User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Registry reveals H. pylori management mistakes
Many patients are receiving inadequate eradication therapy for Helicobacter pylori infection, according to analysis of a European registry.
In their analysis, published in the Journal of Clinical Gastroenterology, Olga P. Nyssen, BSc, PhD, of the Autonomous University of Madrid and colleagues discussed seven errors, which included prescribing a triple instead of quadruple regimen, prescribing therapy for too short of a duration, and prescribing a low dose of proton pump inhibitors (PPIs).
“[E]ven after more than 30 years of experience in H. pylori treatment, the ideal regimen to treat this infection remains undefined,” the investigators wrote. The European Registry on Helicobacter pylori management “represents a good mapping overview of the current situation regarding H. pylori management, allowing not only continuous assessment of the integration of clinical recommendations agreed on medical consensus, but also of the possible strategies for improvement.”
Patient data were drawn from registry-participating countries that each had more than 1,000 cases of H. pylori available; most came from Spain, followed by Russia, Italy, Slovenia, and Lithuania. Of these patients, data for 26,340 patients were analyzed, which ultimately represented 80% of the total registry from 2013 to 2019.
The first mistake discussed in the paper regarded use of less-effective triple therapies (typically PPI plus two antibiotics); one review showed that these regimens fail in 20%-40% of cases. Increasing antibiotic resistances have only worsened the success rate. According to this study, a triple regimen was given as first-line treatment in 46% of cases. Overall, frequency of triple-therapy prescriptions decreased from more than 50% in 2013 to about 40% in 2019. More significant improvements in this area were achieved in Spain, where use of triple therapies decreased from 24% in 2014 to 0% in 2019. According to the investigators, this finding serves as a “paradigmatic example of improvement with time.”
The authors pointed out that “overwhelming evidence” supports 14-day treatment; however, 69% of triple-therapy durations and 58% of quadruple therapy cases were for 7 or 10 days. Triple therapy at this duration showed only 81% cure rate, while it was 88% with 14 days, and quadruple therapy was only 80% effective at 7-10 days but 90% effective at 14 days.
“Fortunately,” the investigators wrote, “this mistake was progressively found less frequently and, at present, the prescription of 7-day standard triple therapy regimens has almost disappeared.”
The authors noted acid suppression via PPIs improves cure rates: In one meta-analysis, the cure rate of triple therapy regimens increased by 6%-10% with high doses of PPIs. However, the current study found that 48% of triple therapies included low-dose PPIs. This number decreased over time, the authors noted: from 67% in 2013 to 20% in 2019.
“From another perspective, the daily PPI dose has increased from a dose equivalent to 54 mg of omeprazole in 2013 to 104 mg in 2019,” they wrote.
The other four errors they discussed were failing to adequately consider penicillin allergies in prescription choices, failing to consider the importance of treatment compliance, repeating certain antibiotics after failures, and not checking eradication success after treatment.
Based on these findings, Dr. Nyssen and colleagues suggested that “penetration of recommendations in the participating European countries is still poor and delayed, even though some improvements from guidelines have been partially incorporated.”
According to Grigorios I. Leontiadis, MD, PhD, of McMaster University, Hamilton, Ont., who coauthored the 2017 American College of Gastroenterology H. pylori management guidelines and the Canadian Association of Gastroenterology “Toronto Consensus” in 2016, “This study is important and timely given the steadily increasing antibiotic resistance of H. pylori worldwide.”
Although Dr. Leontiadias described the results as “suboptimal,” he was partially reassured by the improvements over time, “especially following publication of the 2016 European clinical practice guidelines.” He also noted that some older clinical practice guidelines issued conditional recommendations, which could “justify the lower adherence seen in the early period of this study.”
“The unanswered question,” Dr. Leontiadias went on, “is whether the practice of gastroenterologists who volunteered to participate in this prospective registry is truly representative of how H. pylori is managed in Europe. Most likely it isn’t. Nonparticipating gastroenterologists and nongastroenterologist health care practitioners are probably less aware of and less adherent to clinical practice guidelines. This means that the actual situation in the real world is probably grimmer than what this study shows.”
William D. Chey, MD, Nostrant Collegiate Professor of Gastroenterology at the University of Michigan, Ann Arbor, considered the results “not entirely surprising, but nonetheless, noteworthy.”
Dr. Chey noted that the United States lacks a similar registry to compare real-world H. pylori management; even so, he suggested several findings that “bear reiteration” for clinicians in the United States.
“U.S. providers should consider regimens other than clarithromycin triple therapy when treating H. pylori infection,” Dr. Chey said. “Since U.S. providers do not have reliable data on H. pylori antimicrobial resistance, it is useful to ask about prior macrolide antibiotic exposure, and if a patient has received a macrolide for any reason, clarithromycin triple therapy should be avoided. Bismuth quadruple therapy remains a reliable first-line treatment option in the U.S. Another recently approved first-line treatment option is the combination of a proton pump inhibitor, rifabutin, and amoxicillin. Treatment regimens in the U.S. should be given for a minimum of 10 days and, preferably, for 14 days. Another point made by the article is that providers should be maximizing gastric acid suppression by using higher doses of proton pump inhibitors when treating H. pylori.”
Dr. Chey also noted an emerging treatment option that could soon be available. “Results from phase 3 trials in North America and Europe with the potassium-competitive acid blocker vonoprazan combined with amoxicillin, with and without clarithromycin, are expected in 2021 and may provide another novel first-line treatment option.”
Dr. Nyssen and colleagues disclosed relationships with Allergan, Mayoly, Janssen, and others. Dr. Chey is a consultant for Redhill, Phathom, and Takeda, which is developing vonoprazan. Dr. Leontiadias disclosed no conflicts of interest.
This article was updated 2/16/21.
Many patients are receiving inadequate eradication therapy for Helicobacter pylori infection, according to analysis of a European registry.
In their analysis, published in the Journal of Clinical Gastroenterology, Olga P. Nyssen, BSc, PhD, of the Autonomous University of Madrid and colleagues discussed seven errors, which included prescribing a triple instead of quadruple regimen, prescribing therapy for too short of a duration, and prescribing a low dose of proton pump inhibitors (PPIs).
“[E]ven after more than 30 years of experience in H. pylori treatment, the ideal regimen to treat this infection remains undefined,” the investigators wrote. The European Registry on Helicobacter pylori management “represents a good mapping overview of the current situation regarding H. pylori management, allowing not only continuous assessment of the integration of clinical recommendations agreed on medical consensus, but also of the possible strategies for improvement.”
Patient data were drawn from registry-participating countries that each had more than 1,000 cases of H. pylori available; most came from Spain, followed by Russia, Italy, Slovenia, and Lithuania. Of these patients, data for 26,340 patients were analyzed, which ultimately represented 80% of the total registry from 2013 to 2019.
The first mistake discussed in the paper regarded use of less-effective triple therapies (typically PPI plus two antibiotics); one review showed that these regimens fail in 20%-40% of cases. Increasing antibiotic resistances have only worsened the success rate. According to this study, a triple regimen was given as first-line treatment in 46% of cases. Overall, frequency of triple-therapy prescriptions decreased from more than 50% in 2013 to about 40% in 2019. More significant improvements in this area were achieved in Spain, where use of triple therapies decreased from 24% in 2014 to 0% in 2019. According to the investigators, this finding serves as a “paradigmatic example of improvement with time.”
The authors pointed out that “overwhelming evidence” supports 14-day treatment; however, 69% of triple-therapy durations and 58% of quadruple therapy cases were for 7 or 10 days. Triple therapy at this duration showed only 81% cure rate, while it was 88% with 14 days, and quadruple therapy was only 80% effective at 7-10 days but 90% effective at 14 days.
“Fortunately,” the investigators wrote, “this mistake was progressively found less frequently and, at present, the prescription of 7-day standard triple therapy regimens has almost disappeared.”
The authors noted acid suppression via PPIs improves cure rates: In one meta-analysis, the cure rate of triple therapy regimens increased by 6%-10% with high doses of PPIs. However, the current study found that 48% of triple therapies included low-dose PPIs. This number decreased over time, the authors noted: from 67% in 2013 to 20% in 2019.
“From another perspective, the daily PPI dose has increased from a dose equivalent to 54 mg of omeprazole in 2013 to 104 mg in 2019,” they wrote.
The other four errors they discussed were failing to adequately consider penicillin allergies in prescription choices, failing to consider the importance of treatment compliance, repeating certain antibiotics after failures, and not checking eradication success after treatment.
Based on these findings, Dr. Nyssen and colleagues suggested that “penetration of recommendations in the participating European countries is still poor and delayed, even though some improvements from guidelines have been partially incorporated.”
According to Grigorios I. Leontiadis, MD, PhD, of McMaster University, Hamilton, Ont., who coauthored the 2017 American College of Gastroenterology H. pylori management guidelines and the Canadian Association of Gastroenterology “Toronto Consensus” in 2016, “This study is important and timely given the steadily increasing antibiotic resistance of H. pylori worldwide.”
Although Dr. Leontiadias described the results as “suboptimal,” he was partially reassured by the improvements over time, “especially following publication of the 2016 European clinical practice guidelines.” He also noted that some older clinical practice guidelines issued conditional recommendations, which could “justify the lower adherence seen in the early period of this study.”
“The unanswered question,” Dr. Leontiadias went on, “is whether the practice of gastroenterologists who volunteered to participate in this prospective registry is truly representative of how H. pylori is managed in Europe. Most likely it isn’t. Nonparticipating gastroenterologists and nongastroenterologist health care practitioners are probably less aware of and less adherent to clinical practice guidelines. This means that the actual situation in the real world is probably grimmer than what this study shows.”
William D. Chey, MD, Nostrant Collegiate Professor of Gastroenterology at the University of Michigan, Ann Arbor, considered the results “not entirely surprising, but nonetheless, noteworthy.”
Dr. Chey noted that the United States lacks a similar registry to compare real-world H. pylori management; even so, he suggested several findings that “bear reiteration” for clinicians in the United States.
“U.S. providers should consider regimens other than clarithromycin triple therapy when treating H. pylori infection,” Dr. Chey said. “Since U.S. providers do not have reliable data on H. pylori antimicrobial resistance, it is useful to ask about prior macrolide antibiotic exposure, and if a patient has received a macrolide for any reason, clarithromycin triple therapy should be avoided. Bismuth quadruple therapy remains a reliable first-line treatment option in the U.S. Another recently approved first-line treatment option is the combination of a proton pump inhibitor, rifabutin, and amoxicillin. Treatment regimens in the U.S. should be given for a minimum of 10 days and, preferably, for 14 days. Another point made by the article is that providers should be maximizing gastric acid suppression by using higher doses of proton pump inhibitors when treating H. pylori.”
Dr. Chey also noted an emerging treatment option that could soon be available. “Results from phase 3 trials in North America and Europe with the potassium-competitive acid blocker vonoprazan combined with amoxicillin, with and without clarithromycin, are expected in 2021 and may provide another novel first-line treatment option.”
Dr. Nyssen and colleagues disclosed relationships with Allergan, Mayoly, Janssen, and others. Dr. Chey is a consultant for Redhill, Phathom, and Takeda, which is developing vonoprazan. Dr. Leontiadias disclosed no conflicts of interest.
This article was updated 2/16/21.
Many patients are receiving inadequate eradication therapy for Helicobacter pylori infection, according to analysis of a European registry.
In their analysis, published in the Journal of Clinical Gastroenterology, Olga P. Nyssen, BSc, PhD, of the Autonomous University of Madrid and colleagues discussed seven errors, which included prescribing a triple instead of quadruple regimen, prescribing therapy for too short of a duration, and prescribing a low dose of proton pump inhibitors (PPIs).
“[E]ven after more than 30 years of experience in H. pylori treatment, the ideal regimen to treat this infection remains undefined,” the investigators wrote. The European Registry on Helicobacter pylori management “represents a good mapping overview of the current situation regarding H. pylori management, allowing not only continuous assessment of the integration of clinical recommendations agreed on medical consensus, but also of the possible strategies for improvement.”
Patient data were drawn from registry-participating countries that each had more than 1,000 cases of H. pylori available; most came from Spain, followed by Russia, Italy, Slovenia, and Lithuania. Of these patients, data for 26,340 patients were analyzed, which ultimately represented 80% of the total registry from 2013 to 2019.
The first mistake discussed in the paper regarded use of less-effective triple therapies (typically PPI plus two antibiotics); one review showed that these regimens fail in 20%-40% of cases. Increasing antibiotic resistances have only worsened the success rate. According to this study, a triple regimen was given as first-line treatment in 46% of cases. Overall, frequency of triple-therapy prescriptions decreased from more than 50% in 2013 to about 40% in 2019. More significant improvements in this area were achieved in Spain, where use of triple therapies decreased from 24% in 2014 to 0% in 2019. According to the investigators, this finding serves as a “paradigmatic example of improvement with time.”
The authors pointed out that “overwhelming evidence” supports 14-day treatment; however, 69% of triple-therapy durations and 58% of quadruple therapy cases were for 7 or 10 days. Triple therapy at this duration showed only 81% cure rate, while it was 88% with 14 days, and quadruple therapy was only 80% effective at 7-10 days but 90% effective at 14 days.
“Fortunately,” the investigators wrote, “this mistake was progressively found less frequently and, at present, the prescription of 7-day standard triple therapy regimens has almost disappeared.”
The authors noted acid suppression via PPIs improves cure rates: In one meta-analysis, the cure rate of triple therapy regimens increased by 6%-10% with high doses of PPIs. However, the current study found that 48% of triple therapies included low-dose PPIs. This number decreased over time, the authors noted: from 67% in 2013 to 20% in 2019.
“From another perspective, the daily PPI dose has increased from a dose equivalent to 54 mg of omeprazole in 2013 to 104 mg in 2019,” they wrote.
The other four errors they discussed were failing to adequately consider penicillin allergies in prescription choices, failing to consider the importance of treatment compliance, repeating certain antibiotics after failures, and not checking eradication success after treatment.
Based on these findings, Dr. Nyssen and colleagues suggested that “penetration of recommendations in the participating European countries is still poor and delayed, even though some improvements from guidelines have been partially incorporated.”
According to Grigorios I. Leontiadis, MD, PhD, of McMaster University, Hamilton, Ont., who coauthored the 2017 American College of Gastroenterology H. pylori management guidelines and the Canadian Association of Gastroenterology “Toronto Consensus” in 2016, “This study is important and timely given the steadily increasing antibiotic resistance of H. pylori worldwide.”
Although Dr. Leontiadias described the results as “suboptimal,” he was partially reassured by the improvements over time, “especially following publication of the 2016 European clinical practice guidelines.” He also noted that some older clinical practice guidelines issued conditional recommendations, which could “justify the lower adherence seen in the early period of this study.”
“The unanswered question,” Dr. Leontiadias went on, “is whether the practice of gastroenterologists who volunteered to participate in this prospective registry is truly representative of how H. pylori is managed in Europe. Most likely it isn’t. Nonparticipating gastroenterologists and nongastroenterologist health care practitioners are probably less aware of and less adherent to clinical practice guidelines. This means that the actual situation in the real world is probably grimmer than what this study shows.”
William D. Chey, MD, Nostrant Collegiate Professor of Gastroenterology at the University of Michigan, Ann Arbor, considered the results “not entirely surprising, but nonetheless, noteworthy.”
Dr. Chey noted that the United States lacks a similar registry to compare real-world H. pylori management; even so, he suggested several findings that “bear reiteration” for clinicians in the United States.
“U.S. providers should consider regimens other than clarithromycin triple therapy when treating H. pylori infection,” Dr. Chey said. “Since U.S. providers do not have reliable data on H. pylori antimicrobial resistance, it is useful to ask about prior macrolide antibiotic exposure, and if a patient has received a macrolide for any reason, clarithromycin triple therapy should be avoided. Bismuth quadruple therapy remains a reliable first-line treatment option in the U.S. Another recently approved first-line treatment option is the combination of a proton pump inhibitor, rifabutin, and amoxicillin. Treatment regimens in the U.S. should be given for a minimum of 10 days and, preferably, for 14 days. Another point made by the article is that providers should be maximizing gastric acid suppression by using higher doses of proton pump inhibitors when treating H. pylori.”
Dr. Chey also noted an emerging treatment option that could soon be available. “Results from phase 3 trials in North America and Europe with the potassium-competitive acid blocker vonoprazan combined with amoxicillin, with and without clarithromycin, are expected in 2021 and may provide another novel first-line treatment option.”
Dr. Nyssen and colleagues disclosed relationships with Allergan, Mayoly, Janssen, and others. Dr. Chey is a consultant for Redhill, Phathom, and Takeda, which is developing vonoprazan. Dr. Leontiadias disclosed no conflicts of interest.
This article was updated 2/16/21.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
What we know and don’t know about virus variants and vaccines
About 20 states across the country have detected the more transmissible B.1.1.7 SARS-CoV-2 variant to date. Given the unknowns of the emerging situation, experts with the Infectious Diseases Society of America addressed vaccine effectiveness, how well equipped the United States is to track new mutations, and shared their impressions of President Joe Biden’s COVID-19 executive orders.
One of the major concerns remains the ability of COVID-19 vaccines to work on new strains. “All of our vaccines target the spike protein and try to elicit neutralizing antibodies that bind to that protein,” Mirella Salvatore, MD, assistant professor of medicine and population health sciences at Weill Cornell Medicine, New York, said during an IDSA press briefing on Thursday.
The B.1.1.7 mutation occurs in the “very important” spike protein, a component of the SARS-CoV-2 virus necessary for binding, which allows the virus to enter cells, added Dr. Salvatore, an IDSA fellow.
The evidence suggests that SARS-CoV-2 should be capable of producing one or two mutations per month. However, the B.1.1.7 variant surprised investigators in the United Kingdom when they first discovered the strain had 17 mutations, Dr. Salvatore said.
It’s still unknown why this particular strain is more transmissible, but Dr. Salvatore speculated that the mutation gives the virus an advantage and increases binding, allowing it to enter cells more easily. She added that the mutations might have arisen among immunocompromised people infected with SARS-CoV-2, but “that is just a hypothesis.”
On a positive note, Kathryn M. Edwards, MD, another IDSA fellow, explained at the briefing that the existing vaccines target more than one location on the virus’ spike protein. Therefore, “if there is a mutation that changes one structure of the spike protein, there will be other areas where the binding can occur.”
This polyclonal response “is why the vaccine can still be effective against this virus,” added Dr. Edwards, scientific director of the Vanderbilt Vaccine Research Program and professor of pediatrics at Vanderbilt University, Nashville, Tenn.
Dr. Salvatore emphasized that, although the new variant is more transmissible, it doesn’t appear to be more lethal. “This might affect overall mortality but not for the individual who gets the infection.”
Staying one step ahead
When asked for assurance that COVID-19 vaccines will work against emerging variants, Dr. Edwards said, “It may be we will have to change the vaccine so it is more responsive to new variants, but at this point that does not seem to be the case.”
Should the vaccines require an update, the messenger RNA vaccines have an advantage – researchers can rapidly revise them. “All you need to do is put all the little nucleotides together,” Dr. Edwards said.
“A number of us are looking at how this will work, and we look to influenza,” she added. Dr. Edwards drew an analogy to choosing – and sometimes updating – the influenza strains each year for the annual flu vaccine. With appropriate funding, the same system could be replicated to address any evolving changes to SARS-CoV-2.
On funding, Dr. Salvatore said more money would be required to optimize the surveillance system for emerging strains in the United States.
“We actually have this system – there is a wonderful network that sequences the influenza strains,” she said. “The structure exists, we just need the funding.”
“The CDC is getting the system tooled up to get more viruses to be sequenced,” Dr. Edwards said.
Both experts praised the CDC for its website with up-to-date surveillance information on emerging strains of SARS-CoV-2.
President Biden’s backing of science
A reporter asked each infectious disease expert to share their impression of President Biden’s newly signed COVID-19 executive orders.
“The biggest takeaway is the role of science and the lessons we’ve learned from masks, handwashing, and distancing,” Dr. Edwards said. “We need to heed the advice ... [especially] with a variant that is more contagious.
“It is encouraging that science will be listened to – that is the overall message,” she added.
Dr. Salvatore agreed, saying that the orders give “the feeling that we can now act by following science.”
“We have plenty of papers that show the effectiveness of masking,” for example, she said. Dr. Salvatore acknowledged that there are “a lot of contrasting ideas about masking” across the United States but stressed their importance.
“We should follow measures that we know work,” she said.
Both experts said more research is needed to stay ahead of this evolving scenario. “We still need a lot of basic science showing how this virus replicates in the cell,” Dr. Salvatore said. “We need to really characterize all these mutations and their functions.”
“We need to be concerned, do follow-up studies,” she added, “but we don’t need to panic.”
This article was based on an Infectious Diseases Society of America Media Briefing on Jan. 21, 2021. Dr. Salvatore disclosed that she is a site principal investigator on a study from Verily Life Sciences/Brin Foundation on Predictors of Severe COVID-19 Outcomes and principal investigator for an investigator-initiated study sponsored by Genentech on combination therapy in influenza. Dr. Edwards disclosed National Institutes of Health and Centers for Disease Control and Prevention grants; consulting for Bionet and IBM; and being a member of data safety and monitoring committees for Sanofi, X-4 Pharma, Seqirus, Moderna, Pfizer, and Merck.
A version of this article first appeared on Medscape.com.
About 20 states across the country have detected the more transmissible B.1.1.7 SARS-CoV-2 variant to date. Given the unknowns of the emerging situation, experts with the Infectious Diseases Society of America addressed vaccine effectiveness, how well equipped the United States is to track new mutations, and shared their impressions of President Joe Biden’s COVID-19 executive orders.
One of the major concerns remains the ability of COVID-19 vaccines to work on new strains. “All of our vaccines target the spike protein and try to elicit neutralizing antibodies that bind to that protein,” Mirella Salvatore, MD, assistant professor of medicine and population health sciences at Weill Cornell Medicine, New York, said during an IDSA press briefing on Thursday.
The B.1.1.7 mutation occurs in the “very important” spike protein, a component of the SARS-CoV-2 virus necessary for binding, which allows the virus to enter cells, added Dr. Salvatore, an IDSA fellow.
The evidence suggests that SARS-CoV-2 should be capable of producing one or two mutations per month. However, the B.1.1.7 variant surprised investigators in the United Kingdom when they first discovered the strain had 17 mutations, Dr. Salvatore said.
It’s still unknown why this particular strain is more transmissible, but Dr. Salvatore speculated that the mutation gives the virus an advantage and increases binding, allowing it to enter cells more easily. She added that the mutations might have arisen among immunocompromised people infected with SARS-CoV-2, but “that is just a hypothesis.”
On a positive note, Kathryn M. Edwards, MD, another IDSA fellow, explained at the briefing that the existing vaccines target more than one location on the virus’ spike protein. Therefore, “if there is a mutation that changes one structure of the spike protein, there will be other areas where the binding can occur.”
This polyclonal response “is why the vaccine can still be effective against this virus,” added Dr. Edwards, scientific director of the Vanderbilt Vaccine Research Program and professor of pediatrics at Vanderbilt University, Nashville, Tenn.
Dr. Salvatore emphasized that, although the new variant is more transmissible, it doesn’t appear to be more lethal. “This might affect overall mortality but not for the individual who gets the infection.”
Staying one step ahead
When asked for assurance that COVID-19 vaccines will work against emerging variants, Dr. Edwards said, “It may be we will have to change the vaccine so it is more responsive to new variants, but at this point that does not seem to be the case.”
Should the vaccines require an update, the messenger RNA vaccines have an advantage – researchers can rapidly revise them. “All you need to do is put all the little nucleotides together,” Dr. Edwards said.
“A number of us are looking at how this will work, and we look to influenza,” she added. Dr. Edwards drew an analogy to choosing – and sometimes updating – the influenza strains each year for the annual flu vaccine. With appropriate funding, the same system could be replicated to address any evolving changes to SARS-CoV-2.
On funding, Dr. Salvatore said more money would be required to optimize the surveillance system for emerging strains in the United States.
“We actually have this system – there is a wonderful network that sequences the influenza strains,” she said. “The structure exists, we just need the funding.”
“The CDC is getting the system tooled up to get more viruses to be sequenced,” Dr. Edwards said.
Both experts praised the CDC for its website with up-to-date surveillance information on emerging strains of SARS-CoV-2.
President Biden’s backing of science
A reporter asked each infectious disease expert to share their impression of President Biden’s newly signed COVID-19 executive orders.
“The biggest takeaway is the role of science and the lessons we’ve learned from masks, handwashing, and distancing,” Dr. Edwards said. “We need to heed the advice ... [especially] with a variant that is more contagious.
“It is encouraging that science will be listened to – that is the overall message,” she added.
Dr. Salvatore agreed, saying that the orders give “the feeling that we can now act by following science.”
“We have plenty of papers that show the effectiveness of masking,” for example, she said. Dr. Salvatore acknowledged that there are “a lot of contrasting ideas about masking” across the United States but stressed their importance.
“We should follow measures that we know work,” she said.
Both experts said more research is needed to stay ahead of this evolving scenario. “We still need a lot of basic science showing how this virus replicates in the cell,” Dr. Salvatore said. “We need to really characterize all these mutations and their functions.”
“We need to be concerned, do follow-up studies,” she added, “but we don’t need to panic.”
This article was based on an Infectious Diseases Society of America Media Briefing on Jan. 21, 2021. Dr. Salvatore disclosed that she is a site principal investigator on a study from Verily Life Sciences/Brin Foundation on Predictors of Severe COVID-19 Outcomes and principal investigator for an investigator-initiated study sponsored by Genentech on combination therapy in influenza. Dr. Edwards disclosed National Institutes of Health and Centers for Disease Control and Prevention grants; consulting for Bionet and IBM; and being a member of data safety and monitoring committees for Sanofi, X-4 Pharma, Seqirus, Moderna, Pfizer, and Merck.
A version of this article first appeared on Medscape.com.
About 20 states across the country have detected the more transmissible B.1.1.7 SARS-CoV-2 variant to date. Given the unknowns of the emerging situation, experts with the Infectious Diseases Society of America addressed vaccine effectiveness, how well equipped the United States is to track new mutations, and shared their impressions of President Joe Biden’s COVID-19 executive orders.
One of the major concerns remains the ability of COVID-19 vaccines to work on new strains. “All of our vaccines target the spike protein and try to elicit neutralizing antibodies that bind to that protein,” Mirella Salvatore, MD, assistant professor of medicine and population health sciences at Weill Cornell Medicine, New York, said during an IDSA press briefing on Thursday.
The B.1.1.7 mutation occurs in the “very important” spike protein, a component of the SARS-CoV-2 virus necessary for binding, which allows the virus to enter cells, added Dr. Salvatore, an IDSA fellow.
The evidence suggests that SARS-CoV-2 should be capable of producing one or two mutations per month. However, the B.1.1.7 variant surprised investigators in the United Kingdom when they first discovered the strain had 17 mutations, Dr. Salvatore said.
It’s still unknown why this particular strain is more transmissible, but Dr. Salvatore speculated that the mutation gives the virus an advantage and increases binding, allowing it to enter cells more easily. She added that the mutations might have arisen among immunocompromised people infected with SARS-CoV-2, but “that is just a hypothesis.”
On a positive note, Kathryn M. Edwards, MD, another IDSA fellow, explained at the briefing that the existing vaccines target more than one location on the virus’ spike protein. Therefore, “if there is a mutation that changes one structure of the spike protein, there will be other areas where the binding can occur.”
This polyclonal response “is why the vaccine can still be effective against this virus,” added Dr. Edwards, scientific director of the Vanderbilt Vaccine Research Program and professor of pediatrics at Vanderbilt University, Nashville, Tenn.
Dr. Salvatore emphasized that, although the new variant is more transmissible, it doesn’t appear to be more lethal. “This might affect overall mortality but not for the individual who gets the infection.”
Staying one step ahead
When asked for assurance that COVID-19 vaccines will work against emerging variants, Dr. Edwards said, “It may be we will have to change the vaccine so it is more responsive to new variants, but at this point that does not seem to be the case.”
Should the vaccines require an update, the messenger RNA vaccines have an advantage – researchers can rapidly revise them. “All you need to do is put all the little nucleotides together,” Dr. Edwards said.
“A number of us are looking at how this will work, and we look to influenza,” she added. Dr. Edwards drew an analogy to choosing – and sometimes updating – the influenza strains each year for the annual flu vaccine. With appropriate funding, the same system could be replicated to address any evolving changes to SARS-CoV-2.
On funding, Dr. Salvatore said more money would be required to optimize the surveillance system for emerging strains in the United States.
“We actually have this system – there is a wonderful network that sequences the influenza strains,” she said. “The structure exists, we just need the funding.”
“The CDC is getting the system tooled up to get more viruses to be sequenced,” Dr. Edwards said.
Both experts praised the CDC for its website with up-to-date surveillance information on emerging strains of SARS-CoV-2.
President Biden’s backing of science
A reporter asked each infectious disease expert to share their impression of President Biden’s newly signed COVID-19 executive orders.
“The biggest takeaway is the role of science and the lessons we’ve learned from masks, handwashing, and distancing,” Dr. Edwards said. “We need to heed the advice ... [especially] with a variant that is more contagious.
“It is encouraging that science will be listened to – that is the overall message,” she added.
Dr. Salvatore agreed, saying that the orders give “the feeling that we can now act by following science.”
“We have plenty of papers that show the effectiveness of masking,” for example, she said. Dr. Salvatore acknowledged that there are “a lot of contrasting ideas about masking” across the United States but stressed their importance.
“We should follow measures that we know work,” she said.
Both experts said more research is needed to stay ahead of this evolving scenario. “We still need a lot of basic science showing how this virus replicates in the cell,” Dr. Salvatore said. “We need to really characterize all these mutations and their functions.”
“We need to be concerned, do follow-up studies,” she added, “but we don’t need to panic.”
This article was based on an Infectious Diseases Society of America Media Briefing on Jan. 21, 2021. Dr. Salvatore disclosed that she is a site principal investigator on a study from Verily Life Sciences/Brin Foundation on Predictors of Severe COVID-19 Outcomes and principal investigator for an investigator-initiated study sponsored by Genentech on combination therapy in influenza. Dr. Edwards disclosed National Institutes of Health and Centers for Disease Control and Prevention grants; consulting for Bionet and IBM; and being a member of data safety and monitoring committees for Sanofi, X-4 Pharma, Seqirus, Moderna, Pfizer, and Merck.
A version of this article first appeared on Medscape.com.
Dermatologist survey spotlights psoriasis care deficiencies in reproductive-age women
In a , Jenny Murase, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
“In Germany, the UK, and the United States, dermatologists face challenges in discussing pregnancy and child-bearing aspiration with women of reproductive age, in recommending compatible treatments during pregnancy, and engaging patients in the shared decision-making process. These challenges may exist due to suboptimal knowledge, skills, confidence, and attitude in respective areas of care,” said Dr. Murase, a dermatologist at the University of California, San Francisco, and coeditor-in-chief of the International Journal of Women’s Dermatology.
These shortcomings were documented in a survey, which began with Dr. Murase and her coinvestigators conducting detailed, 45-minute-long, semistructured telephone interviews with 24 dermatologists in the three countries. Those interviews provided the basis for subsequent development of a 20-minute online survey on psoriasis and pregnancy completed by 167 American, German, and UK dermatologists. The survey incorporated multiple choice questions and quantitative rating scales.
“Participants expressed challenges engaging in family planning counseling and reproductive health care as part of risk assessments for psoriasis,” Dr. Murase said.
Among the key findings:
- Forty-seven percent of respondents considered their knowledge of the impact of psoriasis on women’s reproductive health to be suboptimal. This knowledge gap was most common among American dermatologists, 59% of whom rated themselves as having suboptimal knowledge, and least common among German practitioners, only 27% of whom reported deficiencies in this area.
Fifty percent of dermatologists rated themselves as having suboptimal skills in discussing contraceptive methods with their psoriasis patients of childbearing potential.
- Forty-eight percent of respondents – and 59% of the American dermatologists – indicated they prefer to leave pregnancy-related discussions to ob.gyns.
- Fifty-five percent of dermatologists had only limited knowledge of the safety data and indications for prescribing biologic therapies before, during, and after pregnancy. Respondents gave themselves an average score of 58 out of 100 in terms of their confidence in prescribing biologics during pregnancy, compared to 74 out of 100 when prescribing before or after pregnancy.
- Forty-eight percent of participants indicated they had suboptimal skills in helping patients counter obstacles to treatment adherence.
Consideration of treatment of psoriasis in pregnancy requires balancing potential medication risks to the fetus versus the possible maternal and fetal harms of under- or nontreatment of their chronic inflammatory skin disease. It’s a matter that calls for shared decision-making between dermatologist and patient. But the survey showed that shared decision-making was often poorly integrated into clinical practice. Ninety-seven percent of the U.S. dermatologists were unaware of the existence of shared decision-making practice guidelines or models, as were 80% of UK respondents and 85% of the Germans. Of the relatively few dermatologists who were aware of such guidance, nearly half dismissed it as inapplicable to their clinical practice. More than one-third of respondents admitted having suboptimal skills in assessing their patients’ desired level of involvement in medical decisions. And one-third of the German dermatologists and roughly one-quarter of those from the United States and United Kingdom reported feeling pressure to make treatment decisions quickly and without patient input.
Dr. Murase added that the survey findings make a strong case for future interventions designed to help dermatologists appreciate the value of shared decision-making and develop the requisite patient-engagement skills. Dr. Murase reported serving as a paid consultant to UCB Pharma, which funded the survey via an educational grant.
In a , Jenny Murase, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
“In Germany, the UK, and the United States, dermatologists face challenges in discussing pregnancy and child-bearing aspiration with women of reproductive age, in recommending compatible treatments during pregnancy, and engaging patients in the shared decision-making process. These challenges may exist due to suboptimal knowledge, skills, confidence, and attitude in respective areas of care,” said Dr. Murase, a dermatologist at the University of California, San Francisco, and coeditor-in-chief of the International Journal of Women’s Dermatology.
These shortcomings were documented in a survey, which began with Dr. Murase and her coinvestigators conducting detailed, 45-minute-long, semistructured telephone interviews with 24 dermatologists in the three countries. Those interviews provided the basis for subsequent development of a 20-minute online survey on psoriasis and pregnancy completed by 167 American, German, and UK dermatologists. The survey incorporated multiple choice questions and quantitative rating scales.
“Participants expressed challenges engaging in family planning counseling and reproductive health care as part of risk assessments for psoriasis,” Dr. Murase said.
Among the key findings:
- Forty-seven percent of respondents considered their knowledge of the impact of psoriasis on women’s reproductive health to be suboptimal. This knowledge gap was most common among American dermatologists, 59% of whom rated themselves as having suboptimal knowledge, and least common among German practitioners, only 27% of whom reported deficiencies in this area.
Fifty percent of dermatologists rated themselves as having suboptimal skills in discussing contraceptive methods with their psoriasis patients of childbearing potential.
- Forty-eight percent of respondents – and 59% of the American dermatologists – indicated they prefer to leave pregnancy-related discussions to ob.gyns.
- Fifty-five percent of dermatologists had only limited knowledge of the safety data and indications for prescribing biologic therapies before, during, and after pregnancy. Respondents gave themselves an average score of 58 out of 100 in terms of their confidence in prescribing biologics during pregnancy, compared to 74 out of 100 when prescribing before or after pregnancy.
- Forty-eight percent of participants indicated they had suboptimal skills in helping patients counter obstacles to treatment adherence.
Consideration of treatment of psoriasis in pregnancy requires balancing potential medication risks to the fetus versus the possible maternal and fetal harms of under- or nontreatment of their chronic inflammatory skin disease. It’s a matter that calls for shared decision-making between dermatologist and patient. But the survey showed that shared decision-making was often poorly integrated into clinical practice. Ninety-seven percent of the U.S. dermatologists were unaware of the existence of shared decision-making practice guidelines or models, as were 80% of UK respondents and 85% of the Germans. Of the relatively few dermatologists who were aware of such guidance, nearly half dismissed it as inapplicable to their clinical practice. More than one-third of respondents admitted having suboptimal skills in assessing their patients’ desired level of involvement in medical decisions. And one-third of the German dermatologists and roughly one-quarter of those from the United States and United Kingdom reported feeling pressure to make treatment decisions quickly and without patient input.
Dr. Murase added that the survey findings make a strong case for future interventions designed to help dermatologists appreciate the value of shared decision-making and develop the requisite patient-engagement skills. Dr. Murase reported serving as a paid consultant to UCB Pharma, which funded the survey via an educational grant.
In a , Jenny Murase, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
“In Germany, the UK, and the United States, dermatologists face challenges in discussing pregnancy and child-bearing aspiration with women of reproductive age, in recommending compatible treatments during pregnancy, and engaging patients in the shared decision-making process. These challenges may exist due to suboptimal knowledge, skills, confidence, and attitude in respective areas of care,” said Dr. Murase, a dermatologist at the University of California, San Francisco, and coeditor-in-chief of the International Journal of Women’s Dermatology.
These shortcomings were documented in a survey, which began with Dr. Murase and her coinvestigators conducting detailed, 45-minute-long, semistructured telephone interviews with 24 dermatologists in the three countries. Those interviews provided the basis for subsequent development of a 20-minute online survey on psoriasis and pregnancy completed by 167 American, German, and UK dermatologists. The survey incorporated multiple choice questions and quantitative rating scales.
“Participants expressed challenges engaging in family planning counseling and reproductive health care as part of risk assessments for psoriasis,” Dr. Murase said.
Among the key findings:
- Forty-seven percent of respondents considered their knowledge of the impact of psoriasis on women’s reproductive health to be suboptimal. This knowledge gap was most common among American dermatologists, 59% of whom rated themselves as having suboptimal knowledge, and least common among German practitioners, only 27% of whom reported deficiencies in this area.
Fifty percent of dermatologists rated themselves as having suboptimal skills in discussing contraceptive methods with their psoriasis patients of childbearing potential.
- Forty-eight percent of respondents – and 59% of the American dermatologists – indicated they prefer to leave pregnancy-related discussions to ob.gyns.
- Fifty-five percent of dermatologists had only limited knowledge of the safety data and indications for prescribing biologic therapies before, during, and after pregnancy. Respondents gave themselves an average score of 58 out of 100 in terms of their confidence in prescribing biologics during pregnancy, compared to 74 out of 100 when prescribing before or after pregnancy.
- Forty-eight percent of participants indicated they had suboptimal skills in helping patients counter obstacles to treatment adherence.
Consideration of treatment of psoriasis in pregnancy requires balancing potential medication risks to the fetus versus the possible maternal and fetal harms of under- or nontreatment of their chronic inflammatory skin disease. It’s a matter that calls for shared decision-making between dermatologist and patient. But the survey showed that shared decision-making was often poorly integrated into clinical practice. Ninety-seven percent of the U.S. dermatologists were unaware of the existence of shared decision-making practice guidelines or models, as were 80% of UK respondents and 85% of the Germans. Of the relatively few dermatologists who were aware of such guidance, nearly half dismissed it as inapplicable to their clinical practice. More than one-third of respondents admitted having suboptimal skills in assessing their patients’ desired level of involvement in medical decisions. And one-third of the German dermatologists and roughly one-quarter of those from the United States and United Kingdom reported feeling pressure to make treatment decisions quickly and without patient input.
Dr. Murase added that the survey findings make a strong case for future interventions designed to help dermatologists appreciate the value of shared decision-making and develop the requisite patient-engagement skills. Dr. Murase reported serving as a paid consultant to UCB Pharma, which funded the survey via an educational grant.
FROM THE EADV CONGRESS
Widespread liver disease missed in patients with T2D
Among these calls is a pending statement from the Endocrine Society, the American Association of Clinical Endocrinologists, the American Gastroenterology Association, and other groups on what the growing appreciation of highly prevalent liver disease in patients with type 2 diabetes (T2D) means for assessing and managing patients. Publication of the statement is expected by spring 2021, said Christos S. Mantzoros, MD, DSc, PhD, chief of endocrinology for the Veterans Affairs Boston Healthcare System and a representative from the Endocrine Society to the statement-writing panel.
This upcoming “Call to Action” from these groups argues for a “need to collaborate across disciplines, and work together on establishing clinical guidelines, and creating new diagnostics and therapeutics,” said Dr. Mantzoros in an interview.
“Over time, it is becoming clearer that management of NAFLD [nonalcoholic fatty liver disease]/NASH [nonalcoholic steatohepatitis] requires a multidisciplinary panel of doctors ranging from primary care practitioners, to endocrinologists, and hepatologists. Given that the nature of the disease crosses scientific discipline boundaries, and that the number of patients is so large (it is estimated that about one in four U.S. adults have NAFLD), not all patients can be treated at the limited number of hepatology centers.
“However, not all stakeholders have fully realized this fact, and no effort had been undertaken so far by any professional society to develop a coordinated approach and clinical care pathway for NAFLD/NASH. The ‘Call to Action’ meeting can be considered as a starting point for such an important effort,” said Dr. Mantzoros, who is also a professor of medicine at Harvard Medical School and director of the human nutrition unit at Beth Israel Deaconess Medical Center, both in Boston.
Dramatic prevalence rates in patients with T2D
Results from two independent epidemiology reports, published in December 2020, documented steatosis (the fatty liver of NAFLD) in 70%-74% of unselected U.S. patients with T2D, advanced liver fibrosis accompanying this disease in 6%-15%, and previously unrecognized cirrhosis in 3%-8%.
One of these reports analyzed 825 patients with T2D included in the National Health and Nutritional Examination Survey of 2017-2018 run by the Centers for Disease Control and Prevention. All these patients, selected to be representative of the overall U.S. adult population with T2D, underwent transient elastography to identify steatosis and fibrosis, the first U.S. National Health Survey to run this type of population-based survey. The results showed an overall steatosis prevalence of 74% with grade 3 steatosis in 58%, advanced liver fibrosis in 15%, and cirrhosis in 8%, reported the team of Italian researchers who analyzed the data .
The second study focused on a single-center series of 561 patients with T2D who also underwent screening by transient elastography during 2018-2020 and had no history of NAFLD or other liver disease, or alcohol abuse. The imaging results showed a NAFLD prevalence of 70%, with 54% of the entire group diagnosed with severe steatosis, severe fibrosis in 6%, and cirrhosis in 3%. Among the 54% of patients with severe steatosis, 30% also had severe liver fibrosis. About 70% of the 561 patients assessed came from either the family medicine or general internal medicine clinics of the University of Florida, Gainesville, with the remaining 30% enrolled from the center’s endocrinology/diabetes outpatient clinic.
Neither report documented a NASH prevalence, which cannot receive definitive diagnosis by imaging alone. “This is the first study of its kind in the U.S. to establish the magnitude of [liver] disease burden in random patients with T2D seeking regular outpatient care,” wrote the University of Florida research team, led by Kenneth Cusi, MD, professor and chief of the university’s division of endocrinology, diabetes, and metabolism. Their finding that patients with T2D and previously unknown to have NAFLD had a 15% prevalence of moderate or advanced liver fibrosis “should trigger a call to action by all clinicians taking care of patients with T2D. Patient and physician awareness of the hepatic and extrahepatic complications of NASH, and reversing current diagnosis and treatment inertia will be the only way to avert the looming epidemic of cirrhosis in patients with diabetes.”
“Endocrinologists don’t ‘see’ NAFLD and NASH” in their patients with T2D “ because they don’t think about it,” Dr. Mantzoros declared.
“Why is NASH underdiagnosed and undertreated? Because many physicians aren’t aware of it,” agreed Dr. Cusi during a talk in December 2020 at the 18th World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease (WCIRDC). “You never find what you don’t look for.”
“Endocrinologists should do the tests for NASH [in patients with T2D], but we’re all guilty of not doing it enough,” Tracey McLaughlin, MD, an endocrinologist and professor of medicine at Stanford (Calif.) University, commented during the WCIRDC.
These prevalence numbers demand that clinicians suspect liver disease “in any patient with diabetes, especially patients with obesity who are older and have components of metabolic syndrome,” said Dr. Mantzoros. “We need to screen, refer the most advanced cases, and treat the early- and mid-stage cases.”
How to find NASH
Both the American Diabetes Association and the European Association for the Study of Diabetes call for routine screening of patients with T2D, starting with a check of liver enzymes, such as ALT, but no clear consensus exists for the specifics of screening beyond that. Dr. Mantzoros, Dr. Cusi, and other experts agree that the scheme for assessing liver disease in patients with T2D starts with regular monitoring of elevations in liver enzymes including ALT. Next is noninvasive ultrasound assessment of the extent of liver fibrosis inferred from the organ’s stiffness using transient elastography. Another frequently cited initial screening tool is the Fibrosis-4 (FIB-4) score, which incorporates a patient’s age, platelet count, and levels of ALT and a second liver enzyme, AST.
“There is more consensus about FIB-4 and then elastography, but some people use tests other than FIB-4. Unfortunately there is no perfect diagnostic test today. A top priority is to define the best diagnostic test,” said Dr. Mantzoros, who is leading an effort to try to refine screening using artificial intelligence.
“FIB-4 is simple, easy, and well validated,” commented Dr. Cusi during the WCIRDC last December. “FIB-4 and elastography should get you pretty close” to identifying patients with T2D and significant liver disease.
But in a recent editorial, Dr. Cusi agreed on the need for “more reliable tests for the diagnosis of NASH and advanced fibrosis in patients with T2D. Significant work is being done in the field to validate novel and more sophisticated fibrosis biomarkers. Future studies will help us enter a new era of precision medicine where biomarkers will identify and target therapy to those with more active disease at risk for cirrhosis,” he wrote.
“The ultimate goal is to diagnose fibrosis at an early stage to prevent people from developing cirrhosis,” Dr. Cusi said in a recent written statement. “We’re trying to identify these problems before they’re unfixable. Once someone has cirrhosis, there isn’t a whole lot you can do.”
Pioglitazone remains the best-documented treatment
Perhaps some of the inertia in diagnosing NAFLD, NASH, and liver fibrosis in patients with T2D is dissatisfaction with current treatment options, although several proven options exist, notably weight loss and diet, and thiazolidinedione (TZD) pioglitazone. But weight loss and diet pose issues for patient compliance and durability of the intervention, and many clinicians consider pioglitazone flawed by its potential adverse effects.
“When we don’t have an established treatment for something, we tend to not measure it or go after it. That’s been true of liver disease” in patients with T2D, said Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of the Metabolic Institute of America in Tarzana, Calif., during the WCIRDC.
Treatment with pioglitazone has resolved NASH in about a third of patients compared with placebo, prevented fibrosis progression, and cut cardiovascular disease events, noted Dr. Cusi during the WCIRDC.
“Pioglitazone is used in only 8% of patients with T2D, or less, but we need to use it more often because of its proven efficacy in patients with T2D and NASH” said Dr. Mantzoros. “The problem is that pioglitazone has side effects, including weight gain and fluid retention, that makes it less attractive unless one thinks about the diagnosis of NASH.”
Others highlight that the adverse effects of pioglitazone have been either misunderstood, or can be effectively minimized with careful dosing.
“The data with the TZDs are much stronger than the data from anything else. TZDs have gotten a bad name because they also work in the kidney and enhance fluid reabsorption. We use modest dosages of pioglitazone, 15 mg or 30 mg a day, to avoid excess fluid retention,” Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio, said during the WCIRDC. “The best drug for NASH is pioglitazone. No other drug beats it” based on current data, Dr. DeFronzo asserted.
Other strategies include the potential to pair pioglitazone with other interventions that can blunt a weight-gain effect. One intriguing combination would combine pioglitazone with a GLP-1 receptor agonist, a drug class that can produce significant weight loss. Results from a phase 2 study showed promise for semaglutide (Rybelsus) in treating patients with NASH.
Getting the name right
Another factor that may be keeping NAFLD and NASH from achieving a higher profile for patients with T2D are those names, which focus on what the diseases are not – nonalcoholic – rather than what they are.
A series of recent publications in both the endocrinology and hepatology literature have called for renaming these disorders either “metabolic (dysfunction)–associated fatty liver disease (MALFD)”, or “dysmetabolism-associated fatty liver disease (DALFD)”.
“The names NAFLD and NASH indicate absence of alcohol as a cause, but the disease is also characterized by the absence of other causes, such as autoimmune disorders or hepatitis. The names were coined when we did not know much about these diseases. We now know that it is dysmetabolism that causes these conditions, and so we need to adopt a new, more accurate name,” explained Dr. Mantzoros, who has published support for a name change.
While many agree, some have raised concerns as to whether a name change now is premature. A group of hepatologists recently published a rebuttal to an immediate name change , saying that, “although we are in agreement that metabolic fatty liver disease may more accurately and positively reflect the relevant risk factors better than the age-old term nonalcoholic fatty liver disease, the term still leaves a great deal of ambiguity. A name change will be appropriate when informed by a new understanding of the molecular basis of the disease entity, insights that fundamentally change risk stratification, or other important aspects of the disease. We may be on the cusp of this, but we are not there yet.”
Dr. Mantzoros agreed, but for somewhat different reasons.
“We need to be careful and deliberate, because there is a significant body of knowledge and a lot of data from clinical trials collected using the old definitions. We need to find an appropriate time frame for a [name] transition. We need to find a nice and robust way to productively bridge the old to the new,” he said. “We also need new diagnostic criteria, and new therapies. A new name and definition will facilitate progress.”
Dr. Mantzoros been a shareholder of and consultant to Coherus and Pangea, he has been a consultant to AstraZeneca, Eisai, Genfit, Intercept, Novo Nordisk, P.E.S., and Regeneron, and has received travel support from the Metabolic Institute of America and the California Walnut Commission. Dr. Cusi has been a consultant to and has received research funding from numerous drug companies. Dr. McLaughlin is a consultant to January AI. Dr. Handelsman has been a consultant to numerous drug companies. Dr. DeFronzo received research grants from AstraZeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk.
Among these calls is a pending statement from the Endocrine Society, the American Association of Clinical Endocrinologists, the American Gastroenterology Association, and other groups on what the growing appreciation of highly prevalent liver disease in patients with type 2 diabetes (T2D) means for assessing and managing patients. Publication of the statement is expected by spring 2021, said Christos S. Mantzoros, MD, DSc, PhD, chief of endocrinology for the Veterans Affairs Boston Healthcare System and a representative from the Endocrine Society to the statement-writing panel.
This upcoming “Call to Action” from these groups argues for a “need to collaborate across disciplines, and work together on establishing clinical guidelines, and creating new diagnostics and therapeutics,” said Dr. Mantzoros in an interview.
“Over time, it is becoming clearer that management of NAFLD [nonalcoholic fatty liver disease]/NASH [nonalcoholic steatohepatitis] requires a multidisciplinary panel of doctors ranging from primary care practitioners, to endocrinologists, and hepatologists. Given that the nature of the disease crosses scientific discipline boundaries, and that the number of patients is so large (it is estimated that about one in four U.S. adults have NAFLD), not all patients can be treated at the limited number of hepatology centers.
“However, not all stakeholders have fully realized this fact, and no effort had been undertaken so far by any professional society to develop a coordinated approach and clinical care pathway for NAFLD/NASH. The ‘Call to Action’ meeting can be considered as a starting point for such an important effort,” said Dr. Mantzoros, who is also a professor of medicine at Harvard Medical School and director of the human nutrition unit at Beth Israel Deaconess Medical Center, both in Boston.
Dramatic prevalence rates in patients with T2D
Results from two independent epidemiology reports, published in December 2020, documented steatosis (the fatty liver of NAFLD) in 70%-74% of unselected U.S. patients with T2D, advanced liver fibrosis accompanying this disease in 6%-15%, and previously unrecognized cirrhosis in 3%-8%.
One of these reports analyzed 825 patients with T2D included in the National Health and Nutritional Examination Survey of 2017-2018 run by the Centers for Disease Control and Prevention. All these patients, selected to be representative of the overall U.S. adult population with T2D, underwent transient elastography to identify steatosis and fibrosis, the first U.S. National Health Survey to run this type of population-based survey. The results showed an overall steatosis prevalence of 74% with grade 3 steatosis in 58%, advanced liver fibrosis in 15%, and cirrhosis in 8%, reported the team of Italian researchers who analyzed the data .
The second study focused on a single-center series of 561 patients with T2D who also underwent screening by transient elastography during 2018-2020 and had no history of NAFLD or other liver disease, or alcohol abuse. The imaging results showed a NAFLD prevalence of 70%, with 54% of the entire group diagnosed with severe steatosis, severe fibrosis in 6%, and cirrhosis in 3%. Among the 54% of patients with severe steatosis, 30% also had severe liver fibrosis. About 70% of the 561 patients assessed came from either the family medicine or general internal medicine clinics of the University of Florida, Gainesville, with the remaining 30% enrolled from the center’s endocrinology/diabetes outpatient clinic.
Neither report documented a NASH prevalence, which cannot receive definitive diagnosis by imaging alone. “This is the first study of its kind in the U.S. to establish the magnitude of [liver] disease burden in random patients with T2D seeking regular outpatient care,” wrote the University of Florida research team, led by Kenneth Cusi, MD, professor and chief of the university’s division of endocrinology, diabetes, and metabolism. Their finding that patients with T2D and previously unknown to have NAFLD had a 15% prevalence of moderate or advanced liver fibrosis “should trigger a call to action by all clinicians taking care of patients with T2D. Patient and physician awareness of the hepatic and extrahepatic complications of NASH, and reversing current diagnosis and treatment inertia will be the only way to avert the looming epidemic of cirrhosis in patients with diabetes.”
“Endocrinologists don’t ‘see’ NAFLD and NASH” in their patients with T2D “ because they don’t think about it,” Dr. Mantzoros declared.
“Why is NASH underdiagnosed and undertreated? Because many physicians aren’t aware of it,” agreed Dr. Cusi during a talk in December 2020 at the 18th World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease (WCIRDC). “You never find what you don’t look for.”
“Endocrinologists should do the tests for NASH [in patients with T2D], but we’re all guilty of not doing it enough,” Tracey McLaughlin, MD, an endocrinologist and professor of medicine at Stanford (Calif.) University, commented during the WCIRDC.
These prevalence numbers demand that clinicians suspect liver disease “in any patient with diabetes, especially patients with obesity who are older and have components of metabolic syndrome,” said Dr. Mantzoros. “We need to screen, refer the most advanced cases, and treat the early- and mid-stage cases.”
How to find NASH
Both the American Diabetes Association and the European Association for the Study of Diabetes call for routine screening of patients with T2D, starting with a check of liver enzymes, such as ALT, but no clear consensus exists for the specifics of screening beyond that. Dr. Mantzoros, Dr. Cusi, and other experts agree that the scheme for assessing liver disease in patients with T2D starts with regular monitoring of elevations in liver enzymes including ALT. Next is noninvasive ultrasound assessment of the extent of liver fibrosis inferred from the organ’s stiffness using transient elastography. Another frequently cited initial screening tool is the Fibrosis-4 (FIB-4) score, which incorporates a patient’s age, platelet count, and levels of ALT and a second liver enzyme, AST.
“There is more consensus about FIB-4 and then elastography, but some people use tests other than FIB-4. Unfortunately there is no perfect diagnostic test today. A top priority is to define the best diagnostic test,” said Dr. Mantzoros, who is leading an effort to try to refine screening using artificial intelligence.
“FIB-4 is simple, easy, and well validated,” commented Dr. Cusi during the WCIRDC last December. “FIB-4 and elastography should get you pretty close” to identifying patients with T2D and significant liver disease.
But in a recent editorial, Dr. Cusi agreed on the need for “more reliable tests for the diagnosis of NASH and advanced fibrosis in patients with T2D. Significant work is being done in the field to validate novel and more sophisticated fibrosis biomarkers. Future studies will help us enter a new era of precision medicine where biomarkers will identify and target therapy to those with more active disease at risk for cirrhosis,” he wrote.
“The ultimate goal is to diagnose fibrosis at an early stage to prevent people from developing cirrhosis,” Dr. Cusi said in a recent written statement. “We’re trying to identify these problems before they’re unfixable. Once someone has cirrhosis, there isn’t a whole lot you can do.”
Pioglitazone remains the best-documented treatment
Perhaps some of the inertia in diagnosing NAFLD, NASH, and liver fibrosis in patients with T2D is dissatisfaction with current treatment options, although several proven options exist, notably weight loss and diet, and thiazolidinedione (TZD) pioglitazone. But weight loss and diet pose issues for patient compliance and durability of the intervention, and many clinicians consider pioglitazone flawed by its potential adverse effects.
“When we don’t have an established treatment for something, we tend to not measure it or go after it. That’s been true of liver disease” in patients with T2D, said Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of the Metabolic Institute of America in Tarzana, Calif., during the WCIRDC.
Treatment with pioglitazone has resolved NASH in about a third of patients compared with placebo, prevented fibrosis progression, and cut cardiovascular disease events, noted Dr. Cusi during the WCIRDC.
“Pioglitazone is used in only 8% of patients with T2D, or less, but we need to use it more often because of its proven efficacy in patients with T2D and NASH” said Dr. Mantzoros. “The problem is that pioglitazone has side effects, including weight gain and fluid retention, that makes it less attractive unless one thinks about the diagnosis of NASH.”
Others highlight that the adverse effects of pioglitazone have been either misunderstood, or can be effectively minimized with careful dosing.
“The data with the TZDs are much stronger than the data from anything else. TZDs have gotten a bad name because they also work in the kidney and enhance fluid reabsorption. We use modest dosages of pioglitazone, 15 mg or 30 mg a day, to avoid excess fluid retention,” Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio, said during the WCIRDC. “The best drug for NASH is pioglitazone. No other drug beats it” based on current data, Dr. DeFronzo asserted.
Other strategies include the potential to pair pioglitazone with other interventions that can blunt a weight-gain effect. One intriguing combination would combine pioglitazone with a GLP-1 receptor agonist, a drug class that can produce significant weight loss. Results from a phase 2 study showed promise for semaglutide (Rybelsus) in treating patients with NASH.
Getting the name right
Another factor that may be keeping NAFLD and NASH from achieving a higher profile for patients with T2D are those names, which focus on what the diseases are not – nonalcoholic – rather than what they are.
A series of recent publications in both the endocrinology and hepatology literature have called for renaming these disorders either “metabolic (dysfunction)–associated fatty liver disease (MALFD)”, or “dysmetabolism-associated fatty liver disease (DALFD)”.
“The names NAFLD and NASH indicate absence of alcohol as a cause, but the disease is also characterized by the absence of other causes, such as autoimmune disorders or hepatitis. The names were coined when we did not know much about these diseases. We now know that it is dysmetabolism that causes these conditions, and so we need to adopt a new, more accurate name,” explained Dr. Mantzoros, who has published support for a name change.
While many agree, some have raised concerns as to whether a name change now is premature. A group of hepatologists recently published a rebuttal to an immediate name change , saying that, “although we are in agreement that metabolic fatty liver disease may more accurately and positively reflect the relevant risk factors better than the age-old term nonalcoholic fatty liver disease, the term still leaves a great deal of ambiguity. A name change will be appropriate when informed by a new understanding of the molecular basis of the disease entity, insights that fundamentally change risk stratification, or other important aspects of the disease. We may be on the cusp of this, but we are not there yet.”
Dr. Mantzoros agreed, but for somewhat different reasons.
“We need to be careful and deliberate, because there is a significant body of knowledge and a lot of data from clinical trials collected using the old definitions. We need to find an appropriate time frame for a [name] transition. We need to find a nice and robust way to productively bridge the old to the new,” he said. “We also need new diagnostic criteria, and new therapies. A new name and definition will facilitate progress.”
Dr. Mantzoros been a shareholder of and consultant to Coherus and Pangea, he has been a consultant to AstraZeneca, Eisai, Genfit, Intercept, Novo Nordisk, P.E.S., and Regeneron, and has received travel support from the Metabolic Institute of America and the California Walnut Commission. Dr. Cusi has been a consultant to and has received research funding from numerous drug companies. Dr. McLaughlin is a consultant to January AI. Dr. Handelsman has been a consultant to numerous drug companies. Dr. DeFronzo received research grants from AstraZeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk.
Among these calls is a pending statement from the Endocrine Society, the American Association of Clinical Endocrinologists, the American Gastroenterology Association, and other groups on what the growing appreciation of highly prevalent liver disease in patients with type 2 diabetes (T2D) means for assessing and managing patients. Publication of the statement is expected by spring 2021, said Christos S. Mantzoros, MD, DSc, PhD, chief of endocrinology for the Veterans Affairs Boston Healthcare System and a representative from the Endocrine Society to the statement-writing panel.
This upcoming “Call to Action” from these groups argues for a “need to collaborate across disciplines, and work together on establishing clinical guidelines, and creating new diagnostics and therapeutics,” said Dr. Mantzoros in an interview.
“Over time, it is becoming clearer that management of NAFLD [nonalcoholic fatty liver disease]/NASH [nonalcoholic steatohepatitis] requires a multidisciplinary panel of doctors ranging from primary care practitioners, to endocrinologists, and hepatologists. Given that the nature of the disease crosses scientific discipline boundaries, and that the number of patients is so large (it is estimated that about one in four U.S. adults have NAFLD), not all patients can be treated at the limited number of hepatology centers.
“However, not all stakeholders have fully realized this fact, and no effort had been undertaken so far by any professional society to develop a coordinated approach and clinical care pathway for NAFLD/NASH. The ‘Call to Action’ meeting can be considered as a starting point for such an important effort,” said Dr. Mantzoros, who is also a professor of medicine at Harvard Medical School and director of the human nutrition unit at Beth Israel Deaconess Medical Center, both in Boston.
Dramatic prevalence rates in patients with T2D
Results from two independent epidemiology reports, published in December 2020, documented steatosis (the fatty liver of NAFLD) in 70%-74% of unselected U.S. patients with T2D, advanced liver fibrosis accompanying this disease in 6%-15%, and previously unrecognized cirrhosis in 3%-8%.
One of these reports analyzed 825 patients with T2D included in the National Health and Nutritional Examination Survey of 2017-2018 run by the Centers for Disease Control and Prevention. All these patients, selected to be representative of the overall U.S. adult population with T2D, underwent transient elastography to identify steatosis and fibrosis, the first U.S. National Health Survey to run this type of population-based survey. The results showed an overall steatosis prevalence of 74% with grade 3 steatosis in 58%, advanced liver fibrosis in 15%, and cirrhosis in 8%, reported the team of Italian researchers who analyzed the data .
The second study focused on a single-center series of 561 patients with T2D who also underwent screening by transient elastography during 2018-2020 and had no history of NAFLD or other liver disease, or alcohol abuse. The imaging results showed a NAFLD prevalence of 70%, with 54% of the entire group diagnosed with severe steatosis, severe fibrosis in 6%, and cirrhosis in 3%. Among the 54% of patients with severe steatosis, 30% also had severe liver fibrosis. About 70% of the 561 patients assessed came from either the family medicine or general internal medicine clinics of the University of Florida, Gainesville, with the remaining 30% enrolled from the center’s endocrinology/diabetes outpatient clinic.
Neither report documented a NASH prevalence, which cannot receive definitive diagnosis by imaging alone. “This is the first study of its kind in the U.S. to establish the magnitude of [liver] disease burden in random patients with T2D seeking regular outpatient care,” wrote the University of Florida research team, led by Kenneth Cusi, MD, professor and chief of the university’s division of endocrinology, diabetes, and metabolism. Their finding that patients with T2D and previously unknown to have NAFLD had a 15% prevalence of moderate or advanced liver fibrosis “should trigger a call to action by all clinicians taking care of patients with T2D. Patient and physician awareness of the hepatic and extrahepatic complications of NASH, and reversing current diagnosis and treatment inertia will be the only way to avert the looming epidemic of cirrhosis in patients with diabetes.”
“Endocrinologists don’t ‘see’ NAFLD and NASH” in their patients with T2D “ because they don’t think about it,” Dr. Mantzoros declared.
“Why is NASH underdiagnosed and undertreated? Because many physicians aren’t aware of it,” agreed Dr. Cusi during a talk in December 2020 at the 18th World Congress on Insulin Resistance, Diabetes, and Cardiovascular Disease (WCIRDC). “You never find what you don’t look for.”
“Endocrinologists should do the tests for NASH [in patients with T2D], but we’re all guilty of not doing it enough,” Tracey McLaughlin, MD, an endocrinologist and professor of medicine at Stanford (Calif.) University, commented during the WCIRDC.
These prevalence numbers demand that clinicians suspect liver disease “in any patient with diabetes, especially patients with obesity who are older and have components of metabolic syndrome,” said Dr. Mantzoros. “We need to screen, refer the most advanced cases, and treat the early- and mid-stage cases.”
How to find NASH
Both the American Diabetes Association and the European Association for the Study of Diabetes call for routine screening of patients with T2D, starting with a check of liver enzymes, such as ALT, but no clear consensus exists for the specifics of screening beyond that. Dr. Mantzoros, Dr. Cusi, and other experts agree that the scheme for assessing liver disease in patients with T2D starts with regular monitoring of elevations in liver enzymes including ALT. Next is noninvasive ultrasound assessment of the extent of liver fibrosis inferred from the organ’s stiffness using transient elastography. Another frequently cited initial screening tool is the Fibrosis-4 (FIB-4) score, which incorporates a patient’s age, platelet count, and levels of ALT and a second liver enzyme, AST.
“There is more consensus about FIB-4 and then elastography, but some people use tests other than FIB-4. Unfortunately there is no perfect diagnostic test today. A top priority is to define the best diagnostic test,” said Dr. Mantzoros, who is leading an effort to try to refine screening using artificial intelligence.
“FIB-4 is simple, easy, and well validated,” commented Dr. Cusi during the WCIRDC last December. “FIB-4 and elastography should get you pretty close” to identifying patients with T2D and significant liver disease.
But in a recent editorial, Dr. Cusi agreed on the need for “more reliable tests for the diagnosis of NASH and advanced fibrosis in patients with T2D. Significant work is being done in the field to validate novel and more sophisticated fibrosis biomarkers. Future studies will help us enter a new era of precision medicine where biomarkers will identify and target therapy to those with more active disease at risk for cirrhosis,” he wrote.
“The ultimate goal is to diagnose fibrosis at an early stage to prevent people from developing cirrhosis,” Dr. Cusi said in a recent written statement. “We’re trying to identify these problems before they’re unfixable. Once someone has cirrhosis, there isn’t a whole lot you can do.”
Pioglitazone remains the best-documented treatment
Perhaps some of the inertia in diagnosing NAFLD, NASH, and liver fibrosis in patients with T2D is dissatisfaction with current treatment options, although several proven options exist, notably weight loss and diet, and thiazolidinedione (TZD) pioglitazone. But weight loss and diet pose issues for patient compliance and durability of the intervention, and many clinicians consider pioglitazone flawed by its potential adverse effects.
“When we don’t have an established treatment for something, we tend to not measure it or go after it. That’s been true of liver disease” in patients with T2D, said Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of the Metabolic Institute of America in Tarzana, Calif., during the WCIRDC.
Treatment with pioglitazone has resolved NASH in about a third of patients compared with placebo, prevented fibrosis progression, and cut cardiovascular disease events, noted Dr. Cusi during the WCIRDC.
“Pioglitazone is used in only 8% of patients with T2D, or less, but we need to use it more often because of its proven efficacy in patients with T2D and NASH” said Dr. Mantzoros. “The problem is that pioglitazone has side effects, including weight gain and fluid retention, that makes it less attractive unless one thinks about the diagnosis of NASH.”
Others highlight that the adverse effects of pioglitazone have been either misunderstood, or can be effectively minimized with careful dosing.
“The data with the TZDs are much stronger than the data from anything else. TZDs have gotten a bad name because they also work in the kidney and enhance fluid reabsorption. We use modest dosages of pioglitazone, 15 mg or 30 mg a day, to avoid excess fluid retention,” Ralph A. DeFronzo, MD, chief of the diabetes division and professor of medicine at the University of Texas Health Science Center, San Antonio, said during the WCIRDC. “The best drug for NASH is pioglitazone. No other drug beats it” based on current data, Dr. DeFronzo asserted.
Other strategies include the potential to pair pioglitazone with other interventions that can blunt a weight-gain effect. One intriguing combination would combine pioglitazone with a GLP-1 receptor agonist, a drug class that can produce significant weight loss. Results from a phase 2 study showed promise for semaglutide (Rybelsus) in treating patients with NASH.
Getting the name right
Another factor that may be keeping NAFLD and NASH from achieving a higher profile for patients with T2D are those names, which focus on what the diseases are not – nonalcoholic – rather than what they are.
A series of recent publications in both the endocrinology and hepatology literature have called for renaming these disorders either “metabolic (dysfunction)–associated fatty liver disease (MALFD)”, or “dysmetabolism-associated fatty liver disease (DALFD)”.
“The names NAFLD and NASH indicate absence of alcohol as a cause, but the disease is also characterized by the absence of other causes, such as autoimmune disorders or hepatitis. The names were coined when we did not know much about these diseases. We now know that it is dysmetabolism that causes these conditions, and so we need to adopt a new, more accurate name,” explained Dr. Mantzoros, who has published support for a name change.
While many agree, some have raised concerns as to whether a name change now is premature. A group of hepatologists recently published a rebuttal to an immediate name change , saying that, “although we are in agreement that metabolic fatty liver disease may more accurately and positively reflect the relevant risk factors better than the age-old term nonalcoholic fatty liver disease, the term still leaves a great deal of ambiguity. A name change will be appropriate when informed by a new understanding of the molecular basis of the disease entity, insights that fundamentally change risk stratification, or other important aspects of the disease. We may be on the cusp of this, but we are not there yet.”
Dr. Mantzoros agreed, but for somewhat different reasons.
“We need to be careful and deliberate, because there is a significant body of knowledge and a lot of data from clinical trials collected using the old definitions. We need to find an appropriate time frame for a [name] transition. We need to find a nice and robust way to productively bridge the old to the new,” he said. “We also need new diagnostic criteria, and new therapies. A new name and definition will facilitate progress.”
Dr. Mantzoros been a shareholder of and consultant to Coherus and Pangea, he has been a consultant to AstraZeneca, Eisai, Genfit, Intercept, Novo Nordisk, P.E.S., and Regeneron, and has received travel support from the Metabolic Institute of America and the California Walnut Commission. Dr. Cusi has been a consultant to and has received research funding from numerous drug companies. Dr. McLaughlin is a consultant to January AI. Dr. Handelsman has been a consultant to numerous drug companies. Dr. DeFronzo received research grants from AstraZeneca, Janssen, and Merck; he has been an adviser to AstraZeneca, Boehringer Ingelheim, Intarcia, Janssen, and Novo Nordisk; and he has been a speaker on behalf of AstraZeneca and Novo Nordisk.
Generalized pruritic blisters and bullous lesions
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
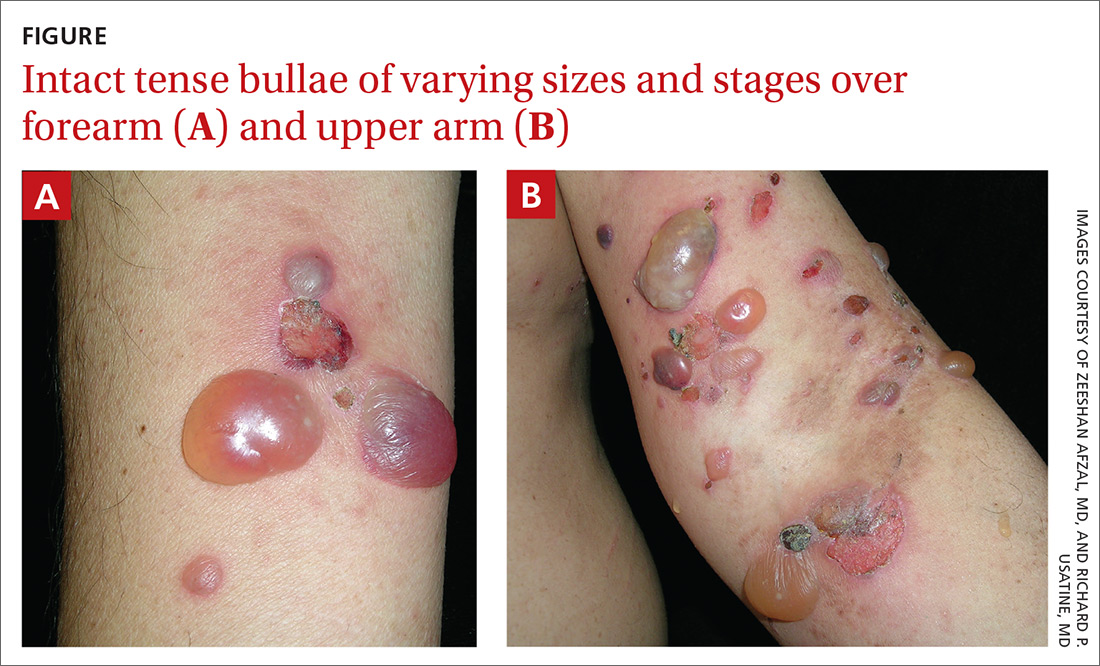
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
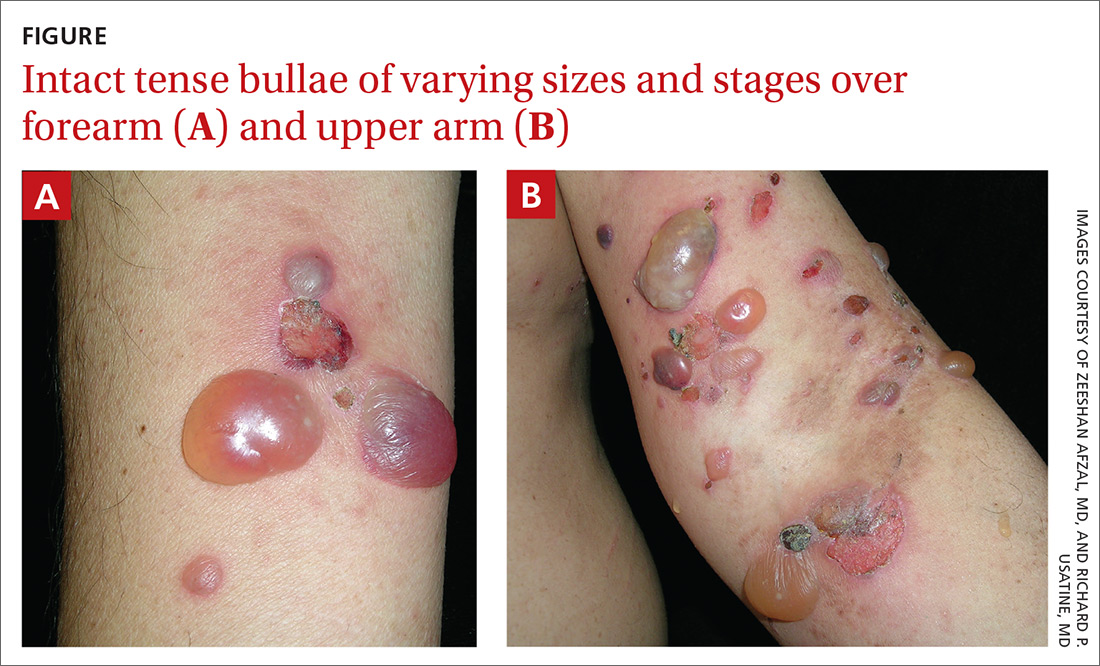
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
A 62-year-old man presented to our skin clinic with multiple pruritic, tense, bullous lesions that manifested on his arms, abdomen, back, and upper thighs over a 1-month period. There were no lesions in his oral cavity or around his eyes, nose, or penile region. He denied dysphagia.
The patient had multiple comorbidities, including diabetes, hypertension, recent stroke, and end-stage renal disease. He was being prepared for dialysis. His medications included torsemide, warfarin, amiodarone, metoprolol, pantoprozole, atorvastatin, and nifedipine. About 3 months prior to this presentation, he was started on oral linaglipton 5 mg/d, an oral antihyperglycemic medication. He had no history of skin disease or cancer, and his family history was not significant.
Physical examination showed multiple 5-mm to 2-cm blisters and bullae on the flexural surface of both of his arms (FIGURE), back, lower abdomen, and upper thighs. His palms and soles were not involved. The lesions were nontender, tense, and filled with clear fluid. Some were intact and others were rupturing. There was no mucocutaneous involvement. Nikolsky sign was negative. There were no signs of bleeding.
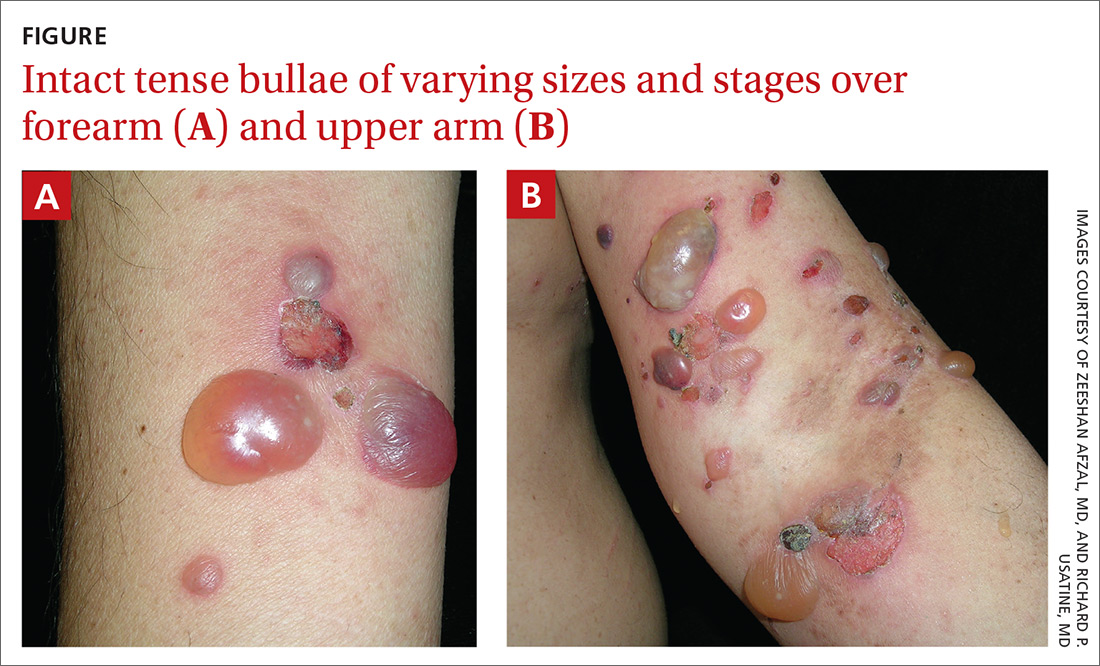
The family physician (FP) obtained a 4-mm punch biopsy at the edge of a 6-mm blister for light microscopy and a 3-mm perilesional punch biopsy for direct immunofluorescence (DIF) microscopy.
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Dx: Bullous pemphigoid secondary to linagliptin use
DIF of the biopsy sample demonstrated linear deposition of complement 3 (C3) and immunoglobulin (Ig) G along the basement membrane zone. Indirect immunofluorescence on salt-split skin demonstrated linear deposition of IgG and C3 on both the roof and floor of the induced blisters. These findings and the patient’s clinical presentation met the criteria for bullous pemphigoid (BP), which is the most common autoimmune skin-blistering disease.1
BP is associated with subepidermal blistering, which can occur in reaction to a variety of triggers. Pathogenesis of this condition involves IgG anti-basement membrane autoantibody complex formation with the hemidesmosomal antigens BP230 and BP180—a process that activates C3 and the release of proteases that can be destructive to tissue along the dermo-epidermal junction.1
Growing incidence. BP usually occurs in patients > 60 years, with no racial or gender preference.1 The incidence rate of BP ranges from 2.4 to 21.7 new cases per 1 million individuals among various worldwide populations.2 The incidence appears to have increased 1.9- to 4.3-fold over the past 2 decades.2
What you’ll see, who’s at risk
Symptoms of BP include localized areas of erythema or pruritic urticarial plaques that gradually become more extensive. A patient may have pruritis alone for an extended period prior to developing blisters and bullae. The bullae are tense and normally 1 to 7 cm in size.1 Eruption is generalized, mostly affecting the lower abdomen, as well as the flexural parts of the extremities. The palms and soles also can be affected.
FPs should be aware of the atypical clinical variants of BP. In a review by Kridin and Ludwig, variants can be prurigo-like, eczema-like, urticaria-like, dyshidrosiform type, erosive type, and erythema annulare centrifugum–like type.2 At-risk populations, such as elderly patients (> 70 years), whose pruritis manifests with or without bullous formation, should be screened for BP.3,4
Continue to: Risk factors for BP
Risk factors for BP. Certain conditions linked to developing BP include neurologic disorders (dementia and Parkinson disease) and psychiatric disorders (unipolar and bipolar disorder).4 Further, it is important to note any medications that could be the cause of a patient’s BP, including dipeptidyl peptidase-4 (DPP-4) inhibitors, psychotropic medications, spironolactone, furosemide, beta-blockers, and antibiotics.3 This patient was taking a beta-blocker (metoprolol) and a DPP-4 inhibitor (linagliptin). Because he was most recently started on linagliptin, we suspected it may have had a causal role in the development of BP.
The association of DPP-4 inhibitors and BP
FPs are increasingly using DPP-4 inhibitors—including sitagliptin, vildagliptin, and linagliptin—as oral antihyperglycemic agents for type 2 diabetes mellitus. Therefore, it’s important to recognize this medication class’s association with BP.5 In a case-control study of 165 patients with BP, Benzaquen et al reported that 28 patients who were taking DPP-4 inhibitors had an associated increased risk for BP (adjusted odds ratio = 2.64; 95% confidence interval [CI], 1.19-5.85).3
The pathophysiology of BP associated with DPP-4 inhibitors remains unclear, but mechanisms have been proposed. The DPP-4 enzyme is expressed on many cells, including keratinocytes, T cells, and endothelial cells.3 It is possible that DPP-4 inhibition at these cells could stimulate activity of inflammatory cytokines, which can lead to enhanced local eosinophil activation and trigger bullous formation. DPP-4 enzymes are also involved in forming plasmin, which is a protease that cleaves BP180.3 Inhibition of this process can affect proper cleavage of BP180, impacting its function and antigenicity.3,6
Other conditions that also exhibit blisters
There are some skin conditions with similar presentations that need to be ruled out in the work-up.
Bullous diabeticorum is a rare, spontaneous, noninflammatory condition found in patients with diabetes.1 Blisters usually manifest as large, tense, asymmetrical, mildly tender lesions that commonly affect the feet and lower legs but can involve the trunk. These usually develop overnight without preceding trauma. Biopsy would show both intra-epidermal and subepidermal bulla with normal DIF findings.1 This condition usually has an excellent prognosis.
Continue to: Pemphigus vulgaris
Pemphigus vulgaris is characterized by nonpruritic, flaccid, painful blisters. This condition usually begins with manifestation of painful oral lesions that evolve into skin blisters. Some patients can develop mucocutaneous lesions.1 Nikolsky sign is positive in these cases. Light microscopy would show intra-epidermal bullae.
Dermatitis herpetiformis. This condition—usually affecting middle-age patients—is associated with severe pruritis and burning. It may start with a few pruritic papules or vesicles that later evolve into urticarial papules, vesicles, or bullae. Dermatitis herpetiformis can resemble herpes simplex virus. It can also be associated with gluten-sensitive enteropathy and small bowel lymphoma.1 DIF of a biopsy sample would show granular deposition of IgA within the tips of the dermal papillae and along the basement membrane of perilesional skin.1
Epidermolysis bullosa acquisita is a rare, severe, chronic condition with subepidermal mucocutaneous blistering.1 It is associated with skin fragility and spontaneous trauma-induced blisters that heal with scar formation and milia. IgG autoantibodies reacting to proteins in the basement membrane zone can cause the disease. It is also associated with Crohn disease.1 DIF findings are similar in BP, but they are differentiated by location of IgG deposits; they can be found on the dermal side of separation in epidermolysis bullosa acquisita, as compared with the epidermal side in BP.1
How to make the Dx in 3 steps
To effectively diagnose and classify BP, use the following 3-step method:
- Establish the presence of 3 of 4 clinical characteristics: patient’s age > 60 years, absence of atrophic scars, absence of mucosal involvement, and absence of bullous lesions on the head and neck.
- Order light microscopy. Findings should be consistent with eosinophils and neutrophils containing subepidermal bullae.
- Order a punch biopsy to obtain a perilesional specimen. DIF of the biopsy findings should feature linear deposits of IgG with or without C3 along the dermo-epidermal junction. This step is essential for an accurate diagnosis.
There also is benefit in ordering supplemental studies, such as an enzyme-linked immunosorbent assay for the detection of anti-BP180 or anti-BP230 IgG autoantibodies.7 However, for this patient, we did not order this study.
Continue to: Management focuses on steroids
Management focuses on steroids
The offending agent should be discontinued immediately. Depending on the severity of disease, treatment can include the use of potent topical corticosteroids alone or in combination with systemic corticosteroids and anti-inflammatory antibiotics (eg, doxycycline, minocycline, erythromycin).1,7 For patients with resistant or refractory disease, consider azathioprine, methotrexate, dapsone, and chlorambucil.1,7 Exceptional cases may benefit from the use of mycophenolate mofetil, intravenous immunoglobulin, or plasmapheresis.1,7
For this patient, initial treatment included discontinuation of linagliption and introduction of topical clobetasol 0.05% and oral prednisone 40 mg/d for 7 days, followed by prednisone 20 mg for 7 days. He was also started on oral doxycycline 100 mg bid and oral nicotinamide 500 mg bid.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
1. Habif TP. Vesicular and bullous diseases. In: Habif TP, ed. Clinical Dermatology: a Color Guide to Diagnosis and Therapy. 6th ed. Elsevier; 2016:635-666.
2. Kridin K, Ludwig RJ. The growing incidence of bullous pemphigoid: overview and potential explanations. Front Med (Lausanne). 2018;5:220.
3. Benzaquen M, Borradori L, Berbis P, et al. Dipeptidyl peptidase IV inhibitors, a risk factor for bullous pemphigoid: retrospective multicenter case-control study from France and Switzerland. J Am Acad Dermatol. 2017;78:1090-1096.
4. Bastuji-Garin S, Joly P, Lemordant P, et al. Risk factors for bullous pemphigoid in the elderly: a prospective case-control study. J Invest Dermatol. 2011;131:637-643.
5. Kridin K, Bergman R. Association of bullous pemphigoid with dipeptidyl-peptidase 4 inhibitors in patients with diabetes: estimating the risk of the new agents and characterizing the patients. JAMA Dermatol. 2018;154:1152-1158.
6. Haber R, Fayad AM, Stephan F, et al. Bullous pemphigoid associated with linagliptin treatment. JAMA Dermatol. 2016;152:224-226.Management of bullous pemphigoid: the European Dermatology Forum consensus in collaboration with the European Academy of Dermatology and Venereology. Br J Dermatol. 2015;172:867-877.
Low-carb diets boost diabetes remission rates, at least short term
Patients with type 2 diabetes who follow a low-carbohydrate diet (LCD) for at least 6 months appear to have significantly higher remission rates than those following other diets, although the benefits diminish by 12 months, suggests a new analysis of trial data from over 1,300 individuals.
“Based on other evidence, it is likely the degree of weight loss would have been a contributing factor, combined with the lower intake of dietary carbohydrates,” study coauthor Grant D. Brinkworth, PhD, Commonwealth Scientific and Industrial Research Organisation, Sydney, , said in an interview.
He acknowledged, however, that “diets in general can be difficult to sustain over the long term. ... We need to provide patients with easy-to-use support tools and convenient solutions to help them adhere to a low-carb diet long term to gain these greater health improvements.
“In addition, more long-term, well-controlled, randomized trials are needed to determine the effects of low-carb diets on sustained weight loss, diabetes remission, and health outcomes,” Dr. Brinkworth added.
The research was published on Janu. 13 in the BMJ by a consortium of international scientists, led by Joshua Z. Goldenberg, PhD, department of nutrition, Texas A&M University, College Station.
Confusion as to best diet for those with diabetes
Type 2 diabetes is a “significant and worsening” worldwide health problem, wrote Dr. Goldenberg and coauthors, in spite of “many pharmaceutical developments and a global emphasis on glycemic control.”
Although structured diets are “recognized as an essential component of treating diabetes, confusion remains about which diet to choose,” with multiple systemic reviews and meta-analyses of carbohydrate-restricted diets “reporting mixed results,” they noted.
They therefore undertook a systematic review of randomized, controlled trials on the efficacy and safety of LCDs and very-low-carbohydrate diets (VLCDs) using the CENTRAL, Medline, CINAHL, and CAB databases, as well as other literature sources.
Researchers defined LCDs as less than 130 g/day of carbohydrates or less than 26% of calories from carbohydrates as part of a 2,000 kcal/day diet and VLCDs as less than 50 g/day or less than 10% of daily calories. They focused on interventions that lasted at least 12 weeks in adults with type 2 diabetes.
Overall, 23 trials involving 1,357 participants met the inclusion criteria; 52% used VLCDs and the control comparator was a low-fat diet in 78% of the studies. The mean age range of patients was 47-67 years, and treatment duration spanned from 3 months to 2 years.
LCDs were associated with a higher rate of diabetes remission when defined as a hemoglobin A1c level of less than 6.5%, compared with control diets at 6 months, at 57% versus 31% – an increase in remission of 32% associated with LCDs (P < .001 for overall effect).
But when defined more tightly as an A1c level of less than 6.5% in the absence of diabetes medications, remission with LCDs was reduced to a nonsignificant 5% versus control diets at 6 months.
At 12 months, data on remission were sparse, ranging from a small effect to a trivial increased risk of diabetes.
Subgroup analysis demonstrated that patients on an LCD achieved greater weight loss at 6 months than those on a control diet, at a mean reduction of 3.46 kg (approximately 7.6 lb). However, the researchers noted that, at 12 months, any weight-loss benefit was “trivial and nonsignificant.”
A similar pattern was seen for reductions in A1c and fasting glucose levels with LCDs: Notable reductions at 6 months largely disappeared by 12 months.
LCDs were also associated with “greater reductions in diabetes medication and clinically important benefits” in triglycerides and insulin resistance at 6 and 12 months, the team wrote.
VLCDs: Adherence Is key
Finally, the team looked at weight loss achieved with VLCDs.
VLCDs were less effective for weight loss at 6 months than less restrictive LCDs. However, this effect was explained by diet adherence, the researchers noted.
Restricting the analysis to “credible” studies, VLCDs were associated with a larger “clinically important” weight-loss versus control diets when patients were highly adherent to the diet, at a mean reduction of 4.47 kg (9.9 lb) versus a mean increase of 0.55 kg (1.2 lb) among patients who were less adherent.
The team noted that their review has a number of limitations, not least of which is the definition of diabetes remission used, which “is the subject of considerable debate,” as well as the safety concerns raised over LCDs.
Given the latter concerns, “clinicians might consider short-term LCDs for management of type 2 diabetes, while actively monitoring and adjusting diabetes medication as needed,” they concluded.
This study was funded in part by Texas A&M University. One coauthor reported receiving funding from Texas A&M AgriLife Research for a separate research project. Dr. Brinkworth is author of the book “The CSIRO Low Carb Diet,” but does not receive financial royalties or funds either directly or indirectly.
A version of this article first appeared on Medscape.com.
Patients with type 2 diabetes who follow a low-carbohydrate diet (LCD) for at least 6 months appear to have significantly higher remission rates than those following other diets, although the benefits diminish by 12 months, suggests a new analysis of trial data from over 1,300 individuals.
“Based on other evidence, it is likely the degree of weight loss would have been a contributing factor, combined with the lower intake of dietary carbohydrates,” study coauthor Grant D. Brinkworth, PhD, Commonwealth Scientific and Industrial Research Organisation, Sydney, , said in an interview.
He acknowledged, however, that “diets in general can be difficult to sustain over the long term. ... We need to provide patients with easy-to-use support tools and convenient solutions to help them adhere to a low-carb diet long term to gain these greater health improvements.
“In addition, more long-term, well-controlled, randomized trials are needed to determine the effects of low-carb diets on sustained weight loss, diabetes remission, and health outcomes,” Dr. Brinkworth added.
The research was published on Janu. 13 in the BMJ by a consortium of international scientists, led by Joshua Z. Goldenberg, PhD, department of nutrition, Texas A&M University, College Station.
Confusion as to best diet for those with diabetes
Type 2 diabetes is a “significant and worsening” worldwide health problem, wrote Dr. Goldenberg and coauthors, in spite of “many pharmaceutical developments and a global emphasis on glycemic control.”
Although structured diets are “recognized as an essential component of treating diabetes, confusion remains about which diet to choose,” with multiple systemic reviews and meta-analyses of carbohydrate-restricted diets “reporting mixed results,” they noted.
They therefore undertook a systematic review of randomized, controlled trials on the efficacy and safety of LCDs and very-low-carbohydrate diets (VLCDs) using the CENTRAL, Medline, CINAHL, and CAB databases, as well as other literature sources.
Researchers defined LCDs as less than 130 g/day of carbohydrates or less than 26% of calories from carbohydrates as part of a 2,000 kcal/day diet and VLCDs as less than 50 g/day or less than 10% of daily calories. They focused on interventions that lasted at least 12 weeks in adults with type 2 diabetes.
Overall, 23 trials involving 1,357 participants met the inclusion criteria; 52% used VLCDs and the control comparator was a low-fat diet in 78% of the studies. The mean age range of patients was 47-67 years, and treatment duration spanned from 3 months to 2 years.
LCDs were associated with a higher rate of diabetes remission when defined as a hemoglobin A1c level of less than 6.5%, compared with control diets at 6 months, at 57% versus 31% – an increase in remission of 32% associated with LCDs (P < .001 for overall effect).
But when defined more tightly as an A1c level of less than 6.5% in the absence of diabetes medications, remission with LCDs was reduced to a nonsignificant 5% versus control diets at 6 months.
At 12 months, data on remission were sparse, ranging from a small effect to a trivial increased risk of diabetes.
Subgroup analysis demonstrated that patients on an LCD achieved greater weight loss at 6 months than those on a control diet, at a mean reduction of 3.46 kg (approximately 7.6 lb). However, the researchers noted that, at 12 months, any weight-loss benefit was “trivial and nonsignificant.”
A similar pattern was seen for reductions in A1c and fasting glucose levels with LCDs: Notable reductions at 6 months largely disappeared by 12 months.
LCDs were also associated with “greater reductions in diabetes medication and clinically important benefits” in triglycerides and insulin resistance at 6 and 12 months, the team wrote.
VLCDs: Adherence Is key
Finally, the team looked at weight loss achieved with VLCDs.
VLCDs were less effective for weight loss at 6 months than less restrictive LCDs. However, this effect was explained by diet adherence, the researchers noted.
Restricting the analysis to “credible” studies, VLCDs were associated with a larger “clinically important” weight-loss versus control diets when patients were highly adherent to the diet, at a mean reduction of 4.47 kg (9.9 lb) versus a mean increase of 0.55 kg (1.2 lb) among patients who were less adherent.
The team noted that their review has a number of limitations, not least of which is the definition of diabetes remission used, which “is the subject of considerable debate,” as well as the safety concerns raised over LCDs.
Given the latter concerns, “clinicians might consider short-term LCDs for management of type 2 diabetes, while actively monitoring and adjusting diabetes medication as needed,” they concluded.
This study was funded in part by Texas A&M University. One coauthor reported receiving funding from Texas A&M AgriLife Research for a separate research project. Dr. Brinkworth is author of the book “The CSIRO Low Carb Diet,” but does not receive financial royalties or funds either directly or indirectly.
A version of this article first appeared on Medscape.com.
Patients with type 2 diabetes who follow a low-carbohydrate diet (LCD) for at least 6 months appear to have significantly higher remission rates than those following other diets, although the benefits diminish by 12 months, suggests a new analysis of trial data from over 1,300 individuals.
“Based on other evidence, it is likely the degree of weight loss would have been a contributing factor, combined with the lower intake of dietary carbohydrates,” study coauthor Grant D. Brinkworth, PhD, Commonwealth Scientific and Industrial Research Organisation, Sydney, , said in an interview.
He acknowledged, however, that “diets in general can be difficult to sustain over the long term. ... We need to provide patients with easy-to-use support tools and convenient solutions to help them adhere to a low-carb diet long term to gain these greater health improvements.
“In addition, more long-term, well-controlled, randomized trials are needed to determine the effects of low-carb diets on sustained weight loss, diabetes remission, and health outcomes,” Dr. Brinkworth added.
The research was published on Janu. 13 in the BMJ by a consortium of international scientists, led by Joshua Z. Goldenberg, PhD, department of nutrition, Texas A&M University, College Station.
Confusion as to best diet for those with diabetes
Type 2 diabetes is a “significant and worsening” worldwide health problem, wrote Dr. Goldenberg and coauthors, in spite of “many pharmaceutical developments and a global emphasis on glycemic control.”
Although structured diets are “recognized as an essential component of treating diabetes, confusion remains about which diet to choose,” with multiple systemic reviews and meta-analyses of carbohydrate-restricted diets “reporting mixed results,” they noted.
They therefore undertook a systematic review of randomized, controlled trials on the efficacy and safety of LCDs and very-low-carbohydrate diets (VLCDs) using the CENTRAL, Medline, CINAHL, and CAB databases, as well as other literature sources.
Researchers defined LCDs as less than 130 g/day of carbohydrates or less than 26% of calories from carbohydrates as part of a 2,000 kcal/day diet and VLCDs as less than 50 g/day or less than 10% of daily calories. They focused on interventions that lasted at least 12 weeks in adults with type 2 diabetes.
Overall, 23 trials involving 1,357 participants met the inclusion criteria; 52% used VLCDs and the control comparator was a low-fat diet in 78% of the studies. The mean age range of patients was 47-67 years, and treatment duration spanned from 3 months to 2 years.
LCDs were associated with a higher rate of diabetes remission when defined as a hemoglobin A1c level of less than 6.5%, compared with control diets at 6 months, at 57% versus 31% – an increase in remission of 32% associated with LCDs (P < .001 for overall effect).
But when defined more tightly as an A1c level of less than 6.5% in the absence of diabetes medications, remission with LCDs was reduced to a nonsignificant 5% versus control diets at 6 months.
At 12 months, data on remission were sparse, ranging from a small effect to a trivial increased risk of diabetes.
Subgroup analysis demonstrated that patients on an LCD achieved greater weight loss at 6 months than those on a control diet, at a mean reduction of 3.46 kg (approximately 7.6 lb). However, the researchers noted that, at 12 months, any weight-loss benefit was “trivial and nonsignificant.”
A similar pattern was seen for reductions in A1c and fasting glucose levels with LCDs: Notable reductions at 6 months largely disappeared by 12 months.
LCDs were also associated with “greater reductions in diabetes medication and clinically important benefits” in triglycerides and insulin resistance at 6 and 12 months, the team wrote.
VLCDs: Adherence Is key
Finally, the team looked at weight loss achieved with VLCDs.
VLCDs were less effective for weight loss at 6 months than less restrictive LCDs. However, this effect was explained by diet adherence, the researchers noted.
Restricting the analysis to “credible” studies, VLCDs were associated with a larger “clinically important” weight-loss versus control diets when patients were highly adherent to the diet, at a mean reduction of 4.47 kg (9.9 lb) versus a mean increase of 0.55 kg (1.2 lb) among patients who were less adherent.
The team noted that their review has a number of limitations, not least of which is the definition of diabetes remission used, which “is the subject of considerable debate,” as well as the safety concerns raised over LCDs.
Given the latter concerns, “clinicians might consider short-term LCDs for management of type 2 diabetes, while actively monitoring and adjusting diabetes medication as needed,” they concluded.
This study was funded in part by Texas A&M University. One coauthor reported receiving funding from Texas A&M AgriLife Research for a separate research project. Dr. Brinkworth is author of the book “The CSIRO Low Carb Diet,” but does not receive financial royalties or funds either directly or indirectly.
A version of this article first appeared on Medscape.com.
Meta-analysis: No evidence that SNRIs relieve back pain
While some guidelines support serotonin norepinephrine reuptake inhibitors (SNRIs) as treatments for back pain, a new systematic review and meta-analysis of existing research found no firm evidence of a benefit. Adverse effects, however, are common.
“Our review shows that, although these medicines are effective, the effect is small and unlikely to be considered clinically important by most patients,” wrote the authors of the review, which appeared Jan. 20 in the BMJ. “Our review also showed that about two-thirds of patients using SNRIs experience adverse events.”
However, the report hinted that certain classes of antidepressants may provide significant relief in knee OA and sciatica.
According to a 2018 review, 10 of 15 clinical guidelines from around the world – including those of the American College of Physicians – recommended antidepressants as treatments for low back pain, and 2 advised against them. “Evidence supporting the use of antidepressants is, however, uncertain,” wrote the authors of the new review, led by Giovanni E. Ferreira, PhD, of the University of Sydney. “Systematic reviews of antidepressants for back pain and osteoarthritis have either not included several published trials, considered only one type of antidepressant (e.g., duloxetine), or failed to assess the certainty of evidence.”
For the new review, the authors analyzed 33 randomized, controlled trials with a total of 5,318 subjects. Both published data and unpublished data from clinical trial registries were included.
Back pain trials
A total of 19 trials examined back pain, mostly lower back pain (16 trials), and none lasted more than 1 year. Fifteen examined SNRIs while others looked at other kinds of antidepressants.
The researchers found that “the effect of SNRIs was small [on back pain] and below this review’s predetermined threshold of clinical importance. ... Evidence ranging from low to very low certainty showed no benefit of a range of antidepressant classes, including SSRIs [selective serotonin reuptake inhibitors], tetracyclic antidepressants, SARIs [serotonin antagonist and reuptake inhibitors], and NDRIs [norepinephrine and dopamine reuptake inhibitors] for pain and disability across follow-ups of 2 weeks or less, 3-13 weeks, and 3-12 months.”
Sciatica trials
Six trials examined antidepressants as treatments for sciatica. Very-low-certainty evidence suggested that SNRIs reduced pain at up to 2 weeks (1 trial, n = 50) but not at 3-13 weeks (3 trials, n = 96). The results of trials of tricyclic antidepressants (TCAs) were the opposite: low- to very-low-certainty evidence suggested the drugs didn’t reduce pain at up to 2 weeks (2 trials, n = 94) but did at 3-13 weeks (2 trials, n = 114) and 3-12 months (1 trial, n = 60).
“All sciatica trials were small, had imprecise estimates, and were at high risk of bias, which reduced the certainty of evidence to low and very low,” the authors cautioned. “This level of uncertainty indicates that the true estimate of effect of TCAs and SNRIs for sciatica is likely to be substantially different from what we estimated in our review.”
Knee OA trials
Eight trials examined SNRIs in knee OA. Moderate-certainty evidence linked the drugs to less pain at up to 2 weeks (four trials, n = 1,328) and low-certainty evidence linked them to less pain at 3-13 weeks (eight trials, n = 1,941). Low-certainty evidence also linked the drugs to less disability at 2 weeks or less (one trial, n = 353) and 3-13 weeks (seven trials, n = 1,810).
In knee OA, “the effect of SNRIs was small and below this review’s predetermined threshold of clinical importance,” the researchers wrote. “However, the lower limit of the confidence interval did contain clinically important effects for pain, but not for disability.”
Antidepressant side effects in trials
A total of 21 trials (n = 4,107) looked at side effects when antidepressants were studied as treatments for back pain and OA. Low-certainty evidence in 13 SNRI trials (n = 3,447) suggested a higher risk of any adverse events in antidepressant versus placebo (62.5% vs. 49.7%; relative risk, 1.23, 95% confidence interval, 1.16-1.30), but there was no significantly higher risk of serious adverse events in 10 SNRI trials with 3,309 subjects (1.6% vs. 1.3%; RR, 1.12, 95% CI, 0.61-2.07).
As for adverse effects of non-SNRIs, “the number of studies evaluating the safety of other antidepressant classes was small, trials were underpowered to detect harm, and the certainty of evidence ranged from low to very low,” the researchers wrote.
Going forward, the authors said that “large, definitive randomized trials that are free of industry ties are urgently needed to resolve uncertainties about the efficacy of antidepressants for sciatica and osteoarthritis highlighted by this review.”
‘Largely ineffective’ drug treatments
In an accompanying commentary, Martin Underwood, of the University of Warwick in Coventry, England, and Colin Tysall, of the University Hospitals of Coventry and Warwickshire, also in Coventry, noted that “drug treatments are largely ineffective for back pain and osteoarthritis and have the potential for serious harm. We need to work harder to help people with these disorders to live better with their pain without recourse to the prescription pad.”
However, they noted that SNRIs may still be helpful for patients with back pain or OA. “Absolute effect sizes for physical treatments for low-back pain are of similar magnitudes to those reported here and translate into numbers needed to treat of between five and nine. If the same were true for SNRIs, some people might choose to a try that option for a 1 in 10 chance of a worthwhile reduction in pain after 3 months. They can easily stop if treatment is ineffective or does not suit them.”
The research received no specific funding. The review authors disclosed relationships with GlaxoSmithKline (postgraduate scholarship), Pfizer (investigational product for two trials), and Flexeze (provision of heat wraps for a trial). Mr. Underwood reported being a director and shareholder of Clinvivo. Mr. Tysall reported no disclosures.
While some guidelines support serotonin norepinephrine reuptake inhibitors (SNRIs) as treatments for back pain, a new systematic review and meta-analysis of existing research found no firm evidence of a benefit. Adverse effects, however, are common.
“Our review shows that, although these medicines are effective, the effect is small and unlikely to be considered clinically important by most patients,” wrote the authors of the review, which appeared Jan. 20 in the BMJ. “Our review also showed that about two-thirds of patients using SNRIs experience adverse events.”
However, the report hinted that certain classes of antidepressants may provide significant relief in knee OA and sciatica.
According to a 2018 review, 10 of 15 clinical guidelines from around the world – including those of the American College of Physicians – recommended antidepressants as treatments for low back pain, and 2 advised against them. “Evidence supporting the use of antidepressants is, however, uncertain,” wrote the authors of the new review, led by Giovanni E. Ferreira, PhD, of the University of Sydney. “Systematic reviews of antidepressants for back pain and osteoarthritis have either not included several published trials, considered only one type of antidepressant (e.g., duloxetine), or failed to assess the certainty of evidence.”
For the new review, the authors analyzed 33 randomized, controlled trials with a total of 5,318 subjects. Both published data and unpublished data from clinical trial registries were included.
Back pain trials
A total of 19 trials examined back pain, mostly lower back pain (16 trials), and none lasted more than 1 year. Fifteen examined SNRIs while others looked at other kinds of antidepressants.
The researchers found that “the effect of SNRIs was small [on back pain] and below this review’s predetermined threshold of clinical importance. ... Evidence ranging from low to very low certainty showed no benefit of a range of antidepressant classes, including SSRIs [selective serotonin reuptake inhibitors], tetracyclic antidepressants, SARIs [serotonin antagonist and reuptake inhibitors], and NDRIs [norepinephrine and dopamine reuptake inhibitors] for pain and disability across follow-ups of 2 weeks or less, 3-13 weeks, and 3-12 months.”
Sciatica trials
Six trials examined antidepressants as treatments for sciatica. Very-low-certainty evidence suggested that SNRIs reduced pain at up to 2 weeks (1 trial, n = 50) but not at 3-13 weeks (3 trials, n = 96). The results of trials of tricyclic antidepressants (TCAs) were the opposite: low- to very-low-certainty evidence suggested the drugs didn’t reduce pain at up to 2 weeks (2 trials, n = 94) but did at 3-13 weeks (2 trials, n = 114) and 3-12 months (1 trial, n = 60).
“All sciatica trials were small, had imprecise estimates, and were at high risk of bias, which reduced the certainty of evidence to low and very low,” the authors cautioned. “This level of uncertainty indicates that the true estimate of effect of TCAs and SNRIs for sciatica is likely to be substantially different from what we estimated in our review.”
Knee OA trials
Eight trials examined SNRIs in knee OA. Moderate-certainty evidence linked the drugs to less pain at up to 2 weeks (four trials, n = 1,328) and low-certainty evidence linked them to less pain at 3-13 weeks (eight trials, n = 1,941). Low-certainty evidence also linked the drugs to less disability at 2 weeks or less (one trial, n = 353) and 3-13 weeks (seven trials, n = 1,810).
In knee OA, “the effect of SNRIs was small and below this review’s predetermined threshold of clinical importance,” the researchers wrote. “However, the lower limit of the confidence interval did contain clinically important effects for pain, but not for disability.”
Antidepressant side effects in trials
A total of 21 trials (n = 4,107) looked at side effects when antidepressants were studied as treatments for back pain and OA. Low-certainty evidence in 13 SNRI trials (n = 3,447) suggested a higher risk of any adverse events in antidepressant versus placebo (62.5% vs. 49.7%; relative risk, 1.23, 95% confidence interval, 1.16-1.30), but there was no significantly higher risk of serious adverse events in 10 SNRI trials with 3,309 subjects (1.6% vs. 1.3%; RR, 1.12, 95% CI, 0.61-2.07).
As for adverse effects of non-SNRIs, “the number of studies evaluating the safety of other antidepressant classes was small, trials were underpowered to detect harm, and the certainty of evidence ranged from low to very low,” the researchers wrote.
Going forward, the authors said that “large, definitive randomized trials that are free of industry ties are urgently needed to resolve uncertainties about the efficacy of antidepressants for sciatica and osteoarthritis highlighted by this review.”
‘Largely ineffective’ drug treatments
In an accompanying commentary, Martin Underwood, of the University of Warwick in Coventry, England, and Colin Tysall, of the University Hospitals of Coventry and Warwickshire, also in Coventry, noted that “drug treatments are largely ineffective for back pain and osteoarthritis and have the potential for serious harm. We need to work harder to help people with these disorders to live better with their pain without recourse to the prescription pad.”
However, they noted that SNRIs may still be helpful for patients with back pain or OA. “Absolute effect sizes for physical treatments for low-back pain are of similar magnitudes to those reported here and translate into numbers needed to treat of between five and nine. If the same were true for SNRIs, some people might choose to a try that option for a 1 in 10 chance of a worthwhile reduction in pain after 3 months. They can easily stop if treatment is ineffective or does not suit them.”
The research received no specific funding. The review authors disclosed relationships with GlaxoSmithKline (postgraduate scholarship), Pfizer (investigational product for two trials), and Flexeze (provision of heat wraps for a trial). Mr. Underwood reported being a director and shareholder of Clinvivo. Mr. Tysall reported no disclosures.
While some guidelines support serotonin norepinephrine reuptake inhibitors (SNRIs) as treatments for back pain, a new systematic review and meta-analysis of existing research found no firm evidence of a benefit. Adverse effects, however, are common.
“Our review shows that, although these medicines are effective, the effect is small and unlikely to be considered clinically important by most patients,” wrote the authors of the review, which appeared Jan. 20 in the BMJ. “Our review also showed that about two-thirds of patients using SNRIs experience adverse events.”
However, the report hinted that certain classes of antidepressants may provide significant relief in knee OA and sciatica.
According to a 2018 review, 10 of 15 clinical guidelines from around the world – including those of the American College of Physicians – recommended antidepressants as treatments for low back pain, and 2 advised against them. “Evidence supporting the use of antidepressants is, however, uncertain,” wrote the authors of the new review, led by Giovanni E. Ferreira, PhD, of the University of Sydney. “Systematic reviews of antidepressants for back pain and osteoarthritis have either not included several published trials, considered only one type of antidepressant (e.g., duloxetine), or failed to assess the certainty of evidence.”
For the new review, the authors analyzed 33 randomized, controlled trials with a total of 5,318 subjects. Both published data and unpublished data from clinical trial registries were included.
Back pain trials
A total of 19 trials examined back pain, mostly lower back pain (16 trials), and none lasted more than 1 year. Fifteen examined SNRIs while others looked at other kinds of antidepressants.
The researchers found that “the effect of SNRIs was small [on back pain] and below this review’s predetermined threshold of clinical importance. ... Evidence ranging from low to very low certainty showed no benefit of a range of antidepressant classes, including SSRIs [selective serotonin reuptake inhibitors], tetracyclic antidepressants, SARIs [serotonin antagonist and reuptake inhibitors], and NDRIs [norepinephrine and dopamine reuptake inhibitors] for pain and disability across follow-ups of 2 weeks or less, 3-13 weeks, and 3-12 months.”
Sciatica trials
Six trials examined antidepressants as treatments for sciatica. Very-low-certainty evidence suggested that SNRIs reduced pain at up to 2 weeks (1 trial, n = 50) but not at 3-13 weeks (3 trials, n = 96). The results of trials of tricyclic antidepressants (TCAs) were the opposite: low- to very-low-certainty evidence suggested the drugs didn’t reduce pain at up to 2 weeks (2 trials, n = 94) but did at 3-13 weeks (2 trials, n = 114) and 3-12 months (1 trial, n = 60).
“All sciatica trials were small, had imprecise estimates, and were at high risk of bias, which reduced the certainty of evidence to low and very low,” the authors cautioned. “This level of uncertainty indicates that the true estimate of effect of TCAs and SNRIs for sciatica is likely to be substantially different from what we estimated in our review.”
Knee OA trials
Eight trials examined SNRIs in knee OA. Moderate-certainty evidence linked the drugs to less pain at up to 2 weeks (four trials, n = 1,328) and low-certainty evidence linked them to less pain at 3-13 weeks (eight trials, n = 1,941). Low-certainty evidence also linked the drugs to less disability at 2 weeks or less (one trial, n = 353) and 3-13 weeks (seven trials, n = 1,810).
In knee OA, “the effect of SNRIs was small and below this review’s predetermined threshold of clinical importance,” the researchers wrote. “However, the lower limit of the confidence interval did contain clinically important effects for pain, but not for disability.”
Antidepressant side effects in trials
A total of 21 trials (n = 4,107) looked at side effects when antidepressants were studied as treatments for back pain and OA. Low-certainty evidence in 13 SNRI trials (n = 3,447) suggested a higher risk of any adverse events in antidepressant versus placebo (62.5% vs. 49.7%; relative risk, 1.23, 95% confidence interval, 1.16-1.30), but there was no significantly higher risk of serious adverse events in 10 SNRI trials with 3,309 subjects (1.6% vs. 1.3%; RR, 1.12, 95% CI, 0.61-2.07).
As for adverse effects of non-SNRIs, “the number of studies evaluating the safety of other antidepressant classes was small, trials were underpowered to detect harm, and the certainty of evidence ranged from low to very low,” the researchers wrote.
Going forward, the authors said that “large, definitive randomized trials that are free of industry ties are urgently needed to resolve uncertainties about the efficacy of antidepressants for sciatica and osteoarthritis highlighted by this review.”
‘Largely ineffective’ drug treatments
In an accompanying commentary, Martin Underwood, of the University of Warwick in Coventry, England, and Colin Tysall, of the University Hospitals of Coventry and Warwickshire, also in Coventry, noted that “drug treatments are largely ineffective for back pain and osteoarthritis and have the potential for serious harm. We need to work harder to help people with these disorders to live better with their pain without recourse to the prescription pad.”
However, they noted that SNRIs may still be helpful for patients with back pain or OA. “Absolute effect sizes for physical treatments for low-back pain are of similar magnitudes to those reported here and translate into numbers needed to treat of between five and nine. If the same were true for SNRIs, some people might choose to a try that option for a 1 in 10 chance of a worthwhile reduction in pain after 3 months. They can easily stop if treatment is ineffective or does not suit them.”
The research received no specific funding. The review authors disclosed relationships with GlaxoSmithKline (postgraduate scholarship), Pfizer (investigational product for two trials), and Flexeze (provision of heat wraps for a trial). Mr. Underwood reported being a director and shareholder of Clinvivo. Mr. Tysall reported no disclosures.
FROM THE BMJ
Face masks can aggravate rosacea
The “maskne” phenomenon – that is, new onset or exacerbation of preexisting acne due to prolonged wearing of protective face masks – has become commonplace during the COVID-19 pandemic. Less well appreciated is that rosacea often markedly worsens, too, Giovanni Damiani, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is particularly interesting because two inflammatory dermatoses with different pathogenesis are both mechanically and microbiologically triggered by mask use,” observed Dr. Damiani, a dermatologist at the University of Milan.
He presented . These patients – 23 with papulopustular and 13 with erythematotelangiectatic rosacea – were wearing face masks for at least 6 hours per day during quarantine. Most were using what Dr. Damiani termed “community masks,” meaning they weren’t approved by the European regulatory agency as personal protective equipment.
Every yardstick Dr. Damiani and coinvestigators employed to characterize the patients’ rosacea demonstrated that the dermatosis was significantly worse during the prolonged mask-wearing period. For example, the average prequarantine score on the Global Flushing Severity Scale was 2.56, jumping to 3.97 after a month of masked quarantine. The flushing score climbed from 1.83 to 2.78 in the subgroup with papulopustular rosacea, and from 3.85 to 6.08 in patients with erythematotelangiectatic rosacea. Scores on the Clinician’s Erythema Assessment rose from 1.09 to 1.7 in the papulopustular rosacea patients, and from 2.46 to 3.54 in those with erythematotelangiectatic rosacea.
Scores on the Dermatology Life Quality Index climbed from 7.35 prequarantine to 10.65 in the subgroup with papulopustular rosacea and from 5.15 to 8.69 in patients with erythematotelangiectatic rosacea. Investigator Global Assessment and Patient’s Self-Assessment scores also deteriorated significantly after a month in masked quarantine.
Clinically, the mask-aggravated rosacea, or “maskacea,” was mainly localized to the dorsal lower third of the nose as well as the cheeks. The ocular and perioral areas and the chin were least affected.
Dr. Damiani advised his colleagues to intensify therapy promptly when patients report any worsening of their preexisting rosacea in connection with use of face masks. He has found this condition is often relatively treatment resistant so long as affected patients continue to wear face masks as an essential tool in preventing transmission of COVID-19.
The dermatologist noted that not all face masks are equal offenders when it comes to aggravating common facial dermatoses. During the spring 2020 pandemic quarantine in Milan, 11.6% of 318 mask wearers, none health care professionals, presented to Dr. Damiani and coinvestigators for treatment of facial dermatoses. The facial dermatosis rate was 5.4% among 168 users of masks bearing the European Union CE mark signifying the devices met relevant safety and performance standards, compared with 18.7% in 150 users of community masks with no CE mark. The rate of irritant contact dermatitis was zero with the CE mark masks and 4.7% with the community masks.
During quarantine, however, these patients wore their protective face masks for only a limited time, since for the most part they were restricted to home. In contrast, during the first week after the quarantine was lifted in early May and the daily hours of mask use increased, facial dermatoses were diagnosed in 8.7% of 23 users of CE-approved masks, compared with 45% of 71 wearers of community masks. Dr. Damiani and colleagues diagnosed irritant contact dermatitis in 16% of the community mask wearers post quarantine, but in not a single user of a mask bearing the CE mark.
The National Rosacea Society has issued patient guidance on avoiding rosacea flare-ups during the Covid-19 pandemic.
Dr. Damiani reported having no financial conflicts regarding his study.
The “maskne” phenomenon – that is, new onset or exacerbation of preexisting acne due to prolonged wearing of protective face masks – has become commonplace during the COVID-19 pandemic. Less well appreciated is that rosacea often markedly worsens, too, Giovanni Damiani, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is particularly interesting because two inflammatory dermatoses with different pathogenesis are both mechanically and microbiologically triggered by mask use,” observed Dr. Damiani, a dermatologist at the University of Milan.
He presented . These patients – 23 with papulopustular and 13 with erythematotelangiectatic rosacea – were wearing face masks for at least 6 hours per day during quarantine. Most were using what Dr. Damiani termed “community masks,” meaning they weren’t approved by the European regulatory agency as personal protective equipment.
Every yardstick Dr. Damiani and coinvestigators employed to characterize the patients’ rosacea demonstrated that the dermatosis was significantly worse during the prolonged mask-wearing period. For example, the average prequarantine score on the Global Flushing Severity Scale was 2.56, jumping to 3.97 after a month of masked quarantine. The flushing score climbed from 1.83 to 2.78 in the subgroup with papulopustular rosacea, and from 3.85 to 6.08 in patients with erythematotelangiectatic rosacea. Scores on the Clinician’s Erythema Assessment rose from 1.09 to 1.7 in the papulopustular rosacea patients, and from 2.46 to 3.54 in those with erythematotelangiectatic rosacea.
Scores on the Dermatology Life Quality Index climbed from 7.35 prequarantine to 10.65 in the subgroup with papulopustular rosacea and from 5.15 to 8.69 in patients with erythematotelangiectatic rosacea. Investigator Global Assessment and Patient’s Self-Assessment scores also deteriorated significantly after a month in masked quarantine.
Clinically, the mask-aggravated rosacea, or “maskacea,” was mainly localized to the dorsal lower third of the nose as well as the cheeks. The ocular and perioral areas and the chin were least affected.
Dr. Damiani advised his colleagues to intensify therapy promptly when patients report any worsening of their preexisting rosacea in connection with use of face masks. He has found this condition is often relatively treatment resistant so long as affected patients continue to wear face masks as an essential tool in preventing transmission of COVID-19.
The dermatologist noted that not all face masks are equal offenders when it comes to aggravating common facial dermatoses. During the spring 2020 pandemic quarantine in Milan, 11.6% of 318 mask wearers, none health care professionals, presented to Dr. Damiani and coinvestigators for treatment of facial dermatoses. The facial dermatosis rate was 5.4% among 168 users of masks bearing the European Union CE mark signifying the devices met relevant safety and performance standards, compared with 18.7% in 150 users of community masks with no CE mark. The rate of irritant contact dermatitis was zero with the CE mark masks and 4.7% with the community masks.
During quarantine, however, these patients wore their protective face masks for only a limited time, since for the most part they were restricted to home. In contrast, during the first week after the quarantine was lifted in early May and the daily hours of mask use increased, facial dermatoses were diagnosed in 8.7% of 23 users of CE-approved masks, compared with 45% of 71 wearers of community masks. Dr. Damiani and colleagues diagnosed irritant contact dermatitis in 16% of the community mask wearers post quarantine, but in not a single user of a mask bearing the CE mark.
The National Rosacea Society has issued patient guidance on avoiding rosacea flare-ups during the Covid-19 pandemic.
Dr. Damiani reported having no financial conflicts regarding his study.
The “maskne” phenomenon – that is, new onset or exacerbation of preexisting acne due to prolonged wearing of protective face masks – has become commonplace during the COVID-19 pandemic. Less well appreciated is that rosacea often markedly worsens, too, Giovanni Damiani, MD, reported at the annual congress of the European Academy of Dermatology and Venereology.
“This is particularly interesting because two inflammatory dermatoses with different pathogenesis are both mechanically and microbiologically triggered by mask use,” observed Dr. Damiani, a dermatologist at the University of Milan.
He presented . These patients – 23 with papulopustular and 13 with erythematotelangiectatic rosacea – were wearing face masks for at least 6 hours per day during quarantine. Most were using what Dr. Damiani termed “community masks,” meaning they weren’t approved by the European regulatory agency as personal protective equipment.
Every yardstick Dr. Damiani and coinvestigators employed to characterize the patients’ rosacea demonstrated that the dermatosis was significantly worse during the prolonged mask-wearing period. For example, the average prequarantine score on the Global Flushing Severity Scale was 2.56, jumping to 3.97 after a month of masked quarantine. The flushing score climbed from 1.83 to 2.78 in the subgroup with papulopustular rosacea, and from 3.85 to 6.08 in patients with erythematotelangiectatic rosacea. Scores on the Clinician’s Erythema Assessment rose from 1.09 to 1.7 in the papulopustular rosacea patients, and from 2.46 to 3.54 in those with erythematotelangiectatic rosacea.
Scores on the Dermatology Life Quality Index climbed from 7.35 prequarantine to 10.65 in the subgroup with papulopustular rosacea and from 5.15 to 8.69 in patients with erythematotelangiectatic rosacea. Investigator Global Assessment and Patient’s Self-Assessment scores also deteriorated significantly after a month in masked quarantine.
Clinically, the mask-aggravated rosacea, or “maskacea,” was mainly localized to the dorsal lower third of the nose as well as the cheeks. The ocular and perioral areas and the chin were least affected.
Dr. Damiani advised his colleagues to intensify therapy promptly when patients report any worsening of their preexisting rosacea in connection with use of face masks. He has found this condition is often relatively treatment resistant so long as affected patients continue to wear face masks as an essential tool in preventing transmission of COVID-19.
The dermatologist noted that not all face masks are equal offenders when it comes to aggravating common facial dermatoses. During the spring 2020 pandemic quarantine in Milan, 11.6% of 318 mask wearers, none health care professionals, presented to Dr. Damiani and coinvestigators for treatment of facial dermatoses. The facial dermatosis rate was 5.4% among 168 users of masks bearing the European Union CE mark signifying the devices met relevant safety and performance standards, compared with 18.7% in 150 users of community masks with no CE mark. The rate of irritant contact dermatitis was zero with the CE mark masks and 4.7% with the community masks.
During quarantine, however, these patients wore their protective face masks for only a limited time, since for the most part they were restricted to home. In contrast, during the first week after the quarantine was lifted in early May and the daily hours of mask use increased, facial dermatoses were diagnosed in 8.7% of 23 users of CE-approved masks, compared with 45% of 71 wearers of community masks. Dr. Damiani and colleagues diagnosed irritant contact dermatitis in 16% of the community mask wearers post quarantine, but in not a single user of a mask bearing the CE mark.
The National Rosacea Society has issued patient guidance on avoiding rosacea flare-ups during the Covid-19 pandemic.
Dr. Damiani reported having no financial conflicts regarding his study.
FROM THE EADV CONGRESS
Early Head Start program boosts healthy eating, self-regulation
Home-based preventive interventions not only improve healthy eating habits and self-regulation in toddlers but also guide their parents toward better food presentation and response to picky behaviors, reported Robert L. Nix, PhD, of the University of Wisconsin, Madison, and his associates.
In a small, randomized controlled trial of 73 families with toddlers aged 18-36 months enrolled in home-based Early Head Start (EHS), the researchers evaluated four protective factors, including toddlers’ healthy eating habits, toddlers’ self-regulation, parents’ responsive feeding practices, and parents’ sensitive scaffolding. The study, conducted from April to October 2013, is the first clinical trial of Recipe 4 Success, a preschool-focused intervention created by administrators and home visitors of EHS that promotes healthy eating and self-regulation in toddlers living in poverty who may otherwise face weight challenges and obesity later in life. Integrating the intervention into EHS allowed the researchers to take full advantage of its national infrastructure and to make dissemination more efficient.
Of the families selected to participate, all of whom were living below the Federal poverty threshold, 66 were retained through post treatment. Most participating parents were biological mothers; 61% were single; 29% were not high school graduates; just 11% were employed full time. The toddlers averaged 30.72 months; 44% were female. Roughly 48% of families were non-Hispanic White; 29% were Black; and 23% were Hispanic or Latinx, the investigators reported in Pediatrics. More than three-quarters of participants were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children or the Supplemental Nutrition Assistance Program.
The program allowed parents to transform toddler eating habits quickly
The study, which was designed to evaluate for posttreatment differences in the primary outcomes, involved 10 consecutive weekly lessons implemented by regularly assigned EHS home visitors. Parents were required to adhere to feeding practices carefully targeted with sensitive, structured scaffolding designed to keep toddlers from becoming overwhelmed. Parents were guided to understand, for instance, that toddlers frequently need to be exposed to a new food 10-20 times before eating it, and that poor sleep can have a detrimental influence on emotional and behavioral controls that can progress to weight gain.
Parent recall of what food and drinks their toddlers consumed in the previous 24-hour period was collected by interviewers. The percentage of all meals that included a fruit and/or vegetable, a protein source, and the absence of sweets and junk food were noted. Toddler self-regulation was assessed in accordance with delay of gratification, task orientation, and emotional/behavioral control. Parents were asked to rate toddler ability to cease desired activities to comply with parental requests. Parental responsive feeding practices were also recorded to observe how they introduce unique healthy foods and how they responded to their toddlers’ reactions. Parental sensitive scaffolding was similarly observed for their ability to structure activities in a developmentally appropriate manner promoting self-regulation.
The researchers noted no statistically significant differences between families in the treatment and control groups, nor were there differences in outcome measures or covariates. Study findings showed that, compared with toddlers who continued to receive just EHS support, the toddlers randomly assigned to Recipe 4 Success were more likely to consume snacks and meals that contained fruits, vegetables, protein, and no sweets or junk food.
As the results of this study and others have shown, early food preferences offer the strongest indication of later diet and healthy eating habits throughout life. The program targeted in this study is significant in its ability to accelerate the adoption of better toddler eating habits in just a 10-week period.
Recipe 4 Success along with other successful preventive interventions for young children are most effective when parents drive the change. “In the present trial, the quality of parenting was most highly related to healthy eating habits and self-regulation at baseline,” the researchers noted.
Specifically, the authors attributed the success of the program to “targeting specific interrelated outcomes with an integrated, theoretically driven intervention model,” which allowed Recipe 4 Success to boost the effectiveness of EHS substantially “in just 10 weeks with a minimal increase in funding,” the authors added.
The authors noted several weaknesses as well as strengths of the study. Its primary weakness was a baseline-posttreatment design, which made it impossible to assert that intervention effects can be sustained. The study was also limited to English-speaking families. Given that most home visitors attended to families in both Recipe 4 Success and EHS, the researchers noted the possibility for contamination across conditions, but they added that this would have actually reduced the intervention effects. The study’s primary strength was the evidenced-based nature of the randomized control. That Recipe 4 Success was operated as an intervention only strengthen the benefits of normal EHS visits.
Patient parents who promote self-regulation have the best chance of success
“This small study emphasizes the importance of parent education and support in setting the toddlers’ palate for lifelong eating habits and self-regulation,” observed Silver Spring, MD, private practice pediatrician and associate clinical professor of pediatrics at George Washington University, Washington, Lillian M. Beard, MD, in a separate interview.
“With the goal of promoting eating habits and self-regulation, I try to guide parents’ choices of what they offer to their toddler. I applaud parents’ patience as I encourage them not to give in and quickly resort to offering salty or sweet snacks. I suggest that if during the course of a day, a palette of colorful healthy choices is offered, most toddlers will graze independently as they go about their play. The challenge is to really support the parent through this quirky stage of their child’s development,” she explained.
“The ultimate challenge today with so much food insecurity, COVID-19 related job losses, and shrinking dollars to feed families is that too many families are feeling a food crisis! A program such as Recipe 4 Success can provide invaluable education for families on how to best stretch their few dollars, with knowledge of which items to seek from their community food pantries, how to best utilize items from the State WIC programs and still seek nutrition tips from their pediatricians while avoiding expensive fast foods that only offer immediate satiety and gratification. The Recipe 4 Success educator, pediatrician, or any community educator can give recommendations about which fresh produce may be inexpensive, but nutritional,” Dr. Beard suggested.
Dr. Nix and colleagues as well as Dr. Beard had no conflicts of interest and no relevant financial disclosures.
Home-based preventive interventions not only improve healthy eating habits and self-regulation in toddlers but also guide their parents toward better food presentation and response to picky behaviors, reported Robert L. Nix, PhD, of the University of Wisconsin, Madison, and his associates.
In a small, randomized controlled trial of 73 families with toddlers aged 18-36 months enrolled in home-based Early Head Start (EHS), the researchers evaluated four protective factors, including toddlers’ healthy eating habits, toddlers’ self-regulation, parents’ responsive feeding practices, and parents’ sensitive scaffolding. The study, conducted from April to October 2013, is the first clinical trial of Recipe 4 Success, a preschool-focused intervention created by administrators and home visitors of EHS that promotes healthy eating and self-regulation in toddlers living in poverty who may otherwise face weight challenges and obesity later in life. Integrating the intervention into EHS allowed the researchers to take full advantage of its national infrastructure and to make dissemination more efficient.
Of the families selected to participate, all of whom were living below the Federal poverty threshold, 66 were retained through post treatment. Most participating parents were biological mothers; 61% were single; 29% were not high school graduates; just 11% were employed full time. The toddlers averaged 30.72 months; 44% were female. Roughly 48% of families were non-Hispanic White; 29% were Black; and 23% were Hispanic or Latinx, the investigators reported in Pediatrics. More than three-quarters of participants were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children or the Supplemental Nutrition Assistance Program.
The program allowed parents to transform toddler eating habits quickly
The study, which was designed to evaluate for posttreatment differences in the primary outcomes, involved 10 consecutive weekly lessons implemented by regularly assigned EHS home visitors. Parents were required to adhere to feeding practices carefully targeted with sensitive, structured scaffolding designed to keep toddlers from becoming overwhelmed. Parents were guided to understand, for instance, that toddlers frequently need to be exposed to a new food 10-20 times before eating it, and that poor sleep can have a detrimental influence on emotional and behavioral controls that can progress to weight gain.
Parent recall of what food and drinks their toddlers consumed in the previous 24-hour period was collected by interviewers. The percentage of all meals that included a fruit and/or vegetable, a protein source, and the absence of sweets and junk food were noted. Toddler self-regulation was assessed in accordance with delay of gratification, task orientation, and emotional/behavioral control. Parents were asked to rate toddler ability to cease desired activities to comply with parental requests. Parental responsive feeding practices were also recorded to observe how they introduce unique healthy foods and how they responded to their toddlers’ reactions. Parental sensitive scaffolding was similarly observed for their ability to structure activities in a developmentally appropriate manner promoting self-regulation.
The researchers noted no statistically significant differences between families in the treatment and control groups, nor were there differences in outcome measures or covariates. Study findings showed that, compared with toddlers who continued to receive just EHS support, the toddlers randomly assigned to Recipe 4 Success were more likely to consume snacks and meals that contained fruits, vegetables, protein, and no sweets or junk food.
As the results of this study and others have shown, early food preferences offer the strongest indication of later diet and healthy eating habits throughout life. The program targeted in this study is significant in its ability to accelerate the adoption of better toddler eating habits in just a 10-week period.
Recipe 4 Success along with other successful preventive interventions for young children are most effective when parents drive the change. “In the present trial, the quality of parenting was most highly related to healthy eating habits and self-regulation at baseline,” the researchers noted.
Specifically, the authors attributed the success of the program to “targeting specific interrelated outcomes with an integrated, theoretically driven intervention model,” which allowed Recipe 4 Success to boost the effectiveness of EHS substantially “in just 10 weeks with a minimal increase in funding,” the authors added.
The authors noted several weaknesses as well as strengths of the study. Its primary weakness was a baseline-posttreatment design, which made it impossible to assert that intervention effects can be sustained. The study was also limited to English-speaking families. Given that most home visitors attended to families in both Recipe 4 Success and EHS, the researchers noted the possibility for contamination across conditions, but they added that this would have actually reduced the intervention effects. The study’s primary strength was the evidenced-based nature of the randomized control. That Recipe 4 Success was operated as an intervention only strengthen the benefits of normal EHS visits.
Patient parents who promote self-regulation have the best chance of success
“This small study emphasizes the importance of parent education and support in setting the toddlers’ palate for lifelong eating habits and self-regulation,” observed Silver Spring, MD, private practice pediatrician and associate clinical professor of pediatrics at George Washington University, Washington, Lillian M. Beard, MD, in a separate interview.
“With the goal of promoting eating habits and self-regulation, I try to guide parents’ choices of what they offer to their toddler. I applaud parents’ patience as I encourage them not to give in and quickly resort to offering salty or sweet snacks. I suggest that if during the course of a day, a palette of colorful healthy choices is offered, most toddlers will graze independently as they go about their play. The challenge is to really support the parent through this quirky stage of their child’s development,” she explained.
“The ultimate challenge today with so much food insecurity, COVID-19 related job losses, and shrinking dollars to feed families is that too many families are feeling a food crisis! A program such as Recipe 4 Success can provide invaluable education for families on how to best stretch their few dollars, with knowledge of which items to seek from their community food pantries, how to best utilize items from the State WIC programs and still seek nutrition tips from their pediatricians while avoiding expensive fast foods that only offer immediate satiety and gratification. The Recipe 4 Success educator, pediatrician, or any community educator can give recommendations about which fresh produce may be inexpensive, but nutritional,” Dr. Beard suggested.
Dr. Nix and colleagues as well as Dr. Beard had no conflicts of interest and no relevant financial disclosures.
Home-based preventive interventions not only improve healthy eating habits and self-regulation in toddlers but also guide their parents toward better food presentation and response to picky behaviors, reported Robert L. Nix, PhD, of the University of Wisconsin, Madison, and his associates.
In a small, randomized controlled trial of 73 families with toddlers aged 18-36 months enrolled in home-based Early Head Start (EHS), the researchers evaluated four protective factors, including toddlers’ healthy eating habits, toddlers’ self-regulation, parents’ responsive feeding practices, and parents’ sensitive scaffolding. The study, conducted from April to October 2013, is the first clinical trial of Recipe 4 Success, a preschool-focused intervention created by administrators and home visitors of EHS that promotes healthy eating and self-regulation in toddlers living in poverty who may otherwise face weight challenges and obesity later in life. Integrating the intervention into EHS allowed the researchers to take full advantage of its national infrastructure and to make dissemination more efficient.
Of the families selected to participate, all of whom were living below the Federal poverty threshold, 66 were retained through post treatment. Most participating parents were biological mothers; 61% were single; 29% were not high school graduates; just 11% were employed full time. The toddlers averaged 30.72 months; 44% were female. Roughly 48% of families were non-Hispanic White; 29% were Black; and 23% were Hispanic or Latinx, the investigators reported in Pediatrics. More than three-quarters of participants were enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children or the Supplemental Nutrition Assistance Program.
The program allowed parents to transform toddler eating habits quickly
The study, which was designed to evaluate for posttreatment differences in the primary outcomes, involved 10 consecutive weekly lessons implemented by regularly assigned EHS home visitors. Parents were required to adhere to feeding practices carefully targeted with sensitive, structured scaffolding designed to keep toddlers from becoming overwhelmed. Parents were guided to understand, for instance, that toddlers frequently need to be exposed to a new food 10-20 times before eating it, and that poor sleep can have a detrimental influence on emotional and behavioral controls that can progress to weight gain.
Parent recall of what food and drinks their toddlers consumed in the previous 24-hour period was collected by interviewers. The percentage of all meals that included a fruit and/or vegetable, a protein source, and the absence of sweets and junk food were noted. Toddler self-regulation was assessed in accordance with delay of gratification, task orientation, and emotional/behavioral control. Parents were asked to rate toddler ability to cease desired activities to comply with parental requests. Parental responsive feeding practices were also recorded to observe how they introduce unique healthy foods and how they responded to their toddlers’ reactions. Parental sensitive scaffolding was similarly observed for their ability to structure activities in a developmentally appropriate manner promoting self-regulation.
The researchers noted no statistically significant differences between families in the treatment and control groups, nor were there differences in outcome measures or covariates. Study findings showed that, compared with toddlers who continued to receive just EHS support, the toddlers randomly assigned to Recipe 4 Success were more likely to consume snacks and meals that contained fruits, vegetables, protein, and no sweets or junk food.
As the results of this study and others have shown, early food preferences offer the strongest indication of later diet and healthy eating habits throughout life. The program targeted in this study is significant in its ability to accelerate the adoption of better toddler eating habits in just a 10-week period.
Recipe 4 Success along with other successful preventive interventions for young children are most effective when parents drive the change. “In the present trial, the quality of parenting was most highly related to healthy eating habits and self-regulation at baseline,” the researchers noted.
Specifically, the authors attributed the success of the program to “targeting specific interrelated outcomes with an integrated, theoretically driven intervention model,” which allowed Recipe 4 Success to boost the effectiveness of EHS substantially “in just 10 weeks with a minimal increase in funding,” the authors added.
The authors noted several weaknesses as well as strengths of the study. Its primary weakness was a baseline-posttreatment design, which made it impossible to assert that intervention effects can be sustained. The study was also limited to English-speaking families. Given that most home visitors attended to families in both Recipe 4 Success and EHS, the researchers noted the possibility for contamination across conditions, but they added that this would have actually reduced the intervention effects. The study’s primary strength was the evidenced-based nature of the randomized control. That Recipe 4 Success was operated as an intervention only strengthen the benefits of normal EHS visits.
Patient parents who promote self-regulation have the best chance of success
“This small study emphasizes the importance of parent education and support in setting the toddlers’ palate for lifelong eating habits and self-regulation,” observed Silver Spring, MD, private practice pediatrician and associate clinical professor of pediatrics at George Washington University, Washington, Lillian M. Beard, MD, in a separate interview.
“With the goal of promoting eating habits and self-regulation, I try to guide parents’ choices of what they offer to their toddler. I applaud parents’ patience as I encourage them not to give in and quickly resort to offering salty or sweet snacks. I suggest that if during the course of a day, a palette of colorful healthy choices is offered, most toddlers will graze independently as they go about their play. The challenge is to really support the parent through this quirky stage of their child’s development,” she explained.
“The ultimate challenge today with so much food insecurity, COVID-19 related job losses, and shrinking dollars to feed families is that too many families are feeling a food crisis! A program such as Recipe 4 Success can provide invaluable education for families on how to best stretch their few dollars, with knowledge of which items to seek from their community food pantries, how to best utilize items from the State WIC programs and still seek nutrition tips from their pediatricians while avoiding expensive fast foods that only offer immediate satiety and gratification. The Recipe 4 Success educator, pediatrician, or any community educator can give recommendations about which fresh produce may be inexpensive, but nutritional,” Dr. Beard suggested.
Dr. Nix and colleagues as well as Dr. Beard had no conflicts of interest and no relevant financial disclosures.
FROM PEDIATRICS
Further warning on SGLT2 inhibitor use and DKA risk in COVID-19
a new case series suggests.
Five patients with type 2 diabetes who were taking SGLT2 inhibitors presented in DKA despite having glucose levels below 300 mg/dL. The report was published online last month in AACE Clinical Case Reports by Rebecca J. Vitale, MD, and colleagues at Brigham and Women’s Hospital, Boston.
“A cluster of euglycemic DKA cases at our hospital during the first wave of the pandemic suggests that patients with diabetes taking SGLT2 inhibitors may be at enhanced risk for euDKA when they contract COVID-19,” senior author Naomi D.L. Fisher, MD, said in an interview.
Dr. Fisher, an endocrinologist, added: “This complication is preventable with the simple measure of holding the drug. We are hopeful that widespread patient and physician education will prevent future cases of euDKA as COVID-19 infections continue to surge.”
These cases underscore recommendations published early in the COVID-19 pandemic by an international panel, she noted.
“Patients who are acutely ill with nausea, vomiting, abdominal pain, or diarrhea, or who are experiencing loss of appetite with reduced food and fluid intake, should be advised to hold their SGLT2 inhibitor. This medication should not be resumed until patients are feeling better and eating and drinking normally.”
On the other hand, “If patients with asymptomatic or mild COVID-19 infection are otherwise well, and are eating and drinking normally, there is no evidence that SGLT2 inhibitors need to be stopped. These patients should monitor [themselves] closely for worsening symptoms, especially resulting in poor hydration and nutrition, which would be reason to discontinue their medication.”
Pay special attention to the elderly, those with complications
However, special consideration should be given to elderly patients and those with medical conditions known to increase the likelihood of severe infection, like heart failure and chronic obstructive pulmonary disease, Dr. Fisher added.
The SGLT2 inhibitor class of drugs causes significant urinary glucose excretion, and they are also diuretics. A decrease in available glucose and volume depletion are probably both important contributors to euDKA, she explained.
With COVID-19 infection the euDKA risk is compounded by several mechanisms. Most cases of euDKA are associated with an underlying state of starvation that can be triggered by vomiting, diarrhea, loss of appetite, and poor oral intake.
In addition – although not yet known for certain – SARS-CoV-2 may also be toxic to pancreatic beta cells and thus reduce insulin secretion. The maladaptive inflammatory response seen with COVID-19 may also contribute, she said.
The patients in the current case series were three men and two women seen between March and May 2020. They ranged in age from 52 to 79 years.
None had a prior history of DKA or any known diabetes complications. In all of them, antihyperglycemic medications, including SGLT2 inhibitors, were stopped on hospital admission. The patients were initially treated with intravenous insulin, and then subcutaneous insulin after the DKA diagnosis.
Three of the patients were discharged to rehabilitation facilities on hospital days 28-47 and one (age 53 years) was discharged home on day 11. The other patient also had hypertension and nonalcoholic steatohepatitis.
A version of this article first appeared on Medscape.com.
a new case series suggests.
Five patients with type 2 diabetes who were taking SGLT2 inhibitors presented in DKA despite having glucose levels below 300 mg/dL. The report was published online last month in AACE Clinical Case Reports by Rebecca J. Vitale, MD, and colleagues at Brigham and Women’s Hospital, Boston.
“A cluster of euglycemic DKA cases at our hospital during the first wave of the pandemic suggests that patients with diabetes taking SGLT2 inhibitors may be at enhanced risk for euDKA when they contract COVID-19,” senior author Naomi D.L. Fisher, MD, said in an interview.
Dr. Fisher, an endocrinologist, added: “This complication is preventable with the simple measure of holding the drug. We are hopeful that widespread patient and physician education will prevent future cases of euDKA as COVID-19 infections continue to surge.”
These cases underscore recommendations published early in the COVID-19 pandemic by an international panel, she noted.
“Patients who are acutely ill with nausea, vomiting, abdominal pain, or diarrhea, or who are experiencing loss of appetite with reduced food and fluid intake, should be advised to hold their SGLT2 inhibitor. This medication should not be resumed until patients are feeling better and eating and drinking normally.”
On the other hand, “If patients with asymptomatic or mild COVID-19 infection are otherwise well, and are eating and drinking normally, there is no evidence that SGLT2 inhibitors need to be stopped. These patients should monitor [themselves] closely for worsening symptoms, especially resulting in poor hydration and nutrition, which would be reason to discontinue their medication.”
Pay special attention to the elderly, those with complications
However, special consideration should be given to elderly patients and those with medical conditions known to increase the likelihood of severe infection, like heart failure and chronic obstructive pulmonary disease, Dr. Fisher added.
The SGLT2 inhibitor class of drugs causes significant urinary glucose excretion, and they are also diuretics. A decrease in available glucose and volume depletion are probably both important contributors to euDKA, she explained.
With COVID-19 infection the euDKA risk is compounded by several mechanisms. Most cases of euDKA are associated with an underlying state of starvation that can be triggered by vomiting, diarrhea, loss of appetite, and poor oral intake.
In addition – although not yet known for certain – SARS-CoV-2 may also be toxic to pancreatic beta cells and thus reduce insulin secretion. The maladaptive inflammatory response seen with COVID-19 may also contribute, she said.
The patients in the current case series were three men and two women seen between March and May 2020. They ranged in age from 52 to 79 years.
None had a prior history of DKA or any known diabetes complications. In all of them, antihyperglycemic medications, including SGLT2 inhibitors, were stopped on hospital admission. The patients were initially treated with intravenous insulin, and then subcutaneous insulin after the DKA diagnosis.
Three of the patients were discharged to rehabilitation facilities on hospital days 28-47 and one (age 53 years) was discharged home on day 11. The other patient also had hypertension and nonalcoholic steatohepatitis.
A version of this article first appeared on Medscape.com.
a new case series suggests.
Five patients with type 2 diabetes who were taking SGLT2 inhibitors presented in DKA despite having glucose levels below 300 mg/dL. The report was published online last month in AACE Clinical Case Reports by Rebecca J. Vitale, MD, and colleagues at Brigham and Women’s Hospital, Boston.
“A cluster of euglycemic DKA cases at our hospital during the first wave of the pandemic suggests that patients with diabetes taking SGLT2 inhibitors may be at enhanced risk for euDKA when they contract COVID-19,” senior author Naomi D.L. Fisher, MD, said in an interview.
Dr. Fisher, an endocrinologist, added: “This complication is preventable with the simple measure of holding the drug. We are hopeful that widespread patient and physician education will prevent future cases of euDKA as COVID-19 infections continue to surge.”
These cases underscore recommendations published early in the COVID-19 pandemic by an international panel, she noted.
“Patients who are acutely ill with nausea, vomiting, abdominal pain, or diarrhea, or who are experiencing loss of appetite with reduced food and fluid intake, should be advised to hold their SGLT2 inhibitor. This medication should not be resumed until patients are feeling better and eating and drinking normally.”
On the other hand, “If patients with asymptomatic or mild COVID-19 infection are otherwise well, and are eating and drinking normally, there is no evidence that SGLT2 inhibitors need to be stopped. These patients should monitor [themselves] closely for worsening symptoms, especially resulting in poor hydration and nutrition, which would be reason to discontinue their medication.”
Pay special attention to the elderly, those with complications
However, special consideration should be given to elderly patients and those with medical conditions known to increase the likelihood of severe infection, like heart failure and chronic obstructive pulmonary disease, Dr. Fisher added.
The SGLT2 inhibitor class of drugs causes significant urinary glucose excretion, and they are also diuretics. A decrease in available glucose and volume depletion are probably both important contributors to euDKA, she explained.
With COVID-19 infection the euDKA risk is compounded by several mechanisms. Most cases of euDKA are associated with an underlying state of starvation that can be triggered by vomiting, diarrhea, loss of appetite, and poor oral intake.
In addition – although not yet known for certain – SARS-CoV-2 may also be toxic to pancreatic beta cells and thus reduce insulin secretion. The maladaptive inflammatory response seen with COVID-19 may also contribute, she said.
The patients in the current case series were three men and two women seen between March and May 2020. They ranged in age from 52 to 79 years.
None had a prior history of DKA or any known diabetes complications. In all of them, antihyperglycemic medications, including SGLT2 inhibitors, were stopped on hospital admission. The patients were initially treated with intravenous insulin, and then subcutaneous insulin after the DKA diagnosis.
Three of the patients were discharged to rehabilitation facilities on hospital days 28-47 and one (age 53 years) was discharged home on day 11. The other patient also had hypertension and nonalcoholic steatohepatitis.
A version of this article first appeared on Medscape.com.









