User login
Manual dexterity may decline more rapidly in pediatric-onset MS
WEST PALM BEACH, FLA. – (AOMS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
When MS onset occurs before the patient is age 18 years, the patient is considered to have POMS. Compared with AOMS, POMS is less prevalent and has distinct features. To determine whether changes in physical performance differ between POMS and AOMS, Sarah M. Planchon, PhD, a project scientist at the Mellen Center for MS at the Cleveland Clinic, and colleagues analyzed data cut 9 from the MS PATHS (MS Partners Advancing Technology and Health Solutions) initiative. As part of this initiative, which is sponsored by Biogen, investigators collect MS performance measures longitudinally at each patient visit. Among these measures are the manual dexterity test (MDT), an iPad version of the Nine-Hole Peg Test, and the walking speed test (WST), which is the iPad version of the Timed 25-Foot Walk.
Dr. Planchon and colleagues matched each patient with POMS to five patients with AOMS according to disease duration. They calculated descriptive statistics for the sample and performed Tukey’s honestly significant difference test to compare patient groups on several categorical variables.
Overall, function was better in POMS than in AOMS
The investigators included 3 years’ worth of data from 6,457 patients in their analysis. The average age was approximately 50 years for patients with AOMS and 31 years for patients with POMS. The time elapsed since diagnosis was approximately 14 years in the AOMS group and 17 years in the POMS group. The proportion of female patients was about 74% in the AOMS group and 73% in the POMS group. Compared with the AOMS group, the POMS group had higher proportions of patients who were Asian (0.5% vs 2.6%), black (9.3% vs 11.5%), and other race (2.8% vs 9.3%).
Overall, patients with POMS performed better than patients with AOMS by 1.39 seconds on the MDT and by 0.79 seconds on the WST. Regression analyses indicated that with increasing age, patients with AOMS declined more quickly on the MDT and the WST than patients with POMS did. When the investigators stratified the results by disease duration, however, patients with POMS declined more rapidly on the MDT than did patients with AOMS. There was no significant difference between groups in WST in this analysis. When Dr. Planchon and colleagues performed linear regression and adjusted for variables such as age, sex, race, education, insurance, employment, MS phenotype, disease duration, number of relapses, and Patient-Determined Disease Steps (PDDS), the MS onset type did not significantly affect outcomes. Age, sex, PDDS, and MS type were significant covariates for both tests.
The role of occupational and physical therapy
“POMS patients tend to have a greater dysfunction of the cerebellar and brainstem regions of the brain, both of which may impact motor skills to a greater degree than other regions of the brain,” said Dr. Planchon. The increased rate of manual impairment in POMS, compared with AOMS, does not necessarily indicate more severe disease, she added. Getting a true picture of disease severity would require consideration of factors such as ambulation, cognitive functioning, vision, fatigue, and depression.
“We would recommend introducing POMS patients to occupational and physical therapy early in their disease course, before significant deficits accrue,” said Dr. Planchon. “Early familiarity with rehabilitation services should help the patient and family optimize what exercises are being done to improve and maintain function.”
The optimal pharmacologic treatment for POMS is unknown. One therapy (i.e., fingolimod) has Food and Drug Administration approval, and clinical trials of other treatments are ongoing. Some MS treatments not indicated for a pediatric population are used off label in children.
“We plan to delve deeper into the data set, including using regression modeling to try to better define differences between individuals with POMS and AOMS that may lead to the functional outcome changes we have already observed,” said Dr. Planchon. “We also plan to investigate further the impact of POMS on cognition and quality of life measures and to better understand disease-modifying therapy prescribing patterns and benefits in individuals with POMS. We will look for associations in the MRI imaging findings and various biomarkers to help us understand the disease process in this special population of MS.”
Dr. Planchon has received research support from the Guthy-Jackson Charitable Foundation. Her coinvestigators received funding from Biogen, Genentech, Genzyme, MedImmune, Novartis, Serono, and Teva.
SOURCE: Planchon SM et al. ACTRIMS 2020. Abstract P043.
WEST PALM BEACH, FLA. – (AOMS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
When MS onset occurs before the patient is age 18 years, the patient is considered to have POMS. Compared with AOMS, POMS is less prevalent and has distinct features. To determine whether changes in physical performance differ between POMS and AOMS, Sarah M. Planchon, PhD, a project scientist at the Mellen Center for MS at the Cleveland Clinic, and colleagues analyzed data cut 9 from the MS PATHS (MS Partners Advancing Technology and Health Solutions) initiative. As part of this initiative, which is sponsored by Biogen, investigators collect MS performance measures longitudinally at each patient visit. Among these measures are the manual dexterity test (MDT), an iPad version of the Nine-Hole Peg Test, and the walking speed test (WST), which is the iPad version of the Timed 25-Foot Walk.
Dr. Planchon and colleagues matched each patient with POMS to five patients with AOMS according to disease duration. They calculated descriptive statistics for the sample and performed Tukey’s honestly significant difference test to compare patient groups on several categorical variables.
Overall, function was better in POMS than in AOMS
The investigators included 3 years’ worth of data from 6,457 patients in their analysis. The average age was approximately 50 years for patients with AOMS and 31 years for patients with POMS. The time elapsed since diagnosis was approximately 14 years in the AOMS group and 17 years in the POMS group. The proportion of female patients was about 74% in the AOMS group and 73% in the POMS group. Compared with the AOMS group, the POMS group had higher proportions of patients who were Asian (0.5% vs 2.6%), black (9.3% vs 11.5%), and other race (2.8% vs 9.3%).
Overall, patients with POMS performed better than patients with AOMS by 1.39 seconds on the MDT and by 0.79 seconds on the WST. Regression analyses indicated that with increasing age, patients with AOMS declined more quickly on the MDT and the WST than patients with POMS did. When the investigators stratified the results by disease duration, however, patients with POMS declined more rapidly on the MDT than did patients with AOMS. There was no significant difference between groups in WST in this analysis. When Dr. Planchon and colleagues performed linear regression and adjusted for variables such as age, sex, race, education, insurance, employment, MS phenotype, disease duration, number of relapses, and Patient-Determined Disease Steps (PDDS), the MS onset type did not significantly affect outcomes. Age, sex, PDDS, and MS type were significant covariates for both tests.
The role of occupational and physical therapy
“POMS patients tend to have a greater dysfunction of the cerebellar and brainstem regions of the brain, both of which may impact motor skills to a greater degree than other regions of the brain,” said Dr. Planchon. The increased rate of manual impairment in POMS, compared with AOMS, does not necessarily indicate more severe disease, she added. Getting a true picture of disease severity would require consideration of factors such as ambulation, cognitive functioning, vision, fatigue, and depression.
“We would recommend introducing POMS patients to occupational and physical therapy early in their disease course, before significant deficits accrue,” said Dr. Planchon. “Early familiarity with rehabilitation services should help the patient and family optimize what exercises are being done to improve and maintain function.”
The optimal pharmacologic treatment for POMS is unknown. One therapy (i.e., fingolimod) has Food and Drug Administration approval, and clinical trials of other treatments are ongoing. Some MS treatments not indicated for a pediatric population are used off label in children.
“We plan to delve deeper into the data set, including using regression modeling to try to better define differences between individuals with POMS and AOMS that may lead to the functional outcome changes we have already observed,” said Dr. Planchon. “We also plan to investigate further the impact of POMS on cognition and quality of life measures and to better understand disease-modifying therapy prescribing patterns and benefits in individuals with POMS. We will look for associations in the MRI imaging findings and various biomarkers to help us understand the disease process in this special population of MS.”
Dr. Planchon has received research support from the Guthy-Jackson Charitable Foundation. Her coinvestigators received funding from Biogen, Genentech, Genzyme, MedImmune, Novartis, Serono, and Teva.
SOURCE: Planchon SM et al. ACTRIMS 2020. Abstract P043.
WEST PALM BEACH, FLA. – (AOMS), according to an analysis presented at the meeting held by the Americas Committee for Treatment and Research in Multiple Sclerosis.
When MS onset occurs before the patient is age 18 years, the patient is considered to have POMS. Compared with AOMS, POMS is less prevalent and has distinct features. To determine whether changes in physical performance differ between POMS and AOMS, Sarah M. Planchon, PhD, a project scientist at the Mellen Center for MS at the Cleveland Clinic, and colleagues analyzed data cut 9 from the MS PATHS (MS Partners Advancing Technology and Health Solutions) initiative. As part of this initiative, which is sponsored by Biogen, investigators collect MS performance measures longitudinally at each patient visit. Among these measures are the manual dexterity test (MDT), an iPad version of the Nine-Hole Peg Test, and the walking speed test (WST), which is the iPad version of the Timed 25-Foot Walk.
Dr. Planchon and colleagues matched each patient with POMS to five patients with AOMS according to disease duration. They calculated descriptive statistics for the sample and performed Tukey’s honestly significant difference test to compare patient groups on several categorical variables.
Overall, function was better in POMS than in AOMS
The investigators included 3 years’ worth of data from 6,457 patients in their analysis. The average age was approximately 50 years for patients with AOMS and 31 years for patients with POMS. The time elapsed since diagnosis was approximately 14 years in the AOMS group and 17 years in the POMS group. The proportion of female patients was about 74% in the AOMS group and 73% in the POMS group. Compared with the AOMS group, the POMS group had higher proportions of patients who were Asian (0.5% vs 2.6%), black (9.3% vs 11.5%), and other race (2.8% vs 9.3%).
Overall, patients with POMS performed better than patients with AOMS by 1.39 seconds on the MDT and by 0.79 seconds on the WST. Regression analyses indicated that with increasing age, patients with AOMS declined more quickly on the MDT and the WST than patients with POMS did. When the investigators stratified the results by disease duration, however, patients with POMS declined more rapidly on the MDT than did patients with AOMS. There was no significant difference between groups in WST in this analysis. When Dr. Planchon and colleagues performed linear regression and adjusted for variables such as age, sex, race, education, insurance, employment, MS phenotype, disease duration, number of relapses, and Patient-Determined Disease Steps (PDDS), the MS onset type did not significantly affect outcomes. Age, sex, PDDS, and MS type were significant covariates for both tests.
The role of occupational and physical therapy
“POMS patients tend to have a greater dysfunction of the cerebellar and brainstem regions of the brain, both of which may impact motor skills to a greater degree than other regions of the brain,” said Dr. Planchon. The increased rate of manual impairment in POMS, compared with AOMS, does not necessarily indicate more severe disease, she added. Getting a true picture of disease severity would require consideration of factors such as ambulation, cognitive functioning, vision, fatigue, and depression.
“We would recommend introducing POMS patients to occupational and physical therapy early in their disease course, before significant deficits accrue,” said Dr. Planchon. “Early familiarity with rehabilitation services should help the patient and family optimize what exercises are being done to improve and maintain function.”
The optimal pharmacologic treatment for POMS is unknown. One therapy (i.e., fingolimod) has Food and Drug Administration approval, and clinical trials of other treatments are ongoing. Some MS treatments not indicated for a pediatric population are used off label in children.
“We plan to delve deeper into the data set, including using regression modeling to try to better define differences between individuals with POMS and AOMS that may lead to the functional outcome changes we have already observed,” said Dr. Planchon. “We also plan to investigate further the impact of POMS on cognition and quality of life measures and to better understand disease-modifying therapy prescribing patterns and benefits in individuals with POMS. We will look for associations in the MRI imaging findings and various biomarkers to help us understand the disease process in this special population of MS.”
Dr. Planchon has received research support from the Guthy-Jackson Charitable Foundation. Her coinvestigators received funding from Biogen, Genentech, Genzyme, MedImmune, Novartis, Serono, and Teva.
SOURCE: Planchon SM et al. ACTRIMS 2020. Abstract P043.
REPORTING FROM ACTRIMS FORUM 2020
Managing children’s fear, anxiety in the age of COVID-19
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
With coronavirus disease (COVID-19) reaching epidemic proportions, many US children are growing increasingly anxious about what this means for their own health and safety and that of their friends and family.
The constantly changing numbers of people affected by the virus and the evolving situation mean daily life for many children is affected in some way, with school trips, sports tournaments, and family vacations being postponed or canceled.
All children may have a heightened level of worry, and some who are normally anxious might be obsessing more about handwashing or getting sick.
Experts say there are ways to manage this fear to help children feel safe and appropriately informed.
Clinicians and other adults should provide children with honest and accurate information geared to their age and developmental level, said David Fassler, MD, clinical professor of psychiatry, University of Vermont Larner College of Medicine, Burlington, and member of the Consumer Issues Committee of the American Academy of Child and Adolescent Psychiatry.
That said, it’s also acceptable to let children know that some questions can’t be answered, said Fassler.
Be truthful, calm
“This is partly because the information keeps changing as we learn more about how the virus spreads, how to best protect communities, and how to treat people who get sick,” he added.
Clinicians and parents should remind children “that there are a lot of adults who are working very hard to keep them safe,” said Eli R. Lebowitz, PhD, associate professor in the Child Study Center, Yale School of Medicine, New Haven, Connecticut, who directs a program for anxiety.
It’s important for adults to pay attention not only to what they say to children but also how they say it, said Lebowitz. He highlighted the importance of talking about the virus “in a calm and matter-of-fact way” rather than in an anxious way.
“If you look scared or tense or your voice is conveying that you’re really scared, the child is going to absorb that and feel anxious as well,” he noted.
This advice also applies when adults are discussing the issue among themselves. They should be aware that “children are listening” and are picking up any anxiety or panic adults are expressing.
Children are soaking up information about this virus from the Internet, the media, friends, teachers, and elsewhere. Lebowitz suggests asking children what they have already heard, which provides an opportunity to correct rumors and inaccurate information.
“A child might have a very inflated sense of what the actual risk is. For example, they may think that anyone who gets the virus dies,” he said.
Myth busting
Adults should let children know that not everything they hear from friends or on the Internet “is necessarily correct,” he added.
Some children who have experienced serious illness or losses may be particularly vulnerable to experiencing intense reactions to graphic news reports or images of illness or death and may need extra support, said Fassler.
Adults could use the “framework of knowledge” that children already have, said Lebowitz. He noted that all children are aware of sickness.
“They know people get sick, and they themselves have probably been sick, so you can tell them that this is a sickness like a bad flu,” he said.
Children should be encouraged to approach adults they trust, such as their pediatrician, a parent, or a teacher, with their questions, said Lebowitz. “Those are the people who are able to give them the most accurate information.”
Fassler noted that accurate, up-to-date information is available via fact sheets developed by the Centers for Disease Control and Prevention and the World Health Organization.
Although it’s helpful and appropriate to be reassuring, Fassler advises not to make unrealistic promises.
“It’s fine to tell kids that you’ll deal with whatever happens, even if it means altering travel plans or work schedules, but you can’t promise that no one in your state or community will get sick,” he said.
Maintain healthy habits
Physicians and other adults can tell children “in an age-appropriate way” how the virus is transmitted and what the symptoms are, but it’s important to emphasize that most people who are sick don’t have COVID-19, said Lebowitz.
“I would emphasize that the people who are the sickest are the elderly who are already sick, rather than healthy younger people,” he said.
Lebowitz recommends continuing to follow guidelines on staying healthy, including coughing into a sleeve instead of your hand and regular handwashing.
It’s also important at this time for children to maintain healthy habits – getting enough physical activity and sleep, eating well, and being outside – because this regime will go a long way toward reducing anxiety, said Lebowitz. Deep breathing and muscle-relaxing exercises can also help, he said.
Lebowitz also suggests maintaining a supportive attitude and showing “some acceptance and validation of what children are feeling, as well as some confidence that they can cope and tolerate feeling uncomfortable sometimes, that they can handle some anxiety.”
While accepting that the child could be anxious, it’s important not to encourage excessive avoidance or unhealthy coping strategies. Fassler and Lebowitz agree that children who are overly anxious or preoccupied with concerns about the coronavirus should be evaluated by a trained, qualified mental health professional.
Signs that a child may need additional help include ongoing sleep difficulties, intrusive thoughts or worries, obsessive-compulsive behaviors, or reluctance or refusal to go to school, said Fassler.
The good news is that most children are resilient, said Fassler. “They’ll adjust, adapt, and go on with their lives.”
This article first appeared on Medscape.com.
Under the influence
I don’t know how successful you have been at getting your adolescent patients to follow your suggestions, but I would guess that my batting average was in the low 100s. Even when I try stepping off my soapbox to involve the patient in a nonjudgmental dialogue, my successes pale in comparison to my failures.
Just looking at our national statistics for obesity, it’s pretty obvious that we are all doing a pretty rotten job of modifying our patients behaviors. You could point to a few encouraging numbers but they are few and far between. You could claim correctly that by the time a child reaches preschool, the die is already cast, throw up your arms, and not even raise the subject of diet with your overweight teenage patients.
A recent article in the journal Appetite hints at a group of strategies for molding patient behavior that so far have gotten very little attention from physicians (“Do perceived norms of social media users eating habits and preferences predict our own food consumption and BMI?” Appetite. 2020 Jan 18. doi: 10.1016/j.appet.2020.104611). Researchers at the department of psychology at Ashton University in Birmingham, England, surveyed more than 350 college-age students asking them about the dietary preference of their Facebook contacts and their own dietary habits. What the investigators found was that respondents who perceived their peers ate a healthy diet ate a healthier diet. Conversely, if the respondents thought their social media contacts ate junk food, they reported eating more of an unhealthy diet themselves.
In other words, it appears that, through social media, we have the potential to influence the eating habits of our patients’ peers. Before we get too excited, it should be pointed out that this study from England wasn’t of a long enough duration to demonstrate an effect on body mass index. And another study of 176 children recently published in Pediatrics found that while influencer marketing of unhealthy foods increased children’s immediate food intake, the equivalent marketing of healthy foods had no effect (“Social influencer marketing and children’s food intake: A randomized trial.” Pediatrics. 2019 Apr 1. doi: 10.1542/peds.2018-2554).
Not being terribly aware of the whos, whats, and wheres of influencers, I did a little bit of Internet searching at the Influencer Marketing hub and learned that influencers comes in all shapes and sizes, from “nanoinfluencers” who have acknowledged expertise and a very small Internet following numbering as few as a hundred to “megainfluencers” who have more than a million followers and might charge large entities a million dollars for a single post. The influencer’s content could appear as a blog, a YouTube video, a podcast, or simply a social media post.
The field of influencer marketing is new and growing exponentially. This initiative could come in the form of an office dedicated to Influencer Marketing created by the American Academy of Pediatrics. That group could search for megainfluencers who might be funded by the academy. But it also could develop a handbook for individual practitioners and groups to help them identify nano- and micro- (1,000-40,000 followers) influencers in their own practices.
You probably don’t ask your patients about their social media habits other than to caution them about time management. Maybe it’s time to dig a little deeper. You may find that you have a potent influencer hidden in your practice. She or he might just be willing to spread a good word or two for you.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I don’t know how successful you have been at getting your adolescent patients to follow your suggestions, but I would guess that my batting average was in the low 100s. Even when I try stepping off my soapbox to involve the patient in a nonjudgmental dialogue, my successes pale in comparison to my failures.
Just looking at our national statistics for obesity, it’s pretty obvious that we are all doing a pretty rotten job of modifying our patients behaviors. You could point to a few encouraging numbers but they are few and far between. You could claim correctly that by the time a child reaches preschool, the die is already cast, throw up your arms, and not even raise the subject of diet with your overweight teenage patients.
A recent article in the journal Appetite hints at a group of strategies for molding patient behavior that so far have gotten very little attention from physicians (“Do perceived norms of social media users eating habits and preferences predict our own food consumption and BMI?” Appetite. 2020 Jan 18. doi: 10.1016/j.appet.2020.104611). Researchers at the department of psychology at Ashton University in Birmingham, England, surveyed more than 350 college-age students asking them about the dietary preference of their Facebook contacts and their own dietary habits. What the investigators found was that respondents who perceived their peers ate a healthy diet ate a healthier diet. Conversely, if the respondents thought their social media contacts ate junk food, they reported eating more of an unhealthy diet themselves.
In other words, it appears that, through social media, we have the potential to influence the eating habits of our patients’ peers. Before we get too excited, it should be pointed out that this study from England wasn’t of a long enough duration to demonstrate an effect on body mass index. And another study of 176 children recently published in Pediatrics found that while influencer marketing of unhealthy foods increased children’s immediate food intake, the equivalent marketing of healthy foods had no effect (“Social influencer marketing and children’s food intake: A randomized trial.” Pediatrics. 2019 Apr 1. doi: 10.1542/peds.2018-2554).
Not being terribly aware of the whos, whats, and wheres of influencers, I did a little bit of Internet searching at the Influencer Marketing hub and learned that influencers comes in all shapes and sizes, from “nanoinfluencers” who have acknowledged expertise and a very small Internet following numbering as few as a hundred to “megainfluencers” who have more than a million followers and might charge large entities a million dollars for a single post. The influencer’s content could appear as a blog, a YouTube video, a podcast, or simply a social media post.
The field of influencer marketing is new and growing exponentially. This initiative could come in the form of an office dedicated to Influencer Marketing created by the American Academy of Pediatrics. That group could search for megainfluencers who might be funded by the academy. But it also could develop a handbook for individual practitioners and groups to help them identify nano- and micro- (1,000-40,000 followers) influencers in their own practices.
You probably don’t ask your patients about their social media habits other than to caution them about time management. Maybe it’s time to dig a little deeper. You may find that you have a potent influencer hidden in your practice. She or he might just be willing to spread a good word or two for you.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I don’t know how successful you have been at getting your adolescent patients to follow your suggestions, but I would guess that my batting average was in the low 100s. Even when I try stepping off my soapbox to involve the patient in a nonjudgmental dialogue, my successes pale in comparison to my failures.
Just looking at our national statistics for obesity, it’s pretty obvious that we are all doing a pretty rotten job of modifying our patients behaviors. You could point to a few encouraging numbers but they are few and far between. You could claim correctly that by the time a child reaches preschool, the die is already cast, throw up your arms, and not even raise the subject of diet with your overweight teenage patients.
A recent article in the journal Appetite hints at a group of strategies for molding patient behavior that so far have gotten very little attention from physicians (“Do perceived norms of social media users eating habits and preferences predict our own food consumption and BMI?” Appetite. 2020 Jan 18. doi: 10.1016/j.appet.2020.104611). Researchers at the department of psychology at Ashton University in Birmingham, England, surveyed more than 350 college-age students asking them about the dietary preference of their Facebook contacts and their own dietary habits. What the investigators found was that respondents who perceived their peers ate a healthy diet ate a healthier diet. Conversely, if the respondents thought their social media contacts ate junk food, they reported eating more of an unhealthy diet themselves.
In other words, it appears that, through social media, we have the potential to influence the eating habits of our patients’ peers. Before we get too excited, it should be pointed out that this study from England wasn’t of a long enough duration to demonstrate an effect on body mass index. And another study of 176 children recently published in Pediatrics found that while influencer marketing of unhealthy foods increased children’s immediate food intake, the equivalent marketing of healthy foods had no effect (“Social influencer marketing and children’s food intake: A randomized trial.” Pediatrics. 2019 Apr 1. doi: 10.1542/peds.2018-2554).
Not being terribly aware of the whos, whats, and wheres of influencers, I did a little bit of Internet searching at the Influencer Marketing hub and learned that influencers comes in all shapes and sizes, from “nanoinfluencers” who have acknowledged expertise and a very small Internet following numbering as few as a hundred to “megainfluencers” who have more than a million followers and might charge large entities a million dollars for a single post. The influencer’s content could appear as a blog, a YouTube video, a podcast, or simply a social media post.
The field of influencer marketing is new and growing exponentially. This initiative could come in the form of an office dedicated to Influencer Marketing created by the American Academy of Pediatrics. That group could search for megainfluencers who might be funded by the academy. But it also could develop a handbook for individual practitioners and groups to help them identify nano- and micro- (1,000-40,000 followers) influencers in their own practices.
You probably don’t ask your patients about their social media habits other than to caution them about time management. Maybe it’s time to dig a little deeper. You may find that you have a potent influencer hidden in your practice. She or he might just be willing to spread a good word or two for you.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Is there empathy erosion?
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
You learned a lot of things in medical school. But there must have been some things that you unlearned on the way to your degree. For instance, you unlearned that you could catch a cold by playing outside on a cold damp day without your jacket. You unlearned that handling a toad would give you warts.
The authors of a recent study suggest that over your 4 years in medical school you also unlearned how to be empathetic (“Does Empathy Decline in the Clinical Phase of Medical Education? A Nationwide, Multi-institutional, Cross-Sectional Study of Students at DO-Granting Medical Schools,” Acad Med. 2020 Jan 21. doi: 10.1097/ACM.0000000000003175). The researchers surveyed more than 10,000 medical students at nearly 50 DO-granting medical schools using standardized questionnaire called the Jefferson Scale of Empathy. They discovered that the students in the clinical phase (years 3 and 4) had lower “empathy scores” than the students in the preclinical phase of their education (years 1 and 2). This decline was statistically significant but “negligible” in magnitude. One wonders why they even chose to publish their results, particularly when the number of respondents to the web-based survey declined with each successive year in medical school. Having looked at the a sample of some of the questions being asked, I can understand why third- and fourth-year students couldn’t be bothered to respond. They were too busy to answer a few dozen “lame” questions.
There may be a decline in empathy over the course our medical training, but I’m not sure that this study can speak to it. An older study found that although medical students scores on a self-administered scale declined between the second and third year, the observed empathetic behavior actually increased. If I had to choose, I would lean more heavily on the results of the behavioral observations.
Certainly, we all changed over the course of our medical education. Including postgraduate training, it may have lasted a decade or more. We saw hundreds of patients, observed life and death on a scale and with an intensity that most of us previously had never experienced. Our perspective changed from being a naive observer to playing the role of an active participant. Did that change include a decline in our capacity for empathy?
Something had to change. We found quickly that we didn’t have the time or emotional energy to learn as much about the person hiding behind every complaint as we once thought we should. We had to cut corners. Sometimes we cut too many. On the other hand, as we saw more patients we may have learned more efficient ways of discovering what we needed to know about them to become an effective and caring physician. If we found ourselves in a specialty in which patients have a high mortality, we were forced to learn ways of protecting ourselves from the emotional damage.
What would you call this process? Was it empathy erosion? Was it a hardening or toughening? Or was it simply maturation? Whatever term you use, it was an obligatory process if we hoped to survive. However, not all of us have done it well. Some of us have narrowed our focus to see only the complaint and the diagnosis, and we too often fail to see the human hiding in plain sight.
For those of us who completed our training with our empathy intact, was this the result of a genetic gift or the atmosphere our parents had created at home? I suspect that in most cases our capacity for empathy as physicians was nurtured and enhanced by the role models we encountered during our training. The mentors we most revered were those who had already been through the annealing process of medical school and specialty training and become even more skilled at caring than when they left college. It is an intangible that can’t be taught. Sadly, there is no way of guaranteeing that everyone who enters medical school will be exposed to or benefit from even one of these master physicians.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Sexual-minority youth at greater risk for physical, sexual violence
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
U.S. high school students who identify as gay, lesbian, bisexual, or questioning – “sexual minorities” – faced twice the risk of physical or sexual assault in the past year compared with their heterosexual peers, according to findings reported in a research letter.
Sexual-minority females were particularly more likely to experience physical violence while sexual-minority boys had a fourfold increased risk of sexual violence.
“The results of our study suggest the existence of a crisis of violence against sexual minority adolescents,” Theodore L. Caputi, MPH, of Harvard Medical School, Boston, and colleagues reported in JAMA Pediatrics. “Given the substantial physical and emotional consequences of violence for those subjected to it and the large existing health disparities among sexual minority adolescents, addressing both physical and sexual violence against sexual minority adolescents should become a public health priority.”
Joshua D. Safer, MD, executive director of the Center for Transgender Medicine and Surgery in the Mount Sinai Health System, New York, said he was not surprised by the findings because adolescents who may feel more vulnerable relative to their peers are likely to be more of a target. They may not have the supports they need, he said, which will affect their resiliency and their ability to push back.
“These patients are at ages where their parents might be among their supporters,” Dr. Safer said in an interview. “People in their circle may not be aware of their circumstances.”
He emphasized the need for physicians to ensure their offices are safe places for sexual-minority youth to talk to adolescent patients about their gender and sexual identity as well as any history of victimization, and to involve parents in being an ally of their child.
The researchers analyzed data from the nationally representative 2015 and 2017 National Youth Risk Behavior Surveys administered to public and private high school students in grades 9-12 by the Centers for Disease Control and Prevention. The 28,811 total respondents represented a 60% response rate both years.
After indicating their sex as male or female and their sexual orientation, respondents reported whether, in the past year, they had experienced a physical fight at school, a physical fight anywhere, or physical violence from a romantic partner. They also reported whether they had been sexually assaulted in the past year by a romantic partner or ever been forced to have intercourse. The 2017 survey included an additional question about sexual assault by anyone in the past year.
Most youth (87%) identified themselves as heterosexual while 2% were gay/lesbian, 7% were bisexual, and 4% were unsure. Sexual minorities reported a higher prevalence of all forms of violence and assault, compared with their heterosexual counterparts. Although risk of a physical fight in the past year differed by a small amount (28% of sexual-minority youth vs. 22% of heterosexual youth), the gap was considerably greater for risk of physical violence by a romantic partner (12% of sexual-minority youth vs. 5% of heterosexual youth).
More than three times as many sexual-minority adolescents (18%) as heterosexual adolescents (5%) said they had ever been forced to have intercourse, and a similarly high proportion of sexual-minority students (21%) had been sexually assaulted in the past year, compared with heterosexual students (8%). After accounting for survey year, sex, age, race/ethnicity, English language proficiency, and grade level, youth who identified as anything other than heterosexual were about twice as likely as their heterosexual counterparts to have experienced physical or sexual violence, including physical violence by a romantic partner (adjusted risk ratio, 1.97) or sexual assault by anyone (aRR, 2.10), in the past year. The risk of physical violence by a romantic partner or sexual assault by anyone was even greater for bisexual youth (aRR, 2.22 and aRR, 2.36, respectively).
The increased likelihood of physical violence and sexual violence differed by sex. Girls who identified as lesbian, bisexual, or questioning were more likely than heterosexual girls to have been in a fight at school or anywhere else (aRR, 1.91 and aRR, 1.74, respectively). Boys who were gay, bisexual, or questioning, meanwhile, were over four times more likely than heterosexual boys to have had forced intercourse or any kind of sexual assault (aRR, 4.70 and aRR, 4.64, respectively).
These findings point to the need for physicians to be “specifically talking to youth about gender identity and sexual orientation. Validating what kids are feeling is important,” Dr. Safer said in an interview.
Key to that process is making sure the physician’s office feels like a safe place for LGBTQ youth to have these kinds of conversations. “Most primary care and pediatric and adolescent care practices are not feeling well equipped to take care of these kids and are not necessarily serving as a good resource for these kids,” Dr. Safer said.
It’s also important for physicians to ask youth about potential violence or abuse they have experienced, including depression and sequelae from lack of support, for which gender- and sexual-minority youth are at greater risk, he said. Finally, doctors need to engage parents in the conversation.
“As a medical professional, you need to be asking the questions and really be out there as an ally, especially for pediatric and adolescent patients, and you need to be helping the parents of your patients be allies too,” Dr. Safer said.
The study was limited by having a binary question only about respondent’s sex and no data collection about transgender youth. The study’s cross-sectional design also precludes the ability to claim causation about any of the associations.
The research was funded by the Marshall Aid Commemoration Commission, Stanford (Calif.) University, and the National Institutes of Health. The authors had no disclosures.
SOURCE: Caputi TL et al. JAMA Pediatr. 2019 Mar 9. doi: 10.1001/jamapediatrics.2019.6291.
FROM JAMA PEDIATRICS
Rotavirus vaccination is not a risk factor for type 1 diabetes
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
published in JAMA Pediatrics.
Previous findings from a number of studies have indicated a possible association between rotavirus and type 1 diabetes, according to Jason M. Glanz, PhD, and colleagues. “Epidemiologic data suggest an association between gastrointestinal infection and incidence of type 1 diabetes in children followed from birth to age 10 years. Given these findings, it is biologically plausible that live, attenuated rotavirus vaccine could either increase or decrease the risk for type 1 diabetes in early childhood,” they wrote.
To examine the association between rotavirus vaccination and the incidence of type 1 diabetes in a cohort of U.S. children, Dr. Glanz, a senior investigator at the Kaiser Permanente Colorado Institute for Health Research in Aurora, and colleagues retrospectively analyzed data from seven health care organizations that participate in the Vaccine Safety Datalink.
The researchers identified children born between 2006 and 2014 who had continuous enrollment from age 6 weeks to 2 years. They excluded children with a medical contraindication to vaccination or fewer than two well-child visits by age 12 months. They followed children until a type 1 diabetes diagnosis, disenrollment, or Dec. 31, 2017. The researchers adjusted for sex, birth year, mother’s age, birth weight, gestational age, and race or ethnicity.
The cohort included 386,937 children who were followed up a median of 5.4 years for a total person-time follow-up of 2,253,879 years. In all, 386,937 children (93.1%) were fully exposed to rotavirus vaccination; 15,765 (4.1%) were partially exposed to rotavirus vaccination, meaning that they received some, but not all, vaccine doses; and 11,003 (2.8%) were unexposed to rotavirus vaccination but had received all other recommended vaccines.
There were 464 cases of type 1 diabetes in the cohort, with an incidence rate of 20 cases per 100,000 person-years in the fully exposed group, 31.2 cases per 100,000 person-years in the partially exposed group, and 22.4 cases per 100,000 person-years in the unexposed group.
The incidence of type 1 diabetes was not significantly different across the rotavirus vaccine–exposure groups. The researchers reported that, compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for children fully exposed to rotavirus vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to the vaccination, it was 1.50 (95% CI, 0.81-2.77).
“Since licensure, rotavirus vaccination has been associated with a reduction in morbidity and mortality due to rotavirus infection in the United States and worldwide. ... Although rotavirus vaccination may not prevent type 1 diabetes, these results should provide additional reassurance to the public that rotavirus vaccination can be safely administered to infants,” they wrote.
The limited follow-up duration and relatively small proportion of patients unexposed to rotavirus vaccination are limitations of the study, the authors noted.
The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
SOURCE: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
FROM JAMA PEDIATRICS
Key clinical point: Rotavirus vaccination is not associated with the incidence of type 1 diabetes and can be safely administered to infants.
Major finding: Compared with children unexposed to rotavirus vaccination, the adjusted hazard ratio for developing type 1 diabetes for children fully exposed to the vaccination was 1.03 (95% confidence interval, 0.62-1.72), and for those partially exposed to it, the aHR was 1.50 (95% CI, 0.81-2.77).
Study details: A retrospective cohort study of 386,937 children using data from the Vaccine Safety Datalink.
Disclosures: The Centers for Disease Control and Prevention funded the study. Several authors reported having received grants from the CDC. One author received grants from the National Institute of Diabetes and Digestive and Kidney Diseases, and another from pharmaceutical companies not involved in the study.
Source: Glanz JM et al. JAMA Pediatr. 2020 Mar 9. doi: 10.1001/jamapediatrics.2019.6324.
More inclusive assessment better predicts cognitive impairment in very preterm children
rather than just severe impairment, in ongoing monitoring, according to a study published in Pediatrics.
Carmina Erdei, MD, of Brigham and Women’s Hospital and the department of pediatrics at Harvard Medical school, both in Boston, and colleagues prospectively studied 103 children born VPT (32 weeks’ or less gestation) and 109 children born term. Exclusion criteria included congenital abnormalities and having non–English-speaking parents.
The investigators assessed the children’s cognitive abilities and neurodevelopment with age-appropriate measures at various ages: Bayley Scales of Infant Development (2nd ed.) at age 2 years, Wechsler Preschool and Primary Scale of Intelligence at age 4 and 6 years, and Wechsler Intelligence Scale for Children (4th ed.) at age 9 and 12 years.
When only severe cognitive impairment at ages 2, 4, and 6 years was used as the criterion for ongoing monitoring, between 18% and 44% of severely impaired children at 12 years were missed – and would not have received continued monitoring and support. However, when any cognitive impairment at the younger ages was the criterion for continued monitoring, 100% of cases of severe impairment at age 12 years were correctly predicted.
The authors suggest that adoption of this more inclusive approach may be warranted, given the long-term ramifications of even mild cognitive impairment.
Positive predictive value (66%), negative predictive value (89%), and specificity (73%) intersected in assessments performed at age 6 years, such that they had the best predictive ability for any cognitive impairment at age 12 years.
“Our findings highlight the potential benefit of monitoring children at high risk with early delay until elementary school,” the authors wrote. “We acknowledge that this would result in a higher number of referrals and potentially increased short-term costs. Developmental follow-up is costly, yet early developmental services are valuable and positively impact preterm children’s cognitive and preacademic skills.”
The investigators also assessed family-social risks, such as socioeconomic status and maternal education, and found that children born VPT were more than twice as likely to be raised in families with more risks than were those born term (33% vs. 13%, respectively).
Limitations of the study include the high false-positive rate (34%) seen with the assessments at age 6 years, but the authors suggested that could be mitigated with risk stratification.
The study was funded by the Neurological Foundation, Lottery Grants Board, Canterbury Medical Research Foundation, and Health Research Council of New Zealand. The authors reported having no relevant financial relationships or conflicts of interest.
SOURCE: Erdei C et al. Pediatrics. 2020 Mar 6. doi: 10.1542/peds.2019-1982.
rather than just severe impairment, in ongoing monitoring, according to a study published in Pediatrics.
Carmina Erdei, MD, of Brigham and Women’s Hospital and the department of pediatrics at Harvard Medical school, both in Boston, and colleagues prospectively studied 103 children born VPT (32 weeks’ or less gestation) and 109 children born term. Exclusion criteria included congenital abnormalities and having non–English-speaking parents.
The investigators assessed the children’s cognitive abilities and neurodevelopment with age-appropriate measures at various ages: Bayley Scales of Infant Development (2nd ed.) at age 2 years, Wechsler Preschool and Primary Scale of Intelligence at age 4 and 6 years, and Wechsler Intelligence Scale for Children (4th ed.) at age 9 and 12 years.
When only severe cognitive impairment at ages 2, 4, and 6 years was used as the criterion for ongoing monitoring, between 18% and 44% of severely impaired children at 12 years were missed – and would not have received continued monitoring and support. However, when any cognitive impairment at the younger ages was the criterion for continued monitoring, 100% of cases of severe impairment at age 12 years were correctly predicted.
The authors suggest that adoption of this more inclusive approach may be warranted, given the long-term ramifications of even mild cognitive impairment.
Positive predictive value (66%), negative predictive value (89%), and specificity (73%) intersected in assessments performed at age 6 years, such that they had the best predictive ability for any cognitive impairment at age 12 years.
“Our findings highlight the potential benefit of monitoring children at high risk with early delay until elementary school,” the authors wrote. “We acknowledge that this would result in a higher number of referrals and potentially increased short-term costs. Developmental follow-up is costly, yet early developmental services are valuable and positively impact preterm children’s cognitive and preacademic skills.”
The investigators also assessed family-social risks, such as socioeconomic status and maternal education, and found that children born VPT were more than twice as likely to be raised in families with more risks than were those born term (33% vs. 13%, respectively).
Limitations of the study include the high false-positive rate (34%) seen with the assessments at age 6 years, but the authors suggested that could be mitigated with risk stratification.
The study was funded by the Neurological Foundation, Lottery Grants Board, Canterbury Medical Research Foundation, and Health Research Council of New Zealand. The authors reported having no relevant financial relationships or conflicts of interest.
SOURCE: Erdei C et al. Pediatrics. 2020 Mar 6. doi: 10.1542/peds.2019-1982.
rather than just severe impairment, in ongoing monitoring, according to a study published in Pediatrics.
Carmina Erdei, MD, of Brigham and Women’s Hospital and the department of pediatrics at Harvard Medical school, both in Boston, and colleagues prospectively studied 103 children born VPT (32 weeks’ or less gestation) and 109 children born term. Exclusion criteria included congenital abnormalities and having non–English-speaking parents.
The investigators assessed the children’s cognitive abilities and neurodevelopment with age-appropriate measures at various ages: Bayley Scales of Infant Development (2nd ed.) at age 2 years, Wechsler Preschool and Primary Scale of Intelligence at age 4 and 6 years, and Wechsler Intelligence Scale for Children (4th ed.) at age 9 and 12 years.
When only severe cognitive impairment at ages 2, 4, and 6 years was used as the criterion for ongoing monitoring, between 18% and 44% of severely impaired children at 12 years were missed – and would not have received continued monitoring and support. However, when any cognitive impairment at the younger ages was the criterion for continued monitoring, 100% of cases of severe impairment at age 12 years were correctly predicted.
The authors suggest that adoption of this more inclusive approach may be warranted, given the long-term ramifications of even mild cognitive impairment.
Positive predictive value (66%), negative predictive value (89%), and specificity (73%) intersected in assessments performed at age 6 years, such that they had the best predictive ability for any cognitive impairment at age 12 years.
“Our findings highlight the potential benefit of monitoring children at high risk with early delay until elementary school,” the authors wrote. “We acknowledge that this would result in a higher number of referrals and potentially increased short-term costs. Developmental follow-up is costly, yet early developmental services are valuable and positively impact preterm children’s cognitive and preacademic skills.”
The investigators also assessed family-social risks, such as socioeconomic status and maternal education, and found that children born VPT were more than twice as likely to be raised in families with more risks than were those born term (33% vs. 13%, respectively).
Limitations of the study include the high false-positive rate (34%) seen with the assessments at age 6 years, but the authors suggested that could be mitigated with risk stratification.
The study was funded by the Neurological Foundation, Lottery Grants Board, Canterbury Medical Research Foundation, and Health Research Council of New Zealand. The authors reported having no relevant financial relationships or conflicts of interest.
SOURCE: Erdei C et al. Pediatrics. 2020 Mar 6. doi: 10.1542/peds.2019-1982.
FROM PEDIATRICS
Breaking bacterial communication may heal EB wounds
LONDON – Disrupting how microorganisms communicate with each other could be a way to overcome antibiotic resistance and to help heal chronic wounds in patients with epidermolysis bullosa (EB), according to presenters at the EB World Congress, organized by the Dystrophic Epidermolysis Bullosa Association (DEBRA).
The majority of chronic wounds in patients with EB are colonized with microorganisms, with a predominance of Staphylococcus species, said Erik Gerner, an industrial PhD student at Mölnlycke Health Care in Gothenburg, Sweden, and Gothenburg University.
Because of the growing problem of antibiotic resistance, alternative treatments are needed, and one possible alternative for treating infected wounds could be interfering with quorum sensing, the cell-to-cell communication used by bacteria, he said. He is hoping to explore this possibility as a novel treatment strategy for infected wounds.
“Quorum sensing is defined as the ability to detect and respond to population density,” Mr. Gerner said, noting that, when there is a sufficient density of bacteria, “they start to communicate with each other.” This enables them to act as a community and perform actions that they could not do as individual cells. Such actions include forming biofilms, which helps protect bacteria from their environment, such as the immune system. Other actions include collectively switching on the production of virulence factors and becoming resistant to treatments.
“Bacteria use quorum sensing to act collectively,” Mr. Gerner said. “If we could shut down this quorum sensing system, it would be very beneficial … and increase the chances to heal the wound.”
The quorum sensing system is based on the production of signaling molecules called AHL (N-acyl homoserine lactones), which are constantly produced at a low rate. This isn’t a problem until the level of bacteria increases and the level of quorum sensing breaches a threshold, he explained.
There are several benefits of inhibiting bacterial communication through disrupting quorum sensing, namely, “a low risk of resistance,” Mr. Gerner said. There is also potentially less toxin production by bacteria, and this could help the immune system in killing the invading bacteria.
One approach to disrupting quorum testing that Mr. Gerner has been investigating is the use of sodium salicylate (NaSa). So far, preclinical work shows that NaSa can reduce toxin production but not the growth rate of bacteria. The advantage of using NaSa is that it is nontoxic to human dermal fibroblasts, with similar results seen in human keratinocytes and immune cells. His work to date has shown that NaSa reduced activity of NF-kB (a proinflammatory signaling pathway) in differentiated and lipopolysaccharide-stimulated monocytes; NF-kB activated production of proinflammatory cytokines (such as interleukin-1 beta and IL-6) are elevated in EB wounds. “My studies support the bodies of evidence that bacteria use quorum sensing to coordinate … and to produce a large number of toxic factors,” Mr. Gerner concluded. Future studies will look at the potential of NaSa to disrupt this activity.
Skin microbiome of EB wounds
Liat Samuelov, MD, of the department of molecular dermatology at Tel Aviv (Israel) Sourasky Medical Center, presented data on skin microbiome characteristics in eight patients with recessive dystrophic EB (RDEB). This showed that there was reduced bacterial diversity in wounds, and a “progressive development of dysbiosis across different stages of DEB wound formation.”
The skin microbiome has been implicated in several skin diseases, Dr. Samuelov and associates observed in a poster presentation. That includes the autoimmune blistering disease bullous pemphigoid (Exp Dermatol. 2017 Dec;26[12]:1221-7). “Colonization of DEB chronic wounds may lead to systemic infections, result in delayed healing, and possibly be involved in the development of squamous cell carcinoma,” they noted in the poster, “thus accurate delineation of the dysbiotic profile … may point to corrective measures of great therapeutic potential.”
The aim was to see what microorganisms were present in the chronic wounds of the patients. To be included in the study, patients must not have had any antibiotic treatment – oral or topical – in the past 6 months. Samples were taken from an untreated wound, around the wound, and from uninvolved skin, which were compared with samples taken from similar areas in age-matched controls.
Reduced bacterial diversity was observed in RDEB wounds, compared with uninvolved or perilesional areas and the skin of control subjects, Dr. Samuelov said in an oral presentation of the study results. There was increased abundance of Staphylococcus epidermidis and decreased Cutibacterium acnes, which she noted was in contrast to other studies where S. aureus was the most common colonizer in RDEB wounds.
Bacterial composition in each group was calculated using the beta-diversity score, while control samples showed similar microbial composition, the DEB samples had no microbial similarities among different samples. These data “suggest the need to ascertain the potential therapeutic benefit of interventions aimed at restoring normal microbiome composition in DEB,” Dr. Samuelov concluded.
Wound colonization and squamous cell carcinoma
Other research on wound microbiology was presented by Laura E. Levin, MD, a dermatologist at New York–Presbyterian, and associates. “Given the potential role of bacteria-induced inflammation in the development of wound-associated SCC [squamous cell carcinoma] in a subset of patients, we sought to improve our understanding of what microbes colonize and infect the wounds of patients with epidermolysis bullosa,” they explained in their poster.
The researchers, from New York–Presbyterian Morgan Stanley Children’s Hospital and Columbia University Irvine Medical Center, New York, presented data from a retrospective analysis of 739 wound cultures taken between 2001 and 2017 from 158 patients enrolled in the Epidermolysis Bullosa Clinical Characterization and Outcomes Database. In the analysis, just under 70% of patients had DEB, of which 90% were of the RDEB subtype; 13% had EB simplex, 14% had junctional EB, and 3% had an unknown EB subtype.
At least one organism grew in 87% of cultures, with the most common microorganism isolated being Staphylococcus aureus (84% of cultures). Other commonly isolated microbes were Pseudomonas aeruginosa in 35% of cultures, Streptococcus group A in 34% of cultures (of which 22% were Streptococcus pyogenes), Corynebacterium species in 31% of cultures, and Proteus species in 18% of cultures.
“Improved understanding of what microbes are colonizing the wounds of our patients may help improve antibiotic stewardship,” the researchers stated.
Looking at the antibiotic susceptibilities, Dr. Levin and associates found that 68% of 115 cultures were sensitive to methicillin and 60% of 15 cultures were sensitive to mupirocin. “Resistance to many systemic and topical antibiotic agents in EB patients supports surveillance cultures with routine testing for mupirocin susceptibility,” they suggested.
A total of 23 patients developed SCC of whom 10 had cultures that grew S. aureus (90%) and P. aeruginosa (50%), and Proteus species (20%). Among the patients who did not develop SCC, the respective cultures positive for each of those microorganisms were 83%, 34%, and 11%. Perhaps “gram-negative and flagellated organisms may be more common in wounds of patients at risk for SCC,” they observed, adding that further studies were needed to determine if “wound microbiome interventions inhibit the risk of development of SCC and improve outcomes.”
Mr. Gerner’s research is supported by Mölnlycke Health Care. Dr. Samuelov had no disclosures. The work by Dr. Levin and associates is supported by the Pediatric Dermatology Research Alliance, EB Research Partnership, and the Epidermolysis Bullosa Medical Research Foundation.
LONDON – Disrupting how microorganisms communicate with each other could be a way to overcome antibiotic resistance and to help heal chronic wounds in patients with epidermolysis bullosa (EB), according to presenters at the EB World Congress, organized by the Dystrophic Epidermolysis Bullosa Association (DEBRA).
The majority of chronic wounds in patients with EB are colonized with microorganisms, with a predominance of Staphylococcus species, said Erik Gerner, an industrial PhD student at Mölnlycke Health Care in Gothenburg, Sweden, and Gothenburg University.
Because of the growing problem of antibiotic resistance, alternative treatments are needed, and one possible alternative for treating infected wounds could be interfering with quorum sensing, the cell-to-cell communication used by bacteria, he said. He is hoping to explore this possibility as a novel treatment strategy for infected wounds.
“Quorum sensing is defined as the ability to detect and respond to population density,” Mr. Gerner said, noting that, when there is a sufficient density of bacteria, “they start to communicate with each other.” This enables them to act as a community and perform actions that they could not do as individual cells. Such actions include forming biofilms, which helps protect bacteria from their environment, such as the immune system. Other actions include collectively switching on the production of virulence factors and becoming resistant to treatments.
“Bacteria use quorum sensing to act collectively,” Mr. Gerner said. “If we could shut down this quorum sensing system, it would be very beneficial … and increase the chances to heal the wound.”
The quorum sensing system is based on the production of signaling molecules called AHL (N-acyl homoserine lactones), which are constantly produced at a low rate. This isn’t a problem until the level of bacteria increases and the level of quorum sensing breaches a threshold, he explained.
There are several benefits of inhibiting bacterial communication through disrupting quorum sensing, namely, “a low risk of resistance,” Mr. Gerner said. There is also potentially less toxin production by bacteria, and this could help the immune system in killing the invading bacteria.
One approach to disrupting quorum testing that Mr. Gerner has been investigating is the use of sodium salicylate (NaSa). So far, preclinical work shows that NaSa can reduce toxin production but not the growth rate of bacteria. The advantage of using NaSa is that it is nontoxic to human dermal fibroblasts, with similar results seen in human keratinocytes and immune cells. His work to date has shown that NaSa reduced activity of NF-kB (a proinflammatory signaling pathway) in differentiated and lipopolysaccharide-stimulated monocytes; NF-kB activated production of proinflammatory cytokines (such as interleukin-1 beta and IL-6) are elevated in EB wounds. “My studies support the bodies of evidence that bacteria use quorum sensing to coordinate … and to produce a large number of toxic factors,” Mr. Gerner concluded. Future studies will look at the potential of NaSa to disrupt this activity.
Skin microbiome of EB wounds
Liat Samuelov, MD, of the department of molecular dermatology at Tel Aviv (Israel) Sourasky Medical Center, presented data on skin microbiome characteristics in eight patients with recessive dystrophic EB (RDEB). This showed that there was reduced bacterial diversity in wounds, and a “progressive development of dysbiosis across different stages of DEB wound formation.”
The skin microbiome has been implicated in several skin diseases, Dr. Samuelov and associates observed in a poster presentation. That includes the autoimmune blistering disease bullous pemphigoid (Exp Dermatol. 2017 Dec;26[12]:1221-7). “Colonization of DEB chronic wounds may lead to systemic infections, result in delayed healing, and possibly be involved in the development of squamous cell carcinoma,” they noted in the poster, “thus accurate delineation of the dysbiotic profile … may point to corrective measures of great therapeutic potential.”
The aim was to see what microorganisms were present in the chronic wounds of the patients. To be included in the study, patients must not have had any antibiotic treatment – oral or topical – in the past 6 months. Samples were taken from an untreated wound, around the wound, and from uninvolved skin, which were compared with samples taken from similar areas in age-matched controls.
Reduced bacterial diversity was observed in RDEB wounds, compared with uninvolved or perilesional areas and the skin of control subjects, Dr. Samuelov said in an oral presentation of the study results. There was increased abundance of Staphylococcus epidermidis and decreased Cutibacterium acnes, which she noted was in contrast to other studies where S. aureus was the most common colonizer in RDEB wounds.
Bacterial composition in each group was calculated using the beta-diversity score, while control samples showed similar microbial composition, the DEB samples had no microbial similarities among different samples. These data “suggest the need to ascertain the potential therapeutic benefit of interventions aimed at restoring normal microbiome composition in DEB,” Dr. Samuelov concluded.
Wound colonization and squamous cell carcinoma
Other research on wound microbiology was presented by Laura E. Levin, MD, a dermatologist at New York–Presbyterian, and associates. “Given the potential role of bacteria-induced inflammation in the development of wound-associated SCC [squamous cell carcinoma] in a subset of patients, we sought to improve our understanding of what microbes colonize and infect the wounds of patients with epidermolysis bullosa,” they explained in their poster.
The researchers, from New York–Presbyterian Morgan Stanley Children’s Hospital and Columbia University Irvine Medical Center, New York, presented data from a retrospective analysis of 739 wound cultures taken between 2001 and 2017 from 158 patients enrolled in the Epidermolysis Bullosa Clinical Characterization and Outcomes Database. In the analysis, just under 70% of patients had DEB, of which 90% were of the RDEB subtype; 13% had EB simplex, 14% had junctional EB, and 3% had an unknown EB subtype.
At least one organism grew in 87% of cultures, with the most common microorganism isolated being Staphylococcus aureus (84% of cultures). Other commonly isolated microbes were Pseudomonas aeruginosa in 35% of cultures, Streptococcus group A in 34% of cultures (of which 22% were Streptococcus pyogenes), Corynebacterium species in 31% of cultures, and Proteus species in 18% of cultures.
“Improved understanding of what microbes are colonizing the wounds of our patients may help improve antibiotic stewardship,” the researchers stated.
Looking at the antibiotic susceptibilities, Dr. Levin and associates found that 68% of 115 cultures were sensitive to methicillin and 60% of 15 cultures were sensitive to mupirocin. “Resistance to many systemic and topical antibiotic agents in EB patients supports surveillance cultures with routine testing for mupirocin susceptibility,” they suggested.
A total of 23 patients developed SCC of whom 10 had cultures that grew S. aureus (90%) and P. aeruginosa (50%), and Proteus species (20%). Among the patients who did not develop SCC, the respective cultures positive for each of those microorganisms were 83%, 34%, and 11%. Perhaps “gram-negative and flagellated organisms may be more common in wounds of patients at risk for SCC,” they observed, adding that further studies were needed to determine if “wound microbiome interventions inhibit the risk of development of SCC and improve outcomes.”
Mr. Gerner’s research is supported by Mölnlycke Health Care. Dr. Samuelov had no disclosures. The work by Dr. Levin and associates is supported by the Pediatric Dermatology Research Alliance, EB Research Partnership, and the Epidermolysis Bullosa Medical Research Foundation.
LONDON – Disrupting how microorganisms communicate with each other could be a way to overcome antibiotic resistance and to help heal chronic wounds in patients with epidermolysis bullosa (EB), according to presenters at the EB World Congress, organized by the Dystrophic Epidermolysis Bullosa Association (DEBRA).
The majority of chronic wounds in patients with EB are colonized with microorganisms, with a predominance of Staphylococcus species, said Erik Gerner, an industrial PhD student at Mölnlycke Health Care in Gothenburg, Sweden, and Gothenburg University.
Because of the growing problem of antibiotic resistance, alternative treatments are needed, and one possible alternative for treating infected wounds could be interfering with quorum sensing, the cell-to-cell communication used by bacteria, he said. He is hoping to explore this possibility as a novel treatment strategy for infected wounds.
“Quorum sensing is defined as the ability to detect and respond to population density,” Mr. Gerner said, noting that, when there is a sufficient density of bacteria, “they start to communicate with each other.” This enables them to act as a community and perform actions that they could not do as individual cells. Such actions include forming biofilms, which helps protect bacteria from their environment, such as the immune system. Other actions include collectively switching on the production of virulence factors and becoming resistant to treatments.
“Bacteria use quorum sensing to act collectively,” Mr. Gerner said. “If we could shut down this quorum sensing system, it would be very beneficial … and increase the chances to heal the wound.”
The quorum sensing system is based on the production of signaling molecules called AHL (N-acyl homoserine lactones), which are constantly produced at a low rate. This isn’t a problem until the level of bacteria increases and the level of quorum sensing breaches a threshold, he explained.
There are several benefits of inhibiting bacterial communication through disrupting quorum sensing, namely, “a low risk of resistance,” Mr. Gerner said. There is also potentially less toxin production by bacteria, and this could help the immune system in killing the invading bacteria.
One approach to disrupting quorum testing that Mr. Gerner has been investigating is the use of sodium salicylate (NaSa). So far, preclinical work shows that NaSa can reduce toxin production but not the growth rate of bacteria. The advantage of using NaSa is that it is nontoxic to human dermal fibroblasts, with similar results seen in human keratinocytes and immune cells. His work to date has shown that NaSa reduced activity of NF-kB (a proinflammatory signaling pathway) in differentiated and lipopolysaccharide-stimulated monocytes; NF-kB activated production of proinflammatory cytokines (such as interleukin-1 beta and IL-6) are elevated in EB wounds. “My studies support the bodies of evidence that bacteria use quorum sensing to coordinate … and to produce a large number of toxic factors,” Mr. Gerner concluded. Future studies will look at the potential of NaSa to disrupt this activity.
Skin microbiome of EB wounds
Liat Samuelov, MD, of the department of molecular dermatology at Tel Aviv (Israel) Sourasky Medical Center, presented data on skin microbiome characteristics in eight patients with recessive dystrophic EB (RDEB). This showed that there was reduced bacterial diversity in wounds, and a “progressive development of dysbiosis across different stages of DEB wound formation.”
The skin microbiome has been implicated in several skin diseases, Dr. Samuelov and associates observed in a poster presentation. That includes the autoimmune blistering disease bullous pemphigoid (Exp Dermatol. 2017 Dec;26[12]:1221-7). “Colonization of DEB chronic wounds may lead to systemic infections, result in delayed healing, and possibly be involved in the development of squamous cell carcinoma,” they noted in the poster, “thus accurate delineation of the dysbiotic profile … may point to corrective measures of great therapeutic potential.”
The aim was to see what microorganisms were present in the chronic wounds of the patients. To be included in the study, patients must not have had any antibiotic treatment – oral or topical – in the past 6 months. Samples were taken from an untreated wound, around the wound, and from uninvolved skin, which were compared with samples taken from similar areas in age-matched controls.
Reduced bacterial diversity was observed in RDEB wounds, compared with uninvolved or perilesional areas and the skin of control subjects, Dr. Samuelov said in an oral presentation of the study results. There was increased abundance of Staphylococcus epidermidis and decreased Cutibacterium acnes, which she noted was in contrast to other studies where S. aureus was the most common colonizer in RDEB wounds.
Bacterial composition in each group was calculated using the beta-diversity score, while control samples showed similar microbial composition, the DEB samples had no microbial similarities among different samples. These data “suggest the need to ascertain the potential therapeutic benefit of interventions aimed at restoring normal microbiome composition in DEB,” Dr. Samuelov concluded.
Wound colonization and squamous cell carcinoma
Other research on wound microbiology was presented by Laura E. Levin, MD, a dermatologist at New York–Presbyterian, and associates. “Given the potential role of bacteria-induced inflammation in the development of wound-associated SCC [squamous cell carcinoma] in a subset of patients, we sought to improve our understanding of what microbes colonize and infect the wounds of patients with epidermolysis bullosa,” they explained in their poster.
The researchers, from New York–Presbyterian Morgan Stanley Children’s Hospital and Columbia University Irvine Medical Center, New York, presented data from a retrospective analysis of 739 wound cultures taken between 2001 and 2017 from 158 patients enrolled in the Epidermolysis Bullosa Clinical Characterization and Outcomes Database. In the analysis, just under 70% of patients had DEB, of which 90% were of the RDEB subtype; 13% had EB simplex, 14% had junctional EB, and 3% had an unknown EB subtype.
At least one organism grew in 87% of cultures, with the most common microorganism isolated being Staphylococcus aureus (84% of cultures). Other commonly isolated microbes were Pseudomonas aeruginosa in 35% of cultures, Streptococcus group A in 34% of cultures (of which 22% were Streptococcus pyogenes), Corynebacterium species in 31% of cultures, and Proteus species in 18% of cultures.
“Improved understanding of what microbes are colonizing the wounds of our patients may help improve antibiotic stewardship,” the researchers stated.
Looking at the antibiotic susceptibilities, Dr. Levin and associates found that 68% of 115 cultures were sensitive to methicillin and 60% of 15 cultures were sensitive to mupirocin. “Resistance to many systemic and topical antibiotic agents in EB patients supports surveillance cultures with routine testing for mupirocin susceptibility,” they suggested.
A total of 23 patients developed SCC of whom 10 had cultures that grew S. aureus (90%) and P. aeruginosa (50%), and Proteus species (20%). Among the patients who did not develop SCC, the respective cultures positive for each of those microorganisms were 83%, 34%, and 11%. Perhaps “gram-negative and flagellated organisms may be more common in wounds of patients at risk for SCC,” they observed, adding that further studies were needed to determine if “wound microbiome interventions inhibit the risk of development of SCC and improve outcomes.”
Mr. Gerner’s research is supported by Mölnlycke Health Care. Dr. Samuelov had no disclosures. The work by Dr. Levin and associates is supported by the Pediatric Dermatology Research Alliance, EB Research Partnership, and the Epidermolysis Bullosa Medical Research Foundation.
REPORTING FROM EB 2020
Flu activity declines again but remains high
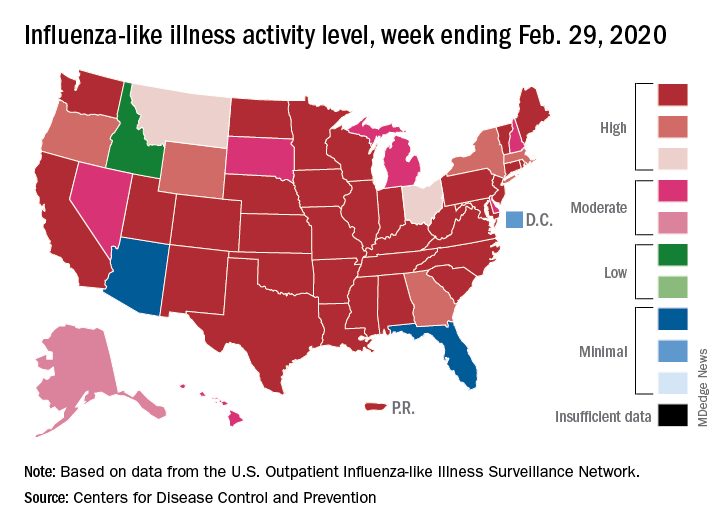
Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.
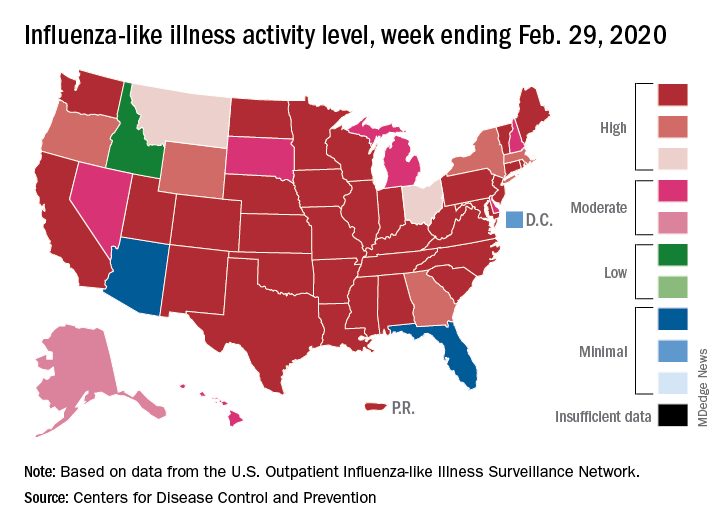
Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.
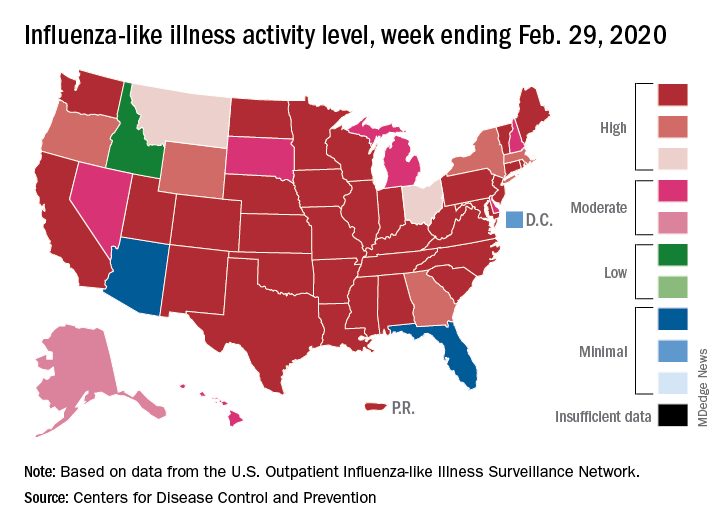
Outpatient visits to health care providers for influenza-like illness dropped from 5.5% the previous week to 5.3% of all visits for the week ending Feb. 29, the Centers for Disease Control and Prevention said on March 6.
The national baseline rate of 2.4% was first reached during the week of Nov. 9, 2019 – marking the start of flu season – and has remained at or above that level for 17 consecutive weeks. Last year’s season, which also was the longest in a decade, lasted 21 consecutive weeks but started 2 weeks later than the current season and had a lower outpatient-visit rate (4.5%) for the last week of February, CDC data show.
This season’s earlier start could mean that even a somewhat steep decline in visits to below the baseline rate – marking the end of the season – might take 5 or 6 weeks and would make 2019-2020 even longer than 2018-2019.
The activity situation on the state level reflects the small national decline. For the week ending Feb. 29, there were 33 states at level 10 on the CDC’s 1-10 activity scale, compared with 37 the week before, and a total of 40 in the “high” range of 8-10, compared with 43 the week before, the CDC’s influenza division reported.
The other main measure of influenza activity, percentage of respiratory specimens testing positive, also declined for the third week in a row and is now at 24.3% after reaching a high of 30.3% during the week of Feb. 2-8, the influenza division said.
The overall cumulative hospitalization rate continues to remain at a fairly typical 57.9 per 100,000 population, but rates for school-aged children (84.9 per 100,000) and young adults (31.2 per 100,000) are among the highest ever recorded at this point in the season. Mortality among children – now at 136 for 2019-2020 – is higher than for any season since reporting began in 2004, with the exception of the 2009 pandemic, the CDC said.
Arsenic levels in infant rice cereal are down
according to test results released by the Food and Drug Administration.
In April 2016, the FDA issued draft guidance calling for manufacturers of the product to reduce the level of arsenic in their cereals by establishing an action level of arsenic of 100 mcg/kg or 100 parts per billion.
Seventy-six percent of samples of infant rice cereal tested in 2018 had levels of arsenic at or below 100 parts per billion versus 47% of samples tested in 2014, according to a statement from the FDA. In 2011-2013, an even lower percentage of samples tested contained amounts of inorganic arsenic at or below the FDA’s current action level for this element, whose consumption has been associated with cancer, skin lesions, cardiovascular diseases, and diabetes.
The 2018 data is based on the testing of 149 samples of infant white and brown rice cereal samples.
“Results from our tests show that manufacturers have made significant progress in ensuring lower levels of inorganic arsenic in infant rice cereal,” Susan Mayne, PhD, director of the Center for Food Safety and Applied Nutrition, said in the FDA statement.
“Both white rice and brown rice cereals showed improvement in meeting the FDA’s 100 ppb proposed action level, but the improvement was greatest for white rice cereals, which tend to have lower levels of inorganic arsenic overall,” according to the statement.
according to test results released by the Food and Drug Administration.
In April 2016, the FDA issued draft guidance calling for manufacturers of the product to reduce the level of arsenic in their cereals by establishing an action level of arsenic of 100 mcg/kg or 100 parts per billion.
Seventy-six percent of samples of infant rice cereal tested in 2018 had levels of arsenic at or below 100 parts per billion versus 47% of samples tested in 2014, according to a statement from the FDA. In 2011-2013, an even lower percentage of samples tested contained amounts of inorganic arsenic at or below the FDA’s current action level for this element, whose consumption has been associated with cancer, skin lesions, cardiovascular diseases, and diabetes.
The 2018 data is based on the testing of 149 samples of infant white and brown rice cereal samples.
“Results from our tests show that manufacturers have made significant progress in ensuring lower levels of inorganic arsenic in infant rice cereal,” Susan Mayne, PhD, director of the Center for Food Safety and Applied Nutrition, said in the FDA statement.
“Both white rice and brown rice cereals showed improvement in meeting the FDA’s 100 ppb proposed action level, but the improvement was greatest for white rice cereals, which tend to have lower levels of inorganic arsenic overall,” according to the statement.
according to test results released by the Food and Drug Administration.
In April 2016, the FDA issued draft guidance calling for manufacturers of the product to reduce the level of arsenic in their cereals by establishing an action level of arsenic of 100 mcg/kg or 100 parts per billion.
Seventy-six percent of samples of infant rice cereal tested in 2018 had levels of arsenic at or below 100 parts per billion versus 47% of samples tested in 2014, according to a statement from the FDA. In 2011-2013, an even lower percentage of samples tested contained amounts of inorganic arsenic at or below the FDA’s current action level for this element, whose consumption has been associated with cancer, skin lesions, cardiovascular diseases, and diabetes.
The 2018 data is based on the testing of 149 samples of infant white and brown rice cereal samples.
“Results from our tests show that manufacturers have made significant progress in ensuring lower levels of inorganic arsenic in infant rice cereal,” Susan Mayne, PhD, director of the Center for Food Safety and Applied Nutrition, said in the FDA statement.
“Both white rice and brown rice cereals showed improvement in meeting the FDA’s 100 ppb proposed action level, but the improvement was greatest for white rice cereals, which tend to have lower levels of inorganic arsenic overall,” according to the statement.






