User login
New advice on artificial pancreas insulin delivery systems
A new consensus statement summarizes the benefits, limitations, and challenges of using automated insulin delivery (AID) systems and provides recommendations for use by people with diabetes.
“Automated insulin delivery systems” is becoming the standard terminology – including by the U.S. Food and Drug Administration – to refer to systems that integrate data from a continuous glucose monitoring (CGM) system via a control algorithm into an insulin pump in order to automate subcutaneous insulin delivery. “Hybrid AID” or “hybrid closed-loop” refers to the current status of these systems, which still require some degree of user input to control glucose levels.
The term “artificial pancreas” was used interchangeably with AID in the past, but it doesn’t take into account exocrine pancreatic function. The term “bionic pancreas” refers to a specific system in development that would ultimately include glucagon along with insulin.
The new consensus report, titled “Automated insulin delivery: Benefits, challenges, and recommendations,” was published online in Diabetes Care and Diabetologia.
The document is geared toward not only diabetologists and other specialists, but also diabetes nurses and specialist dietitians. Colleagues working at regulatory agencies, health care organizations, and related media might also benefit from reading it.
It is endorsed by two professional societies – the European Association for the Study of Diabetes and the American Diabetes Association – and contrasts with other statements about AID systems that are sponsored by their manufacturers, noted document co-author Mark Evans, PhD, professor of diabetic medicine, University of Cambridge, England, in a statement.
“Many clinically relevant aspects, including safety, are addressed in this report. The aim ... is to encourage ongoing improvement of this technology, its safe and effective use, and its accessibility to all who can benefit from it,” Dr. Evans said.
Lead author Jennifer Sherr, MD, PhD, pediatric endocrinology, Yale University, New Haven, Conn., commented that the report “addresses the clinical usage of AID systems from a practical point of view rather than as ... a meta-analysis or a review of all relevant clinical studies. ... As such, the benefits and limitations of systems are discussed while also considering safety, regulatory pathways, and access to this technology.”
AID systems do not mean diabetes is “cured”
Separate recommendations provided at the end of the document are aimed at specific stakeholders, including health care providers, patients and their caregivers, manufacturers, regulatory agencies, and the research community.
The authors make clear in the introduction that, while representing “a significant movement toward optimizing glucose management for individuals with diabetes,” the use of AID systems doesn’t mean that diabetes is “cured.” Rather, “expectations need to be set adequately so that individuals with diabetes and providers understand what such systems can and cannot do.”
In particular, current commercially available AID systems require user input for mealtime insulin dosing and sometimes for correction doses of high blood glucose levels, although the systems at least partially automate that.
“When integrated into care, AID systems hold promise to relieve some of the daily burdens of diabetes care,” the authors write.
The statement also details problems that may arise with the physical devices, including skin irritation from adhesives, occlusion of insulin infusion sets, early CGM sensor failure, and inadequate dosing algorithms.
“Individuals with diabetes who are considering this type of advanced diabetes therapy should not only have appropriate technical understanding of the system but also be able to revert to standard diabetes treatment (that is, nonautomated subcutaneous insulin delivery by pump or injections) in case the AID system fails. They should be able to independently troubleshoot and have access to their health care provider if needed.”
To monitor the impact of the technology, the authors emphasize the importance of the time-in-range metric derived from CGM, with the goal of achieving 70% or greater time in target blood glucose range.
Separate sections of the document address the benefits and limitations of AID systems, education and expectations for both patients and providers, and patient and provider perspectives, including how to handle urgent questions.
Other sections cover special populations such as pregnant women and people with type 2 diabetes, considerations for patient selection for current AID systems, safety, improving access to the technology, liability, and do-it-yourself systems.
Recommendations for health care professionals
A table near the end of the document provides specific recommendations for health care professionals, including the following:
- Be knowledgeable about AID systems and nuances of different systems, including their distinguishing features as well as strengths and weaknesses.
- Inform patients with diabetes about AID systems, including review of currently available systems, and create realistic expectations for device use.
- Involve patients with diabetes in shared decision-making when considering use of AID systems.
- Share information with patients with diabetes, as well as their peers, about general standards set by national and international guidelines on AID systems.
- Provide an on-call number or method by which a person with diabetes can always access support from a health care provider at the practice, including weekends and nights.
- Implement, potentially, protocols on times when AID systems should not be used.
- Use an individual’s health data to improve quality of care and health outcomes.
Most members of the ADA/EASD Diabetes Technology Working Group work with industry, but industry had no input on the project. Dr. Sherr has reported conducting clinical trials for Eli Lilly, Insulet, and Medtronic, and has received in-kind support for research studies from Dexcom and Medtronic. She has also reported consulting for Eli Lilly, Lexicon, Medtronic, and Sanofi, and being an advisory board member for Bigfoot Biomedical, Cecelia Health, Eli Lilly, Insulet, T1D Fund, and Vertex Pharmaceuticals. Dr. Evans has reported conducting clinical trials or research collaborations for, serving on advisory boards for, or receiving speakers fees or travel support from Medtronic, Roche, Abbott Diabetes Care, Dexcom, Novo Nordisk, Eli Lilly, Sanofi, Zucara Therapeutics, Pila Pharma, and AstraZeneca. The University of Cambridge has received salary support for Dr. Evans from the National Health Service.
A version of this article first appeared on Medscape.com.
A new consensus statement summarizes the benefits, limitations, and challenges of using automated insulin delivery (AID) systems and provides recommendations for use by people with diabetes.
“Automated insulin delivery systems” is becoming the standard terminology – including by the U.S. Food and Drug Administration – to refer to systems that integrate data from a continuous glucose monitoring (CGM) system via a control algorithm into an insulin pump in order to automate subcutaneous insulin delivery. “Hybrid AID” or “hybrid closed-loop” refers to the current status of these systems, which still require some degree of user input to control glucose levels.
The term “artificial pancreas” was used interchangeably with AID in the past, but it doesn’t take into account exocrine pancreatic function. The term “bionic pancreas” refers to a specific system in development that would ultimately include glucagon along with insulin.
The new consensus report, titled “Automated insulin delivery: Benefits, challenges, and recommendations,” was published online in Diabetes Care and Diabetologia.
The document is geared toward not only diabetologists and other specialists, but also diabetes nurses and specialist dietitians. Colleagues working at regulatory agencies, health care organizations, and related media might also benefit from reading it.
It is endorsed by two professional societies – the European Association for the Study of Diabetes and the American Diabetes Association – and contrasts with other statements about AID systems that are sponsored by their manufacturers, noted document co-author Mark Evans, PhD, professor of diabetic medicine, University of Cambridge, England, in a statement.
“Many clinically relevant aspects, including safety, are addressed in this report. The aim ... is to encourage ongoing improvement of this technology, its safe and effective use, and its accessibility to all who can benefit from it,” Dr. Evans said.
Lead author Jennifer Sherr, MD, PhD, pediatric endocrinology, Yale University, New Haven, Conn., commented that the report “addresses the clinical usage of AID systems from a practical point of view rather than as ... a meta-analysis or a review of all relevant clinical studies. ... As such, the benefits and limitations of systems are discussed while also considering safety, regulatory pathways, and access to this technology.”
AID systems do not mean diabetes is “cured”
Separate recommendations provided at the end of the document are aimed at specific stakeholders, including health care providers, patients and their caregivers, manufacturers, regulatory agencies, and the research community.
The authors make clear in the introduction that, while representing “a significant movement toward optimizing glucose management for individuals with diabetes,” the use of AID systems doesn’t mean that diabetes is “cured.” Rather, “expectations need to be set adequately so that individuals with diabetes and providers understand what such systems can and cannot do.”
In particular, current commercially available AID systems require user input for mealtime insulin dosing and sometimes for correction doses of high blood glucose levels, although the systems at least partially automate that.
“When integrated into care, AID systems hold promise to relieve some of the daily burdens of diabetes care,” the authors write.
The statement also details problems that may arise with the physical devices, including skin irritation from adhesives, occlusion of insulin infusion sets, early CGM sensor failure, and inadequate dosing algorithms.
“Individuals with diabetes who are considering this type of advanced diabetes therapy should not only have appropriate technical understanding of the system but also be able to revert to standard diabetes treatment (that is, nonautomated subcutaneous insulin delivery by pump or injections) in case the AID system fails. They should be able to independently troubleshoot and have access to their health care provider if needed.”
To monitor the impact of the technology, the authors emphasize the importance of the time-in-range metric derived from CGM, with the goal of achieving 70% or greater time in target blood glucose range.
Separate sections of the document address the benefits and limitations of AID systems, education and expectations for both patients and providers, and patient and provider perspectives, including how to handle urgent questions.
Other sections cover special populations such as pregnant women and people with type 2 diabetes, considerations for patient selection for current AID systems, safety, improving access to the technology, liability, and do-it-yourself systems.
Recommendations for health care professionals
A table near the end of the document provides specific recommendations for health care professionals, including the following:
- Be knowledgeable about AID systems and nuances of different systems, including their distinguishing features as well as strengths and weaknesses.
- Inform patients with diabetes about AID systems, including review of currently available systems, and create realistic expectations for device use.
- Involve patients with diabetes in shared decision-making when considering use of AID systems.
- Share information with patients with diabetes, as well as their peers, about general standards set by national and international guidelines on AID systems.
- Provide an on-call number or method by which a person with diabetes can always access support from a health care provider at the practice, including weekends and nights.
- Implement, potentially, protocols on times when AID systems should not be used.
- Use an individual’s health data to improve quality of care and health outcomes.
Most members of the ADA/EASD Diabetes Technology Working Group work with industry, but industry had no input on the project. Dr. Sherr has reported conducting clinical trials for Eli Lilly, Insulet, and Medtronic, and has received in-kind support for research studies from Dexcom and Medtronic. She has also reported consulting for Eli Lilly, Lexicon, Medtronic, and Sanofi, and being an advisory board member for Bigfoot Biomedical, Cecelia Health, Eli Lilly, Insulet, T1D Fund, and Vertex Pharmaceuticals. Dr. Evans has reported conducting clinical trials or research collaborations for, serving on advisory boards for, or receiving speakers fees or travel support from Medtronic, Roche, Abbott Diabetes Care, Dexcom, Novo Nordisk, Eli Lilly, Sanofi, Zucara Therapeutics, Pila Pharma, and AstraZeneca. The University of Cambridge has received salary support for Dr. Evans from the National Health Service.
A version of this article first appeared on Medscape.com.
A new consensus statement summarizes the benefits, limitations, and challenges of using automated insulin delivery (AID) systems and provides recommendations for use by people with diabetes.
“Automated insulin delivery systems” is becoming the standard terminology – including by the U.S. Food and Drug Administration – to refer to systems that integrate data from a continuous glucose monitoring (CGM) system via a control algorithm into an insulin pump in order to automate subcutaneous insulin delivery. “Hybrid AID” or “hybrid closed-loop” refers to the current status of these systems, which still require some degree of user input to control glucose levels.
The term “artificial pancreas” was used interchangeably with AID in the past, but it doesn’t take into account exocrine pancreatic function. The term “bionic pancreas” refers to a specific system in development that would ultimately include glucagon along with insulin.
The new consensus report, titled “Automated insulin delivery: Benefits, challenges, and recommendations,” was published online in Diabetes Care and Diabetologia.
The document is geared toward not only diabetologists and other specialists, but also diabetes nurses and specialist dietitians. Colleagues working at regulatory agencies, health care organizations, and related media might also benefit from reading it.
It is endorsed by two professional societies – the European Association for the Study of Diabetes and the American Diabetes Association – and contrasts with other statements about AID systems that are sponsored by their manufacturers, noted document co-author Mark Evans, PhD, professor of diabetic medicine, University of Cambridge, England, in a statement.
“Many clinically relevant aspects, including safety, are addressed in this report. The aim ... is to encourage ongoing improvement of this technology, its safe and effective use, and its accessibility to all who can benefit from it,” Dr. Evans said.
Lead author Jennifer Sherr, MD, PhD, pediatric endocrinology, Yale University, New Haven, Conn., commented that the report “addresses the clinical usage of AID systems from a practical point of view rather than as ... a meta-analysis or a review of all relevant clinical studies. ... As such, the benefits and limitations of systems are discussed while also considering safety, regulatory pathways, and access to this technology.”
AID systems do not mean diabetes is “cured”
Separate recommendations provided at the end of the document are aimed at specific stakeholders, including health care providers, patients and their caregivers, manufacturers, regulatory agencies, and the research community.
The authors make clear in the introduction that, while representing “a significant movement toward optimizing glucose management for individuals with diabetes,” the use of AID systems doesn’t mean that diabetes is “cured.” Rather, “expectations need to be set adequately so that individuals with diabetes and providers understand what such systems can and cannot do.”
In particular, current commercially available AID systems require user input for mealtime insulin dosing and sometimes for correction doses of high blood glucose levels, although the systems at least partially automate that.
“When integrated into care, AID systems hold promise to relieve some of the daily burdens of diabetes care,” the authors write.
The statement also details problems that may arise with the physical devices, including skin irritation from adhesives, occlusion of insulin infusion sets, early CGM sensor failure, and inadequate dosing algorithms.
“Individuals with diabetes who are considering this type of advanced diabetes therapy should not only have appropriate technical understanding of the system but also be able to revert to standard diabetes treatment (that is, nonautomated subcutaneous insulin delivery by pump or injections) in case the AID system fails. They should be able to independently troubleshoot and have access to their health care provider if needed.”
To monitor the impact of the technology, the authors emphasize the importance of the time-in-range metric derived from CGM, with the goal of achieving 70% or greater time in target blood glucose range.
Separate sections of the document address the benefits and limitations of AID systems, education and expectations for both patients and providers, and patient and provider perspectives, including how to handle urgent questions.
Other sections cover special populations such as pregnant women and people with type 2 diabetes, considerations for patient selection for current AID systems, safety, improving access to the technology, liability, and do-it-yourself systems.
Recommendations for health care professionals
A table near the end of the document provides specific recommendations for health care professionals, including the following:
- Be knowledgeable about AID systems and nuances of different systems, including their distinguishing features as well as strengths and weaknesses.
- Inform patients with diabetes about AID systems, including review of currently available systems, and create realistic expectations for device use.
- Involve patients with diabetes in shared decision-making when considering use of AID systems.
- Share information with patients with diabetes, as well as their peers, about general standards set by national and international guidelines on AID systems.
- Provide an on-call number or method by which a person with diabetes can always access support from a health care provider at the practice, including weekends and nights.
- Implement, potentially, protocols on times when AID systems should not be used.
- Use an individual’s health data to improve quality of care and health outcomes.
Most members of the ADA/EASD Diabetes Technology Working Group work with industry, but industry had no input on the project. Dr. Sherr has reported conducting clinical trials for Eli Lilly, Insulet, and Medtronic, and has received in-kind support for research studies from Dexcom and Medtronic. She has also reported consulting for Eli Lilly, Lexicon, Medtronic, and Sanofi, and being an advisory board member for Bigfoot Biomedical, Cecelia Health, Eli Lilly, Insulet, T1D Fund, and Vertex Pharmaceuticals. Dr. Evans has reported conducting clinical trials or research collaborations for, serving on advisory boards for, or receiving speakers fees or travel support from Medtronic, Roche, Abbott Diabetes Care, Dexcom, Novo Nordisk, Eli Lilly, Sanofi, Zucara Therapeutics, Pila Pharma, and AstraZeneca. The University of Cambridge has received salary support for Dr. Evans from the National Health Service.
A version of this article first appeared on Medscape.com.
FROM DIABETES CARE AND DIABETOLOGIA
Looking for the source of neuroendocrine tumors
The diversity of neuroendocrine tumors (NETs) – which includes variation in location, mutational profile, and response to therapy – may be due to divergent cellular origins in different tissue sites, according to a new study.
The pathogenesis of gastroenteropancreatic neoplasms (GEP-NENs) is poorly understood, in part because of a lack of modeling systems, according to Suzann Duan, PhD, and colleagues. They are a heterogeneous group of tumors that are increasingly prevalent in the United States. GEP-NENs arise from endocrine-producing cells and include gastric carcinoids, gastrinomas, and pancreatic NETs.
Despite the general mystery surrounding GEP-NENs, there is at least one clue in the form of the MEN1 gene. Both inherited and sporadic mutations of this gene are associated with GEP-NENs. Menin is a tumor suppressor protein, and previous studies have shown that inactivation of MEN1 leads to loss of that protein and is associated with endocrine tumors in the pancreas, pituitary, and upper GI tract.
In new research published in Cellular and Molecular Gastroenterology and Hepatology, researchers investigated the role of MEN1 in neuroendocrine cell development and traced it to a potential role in the development of NETs.
Patients with MEN1 mutations are at increased risk of gastrinomas, which lead to increased production of the peptide hormone gastrin. Gastrin increases acid production and can lead to hyperplasia in parietal and enterochromaffin cells. These generally develop in Brunner’s glands within the submucosa of the duodenum. At time of diagnosis, more than half of such tumors have developed lymph node metastases.
It remains unclear how loss of MEN1 suppresses gastrin production. Previous research showed that homozygous MEN1 deletion in mice is lethal to embryos, while leaving one copy intact leads to heightened risk of endocrine tumors in the pancreas and pituitary gland, but not in the GI tract. The studies did not reveal the tumor’s origin cell.
The researchers developed a novel mouse model in which MEN1 is conditionally deleted from the GI tract epithelium. This led to hyperplasia of gastrin-producing cells (G cells) in the antrum, as well as hypergastrinemia and development of gastric NETs. Exposure to a proton pump inhibitor accelerated gastric NET development, and the researchers identified expansion of enteric glial cells that expressed gastrin and GFAP. Glial cells that differentiated into endocrine phenotype were associated with a reversible loss of menin. “Taken together, these observations suggest that hyperplastic G cells might emerge from reprogrammed neural crest–derived cells in addition to endoderm-derived enteroendocrine cells,” the authors wrote.
That idea is supported by previous research indicating that multipotent glial cells expressing GFAP or SOX10 may play a developmental role in formation of neuroendocrine cells.
With this in mind, the researchers deleted MEN1 in GFAP-expressing cells to see if it would promote neuroendocrine cell development.
The result was hyperplasia in the gastric antrum and NETs in the pituitary and pancreas. To the researchers’ surprise, NET development was associated with loss of GFAP expression as well as activation of neuronal and neuroendocrine-related genes in the stomach, pancreas, and pituitary. There was universal reduction of GFAP protein expression in pituitary and pancreatic NETs, but GFAP transcript levels stayed steady in the gastric antra despite a reduction in GFAP-reporter expression. This could indicate that the menin protein interacts with GFAP. If so, eliminating menin in GFAP-positive cells could change the localization of GFAP, which may in turn lead to changes in glial cell identity.
When the researchers compared transcriptomes of hyperplastic antral tissues to well-differentiated NETs, they found that NETs exhibited a greater loss of glial-restricted progenitor lineage–associated genes as well as more downregulation of gliogenesis-directing factors. “Thus, the transition from a glial-to-neuronal cell phenotype appears to promote the progression from neuroendocrine cell hyperplasia to tumor development,” the authors wrote. They also found that NETs have higher levels of expression of genes associated with neural stem and progenitor cells, as well as upregulation of factors secreted from neural crest cells that promote neurogenesis and restrict the glial cell fate. Many of these factors are part of the Hedgehog signaling pathway, and menin is known to repress Hedgehog signaling.
Intestinal glial cells have a high degree of plasticity. They can become neuronal progenitor cells and yet they can dedifferentiate to differentiate again into other cell lineages.
The research could eventually lead to identification of unique cells-of-origin for these tumors. The authors say that the diversity of the tumors – which includes variation in location, mutational profile, and response to therapy – may be due to divergent cellular origins in different tissue sites. “Defining the cells-of-origin and the events preceding neoplastic transformation will be critical to informing molecular signaling pathways that can then be targeted therapeutically,” the authors wrote.
The authors disclosed no conflicts of interest.
Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) share endocrine and neural features but are diverse in terms of their location, behaviors, and response to therapies. One explanation for heterogeneity in GEP-NENs is that they have diverse cellular origins. The study by Duan and colleagues suggests that glia could be a potential cell of origin in GEP-NENs. GEP-NEN development in the pancreas, pituitary, and upper gastrointestinal tract is associated with mutations in the Multiple Endocrine Neoplasia I (MEN1) gene that cause a loss of the tumor suppressor protein menin.
The tumorigenic potential of GFAP-positive cells differs even between the pituitary, pancreas, and stomach since mice lacking Men1 in GFAP-positive cells did not develop gastrinomas while tumors were observed in the pituitary and pancreas. This could indicate that additional drivers are necessary to promote NENs in the intestine which are not required in other locations. These differences could be important when considering treatment strategies given the diverse nature of the cells and mechanisms involved.
Brian D. Gulbransen, PhD, is an associate professor in the department of physiology and an MSU Foundation Professor at Michigan State University, East Lansing. He has no conflicts.
Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) share endocrine and neural features but are diverse in terms of their location, behaviors, and response to therapies. One explanation for heterogeneity in GEP-NENs is that they have diverse cellular origins. The study by Duan and colleagues suggests that glia could be a potential cell of origin in GEP-NENs. GEP-NEN development in the pancreas, pituitary, and upper gastrointestinal tract is associated with mutations in the Multiple Endocrine Neoplasia I (MEN1) gene that cause a loss of the tumor suppressor protein menin.
The tumorigenic potential of GFAP-positive cells differs even between the pituitary, pancreas, and stomach since mice lacking Men1 in GFAP-positive cells did not develop gastrinomas while tumors were observed in the pituitary and pancreas. This could indicate that additional drivers are necessary to promote NENs in the intestine which are not required in other locations. These differences could be important when considering treatment strategies given the diverse nature of the cells and mechanisms involved.
Brian D. Gulbransen, PhD, is an associate professor in the department of physiology and an MSU Foundation Professor at Michigan State University, East Lansing. He has no conflicts.
Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs) share endocrine and neural features but are diverse in terms of their location, behaviors, and response to therapies. One explanation for heterogeneity in GEP-NENs is that they have diverse cellular origins. The study by Duan and colleagues suggests that glia could be a potential cell of origin in GEP-NENs. GEP-NEN development in the pancreas, pituitary, and upper gastrointestinal tract is associated with mutations in the Multiple Endocrine Neoplasia I (MEN1) gene that cause a loss of the tumor suppressor protein menin.
The tumorigenic potential of GFAP-positive cells differs even between the pituitary, pancreas, and stomach since mice lacking Men1 in GFAP-positive cells did not develop gastrinomas while tumors were observed in the pituitary and pancreas. This could indicate that additional drivers are necessary to promote NENs in the intestine which are not required in other locations. These differences could be important when considering treatment strategies given the diverse nature of the cells and mechanisms involved.
Brian D. Gulbransen, PhD, is an associate professor in the department of physiology and an MSU Foundation Professor at Michigan State University, East Lansing. He has no conflicts.
The diversity of neuroendocrine tumors (NETs) – which includes variation in location, mutational profile, and response to therapy – may be due to divergent cellular origins in different tissue sites, according to a new study.
The pathogenesis of gastroenteropancreatic neoplasms (GEP-NENs) is poorly understood, in part because of a lack of modeling systems, according to Suzann Duan, PhD, and colleagues. They are a heterogeneous group of tumors that are increasingly prevalent in the United States. GEP-NENs arise from endocrine-producing cells and include gastric carcinoids, gastrinomas, and pancreatic NETs.
Despite the general mystery surrounding GEP-NENs, there is at least one clue in the form of the MEN1 gene. Both inherited and sporadic mutations of this gene are associated with GEP-NENs. Menin is a tumor suppressor protein, and previous studies have shown that inactivation of MEN1 leads to loss of that protein and is associated with endocrine tumors in the pancreas, pituitary, and upper GI tract.
In new research published in Cellular and Molecular Gastroenterology and Hepatology, researchers investigated the role of MEN1 in neuroendocrine cell development and traced it to a potential role in the development of NETs.
Patients with MEN1 mutations are at increased risk of gastrinomas, which lead to increased production of the peptide hormone gastrin. Gastrin increases acid production and can lead to hyperplasia in parietal and enterochromaffin cells. These generally develop in Brunner’s glands within the submucosa of the duodenum. At time of diagnosis, more than half of such tumors have developed lymph node metastases.
It remains unclear how loss of MEN1 suppresses gastrin production. Previous research showed that homozygous MEN1 deletion in mice is lethal to embryos, while leaving one copy intact leads to heightened risk of endocrine tumors in the pancreas and pituitary gland, but not in the GI tract. The studies did not reveal the tumor’s origin cell.
The researchers developed a novel mouse model in which MEN1 is conditionally deleted from the GI tract epithelium. This led to hyperplasia of gastrin-producing cells (G cells) in the antrum, as well as hypergastrinemia and development of gastric NETs. Exposure to a proton pump inhibitor accelerated gastric NET development, and the researchers identified expansion of enteric glial cells that expressed gastrin and GFAP. Glial cells that differentiated into endocrine phenotype were associated with a reversible loss of menin. “Taken together, these observations suggest that hyperplastic G cells might emerge from reprogrammed neural crest–derived cells in addition to endoderm-derived enteroendocrine cells,” the authors wrote.
That idea is supported by previous research indicating that multipotent glial cells expressing GFAP or SOX10 may play a developmental role in formation of neuroendocrine cells.
With this in mind, the researchers deleted MEN1 in GFAP-expressing cells to see if it would promote neuroendocrine cell development.
The result was hyperplasia in the gastric antrum and NETs in the pituitary and pancreas. To the researchers’ surprise, NET development was associated with loss of GFAP expression as well as activation of neuronal and neuroendocrine-related genes in the stomach, pancreas, and pituitary. There was universal reduction of GFAP protein expression in pituitary and pancreatic NETs, but GFAP transcript levels stayed steady in the gastric antra despite a reduction in GFAP-reporter expression. This could indicate that the menin protein interacts with GFAP. If so, eliminating menin in GFAP-positive cells could change the localization of GFAP, which may in turn lead to changes in glial cell identity.
When the researchers compared transcriptomes of hyperplastic antral tissues to well-differentiated NETs, they found that NETs exhibited a greater loss of glial-restricted progenitor lineage–associated genes as well as more downregulation of gliogenesis-directing factors. “Thus, the transition from a glial-to-neuronal cell phenotype appears to promote the progression from neuroendocrine cell hyperplasia to tumor development,” the authors wrote. They also found that NETs have higher levels of expression of genes associated with neural stem and progenitor cells, as well as upregulation of factors secreted from neural crest cells that promote neurogenesis and restrict the glial cell fate. Many of these factors are part of the Hedgehog signaling pathway, and menin is known to repress Hedgehog signaling.
Intestinal glial cells have a high degree of plasticity. They can become neuronal progenitor cells and yet they can dedifferentiate to differentiate again into other cell lineages.
The research could eventually lead to identification of unique cells-of-origin for these tumors. The authors say that the diversity of the tumors – which includes variation in location, mutational profile, and response to therapy – may be due to divergent cellular origins in different tissue sites. “Defining the cells-of-origin and the events preceding neoplastic transformation will be critical to informing molecular signaling pathways that can then be targeted therapeutically,” the authors wrote.
The authors disclosed no conflicts of interest.
The diversity of neuroendocrine tumors (NETs) – which includes variation in location, mutational profile, and response to therapy – may be due to divergent cellular origins in different tissue sites, according to a new study.
The pathogenesis of gastroenteropancreatic neoplasms (GEP-NENs) is poorly understood, in part because of a lack of modeling systems, according to Suzann Duan, PhD, and colleagues. They are a heterogeneous group of tumors that are increasingly prevalent in the United States. GEP-NENs arise from endocrine-producing cells and include gastric carcinoids, gastrinomas, and pancreatic NETs.
Despite the general mystery surrounding GEP-NENs, there is at least one clue in the form of the MEN1 gene. Both inherited and sporadic mutations of this gene are associated with GEP-NENs. Menin is a tumor suppressor protein, and previous studies have shown that inactivation of MEN1 leads to loss of that protein and is associated with endocrine tumors in the pancreas, pituitary, and upper GI tract.
In new research published in Cellular and Molecular Gastroenterology and Hepatology, researchers investigated the role of MEN1 in neuroendocrine cell development and traced it to a potential role in the development of NETs.
Patients with MEN1 mutations are at increased risk of gastrinomas, which lead to increased production of the peptide hormone gastrin. Gastrin increases acid production and can lead to hyperplasia in parietal and enterochromaffin cells. These generally develop in Brunner’s glands within the submucosa of the duodenum. At time of diagnosis, more than half of such tumors have developed lymph node metastases.
It remains unclear how loss of MEN1 suppresses gastrin production. Previous research showed that homozygous MEN1 deletion in mice is lethal to embryos, while leaving one copy intact leads to heightened risk of endocrine tumors in the pancreas and pituitary gland, but not in the GI tract. The studies did not reveal the tumor’s origin cell.
The researchers developed a novel mouse model in which MEN1 is conditionally deleted from the GI tract epithelium. This led to hyperplasia of gastrin-producing cells (G cells) in the antrum, as well as hypergastrinemia and development of gastric NETs. Exposure to a proton pump inhibitor accelerated gastric NET development, and the researchers identified expansion of enteric glial cells that expressed gastrin and GFAP. Glial cells that differentiated into endocrine phenotype were associated with a reversible loss of menin. “Taken together, these observations suggest that hyperplastic G cells might emerge from reprogrammed neural crest–derived cells in addition to endoderm-derived enteroendocrine cells,” the authors wrote.
That idea is supported by previous research indicating that multipotent glial cells expressing GFAP or SOX10 may play a developmental role in formation of neuroendocrine cells.
With this in mind, the researchers deleted MEN1 in GFAP-expressing cells to see if it would promote neuroendocrine cell development.
The result was hyperplasia in the gastric antrum and NETs in the pituitary and pancreas. To the researchers’ surprise, NET development was associated with loss of GFAP expression as well as activation of neuronal and neuroendocrine-related genes in the stomach, pancreas, and pituitary. There was universal reduction of GFAP protein expression in pituitary and pancreatic NETs, but GFAP transcript levels stayed steady in the gastric antra despite a reduction in GFAP-reporter expression. This could indicate that the menin protein interacts with GFAP. If so, eliminating menin in GFAP-positive cells could change the localization of GFAP, which may in turn lead to changes in glial cell identity.
When the researchers compared transcriptomes of hyperplastic antral tissues to well-differentiated NETs, they found that NETs exhibited a greater loss of glial-restricted progenitor lineage–associated genes as well as more downregulation of gliogenesis-directing factors. “Thus, the transition from a glial-to-neuronal cell phenotype appears to promote the progression from neuroendocrine cell hyperplasia to tumor development,” the authors wrote. They also found that NETs have higher levels of expression of genes associated with neural stem and progenitor cells, as well as upregulation of factors secreted from neural crest cells that promote neurogenesis and restrict the glial cell fate. Many of these factors are part of the Hedgehog signaling pathway, and menin is known to repress Hedgehog signaling.
Intestinal glial cells have a high degree of plasticity. They can become neuronal progenitor cells and yet they can dedifferentiate to differentiate again into other cell lineages.
The research could eventually lead to identification of unique cells-of-origin for these tumors. The authors say that the diversity of the tumors – which includes variation in location, mutational profile, and response to therapy – may be due to divergent cellular origins in different tissue sites. “Defining the cells-of-origin and the events preceding neoplastic transformation will be critical to informing molecular signaling pathways that can then be targeted therapeutically,” the authors wrote.
The authors disclosed no conflicts of interest.
FROM CELLULAR AND MOLECULAR GASTROENTEROLOGY AND HEPATOLOGY
Opioids leading cause of poisoning deaths in young children
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
ANAHEIM, CALIF. – Opioids are the most common cause of fatal poisonings in young children, and their contribution to children’s deaths has been increasing, according to research presented at the American Academy of Pediatrics National Conference.
The study found that the proportion of deaths in U.S. children linked to opioids has doubled since the mid-2000s, tracking the course of the epidemic in adults in this country.
“What is striking about our study is how the opioid epidemic has not spared our nation’s infants or young children,” Christopher Gaw, MD, MA, a pediatric emergency medicine fellow physician at Children’s Hospital of Philadelphia, said in an interview. “There is important work being done to reduce unnecessary opioid prescribing, drug diversion, and treatment of substance use disorders. These efforts – though not directly related to children – also help protect them, since they can reduce the chance of exposure to opioids in the home.”
Dr. Gaw and his colleagues analyzed data in Child Death Reviews from 40 states that participate in the National Fatality Review Case Reporting System, focusing on children aged 5 years and younger who died from a poisoning between 2005 and 2018. During that time, 731 child poisoning deaths were reported to the system – of which nearly half (47%) involved opioids as the poisoning agent – up from 24% in 2005. More than 4 in 10 deaths (42%) involved children under age 1.
Most of the deaths (61%) occurred in the child’s home, and in even more cases (71%) the child was being supervised when the poisoning occurred, most often by a parent (58.5%). The others supervising children were usually a grandparent (11%) or another relative (5.5%). The child was in view of the supervising individual in 28.5% of the deaths. A child protective services case was opened in 13% of the cases.
“Supervising a child is hard. Kids are constantly exploring and moving,” Dr. Gaw said. “A child may find a dropped medication on the floor that a caregiver doesn’t see, or a child may get into a bag or a purse when a caregiver is looking the other way. Poisonings can happen in a split second.”
Expecting caregivers to be able to watch kids every moment and always be within arm’s reach to prevent an accident is unrealistic, Dr. Gaw said, so families should focus on preparedness.
“Young children can’t tell the difference between a deadly substance versus a substance that is harmless or would only cause some harm. The best way to protect children is to prevent the poisoning from happening in the first place,” Dr. Gaw said. ”
It is recommended that caregivers keep the Poison Control Center’s national 24/7 hotline in their phones: (800) 222-1222.
Two-thirds of the cases Dr. Gaw examined did not involve a call to a poison control center, but most did involve a call to 911.
“My guess is that caregivers likely called 911 instead of poison control because the child was likely critically ill or deceased when found,” Dr. Gaw said, noting that his group did not have access to descriptive information about 911 calls. “If a child is critically ill and a caregiver called poison control first, they would be referred to 911.”
If a child looks healthy but has just swallowed something dangerous or deadly, Dr. Gaw said poison control can guide the family to getting prompt medical attention that could be lifesaving.
“We don’t expect the public to know what substances are harmless, harmful, or deadly,” he said. “People should always call poison control if there is any concern, even if the child looks well.”
Some poison control centers are working to increase the ways people can reach them, including through texting, apps, or online chat, he added.
Gary A. Smith, MD, DrPH, president of the nonprofit Child Injury Prevention Alliance in Columbus, Ohio, and director of the Center for Injury Research and Policy at Nationwide Children’s Hospital, said the high level of supervision in these cases was not surprising.
”We have shown that most children are being directly supervised at the moment of injury for baby walker–related injuries, firework-related injuries, and other types of injuries that we have studied,” Dr. Smith said in an interview. “Injuries happen quickly and generally do not give a parent or caregiver time to react.”
“This dispels the myth that parental supervision is the key to injury prevention,” Dr. Smith said. “Although supervision helps, it is not adequate. These injuries occur to children of good and caring parents. The message for pediatricians is that we must create safe environments for children and design hazards out of existence to effectively prevent poisoning and other injuries.”
That preventive approach has been used for infectious disease and other public health problems, he added.
“Prescription opioids must be kept in their original containers with children-resistant closures and be stored up, away, and out of sight of children, preferably in a locked location,” Dr. Smith said. “If adults use illicit opioids or any other illicit substances – which are commonly laced with fentanyl – they should not use or store them in the home where children can access them.”
Over-the-counter pain, cold, and allergy medications were the second most common cause of death, occurring in 15% of cases.
“There has been a lot of work over the years among health care providers to counsel families on the proper dosing and use of medications such as Tylenol, Motrin, and Benadryl,” Dr. Gaw said. “There has also been a push to educate families that using antihistamines, such as Benadryl, to sedate their children can be dangerous and, depending on the dose, potentially deadly.”
Another 14% of cases were an unspecified illicit drug, and 10% were an unspecified over-the-counter or prescription medication. Carbon monoxide poisoning made up 6% of cases, and the remaining substances included amphetamines, antidepressants, cocaine, and alcohol.
Over half the deaths in 1-year-olds (61%) and children aged 2-5 (54%) were due to opioid poisoning, as were a third of deaths in infants (34%). Most of the poisonings involving amphetamines (81%), cocaine (84%), and alcohol (61.5%) occurred in infants under age 1.
Dr. Smith said that harm-reduction strategies, such as having naloxone on hand and using fentanyl test strips, can reduce the likelihood of death from illicit drugs.
Reducing stigma can save lives
“Referring parents to services for individuals who use drugs is key,” Dr. Smith said. “Treating this as a public health problem without stigmatizing the behavior is something that pediatricians and other health care professionals must remember.” As a resource for other pediatricians, Dr. Gaw noted that CHOP’s poison control center medical director Kevin Osterhoudt, MD produced a 25-minute podcast that covers common causes of poisonings, use of naloxone in children, and prevention tips.
“Naloxone is an effective antidote to opioid poisonings,” Dr. Gaw said. “We often think of using it in adults, but this is also a lifesaving medication for children poisoned by opioids. Educating people on recognizing the signs and symptoms of opioid poisoning and helping them feel empowered to use naloxone is something the public health world is working on.”
Dr. Gaw and Dr. Smith had no relevant disclosures. No external funding was noted for the study.
AT AAP 2022
At the front lines of long COVID, local clinics prove vital
Big-name hospital chains across the United States are opening dedicated centers to help patients dealing with long COVID. But so are the lower-profile clinics and hospitals run by cities, counties and states – including Harborview Medical Center in Seattle.
They serve areas ranging from Campbell County, Wyo., with 47,000 residents, to New York City, with its 8.4 million people. Many providers working there are searching for innovative ways to approach this lingering illness with its variety of symptoms, from brain fog to shortness of breath to depression and more.
Their efforts often fall below the radar, with still-scant serious media attention to long COVID or the public health employees working to treat ailing patients.
Why are state and local health agencies taking on these duties?
They’re leading the way in part because the federal government has made only limited efforts, said Lisa McCorkell, a cofounder of the Patient-Led Research Collaborative. The international group was founded in spring 2020 by researchers who are also long COVID patients.
“It’s a big reason why long COVID isn’t talked about as much,” Ms. McCorkell said. “It’s definitely a national issue. But it trickles down to state and local health departments, and there’s not enough resources.”
The government clinics may be accessible to people without insurance and often are cheaper than clinics at private hospitals.
Harborview has treated more than 1,000 patients with long COVID, and another 200 patients are awaiting treatment, said Jessica Bender, MD, a codirector of the University of Washington Post-COVID Rehabilitation and Recovery Clinic in Seattle’s First Hill neighborhood.
The group Survivor Corps offers lists by states of clinics. While the publicly run clinics may be less expensive or even free for some patients, methods of payment vary from clinic to clinic. Federally qualified health clinics offer treatment on a sliding scale. For instance, the Riverside University Health System in California has federally qualified centers. And other providers who are not federally qualified also offer care paid for on a sliding scale. They include Campbell County Health, where some residents are eligible for discounts of 25%-100%, said spokesperson Norberto Orellana.
At Harborview, Dr. Bender said the public hospital’s post-COVID clinic initially began with a staff of rehabilitation doctors but expanded in 2021 to include family and internal medicine doctors. And it offers mental health programs with rehabilitation psychologists who instruct on how to deal with doctors or loved ones who don’t believe that long COVID exists.
“I have patients who really have been devastated by the lack of support from coworkers [and] family,” Dr. Bender said.
In Campbell County, Wyo., the pandemic surge did not arrive in earnest until late 2021. Physical therapists at Campbell County’s Health Rehabilitation Services organized a rehabilitation program for residents with long COVID after recognizing the need, said Shannon Sorensen, rehabilitation director at Campbell County Health.
“We had patients coming in showing chest pain, or heart palpitations. There were people trying to get back to work. They were frustrated,” Ms. Sorensen said.
Myalgic encephalomyelitis and chronic fatigue syndrome activists have embraced the fight to recognize and help long COVID patients, noting the similarities between the conditions, and hope to help kickstart more organized research, treatment and benefits for long COVID sufferers and myalgic encephalomyelitis/chronic fatigue syndrome patients alike.
In Ft. Collins, Colo., disability activist Alison Sbrana has long had myalgic encephalomyelitis. She and other members of the local chapter of ME Action have met with state officials for several years and are finally seeing the results of those efforts.
Colorado Gov. Jared Polis has created the full-time position of policy adviser for long COVID and post–viral infection planning.
“This is one way forward of how state governments are (finally) paying attention to infection-triggered chronic illnesses and starting to think ahead on them,” Ms. Sbrana said.
New York City’s Health + Hospitals launched what may be the most expansive long COVID treatment program in the nation in April 2021. Called AfterCare, it provides physical and mental health services as well as community support systems and financial assistance.
A persistent issue for patients is that there isn’t yet a test for long COVID, like there is for COVID-19, said Amanda Johnson, MD, assistant vice president for ambulatory care and population health at New York Health + Hospitals. “It’s in many ways a diagnosis of exclusion. You have to make sure their shortness of breath isn’t caused by something else. The same with anemia,” she said.
California’s Department of Public Health has a detailed website devoted to the topic, including videos of “long haulers” describing their experiences.
Vermont is one of several states studying long COVID, said Mark Levine, MD, the state health commissioner. The state, in collaboration with the University of Vermont, has established a surveillance project to determine how many people have long COVID, as well as how severe it is, how long it lasts, and potential predispositions.
The University of Utah, Salt Lake City, established a comprehensive COVID-19 clinic more than a year ago that also handles long COVID patients, said Jeannette Brown, MD, PhD, an associate professor at the school and director of the COVID-19 clinic.
Jennifer Chevinsky, MD, MPH, already had a deep understanding of long COVID when she landed in Riverside County, Calif., in the summer of 2021. She came from Atlanta, where as part of her job as an epidemic intelligence service officer at the CDC, she heard stories of COVID-19 patients who were not getting better.
Now she is a deputy public health officer for Riverside County, in a region known for its deserts, sizzling summer temperatures and diverse populations. She said her department has helped launch programs such as post–COVID-19 follow-up phone calls and long COVID training programs that reach out to the many Latino residents in this county of 2.4 million people. It also includes Black and Native American residents.
“We’re making sure information is circulated with community and faith-based organizations, and community health workers,” she said.
Ms. McCorkell said there is still much work to do to raise public awareness of the risks of long COVID and how to obtain care for patients. She would like to see a national public health campaign about long COVID, possibly spearheaded by the Centers for Disease Control and Prevention in partnership with local health workers and community-based organizations.
“That,” she said, “could make a big difference.”
A version of this article first appeared on WebMD.com.
Big-name hospital chains across the United States are opening dedicated centers to help patients dealing with long COVID. But so are the lower-profile clinics and hospitals run by cities, counties and states – including Harborview Medical Center in Seattle.
They serve areas ranging from Campbell County, Wyo., with 47,000 residents, to New York City, with its 8.4 million people. Many providers working there are searching for innovative ways to approach this lingering illness with its variety of symptoms, from brain fog to shortness of breath to depression and more.
Their efforts often fall below the radar, with still-scant serious media attention to long COVID or the public health employees working to treat ailing patients.
Why are state and local health agencies taking on these duties?
They’re leading the way in part because the federal government has made only limited efforts, said Lisa McCorkell, a cofounder of the Patient-Led Research Collaborative. The international group was founded in spring 2020 by researchers who are also long COVID patients.
“It’s a big reason why long COVID isn’t talked about as much,” Ms. McCorkell said. “It’s definitely a national issue. But it trickles down to state and local health departments, and there’s not enough resources.”
The government clinics may be accessible to people without insurance and often are cheaper than clinics at private hospitals.
Harborview has treated more than 1,000 patients with long COVID, and another 200 patients are awaiting treatment, said Jessica Bender, MD, a codirector of the University of Washington Post-COVID Rehabilitation and Recovery Clinic in Seattle’s First Hill neighborhood.
The group Survivor Corps offers lists by states of clinics. While the publicly run clinics may be less expensive or even free for some patients, methods of payment vary from clinic to clinic. Federally qualified health clinics offer treatment on a sliding scale. For instance, the Riverside University Health System in California has federally qualified centers. And other providers who are not federally qualified also offer care paid for on a sliding scale. They include Campbell County Health, where some residents are eligible for discounts of 25%-100%, said spokesperson Norberto Orellana.
At Harborview, Dr. Bender said the public hospital’s post-COVID clinic initially began with a staff of rehabilitation doctors but expanded in 2021 to include family and internal medicine doctors. And it offers mental health programs with rehabilitation psychologists who instruct on how to deal with doctors or loved ones who don’t believe that long COVID exists.
“I have patients who really have been devastated by the lack of support from coworkers [and] family,” Dr. Bender said.
In Campbell County, Wyo., the pandemic surge did not arrive in earnest until late 2021. Physical therapists at Campbell County’s Health Rehabilitation Services organized a rehabilitation program for residents with long COVID after recognizing the need, said Shannon Sorensen, rehabilitation director at Campbell County Health.
“We had patients coming in showing chest pain, or heart palpitations. There were people trying to get back to work. They were frustrated,” Ms. Sorensen said.
Myalgic encephalomyelitis and chronic fatigue syndrome activists have embraced the fight to recognize and help long COVID patients, noting the similarities between the conditions, and hope to help kickstart more organized research, treatment and benefits for long COVID sufferers and myalgic encephalomyelitis/chronic fatigue syndrome patients alike.
In Ft. Collins, Colo., disability activist Alison Sbrana has long had myalgic encephalomyelitis. She and other members of the local chapter of ME Action have met with state officials for several years and are finally seeing the results of those efforts.
Colorado Gov. Jared Polis has created the full-time position of policy adviser for long COVID and post–viral infection planning.
“This is one way forward of how state governments are (finally) paying attention to infection-triggered chronic illnesses and starting to think ahead on them,” Ms. Sbrana said.
New York City’s Health + Hospitals launched what may be the most expansive long COVID treatment program in the nation in April 2021. Called AfterCare, it provides physical and mental health services as well as community support systems and financial assistance.
A persistent issue for patients is that there isn’t yet a test for long COVID, like there is for COVID-19, said Amanda Johnson, MD, assistant vice president for ambulatory care and population health at New York Health + Hospitals. “It’s in many ways a diagnosis of exclusion. You have to make sure their shortness of breath isn’t caused by something else. The same with anemia,” she said.
California’s Department of Public Health has a detailed website devoted to the topic, including videos of “long haulers” describing their experiences.
Vermont is one of several states studying long COVID, said Mark Levine, MD, the state health commissioner. The state, in collaboration with the University of Vermont, has established a surveillance project to determine how many people have long COVID, as well as how severe it is, how long it lasts, and potential predispositions.
The University of Utah, Salt Lake City, established a comprehensive COVID-19 clinic more than a year ago that also handles long COVID patients, said Jeannette Brown, MD, PhD, an associate professor at the school and director of the COVID-19 clinic.
Jennifer Chevinsky, MD, MPH, already had a deep understanding of long COVID when she landed in Riverside County, Calif., in the summer of 2021. She came from Atlanta, where as part of her job as an epidemic intelligence service officer at the CDC, she heard stories of COVID-19 patients who were not getting better.
Now she is a deputy public health officer for Riverside County, in a region known for its deserts, sizzling summer temperatures and diverse populations. She said her department has helped launch programs such as post–COVID-19 follow-up phone calls and long COVID training programs that reach out to the many Latino residents in this county of 2.4 million people. It also includes Black and Native American residents.
“We’re making sure information is circulated with community and faith-based organizations, and community health workers,” she said.
Ms. McCorkell said there is still much work to do to raise public awareness of the risks of long COVID and how to obtain care for patients. She would like to see a national public health campaign about long COVID, possibly spearheaded by the Centers for Disease Control and Prevention in partnership with local health workers and community-based organizations.
“That,” she said, “could make a big difference.”
A version of this article first appeared on WebMD.com.
Big-name hospital chains across the United States are opening dedicated centers to help patients dealing with long COVID. But so are the lower-profile clinics and hospitals run by cities, counties and states – including Harborview Medical Center in Seattle.
They serve areas ranging from Campbell County, Wyo., with 47,000 residents, to New York City, with its 8.4 million people. Many providers working there are searching for innovative ways to approach this lingering illness with its variety of symptoms, from brain fog to shortness of breath to depression and more.
Their efforts often fall below the radar, with still-scant serious media attention to long COVID or the public health employees working to treat ailing patients.
Why are state and local health agencies taking on these duties?
They’re leading the way in part because the federal government has made only limited efforts, said Lisa McCorkell, a cofounder of the Patient-Led Research Collaborative. The international group was founded in spring 2020 by researchers who are also long COVID patients.
“It’s a big reason why long COVID isn’t talked about as much,” Ms. McCorkell said. “It’s definitely a national issue. But it trickles down to state and local health departments, and there’s not enough resources.”
The government clinics may be accessible to people without insurance and often are cheaper than clinics at private hospitals.
Harborview has treated more than 1,000 patients with long COVID, and another 200 patients are awaiting treatment, said Jessica Bender, MD, a codirector of the University of Washington Post-COVID Rehabilitation and Recovery Clinic in Seattle’s First Hill neighborhood.
The group Survivor Corps offers lists by states of clinics. While the publicly run clinics may be less expensive or even free for some patients, methods of payment vary from clinic to clinic. Federally qualified health clinics offer treatment on a sliding scale. For instance, the Riverside University Health System in California has federally qualified centers. And other providers who are not federally qualified also offer care paid for on a sliding scale. They include Campbell County Health, where some residents are eligible for discounts of 25%-100%, said spokesperson Norberto Orellana.
At Harborview, Dr. Bender said the public hospital’s post-COVID clinic initially began with a staff of rehabilitation doctors but expanded in 2021 to include family and internal medicine doctors. And it offers mental health programs with rehabilitation psychologists who instruct on how to deal with doctors or loved ones who don’t believe that long COVID exists.
“I have patients who really have been devastated by the lack of support from coworkers [and] family,” Dr. Bender said.
In Campbell County, Wyo., the pandemic surge did not arrive in earnest until late 2021. Physical therapists at Campbell County’s Health Rehabilitation Services organized a rehabilitation program for residents with long COVID after recognizing the need, said Shannon Sorensen, rehabilitation director at Campbell County Health.
“We had patients coming in showing chest pain, or heart palpitations. There were people trying to get back to work. They were frustrated,” Ms. Sorensen said.
Myalgic encephalomyelitis and chronic fatigue syndrome activists have embraced the fight to recognize and help long COVID patients, noting the similarities between the conditions, and hope to help kickstart more organized research, treatment and benefits for long COVID sufferers and myalgic encephalomyelitis/chronic fatigue syndrome patients alike.
In Ft. Collins, Colo., disability activist Alison Sbrana has long had myalgic encephalomyelitis. She and other members of the local chapter of ME Action have met with state officials for several years and are finally seeing the results of those efforts.
Colorado Gov. Jared Polis has created the full-time position of policy adviser for long COVID and post–viral infection planning.
“This is one way forward of how state governments are (finally) paying attention to infection-triggered chronic illnesses and starting to think ahead on them,” Ms. Sbrana said.
New York City’s Health + Hospitals launched what may be the most expansive long COVID treatment program in the nation in April 2021. Called AfterCare, it provides physical and mental health services as well as community support systems and financial assistance.
A persistent issue for patients is that there isn’t yet a test for long COVID, like there is for COVID-19, said Amanda Johnson, MD, assistant vice president for ambulatory care and population health at New York Health + Hospitals. “It’s in many ways a diagnosis of exclusion. You have to make sure their shortness of breath isn’t caused by something else. The same with anemia,” she said.
California’s Department of Public Health has a detailed website devoted to the topic, including videos of “long haulers” describing their experiences.
Vermont is one of several states studying long COVID, said Mark Levine, MD, the state health commissioner. The state, in collaboration with the University of Vermont, has established a surveillance project to determine how many people have long COVID, as well as how severe it is, how long it lasts, and potential predispositions.
The University of Utah, Salt Lake City, established a comprehensive COVID-19 clinic more than a year ago that also handles long COVID patients, said Jeannette Brown, MD, PhD, an associate professor at the school and director of the COVID-19 clinic.
Jennifer Chevinsky, MD, MPH, already had a deep understanding of long COVID when she landed in Riverside County, Calif., in the summer of 2021. She came from Atlanta, where as part of her job as an epidemic intelligence service officer at the CDC, she heard stories of COVID-19 patients who were not getting better.
Now she is a deputy public health officer for Riverside County, in a region known for its deserts, sizzling summer temperatures and diverse populations. She said her department has helped launch programs such as post–COVID-19 follow-up phone calls and long COVID training programs that reach out to the many Latino residents in this county of 2.4 million people. It also includes Black and Native American residents.
“We’re making sure information is circulated with community and faith-based organizations, and community health workers,” she said.
Ms. McCorkell said there is still much work to do to raise public awareness of the risks of long COVID and how to obtain care for patients. She would like to see a national public health campaign about long COVID, possibly spearheaded by the Centers for Disease Control and Prevention in partnership with local health workers and community-based organizations.
“That,” she said, “could make a big difference.”
A version of this article first appeared on WebMD.com.
Children and COVID: Downward trend reverses with small increase in new cases
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.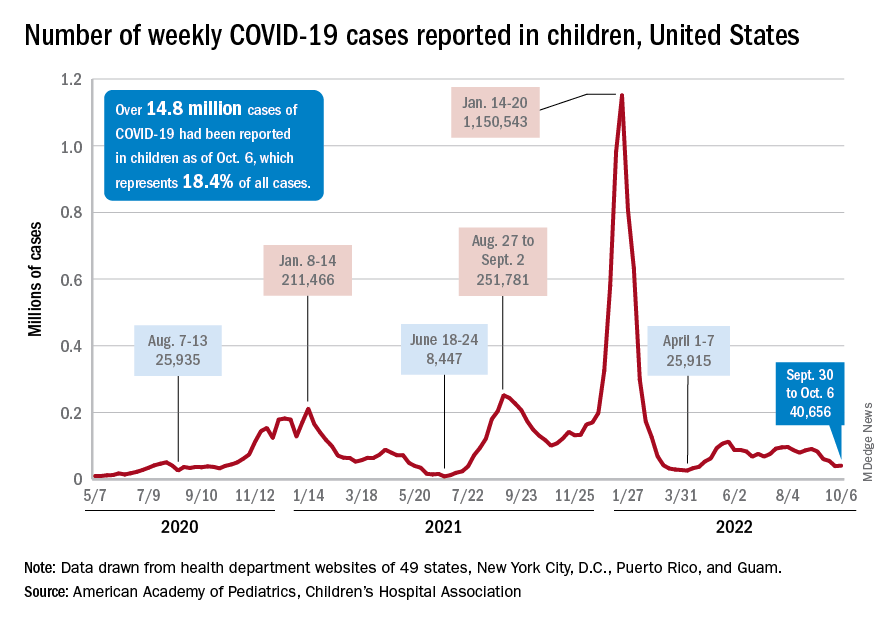
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
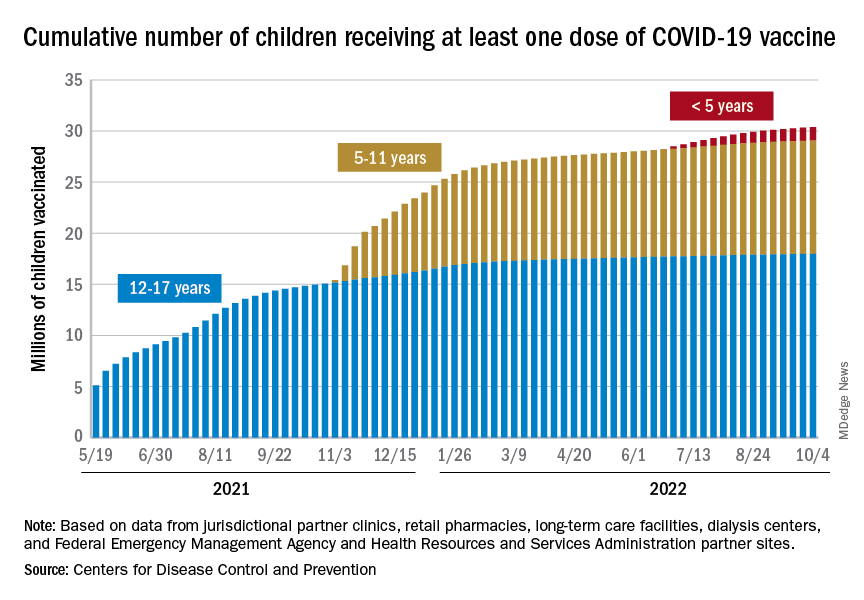
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.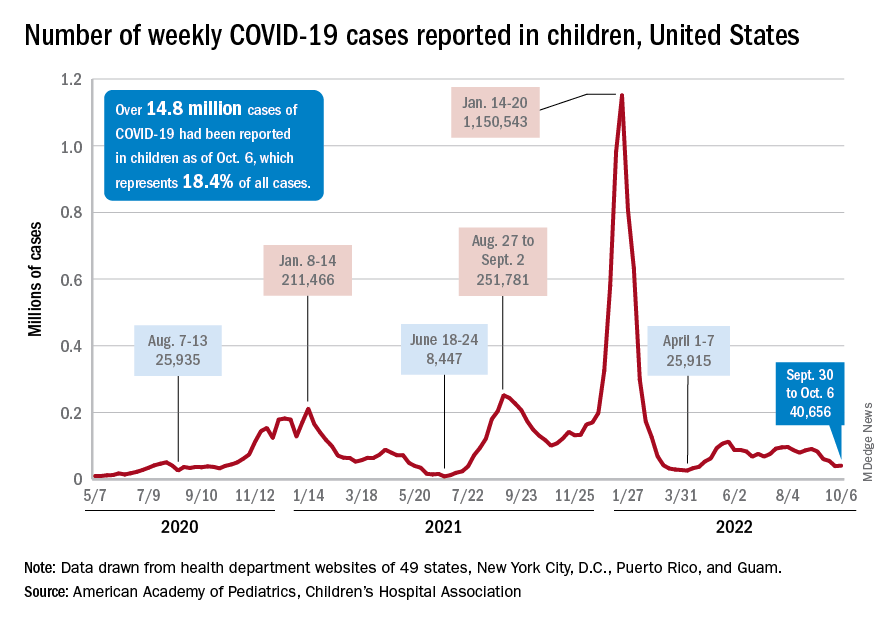
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
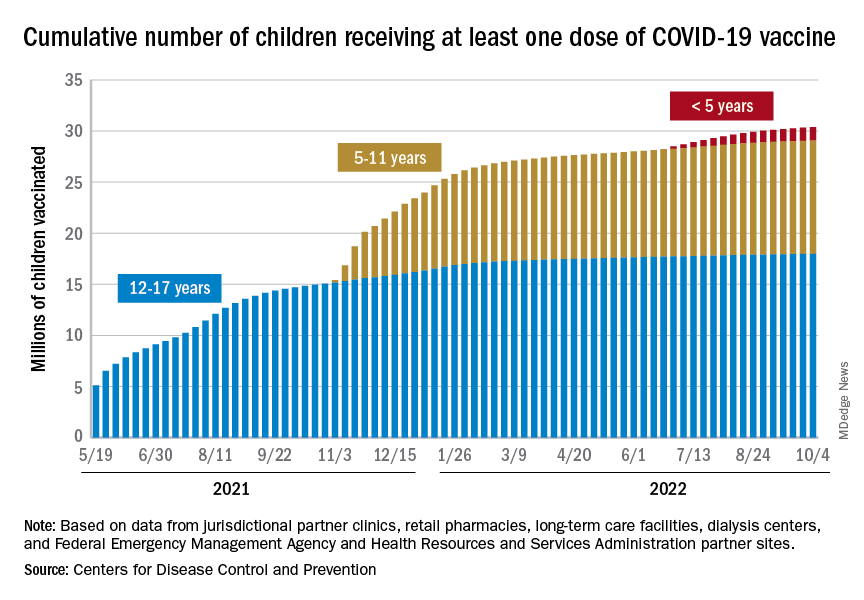
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
A small increase in new cases brought COVID-19’s latest losing streak to an end at 4 weeks, based on data from the American Academy of Pediatrics and the Children’s Hospital Association.
The 40,656 new cases reported bring the U.S. cumulative count of child COVID-19 cases to over 14.8 million since the pandemic began, which represents 18.4% of all cases, the AAP and CHA said in their weekly report based on state-level data.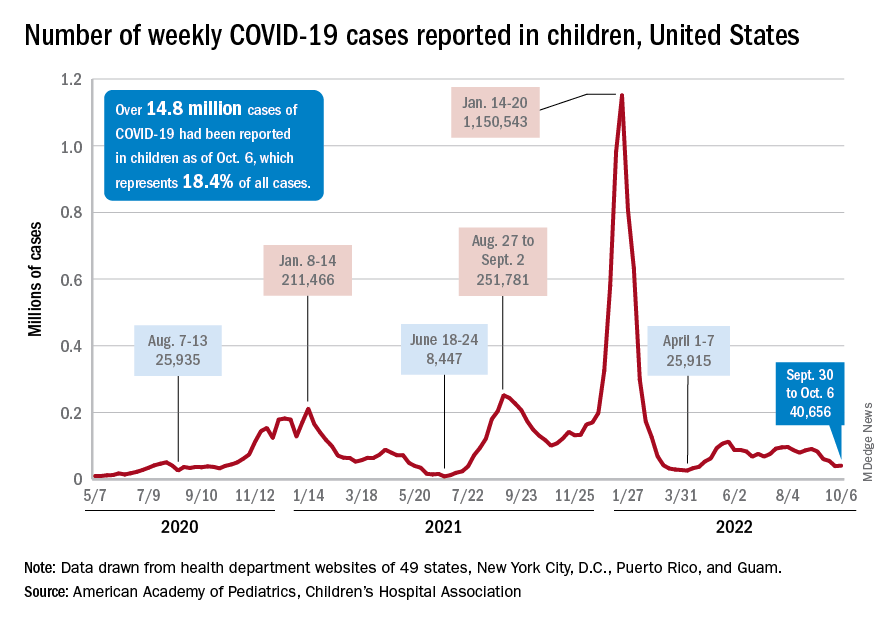
The increase in new cases was not reflected in emergency department visits or hospital admissions, which both continued sustained declines that started in August. In the week from Sept. 27 to Oct. 4, the 7-day averages for ED visits with diagnosed COVID were down by 21.5% (age 0-11), 27.3% (12-15), and 18.2% (16-17), the Centers for Disease Control and Prevention said, while the most recent 7-day average for new admissions – 127 per day for Oct. 2-8 – among children aged 0-17 years with confirmed COVID was down from 161 per day the previous week, a drop of over 21%.
The state-level data that are currently available (several states are no longer reporting) show Alaska (25.5%) and Vermont (25.4%) have the highest proportions of cumulative cases in children, and Florida (12.3%) and Utah (13.5%) have the lowest. Rhode Island has the highest rate of COVID-19 per 100,000 children at 40,427, while Missouri has the lowest at 14,252. The national average is 19,687 per 100,000, the AAP and CHA reported.
Taking a look at vaccination
Vaccinations were up slightly in children aged 12-17 years, as 20,000 initial doses were given during the week of Sept. 29 to Oct. 5, compared with 17,000 and 18,000 the previous 2 weeks. Initial vaccinations in younger children, however, continued declines dating back to August, the AAP said in its weekly vaccination trends report.
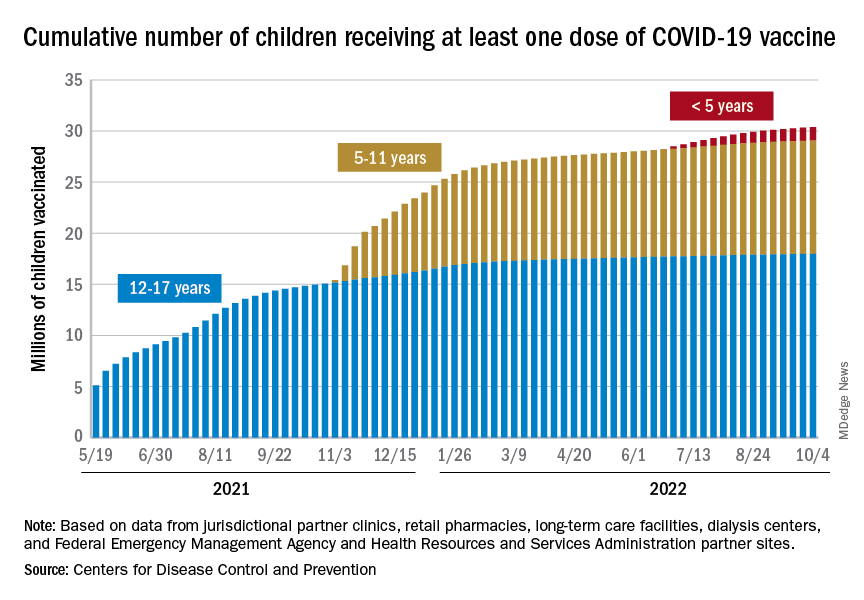
The District of Columbia and Massachusetts have the most highly vaccinated groups of 12- to 17-year-olds, as 100% and 95%, respectively, have received initial doses, while Wyoming (39%) and Idaho (42%) have the lowest. D.C. (73%) and Vermont (68%) have the highest proportions of vaccinated 5- to 11-year-olds, and Alabama (17%) and Mississippi (18%) have the lowest. For children under age 5 years, those in D.C. (33%) and Vermont (26%) are the most likely to have received an initial COVID vaccination, while Alabama, Louisiana, and Mississippi share national-low rates of 2%, the AAP said its report, which is based on CDC data.
When all states and territories are combined, 71% of children aged 12-17 have received at least one dose of vaccine, as have 38.6% of all children 5-11 years old and 6.7% of those under age 5. Almost 61% of the nation’s 16- to 17-year-olds have been fully vaccinated, along with 31.5% of those aged 5-11 and 2.4% of children younger than 5 years, the CDC said on its COVID Data Tracker.
About 42 million children – 58% of the population under the age of 18 years – have not received any vaccine yet, the AAP noted. Meanwhile, CDC data indicate that 36 children died of COVID in the last week, with pediatric deaths now totaling 1,781 over the course of the pandemic.
Pregnant, postpartum women with disabilities at higher risk for violence
Pregnant or postpartum women with disabilities are at relatively high risk of experiencing violence, often from the people closest to them, new research suggests.
The researchers set out to measure risk of interpersonal violence, which the World Health Organization defines as “the intentional use of physical force or power against an individual by an intimate partner, family member, or other community member.”
Hilary K. Brown, PhD, with the department of health & society, University of Toronto, led the study published online in Obstetrics and Gynecology.
Large, population-based dataset
The population study included people 15-49 years old with births in Ontario from 2004 to 2019. They included 147,414 people with physical disabilities; 47,459 people with intellectual disabilities; 2,557 with developmental disabilities; and 9,598 with multiple disabilities.
The control group was 1,594,441 million people without disabilities.
The outcome measured was “any emergency department visit, hospital admission, or death related to physical, sexual, or psychological violence between fertilization and 365 days post partum.”
Researchers found that the adjusted relative risk of interpersonal violence for those with disabilities, compared with those with no disabilities was 1.40 (95% confidence interval, 1.31-1.50) in those with physical disabilities; 2.39 (95% CI, 1.98-2.88) in those with intellectual or developmental disabilities; and 1.96 (95% CI, 1.66-2.30) in those with multiple disabilities.
History of violence means higher risk
Those with a history of interpersonal violence and a disability were at particularly high risk for perinatal violence.
The authors note that pregnancy is a high-risk period for interpersonal violence for all women, particularly by an intimate partner.
“More than 30% of intimate partner violence begins during pregnancy, and preexisting violence tends to escalate perinatally,” they write.
The authors cite previous research that found women with disabilities experience higher rates of abuse overall and by an intimate partner – two to four times rates reported by those without disabilities.
Opportunities for provider intervention
Since the period surrounding pregnancy is a time of increased contact with medical providers and resources, there may be opportunities for identifying abuse and providing interventions.
Those might include better screening, access to violence-related information and services, and education of health care professionals to support people with disabilities. For example, “Tools used for violence screening perinatally do not include items about forms of violence that are unique to individuals with disabilities, such as refusal to assist with activities of daily living.”
The authors add: “[G]iven that the strongest risk factor for interpersonal violence in the perinatal period, particularly in those with disabilities, was a prepregnancy history of interpersonal violence, our findings suggest that more could be done before pregnancy to offer screening and support at the index encounter.”
Violence can lead to adverse outcomes
Implications are important as the violence can result in barriers to care and adverse perinatal outcomes.
Jeanne L. Alhusen, PhD, CRNP, RN, University of Virginia Medical Center professor of nursing and associate dean for research, was not part of this research but wrote a paper earlier this year on the subject and had similar conclusions.
She said before this study by Brown et al., “our understanding of the risk of violence by disability type throughout the perinatal period, on a population-based level, was quite limited.”
With the size of this dataset, she said, this paper provides critical information for health care providers. It extends physicians’ ability to examine risk of violence by disability type as well as these patients’ risk of experiencing different types of violence.
She pointed out that the Pregnancy Risk Assessment Monitoring System (PRAMS) recently incorporated a disability supplement that allows better understanding of pregnancy risks in people with disabilities.
“It will be critical that U.S. states continue to incorporate the disability questions into their PRAMS administration [because] without that information, persons with disabilities will continue to experience unconscionable inequities,” she said.
Barriers to equitable care
Dr. Alhusen added that people with disabilities experience significant barriers in accessing equitable care – both at the provider and the system level.
She said it is critical that we recognize and address the sexual and reproductive health needs of all persons with disability. “This includes screening every person for violence and [ensuring] the tools we utilize are accessible and include items specific to disability-related abuse. In our qualitative studies, we have heard from pregnant persons that they were never screened or that they were screened with their abusive partner sitting next to them.”
Screening questions to ask
The American College of Obstetricians and Gynecologists provides examples of screening questions that are specific to people with disabilities such as asking if a partner has ever prevented the individual from using an assistive device (for example, a wheelchair, cane, or respirator) or refused to help with an important personal need, such as taking medication or getting out of bed.
“For many reasons, people with disabilities are less likely to disclose violence, and health care professionals are less likely to ask them about it,” said coauthor of the current study, Yona Lunsky, PhD, clinician-scientist, Centre for Addiction and Mental Health, Toronto, in a statement. Based on the findings, she said, she hopes clinicians will see the need to develop disability-informed screening tools to capture abuse and identify the appropriate resources for this population before, during, and after pregnancy.
Coauthor Dr. Natasha Saunders receives an honorarium from the BMJ Group (Archives of Diseases in Childhood). Coauthor Dr. Simone N. Vigod receives royalties from UpToDate for authorship of materials related to depression and pregnancy. The other authors did not report any potential conflicts of interest. Dr. Alhusen reported no relevant financial relationships.
Pregnant or postpartum women with disabilities are at relatively high risk of experiencing violence, often from the people closest to them, new research suggests.
The researchers set out to measure risk of interpersonal violence, which the World Health Organization defines as “the intentional use of physical force or power against an individual by an intimate partner, family member, or other community member.”
Hilary K. Brown, PhD, with the department of health & society, University of Toronto, led the study published online in Obstetrics and Gynecology.
Large, population-based dataset
The population study included people 15-49 years old with births in Ontario from 2004 to 2019. They included 147,414 people with physical disabilities; 47,459 people with intellectual disabilities; 2,557 with developmental disabilities; and 9,598 with multiple disabilities.
The control group was 1,594,441 million people without disabilities.
The outcome measured was “any emergency department visit, hospital admission, or death related to physical, sexual, or psychological violence between fertilization and 365 days post partum.”
Researchers found that the adjusted relative risk of interpersonal violence for those with disabilities, compared with those with no disabilities was 1.40 (95% confidence interval, 1.31-1.50) in those with physical disabilities; 2.39 (95% CI, 1.98-2.88) in those with intellectual or developmental disabilities; and 1.96 (95% CI, 1.66-2.30) in those with multiple disabilities.
History of violence means higher risk
Those with a history of interpersonal violence and a disability were at particularly high risk for perinatal violence.
The authors note that pregnancy is a high-risk period for interpersonal violence for all women, particularly by an intimate partner.
“More than 30% of intimate partner violence begins during pregnancy, and preexisting violence tends to escalate perinatally,” they write.
The authors cite previous research that found women with disabilities experience higher rates of abuse overall and by an intimate partner – two to four times rates reported by those without disabilities.
Opportunities for provider intervention
Since the period surrounding pregnancy is a time of increased contact with medical providers and resources, there may be opportunities for identifying abuse and providing interventions.
Those might include better screening, access to violence-related information and services, and education of health care professionals to support people with disabilities. For example, “Tools used for violence screening perinatally do not include items about forms of violence that are unique to individuals with disabilities, such as refusal to assist with activities of daily living.”
The authors add: “[G]iven that the strongest risk factor for interpersonal violence in the perinatal period, particularly in those with disabilities, was a prepregnancy history of interpersonal violence, our findings suggest that more could be done before pregnancy to offer screening and support at the index encounter.”
Violence can lead to adverse outcomes
Implications are important as the violence can result in barriers to care and adverse perinatal outcomes.
Jeanne L. Alhusen, PhD, CRNP, RN, University of Virginia Medical Center professor of nursing and associate dean for research, was not part of this research but wrote a paper earlier this year on the subject and had similar conclusions.
She said before this study by Brown et al., “our understanding of the risk of violence by disability type throughout the perinatal period, on a population-based level, was quite limited.”
With the size of this dataset, she said, this paper provides critical information for health care providers. It extends physicians’ ability to examine risk of violence by disability type as well as these patients’ risk of experiencing different types of violence.
She pointed out that the Pregnancy Risk Assessment Monitoring System (PRAMS) recently incorporated a disability supplement that allows better understanding of pregnancy risks in people with disabilities.
“It will be critical that U.S. states continue to incorporate the disability questions into their PRAMS administration [because] without that information, persons with disabilities will continue to experience unconscionable inequities,” she said.
Barriers to equitable care
Dr. Alhusen added that people with disabilities experience significant barriers in accessing equitable care – both at the provider and the system level.
She said it is critical that we recognize and address the sexual and reproductive health needs of all persons with disability. “This includes screening every person for violence and [ensuring] the tools we utilize are accessible and include items specific to disability-related abuse. In our qualitative studies, we have heard from pregnant persons that they were never screened or that they were screened with their abusive partner sitting next to them.”
Screening questions to ask
The American College of Obstetricians and Gynecologists provides examples of screening questions that are specific to people with disabilities such as asking if a partner has ever prevented the individual from using an assistive device (for example, a wheelchair, cane, or respirator) or refused to help with an important personal need, such as taking medication or getting out of bed.
“For many reasons, people with disabilities are less likely to disclose violence, and health care professionals are less likely to ask them about it,” said coauthor of the current study, Yona Lunsky, PhD, clinician-scientist, Centre for Addiction and Mental Health, Toronto, in a statement. Based on the findings, she said, she hopes clinicians will see the need to develop disability-informed screening tools to capture abuse and identify the appropriate resources for this population before, during, and after pregnancy.
Coauthor Dr. Natasha Saunders receives an honorarium from the BMJ Group (Archives of Diseases in Childhood). Coauthor Dr. Simone N. Vigod receives royalties from UpToDate for authorship of materials related to depression and pregnancy. The other authors did not report any potential conflicts of interest. Dr. Alhusen reported no relevant financial relationships.
Pregnant or postpartum women with disabilities are at relatively high risk of experiencing violence, often from the people closest to them, new research suggests.
The researchers set out to measure risk of interpersonal violence, which the World Health Organization defines as “the intentional use of physical force or power against an individual by an intimate partner, family member, or other community member.”
Hilary K. Brown, PhD, with the department of health & society, University of Toronto, led the study published online in Obstetrics and Gynecology.
Large, population-based dataset
The population study included people 15-49 years old with births in Ontario from 2004 to 2019. They included 147,414 people with physical disabilities; 47,459 people with intellectual disabilities; 2,557 with developmental disabilities; and 9,598 with multiple disabilities.
The control group was 1,594,441 million people without disabilities.
The outcome measured was “any emergency department visit, hospital admission, or death related to physical, sexual, or psychological violence between fertilization and 365 days post partum.”
Researchers found that the adjusted relative risk of interpersonal violence for those with disabilities, compared with those with no disabilities was 1.40 (95% confidence interval, 1.31-1.50) in those with physical disabilities; 2.39 (95% CI, 1.98-2.88) in those with intellectual or developmental disabilities; and 1.96 (95% CI, 1.66-2.30) in those with multiple disabilities.
History of violence means higher risk
Those with a history of interpersonal violence and a disability were at particularly high risk for perinatal violence.
The authors note that pregnancy is a high-risk period for interpersonal violence for all women, particularly by an intimate partner.
“More than 30% of intimate partner violence begins during pregnancy, and preexisting violence tends to escalate perinatally,” they write.
The authors cite previous research that found women with disabilities experience higher rates of abuse overall and by an intimate partner – two to four times rates reported by those without disabilities.
Opportunities for provider intervention
Since the period surrounding pregnancy is a time of increased contact with medical providers and resources, there may be opportunities for identifying abuse and providing interventions.
Those might include better screening, access to violence-related information and services, and education of health care professionals to support people with disabilities. For example, “Tools used for violence screening perinatally do not include items about forms of violence that are unique to individuals with disabilities, such as refusal to assist with activities of daily living.”
The authors add: “[G]iven that the strongest risk factor for interpersonal violence in the perinatal period, particularly in those with disabilities, was a prepregnancy history of interpersonal violence, our findings suggest that more could be done before pregnancy to offer screening and support at the index encounter.”
Violence can lead to adverse outcomes
Implications are important as the violence can result in barriers to care and adverse perinatal outcomes.
Jeanne L. Alhusen, PhD, CRNP, RN, University of Virginia Medical Center professor of nursing and associate dean for research, was not part of this research but wrote a paper earlier this year on the subject and had similar conclusions.
She said before this study by Brown et al., “our understanding of the risk of violence by disability type throughout the perinatal period, on a population-based level, was quite limited.”
With the size of this dataset, she said, this paper provides critical information for health care providers. It extends physicians’ ability to examine risk of violence by disability type as well as these patients’ risk of experiencing different types of violence.
She pointed out that the Pregnancy Risk Assessment Monitoring System (PRAMS) recently incorporated a disability supplement that allows better understanding of pregnancy risks in people with disabilities.
“It will be critical that U.S. states continue to incorporate the disability questions into their PRAMS administration [because] without that information, persons with disabilities will continue to experience unconscionable inequities,” she said.
Barriers to equitable care
Dr. Alhusen added that people with disabilities experience significant barriers in accessing equitable care – both at the provider and the system level.
She said it is critical that we recognize and address the sexual and reproductive health needs of all persons with disability. “This includes screening every person for violence and [ensuring] the tools we utilize are accessible and include items specific to disability-related abuse. In our qualitative studies, we have heard from pregnant persons that they were never screened or that they were screened with their abusive partner sitting next to them.”
Screening questions to ask
The American College of Obstetricians and Gynecologists provides examples of screening questions that are specific to people with disabilities such as asking if a partner has ever prevented the individual from using an assistive device (for example, a wheelchair, cane, or respirator) or refused to help with an important personal need, such as taking medication or getting out of bed.
“For many reasons, people with disabilities are less likely to disclose violence, and health care professionals are less likely to ask them about it,” said coauthor of the current study, Yona Lunsky, PhD, clinician-scientist, Centre for Addiction and Mental Health, Toronto, in a statement. Based on the findings, she said, she hopes clinicians will see the need to develop disability-informed screening tools to capture abuse and identify the appropriate resources for this population before, during, and after pregnancy.
Coauthor Dr. Natasha Saunders receives an honorarium from the BMJ Group (Archives of Diseases in Childhood). Coauthor Dr. Simone N. Vigod receives royalties from UpToDate for authorship of materials related to depression and pregnancy. The other authors did not report any potential conflicts of interest. Dr. Alhusen reported no relevant financial relationships.
FROM OBSTETRICS AND GYNECOLOGY
Previous endemic coronavirus encounters linked with long COVID
People who develop long COVID may be responding more strongly to a non–SARS-CoV-2 virus they encountered in the past than to SARS-CoV-2, a study by researchers at Harvard Medical School suggests.
Long COVID, also called postacute sequelae of COVID-19 (PASC), causes various symptoms that persist at least 4 weeks after the initial SARS-CoV-2 infection, they write in the preprint server medRxiv. Four authors explained their research into possible mechanisms of long COVID in an interview.
“Immunity to non-COVID endemic coronaviruses may play a role in who develops PASC,” co–lead author Jonathan D. Herman, MD, PhD, said. “There’s still so much more we need to understand, but it is striking that back-boosting of immune responses to coronavirus OC43 was uniquely enriched in individuals with PASC.”
“In the study, individuals with PASC preferentially generated stronger responses to previously encountered cold-causing coronaviruses,” co–senior author Galit Alter, PhD, said.
“Instead of generating strong SARS-CoV-2 immunity, they bolstered a response to a different coronavirus, potentially making their response less effective in clearing SARS-CoV-2. Surprisingly, most of the individuals had been vaccinated – and they still maintained this unusual antibody response – pointing to new therapeutic pathways to treat PASC,” Dr. Alter said.
Humoral immunity offers a clue to long-COVID origins
One-fifth of COVID-19 patients progress to long COVID, but which patients develop PASC and why are not well understood, the authors write.
“Antibodies represent powerful biomarkers that have been used for decades to diagnose disease. However, antibodies also provide a powerful source of information on previous infections. The use of antibody profiling, here, pointed to the presence of incomplete antibody responses to SARS-CoV-2 in individuals with PASC,” Dr. Alter said.
The researchers reviewed the medical records of patients in the Mass General Brigham health care system in Boston, including referrals from rheumatologists of participants diagnosed with COVID-19 outside the MGB system, starting on March 1, 2020.
They focused on patients with systemic autoimmune rheumatic diseases (SARDs) because their tendency toward inflammation and autoantibody production may make them more susceptible to PASC and enrich for specific inflammatory-driven endotypes.
All 43 participants had COVID-19 without hospital admission and SARDs. Patients treated only for fibromyalgia, osteoarthritis, mechanical back pain, gout, or pseudogout without a SARD were excluded from the study.
Overall, 79% of participants were female, 35% had rheumatoid arthritis, 19% had psoriatic arthritis, and 95% had received a COVID-19 vaccine.
The researchers used systems serology to perform comprehensive antibody profiling against SARS-CoV-2 and a panel of endemic pathogens or routine vaccine antigens.
Long-COVID patients had a distinct immune response
Overall, 17 patients developed PASC and 26 did not, and in those with PASC, they found a distinct humoral immune response. Patients with PASC:
- harbored less inflamed and weaker Fc-gamma receptor–binding anti–SARS-CoV-2 antibodies;
- showed a significantly expanded and more inflamed antibody response against endemic coronavirus OC43; and
- mounted more avid IgM responses and developed expanded inflammatory OC43 S2–specific Fc-receptor–binding responses, which were linked to cross reactivity across SARS-CoV-2 and common coronaviruses.
“Strengths of the study include the detailed phenotypes of cases after COVID-19, particularly to classify PASC presence or absence, as well as the depth and breadth of antibody profiling. This allowed us to identify a humoral immune signature of PASC,” said co–senior author Jeffrey A. Sparks, MD, MMSc.
“However, the study was limited in its size to investigate different types of PASC, such as fatigue or lung symptoms, that may have biologic differences. Also, all patients in the study had a preexisting rheumatic disease,” he acknowledged.
“A substantial portion of patients with COVID-19 will develop PASC, which can have substantial impact on health and quality of life,” said co–senior author Zachary S. Wallace, MD, MS. “Given the higher risk of COVID-19 in many patients with rheumatic disease, it is important to understand the etiology of PASC in this vulnerable population, to enable future diagnostic and therapeutic advances.”
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California, San Diego, in La Jolla, who was not involved in the study, called the findings interesting even though the results will not immediately affect patient care.
“There may be a link between previous non–SARS-CoV-2 coronavirus infection and PASC,” he added. “Perhaps, by understanding why some people do and do not get PASC, we can develop treatments for the condition.
“This paper is a preprint and will need to go through peer review,” Dr. Smith said. “There are many elements that need to be scrutinized. For example, there is no definition of PASC that is universally accepted, so how did that play into this study?”
Mark Cameron, PhD, associate professor in the department of population and quantitative health sciences at Case Western Reserve University, Cleveland, called this a strong study from a strong group, although it is a preprint prior to peer review.
“In this initial study, the scientists focused on people who had rheumatic disease before getting COVID-19, knowing they are at higher risk for lasting complications and hopefully are more immunologically similar when diagnosed with long COVID – a single ‘endotype’ or group of patients with similar clinical symptoms and background,” he noted.
“Our immune system’s memory sometimes fails to effectively fight a new virus that looks too much like a virus it saw before. This ineffective immune response can set up various problems, including the poor recoveries we see in people with long COVID,” he said.
“OC43 probably emerged in the late 1800s and probably caused a pandemic of severe respiratory illness between 1889 and 1890, previously thought to be a flu,” Dr. Cameron recalled. “OC43 is still around as an endemic coronavirus, usually causing mild or moderate upper-respiratory infections.”
COVID-19 immunity is complex, and previous SARS-CoV-2 infection doesn’t guarantee we won't get COVID-19 again, especially as new variants emerge, added Dr. Cameron, who also was not involved in the study.
“This study may help us better understand the risks and possible mechanisms associated with COVID-19 and long COVID in the face of previous coronavirus infections,” he said. “It may also help guide future COVID-19 therapies and vaccines.”
The authors plan further related research.
The study received grant support and an anonymous donation. Dr. Alter, Dr. Sparks, and Dr. Wallace report financial relationships with the pharmaceutical industry. All other authors, and Dr. Davey and Dr. Cameron, report no conflicts of interest with the study. All experts commented by email.
* This story was updated 10/12/2022.
People who develop long COVID may be responding more strongly to a non–SARS-CoV-2 virus they encountered in the past than to SARS-CoV-2, a study by researchers at Harvard Medical School suggests.
Long COVID, also called postacute sequelae of COVID-19 (PASC), causes various symptoms that persist at least 4 weeks after the initial SARS-CoV-2 infection, they write in the preprint server medRxiv. Four authors explained their research into possible mechanisms of long COVID in an interview.
“Immunity to non-COVID endemic coronaviruses may play a role in who develops PASC,” co–lead author Jonathan D. Herman, MD, PhD, said. “There’s still so much more we need to understand, but it is striking that back-boosting of immune responses to coronavirus OC43 was uniquely enriched in individuals with PASC.”
“In the study, individuals with PASC preferentially generated stronger responses to previously encountered cold-causing coronaviruses,” co–senior author Galit Alter, PhD, said.
“Instead of generating strong SARS-CoV-2 immunity, they bolstered a response to a different coronavirus, potentially making their response less effective in clearing SARS-CoV-2. Surprisingly, most of the individuals had been vaccinated – and they still maintained this unusual antibody response – pointing to new therapeutic pathways to treat PASC,” Dr. Alter said.
Humoral immunity offers a clue to long-COVID origins
One-fifth of COVID-19 patients progress to long COVID, but which patients develop PASC and why are not well understood, the authors write.
“Antibodies represent powerful biomarkers that have been used for decades to diagnose disease. However, antibodies also provide a powerful source of information on previous infections. The use of antibody profiling, here, pointed to the presence of incomplete antibody responses to SARS-CoV-2 in individuals with PASC,” Dr. Alter said.
The researchers reviewed the medical records of patients in the Mass General Brigham health care system in Boston, including referrals from rheumatologists of participants diagnosed with COVID-19 outside the MGB system, starting on March 1, 2020.
They focused on patients with systemic autoimmune rheumatic diseases (SARDs) because their tendency toward inflammation and autoantibody production may make them more susceptible to PASC and enrich for specific inflammatory-driven endotypes.
All 43 participants had COVID-19 without hospital admission and SARDs. Patients treated only for fibromyalgia, osteoarthritis, mechanical back pain, gout, or pseudogout without a SARD were excluded from the study.
Overall, 79% of participants were female, 35% had rheumatoid arthritis, 19% had psoriatic arthritis, and 95% had received a COVID-19 vaccine.
The researchers used systems serology to perform comprehensive antibody profiling against SARS-CoV-2 and a panel of endemic pathogens or routine vaccine antigens.
Long-COVID patients had a distinct immune response
Overall, 17 patients developed PASC and 26 did not, and in those with PASC, they found a distinct humoral immune response. Patients with PASC:
- harbored less inflamed and weaker Fc-gamma receptor–binding anti–SARS-CoV-2 antibodies;
- showed a significantly expanded and more inflamed antibody response against endemic coronavirus OC43; and
- mounted more avid IgM responses and developed expanded inflammatory OC43 S2–specific Fc-receptor–binding responses, which were linked to cross reactivity across SARS-CoV-2 and common coronaviruses.
“Strengths of the study include the detailed phenotypes of cases after COVID-19, particularly to classify PASC presence or absence, as well as the depth and breadth of antibody profiling. This allowed us to identify a humoral immune signature of PASC,” said co–senior author Jeffrey A. Sparks, MD, MMSc.
“However, the study was limited in its size to investigate different types of PASC, such as fatigue or lung symptoms, that may have biologic differences. Also, all patients in the study had a preexisting rheumatic disease,” he acknowledged.
“A substantial portion of patients with COVID-19 will develop PASC, which can have substantial impact on health and quality of life,” said co–senior author Zachary S. Wallace, MD, MS. “Given the higher risk of COVID-19 in many patients with rheumatic disease, it is important to understand the etiology of PASC in this vulnerable population, to enable future diagnostic and therapeutic advances.”
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California, San Diego, in La Jolla, who was not involved in the study, called the findings interesting even though the results will not immediately affect patient care.
“There may be a link between previous non–SARS-CoV-2 coronavirus infection and PASC,” he added. “Perhaps, by understanding why some people do and do not get PASC, we can develop treatments for the condition.
“This paper is a preprint and will need to go through peer review,” Dr. Smith said. “There are many elements that need to be scrutinized. For example, there is no definition of PASC that is universally accepted, so how did that play into this study?”
Mark Cameron, PhD, associate professor in the department of population and quantitative health sciences at Case Western Reserve University, Cleveland, called this a strong study from a strong group, although it is a preprint prior to peer review.
“In this initial study, the scientists focused on people who had rheumatic disease before getting COVID-19, knowing they are at higher risk for lasting complications and hopefully are more immunologically similar when diagnosed with long COVID – a single ‘endotype’ or group of patients with similar clinical symptoms and background,” he noted.
“Our immune system’s memory sometimes fails to effectively fight a new virus that looks too much like a virus it saw before. This ineffective immune response can set up various problems, including the poor recoveries we see in people with long COVID,” he said.
“OC43 probably emerged in the late 1800s and probably caused a pandemic of severe respiratory illness between 1889 and 1890, previously thought to be a flu,” Dr. Cameron recalled. “OC43 is still around as an endemic coronavirus, usually causing mild or moderate upper-respiratory infections.”
COVID-19 immunity is complex, and previous SARS-CoV-2 infection doesn’t guarantee we won't get COVID-19 again, especially as new variants emerge, added Dr. Cameron, who also was not involved in the study.
“This study may help us better understand the risks and possible mechanisms associated with COVID-19 and long COVID in the face of previous coronavirus infections,” he said. “It may also help guide future COVID-19 therapies and vaccines.”
The authors plan further related research.
The study received grant support and an anonymous donation. Dr. Alter, Dr. Sparks, and Dr. Wallace report financial relationships with the pharmaceutical industry. All other authors, and Dr. Davey and Dr. Cameron, report no conflicts of interest with the study. All experts commented by email.
* This story was updated 10/12/2022.
People who develop long COVID may be responding more strongly to a non–SARS-CoV-2 virus they encountered in the past than to SARS-CoV-2, a study by researchers at Harvard Medical School suggests.
Long COVID, also called postacute sequelae of COVID-19 (PASC), causes various symptoms that persist at least 4 weeks after the initial SARS-CoV-2 infection, they write in the preprint server medRxiv. Four authors explained their research into possible mechanisms of long COVID in an interview.
“Immunity to non-COVID endemic coronaviruses may play a role in who develops PASC,” co–lead author Jonathan D. Herman, MD, PhD, said. “There’s still so much more we need to understand, but it is striking that back-boosting of immune responses to coronavirus OC43 was uniquely enriched in individuals with PASC.”
“In the study, individuals with PASC preferentially generated stronger responses to previously encountered cold-causing coronaviruses,” co–senior author Galit Alter, PhD, said.
“Instead of generating strong SARS-CoV-2 immunity, they bolstered a response to a different coronavirus, potentially making their response less effective in clearing SARS-CoV-2. Surprisingly, most of the individuals had been vaccinated – and they still maintained this unusual antibody response – pointing to new therapeutic pathways to treat PASC,” Dr. Alter said.
Humoral immunity offers a clue to long-COVID origins
One-fifth of COVID-19 patients progress to long COVID, but which patients develop PASC and why are not well understood, the authors write.
“Antibodies represent powerful biomarkers that have been used for decades to diagnose disease. However, antibodies also provide a powerful source of information on previous infections. The use of antibody profiling, here, pointed to the presence of incomplete antibody responses to SARS-CoV-2 in individuals with PASC,” Dr. Alter said.
The researchers reviewed the medical records of patients in the Mass General Brigham health care system in Boston, including referrals from rheumatologists of participants diagnosed with COVID-19 outside the MGB system, starting on March 1, 2020.
They focused on patients with systemic autoimmune rheumatic diseases (SARDs) because their tendency toward inflammation and autoantibody production may make them more susceptible to PASC and enrich for specific inflammatory-driven endotypes.
All 43 participants had COVID-19 without hospital admission and SARDs. Patients treated only for fibromyalgia, osteoarthritis, mechanical back pain, gout, or pseudogout without a SARD were excluded from the study.
Overall, 79% of participants were female, 35% had rheumatoid arthritis, 19% had psoriatic arthritis, and 95% had received a COVID-19 vaccine.
The researchers used systems serology to perform comprehensive antibody profiling against SARS-CoV-2 and a panel of endemic pathogens or routine vaccine antigens.
Long-COVID patients had a distinct immune response
Overall, 17 patients developed PASC and 26 did not, and in those with PASC, they found a distinct humoral immune response. Patients with PASC:
- harbored less inflamed and weaker Fc-gamma receptor–binding anti–SARS-CoV-2 antibodies;
- showed a significantly expanded and more inflamed antibody response against endemic coronavirus OC43; and
- mounted more avid IgM responses and developed expanded inflammatory OC43 S2–specific Fc-receptor–binding responses, which were linked to cross reactivity across SARS-CoV-2 and common coronaviruses.
“Strengths of the study include the detailed phenotypes of cases after COVID-19, particularly to classify PASC presence or absence, as well as the depth and breadth of antibody profiling. This allowed us to identify a humoral immune signature of PASC,” said co–senior author Jeffrey A. Sparks, MD, MMSc.
“However, the study was limited in its size to investigate different types of PASC, such as fatigue or lung symptoms, that may have biologic differences. Also, all patients in the study had a preexisting rheumatic disease,” he acknowledged.
“A substantial portion of patients with COVID-19 will develop PASC, which can have substantial impact on health and quality of life,” said co–senior author Zachary S. Wallace, MD, MS. “Given the higher risk of COVID-19 in many patients with rheumatic disease, it is important to understand the etiology of PASC in this vulnerable population, to enable future diagnostic and therapeutic advances.”
Davey Smith, MD, professor of medicine and head of infectious diseases and global public health at the University of California, San Diego, in La Jolla, who was not involved in the study, called the findings interesting even though the results will not immediately affect patient care.
“There may be a link between previous non–SARS-CoV-2 coronavirus infection and PASC,” he added. “Perhaps, by understanding why some people do and do not get PASC, we can develop treatments for the condition.
“This paper is a preprint and will need to go through peer review,” Dr. Smith said. “There are many elements that need to be scrutinized. For example, there is no definition of PASC that is universally accepted, so how did that play into this study?”
Mark Cameron, PhD, associate professor in the department of population and quantitative health sciences at Case Western Reserve University, Cleveland, called this a strong study from a strong group, although it is a preprint prior to peer review.
“In this initial study, the scientists focused on people who had rheumatic disease before getting COVID-19, knowing they are at higher risk for lasting complications and hopefully are more immunologically similar when diagnosed with long COVID – a single ‘endotype’ or group of patients with similar clinical symptoms and background,” he noted.
“Our immune system’s memory sometimes fails to effectively fight a new virus that looks too much like a virus it saw before. This ineffective immune response can set up various problems, including the poor recoveries we see in people with long COVID,” he said.
“OC43 probably emerged in the late 1800s and probably caused a pandemic of severe respiratory illness between 1889 and 1890, previously thought to be a flu,” Dr. Cameron recalled. “OC43 is still around as an endemic coronavirus, usually causing mild or moderate upper-respiratory infections.”
COVID-19 immunity is complex, and previous SARS-CoV-2 infection doesn’t guarantee we won't get COVID-19 again, especially as new variants emerge, added Dr. Cameron, who also was not involved in the study.
“This study may help us better understand the risks and possible mechanisms associated with COVID-19 and long COVID in the face of previous coronavirus infections,” he said. “It may also help guide future COVID-19 therapies and vaccines.”
The authors plan further related research.
The study received grant support and an anonymous donation. Dr. Alter, Dr. Sparks, and Dr. Wallace report financial relationships with the pharmaceutical industry. All other authors, and Dr. Davey and Dr. Cameron, report no conflicts of interest with the study. All experts commented by email.
* This story was updated 10/12/2022.
FROM MEDRXIV
Soccer player with painful toe
A 13-YEAR-OLD GIRL presented to the clinic with a 1-year history of a slow-growing mass on the third toe of her right foot. As a soccer player, she experienced associated pain when kicking the ball or when wearing tight-fitting shoes. The lesion was otherwise asymptomatic. She denied any overt trauma to the area and indicated that the mass had enlarged over the previous year.
On exam, there was a nontender 8 × 8-mm firm nodule underneath the nail with associated nail dystrophy (FIGURE 1). The toe had full mobility, sensation was intact, and capillary refill time was < 2 seconds.
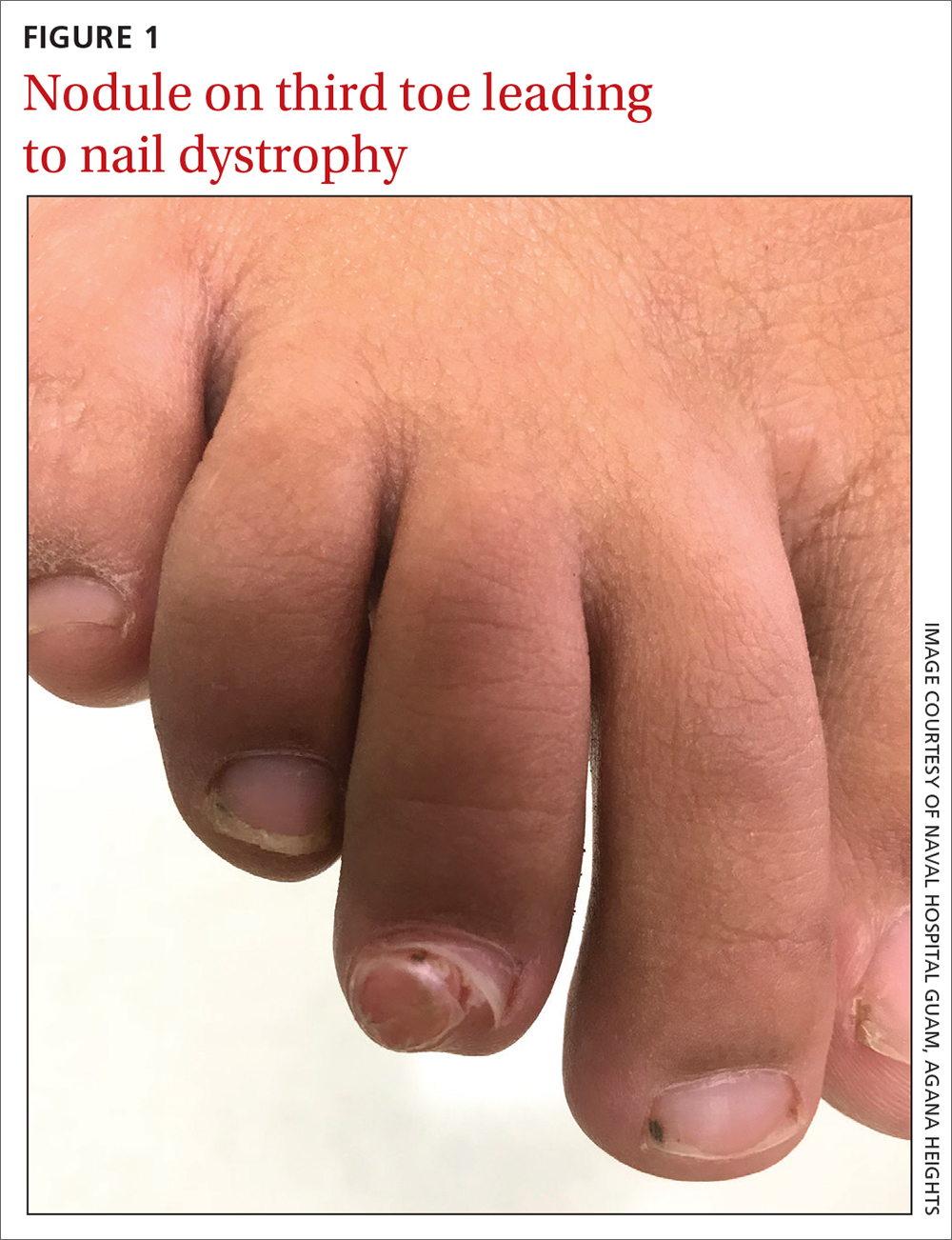
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Subungual exostosis
A plain radiograph of the patient’s foot showed continuity with the bony cortex and medullary space, confirming the diagnosis of subungual exostosis (FIGURE 2).1 An exostosis, or osteochondroma, is a form of benign bone tumor in which trabecular bone overgrows its normal border in a nodular pattern. When this occurs under the nail bed, it is called subungual exostosis.2 Exostosis represents 10% to 15% of all benign bone tumors, making it the most common benign bone tumor.3 Generally, the age of occurrence is 10 to 15 years.3

Repetitive trauma can be a culprit. Up to 8% of exostoses occur in the foot, with the most commonly affected area being the distal medial portion of the big toe.3,4 Repetitive trauma and infection are potential risk factors.3,4 The affected toe may be painful, but that is not always the case.4 Typically, lesions are solitary; however, multiple lesions can occur.4
Most pediatric foot lesions are benign and involve soft tissue
Benign soft-tissue masses make up the overwhelming majority of pediatric foot lesions, accounting for 61% to 87% of all foot lesions.3 Malignancies such as chondrosarcoma can occur and can be difficult to diagnose. Rapid growth, family history, size > 5 cm, heterogenous appearance on magnetic resonance imaging, and poorly defined margins are a few characteristics that should increase suspicion for possible malignancy.5
The differential diagnosis for a growth on the toe similar to the one our patient had would include pyogenic granuloma,
Pyogenic granulomas are benign vascular lesions that occur in patients of all ages. They tend to be dome-shaped and flesh-toned to violaceous red, and they are usually found on the head, neck, and extremities—especially fingers.6 They are associated with trauma and are classically tender with a propensity to bleed.6
Acral fibromyxoma is a benign, slow-growing, predominately painless, firm mass with an affinity for the great toe; the affected area includes the nail in 50% of cases.7 A radiograph may show bony erosion or scalloping due to mass effect; however, there will be no continuity with the bony matrix. (Such continuity would suggest exostosis.)
Periungual fibromas are benign soft-tissue masses, which are pink to red and firm, and emerge from underneath the nails, potentially resulting in dystrophy.8 They can bleed and cause pain, and are strongly associated with tuberous sclerosis.5
Continue to: Verruca vulgaris
Verruca vulgaris, the common wart, can also manifest in the subungual region as a firm, generally painless mass. It is the most common neoplasm of the hand and fingers.6 Tiny black dots that correspond to thrombosed capillaries are key to identifying this lesion.
Surgical excision when patient reaches maturity
The definitive treatment for subungual exostosis is surgical excision, preferably once the patient has reached skeletal maturity. Surgery at this point is associated with decreased recurrence rates.3,4 That said, excision may need to be performed sooner if the lesion is painful and leading to deformity.3
Our patient’s persistent pain prompted us to recommend surgical excision. She underwent a third digit exostectomy, which she tolerated without any issues. The patient was fitted with a postoperative shoe that she wore until her 2-week follow-up appointment, when her sutures were removed. The patient’s activity level progressed as tolerated. She regained full function and returned to playing soccer, without any pain, 3 months after her surgery.
1. Das PC, Hassan S, Kumar P. Subungual exostosis – clinical, radiological, and histological findings. Indian Dermatol Online J. 2019;10:202-203. doi: 10.4103/idoj.IDOJ_104_18
2. Yousefian F, Davis B, Browning JC. Pediatric subungual exostosis. Cutis. 2021;108:256-257. doi:10.12788/cutis.0380
3. Bouchard B, Bartlett M, Donnan L. Assessment of the pediatric foot mass. J Am Acad Orthop Surg. 2017;25:32-41. doi: 10.5435/JAAOS-D-15-00397
4. DaCambra MP, Gupta SK, Ferri-de-Barros F. Subungual exostosis of the toes: a systematic review. Clin Orthop Relat Res. 2014;472:1251-1259. doi: 10.1007/s11999-013-3345-4
5. Shah SH, Callahan MJ. Ultrasound evaluation of superficial lumps and bumps of the extremities in children: a 5-year retrospective review. Pediatr Radiol. 2013;43 suppl 1:S23-S40. doi: 10.1007/s00247-012-2590-0
6. Habif, Thomas P. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 6th ed. Mosby/Elsevier, 2016.
7. Ramya C, Nayak C, Tambe S. Superficial acral fibromyxoma. Indian J Dermatol. 2016;61:457-459. doi: 10.4103/0019-5154.185734
8. Ma D, Darling T, Moss J, et al. Histologic variants of periungual fibromas in tuberous sclerosis complex. J Am Acad Dermatol. 2011;64:442-444. doi: 10.1016/j.jaad.2010.03.002
A 13-YEAR-OLD GIRL presented to the clinic with a 1-year history of a slow-growing mass on the third toe of her right foot. As a soccer player, she experienced associated pain when kicking the ball or when wearing tight-fitting shoes. The lesion was otherwise asymptomatic. She denied any overt trauma to the area and indicated that the mass had enlarged over the previous year.
On exam, there was a nontender 8 × 8-mm firm nodule underneath the nail with associated nail dystrophy (FIGURE 1). The toe had full mobility, sensation was intact, and capillary refill time was < 2 seconds.
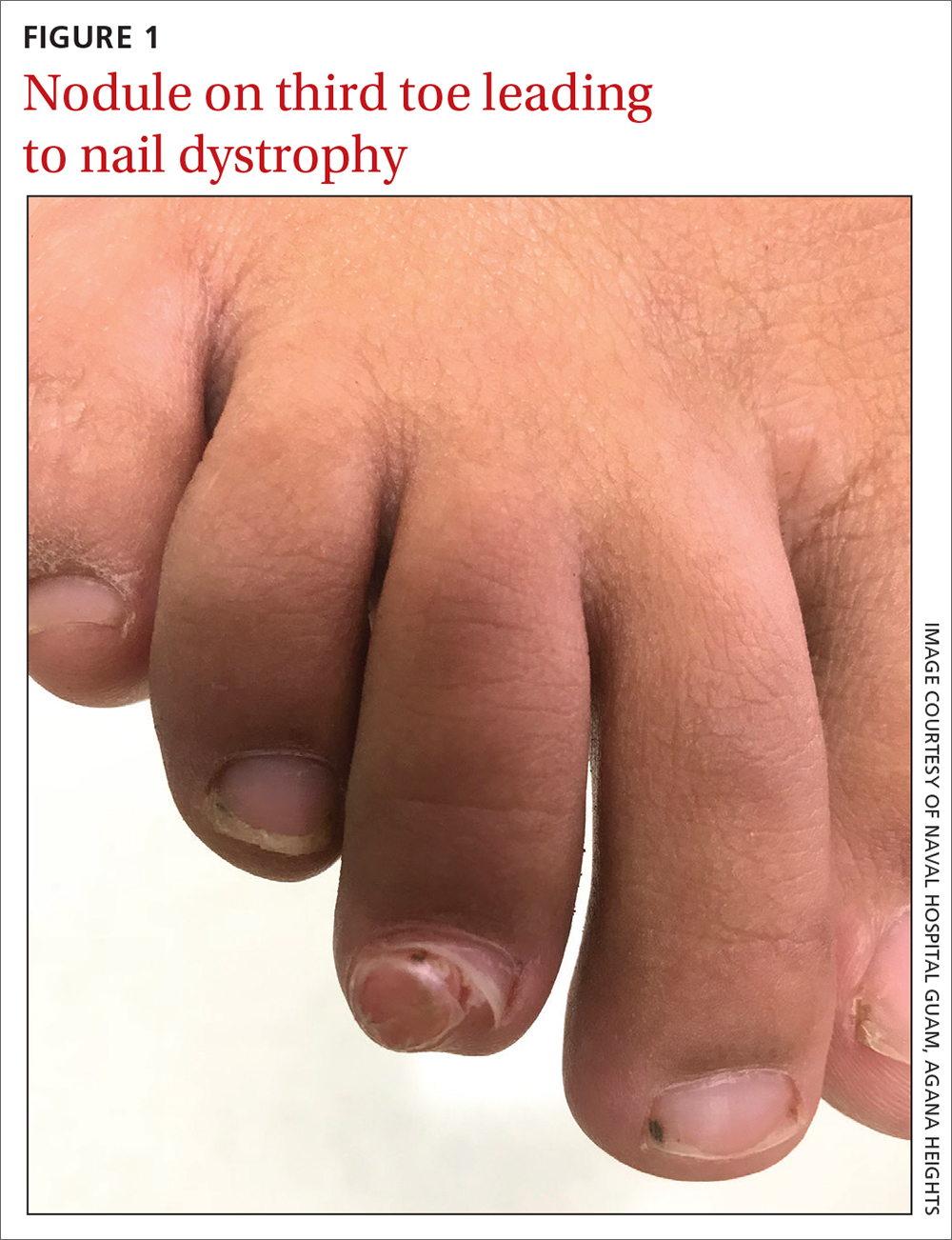
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Subungual exostosis
A plain radiograph of the patient’s foot showed continuity with the bony cortex and medullary space, confirming the diagnosis of subungual exostosis (FIGURE 2).1 An exostosis, or osteochondroma, is a form of benign bone tumor in which trabecular bone overgrows its normal border in a nodular pattern. When this occurs under the nail bed, it is called subungual exostosis.2 Exostosis represents 10% to 15% of all benign bone tumors, making it the most common benign bone tumor.3 Generally, the age of occurrence is 10 to 15 years.3

Repetitive trauma can be a culprit. Up to 8% of exostoses occur in the foot, with the most commonly affected area being the distal medial portion of the big toe.3,4 Repetitive trauma and infection are potential risk factors.3,4 The affected toe may be painful, but that is not always the case.4 Typically, lesions are solitary; however, multiple lesions can occur.4
Most pediatric foot lesions are benign and involve soft tissue
Benign soft-tissue masses make up the overwhelming majority of pediatric foot lesions, accounting for 61% to 87% of all foot lesions.3 Malignancies such as chondrosarcoma can occur and can be difficult to diagnose. Rapid growth, family history, size > 5 cm, heterogenous appearance on magnetic resonance imaging, and poorly defined margins are a few characteristics that should increase suspicion for possible malignancy.5
The differential diagnosis for a growth on the toe similar to the one our patient had would include pyogenic granuloma,
Pyogenic granulomas are benign vascular lesions that occur in patients of all ages. They tend to be dome-shaped and flesh-toned to violaceous red, and they are usually found on the head, neck, and extremities—especially fingers.6 They are associated with trauma and are classically tender with a propensity to bleed.6
Acral fibromyxoma is a benign, slow-growing, predominately painless, firm mass with an affinity for the great toe; the affected area includes the nail in 50% of cases.7 A radiograph may show bony erosion or scalloping due to mass effect; however, there will be no continuity with the bony matrix. (Such continuity would suggest exostosis.)
Periungual fibromas are benign soft-tissue masses, which are pink to red and firm, and emerge from underneath the nails, potentially resulting in dystrophy.8 They can bleed and cause pain, and are strongly associated with tuberous sclerosis.5
Continue to: Verruca vulgaris
Verruca vulgaris, the common wart, can also manifest in the subungual region as a firm, generally painless mass. It is the most common neoplasm of the hand and fingers.6 Tiny black dots that correspond to thrombosed capillaries are key to identifying this lesion.
Surgical excision when patient reaches maturity
The definitive treatment for subungual exostosis is surgical excision, preferably once the patient has reached skeletal maturity. Surgery at this point is associated with decreased recurrence rates.3,4 That said, excision may need to be performed sooner if the lesion is painful and leading to deformity.3
Our patient’s persistent pain prompted us to recommend surgical excision. She underwent a third digit exostectomy, which she tolerated without any issues. The patient was fitted with a postoperative shoe that she wore until her 2-week follow-up appointment, when her sutures were removed. The patient’s activity level progressed as tolerated. She regained full function and returned to playing soccer, without any pain, 3 months after her surgery.
A 13-YEAR-OLD GIRL presented to the clinic with a 1-year history of a slow-growing mass on the third toe of her right foot. As a soccer player, she experienced associated pain when kicking the ball or when wearing tight-fitting shoes. The lesion was otherwise asymptomatic. She denied any overt trauma to the area and indicated that the mass had enlarged over the previous year.
On exam, there was a nontender 8 × 8-mm firm nodule underneath the nail with associated nail dystrophy (FIGURE 1). The toe had full mobility, sensation was intact, and capillary refill time was < 2 seconds.
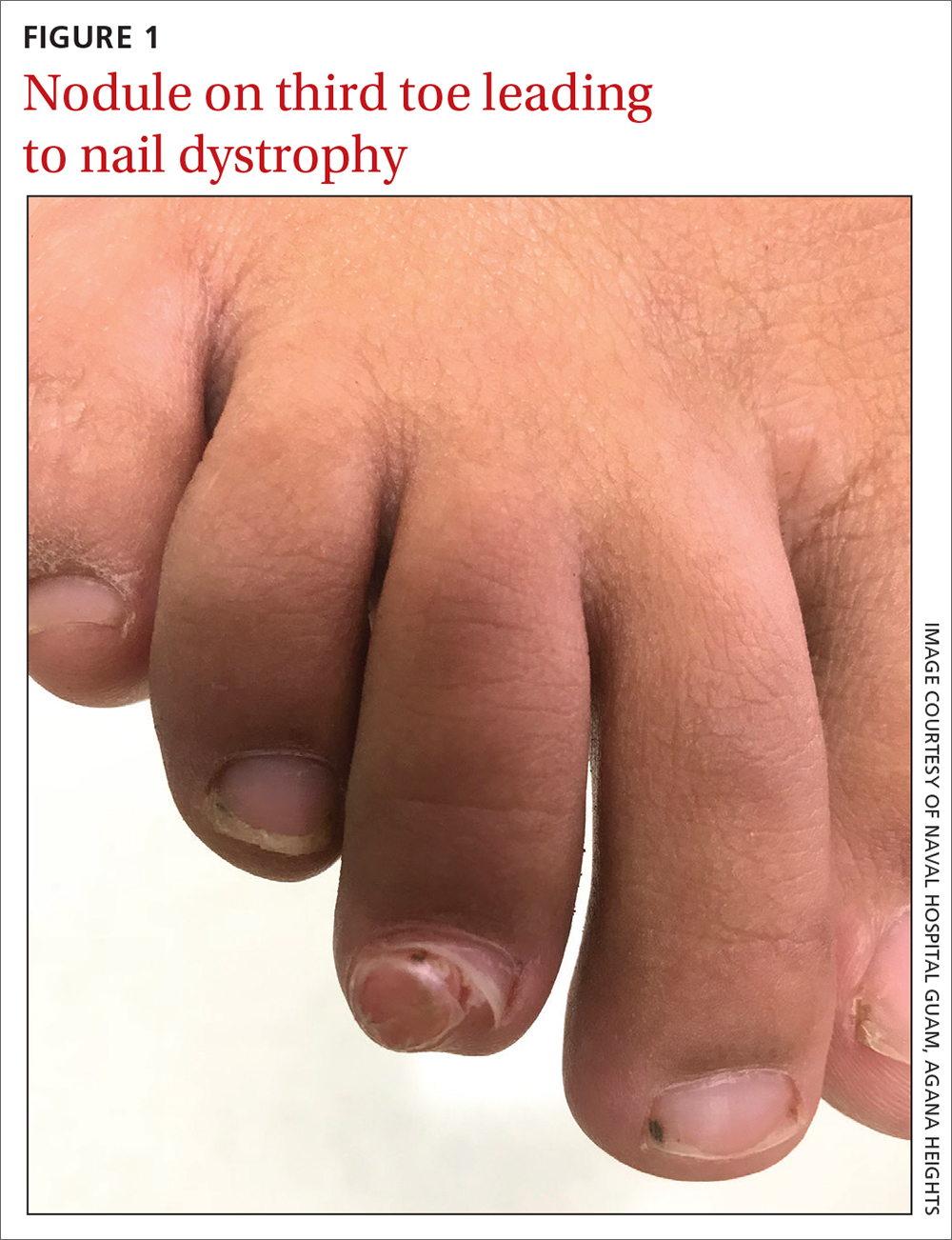
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Subungual exostosis
A plain radiograph of the patient’s foot showed continuity with the bony cortex and medullary space, confirming the diagnosis of subungual exostosis (FIGURE 2).1 An exostosis, or osteochondroma, is a form of benign bone tumor in which trabecular bone overgrows its normal border in a nodular pattern. When this occurs under the nail bed, it is called subungual exostosis.2 Exostosis represents 10% to 15% of all benign bone tumors, making it the most common benign bone tumor.3 Generally, the age of occurrence is 10 to 15 years.3

Repetitive trauma can be a culprit. Up to 8% of exostoses occur in the foot, with the most commonly affected area being the distal medial portion of the big toe.3,4 Repetitive trauma and infection are potential risk factors.3,4 The affected toe may be painful, but that is not always the case.4 Typically, lesions are solitary; however, multiple lesions can occur.4
Most pediatric foot lesions are benign and involve soft tissue
Benign soft-tissue masses make up the overwhelming majority of pediatric foot lesions, accounting for 61% to 87% of all foot lesions.3 Malignancies such as chondrosarcoma can occur and can be difficult to diagnose. Rapid growth, family history, size > 5 cm, heterogenous appearance on magnetic resonance imaging, and poorly defined margins are a few characteristics that should increase suspicion for possible malignancy.5
The differential diagnosis for a growth on the toe similar to the one our patient had would include pyogenic granuloma,
Pyogenic granulomas are benign vascular lesions that occur in patients of all ages. They tend to be dome-shaped and flesh-toned to violaceous red, and they are usually found on the head, neck, and extremities—especially fingers.6 They are associated with trauma and are classically tender with a propensity to bleed.6
Acral fibromyxoma is a benign, slow-growing, predominately painless, firm mass with an affinity for the great toe; the affected area includes the nail in 50% of cases.7 A radiograph may show bony erosion or scalloping due to mass effect; however, there will be no continuity with the bony matrix. (Such continuity would suggest exostosis.)
Periungual fibromas are benign soft-tissue masses, which are pink to red and firm, and emerge from underneath the nails, potentially resulting in dystrophy.8 They can bleed and cause pain, and are strongly associated with tuberous sclerosis.5
Continue to: Verruca vulgaris
Verruca vulgaris, the common wart, can also manifest in the subungual region as a firm, generally painless mass. It is the most common neoplasm of the hand and fingers.6 Tiny black dots that correspond to thrombosed capillaries are key to identifying this lesion.
Surgical excision when patient reaches maturity
The definitive treatment for subungual exostosis is surgical excision, preferably once the patient has reached skeletal maturity. Surgery at this point is associated with decreased recurrence rates.3,4 That said, excision may need to be performed sooner if the lesion is painful and leading to deformity.3
Our patient’s persistent pain prompted us to recommend surgical excision. She underwent a third digit exostectomy, which she tolerated without any issues. The patient was fitted with a postoperative shoe that she wore until her 2-week follow-up appointment, when her sutures were removed. The patient’s activity level progressed as tolerated. She regained full function and returned to playing soccer, without any pain, 3 months after her surgery.
1. Das PC, Hassan S, Kumar P. Subungual exostosis – clinical, radiological, and histological findings. Indian Dermatol Online J. 2019;10:202-203. doi: 10.4103/idoj.IDOJ_104_18
2. Yousefian F, Davis B, Browning JC. Pediatric subungual exostosis. Cutis. 2021;108:256-257. doi:10.12788/cutis.0380
3. Bouchard B, Bartlett M, Donnan L. Assessment of the pediatric foot mass. J Am Acad Orthop Surg. 2017;25:32-41. doi: 10.5435/JAAOS-D-15-00397
4. DaCambra MP, Gupta SK, Ferri-de-Barros F. Subungual exostosis of the toes: a systematic review. Clin Orthop Relat Res. 2014;472:1251-1259. doi: 10.1007/s11999-013-3345-4
5. Shah SH, Callahan MJ. Ultrasound evaluation of superficial lumps and bumps of the extremities in children: a 5-year retrospective review. Pediatr Radiol. 2013;43 suppl 1:S23-S40. doi: 10.1007/s00247-012-2590-0
6. Habif, Thomas P. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 6th ed. Mosby/Elsevier, 2016.
7. Ramya C, Nayak C, Tambe S. Superficial acral fibromyxoma. Indian J Dermatol. 2016;61:457-459. doi: 10.4103/0019-5154.185734
8. Ma D, Darling T, Moss J, et al. Histologic variants of periungual fibromas in tuberous sclerosis complex. J Am Acad Dermatol. 2011;64:442-444. doi: 10.1016/j.jaad.2010.03.002
1. Das PC, Hassan S, Kumar P. Subungual exostosis – clinical, radiological, and histological findings. Indian Dermatol Online J. 2019;10:202-203. doi: 10.4103/idoj.IDOJ_104_18
2. Yousefian F, Davis B, Browning JC. Pediatric subungual exostosis. Cutis. 2021;108:256-257. doi:10.12788/cutis.0380
3. Bouchard B, Bartlett M, Donnan L. Assessment of the pediatric foot mass. J Am Acad Orthop Surg. 2017;25:32-41. doi: 10.5435/JAAOS-D-15-00397
4. DaCambra MP, Gupta SK, Ferri-de-Barros F. Subungual exostosis of the toes: a systematic review. Clin Orthop Relat Res. 2014;472:1251-1259. doi: 10.1007/s11999-013-3345-4
5. Shah SH, Callahan MJ. Ultrasound evaluation of superficial lumps and bumps of the extremities in children: a 5-year retrospective review. Pediatr Radiol. 2013;43 suppl 1:S23-S40. doi: 10.1007/s00247-012-2590-0
6. Habif, Thomas P. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 6th ed. Mosby/Elsevier, 2016.
7. Ramya C, Nayak C, Tambe S. Superficial acral fibromyxoma. Indian J Dermatol. 2016;61:457-459. doi: 10.4103/0019-5154.185734
8. Ma D, Darling T, Moss J, et al. Histologic variants of periungual fibromas in tuberous sclerosis complex. J Am Acad Dermatol. 2011;64:442-444. doi: 10.1016/j.jaad.2010.03.002
Would your patient benefit from a monoclonal antibody?
Small-molecule drugs such as aspirin, albuterol, atorvastatin, and lisinopril are the backbone of disease management in family medicine.1 However, large-molecule biological drugs such as monoclonal antibodies (MAbs) are increasingly prescribed to treat common conditions. In the past decade, MAbs comprised 20% of all drug approvals by the US Food and Drug Administration (FDA), and today they represent more than half of drugs currently in development.2 Fifteen MAbs have been approved by the FDA over the past decade for asthma, atopic dermatitis (AD), hyperlipidemia, osteoporosis, and migraine prevention.3 This review details what makes MAbs unique and what you should know about them.
The uniqueness of monoclonal antibodies
MAbs are biologics, but not all biologics are MAbs—eg, adalimumab (Humira) is a MAb, but etanercept (Enbrel) is not. MAbs are therapeutic proteins made possible by hybridoma technology used to create an antibody with single specificity.4-6 Monoclonal antibodies differ from small-molecule drugs in structure, dosing, route of administration, manufacturing, metabolism, drug interactions, and elimination (TABLE 17-9).
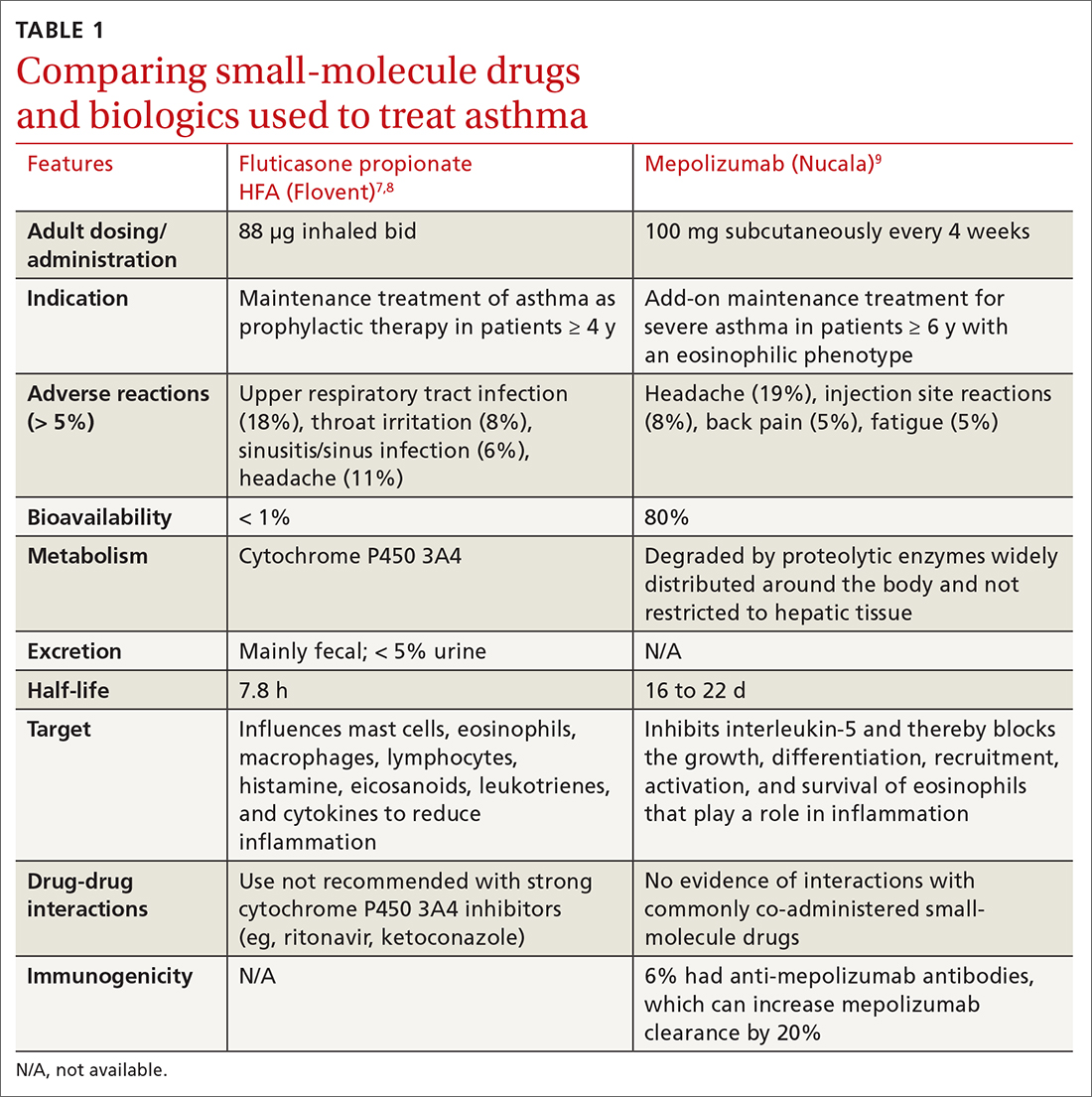
MAbs can be classified as naked, “without any drug or radioactive material attached to them,” or conjugated, “joined to a chemotherapy drug, radioactive isotope, or toxin.”10 MAbs work in several ways, including competitively inhibiting ligand-receptor binding, receptor blockade, or cell elimination from indirect immune system activities such as antibody-dependent cell-mediated cytotoxicity.11,12
Monoclonal antibody uses in family medicine
Asthma
Several MAbs have been approved for use in severe asthma, including but not limited to: omalizumab (Xolair),13 mepolizumab (Nucala),9,14 and dupilumab (Dupixent).15
Omalizumab is a humanized MAb that prevents IgE antibodies from binding to mast cells and basophils, thereby reducing inflammatory mediators.13 A systematic review found that, compared with placebo, omalizumab used in patients with inadequately controlled moderate-to-severe asthma led to significantly fewer asthma exacerbations (absolute risk reduction [ARR], 16% vs 26%; odds ratio [OR] = 0.55; 95% CI, 0.42-0.60; number needed to treat [NNT] = 10) and fewer hospitalizations (ARR, 0.5% vs 3%; OR = 0.16; 95% CI, 0.06-0.42; NNT = 40).13
Significantly more patients in the omalizumab group were able to withdraw from, or reduce, the dose of ICS. GINA recommends omalizumab for patients with positive skin sensitization, total serum IgE ≥ 30 IU/mL, weight within 30 kg to 150 kg, history of childhood asthma and recent exacerbations, and blood eosinophils ≥ 260/mcL.16 Omalizumab is also approved for use in chronic spontaneous urticaria and nasal polyps.
Mepolizumab
Continue to: Another trial found that...
Another trial found that mepolizumab reduced total OCS doses in patients with severe asthma by 50% without increasing exacerbations or worsening asthma control.18 All 3 anti-IL-5 drugs—including not only mepolizumab, but also benralizumab (Fasenra) and reslizumab (Cinqair)—appear to yield similar improvements. A 2017 systematic review found all anti-IL-5 treatments reduced rates of clinically significant asthma exacerbations (treatment with OCS for ≥ 3 days) by roughly 50% in patients with severe eosinophilic asthma and a history of ≥ 2 exacerbations in the past year.
Dupilumab is a humanized MAb that inhibits IL-4 and IL-13, which influence multiple cell types involved in inflammation (eg, mast cells, eosinophils) and inflammatory mediators (histamine, leukotrienes, cytokines).15 In a recent study of patients with uncontrolled asthma, dupilumab 200 mg every 2 weeks compared with placebo showed a modest reduction in the annualized rate of severe asthma exacerbations (0.46 exacerbations vs 0.87, respectively). Dupilumab was effective in patients with blood eosinophil counts ≥ 150/μL but was ineffective in patients with eosinophil counts < 150/μL.15
For patients ≥ 12 years old with severe eosinophilic asthma, GINA recommends using dupilumab as add-on therapy for an initial trial of 4 months at doses of 200 or 300 mg SC every 2 weeks, with preference for 300 mg SC every 2 weeks for OCS-dependent asthma. Dupilumab is approved for use in AD and chronic rhinosinusitis with nasal polyposis. If a biologic agent is not successful after a 4-month trial, consider a 6- to 12-month trial. If efficacy is still minimal, consider switching to an alternative biologic therapy approved for asthma.16
❯ Asthma: Test your skills
Subjective findings: A 19-year-old man presents to your clinic. He has a history of nasal polyps and allergic asthma. At age 18, he was given a diagnosis of severe persistent asthma. He has shortness of breath during waking hours 4 times per week, and treats each of these episodes with albuterol. He also wakes up about twice a week with shortness of breath and has some limitations in normal activities. He reports missing his prescribed fluticasone/salmeterol 500/50 μg, 1 inhalation bid, only once each month. In the last year, he has had 2 exacerbations requiring oral steroids.
Medications: Albuterol 90 μg, 1-2 inhalations, q6h prn; fluticasone/salmeterol 500/50 μg, 1 inhalation bid; tiotropium 1.25 μg, 2 puffs/d; montelukast 10 mg every morning; prednisone 10 mg/d.
Continue to: Objective data
Objective data: Patient is in no apparent distress and afebrile, and oxygen saturation on room air is 97%. Ht, 70 inches; wt, 75 kg. Labs: IgE, 15 IU/mL; serum eosinophils, 315/μL.
Which MAb would be appropriate for this patient? Given that the patient has a blood eosinophil level ≥ 300/μL and severe exacerbations, adult-onset asthma, nasal polyposis, and maintenance OCS at baseline, it would be reasonable to initiate mepolizumab 100 mg SC every 4 weeks, or dupilumab 600 mg once, then 300 mg SC every 2 weeks. Both agents can be self-administered.
Atopic dermatitis
Two MAbs—dupilumab and tralokinumab (Adbry; inhibits IL-13)—are approved for treatment of AD in adults that is uncontrolled with conventional therapy.15,19 Dupilumab is also approved for children ≥ 6 months old.20 Both MAbs are dosed at 600 mg SC, followed by 300 mg every 2 weeks. Dupilumab was compared with placebo in adult patients who had moderate-to-severe AD inadequately controlled on topical corticosteroids (TCSs), to determine the proportion of patients in each group achieving improvement of either 0 or 1 points or ≥ 2 points in the 5-point Investigator Global Assessment (IGA) score from baseline to 16 weeks.21 Thirty-seven percent of patients receiving dupilumab 300 mg SC weekly and 38% of patients receiving dupilumab 300 mg SC every 2 weeks achieved the primary outcome, compared with 10% of those receiving placebo (P < .001).21 Similar IGA scores were reported when dupilumab was combined with TCS, compared with placebo.22
It would be reasonable to consider dupilumab or tralokinumab in patients with: cutaneous atrophy or hypothalamic-pituitary-adrenal axis suppression with TCS, concerns of malignancy with topical calcineurin inhibitors, or problems with the alternative systemic therapies (cyclosporine-induced hypertension, nephrotoxicity, or immunosuppression; azathioprine-induced malignancy; or methotrexate-induced bone marrow suppression, renal impairment, hepatotoxicity, pneumonitis, or gastrointestinal toxicity).23
A distinct advantage of MAbs over other systemic agents in the management of AD is that MAbs do not require frequent monitoring of blood pressure, renal or liver function, complete blood count with differential, electrolytes, or uric acid. Additionally, MAbs have fewer black box warnings and adverse reactions when compared with other systemic agents.
Continue to: Hyperlipidemia
Hyperlipidemia
Three MAbs are approved for use in hyperlipidemia: the angiopoietin-like protein 3 (ANGPTL3) inhibitor evinacumab (Evkeeza)24 and 2 proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, evolocumab (Repatha)25 and alirocumab (Praluent).26
ANGPTL3 inhibitors block ANGPTL3 and reduce endothelial lipase and lipoprotein lipase activity, which in turn decreases low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglyceride formation. PCSK9 inhibitors prevent PCSK9 from binding to LDL receptors, thereby maintaining the number of active LDL receptors and increasing LDL-C removal.
Evinacumab is indicated for homozygous familial hypercholesterolemia and is administered intravenously every 4 weeks. Evinacumab has not been evaluated for effects on cardiovascular morbidity and mortality.
Evolocumab 140 mg SC every 2 weeks or 420 mg SC monthly has been studied in patients on statin therapy with LDL-C ≥ 70 mg/dL. Patients on evolocumab experienced significantly less of the composite endpoint of cardiovascular death, myocardial infarction (MI), stroke, hospitalization for unstable angina, or coronary revascularization compared with placebo (9.8% vs 11.3%; hazard ratio [HR] = 0.85; 95% CI, 0.79-0.92; NNT = 67.27
Alirocumab 75 mg SC every 2 weeks has also been studied in patients receiving statin therapy with LDL-C ≥ 70 mg/dL. Patients taking alirocumab experienced significantly less of the composite endpoint of death from coronary heart disease, nonfatal MI, ischemic stroke, or hospitalization for unstable angina compared with placebo (9.5% vs 11.1%; HR = 0.85; 95% CI, 0.78-0.93; NNT = 63).
Continue to: According to the 2018...
According to the 2018 AHA Cholesterol Guidelines, PCSK9 inhibitors are indicated for patients receiving maximally tolerated LDL-C-lowering therapy (statin and ezetimibe) with LDL-C ≥ 70 mg/dL, if they have had multiple atherosclerotic cardiovascular disease (ASCVD) events or 1 major ASCVD event with multiple high-risk conditions (eg, heterozygous familial hypercholesterolemia, history of coronary artery bypass grafting or percutaneous coronary intervention, hypertension, estimated glomerular filtration rate of 15 to 59 mL/min/1.73m2).29 For patients without prior ASCVD events or high-risk conditions who are receiving maximally tolerated LDL-C-lowering therapy (statin and ezetimibe), PCSK9 inhibitors are indicated if the LDL-C remains ≥ 100 mg/dL.
Osteoporosis
The 2 MAbs approved for use in osteoporosis are the receptor activator of nuclear factor kB ligand (RANKL) inhibitor denosumab (Prolia)30 and the sclerostin inhibitor romosozumab (Evenity).31
Denosumab prevents RANKL from binding to the RANK receptor, thereby inhibiting osteoclast formation and decreasing bone resorption. Denosumab is approved for use in women and men who are at high risk of osteoporotic fracture, including those taking OCSs, men receiving androgen deprivation therapy for prostate cancer, and women receiving adjuvant aromatase inhibitor therapy for breast cancer.
In a 3-year randomized trial, denosumab 60 mg SC every 6 months was compared with placebo in postmenopausal women with T-scores < –2.5, but not < –4.0 at the lumbar spine or total hip. Denosumab significantly reduced new radiographic vertebral fractures (2.3% vs 7.2%; risk ratio [RR] = 0.32; 95% CI, 0.26-0.41; NNT = 21), hip fracture (0.7% vs 1.2%), and nonvertebral fracture (6.5% vs 8.0%).32 Denosumab carries an increased risk of multiple vertebral fractures following discontinuation, skin infections, dermatologic reactions, and severe bone, joint, and muscle pain.
Romosozumab inhibits sclerostin, thereby increasing bone formation and, to a lesser degree, decreasing bone resorption. Romosozumab is approved for use in postmenopausal women at high risk for fracture (ie, those with a history of osteoporotic fracture or multiple risk factors for fracture) or in patients who have not benefited from or are intolerant of other therapies. In one study, postmenopausal women with a T-score of –2.5 to –3.5 at the total hip or femoral neck were randomly assigned to receive either romosozumab 210 mg SC or placebo for 12 months, then each group was switched to denosumab 60 mg SC for 12 months. After the first year, prior to initiating denosumab, patients taking romosozumab experienced significantly fewer new vertebral fractures than patients taking placebo (0.5% vs 1.8%; RR = 0.27; 95% CI, 0.16-0.47; NNT = 77); however, there was no significant difference between the 2 groups with nonvertebral fractures (HR = 0.75; 95% CI, 0.53-1.05).33
Continue to: In another study...
In another study, romosozumab 210 mg SC was compared with alendronate 70 mg weekly, followed by alendronate 70 mg weekly in both groups. Over the first 12 months, patients treated with romosozumab saw a significant reduction in the incidence of new vertebral fractures (4% vs 6.3%; RR = 0.63, P < .003; NNT = 44). Patients treated with romosozumab with alendronate added for another 12 months also saw a significant reduction in new incidence of vertebral fractures (6.2% vs 11.9%; RR = 0.52; P < .001; NNT = 18).34 There was a higher risk of cardiovascular events among patients receiving romosozumab compared with those treated with alendronate, so romosozumab should not be used in individuals who have had an MI or stroke within the previous year.34 Denosumab and romosozumab offer an advantage over some bisphosphonates in that they require less frequent dosing and can be used in patients with renal impairment (creatinine clearance < 35 mL/min, in which zoledronic acid is contraindicated and alendronate is not recommended; < 30 mL/min, in which risedronate and ibandronate are not recommended).
Migraine prevention
Four
Erenumab, fremanezumab, and galcanezumab are all available in subcutaneous autoinjectors (or syringe with fremanezumab). Eptinezumab is an intravenous (IV) infusion given every 3 months.
Erenumab is available in both 70-mg and 140-mg dosing options. Fremanezumab can be given as 225 mg monthly or 675 mg quarterly. Galcanezumab has an initial loading dose of 240 mg followed by 120 mg given monthly. Erenumab targets the CGRP receptor; the others target the CGRP ligand. Eptinezumab has 100% bioavailability and reaches maximum serum concentration sooner than the other antagonists (due to its route of administration), but it must be given in an infusion center. Few insurers approve the use of eptinezumab unless a trial of least 1 of the monthly injectables has failed.
There are no head-to-head studies of the medications in this class. Additionally, differing study designs, definitions, statistical analyses, endpoints, and responder-rate calculations make it challenging to compare them directly against one another. At the very least, all of the CGRP MAbs have efficacy comparable to conventional preventive migraine medications such as propranolol, amitriptyline, and topiramate.40
Continue to: The most commonly reported adverse...
The most commonly reported adverse effect for all 4 CGRPs is injection site reaction, which was highest with the quarterly fremanezumab dose (45%).37 Constipation was most notable with the 140-mg dose of erenumab (3%)35; with the other CGRP MAbs it is comparable to that seen with placebo (< 1%).
Erenumab-induced hypertension has been identified in 61 cases reported through the FDA Adverse Event Reporting System (FAERS) as of 2021.41 This was not reported during MAb development programs, nor was it noted during clinical trials. Blood pressure elevation was seen within 1 week of injection in nearly 50% of the cases, and nearly one-third had pre-existing hypertension.41 Due to these findings, the erenumab prescribing information was updated to include hypertension in its warnings and precautions. It is possible that hypertension could be a class effect, although trial data and posthoc studies have yet to bear that out. Since erenumab was the first CGRP antagonist brought to market (May 2018 vs September 2018 for fremanezumab and galcanezumab), it may have accumulated more FAERS reports. Nearly all studies exclude patients with older age, uncontrolled hypertension, and unstable cardiovascular disease, which could impact data.41
Overall, this class of medications is very well tolerated, easy to use (again, excluding eptinezumab), and maintains a low adverse effect profile, giving added value compared with conventional preventive migraine medications.
The American Headache Society recommends a preventive oral therapy for at least 3 months before trying an alternative medication. After treatment failure with at least 2 oral agents, CGRP MAbs are recommended.42 CGRP antagonists offer convenient dosing, bypass gastrointestinal metabolism (which is useful in patients with nausea/vomiting), and have fewer adverse effects than traditional oral medications.
Worth noting. Several newer oral agents have been recently approved for migraine prevention, including atogepant (Qulipta) and rimegepant (Nurtec), which are also CGRP antagonists. Rimegepant is approved for both acute migraine treatment and prevention.
Continue to: Migraine
❯ Migraine: Test your skills
Subjective findings: A 25-year-old woman presents to your clinic for management of episodic migraines with aura. Her baseline average migraine frequency is 9 headache days/month. Her migraines are becoming more frequent despite treatment. She fears IV medication use and avoids hospitals.
History: Hypertension, irritable bowel syndrome with constipation (IBS-C), and depression. The patient is not pregnant or trying to get pregnant.
Medications: Current medications (for previous 4 months) include propranolol 40 mg at bedtime, linaclotide 145 μg/d, citalopram 20 mg/d, and sumatriptan 50 mg prn. Past medications include venlafaxine 150 mg po bid for 5 months.
What would be appropriate for this patient? This patient meets the criteria for using a CGRP antagonist because she has tried 2 preventive treatments for more than 60 to 90 days. Erenumab is not the best option, given the patient’s history of hypertension and IBS-C. The patient fears hospitals and IV medications, making eptinezumab a less-than-ideal choice. Depending on her insurance, fremanezumab or galcanezumab would be good options at this time.
CGRP antagonists have not been studied or evaluated in pregnancy, but if this patient becomes pregnant, a first-line agent for prevention would be propranolol, and a second-line agent would be a tricyclic antidepressant, memantine, or verapamil. Avoid ergotamines and antiepileptics (topiramate or valproate) in pregnancy.43,44
Continue to: The challenges associated with MAbs
The challenges associated with MAbs
MAbs can be expensive (TABLE 2),45 some prohibitively so. On a population scale, biologics account for around 40% of prescription drug spending and may cost 22 times more than small-molecule drugs.46 Estimates in 2016 showed that MAbs comprise $90.2 billion (43%) of the biologic market.46
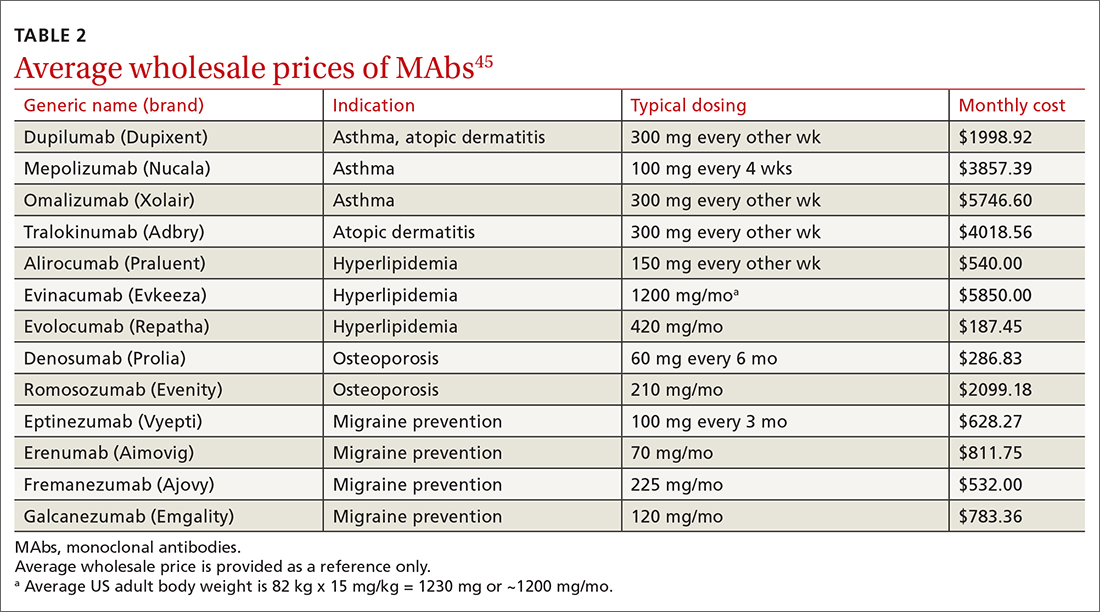
MAbs also require prior authorization forms to be submitted. Prior authorization criteria vary by state and by insurance plan. In my (ES) experience, submitting letters of medical necessity justifying the need for therapy or expertise in the disease states for which the MAb is being prescribed help your patient get the medication they need.
Expect to see additional MAbs approved in the future. If the costs come down, adoption of these agents into practice will likely increase.
CORRESPONDENCE
Evelyn Sbar, MD, Texas Tech University Health Sciences Center, 1400 South Coulter Street, Suite 5100, Amarillo, TX 79106; [email protected]
1. Rui P, Okeyode T. National Ambulatory Medical Care Survey: 2016 national summary tables. National Center for Health Statistics. Accessed June 15, 2022. www.cdc.gov/nchs/data/ahcd/namcs_summary/2016_namcs_web_tables.pdf
2. IDBS. The future of biologics drug development is today. June 27, 2018. Accessed June 15, 2022. www.idbs.com/blog/2018/06/the-future-of-biologics-drug-development-is-today/
3. Antibody therapeutics approved or in regulatory review in the EU or US. Antibody Society. Accessed June 15, 2022. www.antibodysociety.org/resources/approved-antibodies/
4. FDA. Code of Federal Regulations, Title 21, Chapter I, Subchapter F biologics. March 29, 2022. Accessed June 15, 2022. www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=600.3
5. Köhler G, Milstein C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature. 1975;256:495-497. doi: 10.1038/256495a0
6. Raejewsky K. The advent and rise of monoclonal antibodies. Nature. November 4, 2019. Accessed June 15, 2022. www.nature.com/articles/d41586-019-02840-w
7. Flovent. Prescribing information. GlaxoSmithKline; 2010. Accessed June 15, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2010/021433s015lbl.pdf
8. NLM. National Center for Biotechnology Information. PubChem. Method for the preparation of fluticasone and related 17beta-carbothioic esters using a novel carbothioic acid synthesis and novel purification methods. Accessed June 15, 2022. pubchem.ncbi.nlm.nih.gov/patent/WO-0162722-A2
9. Nucala. Prescribing information. GlaxoSmithKline; 2019. Accessed June 15, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2019/761122s000lbl.pdf
10. Argyriou AA, Kalofonos HP. Recent advances relating to the clinical application of naked monoclonal antibodies in solid tumors. Mol Med. 2009;15:183-191. doi: 10.2119/molmed.2009.00007
11. Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84:548-558. doi: 10.1038/clpt.2008.170
12. Zahavi D, AlDeghaither D, O’Connell A, et al. Enhancing antibody-dependent cell-mediated cytotoxicity: a strategy for improving antibody-based immunotherapy. Antib Ther. 2018;1:7-12. doi: 10.1093/abt/tby002
13. Normansell R, Walker S, Milan SJ, et al. Omalizumab for asthma in adults and children. Cochrane Database Syst Rev. 2014:CD003559. doi: 10.1002/14651858.CD003559.pub4
14. Farne HA, Wilson A, Powell C, et al. Anti-IL5 therapies for asthma. Cochrane Database Syst Rev. 2017;9:CD010834. doi: 10.1002/14651858.CD010834.pub3
15. Castro M, Corren J, Pavord ID, et al. Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. N Engl J Med. 2018;378:2486-2496. doi: 10.1056/NEJMoa1804092
16. GINA. Global strategy for asthma management and prevention. 2022 Difficult-to-treat and severe asthma guide—slide set. Accessed June 23, 2022. https://ginasthma.org/severeasthma/
17. Ortega HG, Liu MC, Pavord ID, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371:1198-1207. doi: 10.1056/NEJMoa1403290
18. Bel EH, Wenzel SE, Thompson PJ, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med. 2014;371:1189-1197. doi: 10.1056/NEJMoa1403291
19. Adbry. Prescribing information. Leo Pharma Inc; 2021. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/nda/2022/761180Orig1s000lbl.pdf
20. Dupixent. Prescribing information. Regeneron Pharmaceuticals; 2022. Accessed October 5, 2022. https://www.regeneron.com/downloads/dupixent_fpi.pdf
21. Simpson EL, Bieber T, Guttman-Yassky E, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375:2335-2348. doi: 10.1056/NEJMoa1610020
22. Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial. Lancet. 2017;389:2287-2303. doi: 10.1016/s0140-6736(17)31191-1
23. Sidbury R, Davis DM, Cohen DE, et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71:327-349. doi: 10.1016/j.jaad.2014.03.030
24. Evkeeza. Prescribing information. Regeneron Pharmaceuticals; 2021. Accessed June 24, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761181s000lbl.pdf
25. Repatha. Prescribing information. Amgen; 2015. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2017/125522s014lbl.pdf
26. Praluent. Prescribing information. Sanofi Aventis and Regeneron Pharmaceuticals. 2015. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2017/125559s002lbl.pdf
27. Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713-1722. doi: 10.1056/NEJMoa1615664
28. Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097-2107. doi:10.1056/NEJMoa1801174
29. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2019;73:e285-e350. doi: 10.1016/j.jacc.2018.11.003
30. Prolia. Prescribing information. Amgen; 2010. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2013/125320s094lbl.pdf
31. Evenity. Prescribing information. Amgen; 2019. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2019/761062s000lbl.pdf
32. Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756-765. doi: 10.1056/NEJMoa0809493
33. Cosman F, Crittenden DB, Adachi JD, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375:1532-1543. doi: 10.1056/NEJMoa1607948
34. Saag KG, Petersen J, Brandi ML, et al. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377:1417-1427. doi: 10.1056/NEJMoa1708322
35. Aimovig. Prescribing information. Amgen; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761077s000lbl.pdf
36. Vyepti. Prescribing information. Lundbeck Seattle BioPharmaceuticals; 2020. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2020/761119s000lbl.pdf
37. Ajovy. Prescribing information. Teva Pharmaceuticals; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761089s000lbl.pdf
38. Emgality. Prescribing information. Eli Lilly and Co.; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761063s000lbl.pdf
39. Edvinsson L, Haanes KA, Warfvinge K, et al. CGRP as the target of new migraine therapies - successful translation from bench to clinic. Nat Rev Neurol. 2018;14:338-350. doi: 10.1038/s41582-018-0003-1
40. Vandervorst F. Van Deun L, Van Dycke A, et al. CGRP monoclonal antibodies in migraine: an efficacy and tolerability comparison with standard prophylactic drugs. J Headache Pain. 2021;22:128. doi: 10.1186/s10194-021-01335-2
41. Saely S, Croteau D, Jawidzik L, et al. Hypertension: a new safety risk for patients treated with erenumab. Headache. 2021;61:202-208. doi: 10.1111/head.14051
42. American Headache Society. The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache. 2019;59:1-18. doi: 10.1111/head.13456
43. Burch R. Headache in pregnancy and the puerperium. Neurol Clin. 2019;37:31-51. doi: 10.1016/j.ncl.2018.09.004
44. Burch R. Epidemiology and treatment of menstrual migraine and migraine during pregnancy and lactation: a narrative review. Headache. 2020;60:200-216. doi: 10.1111/head.13665
45. Lexi-Comp. Lexi-drug database. Accessed April 4, 2022. https://online.lexi.com/lco/action/login
46. Walker N. Biologics: driving force in pharma. Pharma’s Almanac. June 5, 2017. Accessed June 15, 2020. www.pharmasalmanac.com/articles/biologics-driving-force-in-pharma
Small-molecule drugs such as aspirin, albuterol, atorvastatin, and lisinopril are the backbone of disease management in family medicine.1 However, large-molecule biological drugs such as monoclonal antibodies (MAbs) are increasingly prescribed to treat common conditions. In the past decade, MAbs comprised 20% of all drug approvals by the US Food and Drug Administration (FDA), and today they represent more than half of drugs currently in development.2 Fifteen MAbs have been approved by the FDA over the past decade for asthma, atopic dermatitis (AD), hyperlipidemia, osteoporosis, and migraine prevention.3 This review details what makes MAbs unique and what you should know about them.
The uniqueness of monoclonal antibodies
MAbs are biologics, but not all biologics are MAbs—eg, adalimumab (Humira) is a MAb, but etanercept (Enbrel) is not. MAbs are therapeutic proteins made possible by hybridoma technology used to create an antibody with single specificity.4-6 Monoclonal antibodies differ from small-molecule drugs in structure, dosing, route of administration, manufacturing, metabolism, drug interactions, and elimination (TABLE 17-9).
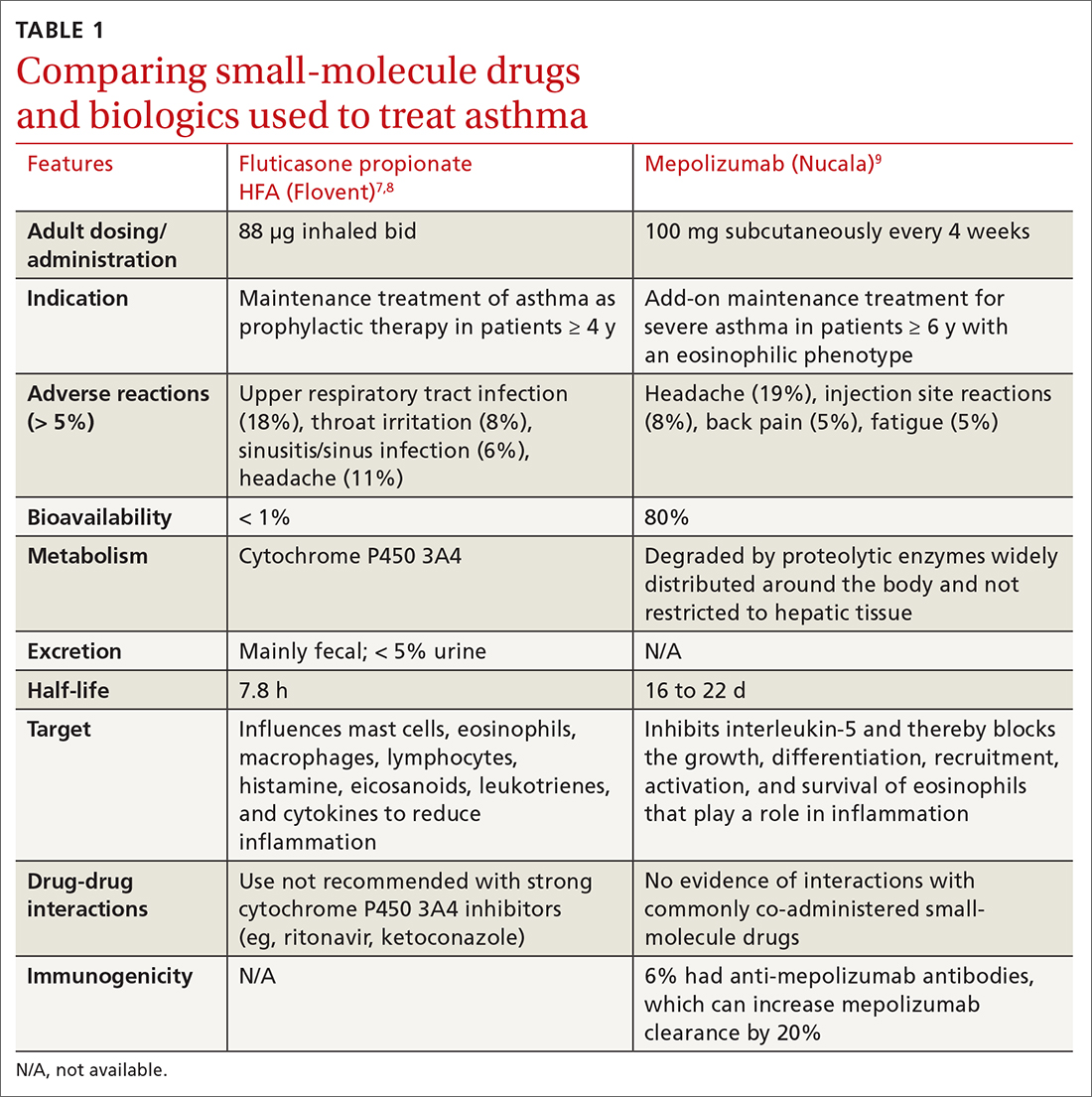
MAbs can be classified as naked, “without any drug or radioactive material attached to them,” or conjugated, “joined to a chemotherapy drug, radioactive isotope, or toxin.”10 MAbs work in several ways, including competitively inhibiting ligand-receptor binding, receptor blockade, or cell elimination from indirect immune system activities such as antibody-dependent cell-mediated cytotoxicity.11,12
Monoclonal antibody uses in family medicine
Asthma
Several MAbs have been approved for use in severe asthma, including but not limited to: omalizumab (Xolair),13 mepolizumab (Nucala),9,14 and dupilumab (Dupixent).15
Omalizumab is a humanized MAb that prevents IgE antibodies from binding to mast cells and basophils, thereby reducing inflammatory mediators.13 A systematic review found that, compared with placebo, omalizumab used in patients with inadequately controlled moderate-to-severe asthma led to significantly fewer asthma exacerbations (absolute risk reduction [ARR], 16% vs 26%; odds ratio [OR] = 0.55; 95% CI, 0.42-0.60; number needed to treat [NNT] = 10) and fewer hospitalizations (ARR, 0.5% vs 3%; OR = 0.16; 95% CI, 0.06-0.42; NNT = 40).13
Significantly more patients in the omalizumab group were able to withdraw from, or reduce, the dose of ICS. GINA recommends omalizumab for patients with positive skin sensitization, total serum IgE ≥ 30 IU/mL, weight within 30 kg to 150 kg, history of childhood asthma and recent exacerbations, and blood eosinophils ≥ 260/mcL.16 Omalizumab is also approved for use in chronic spontaneous urticaria and nasal polyps.
Mepolizumab
Continue to: Another trial found that...
Another trial found that mepolizumab reduced total OCS doses in patients with severe asthma by 50% without increasing exacerbations or worsening asthma control.18 All 3 anti-IL-5 drugs—including not only mepolizumab, but also benralizumab (Fasenra) and reslizumab (Cinqair)—appear to yield similar improvements. A 2017 systematic review found all anti-IL-5 treatments reduced rates of clinically significant asthma exacerbations (treatment with OCS for ≥ 3 days) by roughly 50% in patients with severe eosinophilic asthma and a history of ≥ 2 exacerbations in the past year.
Dupilumab is a humanized MAb that inhibits IL-4 and IL-13, which influence multiple cell types involved in inflammation (eg, mast cells, eosinophils) and inflammatory mediators (histamine, leukotrienes, cytokines).15 In a recent study of patients with uncontrolled asthma, dupilumab 200 mg every 2 weeks compared with placebo showed a modest reduction in the annualized rate of severe asthma exacerbations (0.46 exacerbations vs 0.87, respectively). Dupilumab was effective in patients with blood eosinophil counts ≥ 150/μL but was ineffective in patients with eosinophil counts < 150/μL.15
For patients ≥ 12 years old with severe eosinophilic asthma, GINA recommends using dupilumab as add-on therapy for an initial trial of 4 months at doses of 200 or 300 mg SC every 2 weeks, with preference for 300 mg SC every 2 weeks for OCS-dependent asthma. Dupilumab is approved for use in AD and chronic rhinosinusitis with nasal polyposis. If a biologic agent is not successful after a 4-month trial, consider a 6- to 12-month trial. If efficacy is still minimal, consider switching to an alternative biologic therapy approved for asthma.16
❯ Asthma: Test your skills
Subjective findings: A 19-year-old man presents to your clinic. He has a history of nasal polyps and allergic asthma. At age 18, he was given a diagnosis of severe persistent asthma. He has shortness of breath during waking hours 4 times per week, and treats each of these episodes with albuterol. He also wakes up about twice a week with shortness of breath and has some limitations in normal activities. He reports missing his prescribed fluticasone/salmeterol 500/50 μg, 1 inhalation bid, only once each month. In the last year, he has had 2 exacerbations requiring oral steroids.
Medications: Albuterol 90 μg, 1-2 inhalations, q6h prn; fluticasone/salmeterol 500/50 μg, 1 inhalation bid; tiotropium 1.25 μg, 2 puffs/d; montelukast 10 mg every morning; prednisone 10 mg/d.
Continue to: Objective data
Objective data: Patient is in no apparent distress and afebrile, and oxygen saturation on room air is 97%. Ht, 70 inches; wt, 75 kg. Labs: IgE, 15 IU/mL; serum eosinophils, 315/μL.
Which MAb would be appropriate for this patient? Given that the patient has a blood eosinophil level ≥ 300/μL and severe exacerbations, adult-onset asthma, nasal polyposis, and maintenance OCS at baseline, it would be reasonable to initiate mepolizumab 100 mg SC every 4 weeks, or dupilumab 600 mg once, then 300 mg SC every 2 weeks. Both agents can be self-administered.
Atopic dermatitis
Two MAbs—dupilumab and tralokinumab (Adbry; inhibits IL-13)—are approved for treatment of AD in adults that is uncontrolled with conventional therapy.15,19 Dupilumab is also approved for children ≥ 6 months old.20 Both MAbs are dosed at 600 mg SC, followed by 300 mg every 2 weeks. Dupilumab was compared with placebo in adult patients who had moderate-to-severe AD inadequately controlled on topical corticosteroids (TCSs), to determine the proportion of patients in each group achieving improvement of either 0 or 1 points or ≥ 2 points in the 5-point Investigator Global Assessment (IGA) score from baseline to 16 weeks.21 Thirty-seven percent of patients receiving dupilumab 300 mg SC weekly and 38% of patients receiving dupilumab 300 mg SC every 2 weeks achieved the primary outcome, compared with 10% of those receiving placebo (P < .001).21 Similar IGA scores were reported when dupilumab was combined with TCS, compared with placebo.22
It would be reasonable to consider dupilumab or tralokinumab in patients with: cutaneous atrophy or hypothalamic-pituitary-adrenal axis suppression with TCS, concerns of malignancy with topical calcineurin inhibitors, or problems with the alternative systemic therapies (cyclosporine-induced hypertension, nephrotoxicity, or immunosuppression; azathioprine-induced malignancy; or methotrexate-induced bone marrow suppression, renal impairment, hepatotoxicity, pneumonitis, or gastrointestinal toxicity).23
A distinct advantage of MAbs over other systemic agents in the management of AD is that MAbs do not require frequent monitoring of blood pressure, renal or liver function, complete blood count with differential, electrolytes, or uric acid. Additionally, MAbs have fewer black box warnings and adverse reactions when compared with other systemic agents.
Continue to: Hyperlipidemia
Hyperlipidemia
Three MAbs are approved for use in hyperlipidemia: the angiopoietin-like protein 3 (ANGPTL3) inhibitor evinacumab (Evkeeza)24 and 2 proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, evolocumab (Repatha)25 and alirocumab (Praluent).26
ANGPTL3 inhibitors block ANGPTL3 and reduce endothelial lipase and lipoprotein lipase activity, which in turn decreases low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglyceride formation. PCSK9 inhibitors prevent PCSK9 from binding to LDL receptors, thereby maintaining the number of active LDL receptors and increasing LDL-C removal.
Evinacumab is indicated for homozygous familial hypercholesterolemia and is administered intravenously every 4 weeks. Evinacumab has not been evaluated for effects on cardiovascular morbidity and mortality.
Evolocumab 140 mg SC every 2 weeks or 420 mg SC monthly has been studied in patients on statin therapy with LDL-C ≥ 70 mg/dL. Patients on evolocumab experienced significantly less of the composite endpoint of cardiovascular death, myocardial infarction (MI), stroke, hospitalization for unstable angina, or coronary revascularization compared with placebo (9.8% vs 11.3%; hazard ratio [HR] = 0.85; 95% CI, 0.79-0.92; NNT = 67.27
Alirocumab 75 mg SC every 2 weeks has also been studied in patients receiving statin therapy with LDL-C ≥ 70 mg/dL. Patients taking alirocumab experienced significantly less of the composite endpoint of death from coronary heart disease, nonfatal MI, ischemic stroke, or hospitalization for unstable angina compared with placebo (9.5% vs 11.1%; HR = 0.85; 95% CI, 0.78-0.93; NNT = 63).
Continue to: According to the 2018...
According to the 2018 AHA Cholesterol Guidelines, PCSK9 inhibitors are indicated for patients receiving maximally tolerated LDL-C-lowering therapy (statin and ezetimibe) with LDL-C ≥ 70 mg/dL, if they have had multiple atherosclerotic cardiovascular disease (ASCVD) events or 1 major ASCVD event with multiple high-risk conditions (eg, heterozygous familial hypercholesterolemia, history of coronary artery bypass grafting or percutaneous coronary intervention, hypertension, estimated glomerular filtration rate of 15 to 59 mL/min/1.73m2).29 For patients without prior ASCVD events or high-risk conditions who are receiving maximally tolerated LDL-C-lowering therapy (statin and ezetimibe), PCSK9 inhibitors are indicated if the LDL-C remains ≥ 100 mg/dL.
Osteoporosis
The 2 MAbs approved for use in osteoporosis are the receptor activator of nuclear factor kB ligand (RANKL) inhibitor denosumab (Prolia)30 and the sclerostin inhibitor romosozumab (Evenity).31
Denosumab prevents RANKL from binding to the RANK receptor, thereby inhibiting osteoclast formation and decreasing bone resorption. Denosumab is approved for use in women and men who are at high risk of osteoporotic fracture, including those taking OCSs, men receiving androgen deprivation therapy for prostate cancer, and women receiving adjuvant aromatase inhibitor therapy for breast cancer.
In a 3-year randomized trial, denosumab 60 mg SC every 6 months was compared with placebo in postmenopausal women with T-scores < –2.5, but not < –4.0 at the lumbar spine or total hip. Denosumab significantly reduced new radiographic vertebral fractures (2.3% vs 7.2%; risk ratio [RR] = 0.32; 95% CI, 0.26-0.41; NNT = 21), hip fracture (0.7% vs 1.2%), and nonvertebral fracture (6.5% vs 8.0%).32 Denosumab carries an increased risk of multiple vertebral fractures following discontinuation, skin infections, dermatologic reactions, and severe bone, joint, and muscle pain.
Romosozumab inhibits sclerostin, thereby increasing bone formation and, to a lesser degree, decreasing bone resorption. Romosozumab is approved for use in postmenopausal women at high risk for fracture (ie, those with a history of osteoporotic fracture or multiple risk factors for fracture) or in patients who have not benefited from or are intolerant of other therapies. In one study, postmenopausal women with a T-score of –2.5 to –3.5 at the total hip or femoral neck were randomly assigned to receive either romosozumab 210 mg SC or placebo for 12 months, then each group was switched to denosumab 60 mg SC for 12 months. After the first year, prior to initiating denosumab, patients taking romosozumab experienced significantly fewer new vertebral fractures than patients taking placebo (0.5% vs 1.8%; RR = 0.27; 95% CI, 0.16-0.47; NNT = 77); however, there was no significant difference between the 2 groups with nonvertebral fractures (HR = 0.75; 95% CI, 0.53-1.05).33
Continue to: In another study...
In another study, romosozumab 210 mg SC was compared with alendronate 70 mg weekly, followed by alendronate 70 mg weekly in both groups. Over the first 12 months, patients treated with romosozumab saw a significant reduction in the incidence of new vertebral fractures (4% vs 6.3%; RR = 0.63, P < .003; NNT = 44). Patients treated with romosozumab with alendronate added for another 12 months also saw a significant reduction in new incidence of vertebral fractures (6.2% vs 11.9%; RR = 0.52; P < .001; NNT = 18).34 There was a higher risk of cardiovascular events among patients receiving romosozumab compared with those treated with alendronate, so romosozumab should not be used in individuals who have had an MI or stroke within the previous year.34 Denosumab and romosozumab offer an advantage over some bisphosphonates in that they require less frequent dosing and can be used in patients with renal impairment (creatinine clearance < 35 mL/min, in which zoledronic acid is contraindicated and alendronate is not recommended; < 30 mL/min, in which risedronate and ibandronate are not recommended).
Migraine prevention
Four
Erenumab, fremanezumab, and galcanezumab are all available in subcutaneous autoinjectors (or syringe with fremanezumab). Eptinezumab is an intravenous (IV) infusion given every 3 months.
Erenumab is available in both 70-mg and 140-mg dosing options. Fremanezumab can be given as 225 mg monthly or 675 mg quarterly. Galcanezumab has an initial loading dose of 240 mg followed by 120 mg given monthly. Erenumab targets the CGRP receptor; the others target the CGRP ligand. Eptinezumab has 100% bioavailability and reaches maximum serum concentration sooner than the other antagonists (due to its route of administration), but it must be given in an infusion center. Few insurers approve the use of eptinezumab unless a trial of least 1 of the monthly injectables has failed.
There are no head-to-head studies of the medications in this class. Additionally, differing study designs, definitions, statistical analyses, endpoints, and responder-rate calculations make it challenging to compare them directly against one another. At the very least, all of the CGRP MAbs have efficacy comparable to conventional preventive migraine medications such as propranolol, amitriptyline, and topiramate.40
Continue to: The most commonly reported adverse...
The most commonly reported adverse effect for all 4 CGRPs is injection site reaction, which was highest with the quarterly fremanezumab dose (45%).37 Constipation was most notable with the 140-mg dose of erenumab (3%)35; with the other CGRP MAbs it is comparable to that seen with placebo (< 1%).
Erenumab-induced hypertension has been identified in 61 cases reported through the FDA Adverse Event Reporting System (FAERS) as of 2021.41 This was not reported during MAb development programs, nor was it noted during clinical trials. Blood pressure elevation was seen within 1 week of injection in nearly 50% of the cases, and nearly one-third had pre-existing hypertension.41 Due to these findings, the erenumab prescribing information was updated to include hypertension in its warnings and precautions. It is possible that hypertension could be a class effect, although trial data and posthoc studies have yet to bear that out. Since erenumab was the first CGRP antagonist brought to market (May 2018 vs September 2018 for fremanezumab and galcanezumab), it may have accumulated more FAERS reports. Nearly all studies exclude patients with older age, uncontrolled hypertension, and unstable cardiovascular disease, which could impact data.41
Overall, this class of medications is very well tolerated, easy to use (again, excluding eptinezumab), and maintains a low adverse effect profile, giving added value compared with conventional preventive migraine medications.
The American Headache Society recommends a preventive oral therapy for at least 3 months before trying an alternative medication. After treatment failure with at least 2 oral agents, CGRP MAbs are recommended.42 CGRP antagonists offer convenient dosing, bypass gastrointestinal metabolism (which is useful in patients with nausea/vomiting), and have fewer adverse effects than traditional oral medications.
Worth noting. Several newer oral agents have been recently approved for migraine prevention, including atogepant (Qulipta) and rimegepant (Nurtec), which are also CGRP antagonists. Rimegepant is approved for both acute migraine treatment and prevention.
Continue to: Migraine
❯ Migraine: Test your skills
Subjective findings: A 25-year-old woman presents to your clinic for management of episodic migraines with aura. Her baseline average migraine frequency is 9 headache days/month. Her migraines are becoming more frequent despite treatment. She fears IV medication use and avoids hospitals.
History: Hypertension, irritable bowel syndrome with constipation (IBS-C), and depression. The patient is not pregnant or trying to get pregnant.
Medications: Current medications (for previous 4 months) include propranolol 40 mg at bedtime, linaclotide 145 μg/d, citalopram 20 mg/d, and sumatriptan 50 mg prn. Past medications include venlafaxine 150 mg po bid for 5 months.
What would be appropriate for this patient? This patient meets the criteria for using a CGRP antagonist because she has tried 2 preventive treatments for more than 60 to 90 days. Erenumab is not the best option, given the patient’s history of hypertension and IBS-C. The patient fears hospitals and IV medications, making eptinezumab a less-than-ideal choice. Depending on her insurance, fremanezumab or galcanezumab would be good options at this time.
CGRP antagonists have not been studied or evaluated in pregnancy, but if this patient becomes pregnant, a first-line agent for prevention would be propranolol, and a second-line agent would be a tricyclic antidepressant, memantine, or verapamil. Avoid ergotamines and antiepileptics (topiramate or valproate) in pregnancy.43,44
Continue to: The challenges associated with MAbs
The challenges associated with MAbs
MAbs can be expensive (TABLE 2),45 some prohibitively so. On a population scale, biologics account for around 40% of prescription drug spending and may cost 22 times more than small-molecule drugs.46 Estimates in 2016 showed that MAbs comprise $90.2 billion (43%) of the biologic market.46
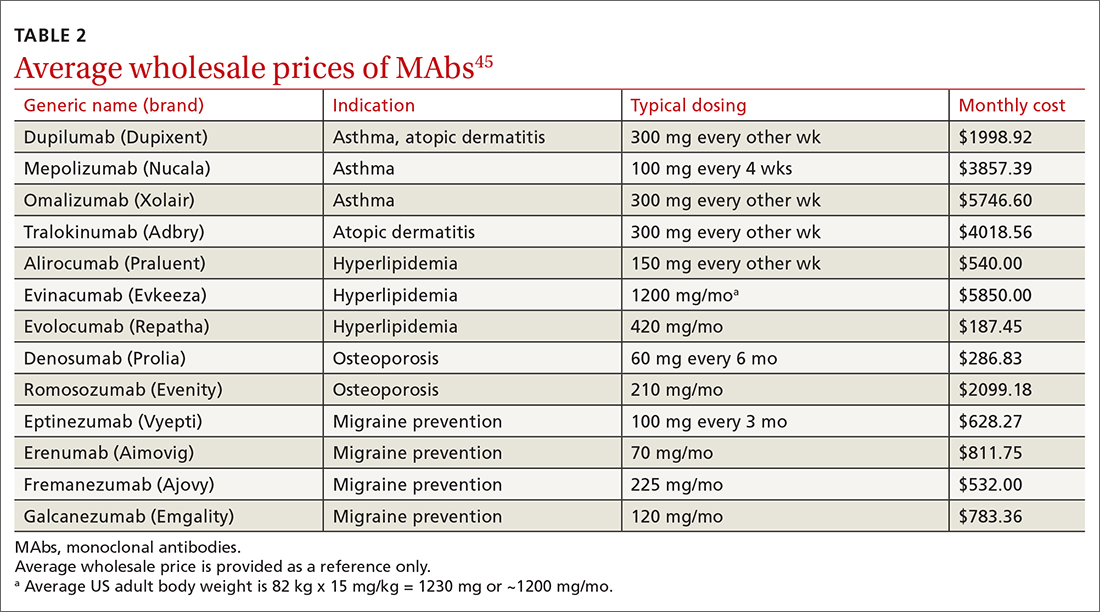
MAbs also require prior authorization forms to be submitted. Prior authorization criteria vary by state and by insurance plan. In my (ES) experience, submitting letters of medical necessity justifying the need for therapy or expertise in the disease states for which the MAb is being prescribed help your patient get the medication they need.
Expect to see additional MAbs approved in the future. If the costs come down, adoption of these agents into practice will likely increase.
CORRESPONDENCE
Evelyn Sbar, MD, Texas Tech University Health Sciences Center, 1400 South Coulter Street, Suite 5100, Amarillo, TX 79106; [email protected]
Small-molecule drugs such as aspirin, albuterol, atorvastatin, and lisinopril are the backbone of disease management in family medicine.1 However, large-molecule biological drugs such as monoclonal antibodies (MAbs) are increasingly prescribed to treat common conditions. In the past decade, MAbs comprised 20% of all drug approvals by the US Food and Drug Administration (FDA), and today they represent more than half of drugs currently in development.2 Fifteen MAbs have been approved by the FDA over the past decade for asthma, atopic dermatitis (AD), hyperlipidemia, osteoporosis, and migraine prevention.3 This review details what makes MAbs unique and what you should know about them.
The uniqueness of monoclonal antibodies
MAbs are biologics, but not all biologics are MAbs—eg, adalimumab (Humira) is a MAb, but etanercept (Enbrel) is not. MAbs are therapeutic proteins made possible by hybridoma technology used to create an antibody with single specificity.4-6 Monoclonal antibodies differ from small-molecule drugs in structure, dosing, route of administration, manufacturing, metabolism, drug interactions, and elimination (TABLE 17-9).
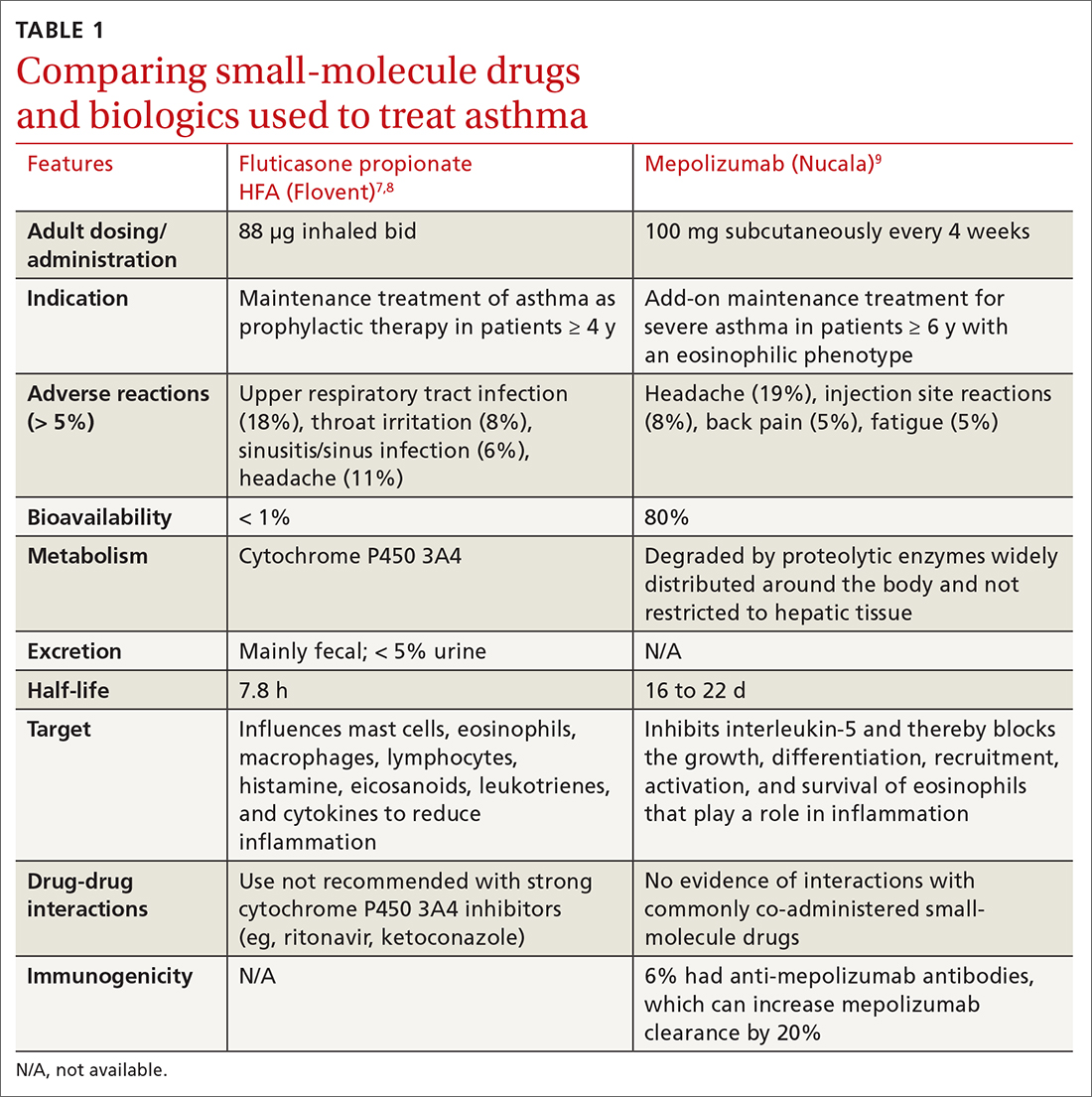
MAbs can be classified as naked, “without any drug or radioactive material attached to them,” or conjugated, “joined to a chemotherapy drug, radioactive isotope, or toxin.”10 MAbs work in several ways, including competitively inhibiting ligand-receptor binding, receptor blockade, or cell elimination from indirect immune system activities such as antibody-dependent cell-mediated cytotoxicity.11,12
Monoclonal antibody uses in family medicine
Asthma
Several MAbs have been approved for use in severe asthma, including but not limited to: omalizumab (Xolair),13 mepolizumab (Nucala),9,14 and dupilumab (Dupixent).15
Omalizumab is a humanized MAb that prevents IgE antibodies from binding to mast cells and basophils, thereby reducing inflammatory mediators.13 A systematic review found that, compared with placebo, omalizumab used in patients with inadequately controlled moderate-to-severe asthma led to significantly fewer asthma exacerbations (absolute risk reduction [ARR], 16% vs 26%; odds ratio [OR] = 0.55; 95% CI, 0.42-0.60; number needed to treat [NNT] = 10) and fewer hospitalizations (ARR, 0.5% vs 3%; OR = 0.16; 95% CI, 0.06-0.42; NNT = 40).13
Significantly more patients in the omalizumab group were able to withdraw from, or reduce, the dose of ICS. GINA recommends omalizumab for patients with positive skin sensitization, total serum IgE ≥ 30 IU/mL, weight within 30 kg to 150 kg, history of childhood asthma and recent exacerbations, and blood eosinophils ≥ 260/mcL.16 Omalizumab is also approved for use in chronic spontaneous urticaria and nasal polyps.
Mepolizumab
Continue to: Another trial found that...
Another trial found that mepolizumab reduced total OCS doses in patients with severe asthma by 50% without increasing exacerbations or worsening asthma control.18 All 3 anti-IL-5 drugs—including not only mepolizumab, but also benralizumab (Fasenra) and reslizumab (Cinqair)—appear to yield similar improvements. A 2017 systematic review found all anti-IL-5 treatments reduced rates of clinically significant asthma exacerbations (treatment with OCS for ≥ 3 days) by roughly 50% in patients with severe eosinophilic asthma and a history of ≥ 2 exacerbations in the past year.
Dupilumab is a humanized MAb that inhibits IL-4 and IL-13, which influence multiple cell types involved in inflammation (eg, mast cells, eosinophils) and inflammatory mediators (histamine, leukotrienes, cytokines).15 In a recent study of patients with uncontrolled asthma, dupilumab 200 mg every 2 weeks compared with placebo showed a modest reduction in the annualized rate of severe asthma exacerbations (0.46 exacerbations vs 0.87, respectively). Dupilumab was effective in patients with blood eosinophil counts ≥ 150/μL but was ineffective in patients with eosinophil counts < 150/μL.15
For patients ≥ 12 years old with severe eosinophilic asthma, GINA recommends using dupilumab as add-on therapy for an initial trial of 4 months at doses of 200 or 300 mg SC every 2 weeks, with preference for 300 mg SC every 2 weeks for OCS-dependent asthma. Dupilumab is approved for use in AD and chronic rhinosinusitis with nasal polyposis. If a biologic agent is not successful after a 4-month trial, consider a 6- to 12-month trial. If efficacy is still minimal, consider switching to an alternative biologic therapy approved for asthma.16
❯ Asthma: Test your skills
Subjective findings: A 19-year-old man presents to your clinic. He has a history of nasal polyps and allergic asthma. At age 18, he was given a diagnosis of severe persistent asthma. He has shortness of breath during waking hours 4 times per week, and treats each of these episodes with albuterol. He also wakes up about twice a week with shortness of breath and has some limitations in normal activities. He reports missing his prescribed fluticasone/salmeterol 500/50 μg, 1 inhalation bid, only once each month. In the last year, he has had 2 exacerbations requiring oral steroids.
Medications: Albuterol 90 μg, 1-2 inhalations, q6h prn; fluticasone/salmeterol 500/50 μg, 1 inhalation bid; tiotropium 1.25 μg, 2 puffs/d; montelukast 10 mg every morning; prednisone 10 mg/d.
Continue to: Objective data
Objective data: Patient is in no apparent distress and afebrile, and oxygen saturation on room air is 97%. Ht, 70 inches; wt, 75 kg. Labs: IgE, 15 IU/mL; serum eosinophils, 315/μL.
Which MAb would be appropriate for this patient? Given that the patient has a blood eosinophil level ≥ 300/μL and severe exacerbations, adult-onset asthma, nasal polyposis, and maintenance OCS at baseline, it would be reasonable to initiate mepolizumab 100 mg SC every 4 weeks, or dupilumab 600 mg once, then 300 mg SC every 2 weeks. Both agents can be self-administered.
Atopic dermatitis
Two MAbs—dupilumab and tralokinumab (Adbry; inhibits IL-13)—are approved for treatment of AD in adults that is uncontrolled with conventional therapy.15,19 Dupilumab is also approved for children ≥ 6 months old.20 Both MAbs are dosed at 600 mg SC, followed by 300 mg every 2 weeks. Dupilumab was compared with placebo in adult patients who had moderate-to-severe AD inadequately controlled on topical corticosteroids (TCSs), to determine the proportion of patients in each group achieving improvement of either 0 or 1 points or ≥ 2 points in the 5-point Investigator Global Assessment (IGA) score from baseline to 16 weeks.21 Thirty-seven percent of patients receiving dupilumab 300 mg SC weekly and 38% of patients receiving dupilumab 300 mg SC every 2 weeks achieved the primary outcome, compared with 10% of those receiving placebo (P < .001).21 Similar IGA scores were reported when dupilumab was combined with TCS, compared with placebo.22
It would be reasonable to consider dupilumab or tralokinumab in patients with: cutaneous atrophy or hypothalamic-pituitary-adrenal axis suppression with TCS, concerns of malignancy with topical calcineurin inhibitors, or problems with the alternative systemic therapies (cyclosporine-induced hypertension, nephrotoxicity, or immunosuppression; azathioprine-induced malignancy; or methotrexate-induced bone marrow suppression, renal impairment, hepatotoxicity, pneumonitis, or gastrointestinal toxicity).23
A distinct advantage of MAbs over other systemic agents in the management of AD is that MAbs do not require frequent monitoring of blood pressure, renal or liver function, complete blood count with differential, electrolytes, or uric acid. Additionally, MAbs have fewer black box warnings and adverse reactions when compared with other systemic agents.
Continue to: Hyperlipidemia
Hyperlipidemia
Three MAbs are approved for use in hyperlipidemia: the angiopoietin-like protein 3 (ANGPTL3) inhibitor evinacumab (Evkeeza)24 and 2 proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors, evolocumab (Repatha)25 and alirocumab (Praluent).26
ANGPTL3 inhibitors block ANGPTL3 and reduce endothelial lipase and lipoprotein lipase activity, which in turn decreases low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and triglyceride formation. PCSK9 inhibitors prevent PCSK9 from binding to LDL receptors, thereby maintaining the number of active LDL receptors and increasing LDL-C removal.
Evinacumab is indicated for homozygous familial hypercholesterolemia and is administered intravenously every 4 weeks. Evinacumab has not been evaluated for effects on cardiovascular morbidity and mortality.
Evolocumab 140 mg SC every 2 weeks or 420 mg SC monthly has been studied in patients on statin therapy with LDL-C ≥ 70 mg/dL. Patients on evolocumab experienced significantly less of the composite endpoint of cardiovascular death, myocardial infarction (MI), stroke, hospitalization for unstable angina, or coronary revascularization compared with placebo (9.8% vs 11.3%; hazard ratio [HR] = 0.85; 95% CI, 0.79-0.92; NNT = 67.27
Alirocumab 75 mg SC every 2 weeks has also been studied in patients receiving statin therapy with LDL-C ≥ 70 mg/dL. Patients taking alirocumab experienced significantly less of the composite endpoint of death from coronary heart disease, nonfatal MI, ischemic stroke, or hospitalization for unstable angina compared with placebo (9.5% vs 11.1%; HR = 0.85; 95% CI, 0.78-0.93; NNT = 63).
Continue to: According to the 2018...
According to the 2018 AHA Cholesterol Guidelines, PCSK9 inhibitors are indicated for patients receiving maximally tolerated LDL-C-lowering therapy (statin and ezetimibe) with LDL-C ≥ 70 mg/dL, if they have had multiple atherosclerotic cardiovascular disease (ASCVD) events or 1 major ASCVD event with multiple high-risk conditions (eg, heterozygous familial hypercholesterolemia, history of coronary artery bypass grafting or percutaneous coronary intervention, hypertension, estimated glomerular filtration rate of 15 to 59 mL/min/1.73m2).29 For patients without prior ASCVD events or high-risk conditions who are receiving maximally tolerated LDL-C-lowering therapy (statin and ezetimibe), PCSK9 inhibitors are indicated if the LDL-C remains ≥ 100 mg/dL.
Osteoporosis
The 2 MAbs approved for use in osteoporosis are the receptor activator of nuclear factor kB ligand (RANKL) inhibitor denosumab (Prolia)30 and the sclerostin inhibitor romosozumab (Evenity).31
Denosumab prevents RANKL from binding to the RANK receptor, thereby inhibiting osteoclast formation and decreasing bone resorption. Denosumab is approved for use in women and men who are at high risk of osteoporotic fracture, including those taking OCSs, men receiving androgen deprivation therapy for prostate cancer, and women receiving adjuvant aromatase inhibitor therapy for breast cancer.
In a 3-year randomized trial, denosumab 60 mg SC every 6 months was compared with placebo in postmenopausal women with T-scores < –2.5, but not < –4.0 at the lumbar spine or total hip. Denosumab significantly reduced new radiographic vertebral fractures (2.3% vs 7.2%; risk ratio [RR] = 0.32; 95% CI, 0.26-0.41; NNT = 21), hip fracture (0.7% vs 1.2%), and nonvertebral fracture (6.5% vs 8.0%).32 Denosumab carries an increased risk of multiple vertebral fractures following discontinuation, skin infections, dermatologic reactions, and severe bone, joint, and muscle pain.
Romosozumab inhibits sclerostin, thereby increasing bone formation and, to a lesser degree, decreasing bone resorption. Romosozumab is approved for use in postmenopausal women at high risk for fracture (ie, those with a history of osteoporotic fracture or multiple risk factors for fracture) or in patients who have not benefited from or are intolerant of other therapies. In one study, postmenopausal women with a T-score of –2.5 to –3.5 at the total hip or femoral neck were randomly assigned to receive either romosozumab 210 mg SC or placebo for 12 months, then each group was switched to denosumab 60 mg SC for 12 months. After the first year, prior to initiating denosumab, patients taking romosozumab experienced significantly fewer new vertebral fractures than patients taking placebo (0.5% vs 1.8%; RR = 0.27; 95% CI, 0.16-0.47; NNT = 77); however, there was no significant difference between the 2 groups with nonvertebral fractures (HR = 0.75; 95% CI, 0.53-1.05).33
Continue to: In another study...
In another study, romosozumab 210 mg SC was compared with alendronate 70 mg weekly, followed by alendronate 70 mg weekly in both groups. Over the first 12 months, patients treated with romosozumab saw a significant reduction in the incidence of new vertebral fractures (4% vs 6.3%; RR = 0.63, P < .003; NNT = 44). Patients treated with romosozumab with alendronate added for another 12 months also saw a significant reduction in new incidence of vertebral fractures (6.2% vs 11.9%; RR = 0.52; P < .001; NNT = 18).34 There was a higher risk of cardiovascular events among patients receiving romosozumab compared with those treated with alendronate, so romosozumab should not be used in individuals who have had an MI or stroke within the previous year.34 Denosumab and romosozumab offer an advantage over some bisphosphonates in that they require less frequent dosing and can be used in patients with renal impairment (creatinine clearance < 35 mL/min, in which zoledronic acid is contraindicated and alendronate is not recommended; < 30 mL/min, in which risedronate and ibandronate are not recommended).
Migraine prevention
Four
Erenumab, fremanezumab, and galcanezumab are all available in subcutaneous autoinjectors (or syringe with fremanezumab). Eptinezumab is an intravenous (IV) infusion given every 3 months.
Erenumab is available in both 70-mg and 140-mg dosing options. Fremanezumab can be given as 225 mg monthly or 675 mg quarterly. Galcanezumab has an initial loading dose of 240 mg followed by 120 mg given monthly. Erenumab targets the CGRP receptor; the others target the CGRP ligand. Eptinezumab has 100% bioavailability and reaches maximum serum concentration sooner than the other antagonists (due to its route of administration), but it must be given in an infusion center. Few insurers approve the use of eptinezumab unless a trial of least 1 of the monthly injectables has failed.
There are no head-to-head studies of the medications in this class. Additionally, differing study designs, definitions, statistical analyses, endpoints, and responder-rate calculations make it challenging to compare them directly against one another. At the very least, all of the CGRP MAbs have efficacy comparable to conventional preventive migraine medications such as propranolol, amitriptyline, and topiramate.40
Continue to: The most commonly reported adverse...
The most commonly reported adverse effect for all 4 CGRPs is injection site reaction, which was highest with the quarterly fremanezumab dose (45%).37 Constipation was most notable with the 140-mg dose of erenumab (3%)35; with the other CGRP MAbs it is comparable to that seen with placebo (< 1%).
Erenumab-induced hypertension has been identified in 61 cases reported through the FDA Adverse Event Reporting System (FAERS) as of 2021.41 This was not reported during MAb development programs, nor was it noted during clinical trials. Blood pressure elevation was seen within 1 week of injection in nearly 50% of the cases, and nearly one-third had pre-existing hypertension.41 Due to these findings, the erenumab prescribing information was updated to include hypertension in its warnings and precautions. It is possible that hypertension could be a class effect, although trial data and posthoc studies have yet to bear that out. Since erenumab was the first CGRP antagonist brought to market (May 2018 vs September 2018 for fremanezumab and galcanezumab), it may have accumulated more FAERS reports. Nearly all studies exclude patients with older age, uncontrolled hypertension, and unstable cardiovascular disease, which could impact data.41
Overall, this class of medications is very well tolerated, easy to use (again, excluding eptinezumab), and maintains a low adverse effect profile, giving added value compared with conventional preventive migraine medications.
The American Headache Society recommends a preventive oral therapy for at least 3 months before trying an alternative medication. After treatment failure with at least 2 oral agents, CGRP MAbs are recommended.42 CGRP antagonists offer convenient dosing, bypass gastrointestinal metabolism (which is useful in patients with nausea/vomiting), and have fewer adverse effects than traditional oral medications.
Worth noting. Several newer oral agents have been recently approved for migraine prevention, including atogepant (Qulipta) and rimegepant (Nurtec), which are also CGRP antagonists. Rimegepant is approved for both acute migraine treatment and prevention.
Continue to: Migraine
❯ Migraine: Test your skills
Subjective findings: A 25-year-old woman presents to your clinic for management of episodic migraines with aura. Her baseline average migraine frequency is 9 headache days/month. Her migraines are becoming more frequent despite treatment. She fears IV medication use and avoids hospitals.
History: Hypertension, irritable bowel syndrome with constipation (IBS-C), and depression. The patient is not pregnant or trying to get pregnant.
Medications: Current medications (for previous 4 months) include propranolol 40 mg at bedtime, linaclotide 145 μg/d, citalopram 20 mg/d, and sumatriptan 50 mg prn. Past medications include venlafaxine 150 mg po bid for 5 months.
What would be appropriate for this patient? This patient meets the criteria for using a CGRP antagonist because she has tried 2 preventive treatments for more than 60 to 90 days. Erenumab is not the best option, given the patient’s history of hypertension and IBS-C. The patient fears hospitals and IV medications, making eptinezumab a less-than-ideal choice. Depending on her insurance, fremanezumab or galcanezumab would be good options at this time.
CGRP antagonists have not been studied or evaluated in pregnancy, but if this patient becomes pregnant, a first-line agent for prevention would be propranolol, and a second-line agent would be a tricyclic antidepressant, memantine, or verapamil. Avoid ergotamines and antiepileptics (topiramate or valproate) in pregnancy.43,44
Continue to: The challenges associated with MAbs
The challenges associated with MAbs
MAbs can be expensive (TABLE 2),45 some prohibitively so. On a population scale, biologics account for around 40% of prescription drug spending and may cost 22 times more than small-molecule drugs.46 Estimates in 2016 showed that MAbs comprise $90.2 billion (43%) of the biologic market.46
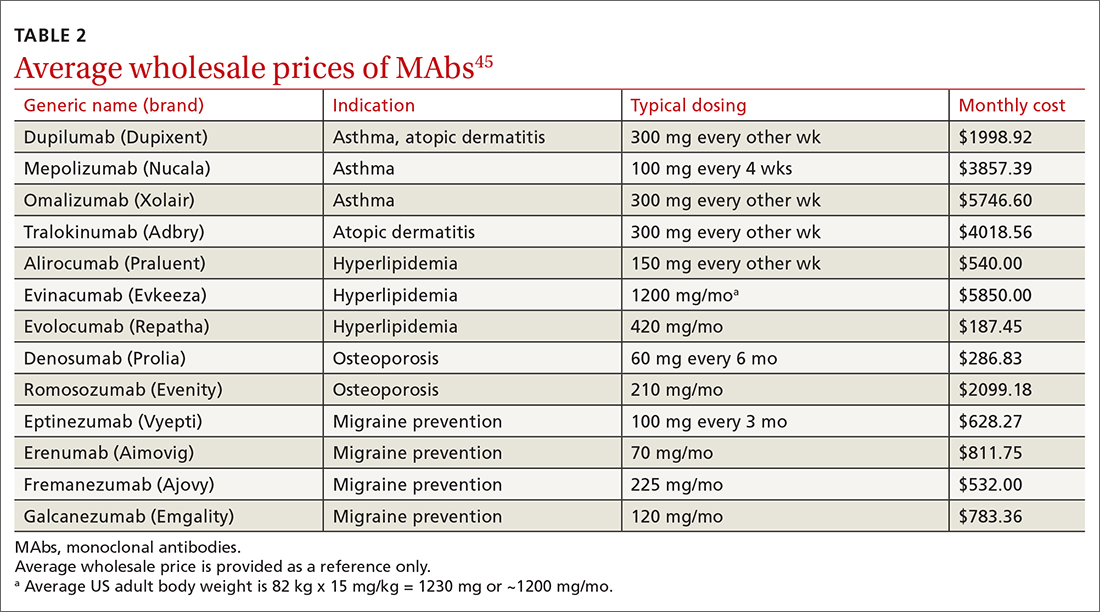
MAbs also require prior authorization forms to be submitted. Prior authorization criteria vary by state and by insurance plan. In my (ES) experience, submitting letters of medical necessity justifying the need for therapy or expertise in the disease states for which the MAb is being prescribed help your patient get the medication they need.
Expect to see additional MAbs approved in the future. If the costs come down, adoption of these agents into practice will likely increase.
CORRESPONDENCE
Evelyn Sbar, MD, Texas Tech University Health Sciences Center, 1400 South Coulter Street, Suite 5100, Amarillo, TX 79106; [email protected]
1. Rui P, Okeyode T. National Ambulatory Medical Care Survey: 2016 national summary tables. National Center for Health Statistics. Accessed June 15, 2022. www.cdc.gov/nchs/data/ahcd/namcs_summary/2016_namcs_web_tables.pdf
2. IDBS. The future of biologics drug development is today. June 27, 2018. Accessed June 15, 2022. www.idbs.com/blog/2018/06/the-future-of-biologics-drug-development-is-today/
3. Antibody therapeutics approved or in regulatory review in the EU or US. Antibody Society. Accessed June 15, 2022. www.antibodysociety.org/resources/approved-antibodies/
4. FDA. Code of Federal Regulations, Title 21, Chapter I, Subchapter F biologics. March 29, 2022. Accessed June 15, 2022. www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=600.3
5. Köhler G, Milstein C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature. 1975;256:495-497. doi: 10.1038/256495a0
6. Raejewsky K. The advent and rise of monoclonal antibodies. Nature. November 4, 2019. Accessed June 15, 2022. www.nature.com/articles/d41586-019-02840-w
7. Flovent. Prescribing information. GlaxoSmithKline; 2010. Accessed June 15, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2010/021433s015lbl.pdf
8. NLM. National Center for Biotechnology Information. PubChem. Method for the preparation of fluticasone and related 17beta-carbothioic esters using a novel carbothioic acid synthesis and novel purification methods. Accessed June 15, 2022. pubchem.ncbi.nlm.nih.gov/patent/WO-0162722-A2
9. Nucala. Prescribing information. GlaxoSmithKline; 2019. Accessed June 15, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2019/761122s000lbl.pdf
10. Argyriou AA, Kalofonos HP. Recent advances relating to the clinical application of naked monoclonal antibodies in solid tumors. Mol Med. 2009;15:183-191. doi: 10.2119/molmed.2009.00007
11. Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84:548-558. doi: 10.1038/clpt.2008.170
12. Zahavi D, AlDeghaither D, O’Connell A, et al. Enhancing antibody-dependent cell-mediated cytotoxicity: a strategy for improving antibody-based immunotherapy. Antib Ther. 2018;1:7-12. doi: 10.1093/abt/tby002
13. Normansell R, Walker S, Milan SJ, et al. Omalizumab for asthma in adults and children. Cochrane Database Syst Rev. 2014:CD003559. doi: 10.1002/14651858.CD003559.pub4
14. Farne HA, Wilson A, Powell C, et al. Anti-IL5 therapies for asthma. Cochrane Database Syst Rev. 2017;9:CD010834. doi: 10.1002/14651858.CD010834.pub3
15. Castro M, Corren J, Pavord ID, et al. Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. N Engl J Med. 2018;378:2486-2496. doi: 10.1056/NEJMoa1804092
16. GINA. Global strategy for asthma management and prevention. 2022 Difficult-to-treat and severe asthma guide—slide set. Accessed June 23, 2022. https://ginasthma.org/severeasthma/
17. Ortega HG, Liu MC, Pavord ID, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371:1198-1207. doi: 10.1056/NEJMoa1403290
18. Bel EH, Wenzel SE, Thompson PJ, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med. 2014;371:1189-1197. doi: 10.1056/NEJMoa1403291
19. Adbry. Prescribing information. Leo Pharma Inc; 2021. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/nda/2022/761180Orig1s000lbl.pdf
20. Dupixent. Prescribing information. Regeneron Pharmaceuticals; 2022. Accessed October 5, 2022. https://www.regeneron.com/downloads/dupixent_fpi.pdf
21. Simpson EL, Bieber T, Guttman-Yassky E, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375:2335-2348. doi: 10.1056/NEJMoa1610020
22. Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial. Lancet. 2017;389:2287-2303. doi: 10.1016/s0140-6736(17)31191-1
23. Sidbury R, Davis DM, Cohen DE, et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71:327-349. doi: 10.1016/j.jaad.2014.03.030
24. Evkeeza. Prescribing information. Regeneron Pharmaceuticals; 2021. Accessed June 24, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761181s000lbl.pdf
25. Repatha. Prescribing information. Amgen; 2015. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2017/125522s014lbl.pdf
26. Praluent. Prescribing information. Sanofi Aventis and Regeneron Pharmaceuticals. 2015. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2017/125559s002lbl.pdf
27. Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713-1722. doi: 10.1056/NEJMoa1615664
28. Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097-2107. doi:10.1056/NEJMoa1801174
29. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2019;73:e285-e350. doi: 10.1016/j.jacc.2018.11.003
30. Prolia. Prescribing information. Amgen; 2010. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2013/125320s094lbl.pdf
31. Evenity. Prescribing information. Amgen; 2019. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2019/761062s000lbl.pdf
32. Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756-765. doi: 10.1056/NEJMoa0809493
33. Cosman F, Crittenden DB, Adachi JD, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375:1532-1543. doi: 10.1056/NEJMoa1607948
34. Saag KG, Petersen J, Brandi ML, et al. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377:1417-1427. doi: 10.1056/NEJMoa1708322
35. Aimovig. Prescribing information. Amgen; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761077s000lbl.pdf
36. Vyepti. Prescribing information. Lundbeck Seattle BioPharmaceuticals; 2020. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2020/761119s000lbl.pdf
37. Ajovy. Prescribing information. Teva Pharmaceuticals; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761089s000lbl.pdf
38. Emgality. Prescribing information. Eli Lilly and Co.; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761063s000lbl.pdf
39. Edvinsson L, Haanes KA, Warfvinge K, et al. CGRP as the target of new migraine therapies - successful translation from bench to clinic. Nat Rev Neurol. 2018;14:338-350. doi: 10.1038/s41582-018-0003-1
40. Vandervorst F. Van Deun L, Van Dycke A, et al. CGRP monoclonal antibodies in migraine: an efficacy and tolerability comparison with standard prophylactic drugs. J Headache Pain. 2021;22:128. doi: 10.1186/s10194-021-01335-2
41. Saely S, Croteau D, Jawidzik L, et al. Hypertension: a new safety risk for patients treated with erenumab. Headache. 2021;61:202-208. doi: 10.1111/head.14051
42. American Headache Society. The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache. 2019;59:1-18. doi: 10.1111/head.13456
43. Burch R. Headache in pregnancy and the puerperium. Neurol Clin. 2019;37:31-51. doi: 10.1016/j.ncl.2018.09.004
44. Burch R. Epidemiology and treatment of menstrual migraine and migraine during pregnancy and lactation: a narrative review. Headache. 2020;60:200-216. doi: 10.1111/head.13665
45. Lexi-Comp. Lexi-drug database. Accessed April 4, 2022. https://online.lexi.com/lco/action/login
46. Walker N. Biologics: driving force in pharma. Pharma’s Almanac. June 5, 2017. Accessed June 15, 2020. www.pharmasalmanac.com/articles/biologics-driving-force-in-pharma
1. Rui P, Okeyode T. National Ambulatory Medical Care Survey: 2016 national summary tables. National Center for Health Statistics. Accessed June 15, 2022. www.cdc.gov/nchs/data/ahcd/namcs_summary/2016_namcs_web_tables.pdf
2. IDBS. The future of biologics drug development is today. June 27, 2018. Accessed June 15, 2022. www.idbs.com/blog/2018/06/the-future-of-biologics-drug-development-is-today/
3. Antibody therapeutics approved or in regulatory review in the EU or US. Antibody Society. Accessed June 15, 2022. www.antibodysociety.org/resources/approved-antibodies/
4. FDA. Code of Federal Regulations, Title 21, Chapter I, Subchapter F biologics. March 29, 2022. Accessed June 15, 2022. www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=600.3
5. Köhler G, Milstein C. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature. 1975;256:495-497. doi: 10.1038/256495a0
6. Raejewsky K. The advent and rise of monoclonal antibodies. Nature. November 4, 2019. Accessed June 15, 2022. www.nature.com/articles/d41586-019-02840-w
7. Flovent. Prescribing information. GlaxoSmithKline; 2010. Accessed June 15, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2010/021433s015lbl.pdf
8. NLM. National Center for Biotechnology Information. PubChem. Method for the preparation of fluticasone and related 17beta-carbothioic esters using a novel carbothioic acid synthesis and novel purification methods. Accessed June 15, 2022. pubchem.ncbi.nlm.nih.gov/patent/WO-0162722-A2
9. Nucala. Prescribing information. GlaxoSmithKline; 2019. Accessed June 15, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2019/761122s000lbl.pdf
10. Argyriou AA, Kalofonos HP. Recent advances relating to the clinical application of naked monoclonal antibodies in solid tumors. Mol Med. 2009;15:183-191. doi: 10.2119/molmed.2009.00007
11. Wang W, Wang EQ, Balthasar JP. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84:548-558. doi: 10.1038/clpt.2008.170
12. Zahavi D, AlDeghaither D, O’Connell A, et al. Enhancing antibody-dependent cell-mediated cytotoxicity: a strategy for improving antibody-based immunotherapy. Antib Ther. 2018;1:7-12. doi: 10.1093/abt/tby002
13. Normansell R, Walker S, Milan SJ, et al. Omalizumab for asthma in adults and children. Cochrane Database Syst Rev. 2014:CD003559. doi: 10.1002/14651858.CD003559.pub4
14. Farne HA, Wilson A, Powell C, et al. Anti-IL5 therapies for asthma. Cochrane Database Syst Rev. 2017;9:CD010834. doi: 10.1002/14651858.CD010834.pub3
15. Castro M, Corren J, Pavord ID, et al. Dupilumab efficacy and safety in moderate-to-severe uncontrolled asthma. N Engl J Med. 2018;378:2486-2496. doi: 10.1056/NEJMoa1804092
16. GINA. Global strategy for asthma management and prevention. 2022 Difficult-to-treat and severe asthma guide—slide set. Accessed June 23, 2022. https://ginasthma.org/severeasthma/
17. Ortega HG, Liu MC, Pavord ID, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371:1198-1207. doi: 10.1056/NEJMoa1403290
18. Bel EH, Wenzel SE, Thompson PJ, et al. Oral glucocorticoid-sparing effect of mepolizumab in eosinophilic asthma. N Engl J Med. 2014;371:1189-1197. doi: 10.1056/NEJMoa1403291
19. Adbry. Prescribing information. Leo Pharma Inc; 2021. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/nda/2022/761180Orig1s000lbl.pdf
20. Dupixent. Prescribing information. Regeneron Pharmaceuticals; 2022. Accessed October 5, 2022. https://www.regeneron.com/downloads/dupixent_fpi.pdf
21. Simpson EL, Bieber T, Guttman-Yassky E, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375:2335-2348. doi: 10.1056/NEJMoa1610020
22. Blauvelt A, de Bruin-Weller M, Gooderham M, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial. Lancet. 2017;389:2287-2303. doi: 10.1016/s0140-6736(17)31191-1
23. Sidbury R, Davis DM, Cohen DE, et al. Guidelines of care for the management of atopic dermatitis: section 3. Management and treatment with phototherapy and systemic agents. J Am Acad Dermatol. 2014;71:327-349. doi: 10.1016/j.jaad.2014.03.030
24. Evkeeza. Prescribing information. Regeneron Pharmaceuticals; 2021. Accessed June 24, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/761181s000lbl.pdf
25. Repatha. Prescribing information. Amgen; 2015. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2017/125522s014lbl.pdf
26. Praluent. Prescribing information. Sanofi Aventis and Regeneron Pharmaceuticals. 2015. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2017/125559s002lbl.pdf
27. Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713-1722. doi: 10.1056/NEJMoa1615664
28. Schwartz GG, Steg PG, Szarek M, et al. Alirocumab and cardiovascular outcomes after acute coronary syndrome. N Engl J Med. 2018;379:2097-2107. doi:10.1056/NEJMoa1801174
29. Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. J Am Coll Cardiol. 2019;73:e285-e350. doi: 10.1016/j.jacc.2018.11.003
30. Prolia. Prescribing information. Amgen; 2010. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2013/125320s094lbl.pdf
31. Evenity. Prescribing information. Amgen; 2019. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2019/761062s000lbl.pdf
32. Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361:756-765. doi: 10.1056/NEJMoa0809493
33. Cosman F, Crittenden DB, Adachi JD, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375:1532-1543. doi: 10.1056/NEJMoa1607948
34. Saag KG, Petersen J, Brandi ML, et al. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377:1417-1427. doi: 10.1056/NEJMoa1708322
35. Aimovig. Prescribing information. Amgen; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761077s000lbl.pdf
36. Vyepti. Prescribing information. Lundbeck Seattle BioPharmaceuticals; 2020. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2020/761119s000lbl.pdf
37. Ajovy. Prescribing information. Teva Pharmaceuticals; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761089s000lbl.pdf
38. Emgality. Prescribing information. Eli Lilly and Co.; 2018. Accessed June 24, 2022. www.accessdata.fda.gov/drugsatfda_docs/label/2018/761063s000lbl.pdf
39. Edvinsson L, Haanes KA, Warfvinge K, et al. CGRP as the target of new migraine therapies - successful translation from bench to clinic. Nat Rev Neurol. 2018;14:338-350. doi: 10.1038/s41582-018-0003-1
40. Vandervorst F. Van Deun L, Van Dycke A, et al. CGRP monoclonal antibodies in migraine: an efficacy and tolerability comparison with standard prophylactic drugs. J Headache Pain. 2021;22:128. doi: 10.1186/s10194-021-01335-2
41. Saely S, Croteau D, Jawidzik L, et al. Hypertension: a new safety risk for patients treated with erenumab. Headache. 2021;61:202-208. doi: 10.1111/head.14051
42. American Headache Society. The American Headache Society position statement on integrating new migraine treatments into clinical practice. Headache. 2019;59:1-18. doi: 10.1111/head.13456
43. Burch R. Headache in pregnancy and the puerperium. Neurol Clin. 2019;37:31-51. doi: 10.1016/j.ncl.2018.09.004
44. Burch R. Epidemiology and treatment of menstrual migraine and migraine during pregnancy and lactation: a narrative review. Headache. 2020;60:200-216. doi: 10.1111/head.13665
45. Lexi-Comp. Lexi-drug database. Accessed April 4, 2022. https://online.lexi.com/lco/action/login
46. Walker N. Biologics: driving force in pharma. Pharma’s Almanac. June 5, 2017. Accessed June 15, 2020. www.pharmasalmanac.com/articles/biologics-driving-force-in-pharma
PRACTICE RECOMMENDATIONS
› Consider anti-immunoglobulin E, anti-interleukin 5, or anti-interleukin 4/interleukin 13 for patients with moderate-to-severe asthma and type 2 airway inflammation. B
› Consider dupilumab for patients with moderate-to-severe atopic dermatitis (with or without topical corticosteroids), or when traditional oral therapies are inadequate or contraindicated. B
› Consider proprotein convertase subtilisin/kexin type 9 inhibitors for patients with heterozygous familial hypercholesterolemia or clinical atherosclerotic cardiovascular disease when maximally tolerated statins or ezetimibe have not lowered low-density lipoprotein cholesterol levels far enough. A
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Going the distance with our patients
Many years ago, I had a patient I’ll call “Hannah,” who was well into her 80s and always came into the office with her daughter. She was a heavy smoker and had hypertension and type 2 diabetes.
At each visit, I would ask her if she still smoked and if she was interested in talking about quitting. At every visit, she would say that she was still smoking and didn’t want to quit. My response was always something along the lines of: “When you’re ready, we can talk more. But I think it is the most important thing you can do to improve your health.” From there, we would discuss any concerns she or her daughter had.
A few years shy of her 100th birthday, Hannah told me she had quit smoking. I was amazed and asked her why, after all these years, she’d done it.
“I quit,” she said, “because I was tired of you nagging me, sonny!” And we both had a good laugh about that.
Hannah’s story reminds me that, as family physicians, we often have an impact on our patients in ways we don’t see in the short term. It is our longitudinal relationships with patients that allow us to plant seeds and reap the benefits over time.
It is these relationships that we can draw upon when counseling our patients with type 2 diabetes to address lifestyle issues such as exercise and a healthy diet. In this issue, McMullan et al1 provide us with a rather hopeful review of the evidence in support of lifestyle changes. For our patients with type 2 diabetes, lifestyle changes can decrease A1C levels by 0.5% (with environmental changes related to diet)2 and 0.7% (with moderate aerobic exercise).3 This is comparable to what is reported for the starting doses of most medications.4 In fact, a meta-analysis showed that a low-carbohydrate diet induced remission at 6 months in 32% of patients.5 (Caveat: The result was not controlled for weight loss as a possible confounding factor and an A1C cutoff of 6.5% was used.)
And yet, we often focus more on the various medications we can prescribe, with professional guidelines pointing the way.
Continue to: The National Institute for Health and Care Excellence
The National Institute for Health and Care Excellence,6 American Diabetes Association,7 American College of Physicians,8 and American Academy of Family Physicians8 have followed the accumulating evidence that various medications improve outcomes—especially in patients at high risk or with established atherosclerotic cardiovascular disease. They have endorsed a stepwise pharmacologic approach beginning with metformin and recommend assessing each patient’s comorbidities to guide whether to add a sodium glucose co-transporter 2 (SGLT2) inhibitor or another agent. Where the groups diverge is what that second agent should be (glucagon-like peptide 1 receptor agonist, SGLT2 inhibitor, or dipeptidyl peptidase-4 inhibitor).
But what about lifestyle? Each organization’s guidelines address lifestyle changes as a foundation for managing patients with type 2 diabetes. But is that call loud enough? Do we heed it well enough?
Implementing lifestyle changes in office practice can be time consuming. Many clinicians lack adequate training or experience to gain any traction with it. Also, there is skepticism about success and sustainability.
I believe change starts when we recognize that while we have a priority list for each patient encounter, so do our patients. But they may not share that list with us unless we open the door by asking questions, such as:
- Of all the things you have heard about caring for your diabetes, what would you like to work on?
- What are you currently doing and what prevents you from meeting your goals?
- How would you like me to help you?
From there, we can start small and build on successes over time. We can go the distance with our patients. In the case of Hannah, I had the honor of caring for her until she died at age 104.
1. McMullan S, Smith DK, Kimsey J. Maximizing lifestyle changes to manage type 2 diabetes. J Fam Pract. 2022;71;342-348. doi: 10.12788/jfp.0482
2. Cradock KA, ÓLaighin G, Finucane FM, et al. Diet behavior change techniques in type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2017;40:1800-1810. doi: 10.2337/dc17-0462
3. Grace A, Chan E, Giallauria F, et al. Clinical outcomes and glycaemic responses to different aerobic exercise training intensities in type II diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. 2017;16:37. doi: 10.1186/s12933-017-0518-6
Many years ago, I had a patient I’ll call “Hannah,” who was well into her 80s and always came into the office with her daughter. She was a heavy smoker and had hypertension and type 2 diabetes.
At each visit, I would ask her if she still smoked and if she was interested in talking about quitting. At every visit, she would say that she was still smoking and didn’t want to quit. My response was always something along the lines of: “When you’re ready, we can talk more. But I think it is the most important thing you can do to improve your health.” From there, we would discuss any concerns she or her daughter had.
A few years shy of her 100th birthday, Hannah told me she had quit smoking. I was amazed and asked her why, after all these years, she’d done it.
“I quit,” she said, “because I was tired of you nagging me, sonny!” And we both had a good laugh about that.
Hannah’s story reminds me that, as family physicians, we often have an impact on our patients in ways we don’t see in the short term. It is our longitudinal relationships with patients that allow us to plant seeds and reap the benefits over time.
It is these relationships that we can draw upon when counseling our patients with type 2 diabetes to address lifestyle issues such as exercise and a healthy diet. In this issue, McMullan et al1 provide us with a rather hopeful review of the evidence in support of lifestyle changes. For our patients with type 2 diabetes, lifestyle changes can decrease A1C levels by 0.5% (with environmental changes related to diet)2 and 0.7% (with moderate aerobic exercise).3 This is comparable to what is reported for the starting doses of most medications.4 In fact, a meta-analysis showed that a low-carbohydrate diet induced remission at 6 months in 32% of patients.5 (Caveat: The result was not controlled for weight loss as a possible confounding factor and an A1C cutoff of 6.5% was used.)
And yet, we often focus more on the various medications we can prescribe, with professional guidelines pointing the way.
Continue to: The National Institute for Health and Care Excellence
The National Institute for Health and Care Excellence,6 American Diabetes Association,7 American College of Physicians,8 and American Academy of Family Physicians8 have followed the accumulating evidence that various medications improve outcomes—especially in patients at high risk or with established atherosclerotic cardiovascular disease. They have endorsed a stepwise pharmacologic approach beginning with metformin and recommend assessing each patient’s comorbidities to guide whether to add a sodium glucose co-transporter 2 (SGLT2) inhibitor or another agent. Where the groups diverge is what that second agent should be (glucagon-like peptide 1 receptor agonist, SGLT2 inhibitor, or dipeptidyl peptidase-4 inhibitor).
But what about lifestyle? Each organization’s guidelines address lifestyle changes as a foundation for managing patients with type 2 diabetes. But is that call loud enough? Do we heed it well enough?
Implementing lifestyle changes in office practice can be time consuming. Many clinicians lack adequate training or experience to gain any traction with it. Also, there is skepticism about success and sustainability.
I believe change starts when we recognize that while we have a priority list for each patient encounter, so do our patients. But they may not share that list with us unless we open the door by asking questions, such as:
- Of all the things you have heard about caring for your diabetes, what would you like to work on?
- What are you currently doing and what prevents you from meeting your goals?
- How would you like me to help you?
From there, we can start small and build on successes over time. We can go the distance with our patients. In the case of Hannah, I had the honor of caring for her until she died at age 104.
Many years ago, I had a patient I’ll call “Hannah,” who was well into her 80s and always came into the office with her daughter. She was a heavy smoker and had hypertension and type 2 diabetes.
At each visit, I would ask her if she still smoked and if she was interested in talking about quitting. At every visit, she would say that she was still smoking and didn’t want to quit. My response was always something along the lines of: “When you’re ready, we can talk more. But I think it is the most important thing you can do to improve your health.” From there, we would discuss any concerns she or her daughter had.
A few years shy of her 100th birthday, Hannah told me she had quit smoking. I was amazed and asked her why, after all these years, she’d done it.
“I quit,” she said, “because I was tired of you nagging me, sonny!” And we both had a good laugh about that.
Hannah’s story reminds me that, as family physicians, we often have an impact on our patients in ways we don’t see in the short term. It is our longitudinal relationships with patients that allow us to plant seeds and reap the benefits over time.
It is these relationships that we can draw upon when counseling our patients with type 2 diabetes to address lifestyle issues such as exercise and a healthy diet. In this issue, McMullan et al1 provide us with a rather hopeful review of the evidence in support of lifestyle changes. For our patients with type 2 diabetes, lifestyle changes can decrease A1C levels by 0.5% (with environmental changes related to diet)2 and 0.7% (with moderate aerobic exercise).3 This is comparable to what is reported for the starting doses of most medications.4 In fact, a meta-analysis showed that a low-carbohydrate diet induced remission at 6 months in 32% of patients.5 (Caveat: The result was not controlled for weight loss as a possible confounding factor and an A1C cutoff of 6.5% was used.)
And yet, we often focus more on the various medications we can prescribe, with professional guidelines pointing the way.
Continue to: The National Institute for Health and Care Excellence
The National Institute for Health and Care Excellence,6 American Diabetes Association,7 American College of Physicians,8 and American Academy of Family Physicians8 have followed the accumulating evidence that various medications improve outcomes—especially in patients at high risk or with established atherosclerotic cardiovascular disease. They have endorsed a stepwise pharmacologic approach beginning with metformin and recommend assessing each patient’s comorbidities to guide whether to add a sodium glucose co-transporter 2 (SGLT2) inhibitor or another agent. Where the groups diverge is what that second agent should be (glucagon-like peptide 1 receptor agonist, SGLT2 inhibitor, or dipeptidyl peptidase-4 inhibitor).
But what about lifestyle? Each organization’s guidelines address lifestyle changes as a foundation for managing patients with type 2 diabetes. But is that call loud enough? Do we heed it well enough?
Implementing lifestyle changes in office practice can be time consuming. Many clinicians lack adequate training or experience to gain any traction with it. Also, there is skepticism about success and sustainability.
I believe change starts when we recognize that while we have a priority list for each patient encounter, so do our patients. But they may not share that list with us unless we open the door by asking questions, such as:
- Of all the things you have heard about caring for your diabetes, what would you like to work on?
- What are you currently doing and what prevents you from meeting your goals?
- How would you like me to help you?
From there, we can start small and build on successes over time. We can go the distance with our patients. In the case of Hannah, I had the honor of caring for her until she died at age 104.
1. McMullan S, Smith DK, Kimsey J. Maximizing lifestyle changes to manage type 2 diabetes. J Fam Pract. 2022;71;342-348. doi: 10.12788/jfp.0482
2. Cradock KA, ÓLaighin G, Finucane FM, et al. Diet behavior change techniques in type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2017;40:1800-1810. doi: 10.2337/dc17-0462
3. Grace A, Chan E, Giallauria F, et al. Clinical outcomes and glycaemic responses to different aerobic exercise training intensities in type II diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. 2017;16:37. doi: 10.1186/s12933-017-0518-6
1. McMullan S, Smith DK, Kimsey J. Maximizing lifestyle changes to manage type 2 diabetes. J Fam Pract. 2022;71;342-348. doi: 10.12788/jfp.0482
2. Cradock KA, ÓLaighin G, Finucane FM, et al. Diet behavior change techniques in type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2017;40:1800-1810. doi: 10.2337/dc17-0462
3. Grace A, Chan E, Giallauria F, et al. Clinical outcomes and glycaemic responses to different aerobic exercise training intensities in type II diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. 2017;16:37. doi: 10.1186/s12933-017-0518-6













