User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Add magnesium to treatment of AF with rapid ventricular response
Background: Most large studies of magnesium sulfate for assistance with rate control in AF occurred in the postoperative setting. This study compared rate control in the ED using magnesium sulfate at high (9 g) and low (4.5 g) doses vs. placebo in combination with usual treatment with atrioventricular nodal-blocking agents.
Study design: Double-blind, prospective, randomized, controlled trial.
Setting: Three tertiary Tunisian EDs.
Synopsis: This trial in Tunisian EDs enrolled 450 patients who presented with AF with rapid ventricular response and were divided into three groups: placebo, low-dose magnesium, and high-dose magnesium. Each patient’s trial medication was given as a 100-cc infusion. Patients were then treated with AV nodal-blocking agents at the discretion of the ED physician. The primary outcome was 20% reduction in rate or heart rate of less than 90 beats per minute. Notable exclusion criteria included hypotension, altered consciousness, decompensated heart failure, MI, and renal failure.
Rate control was achieved at 4 hours in 64% of patients with low-dose magnesium, 59% with high-dose magnesium, and 43% with placebo. At 24 hours, reduction in rate was controlled for 97% of patients on the low dose, 94% on the high dose, and 83% on placebo. Adverse events were mostly flushing, which occurred more frequently with the high dose than the low dose. Major limitations of the study included a lack of statistical assessment regarding baseline similarity between the two groups and that generalizability was limited by a preference for digoxin as the AV nodal agent.
Bottom line: This trial demonstrated that 4.5 g of magnesium sulfate was a useful addition to AV nodal blockers in achieving faster rate control for atrial fibrillation with rapid ventricular response in selected ED patients.
Citation: Bouida W et al. Low-dose magnesium sulfate versus high dose in the early management of rapid atrial fibrillation: Randomized controlled double blind study. Acad Emerg Med. 2018 Jul 19. doi: 10.1111/acem.13522.
Dr. Scott is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: Most large studies of magnesium sulfate for assistance with rate control in AF occurred in the postoperative setting. This study compared rate control in the ED using magnesium sulfate at high (9 g) and low (4.5 g) doses vs. placebo in combination with usual treatment with atrioventricular nodal-blocking agents.
Study design: Double-blind, prospective, randomized, controlled trial.
Setting: Three tertiary Tunisian EDs.
Synopsis: This trial in Tunisian EDs enrolled 450 patients who presented with AF with rapid ventricular response and were divided into three groups: placebo, low-dose magnesium, and high-dose magnesium. Each patient’s trial medication was given as a 100-cc infusion. Patients were then treated with AV nodal-blocking agents at the discretion of the ED physician. The primary outcome was 20% reduction in rate or heart rate of less than 90 beats per minute. Notable exclusion criteria included hypotension, altered consciousness, decompensated heart failure, MI, and renal failure.
Rate control was achieved at 4 hours in 64% of patients with low-dose magnesium, 59% with high-dose magnesium, and 43% with placebo. At 24 hours, reduction in rate was controlled for 97% of patients on the low dose, 94% on the high dose, and 83% on placebo. Adverse events were mostly flushing, which occurred more frequently with the high dose than the low dose. Major limitations of the study included a lack of statistical assessment regarding baseline similarity between the two groups and that generalizability was limited by a preference for digoxin as the AV nodal agent.
Bottom line: This trial demonstrated that 4.5 g of magnesium sulfate was a useful addition to AV nodal blockers in achieving faster rate control for atrial fibrillation with rapid ventricular response in selected ED patients.
Citation: Bouida W et al. Low-dose magnesium sulfate versus high dose in the early management of rapid atrial fibrillation: Randomized controlled double blind study. Acad Emerg Med. 2018 Jul 19. doi: 10.1111/acem.13522.
Dr. Scott is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: Most large studies of magnesium sulfate for assistance with rate control in AF occurred in the postoperative setting. This study compared rate control in the ED using magnesium sulfate at high (9 g) and low (4.5 g) doses vs. placebo in combination with usual treatment with atrioventricular nodal-blocking agents.
Study design: Double-blind, prospective, randomized, controlled trial.
Setting: Three tertiary Tunisian EDs.
Synopsis: This trial in Tunisian EDs enrolled 450 patients who presented with AF with rapid ventricular response and were divided into three groups: placebo, low-dose magnesium, and high-dose magnesium. Each patient’s trial medication was given as a 100-cc infusion. Patients were then treated with AV nodal-blocking agents at the discretion of the ED physician. The primary outcome was 20% reduction in rate or heart rate of less than 90 beats per minute. Notable exclusion criteria included hypotension, altered consciousness, decompensated heart failure, MI, and renal failure.
Rate control was achieved at 4 hours in 64% of patients with low-dose magnesium, 59% with high-dose magnesium, and 43% with placebo. At 24 hours, reduction in rate was controlled for 97% of patients on the low dose, 94% on the high dose, and 83% on placebo. Adverse events were mostly flushing, which occurred more frequently with the high dose than the low dose. Major limitations of the study included a lack of statistical assessment regarding baseline similarity between the two groups and that generalizability was limited by a preference for digoxin as the AV nodal agent.
Bottom line: This trial demonstrated that 4.5 g of magnesium sulfate was a useful addition to AV nodal blockers in achieving faster rate control for atrial fibrillation with rapid ventricular response in selected ED patients.
Citation: Bouida W et al. Low-dose magnesium sulfate versus high dose in the early management of rapid atrial fibrillation: Randomized controlled double blind study. Acad Emerg Med. 2018 Jul 19. doi: 10.1111/acem.13522.
Dr. Scott is an assistant professor in the division of hospital medicine, University of New Mexico.
New recommendations on TB screening for health care workers
U.S. health care personnel no longer need to undergo routine tuberculosis testing in the absence of known exposure, according to new screening guidelines from the National Tuberculosis Controllers Association and CDC.
The revised guidelines on tuberculosis screening, testing, and treatment of U.S. health care personnel, published in Morbidity and Mortality Weekly Report, are the first update since 2005. The new recommendations reflect a reduction in concern about U.S. health care personnel’s risk of occupational exposure to latent and active tuberculosis infection.
Lynn E. Sosa, MD, from the Connecticut Department of Public Health and National Tuberculosis Controllers Association, and coauthors wrote that rates of tuberculosis infection in the United States have declined by 73% since 1991, from 10.4/100,000 population in 1991 to 2.8/100,000 in 2017. This has been matched by similar declines among health care workers, which the authors said raised questions about the cost-effectiveness of the previously recommended routine serial occupational testing.
“In addition, a recent retrospective cohort study of approximately 40,000 health care personnel at a tertiary U.S. medical center in a low TB-incidence state found an extremely low rate of TST conversion (0.3%) during 1998-2014, with a limited proportion attributable to occupational exposure,” they wrote.
The new guidelines recommend health care personnel undergo baseline or preplacement tuberculosis testing with an interferon-gamma release assay (IGRA) or a tuberculin skin test (TST), as well as individual risk assessment and symptom evaluation.
The individual risk assessment considers whether the person has lived in a country with a high tuberculosis rate, whether they are immunosuppressed, or whether they have had close contact with someone with infectious tuberculosis.
This risk assessment can help decide how to interpret an initial positive test result, the authors said.
“For example, health care personnel with a positive test who are asymptomatic, unlikely to be infected with M. [Mycobacterium] tuberculosis, and at low risk for progression on the basis of their risk assessment should have a second test (either an IGRA or a TST) as recommended in the 2017 TB diagnostic guidelines of the American Thoracic Society, Infectious Diseases Society of America, and CDC,” they wrote. “In this example, the health care personnel should be considered infected with M. tuberculosis only if both the first and second tests are positive.”
After that baseline testing, personnel do not need to undergo routine serial testing except in the case of known exposure or ongoing transmission. The guideline authors suggested serial screening might be considered for health care workers whose work puts them at greater risk – for example, pulmonologists or respiratory therapists – or for those working in settings in which transmission has happened in the past.
For personnel with latent tuberculosis infection, the guidelines recommend “encouragement of treatment” unless it is contraindicated, and annual symptom screening in those not undergoing treatment.
The guideline committee also advocated for annual tuberculosis education for all health care workers.
The new recommendations were based on a systematic review of 36 studies of tuberculosis screening and testing among health care personnel, 16 of which were performed in the United States, and all but two of which were conducted in a hospital setting.
The authors stressed that recommendations from the 2005 CDC guidelines – which do not pertain to health care personnel screening, testing, treatment and education – remain unchanged.
One author declared personal fees from the National Tuberculosis Controllers Association during the conduct of the study. Two others reported unrelated grants and personal fees from private industry. No other conflicts of interest were disclosed.
SOURCE: Sosa L et al. MMWR. 2019;68:439-43.
U.S. health care personnel no longer need to undergo routine tuberculosis testing in the absence of known exposure, according to new screening guidelines from the National Tuberculosis Controllers Association and CDC.
The revised guidelines on tuberculosis screening, testing, and treatment of U.S. health care personnel, published in Morbidity and Mortality Weekly Report, are the first update since 2005. The new recommendations reflect a reduction in concern about U.S. health care personnel’s risk of occupational exposure to latent and active tuberculosis infection.
Lynn E. Sosa, MD, from the Connecticut Department of Public Health and National Tuberculosis Controllers Association, and coauthors wrote that rates of tuberculosis infection in the United States have declined by 73% since 1991, from 10.4/100,000 population in 1991 to 2.8/100,000 in 2017. This has been matched by similar declines among health care workers, which the authors said raised questions about the cost-effectiveness of the previously recommended routine serial occupational testing.
“In addition, a recent retrospective cohort study of approximately 40,000 health care personnel at a tertiary U.S. medical center in a low TB-incidence state found an extremely low rate of TST conversion (0.3%) during 1998-2014, with a limited proportion attributable to occupational exposure,” they wrote.
The new guidelines recommend health care personnel undergo baseline or preplacement tuberculosis testing with an interferon-gamma release assay (IGRA) or a tuberculin skin test (TST), as well as individual risk assessment and symptom evaluation.
The individual risk assessment considers whether the person has lived in a country with a high tuberculosis rate, whether they are immunosuppressed, or whether they have had close contact with someone with infectious tuberculosis.
This risk assessment can help decide how to interpret an initial positive test result, the authors said.
“For example, health care personnel with a positive test who are asymptomatic, unlikely to be infected with M. [Mycobacterium] tuberculosis, and at low risk for progression on the basis of their risk assessment should have a second test (either an IGRA or a TST) as recommended in the 2017 TB diagnostic guidelines of the American Thoracic Society, Infectious Diseases Society of America, and CDC,” they wrote. “In this example, the health care personnel should be considered infected with M. tuberculosis only if both the first and second tests are positive.”
After that baseline testing, personnel do not need to undergo routine serial testing except in the case of known exposure or ongoing transmission. The guideline authors suggested serial screening might be considered for health care workers whose work puts them at greater risk – for example, pulmonologists or respiratory therapists – or for those working in settings in which transmission has happened in the past.
For personnel with latent tuberculosis infection, the guidelines recommend “encouragement of treatment” unless it is contraindicated, and annual symptom screening in those not undergoing treatment.
The guideline committee also advocated for annual tuberculosis education for all health care workers.
The new recommendations were based on a systematic review of 36 studies of tuberculosis screening and testing among health care personnel, 16 of which were performed in the United States, and all but two of which were conducted in a hospital setting.
The authors stressed that recommendations from the 2005 CDC guidelines – which do not pertain to health care personnel screening, testing, treatment and education – remain unchanged.
One author declared personal fees from the National Tuberculosis Controllers Association during the conduct of the study. Two others reported unrelated grants and personal fees from private industry. No other conflicts of interest were disclosed.
SOURCE: Sosa L et al. MMWR. 2019;68:439-43.
U.S. health care personnel no longer need to undergo routine tuberculosis testing in the absence of known exposure, according to new screening guidelines from the National Tuberculosis Controllers Association and CDC.
The revised guidelines on tuberculosis screening, testing, and treatment of U.S. health care personnel, published in Morbidity and Mortality Weekly Report, are the first update since 2005. The new recommendations reflect a reduction in concern about U.S. health care personnel’s risk of occupational exposure to latent and active tuberculosis infection.
Lynn E. Sosa, MD, from the Connecticut Department of Public Health and National Tuberculosis Controllers Association, and coauthors wrote that rates of tuberculosis infection in the United States have declined by 73% since 1991, from 10.4/100,000 population in 1991 to 2.8/100,000 in 2017. This has been matched by similar declines among health care workers, which the authors said raised questions about the cost-effectiveness of the previously recommended routine serial occupational testing.
“In addition, a recent retrospective cohort study of approximately 40,000 health care personnel at a tertiary U.S. medical center in a low TB-incidence state found an extremely low rate of TST conversion (0.3%) during 1998-2014, with a limited proportion attributable to occupational exposure,” they wrote.
The new guidelines recommend health care personnel undergo baseline or preplacement tuberculosis testing with an interferon-gamma release assay (IGRA) or a tuberculin skin test (TST), as well as individual risk assessment and symptom evaluation.
The individual risk assessment considers whether the person has lived in a country with a high tuberculosis rate, whether they are immunosuppressed, or whether they have had close contact with someone with infectious tuberculosis.
This risk assessment can help decide how to interpret an initial positive test result, the authors said.
“For example, health care personnel with a positive test who are asymptomatic, unlikely to be infected with M. [Mycobacterium] tuberculosis, and at low risk for progression on the basis of their risk assessment should have a second test (either an IGRA or a TST) as recommended in the 2017 TB diagnostic guidelines of the American Thoracic Society, Infectious Diseases Society of America, and CDC,” they wrote. “In this example, the health care personnel should be considered infected with M. tuberculosis only if both the first and second tests are positive.”
After that baseline testing, personnel do not need to undergo routine serial testing except in the case of known exposure or ongoing transmission. The guideline authors suggested serial screening might be considered for health care workers whose work puts them at greater risk – for example, pulmonologists or respiratory therapists – or for those working in settings in which transmission has happened in the past.
For personnel with latent tuberculosis infection, the guidelines recommend “encouragement of treatment” unless it is contraindicated, and annual symptom screening in those not undergoing treatment.
The guideline committee also advocated for annual tuberculosis education for all health care workers.
The new recommendations were based on a systematic review of 36 studies of tuberculosis screening and testing among health care personnel, 16 of which were performed in the United States, and all but two of which were conducted in a hospital setting.
The authors stressed that recommendations from the 2005 CDC guidelines – which do not pertain to health care personnel screening, testing, treatment and education – remain unchanged.
One author declared personal fees from the National Tuberculosis Controllers Association during the conduct of the study. Two others reported unrelated grants and personal fees from private industry. No other conflicts of interest were disclosed.
SOURCE: Sosa L et al. MMWR. 2019;68:439-43.
FROM MMWR
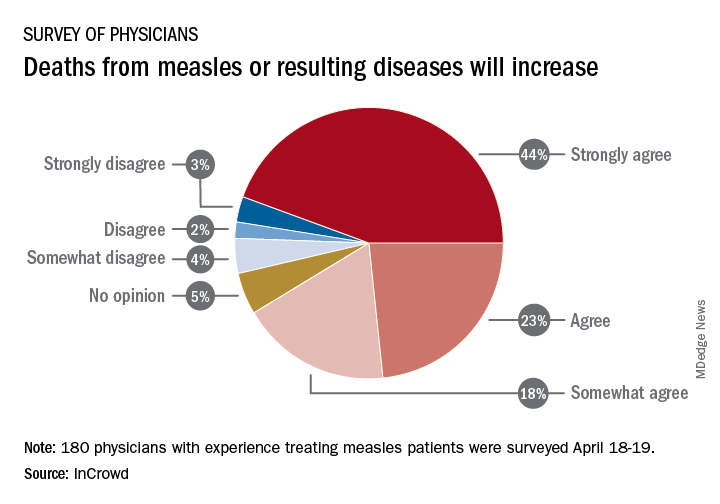
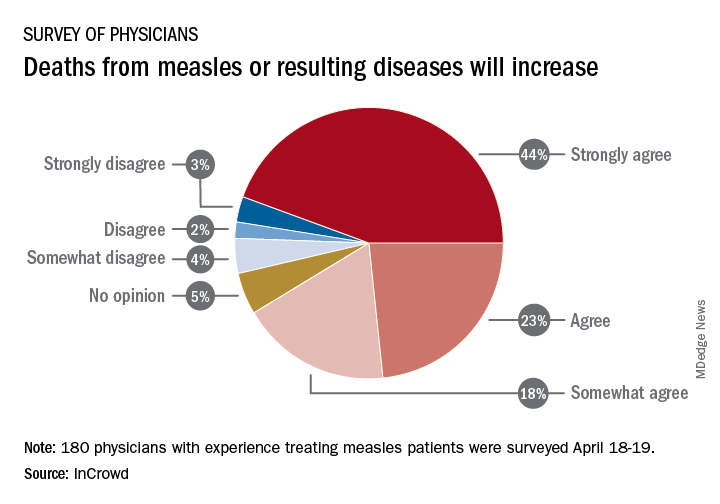
Survey: Physicians predict increase in measles deaths
by real-time market insights technology firm InCrowd.
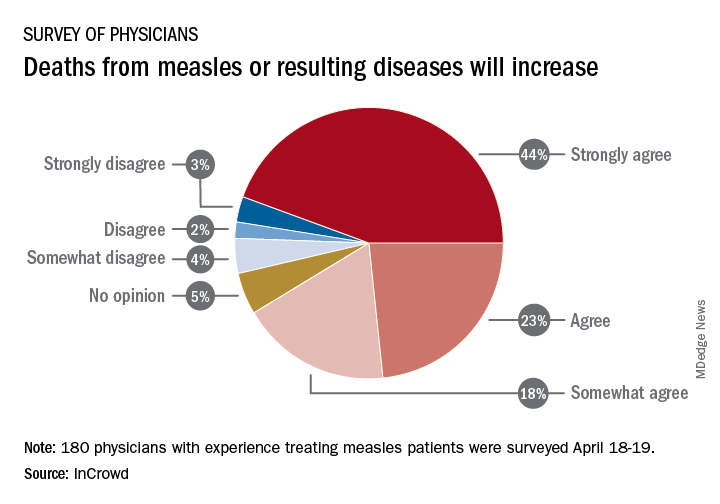
Among the 180 physicians with experience treating measles, 23% agreed and 44% said that they strongly agreed with the statement that measles deaths would increase, and another 18% said that they somewhat agreed. Only 9% expressed some level of disagreement, InCrowd said.
Most of those respondents also believe that summer travel will increase measles outbreaks (29% agreed and 30% strongly agreed) and that more communities will adopt requirements for measles vaccinations (26% and 36%). A majority also said that education about vaccinations will improve (26% agreed and 29% strongly agreed), but almost half of the physicians surveyed also expect vaccination misinformation to get worse (29% and 19%), InCrowd reported.
“With 44% of respondents predicting a high likelihood that deaths caused by measles will increase, the data show the imperative for physicians and patients to keep up the dialogue. … We have a long way to go before declaring victory,” said Diane Hayes, PhD, president and cofounder of InCrowd.
The InCrowd 5-minute microsurvey was conducted on April 18-19, 2019, and included 455 primary care physicians, of whom 40% said that they have treated or knew of colleagues in their facility or community who have treated patients with measles. Of those 180 respondents, 89 were pediatricians and 91 were in other primary care specialties.
by real-time market insights technology firm InCrowd.
Among the 180 physicians with experience treating measles, 23% agreed and 44% said that they strongly agreed with the statement that measles deaths would increase, and another 18% said that they somewhat agreed. Only 9% expressed some level of disagreement, InCrowd said.
Most of those respondents also believe that summer travel will increase measles outbreaks (29% agreed and 30% strongly agreed) and that more communities will adopt requirements for measles vaccinations (26% and 36%). A majority also said that education about vaccinations will improve (26% agreed and 29% strongly agreed), but almost half of the physicians surveyed also expect vaccination misinformation to get worse (29% and 19%), InCrowd reported.
“With 44% of respondents predicting a high likelihood that deaths caused by measles will increase, the data show the imperative for physicians and patients to keep up the dialogue. … We have a long way to go before declaring victory,” said Diane Hayes, PhD, president and cofounder of InCrowd.
The InCrowd 5-minute microsurvey was conducted on April 18-19, 2019, and included 455 primary care physicians, of whom 40% said that they have treated or knew of colleagues in their facility or community who have treated patients with measles. Of those 180 respondents, 89 were pediatricians and 91 were in other primary care specialties.
by real-time market insights technology firm InCrowd.
Among the 180 physicians with experience treating measles, 23% agreed and 44% said that they strongly agreed with the statement that measles deaths would increase, and another 18% said that they somewhat agreed. Only 9% expressed some level of disagreement, InCrowd said.
Most of those respondents also believe that summer travel will increase measles outbreaks (29% agreed and 30% strongly agreed) and that more communities will adopt requirements for measles vaccinations (26% and 36%). A majority also said that education about vaccinations will improve (26% agreed and 29% strongly agreed), but almost half of the physicians surveyed also expect vaccination misinformation to get worse (29% and 19%), InCrowd reported.
“With 44% of respondents predicting a high likelihood that deaths caused by measles will increase, the data show the imperative for physicians and patients to keep up the dialogue. … We have a long way to go before declaring victory,” said Diane Hayes, PhD, president and cofounder of InCrowd.
The InCrowd 5-minute microsurvey was conducted on April 18-19, 2019, and included 455 primary care physicians, of whom 40% said that they have treated or knew of colleagues in their facility or community who have treated patients with measles. Of those 180 respondents, 89 were pediatricians and 91 were in other primary care specialties.
Measles complications in the U.S. unchanged in posteradication era
CHICAGO – An evaluation of the measles threat in the modern era gives no indication that the risk of complications or death is any different than it was before a vaccine became available, according to an analysis of inpatient complications between 2002 and 2013.
In 2000, measles was declared eliminated in the United States, but for those who have been infected since that time, the risk of serious complications and death has not diminished, noted Raj Chovatiya, MD, PhD, in a session at the annual meeting of the Society for Investigative Dermatology.
By eliminated, the Centers of Disease Control and Prevention – which reported 86 confirmed cases of measles in 2000 – was referring to a technical definition of no new endemic or continuous transmissions in the previous 12 months. It was expected that a modest number of cases of this reportable disease would continue to accrue for an infection that remains common elsewhere in the world.
“Worldwide there are about 20 million cases of measles annually with an estimated 100,000 deaths attributed to this cause,” said Dr. Chovatiya, who is a dermatology resident at Northwestern University, Chicago.
In the United States, posteradication infection rates remained at low levels for several years but were already rising from 2002 to 2013, when Dr. Chovatiya and his coinvestigators sought to describe the incidence, associations, comorbidities, and outcomes of hospitalizations for measles. Toward the end of the period the researchers were examining the incidence rates climbed more steeply.
“So far this year, 764 CDC cases of measles [were] reported. That is the most we have seen in the U.S. since 1994,” Dr. Chovatiya said.
Based on his analysis of hospitalizations from 2002 to 2013, the threat of these outbreaks is no different then that before the disease was declared eliminated or before a vaccine became available.
The cross-sectional study was conducted with data from the Nationwide Inpatient Sample, an all-payer database that is considered to be a representative of national trends.
Characteristic of measles, the majority of the 582 hospitalizations evaluated over this period occurred in children aged between 1 and 9 years. The proportion of patients with preexisting chronic comorbid conditions was low. Rather, “most were pretty healthy” prior to admission, according to Dr. Chovatiya, who said that the majority of admissions were from an emergency department.
Measles, which targets epithelial cells and depresses the immune system, is a potentially serious disease because of its ability to produce complications in essentially every organ of the body, including the lungs, kidneys, blood, and central nervous system. Consistent with past studies, the most common complication in this series was pneumonia, observed in 20% of patients. The list of other serious complications identified in this study period, including encephalitis and acute renal failure, was long.
“We observed death in 4.3% of our 582 cases, or about 25 cases,” reported Dr. Chovatiya. He indicated that this is a high percentage among a population composed largely of children who were well before hospitalization.
The mortality rate from measles was numerically but not statistically higher than that of overall hospital admissions during this period, but an admission for measles was associated with significantly longer average length of stay (3.7 vs. 3.5 days) and slightly but significantly higher direct costs ($18,907 vs. $18,474).
“I want to point out that these are just direct inpatient costs,” Dr. Chovatiya said. Extrapolating from published data about indirect expenses, he said that the total health cost burden “is absolutely staggering.”
Previous studies have suggested that about 25% of patients with measles require hospitalization and 1 in every 1,000 patients will die. The data collected by Dr. Chovatiya support these often-cited figures, indicating that they remain unchanged in the modern era.
particularly insufficient penetration of vaccination in many communities.
The vaccine “is inexpensive, extremely effective, and lifesaving,” said Dr. Chovatiya, making the point that all of the morbidity, mortality, and costs he described are largely avoidable.
Attempting to provide perspective of the measles threat and the impact of the vaccine, Dr. Chovatiya cited a hypothetical calculation that 732,000 deaths from measles would have been expected in the United States among the pool of children born between 1994 and 2013 had no vaccine been offered. Again, most of these deaths would have occurred in otherwise healthy children.
Dr. Chovatiya reported no potential conflicts of interest.
CHICAGO – An evaluation of the measles threat in the modern era gives no indication that the risk of complications or death is any different than it was before a vaccine became available, according to an analysis of inpatient complications between 2002 and 2013.
In 2000, measles was declared eliminated in the United States, but for those who have been infected since that time, the risk of serious complications and death has not diminished, noted Raj Chovatiya, MD, PhD, in a session at the annual meeting of the Society for Investigative Dermatology.
By eliminated, the Centers of Disease Control and Prevention – which reported 86 confirmed cases of measles in 2000 – was referring to a technical definition of no new endemic or continuous transmissions in the previous 12 months. It was expected that a modest number of cases of this reportable disease would continue to accrue for an infection that remains common elsewhere in the world.
“Worldwide there are about 20 million cases of measles annually with an estimated 100,000 deaths attributed to this cause,” said Dr. Chovatiya, who is a dermatology resident at Northwestern University, Chicago.
In the United States, posteradication infection rates remained at low levels for several years but were already rising from 2002 to 2013, when Dr. Chovatiya and his coinvestigators sought to describe the incidence, associations, comorbidities, and outcomes of hospitalizations for measles. Toward the end of the period the researchers were examining the incidence rates climbed more steeply.
“So far this year, 764 CDC cases of measles [were] reported. That is the most we have seen in the U.S. since 1994,” Dr. Chovatiya said.
Based on his analysis of hospitalizations from 2002 to 2013, the threat of these outbreaks is no different then that before the disease was declared eliminated or before a vaccine became available.
The cross-sectional study was conducted with data from the Nationwide Inpatient Sample, an all-payer database that is considered to be a representative of national trends.
Characteristic of measles, the majority of the 582 hospitalizations evaluated over this period occurred in children aged between 1 and 9 years. The proportion of patients with preexisting chronic comorbid conditions was low. Rather, “most were pretty healthy” prior to admission, according to Dr. Chovatiya, who said that the majority of admissions were from an emergency department.
Measles, which targets epithelial cells and depresses the immune system, is a potentially serious disease because of its ability to produce complications in essentially every organ of the body, including the lungs, kidneys, blood, and central nervous system. Consistent with past studies, the most common complication in this series was pneumonia, observed in 20% of patients. The list of other serious complications identified in this study period, including encephalitis and acute renal failure, was long.
“We observed death in 4.3% of our 582 cases, or about 25 cases,” reported Dr. Chovatiya. He indicated that this is a high percentage among a population composed largely of children who were well before hospitalization.
The mortality rate from measles was numerically but not statistically higher than that of overall hospital admissions during this period, but an admission for measles was associated with significantly longer average length of stay (3.7 vs. 3.5 days) and slightly but significantly higher direct costs ($18,907 vs. $18,474).
“I want to point out that these are just direct inpatient costs,” Dr. Chovatiya said. Extrapolating from published data about indirect expenses, he said that the total health cost burden “is absolutely staggering.”
Previous studies have suggested that about 25% of patients with measles require hospitalization and 1 in every 1,000 patients will die. The data collected by Dr. Chovatiya support these often-cited figures, indicating that they remain unchanged in the modern era.
particularly insufficient penetration of vaccination in many communities.
The vaccine “is inexpensive, extremely effective, and lifesaving,” said Dr. Chovatiya, making the point that all of the morbidity, mortality, and costs he described are largely avoidable.
Attempting to provide perspective of the measles threat and the impact of the vaccine, Dr. Chovatiya cited a hypothetical calculation that 732,000 deaths from measles would have been expected in the United States among the pool of children born between 1994 and 2013 had no vaccine been offered. Again, most of these deaths would have occurred in otherwise healthy children.
Dr. Chovatiya reported no potential conflicts of interest.
CHICAGO – An evaluation of the measles threat in the modern era gives no indication that the risk of complications or death is any different than it was before a vaccine became available, according to an analysis of inpatient complications between 2002 and 2013.
In 2000, measles was declared eliminated in the United States, but for those who have been infected since that time, the risk of serious complications and death has not diminished, noted Raj Chovatiya, MD, PhD, in a session at the annual meeting of the Society for Investigative Dermatology.
By eliminated, the Centers of Disease Control and Prevention – which reported 86 confirmed cases of measles in 2000 – was referring to a technical definition of no new endemic or continuous transmissions in the previous 12 months. It was expected that a modest number of cases of this reportable disease would continue to accrue for an infection that remains common elsewhere in the world.
“Worldwide there are about 20 million cases of measles annually with an estimated 100,000 deaths attributed to this cause,” said Dr. Chovatiya, who is a dermatology resident at Northwestern University, Chicago.
In the United States, posteradication infection rates remained at low levels for several years but were already rising from 2002 to 2013, when Dr. Chovatiya and his coinvestigators sought to describe the incidence, associations, comorbidities, and outcomes of hospitalizations for measles. Toward the end of the period the researchers were examining the incidence rates climbed more steeply.
“So far this year, 764 CDC cases of measles [were] reported. That is the most we have seen in the U.S. since 1994,” Dr. Chovatiya said.
Based on his analysis of hospitalizations from 2002 to 2013, the threat of these outbreaks is no different then that before the disease was declared eliminated or before a vaccine became available.
The cross-sectional study was conducted with data from the Nationwide Inpatient Sample, an all-payer database that is considered to be a representative of national trends.
Characteristic of measles, the majority of the 582 hospitalizations evaluated over this period occurred in children aged between 1 and 9 years. The proportion of patients with preexisting chronic comorbid conditions was low. Rather, “most were pretty healthy” prior to admission, according to Dr. Chovatiya, who said that the majority of admissions were from an emergency department.
Measles, which targets epithelial cells and depresses the immune system, is a potentially serious disease because of its ability to produce complications in essentially every organ of the body, including the lungs, kidneys, blood, and central nervous system. Consistent with past studies, the most common complication in this series was pneumonia, observed in 20% of patients. The list of other serious complications identified in this study period, including encephalitis and acute renal failure, was long.
“We observed death in 4.3% of our 582 cases, or about 25 cases,” reported Dr. Chovatiya. He indicated that this is a high percentage among a population composed largely of children who were well before hospitalization.
The mortality rate from measles was numerically but not statistically higher than that of overall hospital admissions during this period, but an admission for measles was associated with significantly longer average length of stay (3.7 vs. 3.5 days) and slightly but significantly higher direct costs ($18,907 vs. $18,474).
“I want to point out that these are just direct inpatient costs,” Dr. Chovatiya said. Extrapolating from published data about indirect expenses, he said that the total health cost burden “is absolutely staggering.”
Previous studies have suggested that about 25% of patients with measles require hospitalization and 1 in every 1,000 patients will die. The data collected by Dr. Chovatiya support these often-cited figures, indicating that they remain unchanged in the modern era.
particularly insufficient penetration of vaccination in many communities.
The vaccine “is inexpensive, extremely effective, and lifesaving,” said Dr. Chovatiya, making the point that all of the morbidity, mortality, and costs he described are largely avoidable.
Attempting to provide perspective of the measles threat and the impact of the vaccine, Dr. Chovatiya cited a hypothetical calculation that 732,000 deaths from measles would have been expected in the United States among the pool of children born between 1994 and 2013 had no vaccine been offered. Again, most of these deaths would have occurred in otherwise healthy children.
Dr. Chovatiya reported no potential conflicts of interest.
REPORTING FROM SID 2019
Aspirin shows little benefit for primary prevention of vascular disease in diabetes
Background: Multiple large, randomized, controlled trials and meta-analyses that used aspirin as primary prevention for vascular events showed decreased vascular events, but a significant counterbalanced risk of bleeding. Since diabetes carries a higher risk of vascular events, this study examines aspirin for primary prevention of vascular events in diabetic patients.
Study design: Large, randomized, controlled trial.
Setting: British registry-based study.
Synopsis: This is a 9-year randomized, controlled trial that included 15,480 British patients with diabetes without known vascular disease who were randomized to receive a 100-mg aspirin daily or placebo. Participants in each group were closely matched patients with diabetes who were recruited using registry data and were aged 40 years and older with no alternative strong indication for aspirin.
Overall, aspirin provided no difference in mortality but showed an absolute 1.3% decrease in first vascular events or revascularization procedures with an absolute 1.1% increase in first occurrence of major bleeding event. Approximately 60% of the bleeding events were gastrointestinal or “other” urinary/nose bleeding, and there was no statistically significant increase in intracranial hemorrhage, hemorrhagic stroke, or vision-threatening eye bleeding. Vascular events were defined as transient ischemic attack (TIA), nonfatal MI, nonfatal ischemic stroke, or vascular death excluding intracranial hemorrhage. The major limitation of this study is that it had a composite of endpoints of different clinical significance. Furthermore, TIA as a major vascular event was added after the study began to increase statistical power, and when it is excluded, the difference for vascular events is not statistically significant.
Bottom line: Aspirin when used in primary prevention of vascular events in diabetes provides no improvement in mortality, and the benefit of prevention of vascular events must be weighed against the risks of bleeding.
Citation: The ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in diabetes. N Eng J Med. 2018 Oct 18;379(16):1529-39.
Dr. Scott is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: Multiple large, randomized, controlled trials and meta-analyses that used aspirin as primary prevention for vascular events showed decreased vascular events, but a significant counterbalanced risk of bleeding. Since diabetes carries a higher risk of vascular events, this study examines aspirin for primary prevention of vascular events in diabetic patients.
Study design: Large, randomized, controlled trial.
Setting: British registry-based study.
Synopsis: This is a 9-year randomized, controlled trial that included 15,480 British patients with diabetes without known vascular disease who were randomized to receive a 100-mg aspirin daily or placebo. Participants in each group were closely matched patients with diabetes who were recruited using registry data and were aged 40 years and older with no alternative strong indication for aspirin.
Overall, aspirin provided no difference in mortality but showed an absolute 1.3% decrease in first vascular events or revascularization procedures with an absolute 1.1% increase in first occurrence of major bleeding event. Approximately 60% of the bleeding events were gastrointestinal or “other” urinary/nose bleeding, and there was no statistically significant increase in intracranial hemorrhage, hemorrhagic stroke, or vision-threatening eye bleeding. Vascular events were defined as transient ischemic attack (TIA), nonfatal MI, nonfatal ischemic stroke, or vascular death excluding intracranial hemorrhage. The major limitation of this study is that it had a composite of endpoints of different clinical significance. Furthermore, TIA as a major vascular event was added after the study began to increase statistical power, and when it is excluded, the difference for vascular events is not statistically significant.
Bottom line: Aspirin when used in primary prevention of vascular events in diabetes provides no improvement in mortality, and the benefit of prevention of vascular events must be weighed against the risks of bleeding.
Citation: The ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in diabetes. N Eng J Med. 2018 Oct 18;379(16):1529-39.
Dr. Scott is an assistant professor in the division of hospital medicine, University of New Mexico.
Background: Multiple large, randomized, controlled trials and meta-analyses that used aspirin as primary prevention for vascular events showed decreased vascular events, but a significant counterbalanced risk of bleeding. Since diabetes carries a higher risk of vascular events, this study examines aspirin for primary prevention of vascular events in diabetic patients.
Study design: Large, randomized, controlled trial.
Setting: British registry-based study.
Synopsis: This is a 9-year randomized, controlled trial that included 15,480 British patients with diabetes without known vascular disease who were randomized to receive a 100-mg aspirin daily or placebo. Participants in each group were closely matched patients with diabetes who were recruited using registry data and were aged 40 years and older with no alternative strong indication for aspirin.
Overall, aspirin provided no difference in mortality but showed an absolute 1.3% decrease in first vascular events or revascularization procedures with an absolute 1.1% increase in first occurrence of major bleeding event. Approximately 60% of the bleeding events were gastrointestinal or “other” urinary/nose bleeding, and there was no statistically significant increase in intracranial hemorrhage, hemorrhagic stroke, or vision-threatening eye bleeding. Vascular events were defined as transient ischemic attack (TIA), nonfatal MI, nonfatal ischemic stroke, or vascular death excluding intracranial hemorrhage. The major limitation of this study is that it had a composite of endpoints of different clinical significance. Furthermore, TIA as a major vascular event was added after the study began to increase statistical power, and when it is excluded, the difference for vascular events is not statistically significant.
Bottom line: Aspirin when used in primary prevention of vascular events in diabetes provides no improvement in mortality, and the benefit of prevention of vascular events must be weighed against the risks of bleeding.
Citation: The ASCEND Study Collaborative Group. Effects of aspirin for primary prevention in diabetes. N Eng J Med. 2018 Oct 18;379(16):1529-39.
Dr. Scott is an assistant professor in the division of hospital medicine, University of New Mexico.
Comorbid depression worsens many pediatric hospital outcomes
according to a study in the Journal of Affective Disorders.
The investigators led by Mayowa Olusunmade, MD, MPH, of New Jersey Medical School, Newark, found that, compared with those among nondepressed pediatric patients, hospitalization costs were $2,961 higher (P less than .001), length of stay was 0.89 days longer (P less than .001), and odds of death as an outcome while hospitalized was 1.77 times higher (P = .013) among depressed pediatric patients. On the other hand, depressed patients had 0.3 fewer procedures (P less than .001) than nondepressed patients.
This analysis is based on 17,073 pairs of patients with and without depression that were created through one-to-one propensity score matching. The investigators drew these pairs from an estimated 937,971 patients in the Kids’ Inpatient Database for 2012 who were identified as being aged 6 years and older and having any of the 10 of the most common diagnoses other than affective disorders. The investigators then determined which children among those identified had comorbid depression (2.9%) and which did not (97.1%) to create the propensity score–matched pairs.
One limitation in this study is that the mean age was 17.5 years because depression diagnosis is more atypical among younger patients such that adolescents were disproportionately represented.
The study did not receive funding, and the authors declared there are no conflicts of interest.
SOURCE: Olusunmade M et al. J Affect Disord. 2019 Mar 27. doi: 10.1016/j.jad.2019.03.073.
according to a study in the Journal of Affective Disorders.
The investigators led by Mayowa Olusunmade, MD, MPH, of New Jersey Medical School, Newark, found that, compared with those among nondepressed pediatric patients, hospitalization costs were $2,961 higher (P less than .001), length of stay was 0.89 days longer (P less than .001), and odds of death as an outcome while hospitalized was 1.77 times higher (P = .013) among depressed pediatric patients. On the other hand, depressed patients had 0.3 fewer procedures (P less than .001) than nondepressed patients.
This analysis is based on 17,073 pairs of patients with and without depression that were created through one-to-one propensity score matching. The investigators drew these pairs from an estimated 937,971 patients in the Kids’ Inpatient Database for 2012 who were identified as being aged 6 years and older and having any of the 10 of the most common diagnoses other than affective disorders. The investigators then determined which children among those identified had comorbid depression (2.9%) and which did not (97.1%) to create the propensity score–matched pairs.
One limitation in this study is that the mean age was 17.5 years because depression diagnosis is more atypical among younger patients such that adolescents were disproportionately represented.
The study did not receive funding, and the authors declared there are no conflicts of interest.
SOURCE: Olusunmade M et al. J Affect Disord. 2019 Mar 27. doi: 10.1016/j.jad.2019.03.073.
according to a study in the Journal of Affective Disorders.
The investigators led by Mayowa Olusunmade, MD, MPH, of New Jersey Medical School, Newark, found that, compared with those among nondepressed pediatric patients, hospitalization costs were $2,961 higher (P less than .001), length of stay was 0.89 days longer (P less than .001), and odds of death as an outcome while hospitalized was 1.77 times higher (P = .013) among depressed pediatric patients. On the other hand, depressed patients had 0.3 fewer procedures (P less than .001) than nondepressed patients.
This analysis is based on 17,073 pairs of patients with and without depression that were created through one-to-one propensity score matching. The investigators drew these pairs from an estimated 937,971 patients in the Kids’ Inpatient Database for 2012 who were identified as being aged 6 years and older and having any of the 10 of the most common diagnoses other than affective disorders. The investigators then determined which children among those identified had comorbid depression (2.9%) and which did not (97.1%) to create the propensity score–matched pairs.
One limitation in this study is that the mean age was 17.5 years because depression diagnosis is more atypical among younger patients such that adolescents were disproportionately represented.
The study did not receive funding, and the authors declared there are no conflicts of interest.
SOURCE: Olusunmade M et al. J Affect Disord. 2019 Mar 27. doi: 10.1016/j.jad.2019.03.073.
FROM THE JOURNAL OF AFFECTIVE DISORDERS
HM19: Interprofessional rounds
Better process, outcomes
Session presenters
Surekha Bhamidipati, MD, FACP; Preetham Talari, MD, FACP, SFHM; Mark V. Williams, MD, FACP, MHM
Session title
Interprofessional rounds: What’s the right way?
Session summary
Interprofessional or multidisciplinary rounds involve all members of the care delivery team, including physicians, nurses, case managers, social workers, pharmacists, nurse facilitators, and of course, patients. The primary goal for these rounds is patient-centered care, and to improve communication among the health care team members, as well as with patients and their families.
At HM19, Dr. Preetham Talari and Dr. Mark Williams of the University of Kentucky, and Dr. Surekha Bhamidipati of Christiana Care Health System in Newark, Del., discussed their system-based efforts to try to implement interprofessional rounds, and the role of these rounds in improving patient outcome measures.
The presenters noted that the purpose of these rounds is effective communication and efficient patient care. As shown by multiple studies, there is significant impact in team member satisfaction, decrease in length of stay,1 reduction in adverse events2 and improvement in patient experience.3 They emphasized the importance of implementing these rounds at the bedside, so that patients and families can be engaged in the patient’s care, thereby improving closed communication among the team and the patient. These rounds always offer an opportunity for the patient to ask questions of multiple health care team members as they are gathered together at the same time.
The University of Kentucky named these rounds the “Interprofessional Teamwork Innovation Model (ITIM),” to promote communication and patient-centered coordinated care. Their model showed a significant reduction in readmission rates, and no increase in costs despite adding pharmacy and case managers to the rounds.
Dr. Bhamidipati described how Christiana Care Health System designed multidisciplinary rounds based on the application of Team STEPPS 2.0, a teamwork system developed by the Department of Defense and the Agency for Healthcare Research and Quality to improve the institutional collaboration and communication relating to patient safety.
The Christiana Care model is based on a few principles of team structure, communication, leadership, situation monitoring, and mutual support. The interprofessional team was trained and observed, and a short video recording was made. This video was used as an educational tool in coaching the rest of the team. Dr. Bhamidipati described the importance of interprofessional leaders as coaches to train other team members, and highlighted the engagement of unit leaders in successfully implementing these rounds. The Christiana Care team used its informational technology system to collect real-time data, which was then used for team review.
In summary, the presenters from both the University of Kentucky and Christiana Care highlighted the importance of interprofessional rounds, as well as the need for continued measurement of process and outcome metrics.
Dr. Jonnalagadda is a physician advisor, and Dr. Medarametla is medical director, Hospital Medicine, at Baystate Medical Center, Springfield, Mass.
References
1. Yoo JW et al. Effects of an internal medicine floor interdisciplinary team on hospital and clinical outcomes of seniors with acute medical illness. Geriatr Gerontol Int. 2013 Oct;13(4):942-8. doi: 10.1111/ggi.12035. Epub 2013 Feb 26.
2. O’Leary KJ et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011 Apr 11;171(7):678-84. doi: 10.1001/archinternmed.2011.128.
3. Ratelle JT et al. Implementing bedside rounds to improve patient-centred outcomes: a systematic review. BMJ Qual Saf. 2019;28:317-326.
Better process, outcomes
Better process, outcomes
Session presenters
Surekha Bhamidipati, MD, FACP; Preetham Talari, MD, FACP, SFHM; Mark V. Williams, MD, FACP, MHM
Session title
Interprofessional rounds: What’s the right way?
Session summary
Interprofessional or multidisciplinary rounds involve all members of the care delivery team, including physicians, nurses, case managers, social workers, pharmacists, nurse facilitators, and of course, patients. The primary goal for these rounds is patient-centered care, and to improve communication among the health care team members, as well as with patients and their families.
At HM19, Dr. Preetham Talari and Dr. Mark Williams of the University of Kentucky, and Dr. Surekha Bhamidipati of Christiana Care Health System in Newark, Del., discussed their system-based efforts to try to implement interprofessional rounds, and the role of these rounds in improving patient outcome measures.
The presenters noted that the purpose of these rounds is effective communication and efficient patient care. As shown by multiple studies, there is significant impact in team member satisfaction, decrease in length of stay,1 reduction in adverse events2 and improvement in patient experience.3 They emphasized the importance of implementing these rounds at the bedside, so that patients and families can be engaged in the patient’s care, thereby improving closed communication among the team and the patient. These rounds always offer an opportunity for the patient to ask questions of multiple health care team members as they are gathered together at the same time.
The University of Kentucky named these rounds the “Interprofessional Teamwork Innovation Model (ITIM),” to promote communication and patient-centered coordinated care. Their model showed a significant reduction in readmission rates, and no increase in costs despite adding pharmacy and case managers to the rounds.
Dr. Bhamidipati described how Christiana Care Health System designed multidisciplinary rounds based on the application of Team STEPPS 2.0, a teamwork system developed by the Department of Defense and the Agency for Healthcare Research and Quality to improve the institutional collaboration and communication relating to patient safety.
The Christiana Care model is based on a few principles of team structure, communication, leadership, situation monitoring, and mutual support. The interprofessional team was trained and observed, and a short video recording was made. This video was used as an educational tool in coaching the rest of the team. Dr. Bhamidipati described the importance of interprofessional leaders as coaches to train other team members, and highlighted the engagement of unit leaders in successfully implementing these rounds. The Christiana Care team used its informational technology system to collect real-time data, which was then used for team review.
In summary, the presenters from both the University of Kentucky and Christiana Care highlighted the importance of interprofessional rounds, as well as the need for continued measurement of process and outcome metrics.
Dr. Jonnalagadda is a physician advisor, and Dr. Medarametla is medical director, Hospital Medicine, at Baystate Medical Center, Springfield, Mass.
References
1. Yoo JW et al. Effects of an internal medicine floor interdisciplinary team on hospital and clinical outcomes of seniors with acute medical illness. Geriatr Gerontol Int. 2013 Oct;13(4):942-8. doi: 10.1111/ggi.12035. Epub 2013 Feb 26.
2. O’Leary KJ et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011 Apr 11;171(7):678-84. doi: 10.1001/archinternmed.2011.128.
3. Ratelle JT et al. Implementing bedside rounds to improve patient-centred outcomes: a systematic review. BMJ Qual Saf. 2019;28:317-326.
Session presenters
Surekha Bhamidipati, MD, FACP; Preetham Talari, MD, FACP, SFHM; Mark V. Williams, MD, FACP, MHM
Session title
Interprofessional rounds: What’s the right way?
Session summary
Interprofessional or multidisciplinary rounds involve all members of the care delivery team, including physicians, nurses, case managers, social workers, pharmacists, nurse facilitators, and of course, patients. The primary goal for these rounds is patient-centered care, and to improve communication among the health care team members, as well as with patients and their families.
At HM19, Dr. Preetham Talari and Dr. Mark Williams of the University of Kentucky, and Dr. Surekha Bhamidipati of Christiana Care Health System in Newark, Del., discussed their system-based efforts to try to implement interprofessional rounds, and the role of these rounds in improving patient outcome measures.
The presenters noted that the purpose of these rounds is effective communication and efficient patient care. As shown by multiple studies, there is significant impact in team member satisfaction, decrease in length of stay,1 reduction in adverse events2 and improvement in patient experience.3 They emphasized the importance of implementing these rounds at the bedside, so that patients and families can be engaged in the patient’s care, thereby improving closed communication among the team and the patient. These rounds always offer an opportunity for the patient to ask questions of multiple health care team members as they are gathered together at the same time.
The University of Kentucky named these rounds the “Interprofessional Teamwork Innovation Model (ITIM),” to promote communication and patient-centered coordinated care. Their model showed a significant reduction in readmission rates, and no increase in costs despite adding pharmacy and case managers to the rounds.
Dr. Bhamidipati described how Christiana Care Health System designed multidisciplinary rounds based on the application of Team STEPPS 2.0, a teamwork system developed by the Department of Defense and the Agency for Healthcare Research and Quality to improve the institutional collaboration and communication relating to patient safety.
The Christiana Care model is based on a few principles of team structure, communication, leadership, situation monitoring, and mutual support. The interprofessional team was trained and observed, and a short video recording was made. This video was used as an educational tool in coaching the rest of the team. Dr. Bhamidipati described the importance of interprofessional leaders as coaches to train other team members, and highlighted the engagement of unit leaders in successfully implementing these rounds. The Christiana Care team used its informational technology system to collect real-time data, which was then used for team review.
In summary, the presenters from both the University of Kentucky and Christiana Care highlighted the importance of interprofessional rounds, as well as the need for continued measurement of process and outcome metrics.
Dr. Jonnalagadda is a physician advisor, and Dr. Medarametla is medical director, Hospital Medicine, at Baystate Medical Center, Springfield, Mass.
References
1. Yoo JW et al. Effects of an internal medicine floor interdisciplinary team on hospital and clinical outcomes of seniors with acute medical illness. Geriatr Gerontol Int. 2013 Oct;13(4):942-8. doi: 10.1111/ggi.12035. Epub 2013 Feb 26.
2. O’Leary KJ et al. Structured interdisciplinary rounds in a medical teaching unit: improving patient safety. Arch Intern Med. 2011 Apr 11;171(7):678-84. doi: 10.1001/archinternmed.2011.128.
3. Ratelle JT et al. Implementing bedside rounds to improve patient-centred outcomes: a systematic review. BMJ Qual Saf. 2019;28:317-326.
Living into your legacy
What I learned from women of impact
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
What I learned from women of impact
What I learned from women of impact
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
The word legacy has been synonymous with death to me. When so and so dies, we discuss their legacy. I had a powerful experience that changed my mind on this word that is befitting for this Legacies column.
Seven years ago, I was sitting in a room of powerful women and I was the youngest one there. I wasn’t sure how I got there, but I was glad I did because it changed my life. At the time, I was panicked. The exercise was called “Craft your legacy statement.”
But, this exercise was different. The ask was to “live into your legacy.” Craft a legacy statement in THREE minutes that summarizes what you want your legacy to be … and then decide the three things you need to do now to get there. So, here is my exact legacy 3-minute statement: I am an innovator pushing teaching hospitals to optimize training and patient care delivery through novel technologies and systems science. Clearly, I did not aim high enough. One of the other attendees stated her legacy simply as “Unleash the impossible!” So clearly, I was not able to think big at that moment, but I trudged on.
Next, I had to write the three things I was going to do to enact my legacy today. Things went from bad to worse quickly since I knew this was not going to be easy. The #1 thing had to be something I was going to stop doing because it did not fit with my legacy; #2 was what I was going to start doing to enact this legacy now; and, #3 was something I was going to do to get me closer to what I wanted to be doing. So, my #1, resign my current leadership role that I had had for 8 years; #2, start joining national committees that bridge education and quality; and #3, meet with senior leadership to pitch this new role as a bridging leader, aligning education and quality.
Like all conferences, I went home and forgot what I had done and learned. I settled back into my old life and routines. A few weeks later, a plain looking envelope with awful penmanship showed up at my doorstep addressed to me. It wasn’t until after I opened it and read what was inside that I realized I was the one with horrible penmanship! I completely forgot that I wrote this letter to myself even though they told me it would come and I would forget I wrote it! So, how did I do? Let’s just say if the letter did not arrive, I am not sure where I would be. Fortunately, it did come, and I followed my own orders. Fast forward to present day and I recently stepped into a new role – associate chief medical officer: clinical learning environment – a bridging leader who aligns education and clinical care missions for our health system. Let’s just say again, had that letter not arrived, I am not sure where I would be now.
I have been fortunate to do many things in hospital medicine – clinician, researcher, educator, and my latest role as a leader. Through it all, I would say that there are some lessons that I have picked up along the way that helped me advance, in ways I did not realize:
- Be bold. Years ago, when I was asked by my chair who they should pick to be chief resident, I thought “This must be a trick question – I should definitely tell him why I should be chosen – and then pick the next best person who I want to work with.” Apparently, I was the only person who did that, and that is why my chair chose me. Everyone else picked two other people. So the take-home point here is do not sell yourself short … ever.
- Look for the hidden gateways. A few years ago, I was asked if I wanted to be an institutional leader by the person who currently had that role. I was kind of thrown for a loop, since of course I would not want to appear like I wanted to take his job. I said everything was fine and I felt pretty good about my current positions. It was only a few weeks later that I realized that he was ascertaining my interest in his job since he was leaving. They gave the job to someone else and the word on the street was I was not interested. I totally missed the gate! While it wasn’t necessarily the job I missed out on, it was the opportunity to consider the job because I was afraid. So, don’t miss the gate. It’s the wormhole to a different life that may be the right one for you, but you need to “see it” to seize it.
- Work hard for the money and for the fun. There are many things Gwyneth Paltrow does that I do not agree with, but I will give her credit for one important lesson: she divides her movie roles into those she does for love (for example, The Royal Tenenbaums) and those she does for money (for example, Shallow Hal). It made me realize that even a Hollywood starlet has to do the stuff she may not want to do for the money. So, as a young person, you have to work hard for the money, but ideally it will help you take on a project you love, whatever it is. You’ve won the game when you’re mostly paid to work for the fun ... but that may take some time.
- Always optimize what is best for you personally AND professionally. While I was on maternity leave, the job of my dreams presented itself – or so I thought it did. It was at the intersection of policy, quality, and education, with a national stage, and I would not need to move. But, I knew I could not accept the travel commitment with a young child. While I wondered if I would have regrets, it turns out the right decision professionally also has to work personally. Likewise, there are professional obligations that I take on because it works personally.
- Figure out who your tea house pals are. A few years ago, I was in San Francisco with two close friends having an epic moment about what to do with our lives as adults. We were all on the cusp of changing our directions. Not surprisingly, we could see what the other needed to do, but we could not see it for ourselves. We still text each other sometimes about the need to go back to the Tea House. Sometimes your “tea house pals” are not necessarily those around you every day. They know you, but not everyone in your work place. This “arm’s length” or distance gives them the rational, unbiased perspective to advise you, that you or your colleagues will never have.
- Look for ways to enjoy the journey. Medicine is a very long road. I routinely think about this working with all the trainees and junior faculty I encounter. You can’t be in this solely for the end of the journey. The key is to find the joy in the journey. For me, that has always come from seeking out like-minded fellow travelers to share my highs and lows. While I tweet for many reasons, a big reason is that I take pleasure in watching others on the journey and also sharing my own journey.
Here’s to your journey and living your legacy!
Dr. Arora is associate chief medical officer, clinical learning environment, at University of Chicago Medicine, and assistant dean for scholarship and discovery at the University of Chicago Pritzker School of Medicine. You can follow her journey on Twitter.
Severe OSA increases cardiovascular risk after surgery
Unrecognized severe obstructive sleep apnea is a risk factor for cardiovascular complications after major noncardiac surgery, according to a study published in JAMA.
The researchers state that perioperative mismanagement of obstructive sleep apnea can lead to serious medical consequences. “General anesthetics, sedatives, and postoperative analgesics are potent respiratory depressants that relax the upper airway dilator muscles and impair ventilatory response to hypoxemia and hypercapnia. Each of these events exacerbates [obstructive sleep apnea] and may predispose patients to postoperative cardiovascular complications,” said researchers who conducted the The Postoperative vascular complications in unrecognised Obstructive Sleep apnoea (POSA) study (NCT01494181).
They undertook a prospective observational cohort study involving 1,218 patients undergoing major noncardiac surgery, who were already considered at high risk of postoperative cardiovascular events – having, for example, a history of coronary artery disease, stroke, diabetes, or renal impairment. However, none had a prior diagnosis of obstructive sleep apnea.
Preoperative sleep monitoring revealed that two-thirds of the cohort had unrecognized and untreated obstructive sleep apnea, including 11.2% with severe obstructive sleep apnea.
At 30 days after surgery, patients with obstructive sleep apnea had a 49% higher risk of the primary outcome of myocardial injury, cardiac death, heart failure, thromboembolism, atrial fibrillation, or stroke, compared with those without obstructive sleep apnea.
However, this association was largely due to a significant 2.23-fold higher risk among patients with severe obstructive sleep apnea, while those with only moderate or mild sleep apnea did not show a significant increased risk of cardiovascular complications.
Patients in this study with severe obstructive sleep apnea had a 13-fold higher risk of cardiac death, 80% higher risk of myocardial injury, more than sixfold higher risk of heart failure, and nearly fourfold higher risk of atrial fibrillation.
Researchers also saw an association between obstructive sleep apnea and increased risk of infective outcomes, unplanned tracheal intubation, postoperative lung ventilation, and readmission to the ICU.
The majority of patients received nocturnal oximetry monitoring during their first 3 nights after surgery. This revealed that patients without obstructive sleep apnea had significant increases in oxygen desaturation index during their first night after surgery, while those with sleep apnea did not return to their baseline oxygen desaturation index until the third night after surgery.
“Despite a substantial decrease in ODI [oxygen desaturation index] with oxygen therapy in patients with OSA during the first 3 postoperative nights, supplemental oxygen did not modify the association between OSA and postoperative cardiovascular event,” wrote Matthew T.V. Chan, MD, of Chinese University of Hong Kong, Prince of Wales Hospital, and coauthors.
Given that the events were associated with longer durations of severe oxyhemoglobin desaturation, more aggressive interventions such as positive airway pressure or oral appliances may be required, they noted.
“However, high-level evidence demonstrating the effect of these measures on perioperative outcomes is lacking [and] further clinical trials are now required to test if additional monitoring or alternative interventions would reduce the risk,” they wrote.
The study was supported by the Health and Medical Research Fund (Hong Kong), National Healthcare Group–Khoo Teck Puat Hospital, University Health Network Foundation, University of Malaya, Malaysian Society of Anaesthesiologists, Auckland Medical Research Foundation, and ResMed. One author declared grants from private industry and a patent pending on an obstructive sleep apnea risk questionnaire used in the study.
SOURCE: Chan M et al. JAMA 2019;321[18]:1788-98. doi: 10.1001/jama.2019.4783.
This study is large, prospective, and rigorous and adds important new information to the puzzle of the impact of sleep apnea on postoperative risk, Dennis Auckley, MD, and Stavros Memtsoudis, MD, wrote in an editorial accompanying this study. The study focused on predetermined clinically significant and measurable events, used standardized and objective sleep apnea testing, and attempted to control for many of the confounders that might have influenced outcomes.
The results suggest that obstructive sleep apnea should be recognized as a major perioperative risk factor, and it should receive the same attention and optimization efforts as comorbidities such as diabetes.
Dr. Auckley is from the division of pulmonary, critical care and sleep medicine at MetroHealth Medical Center, Case Western Reserve University, Cleveland, and Dr. Memtsoudis is clinical professor of anesthesiology at Cornell University, New York. These comments are adapted from an editorial (JAMA 2019;231[18]:1775-6). Both declared board and executive positions with the Society of Anesthesia and Sleep Medicine. Dr. Auckley declared research funding from Medtronic, and Dr. Memtsoudis declared personal fees from Teikoku and Sandoz.
This study is large, prospective, and rigorous and adds important new information to the puzzle of the impact of sleep apnea on postoperative risk, Dennis Auckley, MD, and Stavros Memtsoudis, MD, wrote in an editorial accompanying this study. The study focused on predetermined clinically significant and measurable events, used standardized and objective sleep apnea testing, and attempted to control for many of the confounders that might have influenced outcomes.
The results suggest that obstructive sleep apnea should be recognized as a major perioperative risk factor, and it should receive the same attention and optimization efforts as comorbidities such as diabetes.
Dr. Auckley is from the division of pulmonary, critical care and sleep medicine at MetroHealth Medical Center, Case Western Reserve University, Cleveland, and Dr. Memtsoudis is clinical professor of anesthesiology at Cornell University, New York. These comments are adapted from an editorial (JAMA 2019;231[18]:1775-6). Both declared board and executive positions with the Society of Anesthesia and Sleep Medicine. Dr. Auckley declared research funding from Medtronic, and Dr. Memtsoudis declared personal fees from Teikoku and Sandoz.
This study is large, prospective, and rigorous and adds important new information to the puzzle of the impact of sleep apnea on postoperative risk, Dennis Auckley, MD, and Stavros Memtsoudis, MD, wrote in an editorial accompanying this study. The study focused on predetermined clinically significant and measurable events, used standardized and objective sleep apnea testing, and attempted to control for many of the confounders that might have influenced outcomes.
The results suggest that obstructive sleep apnea should be recognized as a major perioperative risk factor, and it should receive the same attention and optimization efforts as comorbidities such as diabetes.
Dr. Auckley is from the division of pulmonary, critical care and sleep medicine at MetroHealth Medical Center, Case Western Reserve University, Cleveland, and Dr. Memtsoudis is clinical professor of anesthesiology at Cornell University, New York. These comments are adapted from an editorial (JAMA 2019;231[18]:1775-6). Both declared board and executive positions with the Society of Anesthesia and Sleep Medicine. Dr. Auckley declared research funding from Medtronic, and Dr. Memtsoudis declared personal fees from Teikoku and Sandoz.
Unrecognized severe obstructive sleep apnea is a risk factor for cardiovascular complications after major noncardiac surgery, according to a study published in JAMA.
The researchers state that perioperative mismanagement of obstructive sleep apnea can lead to serious medical consequences. “General anesthetics, sedatives, and postoperative analgesics are potent respiratory depressants that relax the upper airway dilator muscles and impair ventilatory response to hypoxemia and hypercapnia. Each of these events exacerbates [obstructive sleep apnea] and may predispose patients to postoperative cardiovascular complications,” said researchers who conducted the The Postoperative vascular complications in unrecognised Obstructive Sleep apnoea (POSA) study (NCT01494181).
They undertook a prospective observational cohort study involving 1,218 patients undergoing major noncardiac surgery, who were already considered at high risk of postoperative cardiovascular events – having, for example, a history of coronary artery disease, stroke, diabetes, or renal impairment. However, none had a prior diagnosis of obstructive sleep apnea.
Preoperative sleep monitoring revealed that two-thirds of the cohort had unrecognized and untreated obstructive sleep apnea, including 11.2% with severe obstructive sleep apnea.
At 30 days after surgery, patients with obstructive sleep apnea had a 49% higher risk of the primary outcome of myocardial injury, cardiac death, heart failure, thromboembolism, atrial fibrillation, or stroke, compared with those without obstructive sleep apnea.
However, this association was largely due to a significant 2.23-fold higher risk among patients with severe obstructive sleep apnea, while those with only moderate or mild sleep apnea did not show a significant increased risk of cardiovascular complications.
Patients in this study with severe obstructive sleep apnea had a 13-fold higher risk of cardiac death, 80% higher risk of myocardial injury, more than sixfold higher risk of heart failure, and nearly fourfold higher risk of atrial fibrillation.
Researchers also saw an association between obstructive sleep apnea and increased risk of infective outcomes, unplanned tracheal intubation, postoperative lung ventilation, and readmission to the ICU.
The majority of patients received nocturnal oximetry monitoring during their first 3 nights after surgery. This revealed that patients without obstructive sleep apnea had significant increases in oxygen desaturation index during their first night after surgery, while those with sleep apnea did not return to their baseline oxygen desaturation index until the third night after surgery.
“Despite a substantial decrease in ODI [oxygen desaturation index] with oxygen therapy in patients with OSA during the first 3 postoperative nights, supplemental oxygen did not modify the association between OSA and postoperative cardiovascular event,” wrote Matthew T.V. Chan, MD, of Chinese University of Hong Kong, Prince of Wales Hospital, and coauthors.
Given that the events were associated with longer durations of severe oxyhemoglobin desaturation, more aggressive interventions such as positive airway pressure or oral appliances may be required, they noted.
“However, high-level evidence demonstrating the effect of these measures on perioperative outcomes is lacking [and] further clinical trials are now required to test if additional monitoring or alternative interventions would reduce the risk,” they wrote.
The study was supported by the Health and Medical Research Fund (Hong Kong), National Healthcare Group–Khoo Teck Puat Hospital, University Health Network Foundation, University of Malaya, Malaysian Society of Anaesthesiologists, Auckland Medical Research Foundation, and ResMed. One author declared grants from private industry and a patent pending on an obstructive sleep apnea risk questionnaire used in the study.
SOURCE: Chan M et al. JAMA 2019;321[18]:1788-98. doi: 10.1001/jama.2019.4783.
Unrecognized severe obstructive sleep apnea is a risk factor for cardiovascular complications after major noncardiac surgery, according to a study published in JAMA.
The researchers state that perioperative mismanagement of obstructive sleep apnea can lead to serious medical consequences. “General anesthetics, sedatives, and postoperative analgesics are potent respiratory depressants that relax the upper airway dilator muscles and impair ventilatory response to hypoxemia and hypercapnia. Each of these events exacerbates [obstructive sleep apnea] and may predispose patients to postoperative cardiovascular complications,” said researchers who conducted the The Postoperative vascular complications in unrecognised Obstructive Sleep apnoea (POSA) study (NCT01494181).
They undertook a prospective observational cohort study involving 1,218 patients undergoing major noncardiac surgery, who were already considered at high risk of postoperative cardiovascular events – having, for example, a history of coronary artery disease, stroke, diabetes, or renal impairment. However, none had a prior diagnosis of obstructive sleep apnea.
Preoperative sleep monitoring revealed that two-thirds of the cohort had unrecognized and untreated obstructive sleep apnea, including 11.2% with severe obstructive sleep apnea.
At 30 days after surgery, patients with obstructive sleep apnea had a 49% higher risk of the primary outcome of myocardial injury, cardiac death, heart failure, thromboembolism, atrial fibrillation, or stroke, compared with those without obstructive sleep apnea.
However, this association was largely due to a significant 2.23-fold higher risk among patients with severe obstructive sleep apnea, while those with only moderate or mild sleep apnea did not show a significant increased risk of cardiovascular complications.
Patients in this study with severe obstructive sleep apnea had a 13-fold higher risk of cardiac death, 80% higher risk of myocardial injury, more than sixfold higher risk of heart failure, and nearly fourfold higher risk of atrial fibrillation.
Researchers also saw an association between obstructive sleep apnea and increased risk of infective outcomes, unplanned tracheal intubation, postoperative lung ventilation, and readmission to the ICU.
The majority of patients received nocturnal oximetry monitoring during their first 3 nights after surgery. This revealed that patients without obstructive sleep apnea had significant increases in oxygen desaturation index during their first night after surgery, while those with sleep apnea did not return to their baseline oxygen desaturation index until the third night after surgery.
“Despite a substantial decrease in ODI [oxygen desaturation index] with oxygen therapy in patients with OSA during the first 3 postoperative nights, supplemental oxygen did not modify the association between OSA and postoperative cardiovascular event,” wrote Matthew T.V. Chan, MD, of Chinese University of Hong Kong, Prince of Wales Hospital, and coauthors.
Given that the events were associated with longer durations of severe oxyhemoglobin desaturation, more aggressive interventions such as positive airway pressure or oral appliances may be required, they noted.
“However, high-level evidence demonstrating the effect of these measures on perioperative outcomes is lacking [and] further clinical trials are now required to test if additional monitoring or alternative interventions would reduce the risk,” they wrote.
The study was supported by the Health and Medical Research Fund (Hong Kong), National Healthcare Group–Khoo Teck Puat Hospital, University Health Network Foundation, University of Malaya, Malaysian Society of Anaesthesiologists, Auckland Medical Research Foundation, and ResMed. One author declared grants from private industry and a patent pending on an obstructive sleep apnea risk questionnaire used in the study.
SOURCE: Chan M et al. JAMA 2019;321[18]:1788-98. doi: 10.1001/jama.2019.4783.
FROM JAMA
Pilot program trains residents in telemedicine
WASHINGTON – while still providing the same quality of care during clinic visits, according to the results of a new pilot program.
While telephone visits have been shown to be an effective alternative to face-to-face visits for physicians, residents are not trained to perform telemedicine.
“We have no structured training program on how to teach these residents these skills. We assume that the same skills needed in the clinic are applicable through telephone medicine and we’re not sure about that yet,” Jenna L. Laughlin, DO, said at the annual meeting of the Society of General Internal Medicine.
The pilot study took place at Christiana Care Health System, Wilmington, Del., from October 2016 through December 2018. Nine residents were enrolled in the study, but only six participated.
The objective of the pilot was to demonstrate the feasibility of adding telephone visits into the internal medicine residency practice. This feasibility was measured by templating, scheduling, and supervision, noted Dr. Laughlin, an internist at Christiana Care Health System in Newark, Del. Templating was a term used to describe the designing of the program. For example, the researcher templated 1-hour telephone visit blocks, meaning they designed this structure to integrate into the resident’s training program.
Each resident had 1 hour within the weekly schedule to conduct telephone visits. First-year residents were allowed to do one telephone visit during that hour, second-year residents could do two telephone visits within the hour, and third-year residents could do three telephone visits in that hour.
“There were some challenges associated with scheduling and templating, such as initial schedule templates and a high utilization learning curve,” said Dr. Laughlin, lead author of the study and the program’s leader.
Some didn’t schedule enough telemedicine visits; those residents were assigned to acute clinic visits during the times that they should have been practicing telemedicine.
The program’s second objective was to evaluate the resident experience of scheduled telemedicine visits. This included provider-patient continuity and patient ownership.
The six residents who were surveyed about their experiences said these telephone visits increased their patient ownership and allowed them to build rapport with patients. They said the level of supervision they received was appropriate.
In terms of continuity of care, out the 273 telephone visits scheduled, 179 (65%) were with the patient’s primary care provider and 71 (26.0%) were within the primary care provider’s firm.
“As we build primary care practices in the future, there will be many alternative methods of working with our patients, compared to the traditional face-to-face encounters. I think these are increasingly going to be something that our medical residents need for their future,” Dr. Laughlin said.
The authors reported no conflicts of interest.
WASHINGTON – while still providing the same quality of care during clinic visits, according to the results of a new pilot program.
While telephone visits have been shown to be an effective alternative to face-to-face visits for physicians, residents are not trained to perform telemedicine.
“We have no structured training program on how to teach these residents these skills. We assume that the same skills needed in the clinic are applicable through telephone medicine and we’re not sure about that yet,” Jenna L. Laughlin, DO, said at the annual meeting of the Society of General Internal Medicine.
The pilot study took place at Christiana Care Health System, Wilmington, Del., from October 2016 through December 2018. Nine residents were enrolled in the study, but only six participated.
The objective of the pilot was to demonstrate the feasibility of adding telephone visits into the internal medicine residency practice. This feasibility was measured by templating, scheduling, and supervision, noted Dr. Laughlin, an internist at Christiana Care Health System in Newark, Del. Templating was a term used to describe the designing of the program. For example, the researcher templated 1-hour telephone visit blocks, meaning they designed this structure to integrate into the resident’s training program.
Each resident had 1 hour within the weekly schedule to conduct telephone visits. First-year residents were allowed to do one telephone visit during that hour, second-year residents could do two telephone visits within the hour, and third-year residents could do three telephone visits in that hour.
“There were some challenges associated with scheduling and templating, such as initial schedule templates and a high utilization learning curve,” said Dr. Laughlin, lead author of the study and the program’s leader.
Some didn’t schedule enough telemedicine visits; those residents were assigned to acute clinic visits during the times that they should have been practicing telemedicine.
The program’s second objective was to evaluate the resident experience of scheduled telemedicine visits. This included provider-patient continuity and patient ownership.
The six residents who were surveyed about their experiences said these telephone visits increased their patient ownership and allowed them to build rapport with patients. They said the level of supervision they received was appropriate.
In terms of continuity of care, out the 273 telephone visits scheduled, 179 (65%) were with the patient’s primary care provider and 71 (26.0%) were within the primary care provider’s firm.
“As we build primary care practices in the future, there will be many alternative methods of working with our patients, compared to the traditional face-to-face encounters. I think these are increasingly going to be something that our medical residents need for their future,” Dr. Laughlin said.
The authors reported no conflicts of interest.
WASHINGTON – while still providing the same quality of care during clinic visits, according to the results of a new pilot program.
While telephone visits have been shown to be an effective alternative to face-to-face visits for physicians, residents are not trained to perform telemedicine.
“We have no structured training program on how to teach these residents these skills. We assume that the same skills needed in the clinic are applicable through telephone medicine and we’re not sure about that yet,” Jenna L. Laughlin, DO, said at the annual meeting of the Society of General Internal Medicine.
The pilot study took place at Christiana Care Health System, Wilmington, Del., from October 2016 through December 2018. Nine residents were enrolled in the study, but only six participated.
The objective of the pilot was to demonstrate the feasibility of adding telephone visits into the internal medicine residency practice. This feasibility was measured by templating, scheduling, and supervision, noted Dr. Laughlin, an internist at Christiana Care Health System in Newark, Del. Templating was a term used to describe the designing of the program. For example, the researcher templated 1-hour telephone visit blocks, meaning they designed this structure to integrate into the resident’s training program.
Each resident had 1 hour within the weekly schedule to conduct telephone visits. First-year residents were allowed to do one telephone visit during that hour, second-year residents could do two telephone visits within the hour, and third-year residents could do three telephone visits in that hour.
“There were some challenges associated with scheduling and templating, such as initial schedule templates and a high utilization learning curve,” said Dr. Laughlin, lead author of the study and the program’s leader.
Some didn’t schedule enough telemedicine visits; those residents were assigned to acute clinic visits during the times that they should have been practicing telemedicine.
The program’s second objective was to evaluate the resident experience of scheduled telemedicine visits. This included provider-patient continuity and patient ownership.
The six residents who were surveyed about their experiences said these telephone visits increased their patient ownership and allowed them to build rapport with patients. They said the level of supervision they received was appropriate.
In terms of continuity of care, out the 273 telephone visits scheduled, 179 (65%) were with the patient’s primary care provider and 71 (26.0%) were within the primary care provider’s firm.
“As we build primary care practices in the future, there will be many alternative methods of working with our patients, compared to the traditional face-to-face encounters. I think these are increasingly going to be something that our medical residents need for their future,” Dr. Laughlin said.
The authors reported no conflicts of interest.
REPORTING FROM SGIM 2019
















