User login
BMI compares favorably with body scanning for ID of cardiometabolic traits
Although body mass index is criticized for not distinguishing fat from lean mass, its ability to detect subclinical cardiometabolic abnormalities was on par with more sophisticated body scanning technology, according a recent analysis.
BMI and dual-energy x-ray absorptiometry (DXA) had similar associations with cardiometabolic traits associated with coronary heart disease in individuals evaluated at 10 and 18 years of age in a population-based birth cohort study, the study investigators said.
Changes over time in BMI and DXA also were strongly associated with changes in blood pressure, cholesterol, and other markers, according to Joshua A. Bell, PhD, of MRC Integrative Epidemiology Unit, University of Bristol, England, and his coinvestigators.
“Altogether, the results support abdominal fatness as a primary driver of cardiometabolic dysfunction and BMI as a useful tool for detecting its effects,” Dr. Bell and his colleagues said in a report on the study appearing in the Journal of the American College of Cardiology.
In their analysis, Dr. Bell and coinvestigators used Pearson correlation coefficients to compare BMI and total and regional fat indexes from DXA in offspring participants from ALSPAC, (the Avon Longitudinal Study of Parents and Children), in which BMI and DXA measurements were collected at 10 and 18 years of age.
Researchers identified a total of 2,840 participants with at least one measurement at each of those time points. The mean BMI was 17.5 kg/m2 at 10 years of age and 22.7 kg/m2 at 18 years of age, with greater than 10% of participants classified as obese at each of those time points.
High BMI and high total fat mass index were similarly associated with a variety of cardiometabolic traits, including systolic and diastolic blood pressure, higher low-density lipoprotein (LDL) and very-low-density lipoprotein (VLDL) cholesterol levels and lower high-density lipoprotein (HDL) cholesterol levels, and more inflammation, investigators found.
BMI was strongly correlated with DXA total and regional fat indexes at 10 years of age, and again at 18 years of age, they reported.
Moreover, gains in BMI from 10 to 18 years of age were strongly associated with higher blood pressure, higher LDL and VLDL cholesterol, lower HDL cholesterol, and other cardiometabolic traits, while associations between DXA measurements and those traits closely tracked those of BMI in pattern and magnitude, investigators added.
Fatness is most often measured in populations using BMI, and causal analyses suggest linkage between higher BMI and coronary heart disease and its intermediates, including blood pressure, LDL and remnant cholesterol, and glucose; despite that, BMI is often disparaged as a tool for assessing cardiometabolic abnormalities because it does not distinguish fat from lean mass and cannot quantify fat distribution, investigators said.
However, based on results of this analysis, it is reasonable to depend on BMI to indirectly measure body and abdominal fatness in future studies, they said in their report.
Dr. Bell and his colleagues reported that they had no relationships relevant to the study publication.
SOURCE: Bell JA et al. J Am Coll Cardiol. 2018 Dec 18;72(24):3142-54.
This study reinforces fatness, quantified by body mass index, as the key modifiable factor for maintaining healthy metabolism in young people, according to Ville-Petteri Mäkinen, ScD.
“The good news is that a single BMI measurement may be enough to capture the same essential information as a detailed body scan and serial measurements,” Dr. Mäkinen wrote in an accompanying editorial.
One other important take-home message of the study is that fat gain is not beneficial in any body region; that finding is important with respect to changes in BMI and fat mass index observed in the second decade of life that were associated with cardiometabolic risk factors in the late teens, he noted.
However, the broader take-home message for society is that children are being exposed to an “adverse metabolic milieu” that predicts cardiovascular disease in adulthood, according to Dr. Mäkinen.
“Childhood obesity must not be seen as a phase that passes but as a looming public health crisis that needs to be addressed by all of us,” he concluded.
Dr. Mäkinen is with the South Australian Health and Medical Research Institute, Adelaide. He had no relationships relevant to the contents of his editorial (J Am College Cardiol. 2018 Dec 18;74[24]3155-7).
This study reinforces fatness, quantified by body mass index, as the key modifiable factor for maintaining healthy metabolism in young people, according to Ville-Petteri Mäkinen, ScD.
“The good news is that a single BMI measurement may be enough to capture the same essential information as a detailed body scan and serial measurements,” Dr. Mäkinen wrote in an accompanying editorial.
One other important take-home message of the study is that fat gain is not beneficial in any body region; that finding is important with respect to changes in BMI and fat mass index observed in the second decade of life that were associated with cardiometabolic risk factors in the late teens, he noted.
However, the broader take-home message for society is that children are being exposed to an “adverse metabolic milieu” that predicts cardiovascular disease in adulthood, according to Dr. Mäkinen.
“Childhood obesity must not be seen as a phase that passes but as a looming public health crisis that needs to be addressed by all of us,” he concluded.
Dr. Mäkinen is with the South Australian Health and Medical Research Institute, Adelaide. He had no relationships relevant to the contents of his editorial (J Am College Cardiol. 2018 Dec 18;74[24]3155-7).
This study reinforces fatness, quantified by body mass index, as the key modifiable factor for maintaining healthy metabolism in young people, according to Ville-Petteri Mäkinen, ScD.
“The good news is that a single BMI measurement may be enough to capture the same essential information as a detailed body scan and serial measurements,” Dr. Mäkinen wrote in an accompanying editorial.
One other important take-home message of the study is that fat gain is not beneficial in any body region; that finding is important with respect to changes in BMI and fat mass index observed in the second decade of life that were associated with cardiometabolic risk factors in the late teens, he noted.
However, the broader take-home message for society is that children are being exposed to an “adverse metabolic milieu” that predicts cardiovascular disease in adulthood, according to Dr. Mäkinen.
“Childhood obesity must not be seen as a phase that passes but as a looming public health crisis that needs to be addressed by all of us,” he concluded.
Dr. Mäkinen is with the South Australian Health and Medical Research Institute, Adelaide. He had no relationships relevant to the contents of his editorial (J Am College Cardiol. 2018 Dec 18;74[24]3155-7).
Although body mass index is criticized for not distinguishing fat from lean mass, its ability to detect subclinical cardiometabolic abnormalities was on par with more sophisticated body scanning technology, according a recent analysis.
BMI and dual-energy x-ray absorptiometry (DXA) had similar associations with cardiometabolic traits associated with coronary heart disease in individuals evaluated at 10 and 18 years of age in a population-based birth cohort study, the study investigators said.
Changes over time in BMI and DXA also were strongly associated with changes in blood pressure, cholesterol, and other markers, according to Joshua A. Bell, PhD, of MRC Integrative Epidemiology Unit, University of Bristol, England, and his coinvestigators.
“Altogether, the results support abdominal fatness as a primary driver of cardiometabolic dysfunction and BMI as a useful tool for detecting its effects,” Dr. Bell and his colleagues said in a report on the study appearing in the Journal of the American College of Cardiology.
In their analysis, Dr. Bell and coinvestigators used Pearson correlation coefficients to compare BMI and total and regional fat indexes from DXA in offspring participants from ALSPAC, (the Avon Longitudinal Study of Parents and Children), in which BMI and DXA measurements were collected at 10 and 18 years of age.
Researchers identified a total of 2,840 participants with at least one measurement at each of those time points. The mean BMI was 17.5 kg/m2 at 10 years of age and 22.7 kg/m2 at 18 years of age, with greater than 10% of participants classified as obese at each of those time points.
High BMI and high total fat mass index were similarly associated with a variety of cardiometabolic traits, including systolic and diastolic blood pressure, higher low-density lipoprotein (LDL) and very-low-density lipoprotein (VLDL) cholesterol levels and lower high-density lipoprotein (HDL) cholesterol levels, and more inflammation, investigators found.
BMI was strongly correlated with DXA total and regional fat indexes at 10 years of age, and again at 18 years of age, they reported.
Moreover, gains in BMI from 10 to 18 years of age were strongly associated with higher blood pressure, higher LDL and VLDL cholesterol, lower HDL cholesterol, and other cardiometabolic traits, while associations between DXA measurements and those traits closely tracked those of BMI in pattern and magnitude, investigators added.
Fatness is most often measured in populations using BMI, and causal analyses suggest linkage between higher BMI and coronary heart disease and its intermediates, including blood pressure, LDL and remnant cholesterol, and glucose; despite that, BMI is often disparaged as a tool for assessing cardiometabolic abnormalities because it does not distinguish fat from lean mass and cannot quantify fat distribution, investigators said.
However, based on results of this analysis, it is reasonable to depend on BMI to indirectly measure body and abdominal fatness in future studies, they said in their report.
Dr. Bell and his colleagues reported that they had no relationships relevant to the study publication.
SOURCE: Bell JA et al. J Am Coll Cardiol. 2018 Dec 18;72(24):3142-54.
Although body mass index is criticized for not distinguishing fat from lean mass, its ability to detect subclinical cardiometabolic abnormalities was on par with more sophisticated body scanning technology, according a recent analysis.
BMI and dual-energy x-ray absorptiometry (DXA) had similar associations with cardiometabolic traits associated with coronary heart disease in individuals evaluated at 10 and 18 years of age in a population-based birth cohort study, the study investigators said.
Changes over time in BMI and DXA also were strongly associated with changes in blood pressure, cholesterol, and other markers, according to Joshua A. Bell, PhD, of MRC Integrative Epidemiology Unit, University of Bristol, England, and his coinvestigators.
“Altogether, the results support abdominal fatness as a primary driver of cardiometabolic dysfunction and BMI as a useful tool for detecting its effects,” Dr. Bell and his colleagues said in a report on the study appearing in the Journal of the American College of Cardiology.
In their analysis, Dr. Bell and coinvestigators used Pearson correlation coefficients to compare BMI and total and regional fat indexes from DXA in offspring participants from ALSPAC, (the Avon Longitudinal Study of Parents and Children), in which BMI and DXA measurements were collected at 10 and 18 years of age.
Researchers identified a total of 2,840 participants with at least one measurement at each of those time points. The mean BMI was 17.5 kg/m2 at 10 years of age and 22.7 kg/m2 at 18 years of age, with greater than 10% of participants classified as obese at each of those time points.
High BMI and high total fat mass index were similarly associated with a variety of cardiometabolic traits, including systolic and diastolic blood pressure, higher low-density lipoprotein (LDL) and very-low-density lipoprotein (VLDL) cholesterol levels and lower high-density lipoprotein (HDL) cholesterol levels, and more inflammation, investigators found.
BMI was strongly correlated with DXA total and regional fat indexes at 10 years of age, and again at 18 years of age, they reported.
Moreover, gains in BMI from 10 to 18 years of age were strongly associated with higher blood pressure, higher LDL and VLDL cholesterol, lower HDL cholesterol, and other cardiometabolic traits, while associations between DXA measurements and those traits closely tracked those of BMI in pattern and magnitude, investigators added.
Fatness is most often measured in populations using BMI, and causal analyses suggest linkage between higher BMI and coronary heart disease and its intermediates, including blood pressure, LDL and remnant cholesterol, and glucose; despite that, BMI is often disparaged as a tool for assessing cardiometabolic abnormalities because it does not distinguish fat from lean mass and cannot quantify fat distribution, investigators said.
However, based on results of this analysis, it is reasonable to depend on BMI to indirectly measure body and abdominal fatness in future studies, they said in their report.
Dr. Bell and his colleagues reported that they had no relationships relevant to the study publication.
SOURCE: Bell JA et al. J Am Coll Cardiol. 2018 Dec 18;72(24):3142-54.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: Body mass index and dual-energy x-ray absorptiometry had similar associations with cardiometabolic abnormalities in individuals evaluated at 10 and 18 years of age.
Major finding: BMI was strongly correlated with DXA total and regional fat indexes at age 10 years (0.9) and age 18 years.
Study details: Analysis of 2,840 offspring participants in ALSPAC (the Avon Longitudinal Study of Parents and Children).
Disclosures: Study authors reported that they had no relationships relevant to the study or its publication.
Source: Bell JA et al. J Am Coll Cardiol. 2018 Dec 10;72(24):3142-54.
ACA in peril after Texas ruling
Also today, baracitinib findings have immediate clinical relevance for patients with RA, a look at how often epileptic patients have treatment delayed, and the FDA issues an alert after e-cigarette liquids were found containing erectile dysfunction medication.
Also today, baracitinib findings have immediate clinical relevance for patients with RA, a look at how often epileptic patients have treatment delayed, and the FDA issues an alert after e-cigarette liquids were found containing erectile dysfunction medication.
Also today, baracitinib findings have immediate clinical relevance for patients with RA, a look at how often epileptic patients have treatment delayed, and the FDA issues an alert after e-cigarette liquids were found containing erectile dysfunction medication.
Health Canada approves new indication for daratumumab
Health Canada has approved a third indication for daratumumab (Darzalex®) in multiple myeloma (MM).
The drug is now approved for use in combination with bortezomib, melphalan, and prednisone (VMP) to treat patients with newly diagnosed MM who are ineligible for autologous stem cell transplant.
Health Canada previously approved daratumumab in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat MM patients who have received at least one prior therapy.
Health Canada also approved daratumumab as monotherapy for MM patients who have received at least three prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are refractory to both a proteasome inhibitor and an immunomodulatory agent.
For the product monograph and more information about daratumumab, visit https://www.janssen.com/canada/products.
Trial results
Health Canada’s latest approval of daratumumab is supported by data from the phase 3 ALCYONE study (NCT02195479), which were presented at the 2017 ASH Annual Meeting and simultaneously published in The New England Journal of Medicine.
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant. Patients were randomized to receive VMP or daratumumab plus VMP (D-VMP).
The overall response rates were 91% in the D-VMP arm and 74% in the VMP arm (P<0.0001). Rates of complete response were 43% and 24%, respectively. Rates of minimal residual disease negativity were 22% and 6%, respectively.
The median progression-free survival (PFS) was not reached in the D-VMP arm and was 18.1 months in the VMP arm. The 12-month PFS was 87% and 76%, respectively. The 18-month PFS was 72% and 50%, respectively.
The most common treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
Infusion-related reactions occurred in 28% of patients in the D-VMP arm and 0% of those in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. In both arms, most infections resolved.
The most common grade 3/4 treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
The rate of discontinuation due to adverse events was 5% in the D-VMP arm and 9% in the VMP arm.
The ALCYONE trial was sponsored by Janssen Research & Development, LLC.
Health Canada has approved a third indication for daratumumab (Darzalex®) in multiple myeloma (MM).
The drug is now approved for use in combination with bortezomib, melphalan, and prednisone (VMP) to treat patients with newly diagnosed MM who are ineligible for autologous stem cell transplant.
Health Canada previously approved daratumumab in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat MM patients who have received at least one prior therapy.
Health Canada also approved daratumumab as monotherapy for MM patients who have received at least three prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are refractory to both a proteasome inhibitor and an immunomodulatory agent.
For the product monograph and more information about daratumumab, visit https://www.janssen.com/canada/products.
Trial results
Health Canada’s latest approval of daratumumab is supported by data from the phase 3 ALCYONE study (NCT02195479), which were presented at the 2017 ASH Annual Meeting and simultaneously published in The New England Journal of Medicine.
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant. Patients were randomized to receive VMP or daratumumab plus VMP (D-VMP).
The overall response rates were 91% in the D-VMP arm and 74% in the VMP arm (P<0.0001). Rates of complete response were 43% and 24%, respectively. Rates of minimal residual disease negativity were 22% and 6%, respectively.
The median progression-free survival (PFS) was not reached in the D-VMP arm and was 18.1 months in the VMP arm. The 12-month PFS was 87% and 76%, respectively. The 18-month PFS was 72% and 50%, respectively.
The most common treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
Infusion-related reactions occurred in 28% of patients in the D-VMP arm and 0% of those in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. In both arms, most infections resolved.
The most common grade 3/4 treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
The rate of discontinuation due to adverse events was 5% in the D-VMP arm and 9% in the VMP arm.
The ALCYONE trial was sponsored by Janssen Research & Development, LLC.
Health Canada has approved a third indication for daratumumab (Darzalex®) in multiple myeloma (MM).
The drug is now approved for use in combination with bortezomib, melphalan, and prednisone (VMP) to treat patients with newly diagnosed MM who are ineligible for autologous stem cell transplant.
Health Canada previously approved daratumumab in combination with lenalidomide and dexamethasone or bortezomib and dexamethasone to treat MM patients who have received at least one prior therapy.
Health Canada also approved daratumumab as monotherapy for MM patients who have received at least three prior lines of therapy, including a proteasome inhibitor and an immunomodulatory agent, or who are refractory to both a proteasome inhibitor and an immunomodulatory agent.
For the product monograph and more information about daratumumab, visit https://www.janssen.com/canada/products.
Trial results
Health Canada’s latest approval of daratumumab is supported by data from the phase 3 ALCYONE study (NCT02195479), which were presented at the 2017 ASH Annual Meeting and simultaneously published in The New England Journal of Medicine.
ALCYONE enrolled 706 patients with newly diagnosed MM who were not eligible for high-dose chemotherapy with autologous stem cell transplant. Patients were randomized to receive VMP or daratumumab plus VMP (D-VMP).
The overall response rates were 91% in the D-VMP arm and 74% in the VMP arm (P<0.0001). Rates of complete response were 43% and 24%, respectively. Rates of minimal residual disease negativity were 22% and 6%, respectively.
The median progression-free survival (PFS) was not reached in the D-VMP arm and was 18.1 months in the VMP arm. The 12-month PFS was 87% and 76%, respectively. The 18-month PFS was 72% and 50%, respectively.
The most common treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (50% and 53%), thrombocytopenia (49% and 54%), anemia (28% and 38%), peripheral sensory neuropathy (28% and 34%), upper respiratory tract infection (26% and 14%), diarrhea (24% and 25%), pyrexia (23% and 21%), and nausea (21% and 22%).
Infusion-related reactions occurred in 28% of patients in the D-VMP arm and 0% of those in the VMP arm.
The rate of grade 3/4 infections was higher in the D-VMP arm than the VMP arm—23% and 15%, respectively. In both arms, most infections resolved.
The most common grade 3/4 treatment-emergent adverse events (in the D-VMP and VMP arms, respectively) were neutropenia (40% and 39%), thrombocytopenia (34% and 38%), and anemia (16% and 20%).
The rate of discontinuation due to adverse events was 5% in the D-VMP arm and 9% in the VMP arm.
The ALCYONE trial was sponsored by Janssen Research & Development, LLC.
CHMP recommends BV+AVD for Hodgkin lymphoma
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for brentuximab vedotin (BV).
The CHMP has recommended approval for BV (Adcetris) in combination with doxorubicin, vinblastine, and dacarbazine (AVD) to treat adults with previously untreated, CD30+, stage IV Hodgkin lymphoma (HL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of a CHMP recommendation.
BV is already EC-approved to treat adults with:
- CD30+ HL at increased risk of relapse or progression following autologous stem cell transplant (ASCT)
- Relapsed or refractory, CD30+ HL following ASCT or following at least two prior therapies when ASCT or multi-agent chemotherapy is not a treatment option
- Relapsed or refractory systemic anaplastic large-cell lymphoma
- CD30+ cutaneous T-cell lymphoma after at least one prior systemic therapy.
Phase 3 trial
The CHMP’s recommendation to approve BV in combination with AVD is supported by the phase 3 ECHELON-1 trial (NCT01712490).
Result from ECHELON-1 were presented at the 2017 ASH Annual Meeting and simultaneously published in The New England Journal of Medicine.
In this trial, researchers compared BV plus AVD (BV+AVD) to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for 1334 patients with advanced HL.
The primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review committee, BV+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
The 2-year modified PFS rate was 82.1% in the BV+AVD arm and 77.2% in the ABVD arm.
There was no significant difference between the treatment arms when it came to response rates or overall survival.
The objective response rate was 86% in the BV+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The interim 2-year overall survival rate was 97% in the BV+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
The overall incidence of adverse events (AEs) was 99% in the BV+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with BV+AVD, while pulmonary toxicity was more common with ABVD.
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals, Inc. (a Takeda company) in collaboration with Seattle Genetics, Inc.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for brentuximab vedotin (BV).
The CHMP has recommended approval for BV (Adcetris) in combination with doxorubicin, vinblastine, and dacarbazine (AVD) to treat adults with previously untreated, CD30+, stage IV Hodgkin lymphoma (HL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of a CHMP recommendation.
BV is already EC-approved to treat adults with:
- CD30+ HL at increased risk of relapse or progression following autologous stem cell transplant (ASCT)
- Relapsed or refractory, CD30+ HL following ASCT or following at least two prior therapies when ASCT or multi-agent chemotherapy is not a treatment option
- Relapsed or refractory systemic anaplastic large-cell lymphoma
- CD30+ cutaneous T-cell lymphoma after at least one prior systemic therapy.
Phase 3 trial
The CHMP’s recommendation to approve BV in combination with AVD is supported by the phase 3 ECHELON-1 trial (NCT01712490).
Result from ECHELON-1 were presented at the 2017 ASH Annual Meeting and simultaneously published in The New England Journal of Medicine.
In this trial, researchers compared BV plus AVD (BV+AVD) to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for 1334 patients with advanced HL.
The primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review committee, BV+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
The 2-year modified PFS rate was 82.1% in the BV+AVD arm and 77.2% in the ABVD arm.
There was no significant difference between the treatment arms when it came to response rates or overall survival.
The objective response rate was 86% in the BV+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The interim 2-year overall survival rate was 97% in the BV+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
The overall incidence of adverse events (AEs) was 99% in the BV+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with BV+AVD, while pulmonary toxicity was more common with ABVD.
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals, Inc. (a Takeda company) in collaboration with Seattle Genetics, Inc.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for brentuximab vedotin (BV).
The CHMP has recommended approval for BV (Adcetris) in combination with doxorubicin, vinblastine, and dacarbazine (AVD) to treat adults with previously untreated, CD30+, stage IV Hodgkin lymphoma (HL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of a CHMP recommendation.
BV is already EC-approved to treat adults with:
- CD30+ HL at increased risk of relapse or progression following autologous stem cell transplant (ASCT)
- Relapsed or refractory, CD30+ HL following ASCT or following at least two prior therapies when ASCT or multi-agent chemotherapy is not a treatment option
- Relapsed or refractory systemic anaplastic large-cell lymphoma
- CD30+ cutaneous T-cell lymphoma after at least one prior systemic therapy.
Phase 3 trial
The CHMP’s recommendation to approve BV in combination with AVD is supported by the phase 3 ECHELON-1 trial (NCT01712490).
Result from ECHELON-1 were presented at the 2017 ASH Annual Meeting and simultaneously published in The New England Journal of Medicine.
In this trial, researchers compared BV plus AVD (BV+AVD) to doxorubicin, bleomycin, vinblastine, and dacarbazine (ABVD) as frontline treatment for 1334 patients with advanced HL.
The primary endpoint was modified progression-free survival (PFS), which was defined as time to progression, death, or evidence of non-complete response after completion of frontline therapy followed by subsequent anticancer therapy.
According to an independent review committee, BV+AVD provided a significant improvement in modified PFS compared to ABVD. The hazard ratio was 0.77 (P=0.035), which corresponds to a 23% reduction in the risk of progression, death, or the need for additional anticancer therapy.
The 2-year modified PFS rate was 82.1% in the BV+AVD arm and 77.2% in the ABVD arm.
There was no significant difference between the treatment arms when it came to response rates or overall survival.
The objective response rate was 86% in the BV+AVD arm and 83% in the ABVD arm (P=0.12). The complete response rate was 73% and 70%, respectively (P=0.22).
The interim 2-year overall survival rate was 97% in the BV+AVD arm and 95% in the ABVD arm (hazard ratio=0.72; P=0.19).
The overall incidence of adverse events (AEs) was 99% in the BV+AVD arm and 98% in the ABVD arm. The incidence of grade 3 or higher AEs was 83% and 66%, respectively, and the incidence of serious AEs was 43% and 27%, respectively.
Neutropenia, febrile neutropenia, and peripheral neuropathy were more common with BV+AVD, while pulmonary toxicity was more common with ABVD.
The ECHELON-1 trial was sponsored by Millennium Pharmaceuticals, Inc. (a Takeda company) in collaboration with Seattle Genetics, Inc.
Avoiding the Pitfalls of “Half-visits”
A 3-and-a-half-year-old girl presented to a pediatrician’s office with complaints of vomiting and high fever (103.3°). She was seen by a nurse practitioner, who diagnosed gastroenteritis, prescribed fluid replacement and acetaminophen, and sent the child home.
The NP did not chart the child’s blood pressure, pulse, or respiratory rate. She did note swollen lymph nodes and absence of diarrhea. The NP performed a flu screen but did not order a rapid strep test or urinalysis.
Several hours later, the child was taken to the emergency department with shortness of breath, cough, congestion, tachycardia, hypoxia, dehydration, and lethargy. She was admitted to the pediatric ICU with diagnoses of pneumonia, acute respiratory distress, hypoxemia, neutropenia, and sepsis. She was given IV antibiotics.
Several hours later, the decision was made to transfer the patient to a regional medical center. During transfer, she suffered cardiopulmonary arrest while being placed on a ventilator for transport. Upon arrival at the hospital, she arrested again and required resuscitation for several hours until spontaneous circulation could not be restored.
An autopsy concluded the child died of sepsis and shock from Group A beta-hemolytic streptococcal infection.
It was argued that the NP failed to diagnose and treat streptococcal toxic shock syndrome at the time of the child’s presentation. In support of this contention, it was argued that the NP had failed to perform basic follow-up when the child’s flu test came back negative and that the child’s swollen lymph nodes and lack of diarrhea both mitigated against the NP’s diagnosis of gastroenteritis.
VERDICT
The parties in this case reached a $950,000 settlement.
Continue to: DISCUSSION
DISCUSSION
Every headache and fever could be an early meningitis, every vague abdominal pain an early appendicitis. So how do we handle innocuous-appearing cases with early, nonspecific symptoms of a very serious illness about to unfold?
We must start by following the Miyagi rule. In The Karate Kid, Mr. Miyagi advised that walking on the left or the right side of the road was safe, but walking in the middle would result, sooner or later, in “squish, just like grape.” Although he related this premise to karate, we can also apply it to medicine: See a patient or do not see a patient; but if you see a patient “so-so,” you will be squished—by the patient, by a plaintiff’s attorney, and/or by your state’s medical board.
A case such as this one strikes fear in the heart of anyone who has seen patients in an ambulatory setting. The initial presentation was modest: a toddler with vomiting and fever. We do not know what the other vital signs were, and we do not know whether the child appeared toxic. The lack of vital signs or recorded vital signs represent half-measures. The patient’s vitals could have been normal, and the NP’s actions could have been fully defensible. The problem is, we don’t know—and the clinician is on the hook.
All patients require vital signs. They must be done; they must be complete, and they must be recorded. At a minimum, temperature, blood pressure, respiratory rate, and (generally) O2 saturation are required. Some specialties may have other requirements (eg, fingerstick glucose for patients with diabetes, visual acuity testing for those with eye complaints). A full list of data you should be obtaining is practice specific and beyond the scope of this article; the point is, decide on the relevant set of vitals and intake data and be sure it is recorded at every visit.
Failure to obtain and record vital signs—as seen in this case—is sloppy practice, difficult to defend, and sets up an inference of negligence. Even when the care is perfect (and without bad outcome), if the medical board reviews the record for any reason, you will be sanctioned for “failure to keep adequate and accurate medical records” and your license burdened. Here, we are told the defendant NP “did not chart the child’s blood pressure, pulse, or respiratory rate.” I am willing to bet the NP was not responsible for charting the values in the normal course of practice, but see how responsibility is parked with the clinician? If intake staff do not record vital signs, politely (yet firmly) insist they do so.
Continue to: Furthermore, the disposition of many child visits...
Furthermore, the disposition of many child visits turns on whether the patient “appeared toxic.” Any child’s condition could worsen after evaluation—and in litigation, parents, friends, and family will testify the patient was extremely ill, they “knew something was wrong,” and the clinician ignored their loved one. Thus, the jury will be invited to reconstruct how the child appeared.
When assessing children and the question of “toxic appearance” arises, don’t state a conclusion—paint a picture. Don’t merely state “child appeared nontoxic.” Use your powers of observation to record why they appear nontoxic: “Child sitting up, watching Moana on parent’s phone, smiling and laughing appropriately.” Get interactive; some pediatric providers carry a small vial of bubbles with them and record the child’s response to bubble-making (“Child appropriately reaching for bubbles, smiling, holding one on finger”). The cost is less than $1 for the bubbles, plus the documentation time. The benefit is that it paints a clear picture for the jury of a child responding appropriately. And if your observations suggest a child who is at least unwell—if the movie is poorly received or the bubbles prompt the child to scream or bury her face in her mom’s shoulder—you can consider oral antipyretics/analgesics, fluid, and re-observation.
Another way to create a strong and defensible record is to use patient quotations. These can be extremely helpful to your defense in a malpractice action; as an attorney, I have searched 8,000 pages of records in a medical malpractice case, hoping to find a clear description from a human (not a template) of how a patient looked. Make it clear by adding patient remarks to the chart—just remember that “the only thing that belongs in quotes is what comes out of the patient’s mouth.” Words from an 8-year-old boy— such as “My brother found a legendary scar [a reference to Fortnite] and almost won”—may seem silly, but this documentation itself could win your case.
With teenagers, you may have to ask more questions to glean something suitable; you could ask a 13-year-old her favorite sport and when her one-word answer is “Lacrosse,” ask why. Even if the response is “Because, I don’t know, it’s exciting. There are a lot of goals,” write that down exactly (along with any other observations, such as Teen texting on her phone). These notations tell the plaintiff’s attorney, the judge, and the jury that the patient was behaving normally and interacting with the environment. Should this teen later deteriorate with meningitis, the plaintiff will claim she was toxic in the office. The medical record, however, will show that the patient’s condition changed, and it was a departure from how she looked in your office.
Also, it never hurts to get backup. In any close call, ask the nurse to reevaluate the patient as to whether he or she is “toxic appearing” or is interacting normally with the environment. Have the nurse or medical assistant record facts, such as “patient trying to make a plane out of two tongue depressors, pretending to land it on sister’s leg.” This will create a strong and defensible record: two clinicians relaying two sets of detailed observations.
Continue to: Likewise, encourage intake staff to document...
Likewise, encourage intake staff to document what they see rather than what they conclude from it. Buzzwords (eg, listless, lethargic) should be avoided. If such characterizations find their way into the record, you must take active steps to address them. Either agree with the characterization and perform appropriate work-up, or establish why you do not agree using the methods described (detailed description, verification by another clinician).
Taking these steps will help to protect you in the event of a changing clinical course. But also be wary of those predictable circumstances that lead you into Mr. Miyagi’s middle of the road (what I call “half-visits”): a quick look at a sibling in the room during a patient’s appointment; a “curbside consult” on the medical assistant’s child; the neighborhood acquaintance who asks you to “just take a look.” Why are these dangerous? Because they remove the clinician from his or her usual routine: proper examination on a properly undressed patient, formal assessment of vital signs, and review of relevant history in the chart, among other things. (In this way, phone and email communications with patients require similar caution.) Skipping the routine leads to shortcuts, and shortcuts lead to bad medicine. And if that doesn’t worry you, remember: All these scenarios create a full legal duty and clinician/patient relationship—making them potential pathways to misdiagnosis and eventual loss of license.
IN SUMMARY
Don’t be party to a “half-visit”; insist on full vital signs and a complete visit following your usual routine. Use observational powers and patient quotations to paint a picture of how a patient looked, get backup from another clinician with similar observations. If you can’t document a reassuring record, protect the patient and make the required intervention.
A 3-and-a-half-year-old girl presented to a pediatrician’s office with complaints of vomiting and high fever (103.3°). She was seen by a nurse practitioner, who diagnosed gastroenteritis, prescribed fluid replacement and acetaminophen, and sent the child home.
The NP did not chart the child’s blood pressure, pulse, or respiratory rate. She did note swollen lymph nodes and absence of diarrhea. The NP performed a flu screen but did not order a rapid strep test or urinalysis.
Several hours later, the child was taken to the emergency department with shortness of breath, cough, congestion, tachycardia, hypoxia, dehydration, and lethargy. She was admitted to the pediatric ICU with diagnoses of pneumonia, acute respiratory distress, hypoxemia, neutropenia, and sepsis. She was given IV antibiotics.
Several hours later, the decision was made to transfer the patient to a regional medical center. During transfer, she suffered cardiopulmonary arrest while being placed on a ventilator for transport. Upon arrival at the hospital, she arrested again and required resuscitation for several hours until spontaneous circulation could not be restored.
An autopsy concluded the child died of sepsis and shock from Group A beta-hemolytic streptococcal infection.
It was argued that the NP failed to diagnose and treat streptococcal toxic shock syndrome at the time of the child’s presentation. In support of this contention, it was argued that the NP had failed to perform basic follow-up when the child’s flu test came back negative and that the child’s swollen lymph nodes and lack of diarrhea both mitigated against the NP’s diagnosis of gastroenteritis.
VERDICT
The parties in this case reached a $950,000 settlement.
Continue to: DISCUSSION
DISCUSSION
Every headache and fever could be an early meningitis, every vague abdominal pain an early appendicitis. So how do we handle innocuous-appearing cases with early, nonspecific symptoms of a very serious illness about to unfold?
We must start by following the Miyagi rule. In The Karate Kid, Mr. Miyagi advised that walking on the left or the right side of the road was safe, but walking in the middle would result, sooner or later, in “squish, just like grape.” Although he related this premise to karate, we can also apply it to medicine: See a patient or do not see a patient; but if you see a patient “so-so,” you will be squished—by the patient, by a plaintiff’s attorney, and/or by your state’s medical board.
A case such as this one strikes fear in the heart of anyone who has seen patients in an ambulatory setting. The initial presentation was modest: a toddler with vomiting and fever. We do not know what the other vital signs were, and we do not know whether the child appeared toxic. The lack of vital signs or recorded vital signs represent half-measures. The patient’s vitals could have been normal, and the NP’s actions could have been fully defensible. The problem is, we don’t know—and the clinician is on the hook.
All patients require vital signs. They must be done; they must be complete, and they must be recorded. At a minimum, temperature, blood pressure, respiratory rate, and (generally) O2 saturation are required. Some specialties may have other requirements (eg, fingerstick glucose for patients with diabetes, visual acuity testing for those with eye complaints). A full list of data you should be obtaining is practice specific and beyond the scope of this article; the point is, decide on the relevant set of vitals and intake data and be sure it is recorded at every visit.
Failure to obtain and record vital signs—as seen in this case—is sloppy practice, difficult to defend, and sets up an inference of negligence. Even when the care is perfect (and without bad outcome), if the medical board reviews the record for any reason, you will be sanctioned for “failure to keep adequate and accurate medical records” and your license burdened. Here, we are told the defendant NP “did not chart the child’s blood pressure, pulse, or respiratory rate.” I am willing to bet the NP was not responsible for charting the values in the normal course of practice, but see how responsibility is parked with the clinician? If intake staff do not record vital signs, politely (yet firmly) insist they do so.
Continue to: Furthermore, the disposition of many child visits...
Furthermore, the disposition of many child visits turns on whether the patient “appeared toxic.” Any child’s condition could worsen after evaluation—and in litigation, parents, friends, and family will testify the patient was extremely ill, they “knew something was wrong,” and the clinician ignored their loved one. Thus, the jury will be invited to reconstruct how the child appeared.
When assessing children and the question of “toxic appearance” arises, don’t state a conclusion—paint a picture. Don’t merely state “child appeared nontoxic.” Use your powers of observation to record why they appear nontoxic: “Child sitting up, watching Moana on parent’s phone, smiling and laughing appropriately.” Get interactive; some pediatric providers carry a small vial of bubbles with them and record the child’s response to bubble-making (“Child appropriately reaching for bubbles, smiling, holding one on finger”). The cost is less than $1 for the bubbles, plus the documentation time. The benefit is that it paints a clear picture for the jury of a child responding appropriately. And if your observations suggest a child who is at least unwell—if the movie is poorly received or the bubbles prompt the child to scream or bury her face in her mom’s shoulder—you can consider oral antipyretics/analgesics, fluid, and re-observation.
Another way to create a strong and defensible record is to use patient quotations. These can be extremely helpful to your defense in a malpractice action; as an attorney, I have searched 8,000 pages of records in a medical malpractice case, hoping to find a clear description from a human (not a template) of how a patient looked. Make it clear by adding patient remarks to the chart—just remember that “the only thing that belongs in quotes is what comes out of the patient’s mouth.” Words from an 8-year-old boy— such as “My brother found a legendary scar [a reference to Fortnite] and almost won”—may seem silly, but this documentation itself could win your case.
With teenagers, you may have to ask more questions to glean something suitable; you could ask a 13-year-old her favorite sport and when her one-word answer is “Lacrosse,” ask why. Even if the response is “Because, I don’t know, it’s exciting. There are a lot of goals,” write that down exactly (along with any other observations, such as Teen texting on her phone). These notations tell the plaintiff’s attorney, the judge, and the jury that the patient was behaving normally and interacting with the environment. Should this teen later deteriorate with meningitis, the plaintiff will claim she was toxic in the office. The medical record, however, will show that the patient’s condition changed, and it was a departure from how she looked in your office.
Also, it never hurts to get backup. In any close call, ask the nurse to reevaluate the patient as to whether he or she is “toxic appearing” or is interacting normally with the environment. Have the nurse or medical assistant record facts, such as “patient trying to make a plane out of two tongue depressors, pretending to land it on sister’s leg.” This will create a strong and defensible record: two clinicians relaying two sets of detailed observations.
Continue to: Likewise, encourage intake staff to document...
Likewise, encourage intake staff to document what they see rather than what they conclude from it. Buzzwords (eg, listless, lethargic) should be avoided. If such characterizations find their way into the record, you must take active steps to address them. Either agree with the characterization and perform appropriate work-up, or establish why you do not agree using the methods described (detailed description, verification by another clinician).
Taking these steps will help to protect you in the event of a changing clinical course. But also be wary of those predictable circumstances that lead you into Mr. Miyagi’s middle of the road (what I call “half-visits”): a quick look at a sibling in the room during a patient’s appointment; a “curbside consult” on the medical assistant’s child; the neighborhood acquaintance who asks you to “just take a look.” Why are these dangerous? Because they remove the clinician from his or her usual routine: proper examination on a properly undressed patient, formal assessment of vital signs, and review of relevant history in the chart, among other things. (In this way, phone and email communications with patients require similar caution.) Skipping the routine leads to shortcuts, and shortcuts lead to bad medicine. And if that doesn’t worry you, remember: All these scenarios create a full legal duty and clinician/patient relationship—making them potential pathways to misdiagnosis and eventual loss of license.
IN SUMMARY
Don’t be party to a “half-visit”; insist on full vital signs and a complete visit following your usual routine. Use observational powers and patient quotations to paint a picture of how a patient looked, get backup from another clinician with similar observations. If you can’t document a reassuring record, protect the patient and make the required intervention.
A 3-and-a-half-year-old girl presented to a pediatrician’s office with complaints of vomiting and high fever (103.3°). She was seen by a nurse practitioner, who diagnosed gastroenteritis, prescribed fluid replacement and acetaminophen, and sent the child home.
The NP did not chart the child’s blood pressure, pulse, or respiratory rate. She did note swollen lymph nodes and absence of diarrhea. The NP performed a flu screen but did not order a rapid strep test or urinalysis.
Several hours later, the child was taken to the emergency department with shortness of breath, cough, congestion, tachycardia, hypoxia, dehydration, and lethargy. She was admitted to the pediatric ICU with diagnoses of pneumonia, acute respiratory distress, hypoxemia, neutropenia, and sepsis. She was given IV antibiotics.
Several hours later, the decision was made to transfer the patient to a regional medical center. During transfer, she suffered cardiopulmonary arrest while being placed on a ventilator for transport. Upon arrival at the hospital, she arrested again and required resuscitation for several hours until spontaneous circulation could not be restored.
An autopsy concluded the child died of sepsis and shock from Group A beta-hemolytic streptococcal infection.
It was argued that the NP failed to diagnose and treat streptococcal toxic shock syndrome at the time of the child’s presentation. In support of this contention, it was argued that the NP had failed to perform basic follow-up when the child’s flu test came back negative and that the child’s swollen lymph nodes and lack of diarrhea both mitigated against the NP’s diagnosis of gastroenteritis.
VERDICT
The parties in this case reached a $950,000 settlement.
Continue to: DISCUSSION
DISCUSSION
Every headache and fever could be an early meningitis, every vague abdominal pain an early appendicitis. So how do we handle innocuous-appearing cases with early, nonspecific symptoms of a very serious illness about to unfold?
We must start by following the Miyagi rule. In The Karate Kid, Mr. Miyagi advised that walking on the left or the right side of the road was safe, but walking in the middle would result, sooner or later, in “squish, just like grape.” Although he related this premise to karate, we can also apply it to medicine: See a patient or do not see a patient; but if you see a patient “so-so,” you will be squished—by the patient, by a plaintiff’s attorney, and/or by your state’s medical board.
A case such as this one strikes fear in the heart of anyone who has seen patients in an ambulatory setting. The initial presentation was modest: a toddler with vomiting and fever. We do not know what the other vital signs were, and we do not know whether the child appeared toxic. The lack of vital signs or recorded vital signs represent half-measures. The patient’s vitals could have been normal, and the NP’s actions could have been fully defensible. The problem is, we don’t know—and the clinician is on the hook.
All patients require vital signs. They must be done; they must be complete, and they must be recorded. At a minimum, temperature, blood pressure, respiratory rate, and (generally) O2 saturation are required. Some specialties may have other requirements (eg, fingerstick glucose for patients with diabetes, visual acuity testing for those with eye complaints). A full list of data you should be obtaining is practice specific and beyond the scope of this article; the point is, decide on the relevant set of vitals and intake data and be sure it is recorded at every visit.
Failure to obtain and record vital signs—as seen in this case—is sloppy practice, difficult to defend, and sets up an inference of negligence. Even when the care is perfect (and without bad outcome), if the medical board reviews the record for any reason, you will be sanctioned for “failure to keep adequate and accurate medical records” and your license burdened. Here, we are told the defendant NP “did not chart the child’s blood pressure, pulse, or respiratory rate.” I am willing to bet the NP was not responsible for charting the values in the normal course of practice, but see how responsibility is parked with the clinician? If intake staff do not record vital signs, politely (yet firmly) insist they do so.
Continue to: Furthermore, the disposition of many child visits...
Furthermore, the disposition of many child visits turns on whether the patient “appeared toxic.” Any child’s condition could worsen after evaluation—and in litigation, parents, friends, and family will testify the patient was extremely ill, they “knew something was wrong,” and the clinician ignored their loved one. Thus, the jury will be invited to reconstruct how the child appeared.
When assessing children and the question of “toxic appearance” arises, don’t state a conclusion—paint a picture. Don’t merely state “child appeared nontoxic.” Use your powers of observation to record why they appear nontoxic: “Child sitting up, watching Moana on parent’s phone, smiling and laughing appropriately.” Get interactive; some pediatric providers carry a small vial of bubbles with them and record the child’s response to bubble-making (“Child appropriately reaching for bubbles, smiling, holding one on finger”). The cost is less than $1 for the bubbles, plus the documentation time. The benefit is that it paints a clear picture for the jury of a child responding appropriately. And if your observations suggest a child who is at least unwell—if the movie is poorly received or the bubbles prompt the child to scream or bury her face in her mom’s shoulder—you can consider oral antipyretics/analgesics, fluid, and re-observation.
Another way to create a strong and defensible record is to use patient quotations. These can be extremely helpful to your defense in a malpractice action; as an attorney, I have searched 8,000 pages of records in a medical malpractice case, hoping to find a clear description from a human (not a template) of how a patient looked. Make it clear by adding patient remarks to the chart—just remember that “the only thing that belongs in quotes is what comes out of the patient’s mouth.” Words from an 8-year-old boy— such as “My brother found a legendary scar [a reference to Fortnite] and almost won”—may seem silly, but this documentation itself could win your case.
With teenagers, you may have to ask more questions to glean something suitable; you could ask a 13-year-old her favorite sport and when her one-word answer is “Lacrosse,” ask why. Even if the response is “Because, I don’t know, it’s exciting. There are a lot of goals,” write that down exactly (along with any other observations, such as Teen texting on her phone). These notations tell the plaintiff’s attorney, the judge, and the jury that the patient was behaving normally and interacting with the environment. Should this teen later deteriorate with meningitis, the plaintiff will claim she was toxic in the office. The medical record, however, will show that the patient’s condition changed, and it was a departure from how she looked in your office.
Also, it never hurts to get backup. In any close call, ask the nurse to reevaluate the patient as to whether he or she is “toxic appearing” or is interacting normally with the environment. Have the nurse or medical assistant record facts, such as “patient trying to make a plane out of two tongue depressors, pretending to land it on sister’s leg.” This will create a strong and defensible record: two clinicians relaying two sets of detailed observations.
Continue to: Likewise, encourage intake staff to document...
Likewise, encourage intake staff to document what they see rather than what they conclude from it. Buzzwords (eg, listless, lethargic) should be avoided. If such characterizations find their way into the record, you must take active steps to address them. Either agree with the characterization and perform appropriate work-up, or establish why you do not agree using the methods described (detailed description, verification by another clinician).
Taking these steps will help to protect you in the event of a changing clinical course. But also be wary of those predictable circumstances that lead you into Mr. Miyagi’s middle of the road (what I call “half-visits”): a quick look at a sibling in the room during a patient’s appointment; a “curbside consult” on the medical assistant’s child; the neighborhood acquaintance who asks you to “just take a look.” Why are these dangerous? Because they remove the clinician from his or her usual routine: proper examination on a properly undressed patient, formal assessment of vital signs, and review of relevant history in the chart, among other things. (In this way, phone and email communications with patients require similar caution.) Skipping the routine leads to shortcuts, and shortcuts lead to bad medicine. And if that doesn’t worry you, remember: All these scenarios create a full legal duty and clinician/patient relationship—making them potential pathways to misdiagnosis and eventual loss of license.
IN SUMMARY
Don’t be party to a “half-visit”; insist on full vital signs and a complete visit following your usual routine. Use observational powers and patient quotations to paint a picture of how a patient looked, get backup from another clinician with similar observations. If you can’t document a reassuring record, protect the patient and make the required intervention.
Recommended reading: Board picks the ‘best of 2018’
Recommended Reading lists have been over the years among the most popular features in this publication. It is therefore fitting that for this last issue of ACS Surgery News, we have once again imposed upon our Editorial Advisory Board to come up with their choice of the most important studies published in 2018. They were asked to choose a few studies that they consider most significant in their subspecialties and to explain why these studies should matter to all surgeons.
Some editorial advisers for some publications fill honorary positions with no real responsibility or work involved. Not so for the Editorial Advisory Board of ACS Surgery News. Each member provided a steady stream of commentaries, recommendations, and advice. The publication and the managing editor would have been lost without their kind and willing assistance. In their busy professional lives, they somehow found the time to contribute their expertise to assist their colleagues and their profession. We all owe them a debt of gratitude for their many years of service.
We hope our readers will find the list and the comments of interest.
Otolaryngology
St. Laurent J et al. HPV vaccination and the effects on rates of HPV-related cancers. Curr Probl Cancer 2018; https://doi.org/10.1016/j.currproblcancer.2018.06.004
As a head and neck surgeon over the past 30+ years, I have seen the dramaticrise of one form of HPV-related cancer in the United States, namely, HPV-associated oropharyngeal cancer. This is a true epidemic. It is also a cancer that may well be preventable through vaccination. We have slowly made progress over the past 4 decades in reducing the number of tobacco- and alcohol-related cancers. Here is another cancer that truly falls within the category of a public health problem for which public health solution of vaccination is clearly the most rational approach. Everyone should be aware of these virally induced cancers and what can be done to prevent them. This article presents the “state of the art” knowledge about these cancers and what we can hopefully accomplish through worldwide public health initiatives.
Mark C. Weissler, MD, FACS
Palliative Care
Kopecky KE et al. Third-year medical students’ reactions to surgical patients in pain: Doubt, distress, and depersonalization. J Pain and Symptom Manage. 2018;56(5):719-26.
This insightful study done by surgeons, two of them possessing palliative care and bioethics expertise, is a qualitative analysis of the content of 341 essays written by third-year medical students who described their experiences with surgical patients in pain. Students found it difficult to reconcile patient suffering with the therapeutic objective of treatment. As a result they learned constrained empathy and preference for technical solutions and because they feared an empathic response to pain might compromise the fortitude and efficiency required to be a doctor they pursued strategies to distance themselves from these feelings. The authors note, “Although doctors frequently interact with patients who have serious emotional and physical pain, few have received formal instruction on how to attend to these needs or developed a personal approach to cope with the tragedy of patient illness. Instead, the physician’s response to patients in pain is learned passively and perpetuated through generations. Students now seek to suppress empathy to get the job done. These observations have important implications for physicians, patients, and educators.” For me the study is like a parachute flare illuminating the landscape of early surgical educational experience during which the seeds for future problems such as lost patient trust and burnout are sown. It offers the hope that structured introspective activities may mitigate this.
Su A et al. Beyond pain: Nurses’ assessment of patient suffering, dignity, and dying in the intensive care unit. J Pain Symptom Manage. 2018;55:1591-98.
After reading this sobering study, my reaction was, “If the gold rusts what will happen to the iron?” In this study using chart abstraction, nurses caring for 200 patients in a tertiary care cardiac ICU and a surgical ICU were interviewed about their assessment and perception of the physical and psychosocial dimensions of ICU patients’ experiences in their final week of life. The authors note that nursing symptom assessments have been previously shown to be highly reliable and end-of-life comfort and dignity have been shown to be compatible with ICU level of care. Despite this and the availability of extensive interdisciplinary support from palliative care teams, chaplains, and social workers, dying ICU patients are perceived by nurses to experience extreme indignities and suffer beyond physical pain. The study found that attention to symptoms such as dyspnea and edema might improve the quality of death in the ICU. It is small wonder that moral fatigue and burnout have become prevalent themes of ICU caring.
Balboni T et al. The spiritual event of serious illness. J Pain Symptom Manage. 2018;56(5):816-22.
An ashen-faced dear friend gently reminded me as he was hemorrhaging from an advanced gastric cancer, “Geoff, lets make this a spiritual event, not a medical one.” This paper conjured up this memory with the thoughtful, in-depth account and analysis of patients’ experiences and attitudes that shaped the authors concept of illness as a spiritual event. The idea of spirituality as a basic component of consciousness, especially as it relates to suffering, has been present from the very beginning of modern palliative care and can be traced back to the concept of “total pain” introduced by Dame Cicely Saunders in 1963. The capacity to reframe biophysical calamity as spiritual opportunity is the signature of the most skilled and adroit supportive care we can offer our patients and their families.
Geoffrey P. Dunn, MD, FACS
Colorectal Surgery
Cercek A et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4(6):e180071. doi:10.1001/jamaoncol.2018.0071.
This moderate sized retrospective study demonstrates a single-institution’s experience with total neoadjuvant therapy (TNT) with chemoradiation and chemotherapy as opposed to traditional chemoradiation, surgery, and chemotherapy in patients with locally advanced rectal cancer. They demonstrate equivalent or potentially better outcomes including better complete response rate – 36% versus 21% and rates of chemotherapy completion. While further studies are needed to understand long term outcomes, this study support the use of TNT for locally advanced rectal cancer as now supported by the National Comprehensive Cancer Network guidelines.
Brouquet A et al. Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: Results of a prospective nationwide cohort. Ann Surg. 2018 Feb;267(2):221-228. doi: 10.1097/SLA.0000000000002017.
This large prospective study of almost 600 consecutive Crohn’s disease patients with surgery at 19 French specialty centers demonstrates that anti-TNF therapy less than 3 months prior to ileocolic surgery to be an independent risk factor of the overall postoperative morbidity, preoperative hemoglobin less than10 g/dL, operative time more than180 min, and recurrent Crohn’s disease, as well as a higher risk of overall and intra-abdominal septic postoperative morbidities.
Howard R et al. Taking control of your surgery: Impact of a prehabilitation program on major abdominal surgery. J Am Coll Surg. 2018 Oct 22; https://doi.org/10.1016/j.jamcollsurg.2018.09.018
Results from the Michigan Surgical and Health Optimization Program (MSHOP) are reported in colectomy patients. This prehabilitation program engages patients in four activities before surgery: physical activity, pulmonary rehabilitation, nutritional optimization, and stress reduction. MSHOP patients were matched to emergency and elective, non-MSHOP patients. Overall, 70% of MSHOP patients complied with the program. MSHOP patients were more likely to have improved blood pressure and heart rate intraoperatively, reduction in Clavien-Dindo class 3-4 complications in the MSHOP group (30%), compared with the nonprehabilitation (38%) and emergency (48%) groups (P = .05), as well as average savings of $21,946 per patient.
Genevieve Melton-Meaux, MD, PhD, FACS
Bariatric Surgery
Kalff MC et al. Diagnostic value of computed tomography for detecting anastomotic or staple line leakage after bariatric surgery. Surg Obes Relat Dis. 2018;14(9):1310-16
The most dreaded complication in the current era of metabolic and bariatric surgery, from a technical point of view, remains an anastomotic or staple-line leak. The authors present their findings corresponding to a multivariable regression analysis of a retrospective review of all CT abdomen and pelvis scans conducted from November 2007 to August 2016 at their large teaching hospital and Bariatric Center of Excellence. A CT is especially useful at ruling out low-suspicion cases of leaks, when the surgeon is trying to decide if a diagnostic laparoscopy is indicated, with a sensitivity of 90%-100%, and a negative predictive value of 97%-100%. A negative CT scan is highly accurate for ruling out a leak, especially in those patients without co-existing tachycardia and tachypnea. With caution based on clinical expertise, it may serve to prevent unnecessary diagnostic laparoscopy when appropriately indicated.
Alizadeh RF et al. Risk factors for gastrointestinal leak after bariatric surgery: MBSAQIP analysis. J Am Coll Surg. 2018;227(1):135-141.
The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 database of accredited centers was the object of study. Multivariate logistic regression analysis was used to examine risk factors for GI leaks that are not typically included in similar studies. Of particular interest is finding that Roux-en-Y gastric bypass comes with a higher risk for leak, compared with a sleeve gastrectomy, but with an overall leak rate for both of 0.7% based on current results. In addition, the study found that use of an intraoperative provocative leak test and placement of a surgical drain are associated with a higher leak rate. The same is not true of a postoperative swallow contrast study, which has no effect on the incidence of leaks.
Altieri MS et al. Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc. 2018;32(12):4805-4812.
The field of venous thromboembolism prevention after bariatric surgery remains a challenging one due to the lack of consensus among surgeons. This study analyzes the Cerner Health Facts database from 2003 to 2013, particularly with ICD-9 codes, for patients undergoing Roux-en-Y gastric bypass and sleeve gastrectomy. While the authors confirm the statement that there is a lack of consistency and, therefore, there is ample variability among bariatric centers and surgeons, the use of postoperative VTE chemoprophylaxis leads to a lower incidence of VTE events, and less frequent bleeding episodes, compared with pre-operative chemoprophylaxis. Finally, mixed therapy using heparin and enoxaparin led to more bleeding complications and blood transfusion requirements.
Rodolfo J. Oviedo, MD, FACS, FASMBS
Cardiothoracic Surgery
Stone GW et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018 Sep 23; doi:10.1056/NEJMoa1806640.
This study, known as the COAPT trial, assessed the value of adding transcatheter mitral valve repair to best medical therapy for the treatment of moderate-to-severe or severe functional mitral regurgitation in patients with symptomatic heart failure. Not only was transcatheter mitral valve repair exceedingly safe (more than 96% freedom from device-related complications at 12 months), patients were hospitalized less for heart failure management and had lower all-cause mortality compared with best medical therapy alone. The results of the COAPT trial are an important step forward for transcatheter therapies, which are rapidly becoming an integral part of the treatment algorithms for structural heart disease.
Gaudino M et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 2018;378(22):2069-77.
This analysis of randomized trials comparing radial artery to saphenous vein grafts for coronary artery bypass surgery is quite possibly a practice-changing publication. Routine use of the left internal thoracic (mammary) artery is commonplace among cardiac surgeons; however, the debate over conduit choice for additional bypass grafts is a “tale as old as time.” This study, part of the RADIAL project, combined patient-level data from six trials in order to achieve adequate power to identify differences in clinical outcomes. The use of radial artery grafts as opposed to saphenous vein grafts was associated with less adverse cardiac events, a lower incidence of repeat revascularization, and a higher patency rate at 5 years. Although there was no difference in all-cause mortality, the results of this study support the use of radial artery grafts when additional conduits are needed in coronary artery bypass surgery.
Irving L. Kron, MD, FACS, and Eric J. Charles, MD, PhD
Vascular Surgery
Anand SS. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: An international, randomised, double-blind, placebo-controlled trial. Lancet 2018;391(10117):219-29.
This landmark study was terminated early due to a significant difference in outcomes. Prior to this point, aspirin and statins have been the mainstay of decreasing long-term adverse outcomes for patients with vascular disease. The COMPASS study has found a decrease in combined cardiovascular adverse events when rivaroxaban 2.5 mg was combined with low-dose aspirin in patients with stable PAD or CAD over aspirin alone. This is the first major change supporting use of additional medications for PAD in over 2 decades, when statins were found to impact outcomes. The differences were not impacted by gender, age, or race. Patients with end-tage renal disease were excluded, so it is unclear whether it would be beneficial in this population. The higher rate of bleeding, 3.1% vs 1.9%, was primarily GI, so caution should be used if patients are felt to be at increased risk of bleeding.
These findings suggest the need for a major change in the guidelines and management for the majority of our patients with PAD. Certainly we should look to add this data point to the Vascular Quality Initiative to gather further data and confirm the findings in real world use. It is unclear whether this benefit will be unique to rivaroxaban, or whether other Direct Xa inhibitors will have similar effects. I will certainly be adding ribaroxaban to patients at low risk for bleeding based on this data. Further, rivaroxaban alone did not reduce major cardiovascular adverse events, but did reduce major adverse limb events.
Gohel MS et al. A randomized trial of early endovenous ablation in venous ulceration. N Engl J Med. 2018;378:2105-14.
This multicenter study in the UK looked at over 450 patients with venous ulceration. Deep-venous reflux was also present in one-third of patients in each group. The median time to ulcer healing was decreased significantly from 82 days to 56 days. This study demonstrates the importance of early intervention for superficial reflux to enhance ulcer healing and decrease risk of recurrence. This study found that early endovenous ablation resulted in faster healing of venous ulcers, and more ulcer-free time than delayed intervention in patients treated with maximal medical therapy, including appropriate compression therapy. Previously, ablation was typically planned after ulcers healed to decrease risk of recurrence. Based on these findings, ablation should be offered to patients with nonhealing venous ulcers early in the course of therapy, in addition to standard wound care.
Linda Harris, MD, FACS
Surgical Education
Ellison EC. Ten-year reassessment of the shortage of general surgeons: Increases in graduation numbers of general surgery residents are insufficient to meet the future demand for general surgeons. Surgery. 2018 Oct;164(4):726-32.
Ellison EC et al. The impact of the aging population and incidence of cancer on future projections of general surgery workforce needs. Surgery. 2018 Mar;163(3):553-59.
In 2008, Ellison et al. projected that a deficit in the general surgery workforce would grow to 19% by 2050. The group recently re-examined this projection by reviewing Census Bureau data, the available pool of surgeons with both allopathic and osteopathic degrees and factored in the losses of new surgeons who subspecialize and older surgeons who retire every year. Their conclusion states that, without increasing future general surgeons training numbers, the projected future general surgery workforce shortage will continue to grow.
A second paper by the same group reviewed population and age-adjusted incidence of cancer to estimate the number of general surgeons needed for initial surgical treatment of the patient with cancer in the year 2035 compared with 2010. The total number of new patients with cancers treated by general surgeons is projected to increase 56% in that time span. This would require an increase of over 9,000 general surgeons over that based on current training numbers. Together, the papers predict that there will be an ever-increasing demand for general surgeons in the near future and that general surgeons, currently caring for over 50% of cancer patients in the US, will play an even more important role in surgical cancer treatment.
Michael D. Sarap, MD, FACS
General Surgery
Takada T. Tokyo Guidelines 2018 (TG18). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):1-2.
This is the updated set of guidelines, awaited since 2013, regarding treatment of acute cholecystitis and cholangitis, with updated management strategies from an international panel of experts. The most significant change, and considered overdue by some surgeons, is the modification of the management algorithm to propose that some patients with Grade III acute cholecystitis (severe cholecystitis with evidence of organ dysfunction) may be treated with immediate laparoscopic cholecystectomy, rather than percutaneous cholecystostomy, “when performed at advanced centers with specialized surgeons experienced in this procedure.” As cholecystectomy is the most common general surgery procedure in the United States, most community surgeons have expertise. Whether there is truly need of a specialized gallbladder surgeon at an advanced center to safely complete a laparoscopic cholecystectomy can still be debated. But the change in recommendation from the experts is welcome.
Acuna SA. Operative strategies for perforated diverticulitis: A systematic review and meta-analysis. Dis Colon Rectum. 2018 Dec; 61(12):1442-53.
This analysis of the literature considers the three predominant operations for Hinchey III and Hinchey IV perforated diverticulitis: Hartmann procedure, resection and primary anastomosis, and laparoscopic lavage. The importance of this review is that it considers the initial operation and the downstream procedures when determining overall morbidity and mortality. Laparoscopic lavage did not fare well in this review of randomized controlled trials, resulting in higher morbidity than resection in Hinchey III patients. Interestingly, none of the individual studies analyzed had shown a statistical difference, but in the meta-analysis, the number of patients was sufficient to show statistical significance. The other important conclusion was that primary resection with anastomosis (possibly with diverting ileostomy) was superior to Hartmann procedure, when the likelihood of stoma reversal and the morbidity of the second operation was taken into account.
Mark Savarise, MD, FACS
Foregut
Alicuben ET. Worldwide experience with erosion of the magnetic sphincter augmentation device. J Gastrointest Surg. 2018; 22(8):1442-47.
Although magnetic sphincter augmentation of the lower esophageal sphincter initially appeared to provide excellent reflux control with essentially no risk of erosion, there have now been multiple reports throughout the world of device erosion over time. Fortunately, most erosions occurred with the smallest available device which is no longer on the market and the erosions currently being treated are usually done so with endoscopic/laparoscopic removal without the need for major esophageal resection.
Xiong YQ. Comparison of narrow-band imaging and confocal laser endomicroscopy for the detection of neoplasia in Barrett’s esophagus: A meta-analysis. Clin Res Hepatol Gastroenterol. 2018 Feb;42(1):31-9.
The days of endoscopic screening and surveillance of patients at risk for the development of Barrett’s esophagus via four-quadrant biopsy every couple of centimeters are numbered. The use of confocal laser microscopy to provide accurate real-time visual data regarding the areas of interest in the esophagus is showing promise and gaining traction compared to standard biopsy techniques and narrow-band imaging.
Borbély Y. Electrical stimulation of the lower esophageal sphincter to address gastroesophageal reflux disease after sleeve gastrectomy. Surg Obes Relat Dis. 2018 May;14(5):611-5.
The development of GERD following sleeve gastrectomy is a real problem in a substantial minority of patients due to structural compromise of the lower esophageal sphincter during the procedure. Conversion to gastric bypass as a way to alleviate acid regurgitation has been the mainstay of treatment; however, many patients selected sleeve gastrectomy specifically because they did not want to undergo gastric bypass. For those patients a sleeve preserving procedure such as magnetic sphincter augmentation (currently in clinical trial), Hill procedure, or remnant gastric fundoplication are potential options. Electrical stimulation of the lower esophageal sphincter is revealing itself to be another exciting option (currently in clinical trial) which can be used in patients with as few as 30% peristaltic swallows thus expanding the treatment options for these deserving patients.
Kevin M. Reavis, MD, FACS
Trauma/Critical Care
Teixeira PGR et al. Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury . J Am Coll Surg. 2018;226(5):769-76.
The use of tourniquets for hemorrhage control in trauma patients has been widely condemned in the past because of concerns regarding complications and potential limb loss. However, evidence from liberal tourniquet use in combat situations documenting survival benefits has continued to accumulate. Prompt hemorrhage control in trauma patients, including the use of tourniquets where applicable, has been validated by recent combat zone studies but improved survival hasn’t yet been shown in the civilian setting. In this multicenter, retrospective study of 1,026 patients with peripheral vascular injuries, only a relatively small number (17.6%) had pre-hospital tourniquets applied, yet multivariable analysis showed a significant survival benefit (odds ratio, 5.86). Importantly, no difference was seen in delayed amputation rates, of approximately 1% in both groups. This study helps to emphasize the importance of the Stop the Bleed (STB) campaign which includes education on the effective and safe use of tourniquets for prehospital hemorrhage. The STB program offers surgeons the opportunity to educate members of their own communities in effective bystander first aid.
Pileggi C et al. Ventilator bundle and its effects on mortality among ICU patients: A meta-analysis. Crit Care Med. 2018;46(7):1167-74.
Critically ill patients requiring mechanical ventilation are at risk for a number of complications, including ventilator-associated pneumonia (VAP) (now a subset of ventilator-associated events (VAE) which prolong ventilator and ICU time and contribute to further complication. Ventilator “bundles,” incorporating simple measures such as elevation of the head of the bed; daily “sedation holidays”; and evaluation of readiness for extubation, peptic ulcer, and DVT prophylaxis have been widely used in ICUs for nearly 20 years. Effective implementation has also emphasized multidisciplinary teamwork. Reductions in ventilator-associated pneumonia (VAP) incidence have been widely demonstrated but mortality benefits have been inconsistent. In this meta-analysis of 13 studies, 6 in Europe, 6 in the US and 1 in Brazil, an overall reduction in mortality (odds ratio, 0.9) was demonstrated. The effect was even larger when limited to studies with patients with VAP (OR, 0.71). This study both validates the effectiveness of relatively simple and inexpensive measures and emphasizes the benefits of a team approach to the care of ICU patients.
Krista L. Kaups, MD, FACS
Recommended Reading lists have been over the years among the most popular features in this publication. It is therefore fitting that for this last issue of ACS Surgery News, we have once again imposed upon our Editorial Advisory Board to come up with their choice of the most important studies published in 2018. They were asked to choose a few studies that they consider most significant in their subspecialties and to explain why these studies should matter to all surgeons.
Some editorial advisers for some publications fill honorary positions with no real responsibility or work involved. Not so for the Editorial Advisory Board of ACS Surgery News. Each member provided a steady stream of commentaries, recommendations, and advice. The publication and the managing editor would have been lost without their kind and willing assistance. In their busy professional lives, they somehow found the time to contribute their expertise to assist their colleagues and their profession. We all owe them a debt of gratitude for their many years of service.
We hope our readers will find the list and the comments of interest.
Otolaryngology
St. Laurent J et al. HPV vaccination and the effects on rates of HPV-related cancers. Curr Probl Cancer 2018; https://doi.org/10.1016/j.currproblcancer.2018.06.004
As a head and neck surgeon over the past 30+ years, I have seen the dramaticrise of one form of HPV-related cancer in the United States, namely, HPV-associated oropharyngeal cancer. This is a true epidemic. It is also a cancer that may well be preventable through vaccination. We have slowly made progress over the past 4 decades in reducing the number of tobacco- and alcohol-related cancers. Here is another cancer that truly falls within the category of a public health problem for which public health solution of vaccination is clearly the most rational approach. Everyone should be aware of these virally induced cancers and what can be done to prevent them. This article presents the “state of the art” knowledge about these cancers and what we can hopefully accomplish through worldwide public health initiatives.
Mark C. Weissler, MD, FACS
Palliative Care
Kopecky KE et al. Third-year medical students’ reactions to surgical patients in pain: Doubt, distress, and depersonalization. J Pain and Symptom Manage. 2018;56(5):719-26.
This insightful study done by surgeons, two of them possessing palliative care and bioethics expertise, is a qualitative analysis of the content of 341 essays written by third-year medical students who described their experiences with surgical patients in pain. Students found it difficult to reconcile patient suffering with the therapeutic objective of treatment. As a result they learned constrained empathy and preference for technical solutions and because they feared an empathic response to pain might compromise the fortitude and efficiency required to be a doctor they pursued strategies to distance themselves from these feelings. The authors note, “Although doctors frequently interact with patients who have serious emotional and physical pain, few have received formal instruction on how to attend to these needs or developed a personal approach to cope with the tragedy of patient illness. Instead, the physician’s response to patients in pain is learned passively and perpetuated through generations. Students now seek to suppress empathy to get the job done. These observations have important implications for physicians, patients, and educators.” For me the study is like a parachute flare illuminating the landscape of early surgical educational experience during which the seeds for future problems such as lost patient trust and burnout are sown. It offers the hope that structured introspective activities may mitigate this.
Su A et al. Beyond pain: Nurses’ assessment of patient suffering, dignity, and dying in the intensive care unit. J Pain Symptom Manage. 2018;55:1591-98.
After reading this sobering study, my reaction was, “If the gold rusts what will happen to the iron?” In this study using chart abstraction, nurses caring for 200 patients in a tertiary care cardiac ICU and a surgical ICU were interviewed about their assessment and perception of the physical and psychosocial dimensions of ICU patients’ experiences in their final week of life. The authors note that nursing symptom assessments have been previously shown to be highly reliable and end-of-life comfort and dignity have been shown to be compatible with ICU level of care. Despite this and the availability of extensive interdisciplinary support from palliative care teams, chaplains, and social workers, dying ICU patients are perceived by nurses to experience extreme indignities and suffer beyond physical pain. The study found that attention to symptoms such as dyspnea and edema might improve the quality of death in the ICU. It is small wonder that moral fatigue and burnout have become prevalent themes of ICU caring.
Balboni T et al. The spiritual event of serious illness. J Pain Symptom Manage. 2018;56(5):816-22.
An ashen-faced dear friend gently reminded me as he was hemorrhaging from an advanced gastric cancer, “Geoff, lets make this a spiritual event, not a medical one.” This paper conjured up this memory with the thoughtful, in-depth account and analysis of patients’ experiences and attitudes that shaped the authors concept of illness as a spiritual event. The idea of spirituality as a basic component of consciousness, especially as it relates to suffering, has been present from the very beginning of modern palliative care and can be traced back to the concept of “total pain” introduced by Dame Cicely Saunders in 1963. The capacity to reframe biophysical calamity as spiritual opportunity is the signature of the most skilled and adroit supportive care we can offer our patients and their families.
Geoffrey P. Dunn, MD, FACS
Colorectal Surgery
Cercek A et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4(6):e180071. doi:10.1001/jamaoncol.2018.0071.
This moderate sized retrospective study demonstrates a single-institution’s experience with total neoadjuvant therapy (TNT) with chemoradiation and chemotherapy as opposed to traditional chemoradiation, surgery, and chemotherapy in patients with locally advanced rectal cancer. They demonstrate equivalent or potentially better outcomes including better complete response rate – 36% versus 21% and rates of chemotherapy completion. While further studies are needed to understand long term outcomes, this study support the use of TNT for locally advanced rectal cancer as now supported by the National Comprehensive Cancer Network guidelines.
Brouquet A et al. Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: Results of a prospective nationwide cohort. Ann Surg. 2018 Feb;267(2):221-228. doi: 10.1097/SLA.0000000000002017.
This large prospective study of almost 600 consecutive Crohn’s disease patients with surgery at 19 French specialty centers demonstrates that anti-TNF therapy less than 3 months prior to ileocolic surgery to be an independent risk factor of the overall postoperative morbidity, preoperative hemoglobin less than10 g/dL, operative time more than180 min, and recurrent Crohn’s disease, as well as a higher risk of overall and intra-abdominal septic postoperative morbidities.
Howard R et al. Taking control of your surgery: Impact of a prehabilitation program on major abdominal surgery. J Am Coll Surg. 2018 Oct 22; https://doi.org/10.1016/j.jamcollsurg.2018.09.018
Results from the Michigan Surgical and Health Optimization Program (MSHOP) are reported in colectomy patients. This prehabilitation program engages patients in four activities before surgery: physical activity, pulmonary rehabilitation, nutritional optimization, and stress reduction. MSHOP patients were matched to emergency and elective, non-MSHOP patients. Overall, 70% of MSHOP patients complied with the program. MSHOP patients were more likely to have improved blood pressure and heart rate intraoperatively, reduction in Clavien-Dindo class 3-4 complications in the MSHOP group (30%), compared with the nonprehabilitation (38%) and emergency (48%) groups (P = .05), as well as average savings of $21,946 per patient.
Genevieve Melton-Meaux, MD, PhD, FACS
Bariatric Surgery
Kalff MC et al. Diagnostic value of computed tomography for detecting anastomotic or staple line leakage after bariatric surgery. Surg Obes Relat Dis. 2018;14(9):1310-16
The most dreaded complication in the current era of metabolic and bariatric surgery, from a technical point of view, remains an anastomotic or staple-line leak. The authors present their findings corresponding to a multivariable regression analysis of a retrospective review of all CT abdomen and pelvis scans conducted from November 2007 to August 2016 at their large teaching hospital and Bariatric Center of Excellence. A CT is especially useful at ruling out low-suspicion cases of leaks, when the surgeon is trying to decide if a diagnostic laparoscopy is indicated, with a sensitivity of 90%-100%, and a negative predictive value of 97%-100%. A negative CT scan is highly accurate for ruling out a leak, especially in those patients without co-existing tachycardia and tachypnea. With caution based on clinical expertise, it may serve to prevent unnecessary diagnostic laparoscopy when appropriately indicated.
Alizadeh RF et al. Risk factors for gastrointestinal leak after bariatric surgery: MBSAQIP analysis. J Am Coll Surg. 2018;227(1):135-141.
The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 database of accredited centers was the object of study. Multivariate logistic regression analysis was used to examine risk factors for GI leaks that are not typically included in similar studies. Of particular interest is finding that Roux-en-Y gastric bypass comes with a higher risk for leak, compared with a sleeve gastrectomy, but with an overall leak rate for both of 0.7% based on current results. In addition, the study found that use of an intraoperative provocative leak test and placement of a surgical drain are associated with a higher leak rate. The same is not true of a postoperative swallow contrast study, which has no effect on the incidence of leaks.
Altieri MS et al. Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc. 2018;32(12):4805-4812.
The field of venous thromboembolism prevention after bariatric surgery remains a challenging one due to the lack of consensus among surgeons. This study analyzes the Cerner Health Facts database from 2003 to 2013, particularly with ICD-9 codes, for patients undergoing Roux-en-Y gastric bypass and sleeve gastrectomy. While the authors confirm the statement that there is a lack of consistency and, therefore, there is ample variability among bariatric centers and surgeons, the use of postoperative VTE chemoprophylaxis leads to a lower incidence of VTE events, and less frequent bleeding episodes, compared with pre-operative chemoprophylaxis. Finally, mixed therapy using heparin and enoxaparin led to more bleeding complications and blood transfusion requirements.
Rodolfo J. Oviedo, MD, FACS, FASMBS
Cardiothoracic Surgery
Stone GW et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018 Sep 23; doi:10.1056/NEJMoa1806640.
This study, known as the COAPT trial, assessed the value of adding transcatheter mitral valve repair to best medical therapy for the treatment of moderate-to-severe or severe functional mitral regurgitation in patients with symptomatic heart failure. Not only was transcatheter mitral valve repair exceedingly safe (more than 96% freedom from device-related complications at 12 months), patients were hospitalized less for heart failure management and had lower all-cause mortality compared with best medical therapy alone. The results of the COAPT trial are an important step forward for transcatheter therapies, which are rapidly becoming an integral part of the treatment algorithms for structural heart disease.
Gaudino M et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 2018;378(22):2069-77.
This analysis of randomized trials comparing radial artery to saphenous vein grafts for coronary artery bypass surgery is quite possibly a practice-changing publication. Routine use of the left internal thoracic (mammary) artery is commonplace among cardiac surgeons; however, the debate over conduit choice for additional bypass grafts is a “tale as old as time.” This study, part of the RADIAL project, combined patient-level data from six trials in order to achieve adequate power to identify differences in clinical outcomes. The use of radial artery grafts as opposed to saphenous vein grafts was associated with less adverse cardiac events, a lower incidence of repeat revascularization, and a higher patency rate at 5 years. Although there was no difference in all-cause mortality, the results of this study support the use of radial artery grafts when additional conduits are needed in coronary artery bypass surgery.
Irving L. Kron, MD, FACS, and Eric J. Charles, MD, PhD
Vascular Surgery
Anand SS. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: An international, randomised, double-blind, placebo-controlled trial. Lancet 2018;391(10117):219-29.
This landmark study was terminated early due to a significant difference in outcomes. Prior to this point, aspirin and statins have been the mainstay of decreasing long-term adverse outcomes for patients with vascular disease. The COMPASS study has found a decrease in combined cardiovascular adverse events when rivaroxaban 2.5 mg was combined with low-dose aspirin in patients with stable PAD or CAD over aspirin alone. This is the first major change supporting use of additional medications for PAD in over 2 decades, when statins were found to impact outcomes. The differences were not impacted by gender, age, or race. Patients with end-tage renal disease were excluded, so it is unclear whether it would be beneficial in this population. The higher rate of bleeding, 3.1% vs 1.9%, was primarily GI, so caution should be used if patients are felt to be at increased risk of bleeding.
These findings suggest the need for a major change in the guidelines and management for the majority of our patients with PAD. Certainly we should look to add this data point to the Vascular Quality Initiative to gather further data and confirm the findings in real world use. It is unclear whether this benefit will be unique to rivaroxaban, or whether other Direct Xa inhibitors will have similar effects. I will certainly be adding ribaroxaban to patients at low risk for bleeding based on this data. Further, rivaroxaban alone did not reduce major cardiovascular adverse events, but did reduce major adverse limb events.
Gohel MS et al. A randomized trial of early endovenous ablation in venous ulceration. N Engl J Med. 2018;378:2105-14.
This multicenter study in the UK looked at over 450 patients with venous ulceration. Deep-venous reflux was also present in one-third of patients in each group. The median time to ulcer healing was decreased significantly from 82 days to 56 days. This study demonstrates the importance of early intervention for superficial reflux to enhance ulcer healing and decrease risk of recurrence. This study found that early endovenous ablation resulted in faster healing of venous ulcers, and more ulcer-free time than delayed intervention in patients treated with maximal medical therapy, including appropriate compression therapy. Previously, ablation was typically planned after ulcers healed to decrease risk of recurrence. Based on these findings, ablation should be offered to patients with nonhealing venous ulcers early in the course of therapy, in addition to standard wound care.
Linda Harris, MD, FACS
Surgical Education
Ellison EC. Ten-year reassessment of the shortage of general surgeons: Increases in graduation numbers of general surgery residents are insufficient to meet the future demand for general surgeons. Surgery. 2018 Oct;164(4):726-32.
Ellison EC et al. The impact of the aging population and incidence of cancer on future projections of general surgery workforce needs. Surgery. 2018 Mar;163(3):553-59.
In 2008, Ellison et al. projected that a deficit in the general surgery workforce would grow to 19% by 2050. The group recently re-examined this projection by reviewing Census Bureau data, the available pool of surgeons with both allopathic and osteopathic degrees and factored in the losses of new surgeons who subspecialize and older surgeons who retire every year. Their conclusion states that, without increasing future general surgeons training numbers, the projected future general surgery workforce shortage will continue to grow.
A second paper by the same group reviewed population and age-adjusted incidence of cancer to estimate the number of general surgeons needed for initial surgical treatment of the patient with cancer in the year 2035 compared with 2010. The total number of new patients with cancers treated by general surgeons is projected to increase 56% in that time span. This would require an increase of over 9,000 general surgeons over that based on current training numbers. Together, the papers predict that there will be an ever-increasing demand for general surgeons in the near future and that general surgeons, currently caring for over 50% of cancer patients in the US, will play an even more important role in surgical cancer treatment.
Michael D. Sarap, MD, FACS
General Surgery
Takada T. Tokyo Guidelines 2018 (TG18). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):1-2.
This is the updated set of guidelines, awaited since 2013, regarding treatment of acute cholecystitis and cholangitis, with updated management strategies from an international panel of experts. The most significant change, and considered overdue by some surgeons, is the modification of the management algorithm to propose that some patients with Grade III acute cholecystitis (severe cholecystitis with evidence of organ dysfunction) may be treated with immediate laparoscopic cholecystectomy, rather than percutaneous cholecystostomy, “when performed at advanced centers with specialized surgeons experienced in this procedure.” As cholecystectomy is the most common general surgery procedure in the United States, most community surgeons have expertise. Whether there is truly need of a specialized gallbladder surgeon at an advanced center to safely complete a laparoscopic cholecystectomy can still be debated. But the change in recommendation from the experts is welcome.
Acuna SA. Operative strategies for perforated diverticulitis: A systematic review and meta-analysis. Dis Colon Rectum. 2018 Dec; 61(12):1442-53.
This analysis of the literature considers the three predominant operations for Hinchey III and Hinchey IV perforated diverticulitis: Hartmann procedure, resection and primary anastomosis, and laparoscopic lavage. The importance of this review is that it considers the initial operation and the downstream procedures when determining overall morbidity and mortality. Laparoscopic lavage did not fare well in this review of randomized controlled trials, resulting in higher morbidity than resection in Hinchey III patients. Interestingly, none of the individual studies analyzed had shown a statistical difference, but in the meta-analysis, the number of patients was sufficient to show statistical significance. The other important conclusion was that primary resection with anastomosis (possibly with diverting ileostomy) was superior to Hartmann procedure, when the likelihood of stoma reversal and the morbidity of the second operation was taken into account.
Mark Savarise, MD, FACS
Foregut
Alicuben ET. Worldwide experience with erosion of the magnetic sphincter augmentation device. J Gastrointest Surg. 2018; 22(8):1442-47.
Although magnetic sphincter augmentation of the lower esophageal sphincter initially appeared to provide excellent reflux control with essentially no risk of erosion, there have now been multiple reports throughout the world of device erosion over time. Fortunately, most erosions occurred with the smallest available device which is no longer on the market and the erosions currently being treated are usually done so with endoscopic/laparoscopic removal without the need for major esophageal resection.
Xiong YQ. Comparison of narrow-band imaging and confocal laser endomicroscopy for the detection of neoplasia in Barrett’s esophagus: A meta-analysis. Clin Res Hepatol Gastroenterol. 2018 Feb;42(1):31-9.
The days of endoscopic screening and surveillance of patients at risk for the development of Barrett’s esophagus via four-quadrant biopsy every couple of centimeters are numbered. The use of confocal laser microscopy to provide accurate real-time visual data regarding the areas of interest in the esophagus is showing promise and gaining traction compared to standard biopsy techniques and narrow-band imaging.
Borbély Y. Electrical stimulation of the lower esophageal sphincter to address gastroesophageal reflux disease after sleeve gastrectomy. Surg Obes Relat Dis. 2018 May;14(5):611-5.
The development of GERD following sleeve gastrectomy is a real problem in a substantial minority of patients due to structural compromise of the lower esophageal sphincter during the procedure. Conversion to gastric bypass as a way to alleviate acid regurgitation has been the mainstay of treatment; however, many patients selected sleeve gastrectomy specifically because they did not want to undergo gastric bypass. For those patients a sleeve preserving procedure such as magnetic sphincter augmentation (currently in clinical trial), Hill procedure, or remnant gastric fundoplication are potential options. Electrical stimulation of the lower esophageal sphincter is revealing itself to be another exciting option (currently in clinical trial) which can be used in patients with as few as 30% peristaltic swallows thus expanding the treatment options for these deserving patients.
Kevin M. Reavis, MD, FACS
Trauma/Critical Care
Teixeira PGR et al. Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury . J Am Coll Surg. 2018;226(5):769-76.
The use of tourniquets for hemorrhage control in trauma patients has been widely condemned in the past because of concerns regarding complications and potential limb loss. However, evidence from liberal tourniquet use in combat situations documenting survival benefits has continued to accumulate. Prompt hemorrhage control in trauma patients, including the use of tourniquets where applicable, has been validated by recent combat zone studies but improved survival hasn’t yet been shown in the civilian setting. In this multicenter, retrospective study of 1,026 patients with peripheral vascular injuries, only a relatively small number (17.6%) had pre-hospital tourniquets applied, yet multivariable analysis showed a significant survival benefit (odds ratio, 5.86). Importantly, no difference was seen in delayed amputation rates, of approximately 1% in both groups. This study helps to emphasize the importance of the Stop the Bleed (STB) campaign which includes education on the effective and safe use of tourniquets for prehospital hemorrhage. The STB program offers surgeons the opportunity to educate members of their own communities in effective bystander first aid.
Pileggi C et al. Ventilator bundle and its effects on mortality among ICU patients: A meta-analysis. Crit Care Med. 2018;46(7):1167-74.
Critically ill patients requiring mechanical ventilation are at risk for a number of complications, including ventilator-associated pneumonia (VAP) (now a subset of ventilator-associated events (VAE) which prolong ventilator and ICU time and contribute to further complication. Ventilator “bundles,” incorporating simple measures such as elevation of the head of the bed; daily “sedation holidays”; and evaluation of readiness for extubation, peptic ulcer, and DVT prophylaxis have been widely used in ICUs for nearly 20 years. Effective implementation has also emphasized multidisciplinary teamwork. Reductions in ventilator-associated pneumonia (VAP) incidence have been widely demonstrated but mortality benefits have been inconsistent. In this meta-analysis of 13 studies, 6 in Europe, 6 in the US and 1 in Brazil, an overall reduction in mortality (odds ratio, 0.9) was demonstrated. The effect was even larger when limited to studies with patients with VAP (OR, 0.71). This study both validates the effectiveness of relatively simple and inexpensive measures and emphasizes the benefits of a team approach to the care of ICU patients.
Krista L. Kaups, MD, FACS
Recommended Reading lists have been over the years among the most popular features in this publication. It is therefore fitting that for this last issue of ACS Surgery News, we have once again imposed upon our Editorial Advisory Board to come up with their choice of the most important studies published in 2018. They were asked to choose a few studies that they consider most significant in their subspecialties and to explain why these studies should matter to all surgeons.
Some editorial advisers for some publications fill honorary positions with no real responsibility or work involved. Not so for the Editorial Advisory Board of ACS Surgery News. Each member provided a steady stream of commentaries, recommendations, and advice. The publication and the managing editor would have been lost without their kind and willing assistance. In their busy professional lives, they somehow found the time to contribute their expertise to assist their colleagues and their profession. We all owe them a debt of gratitude for their many years of service.
We hope our readers will find the list and the comments of interest.
Otolaryngology
St. Laurent J et al. HPV vaccination and the effects on rates of HPV-related cancers. Curr Probl Cancer 2018; https://doi.org/10.1016/j.currproblcancer.2018.06.004
As a head and neck surgeon over the past 30+ years, I have seen the dramaticrise of one form of HPV-related cancer in the United States, namely, HPV-associated oropharyngeal cancer. This is a true epidemic. It is also a cancer that may well be preventable through vaccination. We have slowly made progress over the past 4 decades in reducing the number of tobacco- and alcohol-related cancers. Here is another cancer that truly falls within the category of a public health problem for which public health solution of vaccination is clearly the most rational approach. Everyone should be aware of these virally induced cancers and what can be done to prevent them. This article presents the “state of the art” knowledge about these cancers and what we can hopefully accomplish through worldwide public health initiatives.
Mark C. Weissler, MD, FACS
Palliative Care
Kopecky KE et al. Third-year medical students’ reactions to surgical patients in pain: Doubt, distress, and depersonalization. J Pain and Symptom Manage. 2018;56(5):719-26.
This insightful study done by surgeons, two of them possessing palliative care and bioethics expertise, is a qualitative analysis of the content of 341 essays written by third-year medical students who described their experiences with surgical patients in pain. Students found it difficult to reconcile patient suffering with the therapeutic objective of treatment. As a result they learned constrained empathy and preference for technical solutions and because they feared an empathic response to pain might compromise the fortitude and efficiency required to be a doctor they pursued strategies to distance themselves from these feelings. The authors note, “Although doctors frequently interact with patients who have serious emotional and physical pain, few have received formal instruction on how to attend to these needs or developed a personal approach to cope with the tragedy of patient illness. Instead, the physician’s response to patients in pain is learned passively and perpetuated through generations. Students now seek to suppress empathy to get the job done. These observations have important implications for physicians, patients, and educators.” For me the study is like a parachute flare illuminating the landscape of early surgical educational experience during which the seeds for future problems such as lost patient trust and burnout are sown. It offers the hope that structured introspective activities may mitigate this.
Su A et al. Beyond pain: Nurses’ assessment of patient suffering, dignity, and dying in the intensive care unit. J Pain Symptom Manage. 2018;55:1591-98.
After reading this sobering study, my reaction was, “If the gold rusts what will happen to the iron?” In this study using chart abstraction, nurses caring for 200 patients in a tertiary care cardiac ICU and a surgical ICU were interviewed about their assessment and perception of the physical and psychosocial dimensions of ICU patients’ experiences in their final week of life. The authors note that nursing symptom assessments have been previously shown to be highly reliable and end-of-life comfort and dignity have been shown to be compatible with ICU level of care. Despite this and the availability of extensive interdisciplinary support from palliative care teams, chaplains, and social workers, dying ICU patients are perceived by nurses to experience extreme indignities and suffer beyond physical pain. The study found that attention to symptoms such as dyspnea and edema might improve the quality of death in the ICU. It is small wonder that moral fatigue and burnout have become prevalent themes of ICU caring.
Balboni T et al. The spiritual event of serious illness. J Pain Symptom Manage. 2018;56(5):816-22.
An ashen-faced dear friend gently reminded me as he was hemorrhaging from an advanced gastric cancer, “Geoff, lets make this a spiritual event, not a medical one.” This paper conjured up this memory with the thoughtful, in-depth account and analysis of patients’ experiences and attitudes that shaped the authors concept of illness as a spiritual event. The idea of spirituality as a basic component of consciousness, especially as it relates to suffering, has been present from the very beginning of modern palliative care and can be traced back to the concept of “total pain” introduced by Dame Cicely Saunders in 1963. The capacity to reframe biophysical calamity as spiritual opportunity is the signature of the most skilled and adroit supportive care we can offer our patients and their families.
Geoffrey P. Dunn, MD, FACS
Colorectal Surgery
Cercek A et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4(6):e180071. doi:10.1001/jamaoncol.2018.0071.
This moderate sized retrospective study demonstrates a single-institution’s experience with total neoadjuvant therapy (TNT) with chemoradiation and chemotherapy as opposed to traditional chemoradiation, surgery, and chemotherapy in patients with locally advanced rectal cancer. They demonstrate equivalent or potentially better outcomes including better complete response rate – 36% versus 21% and rates of chemotherapy completion. While further studies are needed to understand long term outcomes, this study support the use of TNT for locally advanced rectal cancer as now supported by the National Comprehensive Cancer Network guidelines.
Brouquet A et al. Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: Results of a prospective nationwide cohort. Ann Surg. 2018 Feb;267(2):221-228. doi: 10.1097/SLA.0000000000002017.
This large prospective study of almost 600 consecutive Crohn’s disease patients with surgery at 19 French specialty centers demonstrates that anti-TNF therapy less than 3 months prior to ileocolic surgery to be an independent risk factor of the overall postoperative morbidity, preoperative hemoglobin less than10 g/dL, operative time more than180 min, and recurrent Crohn’s disease, as well as a higher risk of overall and intra-abdominal septic postoperative morbidities.
Howard R et al. Taking control of your surgery: Impact of a prehabilitation program on major abdominal surgery. J Am Coll Surg. 2018 Oct 22; https://doi.org/10.1016/j.jamcollsurg.2018.09.018
Results from the Michigan Surgical and Health Optimization Program (MSHOP) are reported in colectomy patients. This prehabilitation program engages patients in four activities before surgery: physical activity, pulmonary rehabilitation, nutritional optimization, and stress reduction. MSHOP patients were matched to emergency and elective, non-MSHOP patients. Overall, 70% of MSHOP patients complied with the program. MSHOP patients were more likely to have improved blood pressure and heart rate intraoperatively, reduction in Clavien-Dindo class 3-4 complications in the MSHOP group (30%), compared with the nonprehabilitation (38%) and emergency (48%) groups (P = .05), as well as average savings of $21,946 per patient.
Genevieve Melton-Meaux, MD, PhD, FACS
Bariatric Surgery
Kalff MC et al. Diagnostic value of computed tomography for detecting anastomotic or staple line leakage after bariatric surgery. Surg Obes Relat Dis. 2018;14(9):1310-16
The most dreaded complication in the current era of metabolic and bariatric surgery, from a technical point of view, remains an anastomotic or staple-line leak. The authors present their findings corresponding to a multivariable regression analysis of a retrospective review of all CT abdomen and pelvis scans conducted from November 2007 to August 2016 at their large teaching hospital and Bariatric Center of Excellence. A CT is especially useful at ruling out low-suspicion cases of leaks, when the surgeon is trying to decide if a diagnostic laparoscopy is indicated, with a sensitivity of 90%-100%, and a negative predictive value of 97%-100%. A negative CT scan is highly accurate for ruling out a leak, especially in those patients without co-existing tachycardia and tachypnea. With caution based on clinical expertise, it may serve to prevent unnecessary diagnostic laparoscopy when appropriately indicated.
Alizadeh RF et al. Risk factors for gastrointestinal leak after bariatric surgery: MBSAQIP analysis. J Am Coll Surg. 2018;227(1):135-141.
The Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) 2015 database of accredited centers was the object of study. Multivariate logistic regression analysis was used to examine risk factors for GI leaks that are not typically included in similar studies. Of particular interest is finding that Roux-en-Y gastric bypass comes with a higher risk for leak, compared with a sleeve gastrectomy, but with an overall leak rate for both of 0.7% based on current results. In addition, the study found that use of an intraoperative provocative leak test and placement of a surgical drain are associated with a higher leak rate. The same is not true of a postoperative swallow contrast study, which has no effect on the incidence of leaks.
Altieri MS et al. Evaluation of VTE prophylaxis and the impact of alternate regimens on post-operative bleeding and thrombotic complications following bariatric procedures. Surg Endosc. 2018;32(12):4805-4812.
The field of venous thromboembolism prevention after bariatric surgery remains a challenging one due to the lack of consensus among surgeons. This study analyzes the Cerner Health Facts database from 2003 to 2013, particularly with ICD-9 codes, for patients undergoing Roux-en-Y gastric bypass and sleeve gastrectomy. While the authors confirm the statement that there is a lack of consistency and, therefore, there is ample variability among bariatric centers and surgeons, the use of postoperative VTE chemoprophylaxis leads to a lower incidence of VTE events, and less frequent bleeding episodes, compared with pre-operative chemoprophylaxis. Finally, mixed therapy using heparin and enoxaparin led to more bleeding complications and blood transfusion requirements.
Rodolfo J. Oviedo, MD, FACS, FASMBS
Cardiothoracic Surgery
Stone GW et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med. 2018 Sep 23; doi:10.1056/NEJMoa1806640.
This study, known as the COAPT trial, assessed the value of adding transcatheter mitral valve repair to best medical therapy for the treatment of moderate-to-severe or severe functional mitral regurgitation in patients with symptomatic heart failure. Not only was transcatheter mitral valve repair exceedingly safe (more than 96% freedom from device-related complications at 12 months), patients were hospitalized less for heart failure management and had lower all-cause mortality compared with best medical therapy alone. The results of the COAPT trial are an important step forward for transcatheter therapies, which are rapidly becoming an integral part of the treatment algorithms for structural heart disease.
Gaudino M et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N Engl J Med. 2018;378(22):2069-77.
This analysis of randomized trials comparing radial artery to saphenous vein grafts for coronary artery bypass surgery is quite possibly a practice-changing publication. Routine use of the left internal thoracic (mammary) artery is commonplace among cardiac surgeons; however, the debate over conduit choice for additional bypass grafts is a “tale as old as time.” This study, part of the RADIAL project, combined patient-level data from six trials in order to achieve adequate power to identify differences in clinical outcomes. The use of radial artery grafts as opposed to saphenous vein grafts was associated with less adverse cardiac events, a lower incidence of repeat revascularization, and a higher patency rate at 5 years. Although there was no difference in all-cause mortality, the results of this study support the use of radial artery grafts when additional conduits are needed in coronary artery bypass surgery.
Irving L. Kron, MD, FACS, and Eric J. Charles, MD, PhD
Vascular Surgery
Anand SS. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: An international, randomised, double-blind, placebo-controlled trial. Lancet 2018;391(10117):219-29.
This landmark study was terminated early due to a significant difference in outcomes. Prior to this point, aspirin and statins have been the mainstay of decreasing long-term adverse outcomes for patients with vascular disease. The COMPASS study has found a decrease in combined cardiovascular adverse events when rivaroxaban 2.5 mg was combined with low-dose aspirin in patients with stable PAD or CAD over aspirin alone. This is the first major change supporting use of additional medications for PAD in over 2 decades, when statins were found to impact outcomes. The differences were not impacted by gender, age, or race. Patients with end-tage renal disease were excluded, so it is unclear whether it would be beneficial in this population. The higher rate of bleeding, 3.1% vs 1.9%, was primarily GI, so caution should be used if patients are felt to be at increased risk of bleeding.
These findings suggest the need for a major change in the guidelines and management for the majority of our patients with PAD. Certainly we should look to add this data point to the Vascular Quality Initiative to gather further data and confirm the findings in real world use. It is unclear whether this benefit will be unique to rivaroxaban, or whether other Direct Xa inhibitors will have similar effects. I will certainly be adding ribaroxaban to patients at low risk for bleeding based on this data. Further, rivaroxaban alone did not reduce major cardiovascular adverse events, but did reduce major adverse limb events.
Gohel MS et al. A randomized trial of early endovenous ablation in venous ulceration. N Engl J Med. 2018;378:2105-14.
This multicenter study in the UK looked at over 450 patients with venous ulceration. Deep-venous reflux was also present in one-third of patients in each group. The median time to ulcer healing was decreased significantly from 82 days to 56 days. This study demonstrates the importance of early intervention for superficial reflux to enhance ulcer healing and decrease risk of recurrence. This study found that early endovenous ablation resulted in faster healing of venous ulcers, and more ulcer-free time than delayed intervention in patients treated with maximal medical therapy, including appropriate compression therapy. Previously, ablation was typically planned after ulcers healed to decrease risk of recurrence. Based on these findings, ablation should be offered to patients with nonhealing venous ulcers early in the course of therapy, in addition to standard wound care.
Linda Harris, MD, FACS
Surgical Education
Ellison EC. Ten-year reassessment of the shortage of general surgeons: Increases in graduation numbers of general surgery residents are insufficient to meet the future demand for general surgeons. Surgery. 2018 Oct;164(4):726-32.
Ellison EC et al. The impact of the aging population and incidence of cancer on future projections of general surgery workforce needs. Surgery. 2018 Mar;163(3):553-59.
In 2008, Ellison et al. projected that a deficit in the general surgery workforce would grow to 19% by 2050. The group recently re-examined this projection by reviewing Census Bureau data, the available pool of surgeons with both allopathic and osteopathic degrees and factored in the losses of new surgeons who subspecialize and older surgeons who retire every year. Their conclusion states that, without increasing future general surgeons training numbers, the projected future general surgery workforce shortage will continue to grow.
A second paper by the same group reviewed population and age-adjusted incidence of cancer to estimate the number of general surgeons needed for initial surgical treatment of the patient with cancer in the year 2035 compared with 2010. The total number of new patients with cancers treated by general surgeons is projected to increase 56% in that time span. This would require an increase of over 9,000 general surgeons over that based on current training numbers. Together, the papers predict that there will be an ever-increasing demand for general surgeons in the near future and that general surgeons, currently caring for over 50% of cancer patients in the US, will play an even more important role in surgical cancer treatment.
Michael D. Sarap, MD, FACS
General Surgery
Takada T. Tokyo Guidelines 2018 (TG18). J Hepatobiliary Pancreat Sci. 2018 Jan;25(1):1-2.
This is the updated set of guidelines, awaited since 2013, regarding treatment of acute cholecystitis and cholangitis, with updated management strategies from an international panel of experts. The most significant change, and considered overdue by some surgeons, is the modification of the management algorithm to propose that some patients with Grade III acute cholecystitis (severe cholecystitis with evidence of organ dysfunction) may be treated with immediate laparoscopic cholecystectomy, rather than percutaneous cholecystostomy, “when performed at advanced centers with specialized surgeons experienced in this procedure.” As cholecystectomy is the most common general surgery procedure in the United States, most community surgeons have expertise. Whether there is truly need of a specialized gallbladder surgeon at an advanced center to safely complete a laparoscopic cholecystectomy can still be debated. But the change in recommendation from the experts is welcome.
Acuna SA. Operative strategies for perforated diverticulitis: A systematic review and meta-analysis. Dis Colon Rectum. 2018 Dec; 61(12):1442-53.
This analysis of the literature considers the three predominant operations for Hinchey III and Hinchey IV perforated diverticulitis: Hartmann procedure, resection and primary anastomosis, and laparoscopic lavage. The importance of this review is that it considers the initial operation and the downstream procedures when determining overall morbidity and mortality. Laparoscopic lavage did not fare well in this review of randomized controlled trials, resulting in higher morbidity than resection in Hinchey III patients. Interestingly, none of the individual studies analyzed had shown a statistical difference, but in the meta-analysis, the number of patients was sufficient to show statistical significance. The other important conclusion was that primary resection with anastomosis (possibly with diverting ileostomy) was superior to Hartmann procedure, when the likelihood of stoma reversal and the morbidity of the second operation was taken into account.
Mark Savarise, MD, FACS
Foregut
Alicuben ET. Worldwide experience with erosion of the magnetic sphincter augmentation device. J Gastrointest Surg. 2018; 22(8):1442-47.
Although magnetic sphincter augmentation of the lower esophageal sphincter initially appeared to provide excellent reflux control with essentially no risk of erosion, there have now been multiple reports throughout the world of device erosion over time. Fortunately, most erosions occurred with the smallest available device which is no longer on the market and the erosions currently being treated are usually done so with endoscopic/laparoscopic removal without the need for major esophageal resection.
Xiong YQ. Comparison of narrow-band imaging and confocal laser endomicroscopy for the detection of neoplasia in Barrett’s esophagus: A meta-analysis. Clin Res Hepatol Gastroenterol. 2018 Feb;42(1):31-9.
The days of endoscopic screening and surveillance of patients at risk for the development of Barrett’s esophagus via four-quadrant biopsy every couple of centimeters are numbered. The use of confocal laser microscopy to provide accurate real-time visual data regarding the areas of interest in the esophagus is showing promise and gaining traction compared to standard biopsy techniques and narrow-band imaging.
Borbély Y. Electrical stimulation of the lower esophageal sphincter to address gastroesophageal reflux disease after sleeve gastrectomy. Surg Obes Relat Dis. 2018 May;14(5):611-5.
The development of GERD following sleeve gastrectomy is a real problem in a substantial minority of patients due to structural compromise of the lower esophageal sphincter during the procedure. Conversion to gastric bypass as a way to alleviate acid regurgitation has been the mainstay of treatment; however, many patients selected sleeve gastrectomy specifically because they did not want to undergo gastric bypass. For those patients a sleeve preserving procedure such as magnetic sphincter augmentation (currently in clinical trial), Hill procedure, or remnant gastric fundoplication are potential options. Electrical stimulation of the lower esophageal sphincter is revealing itself to be another exciting option (currently in clinical trial) which can be used in patients with as few as 30% peristaltic swallows thus expanding the treatment options for these deserving patients.
Kevin M. Reavis, MD, FACS
Trauma/Critical Care
Teixeira PGR et al. Civilian prehospital tourniquet use is associated with improved survival in patients with peripheral vascular injury . J Am Coll Surg. 2018;226(5):769-76.
The use of tourniquets for hemorrhage control in trauma patients has been widely condemned in the past because of concerns regarding complications and potential limb loss. However, evidence from liberal tourniquet use in combat situations documenting survival benefits has continued to accumulate. Prompt hemorrhage control in trauma patients, including the use of tourniquets where applicable, has been validated by recent combat zone studies but improved survival hasn’t yet been shown in the civilian setting. In this multicenter, retrospective study of 1,026 patients with peripheral vascular injuries, only a relatively small number (17.6%) had pre-hospital tourniquets applied, yet multivariable analysis showed a significant survival benefit (odds ratio, 5.86). Importantly, no difference was seen in delayed amputation rates, of approximately 1% in both groups. This study helps to emphasize the importance of the Stop the Bleed (STB) campaign which includes education on the effective and safe use of tourniquets for prehospital hemorrhage. The STB program offers surgeons the opportunity to educate members of their own communities in effective bystander first aid.
Pileggi C et al. Ventilator bundle and its effects on mortality among ICU patients: A meta-analysis. Crit Care Med. 2018;46(7):1167-74.
Critically ill patients requiring mechanical ventilation are at risk for a number of complications, including ventilator-associated pneumonia (VAP) (now a subset of ventilator-associated events (VAE) which prolong ventilator and ICU time and contribute to further complication. Ventilator “bundles,” incorporating simple measures such as elevation of the head of the bed; daily “sedation holidays”; and evaluation of readiness for extubation, peptic ulcer, and DVT prophylaxis have been widely used in ICUs for nearly 20 years. Effective implementation has also emphasized multidisciplinary teamwork. Reductions in ventilator-associated pneumonia (VAP) incidence have been widely demonstrated but mortality benefits have been inconsistent. In this meta-analysis of 13 studies, 6 in Europe, 6 in the US and 1 in Brazil, an overall reduction in mortality (odds ratio, 0.9) was demonstrated. The effect was even larger when limited to studies with patients with VAP (OR, 0.71). This study both validates the effectiveness of relatively simple and inexpensive measures and emphasizes the benefits of a team approach to the care of ICU patients.
Krista L. Kaups, MD, FACS
NAMDRC update
NAMDRC focuses on keeping its members informed on legislative and regulatory issues impacting their practices.
Today, those agreements have been replaced by employment contracts or simply disappeared entirely, replaced by various business models that have invariably shifted the focus of coverage and payment issues away from the group practice into significantly different financial incentives. The challenge for NAMDRC is to keep its members informed about structural changes in coverage and payment rules that could impact their decision making. In November 2018, CMS published three distinctly separate sets of rules slated to take effect in 2019, all of which affect physicians in the pulmonary, critical care, and sleep landscapes. Through the monthly membership publication, the Washington Watchline, members get timely information that impact their practices. Excerpts from a recent Watchline include:
Physician fee schedule: As most physicians know, CMS had proposed dramatic changes to payment for Level 4 and Level 5 E&M codes, but due to strong reaction from many within the medical community, CMS is withdrawing that specific proposal, at least in the short term. Related provisions include:
• For CY 2019 and 2020, CMS will continue the current coding and payment structure for E/M office/outpatient visits,
• Effective January 1, 2019, for new and established patients for E/M office/outpatient visits, practitioners need not re-enter in the medical record information on the patient’s chief complaint and history that has already been entered by ancillary staff or the beneficiary. The practitioner may simply indicate in the medical record that he or she reviewed and verified this information.
• For 2021, CMS is finalizing a significant reduction in the current payment variation in office/outpatient E/M visit levels by paying a single rate for E/M office/outpatient visit levels 2, 3, and 4 (one for established and another for new patients) beginning in 2021. However, CMS is not finalizing the inclusion of E/M office/outpatient level 5 visits in the single payment rate, to better account for the care and needs of particularly complex patients.
• CMS policy for 2021 will adopt add-on codes that describe the additional resources inherent in visits for primary care and particular kinds of specialized medical care. As discussed further below, these codes will only be reportable with E/M office/outpatient level 2 through 4 visits, and their use generally will not impose new per-visit documentation requirements.
Hospital outpatient rules: There are two particularly relevant issues addressed in this final regulation. The payment rates for pulmonary rehab are:
Pulmonary Rehab via G0424 – APC 5733, $55.90 with co-pay of $11.18
Pulmonary Rehab via G0237, 38, 39 – APC 5732, $32.12 with co-pay of $6.43
This regulation is also the vehicle for CMS addressing issues related to Section 603/site of service payment issues. As physicians know, CMS enacted Section 603 of the 23015 Budget Act that puts notable restrictions on payment for certain hospital outpatient services provided off campus (more than 250 yards from main campus of the hospital). NAMDRC is most concerned about the impact on pulmonary rehab – under the rules, off-campus programs that are grandfathered (“excepted” is the CMS term) as long as they were billing for those services at that location November 2015. However, if a hospital chooses to open a new program, or relocate an existing program to a different location, the payment principles that apply are physician fee schedule rates rather than hospital outpatient rates. In the proposed rule posted this past July, CMS had proposed that even a new service provided in an excepted (grandfathered) setting would be subject to PFS payment rates rather than hospital outpatient rates. CMS has withdrawn that proposal for the coming year, so new services in excepted settings will be covered. “Excepted” is actually CMS’ terminology, which is used to refer to off-campus outpatient facilities that were offering services in November 2015. Services that do not meet that singular criterion are considered nonexcepted (not grandfathered), and those services are paid at the physician fee schedule rate.
DME: In its proposed rule this past summer, CMS actually acknowledged flaws in the structure of the competitive bidding system for DME (including oxygen, CPAP, and certain ventilators referred to by CMS as respiratory assist devices). Specifically, related to oxygen, there is also acknowledgement of reductions in liquid oxygen utilization, a story we have been pushing for years. The CMS proposed rule would have tied liquid portable payment rates to portable concentrator and transfill system payment rates, a genuine bump in actual $$. More than a dozen societies joined to respond to the proposed rule, including NAMDRC, CHEST, and ATS.
In the final rule, CMS is moving forward with its proposal, acknowledging that it will need to monitor shifts in the oxygen marketplace and adjust their payment policies accordingly.
NAMDRC focuses on keeping its members informed on legislative and regulatory issues impacting their practices.
Today, those agreements have been replaced by employment contracts or simply disappeared entirely, replaced by various business models that have invariably shifted the focus of coverage and payment issues away from the group practice into significantly different financial incentives. The challenge for NAMDRC is to keep its members informed about structural changes in coverage and payment rules that could impact their decision making. In November 2018, CMS published three distinctly separate sets of rules slated to take effect in 2019, all of which affect physicians in the pulmonary, critical care, and sleep landscapes. Through the monthly membership publication, the Washington Watchline, members get timely information that impact their practices. Excerpts from a recent Watchline include:
Physician fee schedule: As most physicians know, CMS had proposed dramatic changes to payment for Level 4 and Level 5 E&M codes, but due to strong reaction from many within the medical community, CMS is withdrawing that specific proposal, at least in the short term. Related provisions include:
• For CY 2019 and 2020, CMS will continue the current coding and payment structure for E/M office/outpatient visits,
• Effective January 1, 2019, for new and established patients for E/M office/outpatient visits, practitioners need not re-enter in the medical record information on the patient’s chief complaint and history that has already been entered by ancillary staff or the beneficiary. The practitioner may simply indicate in the medical record that he or she reviewed and verified this information.
• For 2021, CMS is finalizing a significant reduction in the current payment variation in office/outpatient E/M visit levels by paying a single rate for E/M office/outpatient visit levels 2, 3, and 4 (one for established and another for new patients) beginning in 2021. However, CMS is not finalizing the inclusion of E/M office/outpatient level 5 visits in the single payment rate, to better account for the care and needs of particularly complex patients.
• CMS policy for 2021 will adopt add-on codes that describe the additional resources inherent in visits for primary care and particular kinds of specialized medical care. As discussed further below, these codes will only be reportable with E/M office/outpatient level 2 through 4 visits, and their use generally will not impose new per-visit documentation requirements.
Hospital outpatient rules: There are two particularly relevant issues addressed in this final regulation. The payment rates for pulmonary rehab are:
Pulmonary Rehab via G0424 – APC 5733, $55.90 with co-pay of $11.18
Pulmonary Rehab via G0237, 38, 39 – APC 5732, $32.12 with co-pay of $6.43
This regulation is also the vehicle for CMS addressing issues related to Section 603/site of service payment issues. As physicians know, CMS enacted Section 603 of the 23015 Budget Act that puts notable restrictions on payment for certain hospital outpatient services provided off campus (more than 250 yards from main campus of the hospital). NAMDRC is most concerned about the impact on pulmonary rehab – under the rules, off-campus programs that are grandfathered (“excepted” is the CMS term) as long as they were billing for those services at that location November 2015. However, if a hospital chooses to open a new program, or relocate an existing program to a different location, the payment principles that apply are physician fee schedule rates rather than hospital outpatient rates. In the proposed rule posted this past July, CMS had proposed that even a new service provided in an excepted (grandfathered) setting would be subject to PFS payment rates rather than hospital outpatient rates. CMS has withdrawn that proposal for the coming year, so new services in excepted settings will be covered. “Excepted” is actually CMS’ terminology, which is used to refer to off-campus outpatient facilities that were offering services in November 2015. Services that do not meet that singular criterion are considered nonexcepted (not grandfathered), and those services are paid at the physician fee schedule rate.
DME: In its proposed rule this past summer, CMS actually acknowledged flaws in the structure of the competitive bidding system for DME (including oxygen, CPAP, and certain ventilators referred to by CMS as respiratory assist devices). Specifically, related to oxygen, there is also acknowledgement of reductions in liquid oxygen utilization, a story we have been pushing for years. The CMS proposed rule would have tied liquid portable payment rates to portable concentrator and transfill system payment rates, a genuine bump in actual $$. More than a dozen societies joined to respond to the proposed rule, including NAMDRC, CHEST, and ATS.
In the final rule, CMS is moving forward with its proposal, acknowledging that it will need to monitor shifts in the oxygen marketplace and adjust their payment policies accordingly.
NAMDRC focuses on keeping its members informed on legislative and regulatory issues impacting their practices.
Today, those agreements have been replaced by employment contracts or simply disappeared entirely, replaced by various business models that have invariably shifted the focus of coverage and payment issues away from the group practice into significantly different financial incentives. The challenge for NAMDRC is to keep its members informed about structural changes in coverage and payment rules that could impact their decision making. In November 2018, CMS published three distinctly separate sets of rules slated to take effect in 2019, all of which affect physicians in the pulmonary, critical care, and sleep landscapes. Through the monthly membership publication, the Washington Watchline, members get timely information that impact their practices. Excerpts from a recent Watchline include:
Physician fee schedule: As most physicians know, CMS had proposed dramatic changes to payment for Level 4 and Level 5 E&M codes, but due to strong reaction from many within the medical community, CMS is withdrawing that specific proposal, at least in the short term. Related provisions include:
• For CY 2019 and 2020, CMS will continue the current coding and payment structure for E/M office/outpatient visits,
• Effective January 1, 2019, for new and established patients for E/M office/outpatient visits, practitioners need not re-enter in the medical record information on the patient’s chief complaint and history that has already been entered by ancillary staff or the beneficiary. The practitioner may simply indicate in the medical record that he or she reviewed and verified this information.
• For 2021, CMS is finalizing a significant reduction in the current payment variation in office/outpatient E/M visit levels by paying a single rate for E/M office/outpatient visit levels 2, 3, and 4 (one for established and another for new patients) beginning in 2021. However, CMS is not finalizing the inclusion of E/M office/outpatient level 5 visits in the single payment rate, to better account for the care and needs of particularly complex patients.
• CMS policy for 2021 will adopt add-on codes that describe the additional resources inherent in visits for primary care and particular kinds of specialized medical care. As discussed further below, these codes will only be reportable with E/M office/outpatient level 2 through 4 visits, and their use generally will not impose new per-visit documentation requirements.
Hospital outpatient rules: There are two particularly relevant issues addressed in this final regulation. The payment rates for pulmonary rehab are:
Pulmonary Rehab via G0424 – APC 5733, $55.90 with co-pay of $11.18
Pulmonary Rehab via G0237, 38, 39 – APC 5732, $32.12 with co-pay of $6.43
This regulation is also the vehicle for CMS addressing issues related to Section 603/site of service payment issues. As physicians know, CMS enacted Section 603 of the 23015 Budget Act that puts notable restrictions on payment for certain hospital outpatient services provided off campus (more than 250 yards from main campus of the hospital). NAMDRC is most concerned about the impact on pulmonary rehab – under the rules, off-campus programs that are grandfathered (“excepted” is the CMS term) as long as they were billing for those services at that location November 2015. However, if a hospital chooses to open a new program, or relocate an existing program to a different location, the payment principles that apply are physician fee schedule rates rather than hospital outpatient rates. In the proposed rule posted this past July, CMS had proposed that even a new service provided in an excepted (grandfathered) setting would be subject to PFS payment rates rather than hospital outpatient rates. CMS has withdrawn that proposal for the coming year, so new services in excepted settings will be covered. “Excepted” is actually CMS’ terminology, which is used to refer to off-campus outpatient facilities that were offering services in November 2015. Services that do not meet that singular criterion are considered nonexcepted (not grandfathered), and those services are paid at the physician fee schedule rate.
DME: In its proposed rule this past summer, CMS actually acknowledged flaws in the structure of the competitive bidding system for DME (including oxygen, CPAP, and certain ventilators referred to by CMS as respiratory assist devices). Specifically, related to oxygen, there is also acknowledgement of reductions in liquid oxygen utilization, a story we have been pushing for years. The CMS proposed rule would have tied liquid portable payment rates to portable concentrator and transfill system payment rates, a genuine bump in actual $$. More than a dozen societies joined to respond to the proposed rule, including NAMDRC, CHEST, and ATS.
In the final rule, CMS is moving forward with its proposal, acknowledging that it will need to monitor shifts in the oxygen marketplace and adjust their payment policies accordingly.
Current Concepts: Evaluation and Treatment of Discoid Meniscus in the Pediatric Athlete
ABSTRACT
Discoid meniscus is a rare anatomical variant with altered morphology and structure that can sometimes present symptomatically, typically in the pediatric population. The discoid meniscus is usually in the lateral compartment of the knee and is characterized by a partial or complete filling-in of central meniscal tissue, increased meniscal thickness, disorganization of longitudinal collagen fibers, and sometimes lack of peripheral attachments. These changes to both the macro- and micro-structure of the meniscus predispose affected patients to increased rates of both meniscal tears and mechanical symptoms. Surgical management of symptomatic discoid meniscus is directed toward symptom resolution while preserving sufficient functional meniscal tissue to delay or prevent the development of osteoarthritis. Modern surgical techniques consist of arthroscopic saucerization of the discoid meniscus with repair of associated meniscal tears and stabilization of peripheral attachments. Although long-term outcome data are lacking, short- and mid-term outcomes for patients treated with arthroscopic partial meniscectomy and meniscal repair and/or stabilization as needed are generally good.
Continue to: The discoid meniscus...
The discoid meniscus is an uncommon anatomical meniscal variant that may present with pain, snapping, motion loss, swelling, and locking of the affected knee, typically during childhood or adolescence.1 Although the etiology of discoid meniscus is not completely understood, it is considered a congenital anomaly with a possible genetic component.2, 3 Incidence is estimated at 0.4% to 5.2% in the Western European population but is reportedly much higher (roughly 17%) in Asian populations.4-6, Discoid menisci, when present, are almost always in the lateral compartment, although cases of medial discoid meniscus have also been reported. The overall incidence of medial discoid meniscus has been estimated to be between 0.06% and 0.3% while that of lateral discoid meniscus, as detailed above, is significantly higher.7-11
ANATOMY AND MORPHOLOGY
The menisci differentiate from mesenchymal tissue early during fetal development with a clear definition by 8 weeks and a mature anatomical shape by 14 weeks in utero.12 Interestingly, menisci never possess a discoid shape during the normal course of development.13,14 The meniscus is fully vascularized at birth, with the central one-third becoming avascular by 9 months as the vascular supply regresses.14 By 10 years, only the peripheral one-third maintains its vascular supply, and the menisci have adult-like characteristics with tissue composed mainly of circumferential collagen fibers.4,14-16
A normal meniscus is wedge-shaped in the coronal plane and crescent-shaped in the axial plane. The medial meniscus is shaped like the letter “C,” is connected firmly to the joint capsule, and covers approximately 50% of the medial tibial plateau. The normal lateral meniscus covers 70% of the lateral tibial plateau and has firm anterior and posterior attachments while the lateral portion is less securely tethered.17 A discoid meniscus is characterized by an atypical shape—the center being partially or completely filled in (or “disc-like”)—often associated with anomalous attachments to the tibia, femur, and surrounding joint capsule. In addition to an atypical morphology, the discoid meniscus may also be much thicker than normal, resulting in a “block-like” appearance. The increased thickness may be responsible for the pathognomonic snapping of the knee as it is brought passively into flexion or extension (hence, the term “snapping knee” was traditionally used to describe a symptomatic discoid lateral meniscus). While the discoid shape is relatively straightforward to address, the increased meniscal thickness may be quite difficult to correct surgically.4-6,18
In addition to the macromorphological differences characteristic of discoid menisci, histological differences have also been described, including differences in collagen density and disorganization of the circumferential collagen network.19-21 Taken together, these differences may compromise the ability of the discoid meniscus to withstand normal forces placed across the knee and predispose it to tear. This is important because the normal meniscus plays a critical role in facilitating load distribution across the knee joint, in addition to assisting with functions including shock absorption, proprioception, and stabilization of the knee. Torn and/or unstable discoid menisci are unable to perform these functions adequately, which may ultimately result in degenerative joint disease and progress to end-stage osteoarthritis (OA).
CLASSIFICATION
The traditional Watanabe classification of discoid meniscus consists of 3 variants: type I, a complete discoid shape; type II, an incomplete discoid shape; and type III, the Wrisberg variant.22 The Wrisberg variant is described as a more normal-appearing meniscus but lacks normal peripheral attachments.5, 6, 15 This classification system was expanded by Monllau and colleagues, 23 who described a ring-type meniscus variant with normal posterior tibial attachments. Although the Watanabe classification is commonly used, its utility in assisting with clinical decision-making may be limited.
Continue to: Several other classification schemes...
Several other classification schemes exist. Jordan and colleagues24 described a classification scheme defining a meniscal type as complete or incomplete, also noting the presence of symptoms, tearing, and peripheral rim instability. They grouped stable types together, regardless of morphology, and then further classified them based on the presence of symptoms and tears. Similarly, the unstable types were grouped together and then subclassified in the same manner.17,24 Klingele and colleagues25 also described a contemporary classification scheme of discoid meniscus evaluating peripheral stability patterns that may be more clinically and surgically relevant. This classification is based on the type of discoid morphology (complete vs incomplete), the presence or absence of peripheral rim stability (stable vs unstable), and the presence or absence of a meniscal tear (torn vs untorn).5,25
EVALUATION
A stable discoid meniscus is often an incidental finding, seen either on advanced diagnostic imaging performed for another reason or at the time of arthroscopy to address another problem. Younger children with discoid meniscus tend to present with symptoms such as popping and snapping related to instability and the abnormal morphology of the discoid meniscus. Older patients tend to present with symptoms related to acute tears through the abnormal meniscal tissue. Although discoid menisci can become acutely symptomatic in the presence of a tear, the onset of symptoms may occur in the absence of a discrete traumatic event.1 Alternatively, some patients will report a clear history of injury, often a noncontact, rotational injury mechanism related to an athletic activity. Patients with torn discoid menisci may report pain, catching, locking, and/or giving way of the knee, and on examination may have limited extension, snapping, effusion, quadriceps atrophy, and joint line tenderness. Eponymous meniscal compression tests including the McMurray, Apley, and Thessaly tests, may also be performed when meniscal tear is suspected, although this may be tricky for younger children.1
Considering the high association of meniscal tears with ligamentous injuries, examination of knee stability is important. Plain radiographs of the knee should be taken, although the results will often be negative for osseous injury in the case of an isolated meniscal tear. Radiographs of a discoid knee may show subtle differences compared with radiographs of a non-discoid knee. A recent comparison of children with symptomatic lateral discoid menisci with age-matched controls found statistically significant increased lateral joint space, elevated fibular head, increased height of the lateral tibial spine, and increased obliquity of the tibial plateau.26 They did not find statistically significant increased squaring of the lateral femoral condyle or cupping of the lateral tibial plateau. Radiographic signs can be subtle and may not all be present in a patient with a discoid meniscus.
Magnetic resonance imaging (MRI) is the assessment technique of choice for the diagnosis of discoid meniscus, although MRI may not reliably identify a Wrisberg variant or incomplete discoid menisci (Figure 1).
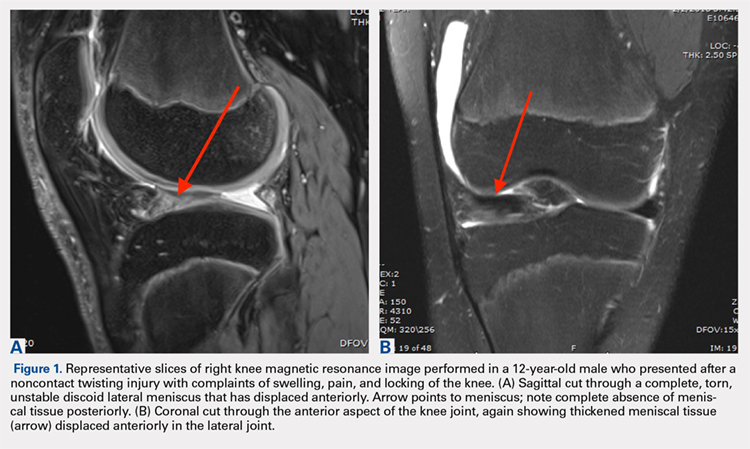
Gans and colleagues27 examined preoperative MRI and clinical examination compared with pathology found during arthroscopy. Although they found that MRI and clinical examination had excellent diagnostic accuracy of 92.7% and 95.3%, respectively, the most common missed pathology on MRI later found on diagnostic arthroscopy was the presence of a lateral discoid meniscus, which occurred in 26.7% of missed diagnoses. Adult diagnostic criteria of discoid meniscus include ≥3 contiguous 5-mm sagittal cuts showing continuity between the anterior and posterior horns of the meniscus. Other criteria include a minimal meniscal width >15 mm on the coronal view or a minimum meniscal width that is >20% of the width of the maximal tibial width.28 These criteria are often applied to children as well. Additionally, if >50% of the lateral joint space is covered by meniscal tissue, a diagnosis of discoid meniscus should be considered.6
Continue to: TREATMENT
TREATMENT
Management of symptomatic discoid meniscus is directed toward resolving symptoms while preserving meniscal tissue and preventing the development of OA. Incidentally found discoid menisci in asymptomatic patients should not be treated surgically and can have periodic follow-ups for detection of any functional deterioration or symptom development. Surgical treatment may be beneficial for patients with symptoms related to their discoid menisci such as pain, recurrent effusion, limited knee motion, mechanical symptoms (e.g., locking and catching), and activity restrictions.
Traditionally, surgical treatment of a symptomatic discoid meniscus consisted of subtotal (meaning nearly complete, or <3mm of peripheral rim remaining) or complete meniscectomy, often performed in an open fashion. Surgical techniques have evolved; current surgical approaches typically include diagnostic arthroscopy followed by arthroscopic saucerization (also called partial meniscectomy) of the central portion of the “disc,” leaving a peripheral rim of 6 mm to 8 mm to approximate that of the normal meniscus (Figure 2).29,30 Saucerization removes the redundant central meniscal tissue in an attempt to create a more “normal” C-shaped morphology, although it does not address the increased thickness characteristic of many discoid menisci. It may be particularly difficult to “debulk” an abnormally thick discoid meniscus in the coronal plane, and there is little in the outcomes literature to support this approach. Following partial meniscectomy, the remaining meniscal tissue should be inspected thoroughly both for the presence of instability and for residual tears. Meniscal tears should be repaired in standard fashion; commonly, this may be a combination of all-inside sutures placed into the posterior horn, inside-out sutures placed into the midbody, and outside-in sutures placed into the anterior horn. Peripheral rim instability—identified, for example, by the ability to translate the posterior horn of the meniscus fully onto the anterior tibial plateau—should be addressed by suturing the meniscus to the adjacent capsule (Figure 2).25, 31 Menisci that have residual complex tears that are not amenable to repair may be treated by subtotal meniscectomy. These patients may be candidates for subsequent meniscal allograft transplantation.32,33
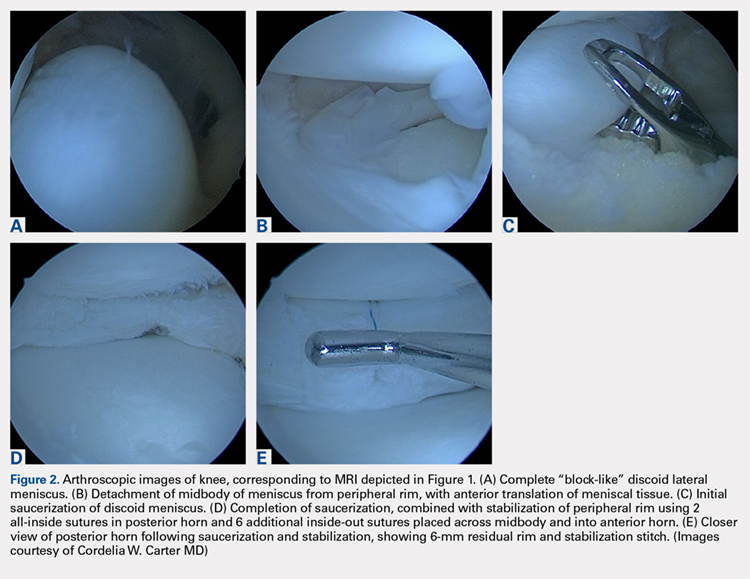
TREATMENT OUTCOMES
Performing a partial meniscectomy has consistently been shown in the laboratory to increase contact stresses proportionally to the percentage of tissue removed.34 It follows logically that performing a subtotal or complete meniscectomy in a young patient would yield increased, abnormal contact stresses throughout the knee with resultant degenerative changes and progression to OA over time. While long-term outcome studies of subtotal or complete meniscectomy have shown somewhat variable results, the majority report the development of pain, instability, poor function, osteoarthritic changes and even the development of osteochondritis desiccans.5,35
In an early investigation of long-term outcomes associated with surgical resection of a discoid lateral meniscus, Räber and colleagues36 retrospectively examined 17 knees that had undergone total meniscectomy for the lateral discoid meniscus. At a mean follow-up of 19.8 years, these authors reported that patients accounting for 10 of 17 operative knees had developed symptoms of osteoarthrosis such as pain. In addition, two-thirds of the knees that had follow-up radiographs performed (10 of 15 knees) had visible osteoarthritic changes present.
In 2011, Stilli and colleagues37 conducted a mid-term follow-up study examining 104 knees over an average follow-up of 8.5 years, with an average age of 8 years at the time of surgery. Younger patients, 2 to 7 years, underwent subtotal meniscectomy whereas patients, 8 to 14 years, underwent arthroscopic partial meniscectomy. Patients with a Wrisberg variant underwent removal of the posterior horn. The authors of this study reported that younger patients who had undergone subtotal meniscectomy had the best outcomes (defined by self-reported questionnaire responses and clinical evaluation). However, these results should be interpreted with caution: at the time of follow-up, patients in this study would still have been in adolescence and may not yet have developed the symptomatic degenerative changes in the knee joint that are strongly associated with meniscectomy.
Continue to: There are a few long-term...
There are few long-term outcome studies for arthroscopic saucerization. In 2014, Ahn and colleagues38 examined patient-reported outcomes and radiographic changes for 48 knees in pediatric patients treated arthroscopically for a symptomatic discoid meniscus. Patients were treated with partial meniscectomy (22 knees), partial meniscectomy with meniscal repair (18 knees), or subtotal meniscectomy (8 knees). Out of 48 knees evaluated, 45 knees (94%) were rated as “excellent” or “good” at an average 10-year follow-up. However, a significant percentage of patients had evidence of degenerative changes on follow-up radiographs, specifically: 88% of the subtotal meniscectomy group, 39% of the partial meniscectomy with repair group, and 23% in the partial meniscectomy-alone group. This finding suggests that the early appearance of radiographic changes suggestive of OA does not necessarily correlate with the development of knee symptoms in this cohort, although longer-term follow-up of these patients into adulthood and middle age is clearly needed.
Recently, short-term outcomes have been reported for contemporary arthroscopic saucerization of discoid menisci with peripheral rim stabilization performed as deemed necessary at the time of surgery. In 2012, Carter and colleagues39 examined 57 knees that underwent saucerization alone or saucerization with peripheral rim stabilization. At an average follow-up of 15 months, both patient populations had equivalent self-reported outcomes and clinical examination findings. The authors concluded that peripheral stabilization does not negatively affect short-term outcomes if instability is recognized and treated.
Yoo and colleagues40 found equivalent results between patients undergoing saucerization, saucerization with rim stabilization, and subtotal meniscectomy for 100 pediatric knees with an average follow-up of 4.7 years. Subtotal meniscectomy was defined as <3 mm of peripheral rim remaining and was performed when there was severe degeneration or complex tearing of the remnant rim following arthroscopic saucerization. Taken together, these data seem to suggest that short- and mid-term outcomes for pediatric patients treated surgically are generally good in terms of reported clinical function and development of OA, although long-term follow-up studies will be essential for understanding the true impact of surgical interventions.
Shieh and colleagues41,42 investigated risk factors for failed meniscal surgery in 324 menisci from 2008 to 2012, including in 46 discoid saucerization procedures with or without stabilization. At a mean of 40 months, 15% of the discoid saucerization cohort required a revision procedure, with increased odds of revision surgeries in patients who had undergone meniscal tear repair. The most frequent indication of revision surgery was sustaining a meniscal tear during intense physical activity in the first year after the index procedure, and patients underwent either debridement or repair for their revision procedure.
SUMMARY
Discoid meniscus is a rare anatomical meniscal variant characterized by an abnormal “O-like” shape, increased meniscal thickness, disorganization of collagen fibers, and variable absence of peripheral attachments. These morphological changes predispose patients with discoid menisci to increased rates of symptomatic meniscal instability and tearing. An MRI remains the most sensitive imaging modality for the diagnosis of a discoid meniscus, with ≥3 contiguous 5-mm sagittal cuts showing continuity between the anterior and posterior horns indicative of a discoid variant. Surgical treatment for symptomatic discoid menisci has evolved from subtotal meniscectomy to contemporary arthroscopic saucerization techniques with repair of meniscal tears and peripheral stabilization performed as needed. Long-term outcome studies for patients who undergo subtotal or complete meniscectomy reveal an association with osteoarthritic changes of the knee. Short- and mid-term outcome studies for patients who undergo arthroscopic saucerization with or without repair and/or peripheral stabilization are generally good, although reoperation rates have been estimated at 15% in the first 3 to 4 years. Longer-term follow-up, with the inclusion of validated functional outcomes measures, will be essential for understanding the true impact of various surgical interventions over time.
1. Yaniv M, Blumberg N. The discoid meniscus. J Child Orthop. 2007;1(2):89-96. doi: 10.1007/s11832-007-0029-1.
2. Gebhardt M, Rosenthal R. Bilateral lateral discoid meniscus in identical twins. J Bone Joint Surg Am. 1979;61(7):1110-1111. doi: 10.2106/00004623-197961070-00027.
3. Dashefsky JH. Discoid lateral meniscus in three members of a family. J Bone Joint Surg, (Am.). 1971;53(6):1208-1210. doi: 10.2106/00004623-197153060-00018.
4. Francavilla ML, Restrepo R, Zamora KW, Sarode V, Swirsky SM, Mintz D. Meniscal pathology in children: differences and similarities with the adult meniscus. Pediatr Radiol. 2014;44(8):910-925. doi: 10.1007/s00247-014-3022-0.
5. Kushare I, Klingele K, Samora W. Discoid meniscus: diagnosis and management. Orthop Clin North Am. 2015;46(4):533-540. doi: 10.1016/j.ocl.2015.06.007.
6. McKay S, Chen C, Rosenfeld S. Orthopedic perspective on selected pediatric and adolescent knee conditions. Pediatr Radiol. 2013;43(1):99-106. doi: 10.1007/s00247-012-2587-8.
7. Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10(3):168-176. doi: 10.5435/00124635-200205000-00003.
8. Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus. Technique and long-term results. Clin Orthop Relat Res. 1982;167(167):19-28.
9. Nathan PA, Cole SC. 12 Discoid meniscus: a clinical and pathologic study. Clin Orthop Relat Res: SC: Cole. 1969;64:107-113.
10. Jeannopoulos CL. Observations on discoid menisci. J Bone Joint Surg, (Am.). 1950;32(3):649-652. doi: 10.2106/00004623-195032030-00019.
11. Dickason J, Del WP, Blazina ME, Fox JM, Friedman MJ, Snyder SJ. A series of ten discoid medial menisci. Clin Orthop Relat Res. 1982;168:75-79. doi: 10.1097/00003086-198208000-00014
12. Andrish JT. Meniscal injuries in children and adolescents: diagnosis and management. J Am Acad Orthop Surg. 1996;4(5):231-237. doi: 10.5435/00124635-199609000-00001.
13. Kaplan E. The embryology of the menisci of the knee joint. Bull Hosp Joint Dis. 1955;16(2):111-124.
14. Clark C, Ogden J. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg, (Am.). 1983;65(4):538-547 doi: 10.2106/00004623-198365040-00018.
15. Carter CW, Kocher MS. Meniscus repair in children. Clin Sports Med. 2012;31(1):135-154. doi: 10.1016/j.csm.2011.09.002.
16. Shieh A, Bastrom T, Roocroft J, Edmonds EW, Pennock AT. Meniscus tear patterns in relation to skeletal immaturity: children versus adolescents. Am J Sports Med. 2013;41(12):2779-2783. doi: 10.1177/0363546513504286.
17. Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthopsurg. 1996;4(4):191-200. doi: 10.5435/00124635-199607000-00003.
18. Flouzat-Lachaniette C, Pujol N, Boisrenoult P, Beaufils P. Discoid medial meniscus: report of four cases and literature review. Orthop Traumatol Surg Res. 2011;97(8):826-832. doi: 10.1016/j.otsr.2011.07.011.
19. Choi Y-H, Seo Y-J, Ha JM, Jung KH, Kim J, Song SY. Collagenous ultrastructure of the discoid meniscus: A Transmission Electron Microscopy Study. Am J Sports Med. 2017;45(3):598-603. doi: 10.1177/0363546516674181.
20. Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL. Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med. 2007;35(3):475-478. doi: 10.1177/0363546506294678.
21. Papadopoulos A, Kirkos JM, Kapetanos GA. Histomorphologic study of discoid meniscus. Arthroscopy. 2009;25(3):262-268. doi: 10.1016/j.arthro.2008.10.006.
22. Watanabe M, Takeda S, Ikeuchi H. Atlas of Arthroscopy. Tokyo: Igaku-Shoin Ltd; 1969.
23. Monllau JC, León A, Cugat R, Ballester J. Ring-shaped lateral meniscus. Arthroscopy. 1998;14(5):502-504. doi: 10.1016/S0749-8063(98)70079-9.
24. Jordan M, Duncan J, Bertrand S. Discoid lateral meniscus: a review. S Orthop J. 1993;2(4):239-253.
25. Klingele KE, Kocher MS, Hresko MT, Gerbino P, Micheli LJ. Discoid lateral meniscus: prevalence of peripheral rim instability. J Pediatr Orthop. 2004;24(1):79-82. doi: 10.1097/01241398-200401000-00015.
26. Choi SH, Ahn JH, Kim KI, et al. Do the radiographic findings of symptomatic discoid lateral meniscus in children differ from normal control subjects? Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1128-1134. doi: 10.1007/s00167-014-2924-6.
27. Gans I, Bedoya MA, Ho-Fung V, Ganley TJ. Diagnostic performance of magnetic resonance imaging and pre-surgical evaluation in the assessment of traumatic intra-articular knee disorders in children and adolescents: what conditions still pose diagnostic challenges? Pediatr Radiol. 2015;45(2):194-202. doi: 10.1007/s00247-014-3127-5.
28. Samoto N, Kozuma M, Tokuhisa T, Kobayashi K. Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging. 2002;20(1):59-64. doi: 10.1016/S0730-725X(02)00473-3.
29. Hayashi LK, Yamaga H, Ida K, Miura T. Arthroscopic meniscectomy for discoid lateral meniscus in children. J Bone Joint Surg, (Am.). 1988;70(10):1495-1500. doi: 10.2106/00004623-198870100-00009.
30. Kim S-J, Kim D-W, Min B-H. Discoid lateral meniscus associated with anomalous insertion of the medial meniscus. Clin Orthop Rel Res. 1995;315(315):234-237 doi: 10.1097/00003086-199506000-00026.
31. Adachi N, Ochi M, Uchio Y, Kuriwaka M, Shinomiya R. Torn discoid lateral meniscus treated using partial central meniscectomy and suture of the peripheral tear. Arthroscopy. 2004;20(5):536-542. doi: 10.1016/j.arthro.2004.01.028.
32. Kim J-M, Bin S-I. Meniscal allograft transplantation after total meniscectomy of torn discoid lateral meniscus. Arthroscopy. 2006;22(12):1344-1350.e1. doi: 10.1016/j.arthro.2006.07.048.
33. Ramme AJ, Strauss EJ, Jazrawi L, Gold HT. Cost effectiveness of meniscal allograft for torn discoid lateral meniscus in young women. Phys Sportsmed. 2016;44(3):278-282. doi: 10.1080/00913847.2016.1197762.
34. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med. 1986;14(4):270-275. doi: 10.1177/036354658601400405.
35. Wroble RR, Henderson RC, Campion ER, el-Khoury GY, Albright JP. Meniscectomy in children and adolescents. A long-term follow-up study. Clin Orthop Relat Res. 1992;279(279):180-189.
36. Räber D, Friederich N, Hefti F. Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg, (Am.). 1998;80(11):1579-1586. doi: 10.2106/00004623-199811000-00003.
37. Stilli S, Reggiani LM, Muccioli GMM, Cappella M, Donzelli O. Arthroscopic treatment for symptomatic discoid lateral meniscus during childhood. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1337-1342. doi: 10.1007/s00167-011-1440-1.
38. Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH. Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy. 2015;31(5):867-873. doi: 10.1016/j.arthro.2014.12.012.
39. Carter CW, Hoellwarth J, Weiss JM. Clinical outcomes as a function of meniscal stability in the discoid meniscus: a preliminary report. J Pediatr Orthop. 2012;32(1):9-14. doi: 10.1097/BPO.0b013e31823d8338.
40. Yoo WJ, Jang WY, Park MS, et al. Arthroscopic treatment for symptomatic discoid meniscus in children: midterm outcomes and prognostic factors. Arthroscopy. 2015;31(12):2327-2334. doi: 10.1016/j.arthro.2015.06.032.
41. Shieh A, Edmonds EW, Pennock AT. Revision meniscus surgery in children and adolescents: the effect of skeletal immaturity. Orthop J Sports Med. 2015;3(7):S00075:2325967115. doi: 10.1177/2325967115S00075.
42. Shieh AK, Edmonds EW, Pennock AT. Revision meniscal surgery in children and adolescents: risk factors and mechanisms for failure and subsequent management. Am J Sports Med. 2016;44(4):838-843. doi: 10.1177/0363546515623511.
ABSTRACT
Discoid meniscus is a rare anatomical variant with altered morphology and structure that can sometimes present symptomatically, typically in the pediatric population. The discoid meniscus is usually in the lateral compartment of the knee and is characterized by a partial or complete filling-in of central meniscal tissue, increased meniscal thickness, disorganization of longitudinal collagen fibers, and sometimes lack of peripheral attachments. These changes to both the macro- and micro-structure of the meniscus predispose affected patients to increased rates of both meniscal tears and mechanical symptoms. Surgical management of symptomatic discoid meniscus is directed toward symptom resolution while preserving sufficient functional meniscal tissue to delay or prevent the development of osteoarthritis. Modern surgical techniques consist of arthroscopic saucerization of the discoid meniscus with repair of associated meniscal tears and stabilization of peripheral attachments. Although long-term outcome data are lacking, short- and mid-term outcomes for patients treated with arthroscopic partial meniscectomy and meniscal repair and/or stabilization as needed are generally good.
Continue to: The discoid meniscus...
The discoid meniscus is an uncommon anatomical meniscal variant that may present with pain, snapping, motion loss, swelling, and locking of the affected knee, typically during childhood or adolescence.1 Although the etiology of discoid meniscus is not completely understood, it is considered a congenital anomaly with a possible genetic component.2, 3 Incidence is estimated at 0.4% to 5.2% in the Western European population but is reportedly much higher (roughly 17%) in Asian populations.4-6, Discoid menisci, when present, are almost always in the lateral compartment, although cases of medial discoid meniscus have also been reported. The overall incidence of medial discoid meniscus has been estimated to be between 0.06% and 0.3% while that of lateral discoid meniscus, as detailed above, is significantly higher.7-11
ANATOMY AND MORPHOLOGY
The menisci differentiate from mesenchymal tissue early during fetal development with a clear definition by 8 weeks and a mature anatomical shape by 14 weeks in utero.12 Interestingly, menisci never possess a discoid shape during the normal course of development.13,14 The meniscus is fully vascularized at birth, with the central one-third becoming avascular by 9 months as the vascular supply regresses.14 By 10 years, only the peripheral one-third maintains its vascular supply, and the menisci have adult-like characteristics with tissue composed mainly of circumferential collagen fibers.4,14-16
A normal meniscus is wedge-shaped in the coronal plane and crescent-shaped in the axial plane. The medial meniscus is shaped like the letter “C,” is connected firmly to the joint capsule, and covers approximately 50% of the medial tibial plateau. The normal lateral meniscus covers 70% of the lateral tibial plateau and has firm anterior and posterior attachments while the lateral portion is less securely tethered.17 A discoid meniscus is characterized by an atypical shape—the center being partially or completely filled in (or “disc-like”)—often associated with anomalous attachments to the tibia, femur, and surrounding joint capsule. In addition to an atypical morphology, the discoid meniscus may also be much thicker than normal, resulting in a “block-like” appearance. The increased thickness may be responsible for the pathognomonic snapping of the knee as it is brought passively into flexion or extension (hence, the term “snapping knee” was traditionally used to describe a symptomatic discoid lateral meniscus). While the discoid shape is relatively straightforward to address, the increased meniscal thickness may be quite difficult to correct surgically.4-6,18
In addition to the macromorphological differences characteristic of discoid menisci, histological differences have also been described, including differences in collagen density and disorganization of the circumferential collagen network.19-21 Taken together, these differences may compromise the ability of the discoid meniscus to withstand normal forces placed across the knee and predispose it to tear. This is important because the normal meniscus plays a critical role in facilitating load distribution across the knee joint, in addition to assisting with functions including shock absorption, proprioception, and stabilization of the knee. Torn and/or unstable discoid menisci are unable to perform these functions adequately, which may ultimately result in degenerative joint disease and progress to end-stage osteoarthritis (OA).
CLASSIFICATION
The traditional Watanabe classification of discoid meniscus consists of 3 variants: type I, a complete discoid shape; type II, an incomplete discoid shape; and type III, the Wrisberg variant.22 The Wrisberg variant is described as a more normal-appearing meniscus but lacks normal peripheral attachments.5, 6, 15 This classification system was expanded by Monllau and colleagues, 23 who described a ring-type meniscus variant with normal posterior tibial attachments. Although the Watanabe classification is commonly used, its utility in assisting with clinical decision-making may be limited.
Continue to: Several other classification schemes...
Several other classification schemes exist. Jordan and colleagues24 described a classification scheme defining a meniscal type as complete or incomplete, also noting the presence of symptoms, tearing, and peripheral rim instability. They grouped stable types together, regardless of morphology, and then further classified them based on the presence of symptoms and tears. Similarly, the unstable types were grouped together and then subclassified in the same manner.17,24 Klingele and colleagues25 also described a contemporary classification scheme of discoid meniscus evaluating peripheral stability patterns that may be more clinically and surgically relevant. This classification is based on the type of discoid morphology (complete vs incomplete), the presence or absence of peripheral rim stability (stable vs unstable), and the presence or absence of a meniscal tear (torn vs untorn).5,25
EVALUATION
A stable discoid meniscus is often an incidental finding, seen either on advanced diagnostic imaging performed for another reason or at the time of arthroscopy to address another problem. Younger children with discoid meniscus tend to present with symptoms such as popping and snapping related to instability and the abnormal morphology of the discoid meniscus. Older patients tend to present with symptoms related to acute tears through the abnormal meniscal tissue. Although discoid menisci can become acutely symptomatic in the presence of a tear, the onset of symptoms may occur in the absence of a discrete traumatic event.1 Alternatively, some patients will report a clear history of injury, often a noncontact, rotational injury mechanism related to an athletic activity. Patients with torn discoid menisci may report pain, catching, locking, and/or giving way of the knee, and on examination may have limited extension, snapping, effusion, quadriceps atrophy, and joint line tenderness. Eponymous meniscal compression tests including the McMurray, Apley, and Thessaly tests, may also be performed when meniscal tear is suspected, although this may be tricky for younger children.1
Considering the high association of meniscal tears with ligamentous injuries, examination of knee stability is important. Plain radiographs of the knee should be taken, although the results will often be negative for osseous injury in the case of an isolated meniscal tear. Radiographs of a discoid knee may show subtle differences compared with radiographs of a non-discoid knee. A recent comparison of children with symptomatic lateral discoid menisci with age-matched controls found statistically significant increased lateral joint space, elevated fibular head, increased height of the lateral tibial spine, and increased obliquity of the tibial plateau.26 They did not find statistically significant increased squaring of the lateral femoral condyle or cupping of the lateral tibial plateau. Radiographic signs can be subtle and may not all be present in a patient with a discoid meniscus.
Magnetic resonance imaging (MRI) is the assessment technique of choice for the diagnosis of discoid meniscus, although MRI may not reliably identify a Wrisberg variant or incomplete discoid menisci (Figure 1).
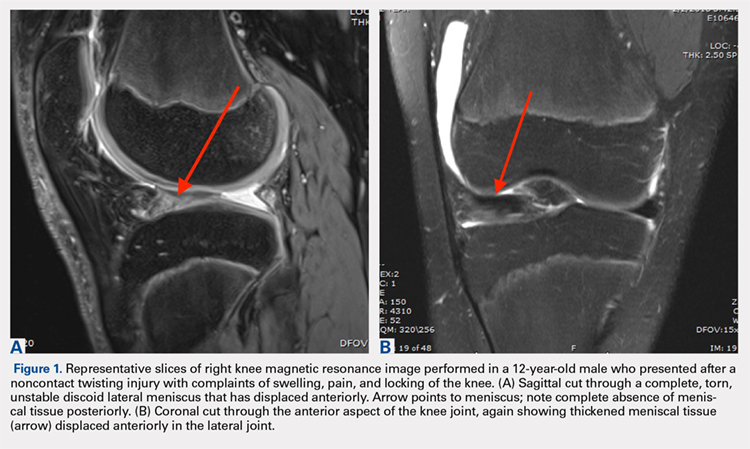
Gans and colleagues27 examined preoperative MRI and clinical examination compared with pathology found during arthroscopy. Although they found that MRI and clinical examination had excellent diagnostic accuracy of 92.7% and 95.3%, respectively, the most common missed pathology on MRI later found on diagnostic arthroscopy was the presence of a lateral discoid meniscus, which occurred in 26.7% of missed diagnoses. Adult diagnostic criteria of discoid meniscus include ≥3 contiguous 5-mm sagittal cuts showing continuity between the anterior and posterior horns of the meniscus. Other criteria include a minimal meniscal width >15 mm on the coronal view or a minimum meniscal width that is >20% of the width of the maximal tibial width.28 These criteria are often applied to children as well. Additionally, if >50% of the lateral joint space is covered by meniscal tissue, a diagnosis of discoid meniscus should be considered.6
Continue to: TREATMENT
TREATMENT
Management of symptomatic discoid meniscus is directed toward resolving symptoms while preserving meniscal tissue and preventing the development of OA. Incidentally found discoid menisci in asymptomatic patients should not be treated surgically and can have periodic follow-ups for detection of any functional deterioration or symptom development. Surgical treatment may be beneficial for patients with symptoms related to their discoid menisci such as pain, recurrent effusion, limited knee motion, mechanical symptoms (e.g., locking and catching), and activity restrictions.
Traditionally, surgical treatment of a symptomatic discoid meniscus consisted of subtotal (meaning nearly complete, or <3mm of peripheral rim remaining) or complete meniscectomy, often performed in an open fashion. Surgical techniques have evolved; current surgical approaches typically include diagnostic arthroscopy followed by arthroscopic saucerization (also called partial meniscectomy) of the central portion of the “disc,” leaving a peripheral rim of 6 mm to 8 mm to approximate that of the normal meniscus (Figure 2).29,30 Saucerization removes the redundant central meniscal tissue in an attempt to create a more “normal” C-shaped morphology, although it does not address the increased thickness characteristic of many discoid menisci. It may be particularly difficult to “debulk” an abnormally thick discoid meniscus in the coronal plane, and there is little in the outcomes literature to support this approach. Following partial meniscectomy, the remaining meniscal tissue should be inspected thoroughly both for the presence of instability and for residual tears. Meniscal tears should be repaired in standard fashion; commonly, this may be a combination of all-inside sutures placed into the posterior horn, inside-out sutures placed into the midbody, and outside-in sutures placed into the anterior horn. Peripheral rim instability—identified, for example, by the ability to translate the posterior horn of the meniscus fully onto the anterior tibial plateau—should be addressed by suturing the meniscus to the adjacent capsule (Figure 2).25, 31 Menisci that have residual complex tears that are not amenable to repair may be treated by subtotal meniscectomy. These patients may be candidates for subsequent meniscal allograft transplantation.32,33
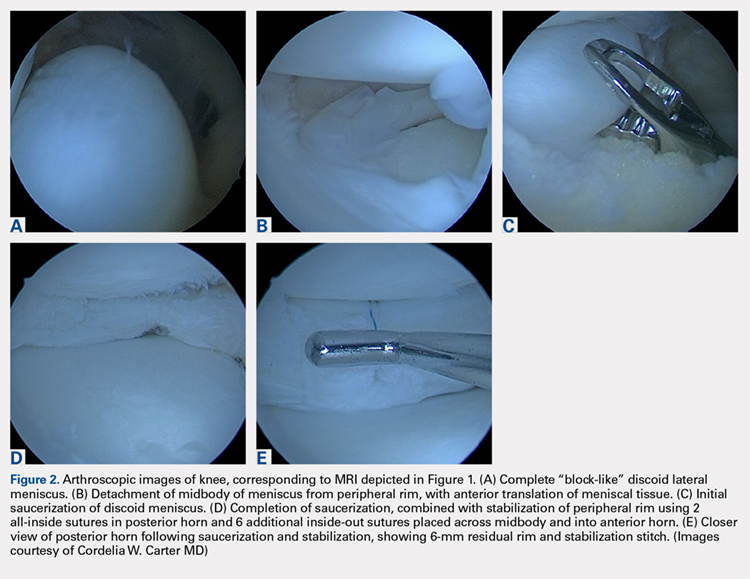
TREATMENT OUTCOMES
Performing a partial meniscectomy has consistently been shown in the laboratory to increase contact stresses proportionally to the percentage of tissue removed.34 It follows logically that performing a subtotal or complete meniscectomy in a young patient would yield increased, abnormal contact stresses throughout the knee with resultant degenerative changes and progression to OA over time. While long-term outcome studies of subtotal or complete meniscectomy have shown somewhat variable results, the majority report the development of pain, instability, poor function, osteoarthritic changes and even the development of osteochondritis desiccans.5,35
In an early investigation of long-term outcomes associated with surgical resection of a discoid lateral meniscus, Räber and colleagues36 retrospectively examined 17 knees that had undergone total meniscectomy for the lateral discoid meniscus. At a mean follow-up of 19.8 years, these authors reported that patients accounting for 10 of 17 operative knees had developed symptoms of osteoarthrosis such as pain. In addition, two-thirds of the knees that had follow-up radiographs performed (10 of 15 knees) had visible osteoarthritic changes present.
In 2011, Stilli and colleagues37 conducted a mid-term follow-up study examining 104 knees over an average follow-up of 8.5 years, with an average age of 8 years at the time of surgery. Younger patients, 2 to 7 years, underwent subtotal meniscectomy whereas patients, 8 to 14 years, underwent arthroscopic partial meniscectomy. Patients with a Wrisberg variant underwent removal of the posterior horn. The authors of this study reported that younger patients who had undergone subtotal meniscectomy had the best outcomes (defined by self-reported questionnaire responses and clinical evaluation). However, these results should be interpreted with caution: at the time of follow-up, patients in this study would still have been in adolescence and may not yet have developed the symptomatic degenerative changes in the knee joint that are strongly associated with meniscectomy.
Continue to: There are a few long-term...
There are few long-term outcome studies for arthroscopic saucerization. In 2014, Ahn and colleagues38 examined patient-reported outcomes and radiographic changes for 48 knees in pediatric patients treated arthroscopically for a symptomatic discoid meniscus. Patients were treated with partial meniscectomy (22 knees), partial meniscectomy with meniscal repair (18 knees), or subtotal meniscectomy (8 knees). Out of 48 knees evaluated, 45 knees (94%) were rated as “excellent” or “good” at an average 10-year follow-up. However, a significant percentage of patients had evidence of degenerative changes on follow-up radiographs, specifically: 88% of the subtotal meniscectomy group, 39% of the partial meniscectomy with repair group, and 23% in the partial meniscectomy-alone group. This finding suggests that the early appearance of radiographic changes suggestive of OA does not necessarily correlate with the development of knee symptoms in this cohort, although longer-term follow-up of these patients into adulthood and middle age is clearly needed.
Recently, short-term outcomes have been reported for contemporary arthroscopic saucerization of discoid menisci with peripheral rim stabilization performed as deemed necessary at the time of surgery. In 2012, Carter and colleagues39 examined 57 knees that underwent saucerization alone or saucerization with peripheral rim stabilization. At an average follow-up of 15 months, both patient populations had equivalent self-reported outcomes and clinical examination findings. The authors concluded that peripheral stabilization does not negatively affect short-term outcomes if instability is recognized and treated.
Yoo and colleagues40 found equivalent results between patients undergoing saucerization, saucerization with rim stabilization, and subtotal meniscectomy for 100 pediatric knees with an average follow-up of 4.7 years. Subtotal meniscectomy was defined as <3 mm of peripheral rim remaining and was performed when there was severe degeneration or complex tearing of the remnant rim following arthroscopic saucerization. Taken together, these data seem to suggest that short- and mid-term outcomes for pediatric patients treated surgically are generally good in terms of reported clinical function and development of OA, although long-term follow-up studies will be essential for understanding the true impact of surgical interventions.
Shieh and colleagues41,42 investigated risk factors for failed meniscal surgery in 324 menisci from 2008 to 2012, including in 46 discoid saucerization procedures with or without stabilization. At a mean of 40 months, 15% of the discoid saucerization cohort required a revision procedure, with increased odds of revision surgeries in patients who had undergone meniscal tear repair. The most frequent indication of revision surgery was sustaining a meniscal tear during intense physical activity in the first year after the index procedure, and patients underwent either debridement or repair for their revision procedure.
SUMMARY
Discoid meniscus is a rare anatomical meniscal variant characterized by an abnormal “O-like” shape, increased meniscal thickness, disorganization of collagen fibers, and variable absence of peripheral attachments. These morphological changes predispose patients with discoid menisci to increased rates of symptomatic meniscal instability and tearing. An MRI remains the most sensitive imaging modality for the diagnosis of a discoid meniscus, with ≥3 contiguous 5-mm sagittal cuts showing continuity between the anterior and posterior horns indicative of a discoid variant. Surgical treatment for symptomatic discoid menisci has evolved from subtotal meniscectomy to contemporary arthroscopic saucerization techniques with repair of meniscal tears and peripheral stabilization performed as needed. Long-term outcome studies for patients who undergo subtotal or complete meniscectomy reveal an association with osteoarthritic changes of the knee. Short- and mid-term outcome studies for patients who undergo arthroscopic saucerization with or without repair and/or peripheral stabilization are generally good, although reoperation rates have been estimated at 15% in the first 3 to 4 years. Longer-term follow-up, with the inclusion of validated functional outcomes measures, will be essential for understanding the true impact of various surgical interventions over time.
ABSTRACT
Discoid meniscus is a rare anatomical variant with altered morphology and structure that can sometimes present symptomatically, typically in the pediatric population. The discoid meniscus is usually in the lateral compartment of the knee and is characterized by a partial or complete filling-in of central meniscal tissue, increased meniscal thickness, disorganization of longitudinal collagen fibers, and sometimes lack of peripheral attachments. These changes to both the macro- and micro-structure of the meniscus predispose affected patients to increased rates of both meniscal tears and mechanical symptoms. Surgical management of symptomatic discoid meniscus is directed toward symptom resolution while preserving sufficient functional meniscal tissue to delay or prevent the development of osteoarthritis. Modern surgical techniques consist of arthroscopic saucerization of the discoid meniscus with repair of associated meniscal tears and stabilization of peripheral attachments. Although long-term outcome data are lacking, short- and mid-term outcomes for patients treated with arthroscopic partial meniscectomy and meniscal repair and/or stabilization as needed are generally good.
Continue to: The discoid meniscus...
The discoid meniscus is an uncommon anatomical meniscal variant that may present with pain, snapping, motion loss, swelling, and locking of the affected knee, typically during childhood or adolescence.1 Although the etiology of discoid meniscus is not completely understood, it is considered a congenital anomaly with a possible genetic component.2, 3 Incidence is estimated at 0.4% to 5.2% in the Western European population but is reportedly much higher (roughly 17%) in Asian populations.4-6, Discoid menisci, when present, are almost always in the lateral compartment, although cases of medial discoid meniscus have also been reported. The overall incidence of medial discoid meniscus has been estimated to be between 0.06% and 0.3% while that of lateral discoid meniscus, as detailed above, is significantly higher.7-11
ANATOMY AND MORPHOLOGY
The menisci differentiate from mesenchymal tissue early during fetal development with a clear definition by 8 weeks and a mature anatomical shape by 14 weeks in utero.12 Interestingly, menisci never possess a discoid shape during the normal course of development.13,14 The meniscus is fully vascularized at birth, with the central one-third becoming avascular by 9 months as the vascular supply regresses.14 By 10 years, only the peripheral one-third maintains its vascular supply, and the menisci have adult-like characteristics with tissue composed mainly of circumferential collagen fibers.4,14-16
A normal meniscus is wedge-shaped in the coronal plane and crescent-shaped in the axial plane. The medial meniscus is shaped like the letter “C,” is connected firmly to the joint capsule, and covers approximately 50% of the medial tibial plateau. The normal lateral meniscus covers 70% of the lateral tibial plateau and has firm anterior and posterior attachments while the lateral portion is less securely tethered.17 A discoid meniscus is characterized by an atypical shape—the center being partially or completely filled in (or “disc-like”)—often associated with anomalous attachments to the tibia, femur, and surrounding joint capsule. In addition to an atypical morphology, the discoid meniscus may also be much thicker than normal, resulting in a “block-like” appearance. The increased thickness may be responsible for the pathognomonic snapping of the knee as it is brought passively into flexion or extension (hence, the term “snapping knee” was traditionally used to describe a symptomatic discoid lateral meniscus). While the discoid shape is relatively straightforward to address, the increased meniscal thickness may be quite difficult to correct surgically.4-6,18
In addition to the macromorphological differences characteristic of discoid menisci, histological differences have also been described, including differences in collagen density and disorganization of the circumferential collagen network.19-21 Taken together, these differences may compromise the ability of the discoid meniscus to withstand normal forces placed across the knee and predispose it to tear. This is important because the normal meniscus plays a critical role in facilitating load distribution across the knee joint, in addition to assisting with functions including shock absorption, proprioception, and stabilization of the knee. Torn and/or unstable discoid menisci are unable to perform these functions adequately, which may ultimately result in degenerative joint disease and progress to end-stage osteoarthritis (OA).
CLASSIFICATION
The traditional Watanabe classification of discoid meniscus consists of 3 variants: type I, a complete discoid shape; type II, an incomplete discoid shape; and type III, the Wrisberg variant.22 The Wrisberg variant is described as a more normal-appearing meniscus but lacks normal peripheral attachments.5, 6, 15 This classification system was expanded by Monllau and colleagues, 23 who described a ring-type meniscus variant with normal posterior tibial attachments. Although the Watanabe classification is commonly used, its utility in assisting with clinical decision-making may be limited.
Continue to: Several other classification schemes...
Several other classification schemes exist. Jordan and colleagues24 described a classification scheme defining a meniscal type as complete or incomplete, also noting the presence of symptoms, tearing, and peripheral rim instability. They grouped stable types together, regardless of morphology, and then further classified them based on the presence of symptoms and tears. Similarly, the unstable types were grouped together and then subclassified in the same manner.17,24 Klingele and colleagues25 also described a contemporary classification scheme of discoid meniscus evaluating peripheral stability patterns that may be more clinically and surgically relevant. This classification is based on the type of discoid morphology (complete vs incomplete), the presence or absence of peripheral rim stability (stable vs unstable), and the presence or absence of a meniscal tear (torn vs untorn).5,25
EVALUATION
A stable discoid meniscus is often an incidental finding, seen either on advanced diagnostic imaging performed for another reason or at the time of arthroscopy to address another problem. Younger children with discoid meniscus tend to present with symptoms such as popping and snapping related to instability and the abnormal morphology of the discoid meniscus. Older patients tend to present with symptoms related to acute tears through the abnormal meniscal tissue. Although discoid menisci can become acutely symptomatic in the presence of a tear, the onset of symptoms may occur in the absence of a discrete traumatic event.1 Alternatively, some patients will report a clear history of injury, often a noncontact, rotational injury mechanism related to an athletic activity. Patients with torn discoid menisci may report pain, catching, locking, and/or giving way of the knee, and on examination may have limited extension, snapping, effusion, quadriceps atrophy, and joint line tenderness. Eponymous meniscal compression tests including the McMurray, Apley, and Thessaly tests, may also be performed when meniscal tear is suspected, although this may be tricky for younger children.1
Considering the high association of meniscal tears with ligamentous injuries, examination of knee stability is important. Plain radiographs of the knee should be taken, although the results will often be negative for osseous injury in the case of an isolated meniscal tear. Radiographs of a discoid knee may show subtle differences compared with radiographs of a non-discoid knee. A recent comparison of children with symptomatic lateral discoid menisci with age-matched controls found statistically significant increased lateral joint space, elevated fibular head, increased height of the lateral tibial spine, and increased obliquity of the tibial plateau.26 They did not find statistically significant increased squaring of the lateral femoral condyle or cupping of the lateral tibial plateau. Radiographic signs can be subtle and may not all be present in a patient with a discoid meniscus.
Magnetic resonance imaging (MRI) is the assessment technique of choice for the diagnosis of discoid meniscus, although MRI may not reliably identify a Wrisberg variant or incomplete discoid menisci (Figure 1).
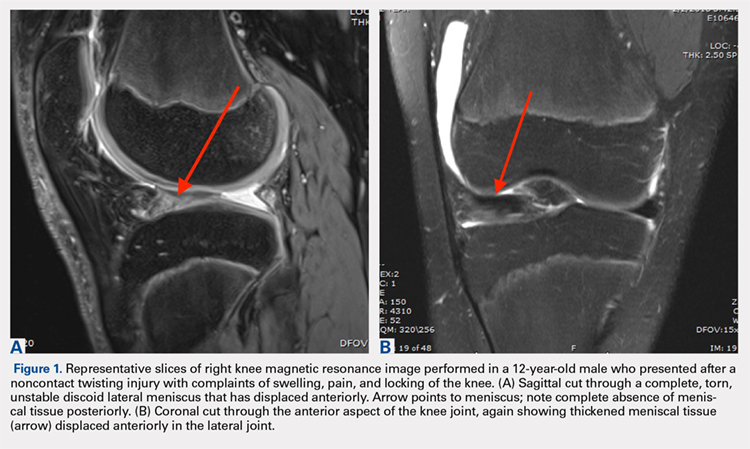
Gans and colleagues27 examined preoperative MRI and clinical examination compared with pathology found during arthroscopy. Although they found that MRI and clinical examination had excellent diagnostic accuracy of 92.7% and 95.3%, respectively, the most common missed pathology on MRI later found on diagnostic arthroscopy was the presence of a lateral discoid meniscus, which occurred in 26.7% of missed diagnoses. Adult diagnostic criteria of discoid meniscus include ≥3 contiguous 5-mm sagittal cuts showing continuity between the anterior and posterior horns of the meniscus. Other criteria include a minimal meniscal width >15 mm on the coronal view or a minimum meniscal width that is >20% of the width of the maximal tibial width.28 These criteria are often applied to children as well. Additionally, if >50% of the lateral joint space is covered by meniscal tissue, a diagnosis of discoid meniscus should be considered.6
Continue to: TREATMENT
TREATMENT
Management of symptomatic discoid meniscus is directed toward resolving symptoms while preserving meniscal tissue and preventing the development of OA. Incidentally found discoid menisci in asymptomatic patients should not be treated surgically and can have periodic follow-ups for detection of any functional deterioration or symptom development. Surgical treatment may be beneficial for patients with symptoms related to their discoid menisci such as pain, recurrent effusion, limited knee motion, mechanical symptoms (e.g., locking and catching), and activity restrictions.
Traditionally, surgical treatment of a symptomatic discoid meniscus consisted of subtotal (meaning nearly complete, or <3mm of peripheral rim remaining) or complete meniscectomy, often performed in an open fashion. Surgical techniques have evolved; current surgical approaches typically include diagnostic arthroscopy followed by arthroscopic saucerization (also called partial meniscectomy) of the central portion of the “disc,” leaving a peripheral rim of 6 mm to 8 mm to approximate that of the normal meniscus (Figure 2).29,30 Saucerization removes the redundant central meniscal tissue in an attempt to create a more “normal” C-shaped morphology, although it does not address the increased thickness characteristic of many discoid menisci. It may be particularly difficult to “debulk” an abnormally thick discoid meniscus in the coronal plane, and there is little in the outcomes literature to support this approach. Following partial meniscectomy, the remaining meniscal tissue should be inspected thoroughly both for the presence of instability and for residual tears. Meniscal tears should be repaired in standard fashion; commonly, this may be a combination of all-inside sutures placed into the posterior horn, inside-out sutures placed into the midbody, and outside-in sutures placed into the anterior horn. Peripheral rim instability—identified, for example, by the ability to translate the posterior horn of the meniscus fully onto the anterior tibial plateau—should be addressed by suturing the meniscus to the adjacent capsule (Figure 2).25, 31 Menisci that have residual complex tears that are not amenable to repair may be treated by subtotal meniscectomy. These patients may be candidates for subsequent meniscal allograft transplantation.32,33
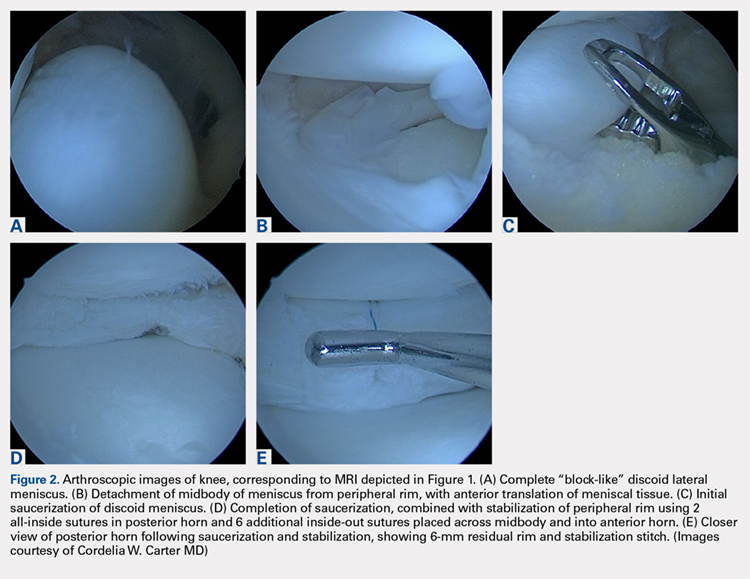
TREATMENT OUTCOMES
Performing a partial meniscectomy has consistently been shown in the laboratory to increase contact stresses proportionally to the percentage of tissue removed.34 It follows logically that performing a subtotal or complete meniscectomy in a young patient would yield increased, abnormal contact stresses throughout the knee with resultant degenerative changes and progression to OA over time. While long-term outcome studies of subtotal or complete meniscectomy have shown somewhat variable results, the majority report the development of pain, instability, poor function, osteoarthritic changes and even the development of osteochondritis desiccans.5,35
In an early investigation of long-term outcomes associated with surgical resection of a discoid lateral meniscus, Räber and colleagues36 retrospectively examined 17 knees that had undergone total meniscectomy for the lateral discoid meniscus. At a mean follow-up of 19.8 years, these authors reported that patients accounting for 10 of 17 operative knees had developed symptoms of osteoarthrosis such as pain. In addition, two-thirds of the knees that had follow-up radiographs performed (10 of 15 knees) had visible osteoarthritic changes present.
In 2011, Stilli and colleagues37 conducted a mid-term follow-up study examining 104 knees over an average follow-up of 8.5 years, with an average age of 8 years at the time of surgery. Younger patients, 2 to 7 years, underwent subtotal meniscectomy whereas patients, 8 to 14 years, underwent arthroscopic partial meniscectomy. Patients with a Wrisberg variant underwent removal of the posterior horn. The authors of this study reported that younger patients who had undergone subtotal meniscectomy had the best outcomes (defined by self-reported questionnaire responses and clinical evaluation). However, these results should be interpreted with caution: at the time of follow-up, patients in this study would still have been in adolescence and may not yet have developed the symptomatic degenerative changes in the knee joint that are strongly associated with meniscectomy.
Continue to: There are a few long-term...
There are few long-term outcome studies for arthroscopic saucerization. In 2014, Ahn and colleagues38 examined patient-reported outcomes and radiographic changes for 48 knees in pediatric patients treated arthroscopically for a symptomatic discoid meniscus. Patients were treated with partial meniscectomy (22 knees), partial meniscectomy with meniscal repair (18 knees), or subtotal meniscectomy (8 knees). Out of 48 knees evaluated, 45 knees (94%) were rated as “excellent” or “good” at an average 10-year follow-up. However, a significant percentage of patients had evidence of degenerative changes on follow-up radiographs, specifically: 88% of the subtotal meniscectomy group, 39% of the partial meniscectomy with repair group, and 23% in the partial meniscectomy-alone group. This finding suggests that the early appearance of radiographic changes suggestive of OA does not necessarily correlate with the development of knee symptoms in this cohort, although longer-term follow-up of these patients into adulthood and middle age is clearly needed.
Recently, short-term outcomes have been reported for contemporary arthroscopic saucerization of discoid menisci with peripheral rim stabilization performed as deemed necessary at the time of surgery. In 2012, Carter and colleagues39 examined 57 knees that underwent saucerization alone or saucerization with peripheral rim stabilization. At an average follow-up of 15 months, both patient populations had equivalent self-reported outcomes and clinical examination findings. The authors concluded that peripheral stabilization does not negatively affect short-term outcomes if instability is recognized and treated.
Yoo and colleagues40 found equivalent results between patients undergoing saucerization, saucerization with rim stabilization, and subtotal meniscectomy for 100 pediatric knees with an average follow-up of 4.7 years. Subtotal meniscectomy was defined as <3 mm of peripheral rim remaining and was performed when there was severe degeneration or complex tearing of the remnant rim following arthroscopic saucerization. Taken together, these data seem to suggest that short- and mid-term outcomes for pediatric patients treated surgically are generally good in terms of reported clinical function and development of OA, although long-term follow-up studies will be essential for understanding the true impact of surgical interventions.
Shieh and colleagues41,42 investigated risk factors for failed meniscal surgery in 324 menisci from 2008 to 2012, including in 46 discoid saucerization procedures with or without stabilization. At a mean of 40 months, 15% of the discoid saucerization cohort required a revision procedure, with increased odds of revision surgeries in patients who had undergone meniscal tear repair. The most frequent indication of revision surgery was sustaining a meniscal tear during intense physical activity in the first year after the index procedure, and patients underwent either debridement or repair for their revision procedure.
SUMMARY
Discoid meniscus is a rare anatomical meniscal variant characterized by an abnormal “O-like” shape, increased meniscal thickness, disorganization of collagen fibers, and variable absence of peripheral attachments. These morphological changes predispose patients with discoid menisci to increased rates of symptomatic meniscal instability and tearing. An MRI remains the most sensitive imaging modality for the diagnosis of a discoid meniscus, with ≥3 contiguous 5-mm sagittal cuts showing continuity between the anterior and posterior horns indicative of a discoid variant. Surgical treatment for symptomatic discoid menisci has evolved from subtotal meniscectomy to contemporary arthroscopic saucerization techniques with repair of meniscal tears and peripheral stabilization performed as needed. Long-term outcome studies for patients who undergo subtotal or complete meniscectomy reveal an association with osteoarthritic changes of the knee. Short- and mid-term outcome studies for patients who undergo arthroscopic saucerization with or without repair and/or peripheral stabilization are generally good, although reoperation rates have been estimated at 15% in the first 3 to 4 years. Longer-term follow-up, with the inclusion of validated functional outcomes measures, will be essential for understanding the true impact of various surgical interventions over time.
1. Yaniv M, Blumberg N. The discoid meniscus. J Child Orthop. 2007;1(2):89-96. doi: 10.1007/s11832-007-0029-1.
2. Gebhardt M, Rosenthal R. Bilateral lateral discoid meniscus in identical twins. J Bone Joint Surg Am. 1979;61(7):1110-1111. doi: 10.2106/00004623-197961070-00027.
3. Dashefsky JH. Discoid lateral meniscus in three members of a family. J Bone Joint Surg, (Am.). 1971;53(6):1208-1210. doi: 10.2106/00004623-197153060-00018.
4. Francavilla ML, Restrepo R, Zamora KW, Sarode V, Swirsky SM, Mintz D. Meniscal pathology in children: differences and similarities with the adult meniscus. Pediatr Radiol. 2014;44(8):910-925. doi: 10.1007/s00247-014-3022-0.
5. Kushare I, Klingele K, Samora W. Discoid meniscus: diagnosis and management. Orthop Clin North Am. 2015;46(4):533-540. doi: 10.1016/j.ocl.2015.06.007.
6. McKay S, Chen C, Rosenfeld S. Orthopedic perspective on selected pediatric and adolescent knee conditions. Pediatr Radiol. 2013;43(1):99-106. doi: 10.1007/s00247-012-2587-8.
7. Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10(3):168-176. doi: 10.5435/00124635-200205000-00003.
8. Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus. Technique and long-term results. Clin Orthop Relat Res. 1982;167(167):19-28.
9. Nathan PA, Cole SC. 12 Discoid meniscus: a clinical and pathologic study. Clin Orthop Relat Res: SC: Cole. 1969;64:107-113.
10. Jeannopoulos CL. Observations on discoid menisci. J Bone Joint Surg, (Am.). 1950;32(3):649-652. doi: 10.2106/00004623-195032030-00019.
11. Dickason J, Del WP, Blazina ME, Fox JM, Friedman MJ, Snyder SJ. A series of ten discoid medial menisci. Clin Orthop Relat Res. 1982;168:75-79. doi: 10.1097/00003086-198208000-00014
12. Andrish JT. Meniscal injuries in children and adolescents: diagnosis and management. J Am Acad Orthop Surg. 1996;4(5):231-237. doi: 10.5435/00124635-199609000-00001.
13. Kaplan E. The embryology of the menisci of the knee joint. Bull Hosp Joint Dis. 1955;16(2):111-124.
14. Clark C, Ogden J. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg, (Am.). 1983;65(4):538-547 doi: 10.2106/00004623-198365040-00018.
15. Carter CW, Kocher MS. Meniscus repair in children. Clin Sports Med. 2012;31(1):135-154. doi: 10.1016/j.csm.2011.09.002.
16. Shieh A, Bastrom T, Roocroft J, Edmonds EW, Pennock AT. Meniscus tear patterns in relation to skeletal immaturity: children versus adolescents. Am J Sports Med. 2013;41(12):2779-2783. doi: 10.1177/0363546513504286.
17. Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthopsurg. 1996;4(4):191-200. doi: 10.5435/00124635-199607000-00003.
18. Flouzat-Lachaniette C, Pujol N, Boisrenoult P, Beaufils P. Discoid medial meniscus: report of four cases and literature review. Orthop Traumatol Surg Res. 2011;97(8):826-832. doi: 10.1016/j.otsr.2011.07.011.
19. Choi Y-H, Seo Y-J, Ha JM, Jung KH, Kim J, Song SY. Collagenous ultrastructure of the discoid meniscus: A Transmission Electron Microscopy Study. Am J Sports Med. 2017;45(3):598-603. doi: 10.1177/0363546516674181.
20. Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL. Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med. 2007;35(3):475-478. doi: 10.1177/0363546506294678.
21. Papadopoulos A, Kirkos JM, Kapetanos GA. Histomorphologic study of discoid meniscus. Arthroscopy. 2009;25(3):262-268. doi: 10.1016/j.arthro.2008.10.006.
22. Watanabe M, Takeda S, Ikeuchi H. Atlas of Arthroscopy. Tokyo: Igaku-Shoin Ltd; 1969.
23. Monllau JC, León A, Cugat R, Ballester J. Ring-shaped lateral meniscus. Arthroscopy. 1998;14(5):502-504. doi: 10.1016/S0749-8063(98)70079-9.
24. Jordan M, Duncan J, Bertrand S. Discoid lateral meniscus: a review. S Orthop J. 1993;2(4):239-253.
25. Klingele KE, Kocher MS, Hresko MT, Gerbino P, Micheli LJ. Discoid lateral meniscus: prevalence of peripheral rim instability. J Pediatr Orthop. 2004;24(1):79-82. doi: 10.1097/01241398-200401000-00015.
26. Choi SH, Ahn JH, Kim KI, et al. Do the radiographic findings of symptomatic discoid lateral meniscus in children differ from normal control subjects? Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1128-1134. doi: 10.1007/s00167-014-2924-6.
27. Gans I, Bedoya MA, Ho-Fung V, Ganley TJ. Diagnostic performance of magnetic resonance imaging and pre-surgical evaluation in the assessment of traumatic intra-articular knee disorders in children and adolescents: what conditions still pose diagnostic challenges? Pediatr Radiol. 2015;45(2):194-202. doi: 10.1007/s00247-014-3127-5.
28. Samoto N, Kozuma M, Tokuhisa T, Kobayashi K. Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging. 2002;20(1):59-64. doi: 10.1016/S0730-725X(02)00473-3.
29. Hayashi LK, Yamaga H, Ida K, Miura T. Arthroscopic meniscectomy for discoid lateral meniscus in children. J Bone Joint Surg, (Am.). 1988;70(10):1495-1500. doi: 10.2106/00004623-198870100-00009.
30. Kim S-J, Kim D-W, Min B-H. Discoid lateral meniscus associated with anomalous insertion of the medial meniscus. Clin Orthop Rel Res. 1995;315(315):234-237 doi: 10.1097/00003086-199506000-00026.
31. Adachi N, Ochi M, Uchio Y, Kuriwaka M, Shinomiya R. Torn discoid lateral meniscus treated using partial central meniscectomy and suture of the peripheral tear. Arthroscopy. 2004;20(5):536-542. doi: 10.1016/j.arthro.2004.01.028.
32. Kim J-M, Bin S-I. Meniscal allograft transplantation after total meniscectomy of torn discoid lateral meniscus. Arthroscopy. 2006;22(12):1344-1350.e1. doi: 10.1016/j.arthro.2006.07.048.
33. Ramme AJ, Strauss EJ, Jazrawi L, Gold HT. Cost effectiveness of meniscal allograft for torn discoid lateral meniscus in young women. Phys Sportsmed. 2016;44(3):278-282. doi: 10.1080/00913847.2016.1197762.
34. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med. 1986;14(4):270-275. doi: 10.1177/036354658601400405.
35. Wroble RR, Henderson RC, Campion ER, el-Khoury GY, Albright JP. Meniscectomy in children and adolescents. A long-term follow-up study. Clin Orthop Relat Res. 1992;279(279):180-189.
36. Räber D, Friederich N, Hefti F. Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg, (Am.). 1998;80(11):1579-1586. doi: 10.2106/00004623-199811000-00003.
37. Stilli S, Reggiani LM, Muccioli GMM, Cappella M, Donzelli O. Arthroscopic treatment for symptomatic discoid lateral meniscus during childhood. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1337-1342. doi: 10.1007/s00167-011-1440-1.
38. Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH. Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy. 2015;31(5):867-873. doi: 10.1016/j.arthro.2014.12.012.
39. Carter CW, Hoellwarth J, Weiss JM. Clinical outcomes as a function of meniscal stability in the discoid meniscus: a preliminary report. J Pediatr Orthop. 2012;32(1):9-14. doi: 10.1097/BPO.0b013e31823d8338.
40. Yoo WJ, Jang WY, Park MS, et al. Arthroscopic treatment for symptomatic discoid meniscus in children: midterm outcomes and prognostic factors. Arthroscopy. 2015;31(12):2327-2334. doi: 10.1016/j.arthro.2015.06.032.
41. Shieh A, Edmonds EW, Pennock AT. Revision meniscus surgery in children and adolescents: the effect of skeletal immaturity. Orthop J Sports Med. 2015;3(7):S00075:2325967115. doi: 10.1177/2325967115S00075.
42. Shieh AK, Edmonds EW, Pennock AT. Revision meniscal surgery in children and adolescents: risk factors and mechanisms for failure and subsequent management. Am J Sports Med. 2016;44(4):838-843. doi: 10.1177/0363546515623511.
1. Yaniv M, Blumberg N. The discoid meniscus. J Child Orthop. 2007;1(2):89-96. doi: 10.1007/s11832-007-0029-1.
2. Gebhardt M, Rosenthal R. Bilateral lateral discoid meniscus in identical twins. J Bone Joint Surg Am. 1979;61(7):1110-1111. doi: 10.2106/00004623-197961070-00027.
3. Dashefsky JH. Discoid lateral meniscus in three members of a family. J Bone Joint Surg, (Am.). 1971;53(6):1208-1210. doi: 10.2106/00004623-197153060-00018.
4. Francavilla ML, Restrepo R, Zamora KW, Sarode V, Swirsky SM, Mintz D. Meniscal pathology in children: differences and similarities with the adult meniscus. Pediatr Radiol. 2014;44(8):910-925. doi: 10.1007/s00247-014-3022-0.
5. Kushare I, Klingele K, Samora W. Discoid meniscus: diagnosis and management. Orthop Clin North Am. 2015;46(4):533-540. doi: 10.1016/j.ocl.2015.06.007.
6. McKay S, Chen C, Rosenfeld S. Orthopedic perspective on selected pediatric and adolescent knee conditions. Pediatr Radiol. 2013;43(1):99-106. doi: 10.1007/s00247-012-2587-8.
7. Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002;10(3):168-176. doi: 10.5435/00124635-200205000-00003.
8. Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus. Technique and long-term results. Clin Orthop Relat Res. 1982;167(167):19-28.
9. Nathan PA, Cole SC. 12 Discoid meniscus: a clinical and pathologic study. Clin Orthop Relat Res: SC: Cole. 1969;64:107-113.
10. Jeannopoulos CL. Observations on discoid menisci. J Bone Joint Surg, (Am.). 1950;32(3):649-652. doi: 10.2106/00004623-195032030-00019.
11. Dickason J, Del WP, Blazina ME, Fox JM, Friedman MJ, Snyder SJ. A series of ten discoid medial menisci. Clin Orthop Relat Res. 1982;168:75-79. doi: 10.1097/00003086-198208000-00014
12. Andrish JT. Meniscal injuries in children and adolescents: diagnosis and management. J Am Acad Orthop Surg. 1996;4(5):231-237. doi: 10.5435/00124635-199609000-00001.
13. Kaplan E. The embryology of the menisci of the knee joint. Bull Hosp Joint Dis. 1955;16(2):111-124.
14. Clark C, Ogden J. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg, (Am.). 1983;65(4):538-547 doi: 10.2106/00004623-198365040-00018.
15. Carter CW, Kocher MS. Meniscus repair in children. Clin Sports Med. 2012;31(1):135-154. doi: 10.1016/j.csm.2011.09.002.
16. Shieh A, Bastrom T, Roocroft J, Edmonds EW, Pennock AT. Meniscus tear patterns in relation to skeletal immaturity: children versus adolescents. Am J Sports Med. 2013;41(12):2779-2783. doi: 10.1177/0363546513504286.
17. Jordan MR. Lateral meniscal variants: evaluation and treatment. J Am Acad Orthopsurg. 1996;4(4):191-200. doi: 10.5435/00124635-199607000-00003.
18. Flouzat-Lachaniette C, Pujol N, Boisrenoult P, Beaufils P. Discoid medial meniscus: report of four cases and literature review. Orthop Traumatol Surg Res. 2011;97(8):826-832. doi: 10.1016/j.otsr.2011.07.011.
19. Choi Y-H, Seo Y-J, Ha JM, Jung KH, Kim J, Song SY. Collagenous ultrastructure of the discoid meniscus: A Transmission Electron Microscopy Study. Am J Sports Med. 2017;45(3):598-603. doi: 10.1177/0363546516674181.
20. Atay OA, Pekmezci M, Doral MN, Sargon MF, Ayvaz M, Johnson DL. Discoid meniscus: an ultrastructural study with transmission electron microscopy. Am J Sports Med. 2007;35(3):475-478. doi: 10.1177/0363546506294678.
21. Papadopoulos A, Kirkos JM, Kapetanos GA. Histomorphologic study of discoid meniscus. Arthroscopy. 2009;25(3):262-268. doi: 10.1016/j.arthro.2008.10.006.
22. Watanabe M, Takeda S, Ikeuchi H. Atlas of Arthroscopy. Tokyo: Igaku-Shoin Ltd; 1969.
23. Monllau JC, León A, Cugat R, Ballester J. Ring-shaped lateral meniscus. Arthroscopy. 1998;14(5):502-504. doi: 10.1016/S0749-8063(98)70079-9.
24. Jordan M, Duncan J, Bertrand S. Discoid lateral meniscus: a review. S Orthop J. 1993;2(4):239-253.
25. Klingele KE, Kocher MS, Hresko MT, Gerbino P, Micheli LJ. Discoid lateral meniscus: prevalence of peripheral rim instability. J Pediatr Orthop. 2004;24(1):79-82. doi: 10.1097/01241398-200401000-00015.
26. Choi SH, Ahn JH, Kim KI, et al. Do the radiographic findings of symptomatic discoid lateral meniscus in children differ from normal control subjects? Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1128-1134. doi: 10.1007/s00167-014-2924-6.
27. Gans I, Bedoya MA, Ho-Fung V, Ganley TJ. Diagnostic performance of magnetic resonance imaging and pre-surgical evaluation in the assessment of traumatic intra-articular knee disorders in children and adolescents: what conditions still pose diagnostic challenges? Pediatr Radiol. 2015;45(2):194-202. doi: 10.1007/s00247-014-3127-5.
28. Samoto N, Kozuma M, Tokuhisa T, Kobayashi K. Diagnosis of discoid lateral meniscus of the knee on MR imaging. Magn Reson Imaging. 2002;20(1):59-64. doi: 10.1016/S0730-725X(02)00473-3.
29. Hayashi LK, Yamaga H, Ida K, Miura T. Arthroscopic meniscectomy for discoid lateral meniscus in children. J Bone Joint Surg, (Am.). 1988;70(10):1495-1500. doi: 10.2106/00004623-198870100-00009.
30. Kim S-J, Kim D-W, Min B-H. Discoid lateral meniscus associated with anomalous insertion of the medial meniscus. Clin Orthop Rel Res. 1995;315(315):234-237 doi: 10.1097/00003086-199506000-00026.
31. Adachi N, Ochi M, Uchio Y, Kuriwaka M, Shinomiya R. Torn discoid lateral meniscus treated using partial central meniscectomy and suture of the peripheral tear. Arthroscopy. 2004;20(5):536-542. doi: 10.1016/j.arthro.2004.01.028.
32. Kim J-M, Bin S-I. Meniscal allograft transplantation after total meniscectomy of torn discoid lateral meniscus. Arthroscopy. 2006;22(12):1344-1350.e1. doi: 10.1016/j.arthro.2006.07.048.
33. Ramme AJ, Strauss EJ, Jazrawi L, Gold HT. Cost effectiveness of meniscal allograft for torn discoid lateral meniscus in young women. Phys Sportsmed. 2016;44(3):278-282. doi: 10.1080/00913847.2016.1197762.
34. Baratz ME, Fu FH, Mengato R. Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: a preliminary report. Am J Sports Med. 1986;14(4):270-275. doi: 10.1177/036354658601400405.
35. Wroble RR, Henderson RC, Campion ER, el-Khoury GY, Albright JP. Meniscectomy in children and adolescents. A long-term follow-up study. Clin Orthop Relat Res. 1992;279(279):180-189.
36. Räber D, Friederich N, Hefti F. Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg, (Am.). 1998;80(11):1579-1586. doi: 10.2106/00004623-199811000-00003.
37. Stilli S, Reggiani LM, Muccioli GMM, Cappella M, Donzelli O. Arthroscopic treatment for symptomatic discoid lateral meniscus during childhood. Knee Surg Sports Traumatol Arthrosc. 2011;19(8):1337-1342. doi: 10.1007/s00167-011-1440-1.
38. Ahn JH, Kim KI, Wang JH, Jeon JW, Cho YC, Lee SH. Long-term results of arthroscopic reshaping for symptomatic discoid lateral meniscus in children. Arthroscopy. 2015;31(5):867-873. doi: 10.1016/j.arthro.2014.12.012.
39. Carter CW, Hoellwarth J, Weiss JM. Clinical outcomes as a function of meniscal stability in the discoid meniscus: a preliminary report. J Pediatr Orthop. 2012;32(1):9-14. doi: 10.1097/BPO.0b013e31823d8338.
40. Yoo WJ, Jang WY, Park MS, et al. Arthroscopic treatment for symptomatic discoid meniscus in children: midterm outcomes and prognostic factors. Arthroscopy. 2015;31(12):2327-2334. doi: 10.1016/j.arthro.2015.06.032.
41. Shieh A, Edmonds EW, Pennock AT. Revision meniscus surgery in children and adolescents: the effect of skeletal immaturity. Orthop J Sports Med. 2015;3(7):S00075:2325967115. doi: 10.1177/2325967115S00075.
42. Shieh AK, Edmonds EW, Pennock AT. Revision meniscal surgery in children and adolescents: risk factors and mechanisms for failure and subsequent management. Am J Sports Med. 2016;44(4):838-843. doi: 10.1177/0363546515623511.
TAKE-HOME POINTS
- The discoid meniscus is a congenital variant that is present from birth and may or not become symptomatic as a child matures.
- MRI may be used to make the diagnosis of discoid lateral meniscus, defined as 3 or more consecutive sagittal 5-mm cuts demonstrating contiguity of the anterior and posterior horns.
- A useful classification system for discoid meniscus describes the shape of the meniscus (complete or partial disc), whether it is torn (torn or intact), and whether it has peripheral instability (stable or unstable).
- Surgical treatment of symptomatic discoid lateral meniscus is aimed at restoring normal morphology and stability to the abnormal meniscus.
- Short- and mid-term outcomes following partial meniscectomy with repair and/or stabilization as needed are generally good; long-term outcomes following subtotal or complete meniscectomy are poor, demonstrating progression to early arthritis.
Barbershop BP intervention going strong at 12 months
for a black male cohort of participants, according to 12-month data from the project.
Of the 319 black, non-Hispanic male participants, 180 were randomized to participate in an intensive 6-month hypertension intervention. The study protocol allowed pharmacists, who visited participants at their barbershops, to prescribe hypertension medication under collaborative practice agreements with participants’ primary care providers (PCPs).
Compared with an active control group who received instruction about blood pressure and lifestyle modification, participants receiving the intervention saw significant reductions in systolic BP at 6 months (N Engl J Med. 2018 Apr 5;378:1291-391). From 6 months onward, participants in the intervention arm received fewer visits from pharmacists, though they still regularly visited the barbershop, where blood pressure was recorded. At the end of 12 months, systolic BP – at least 140 mm Hg at enrollment – dropped by 28.6 mm Hg from baseline in the intervention group to a mean 123.8 mm Hg. For those in the control group, the reduction in systolic BP was 7.2 mm Hg, to a mean 147.4 mm Hg. This 20.8-point difference between the two groups was highly statistically significant (P less than .0001).
“These new 12-month efficacy data are statistically indistinguishable from our previously reported 6-month data,” wrote Ciantal Blyler, PharmD, a clinical pharmacist at Cedars-Sinai Medical Center, Los Angeles, and her coauthors.
Diastolic BP, a secondary outcome measure, fell in the intervention group by 14.5 mm Hg more than in the active controls. In the intervention arm, 68% of participants reached the prespecified goal blood pressure of less than 130/80 mm Hg, while just 11% of the control group hit this target, a significant difference.
No trial participants experienced treatment-related adverse events or deaths during the 6-month extension phase.
Compared with men in the active control arm, those receiving the intervention were on a greater number of antihypertensive classes per regimen. Also, patients receiving the intervention were more likely to receive first-line drugs as add-on therapy. At the end of the 12-month period, all participants in the intensive arm were on antihypertensives, up from 57% at baseline. For the control group, antihypertensive medication use went from 53% at baseline to 65% at 6 months (P less than .001).
The intervention group saw their PCP more frequently than did the control group during the study; there was no difference in PCP visit frequency at baseline. “This suggests that the pharmacist intervention did not interfere with the patient-PCP relationship, and perhaps influenced the increase in PCP visits,” noted Dr. Blyler and her colleagues.
The investigators noted that the pharmacists’ ability to begin, titrate, and change hypertension medication under a collaborative agreement with physicians was an essential part of the program’s initial and continued success. “Perhaps the most critical first step toward widespread dissemination of our model is the expansion of collaborative practice between pharmacists and physicians, or the elimination of the requirement altogether (as in Canada and the UK),” wrote Dr. Blyler and her coauthors.
Beyond that, Dr. Blyler and her colleagues said that scalability will depend on the ability to adapt the model to create operational efficiencies while maintaining intervention potency. The time it took pharmacists to get to and from barbershops was significant, and some form of telemonitoring may work well going forward as “an appropriate means of maintaining/sustaining the intervention effect whilst also addressing this logistical inefficiency,” they said.
The study was funded by the National Institutes of Health, the California Endowment, the Lincy Foundation, the Harriet and Steven Nichols Foundation, the Smidt Heart Institute, and the Division of Community Relations and Development at Cedars-Sinai Medical Center, Los Angeles. One coauthor reported being a consultant for Recor Medical; other authors reported that they had no disclosures.
SOURCE: Blyler C et al. Circulation. 2018 Dec 17.
for a black male cohort of participants, according to 12-month data from the project.
Of the 319 black, non-Hispanic male participants, 180 were randomized to participate in an intensive 6-month hypertension intervention. The study protocol allowed pharmacists, who visited participants at their barbershops, to prescribe hypertension medication under collaborative practice agreements with participants’ primary care providers (PCPs).
Compared with an active control group who received instruction about blood pressure and lifestyle modification, participants receiving the intervention saw significant reductions in systolic BP at 6 months (N Engl J Med. 2018 Apr 5;378:1291-391). From 6 months onward, participants in the intervention arm received fewer visits from pharmacists, though they still regularly visited the barbershop, where blood pressure was recorded. At the end of 12 months, systolic BP – at least 140 mm Hg at enrollment – dropped by 28.6 mm Hg from baseline in the intervention group to a mean 123.8 mm Hg. For those in the control group, the reduction in systolic BP was 7.2 mm Hg, to a mean 147.4 mm Hg. This 20.8-point difference between the two groups was highly statistically significant (P less than .0001).
“These new 12-month efficacy data are statistically indistinguishable from our previously reported 6-month data,” wrote Ciantal Blyler, PharmD, a clinical pharmacist at Cedars-Sinai Medical Center, Los Angeles, and her coauthors.
Diastolic BP, a secondary outcome measure, fell in the intervention group by 14.5 mm Hg more than in the active controls. In the intervention arm, 68% of participants reached the prespecified goal blood pressure of less than 130/80 mm Hg, while just 11% of the control group hit this target, a significant difference.
No trial participants experienced treatment-related adverse events or deaths during the 6-month extension phase.
Compared with men in the active control arm, those receiving the intervention were on a greater number of antihypertensive classes per regimen. Also, patients receiving the intervention were more likely to receive first-line drugs as add-on therapy. At the end of the 12-month period, all participants in the intensive arm were on antihypertensives, up from 57% at baseline. For the control group, antihypertensive medication use went from 53% at baseline to 65% at 6 months (P less than .001).
The intervention group saw their PCP more frequently than did the control group during the study; there was no difference in PCP visit frequency at baseline. “This suggests that the pharmacist intervention did not interfere with the patient-PCP relationship, and perhaps influenced the increase in PCP visits,” noted Dr. Blyler and her colleagues.
The investigators noted that the pharmacists’ ability to begin, titrate, and change hypertension medication under a collaborative agreement with physicians was an essential part of the program’s initial and continued success. “Perhaps the most critical first step toward widespread dissemination of our model is the expansion of collaborative practice between pharmacists and physicians, or the elimination of the requirement altogether (as in Canada and the UK),” wrote Dr. Blyler and her coauthors.
Beyond that, Dr. Blyler and her colleagues said that scalability will depend on the ability to adapt the model to create operational efficiencies while maintaining intervention potency. The time it took pharmacists to get to and from barbershops was significant, and some form of telemonitoring may work well going forward as “an appropriate means of maintaining/sustaining the intervention effect whilst also addressing this logistical inefficiency,” they said.
The study was funded by the National Institutes of Health, the California Endowment, the Lincy Foundation, the Harriet and Steven Nichols Foundation, the Smidt Heart Institute, and the Division of Community Relations and Development at Cedars-Sinai Medical Center, Los Angeles. One coauthor reported being a consultant for Recor Medical; other authors reported that they had no disclosures.
SOURCE: Blyler C et al. Circulation. 2018 Dec 17.
for a black male cohort of participants, according to 12-month data from the project.
Of the 319 black, non-Hispanic male participants, 180 were randomized to participate in an intensive 6-month hypertension intervention. The study protocol allowed pharmacists, who visited participants at their barbershops, to prescribe hypertension medication under collaborative practice agreements with participants’ primary care providers (PCPs).
Compared with an active control group who received instruction about blood pressure and lifestyle modification, participants receiving the intervention saw significant reductions in systolic BP at 6 months (N Engl J Med. 2018 Apr 5;378:1291-391). From 6 months onward, participants in the intervention arm received fewer visits from pharmacists, though they still regularly visited the barbershop, where blood pressure was recorded. At the end of 12 months, systolic BP – at least 140 mm Hg at enrollment – dropped by 28.6 mm Hg from baseline in the intervention group to a mean 123.8 mm Hg. For those in the control group, the reduction in systolic BP was 7.2 mm Hg, to a mean 147.4 mm Hg. This 20.8-point difference between the two groups was highly statistically significant (P less than .0001).
“These new 12-month efficacy data are statistically indistinguishable from our previously reported 6-month data,” wrote Ciantal Blyler, PharmD, a clinical pharmacist at Cedars-Sinai Medical Center, Los Angeles, and her coauthors.
Diastolic BP, a secondary outcome measure, fell in the intervention group by 14.5 mm Hg more than in the active controls. In the intervention arm, 68% of participants reached the prespecified goal blood pressure of less than 130/80 mm Hg, while just 11% of the control group hit this target, a significant difference.
No trial participants experienced treatment-related adverse events or deaths during the 6-month extension phase.
Compared with men in the active control arm, those receiving the intervention were on a greater number of antihypertensive classes per regimen. Also, patients receiving the intervention were more likely to receive first-line drugs as add-on therapy. At the end of the 12-month period, all participants in the intensive arm were on antihypertensives, up from 57% at baseline. For the control group, antihypertensive medication use went from 53% at baseline to 65% at 6 months (P less than .001).
The intervention group saw their PCP more frequently than did the control group during the study; there was no difference in PCP visit frequency at baseline. “This suggests that the pharmacist intervention did not interfere with the patient-PCP relationship, and perhaps influenced the increase in PCP visits,” noted Dr. Blyler and her colleagues.
The investigators noted that the pharmacists’ ability to begin, titrate, and change hypertension medication under a collaborative agreement with physicians was an essential part of the program’s initial and continued success. “Perhaps the most critical first step toward widespread dissemination of our model is the expansion of collaborative practice between pharmacists and physicians, or the elimination of the requirement altogether (as in Canada and the UK),” wrote Dr. Blyler and her coauthors.
Beyond that, Dr. Blyler and her colleagues said that scalability will depend on the ability to adapt the model to create operational efficiencies while maintaining intervention potency. The time it took pharmacists to get to and from barbershops was significant, and some form of telemonitoring may work well going forward as “an appropriate means of maintaining/sustaining the intervention effect whilst also addressing this logistical inefficiency,” they said.
The study was funded by the National Institutes of Health, the California Endowment, the Lincy Foundation, the Harriet and Steven Nichols Foundation, the Smidt Heart Institute, and the Division of Community Relations and Development at Cedars-Sinai Medical Center, Los Angeles. One coauthor reported being a consultant for Recor Medical; other authors reported that they had no disclosures.
SOURCE: Blyler C et al. Circulation. 2018 Dec 17.
FROM CIRCULATION
Key clinical point:
Major finding: Systolic BP fell by 28.6 vs. 7.2 mm Hg for those receiving the intervention (P less than .0001).
Study details: Cluster-randomized cohort study of 319 non-Hispanic African American males with hypertension.
Disclosures: The study was funded by the National Institutes of Health, the California Endowment, the Lincy Foundation, the Harriet and Steven Nichols Foundation, the Smidt Heart Institute, and the Division of Community Relations and Development at Cedars-Sinai Medical Center, Los Angeles. One coauthor reported being a consultant for Recor Medical; other authors reported that they had no disclosures.
Source: Blyler C et al. Circulation. 2018 Dec 17.
2018 REVIEWER APPRECIATION
The JCSO Editors and editorial staff thank all those who generously contributed to the peer-review process this past year. We are mindful of the many demands on you and value the time and expertise you put in to reviewing submissions.
Click on the PDF icon at the top of this introduction for a complete list of the names of all the reviewers.
The JCSO Editors and editorial staff thank all those who generously contributed to the peer-review process this past year. We are mindful of the many demands on you and value the time and expertise you put in to reviewing submissions.
Click on the PDF icon at the top of this introduction for a complete list of the names of all the reviewers.
The JCSO Editors and editorial staff thank all those who generously contributed to the peer-review process this past year. We are mindful of the many demands on you and value the time and expertise you put in to reviewing submissions.
Click on the PDF icon at the top of this introduction for a complete list of the names of all the reviewers.