User login
Hospital guards snoop through patient records, cost hospital $240K
Yakima Valley Memorial Hospital agreed to the voluntary settlement after an investigation into the actions of 23 emergency department security guards who allegedly used their login credentials to access the patient medical records of 419 patients.
The information accessed included names, dates of birth, medical record numbers, addresses, certain notes related to treatment, and insurance information, according to a release by the U.S .Department of Health & Human Services’ Office for Civil Rights (OCR). A breach notification report alerted OCR to the snooping.
As part of the agreement, OCR will monitor Yakima Valley Memorial Hospital for 2 years and the hospital must conduct a thorough risk analysis as well as develop a risk management plan to address and mitigate identified security risks and vulnerabilities. The settlement is not considered an admission of guilt by the hospital.
Is such snooping common?
The incident highlights the frequent practice of employees snooping through medical records and the steep consequences that can result for providers, said Paul Redding, vice president of partner engagement and cybersecurity at Compliancy Group, a company that offers guided HIPAA compliance software for healthcare providers and vendors.
“I think the problem is absolutely growing,” he said. “What’s crazy about this case is it’s actually a really small HIPAA violation. Less than 500 people were affected, and the hospital still must pay a quarter-of-a-million-dollar settlement. If you take the average HIPAA violation, which is in the thousands and thousands of [patients], this amount would be magnified many times over.”
In general, employees snoop through records out of curiosity or to find out information about people they know – or want to learn about, said J. David Sims, a cybersecurity expert and CEO of Security First IT, a company that provides cybersecurity solutions and IT support to health care businesses.
Mr. Sims says he has heard of cases where health professionals snooped through records to find information about the new love interests of ex-partners or to learn about people on dating websites whom they’re interested in dating.
“Most of the time, it’s people being nosy,” he said. “In a lot of cases, it’s curiosity about famous people. You see it a lot in areas where you have football players who come in with injuries or you have an actor or actress who come in for something.”
“Data breaches caused by current and former workforce members impermissibly accessing patient records are a recurring issue across the health care industry. Health care organizations must ensure that workforce members can only access the patient information needed to do their jobs,” OCR director Melanie Fontes Rainer said in a June statement. “HIPAA-covered entities must have robust policies and procedures in place to ensure patient health information is protected from identify theft and fraud.”
Yakima Valley Memorial Hospital did not return a message seeking comment.
According to OCR’s latest report to Congress, complaints about HIPAA violations increased by 39% between 2017 and 2021. Breaches affecting fewer than 500 individuals rose by 5% during the same time period, and breaches impacting 500 or more individuals increased by 58%.
Common reasons employees snoop
The OCR announcement does not specify why the 23 security guards were accessing the medical records, but the incident raises questions about why the security guards had access to protected health information (PHI) in the first place, Mr. Redding said.
“I have yet to have anyone explain to me why the security guards would have access to PHI at all, at any level,” he said. “Was it by design or was it by error?”
In 2019 for instance, dozens of employees at Northwestern Memorial Hospital in Chicago were fired for accessing the health records of former Empire actor Jussie Smollett. In another high-profile case, nearly a dozen emergency medical service employees were caught snooping through 911 records connected to the treatment and, later, death of Joan Rivers.
“Sadly, there is a lack of education around what compliance really means inside the medical industry as a whole,” Mr. Redding said. “There is a lack of employee training and a lack of emphasis on accountability for employees.”
Privacy breaches fuel lawsuits
Health professionals caught snooping through records are frequently terminated and employers can face a range of ramifications, including civil and criminal penalties.
A growing trend is class action lawsuits associated with privacy violations, Mr. Redding adds.
Because patients are unable to sue in civil court for HIPAA breaches, they frequently sue for “breach of an implied contract,” he explained. In such cases, patients allege that the privacy documents they signed with health care providers established an implied contract, and their records being exposed constituted a contract breach.
“Class action lawsuits are starting to become extremely common,” Mr. Redding said. “It’s happening in many cases, even sometimes before Health & Human Services issue a fine, that [providers] are being wrapped into a class action lawsuit.”
Mayo Clinic, for example, was recently slapped with a class action suit after a former employee inappropriately accessed the records of 1,600 patients. Mayo settled the suit in January 2023, the terms of which were not publicly disclosed.
Multiple patients also filed a class action suit against San Diego–based Scripps Health after its data were hit with a cyberattack and subsequent breach that impacted close to 2 million people. Scripps reached a $3.5 million settlement with the plaintiffs in 2023.
Some practices and employers may also face state penalties for data privacy breaches, depending on their jurisdiction. In July, Connecticut became the fifth state to enact a comprehensive data privacy law. The measure, which creates a robust framework for protecting health-related records and other data, includes civil penalties of up to $5,000 for violations. Other states, including California, Virginia, Utah, and Colorado, also have state data privacy laws on the books.
How can practices stop snooping?
A first step to preventing snooping is conducting a thorough risk assessment, said David Harlow, a health care attorney and chief compliance and privacy officer for Insulet Corporation, a medical device company. The analysis should address who has access to what data and whether they really need such access, he said.
“Then it’s putting in place the proper controls to ensure access is limited and use is limited to the appropriate individuals and circumstances,” Mr. Harlow said.
Regulators don’t expect a giant academic medical center and a small private physician practice to take an identical HIPAA compliance approach, he stressed. The ideal approach will vary by entity. Providers just need to address the standards in a way that makes sense for their operation, he said.
Training is also a critical component, adds Mr. Sims.
“Having training is key,” he said. “Oftentimes, an employee might think, ‘Well, if I can click on this data and it comes up, obviously, I can look at it.’ They need to understand what information they are and are not allowed to access.”
Keep in mind that settings or controls might change when larger transitions take place, such as moving to a new electronic health record system, Mr. Sims said. It’s essential to reevaluate controls when changes in the practice take place to ensure that everything is functioning correctly.
Mr. Sims also suggests that practices create a type of “If you see something, say something,” policy that encourages fellow physicians and employees to report anything that looks suspicious within electronic logs. If an employee, for instance, is suddenly looking at many more records than usual or at odd times of the day or night, this should raise red flags.
“It’s great to stop it early so that it doesn’t become a bigger issue for the practice to deal with, but also, from a legal standpoint, you want to have a defensible argument that you were doing all you could to stop this as quickly as possible,” he said. “It puts you in a better position to defend yourself.”
The snooping security guards case holds an important lesson for all health providers, Mr. Harlow said.
“This is a message to all of us, that you need to have done the assessment up front,” he said. You need to have the right controls in place up front. This is not a situation where somebody managed to hack into a system for some devious means. This is someone who was given keys. Why were they given the keys?”
A version of this article first appeared on Medscape.com.
Yakima Valley Memorial Hospital agreed to the voluntary settlement after an investigation into the actions of 23 emergency department security guards who allegedly used their login credentials to access the patient medical records of 419 patients.
The information accessed included names, dates of birth, medical record numbers, addresses, certain notes related to treatment, and insurance information, according to a release by the U.S .Department of Health & Human Services’ Office for Civil Rights (OCR). A breach notification report alerted OCR to the snooping.
As part of the agreement, OCR will monitor Yakima Valley Memorial Hospital for 2 years and the hospital must conduct a thorough risk analysis as well as develop a risk management plan to address and mitigate identified security risks and vulnerabilities. The settlement is not considered an admission of guilt by the hospital.
Is such snooping common?
The incident highlights the frequent practice of employees snooping through medical records and the steep consequences that can result for providers, said Paul Redding, vice president of partner engagement and cybersecurity at Compliancy Group, a company that offers guided HIPAA compliance software for healthcare providers and vendors.
“I think the problem is absolutely growing,” he said. “What’s crazy about this case is it’s actually a really small HIPAA violation. Less than 500 people were affected, and the hospital still must pay a quarter-of-a-million-dollar settlement. If you take the average HIPAA violation, which is in the thousands and thousands of [patients], this amount would be magnified many times over.”
In general, employees snoop through records out of curiosity or to find out information about people they know – or want to learn about, said J. David Sims, a cybersecurity expert and CEO of Security First IT, a company that provides cybersecurity solutions and IT support to health care businesses.
Mr. Sims says he has heard of cases where health professionals snooped through records to find information about the new love interests of ex-partners or to learn about people on dating websites whom they’re interested in dating.
“Most of the time, it’s people being nosy,” he said. “In a lot of cases, it’s curiosity about famous people. You see it a lot in areas where you have football players who come in with injuries or you have an actor or actress who come in for something.”
“Data breaches caused by current and former workforce members impermissibly accessing patient records are a recurring issue across the health care industry. Health care organizations must ensure that workforce members can only access the patient information needed to do their jobs,” OCR director Melanie Fontes Rainer said in a June statement. “HIPAA-covered entities must have robust policies and procedures in place to ensure patient health information is protected from identify theft and fraud.”
Yakima Valley Memorial Hospital did not return a message seeking comment.
According to OCR’s latest report to Congress, complaints about HIPAA violations increased by 39% between 2017 and 2021. Breaches affecting fewer than 500 individuals rose by 5% during the same time period, and breaches impacting 500 or more individuals increased by 58%.
Common reasons employees snoop
The OCR announcement does not specify why the 23 security guards were accessing the medical records, but the incident raises questions about why the security guards had access to protected health information (PHI) in the first place, Mr. Redding said.
“I have yet to have anyone explain to me why the security guards would have access to PHI at all, at any level,” he said. “Was it by design or was it by error?”
In 2019 for instance, dozens of employees at Northwestern Memorial Hospital in Chicago were fired for accessing the health records of former Empire actor Jussie Smollett. In another high-profile case, nearly a dozen emergency medical service employees were caught snooping through 911 records connected to the treatment and, later, death of Joan Rivers.
“Sadly, there is a lack of education around what compliance really means inside the medical industry as a whole,” Mr. Redding said. “There is a lack of employee training and a lack of emphasis on accountability for employees.”
Privacy breaches fuel lawsuits
Health professionals caught snooping through records are frequently terminated and employers can face a range of ramifications, including civil and criminal penalties.
A growing trend is class action lawsuits associated with privacy violations, Mr. Redding adds.
Because patients are unable to sue in civil court for HIPAA breaches, they frequently sue for “breach of an implied contract,” he explained. In such cases, patients allege that the privacy documents they signed with health care providers established an implied contract, and their records being exposed constituted a contract breach.
“Class action lawsuits are starting to become extremely common,” Mr. Redding said. “It’s happening in many cases, even sometimes before Health & Human Services issue a fine, that [providers] are being wrapped into a class action lawsuit.”
Mayo Clinic, for example, was recently slapped with a class action suit after a former employee inappropriately accessed the records of 1,600 patients. Mayo settled the suit in January 2023, the terms of which were not publicly disclosed.
Multiple patients also filed a class action suit against San Diego–based Scripps Health after its data were hit with a cyberattack and subsequent breach that impacted close to 2 million people. Scripps reached a $3.5 million settlement with the plaintiffs in 2023.
Some practices and employers may also face state penalties for data privacy breaches, depending on their jurisdiction. In July, Connecticut became the fifth state to enact a comprehensive data privacy law. The measure, which creates a robust framework for protecting health-related records and other data, includes civil penalties of up to $5,000 for violations. Other states, including California, Virginia, Utah, and Colorado, also have state data privacy laws on the books.
How can practices stop snooping?
A first step to preventing snooping is conducting a thorough risk assessment, said David Harlow, a health care attorney and chief compliance and privacy officer for Insulet Corporation, a medical device company. The analysis should address who has access to what data and whether they really need such access, he said.
“Then it’s putting in place the proper controls to ensure access is limited and use is limited to the appropriate individuals and circumstances,” Mr. Harlow said.
Regulators don’t expect a giant academic medical center and a small private physician practice to take an identical HIPAA compliance approach, he stressed. The ideal approach will vary by entity. Providers just need to address the standards in a way that makes sense for their operation, he said.
Training is also a critical component, adds Mr. Sims.
“Having training is key,” he said. “Oftentimes, an employee might think, ‘Well, if I can click on this data and it comes up, obviously, I can look at it.’ They need to understand what information they are and are not allowed to access.”
Keep in mind that settings or controls might change when larger transitions take place, such as moving to a new electronic health record system, Mr. Sims said. It’s essential to reevaluate controls when changes in the practice take place to ensure that everything is functioning correctly.
Mr. Sims also suggests that practices create a type of “If you see something, say something,” policy that encourages fellow physicians and employees to report anything that looks suspicious within electronic logs. If an employee, for instance, is suddenly looking at many more records than usual or at odd times of the day or night, this should raise red flags.
“It’s great to stop it early so that it doesn’t become a bigger issue for the practice to deal with, but also, from a legal standpoint, you want to have a defensible argument that you were doing all you could to stop this as quickly as possible,” he said. “It puts you in a better position to defend yourself.”
The snooping security guards case holds an important lesson for all health providers, Mr. Harlow said.
“This is a message to all of us, that you need to have done the assessment up front,” he said. You need to have the right controls in place up front. This is not a situation where somebody managed to hack into a system for some devious means. This is someone who was given keys. Why were they given the keys?”
A version of this article first appeared on Medscape.com.
Yakima Valley Memorial Hospital agreed to the voluntary settlement after an investigation into the actions of 23 emergency department security guards who allegedly used their login credentials to access the patient medical records of 419 patients.
The information accessed included names, dates of birth, medical record numbers, addresses, certain notes related to treatment, and insurance information, according to a release by the U.S .Department of Health & Human Services’ Office for Civil Rights (OCR). A breach notification report alerted OCR to the snooping.
As part of the agreement, OCR will monitor Yakima Valley Memorial Hospital for 2 years and the hospital must conduct a thorough risk analysis as well as develop a risk management plan to address and mitigate identified security risks and vulnerabilities. The settlement is not considered an admission of guilt by the hospital.
Is such snooping common?
The incident highlights the frequent practice of employees snooping through medical records and the steep consequences that can result for providers, said Paul Redding, vice president of partner engagement and cybersecurity at Compliancy Group, a company that offers guided HIPAA compliance software for healthcare providers and vendors.
“I think the problem is absolutely growing,” he said. “What’s crazy about this case is it’s actually a really small HIPAA violation. Less than 500 people were affected, and the hospital still must pay a quarter-of-a-million-dollar settlement. If you take the average HIPAA violation, which is in the thousands and thousands of [patients], this amount would be magnified many times over.”
In general, employees snoop through records out of curiosity or to find out information about people they know – or want to learn about, said J. David Sims, a cybersecurity expert and CEO of Security First IT, a company that provides cybersecurity solutions and IT support to health care businesses.
Mr. Sims says he has heard of cases where health professionals snooped through records to find information about the new love interests of ex-partners or to learn about people on dating websites whom they’re interested in dating.
“Most of the time, it’s people being nosy,” he said. “In a lot of cases, it’s curiosity about famous people. You see it a lot in areas where you have football players who come in with injuries or you have an actor or actress who come in for something.”
“Data breaches caused by current and former workforce members impermissibly accessing patient records are a recurring issue across the health care industry. Health care organizations must ensure that workforce members can only access the patient information needed to do their jobs,” OCR director Melanie Fontes Rainer said in a June statement. “HIPAA-covered entities must have robust policies and procedures in place to ensure patient health information is protected from identify theft and fraud.”
Yakima Valley Memorial Hospital did not return a message seeking comment.
According to OCR’s latest report to Congress, complaints about HIPAA violations increased by 39% between 2017 and 2021. Breaches affecting fewer than 500 individuals rose by 5% during the same time period, and breaches impacting 500 or more individuals increased by 58%.
Common reasons employees snoop
The OCR announcement does not specify why the 23 security guards were accessing the medical records, but the incident raises questions about why the security guards had access to protected health information (PHI) in the first place, Mr. Redding said.
“I have yet to have anyone explain to me why the security guards would have access to PHI at all, at any level,” he said. “Was it by design or was it by error?”
In 2019 for instance, dozens of employees at Northwestern Memorial Hospital in Chicago were fired for accessing the health records of former Empire actor Jussie Smollett. In another high-profile case, nearly a dozen emergency medical service employees were caught snooping through 911 records connected to the treatment and, later, death of Joan Rivers.
“Sadly, there is a lack of education around what compliance really means inside the medical industry as a whole,” Mr. Redding said. “There is a lack of employee training and a lack of emphasis on accountability for employees.”
Privacy breaches fuel lawsuits
Health professionals caught snooping through records are frequently terminated and employers can face a range of ramifications, including civil and criminal penalties.
A growing trend is class action lawsuits associated with privacy violations, Mr. Redding adds.
Because patients are unable to sue in civil court for HIPAA breaches, they frequently sue for “breach of an implied contract,” he explained. In such cases, patients allege that the privacy documents they signed with health care providers established an implied contract, and their records being exposed constituted a contract breach.
“Class action lawsuits are starting to become extremely common,” Mr. Redding said. “It’s happening in many cases, even sometimes before Health & Human Services issue a fine, that [providers] are being wrapped into a class action lawsuit.”
Mayo Clinic, for example, was recently slapped with a class action suit after a former employee inappropriately accessed the records of 1,600 patients. Mayo settled the suit in January 2023, the terms of which were not publicly disclosed.
Multiple patients also filed a class action suit against San Diego–based Scripps Health after its data were hit with a cyberattack and subsequent breach that impacted close to 2 million people. Scripps reached a $3.5 million settlement with the plaintiffs in 2023.
Some practices and employers may also face state penalties for data privacy breaches, depending on their jurisdiction. In July, Connecticut became the fifth state to enact a comprehensive data privacy law. The measure, which creates a robust framework for protecting health-related records and other data, includes civil penalties of up to $5,000 for violations. Other states, including California, Virginia, Utah, and Colorado, also have state data privacy laws on the books.
How can practices stop snooping?
A first step to preventing snooping is conducting a thorough risk assessment, said David Harlow, a health care attorney and chief compliance and privacy officer for Insulet Corporation, a medical device company. The analysis should address who has access to what data and whether they really need such access, he said.
“Then it’s putting in place the proper controls to ensure access is limited and use is limited to the appropriate individuals and circumstances,” Mr. Harlow said.
Regulators don’t expect a giant academic medical center and a small private physician practice to take an identical HIPAA compliance approach, he stressed. The ideal approach will vary by entity. Providers just need to address the standards in a way that makes sense for their operation, he said.
Training is also a critical component, adds Mr. Sims.
“Having training is key,” he said. “Oftentimes, an employee might think, ‘Well, if I can click on this data and it comes up, obviously, I can look at it.’ They need to understand what information they are and are not allowed to access.”
Keep in mind that settings or controls might change when larger transitions take place, such as moving to a new electronic health record system, Mr. Sims said. It’s essential to reevaluate controls when changes in the practice take place to ensure that everything is functioning correctly.
Mr. Sims also suggests that practices create a type of “If you see something, say something,” policy that encourages fellow physicians and employees to report anything that looks suspicious within electronic logs. If an employee, for instance, is suddenly looking at many more records than usual or at odd times of the day or night, this should raise red flags.
“It’s great to stop it early so that it doesn’t become a bigger issue for the practice to deal with, but also, from a legal standpoint, you want to have a defensible argument that you were doing all you could to stop this as quickly as possible,” he said. “It puts you in a better position to defend yourself.”
The snooping security guards case holds an important lesson for all health providers, Mr. Harlow said.
“This is a message to all of us, that you need to have done the assessment up front,” he said. You need to have the right controls in place up front. This is not a situation where somebody managed to hack into a system for some devious means. This is someone who was given keys. Why were they given the keys?”
A version of this article first appeared on Medscape.com.
Time to end direct-to-consumer ads, says physician
One has to be living off the grid to not be bombarded with direct-to-consumer (DTC) pharmaceutical advertising. Since 1997, when the Food and Drug Administration eased restrictions on this prohibition and allowed pharmaceutical companies to promote prescription-only medications to the public, there has been a deluge of ads in magazines, on the Internet, and, most annoying, on commercial television.
These television ads are quite formulaic:
We are initially introduced to a number of highly functioning patients (typically actors) who are engaged in rewarding pursuits. A voiceover narration then presents the pharmaceutical to be promoted, suggesting (not so subtly) to consumers that taking the advertised drug will improve one’s disease outlook or quality of life such that they too, just like the actors in the minidrama, can lead such highly productive lives.
The potential best-case scenarios of these new treatments may be stated. There then follows a litany of side effects – some of them life threatening – warnings, and contraindications. We’re again treated to another 5 or 10 seconds of patients leading “the good life,” and almost all of the ads end with the narrator concluding: “Ask your doctor (sometimes ‘provider’) if _____ is right for you.”
Americans spend more money on their prescriptions than do citizens of any other highly developed nation. I have personally heard from patients who get their prescriptions from other countries, where they are more affordable. These patients will also cut their pills in half or take a medication every other day instead of every day, to economize on drug costs.
Another “trick” they use to save money – and I have heard pharmacists and pharmaceutical reps themselves recommend this – is to ask for a higher dose of a medication, usually double, and then use a pill cutter to divide a tablet in half, thus making their prescription last twice as long. Why do Americans have to resort to such “workarounds”?
Many of the medications advertised are for relatively rare conditions, such as thyroid eye disease or myasthenia gravis (which affects up to about 60,000 patients in the United States). Why not spend these advertising dollars on programs to make drugs taken by the millions of Americans with common conditions (for example, hypertension, diabetes, heart failure) more affordable?
Very often the television ads contain medical jargon, such as: “If you have the EGFR mutation, or if your cancer is HER2 negative ...”
Do most patients truly understand what these terms mean? And what happens when a patient’s physician doesn’t prescribe a medication that a patient has seen on TV and asks for, or when the physician believes that a generic (nonadvertised) medication might work just as well? This creates conflict and potential discord, adversely affecting the doctor-patient relationship.
An oncologist colleague related to me that he often has to spend time correcting patients’ misperceptions of potential miracle cures offered by these ads, and that several patients have left his practice because he would not prescribe a drug they saw advertised.
Further, while these ads urge patients to try expensive “newest and latest” treatments, pharmacy benefit plans are working with health care insurance conglomerates to reduce costs of pharmaceuticals.
How does this juxtaposition of opposing forces make any sense?
It is time for us to put an end to DTC advertising, at least on television. It will require legislative action by our federal government to end this practice (legal, by the way, only in the United States and New Zealand), and hence the willingness of our politicians to get behind legislation to do so.
Just as a law was passed to prohibit tobacco advertising on television, so should a law be passed to regulate DTC pharmaceutical advertising.
The time to end DTC advertising has come!
Lloyd Alterman, MD, is a retired physician and chairman of the New Jersey Universal Healthcare Coalition. He disclosed having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
One has to be living off the grid to not be bombarded with direct-to-consumer (DTC) pharmaceutical advertising. Since 1997, when the Food and Drug Administration eased restrictions on this prohibition and allowed pharmaceutical companies to promote prescription-only medications to the public, there has been a deluge of ads in magazines, on the Internet, and, most annoying, on commercial television.
These television ads are quite formulaic:
We are initially introduced to a number of highly functioning patients (typically actors) who are engaged in rewarding pursuits. A voiceover narration then presents the pharmaceutical to be promoted, suggesting (not so subtly) to consumers that taking the advertised drug will improve one’s disease outlook or quality of life such that they too, just like the actors in the minidrama, can lead such highly productive lives.
The potential best-case scenarios of these new treatments may be stated. There then follows a litany of side effects – some of them life threatening – warnings, and contraindications. We’re again treated to another 5 or 10 seconds of patients leading “the good life,” and almost all of the ads end with the narrator concluding: “Ask your doctor (sometimes ‘provider’) if _____ is right for you.”
Americans spend more money on their prescriptions than do citizens of any other highly developed nation. I have personally heard from patients who get their prescriptions from other countries, where they are more affordable. These patients will also cut their pills in half or take a medication every other day instead of every day, to economize on drug costs.
Another “trick” they use to save money – and I have heard pharmacists and pharmaceutical reps themselves recommend this – is to ask for a higher dose of a medication, usually double, and then use a pill cutter to divide a tablet in half, thus making their prescription last twice as long. Why do Americans have to resort to such “workarounds”?
Many of the medications advertised are for relatively rare conditions, such as thyroid eye disease or myasthenia gravis (which affects up to about 60,000 patients in the United States). Why not spend these advertising dollars on programs to make drugs taken by the millions of Americans with common conditions (for example, hypertension, diabetes, heart failure) more affordable?
Very often the television ads contain medical jargon, such as: “If you have the EGFR mutation, or if your cancer is HER2 negative ...”
Do most patients truly understand what these terms mean? And what happens when a patient’s physician doesn’t prescribe a medication that a patient has seen on TV and asks for, or when the physician believes that a generic (nonadvertised) medication might work just as well? This creates conflict and potential discord, adversely affecting the doctor-patient relationship.
An oncologist colleague related to me that he often has to spend time correcting patients’ misperceptions of potential miracle cures offered by these ads, and that several patients have left his practice because he would not prescribe a drug they saw advertised.
Further, while these ads urge patients to try expensive “newest and latest” treatments, pharmacy benefit plans are working with health care insurance conglomerates to reduce costs of pharmaceuticals.
How does this juxtaposition of opposing forces make any sense?
It is time for us to put an end to DTC advertising, at least on television. It will require legislative action by our federal government to end this practice (legal, by the way, only in the United States and New Zealand), and hence the willingness of our politicians to get behind legislation to do so.
Just as a law was passed to prohibit tobacco advertising on television, so should a law be passed to regulate DTC pharmaceutical advertising.
The time to end DTC advertising has come!
Lloyd Alterman, MD, is a retired physician and chairman of the New Jersey Universal Healthcare Coalition. He disclosed having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
One has to be living off the grid to not be bombarded with direct-to-consumer (DTC) pharmaceutical advertising. Since 1997, when the Food and Drug Administration eased restrictions on this prohibition and allowed pharmaceutical companies to promote prescription-only medications to the public, there has been a deluge of ads in magazines, on the Internet, and, most annoying, on commercial television.
These television ads are quite formulaic:
We are initially introduced to a number of highly functioning patients (typically actors) who are engaged in rewarding pursuits. A voiceover narration then presents the pharmaceutical to be promoted, suggesting (not so subtly) to consumers that taking the advertised drug will improve one’s disease outlook or quality of life such that they too, just like the actors in the minidrama, can lead such highly productive lives.
The potential best-case scenarios of these new treatments may be stated. There then follows a litany of side effects – some of them life threatening – warnings, and contraindications. We’re again treated to another 5 or 10 seconds of patients leading “the good life,” and almost all of the ads end with the narrator concluding: “Ask your doctor (sometimes ‘provider’) if _____ is right for you.”
Americans spend more money on their prescriptions than do citizens of any other highly developed nation. I have personally heard from patients who get their prescriptions from other countries, where they are more affordable. These patients will also cut their pills in half or take a medication every other day instead of every day, to economize on drug costs.
Another “trick” they use to save money – and I have heard pharmacists and pharmaceutical reps themselves recommend this – is to ask for a higher dose of a medication, usually double, and then use a pill cutter to divide a tablet in half, thus making their prescription last twice as long. Why do Americans have to resort to such “workarounds”?
Many of the medications advertised are for relatively rare conditions, such as thyroid eye disease or myasthenia gravis (which affects up to about 60,000 patients in the United States). Why not spend these advertising dollars on programs to make drugs taken by the millions of Americans with common conditions (for example, hypertension, diabetes, heart failure) more affordable?
Very often the television ads contain medical jargon, such as: “If you have the EGFR mutation, or if your cancer is HER2 negative ...”
Do most patients truly understand what these terms mean? And what happens when a patient’s physician doesn’t prescribe a medication that a patient has seen on TV and asks for, or when the physician believes that a generic (nonadvertised) medication might work just as well? This creates conflict and potential discord, adversely affecting the doctor-patient relationship.
An oncologist colleague related to me that he often has to spend time correcting patients’ misperceptions of potential miracle cures offered by these ads, and that several patients have left his practice because he would not prescribe a drug they saw advertised.
Further, while these ads urge patients to try expensive “newest and latest” treatments, pharmacy benefit plans are working with health care insurance conglomerates to reduce costs of pharmaceuticals.
How does this juxtaposition of opposing forces make any sense?
It is time for us to put an end to DTC advertising, at least on television. It will require legislative action by our federal government to end this practice (legal, by the way, only in the United States and New Zealand), and hence the willingness of our politicians to get behind legislation to do so.
Just as a law was passed to prohibit tobacco advertising on television, so should a law be passed to regulate DTC pharmaceutical advertising.
The time to end DTC advertising has come!
Lloyd Alterman, MD, is a retired physician and chairman of the New Jersey Universal Healthcare Coalition. He disclosed having no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Rising patient costs tied to private equity ownership
The report was a collaboration of University of California, Berkeley, staff and researchers from two nonprofits, the American Antitrust Institute and the Washington Center for Equitable Growth. It provides “convincing evidence that incentives to put profits before patients have grown stronger with an increase in private equity ownership of physician practices,” lead author Richard Scheffler, PhD, of UC Berkeley said in a statement.
The report also noted that private equity acquisitions of physician groups have risen sixfold in just a decade, increasing from 75 deals in 2012 to 484 deals in 2021.
Separately, the American Medical Association earlier released a separate report on trends in physician practice arrangements, finding that the percentage of physicians working in private equity–owned groups was 4.5% in 2022, the same as in its previous 2020 report. The share of physicians working in private practices fell by 13 percentage points from 60.1% to 46.7% between 2012 and 2022, the AMA reported.
The Berkeley report and the AMA update come amid rising concerns about the effects of the decline of independent physician practices. The U.S. Senate Finance Committee, which oversees most federal health spending, held a June hearing examining the causes and consequences of increased corporate ownership in health care, including a look at physician practices.
“It’s increasingly clear that consolidation in health care is not lowering costs or increasing the quality of Americans’ health care,” Senate Finance Chairman Ron Wyden (D-Ore.) said in an email. “For private equity in health care in particular, there needs to be more transparency around ownership so the effect on these business relationships can be better understood.”
Federal and state agencies do not generally track acquisitions of physician practices.
The UC Berkeley report impressively documents the rising influence of private equity in health care, for which it’s tough to find good data, said Karen Joynt Maddox, MD, MPH, of Washington University in St. Louis. Dr. Maddox, a cardiologist and policy researcher who also has studied the effects of consolidation in health care, examined the new report at the request of this news organization.
“They did a great job with the data,” Dr. Maddox said. “One of the big issues around private equity, and in general, ‘corporatization’ and consolidation of health care, is that there’s not a great way to track ownership changes. It’s really difficult to study.”
Dr. Scheffler and colleagues used data from the commercial firm PitchBook to identify acquisitions of physician practices by private equity firms. They consulted IQVIA’s physician databases – OneKey and SK&A Office-Based Physicians Database – to learn about the location, size, and specialties of acquired practices. They also used data from the nonprofit Health Care Cost Institute, which tracks commercial health plan claims, to assess how private equity acquisitions affected prices.
The researchers then matched the findings for practices acquired by private equity firms from 2015 to 2021 against those for comparable physician practices that remained independent from 2012 to 2021.
The authors then tied private-equity ownership to the following price increases:
- Gastroenterology (14%; 95% confidence interval, 7.9%-20.4%
- Oncology (16.4%; 95% CI, 5.5%-28.4%)
- Dermatology (4.0%; 95% CI, 1%-7.1%)
- Ob.gyn. (8.8%; 95% CI, 3.8%-14%)
- Ophthalmology (8.7%; 95% CI, 5.1%-12.3%)
- Radiology (8.2%; 95% CI, 0.8%-16.1%)
- Orthopedics (7.1%; 95% CI, 2.2%-12.3%)
- Primary care (4.1%; 95% CI, 1.3%-7%)
The analysis also found higher prices for cardiology (8.7%; 95% CI, –6.4% to 26.1%) and urology (4.2%; 95% CI, –2.3% to 11.1%), but neither of these findings was statistically significant, one of the authors, Daniel R. Arnold, PhD, of UC Berkeley, said in an email. This was most likely caused by smaller sample sizes for these fields.
Factors driving consolidation
The two reports and the Senate Finance consolidation hearing raised similar issues, including calls to look at the factors driving more physicians out of independent practice, including Medicare reimbursement that may not keep up with rising inflation.
The Berkeley report authors called for Congress to add a broad inflation component to the Medicare physician fee schedule. It also called on Congress to add cases where Medicare, the biggest U.S. purchaser of health care, pays less for services when performed in independent practices than in hospital-affiliated ones.
Shawn Martin, executive vice president and CEO of the American Academy of Family Physicians, said his group appreciates how the report from UC Berkeley and nonprofit groups echoed recommendations many clinicians have made, including the call for a broad inflation adjustment for the fee schedule.
“To move the needle forward, Congress must advance site-neutral payment policies while also addressing the administrative requirements that take physicians away from the important work of caring for patients,” Mr. Martin said in an email.
Arnold Ventures provided funding for the report, which was a joint project of the American Antitrust Institute, the Nicholas C. Petris Center on Health Care Markets and Consumer Welfare, UC Berkeley, and the Washington Center for Equitable Growth.
A version of this article appeared on Medscape.com.
The report was a collaboration of University of California, Berkeley, staff and researchers from two nonprofits, the American Antitrust Institute and the Washington Center for Equitable Growth. It provides “convincing evidence that incentives to put profits before patients have grown stronger with an increase in private equity ownership of physician practices,” lead author Richard Scheffler, PhD, of UC Berkeley said in a statement.
The report also noted that private equity acquisitions of physician groups have risen sixfold in just a decade, increasing from 75 deals in 2012 to 484 deals in 2021.
Separately, the American Medical Association earlier released a separate report on trends in physician practice arrangements, finding that the percentage of physicians working in private equity–owned groups was 4.5% in 2022, the same as in its previous 2020 report. The share of physicians working in private practices fell by 13 percentage points from 60.1% to 46.7% between 2012 and 2022, the AMA reported.
The Berkeley report and the AMA update come amid rising concerns about the effects of the decline of independent physician practices. The U.S. Senate Finance Committee, which oversees most federal health spending, held a June hearing examining the causes and consequences of increased corporate ownership in health care, including a look at physician practices.
“It’s increasingly clear that consolidation in health care is not lowering costs or increasing the quality of Americans’ health care,” Senate Finance Chairman Ron Wyden (D-Ore.) said in an email. “For private equity in health care in particular, there needs to be more transparency around ownership so the effect on these business relationships can be better understood.”
Federal and state agencies do not generally track acquisitions of physician practices.
The UC Berkeley report impressively documents the rising influence of private equity in health care, for which it’s tough to find good data, said Karen Joynt Maddox, MD, MPH, of Washington University in St. Louis. Dr. Maddox, a cardiologist and policy researcher who also has studied the effects of consolidation in health care, examined the new report at the request of this news organization.
“They did a great job with the data,” Dr. Maddox said. “One of the big issues around private equity, and in general, ‘corporatization’ and consolidation of health care, is that there’s not a great way to track ownership changes. It’s really difficult to study.”
Dr. Scheffler and colleagues used data from the commercial firm PitchBook to identify acquisitions of physician practices by private equity firms. They consulted IQVIA’s physician databases – OneKey and SK&A Office-Based Physicians Database – to learn about the location, size, and specialties of acquired practices. They also used data from the nonprofit Health Care Cost Institute, which tracks commercial health plan claims, to assess how private equity acquisitions affected prices.
The researchers then matched the findings for practices acquired by private equity firms from 2015 to 2021 against those for comparable physician practices that remained independent from 2012 to 2021.
The authors then tied private-equity ownership to the following price increases:
- Gastroenterology (14%; 95% confidence interval, 7.9%-20.4%
- Oncology (16.4%; 95% CI, 5.5%-28.4%)
- Dermatology (4.0%; 95% CI, 1%-7.1%)
- Ob.gyn. (8.8%; 95% CI, 3.8%-14%)
- Ophthalmology (8.7%; 95% CI, 5.1%-12.3%)
- Radiology (8.2%; 95% CI, 0.8%-16.1%)
- Orthopedics (7.1%; 95% CI, 2.2%-12.3%)
- Primary care (4.1%; 95% CI, 1.3%-7%)
The analysis also found higher prices for cardiology (8.7%; 95% CI, –6.4% to 26.1%) and urology (4.2%; 95% CI, –2.3% to 11.1%), but neither of these findings was statistically significant, one of the authors, Daniel R. Arnold, PhD, of UC Berkeley, said in an email. This was most likely caused by smaller sample sizes for these fields.
Factors driving consolidation
The two reports and the Senate Finance consolidation hearing raised similar issues, including calls to look at the factors driving more physicians out of independent practice, including Medicare reimbursement that may not keep up with rising inflation.
The Berkeley report authors called for Congress to add a broad inflation component to the Medicare physician fee schedule. It also called on Congress to add cases where Medicare, the biggest U.S. purchaser of health care, pays less for services when performed in independent practices than in hospital-affiliated ones.
Shawn Martin, executive vice president and CEO of the American Academy of Family Physicians, said his group appreciates how the report from UC Berkeley and nonprofit groups echoed recommendations many clinicians have made, including the call for a broad inflation adjustment for the fee schedule.
“To move the needle forward, Congress must advance site-neutral payment policies while also addressing the administrative requirements that take physicians away from the important work of caring for patients,” Mr. Martin said in an email.
Arnold Ventures provided funding for the report, which was a joint project of the American Antitrust Institute, the Nicholas C. Petris Center on Health Care Markets and Consumer Welfare, UC Berkeley, and the Washington Center for Equitable Growth.
A version of this article appeared on Medscape.com.
The report was a collaboration of University of California, Berkeley, staff and researchers from two nonprofits, the American Antitrust Institute and the Washington Center for Equitable Growth. It provides “convincing evidence that incentives to put profits before patients have grown stronger with an increase in private equity ownership of physician practices,” lead author Richard Scheffler, PhD, of UC Berkeley said in a statement.
The report also noted that private equity acquisitions of physician groups have risen sixfold in just a decade, increasing from 75 deals in 2012 to 484 deals in 2021.
Separately, the American Medical Association earlier released a separate report on trends in physician practice arrangements, finding that the percentage of physicians working in private equity–owned groups was 4.5% in 2022, the same as in its previous 2020 report. The share of physicians working in private practices fell by 13 percentage points from 60.1% to 46.7% between 2012 and 2022, the AMA reported.
The Berkeley report and the AMA update come amid rising concerns about the effects of the decline of independent physician practices. The U.S. Senate Finance Committee, which oversees most federal health spending, held a June hearing examining the causes and consequences of increased corporate ownership in health care, including a look at physician practices.
“It’s increasingly clear that consolidation in health care is not lowering costs or increasing the quality of Americans’ health care,” Senate Finance Chairman Ron Wyden (D-Ore.) said in an email. “For private equity in health care in particular, there needs to be more transparency around ownership so the effect on these business relationships can be better understood.”
Federal and state agencies do not generally track acquisitions of physician practices.
The UC Berkeley report impressively documents the rising influence of private equity in health care, for which it’s tough to find good data, said Karen Joynt Maddox, MD, MPH, of Washington University in St. Louis. Dr. Maddox, a cardiologist and policy researcher who also has studied the effects of consolidation in health care, examined the new report at the request of this news organization.
“They did a great job with the data,” Dr. Maddox said. “One of the big issues around private equity, and in general, ‘corporatization’ and consolidation of health care, is that there’s not a great way to track ownership changes. It’s really difficult to study.”
Dr. Scheffler and colleagues used data from the commercial firm PitchBook to identify acquisitions of physician practices by private equity firms. They consulted IQVIA’s physician databases – OneKey and SK&A Office-Based Physicians Database – to learn about the location, size, and specialties of acquired practices. They also used data from the nonprofit Health Care Cost Institute, which tracks commercial health plan claims, to assess how private equity acquisitions affected prices.
The researchers then matched the findings for practices acquired by private equity firms from 2015 to 2021 against those for comparable physician practices that remained independent from 2012 to 2021.
The authors then tied private-equity ownership to the following price increases:
- Gastroenterology (14%; 95% confidence interval, 7.9%-20.4%
- Oncology (16.4%; 95% CI, 5.5%-28.4%)
- Dermatology (4.0%; 95% CI, 1%-7.1%)
- Ob.gyn. (8.8%; 95% CI, 3.8%-14%)
- Ophthalmology (8.7%; 95% CI, 5.1%-12.3%)
- Radiology (8.2%; 95% CI, 0.8%-16.1%)
- Orthopedics (7.1%; 95% CI, 2.2%-12.3%)
- Primary care (4.1%; 95% CI, 1.3%-7%)
The analysis also found higher prices for cardiology (8.7%; 95% CI, –6.4% to 26.1%) and urology (4.2%; 95% CI, –2.3% to 11.1%), but neither of these findings was statistically significant, one of the authors, Daniel R. Arnold, PhD, of UC Berkeley, said in an email. This was most likely caused by smaller sample sizes for these fields.
Factors driving consolidation
The two reports and the Senate Finance consolidation hearing raised similar issues, including calls to look at the factors driving more physicians out of independent practice, including Medicare reimbursement that may not keep up with rising inflation.
The Berkeley report authors called for Congress to add a broad inflation component to the Medicare physician fee schedule. It also called on Congress to add cases where Medicare, the biggest U.S. purchaser of health care, pays less for services when performed in independent practices than in hospital-affiliated ones.
Shawn Martin, executive vice president and CEO of the American Academy of Family Physicians, said his group appreciates how the report from UC Berkeley and nonprofit groups echoed recommendations many clinicians have made, including the call for a broad inflation adjustment for the fee schedule.
“To move the needle forward, Congress must advance site-neutral payment policies while also addressing the administrative requirements that take physicians away from the important work of caring for patients,” Mr. Martin said in an email.
Arnold Ventures provided funding for the report, which was a joint project of the American Antitrust Institute, the Nicholas C. Petris Center on Health Care Markets and Consumer Welfare, UC Berkeley, and the Washington Center for Equitable Growth.
A version of this article appeared on Medscape.com.
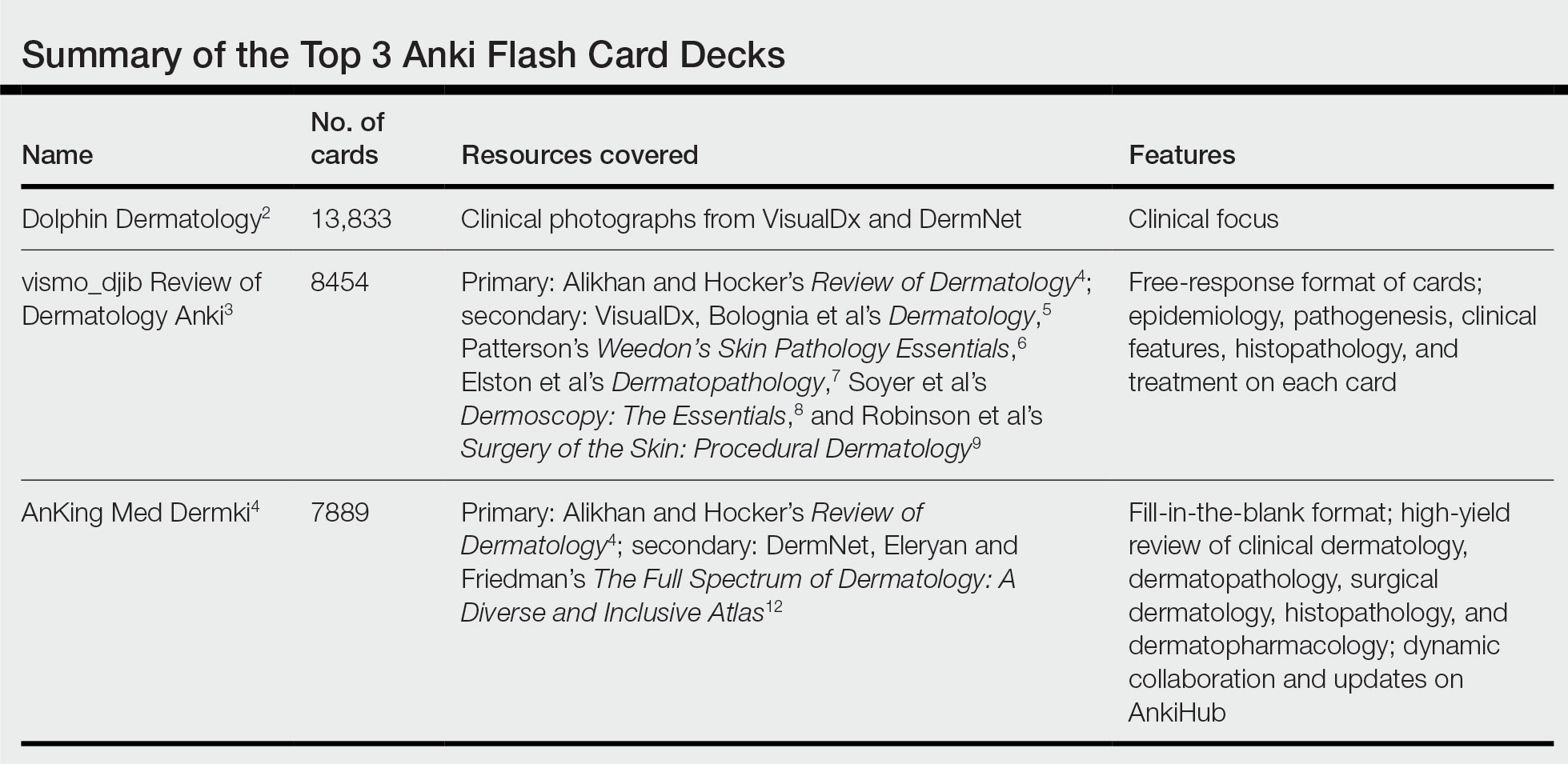
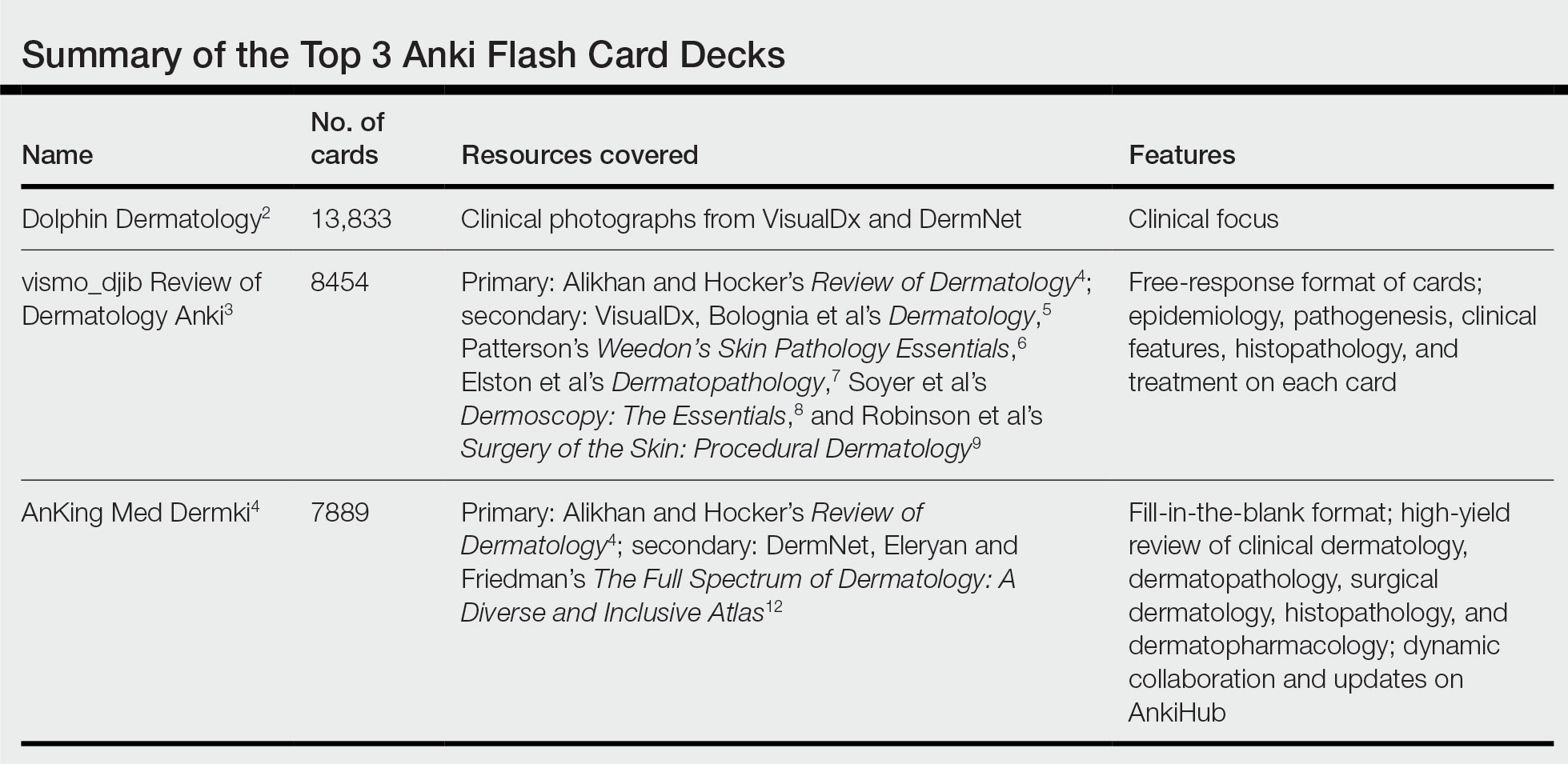
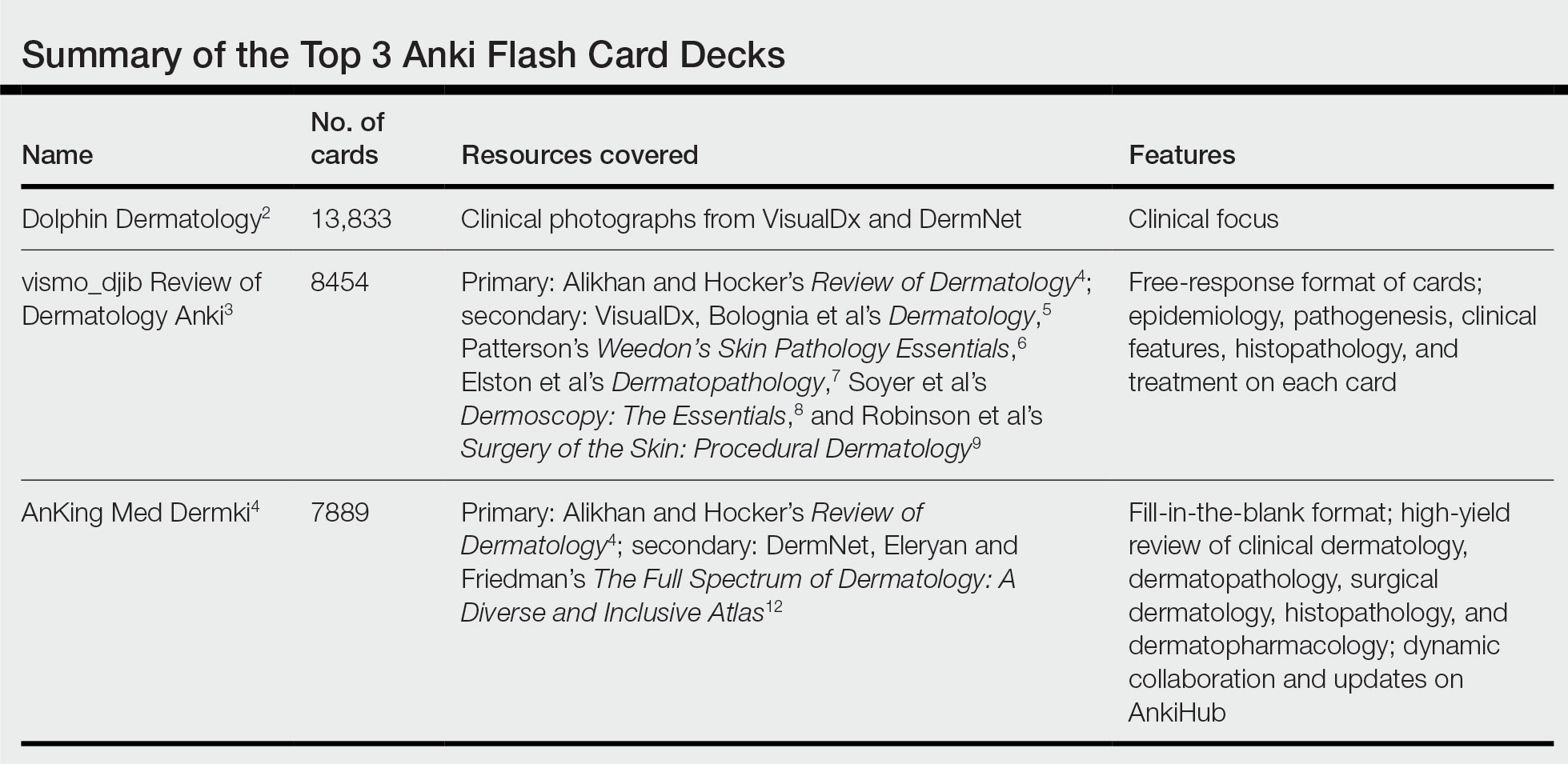
Review of 3 Comprehensive Anki Flash Card Decks for Dermatology Residents
Similar to medical school, residency is a time to drink out of the proverbial firehose of knowledge. Along with clinical duties, there is a plethora of information ranging from clinical management decisions to boards fodder that dermatology residents are expected to know, leaving residents to adopt study habits from medical school. Flash cards remain a popular study tool in the medical education community. The use of Anki, a web-based and mobile flash card application (app) that features custom and premade flash card decks made and shared by users, has become increasingly popular. In a 2021 study, Lu et al1 found that Anki flash card usage was associated with higher US Medical Licensing Examination scores. Herein, I provide an updated review of the top 3 most comprehensive premade Anki decks for dermatology residents, per my assessment.
COMPREHENSIVE DERMATOLOGY DECKS
Dolphin Dermatology
- Creator: Reddit user, Unknown2
- Date created: December 2020
- Last updated: April 2022
- Number of cards: 13,833
- Resources covered: Photographs of common dermatologic diagnoses from online sources such as VisualDx (https://www.visualdx.com/) and DermNet (https://dermnetnz.org/).
- Format of cards: One image or factoid per card.
- Card tags (allow separation of Anki decks into subcategories): Each general dermatology card is tagged by the diagnosis name. Pediatric dermatology cards are tagged by affected body location.
- Advantages: As you may glean by the sheer number of flash cards, this deck is a comprehensive review of clinical dermatology. Most cards feature clinical vignettes with clinical photographs of a dermatologic condition or histologic slide and ask what the diagnosis may be. It features photographs of pathology on a range of skin tones and many different images of each diagnosis. This is a great deck for residents who need to study clinical photographs of dermatologic diagnoses.
- Disadvantages: This deck does not cover dermatopathology, basic science, treatment options, or pharmacology in depth. Additionally, is difficult to find a link to download this resource.
- At the time of publication of this article, users are unable to download this deck.
vismo_djib’s Review of Dermatology Anki
- Creator: Reddit user vismo_djib3
- Date created: June 2020
- Last updated: February 2022
- Number of cards: 8454
- Resources covered: Alikhan and Hocker’s Review of Dermatology4 is the main resource with supplemental images from VisualDx, Bolognia et al’s Dermatology,5 Patterson’s Weedon’s Skin Pathology Essentials,6 Elston et al’s Dermatopathology,7 Soyer et al’s Dermoscopy: The Essentials,8 and Robinson et al’s Surgery of the Skin: Procedural Dermatology.9
- Format of cards: Cards mostly feature a diagnosis with color-coded categories including epidemiology, pathogenesis, clinical features, histopathology, and treatment.
- Card tags (allow separation of Anki decks into subcategories): Cards are tagged with chapter numbers from Alikhan and Hocker’s Review of Dermatology.4
- Advantages: This impressive comprehensive review of dermatology is a great option for residents studying for the American Board of Dermatology CORE examinations and users looking to solidify the information in Alikhan and Hocker’s Review of Dermatology,4 a frequently used resource among dermatology residents. It currently is my favorite deck because it features holistic information on diagnosis, epidemiology, pathogenesis, histopathology, and treatment with excellent clinical photographs.
- Disadvantages: For some purposes, this deck may be too lofty. For maximum benefit, it may require user customization including separating cards by tag and other add-ons that allow only 1 card per note, which will separate the information on each card into smaller increments. The mostly free-response format and lengthy slides may make it difficult to practice recall.
AnKingMed Dermki
- Creator: Reddit user AnKingMed10,11
- Date created: April 2023
- Last updated: This deck features a dynamic add-on and collaboration application called AnkiHub, which allows for real-time updates. At the time this article was written, the deck was last updated on June 19, 2023.
- Number of cards: 7889
- Resources covered: Currently 75% of Alikhan and Hocker’s Review of Dermatology4 with supplemental images from DermNet and Eleryan and Friedman’s The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas.12
- Format of cards: Cards are in a fill-in-the-blank format.
- Card tags (allow separation of Anki decks into subcategories): Cards are tagged by chapter number and subsection of Alikhan and Hocker’s Review of Dermatology.4
- Advantages: As the newest contribution to the dermatology Anki card compendium, this deck is up to date, innovative, and dynamic. It features an optional add-on application—AnkiHub—which allows users to keep up with live updates and collaborations. The deck features a fill-in-the-blank format that may be preferred to a free-response format for information recall. It features Alikhan and Hocker’s Review of Dermatology,4 which is a high-yield review of clinical dermatology, dermatopathology, surgical dermatology, pharmacology, and histopathology for dermatology residents.
- Disadvantages: The deck is still currently in a development phase, covering 75% of Alikhan and Hocker’s Review of Dermatology4 with plans to add the remaining 25%. The add-on to access the most up-to-date version of the flashcards requires a paid monthly or annual subscription; however, the creator announced they will release periodic free updates of the deck.
Final Thoughts
As a collaborative platform, new flash card decks are always being added to Anki. This article is not comprehensive of all dermatologic flash card decks available. There are decks better suited for medical students covering topics such as the American Academy of Dermatology Basic Dermatology Curriculum, UWorld United States Medical Licensing Examination dermatology, and dermatology in internal medicine. Furthermore, specific study tools in dermatology may have their own accompanying Anki decks (ie, The Grenz Zone podcast, Dermnemonics). Flash cards can be a valuable study tool to trainees in medicine, and residents are immensely grateful to our peers who make them for our use.
- Lu M, Farhat JH, Beck Dallaghan GL. Enhanced learning and retention of medical knowledge using the mobile flash card application Anki. Med Sci Educ. 2021;31:1975-1981. doi:10.1007/s40670-021-01386-9
- Unknown. Dolphin Dermatology. Reddit website. Accessed July 19, 2023. https://www.reddit.com/r/medicalschoolanki/comments/116jbpc/dolphin_derm/
- vismo_djib. Review of dermatology Anki. Reddit website. Published June 13, 2020. Accessed June 22, 2023. https://www.reddit.com/r/DermApp/comments/h8gz3d/review_of_dermatology_anki/
- Alikhan A, Hocker TLH. Review of Dermatology. Elsevier; 2016.
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. Elsevier Health Sciences; 2017.
- Patterson JW. Weedon’s Skin Pathology Essentials. Elsevier Health Sciences; 2016.
- Elston D, Ferringer T, Ko CJ, et al. Dermatopathology. Elsevier Health Sciences; 2013.
- Soyer HP, Argenziano G, Hofmann-Wellenhof R, et al. Dermoscopy: The Essentials. Elsevier Health Sciences; 2011.
- Robinson JK, Hanke CW, Siegel DM, et al. Surgery of the Skin: Procedural Dermatology. Elsevier Health Sciences; 2014.
- AnKingMed. Dermki: dermatology residency Anki deck. Reddit website. Published April 8, 2023. Accessed June 22, 2023. https://www.reddit.com/r/medicalschoolanki/comments/12fo9ji/dermki_dermatology_residency_anki_deck/
- Dermki deck for Dermatology Residents. Notion website. Accessed July 10, 2023. https://ankingmed.notion.site/Dermki-deck-for-Dermatology-Residents-9e0b8d8abc2a4bf7941903d80e5b01a2
- Eleryan M, Friedman A. The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas. Sanovaworks; 2021.
Similar to medical school, residency is a time to drink out of the proverbial firehose of knowledge. Along with clinical duties, there is a plethora of information ranging from clinical management decisions to boards fodder that dermatology residents are expected to know, leaving residents to adopt study habits from medical school. Flash cards remain a popular study tool in the medical education community. The use of Anki, a web-based and mobile flash card application (app) that features custom and premade flash card decks made and shared by users, has become increasingly popular. In a 2021 study, Lu et al1 found that Anki flash card usage was associated with higher US Medical Licensing Examination scores. Herein, I provide an updated review of the top 3 most comprehensive premade Anki decks for dermatology residents, per my assessment.
COMPREHENSIVE DERMATOLOGY DECKS
Dolphin Dermatology
- Creator: Reddit user, Unknown2
- Date created: December 2020
- Last updated: April 2022
- Number of cards: 13,833
- Resources covered: Photographs of common dermatologic diagnoses from online sources such as VisualDx (https://www.visualdx.com/) and DermNet (https://dermnetnz.org/).
- Format of cards: One image or factoid per card.
- Card tags (allow separation of Anki decks into subcategories): Each general dermatology card is tagged by the diagnosis name. Pediatric dermatology cards are tagged by affected body location.
- Advantages: As you may glean by the sheer number of flash cards, this deck is a comprehensive review of clinical dermatology. Most cards feature clinical vignettes with clinical photographs of a dermatologic condition or histologic slide and ask what the diagnosis may be. It features photographs of pathology on a range of skin tones and many different images of each diagnosis. This is a great deck for residents who need to study clinical photographs of dermatologic diagnoses.
- Disadvantages: This deck does not cover dermatopathology, basic science, treatment options, or pharmacology in depth. Additionally, is difficult to find a link to download this resource.
- At the time of publication of this article, users are unable to download this deck.
vismo_djib’s Review of Dermatology Anki
- Creator: Reddit user vismo_djib3
- Date created: June 2020
- Last updated: February 2022
- Number of cards: 8454
- Resources covered: Alikhan and Hocker’s Review of Dermatology4 is the main resource with supplemental images from VisualDx, Bolognia et al’s Dermatology,5 Patterson’s Weedon’s Skin Pathology Essentials,6 Elston et al’s Dermatopathology,7 Soyer et al’s Dermoscopy: The Essentials,8 and Robinson et al’s Surgery of the Skin: Procedural Dermatology.9
- Format of cards: Cards mostly feature a diagnosis with color-coded categories including epidemiology, pathogenesis, clinical features, histopathology, and treatment.
- Card tags (allow separation of Anki decks into subcategories): Cards are tagged with chapter numbers from Alikhan and Hocker’s Review of Dermatology.4
- Advantages: This impressive comprehensive review of dermatology is a great option for residents studying for the American Board of Dermatology CORE examinations and users looking to solidify the information in Alikhan and Hocker’s Review of Dermatology,4 a frequently used resource among dermatology residents. It currently is my favorite deck because it features holistic information on diagnosis, epidemiology, pathogenesis, histopathology, and treatment with excellent clinical photographs.
- Disadvantages: For some purposes, this deck may be too lofty. For maximum benefit, it may require user customization including separating cards by tag and other add-ons that allow only 1 card per note, which will separate the information on each card into smaller increments. The mostly free-response format and lengthy slides may make it difficult to practice recall.
AnKingMed Dermki
- Creator: Reddit user AnKingMed10,11
- Date created: April 2023
- Last updated: This deck features a dynamic add-on and collaboration application called AnkiHub, which allows for real-time updates. At the time this article was written, the deck was last updated on June 19, 2023.
- Number of cards: 7889
- Resources covered: Currently 75% of Alikhan and Hocker’s Review of Dermatology4 with supplemental images from DermNet and Eleryan and Friedman’s The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas.12
- Format of cards: Cards are in a fill-in-the-blank format.
- Card tags (allow separation of Anki decks into subcategories): Cards are tagged by chapter number and subsection of Alikhan and Hocker’s Review of Dermatology.4
- Advantages: As the newest contribution to the dermatology Anki card compendium, this deck is up to date, innovative, and dynamic. It features an optional add-on application—AnkiHub—which allows users to keep up with live updates and collaborations. The deck features a fill-in-the-blank format that may be preferred to a free-response format for information recall. It features Alikhan and Hocker’s Review of Dermatology,4 which is a high-yield review of clinical dermatology, dermatopathology, surgical dermatology, pharmacology, and histopathology for dermatology residents.
- Disadvantages: The deck is still currently in a development phase, covering 75% of Alikhan and Hocker’s Review of Dermatology4 with plans to add the remaining 25%. The add-on to access the most up-to-date version of the flashcards requires a paid monthly or annual subscription; however, the creator announced they will release periodic free updates of the deck.
Final Thoughts
As a collaborative platform, new flash card decks are always being added to Anki. This article is not comprehensive of all dermatologic flash card decks available. There are decks better suited for medical students covering topics such as the American Academy of Dermatology Basic Dermatology Curriculum, UWorld United States Medical Licensing Examination dermatology, and dermatology in internal medicine. Furthermore, specific study tools in dermatology may have their own accompanying Anki decks (ie, The Grenz Zone podcast, Dermnemonics). Flash cards can be a valuable study tool to trainees in medicine, and residents are immensely grateful to our peers who make them for our use.
Similar to medical school, residency is a time to drink out of the proverbial firehose of knowledge. Along with clinical duties, there is a plethora of information ranging from clinical management decisions to boards fodder that dermatology residents are expected to know, leaving residents to adopt study habits from medical school. Flash cards remain a popular study tool in the medical education community. The use of Anki, a web-based and mobile flash card application (app) that features custom and premade flash card decks made and shared by users, has become increasingly popular. In a 2021 study, Lu et al1 found that Anki flash card usage was associated with higher US Medical Licensing Examination scores. Herein, I provide an updated review of the top 3 most comprehensive premade Anki decks for dermatology residents, per my assessment.
COMPREHENSIVE DERMATOLOGY DECKS
Dolphin Dermatology
- Creator: Reddit user, Unknown2
- Date created: December 2020
- Last updated: April 2022
- Number of cards: 13,833
- Resources covered: Photographs of common dermatologic diagnoses from online sources such as VisualDx (https://www.visualdx.com/) and DermNet (https://dermnetnz.org/).
- Format of cards: One image or factoid per card.
- Card tags (allow separation of Anki decks into subcategories): Each general dermatology card is tagged by the diagnosis name. Pediatric dermatology cards are tagged by affected body location.
- Advantages: As you may glean by the sheer number of flash cards, this deck is a comprehensive review of clinical dermatology. Most cards feature clinical vignettes with clinical photographs of a dermatologic condition or histologic slide and ask what the diagnosis may be. It features photographs of pathology on a range of skin tones and many different images of each diagnosis. This is a great deck for residents who need to study clinical photographs of dermatologic diagnoses.
- Disadvantages: This deck does not cover dermatopathology, basic science, treatment options, or pharmacology in depth. Additionally, is difficult to find a link to download this resource.
- At the time of publication of this article, users are unable to download this deck.
vismo_djib’s Review of Dermatology Anki
- Creator: Reddit user vismo_djib3
- Date created: June 2020
- Last updated: February 2022
- Number of cards: 8454
- Resources covered: Alikhan and Hocker’s Review of Dermatology4 is the main resource with supplemental images from VisualDx, Bolognia et al’s Dermatology,5 Patterson’s Weedon’s Skin Pathology Essentials,6 Elston et al’s Dermatopathology,7 Soyer et al’s Dermoscopy: The Essentials,8 and Robinson et al’s Surgery of the Skin: Procedural Dermatology.9
- Format of cards: Cards mostly feature a diagnosis with color-coded categories including epidemiology, pathogenesis, clinical features, histopathology, and treatment.
- Card tags (allow separation of Anki decks into subcategories): Cards are tagged with chapter numbers from Alikhan and Hocker’s Review of Dermatology.4
- Advantages: This impressive comprehensive review of dermatology is a great option for residents studying for the American Board of Dermatology CORE examinations and users looking to solidify the information in Alikhan and Hocker’s Review of Dermatology,4 a frequently used resource among dermatology residents. It currently is my favorite deck because it features holistic information on diagnosis, epidemiology, pathogenesis, histopathology, and treatment with excellent clinical photographs.
- Disadvantages: For some purposes, this deck may be too lofty. For maximum benefit, it may require user customization including separating cards by tag and other add-ons that allow only 1 card per note, which will separate the information on each card into smaller increments. The mostly free-response format and lengthy slides may make it difficult to practice recall.
AnKingMed Dermki
- Creator: Reddit user AnKingMed10,11
- Date created: April 2023
- Last updated: This deck features a dynamic add-on and collaboration application called AnkiHub, which allows for real-time updates. At the time this article was written, the deck was last updated on June 19, 2023.
- Number of cards: 7889
- Resources covered: Currently 75% of Alikhan and Hocker’s Review of Dermatology4 with supplemental images from DermNet and Eleryan and Friedman’s The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas.12
- Format of cards: Cards are in a fill-in-the-blank format.
- Card tags (allow separation of Anki decks into subcategories): Cards are tagged by chapter number and subsection of Alikhan and Hocker’s Review of Dermatology.4
- Advantages: As the newest contribution to the dermatology Anki card compendium, this deck is up to date, innovative, and dynamic. It features an optional add-on application—AnkiHub—which allows users to keep up with live updates and collaborations. The deck features a fill-in-the-blank format that may be preferred to a free-response format for information recall. It features Alikhan and Hocker’s Review of Dermatology,4 which is a high-yield review of clinical dermatology, dermatopathology, surgical dermatology, pharmacology, and histopathology for dermatology residents.
- Disadvantages: The deck is still currently in a development phase, covering 75% of Alikhan and Hocker’s Review of Dermatology4 with plans to add the remaining 25%. The add-on to access the most up-to-date version of the flashcards requires a paid monthly or annual subscription; however, the creator announced they will release periodic free updates of the deck.
Final Thoughts
As a collaborative platform, new flash card decks are always being added to Anki. This article is not comprehensive of all dermatologic flash card decks available. There are decks better suited for medical students covering topics such as the American Academy of Dermatology Basic Dermatology Curriculum, UWorld United States Medical Licensing Examination dermatology, and dermatology in internal medicine. Furthermore, specific study tools in dermatology may have their own accompanying Anki decks (ie, The Grenz Zone podcast, Dermnemonics). Flash cards can be a valuable study tool to trainees in medicine, and residents are immensely grateful to our peers who make them for our use.
- Lu M, Farhat JH, Beck Dallaghan GL. Enhanced learning and retention of medical knowledge using the mobile flash card application Anki. Med Sci Educ. 2021;31:1975-1981. doi:10.1007/s40670-021-01386-9
- Unknown. Dolphin Dermatology. Reddit website. Accessed July 19, 2023. https://www.reddit.com/r/medicalschoolanki/comments/116jbpc/dolphin_derm/
- vismo_djib. Review of dermatology Anki. Reddit website. Published June 13, 2020. Accessed June 22, 2023. https://www.reddit.com/r/DermApp/comments/h8gz3d/review_of_dermatology_anki/
- Alikhan A, Hocker TLH. Review of Dermatology. Elsevier; 2016.
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. Elsevier Health Sciences; 2017.
- Patterson JW. Weedon’s Skin Pathology Essentials. Elsevier Health Sciences; 2016.
- Elston D, Ferringer T, Ko CJ, et al. Dermatopathology. Elsevier Health Sciences; 2013.
- Soyer HP, Argenziano G, Hofmann-Wellenhof R, et al. Dermoscopy: The Essentials. Elsevier Health Sciences; 2011.
- Robinson JK, Hanke CW, Siegel DM, et al. Surgery of the Skin: Procedural Dermatology. Elsevier Health Sciences; 2014.
- AnKingMed. Dermki: dermatology residency Anki deck. Reddit website. Published April 8, 2023. Accessed June 22, 2023. https://www.reddit.com/r/medicalschoolanki/comments/12fo9ji/dermki_dermatology_residency_anki_deck/
- Dermki deck for Dermatology Residents. Notion website. Accessed July 10, 2023. https://ankingmed.notion.site/Dermki-deck-for-Dermatology-Residents-9e0b8d8abc2a4bf7941903d80e5b01a2
- Eleryan M, Friedman A. The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas. Sanovaworks; 2021.
- Lu M, Farhat JH, Beck Dallaghan GL. Enhanced learning and retention of medical knowledge using the mobile flash card application Anki. Med Sci Educ. 2021;31:1975-1981. doi:10.1007/s40670-021-01386-9
- Unknown. Dolphin Dermatology. Reddit website. Accessed July 19, 2023. https://www.reddit.com/r/medicalschoolanki/comments/116jbpc/dolphin_derm/
- vismo_djib. Review of dermatology Anki. Reddit website. Published June 13, 2020. Accessed June 22, 2023. https://www.reddit.com/r/DermApp/comments/h8gz3d/review_of_dermatology_anki/
- Alikhan A, Hocker TLH. Review of Dermatology. Elsevier; 2016.
- Bolognia JL, Schaffer JV, Cerroni L. Dermatology. Elsevier Health Sciences; 2017.
- Patterson JW. Weedon’s Skin Pathology Essentials. Elsevier Health Sciences; 2016.
- Elston D, Ferringer T, Ko CJ, et al. Dermatopathology. Elsevier Health Sciences; 2013.
- Soyer HP, Argenziano G, Hofmann-Wellenhof R, et al. Dermoscopy: The Essentials. Elsevier Health Sciences; 2011.
- Robinson JK, Hanke CW, Siegel DM, et al. Surgery of the Skin: Procedural Dermatology. Elsevier Health Sciences; 2014.
- AnKingMed. Dermki: dermatology residency Anki deck. Reddit website. Published April 8, 2023. Accessed June 22, 2023. https://www.reddit.com/r/medicalschoolanki/comments/12fo9ji/dermki_dermatology_residency_anki_deck/
- Dermki deck for Dermatology Residents. Notion website. Accessed July 10, 2023. https://ankingmed.notion.site/Dermki-deck-for-Dermatology-Residents-9e0b8d8abc2a4bf7941903d80e5b01a2
- Eleryan M, Friedman A. The Full Spectrum of Dermatology: A Diverse and Inclusive Atlas. Sanovaworks; 2021.
Resident Pearl
- Publicly available Anki flashcard decks may aid dermatology residents in mastering the learning objectives required during training.
Want to add a new partner to your practice? Here’s what to consider
When the match is right, the benefits can be significant: more hands to share the load of running a medical practice, and increased revenue and expanded patient population. A partner can bring in new, complementary strengths and skills. Adding a partner is also a way to prepare for the future by setting your practice up for a smooth transition if you or another partner is looking toward retirement.
But a mismatched partnership can cost you time and money, not to mention endless amount of conflict, dysfunction, and liability. Mutual trust and a long-term commitment on both sides are critical.
“Just like with marriage, it can be very difficult, traumatic, and expensive to break up with a partner,” said Clifton Straughn, MD, partner at Direct Access MD, a concierge-service model family practice in Anderson, S.C. “So, do your due diligence and take your time.” Picking the right partner is essential.
The basics
Before you begin the process of partnership with a physician, be sure you know what you need, the skill sets you’re looking for to complement your practice, and the personality characteristics and values that are important to you so the person you choose can check all the boxes and not just add a name to the letterhead.
“A lot of times, doctors go into this with just a general idea that they need more doctors or that they would like to be bigger or have more clout,” said Tim Boden, a certified medical practice executive with over 40 years of experience. “But you have to understand that to a certain degree, if you’re bringing somebody in who has basically an identical clinical profile to yours, you’re going to be sacrificing a bit of your lunch for a while until that person builds a name for himself or herself. A new partner’s skill set should match the need that you’re trying to fill.”
Figure out and discuss with your current partners how much it will cost to bring in a partner between their compensation and additional practice expenses. How much revenue will you expect the partner to generate? Will your practice break even the first year or the second? And how will you cover any shortfall?
It’s also essential to understand how the day-to-day operation of your practice will change after you add another partner.
- Will the new partner’s percentage of ownership be the same as that of the other partners?
- Will their ownership include a percentage of the facility, equipment, supplies, and accounts receivable?
- How will you split call and work hours?
- How will decision-making work?
- How would buyout work if a partner were to leave the practice, and is there a minimum obligation, such as a 5-year commitment?
As a team, you may also want to discuss “soft skills,” or the way you’d hope a partner would represent your practice to patients and the community.
“These can be harder to quantify,” said Dr. Straughn. “Evaluating them can take artful questions and simple observation over time.”
It’s a slow process
Many practices offer paths to partnership rather than bringing in a partner straight away. With this process, an incoming physician works toward that goal. If you’re going this route, discuss this during the hiring process, so that both sides are clear about the process. Rule No. 1 is to make sure that new hires understand that partnership is possible, although it’s not a given. The typical partnership track is 2-3 years, but you can set the timeline that works best for your practice.
Mr. Boden recommends at least a year for this period so as to allow you the opportunity to evaluate the new member, how they work, and how they fit with your team. The partnership track method is typically for young or fairly new physicians.
“I would avoid ever promising an ownership position to a recruit,” said Mr. Boden. “I would only show them how it can happen and what it would look like if they qualify.”
Consider professional help
If you want to be sure you weigh all the pros and cons of your new partner, a medical practice consultant may be the way to go. A consultant can identify many situations that you might overlook.
Some services offer a medical practice assessment to help you see where you need the most help and what skills might be best to bring to the table. They might also be able to take over some of the administrative work of a new hire if you like, so you and the other partners can focus solely on interacting with and observing the clinical abilities of a potential partner.
A health care attorney can help you build a sound agreement regarding decision-making and how the fees/costs will be divided and can put legal protections in place for everyone involved.
You’ll need a buy-sell agreement (also called a partnership or shareholder agreement) that spells out the terms and conditions, including buying into and selling out of the practice. A fair agreement respects all parties, while a poor one that offers the new partner a minority share or lessor profit may favor the practice’s current partners but could breed resentment, undermining the practice’s culture and morale.
Takeaway
Ideally, you’ll select someone with excellent credentials and experience with similar goals for the practice who blends well with your staff. It’s best to find someone who fits well culturally with your office and who practices medicine with a similar patient philosophy.
To that end, Mr. Boden encourages out-of-the-box questions for interviews, such as what a potential partner wants to make sure they have room for in their life, or what their ideal work and family life looks like. The more you can assess components such as emotional intelligence, =the fuller picture you’ll get.
“You’re going to be spending major hours every week with this person, and your destiny is going to be tied up with theirs to some degree,” said Mr. Boden. You can teach somebody the job, but if you don’t genuinely like and respect them and want to work with them daily, it may not be the right fit.
A version of this article first appeared on Medscape.com.
When the match is right, the benefits can be significant: more hands to share the load of running a medical practice, and increased revenue and expanded patient population. A partner can bring in new, complementary strengths and skills. Adding a partner is also a way to prepare for the future by setting your practice up for a smooth transition if you or another partner is looking toward retirement.
But a mismatched partnership can cost you time and money, not to mention endless amount of conflict, dysfunction, and liability. Mutual trust and a long-term commitment on both sides are critical.
“Just like with marriage, it can be very difficult, traumatic, and expensive to break up with a partner,” said Clifton Straughn, MD, partner at Direct Access MD, a concierge-service model family practice in Anderson, S.C. “So, do your due diligence and take your time.” Picking the right partner is essential.
The basics
Before you begin the process of partnership with a physician, be sure you know what you need, the skill sets you’re looking for to complement your practice, and the personality characteristics and values that are important to you so the person you choose can check all the boxes and not just add a name to the letterhead.
“A lot of times, doctors go into this with just a general idea that they need more doctors or that they would like to be bigger or have more clout,” said Tim Boden, a certified medical practice executive with over 40 years of experience. “But you have to understand that to a certain degree, if you’re bringing somebody in who has basically an identical clinical profile to yours, you’re going to be sacrificing a bit of your lunch for a while until that person builds a name for himself or herself. A new partner’s skill set should match the need that you’re trying to fill.”
Figure out and discuss with your current partners how much it will cost to bring in a partner between their compensation and additional practice expenses. How much revenue will you expect the partner to generate? Will your practice break even the first year or the second? And how will you cover any shortfall?
It’s also essential to understand how the day-to-day operation of your practice will change after you add another partner.
- Will the new partner’s percentage of ownership be the same as that of the other partners?
- Will their ownership include a percentage of the facility, equipment, supplies, and accounts receivable?
- How will you split call and work hours?
- How will decision-making work?
- How would buyout work if a partner were to leave the practice, and is there a minimum obligation, such as a 5-year commitment?
As a team, you may also want to discuss “soft skills,” or the way you’d hope a partner would represent your practice to patients and the community.
“These can be harder to quantify,” said Dr. Straughn. “Evaluating them can take artful questions and simple observation over time.”
It’s a slow process
Many practices offer paths to partnership rather than bringing in a partner straight away. With this process, an incoming physician works toward that goal. If you’re going this route, discuss this during the hiring process, so that both sides are clear about the process. Rule No. 1 is to make sure that new hires understand that partnership is possible, although it’s not a given. The typical partnership track is 2-3 years, but you can set the timeline that works best for your practice.
Mr. Boden recommends at least a year for this period so as to allow you the opportunity to evaluate the new member, how they work, and how they fit with your team. The partnership track method is typically for young or fairly new physicians.
“I would avoid ever promising an ownership position to a recruit,” said Mr. Boden. “I would only show them how it can happen and what it would look like if they qualify.”
Consider professional help
If you want to be sure you weigh all the pros and cons of your new partner, a medical practice consultant may be the way to go. A consultant can identify many situations that you might overlook.
Some services offer a medical practice assessment to help you see where you need the most help and what skills might be best to bring to the table. They might also be able to take over some of the administrative work of a new hire if you like, so you and the other partners can focus solely on interacting with and observing the clinical abilities of a potential partner.
A health care attorney can help you build a sound agreement regarding decision-making and how the fees/costs will be divided and can put legal protections in place for everyone involved.
You’ll need a buy-sell agreement (also called a partnership or shareholder agreement) that spells out the terms and conditions, including buying into and selling out of the practice. A fair agreement respects all parties, while a poor one that offers the new partner a minority share or lessor profit may favor the practice’s current partners but could breed resentment, undermining the practice’s culture and morale.
Takeaway
Ideally, you’ll select someone with excellent credentials and experience with similar goals for the practice who blends well with your staff. It’s best to find someone who fits well culturally with your office and who practices medicine with a similar patient philosophy.
To that end, Mr. Boden encourages out-of-the-box questions for interviews, such as what a potential partner wants to make sure they have room for in their life, or what their ideal work and family life looks like. The more you can assess components such as emotional intelligence, =the fuller picture you’ll get.
“You’re going to be spending major hours every week with this person, and your destiny is going to be tied up with theirs to some degree,” said Mr. Boden. You can teach somebody the job, but if you don’t genuinely like and respect them and want to work with them daily, it may not be the right fit.
A version of this article first appeared on Medscape.com.
When the match is right, the benefits can be significant: more hands to share the load of running a medical practice, and increased revenue and expanded patient population. A partner can bring in new, complementary strengths and skills. Adding a partner is also a way to prepare for the future by setting your practice up for a smooth transition if you or another partner is looking toward retirement.
But a mismatched partnership can cost you time and money, not to mention endless amount of conflict, dysfunction, and liability. Mutual trust and a long-term commitment on both sides are critical.
“Just like with marriage, it can be very difficult, traumatic, and expensive to break up with a partner,” said Clifton Straughn, MD, partner at Direct Access MD, a concierge-service model family practice in Anderson, S.C. “So, do your due diligence and take your time.” Picking the right partner is essential.
The basics
Before you begin the process of partnership with a physician, be sure you know what you need, the skill sets you’re looking for to complement your practice, and the personality characteristics and values that are important to you so the person you choose can check all the boxes and not just add a name to the letterhead.
“A lot of times, doctors go into this with just a general idea that they need more doctors or that they would like to be bigger or have more clout,” said Tim Boden, a certified medical practice executive with over 40 years of experience. “But you have to understand that to a certain degree, if you’re bringing somebody in who has basically an identical clinical profile to yours, you’re going to be sacrificing a bit of your lunch for a while until that person builds a name for himself or herself. A new partner’s skill set should match the need that you’re trying to fill.”
Figure out and discuss with your current partners how much it will cost to bring in a partner between their compensation and additional practice expenses. How much revenue will you expect the partner to generate? Will your practice break even the first year or the second? And how will you cover any shortfall?
It’s also essential to understand how the day-to-day operation of your practice will change after you add another partner.
- Will the new partner’s percentage of ownership be the same as that of the other partners?
- Will their ownership include a percentage of the facility, equipment, supplies, and accounts receivable?
- How will you split call and work hours?
- How will decision-making work?
- How would buyout work if a partner were to leave the practice, and is there a minimum obligation, such as a 5-year commitment?
As a team, you may also want to discuss “soft skills,” or the way you’d hope a partner would represent your practice to patients and the community.
“These can be harder to quantify,” said Dr. Straughn. “Evaluating them can take artful questions and simple observation over time.”
It’s a slow process
Many practices offer paths to partnership rather than bringing in a partner straight away. With this process, an incoming physician works toward that goal. If you’re going this route, discuss this during the hiring process, so that both sides are clear about the process. Rule No. 1 is to make sure that new hires understand that partnership is possible, although it’s not a given. The typical partnership track is 2-3 years, but you can set the timeline that works best for your practice.
Mr. Boden recommends at least a year for this period so as to allow you the opportunity to evaluate the new member, how they work, and how they fit with your team. The partnership track method is typically for young or fairly new physicians.
“I would avoid ever promising an ownership position to a recruit,” said Mr. Boden. “I would only show them how it can happen and what it would look like if they qualify.”
Consider professional help
If you want to be sure you weigh all the pros and cons of your new partner, a medical practice consultant may be the way to go. A consultant can identify many situations that you might overlook.
Some services offer a medical practice assessment to help you see where you need the most help and what skills might be best to bring to the table. They might also be able to take over some of the administrative work of a new hire if you like, so you and the other partners can focus solely on interacting with and observing the clinical abilities of a potential partner.
A health care attorney can help you build a sound agreement regarding decision-making and how the fees/costs will be divided and can put legal protections in place for everyone involved.
You’ll need a buy-sell agreement (also called a partnership or shareholder agreement) that spells out the terms and conditions, including buying into and selling out of the practice. A fair agreement respects all parties, while a poor one that offers the new partner a minority share or lessor profit may favor the practice’s current partners but could breed resentment, undermining the practice’s culture and morale.
Takeaway
Ideally, you’ll select someone with excellent credentials and experience with similar goals for the practice who blends well with your staff. It’s best to find someone who fits well culturally with your office and who practices medicine with a similar patient philosophy.
To that end, Mr. Boden encourages out-of-the-box questions for interviews, such as what a potential partner wants to make sure they have room for in their life, or what their ideal work and family life looks like. The more you can assess components such as emotional intelligence, =the fuller picture you’ll get.
“You’re going to be spending major hours every week with this person, and your destiny is going to be tied up with theirs to some degree,” said Mr. Boden. You can teach somebody the job, but if you don’t genuinely like and respect them and want to work with them daily, it may not be the right fit.
A version of this article first appeared on Medscape.com.
Doc’s lawsuit tests new crackdown on noncompete clauses
In a test of one of the nation’s most restrictive laws limiting noncompete clauses in medicine, an Indiana pediatric critical-care physician is suing to stop his former hospital employer from controlling his future employment prospects.
David Lankford, DO, acknowledges that he signed a contract with the Lutheran Health Network that included a noncompete clause. However,
Indiana’s law is notable among states because if a physician terminates his/her job for cause, the noncompete may be considered unenforceable.
“When you have physicians who are unable to work in their community, it creates a barrier for access to care for patients,” Dr. Lankford said in an interview. “I’m fighting to decrease barriers and continue to have patients be able to see their doctors in their own hometown or their own county.”
Lutheran Health’s media relations department did not respond to requests for comment.
Noncompete clauses ‘extremely common’
Non-compete clauses – which typically restrict when and where employees can take future jobs – are common in physician contracts, Anu Murthy, JD, who reviews employee contracts for a firm called Contract Diagnostics, said in an interview.
However, the tide has been turning against them.
About a dozen states and the District of Columbia have enacted legislation to limit the use of noncompetes in employment contracts, and about half of states have pending legislation that could dilute noncompete clauses, Ms. Murthy said. In June, the state of New York sent a noncompete ban bill to the governor’s desk.
For more about state-by-state restrictions on noncompete clauses, check this chart.
In his lawsuit, Dr. Lankford said he was hired in 2017 to work at Lutheran Hospital in Fort Wayne.
Dr. Lankford signed an employee renewal contract in 2020 that included a noncompete clause; his attorneys declined to provide details about the clause because of confidentiality restrictions.
In 2022, the lawsuit says, Lutheran Hospital told Dr. Lankford that he’d need to take on more work due to layoffs of pediatric hospitalists. His patient load subsequently grew by 4-5 times, and he quit as of Jan. 7, 2023.
Dr. Lankford wrote that he found a new job at Parkview Regional Medical Center in Fort Wayne, but his former employer threatened to take action under the noncompete clause, and Parkview withdrew its offer.
Among other things, the new Indiana law says that the clauses are not enforceable “if physician terminates the physician’s employment for cause.”
The lawsuit asks for a judge to prevent Lutheran Health Network from enforcing the clause.
Impact on patients
The new Indiana law also bans noncompete clauses for primary care physicians. Kathleen A. DeLaney, JD, one of Dr. Lankford’s attorneys, said in an interview that this provision came about because rural legislators didn’t want to add to the challenges of attracting primary care doctors to move to their communities.
State legislators have become less friendly to noncompete clauses in medicine because they’re wary of the negative effects on patients, Evan Starr, PhD, said in an interview. The clauses prevent doctors from taking new jobs where they could continue to treat their previous patients, said Dr. Starr, associate professor in the department of management and organization at the University of Maryland.
However, he said, hospitals are fighting to preserve the clauses, arguing that they provide a base of patients to physicians in return for their agreement not to go work for a competitor.
The legal landscape may change even more. The Federal Trade Commission has proposed banning the clauses nationally, and a decision is expected in 2024. However, it’s an election year, which may delay a decision, attorney Ms. Murthy said, “and there is also language in the proposed rule that could exempt nonprofit hospitals, which further complicates the issues.”
For now, Ms. Murthy said, “we are still seeing noncompetes and other restrictive covenants in almost every contract we review in all 50 states and across all specialties. We explicitly explain to every client that they should only sign the agreement with the expectation that their specific noncompete will be enforced as written. Large employer groups, including hospital systems, will likely fight any kind of restriction or dilution of noncompetes, and these types of legal challenges could be tied up in court for many years.”
A version of this article first appeared on Medscape.com.
In a test of one of the nation’s most restrictive laws limiting noncompete clauses in medicine, an Indiana pediatric critical-care physician is suing to stop his former hospital employer from controlling his future employment prospects.
David Lankford, DO, acknowledges that he signed a contract with the Lutheran Health Network that included a noncompete clause. However,
Indiana’s law is notable among states because if a physician terminates his/her job for cause, the noncompete may be considered unenforceable.
“When you have physicians who are unable to work in their community, it creates a barrier for access to care for patients,” Dr. Lankford said in an interview. “I’m fighting to decrease barriers and continue to have patients be able to see their doctors in their own hometown or their own county.”
Lutheran Health’s media relations department did not respond to requests for comment.
Noncompete clauses ‘extremely common’
Non-compete clauses – which typically restrict when and where employees can take future jobs – are common in physician contracts, Anu Murthy, JD, who reviews employee contracts for a firm called Contract Diagnostics, said in an interview.
However, the tide has been turning against them.
About a dozen states and the District of Columbia have enacted legislation to limit the use of noncompetes in employment contracts, and about half of states have pending legislation that could dilute noncompete clauses, Ms. Murthy said. In June, the state of New York sent a noncompete ban bill to the governor’s desk.
For more about state-by-state restrictions on noncompete clauses, check this chart.
In his lawsuit, Dr. Lankford said he was hired in 2017 to work at Lutheran Hospital in Fort Wayne.
Dr. Lankford signed an employee renewal contract in 2020 that included a noncompete clause; his attorneys declined to provide details about the clause because of confidentiality restrictions.
In 2022, the lawsuit says, Lutheran Hospital told Dr. Lankford that he’d need to take on more work due to layoffs of pediatric hospitalists. His patient load subsequently grew by 4-5 times, and he quit as of Jan. 7, 2023.
Dr. Lankford wrote that he found a new job at Parkview Regional Medical Center in Fort Wayne, but his former employer threatened to take action under the noncompete clause, and Parkview withdrew its offer.
Among other things, the new Indiana law says that the clauses are not enforceable “if physician terminates the physician’s employment for cause.”
The lawsuit asks for a judge to prevent Lutheran Health Network from enforcing the clause.
Impact on patients
The new Indiana law also bans noncompete clauses for primary care physicians. Kathleen A. DeLaney, JD, one of Dr. Lankford’s attorneys, said in an interview that this provision came about because rural legislators didn’t want to add to the challenges of attracting primary care doctors to move to their communities.
State legislators have become less friendly to noncompete clauses in medicine because they’re wary of the negative effects on patients, Evan Starr, PhD, said in an interview. The clauses prevent doctors from taking new jobs where they could continue to treat their previous patients, said Dr. Starr, associate professor in the department of management and organization at the University of Maryland.
However, he said, hospitals are fighting to preserve the clauses, arguing that they provide a base of patients to physicians in return for their agreement not to go work for a competitor.
The legal landscape may change even more. The Federal Trade Commission has proposed banning the clauses nationally, and a decision is expected in 2024. However, it’s an election year, which may delay a decision, attorney Ms. Murthy said, “and there is also language in the proposed rule that could exempt nonprofit hospitals, which further complicates the issues.”
For now, Ms. Murthy said, “we are still seeing noncompetes and other restrictive covenants in almost every contract we review in all 50 states and across all specialties. We explicitly explain to every client that they should only sign the agreement with the expectation that their specific noncompete will be enforced as written. Large employer groups, including hospital systems, will likely fight any kind of restriction or dilution of noncompetes, and these types of legal challenges could be tied up in court for many years.”
A version of this article first appeared on Medscape.com.
In a test of one of the nation’s most restrictive laws limiting noncompete clauses in medicine, an Indiana pediatric critical-care physician is suing to stop his former hospital employer from controlling his future employment prospects.
David Lankford, DO, acknowledges that he signed a contract with the Lutheran Health Network that included a noncompete clause. However,
Indiana’s law is notable among states because if a physician terminates his/her job for cause, the noncompete may be considered unenforceable.
“When you have physicians who are unable to work in their community, it creates a barrier for access to care for patients,” Dr. Lankford said in an interview. “I’m fighting to decrease barriers and continue to have patients be able to see their doctors in their own hometown or their own county.”
Lutheran Health’s media relations department did not respond to requests for comment.
Noncompete clauses ‘extremely common’
Non-compete clauses – which typically restrict when and where employees can take future jobs – are common in physician contracts, Anu Murthy, JD, who reviews employee contracts for a firm called Contract Diagnostics, said in an interview.
However, the tide has been turning against them.
About a dozen states and the District of Columbia have enacted legislation to limit the use of noncompetes in employment contracts, and about half of states have pending legislation that could dilute noncompete clauses, Ms. Murthy said. In June, the state of New York sent a noncompete ban bill to the governor’s desk.
For more about state-by-state restrictions on noncompete clauses, check this chart.
In his lawsuit, Dr. Lankford said he was hired in 2017 to work at Lutheran Hospital in Fort Wayne.
Dr. Lankford signed an employee renewal contract in 2020 that included a noncompete clause; his attorneys declined to provide details about the clause because of confidentiality restrictions.
In 2022, the lawsuit says, Lutheran Hospital told Dr. Lankford that he’d need to take on more work due to layoffs of pediatric hospitalists. His patient load subsequently grew by 4-5 times, and he quit as of Jan. 7, 2023.
Dr. Lankford wrote that he found a new job at Parkview Regional Medical Center in Fort Wayne, but his former employer threatened to take action under the noncompete clause, and Parkview withdrew its offer.
Among other things, the new Indiana law says that the clauses are not enforceable “if physician terminates the physician’s employment for cause.”
The lawsuit asks for a judge to prevent Lutheran Health Network from enforcing the clause.
Impact on patients
The new Indiana law also bans noncompete clauses for primary care physicians. Kathleen A. DeLaney, JD, one of Dr. Lankford’s attorneys, said in an interview that this provision came about because rural legislators didn’t want to add to the challenges of attracting primary care doctors to move to their communities.
State legislators have become less friendly to noncompete clauses in medicine because they’re wary of the negative effects on patients, Evan Starr, PhD, said in an interview. The clauses prevent doctors from taking new jobs where they could continue to treat their previous patients, said Dr. Starr, associate professor in the department of management and organization at the University of Maryland.
However, he said, hospitals are fighting to preserve the clauses, arguing that they provide a base of patients to physicians in return for their agreement not to go work for a competitor.
The legal landscape may change even more. The Federal Trade Commission has proposed banning the clauses nationally, and a decision is expected in 2024. However, it’s an election year, which may delay a decision, attorney Ms. Murthy said, “and there is also language in the proposed rule that could exempt nonprofit hospitals, which further complicates the issues.”
For now, Ms. Murthy said, “we are still seeing noncompetes and other restrictive covenants in almost every contract we review in all 50 states and across all specialties. We explicitly explain to every client that they should only sign the agreement with the expectation that their specific noncompete will be enforced as written. Large employer groups, including hospital systems, will likely fight any kind of restriction or dilution of noncompetes, and these types of legal challenges could be tied up in court for many years.”
A version of this article first appeared on Medscape.com.
Immunotherapy stewardship could save tens of millions a year
Implementing stewardship strategies for immune checkpoint inhibitor (ICI) therapy, including personalized weight-based dosing, dose rounding, and pharmacy-level vial sharing, could generate savings of as much as $74 million each year for the Veterans Health Administration (VHA), a new analysis suggests.
That $74 million in savings would translate to nearly 14% less spent on ICI therapy annually.
first author Alex Bryant, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published in Health Affairs.
ICI therapy is used in about 40 unique cancer indications and, in 2020, accounted for more than $6 billion in Medicare Part B spending.
Two of the most prescribed ICIs – pembrolizumab and nivolumab – initially received their U.S. approval at personalized weight-based doses. But at the request of the manufacturers, the Food and Drug Administration approved “one-size-fits-all” flat doses, despite a lack of data to support this strategy compared with weight-based dosing.
With a fixed dose strategy, “patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel, told this news organization last year. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
To compare the cost of a weight-based vs. fixed-dose strategy, Dr. Bryant and colleagues conducted a simulation analysis under four stewardship scenarios, using data from the VHA and Medicare drug prices. Strategy one looked at weight-based dosing; strategy two combined weight-based dosing and dose rounding but not single-use vial sharing; strategy three used weight-based dosing and single-use vial sharing but not dose rounding; and strategy four, the most aggressive, combined all three.
ICIs in the VHA national formulary included pembrolizumab, nivolumab, atezolizumab, durvalumab, and cemiplimab-rwlc.
Using an algorithm to extract data, the team identified 49,851 administration events in 8,276 unique patients in 2021 – just over half were pembrolizumab, nearly 23% were nivolumab, and the remaining 26% largely included atezolizumab (12.1%) and durvalumab (11.9%).
The team found that the VHA spends roughly $537 million annually on ICIs. But implementing the stewardship measures that combined weight-based dosing, dose rounding, and vial sharing could save the VHA $74 million, or about 14%, annually on ICIs.
Most of the savings came from dosing changes to pembrolizumab and nivolumab, with greater savings achieved by combining more stewardship strategies. For instance, using strategy one (weight-based dosing alone) could lead to annual pembrolizumab savings of $14 million. Adding dose rounding (strategy two) could reduce pembrolizumab spending by $24 million. And using strategy four, with an unlimited window for vial sharing, could mean annual savings of nearly $60 million.
“Our results should prompt cost-conscious systems and payers to ask whether the amounts of drugs they’re providing to patients and how they go about making those doses are the most cost-effective approaches,” said corresponding author Garth W. Strohbehn, MD, of the University of Michigan and the VA Ann Arbor Healthcare System.
Dr. Strohbehn said the prospect of adopting these strategies hinges on several factors, with financial incentives at the prescriber and medical center level likely being the most influential.
“In fee-for-service systems, reimbursement scales with the amount of drug administered, so there can be a financial disincentive to decreasing overall drug usage,” Dr. Strohbehn explained.
“Conversely, integrated systems such as Kaiser Permanente or the VHA and large self-insured employers are incentivized to contain costs and take great care of patients, so they may be more inclined to promote these strategies,” he added.
However, Adam C. Powell, PhD, president, Payer+Provider Syndicate, who wasn’t involved in the analysis, cautioned that such a shift may come with unintended consequences.
The Infrastructure, Investment, and Jobs Act of 2021 let the Centers for Medicare and Medicaid Services seek reimbursement for discarded drugs – in effect, changing the reimbursement model for medications. That led pharmaceutical manufacturers to respond in kind by changing the dosing model, Dr. Powell said.
“Drugs that previously had personalized weight-based dosing were moved to uniform flat dosing, eliminating the potential for the manufacturer to have to issue a reimbursement if the patient’s personalized dose fell short of the amount in the single-use vial,” Dr. Powell added.
If there is a substantial migration to weight-based dosing, “it is possible that pharmaceutical manufacturers will rethink their dosing and pricing models, just as happened previously,” he cautioned.
However, these strategies could also provide relief for another escalating issue: drug shortages. Especially in the current moment, having a stewardship mindset, “might be helpful in navigating drug shortages,” Dr. Strohbehn said.
This research had no commercial funding. Dr. Bryant, Dr. Strohbehn, and Dr. Powell report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Implementing stewardship strategies for immune checkpoint inhibitor (ICI) therapy, including personalized weight-based dosing, dose rounding, and pharmacy-level vial sharing, could generate savings of as much as $74 million each year for the Veterans Health Administration (VHA), a new analysis suggests.
That $74 million in savings would translate to nearly 14% less spent on ICI therapy annually.
first author Alex Bryant, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published in Health Affairs.
ICI therapy is used in about 40 unique cancer indications and, in 2020, accounted for more than $6 billion in Medicare Part B spending.
Two of the most prescribed ICIs – pembrolizumab and nivolumab – initially received their U.S. approval at personalized weight-based doses. But at the request of the manufacturers, the Food and Drug Administration approved “one-size-fits-all” flat doses, despite a lack of data to support this strategy compared with weight-based dosing.
With a fixed dose strategy, “patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel, told this news organization last year. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
To compare the cost of a weight-based vs. fixed-dose strategy, Dr. Bryant and colleagues conducted a simulation analysis under four stewardship scenarios, using data from the VHA and Medicare drug prices. Strategy one looked at weight-based dosing; strategy two combined weight-based dosing and dose rounding but not single-use vial sharing; strategy three used weight-based dosing and single-use vial sharing but not dose rounding; and strategy four, the most aggressive, combined all three.
ICIs in the VHA national formulary included pembrolizumab, nivolumab, atezolizumab, durvalumab, and cemiplimab-rwlc.
Using an algorithm to extract data, the team identified 49,851 administration events in 8,276 unique patients in 2021 – just over half were pembrolizumab, nearly 23% were nivolumab, and the remaining 26% largely included atezolizumab (12.1%) and durvalumab (11.9%).
The team found that the VHA spends roughly $537 million annually on ICIs. But implementing the stewardship measures that combined weight-based dosing, dose rounding, and vial sharing could save the VHA $74 million, or about 14%, annually on ICIs.
Most of the savings came from dosing changes to pembrolizumab and nivolumab, with greater savings achieved by combining more stewardship strategies. For instance, using strategy one (weight-based dosing alone) could lead to annual pembrolizumab savings of $14 million. Adding dose rounding (strategy two) could reduce pembrolizumab spending by $24 million. And using strategy four, with an unlimited window for vial sharing, could mean annual savings of nearly $60 million.
“Our results should prompt cost-conscious systems and payers to ask whether the amounts of drugs they’re providing to patients and how they go about making those doses are the most cost-effective approaches,” said corresponding author Garth W. Strohbehn, MD, of the University of Michigan and the VA Ann Arbor Healthcare System.
Dr. Strohbehn said the prospect of adopting these strategies hinges on several factors, with financial incentives at the prescriber and medical center level likely being the most influential.
“In fee-for-service systems, reimbursement scales with the amount of drug administered, so there can be a financial disincentive to decreasing overall drug usage,” Dr. Strohbehn explained.
“Conversely, integrated systems such as Kaiser Permanente or the VHA and large self-insured employers are incentivized to contain costs and take great care of patients, so they may be more inclined to promote these strategies,” he added.
However, Adam C. Powell, PhD, president, Payer+Provider Syndicate, who wasn’t involved in the analysis, cautioned that such a shift may come with unintended consequences.
The Infrastructure, Investment, and Jobs Act of 2021 let the Centers for Medicare and Medicaid Services seek reimbursement for discarded drugs – in effect, changing the reimbursement model for medications. That led pharmaceutical manufacturers to respond in kind by changing the dosing model, Dr. Powell said.
“Drugs that previously had personalized weight-based dosing were moved to uniform flat dosing, eliminating the potential for the manufacturer to have to issue a reimbursement if the patient’s personalized dose fell short of the amount in the single-use vial,” Dr. Powell added.
If there is a substantial migration to weight-based dosing, “it is possible that pharmaceutical manufacturers will rethink their dosing and pricing models, just as happened previously,” he cautioned.
However, these strategies could also provide relief for another escalating issue: drug shortages. Especially in the current moment, having a stewardship mindset, “might be helpful in navigating drug shortages,” Dr. Strohbehn said.
This research had no commercial funding. Dr. Bryant, Dr. Strohbehn, and Dr. Powell report no relevant financial relationships.
A version of this article appeared on Medscape.com.
Implementing stewardship strategies for immune checkpoint inhibitor (ICI) therapy, including personalized weight-based dosing, dose rounding, and pharmacy-level vial sharing, could generate savings of as much as $74 million each year for the Veterans Health Administration (VHA), a new analysis suggests.
That $74 million in savings would translate to nearly 14% less spent on ICI therapy annually.
first author Alex Bryant, MD, University of Michigan, Ann Arbor, said in an interview.
The study was published in Health Affairs.
ICI therapy is used in about 40 unique cancer indications and, in 2020, accounted for more than $6 billion in Medicare Part B spending.
Two of the most prescribed ICIs – pembrolizumab and nivolumab – initially received their U.S. approval at personalized weight-based doses. But at the request of the manufacturers, the Food and Drug Administration approved “one-size-fits-all” flat doses, despite a lack of data to support this strategy compared with weight-based dosing.
With a fixed dose strategy, “patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel, told this news organization last year. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
To compare the cost of a weight-based vs. fixed-dose strategy, Dr. Bryant and colleagues conducted a simulation analysis under four stewardship scenarios, using data from the VHA and Medicare drug prices. Strategy one looked at weight-based dosing; strategy two combined weight-based dosing and dose rounding but not single-use vial sharing; strategy three used weight-based dosing and single-use vial sharing but not dose rounding; and strategy four, the most aggressive, combined all three.
ICIs in the VHA national formulary included pembrolizumab, nivolumab, atezolizumab, durvalumab, and cemiplimab-rwlc.
Using an algorithm to extract data, the team identified 49,851 administration events in 8,276 unique patients in 2021 – just over half were pembrolizumab, nearly 23% were nivolumab, and the remaining 26% largely included atezolizumab (12.1%) and durvalumab (11.9%).
The team found that the VHA spends roughly $537 million annually on ICIs. But implementing the stewardship measures that combined weight-based dosing, dose rounding, and vial sharing could save the VHA $74 million, or about 14%, annually on ICIs.
Most of the savings came from dosing changes to pembrolizumab and nivolumab, with greater savings achieved by combining more stewardship strategies. For instance, using strategy one (weight-based dosing alone) could lead to annual pembrolizumab savings of $14 million. Adding dose rounding (strategy two) could reduce pembrolizumab spending by $24 million. And using strategy four, with an unlimited window for vial sharing, could mean annual savings of nearly $60 million.
“Our results should prompt cost-conscious systems and payers to ask whether the amounts of drugs they’re providing to patients and how they go about making those doses are the most cost-effective approaches,” said corresponding author Garth W. Strohbehn, MD, of the University of Michigan and the VA Ann Arbor Healthcare System.
Dr. Strohbehn said the prospect of adopting these strategies hinges on several factors, with financial incentives at the prescriber and medical center level likely being the most influential.
“In fee-for-service systems, reimbursement scales with the amount of drug administered, so there can be a financial disincentive to decreasing overall drug usage,” Dr. Strohbehn explained.
“Conversely, integrated systems such as Kaiser Permanente or the VHA and large self-insured employers are incentivized to contain costs and take great care of patients, so they may be more inclined to promote these strategies,” he added.
However, Adam C. Powell, PhD, president, Payer+Provider Syndicate, who wasn’t involved in the analysis, cautioned that such a shift may come with unintended consequences.
The Infrastructure, Investment, and Jobs Act of 2021 let the Centers for Medicare and Medicaid Services seek reimbursement for discarded drugs – in effect, changing the reimbursement model for medications. That led pharmaceutical manufacturers to respond in kind by changing the dosing model, Dr. Powell said.
“Drugs that previously had personalized weight-based dosing were moved to uniform flat dosing, eliminating the potential for the manufacturer to have to issue a reimbursement if the patient’s personalized dose fell short of the amount in the single-use vial,” Dr. Powell added.
If there is a substantial migration to weight-based dosing, “it is possible that pharmaceutical manufacturers will rethink their dosing and pricing models, just as happened previously,” he cautioned.
However, these strategies could also provide relief for another escalating issue: drug shortages. Especially in the current moment, having a stewardship mindset, “might be helpful in navigating drug shortages,” Dr. Strohbehn said.
This research had no commercial funding. Dr. Bryant, Dr. Strohbehn, and Dr. Powell report no relevant financial relationships.
A version of this article appeared on Medscape.com.
FROM HEALTH AFFAIRS
For love or money: How do doctors choose their specialty?
Medical student loans top hundreds of thousands of dollars, so it’s understandable that physicians may want to select a specialty that pays well.
Moreover, most advised young doctors to follow their hearts rather than their wallets.
“There is no question that many young kids immediately think about money when deciding to pursue medicine, but the thought of a big paycheck will never sustain someone long enough to get them here,” says Sergio Alvarez, MD, a board-certified plastic surgeon based in Miami, Fla., and the CEO and medical director of Mia Aesthetics, which has several national locations.
“Getting into medicine is a long game, and there are many hurdles along the way that only the dedicated overcome,” says Dr. Alvarez.
Unfortunately, he says it may be late in that long game before some realize that the pay rate for certain specialties isn’t commensurate with the immense workload and responsibility they require.
“The short of it is that to become a happy doctor, medicine really needs to be a calling: a passion! There are far easier things to do to make money.”
Here is what physicians said about choosing between love or money.
The lowest-paying subspecialty in a low-paying specialty
Sophia Yen, MD, MPH, cofounder and CEO of Pandia Health, a women-founded, doctor-led birth control delivery service in Sunnyvale, Calif., and clinical associate professor at Stanford (Calif.) University, says you should pursue a specialty because you love the work.
“I chose the lowest-paying subspecialty (adolescent medicine) of a low-paying specialty (pediatrics), but I’d do it all again because I love the patient population – I love what I do.”
Dr. Yen says she chose adolescent medicine because she loves doing “outpatient gynecology” without going through the surgical training of a full ob.gyn. “I love the target population of young adults because you can talk to the patient versus in pediatrics, where you often talk to the parent. With young adults you can catch things – for example, teach a young person about consent, alcohol, marijuana’s effects on the growing brain, prevent unplanned pregnancies and sexually transmitted infections, instill healthy eating, and more.
“Do I wish that I got paid as much as a surgeon?” Dr. Yen says yes. “I hope that someday society will realize the time spent preventing future disease is worth it and pay us accordingly.”
Unfortunately, she says, since the health care system makes more money if you get pregnant, need a cardiac bypass, or need gastric surgery, those who deliver babies or do surgery get paid more than someone who prevents the need for those services.
Money doesn’t buy happiness
Stella Bard, MD, a rheumatologist in McKinney, Tex., says she eats, lives, and breathes rheumatology. “I never regret the decision of choosing this specialty for a single second,” says Dr. Bard. “I feel like it’s a rewarding experience with every single patient encounter.” Dr. Bard notes that money is no guarantee of happiness and that she feels blessed to wake up every morning doing what she loves.
Career or calling?
For Dr. Alvarez, inspiration came when watching his father help change people’s lives. “I saw how impactful a doctor is during a person’s most desperate moments, and that was enough to make medicine my life’s passion at the age of 10.”
He says once you’re in medical school, choosing a specialty is far easier than you think. “Each specialty requires a certain personality or specific characteristics, and some will call to you while others simply won’t.”
“For me, plastics was about finesse, art, and life-changing surgeries that affected people from kids to adults and involved every aspect of the human body. Changing someone’s outward appearance has a profoundly positive impact on their confidence and self-esteem, making plastic surgery a genuinely transformative experience.”
Patricia Celan, MD, a postgraduate psychiatry resident in Canada, also chose psychiatry for the love of the field. “I enjoy helping vulnerable people and exploring what makes a person tick, the source of their difficulties, and how to help people counteract and overcome the difficult cards they’ve been dealt in life.”
She says it’s incredibly rewarding to watch someone turn their life around from severe mental illness, especially those who have been victimized and traumatized, and learn to trust people again.
“I could have made more money in a higher-paying specialty, yes, but I’m not sure I would have felt as fulfilled as psychiatry can make me feel.”
Dr. Celan says everyone has their calling, and some lucky people find their deepest passion in higher-paying specialties. “My calling is psychiatry, and I am at peace with this no matter the money.”
For the love of surgery
“In my experience, most people don’t choose their specialty based on money,” says Nicole Aaronson, MD, MBA, an otolaryngologist and board-certified in the subspecialty of pediatric otolaryngology, an attending surgeon at Nemours Children’s Health of Delaware and clinical associate professor of otolaryngology and pediatrics at Sidney Kimmel Medical College, Philadelphia.
“The first decision point in medical school is usually figuring out if you are a surgery person or a medicine person. I knew very early that I wanted to be a surgeon and wanted to spend time in the OR fixing problems with my hands.”
Part of what attracted Dr. Aaronson to otolaryngology was the variety of conditions managed within the specialty, from head and neck cancer to voice problems to sleep disorders to sinus disease. “I chose my subspecialty because I enjoy working with children and making an impact that will help them live their best possible lives.”
She says a relatively simple surgery like placing ear tubes may help a child’s hearing and allow them to be more successful in school, opening up a new world of opportunities for the child’s future.
“While I don’t think most people choose their specialty based on prospective compensation, I do think all physicians want to be compensated fairly for their time, effort, and level of training,” says Dr. Aaronson.
Choosing a specialty for the money can lead to burnout and dissatisfaction
“For me, the decision to pursue gastroenterology went beyond financial considerations,” says Saurabh Sethi, MD, MPH, a gastroenterologist specializing in hepatology and interventional endoscopy. “While financial stability is undoubtedly important, no doctor enters this field solely for the love of money. The primary driving force for most medical professionals, myself included, is the passion to help people and make a positive difference in their lives.”
Dr. Sethi says the gratification that comes from providing quality care and witnessing patients’ improved well-being is priceless. Moreover, he believes that selecting a specialty based solely on financial gain is likely to lead to burnout and greater dissatisfaction over time.
“By following my love for gut health and prioritizing patient care, I have found a sense of fulfillment and purpose in my career. It has been a rewarding journey, and I’m grateful for the opportunity to contribute to the well-being of my patients through my expertise in gastroenterology.”
Key takeaways: Love or money?
Multiple factors influence doctors’ specialty choices, including genuine love for the work and the future of the specialty. Others include job prospects, hands-on experience they receive, mentors, childhood dreams, parental expectations, complexity of cases, the lifestyle of each specialty, including office hours worked, on-call requirements, and autonomy.
Physicians also mentioned other factors they considered when choosing their specialty:
- Personal interest.
- Intellectual stimulation.
- Work-life balance.
- Patient populations.
- Future opportunities.
- Desire to make a difference.
- Passion.
- Financial stability.
- Being personally fulfilled.
Overwhelmingly, doctors say to pick a specialty you can envision yourself loving 40 years from now and you won’t go wrong.
A version of this article first appeared on Medscape.com.
Medical student loans top hundreds of thousands of dollars, so it’s understandable that physicians may want to select a specialty that pays well.
Moreover, most advised young doctors to follow their hearts rather than their wallets.
“There is no question that many young kids immediately think about money when deciding to pursue medicine, but the thought of a big paycheck will never sustain someone long enough to get them here,” says Sergio Alvarez, MD, a board-certified plastic surgeon based in Miami, Fla., and the CEO and medical director of Mia Aesthetics, which has several national locations.
“Getting into medicine is a long game, and there are many hurdles along the way that only the dedicated overcome,” says Dr. Alvarez.
Unfortunately, he says it may be late in that long game before some realize that the pay rate for certain specialties isn’t commensurate with the immense workload and responsibility they require.
“The short of it is that to become a happy doctor, medicine really needs to be a calling: a passion! There are far easier things to do to make money.”
Here is what physicians said about choosing between love or money.
The lowest-paying subspecialty in a low-paying specialty
Sophia Yen, MD, MPH, cofounder and CEO of Pandia Health, a women-founded, doctor-led birth control delivery service in Sunnyvale, Calif., and clinical associate professor at Stanford (Calif.) University, says you should pursue a specialty because you love the work.
“I chose the lowest-paying subspecialty (adolescent medicine) of a low-paying specialty (pediatrics), but I’d do it all again because I love the patient population – I love what I do.”
Dr. Yen says she chose adolescent medicine because she loves doing “outpatient gynecology” without going through the surgical training of a full ob.gyn. “I love the target population of young adults because you can talk to the patient versus in pediatrics, where you often talk to the parent. With young adults you can catch things – for example, teach a young person about consent, alcohol, marijuana’s effects on the growing brain, prevent unplanned pregnancies and sexually transmitted infections, instill healthy eating, and more.
“Do I wish that I got paid as much as a surgeon?” Dr. Yen says yes. “I hope that someday society will realize the time spent preventing future disease is worth it and pay us accordingly.”
Unfortunately, she says, since the health care system makes more money if you get pregnant, need a cardiac bypass, or need gastric surgery, those who deliver babies or do surgery get paid more than someone who prevents the need for those services.
Money doesn’t buy happiness
Stella Bard, MD, a rheumatologist in McKinney, Tex., says she eats, lives, and breathes rheumatology. “I never regret the decision of choosing this specialty for a single second,” says Dr. Bard. “I feel like it’s a rewarding experience with every single patient encounter.” Dr. Bard notes that money is no guarantee of happiness and that she feels blessed to wake up every morning doing what she loves.
Career or calling?
For Dr. Alvarez, inspiration came when watching his father help change people’s lives. “I saw how impactful a doctor is during a person’s most desperate moments, and that was enough to make medicine my life’s passion at the age of 10.”
He says once you’re in medical school, choosing a specialty is far easier than you think. “Each specialty requires a certain personality or specific characteristics, and some will call to you while others simply won’t.”
“For me, plastics was about finesse, art, and life-changing surgeries that affected people from kids to adults and involved every aspect of the human body. Changing someone’s outward appearance has a profoundly positive impact on their confidence and self-esteem, making plastic surgery a genuinely transformative experience.”
Patricia Celan, MD, a postgraduate psychiatry resident in Canada, also chose psychiatry for the love of the field. “I enjoy helping vulnerable people and exploring what makes a person tick, the source of their difficulties, and how to help people counteract and overcome the difficult cards they’ve been dealt in life.”
She says it’s incredibly rewarding to watch someone turn their life around from severe mental illness, especially those who have been victimized and traumatized, and learn to trust people again.
“I could have made more money in a higher-paying specialty, yes, but I’m not sure I would have felt as fulfilled as psychiatry can make me feel.”
Dr. Celan says everyone has their calling, and some lucky people find their deepest passion in higher-paying specialties. “My calling is psychiatry, and I am at peace with this no matter the money.”
For the love of surgery
“In my experience, most people don’t choose their specialty based on money,” says Nicole Aaronson, MD, MBA, an otolaryngologist and board-certified in the subspecialty of pediatric otolaryngology, an attending surgeon at Nemours Children’s Health of Delaware and clinical associate professor of otolaryngology and pediatrics at Sidney Kimmel Medical College, Philadelphia.
“The first decision point in medical school is usually figuring out if you are a surgery person or a medicine person. I knew very early that I wanted to be a surgeon and wanted to spend time in the OR fixing problems with my hands.”
Part of what attracted Dr. Aaronson to otolaryngology was the variety of conditions managed within the specialty, from head and neck cancer to voice problems to sleep disorders to sinus disease. “I chose my subspecialty because I enjoy working with children and making an impact that will help them live their best possible lives.”
She says a relatively simple surgery like placing ear tubes may help a child’s hearing and allow them to be more successful in school, opening up a new world of opportunities for the child’s future.
“While I don’t think most people choose their specialty based on prospective compensation, I do think all physicians want to be compensated fairly for their time, effort, and level of training,” says Dr. Aaronson.
Choosing a specialty for the money can lead to burnout and dissatisfaction
“For me, the decision to pursue gastroenterology went beyond financial considerations,” says Saurabh Sethi, MD, MPH, a gastroenterologist specializing in hepatology and interventional endoscopy. “While financial stability is undoubtedly important, no doctor enters this field solely for the love of money. The primary driving force for most medical professionals, myself included, is the passion to help people and make a positive difference in their lives.”
Dr. Sethi says the gratification that comes from providing quality care and witnessing patients’ improved well-being is priceless. Moreover, he believes that selecting a specialty based solely on financial gain is likely to lead to burnout and greater dissatisfaction over time.
“By following my love for gut health and prioritizing patient care, I have found a sense of fulfillment and purpose in my career. It has been a rewarding journey, and I’m grateful for the opportunity to contribute to the well-being of my patients through my expertise in gastroenterology.”
Key takeaways: Love or money?
Multiple factors influence doctors’ specialty choices, including genuine love for the work and the future of the specialty. Others include job prospects, hands-on experience they receive, mentors, childhood dreams, parental expectations, complexity of cases, the lifestyle of each specialty, including office hours worked, on-call requirements, and autonomy.
Physicians also mentioned other factors they considered when choosing their specialty:
- Personal interest.
- Intellectual stimulation.
- Work-life balance.
- Patient populations.
- Future opportunities.
- Desire to make a difference.
- Passion.
- Financial stability.
- Being personally fulfilled.
Overwhelmingly, doctors say to pick a specialty you can envision yourself loving 40 years from now and you won’t go wrong.
A version of this article first appeared on Medscape.com.
Medical student loans top hundreds of thousands of dollars, so it’s understandable that physicians may want to select a specialty that pays well.
Moreover, most advised young doctors to follow their hearts rather than their wallets.
“There is no question that many young kids immediately think about money when deciding to pursue medicine, but the thought of a big paycheck will never sustain someone long enough to get them here,” says Sergio Alvarez, MD, a board-certified plastic surgeon based in Miami, Fla., and the CEO and medical director of Mia Aesthetics, which has several national locations.
“Getting into medicine is a long game, and there are many hurdles along the way that only the dedicated overcome,” says Dr. Alvarez.
Unfortunately, he says it may be late in that long game before some realize that the pay rate for certain specialties isn’t commensurate with the immense workload and responsibility they require.
“The short of it is that to become a happy doctor, medicine really needs to be a calling: a passion! There are far easier things to do to make money.”
Here is what physicians said about choosing between love or money.
The lowest-paying subspecialty in a low-paying specialty
Sophia Yen, MD, MPH, cofounder and CEO of Pandia Health, a women-founded, doctor-led birth control delivery service in Sunnyvale, Calif., and clinical associate professor at Stanford (Calif.) University, says you should pursue a specialty because you love the work.
“I chose the lowest-paying subspecialty (adolescent medicine) of a low-paying specialty (pediatrics), but I’d do it all again because I love the patient population – I love what I do.”
Dr. Yen says she chose adolescent medicine because she loves doing “outpatient gynecology” without going through the surgical training of a full ob.gyn. “I love the target population of young adults because you can talk to the patient versus in pediatrics, where you often talk to the parent. With young adults you can catch things – for example, teach a young person about consent, alcohol, marijuana’s effects on the growing brain, prevent unplanned pregnancies and sexually transmitted infections, instill healthy eating, and more.
“Do I wish that I got paid as much as a surgeon?” Dr. Yen says yes. “I hope that someday society will realize the time spent preventing future disease is worth it and pay us accordingly.”
Unfortunately, she says, since the health care system makes more money if you get pregnant, need a cardiac bypass, or need gastric surgery, those who deliver babies or do surgery get paid more than someone who prevents the need for those services.
Money doesn’t buy happiness
Stella Bard, MD, a rheumatologist in McKinney, Tex., says she eats, lives, and breathes rheumatology. “I never regret the decision of choosing this specialty for a single second,” says Dr. Bard. “I feel like it’s a rewarding experience with every single patient encounter.” Dr. Bard notes that money is no guarantee of happiness and that she feels blessed to wake up every morning doing what she loves.
Career or calling?
For Dr. Alvarez, inspiration came when watching his father help change people’s lives. “I saw how impactful a doctor is during a person’s most desperate moments, and that was enough to make medicine my life’s passion at the age of 10.”
He says once you’re in medical school, choosing a specialty is far easier than you think. “Each specialty requires a certain personality or specific characteristics, and some will call to you while others simply won’t.”
“For me, plastics was about finesse, art, and life-changing surgeries that affected people from kids to adults and involved every aspect of the human body. Changing someone’s outward appearance has a profoundly positive impact on their confidence and self-esteem, making plastic surgery a genuinely transformative experience.”
Patricia Celan, MD, a postgraduate psychiatry resident in Canada, also chose psychiatry for the love of the field. “I enjoy helping vulnerable people and exploring what makes a person tick, the source of their difficulties, and how to help people counteract and overcome the difficult cards they’ve been dealt in life.”
She says it’s incredibly rewarding to watch someone turn their life around from severe mental illness, especially those who have been victimized and traumatized, and learn to trust people again.
“I could have made more money in a higher-paying specialty, yes, but I’m not sure I would have felt as fulfilled as psychiatry can make me feel.”
Dr. Celan says everyone has their calling, and some lucky people find their deepest passion in higher-paying specialties. “My calling is psychiatry, and I am at peace with this no matter the money.”
For the love of surgery
“In my experience, most people don’t choose their specialty based on money,” says Nicole Aaronson, MD, MBA, an otolaryngologist and board-certified in the subspecialty of pediatric otolaryngology, an attending surgeon at Nemours Children’s Health of Delaware and clinical associate professor of otolaryngology and pediatrics at Sidney Kimmel Medical College, Philadelphia.
“The first decision point in medical school is usually figuring out if you are a surgery person or a medicine person. I knew very early that I wanted to be a surgeon and wanted to spend time in the OR fixing problems with my hands.”
Part of what attracted Dr. Aaronson to otolaryngology was the variety of conditions managed within the specialty, from head and neck cancer to voice problems to sleep disorders to sinus disease. “I chose my subspecialty because I enjoy working with children and making an impact that will help them live their best possible lives.”
She says a relatively simple surgery like placing ear tubes may help a child’s hearing and allow them to be more successful in school, opening up a new world of opportunities for the child’s future.
“While I don’t think most people choose their specialty based on prospective compensation, I do think all physicians want to be compensated fairly for their time, effort, and level of training,” says Dr. Aaronson.
Choosing a specialty for the money can lead to burnout and dissatisfaction
“For me, the decision to pursue gastroenterology went beyond financial considerations,” says Saurabh Sethi, MD, MPH, a gastroenterologist specializing in hepatology and interventional endoscopy. “While financial stability is undoubtedly important, no doctor enters this field solely for the love of money. The primary driving force for most medical professionals, myself included, is the passion to help people and make a positive difference in their lives.”
Dr. Sethi says the gratification that comes from providing quality care and witnessing patients’ improved well-being is priceless. Moreover, he believes that selecting a specialty based solely on financial gain is likely to lead to burnout and greater dissatisfaction over time.
“By following my love for gut health and prioritizing patient care, I have found a sense of fulfillment and purpose in my career. It has been a rewarding journey, and I’m grateful for the opportunity to contribute to the well-being of my patients through my expertise in gastroenterology.”
Key takeaways: Love or money?
Multiple factors influence doctors’ specialty choices, including genuine love for the work and the future of the specialty. Others include job prospects, hands-on experience they receive, mentors, childhood dreams, parental expectations, complexity of cases, the lifestyle of each specialty, including office hours worked, on-call requirements, and autonomy.
Physicians also mentioned other factors they considered when choosing their specialty:
- Personal interest.
- Intellectual stimulation.
- Work-life balance.
- Patient populations.
- Future opportunities.
- Desire to make a difference.
- Passion.
- Financial stability.
- Being personally fulfilled.
Overwhelmingly, doctors say to pick a specialty you can envision yourself loving 40 years from now and you won’t go wrong.
A version of this article first appeared on Medscape.com.
Gender and racial biases in Press Ganey patient satisfaction surveys

Patient satisfaction questionnaires were developed in the 1980s as part of the movement to better understand the patient’s experience and their perspective of the quality of care. In 1985, the Press Ganey survey—now the most widely used method to assess patient satisfaction—was developed by 2 professors in anthropology and sociology-statistics at Notre Dame. Initially intended for inpatient admissions, the survey was validated based on a few thousand survey results.1 Given the strong interest in improving patient satisfaction at the time, it became widely adopted and quickly expanded into outpatient encounters and ambulatory surgery settings.
Although other surveys have been developed,2 the Press Ganey survey is the most commonly used assessment tool for patient satisfaction metrics in the United States, with approximately 50% of all hospitals and more than 41,000 health care organizations using its services.3,4 The survey consists of 6 domains related to satisfaction with:
1. the care provider
2. the nurse or assistant
3. personal issues
4. overall assessment
5. access
6. moving through the visit.
Survey items are scored using a 5-point Likert scale, with scores ranging from “very poor” (a score of 1) to “very good” (a score of 5). According to the company, because this format is balanced and parallel (unlike a “poor” to “excellent” format), responses can be quantified and used statistically without violating methodologic assumptions. Also, variability in patients’ responses with this format allows for the identification of opportunities to improve, unlike “yes/no” response formats.1 There are limitations to this design, however, which can impact data quality,5 as we will see.
Adoption of the survey as we move toward value-based care
More recently, patients’ satisfaction with their health care has received increased attention as we move to a patient-centered care model and as health care reimbursement models shift toward value-based care. Current trends in health care policy statements include the importance of raising the standard of care and shifting from a “fee-for-service” to a “pay-for-performance” reimbursement model.7,8 As a result, hospitals are establishing systems to measure “performance” that are not nationally standardized or extensively studied with objective measures. The changing standard of health care expectations in the United States is a topic of much public debate.9 And as expectations and new standards are defined, the impact of implementing novel measures of performance should be evaluated prior to widespread adoption and utilization.
Patient satisfaction also has been identified as a driver for hospital finances through loyalty, described as the “likelihood to return to that system for future medical services.”10,11 This measure has contributed to policy changes that reinforce prioritization of patient satisfaction. For example, the Affordable Care Act tied Medicare reimbursement and patient satisfaction together in the Hospital Value-Based Purchasing Program. This program uses measures of clinical processes, efficiency, outcomes, and patient experiences to calculate a total score that results in hospital reimbursement and incentives,12 which creates a direct pathway from patient experience to reimbursement—underscoring hospitals’ desire for ongoing assessment of patient satisfaction.
In 2005, the Centers for Medicare and Medicaid Services and the Agency for Health care Research and Quality developed the Hospital Consumer Assessment of Health care Providers and Systems (HCAHPS) survey in response to criticisms of the Press Ganey survey. The HCAHPS survey consists of 27 questions with 3 broad goals19:
- to produce data about patients’ perspectives of care that allow for objective and meaningful comparisons of hospitals
- to publicly report survey results and create new incentives for hospitals to improve quality of care
- to produce public reports that enhance accountability by increasing transparency.
One difference with the HCAHPS is that it measures frequency, or how often a service was performed (“never”, “sometimes”, “usually”, “always”), whereas Press Ganey measures satisfaction. It also only surveys inpatients and does not address outpatient encounters. Despite the differences, it is a widely used patient satisfaction survey and is subject to similar issues and biases as the Press Ganey survey.
Continue to: Gender, race, and age bias...
Gender, race, and age bias
Although the rationale behind gathering patient input is important, recent data suggest that patient satisfaction surveys are subject to inherent biases.6,13,14 These biases tend to negatively impact women and non-White physicians, adding to the systemic discrimination against women and physicians of color that already exists in health care.
In a single-site retrospective study performed in 2018 by Rogo-Gupta et al, female gynecologists were found to be 47% less likely to receive top patient satisfaction scores than their male counterparts owing to their gender alone, suggesting that gender bias may impact the results of patient satisfaction questionnaires.13 The authors encouraged that the results of patient satisfaction surveys be interpreted with great caution until the impact on female physicians is better understood.
A multi-center study by the same group (Rogo-Gupta et al) assessed the same construct across 5 different geographically diverse institutions.15 This study confirmed that female gynecologists were less likely to receive a top satisfaction score from their patients (19% lower odds when compared with male gynecologists). They also studied the effects of other patient demographics, including age, race/ethnicity, and race concordance. Older patients (aged ≥63 years) had an over-3-fold increase in odds of providing a top satisfaction score than younger patients. Additionally, Asian physicians had significantly lower odds of receiving a top satisfaction score when compared with White physicians, while Asian patients had significantly lower odds of providing a top satisfaction score when compared with White patients. Lastly, in most cases, when underrepresented-in-medicine patients saw an underrepresented-in-medicine physician (race concordance), there was a significant increase in odds of receiving a top satisfaction score. Asian race concordance, however, actually resulted in a lower likelihood of receiving a top satisfaction score.15
Literature from other specialties supports these findings. These results are consistent with emerging data from other medical specialties that also suggest that Press Ganey survey data are subject to inherent biases. For example, data from emergency medicine literature have shown discrepancies between patient satisfaction for providers at tertiary inner-city institutions versus those in affluent suburban populations,16 and that worse mortality is actually correlated with better patient satisfaction scores, and vice versa.17
Another study by Sotto-Santiago in 2019 assessed patient satisfaction scores in multiple specialties at a single institution where quality-related financial incentives were offered based on this metric. They found a significant difference in patient satisfaction scores between underrepresented and White physicians, which suggests a potential bias among patients and institutional practices—ultimately leading to pay inequities through differences in financial incentives.18
Percentile differences reveal small gaps in satisfaction ratings
When examining the difference between raw Press Ganey patient satisfaction data and the percentiles associated with these scores, an interesting finding arises. Looking at the 2023 multicenter study by Rogo-Gupta et al, the difference in the top raw scores between male and female gynecologists appears to be small (3.3%).15 However, in 2020, the difference in top scores separating the top (75th) and bottom (25th) percentile quartiles of physicians was also small, at only 6.9%.
Considering the percentiles, if a provider who scores in the 25th percentile is compared with a colleague who scores in the 75th percentile, they may think the reported satisfaction score differences were quite large. This may potentially invoke feelings of decreased self-worth, negatively impact their professional identity or overall well-being, and they may seek (or be told to seek) improvement opportunities. Now imagine the provider in question realizes the difference between the 25th percentile and 75th percentile is actually only 6.9%. This information may completely change how the results are interpreted and acted upon by administrators. This is further changed with the understanding that 3.3% of the difference may be due to gender alone, narrowing the gap even further. Providers would become understandably frustrated if measures of success such as reimbursement, financial bonus or incentives, promotion, or advancement are linked to these results. It violates the value of fairness and does not offer an equitable starting point.
Evolution of the data distribution. Another consideration, as noted by Robert C. Lloyd, PhD, one of the statisticians who helped develop the percentile statistical analysis mapping in 1985, is that it was based on a classic bell-shaped distribution of patient satisfaction survey scores.19 Because hospitals, medical groups, and physicians have been working these past 20 years to achieve higher Press Ganey scores, the data no longer have a bell-shaped distribution. Rather, there are significant clusters of raw scores at the high end with a very narrow response range. When these data are mapped to the percentile spectrum, they are highly inaccurate.19
Impact of sample size. According to Press Ganey, a minimum of 30 survey responses collected over the designated time period is necessary to draw meaningful conclusions of the data for a specific individual, program, or hospital. Despite this requirement to achieve statistical significance, Sullivan and DeLucia found that the firm often provides comparative data about hospital departments and individual physicians based on a smaller sample size that may create an unacceptably large margin of error.20 Sullivan, for example, said his department may only have 8 to 10 Press Ganey survey responses per month and yet still receives monthly reports from the company analyzing the data. Because of the small sample size, 1 month his department ranked in the 1st percentile and 2 months later it ranked in the 99th percentile.20
The effect of a high ceiling rate. A psychometrics report for the Press Ganey survey is available from the vendor that provides vague assessments of reliability and validity based on 2,762 surveys from 12 practices across 10 states. This report describes a 12-question version of the survey with “no problems encountered” with missingness and response variability. The report further states that the Press Ganey survey demonstrates construct, convergent, divergent, and predictive validities, and high reliability; however, these data are not made available.1
In response to this report, Presson et al analyzed more than 34,000 surveys from one institution to evaluate the reliability and validity of the Press Ganey survey.21 Overall, the survey demonstrated suitable psychometric properties for most metrics. However, Presson et al noted a significantly high ceiling rate of 29.3% for the total score, which ranged from 55.4% to 84.1% across items.21 (Ceiling rates are considered substantial if they occur more than 20% of the time.) Ultimately, a high ceiling rate reduces the power to discriminate between patients who have high satisfaction (everyone is “happy”) with those who are just slightly less than happy, but not dissatisfied. This data quality metric can impact the reliability and validity of a survey—and substantial ceiling rates can notably impact percentile rankings of scores within an institution, offering a possible explanation for the small percentage change between the top and bottom percentiles.
Continue to: Other issues with surveys...
Other issues with surveys
In addition to the limitations associated with percentile groupings, survey data are always subject to nonresponse bias, and small sample size can lead to nonsignificant results. Skewed responses also can make it difficult to identify true outlying providers who may need remediation or may be offering a superior patient experience. Satisfaction surveys also lack an assessment of objective data and instead assess how patients perceive and feel, which introduces subjectivity to the results.
Additionally, focusing on improving patient experience ratings can incentivize unnecessary or inappropriate care (ie, overprescribing of narcotics, prescribing antibiotics when not indicated, or ordering testing that may not change management). Some physicians even state that they are not getting the type of feedback that they are asking for and that the survey is not asking the right questions to elicit patient input that is meaningful to their practice. Lastly, the incorporation of trainees and advanced practice providers in the patient care experience leads to the assessment of an alternative provider being included in the ultimate score and may not be representative of that physician.
Patients’ perception and survey results. In some circumstances, the patient’s understanding of their medical situation may affect their responses. Some may argue that patients may mistake a physician’s confidence for competence, when in reality these two entities are mutually exclusive. In a randomized controlled trial, researchers from Mount Sinai School of Medicine and Columbia University Medical Center surveyed inner-city women with newly diagnosed and surgically treated early-stage breast cancer for their perceived quality of care and the process of getting care, including referrals, test results, and treatments. They compared the responses with patient records to determine the actual quality of care. Of the 374 women who received treatment for early-stage breast cancer, 55% said they received “excellent care,” but most—88%—actually got care that was in line with the best current treatment guidelines. Interestingly, the study found African American women were less likely to report excellent care than White or Hispanic women, less likely to trust their doctor, and more likely to say they experienced bias during the process. However, there was no difference in actual quality of care received in any group.22
You can’t improve what you can’t control. Ultimately, while many providers think patient satisfaction survey results may help inform some aspects of their practice, they cannot improve what they cannot control. For example, the multicenter study by Rogo-Gupta et al found that older patients (≥63 years) have more than a 3-fold increase in odds of giving a top satisfaction score than younger patients (≤33 years), independent of other aspects of the care experience.15 Additionally, they found that older physicians (≥56 years) had a significant increase in odds of receiving a top satisfaction score when compared with physicians who were younger than 55 years old.15 Given that physicians clearly cannot control their own age or the age of their patients, the negative impacts of these biases need to be addressed and remedied at a systems level.
Why might these biases exist?
While we cannot completely understand all of the possible explanations for these biases, it is important to emphasize the long-standing prejudice and discrimination against women and people of color in our society and how this has impacted our behavior. While strides have been made, there clearly still seems to be a difference between what we say and how our biases impact our behavior. Women are still tougher on women in professional evaluations in other fields as well23; it is not unique to medicine. While workplace improvements are slowly changing, women still face inequities. The more research we publish to describe it, the more we hope the conversation continues, allowing us to reduce the impact of bias on our sense of self-worth and identity related to our careers, narrow the pay gap, and see women advance at the same rate as male counterparts. Considerable transformation is crucial to prevent further workforce attrition.
With regard to the lower scores provided by Asian patients, studies suggest that cultural response bias, rather than true differences in quality of care, may account for these discrepancies. Previous literature has found that Asian patients are more likely to select midpoints, rather than extremes, when completing Likert-type studies24 and are not more likely to change medical providers than other race/ethnicities, indicating that lower ratings may not necessarily imply greater dissatisfaction with care.25
Far-reaching effects on finances, income, well-being, job satisfaction, etc.
Depending on how the results are distributed and used, the effects of patient satisfaction surveys can extend well beyond the original intentions. At some institutions, income for physicians is directly tied to their Press Ganey satisfaction scores, which could have profound implications for female and Asian physicians,13,15 who would be paid less—resulting in a wider pay gap than already exists.18
When negative and not constructive, patient evaluations can contribute to physician burnout and a loss of productive members of the workforce.26 This is especially important in obstetrics and gynecology, where physicians are most likely to experience burnout due to multiple factors such as high-risk medical conditions, pressures of the electronic medical record (EMR), the medicolegal environment, and difficulty balancing patient expectations for autonomy with professional judgement.27 Burnout also disproportionately affects women and younger physicians, which is especially concerning given that, in 2017, approximately one-third of practicing obstetrician/gynecologists were women, while that same year more than 80% of trainees matching into the field were women.28 In one survey sent to members of a prominent medical society, 20% of the medical professionals who responded said they have had their employment threatened by low patient satisfaction scores, 78% reported that patient satisfaction surveys moderately or severely affected their job satisfaction, and 28% stated they had considered quitting their job or leaving the medical profession.29Another related effect is the association between malpractice proceedings and a lack of satisfaction with perceived quality of physician-patient communication.30 This may be an important determinant of malpractice lawsuits, and ensuring high patient satisfaction may be a form of defensive medicine.
Continue to: Controlling the narrative for the future: Proposed strategies...
Controlling the narrative for the future: Proposed strategies
The rapid, widespread adoption of the Press Ganey survey across specialties, clinical care settings, and geographic areas may have been largely due to the ease and operational benefits for hospitals rather than after rigorous study and validation. For example, repeated use of a specific measurement tool may facilitate comparison across areas within a hospital but also across institutions, which can help assess performance at a national level. Hospitals also may have a financial incentive to work with a single third-party or vendor instead of using multiple options across multiple vendors. However, the impact of adoption of novel measures of performance should be evaluated prior to widespread adoption and utilization.
A similar example of an emergence of a technological advancement that has changed the field of medicine and how we provide care is the EMR. Epic is now the most commonly used medical record system and holds the market share of the industry, covering 78% of patients in the United States.31 While there are certainly many potential benefits of a common EMR, such as ease of information sharing and standardization of formatting, opportunities are identified in real time and require product adjustment. For example, modifications have been made to accurately represent gender outside of the previously used dichotomous options. Diagnoses such as cervical cancer screening can now be used even if the patient gender is listed as male.
Similarly, the Press Ganey and other patient satisfaction questionnaires should be evaluated and modified to address existing societal biases. The World Health Organization estimates that it will take 300 years to fix gender inequality,32 but we have an opportunity now to control the narrative and improve patient feedback.
Future research avenues
Ultimately, there is a need to further explore currently available methods of evaluating clinical encounters to better understand the inherent biases and limitations. We hope this review will encourage other physicians to examine their specialties and hospitals and require similar analyses from vendors of such satisfaction rating products prior to using them. At the very least, health systems should be willing to partner with vendors and physicians on an ongoing basis to better understand the biases involved in these survey results and make modifications as needed. Patients also obtain information from and contribute to self-reported, publicly available websites; therefore, additional exploration into a nationalized standard for assessing patient satisfaction also may serve as an opportunity to standardize the information patients evaluate.33 Further assessment of the potential financial and emotional impact of using the currently available patient-reported surveys on female physicians, Asian physicians, young physicians, and physicians who see young patients is needed. It is time to put pressure on a broken patient satisfaction system and improve on a national level to avoid undue negative consequences on our physicians. Use of patient satisfaction survey data should be limited until we all understand and account for the biases that are evident. ●
- Appeal to the Press Ganey corporation with the results of recent data and other studies to ensure they are aware of the biases that exist in their product
- Appeal to hospital-level administration to refrain from using Press Ganey scores as a tool to dictate reimbursement; instead rely on other more objective measures of performance (such as publications, presentations, research accomplishments, patient and surgical outcomes, promotion, committees, national leadership roles, etc)
- Apply a “corrective factor” or “adjustment factor” to eliminate the baseline discrepancy between scores for men and women
- Consider moving to an alternative survey methodology
- Provide patient education to define “performance” (ie, frame what a patient can expect from a provider such as being on time, courteous, and empathetic; caution against asking patients to assess competence and knowledge)
- Outpatient Services (OU) Survey Psychometrics Report. Published online 2019.
- Zusman EE. HCAHPS replaces Press Ganey Survey as quality measure for patient hospital experience. Neurosurgery. 2012;71:N21-N24. doi: 10.1227/01.neu.0000417536.07871.ed
- Press Ganey. Company. Accessed April 20, 2023. www.pressganey. com/company/
- Press, Ganey--first year of patient satisfaction measurement. Hosp Guest Relations Rep. 1986;1:4-5.
- DeCastellarnau A. A classification of response scale characteristics that affect data quality: a literature review. Qual Quant. 2018;52:15231559. doi: 10.1007/s11135-017-0533-4
- Tyser AR, Abtahi AM, McFadden M, et al. Evidence of non-response bias in the Press-Ganey patient satisfaction survey. BMC Health Serv Res. 2016;16:350. doi: 10.1186/s12913-016-1595-z
- Duseja R, Durham M, Schreiber M. CMS quality measure development. JAMA. 2020;324:1213-1214. doi: 10.1001/jama.2020.12070
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001. doi: 10.17226/10027
- Parmet WE. Health: policy or law? A population-based analysis of the Supreme Court’s ACA cases. J Health Polit Policy Law. 2016;41:10611081. doi: 10.1215/03616878-3665949
- Richter JP, Muhlestein DB. Patient experience and hospital profitability: is there a link? Health Care Manage Rev. 2017;42:247-257. doi: 10.1097/HMR.0000000000000105
- Huang C-H, Wu H-H, Lee Y-C, et al. What role does patient gratitude play in the relationship between relationship quality and patient loyalty? Inquiry. 2019;56:46958019868324. doi: 10.1177/0046958019868324
- Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; hospital inpatient value-based purchasing program. Final rule. Fed Regist. 2011;76:26490-26547.
- Rogo-Gupta LJ, Haunschild C, Altamirano J, et al. Physician gender is associated with Press Ganey patient satisfaction scores in outpatient gynecology. Womens Health Issues. 2018;28:281-285. doi: 10.1016 /j.whi.2018.01.001
- DeLoughery EP. Physician race and specialty influence Press Ganey survey results. Neth J Med. 2019;77:366-369.
- Homewood L, Altamirano J, Fassiotto M, et al. Women gynecologists receive lower Press Ganey patient satisfaction scores in a multicenter cross-sectional study. Am J Obstet Gynecol. 2023;228:S801. doi: 10.1016/j.ajog.2022.12.025
- Sharp B, Johnson J, Hamedani AG, et al. What are we measuring? Evaluating physician-specific satisfaction scores between emergency departments. West J Emerg Med. 2019;20:454-459. doi: 10.5811 /westjem.2019.4.41040
- Mosley M. Viewpoint: Press Ganey is a worthless tool for the ED. Emerg Med News. 2019;41:3-4. doi: 10.1097/01.EEM.0000616512.68475.69
- Sotto-Santiago S, Slaven JE, Rohr-Kirchgraber T. (Dis)Incentivizing patient satisfaction metrics: the unintended consequences of institutional bias. Health Equity. 2019;3:13-18. doi: 10.1089/heq.2018.0065
- Lloyd RC. Quality Health Care: A Guide to Developing and Using Indicators. 2nd ed. Jones & Bartlett Learning; 2019. Accessed April 23, 2023. www.jblearning.com/catalog/productdetails /9781284023077
- 2+2=7? Seven things you may not know about Press Ganey statistics. Emergency Physicians Monthly. Accessed April 23, 2023. epmonthly. com/article/227-seven-things-you-may-not-know-about-pressgainey-statistics/
- Presson AP, Zhang C, Abtahi AM, et al. Psychometric properties of the Press Ganey® Outpatient Medical Practice Survey. Health Qual Life Outcomes. 2017;15:32. doi: 10.1186/s12955-017-0610-3
- Bickell NA, Neuman J, Fei K, et al. Quality of breast cancer care: perception versus practice. J Clin Oncol. 2012;30:1791-1795. doi: 10.1200 /JCO.2011.38.7605
- Strauss K. Women in the workplace: are women tougher on other women? Forbes. July 18, 2016. Accessed April 27, 2023. www.forbes. com/sites/karstenstrauss/2016/07/18/women-in-the-workplace -are-women-tougher-on-other-women/
- Lee JW, Jones PS, Mineyama Y, et al. Cultural differences in responses to a Likert scale. Res Nurs Health. 2002;25:295-306. doi: 10.1002 /nur.10041
- Saha S, Hickam DH. Explaining low ratings of patient satisfaction among Asian-Americans. Am J Med Qual. 2003;18:256-264. doi: 10.1177/106286060301800606
- Halbesleben JRB, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33:29-39. doi: 10.1097/01. HMR.0000304493.87898.72
- Bradford L, Glaser G. Addressing physician burnout and ensuring high-quality care of the physician workforce. Obstet Gynecol. 2021;137:3-11. doi: 10.1097/AOG.0000000000004197
- Boyle P. Nation’s physician workforce evolves: more women, a bit older, and toward different specialties. AAMCNEWS. February 2, 2021. Accessed April 20, 2023. www.aamc.org/news-insights/nations-physician-workforce-evolves-more-women-bit-older-and-towarddifferent-specialties
- Zgierska A, Rabago D, Miller MM. Impact of patient satisfaction ratings on physicians and clinical care. Patient Prefer Adherence. 2014;8:437-446. doi: 10.2147/PPA.S59077
- Yeh J, Nagel EE. Patient satisfaction in obstetrics and gynecology: individualized patient-centered communication. Clin Med Insights Womens Health. 2010;3:23. doi: 10.4137/CMWH.S5870
- Epic. About us. Accessed April 19, 2023. www.epic.com/about
- United Nations. Without investment, gender equality will take nearly 300 years: UN report. September 7, 2022. Accessed April 19, 2023. news.un.org/en/story/2022/09/1126171
- Ryan T, Specht J, Smith S, et al. Does the Press Ganey Survey correlate to online health grades for a major academic otolaryngology department? Otolaryngol Head Neck Surg. 2016;155:411-415. doi: 10.1177/0194599816652386

Patient satisfaction questionnaires were developed in the 1980s as part of the movement to better understand the patient’s experience and their perspective of the quality of care. In 1985, the Press Ganey survey—now the most widely used method to assess patient satisfaction—was developed by 2 professors in anthropology and sociology-statistics at Notre Dame. Initially intended for inpatient admissions, the survey was validated based on a few thousand survey results.1 Given the strong interest in improving patient satisfaction at the time, it became widely adopted and quickly expanded into outpatient encounters and ambulatory surgery settings.
Although other surveys have been developed,2 the Press Ganey survey is the most commonly used assessment tool for patient satisfaction metrics in the United States, with approximately 50% of all hospitals and more than 41,000 health care organizations using its services.3,4 The survey consists of 6 domains related to satisfaction with:
1. the care provider
2. the nurse or assistant
3. personal issues
4. overall assessment
5. access
6. moving through the visit.
Survey items are scored using a 5-point Likert scale, with scores ranging from “very poor” (a score of 1) to “very good” (a score of 5). According to the company, because this format is balanced and parallel (unlike a “poor” to “excellent” format), responses can be quantified and used statistically without violating methodologic assumptions. Also, variability in patients’ responses with this format allows for the identification of opportunities to improve, unlike “yes/no” response formats.1 There are limitations to this design, however, which can impact data quality,5 as we will see.
Adoption of the survey as we move toward value-based care
More recently, patients’ satisfaction with their health care has received increased attention as we move to a patient-centered care model and as health care reimbursement models shift toward value-based care. Current trends in health care policy statements include the importance of raising the standard of care and shifting from a “fee-for-service” to a “pay-for-performance” reimbursement model.7,8 As a result, hospitals are establishing systems to measure “performance” that are not nationally standardized or extensively studied with objective measures. The changing standard of health care expectations in the United States is a topic of much public debate.9 And as expectations and new standards are defined, the impact of implementing novel measures of performance should be evaluated prior to widespread adoption and utilization.
Patient satisfaction also has been identified as a driver for hospital finances through loyalty, described as the “likelihood to return to that system for future medical services.”10,11 This measure has contributed to policy changes that reinforce prioritization of patient satisfaction. For example, the Affordable Care Act tied Medicare reimbursement and patient satisfaction together in the Hospital Value-Based Purchasing Program. This program uses measures of clinical processes, efficiency, outcomes, and patient experiences to calculate a total score that results in hospital reimbursement and incentives,12 which creates a direct pathway from patient experience to reimbursement—underscoring hospitals’ desire for ongoing assessment of patient satisfaction.
In 2005, the Centers for Medicare and Medicaid Services and the Agency for Health care Research and Quality developed the Hospital Consumer Assessment of Health care Providers and Systems (HCAHPS) survey in response to criticisms of the Press Ganey survey. The HCAHPS survey consists of 27 questions with 3 broad goals19:
- to produce data about patients’ perspectives of care that allow for objective and meaningful comparisons of hospitals
- to publicly report survey results and create new incentives for hospitals to improve quality of care
- to produce public reports that enhance accountability by increasing transparency.
One difference with the HCAHPS is that it measures frequency, or how often a service was performed (“never”, “sometimes”, “usually”, “always”), whereas Press Ganey measures satisfaction. It also only surveys inpatients and does not address outpatient encounters. Despite the differences, it is a widely used patient satisfaction survey and is subject to similar issues and biases as the Press Ganey survey.
Continue to: Gender, race, and age bias...
Gender, race, and age bias
Although the rationale behind gathering patient input is important, recent data suggest that patient satisfaction surveys are subject to inherent biases.6,13,14 These biases tend to negatively impact women and non-White physicians, adding to the systemic discrimination against women and physicians of color that already exists in health care.
In a single-site retrospective study performed in 2018 by Rogo-Gupta et al, female gynecologists were found to be 47% less likely to receive top patient satisfaction scores than their male counterparts owing to their gender alone, suggesting that gender bias may impact the results of patient satisfaction questionnaires.13 The authors encouraged that the results of patient satisfaction surveys be interpreted with great caution until the impact on female physicians is better understood.
A multi-center study by the same group (Rogo-Gupta et al) assessed the same construct across 5 different geographically diverse institutions.15 This study confirmed that female gynecologists were less likely to receive a top satisfaction score from their patients (19% lower odds when compared with male gynecologists). They also studied the effects of other patient demographics, including age, race/ethnicity, and race concordance. Older patients (aged ≥63 years) had an over-3-fold increase in odds of providing a top satisfaction score than younger patients. Additionally, Asian physicians had significantly lower odds of receiving a top satisfaction score when compared with White physicians, while Asian patients had significantly lower odds of providing a top satisfaction score when compared with White patients. Lastly, in most cases, when underrepresented-in-medicine patients saw an underrepresented-in-medicine physician (race concordance), there was a significant increase in odds of receiving a top satisfaction score. Asian race concordance, however, actually resulted in a lower likelihood of receiving a top satisfaction score.15
Literature from other specialties supports these findings. These results are consistent with emerging data from other medical specialties that also suggest that Press Ganey survey data are subject to inherent biases. For example, data from emergency medicine literature have shown discrepancies between patient satisfaction for providers at tertiary inner-city institutions versus those in affluent suburban populations,16 and that worse mortality is actually correlated with better patient satisfaction scores, and vice versa.17
Another study by Sotto-Santiago in 2019 assessed patient satisfaction scores in multiple specialties at a single institution where quality-related financial incentives were offered based on this metric. They found a significant difference in patient satisfaction scores between underrepresented and White physicians, which suggests a potential bias among patients and institutional practices—ultimately leading to pay inequities through differences in financial incentives.18
Percentile differences reveal small gaps in satisfaction ratings
When examining the difference between raw Press Ganey patient satisfaction data and the percentiles associated with these scores, an interesting finding arises. Looking at the 2023 multicenter study by Rogo-Gupta et al, the difference in the top raw scores between male and female gynecologists appears to be small (3.3%).15 However, in 2020, the difference in top scores separating the top (75th) and bottom (25th) percentile quartiles of physicians was also small, at only 6.9%.
Considering the percentiles, if a provider who scores in the 25th percentile is compared with a colleague who scores in the 75th percentile, they may think the reported satisfaction score differences were quite large. This may potentially invoke feelings of decreased self-worth, negatively impact their professional identity or overall well-being, and they may seek (or be told to seek) improvement opportunities. Now imagine the provider in question realizes the difference between the 25th percentile and 75th percentile is actually only 6.9%. This information may completely change how the results are interpreted and acted upon by administrators. This is further changed with the understanding that 3.3% of the difference may be due to gender alone, narrowing the gap even further. Providers would become understandably frustrated if measures of success such as reimbursement, financial bonus or incentives, promotion, or advancement are linked to these results. It violates the value of fairness and does not offer an equitable starting point.
Evolution of the data distribution. Another consideration, as noted by Robert C. Lloyd, PhD, one of the statisticians who helped develop the percentile statistical analysis mapping in 1985, is that it was based on a classic bell-shaped distribution of patient satisfaction survey scores.19 Because hospitals, medical groups, and physicians have been working these past 20 years to achieve higher Press Ganey scores, the data no longer have a bell-shaped distribution. Rather, there are significant clusters of raw scores at the high end with a very narrow response range. When these data are mapped to the percentile spectrum, they are highly inaccurate.19
Impact of sample size. According to Press Ganey, a minimum of 30 survey responses collected over the designated time period is necessary to draw meaningful conclusions of the data for a specific individual, program, or hospital. Despite this requirement to achieve statistical significance, Sullivan and DeLucia found that the firm often provides comparative data about hospital departments and individual physicians based on a smaller sample size that may create an unacceptably large margin of error.20 Sullivan, for example, said his department may only have 8 to 10 Press Ganey survey responses per month and yet still receives monthly reports from the company analyzing the data. Because of the small sample size, 1 month his department ranked in the 1st percentile and 2 months later it ranked in the 99th percentile.20
The effect of a high ceiling rate. A psychometrics report for the Press Ganey survey is available from the vendor that provides vague assessments of reliability and validity based on 2,762 surveys from 12 practices across 10 states. This report describes a 12-question version of the survey with “no problems encountered” with missingness and response variability. The report further states that the Press Ganey survey demonstrates construct, convergent, divergent, and predictive validities, and high reliability; however, these data are not made available.1
In response to this report, Presson et al analyzed more than 34,000 surveys from one institution to evaluate the reliability and validity of the Press Ganey survey.21 Overall, the survey demonstrated suitable psychometric properties for most metrics. However, Presson et al noted a significantly high ceiling rate of 29.3% for the total score, which ranged from 55.4% to 84.1% across items.21 (Ceiling rates are considered substantial if they occur more than 20% of the time.) Ultimately, a high ceiling rate reduces the power to discriminate between patients who have high satisfaction (everyone is “happy”) with those who are just slightly less than happy, but not dissatisfied. This data quality metric can impact the reliability and validity of a survey—and substantial ceiling rates can notably impact percentile rankings of scores within an institution, offering a possible explanation for the small percentage change between the top and bottom percentiles.
Continue to: Other issues with surveys...
Other issues with surveys
In addition to the limitations associated with percentile groupings, survey data are always subject to nonresponse bias, and small sample size can lead to nonsignificant results. Skewed responses also can make it difficult to identify true outlying providers who may need remediation or may be offering a superior patient experience. Satisfaction surveys also lack an assessment of objective data and instead assess how patients perceive and feel, which introduces subjectivity to the results.
Additionally, focusing on improving patient experience ratings can incentivize unnecessary or inappropriate care (ie, overprescribing of narcotics, prescribing antibiotics when not indicated, or ordering testing that may not change management). Some physicians even state that they are not getting the type of feedback that they are asking for and that the survey is not asking the right questions to elicit patient input that is meaningful to their practice. Lastly, the incorporation of trainees and advanced practice providers in the patient care experience leads to the assessment of an alternative provider being included in the ultimate score and may not be representative of that physician.
Patients’ perception and survey results. In some circumstances, the patient’s understanding of their medical situation may affect their responses. Some may argue that patients may mistake a physician’s confidence for competence, when in reality these two entities are mutually exclusive. In a randomized controlled trial, researchers from Mount Sinai School of Medicine and Columbia University Medical Center surveyed inner-city women with newly diagnosed and surgically treated early-stage breast cancer for their perceived quality of care and the process of getting care, including referrals, test results, and treatments. They compared the responses with patient records to determine the actual quality of care. Of the 374 women who received treatment for early-stage breast cancer, 55% said they received “excellent care,” but most—88%—actually got care that was in line with the best current treatment guidelines. Interestingly, the study found African American women were less likely to report excellent care than White or Hispanic women, less likely to trust their doctor, and more likely to say they experienced bias during the process. However, there was no difference in actual quality of care received in any group.22
You can’t improve what you can’t control. Ultimately, while many providers think patient satisfaction survey results may help inform some aspects of their practice, they cannot improve what they cannot control. For example, the multicenter study by Rogo-Gupta et al found that older patients (≥63 years) have more than a 3-fold increase in odds of giving a top satisfaction score than younger patients (≤33 years), independent of other aspects of the care experience.15 Additionally, they found that older physicians (≥56 years) had a significant increase in odds of receiving a top satisfaction score when compared with physicians who were younger than 55 years old.15 Given that physicians clearly cannot control their own age or the age of their patients, the negative impacts of these biases need to be addressed and remedied at a systems level.
Why might these biases exist?
While we cannot completely understand all of the possible explanations for these biases, it is important to emphasize the long-standing prejudice and discrimination against women and people of color in our society and how this has impacted our behavior. While strides have been made, there clearly still seems to be a difference between what we say and how our biases impact our behavior. Women are still tougher on women in professional evaluations in other fields as well23; it is not unique to medicine. While workplace improvements are slowly changing, women still face inequities. The more research we publish to describe it, the more we hope the conversation continues, allowing us to reduce the impact of bias on our sense of self-worth and identity related to our careers, narrow the pay gap, and see women advance at the same rate as male counterparts. Considerable transformation is crucial to prevent further workforce attrition.
With regard to the lower scores provided by Asian patients, studies suggest that cultural response bias, rather than true differences in quality of care, may account for these discrepancies. Previous literature has found that Asian patients are more likely to select midpoints, rather than extremes, when completing Likert-type studies24 and are not more likely to change medical providers than other race/ethnicities, indicating that lower ratings may not necessarily imply greater dissatisfaction with care.25
Far-reaching effects on finances, income, well-being, job satisfaction, etc.
Depending on how the results are distributed and used, the effects of patient satisfaction surveys can extend well beyond the original intentions. At some institutions, income for physicians is directly tied to their Press Ganey satisfaction scores, which could have profound implications for female and Asian physicians,13,15 who would be paid less—resulting in a wider pay gap than already exists.18
When negative and not constructive, patient evaluations can contribute to physician burnout and a loss of productive members of the workforce.26 This is especially important in obstetrics and gynecology, where physicians are most likely to experience burnout due to multiple factors such as high-risk medical conditions, pressures of the electronic medical record (EMR), the medicolegal environment, and difficulty balancing patient expectations for autonomy with professional judgement.27 Burnout also disproportionately affects women and younger physicians, which is especially concerning given that, in 2017, approximately one-third of practicing obstetrician/gynecologists were women, while that same year more than 80% of trainees matching into the field were women.28 In one survey sent to members of a prominent medical society, 20% of the medical professionals who responded said they have had their employment threatened by low patient satisfaction scores, 78% reported that patient satisfaction surveys moderately or severely affected their job satisfaction, and 28% stated they had considered quitting their job or leaving the medical profession.29Another related effect is the association between malpractice proceedings and a lack of satisfaction with perceived quality of physician-patient communication.30 This may be an important determinant of malpractice lawsuits, and ensuring high patient satisfaction may be a form of defensive medicine.
Continue to: Controlling the narrative for the future: Proposed strategies...
Controlling the narrative for the future: Proposed strategies
The rapid, widespread adoption of the Press Ganey survey across specialties, clinical care settings, and geographic areas may have been largely due to the ease and operational benefits for hospitals rather than after rigorous study and validation. For example, repeated use of a specific measurement tool may facilitate comparison across areas within a hospital but also across institutions, which can help assess performance at a national level. Hospitals also may have a financial incentive to work with a single third-party or vendor instead of using multiple options across multiple vendors. However, the impact of adoption of novel measures of performance should be evaluated prior to widespread adoption and utilization.
A similar example of an emergence of a technological advancement that has changed the field of medicine and how we provide care is the EMR. Epic is now the most commonly used medical record system and holds the market share of the industry, covering 78% of patients in the United States.31 While there are certainly many potential benefits of a common EMR, such as ease of information sharing and standardization of formatting, opportunities are identified in real time and require product adjustment. For example, modifications have been made to accurately represent gender outside of the previously used dichotomous options. Diagnoses such as cervical cancer screening can now be used even if the patient gender is listed as male.
Similarly, the Press Ganey and other patient satisfaction questionnaires should be evaluated and modified to address existing societal biases. The World Health Organization estimates that it will take 300 years to fix gender inequality,32 but we have an opportunity now to control the narrative and improve patient feedback.
Future research avenues
Ultimately, there is a need to further explore currently available methods of evaluating clinical encounters to better understand the inherent biases and limitations. We hope this review will encourage other physicians to examine their specialties and hospitals and require similar analyses from vendors of such satisfaction rating products prior to using them. At the very least, health systems should be willing to partner with vendors and physicians on an ongoing basis to better understand the biases involved in these survey results and make modifications as needed. Patients also obtain information from and contribute to self-reported, publicly available websites; therefore, additional exploration into a nationalized standard for assessing patient satisfaction also may serve as an opportunity to standardize the information patients evaluate.33 Further assessment of the potential financial and emotional impact of using the currently available patient-reported surveys on female physicians, Asian physicians, young physicians, and physicians who see young patients is needed. It is time to put pressure on a broken patient satisfaction system and improve on a national level to avoid undue negative consequences on our physicians. Use of patient satisfaction survey data should be limited until we all understand and account for the biases that are evident. ●
- Appeal to the Press Ganey corporation with the results of recent data and other studies to ensure they are aware of the biases that exist in their product
- Appeal to hospital-level administration to refrain from using Press Ganey scores as a tool to dictate reimbursement; instead rely on other more objective measures of performance (such as publications, presentations, research accomplishments, patient and surgical outcomes, promotion, committees, national leadership roles, etc)
- Apply a “corrective factor” or “adjustment factor” to eliminate the baseline discrepancy between scores for men and women
- Consider moving to an alternative survey methodology
- Provide patient education to define “performance” (ie, frame what a patient can expect from a provider such as being on time, courteous, and empathetic; caution against asking patients to assess competence and knowledge)

Patient satisfaction questionnaires were developed in the 1980s as part of the movement to better understand the patient’s experience and their perspective of the quality of care. In 1985, the Press Ganey survey—now the most widely used method to assess patient satisfaction—was developed by 2 professors in anthropology and sociology-statistics at Notre Dame. Initially intended for inpatient admissions, the survey was validated based on a few thousand survey results.1 Given the strong interest in improving patient satisfaction at the time, it became widely adopted and quickly expanded into outpatient encounters and ambulatory surgery settings.
Although other surveys have been developed,2 the Press Ganey survey is the most commonly used assessment tool for patient satisfaction metrics in the United States, with approximately 50% of all hospitals and more than 41,000 health care organizations using its services.3,4 The survey consists of 6 domains related to satisfaction with:
1. the care provider
2. the nurse or assistant
3. personal issues
4. overall assessment
5. access
6. moving through the visit.
Survey items are scored using a 5-point Likert scale, with scores ranging from “very poor” (a score of 1) to “very good” (a score of 5). According to the company, because this format is balanced and parallel (unlike a “poor” to “excellent” format), responses can be quantified and used statistically without violating methodologic assumptions. Also, variability in patients’ responses with this format allows for the identification of opportunities to improve, unlike “yes/no” response formats.1 There are limitations to this design, however, which can impact data quality,5 as we will see.
Adoption of the survey as we move toward value-based care
More recently, patients’ satisfaction with their health care has received increased attention as we move to a patient-centered care model and as health care reimbursement models shift toward value-based care. Current trends in health care policy statements include the importance of raising the standard of care and shifting from a “fee-for-service” to a “pay-for-performance” reimbursement model.7,8 As a result, hospitals are establishing systems to measure “performance” that are not nationally standardized or extensively studied with objective measures. The changing standard of health care expectations in the United States is a topic of much public debate.9 And as expectations and new standards are defined, the impact of implementing novel measures of performance should be evaluated prior to widespread adoption and utilization.
Patient satisfaction also has been identified as a driver for hospital finances through loyalty, described as the “likelihood to return to that system for future medical services.”10,11 This measure has contributed to policy changes that reinforce prioritization of patient satisfaction. For example, the Affordable Care Act tied Medicare reimbursement and patient satisfaction together in the Hospital Value-Based Purchasing Program. This program uses measures of clinical processes, efficiency, outcomes, and patient experiences to calculate a total score that results in hospital reimbursement and incentives,12 which creates a direct pathway from patient experience to reimbursement—underscoring hospitals’ desire for ongoing assessment of patient satisfaction.
In 2005, the Centers for Medicare and Medicaid Services and the Agency for Health care Research and Quality developed the Hospital Consumer Assessment of Health care Providers and Systems (HCAHPS) survey in response to criticisms of the Press Ganey survey. The HCAHPS survey consists of 27 questions with 3 broad goals19:
- to produce data about patients’ perspectives of care that allow for objective and meaningful comparisons of hospitals
- to publicly report survey results and create new incentives for hospitals to improve quality of care
- to produce public reports that enhance accountability by increasing transparency.
One difference with the HCAHPS is that it measures frequency, or how often a service was performed (“never”, “sometimes”, “usually”, “always”), whereas Press Ganey measures satisfaction. It also only surveys inpatients and does not address outpatient encounters. Despite the differences, it is a widely used patient satisfaction survey and is subject to similar issues and biases as the Press Ganey survey.
Continue to: Gender, race, and age bias...
Gender, race, and age bias
Although the rationale behind gathering patient input is important, recent data suggest that patient satisfaction surveys are subject to inherent biases.6,13,14 These biases tend to negatively impact women and non-White physicians, adding to the systemic discrimination against women and physicians of color that already exists in health care.
In a single-site retrospective study performed in 2018 by Rogo-Gupta et al, female gynecologists were found to be 47% less likely to receive top patient satisfaction scores than their male counterparts owing to their gender alone, suggesting that gender bias may impact the results of patient satisfaction questionnaires.13 The authors encouraged that the results of patient satisfaction surveys be interpreted with great caution until the impact on female physicians is better understood.
A multi-center study by the same group (Rogo-Gupta et al) assessed the same construct across 5 different geographically diverse institutions.15 This study confirmed that female gynecologists were less likely to receive a top satisfaction score from their patients (19% lower odds when compared with male gynecologists). They also studied the effects of other patient demographics, including age, race/ethnicity, and race concordance. Older patients (aged ≥63 years) had an over-3-fold increase in odds of providing a top satisfaction score than younger patients. Additionally, Asian physicians had significantly lower odds of receiving a top satisfaction score when compared with White physicians, while Asian patients had significantly lower odds of providing a top satisfaction score when compared with White patients. Lastly, in most cases, when underrepresented-in-medicine patients saw an underrepresented-in-medicine physician (race concordance), there was a significant increase in odds of receiving a top satisfaction score. Asian race concordance, however, actually resulted in a lower likelihood of receiving a top satisfaction score.15
Literature from other specialties supports these findings. These results are consistent with emerging data from other medical specialties that also suggest that Press Ganey survey data are subject to inherent biases. For example, data from emergency medicine literature have shown discrepancies between patient satisfaction for providers at tertiary inner-city institutions versus those in affluent suburban populations,16 and that worse mortality is actually correlated with better patient satisfaction scores, and vice versa.17
Another study by Sotto-Santiago in 2019 assessed patient satisfaction scores in multiple specialties at a single institution where quality-related financial incentives were offered based on this metric. They found a significant difference in patient satisfaction scores between underrepresented and White physicians, which suggests a potential bias among patients and institutional practices—ultimately leading to pay inequities through differences in financial incentives.18
Percentile differences reveal small gaps in satisfaction ratings
When examining the difference between raw Press Ganey patient satisfaction data and the percentiles associated with these scores, an interesting finding arises. Looking at the 2023 multicenter study by Rogo-Gupta et al, the difference in the top raw scores between male and female gynecologists appears to be small (3.3%).15 However, in 2020, the difference in top scores separating the top (75th) and bottom (25th) percentile quartiles of physicians was also small, at only 6.9%.
Considering the percentiles, if a provider who scores in the 25th percentile is compared with a colleague who scores in the 75th percentile, they may think the reported satisfaction score differences were quite large. This may potentially invoke feelings of decreased self-worth, negatively impact their professional identity or overall well-being, and they may seek (or be told to seek) improvement opportunities. Now imagine the provider in question realizes the difference between the 25th percentile and 75th percentile is actually only 6.9%. This information may completely change how the results are interpreted and acted upon by administrators. This is further changed with the understanding that 3.3% of the difference may be due to gender alone, narrowing the gap even further. Providers would become understandably frustrated if measures of success such as reimbursement, financial bonus or incentives, promotion, or advancement are linked to these results. It violates the value of fairness and does not offer an equitable starting point.
Evolution of the data distribution. Another consideration, as noted by Robert C. Lloyd, PhD, one of the statisticians who helped develop the percentile statistical analysis mapping in 1985, is that it was based on a classic bell-shaped distribution of patient satisfaction survey scores.19 Because hospitals, medical groups, and physicians have been working these past 20 years to achieve higher Press Ganey scores, the data no longer have a bell-shaped distribution. Rather, there are significant clusters of raw scores at the high end with a very narrow response range. When these data are mapped to the percentile spectrum, they are highly inaccurate.19
Impact of sample size. According to Press Ganey, a minimum of 30 survey responses collected over the designated time period is necessary to draw meaningful conclusions of the data for a specific individual, program, or hospital. Despite this requirement to achieve statistical significance, Sullivan and DeLucia found that the firm often provides comparative data about hospital departments and individual physicians based on a smaller sample size that may create an unacceptably large margin of error.20 Sullivan, for example, said his department may only have 8 to 10 Press Ganey survey responses per month and yet still receives monthly reports from the company analyzing the data. Because of the small sample size, 1 month his department ranked in the 1st percentile and 2 months later it ranked in the 99th percentile.20
The effect of a high ceiling rate. A psychometrics report for the Press Ganey survey is available from the vendor that provides vague assessments of reliability and validity based on 2,762 surveys from 12 practices across 10 states. This report describes a 12-question version of the survey with “no problems encountered” with missingness and response variability. The report further states that the Press Ganey survey demonstrates construct, convergent, divergent, and predictive validities, and high reliability; however, these data are not made available.1
In response to this report, Presson et al analyzed more than 34,000 surveys from one institution to evaluate the reliability and validity of the Press Ganey survey.21 Overall, the survey demonstrated suitable psychometric properties for most metrics. However, Presson et al noted a significantly high ceiling rate of 29.3% for the total score, which ranged from 55.4% to 84.1% across items.21 (Ceiling rates are considered substantial if they occur more than 20% of the time.) Ultimately, a high ceiling rate reduces the power to discriminate between patients who have high satisfaction (everyone is “happy”) with those who are just slightly less than happy, but not dissatisfied. This data quality metric can impact the reliability and validity of a survey—and substantial ceiling rates can notably impact percentile rankings of scores within an institution, offering a possible explanation for the small percentage change between the top and bottom percentiles.
Continue to: Other issues with surveys...
Other issues with surveys
In addition to the limitations associated with percentile groupings, survey data are always subject to nonresponse bias, and small sample size can lead to nonsignificant results. Skewed responses also can make it difficult to identify true outlying providers who may need remediation or may be offering a superior patient experience. Satisfaction surveys also lack an assessment of objective data and instead assess how patients perceive and feel, which introduces subjectivity to the results.
Additionally, focusing on improving patient experience ratings can incentivize unnecessary or inappropriate care (ie, overprescribing of narcotics, prescribing antibiotics when not indicated, or ordering testing that may not change management). Some physicians even state that they are not getting the type of feedback that they are asking for and that the survey is not asking the right questions to elicit patient input that is meaningful to their practice. Lastly, the incorporation of trainees and advanced practice providers in the patient care experience leads to the assessment of an alternative provider being included in the ultimate score and may not be representative of that physician.
Patients’ perception and survey results. In some circumstances, the patient’s understanding of their medical situation may affect their responses. Some may argue that patients may mistake a physician’s confidence for competence, when in reality these two entities are mutually exclusive. In a randomized controlled trial, researchers from Mount Sinai School of Medicine and Columbia University Medical Center surveyed inner-city women with newly diagnosed and surgically treated early-stage breast cancer for their perceived quality of care and the process of getting care, including referrals, test results, and treatments. They compared the responses with patient records to determine the actual quality of care. Of the 374 women who received treatment for early-stage breast cancer, 55% said they received “excellent care,” but most—88%—actually got care that was in line with the best current treatment guidelines. Interestingly, the study found African American women were less likely to report excellent care than White or Hispanic women, less likely to trust their doctor, and more likely to say they experienced bias during the process. However, there was no difference in actual quality of care received in any group.22
You can’t improve what you can’t control. Ultimately, while many providers think patient satisfaction survey results may help inform some aspects of their practice, they cannot improve what they cannot control. For example, the multicenter study by Rogo-Gupta et al found that older patients (≥63 years) have more than a 3-fold increase in odds of giving a top satisfaction score than younger patients (≤33 years), independent of other aspects of the care experience.15 Additionally, they found that older physicians (≥56 years) had a significant increase in odds of receiving a top satisfaction score when compared with physicians who were younger than 55 years old.15 Given that physicians clearly cannot control their own age or the age of their patients, the negative impacts of these biases need to be addressed and remedied at a systems level.
Why might these biases exist?
While we cannot completely understand all of the possible explanations for these biases, it is important to emphasize the long-standing prejudice and discrimination against women and people of color in our society and how this has impacted our behavior. While strides have been made, there clearly still seems to be a difference between what we say and how our biases impact our behavior. Women are still tougher on women in professional evaluations in other fields as well23; it is not unique to medicine. While workplace improvements are slowly changing, women still face inequities. The more research we publish to describe it, the more we hope the conversation continues, allowing us to reduce the impact of bias on our sense of self-worth and identity related to our careers, narrow the pay gap, and see women advance at the same rate as male counterparts. Considerable transformation is crucial to prevent further workforce attrition.
With regard to the lower scores provided by Asian patients, studies suggest that cultural response bias, rather than true differences in quality of care, may account for these discrepancies. Previous literature has found that Asian patients are more likely to select midpoints, rather than extremes, when completing Likert-type studies24 and are not more likely to change medical providers than other race/ethnicities, indicating that lower ratings may not necessarily imply greater dissatisfaction with care.25
Far-reaching effects on finances, income, well-being, job satisfaction, etc.
Depending on how the results are distributed and used, the effects of patient satisfaction surveys can extend well beyond the original intentions. At some institutions, income for physicians is directly tied to their Press Ganey satisfaction scores, which could have profound implications for female and Asian physicians,13,15 who would be paid less—resulting in a wider pay gap than already exists.18
When negative and not constructive, patient evaluations can contribute to physician burnout and a loss of productive members of the workforce.26 This is especially important in obstetrics and gynecology, where physicians are most likely to experience burnout due to multiple factors such as high-risk medical conditions, pressures of the electronic medical record (EMR), the medicolegal environment, and difficulty balancing patient expectations for autonomy with professional judgement.27 Burnout also disproportionately affects women and younger physicians, which is especially concerning given that, in 2017, approximately one-third of practicing obstetrician/gynecologists were women, while that same year more than 80% of trainees matching into the field were women.28 In one survey sent to members of a prominent medical society, 20% of the medical professionals who responded said they have had their employment threatened by low patient satisfaction scores, 78% reported that patient satisfaction surveys moderately or severely affected their job satisfaction, and 28% stated they had considered quitting their job or leaving the medical profession.29Another related effect is the association between malpractice proceedings and a lack of satisfaction with perceived quality of physician-patient communication.30 This may be an important determinant of malpractice lawsuits, and ensuring high patient satisfaction may be a form of defensive medicine.
Continue to: Controlling the narrative for the future: Proposed strategies...
Controlling the narrative for the future: Proposed strategies
The rapid, widespread adoption of the Press Ganey survey across specialties, clinical care settings, and geographic areas may have been largely due to the ease and operational benefits for hospitals rather than after rigorous study and validation. For example, repeated use of a specific measurement tool may facilitate comparison across areas within a hospital but also across institutions, which can help assess performance at a national level. Hospitals also may have a financial incentive to work with a single third-party or vendor instead of using multiple options across multiple vendors. However, the impact of adoption of novel measures of performance should be evaluated prior to widespread adoption and utilization.
A similar example of an emergence of a technological advancement that has changed the field of medicine and how we provide care is the EMR. Epic is now the most commonly used medical record system and holds the market share of the industry, covering 78% of patients in the United States.31 While there are certainly many potential benefits of a common EMR, such as ease of information sharing and standardization of formatting, opportunities are identified in real time and require product adjustment. For example, modifications have been made to accurately represent gender outside of the previously used dichotomous options. Diagnoses such as cervical cancer screening can now be used even if the patient gender is listed as male.
Similarly, the Press Ganey and other patient satisfaction questionnaires should be evaluated and modified to address existing societal biases. The World Health Organization estimates that it will take 300 years to fix gender inequality,32 but we have an opportunity now to control the narrative and improve patient feedback.
Future research avenues
Ultimately, there is a need to further explore currently available methods of evaluating clinical encounters to better understand the inherent biases and limitations. We hope this review will encourage other physicians to examine their specialties and hospitals and require similar analyses from vendors of such satisfaction rating products prior to using them. At the very least, health systems should be willing to partner with vendors and physicians on an ongoing basis to better understand the biases involved in these survey results and make modifications as needed. Patients also obtain information from and contribute to self-reported, publicly available websites; therefore, additional exploration into a nationalized standard for assessing patient satisfaction also may serve as an opportunity to standardize the information patients evaluate.33 Further assessment of the potential financial and emotional impact of using the currently available patient-reported surveys on female physicians, Asian physicians, young physicians, and physicians who see young patients is needed. It is time to put pressure on a broken patient satisfaction system and improve on a national level to avoid undue negative consequences on our physicians. Use of patient satisfaction survey data should be limited until we all understand and account for the biases that are evident. ●
- Appeal to the Press Ganey corporation with the results of recent data and other studies to ensure they are aware of the biases that exist in their product
- Appeal to hospital-level administration to refrain from using Press Ganey scores as a tool to dictate reimbursement; instead rely on other more objective measures of performance (such as publications, presentations, research accomplishments, patient and surgical outcomes, promotion, committees, national leadership roles, etc)
- Apply a “corrective factor” or “adjustment factor” to eliminate the baseline discrepancy between scores for men and women
- Consider moving to an alternative survey methodology
- Provide patient education to define “performance” (ie, frame what a patient can expect from a provider such as being on time, courteous, and empathetic; caution against asking patients to assess competence and knowledge)
- Outpatient Services (OU) Survey Psychometrics Report. Published online 2019.
- Zusman EE. HCAHPS replaces Press Ganey Survey as quality measure for patient hospital experience. Neurosurgery. 2012;71:N21-N24. doi: 10.1227/01.neu.0000417536.07871.ed
- Press Ganey. Company. Accessed April 20, 2023. www.pressganey. com/company/
- Press, Ganey--first year of patient satisfaction measurement. Hosp Guest Relations Rep. 1986;1:4-5.
- DeCastellarnau A. A classification of response scale characteristics that affect data quality: a literature review. Qual Quant. 2018;52:15231559. doi: 10.1007/s11135-017-0533-4
- Tyser AR, Abtahi AM, McFadden M, et al. Evidence of non-response bias in the Press-Ganey patient satisfaction survey. BMC Health Serv Res. 2016;16:350. doi: 10.1186/s12913-016-1595-z
- Duseja R, Durham M, Schreiber M. CMS quality measure development. JAMA. 2020;324:1213-1214. doi: 10.1001/jama.2020.12070
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001. doi: 10.17226/10027
- Parmet WE. Health: policy or law? A population-based analysis of the Supreme Court’s ACA cases. J Health Polit Policy Law. 2016;41:10611081. doi: 10.1215/03616878-3665949
- Richter JP, Muhlestein DB. Patient experience and hospital profitability: is there a link? Health Care Manage Rev. 2017;42:247-257. doi: 10.1097/HMR.0000000000000105
- Huang C-H, Wu H-H, Lee Y-C, et al. What role does patient gratitude play in the relationship between relationship quality and patient loyalty? Inquiry. 2019;56:46958019868324. doi: 10.1177/0046958019868324
- Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; hospital inpatient value-based purchasing program. Final rule. Fed Regist. 2011;76:26490-26547.
- Rogo-Gupta LJ, Haunschild C, Altamirano J, et al. Physician gender is associated with Press Ganey patient satisfaction scores in outpatient gynecology. Womens Health Issues. 2018;28:281-285. doi: 10.1016 /j.whi.2018.01.001
- DeLoughery EP. Physician race and specialty influence Press Ganey survey results. Neth J Med. 2019;77:366-369.
- Homewood L, Altamirano J, Fassiotto M, et al. Women gynecologists receive lower Press Ganey patient satisfaction scores in a multicenter cross-sectional study. Am J Obstet Gynecol. 2023;228:S801. doi: 10.1016/j.ajog.2022.12.025
- Sharp B, Johnson J, Hamedani AG, et al. What are we measuring? Evaluating physician-specific satisfaction scores between emergency departments. West J Emerg Med. 2019;20:454-459. doi: 10.5811 /westjem.2019.4.41040
- Mosley M. Viewpoint: Press Ganey is a worthless tool for the ED. Emerg Med News. 2019;41:3-4. doi: 10.1097/01.EEM.0000616512.68475.69
- Sotto-Santiago S, Slaven JE, Rohr-Kirchgraber T. (Dis)Incentivizing patient satisfaction metrics: the unintended consequences of institutional bias. Health Equity. 2019;3:13-18. doi: 10.1089/heq.2018.0065
- Lloyd RC. Quality Health Care: A Guide to Developing and Using Indicators. 2nd ed. Jones & Bartlett Learning; 2019. Accessed April 23, 2023. www.jblearning.com/catalog/productdetails /9781284023077
- 2+2=7? Seven things you may not know about Press Ganey statistics. Emergency Physicians Monthly. Accessed April 23, 2023. epmonthly. com/article/227-seven-things-you-may-not-know-about-pressgainey-statistics/
- Presson AP, Zhang C, Abtahi AM, et al. Psychometric properties of the Press Ganey® Outpatient Medical Practice Survey. Health Qual Life Outcomes. 2017;15:32. doi: 10.1186/s12955-017-0610-3
- Bickell NA, Neuman J, Fei K, et al. Quality of breast cancer care: perception versus practice. J Clin Oncol. 2012;30:1791-1795. doi: 10.1200 /JCO.2011.38.7605
- Strauss K. Women in the workplace: are women tougher on other women? Forbes. July 18, 2016. Accessed April 27, 2023. www.forbes. com/sites/karstenstrauss/2016/07/18/women-in-the-workplace -are-women-tougher-on-other-women/
- Lee JW, Jones PS, Mineyama Y, et al. Cultural differences in responses to a Likert scale. Res Nurs Health. 2002;25:295-306. doi: 10.1002 /nur.10041
- Saha S, Hickam DH. Explaining low ratings of patient satisfaction among Asian-Americans. Am J Med Qual. 2003;18:256-264. doi: 10.1177/106286060301800606
- Halbesleben JRB, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33:29-39. doi: 10.1097/01. HMR.0000304493.87898.72
- Bradford L, Glaser G. Addressing physician burnout and ensuring high-quality care of the physician workforce. Obstet Gynecol. 2021;137:3-11. doi: 10.1097/AOG.0000000000004197
- Boyle P. Nation’s physician workforce evolves: more women, a bit older, and toward different specialties. AAMCNEWS. February 2, 2021. Accessed April 20, 2023. www.aamc.org/news-insights/nations-physician-workforce-evolves-more-women-bit-older-and-towarddifferent-specialties
- Zgierska A, Rabago D, Miller MM. Impact of patient satisfaction ratings on physicians and clinical care. Patient Prefer Adherence. 2014;8:437-446. doi: 10.2147/PPA.S59077
- Yeh J, Nagel EE. Patient satisfaction in obstetrics and gynecology: individualized patient-centered communication. Clin Med Insights Womens Health. 2010;3:23. doi: 10.4137/CMWH.S5870
- Epic. About us. Accessed April 19, 2023. www.epic.com/about
- United Nations. Without investment, gender equality will take nearly 300 years: UN report. September 7, 2022. Accessed April 19, 2023. news.un.org/en/story/2022/09/1126171
- Ryan T, Specht J, Smith S, et al. Does the Press Ganey Survey correlate to online health grades for a major academic otolaryngology department? Otolaryngol Head Neck Surg. 2016;155:411-415. doi: 10.1177/0194599816652386
- Outpatient Services (OU) Survey Psychometrics Report. Published online 2019.
- Zusman EE. HCAHPS replaces Press Ganey Survey as quality measure for patient hospital experience. Neurosurgery. 2012;71:N21-N24. doi: 10.1227/01.neu.0000417536.07871.ed
- Press Ganey. Company. Accessed April 20, 2023. www.pressganey. com/company/
- Press, Ganey--first year of patient satisfaction measurement. Hosp Guest Relations Rep. 1986;1:4-5.
- DeCastellarnau A. A classification of response scale characteristics that affect data quality: a literature review. Qual Quant. 2018;52:15231559. doi: 10.1007/s11135-017-0533-4
- Tyser AR, Abtahi AM, McFadden M, et al. Evidence of non-response bias in the Press-Ganey patient satisfaction survey. BMC Health Serv Res. 2016;16:350. doi: 10.1186/s12913-016-1595-z
- Duseja R, Durham M, Schreiber M. CMS quality measure development. JAMA. 2020;324:1213-1214. doi: 10.1001/jama.2020.12070
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press; 2001. doi: 10.17226/10027
- Parmet WE. Health: policy or law? A population-based analysis of the Supreme Court’s ACA cases. J Health Polit Policy Law. 2016;41:10611081. doi: 10.1215/03616878-3665949
- Richter JP, Muhlestein DB. Patient experience and hospital profitability: is there a link? Health Care Manage Rev. 2017;42:247-257. doi: 10.1097/HMR.0000000000000105
- Huang C-H, Wu H-H, Lee Y-C, et al. What role does patient gratitude play in the relationship between relationship quality and patient loyalty? Inquiry. 2019;56:46958019868324. doi: 10.1177/0046958019868324
- Centers for Medicare & Medicaid Services (CMS), HHS. Medicare program; hospital inpatient value-based purchasing program. Final rule. Fed Regist. 2011;76:26490-26547.
- Rogo-Gupta LJ, Haunschild C, Altamirano J, et al. Physician gender is associated with Press Ganey patient satisfaction scores in outpatient gynecology. Womens Health Issues. 2018;28:281-285. doi: 10.1016 /j.whi.2018.01.001
- DeLoughery EP. Physician race and specialty influence Press Ganey survey results. Neth J Med. 2019;77:366-369.
- Homewood L, Altamirano J, Fassiotto M, et al. Women gynecologists receive lower Press Ganey patient satisfaction scores in a multicenter cross-sectional study. Am J Obstet Gynecol. 2023;228:S801. doi: 10.1016/j.ajog.2022.12.025
- Sharp B, Johnson J, Hamedani AG, et al. What are we measuring? Evaluating physician-specific satisfaction scores between emergency departments. West J Emerg Med. 2019;20:454-459. doi: 10.5811 /westjem.2019.4.41040
- Mosley M. Viewpoint: Press Ganey is a worthless tool for the ED. Emerg Med News. 2019;41:3-4. doi: 10.1097/01.EEM.0000616512.68475.69
- Sotto-Santiago S, Slaven JE, Rohr-Kirchgraber T. (Dis)Incentivizing patient satisfaction metrics: the unintended consequences of institutional bias. Health Equity. 2019;3:13-18. doi: 10.1089/heq.2018.0065
- Lloyd RC. Quality Health Care: A Guide to Developing and Using Indicators. 2nd ed. Jones & Bartlett Learning; 2019. Accessed April 23, 2023. www.jblearning.com/catalog/productdetails /9781284023077
- 2+2=7? Seven things you may not know about Press Ganey statistics. Emergency Physicians Monthly. Accessed April 23, 2023. epmonthly. com/article/227-seven-things-you-may-not-know-about-pressgainey-statistics/
- Presson AP, Zhang C, Abtahi AM, et al. Psychometric properties of the Press Ganey® Outpatient Medical Practice Survey. Health Qual Life Outcomes. 2017;15:32. doi: 10.1186/s12955-017-0610-3
- Bickell NA, Neuman J, Fei K, et al. Quality of breast cancer care: perception versus practice. J Clin Oncol. 2012;30:1791-1795. doi: 10.1200 /JCO.2011.38.7605
- Strauss K. Women in the workplace: are women tougher on other women? Forbes. July 18, 2016. Accessed April 27, 2023. www.forbes. com/sites/karstenstrauss/2016/07/18/women-in-the-workplace -are-women-tougher-on-other-women/
- Lee JW, Jones PS, Mineyama Y, et al. Cultural differences in responses to a Likert scale. Res Nurs Health. 2002;25:295-306. doi: 10.1002 /nur.10041
- Saha S, Hickam DH. Explaining low ratings of patient satisfaction among Asian-Americans. Am J Med Qual. 2003;18:256-264. doi: 10.1177/106286060301800606
- Halbesleben JRB, Rathert C. Linking physician burnout and patient outcomes: exploring the dyadic relationship between physicians and patients. Health Care Manage Rev. 2008;33:29-39. doi: 10.1097/01. HMR.0000304493.87898.72
- Bradford L, Glaser G. Addressing physician burnout and ensuring high-quality care of the physician workforce. Obstet Gynecol. 2021;137:3-11. doi: 10.1097/AOG.0000000000004197
- Boyle P. Nation’s physician workforce evolves: more women, a bit older, and toward different specialties. AAMCNEWS. February 2, 2021. Accessed April 20, 2023. www.aamc.org/news-insights/nations-physician-workforce-evolves-more-women-bit-older-and-towarddifferent-specialties
- Zgierska A, Rabago D, Miller MM. Impact of patient satisfaction ratings on physicians and clinical care. Patient Prefer Adherence. 2014;8:437-446. doi: 10.2147/PPA.S59077
- Yeh J, Nagel EE. Patient satisfaction in obstetrics and gynecology: individualized patient-centered communication. Clin Med Insights Womens Health. 2010;3:23. doi: 10.4137/CMWH.S5870
- Epic. About us. Accessed April 19, 2023. www.epic.com/about
- United Nations. Without investment, gender equality will take nearly 300 years: UN report. September 7, 2022. Accessed April 19, 2023. news.un.org/en/story/2022/09/1126171
- Ryan T, Specht J, Smith S, et al. Does the Press Ganey Survey correlate to online health grades for a major academic otolaryngology department? Otolaryngol Head Neck Surg. 2016;155:411-415. doi: 10.1177/0194599816652386
Impostor syndrome is a risk for doctors of all ages
COVID-19 imposed challenges on health care professionals and systems by forcing changes in how doctors organize themselves professionally as well as in their relationships with patients and in their expectations (realistic or not) of their roles. The situation was bound to generate high rates of frustration and discomfort among younger and older physicians. It was compounded by a generational transition of the profession, which was accelerated by the virus. It was not managed by the decision-makers and was painful for doctors and patients.
Impostor syndrome (IS) is a psychological construct characterized by the persistent belief that one’s success is undeserved, rather than stemming from personal effort, skill, and ability. The phenomenon is common among medics for various reasons, including professional burnout. Recent studies have helped to better define the extent and characteristic features of the syndrome, as well as efforts to combat it.
Doctors and burnout
Although occupational burnout among physicians is a systemic issue primarily attributable to problems in the practice environment, professional norms and aspects of medical culture often contribute to the distress that individual physicians experience.
These dimensions have been well characterized and include suggestions that physicians should be impervious to normal human limitations (that is, superhuman), that work should always come first, and that seeking help is a sign of weakness. In aggregate, these attitudes lead many physicians to engage in unhealthy levels of self-sacrifice, manifested by excessive work hours, anxiety about missing something that would benefit their patients, and prioritizing work over personal health. These factors are familiar to many hospital-based and family physicians.
The impostor phenomenon
The impostor phenomenon (IP) is a psychological experience of intellectual and professional fraud. Individuals who suffer from it believe that others have inflated perceptions of the individual’s abilities and fear being judged. This fear persists despite continual proof of the individual’s successes. These people ignore praise, are highly self-critical, and attribute their successes to external factors, such as luck, hard work, or receiving help from others, rather than to qualities such as skill, intelligence, or ability.
IP is common among men and women. Some studies suggest it may be more prevalent among women. Studies across industries suggest that the phenomenon is associated with personal consequences (for example, low emotional well-being, problems with work-life integration, anxiety, depression, suicide) and professional consequences (for example, impaired job performance, occupational burnout). Studies involving U.S. medical students have revealed that more than one in four medical students experience IP and that those who experience it are at higher risk for burnout.
Surveying IS
IS, which is not a formal psychiatric diagnosis, is defined as having feelings of uncertainty, inadequacy, and being undeserving of one’s achievements despite evidence to the contrary. There are five subtypes of IS:
- Perfectionist: insecurity related to self-imposed, unachievable goals
- Expert: feeling inadequate from lacking sufficient knowledge
- Superperson: assuming excessive workloads just to feel okay among peers
- Natural genius: experiencing shame when it takes effort to develop a skill
- Soloist: believing that requesting help is a sign of weakness
Risk factors
Studies suggest that IS is a problem early in the physician training process. There is limited information on IS among physicians in practice.
Because transitions represent a risk factor for IP, the frequent rotation between clerkships and being a “perpetual novice” during medical school training may contribute to the high prevalence. Qualitative studies suggest that, once in practice, other professional experiences (for example, unfavorable patient outcomes, patient complaints, rejection of grants or manuscripts, and poor teaching evaluations or patient satisfaction scores) may contribute to IP.
Impact on doctors
Several methods have been used to classify how much the phenomenon interferes with a person’s life. The Clance Impostor Phenomenon Scale is a 20-item scale that asks respondents to indicate how well each item characterizes their experience on a 5-point scale. Options range from “not at all” to “very true.” The sum of responses to the individual items is used to create an aggregate score (IP score). The higher the score, the more frequently and seriously IP interferes with a person’s life.
A simplified version of the IP score was used in a study of 3,237 U.S. doctors that investigated the association between IS and burnout among doctors and to compare their rates of IS with those of other professionals.
Mean IP scores were higher for female physicians than for male physicians (mean, 10.91 vs. 9.12; P < .001). Scores decreased with age and were lower among those who were married or widowed.
With respect to professional characteristics, IP scores were greater among those in academic practice or who worked in the Veterans Affairs medical system and decreased with years in practice.
The highest IP scores were among pediatric subspecialists, general pediatricians, and emergency medicine physicians. Scores were lowest among ophthalmologists, radiologists, and orthopedic surgeons. IP has been independently associated with the risk of burnout and low professional fulfillment.
Lessening the impact
An article commenting on the study highlighted the following expert practice strategies that doctors can use to reduce the impact of IS in their professional life.
- Review and celebrate feats that have led to your professional role.
- Share concerns with trusted colleagues who can validate your accomplishments and normalize your feelings by reporting their own struggles with IS.
- Combat perfectionism by accepting that it is okay to be good enough when meeting the challenges of a demanding profession.
- Exercise self-compassion as an alternative to relying on an external locus of self-worth.
- Understand that IS may be common, especially during transitions, such as when entering medical school, graduate medical training, or starting a new career.
This article was translated from Univadis Italy. A version appeared on Medscape.com.
COVID-19 imposed challenges on health care professionals and systems by forcing changes in how doctors organize themselves professionally as well as in their relationships with patients and in their expectations (realistic or not) of their roles. The situation was bound to generate high rates of frustration and discomfort among younger and older physicians. It was compounded by a generational transition of the profession, which was accelerated by the virus. It was not managed by the decision-makers and was painful for doctors and patients.
Impostor syndrome (IS) is a psychological construct characterized by the persistent belief that one’s success is undeserved, rather than stemming from personal effort, skill, and ability. The phenomenon is common among medics for various reasons, including professional burnout. Recent studies have helped to better define the extent and characteristic features of the syndrome, as well as efforts to combat it.
Doctors and burnout
Although occupational burnout among physicians is a systemic issue primarily attributable to problems in the practice environment, professional norms and aspects of medical culture often contribute to the distress that individual physicians experience.
These dimensions have been well characterized and include suggestions that physicians should be impervious to normal human limitations (that is, superhuman), that work should always come first, and that seeking help is a sign of weakness. In aggregate, these attitudes lead many physicians to engage in unhealthy levels of self-sacrifice, manifested by excessive work hours, anxiety about missing something that would benefit their patients, and prioritizing work over personal health. These factors are familiar to many hospital-based and family physicians.
The impostor phenomenon
The impostor phenomenon (IP) is a psychological experience of intellectual and professional fraud. Individuals who suffer from it believe that others have inflated perceptions of the individual’s abilities and fear being judged. This fear persists despite continual proof of the individual’s successes. These people ignore praise, are highly self-critical, and attribute their successes to external factors, such as luck, hard work, or receiving help from others, rather than to qualities such as skill, intelligence, or ability.
IP is common among men and women. Some studies suggest it may be more prevalent among women. Studies across industries suggest that the phenomenon is associated with personal consequences (for example, low emotional well-being, problems with work-life integration, anxiety, depression, suicide) and professional consequences (for example, impaired job performance, occupational burnout). Studies involving U.S. medical students have revealed that more than one in four medical students experience IP and that those who experience it are at higher risk for burnout.
Surveying IS
IS, which is not a formal psychiatric diagnosis, is defined as having feelings of uncertainty, inadequacy, and being undeserving of one’s achievements despite evidence to the contrary. There are five subtypes of IS:
- Perfectionist: insecurity related to self-imposed, unachievable goals
- Expert: feeling inadequate from lacking sufficient knowledge
- Superperson: assuming excessive workloads just to feel okay among peers
- Natural genius: experiencing shame when it takes effort to develop a skill
- Soloist: believing that requesting help is a sign of weakness
Risk factors
Studies suggest that IS is a problem early in the physician training process. There is limited information on IS among physicians in practice.
Because transitions represent a risk factor for IP, the frequent rotation between clerkships and being a “perpetual novice” during medical school training may contribute to the high prevalence. Qualitative studies suggest that, once in practice, other professional experiences (for example, unfavorable patient outcomes, patient complaints, rejection of grants or manuscripts, and poor teaching evaluations or patient satisfaction scores) may contribute to IP.
Impact on doctors
Several methods have been used to classify how much the phenomenon interferes with a person’s life. The Clance Impostor Phenomenon Scale is a 20-item scale that asks respondents to indicate how well each item characterizes their experience on a 5-point scale. Options range from “not at all” to “very true.” The sum of responses to the individual items is used to create an aggregate score (IP score). The higher the score, the more frequently and seriously IP interferes with a person’s life.
A simplified version of the IP score was used in a study of 3,237 U.S. doctors that investigated the association between IS and burnout among doctors and to compare their rates of IS with those of other professionals.
Mean IP scores were higher for female physicians than for male physicians (mean, 10.91 vs. 9.12; P < .001). Scores decreased with age and were lower among those who were married or widowed.
With respect to professional characteristics, IP scores were greater among those in academic practice or who worked in the Veterans Affairs medical system and decreased with years in practice.
The highest IP scores were among pediatric subspecialists, general pediatricians, and emergency medicine physicians. Scores were lowest among ophthalmologists, radiologists, and orthopedic surgeons. IP has been independently associated with the risk of burnout and low professional fulfillment.
Lessening the impact
An article commenting on the study highlighted the following expert practice strategies that doctors can use to reduce the impact of IS in their professional life.
- Review and celebrate feats that have led to your professional role.
- Share concerns with trusted colleagues who can validate your accomplishments and normalize your feelings by reporting their own struggles with IS.
- Combat perfectionism by accepting that it is okay to be good enough when meeting the challenges of a demanding profession.
- Exercise self-compassion as an alternative to relying on an external locus of self-worth.
- Understand that IS may be common, especially during transitions, such as when entering medical school, graduate medical training, or starting a new career.
This article was translated from Univadis Italy. A version appeared on Medscape.com.
COVID-19 imposed challenges on health care professionals and systems by forcing changes in how doctors organize themselves professionally as well as in their relationships with patients and in their expectations (realistic or not) of their roles. The situation was bound to generate high rates of frustration and discomfort among younger and older physicians. It was compounded by a generational transition of the profession, which was accelerated by the virus. It was not managed by the decision-makers and was painful for doctors and patients.
Impostor syndrome (IS) is a psychological construct characterized by the persistent belief that one’s success is undeserved, rather than stemming from personal effort, skill, and ability. The phenomenon is common among medics for various reasons, including professional burnout. Recent studies have helped to better define the extent and characteristic features of the syndrome, as well as efforts to combat it.
Doctors and burnout
Although occupational burnout among physicians is a systemic issue primarily attributable to problems in the practice environment, professional norms and aspects of medical culture often contribute to the distress that individual physicians experience.
These dimensions have been well characterized and include suggestions that physicians should be impervious to normal human limitations (that is, superhuman), that work should always come first, and that seeking help is a sign of weakness. In aggregate, these attitudes lead many physicians to engage in unhealthy levels of self-sacrifice, manifested by excessive work hours, anxiety about missing something that would benefit their patients, and prioritizing work over personal health. These factors are familiar to many hospital-based and family physicians.
The impostor phenomenon
The impostor phenomenon (IP) is a psychological experience of intellectual and professional fraud. Individuals who suffer from it believe that others have inflated perceptions of the individual’s abilities and fear being judged. This fear persists despite continual proof of the individual’s successes. These people ignore praise, are highly self-critical, and attribute their successes to external factors, such as luck, hard work, or receiving help from others, rather than to qualities such as skill, intelligence, or ability.
IP is common among men and women. Some studies suggest it may be more prevalent among women. Studies across industries suggest that the phenomenon is associated with personal consequences (for example, low emotional well-being, problems with work-life integration, anxiety, depression, suicide) and professional consequences (for example, impaired job performance, occupational burnout). Studies involving U.S. medical students have revealed that more than one in four medical students experience IP and that those who experience it are at higher risk for burnout.
Surveying IS
IS, which is not a formal psychiatric diagnosis, is defined as having feelings of uncertainty, inadequacy, and being undeserving of one’s achievements despite evidence to the contrary. There are five subtypes of IS:
- Perfectionist: insecurity related to self-imposed, unachievable goals
- Expert: feeling inadequate from lacking sufficient knowledge
- Superperson: assuming excessive workloads just to feel okay among peers
- Natural genius: experiencing shame when it takes effort to develop a skill
- Soloist: believing that requesting help is a sign of weakness
Risk factors
Studies suggest that IS is a problem early in the physician training process. There is limited information on IS among physicians in practice.
Because transitions represent a risk factor for IP, the frequent rotation between clerkships and being a “perpetual novice” during medical school training may contribute to the high prevalence. Qualitative studies suggest that, once in practice, other professional experiences (for example, unfavorable patient outcomes, patient complaints, rejection of grants or manuscripts, and poor teaching evaluations or patient satisfaction scores) may contribute to IP.
Impact on doctors
Several methods have been used to classify how much the phenomenon interferes with a person’s life. The Clance Impostor Phenomenon Scale is a 20-item scale that asks respondents to indicate how well each item characterizes their experience on a 5-point scale. Options range from “not at all” to “very true.” The sum of responses to the individual items is used to create an aggregate score (IP score). The higher the score, the more frequently and seriously IP interferes with a person’s life.
A simplified version of the IP score was used in a study of 3,237 U.S. doctors that investigated the association between IS and burnout among doctors and to compare their rates of IS with those of other professionals.
Mean IP scores were higher for female physicians than for male physicians (mean, 10.91 vs. 9.12; P < .001). Scores decreased with age and were lower among those who were married or widowed.
With respect to professional characteristics, IP scores were greater among those in academic practice or who worked in the Veterans Affairs medical system and decreased with years in practice.
The highest IP scores were among pediatric subspecialists, general pediatricians, and emergency medicine physicians. Scores were lowest among ophthalmologists, radiologists, and orthopedic surgeons. IP has been independently associated with the risk of burnout and low professional fulfillment.
Lessening the impact
An article commenting on the study highlighted the following expert practice strategies that doctors can use to reduce the impact of IS in their professional life.
- Review and celebrate feats that have led to your professional role.
- Share concerns with trusted colleagues who can validate your accomplishments and normalize your feelings by reporting their own struggles with IS.
- Combat perfectionism by accepting that it is okay to be good enough when meeting the challenges of a demanding profession.
- Exercise self-compassion as an alternative to relying on an external locus of self-worth.
- Understand that IS may be common, especially during transitions, such as when entering medical school, graduate medical training, or starting a new career.
This article was translated from Univadis Italy. A version appeared on Medscape.com.

