User login
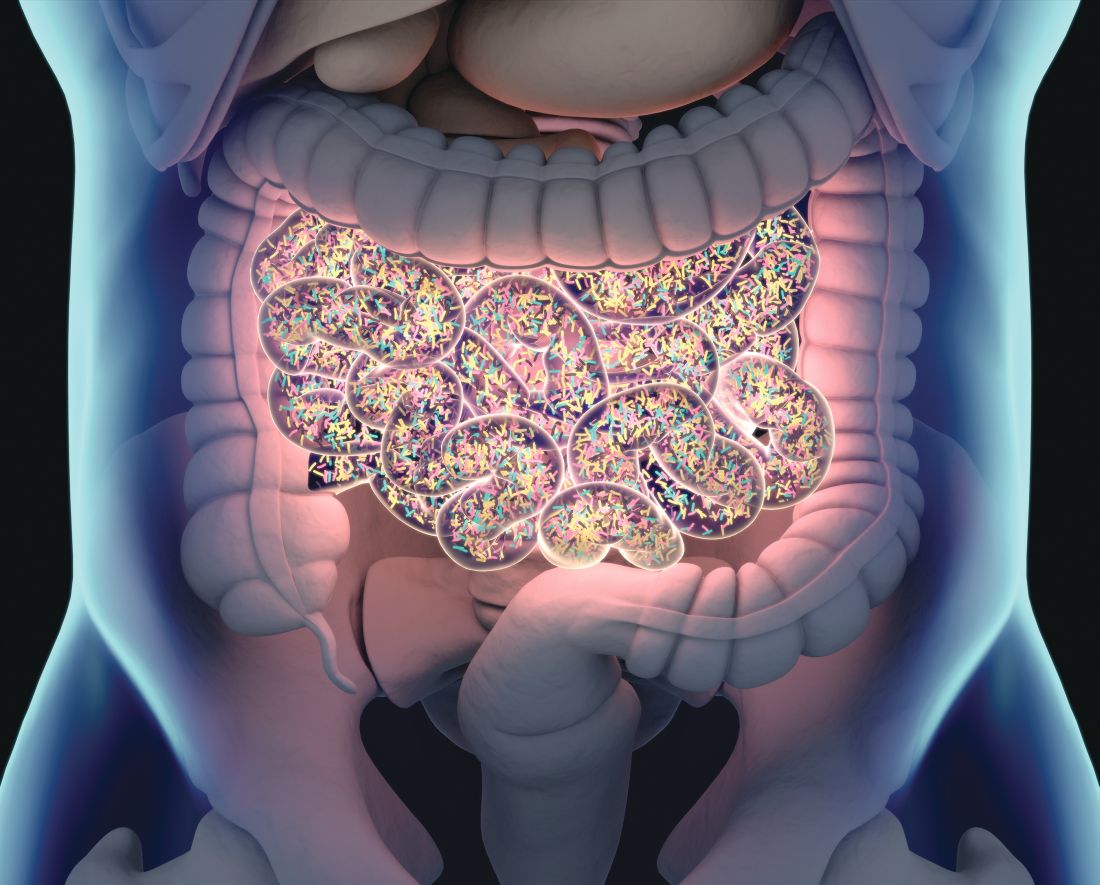
Rising microbiome investigator: Lea Ann Chen, MD
We spoke with Dr. Chen, assistant professor of medicine at New York University and the recipient of the AGA Research Foundation’s 2016 Research Scholar Award, to learn about her work on the gut microbiome and inflammatory bowel disease (IBD).
How would you sum up your research in one sentence?
I study longitudinal changes of the gut microbiome as it relates to gastrointestinal illnesses, particularly IBD.
What impact do you hope your research will have on patients?
I hope that my research will provide greater insights into the role of gut microbes in disease pathogenesis and activity to ultimately inform the development of new diagnostics and treatments.
What inspired you to focus your research career on the gut microbiome?
I’ve long been fascinated by ecological systems and host-microbe interactions. As technologies to study the gut microbiome became more readily available, I was eager, and somewhat relieved, to be able to combine my research interests with my clinical interest in gastroenterology.
What recent publication from your lab best represents your work, if anyone wants to learn more?
In this study, we show that gut bacterial disturbances are resolved after fecal transplantation in children without IBD but are only transiently resolved in those with IBD.
Hourigan S.*, Chen L.A.*, Grigoryan Z., et al. Microbiome changes associated with sustained eradication of Clostridium difficile after fecal microbiota transplantation in children with and without inflammatory bowel disease. Aliment Pharmacol Ther. 2015;42:741-52.
You’re involved with several AGA initiatives including the Future Leaders Program and the FMT National Registry. How has being an AGA member impacted your career?
AGA has provided key mentorship and training opportunities that have been instrumental in my career development. It has further helped me discover a diverse community of clinicians and scientists who are amazing role models, resources and colleagues. I really had no inkling what was in store when I first joined AGA as a trainee, but I feel very lucky that I did and am grateful for how AGA membership has really enriched my life as a gastroenterologist.
We spoke with Dr. Chen, assistant professor of medicine at New York University and the recipient of the AGA Research Foundation’s 2016 Research Scholar Award, to learn about her work on the gut microbiome and inflammatory bowel disease (IBD).
How would you sum up your research in one sentence?
I study longitudinal changes of the gut microbiome as it relates to gastrointestinal illnesses, particularly IBD.
What impact do you hope your research will have on patients?
I hope that my research will provide greater insights into the role of gut microbes in disease pathogenesis and activity to ultimately inform the development of new diagnostics and treatments.
What inspired you to focus your research career on the gut microbiome?
I’ve long been fascinated by ecological systems and host-microbe interactions. As technologies to study the gut microbiome became more readily available, I was eager, and somewhat relieved, to be able to combine my research interests with my clinical interest in gastroenterology.
What recent publication from your lab best represents your work, if anyone wants to learn more?
In this study, we show that gut bacterial disturbances are resolved after fecal transplantation in children without IBD but are only transiently resolved in those with IBD.
Hourigan S.*, Chen L.A.*, Grigoryan Z., et al. Microbiome changes associated with sustained eradication of Clostridium difficile after fecal microbiota transplantation in children with and without inflammatory bowel disease. Aliment Pharmacol Ther. 2015;42:741-52.
You’re involved with several AGA initiatives including the Future Leaders Program and the FMT National Registry. How has being an AGA member impacted your career?
AGA has provided key mentorship and training opportunities that have been instrumental in my career development. It has further helped me discover a diverse community of clinicians and scientists who are amazing role models, resources and colleagues. I really had no inkling what was in store when I first joined AGA as a trainee, but I feel very lucky that I did and am grateful for how AGA membership has really enriched my life as a gastroenterologist.
We spoke with Dr. Chen, assistant professor of medicine at New York University and the recipient of the AGA Research Foundation’s 2016 Research Scholar Award, to learn about her work on the gut microbiome and inflammatory bowel disease (IBD).
How would you sum up your research in one sentence?
I study longitudinal changes of the gut microbiome as it relates to gastrointestinal illnesses, particularly IBD.
What impact do you hope your research will have on patients?
I hope that my research will provide greater insights into the role of gut microbes in disease pathogenesis and activity to ultimately inform the development of new diagnostics and treatments.
What inspired you to focus your research career on the gut microbiome?
I’ve long been fascinated by ecological systems and host-microbe interactions. As technologies to study the gut microbiome became more readily available, I was eager, and somewhat relieved, to be able to combine my research interests with my clinical interest in gastroenterology.
What recent publication from your lab best represents your work, if anyone wants to learn more?
In this study, we show that gut bacterial disturbances are resolved after fecal transplantation in children without IBD but are only transiently resolved in those with IBD.
Hourigan S.*, Chen L.A.*, Grigoryan Z., et al. Microbiome changes associated with sustained eradication of Clostridium difficile after fecal microbiota transplantation in children with and without inflammatory bowel disease. Aliment Pharmacol Ther. 2015;42:741-52.
You’re involved with several AGA initiatives including the Future Leaders Program and the FMT National Registry. How has being an AGA member impacted your career?
AGA has provided key mentorship and training opportunities that have been instrumental in my career development. It has further helped me discover a diverse community of clinicians and scientists who are amazing role models, resources and colleagues. I really had no inkling what was in store when I first joined AGA as a trainee, but I feel very lucky that I did and am grateful for how AGA membership has really enriched my life as a gastroenterologist.
Differences in gut bacteria can distinguish IBD from IBS
Thanks to shotgun metagenomic sequencing of gut microbiota, physicians are on track to more easily distinguish inflammatory bowel disease (IBD) from irritable bowel syndrome (IBS), according to an analysis of stool samples from patients with the two common gastrointestinal diseases.
“The integration of these datasets allowed us to pinpoint key species as targets for functional studies in IBD and IBS and to connect knowledge of the etiology and pathogenesis of IBD and IBS with the gut microbiome to provide potential new targets for treatment,” wrote Arnau Vich Vila, of the University of Groningen, the Netherlands, and his coauthors. The report is in Science Translational Medicine.
Stool samples from 1,792 participants were analyzed: 355 from patients with IBD, 412 from patients with IBS, and 1,025 from the control group. The researchers found 24 bacterial taxa associated with both IBD and IBS and specific species that accompanied specific diseases, such as an abundance of Bacteroides in patients with IBD and Firmicutes in patients with IBS. In addition, their predictive model to distinguish IBD from IBS via gut microbial composition data [area under the curve (AUC) mean = 0.91 (0.81 to 0.99)] proved more accurate than did current fecal biomarker calprotectin [AUC mean = 0.80 (0.71 to 0.88); P = .002].
The authors acknowledged additional evidence that will be needed before these results can be translated to clinical practice, including supporting their described microbial pathways with metatranscriptomics and metabolomics data as well as functional experiments. They also observed that their predictive model will need to be validated through replication of their findings in patients with other gastrointestinal disorders or prediagnostic groups. They noted that their analysis benefited from being able to correct for confounding factors such as medication use, which is “essential for identifying disease-associated microbial features and avoiding false-positive associations due to changes in GI acidity or bowel mobility.”
One author reported receiving speaker fees from AbbVie and was a shareholder of the health care IT company Aceso BV and of Floris Medical Holding BV. Another author declared unrestricted research grants from AbbVie, Takeda, and Ferring Pharmaceuticals, is on the advisory boards for Mundipharma and Pharmacosmos, and has received speaker fees from Takeda and Janssen Pharmaceuticals. A third author declared consulting work for Takeda. The others reported no conflicts of interest.
SOURCE: Vich Vila A et al. Sci Transl Med. 2018 Dec 19. doi: 10.1126/scitranslmed.aap8914.
Thanks to shotgun metagenomic sequencing of gut microbiota, physicians are on track to more easily distinguish inflammatory bowel disease (IBD) from irritable bowel syndrome (IBS), according to an analysis of stool samples from patients with the two common gastrointestinal diseases.
“The integration of these datasets allowed us to pinpoint key species as targets for functional studies in IBD and IBS and to connect knowledge of the etiology and pathogenesis of IBD and IBS with the gut microbiome to provide potential new targets for treatment,” wrote Arnau Vich Vila, of the University of Groningen, the Netherlands, and his coauthors. The report is in Science Translational Medicine.
Stool samples from 1,792 participants were analyzed: 355 from patients with IBD, 412 from patients with IBS, and 1,025 from the control group. The researchers found 24 bacterial taxa associated with both IBD and IBS and specific species that accompanied specific diseases, such as an abundance of Bacteroides in patients with IBD and Firmicutes in patients with IBS. In addition, their predictive model to distinguish IBD from IBS via gut microbial composition data [area under the curve (AUC) mean = 0.91 (0.81 to 0.99)] proved more accurate than did current fecal biomarker calprotectin [AUC mean = 0.80 (0.71 to 0.88); P = .002].
The authors acknowledged additional evidence that will be needed before these results can be translated to clinical practice, including supporting their described microbial pathways with metatranscriptomics and metabolomics data as well as functional experiments. They also observed that their predictive model will need to be validated through replication of their findings in patients with other gastrointestinal disorders or prediagnostic groups. They noted that their analysis benefited from being able to correct for confounding factors such as medication use, which is “essential for identifying disease-associated microbial features and avoiding false-positive associations due to changes in GI acidity or bowel mobility.”
One author reported receiving speaker fees from AbbVie and was a shareholder of the health care IT company Aceso BV and of Floris Medical Holding BV. Another author declared unrestricted research grants from AbbVie, Takeda, and Ferring Pharmaceuticals, is on the advisory boards for Mundipharma and Pharmacosmos, and has received speaker fees from Takeda and Janssen Pharmaceuticals. A third author declared consulting work for Takeda. The others reported no conflicts of interest.
SOURCE: Vich Vila A et al. Sci Transl Med. 2018 Dec 19. doi: 10.1126/scitranslmed.aap8914.
Thanks to shotgun metagenomic sequencing of gut microbiota, physicians are on track to more easily distinguish inflammatory bowel disease (IBD) from irritable bowel syndrome (IBS), according to an analysis of stool samples from patients with the two common gastrointestinal diseases.
“The integration of these datasets allowed us to pinpoint key species as targets for functional studies in IBD and IBS and to connect knowledge of the etiology and pathogenesis of IBD and IBS with the gut microbiome to provide potential new targets for treatment,” wrote Arnau Vich Vila, of the University of Groningen, the Netherlands, and his coauthors. The report is in Science Translational Medicine.
Stool samples from 1,792 participants were analyzed: 355 from patients with IBD, 412 from patients with IBS, and 1,025 from the control group. The researchers found 24 bacterial taxa associated with both IBD and IBS and specific species that accompanied specific diseases, such as an abundance of Bacteroides in patients with IBD and Firmicutes in patients with IBS. In addition, their predictive model to distinguish IBD from IBS via gut microbial composition data [area under the curve (AUC) mean = 0.91 (0.81 to 0.99)] proved more accurate than did current fecal biomarker calprotectin [AUC mean = 0.80 (0.71 to 0.88); P = .002].
The authors acknowledged additional evidence that will be needed before these results can be translated to clinical practice, including supporting their described microbial pathways with metatranscriptomics and metabolomics data as well as functional experiments. They also observed that their predictive model will need to be validated through replication of their findings in patients with other gastrointestinal disorders or prediagnostic groups. They noted that their analysis benefited from being able to correct for confounding factors such as medication use, which is “essential for identifying disease-associated microbial features and avoiding false-positive associations due to changes in GI acidity or bowel mobility.”
One author reported receiving speaker fees from AbbVie and was a shareholder of the health care IT company Aceso BV and of Floris Medical Holding BV. Another author declared unrestricted research grants from AbbVie, Takeda, and Ferring Pharmaceuticals, is on the advisory boards for Mundipharma and Pharmacosmos, and has received speaker fees from Takeda and Janssen Pharmaceuticals. A third author declared consulting work for Takeda. The others reported no conflicts of interest.
SOURCE: Vich Vila A et al. Sci Transl Med. 2018 Dec 19. doi: 10.1126/scitranslmed.aap8914.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point: Shotgun metagenomic sequencing data revealed key differences in gut microbiome composition between patients with inflammatory bowel disease and patients with irritable bowel syndrome.
Major finding: A predictive model to distinguish IBD from IBS based on gut microbial composition data [area under the curve (AUC) mean = 0.91 (0.81-0.99)] proved more accurate than did fecal biomarker calprotectin [AUC mean = 0.80 (0.71-0.88); P = .002].
Study details: A case-control analysis using shotgun metagenomic sequencing of stool samples from 1,792 individuals with IBD, IBS, or neither.
Disclosures: One author reported receiving speaker fees from AbbVie and was a shareholder of the health care IT company Aceso BV and of Floris Medical Holding BV. Another author declared unrestricted research grants from AbbVie, Takeda, and Ferring Pharmaceuticals, is on the advisory boards for Mundipharma and Pharmacosmos, and has received speaker fees from Takeda and Janssen Pharmaceuticals. A third author declared consulting work for Takeda. The others reported no conflicts of interest.
Source: Vich Vila A et al. Sci Transl Med. 2018 Dec 19. doi: 10.1126/scitranslmed.aap8914.
Ingredients for effective team-based care
Changing times for U.S. health care
The current health care environment is undergoing a rapid transformation. In evolutionary biology, a theory exists called punctuated equilibrium. This theory suggests there are long periods of little or no morphological change amongst species and then, geologically speaking, short periods of rapid change in response to pressures within the environment. This rapid period of change adds significant diversity to the landscape of existing species. In health care, we are undergoing a period of “punctuation.”
A testament to the degree of change is a scan of the various consolidation activities occurring across the health care space. Some are more traditional, such as mergers of health systems with different or competing geographical footprints or hospitalist management companies that provide similar services and desire to increase their market share. Others that are more interesting are those that include mergers of seemingly different business lines or offerings, like CVS Health and Aetna; Humana and Kindred; or even organizations such as Amazon, Berkshire Hathaway, and JP Morgan hiring Atul Gawande as the CEO of their newly formed health care venture. The latter examples serve as an illustration of the reorganization that is occurring within health care delivery. This represents, at the very least, a blurring of the lines – if not a deconstruction and complete rebuild – of traditional lines of separation between payers, providers, employers, and retailers.
In other words, the silos are coming down, significant diversity in the landscape of existing species. A common theme across these changes is that most – if not all – participants will share some portion of the financial risk associated with these evolving models. High-deductible health plans, alternative payment models (APMs), and advanced APMs are examples of tactics and models that distribute the financial risk. The consolidations referenced above will likely continue to encourage distribution of the financial risk across patients, providers, employers, and payers.
A key theme coming into focus is that the evolving care delivery system will not be defined by bricks and mortar. Rather, it will follow the patient and go wherever he or she goes to meet his or her specific needs. This is why we’re seeing mergers comprised of a variety of assets, including personnel, technology, critical supplies (such as pharmaceuticals), and funding resources. This very purposeful and deliberate melting pot phenomenon will restructure and reformat the care delivery model.
To be successful within this new landscape, there will need to be a renewed focus on working within a collaborative model. The days of a single entity or provider being able to serve as the “be all” or “do all” is over, and the days of practicing medicine as the Lone Ranger are anachronistic. Instead, there is a need for health care providers to embrace and lead a team-based care model. Team-based care should have the patient at the center of the care delivery model and leverage the expertise of the various team members to practice at the “top of their expertise.”
In hospital medicine, this includes a variety of team members – from physicians, nurse practitioners, physician assistants, and clinical pharmacists to case managers, physical therapists, subject matter experts in quality improvement, and analysts – who identify operational priorities from the data rather than reporting predefined goals on dashboards. Although possibly a good start, this is by no means an exhaustive list of team members. The team will be defined by the goals the health care team aspires to achieve. These goals may include closer alignment with payers, employers, and post-acute partners; the goals will influence the composition of the team. Once the team is defined, the challenge will be to effectively integrate team members, so they are contributing their expertise to the patient care being delivered.
Some ingredients for effective team-based care include the following:
- Developing an effective process for engagement and providing a voice for all team members. Interdisciplinary team rounds where there is an established time for team members to plan and operationalize their plans around patient care can serve as an example of this type of structured process.
- Creating well-defined roles and responsibilities with key performance indicators to promote accountability. The team will have outcomes they are measuring and striving to impact, and each team member will have a role in achieving those goals. Being able to parse out and measure how each team member contributes to the overall outcome can be beneficial. This provides an opportunity for each team member to play a meaningful role in accomplishing the overall goal and allows for a measurement process to track success. For example, an overall team goal may be to have a specific percentage of eligible discharges completed by 11:00 a.m. To accomplish this goal, there may be specific objectives for the clinicians to have discharge orders in the chart by 9:30 a.m. and for case management to have communicated with any post-acute services the day before discharge. These specific accountability measures facilitate accomplishing the larger team goal.
- Developing a culture of safety and transparency. Effective teams promote an environment where all members are empowered and encouraged to speak and share their perspective and knowledge. Communication is based on the value it provides to accomplishing the team’s goals rather than based on a hierarchy which determines who contributes and when.
- Defining and then redefining the competencies required of the team to promote continued development and growth. In this time of dynamic change, the skill sets that helped us get where we are today may be different then the skill sets that are needed for success in the future. There will continue to be a need for functional and knowledge-based competencies in addition to the need to focus on competencies that engender a culture of team-based care. For example, hospitalist leaders will need to understand evidence-based medicine to support appropriate management of a septic patient and simultaneously understand evidence-based management/leadership to affect sepsis care across his or her health care system.
With this change in the health care environment come new and exciting opportunities. Hospital medicine has always elected to assume a leadership role in these times of change, these periods of “punctuation.” Development of effective team-based care is a great place for those of us working in hospital medicine to demonstrate our leadership as we care for our patients.
Dr. Frost is national medical director, hospital-based services, at LifePoint Health, Brentwood, Tenn. He is president-elect of the Society of Hospital Medicine.
Changing times for U.S. health care
Changing times for U.S. health care
The current health care environment is undergoing a rapid transformation. In evolutionary biology, a theory exists called punctuated equilibrium. This theory suggests there are long periods of little or no morphological change amongst species and then, geologically speaking, short periods of rapid change in response to pressures within the environment. This rapid period of change adds significant diversity to the landscape of existing species. In health care, we are undergoing a period of “punctuation.”
A testament to the degree of change is a scan of the various consolidation activities occurring across the health care space. Some are more traditional, such as mergers of health systems with different or competing geographical footprints or hospitalist management companies that provide similar services and desire to increase their market share. Others that are more interesting are those that include mergers of seemingly different business lines or offerings, like CVS Health and Aetna; Humana and Kindred; or even organizations such as Amazon, Berkshire Hathaway, and JP Morgan hiring Atul Gawande as the CEO of their newly formed health care venture. The latter examples serve as an illustration of the reorganization that is occurring within health care delivery. This represents, at the very least, a blurring of the lines – if not a deconstruction and complete rebuild – of traditional lines of separation between payers, providers, employers, and retailers.
In other words, the silos are coming down, significant diversity in the landscape of existing species. A common theme across these changes is that most – if not all – participants will share some portion of the financial risk associated with these evolving models. High-deductible health plans, alternative payment models (APMs), and advanced APMs are examples of tactics and models that distribute the financial risk. The consolidations referenced above will likely continue to encourage distribution of the financial risk across patients, providers, employers, and payers.
A key theme coming into focus is that the evolving care delivery system will not be defined by bricks and mortar. Rather, it will follow the patient and go wherever he or she goes to meet his or her specific needs. This is why we’re seeing mergers comprised of a variety of assets, including personnel, technology, critical supplies (such as pharmaceuticals), and funding resources. This very purposeful and deliberate melting pot phenomenon will restructure and reformat the care delivery model.
To be successful within this new landscape, there will need to be a renewed focus on working within a collaborative model. The days of a single entity or provider being able to serve as the “be all” or “do all” is over, and the days of practicing medicine as the Lone Ranger are anachronistic. Instead, there is a need for health care providers to embrace and lead a team-based care model. Team-based care should have the patient at the center of the care delivery model and leverage the expertise of the various team members to practice at the “top of their expertise.”
In hospital medicine, this includes a variety of team members – from physicians, nurse practitioners, physician assistants, and clinical pharmacists to case managers, physical therapists, subject matter experts in quality improvement, and analysts – who identify operational priorities from the data rather than reporting predefined goals on dashboards. Although possibly a good start, this is by no means an exhaustive list of team members. The team will be defined by the goals the health care team aspires to achieve. These goals may include closer alignment with payers, employers, and post-acute partners; the goals will influence the composition of the team. Once the team is defined, the challenge will be to effectively integrate team members, so they are contributing their expertise to the patient care being delivered.
Some ingredients for effective team-based care include the following:
- Developing an effective process for engagement and providing a voice for all team members. Interdisciplinary team rounds where there is an established time for team members to plan and operationalize their plans around patient care can serve as an example of this type of structured process.
- Creating well-defined roles and responsibilities with key performance indicators to promote accountability. The team will have outcomes they are measuring and striving to impact, and each team member will have a role in achieving those goals. Being able to parse out and measure how each team member contributes to the overall outcome can be beneficial. This provides an opportunity for each team member to play a meaningful role in accomplishing the overall goal and allows for a measurement process to track success. For example, an overall team goal may be to have a specific percentage of eligible discharges completed by 11:00 a.m. To accomplish this goal, there may be specific objectives for the clinicians to have discharge orders in the chart by 9:30 a.m. and for case management to have communicated with any post-acute services the day before discharge. These specific accountability measures facilitate accomplishing the larger team goal.
- Developing a culture of safety and transparency. Effective teams promote an environment where all members are empowered and encouraged to speak and share their perspective and knowledge. Communication is based on the value it provides to accomplishing the team’s goals rather than based on a hierarchy which determines who contributes and when.
- Defining and then redefining the competencies required of the team to promote continued development and growth. In this time of dynamic change, the skill sets that helped us get where we are today may be different then the skill sets that are needed for success in the future. There will continue to be a need for functional and knowledge-based competencies in addition to the need to focus on competencies that engender a culture of team-based care. For example, hospitalist leaders will need to understand evidence-based medicine to support appropriate management of a septic patient and simultaneously understand evidence-based management/leadership to affect sepsis care across his or her health care system.
With this change in the health care environment come new and exciting opportunities. Hospital medicine has always elected to assume a leadership role in these times of change, these periods of “punctuation.” Development of effective team-based care is a great place for those of us working in hospital medicine to demonstrate our leadership as we care for our patients.
Dr. Frost is national medical director, hospital-based services, at LifePoint Health, Brentwood, Tenn. He is president-elect of the Society of Hospital Medicine.
The current health care environment is undergoing a rapid transformation. In evolutionary biology, a theory exists called punctuated equilibrium. This theory suggests there are long periods of little or no morphological change amongst species and then, geologically speaking, short periods of rapid change in response to pressures within the environment. This rapid period of change adds significant diversity to the landscape of existing species. In health care, we are undergoing a period of “punctuation.”
A testament to the degree of change is a scan of the various consolidation activities occurring across the health care space. Some are more traditional, such as mergers of health systems with different or competing geographical footprints or hospitalist management companies that provide similar services and desire to increase their market share. Others that are more interesting are those that include mergers of seemingly different business lines or offerings, like CVS Health and Aetna; Humana and Kindred; or even organizations such as Amazon, Berkshire Hathaway, and JP Morgan hiring Atul Gawande as the CEO of their newly formed health care venture. The latter examples serve as an illustration of the reorganization that is occurring within health care delivery. This represents, at the very least, a blurring of the lines – if not a deconstruction and complete rebuild – of traditional lines of separation between payers, providers, employers, and retailers.
In other words, the silos are coming down, significant diversity in the landscape of existing species. A common theme across these changes is that most – if not all – participants will share some portion of the financial risk associated with these evolving models. High-deductible health plans, alternative payment models (APMs), and advanced APMs are examples of tactics and models that distribute the financial risk. The consolidations referenced above will likely continue to encourage distribution of the financial risk across patients, providers, employers, and payers.
A key theme coming into focus is that the evolving care delivery system will not be defined by bricks and mortar. Rather, it will follow the patient and go wherever he or she goes to meet his or her specific needs. This is why we’re seeing mergers comprised of a variety of assets, including personnel, technology, critical supplies (such as pharmaceuticals), and funding resources. This very purposeful and deliberate melting pot phenomenon will restructure and reformat the care delivery model.
To be successful within this new landscape, there will need to be a renewed focus on working within a collaborative model. The days of a single entity or provider being able to serve as the “be all” or “do all” is over, and the days of practicing medicine as the Lone Ranger are anachronistic. Instead, there is a need for health care providers to embrace and lead a team-based care model. Team-based care should have the patient at the center of the care delivery model and leverage the expertise of the various team members to practice at the “top of their expertise.”
In hospital medicine, this includes a variety of team members – from physicians, nurse practitioners, physician assistants, and clinical pharmacists to case managers, physical therapists, subject matter experts in quality improvement, and analysts – who identify operational priorities from the data rather than reporting predefined goals on dashboards. Although possibly a good start, this is by no means an exhaustive list of team members. The team will be defined by the goals the health care team aspires to achieve. These goals may include closer alignment with payers, employers, and post-acute partners; the goals will influence the composition of the team. Once the team is defined, the challenge will be to effectively integrate team members, so they are contributing their expertise to the patient care being delivered.
Some ingredients for effective team-based care include the following:
- Developing an effective process for engagement and providing a voice for all team members. Interdisciplinary team rounds where there is an established time for team members to plan and operationalize their plans around patient care can serve as an example of this type of structured process.
- Creating well-defined roles and responsibilities with key performance indicators to promote accountability. The team will have outcomes they are measuring and striving to impact, and each team member will have a role in achieving those goals. Being able to parse out and measure how each team member contributes to the overall outcome can be beneficial. This provides an opportunity for each team member to play a meaningful role in accomplishing the overall goal and allows for a measurement process to track success. For example, an overall team goal may be to have a specific percentage of eligible discharges completed by 11:00 a.m. To accomplish this goal, there may be specific objectives for the clinicians to have discharge orders in the chart by 9:30 a.m. and for case management to have communicated with any post-acute services the day before discharge. These specific accountability measures facilitate accomplishing the larger team goal.
- Developing a culture of safety and transparency. Effective teams promote an environment where all members are empowered and encouraged to speak and share their perspective and knowledge. Communication is based on the value it provides to accomplishing the team’s goals rather than based on a hierarchy which determines who contributes and when.
- Defining and then redefining the competencies required of the team to promote continued development and growth. In this time of dynamic change, the skill sets that helped us get where we are today may be different then the skill sets that are needed for success in the future. There will continue to be a need for functional and knowledge-based competencies in addition to the need to focus on competencies that engender a culture of team-based care. For example, hospitalist leaders will need to understand evidence-based medicine to support appropriate management of a septic patient and simultaneously understand evidence-based management/leadership to affect sepsis care across his or her health care system.
With this change in the health care environment come new and exciting opportunities. Hospital medicine has always elected to assume a leadership role in these times of change, these periods of “punctuation.” Development of effective team-based care is a great place for those of us working in hospital medicine to demonstrate our leadership as we care for our patients.
Dr. Frost is national medical director, hospital-based services, at LifePoint Health, Brentwood, Tenn. He is president-elect of the Society of Hospital Medicine.
Real-world weight loss with meds approximates RCT results
NASHVILLE, TENN. –
The results seen with the medication combo – a mean 15.5% total body weight loss at 12 months – bested the 8%-11% seen in randomized controlled trials (RCTs), said Gerardo Calderon, MD, in an interview during a poster session at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. The combination was also the most commonly prescribed weight loss medication at the Mayo Clinic, where Dr. Calderon is a gastroenterology and hepatology research fellow.
Patients taking lorcaserin at the Mayo Clinic also lost more weight loss than RCT participants (8.8% vs. 5%-6%, respectively). Notably, they also had a higher probability of losing at least 10% of their baseline total body weight (40% vs. 17%-23% in clinical trials). In RCTs, 37%-48% of patients taking phentermine/topiramate-ER had a total body weight loss of at least 10%, similar to the Mayo Clinic’s figure of 49%.
The rate of reported adverse events – 23.8% – exceeded that reported in RCTs, noted Dr. Calderon. Gastrointestinal symptoms, such as nausea, vomiting, diarrhea, and constipation, were reported by 2%-20% of patients across the various drugs prescribed. Insomnia and mood changes, along with dizziness or lightheadedness, were reported by 2%-6% of patients. Almost 12% of patients taking phentermine/topiramate-SR reported paresthesias. No patients stopped taking their medication because of side effects, however.
The study was a review of patients seen at the Mayo Clinic during January 2016 – June 2018. Patients were included if they were prescribed weight loss medications and had a body mass index of at least 25 kg/m2 with comorbidities related to adiposity or with a BMI of at least 30 without such comorbidities. To be included, patients had to be followed for at least 3 months and see a Mayo Clinic physician at least twice.
Patients with previous bariatric surgery or other major gastrointestinal surgery, those who didn’t use their medications because of insurance problems or drug costs, and those who were on weight loss medication before being seen for the first time were excluded from the study.
Patients were a mean 49 years old, and most were female (86/118; 72.9%). Mean BMI at enrollment was 41.7, with a mean weight of 117.6 kg.
Of 118 patients, 76 (64.4%) had dyslipidemia. About half of patients reported obstructive sleep apnea, and the same amount had hypertension. About 40% had diabetes, and the same number had degenerative joint disease.
Phentermine/topiramate was prescribed the most frequently, with 43.2% of patients on this medication. Liraglutide was taken by 34.7% of patients, bupropion/naltrexone-SR by 16.1%, and lorcaserin by 5.9%.
Patients taking liraglutide had similar weight loss (7.1%) to that seen in RCTs (6%-8%). For this medication, the real-world Mayo Clinic experience showed less chance of hitting the 10% total body weight loss mark (12% vs. 26%-33% in RCTs).
For bupropion/naltrexone-SR, weight loss was similar among the Mayo Clinic patients (7.2%) and RCT participants (5%-8%), and probability of achieving at least 10% total body weight loss was similar as well (32% vs. 34%).
Weight loss medication was a component of a multidisciplinary weight loss approach at Mayo Clinic. Physicians, dietitians, and psychologists worked together to care for patients with overweight and obesity at his facility, Dr. Calderon said. Overall, patients were followed for a mean 6.7 months, and patients had a mean 3 follow-up visits, with over half of patients attending at least one follow-up appointment in study months 6-12. At 12 months, though, the attrition rate was 57.9%. “We notice an attrition rate of almost 60% at 1 year. People are not coming to their follow-up. ... Definitely, this is something we are concerned about, and we would like to bring these attrition rates lower,” he said.
Most patients (63.6%) saw a dietitian, but on average, patients had just one appointment. “At the Mayo Clinic, we provide dietitians and psychological support. But it’s up to the patients if they want to have it or not,” said Dr. Calderon. “Most of them, they just went once to a dietitian.”
“Overall, these outcomes are similar to those in RCTs and support the concept that weight loss medications can achieve clinically significant weight loss in a multidisciplinary weight loss program,” noted Dr. Calderon and his coauthors.
Dr. Calderon reported no outside sources of funding and no conflicts of interest.
SOURCE: Calderon G et al. Obesity Week, Abstract T-P-3425.
NASHVILLE, TENN. –
The results seen with the medication combo – a mean 15.5% total body weight loss at 12 months – bested the 8%-11% seen in randomized controlled trials (RCTs), said Gerardo Calderon, MD, in an interview during a poster session at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. The combination was also the most commonly prescribed weight loss medication at the Mayo Clinic, where Dr. Calderon is a gastroenterology and hepatology research fellow.
Patients taking lorcaserin at the Mayo Clinic also lost more weight loss than RCT participants (8.8% vs. 5%-6%, respectively). Notably, they also had a higher probability of losing at least 10% of their baseline total body weight (40% vs. 17%-23% in clinical trials). In RCTs, 37%-48% of patients taking phentermine/topiramate-ER had a total body weight loss of at least 10%, similar to the Mayo Clinic’s figure of 49%.
The rate of reported adverse events – 23.8% – exceeded that reported in RCTs, noted Dr. Calderon. Gastrointestinal symptoms, such as nausea, vomiting, diarrhea, and constipation, were reported by 2%-20% of patients across the various drugs prescribed. Insomnia and mood changes, along with dizziness or lightheadedness, were reported by 2%-6% of patients. Almost 12% of patients taking phentermine/topiramate-SR reported paresthesias. No patients stopped taking their medication because of side effects, however.
The study was a review of patients seen at the Mayo Clinic during January 2016 – June 2018. Patients were included if they were prescribed weight loss medications and had a body mass index of at least 25 kg/m2 with comorbidities related to adiposity or with a BMI of at least 30 without such comorbidities. To be included, patients had to be followed for at least 3 months and see a Mayo Clinic physician at least twice.
Patients with previous bariatric surgery or other major gastrointestinal surgery, those who didn’t use their medications because of insurance problems or drug costs, and those who were on weight loss medication before being seen for the first time were excluded from the study.
Patients were a mean 49 years old, and most were female (86/118; 72.9%). Mean BMI at enrollment was 41.7, with a mean weight of 117.6 kg.
Of 118 patients, 76 (64.4%) had dyslipidemia. About half of patients reported obstructive sleep apnea, and the same amount had hypertension. About 40% had diabetes, and the same number had degenerative joint disease.
Phentermine/topiramate was prescribed the most frequently, with 43.2% of patients on this medication. Liraglutide was taken by 34.7% of patients, bupropion/naltrexone-SR by 16.1%, and lorcaserin by 5.9%.
Patients taking liraglutide had similar weight loss (7.1%) to that seen in RCTs (6%-8%). For this medication, the real-world Mayo Clinic experience showed less chance of hitting the 10% total body weight loss mark (12% vs. 26%-33% in RCTs).
For bupropion/naltrexone-SR, weight loss was similar among the Mayo Clinic patients (7.2%) and RCT participants (5%-8%), and probability of achieving at least 10% total body weight loss was similar as well (32% vs. 34%).
Weight loss medication was a component of a multidisciplinary weight loss approach at Mayo Clinic. Physicians, dietitians, and psychologists worked together to care for patients with overweight and obesity at his facility, Dr. Calderon said. Overall, patients were followed for a mean 6.7 months, and patients had a mean 3 follow-up visits, with over half of patients attending at least one follow-up appointment in study months 6-12. At 12 months, though, the attrition rate was 57.9%. “We notice an attrition rate of almost 60% at 1 year. People are not coming to their follow-up. ... Definitely, this is something we are concerned about, and we would like to bring these attrition rates lower,” he said.
Most patients (63.6%) saw a dietitian, but on average, patients had just one appointment. “At the Mayo Clinic, we provide dietitians and psychological support. But it’s up to the patients if they want to have it or not,” said Dr. Calderon. “Most of them, they just went once to a dietitian.”
“Overall, these outcomes are similar to those in RCTs and support the concept that weight loss medications can achieve clinically significant weight loss in a multidisciplinary weight loss program,” noted Dr. Calderon and his coauthors.
Dr. Calderon reported no outside sources of funding and no conflicts of interest.
SOURCE: Calderon G et al. Obesity Week, Abstract T-P-3425.
NASHVILLE, TENN. –
The results seen with the medication combo – a mean 15.5% total body weight loss at 12 months – bested the 8%-11% seen in randomized controlled trials (RCTs), said Gerardo Calderon, MD, in an interview during a poster session at Obesity Week, presented by the Obesity Society and the American Society for Metabolic and Bariatric Surgery. The combination was also the most commonly prescribed weight loss medication at the Mayo Clinic, where Dr. Calderon is a gastroenterology and hepatology research fellow.
Patients taking lorcaserin at the Mayo Clinic also lost more weight loss than RCT participants (8.8% vs. 5%-6%, respectively). Notably, they also had a higher probability of losing at least 10% of their baseline total body weight (40% vs. 17%-23% in clinical trials). In RCTs, 37%-48% of patients taking phentermine/topiramate-ER had a total body weight loss of at least 10%, similar to the Mayo Clinic’s figure of 49%.
The rate of reported adverse events – 23.8% – exceeded that reported in RCTs, noted Dr. Calderon. Gastrointestinal symptoms, such as nausea, vomiting, diarrhea, and constipation, were reported by 2%-20% of patients across the various drugs prescribed. Insomnia and mood changes, along with dizziness or lightheadedness, were reported by 2%-6% of patients. Almost 12% of patients taking phentermine/topiramate-SR reported paresthesias. No patients stopped taking their medication because of side effects, however.
The study was a review of patients seen at the Mayo Clinic during January 2016 – June 2018. Patients were included if they were prescribed weight loss medications and had a body mass index of at least 25 kg/m2 with comorbidities related to adiposity or with a BMI of at least 30 without such comorbidities. To be included, patients had to be followed for at least 3 months and see a Mayo Clinic physician at least twice.
Patients with previous bariatric surgery or other major gastrointestinal surgery, those who didn’t use their medications because of insurance problems or drug costs, and those who were on weight loss medication before being seen for the first time were excluded from the study.
Patients were a mean 49 years old, and most were female (86/118; 72.9%). Mean BMI at enrollment was 41.7, with a mean weight of 117.6 kg.
Of 118 patients, 76 (64.4%) had dyslipidemia. About half of patients reported obstructive sleep apnea, and the same amount had hypertension. About 40% had diabetes, and the same number had degenerative joint disease.
Phentermine/topiramate was prescribed the most frequently, with 43.2% of patients on this medication. Liraglutide was taken by 34.7% of patients, bupropion/naltrexone-SR by 16.1%, and lorcaserin by 5.9%.
Patients taking liraglutide had similar weight loss (7.1%) to that seen in RCTs (6%-8%). For this medication, the real-world Mayo Clinic experience showed less chance of hitting the 10% total body weight loss mark (12% vs. 26%-33% in RCTs).
For bupropion/naltrexone-SR, weight loss was similar among the Mayo Clinic patients (7.2%) and RCT participants (5%-8%), and probability of achieving at least 10% total body weight loss was similar as well (32% vs. 34%).
Weight loss medication was a component of a multidisciplinary weight loss approach at Mayo Clinic. Physicians, dietitians, and psychologists worked together to care for patients with overweight and obesity at his facility, Dr. Calderon said. Overall, patients were followed for a mean 6.7 months, and patients had a mean 3 follow-up visits, with over half of patients attending at least one follow-up appointment in study months 6-12. At 12 months, though, the attrition rate was 57.9%. “We notice an attrition rate of almost 60% at 1 year. People are not coming to their follow-up. ... Definitely, this is something we are concerned about, and we would like to bring these attrition rates lower,” he said.
Most patients (63.6%) saw a dietitian, but on average, patients had just one appointment. “At the Mayo Clinic, we provide dietitians and psychological support. But it’s up to the patients if they want to have it or not,” said Dr. Calderon. “Most of them, they just went once to a dietitian.”
“Overall, these outcomes are similar to those in RCTs and support the concept that weight loss medications can achieve clinically significant weight loss in a multidisciplinary weight loss program,” noted Dr. Calderon and his coauthors.
Dr. Calderon reported no outside sources of funding and no conflicts of interest.
SOURCE: Calderon G et al. Obesity Week, Abstract T-P-3425.
REPORTING FROM OBESITY WEEK 2018
Key clinical point: Patients taking weight loss medications saw real-world results comparable to those seen in RCTs
Major finding: Patients on phertermine-topiramate-ER lost over 15% of their body weight at 12 months.
Study details: Single-center retrospective cohort study of 188 patients taking weight loss medications.
Disclosures: The authors reported no conflicts of interest and no outside sources of funding.
Source: Calderon G et al. Obesity Week 2018, Abstract T-P-3425.
Apply for a VRIC Travel Scholarship
The Vascular Research Initiatives Conference emphasizes emerging vascular science and encourages interactive participation of attendees, including trainees who are aspiring academic vascular surgeons. The SVS Foundation offers the Vascular Research Initiatives Conference Trainee Travel Scholarship for trainees to attend the conference. The trainee authors of top-scoring abstracts will be considered for the award, which includes complimentary registration to VRIC as well as the American Heart Association's Vascular Discover Scientific Sessions, plus $1,000 for conference travel. Applications are accepted until Jan 15, 2019.
The Vascular Research Initiatives Conference emphasizes emerging vascular science and encourages interactive participation of attendees, including trainees who are aspiring academic vascular surgeons. The SVS Foundation offers the Vascular Research Initiatives Conference Trainee Travel Scholarship for trainees to attend the conference. The trainee authors of top-scoring abstracts will be considered for the award, which includes complimentary registration to VRIC as well as the American Heart Association's Vascular Discover Scientific Sessions, plus $1,000 for conference travel. Applications are accepted until Jan 15, 2019.
The Vascular Research Initiatives Conference emphasizes emerging vascular science and encourages interactive participation of attendees, including trainees who are aspiring academic vascular surgeons. The SVS Foundation offers the Vascular Research Initiatives Conference Trainee Travel Scholarship for trainees to attend the conference. The trainee authors of top-scoring abstracts will be considered for the award, which includes complimentary registration to VRIC as well as the American Heart Association's Vascular Discover Scientific Sessions, plus $1,000 for conference travel. Applications are accepted until Jan 15, 2019.
Learn about Workings of Washington
The workings of Congress and other governmental agencies frequently seem obscure and the impact of their decisions unclear. Yet collectively, these entities in Washington, D.C., wield huge power over vascular surgeons’ careers and lives. Do you have questions about what goes on in Washington and the efforts of SVS advocacy staff to shape legislation and policies on your behalf? Email questions to Mindi Walker at [email protected].
The workings of Congress and other governmental agencies frequently seem obscure and the impact of their decisions unclear. Yet collectively, these entities in Washington, D.C., wield huge power over vascular surgeons’ careers and lives. Do you have questions about what goes on in Washington and the efforts of SVS advocacy staff to shape legislation and policies on your behalf? Email questions to Mindi Walker at [email protected].
The workings of Congress and other governmental agencies frequently seem obscure and the impact of their decisions unclear. Yet collectively, these entities in Washington, D.C., wield huge power over vascular surgeons’ careers and lives. Do you have questions about what goes on in Washington and the efforts of SVS advocacy staff to shape legislation and policies on your behalf? Email questions to Mindi Walker at [email protected].
Complete Survey on Regulatory Burdens
The SVS is working to ascertain members' experiences in meeting federal regulatory requirements, with responses due by Dec. 31. Approximately 135 members have already responded – join them. Read more and find the survey link here.
The SVS is working to ascertain members' experiences in meeting federal regulatory requirements, with responses due by Dec. 31. Approximately 135 members have already responded – join them. Read more and find the survey link here.
The SVS is working to ascertain members' experiences in meeting federal regulatory requirements, with responses due by Dec. 31. Approximately 135 members have already responded – join them. Read more and find the survey link here.
Beware “The Great Mimicker” that can lurk in the vulva
LAS VEGAS – Officially a type of precancerous lesion is known as vulvar intraepithelial neoplasia (VIN); unofficially, an obstetrician-gynecologist calls it something else: “The Great Mimicker.” That’s because symptoms of VIN can fool physicians into thinking they’re seeing other vulvar conditions. The good news: A biopsy can offer crucial insight and should be performed on any dysplastic or unusual lesion on the vulva.
Amanda Nickles Fader, MD, of Johns Hopkins Hospital in Baltimore, offered this advice and other tips about this type of precancerous vulvar lesion in a presentation at the Pelvic Anatomy and Gynecologic Surgery Symposium.
According to Dr. Nickles Fader, vulvar cancer accounts for 5% of all gynecologic malignancies, and it appears most in women aged 65-75 years. However, about 15% of all vulvar cancers appear in women under the age of 40 years. “We’re seeing a greater number of premenopausal women with this condition, probably due to HPV [human papillomavirus],” she said, adding that HPV vaccines are crucial to prevention.
The VIN form of precancerous lesion is most common in premenopausal women (75%) and – like vulvar cancer – is linked to HPV infection, HIV infection, cigarette smoking, and weakened or suppressed immune systems, Dr. Nickles Faber said at the meeting jointly provided by Global Academy for Medical Education and the University of Cincinnati. Global Academy and this news organization are owned by the same company.
VIN presents with symptoms such as pruritus, altered vulvar appearance at the site of the lesion, palpable abnormality, and perineal pain or burning. About 40% of cases do not show symptoms and are diagnosed by gynecologists at annual visits.
It’s important to biopsy these lesions, she said, because they can mimic other conditions such as vulvar cancer, condyloma acuminatum (genital warts), lichen sclerosus, lichen planus, and condyloma latum (a lesion linked to syphilis).
“Biopsy, biopsy, biopsy,” she urged.
In fact, one form of VIN – differentiated VIN – is associated with dermatologic conditions such as lichen sclerosus, and treatment of these conditions can prevent development of this VIN type.
As for treatment, Dr. Nickles Faber said surgery is the mainstay. About 90% of the time, wide local excision is the “go-to” approach, although the skinning vulvectomy procedure may be appropriate in lesions that are more extensive or multifocal and confluent. “It’s a lot more disfiguring.”
Laser ablation is a “very reasonable” option when cancer has been eliminated as a possibility, she said. It may be appropriate in multifocal or extensive lesions and can have important cosmetic advantages when excision would be inappropriate.
Off-label use of imiquimod 5%, a topical immune response modifier, can be appropriate in multifocal high-grade VINs, but it’s crucial to exclude invasive squamous cell carcinoma. As she noted, imiquimod is Food and Drug Administration–approved for anogenital warts but not for VIN. Beware of toxicity over the long term.
Dr. Nickles Fader reported no relevant financial disclosures.
LAS VEGAS – Officially a type of precancerous lesion is known as vulvar intraepithelial neoplasia (VIN); unofficially, an obstetrician-gynecologist calls it something else: “The Great Mimicker.” That’s because symptoms of VIN can fool physicians into thinking they’re seeing other vulvar conditions. The good news: A biopsy can offer crucial insight and should be performed on any dysplastic or unusual lesion on the vulva.
Amanda Nickles Fader, MD, of Johns Hopkins Hospital in Baltimore, offered this advice and other tips about this type of precancerous vulvar lesion in a presentation at the Pelvic Anatomy and Gynecologic Surgery Symposium.
According to Dr. Nickles Fader, vulvar cancer accounts for 5% of all gynecologic malignancies, and it appears most in women aged 65-75 years. However, about 15% of all vulvar cancers appear in women under the age of 40 years. “We’re seeing a greater number of premenopausal women with this condition, probably due to HPV [human papillomavirus],” she said, adding that HPV vaccines are crucial to prevention.
The VIN form of precancerous lesion is most common in premenopausal women (75%) and – like vulvar cancer – is linked to HPV infection, HIV infection, cigarette smoking, and weakened or suppressed immune systems, Dr. Nickles Faber said at the meeting jointly provided by Global Academy for Medical Education and the University of Cincinnati. Global Academy and this news organization are owned by the same company.
VIN presents with symptoms such as pruritus, altered vulvar appearance at the site of the lesion, palpable abnormality, and perineal pain or burning. About 40% of cases do not show symptoms and are diagnosed by gynecologists at annual visits.
It’s important to biopsy these lesions, she said, because they can mimic other conditions such as vulvar cancer, condyloma acuminatum (genital warts), lichen sclerosus, lichen planus, and condyloma latum (a lesion linked to syphilis).
“Biopsy, biopsy, biopsy,” she urged.
In fact, one form of VIN – differentiated VIN – is associated with dermatologic conditions such as lichen sclerosus, and treatment of these conditions can prevent development of this VIN type.
As for treatment, Dr. Nickles Faber said surgery is the mainstay. About 90% of the time, wide local excision is the “go-to” approach, although the skinning vulvectomy procedure may be appropriate in lesions that are more extensive or multifocal and confluent. “It’s a lot more disfiguring.”
Laser ablation is a “very reasonable” option when cancer has been eliminated as a possibility, she said. It may be appropriate in multifocal or extensive lesions and can have important cosmetic advantages when excision would be inappropriate.
Off-label use of imiquimod 5%, a topical immune response modifier, can be appropriate in multifocal high-grade VINs, but it’s crucial to exclude invasive squamous cell carcinoma. As she noted, imiquimod is Food and Drug Administration–approved for anogenital warts but not for VIN. Beware of toxicity over the long term.
Dr. Nickles Fader reported no relevant financial disclosures.
LAS VEGAS – Officially a type of precancerous lesion is known as vulvar intraepithelial neoplasia (VIN); unofficially, an obstetrician-gynecologist calls it something else: “The Great Mimicker.” That’s because symptoms of VIN can fool physicians into thinking they’re seeing other vulvar conditions. The good news: A biopsy can offer crucial insight and should be performed on any dysplastic or unusual lesion on the vulva.
Amanda Nickles Fader, MD, of Johns Hopkins Hospital in Baltimore, offered this advice and other tips about this type of precancerous vulvar lesion in a presentation at the Pelvic Anatomy and Gynecologic Surgery Symposium.
According to Dr. Nickles Fader, vulvar cancer accounts for 5% of all gynecologic malignancies, and it appears most in women aged 65-75 years. However, about 15% of all vulvar cancers appear in women under the age of 40 years. “We’re seeing a greater number of premenopausal women with this condition, probably due to HPV [human papillomavirus],” she said, adding that HPV vaccines are crucial to prevention.
The VIN form of precancerous lesion is most common in premenopausal women (75%) and – like vulvar cancer – is linked to HPV infection, HIV infection, cigarette smoking, and weakened or suppressed immune systems, Dr. Nickles Faber said at the meeting jointly provided by Global Academy for Medical Education and the University of Cincinnati. Global Academy and this news organization are owned by the same company.
VIN presents with symptoms such as pruritus, altered vulvar appearance at the site of the lesion, palpable abnormality, and perineal pain or burning. About 40% of cases do not show symptoms and are diagnosed by gynecologists at annual visits.
It’s important to biopsy these lesions, she said, because they can mimic other conditions such as vulvar cancer, condyloma acuminatum (genital warts), lichen sclerosus, lichen planus, and condyloma latum (a lesion linked to syphilis).
“Biopsy, biopsy, biopsy,” she urged.
In fact, one form of VIN – differentiated VIN – is associated with dermatologic conditions such as lichen sclerosus, and treatment of these conditions can prevent development of this VIN type.
As for treatment, Dr. Nickles Faber said surgery is the mainstay. About 90% of the time, wide local excision is the “go-to” approach, although the skinning vulvectomy procedure may be appropriate in lesions that are more extensive or multifocal and confluent. “It’s a lot more disfiguring.”
Laser ablation is a “very reasonable” option when cancer has been eliminated as a possibility, she said. It may be appropriate in multifocal or extensive lesions and can have important cosmetic advantages when excision would be inappropriate.
Off-label use of imiquimod 5%, a topical immune response modifier, can be appropriate in multifocal high-grade VINs, but it’s crucial to exclude invasive squamous cell carcinoma. As she noted, imiquimod is Food and Drug Administration–approved for anogenital warts but not for VIN. Beware of toxicity over the long term.
Dr. Nickles Fader reported no relevant financial disclosures.
EXPERT ANALYSIS FROM PAGS
How does CBD compare and interact with other AEDs?
according to a review published in Developmental Medicine & Child Neurology. “Careful down-titration of benzodiazepines is essential to minimize sedation with adjunctive CBD,” the authors said.
Although CBD’s antiepileptic mechanisms “are not fully elucidated, it is clear that administration of CBD as adjunct therapy decreases seizure frequency in patients with Dravet syndrome and Lennox-Gastaut syndrome,” wrote Shayma Ali, a doctoral student in the department of pediatrics and child health at the University of Otago in Wellington, New Zealand, and her colleagues. “Contrary to public expectation of miraculous results, CBD has a similar antiepileptic and side effect profile to other AEDs. Nevertheless, as individual children with these developmental and epileptic encephalopathies are often refractory to available AEDs, the addition of another potentially effective therapeutic medicine will be warmly welcomed by families and physicians.”
The FDA approved Epidiolex, a pharmaceutical-grade oral solution that is 98% CBD, in June of 2018. In September of 2018, the Drug Enforcement Administration classified it as a Schedule V controlled substance. Patients’ use of nonpharmaceutical grade CBD products, including those combined with tetrahydrocannabinol (THC), “raises concerns about the use of products with THC on the developing brain,” the review authors said.
Randomized trials
Three randomized, controlled, double-blind trials in patients with Dravet syndrome and Lennox-Gastaut syndrome found that CBD, compared with placebo, results in greater median seizure reductions (38%-41% vs. 13%-19%) and responder rates (i.e., the proportion of patients with 50% reductions in convulsive or drop seizures; 39%-46% vs. 14%-27%).
Common adverse effects include somnolence, diarrhea, decreased appetite, fatigue, lethargy, pyrexia, and vomiting. Hepatic transaminases became elevated in some patients, and this result occurred more often in patients taking valproate.
No phase 2 or phase 3 trials have assessed the efficacy of CBD without coadministration of other AEDs, and CBD’s efficacy may relate to its impact on the pharmacokinetics of coadministered AEDs. “The most important clinical interaction is between CBD and clobazam, as [the dose of] clobazam often needs to be lowered because of excessive sedation,” wrote Ms. Ali and her colleagues. CBD inhibits CYP2C19 and CYP3A4 – enzymes that are involved in clobazam metabolism – which results in high plasma concentrations of clobazam’s active metabolite, norclobazam. Plasma levels of topiramate, rufinamide, zonisamide, and eslicarbazepine also may increase when these drugs are taken with CBD.
Challenges and opportunities
Of the hundreds of compounds in the marijuana plant, CBD “has the most evidence of antiepileptic efficacy and does not have the psychoactive effects” of THC, the authors said. Little evidence supports the combination of THC and CBD for the treatment of epilepsy. In addition, research indicates that THC can have a proconvulsive effect in animal models and harm the development of the human brain.
Investigators are evaluating alternative routes of CBD delivery to avoid first-pass metabolism, such as oromucosal sprays, transdermal gels, eye drops, intranasal sprays, and rectal suppositories. “Alternative methods of administration ... deserve consideration, particularly for the developmental and epileptic encephalopathies population, as administration of oral medication can be challenging,” they said.
SOURCE: Ali S et al. Dev Med Child Neurol. 2018. doi: 10.1111/dmcn.14087.
according to a review published in Developmental Medicine & Child Neurology. “Careful down-titration of benzodiazepines is essential to minimize sedation with adjunctive CBD,” the authors said.
Although CBD’s antiepileptic mechanisms “are not fully elucidated, it is clear that administration of CBD as adjunct therapy decreases seizure frequency in patients with Dravet syndrome and Lennox-Gastaut syndrome,” wrote Shayma Ali, a doctoral student in the department of pediatrics and child health at the University of Otago in Wellington, New Zealand, and her colleagues. “Contrary to public expectation of miraculous results, CBD has a similar antiepileptic and side effect profile to other AEDs. Nevertheless, as individual children with these developmental and epileptic encephalopathies are often refractory to available AEDs, the addition of another potentially effective therapeutic medicine will be warmly welcomed by families and physicians.”
The FDA approved Epidiolex, a pharmaceutical-grade oral solution that is 98% CBD, in June of 2018. In September of 2018, the Drug Enforcement Administration classified it as a Schedule V controlled substance. Patients’ use of nonpharmaceutical grade CBD products, including those combined with tetrahydrocannabinol (THC), “raises concerns about the use of products with THC on the developing brain,” the review authors said.
Randomized trials
Three randomized, controlled, double-blind trials in patients with Dravet syndrome and Lennox-Gastaut syndrome found that CBD, compared with placebo, results in greater median seizure reductions (38%-41% vs. 13%-19%) and responder rates (i.e., the proportion of patients with 50% reductions in convulsive or drop seizures; 39%-46% vs. 14%-27%).
Common adverse effects include somnolence, diarrhea, decreased appetite, fatigue, lethargy, pyrexia, and vomiting. Hepatic transaminases became elevated in some patients, and this result occurred more often in patients taking valproate.
No phase 2 or phase 3 trials have assessed the efficacy of CBD without coadministration of other AEDs, and CBD’s efficacy may relate to its impact on the pharmacokinetics of coadministered AEDs. “The most important clinical interaction is between CBD and clobazam, as [the dose of] clobazam often needs to be lowered because of excessive sedation,” wrote Ms. Ali and her colleagues. CBD inhibits CYP2C19 and CYP3A4 – enzymes that are involved in clobazam metabolism – which results in high plasma concentrations of clobazam’s active metabolite, norclobazam. Plasma levels of topiramate, rufinamide, zonisamide, and eslicarbazepine also may increase when these drugs are taken with CBD.
Challenges and opportunities
Of the hundreds of compounds in the marijuana plant, CBD “has the most evidence of antiepileptic efficacy and does not have the psychoactive effects” of THC, the authors said. Little evidence supports the combination of THC and CBD for the treatment of epilepsy. In addition, research indicates that THC can have a proconvulsive effect in animal models and harm the development of the human brain.
Investigators are evaluating alternative routes of CBD delivery to avoid first-pass metabolism, such as oromucosal sprays, transdermal gels, eye drops, intranasal sprays, and rectal suppositories. “Alternative methods of administration ... deserve consideration, particularly for the developmental and epileptic encephalopathies population, as administration of oral medication can be challenging,” they said.
SOURCE: Ali S et al. Dev Med Child Neurol. 2018. doi: 10.1111/dmcn.14087.
according to a review published in Developmental Medicine & Child Neurology. “Careful down-titration of benzodiazepines is essential to minimize sedation with adjunctive CBD,” the authors said.
Although CBD’s antiepileptic mechanisms “are not fully elucidated, it is clear that administration of CBD as adjunct therapy decreases seizure frequency in patients with Dravet syndrome and Lennox-Gastaut syndrome,” wrote Shayma Ali, a doctoral student in the department of pediatrics and child health at the University of Otago in Wellington, New Zealand, and her colleagues. “Contrary to public expectation of miraculous results, CBD has a similar antiepileptic and side effect profile to other AEDs. Nevertheless, as individual children with these developmental and epileptic encephalopathies are often refractory to available AEDs, the addition of another potentially effective therapeutic medicine will be warmly welcomed by families and physicians.”
The FDA approved Epidiolex, a pharmaceutical-grade oral solution that is 98% CBD, in June of 2018. In September of 2018, the Drug Enforcement Administration classified it as a Schedule V controlled substance. Patients’ use of nonpharmaceutical grade CBD products, including those combined with tetrahydrocannabinol (THC), “raises concerns about the use of products with THC on the developing brain,” the review authors said.
Randomized trials
Three randomized, controlled, double-blind trials in patients with Dravet syndrome and Lennox-Gastaut syndrome found that CBD, compared with placebo, results in greater median seizure reductions (38%-41% vs. 13%-19%) and responder rates (i.e., the proportion of patients with 50% reductions in convulsive or drop seizures; 39%-46% vs. 14%-27%).
Common adverse effects include somnolence, diarrhea, decreased appetite, fatigue, lethargy, pyrexia, and vomiting. Hepatic transaminases became elevated in some patients, and this result occurred more often in patients taking valproate.
No phase 2 or phase 3 trials have assessed the efficacy of CBD without coadministration of other AEDs, and CBD’s efficacy may relate to its impact on the pharmacokinetics of coadministered AEDs. “The most important clinical interaction is between CBD and clobazam, as [the dose of] clobazam often needs to be lowered because of excessive sedation,” wrote Ms. Ali and her colleagues. CBD inhibits CYP2C19 and CYP3A4 – enzymes that are involved in clobazam metabolism – which results in high plasma concentrations of clobazam’s active metabolite, norclobazam. Plasma levels of topiramate, rufinamide, zonisamide, and eslicarbazepine also may increase when these drugs are taken with CBD.
Challenges and opportunities
Of the hundreds of compounds in the marijuana plant, CBD “has the most evidence of antiepileptic efficacy and does not have the psychoactive effects” of THC, the authors said. Little evidence supports the combination of THC and CBD for the treatment of epilepsy. In addition, research indicates that THC can have a proconvulsive effect in animal models and harm the development of the human brain.
Investigators are evaluating alternative routes of CBD delivery to avoid first-pass metabolism, such as oromucosal sprays, transdermal gels, eye drops, intranasal sprays, and rectal suppositories. “Alternative methods of administration ... deserve consideration, particularly for the developmental and epileptic encephalopathies population, as administration of oral medication can be challenging,” they said.
SOURCE: Ali S et al. Dev Med Child Neurol. 2018. doi: 10.1111/dmcn.14087.
FROM DEVELOPMENTAL MEDICINE & CHILD NEUROLOGY
Key clinical point: Cannabidiol’s efficacy is similar to that of other antiepileptic drugs.
Major finding: Cannabidiol inhibits CYP2C19 and CYP3A4, which are involved in clobazam metabolism.
Study details: An invited review.
Disclosures: No disclosures were reported.
Source: Ali S et al. Dev Med Child Neurol. 2018. doi: 10.1111/dmcn.14087.
Frontline veliparib/cisplatin/etoposide shows efficacy in advanced SCLC
For patients with extensive-stage small-cell lung cancer (ES-SCLC), the addition of the poly (ADP ribose) polymerase (PARP) inhibitor veliparib to frontline chemotherapy with cisplatin and etoposide resulted in a slight but significant improvement in progression-free survival but not overall survival, compared with cisplatin/etoposide alone, investigators reported in the Journal of Clinical Oncology.
Among 128 patients with newly diagnosed ES-SCLC, the median progression-free survival (PFS; the primary endpoint) for those randomized to veliparib/cisplatin/etoposide was 6.1 months, compared with 5.5 months for patients randomized to cisplatin/etoposide alone.
This translated into an unstratified hazard ratio for PFS with veliparib of 0.75 (one-sided P = .06) and a stratified HR of 0.63 (one-sided P = .01), reported Taofeek K. Owonikoko, MD, PhD, and his colleagues at Emory University in Atlanta.
“Although the initial result of our study is promising, additional confirmation in a larger definitive study is warranted, given the mixed results reported by other studies of PARP inhibitors in this patient population,” they wrote.
Median overall survival (OS) with cisplatin/etoposide in ES-SCLC is approximately 9-11 months, and fewer than 5% of patients survive out to 5 years. To see whether the addition of a PARP inhibitor to the standard of care could improve outcomes, the investigators first demonstrated in a phase 1 trial that the combination of veliparib with a platinum doublet of cisplatin and etoposide was safe (Lung Cancer. 2015 Jul;89[1]:66-70), and in the current study, they evaluated efficacy.
A total of 128 eligible patients (median age, 66 years; 52% men) with ES-SCLC were included in the analysis. Extensive-stage disease was defined as the presence of extrathoracic metastatic disease, malignant pleural effusion, and bilateral or contralateral supraclavicular adenopathy.
The patients were stratified by sex and serum lactate dehydrogenase (LDH) levels and then randomized to receive a maximum of four 3-week cycles of of cisplatin 75 mg/m2 intravenously on day 1 and etoposide 100 mg/m2 on days 1 through 3, plus either oral veliparib 100 mg twice daily on days 1 through 7 or placebo.
The primary endpoint of PFS was as noted before. Median overall survival was 10.3 months in the veliparib arm versus 8.9 months in the cisplatin/etoposide alone arm, a difference that was not statistically significant. The respective overall response rates were 71.9% vs. 65.6%, but this difference was also not significant.
Looking at the treatment effect by strata, the investigators found that men with high serum LDH levels had a significant PFS benefit with veliparib (HR, 0.34; one-sided P less than .001), but no significant benefit was seen in men with normal LDH or in women regardless of LDH status.
Grade 3 or greater hematologic toxicities that occurred more frequently in the veliparib arm included CD4 lymphopenia in 8% vs. 0% and neutropenia in 49% vs. 32%.
The investigators noted that the discrepancy between the magnitude of the risk reduction as measured by the hazard ratio and the actual, modest difference in median PFS between the study arms may be explained by the fact that men with elevated LDH represented the largest patient strata.
“Therefore, we hypothesize that this cohort probably contained a sufficient proportion of patients with SCLC who harbored some biologic vulnerability to this therapeutic strategy,” they wrote.
They acknowledged that although toxicities were higher with veliparib combination, the ability to deliver chemotherapy was equal between the arms.
Further exploration of the combination of veliparib/cisplatin/etoposide may be justified if results of another ongoing phase 2 study (NCT02289690) of a carboplatin-based chemotherapy doublet plus veliparib has similar efficacy results, Dr. Owonikoko and his associates concluded.
The study was coordinated by the Eastern Cooperative Oncology Group–American College of Radiology Imaging Network Cancer Research Group and supported by the National Cancer Institute. Dr. Owonikoko disclosed a consulting or advisory role with AbbVie, developer of veliparib, and other companies, as well as institutional research funding from AbbVie and others.
SOURCE: Owonikoko TK et al. J Clin Oncol. 2018 Dec 5. doi: 10.1200/JCO.18.00264.
For patients with extensive-stage small-cell lung cancer (ES-SCLC), the addition of the poly (ADP ribose) polymerase (PARP) inhibitor veliparib to frontline chemotherapy with cisplatin and etoposide resulted in a slight but significant improvement in progression-free survival but not overall survival, compared with cisplatin/etoposide alone, investigators reported in the Journal of Clinical Oncology.
Among 128 patients with newly diagnosed ES-SCLC, the median progression-free survival (PFS; the primary endpoint) for those randomized to veliparib/cisplatin/etoposide was 6.1 months, compared with 5.5 months for patients randomized to cisplatin/etoposide alone.
This translated into an unstratified hazard ratio for PFS with veliparib of 0.75 (one-sided P = .06) and a stratified HR of 0.63 (one-sided P = .01), reported Taofeek K. Owonikoko, MD, PhD, and his colleagues at Emory University in Atlanta.
“Although the initial result of our study is promising, additional confirmation in a larger definitive study is warranted, given the mixed results reported by other studies of PARP inhibitors in this patient population,” they wrote.
Median overall survival (OS) with cisplatin/etoposide in ES-SCLC is approximately 9-11 months, and fewer than 5% of patients survive out to 5 years. To see whether the addition of a PARP inhibitor to the standard of care could improve outcomes, the investigators first demonstrated in a phase 1 trial that the combination of veliparib with a platinum doublet of cisplatin and etoposide was safe (Lung Cancer. 2015 Jul;89[1]:66-70), and in the current study, they evaluated efficacy.
A total of 128 eligible patients (median age, 66 years; 52% men) with ES-SCLC were included in the analysis. Extensive-stage disease was defined as the presence of extrathoracic metastatic disease, malignant pleural effusion, and bilateral or contralateral supraclavicular adenopathy.
The patients were stratified by sex and serum lactate dehydrogenase (LDH) levels and then randomized to receive a maximum of four 3-week cycles of of cisplatin 75 mg/m2 intravenously on day 1 and etoposide 100 mg/m2 on days 1 through 3, plus either oral veliparib 100 mg twice daily on days 1 through 7 or placebo.
The primary endpoint of PFS was as noted before. Median overall survival was 10.3 months in the veliparib arm versus 8.9 months in the cisplatin/etoposide alone arm, a difference that was not statistically significant. The respective overall response rates were 71.9% vs. 65.6%, but this difference was also not significant.
Looking at the treatment effect by strata, the investigators found that men with high serum LDH levels had a significant PFS benefit with veliparib (HR, 0.34; one-sided P less than .001), but no significant benefit was seen in men with normal LDH or in women regardless of LDH status.
Grade 3 or greater hematologic toxicities that occurred more frequently in the veliparib arm included CD4 lymphopenia in 8% vs. 0% and neutropenia in 49% vs. 32%.
The investigators noted that the discrepancy between the magnitude of the risk reduction as measured by the hazard ratio and the actual, modest difference in median PFS between the study arms may be explained by the fact that men with elevated LDH represented the largest patient strata.
“Therefore, we hypothesize that this cohort probably contained a sufficient proportion of patients with SCLC who harbored some biologic vulnerability to this therapeutic strategy,” they wrote.
They acknowledged that although toxicities were higher with veliparib combination, the ability to deliver chemotherapy was equal between the arms.
Further exploration of the combination of veliparib/cisplatin/etoposide may be justified if results of another ongoing phase 2 study (NCT02289690) of a carboplatin-based chemotherapy doublet plus veliparib has similar efficacy results, Dr. Owonikoko and his associates concluded.
The study was coordinated by the Eastern Cooperative Oncology Group–American College of Radiology Imaging Network Cancer Research Group and supported by the National Cancer Institute. Dr. Owonikoko disclosed a consulting or advisory role with AbbVie, developer of veliparib, and other companies, as well as institutional research funding from AbbVie and others.
SOURCE: Owonikoko TK et al. J Clin Oncol. 2018 Dec 5. doi: 10.1200/JCO.18.00264.
For patients with extensive-stage small-cell lung cancer (ES-SCLC), the addition of the poly (ADP ribose) polymerase (PARP) inhibitor veliparib to frontline chemotherapy with cisplatin and etoposide resulted in a slight but significant improvement in progression-free survival but not overall survival, compared with cisplatin/etoposide alone, investigators reported in the Journal of Clinical Oncology.
Among 128 patients with newly diagnosed ES-SCLC, the median progression-free survival (PFS; the primary endpoint) for those randomized to veliparib/cisplatin/etoposide was 6.1 months, compared with 5.5 months for patients randomized to cisplatin/etoposide alone.
This translated into an unstratified hazard ratio for PFS with veliparib of 0.75 (one-sided P = .06) and a stratified HR of 0.63 (one-sided P = .01), reported Taofeek K. Owonikoko, MD, PhD, and his colleagues at Emory University in Atlanta.
“Although the initial result of our study is promising, additional confirmation in a larger definitive study is warranted, given the mixed results reported by other studies of PARP inhibitors in this patient population,” they wrote.
Median overall survival (OS) with cisplatin/etoposide in ES-SCLC is approximately 9-11 months, and fewer than 5% of patients survive out to 5 years. To see whether the addition of a PARP inhibitor to the standard of care could improve outcomes, the investigators first demonstrated in a phase 1 trial that the combination of veliparib with a platinum doublet of cisplatin and etoposide was safe (Lung Cancer. 2015 Jul;89[1]:66-70), and in the current study, they evaluated efficacy.
A total of 128 eligible patients (median age, 66 years; 52% men) with ES-SCLC were included in the analysis. Extensive-stage disease was defined as the presence of extrathoracic metastatic disease, malignant pleural effusion, and bilateral or contralateral supraclavicular adenopathy.
The patients were stratified by sex and serum lactate dehydrogenase (LDH) levels and then randomized to receive a maximum of four 3-week cycles of of cisplatin 75 mg/m2 intravenously on day 1 and etoposide 100 mg/m2 on days 1 through 3, plus either oral veliparib 100 mg twice daily on days 1 through 7 or placebo.
The primary endpoint of PFS was as noted before. Median overall survival was 10.3 months in the veliparib arm versus 8.9 months in the cisplatin/etoposide alone arm, a difference that was not statistically significant. The respective overall response rates were 71.9% vs. 65.6%, but this difference was also not significant.
Looking at the treatment effect by strata, the investigators found that men with high serum LDH levels had a significant PFS benefit with veliparib (HR, 0.34; one-sided P less than .001), but no significant benefit was seen in men with normal LDH or in women regardless of LDH status.
Grade 3 or greater hematologic toxicities that occurred more frequently in the veliparib arm included CD4 lymphopenia in 8% vs. 0% and neutropenia in 49% vs. 32%.
The investigators noted that the discrepancy between the magnitude of the risk reduction as measured by the hazard ratio and the actual, modest difference in median PFS between the study arms may be explained by the fact that men with elevated LDH represented the largest patient strata.
“Therefore, we hypothesize that this cohort probably contained a sufficient proportion of patients with SCLC who harbored some biologic vulnerability to this therapeutic strategy,” they wrote.
They acknowledged that although toxicities were higher with veliparib combination, the ability to deliver chemotherapy was equal between the arms.
Further exploration of the combination of veliparib/cisplatin/etoposide may be justified if results of another ongoing phase 2 study (NCT02289690) of a carboplatin-based chemotherapy doublet plus veliparib has similar efficacy results, Dr. Owonikoko and his associates concluded.
The study was coordinated by the Eastern Cooperative Oncology Group–American College of Radiology Imaging Network Cancer Research Group and supported by the National Cancer Institute. Dr. Owonikoko disclosed a consulting or advisory role with AbbVie, developer of veliparib, and other companies, as well as institutional research funding from AbbVie and others.
SOURCE: Owonikoko TK et al. J Clin Oncol. 2018 Dec 5. doi: 10.1200/JCO.18.00264.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Adding a PARP inhibitor to standard chemotherapy may improve progression-free survival in patients with extensive-stage small-cell lung cancer (ES-SCLC).
Major finding: The stratified hazard ratio for PFS with veliparib/cisplatin/etoposide was 0.63 (one-sided P = .01).
Study details: Randomized phase 2 trial in 128 patients with newly diagnosed ES-SCLC.
Disclosures: The study was coordinated by the Eastern Cooperative Oncology Group–American College of Radiology Imaging Network Cancer Research Group and supported by the National Cancer Institute. Dr. Owonikoko disclosed a consulting or advisory role with AbbVie, the developer of veliparib, and other companies, as well as institutional research funding from AbbVie and others.
Source: Owonikoko TK et al. J Clin Oncol. 2018 Dec 5. doi: 10.1200/JCO.18.00264.