User login
The amazing brain
Last week, unbeknownst to most people, Dayton, Ohio, hosted the world championships of Winter Drumline. It’s a combination of percussion instruments, dance, and music, with a storyline. Think of it as a very fast-paced half-time show, with only percussion, in 6 minutes or less.
My daughter fell in love with it her second year of high school, and has participated in it through college. Her specialty is the pit – marimba, vibraphone, xylophone. This gives our house a cruise ship atmosphere when she comes home to practice on weekends.
Over the years my wife and I have gone to many of her shows and competitions, streamed others online, and always been amazed by the variety of costumes, choreography, music numbers, and overall themes different teams come up with. We’ve seen shows based on 1930s detective fiction, ocean life, westerns, science fiction, toxic waste, emotions, relationships, flamenco, pirate ships, and many others.
And, as always, I marvel at the human brain.
Only 2-3 pounds but still an amazing thing. The capacity for imagination is endless, and one of the things that got us where we are today. The ability to see things that don’t exist yet, and work out the details on how to get there. The pyramids, Petra, the Great Wall, flight, the steam engine, landing on the moon, the ISS. And, of course, Winter Drumline.
It’s a uniquely (as far as we know) human capacity. To look at a rock and envision what it might be carved into. To look at Jupiter and think of a way to get a probe there. To sit in an empty gym and imagine the floor covered with dozens of percussion instruments and their players, imagining what each will be playing and doing at a given moment.
It’s really a remarkable capacity when you think about it. I’m sure it originally began as a way to figure out where you might find shelter or food, or simply to outwit the other tribe. But it’s become so much more than that. Someone envisioned every movie you see, book you read, and the computer I’m writing this on.
In his 1968 novelization of “2001: A Space Odyssey” Arthur C. Clarke described the thoughts of the unknown civilization that had left the Monolith behind for us as “in all the galaxy they had found nothing more precious than Mind.”
I’d agree with that. Even after 30 years of learning about the 2-3 pounds of semi-solid tissue we all carry upstairs, and doing my best to treat its malfunctions, I’ve never ceased to be amazed by it.
I hope I always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Last week, unbeknownst to most people, Dayton, Ohio, hosted the world championships of Winter Drumline. It’s a combination of percussion instruments, dance, and music, with a storyline. Think of it as a very fast-paced half-time show, with only percussion, in 6 minutes or less.
My daughter fell in love with it her second year of high school, and has participated in it through college. Her specialty is the pit – marimba, vibraphone, xylophone. This gives our house a cruise ship atmosphere when she comes home to practice on weekends.
Over the years my wife and I have gone to many of her shows and competitions, streamed others online, and always been amazed by the variety of costumes, choreography, music numbers, and overall themes different teams come up with. We’ve seen shows based on 1930s detective fiction, ocean life, westerns, science fiction, toxic waste, emotions, relationships, flamenco, pirate ships, and many others.
And, as always, I marvel at the human brain.
Only 2-3 pounds but still an amazing thing. The capacity for imagination is endless, and one of the things that got us where we are today. The ability to see things that don’t exist yet, and work out the details on how to get there. The pyramids, Petra, the Great Wall, flight, the steam engine, landing on the moon, the ISS. And, of course, Winter Drumline.
It’s a uniquely (as far as we know) human capacity. To look at a rock and envision what it might be carved into. To look at Jupiter and think of a way to get a probe there. To sit in an empty gym and imagine the floor covered with dozens of percussion instruments and their players, imagining what each will be playing and doing at a given moment.
It’s really a remarkable capacity when you think about it. I’m sure it originally began as a way to figure out where you might find shelter or food, or simply to outwit the other tribe. But it’s become so much more than that. Someone envisioned every movie you see, book you read, and the computer I’m writing this on.
In his 1968 novelization of “2001: A Space Odyssey” Arthur C. Clarke described the thoughts of the unknown civilization that had left the Monolith behind for us as “in all the galaxy they had found nothing more precious than Mind.”
I’d agree with that. Even after 30 years of learning about the 2-3 pounds of semi-solid tissue we all carry upstairs, and doing my best to treat its malfunctions, I’ve never ceased to be amazed by it.
I hope I always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Last week, unbeknownst to most people, Dayton, Ohio, hosted the world championships of Winter Drumline. It’s a combination of percussion instruments, dance, and music, with a storyline. Think of it as a very fast-paced half-time show, with only percussion, in 6 minutes or less.
My daughter fell in love with it her second year of high school, and has participated in it through college. Her specialty is the pit – marimba, vibraphone, xylophone. This gives our house a cruise ship atmosphere when she comes home to practice on weekends.
Over the years my wife and I have gone to many of her shows and competitions, streamed others online, and always been amazed by the variety of costumes, choreography, music numbers, and overall themes different teams come up with. We’ve seen shows based on 1930s detective fiction, ocean life, westerns, science fiction, toxic waste, emotions, relationships, flamenco, pirate ships, and many others.
And, as always, I marvel at the human brain.
Only 2-3 pounds but still an amazing thing. The capacity for imagination is endless, and one of the things that got us where we are today. The ability to see things that don’t exist yet, and work out the details on how to get there. The pyramids, Petra, the Great Wall, flight, the steam engine, landing on the moon, the ISS. And, of course, Winter Drumline.
It’s a uniquely (as far as we know) human capacity. To look at a rock and envision what it might be carved into. To look at Jupiter and think of a way to get a probe there. To sit in an empty gym and imagine the floor covered with dozens of percussion instruments and their players, imagining what each will be playing and doing at a given moment.
It’s really a remarkable capacity when you think about it. I’m sure it originally began as a way to figure out where you might find shelter or food, or simply to outwit the other tribe. But it’s become so much more than that. Someone envisioned every movie you see, book you read, and the computer I’m writing this on.
In his 1968 novelization of “2001: A Space Odyssey” Arthur C. Clarke described the thoughts of the unknown civilization that had left the Monolith behind for us as “in all the galaxy they had found nothing more precious than Mind.”
I’d agree with that. Even after 30 years of learning about the 2-3 pounds of semi-solid tissue we all carry upstairs, and doing my best to treat its malfunctions, I’ve never ceased to be amazed by it.
I hope I always will be.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Are delayed antibiotic prescriptions futile?
I recently posted a case about a smoker who became angry when I hesitated to prescribe antibiotics for his self-diagnosed bronchitis. He even threatened to retaliate by posting negative online reviews of my practice. In the end, I decided to use the strategy of a delayed prescription for antibiotics, instructing him to fill the prescription only if his symptoms worsened. I asked whether readers agreed with this approach. Thank you for the thoughtful comments regarding a case that certainly seemed familiar to many of you. I very much appreciate the chance to interact and share perspectives in a challenging clinical dilemma.
One theme that emerged through several comments was the perceived futility of the delayed prescriptions for antibiotics. To summarize, the collective logic stated that there is no point in delaying a prescription, because the patient will be very likely to fill that prescription right away despite counseling from the health care provider (HCP).
However, studies of delayed antibiotic prescriptions show that patients generally honor the advice to only fill the prescription if they are not improving clinically. In a study comparing immediate, delayed, or no antibiotic prescriptions among a cohort of children with uncomplicated respiratory infections, the overall rates of use of antibiotics in the three respective groups were 96%, 25.3%, and 12.0%. In another randomized trial exploring different strategies for delayed prescriptions among adults with upper respiratory infections, the rate of antibiotic use was 37% with delayed prescription strategies vs. 97% of patients prescribed antibiotics immediately. Neither of these prospective studies found a significant difference in clinical symptoms or complications in comparing the delayed and immediate antibiotic prescription groups.
Another common theme in the comments on this case focused on the challenge of online reviews of HCPs by patients. Multiple popular websites are devoted to patients’ unedited comments on HCPs and their practices, but there are still certain patterns to the comments. Some reviews describe the professionalism or empathy of the HCP, but others might focus more attention on the overall practice or office. These latter comments might emphasize issues such as timeliness of appointments, interactions with staff, or even parking and traffic. These are issues over which the HCP usually has little control.
HCPs are quite human, and therefore we might feel great about positive comments and dispirited or even angry with negative comments. So what is the best practice for HCPs in managing these online comments? A review by Dr Rebekah Bernard, which was published in the Sept. 25, 2018, issue of Medical Economics, offered some pragmatic advice:
Do not perseverate on one or two negative reviews. In fact, they might help! Dr. Bernard describes the psychological theory of the “pratfall effect,” in which people are more likely to prefer someone who is generally very good but not perfect to someone with nothing but exceptional reviews. HCPs with perfect reviews every time may be seen as intimidating or unapproachable.
Satisfied patients will frequently rally to support an HCP with an unfavorable review. This group may not be very motivated to complete online reviews until they see a comment which does at all match their own experience with the HCP.
Most importantly, HCPs can take an active role in minimizing the impact of negative online reviews while also enhancing their business model. Increasing your presence on the Internet and social media can help dilute negative reviews and push them down the list when someone performs a search on your name or practice. Creating a website for your practice is an effective means to be first on search engine lists, and HCPs should seek search-engine optimization features that promote this outcome. Adding social media contacts for yourself and/or your practice, as many as you can tolerate and maintain, allows HCPs to further control the narrative regarding their practice and central messaging to patients and the community.
In conclusion, delayed antibiotic prescriptions can reduce the use of unnecessary antibiotics for upper respiratory infections among children and adults, and they are not associated with worse clinical outcomes vs. immediate antibiotic prescriptions. They can also improve patient satisfaction for these visits, which can minimize the challenging issue of negative reviews of HCPs. HCPs should therefore consider delayed prescriptions as a strong option among patients without an indication for an antibiotic prescription.
A version of this article first appeared on Medscape.com.
I recently posted a case about a smoker who became angry when I hesitated to prescribe antibiotics for his self-diagnosed bronchitis. He even threatened to retaliate by posting negative online reviews of my practice. In the end, I decided to use the strategy of a delayed prescription for antibiotics, instructing him to fill the prescription only if his symptoms worsened. I asked whether readers agreed with this approach. Thank you for the thoughtful comments regarding a case that certainly seemed familiar to many of you. I very much appreciate the chance to interact and share perspectives in a challenging clinical dilemma.
One theme that emerged through several comments was the perceived futility of the delayed prescriptions for antibiotics. To summarize, the collective logic stated that there is no point in delaying a prescription, because the patient will be very likely to fill that prescription right away despite counseling from the health care provider (HCP).
However, studies of delayed antibiotic prescriptions show that patients generally honor the advice to only fill the prescription if they are not improving clinically. In a study comparing immediate, delayed, or no antibiotic prescriptions among a cohort of children with uncomplicated respiratory infections, the overall rates of use of antibiotics in the three respective groups were 96%, 25.3%, and 12.0%. In another randomized trial exploring different strategies for delayed prescriptions among adults with upper respiratory infections, the rate of antibiotic use was 37% with delayed prescription strategies vs. 97% of patients prescribed antibiotics immediately. Neither of these prospective studies found a significant difference in clinical symptoms or complications in comparing the delayed and immediate antibiotic prescription groups.
Another common theme in the comments on this case focused on the challenge of online reviews of HCPs by patients. Multiple popular websites are devoted to patients’ unedited comments on HCPs and their practices, but there are still certain patterns to the comments. Some reviews describe the professionalism or empathy of the HCP, but others might focus more attention on the overall practice or office. These latter comments might emphasize issues such as timeliness of appointments, interactions with staff, or even parking and traffic. These are issues over which the HCP usually has little control.
HCPs are quite human, and therefore we might feel great about positive comments and dispirited or even angry with negative comments. So what is the best practice for HCPs in managing these online comments? A review by Dr Rebekah Bernard, which was published in the Sept. 25, 2018, issue of Medical Economics, offered some pragmatic advice:
Do not perseverate on one or two negative reviews. In fact, they might help! Dr. Bernard describes the psychological theory of the “pratfall effect,” in which people are more likely to prefer someone who is generally very good but not perfect to someone with nothing but exceptional reviews. HCPs with perfect reviews every time may be seen as intimidating or unapproachable.
Satisfied patients will frequently rally to support an HCP with an unfavorable review. This group may not be very motivated to complete online reviews until they see a comment which does at all match their own experience with the HCP.
Most importantly, HCPs can take an active role in minimizing the impact of negative online reviews while also enhancing their business model. Increasing your presence on the Internet and social media can help dilute negative reviews and push them down the list when someone performs a search on your name or practice. Creating a website for your practice is an effective means to be first on search engine lists, and HCPs should seek search-engine optimization features that promote this outcome. Adding social media contacts for yourself and/or your practice, as many as you can tolerate and maintain, allows HCPs to further control the narrative regarding their practice and central messaging to patients and the community.
In conclusion, delayed antibiotic prescriptions can reduce the use of unnecessary antibiotics for upper respiratory infections among children and adults, and they are not associated with worse clinical outcomes vs. immediate antibiotic prescriptions. They can also improve patient satisfaction for these visits, which can minimize the challenging issue of negative reviews of HCPs. HCPs should therefore consider delayed prescriptions as a strong option among patients without an indication for an antibiotic prescription.
A version of this article first appeared on Medscape.com.
I recently posted a case about a smoker who became angry when I hesitated to prescribe antibiotics for his self-diagnosed bronchitis. He even threatened to retaliate by posting negative online reviews of my practice. In the end, I decided to use the strategy of a delayed prescription for antibiotics, instructing him to fill the prescription only if his symptoms worsened. I asked whether readers agreed with this approach. Thank you for the thoughtful comments regarding a case that certainly seemed familiar to many of you. I very much appreciate the chance to interact and share perspectives in a challenging clinical dilemma.
One theme that emerged through several comments was the perceived futility of the delayed prescriptions for antibiotics. To summarize, the collective logic stated that there is no point in delaying a prescription, because the patient will be very likely to fill that prescription right away despite counseling from the health care provider (HCP).
However, studies of delayed antibiotic prescriptions show that patients generally honor the advice to only fill the prescription if they are not improving clinically. In a study comparing immediate, delayed, or no antibiotic prescriptions among a cohort of children with uncomplicated respiratory infections, the overall rates of use of antibiotics in the three respective groups were 96%, 25.3%, and 12.0%. In another randomized trial exploring different strategies for delayed prescriptions among adults with upper respiratory infections, the rate of antibiotic use was 37% with delayed prescription strategies vs. 97% of patients prescribed antibiotics immediately. Neither of these prospective studies found a significant difference in clinical symptoms or complications in comparing the delayed and immediate antibiotic prescription groups.
Another common theme in the comments on this case focused on the challenge of online reviews of HCPs by patients. Multiple popular websites are devoted to patients’ unedited comments on HCPs and their practices, but there are still certain patterns to the comments. Some reviews describe the professionalism or empathy of the HCP, but others might focus more attention on the overall practice or office. These latter comments might emphasize issues such as timeliness of appointments, interactions with staff, or even parking and traffic. These are issues over which the HCP usually has little control.
HCPs are quite human, and therefore we might feel great about positive comments and dispirited or even angry with negative comments. So what is the best practice for HCPs in managing these online comments? A review by Dr Rebekah Bernard, which was published in the Sept. 25, 2018, issue of Medical Economics, offered some pragmatic advice:
Do not perseverate on one or two negative reviews. In fact, they might help! Dr. Bernard describes the psychological theory of the “pratfall effect,” in which people are more likely to prefer someone who is generally very good but not perfect to someone with nothing but exceptional reviews. HCPs with perfect reviews every time may be seen as intimidating or unapproachable.
Satisfied patients will frequently rally to support an HCP with an unfavorable review. This group may not be very motivated to complete online reviews until they see a comment which does at all match their own experience with the HCP.
Most importantly, HCPs can take an active role in minimizing the impact of negative online reviews while also enhancing their business model. Increasing your presence on the Internet and social media can help dilute negative reviews and push them down the list when someone performs a search on your name or practice. Creating a website for your practice is an effective means to be first on search engine lists, and HCPs should seek search-engine optimization features that promote this outcome. Adding social media contacts for yourself and/or your practice, as many as you can tolerate and maintain, allows HCPs to further control the narrative regarding their practice and central messaging to patients and the community.
In conclusion, delayed antibiotic prescriptions can reduce the use of unnecessary antibiotics for upper respiratory infections among children and adults, and they are not associated with worse clinical outcomes vs. immediate antibiotic prescriptions. They can also improve patient satisfaction for these visits, which can minimize the challenging issue of negative reviews of HCPs. HCPs should therefore consider delayed prescriptions as a strong option among patients without an indication for an antibiotic prescription.
A version of this article first appeared on Medscape.com.
Rabies: How to respond to parents’ questions
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
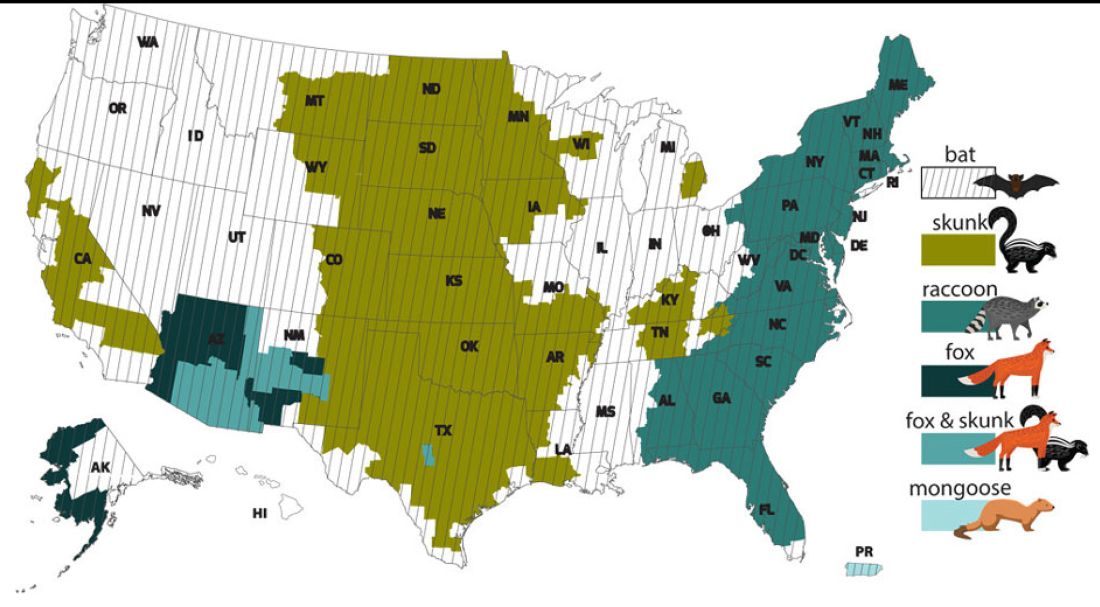
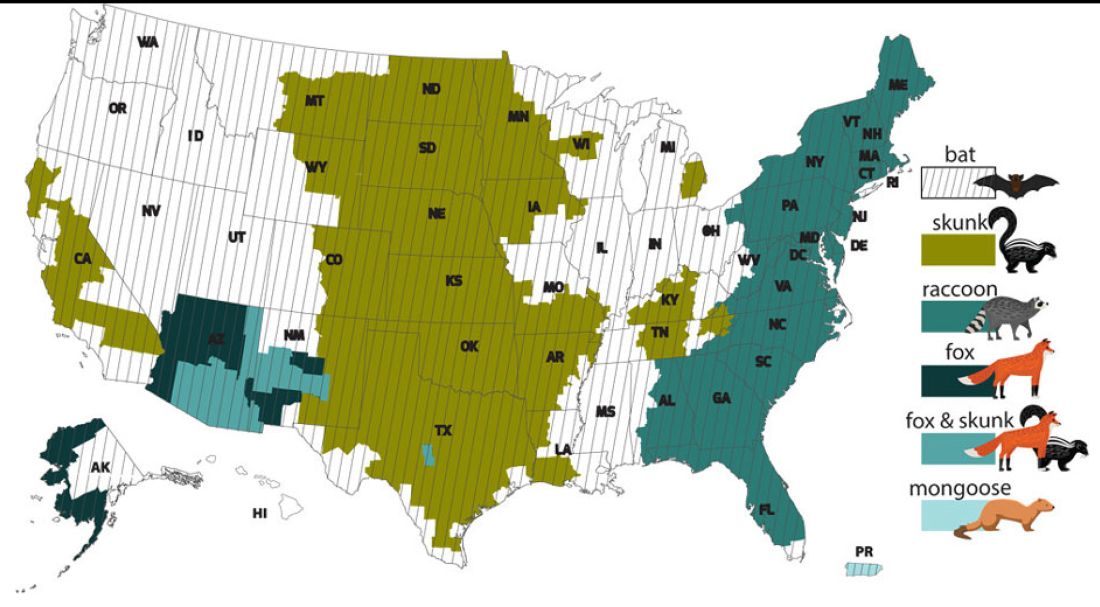
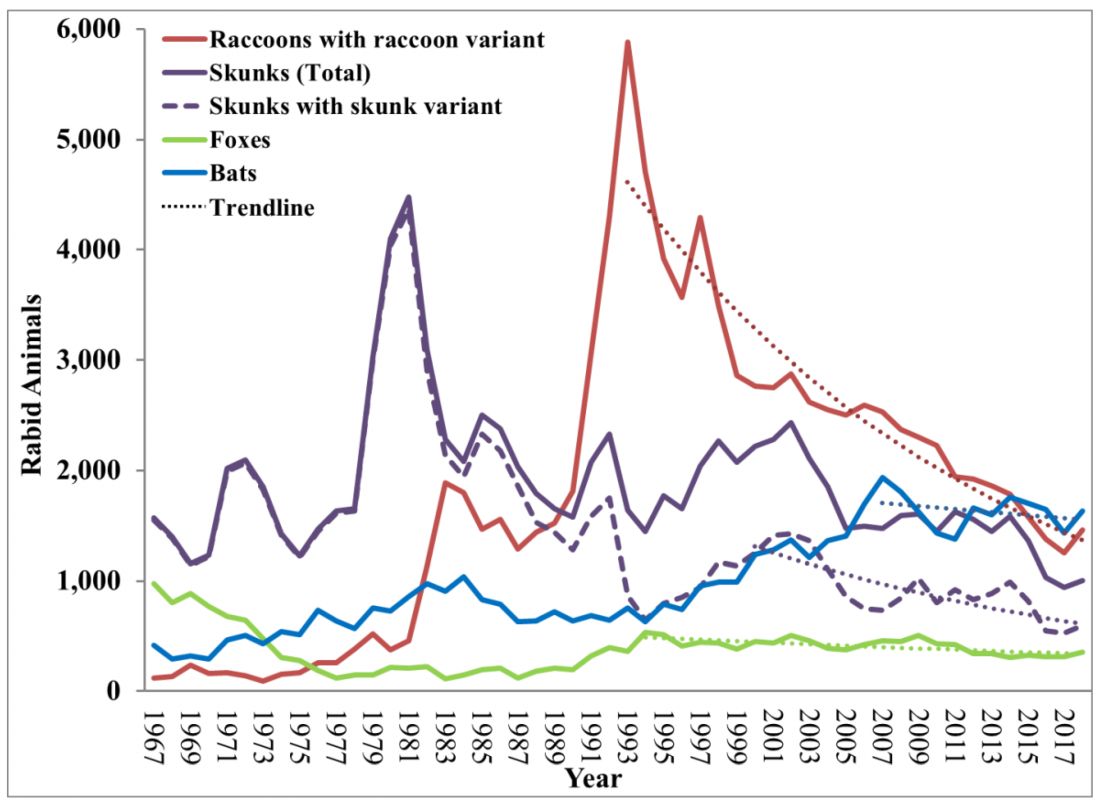
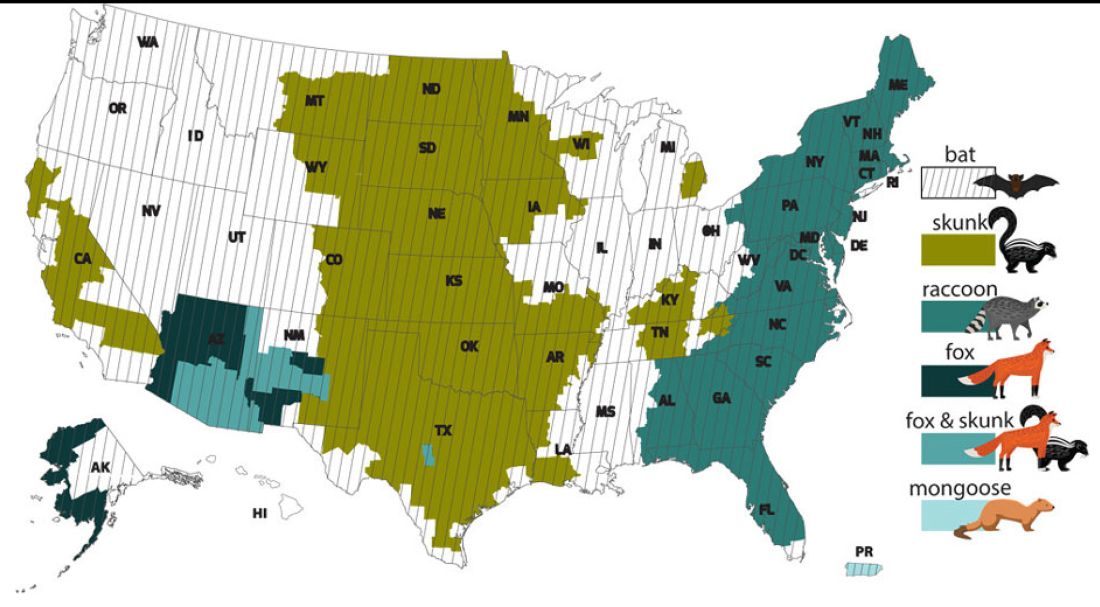
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
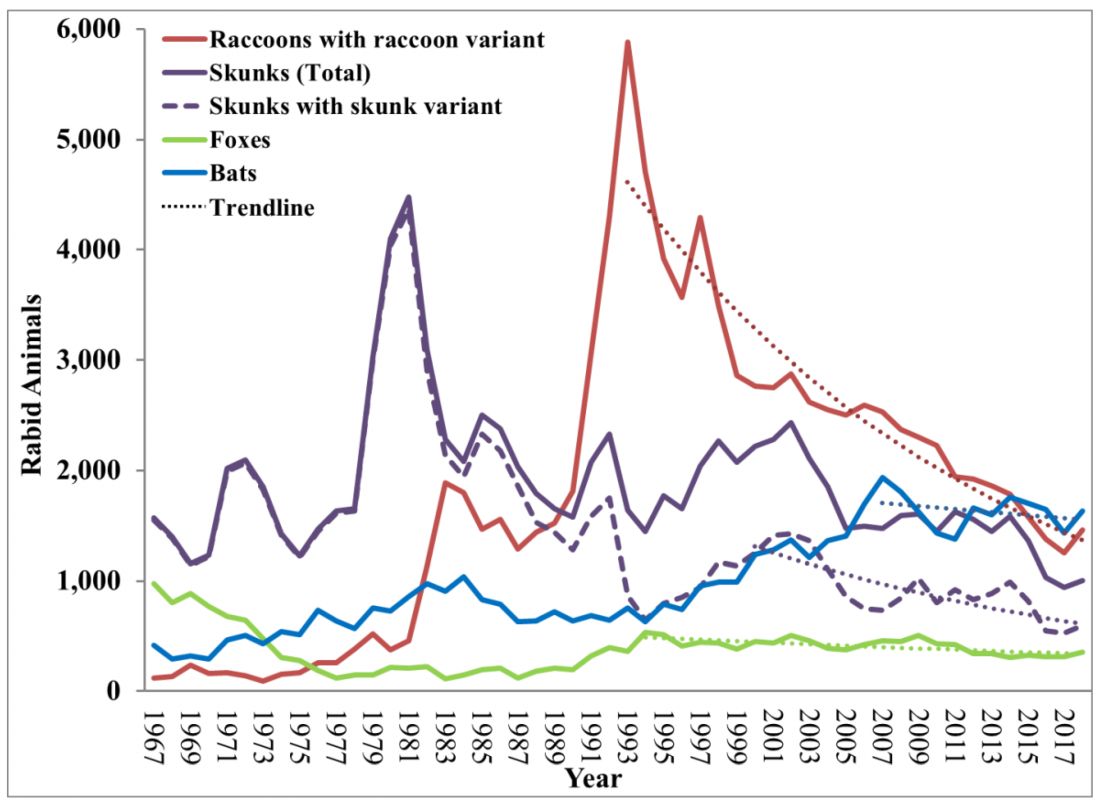
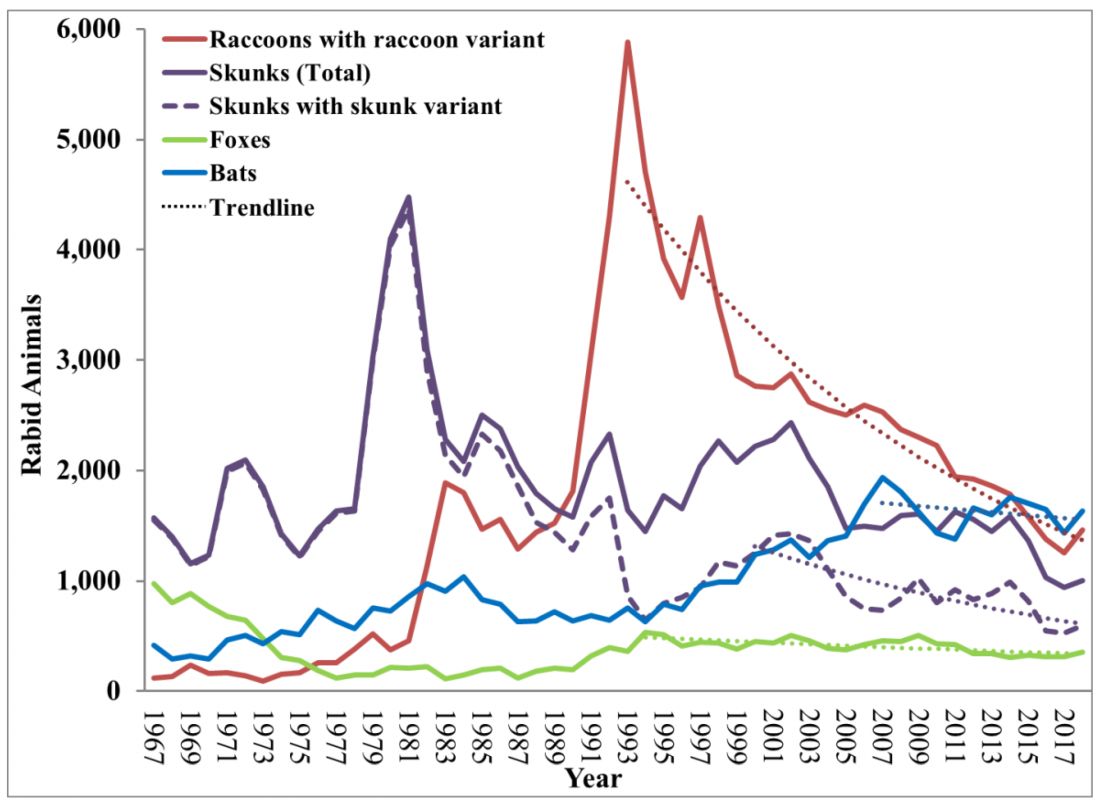
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
When most families hear the word rabies, they envision a dog foaming at the mouth and think about receiving multiple painful, often intra-abdominal injections. However, the epidemiology of rabies has changed in the United States. Postexposure prophylaxis (PEP) may not always be indicated and for certain persons preexposure prophylaxis (PrEP) is available and recommended.
Rabies is a Lyssavirus that is transmitted through saliva most often from the bite or scratch of an infected animal. Sometimes it’s via direct contact with mucous membranes. Although rare, cases have been described in which an undiagnosed donor passed the virus via transplant to recipients and four cases of aerosolized transmission were documented in two spelunkers and two laboratory technicians working with the virus. Worldwide it’s estimated that rabies causes 59,000 deaths annually.
Most cases (98%) are secondary to canine rabies. Prior to 1960, dogs were the major reservoir in the United States; however, after introduction of leash laws and animal vaccination in 1947, there was a drastic decline in cases caused by the canine rabies virus variant (CRVV). By 2004, CRVV was eliminated in the United States.
However, the proportion of strains associated with wildlife including raccoons, skunks, foxes, bats, coyotes, and mongoose now account for most of the cases in humans. Wildlife rabies is found in all states except Hawaii. Between 1960 and 2018, 89 cases were acquired in the United States and 62 (70%) were from bat exposure. Dog bites acquired during international travel were the cause of 36 cases.
Once signs and symptoms of disease develop there is no treatment. Regardless of the species variant, rabies virus infection is fatal in over 99% of cases. However, disease can be prevented with prompt initiation of PEP, which includes administration of rabies immune globulin (RIG) and rabies vaccine. Let’s look at a few different scenarios.
1. A delivery person is bitten by your neighbor’s dog while making a delivery. He was told to get rabies vaccine. What should we advise?
Canine rabies has been eliminated in the United States. However, unvaccinated canines can acquire rabies from wildlife. In this situation, you can determine the immunization status of the dog. Contact your local/state health department to assist with enforcement and management. Bites by cats and ferrets should be managed similarly.
Healthy dog:
1. Observe for 10 days.
2. PEP is not indicated unless the animal develops signs/symptoms of rabies. Then euthanize and begin PEP.
Dog appears rabid or suspected to be rabid:
1. Begin PEP.
2. Animal should be euthanized. If immunofluorescent test is negative discontinue PEP.
Dog unavailable:
Contact local/state health department. They are more familiar with rabies surveillance data.
2. Patient relocating to Malaysia for 3-4 years. Rabies PrEP was recommended but the family wants your opinion before receiving the vaccine. What would you advise?
Canine rabies is felt to be the primary cause of rabies outside of the United States. Canines are not routinely vaccinated in many foreign destinations, and the availability of RIG and rabies vaccine is not guaranteed in developing countries. As noted above, dog bites during international travel accounted for 28% of U.S. cases between 1960 and 2018.
In May 2022 recommendations for a modified two-dose PrEP schedule was published that identifies five risk groups and includes specific timing for checking rabies titers. The third rabies dose can now be administered up until year 3 (Morb Mortal Wkly Rep. 2022 May 6;71[18]:619-27). For individuals relocating to countries where CRVV is present, I prefer the traditional three-dose PrEP schedule administered between 21 and 28 days. However, we now have options. If exposure occurs any time after completion of a three-dose PrEP series or within 3 years after completion of a two-dose PrEP series, RIG would not be required. All patients would receive two doses of rabies vaccine (days 0, 3). If exposure occurs after 3 years in a person who received two doses of PrEP who did not have documentation of a protective rabies titer (> 5 IU/mL), treatment will include RIG plus four doses of vaccine (days 0, 3, 7, 14).
For this relocating patient, supporting PrEP would be strongly recommended.
3. A mother tells you she sees bats flying around her home at night and a few have even gotten into the home. This morning she saw one in her child’s room. He was still sleeping. Is there anything she needs to do?
Bats have become the predominant source of rabies in the United States. In addition to the cases noted above, three fatal cases occurred between Sept. 28 and Nov. 10, 2021, after bat exposures in August 2021 (MMWR Morb Mortal Wkly Rep. 2022 Jan 7;71:31-2). All had recognized contact with a bat 3-7 weeks prior to onset of symptoms and died 2-3 weeks after symptom onset. One declined PEP and the other two did not realize the risk for rabies from their exposure or did not notice a scratch or bite. Bites from bats may be small and unnoticed. Exposure to a bat in a closed room while sleeping is considered an exposure. Hawaii is the only state not reporting rabid bats.
PEP is recommended for her child. She should identify potential areas bats may enter the home and seal them in addition to removal of any bat roosts.
4. A parent realizes a house guest has been feeding raccoons in the backyard. What’s your response?
While bat rabies is the predominant variant associated with disease in the United States, as illustrated in Figure 1, other species of wildlife including raccoons are a major source of rabies. The geographic spread of the raccoon variant of rabies has been limited by oral vaccination via bait. In the situation noted here, the raccoons have returned because food was being offered thus increasing the families chance of a potential rabies exposure. Wildlife including skunks, raccoons, coyotes, foxes, and mongooses are always considered rabid until proven negative by laboratory testing.
You recommend to stop feeding wildlife and never to approach them. Have them contact the local rabies control unit and/or state wildlife services to assist with removal of the raccoons. Depending on the locale, pest control may be required at the owners expense. Inform the family to seek PEP if anyone is bitten or scratched by the raccoons.
As per the Centers for Disease Control and Prevention, about 55,000 residents receive PEP annually with health-associated expenditures including diagnostics, prevention, and control estimated between $245 and $510 million annually. Rabies is one of the most fatal diseases that can be prevented by avoiding contact with wild animals, maintenance of high immunization rates in pets, and keeping people informed of potential sources including bats. One can’t determine if an animal has rabies by looking at it. Rabies remains an urgent disease that we have to remember to address with our patients and their families. For additional information go to www.CDC.gov/rabies.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She has no relevant financial disclosures.
Thirty years of epilepsy therapy: ‘Plus ça change, plus c’est la même chose’?
Although the past 30 years have stirred up a whirlwind of neurological research that has dramatically expanded therapeutic options for patients with epilepsy, historical pioneers in the field might be disappointed at the fact that treatment response has remained stubbornly stagnant. “Plus ça change, plus c’est la même chose,” they might say: The more things change, the more they stay the same. In fact, since 1993, , with roughly two-thirds of patients achieving seizure freedom and a third still struggling with treatment resistance.
But if you widen the lens and look towards the horizon, things are “on the cusp and going like a rocket,” said Jacqueline A. French, MD, professor of neurology in the Comprehensive Epilepsy Center at NYU Langone Health, New York. While treatment response rates may be stuck, adverse effects of those treatments have plummeted, and even treatment-resistant patients dealing with residual seizures live a much freer life with far fewer and less serious episodes.
Simpler times
In the late 1980s, just as Dr. French was finishing her second epilepsy fellowship at Yale, it was “almost laughable that things were so simple,” she recalls. “There were a few major centers that were doing epilepsy surgery … and in the world of medication, there were just five major drugs: phenobarbital, primidone, carbamazepine, phenytoin, and valproate.” That all changed as she was settling in to her first academic position at the University of Pennsylvania, with the “explosive” introduction of felbamate, a new antiseizure drug whose precipitous rise and fall from favor cast a sobering shadow which set the course for future drug development in the field.
“The felbamate story has a lot to do with what came after, but it was a drug that was much more advantageous in regards to a lot of the things that we didn’t like about antiseizure medicines or antiepileptic drugs as we called them at that time,” she said. The older drugs affected the cerebellum, making people sleepy and unable to concentrate. They also came with the risk of serious adverse effects such as hepatic enzyme induction and teratogenicity. Not only was felbamate nonsedating, “it actually was a little bit alerting,” said Dr. French. “People felt so different and so great on it, and it was effective for some seizure types that we didn’t really have good drugs for.” Very quickly, felbamate became a first-line therapy. Within its first year on the market, 150,000 newly diagnosed patients were started on it, “which is unthinkable now,” she said.
Sure enough, it all came crashing down a year later, on Aug. 1, 1994, when the drug was urgently withdrawn by the U.S. Food and Drug Administration after being linked to the development of aplastic anemia. “There was a day that anybody who was there at the time will remember when we all got the news, that everybody had to be taken off the drug,” Dr. French recalled. “We spent the weekend in the chart room, looking chart by chart by chart, for who was on felbamate.”
Until then, Dr. French had been straddling the line between her interests in pharmacologic versus surgical treatments for epilepsy. In fact, during her second epilepsy fellowship, which was dedicated to surgery, she published “Characteristics of medial temporal lobe epilepsy” in Annals of Neurology, one of the most-cited papers of her career. “Epilepsy from the temporal lobe is the biggest and best shot on goal when you’re talking about sending somebody to epilepsy surgery and rendering them completely seizure free,” she said. “Early in my career at the University of Pennsylvania, it was all about identifying those patients. And you know, there is nothing more gratifying than taking somebody whose life has been devastated by frequent seizures, who is injuring themselves and not able to be independent, and doing a surgery, which is very safe, and then all the seizures are gone – which is probably why I was so excited by surgery at the time.”
For a while, in the early 1990s, temporal lobectomy eclipsed many of the other avenues in epilepsy treatment, but it too has given way to a much wider variety of more complex techniques, which may be less curative but more palliative.
More drug options
Meanwhile, the felbamate story had ignited debate in the field about safer drug development – pushing Dr. French into establishing what was then known as the Antiepileptic Drug Trials conference, later renamed the Epilepsy Therapies & Diagnostics Development Symposium – a forum that encouraged safer, but also swifter movement of drugs through the pipeline and onto the market. “After felbamate, came gabapentin, and then came to topiramate and lamotrigine, and very quickly there were many, many, many choices,” she explained. “But once stung, twice shy. Felbamate really gave us a new perspective on which patients we put on the new drugs. Now we have a process of starting them in people with treatment-resistant epilepsy first. The risk-benefit equation is more reasonable because they have lots of risks. And then we work our way back to people with newly diagnosed epilepsy.”
Disease-modifying therapies
Today, the medications used to treat epilepsy are referred to as antiseizure rather than antiepileptic drugs because they simply suppress seizure symptoms and do not address the cause. But the rocket that Dr. French is watching gain speed and momentum is the disease-modifying gene therapies – true antiepileptics that may significantly move the needle on the number and type of patients who can reach seizure freedom. “We spent the last 25 years not even thinking we would ever have antiepileptic therapies, and now in the last 5 years or so, we were pretty sure we will,” she said. “We have gene therapies that can intervene now – none yet that have actually reached approval, these are all currently in trials – but we certainly have high expectations that they will very soon be available.”
Improving patients’ lives
While gene therapy rockets ahead, new device developments are already improving life for patients, even despite ongoing seizures. A drug-delivering pump is still in trials, but could make a big difference to daily medication adherence, and wearable or implantable devices are being developed to track seizures. More accurate tracking has also revealed that many people’s seizures are actually quite predictable, with regular cycles allowing for the possibility of prophylactic medication when increased seizure activity is expected.
Despite 30 years of no change in the proportion of epilepsy patients experiencing treatment resistance, Dr. French said that drugs, devices, and surgeries have improved the lives of all patients – both treatment resistant and treatment sensitive. “The difference between almost seizure free and completely seizure free is a big one because it means you can’t drive, you may have difficulty with your employment, but being able to take a pill every day and feel otherwise completely normal? We’ve come a long way.”
Although the past 30 years have stirred up a whirlwind of neurological research that has dramatically expanded therapeutic options for patients with epilepsy, historical pioneers in the field might be disappointed at the fact that treatment response has remained stubbornly stagnant. “Plus ça change, plus c’est la même chose,” they might say: The more things change, the more they stay the same. In fact, since 1993, , with roughly two-thirds of patients achieving seizure freedom and a third still struggling with treatment resistance.
But if you widen the lens and look towards the horizon, things are “on the cusp and going like a rocket,” said Jacqueline A. French, MD, professor of neurology in the Comprehensive Epilepsy Center at NYU Langone Health, New York. While treatment response rates may be stuck, adverse effects of those treatments have plummeted, and even treatment-resistant patients dealing with residual seizures live a much freer life with far fewer and less serious episodes.
Simpler times
In the late 1980s, just as Dr. French was finishing her second epilepsy fellowship at Yale, it was “almost laughable that things were so simple,” she recalls. “There were a few major centers that were doing epilepsy surgery … and in the world of medication, there were just five major drugs: phenobarbital, primidone, carbamazepine, phenytoin, and valproate.” That all changed as she was settling in to her first academic position at the University of Pennsylvania, with the “explosive” introduction of felbamate, a new antiseizure drug whose precipitous rise and fall from favor cast a sobering shadow which set the course for future drug development in the field.
“The felbamate story has a lot to do with what came after, but it was a drug that was much more advantageous in regards to a lot of the things that we didn’t like about antiseizure medicines or antiepileptic drugs as we called them at that time,” she said. The older drugs affected the cerebellum, making people sleepy and unable to concentrate. They also came with the risk of serious adverse effects such as hepatic enzyme induction and teratogenicity. Not only was felbamate nonsedating, “it actually was a little bit alerting,” said Dr. French. “People felt so different and so great on it, and it was effective for some seizure types that we didn’t really have good drugs for.” Very quickly, felbamate became a first-line therapy. Within its first year on the market, 150,000 newly diagnosed patients were started on it, “which is unthinkable now,” she said.
Sure enough, it all came crashing down a year later, on Aug. 1, 1994, when the drug was urgently withdrawn by the U.S. Food and Drug Administration after being linked to the development of aplastic anemia. “There was a day that anybody who was there at the time will remember when we all got the news, that everybody had to be taken off the drug,” Dr. French recalled. “We spent the weekend in the chart room, looking chart by chart by chart, for who was on felbamate.”
Until then, Dr. French had been straddling the line between her interests in pharmacologic versus surgical treatments for epilepsy. In fact, during her second epilepsy fellowship, which was dedicated to surgery, she published “Characteristics of medial temporal lobe epilepsy” in Annals of Neurology, one of the most-cited papers of her career. “Epilepsy from the temporal lobe is the biggest and best shot on goal when you’re talking about sending somebody to epilepsy surgery and rendering them completely seizure free,” she said. “Early in my career at the University of Pennsylvania, it was all about identifying those patients. And you know, there is nothing more gratifying than taking somebody whose life has been devastated by frequent seizures, who is injuring themselves and not able to be independent, and doing a surgery, which is very safe, and then all the seizures are gone – which is probably why I was so excited by surgery at the time.”
For a while, in the early 1990s, temporal lobectomy eclipsed many of the other avenues in epilepsy treatment, but it too has given way to a much wider variety of more complex techniques, which may be less curative but more palliative.
More drug options
Meanwhile, the felbamate story had ignited debate in the field about safer drug development – pushing Dr. French into establishing what was then known as the Antiepileptic Drug Trials conference, later renamed the Epilepsy Therapies & Diagnostics Development Symposium – a forum that encouraged safer, but also swifter movement of drugs through the pipeline and onto the market. “After felbamate, came gabapentin, and then came to topiramate and lamotrigine, and very quickly there were many, many, many choices,” she explained. “But once stung, twice shy. Felbamate really gave us a new perspective on which patients we put on the new drugs. Now we have a process of starting them in people with treatment-resistant epilepsy first. The risk-benefit equation is more reasonable because they have lots of risks. And then we work our way back to people with newly diagnosed epilepsy.”
Disease-modifying therapies
Today, the medications used to treat epilepsy are referred to as antiseizure rather than antiepileptic drugs because they simply suppress seizure symptoms and do not address the cause. But the rocket that Dr. French is watching gain speed and momentum is the disease-modifying gene therapies – true antiepileptics that may significantly move the needle on the number and type of patients who can reach seizure freedom. “We spent the last 25 years not even thinking we would ever have antiepileptic therapies, and now in the last 5 years or so, we were pretty sure we will,” she said. “We have gene therapies that can intervene now – none yet that have actually reached approval, these are all currently in trials – but we certainly have high expectations that they will very soon be available.”
Improving patients’ lives
While gene therapy rockets ahead, new device developments are already improving life for patients, even despite ongoing seizures. A drug-delivering pump is still in trials, but could make a big difference to daily medication adherence, and wearable or implantable devices are being developed to track seizures. More accurate tracking has also revealed that many people’s seizures are actually quite predictable, with regular cycles allowing for the possibility of prophylactic medication when increased seizure activity is expected.
Despite 30 years of no change in the proportion of epilepsy patients experiencing treatment resistance, Dr. French said that drugs, devices, and surgeries have improved the lives of all patients – both treatment resistant and treatment sensitive. “The difference between almost seizure free and completely seizure free is a big one because it means you can’t drive, you may have difficulty with your employment, but being able to take a pill every day and feel otherwise completely normal? We’ve come a long way.”
Although the past 30 years have stirred up a whirlwind of neurological research that has dramatically expanded therapeutic options for patients with epilepsy, historical pioneers in the field might be disappointed at the fact that treatment response has remained stubbornly stagnant. “Plus ça change, plus c’est la même chose,” they might say: The more things change, the more they stay the same. In fact, since 1993, , with roughly two-thirds of patients achieving seizure freedom and a third still struggling with treatment resistance.
But if you widen the lens and look towards the horizon, things are “on the cusp and going like a rocket,” said Jacqueline A. French, MD, professor of neurology in the Comprehensive Epilepsy Center at NYU Langone Health, New York. While treatment response rates may be stuck, adverse effects of those treatments have plummeted, and even treatment-resistant patients dealing with residual seizures live a much freer life with far fewer and less serious episodes.
Simpler times
In the late 1980s, just as Dr. French was finishing her second epilepsy fellowship at Yale, it was “almost laughable that things were so simple,” she recalls. “There were a few major centers that were doing epilepsy surgery … and in the world of medication, there were just five major drugs: phenobarbital, primidone, carbamazepine, phenytoin, and valproate.” That all changed as she was settling in to her first academic position at the University of Pennsylvania, with the “explosive” introduction of felbamate, a new antiseizure drug whose precipitous rise and fall from favor cast a sobering shadow which set the course for future drug development in the field.
“The felbamate story has a lot to do with what came after, but it was a drug that was much more advantageous in regards to a lot of the things that we didn’t like about antiseizure medicines or antiepileptic drugs as we called them at that time,” she said. The older drugs affected the cerebellum, making people sleepy and unable to concentrate. They also came with the risk of serious adverse effects such as hepatic enzyme induction and teratogenicity. Not only was felbamate nonsedating, “it actually was a little bit alerting,” said Dr. French. “People felt so different and so great on it, and it was effective for some seizure types that we didn’t really have good drugs for.” Very quickly, felbamate became a first-line therapy. Within its first year on the market, 150,000 newly diagnosed patients were started on it, “which is unthinkable now,” she said.
Sure enough, it all came crashing down a year later, on Aug. 1, 1994, when the drug was urgently withdrawn by the U.S. Food and Drug Administration after being linked to the development of aplastic anemia. “There was a day that anybody who was there at the time will remember when we all got the news, that everybody had to be taken off the drug,” Dr. French recalled. “We spent the weekend in the chart room, looking chart by chart by chart, for who was on felbamate.”
Until then, Dr. French had been straddling the line between her interests in pharmacologic versus surgical treatments for epilepsy. In fact, during her second epilepsy fellowship, which was dedicated to surgery, she published “Characteristics of medial temporal lobe epilepsy” in Annals of Neurology, one of the most-cited papers of her career. “Epilepsy from the temporal lobe is the biggest and best shot on goal when you’re talking about sending somebody to epilepsy surgery and rendering them completely seizure free,” she said. “Early in my career at the University of Pennsylvania, it was all about identifying those patients. And you know, there is nothing more gratifying than taking somebody whose life has been devastated by frequent seizures, who is injuring themselves and not able to be independent, and doing a surgery, which is very safe, and then all the seizures are gone – which is probably why I was so excited by surgery at the time.”
For a while, in the early 1990s, temporal lobectomy eclipsed many of the other avenues in epilepsy treatment, but it too has given way to a much wider variety of more complex techniques, which may be less curative but more palliative.
More drug options
Meanwhile, the felbamate story had ignited debate in the field about safer drug development – pushing Dr. French into establishing what was then known as the Antiepileptic Drug Trials conference, later renamed the Epilepsy Therapies & Diagnostics Development Symposium – a forum that encouraged safer, but also swifter movement of drugs through the pipeline and onto the market. “After felbamate, came gabapentin, and then came to topiramate and lamotrigine, and very quickly there were many, many, many choices,” she explained. “But once stung, twice shy. Felbamate really gave us a new perspective on which patients we put on the new drugs. Now we have a process of starting them in people with treatment-resistant epilepsy first. The risk-benefit equation is more reasonable because they have lots of risks. And then we work our way back to people with newly diagnosed epilepsy.”
Disease-modifying therapies
Today, the medications used to treat epilepsy are referred to as antiseizure rather than antiepileptic drugs because they simply suppress seizure symptoms and do not address the cause. But the rocket that Dr. French is watching gain speed and momentum is the disease-modifying gene therapies – true antiepileptics that may significantly move the needle on the number and type of patients who can reach seizure freedom. “We spent the last 25 years not even thinking we would ever have antiepileptic therapies, and now in the last 5 years or so, we were pretty sure we will,” she said. “We have gene therapies that can intervene now – none yet that have actually reached approval, these are all currently in trials – but we certainly have high expectations that they will very soon be available.”
Improving patients’ lives
While gene therapy rockets ahead, new device developments are already improving life for patients, even despite ongoing seizures. A drug-delivering pump is still in trials, but could make a big difference to daily medication adherence, and wearable or implantable devices are being developed to track seizures. More accurate tracking has also revealed that many people’s seizures are actually quite predictable, with regular cycles allowing for the possibility of prophylactic medication when increased seizure activity is expected.
Despite 30 years of no change in the proportion of epilepsy patients experiencing treatment resistance, Dr. French said that drugs, devices, and surgeries have improved the lives of all patients – both treatment resistant and treatment sensitive. “The difference between almost seizure free and completely seizure free is a big one because it means you can’t drive, you may have difficulty with your employment, but being able to take a pill every day and feel otherwise completely normal? We’ve come a long way.”
A 7-month-old male presents with pustules and inflamed papules on the scalp and extremities
The bacterial, fungal, and atypical mycobacterial cultures from the lesions performed at the emergency department were all negative.
Pediatric dermatology was consulted and a punch biopsy of one of the lesions was done. Histopathologic examination showed a mixed perifollicular infiltrate of predominantly eosinophils with some neutrophils and associated microabscesses. Periodic acid Schiff and Fite stains failed to reveal any organisms. CD1 immunostain was negative. Fresh tissue cultures for bacteria, fungi, and atypical mycobacteria were negative.
Given the clinical presentation of chronic recurrent sterile pustules on an infant with associated eosinophilia and the reported histopathologic findings, the patient was diagnosed with eosinophilic pustular folliculitis of infancy (EPFI).
EPFI is a rare and idiopathic cutaneous disorder present in children. About 70% of the cases reported occur in the first 6 month of life and rarely present past 3 years of age. EPF encompasses a group of conditions including the classic adult form, or Ofuji disease. EPF is seen in immunosuppressed patients, mainly HIV positive, and EPF is also seen in infants and children.
In EPFI, males are most commonly affected. The condition presents, as it did in our patient, with recurrent crops of sterile papules and pustules mainly on the scalp, but they can occur in other parts of the body. The lesions go away within a few weeks to months without leaving any scars but it can take months to years to resolve. Histopathologic analysis of the lesions show an eosinophilic infiltrate which can be follicular, perifollicular, or periadnexal with associated flame figures in about 26% of cases.
Aggressive treatment is usually not needed as lesions are self-limited. Lesions can be treated with topical corticosteroids and oral antihistamine medications like cetirizine if symptomatic.
If the lesions start to present during the neonatal period, one may consider in the differential diagnosis, neonatal rashes like transient neonatal pustular melanosis and erythema toxicum neonatorum. Both of these neonatal conditions tend to resolve in the first month of life, compared with EPFI where lesions can come and go for months to years. EPFI lesions can be described as pustules and inflammatory papules, as well as furuncles and vesicles. All of the lesions may be seen in one patient at one time, which will not be typical for transient neonatal pustular melanosis or erythema toxicum. Eosinophils can be seen in erythema toxicum but folliculitis is not present. The inflammatory infiltrate seen in transient neonatal pustular melanosis is polymorphonuclear, not eosinophilic.
Early in the presentation, infectious conditions like staphylococcal or streptococcal folliculitis, cellulitis and furunculosis, tinea capitis, atypical mycobacterial infections, herpes simplex, and parasitic infections like scabies should be considered. In young infants, empiric antibiotic treatment may be started until cultures are finalized. If there is a family history of pruritic papules and pustules, scabies should be considered. A scabies prep can be done to rule out this entity.
Langerhans cell histiocytosis can also present with pustules and papules in early infancy and also has a predilection for the scalp. When this condition is in question, a skin biopsy should be performed which shows a CD1 positive histiocytic infiltrate.
In conclusion, EPFI is a benign rare condition that can present in infants as recurrent pustules and papules, mainly on the scalp, which are self-limited and if symptomatic can be treated with topical corticosteroids and antihistamines.
References
Alonso-Castro L et al. Dermatol Online J. 2012 Oct 15;18(10):6.
Frølunde AS et al. Clin Case Rep. 2021 May 11;9(5):e04167.
Hernández-Martín Á et al. J Am Acad Dermatol. 2013 Jan;68(1):150-5.
The bacterial, fungal, and atypical mycobacterial cultures from the lesions performed at the emergency department were all negative.
Pediatric dermatology was consulted and a punch biopsy of one of the lesions was done. Histopathologic examination showed a mixed perifollicular infiltrate of predominantly eosinophils with some neutrophils and associated microabscesses. Periodic acid Schiff and Fite stains failed to reveal any organisms. CD1 immunostain was negative. Fresh tissue cultures for bacteria, fungi, and atypical mycobacteria were negative.
Given the clinical presentation of chronic recurrent sterile pustules on an infant with associated eosinophilia and the reported histopathologic findings, the patient was diagnosed with eosinophilic pustular folliculitis of infancy (EPFI).
EPFI is a rare and idiopathic cutaneous disorder present in children. About 70% of the cases reported occur in the first 6 month of life and rarely present past 3 years of age. EPF encompasses a group of conditions including the classic adult form, or Ofuji disease. EPF is seen in immunosuppressed patients, mainly HIV positive, and EPF is also seen in infants and children.
In EPFI, males are most commonly affected. The condition presents, as it did in our patient, with recurrent crops of sterile papules and pustules mainly on the scalp, but they can occur in other parts of the body. The lesions go away within a few weeks to months without leaving any scars but it can take months to years to resolve. Histopathologic analysis of the lesions show an eosinophilic infiltrate which can be follicular, perifollicular, or periadnexal with associated flame figures in about 26% of cases.
Aggressive treatment is usually not needed as lesions are self-limited. Lesions can be treated with topical corticosteroids and oral antihistamine medications like cetirizine if symptomatic.
If the lesions start to present during the neonatal period, one may consider in the differential diagnosis, neonatal rashes like transient neonatal pustular melanosis and erythema toxicum neonatorum. Both of these neonatal conditions tend to resolve in the first month of life, compared with EPFI where lesions can come and go for months to years. EPFI lesions can be described as pustules and inflammatory papules, as well as furuncles and vesicles. All of the lesions may be seen in one patient at one time, which will not be typical for transient neonatal pustular melanosis or erythema toxicum. Eosinophils can be seen in erythema toxicum but folliculitis is not present. The inflammatory infiltrate seen in transient neonatal pustular melanosis is polymorphonuclear, not eosinophilic.
Early in the presentation, infectious conditions like staphylococcal or streptococcal folliculitis, cellulitis and furunculosis, tinea capitis, atypical mycobacterial infections, herpes simplex, and parasitic infections like scabies should be considered. In young infants, empiric antibiotic treatment may be started until cultures are finalized. If there is a family history of pruritic papules and pustules, scabies should be considered. A scabies prep can be done to rule out this entity.
Langerhans cell histiocytosis can also present with pustules and papules in early infancy and also has a predilection for the scalp. When this condition is in question, a skin biopsy should be performed which shows a CD1 positive histiocytic infiltrate.
In conclusion, EPFI is a benign rare condition that can present in infants as recurrent pustules and papules, mainly on the scalp, which are self-limited and if symptomatic can be treated with topical corticosteroids and antihistamines.
References
Alonso-Castro L et al. Dermatol Online J. 2012 Oct 15;18(10):6.
Frølunde AS et al. Clin Case Rep. 2021 May 11;9(5):e04167.
Hernández-Martín Á et al. J Am Acad Dermatol. 2013 Jan;68(1):150-5.
The bacterial, fungal, and atypical mycobacterial cultures from the lesions performed at the emergency department were all negative.
Pediatric dermatology was consulted and a punch biopsy of one of the lesions was done. Histopathologic examination showed a mixed perifollicular infiltrate of predominantly eosinophils with some neutrophils and associated microabscesses. Periodic acid Schiff and Fite stains failed to reveal any organisms. CD1 immunostain was negative. Fresh tissue cultures for bacteria, fungi, and atypical mycobacteria were negative.
Given the clinical presentation of chronic recurrent sterile pustules on an infant with associated eosinophilia and the reported histopathologic findings, the patient was diagnosed with eosinophilic pustular folliculitis of infancy (EPFI).
EPFI is a rare and idiopathic cutaneous disorder present in children. About 70% of the cases reported occur in the first 6 month of life and rarely present past 3 years of age. EPF encompasses a group of conditions including the classic adult form, or Ofuji disease. EPF is seen in immunosuppressed patients, mainly HIV positive, and EPF is also seen in infants and children.
In EPFI, males are most commonly affected. The condition presents, as it did in our patient, with recurrent crops of sterile papules and pustules mainly on the scalp, but they can occur in other parts of the body. The lesions go away within a few weeks to months without leaving any scars but it can take months to years to resolve. Histopathologic analysis of the lesions show an eosinophilic infiltrate which can be follicular, perifollicular, or periadnexal with associated flame figures in about 26% of cases.
Aggressive treatment is usually not needed as lesions are self-limited. Lesions can be treated with topical corticosteroids and oral antihistamine medications like cetirizine if symptomatic.
If the lesions start to present during the neonatal period, one may consider in the differential diagnosis, neonatal rashes like transient neonatal pustular melanosis and erythema toxicum neonatorum. Both of these neonatal conditions tend to resolve in the first month of life, compared with EPFI where lesions can come and go for months to years. EPFI lesions can be described as pustules and inflammatory papules, as well as furuncles and vesicles. All of the lesions may be seen in one patient at one time, which will not be typical for transient neonatal pustular melanosis or erythema toxicum. Eosinophils can be seen in erythema toxicum but folliculitis is not present. The inflammatory infiltrate seen in transient neonatal pustular melanosis is polymorphonuclear, not eosinophilic.
Early in the presentation, infectious conditions like staphylococcal or streptococcal folliculitis, cellulitis and furunculosis, tinea capitis, atypical mycobacterial infections, herpes simplex, and parasitic infections like scabies should be considered. In young infants, empiric antibiotic treatment may be started until cultures are finalized. If there is a family history of pruritic papules and pustules, scabies should be considered. A scabies prep can be done to rule out this entity.
Langerhans cell histiocytosis can also present with pustules and papules in early infancy and also has a predilection for the scalp. When this condition is in question, a skin biopsy should be performed which shows a CD1 positive histiocytic infiltrate.
In conclusion, EPFI is a benign rare condition that can present in infants as recurrent pustules and papules, mainly on the scalp, which are self-limited and if symptomatic can be treated with topical corticosteroids and antihistamines.
References
Alonso-Castro L et al. Dermatol Online J. 2012 Oct 15;18(10):6.
Frølunde AS et al. Clin Case Rep. 2021 May 11;9(5):e04167.
Hernández-Martín Á et al. J Am Acad Dermatol. 2013 Jan;68(1):150-5.
A 7-month-old male is brought to the emergency department for evaluation of pustules and inflamed papules on the scalp and extremities for several weeks of duration. The parents report the lesions started about a month prior and he has already been treated with cephalexin, clindamycin, and sulfamethoxazole without any improvement. Cultures sent prior by the child's pediatrician did not reveal any fungus or bacteria. The parents report a low-grade fever for about 3 days.
He was born via natural vaginal delivery with no instrumentation or external monitoring. Mom had prenatal care. Besides the skin lesions, the baby has been healthy and growing well. He has no history of eczema or severe infections. He has not been hospitalized before.
On physical examination the baby was not febrile. On the scalp and forehead, he had diffusely distributed pustules, erythematous papules, and nodules. He also presented with scattered, fine, small, crusted 1-2-mm pink papules on the trunk and extremities. He had no adenopathy or hepatosplenomegaly.
At the emergency department, samples from one of the pustules were sent for bacterial, fungal, and atypical mycobacteria cultures. Laboratory test showed a normal blood count with associated eosinophilia (2.8 x 109 L), and normal liver and kidney function. A head ultrasound showed three ill-defined hypoechoic foci within the scalp.
The patient was admitted for treatment with broad-spectrum antibiotics and dermatology was consulted.
Teen girls are in crisis: A call to action resulting from 2021 CDC data
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
Case: “Where’s my mommy?”
A 13-year-old girl “D” appeared lifeless in her hospital bed, swallowed by tubes, gauze, and crisp white sheets. She seemed fragile next to the giant machines beeping all around her, as they churned and groaned to keep her alive. She was in the pediatric intensive care unit, a place she had only seen once or twice on TV. Her sleeping mother lay next to her in an uncomfortable-looking recliner chair, curled up in a ball. She abruptly woke up when I walked into the room, doing her best to wipe away 5 days’ worth of worry and sadness from her exhausted face. She saw “Child Psychiatrist” written on my hospital badge, desperately searching my face for answers or a sign of hope.
Her daughter – a straight-A middle school student who loved Taylor Swift and soccer – had overdosed on Tylenol after discovering that she did not make the cheerleading team. I reported that her daughter’s liver enzymes were finally trending down and that she would likely not require a liver transplant. She would survive. As tears welled up in this mother’s eyes, I heard a faint whisper from across the room. “Where’s my mommy?” D was awake and frantically searching the room for her mother, someone who could soothe her in this living nightmare. As the two embraced, I felt tears well up in my eyes as I couldn’t help but think of my own 3-year-old daughter at home. How could I protect her from the sadness and despair that this little girl was feeling? How can we collectively protect every little girl from wanting to end their life?
CDC data: Teen girls need help now
The latest biennial Centers for Disease Control and Prevention Youth Risk Behavior Survey, administered in the fall of 2021, resulted in alarming data showing that mental health has worsened for all adolescents, but especially for girls. The survey was administered to more than 17,000 students in 152 public and private schools throughout the United States, showing that “America’s teen girls are engulfed in a growing wave of sadness, violence, and trauma.”1 In particular, rates of sadness, suicidal ideation, suicide attempts, and mental health crisis ED visits among girls are the highest reported in a decade. Nearly 60% of girls felt persistent sadness or hopelessness during the past year, double the rate of boys. More than 25% of girls made a suicide plan; this percentage increased 60% over the past 10 years. Alarmingly, ED visits for suicide attempts for girls increased more than 50% in the past 2 years alone.
Even before the COVID-19 pandemic, experts were sounding the alarm on the growing rates of anxiety and depression in U.S. youth. The pandemic-driven isolation, lack of social connection, and missing of major milestones did not help the situation and only deepened the cracks in a faulty mental health care system. Further, civil unrest and social upheaval in the United States felt – and continues to feel – chaotic and unpredictable. For teens, the current cultural climate represents their not-too-distant future as adults, causing worry and anxiety.
In addition to securing their futures through performance in school and extracurricular activities, teenagers are forming their identities. Establishing a personal identity is a difficult task for all teens, though teenage girls face uniquely difficult challenges in our current society. In particular, teenage girls are expected to conform their behaviors to fit societal expectations that may clash with their desires and self-conceptualization. This conflict is further complicated by heightened beauty standards, online hate and competition, academic pressure, and self-doubt. CDC data show that girls experience sexual harassment and cyberbullying at roughly twice the rate of their male counterparts. Girls also experience higher levels of sexual violence and bullying. Alarmingly, 14% of girls reported being forced to have sex at some point in their lives. The sad truth is that, for every 10 teenage girls you know, at least one of them, and probably more, has likely been raped.
A call to action for providers
As providers, what can we do about these alarming statistics? It’s easy to become overwhelmed by data on a national level. However, regardless of our current clinical practice situation, we cannot lose sight of the humanity behind these numbers. Five extra minutes of truly listening to our patients, normalizing conversations about mental health, and looking for mental health warning signs (that is, increased isolation, declining function in school, maladaptive coping skills such as self-injurious behavior or substance use) can mean the difference between life and death.
As pediatric providers, formally screening for suicide risk is critical. Specifically, the American Academy of Pediatrics recommends that all youth aged 12 years or older be screened for suicide risk.2 In addition to asking families to reduce access to lethal means, it is important to utilize suicide-specific screeners to prevent suicide attempts and deaths in the pediatric community. Pediatric providers must feel prepared to counsel patients and families on suicide prevention and, if this skill set is underdeveloped, appropriate referrals and support must be provided.
At the same time, it is important to note the larger context. This national tragedy has been long-standing and further accelerated by the social isolation and stress of the pandemic. Madigan and colleagues recently showed that the lack of a social outlet resulting from COVID-19 caused an increase in screen time among all children.3 As a result, many teen girls turned to social media to recreate these social connections online.4 This dependence on social media for validation has contributed to increased rates of depression by intensifying unrealistic body standards, comparisons, and competition among peers.5 However, recent pediatric partnership programs have improved mental health access, reduced ED visits, and increased primary care physician’s comfort with managing mental health concerns.6 These programs are called Child Psychiatry Access Programs (CPAPs) and utilize a collaborative care model through which primary care clinicians consult with child and adolescent psychiatrists. CPAPs, while not the entire solution, offer a major step in the right direction toward tackling this mental health crisis in a sustainable, collaborative, and effective way.
As students return to in-person learning, connectedness at school is a powerful protective factor against depression and anxiety. We must infuse resources and support into our schools and teachers, as they stand on the front lines for our children. Specifically, bolstering schools with school counselors and appropriate mental health support staff will help rescue teachers from burnout while also explicitly identifying mental health care as a priority. Finally, modeling positive behavior for families and identifying safe adults at school can help at-risk youth feel more connected. To achieve meaningful improvement in children’s mental health, it is crucial to collaboratively remodel broken systems to ensure that all children are supported early, effectively, and equitably.
Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences, program director of the child and adolescent psychiatry fellowship, and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior in Los Angeles.
References
1. Centers for Disease Control and Prevention. YRBSS Data Summary & Trends. 2023 Feb 13. https://www.cdc.gov/healthyyouth/data/yrbs/yrbs_data_summary_and_trends.htm
2. American Academy of Pediatrics. Screening for Suicide Risk in Clinical Practice. 2023 Feb 22. https://www.aap.org/en/patient-care/blueprint-for-youth-suicide-prevention/strategies-for-clinical-settings-for-youth-suicide-prevention/screening-for-suicide-risk-in-clinical-practice/
3. Madigan S et al. JAMA Pediatr. 2022;176(12):1188-98. doi: 10.1001/JAMAPEDIATRICS.2022.4116
4. Pew Research Center. Teens, Social Media and Technology 2022. 2022 Aug 10. https://www.pewresearch.org/internet/2022/08/10/teens-social-media-and-technology-2022/
5. Hunt MG et al. J Social Clin Psychology. 2018;37(10):751-68. doi: 10.1521/JSCP.2018.37.10.751
6. Godoy L et al. J Pediatr Health Care. 2022 Dec 16. doi: 10.1016/j.pedhc.2022.11.009.
Prior authorizations: Time to rebel?
I imagine I am not alone when I tell you that my blood pressure rises every time I receive an email from CoverMyMeds, or worse, a phone call from a patient to tell me the pharmacist says I need to call their insurance company to get a medication authorized. Prior authorizations (PAs) are the bane of every physician’s existence.
They ask providers to jump through hoops, and no one oversees the placement of these hoops. The process puts patients at risk and sucks the joy from the practice of medicine.
In fall 2021, the legislative committee of the Maryland Psychiatric Society, with the help of Kathy Orellana and Tim Clement from the American Psychiatric Association, drafted a bill to modify the use of PAs. Unfortunately, the bill died in committee during the 2022 Maryland General Assembly legislative session.
Robert Herman, MD, who helped draft the initial legislation, was delighted when he learned that MedChi, the Maryland State Medical Society, had taken the proposed legislation and expanded it. “It was everything we wished for and more,” Dr. Herman said.
During this year’s legislative session, House Bill 305/Senate Bill 308, Health Insurance – Utilization Review – Revisions, was sponsored by 19 delegates and two senators. Fifty medical associations, including dentists and physical therapists, endorsed the bill. Many people, including Dr. Herman, testified before the Health and Government Operations Committee on Feb. 16.
Delegate Kenneth Kerr introduced the legislation to the committee.
“Before I begin, let me make two points. First, the bill does not do away with prior authorization or other utilization review techniques; rather, it tries to make a more balanced approach for both patients and physicians by attempting to reduce the volume that’s subject to prior authorization, by increasing transparency and communication, and by studying how the process can be improved overall. Second, we have over 50 organizations representing health care providers and patient advocacy organizations supporting this legislation. This is a systemic issue across the entire spectrum of healthcare,” said Mr. Kerr.
Mr. Kerr went on to say there were 81,143 denials for treatment in 2021. The three areas with the highest rate of denials were pharmacy, dental, and the combination of labs and radiology.
He further noted that, when consumers filed a complaint with the Maryland Insurance Administration, 72.4% of denials were reversed in 2022.
“This resulted in more benefits that could have, and should have, been given to the patient at the first request. These reversals indicate there is a problem,” Mr. Kerr said. He discussed increased administrative costs, the enormous workload burden this incurs, and the problem of burnout among medical providers.
The proposed legislation includes a ban on PA requirements for generic medications, for dose changes of previously authorized medication, and ends the requirement for yearly authorizations. It requires that a physician of the same specialty be on the panel that denies care and shortens the time periods allowed for responses and appeals.
Testimony began with those supporting the legislation. Doctors highlighted the harm inflicted on their patients by the PA process. An oncologist spoke of how it took weeks to get approval for chemotherapy for a patient with an aggressive cancer, a gastroenterologist discussed a patient who became ill and lost her job when successful treatment for inflammatory bowel disease was stopped while she waited for the yearly medication reapproval, and another physician told of a patient who died of an exacerbation of obstructive lung disease, also while awaiting a yearly reapproval for an effective medication.
A dentist spoke about how he was not authorized to place a crown on a patient’s tooth. Instead, he was instructed to try a filling first, and when the filling failed, he was told he would not be authorized to work on the same tooth twice in one year.
A physical therapist testified that PA was required every two to four sessions, and each request took up half of a session – a significant portion of time that was not used for treatment.
Three people testified in opposition to the bill. Matthew Celantano, executive director of the League of Life and Health Insurers of Maryland, called the legislation “drastic” and testified that the cost would be prohibitive.
“From our end, it’s important for you to hear that prior authorization is care coordination. It’s protection that keeps [patients] safe, but helps control skyrocketing health care costs,” said Mr. Celantano.
Deb Rivkin, vice president of government affairs for CareFirst Blue Cross Blue Shield, testified in favor of using better technology. She cited legislation under consideration in Virginia that would give clinicians more information about the specific medications that require PAs, price information, and real-time authorizations.
Finally, representing the Pharmaceutical Care Management Association, Heather Cascone testified about PAs for generic medications. Her testimony focused on prior authorization for generic medications. She claimed that “... by allowing unrestricted dispensing of generic drugs, or an override based on the subjective opinion of the prescriber, prior authorization can protect patients from drugs with a safety risk; they can catch things like drug-disease contraindications, dosage errors, pregnancy-related contraindications, and a variety of cost-savings protections.”
I found this testimony particularly difficult because the “protector” is generally not a physician and has neither seen, nor examined, the patient. The implication that patients need protection from their doctors who would be unaware aware that they are pregnant, or are ill, was offensive. It also implies that PBMs are lax by not requiring PA on all medications, ignoring the fact that patients often bypass such denials by paying out of pocket for treatment.
If this had been a high school debate, there would be no doubt the enthusiasm for the bill for HB305 was strong, the committee chair was eager, and the arguments in favor of the legislation robust. There are no public minutes for the subsequent meetings with stakeholders, and I was somewhat heartbroken to learn that once again, the bill died in committee.
Annette Hanson, MD, chair of the MPS legislative committee, remains optimistic for the future. “Since then, the APA [American Psychiatric Association] has taken our bill and used it as model legislation now being offered to other district branches. MPS has created something that is going to spread across the country. Change may be slow, but it is not inevitable. And when it happens, I want you to remember that it started here,” she said.
However, the pressure is on. A recent ProPublica article documented how Cigna rejects claims by the batch without ever reviewing them. Soon after that piece was published, it was announced that several of the large insurers, including Cigna, would be cutting back on PA demands. It remains to be seen whether this is a token move to placate legislators, and whether it will provide meaningful relief to physicians and patients. I remain skeptical.
In the meantime, physicians’ ability to help their patients remains compromised and administrative tasks consume valuable time. I have started to wonder whether there may be some other way to push this issue to action. PA is about cost containment, but perhaps there are other ways to economize.
Why do medications cost less in other countries? Why does a medication cost hundreds of dollars more at one pharmacy versus another? Why do medicines sometimes have a copay that is two or three times higher than the cash price? Why do some covered medications have copays of thousands of dollars a year? I wonder if physicians shouldn’t come together and collectively agree not to comply and refuse to complete PAs in organized rebellion.
The fear, of course, is that such an endeavor would hurt patients, but if we all agreed in concert, then for better or for worse, something would have to give. The existing system is already hurting everyone, and physicians, by agreeing to play this awful game, are complicit in letting insurers dictate the care our patients receive.
Dinah Miller, MD, is a coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016) and has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
A version of this article first appeared on Medscape.com.
I imagine I am not alone when I tell you that my blood pressure rises every time I receive an email from CoverMyMeds, or worse, a phone call from a patient to tell me the pharmacist says I need to call their insurance company to get a medication authorized. Prior authorizations (PAs) are the bane of every physician’s existence.
They ask providers to jump through hoops, and no one oversees the placement of these hoops. The process puts patients at risk and sucks the joy from the practice of medicine.
In fall 2021, the legislative committee of the Maryland Psychiatric Society, with the help of Kathy Orellana and Tim Clement from the American Psychiatric Association, drafted a bill to modify the use of PAs. Unfortunately, the bill died in committee during the 2022 Maryland General Assembly legislative session.
Robert Herman, MD, who helped draft the initial legislation, was delighted when he learned that MedChi, the Maryland State Medical Society, had taken the proposed legislation and expanded it. “It was everything we wished for and more,” Dr. Herman said.
During this year’s legislative session, House Bill 305/Senate Bill 308, Health Insurance – Utilization Review – Revisions, was sponsored by 19 delegates and two senators. Fifty medical associations, including dentists and physical therapists, endorsed the bill. Many people, including Dr. Herman, testified before the Health and Government Operations Committee on Feb. 16.
Delegate Kenneth Kerr introduced the legislation to the committee.
“Before I begin, let me make two points. First, the bill does not do away with prior authorization or other utilization review techniques; rather, it tries to make a more balanced approach for both patients and physicians by attempting to reduce the volume that’s subject to prior authorization, by increasing transparency and communication, and by studying how the process can be improved overall. Second, we have over 50 organizations representing health care providers and patient advocacy organizations supporting this legislation. This is a systemic issue across the entire spectrum of healthcare,” said Mr. Kerr.
Mr. Kerr went on to say there were 81,143 denials for treatment in 2021. The three areas with the highest rate of denials were pharmacy, dental, and the combination of labs and radiology.
He further noted that, when consumers filed a complaint with the Maryland Insurance Administration, 72.4% of denials were reversed in 2022.
“This resulted in more benefits that could have, and should have, been given to the patient at the first request. These reversals indicate there is a problem,” Mr. Kerr said. He discussed increased administrative costs, the enormous workload burden this incurs, and the problem of burnout among medical providers.
The proposed legislation includes a ban on PA requirements for generic medications, for dose changes of previously authorized medication, and ends the requirement for yearly authorizations. It requires that a physician of the same specialty be on the panel that denies care and shortens the time periods allowed for responses and appeals.
Testimony began with those supporting the legislation. Doctors highlighted the harm inflicted on their patients by the PA process. An oncologist spoke of how it took weeks to get approval for chemotherapy for a patient with an aggressive cancer, a gastroenterologist discussed a patient who became ill and lost her job when successful treatment for inflammatory bowel disease was stopped while she waited for the yearly medication reapproval, and another physician told of a patient who died of an exacerbation of obstructive lung disease, also while awaiting a yearly reapproval for an effective medication.
A dentist spoke about how he was not authorized to place a crown on a patient’s tooth. Instead, he was instructed to try a filling first, and when the filling failed, he was told he would not be authorized to work on the same tooth twice in one year.
A physical therapist testified that PA was required every two to four sessions, and each request took up half of a session – a significant portion of time that was not used for treatment.
Three people testified in opposition to the bill. Matthew Celantano, executive director of the League of Life and Health Insurers of Maryland, called the legislation “drastic” and testified that the cost would be prohibitive.
“From our end, it’s important for you to hear that prior authorization is care coordination. It’s protection that keeps [patients] safe, but helps control skyrocketing health care costs,” said Mr. Celantano.
Deb Rivkin, vice president of government affairs for CareFirst Blue Cross Blue Shield, testified in favor of using better technology. She cited legislation under consideration in Virginia that would give clinicians more information about the specific medications that require PAs, price information, and real-time authorizations.
Finally, representing the Pharmaceutical Care Management Association, Heather Cascone testified about PAs for generic medications. Her testimony focused on prior authorization for generic medications. She claimed that “... by allowing unrestricted dispensing of generic drugs, or an override based on the subjective opinion of the prescriber, prior authorization can protect patients from drugs with a safety risk; they can catch things like drug-disease contraindications, dosage errors, pregnancy-related contraindications, and a variety of cost-savings protections.”
I found this testimony particularly difficult because the “protector” is generally not a physician and has neither seen, nor examined, the patient. The implication that patients need protection from their doctors who would be unaware aware that they are pregnant, or are ill, was offensive. It also implies that PBMs are lax by not requiring PA on all medications, ignoring the fact that patients often bypass such denials by paying out of pocket for treatment.
If this had been a high school debate, there would be no doubt the enthusiasm for the bill for HB305 was strong, the committee chair was eager, and the arguments in favor of the legislation robust. There are no public minutes for the subsequent meetings with stakeholders, and I was somewhat heartbroken to learn that once again, the bill died in committee.
Annette Hanson, MD, chair of the MPS legislative committee, remains optimistic for the future. “Since then, the APA [American Psychiatric Association] has taken our bill and used it as model legislation now being offered to other district branches. MPS has created something that is going to spread across the country. Change may be slow, but it is not inevitable. And when it happens, I want you to remember that it started here,” she said.
However, the pressure is on. A recent ProPublica article documented how Cigna rejects claims by the batch without ever reviewing them. Soon after that piece was published, it was announced that several of the large insurers, including Cigna, would be cutting back on PA demands. It remains to be seen whether this is a token move to placate legislators, and whether it will provide meaningful relief to physicians and patients. I remain skeptical.
In the meantime, physicians’ ability to help their patients remains compromised and administrative tasks consume valuable time. I have started to wonder whether there may be some other way to push this issue to action. PA is about cost containment, but perhaps there are other ways to economize.
Why do medications cost less in other countries? Why does a medication cost hundreds of dollars more at one pharmacy versus another? Why do medicines sometimes have a copay that is two or three times higher than the cash price? Why do some covered medications have copays of thousands of dollars a year? I wonder if physicians shouldn’t come together and collectively agree not to comply and refuse to complete PAs in organized rebellion.
The fear, of course, is that such an endeavor would hurt patients, but if we all agreed in concert, then for better or for worse, something would have to give. The existing system is already hurting everyone, and physicians, by agreeing to play this awful game, are complicit in letting insurers dictate the care our patients receive.
Dinah Miller, MD, is a coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016) and has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
A version of this article first appeared on Medscape.com.
I imagine I am not alone when I tell you that my blood pressure rises every time I receive an email from CoverMyMeds, or worse, a phone call from a patient to tell me the pharmacist says I need to call their insurance company to get a medication authorized. Prior authorizations (PAs) are the bane of every physician’s existence.
They ask providers to jump through hoops, and no one oversees the placement of these hoops. The process puts patients at risk and sucks the joy from the practice of medicine.
In fall 2021, the legislative committee of the Maryland Psychiatric Society, with the help of Kathy Orellana and Tim Clement from the American Psychiatric Association, drafted a bill to modify the use of PAs. Unfortunately, the bill died in committee during the 2022 Maryland General Assembly legislative session.
Robert Herman, MD, who helped draft the initial legislation, was delighted when he learned that MedChi, the Maryland State Medical Society, had taken the proposed legislation and expanded it. “It was everything we wished for and more,” Dr. Herman said.
During this year’s legislative session, House Bill 305/Senate Bill 308, Health Insurance – Utilization Review – Revisions, was sponsored by 19 delegates and two senators. Fifty medical associations, including dentists and physical therapists, endorsed the bill. Many people, including Dr. Herman, testified before the Health and Government Operations Committee on Feb. 16.
Delegate Kenneth Kerr introduced the legislation to the committee.
“Before I begin, let me make two points. First, the bill does not do away with prior authorization or other utilization review techniques; rather, it tries to make a more balanced approach for both patients and physicians by attempting to reduce the volume that’s subject to prior authorization, by increasing transparency and communication, and by studying how the process can be improved overall. Second, we have over 50 organizations representing health care providers and patient advocacy organizations supporting this legislation. This is a systemic issue across the entire spectrum of healthcare,” said Mr. Kerr.
Mr. Kerr went on to say there were 81,143 denials for treatment in 2021. The three areas with the highest rate of denials were pharmacy, dental, and the combination of labs and radiology.
He further noted that, when consumers filed a complaint with the Maryland Insurance Administration, 72.4% of denials were reversed in 2022.
“This resulted in more benefits that could have, and should have, been given to the patient at the first request. These reversals indicate there is a problem,” Mr. Kerr said. He discussed increased administrative costs, the enormous workload burden this incurs, and the problem of burnout among medical providers.
The proposed legislation includes a ban on PA requirements for generic medications, for dose changes of previously authorized medication, and ends the requirement for yearly authorizations. It requires that a physician of the same specialty be on the panel that denies care and shortens the time periods allowed for responses and appeals.
Testimony began with those supporting the legislation. Doctors highlighted the harm inflicted on their patients by the PA process. An oncologist spoke of how it took weeks to get approval for chemotherapy for a patient with an aggressive cancer, a gastroenterologist discussed a patient who became ill and lost her job when successful treatment for inflammatory bowel disease was stopped while she waited for the yearly medication reapproval, and another physician told of a patient who died of an exacerbation of obstructive lung disease, also while awaiting a yearly reapproval for an effective medication.
A dentist spoke about how he was not authorized to place a crown on a patient’s tooth. Instead, he was instructed to try a filling first, and when the filling failed, he was told he would not be authorized to work on the same tooth twice in one year.
A physical therapist testified that PA was required every two to four sessions, and each request took up half of a session – a significant portion of time that was not used for treatment.
Three people testified in opposition to the bill. Matthew Celantano, executive director of the League of Life and Health Insurers of Maryland, called the legislation “drastic” and testified that the cost would be prohibitive.
“From our end, it’s important for you to hear that prior authorization is care coordination. It’s protection that keeps [patients] safe, but helps control skyrocketing health care costs,” said Mr. Celantano.
Deb Rivkin, vice president of government affairs for CareFirst Blue Cross Blue Shield, testified in favor of using better technology. She cited legislation under consideration in Virginia that would give clinicians more information about the specific medications that require PAs, price information, and real-time authorizations.
Finally, representing the Pharmaceutical Care Management Association, Heather Cascone testified about PAs for generic medications. Her testimony focused on prior authorization for generic medications. She claimed that “... by allowing unrestricted dispensing of generic drugs, or an override based on the subjective opinion of the prescriber, prior authorization can protect patients from drugs with a safety risk; they can catch things like drug-disease contraindications, dosage errors, pregnancy-related contraindications, and a variety of cost-savings protections.”
I found this testimony particularly difficult because the “protector” is generally not a physician and has neither seen, nor examined, the patient. The implication that patients need protection from their doctors who would be unaware aware that they are pregnant, or are ill, was offensive. It also implies that PBMs are lax by not requiring PA on all medications, ignoring the fact that patients often bypass such denials by paying out of pocket for treatment.
If this had been a high school debate, there would be no doubt the enthusiasm for the bill for HB305 was strong, the committee chair was eager, and the arguments in favor of the legislation robust. There are no public minutes for the subsequent meetings with stakeholders, and I was somewhat heartbroken to learn that once again, the bill died in committee.
Annette Hanson, MD, chair of the MPS legislative committee, remains optimistic for the future. “Since then, the APA [American Psychiatric Association] has taken our bill and used it as model legislation now being offered to other district branches. MPS has created something that is going to spread across the country. Change may be slow, but it is not inevitable. And when it happens, I want you to remember that it started here,” she said.
However, the pressure is on. A recent ProPublica article documented how Cigna rejects claims by the batch without ever reviewing them. Soon after that piece was published, it was announced that several of the large insurers, including Cigna, would be cutting back on PA demands. It remains to be seen whether this is a token move to placate legislators, and whether it will provide meaningful relief to physicians and patients. I remain skeptical.
In the meantime, physicians’ ability to help their patients remains compromised and administrative tasks consume valuable time. I have started to wonder whether there may be some other way to push this issue to action. PA is about cost containment, but perhaps there are other ways to economize.
Why do medications cost less in other countries? Why does a medication cost hundreds of dollars more at one pharmacy versus another? Why do medicines sometimes have a copay that is two or three times higher than the cash price? Why do some covered medications have copays of thousands of dollars a year? I wonder if physicians shouldn’t come together and collectively agree not to comply and refuse to complete PAs in organized rebellion.
The fear, of course, is that such an endeavor would hurt patients, but if we all agreed in concert, then for better or for worse, something would have to give. The existing system is already hurting everyone, and physicians, by agreeing to play this awful game, are complicit in letting insurers dictate the care our patients receive.
Dinah Miller, MD, is a coauthor of Committed: The Battle Over Involuntary Psychiatric Care (Johns Hopkins University Press, 2016) and has a private practice and is an assistant professor of psychiatry and behavioral sciences at Johns Hopkins in Baltimore.
A version of this article first appeared on Medscape.com.
LGBTQ+ Youth Consult Questions remain over use of sex hormone therapy
“They Paused Puberty but Is There a Cost?”
“Bone Health: Puberty Blockers Not Fully Reversible.”
Headlines such as these from major national news outlets have begun to cast doubt on one of the medications used in treating gender-diverse adolescents and young adults. GnRH agonists, such as leuprorelin and triptorelin, were first approved by the Food and Drug Administration in the 1980s and have been used since then for a variety of medical indications. In the decades since, these medications have been successfully used with a generally favorable side effect profile.
GnRH agonists and puberty
In the treatment of precocious puberty, GnRH agonists are often started prior to the age of 7, depending on the age at which the affected patient begins showing signs of central puberty. These include breast development, scrotal enlargement, and so on. GnRH agonists typically are continued until age 10-12, depending on the patient and an informed discussion with the patient’s parents about optimal outcomes.1 Therefore, it is not uncommon to see these medications used for anywhere from 1 to 4 years, depending on the age at which precocious puberty started.
GnRH agonists are used in two populations of transgender individuals. The first group is those youths who have just started their natal, or biological, puberty. The medication is not started until the patient has biochemical or physical exam evidence that puberty has started. The medication is then continued until hormones are started. This is usually 2-3 years on average, depending on the age at which the medication was started. This is essentially comparable with cisgender youths who have taken these medications for precocious puberty. The second population of individuals who use GnRH agonists is transgender women who are also on estrogen therapy. In these women, the GnRH agonist is used for androgen (testosterone) suppression.
Concerns over bone health
One of the main concerns recently expressed about long-term use of GnRH agonists is their effect on bone density. Adolescence is a critical time for bone mineral density (BMD) accrual and this is driven by sex hormones. When GnRH agonists are used to delay puberty in transgender adolescents, this then delays the maturation of the adult skeleton until the GnRH agonist is stopped (and natal puberty resumes) or cross-sex hormones are started. In a recent multicenter study2 looking at baseline BMD of transgender youth at the time of GnRH agonist initiation, 30% of those assigned male at birth and 13% of those assigned female at birth had low bone mineral density for age (defined as a BMD z score of <–2). For those with low BMD, their physical activity scores were significantly lower than those with normal BMD. Thus, these adolescents require close follow-up, just like their cisgender peers.
There are currently no long-term data on the risk of developing fractures or osteoporosis in those individuals who were treated with GnRH agonists and then went on to start cross-sex hormone therapy. Some studies suggest that there is a risk that BMD does not recover after being on cross-sex hormones,3 while another study suggested that transgender men recover their BMD after being on testosterone.4 It is still unclear in that study why transgender women did not recover their BMD or why they were low at baseline. Interestingly, a 2012 study5 from Brazil showed that there was no difference in BMD for cisgender girls who had been off their GnRH agonist therapy for at least 3 years, as compared with their age-matched controls who had never been on GnRH agonist therapy. These conflicting data highlight the importance of long-term follow-up, as well as the need to include age-matched, cisgender control subjects, to better understand if there is truly a difference in transgender individuals or if today’s adolescents, in general, have low BMD.
Lingering questions
In summary, the use of GnRH agonists in transgender adolescents remains controversial because of the potential long-term effects on bone mineral density. However, this risk must be balanced against the risks of allowing natal puberty to progress in certain transgender individuals with the development of undesired secondary sex characteristics. More longitudinal studies are needed to better understand the long-term risks of osteoporosis and fractures in those who have undergone GnRH agonist therapy as part of their gender-affirming medical care, as well as any clinical interventions that might help mitigate this risk.
Dr. Cooper is assistant professor of pediatrics at UT Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Harrington J et al. Treatment of precocious puberty. UpToDate. www.uptodate.com/contents/treatment-of-precocious-puberty.
2. Lee JY et al. J Endocr Soc. 2020;4(9):bvaa065. doi: 10.1210/jendso/bvaa065.
3. Klink D et al. J Clin Endocrinol Metab. 2015;100(2):E270-5. doi: 10.1210/jc.2014-2439.
4. Schagen SEE et al. J Clin Endocrinol Metab. 2020;105(12):e4252-e4263. doi: 10.1210/clinem/dgaa604.
5. Alessandri SB et al. Clinics (Sao Paulo). 2012;67(6):591-6. doi: 10.6061/clinics/2012(06)08.
“They Paused Puberty but Is There a Cost?”
“Bone Health: Puberty Blockers Not Fully Reversible.”
Headlines such as these from major national news outlets have begun to cast doubt on one of the medications used in treating gender-diverse adolescents and young adults. GnRH agonists, such as leuprorelin and triptorelin, were first approved by the Food and Drug Administration in the 1980s and have been used since then for a variety of medical indications. In the decades since, these medications have been successfully used with a generally favorable side effect profile.
GnRH agonists and puberty
In the treatment of precocious puberty, GnRH agonists are often started prior to the age of 7, depending on the age at which the affected patient begins showing signs of central puberty. These include breast development, scrotal enlargement, and so on. GnRH agonists typically are continued until age 10-12, depending on the patient and an informed discussion with the patient’s parents about optimal outcomes.1 Therefore, it is not uncommon to see these medications used for anywhere from 1 to 4 years, depending on the age at which precocious puberty started.
GnRH agonists are used in two populations of transgender individuals. The first group is those youths who have just started their natal, or biological, puberty. The medication is not started until the patient has biochemical or physical exam evidence that puberty has started. The medication is then continued until hormones are started. This is usually 2-3 years on average, depending on the age at which the medication was started. This is essentially comparable with cisgender youths who have taken these medications for precocious puberty. The second population of individuals who use GnRH agonists is transgender women who are also on estrogen therapy. In these women, the GnRH agonist is used for androgen (testosterone) suppression.
Concerns over bone health
One of the main concerns recently expressed about long-term use of GnRH agonists is their effect on bone density. Adolescence is a critical time for bone mineral density (BMD) accrual and this is driven by sex hormones. When GnRH agonists are used to delay puberty in transgender adolescents, this then delays the maturation of the adult skeleton until the GnRH agonist is stopped (and natal puberty resumes) or cross-sex hormones are started. In a recent multicenter study2 looking at baseline BMD of transgender youth at the time of GnRH agonist initiation, 30% of those assigned male at birth and 13% of those assigned female at birth had low bone mineral density for age (defined as a BMD z score of <–2). For those with low BMD, their physical activity scores were significantly lower than those with normal BMD. Thus, these adolescents require close follow-up, just like their cisgender peers.
There are currently no long-term data on the risk of developing fractures or osteoporosis in those individuals who were treated with GnRH agonists and then went on to start cross-sex hormone therapy. Some studies suggest that there is a risk that BMD does not recover after being on cross-sex hormones,3 while another study suggested that transgender men recover their BMD after being on testosterone.4 It is still unclear in that study why transgender women did not recover their BMD or why they were low at baseline. Interestingly, a 2012 study5 from Brazil showed that there was no difference in BMD for cisgender girls who had been off their GnRH agonist therapy for at least 3 years, as compared with their age-matched controls who had never been on GnRH agonist therapy. These conflicting data highlight the importance of long-term follow-up, as well as the need to include age-matched, cisgender control subjects, to better understand if there is truly a difference in transgender individuals or if today’s adolescents, in general, have low BMD.
Lingering questions
In summary, the use of GnRH agonists in transgender adolescents remains controversial because of the potential long-term effects on bone mineral density. However, this risk must be balanced against the risks of allowing natal puberty to progress in certain transgender individuals with the development of undesired secondary sex characteristics. More longitudinal studies are needed to better understand the long-term risks of osteoporosis and fractures in those who have undergone GnRH agonist therapy as part of their gender-affirming medical care, as well as any clinical interventions that might help mitigate this risk.
Dr. Cooper is assistant professor of pediatrics at UT Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Harrington J et al. Treatment of precocious puberty. UpToDate. www.uptodate.com/contents/treatment-of-precocious-puberty.
2. Lee JY et al. J Endocr Soc. 2020;4(9):bvaa065. doi: 10.1210/jendso/bvaa065.
3. Klink D et al. J Clin Endocrinol Metab. 2015;100(2):E270-5. doi: 10.1210/jc.2014-2439.
4. Schagen SEE et al. J Clin Endocrinol Metab. 2020;105(12):e4252-e4263. doi: 10.1210/clinem/dgaa604.
5. Alessandri SB et al. Clinics (Sao Paulo). 2012;67(6):591-6. doi: 10.6061/clinics/2012(06)08.
“They Paused Puberty but Is There a Cost?”
“Bone Health: Puberty Blockers Not Fully Reversible.”
Headlines such as these from major national news outlets have begun to cast doubt on one of the medications used in treating gender-diverse adolescents and young adults. GnRH agonists, such as leuprorelin and triptorelin, were first approved by the Food and Drug Administration in the 1980s and have been used since then for a variety of medical indications. In the decades since, these medications have been successfully used with a generally favorable side effect profile.
GnRH agonists and puberty
In the treatment of precocious puberty, GnRH agonists are often started prior to the age of 7, depending on the age at which the affected patient begins showing signs of central puberty. These include breast development, scrotal enlargement, and so on. GnRH agonists typically are continued until age 10-12, depending on the patient and an informed discussion with the patient’s parents about optimal outcomes.1 Therefore, it is not uncommon to see these medications used for anywhere from 1 to 4 years, depending on the age at which precocious puberty started.
GnRH agonists are used in two populations of transgender individuals. The first group is those youths who have just started their natal, or biological, puberty. The medication is not started until the patient has biochemical or physical exam evidence that puberty has started. The medication is then continued until hormones are started. This is usually 2-3 years on average, depending on the age at which the medication was started. This is essentially comparable with cisgender youths who have taken these medications for precocious puberty. The second population of individuals who use GnRH agonists is transgender women who are also on estrogen therapy. In these women, the GnRH agonist is used for androgen (testosterone) suppression.
Concerns over bone health
One of the main concerns recently expressed about long-term use of GnRH agonists is their effect on bone density. Adolescence is a critical time for bone mineral density (BMD) accrual and this is driven by sex hormones. When GnRH agonists are used to delay puberty in transgender adolescents, this then delays the maturation of the adult skeleton until the GnRH agonist is stopped (and natal puberty resumes) or cross-sex hormones are started. In a recent multicenter study2 looking at baseline BMD of transgender youth at the time of GnRH agonist initiation, 30% of those assigned male at birth and 13% of those assigned female at birth had low bone mineral density for age (defined as a BMD z score of <–2). For those with low BMD, their physical activity scores were significantly lower than those with normal BMD. Thus, these adolescents require close follow-up, just like their cisgender peers.
There are currently no long-term data on the risk of developing fractures or osteoporosis in those individuals who were treated with GnRH agonists and then went on to start cross-sex hormone therapy. Some studies suggest that there is a risk that BMD does not recover after being on cross-sex hormones,3 while another study suggested that transgender men recover their BMD after being on testosterone.4 It is still unclear in that study why transgender women did not recover their BMD or why they were low at baseline. Interestingly, a 2012 study5 from Brazil showed that there was no difference in BMD for cisgender girls who had been off their GnRH agonist therapy for at least 3 years, as compared with their age-matched controls who had never been on GnRH agonist therapy. These conflicting data highlight the importance of long-term follow-up, as well as the need to include age-matched, cisgender control subjects, to better understand if there is truly a difference in transgender individuals or if today’s adolescents, in general, have low BMD.
Lingering questions
In summary, the use of GnRH agonists in transgender adolescents remains controversial because of the potential long-term effects on bone mineral density. However, this risk must be balanced against the risks of allowing natal puberty to progress in certain transgender individuals with the development of undesired secondary sex characteristics. More longitudinal studies are needed to better understand the long-term risks of osteoporosis and fractures in those who have undergone GnRH agonist therapy as part of their gender-affirming medical care, as well as any clinical interventions that might help mitigate this risk.
Dr. Cooper is assistant professor of pediatrics at UT Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
References
1. Harrington J et al. Treatment of precocious puberty. UpToDate. www.uptodate.com/contents/treatment-of-precocious-puberty.
2. Lee JY et al. J Endocr Soc. 2020;4(9):bvaa065. doi: 10.1210/jendso/bvaa065.
3. Klink D et al. J Clin Endocrinol Metab. 2015;100(2):E270-5. doi: 10.1210/jc.2014-2439.
4. Schagen SEE et al. J Clin Endocrinol Metab. 2020;105(12):e4252-e4263. doi: 10.1210/clinem/dgaa604.
5. Alessandri SB et al. Clinics (Sao Paulo). 2012;67(6):591-6. doi: 10.6061/clinics/2012(06)08.
Health care in America: Let that tapeworm grow
In my most recent column, “ ‘They All Laughed When I Spoke of Greedy Doctors,’ ” I attempted to provide a global understanding of some of the economic forces that have made American medicine what it is, how that happened, and why it is still happening.
I did not propose a fix. I have been proposing fixes for more than 30 years, on the pages of JAMA until 1999 and then for this news organization, most recently in 2019 with “Healthcare for All in a Land of Special Interests.”
Where you stand depends a lot on where you sit.
Is this good news or bad news? When William Hubbard was the dean of the University of Michigan School of Medicine in 1969, he said that “an academic medical center is the most efficient energy and resource trapping device that has ever been created” (personal communication, 1969).
To me as a faculty member of an academic medical center for many years, that was great news. We could grow faculty, erect buildings, take the best care of sick people, churn out research papers, mint new physicians and specialists, and get paid well in the process for doing “the Lord’s work.” What’s not to like? At that time, the proportion of the country’s gross national product expended for medical and health care was about 7%. And the predicted life span of an American at birth was 70.5 years.
Is this good news or bad news? In 2021, the proportion of our annual gross domestic product (GDP) consumed by health care was 18.3%, totaling $4.3 trillion, or $12,914 per person. For perspective, in 2021, the median income per capita was $37,638. Because quite a few Americans have very high incomes, the mean income per capita is much higher: $63,444. Predicted life span in 2021 was 76.4 years.
Thus, in a span of 53 years (1969-2022), only 5.9 years of life were gained per person born, for how many trillions of dollars expended? To me as a tax-paying citizen and payer of medical insurance premiums, that is bad news.
Is this good news or bad news? If we compare developed societies globally, our medical system does a whole lot of things very well indeed. But we spend a great deal more than any other country for health care and objectively achieve poorer outcomes. Thus, we are neither efficient nor effective. We keep a lot of workers very busy doing stuff, and they are generally well paid. As a worker, that’s good news; as a manager who values efficiency, it’s bad news indeed.
Is this good news or bad news? We’re the leader at finding money to pay people to do “health care work.” More Americans work in health care than any other field. In 2019, the United States employed some 21,000,000 people doing “health care and social assistance.” Among others, these occupations include physicians, dentists, dental hygienists and assistants, pharmacists, registered nurses, LVNs/LPNs, nursing aides, technologists and technicians, home health aides, respiratory therapists, occupational and speech therapists, social workers, childcare workers, and personal and home care aides. For a patient, parent, grandparent, and great-grandparent, it is good news to have all those folks available to take care of us when we need it.
So, while I have cringed at the frequent exposés from Roy Poses of what seem to me to be massive societal betrayals by American health care industry giants, it doesn’t have to be that way. Might it still be possible to do well while doing good?
A jobs program
Consider such common medical procedures as coronary artery stents or bypass grafts for stable angina (when optimal medical therapy is as good, or better than, and much less expensive); PSAs on asymptomatic men followed by unnecessary surgery for localized cancer; excess surgery for low back pain; and the jobs created by managing the people caught up in medical complications of the obesity epidemic.
Don’t forget the number of people employed simply to “follow the money” within our byzantine cockamamie medical billing system. In 2009, this prompted me to describe the bloated system as a “health care bubble” not unlike Enron, the submarket real estate financing debacle, or the dot-com boom and bust. I warned of the downside of bursting that bubble, particularly lost jobs.
The Affordable Care Act (ACA) provided health insurance to some 35 million Americans who had been uninsured. It retarded health care inflation. But it did nothing to trim administrative costs or very high pay for nonclinical executives, or shareholder profits in those companies that were for-profit, or drug and device prices. Without the support of all those groups, the ACA would never have passed Congress. The ACA has clearly been a mixed blessing.
If any large American constituency were ever serious about reducing the percentage of our GDP expended on health care, we have excellent ways to do that while improving the health and well-being of the American people. But remember, one person’s liability (unnecessary work) is another person’s asset (needed job).
The MBAization of medicine
Meanwhile, back at Dean Hubbard’s voracious academic medical center, the high intellect and driven nature of those who are attracted to medicine as a career has had other effects. The resulting organizations reflect not only the glorious calling of caring for the sick and the availability of lots of money to recruit and compensate leaders, but also the necessity to develop strong executive types who won’t be “eaten alive” by the high-powered workforce of demanding physicians and the surrounding environment.
Thus, it came as no great surprise that in its 2021 determination of America’s top 25 Best Large Employers, Forbes included five health care organizations and seven universities. Beating out such giants as NASA, Cisco, Microsoft, Netflix, and Google, the University of Alabama Birmingham Hospital was ranked first. Mayo Clinic and Yale University came in third and fifth, respectively, and at the other end of the list were Duke (23), MIT (24), and MD Anderson (25).
My goodness! Well done.
Yet, as a country attempting to be balanced, Warren Buffett’s descriptive entreaty on the 2021 failure of Haven, the Amazon-Chase-Berkshire Hathaway joint initiative, remains troubling. Calling upon Haven to change the U.S. health care system, Buffet said, “We learned a lot about the difficulty of changing around an industry that’s 17% of the GDP. We were fighting a tapeworm in the American economy, and the tapeworm won.” They had failed to tame the American health care cost beast.
I am on record as despising the “MBAization” of American medicine. Unfairly, I blamed a professional and technical discipline for what I considered misuse. I hereby repent and renounce my earlier condemnations.
Take it all over?
Here’s an idea: If you can’t beat them, join them.
Medical care is important, especially for acute illnesses and injuries, early cancer therapy, and many chronic conditions. But the real determinants of health writ large are social: wealth, education, housing, nutritious food, childcare, climate, clean air and water, meaningful employment, safety from violence, exercise schemes, vaccinations, and so on.
Why doesn’t the American medical-industrial complex simply bestow the label of “health care” on all health-related social determinants? Take it all over. Good “health care” jobs for everyone. Medical professionals will still be blamed for the low health quality and poor outcome scores, the main social determinants of health over which we have no control or influence.
Let that tapeworm grow to encompass all social determinants of health, and measure results by length and quality of life, national human happiness, and, of course, jobs. We can do it. Let that bubble glow. Party time.
And that’s the way it is. That’s my opinion.
George Lundberg, MD, is editor-in-chief at Cancer Commons, president of the Lundberg Institute, executive advisor at Cureus, and a clinical professor of pathology at Northwestern University. Previously, he served as editor-in-chief of JAMA (including 10 specialty journals), American Medical News, and Medscape.
A version of this article first appeared on Medscape.com.
In my most recent column, “ ‘They All Laughed When I Spoke of Greedy Doctors,’ ” I attempted to provide a global understanding of some of the economic forces that have made American medicine what it is, how that happened, and why it is still happening.
I did not propose a fix. I have been proposing fixes for more than 30 years, on the pages of JAMA until 1999 and then for this news organization, most recently in 2019 with “Healthcare for All in a Land of Special Interests.”
Where you stand depends a lot on where you sit.
Is this good news or bad news? When William Hubbard was the dean of the University of Michigan School of Medicine in 1969, he said that “an academic medical center is the most efficient energy and resource trapping device that has ever been created” (personal communication, 1969).
To me as a faculty member of an academic medical center for many years, that was great news. We could grow faculty, erect buildings, take the best care of sick people, churn out research papers, mint new physicians and specialists, and get paid well in the process for doing “the Lord’s work.” What’s not to like? At that time, the proportion of the country’s gross national product expended for medical and health care was about 7%. And the predicted life span of an American at birth was 70.5 years.
Is this good news or bad news? In 2021, the proportion of our annual gross domestic product (GDP) consumed by health care was 18.3%, totaling $4.3 trillion, or $12,914 per person. For perspective, in 2021, the median income per capita was $37,638. Because quite a few Americans have very high incomes, the mean income per capita is much higher: $63,444. Predicted life span in 2021 was 76.4 years.
Thus, in a span of 53 years (1969-2022), only 5.9 years of life were gained per person born, for how many trillions of dollars expended? To me as a tax-paying citizen and payer of medical insurance premiums, that is bad news.
Is this good news or bad news? If we compare developed societies globally, our medical system does a whole lot of things very well indeed. But we spend a great deal more than any other country for health care and objectively achieve poorer outcomes. Thus, we are neither efficient nor effective. We keep a lot of workers very busy doing stuff, and they are generally well paid. As a worker, that’s good news; as a manager who values efficiency, it’s bad news indeed.
Is this good news or bad news? We’re the leader at finding money to pay people to do “health care work.” More Americans work in health care than any other field. In 2019, the United States employed some 21,000,000 people doing “health care and social assistance.” Among others, these occupations include physicians, dentists, dental hygienists and assistants, pharmacists, registered nurses, LVNs/LPNs, nursing aides, technologists and technicians, home health aides, respiratory therapists, occupational and speech therapists, social workers, childcare workers, and personal and home care aides. For a patient, parent, grandparent, and great-grandparent, it is good news to have all those folks available to take care of us when we need it.
So, while I have cringed at the frequent exposés from Roy Poses of what seem to me to be massive societal betrayals by American health care industry giants, it doesn’t have to be that way. Might it still be possible to do well while doing good?
A jobs program
Consider such common medical procedures as coronary artery stents or bypass grafts for stable angina (when optimal medical therapy is as good, or better than, and much less expensive); PSAs on asymptomatic men followed by unnecessary surgery for localized cancer; excess surgery for low back pain; and the jobs created by managing the people caught up in medical complications of the obesity epidemic.
Don’t forget the number of people employed simply to “follow the money” within our byzantine cockamamie medical billing system. In 2009, this prompted me to describe the bloated system as a “health care bubble” not unlike Enron, the submarket real estate financing debacle, or the dot-com boom and bust. I warned of the downside of bursting that bubble, particularly lost jobs.
The Affordable Care Act (ACA) provided health insurance to some 35 million Americans who had been uninsured. It retarded health care inflation. But it did nothing to trim administrative costs or very high pay for nonclinical executives, or shareholder profits in those companies that were for-profit, or drug and device prices. Without the support of all those groups, the ACA would never have passed Congress. The ACA has clearly been a mixed blessing.
If any large American constituency were ever serious about reducing the percentage of our GDP expended on health care, we have excellent ways to do that while improving the health and well-being of the American people. But remember, one person’s liability (unnecessary work) is another person’s asset (needed job).
The MBAization of medicine
Meanwhile, back at Dean Hubbard’s voracious academic medical center, the high intellect and driven nature of those who are attracted to medicine as a career has had other effects. The resulting organizations reflect not only the glorious calling of caring for the sick and the availability of lots of money to recruit and compensate leaders, but also the necessity to develop strong executive types who won’t be “eaten alive” by the high-powered workforce of demanding physicians and the surrounding environment.
Thus, it came as no great surprise that in its 2021 determination of America’s top 25 Best Large Employers, Forbes included five health care organizations and seven universities. Beating out such giants as NASA, Cisco, Microsoft, Netflix, and Google, the University of Alabama Birmingham Hospital was ranked first. Mayo Clinic and Yale University came in third and fifth, respectively, and at the other end of the list were Duke (23), MIT (24), and MD Anderson (25).
My goodness! Well done.
Yet, as a country attempting to be balanced, Warren Buffett’s descriptive entreaty on the 2021 failure of Haven, the Amazon-Chase-Berkshire Hathaway joint initiative, remains troubling. Calling upon Haven to change the U.S. health care system, Buffet said, “We learned a lot about the difficulty of changing around an industry that’s 17% of the GDP. We were fighting a tapeworm in the American economy, and the tapeworm won.” They had failed to tame the American health care cost beast.
I am on record as despising the “MBAization” of American medicine. Unfairly, I blamed a professional and technical discipline for what I considered misuse. I hereby repent and renounce my earlier condemnations.
Take it all over?
Here’s an idea: If you can’t beat them, join them.
Medical care is important, especially for acute illnesses and injuries, early cancer therapy, and many chronic conditions. But the real determinants of health writ large are social: wealth, education, housing, nutritious food, childcare, climate, clean air and water, meaningful employment, safety from violence, exercise schemes, vaccinations, and so on.
Why doesn’t the American medical-industrial complex simply bestow the label of “health care” on all health-related social determinants? Take it all over. Good “health care” jobs for everyone. Medical professionals will still be blamed for the low health quality and poor outcome scores, the main social determinants of health over which we have no control or influence.
Let that tapeworm grow to encompass all social determinants of health, and measure results by length and quality of life, national human happiness, and, of course, jobs. We can do it. Let that bubble glow. Party time.
And that’s the way it is. That’s my opinion.
George Lundberg, MD, is editor-in-chief at Cancer Commons, president of the Lundberg Institute, executive advisor at Cureus, and a clinical professor of pathology at Northwestern University. Previously, he served as editor-in-chief of JAMA (including 10 specialty journals), American Medical News, and Medscape.
A version of this article first appeared on Medscape.com.
In my most recent column, “ ‘They All Laughed When I Spoke of Greedy Doctors,’ ” I attempted to provide a global understanding of some of the economic forces that have made American medicine what it is, how that happened, and why it is still happening.
I did not propose a fix. I have been proposing fixes for more than 30 years, on the pages of JAMA until 1999 and then for this news organization, most recently in 2019 with “Healthcare for All in a Land of Special Interests.”
Where you stand depends a lot on where you sit.
Is this good news or bad news? When William Hubbard was the dean of the University of Michigan School of Medicine in 1969, he said that “an academic medical center is the most efficient energy and resource trapping device that has ever been created” (personal communication, 1969).
To me as a faculty member of an academic medical center for many years, that was great news. We could grow faculty, erect buildings, take the best care of sick people, churn out research papers, mint new physicians and specialists, and get paid well in the process for doing “the Lord’s work.” What’s not to like? At that time, the proportion of the country’s gross national product expended for medical and health care was about 7%. And the predicted life span of an American at birth was 70.5 years.
Is this good news or bad news? In 2021, the proportion of our annual gross domestic product (GDP) consumed by health care was 18.3%, totaling $4.3 trillion, or $12,914 per person. For perspective, in 2021, the median income per capita was $37,638. Because quite a few Americans have very high incomes, the mean income per capita is much higher: $63,444. Predicted life span in 2021 was 76.4 years.
Thus, in a span of 53 years (1969-2022), only 5.9 years of life were gained per person born, for how many trillions of dollars expended? To me as a tax-paying citizen and payer of medical insurance premiums, that is bad news.
Is this good news or bad news? If we compare developed societies globally, our medical system does a whole lot of things very well indeed. But we spend a great deal more than any other country for health care and objectively achieve poorer outcomes. Thus, we are neither efficient nor effective. We keep a lot of workers very busy doing stuff, and they are generally well paid. As a worker, that’s good news; as a manager who values efficiency, it’s bad news indeed.
Is this good news or bad news? We’re the leader at finding money to pay people to do “health care work.” More Americans work in health care than any other field. In 2019, the United States employed some 21,000,000 people doing “health care and social assistance.” Among others, these occupations include physicians, dentists, dental hygienists and assistants, pharmacists, registered nurses, LVNs/LPNs, nursing aides, technologists and technicians, home health aides, respiratory therapists, occupational and speech therapists, social workers, childcare workers, and personal and home care aides. For a patient, parent, grandparent, and great-grandparent, it is good news to have all those folks available to take care of us when we need it.
So, while I have cringed at the frequent exposés from Roy Poses of what seem to me to be massive societal betrayals by American health care industry giants, it doesn’t have to be that way. Might it still be possible to do well while doing good?
A jobs program
Consider such common medical procedures as coronary artery stents or bypass grafts for stable angina (when optimal medical therapy is as good, or better than, and much less expensive); PSAs on asymptomatic men followed by unnecessary surgery for localized cancer; excess surgery for low back pain; and the jobs created by managing the people caught up in medical complications of the obesity epidemic.
Don’t forget the number of people employed simply to “follow the money” within our byzantine cockamamie medical billing system. In 2009, this prompted me to describe the bloated system as a “health care bubble” not unlike Enron, the submarket real estate financing debacle, or the dot-com boom and bust. I warned of the downside of bursting that bubble, particularly lost jobs.
The Affordable Care Act (ACA) provided health insurance to some 35 million Americans who had been uninsured. It retarded health care inflation. But it did nothing to trim administrative costs or very high pay for nonclinical executives, or shareholder profits in those companies that were for-profit, or drug and device prices. Without the support of all those groups, the ACA would never have passed Congress. The ACA has clearly been a mixed blessing.
If any large American constituency were ever serious about reducing the percentage of our GDP expended on health care, we have excellent ways to do that while improving the health and well-being of the American people. But remember, one person’s liability (unnecessary work) is another person’s asset (needed job).
The MBAization of medicine
Meanwhile, back at Dean Hubbard’s voracious academic medical center, the high intellect and driven nature of those who are attracted to medicine as a career has had other effects. The resulting organizations reflect not only the glorious calling of caring for the sick and the availability of lots of money to recruit and compensate leaders, but also the necessity to develop strong executive types who won’t be “eaten alive” by the high-powered workforce of demanding physicians and the surrounding environment.
Thus, it came as no great surprise that in its 2021 determination of America’s top 25 Best Large Employers, Forbes included five health care organizations and seven universities. Beating out such giants as NASA, Cisco, Microsoft, Netflix, and Google, the University of Alabama Birmingham Hospital was ranked first. Mayo Clinic and Yale University came in third and fifth, respectively, and at the other end of the list were Duke (23), MIT (24), and MD Anderson (25).
My goodness! Well done.
Yet, as a country attempting to be balanced, Warren Buffett’s descriptive entreaty on the 2021 failure of Haven, the Amazon-Chase-Berkshire Hathaway joint initiative, remains troubling. Calling upon Haven to change the U.S. health care system, Buffet said, “We learned a lot about the difficulty of changing around an industry that’s 17% of the GDP. We were fighting a tapeworm in the American economy, and the tapeworm won.” They had failed to tame the American health care cost beast.
I am on record as despising the “MBAization” of American medicine. Unfairly, I blamed a professional and technical discipline for what I considered misuse. I hereby repent and renounce my earlier condemnations.
Take it all over?
Here’s an idea: If you can’t beat them, join them.
Medical care is important, especially for acute illnesses and injuries, early cancer therapy, and many chronic conditions. But the real determinants of health writ large are social: wealth, education, housing, nutritious food, childcare, climate, clean air and water, meaningful employment, safety from violence, exercise schemes, vaccinations, and so on.
Why doesn’t the American medical-industrial complex simply bestow the label of “health care” on all health-related social determinants? Take it all over. Good “health care” jobs for everyone. Medical professionals will still be blamed for the low health quality and poor outcome scores, the main social determinants of health over which we have no control or influence.
Let that tapeworm grow to encompass all social determinants of health, and measure results by length and quality of life, national human happiness, and, of course, jobs. We can do it. Let that bubble glow. Party time.
And that’s the way it is. That’s my opinion.
George Lundberg, MD, is editor-in-chief at Cancer Commons, president of the Lundberg Institute, executive advisor at Cureus, and a clinical professor of pathology at Northwestern University. Previously, he served as editor-in-chief of JAMA (including 10 specialty journals), American Medical News, and Medscape.
A version of this article first appeared on Medscape.com.
Addressing the new mortality: Counseling on lethal means
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.
Although I have worked with depressed patients for many years, I have come to realize that
Firearms are now the leading cause of death for U.S. children and youth aged 1-24 years, an increase of 29.5% from 2019 to 2020. Among all youth firearm deaths, homicides (58%), suicides (37%), unintentional shootings (2%), and legal intervention (1%) were causes. These horrific numbers do not even include almost 400,000 child ED visits from 2010 to 2019 for nonfatal firearm injuries that were unintentional (39.4%), assault-related (37.7%), or self-harm (1.7%).
Accidental injury from firearms is greater when the weapon is a handgun or pistol as these are small enough to be fired by a 2-year-old, more likely to be stored loaded with ammunition as “self-protection,” and less likely to be in a gun storage case.
While an overall decline in gun ownership has occurred in homes with children ages 1-5, the proportion of weapons that are handguns has actually increased, posing higher danger to the family itself. We can’t assume hiding a weapon is ever enough as children often know the location of guns and their keys or lock codes.
Many Americans fear for their safety, have doubts about policing as protective, and strongly assert the need to protect themselves. While asking about guns in the home is universally recommended, these beliefs need to be taken into account in the discussion. It is also important to speak with the firearm owner, most often the father. We might ask, “Do you feel that you need a firearm in your home to feel safe?” as a way to nonjudgmentally acknowledge their beliefs. Because women are more likely to be killed by their spouses than by all other types of assailants combined, we can ask, “What dangers worry you the most?” and “Do you feel safe in your current and any past relationships?” If their answer is worrisome, the discussion must first turn to dealing with the family situation. If the perceived threat is outside the family, we can inform families that having a gun in evidence in the home greatly increases the risk of being hurt by an assailant as well as risk for child injury and death. We might ask, “Can you think of any other ways to protect your home (for example, alarm system, outdoor lighting, dog, or pepper spray)?”
If parents insist on keeping a gun, we can strongly and directly recommend that all firearms be stored locked, unloaded, and with ammunition locked and stored separately. We can provide information on such locking and storage options. Programs in which information on devices to disable the gun were provided – such as cables to pass through the chamber or trigger locks – have shown big increases in safe gun storage. It may be worth saying/posting information on the Child Access Prevention (CAP) laws, enacted by many states, making adults owning firearms that are not stored safely unloaded legally responsible for any resulting injuries or deaths. Such laws have reduced injuries of both children and adults by 30%-40%, unintentional gun deaths by 23%, and gun suicides by 11% (for 14- to 17-year-olds).
If the reason for owning a gun is for hunting, the owner is more likely to have had firearm safety training and use a long gun. Long guns are more difficult for a child. Discussing safe hunting gun storage is still worth recommending, as is removing any handguns they may own as these are most dangerous.
Removing or securing firearms is important for everyone’s safety but it is an essential and perhaps more difficult topic of discussion when a child is at risk for suicide or harming others. We need to consider some crucial facts about completed suicide, now the leading cause of death in children and adolescents and largely from guns. Most suicide attempts occur within 10 minutes of having a wave of suicidal thoughts. These waves of thoughts may be acted upon immediately when lethal means are available, with guns by far the most likely to result in death. It is therefore critical to assess access and counsel about lethal means in every family with a child reporting thoughts of killing themselves or others, or a history of violence or substance use. Even without imminent risk of self-harm, we can start a discussion about securing lethal means by saying, “It’s like wearing a seatbelt; you don’t expect a car crash, but if one happens, wearing a safety belt can greatly reduce injury. Guns are the most frequent cause of dying, so let’s make a plan to reduce access to those.”
Creating a written plan to deal with waves of suicidal thoughts is the basis of a Safety Plan. We can accurately remind families and youth that “When someone is struggling like this, sometimes suicidal feelings can show up and get worse fast. There are steps I routinely recommend to make things safer at home.”
It is important to assess the presence of guns in the primary home and other places the child spends time even if we have asked in the past, as things change. If firearms are present, even if locked up appropriately, when a child is having suicidal thoughts we can say, “What some gun owners in your situation do is store weapons elsewhere temporarily with someone they trust, at a self-storage unit, gun or pawn shop, or police department. I’d like to talk over storage options like that with you.” If the child themself owns the firearm, they need to agree with a removal or lock up plan for giving up their access.
If the gun owner is unwilling to remove firearms, even temporarily, we can ask them to lock them up separately from ammunition, a move that alone reduces danger a lot, and ensure the child has no access to the keys or combination. Better yet, we can ask, “Would you be willing to ask someone who doesn’t live in your home to hold the keys or to change the combination temporarily or at least store the ammunition?” They could also remove from the home a critical component of the gun so that it can’t fire, such as the slide or firing pin. If even those steps are not accepted, we can ask, “What other options would you be willing to consider to increase your child’s safety, at least until s/he is doing better?”
Whatever plan we negotiate with the family, as for any health behavior change strategy, it is more likely to be implemented if we summarize the specifics, write them down, and set a time-frame for carrying it out. We might say, “Let’s review who’s doing what and when: Dad will take the guns to his uncle’s house tomorrow and meanwhile, he will put them in the gun safe.” A follow-up call or contact soon, a key part of management of suicidal ideation, also signals how strongly we care about these safety measures and has been shown to increase implementation. We might call to say, “I wanted to check in and see how [you/your child] is doing and also ask how the plan is going that we talked about for gun storage.”
Discussions about firearms can spark strong emotions, especially if the family suspects political motivations. The Florida law prohibiting health care providers from discussing guns with patients was overturned but the thinking remains and may give us pause before having these important conversations. First of all, we need to stay calm and be prepared with key facts. The “sandwich” method is a useful approach to reduce resistance: start with something you can agree on (such as “What we hear on the news can make us all scared about safety”); then add the facts we want to convey (such as “You are actually less likely to get hurt in a break-in if you do not have a gun”); then conclude with a positive (such as “I can see that you are giving a lot of thought to how to keep your family safe”). Families generally trust our intentions and knowledge and appreciate rather than resent safety counseling when it is given in a nonjudgmental manner. Because we are protectors of child health, firearm safety must be an essential part of our anticipatory guidance.
Dr. Howard is assistant professor of pediatrics at Johns Hopkins University, Baltimore, and creator of CHADIS (www.CHADIS.com). She had no other relevant disclosures. Dr. Howard’s contribution to this publication was as a paid expert to MDedge News. E-mail her at [email protected].
*Wording suggestions adapted from https://www.hsph.harvard.edu/means-matter/recommendations/clinicians.















