User login
Promoting confrontation
The optimist says the glass is half-full. The pessimist says it is half-empty. An engineer says the glass is twice as large as needed to contain the specified amount of fluid. To some people, that mindset makes engineers negative people. We focus on weaknesses and inefficiencies. A chain is only as strong as its weakest link. There is no partial credit when building a bridge. 98% right is still wrong.
When I worked as an engineer, critiquing ideas was a daily activity. I am used to conflicting opinions. Industry trains people to be professional and act appropriately when disagreeing with a colleague. Tact is the art of making a point without making an enemy. Engineering has a strong culture of focusing on a problem rather than on personalities. Upper management made it clear that in any turf war, both sides will lose. Academia has a different culture. Turf wars in academia are so bitter because the stakes are so small.
Pediatrics has less confrontation and competitiveness than do other subspecialties. That makes the work environment more pleasant, as long as every other group in the hospital isn’t walking all over you. Pediatricians often view themselves as dedicated to doing what is right for the children, even to the point of martyrdom. Some early pediatric hospitalist programs got into economic trouble because they adopted tasks that benefited the children but that weren’t being performed by other physicians precisely because those tasks were neither valued nor compensated. Learning to say “No” is hard but necessary.
As a clinical ethics consultant, I was consulted when conflict had developed between providers and patients/parents or between different specialties. Ethics consults are rarely about what philosophers would call ethics. They are mostly about miscommunication, empowering voices to be heard and clarifying values. Practical skills in de-escalation and mediation are more important than either law or philosophy degrees.
There are downsides to avoiding confrontation. Truth suffers. Integrity is lost. Goals become corrupted. I will give two examples. One ED had a five-level triage system. Level 1 was reserved for life-threatening situations such as gunshot wounds and resuscitations. So I was surprised to see a “bili” baby triaged at Level 1. He was a good baby with normal vitals. Admission for phototherapy was reasonable, but the urgency of a bilirubin of 19 did not match that of a gunshot wound. A colleague warned me not to even consider challenging the practice. A powerful physician at that institution had made it policy years earlier.
I witnessed a similar dynamic many times at that institution. Residents are even better than 4-year-olds at noticing hypocritical behavior. Once they perceive that the dynamic is political power and not science, they adapt quickly. A couple days later, I asked a resident if he really thought an IV was necessary for a toddler we were admitting. He replied no, but if he hadn’t put an IV in, the hospital wouldn’t get paid for the admission. To him, that was the unspoken policy. The action didn’t even cause him moral distress. I worry about that much cynicism so early in a career. Cognitive dissonance starts small and slowly creeps its way into everything.
The art of managing conflict is particularly important in pediatric hospital medicine because of its heavy investment in reducing overdiagnosis and overtreatment. Many pediatric hospitalists are located at academic institutions and more subject to its turf wars than outpatient colleagues practicing in small groups. The recent conference for pediatric hospital medicine was held in Atlanta, a few blocks from the Center for Civil and Human Rights. That museum evokes powerful images of struggles around the world. My two takeaway lessons: Silence is a form of collaboration. Tyrannical suppression of dissent magnifies suffering.
In poorly managed academic institutions, it can be harmful to one’s career to ask questions, challenge assumptions, and seek truth. A recent report found that the Department of Veterans Affairs health system also has a culture that punishes whistle-blowers. Nationally, politics has become polarized. Splitting, once considered a dysfunctional behavior, has become normalized. So I understand the reluctance to speak up. One must choose one’s battles.
Given the personal and career risks, why confront inaccurate research, wasteful practices, and unjust policies? I believe that there is a balance and a choice each person must make. Canadian engineers wear an iron ring to remind themselves of their professional responsibilities. Doctors wear white coats. Personally, I share a memory with other engineers of my generation. In January 1986, NASA engineers could not convince their managers about a risk. The space shuttle Challenger exploded. I heard about it in the medical school’s cafeteria. So for me, disputation is part of the vocation.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The optimist says the glass is half-full. The pessimist says it is half-empty. An engineer says the glass is twice as large as needed to contain the specified amount of fluid. To some people, that mindset makes engineers negative people. We focus on weaknesses and inefficiencies. A chain is only as strong as its weakest link. There is no partial credit when building a bridge. 98% right is still wrong.
When I worked as an engineer, critiquing ideas was a daily activity. I am used to conflicting opinions. Industry trains people to be professional and act appropriately when disagreeing with a colleague. Tact is the art of making a point without making an enemy. Engineering has a strong culture of focusing on a problem rather than on personalities. Upper management made it clear that in any turf war, both sides will lose. Academia has a different culture. Turf wars in academia are so bitter because the stakes are so small.
Pediatrics has less confrontation and competitiveness than do other subspecialties. That makes the work environment more pleasant, as long as every other group in the hospital isn’t walking all over you. Pediatricians often view themselves as dedicated to doing what is right for the children, even to the point of martyrdom. Some early pediatric hospitalist programs got into economic trouble because they adopted tasks that benefited the children but that weren’t being performed by other physicians precisely because those tasks were neither valued nor compensated. Learning to say “No” is hard but necessary.
As a clinical ethics consultant, I was consulted when conflict had developed between providers and patients/parents or between different specialties. Ethics consults are rarely about what philosophers would call ethics. They are mostly about miscommunication, empowering voices to be heard and clarifying values. Practical skills in de-escalation and mediation are more important than either law or philosophy degrees.
There are downsides to avoiding confrontation. Truth suffers. Integrity is lost. Goals become corrupted. I will give two examples. One ED had a five-level triage system. Level 1 was reserved for life-threatening situations such as gunshot wounds and resuscitations. So I was surprised to see a “bili” baby triaged at Level 1. He was a good baby with normal vitals. Admission for phototherapy was reasonable, but the urgency of a bilirubin of 19 did not match that of a gunshot wound. A colleague warned me not to even consider challenging the practice. A powerful physician at that institution had made it policy years earlier.
I witnessed a similar dynamic many times at that institution. Residents are even better than 4-year-olds at noticing hypocritical behavior. Once they perceive that the dynamic is political power and not science, they adapt quickly. A couple days later, I asked a resident if he really thought an IV was necessary for a toddler we were admitting. He replied no, but if he hadn’t put an IV in, the hospital wouldn’t get paid for the admission. To him, that was the unspoken policy. The action didn’t even cause him moral distress. I worry about that much cynicism so early in a career. Cognitive dissonance starts small and slowly creeps its way into everything.
The art of managing conflict is particularly important in pediatric hospital medicine because of its heavy investment in reducing overdiagnosis and overtreatment. Many pediatric hospitalists are located at academic institutions and more subject to its turf wars than outpatient colleagues practicing in small groups. The recent conference for pediatric hospital medicine was held in Atlanta, a few blocks from the Center for Civil and Human Rights. That museum evokes powerful images of struggles around the world. My two takeaway lessons: Silence is a form of collaboration. Tyrannical suppression of dissent magnifies suffering.
In poorly managed academic institutions, it can be harmful to one’s career to ask questions, challenge assumptions, and seek truth. A recent report found that the Department of Veterans Affairs health system also has a culture that punishes whistle-blowers. Nationally, politics has become polarized. Splitting, once considered a dysfunctional behavior, has become normalized. So I understand the reluctance to speak up. One must choose one’s battles.
Given the personal and career risks, why confront inaccurate research, wasteful practices, and unjust policies? I believe that there is a balance and a choice each person must make. Canadian engineers wear an iron ring to remind themselves of their professional responsibilities. Doctors wear white coats. Personally, I share a memory with other engineers of my generation. In January 1986, NASA engineers could not convince their managers about a risk. The space shuttle Challenger exploded. I heard about it in the medical school’s cafeteria. So for me, disputation is part of the vocation.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
The optimist says the glass is half-full. The pessimist says it is half-empty. An engineer says the glass is twice as large as needed to contain the specified amount of fluid. To some people, that mindset makes engineers negative people. We focus on weaknesses and inefficiencies. A chain is only as strong as its weakest link. There is no partial credit when building a bridge. 98% right is still wrong.
When I worked as an engineer, critiquing ideas was a daily activity. I am used to conflicting opinions. Industry trains people to be professional and act appropriately when disagreeing with a colleague. Tact is the art of making a point without making an enemy. Engineering has a strong culture of focusing on a problem rather than on personalities. Upper management made it clear that in any turf war, both sides will lose. Academia has a different culture. Turf wars in academia are so bitter because the stakes are so small.
Pediatrics has less confrontation and competitiveness than do other subspecialties. That makes the work environment more pleasant, as long as every other group in the hospital isn’t walking all over you. Pediatricians often view themselves as dedicated to doing what is right for the children, even to the point of martyrdom. Some early pediatric hospitalist programs got into economic trouble because they adopted tasks that benefited the children but that weren’t being performed by other physicians precisely because those tasks were neither valued nor compensated. Learning to say “No” is hard but necessary.
As a clinical ethics consultant, I was consulted when conflict had developed between providers and patients/parents or between different specialties. Ethics consults are rarely about what philosophers would call ethics. They are mostly about miscommunication, empowering voices to be heard and clarifying values. Practical skills in de-escalation and mediation are more important than either law or philosophy degrees.
There are downsides to avoiding confrontation. Truth suffers. Integrity is lost. Goals become corrupted. I will give two examples. One ED had a five-level triage system. Level 1 was reserved for life-threatening situations such as gunshot wounds and resuscitations. So I was surprised to see a “bili” baby triaged at Level 1. He was a good baby with normal vitals. Admission for phototherapy was reasonable, but the urgency of a bilirubin of 19 did not match that of a gunshot wound. A colleague warned me not to even consider challenging the practice. A powerful physician at that institution had made it policy years earlier.
I witnessed a similar dynamic many times at that institution. Residents are even better than 4-year-olds at noticing hypocritical behavior. Once they perceive that the dynamic is political power and not science, they adapt quickly. A couple days later, I asked a resident if he really thought an IV was necessary for a toddler we were admitting. He replied no, but if he hadn’t put an IV in, the hospital wouldn’t get paid for the admission. To him, that was the unspoken policy. The action didn’t even cause him moral distress. I worry about that much cynicism so early in a career. Cognitive dissonance starts small and slowly creeps its way into everything.
The art of managing conflict is particularly important in pediatric hospital medicine because of its heavy investment in reducing overdiagnosis and overtreatment. Many pediatric hospitalists are located at academic institutions and more subject to its turf wars than outpatient colleagues practicing in small groups. The recent conference for pediatric hospital medicine was held in Atlanta, a few blocks from the Center for Civil and Human Rights. That museum evokes powerful images of struggles around the world. My two takeaway lessons: Silence is a form of collaboration. Tyrannical suppression of dissent magnifies suffering.
In poorly managed academic institutions, it can be harmful to one’s career to ask questions, challenge assumptions, and seek truth. A recent report found that the Department of Veterans Affairs health system also has a culture that punishes whistle-blowers. Nationally, politics has become polarized. Splitting, once considered a dysfunctional behavior, has become normalized. So I understand the reluctance to speak up. One must choose one’s battles.
Given the personal and career risks, why confront inaccurate research, wasteful practices, and unjust policies? I believe that there is a balance and a choice each person must make. Canadian engineers wear an iron ring to remind themselves of their professional responsibilities. Doctors wear white coats. Personally, I share a memory with other engineers of my generation. In January 1986, NASA engineers could not convince their managers about a risk. The space shuttle Challenger exploded. I heard about it in the medical school’s cafeteria. So for me, disputation is part of the vocation.
Dr. Powell is a pediatric hospitalist and clinical ethics consultant living in St. Louis. Email him at [email protected].
A beautiful diagnosis
Defensive medicine exists. The question is how often it happens and how large a role it plays in making medical care in the United States so costly. When Dr. Tom Price was a congressman, he was quoted as saying that defensive medicine is responsible for more than 25% of every dollar this country spends on health care. (“A Fear of Lawsuits Really Does Seem to Result in Extra Medical Tests” Margot Sanger-Katz, New York Times, July 23, 2018). Neither I nor anyone else had any data to support or refute Dr. Price’s claim in 2010, but based on 50 years of practicing and observing medicine, I don’t find his claim completely unreasonable.
Defensive medicine has been going on for so many generations of physicians that most doctors practicing today don’t realize they are doing it. A physician may order a full battery of chemistries on a patient presenting with mild anemia when only a CBC is necessary because that’s the way he was trained.
However, the evidence to support my suspicion that defensive medicine is a significant financial drain on our economy has been difficult to tease out of the tangled web of confounders that is woven into our patchwork health care system. A recent study by two economists provides a glimpse into the role of defensive medicine in the cost of health care (“Defensive Medicine: Evidence from Military Immunity” Michael D. Frakes and Jonathan Gruber, National Bureau of Economic Research, July 2018). Using the unusual combination of circumstances in which military personnel and their dependents can or cannot sue depending on where they are receiving care, the investigators found that “liability immunity reduces inpatient spending by 5% with no measurable negative effect on patient outcomes.” While that may not be as high as Dr. Price or I think it may be, 5% of three trillion dollars is serious money.
The bigger problem is that defensive medicine is ugly, artless, and intellectually unsatisfying. While the patient may not view your diagnosis of his chronic debilitating or terminal illness as a work of art, there are such things as beautiful diagnoses. One may be beautiful in its simplicity and its ability to unify a variety of previously unexplained symptoms. Another diagnosis may be the intellectually stimulating result of a carefully thought out branching decision tree to solve a puzzling array of complaints using a minimum of costly studies.
Defensive medicine decisions are made primarily to avoid mistakes and omissions. Physicians often behave as though we believe our errors will always be fatal. That may be somewhat true for surgeons, but for the rest of us errors can be an important part of learning. The unfortunate outcome of an error, particularly one of omission, can usually be avoided by following the patient closely, remaining available ... and continuing to exude an aura of caring.
With close and thoughtful follow-up, you are going to discover pretty quickly when you have missed the target. Patients understand that we aren’t going to get the correct diagnosis or prescribe the best treatment on the first try every time. What patients don’t understand and what may prompt them to sue is feeling that they are being ignored.
While practicing defensive medicine isn’t usually listed as one of the cardinal symptoms of physician burnout, it probably deserves more attention. With some introspection and a bit of courage, How many of your decisions are being made to avoid an error? Wouldn’t it be more fun to be making beautiful diagnoses you can be proud of?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].
Defensive medicine exists. The question is how often it happens and how large a role it plays in making medical care in the United States so costly. When Dr. Tom Price was a congressman, he was quoted as saying that defensive medicine is responsible for more than 25% of every dollar this country spends on health care. (“A Fear of Lawsuits Really Does Seem to Result in Extra Medical Tests” Margot Sanger-Katz, New York Times, July 23, 2018). Neither I nor anyone else had any data to support or refute Dr. Price’s claim in 2010, but based on 50 years of practicing and observing medicine, I don’t find his claim completely unreasonable.
Defensive medicine has been going on for so many generations of physicians that most doctors practicing today don’t realize they are doing it. A physician may order a full battery of chemistries on a patient presenting with mild anemia when only a CBC is necessary because that’s the way he was trained.
However, the evidence to support my suspicion that defensive medicine is a significant financial drain on our economy has been difficult to tease out of the tangled web of confounders that is woven into our patchwork health care system. A recent study by two economists provides a glimpse into the role of defensive medicine in the cost of health care (“Defensive Medicine: Evidence from Military Immunity” Michael D. Frakes and Jonathan Gruber, National Bureau of Economic Research, July 2018). Using the unusual combination of circumstances in which military personnel and their dependents can or cannot sue depending on where they are receiving care, the investigators found that “liability immunity reduces inpatient spending by 5% with no measurable negative effect on patient outcomes.” While that may not be as high as Dr. Price or I think it may be, 5% of three trillion dollars is serious money.
The bigger problem is that defensive medicine is ugly, artless, and intellectually unsatisfying. While the patient may not view your diagnosis of his chronic debilitating or terminal illness as a work of art, there are such things as beautiful diagnoses. One may be beautiful in its simplicity and its ability to unify a variety of previously unexplained symptoms. Another diagnosis may be the intellectually stimulating result of a carefully thought out branching decision tree to solve a puzzling array of complaints using a minimum of costly studies.
Defensive medicine decisions are made primarily to avoid mistakes and omissions. Physicians often behave as though we believe our errors will always be fatal. That may be somewhat true for surgeons, but for the rest of us errors can be an important part of learning. The unfortunate outcome of an error, particularly one of omission, can usually be avoided by following the patient closely, remaining available ... and continuing to exude an aura of caring.
With close and thoughtful follow-up, you are going to discover pretty quickly when you have missed the target. Patients understand that we aren’t going to get the correct diagnosis or prescribe the best treatment on the first try every time. What patients don’t understand and what may prompt them to sue is feeling that they are being ignored.
While practicing defensive medicine isn’t usually listed as one of the cardinal symptoms of physician burnout, it probably deserves more attention. With some introspection and a bit of courage, How many of your decisions are being made to avoid an error? Wouldn’t it be more fun to be making beautiful diagnoses you can be proud of?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].
Defensive medicine exists. The question is how often it happens and how large a role it plays in making medical care in the United States so costly. When Dr. Tom Price was a congressman, he was quoted as saying that defensive medicine is responsible for more than 25% of every dollar this country spends on health care. (“A Fear of Lawsuits Really Does Seem to Result in Extra Medical Tests” Margot Sanger-Katz, New York Times, July 23, 2018). Neither I nor anyone else had any data to support or refute Dr. Price’s claim in 2010, but based on 50 years of practicing and observing medicine, I don’t find his claim completely unreasonable.
Defensive medicine has been going on for so many generations of physicians that most doctors practicing today don’t realize they are doing it. A physician may order a full battery of chemistries on a patient presenting with mild anemia when only a CBC is necessary because that’s the way he was trained.
However, the evidence to support my suspicion that defensive medicine is a significant financial drain on our economy has been difficult to tease out of the tangled web of confounders that is woven into our patchwork health care system. A recent study by two economists provides a glimpse into the role of defensive medicine in the cost of health care (“Defensive Medicine: Evidence from Military Immunity” Michael D. Frakes and Jonathan Gruber, National Bureau of Economic Research, July 2018). Using the unusual combination of circumstances in which military personnel and their dependents can or cannot sue depending on where they are receiving care, the investigators found that “liability immunity reduces inpatient spending by 5% with no measurable negative effect on patient outcomes.” While that may not be as high as Dr. Price or I think it may be, 5% of three trillion dollars is serious money.
The bigger problem is that defensive medicine is ugly, artless, and intellectually unsatisfying. While the patient may not view your diagnosis of his chronic debilitating or terminal illness as a work of art, there are such things as beautiful diagnoses. One may be beautiful in its simplicity and its ability to unify a variety of previously unexplained symptoms. Another diagnosis may be the intellectually stimulating result of a carefully thought out branching decision tree to solve a puzzling array of complaints using a minimum of costly studies.
Defensive medicine decisions are made primarily to avoid mistakes and omissions. Physicians often behave as though we believe our errors will always be fatal. That may be somewhat true for surgeons, but for the rest of us errors can be an important part of learning. The unfortunate outcome of an error, particularly one of omission, can usually be avoided by following the patient closely, remaining available ... and continuing to exude an aura of caring.
With close and thoughtful follow-up, you are going to discover pretty quickly when you have missed the target. Patients understand that we aren’t going to get the correct diagnosis or prescribe the best treatment on the first try every time. What patients don’t understand and what may prompt them to sue is feeling that they are being ignored.
While practicing defensive medicine isn’t usually listed as one of the cardinal symptoms of physician burnout, it probably deserves more attention. With some introspection and a bit of courage, How many of your decisions are being made to avoid an error? Wouldn’t it be more fun to be making beautiful diagnoses you can be proud of?
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “Is My Child Overtired?: The Sleep Solution for Raising Happier, Healthier Children.” Email him at [email protected].
Beyond the monoamines: The future of antidepressants
For close to 6 decades, since the approval of imipramine in 1959, all Food and Drug Administration-approved medications for depression worked through the monoamine system, in some ways altering the concentration of serotonin, norepinephrine, or dopamine within synapses or binding to post synaptic receptors. A conservative estimate has at least a third of patients with depression not adequately responsive to these monoaminergic medications.
A host of medications in various stages of development might each offer unique additions to the current therapeutic paradigm. Compounds closest to market include N-methyl-D-aspartate (NMDA) blockers such as esketamine or rapastinel; opioid receptor partial agonists and antagonists, such as Alkermes 5461; and a GABAA receptor modulator, brexanolone. A further off, more speculative intervention involves the use of psychedelic drugs like psilocybin.
NMDA antagonists have gained the highest visibility after some promising results in early studies looking at intravenous ketamine, an anesthetic agent approved by the FDA in 1970 for treatment-resistant depression. This has led to several companies trying to develop a patentable NMDA antagonist for depression. The most likely first candidate is one of the enantiomers of ketamine, esketamine, which, because of higher binding affinity, can be dosed intranasally rather than intravenously. Studies are completed to establish efficacy in TRD2 [treatment-resistant depression] as well as acute suicidality3. Johnson & Johnson plans to submit these results for FDA approval this year.
Another promising NMDA antagonist, rapastinel, is wending its way through clinical trials – but should it be approved, its use might be limited by the requirement for intravenous delivery.
Despite only early evidence for efficacy in depression, the easy availability of ketamine for infusion has created a cadre of independent clinicians as well as some academic clinics offering intravenous ketamine infusions for those with difficult-to-treat depression and adequate finances to pay for off-label treatment (some insurance companies as well have supported its use). It is understandable to try to offer patients suffering with refractory illnesses anything the field has to offer, but the limitations on our knowledge, especially about the efficacy and safety of long-term use of ketamine for depression, need to be taken into account4. There is little to no regulation around providing intravenous ketamine, and clinicians and patients should be aware of the risks, take care in the administration of the drug, and watch for the potential of dissociation or substance abuse along with being clear about the likelihood of benefit being at best around 50%. As more evidence and experience are collected, NMDA antagonists might offer a unique efficacy profile within safe boundaries.
Opioid agonists have some antidepressant activity, but tolerance to it quickly develops – requiring users to take increasingly higher doses. Would a partial opioid agonist coupled with a pure opioid antagonist provide ongoing efficacy at a continuous dose with adequate safety? A combination medication containing buprenorphine, a partial* mu- and kappa-opioid partial agonist, and samidorphan, a mu-opioid antagonist, is currently being reviewed by the FDA. The phase 3 studies are not yet published. However, the phase 2 published trial demonstrated efficacy at low doses (2 mg of buprenorphine with 2 mg of samidorphan) as an adjunctive medication in treatment-resistant depression5. While offering a novel mechanism of action and a reasonable safety profile seen in several poster presentations, though not published articles, the drug – should it receive approval – will require an intensive effort to educate practitioners and the public about the critical differences (especially with regard to risk/benefits of long-term use, abuse potential, and safety) between opiate agonism and opiate modulation/antagonism.
Brexanolone, an intravenous formulation of allopregnanolone, a positive allosteric modulator of gamma-aminobutyric acid (GABAA) receptors, has been studied for the treatment of postpartum depression6. Early development has focused on an intravenous delivery system and a unique target population of postpartum depression, but the novel concept of targeting GABAA receptors might prove fruitful with a wider population of depressed patients with inadequate responses to existing antidepressants. An oral formulation, SAGE-217, is in early clinical trials.
While much earlier in the development for FDA approval, psychedelics, particularly psilocybin, have been investigated for use in treatment-resistant depression. A small double-blind trial in terminal cancer patients showed that psilocybin had a remarkable palliative effect on depression and anxiety7. An open label study of treatment-resistant depressed patients demonstrated lasting benefit over 6 months after two doses of psilocybin8. A neuroimaging study supported the idea that changes in resting state functional connectivity in specific brain regions from exposure to psilocybin might account for alleviation in depressive symptoms9. These findings are preliminary, but they have sparked the commencement of a few phase 2 randomized trials for psychedelic drugs. It should be noted that all these trial to date – and those planned – require dosing to be done in a very controlled and supervised psychologically supportive environment.
Which of these treatments will make it to market? That remains unclear, but it is reassuring that so many different novel paradigms for addressing treatment-resistant depression are in development.
Dr. Aaronson is the director of clinical research programs at the Sheppard Pratt Health System in Baltimore. He serves as a consultant to several companies, including Alkermes, Genomind, LivaNova, Neuronetics, and Sage Therapeutics. He has received honoraria for speaking from Neurocrine, Otsuka, and Sunovion. He has received research support from Neuronetics. Dr. Aaronson also serves as a clinical associate professor of psychiatry at the University of Maryland, Baltimore, and is a Distinguished Fellow of the American Psychiatric Association and a Fellow of the American College of Psychiatrists.
References
1. Am J Psychiatry. 2006;163(11):1905-17.
2. JAMA Psychiatry. 2018 Feb 1;75(2):139-48.
3. Am J Psychiatry. 2018 Jul 1;175(7):620-30.
4. JAMA Psychiatry. 2017;74(4):399-405.
5. Am J Psychiatry. 2016 May 1;173(5):499-508.
6. Lancet. 2017 Jul 29;390(10093):480-9.
7. J Psychopharmacol. 2016;30(12):1181-97.
8. Psychopharmacology (Berl). 2018 Feb;235(2):399-408.
9. Sci Rep. 2017 Oct 13;7(1):13187.
*Correction, 10/18/2019: An earlier version of this story misidentified buprenorphine.
For close to 6 decades, since the approval of imipramine in 1959, all Food and Drug Administration-approved medications for depression worked through the monoamine system, in some ways altering the concentration of serotonin, norepinephrine, or dopamine within synapses or binding to post synaptic receptors. A conservative estimate has at least a third of patients with depression not adequately responsive to these monoaminergic medications.
A host of medications in various stages of development might each offer unique additions to the current therapeutic paradigm. Compounds closest to market include N-methyl-D-aspartate (NMDA) blockers such as esketamine or rapastinel; opioid receptor partial agonists and antagonists, such as Alkermes 5461; and a GABAA receptor modulator, brexanolone. A further off, more speculative intervention involves the use of psychedelic drugs like psilocybin.
NMDA antagonists have gained the highest visibility after some promising results in early studies looking at intravenous ketamine, an anesthetic agent approved by the FDA in 1970 for treatment-resistant depression. This has led to several companies trying to develop a patentable NMDA antagonist for depression. The most likely first candidate is one of the enantiomers of ketamine, esketamine, which, because of higher binding affinity, can be dosed intranasally rather than intravenously. Studies are completed to establish efficacy in TRD2 [treatment-resistant depression] as well as acute suicidality3. Johnson & Johnson plans to submit these results for FDA approval this year.
Another promising NMDA antagonist, rapastinel, is wending its way through clinical trials – but should it be approved, its use might be limited by the requirement for intravenous delivery.
Despite only early evidence for efficacy in depression, the easy availability of ketamine for infusion has created a cadre of independent clinicians as well as some academic clinics offering intravenous ketamine infusions for those with difficult-to-treat depression and adequate finances to pay for off-label treatment (some insurance companies as well have supported its use). It is understandable to try to offer patients suffering with refractory illnesses anything the field has to offer, but the limitations on our knowledge, especially about the efficacy and safety of long-term use of ketamine for depression, need to be taken into account4. There is little to no regulation around providing intravenous ketamine, and clinicians and patients should be aware of the risks, take care in the administration of the drug, and watch for the potential of dissociation or substance abuse along with being clear about the likelihood of benefit being at best around 50%. As more evidence and experience are collected, NMDA antagonists might offer a unique efficacy profile within safe boundaries.
Opioid agonists have some antidepressant activity, but tolerance to it quickly develops – requiring users to take increasingly higher doses. Would a partial opioid agonist coupled with a pure opioid antagonist provide ongoing efficacy at a continuous dose with adequate safety? A combination medication containing buprenorphine, a partial* mu- and kappa-opioid partial agonist, and samidorphan, a mu-opioid antagonist, is currently being reviewed by the FDA. The phase 3 studies are not yet published. However, the phase 2 published trial demonstrated efficacy at low doses (2 mg of buprenorphine with 2 mg of samidorphan) as an adjunctive medication in treatment-resistant depression5. While offering a novel mechanism of action and a reasonable safety profile seen in several poster presentations, though not published articles, the drug – should it receive approval – will require an intensive effort to educate practitioners and the public about the critical differences (especially with regard to risk/benefits of long-term use, abuse potential, and safety) between opiate agonism and opiate modulation/antagonism.
Brexanolone, an intravenous formulation of allopregnanolone, a positive allosteric modulator of gamma-aminobutyric acid (GABAA) receptors, has been studied for the treatment of postpartum depression6. Early development has focused on an intravenous delivery system and a unique target population of postpartum depression, but the novel concept of targeting GABAA receptors might prove fruitful with a wider population of depressed patients with inadequate responses to existing antidepressants. An oral formulation, SAGE-217, is in early clinical trials.
While much earlier in the development for FDA approval, psychedelics, particularly psilocybin, have been investigated for use in treatment-resistant depression. A small double-blind trial in terminal cancer patients showed that psilocybin had a remarkable palliative effect on depression and anxiety7. An open label study of treatment-resistant depressed patients demonstrated lasting benefit over 6 months after two doses of psilocybin8. A neuroimaging study supported the idea that changes in resting state functional connectivity in specific brain regions from exposure to psilocybin might account for alleviation in depressive symptoms9. These findings are preliminary, but they have sparked the commencement of a few phase 2 randomized trials for psychedelic drugs. It should be noted that all these trial to date – and those planned – require dosing to be done in a very controlled and supervised psychologically supportive environment.
Which of these treatments will make it to market? That remains unclear, but it is reassuring that so many different novel paradigms for addressing treatment-resistant depression are in development.
Dr. Aaronson is the director of clinical research programs at the Sheppard Pratt Health System in Baltimore. He serves as a consultant to several companies, including Alkermes, Genomind, LivaNova, Neuronetics, and Sage Therapeutics. He has received honoraria for speaking from Neurocrine, Otsuka, and Sunovion. He has received research support from Neuronetics. Dr. Aaronson also serves as a clinical associate professor of psychiatry at the University of Maryland, Baltimore, and is a Distinguished Fellow of the American Psychiatric Association and a Fellow of the American College of Psychiatrists.
References
1. Am J Psychiatry. 2006;163(11):1905-17.
2. JAMA Psychiatry. 2018 Feb 1;75(2):139-48.
3. Am J Psychiatry. 2018 Jul 1;175(7):620-30.
4. JAMA Psychiatry. 2017;74(4):399-405.
5. Am J Psychiatry. 2016 May 1;173(5):499-508.
6. Lancet. 2017 Jul 29;390(10093):480-9.
7. J Psychopharmacol. 2016;30(12):1181-97.
8. Psychopharmacology (Berl). 2018 Feb;235(2):399-408.
9. Sci Rep. 2017 Oct 13;7(1):13187.
*Correction, 10/18/2019: An earlier version of this story misidentified buprenorphine.
For close to 6 decades, since the approval of imipramine in 1959, all Food and Drug Administration-approved medications for depression worked through the monoamine system, in some ways altering the concentration of serotonin, norepinephrine, or dopamine within synapses or binding to post synaptic receptors. A conservative estimate has at least a third of patients with depression not adequately responsive to these monoaminergic medications.
A host of medications in various stages of development might each offer unique additions to the current therapeutic paradigm. Compounds closest to market include N-methyl-D-aspartate (NMDA) blockers such as esketamine or rapastinel; opioid receptor partial agonists and antagonists, such as Alkermes 5461; and a GABAA receptor modulator, brexanolone. A further off, more speculative intervention involves the use of psychedelic drugs like psilocybin.
NMDA antagonists have gained the highest visibility after some promising results in early studies looking at intravenous ketamine, an anesthetic agent approved by the FDA in 1970 for treatment-resistant depression. This has led to several companies trying to develop a patentable NMDA antagonist for depression. The most likely first candidate is one of the enantiomers of ketamine, esketamine, which, because of higher binding affinity, can be dosed intranasally rather than intravenously. Studies are completed to establish efficacy in TRD2 [treatment-resistant depression] as well as acute suicidality3. Johnson & Johnson plans to submit these results for FDA approval this year.
Another promising NMDA antagonist, rapastinel, is wending its way through clinical trials – but should it be approved, its use might be limited by the requirement for intravenous delivery.
Despite only early evidence for efficacy in depression, the easy availability of ketamine for infusion has created a cadre of independent clinicians as well as some academic clinics offering intravenous ketamine infusions for those with difficult-to-treat depression and adequate finances to pay for off-label treatment (some insurance companies as well have supported its use). It is understandable to try to offer patients suffering with refractory illnesses anything the field has to offer, but the limitations on our knowledge, especially about the efficacy and safety of long-term use of ketamine for depression, need to be taken into account4. There is little to no regulation around providing intravenous ketamine, and clinicians and patients should be aware of the risks, take care in the administration of the drug, and watch for the potential of dissociation or substance abuse along with being clear about the likelihood of benefit being at best around 50%. As more evidence and experience are collected, NMDA antagonists might offer a unique efficacy profile within safe boundaries.
Opioid agonists have some antidepressant activity, but tolerance to it quickly develops – requiring users to take increasingly higher doses. Would a partial opioid agonist coupled with a pure opioid antagonist provide ongoing efficacy at a continuous dose with adequate safety? A combination medication containing buprenorphine, a partial* mu- and kappa-opioid partial agonist, and samidorphan, a mu-opioid antagonist, is currently being reviewed by the FDA. The phase 3 studies are not yet published. However, the phase 2 published trial demonstrated efficacy at low doses (2 mg of buprenorphine with 2 mg of samidorphan) as an adjunctive medication in treatment-resistant depression5. While offering a novel mechanism of action and a reasonable safety profile seen in several poster presentations, though not published articles, the drug – should it receive approval – will require an intensive effort to educate practitioners and the public about the critical differences (especially with regard to risk/benefits of long-term use, abuse potential, and safety) between opiate agonism and opiate modulation/antagonism.
Brexanolone, an intravenous formulation of allopregnanolone, a positive allosteric modulator of gamma-aminobutyric acid (GABAA) receptors, has been studied for the treatment of postpartum depression6. Early development has focused on an intravenous delivery system and a unique target population of postpartum depression, but the novel concept of targeting GABAA receptors might prove fruitful with a wider population of depressed patients with inadequate responses to existing antidepressants. An oral formulation, SAGE-217, is in early clinical trials.
While much earlier in the development for FDA approval, psychedelics, particularly psilocybin, have been investigated for use in treatment-resistant depression. A small double-blind trial in terminal cancer patients showed that psilocybin had a remarkable palliative effect on depression and anxiety7. An open label study of treatment-resistant depressed patients demonstrated lasting benefit over 6 months after two doses of psilocybin8. A neuroimaging study supported the idea that changes in resting state functional connectivity in specific brain regions from exposure to psilocybin might account for alleviation in depressive symptoms9. These findings are preliminary, but they have sparked the commencement of a few phase 2 randomized trials for psychedelic drugs. It should be noted that all these trial to date – and those planned – require dosing to be done in a very controlled and supervised psychologically supportive environment.
Which of these treatments will make it to market? That remains unclear, but it is reassuring that so many different novel paradigms for addressing treatment-resistant depression are in development.
Dr. Aaronson is the director of clinical research programs at the Sheppard Pratt Health System in Baltimore. He serves as a consultant to several companies, including Alkermes, Genomind, LivaNova, Neuronetics, and Sage Therapeutics. He has received honoraria for speaking from Neurocrine, Otsuka, and Sunovion. He has received research support from Neuronetics. Dr. Aaronson also serves as a clinical associate professor of psychiatry at the University of Maryland, Baltimore, and is a Distinguished Fellow of the American Psychiatric Association and a Fellow of the American College of Psychiatrists.
References
1. Am J Psychiatry. 2006;163(11):1905-17.
2. JAMA Psychiatry. 2018 Feb 1;75(2):139-48.
3. Am J Psychiatry. 2018 Jul 1;175(7):620-30.
4. JAMA Psychiatry. 2017;74(4):399-405.
5. Am J Psychiatry. 2016 May 1;173(5):499-508.
6. Lancet. 2017 Jul 29;390(10093):480-9.
7. J Psychopharmacol. 2016;30(12):1181-97.
8. Psychopharmacology (Berl). 2018 Feb;235(2):399-408.
9. Sci Rep. 2017 Oct 13;7(1):13187.
*Correction, 10/18/2019: An earlier version of this story misidentified buprenorphine.
Creating positive patient experiences
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Let’s start with an exercise, shall we? What was the last vacation you went on? How would you rate that vacation on a scale of 1-10?
How you came up with that score is likely not entirely reflective of your actual experience. Understanding how we remember experiences is critical for the work we do everyday.
My last vacation was in Alaska. I’d rate it a 9 out of 10. How did I come up with that score? It is not the mean score of the entire trip as you might expect. Rather, I took a shortcut and thought only about the highlights to come up with a number. We remember, and evaluate, our experiences as a series of discrete events. In considering these events, it is only the highs, the lows, and the transitions that matter. Think about the score you gave your vacation. What specific moments did you remember?
This phenomenon is not specific to vacations. It applies to all service experiences. When your patients evaluate you, they will ignore most of what occurred and focus on only a few moments. Fair or not, it is from these bits only that they will rate their entire experience. This information helps us devise strategies to achieve high satisfaction scores: Focus on the high points, address the low points, if any, and be sure the transitions are pleasant.
For example, a patient might come to see you for a procedure. It could be something positive, such as injection of cosmetic filler or something negative like a colonoscopy. Either way, being finished with the procedure will likely be the best part for them. Don’t rush this time; instead of quickly moving on, take a moment to acknowledge you’re done, how well the patient did, or how much better they will now look or feel. Engaging with your patient at this moment can improve the salience of their experience and increase the likelihood that she or he will remember the appointment favorably and rate you accordingly, if given the opportunity.
In the same way, if you are aware your patient has experienced something negative, try to respond to it right away. Acknowledge if she or he expressed frustration, such as a long wait or pain, then take a minute to address or reframe it. Blunting the severity of the service failure can blunt their recall of it. This will make it less likely that it becomes a memorable part of their experience.
Last, transitions matter. These are the moments when your patient shifts from one setting to another, such as arriving at your office, moving from the waiting room to the exam room, and wrapping up the visit with the receptionist. Many of these moments will be managed by your staff. Therefore, invest time reminding them of their importance and teaching them tips and techniques to help patients transition smoothly and to feel well cared for. There will likely be a wonderful return on investment for them, you and, most importantly, your patients.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Employment practices liability insurance
No matter how complete your insurance portfolio, there is one policy – one you probably have never heard of – that you should definitely consider adding to it.
A while ago, I spoke with a dermatologist in California who experienced every employer’s nightmare: he fired an incompetent employee, who promptly sued him for wrongful termination and accused him of sexual harassment to boot. The charges were completely false, and the employee’s transgressions were well documented; but he was not insured against a suit of that type, and defending it would have been prohibitively expensive. He was forced to settle it for a significant sum of money.
Disasters like that are becoming more common. Plaintiffs’ attorneys know that most small businesses, including medical practices, are not insured against internal liability actions – and that settlements are cheaper than litigation.
Fortunately, there is a relatively inexpensive alternative: not covered by conventional liability insurance. These include wrongful termination, sexual harassment, discrimination, breach of employment contract, negligent hiring or evaluation, failure to promote, wrongful discipline, mismanagement of benefits, and the ever-popular “emotional distress.”
EPLI coverage would have permitted the California dermatologist to mount a proper defense against his employee’s groundless charges. In fact, there is a better than even chance that the lawsuit would have been dropped, or never filed to begin with.
Some liability carriers are beginning to cover some employee-related issues in “umbrella” policies, so before looking into EPLI, check your current coverage. Then, as with all insurance, you should shop around for the best price and carefully read the policies on your short list. All EPLI policies cover litigation against your practice and its owners by employees, but some cover only full-timers. Try to obtain the broadest coverage possible so that claims from part-time, temporary, and seasonal employees, and, if possible, even applicants for employment and former employees, also are covered.
You should also look for the most comprehensive policy in terms of coverage. Almost every EPLI policy covers the allegations mentioned above, but some offer a more comprehensive list of covered acts, such as invasion of privacy and defamation of character.
Also be aware of precisely what each policy does not cover. Most exclude punitive damages and court-imposed fines, as well as criminal acts, fraud, and other clearly illegal conduct. For example, you would not be covered if you fired an employee because he or she refused to falsify insurance claims.
Depending on where you practice, it may be necessary to ask an employment attorney to evaluate your individual EPLI needs. An underwriter cannot anticipate every eventuality for you, particularly if he or she does not live in your area and is not familiar with employment conditions in your community.
As with any liability policy, try to get a clause added that permits you to choose your own defense attorney. Better still, pick a specific attorney or firm that you trust and have that counsel named in an endorsement to the policy. Otherwise, the insurance carrier will select an attorney from its own panel who may not consider your interests a higher priority than those of the insurer itself.
If you must accept the insurer’s choice of counsel, you should find out whether that attorney is experienced in employment law, which is a very specialized area. And just as with your malpractice policy, you will want to maintain as much control as possible over the settlement of claims. Ideally, no claim should be settled without your express permission.
As with any insurance policy you buy, be sure to choose an established carrier with ample experience in the field and solid financial strength. A low premium is no bargain if the carrier is new to EPLI or goes broke.
Above all, as with any insurance policy, make sure that you can live with the claims definition and exclusions in the policy you choose, and seek advice if you are unsure what your specific needs are before signing on the dotted line.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
No matter how complete your insurance portfolio, there is one policy – one you probably have never heard of – that you should definitely consider adding to it.
A while ago, I spoke with a dermatologist in California who experienced every employer’s nightmare: he fired an incompetent employee, who promptly sued him for wrongful termination and accused him of sexual harassment to boot. The charges were completely false, and the employee’s transgressions were well documented; but he was not insured against a suit of that type, and defending it would have been prohibitively expensive. He was forced to settle it for a significant sum of money.
Disasters like that are becoming more common. Plaintiffs’ attorneys know that most small businesses, including medical practices, are not insured against internal liability actions – and that settlements are cheaper than litigation.
Fortunately, there is a relatively inexpensive alternative: not covered by conventional liability insurance. These include wrongful termination, sexual harassment, discrimination, breach of employment contract, negligent hiring or evaluation, failure to promote, wrongful discipline, mismanagement of benefits, and the ever-popular “emotional distress.”
EPLI coverage would have permitted the California dermatologist to mount a proper defense against his employee’s groundless charges. In fact, there is a better than even chance that the lawsuit would have been dropped, or never filed to begin with.
Some liability carriers are beginning to cover some employee-related issues in “umbrella” policies, so before looking into EPLI, check your current coverage. Then, as with all insurance, you should shop around for the best price and carefully read the policies on your short list. All EPLI policies cover litigation against your practice and its owners by employees, but some cover only full-timers. Try to obtain the broadest coverage possible so that claims from part-time, temporary, and seasonal employees, and, if possible, even applicants for employment and former employees, also are covered.
You should also look for the most comprehensive policy in terms of coverage. Almost every EPLI policy covers the allegations mentioned above, but some offer a more comprehensive list of covered acts, such as invasion of privacy and defamation of character.
Also be aware of precisely what each policy does not cover. Most exclude punitive damages and court-imposed fines, as well as criminal acts, fraud, and other clearly illegal conduct. For example, you would not be covered if you fired an employee because he or she refused to falsify insurance claims.
Depending on where you practice, it may be necessary to ask an employment attorney to evaluate your individual EPLI needs. An underwriter cannot anticipate every eventuality for you, particularly if he or she does not live in your area and is not familiar with employment conditions in your community.
As with any liability policy, try to get a clause added that permits you to choose your own defense attorney. Better still, pick a specific attorney or firm that you trust and have that counsel named in an endorsement to the policy. Otherwise, the insurance carrier will select an attorney from its own panel who may not consider your interests a higher priority than those of the insurer itself.
If you must accept the insurer’s choice of counsel, you should find out whether that attorney is experienced in employment law, which is a very specialized area. And just as with your malpractice policy, you will want to maintain as much control as possible over the settlement of claims. Ideally, no claim should be settled without your express permission.
As with any insurance policy you buy, be sure to choose an established carrier with ample experience in the field and solid financial strength. A low premium is no bargain if the carrier is new to EPLI or goes broke.
Above all, as with any insurance policy, make sure that you can live with the claims definition and exclusions in the policy you choose, and seek advice if you are unsure what your specific needs are before signing on the dotted line.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
No matter how complete your insurance portfolio, there is one policy – one you probably have never heard of – that you should definitely consider adding to it.
A while ago, I spoke with a dermatologist in California who experienced every employer’s nightmare: he fired an incompetent employee, who promptly sued him for wrongful termination and accused him of sexual harassment to boot. The charges were completely false, and the employee’s transgressions were well documented; but he was not insured against a suit of that type, and defending it would have been prohibitively expensive. He was forced to settle it for a significant sum of money.
Disasters like that are becoming more common. Plaintiffs’ attorneys know that most small businesses, including medical practices, are not insured against internal liability actions – and that settlements are cheaper than litigation.
Fortunately, there is a relatively inexpensive alternative: not covered by conventional liability insurance. These include wrongful termination, sexual harassment, discrimination, breach of employment contract, negligent hiring or evaluation, failure to promote, wrongful discipline, mismanagement of benefits, and the ever-popular “emotional distress.”
EPLI coverage would have permitted the California dermatologist to mount a proper defense against his employee’s groundless charges. In fact, there is a better than even chance that the lawsuit would have been dropped, or never filed to begin with.
Some liability carriers are beginning to cover some employee-related issues in “umbrella” policies, so before looking into EPLI, check your current coverage. Then, as with all insurance, you should shop around for the best price and carefully read the policies on your short list. All EPLI policies cover litigation against your practice and its owners by employees, but some cover only full-timers. Try to obtain the broadest coverage possible so that claims from part-time, temporary, and seasonal employees, and, if possible, even applicants for employment and former employees, also are covered.
You should also look for the most comprehensive policy in terms of coverage. Almost every EPLI policy covers the allegations mentioned above, but some offer a more comprehensive list of covered acts, such as invasion of privacy and defamation of character.
Also be aware of precisely what each policy does not cover. Most exclude punitive damages and court-imposed fines, as well as criminal acts, fraud, and other clearly illegal conduct. For example, you would not be covered if you fired an employee because he or she refused to falsify insurance claims.
Depending on where you practice, it may be necessary to ask an employment attorney to evaluate your individual EPLI needs. An underwriter cannot anticipate every eventuality for you, particularly if he or she does not live in your area and is not familiar with employment conditions in your community.
As with any liability policy, try to get a clause added that permits you to choose your own defense attorney. Better still, pick a specific attorney or firm that you trust and have that counsel named in an endorsement to the policy. Otherwise, the insurance carrier will select an attorney from its own panel who may not consider your interests a higher priority than those of the insurer itself.
If you must accept the insurer’s choice of counsel, you should find out whether that attorney is experienced in employment law, which is a very specialized area. And just as with your malpractice policy, you will want to maintain as much control as possible over the settlement of claims. Ideally, no claim should be settled without your express permission.
As with any insurance policy you buy, be sure to choose an established carrier with ample experience in the field and solid financial strength. A low premium is no bargain if the carrier is new to EPLI or goes broke.
Above all, as with any insurance policy, make sure that you can live with the claims definition and exclusions in the policy you choose, and seek advice if you are unsure what your specific needs are before signing on the dotted line.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
A Veteran With Fibromyalgia Presenting With Dyspnea
Case Presentation. A 64-year-old US Army veteran with a history of colorectal cancer, melanoma, and fibrinolytic presented with dyspnea to VA Boston Healthcare System (VABHS). Seven years prior to the current presentation, at the time of her diagnosis of colorectal cancer, the patient was found to be HIV negative but to have a positive purified protein derivative (PPD) test. She was treated with isoniazid (INH) therapy for 9 months. Sputum cultures collected prior to initiation of therapy grew Mycobacterium avium complex (MAC) in 1 of 3 samples, with these results reported several months after initiation of therapy. She was a never smoker with no known travel or exposure. At the time of the current presentation, her medications included bupropion, levothyroxine, capsaicin, cyclobenzaprine, ibuprofen, and acetaminophen.
►Lakshmana Swamy, MD, Chief Medical Resident, VABHS and Boston Medical Center. Dr. Monach, this patient is on a variety of pain medications and has a diagnosis of fibromyalgia. This diagnosis often frustrates doctors and patients alike. Can you tell us about fibromyalgia from the rheumatologist’s perspective and what you think of her current treatment regimen?
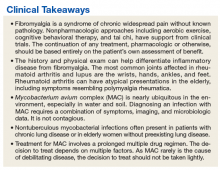
►Paul A. Monach, MD, PhD, Chief, Section of Rheumatology, VABHS and Associate Professor of Medicine, Boston University School of Medicine. Fibromyalgia is a syndrome of chronic widespread pain without known pathology in the musculoskeletal system. It is thought to be caused by chronic dysfunction of pain-processing pathways in the central nervous system (CNS). It is often accompanied by other somatic symptoms such as chronic fatigue, irritable bowel syndrome, and bladder pain. It is a common condition, affecting up to 5% of otherwise healthy women. It is particularly common in persons with chronic nonrestorative sleep or posttraumatic stress disorder from a wide range of causes. However, it also is more common in persons with autoimmune inflammatory diseases, such as lupus, Sjögren syndrome, or rheumatoid arthritis. Concern for one of these diseases is the main reason to consider referring a patient for evaluation by a rheumatologist. Often rheumatologists participate in the management of fibromyalgia. A patient should be given appropriate expectations by the referring physician.
Effectiveness of treatment varies widely among patients. Nonpharmacologic approaches such as aerobic exercise, cognitive behavioral therapy, and tai chi have support from clinical trials, and yoga and aquatherapy also are widely used.1,2 The classes of drugs used are the same as for neuropathic pain: tricyclics, including cyclobenzaprine; serotonin and norepinephrine reuptake inhibitors (SNRIs); and gabapentinoids. In contrast, nonsteroidal anti-inflammatory drugs and opioids are ineffective unless there is a superimposed mechanical or inflammatory cause in the periphery. The key point is that continuation of any treatment should be based entirely on the patient’s own assessment of benefit.
►Dr. Swamy. Seven years later, the patient returned to her primary care provider, reporting increased dyspnea on exertion as well as significant fatigue. She was referred to the pulmonary department and had repeat computed tomography (CT) scans of the chest, which indicated persistent right middle lobe (RML) bronchiectasis. She then underwent bronchoscopy with a subsequent bronchoalveolar lavage (BAL) culture growing MAC. Dr. Fine, please interpret the baseline and follow-up CT scans and help us understand the significance of the MAC on sputum and BAL cultures.
►Alan Fine, MD, Section of Pulmonary and Critical Care, VABHS and Professor of Medicine, Boston University School of Medicine. Prior to this presentation, the patient had a pleural-based area of fibrosis with possible associated RML bronchiectasis. This appears to be a postinflammatory process without classic features of malignant or metastatic disease. She then had a sputum, which grew MAC in only 1 of 3 samples and in liquid media only. Importantly, the sputum was not smear positive. All of this suggests a low organism burden. One possibility is that this could reflect colonization with MAC; it is not uncommon for patients with underlying chronic changes in their lung to grow MAC, and it is often difficult to tell whether it is indicative of active disease. Structural lung disease, such as bronchiectasis, predisposes a patient to MAC, but chronic MAC also may cause bronchiectasis. This chicken-and-egg scenario comes up frequently. She may have a MAC infection, but as she is HIV negative and asymptomatic, there is no urgent indication to treat, especially as the burden of therapy is not insignificant.
►Dr. Swamy. Do we need to worry about Mycobacterium tuberculosis (MTB)?
►Dr. Fine. Although she was previously PPD positive, she had already completed 1 year of isoniazid (INH) therapy, making active MTB less likely. From an infection control standpoint, it is important to distinguish MAC from MTB. The former is not contagious, and there is no need for airborne isolation.
►Dr. Swamy. Dr. Fine, where does MAC come from? Does it commonly cause disease?
►Dr. Fine. In the environment, MAC is nearly ubiquitous , especially in water and soil. In one study, 20% of showerheads were positive for MAC; when patients are infected, we may suggest changing/bleaching the showerhead, but there are no definitive recommendations.3 Because MAC is so common in the environment, it is unlikely that measures to target MAC colonization will be clinically meaningful. On the other hand, the incidence of nontuberculous mycobacterial infections is increasing across the US, and it may be a common and frequently underdiagnosed cause of chronic cough, especially in postmenopausal women.
►Dr. Swamy. Four years prior to the current presentation, the patient developed a cough after an upper respiratory tract infection that persisted for more than 2 weeks. Given her history, she underwent a repeat chest CT, which noted a slight increase in nodularity and ground-glass opacity restricted to the RML. She also reported dyspnea on exertion and was referred to the pulmonary medicine department. By the time she arrived, her dyspnea had largely resolved, but she reported persistent fatigue without other systemic symptoms, such as fevers or chills. Dr. Fine, does MAC explain this patient’s dyspnea?
►Dr. Fine. As her pulmonary symptoms resolved in a short period of time with only azithromycin, it is very unlikely that her symptoms were related to her prior disease. The MAC infection is not likely to cause dyspnea on exertion and fatigue and should be worked up more broadly before attributing it to MAC. In view of this, it would not be unreasonable to follow her clinically and see her again in 6 to 8 weeks. In this context, we also should consider the untoward impact of repeated radiation exposure derived from multiple CT scans. When a patient has an abnormality on CT scan, it often leads to further scans even if the symptoms do not match the previous findings, as in this case.
►Dr. Swamy. Given her ongoing fatigue and systemic symptoms (morning stiffness of the shoulders, legs, and thighs, and leg cramps), she was referred to the rheumatology department where the physical examination revealed muscle tenderness in her proximal arms and legs with normal strength, tender points at the elbows and medial side of the bilateral knees, significant tenderness of lower legs, and no synovitis.
Dr. Monach, can you walk us through your approach to this patient? Are we seeing manifestations of fibromyalgia? What diagnoses concerns you and how would you proceed?
►Dr. Monach. The history and exam are most helpful in raising or reducing suspicion for an underlying inflammatory disease. Areas of tenderness described in her case are typical of fibromyalgia, although it can be difficult to interpret symptoms in the hip girdle and shoulder girdle because objective findings are often absent on exam in patients with inflammatory arthritis or bursitis. Similarly, tenderness at sites of tendon insertion (enthuses) without objective abnormalities is common in different forms of spondyloarthritis, so tenderness at the elbow, knee, lateral hip, and low back can be difficult to interpret. What this patient is lacking is prominent subjective or objective findings in the joints most commonly affected in rheumatoid arthritis and lupus: wrists, hands, ankles, and feet.
►Dr. Swamy. Initial laboratory data include an erythrocyte sedimentation rate of 79 with a normal C-reactive protein. A tentative diagnosis of polymyalgia rheumatic is made with consideration of a trial treatment of prednisone.
Dr. Monach, this patient has an indolent infection and is about to be given glucocorticoids. Could you describe the situations in which you feel that glucocorticoids cause a relative immunosuppression?
►Dr. Monach. Glucocorticoids are considered safe in a patient whose infection is not intrinsically dangerous or who has started appropriate antibiotics for that infection. Although all toxicities of glucocorticoids are dose dependent, the long-standing assertion that doses below 10 mg to 15 mg do not increase risk of infection is contradicted by data published in the past 10 to 15 years, with the caveat that these patients were on long-term treatment.
►Dr. Swamy. The patient was started on prednisone 15 mg per day for 15 days. She returned to the clinic after 1 week of prednisone troutment and noted “significant improvement in fatigue, morning stiffness of shoulders, thighs, leg, back is better, leg cramps resolved, shooting pain in many joints resolved.” Further laboratory results were notable for a negative rheumatoid factor, negative antinuclear antibody, and a cyclic citrullinated peptide of 60. A presumptive diagnosis of rheumatoid arthritis (RA) was made and plaquenil 200 mg twice daily was started.
Dr. Monach, can you explain why RA comes up now on serology but was not considered initially? Why does this presentation fit RA, and was her response to treatment typical? How does this fit in with her previous diagnosis of fibromyalgia? Was that just an atypical, indolent presentation of RA?
►Dr. Monach. Though her presentation is atypical for RA, in elderly patients, RA can present with symptoms resembling polymyalgia rheumatica. The question is whether she had RA all along (in which case “elderly onset” would not apply) or had fibromyalgia and developed RA more recently. The response to empiric glucocorticoid therapy is helpful, since fibromyalgia should not improve with prednisone even in a patient with RA unless treatment of RA would allow better sleep and ability to exercise. Rheumatoid arthritis typically responds very well to prednisone in the 5-mg to 15-mg range.
►Dr. Swamy. Given the new diagnosis of an inflammatory arthritis requiring immunosuppression, bronchoscopy with BAL is performed to evaluate for the presence of MAC. These cultures were positive for MAC.
Dr. Fine, does the positive BAL culture indicate an active MAC infection?
►Dr. Fine. Yes, based on these updated data, the patient has an active MAC infection. Active infection is defined as symptoms or imaging consistent with the diagnosis, supporting microbiology data (either 2 sputum or 1 BAL sample growing MAC) and the exclusion of other causes. Previously, this patient grew MAC in just one expectorated sputum; this did not meet the microbiologic criteria. Now sputum has grown in the BAL sample; along with the CT imaging, this is enough to diagnosis active MAC infection.
Treatment for MAC must consider the details of each case. First, this is not an emergency; treatment decisions should be made with the rheumatologist to consider the planned immunosuppression. For example, we must consider potential drug interactions. A specific point should be made of the use of tumor necrosis factor (TNF)-α inhibition, which data indicate can reactivate TB and may inhibit mechanisms that restrain mycobacterial disease. Serious cases of MAC infection have been reported in the literature in the setting of TNF-α inhibition.5,6 Despite these concerns, there is not a contraindication to using these therapies from the perspective of the active MAC disease. All of these decisions will impact the need to commit the patient to MAC therapy.
►Dr. Swamy. Dr. Fine, what do you consider prior to initiating MAC therapy?
► Dr. Fine. The decision to pursue MAC therapy should not be taken lightly. Therapy often entails prolonged multidrug regimens, usually spanning more than a year, with frequent adverse effects. Outside of very specific cases, such as TNF-β inhibition, MAC is rarely a life-threatening disease, so the benefit may be limited. Treatment for MAC is certainly unlikely to be fruitful without a diligent and motivated patient able to handle the high and prolonged pill burden. Of note, it is also important to keep this patient up-to-date with influenza and pneumonia vaccination given her structural lung disease.
►Dr. Swamy. The decision is made to treat MAC with azithromycin, rifampin, and ethambutol. The disease is noted to be nonfibrocavitary. The patient underwent monthly liver function test monitoring and visual acuity testing, which were unremarkable. Dr. Fine, can you describe the phenotypes of nontuberculous mycobacterial (NTM) disease?
►Dr. Fine. There are 3 main phenotypes of NTM.3 First, we see the elderly man with preexisting lung disease—usually chronic obstructive pulmonary disease—with fibrocavitary and/or reticulonodular appearance. Second, we see the slim, elderly woman often without any preexisting lung disease presenting with focal bronchiectasis and nodular lesions in right middle lobe and lingula—the Lady Windermere syndrome. This eponym is derived from Oscar Wilde’s play “Lady Windermere’s Fan, a Play About a Good Woman,” and was first associated with this disease in 1992.7 At the time, it was thought that the voluntary suppression of cough led to poorly draining lung regions, vulnerable to engraftment by atypical mycobacteria. Infection with atypical mycobacteria are associated with this population; however, it is no longer thought to be due to the voluntary suppression of cough.7,8 Third, we do occasionally see atypical presentations, such as focal masses and solitary nodules.
►Dr. Swamy. At 1-year follow-up she successfully completed MAC therapy and noted ongoing control of rheumatoid symptoms.
1. Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome—a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2018;22(2):242-260.
2. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4:CD011279.
3. Aksamit TR, Philley JV, Griffith DE. Nontuberculous mycobacterial (NTM) lung disease: the top ten essentials. Respir Med. 2014;108(3):417-425.
4. Aucott JN. Glucocorticoids and infection. Endocrinol Metab Clin North Am. 1994;23(3):655-670.
5. Curtis JR, Yang S, Patkar NM, et al. Risk of hospitalized bacterial infections associated with biologic treatment among US veterans with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(7):990-997.
6. Lane MA, McDonald JR, Zeringue AL, et al. TNF-α antagonist use and risk of hospitalization for infection in a national cohort of veterans with rheumatoid arthritis. Medicine (Baltimore). 2011;90(2):139-145.
7. Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest. 1992;101(6):1605-1609.
8. Kasthoori JJ, Liam CK, Wastie ML. Lady Windermere syndrome: an inappropriate eponym for an increasingly important condition. Singapore Med J. 2008;49(2):e47-e49.
Case Presentation. A 64-year-old US Army veteran with a history of colorectal cancer, melanoma, and fibrinolytic presented with dyspnea to VA Boston Healthcare System (VABHS). Seven years prior to the current presentation, at the time of her diagnosis of colorectal cancer, the patient was found to be HIV negative but to have a positive purified protein derivative (PPD) test. She was treated with isoniazid (INH) therapy for 9 months. Sputum cultures collected prior to initiation of therapy grew Mycobacterium avium complex (MAC) in 1 of 3 samples, with these results reported several months after initiation of therapy. She was a never smoker with no known travel or exposure. At the time of the current presentation, her medications included bupropion, levothyroxine, capsaicin, cyclobenzaprine, ibuprofen, and acetaminophen.
►Lakshmana Swamy, MD, Chief Medical Resident, VABHS and Boston Medical Center. Dr. Monach, this patient is on a variety of pain medications and has a diagnosis of fibromyalgia. This diagnosis often frustrates doctors and patients alike. Can you tell us about fibromyalgia from the rheumatologist’s perspective and what you think of her current treatment regimen?
►Paul A. Monach, MD, PhD, Chief, Section of Rheumatology, VABHS and Associate Professor of Medicine, Boston University School of Medicine. Fibromyalgia is a syndrome of chronic widespread pain without known pathology in the musculoskeletal system. It is thought to be caused by chronic dysfunction of pain-processing pathways in the central nervous system (CNS). It is often accompanied by other somatic symptoms such as chronic fatigue, irritable bowel syndrome, and bladder pain. It is a common condition, affecting up to 5% of otherwise healthy women. It is particularly common in persons with chronic nonrestorative sleep or posttraumatic stress disorder from a wide range of causes. However, it also is more common in persons with autoimmune inflammatory diseases, such as lupus, Sjögren syndrome, or rheumatoid arthritis. Concern for one of these diseases is the main reason to consider referring a patient for evaluation by a rheumatologist. Often rheumatologists participate in the management of fibromyalgia. A patient should be given appropriate expectations by the referring physician.
Effectiveness of treatment varies widely among patients. Nonpharmacologic approaches such as aerobic exercise, cognitive behavioral therapy, and tai chi have support from clinical trials, and yoga and aquatherapy also are widely used.1,2 The classes of drugs used are the same as for neuropathic pain: tricyclics, including cyclobenzaprine; serotonin and norepinephrine reuptake inhibitors (SNRIs); and gabapentinoids. In contrast, nonsteroidal anti-inflammatory drugs and opioids are ineffective unless there is a superimposed mechanical or inflammatory cause in the periphery. The key point is that continuation of any treatment should be based entirely on the patient’s own assessment of benefit.
►Dr. Swamy. Seven years later, the patient returned to her primary care provider, reporting increased dyspnea on exertion as well as significant fatigue. She was referred to the pulmonary department and had repeat computed tomography (CT) scans of the chest, which indicated persistent right middle lobe (RML) bronchiectasis. She then underwent bronchoscopy with a subsequent bronchoalveolar lavage (BAL) culture growing MAC. Dr. Fine, please interpret the baseline and follow-up CT scans and help us understand the significance of the MAC on sputum and BAL cultures.
►Alan Fine, MD, Section of Pulmonary and Critical Care, VABHS and Professor of Medicine, Boston University School of Medicine. Prior to this presentation, the patient had a pleural-based area of fibrosis with possible associated RML bronchiectasis. This appears to be a postinflammatory process without classic features of malignant or metastatic disease. She then had a sputum, which grew MAC in only 1 of 3 samples and in liquid media only. Importantly, the sputum was not smear positive. All of this suggests a low organism burden. One possibility is that this could reflect colonization with MAC; it is not uncommon for patients with underlying chronic changes in their lung to grow MAC, and it is often difficult to tell whether it is indicative of active disease. Structural lung disease, such as bronchiectasis, predisposes a patient to MAC, but chronic MAC also may cause bronchiectasis. This chicken-and-egg scenario comes up frequently. She may have a MAC infection, but as she is HIV negative and asymptomatic, there is no urgent indication to treat, especially as the burden of therapy is not insignificant.
►Dr. Swamy. Do we need to worry about Mycobacterium tuberculosis (MTB)?
►Dr. Fine. Although she was previously PPD positive, she had already completed 1 year of isoniazid (INH) therapy, making active MTB less likely. From an infection control standpoint, it is important to distinguish MAC from MTB. The former is not contagious, and there is no need for airborne isolation.
►Dr. Swamy. Dr. Fine, where does MAC come from? Does it commonly cause disease?
►Dr. Fine. In the environment, MAC is nearly ubiquitous , especially in water and soil. In one study, 20% of showerheads were positive for MAC; when patients are infected, we may suggest changing/bleaching the showerhead, but there are no definitive recommendations.3 Because MAC is so common in the environment, it is unlikely that measures to target MAC colonization will be clinically meaningful. On the other hand, the incidence of nontuberculous mycobacterial infections is increasing across the US, and it may be a common and frequently underdiagnosed cause of chronic cough, especially in postmenopausal women.
►Dr. Swamy. Four years prior to the current presentation, the patient developed a cough after an upper respiratory tract infection that persisted for more than 2 weeks. Given her history, she underwent a repeat chest CT, which noted a slight increase in nodularity and ground-glass opacity restricted to the RML. She also reported dyspnea on exertion and was referred to the pulmonary medicine department. By the time she arrived, her dyspnea had largely resolved, but she reported persistent fatigue without other systemic symptoms, such as fevers or chills. Dr. Fine, does MAC explain this patient’s dyspnea?
►Dr. Fine. As her pulmonary symptoms resolved in a short period of time with only azithromycin, it is very unlikely that her symptoms were related to her prior disease. The MAC infection is not likely to cause dyspnea on exertion and fatigue and should be worked up more broadly before attributing it to MAC. In view of this, it would not be unreasonable to follow her clinically and see her again in 6 to 8 weeks. In this context, we also should consider the untoward impact of repeated radiation exposure derived from multiple CT scans. When a patient has an abnormality on CT scan, it often leads to further scans even if the symptoms do not match the previous findings, as in this case.
►Dr. Swamy. Given her ongoing fatigue and systemic symptoms (morning stiffness of the shoulders, legs, and thighs, and leg cramps), she was referred to the rheumatology department where the physical examination revealed muscle tenderness in her proximal arms and legs with normal strength, tender points at the elbows and medial side of the bilateral knees, significant tenderness of lower legs, and no synovitis.
Dr. Monach, can you walk us through your approach to this patient? Are we seeing manifestations of fibromyalgia? What diagnoses concerns you and how would you proceed?
►Dr. Monach. The history and exam are most helpful in raising or reducing suspicion for an underlying inflammatory disease. Areas of tenderness described in her case are typical of fibromyalgia, although it can be difficult to interpret symptoms in the hip girdle and shoulder girdle because objective findings are often absent on exam in patients with inflammatory arthritis or bursitis. Similarly, tenderness at sites of tendon insertion (enthuses) without objective abnormalities is common in different forms of spondyloarthritis, so tenderness at the elbow, knee, lateral hip, and low back can be difficult to interpret. What this patient is lacking is prominent subjective or objective findings in the joints most commonly affected in rheumatoid arthritis and lupus: wrists, hands, ankles, and feet.
►Dr. Swamy. Initial laboratory data include an erythrocyte sedimentation rate of 79 with a normal C-reactive protein. A tentative diagnosis of polymyalgia rheumatic is made with consideration of a trial treatment of prednisone.
Dr. Monach, this patient has an indolent infection and is about to be given glucocorticoids. Could you describe the situations in which you feel that glucocorticoids cause a relative immunosuppression?
►Dr. Monach. Glucocorticoids are considered safe in a patient whose infection is not intrinsically dangerous or who has started appropriate antibiotics for that infection. Although all toxicities of glucocorticoids are dose dependent, the long-standing assertion that doses below 10 mg to 15 mg do not increase risk of infection is contradicted by data published in the past 10 to 15 years, with the caveat that these patients were on long-term treatment.
►Dr. Swamy. The patient was started on prednisone 15 mg per day for 15 days. She returned to the clinic after 1 week of prednisone troutment and noted “significant improvement in fatigue, morning stiffness of shoulders, thighs, leg, back is better, leg cramps resolved, shooting pain in many joints resolved.” Further laboratory results were notable for a negative rheumatoid factor, negative antinuclear antibody, and a cyclic citrullinated peptide of 60. A presumptive diagnosis of rheumatoid arthritis (RA) was made and plaquenil 200 mg twice daily was started.
Dr. Monach, can you explain why RA comes up now on serology but was not considered initially? Why does this presentation fit RA, and was her response to treatment typical? How does this fit in with her previous diagnosis of fibromyalgia? Was that just an atypical, indolent presentation of RA?
►Dr. Monach. Though her presentation is atypical for RA, in elderly patients, RA can present with symptoms resembling polymyalgia rheumatica. The question is whether she had RA all along (in which case “elderly onset” would not apply) or had fibromyalgia and developed RA more recently. The response to empiric glucocorticoid therapy is helpful, since fibromyalgia should not improve with prednisone even in a patient with RA unless treatment of RA would allow better sleep and ability to exercise. Rheumatoid arthritis typically responds very well to prednisone in the 5-mg to 15-mg range.
►Dr. Swamy. Given the new diagnosis of an inflammatory arthritis requiring immunosuppression, bronchoscopy with BAL is performed to evaluate for the presence of MAC. These cultures were positive for MAC.
Dr. Fine, does the positive BAL culture indicate an active MAC infection?
►Dr. Fine. Yes, based on these updated data, the patient has an active MAC infection. Active infection is defined as symptoms or imaging consistent with the diagnosis, supporting microbiology data (either 2 sputum or 1 BAL sample growing MAC) and the exclusion of other causes. Previously, this patient grew MAC in just one expectorated sputum; this did not meet the microbiologic criteria. Now sputum has grown in the BAL sample; along with the CT imaging, this is enough to diagnosis active MAC infection.
Treatment for MAC must consider the details of each case. First, this is not an emergency; treatment decisions should be made with the rheumatologist to consider the planned immunosuppression. For example, we must consider potential drug interactions. A specific point should be made of the use of tumor necrosis factor (TNF)-α inhibition, which data indicate can reactivate TB and may inhibit mechanisms that restrain mycobacterial disease. Serious cases of MAC infection have been reported in the literature in the setting of TNF-α inhibition.5,6 Despite these concerns, there is not a contraindication to using these therapies from the perspective of the active MAC disease. All of these decisions will impact the need to commit the patient to MAC therapy.
►Dr. Swamy. Dr. Fine, what do you consider prior to initiating MAC therapy?
► Dr. Fine. The decision to pursue MAC therapy should not be taken lightly. Therapy often entails prolonged multidrug regimens, usually spanning more than a year, with frequent adverse effects. Outside of very specific cases, such as TNF-β inhibition, MAC is rarely a life-threatening disease, so the benefit may be limited. Treatment for MAC is certainly unlikely to be fruitful without a diligent and motivated patient able to handle the high and prolonged pill burden. Of note, it is also important to keep this patient up-to-date with influenza and pneumonia vaccination given her structural lung disease.
►Dr. Swamy. The decision is made to treat MAC with azithromycin, rifampin, and ethambutol. The disease is noted to be nonfibrocavitary. The patient underwent monthly liver function test monitoring and visual acuity testing, which were unremarkable. Dr. Fine, can you describe the phenotypes of nontuberculous mycobacterial (NTM) disease?
►Dr. Fine. There are 3 main phenotypes of NTM.3 First, we see the elderly man with preexisting lung disease—usually chronic obstructive pulmonary disease—with fibrocavitary and/or reticulonodular appearance. Second, we see the slim, elderly woman often without any preexisting lung disease presenting with focal bronchiectasis and nodular lesions in right middle lobe and lingula—the Lady Windermere syndrome. This eponym is derived from Oscar Wilde’s play “Lady Windermere’s Fan, a Play About a Good Woman,” and was first associated with this disease in 1992.7 At the time, it was thought that the voluntary suppression of cough led to poorly draining lung regions, vulnerable to engraftment by atypical mycobacteria. Infection with atypical mycobacteria are associated with this population; however, it is no longer thought to be due to the voluntary suppression of cough.7,8 Third, we do occasionally see atypical presentations, such as focal masses and solitary nodules.
►Dr. Swamy. At 1-year follow-up she successfully completed MAC therapy and noted ongoing control of rheumatoid symptoms.
Case Presentation. A 64-year-old US Army veteran with a history of colorectal cancer, melanoma, and fibrinolytic presented with dyspnea to VA Boston Healthcare System (VABHS). Seven years prior to the current presentation, at the time of her diagnosis of colorectal cancer, the patient was found to be HIV negative but to have a positive purified protein derivative (PPD) test. She was treated with isoniazid (INH) therapy for 9 months. Sputum cultures collected prior to initiation of therapy grew Mycobacterium avium complex (MAC) in 1 of 3 samples, with these results reported several months after initiation of therapy. She was a never smoker with no known travel or exposure. At the time of the current presentation, her medications included bupropion, levothyroxine, capsaicin, cyclobenzaprine, ibuprofen, and acetaminophen.
►Lakshmana Swamy, MD, Chief Medical Resident, VABHS and Boston Medical Center. Dr. Monach, this patient is on a variety of pain medications and has a diagnosis of fibromyalgia. This diagnosis often frustrates doctors and patients alike. Can you tell us about fibromyalgia from the rheumatologist’s perspective and what you think of her current treatment regimen?
►Paul A. Monach, MD, PhD, Chief, Section of Rheumatology, VABHS and Associate Professor of Medicine, Boston University School of Medicine. Fibromyalgia is a syndrome of chronic widespread pain without known pathology in the musculoskeletal system. It is thought to be caused by chronic dysfunction of pain-processing pathways in the central nervous system (CNS). It is often accompanied by other somatic symptoms such as chronic fatigue, irritable bowel syndrome, and bladder pain. It is a common condition, affecting up to 5% of otherwise healthy women. It is particularly common in persons with chronic nonrestorative sleep or posttraumatic stress disorder from a wide range of causes. However, it also is more common in persons with autoimmune inflammatory diseases, such as lupus, Sjögren syndrome, or rheumatoid arthritis. Concern for one of these diseases is the main reason to consider referring a patient for evaluation by a rheumatologist. Often rheumatologists participate in the management of fibromyalgia. A patient should be given appropriate expectations by the referring physician.
Effectiveness of treatment varies widely among patients. Nonpharmacologic approaches such as aerobic exercise, cognitive behavioral therapy, and tai chi have support from clinical trials, and yoga and aquatherapy also are widely used.1,2 The classes of drugs used are the same as for neuropathic pain: tricyclics, including cyclobenzaprine; serotonin and norepinephrine reuptake inhibitors (SNRIs); and gabapentinoids. In contrast, nonsteroidal anti-inflammatory drugs and opioids are ineffective unless there is a superimposed mechanical or inflammatory cause in the periphery. The key point is that continuation of any treatment should be based entirely on the patient’s own assessment of benefit.
►Dr. Swamy. Seven years later, the patient returned to her primary care provider, reporting increased dyspnea on exertion as well as significant fatigue. She was referred to the pulmonary department and had repeat computed tomography (CT) scans of the chest, which indicated persistent right middle lobe (RML) bronchiectasis. She then underwent bronchoscopy with a subsequent bronchoalveolar lavage (BAL) culture growing MAC. Dr. Fine, please interpret the baseline and follow-up CT scans and help us understand the significance of the MAC on sputum and BAL cultures.
►Alan Fine, MD, Section of Pulmonary and Critical Care, VABHS and Professor of Medicine, Boston University School of Medicine. Prior to this presentation, the patient had a pleural-based area of fibrosis with possible associated RML bronchiectasis. This appears to be a postinflammatory process without classic features of malignant or metastatic disease. She then had a sputum, which grew MAC in only 1 of 3 samples and in liquid media only. Importantly, the sputum was not smear positive. All of this suggests a low organism burden. One possibility is that this could reflect colonization with MAC; it is not uncommon for patients with underlying chronic changes in their lung to grow MAC, and it is often difficult to tell whether it is indicative of active disease. Structural lung disease, such as bronchiectasis, predisposes a patient to MAC, but chronic MAC also may cause bronchiectasis. This chicken-and-egg scenario comes up frequently. She may have a MAC infection, but as she is HIV negative and asymptomatic, there is no urgent indication to treat, especially as the burden of therapy is not insignificant.
►Dr. Swamy. Do we need to worry about Mycobacterium tuberculosis (MTB)?
►Dr. Fine. Although she was previously PPD positive, she had already completed 1 year of isoniazid (INH) therapy, making active MTB less likely. From an infection control standpoint, it is important to distinguish MAC from MTB. The former is not contagious, and there is no need for airborne isolation.
►Dr. Swamy. Dr. Fine, where does MAC come from? Does it commonly cause disease?
►Dr. Fine. In the environment, MAC is nearly ubiquitous , especially in water and soil. In one study, 20% of showerheads were positive for MAC; when patients are infected, we may suggest changing/bleaching the showerhead, but there are no definitive recommendations.3 Because MAC is so common in the environment, it is unlikely that measures to target MAC colonization will be clinically meaningful. On the other hand, the incidence of nontuberculous mycobacterial infections is increasing across the US, and it may be a common and frequently underdiagnosed cause of chronic cough, especially in postmenopausal women.
►Dr. Swamy. Four years prior to the current presentation, the patient developed a cough after an upper respiratory tract infection that persisted for more than 2 weeks. Given her history, she underwent a repeat chest CT, which noted a slight increase in nodularity and ground-glass opacity restricted to the RML. She also reported dyspnea on exertion and was referred to the pulmonary medicine department. By the time she arrived, her dyspnea had largely resolved, but she reported persistent fatigue without other systemic symptoms, such as fevers or chills. Dr. Fine, does MAC explain this patient’s dyspnea?
►Dr. Fine. As her pulmonary symptoms resolved in a short period of time with only azithromycin, it is very unlikely that her symptoms were related to her prior disease. The MAC infection is not likely to cause dyspnea on exertion and fatigue and should be worked up more broadly before attributing it to MAC. In view of this, it would not be unreasonable to follow her clinically and see her again in 6 to 8 weeks. In this context, we also should consider the untoward impact of repeated radiation exposure derived from multiple CT scans. When a patient has an abnormality on CT scan, it often leads to further scans even if the symptoms do not match the previous findings, as in this case.
►Dr. Swamy. Given her ongoing fatigue and systemic symptoms (morning stiffness of the shoulders, legs, and thighs, and leg cramps), she was referred to the rheumatology department where the physical examination revealed muscle tenderness in her proximal arms and legs with normal strength, tender points at the elbows and medial side of the bilateral knees, significant tenderness of lower legs, and no synovitis.
Dr. Monach, can you walk us through your approach to this patient? Are we seeing manifestations of fibromyalgia? What diagnoses concerns you and how would you proceed?
►Dr. Monach. The history and exam are most helpful in raising or reducing suspicion for an underlying inflammatory disease. Areas of tenderness described in her case are typical of fibromyalgia, although it can be difficult to interpret symptoms in the hip girdle and shoulder girdle because objective findings are often absent on exam in patients with inflammatory arthritis or bursitis. Similarly, tenderness at sites of tendon insertion (enthuses) without objective abnormalities is common in different forms of spondyloarthritis, so tenderness at the elbow, knee, lateral hip, and low back can be difficult to interpret. What this patient is lacking is prominent subjective or objective findings in the joints most commonly affected in rheumatoid arthritis and lupus: wrists, hands, ankles, and feet.
►Dr. Swamy. Initial laboratory data include an erythrocyte sedimentation rate of 79 with a normal C-reactive protein. A tentative diagnosis of polymyalgia rheumatic is made with consideration of a trial treatment of prednisone.
Dr. Monach, this patient has an indolent infection and is about to be given glucocorticoids. Could you describe the situations in which you feel that glucocorticoids cause a relative immunosuppression?
►Dr. Monach. Glucocorticoids are considered safe in a patient whose infection is not intrinsically dangerous or who has started appropriate antibiotics for that infection. Although all toxicities of glucocorticoids are dose dependent, the long-standing assertion that doses below 10 mg to 15 mg do not increase risk of infection is contradicted by data published in the past 10 to 15 years, with the caveat that these patients were on long-term treatment.
►Dr. Swamy. The patient was started on prednisone 15 mg per day for 15 days. She returned to the clinic after 1 week of prednisone troutment and noted “significant improvement in fatigue, morning stiffness of shoulders, thighs, leg, back is better, leg cramps resolved, shooting pain in many joints resolved.” Further laboratory results were notable for a negative rheumatoid factor, negative antinuclear antibody, and a cyclic citrullinated peptide of 60. A presumptive diagnosis of rheumatoid arthritis (RA) was made and plaquenil 200 mg twice daily was started.
Dr. Monach, can you explain why RA comes up now on serology but was not considered initially? Why does this presentation fit RA, and was her response to treatment typical? How does this fit in with her previous diagnosis of fibromyalgia? Was that just an atypical, indolent presentation of RA?
►Dr. Monach. Though her presentation is atypical for RA, in elderly patients, RA can present with symptoms resembling polymyalgia rheumatica. The question is whether she had RA all along (in which case “elderly onset” would not apply) or had fibromyalgia and developed RA more recently. The response to empiric glucocorticoid therapy is helpful, since fibromyalgia should not improve with prednisone even in a patient with RA unless treatment of RA would allow better sleep and ability to exercise. Rheumatoid arthritis typically responds very well to prednisone in the 5-mg to 15-mg range.
►Dr. Swamy. Given the new diagnosis of an inflammatory arthritis requiring immunosuppression, bronchoscopy with BAL is performed to evaluate for the presence of MAC. These cultures were positive for MAC.
Dr. Fine, does the positive BAL culture indicate an active MAC infection?
►Dr. Fine. Yes, based on these updated data, the patient has an active MAC infection. Active infection is defined as symptoms or imaging consistent with the diagnosis, supporting microbiology data (either 2 sputum or 1 BAL sample growing MAC) and the exclusion of other causes. Previously, this patient grew MAC in just one expectorated sputum; this did not meet the microbiologic criteria. Now sputum has grown in the BAL sample; along with the CT imaging, this is enough to diagnosis active MAC infection.
Treatment for MAC must consider the details of each case. First, this is not an emergency; treatment decisions should be made with the rheumatologist to consider the planned immunosuppression. For example, we must consider potential drug interactions. A specific point should be made of the use of tumor necrosis factor (TNF)-α inhibition, which data indicate can reactivate TB and may inhibit mechanisms that restrain mycobacterial disease. Serious cases of MAC infection have been reported in the literature in the setting of TNF-α inhibition.5,6 Despite these concerns, there is not a contraindication to using these therapies from the perspective of the active MAC disease. All of these decisions will impact the need to commit the patient to MAC therapy.
►Dr. Swamy. Dr. Fine, what do you consider prior to initiating MAC therapy?
► Dr. Fine. The decision to pursue MAC therapy should not be taken lightly. Therapy often entails prolonged multidrug regimens, usually spanning more than a year, with frequent adverse effects. Outside of very specific cases, such as TNF-β inhibition, MAC is rarely a life-threatening disease, so the benefit may be limited. Treatment for MAC is certainly unlikely to be fruitful without a diligent and motivated patient able to handle the high and prolonged pill burden. Of note, it is also important to keep this patient up-to-date with influenza and pneumonia vaccination given her structural lung disease.
►Dr. Swamy. The decision is made to treat MAC with azithromycin, rifampin, and ethambutol. The disease is noted to be nonfibrocavitary. The patient underwent monthly liver function test monitoring and visual acuity testing, which were unremarkable. Dr. Fine, can you describe the phenotypes of nontuberculous mycobacterial (NTM) disease?
►Dr. Fine. There are 3 main phenotypes of NTM.3 First, we see the elderly man with preexisting lung disease—usually chronic obstructive pulmonary disease—with fibrocavitary and/or reticulonodular appearance. Second, we see the slim, elderly woman often without any preexisting lung disease presenting with focal bronchiectasis and nodular lesions in right middle lobe and lingula—the Lady Windermere syndrome. This eponym is derived from Oscar Wilde’s play “Lady Windermere’s Fan, a Play About a Good Woman,” and was first associated with this disease in 1992.7 At the time, it was thought that the voluntary suppression of cough led to poorly draining lung regions, vulnerable to engraftment by atypical mycobacteria. Infection with atypical mycobacteria are associated with this population; however, it is no longer thought to be due to the voluntary suppression of cough.7,8 Third, we do occasionally see atypical presentations, such as focal masses and solitary nodules.
►Dr. Swamy. At 1-year follow-up she successfully completed MAC therapy and noted ongoing control of rheumatoid symptoms.
1. Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome—a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2018;22(2):242-260.
2. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4:CD011279.
3. Aksamit TR, Philley JV, Griffith DE. Nontuberculous mycobacterial (NTM) lung disease: the top ten essentials. Respir Med. 2014;108(3):417-425.
4. Aucott JN. Glucocorticoids and infection. Endocrinol Metab Clin North Am. 1994;23(3):655-670.
5. Curtis JR, Yang S, Patkar NM, et al. Risk of hospitalized bacterial infections associated with biologic treatment among US veterans with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(7):990-997.
6. Lane MA, McDonald JR, Zeringue AL, et al. TNF-α antagonist use and risk of hospitalization for infection in a national cohort of veterans with rheumatoid arthritis. Medicine (Baltimore). 2011;90(2):139-145.
7. Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest. 1992;101(6):1605-1609.
8. Kasthoori JJ, Liam CK, Wastie ML. Lady Windermere syndrome: an inappropriate eponym for an increasingly important condition. Singapore Med J. 2008;49(2):e47-e49.
1. Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome—a systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2018;22(2):242-260.
2. Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;4:CD011279.
3. Aksamit TR, Philley JV, Griffith DE. Nontuberculous mycobacterial (NTM) lung disease: the top ten essentials. Respir Med. 2014;108(3):417-425.
4. Aucott JN. Glucocorticoids and infection. Endocrinol Metab Clin North Am. 1994;23(3):655-670.
5. Curtis JR, Yang S, Patkar NM, et al. Risk of hospitalized bacterial infections associated with biologic treatment among US veterans with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2014;66(7):990-997.
6. Lane MA, McDonald JR, Zeringue AL, et al. TNF-α antagonist use and risk of hospitalization for infection in a national cohort of veterans with rheumatoid arthritis. Medicine (Baltimore). 2011;90(2):139-145.
7. Reich JM, Johnson RE. Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest. 1992;101(6):1605-1609.
8. Kasthoori JJ, Liam CK, Wastie ML. Lady Windermere syndrome: an inappropriate eponym for an increasingly important condition. Singapore Med J. 2008;49(2):e47-e49.
OTP: Pipe Dream, Smoke Screen, or the Right Thing?
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at [email protected].
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at [email protected].
We live in a world of acronyms. OMG, GOAT, and the like are ubiquitous on social media and increasingly sprinkled into more traditional journalistic formats. But if you’re a PA, the most important acronym for at least the past two years has been OTP—optimal team practice.
In my February 2017 editorial, I opined on the related concept of full practice authority (FPA), discussing the hurdles the NP and PA professions face to achieve this goal (Clinician Reviews. 2017;27[2]:12-14). Both professions, now more than a half-century old, assert that they have demonstrated, through practice and research, a commitment to competent, quality health care. In recent years, these assertions have been increasingly centered around acquiring more autonomy and responsibility—what NPs refer to as the ability to practice to the fullest extent of their education and training. As a profession, the NPs have done an excellent job of breaking down unnecessary barriers to their practice.
PAs, however, continue to have challenges with this concept. To address this, a mere three months after my FPA editorial, the House of Delegates of the American Academy of PAs (AAPA) adopted OTP as a policy. The Academy says OTP is designed to increase access to care and help align the PA profession with modern societal health care needs.1
- Allow PAs to practice without a formal agreement with a particular physician
- Create separate majority-PA regulatory boards (or give authority to boards comprised of PAs and physicians who practice with PAs), and
- Allow PAs to be directly reimbursed by all public and private insurers. (PAs continue to be the only health care professionals who bill Medicare but are not entitled to direct reimbursement.)
These changes encourage PAs to practice to the full extent of their training and remove restrictions that currently obstruct delivery of care.1,2 Yet there are unintended consequences as the profession pursues this path.
The Physician Assistant Education Association (PAEA), while supporting most of the OTP policy, has raised concerns about changing curricula to reflect increased autonomy, which would require longer educational programs and incur higher costs for students.3 A significant part of PA education for the past half-century has been the social integration into the health care realm with physicians. There is also concern that changes to accommodate OTP might ultimately lead to a requirement for PAs to have a doctorate degree in order to practice—although not everyone sees that as a drawback!
Proponents of OTP, on the other hand, insist that times have changed and the profession must change with them—or at least, the rules governing the profession must be amended to reflect practical realities. AAPA leaders believe that physician oversight provisions are no longer necessary, and that PAs must acclimate to the changing health care marketplace to solidify the future of the profession and meet the needs of patients.
Continue to: Barriers to PA recruitment continue to...
Barriers to PA recruitment continue to exist as a result of statutory requirements. In today’s health care system, physicians are more likely to be employed by a large institution. Because of this, they may no longer see a financial benefit to entering into a formal agreement with a PA, which is currently required by statute for PAs to practice. Furthermore, as PAs and physicians increasingly practice in groups, the requirement for PAs to have an agreement with a specific physician is challenging to manage and places all providers involved at risk for disciplinary action for administrative infractions unrelated to patient care or outcomes.
Advocates for OTP also emphasize the perception that our NP colleagues are preferentially hired over PAs. In 22 states and the District of Columbia, NPs are allowed to practice without a collaborative agreement with a specific physician, anecdotally making them easier to hire.4 Even in states where NPs do not have FPA, the perception that hiring an NP is less burdensome than hiring a PA often exists. If accurate, these reports suggest PAs are at a disadvantage relative to NPs, resulting in lost opportunities for employment and advancement. (At least one study—based on a survey of members of the American College of Emergency Physicians council, who have direct experience in hiring NPs and PAs—demonstrated no differences in hiring preferences between the two professions. The same survey also revealed wide variability in supervisory requirements, however.5)
By recommending the elimination of the requirement for PAs to have an agreement with a specific physician in order to practice, AAPA is in effect broadening an evolution already occurring at the state level. In 2016, Michigan removed the supervisory requirement and repealed the stipulation of physician responsibility for PA-provided care; PAs in Michigan now practice with a “participating physician.” In 2017, New Mexico amended its Medical Practice Act to allow PAs who practice primary care to collaborate with a physician, while PAs who practice specialty care must be supervised by a physician.6 Illinois recently signed a 10-year extension of the state’s PA Practice Act that also better reflects the relationship between PAs and physicians, substituting “collaborating physician” for “supervising physician.”7 West Virginia has also adopted legislation referring to the physician/PA relationship as a “collaboration” (terminology Alaska has used since the 1980s).
In supporting the recent changes in Illinois, Dr. Nestor Ramirez, President of the Illinois State Medical Society, noted that “Patients are best served by physician-led teams of professionals practicing within the scope of their licensure, and physicians work collaboratively with PAs and other allied healthcare professionals to ensure that the care provided is of the highest quality.” Changing the terminology to collaboration, he added, simply “brings the language of the Physician Assistant Practice Act in line with that of other licensure acts.”7
Perhaps the larger challenge in implementing OTP will be achieving this level of support from all our physician colleagues. In a small survey on this topic conducted by researchers at the Hofstra Northwell School of Graduate Nursing and Physician Assistant Studies, nearly 80% of physician respondents had no previous knowledge of OTP. The majority (62.8%) agreed with the notion that PAs are committed to team practice (first component of OTP); however, less than half of the respondents (47.3%) said they would support OTP policy. The authors concluded that OTP advocacy efforts should target physician awareness and support.8
Continue to: One thing is clear...
One thing is clear: the OTP train has left the proverbial station. My concern is: Are we on the right track, with the right strategic plan, and with the right people on board? In my opinion, we need to turn to our professional organizational leaders and ask them to carefully evaluate all the unintended consequences of OTP and outline a carefully thought-out plan for the next decade of PA practice. While state efforts are thus far focused on amending supervisory requirements, I think we would be best served focusing on the development of PA-specific regulatory boards (currently, only five states have one). In the long term, this would make the profession responsible for its own practice regulations.
There is no doubt that we must find appropriate responses to the changing practice environment. As we work toward professional solutions, we must take into consideration the needs of all stakeholders, including our physician colleagues, PA educators, PA regulators, current and future students, and patients. How do we best partner with them—and with our NP colleagues—for the sake of continuity of patient care? Send your ideas to me at [email protected].
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.
1. AAPA. Frequently asked questions: optimal team practice. www.aapa.org/wp-content/uploads/2018/01/Core-FAQ.pdf. Accessed July 12, 2018.
2. AAPA. Guidelines for state regulation of PAs. www.aapa.org/download/35030/. Accessed July 12, 2018.
3. Physician Assistant Education Association. Optimal team practice: the right prescription for all PAs? http://paeaonline.org/wp-content/uploads/2017/05/PAEA-OTP-Task-Force-Report_2017_2.pdf. Accessed July 12, 2018.
4. Japsen B. Nurse practitioners boost presence by 43% in rural America. www.forbes.com/sites/brucejapsen/2018/06/05/nurse-practitioners-boost-presence-by-43-in-rural-america/#39542d52648b. Accessed July 12, 2018.
5. Phillips AW, Klauer KM, Kessler CS. Emergency physician evaluation of PA and NP practice patterns. JAAPA. 2018;31(5):38-43.
6. AAPA. New Mexico PAs celebrate the enactment of collaboration bill. April 18, 2017. www.aapa.org/news-central/2017/04/new-mexico-pas-celebrate-enactment-collaboration-bill/. Accessed July 12, 2018.
7. Japsen B. States lift more hurdles to physician assistants. September 8, 2017. Forbes. www.forbes.com/sites/brucejapsen/2017/09/08/states-lift-more-hurdles-to-physician-assistants/#57ec3e822eff. Accessed July 12, 2018.
8. DeForte L, Doerler A, Oliphant A, et al. Assessing physicians’ opinions regarding optimal team practice. Presented at: AAPA 2018 annual conference; May 19-23, 2018; New Orleans, LA. Poster 115.
Childhood Neuromuscular Disease as a Metaphor for the Scientific Advances in Child Neurology of the Last Quarter Century
John B. Bodensteiner, MD
Dr. Bodensteiner is Director of the American Board of Psychiatry and Neurology, Founding Editor and Senior Associate Editor of Seminars in Pediatric Neurology, and Senior Associate Editor of the Journal of Child Neurology.
The impetus for this article is the celebration of 25 years of publication of Neurology Reviews. Child neurology has advanced so much in these years that it is hardly recognizable from the previous state of our understanding. Many components of the discipline include, but are not limited to, epilepsy, headache, demyelinating diseases, autoimmune diseases, neoplastic, neonatal, neuromuscular disease, and developmental conditions. My interest has been related to the neuromuscular diseases of childhood. Thus, I have chosen to describe some of the ways the advances in basic medical science and our understanding of the genetic and molecular mechanisms of disease have altered the way we think about these conditions. For the first time, this knowledge has allowed us to identify targets and techniques for effective intervention and disease modification.
Myotonic Muscular Dystrophy
One example of how the advancement in the discipline of genetics has changed our understanding of disease would be myotonic muscular dystrophy (MyoD1). When I started seeing patients in the mid 1960s, MyoD1, particularly as seen in children, was recognized as an example of autosomal dominant inheritance. The tendency for subsequent generations to be more severely affected than their parents is a phenomenon known as anticipation. Anticipation was recognized, though not explained, with the understanding of the genetic mechanisms of the time. The fact that when the disease affected an infant or newborn it was almost always inherited from the mother was also well established, though the reason for this was also not understood. Actually, during the late 1970s and early 1980s the existence of the phenomenon of anticipation was widely questioned and some publications proposed that anticipation was just an artifact of observation due to the fact that we (medical clinicians) were getting better and thus identifying the disease earlier than in past years. The recognition of the importance of repeated segments of DNA in the pathogenesis of human disease and the subsequent development of the technology to study the phenomenon allowed recognition of this previously unappreciated mechanism of genetic disease causation. This new genetic mechanism explained how anticipation could occur and confirmed it as a real phenomenon. Expanded numbers of tandem repeats probably allowed the explanation of the difference in gene transmission related to the parental gender as well.1
Genetic Insights
Advancements in the understanding of genetic mechanisms of disease have made it possible to begin to identify the molecular mechanisms operating in many previously incomprehensible diseases. The development of laboratory techniques necessary for the identification of these genetic abnormalities has brought the recognition of these disease mechanisms into clinical practice. Twenty-five years ago, the ability to identify alterations in DNA sequences, the presence of deletions/duplications and expansion of trinucleotide repeats, as well as the determination (and recognition of the significance) of gene copy number, was not available to the clinician. This advancement in genetic understanding has, in turn, allowed the identification of therapeutic targets in the hope of being able to moderate or eliminate the consequence of the defective gene.
Spinal Muscular Atrophy
In the last few years, the use of relatively small molecules such as oligonucleotides to alter the transcription of mutated RNA to produce a functioning protein has been developed. Because they are small molecules, they can be delivered with relative ease to the desired site. This technology has been applied to the treatment of spinal muscular atrophy (SMA) with considerable success.
Survival motor neuron gene product is essential for the health of the anterior horn cells of the spinal cord of the central nervous system. In the human genome there are two copies of the survival motor neuron gene, labeled SMN1 and SMN2. SMN1 normally produces a functional protein that is stable and necessary for the anterior horn survival. All patients with SMA have mutations in SMN1 that result in the gene being inactive. The protein product of SMN2 is usually truncated and not very stable, though it has some function. The severity of the resulting disease is influenced by the number of copies of the SMN2 gene present, and thus the available amount of partially functional SMN2 product. The oligonucleotide, in this case delivered via lumbar puncture, serves to alter the splicing of the protein product from SMN2, allowing the production of the more effective and stable protein with properties more similar to the SMN1 protein, thus ameliorating the effect of the SMN1 mutation. The patient, however, requires the administration of the therapeutic oligonucleotide indefinitely.
Gene Editing
The Gold Ring of therapeutic intervention, being able to actually correct the gene defect in any given disease, is still a goal of medical science. For the first time, this is a realistic aspiration due to the identification, development, and application of the gene editing tool Cas9 and CRISPR-Cas9 techniques.2 This new technology allows the production of a custom piece of DNA (cassette) that can repair the defective gene if incorporated into the DNA sequence of the host. The techniques necessary to introduce the therapeutic cassette to the affected cell and encourage the incorporation of the new material into the DNA have largely been developed already. The hurdle has always been the difficulty producing the therapeutic cassette for the given defect. The application of the CRISPR-Cas9 technology offers the promise of being able to produce a custom cassette specific for the given mutation, and thus potentially correcting the mutation involved in a wide variety of diseases.
The last quarter century has seen the expansion of the genetic techniques to allow the recognition and diagnosis of diseases that had resisted definitive diagnosis up to this time. These techniques have also led to the uncovering of disease mechanisms previously opaque to our understanding. The next quarter century promises to produce an explosion of therapeutic possibilities on a scale previously unimaginable. Despite the considerable initial expense of these new therapies, I believe they will be of incalculable value going forward.
References
1. de Koning AP, Gu W, Castoe TA, et al. Repetitive elements may comprise over two-thirds of the human genome. PLoS Genet. 2011;7(12):e1002384.
2. Adli M. The CRISPR tool kit for genome editing and beyond. Nat Commun. 2018;9(1):1911.
John B. Bodensteiner, MD
Dr. Bodensteiner is Director of the American Board of Psychiatry and Neurology, Founding Editor and Senior Associate Editor of Seminars in Pediatric Neurology, and Senior Associate Editor of the Journal of Child Neurology.
The impetus for this article is the celebration of 25 years of publication of Neurology Reviews. Child neurology has advanced so much in these years that it is hardly recognizable from the previous state of our understanding. Many components of the discipline include, but are not limited to, epilepsy, headache, demyelinating diseases, autoimmune diseases, neoplastic, neonatal, neuromuscular disease, and developmental conditions. My interest has been related to the neuromuscular diseases of childhood. Thus, I have chosen to describe some of the ways the advances in basic medical science and our understanding of the genetic and molecular mechanisms of disease have altered the way we think about these conditions. For the first time, this knowledge has allowed us to identify targets and techniques for effective intervention and disease modification.
Myotonic Muscular Dystrophy
One example of how the advancement in the discipline of genetics has changed our understanding of disease would be myotonic muscular dystrophy (MyoD1). When I started seeing patients in the mid 1960s, MyoD1, particularly as seen in children, was recognized as an example of autosomal dominant inheritance. The tendency for subsequent generations to be more severely affected than their parents is a phenomenon known as anticipation. Anticipation was recognized, though not explained, with the understanding of the genetic mechanisms of the time. The fact that when the disease affected an infant or newborn it was almost always inherited from the mother was also well established, though the reason for this was also not understood. Actually, during the late 1970s and early 1980s the existence of the phenomenon of anticipation was widely questioned and some publications proposed that anticipation was just an artifact of observation due to the fact that we (medical clinicians) were getting better and thus identifying the disease earlier than in past years. The recognition of the importance of repeated segments of DNA in the pathogenesis of human disease and the subsequent development of the technology to study the phenomenon allowed recognition of this previously unappreciated mechanism of genetic disease causation. This new genetic mechanism explained how anticipation could occur and confirmed it as a real phenomenon. Expanded numbers of tandem repeats probably allowed the explanation of the difference in gene transmission related to the parental gender as well.1
Genetic Insights
Advancements in the understanding of genetic mechanisms of disease have made it possible to begin to identify the molecular mechanisms operating in many previously incomprehensible diseases. The development of laboratory techniques necessary for the identification of these genetic abnormalities has brought the recognition of these disease mechanisms into clinical practice. Twenty-five years ago, the ability to identify alterations in DNA sequences, the presence of deletions/duplications and expansion of trinucleotide repeats, as well as the determination (and recognition of the significance) of gene copy number, was not available to the clinician. This advancement in genetic understanding has, in turn, allowed the identification of therapeutic targets in the hope of being able to moderate or eliminate the consequence of the defective gene.
Spinal Muscular Atrophy
In the last few years, the use of relatively small molecules such as oligonucleotides to alter the transcription of mutated RNA to produce a functioning protein has been developed. Because they are small molecules, they can be delivered with relative ease to the desired site. This technology has been applied to the treatment of spinal muscular atrophy (SMA) with considerable success.
Survival motor neuron gene product is essential for the health of the anterior horn cells of the spinal cord of the central nervous system. In the human genome there are two copies of the survival motor neuron gene, labeled SMN1 and SMN2. SMN1 normally produces a functional protein that is stable and necessary for the anterior horn survival. All patients with SMA have mutations in SMN1 that result in the gene being inactive. The protein product of SMN2 is usually truncated and not very stable, though it has some function. The severity of the resulting disease is influenced by the number of copies of the SMN2 gene present, and thus the available amount of partially functional SMN2 product. The oligonucleotide, in this case delivered via lumbar puncture, serves to alter the splicing of the protein product from SMN2, allowing the production of the more effective and stable protein with properties more similar to the SMN1 protein, thus ameliorating the effect of the SMN1 mutation. The patient, however, requires the administration of the therapeutic oligonucleotide indefinitely.
Gene Editing
The Gold Ring of therapeutic intervention, being able to actually correct the gene defect in any given disease, is still a goal of medical science. For the first time, this is a realistic aspiration due to the identification, development, and application of the gene editing tool Cas9 and CRISPR-Cas9 techniques.2 This new technology allows the production of a custom piece of DNA (cassette) that can repair the defective gene if incorporated into the DNA sequence of the host. The techniques necessary to introduce the therapeutic cassette to the affected cell and encourage the incorporation of the new material into the DNA have largely been developed already. The hurdle has always been the difficulty producing the therapeutic cassette for the given defect. The application of the CRISPR-Cas9 technology offers the promise of being able to produce a custom cassette specific for the given mutation, and thus potentially correcting the mutation involved in a wide variety of diseases.
The last quarter century has seen the expansion of the genetic techniques to allow the recognition and diagnosis of diseases that had resisted definitive diagnosis up to this time. These techniques have also led to the uncovering of disease mechanisms previously opaque to our understanding. The next quarter century promises to produce an explosion of therapeutic possibilities on a scale previously unimaginable. Despite the considerable initial expense of these new therapies, I believe they will be of incalculable value going forward.
References
1. de Koning AP, Gu W, Castoe TA, et al. Repetitive elements may comprise over two-thirds of the human genome. PLoS Genet. 2011;7(12):e1002384.
2. Adli M. The CRISPR tool kit for genome editing and beyond. Nat Commun. 2018;9(1):1911.
John B. Bodensteiner, MD
Dr. Bodensteiner is Director of the American Board of Psychiatry and Neurology, Founding Editor and Senior Associate Editor of Seminars in Pediatric Neurology, and Senior Associate Editor of the Journal of Child Neurology.
The impetus for this article is the celebration of 25 years of publication of Neurology Reviews. Child neurology has advanced so much in these years that it is hardly recognizable from the previous state of our understanding. Many components of the discipline include, but are not limited to, epilepsy, headache, demyelinating diseases, autoimmune diseases, neoplastic, neonatal, neuromuscular disease, and developmental conditions. My interest has been related to the neuromuscular diseases of childhood. Thus, I have chosen to describe some of the ways the advances in basic medical science and our understanding of the genetic and molecular mechanisms of disease have altered the way we think about these conditions. For the first time, this knowledge has allowed us to identify targets and techniques for effective intervention and disease modification.
Myotonic Muscular Dystrophy
One example of how the advancement in the discipline of genetics has changed our understanding of disease would be myotonic muscular dystrophy (MyoD1). When I started seeing patients in the mid 1960s, MyoD1, particularly as seen in children, was recognized as an example of autosomal dominant inheritance. The tendency for subsequent generations to be more severely affected than their parents is a phenomenon known as anticipation. Anticipation was recognized, though not explained, with the understanding of the genetic mechanisms of the time. The fact that when the disease affected an infant or newborn it was almost always inherited from the mother was also well established, though the reason for this was also not understood. Actually, during the late 1970s and early 1980s the existence of the phenomenon of anticipation was widely questioned and some publications proposed that anticipation was just an artifact of observation due to the fact that we (medical clinicians) were getting better and thus identifying the disease earlier than in past years. The recognition of the importance of repeated segments of DNA in the pathogenesis of human disease and the subsequent development of the technology to study the phenomenon allowed recognition of this previously unappreciated mechanism of genetic disease causation. This new genetic mechanism explained how anticipation could occur and confirmed it as a real phenomenon. Expanded numbers of tandem repeats probably allowed the explanation of the difference in gene transmission related to the parental gender as well.1
Genetic Insights
Advancements in the understanding of genetic mechanisms of disease have made it possible to begin to identify the molecular mechanisms operating in many previously incomprehensible diseases. The development of laboratory techniques necessary for the identification of these genetic abnormalities has brought the recognition of these disease mechanisms into clinical practice. Twenty-five years ago, the ability to identify alterations in DNA sequences, the presence of deletions/duplications and expansion of trinucleotide repeats, as well as the determination (and recognition of the significance) of gene copy number, was not available to the clinician. This advancement in genetic understanding has, in turn, allowed the identification of therapeutic targets in the hope of being able to moderate or eliminate the consequence of the defective gene.
Spinal Muscular Atrophy
In the last few years, the use of relatively small molecules such as oligonucleotides to alter the transcription of mutated RNA to produce a functioning protein has been developed. Because they are small molecules, they can be delivered with relative ease to the desired site. This technology has been applied to the treatment of spinal muscular atrophy (SMA) with considerable success.
Survival motor neuron gene product is essential for the health of the anterior horn cells of the spinal cord of the central nervous system. In the human genome there are two copies of the survival motor neuron gene, labeled SMN1 and SMN2. SMN1 normally produces a functional protein that is stable and necessary for the anterior horn survival. All patients with SMA have mutations in SMN1 that result in the gene being inactive. The protein product of SMN2 is usually truncated and not very stable, though it has some function. The severity of the resulting disease is influenced by the number of copies of the SMN2 gene present, and thus the available amount of partially functional SMN2 product. The oligonucleotide, in this case delivered via lumbar puncture, serves to alter the splicing of the protein product from SMN2, allowing the production of the more effective and stable protein with properties more similar to the SMN1 protein, thus ameliorating the effect of the SMN1 mutation. The patient, however, requires the administration of the therapeutic oligonucleotide indefinitely.
Gene Editing
The Gold Ring of therapeutic intervention, being able to actually correct the gene defect in any given disease, is still a goal of medical science. For the first time, this is a realistic aspiration due to the identification, development, and application of the gene editing tool Cas9 and CRISPR-Cas9 techniques.2 This new technology allows the production of a custom piece of DNA (cassette) that can repair the defective gene if incorporated into the DNA sequence of the host. The techniques necessary to introduce the therapeutic cassette to the affected cell and encourage the incorporation of the new material into the DNA have largely been developed already. The hurdle has always been the difficulty producing the therapeutic cassette for the given defect. The application of the CRISPR-Cas9 technology offers the promise of being able to produce a custom cassette specific for the given mutation, and thus potentially correcting the mutation involved in a wide variety of diseases.
The last quarter century has seen the expansion of the genetic techniques to allow the recognition and diagnosis of diseases that had resisted definitive diagnosis up to this time. These techniques have also led to the uncovering of disease mechanisms previously opaque to our understanding. The next quarter century promises to produce an explosion of therapeutic possibilities on a scale previously unimaginable. Despite the considerable initial expense of these new therapies, I believe they will be of incalculable value going forward.
References
1. de Koning AP, Gu W, Castoe TA, et al. Repetitive elements may comprise over two-thirds of the human genome. PLoS Genet. 2011;7(12):e1002384.
2. Adli M. The CRISPR tool kit for genome editing and beyond. Nat Commun. 2018;9(1):1911.
Melasma Treatment With Oral Tranexamic Acid and a Novel Adjuvant Topical Therapy
To the Editor:
I read with interest the informative article by Sheu1 published online in Cutis in February 2018, which succinctly described the pharmacologic characteristics of tranexamic acid, a synthetic lysine derivative, and its mechanism of action in the management of melasma by mitigating UV radiation-induced melanogenesis and neovascularization by inhibiting plasminogen activation. Additionally, the author summarized a study in which oral tranexamic acid was used to successfully treat melasma patients. After 4 months of treatment, 90% of 561 patients treated at a single center in Singapore demonstrated improvement in melasma severity.2 Sheu1 also discussed daily oral doses of tranexamic acid (500-1500 mg) that demonstrated improvement in melasma patients and reviewed potential adverse events (eg, abdominal pain and bloating, deep venous thrombosis, pulmonary embolism) for which patients should be screened and counseled prior to initiating treatment.
Recently, another study showed oral tranexamic acid to be an effective treatment in women with moderate to severe melasma. An important observation by the investigators was that once the initial phase of their study--250 mg of oral tranexamic acid twice daily and sunscreen applied to the face each morning and every 2 hours during daylight hours for 3 months--concluded and a second phase during which all participants only applied sunscreen for an additional 3 months, those with severe melasma lost most of their improvement.3 An adjuvant topical treatment, such as tranexamic acid or an inhibitor of tyrosinase (hydroquinone), might improve the results; however, initiating therapy with a topical agent whose mode of action is directed toward other melasma etiologic factors, such as the increased expression of estrogen receptors and vascular endothelial growth factor in affected skin, might be more beneficial.4,5
I recently proposed a novel approach for melasma management that would be appropriate as an adjuvant topical therapy for patients concurrently being treated with oral tranexamic acid.6 The therapeutic intervention utilizes active agents that specifically affect etiologic factors in the pathogenesis of melasma--estrogen and angiogenesis--that previously have not been targeted topically. Indeed, the topical agent contains an antiestrogen--either a selective estrogen receptor modulator (eg, tamoxifen, raloxifene), aromatase inhibitor (eg, anastrozole, letrozole, exemestane), or a selective estrogen receptor degrader (eg, fulvestrant)--and a vascular endothelial growth factor inhibitor (eg, bevacizumab).6
In conclusion, the therapeutic armamentarium for managing patients with melasma includes topical agents, oral therapies, and physical modalities. Optimizing the approach to treating melasma patients should incorporate therapies that are specifically directed toward various etiologic factors of the condition. The concurrent use of a topical agent that contains an antiestrogen and an inhibitor of vascular endothelial growth factor in women with melasma who are being treated with oral tranexamic acid warrants further investigation to assess not only for enhanced but also sustained reduction in facial skin pigmentation.
- Sheu SL. Treatment of melasma using tranexamic acid: what's known and what's next. Cutis. 2018;101:E7-E8.
- Lee HC, Thng TG, Goh CL. Oral tranexamic acid (TA) in the treatment of melasma: a retrospective study. J Am Acad Dermatol. 2016;75:385-392.
- Del Rosaria E, Forez-Pollack S, Zapata L Jr, et al. Randomized, placebo-controlled, double-blind study of oral tranexamic acid in the treatment of moderate-to-severe melasma. J Am Acad Dermatol. 2018;78:363-369.
- Jang YH, Lee JY, Kang HY, et al. Oestrogen and progesterone receptor expression in melasma: an immunohistochemical analysis. J Eur Acad Dermatol Venereol. 2010;24:1312-1316.
- Kim EH, Kim YC, Lee ES, et al. The vascular characteristics of melasma. J Dermatol Sci. 2007;46:111-116.
- Cohen PR. Melasma treatment: a novel approach using a topical agent that contains an anti-estrogen and a vascular endothelial growth factor inhibitor [published online February 3, 2017]. Med Hypotheses. 2017;101:1-5.
To the Editor:
I read with interest the informative article by Sheu1 published online in Cutis in February 2018, which succinctly described the pharmacologic characteristics of tranexamic acid, a synthetic lysine derivative, and its mechanism of action in the management of melasma by mitigating UV radiation-induced melanogenesis and neovascularization by inhibiting plasminogen activation. Additionally, the author summarized a study in which oral tranexamic acid was used to successfully treat melasma patients. After 4 months of treatment, 90% of 561 patients treated at a single center in Singapore demonstrated improvement in melasma severity.2 Sheu1 also discussed daily oral doses of tranexamic acid (500-1500 mg) that demonstrated improvement in melasma patients and reviewed potential adverse events (eg, abdominal pain and bloating, deep venous thrombosis, pulmonary embolism) for which patients should be screened and counseled prior to initiating treatment.
Recently, another study showed oral tranexamic acid to be an effective treatment in women with moderate to severe melasma. An important observation by the investigators was that once the initial phase of their study--250 mg of oral tranexamic acid twice daily and sunscreen applied to the face each morning and every 2 hours during daylight hours for 3 months--concluded and a second phase during which all participants only applied sunscreen for an additional 3 months, those with severe melasma lost most of their improvement.3 An adjuvant topical treatment, such as tranexamic acid or an inhibitor of tyrosinase (hydroquinone), might improve the results; however, initiating therapy with a topical agent whose mode of action is directed toward other melasma etiologic factors, such as the increased expression of estrogen receptors and vascular endothelial growth factor in affected skin, might be more beneficial.4,5
I recently proposed a novel approach for melasma management that would be appropriate as an adjuvant topical therapy for patients concurrently being treated with oral tranexamic acid.6 The therapeutic intervention utilizes active agents that specifically affect etiologic factors in the pathogenesis of melasma--estrogen and angiogenesis--that previously have not been targeted topically. Indeed, the topical agent contains an antiestrogen--either a selective estrogen receptor modulator (eg, tamoxifen, raloxifene), aromatase inhibitor (eg, anastrozole, letrozole, exemestane), or a selective estrogen receptor degrader (eg, fulvestrant)--and a vascular endothelial growth factor inhibitor (eg, bevacizumab).6
In conclusion, the therapeutic armamentarium for managing patients with melasma includes topical agents, oral therapies, and physical modalities. Optimizing the approach to treating melasma patients should incorporate therapies that are specifically directed toward various etiologic factors of the condition. The concurrent use of a topical agent that contains an antiestrogen and an inhibitor of vascular endothelial growth factor in women with melasma who are being treated with oral tranexamic acid warrants further investigation to assess not only for enhanced but also sustained reduction in facial skin pigmentation.
To the Editor:
I read with interest the informative article by Sheu1 published online in Cutis in February 2018, which succinctly described the pharmacologic characteristics of tranexamic acid, a synthetic lysine derivative, and its mechanism of action in the management of melasma by mitigating UV radiation-induced melanogenesis and neovascularization by inhibiting plasminogen activation. Additionally, the author summarized a study in which oral tranexamic acid was used to successfully treat melasma patients. After 4 months of treatment, 90% of 561 patients treated at a single center in Singapore demonstrated improvement in melasma severity.2 Sheu1 also discussed daily oral doses of tranexamic acid (500-1500 mg) that demonstrated improvement in melasma patients and reviewed potential adverse events (eg, abdominal pain and bloating, deep venous thrombosis, pulmonary embolism) for which patients should be screened and counseled prior to initiating treatment.
Recently, another study showed oral tranexamic acid to be an effective treatment in women with moderate to severe melasma. An important observation by the investigators was that once the initial phase of their study--250 mg of oral tranexamic acid twice daily and sunscreen applied to the face each morning and every 2 hours during daylight hours for 3 months--concluded and a second phase during which all participants only applied sunscreen for an additional 3 months, those with severe melasma lost most of their improvement.3 An adjuvant topical treatment, such as tranexamic acid or an inhibitor of tyrosinase (hydroquinone), might improve the results; however, initiating therapy with a topical agent whose mode of action is directed toward other melasma etiologic factors, such as the increased expression of estrogen receptors and vascular endothelial growth factor in affected skin, might be more beneficial.4,5
I recently proposed a novel approach for melasma management that would be appropriate as an adjuvant topical therapy for patients concurrently being treated with oral tranexamic acid.6 The therapeutic intervention utilizes active agents that specifically affect etiologic factors in the pathogenesis of melasma--estrogen and angiogenesis--that previously have not been targeted topically. Indeed, the topical agent contains an antiestrogen--either a selective estrogen receptor modulator (eg, tamoxifen, raloxifene), aromatase inhibitor (eg, anastrozole, letrozole, exemestane), or a selective estrogen receptor degrader (eg, fulvestrant)--and a vascular endothelial growth factor inhibitor (eg, bevacizumab).6
In conclusion, the therapeutic armamentarium for managing patients with melasma includes topical agents, oral therapies, and physical modalities. Optimizing the approach to treating melasma patients should incorporate therapies that are specifically directed toward various etiologic factors of the condition. The concurrent use of a topical agent that contains an antiestrogen and an inhibitor of vascular endothelial growth factor in women with melasma who are being treated with oral tranexamic acid warrants further investigation to assess not only for enhanced but also sustained reduction in facial skin pigmentation.
- Sheu SL. Treatment of melasma using tranexamic acid: what's known and what's next. Cutis. 2018;101:E7-E8.
- Lee HC, Thng TG, Goh CL. Oral tranexamic acid (TA) in the treatment of melasma: a retrospective study. J Am Acad Dermatol. 2016;75:385-392.
- Del Rosaria E, Forez-Pollack S, Zapata L Jr, et al. Randomized, placebo-controlled, double-blind study of oral tranexamic acid in the treatment of moderate-to-severe melasma. J Am Acad Dermatol. 2018;78:363-369.
- Jang YH, Lee JY, Kang HY, et al. Oestrogen and progesterone receptor expression in melasma: an immunohistochemical analysis. J Eur Acad Dermatol Venereol. 2010;24:1312-1316.
- Kim EH, Kim YC, Lee ES, et al. The vascular characteristics of melasma. J Dermatol Sci. 2007;46:111-116.
- Cohen PR. Melasma treatment: a novel approach using a topical agent that contains an anti-estrogen and a vascular endothelial growth factor inhibitor [published online February 3, 2017]. Med Hypotheses. 2017;101:1-5.
- Sheu SL. Treatment of melasma using tranexamic acid: what's known and what's next. Cutis. 2018;101:E7-E8.
- Lee HC, Thng TG, Goh CL. Oral tranexamic acid (TA) in the treatment of melasma: a retrospective study. J Am Acad Dermatol. 2016;75:385-392.
- Del Rosaria E, Forez-Pollack S, Zapata L Jr, et al. Randomized, placebo-controlled, double-blind study of oral tranexamic acid in the treatment of moderate-to-severe melasma. J Am Acad Dermatol. 2018;78:363-369.
- Jang YH, Lee JY, Kang HY, et al. Oestrogen and progesterone receptor expression in melasma: an immunohistochemical analysis. J Eur Acad Dermatol Venereol. 2010;24:1312-1316.
- Kim EH, Kim YC, Lee ES, et al. The vascular characteristics of melasma. J Dermatol Sci. 2007;46:111-116.
- Cohen PR. Melasma treatment: a novel approach using a topical agent that contains an anti-estrogen and a vascular endothelial growth factor inhibitor [published online February 3, 2017]. Med Hypotheses. 2017;101:1-5.
Electronic Medical Records in Dermatology: The Good, the Bad, and the Ugly
The American Recovery and Reinvestment Act of 2009 introduced the Health Information Technology for Economic and Clinical Health (HITECH) Act and allocated $19.2 billion to promote the implementation of an electronic medical record (EMR) by hospitals as well as physicians in private practices.1 The EMR stores longitudinal health information and constructs a comprehensive picture of a patient's medical history.2,3 Following its debut, the US Department of Health & Human Services set forth meaningful use (MU) criteria,1 which aimed to increase quality of care, safety, and efficiency. Meaningful use criteria also sought to decrease health disparities; improve coordination of care; engage patients in their care; refine population and public health measures; and finally ensure accessibility, privacy, and security of patient data.1,2
The EMR offers potential gains at multiple levels of the patient-physician-public health hierarchy: a decrease in medical errors and duplicate services, timely access to test results and records, timely notification of patients in need for preventive services, and preservation of medical records in the event of an environmental disaster.1-3 Furthermore, physicians can take advantage of informational reciprocity with other providers, gain remote access to medical records, be reminded of need for service, e-prescribe, monitor for drug interactions, and utilize clinical information for research purposes.1,3 Lastly, public health organizations can use EMRs to improve outcomes by employing surveillance measures and creating patient registries that serve to protect the society at large.1
Although it seems that the broad-scale implementation of EMRs will undoubtedly enhance the quality of patient care in the years to come, many obstacles must be overcome to reach this potential. Certification of EMR systems and implementation of confidentiality measures that are compatible with the Health Insurance Portability and Accountability Act are the forerunning concerns, and the interconnectivity of EMR systems becomes more important as MU enters its later stages (eg, increased electronic transmission of patient data during phases of care, reliance on e-prescribing, population-level analysis of patient data to improve health outcomes). Additionally, the cost to implement and maintain an EMR deters many physicians in smaller practices from shouldering the charges, as they do not necessarily see increased productivity with this technology.2 Last but not least, unintended consequences of EMR implementation can involve the dangers of upcoding and overdocumentation.1
Dermatology is a visually dominant field serving a high volume of patients that require both medical and surgical care. These factors do not preclude the implementation of EMRs in our specialty but rather necessitate the utilization of a system specifically designed to cater to the needs of specialists in dermatology. This editorial will address some fundamental considerations in implementing an EMR in dermatology; discuss what platforms and patient interfaces are most practical; reiterate the importance of interoperability; and highlight the implications of this powerful tool in education, research, training, and monitoring quality of care.
Implementation and Specific Considerations in Dermatology
One of the biggest areas of concern in adopting an EMR is the associated financial burden.2-5 Although government incentives of MU cover a part of the initial cost of purchasing an EMR, expert maintenance costs, changes in workflow dynamics, and a steep learning curve can translate into lost productivity and revenue, discouraging many dermatologists from implementing an EMR.3,5 Furthermore, physicians who are nearing the end of their careers may not realize the longer-term benefits of implementing an EMR and therefore may decline to do so despite the disincentives of lower Medicare reimbursements.2 In fact, when juxtaposing the upfront cost of implementing an EMR against the expected increase in revenue after its implementation, there are general concerns that there will be a net loss on the part of the provider, which is a barrier to adoption of EMRs.3
Beyond the cost-benefit analysis, dermatologists often report multiple lesions in different anatomic sites or identify multiple biopsy sites that have been conveniently recorded on body templates included in their paper-based examination forms. Converting that information into words to be entered into an EMR can be excruciatingly time consuming and not easily comprehensible upon follow-up visits with the patient, which again results in decreased efficiency and productivity.4 Therefore, selecting a dermatology-compatible EMR that aims to make this transition easier is of utmost importance. One developer introduced an EMR with a touch interface containing a human body in all its facets that can be rotated, zoomed, and marked multiple times for accurate and convenient recording of lesions and intended procedure sites. This system automatically produces codes for examinations and procedures; facilitates e-prescription and ordering of laboratory results; prints pathology requests and consent forms; and includes information for patient education regarding their care. For example, the physical examination section of an H&P (history and physical examination) can be generated with a few taps on the screen, translating into increased efficiency and productivity.
The visual nature of dermatology demands the use of images, and as such, photographs have become integral in the diagnosis and follow-up of dermatology patients. Digital and dermatoscopic images not only help to eliminate unnecessary biopsies but also can promote early detection and management of malignancies.6 Thus, the capability to link photographs to a patient's medical record using an EMR is an invaluable gain. However, employing this feature in clinical practice has ethical implications that must be addressed, given that taking photographs can evoke an avoidable fear in patients regarding unlawful dissemination or unnecessary exposure of these images to physicians who do not need to access them.6 Thus, guidelines must be set for uploading, de-identifying, and annotating patient photographs, and only physicians involved in the care of the patient should be allocated access.4,6
EMR Platforms
When computers were first introduced into examination rooms, many physicians were reluctant, as computers were thought to disconnect physicians from patients, arousing a sense of remoteness and further depersonalizing the encounter as physicians spent more time typing and less time making meaningful eye contact with patients.5 The practice of dermatology requires patient-centered communication that serves to enhance the quality of care while at the same time allowing physicians to fulfill professional competencies and reduce medical errors, which may ultimately translate into patient satisfaction.7 In fact, when the patient-physician relationship is interrupted, patients are more likely to pursue legal action in the wake of a bad treatment outcome.5
Employing a tablet-friendly EMR can help circumvent (or at least minimize) this problem by providing the physician with a light, user-friendly device that eliminates the need for laptops or desktop computers.4 Going one step further, the utilization of tablets eliminates the need for accessory digital cameras, as most tablets come with built-in high-resolution cameras for capturing clinical photographs and immediately linking them to the patient's medical record. Lastly, tablet technology allows physicians to access consent forms while in the examination room with the patient to more readily obtain a signature for procedural or research consent.4,8
Interoperability, MU, and Quality of Care
The real goal in nationwide implementation of EMR technology is to accomplish MU criteria. Different EMRs should not only allow data to be imported and exported but ideally should be compatible and interoperable with one another.2 The myriad of different EMR platforms available impedes maximal functionality as MU moves into its final stage. For example, if an academic dermatology program in the setting of a larger hospital is required to use the generic hospital EMR, the dermatologist's specific needs may not be effectively met; on the other hand, if a dermatology-specific EMR is implemented, access to the hospital's larger database of patient information may be sacrificed. Optimal EMR systems should be designed to allow specificity for a given specialty while being able to receive and integrate laboratory values, dermatopathology and radiology results, and notes from consultations by other physicians. Such integration may reduce duplicate services, increase patient satisfaction, and fulfill MU criteria. In fact, the fear of many physicians, especially those in a field such as dermatology, are the unwanted costs that come with implementation of an EMR system that will soon become impractical due to compatibility issues.2 As a result, until a system that can meet the needs of multiple specialties is developed, dermatologists and other physicians upgrading to an EMR should consider implementing a system that is compatible with nearby hospitals, other specialists' offices, and diagnostic centers to maximize interoperability at the local level.2,3
Electronic medical record systems that interoperate also provide the ability to set forth performance measures for physicians aimed at improving quality of care. As our health care system moves toward a pay-for-performance model, EMRs will become a tool to determine if standards of care have been met, unnecessary diagnostic tests have been avoided, and unwanted outcomes have been minimized. These measures will usher in a new era of medicine in which physicians strive to improve the care provided to their patients and receive increases in their reimbursements, while patient outcomes and satisfaction are improved.9
Academics, Education, Research, and Residency
The practicality of EMRs in dermatology may best be appreciated in academic settings. Electronic medical records serve as a repository of coded information that is neatly organized and can be rapidly searched, allowing for use as a powerful research tool. As an example, physicians can use EMR systems to identify patients with specific qualifications and study outcome variables over time.2,3 Additionally, with the rise of interoperable systems, we can expect a new dawn in medical research as more information becomes available to clinical investigators, opening doors to endless possibilities for evidence-based care.2,3,8
Another advantage of EMRs is their utility in residency programs that are charged with the task of ensuring resident competency via exposure to a comprehensive host of clinical encounters. An EMR system uniquely allows residents and attending dermatologists to monitor adequate exposure to general, pediatric, complex medical, procedural, and dermatopathologic cases, and to track the number of procedures performed by the residents by directly linking the information into the Accreditation Council for Graduate Medical Education procedure log.
Furthermore, due to the dominance of digital and dermatoscopic images in the field, interoperable EMRs could be used to construct a database of clinical and dermatopathologic specimens that not only can be used in educating residents but also may serve as a powerful reference tool in the diagnosis of complex and rare cases.8 Another often unrecognized advantage of EMRs is their utility in teledermatology. With the interoperable EMRs within academic institutions, teledermatology can be used locally and nationally for rapid consultation with high diagnostic validity,10 which has the burgeoning potential of providing patients with quicker time to diagnosis considering the dermatologist shortage in various parts of the country.
Lastly, the implementation of EMRs in residency programs has the additional benefit of exposing residents and medical students to emerging technology early on in their careers and fosters a degree of familiarity and comfort that may lead to implementation of EMRs in their future practices.2 For dermatologists in-training, early exposure to these technologies also may serve as a way to develop an interactive interview style and adapt to the presence of EMRs in examination rooms without sacrificing quality of care and meaningful patient interaction.7
Conclusion
Electronic medical records are already becoming an integral part of many hospitals and private dermatology practices. Although EMRs provide potential benefits that can be expected to ultimately outweigh the associated costs in larger settings such as hospitals, residency programs, and multidisciplinary practices, EMRs may not be immediately beneficial to physicians in private practices or those approaching the end of their careers. Although a perfect system may be unattainable, development of interoperable systems designed to meet the needs of specialties such as dermatology are essential in attaining a comprehensive patient medical profile, improving quality of care, minimizing costs, reducing medical errors, and maximizing patient satisfaction.
- Health IT and health information exchange basics. Office of the National Coordinator for Health Information Technology website. http://www.healthit.gov/providers-professionals/learn-ehr-basics. Reviewed January 8, 2018. Accessed July 10, 2018.
- Grosshandler JA, Tulbert B, Kaufmann MD, et al. The electronic medical record in dermatology. Arch Dermatol. 2010;146:1031-1036.
- Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy. 2011;4:47-55.
- Kaufmann MD, Desai S. Special requirements for electronic health records in dermatology. Semin Cutan Med Surg. 2012;31:160-162.
- Wheeland RG. Separating EMR implementation hype from fact. Dermatology Times. http://www.dermatologytimes.com/modern-medicine-now/separating-emr-implementation-hype-fact. Published July 1, 2012. Accessed July 16, 2018.
- Lakdawala N, Bercovitch L, Grant-Kels JM. A picture is worth a thousand words: ethical dilemmas presented by storing digital photographs in electronic health records. J Am Acad Dermatol. 2013;69:473-475.
- Nguyen TV, Hong J, Prose NS. Compassionate care: enhancing physician-patient communication and education in dermatology: part I: patient-centered communication. J Am Acad Dermatol. 2013;68:353.e1-8.
- Ratner D, Thomas CO, Bickers D. The uses of digital photography in dermatology. J Am Acad Dermatol. 1999;41(5, pt 1):749-756.
- Wilson RL, Feldman SR. Physician performance measures in dermatology. J Am Acad Dermatol. 2010;63:E29-E35.
- Vañó-Galván S, Hidalgo A, Aguayo-Leiva I, et al. Store-and-forward teledermatology: assessment of validity in a series of 2000 observations [in Spanish]. Actas Dermosifiliogr. 2011;102:277-283.
The American Recovery and Reinvestment Act of 2009 introduced the Health Information Technology for Economic and Clinical Health (HITECH) Act and allocated $19.2 billion to promote the implementation of an electronic medical record (EMR) by hospitals as well as physicians in private practices.1 The EMR stores longitudinal health information and constructs a comprehensive picture of a patient's medical history.2,3 Following its debut, the US Department of Health & Human Services set forth meaningful use (MU) criteria,1 which aimed to increase quality of care, safety, and efficiency. Meaningful use criteria also sought to decrease health disparities; improve coordination of care; engage patients in their care; refine population and public health measures; and finally ensure accessibility, privacy, and security of patient data.1,2
The EMR offers potential gains at multiple levels of the patient-physician-public health hierarchy: a decrease in medical errors and duplicate services, timely access to test results and records, timely notification of patients in need for preventive services, and preservation of medical records in the event of an environmental disaster.1-3 Furthermore, physicians can take advantage of informational reciprocity with other providers, gain remote access to medical records, be reminded of need for service, e-prescribe, monitor for drug interactions, and utilize clinical information for research purposes.1,3 Lastly, public health organizations can use EMRs to improve outcomes by employing surveillance measures and creating patient registries that serve to protect the society at large.1
Although it seems that the broad-scale implementation of EMRs will undoubtedly enhance the quality of patient care in the years to come, many obstacles must be overcome to reach this potential. Certification of EMR systems and implementation of confidentiality measures that are compatible with the Health Insurance Portability and Accountability Act are the forerunning concerns, and the interconnectivity of EMR systems becomes more important as MU enters its later stages (eg, increased electronic transmission of patient data during phases of care, reliance on e-prescribing, population-level analysis of patient data to improve health outcomes). Additionally, the cost to implement and maintain an EMR deters many physicians in smaller practices from shouldering the charges, as they do not necessarily see increased productivity with this technology.2 Last but not least, unintended consequences of EMR implementation can involve the dangers of upcoding and overdocumentation.1
Dermatology is a visually dominant field serving a high volume of patients that require both medical and surgical care. These factors do not preclude the implementation of EMRs in our specialty but rather necessitate the utilization of a system specifically designed to cater to the needs of specialists in dermatology. This editorial will address some fundamental considerations in implementing an EMR in dermatology; discuss what platforms and patient interfaces are most practical; reiterate the importance of interoperability; and highlight the implications of this powerful tool in education, research, training, and monitoring quality of care.
Implementation and Specific Considerations in Dermatology
One of the biggest areas of concern in adopting an EMR is the associated financial burden.2-5 Although government incentives of MU cover a part of the initial cost of purchasing an EMR, expert maintenance costs, changes in workflow dynamics, and a steep learning curve can translate into lost productivity and revenue, discouraging many dermatologists from implementing an EMR.3,5 Furthermore, physicians who are nearing the end of their careers may not realize the longer-term benefits of implementing an EMR and therefore may decline to do so despite the disincentives of lower Medicare reimbursements.2 In fact, when juxtaposing the upfront cost of implementing an EMR against the expected increase in revenue after its implementation, there are general concerns that there will be a net loss on the part of the provider, which is a barrier to adoption of EMRs.3
Beyond the cost-benefit analysis, dermatologists often report multiple lesions in different anatomic sites or identify multiple biopsy sites that have been conveniently recorded on body templates included in their paper-based examination forms. Converting that information into words to be entered into an EMR can be excruciatingly time consuming and not easily comprehensible upon follow-up visits with the patient, which again results in decreased efficiency and productivity.4 Therefore, selecting a dermatology-compatible EMR that aims to make this transition easier is of utmost importance. One developer introduced an EMR with a touch interface containing a human body in all its facets that can be rotated, zoomed, and marked multiple times for accurate and convenient recording of lesions and intended procedure sites. This system automatically produces codes for examinations and procedures; facilitates e-prescription and ordering of laboratory results; prints pathology requests and consent forms; and includes information for patient education regarding their care. For example, the physical examination section of an H&P (history and physical examination) can be generated with a few taps on the screen, translating into increased efficiency and productivity.
The visual nature of dermatology demands the use of images, and as such, photographs have become integral in the diagnosis and follow-up of dermatology patients. Digital and dermatoscopic images not only help to eliminate unnecessary biopsies but also can promote early detection and management of malignancies.6 Thus, the capability to link photographs to a patient's medical record using an EMR is an invaluable gain. However, employing this feature in clinical practice has ethical implications that must be addressed, given that taking photographs can evoke an avoidable fear in patients regarding unlawful dissemination or unnecessary exposure of these images to physicians who do not need to access them.6 Thus, guidelines must be set for uploading, de-identifying, and annotating patient photographs, and only physicians involved in the care of the patient should be allocated access.4,6
EMR Platforms
When computers were first introduced into examination rooms, many physicians were reluctant, as computers were thought to disconnect physicians from patients, arousing a sense of remoteness and further depersonalizing the encounter as physicians spent more time typing and less time making meaningful eye contact with patients.5 The practice of dermatology requires patient-centered communication that serves to enhance the quality of care while at the same time allowing physicians to fulfill professional competencies and reduce medical errors, which may ultimately translate into patient satisfaction.7 In fact, when the patient-physician relationship is interrupted, patients are more likely to pursue legal action in the wake of a bad treatment outcome.5
Employing a tablet-friendly EMR can help circumvent (or at least minimize) this problem by providing the physician with a light, user-friendly device that eliminates the need for laptops or desktop computers.4 Going one step further, the utilization of tablets eliminates the need for accessory digital cameras, as most tablets come with built-in high-resolution cameras for capturing clinical photographs and immediately linking them to the patient's medical record. Lastly, tablet technology allows physicians to access consent forms while in the examination room with the patient to more readily obtain a signature for procedural or research consent.4,8
Interoperability, MU, and Quality of Care
The real goal in nationwide implementation of EMR technology is to accomplish MU criteria. Different EMRs should not only allow data to be imported and exported but ideally should be compatible and interoperable with one another.2 The myriad of different EMR platforms available impedes maximal functionality as MU moves into its final stage. For example, if an academic dermatology program in the setting of a larger hospital is required to use the generic hospital EMR, the dermatologist's specific needs may not be effectively met; on the other hand, if a dermatology-specific EMR is implemented, access to the hospital's larger database of patient information may be sacrificed. Optimal EMR systems should be designed to allow specificity for a given specialty while being able to receive and integrate laboratory values, dermatopathology and radiology results, and notes from consultations by other physicians. Such integration may reduce duplicate services, increase patient satisfaction, and fulfill MU criteria. In fact, the fear of many physicians, especially those in a field such as dermatology, are the unwanted costs that come with implementation of an EMR system that will soon become impractical due to compatibility issues.2 As a result, until a system that can meet the needs of multiple specialties is developed, dermatologists and other physicians upgrading to an EMR should consider implementing a system that is compatible with nearby hospitals, other specialists' offices, and diagnostic centers to maximize interoperability at the local level.2,3
Electronic medical record systems that interoperate also provide the ability to set forth performance measures for physicians aimed at improving quality of care. As our health care system moves toward a pay-for-performance model, EMRs will become a tool to determine if standards of care have been met, unnecessary diagnostic tests have been avoided, and unwanted outcomes have been minimized. These measures will usher in a new era of medicine in which physicians strive to improve the care provided to their patients and receive increases in their reimbursements, while patient outcomes and satisfaction are improved.9
Academics, Education, Research, and Residency
The practicality of EMRs in dermatology may best be appreciated in academic settings. Electronic medical records serve as a repository of coded information that is neatly organized and can be rapidly searched, allowing for use as a powerful research tool. As an example, physicians can use EMR systems to identify patients with specific qualifications and study outcome variables over time.2,3 Additionally, with the rise of interoperable systems, we can expect a new dawn in medical research as more information becomes available to clinical investigators, opening doors to endless possibilities for evidence-based care.2,3,8
Another advantage of EMRs is their utility in residency programs that are charged with the task of ensuring resident competency via exposure to a comprehensive host of clinical encounters. An EMR system uniquely allows residents and attending dermatologists to monitor adequate exposure to general, pediatric, complex medical, procedural, and dermatopathologic cases, and to track the number of procedures performed by the residents by directly linking the information into the Accreditation Council for Graduate Medical Education procedure log.
Furthermore, due to the dominance of digital and dermatoscopic images in the field, interoperable EMRs could be used to construct a database of clinical and dermatopathologic specimens that not only can be used in educating residents but also may serve as a powerful reference tool in the diagnosis of complex and rare cases.8 Another often unrecognized advantage of EMRs is their utility in teledermatology. With the interoperable EMRs within academic institutions, teledermatology can be used locally and nationally for rapid consultation with high diagnostic validity,10 which has the burgeoning potential of providing patients with quicker time to diagnosis considering the dermatologist shortage in various parts of the country.
Lastly, the implementation of EMRs in residency programs has the additional benefit of exposing residents and medical students to emerging technology early on in their careers and fosters a degree of familiarity and comfort that may lead to implementation of EMRs in their future practices.2 For dermatologists in-training, early exposure to these technologies also may serve as a way to develop an interactive interview style and adapt to the presence of EMRs in examination rooms without sacrificing quality of care and meaningful patient interaction.7
Conclusion
Electronic medical records are already becoming an integral part of many hospitals and private dermatology practices. Although EMRs provide potential benefits that can be expected to ultimately outweigh the associated costs in larger settings such as hospitals, residency programs, and multidisciplinary practices, EMRs may not be immediately beneficial to physicians in private practices or those approaching the end of their careers. Although a perfect system may be unattainable, development of interoperable systems designed to meet the needs of specialties such as dermatology are essential in attaining a comprehensive patient medical profile, improving quality of care, minimizing costs, reducing medical errors, and maximizing patient satisfaction.
The American Recovery and Reinvestment Act of 2009 introduced the Health Information Technology for Economic and Clinical Health (HITECH) Act and allocated $19.2 billion to promote the implementation of an electronic medical record (EMR) by hospitals as well as physicians in private practices.1 The EMR stores longitudinal health information and constructs a comprehensive picture of a patient's medical history.2,3 Following its debut, the US Department of Health & Human Services set forth meaningful use (MU) criteria,1 which aimed to increase quality of care, safety, and efficiency. Meaningful use criteria also sought to decrease health disparities; improve coordination of care; engage patients in their care; refine population and public health measures; and finally ensure accessibility, privacy, and security of patient data.1,2
The EMR offers potential gains at multiple levels of the patient-physician-public health hierarchy: a decrease in medical errors and duplicate services, timely access to test results and records, timely notification of patients in need for preventive services, and preservation of medical records in the event of an environmental disaster.1-3 Furthermore, physicians can take advantage of informational reciprocity with other providers, gain remote access to medical records, be reminded of need for service, e-prescribe, monitor for drug interactions, and utilize clinical information for research purposes.1,3 Lastly, public health organizations can use EMRs to improve outcomes by employing surveillance measures and creating patient registries that serve to protect the society at large.1
Although it seems that the broad-scale implementation of EMRs will undoubtedly enhance the quality of patient care in the years to come, many obstacles must be overcome to reach this potential. Certification of EMR systems and implementation of confidentiality measures that are compatible with the Health Insurance Portability and Accountability Act are the forerunning concerns, and the interconnectivity of EMR systems becomes more important as MU enters its later stages (eg, increased electronic transmission of patient data during phases of care, reliance on e-prescribing, population-level analysis of patient data to improve health outcomes). Additionally, the cost to implement and maintain an EMR deters many physicians in smaller practices from shouldering the charges, as they do not necessarily see increased productivity with this technology.2 Last but not least, unintended consequences of EMR implementation can involve the dangers of upcoding and overdocumentation.1
Dermatology is a visually dominant field serving a high volume of patients that require both medical and surgical care. These factors do not preclude the implementation of EMRs in our specialty but rather necessitate the utilization of a system specifically designed to cater to the needs of specialists in dermatology. This editorial will address some fundamental considerations in implementing an EMR in dermatology; discuss what platforms and patient interfaces are most practical; reiterate the importance of interoperability; and highlight the implications of this powerful tool in education, research, training, and monitoring quality of care.
Implementation and Specific Considerations in Dermatology
One of the biggest areas of concern in adopting an EMR is the associated financial burden.2-5 Although government incentives of MU cover a part of the initial cost of purchasing an EMR, expert maintenance costs, changes in workflow dynamics, and a steep learning curve can translate into lost productivity and revenue, discouraging many dermatologists from implementing an EMR.3,5 Furthermore, physicians who are nearing the end of their careers may not realize the longer-term benefits of implementing an EMR and therefore may decline to do so despite the disincentives of lower Medicare reimbursements.2 In fact, when juxtaposing the upfront cost of implementing an EMR against the expected increase in revenue after its implementation, there are general concerns that there will be a net loss on the part of the provider, which is a barrier to adoption of EMRs.3
Beyond the cost-benefit analysis, dermatologists often report multiple lesions in different anatomic sites or identify multiple biopsy sites that have been conveniently recorded on body templates included in their paper-based examination forms. Converting that information into words to be entered into an EMR can be excruciatingly time consuming and not easily comprehensible upon follow-up visits with the patient, which again results in decreased efficiency and productivity.4 Therefore, selecting a dermatology-compatible EMR that aims to make this transition easier is of utmost importance. One developer introduced an EMR with a touch interface containing a human body in all its facets that can be rotated, zoomed, and marked multiple times for accurate and convenient recording of lesions and intended procedure sites. This system automatically produces codes for examinations and procedures; facilitates e-prescription and ordering of laboratory results; prints pathology requests and consent forms; and includes information for patient education regarding their care. For example, the physical examination section of an H&P (history and physical examination) can be generated with a few taps on the screen, translating into increased efficiency and productivity.
The visual nature of dermatology demands the use of images, and as such, photographs have become integral in the diagnosis and follow-up of dermatology patients. Digital and dermatoscopic images not only help to eliminate unnecessary biopsies but also can promote early detection and management of malignancies.6 Thus, the capability to link photographs to a patient's medical record using an EMR is an invaluable gain. However, employing this feature in clinical practice has ethical implications that must be addressed, given that taking photographs can evoke an avoidable fear in patients regarding unlawful dissemination or unnecessary exposure of these images to physicians who do not need to access them.6 Thus, guidelines must be set for uploading, de-identifying, and annotating patient photographs, and only physicians involved in the care of the patient should be allocated access.4,6
EMR Platforms
When computers were first introduced into examination rooms, many physicians were reluctant, as computers were thought to disconnect physicians from patients, arousing a sense of remoteness and further depersonalizing the encounter as physicians spent more time typing and less time making meaningful eye contact with patients.5 The practice of dermatology requires patient-centered communication that serves to enhance the quality of care while at the same time allowing physicians to fulfill professional competencies and reduce medical errors, which may ultimately translate into patient satisfaction.7 In fact, when the patient-physician relationship is interrupted, patients are more likely to pursue legal action in the wake of a bad treatment outcome.5
Employing a tablet-friendly EMR can help circumvent (or at least minimize) this problem by providing the physician with a light, user-friendly device that eliminates the need for laptops or desktop computers.4 Going one step further, the utilization of tablets eliminates the need for accessory digital cameras, as most tablets come with built-in high-resolution cameras for capturing clinical photographs and immediately linking them to the patient's medical record. Lastly, tablet technology allows physicians to access consent forms while in the examination room with the patient to more readily obtain a signature for procedural or research consent.4,8
Interoperability, MU, and Quality of Care
The real goal in nationwide implementation of EMR technology is to accomplish MU criteria. Different EMRs should not only allow data to be imported and exported but ideally should be compatible and interoperable with one another.2 The myriad of different EMR platforms available impedes maximal functionality as MU moves into its final stage. For example, if an academic dermatology program in the setting of a larger hospital is required to use the generic hospital EMR, the dermatologist's specific needs may not be effectively met; on the other hand, if a dermatology-specific EMR is implemented, access to the hospital's larger database of patient information may be sacrificed. Optimal EMR systems should be designed to allow specificity for a given specialty while being able to receive and integrate laboratory values, dermatopathology and radiology results, and notes from consultations by other physicians. Such integration may reduce duplicate services, increase patient satisfaction, and fulfill MU criteria. In fact, the fear of many physicians, especially those in a field such as dermatology, are the unwanted costs that come with implementation of an EMR system that will soon become impractical due to compatibility issues.2 As a result, until a system that can meet the needs of multiple specialties is developed, dermatologists and other physicians upgrading to an EMR should consider implementing a system that is compatible with nearby hospitals, other specialists' offices, and diagnostic centers to maximize interoperability at the local level.2,3
Electronic medical record systems that interoperate also provide the ability to set forth performance measures for physicians aimed at improving quality of care. As our health care system moves toward a pay-for-performance model, EMRs will become a tool to determine if standards of care have been met, unnecessary diagnostic tests have been avoided, and unwanted outcomes have been minimized. These measures will usher in a new era of medicine in which physicians strive to improve the care provided to their patients and receive increases in their reimbursements, while patient outcomes and satisfaction are improved.9
Academics, Education, Research, and Residency
The practicality of EMRs in dermatology may best be appreciated in academic settings. Electronic medical records serve as a repository of coded information that is neatly organized and can be rapidly searched, allowing for use as a powerful research tool. As an example, physicians can use EMR systems to identify patients with specific qualifications and study outcome variables over time.2,3 Additionally, with the rise of interoperable systems, we can expect a new dawn in medical research as more information becomes available to clinical investigators, opening doors to endless possibilities for evidence-based care.2,3,8
Another advantage of EMRs is their utility in residency programs that are charged with the task of ensuring resident competency via exposure to a comprehensive host of clinical encounters. An EMR system uniquely allows residents and attending dermatologists to monitor adequate exposure to general, pediatric, complex medical, procedural, and dermatopathologic cases, and to track the number of procedures performed by the residents by directly linking the information into the Accreditation Council for Graduate Medical Education procedure log.
Furthermore, due to the dominance of digital and dermatoscopic images in the field, interoperable EMRs could be used to construct a database of clinical and dermatopathologic specimens that not only can be used in educating residents but also may serve as a powerful reference tool in the diagnosis of complex and rare cases.8 Another often unrecognized advantage of EMRs is their utility in teledermatology. With the interoperable EMRs within academic institutions, teledermatology can be used locally and nationally for rapid consultation with high diagnostic validity,10 which has the burgeoning potential of providing patients with quicker time to diagnosis considering the dermatologist shortage in various parts of the country.
Lastly, the implementation of EMRs in residency programs has the additional benefit of exposing residents and medical students to emerging technology early on in their careers and fosters a degree of familiarity and comfort that may lead to implementation of EMRs in their future practices.2 For dermatologists in-training, early exposure to these technologies also may serve as a way to develop an interactive interview style and adapt to the presence of EMRs in examination rooms without sacrificing quality of care and meaningful patient interaction.7
Conclusion
Electronic medical records are already becoming an integral part of many hospitals and private dermatology practices. Although EMRs provide potential benefits that can be expected to ultimately outweigh the associated costs in larger settings such as hospitals, residency programs, and multidisciplinary practices, EMRs may not be immediately beneficial to physicians in private practices or those approaching the end of their careers. Although a perfect system may be unattainable, development of interoperable systems designed to meet the needs of specialties such as dermatology are essential in attaining a comprehensive patient medical profile, improving quality of care, minimizing costs, reducing medical errors, and maximizing patient satisfaction.
- Health IT and health information exchange basics. Office of the National Coordinator for Health Information Technology website. http://www.healthit.gov/providers-professionals/learn-ehr-basics. Reviewed January 8, 2018. Accessed July 10, 2018.
- Grosshandler JA, Tulbert B, Kaufmann MD, et al. The electronic medical record in dermatology. Arch Dermatol. 2010;146:1031-1036.
- Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy. 2011;4:47-55.
- Kaufmann MD, Desai S. Special requirements for electronic health records in dermatology. Semin Cutan Med Surg. 2012;31:160-162.
- Wheeland RG. Separating EMR implementation hype from fact. Dermatology Times. http://www.dermatologytimes.com/modern-medicine-now/separating-emr-implementation-hype-fact. Published July 1, 2012. Accessed July 16, 2018.
- Lakdawala N, Bercovitch L, Grant-Kels JM. A picture is worth a thousand words: ethical dilemmas presented by storing digital photographs in electronic health records. J Am Acad Dermatol. 2013;69:473-475.
- Nguyen TV, Hong J, Prose NS. Compassionate care: enhancing physician-patient communication and education in dermatology: part I: patient-centered communication. J Am Acad Dermatol. 2013;68:353.e1-8.
- Ratner D, Thomas CO, Bickers D. The uses of digital photography in dermatology. J Am Acad Dermatol. 1999;41(5, pt 1):749-756.
- Wilson RL, Feldman SR. Physician performance measures in dermatology. J Am Acad Dermatol. 2010;63:E29-E35.
- Vañó-Galván S, Hidalgo A, Aguayo-Leiva I, et al. Store-and-forward teledermatology: assessment of validity in a series of 2000 observations [in Spanish]. Actas Dermosifiliogr. 2011;102:277-283.
- Health IT and health information exchange basics. Office of the National Coordinator for Health Information Technology website. http://www.healthit.gov/providers-professionals/learn-ehr-basics. Reviewed January 8, 2018. Accessed July 10, 2018.
- Grosshandler JA, Tulbert B, Kaufmann MD, et al. The electronic medical record in dermatology. Arch Dermatol. 2010;146:1031-1036.
- Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy. 2011;4:47-55.
- Kaufmann MD, Desai S. Special requirements for electronic health records in dermatology. Semin Cutan Med Surg. 2012;31:160-162.
- Wheeland RG. Separating EMR implementation hype from fact. Dermatology Times. http://www.dermatologytimes.com/modern-medicine-now/separating-emr-implementation-hype-fact. Published July 1, 2012. Accessed July 16, 2018.
- Lakdawala N, Bercovitch L, Grant-Kels JM. A picture is worth a thousand words: ethical dilemmas presented by storing digital photographs in electronic health records. J Am Acad Dermatol. 2013;69:473-475.
- Nguyen TV, Hong J, Prose NS. Compassionate care: enhancing physician-patient communication and education in dermatology: part I: patient-centered communication. J Am Acad Dermatol. 2013;68:353.e1-8.
- Ratner D, Thomas CO, Bickers D. The uses of digital photography in dermatology. J Am Acad Dermatol. 1999;41(5, pt 1):749-756.
- Wilson RL, Feldman SR. Physician performance measures in dermatology. J Am Acad Dermatol. 2010;63:E29-E35.
- Vañó-Galván S, Hidalgo A, Aguayo-Leiva I, et al. Store-and-forward teledermatology: assessment of validity in a series of 2000 observations [in Spanish]. Actas Dermosifiliogr. 2011;102:277-283.