User login
Meet the JCOM Author with Dr. Barkoudah: A Multidisciplinary Team–Based Clinical Care Pathway for Infective Endocarditis
Is it time to stop treating high triglycerides?
The publication of the PROMINENT trial, where pemafibrate successfully lowered high levels but was not associated with a lower risk for cardiovascular events, reinforced the point. Is it time to stop measuring and treating high triglycerides?
There may be noncardiovascular reasons to treat hypertriglyceridemia. Pancreatitis is the most cited one, given that the risk for pancreatitis increases with increasing triglyceride levels, especially in patients with a prior episode.
There may also be practical reasons to lower trigs. Because most cholesterol panels use the Friedewald equation to calculate low-density lipoprotein cholesterol (LDL-C) rather than measuring it directly, very high triglyceride levels can invalidate the calculation and return error messages on lab reports.
But we now have alternatives to measuring LDL-C, including non–high-density lipoprotein cholesterol (HDL-C) and apolipoprotein B (apoB), that better predict risk and are usable even in the setting of nonfasting samples when triglycerides are elevated.
Independent cardiovascular risk factor?
If we are going to measure and treat high triglycerides for cardiovascular reasons, the relevant question is, are high triglycerides an independent risk factor for cardiovascular disease?
Proponents have a broad swath of supportive literature to point at. Multiple studies have shown an association between triglyceride levels and cardiovascular risk. The evidence even extends beyond traditional epidemiologic analyses, to genetic studies that should be free from some of the problems seen in observational cohorts.
But it is difficult to be certain whether these associations are causal or merely confounding. An unhealthy diet will increase triglycerides, as will alcohol. Patients with diabetes or metabolic syndrome have high triglycerides. So do patients with nephrotic syndrome or hypothyroidism, or hypertensive patients taking thiazide diuretics. Adjusting for these baseline factors is possible but imperfect, and residual confounding is always an issue. An analysis of the Reykjavik and the EPIC-Norfolk studies found an association between triglyceride levels and cardiovascular risk. That risk was attenuated, but not eliminated, when adjusted for traditional risk factors such as age, smoking, blood pressure, diabetes, and cholesterol.
Randomized trials of triglyceride-lowering therapies would help resolve the question of whether hypertriglyceridemia contributes to coronary disease or simply identifies high-risk patients. Early trials seemed to support the idea of a causal link. The Helsinki Heart Study randomized patients to gemfibrozil or placebo and found a 34% relative risk reduction in coronary artery disease with the fibrate. But gemfibrozil didn’t only reduce triglycerides. It also increased HDL-C and lowered LDL-C relative to placebo, which may explain the observed benefit.
Gemfibrozil is rarely used today because we can achieve much greater LDL-C reductions with statins, as well as ezetimibe and PCSK9 inhibitors. The success of these drugs may not leave any room for triglyceride-lowering medications.
The pre- vs. post-statin era
In the 2005 FIELD study, participants were randomized to receive fenofibrate or placebo. Although patients weren’t taking statin at study entry, 17% of the placebo group started taking one during the trial. Fenofibrate wasn’t associated with a reduction in the primary endpoint, a combination of coronary heart disease death or nonfatal myocardial infarction (MI). Among the many secondary endpoints, nonfatal MI was lower but cardiovascular mortality was not in the fibrate-treated patients. In the same vein, the 2010 ACCORD study randomized patients to receive simvastatin plus fenofibrate or simvastatin alone. The composite primary outcome of MI, stroke, and cardiovascular mortality was not lowered nor were any secondary outcomes with the combination therapy. In the statin era, triglyceride-lowering therapies have not shown much benefit.
The final nail in the coffin may very well be the aforementioned PROMINENT trial. The new agent, pemafibrate, fared no better than its predecessor fenofibrate. Pemafibrate had no impact on the study’s primary composite outcome of nonfatal MI, stroke, coronary revascularization, or cardiovascular death despite being very effective at lowering triglycerides (by more than 25%). Patients treated with pemafibrate had increased LDL-C and apoB compared with the placebo group. When you realize that, the results of the study are not very surprising.
Some point to the results of REDUCE-IT as proof that triglycerides are still a valid target for pharmacotherapy. The debate on whether REDUCE-IT tested a good drug or a bad placebo is one for another day. The salient point for today is that the benefits of eicosapentaenoic acid (EPA) were seen regardless of either baseline or final triglyceride level. EPA may lower cardiac risk, but there is no widespread consensus that it does so by lowering triglycerides. There may be other mechanisms at work.
You could still argue that high triglycerides have value as a risk prediction tool even if their role as a target for drug therapy is questionable. There was a time when medications to lower triglycerides had a benefit. But this is the post-statin era, and that time has passed.
If you see patients with high triglycerides, treating them with triglyceride-lowering medication probably isn’t going to reduce their cardiovascular risk. Dietary interventions, encouraging exercise, and reducing alcohol consumption are better options. Not only will they lead to lower cholesterol levels, but they’ll lower cardiovascular risk, too.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, with a degree in epidemiology. He has disclosed no relevant financial relationships. He spends most of his time doing things that he doesn’t get paid for, like research, teaching, and podcasting. Occasionally he finds time to practice cardiology to pay the rent. He realizes that half of his research findings will be disproved in 5 years; he just doesn’t know which half. He is a regular contributor to the Montreal Gazette, CJAD radio, and CTV television in Montreal and is host of the award-winning podcast The Body of Evidence. The Body of Evidence.
A version of this article originally appeared on Medscape.com.
The publication of the PROMINENT trial, where pemafibrate successfully lowered high levels but was not associated with a lower risk for cardiovascular events, reinforced the point. Is it time to stop measuring and treating high triglycerides?
There may be noncardiovascular reasons to treat hypertriglyceridemia. Pancreatitis is the most cited one, given that the risk for pancreatitis increases with increasing triglyceride levels, especially in patients with a prior episode.
There may also be practical reasons to lower trigs. Because most cholesterol panels use the Friedewald equation to calculate low-density lipoprotein cholesterol (LDL-C) rather than measuring it directly, very high triglyceride levels can invalidate the calculation and return error messages on lab reports.
But we now have alternatives to measuring LDL-C, including non–high-density lipoprotein cholesterol (HDL-C) and apolipoprotein B (apoB), that better predict risk and are usable even in the setting of nonfasting samples when triglycerides are elevated.
Independent cardiovascular risk factor?
If we are going to measure and treat high triglycerides for cardiovascular reasons, the relevant question is, are high triglycerides an independent risk factor for cardiovascular disease?
Proponents have a broad swath of supportive literature to point at. Multiple studies have shown an association between triglyceride levels and cardiovascular risk. The evidence even extends beyond traditional epidemiologic analyses, to genetic studies that should be free from some of the problems seen in observational cohorts.
But it is difficult to be certain whether these associations are causal or merely confounding. An unhealthy diet will increase triglycerides, as will alcohol. Patients with diabetes or metabolic syndrome have high triglycerides. So do patients with nephrotic syndrome or hypothyroidism, or hypertensive patients taking thiazide diuretics. Adjusting for these baseline factors is possible but imperfect, and residual confounding is always an issue. An analysis of the Reykjavik and the EPIC-Norfolk studies found an association between triglyceride levels and cardiovascular risk. That risk was attenuated, but not eliminated, when adjusted for traditional risk factors such as age, smoking, blood pressure, diabetes, and cholesterol.
Randomized trials of triglyceride-lowering therapies would help resolve the question of whether hypertriglyceridemia contributes to coronary disease or simply identifies high-risk patients. Early trials seemed to support the idea of a causal link. The Helsinki Heart Study randomized patients to gemfibrozil or placebo and found a 34% relative risk reduction in coronary artery disease with the fibrate. But gemfibrozil didn’t only reduce triglycerides. It also increased HDL-C and lowered LDL-C relative to placebo, which may explain the observed benefit.
Gemfibrozil is rarely used today because we can achieve much greater LDL-C reductions with statins, as well as ezetimibe and PCSK9 inhibitors. The success of these drugs may not leave any room for triglyceride-lowering medications.
The pre- vs. post-statin era
In the 2005 FIELD study, participants were randomized to receive fenofibrate or placebo. Although patients weren’t taking statin at study entry, 17% of the placebo group started taking one during the trial. Fenofibrate wasn’t associated with a reduction in the primary endpoint, a combination of coronary heart disease death or nonfatal myocardial infarction (MI). Among the many secondary endpoints, nonfatal MI was lower but cardiovascular mortality was not in the fibrate-treated patients. In the same vein, the 2010 ACCORD study randomized patients to receive simvastatin plus fenofibrate or simvastatin alone. The composite primary outcome of MI, stroke, and cardiovascular mortality was not lowered nor were any secondary outcomes with the combination therapy. In the statin era, triglyceride-lowering therapies have not shown much benefit.
The final nail in the coffin may very well be the aforementioned PROMINENT trial. The new agent, pemafibrate, fared no better than its predecessor fenofibrate. Pemafibrate had no impact on the study’s primary composite outcome of nonfatal MI, stroke, coronary revascularization, or cardiovascular death despite being very effective at lowering triglycerides (by more than 25%). Patients treated with pemafibrate had increased LDL-C and apoB compared with the placebo group. When you realize that, the results of the study are not very surprising.
Some point to the results of REDUCE-IT as proof that triglycerides are still a valid target for pharmacotherapy. The debate on whether REDUCE-IT tested a good drug or a bad placebo is one for another day. The salient point for today is that the benefits of eicosapentaenoic acid (EPA) were seen regardless of either baseline or final triglyceride level. EPA may lower cardiac risk, but there is no widespread consensus that it does so by lowering triglycerides. There may be other mechanisms at work.
You could still argue that high triglycerides have value as a risk prediction tool even if their role as a target for drug therapy is questionable. There was a time when medications to lower triglycerides had a benefit. But this is the post-statin era, and that time has passed.
If you see patients with high triglycerides, treating them with triglyceride-lowering medication probably isn’t going to reduce their cardiovascular risk. Dietary interventions, encouraging exercise, and reducing alcohol consumption are better options. Not only will they lead to lower cholesterol levels, but they’ll lower cardiovascular risk, too.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, with a degree in epidemiology. He has disclosed no relevant financial relationships. He spends most of his time doing things that he doesn’t get paid for, like research, teaching, and podcasting. Occasionally he finds time to practice cardiology to pay the rent. He realizes that half of his research findings will be disproved in 5 years; he just doesn’t know which half. He is a regular contributor to the Montreal Gazette, CJAD radio, and CTV television in Montreal and is host of the award-winning podcast The Body of Evidence. The Body of Evidence.
A version of this article originally appeared on Medscape.com.
The publication of the PROMINENT trial, where pemafibrate successfully lowered high levels but was not associated with a lower risk for cardiovascular events, reinforced the point. Is it time to stop measuring and treating high triglycerides?
There may be noncardiovascular reasons to treat hypertriglyceridemia. Pancreatitis is the most cited one, given that the risk for pancreatitis increases with increasing triglyceride levels, especially in patients with a prior episode.
There may also be practical reasons to lower trigs. Because most cholesterol panels use the Friedewald equation to calculate low-density lipoprotein cholesterol (LDL-C) rather than measuring it directly, very high triglyceride levels can invalidate the calculation and return error messages on lab reports.
But we now have alternatives to measuring LDL-C, including non–high-density lipoprotein cholesterol (HDL-C) and apolipoprotein B (apoB), that better predict risk and are usable even in the setting of nonfasting samples when triglycerides are elevated.
Independent cardiovascular risk factor?
If we are going to measure and treat high triglycerides for cardiovascular reasons, the relevant question is, are high triglycerides an independent risk factor for cardiovascular disease?
Proponents have a broad swath of supportive literature to point at. Multiple studies have shown an association between triglyceride levels and cardiovascular risk. The evidence even extends beyond traditional epidemiologic analyses, to genetic studies that should be free from some of the problems seen in observational cohorts.
But it is difficult to be certain whether these associations are causal or merely confounding. An unhealthy diet will increase triglycerides, as will alcohol. Patients with diabetes or metabolic syndrome have high triglycerides. So do patients with nephrotic syndrome or hypothyroidism, or hypertensive patients taking thiazide diuretics. Adjusting for these baseline factors is possible but imperfect, and residual confounding is always an issue. An analysis of the Reykjavik and the EPIC-Norfolk studies found an association between triglyceride levels and cardiovascular risk. That risk was attenuated, but not eliminated, when adjusted for traditional risk factors such as age, smoking, blood pressure, diabetes, and cholesterol.
Randomized trials of triglyceride-lowering therapies would help resolve the question of whether hypertriglyceridemia contributes to coronary disease or simply identifies high-risk patients. Early trials seemed to support the idea of a causal link. The Helsinki Heart Study randomized patients to gemfibrozil or placebo and found a 34% relative risk reduction in coronary artery disease with the fibrate. But gemfibrozil didn’t only reduce triglycerides. It also increased HDL-C and lowered LDL-C relative to placebo, which may explain the observed benefit.
Gemfibrozil is rarely used today because we can achieve much greater LDL-C reductions with statins, as well as ezetimibe and PCSK9 inhibitors. The success of these drugs may not leave any room for triglyceride-lowering medications.
The pre- vs. post-statin era
In the 2005 FIELD study, participants were randomized to receive fenofibrate or placebo. Although patients weren’t taking statin at study entry, 17% of the placebo group started taking one during the trial. Fenofibrate wasn’t associated with a reduction in the primary endpoint, a combination of coronary heart disease death or nonfatal myocardial infarction (MI). Among the many secondary endpoints, nonfatal MI was lower but cardiovascular mortality was not in the fibrate-treated patients. In the same vein, the 2010 ACCORD study randomized patients to receive simvastatin plus fenofibrate or simvastatin alone. The composite primary outcome of MI, stroke, and cardiovascular mortality was not lowered nor were any secondary outcomes with the combination therapy. In the statin era, triglyceride-lowering therapies have not shown much benefit.
The final nail in the coffin may very well be the aforementioned PROMINENT trial. The new agent, pemafibrate, fared no better than its predecessor fenofibrate. Pemafibrate had no impact on the study’s primary composite outcome of nonfatal MI, stroke, coronary revascularization, or cardiovascular death despite being very effective at lowering triglycerides (by more than 25%). Patients treated with pemafibrate had increased LDL-C and apoB compared with the placebo group. When you realize that, the results of the study are not very surprising.
Some point to the results of REDUCE-IT as proof that triglycerides are still a valid target for pharmacotherapy. The debate on whether REDUCE-IT tested a good drug or a bad placebo is one for another day. The salient point for today is that the benefits of eicosapentaenoic acid (EPA) were seen regardless of either baseline or final triglyceride level. EPA may lower cardiac risk, but there is no widespread consensus that it does so by lowering triglycerides. There may be other mechanisms at work.
You could still argue that high triglycerides have value as a risk prediction tool even if their role as a target for drug therapy is questionable. There was a time when medications to lower triglycerides had a benefit. But this is the post-statin era, and that time has passed.
If you see patients with high triglycerides, treating them with triglyceride-lowering medication probably isn’t going to reduce their cardiovascular risk. Dietary interventions, encouraging exercise, and reducing alcohol consumption are better options. Not only will they lead to lower cholesterol levels, but they’ll lower cardiovascular risk, too.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal, with a degree in epidemiology. He has disclosed no relevant financial relationships. He spends most of his time doing things that he doesn’t get paid for, like research, teaching, and podcasting. Occasionally he finds time to practice cardiology to pay the rent. He realizes that half of his research findings will be disproved in 5 years; he just doesn’t know which half. He is a regular contributor to the Montreal Gazette, CJAD radio, and CTV television in Montreal and is host of the award-winning podcast The Body of Evidence. The Body of Evidence.
A version of this article originally appeared on Medscape.com.
Commotio cordis underrecognized, undertreated outside of sports
Sudden cardiac arrest (SCA) due to commotio cordis occurs more frequently in non–sport-related settings than is commonly thought, resulting in lower rates of resuscitation and increased mortality, especially among young women, a new review suggests.
The condition is rare, caused by an often fatal arrhythmia secondary to a blunt, nonpenetrating impact over the precordium, without direct structural damage to the heart itself. Common causes in nonsport settings include assault, motor vehicle accidents (MVAs), and daily activities such as occupational accidents.
“We found a stark difference in mortality outcomes between non–sport-related commotio cordis compared to sport-related events,” at 88% vs. 66%, Han S. Lim, MBBS, PhD, of the University of Melbourne, and Austin Health, Heidelberg, Australia, told this news organization. “Rates of cardiopulmonary resuscitation (CPR) (27% vs. 97%) and defibrillation (17% vs. 81%) were considerably lower in the non–sport-related events.”
“Although still being male-predominant, of concern, we saw a higher proportion of females in non–sport-related commotio cordis due to assault, MVAs, and other activities,” he noted. Such events may occur “in secluded domestic settings, may not be witnessed, or may occur as intentional harm, whereby the witness could also be the perpetrator, reducing the likelihood of prompt diagnosis, CPR, and defibrillation administration.”
The study was published online in JACC: Clinical Electrophysiology.
Young women affected
Dr. Lim and colleagues searched the literature through 2021 for all cases of commotio cordis. Three hundred and thirty-four cases from among 53 citations were included in the analysis; of those, 121 (36%) occurred in non–sport-related settings, including assault (76%), MVAs (7%), and daily activities (16%). “Daily activities” comprised activities that were expected in a person’s day-to-day routine such as falls, play fighting (in children), and occupational accidents.
Non–sport-related cases primarily involved nonprojectile etiologies (95%), including bodily contact (79%), such as impacts from fists, feet, and knees; impacts with handlebars or steering wheels; and solid stick-like weapons and flat surfaces.
Sport-related cases involved a significantly higher proportion of projectiles (94% vs. 5%) and occurred across a range of sports, mostly at the competitive level (66%).
Both sport-related and non–sport-related commotio cordis affected a similar younger demographic (mean age, 19; mostly males). No statistically significant differences between the two groups were seen with regard to previous cardiac history or family history of cardiac disease, or in arrhythmias on electrocardiogram, biomarkers, or imaging findings.
However, in non–sport-related events, the proportion of females affected was significantly higher (13% vs. 2%), as was mortality (88% vs. 66%). Rates were lower for CPR (27% vs. 97%) and defibrillation use (17% vs. 81%), and resuscitation was more commonly delayed beyond 3 minutes (80% vs. 5%).
The finding that more than a third of reported cases were non–sport-related “is higher than previously reported, and included data from 15 different countries,” the authors noted.
Study limitations included the use of data only from published studies, inclusion of a case series limited to fatal cases, small sample sizes, and lack of consistent reporting of demographic data, mechanisms, investigation results, management, and outcomes.
Increased awareness ‘essential’
Dr. Lim and colleagues concluded that increased awareness of non–sport-related commotio cordis is “essential” for early recognition, resuscitation, and mortality reduction.
Jim Cheung, MD, chair of the American College of Cardiology’s electrophysiology section, “completely agrees.” Greater awareness among the general population could reduce barriers to CPR and automated external defibrillator (AED) use, he said, which in turn, can lead to improved survival.
Furthermore, Dr. Cheung added, “This study underscores the importance of ensuring that non–cardiology-trained physicians such as emergency medicine physicians and trauma surgeons who might encounter patients with non–sports-related commotio cordis recognize the entity during the course of treatment.”
Because the review relied only on published cases, “it may not represent the true breadth of cases that are occurring in the real world,” he noted. “I suspect that cases that occur outside of sports-related activities, such as MVAs and assault, are more likely to be underreported and that the true proportion of non–sports-related commotio cordis may be significantly higher than 36%.” Increased reporting of cases as part of an international commotio cordis registry would help provide additional insights, he suggested.
“There is a common misperception that SCA only occurs among older patients and patients with known coronary artery disease or heart failure,” he said. “For us to move the needle on improving SCA survival, we will need to tackle the problem from multiple angles including increasing public awareness, training the public on CPR and AED use, and improving access to AEDs by addressing structural barriers.”
Dr. Cheung pointed to ongoing efforts by nonprofit, patient-driven organizations such as the SADS Foundation and Omar Carter Foundation, and professional societies such as the American College of Cardiology, the American Heart Association, and Heart Rhythm Society, to direct public awareness campaigns and legislative proposals to address this problem.
Similar efforts are underway among cardiac societies and SCA awareness groups in Australia, Dr. Lim said.
No funding or relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
Sudden cardiac arrest (SCA) due to commotio cordis occurs more frequently in non–sport-related settings than is commonly thought, resulting in lower rates of resuscitation and increased mortality, especially among young women, a new review suggests.
The condition is rare, caused by an often fatal arrhythmia secondary to a blunt, nonpenetrating impact over the precordium, without direct structural damage to the heart itself. Common causes in nonsport settings include assault, motor vehicle accidents (MVAs), and daily activities such as occupational accidents.
“We found a stark difference in mortality outcomes between non–sport-related commotio cordis compared to sport-related events,” at 88% vs. 66%, Han S. Lim, MBBS, PhD, of the University of Melbourne, and Austin Health, Heidelberg, Australia, told this news organization. “Rates of cardiopulmonary resuscitation (CPR) (27% vs. 97%) and defibrillation (17% vs. 81%) were considerably lower in the non–sport-related events.”
“Although still being male-predominant, of concern, we saw a higher proportion of females in non–sport-related commotio cordis due to assault, MVAs, and other activities,” he noted. Such events may occur “in secluded domestic settings, may not be witnessed, or may occur as intentional harm, whereby the witness could also be the perpetrator, reducing the likelihood of prompt diagnosis, CPR, and defibrillation administration.”
The study was published online in JACC: Clinical Electrophysiology.
Young women affected
Dr. Lim and colleagues searched the literature through 2021 for all cases of commotio cordis. Three hundred and thirty-four cases from among 53 citations were included in the analysis; of those, 121 (36%) occurred in non–sport-related settings, including assault (76%), MVAs (7%), and daily activities (16%). “Daily activities” comprised activities that were expected in a person’s day-to-day routine such as falls, play fighting (in children), and occupational accidents.
Non–sport-related cases primarily involved nonprojectile etiologies (95%), including bodily contact (79%), such as impacts from fists, feet, and knees; impacts with handlebars or steering wheels; and solid stick-like weapons and flat surfaces.
Sport-related cases involved a significantly higher proportion of projectiles (94% vs. 5%) and occurred across a range of sports, mostly at the competitive level (66%).
Both sport-related and non–sport-related commotio cordis affected a similar younger demographic (mean age, 19; mostly males). No statistically significant differences between the two groups were seen with regard to previous cardiac history or family history of cardiac disease, or in arrhythmias on electrocardiogram, biomarkers, or imaging findings.
However, in non–sport-related events, the proportion of females affected was significantly higher (13% vs. 2%), as was mortality (88% vs. 66%). Rates were lower for CPR (27% vs. 97%) and defibrillation use (17% vs. 81%), and resuscitation was more commonly delayed beyond 3 minutes (80% vs. 5%).
The finding that more than a third of reported cases were non–sport-related “is higher than previously reported, and included data from 15 different countries,” the authors noted.
Study limitations included the use of data only from published studies, inclusion of a case series limited to fatal cases, small sample sizes, and lack of consistent reporting of demographic data, mechanisms, investigation results, management, and outcomes.
Increased awareness ‘essential’
Dr. Lim and colleagues concluded that increased awareness of non–sport-related commotio cordis is “essential” for early recognition, resuscitation, and mortality reduction.
Jim Cheung, MD, chair of the American College of Cardiology’s electrophysiology section, “completely agrees.” Greater awareness among the general population could reduce barriers to CPR and automated external defibrillator (AED) use, he said, which in turn, can lead to improved survival.
Furthermore, Dr. Cheung added, “This study underscores the importance of ensuring that non–cardiology-trained physicians such as emergency medicine physicians and trauma surgeons who might encounter patients with non–sports-related commotio cordis recognize the entity during the course of treatment.”
Because the review relied only on published cases, “it may not represent the true breadth of cases that are occurring in the real world,” he noted. “I suspect that cases that occur outside of sports-related activities, such as MVAs and assault, are more likely to be underreported and that the true proportion of non–sports-related commotio cordis may be significantly higher than 36%.” Increased reporting of cases as part of an international commotio cordis registry would help provide additional insights, he suggested.
“There is a common misperception that SCA only occurs among older patients and patients with known coronary artery disease or heart failure,” he said. “For us to move the needle on improving SCA survival, we will need to tackle the problem from multiple angles including increasing public awareness, training the public on CPR and AED use, and improving access to AEDs by addressing structural barriers.”
Dr. Cheung pointed to ongoing efforts by nonprofit, patient-driven organizations such as the SADS Foundation and Omar Carter Foundation, and professional societies such as the American College of Cardiology, the American Heart Association, and Heart Rhythm Society, to direct public awareness campaigns and legislative proposals to address this problem.
Similar efforts are underway among cardiac societies and SCA awareness groups in Australia, Dr. Lim said.
No funding or relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
Sudden cardiac arrest (SCA) due to commotio cordis occurs more frequently in non–sport-related settings than is commonly thought, resulting in lower rates of resuscitation and increased mortality, especially among young women, a new review suggests.
The condition is rare, caused by an often fatal arrhythmia secondary to a blunt, nonpenetrating impact over the precordium, without direct structural damage to the heart itself. Common causes in nonsport settings include assault, motor vehicle accidents (MVAs), and daily activities such as occupational accidents.
“We found a stark difference in mortality outcomes between non–sport-related commotio cordis compared to sport-related events,” at 88% vs. 66%, Han S. Lim, MBBS, PhD, of the University of Melbourne, and Austin Health, Heidelberg, Australia, told this news organization. “Rates of cardiopulmonary resuscitation (CPR) (27% vs. 97%) and defibrillation (17% vs. 81%) were considerably lower in the non–sport-related events.”
“Although still being male-predominant, of concern, we saw a higher proportion of females in non–sport-related commotio cordis due to assault, MVAs, and other activities,” he noted. Such events may occur “in secluded domestic settings, may not be witnessed, or may occur as intentional harm, whereby the witness could also be the perpetrator, reducing the likelihood of prompt diagnosis, CPR, and defibrillation administration.”
The study was published online in JACC: Clinical Electrophysiology.
Young women affected
Dr. Lim and colleagues searched the literature through 2021 for all cases of commotio cordis. Three hundred and thirty-four cases from among 53 citations were included in the analysis; of those, 121 (36%) occurred in non–sport-related settings, including assault (76%), MVAs (7%), and daily activities (16%). “Daily activities” comprised activities that were expected in a person’s day-to-day routine such as falls, play fighting (in children), and occupational accidents.
Non–sport-related cases primarily involved nonprojectile etiologies (95%), including bodily contact (79%), such as impacts from fists, feet, and knees; impacts with handlebars or steering wheels; and solid stick-like weapons and flat surfaces.
Sport-related cases involved a significantly higher proportion of projectiles (94% vs. 5%) and occurred across a range of sports, mostly at the competitive level (66%).
Both sport-related and non–sport-related commotio cordis affected a similar younger demographic (mean age, 19; mostly males). No statistically significant differences between the two groups were seen with regard to previous cardiac history or family history of cardiac disease, or in arrhythmias on electrocardiogram, biomarkers, or imaging findings.
However, in non–sport-related events, the proportion of females affected was significantly higher (13% vs. 2%), as was mortality (88% vs. 66%). Rates were lower for CPR (27% vs. 97%) and defibrillation use (17% vs. 81%), and resuscitation was more commonly delayed beyond 3 minutes (80% vs. 5%).
The finding that more than a third of reported cases were non–sport-related “is higher than previously reported, and included data from 15 different countries,” the authors noted.
Study limitations included the use of data only from published studies, inclusion of a case series limited to fatal cases, small sample sizes, and lack of consistent reporting of demographic data, mechanisms, investigation results, management, and outcomes.
Increased awareness ‘essential’
Dr. Lim and colleagues concluded that increased awareness of non–sport-related commotio cordis is “essential” for early recognition, resuscitation, and mortality reduction.
Jim Cheung, MD, chair of the American College of Cardiology’s electrophysiology section, “completely agrees.” Greater awareness among the general population could reduce barriers to CPR and automated external defibrillator (AED) use, he said, which in turn, can lead to improved survival.
Furthermore, Dr. Cheung added, “This study underscores the importance of ensuring that non–cardiology-trained physicians such as emergency medicine physicians and trauma surgeons who might encounter patients with non–sports-related commotio cordis recognize the entity during the course of treatment.”
Because the review relied only on published cases, “it may not represent the true breadth of cases that are occurring in the real world,” he noted. “I suspect that cases that occur outside of sports-related activities, such as MVAs and assault, are more likely to be underreported and that the true proportion of non–sports-related commotio cordis may be significantly higher than 36%.” Increased reporting of cases as part of an international commotio cordis registry would help provide additional insights, he suggested.
“There is a common misperception that SCA only occurs among older patients and patients with known coronary artery disease or heart failure,” he said. “For us to move the needle on improving SCA survival, we will need to tackle the problem from multiple angles including increasing public awareness, training the public on CPR and AED use, and improving access to AEDs by addressing structural barriers.”
Dr. Cheung pointed to ongoing efforts by nonprofit, patient-driven organizations such as the SADS Foundation and Omar Carter Foundation, and professional societies such as the American College of Cardiology, the American Heart Association, and Heart Rhythm Society, to direct public awareness campaigns and legislative proposals to address this problem.
Similar efforts are underway among cardiac societies and SCA awareness groups in Australia, Dr. Lim said.
No funding or relevant financial relationships were disclosed.
A version of this article first appeared on Medscape.com.
FROM JACC: CLINICAL ELECTROPHYSIOLOGY
One or two high-step days may reduce mortality risks
Taking 8,000 steps or more for just 1 or 2 days a week was linked to a significant reduction in all-cause and cardiovascular mortality, according to a study of about 3,000 adults.
Previous research has shown lower mortality rates among individuals who walk consistently, especially those who log at least 8,000 steps daily, but the benefit of intense walking just once or twice a week on long-term health outcomes has not been examined, wrote Kosuke Inoue, MD, of Kyoto University, Japan, and colleagues.
In a study published in JAMA Network Open, the researchers reviewed 10-year follow-up data for 3,101 adults aged 20 years and older who were part of the 2005 and 2006 National Health and Nutrition Examination Survey (NHANES).
The participants were asked to wear accelerometers to track their steps for 7 consecutive days. The researchers assessed the dose-response relationship between days of taking 8,000 steps or more (about 4 miles) during 1 week, and the primary outcome of all-cause mortality risk after 10 years. Cardiovascular mortality risk after 10 years was a secondary outcome.
The mean age of the participants was 50.5 years and 51% were women. The breakdown by ethnicity was 51% White, 21% Black, 24% Hispanic, and 4% other races/ethnicities. A total of 632 individuals took 8,000 steps or more 0 days a week, 532 took at least 8,000 steps 1-2 days per week, and 1,937 took at least 8,000 steps 3-7 days a week.
During the 10-year follow-up period, overall all-cause mortality was 14.2% and cardiovascular mortality was 5.3% across all step groups.
In an adjusted analysis, individuals who took at least 8,000 steps 1-2 days a week had a 14.9% lower all-cause mortality risk compared with those who never reached 8,000 daily steps. This difference was similar to the 16.5% reduced mortality risk for those who took at least 8,000 steps 3-7 days a week.
Similarly, compared with the group with no days of at least 8,000 steps, cardiovascular mortality risk was 8.1% lower for those who took 8,000 steps 1-2 days per week and 8.4% lower for those who took at least 8,000 steps 3-7 days per week. The decreased mortality risk plateaued at 3-4 days.
These patterns in reduced all-cause mortality risk persisted in a stratified analysis by age (younger than 65 years and 65 years and older) and sex. Similar patterns in reduced mortality also emerged when the researchers used different thresholds of daily steps, such as a minimum of 10,000 steps instead of 8,000. The adjusted all-cause mortality for groups who took at least 10,000 steps 1-2 days a week, 3-7 days a week, and no days a week were 8.1%, 7.3%, and 16.7%, respectively, with corresponding cardiovascular mortality risks of 2.4%, 2.3%, and 7.0%, respectively.
“Given the simplicity and ease of counting daily steps, our findings indicate that the recommended number of steps taken on as few as 1 to 2 days per week may be a feasible option for individuals who are striving to achieve some health benefits through adhering to a recommended daily step count but are unable to accomplish this on a daily basis,” the researchers wrote in their discussion.
The findings were limited by several factors including the use daily step measures for 1 week only at baseline, with no data on how physical activity changes might impact mortality risk, the researchers noted. Other limitations included possible accelerometer error and misclassification of activity, possible selection bias, and lack of data on cause-specific mortality outside of cardiovascular death, they said.
However, the results were strengthened by the use of accelerometers as objective measures of activity and by the availability of 10-year follow-up data for nearly 100% of the participants, they said.
“Although our findings might suffer from residual confounding that should be addressed in future research, they suggest that people may receive substantial health benefits even if a sufficient number of steps are taken on only a couple days of the week,” they concluded.
Proceed with caution
The current study findings should be interpreted cautiously in light of the potential unmeasured confounding factors and selection bias that often occur in studies of physical activity, James Sawalla Guseh, MD, of Massachusetts General Hospital, and Jose F. Figueroa, MD, of Harvard T.H. Chan School of Public Health, Boston, wrote in an accompanying editorial.
The results support previous studies showing some longevity benefits with “weekend warrior” patterns of intense physical activity for only a couple of days; however, “the body of evidence for sporadic activity is not as robust as the evidence for sustained and regular aerobic activity,” the authors emphasized.
The editorial authors also highlighted the limitations of the current study, including the observational design and significant differences in demographics and comorbidities between the 1- to 2-days of 8,000 steps exercise group and the 0-day group, as well as the reliance on only a week’s worth of data to infer 10 years’ mortality.
Although the data are consistent with previous observations that increased exercise volume reduces mortality, more research is needed, as the current study findings may not reflect other dimensions of health, including neurological health, they said.
Despite the need for cautious interpretation of the results, the current study “supports the emerging and popular idea that step counting, which does not require consideration of exercise duration or intensity, can offer guidance toward robust and favorable health outcomes,” and may inform step-based activity goals to improve public health, the editorialists wrote.
The study was supported by the Japan Agency for Medical Research and Development, the Japan Society for the Promotion of Science, the Japan Endocrine Society, and the Meiji Yasuda Life Foundation of Health and Welfare. Dr. Inoue also was supported by the Program for the Development of Next-Generation Leading Scientists With Global Insight sponsored by the Ministry of Education, Culture, Sports, Science and Technology, Japan. The other researchers had no relevant financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
Taking 8,000 steps or more for just 1 or 2 days a week was linked to a significant reduction in all-cause and cardiovascular mortality, according to a study of about 3,000 adults.
Previous research has shown lower mortality rates among individuals who walk consistently, especially those who log at least 8,000 steps daily, but the benefit of intense walking just once or twice a week on long-term health outcomes has not been examined, wrote Kosuke Inoue, MD, of Kyoto University, Japan, and colleagues.
In a study published in JAMA Network Open, the researchers reviewed 10-year follow-up data for 3,101 adults aged 20 years and older who were part of the 2005 and 2006 National Health and Nutrition Examination Survey (NHANES).
The participants were asked to wear accelerometers to track their steps for 7 consecutive days. The researchers assessed the dose-response relationship between days of taking 8,000 steps or more (about 4 miles) during 1 week, and the primary outcome of all-cause mortality risk after 10 years. Cardiovascular mortality risk after 10 years was a secondary outcome.
The mean age of the participants was 50.5 years and 51% were women. The breakdown by ethnicity was 51% White, 21% Black, 24% Hispanic, and 4% other races/ethnicities. A total of 632 individuals took 8,000 steps or more 0 days a week, 532 took at least 8,000 steps 1-2 days per week, and 1,937 took at least 8,000 steps 3-7 days a week.
During the 10-year follow-up period, overall all-cause mortality was 14.2% and cardiovascular mortality was 5.3% across all step groups.
In an adjusted analysis, individuals who took at least 8,000 steps 1-2 days a week had a 14.9% lower all-cause mortality risk compared with those who never reached 8,000 daily steps. This difference was similar to the 16.5% reduced mortality risk for those who took at least 8,000 steps 3-7 days a week.
Similarly, compared with the group with no days of at least 8,000 steps, cardiovascular mortality risk was 8.1% lower for those who took 8,000 steps 1-2 days per week and 8.4% lower for those who took at least 8,000 steps 3-7 days per week. The decreased mortality risk plateaued at 3-4 days.
These patterns in reduced all-cause mortality risk persisted in a stratified analysis by age (younger than 65 years and 65 years and older) and sex. Similar patterns in reduced mortality also emerged when the researchers used different thresholds of daily steps, such as a minimum of 10,000 steps instead of 8,000. The adjusted all-cause mortality for groups who took at least 10,000 steps 1-2 days a week, 3-7 days a week, and no days a week were 8.1%, 7.3%, and 16.7%, respectively, with corresponding cardiovascular mortality risks of 2.4%, 2.3%, and 7.0%, respectively.
“Given the simplicity and ease of counting daily steps, our findings indicate that the recommended number of steps taken on as few as 1 to 2 days per week may be a feasible option for individuals who are striving to achieve some health benefits through adhering to a recommended daily step count but are unable to accomplish this on a daily basis,” the researchers wrote in their discussion.
The findings were limited by several factors including the use daily step measures for 1 week only at baseline, with no data on how physical activity changes might impact mortality risk, the researchers noted. Other limitations included possible accelerometer error and misclassification of activity, possible selection bias, and lack of data on cause-specific mortality outside of cardiovascular death, they said.
However, the results were strengthened by the use of accelerometers as objective measures of activity and by the availability of 10-year follow-up data for nearly 100% of the participants, they said.
“Although our findings might suffer from residual confounding that should be addressed in future research, they suggest that people may receive substantial health benefits even if a sufficient number of steps are taken on only a couple days of the week,” they concluded.
Proceed with caution
The current study findings should be interpreted cautiously in light of the potential unmeasured confounding factors and selection bias that often occur in studies of physical activity, James Sawalla Guseh, MD, of Massachusetts General Hospital, and Jose F. Figueroa, MD, of Harvard T.H. Chan School of Public Health, Boston, wrote in an accompanying editorial.
The results support previous studies showing some longevity benefits with “weekend warrior” patterns of intense physical activity for only a couple of days; however, “the body of evidence for sporadic activity is not as robust as the evidence for sustained and regular aerobic activity,” the authors emphasized.
The editorial authors also highlighted the limitations of the current study, including the observational design and significant differences in demographics and comorbidities between the 1- to 2-days of 8,000 steps exercise group and the 0-day group, as well as the reliance on only a week’s worth of data to infer 10 years’ mortality.
Although the data are consistent with previous observations that increased exercise volume reduces mortality, more research is needed, as the current study findings may not reflect other dimensions of health, including neurological health, they said.
Despite the need for cautious interpretation of the results, the current study “supports the emerging and popular idea that step counting, which does not require consideration of exercise duration or intensity, can offer guidance toward robust and favorable health outcomes,” and may inform step-based activity goals to improve public health, the editorialists wrote.
The study was supported by the Japan Agency for Medical Research and Development, the Japan Society for the Promotion of Science, the Japan Endocrine Society, and the Meiji Yasuda Life Foundation of Health and Welfare. Dr. Inoue also was supported by the Program for the Development of Next-Generation Leading Scientists With Global Insight sponsored by the Ministry of Education, Culture, Sports, Science and Technology, Japan. The other researchers had no relevant financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
Taking 8,000 steps or more for just 1 or 2 days a week was linked to a significant reduction in all-cause and cardiovascular mortality, according to a study of about 3,000 adults.
Previous research has shown lower mortality rates among individuals who walk consistently, especially those who log at least 8,000 steps daily, but the benefit of intense walking just once or twice a week on long-term health outcomes has not been examined, wrote Kosuke Inoue, MD, of Kyoto University, Japan, and colleagues.
In a study published in JAMA Network Open, the researchers reviewed 10-year follow-up data for 3,101 adults aged 20 years and older who were part of the 2005 and 2006 National Health and Nutrition Examination Survey (NHANES).
The participants were asked to wear accelerometers to track their steps for 7 consecutive days. The researchers assessed the dose-response relationship between days of taking 8,000 steps or more (about 4 miles) during 1 week, and the primary outcome of all-cause mortality risk after 10 years. Cardiovascular mortality risk after 10 years was a secondary outcome.
The mean age of the participants was 50.5 years and 51% were women. The breakdown by ethnicity was 51% White, 21% Black, 24% Hispanic, and 4% other races/ethnicities. A total of 632 individuals took 8,000 steps or more 0 days a week, 532 took at least 8,000 steps 1-2 days per week, and 1,937 took at least 8,000 steps 3-7 days a week.
During the 10-year follow-up period, overall all-cause mortality was 14.2% and cardiovascular mortality was 5.3% across all step groups.
In an adjusted analysis, individuals who took at least 8,000 steps 1-2 days a week had a 14.9% lower all-cause mortality risk compared with those who never reached 8,000 daily steps. This difference was similar to the 16.5% reduced mortality risk for those who took at least 8,000 steps 3-7 days a week.
Similarly, compared with the group with no days of at least 8,000 steps, cardiovascular mortality risk was 8.1% lower for those who took 8,000 steps 1-2 days per week and 8.4% lower for those who took at least 8,000 steps 3-7 days per week. The decreased mortality risk plateaued at 3-4 days.
These patterns in reduced all-cause mortality risk persisted in a stratified analysis by age (younger than 65 years and 65 years and older) and sex. Similar patterns in reduced mortality also emerged when the researchers used different thresholds of daily steps, such as a minimum of 10,000 steps instead of 8,000. The adjusted all-cause mortality for groups who took at least 10,000 steps 1-2 days a week, 3-7 days a week, and no days a week were 8.1%, 7.3%, and 16.7%, respectively, with corresponding cardiovascular mortality risks of 2.4%, 2.3%, and 7.0%, respectively.
“Given the simplicity and ease of counting daily steps, our findings indicate that the recommended number of steps taken on as few as 1 to 2 days per week may be a feasible option for individuals who are striving to achieve some health benefits through adhering to a recommended daily step count but are unable to accomplish this on a daily basis,” the researchers wrote in their discussion.
The findings were limited by several factors including the use daily step measures for 1 week only at baseline, with no data on how physical activity changes might impact mortality risk, the researchers noted. Other limitations included possible accelerometer error and misclassification of activity, possible selection bias, and lack of data on cause-specific mortality outside of cardiovascular death, they said.
However, the results were strengthened by the use of accelerometers as objective measures of activity and by the availability of 10-year follow-up data for nearly 100% of the participants, they said.
“Although our findings might suffer from residual confounding that should be addressed in future research, they suggest that people may receive substantial health benefits even if a sufficient number of steps are taken on only a couple days of the week,” they concluded.
Proceed with caution
The current study findings should be interpreted cautiously in light of the potential unmeasured confounding factors and selection bias that often occur in studies of physical activity, James Sawalla Guseh, MD, of Massachusetts General Hospital, and Jose F. Figueroa, MD, of Harvard T.H. Chan School of Public Health, Boston, wrote in an accompanying editorial.
The results support previous studies showing some longevity benefits with “weekend warrior” patterns of intense physical activity for only a couple of days; however, “the body of evidence for sporadic activity is not as robust as the evidence for sustained and regular aerobic activity,” the authors emphasized.
The editorial authors also highlighted the limitations of the current study, including the observational design and significant differences in demographics and comorbidities between the 1- to 2-days of 8,000 steps exercise group and the 0-day group, as well as the reliance on only a week’s worth of data to infer 10 years’ mortality.
Although the data are consistent with previous observations that increased exercise volume reduces mortality, more research is needed, as the current study findings may not reflect other dimensions of health, including neurological health, they said.
Despite the need for cautious interpretation of the results, the current study “supports the emerging and popular idea that step counting, which does not require consideration of exercise duration or intensity, can offer guidance toward robust and favorable health outcomes,” and may inform step-based activity goals to improve public health, the editorialists wrote.
The study was supported by the Japan Agency for Medical Research and Development, the Japan Society for the Promotion of Science, the Japan Endocrine Society, and the Meiji Yasuda Life Foundation of Health and Welfare. Dr. Inoue also was supported by the Program for the Development of Next-Generation Leading Scientists With Global Insight sponsored by the Ministry of Education, Culture, Sports, Science and Technology, Japan. The other researchers had no relevant financial conflicts to disclose. The editorial authors had no financial conflicts to disclose.
FROM JAMA NETWORK OPEN
Disparities in statin use persist in high-risk Americans
Disparities in statin use in minority populations persist regardless of insurance status and 10-year atherosclerotic cardiovascular disease risk.
Those are among the findings of a study that sampled a national population database and has provided robust data and granular details on those disparities.
The researchers reported in JAMA Cardiology that the overall prevalence of statin use was 25.5%, and that it varied significantly between defined ethnic groups: 20% for Blacks, 15.4% for Hispanics, and 27.9% for Whites (P < .001). Statin use rates by Asian participants, at 25.5%, didn’t differ significantly from use by Whites.
“We know that there are racial and ethnic disparities in the use of guideline-indicated statins after having established heart disease, but it was unknown if these disparities existed in the use of guideline-indicated statins for prevention of heart disease in those who just have risk factors,” lead author Joshua Jacobs, PharmD, a clinical pharmacist of cardiovascular medicine at University of Utah Intermountain Healthcare, said in written comments. “Additionally, race is included in the guideline-recommended risk factor calculation in an effort to reduce these disparities.”
Dr. Jacobs and colleagues evaluated statins for use in primary prevention, building upon previous single-center or diabetes-only cohort studies. What makes their study different from previous studies evaluating disparities in statin use is its use of temporal trends or current 10-year predicted ASCVD risk categorization, he said.
Using data from the National Health and Nutrition Examination Survey (NHANES), the researchers performed a serial, cross-sectional analysis of 3,417 participants that they said represented 39.4 million U.S. adults after applying sampling weights for age, gender, and race and ethnicity. In the weighted sample, 62.2% were men. In terms of self-reported race and ethnicity, 4.2% were of Asian descent, 12.7% were Black, 10.1% were Hispanic, and 73% were White.
Study participants completed a standardized questionnaire given by trained interviewers and also went to mobile examination centers where physical, anthropomorphic, and laboratory measurements, including height, weight, LDL cholesterol, and fasting blood glucose were collected. Pill bottle review also verified participants’ self-reported medication use.
The study noted that for primary prevention of atherosclerotic cardiovascular disease (ASCVD), the 2018 American College of Cardiology/American Heart Association Guideline recommends statins for, among other patient factors, elevated 10-year predicted ASCVD risk. The study divided ASCVD risk strata into three groups – 5% to less than 7.5%, 7.5% to less than 20%, and more than 20% – based on the 2018 ACC/AHA guideline and used pooled cohort equation to calculate 10-year ASCVD risk, which the guideline endorses.
Gaps persist despite ASCVD risk
The analysis found no statistically significant difference within each ASCVD risk strata between the White and Asian groups. But although statin use increased proportionately across each higher risk group, the gap widened noticeably in the highest risk group (more than 20% 10-year risk) between Whites, used as the reference at 37.6%, and Blacks (23.8%; prevalence ratio, .90; 95% confidence interval, .82-.98) and Hispanics (23.9%; PR, .90; 95% CI, .81-.99).
The study also evaluated a number of social determinants of health factors. Health insurance and access to routine health care were significantly associated with greater statin use in Black, Hispanic, and White participants; marital status and food insecurity were not. However, even when variables such as education, household income, and health insurance were applied, statin use was still significantly higher in Whites than in Blacks and Hispanics. For those with health insurance, statin use was 28.6% (95% CI, 25-32), 21.1% (95% CI, 17.3-25.4) and 19.9% (95% CI, 15.9-24.5), respectively.
The study noted that the pooled cohort equation-guided approach to statins for primary prevention, which the 2018 ACC/AHA guideline endorsed, should promote greater use of statins among Black patients. “Equitable use of statin therapy for prevention of heart disease is needed for Black and Hispanic adults,” Dr. Jacobs said. “Improvements in access to care, such as having a routine primary care clinician and health insurance, may decrease these health disparities.”
A goal of the study was to identify if disparities in statin use held up across different risk groups, senior author Ambarish Pandey, MD, said in an interview. Use of the NHANES data makes this study unique among analyses of statin use disparities, he said.
“A lot of the work that has been done previously has focused on secondary prevention among patients who have atherosclerotic cardiovascular disease or have focused on single-center or hospital-based cohorts and have not really focused on a national representative cohort like NHANES,” said Dr. Pandey, of the UT Southwestern Medical Center, Dallas.
The next step is to do community-based participatory research focusing on different implementation strategies to increase the uptake of preventive statin use among Black and Hispanic communities, Dr. Jacobs said.
Dr. Jacobs has no relevant relationships to disclose. Dr. Pandey disclosed relationships with Gilead Sciences, Applied Therapeutics, Myovista, Tricog Health, Eli Lilly, Cytokinetics, Rivus, Roche Diagnostics, Pieces Technologies, Palomarin, Emmi Solutions, and Axon.
Disparities in statin use in minority populations persist regardless of insurance status and 10-year atherosclerotic cardiovascular disease risk.
Those are among the findings of a study that sampled a national population database and has provided robust data and granular details on those disparities.
The researchers reported in JAMA Cardiology that the overall prevalence of statin use was 25.5%, and that it varied significantly between defined ethnic groups: 20% for Blacks, 15.4% for Hispanics, and 27.9% for Whites (P < .001). Statin use rates by Asian participants, at 25.5%, didn’t differ significantly from use by Whites.
“We know that there are racial and ethnic disparities in the use of guideline-indicated statins after having established heart disease, but it was unknown if these disparities existed in the use of guideline-indicated statins for prevention of heart disease in those who just have risk factors,” lead author Joshua Jacobs, PharmD, a clinical pharmacist of cardiovascular medicine at University of Utah Intermountain Healthcare, said in written comments. “Additionally, race is included in the guideline-recommended risk factor calculation in an effort to reduce these disparities.”
Dr. Jacobs and colleagues evaluated statins for use in primary prevention, building upon previous single-center or diabetes-only cohort studies. What makes their study different from previous studies evaluating disparities in statin use is its use of temporal trends or current 10-year predicted ASCVD risk categorization, he said.
Using data from the National Health and Nutrition Examination Survey (NHANES), the researchers performed a serial, cross-sectional analysis of 3,417 participants that they said represented 39.4 million U.S. adults after applying sampling weights for age, gender, and race and ethnicity. In the weighted sample, 62.2% were men. In terms of self-reported race and ethnicity, 4.2% were of Asian descent, 12.7% were Black, 10.1% were Hispanic, and 73% were White.
Study participants completed a standardized questionnaire given by trained interviewers and also went to mobile examination centers where physical, anthropomorphic, and laboratory measurements, including height, weight, LDL cholesterol, and fasting blood glucose were collected. Pill bottle review also verified participants’ self-reported medication use.
The study noted that for primary prevention of atherosclerotic cardiovascular disease (ASCVD), the 2018 American College of Cardiology/American Heart Association Guideline recommends statins for, among other patient factors, elevated 10-year predicted ASCVD risk. The study divided ASCVD risk strata into three groups – 5% to less than 7.5%, 7.5% to less than 20%, and more than 20% – based on the 2018 ACC/AHA guideline and used pooled cohort equation to calculate 10-year ASCVD risk, which the guideline endorses.
Gaps persist despite ASCVD risk
The analysis found no statistically significant difference within each ASCVD risk strata between the White and Asian groups. But although statin use increased proportionately across each higher risk group, the gap widened noticeably in the highest risk group (more than 20% 10-year risk) between Whites, used as the reference at 37.6%, and Blacks (23.8%; prevalence ratio, .90; 95% confidence interval, .82-.98) and Hispanics (23.9%; PR, .90; 95% CI, .81-.99).
The study also evaluated a number of social determinants of health factors. Health insurance and access to routine health care were significantly associated with greater statin use in Black, Hispanic, and White participants; marital status and food insecurity were not. However, even when variables such as education, household income, and health insurance were applied, statin use was still significantly higher in Whites than in Blacks and Hispanics. For those with health insurance, statin use was 28.6% (95% CI, 25-32), 21.1% (95% CI, 17.3-25.4) and 19.9% (95% CI, 15.9-24.5), respectively.
The study noted that the pooled cohort equation-guided approach to statins for primary prevention, which the 2018 ACC/AHA guideline endorsed, should promote greater use of statins among Black patients. “Equitable use of statin therapy for prevention of heart disease is needed for Black and Hispanic adults,” Dr. Jacobs said. “Improvements in access to care, such as having a routine primary care clinician and health insurance, may decrease these health disparities.”
A goal of the study was to identify if disparities in statin use held up across different risk groups, senior author Ambarish Pandey, MD, said in an interview. Use of the NHANES data makes this study unique among analyses of statin use disparities, he said.
“A lot of the work that has been done previously has focused on secondary prevention among patients who have atherosclerotic cardiovascular disease or have focused on single-center or hospital-based cohorts and have not really focused on a national representative cohort like NHANES,” said Dr. Pandey, of the UT Southwestern Medical Center, Dallas.
The next step is to do community-based participatory research focusing on different implementation strategies to increase the uptake of preventive statin use among Black and Hispanic communities, Dr. Jacobs said.
Dr. Jacobs has no relevant relationships to disclose. Dr. Pandey disclosed relationships with Gilead Sciences, Applied Therapeutics, Myovista, Tricog Health, Eli Lilly, Cytokinetics, Rivus, Roche Diagnostics, Pieces Technologies, Palomarin, Emmi Solutions, and Axon.
Disparities in statin use in minority populations persist regardless of insurance status and 10-year atherosclerotic cardiovascular disease risk.
Those are among the findings of a study that sampled a national population database and has provided robust data and granular details on those disparities.
The researchers reported in JAMA Cardiology that the overall prevalence of statin use was 25.5%, and that it varied significantly between defined ethnic groups: 20% for Blacks, 15.4% for Hispanics, and 27.9% for Whites (P < .001). Statin use rates by Asian participants, at 25.5%, didn’t differ significantly from use by Whites.
“We know that there are racial and ethnic disparities in the use of guideline-indicated statins after having established heart disease, but it was unknown if these disparities existed in the use of guideline-indicated statins for prevention of heart disease in those who just have risk factors,” lead author Joshua Jacobs, PharmD, a clinical pharmacist of cardiovascular medicine at University of Utah Intermountain Healthcare, said in written comments. “Additionally, race is included in the guideline-recommended risk factor calculation in an effort to reduce these disparities.”
Dr. Jacobs and colleagues evaluated statins for use in primary prevention, building upon previous single-center or diabetes-only cohort studies. What makes their study different from previous studies evaluating disparities in statin use is its use of temporal trends or current 10-year predicted ASCVD risk categorization, he said.
Using data from the National Health and Nutrition Examination Survey (NHANES), the researchers performed a serial, cross-sectional analysis of 3,417 participants that they said represented 39.4 million U.S. adults after applying sampling weights for age, gender, and race and ethnicity. In the weighted sample, 62.2% were men. In terms of self-reported race and ethnicity, 4.2% were of Asian descent, 12.7% were Black, 10.1% were Hispanic, and 73% were White.
Study participants completed a standardized questionnaire given by trained interviewers and also went to mobile examination centers where physical, anthropomorphic, and laboratory measurements, including height, weight, LDL cholesterol, and fasting blood glucose were collected. Pill bottle review also verified participants’ self-reported medication use.
The study noted that for primary prevention of atherosclerotic cardiovascular disease (ASCVD), the 2018 American College of Cardiology/American Heart Association Guideline recommends statins for, among other patient factors, elevated 10-year predicted ASCVD risk. The study divided ASCVD risk strata into three groups – 5% to less than 7.5%, 7.5% to less than 20%, and more than 20% – based on the 2018 ACC/AHA guideline and used pooled cohort equation to calculate 10-year ASCVD risk, which the guideline endorses.
Gaps persist despite ASCVD risk
The analysis found no statistically significant difference within each ASCVD risk strata between the White and Asian groups. But although statin use increased proportionately across each higher risk group, the gap widened noticeably in the highest risk group (more than 20% 10-year risk) between Whites, used as the reference at 37.6%, and Blacks (23.8%; prevalence ratio, .90; 95% confidence interval, .82-.98) and Hispanics (23.9%; PR, .90; 95% CI, .81-.99).
The study also evaluated a number of social determinants of health factors. Health insurance and access to routine health care were significantly associated with greater statin use in Black, Hispanic, and White participants; marital status and food insecurity were not. However, even when variables such as education, household income, and health insurance were applied, statin use was still significantly higher in Whites than in Blacks and Hispanics. For those with health insurance, statin use was 28.6% (95% CI, 25-32), 21.1% (95% CI, 17.3-25.4) and 19.9% (95% CI, 15.9-24.5), respectively.
The study noted that the pooled cohort equation-guided approach to statins for primary prevention, which the 2018 ACC/AHA guideline endorsed, should promote greater use of statins among Black patients. “Equitable use of statin therapy for prevention of heart disease is needed for Black and Hispanic adults,” Dr. Jacobs said. “Improvements in access to care, such as having a routine primary care clinician and health insurance, may decrease these health disparities.”
A goal of the study was to identify if disparities in statin use held up across different risk groups, senior author Ambarish Pandey, MD, said in an interview. Use of the NHANES data makes this study unique among analyses of statin use disparities, he said.
“A lot of the work that has been done previously has focused on secondary prevention among patients who have atherosclerotic cardiovascular disease or have focused on single-center or hospital-based cohorts and have not really focused on a national representative cohort like NHANES,” said Dr. Pandey, of the UT Southwestern Medical Center, Dallas.
The next step is to do community-based participatory research focusing on different implementation strategies to increase the uptake of preventive statin use among Black and Hispanic communities, Dr. Jacobs said.
Dr. Jacobs has no relevant relationships to disclose. Dr. Pandey disclosed relationships with Gilead Sciences, Applied Therapeutics, Myovista, Tricog Health, Eli Lilly, Cytokinetics, Rivus, Roche Diagnostics, Pieces Technologies, Palomarin, Emmi Solutions, and Axon.
FROM JAMA CARDIOLOGY
Does new heart transplant method challenge definition of death?
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
The relatively recent innovation of heart transplantation after circulatory death of the donor is increasing the number of donor hearts available and leading to many more lives on the heart transplant waiting list being saved. Experts agree it’s a major and very welcome advance in medicine.
However, some of the processes involved in one approach to donation after circulatory death has raised ethical concerns and questions about whether they violate the “dead donor rule” – a principle that requires patients be declared dead before removal of life-sustaining organs for transplant.
Experts in the fields of transplantation and medical ethics have yet to reach consensus, causing problems for the transplant community, who worry that this could cause a loss of confidence in the entire transplant process.
A new pathway for heart transplantation
The traditional approach to transplantation is to retrieve organs from a donor who has been declared brain dead, known as “donation after brain death (DBD).” These patients have usually suffered a catastrophic brain injury but survived to get to intensive care.
As the brain swells because of injury, it becomes evident that all brain function is lost, and the patient is declared brain dead. However, breathing is maintained by the ventilator and the heart is still beating. Because the organs are being oxygenated, there is no immediate rush to retrieve the organs and the heart can be evaluated for its suitability for transplant in a calm and methodical way before it is removed.
However, there is a massive shortage of organs, especially hearts, partially because of the limited number of donors who are declared brain dead in that setting.
In recent years, another pathway for organ transplantation has become available: “donation after circulatory death (DCD).” These patients also have suffered a catastrophic brain injury considered to be nonsurvivable, but unlike the DBD situation, the brain still has some function, so the patient does not meet the criteria for brain death.
Still, because the patient is considered to have no chance of a meaningful recovery, the family often recognizes the futility of treatment and agrees to the withdrawal of life support. When this happens, the heart normally stops beating after a period of time. There is then a “stand-off time” – normally 5 minutes – after which death is declared and the organs can be removed.
The difficulty with this approach, however, is that because the heart has been stopped, it has been deprived of oxygen, potentially causing injury. While DCD has been practiced for several years to retrieve organs such as the kidney, liver, lungs, and pancreas, the heart is more difficult as it is more susceptible to oxygen deprivation. And for the heart to be assessed for transplant suitability, it should ideally be beating, so it has to be reperfused and restarted quickly after death has been declared.
For many years it was thought the oxygen deprivation that occurs after circulatory death would be too much to provide a functional organ. But researchers in the United Kingdom and Australia developed techniques to overcome this problem, and early DCD heart transplants took place in 2014 in Australia, and in 2015 in the United Kingdom.
Heart transplantation after circulatory death has now become a routine part of the transplant program in many countries, including the United States, Spain, Belgium, the Netherlands, and Austria.
In the United States, 348 DCD heart transplants were performed in 2022, with numbers expected to reach 700 to 800 this year as more centers come online.
It is expected that most countries with heart transplant programs will follow suit and the number of donor hearts will increase by up to 30% worldwide because of DCD.
Currently, there are about 8,000 heart transplants worldwide each year and with DCD this could rise to about 10,000, potentially an extra 2,000 lives saved each year, experts estimate.
Two different approaches to DCD heart transplantation have been developed.
The direct procurement approach
The Australian group, based at St. Vincent’s Hospital in Sydney, developed a technique referred to as “direct procurement”: after the standoff period and declaration of circulatory death, the chest is opened, and the heart is removed. New technology, the Organ Care System (OCS) heart box (Transmedics), is then used to reperfuse and restart the heart outside the body so its suitability for transplant can be assessed.
The heart is kept perfused and beating in the OCS box while it is being transported to the recipient. This has enabled longer transit times than the traditional way of transporting the nonbeating heart on ice.
Peter MacDonald, MD, PhD, from the St Vincent’s group that developed this approach, said, “Most people thought a heart from a DCD donor would not survive transport – that the injury to the heart from the combination of life support withdrawal, stand-off time, and cold storage would be too much. But we modeled the process in the lab and were able to show that we were able to get the heart beating again after withdrawal of life support.”
Dr. McDonald noted that “the recipient of their first human DCD heart transplant using this machine in 2014 is still alive and well.” The Australian group has now done 85 of these DCD heart transplants, and they have increased the number of heart transplant procedures at St. Vincent’s Hospital by 25%.
Normothermic regional perfusion (NRP)
The U.K. group, based at the Royal Papworth Hospital in Cambridge, England, developed a different approach to DCD: After the standoff period and the declaration of circulatory death, the donor is connected to a heart/lung machine using extracorporeal membrane oxygenation (ECMO) so that the heart is perfused and starts beating again inside the body. This approach is known as normothermic regional perfusion (NRP).
Marius Berman, MD, surgical lead for Transplantation and Mechanical Circulatory Support at Papworth, explained that the NRP approach allows the heart to be perfused and restarted faster than direct procurement, resulting in a shorter ischemic time. The heart can be evaluated thoroughly for suitability for transplantation in situ before committing to transplantation, and because the heart is less damaged, it can be transported on ice without use of the OCS box.
“DCD is more complicated than DBD, because the heart has stopped and has to be restarted. Retrieval teams have to be very experienced,” Dr. Berman noted. “This is more of an issue for the direct procurement approach, where the chest has to be opened and the heart retrieved as fast as possible. It is a rush. The longer time without the heart being perfused correlates to an increased incidence of primary graft dysfunction. With NRP, we can get the heart started again more quickly, which is crucial.”
Stephen Large, MBBS, another cardiothoracic surgeon with the Papworth team, added that they have reduced ischemic time to about 15 minutes. “That’s considerably shorter than reperfusing the heart outside the body,” he said. “This results in a healthier organ for the recipient.”
The NRP approach is also less expensive than direct procurement as one OCS box costs about $75,000.
He pointed out that the NRP approach can also be used for heart transplants in children and even small babies, while currently the direct procurement technique is not typically suitable for children because the OCS box was not designed for small hearts.
DCD, using either technique, has increased the heart transplant rate by 40% at Papworth, and is being used at all seven transplant centers in the United Kingdom, “a world first,” noted Dr. Large.
The Papworth team recently published its 5-year experience with 25 NRP transplants and 85 direct procurement transplants. Survival in recipients was no different, although there was some suggestion that the NRP hearts may have been in slightly better condition, possibly being more resistant to immunological rejection.
Ethical concerns about NRP
Restarting the circulation during the NRP process has raised ethical concerns.
When the NRP technique was first used in the United States, these ethical questions were raised by several groups, including the American College of Physicians (ACP).
Harry Peled, MD, Providence St. Jude Medical Center, Fullerton, Calif., coauthor of a recent Viewpoint on the issue, is board-certified in both cardiology and critical care, and said he is a supporter of DCD using direct procurement, but he does not believe that NRP is ethical at present. He is not part of the ACP, but said his views align with those of the organization.
There are two ethical problems with NRP, he said. The first is whether by restarting the circulation, the NRP process violates the U.S. definition of death, and retrieval of organs would therefore violate the dead donor rule.
“American law states that death is the irreversible cessation of brain function or of circulatory function. But with NRP, the circulation is artificially restored, so the cessation of circulatory function is not irreversible,” Dr. Peled pointed out.
“I have no problem with DCD using direct procurement as we are not restarting the circulation. But NRP is restarting the circulation and that is a problem for me,” Dr. Peled said. “I would argue that by performing NRP, we are resuscitating the patient.”
The second ethical problem with NRP is concern about whether, during the process, there would be any circulation to the brain, and if so, would this be enough to restore some brain function? Before NRP is started, the main arch vessel arteries to the head are clamped to prevent flow to the brain, but there are worries that some blood flow may still be possible through small collateral vessels.
“We have established that these patients do not have enough brain function for a meaningful life, which is why a decision has been made to remove life support, but they have not been declared brain dead,” Dr. Peled said.
With direct procurement, the circulation is not restarted so there is no chance that any brain function will be restored, he said. “But with NRP, because the arch vessels have to be clamped to prevent brain circulation, that is admitting there is concern that brain function may be restored if circulation to the brain is reestablished, and brain function is compatible with life. As we do not know whether there is any meaningful circulation to the brain via the small collaterals, there is, in effect, a risk of bringing the patient back to life.”
The other major concern for some is whether even a very small amount of circulation to the brain would be enough to support consciousness, and “we don’t know that for certain,” Dr. Peled said.
The argument for NRP
Nader Moazami, MD, professor of cardiovascular surgery, NYU Langone Health, New York, is one of the more vocal proponents of NRP for DCD heart transplantation in the United States, and has coauthored responses to these ethical concerns.
“People are confusing many issues to produce an argument against NRP,” he said.
“Our position is that death has already been declared based on the lack of circulatory function for over 5 minutes and this has been with the full agreement of the family, knowing that the patient has no chance of a meaningful life. No one is thinking of trying to resuscitate the patient. It has already been established that any future efforts to resuscitate are futile. In this case, we are not resuscitating the patient by restarting the circulation. It is just regional perfusion of the organs.”
Dr. Moazami pointed out this concept was accepted for the practice of abdominal DCD when it first started in the United States in the 1990s where cold perfusion was used to preserve the abdominal organs before they were retrieved from the body.
“The new approach of using NRP is similar except that it involves circulating warm blood, which will preserve organs better and result in higher quality organs for the recipient.”
On the issue of concern about possible circulation to the brain, Dr. Moazami said: “The ethical critics of NRP are questioning whether the brain may not be dead. We are arguing that the patient has already been declared dead as they have had a circulatory death. You cannot die twice.”
He maintained that the clamping of the arch vessels to the head will ensure that when the circulation is restarted “the natural process of circulatory death leading to brain death will continue to progress.”
On the concerns about possible collateral flow to the brain, Dr. Moazami said there is no evidence that this occurs. “Prominent neurologists have said it is impossible for collaterals to provide any meaningful blood flow to the brain in this situation. And even if there is small amount of blood flow to the brain, this would be insufficient to maintain any meaningful brain function.”
But Dr. Peled argues that this has not been proved. “Even though we don’t think there is enough circulation to the brain for any function with NRP, we don’t know that with 100% certainty,” he said. “In my view, if there is a possibility of even the smallest amount of brain flow, we are going against the dead donor rule. We are rewriting the rules of death.”
Dr. Moazami countered: “Nothing in life is 100%, particularly in medicine. With that argument can you also prove with 100% certainty to me that there is absolutely no brain function with regular direct procurement DCD? We know that brain death has started, but the question is: Has it been completed? We don’t know the answer to this question with 100% certainty, but that is the case for regular direct procurement DCD as well, and that has been accepted by almost everyone.
“The whole issue revolves around when are we comfortable that death has occurred,” he said. “Those against NRP are concerned that organs are being taken before the patient is dead. But the key point is that the patient has already been declared dead.”
Since there is some concern over the ethics of NRP, why not just stick to DCD with direct procurement?
Dr. Moazami argued that NRP results in healthier organs. “NRP allows more successful heart transplants, liver transplants, lung transplants. It preserves all the organs better,” he said. “This will have a big impact on recipients – they would obviously much prefer a healthier organ. In addition, the process is easier and cheaper, so more centers will be able to do it, therefore more transplants will get done and more lives will be saved if NRP is used.”
He added: “I am a physician taking care of sick patients. I believe I have to respect the wishes of the donor and the donor family; make sure I’m not doing any harm to the donor; and ensure the best quality possible of the organ I am retrieving to best serve the recipient. I am happy I am doing this by using NRP for DCD heart transplantation.”
But Dr. Peled argued that while NRP may have some possible advantages over direct procurement, that does not justify allowing a process to go ahead that is unethical.
“The fact that NRP may result in some benefits doesn’t justify violating the dead donor rule or the possibility, however small, of causing pain to the donor. If it’s unethical, it’s unethical. Full stop,” he said.
“I feel that NRP is not respecting the rights of our patients and that the process does not have adequate transparency. We took it to our local ethics committee, and they decided not to approve NRP in our health care system. I agree with this decision,” Dr. Peled said.
“The trouble is different experts and different countries are not in agreement about this,” he added. “Reasonable, well-informed people are in disagreement. I do not believe we can have a standard of care where there is not consensus.”
Cautious nod
In a 2022 consensus statement, the International Society for Heart and Lung Transplantation (ISHLT) gave a cautious nod toward DCD and NRP, dependent on local recommendations.
The ISHLT conclusion reads: “With appropriate consideration of the ethical principles involved in organ donation, DCD can be undertaken in a morally permissible manner. In all cases, the introduction of DCD programs should be in accordance with local legal regulations. Countries lacking a DCD pathway should be encouraged to develop national ethical, professional, and legal frameworks to address both public and professional concerns.”
The author of a recent editorial on the subject, Ulrich P. Jorde, MD, head of the heart transplant program at Montefiore Medical Center, New York, said, “DCD is a great step forward. People regularly die on the heart transplant waiting list. DCD will increase the supply of donor hearts by 20% to 30%.”
However, he noted that while most societies have agreed on a protocol for organ donation based on brain death, the situation is more complicated with circulatory death.
“Different countries have different definitions of circulatory death. How long do we have to wait after the heart has stopped beating before the patient is declared dead? Most countries have agreed on 5 minutes, but other countries have imposed different periods and as such, different definitions of death.
“The ISHLT statement says that restarting the circulation is acceptable if death has been certified according to prevailing law and surgical interventions are undertaken to preclude any restoration of cerebral circulation. But our problem is that different regional societies have different definitions of circulatory, death which makes the situation confusing.”
Dr. Jorde added: “We also have to weigh the wishes of the donor and their family. If family, advocating what are presumed to be the donor’s wishes, have decided that DCD would be acceptable and they understand the concept and wish to donate the organs after circulatory death, this should be strongly considered under the concept of self-determination, a basic human right.”
Variations in practice around the world
This ethical debate has led to large variations in practice around the world, with some countries, such as Spain, allowing both methods of DCD, while Australia allows direct procurement but not NRP, and Germany currently does not allow DCD at all.
In the United States, things are even more complicated, with some states allowing NRP while others don’t. Even within states, some hospitals and transplant organizations allow NRP, and others don’t.
David A. D’Alessandro, MD, cardiac surgeon at Massachusetts General Hospital, Boston, uses only the direct procurement approach as his region does not allow NRP.
“The direct procurement approach is not controversial and to me that’s a big advantage. I believe we need to agree on the ethics first, and then get into a debate about which technique is better,” he told this news organization.
Dr. D’Alessandro and his group recently published the results of their study, with direct procurement DCD heart transplantation showing similar short-term clinical outcomes to DBD.
“We are only doing direct procurement and we are seeing good results that appear to be comparable to DBD. That is good enough for me,” he said.
Dr. D’Alessandro estimates that in the United States both types of DCD procedures are currently being done about equally.
“Anything we can do to increase the amount of hearts available for transplantation is a big deal,” he said. “At the moment, only the very sickest patients get a heart transplant, and many patients die on the transplant waiting list. Very sadly, many young people die every year from a circulatory death after having life support withdrawn. Before DCD, these beautiful functional organs were not able to be used. Now we have a way of saving lives with these organs.”
Dr. D’Alessandro noted that more and more centers in the United States are starting to perform DCD heart transplants.
“Not every transplant center may join in as the DCD procedures are very resource-intensive and time-consuming. For low-volume transplant centers, it may not be worth the expense and anguish to do DCD heart transplants. But bigger centers will need to engage in DCD to remain competitive. My guess is that 50%-70% of U.S. transplant centers will do DCD in future.”
He said he thinks it is a “medical shortcoming” that agreement cannot be reached on the ethics of NRP. “In an ideal world everyone would be on the same page. It makes me a bit uncomfortable that some people think it’s okay and some people don’t.”
Adam DeVore, MD, a cardiologist at Duke University Medical Center, Durham, N.C., the first U.S. center to perform an adult DCD heart transplant, reported that his institution uses both methods, with the choice sometimes depending on how far the heart must travel.
“If the recipient is near, NRP may be chosen as the heart is transported on ice, but if it needs to go further away we are more likely to choose direct procurement and use of the OCS box,” he said.
“I am really proud of what we’ve been able to do, helping to introduce DCD in the U.S.,” Dr. DeVore said. “This is having a massive benefit in increasing the number of hearts for donation with great outcomes.”
But he acknowledged that the whole concept of DCD is somewhat controversial.
“The idea of brain death really came about for the purpose of heart donation. The two things are very intricately tied. Trying to do heart donation without brain death having been declared is foreign to people. Also, in DCD there is the issue of [this]: When life support is removed, how long do we wait before death can be declared? That could be in conflict with how long the organ needs to remain viable. We are going through the process now of looking at these questions. There is a lot of variation in the U.S. about the withdrawal of care and the declaration of death, which is not completely standardized.
“But the concept of circulatory death itself is accepted after the withdrawal of life support. I think it’s the rush to take the organs out that makes it more difficult.”
Dr. DeVore said the field is moving forward now. “As the process has become more common, people have become more comfortable, probably because of the big difference it will make to saving lives. But we do need to try and standardize best practices.”
A recent Canadian review of the ethics of DCD concluded that the direct procurement approach would be in alignment with current medical guidelines, but that further work is required to evaluate the consistency of NRP with current Canadian death determination policy and to ensure the absence of brain perfusion during this process.
In the United Kingdom, the definition of death is brain-based, and brain death is defined on a neurological basis.
Dr. Stephen Large from Papworth explained that this recognizes the presence of brain-stem death through brain stem reflex testing after the withdrawal of life support, cardiorespiratory arrest and 5 further minutes of ischemia. As long as NRP does not restore intracranial (brainstem) perfusion after death has been confirmed, then it is consistent with laws for death determination and therefore both direct procurement and NRP are permissible.
However, the question over possible collateral flow to the brain has led the United Kingdom to pause the NRP technique as routine practice while this is investigated further. So, at the present time, the vast majority of DCD heart transplants are being conducted using the direct procurement approach.
But the United Kingdom is facing the bigger challenge: national funding that will soon end. “The DCD program in the U.K. has been extremely successful, increasing heart transplant rates by up to 28%,” Dr. Berman said. “Everybody wants it to continue. But at present the DCD program only has national funding in the U.K. until March 2023. We don’t know what will happen after that.”
The current model in the United Kingdom consists of three specialized DCD heart retrieval teams, a national protocol of direct organ procurement and delivery of DCD hearts to all seven transplant programs, both adult and pediatric.
If the national funding is not extended, “we will go back to individual hospitals trying to fund their own programs. That will be a serious threat to the program and could result in a large reduction in heart transplants,” said Dr. Berman.
Definition of death
The crux of the issue with regard to NRP seems to be variations in how death is defined and the interpretation of those definitions.
DCD donors will have had many tests indicating severe brain damage, a neurologist will have declared the prognosis is futile, and relatives will have agreed to withdraw life support, Dr. Jorde said. “The heart stops beating, and the stand-off time means that blood flow to the brain ceases completely for at least 5 minutes before circulatory death is declared. This is enough on its own to stop brain function.”
Dr. Large made the point that by the time the circulation is reestablished with NRP, more time has elapsed, and the brain will have been without perfusion for much longer than 5 minutes, so it would be “physiologically almost impossible” for there to be any blood flow to the brain.
“Because these brains are already very damaged before life support was removed, the intracranial pressure is high, which will further discourage blood flow to the brain,” he said. Then the donor goes through a period of anoxic heart arrest, up to 16 minutes at a minimum of no blood supply, enough on its own to stop meaningful brain function.
“It’s asking an awful lot to believe that there might be any brain function left,” he said. “And if, on reestablishing the circulation with NRP, there is any blood in the collaterals, the pressure of such flow is so low it won’t enter the brain.”
Dr. Large also pointed out that the fact that the United Kingdom requires a neurologic definition for brain-stem death makes the process easier.
In Australia, St. Vincent’s cardiologist Dr. MacDonald noted that death is defined as the irreversible cessation of circulation, so the NRP procedure is not allowed.
“With NRP, there is an ethical dilemma over whether the patient has legally died or not. Different countries have different ways of defining death. Perhaps society will have to review of the definition of death,” he suggested. Death is a process, “but for organ donation, we have to choose a moment in time of that process that satisfies everyone – when there is no prospect of recovery of the donor but the organs can still be utilized without harming the donor.”
Dr. MacDonald said the field is in transition. “I don’t want to argue that one technique is better than the other; I think it’s good to have access to both techniques. Anything that will increase the number of transplants we can do is a good thing.”
Collaborative decision
Everyone seems to agree that there should be an effort to try to define death in a uniform way worldwide, and that international, national and local regulations are aligned with each other.
Dr. Jorde said: “It is of critical importance that local guidelines are streamlined, firstly in any one given country and then globally, and these things must be discussed transparently within society with all stakeholders – doctors, patients, citizens.”
Dr. Peled, from Providence St. Jude in California, concurred: “There is the possibility that we could change the definition of death, but that cannot be a decision based solely on transplant organizations. It has to be a collaborative decision with a large input from groups who do not have an interest in the procurement of organs.”
He added: “The dialogue so far has been civil, and everybody is trying to do the right thing. My hope is that as a civilized society we will figure out a way forward. At present, there is significant controversy about NRP, and families need to know that. My main concern is that if there is any lack of transparency in getting informed consent, then this risks people losing trust in the donation system.”
Dr. Moazami, from NYU Langone, said the controversy has cast a cloud over the practice of NRP throughout the world. “We need to get it sorted out.”
He said he believes the way forward is to settle the question of whether there is any meaningful blood flow to the brain with the NRP technique.
“This is where the research has to focus. I believe this concern is hypothetical, but I am happy to do the studies to confirm that. Then, the issue should come to a rest. I think that is the right way forward – to do the studies rather than enforcing a moratorium on the practice because of a hypothetical concern.”
These studies on blood flow to the brain are now getting started in both the United Kingdom and the United States.
The U.K. study is being run by Antonio Rubino, MD, consultant in cardiothoracic anesthesia and intensive care at Papworth Hospital NHS Foundation and clinical lead, organ donation. Dr. Rubino explained that the study will assess cerebral blood flow using CT angiography of the brain. “We hypothesize that this will provide evidence to indicate that brain blood flow is not present during NRP and promote trust in the use of NRP in routine practice,” he said.
Dr. Large said: “Rather than having these tortured arguments, we will do the measurements. For the sake of society in this situation, I think it’s good to stop and take a breath. We must measure this, and we are doing just that.”
If there is any blood flow at all, Dr. Large said they will then have to seek expert guidance. “Say we find there is 50 mL of blood flow and normal blood flow is 1,500 mL/min. We will need expert guidance on whether it is remotely possible to be sentient on that. I would say it would be extraordinarily unlikely.”
Dr. Berman summarized the situation: “DCD is increasing the availability of hearts for transplant. This is saving lives, reducing the number of patients on the waiting list, and reducing hospital stays for patients unable to leave the hospital without a transplant. It is definitely here to stay. It is crucial that it gets funded properly, and it is also crucial that we resolve the NRP ethical issues as soon as possible.”
He is hopeful that some of these issues will be resolved this year.
Dr. MacDonald reported he has received “in-kind” support from Transmedics through provision of research modules for preclinical research studies. Dr. D’Alessandro reported he is on the speakers bureau for Abiomed, not relevant to this article. No other relevant disclosures were reported.
A version of this article first appeared on Medscape.com.
Dabigatran recalled over potential carcinogen
The nationwide recall, to the consumer level, is because of the detection of the nitrosamine impurity, N-nitroso-dabigatran, which may increase the risk of cancer with prolonged exposure to levels higher than acceptable.
To date, Ascend Laboratories has not received any reports of adverse events related to this recall.
The recalled product was distributed nationwide to wholesalers, distributors, and retailers in the United States from June 2022 to October 2022.
Complete details of the recalled product, including national drug code, lot numbers, expiration dates, and configuration/counts, are provided in a company announcement that was posted on the Food and Drug Administration website.
The company is advising patients who have any dabigatran that has been recalled to continue taking their medication and to contact their physician for advice regarding an alternative treatment.
Wholesalers/distributors and pharmacies with an existing inventory of the affected lots should stop use and distribution and quarantine the product immediately. Wholesalers and distributors should also recall the distributed product.
Questions regarding this recall can call Ascend Laboratories at 877.272.7901 (24 hours, 7 days a week).
Problems with this product should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article originally appeared on Medscape.com.
The nationwide recall, to the consumer level, is because of the detection of the nitrosamine impurity, N-nitroso-dabigatran, which may increase the risk of cancer with prolonged exposure to levels higher than acceptable.
To date, Ascend Laboratories has not received any reports of adverse events related to this recall.
The recalled product was distributed nationwide to wholesalers, distributors, and retailers in the United States from June 2022 to October 2022.
Complete details of the recalled product, including national drug code, lot numbers, expiration dates, and configuration/counts, are provided in a company announcement that was posted on the Food and Drug Administration website.
The company is advising patients who have any dabigatran that has been recalled to continue taking their medication and to contact their physician for advice regarding an alternative treatment.
Wholesalers/distributors and pharmacies with an existing inventory of the affected lots should stop use and distribution and quarantine the product immediately. Wholesalers and distributors should also recall the distributed product.
Questions regarding this recall can call Ascend Laboratories at 877.272.7901 (24 hours, 7 days a week).
Problems with this product should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article originally appeared on Medscape.com.
The nationwide recall, to the consumer level, is because of the detection of the nitrosamine impurity, N-nitroso-dabigatran, which may increase the risk of cancer with prolonged exposure to levels higher than acceptable.
To date, Ascend Laboratories has not received any reports of adverse events related to this recall.
The recalled product was distributed nationwide to wholesalers, distributors, and retailers in the United States from June 2022 to October 2022.
Complete details of the recalled product, including national drug code, lot numbers, expiration dates, and configuration/counts, are provided in a company announcement that was posted on the Food and Drug Administration website.
The company is advising patients who have any dabigatran that has been recalled to continue taking their medication and to contact their physician for advice regarding an alternative treatment.
Wholesalers/distributors and pharmacies with an existing inventory of the affected lots should stop use and distribution and quarantine the product immediately. Wholesalers and distributors should also recall the distributed product.
Questions regarding this recall can call Ascend Laboratories at 877.272.7901 (24 hours, 7 days a week).
Problems with this product should be reported to the FDA through MedWatch, its adverse event reporting program.
A version of this article originally appeared on Medscape.com.
Implementation of a Multidisciplinary Team–Based Clinical Care Pathway Is Associated With Increased Surgery Rates for Infective Endocarditis
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
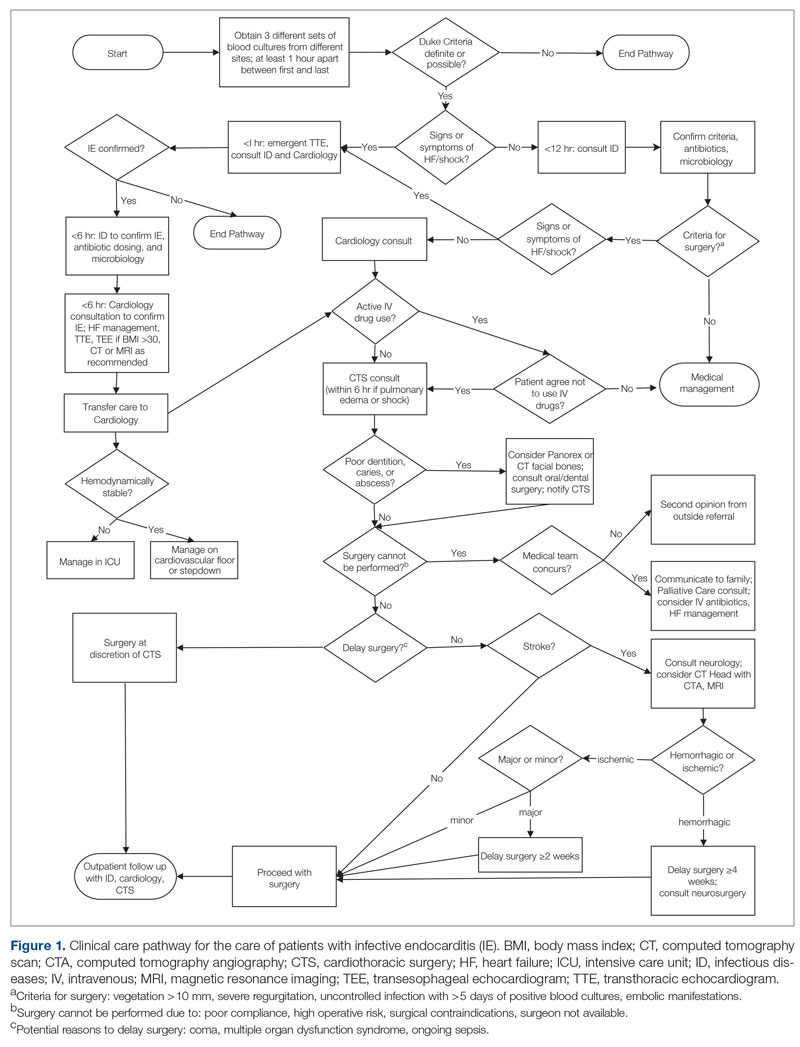
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
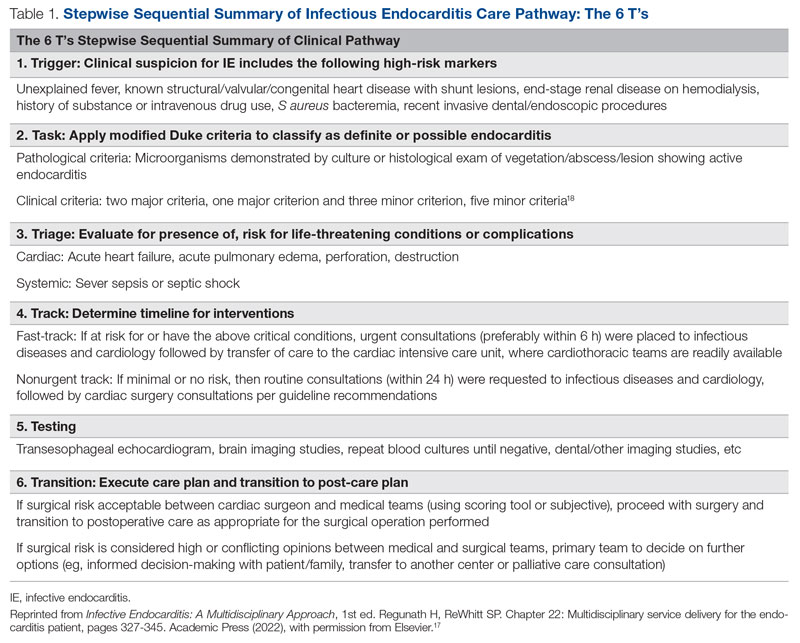
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
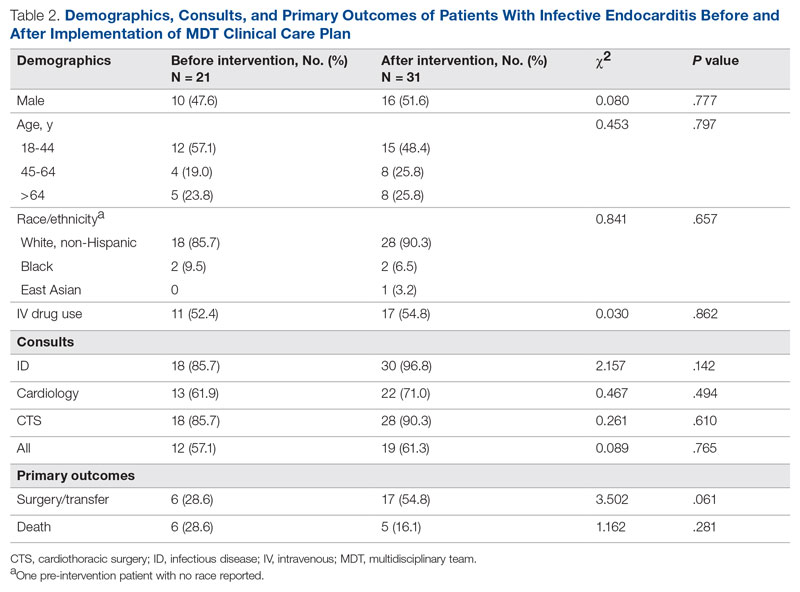
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
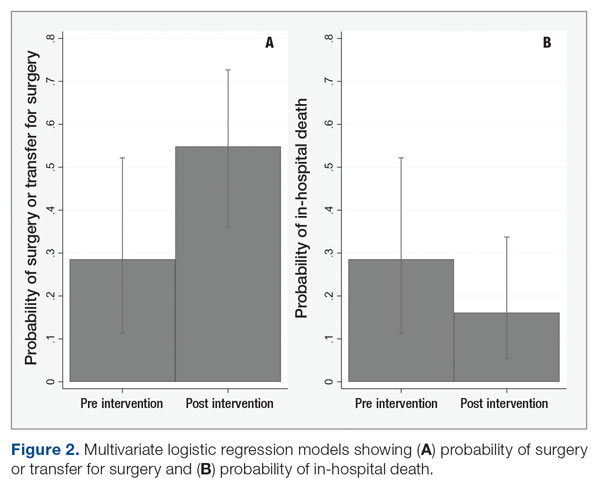
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; [email protected]
Disclosures: None reported.
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
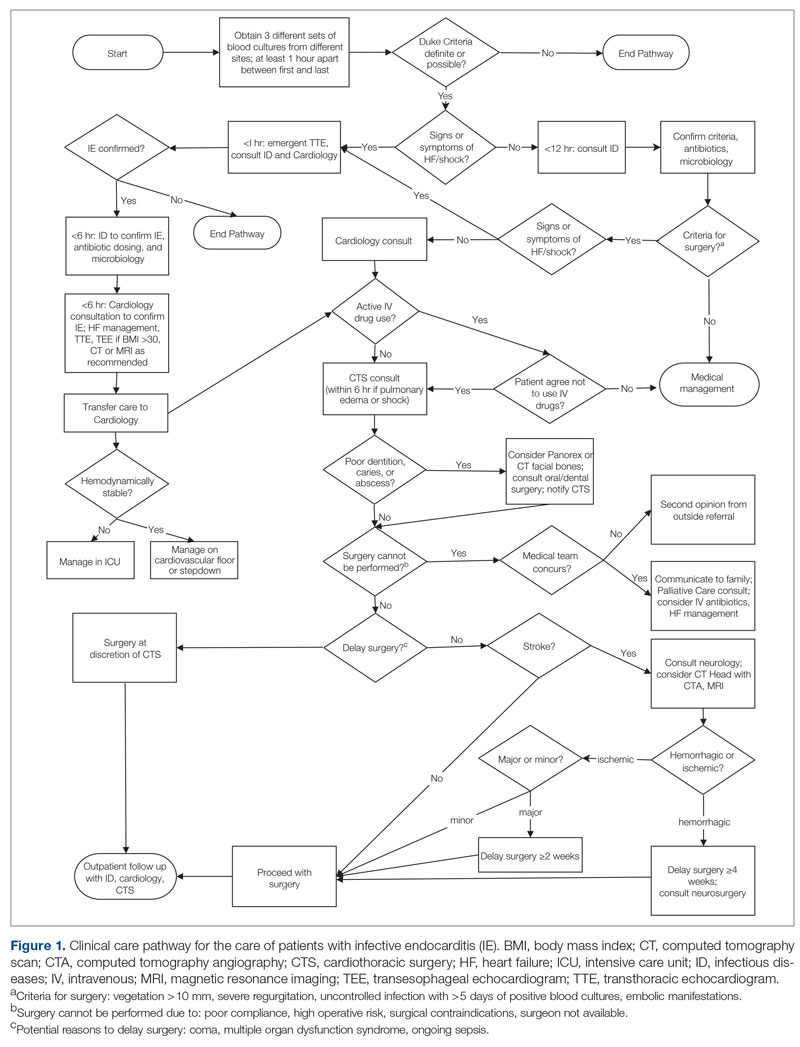
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
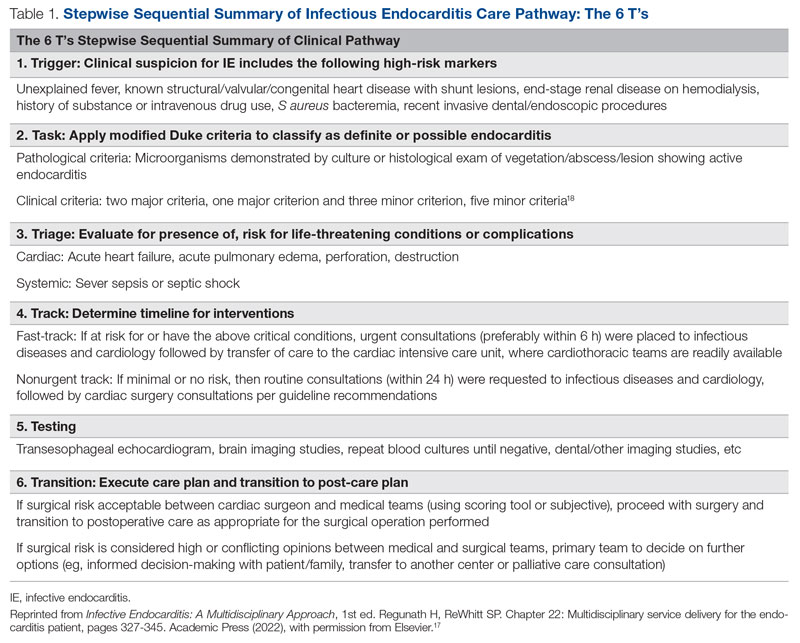
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
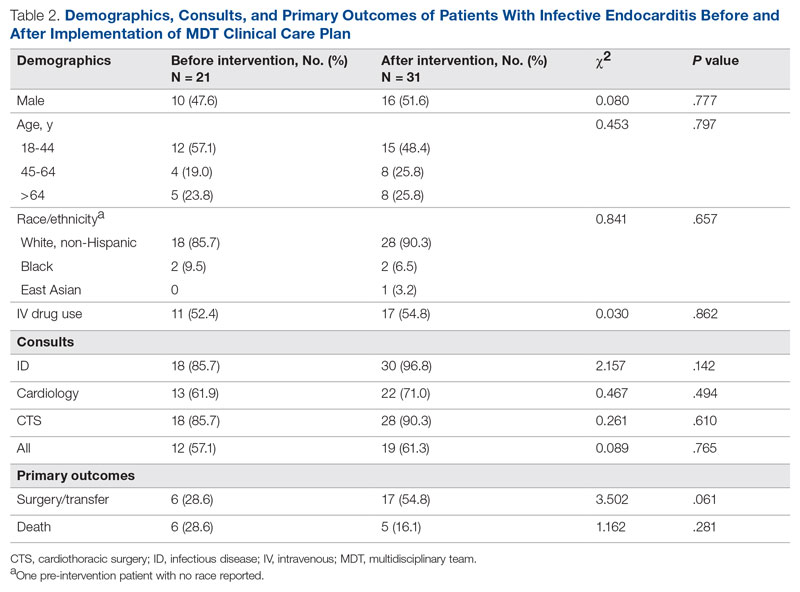
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
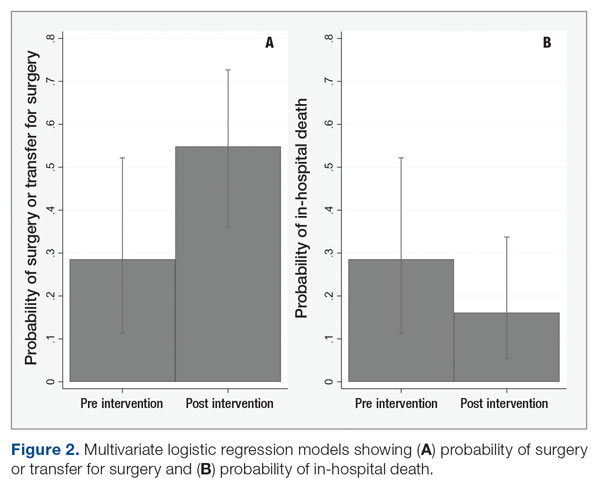
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; [email protected]
Disclosures: None reported.
From the University of Missouri School of Medicine, Columbia, MO (Haley Crosby); Department of Clinical Family and Community Medicine, University of Missouri, Columbia, MO (Dr. Pierce); and Department of Medicine, Divisions of Infectious Diseases and Pulmonary, Critical Care and Environmental Medicine, University of Missouri, Columbia, MO, and Divisions of Pulmonary and Critical Care Medicine and Infectious Diseases, University of Maryland Baltimore Washington Medical Center, Glen Burnie, MD (Dr. Regunath).
ABSTRACT
Objective: Multidisciplinary teams (MDTs) improve outcomes for patients with infective endocarditis (IE), but methods of implementation vary. In our academic medical center, we developed an MDT approach guided by a clinical care pathway and assessed outcomes of patients with IE.
Methods: We compared outcomes of patients with IE and indications for surgery between December 2018 and June 2020 with our prior published data for the period January to December 2016. MDT interventions involved recurring conferences with infectious diseases physicians in team meetings and promoting a clinical care pathway to guide providers on steps in management. Primary outcomes were surgery and in-hospital death.
Results: Prior to the intervention, 6 of 21 (28.6%) patients with indications for surgery underwent surgery or were transferred to higher centers for surgery, and 6 (28.6%) patients died. Post intervention, 17 of 31 (54.8%) patients underwent or were transferred for surgery, and 5 (16.1%) died. After adjusting for age and gender, the odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) compared with the pre-intervention period. The odds ratio for death among patients in the postintervention period was 0.40 (95% CI, 0.09-1.69; P = .21).
Conclusion: An MDT team approach using a clinical pathway was associated with an increased number of surgeries performed for IE and may lower rates of in-hospital mortality.
Keywords: infective endocarditis, clinical pathway, quality improvement, multidisciplinary team, valve surgery.
Infective endocarditis (IE) is associated with significant morbidity and mortality.1 Rates of IE due to Staphylococcus aureus are increasing in the United States.2 Reported in-hospital mortality from IE ranges from 15% to 20%.3
Clinical pathways are defined as “structured, multidisciplinary plans of care used by health services to detail essential steps in the care of patients with a specific clinical problem.”12 In the modern era, these pathways are often developed and implemented via the electronic health record (EHR) system. Studies of clinical pathways generally demonstrate improvements in patient outcomes, quality of care, or resource utilization.13,14 Clinical pathways represent 1 possible approach to the implementation of a MDT in the care of patients with IE.15
In our earlier work, we used quality improvement principles in the design of an MDT approach to IE care at our institution.16 Despite having indications for surgery, 12 of 21 (57.1%) patients with IE did not undergo surgery, and we identified these missed opportunities for surgery as a leverage point for improvement of outcomes. With input from the various specialties and stakeholders, we developed a clinical pathway (algorithm) for the institutional management of IE that guides next steps in clinical care and their timelines, aiming to reduce by 50% (from 57.1% to 28.6%) the number of patients with IE who do not undergo surgery despite guideline indications for early surgical intervention. In this report, we describe the implementation of this clinical pathway as our MDT approach to the care of patients with IE at our institution.
Methods
The University of Missouri, Columbia, is a tertiary care academic health system with 5 hospitals and more than 60 clinic locations across central Missouri. In the spring of 2018, an MDT was developed, with support from administrative leaders, to improve the care of patients with IE at our institution. The work group prioritized one leverage point to improve IE outcomes, which was improving the number of surgeries performed on those IE patients who had guideline indications for surgery. A clinical pathway was developed around this leverage point (Figure 1). The pathway leveraged the 6 T’s (Table 1) to guide providers through the evaluation and management of IE.17 The pathway focused on improving adherence to standards of care and reduction in practice variation by defining indications for referrals and diagnostic interventions, helping to reduce delays in consultation and diagnosis. The pathway also clearly outlined the surgical indications and timing for patients with IE and provided the basis for decisions to proceed with surgery.
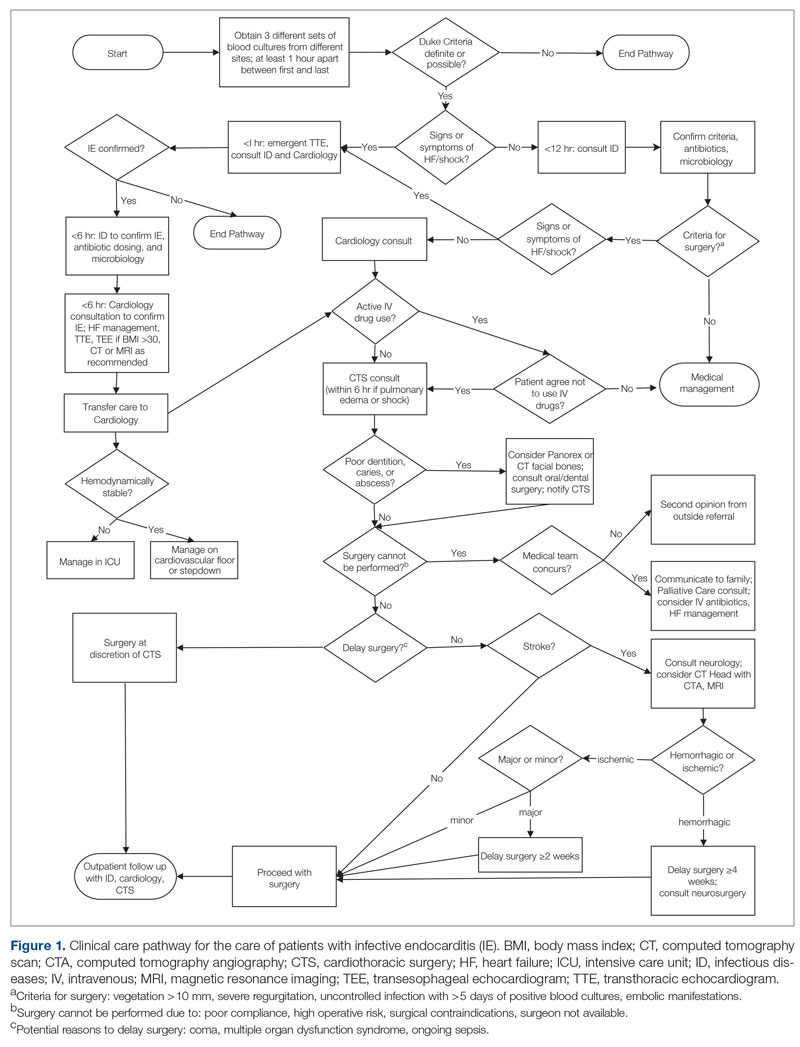
Starting in late 2018, in collaboration with cardiology and CTS teams, ID specialists socialized the clinical pathway to inpatient services that cared for patients with IE. Infectious diseases physicians also provided recurring conferences on the effectiveness of MDTs in IE management and participated in heart-valve team case discussions. Finally, in May 2019, an electronic version of the pathway was embedded in the EHR system using a Cerner PowerChart feature known as Care Pathways. The feature presents the user with algorithm questions in the EHR and provides recommendations, relevant orders, timelines, and other decision support in the clinical pathway. The feature is available to all providers in the health system.
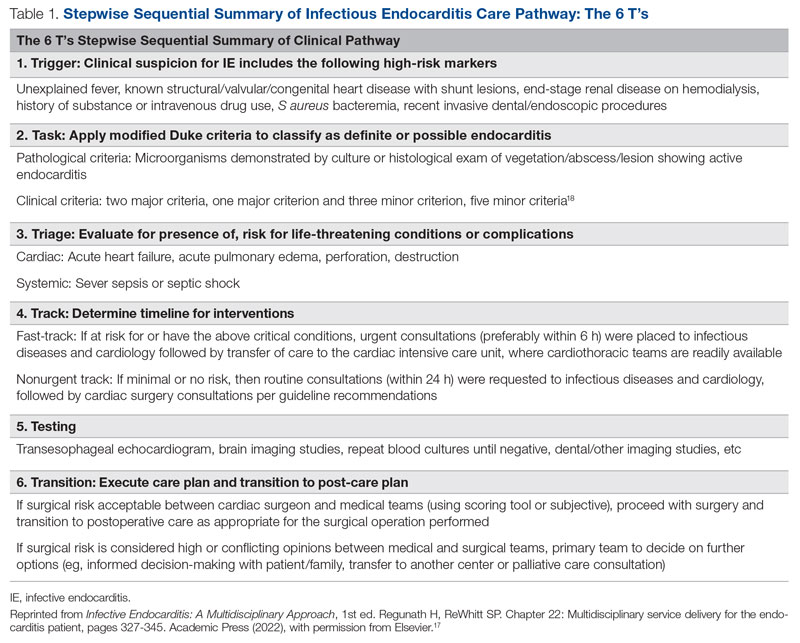
To evaluate the effectiveness of our intervention, we recorded outcomes for patients with IE with surgical indications between December 2018 and June 2020 and compared them with our prior published data from January to December 2016. Cases of IE for the current study period were identified via retrospective chart review. Records from December 2018 to June 2020 were searched using International Statistical Classification of Diseases, Tenth Revision (ICD-10) discharge codes for IE (I33, I33.0, I33.9, I38, I39, M32.11). To select those patients with definitive IE and indications for surgery, the following criteria were applied: age ≥ 18 years; fulfilled modified Duke criteria for definite IE18; and met ≥ 1 American Heart Association (AHA)/Infection Diseases Society of America criteria for recommendation for surgery. Indications for surgery were ≥ 1 of the following: left-sided endocarditis caused by S aureus, fungal, or highly resistant organism; new heart block; annular or aortic abscess; persistent bacteremia or fever despite 5 days of appropriate antimicrobials; vegetation size ≥ 10 mm and evidence of embolic phenomena; recurrence of prosthetic valve infection; recurrent emboli and persistent vegetation despite antimicrobials; and increase in vegetation size despite antimicrobials.16
Age was treated as a categorical variable, using the age groups 18 to 44 years, 45 to 64 years, and 65 years and older. Gender was self-reported. Primary outcomes were surgery or transfer to a higher center for surgery and in-hospital death. Secondary outcomes included consults to teams involved in multidisciplinary care of patients with IE, including ID, cardiology, and CTS. Bivariate analyses were performed using Pearson χ2 tests. Odds ratios for surgery and death were calculated using a multivariate logistic regression model including age and gender covariates. Statistical significance was defined at α = 0.05, and statistical analysis was performed using Stata/IC v16.1 (StataCorp LLC). Our university institutional review board (IRB) reviewed the project (#2010858-QI) and determined that the project was quality-improvement activity, not human subject research, and therefore did not require additional IRB review.
Results
We identified 21 patients in the pre-intervention period and 31 patients in the postintervention period with definitive IE who had guideline indications for surgery. The postintervention cohort was older and had more male patients; this difference was not statistically significant. No differences were noted between the groups for race, gender, or intravenous (IV) drug use (Table 2). Chi-square tests of independence were performed to assess the relationship between age and our primary outcomes. There was a significant relationship between age and the likelihood of receiving or being transferred for surgery (59.3% vs 50% vs 7.7% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 [2, N = 52] = 9.67; P = .008), but not between age and mortality (14.8% vs 25.0% vs 30.8% for 18-44 y, 45-64 y, and ≥ 65 y, respectively; χ2 = 1.48 [2, N = 52; P = .478]. The electronic version of the clinical pathway was activated and used in only 3 of the 31 patients in the postintervention period. Consultations to ID, cardiology, and CTS teams were compared between the study periods (Table 2). Although more consultations were seen in the postintervention period, differences were not statistically significant.
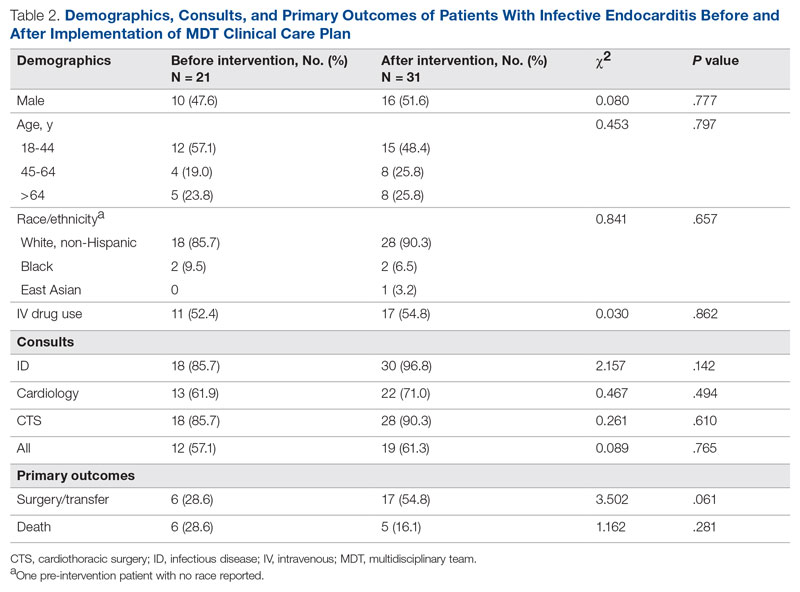
The unadjusted primary outcomes are shown in Table 2. More surgeries were performed per guideline indications, and fewer deaths were noted in the postintervention period than in the pre-intervention period, but the differences were not statistically significant (Table 2).
Because the postintervention period had more male patients and older patients, we evaluated the outcomes using a logistic regression model controlling for both age and gender. The odds of surgery or transfer for surgery for patients in the postintervention period were 4.88 (95% CI, 1.20-19.79; P = .027) as compared with the pre-intervention period, and the odds ratio for death among patients in the postintervention period compared with the pre-intervention period was 0.40 (95% CI, 0.09-1.69; P = .21) (Figure 2).
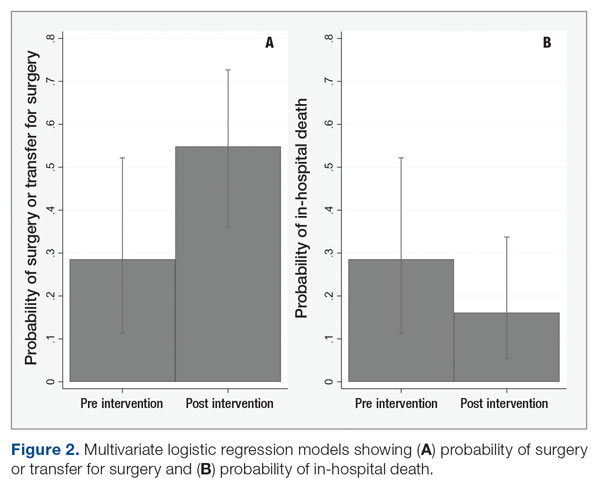
Discussion
In our study, patients with IE with guideline indications for surgery had significantly higher rates of surgery in the postintervention period than in the pre-intervention period. The implementation of an MDT, recurring educational sessions, and efforts to implement and familiarize team members with the clinical pathway approach are the most likely reasons for this change. The increased rates of surgery in the postintervention period were the likely proximate cause of the 60% reduction in in-hospital mortality. This improvement in mortality, while not statistically significant, is very likely to be clinically significant and helps reinforce the value of the MDT intervention used.
Our findings are consistent with existing and mounting literature on the use of MDTs to improve outcomes for patients with IE, including 2 studies that noted an increased rate of surgery for patients with indications.8,19 Several other studies in both Europe and North America have found significant decreases in mortality,6-11,20,21 rates of complications,9 time to diagnosis and treatment,11 and length of stay9,20 for patients with IE managed with an MDT strategy. Although current AHA guidelines for care of patients with IE do suggest an MDT approach, the strategy for this approach is not well established.22 Only 1 study that has implemented a new MDT protocol for care of IE has been conducted in the United States.8
While effective MDTs certainly improve outcomes in patients with IE, there are reported differences in implementation of such an approach. With the MDT model as the core, various implementations included regular case conferences,10,11,19,21,23 formation of a consulting team,6,8 or establishment of a new protocol or algorithm for care.8,9,20 Our approach used a clinical pathway as a basis for improved communication among consulting services, education of learning providers via regular case conferences, and implementation of an electronic clinical care pathway to guide them step by step. Our pathway followed the institutionally standardized algorithm (Figure 1), using what we called the 6 T’s approach (Table 1), that guides providers to evaluate critical cases in a fast track.17
To the best of our knowledge, ours is the first report of an MDT that used an electronic clinical care pathway embedded within the EHR. The electronic version of our clinical pathway went live for only the second half of the postintervention study period, which is the most likely reason for its limited utilization. It is also possible that educational efforts in the first half of the intervention period were sufficient to familiarize providers with the care pathway such that the electronic version was seldom needed. We are exploring other possible ways of improving electronic pathway utilization, such as improving the feature usability and further systemwide educational efforts.
Our study has other limitations. Quasi-experimental before-and-after comparisons are subject to confounding from concurrent interventions. We had a substantial change in cardiothoracic faculty soon after the commencement of our efforts to form the MDT, and thus cannot rule out differences related to their comfort level in considering or offering surgery. We also cannot rule out a Hawthorne effect, where knowledge of the ongoing quality-improvement project changed provider behavior, making surgery more likely. We did not evaluate rates of right- versus left-sided endocarditis, which have been linked to mortality.24 Our study also was performed across a single academic institution, which may limit its generalizability. Finally, our study may not have been adequately powered to detect differences in mortality due to implementation of the MDT approach.
Conclusion
Our work suggests that an MDT for IE can be successfully designed and implemented with a clinical pathway using quality-improvement tools in centers where subspecialty services are available. Our approach was associated with a higher rate of surgery among patients with guideline indications for surgery and may reduce in-hospital mortality. An electronic clinical care pathway embedded in the EHR is feasible and may have a role in MDT implementation.
These data were also accepted as a poster at IDWeek 2022, Washington, DC. The poster abstract is published in an online supplement of Open Forum Infectious Diseases as an abstract publication.
Corresponding author: Haley Crosby; [email protected]
Disclosures: None reported.
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
1. Baddour LM, Wilson WR, Bayer AS, et al. Infective endocarditis in adults: diagnosis, antimicrobial therapy, and management of complications: a scientific statement for healthcare professionals from the American Heart Association. Circulation. 2015;132(15):1435-1486. doi:10.1161/cir.0000000000000296
2. Federspiel JJ, Stearns SC, Peppercorn AF, et al. Increasing US rates of endocarditis with Staphylococcus aureus: 1999-2008. Arch Intern Med. 2012;172(4):363-365. doi:10.1001/archinternmed.2011.1027
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(23):e521-e643. doi:10.1161/cir.0000000000000031
4. Chambers J, Sandoe J, Ray S, et al. The infective endocarditis team: recommendations from an international working group. Heart. 2014;100(7):524-527. doi:10.1136/heartjnl-2013-304354
5. Habib G, Lancellotti P, Antunes MJ, et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36(44):3075-3128. doi:10.1093/eurheartj/ehv319
6. Chirillo F, Scotton P, Rocco F, et al. Impact of a multidisciplinary management strategy on the outcome of patients with native valve infective endocarditis. Am J Cardiol. 2013;112(8):1171-1176. doi:10.1016/j.amjcard.2013.05.060
7. Botelho-Nevers E, Thuny F, Casalta JP, et al. Dramatic reduction in infective endocarditis-related mortality with a management-based approach. Arch Intern Med. 2009;169(14):1290-1298. doi:10.1001/archinternmed.2009.192
8. El-Dalati S, Cronin D, Riddell IV J, et al. The clinical impact of implementation of a multidisciplinary endocarditis team. Ann Thorac Surg. 2022;113(1):118-124.
9. Carrasco-Chinchilla F, Sánchez-Espín G, Ruiz-Morales J, et al. Influence of a multidisciplinary alert strategy on mortality due to left-sided infective endocarditis. Rev Esp Cardiol (Engl Ed). 2014;67(5):380-386. doi:10.1016/j.rec.2013.09.010
10. Issa N, Dijos M, Greib C, et al. Impact of an endocarditis team in the management of 357 infective endocarditis [abstract]. Open Forum Infect Dis. 2016;3(suppl 1):S201. doi:10.1093/ofid/ofw172.825
11. Kaura A, Byrne J, Fife A, et al. Inception of the ‘endocarditis team’ is associated with improved survival in patients with infective endocarditis who are managed medically: findings from a before-and-after study. Open Heart. 2017;4(2):e000699. doi:10.1136/openhrt-2017-000699
12. Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;(3):Cd006632. doi:10.1002/14651858.CD006632.pub2
13. Neame MT, Chacko J, Surace AE, et al. A systematic review of the effects of implementing clinical pathways supported by health information technologies. J Am Med Inform Assoc. 2019;26(4):356-363. doi:10.1093/jamia/ocy176
14. Trimarchi L, Caruso R, Magon G, et al. Clinical pathways and patient-related outcomes in hospital-based settings: a systematic review and meta-analysis of randomized controlled trials. Acta Biomed. 2021;92(1):e2021093. doi:10.23750/abm.v92i1.10639
15. Gibbons EF, Huang G, Aldea G, et al. A multidisciplinary pathway for the diagnosis and treatment of infectious endocarditis. Crit Pathw Cardiol. 2020;19(4):187-194. doi:10.1097/hpc.0000000000000224
16. Regunath H, Vasudevan A, Vyas K, et al. A quality improvement initiative: developing a multi-disciplinary team for infective endocarditis. Mo Med. 2019;116(4):291-296.
17. Regunath H, Whitt SP. Multidisciplinary service delivery for the endocarditis patient. In: Infective Endocarditis: A Multidisciplinary Approach. 1st ed. Kilic A, ed. Academic Press; 2022.
18. Durack DT, Lukes AS, Bright DK. New criteria for diagnosis of infective endocarditis: utilization of specific echocardiographic findings. Duke Endocarditis Service. Am J Med. 1994;96(3):200-209. doi:10.1016/0002-9343(94)90143-0
19. Tan C, Hansen MS, Cohen G, et al. Case conferences for infective endocarditis: a quality improvement initiative. PLoS One. 2018;13(10):e0205528. doi:10.1371/journal.pone.0205528
20. Ruch Y, Mazzucotelli JP, Lefebvre F, et al. Impact of setting up an “endocarditis team” on the management of infective endocarditis. Open Forum Infect Dis. 2019;6(9):ofz308. doi:10.1093/ofid/ofz308
21. Camou F, Dijos M, Barandon L, et al. Management of infective endocarditis and multidisciplinary approach. Med Mal Infect. 2019;49(1):17-22. doi:10.1016/j.medmal.2018.06.007
22. Pettersson GB, Hussain ST. Current AATS guidelines on surgical treatment of infective endocarditis. Ann Cardiothorac Surg. 2019;8(6):630-644. doi:10.21037/acs.2019.10.05
23. Mestres CA, Paré JC, Miró JM. Organization and functioning of a multidisciplinary team for the diagnosis and treatment of infective endocarditis: a 30-year perspective (1985-2014). Rev Esp Cardiol (Engl Ed). 2015;68(5):363-368. doi:10.1016/j.rec.2014.10.006
24. Stavi V, Brandstaetter E, Sagy I, et al. Comparison of clinical characteristics and prognosis in patients with right- and left-sided infective endocarditis. Rambam Maimonides Med J. 2019;10(1):e00003. doi:10.5041/rmmj.10338
The Shifting Landscape of Thrombolytic Therapy for Acute Ischemic Stroke
Study 1 Overview (Menon et al)
Objective: To determine whether a 0.25 mg/kg dose of intravenous tenecteplase is noninferior to intravenous alteplase 0.9 mg/kg for patients with acute ischemic stroke eligible for thrombolytic therapy.
Design: Multicenter, parallel-group, open-label randomized controlled trial.
Setting and participants: The trial was conducted at 22 primary and comprehensive stroke centers across Canada. A primary stroke center was defined as a hospital capable of offering intravenous thrombolysis to patients with acute ischemic stroke, while a comprehensive stroke center was able to offer thrombectomy services in addition. The involved centers also participated in Canadian quality improvement registries (either Quality Improvement and Clinical Research [QuiCR] or Optimizing Patient Treatment in Major Ischemic Stroke with EVT [OPTIMISE]) that track patient outcomes. Patients were eligible for inclusion if they were aged 18 years or older, had a diagnosis of acute ischemic stroke, presented within 4.5 hours of symptom onset, and were eligible for thrombolysis according to Canadian guidelines.
Patients were randomized in a 1:1 fashion to either intravenous tenecteplase (0.25 mg/kg single dose, maximum of 25 mg) or intravenous alteplase (0.9 mg/kg total dose to a maximum of 90 mg, delivered as a bolus followed by a continuous infusion). A total of 1600 patients were enrolled, with 816 randomly assigned to the tenecteplase arm and 784 to the alteplase arm; 1577 patients were included in the intention-to-treat (ITT) analysis (n = 806 tenecteplase; n = 771 alteplase). The median age of enrollees was 74 years, and 52.1% of the ITT population were men.
Main outcome measures: In the ITT population, the primary outcome measure was a modified Rankin score (mRS) of 0 or 1 at 90 to 120 days post treatment. Safety outcomes included symptomatic intracerebral hemorrhage, orolingual angioedema, extracranial bleeding that required blood transfusion (all within 24 hours of thrombolytic administration), and all-cause mortality at 90 days. The noninferiority threshold for intravenous tenecteplase was set as the lower 95% CI of the difference between the tenecteplase and alteplase groups in the proportion of patients who met the primary outcome exceeding –5%.
Main results: The primary outcome of mRS of either 0 or 1 at 90 to 120 days of treatment occurred in 296 (36.9%) of the 802 patients assigned to tenecteplase and 266 (34.8%) of the 765 patients assigned to alteplase (unadjusted risk difference, 2.1%; 95% CI, –2.6 to 6.9). The prespecified noninferiority threshold was met. There were no significant differences between the groups in rates of intracerebral hemorrhage at 24 hours or 90-day all-cause mortality.
Conclusion: Intravenous tenecteplase is a reasonable alternative to alteplase for patients eligible for thrombolytic therapy.
Study 2 Overview (Wang et al)
Objective: To determine whether tenecteplase (dose 0.25 mg/kg) is noninferior to alteplase in patients with acute ischemic stroke who are within 4.5 hours of symptom onset and eligible for thrombolytic therapy but either refused or were ineligible for endovascular thrombectomy.
Design: Multicenter, prospective, open-label, randomized, controlled noninferiority trial.
Setting and participants: This trial was conducted at 53 centers across China and included patients 18 years of age or older who were within 4.5 hours of symptom onset and were thrombolytic eligible, had a mRS ≤ 1 at enrollment, and had a National Institutes of Health Stroke Scale score between 5 and 25. Eligible participants were randomized 1:1 to either tenecteplase 0.25 mg/kg (maximum dose 25 mg) or alteplase 0.9 mg/kg (maximum dose 90 mg, administered as a bolus followed by infusion). During the enrollment period (June 12, 2021, to May 29, 2022), a total of 1430 participants were enrolled, and, of those, 716 were randomly assigned to tenecteplase and 714 to alteplase. Six patients assigned to tenecteplase and 7 assigned to alteplase did not receive drugs. At 90 days, 5 in the tenecteplase group and 11 in the alteplase group were lost to follow up.
Main outcome measures: The primary efficacy outcome was a mRS of 0 or 1 at 90 days. The primary safety outcome was intracranial hemorrhage within 36 hours. Safety outcomes included parenchymal hematoma 2, as defined by the European Cooperative Acute Stroke Study III; any intracranial or significant hemorrhage, as defined by the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries criteria; and death from all causes at 90 days. Noninferiority for tenecteplase would be declared if the lower 97.5% 1-sided CI for the relative risk (RR) for the primary outcome did not cross 0.937.
Main results: In the modified ITT population, the primary outcome occurred in 439 (62%) of the tenecteplase group and 405 (68%) of the alteplase group (RR, 1.07; 95% CI, 0.98-1.16). This met the prespecified margin for noninferiority. Intracranial hemorrhage within 36 hours was experienced by 15 (2%) patients in the tenecteplase group and 13 (2%) in the alteplase group (RR, 1.18; 95% CI, 0.56-2.50). Death at 90 days occurred in 46 (7%) patients in the tenecteplase group and 35 (5%) in the alteplase group (RR, 1.31; 95% CI, 0.86-2.01).
Conclusion: Tenecteplase was noninferior to alteplase in patients with acute ischemic stroke who met criteria for thrombolysis and either refused or were ineligible for endovascular thrombectomy.
Commentary
Alteplase has been FDA-approved for managing acute ischemic stroke since 1996 and has demonstrated positive effects on functional outcomes. Drawbacks of alteplase therapy, however, include bleeding risk as well as cumbersome administration of a bolus dose followed by a 60-minute infusion. In recent years, the question of whether or not tenecteplase could replace alteplase as the preferred thrombolytic for acute ischemic stroke has garnered much attention. Several features of tenecteplase make it an attractive option, including increased fibrin specificity, a longer half-life, and ease of administration as a single, rapid bolus dose. In phase 2 trials that compared tenecteplase 0.25 mg/kg with alteplase, findings suggested the potential for early neurological improvement as well as improved outcomes at 90 days. While the role of tenecteplase in acute myocardial infarction has been well established due to ease of use and a favorable adverse-effect profile,1 there is much less evidence from phase 3 randomized controlled clinical trials to secure the role of tenecteplase in acute ischemic stroke.2
Menon et al attempted to close this gap in the literature by conducting a randomized controlled clinical trial (AcT) comparing tenecteplase to alteplase in a Canadian patient population. The trial's patient population mirrors that of real-world data from global registries in terms of age, sex, and baseline stroke severity. In addition, the eligibility window of 4.5 hours from symptom onset as well as the inclusion and exclusion criteria for therapy are common to those utilized in other countries, making the findings generalizable. There were some limitations to the study, however, including the impact of COVID-19 on recruitment efforts as well as limitations of research infrastructure and staffing, which may have limited enrollment efforts at primary stroke centers. Nonetheless, the authors concluded that their results provide evidence that tenecteplase is comparable to alteplase, with similar functional and safety outcomes.
TRACE-2 focused on an Asian patient population and provided follow up to the dose-ranging TRACE-1 phase 2 trial. TRACE-1 showed that tenecteplase 0.25 mg/kg had a similar safety profile to alteplase 0.9 mg/kg in Chinese patients presenting with acute ischemic stroke. TRACE-2 sought to establish noninferiority of tenecteplase and excluded patients who were ineligible for or refused thrombectomy. Interestingly, the tenecteplase arm, as the authors point out, had numerically greater mortality as well as intracranial hemorrhage, but these differences were not statistically significant between the treatment groups at 90 days. The TRACE-2 results parallel those of AcT, and although there were differences in ethnicity between the 2 trials, the authors cite this as evidence that the results are consistent and provide evidence for the role of tenecteplase in the management of acute ischemic stroke. Limitations of this trial include potential bias from its open-label design, as well as exclusion of patients with more severe strokes eligible for thrombectomy, which may limit generalizability to patients with more disabling strokes who could have a higher risk of intracranial hemorrhage.
Application for Clinical Practice and System Implementation
Across the country, many organizations have adopted the off-label use of tenecteplase for managing fibrinolytic-eligible acute ischemic stroke patients. In most cases, the impetus for change is the ease of dosing and administration of tenecteplase compared to alteplase, while the inclusion and exclusion criteria and overall management remain the same. Timely administration of therapy in stroke is critical. This, along with other time constraints in stroke workflows, the weight-based calculation of alteplase doses, and alteplase’s administration method may lead to medication errors when using this agent to treat patients with acute stroke. The rapid, single-dose administration of tenecteplase removes many barriers that hospitals face when patients may need to be treated and then transferred to another site for further care. Without the worry to “drip and ship,” the completion of administration may allow for timely patient transfer and eliminate the need for monitoring of an infusion during transfer. For some organizations, there may be a potential for drug cost-savings as well as improved metrics, such as door-to-needle time, but the overall effects of switching from alteplase to tenecteplase remain to be seen. Currently, tenecteplase is included in stroke guidelines as a “reasonable choice,” though with a low level of evidence.3 However, these 2 studies support the role of tenecteplase in acute ischemic stroke treatment and may provide a foundation for further studies to establish the role of tenecteplase in the acute ischemic stroke population.
Practice Points
- Tenecteplase may be considered as an alternative to alteplase for acute ischemic stroke for patients who meet eligibility criteria for thrombolytics; this recommendation is included in the most recent stroke guidelines, although tenecteplase has not been demonstrated to be superior to alteplase.
- The ease of administration of tenecteplase as a single intravenous bolus dose represents a benefit compared to alteplase; it is an off-label use, however, and further studies are needed to establish the superiority of tenecteplase in terms of functional and safety outcomes.
– Carol Heunisch, PharmD, BCPS, BCCP
Pharmacy Department, NorthShore–Edward-Elmhurst Health, Evanston, IL
1. Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT-2) Investigators; F Van De Werf, J Adgey, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Lancet. 1999;354(9180):716-722. doi:10.1016/s0140-6736(99)07403-6
2. Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischaemic stroke: meta-analysis of 5 randomized trials. Stroke. 2019;50(8):2156-2162. doi:10.1161/STROKEAHA.119.025080
3. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. doi:10.1161/STR.0000000000000211
Study 1 Overview (Menon et al)
Objective: To determine whether a 0.25 mg/kg dose of intravenous tenecteplase is noninferior to intravenous alteplase 0.9 mg/kg for patients with acute ischemic stroke eligible for thrombolytic therapy.
Design: Multicenter, parallel-group, open-label randomized controlled trial.
Setting and participants: The trial was conducted at 22 primary and comprehensive stroke centers across Canada. A primary stroke center was defined as a hospital capable of offering intravenous thrombolysis to patients with acute ischemic stroke, while a comprehensive stroke center was able to offer thrombectomy services in addition. The involved centers also participated in Canadian quality improvement registries (either Quality Improvement and Clinical Research [QuiCR] or Optimizing Patient Treatment in Major Ischemic Stroke with EVT [OPTIMISE]) that track patient outcomes. Patients were eligible for inclusion if they were aged 18 years or older, had a diagnosis of acute ischemic stroke, presented within 4.5 hours of symptom onset, and were eligible for thrombolysis according to Canadian guidelines.
Patients were randomized in a 1:1 fashion to either intravenous tenecteplase (0.25 mg/kg single dose, maximum of 25 mg) or intravenous alteplase (0.9 mg/kg total dose to a maximum of 90 mg, delivered as a bolus followed by a continuous infusion). A total of 1600 patients were enrolled, with 816 randomly assigned to the tenecteplase arm and 784 to the alteplase arm; 1577 patients were included in the intention-to-treat (ITT) analysis (n = 806 tenecteplase; n = 771 alteplase). The median age of enrollees was 74 years, and 52.1% of the ITT population were men.
Main outcome measures: In the ITT population, the primary outcome measure was a modified Rankin score (mRS) of 0 or 1 at 90 to 120 days post treatment. Safety outcomes included symptomatic intracerebral hemorrhage, orolingual angioedema, extracranial bleeding that required blood transfusion (all within 24 hours of thrombolytic administration), and all-cause mortality at 90 days. The noninferiority threshold for intravenous tenecteplase was set as the lower 95% CI of the difference between the tenecteplase and alteplase groups in the proportion of patients who met the primary outcome exceeding –5%.
Main results: The primary outcome of mRS of either 0 or 1 at 90 to 120 days of treatment occurred in 296 (36.9%) of the 802 patients assigned to tenecteplase and 266 (34.8%) of the 765 patients assigned to alteplase (unadjusted risk difference, 2.1%; 95% CI, –2.6 to 6.9). The prespecified noninferiority threshold was met. There were no significant differences between the groups in rates of intracerebral hemorrhage at 24 hours or 90-day all-cause mortality.
Conclusion: Intravenous tenecteplase is a reasonable alternative to alteplase for patients eligible for thrombolytic therapy.
Study 2 Overview (Wang et al)
Objective: To determine whether tenecteplase (dose 0.25 mg/kg) is noninferior to alteplase in patients with acute ischemic stroke who are within 4.5 hours of symptom onset and eligible for thrombolytic therapy but either refused or were ineligible for endovascular thrombectomy.
Design: Multicenter, prospective, open-label, randomized, controlled noninferiority trial.
Setting and participants: This trial was conducted at 53 centers across China and included patients 18 years of age or older who were within 4.5 hours of symptom onset and were thrombolytic eligible, had a mRS ≤ 1 at enrollment, and had a National Institutes of Health Stroke Scale score between 5 and 25. Eligible participants were randomized 1:1 to either tenecteplase 0.25 mg/kg (maximum dose 25 mg) or alteplase 0.9 mg/kg (maximum dose 90 mg, administered as a bolus followed by infusion). During the enrollment period (June 12, 2021, to May 29, 2022), a total of 1430 participants were enrolled, and, of those, 716 were randomly assigned to tenecteplase and 714 to alteplase. Six patients assigned to tenecteplase and 7 assigned to alteplase did not receive drugs. At 90 days, 5 in the tenecteplase group and 11 in the alteplase group were lost to follow up.
Main outcome measures: The primary efficacy outcome was a mRS of 0 or 1 at 90 days. The primary safety outcome was intracranial hemorrhage within 36 hours. Safety outcomes included parenchymal hematoma 2, as defined by the European Cooperative Acute Stroke Study III; any intracranial or significant hemorrhage, as defined by the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries criteria; and death from all causes at 90 days. Noninferiority for tenecteplase would be declared if the lower 97.5% 1-sided CI for the relative risk (RR) for the primary outcome did not cross 0.937.
Main results: In the modified ITT population, the primary outcome occurred in 439 (62%) of the tenecteplase group and 405 (68%) of the alteplase group (RR, 1.07; 95% CI, 0.98-1.16). This met the prespecified margin for noninferiority. Intracranial hemorrhage within 36 hours was experienced by 15 (2%) patients in the tenecteplase group and 13 (2%) in the alteplase group (RR, 1.18; 95% CI, 0.56-2.50). Death at 90 days occurred in 46 (7%) patients in the tenecteplase group and 35 (5%) in the alteplase group (RR, 1.31; 95% CI, 0.86-2.01).
Conclusion: Tenecteplase was noninferior to alteplase in patients with acute ischemic stroke who met criteria for thrombolysis and either refused or were ineligible for endovascular thrombectomy.
Commentary
Alteplase has been FDA-approved for managing acute ischemic stroke since 1996 and has demonstrated positive effects on functional outcomes. Drawbacks of alteplase therapy, however, include bleeding risk as well as cumbersome administration of a bolus dose followed by a 60-minute infusion. In recent years, the question of whether or not tenecteplase could replace alteplase as the preferred thrombolytic for acute ischemic stroke has garnered much attention. Several features of tenecteplase make it an attractive option, including increased fibrin specificity, a longer half-life, and ease of administration as a single, rapid bolus dose. In phase 2 trials that compared tenecteplase 0.25 mg/kg with alteplase, findings suggested the potential for early neurological improvement as well as improved outcomes at 90 days. While the role of tenecteplase in acute myocardial infarction has been well established due to ease of use and a favorable adverse-effect profile,1 there is much less evidence from phase 3 randomized controlled clinical trials to secure the role of tenecteplase in acute ischemic stroke.2
Menon et al attempted to close this gap in the literature by conducting a randomized controlled clinical trial (AcT) comparing tenecteplase to alteplase in a Canadian patient population. The trial's patient population mirrors that of real-world data from global registries in terms of age, sex, and baseline stroke severity. In addition, the eligibility window of 4.5 hours from symptom onset as well as the inclusion and exclusion criteria for therapy are common to those utilized in other countries, making the findings generalizable. There were some limitations to the study, however, including the impact of COVID-19 on recruitment efforts as well as limitations of research infrastructure and staffing, which may have limited enrollment efforts at primary stroke centers. Nonetheless, the authors concluded that their results provide evidence that tenecteplase is comparable to alteplase, with similar functional and safety outcomes.
TRACE-2 focused on an Asian patient population and provided follow up to the dose-ranging TRACE-1 phase 2 trial. TRACE-1 showed that tenecteplase 0.25 mg/kg had a similar safety profile to alteplase 0.9 mg/kg in Chinese patients presenting with acute ischemic stroke. TRACE-2 sought to establish noninferiority of tenecteplase and excluded patients who were ineligible for or refused thrombectomy. Interestingly, the tenecteplase arm, as the authors point out, had numerically greater mortality as well as intracranial hemorrhage, but these differences were not statistically significant between the treatment groups at 90 days. The TRACE-2 results parallel those of AcT, and although there were differences in ethnicity between the 2 trials, the authors cite this as evidence that the results are consistent and provide evidence for the role of tenecteplase in the management of acute ischemic stroke. Limitations of this trial include potential bias from its open-label design, as well as exclusion of patients with more severe strokes eligible for thrombectomy, which may limit generalizability to patients with more disabling strokes who could have a higher risk of intracranial hemorrhage.
Application for Clinical Practice and System Implementation
Across the country, many organizations have adopted the off-label use of tenecteplase for managing fibrinolytic-eligible acute ischemic stroke patients. In most cases, the impetus for change is the ease of dosing and administration of tenecteplase compared to alteplase, while the inclusion and exclusion criteria and overall management remain the same. Timely administration of therapy in stroke is critical. This, along with other time constraints in stroke workflows, the weight-based calculation of alteplase doses, and alteplase’s administration method may lead to medication errors when using this agent to treat patients with acute stroke. The rapid, single-dose administration of tenecteplase removes many barriers that hospitals face when patients may need to be treated and then transferred to another site for further care. Without the worry to “drip and ship,” the completion of administration may allow for timely patient transfer and eliminate the need for monitoring of an infusion during transfer. For some organizations, there may be a potential for drug cost-savings as well as improved metrics, such as door-to-needle time, but the overall effects of switching from alteplase to tenecteplase remain to be seen. Currently, tenecteplase is included in stroke guidelines as a “reasonable choice,” though with a low level of evidence.3 However, these 2 studies support the role of tenecteplase in acute ischemic stroke treatment and may provide a foundation for further studies to establish the role of tenecteplase in the acute ischemic stroke population.
Practice Points
- Tenecteplase may be considered as an alternative to alteplase for acute ischemic stroke for patients who meet eligibility criteria for thrombolytics; this recommendation is included in the most recent stroke guidelines, although tenecteplase has not been demonstrated to be superior to alteplase.
- The ease of administration of tenecteplase as a single intravenous bolus dose represents a benefit compared to alteplase; it is an off-label use, however, and further studies are needed to establish the superiority of tenecteplase in terms of functional and safety outcomes.
– Carol Heunisch, PharmD, BCPS, BCCP
Pharmacy Department, NorthShore–Edward-Elmhurst Health, Evanston, IL
Study 1 Overview (Menon et al)
Objective: To determine whether a 0.25 mg/kg dose of intravenous tenecteplase is noninferior to intravenous alteplase 0.9 mg/kg for patients with acute ischemic stroke eligible for thrombolytic therapy.
Design: Multicenter, parallel-group, open-label randomized controlled trial.
Setting and participants: The trial was conducted at 22 primary and comprehensive stroke centers across Canada. A primary stroke center was defined as a hospital capable of offering intravenous thrombolysis to patients with acute ischemic stroke, while a comprehensive stroke center was able to offer thrombectomy services in addition. The involved centers also participated in Canadian quality improvement registries (either Quality Improvement and Clinical Research [QuiCR] or Optimizing Patient Treatment in Major Ischemic Stroke with EVT [OPTIMISE]) that track patient outcomes. Patients were eligible for inclusion if they were aged 18 years or older, had a diagnosis of acute ischemic stroke, presented within 4.5 hours of symptom onset, and were eligible for thrombolysis according to Canadian guidelines.
Patients were randomized in a 1:1 fashion to either intravenous tenecteplase (0.25 mg/kg single dose, maximum of 25 mg) or intravenous alteplase (0.9 mg/kg total dose to a maximum of 90 mg, delivered as a bolus followed by a continuous infusion). A total of 1600 patients were enrolled, with 816 randomly assigned to the tenecteplase arm and 784 to the alteplase arm; 1577 patients were included in the intention-to-treat (ITT) analysis (n = 806 tenecteplase; n = 771 alteplase). The median age of enrollees was 74 years, and 52.1% of the ITT population were men.
Main outcome measures: In the ITT population, the primary outcome measure was a modified Rankin score (mRS) of 0 or 1 at 90 to 120 days post treatment. Safety outcomes included symptomatic intracerebral hemorrhage, orolingual angioedema, extracranial bleeding that required blood transfusion (all within 24 hours of thrombolytic administration), and all-cause mortality at 90 days. The noninferiority threshold for intravenous tenecteplase was set as the lower 95% CI of the difference between the tenecteplase and alteplase groups in the proportion of patients who met the primary outcome exceeding –5%.
Main results: The primary outcome of mRS of either 0 or 1 at 90 to 120 days of treatment occurred in 296 (36.9%) of the 802 patients assigned to tenecteplase and 266 (34.8%) of the 765 patients assigned to alteplase (unadjusted risk difference, 2.1%; 95% CI, –2.6 to 6.9). The prespecified noninferiority threshold was met. There were no significant differences between the groups in rates of intracerebral hemorrhage at 24 hours or 90-day all-cause mortality.
Conclusion: Intravenous tenecteplase is a reasonable alternative to alteplase for patients eligible for thrombolytic therapy.
Study 2 Overview (Wang et al)
Objective: To determine whether tenecteplase (dose 0.25 mg/kg) is noninferior to alteplase in patients with acute ischemic stroke who are within 4.5 hours of symptom onset and eligible for thrombolytic therapy but either refused or were ineligible for endovascular thrombectomy.
Design: Multicenter, prospective, open-label, randomized, controlled noninferiority trial.
Setting and participants: This trial was conducted at 53 centers across China and included patients 18 years of age or older who were within 4.5 hours of symptom onset and were thrombolytic eligible, had a mRS ≤ 1 at enrollment, and had a National Institutes of Health Stroke Scale score between 5 and 25. Eligible participants were randomized 1:1 to either tenecteplase 0.25 mg/kg (maximum dose 25 mg) or alteplase 0.9 mg/kg (maximum dose 90 mg, administered as a bolus followed by infusion). During the enrollment period (June 12, 2021, to May 29, 2022), a total of 1430 participants were enrolled, and, of those, 716 were randomly assigned to tenecteplase and 714 to alteplase. Six patients assigned to tenecteplase and 7 assigned to alteplase did not receive drugs. At 90 days, 5 in the tenecteplase group and 11 in the alteplase group were lost to follow up.
Main outcome measures: The primary efficacy outcome was a mRS of 0 or 1 at 90 days. The primary safety outcome was intracranial hemorrhage within 36 hours. Safety outcomes included parenchymal hematoma 2, as defined by the European Cooperative Acute Stroke Study III; any intracranial or significant hemorrhage, as defined by the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries criteria; and death from all causes at 90 days. Noninferiority for tenecteplase would be declared if the lower 97.5% 1-sided CI for the relative risk (RR) for the primary outcome did not cross 0.937.
Main results: In the modified ITT population, the primary outcome occurred in 439 (62%) of the tenecteplase group and 405 (68%) of the alteplase group (RR, 1.07; 95% CI, 0.98-1.16). This met the prespecified margin for noninferiority. Intracranial hemorrhage within 36 hours was experienced by 15 (2%) patients in the tenecteplase group and 13 (2%) in the alteplase group (RR, 1.18; 95% CI, 0.56-2.50). Death at 90 days occurred in 46 (7%) patients in the tenecteplase group and 35 (5%) in the alteplase group (RR, 1.31; 95% CI, 0.86-2.01).
Conclusion: Tenecteplase was noninferior to alteplase in patients with acute ischemic stroke who met criteria for thrombolysis and either refused or were ineligible for endovascular thrombectomy.
Commentary
Alteplase has been FDA-approved for managing acute ischemic stroke since 1996 and has demonstrated positive effects on functional outcomes. Drawbacks of alteplase therapy, however, include bleeding risk as well as cumbersome administration of a bolus dose followed by a 60-minute infusion. In recent years, the question of whether or not tenecteplase could replace alteplase as the preferred thrombolytic for acute ischemic stroke has garnered much attention. Several features of tenecteplase make it an attractive option, including increased fibrin specificity, a longer half-life, and ease of administration as a single, rapid bolus dose. In phase 2 trials that compared tenecteplase 0.25 mg/kg with alteplase, findings suggested the potential for early neurological improvement as well as improved outcomes at 90 days. While the role of tenecteplase in acute myocardial infarction has been well established due to ease of use and a favorable adverse-effect profile,1 there is much less evidence from phase 3 randomized controlled clinical trials to secure the role of tenecteplase in acute ischemic stroke.2
Menon et al attempted to close this gap in the literature by conducting a randomized controlled clinical trial (AcT) comparing tenecteplase to alteplase in a Canadian patient population. The trial's patient population mirrors that of real-world data from global registries in terms of age, sex, and baseline stroke severity. In addition, the eligibility window of 4.5 hours from symptom onset as well as the inclusion and exclusion criteria for therapy are common to those utilized in other countries, making the findings generalizable. There were some limitations to the study, however, including the impact of COVID-19 on recruitment efforts as well as limitations of research infrastructure and staffing, which may have limited enrollment efforts at primary stroke centers. Nonetheless, the authors concluded that their results provide evidence that tenecteplase is comparable to alteplase, with similar functional and safety outcomes.
TRACE-2 focused on an Asian patient population and provided follow up to the dose-ranging TRACE-1 phase 2 trial. TRACE-1 showed that tenecteplase 0.25 mg/kg had a similar safety profile to alteplase 0.9 mg/kg in Chinese patients presenting with acute ischemic stroke. TRACE-2 sought to establish noninferiority of tenecteplase and excluded patients who were ineligible for or refused thrombectomy. Interestingly, the tenecteplase arm, as the authors point out, had numerically greater mortality as well as intracranial hemorrhage, but these differences were not statistically significant between the treatment groups at 90 days. The TRACE-2 results parallel those of AcT, and although there were differences in ethnicity between the 2 trials, the authors cite this as evidence that the results are consistent and provide evidence for the role of tenecteplase in the management of acute ischemic stroke. Limitations of this trial include potential bias from its open-label design, as well as exclusion of patients with more severe strokes eligible for thrombectomy, which may limit generalizability to patients with more disabling strokes who could have a higher risk of intracranial hemorrhage.
Application for Clinical Practice and System Implementation
Across the country, many organizations have adopted the off-label use of tenecteplase for managing fibrinolytic-eligible acute ischemic stroke patients. In most cases, the impetus for change is the ease of dosing and administration of tenecteplase compared to alteplase, while the inclusion and exclusion criteria and overall management remain the same. Timely administration of therapy in stroke is critical. This, along with other time constraints in stroke workflows, the weight-based calculation of alteplase doses, and alteplase’s administration method may lead to medication errors when using this agent to treat patients with acute stroke. The rapid, single-dose administration of tenecteplase removes many barriers that hospitals face when patients may need to be treated and then transferred to another site for further care. Without the worry to “drip and ship,” the completion of administration may allow for timely patient transfer and eliminate the need for monitoring of an infusion during transfer. For some organizations, there may be a potential for drug cost-savings as well as improved metrics, such as door-to-needle time, but the overall effects of switching from alteplase to tenecteplase remain to be seen. Currently, tenecteplase is included in stroke guidelines as a “reasonable choice,” though with a low level of evidence.3 However, these 2 studies support the role of tenecteplase in acute ischemic stroke treatment and may provide a foundation for further studies to establish the role of tenecteplase in the acute ischemic stroke population.
Practice Points
- Tenecteplase may be considered as an alternative to alteplase for acute ischemic stroke for patients who meet eligibility criteria for thrombolytics; this recommendation is included in the most recent stroke guidelines, although tenecteplase has not been demonstrated to be superior to alteplase.
- The ease of administration of tenecteplase as a single intravenous bolus dose represents a benefit compared to alteplase; it is an off-label use, however, and further studies are needed to establish the superiority of tenecteplase in terms of functional and safety outcomes.
– Carol Heunisch, PharmD, BCPS, BCCP
Pharmacy Department, NorthShore–Edward-Elmhurst Health, Evanston, IL
1. Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT-2) Investigators; F Van De Werf, J Adgey, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Lancet. 1999;354(9180):716-722. doi:10.1016/s0140-6736(99)07403-6
2. Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischaemic stroke: meta-analysis of 5 randomized trials. Stroke. 2019;50(8):2156-2162. doi:10.1161/STROKEAHA.119.025080
3. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. doi:10.1161/STR.0000000000000211
1. Assessment of the Safety and Efficacy of a New Thrombolytic (ASSENT-2) Investigators; F Van De Werf, J Adgey, et al. Single-bolus tenecteplase compared with front-loaded alteplase in acute myocardial infarction: the ASSENT-2 double-blind randomised trial. Lancet. 1999;354(9180):716-722. doi:10.1016/s0140-6736(99)07403-6
2. Burgos AM, Saver JL. Evidence that tenecteplase is noninferior to alteplase for acute ischaemic stroke: meta-analysis of 5 randomized trials. Stroke. 2019;50(8):2156-2162. doi:10.1161/STROKEAHA.119.025080
3. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. doi:10.1161/STR.0000000000000211
Dapagliflozin’s HFpEF benefit tied to lower filling pressure
NEW ORLEANS – Treatment of patients with heart failure with preserved ejection fraction (HFpEF) with the SGLT2 inhibitor dapagliflozin (Farxiga) for 24 weeks produced significant and beneficial reductions in left-heart filling pressures in a mechanistic, randomized clinical study.
The findings “provide new insight into the mechanisms underlying the favorable clinical effects of dapagliflozin in patients with HFpEF,” Barry A. Borlaug, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. “Elevations in left heart filling pressures at rest and during exercise are fundamental pathophysiologic features of HFpEF,” he noted.
Results from prior studies documented the benefit of dapagliflozin for improving clinical outcomes in patients with HFpEF in the DELIVER trial, and for the related sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance) in the EMPEROR-Preserved trial. The new findings presented by Dr. Borlaug provide evidence from a placebo-controlled, prospective study for one way by which these SGLT2 inhibitors exert this benefit in patients with HFpEF.
The results of his single-center study showed that, in patients with HFpEF who also exhibited “severe” elevations in pulmonary capillary wedge pressure (PCWP) during exercise, 24 weeks of treatment with dapagliflozin led to a significant reduction in PCWP during exercise. The treatment produced an average 6.1–mm Hg drop from baseline compared with control patients who received placebo. A similar pattern occurred when these patients were at rest, when dapagliflozin treatment linked with a significant average reduction in PCWP from baseline of 3.5 mm Hg compared with controls.
Improving a ‘specific and fundamental’ feature of HFpEF
“This fantastic study looked at one of the fundamental aspects of HFpEF,” said John R. Teerlink, MD, designated discussant for the study. “You’ve shown that dapagliflozin targets a specific and fundamental” manifestation of HFpEF by lowering PCWP, said Dr. Teerlink, director of Heart Failure at the San Francisco Veterans Affairs Medical Center.
However, Dr. Teerlink added, the study did not directly address the related question of what physiologic action of dapagliflozin produces this notable drop in PCWP.
“We’re just starting to look at that,” replied Dr. Borlaug, a cardiologist and professor at the Mayo Clinic in Rochester, Minn.
He reported finding an intriguing correlate in the current study linked to the cut in PCWP with dapagliflozin treatment. The SGLT2 inhibitor at a standard daily 10-mg dose produced an average 3.5-kg drop in body weight in the dapagliflozin-treated patients that significantly linked with the changes in PCWP both at rest and during exercise. Dapagliflozin-treated patients also showed a significant reduction from their baseline plasma volume compared with placebo-treated patients, but this “poorly correlated” with the dapagliflozin-linked cuts in PCWP, Dr. Borlaug said.
“I don’t think this means weight loss is the cause of the hemodynamic benefit, but maybe it’s an indicator. When patients [with HFpEF] lose weight, they are in a metabolic state that leads to good changes in hemodynamics,” he suggested. “My guess is that there is probably a combination of many different little things [caused by dapagliflozin treatment of patients with HFpEF] that together result in the 20%-25% relative improvement we see in filling pressure.”
An ‘obese, cardiometabolic’ HFpEF phenotype
The study enrolled patients with HFpEF and a left ventricular ejection fraction of at least 50%, a New York Heart Association functional class of 2 or 3, and a PCWP during exercise of at least 25 mm Hg. Of the 37 evaluable patients, about two-thirds of the patients were women, more than two-thirds were in functional class 3, about 70% were obese, and their average ejection fraction was about 62%. The study excluded patients with HFpEF who also had type 1 diabetes, cardiomyopathy, pericardial disease, or other causes of dyspnea or heart failure.
Dr. Teerlink asked about the generalizability of the findings, as the study cohort seemed to differ in certain respects from the patients enrolled in the DELIVER trial, and because of the many apparently distinct patient phenotypes that exist within the scope of HFpEF.
An “obese, cardiometabolic phenotype” predominated the study cohort, Dr. Borlaug said. “The patients we enrolled look like the HFpEF patients seen in U.S. clinics.” However, he added that “in reality, many [HFpEF phenotypes] coexist in one patient. It’s not that simple,” that every patient with HFpEF can be categorized into a single HFpEF phenotype.
The researchers monitored PCWP invasively with high-fidelity micromanometer catheters.
The study was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Borlaug has received research funding from AstraZeneca, as well as from Corvia, GlaxoSmithKline, Medtronic, Mesoblast, Novo Nordisk, and Tenax. Dr. Teerlink has had financial relationships with AstraZeneca, as well as with Amgen, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Cytokinetics, Medtronic, Merck, Novartis, Servier, and Windtree Therapeutics.
NEW ORLEANS – Treatment of patients with heart failure with preserved ejection fraction (HFpEF) with the SGLT2 inhibitor dapagliflozin (Farxiga) for 24 weeks produced significant and beneficial reductions in left-heart filling pressures in a mechanistic, randomized clinical study.
The findings “provide new insight into the mechanisms underlying the favorable clinical effects of dapagliflozin in patients with HFpEF,” Barry A. Borlaug, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. “Elevations in left heart filling pressures at rest and during exercise are fundamental pathophysiologic features of HFpEF,” he noted.
Results from prior studies documented the benefit of dapagliflozin for improving clinical outcomes in patients with HFpEF in the DELIVER trial, and for the related sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance) in the EMPEROR-Preserved trial. The new findings presented by Dr. Borlaug provide evidence from a placebo-controlled, prospective study for one way by which these SGLT2 inhibitors exert this benefit in patients with HFpEF.
The results of his single-center study showed that, in patients with HFpEF who also exhibited “severe” elevations in pulmonary capillary wedge pressure (PCWP) during exercise, 24 weeks of treatment with dapagliflozin led to a significant reduction in PCWP during exercise. The treatment produced an average 6.1–mm Hg drop from baseline compared with control patients who received placebo. A similar pattern occurred when these patients were at rest, when dapagliflozin treatment linked with a significant average reduction in PCWP from baseline of 3.5 mm Hg compared with controls.
Improving a ‘specific and fundamental’ feature of HFpEF
“This fantastic study looked at one of the fundamental aspects of HFpEF,” said John R. Teerlink, MD, designated discussant for the study. “You’ve shown that dapagliflozin targets a specific and fundamental” manifestation of HFpEF by lowering PCWP, said Dr. Teerlink, director of Heart Failure at the San Francisco Veterans Affairs Medical Center.
However, Dr. Teerlink added, the study did not directly address the related question of what physiologic action of dapagliflozin produces this notable drop in PCWP.
“We’re just starting to look at that,” replied Dr. Borlaug, a cardiologist and professor at the Mayo Clinic in Rochester, Minn.
He reported finding an intriguing correlate in the current study linked to the cut in PCWP with dapagliflozin treatment. The SGLT2 inhibitor at a standard daily 10-mg dose produced an average 3.5-kg drop in body weight in the dapagliflozin-treated patients that significantly linked with the changes in PCWP both at rest and during exercise. Dapagliflozin-treated patients also showed a significant reduction from their baseline plasma volume compared with placebo-treated patients, but this “poorly correlated” with the dapagliflozin-linked cuts in PCWP, Dr. Borlaug said.
“I don’t think this means weight loss is the cause of the hemodynamic benefit, but maybe it’s an indicator. When patients [with HFpEF] lose weight, they are in a metabolic state that leads to good changes in hemodynamics,” he suggested. “My guess is that there is probably a combination of many different little things [caused by dapagliflozin treatment of patients with HFpEF] that together result in the 20%-25% relative improvement we see in filling pressure.”
An ‘obese, cardiometabolic’ HFpEF phenotype
The study enrolled patients with HFpEF and a left ventricular ejection fraction of at least 50%, a New York Heart Association functional class of 2 or 3, and a PCWP during exercise of at least 25 mm Hg. Of the 37 evaluable patients, about two-thirds of the patients were women, more than two-thirds were in functional class 3, about 70% were obese, and their average ejection fraction was about 62%. The study excluded patients with HFpEF who also had type 1 diabetes, cardiomyopathy, pericardial disease, or other causes of dyspnea or heart failure.
Dr. Teerlink asked about the generalizability of the findings, as the study cohort seemed to differ in certain respects from the patients enrolled in the DELIVER trial, and because of the many apparently distinct patient phenotypes that exist within the scope of HFpEF.
An “obese, cardiometabolic phenotype” predominated the study cohort, Dr. Borlaug said. “The patients we enrolled look like the HFpEF patients seen in U.S. clinics.” However, he added that “in reality, many [HFpEF phenotypes] coexist in one patient. It’s not that simple,” that every patient with HFpEF can be categorized into a single HFpEF phenotype.
The researchers monitored PCWP invasively with high-fidelity micromanometer catheters.
The study was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Borlaug has received research funding from AstraZeneca, as well as from Corvia, GlaxoSmithKline, Medtronic, Mesoblast, Novo Nordisk, and Tenax. Dr. Teerlink has had financial relationships with AstraZeneca, as well as with Amgen, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Cytokinetics, Medtronic, Merck, Novartis, Servier, and Windtree Therapeutics.
NEW ORLEANS – Treatment of patients with heart failure with preserved ejection fraction (HFpEF) with the SGLT2 inhibitor dapagliflozin (Farxiga) for 24 weeks produced significant and beneficial reductions in left-heart filling pressures in a mechanistic, randomized clinical study.
The findings “provide new insight into the mechanisms underlying the favorable clinical effects of dapagliflozin in patients with HFpEF,” Barry A. Borlaug, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation. “Elevations in left heart filling pressures at rest and during exercise are fundamental pathophysiologic features of HFpEF,” he noted.
Results from prior studies documented the benefit of dapagliflozin for improving clinical outcomes in patients with HFpEF in the DELIVER trial, and for the related sodium-glucose cotransporter 2 (SGLT2) inhibitor empagliflozin (Jardiance) in the EMPEROR-Preserved trial. The new findings presented by Dr. Borlaug provide evidence from a placebo-controlled, prospective study for one way by which these SGLT2 inhibitors exert this benefit in patients with HFpEF.
The results of his single-center study showed that, in patients with HFpEF who also exhibited “severe” elevations in pulmonary capillary wedge pressure (PCWP) during exercise, 24 weeks of treatment with dapagliflozin led to a significant reduction in PCWP during exercise. The treatment produced an average 6.1–mm Hg drop from baseline compared with control patients who received placebo. A similar pattern occurred when these patients were at rest, when dapagliflozin treatment linked with a significant average reduction in PCWP from baseline of 3.5 mm Hg compared with controls.
Improving a ‘specific and fundamental’ feature of HFpEF
“This fantastic study looked at one of the fundamental aspects of HFpEF,” said John R. Teerlink, MD, designated discussant for the study. “You’ve shown that dapagliflozin targets a specific and fundamental” manifestation of HFpEF by lowering PCWP, said Dr. Teerlink, director of Heart Failure at the San Francisco Veterans Affairs Medical Center.
However, Dr. Teerlink added, the study did not directly address the related question of what physiologic action of dapagliflozin produces this notable drop in PCWP.
“We’re just starting to look at that,” replied Dr. Borlaug, a cardiologist and professor at the Mayo Clinic in Rochester, Minn.
He reported finding an intriguing correlate in the current study linked to the cut in PCWP with dapagliflozin treatment. The SGLT2 inhibitor at a standard daily 10-mg dose produced an average 3.5-kg drop in body weight in the dapagliflozin-treated patients that significantly linked with the changes in PCWP both at rest and during exercise. Dapagliflozin-treated patients also showed a significant reduction from their baseline plasma volume compared with placebo-treated patients, but this “poorly correlated” with the dapagliflozin-linked cuts in PCWP, Dr. Borlaug said.
“I don’t think this means weight loss is the cause of the hemodynamic benefit, but maybe it’s an indicator. When patients [with HFpEF] lose weight, they are in a metabolic state that leads to good changes in hemodynamics,” he suggested. “My guess is that there is probably a combination of many different little things [caused by dapagliflozin treatment of patients with HFpEF] that together result in the 20%-25% relative improvement we see in filling pressure.”
An ‘obese, cardiometabolic’ HFpEF phenotype
The study enrolled patients with HFpEF and a left ventricular ejection fraction of at least 50%, a New York Heart Association functional class of 2 or 3, and a PCWP during exercise of at least 25 mm Hg. Of the 37 evaluable patients, about two-thirds of the patients were women, more than two-thirds were in functional class 3, about 70% were obese, and their average ejection fraction was about 62%. The study excluded patients with HFpEF who also had type 1 diabetes, cardiomyopathy, pericardial disease, or other causes of dyspnea or heart failure.
Dr. Teerlink asked about the generalizability of the findings, as the study cohort seemed to differ in certain respects from the patients enrolled in the DELIVER trial, and because of the many apparently distinct patient phenotypes that exist within the scope of HFpEF.
An “obese, cardiometabolic phenotype” predominated the study cohort, Dr. Borlaug said. “The patients we enrolled look like the HFpEF patients seen in U.S. clinics.” However, he added that “in reality, many [HFpEF phenotypes] coexist in one patient. It’s not that simple,” that every patient with HFpEF can be categorized into a single HFpEF phenotype.
The researchers monitored PCWP invasively with high-fidelity micromanometer catheters.
The study was sponsored by AstraZeneca, the company that markets dapagliflozin (Farxiga). Dr. Borlaug has received research funding from AstraZeneca, as well as from Corvia, GlaxoSmithKline, Medtronic, Mesoblast, Novo Nordisk, and Tenax. Dr. Teerlink has had financial relationships with AstraZeneca, as well as with Amgen, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, Cytokinetics, Medtronic, Merck, Novartis, Servier, and Windtree Therapeutics.
AT ACC 2023