User login
Early breast cancer: Patients report favorable quality of life after partial breast irradiation
In women with breast cancer undergoing breast-conserving surgery, accelerated partial breast irradiation (APBI) using multicatheter brachytherapy does not negatively affect quality of life, compared with standard whole breast irradiation, investigators have reported.
Patients reported similar quality of life scores for multicatheter brachytherapy–based APBI and whole breast irradiation in the study by the Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology (GEC-ESTRO).
Moreover, breast symptom scores were significantly worse for whole-breast radiation, Rebekka Schäfer, MD, of the department of radiation oncology at the University Hospital Würzburg (Germany) and colleagues reported in Lancet Oncology.
“This trial provides further clinical evidence that APBI with interstitial brachytherapy can be considered as an alternative treatment option after breast-conserving surgery for patients with low-risk breast cancer,” Dr. Schäfer and coauthors wrote.
In several previous studies, APBI has been shown to have clinical outcomes equivalent to those of whole breast irradiation in terms of disease recurrence, survival, and treatment side effects, they added.
The quality of life findings in the present report come from long-term follow-up of a randomized, controlled, phase 3 trial conducted at 16 European centers. This study included 1,184 women with early breast cancer randomly who, after receiving breast-conserving surgery, were assigned either to APBI that used multicatheter brachytherapy or to whole breast irradiation.
Women in the study completed validated quality of life questionnaires right before and right after radiotherapy, as well as during follow-up.
A little more than half of the women in each group completed the quality of life questionnaires after the treatment and again at follow-up, investigators said.
Global health status was stable over time in both groups, investigators reported. In the APBI group, global health status score on a scale of 0-100 was 65.6 right after the procedure and 66.2 at 5 years; similarly, scores in the whole breast irradiation group were 64.6 after radiotherapy and 66.0 at 5 years.
The only quality of life difference between arms that investigators characterized as moderately clinically relevant was in breast symptom scores, which were significantly worse in the whole breast radiation group right after radiotherapy (difference of means, 13.6; 95% CI, 9.7-17.5; P less than .0001) and at 3-month follow-up (difference of means, 12.7; 95% CI, 9.8-15.6; P less than .0001).
Emotional functioning, fatigue, and financial difficulty scores in the APBI group were “slightly better” than in the whole breast radiation group right after radiotherapy and at a 3-month follow-up, investigators reported; however, at 5 year follow-up, there were no significant differences between arms in those measures.
“Our findings show that APBI using multicatheter interstitial brachytherapy does not result in clinically significant deterioration of overall quality of life and that the different domains of quality of life after APBI were not worse in comparison with whole breast irradiation in terms of clinically relevant differences,” Dr. Schäfer and colleagues concluded in their report.
Dr. Schäfer reported no conflicts of interest. Coauthors reported disclosures outside of the submitted work including Nucletron Operations BV, Elekta Company, Merck Serono, Novocure, AstraZeneca, and Bristol-Myers Squibb, among others.
SOURCE: Schäfer R et al. Lancet Oncol. 2018 Apr 22. doi: 10.1016/S1470-2045(18)30195-5.
This study by Schäfer and colleagues supports results of earlier and smaller studies showing promising quality of life results following accelerated partial breast irradiation (APBI) using multicatheter brachytherapy, according to Reshma Jagsi, MD.
“The results suggest that for quality of life, multicatheter brachytherapy-based APBI does not adversely affect outcomes, compared with whole breast irradiation,” Dr. Jagsi wrote in an editorial accompanying the article.
In previous trials, APBI using external radiation beam techniques has likewise shown favorable and promising quality of life outcomes.
There are now eagerly anticipated studies of APBI delivered primarily using external beam techniques that have included rigorous collection of quality of life outcomes, Dr. Jagsi added.
Those trials, which include RAPID and RTOG 0413/NSABP B39, will provide additional evidence to consider alongside those of the trial reported by Schäfer and colleagues on behalf of the Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology (GEC-ESTRO).
“Together with the results from the GEC-ESTRO trial, results from these trials will be meaningful to the many tens of thousands of women who undergo breast-conserving surgery and adjuvant radiotherapy each year,” Dr. Jagsi wrote.
Reshma Jagsi, MD, is with the department of radiation oncology at the University of Michigan, Ann Arbor. These comments are derived from editorial in Lancet Oncology . Dr. Jagsi reported receiving personal fees from Amgen.
This study by Schäfer and colleagues supports results of earlier and smaller studies showing promising quality of life results following accelerated partial breast irradiation (APBI) using multicatheter brachytherapy, according to Reshma Jagsi, MD.
“The results suggest that for quality of life, multicatheter brachytherapy-based APBI does not adversely affect outcomes, compared with whole breast irradiation,” Dr. Jagsi wrote in an editorial accompanying the article.
In previous trials, APBI using external radiation beam techniques has likewise shown favorable and promising quality of life outcomes.
There are now eagerly anticipated studies of APBI delivered primarily using external beam techniques that have included rigorous collection of quality of life outcomes, Dr. Jagsi added.
Those trials, which include RAPID and RTOG 0413/NSABP B39, will provide additional evidence to consider alongside those of the trial reported by Schäfer and colleagues on behalf of the Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology (GEC-ESTRO).
“Together with the results from the GEC-ESTRO trial, results from these trials will be meaningful to the many tens of thousands of women who undergo breast-conserving surgery and adjuvant radiotherapy each year,” Dr. Jagsi wrote.
Reshma Jagsi, MD, is with the department of radiation oncology at the University of Michigan, Ann Arbor. These comments are derived from editorial in Lancet Oncology . Dr. Jagsi reported receiving personal fees from Amgen.
This study by Schäfer and colleagues supports results of earlier and smaller studies showing promising quality of life results following accelerated partial breast irradiation (APBI) using multicatheter brachytherapy, according to Reshma Jagsi, MD.
“The results suggest that for quality of life, multicatheter brachytherapy-based APBI does not adversely affect outcomes, compared with whole breast irradiation,” Dr. Jagsi wrote in an editorial accompanying the article.
In previous trials, APBI using external radiation beam techniques has likewise shown favorable and promising quality of life outcomes.
There are now eagerly anticipated studies of APBI delivered primarily using external beam techniques that have included rigorous collection of quality of life outcomes, Dr. Jagsi added.
Those trials, which include RAPID and RTOG 0413/NSABP B39, will provide additional evidence to consider alongside those of the trial reported by Schäfer and colleagues on behalf of the Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology (GEC-ESTRO).
“Together with the results from the GEC-ESTRO trial, results from these trials will be meaningful to the many tens of thousands of women who undergo breast-conserving surgery and adjuvant radiotherapy each year,” Dr. Jagsi wrote.
Reshma Jagsi, MD, is with the department of radiation oncology at the University of Michigan, Ann Arbor. These comments are derived from editorial in Lancet Oncology . Dr. Jagsi reported receiving personal fees from Amgen.
In women with breast cancer undergoing breast-conserving surgery, accelerated partial breast irradiation (APBI) using multicatheter brachytherapy does not negatively affect quality of life, compared with standard whole breast irradiation, investigators have reported.
Patients reported similar quality of life scores for multicatheter brachytherapy–based APBI and whole breast irradiation in the study by the Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology (GEC-ESTRO).
Moreover, breast symptom scores were significantly worse for whole-breast radiation, Rebekka Schäfer, MD, of the department of radiation oncology at the University Hospital Würzburg (Germany) and colleagues reported in Lancet Oncology.
“This trial provides further clinical evidence that APBI with interstitial brachytherapy can be considered as an alternative treatment option after breast-conserving surgery for patients with low-risk breast cancer,” Dr. Schäfer and coauthors wrote.
In several previous studies, APBI has been shown to have clinical outcomes equivalent to those of whole breast irradiation in terms of disease recurrence, survival, and treatment side effects, they added.
The quality of life findings in the present report come from long-term follow-up of a randomized, controlled, phase 3 trial conducted at 16 European centers. This study included 1,184 women with early breast cancer randomly who, after receiving breast-conserving surgery, were assigned either to APBI that used multicatheter brachytherapy or to whole breast irradiation.
Women in the study completed validated quality of life questionnaires right before and right after radiotherapy, as well as during follow-up.
A little more than half of the women in each group completed the quality of life questionnaires after the treatment and again at follow-up, investigators said.
Global health status was stable over time in both groups, investigators reported. In the APBI group, global health status score on a scale of 0-100 was 65.6 right after the procedure and 66.2 at 5 years; similarly, scores in the whole breast irradiation group were 64.6 after radiotherapy and 66.0 at 5 years.
The only quality of life difference between arms that investigators characterized as moderately clinically relevant was in breast symptom scores, which were significantly worse in the whole breast radiation group right after radiotherapy (difference of means, 13.6; 95% CI, 9.7-17.5; P less than .0001) and at 3-month follow-up (difference of means, 12.7; 95% CI, 9.8-15.6; P less than .0001).
Emotional functioning, fatigue, and financial difficulty scores in the APBI group were “slightly better” than in the whole breast radiation group right after radiotherapy and at a 3-month follow-up, investigators reported; however, at 5 year follow-up, there were no significant differences between arms in those measures.
“Our findings show that APBI using multicatheter interstitial brachytherapy does not result in clinically significant deterioration of overall quality of life and that the different domains of quality of life after APBI were not worse in comparison with whole breast irradiation in terms of clinically relevant differences,” Dr. Schäfer and colleagues concluded in their report.
Dr. Schäfer reported no conflicts of interest. Coauthors reported disclosures outside of the submitted work including Nucletron Operations BV, Elekta Company, Merck Serono, Novocure, AstraZeneca, and Bristol-Myers Squibb, among others.
SOURCE: Schäfer R et al. Lancet Oncol. 2018 Apr 22. doi: 10.1016/S1470-2045(18)30195-5.
In women with breast cancer undergoing breast-conserving surgery, accelerated partial breast irradiation (APBI) using multicatheter brachytherapy does not negatively affect quality of life, compared with standard whole breast irradiation, investigators have reported.
Patients reported similar quality of life scores for multicatheter brachytherapy–based APBI and whole breast irradiation in the study by the Groupe Européen de Curiethérapie of European Society for Radiotherapy and Oncology (GEC-ESTRO).
Moreover, breast symptom scores were significantly worse for whole-breast radiation, Rebekka Schäfer, MD, of the department of radiation oncology at the University Hospital Würzburg (Germany) and colleagues reported in Lancet Oncology.
“This trial provides further clinical evidence that APBI with interstitial brachytherapy can be considered as an alternative treatment option after breast-conserving surgery for patients with low-risk breast cancer,” Dr. Schäfer and coauthors wrote.
In several previous studies, APBI has been shown to have clinical outcomes equivalent to those of whole breast irradiation in terms of disease recurrence, survival, and treatment side effects, they added.
The quality of life findings in the present report come from long-term follow-up of a randomized, controlled, phase 3 trial conducted at 16 European centers. This study included 1,184 women with early breast cancer randomly who, after receiving breast-conserving surgery, were assigned either to APBI that used multicatheter brachytherapy or to whole breast irradiation.
Women in the study completed validated quality of life questionnaires right before and right after radiotherapy, as well as during follow-up.
A little more than half of the women in each group completed the quality of life questionnaires after the treatment and again at follow-up, investigators said.
Global health status was stable over time in both groups, investigators reported. In the APBI group, global health status score on a scale of 0-100 was 65.6 right after the procedure and 66.2 at 5 years; similarly, scores in the whole breast irradiation group were 64.6 after radiotherapy and 66.0 at 5 years.
The only quality of life difference between arms that investigators characterized as moderately clinically relevant was in breast symptom scores, which were significantly worse in the whole breast radiation group right after radiotherapy (difference of means, 13.6; 95% CI, 9.7-17.5; P less than .0001) and at 3-month follow-up (difference of means, 12.7; 95% CI, 9.8-15.6; P less than .0001).
Emotional functioning, fatigue, and financial difficulty scores in the APBI group were “slightly better” than in the whole breast radiation group right after radiotherapy and at a 3-month follow-up, investigators reported; however, at 5 year follow-up, there were no significant differences between arms in those measures.
“Our findings show that APBI using multicatheter interstitial brachytherapy does not result in clinically significant deterioration of overall quality of life and that the different domains of quality of life after APBI were not worse in comparison with whole breast irradiation in terms of clinically relevant differences,” Dr. Schäfer and colleagues concluded in their report.
Dr. Schäfer reported no conflicts of interest. Coauthors reported disclosures outside of the submitted work including Nucletron Operations BV, Elekta Company, Merck Serono, Novocure, AstraZeneca, and Bristol-Myers Squibb, among others.
SOURCE: Schäfer R et al. Lancet Oncol. 2018 Apr 22. doi: 10.1016/S1470-2045(18)30195-5.
FROM LANCET ONCOLOGY
Key clinical point: Quality of life results support the use of accelerated partial breast irradiation (APBI) using multicatheter brachytherapy as an alternative to whole breast radiation after breast-conserving surgery.
Major finding: Patients reported similar quality of life scores for the two modalities, while breast symptom scores for whole breast radiation were significantly worse right after radiotherapy (difference of means, 13.6; 95% confidence interval, 9.7-17.5; P less than .0001) and at 3-month follow-up (difference of means, 12.7; 95% CI, 9.8-15.6; P less than .0001), compared with those for APBI.
Study details: 5-year quality of life results from a European phase 3 trial including 1,184 women with early breast cancer who, after undergoing breast-conserving surgery, received either whole breast irradiation or APBI using multicatheter brachytherapy.
Disclosures: Authors reported disclosures outside of the submitted work including Nucletron Operations BV, Elekta Company, Merck Serono, Novocure, AstraZeneca, and Bristol-Myers Squibb, among others.
Source: Schäfer R et al. Lancet Oncol. 2018 Apr 22. doi: 10.1016/S1470-2045(18)30195-5.
Nation’s Top Doc Wants The Overdose Antidote Widely On Hand. Is That Feasible?
When Surgeon General Jerome Adams issued an advisory calling for more people to carry naloxone — not just people at overdose risk, but also friends and family — experts and advocates were almost giddy.
This is an “unequivocally positive” step forward, said Leo Beletsky, an associate professor of law and health sciences at Northeastern University.
And not necessarily a surprise. Adams, who previously was Indiana’s health commissioner, was recruited to be the nation’s top doctor in part because of his work with then-Gov. Mike Pence, now the vice president. In Indiana, Adams pushed for harm-reduction approaches, which included expanded access to naloxone and the implementation of a needle exchange to combat the state’s much-publicized HIV outbreak, which began in 2015 and was linked to injection drug use.
Others cautioned, though, that his have-naloxone-will-carry recommendation is at best limited in what it can achieve, in part because the drug is relatively expensive.
Kaiser Health News breaks down what the advisory means, experts’ concerns and what policy approaches may be in the pipeline.
Many public health advocates applaud the surgeon general’s position.
Naloxone, which is a drug that can keep drug users alive by reversing opioid overdoses, is viewed by many as the cornerstone of the harm-reduction approach to the epidemic. Experts say people with addiction problems should carry it, and so should their family, friends and acquaintances.
“We want to put it more in reach,” said Traci Green, an associate professor of emergency medicine and community health sciences at Boston University, who has extensively researched the opioid abuse crisis. “It could not have been a better endorsement.”
Others, including Diane Goodman, who penned a recent Medscape commentary reflecting on the advisory, wonder whether this is a “rational” response to the scourge, since opioid addiction is one of many health problems people might encounter in everyday life and for which treatment options are still limited.
“I’m not sure it makes much more sense than any of us carrying a bottle of nitroglycerin to treat patients with end-stage angina,” wrote Goodman, an acute-care nurse practitioner, referring to chest pain.
“What, exactly, are we offering to addicts once their condition has been reversed?” she asked, noting that without treatment and therapy programs that help wean people from addiction “the odds of survival for any length of time remain low, no matter how much reversal medication is kept nearby.”
Results would likely be limited by naloxone’s price tag.
Take Baltimore, which has been hit particularly hard by the opioid epidemic. Its health department already has pushed for more people to carry naloxone.
But the drug’s price is an issue, said Dr. Leana Wen, the city’s health commissioner, and an emergency physician. She suggested that the federal government negotiate directly for a lower price, or give more money to organizations and agencies like hers so they can afford to maintain an adequate supply.
“Every day, people are calling us at the Baltimore City Health Department and requesting naloxone, and I have to tell them I can’t afford for them to have it,” Wen said.
The drug is available in generic form, which can be stored in a vial and injected via a needle, as well as in patented products, such as the nasal spray Narcan, sold by ADAPT Pharmaceuticals, and Kaleo’s Evzio, a talking auto-injector.
Generic naloxone costs $20 to $40 per dose. Narcan, the nasal spray, costs $125 for a two-dose carton, according to ADAPT’s website. A two-pack of Evzio costs close to $4,000, according to GoodRx.
Health departments and first responders qualify for a discounted rate of $75 per carton of Narcan. Kaleo has made Evzio coupons available to consumers, so that some will not have a copay, and it advertises a discount for federal and state agencies.
Skeptics point out that similar methods have been used to build brand loyalty and potentially make a particular product a household name. That’s how Epi-Pen became synonymous with epinephrine for the treatment of anaphylactic shock.
“There’s clearly some overlap” here between the pricing strategies used by naloxone manufacturers and Epi-Pen distributor Mylan, said Richard Evans, co-founder of SSR Health, which tracks the pharmaceutical industry.
But it’s not a perfect comparison. The presence of low-cost generics changes the calculus, he said, as does the different level of demand.
Nonprofit organizations and health care providers keenly feel the pressures of increasing demand and cost.
Experts say price breaks on naloxone are not sufficient to cover the costs on the ground.
“Sixty-four thousand people lost their lives [nationally in 2016] — that’s someone every 12 minutes,” said Justin Phillips, executive director of Overdose Lifeline, an Indianapolis-based nonprofit. “Ten free kits is not going to be enough.”
Phillips said her organization relies on generic naloxone, which is the least expensive formulation. It’s the only feasible option, using dedicated grant money the group received from the state attorney general’s office as part of a program funded by a settlement with pharmaceutical companies.
But that money is almost dried up. “We need to be able to access naloxone — which I’m told is pennies to make — for the pennies it cost to make it,” Phillips said.
Phillips, who worked with Adams when he ran Indiana’s health department, said she has discussed the need for naloxone funding with the surgeon general, but never its price.
Pharmacies assess the hurdles of distribution.
Local pharmacies are key in this chain, but the overdose antidote is new territory for many pharmacists, said Randy Hitchens, the executive vice president of the Indiana Pharmacists Alliance. He said in 2015, when Adams began his push to get naloxone into the hands of drug users and their families, only one or two retail pharmacies carried it.
“This has always been an emergency room drug. Retail pharmacists typically were not used to dealing with [it],” Hitchens said. “A lot were probably saying, ‘What in the devil is naloxone?’”
Today, he estimates 60 to 70 percent of Indiana’s more than 1,100 retail pharmacies carry the drug. Walgreens, the pharmacy chain, has committed to stocking Narcan.
Access, though, is always subject to retail pressures.
“If pharmacies are not seeing a steady stream coming in asking for it, they won’t be incentivized to carry it on their shelves,” said Daniel Raymond, the deputy director of policy and planning for the Harm Reduction Coalition.
A patchwork of other decentralized sources for naloxone exist: syringe-exchange vans, county and state health departments, churches and community centers, all trying to find ways to get overdose medication into the hands of people who need it.
That supply stream “meets people where they are,” Raymond said, but those little programs don’t have the muscle to negotiate discounted prices.
“Individual health programs are trying to navigate the crisis on their own, but when you see … growing demand and limited supply, it’s a role for federal intervention,” Raymond said.
He’d like to see the federal government step in to negotiate prices where smaller programs can’t.
The surgeon general’s message is one part of Washington’s broader response to the epidemic. But even as Congress crafts an opioid epidemic response package, it’s not clear it will tackle these concerns.
In the House of Representatives’ Energy and Commerce Committee, one bill being discussed would require all state Medicaid programs to cover at least one form of naloxone. Currently, not all state Medicaid programs do so.
A Senate bill would authorize $300 million annually to equip first responders with naloxone.
But critics say those approaches still don’t address the underlying problems: cost and funding.
“You can either make naloxone available, at a much discounted price, or we need to have a lot more resources in order to purchase it,” Wen said. “I don’t care which one. My only concern is the health and well-being of our residents.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
When Surgeon General Jerome Adams issued an advisory calling for more people to carry naloxone — not just people at overdose risk, but also friends and family — experts and advocates were almost giddy.
This is an “unequivocally positive” step forward, said Leo Beletsky, an associate professor of law and health sciences at Northeastern University.
And not necessarily a surprise. Adams, who previously was Indiana’s health commissioner, was recruited to be the nation’s top doctor in part because of his work with then-Gov. Mike Pence, now the vice president. In Indiana, Adams pushed for harm-reduction approaches, which included expanded access to naloxone and the implementation of a needle exchange to combat the state’s much-publicized HIV outbreak, which began in 2015 and was linked to injection drug use.
Others cautioned, though, that his have-naloxone-will-carry recommendation is at best limited in what it can achieve, in part because the drug is relatively expensive.
Kaiser Health News breaks down what the advisory means, experts’ concerns and what policy approaches may be in the pipeline.
Many public health advocates applaud the surgeon general’s position.
Naloxone, which is a drug that can keep drug users alive by reversing opioid overdoses, is viewed by many as the cornerstone of the harm-reduction approach to the epidemic. Experts say people with addiction problems should carry it, and so should their family, friends and acquaintances.
“We want to put it more in reach,” said Traci Green, an associate professor of emergency medicine and community health sciences at Boston University, who has extensively researched the opioid abuse crisis. “It could not have been a better endorsement.”
Others, including Diane Goodman, who penned a recent Medscape commentary reflecting on the advisory, wonder whether this is a “rational” response to the scourge, since opioid addiction is one of many health problems people might encounter in everyday life and for which treatment options are still limited.
“I’m not sure it makes much more sense than any of us carrying a bottle of nitroglycerin to treat patients with end-stage angina,” wrote Goodman, an acute-care nurse practitioner, referring to chest pain.
“What, exactly, are we offering to addicts once their condition has been reversed?” she asked, noting that without treatment and therapy programs that help wean people from addiction “the odds of survival for any length of time remain low, no matter how much reversal medication is kept nearby.”
Results would likely be limited by naloxone’s price tag.
Take Baltimore, which has been hit particularly hard by the opioid epidemic. Its health department already has pushed for more people to carry naloxone.
But the drug’s price is an issue, said Dr. Leana Wen, the city’s health commissioner, and an emergency physician. She suggested that the federal government negotiate directly for a lower price, or give more money to organizations and agencies like hers so they can afford to maintain an adequate supply.
“Every day, people are calling us at the Baltimore City Health Department and requesting naloxone, and I have to tell them I can’t afford for them to have it,” Wen said.
The drug is available in generic form, which can be stored in a vial and injected via a needle, as well as in patented products, such as the nasal spray Narcan, sold by ADAPT Pharmaceuticals, and Kaleo’s Evzio, a talking auto-injector.
Generic naloxone costs $20 to $40 per dose. Narcan, the nasal spray, costs $125 for a two-dose carton, according to ADAPT’s website. A two-pack of Evzio costs close to $4,000, according to GoodRx.
Health departments and first responders qualify for a discounted rate of $75 per carton of Narcan. Kaleo has made Evzio coupons available to consumers, so that some will not have a copay, and it advertises a discount for federal and state agencies.
Skeptics point out that similar methods have been used to build brand loyalty and potentially make a particular product a household name. That’s how Epi-Pen became synonymous with epinephrine for the treatment of anaphylactic shock.
“There’s clearly some overlap” here between the pricing strategies used by naloxone manufacturers and Epi-Pen distributor Mylan, said Richard Evans, co-founder of SSR Health, which tracks the pharmaceutical industry.
But it’s not a perfect comparison. The presence of low-cost generics changes the calculus, he said, as does the different level of demand.
Nonprofit organizations and health care providers keenly feel the pressures of increasing demand and cost.
Experts say price breaks on naloxone are not sufficient to cover the costs on the ground.
“Sixty-four thousand people lost their lives [nationally in 2016] — that’s someone every 12 minutes,” said Justin Phillips, executive director of Overdose Lifeline, an Indianapolis-based nonprofit. “Ten free kits is not going to be enough.”
Phillips said her organization relies on generic naloxone, which is the least expensive formulation. It’s the only feasible option, using dedicated grant money the group received from the state attorney general’s office as part of a program funded by a settlement with pharmaceutical companies.
But that money is almost dried up. “We need to be able to access naloxone — which I’m told is pennies to make — for the pennies it cost to make it,” Phillips said.
Phillips, who worked with Adams when he ran Indiana’s health department, said she has discussed the need for naloxone funding with the surgeon general, but never its price.
Pharmacies assess the hurdles of distribution.
Local pharmacies are key in this chain, but the overdose antidote is new territory for many pharmacists, said Randy Hitchens, the executive vice president of the Indiana Pharmacists Alliance. He said in 2015, when Adams began his push to get naloxone into the hands of drug users and their families, only one or two retail pharmacies carried it.
“This has always been an emergency room drug. Retail pharmacists typically were not used to dealing with [it],” Hitchens said. “A lot were probably saying, ‘What in the devil is naloxone?’”
Today, he estimates 60 to 70 percent of Indiana’s more than 1,100 retail pharmacies carry the drug. Walgreens, the pharmacy chain, has committed to stocking Narcan.
Access, though, is always subject to retail pressures.
“If pharmacies are not seeing a steady stream coming in asking for it, they won’t be incentivized to carry it on their shelves,” said Daniel Raymond, the deputy director of policy and planning for the Harm Reduction Coalition.
A patchwork of other decentralized sources for naloxone exist: syringe-exchange vans, county and state health departments, churches and community centers, all trying to find ways to get overdose medication into the hands of people who need it.
That supply stream “meets people where they are,” Raymond said, but those little programs don’t have the muscle to negotiate discounted prices.
“Individual health programs are trying to navigate the crisis on their own, but when you see … growing demand and limited supply, it’s a role for federal intervention,” Raymond said.
He’d like to see the federal government step in to negotiate prices where smaller programs can’t.
The surgeon general’s message is one part of Washington’s broader response to the epidemic. But even as Congress crafts an opioid epidemic response package, it’s not clear it will tackle these concerns.
In the House of Representatives’ Energy and Commerce Committee, one bill being discussed would require all state Medicaid programs to cover at least one form of naloxone. Currently, not all state Medicaid programs do so.
A Senate bill would authorize $300 million annually to equip first responders with naloxone.
But critics say those approaches still don’t address the underlying problems: cost and funding.
“You can either make naloxone available, at a much discounted price, or we need to have a lot more resources in order to purchase it,” Wen said. “I don’t care which one. My only concern is the health and well-being of our residents.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
When Surgeon General Jerome Adams issued an advisory calling for more people to carry naloxone — not just people at overdose risk, but also friends and family — experts and advocates were almost giddy.
This is an “unequivocally positive” step forward, said Leo Beletsky, an associate professor of law and health sciences at Northeastern University.
And not necessarily a surprise. Adams, who previously was Indiana’s health commissioner, was recruited to be the nation’s top doctor in part because of his work with then-Gov. Mike Pence, now the vice president. In Indiana, Adams pushed for harm-reduction approaches, which included expanded access to naloxone and the implementation of a needle exchange to combat the state’s much-publicized HIV outbreak, which began in 2015 and was linked to injection drug use.
Others cautioned, though, that his have-naloxone-will-carry recommendation is at best limited in what it can achieve, in part because the drug is relatively expensive.
Kaiser Health News breaks down what the advisory means, experts’ concerns and what policy approaches may be in the pipeline.
Many public health advocates applaud the surgeon general’s position.
Naloxone, which is a drug that can keep drug users alive by reversing opioid overdoses, is viewed by many as the cornerstone of the harm-reduction approach to the epidemic. Experts say people with addiction problems should carry it, and so should their family, friends and acquaintances.
“We want to put it more in reach,” said Traci Green, an associate professor of emergency medicine and community health sciences at Boston University, who has extensively researched the opioid abuse crisis. “It could not have been a better endorsement.”
Others, including Diane Goodman, who penned a recent Medscape commentary reflecting on the advisory, wonder whether this is a “rational” response to the scourge, since opioid addiction is one of many health problems people might encounter in everyday life and for which treatment options are still limited.
“I’m not sure it makes much more sense than any of us carrying a bottle of nitroglycerin to treat patients with end-stage angina,” wrote Goodman, an acute-care nurse practitioner, referring to chest pain.
“What, exactly, are we offering to addicts once their condition has been reversed?” she asked, noting that without treatment and therapy programs that help wean people from addiction “the odds of survival for any length of time remain low, no matter how much reversal medication is kept nearby.”
Results would likely be limited by naloxone’s price tag.
Take Baltimore, which has been hit particularly hard by the opioid epidemic. Its health department already has pushed for more people to carry naloxone.
But the drug’s price is an issue, said Dr. Leana Wen, the city’s health commissioner, and an emergency physician. She suggested that the federal government negotiate directly for a lower price, or give more money to organizations and agencies like hers so they can afford to maintain an adequate supply.
“Every day, people are calling us at the Baltimore City Health Department and requesting naloxone, and I have to tell them I can’t afford for them to have it,” Wen said.
The drug is available in generic form, which can be stored in a vial and injected via a needle, as well as in patented products, such as the nasal spray Narcan, sold by ADAPT Pharmaceuticals, and Kaleo’s Evzio, a talking auto-injector.
Generic naloxone costs $20 to $40 per dose. Narcan, the nasal spray, costs $125 for a two-dose carton, according to ADAPT’s website. A two-pack of Evzio costs close to $4,000, according to GoodRx.
Health departments and first responders qualify for a discounted rate of $75 per carton of Narcan. Kaleo has made Evzio coupons available to consumers, so that some will not have a copay, and it advertises a discount for federal and state agencies.
Skeptics point out that similar methods have been used to build brand loyalty and potentially make a particular product a household name. That’s how Epi-Pen became synonymous with epinephrine for the treatment of anaphylactic shock.
“There’s clearly some overlap” here between the pricing strategies used by naloxone manufacturers and Epi-Pen distributor Mylan, said Richard Evans, co-founder of SSR Health, which tracks the pharmaceutical industry.
But it’s not a perfect comparison. The presence of low-cost generics changes the calculus, he said, as does the different level of demand.
Nonprofit organizations and health care providers keenly feel the pressures of increasing demand and cost.
Experts say price breaks on naloxone are not sufficient to cover the costs on the ground.
“Sixty-four thousand people lost their lives [nationally in 2016] — that’s someone every 12 minutes,” said Justin Phillips, executive director of Overdose Lifeline, an Indianapolis-based nonprofit. “Ten free kits is not going to be enough.”
Phillips said her organization relies on generic naloxone, which is the least expensive formulation. It’s the only feasible option, using dedicated grant money the group received from the state attorney general’s office as part of a program funded by a settlement with pharmaceutical companies.
But that money is almost dried up. “We need to be able to access naloxone — which I’m told is pennies to make — for the pennies it cost to make it,” Phillips said.
Phillips, who worked with Adams when he ran Indiana’s health department, said she has discussed the need for naloxone funding with the surgeon general, but never its price.
Pharmacies assess the hurdles of distribution.
Local pharmacies are key in this chain, but the overdose antidote is new territory for many pharmacists, said Randy Hitchens, the executive vice president of the Indiana Pharmacists Alliance. He said in 2015, when Adams began his push to get naloxone into the hands of drug users and their families, only one or two retail pharmacies carried it.
“This has always been an emergency room drug. Retail pharmacists typically were not used to dealing with [it],” Hitchens said. “A lot were probably saying, ‘What in the devil is naloxone?’”
Today, he estimates 60 to 70 percent of Indiana’s more than 1,100 retail pharmacies carry the drug. Walgreens, the pharmacy chain, has committed to stocking Narcan.
Access, though, is always subject to retail pressures.
“If pharmacies are not seeing a steady stream coming in asking for it, they won’t be incentivized to carry it on their shelves,” said Daniel Raymond, the deputy director of policy and planning for the Harm Reduction Coalition.
A patchwork of other decentralized sources for naloxone exist: syringe-exchange vans, county and state health departments, churches and community centers, all trying to find ways to get overdose medication into the hands of people who need it.
That supply stream “meets people where they are,” Raymond said, but those little programs don’t have the muscle to negotiate discounted prices.
“Individual health programs are trying to navigate the crisis on their own, but when you see … growing demand and limited supply, it’s a role for federal intervention,” Raymond said.
He’d like to see the federal government step in to negotiate prices where smaller programs can’t.
The surgeon general’s message is one part of Washington’s broader response to the epidemic. But even as Congress crafts an opioid epidemic response package, it’s not clear it will tackle these concerns.
In the House of Representatives’ Energy and Commerce Committee, one bill being discussed would require all state Medicaid programs to cover at least one form of naloxone. Currently, not all state Medicaid programs do so.
A Senate bill would authorize $300 million annually to equip first responders with naloxone.
But critics say those approaches still don’t address the underlying problems: cost and funding.
“You can either make naloxone available, at a much discounted price, or we need to have a lot more resources in order to purchase it,” Wen said. “I don’t care which one. My only concern is the health and well-being of our residents.”
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.
Screening tool IDs older NSCLC patients suitable for SBRT
A validated screening tool may help to identify older adults with early-stage non–small cell lung cancer who could benefit from stereotactic body radiotherapy with curative intent, investigators contend,
Among 43 patients aged 65-89 years (median age 78) with stage T1 or T2 non–small cell lung cancer tumors who underwent stereotactic body radiotherapy (SBRT), scores of 13 or higher on the Geriatric 8 (G8) screening tool were associated with high 2- and 5-year survival rates, reported Toshiya Maebayashi, MD, PhD, from Nihon University in Tokyo, and colleagues.
“Regardless of age, the G8 screening tool may enable us to identify relatively healthy seniors who would be likely to have longer survival times after SBRT for early lung cancer,” they wrote in a study published in the Journal of Geriatric Oncology.
The G8 Screening tool assesses the health status of older patients according to their food intake, recent weight loss, mobility, neuropsychological problems, body mass index, prescription drug use, and age. Higher scores on the scale, which can range from 0 to 17, are indicative of better health status.
To see whether the G8 tool could predict the benefits of SBRT, the investigators performed a retrospective study of long-term outcomes in older patients with early-stage non–small cell lung cancer.
They included 34 patients with T1 tumors and 9 patients with T2 tumors who underwent SBRT from 2004 to 2011 at their center. The median follow-up was 46 months (range, 3-112 months).
Patients with T1 tumors had G8 scores ranging from 9 to 16 (median 13). Patients with T2 tumors had scores ranging from 8 to 15 (median 12).
For patients with G8 scores of 12 or lower, the overall survival rate after 2 years was 56.1%, and 28% after 5 years. In contrast, the respective 2- and 5-year overall survival rates for patients with G8 scores of 13 or higher were 94.1% and 68.4% (P = .0014).
In univariate analysis, factors significantly associated with survival included T-stage (P = .034), pathology (P = .004), and G8 score (P = .001). G8 score was also significantly associated with overall survival in multivariate analysis (P = .006).
Adverse events included rib fractures in nine patients, grade 2 pneumonitis in four and grade 3 pneumonitis in two patients. There were no cases of hemoptysis. Neither G8 score nor age were related to adverse events.
“We anticipate that functional evaluation of older patients will allow us to actively recommend SBRT [an approach less likely than other current treatments to cause adverse events] to older patients who are in relatively good condition but hesitant to receive treatment,” the investigators wrote.
The authors did not receive special funding for the study, and had no conflicts of interest.
SOURCE: Maebayashi T et al. J Geriatr Oncol. 2018 Mar 22. doi: 10.1016/j.jgo.2018.03.005.
A validated screening tool may help to identify older adults with early-stage non–small cell lung cancer who could benefit from stereotactic body radiotherapy with curative intent, investigators contend,
Among 43 patients aged 65-89 years (median age 78) with stage T1 or T2 non–small cell lung cancer tumors who underwent stereotactic body radiotherapy (SBRT), scores of 13 or higher on the Geriatric 8 (G8) screening tool were associated with high 2- and 5-year survival rates, reported Toshiya Maebayashi, MD, PhD, from Nihon University in Tokyo, and colleagues.
“Regardless of age, the G8 screening tool may enable us to identify relatively healthy seniors who would be likely to have longer survival times after SBRT for early lung cancer,” they wrote in a study published in the Journal of Geriatric Oncology.
The G8 Screening tool assesses the health status of older patients according to their food intake, recent weight loss, mobility, neuropsychological problems, body mass index, prescription drug use, and age. Higher scores on the scale, which can range from 0 to 17, are indicative of better health status.
To see whether the G8 tool could predict the benefits of SBRT, the investigators performed a retrospective study of long-term outcomes in older patients with early-stage non–small cell lung cancer.
They included 34 patients with T1 tumors and 9 patients with T2 tumors who underwent SBRT from 2004 to 2011 at their center. The median follow-up was 46 months (range, 3-112 months).
Patients with T1 tumors had G8 scores ranging from 9 to 16 (median 13). Patients with T2 tumors had scores ranging from 8 to 15 (median 12).
For patients with G8 scores of 12 or lower, the overall survival rate after 2 years was 56.1%, and 28% after 5 years. In contrast, the respective 2- and 5-year overall survival rates for patients with G8 scores of 13 or higher were 94.1% and 68.4% (P = .0014).
In univariate analysis, factors significantly associated with survival included T-stage (P = .034), pathology (P = .004), and G8 score (P = .001). G8 score was also significantly associated with overall survival in multivariate analysis (P = .006).
Adverse events included rib fractures in nine patients, grade 2 pneumonitis in four and grade 3 pneumonitis in two patients. There were no cases of hemoptysis. Neither G8 score nor age were related to adverse events.
“We anticipate that functional evaluation of older patients will allow us to actively recommend SBRT [an approach less likely than other current treatments to cause adverse events] to older patients who are in relatively good condition but hesitant to receive treatment,” the investigators wrote.
The authors did not receive special funding for the study, and had no conflicts of interest.
SOURCE: Maebayashi T et al. J Geriatr Oncol. 2018 Mar 22. doi: 10.1016/j.jgo.2018.03.005.
A validated screening tool may help to identify older adults with early-stage non–small cell lung cancer who could benefit from stereotactic body radiotherapy with curative intent, investigators contend,
Among 43 patients aged 65-89 years (median age 78) with stage T1 or T2 non–small cell lung cancer tumors who underwent stereotactic body radiotherapy (SBRT), scores of 13 or higher on the Geriatric 8 (G8) screening tool were associated with high 2- and 5-year survival rates, reported Toshiya Maebayashi, MD, PhD, from Nihon University in Tokyo, and colleagues.
“Regardless of age, the G8 screening tool may enable us to identify relatively healthy seniors who would be likely to have longer survival times after SBRT for early lung cancer,” they wrote in a study published in the Journal of Geriatric Oncology.
The G8 Screening tool assesses the health status of older patients according to their food intake, recent weight loss, mobility, neuropsychological problems, body mass index, prescription drug use, and age. Higher scores on the scale, which can range from 0 to 17, are indicative of better health status.
To see whether the G8 tool could predict the benefits of SBRT, the investigators performed a retrospective study of long-term outcomes in older patients with early-stage non–small cell lung cancer.
They included 34 patients with T1 tumors and 9 patients with T2 tumors who underwent SBRT from 2004 to 2011 at their center. The median follow-up was 46 months (range, 3-112 months).
Patients with T1 tumors had G8 scores ranging from 9 to 16 (median 13). Patients with T2 tumors had scores ranging from 8 to 15 (median 12).
For patients with G8 scores of 12 or lower, the overall survival rate after 2 years was 56.1%, and 28% after 5 years. In contrast, the respective 2- and 5-year overall survival rates for patients with G8 scores of 13 or higher were 94.1% and 68.4% (P = .0014).
In univariate analysis, factors significantly associated with survival included T-stage (P = .034), pathology (P = .004), and G8 score (P = .001). G8 score was also significantly associated with overall survival in multivariate analysis (P = .006).
Adverse events included rib fractures in nine patients, grade 2 pneumonitis in four and grade 3 pneumonitis in two patients. There were no cases of hemoptysis. Neither G8 score nor age were related to adverse events.
“We anticipate that functional evaluation of older patients will allow us to actively recommend SBRT [an approach less likely than other current treatments to cause adverse events] to older patients who are in relatively good condition but hesitant to receive treatment,” the investigators wrote.
The authors did not receive special funding for the study, and had no conflicts of interest.
SOURCE: Maebayashi T et al. J Geriatr Oncol. 2018 Mar 22. doi: 10.1016/j.jgo.2018.03.005.
FROM THE JOURNAL OF GERIATRIC ONCOLOGY
Key clinical point: The Geriatric 8 screening tool may identify older patients with non–small cell lung cancer who could benefit from stereotactic body radiotherapy.
Major finding: Geriatric 8 scores of 13 or higher were associated with better 2- and 5-year overall survival.
Study details: A retrospective analysis of 43 patients aged 65-89 years with stage T1 or T2 non–small cell lung cancer.
Disclosures: The authors did not receive special funding for the study, and had no conflicts of interest to disclose.
Source: Maebayashi T et al. J Geriatr Oncol. 2018 Mar 22. doi: 10.1016/j.jgo.2018.03.005.
Colchicine looks promising for treating prurigo pigmentosa in case report
said Isa An, MD of Dicle University, Diyarbakır, Turkey, and associates.
They described a 16-year-old Turkish girl who presented with an itchy rash on her back of 4 weeks’ duration. Treatment with oral antihistamines, and topical and systemic steroids were ineffective. On physical examination, there were erythematous macules, sporadic excoriated papules, and reticulate hyperpigmentation on her back. Complete blood count and liver function tests were normal.
Histopathologic examination showed “infrequent necrotic keratinocytes with marked acanthosis and spongiosis on the epidermis, increased basal layer pigmentation, and perivascular lymphocytic infiltrate on the upper dermis.” Because of these findings, a diagnosis of prurigo pigmentosa was made, they wrote in Pediatric Dermatology.
Treatment with colchicine 1.5 g/day was started, and while the lesions resolved in the second week of treatment, the reticulate hyperpigmentation remained, Dr. An and her associates reported. The reticulate hyperpigmentation did not regress during the first month of treatment. At 6-month follow-up, there were no more symptoms of itch or recurrence of the original lesions. The reticulate hyperpigmentation was not treated.
A rare inflammatory skin disease seen principally in young Japanese women, prurigo pigmentosa has been reported in both men and women of other ethnicities, they said. Generally, macrolide antibiotics, such as clarithromycin, dapsone, and isotretinoin have been used effectively to treat prurigo pigmentosa. Minocycline and doxycycline are considered to be effective in treating this skin disease because of their anti-inflammatory effects and because they have “been shown to inhibit the synthesis of cytokines and chemokines that regulate leukocyte differentiation and activation.” Leukocyte differentiation and activation “are key pathologic features of prurigo pigmentosa,” the authors added.
Colchicine, a neutral, liposoluble tricyclic alkaloid, “exerts an anti-inflammatory effect by inhibiting neutrophil chemotaxis,” said Dr. An and her associates, which is why it is thought to be a potentially effective drug for treating prurigo pigmentosa, as shown in this case study. “Further studies are required to verify whether colchicine is an effective treatment option,” for prurigo pigmentosa, they added.
SOURCE: An I et al. Pediatr Dermatol. 2018 Apr 11. doi: 10.1111/pde.13480.
said Isa An, MD of Dicle University, Diyarbakır, Turkey, and associates.
They described a 16-year-old Turkish girl who presented with an itchy rash on her back of 4 weeks’ duration. Treatment with oral antihistamines, and topical and systemic steroids were ineffective. On physical examination, there were erythematous macules, sporadic excoriated papules, and reticulate hyperpigmentation on her back. Complete blood count and liver function tests were normal.
Histopathologic examination showed “infrequent necrotic keratinocytes with marked acanthosis and spongiosis on the epidermis, increased basal layer pigmentation, and perivascular lymphocytic infiltrate on the upper dermis.” Because of these findings, a diagnosis of prurigo pigmentosa was made, they wrote in Pediatric Dermatology.
Treatment with colchicine 1.5 g/day was started, and while the lesions resolved in the second week of treatment, the reticulate hyperpigmentation remained, Dr. An and her associates reported. The reticulate hyperpigmentation did not regress during the first month of treatment. At 6-month follow-up, there were no more symptoms of itch or recurrence of the original lesions. The reticulate hyperpigmentation was not treated.
A rare inflammatory skin disease seen principally in young Japanese women, prurigo pigmentosa has been reported in both men and women of other ethnicities, they said. Generally, macrolide antibiotics, such as clarithromycin, dapsone, and isotretinoin have been used effectively to treat prurigo pigmentosa. Minocycline and doxycycline are considered to be effective in treating this skin disease because of their anti-inflammatory effects and because they have “been shown to inhibit the synthesis of cytokines and chemokines that regulate leukocyte differentiation and activation.” Leukocyte differentiation and activation “are key pathologic features of prurigo pigmentosa,” the authors added.
Colchicine, a neutral, liposoluble tricyclic alkaloid, “exerts an anti-inflammatory effect by inhibiting neutrophil chemotaxis,” said Dr. An and her associates, which is why it is thought to be a potentially effective drug for treating prurigo pigmentosa, as shown in this case study. “Further studies are required to verify whether colchicine is an effective treatment option,” for prurigo pigmentosa, they added.
SOURCE: An I et al. Pediatr Dermatol. 2018 Apr 11. doi: 10.1111/pde.13480.
said Isa An, MD of Dicle University, Diyarbakır, Turkey, and associates.
They described a 16-year-old Turkish girl who presented with an itchy rash on her back of 4 weeks’ duration. Treatment with oral antihistamines, and topical and systemic steroids were ineffective. On physical examination, there were erythematous macules, sporadic excoriated papules, and reticulate hyperpigmentation on her back. Complete blood count and liver function tests were normal.
Histopathologic examination showed “infrequent necrotic keratinocytes with marked acanthosis and spongiosis on the epidermis, increased basal layer pigmentation, and perivascular lymphocytic infiltrate on the upper dermis.” Because of these findings, a diagnosis of prurigo pigmentosa was made, they wrote in Pediatric Dermatology.
Treatment with colchicine 1.5 g/day was started, and while the lesions resolved in the second week of treatment, the reticulate hyperpigmentation remained, Dr. An and her associates reported. The reticulate hyperpigmentation did not regress during the first month of treatment. At 6-month follow-up, there were no more symptoms of itch or recurrence of the original lesions. The reticulate hyperpigmentation was not treated.
A rare inflammatory skin disease seen principally in young Japanese women, prurigo pigmentosa has been reported in both men and women of other ethnicities, they said. Generally, macrolide antibiotics, such as clarithromycin, dapsone, and isotretinoin have been used effectively to treat prurigo pigmentosa. Minocycline and doxycycline are considered to be effective in treating this skin disease because of their anti-inflammatory effects and because they have “been shown to inhibit the synthesis of cytokines and chemokines that regulate leukocyte differentiation and activation.” Leukocyte differentiation and activation “are key pathologic features of prurigo pigmentosa,” the authors added.
Colchicine, a neutral, liposoluble tricyclic alkaloid, “exerts an anti-inflammatory effect by inhibiting neutrophil chemotaxis,” said Dr. An and her associates, which is why it is thought to be a potentially effective drug for treating prurigo pigmentosa, as shown in this case study. “Further studies are required to verify whether colchicine is an effective treatment option,” for prurigo pigmentosa, they added.
SOURCE: An I et al. Pediatr Dermatol. 2018 Apr 11. doi: 10.1111/pde.13480.
FROM PEDIATRIC DERMATOLOGY
Ideal sun protection practices by parents low in Toronto
according to Marcus G. Tan, MD, of the University of Toronto, and his associates.
Too much sun exposure as a child is a known risk factor for skin cancer, and “it has been estimated that approximately half of cumulative ultraviolet exposure by age 60 occurs before age 20.” So it is important that children be protected from excessive sun exposure, the investigators wrote, underscoring the reason for their study of parental sun protection by Canadian parents in Toronto, which has a multiracial population.
Parental sun protection efforts were considered ideal if they used sun protection every day; on sunny days all year round; or during the summer, using at least SPF 30, and reapplying sunscreen at least every 2 hours. Parental efforts would be considered nonideal if they did not meet any of these three criteria.
Of 183 parents, 17% used ideal sun protection for their children; 28% were in the lighter-skinned group (Fitzpatrick phototype I-III) and 5% in the darker-skinned group (Fitzpatrick phototype IV-V), The greater likelihood of using ideal sun protection among those in the lighter-skinned group was statistically significant (odds ratio, 7.4; P less than .001). As each child grew 1 year older, parents were 31% less likely to use ideal sun protection (OR, 0.69; P = .007).
Parents whose children were in the lighter-skinned group were “more likely to believe that sun exposure was harmful” for their children (OR, 17.2), and “to perceive value in sun protection,” (OR, 11.4) the researchers said. The parents whose children were in the darker-skinned group were more likely to consider sun protection as having drawbacks (OR, 9.2), and to believe that darker skin tone provides more sun protection (OR, 12.4). Neither of the two groups was more likely to consider that sun exposure provided health benefits or that it improved appearance.
Parents whose children were in the lighter-skinned group reported significantly more frequent use of sunscreen (OR, 3.6), sunglasses (OR, 2.3), and sun suits (OR, 2.7). The parents of the children in this group reported similar or higher rates of use of hats, long-sleeved clothing, and umbrellas; seeking shade; and staying indoors between 12 pm and 2 pm, but these rates were not statistically significantly different from those reported by the parents of children in the darker-skinned group, the investigators said.
“Our study suggests that more targeted education guidelines are necessary to ensure sun safety for all children, especially in a multiracial population,” said Dr. Tan and his colleagues. “Dermatologists and primary care physicians are in ideal positions to initiate personalized efforts to improve overall rates of sun protection.”
Dr. Tan reported no relevant financial disclosures. Dr. Miriam Weinstein has worked as an advisory board member for Johnson & Johnson, which manufactures sunscreen; and Dr. Shudeshna Nag consults for Valeant, which manufactures sunscreen.
SOURCE: Tan MG et al. Pediatr Dermatol. 2018 Feb 13. doi: 10.1111/pde.13433.
according to Marcus G. Tan, MD, of the University of Toronto, and his associates.
Too much sun exposure as a child is a known risk factor for skin cancer, and “it has been estimated that approximately half of cumulative ultraviolet exposure by age 60 occurs before age 20.” So it is important that children be protected from excessive sun exposure, the investigators wrote, underscoring the reason for their study of parental sun protection by Canadian parents in Toronto, which has a multiracial population.
Parental sun protection efforts were considered ideal if they used sun protection every day; on sunny days all year round; or during the summer, using at least SPF 30, and reapplying sunscreen at least every 2 hours. Parental efforts would be considered nonideal if they did not meet any of these three criteria.
Of 183 parents, 17% used ideal sun protection for their children; 28% were in the lighter-skinned group (Fitzpatrick phototype I-III) and 5% in the darker-skinned group (Fitzpatrick phototype IV-V), The greater likelihood of using ideal sun protection among those in the lighter-skinned group was statistically significant (odds ratio, 7.4; P less than .001). As each child grew 1 year older, parents were 31% less likely to use ideal sun protection (OR, 0.69; P = .007).
Parents whose children were in the lighter-skinned group were “more likely to believe that sun exposure was harmful” for their children (OR, 17.2), and “to perceive value in sun protection,” (OR, 11.4) the researchers said. The parents whose children were in the darker-skinned group were more likely to consider sun protection as having drawbacks (OR, 9.2), and to believe that darker skin tone provides more sun protection (OR, 12.4). Neither of the two groups was more likely to consider that sun exposure provided health benefits or that it improved appearance.
Parents whose children were in the lighter-skinned group reported significantly more frequent use of sunscreen (OR, 3.6), sunglasses (OR, 2.3), and sun suits (OR, 2.7). The parents of the children in this group reported similar or higher rates of use of hats, long-sleeved clothing, and umbrellas; seeking shade; and staying indoors between 12 pm and 2 pm, but these rates were not statistically significantly different from those reported by the parents of children in the darker-skinned group, the investigators said.
“Our study suggests that more targeted education guidelines are necessary to ensure sun safety for all children, especially in a multiracial population,” said Dr. Tan and his colleagues. “Dermatologists and primary care physicians are in ideal positions to initiate personalized efforts to improve overall rates of sun protection.”
Dr. Tan reported no relevant financial disclosures. Dr. Miriam Weinstein has worked as an advisory board member for Johnson & Johnson, which manufactures sunscreen; and Dr. Shudeshna Nag consults for Valeant, which manufactures sunscreen.
SOURCE: Tan MG et al. Pediatr Dermatol. 2018 Feb 13. doi: 10.1111/pde.13433.
according to Marcus G. Tan, MD, of the University of Toronto, and his associates.
Too much sun exposure as a child is a known risk factor for skin cancer, and “it has been estimated that approximately half of cumulative ultraviolet exposure by age 60 occurs before age 20.” So it is important that children be protected from excessive sun exposure, the investigators wrote, underscoring the reason for their study of parental sun protection by Canadian parents in Toronto, which has a multiracial population.
Parental sun protection efforts were considered ideal if they used sun protection every day; on sunny days all year round; or during the summer, using at least SPF 30, and reapplying sunscreen at least every 2 hours. Parental efforts would be considered nonideal if they did not meet any of these three criteria.
Of 183 parents, 17% used ideal sun protection for their children; 28% were in the lighter-skinned group (Fitzpatrick phototype I-III) and 5% in the darker-skinned group (Fitzpatrick phototype IV-V), The greater likelihood of using ideal sun protection among those in the lighter-skinned group was statistically significant (odds ratio, 7.4; P less than .001). As each child grew 1 year older, parents were 31% less likely to use ideal sun protection (OR, 0.69; P = .007).
Parents whose children were in the lighter-skinned group were “more likely to believe that sun exposure was harmful” for their children (OR, 17.2), and “to perceive value in sun protection,” (OR, 11.4) the researchers said. The parents whose children were in the darker-skinned group were more likely to consider sun protection as having drawbacks (OR, 9.2), and to believe that darker skin tone provides more sun protection (OR, 12.4). Neither of the two groups was more likely to consider that sun exposure provided health benefits or that it improved appearance.
Parents whose children were in the lighter-skinned group reported significantly more frequent use of sunscreen (OR, 3.6), sunglasses (OR, 2.3), and sun suits (OR, 2.7). The parents of the children in this group reported similar or higher rates of use of hats, long-sleeved clothing, and umbrellas; seeking shade; and staying indoors between 12 pm and 2 pm, but these rates were not statistically significantly different from those reported by the parents of children in the darker-skinned group, the investigators said.
“Our study suggests that more targeted education guidelines are necessary to ensure sun safety for all children, especially in a multiracial population,” said Dr. Tan and his colleagues. “Dermatologists and primary care physicians are in ideal positions to initiate personalized efforts to improve overall rates of sun protection.”
Dr. Tan reported no relevant financial disclosures. Dr. Miriam Weinstein has worked as an advisory board member for Johnson & Johnson, which manufactures sunscreen; and Dr. Shudeshna Nag consults for Valeant, which manufactures sunscreen.
SOURCE: Tan MG et al. Pediatr Dermatol. 2018 Feb 13. doi: 10.1111/pde.13433.
FROM PEDIATRIC DERMATOLOGY
Key clinical point: More targeted education of parents regarding sun protection practices may be needed.
Major finding: Of 183 parents, 17% used ideal sun protection; 28% were in the lighter-skinned group and 5% in the darker-skinned group (odds ratio, 7.4; P less than .001).
Study details: The parents of 183 children aged from 6 months to 6 years in Toronto completed a questionnaire about their sun protection practices.
Disclosures: Dr. Marcus G. Tan reported no relevant financial disclosures. Dr.Miriam Weinstein has worked as an advisory board member for Johnson & Johnson, which manufactures sunscreen; and Dr. Shudeshna Nag consults for Valeant, which manufactures sunscreen.
Source: Tan MG et al. Pediatr Dermatol. 2018 Feb 13. doi: 10.1111/pde.13433.
Beware nonopiate meds with high street value
NEW ORLEANS – Gabapentin heads the short list of prescription drugs other than opioids and benzodiazepines with substantial black-market abuse potential, according to Alexander Y. Walley, MD.
“At least in Massachusetts, where I see patients, these are the pills that people are using and trading on the street. Your part of the country might have others,” noted Dr. Walley, director of the addiction medicine fellowship program at Boston Medical Center.
“I’m not telling you to never prescribe these medications – they are clinically indicated in certain cases and should certainly be used,” Dr. Walley said at the annual meeting of the American College of Physicians. “But now that you know that they might be misused, you should use safeguards.
“A lot of these medications – gabapentin is an example – are a problem primarily in people with other substance use disorders,” he added. “That’s really where I think you need to have the greatest caution.”
Gabapentinoids
Gabapentin and pregabalin are not addictive in the sense that it’s easy to get laboratory animals or healthy volunteers to self-administer them. However, gabapentinoid use disorder is extremely common among people with opioid use disorder, who report that the combination boosts the euphoric effects of opioids and reduces opioid withdrawal symptoms without causing side effects.
Indeed, a recent systematic review of 106 studies found that gabapentinoid use disorder was present in up to 26% of opioid users (Eur Neuropsychopharmacol. 2017 Dec;27[12]:1185-1215).
Overdoses involving gabapentinoids alone are uncommon because they require consumption at up to 25 times the maximum recommended dose. Moreover, these overdoses are rarely fatal.
“You almost can’t overdose on a gabapentinoid, because you have to take lots and lots of it to do so, and you’ll usually survive. But if you add it to an opioid or other sedative, then you’re really in dangerous territory. That’s where all the deaths are clustered,” Dr. Walley explained.
A recent Canadian/Dutch population-based, nested, case-control study concluded that concomitant prescription of opioids and gabapentin was associated with a 49% greater chance of fatal overdose, compared with opioid prescription alone, in an analysis extensively adjusted for potential confounders. A dose-response effect was noted, such that coprescription of high-dose gabapentin was linked to an adjusted 58% increased risk (PLoS Med. 2017 Oct 3;14[10]:e1002396).
Complicating the picture, however, is solid evidence from a randomized, placebo-controlled, crossover trial that gabapentin and opioids are synergistic for relief from neuropathic pain, which can be notoriously difficult to control (N Engl J Med. 2005 Mar 31;352[13]:1324-34).
“It’s tricky, because you can potentially spare having to use high-dose opioids by adding gabapentin,” Dr. Walley observed. “So, as prescribers, you’re in a difficult position, because there’s a mixed message here: When gabapentin is combined with opioids, that’s when it’s dangerous – but that’s also when they’re potentially more effective for pain.”
Promethazine
This drug has a host of neurobiologic actions, which collectively provide sedative and antiemetic effects. Promethazine jacks up opioid-induced euphoria and alleviates withdrawal symptoms. It’s commonly detected in toxicology testing of patients on prescription opioids for chronic pain or on methadone therapy for opioid use disorder.
National Poison Data System figures show an unwelcome trend: A sharp uptick in promethazine abuse/misuse beginning in 2008, even while the total number of poisoning events of all kinds reported to the system began a steady decline (J Addict Med. 2015 May-Jun;9[3]:233-7).
Clonidine
This centrally acting alpha2-adrenoreceptor and imidazoline-receptor agonist is indicated for treatment of hypertension. However, it’s also extensively used off-label to treat anxiety, as well as for alcohol and opioid withdrawal symptoms. The problem is, clonidine boosts opioid-induced euphoria.
A retrospective study of clonidine-overdose patients characterized the clonidine overdose syndrome as marked by sedation, hypotension, bradycardia, and excessive pupillary constriction (Clin Toxicol [Phila]. 2017 Mar;55[3]:187-92).
“The combination of clonidine and opioids is particularly dangerous,” according to Dr. Walley. “Even though it mimics what an opioid overdose looks like, a clonidine overdose is not responsive to naloxone.”
Stimulants
One-quarter of patients who are prescribed methylphenidate or amphetamine for ADHD report being asked to divert their medication, and 11%-29% sell or give it to others seeking to use it recreationally or as a performance aid.
It’s common for prescription seekers to misrepresent symptoms of ADHD, and this play-acting is often tough to detect. In contrast, the nonstimulant atomoxetine (Strattera) and the alpha-adrenergic agonists prescribed for ADHD aren’t linked to misuse or diversion (Postgrad Med. 2014 Sep;126[5]:64-81).
Bupropion
This norepinephrine and dopamine reuptake inhibitor is generally assumed to have low abuse potential. That’s usually true – except in jail and prisons.
“In my patient population, where I have a keen eye to what’s being used on the street, bupropion is not one of the medications that I see very often in my patients who are not incarcerated,” Dr. Walley said. “But in incarcerated settings, it does have a street value.”
Consider safeguards
None of the prescription drugs on Dr. Walley’s problem list is included in prescription monitoring programs, nor are they detectable with standard toxicology testing. This poses a challenge for prescribing physicians.
Before prescribing any of these potentially abusable medications for a given patient, therefore, Dr. Walley considers the underlying risks. For example, an addiction history is a big red flag. So is coprescription of an opioid or another drug that might have synergistic adverse effects. Dr. Walley makes sure there is a solid indication for the medication, and, having prescribed the drug, he wants to see and document clear functional benefit.
Drug-specific toxicology screening is worthy of consideration as a means of confirming the presence of the prescribed medication, along with the absence of opioids or other drugs that shouldn’t be on board.
“I do this with gabapentin, because I see a lot of diversion,” he explained. “If gabapentin doesn’t show up in the toxicology screen, I stop prescribing it. Or if I detect it and it hasn’t been prescribed, that allows me to have a safety discussion with the patient.”
Dr. Walley reported no financial conflicts of interest regarding his presentation.
NEW ORLEANS – Gabapentin heads the short list of prescription drugs other than opioids and benzodiazepines with substantial black-market abuse potential, according to Alexander Y. Walley, MD.
“At least in Massachusetts, where I see patients, these are the pills that people are using and trading on the street. Your part of the country might have others,” noted Dr. Walley, director of the addiction medicine fellowship program at Boston Medical Center.
“I’m not telling you to never prescribe these medications – they are clinically indicated in certain cases and should certainly be used,” Dr. Walley said at the annual meeting of the American College of Physicians. “But now that you know that they might be misused, you should use safeguards.
“A lot of these medications – gabapentin is an example – are a problem primarily in people with other substance use disorders,” he added. “That’s really where I think you need to have the greatest caution.”
Gabapentinoids
Gabapentin and pregabalin are not addictive in the sense that it’s easy to get laboratory animals or healthy volunteers to self-administer them. However, gabapentinoid use disorder is extremely common among people with opioid use disorder, who report that the combination boosts the euphoric effects of opioids and reduces opioid withdrawal symptoms without causing side effects.
Indeed, a recent systematic review of 106 studies found that gabapentinoid use disorder was present in up to 26% of opioid users (Eur Neuropsychopharmacol. 2017 Dec;27[12]:1185-1215).
Overdoses involving gabapentinoids alone are uncommon because they require consumption at up to 25 times the maximum recommended dose. Moreover, these overdoses are rarely fatal.
“You almost can’t overdose on a gabapentinoid, because you have to take lots and lots of it to do so, and you’ll usually survive. But if you add it to an opioid or other sedative, then you’re really in dangerous territory. That’s where all the deaths are clustered,” Dr. Walley explained.
A recent Canadian/Dutch population-based, nested, case-control study concluded that concomitant prescription of opioids and gabapentin was associated with a 49% greater chance of fatal overdose, compared with opioid prescription alone, in an analysis extensively adjusted for potential confounders. A dose-response effect was noted, such that coprescription of high-dose gabapentin was linked to an adjusted 58% increased risk (PLoS Med. 2017 Oct 3;14[10]:e1002396).
Complicating the picture, however, is solid evidence from a randomized, placebo-controlled, crossover trial that gabapentin and opioids are synergistic for relief from neuropathic pain, which can be notoriously difficult to control (N Engl J Med. 2005 Mar 31;352[13]:1324-34).
“It’s tricky, because you can potentially spare having to use high-dose opioids by adding gabapentin,” Dr. Walley observed. “So, as prescribers, you’re in a difficult position, because there’s a mixed message here: When gabapentin is combined with opioids, that’s when it’s dangerous – but that’s also when they’re potentially more effective for pain.”
Promethazine
This drug has a host of neurobiologic actions, which collectively provide sedative and antiemetic effects. Promethazine jacks up opioid-induced euphoria and alleviates withdrawal symptoms. It’s commonly detected in toxicology testing of patients on prescription opioids for chronic pain or on methadone therapy for opioid use disorder.
National Poison Data System figures show an unwelcome trend: A sharp uptick in promethazine abuse/misuse beginning in 2008, even while the total number of poisoning events of all kinds reported to the system began a steady decline (J Addict Med. 2015 May-Jun;9[3]:233-7).
Clonidine
This centrally acting alpha2-adrenoreceptor and imidazoline-receptor agonist is indicated for treatment of hypertension. However, it’s also extensively used off-label to treat anxiety, as well as for alcohol and opioid withdrawal symptoms. The problem is, clonidine boosts opioid-induced euphoria.
A retrospective study of clonidine-overdose patients characterized the clonidine overdose syndrome as marked by sedation, hypotension, bradycardia, and excessive pupillary constriction (Clin Toxicol [Phila]. 2017 Mar;55[3]:187-92).
“The combination of clonidine and opioids is particularly dangerous,” according to Dr. Walley. “Even though it mimics what an opioid overdose looks like, a clonidine overdose is not responsive to naloxone.”
Stimulants
One-quarter of patients who are prescribed methylphenidate or amphetamine for ADHD report being asked to divert their medication, and 11%-29% sell or give it to others seeking to use it recreationally or as a performance aid.
It’s common for prescription seekers to misrepresent symptoms of ADHD, and this play-acting is often tough to detect. In contrast, the nonstimulant atomoxetine (Strattera) and the alpha-adrenergic agonists prescribed for ADHD aren’t linked to misuse or diversion (Postgrad Med. 2014 Sep;126[5]:64-81).
Bupropion
This norepinephrine and dopamine reuptake inhibitor is generally assumed to have low abuse potential. That’s usually true – except in jail and prisons.
“In my patient population, where I have a keen eye to what’s being used on the street, bupropion is not one of the medications that I see very often in my patients who are not incarcerated,” Dr. Walley said. “But in incarcerated settings, it does have a street value.”
Consider safeguards
None of the prescription drugs on Dr. Walley’s problem list is included in prescription monitoring programs, nor are they detectable with standard toxicology testing. This poses a challenge for prescribing physicians.
Before prescribing any of these potentially abusable medications for a given patient, therefore, Dr. Walley considers the underlying risks. For example, an addiction history is a big red flag. So is coprescription of an opioid or another drug that might have synergistic adverse effects. Dr. Walley makes sure there is a solid indication for the medication, and, having prescribed the drug, he wants to see and document clear functional benefit.
Drug-specific toxicology screening is worthy of consideration as a means of confirming the presence of the prescribed medication, along with the absence of opioids or other drugs that shouldn’t be on board.
“I do this with gabapentin, because I see a lot of diversion,” he explained. “If gabapentin doesn’t show up in the toxicology screen, I stop prescribing it. Or if I detect it and it hasn’t been prescribed, that allows me to have a safety discussion with the patient.”
Dr. Walley reported no financial conflicts of interest regarding his presentation.
NEW ORLEANS – Gabapentin heads the short list of prescription drugs other than opioids and benzodiazepines with substantial black-market abuse potential, according to Alexander Y. Walley, MD.
“At least in Massachusetts, where I see patients, these are the pills that people are using and trading on the street. Your part of the country might have others,” noted Dr. Walley, director of the addiction medicine fellowship program at Boston Medical Center.
“I’m not telling you to never prescribe these medications – they are clinically indicated in certain cases and should certainly be used,” Dr. Walley said at the annual meeting of the American College of Physicians. “But now that you know that they might be misused, you should use safeguards.
“A lot of these medications – gabapentin is an example – are a problem primarily in people with other substance use disorders,” he added. “That’s really where I think you need to have the greatest caution.”
Gabapentinoids
Gabapentin and pregabalin are not addictive in the sense that it’s easy to get laboratory animals or healthy volunteers to self-administer them. However, gabapentinoid use disorder is extremely common among people with opioid use disorder, who report that the combination boosts the euphoric effects of opioids and reduces opioid withdrawal symptoms without causing side effects.
Indeed, a recent systematic review of 106 studies found that gabapentinoid use disorder was present in up to 26% of opioid users (Eur Neuropsychopharmacol. 2017 Dec;27[12]:1185-1215).
Overdoses involving gabapentinoids alone are uncommon because they require consumption at up to 25 times the maximum recommended dose. Moreover, these overdoses are rarely fatal.
“You almost can’t overdose on a gabapentinoid, because you have to take lots and lots of it to do so, and you’ll usually survive. But if you add it to an opioid or other sedative, then you’re really in dangerous territory. That’s where all the deaths are clustered,” Dr. Walley explained.
A recent Canadian/Dutch population-based, nested, case-control study concluded that concomitant prescription of opioids and gabapentin was associated with a 49% greater chance of fatal overdose, compared with opioid prescription alone, in an analysis extensively adjusted for potential confounders. A dose-response effect was noted, such that coprescription of high-dose gabapentin was linked to an adjusted 58% increased risk (PLoS Med. 2017 Oct 3;14[10]:e1002396).
Complicating the picture, however, is solid evidence from a randomized, placebo-controlled, crossover trial that gabapentin and opioids are synergistic for relief from neuropathic pain, which can be notoriously difficult to control (N Engl J Med. 2005 Mar 31;352[13]:1324-34).
“It’s tricky, because you can potentially spare having to use high-dose opioids by adding gabapentin,” Dr. Walley observed. “So, as prescribers, you’re in a difficult position, because there’s a mixed message here: When gabapentin is combined with opioids, that’s when it’s dangerous – but that’s also when they’re potentially more effective for pain.”
Promethazine
This drug has a host of neurobiologic actions, which collectively provide sedative and antiemetic effects. Promethazine jacks up opioid-induced euphoria and alleviates withdrawal symptoms. It’s commonly detected in toxicology testing of patients on prescription opioids for chronic pain or on methadone therapy for opioid use disorder.
National Poison Data System figures show an unwelcome trend: A sharp uptick in promethazine abuse/misuse beginning in 2008, even while the total number of poisoning events of all kinds reported to the system began a steady decline (J Addict Med. 2015 May-Jun;9[3]:233-7).
Clonidine
This centrally acting alpha2-adrenoreceptor and imidazoline-receptor agonist is indicated for treatment of hypertension. However, it’s also extensively used off-label to treat anxiety, as well as for alcohol and opioid withdrawal symptoms. The problem is, clonidine boosts opioid-induced euphoria.
A retrospective study of clonidine-overdose patients characterized the clonidine overdose syndrome as marked by sedation, hypotension, bradycardia, and excessive pupillary constriction (Clin Toxicol [Phila]. 2017 Mar;55[3]:187-92).
“The combination of clonidine and opioids is particularly dangerous,” according to Dr. Walley. “Even though it mimics what an opioid overdose looks like, a clonidine overdose is not responsive to naloxone.”
Stimulants
One-quarter of patients who are prescribed methylphenidate or amphetamine for ADHD report being asked to divert their medication, and 11%-29% sell or give it to others seeking to use it recreationally or as a performance aid.
It’s common for prescription seekers to misrepresent symptoms of ADHD, and this play-acting is often tough to detect. In contrast, the nonstimulant atomoxetine (Strattera) and the alpha-adrenergic agonists prescribed for ADHD aren’t linked to misuse or diversion (Postgrad Med. 2014 Sep;126[5]:64-81).
Bupropion
This norepinephrine and dopamine reuptake inhibitor is generally assumed to have low abuse potential. That’s usually true – except in jail and prisons.
“In my patient population, where I have a keen eye to what’s being used on the street, bupropion is not one of the medications that I see very often in my patients who are not incarcerated,” Dr. Walley said. “But in incarcerated settings, it does have a street value.”
Consider safeguards
None of the prescription drugs on Dr. Walley’s problem list is included in prescription monitoring programs, nor are they detectable with standard toxicology testing. This poses a challenge for prescribing physicians.
Before prescribing any of these potentially abusable medications for a given patient, therefore, Dr. Walley considers the underlying risks. For example, an addiction history is a big red flag. So is coprescription of an opioid or another drug that might have synergistic adverse effects. Dr. Walley makes sure there is a solid indication for the medication, and, having prescribed the drug, he wants to see and document clear functional benefit.
Drug-specific toxicology screening is worthy of consideration as a means of confirming the presence of the prescribed medication, along with the absence of opioids or other drugs that shouldn’t be on board.
“I do this with gabapentin, because I see a lot of diversion,” he explained. “If gabapentin doesn’t show up in the toxicology screen, I stop prescribing it. Or if I detect it and it hasn’t been prescribed, that allows me to have a safety discussion with the patient.”
Dr. Walley reported no financial conflicts of interest regarding his presentation.
EXPERT ANALYSIS FROM ACP INTERNAL MEDICINE
Substance use linked to conversion to schizophrenia
People with schizotypal disorder who use cannabis, amphetamines, and opioids might be more likely to convert to schizophrenia, according to a prospective cohort study.
The study, published online April 25 by JAMA Psychiatry, involved 2,539 Danish individuals with incident schizotypal disorder – but without a diagnosis of schizophrenia – who had been followed from birth.
After 20 years of follow-up, about one-third (33.1%) of the total cohort had converted to schizophrenia. Among individuals without any substance use disorder, the conversion rate was 30.6%, while among individuals with cannabis use disorders, the conversion rate was 58.2%. Meanwhile, those with alcohol use disorder had a conversion rate of 47%, reported Carsten Hjorthøj, PhD, of Copenhagen University Hospital, Mental Health Center Copenhagen, and coauthors.
Participants with any substance use disorder had a 34% higher risk of converting to schizophrenia, but the risk was more than twofold higher with opioid use disorder (hazard ratio, 2.74; 95% confidence interval, 1.38-5.45), 30% higher with cannabis use disorder, and 90% higher with amphetamine use disorder.
Patients who had been prescribed antipsychotics also showed a higher risk of converting to schizophrenia (HR, 1.42; 95% CI, 1.18-1.70), which the authors suggested might reflect the fact that these patients were likely to be the most severely ill.
These associations were found even after adjustment for factors such as sex, birth year, all other individual types of substance use disorders, and parental mental disorders.
Dr. Hjorthøj and coauthors said the association between cannabis use and conversion to schizophrenia might be causal. “First, the association appears to be dose-dependent; second, the association is stronger for more potent types of cannabis; third, cannabis use is associated with earlier onset of psychosis; and fourth, age at onset of cannabis use is associated with age at onset of schizophrenia,” they wrote.
However, they also acknowledged that schizophrenia itself might increase the risk of individuals starting to use cannabis and other substances – a theory supported by the wide range of substances associated with conversion to schizophrenia.
“In our study, the first registered date of substance use disorder came before the first registered date of schizophrenia, but delays in diagnoses may have caused schizophrenia or its preclinical symptoms to predate substance use.”
The association between alcohol use disorder and conversion to schizophrenia was seen only in sensitivity analyses that ignored the birth year of the cohort, which the authors suggested may have been the result of increased power in this analysis.
Among the limitations cited by the authors was their inability to validate the schizotypal disorder diagnoses. Also, they wrote, the participants’ diagnoses were based on ICD-8 and ICD-10 criteria, and it was unclear whether the study results are generalizable to DSM-5 diagnoses.
The Lundbeck Foundation supported the study. No conflicts of interest were declared.
SOURCE: Hjorthøj C et al. JAMA Psychiatry. 2018 Apr 25. doi: 10.1001/jamapsychiatry.2018.0568.
People with schizotypal disorder who use cannabis, amphetamines, and opioids might be more likely to convert to schizophrenia, according to a prospective cohort study.
The study, published online April 25 by JAMA Psychiatry, involved 2,539 Danish individuals with incident schizotypal disorder – but without a diagnosis of schizophrenia – who had been followed from birth.
After 20 years of follow-up, about one-third (33.1%) of the total cohort had converted to schizophrenia. Among individuals without any substance use disorder, the conversion rate was 30.6%, while among individuals with cannabis use disorders, the conversion rate was 58.2%. Meanwhile, those with alcohol use disorder had a conversion rate of 47%, reported Carsten Hjorthøj, PhD, of Copenhagen University Hospital, Mental Health Center Copenhagen, and coauthors.
Participants with any substance use disorder had a 34% higher risk of converting to schizophrenia, but the risk was more than twofold higher with opioid use disorder (hazard ratio, 2.74; 95% confidence interval, 1.38-5.45), 30% higher with cannabis use disorder, and 90% higher with amphetamine use disorder.
Patients who had been prescribed antipsychotics also showed a higher risk of converting to schizophrenia (HR, 1.42; 95% CI, 1.18-1.70), which the authors suggested might reflect the fact that these patients were likely to be the most severely ill.
These associations were found even after adjustment for factors such as sex, birth year, all other individual types of substance use disorders, and parental mental disorders.
Dr. Hjorthøj and coauthors said the association between cannabis use and conversion to schizophrenia might be causal. “First, the association appears to be dose-dependent; second, the association is stronger for more potent types of cannabis; third, cannabis use is associated with earlier onset of psychosis; and fourth, age at onset of cannabis use is associated with age at onset of schizophrenia,” they wrote.
However, they also acknowledged that schizophrenia itself might increase the risk of individuals starting to use cannabis and other substances – a theory supported by the wide range of substances associated with conversion to schizophrenia.
“In our study, the first registered date of substance use disorder came before the first registered date of schizophrenia, but delays in diagnoses may have caused schizophrenia or its preclinical symptoms to predate substance use.”
The association between alcohol use disorder and conversion to schizophrenia was seen only in sensitivity analyses that ignored the birth year of the cohort, which the authors suggested may have been the result of increased power in this analysis.
Among the limitations cited by the authors was their inability to validate the schizotypal disorder diagnoses. Also, they wrote, the participants’ diagnoses were based on ICD-8 and ICD-10 criteria, and it was unclear whether the study results are generalizable to DSM-5 diagnoses.
The Lundbeck Foundation supported the study. No conflicts of interest were declared.
SOURCE: Hjorthøj C et al. JAMA Psychiatry. 2018 Apr 25. doi: 10.1001/jamapsychiatry.2018.0568.
People with schizotypal disorder who use cannabis, amphetamines, and opioids might be more likely to convert to schizophrenia, according to a prospective cohort study.
The study, published online April 25 by JAMA Psychiatry, involved 2,539 Danish individuals with incident schizotypal disorder – but without a diagnosis of schizophrenia – who had been followed from birth.
After 20 years of follow-up, about one-third (33.1%) of the total cohort had converted to schizophrenia. Among individuals without any substance use disorder, the conversion rate was 30.6%, while among individuals with cannabis use disorders, the conversion rate was 58.2%. Meanwhile, those with alcohol use disorder had a conversion rate of 47%, reported Carsten Hjorthøj, PhD, of Copenhagen University Hospital, Mental Health Center Copenhagen, and coauthors.
Participants with any substance use disorder had a 34% higher risk of converting to schizophrenia, but the risk was more than twofold higher with opioid use disorder (hazard ratio, 2.74; 95% confidence interval, 1.38-5.45), 30% higher with cannabis use disorder, and 90% higher with amphetamine use disorder.
Patients who had been prescribed antipsychotics also showed a higher risk of converting to schizophrenia (HR, 1.42; 95% CI, 1.18-1.70), which the authors suggested might reflect the fact that these patients were likely to be the most severely ill.
These associations were found even after adjustment for factors such as sex, birth year, all other individual types of substance use disorders, and parental mental disorders.
Dr. Hjorthøj and coauthors said the association between cannabis use and conversion to schizophrenia might be causal. “First, the association appears to be dose-dependent; second, the association is stronger for more potent types of cannabis; third, cannabis use is associated with earlier onset of psychosis; and fourth, age at onset of cannabis use is associated with age at onset of schizophrenia,” they wrote.
However, they also acknowledged that schizophrenia itself might increase the risk of individuals starting to use cannabis and other substances – a theory supported by the wide range of substances associated with conversion to schizophrenia.
“In our study, the first registered date of substance use disorder came before the first registered date of schizophrenia, but delays in diagnoses may have caused schizophrenia or its preclinical symptoms to predate substance use.”
The association between alcohol use disorder and conversion to schizophrenia was seen only in sensitivity analyses that ignored the birth year of the cohort, which the authors suggested may have been the result of increased power in this analysis.
Among the limitations cited by the authors was their inability to validate the schizotypal disorder diagnoses. Also, they wrote, the participants’ diagnoses were based on ICD-8 and ICD-10 criteria, and it was unclear whether the study results are generalizable to DSM-5 diagnoses.
The Lundbeck Foundation supported the study. No conflicts of interest were declared.
SOURCE: Hjorthøj C et al. JAMA Psychiatry. 2018 Apr 25. doi: 10.1001/jamapsychiatry.2018.0568.
FROM JAMA PSYCHIATRY
Key clinical point: Patients with schizotypal disorder who have substance use disorders are more likely to convert to schizophrenia.
Major finding: The conversion rate from schizotypal disorder to schizophrenia was 58.2% in individuals with substance use disorder.
Study details: Prospective cohort study in 2,539 individuals with schizotypal disorder.
Disclosures: The Lundbeck Foundation supported the study. No conflicts of interest were declared.
Source: Hjorthøj C et al. JAMA Psychiatry. 2018 Apr 25. doi: 10.1001/jamapsychiatry.2018.0568.
FDA advisory committee votes to recommend update to celecoxib safety labeling
SILVER SPRING, MD. – An FDA advisory committee voted (15 yes, 5 no, 1 abstention) to update the safety information in the label of celecoxib, a nonsteroidal anti-inflammatory drug (NSAID), for use in patients with osteoarthritis (OA) and rheumatoid arthritis, on the basis of results of the PRECISION trial.
A Joint Meeting ofthe Arthritis Advisory Committee and the Drug Safety and Risk Management Advisory Committee was convened April 24-25 to address two issues, the first being the consideration of Pfizer’s application for celecoxib and the second, to assess the safety of celecoxib and other common NSAIDs like ibuprofen and naproxen.
The randomized controlled PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs. Ibuprofen or Naproxen) trial compared celecoxib, naproxen, and ibuprofen and their cardiovascular outcomes. The PRECISION trial was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that the rates of cardiovascular events (cardiovascular death, myocardial infarction, or stroke) were 2.3% with celecoxib, 2.5% with naproxen, and 2.7% with ibuprofen during a follow-up approaching 3 years, showing noninferiority for celecoxib.
In a post hoc analysis presented by Steven Nissen, MD, patients taking ibuprofen and naproxen experienced adjudicated cardiovascular, GI, or renal events 28% and 15% more than did patients taking celecoxib.
The results of the study could inform clinical strategy, said Dr. Nissen, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “For arthritis patients who require NSAIDs to achieve an acceptable quality of life, particularly those at high cardiovascular, GI, or renal risk, the PRECISION trial suggests that a clinical strategy of starting patients on celecoxib 200 mg daily may be the safest approach, reserving full therapeutic doses of ibuprofen and naproxen for patients who do not respond to celecoxib."
SILVER SPRING, MD. – An FDA advisory committee voted (15 yes, 5 no, 1 abstention) to update the safety information in the label of celecoxib, a nonsteroidal anti-inflammatory drug (NSAID), for use in patients with osteoarthritis (OA) and rheumatoid arthritis, on the basis of results of the PRECISION trial.
A Joint Meeting ofthe Arthritis Advisory Committee and the Drug Safety and Risk Management Advisory Committee was convened April 24-25 to address two issues, the first being the consideration of Pfizer’s application for celecoxib and the second, to assess the safety of celecoxib and other common NSAIDs like ibuprofen and naproxen.
The randomized controlled PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs. Ibuprofen or Naproxen) trial compared celecoxib, naproxen, and ibuprofen and their cardiovascular outcomes. The PRECISION trial was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that the rates of cardiovascular events (cardiovascular death, myocardial infarction, or stroke) were 2.3% with celecoxib, 2.5% with naproxen, and 2.7% with ibuprofen during a follow-up approaching 3 years, showing noninferiority for celecoxib.
In a post hoc analysis presented by Steven Nissen, MD, patients taking ibuprofen and naproxen experienced adjudicated cardiovascular, GI, or renal events 28% and 15% more than did patients taking celecoxib.
The results of the study could inform clinical strategy, said Dr. Nissen, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “For arthritis patients who require NSAIDs to achieve an acceptable quality of life, particularly those at high cardiovascular, GI, or renal risk, the PRECISION trial suggests that a clinical strategy of starting patients on celecoxib 200 mg daily may be the safest approach, reserving full therapeutic doses of ibuprofen and naproxen for patients who do not respond to celecoxib."
SILVER SPRING, MD. – An FDA advisory committee voted (15 yes, 5 no, 1 abstention) to update the safety information in the label of celecoxib, a nonsteroidal anti-inflammatory drug (NSAID), for use in patients with osteoarthritis (OA) and rheumatoid arthritis, on the basis of results of the PRECISION trial.
A Joint Meeting ofthe Arthritis Advisory Committee and the Drug Safety and Risk Management Advisory Committee was convened April 24-25 to address two issues, the first being the consideration of Pfizer’s application for celecoxib and the second, to assess the safety of celecoxib and other common NSAIDs like ibuprofen and naproxen.
The randomized controlled PRECISION (Prospective Randomized Evaluation of Celecoxib Integrated Safety vs. Ibuprofen or Naproxen) trial compared celecoxib, naproxen, and ibuprofen and their cardiovascular outcomes. The PRECISION trial was undertaken after another selective COX-2 inhibitor, rofecoxib (Vioxx), was withdrawn from the market because of associated cardiovascular events. It compared the three drugs among more than 24,000 patients with painful arthritis and elevated cardiovascular risk.
Main results showed that the rates of cardiovascular events (cardiovascular death, myocardial infarction, or stroke) were 2.3% with celecoxib, 2.5% with naproxen, and 2.7% with ibuprofen during a follow-up approaching 3 years, showing noninferiority for celecoxib.
In a post hoc analysis presented by Steven Nissen, MD, patients taking ibuprofen and naproxen experienced adjudicated cardiovascular, GI, or renal events 28% and 15% more than did patients taking celecoxib.
The results of the study could inform clinical strategy, said Dr. Nissen, chair of cardiovascular medicine at the Cleveland Clinic in Ohio. “For arthritis patients who require NSAIDs to achieve an acceptable quality of life, particularly those at high cardiovascular, GI, or renal risk, the PRECISION trial suggests that a clinical strategy of starting patients on celecoxib 200 mg daily may be the safest approach, reserving full therapeutic doses of ibuprofen and naproxen for patients who do not respond to celecoxib."
REPORTING FROM AN FDA ADVISORY COMMITTEE MEETING
FDA places partial hold on trials after secondary lymphoma
The drugmaker after a pediatric patient developed a secondary T-cell lymphoma.
The Food and Drug Administration had issued a partial clinical hold in April on new enrollment of any patients with genetically defined solid tumors and hematologic malignancies. Patients already enrolled who have not had disease progression can continue to receive tazemetostat.
Tazemetostat is a first-in-class EZH2 inhibitor being studied as monotherapy in phase 1 and 2 trials for certain molecularly defined solid tumors, follicular lymphoma and diffuse large B-cell lymphoma, mesothelioma, and in combination studies of DLBCL and non–small cell lung cancer.
Epizyme is currently working to update informed consent, the investigator’s brochure, and study protocols, the company said in a statement.
The drugmaker after a pediatric patient developed a secondary T-cell lymphoma.
The Food and Drug Administration had issued a partial clinical hold in April on new enrollment of any patients with genetically defined solid tumors and hematologic malignancies. Patients already enrolled who have not had disease progression can continue to receive tazemetostat.
Tazemetostat is a first-in-class EZH2 inhibitor being studied as monotherapy in phase 1 and 2 trials for certain molecularly defined solid tumors, follicular lymphoma and diffuse large B-cell lymphoma, mesothelioma, and in combination studies of DLBCL and non–small cell lung cancer.
Epizyme is currently working to update informed consent, the investigator’s brochure, and study protocols, the company said in a statement.
The drugmaker after a pediatric patient developed a secondary T-cell lymphoma.
The Food and Drug Administration had issued a partial clinical hold in April on new enrollment of any patients with genetically defined solid tumors and hematologic malignancies. Patients already enrolled who have not had disease progression can continue to receive tazemetostat.
Tazemetostat is a first-in-class EZH2 inhibitor being studied as monotherapy in phase 1 and 2 trials for certain molecularly defined solid tumors, follicular lymphoma and diffuse large B-cell lymphoma, mesothelioma, and in combination studies of DLBCL and non–small cell lung cancer.
Epizyme is currently working to update informed consent, the investigator’s brochure, and study protocols, the company said in a statement.
Hidradenitis suppurativa packs mighty QOL impact
KAUAI, HAWAII – Anyone who has treated patients with hidradenitis suppurativa (HS) recognizes that this can be a debilitating disease. Helping put that into fuller perspective, recent evidence has shown that the quality of life effects of moderate to severe HS are objectively worse than those of moderate to severe psoriasis, according to Iltefat H. Hamzavi, MD, president of the Hidradenitis Suppurativa Foundation and a dermatologist at Henry Ford Hospital in Detroit.
He was lead author of a study in which he and his coinvestigators compared weighted averages of a variety of quality of life measures in patients with moderate to severe HS or psoriasis who participated in five AbbVie-sponsored randomized clinical trials of biologic agents (J Am Acad Dermatol. 2017 Dec;77[6]:1038-46).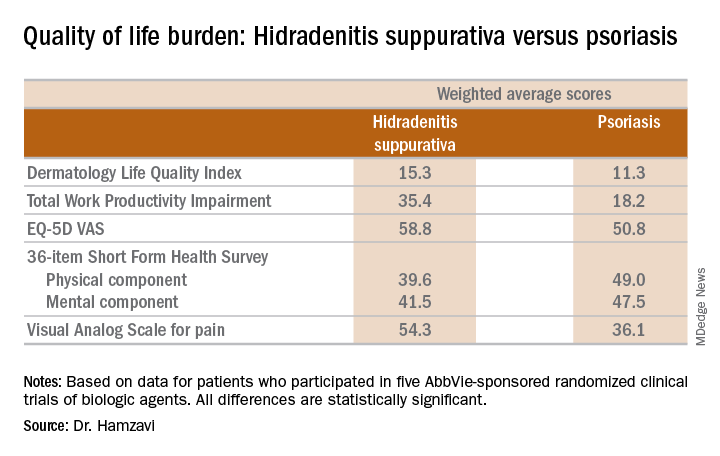
“The number of HS patients who experience downward drift – losing their job and their health insurance and ultimately being unable to move out of a lower socioeconomic group – is staggering,” the dermatologist said.
which underscores the importance of a psychiatric evaluation as part of routine care for patients with this dermatologic disease. “Suicide is much more common in the HS population than in almost any other dermatologic disease,” Dr. Hamzavi added.
He reported serving as a consultant for AbbVie, Incyte, and UCB.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII – Anyone who has treated patients with hidradenitis suppurativa (HS) recognizes that this can be a debilitating disease. Helping put that into fuller perspective, recent evidence has shown that the quality of life effects of moderate to severe HS are objectively worse than those of moderate to severe psoriasis, according to Iltefat H. Hamzavi, MD, president of the Hidradenitis Suppurativa Foundation and a dermatologist at Henry Ford Hospital in Detroit.
He was lead author of a study in which he and his coinvestigators compared weighted averages of a variety of quality of life measures in patients with moderate to severe HS or psoriasis who participated in five AbbVie-sponsored randomized clinical trials of biologic agents (J Am Acad Dermatol. 2017 Dec;77[6]:1038-46).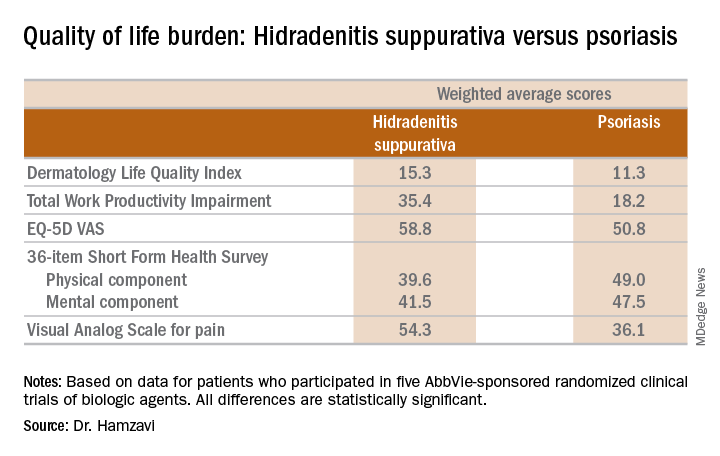
“The number of HS patients who experience downward drift – losing their job and their health insurance and ultimately being unable to move out of a lower socioeconomic group – is staggering,” the dermatologist said.
which underscores the importance of a psychiatric evaluation as part of routine care for patients with this dermatologic disease. “Suicide is much more common in the HS population than in almost any other dermatologic disease,” Dr. Hamzavi added.
He reported serving as a consultant for AbbVie, Incyte, and UCB.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
KAUAI, HAWAII – Anyone who has treated patients with hidradenitis suppurativa (HS) recognizes that this can be a debilitating disease. Helping put that into fuller perspective, recent evidence has shown that the quality of life effects of moderate to severe HS are objectively worse than those of moderate to severe psoriasis, according to Iltefat H. Hamzavi, MD, president of the Hidradenitis Suppurativa Foundation and a dermatologist at Henry Ford Hospital in Detroit.
He was lead author of a study in which he and his coinvestigators compared weighted averages of a variety of quality of life measures in patients with moderate to severe HS or psoriasis who participated in five AbbVie-sponsored randomized clinical trials of biologic agents (J Am Acad Dermatol. 2017 Dec;77[6]:1038-46).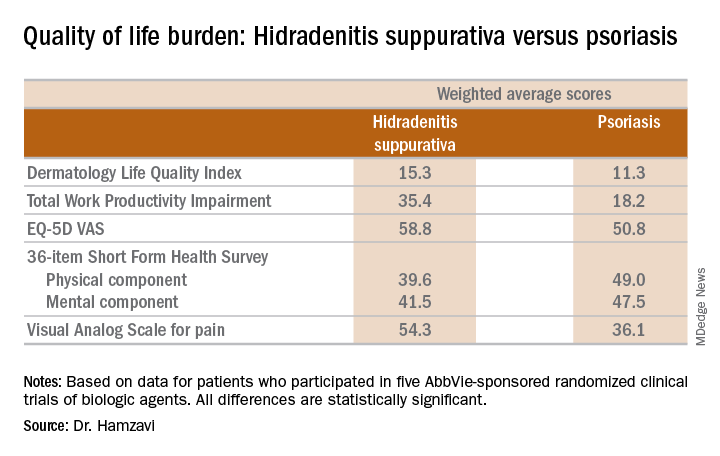
“The number of HS patients who experience downward drift – losing their job and their health insurance and ultimately being unable to move out of a lower socioeconomic group – is staggering,” the dermatologist said.
which underscores the importance of a psychiatric evaluation as part of routine care for patients with this dermatologic disease. “Suicide is much more common in the HS population than in almost any other dermatologic disease,” Dr. Hamzavi added.
He reported serving as a consultant for AbbVie, Incyte, and UCB.
SDEF/Global Academy for Medical Education and this news organization are owned by the same parent company.
EXPERT ANALYSIS FROM SDEF HAWAII DERMATOLOGY SEMINAR







