User login
Young children quickly outgrow the need for ear tubes
About half a million children between the ages of 1 and 3 years old have ear tube surgery in the United States every year at an annual cost exceeding $2 billion. It is the most common childhood surgery performed with anesthesia. It is a surgery commonly performed on children in most other high- and middle-income countries.
My group recently published a paper on the timing and necessity of tympanostomy tubes for recurrent otitis media in young children. The primary objective was to quantitatively examine recurrent acute otitis media (AOM) incidence with respect to age of occurrence, the influence of daycare attendance, and other risk factors in individual children. We introduced the concept of a “window of susceptibility” to AOM as new terminology referring to a child who has two or more closely spaced AOM occurrences during a window of time. We sought to know what to expect and how to advise the parent when a child presents with closely spaced AOMs.
A secondary objective was to develop models to predict the risk and timing of AOM recurrences based on the natural history of disease in young children who do not get tympanostomy tubes. Prediction models were developed to assist clinicians in understanding and explaining to parents the benefit of tympanostomy tubes based on the child’s age and number of AOMs.
The children were all from a primary care pediatric practice in Rochester, N.Y., which comprised a typical mixed demographic of largely middle-class, health care–insured families that was broadly representative of the racial/ethnic diversity in the community. The sample included both wealthy families and those living below the poverty line. The diagnosis of AOM was made based on the American Academy of Pediatrics guidance in which a presumed middle ear effusion and a full or bulging tympanic membrane were required. Almost all episodes (> 85%) of clinically diagnosed AOM cases were confirmed by culture of middle ear fluid collected by tympanocentesis to ensure diagnostic accuracy.
286 children who had ear infections were studied. We found that 80% of ear infections occurred during a very narrow window of susceptibility – age 6-21 months. About 72% of children had a window of susceptibility to ear infections that lasted 5 months or less; 97% of children had a window of susceptibility that lasted 10 months or less.
From this result, we observed that about 90% of children have a window of time lasting about 10 months when they get repeated ear infections. By the time a child gets three ear infections in 6 months (a period of time recommended by the AAP and American Academy of Otolaryngology–Head and Neck Surgery when ear tubes might be considered) and then a referral for ear tubes is made and the child gets an appointment with the ear, nose, and throat doctor, and surgery is scheduled, the ear infections were going to stop anyway.
In other words, millions of children worldwide have been getting ear tubes and physicians and parents saw that the ear infections stopped. So they concluded the ear tubes stopped the infections. We found the infections were going to stop anyway even if the child did not receive ear tubes because their susceptibility to ear infections is over by the time the surgery is performed. The child outgrew ear infections.
An exception was children in daycare at an early age. Our study found that children in daycare who are around 6 months old and start getting ear infections at that age are likely destined to have three or more ear infections in the first year of life. If children are going to be in daycare, perhaps those who need them should receive ear tubes early. Analysis of other demographic and risk factor covariates – sex, race/ethnicity, breastfeeding, siblings in the home, smoking in the home, atopy, and family history of otitis media – were not significantly associated with the number of AOMs in the child population we studied.
We developed a prediction model for doctors, so they could input a child’s age, number of ear infections, and daycare attendance and receive back an estimate of the number of likely future ear infections for that child. With that knowledge, physicians and parents can make more informed decisions.
Our message to clinicians and parents is to reconsider the necessity and timing of ear tube surgery for children with recurrent ear infections because the future is not predicted by the past. Children having several ear infections in a short time does not predict that they will have a similar number of ear infections in the future.
The study was supported by the National Institutes of Health awarded to Rochester Regional Health. Dr. Pichichero was principal investigator for the award.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
About half a million children between the ages of 1 and 3 years old have ear tube surgery in the United States every year at an annual cost exceeding $2 billion. It is the most common childhood surgery performed with anesthesia. It is a surgery commonly performed on children in most other high- and middle-income countries.
My group recently published a paper on the timing and necessity of tympanostomy tubes for recurrent otitis media in young children. The primary objective was to quantitatively examine recurrent acute otitis media (AOM) incidence with respect to age of occurrence, the influence of daycare attendance, and other risk factors in individual children. We introduced the concept of a “window of susceptibility” to AOM as new terminology referring to a child who has two or more closely spaced AOM occurrences during a window of time. We sought to know what to expect and how to advise the parent when a child presents with closely spaced AOMs.
A secondary objective was to develop models to predict the risk and timing of AOM recurrences based on the natural history of disease in young children who do not get tympanostomy tubes. Prediction models were developed to assist clinicians in understanding and explaining to parents the benefit of tympanostomy tubes based on the child’s age and number of AOMs.
The children were all from a primary care pediatric practice in Rochester, N.Y., which comprised a typical mixed demographic of largely middle-class, health care–insured families that was broadly representative of the racial/ethnic diversity in the community. The sample included both wealthy families and those living below the poverty line. The diagnosis of AOM was made based on the American Academy of Pediatrics guidance in which a presumed middle ear effusion and a full or bulging tympanic membrane were required. Almost all episodes (> 85%) of clinically diagnosed AOM cases were confirmed by culture of middle ear fluid collected by tympanocentesis to ensure diagnostic accuracy.
286 children who had ear infections were studied. We found that 80% of ear infections occurred during a very narrow window of susceptibility – age 6-21 months. About 72% of children had a window of susceptibility to ear infections that lasted 5 months or less; 97% of children had a window of susceptibility that lasted 10 months or less.
From this result, we observed that about 90% of children have a window of time lasting about 10 months when they get repeated ear infections. By the time a child gets three ear infections in 6 months (a period of time recommended by the AAP and American Academy of Otolaryngology–Head and Neck Surgery when ear tubes might be considered) and then a referral for ear tubes is made and the child gets an appointment with the ear, nose, and throat doctor, and surgery is scheduled, the ear infections were going to stop anyway.
In other words, millions of children worldwide have been getting ear tubes and physicians and parents saw that the ear infections stopped. So they concluded the ear tubes stopped the infections. We found the infections were going to stop anyway even if the child did not receive ear tubes because their susceptibility to ear infections is over by the time the surgery is performed. The child outgrew ear infections.
An exception was children in daycare at an early age. Our study found that children in daycare who are around 6 months old and start getting ear infections at that age are likely destined to have three or more ear infections in the first year of life. If children are going to be in daycare, perhaps those who need them should receive ear tubes early. Analysis of other demographic and risk factor covariates – sex, race/ethnicity, breastfeeding, siblings in the home, smoking in the home, atopy, and family history of otitis media – were not significantly associated with the number of AOMs in the child population we studied.
We developed a prediction model for doctors, so they could input a child’s age, number of ear infections, and daycare attendance and receive back an estimate of the number of likely future ear infections for that child. With that knowledge, physicians and parents can make more informed decisions.
Our message to clinicians and parents is to reconsider the necessity and timing of ear tube surgery for children with recurrent ear infections because the future is not predicted by the past. Children having several ear infections in a short time does not predict that they will have a similar number of ear infections in the future.
The study was supported by the National Institutes of Health awarded to Rochester Regional Health. Dr. Pichichero was principal investigator for the award.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
About half a million children between the ages of 1 and 3 years old have ear tube surgery in the United States every year at an annual cost exceeding $2 billion. It is the most common childhood surgery performed with anesthesia. It is a surgery commonly performed on children in most other high- and middle-income countries.
My group recently published a paper on the timing and necessity of tympanostomy tubes for recurrent otitis media in young children. The primary objective was to quantitatively examine recurrent acute otitis media (AOM) incidence with respect to age of occurrence, the influence of daycare attendance, and other risk factors in individual children. We introduced the concept of a “window of susceptibility” to AOM as new terminology referring to a child who has two or more closely spaced AOM occurrences during a window of time. We sought to know what to expect and how to advise the parent when a child presents with closely spaced AOMs.
A secondary objective was to develop models to predict the risk and timing of AOM recurrences based on the natural history of disease in young children who do not get tympanostomy tubes. Prediction models were developed to assist clinicians in understanding and explaining to parents the benefit of tympanostomy tubes based on the child’s age and number of AOMs.
The children were all from a primary care pediatric practice in Rochester, N.Y., which comprised a typical mixed demographic of largely middle-class, health care–insured families that was broadly representative of the racial/ethnic diversity in the community. The sample included both wealthy families and those living below the poverty line. The diagnosis of AOM was made based on the American Academy of Pediatrics guidance in which a presumed middle ear effusion and a full or bulging tympanic membrane were required. Almost all episodes (> 85%) of clinically diagnosed AOM cases were confirmed by culture of middle ear fluid collected by tympanocentesis to ensure diagnostic accuracy.
286 children who had ear infections were studied. We found that 80% of ear infections occurred during a very narrow window of susceptibility – age 6-21 months. About 72% of children had a window of susceptibility to ear infections that lasted 5 months or less; 97% of children had a window of susceptibility that lasted 10 months or less.
From this result, we observed that about 90% of children have a window of time lasting about 10 months when they get repeated ear infections. By the time a child gets three ear infections in 6 months (a period of time recommended by the AAP and American Academy of Otolaryngology–Head and Neck Surgery when ear tubes might be considered) and then a referral for ear tubes is made and the child gets an appointment with the ear, nose, and throat doctor, and surgery is scheduled, the ear infections were going to stop anyway.
In other words, millions of children worldwide have been getting ear tubes and physicians and parents saw that the ear infections stopped. So they concluded the ear tubes stopped the infections. We found the infections were going to stop anyway even if the child did not receive ear tubes because their susceptibility to ear infections is over by the time the surgery is performed. The child outgrew ear infections.
An exception was children in daycare at an early age. Our study found that children in daycare who are around 6 months old and start getting ear infections at that age are likely destined to have three or more ear infections in the first year of life. If children are going to be in daycare, perhaps those who need them should receive ear tubes early. Analysis of other demographic and risk factor covariates – sex, race/ethnicity, breastfeeding, siblings in the home, smoking in the home, atopy, and family history of otitis media – were not significantly associated with the number of AOMs in the child population we studied.
We developed a prediction model for doctors, so they could input a child’s age, number of ear infections, and daycare attendance and receive back an estimate of the number of likely future ear infections for that child. With that knowledge, physicians and parents can make more informed decisions.
Our message to clinicians and parents is to reconsider the necessity and timing of ear tube surgery for children with recurrent ear infections because the future is not predicted by the past. Children having several ear infections in a short time does not predict that they will have a similar number of ear infections in the future.
The study was supported by the National Institutes of Health awarded to Rochester Regional Health. Dr. Pichichero was principal investigator for the award.
Dr. Pichichero is a specialist in pediatric infectious diseases, Center for Infectious Diseases and Immunology, and director of the Research Institute, at Rochester (N.Y.) General Hospital. He has no conflicts of interest to declare.
USPSTF backs screening for hypertensive disorders of pregnancy
The U.S. Preventive Services Task Force (USPSTF) recommends that clinicians screen for hypertensive disorders of pregnancy, which can cause serious and fatal complications, according to a new draft statement.
All pregnant people should have their blood pressure measured at each prenatal visit to identify and prevent serious health problems. The grade B recommendation expands on the task force’s 2017 recommendation on screening for preeclampsia to include all hypertensive disorders of pregnancy.
“Hypertensive disorders of pregnancy are some of the leading causes of serious complications and death for pregnant people,” Esa Davis, MD, a USPSTF member and associate professor of medicine and clinical and translational science at the University of Pittsburgh School of Medicine, told this news organization.
In the U.S., the rate of hypertensive disorders of pregnancy has increased in recent decades, jumping from about 500 cases per 10,000 deliveries in the early 1990s to more than 1,000 cases per 10,000 deliveries in the mid-2010s.
“The U.S. Preventive Services Task Force wants to help save the lives of pregnant people and their babies by ensuring that clinicians have the most up-to-date guidance on how to find these conditions early,” she said.
The draft recommendation statement was published online .
Screening recommendation
Hypertensive disorders of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and chronic hypertension with and without superimposed preeclampsia, are marked by elevated blood pressure during pregnancy.
The disorders can lead to complications for the pregnant person, such as stroke, retinal detachment, organ damage or failure, and seizures, as well as for the baby, including restricted growth, low birth weight, and stillbirth. Many complications can lead to early induction of labor, cesarean delivery, and preterm birth.
After commissioning a systematic evidence review, the USPSTF provided a grade B recommendation for clinicians to offer or provide screening for hypertensive disorders of pregnancy. The recommendation concludes with “moderate certainty” that screening with blood pressure measurements has “substantial net benefit.”
The task force notes that it is “essential” for all pregnant women and pregnant people of all genders to be screened and that those who screen positive receive evidence-based management of their condition.
Risk factors include a history of eclampsia or preeclampsia, a family history of preeclampsia, a previous adverse pregnancy outcome, having gestational diabetes or chronic hypertension, being pregnant with more than one baby, having a first pregnancy, having a high body mass index prior to pregnancy, and being 35 years of age or older.
In addition, Black, American Indian, and Alaska Native people face higher risks and are more likely both to have and to die from a hypertensive disorder of pregnancy. In particular, Black people experience higher rates of maternal and infant morbidity and perinatal mortality than other racial and ethnic groups, and hypertensive disorders of pregnancy account for a larger proportion of these outcomes.
Although measuring blood pressure throughout pregnancy is an important first step, it’s not enough to improve inequities in health outcomes, the task force notes. Identifying hypertensive disorders of pregnancy requires adequate prenatal follow-up visits, surveillance, and evidence-based care, which can be a barrier for some pregnant people.
Follow-up visits with health care providers such as nurses, nurse midwives, pediatricians, and lactation consultants could help, as well as screening and monitoring during the postpartum period. Other approaches include telehealth, connections to community resources during the perinatal period, collaborative care provided in medical homes, and multilevel interventions to address underlying health inequities that increase health risks during pregnancy.
“Since screening is not enough to address the health disparities experienced by Black, American Indian, and Alaska Native people, health care professionals should also do what they can to help address these inequities,” Dr. Davis said. “For example, the task force identified a few promising approaches, including using standardized clinical bundles of best practices for disease management to help ensure that all pregnant persons receive appropriate, equitable care.”
Additional considerations
The USPSTF looked at the evidence on additional methods of screening but continued to find that measuring blood pressure at each prenatal visit is the best approach. Other evaluations, such as testing for proteinuria when preeclampsia is suspected, have low accuracy for detecting proteinuria in pregnancy.
Although there is no currently available treatment for preeclampsia except delivery, management strategies for diagnosed hypertensive disorders of pregnancy include close fetal and maternal monitoring, antihypertension medications, and magnesium sulfate for seizure prophylaxis when indicated.
Previously, the USPSTF also recommended that pregnant Black people be considered for treatment with low-dose aspirin to prevent preeclampsia, with aspirin use recommended for those with at least one additional moderate risk factor. Clinicians should also be aware of the complications of poor health outcomes among populations who face higher risks.
The USPSTF noted several gaps for future research, including the best approaches for blood pressure monitoring during pregnancy and the postpartum period, how to address health inequities through multilevel interventions, how to increase access to care through telehealth services, and how to mitigate cardiovascular complications later in life in patients diagnosed with hypertensive disorders of pregnancy.
“Continued research is needed in these promising areas,” Dr. Davis said. “We hope all clinicians will join us in helping ensure that all parents and babies have access to the care they need to be as healthy as possible.”
The draft recommendation statement and draft evidence review were posted for public comment on the USPSTF website. Comments can be submitted until March 6.
No relevant financial relationships have been disclosed.
A version of this article originally appeared on Medscape.com.
The U.S. Preventive Services Task Force (USPSTF) recommends that clinicians screen for hypertensive disorders of pregnancy, which can cause serious and fatal complications, according to a new draft statement.
All pregnant people should have their blood pressure measured at each prenatal visit to identify and prevent serious health problems. The grade B recommendation expands on the task force’s 2017 recommendation on screening for preeclampsia to include all hypertensive disorders of pregnancy.
“Hypertensive disorders of pregnancy are some of the leading causes of serious complications and death for pregnant people,” Esa Davis, MD, a USPSTF member and associate professor of medicine and clinical and translational science at the University of Pittsburgh School of Medicine, told this news organization.
In the U.S., the rate of hypertensive disorders of pregnancy has increased in recent decades, jumping from about 500 cases per 10,000 deliveries in the early 1990s to more than 1,000 cases per 10,000 deliveries in the mid-2010s.
“The U.S. Preventive Services Task Force wants to help save the lives of pregnant people and their babies by ensuring that clinicians have the most up-to-date guidance on how to find these conditions early,” she said.
The draft recommendation statement was published online .
Screening recommendation
Hypertensive disorders of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and chronic hypertension with and without superimposed preeclampsia, are marked by elevated blood pressure during pregnancy.
The disorders can lead to complications for the pregnant person, such as stroke, retinal detachment, organ damage or failure, and seizures, as well as for the baby, including restricted growth, low birth weight, and stillbirth. Many complications can lead to early induction of labor, cesarean delivery, and preterm birth.
After commissioning a systematic evidence review, the USPSTF provided a grade B recommendation for clinicians to offer or provide screening for hypertensive disorders of pregnancy. The recommendation concludes with “moderate certainty” that screening with blood pressure measurements has “substantial net benefit.”
The task force notes that it is “essential” for all pregnant women and pregnant people of all genders to be screened and that those who screen positive receive evidence-based management of their condition.
Risk factors include a history of eclampsia or preeclampsia, a family history of preeclampsia, a previous adverse pregnancy outcome, having gestational diabetes or chronic hypertension, being pregnant with more than one baby, having a first pregnancy, having a high body mass index prior to pregnancy, and being 35 years of age or older.
In addition, Black, American Indian, and Alaska Native people face higher risks and are more likely both to have and to die from a hypertensive disorder of pregnancy. In particular, Black people experience higher rates of maternal and infant morbidity and perinatal mortality than other racial and ethnic groups, and hypertensive disorders of pregnancy account for a larger proportion of these outcomes.
Although measuring blood pressure throughout pregnancy is an important first step, it’s not enough to improve inequities in health outcomes, the task force notes. Identifying hypertensive disorders of pregnancy requires adequate prenatal follow-up visits, surveillance, and evidence-based care, which can be a barrier for some pregnant people.
Follow-up visits with health care providers such as nurses, nurse midwives, pediatricians, and lactation consultants could help, as well as screening and monitoring during the postpartum period. Other approaches include telehealth, connections to community resources during the perinatal period, collaborative care provided in medical homes, and multilevel interventions to address underlying health inequities that increase health risks during pregnancy.
“Since screening is not enough to address the health disparities experienced by Black, American Indian, and Alaska Native people, health care professionals should also do what they can to help address these inequities,” Dr. Davis said. “For example, the task force identified a few promising approaches, including using standardized clinical bundles of best practices for disease management to help ensure that all pregnant persons receive appropriate, equitable care.”
Additional considerations
The USPSTF looked at the evidence on additional methods of screening but continued to find that measuring blood pressure at each prenatal visit is the best approach. Other evaluations, such as testing for proteinuria when preeclampsia is suspected, have low accuracy for detecting proteinuria in pregnancy.
Although there is no currently available treatment for preeclampsia except delivery, management strategies for diagnosed hypertensive disorders of pregnancy include close fetal and maternal monitoring, antihypertension medications, and magnesium sulfate for seizure prophylaxis when indicated.
Previously, the USPSTF also recommended that pregnant Black people be considered for treatment with low-dose aspirin to prevent preeclampsia, with aspirin use recommended for those with at least one additional moderate risk factor. Clinicians should also be aware of the complications of poor health outcomes among populations who face higher risks.
The USPSTF noted several gaps for future research, including the best approaches for blood pressure monitoring during pregnancy and the postpartum period, how to address health inequities through multilevel interventions, how to increase access to care through telehealth services, and how to mitigate cardiovascular complications later in life in patients diagnosed with hypertensive disorders of pregnancy.
“Continued research is needed in these promising areas,” Dr. Davis said. “We hope all clinicians will join us in helping ensure that all parents and babies have access to the care they need to be as healthy as possible.”
The draft recommendation statement and draft evidence review were posted for public comment on the USPSTF website. Comments can be submitted until March 6.
No relevant financial relationships have been disclosed.
A version of this article originally appeared on Medscape.com.
The U.S. Preventive Services Task Force (USPSTF) recommends that clinicians screen for hypertensive disorders of pregnancy, which can cause serious and fatal complications, according to a new draft statement.
All pregnant people should have their blood pressure measured at each prenatal visit to identify and prevent serious health problems. The grade B recommendation expands on the task force’s 2017 recommendation on screening for preeclampsia to include all hypertensive disorders of pregnancy.
“Hypertensive disorders of pregnancy are some of the leading causes of serious complications and death for pregnant people,” Esa Davis, MD, a USPSTF member and associate professor of medicine and clinical and translational science at the University of Pittsburgh School of Medicine, told this news organization.
In the U.S., the rate of hypertensive disorders of pregnancy has increased in recent decades, jumping from about 500 cases per 10,000 deliveries in the early 1990s to more than 1,000 cases per 10,000 deliveries in the mid-2010s.
“The U.S. Preventive Services Task Force wants to help save the lives of pregnant people and their babies by ensuring that clinicians have the most up-to-date guidance on how to find these conditions early,” she said.
The draft recommendation statement was published online .
Screening recommendation
Hypertensive disorders of pregnancy, including gestational hypertension, preeclampsia, eclampsia, and chronic hypertension with and without superimposed preeclampsia, are marked by elevated blood pressure during pregnancy.
The disorders can lead to complications for the pregnant person, such as stroke, retinal detachment, organ damage or failure, and seizures, as well as for the baby, including restricted growth, low birth weight, and stillbirth. Many complications can lead to early induction of labor, cesarean delivery, and preterm birth.
After commissioning a systematic evidence review, the USPSTF provided a grade B recommendation for clinicians to offer or provide screening for hypertensive disorders of pregnancy. The recommendation concludes with “moderate certainty” that screening with blood pressure measurements has “substantial net benefit.”
The task force notes that it is “essential” for all pregnant women and pregnant people of all genders to be screened and that those who screen positive receive evidence-based management of their condition.
Risk factors include a history of eclampsia or preeclampsia, a family history of preeclampsia, a previous adverse pregnancy outcome, having gestational diabetes or chronic hypertension, being pregnant with more than one baby, having a first pregnancy, having a high body mass index prior to pregnancy, and being 35 years of age or older.
In addition, Black, American Indian, and Alaska Native people face higher risks and are more likely both to have and to die from a hypertensive disorder of pregnancy. In particular, Black people experience higher rates of maternal and infant morbidity and perinatal mortality than other racial and ethnic groups, and hypertensive disorders of pregnancy account for a larger proportion of these outcomes.
Although measuring blood pressure throughout pregnancy is an important first step, it’s not enough to improve inequities in health outcomes, the task force notes. Identifying hypertensive disorders of pregnancy requires adequate prenatal follow-up visits, surveillance, and evidence-based care, which can be a barrier for some pregnant people.
Follow-up visits with health care providers such as nurses, nurse midwives, pediatricians, and lactation consultants could help, as well as screening and monitoring during the postpartum period. Other approaches include telehealth, connections to community resources during the perinatal period, collaborative care provided in medical homes, and multilevel interventions to address underlying health inequities that increase health risks during pregnancy.
“Since screening is not enough to address the health disparities experienced by Black, American Indian, and Alaska Native people, health care professionals should also do what they can to help address these inequities,” Dr. Davis said. “For example, the task force identified a few promising approaches, including using standardized clinical bundles of best practices for disease management to help ensure that all pregnant persons receive appropriate, equitable care.”
Additional considerations
The USPSTF looked at the evidence on additional methods of screening but continued to find that measuring blood pressure at each prenatal visit is the best approach. Other evaluations, such as testing for proteinuria when preeclampsia is suspected, have low accuracy for detecting proteinuria in pregnancy.
Although there is no currently available treatment for preeclampsia except delivery, management strategies for diagnosed hypertensive disorders of pregnancy include close fetal and maternal monitoring, antihypertension medications, and magnesium sulfate for seizure prophylaxis when indicated.
Previously, the USPSTF also recommended that pregnant Black people be considered for treatment with low-dose aspirin to prevent preeclampsia, with aspirin use recommended for those with at least one additional moderate risk factor. Clinicians should also be aware of the complications of poor health outcomes among populations who face higher risks.
The USPSTF noted several gaps for future research, including the best approaches for blood pressure monitoring during pregnancy and the postpartum period, how to address health inequities through multilevel interventions, how to increase access to care through telehealth services, and how to mitigate cardiovascular complications later in life in patients diagnosed with hypertensive disorders of pregnancy.
“Continued research is needed in these promising areas,” Dr. Davis said. “We hope all clinicians will join us in helping ensure that all parents and babies have access to the care they need to be as healthy as possible.”
The draft recommendation statement and draft evidence review were posted for public comment on the USPSTF website. Comments can be submitted until March 6.
No relevant financial relationships have been disclosed.
A version of this article originally appeared on Medscape.com.
Dapagliflozin gets expanded heart failure indication in Europe
The European Commission has expanded the indication for dapagliflozin (Forxiga) to include heart failure across the full spectrum of left ventricular ejection fraction – including HF with mildly reduced and preserved ejection fraction, AstraZeneca has announced.
The EC nod for the sodium-glucose cotransporter 2 (SGLT2) inhibitor (known as Farxiga in the United States) follows the positive opinion of the Committee for Medicinal Products for Human Use of the European Medicines Agency in December 2022.
The committee’s decision was based on results from the DELIVER phase 3 trial, which showed clear clinical benefits of the SGLT2 inhibitor in patients with HF regardless of their left ventricular function.
The study was published in the New England Journal of Medicine and presented at the European Society of Cardiology’s annual congress.
The data support the use of SGLT2 inhibitors as “foundational agents for virtually all patients with heart failure” regardless of their ejection fraction or whether or not they have type 2 diabetes, said study presenter Scott D. Solomon, MD, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston.
The Food and Drug Administration is currently reviewing AstraZeneca’s application to expand the HF indication for dapagliflozin in the United States.
A version of this article first appeared on Medscape.com.
The European Commission has expanded the indication for dapagliflozin (Forxiga) to include heart failure across the full spectrum of left ventricular ejection fraction – including HF with mildly reduced and preserved ejection fraction, AstraZeneca has announced.
The EC nod for the sodium-glucose cotransporter 2 (SGLT2) inhibitor (known as Farxiga in the United States) follows the positive opinion of the Committee for Medicinal Products for Human Use of the European Medicines Agency in December 2022.
The committee’s decision was based on results from the DELIVER phase 3 trial, which showed clear clinical benefits of the SGLT2 inhibitor in patients with HF regardless of their left ventricular function.
The study was published in the New England Journal of Medicine and presented at the European Society of Cardiology’s annual congress.
The data support the use of SGLT2 inhibitors as “foundational agents for virtually all patients with heart failure” regardless of their ejection fraction or whether or not they have type 2 diabetes, said study presenter Scott D. Solomon, MD, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston.
The Food and Drug Administration is currently reviewing AstraZeneca’s application to expand the HF indication for dapagliflozin in the United States.
A version of this article first appeared on Medscape.com.
The European Commission has expanded the indication for dapagliflozin (Forxiga) to include heart failure across the full spectrum of left ventricular ejection fraction – including HF with mildly reduced and preserved ejection fraction, AstraZeneca has announced.
The EC nod for the sodium-glucose cotransporter 2 (SGLT2) inhibitor (known as Farxiga in the United States) follows the positive opinion of the Committee for Medicinal Products for Human Use of the European Medicines Agency in December 2022.
The committee’s decision was based on results from the DELIVER phase 3 trial, which showed clear clinical benefits of the SGLT2 inhibitor in patients with HF regardless of their left ventricular function.
The study was published in the New England Journal of Medicine and presented at the European Society of Cardiology’s annual congress.
The data support the use of SGLT2 inhibitors as “foundational agents for virtually all patients with heart failure” regardless of their ejection fraction or whether or not they have type 2 diabetes, said study presenter Scott D. Solomon, MD, of Harvard Medical School and Brigham and Women’s Hospital, both in Boston.
The Food and Drug Administration is currently reviewing AstraZeneca’s application to expand the HF indication for dapagliflozin in the United States.
A version of this article first appeared on Medscape.com.
Cardiac monitoring company settles DOJ false claims allegations
Beyond Reps (dba IronRod Health and Cardiac Monitoring Services) has agreed to pay $673,200 to resolve allegations that it submitted false claims to federal health care programs relating to remote cardiac monitoring services.
The U.S. Department of Justice alleges that between Jan. 1, 2018, and April 30, 2021, IronRod, with headquarters in Phoenix, used technicians who lacked required credentials to conduct remote cardiac monitoring readings.
The government further alleges that between June 1, 2018, and Aug. 20, 2018, the company misrepresented that it performed services in New York state in order to get higher reimbursements from Medicare for remote cardiac monitoring services.
“Providers that seek payment from federal health programs are required to follow laws meant to protect beneficiaries, as well as to protect the integrity of those programs,” U.S. Attorney Trini E. Ross said in a statement.
“Our office is committed to pursuing cases against any provider that cuts corners or seeks to obtain payments for which they are not entitled,” Ms. Ross said.
A request to Beyond Reps for comment was not returned.
The civil settlement resolves claims brought under the qui tam (whistleblower) provisions of the False Claims Act by Coleen DeGroat.
Under those provisions, a private party can file an action on behalf of the United States and receive a portion of any recovery. Ms. DeGroat will receive a share of the settlement.
A version of this article first appeared on Medscape.com.
Beyond Reps (dba IronRod Health and Cardiac Monitoring Services) has agreed to pay $673,200 to resolve allegations that it submitted false claims to federal health care programs relating to remote cardiac monitoring services.
The U.S. Department of Justice alleges that between Jan. 1, 2018, and April 30, 2021, IronRod, with headquarters in Phoenix, used technicians who lacked required credentials to conduct remote cardiac monitoring readings.
The government further alleges that between June 1, 2018, and Aug. 20, 2018, the company misrepresented that it performed services in New York state in order to get higher reimbursements from Medicare for remote cardiac monitoring services.
“Providers that seek payment from federal health programs are required to follow laws meant to protect beneficiaries, as well as to protect the integrity of those programs,” U.S. Attorney Trini E. Ross said in a statement.
“Our office is committed to pursuing cases against any provider that cuts corners or seeks to obtain payments for which they are not entitled,” Ms. Ross said.
A request to Beyond Reps for comment was not returned.
The civil settlement resolves claims brought under the qui tam (whistleblower) provisions of the False Claims Act by Coleen DeGroat.
Under those provisions, a private party can file an action on behalf of the United States and receive a portion of any recovery. Ms. DeGroat will receive a share of the settlement.
A version of this article first appeared on Medscape.com.
Beyond Reps (dba IronRod Health and Cardiac Monitoring Services) has agreed to pay $673,200 to resolve allegations that it submitted false claims to federal health care programs relating to remote cardiac monitoring services.
The U.S. Department of Justice alleges that between Jan. 1, 2018, and April 30, 2021, IronRod, with headquarters in Phoenix, used technicians who lacked required credentials to conduct remote cardiac monitoring readings.
The government further alleges that between June 1, 2018, and Aug. 20, 2018, the company misrepresented that it performed services in New York state in order to get higher reimbursements from Medicare for remote cardiac monitoring services.
“Providers that seek payment from federal health programs are required to follow laws meant to protect beneficiaries, as well as to protect the integrity of those programs,” U.S. Attorney Trini E. Ross said in a statement.
“Our office is committed to pursuing cases against any provider that cuts corners or seeks to obtain payments for which they are not entitled,” Ms. Ross said.
A request to Beyond Reps for comment was not returned.
The civil settlement resolves claims brought under the qui tam (whistleblower) provisions of the False Claims Act by Coleen DeGroat.
Under those provisions, a private party can file an action on behalf of the United States and receive a portion of any recovery. Ms. DeGroat will receive a share of the settlement.
A version of this article first appeared on Medscape.com.
What happened to surgical mitral valve repair in the MitraClip era?
The overall case volume for surgical mitral valve (MV) repair of degenerative mitral regurgitation (DMR) hasn’t changed much nearly a decade into the age of transcatheter edge-to-edge repair (TEER). But, over the same period, there’s been a shift in the surgical–MV repair case mix at centers that have offered both the surgical option and TEER, a new study suggests.
Once TEER was introduced, those centers over time used the operative approach less in higher– and intermediate–surgical risk patients and more often in those deemed low risk for surgery. And that trend – at centers offering both approaches – paralleled improved risk-adjusted surgical repair short-term complications and 30-day and 5-year mortality.
The findings come from an analysis based on Society of Thoracic Surgeons and Medicare claims data collected from 2011 through 2018 at surgical–MV repair centers that also offered TEER for DMR after its 2013 approval. The transcatheter procedure, until only recently the exclusive domain of Abbott’s MitraClip in various incarnations, is officially indicated for patients judged too high risk for surgical MV repair.
A shift in surgical MV repair to predominantly lower-risk patients would be expected to improve outcomes. But the improvements seen in the current study seem to have a more complex explanation, Sreekanth Vemulapalli, MD, told this news organization.
The data seem to show TEER indication creep from higher-risk cases, for which there is clinical trial support, to intermediate-risk patients, that lack such evidence in favor of TEER. That seemed to push surgical repair toward even lower-risk cases. “I think that’s exactly right,” said Dr. Vemulapalli, Duke Clinical Research Institute, Durham, N.C.
Still, he observed, the analysis was adjusted for surgical risk, and “Even after that adjustment, it looked like surgical outcomes were getting better after the availability of transcatheter mitral repair techniques.”
That observation may be explained by an increasingly sharp, “more careful” process for selecting patients for surgical repair vs. TEER, said Dr. Vemulapalli, who is senior author of the study published in the Journal of the American College of Cardiology. Angela M. Lowenstern, MD, Vanderbilt University, Nashville, and Andrew M. Vekstein, MD, Duke Clinical Research Institute, were the lead authors.
Indeed, the report states, the analysis supports the view that “a systematic evaluation by a heart team able to direct patients towards either surgical or transcatheter approaches enhances both short-term and long-term surgical outcomes.”
“In a world where both surgical and transcatheter techniques are going to be available,” Dr. Vemulapalli said, “patient selection becomes very, very important.”
An accompanying editorial acknowledges the heart-team approach’s potential for improving the selection of patients for surgery and perhaps therefore outcomes. But it also cites issues with that interpretation of the data.
For example, the heart-team approach is not used in consistent ways across the United States. And “although the heart team is recommended in multiple guidelines for valvular heart therapies, there is little evidence for its efficacy, specifically regarding improving clinical outcomes,” write Matthew W. Sherwood, MD, MHS, and Wayne B. Batchelor, MD, MHS, Inova Heart and Vascular Institute, Falls Church, Va.
The editorialists highlight the study’s “significant downtrend in both high-risk and intermediate-risk surgical cases, with a concomitant increase in low-risk cases,” after introduction of TEER. That shift in case mix, they write, “would seem to be a more likely explanation for the modest improvement in outcomes for surgical MV repair.”
Also, importantly, the analysis didn’t include data on TEER procedures, only indirect evidence for TEER’s effect on surgical MV repair, the editorialists observe, and study authors acknowledge.
Still, the analysis looked at nearly 14,000 patients at 278 U.S. sites with surgical MV repair that launched TEER programs during the study period. They accounted for 6,806 surgical cases before and 7,153 surgical cases after the advent of TEER.
Their median annualized institutional surgical MV repair volume was 32 before and 29 after TEER availability (P = .06).
The risk-adjusted odds ratio for 30-day mortality after vs. before TEER became an option was 0.73 (95% confidence interval, 0.54-0.99). The corresponding hazard ratio for mortality at 5 years was 0.75 (95% CI, 0.66-0.86).
Other risk-adjusted surgical outcomes improved once TEER became available, including MV adverse outcomes (OR, 0.71; 95% CI, 0.58-0.86; P < .001), operative mortality (OR, 0.73; 95% CI, 0.54-0.99; P = .041), and major morbidity (OR, 0.85; 95% CI, 0.73-0.98; P = .026)
Despite the data’s suggestion of TEER indication creep from solely high–surgical risk patients to those at intermediate risk, Dr. Vemulapalli said, “I don’t think that people should be doing transcatheter mitral repair in intermediate- or low-risk patients as a general rule.” Although, he added, “there will always be certain exceptions, depending on the patient’s specific situation.”
Dr. Vemulapalli pointed to several ongoing trials comparing TEER vs. surgical MR repair in patients with DMR at intermediate surgical risk, including REPAIR MR and PRIMARY.
The study was supported by the National Institutes of Health and Abbott. Dr. Vemulapalli discloses receiving grants or contracts from the American College of Cardiology, the Society of Thoracic Surgeons, Cytokinetics, Abbott Vascular, the National Institutes of Health, and Boston Scientific; and consulting or serving on an advisory board for Janssen, the American College of Physicians, HeartFlow, and Edwards LifeSciences. Dr. Sherwood discloses receiving honoraria or consulting fees from Medtronic and Boston Scientific. Dr. Batchelor discloses receiving consulting fees from Medtronic, Boston Scientific, Edwards Lifesciences, and Abbott.
A version of this article first appeared on Medscape.com.
The overall case volume for surgical mitral valve (MV) repair of degenerative mitral regurgitation (DMR) hasn’t changed much nearly a decade into the age of transcatheter edge-to-edge repair (TEER). But, over the same period, there’s been a shift in the surgical–MV repair case mix at centers that have offered both the surgical option and TEER, a new study suggests.
Once TEER was introduced, those centers over time used the operative approach less in higher– and intermediate–surgical risk patients and more often in those deemed low risk for surgery. And that trend – at centers offering both approaches – paralleled improved risk-adjusted surgical repair short-term complications and 30-day and 5-year mortality.
The findings come from an analysis based on Society of Thoracic Surgeons and Medicare claims data collected from 2011 through 2018 at surgical–MV repair centers that also offered TEER for DMR after its 2013 approval. The transcatheter procedure, until only recently the exclusive domain of Abbott’s MitraClip in various incarnations, is officially indicated for patients judged too high risk for surgical MV repair.
A shift in surgical MV repair to predominantly lower-risk patients would be expected to improve outcomes. But the improvements seen in the current study seem to have a more complex explanation, Sreekanth Vemulapalli, MD, told this news organization.
The data seem to show TEER indication creep from higher-risk cases, for which there is clinical trial support, to intermediate-risk patients, that lack such evidence in favor of TEER. That seemed to push surgical repair toward even lower-risk cases. “I think that’s exactly right,” said Dr. Vemulapalli, Duke Clinical Research Institute, Durham, N.C.
Still, he observed, the analysis was adjusted for surgical risk, and “Even after that adjustment, it looked like surgical outcomes were getting better after the availability of transcatheter mitral repair techniques.”
That observation may be explained by an increasingly sharp, “more careful” process for selecting patients for surgical repair vs. TEER, said Dr. Vemulapalli, who is senior author of the study published in the Journal of the American College of Cardiology. Angela M. Lowenstern, MD, Vanderbilt University, Nashville, and Andrew M. Vekstein, MD, Duke Clinical Research Institute, were the lead authors.
Indeed, the report states, the analysis supports the view that “a systematic evaluation by a heart team able to direct patients towards either surgical or transcatheter approaches enhances both short-term and long-term surgical outcomes.”
“In a world where both surgical and transcatheter techniques are going to be available,” Dr. Vemulapalli said, “patient selection becomes very, very important.”
An accompanying editorial acknowledges the heart-team approach’s potential for improving the selection of patients for surgery and perhaps therefore outcomes. But it also cites issues with that interpretation of the data.
For example, the heart-team approach is not used in consistent ways across the United States. And “although the heart team is recommended in multiple guidelines for valvular heart therapies, there is little evidence for its efficacy, specifically regarding improving clinical outcomes,” write Matthew W. Sherwood, MD, MHS, and Wayne B. Batchelor, MD, MHS, Inova Heart and Vascular Institute, Falls Church, Va.
The editorialists highlight the study’s “significant downtrend in both high-risk and intermediate-risk surgical cases, with a concomitant increase in low-risk cases,” after introduction of TEER. That shift in case mix, they write, “would seem to be a more likely explanation for the modest improvement in outcomes for surgical MV repair.”
Also, importantly, the analysis didn’t include data on TEER procedures, only indirect evidence for TEER’s effect on surgical MV repair, the editorialists observe, and study authors acknowledge.
Still, the analysis looked at nearly 14,000 patients at 278 U.S. sites with surgical MV repair that launched TEER programs during the study period. They accounted for 6,806 surgical cases before and 7,153 surgical cases after the advent of TEER.
Their median annualized institutional surgical MV repair volume was 32 before and 29 after TEER availability (P = .06).
The risk-adjusted odds ratio for 30-day mortality after vs. before TEER became an option was 0.73 (95% confidence interval, 0.54-0.99). The corresponding hazard ratio for mortality at 5 years was 0.75 (95% CI, 0.66-0.86).
Other risk-adjusted surgical outcomes improved once TEER became available, including MV adverse outcomes (OR, 0.71; 95% CI, 0.58-0.86; P < .001), operative mortality (OR, 0.73; 95% CI, 0.54-0.99; P = .041), and major morbidity (OR, 0.85; 95% CI, 0.73-0.98; P = .026)
Despite the data’s suggestion of TEER indication creep from solely high–surgical risk patients to those at intermediate risk, Dr. Vemulapalli said, “I don’t think that people should be doing transcatheter mitral repair in intermediate- or low-risk patients as a general rule.” Although, he added, “there will always be certain exceptions, depending on the patient’s specific situation.”
Dr. Vemulapalli pointed to several ongoing trials comparing TEER vs. surgical MR repair in patients with DMR at intermediate surgical risk, including REPAIR MR and PRIMARY.
The study was supported by the National Institutes of Health and Abbott. Dr. Vemulapalli discloses receiving grants or contracts from the American College of Cardiology, the Society of Thoracic Surgeons, Cytokinetics, Abbott Vascular, the National Institutes of Health, and Boston Scientific; and consulting or serving on an advisory board for Janssen, the American College of Physicians, HeartFlow, and Edwards LifeSciences. Dr. Sherwood discloses receiving honoraria or consulting fees from Medtronic and Boston Scientific. Dr. Batchelor discloses receiving consulting fees from Medtronic, Boston Scientific, Edwards Lifesciences, and Abbott.
A version of this article first appeared on Medscape.com.
The overall case volume for surgical mitral valve (MV) repair of degenerative mitral regurgitation (DMR) hasn’t changed much nearly a decade into the age of transcatheter edge-to-edge repair (TEER). But, over the same period, there’s been a shift in the surgical–MV repair case mix at centers that have offered both the surgical option and TEER, a new study suggests.
Once TEER was introduced, those centers over time used the operative approach less in higher– and intermediate–surgical risk patients and more often in those deemed low risk for surgery. And that trend – at centers offering both approaches – paralleled improved risk-adjusted surgical repair short-term complications and 30-day and 5-year mortality.
The findings come from an analysis based on Society of Thoracic Surgeons and Medicare claims data collected from 2011 through 2018 at surgical–MV repair centers that also offered TEER for DMR after its 2013 approval. The transcatheter procedure, until only recently the exclusive domain of Abbott’s MitraClip in various incarnations, is officially indicated for patients judged too high risk for surgical MV repair.
A shift in surgical MV repair to predominantly lower-risk patients would be expected to improve outcomes. But the improvements seen in the current study seem to have a more complex explanation, Sreekanth Vemulapalli, MD, told this news organization.
The data seem to show TEER indication creep from higher-risk cases, for which there is clinical trial support, to intermediate-risk patients, that lack such evidence in favor of TEER. That seemed to push surgical repair toward even lower-risk cases. “I think that’s exactly right,” said Dr. Vemulapalli, Duke Clinical Research Institute, Durham, N.C.
Still, he observed, the analysis was adjusted for surgical risk, and “Even after that adjustment, it looked like surgical outcomes were getting better after the availability of transcatheter mitral repair techniques.”
That observation may be explained by an increasingly sharp, “more careful” process for selecting patients for surgical repair vs. TEER, said Dr. Vemulapalli, who is senior author of the study published in the Journal of the American College of Cardiology. Angela M. Lowenstern, MD, Vanderbilt University, Nashville, and Andrew M. Vekstein, MD, Duke Clinical Research Institute, were the lead authors.
Indeed, the report states, the analysis supports the view that “a systematic evaluation by a heart team able to direct patients towards either surgical or transcatheter approaches enhances both short-term and long-term surgical outcomes.”
“In a world where both surgical and transcatheter techniques are going to be available,” Dr. Vemulapalli said, “patient selection becomes very, very important.”
An accompanying editorial acknowledges the heart-team approach’s potential for improving the selection of patients for surgery and perhaps therefore outcomes. But it also cites issues with that interpretation of the data.
For example, the heart-team approach is not used in consistent ways across the United States. And “although the heart team is recommended in multiple guidelines for valvular heart therapies, there is little evidence for its efficacy, specifically regarding improving clinical outcomes,” write Matthew W. Sherwood, MD, MHS, and Wayne B. Batchelor, MD, MHS, Inova Heart and Vascular Institute, Falls Church, Va.
The editorialists highlight the study’s “significant downtrend in both high-risk and intermediate-risk surgical cases, with a concomitant increase in low-risk cases,” after introduction of TEER. That shift in case mix, they write, “would seem to be a more likely explanation for the modest improvement in outcomes for surgical MV repair.”
Also, importantly, the analysis didn’t include data on TEER procedures, only indirect evidence for TEER’s effect on surgical MV repair, the editorialists observe, and study authors acknowledge.
Still, the analysis looked at nearly 14,000 patients at 278 U.S. sites with surgical MV repair that launched TEER programs during the study period. They accounted for 6,806 surgical cases before and 7,153 surgical cases after the advent of TEER.
Their median annualized institutional surgical MV repair volume was 32 before and 29 after TEER availability (P = .06).
The risk-adjusted odds ratio for 30-day mortality after vs. before TEER became an option was 0.73 (95% confidence interval, 0.54-0.99). The corresponding hazard ratio for mortality at 5 years was 0.75 (95% CI, 0.66-0.86).
Other risk-adjusted surgical outcomes improved once TEER became available, including MV adverse outcomes (OR, 0.71; 95% CI, 0.58-0.86; P < .001), operative mortality (OR, 0.73; 95% CI, 0.54-0.99; P = .041), and major morbidity (OR, 0.85; 95% CI, 0.73-0.98; P = .026)
Despite the data’s suggestion of TEER indication creep from solely high–surgical risk patients to those at intermediate risk, Dr. Vemulapalli said, “I don’t think that people should be doing transcatheter mitral repair in intermediate- or low-risk patients as a general rule.” Although, he added, “there will always be certain exceptions, depending on the patient’s specific situation.”
Dr. Vemulapalli pointed to several ongoing trials comparing TEER vs. surgical MR repair in patients with DMR at intermediate surgical risk, including REPAIR MR and PRIMARY.
The study was supported by the National Institutes of Health and Abbott. Dr. Vemulapalli discloses receiving grants or contracts from the American College of Cardiology, the Society of Thoracic Surgeons, Cytokinetics, Abbott Vascular, the National Institutes of Health, and Boston Scientific; and consulting or serving on an advisory board for Janssen, the American College of Physicians, HeartFlow, and Edwards LifeSciences. Dr. Sherwood discloses receiving honoraria or consulting fees from Medtronic and Boston Scientific. Dr. Batchelor discloses receiving consulting fees from Medtronic, Boston Scientific, Edwards Lifesciences, and Abbott.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Nature, not nurture, the culprit in OCD
new research suggests.
This finding from a large, register-based study is particularly surprising because results from previous studies of major depression and anxiety disorder have shown a significant effect of parenting and a child’s home environment on the risk for these disorders, the investigators noted.
While the results likely won’t change patient treatment, one expert said it could alleviate concerns of some parents with OCD who fear that witnessing their obsessive behaviors might put their children at higher risk for the disorder.
“The evidence is consistent with the idea that the psychological transmission of OCD from parent to child, if it exists, is really pretty weak,” lead author Kenneth S. Kendler, MD, professor of psychiatry and director of the Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said in an interview.
The findings were published online in JAMA Psychiatry.
Family analysis
The study is the first to include adoptive parents in an analysis of OCD transmission, which allowed investigators to answer the nature versus nurture question that is often difficult to decipher.
Working with Swedish population registries, researchers identified more than 2.4 million offspring. Of these, 27,141 individuals (1.1%) had a lifetime diagnosis of OCD.
Families were divided into four types: intact families, with kids who lived at home with their biological parents from birth to at least age 15 years; families with kids who never lived with their biological father; families with children who did not live with their biological fathers between birth and age 15 years but who lived with a stepfather for at least 10 of those years; and families with children who were adopted before the age of 5 by people with no biological connection to the child.
After analyzing data from all parent-child relationships, researchers found that genes plus rearing (odds ratio, 3.94; 95% confidence interval, 3.58-4.33) and genes only (OR, 3.34; 95% CI, 2.27-4.93) were significantly more likely to be correlated to transmission of OCD from parent to offspring than rearing alone. Rearing only (OR, 1.4; 95% CI, 0.45-4.39) was not significantly correlated with OCD transmission
“It appears from our data that the only substantial transmission that occurs is in the genes parents transmit, not by the modeling of behavior,” Dr. Kendler said.
“There’s an idea that you can learn some things from your parents from psychopathology, but we didn’t see that kids picked that up much in the case of OCD,” he added.
However, there was one outlier: Children raised by stepparents or adoptive parents with an anxiety disorder had a greater risk of developing OCD.
Given the lack of evidence of a strong rearing effect in other analyses, Dr. Kendler noted that this rogue finding could be caused by an underpowered sample; the researchers plan to study the data further.
“Psychiatric disorders, like many other conditions, are often correlated with neighboring conditions,” he said. “Our study would suggest that some of the molecular genetic variants between OCD and generalized anxiety disorder or other anxiety disorders would be shared, but some would be unique.”
Answers an old question
In a comment, Jon Grant, JD, MD, MPH, professor of psychiatry and director of the Addictive, Compulsive, and Impulsive Disorders Research Lab at the University of Chicago, said the findings fill an important gap in what is known about OCD.
“I think the findings are really answering this old question of: ‘Is OCD due to the rearing patterns in a family versus genetics?’ This was able to get at that information showing that it’s virtually all due to genetics within families, and that’s really good to know,” said Dr. Grant, who was not a part of the study.
He was also struck by the finding of a strong genetic relationship between OCD and generalized anxiety disorder (GAD).
While identifying that OCD and GAD are genetically linked likely won’t change clinical care, “I think it at least allows clinicians to know when we see that comorbidity that it may be much more genetically linked in the case of GAD,” Dr. Grant said.
The study was funded by the Swedish Research Council, as well as Avtal om Läkarutbildning och Forskning funding from Region Skåne. Dr. Kendler and Dr. Grant reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
This finding from a large, register-based study is particularly surprising because results from previous studies of major depression and anxiety disorder have shown a significant effect of parenting and a child’s home environment on the risk for these disorders, the investigators noted.
While the results likely won’t change patient treatment, one expert said it could alleviate concerns of some parents with OCD who fear that witnessing their obsessive behaviors might put their children at higher risk for the disorder.
“The evidence is consistent with the idea that the psychological transmission of OCD from parent to child, if it exists, is really pretty weak,” lead author Kenneth S. Kendler, MD, professor of psychiatry and director of the Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said in an interview.
The findings were published online in JAMA Psychiatry.
Family analysis
The study is the first to include adoptive parents in an analysis of OCD transmission, which allowed investigators to answer the nature versus nurture question that is often difficult to decipher.
Working with Swedish population registries, researchers identified more than 2.4 million offspring. Of these, 27,141 individuals (1.1%) had a lifetime diagnosis of OCD.
Families were divided into four types: intact families, with kids who lived at home with their biological parents from birth to at least age 15 years; families with kids who never lived with their biological father; families with children who did not live with their biological fathers between birth and age 15 years but who lived with a stepfather for at least 10 of those years; and families with children who were adopted before the age of 5 by people with no biological connection to the child.
After analyzing data from all parent-child relationships, researchers found that genes plus rearing (odds ratio, 3.94; 95% confidence interval, 3.58-4.33) and genes only (OR, 3.34; 95% CI, 2.27-4.93) were significantly more likely to be correlated to transmission of OCD from parent to offspring than rearing alone. Rearing only (OR, 1.4; 95% CI, 0.45-4.39) was not significantly correlated with OCD transmission
“It appears from our data that the only substantial transmission that occurs is in the genes parents transmit, not by the modeling of behavior,” Dr. Kendler said.
“There’s an idea that you can learn some things from your parents from psychopathology, but we didn’t see that kids picked that up much in the case of OCD,” he added.
However, there was one outlier: Children raised by stepparents or adoptive parents with an anxiety disorder had a greater risk of developing OCD.
Given the lack of evidence of a strong rearing effect in other analyses, Dr. Kendler noted that this rogue finding could be caused by an underpowered sample; the researchers plan to study the data further.
“Psychiatric disorders, like many other conditions, are often correlated with neighboring conditions,” he said. “Our study would suggest that some of the molecular genetic variants between OCD and generalized anxiety disorder or other anxiety disorders would be shared, but some would be unique.”
Answers an old question
In a comment, Jon Grant, JD, MD, MPH, professor of psychiatry and director of the Addictive, Compulsive, and Impulsive Disorders Research Lab at the University of Chicago, said the findings fill an important gap in what is known about OCD.
“I think the findings are really answering this old question of: ‘Is OCD due to the rearing patterns in a family versus genetics?’ This was able to get at that information showing that it’s virtually all due to genetics within families, and that’s really good to know,” said Dr. Grant, who was not a part of the study.
He was also struck by the finding of a strong genetic relationship between OCD and generalized anxiety disorder (GAD).
While identifying that OCD and GAD are genetically linked likely won’t change clinical care, “I think it at least allows clinicians to know when we see that comorbidity that it may be much more genetically linked in the case of GAD,” Dr. Grant said.
The study was funded by the Swedish Research Council, as well as Avtal om Läkarutbildning och Forskning funding from Region Skåne. Dr. Kendler and Dr. Grant reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
This finding from a large, register-based study is particularly surprising because results from previous studies of major depression and anxiety disorder have shown a significant effect of parenting and a child’s home environment on the risk for these disorders, the investigators noted.
While the results likely won’t change patient treatment, one expert said it could alleviate concerns of some parents with OCD who fear that witnessing their obsessive behaviors might put their children at higher risk for the disorder.
“The evidence is consistent with the idea that the psychological transmission of OCD from parent to child, if it exists, is really pretty weak,” lead author Kenneth S. Kendler, MD, professor of psychiatry and director of the Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, said in an interview.
The findings were published online in JAMA Psychiatry.
Family analysis
The study is the first to include adoptive parents in an analysis of OCD transmission, which allowed investigators to answer the nature versus nurture question that is often difficult to decipher.
Working with Swedish population registries, researchers identified more than 2.4 million offspring. Of these, 27,141 individuals (1.1%) had a lifetime diagnosis of OCD.
Families were divided into four types: intact families, with kids who lived at home with their biological parents from birth to at least age 15 years; families with kids who never lived with their biological father; families with children who did not live with their biological fathers between birth and age 15 years but who lived with a stepfather for at least 10 of those years; and families with children who were adopted before the age of 5 by people with no biological connection to the child.
After analyzing data from all parent-child relationships, researchers found that genes plus rearing (odds ratio, 3.94; 95% confidence interval, 3.58-4.33) and genes only (OR, 3.34; 95% CI, 2.27-4.93) were significantly more likely to be correlated to transmission of OCD from parent to offspring than rearing alone. Rearing only (OR, 1.4; 95% CI, 0.45-4.39) was not significantly correlated with OCD transmission
“It appears from our data that the only substantial transmission that occurs is in the genes parents transmit, not by the modeling of behavior,” Dr. Kendler said.
“There’s an idea that you can learn some things from your parents from psychopathology, but we didn’t see that kids picked that up much in the case of OCD,” he added.
However, there was one outlier: Children raised by stepparents or adoptive parents with an anxiety disorder had a greater risk of developing OCD.
Given the lack of evidence of a strong rearing effect in other analyses, Dr. Kendler noted that this rogue finding could be caused by an underpowered sample; the researchers plan to study the data further.
“Psychiatric disorders, like many other conditions, are often correlated with neighboring conditions,” he said. “Our study would suggest that some of the molecular genetic variants between OCD and generalized anxiety disorder or other anxiety disorders would be shared, but some would be unique.”
Answers an old question
In a comment, Jon Grant, JD, MD, MPH, professor of psychiatry and director of the Addictive, Compulsive, and Impulsive Disorders Research Lab at the University of Chicago, said the findings fill an important gap in what is known about OCD.
“I think the findings are really answering this old question of: ‘Is OCD due to the rearing patterns in a family versus genetics?’ This was able to get at that information showing that it’s virtually all due to genetics within families, and that’s really good to know,” said Dr. Grant, who was not a part of the study.
He was also struck by the finding of a strong genetic relationship between OCD and generalized anxiety disorder (GAD).
While identifying that OCD and GAD are genetically linked likely won’t change clinical care, “I think it at least allows clinicians to know when we see that comorbidity that it may be much more genetically linked in the case of GAD,” Dr. Grant said.
The study was funded by the Swedish Research Council, as well as Avtal om Läkarutbildning och Forskning funding from Region Skåne. Dr. Kendler and Dr. Grant reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Three wild technologies about to change health care
When I was a child, I watched syndicated episodes of the original “Star Trek.” I was dazzled by the space travel, sure, but also the medical technology.
A handheld “tricorder” detected diseases, while an intramuscular injector (“hypospray”) could treat them. Sickbay “biobeds” came with real-time health monitors that looked futuristic at the time but seem primitive today.
Such visions inspired a lot of us kids to pursue science. Little did we know the real-life advances many of us would see in our lifetimes.
Artificial intelligence helping to spot disease, robots performing surgery, even video calls between doctor and patient – all these once sounded fantastical but now happen in clinical care.
Now, in the 23rd year of the 21st century, you might not believe wht we’ll be capable of next. Three especially wild examples are moving closer to clinical reality.
Human hibernation
Captain America, Han Solo, and “Star Trek” villain Khan – all were preserved at low temperatures and then revived, waking up alive and well months, decades, or centuries later. These are fictional examples, to be sure, but the science they’re rooted in is real.
(In one extreme case, a climber survived after almost 9 hours of efforts to revive him.)
Useful for a space traveler? Maybe not. But it’s potentially huge for someone with life-threatening injuries from a car accident or a gunshot wound.
That’s the thinking behind a breakthrough procedure that came after decades of research on pigs and dogs, now in a clinical trial. The idea: A person with massive blood loss whose heart has stopped is injected with an ice-cold fluid, cooling them from the inside, down to about 50° F.
Doctors already induce more modest hypothermia to protect the brain and other organs after cardiac arrest and during surgery on the aortic arch (the main artery carrying blood from the heart).
But this experimental procedure – called emergency preservation and resuscitation (EPR) – goes far beyond that, dramatically “decreasing the body’s need for oxygen and blood flow,” says Samuel Tisherman, MD, a trauma surgeon at the University of Maryland Medical Center and the trial’s lead researcher. This puts the patient in a state of suspended animation that “could buy time for surgeons to stop the bleeding and save more of these patients.”
The technique has been done on at least six patients, though none were reported to survive. The trial is expected to include 20 people by the time it wraps up in December, according to the listing on the U.S. clinical trials database. Though given the strict requirements for candidates (emergency trauma victims who are not likely to survive), one can’t exactly rely on a set schedule.
Still, the technology is promising. Someday we may even use it to keep patients in suspended animation for months or years, experts predict, helping astronauts through decades-long spaceflights, or stalling death in sick patients awaiting a cure.
Artificial womb
Another sci-fi classic: growing human babies outside the womb. Think the fetus fields from “The Matrix,” or the frozen embryos in “Alien: Covenant.”
In 1923, British biologist J.B.S. Haldane coined a term for that – ectogenesis. He predicted that 70% of pregnancies would take place, from fertilization to birth, in artificial wombs by 2074. That many seems unlikely, but the timeline is on track.
Developing an embryo outside the womb is already routine in in vitro fertilization. And technology enables preterm babies to survive through much of the second half of gestation. Normal human pregnancy is 40 weeks, and the youngest preterm baby ever to survive was 21 weeks and 1 day old, just a few days younger than a smattering of others who lived.
The biggest obstacle for babies younger than that is lung viability. Mechanical ventilation can damage the lungs and lead to a chronic (sometimes fatal) lung disease known as bronchopulmonary dysplasia. Avoiding this would mean figuring out a way to maintain fetal circulation – the intricate system that delivers oxygenated blood from the placenta to the fetus via the umbilical cord. Researchers at Children’s Hospital of Philadelphia have done this using a fetal lamb.
The key to their invention is a substitute placenta: an oxygenator connected to the lamb’s umbilical cord. Tubes inserted through the umbilical vein and arteries carry oxygenated blood from the “placenta” to the fetus, and deoxygenated blood back out. The lamb resides in an artificial, fluid-filled amniotic sac until its lungs and other organs are developed.
Fertility treatment could benefit, too. “An artificial womb may substitute in situations in which a gestational carrier – surrogate – is indicated,” says Paula Amato, MD, a professor of obstetrics and gynecology at Oregon Health and Science University, Portland. (Dr. Amato is not involved in the CHOP research.) For example: when the mother is missing a uterus or can’t carry a pregnancy safely.
No date is set for clinical trials yet. But according to the research, the main difference between human and lamb may come down to size. A lamb’s umbilical vessels are larger, so feeding in a tube is easier. With today’s advances in miniaturizing surgical methods, that seems like a challenge scientists can overcome.
Messenger RNA therapeutics
Back to “Star Trek.” The hypospray injector’s contents could cure just about any disease, even one newly discovered on a strange planet. That’s not unlike messenger RNA (mRNA) technology, a breakthrough that enabled scientists to quickly develop some of the first COVID-19 vaccines.
But vaccines are just the beginning of what this technology can do.
A whole field of immunotherapy is emerging that uses mRNA to deliver instructions to produce chimeric antigen receptor–modified immune cells (CAR-modified immune cells). These cells are engineered to target diseased cells and tissues, like cancer cells and harmful fibroblasts (scar tissue) that promote fibrosis in, for example, the heart and lungs.
The field is bursting with rodent research, and clinical trials have started for treating some advanced-stage malignancies.
Actual clinical use may be years away, but if all goes well, these medicines could help treat or even cure the core medical problems facing humanity. We’re talking cancer, heart disease, neurodegenerative disease – transforming one therapy into another by simply changing the mRNA’s “nucleotide sequence,” the blueprint containing instructions telling it what to do, and what disease to attack.
As this technology matures, we may start to feel as if we’re really on “Star Trek,” where Dr. Leonard “Bones” McCoy pulls out the same device to treat just about every disease or injury.
A version of this article first appeared on WebMD.com.
When I was a child, I watched syndicated episodes of the original “Star Trek.” I was dazzled by the space travel, sure, but also the medical technology.
A handheld “tricorder” detected diseases, while an intramuscular injector (“hypospray”) could treat them. Sickbay “biobeds” came with real-time health monitors that looked futuristic at the time but seem primitive today.
Such visions inspired a lot of us kids to pursue science. Little did we know the real-life advances many of us would see in our lifetimes.
Artificial intelligence helping to spot disease, robots performing surgery, even video calls between doctor and patient – all these once sounded fantastical but now happen in clinical care.
Now, in the 23rd year of the 21st century, you might not believe wht we’ll be capable of next. Three especially wild examples are moving closer to clinical reality.
Human hibernation
Captain America, Han Solo, and “Star Trek” villain Khan – all were preserved at low temperatures and then revived, waking up alive and well months, decades, or centuries later. These are fictional examples, to be sure, but the science they’re rooted in is real.
(In one extreme case, a climber survived after almost 9 hours of efforts to revive him.)
Useful for a space traveler? Maybe not. But it’s potentially huge for someone with life-threatening injuries from a car accident or a gunshot wound.
That’s the thinking behind a breakthrough procedure that came after decades of research on pigs and dogs, now in a clinical trial. The idea: A person with massive blood loss whose heart has stopped is injected with an ice-cold fluid, cooling them from the inside, down to about 50° F.
Doctors already induce more modest hypothermia to protect the brain and other organs after cardiac arrest and during surgery on the aortic arch (the main artery carrying blood from the heart).
But this experimental procedure – called emergency preservation and resuscitation (EPR) – goes far beyond that, dramatically “decreasing the body’s need for oxygen and blood flow,” says Samuel Tisherman, MD, a trauma surgeon at the University of Maryland Medical Center and the trial’s lead researcher. This puts the patient in a state of suspended animation that “could buy time for surgeons to stop the bleeding and save more of these patients.”
The technique has been done on at least six patients, though none were reported to survive. The trial is expected to include 20 people by the time it wraps up in December, according to the listing on the U.S. clinical trials database. Though given the strict requirements for candidates (emergency trauma victims who are not likely to survive), one can’t exactly rely on a set schedule.
Still, the technology is promising. Someday we may even use it to keep patients in suspended animation for months or years, experts predict, helping astronauts through decades-long spaceflights, or stalling death in sick patients awaiting a cure.
Artificial womb
Another sci-fi classic: growing human babies outside the womb. Think the fetus fields from “The Matrix,” or the frozen embryos in “Alien: Covenant.”
In 1923, British biologist J.B.S. Haldane coined a term for that – ectogenesis. He predicted that 70% of pregnancies would take place, from fertilization to birth, in artificial wombs by 2074. That many seems unlikely, but the timeline is on track.
Developing an embryo outside the womb is already routine in in vitro fertilization. And technology enables preterm babies to survive through much of the second half of gestation. Normal human pregnancy is 40 weeks, and the youngest preterm baby ever to survive was 21 weeks and 1 day old, just a few days younger than a smattering of others who lived.
The biggest obstacle for babies younger than that is lung viability. Mechanical ventilation can damage the lungs and lead to a chronic (sometimes fatal) lung disease known as bronchopulmonary dysplasia. Avoiding this would mean figuring out a way to maintain fetal circulation – the intricate system that delivers oxygenated blood from the placenta to the fetus via the umbilical cord. Researchers at Children’s Hospital of Philadelphia have done this using a fetal lamb.
The key to their invention is a substitute placenta: an oxygenator connected to the lamb’s umbilical cord. Tubes inserted through the umbilical vein and arteries carry oxygenated blood from the “placenta” to the fetus, and deoxygenated blood back out. The lamb resides in an artificial, fluid-filled amniotic sac until its lungs and other organs are developed.
Fertility treatment could benefit, too. “An artificial womb may substitute in situations in which a gestational carrier – surrogate – is indicated,” says Paula Amato, MD, a professor of obstetrics and gynecology at Oregon Health and Science University, Portland. (Dr. Amato is not involved in the CHOP research.) For example: when the mother is missing a uterus or can’t carry a pregnancy safely.
No date is set for clinical trials yet. But according to the research, the main difference between human and lamb may come down to size. A lamb’s umbilical vessels are larger, so feeding in a tube is easier. With today’s advances in miniaturizing surgical methods, that seems like a challenge scientists can overcome.
Messenger RNA therapeutics
Back to “Star Trek.” The hypospray injector’s contents could cure just about any disease, even one newly discovered on a strange planet. That’s not unlike messenger RNA (mRNA) technology, a breakthrough that enabled scientists to quickly develop some of the first COVID-19 vaccines.
But vaccines are just the beginning of what this technology can do.
A whole field of immunotherapy is emerging that uses mRNA to deliver instructions to produce chimeric antigen receptor–modified immune cells (CAR-modified immune cells). These cells are engineered to target diseased cells and tissues, like cancer cells and harmful fibroblasts (scar tissue) that promote fibrosis in, for example, the heart and lungs.
The field is bursting with rodent research, and clinical trials have started for treating some advanced-stage malignancies.
Actual clinical use may be years away, but if all goes well, these medicines could help treat or even cure the core medical problems facing humanity. We’re talking cancer, heart disease, neurodegenerative disease – transforming one therapy into another by simply changing the mRNA’s “nucleotide sequence,” the blueprint containing instructions telling it what to do, and what disease to attack.
As this technology matures, we may start to feel as if we’re really on “Star Trek,” where Dr. Leonard “Bones” McCoy pulls out the same device to treat just about every disease or injury.
A version of this article first appeared on WebMD.com.
When I was a child, I watched syndicated episodes of the original “Star Trek.” I was dazzled by the space travel, sure, but also the medical technology.
A handheld “tricorder” detected diseases, while an intramuscular injector (“hypospray”) could treat them. Sickbay “biobeds” came with real-time health monitors that looked futuristic at the time but seem primitive today.
Such visions inspired a lot of us kids to pursue science. Little did we know the real-life advances many of us would see in our lifetimes.
Artificial intelligence helping to spot disease, robots performing surgery, even video calls between doctor and patient – all these once sounded fantastical but now happen in clinical care.
Now, in the 23rd year of the 21st century, you might not believe wht we’ll be capable of next. Three especially wild examples are moving closer to clinical reality.
Human hibernation
Captain America, Han Solo, and “Star Trek” villain Khan – all were preserved at low temperatures and then revived, waking up alive and well months, decades, or centuries later. These are fictional examples, to be sure, but the science they’re rooted in is real.
(In one extreme case, a climber survived after almost 9 hours of efforts to revive him.)
Useful for a space traveler? Maybe not. But it’s potentially huge for someone with life-threatening injuries from a car accident or a gunshot wound.
That’s the thinking behind a breakthrough procedure that came after decades of research on pigs and dogs, now in a clinical trial. The idea: A person with massive blood loss whose heart has stopped is injected with an ice-cold fluid, cooling them from the inside, down to about 50° F.
Doctors already induce more modest hypothermia to protect the brain and other organs after cardiac arrest and during surgery on the aortic arch (the main artery carrying blood from the heart).
But this experimental procedure – called emergency preservation and resuscitation (EPR) – goes far beyond that, dramatically “decreasing the body’s need for oxygen and blood flow,” says Samuel Tisherman, MD, a trauma surgeon at the University of Maryland Medical Center and the trial’s lead researcher. This puts the patient in a state of suspended animation that “could buy time for surgeons to stop the bleeding and save more of these patients.”
The technique has been done on at least six patients, though none were reported to survive. The trial is expected to include 20 people by the time it wraps up in December, according to the listing on the U.S. clinical trials database. Though given the strict requirements for candidates (emergency trauma victims who are not likely to survive), one can’t exactly rely on a set schedule.
Still, the technology is promising. Someday we may even use it to keep patients in suspended animation for months or years, experts predict, helping astronauts through decades-long spaceflights, or stalling death in sick patients awaiting a cure.
Artificial womb
Another sci-fi classic: growing human babies outside the womb. Think the fetus fields from “The Matrix,” or the frozen embryos in “Alien: Covenant.”
In 1923, British biologist J.B.S. Haldane coined a term for that – ectogenesis. He predicted that 70% of pregnancies would take place, from fertilization to birth, in artificial wombs by 2074. That many seems unlikely, but the timeline is on track.
Developing an embryo outside the womb is already routine in in vitro fertilization. And technology enables preterm babies to survive through much of the second half of gestation. Normal human pregnancy is 40 weeks, and the youngest preterm baby ever to survive was 21 weeks and 1 day old, just a few days younger than a smattering of others who lived.
The biggest obstacle for babies younger than that is lung viability. Mechanical ventilation can damage the lungs and lead to a chronic (sometimes fatal) lung disease known as bronchopulmonary dysplasia. Avoiding this would mean figuring out a way to maintain fetal circulation – the intricate system that delivers oxygenated blood from the placenta to the fetus via the umbilical cord. Researchers at Children’s Hospital of Philadelphia have done this using a fetal lamb.
The key to their invention is a substitute placenta: an oxygenator connected to the lamb’s umbilical cord. Tubes inserted through the umbilical vein and arteries carry oxygenated blood from the “placenta” to the fetus, and deoxygenated blood back out. The lamb resides in an artificial, fluid-filled amniotic sac until its lungs and other organs are developed.
Fertility treatment could benefit, too. “An artificial womb may substitute in situations in which a gestational carrier – surrogate – is indicated,” says Paula Amato, MD, a professor of obstetrics and gynecology at Oregon Health and Science University, Portland. (Dr. Amato is not involved in the CHOP research.) For example: when the mother is missing a uterus or can’t carry a pregnancy safely.
No date is set for clinical trials yet. But according to the research, the main difference between human and lamb may come down to size. A lamb’s umbilical vessels are larger, so feeding in a tube is easier. With today’s advances in miniaturizing surgical methods, that seems like a challenge scientists can overcome.
Messenger RNA therapeutics
Back to “Star Trek.” The hypospray injector’s contents could cure just about any disease, even one newly discovered on a strange planet. That’s not unlike messenger RNA (mRNA) technology, a breakthrough that enabled scientists to quickly develop some of the first COVID-19 vaccines.
But vaccines are just the beginning of what this technology can do.
A whole field of immunotherapy is emerging that uses mRNA to deliver instructions to produce chimeric antigen receptor–modified immune cells (CAR-modified immune cells). These cells are engineered to target diseased cells and tissues, like cancer cells and harmful fibroblasts (scar tissue) that promote fibrosis in, for example, the heart and lungs.
The field is bursting with rodent research, and clinical trials have started for treating some advanced-stage malignancies.
Actual clinical use may be years away, but if all goes well, these medicines could help treat or even cure the core medical problems facing humanity. We’re talking cancer, heart disease, neurodegenerative disease – transforming one therapy into another by simply changing the mRNA’s “nucleotide sequence,” the blueprint containing instructions telling it what to do, and what disease to attack.
As this technology matures, we may start to feel as if we’re really on “Star Trek,” where Dr. Leonard “Bones” McCoy pulls out the same device to treat just about every disease or injury.
A version of this article first appeared on WebMD.com.
A new (old) drug joins the COVID fray, and guess what? It works
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
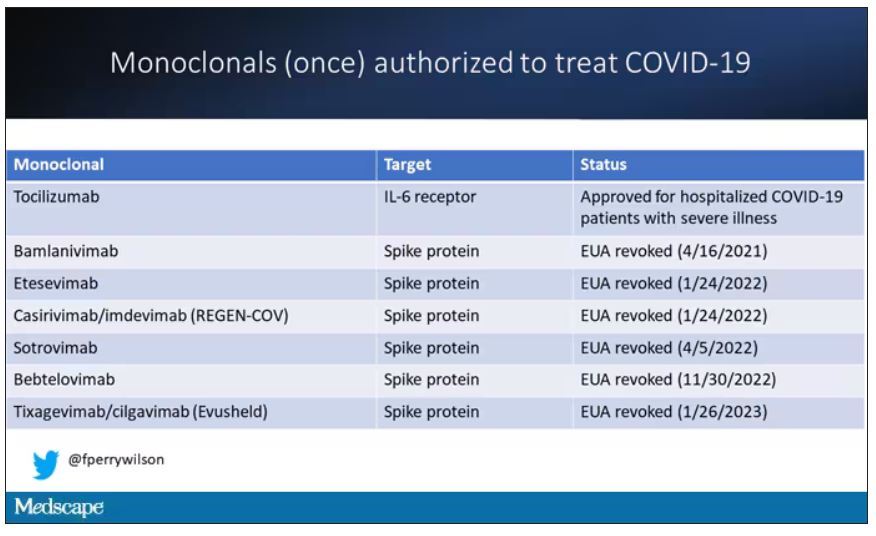
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.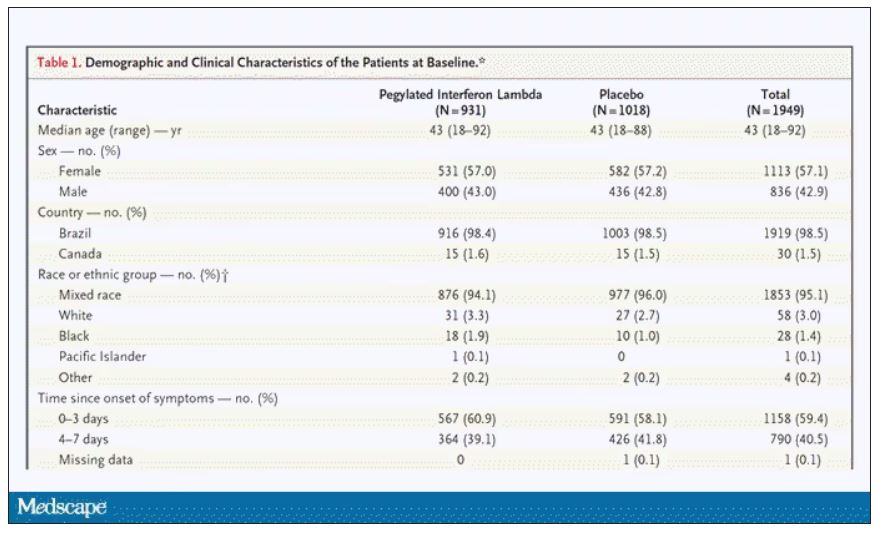
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.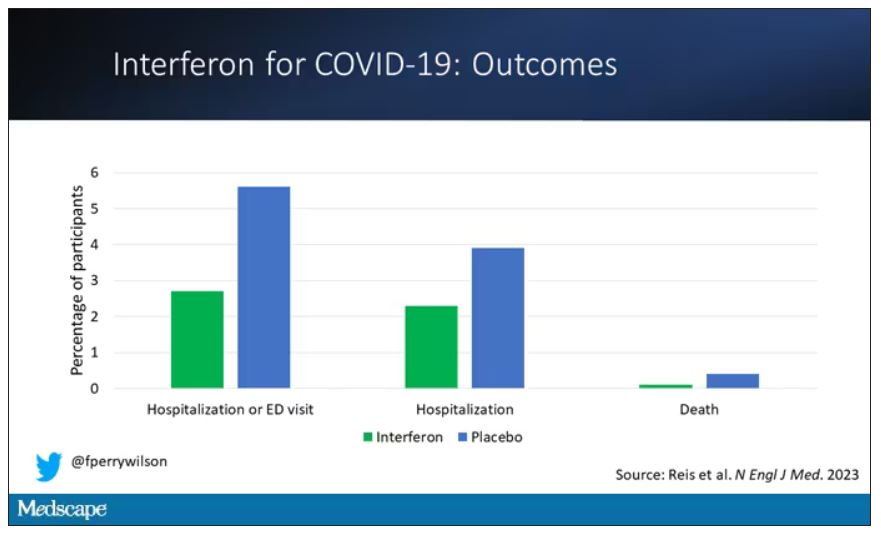
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.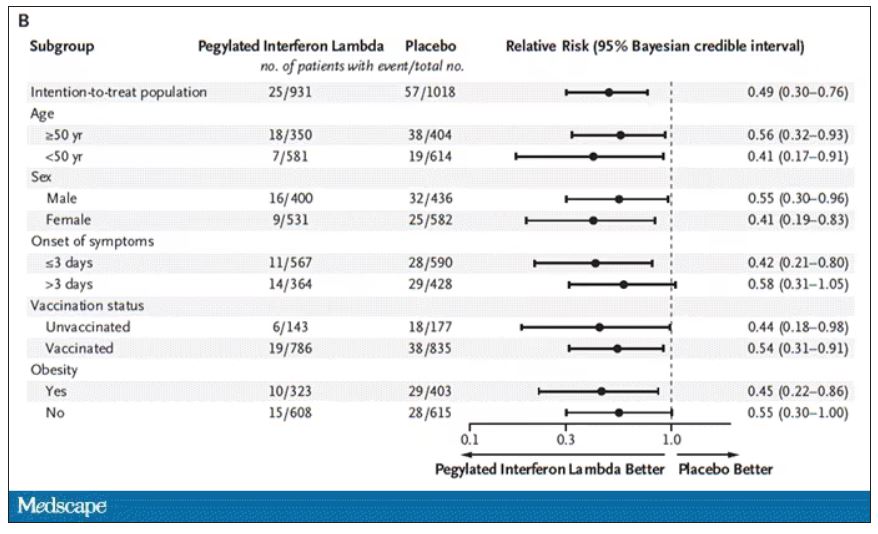
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.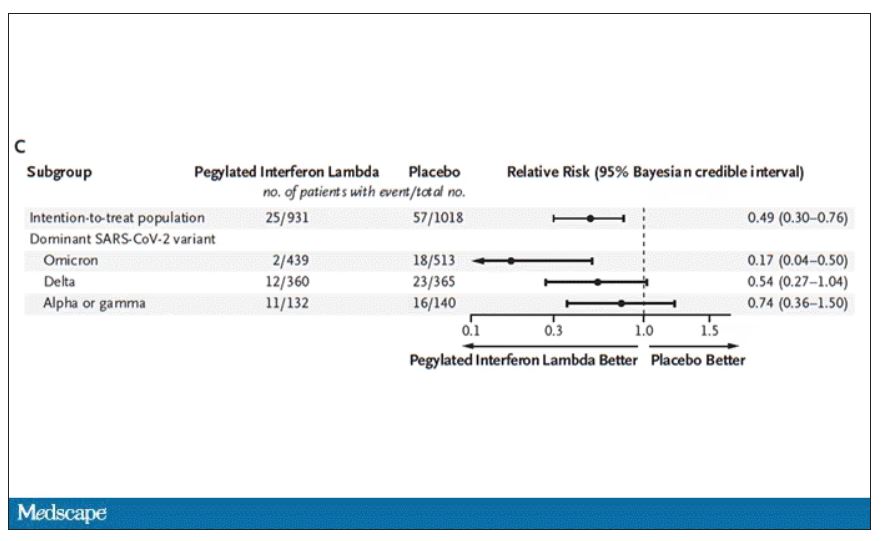
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.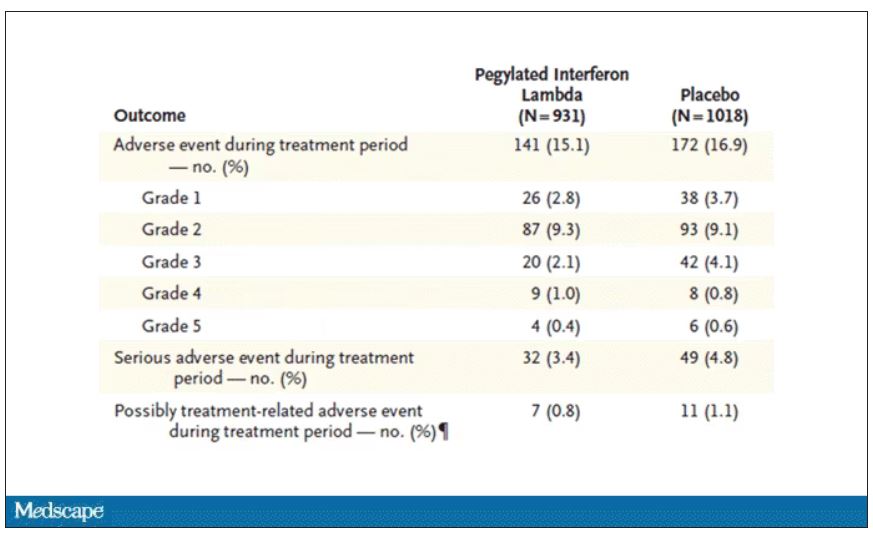
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
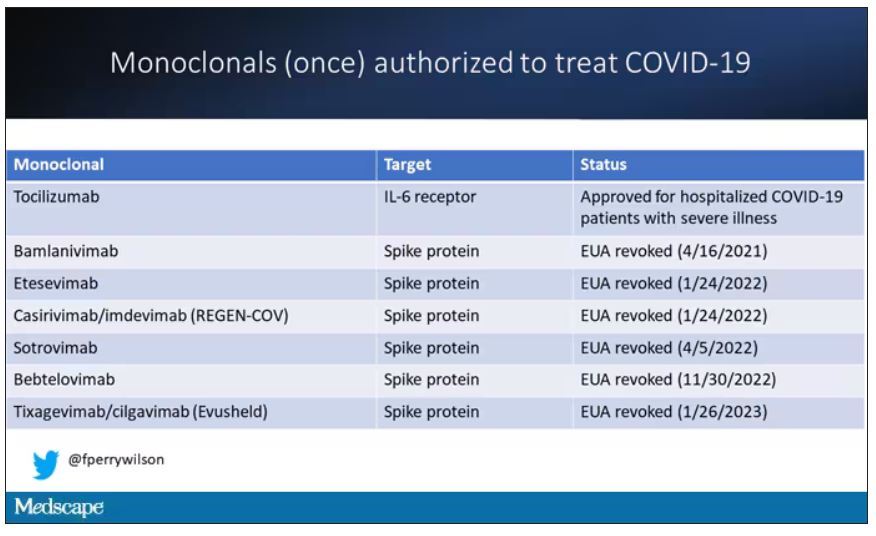
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.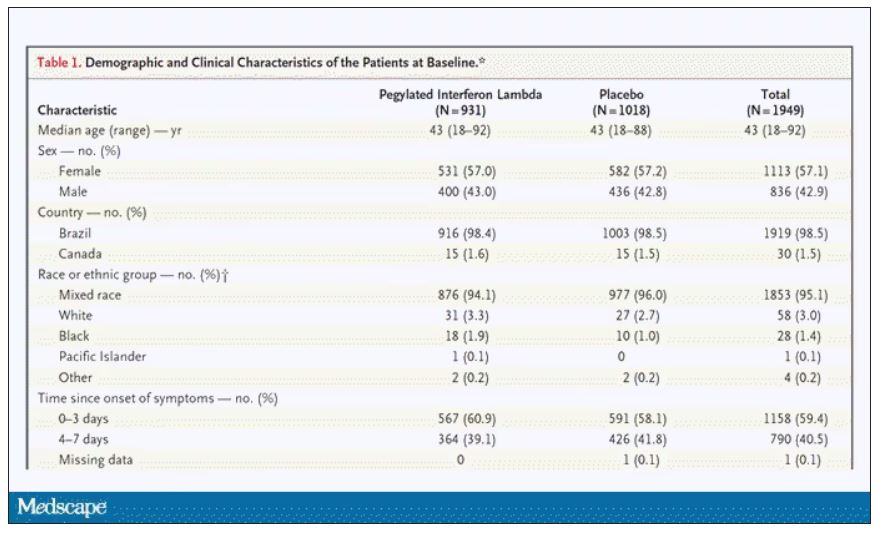
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.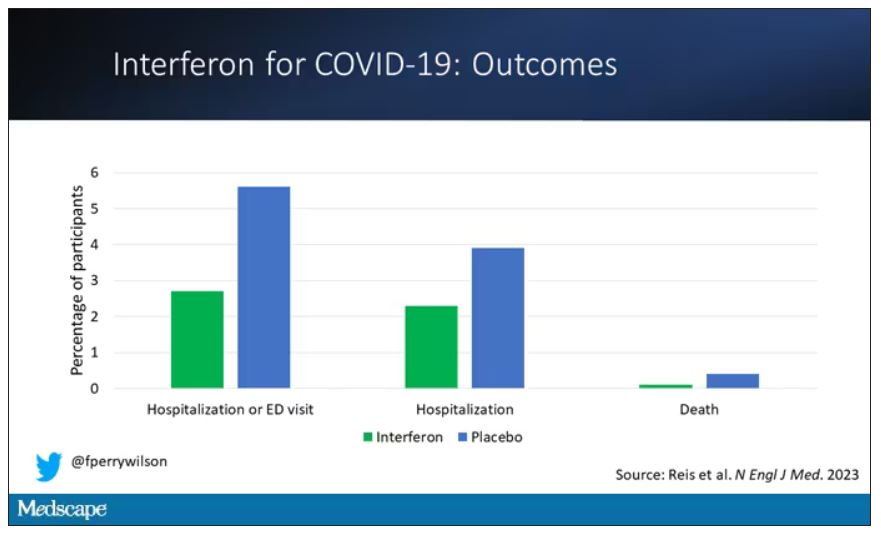
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.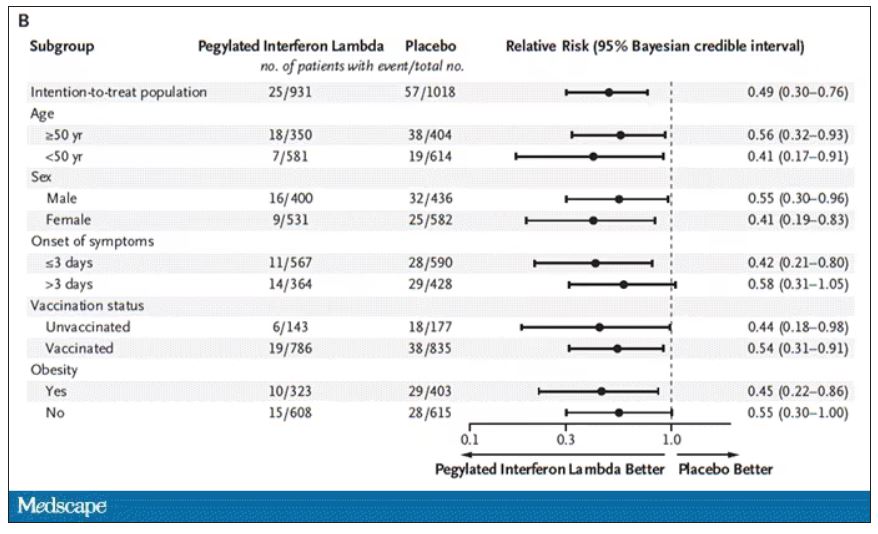
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.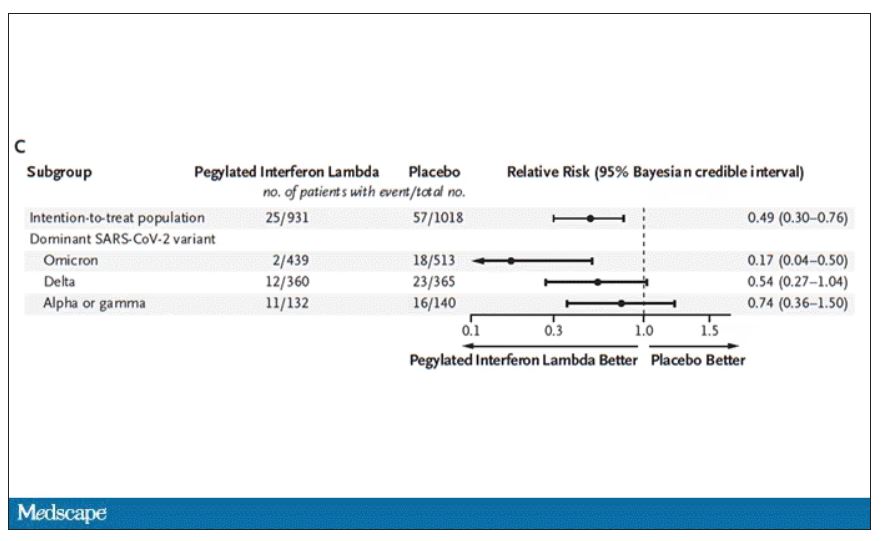
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.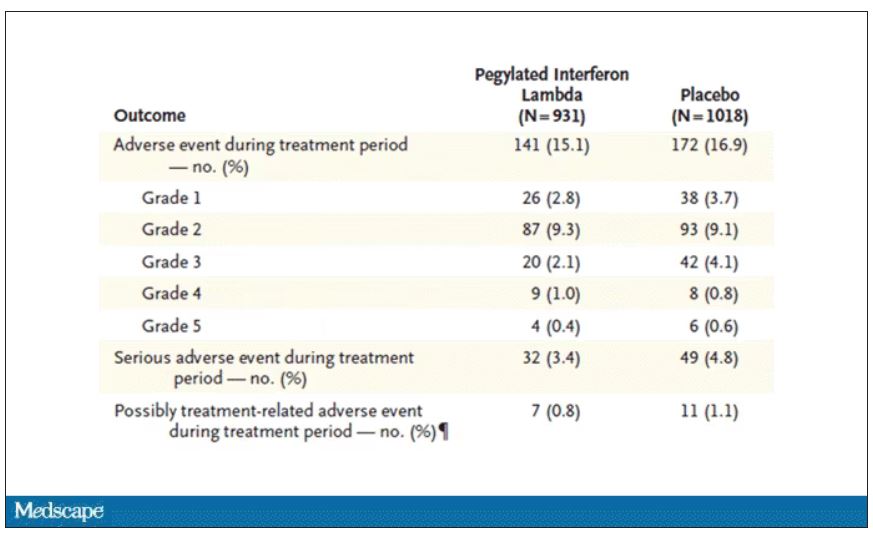
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
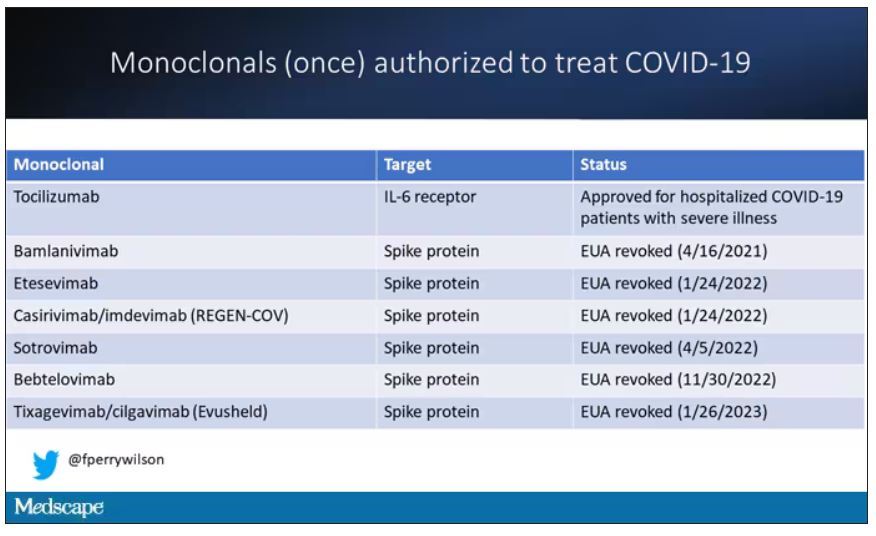
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.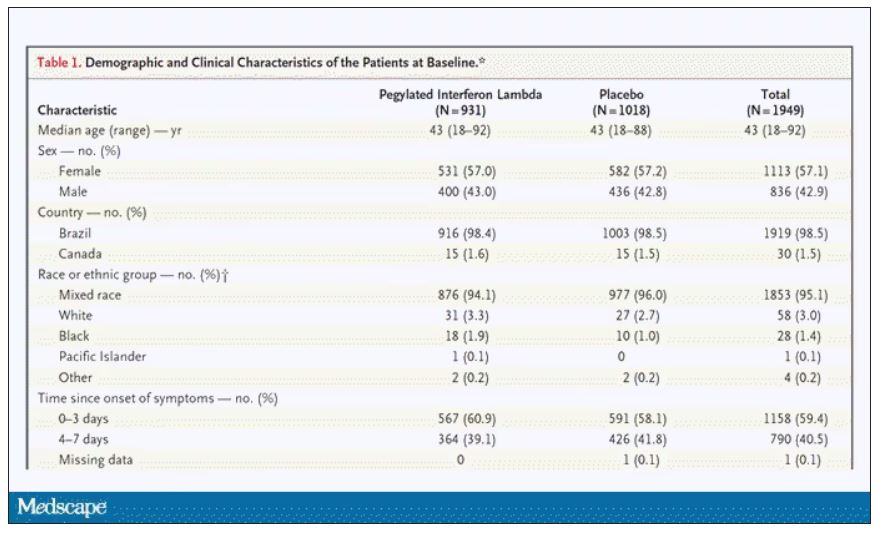
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.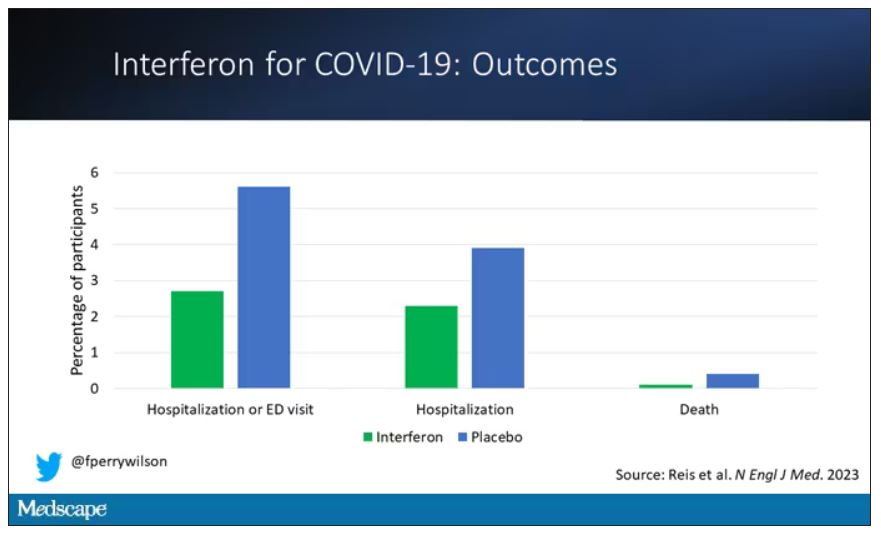
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.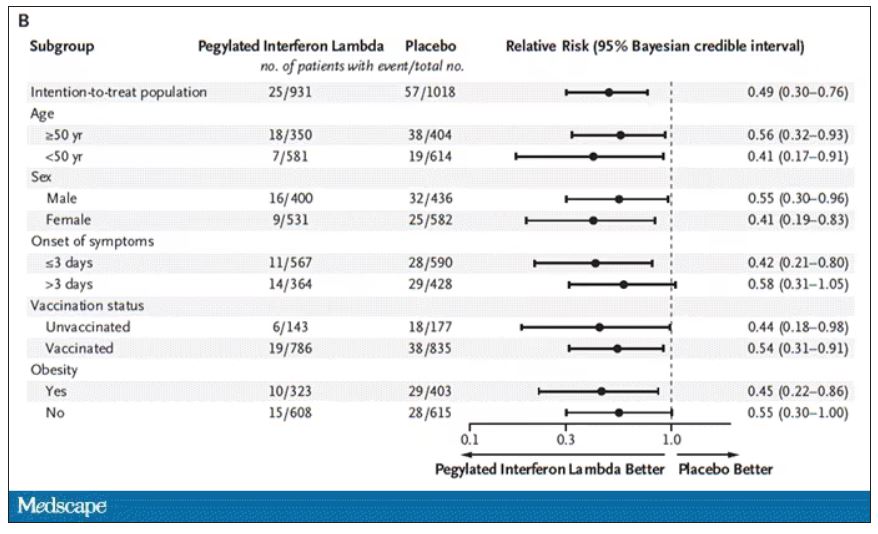
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.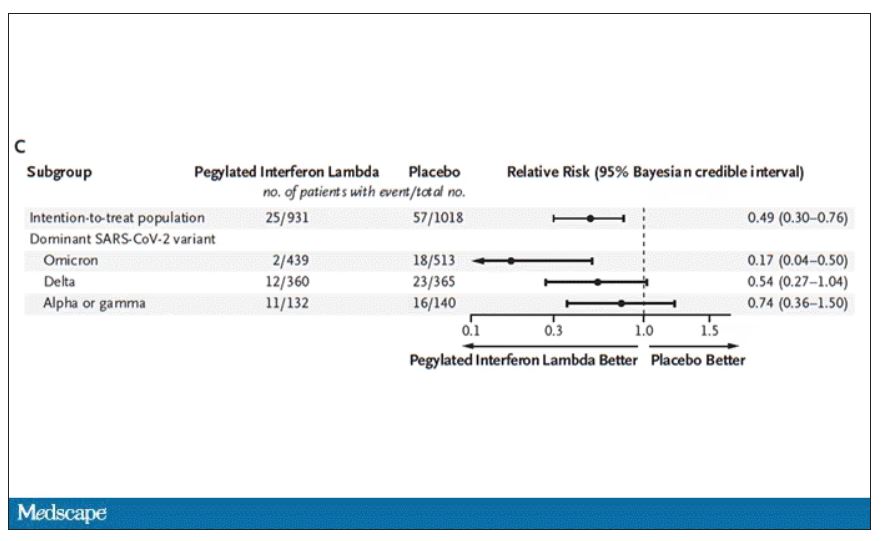
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.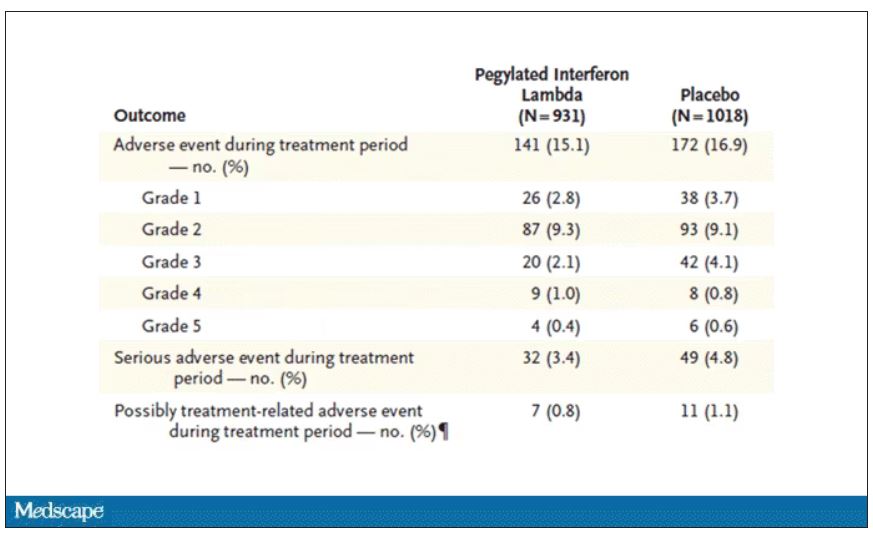
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Can a hormone shot rescue low libido?
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN

