time points throughout isotretinoin treatment allows for more realistic expectations during therapy. Therefore, it is only fitting that instructive imagery would serve to benefit patient education.
In conclusion, communication between dermatologists and their patients involves multiple variables that can contribute to successful patient instruction for the management of dermatologic disease. Indeed, successful interaction not only includes mutual awareness of words or phrases that can otherwise be misconstrued but also attention to the readability of written materials and the benefits of visual instruction in the clinic setting. Integrating these aspects of health literacy can optimize rapport, treatment adherence, and health outcomes.
To the Editor:
We read with interest the Cutis Resident Corner column by Tracey1 on miscommunication with dermatology patients in which the author highlighted how seemingly straightforward language can deceivingly complicate effective communication between dermatologists and their patients. The examples she provided, including subtleties in describing what constitutes the “affected area” for proper application of a topical treatment or the inconsistent use of trade names for medications, underscore how misperceptions of verbal instruction can lead to poor treatment adherence and unintended health outcomes.1
In addition to how dermatologists deliver treatment information to their patients, a broader aspect of physician-patient communication is health literacy, which is defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”2 Health literacy involves reading, listening, numeracy, decision-making, and health knowledge; patients who are potentially at risk for having limited skills in these areas include the elderly, those with poor English language proficiency, and those of lower socioeconomic status.3
In 2003, the National Assessment of Adult Literacy found that only 12% of individuals older than 16 years had a proficient level of health literacy.4 In an effort to address gaps in communication between health care providers and patients, the American Medical Association, National Institutes of Health, and the US Department of Health & Human Services recommend that educational materials be written at no higher than a 6th grade reading level.5,6 Currently, only 2% of dermatology educational materials meet this recommendation; the average reading level of patient dermatology materials is at a 12th grade level, despite the average American adult reading at an 8th grade level.7
It is imperative that dermatologists seek to improve both their verbal and nonverbal communication skills to effectively reach a broader patient population. Visual cues, such as pamphlets to illustrate what is meant by a “pea-sized” amount of adapalene or a photograph demonstrating “border asymmetry” in a melanoma, may be more effective than verbal or written communication alone. In addition, when certain drugs or treatments may be called by various names or when different drug names sound similar
The visual nature of dermatology creates unique psychosocial scenarios that may inherently motivate patients to understand their cutaneous disease; for example, providing photographs that depict acne improvement at different time points throughout isotretinoin treatment allows for more realistic expectations during therapy. Therefore, it is only fitting that instructive imagery would serve to benefit patient education.
In conclusion, communication between dermatologists and their patients involves multiple variables that can contribute to successful patient instruction for the management of dermatologic disease. Indeed, successful interaction not only includes mutual awareness of words or phrases that can otherwise be misconstrued but also attention to the readability of written materials and the benefits of visual instruction in the clinic setting. Integrating these aspects of health literacy can optimize rapport, treatment adherence, and health outcomes.
- Tracey E. Miscommunication with dermatology patients: are we speaking the same language? Cutis. 2018;102:E27-E28.
- Selden CR, Zorn M, Ratzan SC, et al, eds. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services; 2000.
- Institute of Medicine (US) Committee on Health Literacy; Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
- Kutner M, Greenberg E, Baer J. A First Look at the Literacy of America’s Adults in the 21st Century. Jessup, MD: National Center for Education Statistics, US Department of Education, Institute of Education Sciences; 2006. http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006470. Published December 15, 2005. Accessed May 21, 2019.
- Weiss BD. Health Literacy: A Manual for Clinicians. Chicago, IL: American Medical Association Foundation and American Medical Association; 2003.
- How to write easy-to-read health materials. National Library of Medicine website. http://www.nlm.nih.gov/medlineplus/etr.html. Accessed May 21, 2019.
- Prabhu AV, Gupta R, Kim C, et al. Patient education materials in dermatology: addressing the health literacy needs of patients. JAMA Dermatol. 2016;152:946-947.
- Tracey E. Miscommunication with dermatology patients: are we speaking the same language? Cutis. 2018;102:E27-E28.
- Selden CR, Zorn M, Ratzan SC, et al, eds. National Library of Medicine Current Bibliographies in Medicine: Health Literacy. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services; 2000.
- Institute of Medicine (US) Committee on Health Literacy; Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
- Kutner M, Greenberg E, Baer J. A First Look at the Literacy of America’s Adults in the 21st Century. Jessup, MD: National Center for Education Statistics, US Department of Education, Institute of Education Sciences; 2006. http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006470. Published December 15, 2005. Accessed May 21, 2019.
- Weiss BD. Health Literacy: A Manual for Clinicians. Chicago, IL: American Medical Association Foundation and American Medical Association; 2003.
- How to write easy-to-read health materials. National Library of Medicine website. http://www.nlm.nih.gov/medlineplus/etr.html. Accessed May 21, 2019.
- Prabhu AV, Gupta R, Kim C, et al. Patient education materials in dermatology: addressing the health literacy needs of patients. JAMA Dermatol. 2016;152:946-947.
Analysis: Why Alexa’s bedside manner is bad for health care
Amazon has opened a new health care frontier: Now Alexa can be used to transmit patient data. Using this new feature – which Amazon labeled as a “skill” – a company named Livongo will allow diabetes patients – which it calls “members” – to use the device to “query their last blood sugar reading, blood sugar measurement trends, and receive insights and Health Nudges that are personalized to them.”
Private equity and venture capital firms are in love with a legion of companies and startups touting the benefits of virtual doctors’ visits and telemedicine to revolutionize health care, investing almost $10 billion in 2018, a record for the sector. Without stepping into a gym or a clinic, a startup called Kinetxx will provide patients with virtual physical therapy, along with messaging and exercise logging. And Maven Clinic (which is not actually a physical place) offers online medical guidance and personal advice focusing on women’s health needs.
In April, at Fortune’s Brainstorm Health conference in San Diego, Bruce Broussard, CEO of health insurer Humana, said he believes technology will help patients receive help during medical crises, citing the benefits of home monitoring and the ability of doctors’ visits to be conducted by video conference.
But when I returned from Brainstorm Health, I was confronted by an alternative reality of virtual medicine: a $235 medical bill for a telehealth visit that resulted from one of my kids calling a longtime doctor’s office. It was for a five-minute phone call answering a question about a possible infection.
Virtual communications have streamlined life and transformed many of our relationships for the better. There is little need anymore to sit across the desk from a tax accountant or travel agent or to stand in a queue for a bank teller. And there is certainly room for disruptive digital innovation in our confusing and overpriced health care system.
But it remains an open question whether virtual medicine will prove a valuable, convenient adjunct to health care. Or, instead, will it be a way for the U.S. profit-driven health care system to make big bucks by outsourcing core duties – while providing a paler version of actual medical treatment?
After all, my doctors have long answered my questions and dispensed phone and email advice for free – as part of our doctor-patient relationship – though it didn’t have a cool branding moniker like telehealth. And my obstetrician’s office offered great support and advice through two difficult pregnancies – maybe they should have been paid for that valuable service. But $235 for a phone call (which works out to over $2,000 per hour)? Not even a corporate lawyer bills that.
Logic holds that some digital health tools have tremendous potential: A neurologist can view a patient by video to see if lopsided facial movements suggest a stroke. A patient with an irregular heart rhythm could send in digital tracings to see if a new prescription drug is working. But the tangible benefit of many other virtual services offered is less certain. Some people may like receiving feedback about their sleep from an Apple Watch, but I’m not sure that’s medicine.
And if virtual medicine is pursued in the name of business efficiency or just profit, it has enormous potential to make health care worse.
My doctor’s nurse is far better equipped to answer a question about my ongoing health problem than someone at a call center reading from a script. And, however thorough a virtual visit may be, it forsakes some of the diagnostic information that comes when you see and touch the patient.
A study published recently in Pediatrics found that children who had a telemedicine visit for an upper respiratory infection were far more likely to get an antibiotic than those who physically saw a doctor, suggesting overprescribing is at work. It makes sense: A doctor can’t use a stethoscope to listen to lungs or wiggle an otoscope into a kid’s ear by video. Similarly, a virtual physical therapist can’t feel the knots in muscle or notice a fleeting wince on a patient’s face via camera.
More important, perhaps, virtual medicine means losing the support that has long been a crucial part of the profession. There are programs to provide iPads to people in home hospice for resources about grief and chatbots that purport to treat depression. Maybe people at such challenging moments need – and deserve – human contact.
Of course, companies like those mentioned are expecting to be reimbursed for the remote monitoring and virtual advice they provide. Investors, in turn, get generous payback without having to employ so many actual doctors or other health professionals. Livongo, for instance, has raised a total of $235 million in funding over six rounds. And, as of 2018, Medicare announced it would allow such digital monitoring tools to “qualify for reimbursement,” if they are “clinically endorsed.” But, ultimately, will the well-being of patients or investors decide which tools are clinically endorsed?
So far, with its new so-called skill, Alexa will be able to perform a half-dozen health-related services. In addition to diabetes coaching, it can find the earliest urgent care appointment in a given area and check the status of a prescription drug delivery.
But it will not provide many things patients desperately want, which technology should be able to readily deliver, such as a reliable price estimate for an upcoming surgery, the infection rates at the local hospital, the location of the cheapest cholesterol test nearby. And if we’re trying to bring health care into the tech-enabled 21st century, how about starting with low-hanging fruit: Does any other sector still use paper bills and faxes?
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Amazon has opened a new health care frontier: Now Alexa can be used to transmit patient data. Using this new feature – which Amazon labeled as a “skill” – a company named Livongo will allow diabetes patients – which it calls “members” – to use the device to “query their last blood sugar reading, blood sugar measurement trends, and receive insights and Health Nudges that are personalized to them.”
Private equity and venture capital firms are in love with a legion of companies and startups touting the benefits of virtual doctors’ visits and telemedicine to revolutionize health care, investing almost $10 billion in 2018, a record for the sector. Without stepping into a gym or a clinic, a startup called Kinetxx will provide patients with virtual physical therapy, along with messaging and exercise logging. And Maven Clinic (which is not actually a physical place) offers online medical guidance and personal advice focusing on women’s health needs.
In April, at Fortune’s Brainstorm Health conference in San Diego, Bruce Broussard, CEO of health insurer Humana, said he believes technology will help patients receive help during medical crises, citing the benefits of home monitoring and the ability of doctors’ visits to be conducted by video conference.
But when I returned from Brainstorm Health, I was confronted by an alternative reality of virtual medicine: a $235 medical bill for a telehealth visit that resulted from one of my kids calling a longtime doctor’s office. It was for a five-minute phone call answering a question about a possible infection.
Virtual communications have streamlined life and transformed many of our relationships for the better. There is little need anymore to sit across the desk from a tax accountant or travel agent or to stand in a queue for a bank teller. And there is certainly room for disruptive digital innovation in our confusing and overpriced health care system.
But it remains an open question whether virtual medicine will prove a valuable, convenient adjunct to health care. Or, instead, will it be a way for the U.S. profit-driven health care system to make big bucks by outsourcing core duties – while providing a paler version of actual medical treatment?
After all, my doctors have long answered my questions and dispensed phone and email advice for free – as part of our doctor-patient relationship – though it didn’t have a cool branding moniker like telehealth. And my obstetrician’s office offered great support and advice through two difficult pregnancies – maybe they should have been paid for that valuable service. But $235 for a phone call (which works out to over $2,000 per hour)? Not even a corporate lawyer bills that.
Logic holds that some digital health tools have tremendous potential: A neurologist can view a patient by video to see if lopsided facial movements suggest a stroke. A patient with an irregular heart rhythm could send in digital tracings to see if a new prescription drug is working. But the tangible benefit of many other virtual services offered is less certain. Some people may like receiving feedback about their sleep from an Apple Watch, but I’m not sure that’s medicine.
And if virtual medicine is pursued in the name of business efficiency or just profit, it has enormous potential to make health care worse.
My doctor’s nurse is far better equipped to answer a question about my ongoing health problem than someone at a call center reading from a script. And, however thorough a virtual visit may be, it forsakes some of the diagnostic information that comes when you see and touch the patient.
A study published recently in Pediatrics found that children who had a telemedicine visit for an upper respiratory infection were far more likely to get an antibiotic than those who physically saw a doctor, suggesting overprescribing is at work. It makes sense: A doctor can’t use a stethoscope to listen to lungs or wiggle an otoscope into a kid’s ear by video. Similarly, a virtual physical therapist can’t feel the knots in muscle or notice a fleeting wince on a patient’s face via camera.
More important, perhaps, virtual medicine means losing the support that has long been a crucial part of the profession. There are programs to provide iPads to people in home hospice for resources about grief and chatbots that purport to treat depression. Maybe people at such challenging moments need – and deserve – human contact.
Of course, companies like those mentioned are expecting to be reimbursed for the remote monitoring and virtual advice they provide. Investors, in turn, get generous payback without having to employ so many actual doctors or other health professionals. Livongo, for instance, has raised a total of $235 million in funding over six rounds. And, as of 2018, Medicare announced it would allow such digital monitoring tools to “qualify for reimbursement,” if they are “clinically endorsed.” But, ultimately, will the well-being of patients or investors decide which tools are clinically endorsed?
So far, with its new so-called skill, Alexa will be able to perform a half-dozen health-related services. In addition to diabetes coaching, it can find the earliest urgent care appointment in a given area and check the status of a prescription drug delivery.
But it will not provide many things patients desperately want, which technology should be able to readily deliver, such as a reliable price estimate for an upcoming surgery, the infection rates at the local hospital, the location of the cheapest cholesterol test nearby. And if we’re trying to bring health care into the tech-enabled 21st century, how about starting with low-hanging fruit: Does any other sector still use paper bills and faxes?
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Amazon has opened a new health care frontier: Now Alexa can be used to transmit patient data. Using this new feature – which Amazon labeled as a “skill” – a company named Livongo will allow diabetes patients – which it calls “members” – to use the device to “query their last blood sugar reading, blood sugar measurement trends, and receive insights and Health Nudges that are personalized to them.”
Private equity and venture capital firms are in love with a legion of companies and startups touting the benefits of virtual doctors’ visits and telemedicine to revolutionize health care, investing almost $10 billion in 2018, a record for the sector. Without stepping into a gym or a clinic, a startup called Kinetxx will provide patients with virtual physical therapy, along with messaging and exercise logging. And Maven Clinic (which is not actually a physical place) offers online medical guidance and personal advice focusing on women’s health needs.
In April, at Fortune’s Brainstorm Health conference in San Diego, Bruce Broussard, CEO of health insurer Humana, said he believes technology will help patients receive help during medical crises, citing the benefits of home monitoring and the ability of doctors’ visits to be conducted by video conference.
But when I returned from Brainstorm Health, I was confronted by an alternative reality of virtual medicine: a $235 medical bill for a telehealth visit that resulted from one of my kids calling a longtime doctor’s office. It was for a five-minute phone call answering a question about a possible infection.
Virtual communications have streamlined life and transformed many of our relationships for the better. There is little need anymore to sit across the desk from a tax accountant or travel agent or to stand in a queue for a bank teller. And there is certainly room for disruptive digital innovation in our confusing and overpriced health care system.
But it remains an open question whether virtual medicine will prove a valuable, convenient adjunct to health care. Or, instead, will it be a way for the U.S. profit-driven health care system to make big bucks by outsourcing core duties – while providing a paler version of actual medical treatment?
After all, my doctors have long answered my questions and dispensed phone and email advice for free – as part of our doctor-patient relationship – though it didn’t have a cool branding moniker like telehealth. And my obstetrician’s office offered great support and advice through two difficult pregnancies – maybe they should have been paid for that valuable service. But $235 for a phone call (which works out to over $2,000 per hour)? Not even a corporate lawyer bills that.
Logic holds that some digital health tools have tremendous potential: A neurologist can view a patient by video to see if lopsided facial movements suggest a stroke. A patient with an irregular heart rhythm could send in digital tracings to see if a new prescription drug is working. But the tangible benefit of many other virtual services offered is less certain. Some people may like receiving feedback about their sleep from an Apple Watch, but I’m not sure that’s medicine.
And if virtual medicine is pursued in the name of business efficiency or just profit, it has enormous potential to make health care worse.
My doctor’s nurse is far better equipped to answer a question about my ongoing health problem than someone at a call center reading from a script. And, however thorough a virtual visit may be, it forsakes some of the diagnostic information that comes when you see and touch the patient.
A study published recently in Pediatrics found that children who had a telemedicine visit for an upper respiratory infection were far more likely to get an antibiotic than those who physically saw a doctor, suggesting overprescribing is at work. It makes sense: A doctor can’t use a stethoscope to listen to lungs or wiggle an otoscope into a kid’s ear by video. Similarly, a virtual physical therapist can’t feel the knots in muscle or notice a fleeting wince on a patient’s face via camera.
More important, perhaps, virtual medicine means losing the support that has long been a crucial part of the profession. There are programs to provide iPads to people in home hospice for resources about grief and chatbots that purport to treat depression. Maybe people at such challenging moments need – and deserve – human contact.
Of course, companies like those mentioned are expecting to be reimbursed for the remote monitoring and virtual advice they provide. Investors, in turn, get generous payback without having to employ so many actual doctors or other health professionals. Livongo, for instance, has raised a total of $235 million in funding over six rounds. And, as of 2018, Medicare announced it would allow such digital monitoring tools to “qualify for reimbursement,” if they are “clinically endorsed.” But, ultimately, will the well-being of patients or investors decide which tools are clinically endorsed?
So far, with its new so-called skill, Alexa will be able to perform a half-dozen health-related services. In addition to diabetes coaching, it can find the earliest urgent care appointment in a given area and check the status of a prescription drug delivery.
But it will not provide many things patients desperately want, which technology should be able to readily deliver, such as a reliable price estimate for an upcoming surgery, the infection rates at the local hospital, the location of the cheapest cholesterol test nearby. And if we’re trying to bring health care into the tech-enabled 21st century, how about starting with low-hanging fruit: Does any other sector still use paper bills and faxes?
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Gone But Not Forgotten: How VA Remembers
Caring for veterans at the end of their lives is a great honor. The US Department of Veterans Affairs (VA) health care professionals (HCPs) find meaning and take pride in providing this care. We are there to support the patient and their family and loved ones around the time of death. When our patients die, we feel the loss and grieve as well. VA health care providers look to our teams to set up rituals that pay tribute to the veteran and to show respect and gratitude for our role in these moments. It is important to recognize the bonds we share and the grief we feel when a veteran dies. The relationships we form, the recognition of loss, and the honoring of the veterans help nourish and maintain us.
Although the number of VA inpatient deaths nationwide has been declining steadily for years, internal reporting by the Palliative and Hospice Care Program Office has shown that the percentage of VA inpatient deaths that occur in hospice settings has steadily grown. Since 2013, more veterans die in VA inpatient hospice beds than in any other hospital setting. Therefore, it is useful to take stock of the way hospice and palliative care providers and staff process and provide support so that they can continue to provide service to veterans.
In the same way that all loss and grief are unique, there are many diverse rituals across VA facilities. This article highlights some of the unique traditions that hospice and palliative care teams have adopted to embrace this remembrance. We hope that by sharing these practices others will be inspired to find ways to reflect on their work and honor the lives of veterans.
The authors reached out to VA palliative care colleagues across the country via the Veterans Health Administration National Hospice and Palliative Care listserve to ask: How does your team practice remembrance? Palliative care providers responded and shared the unique ways they and their teams reflect on these losses.
There are many moments for reflection from the time of death to the weeks and months after, to the entire year of cumulative loss. Some observances start around the time of death. Susan MacDonald, RN, GEC, from Erie VA Medical Center (VAMC) in Pennsylvania reported that following the death of a veteran in the hospice unit, there is a bedside remembrance that includes the chaplain, care team, family, and other loved ones. At the John D. Dingell VAMC in Detroit, Michigan, the clinical chaplain leads a memorial service after a community living center (CLC) resident dies.
Several VAMCs, such as Detroit and Erie, have an Honors Escort or Final Salute. In these ceremonies, family, employees, residents, and other veterans line the hallways to honor the veteran on their departure from the building.1 At the VA Maine Healthcare System, Kate MacFawn, nurse manager, Inpatient Hospice Unit, explained, “We debrief every death the day after it occurs. The doc[tor]s check in with the nursing staff on each shift, and the rest of the multidisciplinary team discusses [it] in our morning report.”
Palliative care providers consider the physical spaces where the veteran has spent those last moments and the void that is left. Karen Pickler, staff chaplain at Northport VAMC Hospice Unit recounts:
At the time of death, we decorate the tray table with the veteran’s picture, a flag, and an angel. In the CLC they will have a memorial service on Friday if a resident has died that week. This is for the unit and staff. In the past, other residents were not informed of the death. This way, the relationships between residents are honored as well as their natural families.
At VA Boston Healthcare System (VABHS) in Massachusetts in the Inpatient Hospice Unit-CLC, after a veteran dies, a flag, a strand of lights, and a rose in a vase are placed outside the veteran’s room to mark the absence. The VABHS remembrance practice has evolved over time based on input from the team. According to Noah Whiddon, LICSW, CLC complex case coordinator, at a weekly interdisciplinary team (IDT) meeting, the names of veterans who have died in the past week are read, and there is a commemorative ribbon cutting. “Any team member may write the last name of the deceased veteran on the ribbon and place it into a vase,” he said. “One of the nurse team members felt that a moment of silence would be appropriate, and we have added that.”
Every 6 months, VABHS holds a flag burning ceremony to appropriately dispose of worn out flags. Veterans and families are invited. The commemorative ribbons are packaged and burned at this ceremony with the following explanation of the ritual:
We’d like to take a moment to reflect on the lives of veterans we’ve lost in the last 6 months. Each week we remember the veterans for whom we have cared who have passed away. As part of this, we cut a ribbon and inscribe their name on it to commemorate their memory. We might have known these veterans for a few days or for a few years, but each of their lives had meaning for us. The courage that our veterans demonstrate at the end of their lives is an extension of the bravery they displayed in their service to our country. Today we will burn their commemorative ribbons with our country’s flag in tribute to and respect for their selflessness to our country. Please join us in a few moments of silence as their ribbons burn together with our flag.
In the VABHS acute care hospital, the palliative care IDT reserves 30 minutes, twice monthly for a chaplain-led remembrance. A large bowl-shaped shell is placed in the center of the table with smaller shells around it. Any team member can read the names of veterans who have died in prior weeks and share a memory of the patient or family, and then place a smaller shell into the larger bowl. This represents the transition from the smallest part of the universe back into the larger part. At the end, a moment of silence is observed or a poem is read. This tradition was brought to the team by the palliative care chaplain, Douglas Falls, MDiv.
Bimonthly bereavement meetings are held at the James A. Haley Veterans’ Hospital-Pasco County branch, and each veteran who has died is remembered. Whoever wants to share is welcome. “We conclude with a poem, usually shared by the physician, but it can be any team member,” explained Linda Falzetta-Gross, ARNP-BC. “This process is led by the team social worker. In the past, we used to ring a bell prior to each name.”
Bells also are used at the Greater West Los Angeles VAMC in California. At the weekly clinic, veterans who have died are remembered, and each team member has an opportunity to share memories. “We ring a Tibetan bell for a moment without words,” explains Geoffrey Tyrell, palliative care chaplain. “It is introduced with a few words to allow new staff members in our clinic to participate, as a moment of mindfulness to let go of our words and to go inside, to see what we might need for our own wellness.” Afterward the chaplain says a few words and wishes for peace for the veterans and their families. The team also has responded well to more participatory group activities, such as placing rocks in a bowl of water, to symbolize letting go of something that has been difficult.
Additionally, there are practices of a larger scope. Many VAMCs have established facility-wide memorial services annually, biannually, or quarterly. At this time, families and staff come together to remember and honor veterans who have died within the VAMC. These memorials might involve a variety of service lines, such as chaplaincy, voluntary services, nursing, and social work and may consist of an honor guard, music, and readings. In accordance with the Health Insurance Portability and Accountability Act (HIPAA) and privacy regulations, only family members of deceased veterans may speak the names at the ceremony unless written consent is given. At the Tennessee Valley Healthcare System in Nashville, family members may stand and give the name of the person they are honoring. Balloons are released, stories are told, and a poem or appropriate passage is read. Families are given a book pinned with a flag, according to Jennifer C. Crenshaw, clinical staff chaplain. Family members are moved knowing that the VA remembers their loved ones even months after they are gone.
Due to the overwhelming positive feedback from veterans’ families who participated in these ceremonies, on January 24, 2018, Carolyn Clancy, MD, VHA Executive-in-Charge, Office of the Under Secretary for Health issued a memorandum requesting that all VAMCs immediately adopt this best practice: to host periodic ceremonies to publicly recognize and honor deceased veterans in the presence of their families, VA care providers, veterans service organizations and community members. Clancy recommended calling the ceremonies “The Last Roll Call Ceremony of Remembrance.”2
These rituals are a small sample of the rich diversity of practice in VAs across the country. What unifies VA palliative care providers is our mission to serve the veterans, honor their deaths, show respect and gratitude, and recognize that we, too, feel the pain of loss. We mark these moments with solemnity and beauty—a bell, a poem, a prayer—to honor our shared experience caring for veterans.
1. Saint S. A VA hospital you may not know: The Final Salute, and how much we doctors care. https://theconversation.com/a-va-hospital-you-may-not-know-the-final-salute-and-how-much-we-doctors-care-94217. Published March 30, 2018. Accessed May 8, 2019.
2. Clancy CM. VAIQ Memorandum 7866347: Implementation of the last roll call ceremony of remembrance at all Veterans Affairs medical centers. Published 2018.
Caring for veterans at the end of their lives is a great honor. The US Department of Veterans Affairs (VA) health care professionals (HCPs) find meaning and take pride in providing this care. We are there to support the patient and their family and loved ones around the time of death. When our patients die, we feel the loss and grieve as well. VA health care providers look to our teams to set up rituals that pay tribute to the veteran and to show respect and gratitude for our role in these moments. It is important to recognize the bonds we share and the grief we feel when a veteran dies. The relationships we form, the recognition of loss, and the honoring of the veterans help nourish and maintain us.
Although the number of VA inpatient deaths nationwide has been declining steadily for years, internal reporting by the Palliative and Hospice Care Program Office has shown that the percentage of VA inpatient deaths that occur in hospice settings has steadily grown. Since 2013, more veterans die in VA inpatient hospice beds than in any other hospital setting. Therefore, it is useful to take stock of the way hospice and palliative care providers and staff process and provide support so that they can continue to provide service to veterans.
In the same way that all loss and grief are unique, there are many diverse rituals across VA facilities. This article highlights some of the unique traditions that hospice and palliative care teams have adopted to embrace this remembrance. We hope that by sharing these practices others will be inspired to find ways to reflect on their work and honor the lives of veterans.
The authors reached out to VA palliative care colleagues across the country via the Veterans Health Administration National Hospice and Palliative Care listserve to ask: How does your team practice remembrance? Palliative care providers responded and shared the unique ways they and their teams reflect on these losses.
There are many moments for reflection from the time of death to the weeks and months after, to the entire year of cumulative loss. Some observances start around the time of death. Susan MacDonald, RN, GEC, from Erie VA Medical Center (VAMC) in Pennsylvania reported that following the death of a veteran in the hospice unit, there is a bedside remembrance that includes the chaplain, care team, family, and other loved ones. At the John D. Dingell VAMC in Detroit, Michigan, the clinical chaplain leads a memorial service after a community living center (CLC) resident dies.
Several VAMCs, such as Detroit and Erie, have an Honors Escort or Final Salute. In these ceremonies, family, employees, residents, and other veterans line the hallways to honor the veteran on their departure from the building.1 At the VA Maine Healthcare System, Kate MacFawn, nurse manager, Inpatient Hospice Unit, explained, “We debrief every death the day after it occurs. The doc[tor]s check in with the nursing staff on each shift, and the rest of the multidisciplinary team discusses [it] in our morning report.”
Palliative care providers consider the physical spaces where the veteran has spent those last moments and the void that is left. Karen Pickler, staff chaplain at Northport VAMC Hospice Unit recounts:
At the time of death, we decorate the tray table with the veteran’s picture, a flag, and an angel. In the CLC they will have a memorial service on Friday if a resident has died that week. This is for the unit and staff. In the past, other residents were not informed of the death. This way, the relationships between residents are honored as well as their natural families.
At VA Boston Healthcare System (VABHS) in Massachusetts in the Inpatient Hospice Unit-CLC, after a veteran dies, a flag, a strand of lights, and a rose in a vase are placed outside the veteran’s room to mark the absence. The VABHS remembrance practice has evolved over time based on input from the team. According to Noah Whiddon, LICSW, CLC complex case coordinator, at a weekly interdisciplinary team (IDT) meeting, the names of veterans who have died in the past week are read, and there is a commemorative ribbon cutting. “Any team member may write the last name of the deceased veteran on the ribbon and place it into a vase,” he said. “One of the nurse team members felt that a moment of silence would be appropriate, and we have added that.”
Every 6 months, VABHS holds a flag burning ceremony to appropriately dispose of worn out flags. Veterans and families are invited. The commemorative ribbons are packaged and burned at this ceremony with the following explanation of the ritual:
We’d like to take a moment to reflect on the lives of veterans we’ve lost in the last 6 months. Each week we remember the veterans for whom we have cared who have passed away. As part of this, we cut a ribbon and inscribe their name on it to commemorate their memory. We might have known these veterans for a few days or for a few years, but each of their lives had meaning for us. The courage that our veterans demonstrate at the end of their lives is an extension of the bravery they displayed in their service to our country. Today we will burn their commemorative ribbons with our country’s flag in tribute to and respect for their selflessness to our country. Please join us in a few moments of silence as their ribbons burn together with our flag.
In the VABHS acute care hospital, the palliative care IDT reserves 30 minutes, twice monthly for a chaplain-led remembrance. A large bowl-shaped shell is placed in the center of the table with smaller shells around it. Any team member can read the names of veterans who have died in prior weeks and share a memory of the patient or family, and then place a smaller shell into the larger bowl. This represents the transition from the smallest part of the universe back into the larger part. At the end, a moment of silence is observed or a poem is read. This tradition was brought to the team by the palliative care chaplain, Douglas Falls, MDiv.
Bimonthly bereavement meetings are held at the James A. Haley Veterans’ Hospital-Pasco County branch, and each veteran who has died is remembered. Whoever wants to share is welcome. “We conclude with a poem, usually shared by the physician, but it can be any team member,” explained Linda Falzetta-Gross, ARNP-BC. “This process is led by the team social worker. In the past, we used to ring a bell prior to each name.”
Bells also are used at the Greater West Los Angeles VAMC in California. At the weekly clinic, veterans who have died are remembered, and each team member has an opportunity to share memories. “We ring a Tibetan bell for a moment without words,” explains Geoffrey Tyrell, palliative care chaplain. “It is introduced with a few words to allow new staff members in our clinic to participate, as a moment of mindfulness to let go of our words and to go inside, to see what we might need for our own wellness.” Afterward the chaplain says a few words and wishes for peace for the veterans and their families. The team also has responded well to more participatory group activities, such as placing rocks in a bowl of water, to symbolize letting go of something that has been difficult.
Additionally, there are practices of a larger scope. Many VAMCs have established facility-wide memorial services annually, biannually, or quarterly. At this time, families and staff come together to remember and honor veterans who have died within the VAMC. These memorials might involve a variety of service lines, such as chaplaincy, voluntary services, nursing, and social work and may consist of an honor guard, music, and readings. In accordance with the Health Insurance Portability and Accountability Act (HIPAA) and privacy regulations, only family members of deceased veterans may speak the names at the ceremony unless written consent is given. At the Tennessee Valley Healthcare System in Nashville, family members may stand and give the name of the person they are honoring. Balloons are released, stories are told, and a poem or appropriate passage is read. Families are given a book pinned with a flag, according to Jennifer C. Crenshaw, clinical staff chaplain. Family members are moved knowing that the VA remembers their loved ones even months after they are gone.
Due to the overwhelming positive feedback from veterans’ families who participated in these ceremonies, on January 24, 2018, Carolyn Clancy, MD, VHA Executive-in-Charge, Office of the Under Secretary for Health issued a memorandum requesting that all VAMCs immediately adopt this best practice: to host periodic ceremonies to publicly recognize and honor deceased veterans in the presence of their families, VA care providers, veterans service organizations and community members. Clancy recommended calling the ceremonies “The Last Roll Call Ceremony of Remembrance.”2
These rituals are a small sample of the rich diversity of practice in VAs across the country. What unifies VA palliative care providers is our mission to serve the veterans, honor their deaths, show respect and gratitude, and recognize that we, too, feel the pain of loss. We mark these moments with solemnity and beauty—a bell, a poem, a prayer—to honor our shared experience caring for veterans.
Caring for veterans at the end of their lives is a great honor. The US Department of Veterans Affairs (VA) health care professionals (HCPs) find meaning and take pride in providing this care. We are there to support the patient and their family and loved ones around the time of death. When our patients die, we feel the loss and grieve as well. VA health care providers look to our teams to set up rituals that pay tribute to the veteran and to show respect and gratitude for our role in these moments. It is important to recognize the bonds we share and the grief we feel when a veteran dies. The relationships we form, the recognition of loss, and the honoring of the veterans help nourish and maintain us.
Although the number of VA inpatient deaths nationwide has been declining steadily for years, internal reporting by the Palliative and Hospice Care Program Office has shown that the percentage of VA inpatient deaths that occur in hospice settings has steadily grown. Since 2013, more veterans die in VA inpatient hospice beds than in any other hospital setting. Therefore, it is useful to take stock of the way hospice and palliative care providers and staff process and provide support so that they can continue to provide service to veterans.
In the same way that all loss and grief are unique, there are many diverse rituals across VA facilities. This article highlights some of the unique traditions that hospice and palliative care teams have adopted to embrace this remembrance. We hope that by sharing these practices others will be inspired to find ways to reflect on their work and honor the lives of veterans.
The authors reached out to VA palliative care colleagues across the country via the Veterans Health Administration National Hospice and Palliative Care listserve to ask: How does your team practice remembrance? Palliative care providers responded and shared the unique ways they and their teams reflect on these losses.
There are many moments for reflection from the time of death to the weeks and months after, to the entire year of cumulative loss. Some observances start around the time of death. Susan MacDonald, RN, GEC, from Erie VA Medical Center (VAMC) in Pennsylvania reported that following the death of a veteran in the hospice unit, there is a bedside remembrance that includes the chaplain, care team, family, and other loved ones. At the John D. Dingell VAMC in Detroit, Michigan, the clinical chaplain leads a memorial service after a community living center (CLC) resident dies.
Several VAMCs, such as Detroit and Erie, have an Honors Escort or Final Salute. In these ceremonies, family, employees, residents, and other veterans line the hallways to honor the veteran on their departure from the building.1 At the VA Maine Healthcare System, Kate MacFawn, nurse manager, Inpatient Hospice Unit, explained, “We debrief every death the day after it occurs. The doc[tor]s check in with the nursing staff on each shift, and the rest of the multidisciplinary team discusses [it] in our morning report.”
Palliative care providers consider the physical spaces where the veteran has spent those last moments and the void that is left. Karen Pickler, staff chaplain at Northport VAMC Hospice Unit recounts:
At the time of death, we decorate the tray table with the veteran’s picture, a flag, and an angel. In the CLC they will have a memorial service on Friday if a resident has died that week. This is for the unit and staff. In the past, other residents were not informed of the death. This way, the relationships between residents are honored as well as their natural families.
At VA Boston Healthcare System (VABHS) in Massachusetts in the Inpatient Hospice Unit-CLC, after a veteran dies, a flag, a strand of lights, and a rose in a vase are placed outside the veteran’s room to mark the absence. The VABHS remembrance practice has evolved over time based on input from the team. According to Noah Whiddon, LICSW, CLC complex case coordinator, at a weekly interdisciplinary team (IDT) meeting, the names of veterans who have died in the past week are read, and there is a commemorative ribbon cutting. “Any team member may write the last name of the deceased veteran on the ribbon and place it into a vase,” he said. “One of the nurse team members felt that a moment of silence would be appropriate, and we have added that.”
Every 6 months, VABHS holds a flag burning ceremony to appropriately dispose of worn out flags. Veterans and families are invited. The commemorative ribbons are packaged and burned at this ceremony with the following explanation of the ritual:
We’d like to take a moment to reflect on the lives of veterans we’ve lost in the last 6 months. Each week we remember the veterans for whom we have cared who have passed away. As part of this, we cut a ribbon and inscribe their name on it to commemorate their memory. We might have known these veterans for a few days or for a few years, but each of their lives had meaning for us. The courage that our veterans demonstrate at the end of their lives is an extension of the bravery they displayed in their service to our country. Today we will burn their commemorative ribbons with our country’s flag in tribute to and respect for their selflessness to our country. Please join us in a few moments of silence as their ribbons burn together with our flag.
In the VABHS acute care hospital, the palliative care IDT reserves 30 minutes, twice monthly for a chaplain-led remembrance. A large bowl-shaped shell is placed in the center of the table with smaller shells around it. Any team member can read the names of veterans who have died in prior weeks and share a memory of the patient or family, and then place a smaller shell into the larger bowl. This represents the transition from the smallest part of the universe back into the larger part. At the end, a moment of silence is observed or a poem is read. This tradition was brought to the team by the palliative care chaplain, Douglas Falls, MDiv.
Bimonthly bereavement meetings are held at the James A. Haley Veterans’ Hospital-Pasco County branch, and each veteran who has died is remembered. Whoever wants to share is welcome. “We conclude with a poem, usually shared by the physician, but it can be any team member,” explained Linda Falzetta-Gross, ARNP-BC. “This process is led by the team social worker. In the past, we used to ring a bell prior to each name.”
Bells also are used at the Greater West Los Angeles VAMC in California. At the weekly clinic, veterans who have died are remembered, and each team member has an opportunity to share memories. “We ring a Tibetan bell for a moment without words,” explains Geoffrey Tyrell, palliative care chaplain. “It is introduced with a few words to allow new staff members in our clinic to participate, as a moment of mindfulness to let go of our words and to go inside, to see what we might need for our own wellness.” Afterward the chaplain says a few words and wishes for peace for the veterans and their families. The team also has responded well to more participatory group activities, such as placing rocks in a bowl of water, to symbolize letting go of something that has been difficult.
Additionally, there are practices of a larger scope. Many VAMCs have established facility-wide memorial services annually, biannually, or quarterly. At this time, families and staff come together to remember and honor veterans who have died within the VAMC. These memorials might involve a variety of service lines, such as chaplaincy, voluntary services, nursing, and social work and may consist of an honor guard, music, and readings. In accordance with the Health Insurance Portability and Accountability Act (HIPAA) and privacy regulations, only family members of deceased veterans may speak the names at the ceremony unless written consent is given. At the Tennessee Valley Healthcare System in Nashville, family members may stand and give the name of the person they are honoring. Balloons are released, stories are told, and a poem or appropriate passage is read. Families are given a book pinned with a flag, according to Jennifer C. Crenshaw, clinical staff chaplain. Family members are moved knowing that the VA remembers their loved ones even months after they are gone.
Due to the overwhelming positive feedback from veterans’ families who participated in these ceremonies, on January 24, 2018, Carolyn Clancy, MD, VHA Executive-in-Charge, Office of the Under Secretary for Health issued a memorandum requesting that all VAMCs immediately adopt this best practice: to host periodic ceremonies to publicly recognize and honor deceased veterans in the presence of their families, VA care providers, veterans service organizations and community members. Clancy recommended calling the ceremonies “The Last Roll Call Ceremony of Remembrance.”2
These rituals are a small sample of the rich diversity of practice in VAs across the country. What unifies VA palliative care providers is our mission to serve the veterans, honor their deaths, show respect and gratitude, and recognize that we, too, feel the pain of loss. We mark these moments with solemnity and beauty—a bell, a poem, a prayer—to honor our shared experience caring for veterans.
1. Saint S. A VA hospital you may not know: The Final Salute, and how much we doctors care. https://theconversation.com/a-va-hospital-you-may-not-know-the-final-salute-and-how-much-we-doctors-care-94217. Published March 30, 2018. Accessed May 8, 2019.
2. Clancy CM. VAIQ Memorandum 7866347: Implementation of the last roll call ceremony of remembrance at all Veterans Affairs medical centers. Published 2018.
1. Saint S. A VA hospital you may not know: The Final Salute, and how much we doctors care. https://theconversation.com/a-va-hospital-you-may-not-know-the-final-salute-and-how-much-we-doctors-care-94217. Published March 30, 2018. Accessed May 8, 2019.
2. Clancy CM. VAIQ Memorandum 7866347: Implementation of the last roll call ceremony of remembrance at all Veterans Affairs medical centers. Published 2018.
GI practice consolidation continues
Digestive Disease Week® (DDW) 2019 is now history. This was the 50th anniversary of DDW and again, it lived up to its reputation as the world’s foremost meeting dedicated to digestive diseases. GI & Hepatology News will publish multiple articles highlighting the best of DDW in the coming months.
The AGA Presidential Plenary session is an annual DDW highlight. This year’s session did not disappoint and was attended by a large crowd. David Lieberman, MD, AGAF (outgoing AGA president) and Hashem B. El-Serag MD, MPH, AGAF (incoming AGA president) moderated the session. Outstanding presentations about management of obesity, new findings in IBD, the use of virtual reality in the treatment of functional abdominal pain, and findings from a long-term colorectal cancer screening trial were some of the key presentations.
Recent behind-the-scenes work by the AGA is paying off for its members and the larger GI community. The AGA was again awarded an NIH-funded grant to advance its education and training of under-represented minorities. This is the second NIH grant given to the AGA, who now has become a leader in diversity and inclusive education. The AGA has strengthened its close bond with the Crohn's and Colitis Foundation, adding to its portfolio of scientific and clinical offerings focused on IBD. The AGA Center for Gut Microbiome Research and Education has emerged as one of the best sources of education and research about the microbiome’s impact on digestive health.
On the business front, there are tectonic changes occurring. In 2018, three large GI practices were sold to private equity companies and each has completed multiple arbitrage plays (acquisition of smaller practices), growing to over 200 physicians. This year we will see 6-10 additional private equity acquisitions and will likely see one or more GI practices of 500-1000 providers. This consolidation will have profound implications for the practice of gastroenterology and will provide some interesting opportunities to conduct population-based research for physicians who can capture that potential through academic-community partnerships.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Digestive Disease Week® (DDW) 2019 is now history. This was the 50th anniversary of DDW and again, it lived up to its reputation as the world’s foremost meeting dedicated to digestive diseases. GI & Hepatology News will publish multiple articles highlighting the best of DDW in the coming months.
The AGA Presidential Plenary session is an annual DDW highlight. This year’s session did not disappoint and was attended by a large crowd. David Lieberman, MD, AGAF (outgoing AGA president) and Hashem B. El-Serag MD, MPH, AGAF (incoming AGA president) moderated the session. Outstanding presentations about management of obesity, new findings in IBD, the use of virtual reality in the treatment of functional abdominal pain, and findings from a long-term colorectal cancer screening trial were some of the key presentations.
Recent behind-the-scenes work by the AGA is paying off for its members and the larger GI community. The AGA was again awarded an NIH-funded grant to advance its education and training of under-represented minorities. This is the second NIH grant given to the AGA, who now has become a leader in diversity and inclusive education. The AGA has strengthened its close bond with the Crohn's and Colitis Foundation, adding to its portfolio of scientific and clinical offerings focused on IBD. The AGA Center for Gut Microbiome Research and Education has emerged as one of the best sources of education and research about the microbiome’s impact on digestive health.
On the business front, there are tectonic changes occurring. In 2018, three large GI practices were sold to private equity companies and each has completed multiple arbitrage plays (acquisition of smaller practices), growing to over 200 physicians. This year we will see 6-10 additional private equity acquisitions and will likely see one or more GI practices of 500-1000 providers. This consolidation will have profound implications for the practice of gastroenterology and will provide some interesting opportunities to conduct population-based research for physicians who can capture that potential through academic-community partnerships.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Digestive Disease Week® (DDW) 2019 is now history. This was the 50th anniversary of DDW and again, it lived up to its reputation as the world’s foremost meeting dedicated to digestive diseases. GI & Hepatology News will publish multiple articles highlighting the best of DDW in the coming months.
The AGA Presidential Plenary session is an annual DDW highlight. This year’s session did not disappoint and was attended by a large crowd. David Lieberman, MD, AGAF (outgoing AGA president) and Hashem B. El-Serag MD, MPH, AGAF (incoming AGA president) moderated the session. Outstanding presentations about management of obesity, new findings in IBD, the use of virtual reality in the treatment of functional abdominal pain, and findings from a long-term colorectal cancer screening trial were some of the key presentations.
Recent behind-the-scenes work by the AGA is paying off for its members and the larger GI community. The AGA was again awarded an NIH-funded grant to advance its education and training of under-represented minorities. This is the second NIH grant given to the AGA, who now has become a leader in diversity and inclusive education. The AGA has strengthened its close bond with the Crohn's and Colitis Foundation, adding to its portfolio of scientific and clinical offerings focused on IBD. The AGA Center for Gut Microbiome Research and Education has emerged as one of the best sources of education and research about the microbiome’s impact on digestive health.
On the business front, there are tectonic changes occurring. In 2018, three large GI practices were sold to private equity companies and each has completed multiple arbitrage plays (acquisition of smaller practices), growing to over 200 physicians. This year we will see 6-10 additional private equity acquisitions and will likely see one or more GI practices of 500-1000 providers. This consolidation will have profound implications for the practice of gastroenterology and will provide some interesting opportunities to conduct population-based research for physicians who can capture that potential through academic-community partnerships.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Psychiatry and neurology, more
Dr. Nasrallah’s “Psychiatry and neurology: Sister neuroscience specialties with different approaches to the brain” (From the Editor,
In mathematics, chaos theory deals with the impossible complexity of simplicity. From primitive initial states, self-interacting systems give rise to short-term predictability, but an unpredictable long-term. Classically, this is illustrated as a hurricane born from the flapping of a butterfly’s wings. Neurology has found great clinical utility in understanding butterfly wings. However, psychiatry forsakes simplicity for complexity: it dives into the emergent systems that arise from self-interacting neurons, asking us to stand within the eye of the hurricane and understand it in its entirety. Psychiatry asks us to transcend the traditional medical focus of discrete physiological mechanisms, and ask—from the standpoint of biologic, social, and spiritual well-being—how can we calm the hurricane?
Psychiatry once had a widely-encompassing understanding of its remit: to appreciate the multifaceted experience of the human life and grant succor to the fractured or anguished soul. In such times, psychiatry was a popular destination for seniors graduating in the United States. Annually, 7% to 10% of US graduates chose psychiatry as a career, and continued to do so until the late 1970s.1 In the 1970s, the reductive understanding of the mind increased in prominence, and the role of psychiatry transitioned to one similar to that of other medical specialties: putting patients in boxes, and chronically titrating their medications. The interest of graduating seniors waned alongside the scope of our interest: in 1977, only 4.4% of US graduates pursued psychiatry.2 In 2019, 4.06% of graduating senior applications were to the field of psychiatry.3 (This is not meant to undervalue the quality of international medical graduates, but to focus on local trends in cultural values.)
Psychiatry offers diagnostic and therapeutic avenues that are traditionally undervalued in other fields of medicine. Nephrosis may not care if a patient feels that his or her life is spiritually satisfying and their actions meaningful. However, a patient’s anguish at his reduced functional status does not care for whether his albumin level is normalized—he requires that his suffering be recognized, and that we make an earnest effort to cloak “the shameful nakedness of pain.”4
Psychiatry also makes unique demands of, and offers benefits to, the practitioner. Neurologists complete their residencies feeling that their clinical acumen has increased: “I can formulate a thorough differential now.” Psychiatry asks us not only to cultivate technical proficiency, but also wisdom. The prolonged reflection on the quality and nature of human experience, and the need to guide such patients in a manner far wider and more meaningful in scope than their serotonin pathways, offers the opportunity to emerge from residency a more mindful and grateful human being.
Ultimately, the loss of this sense of scope has not been a failure of medical education. It has been a surrender of the current generation of psychiatry attendings. We have ceded responsibility for the social and spiritual care of our patients to other fields, or to no one at all. If we give up on understanding the hurricane, how can we be surprised that students prefer to chase butterflies?
James Steinberg, MPH, OMS-IV
New York Institute of Technology
College of Osteopathic Medicine
Old Westbury, New York
Robert Barris, MD
Director
Inpatient Psychiatric Services
Nassau University Medical Center
East Meadow, New York
References
1. Sierles FS, Taylor MA. Decline of U.S. medical student career choice of psychiatry and what to do about it. Am J Psychiatry. 1995;152(10):1416-1426.
2. Results and data: main residency match. NRMP data. The National Resident Matching Program. https://mk0nrmpcikgb8jxyd19h.kinstacdn.com/wp-content/uploads/2013/08/resultsanddata1984.pdf. Published May 1984. Accessed May 8, 2019.
3. Advanced Data Tables. The Match 2019. The National Resident Matching Program. https://mk0nrmpcikgb8jxyd19h.kinstacdn.com/wp-content/uploads/2019/03/Advance-Data-Tables-2019_WWW.pdf. Published March 2019. Accessed May 8, 2019.
4. Kipling R. Doctors. In: Kipling: poems (Everyman’s Library Pocket Poets Series). New York, NY: Random House. 2007:234.
Dr. Nasrallah responds
Thank you, Mr. Steinberg and Dr. Barris, for your comments about my editorial. I genuinely enjoyed the eloquence of your letter. In computers, which we all own and use, hardware is indispensable because it enables us to exploit the software, but the richness of the software is far more interesting than the hardware for the creative productivity of humans. So what you say is correct: T
Henry A. Nasrallah, MD
Editor-in-Chief
The Sydney W. Souers Endowed Chair
Professor and Chairman
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
Continue to: Perspectives on motherhood and psychiatry
Perspectives on motherhood and psychiatry
I very much enjoyed Drs. Helen M. Farrell’s and Katherine A. Kosman’s recent article “Motherhood and the working psychiatrist” (Psychiatry 2.0,
Christina Ford, MD
Private psychiatric practice
Los Angeles, California
I doubt that anyone—male or female—would argue against the points made by Drs. Farrell and Kosman’s “Motherhood and the working psychiatrist,” which emphasized the need for breaking down the barriers that continue to exist for female physicians who choose to balance their careers with motherhood. As a female psychiatrist who has known since high school that I would choose to remain child-free, I would like to add a different perspective to this discussion and possibly help represent the 20% of women, age 40 to 44, with an MD or PhD who are also child-free.1
While Drs. Farrell and Kosman referenced many assumptions made about working physician mothers, I have not been able to move through medical school, residency, and my career without battling certain assumptions as well. Although every mother is a woman, logic dictates that the converse—every woman is a mother—is certainly not true. However, when interviewing for residency, I was paired specifically with a female attending who had children, and I was told that I could ask her questions about how to balance work-life and raising a family, despite the fact that I did not say or indicate that I had any interest in having such a conversation. There is also the assumption (sometimes more explicit than others) that those of us without children are missing out on something—that we are not included in the “having it all” category. However, in my mind, “having it all” means having the choice to remain child-free, to focus more intensely on my career, to travel when I want, and to own a white couch—without feeling the social obligation to fulfill a role in which I really have no interest.
Cherishing that ability to focus more on my career, however, does not imply that I am boundlessly able and willing to take extra calls, work holidays, or cover for all my colleagues with children (which is also a common assumption). And while I may not be a caregiver to children, that should not detract from the devotion and time I want to spend helping my parents, relatives, and friends.
The article also made the case that facilities, medical schools, and residency programs need to implement policies and procedures that guide the development of accommodations, such as flexible scheduling and lactation rooms, to meet the needs of trainees and physicians without having to jump through hoops or rely on colleagues for coverage and other assistance. Having been in situations where such policies and procedures were not in place, I can affirm that the absence of such guidelines leads not only parents but also child-free physicians to feeling unnecessarily stressed. There was no clear coverage in place when fellow classmates in my residency program went on maternity leave. Essentially, everyone else was expected to step up and take on the additional caseloads, leading the pregnant classmates to try to time things around rotations where there were lighter demands or more residents assigned—not a simple task by any means.
Post-residency, there have been continued challenges. At one point, I was working in a clinic with 2 other female psychiatrists, one of whom was making plans to take maternity leave. During a meeting with our supervisors, the other physician and I were told that we were taking on the third doctor’s patients (without any extension of our own hours or reimbursement) while she was on leave. In addition to disgruntlement over the extra work being sprung on us, I pointed out that this would, in effect, make the third physician’s role obsolete. If 2 of us were able to do the work of 3, what would be the point in keeping her position when she returned? I was assured that this wouldn’t be the case. We dealt with the weeks of covering additional patients, and when she returned from leave, she was asked to shift some of her hours to a different (and, in my opinion, less desirable) clinic.
So, yes, it is incumbent upon facilities and training programs to take responsibility and to remove the barriers that make the jobs of female physicians with children even more challenging than they need to be. This can benefit not only those physicians and their children, but also their colleagues and, ultimately, the patients, who often bear the brunt of stressed, burnt-out physicians and disorganized programs. While I am not going to take a stance on whether it truly takes a village to raise a child, I certainly do not think that it should take a village to organize maternity leave and lactation rooms.
Jessica L. Langenhan, MD, MBA, CHCQM
Medical DirectorBeacon Health Options
Cypress, California
Reference
1. Livingston G. Childlessness. Pew Research Center. https://www.pewsocialtrends.org/2015/05/07/childlessness/. Published May 7, 2015. Accessed May 9, 2019.
Dr. Nasrallah’s “Psychiatry and neurology: Sister neuroscience specialties with different approaches to the brain” (From the Editor,
In mathematics, chaos theory deals with the impossible complexity of simplicity. From primitive initial states, self-interacting systems give rise to short-term predictability, but an unpredictable long-term. Classically, this is illustrated as a hurricane born from the flapping of a butterfly’s wings. Neurology has found great clinical utility in understanding butterfly wings. However, psychiatry forsakes simplicity for complexity: it dives into the emergent systems that arise from self-interacting neurons, asking us to stand within the eye of the hurricane and understand it in its entirety. Psychiatry asks us to transcend the traditional medical focus of discrete physiological mechanisms, and ask—from the standpoint of biologic, social, and spiritual well-being—how can we calm the hurricane?
Psychiatry once had a widely-encompassing understanding of its remit: to appreciate the multifaceted experience of the human life and grant succor to the fractured or anguished soul. In such times, psychiatry was a popular destination for seniors graduating in the United States. Annually, 7% to 10% of US graduates chose psychiatry as a career, and continued to do so until the late 1970s.1 In the 1970s, the reductive understanding of the mind increased in prominence, and the role of psychiatry transitioned to one similar to that of other medical specialties: putting patients in boxes, and chronically titrating their medications. The interest of graduating seniors waned alongside the scope of our interest: in 1977, only 4.4% of US graduates pursued psychiatry.2 In 2019, 4.06% of graduating senior applications were to the field of psychiatry.3 (This is not meant to undervalue the quality of international medical graduates, but to focus on local trends in cultural values.)
Psychiatry offers diagnostic and therapeutic avenues that are traditionally undervalued in other fields of medicine. Nephrosis may not care if a patient feels that his or her life is spiritually satisfying and their actions meaningful. However, a patient’s anguish at his reduced functional status does not care for whether his albumin level is normalized—he requires that his suffering be recognized, and that we make an earnest effort to cloak “the shameful nakedness of pain.”4
Psychiatry also makes unique demands of, and offers benefits to, the practitioner. Neurologists complete their residencies feeling that their clinical acumen has increased: “I can formulate a thorough differential now.” Psychiatry asks us not only to cultivate technical proficiency, but also wisdom. The prolonged reflection on the quality and nature of human experience, and the need to guide such patients in a manner far wider and more meaningful in scope than their serotonin pathways, offers the opportunity to emerge from residency a more mindful and grateful human being.
Ultimately, the loss of this sense of scope has not been a failure of medical education. It has been a surrender of the current generation of psychiatry attendings. We have ceded responsibility for the social and spiritual care of our patients to other fields, or to no one at all. If we give up on understanding the hurricane, how can we be surprised that students prefer to chase butterflies?
James Steinberg, MPH, OMS-IV
New York Institute of Technology
College of Osteopathic Medicine
Old Westbury, New York
Robert Barris, MD
Director
Inpatient Psychiatric Services
Nassau University Medical Center
East Meadow, New York
References
1. Sierles FS, Taylor MA. Decline of U.S. medical student career choice of psychiatry and what to do about it. Am J Psychiatry. 1995;152(10):1416-1426.
2. Results and data: main residency match. NRMP data. The National Resident Matching Program. https://mk0nrmpcikgb8jxyd19h.kinstacdn.com/wp-content/uploads/2013/08/resultsanddata1984.pdf. Published May 1984. Accessed May 8, 2019.
3. Advanced Data Tables. The Match 2019. The National Resident Matching Program. https://mk0nrmpcikgb8jxyd19h.kinstacdn.com/wp-content/uploads/2019/03/Advance-Data-Tables-2019_WWW.pdf. Published March 2019. Accessed May 8, 2019.
4. Kipling R. Doctors. In: Kipling: poems (Everyman’s Library Pocket Poets Series). New York, NY: Random House. 2007:234.
Dr. Nasrallah responds
Thank you, Mr. Steinberg and Dr. Barris, for your comments about my editorial. I genuinely enjoyed the eloquence of your letter. In computers, which we all own and use, hardware is indispensable because it enables us to exploit the software, but the richness of the software is far more interesting than the hardware for the creative productivity of humans. So what you say is correct: T
Henry A. Nasrallah, MD
Editor-in-Chief
The Sydney W. Souers Endowed Chair
Professor and Chairman
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
Continue to: Perspectives on motherhood and psychiatry
Perspectives on motherhood and psychiatry
I very much enjoyed Drs. Helen M. Farrell’s and Katherine A. Kosman’s recent article “Motherhood and the working psychiatrist” (Psychiatry 2.0,
Christina Ford, MD
Private psychiatric practice
Los Angeles, California
I doubt that anyone—male or female—would argue against the points made by Drs. Farrell and Kosman’s “Motherhood and the working psychiatrist,” which emphasized the need for breaking down the barriers that continue to exist for female physicians who choose to balance their careers with motherhood. As a female psychiatrist who has known since high school that I would choose to remain child-free, I would like to add a different perspective to this discussion and possibly help represent the 20% of women, age 40 to 44, with an MD or PhD who are also child-free.1
While Drs. Farrell and Kosman referenced many assumptions made about working physician mothers, I have not been able to move through medical school, residency, and my career without battling certain assumptions as well. Although every mother is a woman, logic dictates that the converse—every woman is a mother—is certainly not true. However, when interviewing for residency, I was paired specifically with a female attending who had children, and I was told that I could ask her questions about how to balance work-life and raising a family, despite the fact that I did not say or indicate that I had any interest in having such a conversation. There is also the assumption (sometimes more explicit than others) that those of us without children are missing out on something—that we are not included in the “having it all” category. However, in my mind, “having it all” means having the choice to remain child-free, to focus more intensely on my career, to travel when I want, and to own a white couch—without feeling the social obligation to fulfill a role in which I really have no interest.
Cherishing that ability to focus more on my career, however, does not imply that I am boundlessly able and willing to take extra calls, work holidays, or cover for all my colleagues with children (which is also a common assumption). And while I may not be a caregiver to children, that should not detract from the devotion and time I want to spend helping my parents, relatives, and friends.
The article also made the case that facilities, medical schools, and residency programs need to implement policies and procedures that guide the development of accommodations, such as flexible scheduling and lactation rooms, to meet the needs of trainees and physicians without having to jump through hoops or rely on colleagues for coverage and other assistance. Having been in situations where such policies and procedures were not in place, I can affirm that the absence of such guidelines leads not only parents but also child-free physicians to feeling unnecessarily stressed. There was no clear coverage in place when fellow classmates in my residency program went on maternity leave. Essentially, everyone else was expected to step up and take on the additional caseloads, leading the pregnant classmates to try to time things around rotations where there were lighter demands or more residents assigned—not a simple task by any means.
Post-residency, there have been continued challenges. At one point, I was working in a clinic with 2 other female psychiatrists, one of whom was making plans to take maternity leave. During a meeting with our supervisors, the other physician and I were told that we were taking on the third doctor’s patients (without any extension of our own hours or reimbursement) while she was on leave. In addition to disgruntlement over the extra work being sprung on us, I pointed out that this would, in effect, make the third physician’s role obsolete. If 2 of us were able to do the work of 3, what would be the point in keeping her position when she returned? I was assured that this wouldn’t be the case. We dealt with the weeks of covering additional patients, and when she returned from leave, she was asked to shift some of her hours to a different (and, in my opinion, less desirable) clinic.
So, yes, it is incumbent upon facilities and training programs to take responsibility and to remove the barriers that make the jobs of female physicians with children even more challenging than they need to be. This can benefit not only those physicians and their children, but also their colleagues and, ultimately, the patients, who often bear the brunt of stressed, burnt-out physicians and disorganized programs. While I am not going to take a stance on whether it truly takes a village to raise a child, I certainly do not think that it should take a village to organize maternity leave and lactation rooms.
Jessica L. Langenhan, MD, MBA, CHCQM
Medical DirectorBeacon Health Options
Cypress, California
Reference
1. Livingston G. Childlessness. Pew Research Center. https://www.pewsocialtrends.org/2015/05/07/childlessness/. Published May 7, 2015. Accessed May 9, 2019.
Dr. Nasrallah’s “Psychiatry and neurology: Sister neuroscience specialties with different approaches to the brain” (From the Editor,
In mathematics, chaos theory deals with the impossible complexity of simplicity. From primitive initial states, self-interacting systems give rise to short-term predictability, but an unpredictable long-term. Classically, this is illustrated as a hurricane born from the flapping of a butterfly’s wings. Neurology has found great clinical utility in understanding butterfly wings. However, psychiatry forsakes simplicity for complexity: it dives into the emergent systems that arise from self-interacting neurons, asking us to stand within the eye of the hurricane and understand it in its entirety. Psychiatry asks us to transcend the traditional medical focus of discrete physiological mechanisms, and ask—from the standpoint of biologic, social, and spiritual well-being—how can we calm the hurricane?
Psychiatry once had a widely-encompassing understanding of its remit: to appreciate the multifaceted experience of the human life and grant succor to the fractured or anguished soul. In such times, psychiatry was a popular destination for seniors graduating in the United States. Annually, 7% to 10% of US graduates chose psychiatry as a career, and continued to do so until the late 1970s.1 In the 1970s, the reductive understanding of the mind increased in prominence, and the role of psychiatry transitioned to one similar to that of other medical specialties: putting patients in boxes, and chronically titrating their medications. The interest of graduating seniors waned alongside the scope of our interest: in 1977, only 4.4% of US graduates pursued psychiatry.2 In 2019, 4.06% of graduating senior applications were to the field of psychiatry.3 (This is not meant to undervalue the quality of international medical graduates, but to focus on local trends in cultural values.)
Psychiatry offers diagnostic and therapeutic avenues that are traditionally undervalued in other fields of medicine. Nephrosis may not care if a patient feels that his or her life is spiritually satisfying and their actions meaningful. However, a patient’s anguish at his reduced functional status does not care for whether his albumin level is normalized—he requires that his suffering be recognized, and that we make an earnest effort to cloak “the shameful nakedness of pain.”4
Psychiatry also makes unique demands of, and offers benefits to, the practitioner. Neurologists complete their residencies feeling that their clinical acumen has increased: “I can formulate a thorough differential now.” Psychiatry asks us not only to cultivate technical proficiency, but also wisdom. The prolonged reflection on the quality and nature of human experience, and the need to guide such patients in a manner far wider and more meaningful in scope than their serotonin pathways, offers the opportunity to emerge from residency a more mindful and grateful human being.
Ultimately, the loss of this sense of scope has not been a failure of medical education. It has been a surrender of the current generation of psychiatry attendings. We have ceded responsibility for the social and spiritual care of our patients to other fields, or to no one at all. If we give up on understanding the hurricane, how can we be surprised that students prefer to chase butterflies?
James Steinberg, MPH, OMS-IV
New York Institute of Technology
College of Osteopathic Medicine
Old Westbury, New York
Robert Barris, MD
Director
Inpatient Psychiatric Services
Nassau University Medical Center
East Meadow, New York
References
1. Sierles FS, Taylor MA. Decline of U.S. medical student career choice of psychiatry and what to do about it. Am J Psychiatry. 1995;152(10):1416-1426.
2. Results and data: main residency match. NRMP data. The National Resident Matching Program. https://mk0nrmpcikgb8jxyd19h.kinstacdn.com/wp-content/uploads/2013/08/resultsanddata1984.pdf. Published May 1984. Accessed May 8, 2019.
3. Advanced Data Tables. The Match 2019. The National Resident Matching Program. https://mk0nrmpcikgb8jxyd19h.kinstacdn.com/wp-content/uploads/2019/03/Advance-Data-Tables-2019_WWW.pdf. Published March 2019. Accessed May 8, 2019.
4. Kipling R. Doctors. In: Kipling: poems (Everyman’s Library Pocket Poets Series). New York, NY: Random House. 2007:234.
Dr. Nasrallah responds
Thank you, Mr. Steinberg and Dr. Barris, for your comments about my editorial. I genuinely enjoyed the eloquence of your letter. In computers, which we all own and use, hardware is indispensable because it enables us to exploit the software, but the richness of the software is far more interesting than the hardware for the creative productivity of humans. So what you say is correct: T
Henry A. Nasrallah, MD
Editor-in-Chief
The Sydney W. Souers Endowed Chair
Professor and Chairman
Department of Psychiatry and Behavioral Neuroscience
Saint Louis University School of Medicine
St. Louis, Missouri
Continue to: Perspectives on motherhood and psychiatry
Perspectives on motherhood and psychiatry
I very much enjoyed Drs. Helen M. Farrell’s and Katherine A. Kosman’s recent article “Motherhood and the working psychiatrist” (Psychiatry 2.0,
Christina Ford, MD
Private psychiatric practice
Los Angeles, California
I doubt that anyone—male or female—would argue against the points made by Drs. Farrell and Kosman’s “Motherhood and the working psychiatrist,” which emphasized the need for breaking down the barriers that continue to exist for female physicians who choose to balance their careers with motherhood. As a female psychiatrist who has known since high school that I would choose to remain child-free, I would like to add a different perspective to this discussion and possibly help represent the 20% of women, age 40 to 44, with an MD or PhD who are also child-free.1
While Drs. Farrell and Kosman referenced many assumptions made about working physician mothers, I have not been able to move through medical school, residency, and my career without battling certain assumptions as well. Although every mother is a woman, logic dictates that the converse—every woman is a mother—is certainly not true. However, when interviewing for residency, I was paired specifically with a female attending who had children, and I was told that I could ask her questions about how to balance work-life and raising a family, despite the fact that I did not say or indicate that I had any interest in having such a conversation. There is also the assumption (sometimes more explicit than others) that those of us without children are missing out on something—that we are not included in the “having it all” category. However, in my mind, “having it all” means having the choice to remain child-free, to focus more intensely on my career, to travel when I want, and to own a white couch—without feeling the social obligation to fulfill a role in which I really have no interest.
Cherishing that ability to focus more on my career, however, does not imply that I am boundlessly able and willing to take extra calls, work holidays, or cover for all my colleagues with children (which is also a common assumption). And while I may not be a caregiver to children, that should not detract from the devotion and time I want to spend helping my parents, relatives, and friends.
The article also made the case that facilities, medical schools, and residency programs need to implement policies and procedures that guide the development of accommodations, such as flexible scheduling and lactation rooms, to meet the needs of trainees and physicians without having to jump through hoops or rely on colleagues for coverage and other assistance. Having been in situations where such policies and procedures were not in place, I can affirm that the absence of such guidelines leads not only parents but also child-free physicians to feeling unnecessarily stressed. There was no clear coverage in place when fellow classmates in my residency program went on maternity leave. Essentially, everyone else was expected to step up and take on the additional caseloads, leading the pregnant classmates to try to time things around rotations where there were lighter demands or more residents assigned—not a simple task by any means.
Post-residency, there have been continued challenges. At one point, I was working in a clinic with 2 other female psychiatrists, one of whom was making plans to take maternity leave. During a meeting with our supervisors, the other physician and I were told that we were taking on the third doctor’s patients (without any extension of our own hours or reimbursement) while she was on leave. In addition to disgruntlement over the extra work being sprung on us, I pointed out that this would, in effect, make the third physician’s role obsolete. If 2 of us were able to do the work of 3, what would be the point in keeping her position when she returned? I was assured that this wouldn’t be the case. We dealt with the weeks of covering additional patients, and when she returned from leave, she was asked to shift some of her hours to a different (and, in my opinion, less desirable) clinic.
So, yes, it is incumbent upon facilities and training programs to take responsibility and to remove the barriers that make the jobs of female physicians with children even more challenging than they need to be. This can benefit not only those physicians and their children, but also their colleagues and, ultimately, the patients, who often bear the brunt of stressed, burnt-out physicians and disorganized programs. While I am not going to take a stance on whether it truly takes a village to raise a child, I certainly do not think that it should take a village to organize maternity leave and lactation rooms.
Jessica L. Langenhan, MD, MBA, CHCQM
Medical DirectorBeacon Health Options
Cypress, California
Reference
1. Livingston G. Childlessness. Pew Research Center. https://www.pewsocialtrends.org/2015/05/07/childlessness/. Published May 7, 2015. Accessed May 9, 2019.
Mobile apps and mental health: Using technology to quantify real-time clinical risk
In today’s global society, smartphones are ubiquitous, used by >2.5 billion people.1 They provide limitless availability of on-demand services and resources, unparalleled computing power by size, and the ability to connect with anyone in the world.
Digital applications and new mobile technologies can be used to change the nature of the psychiatrist–patient relationship. The future of clinical practice is changing with the help of smartphones and apps. Diagnosis, follow-up, and treatment will never look the same as we come to better understand and apply emerging technologies.2
Both Android and iOS—the 2 largest mobile operating systems by market share3—provide outlets for the dissemination of mobile applications. There are currently >10,000 mental health–related apps available for download.4 One particular use case of mental health–related apps is digital phenotyping.
In this article, we aim to:
- define digital phenotyping
- explore the potential advances in patient care afforded by emerging technology
- discuss the ethical dilemmas and future of mental health apps.
The possibilities of digital phenotyping
Digital phenotyping is capturing a patient’s real-time clinical state using digital technology to better understand the patient’s state outside of the clinic. While digital phenotyping may seem new, the concepts behind it are grounded in good clinical care.
For example, it is important to assess sleep and physical activity for nearly all patients, regardless of diagnosis. However, the patient’s retrospective recollection of sleep, mood, and other clinically relevant metrics is often unreliable, especially when visits are months apart. With smartphones, it is possible to automatically collect metrics for sleep, activity, mood, and much more in real time from the convenience of our patients’ personal devices (Figure 1).
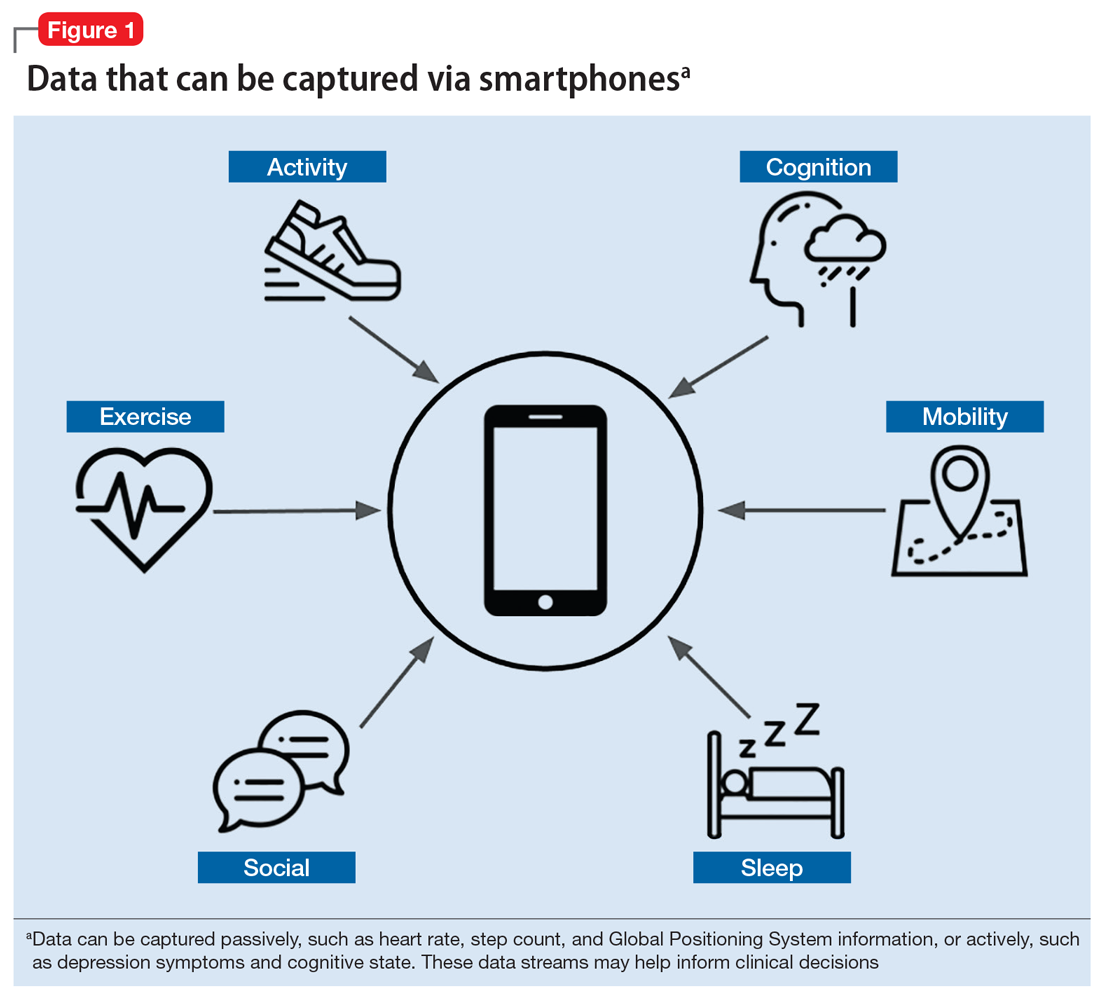
Smartphones can capture a seemingly endless number of data streams, from patient-interfacing active data, such as journal entries, messaging, and games, to data that is captured passively, such as screen time, Global Positioning System information, and step count. Clinicians can work with patients to customize which digital phenotyping data they would like to capture. In one study, researchers worked with 17 patients with schizophrenia by capturing self-reported surveys, anonymized phone call logs, and location data to see if they could predict relapse by observing variations in how patients interact with their smartphones.5 They observed that the rate of behavioral anomalies was 71% higher in the 2 weeks prior to relapse than during other periods. The data captured by the smartphone will depend on the patient and the clinical needs. Some clinicians may only want to collect data on step count and screen time to learn if a patient is overusing his or her smartphone, which might be related to becoming less physically active.
Continue to: One novel data stream...
One novel data stream offered by smartphone digital phenotyping is cognition. While we know that impaired cognition is a core symptom of schizophrenia, and that cognition is affected by depression and anxiety, cognitive symptoms are clinically challenging to quantify. Thus, the cognitive burden of mental illness and the cognitive effects of treatment are often overlooked. However, smartphones are beginning to offer a novel means of capturing a patient’s cognitive state through the use of common clinical tests. For example, the Trail Making Test measures visual attention and executive function by having participants connect dots that differ in number, color, or shape in an ascending pattern.6 By having patients perform this test on a smartphone, clinicians can utilize the touchscreen to capture the user’s discrete actions, such as time to completion and misclicks. These data can be used to build novel measures of cognitive performance that can account for learning bias and other confounding variables.7 While these digital cognitive biomarkers are still in active research, it is likely that they will quickly be developed for broad clinical use.
In addition to the novel data offered by digital phenotyping, another benefit is the low cost and ease of use. Unlike wearable devices such as smartwatches, which can also offer data on steps and sleep, smartphone-based digital phenotyping does not require patients to purchase or use additional devices. Running on patients’ smartphones, digital phenotyping offers the ability to capture rich and continuous health data without added effort or cost. Given that the average person interacts with their phone more than 2,600 times per day,8 smartphones are well suited for capturing large amounts of information that may provide insights into patients’ mental health.
For illnesses such as depression and anxiety, the clinical relevance of digital phenotyping is in the ability to capture symptoms as they occur in context. Figure 2 provides a simplified example of how we can learn that for this fictitious patient, exercise greatly improves anxiety, whereas being in a certain environment worsens it. Other insights about sleep and social settings could also provide further information about the context of the patient’s symptoms. While these correlations alone will not lead to better clinical outcomes, it is easy to imagine how such data could help a patient and clinician start a conversation about making impactful changes.
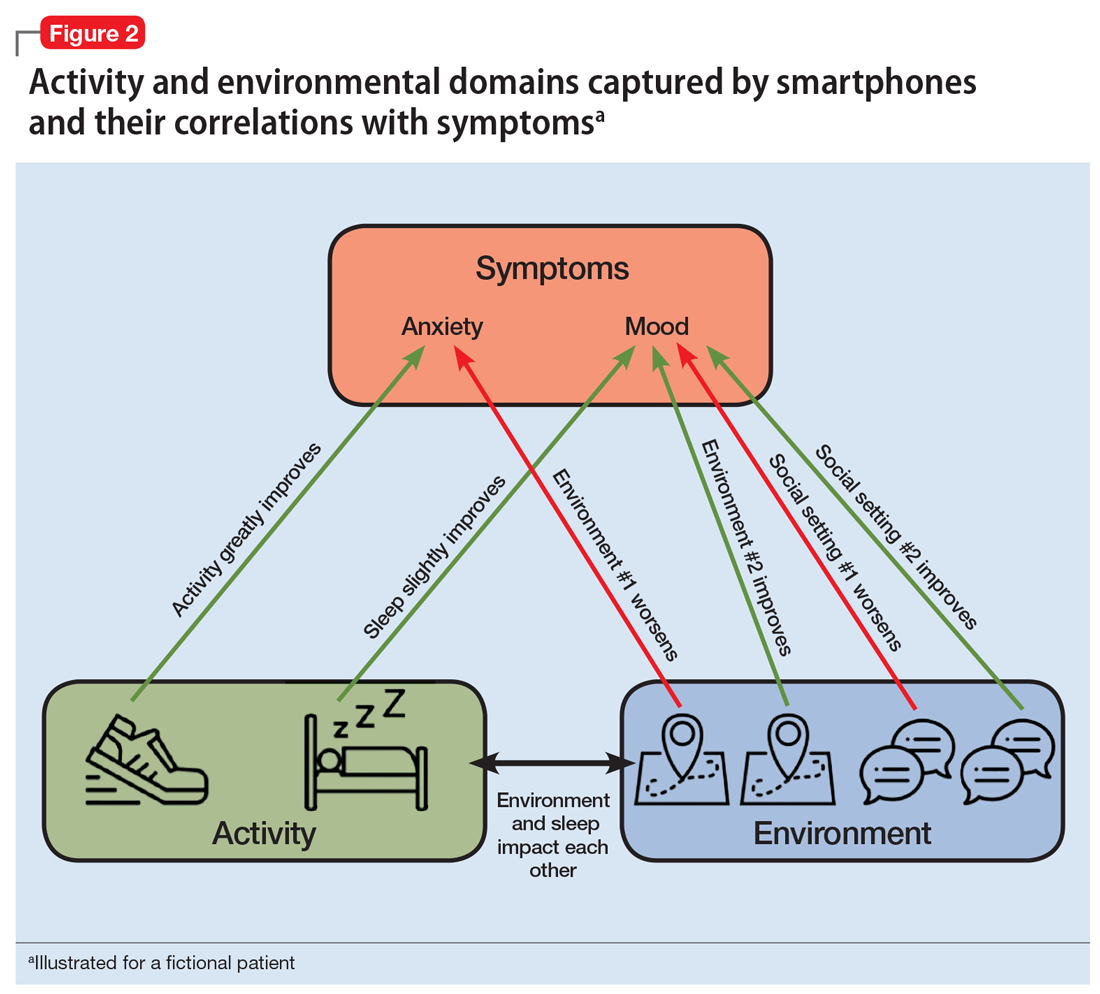
Continue to: Case report...
Case report: Digital phenotyping
To illustrate how digital phenotyping could be put to clinical use, we created the following case report of a fictional patient who agrees to be monitored via her smartphone.
Consider a hypothetical patient we will call Ms. T who is in her mid-20s and has been diagnosed with schizophrenia. On a follow-up visit, she says she has insomnia. She also reports having a recent loss of appetite and higher levels of anxiety. After reviewing her smartphone data (Figure 3), the clinician sees an inversely proportional relationship between her sleep quality and symptoms of anxiety, psychosis, and depression, which suggests that these symptoms might be due to poor sleep. Her step count has been fairly stable, indicating that there is no significant correlation between physical activity and her other symptoms.
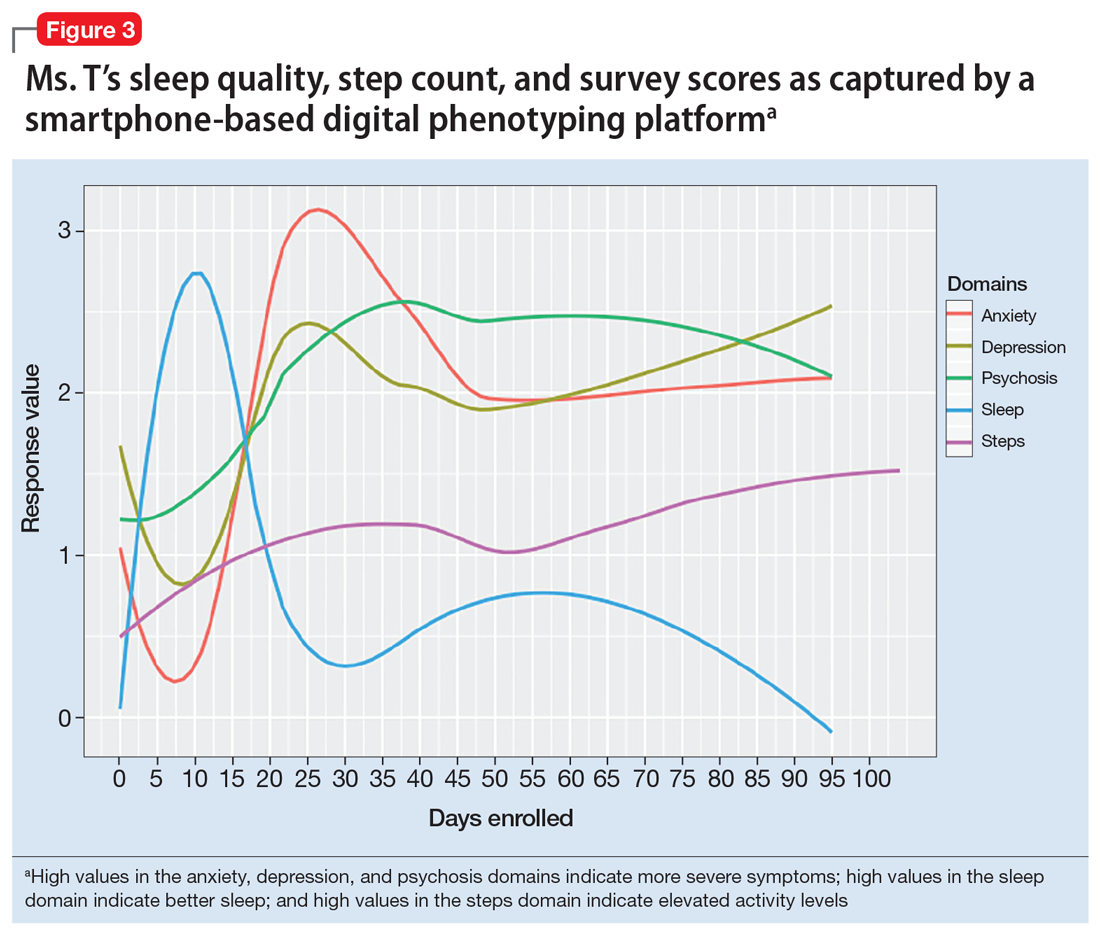
Continue to: The clinician shows...
The clinician shows Ms. T the data to help her understand why a trial of cognitive-behavioral therapy for insomnia, or at least improving sleep hygiene, may offer several benefits. The clinician advises her to continue to use the app to help assess her response to these interventions and monitor her progress in real time.
Dilemma: The ethics of continuous observation
The rich data captured by digital phenotyping afford many clinical opportunities, but also raise concerns. Among these are 3 significant ethical implications.
Firstly, the same data that may help a clinician learn about what environments are associated with less anxiety for the patient may also reveal personal details about where that patient has been or with whom they have interacted. In the wrong hands, such personal data could cause harm. And even in the hands of a trusted clinician, a breach in the patient’s privacy begs the question: “Should such information be anyone’s business at all?”
Secondly, many apps that offer digital phenotyping could also store patient data—something that currently pervades social media and causes reasonable discomfort for many people. You might have personally encountered this with social media platforms such as Facebook. When it comes to mobile mental health apps, clinicians should carefully understand the data usage agreement of any digital phenotyping app they wish to use and then share this information with their patients.
Finally, while it is possible to collect the types of data outlined in this article, less is known about how to use it directly in clinical care. Understanding for each patient which data streams are most meaningful and which data streams are noise that should be ignored is an area of ongoing research. A good first step may be to begin with data streams that are known to be clinically relevant and valuable, such as sleep and physical activity.9-11
Continue to: Discussion...
Discussion: Genomic sequencing and digital phenotyping
Although smartphones can gather a wide range of active and passive data, other data streams hold potential for predicting relapse and performing other clinically relevant actions. One data stream that could be of clinical use is genomic sequencing.12 The genotyping of patients provides a wealth of information about the underlying biology, and genomic sequencing has never been cheaper.13
Combining the data gathered via digital phenotyping with that of genotyping could help elucidate the mechanisms by which specific diseases and symptoms occur. This could be very promising to better understand and treat our patients. However, as is the case with genomics, digital phenotyping has important ethical implications. If used in the proper way to benefit our patients, the future for this new method is bright.
1. Statista. Number of smartphone users worldwide from 2014 to 2020 (in billions). https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Accessed April 29, 2019.
2. Thibaut F. Digital applications: the future in psychiatry? Dialogues Clin Neurosci. 2016;18(2):123.
3. Statista. Global market share held by the leading smartphone operating systems in sales to end users from 1st quarter 2009 to 2nd quarter 2018. https://www.statista.com/statistics/266136/global-market-share-held-by-smartphone-operating-systems/. Accessed April 19, 2019.
4. Torous J, Roberts L. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74(5):437-438.
5. Barnett I, Torous J, Staples P, et al. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018;43(8):1660-1666.
6. Arnett JA, Labovitz SS. Effect of physical layout in performance of the Trail Making Test. Psychological Assessment. 1995;7(2):220-221.
7. Brouillette RM, Foil H, Fontenot S, et al. Feasibility, reliability, and validity of a smartphone based application for the assessment of cognitive function in the elderly. PloS One. 2013;8(6):e65925. doi: 10.1371/journal.pone.0065925.
8. Winnick W. Putting a finger on our phone obsession. dscout. https://blog.dscout.com/mobile-touches. Published June 16, 2016. Accessed April 29, 2019.
9. Waite F, Myers E, Harvey AG, et al. Treating sleep problems in patients with schizophrenia. Behav Cogn Psychother. 2016;44(3):273-287.
10. Mcgurk SR, Mueser KT, Xie H, et al. (2015). Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial. Am J Psychiatry. 2015;172(9):852-861.
11. Firth J, Stubbs B, Rosenbaum S, et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2017;43(3):546-556.
12. Manolio TA, Chisholm RL, Ozenberger B, et al. Implementing genomic medicine in the clinic: the future is here. Genet Med. 2013;15(4):258-267.
13. National Human Genome Research Institute. The cost of sequencing a human genome. https://www.genome.gov/27565109/the-cost-of-sequencing-a-human-genome/. Updated July 6, 2016. Accessed April 29, 2019.
In today’s global society, smartphones are ubiquitous, used by >2.5 billion people.1 They provide limitless availability of on-demand services and resources, unparalleled computing power by size, and the ability to connect with anyone in the world.
Digital applications and new mobile technologies can be used to change the nature of the psychiatrist–patient relationship. The future of clinical practice is changing with the help of smartphones and apps. Diagnosis, follow-up, and treatment will never look the same as we come to better understand and apply emerging technologies.2
Both Android and iOS—the 2 largest mobile operating systems by market share3—provide outlets for the dissemination of mobile applications. There are currently >10,000 mental health–related apps available for download.4 One particular use case of mental health–related apps is digital phenotyping.
In this article, we aim to:
- define digital phenotyping
- explore the potential advances in patient care afforded by emerging technology
- discuss the ethical dilemmas and future of mental health apps.
The possibilities of digital phenotyping
Digital phenotyping is capturing a patient’s real-time clinical state using digital technology to better understand the patient’s state outside of the clinic. While digital phenotyping may seem new, the concepts behind it are grounded in good clinical care.
For example, it is important to assess sleep and physical activity for nearly all patients, regardless of diagnosis. However, the patient’s retrospective recollection of sleep, mood, and other clinically relevant metrics is often unreliable, especially when visits are months apart. With smartphones, it is possible to automatically collect metrics for sleep, activity, mood, and much more in real time from the convenience of our patients’ personal devices (Figure 1).
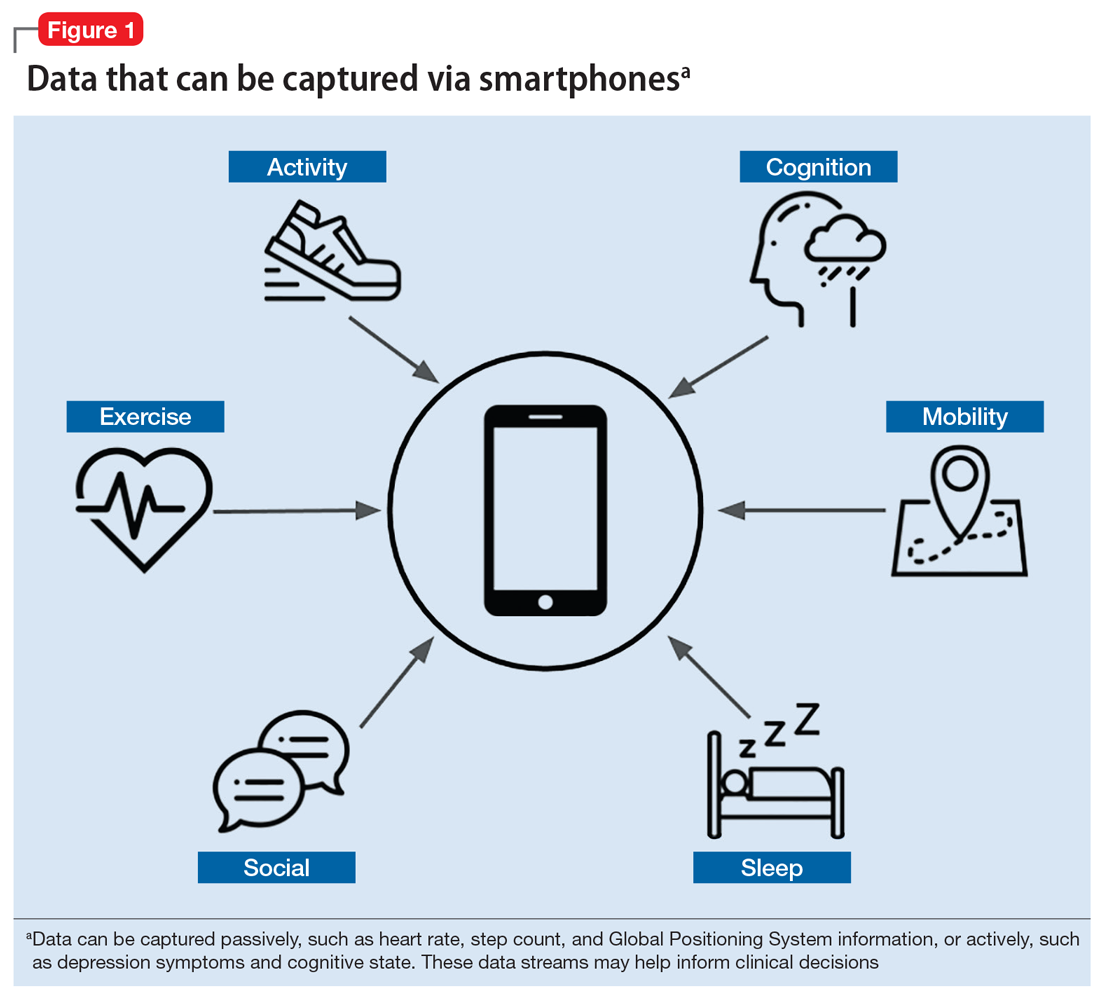
Smartphones can capture a seemingly endless number of data streams, from patient-interfacing active data, such as journal entries, messaging, and games, to data that is captured passively, such as screen time, Global Positioning System information, and step count. Clinicians can work with patients to customize which digital phenotyping data they would like to capture. In one study, researchers worked with 17 patients with schizophrenia by capturing self-reported surveys, anonymized phone call logs, and location data to see if they could predict relapse by observing variations in how patients interact with their smartphones.5 They observed that the rate of behavioral anomalies was 71% higher in the 2 weeks prior to relapse than during other periods. The data captured by the smartphone will depend on the patient and the clinical needs. Some clinicians may only want to collect data on step count and screen time to learn if a patient is overusing his or her smartphone, which might be related to becoming less physically active.
Continue to: One novel data stream...
One novel data stream offered by smartphone digital phenotyping is cognition. While we know that impaired cognition is a core symptom of schizophrenia, and that cognition is affected by depression and anxiety, cognitive symptoms are clinically challenging to quantify. Thus, the cognitive burden of mental illness and the cognitive effects of treatment are often overlooked. However, smartphones are beginning to offer a novel means of capturing a patient’s cognitive state through the use of common clinical tests. For example, the Trail Making Test measures visual attention and executive function by having participants connect dots that differ in number, color, or shape in an ascending pattern.6 By having patients perform this test on a smartphone, clinicians can utilize the touchscreen to capture the user’s discrete actions, such as time to completion and misclicks. These data can be used to build novel measures of cognitive performance that can account for learning bias and other confounding variables.7 While these digital cognitive biomarkers are still in active research, it is likely that they will quickly be developed for broad clinical use.
In addition to the novel data offered by digital phenotyping, another benefit is the low cost and ease of use. Unlike wearable devices such as smartwatches, which can also offer data on steps and sleep, smartphone-based digital phenotyping does not require patients to purchase or use additional devices. Running on patients’ smartphones, digital phenotyping offers the ability to capture rich and continuous health data without added effort or cost. Given that the average person interacts with their phone more than 2,600 times per day,8 smartphones are well suited for capturing large amounts of information that may provide insights into patients’ mental health.
For illnesses such as depression and anxiety, the clinical relevance of digital phenotyping is in the ability to capture symptoms as they occur in context. Figure 2 provides a simplified example of how we can learn that for this fictitious patient, exercise greatly improves anxiety, whereas being in a certain environment worsens it. Other insights about sleep and social settings could also provide further information about the context of the patient’s symptoms. While these correlations alone will not lead to better clinical outcomes, it is easy to imagine how such data could help a patient and clinician start a conversation about making impactful changes.
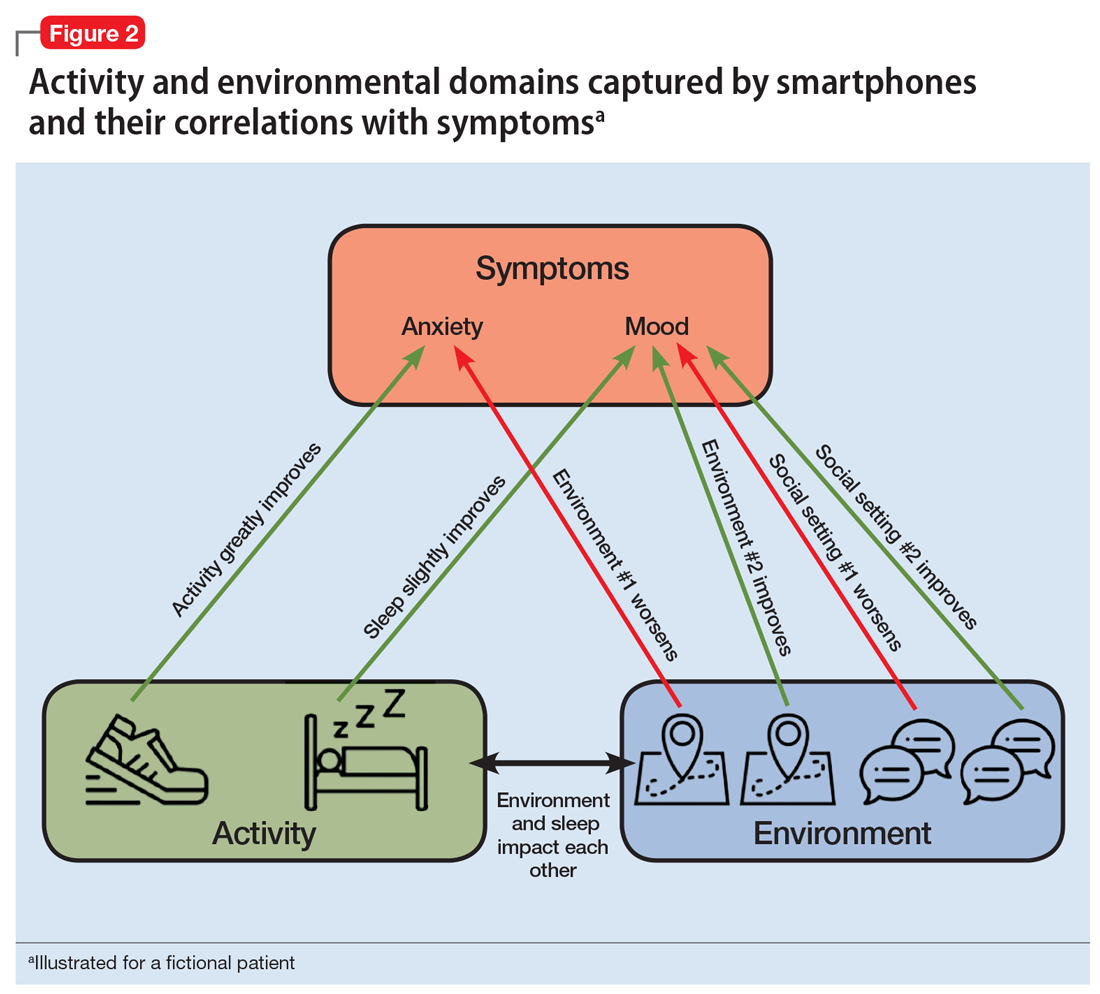
Continue to: Case report...
Case report: Digital phenotyping
To illustrate how digital phenotyping could be put to clinical use, we created the following case report of a fictional patient who agrees to be monitored via her smartphone.
Consider a hypothetical patient we will call Ms. T who is in her mid-20s and has been diagnosed with schizophrenia. On a follow-up visit, she says she has insomnia. She also reports having a recent loss of appetite and higher levels of anxiety. After reviewing her smartphone data (Figure 3), the clinician sees an inversely proportional relationship between her sleep quality and symptoms of anxiety, psychosis, and depression, which suggests that these symptoms might be due to poor sleep. Her step count has been fairly stable, indicating that there is no significant correlation between physical activity and her other symptoms.
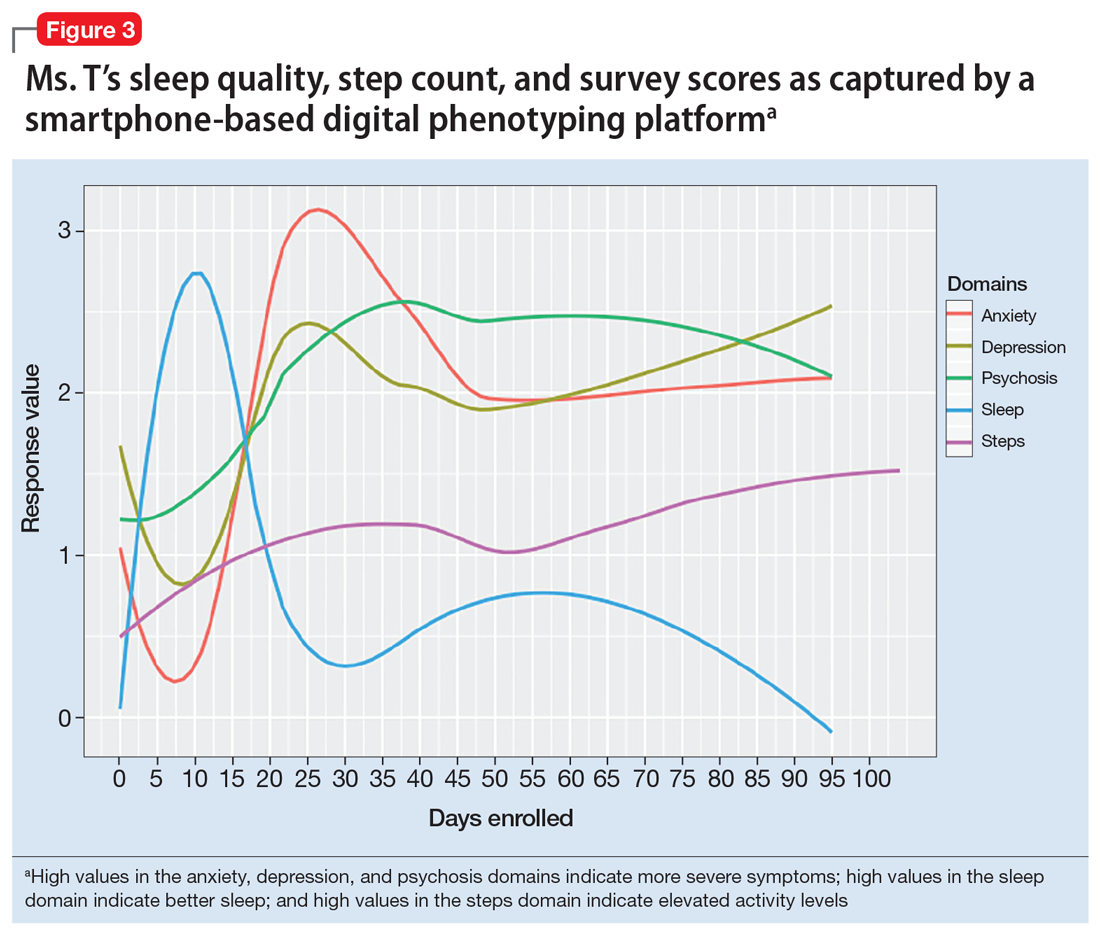
Continue to: The clinician shows...
The clinician shows Ms. T the data to help her understand why a trial of cognitive-behavioral therapy for insomnia, or at least improving sleep hygiene, may offer several benefits. The clinician advises her to continue to use the app to help assess her response to these interventions and monitor her progress in real time.
Dilemma: The ethics of continuous observation
The rich data captured by digital phenotyping afford many clinical opportunities, but also raise concerns. Among these are 3 significant ethical implications.
Firstly, the same data that may help a clinician learn about what environments are associated with less anxiety for the patient may also reveal personal details about where that patient has been or with whom they have interacted. In the wrong hands, such personal data could cause harm. And even in the hands of a trusted clinician, a breach in the patient’s privacy begs the question: “Should such information be anyone’s business at all?”
Secondly, many apps that offer digital phenotyping could also store patient data—something that currently pervades social media and causes reasonable discomfort for many people. You might have personally encountered this with social media platforms such as Facebook. When it comes to mobile mental health apps, clinicians should carefully understand the data usage agreement of any digital phenotyping app they wish to use and then share this information with their patients.
Finally, while it is possible to collect the types of data outlined in this article, less is known about how to use it directly in clinical care. Understanding for each patient which data streams are most meaningful and which data streams are noise that should be ignored is an area of ongoing research. A good first step may be to begin with data streams that are known to be clinically relevant and valuable, such as sleep and physical activity.9-11
Continue to: Discussion...
Discussion: Genomic sequencing and digital phenotyping
Although smartphones can gather a wide range of active and passive data, other data streams hold potential for predicting relapse and performing other clinically relevant actions. One data stream that could be of clinical use is genomic sequencing.12 The genotyping of patients provides a wealth of information about the underlying biology, and genomic sequencing has never been cheaper.13
Combining the data gathered via digital phenotyping with that of genotyping could help elucidate the mechanisms by which specific diseases and symptoms occur. This could be very promising to better understand and treat our patients. However, as is the case with genomics, digital phenotyping has important ethical implications. If used in the proper way to benefit our patients, the future for this new method is bright.
In today’s global society, smartphones are ubiquitous, used by >2.5 billion people.1 They provide limitless availability of on-demand services and resources, unparalleled computing power by size, and the ability to connect with anyone in the world.
Digital applications and new mobile technologies can be used to change the nature of the psychiatrist–patient relationship. The future of clinical practice is changing with the help of smartphones and apps. Diagnosis, follow-up, and treatment will never look the same as we come to better understand and apply emerging technologies.2
Both Android and iOS—the 2 largest mobile operating systems by market share3—provide outlets for the dissemination of mobile applications. There are currently >10,000 mental health–related apps available for download.4 One particular use case of mental health–related apps is digital phenotyping.
In this article, we aim to:
- define digital phenotyping
- explore the potential advances in patient care afforded by emerging technology
- discuss the ethical dilemmas and future of mental health apps.
The possibilities of digital phenotyping
Digital phenotyping is capturing a patient’s real-time clinical state using digital technology to better understand the patient’s state outside of the clinic. While digital phenotyping may seem new, the concepts behind it are grounded in good clinical care.
For example, it is important to assess sleep and physical activity for nearly all patients, regardless of diagnosis. However, the patient’s retrospective recollection of sleep, mood, and other clinically relevant metrics is often unreliable, especially when visits are months apart. With smartphones, it is possible to automatically collect metrics for sleep, activity, mood, and much more in real time from the convenience of our patients’ personal devices (Figure 1).
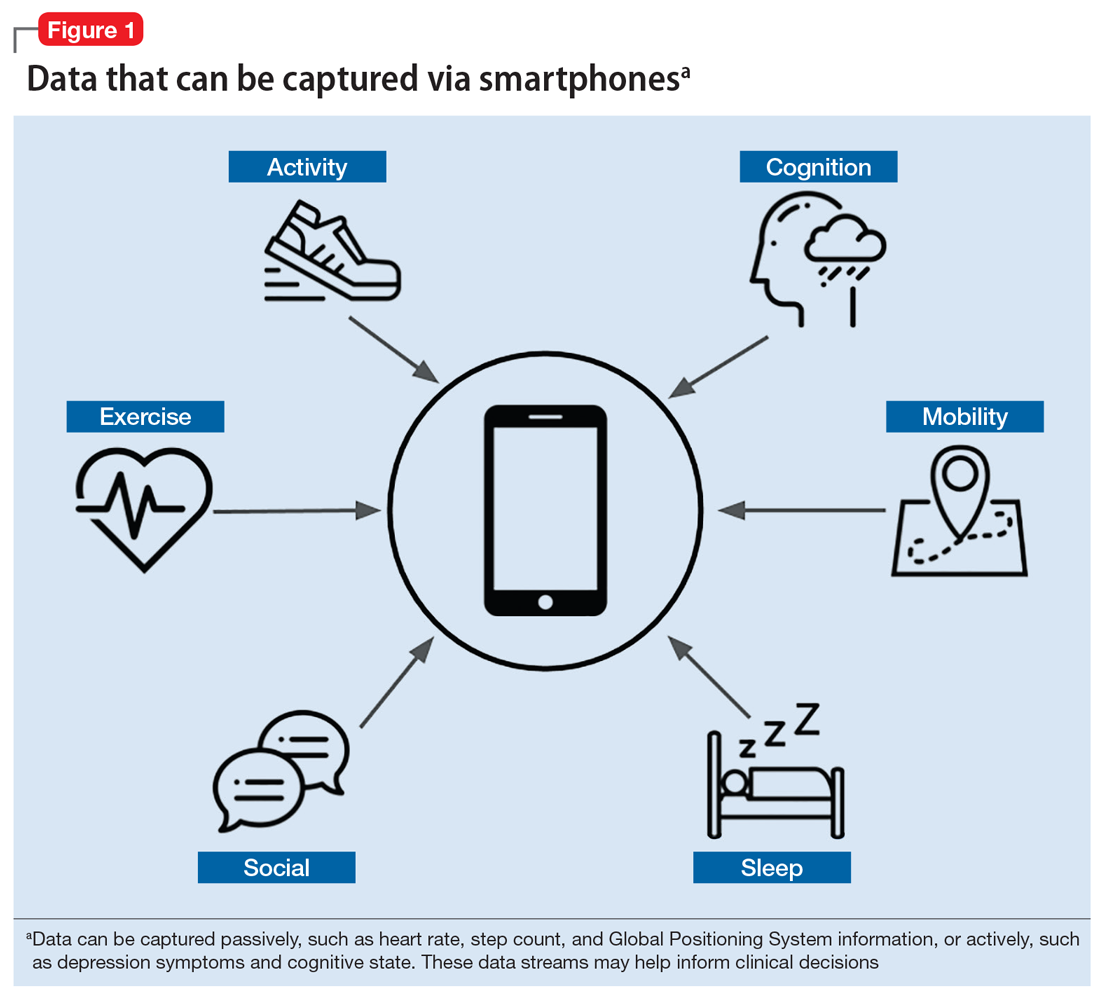
Smartphones can capture a seemingly endless number of data streams, from patient-interfacing active data, such as journal entries, messaging, and games, to data that is captured passively, such as screen time, Global Positioning System information, and step count. Clinicians can work with patients to customize which digital phenotyping data they would like to capture. In one study, researchers worked with 17 patients with schizophrenia by capturing self-reported surveys, anonymized phone call logs, and location data to see if they could predict relapse by observing variations in how patients interact with their smartphones.5 They observed that the rate of behavioral anomalies was 71% higher in the 2 weeks prior to relapse than during other periods. The data captured by the smartphone will depend on the patient and the clinical needs. Some clinicians may only want to collect data on step count and screen time to learn if a patient is overusing his or her smartphone, which might be related to becoming less physically active.
Continue to: One novel data stream...
One novel data stream offered by smartphone digital phenotyping is cognition. While we know that impaired cognition is a core symptom of schizophrenia, and that cognition is affected by depression and anxiety, cognitive symptoms are clinically challenging to quantify. Thus, the cognitive burden of mental illness and the cognitive effects of treatment are often overlooked. However, smartphones are beginning to offer a novel means of capturing a patient’s cognitive state through the use of common clinical tests. For example, the Trail Making Test measures visual attention and executive function by having participants connect dots that differ in number, color, or shape in an ascending pattern.6 By having patients perform this test on a smartphone, clinicians can utilize the touchscreen to capture the user’s discrete actions, such as time to completion and misclicks. These data can be used to build novel measures of cognitive performance that can account for learning bias and other confounding variables.7 While these digital cognitive biomarkers are still in active research, it is likely that they will quickly be developed for broad clinical use.
In addition to the novel data offered by digital phenotyping, another benefit is the low cost and ease of use. Unlike wearable devices such as smartwatches, which can also offer data on steps and sleep, smartphone-based digital phenotyping does not require patients to purchase or use additional devices. Running on patients’ smartphones, digital phenotyping offers the ability to capture rich and continuous health data without added effort or cost. Given that the average person interacts with their phone more than 2,600 times per day,8 smartphones are well suited for capturing large amounts of information that may provide insights into patients’ mental health.
For illnesses such as depression and anxiety, the clinical relevance of digital phenotyping is in the ability to capture symptoms as they occur in context. Figure 2 provides a simplified example of how we can learn that for this fictitious patient, exercise greatly improves anxiety, whereas being in a certain environment worsens it. Other insights about sleep and social settings could also provide further information about the context of the patient’s symptoms. While these correlations alone will not lead to better clinical outcomes, it is easy to imagine how such data could help a patient and clinician start a conversation about making impactful changes.
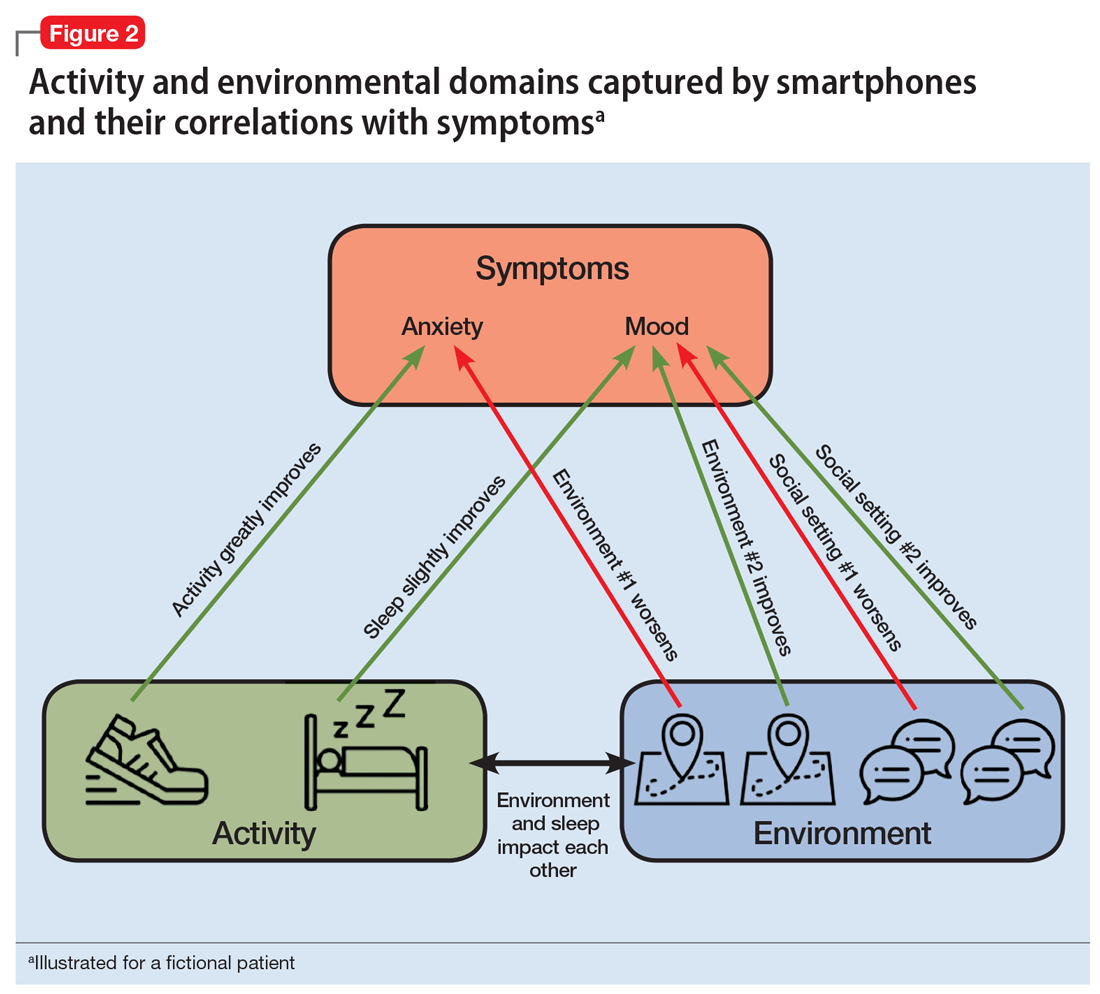
Continue to: Case report...
Case report: Digital phenotyping
To illustrate how digital phenotyping could be put to clinical use, we created the following case report of a fictional patient who agrees to be monitored via her smartphone.
Consider a hypothetical patient we will call Ms. T who is in her mid-20s and has been diagnosed with schizophrenia. On a follow-up visit, she says she has insomnia. She also reports having a recent loss of appetite and higher levels of anxiety. After reviewing her smartphone data (Figure 3), the clinician sees an inversely proportional relationship between her sleep quality and symptoms of anxiety, psychosis, and depression, which suggests that these symptoms might be due to poor sleep. Her step count has been fairly stable, indicating that there is no significant correlation between physical activity and her other symptoms.
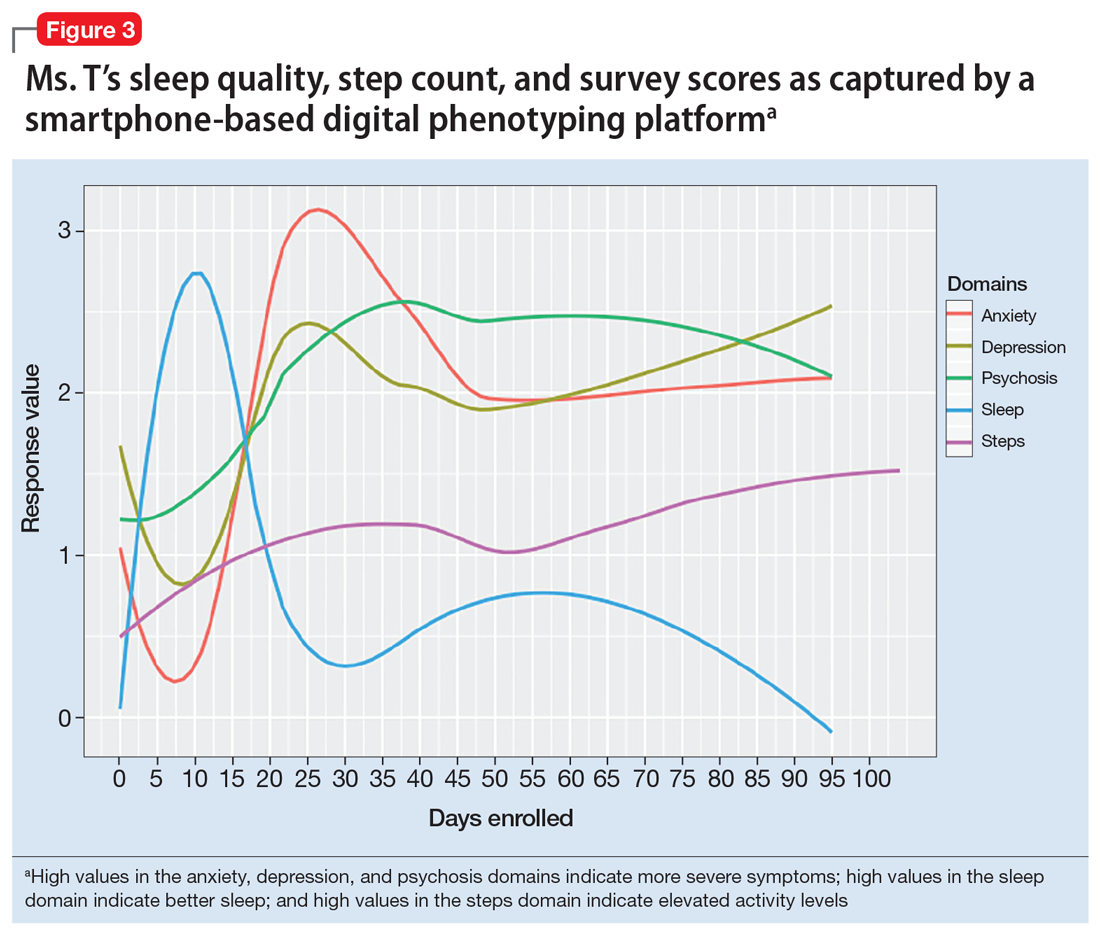
Continue to: The clinician shows...
The clinician shows Ms. T the data to help her understand why a trial of cognitive-behavioral therapy for insomnia, or at least improving sleep hygiene, may offer several benefits. The clinician advises her to continue to use the app to help assess her response to these interventions and monitor her progress in real time.
Dilemma: The ethics of continuous observation
The rich data captured by digital phenotyping afford many clinical opportunities, but also raise concerns. Among these are 3 significant ethical implications.
Firstly, the same data that may help a clinician learn about what environments are associated with less anxiety for the patient may also reveal personal details about where that patient has been or with whom they have interacted. In the wrong hands, such personal data could cause harm. And even in the hands of a trusted clinician, a breach in the patient’s privacy begs the question: “Should such information be anyone’s business at all?”
Secondly, many apps that offer digital phenotyping could also store patient data—something that currently pervades social media and causes reasonable discomfort for many people. You might have personally encountered this with social media platforms such as Facebook. When it comes to mobile mental health apps, clinicians should carefully understand the data usage agreement of any digital phenotyping app they wish to use and then share this information with their patients.
Finally, while it is possible to collect the types of data outlined in this article, less is known about how to use it directly in clinical care. Understanding for each patient which data streams are most meaningful and which data streams are noise that should be ignored is an area of ongoing research. A good first step may be to begin with data streams that are known to be clinically relevant and valuable, such as sleep and physical activity.9-11
Continue to: Discussion...
Discussion: Genomic sequencing and digital phenotyping
Although smartphones can gather a wide range of active and passive data, other data streams hold potential for predicting relapse and performing other clinically relevant actions. One data stream that could be of clinical use is genomic sequencing.12 The genotyping of patients provides a wealth of information about the underlying biology, and genomic sequencing has never been cheaper.13
Combining the data gathered via digital phenotyping with that of genotyping could help elucidate the mechanisms by which specific diseases and symptoms occur. This could be very promising to better understand and treat our patients. However, as is the case with genomics, digital phenotyping has important ethical implications. If used in the proper way to benefit our patients, the future for this new method is bright.
1. Statista. Number of smartphone users worldwide from 2014 to 2020 (in billions). https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Accessed April 29, 2019.
2. Thibaut F. Digital applications: the future in psychiatry? Dialogues Clin Neurosci. 2016;18(2):123.
3. Statista. Global market share held by the leading smartphone operating systems in sales to end users from 1st quarter 2009 to 2nd quarter 2018. https://www.statista.com/statistics/266136/global-market-share-held-by-smartphone-operating-systems/. Accessed April 19, 2019.
4. Torous J, Roberts L. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74(5):437-438.
5. Barnett I, Torous J, Staples P, et al. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018;43(8):1660-1666.
6. Arnett JA, Labovitz SS. Effect of physical layout in performance of the Trail Making Test. Psychological Assessment. 1995;7(2):220-221.
7. Brouillette RM, Foil H, Fontenot S, et al. Feasibility, reliability, and validity of a smartphone based application for the assessment of cognitive function in the elderly. PloS One. 2013;8(6):e65925. doi: 10.1371/journal.pone.0065925.
8. Winnick W. Putting a finger on our phone obsession. dscout. https://blog.dscout.com/mobile-touches. Published June 16, 2016. Accessed April 29, 2019.
9. Waite F, Myers E, Harvey AG, et al. Treating sleep problems in patients with schizophrenia. Behav Cogn Psychother. 2016;44(3):273-287.
10. Mcgurk SR, Mueser KT, Xie H, et al. (2015). Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial. Am J Psychiatry. 2015;172(9):852-861.
11. Firth J, Stubbs B, Rosenbaum S, et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2017;43(3):546-556.
12. Manolio TA, Chisholm RL, Ozenberger B, et al. Implementing genomic medicine in the clinic: the future is here. Genet Med. 2013;15(4):258-267.
13. National Human Genome Research Institute. The cost of sequencing a human genome. https://www.genome.gov/27565109/the-cost-of-sequencing-a-human-genome/. Updated July 6, 2016. Accessed April 29, 2019.
1. Statista. Number of smartphone users worldwide from 2014 to 2020 (in billions). https://www.statista.com/statistics/330695/number-of-smartphone-users-worldwide/. Accessed April 29, 2019.
2. Thibaut F. Digital applications: the future in psychiatry? Dialogues Clin Neurosci. 2016;18(2):123.
3. Statista. Global market share held by the leading smartphone operating systems in sales to end users from 1st quarter 2009 to 2nd quarter 2018. https://www.statista.com/statistics/266136/global-market-share-held-by-smartphone-operating-systems/. Accessed April 19, 2019.
4. Torous J, Roberts L. Needed innovation in digital health and smartphone applications for mental health: transparency and trust. JAMA Psychiatry. 2017;74(5):437-438.
5. Barnett I, Torous J, Staples P, et al. Relapse prediction in schizophrenia through digital phenotyping: a pilot study. Neuropsychopharmacology. 2018;43(8):1660-1666.
6. Arnett JA, Labovitz SS. Effect of physical layout in performance of the Trail Making Test. Psychological Assessment. 1995;7(2):220-221.
7. Brouillette RM, Foil H, Fontenot S, et al. Feasibility, reliability, and validity of a smartphone based application for the assessment of cognitive function in the elderly. PloS One. 2013;8(6):e65925. doi: 10.1371/journal.pone.0065925.
8. Winnick W. Putting a finger on our phone obsession. dscout. https://blog.dscout.com/mobile-touches. Published June 16, 2016. Accessed April 29, 2019.
9. Waite F, Myers E, Harvey AG, et al. Treating sleep problems in patients with schizophrenia. Behav Cogn Psychother. 2016;44(3):273-287.
10. Mcgurk SR, Mueser KT, Xie H, et al. (2015). Cognitive enhancement treatment for people with mental illness who do not respond to supported employment: a randomized controlled trial. Am J Psychiatry. 2015;172(9):852-861.
11. Firth J, Stubbs B, Rosenbaum S, et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull. 2017;43(3):546-556.
12. Manolio TA, Chisholm RL, Ozenberger B, et al. Implementing genomic medicine in the clinic: the future is here. Genet Med. 2013;15(4):258-267.
13. National Human Genome Research Institute. The cost of sequencing a human genome. https://www.genome.gov/27565109/the-cost-of-sequencing-a-human-genome/. Updated July 6, 2016. Accessed April 29, 2019.
A longing for belonging
As I watched my grandson and his team warm up for their Saturday morning lacrosse game, a long parade of mostly purple-shirted adults and children of all ages began to weave its way around the periphery of the athletic field complex. A quick reading of the hand-lettered and machine-printed shirts made it clear that I was watching a charity walk for cystic fibrosis. There must have been several hundred walkers strolling by, laughing and chatting with one another. It lent a festive atmosphere to the park. I suspect that for most of the participants this was not their first fundraising event for cystic fibrosis.
The motley mix of marchers probably included several handfuls of parents of children with cystic fibrosis. I wonder how many of those parents realized how fortunate they were. Cystic fibrosis isn’t a great diagnosis. But at least it is a diagnosis, and with the diagnosis comes a community.
Reading a front-page article on DNA testing in a recent Wall Street Journal issue had primed me to reconsider how even an unfortunate diagnosis can be extremely valuable for a family (“The Unfulfilled Promise of DNA Testing,” by Amy Dockser Marcus, May 18, 2019).The focus of the article was on the confusion and disappointment that are the predictable consequences of our current inability to accurately correlate genetic code “mistakes” with phenotypic abnormalities. Of course there have been a few successes, but we aren’t even close to the promise that many have predicted in the wake of sequencing the human genome. The family featured in the article has a ridden roller coaster ride through two failed attributions of genetic syndromes that appeared to provide their now 8-year-old daughter with a diagnosis for her epilepsy and developmental delay.
In each case, the mother had searched out other families with children who shared the same genetic code errors. She formed support groups and created foundations to promote research for these rare disorders only to learn that her daughter didn’t really fit into the phenotype exhibited by the other children. As the article indicates this mother had “found a genetic home, only to feel that she no longer belonged.” She had made “intense friendships” and for “2 years, the community was her main emotional support.” Since the second diagnosis has evaporated, she has struggled with whether to remain with that community, having already left one behind. She has been encouraged to stay involved by another mother whose son does have the diagnosis. Understandably, she is still seeking the correct diagnosis, and I suspect will form or join a new community when she finds it.
We all want to belong to a community. And with that ticket comes the opportunity to share the frustrations and difficulties unique to children with that diagnosis, and the comfort that there are other people who look, behave, and feel the way we do. We hear repeatedly about the value of diversity and how wonderful it is to be all inclusive. And certainly we should continue to be as accepting as we can of people who are different. But the truth is that we will always fall short because we seem to be hardwired to notice what is different. And the power of the longing to belong is often stronger than our will to be inclusive.
The revolution that resulted in the disappearance of the label “mental retardation” and the widespread adoption of the diagnosis of autism are examples of how a community can form around a diagnosis. But not every child who is labeled as autistic will actually fit the diagnosis. Yet even a less-than-perfect attribution can provide a place where a family and a patient can feel that they belong.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
As I watched my grandson and his team warm up for their Saturday morning lacrosse game, a long parade of mostly purple-shirted adults and children of all ages began to weave its way around the periphery of the athletic field complex. A quick reading of the hand-lettered and machine-printed shirts made it clear that I was watching a charity walk for cystic fibrosis. There must have been several hundred walkers strolling by, laughing and chatting with one another. It lent a festive atmosphere to the park. I suspect that for most of the participants this was not their first fundraising event for cystic fibrosis.
The motley mix of marchers probably included several handfuls of parents of children with cystic fibrosis. I wonder how many of those parents realized how fortunate they were. Cystic fibrosis isn’t a great diagnosis. But at least it is a diagnosis, and with the diagnosis comes a community.
Reading a front-page article on DNA testing in a recent Wall Street Journal issue had primed me to reconsider how even an unfortunate diagnosis can be extremely valuable for a family (“The Unfulfilled Promise of DNA Testing,” by Amy Dockser Marcus, May 18, 2019).The focus of the article was on the confusion and disappointment that are the predictable consequences of our current inability to accurately correlate genetic code “mistakes” with phenotypic abnormalities. Of course there have been a few successes, but we aren’t even close to the promise that many have predicted in the wake of sequencing the human genome. The family featured in the article has a ridden roller coaster ride through two failed attributions of genetic syndromes that appeared to provide their now 8-year-old daughter with a diagnosis for her epilepsy and developmental delay.
In each case, the mother had searched out other families with children who shared the same genetic code errors. She formed support groups and created foundations to promote research for these rare disorders only to learn that her daughter didn’t really fit into the phenotype exhibited by the other children. As the article indicates this mother had “found a genetic home, only to feel that she no longer belonged.” She had made “intense friendships” and for “2 years, the community was her main emotional support.” Since the second diagnosis has evaporated, she has struggled with whether to remain with that community, having already left one behind. She has been encouraged to stay involved by another mother whose son does have the diagnosis. Understandably, she is still seeking the correct diagnosis, and I suspect will form or join a new community when she finds it.
We all want to belong to a community. And with that ticket comes the opportunity to share the frustrations and difficulties unique to children with that diagnosis, and the comfort that there are other people who look, behave, and feel the way we do. We hear repeatedly about the value of diversity and how wonderful it is to be all inclusive. And certainly we should continue to be as accepting as we can of people who are different. But the truth is that we will always fall short because we seem to be hardwired to notice what is different. And the power of the longing to belong is often stronger than our will to be inclusive.
The revolution that resulted in the disappearance of the label “mental retardation” and the widespread adoption of the diagnosis of autism are examples of how a community can form around a diagnosis. But not every child who is labeled as autistic will actually fit the diagnosis. Yet even a less-than-perfect attribution can provide a place where a family and a patient can feel that they belong.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
As I watched my grandson and his team warm up for their Saturday morning lacrosse game, a long parade of mostly purple-shirted adults and children of all ages began to weave its way around the periphery of the athletic field complex. A quick reading of the hand-lettered and machine-printed shirts made it clear that I was watching a charity walk for cystic fibrosis. There must have been several hundred walkers strolling by, laughing and chatting with one another. It lent a festive atmosphere to the park. I suspect that for most of the participants this was not their first fundraising event for cystic fibrosis.
The motley mix of marchers probably included several handfuls of parents of children with cystic fibrosis. I wonder how many of those parents realized how fortunate they were. Cystic fibrosis isn’t a great diagnosis. But at least it is a diagnosis, and with the diagnosis comes a community.
Reading a front-page article on DNA testing in a recent Wall Street Journal issue had primed me to reconsider how even an unfortunate diagnosis can be extremely valuable for a family (“The Unfulfilled Promise of DNA Testing,” by Amy Dockser Marcus, May 18, 2019).The focus of the article was on the confusion and disappointment that are the predictable consequences of our current inability to accurately correlate genetic code “mistakes” with phenotypic abnormalities. Of course there have been a few successes, but we aren’t even close to the promise that many have predicted in the wake of sequencing the human genome. The family featured in the article has a ridden roller coaster ride through two failed attributions of genetic syndromes that appeared to provide their now 8-year-old daughter with a diagnosis for her epilepsy and developmental delay.
In each case, the mother had searched out other families with children who shared the same genetic code errors. She formed support groups and created foundations to promote research for these rare disorders only to learn that her daughter didn’t really fit into the phenotype exhibited by the other children. As the article indicates this mother had “found a genetic home, only to feel that she no longer belonged.” She had made “intense friendships” and for “2 years, the community was her main emotional support.” Since the second diagnosis has evaporated, she has struggled with whether to remain with that community, having already left one behind. She has been encouraged to stay involved by another mother whose son does have the diagnosis. Understandably, she is still seeking the correct diagnosis, and I suspect will form or join a new community when she finds it.
We all want to belong to a community. And with that ticket comes the opportunity to share the frustrations and difficulties unique to children with that diagnosis, and the comfort that there are other people who look, behave, and feel the way we do. We hear repeatedly about the value of diversity and how wonderful it is to be all inclusive. And certainly we should continue to be as accepting as we can of people who are different. But the truth is that we will always fall short because we seem to be hardwired to notice what is different. And the power of the longing to belong is often stronger than our will to be inclusive.
The revolution that resulted in the disappearance of the label “mental retardation” and the widespread adoption of the diagnosis of autism are examples of how a community can form around a diagnosis. But not every child who is labeled as autistic will actually fit the diagnosis. Yet even a less-than-perfect attribution can provide a place where a family and a patient can feel that they belong.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].







