User login
SHM’s Center for Quality Improvement to partner on NIH grant
The Society of Hospital Medicine has announced that its award-winning Center for Quality Improvement will partner on the National Institutes of Health National, Heart, Lung, and Blood Institute study, “The SIP Study: Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children” (NIH R61HL157804). The core objectives of the planned 5-year study are to identify and test practical, sustainable strategies for implementing a multicondition clinical pathway intervention for children hospitalized with asthma, pneumonia, or bronchiolitis in community hospitals.
Under the leadership of principal investigator Sunitha Kaiser, MD, MSc, a pediatric hospitalist at the University of California, San Francisco, the study will employ rigorous implementation science methods and SHM’s mentored implementation model.
“The lessons learned from this study could inform improved care delivery strategies for the millions of children hospitalized with respiratory illnesses across the U.S. each year,” said Jenna Goldstein, chief of strategic partnerships at SHM and director of SHM’s Center for Quality Improvement.
The team will recruit a diverse group of community hospitals in partnership with SHM, the Value in Inpatient Pediatrics Network (within the American Academy of Pediatrics), the Pediatric Research in Inpatient Settings Network, America’s Hospital Essentials, and the National Improvement Partnership Network. In collaboration with these national organizations and the participating hospitals, the team seeks to realize the following aims:
- Aim 1. (Preimplementation) Identify barriers and facilitators of implementing a multicondition pathway intervention and refine the intervention for community hospitals.
- Aim 2a. Determine the effects of the intervention, compared with control via chart reviews of children hospitalized with asthma, pneumonia, or bronchiolitis.
- Aim 2b. Determine if the core implementation strategies (audit and feedback, electronic order sets, Plan-Do-Study-Act cycles) are associated with clinicians’ guideline adoption.
“SHM’s Center for Quality Improvement is a recognized partner in facilitating process and culture change in the hospital to improve outcomes for patients,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “SHM is committed to supporting quality-improvement research, and we look forward to contributing to improved care for hospitalized pediatric patients through this study and beyond.”
To learn more about SHM’s Center for Quality Improvement, visit hospitalmedicine.org/qi.
The Society of Hospital Medicine has announced that its award-winning Center for Quality Improvement will partner on the National Institutes of Health National, Heart, Lung, and Blood Institute study, “The SIP Study: Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children” (NIH R61HL157804). The core objectives of the planned 5-year study are to identify and test practical, sustainable strategies for implementing a multicondition clinical pathway intervention for children hospitalized with asthma, pneumonia, or bronchiolitis in community hospitals.
Under the leadership of principal investigator Sunitha Kaiser, MD, MSc, a pediatric hospitalist at the University of California, San Francisco, the study will employ rigorous implementation science methods and SHM’s mentored implementation model.
“The lessons learned from this study could inform improved care delivery strategies for the millions of children hospitalized with respiratory illnesses across the U.S. each year,” said Jenna Goldstein, chief of strategic partnerships at SHM and director of SHM’s Center for Quality Improvement.
The team will recruit a diverse group of community hospitals in partnership with SHM, the Value in Inpatient Pediatrics Network (within the American Academy of Pediatrics), the Pediatric Research in Inpatient Settings Network, America’s Hospital Essentials, and the National Improvement Partnership Network. In collaboration with these national organizations and the participating hospitals, the team seeks to realize the following aims:
- Aim 1. (Preimplementation) Identify barriers and facilitators of implementing a multicondition pathway intervention and refine the intervention for community hospitals.
- Aim 2a. Determine the effects of the intervention, compared with control via chart reviews of children hospitalized with asthma, pneumonia, or bronchiolitis.
- Aim 2b. Determine if the core implementation strategies (audit and feedback, electronic order sets, Plan-Do-Study-Act cycles) are associated with clinicians’ guideline adoption.
“SHM’s Center for Quality Improvement is a recognized partner in facilitating process and culture change in the hospital to improve outcomes for patients,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “SHM is committed to supporting quality-improvement research, and we look forward to contributing to improved care for hospitalized pediatric patients through this study and beyond.”
To learn more about SHM’s Center for Quality Improvement, visit hospitalmedicine.org/qi.
The Society of Hospital Medicine has announced that its award-winning Center for Quality Improvement will partner on the National Institutes of Health National, Heart, Lung, and Blood Institute study, “The SIP Study: Simultaneously Implementing Pathways for Improving Asthma, Pneumonia, and Bronchiolitis Care for Hospitalized Children” (NIH R61HL157804). The core objectives of the planned 5-year study are to identify and test practical, sustainable strategies for implementing a multicondition clinical pathway intervention for children hospitalized with asthma, pneumonia, or bronchiolitis in community hospitals.
Under the leadership of principal investigator Sunitha Kaiser, MD, MSc, a pediatric hospitalist at the University of California, San Francisco, the study will employ rigorous implementation science methods and SHM’s mentored implementation model.
“The lessons learned from this study could inform improved care delivery strategies for the millions of children hospitalized with respiratory illnesses across the U.S. each year,” said Jenna Goldstein, chief of strategic partnerships at SHM and director of SHM’s Center for Quality Improvement.
The team will recruit a diverse group of community hospitals in partnership with SHM, the Value in Inpatient Pediatrics Network (within the American Academy of Pediatrics), the Pediatric Research in Inpatient Settings Network, America’s Hospital Essentials, and the National Improvement Partnership Network. In collaboration with these national organizations and the participating hospitals, the team seeks to realize the following aims:
- Aim 1. (Preimplementation) Identify barriers and facilitators of implementing a multicondition pathway intervention and refine the intervention for community hospitals.
- Aim 2a. Determine the effects of the intervention, compared with control via chart reviews of children hospitalized with asthma, pneumonia, or bronchiolitis.
- Aim 2b. Determine if the core implementation strategies (audit and feedback, electronic order sets, Plan-Do-Study-Act cycles) are associated with clinicians’ guideline adoption.
“SHM’s Center for Quality Improvement is a recognized partner in facilitating process and culture change in the hospital to improve outcomes for patients,” said Eric E. Howell, MD, MHM, chief executive officer of SHM. “SHM is committed to supporting quality-improvement research, and we look forward to contributing to improved care for hospitalized pediatric patients through this study and beyond.”
To learn more about SHM’s Center for Quality Improvement, visit hospitalmedicine.org/qi.
Hep B vaccine response varied among youth with inflammatory, autoimmune disorders
“Hepatitis B is a common viral infection with 2 billion people worldwide having evidence of prior or current infection, and it can present as an acute or chronic infection,” or with chronic sequelae, including cirrhosis and hepatocellular carcinoma, Alexandra Ritter said during the annual meeting of the Society for Pediatric Dermatology. A three-dose vaccination series is recommended beginning at birth, and in 2016, the Centers for Disease Control and Prevention reported that 90.5% of U.S. children aged 19-35 months had completed the series.
While the vaccine series provides protection in healthy individuals more than 95% of the time, a decreased response has been noted in specific pediatric populations, including those with inflammatory and autoimmune diseases. “This is important to note and investigate further because a decreased vaccine response increases the risk for this high-risk population, and the use of boosters is currently debated,” said Ms. Ritter, who is a fourth-year student at the Medical University of South Carolina, Charleston.
To determine the percent of pediatric patients with inflammatory or autoimmune disease who lack evidence of immunity following the hepatitis B vaccine series, Ms. Ritter and colleagues Abigail Truitt and pediatric dermatologist Lara Wine Lee, MD, PhD, of MUSC, retrospectively reviewed the charts of 160 patients between the ages of 6 months and 21 years, who were diagnosed with an autoimmune or autoinflammatory disease, or inflammatory bowel disease (IBD), and had documented evidence of vaccination and serologic testing prior to the start of immunosuppressive therapy.
Of the 160 patients, 100 (63%) had IBD, 34 (21%) had an autoimmune disease, 26 (16%) had an autoinflammatory disease, 89 (56%) were female, and their mean age was 15 years.
The researchers observed variation in the testing ordered between the three patient groups. Specifically, 88.2% of autoimmune patients had hepatitis B surface antigen (HBsAg) testing, compared with 96.15% of patients with an autoinflammatory disease and 67% of patients with IBD, while 76.47% of patients with an autoimmune disease had hepatitis B core antibody (anti-HBc) testing, compared with 88.46% of patients with an autoinflammatory disease and 31% of patients with IBD.
In addition, 82.35% of patients with an autoimmune disease had HBsAg testing, compared with 100% of patients with an autoinflammatory disease and 94% of patients with IBD.
Of the 148 patients who had HBsAg testing ordered and completed prior to starting an immunosuppressive drug, there was no statistically significant difference in the percent of patients showing evidence of an immune response to the hepatitis B vaccine (32.14% among patients with an autoimmune disease, 34.62% among patients with an autoinflammatory disease, and 31.91% among patients with IBD). Combined, 67.57% of tested negative for the hepatitis B surface antibody.
“Our study showed that the majority of these patients did not show serologic evidence of immunity despite being fully vaccinated,” Ms. Ritter said. “There was also variation in the testing ordered and a more standardized approach is needed in this high-risk population.” She acknowledged certain limitations of the study, including its retrospective design and lack of a control group.
“This brings us to our next question of whether this indicates a failure of the vaccine, or the way immunity is tested,” she continued. “The CDC and the European Consensus Group on Hepatitis B Immunity recommend a cutoff of greater than 10 mIU/mL. Those that achieve immunity are protected for up to 20 years due to immune memory, even if their antibody levels later drop. There have been rare cases of immunocompetent individuals having evidence of transient asymptomatic infections when antibody levels drop. The chronic disease has only been documented in infants born to positive mothers. In hemodialysis patients, however, clinically significant infections have been documented when antibody levels drop.”
The CDC only recommends postvaccination testing to infants born to positive mothers, health care workers at high risk, hemodialysis patients, people with HIV and other immunocompromised people, and needle-sharing partners of chronically infected people. This is completed 1-2 months following the third vaccine dose, and those with antibody levels less than 10 mIU/mL should be revaccinated. “As some groups do not respond to the vaccine series, alternative dosing and the intradermal vaccine have been studied and shown to be effective in certain groups,” she said.
When it comes to monitoring immunocompromised individuals and giving booster shots, however, there are conflicting recommendations. The CDC recommends yearly testing and booster shots when levels drop below 10 mIU/mL only in hemodialysis patients, while the European Consensus Group recommends testing every 6-12 months for immunocompromised individuals and boosters when their levels drop below 10 mIU/mL.
“The CDC has not yet determined if other immunocompromised individuals should receive a booster, with more research required, but studies have shown it to be effective,” Ms. Ritter said. In a similar study looking at evidence of immunity in children with connective tissue disease who were on immunosuppressive treatment, 50% had no evidence of protective antibodies, compared with 96% in the control group. “In that study, a booster shot was given, and protective antibody concentrations were found at follow-up,” she said.
The researchers reported having no financial disclosures.
[email protected]
“Hepatitis B is a common viral infection with 2 billion people worldwide having evidence of prior or current infection, and it can present as an acute or chronic infection,” or with chronic sequelae, including cirrhosis and hepatocellular carcinoma, Alexandra Ritter said during the annual meeting of the Society for Pediatric Dermatology. A three-dose vaccination series is recommended beginning at birth, and in 2016, the Centers for Disease Control and Prevention reported that 90.5% of U.S. children aged 19-35 months had completed the series.
While the vaccine series provides protection in healthy individuals more than 95% of the time, a decreased response has been noted in specific pediatric populations, including those with inflammatory and autoimmune diseases. “This is important to note and investigate further because a decreased vaccine response increases the risk for this high-risk population, and the use of boosters is currently debated,” said Ms. Ritter, who is a fourth-year student at the Medical University of South Carolina, Charleston.
To determine the percent of pediatric patients with inflammatory or autoimmune disease who lack evidence of immunity following the hepatitis B vaccine series, Ms. Ritter and colleagues Abigail Truitt and pediatric dermatologist Lara Wine Lee, MD, PhD, of MUSC, retrospectively reviewed the charts of 160 patients between the ages of 6 months and 21 years, who were diagnosed with an autoimmune or autoinflammatory disease, or inflammatory bowel disease (IBD), and had documented evidence of vaccination and serologic testing prior to the start of immunosuppressive therapy.
Of the 160 patients, 100 (63%) had IBD, 34 (21%) had an autoimmune disease, 26 (16%) had an autoinflammatory disease, 89 (56%) were female, and their mean age was 15 years.
The researchers observed variation in the testing ordered between the three patient groups. Specifically, 88.2% of autoimmune patients had hepatitis B surface antigen (HBsAg) testing, compared with 96.15% of patients with an autoinflammatory disease and 67% of patients with IBD, while 76.47% of patients with an autoimmune disease had hepatitis B core antibody (anti-HBc) testing, compared with 88.46% of patients with an autoinflammatory disease and 31% of patients with IBD.
In addition, 82.35% of patients with an autoimmune disease had HBsAg testing, compared with 100% of patients with an autoinflammatory disease and 94% of patients with IBD.
Of the 148 patients who had HBsAg testing ordered and completed prior to starting an immunosuppressive drug, there was no statistically significant difference in the percent of patients showing evidence of an immune response to the hepatitis B vaccine (32.14% among patients with an autoimmune disease, 34.62% among patients with an autoinflammatory disease, and 31.91% among patients with IBD). Combined, 67.57% of tested negative for the hepatitis B surface antibody.
“Our study showed that the majority of these patients did not show serologic evidence of immunity despite being fully vaccinated,” Ms. Ritter said. “There was also variation in the testing ordered and a more standardized approach is needed in this high-risk population.” She acknowledged certain limitations of the study, including its retrospective design and lack of a control group.
“This brings us to our next question of whether this indicates a failure of the vaccine, or the way immunity is tested,” she continued. “The CDC and the European Consensus Group on Hepatitis B Immunity recommend a cutoff of greater than 10 mIU/mL. Those that achieve immunity are protected for up to 20 years due to immune memory, even if their antibody levels later drop. There have been rare cases of immunocompetent individuals having evidence of transient asymptomatic infections when antibody levels drop. The chronic disease has only been documented in infants born to positive mothers. In hemodialysis patients, however, clinically significant infections have been documented when antibody levels drop.”
The CDC only recommends postvaccination testing to infants born to positive mothers, health care workers at high risk, hemodialysis patients, people with HIV and other immunocompromised people, and needle-sharing partners of chronically infected people. This is completed 1-2 months following the third vaccine dose, and those with antibody levels less than 10 mIU/mL should be revaccinated. “As some groups do not respond to the vaccine series, alternative dosing and the intradermal vaccine have been studied and shown to be effective in certain groups,” she said.
When it comes to monitoring immunocompromised individuals and giving booster shots, however, there are conflicting recommendations. The CDC recommends yearly testing and booster shots when levels drop below 10 mIU/mL only in hemodialysis patients, while the European Consensus Group recommends testing every 6-12 months for immunocompromised individuals and boosters when their levels drop below 10 mIU/mL.
“The CDC has not yet determined if other immunocompromised individuals should receive a booster, with more research required, but studies have shown it to be effective,” Ms. Ritter said. In a similar study looking at evidence of immunity in children with connective tissue disease who were on immunosuppressive treatment, 50% had no evidence of protective antibodies, compared with 96% in the control group. “In that study, a booster shot was given, and protective antibody concentrations were found at follow-up,” she said.
The researchers reported having no financial disclosures.
[email protected]
“Hepatitis B is a common viral infection with 2 billion people worldwide having evidence of prior or current infection, and it can present as an acute or chronic infection,” or with chronic sequelae, including cirrhosis and hepatocellular carcinoma, Alexandra Ritter said during the annual meeting of the Society for Pediatric Dermatology. A three-dose vaccination series is recommended beginning at birth, and in 2016, the Centers for Disease Control and Prevention reported that 90.5% of U.S. children aged 19-35 months had completed the series.
While the vaccine series provides protection in healthy individuals more than 95% of the time, a decreased response has been noted in specific pediatric populations, including those with inflammatory and autoimmune diseases. “This is important to note and investigate further because a decreased vaccine response increases the risk for this high-risk population, and the use of boosters is currently debated,” said Ms. Ritter, who is a fourth-year student at the Medical University of South Carolina, Charleston.
To determine the percent of pediatric patients with inflammatory or autoimmune disease who lack evidence of immunity following the hepatitis B vaccine series, Ms. Ritter and colleagues Abigail Truitt and pediatric dermatologist Lara Wine Lee, MD, PhD, of MUSC, retrospectively reviewed the charts of 160 patients between the ages of 6 months and 21 years, who were diagnosed with an autoimmune or autoinflammatory disease, or inflammatory bowel disease (IBD), and had documented evidence of vaccination and serologic testing prior to the start of immunosuppressive therapy.
Of the 160 patients, 100 (63%) had IBD, 34 (21%) had an autoimmune disease, 26 (16%) had an autoinflammatory disease, 89 (56%) were female, and their mean age was 15 years.
The researchers observed variation in the testing ordered between the three patient groups. Specifically, 88.2% of autoimmune patients had hepatitis B surface antigen (HBsAg) testing, compared with 96.15% of patients with an autoinflammatory disease and 67% of patients with IBD, while 76.47% of patients with an autoimmune disease had hepatitis B core antibody (anti-HBc) testing, compared with 88.46% of patients with an autoinflammatory disease and 31% of patients with IBD.
In addition, 82.35% of patients with an autoimmune disease had HBsAg testing, compared with 100% of patients with an autoinflammatory disease and 94% of patients with IBD.
Of the 148 patients who had HBsAg testing ordered and completed prior to starting an immunosuppressive drug, there was no statistically significant difference in the percent of patients showing evidence of an immune response to the hepatitis B vaccine (32.14% among patients with an autoimmune disease, 34.62% among patients with an autoinflammatory disease, and 31.91% among patients with IBD). Combined, 67.57% of tested negative for the hepatitis B surface antibody.
“Our study showed that the majority of these patients did not show serologic evidence of immunity despite being fully vaccinated,” Ms. Ritter said. “There was also variation in the testing ordered and a more standardized approach is needed in this high-risk population.” She acknowledged certain limitations of the study, including its retrospective design and lack of a control group.
“This brings us to our next question of whether this indicates a failure of the vaccine, or the way immunity is tested,” she continued. “The CDC and the European Consensus Group on Hepatitis B Immunity recommend a cutoff of greater than 10 mIU/mL. Those that achieve immunity are protected for up to 20 years due to immune memory, even if their antibody levels later drop. There have been rare cases of immunocompetent individuals having evidence of transient asymptomatic infections when antibody levels drop. The chronic disease has only been documented in infants born to positive mothers. In hemodialysis patients, however, clinically significant infections have been documented when antibody levels drop.”
The CDC only recommends postvaccination testing to infants born to positive mothers, health care workers at high risk, hemodialysis patients, people with HIV and other immunocompromised people, and needle-sharing partners of chronically infected people. This is completed 1-2 months following the third vaccine dose, and those with antibody levels less than 10 mIU/mL should be revaccinated. “As some groups do not respond to the vaccine series, alternative dosing and the intradermal vaccine have been studied and shown to be effective in certain groups,” she said.
When it comes to monitoring immunocompromised individuals and giving booster shots, however, there are conflicting recommendations. The CDC recommends yearly testing and booster shots when levels drop below 10 mIU/mL only in hemodialysis patients, while the European Consensus Group recommends testing every 6-12 months for immunocompromised individuals and boosters when their levels drop below 10 mIU/mL.
“The CDC has not yet determined if other immunocompromised individuals should receive a booster, with more research required, but studies have shown it to be effective,” Ms. Ritter said. In a similar study looking at evidence of immunity in children with connective tissue disease who were on immunosuppressive treatment, 50% had no evidence of protective antibodies, compared with 96% in the control group. “In that study, a booster shot was given, and protective antibody concentrations were found at follow-up,” she said.
The researchers reported having no financial disclosures.
[email protected]
FROM SPD 2021
Febrile infant guideline allows wiggle room on hospital admission, testing
The long-anticipated American Academy of Pediatrics guidelines for the treatment of well-appearing febrile infants have arrived, and key points include updated guidance for cerebrospinal fluid testing and urine cultures, according to Robert Pantell, MD, and Kenneth Roberts, MD, who presented the guidelines at the virtual Pediatric Hospital Medicine annual conference.
The AAP guideline was published in the August 2021 issue of Pediatrics. The guideline includes 21 key action statements and 40 total recommendations, and describes separate management algorithms for three age groups: infants aged 8-21 days, 22-28 days, and 29-60 days.
Dr. Roberts, of the University of North Carolina at Chapel Hill, and Dr. Pantell, of the University of California, San Francisco, emphasized that all pediatricians should read the full guideline, but they offered an overview of some of the notable points.
Some changes that drove the development of evidence-based guideline included changes in technology, such as the increased use of procalcitonin, the development of large research networks for studies of sufficient size, and a need to reduce the costs of unnecessary care and unnecessary trauma for infants, Dr. Roberts said. Use of data from large networks such as the Pediatric Emergency Care Applied Research Network provided enough evidence to support dividing the aged 8- to 60-day population into three groups.
The guideline applies to well-appearing term infants aged 8-60 days and at least 37 weeks’ gestation, with fever of 38° C (100.4° F) or higher in the past 24 hours in the home or clinical setting. The decision to exclude infants in the first week of life from the guideline was because at this age, infants “are sufficiently different in rates and types of illness, including early-onset bacterial infection,” according to the authors.
Dr. Roberts emphasized that the guidelines apply to “well-appearing infants,” which is not always obvious. “If a clinician is not confident an infant is well appearing, the clinical practice guideline should not be applied,” he said.
The guideline also includes a visual algorithm for each age group.
Dr. Pantell summarized the key action statements for the three age groups, and encouraged pediatricians to review the visual algorithms and footnotes available in the full text of the guideline.
The guideline includes seven key action statements for each of the three age groups. Four of these address evaluations, using urine, blood culture, inflammatory markers (IM), and cerebrospinal fluid (CSF). One action statement focuses on initial treatment, and two on management: hospital admission versus monitoring at home, and treatment cessation.
Infants aged 8-21 days
The key action statements for well-appearing infants aged 8-21 days are similar to what clinicians likely would do for ill-appearing infants, the authors noted, based in part on the challenge of assessing an infant this age as “well appearing,” because they don’t yet have the ability to interact with the clinician.
For the 8- to 21-day group, the first two key actions are to obtain a urine specimen and blood culture, Dr. Pantell said. Also, clinicians “should” obtain a CSF for analysis and culture. “We recognize that the ability to get CSF quickly is a challenge,” he added. However, for the 8- to 21-day age group, a new feature is that these infants may be discharged if the CSF is negative. Evaluation in this youngest group states that clinicians “may assess inflammatory markers” including height of fever, absolute neutrophil count, C-reactive protein, and procalcitonin.
Treatment of infants in the 8- to 21-day group “should” include parenteral antimicrobial therapy, according to the guideline, and these infants “should” be actively monitored in the hospital by nurses and staff experienced in neonatal care, Dr. Pantell said. The guideline also includes a key action statement to stop antimicrobials at 24-36 hours if cultures are negative, but to treat identified organisms.
Infants aged 22-28 days
In both the 22- to 28-day-old and 29- to 60-day-old groups, the guideline offers opportunities for less testing and treatment, such as avoiding a lumbar puncture, and fewer hospitalizations. The development of a separate guideline for the 22- to 28-day group is something new, said Dr. Pantell. The guideline states that clinicians should obtain urine specimens and blood culture, and should assess IM in this group. Further key action statements note that clinicians “should obtain a CSF if any IM is positive,” but “may” obtain CSF if the infant is hospitalized, if blood and urine cultures have been obtained, and if none of the IMs are abnormal.
As with younger patients, those with a negative CSF can go home, he said. As for treatment, clinicians “should” administer parenteral antimicrobial therapy to infants managed at home even if they have a negative CSF and urinalysis (UA), and no abnormal inflammatory markers Other points for management of infants in this age group at home include verbal teaching and written instructions for caregivers, plans for a re-evaluation at home in 24 hours, and a plan for communication and access to emergency care in case of a change in clinical status, Dr. Pantell explained. The guideline states that infants “should” be hospitalized if CSF is either not obtained or not interpretable, which leaves room for clinical judgment and individual circumstances. Antimicrobials “should” be discontinued in this group once all cultures are negative after 24-36 hours and no other infection requires treatment.
Infants aged 29-60 days
For the 29- to 60-day group, there are some differences, the main one is the recommendation of blood cultures in this group, said Dr. Pantell. “We are seeing a lot of UTIs [urinary tract infections], and we would like those treated.” However, clinicians need not obtain a CSF if other IMs are normal, but may do so if any IM is abnormal. Antimicrobial therapy may include ceftriaxone or cephalexin for UTIs, or vancomycin for bacteremia.
Although antimicrobial therapy is an option for UTIs and bacterial meningitis, clinicians “need not” use antimicrobials if CSF is normal, if UA is negative, and if no IMs are abnormal, Dr. Pantell added. Overall, further management of infants in this oldest age group should focus on discharge to home in the absence of abnormal findings, but hospitalization in the presence of abnormal CSF, IMs, or other concerns.
During a question-and-answer session, Dr. Roberts said that, while rectal temperature is preferable, any method is acceptable as a starting point for applying the guideline. Importantly, the guideline still leaves room for clinical judgment. “We hope this will change some thinking as far as whether one model fits all,” he noted. The authors tried to temper the word “should” with the word “may” when possible, so clinicians can say: “I’m going to individualize my decision to the infant in front of me.”
Ultimately, the guideline is meant as a guide, and not an absolute standard of care, the authors said. The language of the key action statements includes the words “should, may, need not” in place of “must, must not.” The guideline recommends factoring family values and preferences into any treatment decisions. “Variations, taking into account individual circumstances, may be appropriate.”
The guideline received no outside funding. The authors had no financial conflicts to disclose.
The long-anticipated American Academy of Pediatrics guidelines for the treatment of well-appearing febrile infants have arrived, and key points include updated guidance for cerebrospinal fluid testing and urine cultures, according to Robert Pantell, MD, and Kenneth Roberts, MD, who presented the guidelines at the virtual Pediatric Hospital Medicine annual conference.
The AAP guideline was published in the August 2021 issue of Pediatrics. The guideline includes 21 key action statements and 40 total recommendations, and describes separate management algorithms for three age groups: infants aged 8-21 days, 22-28 days, and 29-60 days.
Dr. Roberts, of the University of North Carolina at Chapel Hill, and Dr. Pantell, of the University of California, San Francisco, emphasized that all pediatricians should read the full guideline, but they offered an overview of some of the notable points.
Some changes that drove the development of evidence-based guideline included changes in technology, such as the increased use of procalcitonin, the development of large research networks for studies of sufficient size, and a need to reduce the costs of unnecessary care and unnecessary trauma for infants, Dr. Roberts said. Use of data from large networks such as the Pediatric Emergency Care Applied Research Network provided enough evidence to support dividing the aged 8- to 60-day population into three groups.
The guideline applies to well-appearing term infants aged 8-60 days and at least 37 weeks’ gestation, with fever of 38° C (100.4° F) or higher in the past 24 hours in the home or clinical setting. The decision to exclude infants in the first week of life from the guideline was because at this age, infants “are sufficiently different in rates and types of illness, including early-onset bacterial infection,” according to the authors.
Dr. Roberts emphasized that the guidelines apply to “well-appearing infants,” which is not always obvious. “If a clinician is not confident an infant is well appearing, the clinical practice guideline should not be applied,” he said.
The guideline also includes a visual algorithm for each age group.
Dr. Pantell summarized the key action statements for the three age groups, and encouraged pediatricians to review the visual algorithms and footnotes available in the full text of the guideline.
The guideline includes seven key action statements for each of the three age groups. Four of these address evaluations, using urine, blood culture, inflammatory markers (IM), and cerebrospinal fluid (CSF). One action statement focuses on initial treatment, and two on management: hospital admission versus monitoring at home, and treatment cessation.
Infants aged 8-21 days
The key action statements for well-appearing infants aged 8-21 days are similar to what clinicians likely would do for ill-appearing infants, the authors noted, based in part on the challenge of assessing an infant this age as “well appearing,” because they don’t yet have the ability to interact with the clinician.
For the 8- to 21-day group, the first two key actions are to obtain a urine specimen and blood culture, Dr. Pantell said. Also, clinicians “should” obtain a CSF for analysis and culture. “We recognize that the ability to get CSF quickly is a challenge,” he added. However, for the 8- to 21-day age group, a new feature is that these infants may be discharged if the CSF is negative. Evaluation in this youngest group states that clinicians “may assess inflammatory markers” including height of fever, absolute neutrophil count, C-reactive protein, and procalcitonin.
Treatment of infants in the 8- to 21-day group “should” include parenteral antimicrobial therapy, according to the guideline, and these infants “should” be actively monitored in the hospital by nurses and staff experienced in neonatal care, Dr. Pantell said. The guideline also includes a key action statement to stop antimicrobials at 24-36 hours if cultures are negative, but to treat identified organisms.
Infants aged 22-28 days
In both the 22- to 28-day-old and 29- to 60-day-old groups, the guideline offers opportunities for less testing and treatment, such as avoiding a lumbar puncture, and fewer hospitalizations. The development of a separate guideline for the 22- to 28-day group is something new, said Dr. Pantell. The guideline states that clinicians should obtain urine specimens and blood culture, and should assess IM in this group. Further key action statements note that clinicians “should obtain a CSF if any IM is positive,” but “may” obtain CSF if the infant is hospitalized, if blood and urine cultures have been obtained, and if none of the IMs are abnormal.
As with younger patients, those with a negative CSF can go home, he said. As for treatment, clinicians “should” administer parenteral antimicrobial therapy to infants managed at home even if they have a negative CSF and urinalysis (UA), and no abnormal inflammatory markers Other points for management of infants in this age group at home include verbal teaching and written instructions for caregivers, plans for a re-evaluation at home in 24 hours, and a plan for communication and access to emergency care in case of a change in clinical status, Dr. Pantell explained. The guideline states that infants “should” be hospitalized if CSF is either not obtained or not interpretable, which leaves room for clinical judgment and individual circumstances. Antimicrobials “should” be discontinued in this group once all cultures are negative after 24-36 hours and no other infection requires treatment.
Infants aged 29-60 days
For the 29- to 60-day group, there are some differences, the main one is the recommendation of blood cultures in this group, said Dr. Pantell. “We are seeing a lot of UTIs [urinary tract infections], and we would like those treated.” However, clinicians need not obtain a CSF if other IMs are normal, but may do so if any IM is abnormal. Antimicrobial therapy may include ceftriaxone or cephalexin for UTIs, or vancomycin for bacteremia.
Although antimicrobial therapy is an option for UTIs and bacterial meningitis, clinicians “need not” use antimicrobials if CSF is normal, if UA is negative, and if no IMs are abnormal, Dr. Pantell added. Overall, further management of infants in this oldest age group should focus on discharge to home in the absence of abnormal findings, but hospitalization in the presence of abnormal CSF, IMs, or other concerns.
During a question-and-answer session, Dr. Roberts said that, while rectal temperature is preferable, any method is acceptable as a starting point for applying the guideline. Importantly, the guideline still leaves room for clinical judgment. “We hope this will change some thinking as far as whether one model fits all,” he noted. The authors tried to temper the word “should” with the word “may” when possible, so clinicians can say: “I’m going to individualize my decision to the infant in front of me.”
Ultimately, the guideline is meant as a guide, and not an absolute standard of care, the authors said. The language of the key action statements includes the words “should, may, need not” in place of “must, must not.” The guideline recommends factoring family values and preferences into any treatment decisions. “Variations, taking into account individual circumstances, may be appropriate.”
The guideline received no outside funding. The authors had no financial conflicts to disclose.
The long-anticipated American Academy of Pediatrics guidelines for the treatment of well-appearing febrile infants have arrived, and key points include updated guidance for cerebrospinal fluid testing and urine cultures, according to Robert Pantell, MD, and Kenneth Roberts, MD, who presented the guidelines at the virtual Pediatric Hospital Medicine annual conference.
The AAP guideline was published in the August 2021 issue of Pediatrics. The guideline includes 21 key action statements and 40 total recommendations, and describes separate management algorithms for three age groups: infants aged 8-21 days, 22-28 days, and 29-60 days.
Dr. Roberts, of the University of North Carolina at Chapel Hill, and Dr. Pantell, of the University of California, San Francisco, emphasized that all pediatricians should read the full guideline, but they offered an overview of some of the notable points.
Some changes that drove the development of evidence-based guideline included changes in technology, such as the increased use of procalcitonin, the development of large research networks for studies of sufficient size, and a need to reduce the costs of unnecessary care and unnecessary trauma for infants, Dr. Roberts said. Use of data from large networks such as the Pediatric Emergency Care Applied Research Network provided enough evidence to support dividing the aged 8- to 60-day population into three groups.
The guideline applies to well-appearing term infants aged 8-60 days and at least 37 weeks’ gestation, with fever of 38° C (100.4° F) or higher in the past 24 hours in the home or clinical setting. The decision to exclude infants in the first week of life from the guideline was because at this age, infants “are sufficiently different in rates and types of illness, including early-onset bacterial infection,” according to the authors.
Dr. Roberts emphasized that the guidelines apply to “well-appearing infants,” which is not always obvious. “If a clinician is not confident an infant is well appearing, the clinical practice guideline should not be applied,” he said.
The guideline also includes a visual algorithm for each age group.
Dr. Pantell summarized the key action statements for the three age groups, and encouraged pediatricians to review the visual algorithms and footnotes available in the full text of the guideline.
The guideline includes seven key action statements for each of the three age groups. Four of these address evaluations, using urine, blood culture, inflammatory markers (IM), and cerebrospinal fluid (CSF). One action statement focuses on initial treatment, and two on management: hospital admission versus monitoring at home, and treatment cessation.
Infants aged 8-21 days
The key action statements for well-appearing infants aged 8-21 days are similar to what clinicians likely would do for ill-appearing infants, the authors noted, based in part on the challenge of assessing an infant this age as “well appearing,” because they don’t yet have the ability to interact with the clinician.
For the 8- to 21-day group, the first two key actions are to obtain a urine specimen and blood culture, Dr. Pantell said. Also, clinicians “should” obtain a CSF for analysis and culture. “We recognize that the ability to get CSF quickly is a challenge,” he added. However, for the 8- to 21-day age group, a new feature is that these infants may be discharged if the CSF is negative. Evaluation in this youngest group states that clinicians “may assess inflammatory markers” including height of fever, absolute neutrophil count, C-reactive protein, and procalcitonin.
Treatment of infants in the 8- to 21-day group “should” include parenteral antimicrobial therapy, according to the guideline, and these infants “should” be actively monitored in the hospital by nurses and staff experienced in neonatal care, Dr. Pantell said. The guideline also includes a key action statement to stop antimicrobials at 24-36 hours if cultures are negative, but to treat identified organisms.
Infants aged 22-28 days
In both the 22- to 28-day-old and 29- to 60-day-old groups, the guideline offers opportunities for less testing and treatment, such as avoiding a lumbar puncture, and fewer hospitalizations. The development of a separate guideline for the 22- to 28-day group is something new, said Dr. Pantell. The guideline states that clinicians should obtain urine specimens and blood culture, and should assess IM in this group. Further key action statements note that clinicians “should obtain a CSF if any IM is positive,” but “may” obtain CSF if the infant is hospitalized, if blood and urine cultures have been obtained, and if none of the IMs are abnormal.
As with younger patients, those with a negative CSF can go home, he said. As for treatment, clinicians “should” administer parenteral antimicrobial therapy to infants managed at home even if they have a negative CSF and urinalysis (UA), and no abnormal inflammatory markers Other points for management of infants in this age group at home include verbal teaching and written instructions for caregivers, plans for a re-evaluation at home in 24 hours, and a plan for communication and access to emergency care in case of a change in clinical status, Dr. Pantell explained. The guideline states that infants “should” be hospitalized if CSF is either not obtained or not interpretable, which leaves room for clinical judgment and individual circumstances. Antimicrobials “should” be discontinued in this group once all cultures are negative after 24-36 hours and no other infection requires treatment.
Infants aged 29-60 days
For the 29- to 60-day group, there are some differences, the main one is the recommendation of blood cultures in this group, said Dr. Pantell. “We are seeing a lot of UTIs [urinary tract infections], and we would like those treated.” However, clinicians need not obtain a CSF if other IMs are normal, but may do so if any IM is abnormal. Antimicrobial therapy may include ceftriaxone or cephalexin for UTIs, or vancomycin for bacteremia.
Although antimicrobial therapy is an option for UTIs and bacterial meningitis, clinicians “need not” use antimicrobials if CSF is normal, if UA is negative, and if no IMs are abnormal, Dr. Pantell added. Overall, further management of infants in this oldest age group should focus on discharge to home in the absence of abnormal findings, but hospitalization in the presence of abnormal CSF, IMs, or other concerns.
During a question-and-answer session, Dr. Roberts said that, while rectal temperature is preferable, any method is acceptable as a starting point for applying the guideline. Importantly, the guideline still leaves room for clinical judgment. “We hope this will change some thinking as far as whether one model fits all,” he noted. The authors tried to temper the word “should” with the word “may” when possible, so clinicians can say: “I’m going to individualize my decision to the infant in front of me.”
Ultimately, the guideline is meant as a guide, and not an absolute standard of care, the authors said. The language of the key action statements includes the words “should, may, need not” in place of “must, must not.” The guideline recommends factoring family values and preferences into any treatment decisions. “Variations, taking into account individual circumstances, may be appropriate.”
The guideline received no outside funding. The authors had no financial conflicts to disclose.
FROM PHM 2021
Masking in school: A battle of the op-eds
Traditionally, as the ides of August descend upon us we expect to be bombarded with advertisements encouraging parents and students to finish up their back-to-school shopping. But, this year the question on every parent and school administrator’s mind is not which color back pack will be the most popular this year but whether a mask should be a required part of the back-to-school ensemble.
The American Academy of Pediatrics has recommended that “All students older than 2 years and all school staff should wear a mask at school” (“American Academy of Pediatrics Updates Recommendations for Opening Schools in Fall 2021.” 2021 Jul 19). The academy’s statement includes a generous list of common sense caveats but it does not include a statement that masks have been shown to be protective for children in school environments. The Centers for Disease Control and Prevention “recommends” universal indoor masking along with keeping a 3-foot separation but again fails to include any references to support the effectiveness of masks (“Guidance for COVID-19 Prevention in K-12 Schools.” 2021 Aug 5).
Not surprisingly, into this void have stepped two pairs of experts – one group purporting to have evidence that masking is effective in school environments and the other warning that masks may not only be ineffective but that they also carry some significant downsides. And, where can you find these opposing positions? Not in The Lancet. Not in the New England Journal of Medicine. We don’t have time for any of that peer-reviewed monkey business. No, this is pandemic-era science where we have an abundance of opinions and paucity of facts. You will find these opposing articles on the op-ed pages of two of this country’s major newspapers.
In the Aug. 10, 2021, edition of the New York Times you will find an article (“We Studied One Million Students. This Is What We Learned About Masking”) by two pediatricians, Kanecia Zimmerman, MD, and Danny Benjamin Jr., MD, who have “studied” a million students in North Carolina school systems and tell us universal masking is “one of the most effective and efficient strategies for preventing SARS-CoV-2 transmission in schools. These investigators write that they “believe” the low rate of in school transmission they observed in North Carolina was “because of the mask-on-mask school environment.”
However, in the next paragraph the authors admit, “Because North Carolina had a mask mandate for all K-12 schools, we could not compare masked schools with unmasked schools.” They lean instead on studies from three other states with mask mandates that also had low transmission rates and a single report of an outbreak in Israel that employed neither masking nor safe distancing.
On the other side of the divide is an article in the Wall Street Journal titled “The Case Against Masks for Children” by Marty Makary, MD, and H. Cody Meissner, MD, (2021 Aug 9). The authors, one a pediatric infectious disease specialist, argue that there is “no science behind mask mandates for children.” And, observe that, of the $46 billion spent on research grants by the National Institutes of Health, “not a single grant was dedicated to studying masking in children.”
Dr. Makary and Dr. Meissner present a variety of concerns about the effects of masking including those on the development and communication skills of young children. None of their theoretical concerns of course are supported by controlled studies. They also observe that in previous studies children seem to be less likely to transmit COVID-19 than adults. Although we all know the landscape is changing with the emergence of the delta strain. In their strongest statement the authors claim, “It is abusive to force kids who struggle with them [masks] to sacrifice for the sake of unvaccinated adults.”
So there you have it. It is a situation we have come to expect over the last 2 years – plenty of opinions and too few facts supported by controlled studies. Both pairs of authors, however, agree on two things: Vaccination should continue to be considered our primary tool in prevention and control of COVID-19. and children need to be in school. Based on nothing more than a hunch and 7 decades of hunching, I tend to side with Dr. Makary and Dr. Meissner. Depending on the situation, I suggest masking but wouldn’t mandate it for children in school.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Traditionally, as the ides of August descend upon us we expect to be bombarded with advertisements encouraging parents and students to finish up their back-to-school shopping. But, this year the question on every parent and school administrator’s mind is not which color back pack will be the most popular this year but whether a mask should be a required part of the back-to-school ensemble.
The American Academy of Pediatrics has recommended that “All students older than 2 years and all school staff should wear a mask at school” (“American Academy of Pediatrics Updates Recommendations for Opening Schools in Fall 2021.” 2021 Jul 19). The academy’s statement includes a generous list of common sense caveats but it does not include a statement that masks have been shown to be protective for children in school environments. The Centers for Disease Control and Prevention “recommends” universal indoor masking along with keeping a 3-foot separation but again fails to include any references to support the effectiveness of masks (“Guidance for COVID-19 Prevention in K-12 Schools.” 2021 Aug 5).
Not surprisingly, into this void have stepped two pairs of experts – one group purporting to have evidence that masking is effective in school environments and the other warning that masks may not only be ineffective but that they also carry some significant downsides. And, where can you find these opposing positions? Not in The Lancet. Not in the New England Journal of Medicine. We don’t have time for any of that peer-reviewed monkey business. No, this is pandemic-era science where we have an abundance of opinions and paucity of facts. You will find these opposing articles on the op-ed pages of two of this country’s major newspapers.
In the Aug. 10, 2021, edition of the New York Times you will find an article (“We Studied One Million Students. This Is What We Learned About Masking”) by two pediatricians, Kanecia Zimmerman, MD, and Danny Benjamin Jr., MD, who have “studied” a million students in North Carolina school systems and tell us universal masking is “one of the most effective and efficient strategies for preventing SARS-CoV-2 transmission in schools. These investigators write that they “believe” the low rate of in school transmission they observed in North Carolina was “because of the mask-on-mask school environment.”
However, in the next paragraph the authors admit, “Because North Carolina had a mask mandate for all K-12 schools, we could not compare masked schools with unmasked schools.” They lean instead on studies from three other states with mask mandates that also had low transmission rates and a single report of an outbreak in Israel that employed neither masking nor safe distancing.
On the other side of the divide is an article in the Wall Street Journal titled “The Case Against Masks for Children” by Marty Makary, MD, and H. Cody Meissner, MD, (2021 Aug 9). The authors, one a pediatric infectious disease specialist, argue that there is “no science behind mask mandates for children.” And, observe that, of the $46 billion spent on research grants by the National Institutes of Health, “not a single grant was dedicated to studying masking in children.”
Dr. Makary and Dr. Meissner present a variety of concerns about the effects of masking including those on the development and communication skills of young children. None of their theoretical concerns of course are supported by controlled studies. They also observe that in previous studies children seem to be less likely to transmit COVID-19 than adults. Although we all know the landscape is changing with the emergence of the delta strain. In their strongest statement the authors claim, “It is abusive to force kids who struggle with them [masks] to sacrifice for the sake of unvaccinated adults.”
So there you have it. It is a situation we have come to expect over the last 2 years – plenty of opinions and too few facts supported by controlled studies. Both pairs of authors, however, agree on two things: Vaccination should continue to be considered our primary tool in prevention and control of COVID-19. and children need to be in school. Based on nothing more than a hunch and 7 decades of hunching, I tend to side with Dr. Makary and Dr. Meissner. Depending on the situation, I suggest masking but wouldn’t mandate it for children in school.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Traditionally, as the ides of August descend upon us we expect to be bombarded with advertisements encouraging parents and students to finish up their back-to-school shopping. But, this year the question on every parent and school administrator’s mind is not which color back pack will be the most popular this year but whether a mask should be a required part of the back-to-school ensemble.
The American Academy of Pediatrics has recommended that “All students older than 2 years and all school staff should wear a mask at school” (“American Academy of Pediatrics Updates Recommendations for Opening Schools in Fall 2021.” 2021 Jul 19). The academy’s statement includes a generous list of common sense caveats but it does not include a statement that masks have been shown to be protective for children in school environments. The Centers for Disease Control and Prevention “recommends” universal indoor masking along with keeping a 3-foot separation but again fails to include any references to support the effectiveness of masks (“Guidance for COVID-19 Prevention in K-12 Schools.” 2021 Aug 5).
Not surprisingly, into this void have stepped two pairs of experts – one group purporting to have evidence that masking is effective in school environments and the other warning that masks may not only be ineffective but that they also carry some significant downsides. And, where can you find these opposing positions? Not in The Lancet. Not in the New England Journal of Medicine. We don’t have time for any of that peer-reviewed monkey business. No, this is pandemic-era science where we have an abundance of opinions and paucity of facts. You will find these opposing articles on the op-ed pages of two of this country’s major newspapers.
In the Aug. 10, 2021, edition of the New York Times you will find an article (“We Studied One Million Students. This Is What We Learned About Masking”) by two pediatricians, Kanecia Zimmerman, MD, and Danny Benjamin Jr., MD, who have “studied” a million students in North Carolina school systems and tell us universal masking is “one of the most effective and efficient strategies for preventing SARS-CoV-2 transmission in schools. These investigators write that they “believe” the low rate of in school transmission they observed in North Carolina was “because of the mask-on-mask school environment.”
However, in the next paragraph the authors admit, “Because North Carolina had a mask mandate for all K-12 schools, we could not compare masked schools with unmasked schools.” They lean instead on studies from three other states with mask mandates that also had low transmission rates and a single report of an outbreak in Israel that employed neither masking nor safe distancing.
On the other side of the divide is an article in the Wall Street Journal titled “The Case Against Masks for Children” by Marty Makary, MD, and H. Cody Meissner, MD, (2021 Aug 9). The authors, one a pediatric infectious disease specialist, argue that there is “no science behind mask mandates for children.” And, observe that, of the $46 billion spent on research grants by the National Institutes of Health, “not a single grant was dedicated to studying masking in children.”
Dr. Makary and Dr. Meissner present a variety of concerns about the effects of masking including those on the development and communication skills of young children. None of their theoretical concerns of course are supported by controlled studies. They also observe that in previous studies children seem to be less likely to transmit COVID-19 than adults. Although we all know the landscape is changing with the emergence of the delta strain. In their strongest statement the authors claim, “It is abusive to force kids who struggle with them [masks] to sacrifice for the sake of unvaccinated adults.”
So there you have it. It is a situation we have come to expect over the last 2 years – plenty of opinions and too few facts supported by controlled studies. Both pairs of authors, however, agree on two things: Vaccination should continue to be considered our primary tool in prevention and control of COVID-19. and children need to be in school. Based on nothing more than a hunch and 7 decades of hunching, I tend to side with Dr. Makary and Dr. Meissner. Depending on the situation, I suggest masking but wouldn’t mandate it for children in school.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Major musculoskeletal surgery in children with medically complex conditions
A review of the International Committee’s guide
The International Committee on Perioperative Care for Children with Medical Complexity developed an online guide, “Deciding on and Preparing for Major Musculoskeletal Surgery in Children with Cerebral Palsy, Neurodevelopmental Disorders, and Other Medically Complex Conditions,” published on Dec. 20, 2020, detailing how to prepare pediatric patients with medical complexity prior to musculoskeletal surgery. The guide was developed from a dearth of information regarding optimal care practices for these patients.
The multidisciplinary committee included members from orthopedic surgery, general pediatrics, pediatric hospital medicine, anesthesiology, critical care medicine, pain medicine, physiotherapy, developmental and behavioral pediatrics, and families of children with cerebral palsy. Mirna Giordano, MD, FAAP, FHM, associate professor of pediatrics at Columbia University, New York, and International Committee member, helped develop these recommendations to “improve quality of care in the perioperative period for children with medical complexities and neurodisabilities all over the world.”
The guide meticulously details the steps required to successfully prepare for an operation and postoperative recovery. It includes an algorithm and comprehensive assessment plan that can be implemented to assess and optimize the child’s health and wellbeing prior to surgery. It encourages shared decision making and highlights the need for ongoing, open communication between providers, patients, and families to set goals and expectations, discuss potential complications, and describe outcomes and the recovery process.
The module elaborates on several key factors that must be evaluated and addressed long before surgery to ensure success. Baseline nutrition is critical and must be evaluated with body composition and anthropometric measurements. Respiratory health must be assessed with consideration of pulmonology consultation, specific testing, and ventilator or assistive-device optimization. Moreover, children with innate muscular weakness or restrictive lung disease should have baseline physiology evaluated in anticipation of potential postoperative complications, including atelectasis, hypoventilation, and pneumonia. Coexisting chronic medical conditions must also be optimized in anticipation of expected deviations from baseline.
In anticipation of peri- and postoperative care, the medical team should also be aware of details surrounding patients’ indwelling medical devices, such as cardiac implantable devices and tracheostomies. Particular attention should be paid to baclofen pumps, as malfunction or mistitration can lead to periprocedural hypotension or withdrawal.
Of paramount importance is understanding how the child appears and responds when in pain or discomfort, especially for a child with limited verbal communication. The module provides pain assessment tools, tailored to verbal and nonverbal patients in both the inpatient and outpatient settings. The module also shares guidance on establishing communication and goals with the family and within the care team on how the child appears when in distress and how he/she/they respond to pain medications. The pain plan should encompass both pharmacologic and nonpharmacologic therapeutics. Furthermore, as pain and discomfort may present from multiple sources, not limited to the regions involved in the procedure, understanding how the child responds to urinary retention, constipation, dyspnea, and uncomfortable positions is important to care. Postoperative immobilization must also be addressed as it may lead to pressure injury, manifesting as behavioral changes.
The module also presents laboratory testing as part of the preoperative health assessment. It details the utility or lack thereof of several common practices and provides recommendations on components that should be part of each patient’s assessment. It also contains videos showcased from the Courage Parents Network on family and provider perceptions of spinal fusion.
Family and social assessments must not be neglected prior to surgery, as these areas may also affect surgical outcomes. The module shares several screening tools that care team members can use to screen for family and social issues. Challenges to discharge planning are also discussed, including how to approach transportation, medical equipment, and school transitions needs.
The module is available for review in OPEN Pediatrics (www.openpediatrics.org), an online community for pediatric health professionals who share peer-reviewed best practices. “Our aim is to disseminate the recommendations as widely as possible to bring about the maximum good to the most,” Dr. Giordano said. The International Committee on Perioperative Care for Children with Medical Complexity is planning further guides regarding perioperative care, particularly for intraoperative and postoperative considerations.
Dr. Tantoco is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago, and instructor of medicine (hospital medicine) and pediatrics in Northwestern University, in Chicago. She is also a member of the SHM Pediatrics Special Interest Group Executive Committee. Dr. Bhasin is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital, and assistant professor of medicine (hospital medicine) and pediatrics in Northwestern University.
A review of the International Committee’s guide
A review of the International Committee’s guide
The International Committee on Perioperative Care for Children with Medical Complexity developed an online guide, “Deciding on and Preparing for Major Musculoskeletal Surgery in Children with Cerebral Palsy, Neurodevelopmental Disorders, and Other Medically Complex Conditions,” published on Dec. 20, 2020, detailing how to prepare pediatric patients with medical complexity prior to musculoskeletal surgery. The guide was developed from a dearth of information regarding optimal care practices for these patients.
The multidisciplinary committee included members from orthopedic surgery, general pediatrics, pediatric hospital medicine, anesthesiology, critical care medicine, pain medicine, physiotherapy, developmental and behavioral pediatrics, and families of children with cerebral palsy. Mirna Giordano, MD, FAAP, FHM, associate professor of pediatrics at Columbia University, New York, and International Committee member, helped develop these recommendations to “improve quality of care in the perioperative period for children with medical complexities and neurodisabilities all over the world.”
The guide meticulously details the steps required to successfully prepare for an operation and postoperative recovery. It includes an algorithm and comprehensive assessment plan that can be implemented to assess and optimize the child’s health and wellbeing prior to surgery. It encourages shared decision making and highlights the need for ongoing, open communication between providers, patients, and families to set goals and expectations, discuss potential complications, and describe outcomes and the recovery process.
The module elaborates on several key factors that must be evaluated and addressed long before surgery to ensure success. Baseline nutrition is critical and must be evaluated with body composition and anthropometric measurements. Respiratory health must be assessed with consideration of pulmonology consultation, specific testing, and ventilator or assistive-device optimization. Moreover, children with innate muscular weakness or restrictive lung disease should have baseline physiology evaluated in anticipation of potential postoperative complications, including atelectasis, hypoventilation, and pneumonia. Coexisting chronic medical conditions must also be optimized in anticipation of expected deviations from baseline.
In anticipation of peri- and postoperative care, the medical team should also be aware of details surrounding patients’ indwelling medical devices, such as cardiac implantable devices and tracheostomies. Particular attention should be paid to baclofen pumps, as malfunction or mistitration can lead to periprocedural hypotension or withdrawal.
Of paramount importance is understanding how the child appears and responds when in pain or discomfort, especially for a child with limited verbal communication. The module provides pain assessment tools, tailored to verbal and nonverbal patients in both the inpatient and outpatient settings. The module also shares guidance on establishing communication and goals with the family and within the care team on how the child appears when in distress and how he/she/they respond to pain medications. The pain plan should encompass both pharmacologic and nonpharmacologic therapeutics. Furthermore, as pain and discomfort may present from multiple sources, not limited to the regions involved in the procedure, understanding how the child responds to urinary retention, constipation, dyspnea, and uncomfortable positions is important to care. Postoperative immobilization must also be addressed as it may lead to pressure injury, manifesting as behavioral changes.
The module also presents laboratory testing as part of the preoperative health assessment. It details the utility or lack thereof of several common practices and provides recommendations on components that should be part of each patient’s assessment. It also contains videos showcased from the Courage Parents Network on family and provider perceptions of spinal fusion.
Family and social assessments must not be neglected prior to surgery, as these areas may also affect surgical outcomes. The module shares several screening tools that care team members can use to screen for family and social issues. Challenges to discharge planning are also discussed, including how to approach transportation, medical equipment, and school transitions needs.
The module is available for review in OPEN Pediatrics (www.openpediatrics.org), an online community for pediatric health professionals who share peer-reviewed best practices. “Our aim is to disseminate the recommendations as widely as possible to bring about the maximum good to the most,” Dr. Giordano said. The International Committee on Perioperative Care for Children with Medical Complexity is planning further guides regarding perioperative care, particularly for intraoperative and postoperative considerations.
Dr. Tantoco is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago, and instructor of medicine (hospital medicine) and pediatrics in Northwestern University, in Chicago. She is also a member of the SHM Pediatrics Special Interest Group Executive Committee. Dr. Bhasin is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital, and assistant professor of medicine (hospital medicine) and pediatrics in Northwestern University.
The International Committee on Perioperative Care for Children with Medical Complexity developed an online guide, “Deciding on and Preparing for Major Musculoskeletal Surgery in Children with Cerebral Palsy, Neurodevelopmental Disorders, and Other Medically Complex Conditions,” published on Dec. 20, 2020, detailing how to prepare pediatric patients with medical complexity prior to musculoskeletal surgery. The guide was developed from a dearth of information regarding optimal care practices for these patients.
The multidisciplinary committee included members from orthopedic surgery, general pediatrics, pediatric hospital medicine, anesthesiology, critical care medicine, pain medicine, physiotherapy, developmental and behavioral pediatrics, and families of children with cerebral palsy. Mirna Giordano, MD, FAAP, FHM, associate professor of pediatrics at Columbia University, New York, and International Committee member, helped develop these recommendations to “improve quality of care in the perioperative period for children with medical complexities and neurodisabilities all over the world.”
The guide meticulously details the steps required to successfully prepare for an operation and postoperative recovery. It includes an algorithm and comprehensive assessment plan that can be implemented to assess and optimize the child’s health and wellbeing prior to surgery. It encourages shared decision making and highlights the need for ongoing, open communication between providers, patients, and families to set goals and expectations, discuss potential complications, and describe outcomes and the recovery process.
The module elaborates on several key factors that must be evaluated and addressed long before surgery to ensure success. Baseline nutrition is critical and must be evaluated with body composition and anthropometric measurements. Respiratory health must be assessed with consideration of pulmonology consultation, specific testing, and ventilator or assistive-device optimization. Moreover, children with innate muscular weakness or restrictive lung disease should have baseline physiology evaluated in anticipation of potential postoperative complications, including atelectasis, hypoventilation, and pneumonia. Coexisting chronic medical conditions must also be optimized in anticipation of expected deviations from baseline.
In anticipation of peri- and postoperative care, the medical team should also be aware of details surrounding patients’ indwelling medical devices, such as cardiac implantable devices and tracheostomies. Particular attention should be paid to baclofen pumps, as malfunction or mistitration can lead to periprocedural hypotension or withdrawal.
Of paramount importance is understanding how the child appears and responds when in pain or discomfort, especially for a child with limited verbal communication. The module provides pain assessment tools, tailored to verbal and nonverbal patients in both the inpatient and outpatient settings. The module also shares guidance on establishing communication and goals with the family and within the care team on how the child appears when in distress and how he/she/they respond to pain medications. The pain plan should encompass both pharmacologic and nonpharmacologic therapeutics. Furthermore, as pain and discomfort may present from multiple sources, not limited to the regions involved in the procedure, understanding how the child responds to urinary retention, constipation, dyspnea, and uncomfortable positions is important to care. Postoperative immobilization must also be addressed as it may lead to pressure injury, manifesting as behavioral changes.
The module also presents laboratory testing as part of the preoperative health assessment. It details the utility or lack thereof of several common practices and provides recommendations on components that should be part of each patient’s assessment. It also contains videos showcased from the Courage Parents Network on family and provider perceptions of spinal fusion.
Family and social assessments must not be neglected prior to surgery, as these areas may also affect surgical outcomes. The module shares several screening tools that care team members can use to screen for family and social issues. Challenges to discharge planning are also discussed, including how to approach transportation, medical equipment, and school transitions needs.
The module is available for review in OPEN Pediatrics (www.openpediatrics.org), an online community for pediatric health professionals who share peer-reviewed best practices. “Our aim is to disseminate the recommendations as widely as possible to bring about the maximum good to the most,” Dr. Giordano said. The International Committee on Perioperative Care for Children with Medical Complexity is planning further guides regarding perioperative care, particularly for intraoperative and postoperative considerations.
Dr. Tantoco is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital of Chicago, and instructor of medicine (hospital medicine) and pediatrics in Northwestern University, in Chicago. She is also a member of the SHM Pediatrics Special Interest Group Executive Committee. Dr. Bhasin is a med-peds hospitalist at Northwestern Memorial Hospital and Ann & Robert H. Lurie Children’s Hospital, and assistant professor of medicine (hospital medicine) and pediatrics in Northwestern University.
Ultraprocessed foods comprise most of the calories for youths
In the 2 decades from 1999 to 2018, ultraprocessed foods consistently accounted for the majority of energy intake by American young people, a large cross-sectional study of National Health and Nutrition Examination Survey (NHANES) data shows.
In young people aged 2-19 years, the estimated percentage of total energy from consumption of ultraprocessed foods increased from 61.4% to 67.0%, for a difference of 5.6% (95% confidence interval [CI] 3.5-7.7, P < .001 for trend), according to Lu Wang, PhD, MPH, a postdoctoral fellow at the Friedman School of Nutrition Science and Policy at Tufts University in Boston, and colleagues.
In contrast, total energy from non- or minimally processed foods decreased from 28.8% to 23.5% (difference −5.3%, 95% CI, −7.5 to −3.2, P < .001 for trend).
“The estimated percentage of energy consumed from ultraprocessed foods increased from 1999 to 2018, with an increasing trend in ready-to-heat and -eat mixed dishes and a decreasing trend in sugar-sweetened beverages,” the authors wrote. The report was published online Aug. 10 in JAMA.
The findings held regardless of the educational and socioeconomic status of the children’s parents.
Significant disparities by race and ethnicity emerged, however, with the ultraprocessed food phenomenon more marked in non-Hispanic Black youths and Mexican-American youths than in their non-Hispanic White counterparts. “Targeted marketing of junk foods toward racial/ethnic minority youths may partly contribute to such differences,” the authors wrote. “However, persistently lower consumption of ultraprocessed foods among Mexican-American youths may reflect more home cooking among Hispanic families.”
Among non-Hispanic Black youths consumption rose from 62.2% to 72.5% (difference 10.3%, 95% CI, 6.8-13.8) and among Mexican-American youths from 55.8% to 63.5% (difference 7.6%, 95% CI, 4.4-10.9). In non-Hispanic White youths intake rose from 63.4% to 68.6% (difference 5.2%, 95% CI, 2.1-8.3, P = .04 for trends).
In addition, a higher consumption of ultraprocessed foods among school-aged youths than among preschool children aged 2-5 years may reflect increased marketing, availability, and selection of ultraprocessed foods for older youths, the authors noted.
Food processing, with its potential adverse effects, may need to be considered as a food dimension in addition to nutrients and food groups in future dietary recommendations and food policies, they added.
“An increasing number of studies are showing a link between ultraprocessed food consumption and adverse health outcomes in children,” corresponding author Fang Fang Zhang, MD, PhD, Neely Family Professor and associate professor at Tufts’ Friedman School of Nutrition Science and Policy, said in an interview. “Health care providers can play a larger role in encouraging patients – and their parents – to replace unhealthy ultraprocessed foods such as ultraprocessed sweet bakery products with healthy unprocessed or minimally processed foods in their diet such as less processed whole grains. “
In Dr. Zhang’s view, teachers also have a part to play in promoting nutrition literacy. “Schools can play an important role in empowering children with knowledge and skills to make healthy food choices,” she said. “Nutrition literacy should be an integral part of the health education curriculum in all K-12 schools.”
Commenting on the study but not involved in it, Michelle Katzow, MD, a pediatrician/obesity medicine specialist and assistant professor at the Feinstein Institutes for Medical Research in Manhasset, N.Y., said the work highlights an often overlooked aspect of the modern American diet that may well be contributing to poor health outcomes in young people.
“It suggests that even as the science advances and we learn more about the adverse health effects of ultraprocessed foods, public health efforts to improve nutrition and food quality in children have not been successful,” she said in an interview. “This is because it is so hard for public health advocates to compete with the food industry, which stands to really benefit financially from hooking kids on processed foods that are not good for their health.”
Dr. Katzow added that the observed racial/ethnic disparities are not surprising in light of a growing body of evidence that racism exists in food marketing. “We need to put forward policies that regulate the food industry, particularly in relation to its most susceptible targets, our kids.”
Study details
The serial cross-sectional analysis used 24-hour dietary recall data from a nationally representative sample from 10 NHANES cycles for the range of 1999-2000 to 2017-2018. The weighted mean age of the cohort was 10.7 years and 49.1% were girls.
Among the subgroups of ultraprocessed foods, the estimated percentage of energy from ready-to-heat and ready-to-eat mixed dishes increased from 2.2% to 11.2% (difference 8.9%; 95%, CI, 7.7-10.2).
Energy from sweets and sweet snacks increased from 10.7% to 12.9% (difference 2.3%; 95% CI, 1.0-3.6), but the estimated percentage of energy decreased for sugar-sweetened beverages from 10.8% to 5.3% (difference −5.5%; 95% CI, −6.5 to −4.5).
In other categories, estimated energy intake from processed fats and oils, condiments, and sauces fell from 7.1% to 4.0% (difference −3.1%; 95% CI, −3.7 to −2.6, all P < .05 for trend).
Not surprisingly, ultraprocessed foods had an overall poorer nutrient profile than that of nonultraprocessed, although they often contained less saturated fat, and they also contained more carbohydrates, mostly from low-quality sources with added sugars and low levels of dietary fiber and protein.
And despite a higher total folate content in ultraprocessed foods because of fortification, higher-level consumers took in less total folate owing to their lower consumption of whole foods.
The authors cautioned that in addition to poor nutrient profiles, processing itself may harm health by changing the physical structure and chemical composition of food, which could lead to elevated glycemic response and reduced satiety. Furthermore, recent research has linked food additives such as emulsifiers, stabilizers, and artificial sweeteners to adverse metabolomic effects and obesity risk. Pointing to the recent success of efforts to reduce consumption of sugary beverages, Dr. Zhang said, “We need to mobilize the same energy and level of commitment when it comes to other unhealthy ultraprocessed foods such as cakes, cookies, doughnuts, and brownies.”
The trends identified by the Tufts study “are concerning and potentially have major public health significance,” according to an accompanying JAMA editorial.
“Better dietary assessment methods are needed to document trends and understand the unique role of ultraprocessed foods to inform future evidence-based policy and dietary recommendations,” wrote Katie A. Meyer, ScD, and Lindsey Smith Taillie, PhD, of the Gillings School of Global Public Health at the University of North Carolina in Chapel Hill.
The editorialists share the authors’ view that “a conceptual advancement would be to consider the level and characteristics of processing as just one of multiple dimensions (including nutrients and food groups) used to classify foods as healthy or unhealthy.” They pointed out that the Pan American Health Organization already recommends targeting products that are ultraprocessed and high in concerning add-in nutrients.
They cautioned, however, that the classification of ultraprocessed foods will not be easy because it requires data on a full list of ingredients, and the effects of processing generally cannot be separated from the composite nutrients of ultraprocessed foods.
This presents a challenge for national food consumption research “given that most large epidemiological studies rely on food frequency questionnaires that lack the information necessary to classify processing levels,” they wrote.
This study was supported by the National Institutes of Health and the São Paulo Research Foundation. Coauthor Dariush Mozaffarian, MD, a cardiologist at Tufts University, disclosed support from the Bill & Melinda Gates Foundation, the National Institutes of Health, and the Rockefeller Foundation as well as personal fees from several commercial companies. He has served on several scientific advisory boards and received royalties from UpToDate, all outside of the submitted work. Dr. Meyer reported a grant from choline manufacturer Balchem. Dr. Taillie reported funding from Bloomberg Philanthropies. Dr. Zhang had no disclosures. Dr. Katzow disclosed no competing interests.
In the 2 decades from 1999 to 2018, ultraprocessed foods consistently accounted for the majority of energy intake by American young people, a large cross-sectional study of National Health and Nutrition Examination Survey (NHANES) data shows.
In young people aged 2-19 years, the estimated percentage of total energy from consumption of ultraprocessed foods increased from 61.4% to 67.0%, for a difference of 5.6% (95% confidence interval [CI] 3.5-7.7, P < .001 for trend), according to Lu Wang, PhD, MPH, a postdoctoral fellow at the Friedman School of Nutrition Science and Policy at Tufts University in Boston, and colleagues.
In contrast, total energy from non- or minimally processed foods decreased from 28.8% to 23.5% (difference −5.3%, 95% CI, −7.5 to −3.2, P < .001 for trend).
“The estimated percentage of energy consumed from ultraprocessed foods increased from 1999 to 2018, with an increasing trend in ready-to-heat and -eat mixed dishes and a decreasing trend in sugar-sweetened beverages,” the authors wrote. The report was published online Aug. 10 in JAMA.
The findings held regardless of the educational and socioeconomic status of the children’s parents.
Significant disparities by race and ethnicity emerged, however, with the ultraprocessed food phenomenon more marked in non-Hispanic Black youths and Mexican-American youths than in their non-Hispanic White counterparts. “Targeted marketing of junk foods toward racial/ethnic minority youths may partly contribute to such differences,” the authors wrote. “However, persistently lower consumption of ultraprocessed foods among Mexican-American youths may reflect more home cooking among Hispanic families.”
Among non-Hispanic Black youths consumption rose from 62.2% to 72.5% (difference 10.3%, 95% CI, 6.8-13.8) and among Mexican-American youths from 55.8% to 63.5% (difference 7.6%, 95% CI, 4.4-10.9). In non-Hispanic White youths intake rose from 63.4% to 68.6% (difference 5.2%, 95% CI, 2.1-8.3, P = .04 for trends).
In addition, a higher consumption of ultraprocessed foods among school-aged youths than among preschool children aged 2-5 years may reflect increased marketing, availability, and selection of ultraprocessed foods for older youths, the authors noted.
Food processing, with its potential adverse effects, may need to be considered as a food dimension in addition to nutrients and food groups in future dietary recommendations and food policies, they added.
“An increasing number of studies are showing a link between ultraprocessed food consumption and adverse health outcomes in children,” corresponding author Fang Fang Zhang, MD, PhD, Neely Family Professor and associate professor at Tufts’ Friedman School of Nutrition Science and Policy, said in an interview. “Health care providers can play a larger role in encouraging patients – and their parents – to replace unhealthy ultraprocessed foods such as ultraprocessed sweet bakery products with healthy unprocessed or minimally processed foods in their diet such as less processed whole grains. “
In Dr. Zhang’s view, teachers also have a part to play in promoting nutrition literacy. “Schools can play an important role in empowering children with knowledge and skills to make healthy food choices,” she said. “Nutrition literacy should be an integral part of the health education curriculum in all K-12 schools.”
Commenting on the study but not involved in it, Michelle Katzow, MD, a pediatrician/obesity medicine specialist and assistant professor at the Feinstein Institutes for Medical Research in Manhasset, N.Y., said the work highlights an often overlooked aspect of the modern American diet that may well be contributing to poor health outcomes in young people.
“It suggests that even as the science advances and we learn more about the adverse health effects of ultraprocessed foods, public health efforts to improve nutrition and food quality in children have not been successful,” she said in an interview. “This is because it is so hard for public health advocates to compete with the food industry, which stands to really benefit financially from hooking kids on processed foods that are not good for their health.”
Dr. Katzow added that the observed racial/ethnic disparities are not surprising in light of a growing body of evidence that racism exists in food marketing. “We need to put forward policies that regulate the food industry, particularly in relation to its most susceptible targets, our kids.”
Study details
The serial cross-sectional analysis used 24-hour dietary recall data from a nationally representative sample from 10 NHANES cycles for the range of 1999-2000 to 2017-2018. The weighted mean age of the cohort was 10.7 years and 49.1% were girls.
Among the subgroups of ultraprocessed foods, the estimated percentage of energy from ready-to-heat and ready-to-eat mixed dishes increased from 2.2% to 11.2% (difference 8.9%; 95%, CI, 7.7-10.2).
Energy from sweets and sweet snacks increased from 10.7% to 12.9% (difference 2.3%; 95% CI, 1.0-3.6), but the estimated percentage of energy decreased for sugar-sweetened beverages from 10.8% to 5.3% (difference −5.5%; 95% CI, −6.5 to −4.5).
In other categories, estimated energy intake from processed fats and oils, condiments, and sauces fell from 7.1% to 4.0% (difference −3.1%; 95% CI, −3.7 to −2.6, all P < .05 for trend).
Not surprisingly, ultraprocessed foods had an overall poorer nutrient profile than that of nonultraprocessed, although they often contained less saturated fat, and they also contained more carbohydrates, mostly from low-quality sources with added sugars and low levels of dietary fiber and protein.
And despite a higher total folate content in ultraprocessed foods because of fortification, higher-level consumers took in less total folate owing to their lower consumption of whole foods.
The authors cautioned that in addition to poor nutrient profiles, processing itself may harm health by changing the physical structure and chemical composition of food, which could lead to elevated glycemic response and reduced satiety. Furthermore, recent research has linked food additives such as emulsifiers, stabilizers, and artificial sweeteners to adverse metabolomic effects and obesity risk. Pointing to the recent success of efforts to reduce consumption of sugary beverages, Dr. Zhang said, “We need to mobilize the same energy and level of commitment when it comes to other unhealthy ultraprocessed foods such as cakes, cookies, doughnuts, and brownies.”
The trends identified by the Tufts study “are concerning and potentially have major public health significance,” according to an accompanying JAMA editorial.
“Better dietary assessment methods are needed to document trends and understand the unique role of ultraprocessed foods to inform future evidence-based policy and dietary recommendations,” wrote Katie A. Meyer, ScD, and Lindsey Smith Taillie, PhD, of the Gillings School of Global Public Health at the University of North Carolina in Chapel Hill.
The editorialists share the authors’ view that “a conceptual advancement would be to consider the level and characteristics of processing as just one of multiple dimensions (including nutrients and food groups) used to classify foods as healthy or unhealthy.” They pointed out that the Pan American Health Organization already recommends targeting products that are ultraprocessed and high in concerning add-in nutrients.
They cautioned, however, that the classification of ultraprocessed foods will not be easy because it requires data on a full list of ingredients, and the effects of processing generally cannot be separated from the composite nutrients of ultraprocessed foods.
This presents a challenge for national food consumption research “given that most large epidemiological studies rely on food frequency questionnaires that lack the information necessary to classify processing levels,” they wrote.
This study was supported by the National Institutes of Health and the São Paulo Research Foundation. Coauthor Dariush Mozaffarian, MD, a cardiologist at Tufts University, disclosed support from the Bill & Melinda Gates Foundation, the National Institutes of Health, and the Rockefeller Foundation as well as personal fees from several commercial companies. He has served on several scientific advisory boards and received royalties from UpToDate, all outside of the submitted work. Dr. Meyer reported a grant from choline manufacturer Balchem. Dr. Taillie reported funding from Bloomberg Philanthropies. Dr. Zhang had no disclosures. Dr. Katzow disclosed no competing interests.
In the 2 decades from 1999 to 2018, ultraprocessed foods consistently accounted for the majority of energy intake by American young people, a large cross-sectional study of National Health and Nutrition Examination Survey (NHANES) data shows.
In young people aged 2-19 years, the estimated percentage of total energy from consumption of ultraprocessed foods increased from 61.4% to 67.0%, for a difference of 5.6% (95% confidence interval [CI] 3.5-7.7, P < .001 for trend), according to Lu Wang, PhD, MPH, a postdoctoral fellow at the Friedman School of Nutrition Science and Policy at Tufts University in Boston, and colleagues.
In contrast, total energy from non- or minimally processed foods decreased from 28.8% to 23.5% (difference −5.3%, 95% CI, −7.5 to −3.2, P < .001 for trend).
“The estimated percentage of energy consumed from ultraprocessed foods increased from 1999 to 2018, with an increasing trend in ready-to-heat and -eat mixed dishes and a decreasing trend in sugar-sweetened beverages,” the authors wrote. The report was published online Aug. 10 in JAMA.
The findings held regardless of the educational and socioeconomic status of the children’s parents.
Significant disparities by race and ethnicity emerged, however, with the ultraprocessed food phenomenon more marked in non-Hispanic Black youths and Mexican-American youths than in their non-Hispanic White counterparts. “Targeted marketing of junk foods toward racial/ethnic minority youths may partly contribute to such differences,” the authors wrote. “However, persistently lower consumption of ultraprocessed foods among Mexican-American youths may reflect more home cooking among Hispanic families.”
Among non-Hispanic Black youths consumption rose from 62.2% to 72.5% (difference 10.3%, 95% CI, 6.8-13.8) and among Mexican-American youths from 55.8% to 63.5% (difference 7.6%, 95% CI, 4.4-10.9). In non-Hispanic White youths intake rose from 63.4% to 68.6% (difference 5.2%, 95% CI, 2.1-8.3, P = .04 for trends).
In addition, a higher consumption of ultraprocessed foods among school-aged youths than among preschool children aged 2-5 years may reflect increased marketing, availability, and selection of ultraprocessed foods for older youths, the authors noted.
Food processing, with its potential adverse effects, may need to be considered as a food dimension in addition to nutrients and food groups in future dietary recommendations and food policies, they added.
“An increasing number of studies are showing a link between ultraprocessed food consumption and adverse health outcomes in children,” corresponding author Fang Fang Zhang, MD, PhD, Neely Family Professor and associate professor at Tufts’ Friedman School of Nutrition Science and Policy, said in an interview. “Health care providers can play a larger role in encouraging patients – and their parents – to replace unhealthy ultraprocessed foods such as ultraprocessed sweet bakery products with healthy unprocessed or minimally processed foods in their diet such as less processed whole grains. “
In Dr. Zhang’s view, teachers also have a part to play in promoting nutrition literacy. “Schools can play an important role in empowering children with knowledge and skills to make healthy food choices,” she said. “Nutrition literacy should be an integral part of the health education curriculum in all K-12 schools.”
Commenting on the study but not involved in it, Michelle Katzow, MD, a pediatrician/obesity medicine specialist and assistant professor at the Feinstein Institutes for Medical Research in Manhasset, N.Y., said the work highlights an often overlooked aspect of the modern American diet that may well be contributing to poor health outcomes in young people.
“It suggests that even as the science advances and we learn more about the adverse health effects of ultraprocessed foods, public health efforts to improve nutrition and food quality in children have not been successful,” she said in an interview. “This is because it is so hard for public health advocates to compete with the food industry, which stands to really benefit financially from hooking kids on processed foods that are not good for their health.”
Dr. Katzow added that the observed racial/ethnic disparities are not surprising in light of a growing body of evidence that racism exists in food marketing. “We need to put forward policies that regulate the food industry, particularly in relation to its most susceptible targets, our kids.”
Study details
The serial cross-sectional analysis used 24-hour dietary recall data from a nationally representative sample from 10 NHANES cycles for the range of 1999-2000 to 2017-2018. The weighted mean age of the cohort was 10.7 years and 49.1% were girls.
Among the subgroups of ultraprocessed foods, the estimated percentage of energy from ready-to-heat and ready-to-eat mixed dishes increased from 2.2% to 11.2% (difference 8.9%; 95%, CI, 7.7-10.2).
Energy from sweets and sweet snacks increased from 10.7% to 12.9% (difference 2.3%; 95% CI, 1.0-3.6), but the estimated percentage of energy decreased for sugar-sweetened beverages from 10.8% to 5.3% (difference −5.5%; 95% CI, −6.5 to −4.5).
In other categories, estimated energy intake from processed fats and oils, condiments, and sauces fell from 7.1% to 4.0% (difference −3.1%; 95% CI, −3.7 to −2.6, all P < .05 for trend).
Not surprisingly, ultraprocessed foods had an overall poorer nutrient profile than that of nonultraprocessed, although they often contained less saturated fat, and they also contained more carbohydrates, mostly from low-quality sources with added sugars and low levels of dietary fiber and protein.
And despite a higher total folate content in ultraprocessed foods because of fortification, higher-level consumers took in less total folate owing to their lower consumption of whole foods.
The authors cautioned that in addition to poor nutrient profiles, processing itself may harm health by changing the physical structure and chemical composition of food, which could lead to elevated glycemic response and reduced satiety. Furthermore, recent research has linked food additives such as emulsifiers, stabilizers, and artificial sweeteners to adverse metabolomic effects and obesity risk. Pointing to the recent success of efforts to reduce consumption of sugary beverages, Dr. Zhang said, “We need to mobilize the same energy and level of commitment when it comes to other unhealthy ultraprocessed foods such as cakes, cookies, doughnuts, and brownies.”
The trends identified by the Tufts study “are concerning and potentially have major public health significance,” according to an accompanying JAMA editorial.
“Better dietary assessment methods are needed to document trends and understand the unique role of ultraprocessed foods to inform future evidence-based policy and dietary recommendations,” wrote Katie A. Meyer, ScD, and Lindsey Smith Taillie, PhD, of the Gillings School of Global Public Health at the University of North Carolina in Chapel Hill.
The editorialists share the authors’ view that “a conceptual advancement would be to consider the level and characteristics of processing as just one of multiple dimensions (including nutrients and food groups) used to classify foods as healthy or unhealthy.” They pointed out that the Pan American Health Organization already recommends targeting products that are ultraprocessed and high in concerning add-in nutrients.
They cautioned, however, that the classification of ultraprocessed foods will not be easy because it requires data on a full list of ingredients, and the effects of processing generally cannot be separated from the composite nutrients of ultraprocessed foods.
This presents a challenge for national food consumption research “given that most large epidemiological studies rely on food frequency questionnaires that lack the information necessary to classify processing levels,” they wrote.
This study was supported by the National Institutes of Health and the São Paulo Research Foundation. Coauthor Dariush Mozaffarian, MD, a cardiologist at Tufts University, disclosed support from the Bill & Melinda Gates Foundation, the National Institutes of Health, and the Rockefeller Foundation as well as personal fees from several commercial companies. He has served on several scientific advisory boards and received royalties from UpToDate, all outside of the submitted work. Dr. Meyer reported a grant from choline manufacturer Balchem. Dr. Taillie reported funding from Bloomberg Philanthropies. Dr. Zhang had no disclosures. Dr. Katzow disclosed no competing interests.
FROM JAMA
Surge of new child COVID cases continues for 6th consecutive week
The current COVID-19 surge has brought new cases in children to their highest level since February, according to a new report.
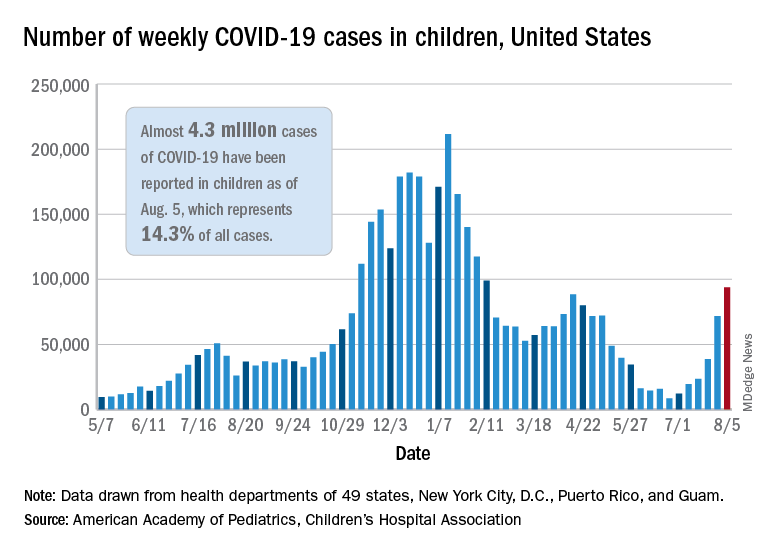
New pediatric cases rose for the 6th straight week, with almost 94,000 reported for the week ending Aug. 5.
That weekly total was up by 31% over the previous week and by over 1,000% since late June, when the new-case figure was at its lowest point (8,447) since early in the pandemic, the American Academy of Pediatrics and the Children’s Hospital Association said. COVID-related deaths – 13 for the week – were also higher than at any time since March 2021.
Almost 4.3 million children have been infected with SARS-CoV-2, which is 14.3% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. Children represented 15.0% of the new cases reported in those jurisdictions during the week ending Aug. 5, the AAP and CHA said in their weekly report.
Another measure that has been trending upward recently is vaccine initiation among 12- to 15-year-olds, although the latest weekly total is still well below the high of 1.4 million seen in May. First-time vaccinations reached almost 411,000 for the week of Aug. 3-9, marking the fourth consecutive increase in that age group, the Centers for Disease Control and Prevention said on its COVID Data Tracker. Vaccinations also increased, although more modestly, for 16- and 17-year-olds in the most recent week.
Cumulative figures for children aged 12-17 show that almost 10.4 million have received at least one dose and that 7.7 million are fully vaccinated as of Aug. 9. By age group, 42.2% of those aged 12-15 have received at least one dose, and 30.4% have completed the vaccine regimen. Among those aged 16-17 years, 52.2% have gotten their first dose, and 41.4% are fully vaccinated, according to the COVID Data Tracker.
Looking at vaccination rates on the state level shows that only 20% of children aged 12-17 in Wyoming and 21% in Mississippi have gotten at least one dose as of Aug. 4, while Massachusetts is up to 68% and Vermont reports 70%. Rates for full vaccination range from 11% in Mississippi and Alabama to 61% in Vermont, based on an AAP analysis of CDC data, which is not available for Idaho.
The current COVID-19 surge has brought new cases in children to their highest level since February, according to a new report.
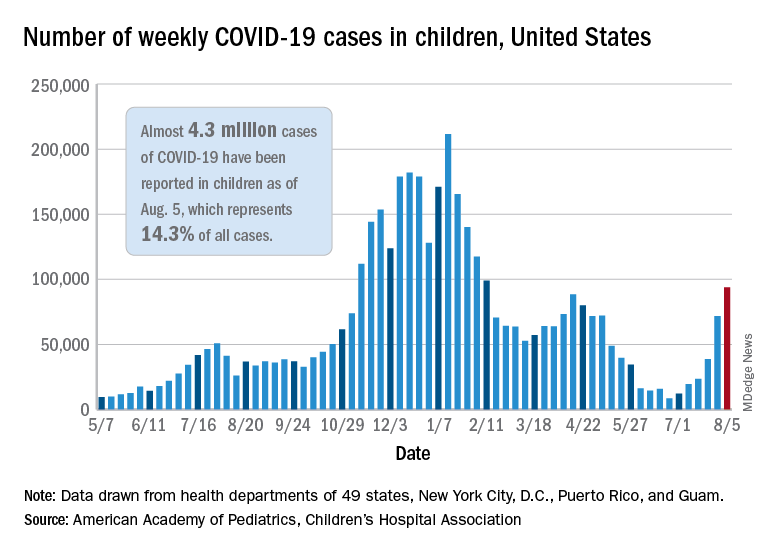
New pediatric cases rose for the 6th straight week, with almost 94,000 reported for the week ending Aug. 5.
That weekly total was up by 31% over the previous week and by over 1,000% since late June, when the new-case figure was at its lowest point (8,447) since early in the pandemic, the American Academy of Pediatrics and the Children’s Hospital Association said. COVID-related deaths – 13 for the week – were also higher than at any time since March 2021.
Almost 4.3 million children have been infected with SARS-CoV-2, which is 14.3% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. Children represented 15.0% of the new cases reported in those jurisdictions during the week ending Aug. 5, the AAP and CHA said in their weekly report.
Another measure that has been trending upward recently is vaccine initiation among 12- to 15-year-olds, although the latest weekly total is still well below the high of 1.4 million seen in May. First-time vaccinations reached almost 411,000 for the week of Aug. 3-9, marking the fourth consecutive increase in that age group, the Centers for Disease Control and Prevention said on its COVID Data Tracker. Vaccinations also increased, although more modestly, for 16- and 17-year-olds in the most recent week.
Cumulative figures for children aged 12-17 show that almost 10.4 million have received at least one dose and that 7.7 million are fully vaccinated as of Aug. 9. By age group, 42.2% of those aged 12-15 have received at least one dose, and 30.4% have completed the vaccine regimen. Among those aged 16-17 years, 52.2% have gotten their first dose, and 41.4% are fully vaccinated, according to the COVID Data Tracker.
Looking at vaccination rates on the state level shows that only 20% of children aged 12-17 in Wyoming and 21% in Mississippi have gotten at least one dose as of Aug. 4, while Massachusetts is up to 68% and Vermont reports 70%. Rates for full vaccination range from 11% in Mississippi and Alabama to 61% in Vermont, based on an AAP analysis of CDC data, which is not available for Idaho.
The current COVID-19 surge has brought new cases in children to their highest level since February, according to a new report.
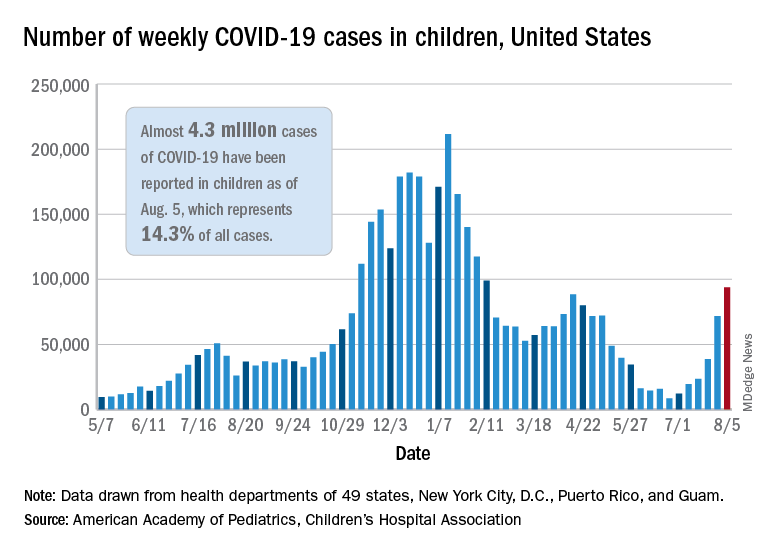
New pediatric cases rose for the 6th straight week, with almost 94,000 reported for the week ending Aug. 5.
That weekly total was up by 31% over the previous week and by over 1,000% since late June, when the new-case figure was at its lowest point (8,447) since early in the pandemic, the American Academy of Pediatrics and the Children’s Hospital Association said. COVID-related deaths – 13 for the week – were also higher than at any time since March 2021.
Almost 4.3 million children have been infected with SARS-CoV-2, which is 14.3% of all cases reported in 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam. Children represented 15.0% of the new cases reported in those jurisdictions during the week ending Aug. 5, the AAP and CHA said in their weekly report.
Another measure that has been trending upward recently is vaccine initiation among 12- to 15-year-olds, although the latest weekly total is still well below the high of 1.4 million seen in May. First-time vaccinations reached almost 411,000 for the week of Aug. 3-9, marking the fourth consecutive increase in that age group, the Centers for Disease Control and Prevention said on its COVID Data Tracker. Vaccinations also increased, although more modestly, for 16- and 17-year-olds in the most recent week.
Cumulative figures for children aged 12-17 show that almost 10.4 million have received at least one dose and that 7.7 million are fully vaccinated as of Aug. 9. By age group, 42.2% of those aged 12-15 have received at least one dose, and 30.4% have completed the vaccine regimen. Among those aged 16-17 years, 52.2% have gotten their first dose, and 41.4% are fully vaccinated, according to the COVID Data Tracker.
Looking at vaccination rates on the state level shows that only 20% of children aged 12-17 in Wyoming and 21% in Mississippi have gotten at least one dose as of Aug. 4, while Massachusetts is up to 68% and Vermont reports 70%. Rates for full vaccination range from 11% in Mississippi and Alabama to 61% in Vermont, based on an AAP analysis of CDC data, which is not available for Idaho.
Better CNS control in children with ALL: ‘Goldilocks’ approach
Treatment of central nervous system involvement in pediatric acute lymphoblastic leukemia (ALL) needs to be based on risk, and should no longer be applied in a one-size-fits all approach, say experts writing in an editorial published July 29 in the journal Blood.
“Because cure rates now exceed 90%, using neurotoxic drugs in non–risk-adapted protocols is unacceptable and a paradigm shift in treating CNS ALL is required,” write pediatric leukemia researchers Christina Halsey, PhD, of the University of Glasgow and Gabriele Escherich, MD, of the University Medical Center Hamburg-Eppendorf (Germany).
“We want to reach a Goldilocks point: not too much, not too little, but just right for every child,” they write.
The problem is that “the absence of clinically useful biomarkers prevents accurate risk stratification, resulting in universal use of intensive CNS-directed therapy. This therapy is likely to overtreat many children, exposing them to an unnecessary risk of toxicity,” including long-term cognitive deficits in 20%-40% of them, they point out.
The editorial accompanied a new study in which investigators in China focused on improving CNS control in children with ALL, which the editorialists said was step in the right direction.
In the Chinese Children’s Cancer Group ALL-2015 trial, investigators found that prephase dexamethasone, delayed intrathecal therapy, intravenous anesthesia to reduce traumatic lumbar punctures, and flow cytometry to accurately ascertain initial CNS involvement may improve CNS control.
The trial included 7,640 consecutive children up to age 18 treated from 2015 to 2019 across 20 major medical centers in China. Children received conventional remission induction and subsequent risk-directed therapy, including 16-22 triple intrathecal treatments. Prophylactic cranial irradiation was not used.
The 5-year event-free survival was 80.3% and overall survival 91.1%. The cumulative risk of isolated CNS relapse was 1.9% and of any CNS relapse 2.7%, comparable to reports from other major study groups, both with and without cranial radiation.
“We attributed our relatively good CNS control to the prephase treatment with dexamethasone, which reduced leukemia cells in blood and the CNS, and to the delayed intrathecal therapy until all (or a large proportion) of circulating leukemic blasts were cleared, thus reducing the consequence of traumatic lumbar puncture with blasts,” said the investigators, led by Jingyan Tang, MD, a hematologist/oncologist at the Shanghai (China) Children’s Medical Center.
“This approach of delayed administration of initial intrathecal therapy after prephase steroid treatment, if confirmed successful by additional studies, can be adopted readily,” they say.
The editorialists concur. The low rates of CNS relapse, despite omission of radiotherapy and inclusion of high-risk subgroups, “might suggest a potential protective effect of steroids before diagnostic lumbar puncture,” they said.
“However, flow cytometry is not sensitive enough to track disease response over time. In the bone marrow, minimal residual disease (MRD) is used to identify children at high or low risk of relapse and modify therapy accordingly. We desperately need a minimal residual disease equivalent for CNS leukemia to allow us to tailor therapy,” Dr. Halsey and Dr. Escherich say.
It’s not surprising that the use of anesthesia led to fewer traumatic lumbar punctures than in “frightened child[ren] undergoing such a painful procedure without anesthesia,” the study team notes. Its correlation with lower CNS relapses is probably because drug delivery was more accurate in sedated children, the editorialists add.
Female sex was also protective against relapse in cases where general anesthesia wasn’t used for lumbar puncture. “One could speculate that it is more difficult to restrict male patients than female patients for successful intrathecal therapy if they were not undergoing anesthesia during the procedure,” the investigators write.
“Unfortunately,” the editorialists add, rapid adoption of anesthesia for lumbar punctures “is tempered by the recent observation that repeated general anesthesia in children with ALL is associated with increased neurotoxicity.”
The work was supported by grants from the National Natural Science Foundation of China, National Cancer Institute, and others. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treatment of central nervous system involvement in pediatric acute lymphoblastic leukemia (ALL) needs to be based on risk, and should no longer be applied in a one-size-fits all approach, say experts writing in an editorial published July 29 in the journal Blood.
“Because cure rates now exceed 90%, using neurotoxic drugs in non–risk-adapted protocols is unacceptable and a paradigm shift in treating CNS ALL is required,” write pediatric leukemia researchers Christina Halsey, PhD, of the University of Glasgow and Gabriele Escherich, MD, of the University Medical Center Hamburg-Eppendorf (Germany).
“We want to reach a Goldilocks point: not too much, not too little, but just right for every child,” they write.
The problem is that “the absence of clinically useful biomarkers prevents accurate risk stratification, resulting in universal use of intensive CNS-directed therapy. This therapy is likely to overtreat many children, exposing them to an unnecessary risk of toxicity,” including long-term cognitive deficits in 20%-40% of them, they point out.
The editorial accompanied a new study in which investigators in China focused on improving CNS control in children with ALL, which the editorialists said was step in the right direction.
In the Chinese Children’s Cancer Group ALL-2015 trial, investigators found that prephase dexamethasone, delayed intrathecal therapy, intravenous anesthesia to reduce traumatic lumbar punctures, and flow cytometry to accurately ascertain initial CNS involvement may improve CNS control.
The trial included 7,640 consecutive children up to age 18 treated from 2015 to 2019 across 20 major medical centers in China. Children received conventional remission induction and subsequent risk-directed therapy, including 16-22 triple intrathecal treatments. Prophylactic cranial irradiation was not used.
The 5-year event-free survival was 80.3% and overall survival 91.1%. The cumulative risk of isolated CNS relapse was 1.9% and of any CNS relapse 2.7%, comparable to reports from other major study groups, both with and without cranial radiation.
“We attributed our relatively good CNS control to the prephase treatment with dexamethasone, which reduced leukemia cells in blood and the CNS, and to the delayed intrathecal therapy until all (or a large proportion) of circulating leukemic blasts were cleared, thus reducing the consequence of traumatic lumbar puncture with blasts,” said the investigators, led by Jingyan Tang, MD, a hematologist/oncologist at the Shanghai (China) Children’s Medical Center.
“This approach of delayed administration of initial intrathecal therapy after prephase steroid treatment, if confirmed successful by additional studies, can be adopted readily,” they say.
The editorialists concur. The low rates of CNS relapse, despite omission of radiotherapy and inclusion of high-risk subgroups, “might suggest a potential protective effect of steroids before diagnostic lumbar puncture,” they said.
“However, flow cytometry is not sensitive enough to track disease response over time. In the bone marrow, minimal residual disease (MRD) is used to identify children at high or low risk of relapse and modify therapy accordingly. We desperately need a minimal residual disease equivalent for CNS leukemia to allow us to tailor therapy,” Dr. Halsey and Dr. Escherich say.
It’s not surprising that the use of anesthesia led to fewer traumatic lumbar punctures than in “frightened child[ren] undergoing such a painful procedure without anesthesia,” the study team notes. Its correlation with lower CNS relapses is probably because drug delivery was more accurate in sedated children, the editorialists add.
Female sex was also protective against relapse in cases where general anesthesia wasn’t used for lumbar puncture. “One could speculate that it is more difficult to restrict male patients than female patients for successful intrathecal therapy if they were not undergoing anesthesia during the procedure,” the investigators write.
“Unfortunately,” the editorialists add, rapid adoption of anesthesia for lumbar punctures “is tempered by the recent observation that repeated general anesthesia in children with ALL is associated with increased neurotoxicity.”
The work was supported by grants from the National Natural Science Foundation of China, National Cancer Institute, and others. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Treatment of central nervous system involvement in pediatric acute lymphoblastic leukemia (ALL) needs to be based on risk, and should no longer be applied in a one-size-fits all approach, say experts writing in an editorial published July 29 in the journal Blood.
“Because cure rates now exceed 90%, using neurotoxic drugs in non–risk-adapted protocols is unacceptable and a paradigm shift in treating CNS ALL is required,” write pediatric leukemia researchers Christina Halsey, PhD, of the University of Glasgow and Gabriele Escherich, MD, of the University Medical Center Hamburg-Eppendorf (Germany).
“We want to reach a Goldilocks point: not too much, not too little, but just right for every child,” they write.
The problem is that “the absence of clinically useful biomarkers prevents accurate risk stratification, resulting in universal use of intensive CNS-directed therapy. This therapy is likely to overtreat many children, exposing them to an unnecessary risk of toxicity,” including long-term cognitive deficits in 20%-40% of them, they point out.
The editorial accompanied a new study in which investigators in China focused on improving CNS control in children with ALL, which the editorialists said was step in the right direction.
In the Chinese Children’s Cancer Group ALL-2015 trial, investigators found that prephase dexamethasone, delayed intrathecal therapy, intravenous anesthesia to reduce traumatic lumbar punctures, and flow cytometry to accurately ascertain initial CNS involvement may improve CNS control.
The trial included 7,640 consecutive children up to age 18 treated from 2015 to 2019 across 20 major medical centers in China. Children received conventional remission induction and subsequent risk-directed therapy, including 16-22 triple intrathecal treatments. Prophylactic cranial irradiation was not used.
The 5-year event-free survival was 80.3% and overall survival 91.1%. The cumulative risk of isolated CNS relapse was 1.9% and of any CNS relapse 2.7%, comparable to reports from other major study groups, both with and without cranial radiation.
“We attributed our relatively good CNS control to the prephase treatment with dexamethasone, which reduced leukemia cells in blood and the CNS, and to the delayed intrathecal therapy until all (or a large proportion) of circulating leukemic blasts were cleared, thus reducing the consequence of traumatic lumbar puncture with blasts,” said the investigators, led by Jingyan Tang, MD, a hematologist/oncologist at the Shanghai (China) Children’s Medical Center.
“This approach of delayed administration of initial intrathecal therapy after prephase steroid treatment, if confirmed successful by additional studies, can be adopted readily,” they say.
The editorialists concur. The low rates of CNS relapse, despite omission of radiotherapy and inclusion of high-risk subgroups, “might suggest a potential protective effect of steroids before diagnostic lumbar puncture,” they said.
“However, flow cytometry is not sensitive enough to track disease response over time. In the bone marrow, minimal residual disease (MRD) is used to identify children at high or low risk of relapse and modify therapy accordingly. We desperately need a minimal residual disease equivalent for CNS leukemia to allow us to tailor therapy,” Dr. Halsey and Dr. Escherich say.
It’s not surprising that the use of anesthesia led to fewer traumatic lumbar punctures than in “frightened child[ren] undergoing such a painful procedure without anesthesia,” the study team notes. Its correlation with lower CNS relapses is probably because drug delivery was more accurate in sedated children, the editorialists add.
Female sex was also protective against relapse in cases where general anesthesia wasn’t used for lumbar puncture. “One could speculate that it is more difficult to restrict male patients than female patients for successful intrathecal therapy if they were not undergoing anesthesia during the procedure,” the investigators write.
“Unfortunately,” the editorialists add, rapid adoption of anesthesia for lumbar punctures “is tempered by the recent observation that repeated general anesthesia in children with ALL is associated with increased neurotoxicity.”
The work was supported by grants from the National Natural Science Foundation of China, National Cancer Institute, and others. The study authors and editorialists have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Global youth depression and anxiety doubled during pandemic
The COVID-19 pandemic doubled international rates of child and adolescent psychological disorders, according to results of a meta-analysis.
In the first year of the pandemic, an estimated one in four youth across various regions of the globe experienced clinically elevated depression symptoms, while one in five experienced clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double prepandemic estimates, according to Nicole Racine, PhD, RPsych, a clinical psychologist at the University of Calgary (Alta.) and colleagues.
Their meta-analysis of 29 studies, comprising 80,879 young people worldwide aged 18 years or less, found pooled prevalence estimates of clinically elevated youth depression and anxiety of 25.2% (95% confidence interval, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively.
“The prevalence of depression and anxiety symptoms during COVID-19 [has] doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls,” the researchers write online in JAMA Pediatrics.
Prepandemic estimates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% and 12.9%, respectively, the authors say.
The increases revealed in these international findings have implications for targeted mental health resource planning.
“One difficulty in the literature is that there are large discrepancies on the prevalence of child depression and anxiety during the COVID-19 pandemic, with published rates between 2% and 68%,” corresponding author Sheri Madigan, PhD, RPsych, of the University of Calgary department of psychology, said in an interview. “By conducting a synthesis of the 29 studies on over 80,000 children, we were able to determine that, on average across these studies, 25% of youth are experiencing depression and 20% are experiencing anxiety during the COVID-19 pandemic.”
The cohort
The mean age in the combined global cohort was 13 years (range 4.1-17.6 ), and the mean proportion of females was 52.7% (standard deviation) 12.3%). The findings were based on international data published from Jan. 1, 2020, to Feb. 16, 2021, in studies conducted in the Middle East (n = 1), Europe (n = 4), South America (n = 2), North America (n = 6), and East Asia (n = 16). Notably absent were data from most of Latin America and the Middle East, Africa, South East Asia, and the Pacific Islands.
As the year progressed, the prevalence of depressive symptoms rose (b = .26; 95% CI, .06-46) with the number of months elapsed. Prevalence rates also rose as both age (b = 0.08, 95% CI, 0.01-0.15), and the percentage of females in samples increased (b = .03; 95% CI, 0.01-0.05).
The authors surmise that this cumulative worsening might be because of prolonged social isolation, family financial difficulties, missed milestones, and school disruptions, which are compounded over time. A second possibility is that studies conducted in the earlier months of the pandemic were more likely to be conducted in East Asia, where the self-reported prevalence of mental health symptoms tends to be lower.
The findings highlight an urgent need for intervention and recovery efforts and also indicate the need to consider individual differences when determining targets for intervention, including age, sex, and exposure to COVID-19 stressors), they add.
Even more concerning, recent data from the Centers for Disease Control and Prevention suggest that the pandemic spurred an increase in suspected suicide attempts by teenage girls. In the United Kingdom, acute mental health presentations to emergency care tripled over 2019 at one pediatric facility during the pandemic.
The authors attribute the toll on the psychological well-being of the world’s young people to pandemic-mandated restrictions. Those entailed loss of peer interactions, social isolation, and reduced contact with support figures such as teachers, and, “In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs.” For many children, these services were rendered unavailable owing to school closures, Dr. Madigan and associates write.
In the context of clinical practice, doctors play a critical role. “With school closures, the physician’s office may be the only mental health checkpoint for youth,” Dr. Madigan said “So I recommend that family physicians screen for, and/or ask children and youth, about their mental health.”
On the home front, emerging research suggests that a predictable home environment can protect children’s mental well-being, with less depression and fewer behavioral problems observed in families adhering to regular routines during COVID-19. “Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity,” the authors write.
They also point to the need for research on the long-term effects of the pandemic on mental health, including studies in order to “augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth.”
In an accompanying editorial, Tami D. Benton, MD, psychiatrist-in-chief at Children’s Hospital of Philadelphia, and colleagues, who were not involved in the meta-analysis, note certain limitations to the study. First, the included studies are based on self- or parent-reported symptoms. Second, the studies, more than half of which (55.2%) were done in China, may not be generalizable to all regions of the world, where 90% of children live in low- or middle-income countries.
Still, they write,“The increased mental health needs identified in the meta-analysis call for immediate action for every country. Our responses must consider the range of child mental health infrastructures available, which vary across countries, with some having well-developed and coordinated mental health services, while others have informal, limited, underfunded, or fragmented systems of care.”
Empirically supported and culturally appropriate intervention strategies for children and families according to countries and communities will be crucial, they stress.
“This meta-analysis provides the most complete evidence to date on the toll the COVID-19 pandemic has taken on child and adolescent mental health,” said Katie A. McLaughlin, PhD, a professor of psychology at Harvard University in Boston, who was not involved in the study. “The results confirm the substantial increases in symptoms of youth depression and anxiety that many clinicians and researchers have observed during the pandemic and highlight the critical need for greater investments in mental health services for children and adolescents.”
This study received no specific funding other than research support to the investigators from nonprivate entities. The authors disclosed no relevant conflicts of interest. Dr. Benton and associates and Dr. McLaughlin declared no competing interests.
The COVID-19 pandemic doubled international rates of child and adolescent psychological disorders, according to results of a meta-analysis.
In the first year of the pandemic, an estimated one in four youth across various regions of the globe experienced clinically elevated depression symptoms, while one in five experienced clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double prepandemic estimates, according to Nicole Racine, PhD, RPsych, a clinical psychologist at the University of Calgary (Alta.) and colleagues.
Their meta-analysis of 29 studies, comprising 80,879 young people worldwide aged 18 years or less, found pooled prevalence estimates of clinically elevated youth depression and anxiety of 25.2% (95% confidence interval, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively.
“The prevalence of depression and anxiety symptoms during COVID-19 [has] doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls,” the researchers write online in JAMA Pediatrics.
Prepandemic estimates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% and 12.9%, respectively, the authors say.
The increases revealed in these international findings have implications for targeted mental health resource planning.
“One difficulty in the literature is that there are large discrepancies on the prevalence of child depression and anxiety during the COVID-19 pandemic, with published rates between 2% and 68%,” corresponding author Sheri Madigan, PhD, RPsych, of the University of Calgary department of psychology, said in an interview. “By conducting a synthesis of the 29 studies on over 80,000 children, we were able to determine that, on average across these studies, 25% of youth are experiencing depression and 20% are experiencing anxiety during the COVID-19 pandemic.”
The cohort
The mean age in the combined global cohort was 13 years (range 4.1-17.6 ), and the mean proportion of females was 52.7% (standard deviation) 12.3%). The findings were based on international data published from Jan. 1, 2020, to Feb. 16, 2021, in studies conducted in the Middle East (n = 1), Europe (n = 4), South America (n = 2), North America (n = 6), and East Asia (n = 16). Notably absent were data from most of Latin America and the Middle East, Africa, South East Asia, and the Pacific Islands.
As the year progressed, the prevalence of depressive symptoms rose (b = .26; 95% CI, .06-46) with the number of months elapsed. Prevalence rates also rose as both age (b = 0.08, 95% CI, 0.01-0.15), and the percentage of females in samples increased (b = .03; 95% CI, 0.01-0.05).
The authors surmise that this cumulative worsening might be because of prolonged social isolation, family financial difficulties, missed milestones, and school disruptions, which are compounded over time. A second possibility is that studies conducted in the earlier months of the pandemic were more likely to be conducted in East Asia, where the self-reported prevalence of mental health symptoms tends to be lower.
The findings highlight an urgent need for intervention and recovery efforts and also indicate the need to consider individual differences when determining targets for intervention, including age, sex, and exposure to COVID-19 stressors), they add.
Even more concerning, recent data from the Centers for Disease Control and Prevention suggest that the pandemic spurred an increase in suspected suicide attempts by teenage girls. In the United Kingdom, acute mental health presentations to emergency care tripled over 2019 at one pediatric facility during the pandemic.
The authors attribute the toll on the psychological well-being of the world’s young people to pandemic-mandated restrictions. Those entailed loss of peer interactions, social isolation, and reduced contact with support figures such as teachers, and, “In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs.” For many children, these services were rendered unavailable owing to school closures, Dr. Madigan and associates write.
In the context of clinical practice, doctors play a critical role. “With school closures, the physician’s office may be the only mental health checkpoint for youth,” Dr. Madigan said “So I recommend that family physicians screen for, and/or ask children and youth, about their mental health.”
On the home front, emerging research suggests that a predictable home environment can protect children’s mental well-being, with less depression and fewer behavioral problems observed in families adhering to regular routines during COVID-19. “Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity,” the authors write.
They also point to the need for research on the long-term effects of the pandemic on mental health, including studies in order to “augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth.”
In an accompanying editorial, Tami D. Benton, MD, psychiatrist-in-chief at Children’s Hospital of Philadelphia, and colleagues, who were not involved in the meta-analysis, note certain limitations to the study. First, the included studies are based on self- or parent-reported symptoms. Second, the studies, more than half of which (55.2%) were done in China, may not be generalizable to all regions of the world, where 90% of children live in low- or middle-income countries.
Still, they write,“The increased mental health needs identified in the meta-analysis call for immediate action for every country. Our responses must consider the range of child mental health infrastructures available, which vary across countries, with some having well-developed and coordinated mental health services, while others have informal, limited, underfunded, or fragmented systems of care.”
Empirically supported and culturally appropriate intervention strategies for children and families according to countries and communities will be crucial, they stress.
“This meta-analysis provides the most complete evidence to date on the toll the COVID-19 pandemic has taken on child and adolescent mental health,” said Katie A. McLaughlin, PhD, a professor of psychology at Harvard University in Boston, who was not involved in the study. “The results confirm the substantial increases in symptoms of youth depression and anxiety that many clinicians and researchers have observed during the pandemic and highlight the critical need for greater investments in mental health services for children and adolescents.”
This study received no specific funding other than research support to the investigators from nonprivate entities. The authors disclosed no relevant conflicts of interest. Dr. Benton and associates and Dr. McLaughlin declared no competing interests.
The COVID-19 pandemic doubled international rates of child and adolescent psychological disorders, according to results of a meta-analysis.
In the first year of the pandemic, an estimated one in four youth across various regions of the globe experienced clinically elevated depression symptoms, while one in five experienced clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double prepandemic estimates, according to Nicole Racine, PhD, RPsych, a clinical psychologist at the University of Calgary (Alta.) and colleagues.
Their meta-analysis of 29 studies, comprising 80,879 young people worldwide aged 18 years or less, found pooled prevalence estimates of clinically elevated youth depression and anxiety of 25.2% (95% confidence interval, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively.
“The prevalence of depression and anxiety symptoms during COVID-19 [has] doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls,” the researchers write online in JAMA Pediatrics.
Prepandemic estimates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% and 12.9%, respectively, the authors say.
The increases revealed in these international findings have implications for targeted mental health resource planning.
“One difficulty in the literature is that there are large discrepancies on the prevalence of child depression and anxiety during the COVID-19 pandemic, with published rates between 2% and 68%,” corresponding author Sheri Madigan, PhD, RPsych, of the University of Calgary department of psychology, said in an interview. “By conducting a synthesis of the 29 studies on over 80,000 children, we were able to determine that, on average across these studies, 25% of youth are experiencing depression and 20% are experiencing anxiety during the COVID-19 pandemic.”
The cohort
The mean age in the combined global cohort was 13 years (range 4.1-17.6 ), and the mean proportion of females was 52.7% (standard deviation) 12.3%). The findings were based on international data published from Jan. 1, 2020, to Feb. 16, 2021, in studies conducted in the Middle East (n = 1), Europe (n = 4), South America (n = 2), North America (n = 6), and East Asia (n = 16). Notably absent were data from most of Latin America and the Middle East, Africa, South East Asia, and the Pacific Islands.
As the year progressed, the prevalence of depressive symptoms rose (b = .26; 95% CI, .06-46) with the number of months elapsed. Prevalence rates also rose as both age (b = 0.08, 95% CI, 0.01-0.15), and the percentage of females in samples increased (b = .03; 95% CI, 0.01-0.05).
The authors surmise that this cumulative worsening might be because of prolonged social isolation, family financial difficulties, missed milestones, and school disruptions, which are compounded over time. A second possibility is that studies conducted in the earlier months of the pandemic were more likely to be conducted in East Asia, where the self-reported prevalence of mental health symptoms tends to be lower.
The findings highlight an urgent need for intervention and recovery efforts and also indicate the need to consider individual differences when determining targets for intervention, including age, sex, and exposure to COVID-19 stressors), they add.
Even more concerning, recent data from the Centers for Disease Control and Prevention suggest that the pandemic spurred an increase in suspected suicide attempts by teenage girls. In the United Kingdom, acute mental health presentations to emergency care tripled over 2019 at one pediatric facility during the pandemic.
The authors attribute the toll on the psychological well-being of the world’s young people to pandemic-mandated restrictions. Those entailed loss of peer interactions, social isolation, and reduced contact with support figures such as teachers, and, “In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs.” For many children, these services were rendered unavailable owing to school closures, Dr. Madigan and associates write.
In the context of clinical practice, doctors play a critical role. “With school closures, the physician’s office may be the only mental health checkpoint for youth,” Dr. Madigan said “So I recommend that family physicians screen for, and/or ask children and youth, about their mental health.”
On the home front, emerging research suggests that a predictable home environment can protect children’s mental well-being, with less depression and fewer behavioral problems observed in families adhering to regular routines during COVID-19. “Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity,” the authors write.
They also point to the need for research on the long-term effects of the pandemic on mental health, including studies in order to “augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth.”
In an accompanying editorial, Tami D. Benton, MD, psychiatrist-in-chief at Children’s Hospital of Philadelphia, and colleagues, who were not involved in the meta-analysis, note certain limitations to the study. First, the included studies are based on self- or parent-reported symptoms. Second, the studies, more than half of which (55.2%) were done in China, may not be generalizable to all regions of the world, where 90% of children live in low- or middle-income countries.
Still, they write,“The increased mental health needs identified in the meta-analysis call for immediate action for every country. Our responses must consider the range of child mental health infrastructures available, which vary across countries, with some having well-developed and coordinated mental health services, while others have informal, limited, underfunded, or fragmented systems of care.”
Empirically supported and culturally appropriate intervention strategies for children and families according to countries and communities will be crucial, they stress.
“This meta-analysis provides the most complete evidence to date on the toll the COVID-19 pandemic has taken on child and adolescent mental health,” said Katie A. McLaughlin, PhD, a professor of psychology at Harvard University in Boston, who was not involved in the study. “The results confirm the substantial increases in symptoms of youth depression and anxiety that many clinicians and researchers have observed during the pandemic and highlight the critical need for greater investments in mental health services for children and adolescents.”
This study received no specific funding other than research support to the investigators from nonprivate entities. The authors disclosed no relevant conflicts of interest. Dr. Benton and associates and Dr. McLaughlin declared no competing interests.
Exposure to marijuana smoke linked to increased risk of respiratory infections in children
Exposure to secondhand marijuana smoke is more strongly associated with viral respiratory infections in children, compared with children who were exposed to tobacco smoke and those with no smoke exposure, new research shows.
“The findings of this study are interesting and pleasantly raise further questions,” said Kristen Miller, MD, attending physician in the division of pulmonary and sleep medicine at Children’s Hospital of Philadelphia, who was not involved in the study. “Given the robust literature regarding secondhand smoke exposure and the current landscape surrounding marijuana, this is a timely study to evaluate the prevalence of marijuana use and the associated effects of marijuana exposure among children.”
Prior research has linked primary marijuana use with respiratory effects. A 2020 study associated cannabis use with an increased risk of severe bronchitis, lung hyperinflation, and increased central airway resistance. However, according to the Centers for Disease Control and Prevention, there are still a lot of unanswered questions surrounding secondhand marijuana smoke exposure and its effects.
“If kids are exposed to enough secondhand smoke, regardless of what the substance is, they’re going to have some negative health outcomes with it,” study author Adam Johnson, MD, of Wake Forest University, Winston-Salem, N.C., said in an interview.
The study, published in Pediatric Research, looked at rates of reported ED and urgent care visits and specific illnesses – such as otitis media, viral respiratory infections, and asthma exacerbations – among children with marijuana exposure and tobacco exposure.
For the study, Dr. Johnson and colleagues surveyed 1,500 parents and caregivers who went to an academic children’s hospital between Dec. 1, 2015, and July 30, 2017. Researchers found that children exposed to marijuana smoke had higher rates of ED visits at 2.21 within the past 12 months, compared with those exposed to tobacco smoke (2.14 within the past 12 months) and those with no smoke exposure (1.94 within the past 12 months). However, the difference in these visits were not statistically significant.
Researchers saw that children exposed to secondhand marijuana smoke saw a 30% increase in viral respiratory infections, compared with those who were not exposed to tobacco or marijuana smoke, Dr. Johnson said. Caregivers who smoked marijuana reported a rate of 1.31 viral infections in their children within the last year. Meanwhile those who smoked tobacco reported a rate of 1.00 infections within the last 12 months and caregivers who did not smoke reported 1.04 infections within the year.
“It suggests that components in marijuana smoke may depress the body’s immune responses to viral infections in children,” Dr. Miller said in an interview.
When it came to otitis media episodes, children exposed to marijuana had a rate of 0.96 episodes within the past 12 months. Children experiencing secondhand tobacco smoke had a rate of 0.83 episodes and those with no smoke exposure had 0.75 episodes within the past 12 months. Researchers did not note this difference as statistically significant.
When it came to asthma exacerbations, children exposed to marijuana smoke also had statistically insignificantly higher rates of exacerbations, compared with those exposed to tobacco smoke and those not exposed to smoke.
“I think it was surprising that the survey results found that marijuana seemed to be more strongly associated with the viral respiratory infections than tobacco,” Dr. Johnson said. “We know that secondhand tobacco smoke exposure in kids does lead to things like otitis media or ear infections, asthma attacks, and other processes, including colds. It was interesting that we didn’t find that association [in the new study], but we found that with marijuana.”
Dr. Johnson said the findings are especially concerning with increases in the acceptance and accessibility of marijuana as it becomes legalized in many states.
A 2015 study examined the effect of secondhand marijuana smoke exposure. Researchers found that exposure to secondhand marijuana smoke can increase heart rate, have mild to moderate sedative effects and can produce detectable cannabinoid levels in blood and urine. However, another study published in 2012 found that low to moderate primary marijuana use is less harmful to users’ lungs than tobacco exposure.
Dr. Miller added that little is known about how exposure to marijuana smoke can affect the innate responses to pathogens and there is a need to “study this in more detail” to figure out if secondhand marijuana smoke is a risk factor for either an increase in respiratory virus infections or their severity.
“These questions could have considerable implications for the health of our children and public health measures regarding marijuana use,” she explained. “As documented marijuana use increases, health care providers need to be aware of the effects of marijuana use and exposure.”
Neither Dr. Johnson nor Dr. Miller has any relevant financial disclosures.
Exposure to secondhand marijuana smoke is more strongly associated with viral respiratory infections in children, compared with children who were exposed to tobacco smoke and those with no smoke exposure, new research shows.
“The findings of this study are interesting and pleasantly raise further questions,” said Kristen Miller, MD, attending physician in the division of pulmonary and sleep medicine at Children’s Hospital of Philadelphia, who was not involved in the study. “Given the robust literature regarding secondhand smoke exposure and the current landscape surrounding marijuana, this is a timely study to evaluate the prevalence of marijuana use and the associated effects of marijuana exposure among children.”
Prior research has linked primary marijuana use with respiratory effects. A 2020 study associated cannabis use with an increased risk of severe bronchitis, lung hyperinflation, and increased central airway resistance. However, according to the Centers for Disease Control and Prevention, there are still a lot of unanswered questions surrounding secondhand marijuana smoke exposure and its effects.
“If kids are exposed to enough secondhand smoke, regardless of what the substance is, they’re going to have some negative health outcomes with it,” study author Adam Johnson, MD, of Wake Forest University, Winston-Salem, N.C., said in an interview.
The study, published in Pediatric Research, looked at rates of reported ED and urgent care visits and specific illnesses – such as otitis media, viral respiratory infections, and asthma exacerbations – among children with marijuana exposure and tobacco exposure.
For the study, Dr. Johnson and colleagues surveyed 1,500 parents and caregivers who went to an academic children’s hospital between Dec. 1, 2015, and July 30, 2017. Researchers found that children exposed to marijuana smoke had higher rates of ED visits at 2.21 within the past 12 months, compared with those exposed to tobacco smoke (2.14 within the past 12 months) and those with no smoke exposure (1.94 within the past 12 months). However, the difference in these visits were not statistically significant.
Researchers saw that children exposed to secondhand marijuana smoke saw a 30% increase in viral respiratory infections, compared with those who were not exposed to tobacco or marijuana smoke, Dr. Johnson said. Caregivers who smoked marijuana reported a rate of 1.31 viral infections in their children within the last year. Meanwhile those who smoked tobacco reported a rate of 1.00 infections within the last 12 months and caregivers who did not smoke reported 1.04 infections within the year.
“It suggests that components in marijuana smoke may depress the body’s immune responses to viral infections in children,” Dr. Miller said in an interview.
When it came to otitis media episodes, children exposed to marijuana had a rate of 0.96 episodes within the past 12 months. Children experiencing secondhand tobacco smoke had a rate of 0.83 episodes and those with no smoke exposure had 0.75 episodes within the past 12 months. Researchers did not note this difference as statistically significant.
When it came to asthma exacerbations, children exposed to marijuana smoke also had statistically insignificantly higher rates of exacerbations, compared with those exposed to tobacco smoke and those not exposed to smoke.
“I think it was surprising that the survey results found that marijuana seemed to be more strongly associated with the viral respiratory infections than tobacco,” Dr. Johnson said. “We know that secondhand tobacco smoke exposure in kids does lead to things like otitis media or ear infections, asthma attacks, and other processes, including colds. It was interesting that we didn’t find that association [in the new study], but we found that with marijuana.”
Dr. Johnson said the findings are especially concerning with increases in the acceptance and accessibility of marijuana as it becomes legalized in many states.
A 2015 study examined the effect of secondhand marijuana smoke exposure. Researchers found that exposure to secondhand marijuana smoke can increase heart rate, have mild to moderate sedative effects and can produce detectable cannabinoid levels in blood and urine. However, another study published in 2012 found that low to moderate primary marijuana use is less harmful to users’ lungs than tobacco exposure.
Dr. Miller added that little is known about how exposure to marijuana smoke can affect the innate responses to pathogens and there is a need to “study this in more detail” to figure out if secondhand marijuana smoke is a risk factor for either an increase in respiratory virus infections or their severity.
“These questions could have considerable implications for the health of our children and public health measures regarding marijuana use,” she explained. “As documented marijuana use increases, health care providers need to be aware of the effects of marijuana use and exposure.”
Neither Dr. Johnson nor Dr. Miller has any relevant financial disclosures.
Exposure to secondhand marijuana smoke is more strongly associated with viral respiratory infections in children, compared with children who were exposed to tobacco smoke and those with no smoke exposure, new research shows.
“The findings of this study are interesting and pleasantly raise further questions,” said Kristen Miller, MD, attending physician in the division of pulmonary and sleep medicine at Children’s Hospital of Philadelphia, who was not involved in the study. “Given the robust literature regarding secondhand smoke exposure and the current landscape surrounding marijuana, this is a timely study to evaluate the prevalence of marijuana use and the associated effects of marijuana exposure among children.”
Prior research has linked primary marijuana use with respiratory effects. A 2020 study associated cannabis use with an increased risk of severe bronchitis, lung hyperinflation, and increased central airway resistance. However, according to the Centers for Disease Control and Prevention, there are still a lot of unanswered questions surrounding secondhand marijuana smoke exposure and its effects.
“If kids are exposed to enough secondhand smoke, regardless of what the substance is, they’re going to have some negative health outcomes with it,” study author Adam Johnson, MD, of Wake Forest University, Winston-Salem, N.C., said in an interview.
The study, published in Pediatric Research, looked at rates of reported ED and urgent care visits and specific illnesses – such as otitis media, viral respiratory infections, and asthma exacerbations – among children with marijuana exposure and tobacco exposure.
For the study, Dr. Johnson and colleagues surveyed 1,500 parents and caregivers who went to an academic children’s hospital between Dec. 1, 2015, and July 30, 2017. Researchers found that children exposed to marijuana smoke had higher rates of ED visits at 2.21 within the past 12 months, compared with those exposed to tobacco smoke (2.14 within the past 12 months) and those with no smoke exposure (1.94 within the past 12 months). However, the difference in these visits were not statistically significant.
Researchers saw that children exposed to secondhand marijuana smoke saw a 30% increase in viral respiratory infections, compared with those who were not exposed to tobacco or marijuana smoke, Dr. Johnson said. Caregivers who smoked marijuana reported a rate of 1.31 viral infections in their children within the last year. Meanwhile those who smoked tobacco reported a rate of 1.00 infections within the last 12 months and caregivers who did not smoke reported 1.04 infections within the year.
“It suggests that components in marijuana smoke may depress the body’s immune responses to viral infections in children,” Dr. Miller said in an interview.
When it came to otitis media episodes, children exposed to marijuana had a rate of 0.96 episodes within the past 12 months. Children experiencing secondhand tobacco smoke had a rate of 0.83 episodes and those with no smoke exposure had 0.75 episodes within the past 12 months. Researchers did not note this difference as statistically significant.
When it came to asthma exacerbations, children exposed to marijuana smoke also had statistically insignificantly higher rates of exacerbations, compared with those exposed to tobacco smoke and those not exposed to smoke.
“I think it was surprising that the survey results found that marijuana seemed to be more strongly associated with the viral respiratory infections than tobacco,” Dr. Johnson said. “We know that secondhand tobacco smoke exposure in kids does lead to things like otitis media or ear infections, asthma attacks, and other processes, including colds. It was interesting that we didn’t find that association [in the new study], but we found that with marijuana.”
Dr. Johnson said the findings are especially concerning with increases in the acceptance and accessibility of marijuana as it becomes legalized in many states.
A 2015 study examined the effect of secondhand marijuana smoke exposure. Researchers found that exposure to secondhand marijuana smoke can increase heart rate, have mild to moderate sedative effects and can produce detectable cannabinoid levels in blood and urine. However, another study published in 2012 found that low to moderate primary marijuana use is less harmful to users’ lungs than tobacco exposure.
Dr. Miller added that little is known about how exposure to marijuana smoke can affect the innate responses to pathogens and there is a need to “study this in more detail” to figure out if secondhand marijuana smoke is a risk factor for either an increase in respiratory virus infections or their severity.
“These questions could have considerable implications for the health of our children and public health measures regarding marijuana use,” she explained. “As documented marijuana use increases, health care providers need to be aware of the effects of marijuana use and exposure.”
Neither Dr. Johnson nor Dr. Miller has any relevant financial disclosures.
FROM PEDIATRIC RESEARCH