User login
Oral Antibiotics for Infective Endocarditis May Be Safe in Low-Risk Patients
Background: Treating infective endocarditis with four to six weeks of intravenous antibiotics carries a high cost. There are data to support oral antibiotics for right-sided endocarditis due to methicillin-sensitive Staphylococcus aureus (with ciprofloxacin and rifampicin), but experience in using oral antibiotics for infective endocarditis is limited.
Study design: Cohort study.
Setting: Large academic hospital in France.
Synopsis: The researchers included 426 patients with definitive or probable endocarditis by Duke criteria. After an initial period of treatment with intravenous (IV) antibiotics, 50% of the identified group was transitioned to oral antibiotics (amoxicillin alone in 50% and combinations of fluoroquinolones, rifampicin, amoxicillin, and clindamycin in the others).
The risk of death was not increased in the group treated with oral antibiotics when adjusted for the four biggest predictors of death (age >65, type 1 diabetes mellitus, disinsertion of prosthetic valve, and endocarditis due to S. aureus). Nine patients treated with IV antibiotics experienced relapsed endocarditis compared to two patients treated with oral antibiotics.
Patients selected for treatment with oral antibiotics were less likely to have severe disease, significant comorbidities, or infection with S. aureus. The length of treatment with IV antibiotics before switching to oral antibiotics varied widely.
Bottom line: It’s possible low-risk patients with infective endocarditis may be treated with oral antibiotics, but more data are needed.
Citation: Mzabi A, Kernéis S, Richaud C, Podglajen I, Fernandez-Gerlinger MP, Mainardi, JL. Switch to oral antibiotics in the treatment of infective endocarditis is not associated with increased risk of mortality in non-severely ill patients [published online ahead of print April 16, 2016]. Clin Microbiol Infect. doi:10.1016/j.cmi.2016.04.003.
Background: Treating infective endocarditis with four to six weeks of intravenous antibiotics carries a high cost. There are data to support oral antibiotics for right-sided endocarditis due to methicillin-sensitive Staphylococcus aureus (with ciprofloxacin and rifampicin), but experience in using oral antibiotics for infective endocarditis is limited.
Study design: Cohort study.
Setting: Large academic hospital in France.
Synopsis: The researchers included 426 patients with definitive or probable endocarditis by Duke criteria. After an initial period of treatment with intravenous (IV) antibiotics, 50% of the identified group was transitioned to oral antibiotics (amoxicillin alone in 50% and combinations of fluoroquinolones, rifampicin, amoxicillin, and clindamycin in the others).
The risk of death was not increased in the group treated with oral antibiotics when adjusted for the four biggest predictors of death (age >65, type 1 diabetes mellitus, disinsertion of prosthetic valve, and endocarditis due to S. aureus). Nine patients treated with IV antibiotics experienced relapsed endocarditis compared to two patients treated with oral antibiotics.
Patients selected for treatment with oral antibiotics were less likely to have severe disease, significant comorbidities, or infection with S. aureus. The length of treatment with IV antibiotics before switching to oral antibiotics varied widely.
Bottom line: It’s possible low-risk patients with infective endocarditis may be treated with oral antibiotics, but more data are needed.
Citation: Mzabi A, Kernéis S, Richaud C, Podglajen I, Fernandez-Gerlinger MP, Mainardi, JL. Switch to oral antibiotics in the treatment of infective endocarditis is not associated with increased risk of mortality in non-severely ill patients [published online ahead of print April 16, 2016]. Clin Microbiol Infect. doi:10.1016/j.cmi.2016.04.003.
Background: Treating infective endocarditis with four to six weeks of intravenous antibiotics carries a high cost. There are data to support oral antibiotics for right-sided endocarditis due to methicillin-sensitive Staphylococcus aureus (with ciprofloxacin and rifampicin), but experience in using oral antibiotics for infective endocarditis is limited.
Study design: Cohort study.
Setting: Large academic hospital in France.
Synopsis: The researchers included 426 patients with definitive or probable endocarditis by Duke criteria. After an initial period of treatment with intravenous (IV) antibiotics, 50% of the identified group was transitioned to oral antibiotics (amoxicillin alone in 50% and combinations of fluoroquinolones, rifampicin, amoxicillin, and clindamycin in the others).
The risk of death was not increased in the group treated with oral antibiotics when adjusted for the four biggest predictors of death (age >65, type 1 diabetes mellitus, disinsertion of prosthetic valve, and endocarditis due to S. aureus). Nine patients treated with IV antibiotics experienced relapsed endocarditis compared to two patients treated with oral antibiotics.
Patients selected for treatment with oral antibiotics were less likely to have severe disease, significant comorbidities, or infection with S. aureus. The length of treatment with IV antibiotics before switching to oral antibiotics varied widely.
Bottom line: It’s possible low-risk patients with infective endocarditis may be treated with oral antibiotics, but more data are needed.
Citation: Mzabi A, Kernéis S, Richaud C, Podglajen I, Fernandez-Gerlinger MP, Mainardi, JL. Switch to oral antibiotics in the treatment of infective endocarditis is not associated with increased risk of mortality in non-severely ill patients [published online ahead of print April 16, 2016]. Clin Microbiol Infect. doi:10.1016/j.cmi.2016.04.003.
Team devises novel fluorescence microscopy technique

Researchers say they have developed a fluorescence microscopy technique that improves image resolution by acquiring 3 views of a sample at the same time.
The team applied their technique in 2 microscopy modes and used it to image several types of biological samples.
For both modes, the technique demonstrated a volumetric resolution of up to 235 by 235 by 340 nanometers, double the volumetric resolution of traditional methods.
The researchers believe this technique will prove particularly useful for watching the dynamics of biological processes, which can provide insights into the workings of healthy and diseased cells.
They described the technique in the journal Optica.
The researchers noted that most fluorescence microscopy methods fail to capture much of the fluorescence emitted from a sample, which represents lost information and reduces image resolution.
“In our work, we captured this previously neglected fluorescence and fused it with the traditional views used in conventional microscopy,” said study author Yicong Wu, PhD, of the National Institute of Biomedical Imaging and Bioengineering at the National Institutes of Health in Bethesda, Maryland.
“This increases resolution without compromising either temporal resolution or adding additional light to the sample.”
Adding a third objective lens
The new multi-view approach helps improve a technique the researchers previously developed called dual-view plane illumination microscopy (diSPIM). Scientists around the world employ commercial versions of diSPIM, which uses a thin sheet of light and 2 objective lenses to excite and detect fluorescence.
“The main motivation of this new research was that the resolution in diSPIM was limited by the numerical aperture of the upper lenses, and fluorescence emitted in the direction of the coverslip is not captured,” explained study author Hari Shroff, PhD, also of the National Institute of Biomedical Imaging and Bioengineering.
“We reasoned that if we could simultaneously image this neglected signal by adding a higher numerical aperture lens that acquired the bottom view, then we could boost the lateral resolution.”
In the improved diSPIM microscopy technique, each light sheet is tilted at a 45-degree angle relative to an additional lower objective lens.
In its current design, the researchers swept the lower objective’s plane of focus through the sample to image the previously unused fluorescence, but this mechanical scanning could be replaced with a passive optic in future versions of the microscope.
Using the multi-view approach improved the lateral, or horizontal, resolution of diSPIM to about 235 nm.
The researchers also implemented the new technique in wide-field mode by scanning the 3 objectives through a sample simultaneously to produce 3 individual 3D views. With this mode, the multi-view method improved axial, or Z-axis, resolution, to about 340 nm, an increase of 45%.
Merging 3 views into 1
Whether acquired in wide-field or light-sheet mode, the 3 views must be precisely aligned and also cleaned up with an image processing technique known as deconvolution.
“One helpful trick was to deconvolve each view first to increase image quality, contrast, and so forth, which then allowed accurate registration of the 3 views,” Dr Wu said. “In wide-field mode, we further aided registration of the images by adding fluorescent beads to the samples as point of reference.”
The researchers demonstrated the multi-view technique by imaging biological samples and were able to see detailed features not typically observable.
For example, the wide-field multi-view microscope clearly resolved the spherical protein shell present when Bacillus subtilis forms a spore and also allowed the researchers to observe the dynamics of organelles inside cells.
In light-sheet mode, the team clearly saw the 3D dynamic nature of tiny protrusions on living white blood cells when they acquired 150 triple-view images over 40 minutes.
Although other methods have been used to capture multiple views sequentially, the researchers said this new method improves spatial resolution without introducing additional illumination or compromising temporal resolution relative to conventional imaging.
This is important because additional light can be damaging and even deadly to living cells, and the temporal resolution is needed to capture fast processes.
The researchers are now exploring additional biological applications for the new system and are working to extend the method to other microscope modalities, such as confocal microscopy. ![]()

Researchers say they have developed a fluorescence microscopy technique that improves image resolution by acquiring 3 views of a sample at the same time.
The team applied their technique in 2 microscopy modes and used it to image several types of biological samples.
For both modes, the technique demonstrated a volumetric resolution of up to 235 by 235 by 340 nanometers, double the volumetric resolution of traditional methods.
The researchers believe this technique will prove particularly useful for watching the dynamics of biological processes, which can provide insights into the workings of healthy and diseased cells.
They described the technique in the journal Optica.
The researchers noted that most fluorescence microscopy methods fail to capture much of the fluorescence emitted from a sample, which represents lost information and reduces image resolution.
“In our work, we captured this previously neglected fluorescence and fused it with the traditional views used in conventional microscopy,” said study author Yicong Wu, PhD, of the National Institute of Biomedical Imaging and Bioengineering at the National Institutes of Health in Bethesda, Maryland.
“This increases resolution without compromising either temporal resolution or adding additional light to the sample.”
Adding a third objective lens
The new multi-view approach helps improve a technique the researchers previously developed called dual-view plane illumination microscopy (diSPIM). Scientists around the world employ commercial versions of diSPIM, which uses a thin sheet of light and 2 objective lenses to excite and detect fluorescence.
“The main motivation of this new research was that the resolution in diSPIM was limited by the numerical aperture of the upper lenses, and fluorescence emitted in the direction of the coverslip is not captured,” explained study author Hari Shroff, PhD, also of the National Institute of Biomedical Imaging and Bioengineering.
“We reasoned that if we could simultaneously image this neglected signal by adding a higher numerical aperture lens that acquired the bottom view, then we could boost the lateral resolution.”
In the improved diSPIM microscopy technique, each light sheet is tilted at a 45-degree angle relative to an additional lower objective lens.
In its current design, the researchers swept the lower objective’s plane of focus through the sample to image the previously unused fluorescence, but this mechanical scanning could be replaced with a passive optic in future versions of the microscope.
Using the multi-view approach improved the lateral, or horizontal, resolution of diSPIM to about 235 nm.
The researchers also implemented the new technique in wide-field mode by scanning the 3 objectives through a sample simultaneously to produce 3 individual 3D views. With this mode, the multi-view method improved axial, or Z-axis, resolution, to about 340 nm, an increase of 45%.
Merging 3 views into 1
Whether acquired in wide-field or light-sheet mode, the 3 views must be precisely aligned and also cleaned up with an image processing technique known as deconvolution.
“One helpful trick was to deconvolve each view first to increase image quality, contrast, and so forth, which then allowed accurate registration of the 3 views,” Dr Wu said. “In wide-field mode, we further aided registration of the images by adding fluorescent beads to the samples as point of reference.”
The researchers demonstrated the multi-view technique by imaging biological samples and were able to see detailed features not typically observable.
For example, the wide-field multi-view microscope clearly resolved the spherical protein shell present when Bacillus subtilis forms a spore and also allowed the researchers to observe the dynamics of organelles inside cells.
In light-sheet mode, the team clearly saw the 3D dynamic nature of tiny protrusions on living white blood cells when they acquired 150 triple-view images over 40 minutes.
Although other methods have been used to capture multiple views sequentially, the researchers said this new method improves spatial resolution without introducing additional illumination or compromising temporal resolution relative to conventional imaging.
This is important because additional light can be damaging and even deadly to living cells, and the temporal resolution is needed to capture fast processes.
The researchers are now exploring additional biological applications for the new system and are working to extend the method to other microscope modalities, such as confocal microscopy. ![]()

Researchers say they have developed a fluorescence microscopy technique that improves image resolution by acquiring 3 views of a sample at the same time.
The team applied their technique in 2 microscopy modes and used it to image several types of biological samples.
For both modes, the technique demonstrated a volumetric resolution of up to 235 by 235 by 340 nanometers, double the volumetric resolution of traditional methods.
The researchers believe this technique will prove particularly useful for watching the dynamics of biological processes, which can provide insights into the workings of healthy and diseased cells.
They described the technique in the journal Optica.
The researchers noted that most fluorescence microscopy methods fail to capture much of the fluorescence emitted from a sample, which represents lost information and reduces image resolution.
“In our work, we captured this previously neglected fluorescence and fused it with the traditional views used in conventional microscopy,” said study author Yicong Wu, PhD, of the National Institute of Biomedical Imaging and Bioengineering at the National Institutes of Health in Bethesda, Maryland.
“This increases resolution without compromising either temporal resolution or adding additional light to the sample.”
Adding a third objective lens
The new multi-view approach helps improve a technique the researchers previously developed called dual-view plane illumination microscopy (diSPIM). Scientists around the world employ commercial versions of diSPIM, which uses a thin sheet of light and 2 objective lenses to excite and detect fluorescence.
“The main motivation of this new research was that the resolution in diSPIM was limited by the numerical aperture of the upper lenses, and fluorescence emitted in the direction of the coverslip is not captured,” explained study author Hari Shroff, PhD, also of the National Institute of Biomedical Imaging and Bioengineering.
“We reasoned that if we could simultaneously image this neglected signal by adding a higher numerical aperture lens that acquired the bottom view, then we could boost the lateral resolution.”
In the improved diSPIM microscopy technique, each light sheet is tilted at a 45-degree angle relative to an additional lower objective lens.
In its current design, the researchers swept the lower objective’s plane of focus through the sample to image the previously unused fluorescence, but this mechanical scanning could be replaced with a passive optic in future versions of the microscope.
Using the multi-view approach improved the lateral, or horizontal, resolution of diSPIM to about 235 nm.
The researchers also implemented the new technique in wide-field mode by scanning the 3 objectives through a sample simultaneously to produce 3 individual 3D views. With this mode, the multi-view method improved axial, or Z-axis, resolution, to about 340 nm, an increase of 45%.
Merging 3 views into 1
Whether acquired in wide-field or light-sheet mode, the 3 views must be precisely aligned and also cleaned up with an image processing technique known as deconvolution.
“One helpful trick was to deconvolve each view first to increase image quality, contrast, and so forth, which then allowed accurate registration of the 3 views,” Dr Wu said. “In wide-field mode, we further aided registration of the images by adding fluorescent beads to the samples as point of reference.”
The researchers demonstrated the multi-view technique by imaging biological samples and were able to see detailed features not typically observable.
For example, the wide-field multi-view microscope clearly resolved the spherical protein shell present when Bacillus subtilis forms a spore and also allowed the researchers to observe the dynamics of organelles inside cells.
In light-sheet mode, the team clearly saw the 3D dynamic nature of tiny protrusions on living white blood cells when they acquired 150 triple-view images over 40 minutes.
Although other methods have been used to capture multiple views sequentially, the researchers said this new method improves spatial resolution without introducing additional illumination or compromising temporal resolution relative to conventional imaging.
This is important because additional light can be damaging and even deadly to living cells, and the temporal resolution is needed to capture fast processes.
The researchers are now exploring additional biological applications for the new system and are working to extend the method to other microscope modalities, such as confocal microscopy. ![]()
Clean-catch urine method effective in young infants
Urine samples from a noninvasive clean-catch method have no significantly greater contamination rate than do those from urethral catheterization, making clean catch a quick, effective option to attempt before catheterization, a recent study found.
The clean-catch method uses a standard bladder stimulation technique and was most successful in infants less than 90 days old.
“Because the use of urethral catheterization is an invasive method that could be associated with adverse events in up to 20% of children, our findings support the use of the clean-catch urine standardized stimulation technique as an alternative to invasive methods to obtain a urine specimen,” wrote Mélanie Labrosse, MD, PhD, and her associates at the University of Montreal (Pediatrics. 2016 Aug 19. doi: 10.1542/peds.2016-0573). “However, until further studies on proportion and predictive factors of contamination become available, it would be more cautious to perform invasive methods in children who appear ill, who have a positive urinalysis, or before beginning antibiotics.”
The clean-catch method involved providing the infants an opportunity to feed over 20 minutes, after which a practitioner cleaned the genitals and the parent then held the infant by the armpits. Female infants’ hips were flexed and male infants’ legs dangled.
“Examiners then alternated between bladder stimulation maneuvers, which consisted of gentle tapping in the suprapubic area at a frequency of 100 taps per minute for 30 seconds, and lumbar paravertebral massage maneuvers for 30 seconds,” the authors wrote. “These two stimulation maneuvers were repeated until micturition began or for a maximum of 300 seconds.”
The researchers attempted the clean-catch technique with 126 infants under 6 months old. About half were boys, a quarter of whom were circumcised, and the whole sample had a median age of 55 days. The procedure took a median 45 seconds and was effective in 49% of the children (at least 1 mL of urine collected within 5 minutes).
The procedure was more likely to be effective in infants under 3 months old, with three times greater odds of success for those aged 30-59 days and four times greater odds of success for those aged 0-29 days and those aged 60-89 days (odds ratio 3.2, 4.3, and 4.4, respectively). Only 26% of the children aged 91-180 days yielded a successful clean-catch sample, compared with 61% of infants under 30 days and 54% of infants under 90 days old. UTI was present in 11 (9%) children.
Likelihood of a successful clean-catch sample was not affected by infant sex, low oral intake, or recent urination (within an hour).
While 16% of the clean catches were contaminated, this rate was not statistically different from the 6% of contaminated samples among those undergoing the invasive method.
The authors suggested using the clean-catch technique as a first attempt in two situations: ruling out UTI in children aged 2-6 months and in children under 6 months who need a urinalysis in which urine typically would be obtained noninvasively.
“In addition, trying the CCU procedure instead of using a collection bag seems reasonable, considering the wait time associated with this technique and the logistics involved in changing the bag every 30 minutes,” the authors noted.
They reported having no disclosures. No external funding source was noted in the study.
Urine samples from a noninvasive clean-catch method have no significantly greater contamination rate than do those from urethral catheterization, making clean catch a quick, effective option to attempt before catheterization, a recent study found.
The clean-catch method uses a standard bladder stimulation technique and was most successful in infants less than 90 days old.
“Because the use of urethral catheterization is an invasive method that could be associated with adverse events in up to 20% of children, our findings support the use of the clean-catch urine standardized stimulation technique as an alternative to invasive methods to obtain a urine specimen,” wrote Mélanie Labrosse, MD, PhD, and her associates at the University of Montreal (Pediatrics. 2016 Aug 19. doi: 10.1542/peds.2016-0573). “However, until further studies on proportion and predictive factors of contamination become available, it would be more cautious to perform invasive methods in children who appear ill, who have a positive urinalysis, or before beginning antibiotics.”
The clean-catch method involved providing the infants an opportunity to feed over 20 minutes, after which a practitioner cleaned the genitals and the parent then held the infant by the armpits. Female infants’ hips were flexed and male infants’ legs dangled.
“Examiners then alternated between bladder stimulation maneuvers, which consisted of gentle tapping in the suprapubic area at a frequency of 100 taps per minute for 30 seconds, and lumbar paravertebral massage maneuvers for 30 seconds,” the authors wrote. “These two stimulation maneuvers were repeated until micturition began or for a maximum of 300 seconds.”
The researchers attempted the clean-catch technique with 126 infants under 6 months old. About half were boys, a quarter of whom were circumcised, and the whole sample had a median age of 55 days. The procedure took a median 45 seconds and was effective in 49% of the children (at least 1 mL of urine collected within 5 minutes).
The procedure was more likely to be effective in infants under 3 months old, with three times greater odds of success for those aged 30-59 days and four times greater odds of success for those aged 0-29 days and those aged 60-89 days (odds ratio 3.2, 4.3, and 4.4, respectively). Only 26% of the children aged 91-180 days yielded a successful clean-catch sample, compared with 61% of infants under 30 days and 54% of infants under 90 days old. UTI was present in 11 (9%) children.
Likelihood of a successful clean-catch sample was not affected by infant sex, low oral intake, or recent urination (within an hour).
While 16% of the clean catches were contaminated, this rate was not statistically different from the 6% of contaminated samples among those undergoing the invasive method.
The authors suggested using the clean-catch technique as a first attempt in two situations: ruling out UTI in children aged 2-6 months and in children under 6 months who need a urinalysis in which urine typically would be obtained noninvasively.
“In addition, trying the CCU procedure instead of using a collection bag seems reasonable, considering the wait time associated with this technique and the logistics involved in changing the bag every 30 minutes,” the authors noted.
They reported having no disclosures. No external funding source was noted in the study.
Urine samples from a noninvasive clean-catch method have no significantly greater contamination rate than do those from urethral catheterization, making clean catch a quick, effective option to attempt before catheterization, a recent study found.
The clean-catch method uses a standard bladder stimulation technique and was most successful in infants less than 90 days old.
“Because the use of urethral catheterization is an invasive method that could be associated with adverse events in up to 20% of children, our findings support the use of the clean-catch urine standardized stimulation technique as an alternative to invasive methods to obtain a urine specimen,” wrote Mélanie Labrosse, MD, PhD, and her associates at the University of Montreal (Pediatrics. 2016 Aug 19. doi: 10.1542/peds.2016-0573). “However, until further studies on proportion and predictive factors of contamination become available, it would be more cautious to perform invasive methods in children who appear ill, who have a positive urinalysis, or before beginning antibiotics.”
The clean-catch method involved providing the infants an opportunity to feed over 20 minutes, after which a practitioner cleaned the genitals and the parent then held the infant by the armpits. Female infants’ hips were flexed and male infants’ legs dangled.
“Examiners then alternated between bladder stimulation maneuvers, which consisted of gentle tapping in the suprapubic area at a frequency of 100 taps per minute for 30 seconds, and lumbar paravertebral massage maneuvers for 30 seconds,” the authors wrote. “These two stimulation maneuvers were repeated until micturition began or for a maximum of 300 seconds.”
The researchers attempted the clean-catch technique with 126 infants under 6 months old. About half were boys, a quarter of whom were circumcised, and the whole sample had a median age of 55 days. The procedure took a median 45 seconds and was effective in 49% of the children (at least 1 mL of urine collected within 5 minutes).
The procedure was more likely to be effective in infants under 3 months old, with three times greater odds of success for those aged 30-59 days and four times greater odds of success for those aged 0-29 days and those aged 60-89 days (odds ratio 3.2, 4.3, and 4.4, respectively). Only 26% of the children aged 91-180 days yielded a successful clean-catch sample, compared with 61% of infants under 30 days and 54% of infants under 90 days old. UTI was present in 11 (9%) children.
Likelihood of a successful clean-catch sample was not affected by infant sex, low oral intake, or recent urination (within an hour).
While 16% of the clean catches were contaminated, this rate was not statistically different from the 6% of contaminated samples among those undergoing the invasive method.
The authors suggested using the clean-catch technique as a first attempt in two situations: ruling out UTI in children aged 2-6 months and in children under 6 months who need a urinalysis in which urine typically would be obtained noninvasively.
“In addition, trying the CCU procedure instead of using a collection bag seems reasonable, considering the wait time associated with this technique and the logistics involved in changing the bag every 30 minutes,” the authors noted.
They reported having no disclosures. No external funding source was noted in the study.
FROM PEDIATRICS
Key clinical point: A noninvasive clean-catch urine sample method can be effective in infants under 90 days old.
Major finding: Forty-nine percent of infants under 6 months old produced a successful clean catch; odds of success were 3-4 times greater in infants under 90 days.
Data source: A prospective cohort study of 126 infants under 6 months old in a Montreal pediatric emergency department between May and October 2015.
Disclosures: The authors reported having no disclosures. No external funding source was noted in the study.
The Missing Element
A 57‐year‐old man presented to an emergency department with 1 month of progressive, bilateral lower extremity pain and weakness.
The first step in evaluating weakness is to determine whether it is objective (ie, decreased muscle strength due to pathology along the neuromuscular axis) or subjective. The sensation of weakness without loss of muscle strength may result from a debilitating chronic disease (eg, congestive heart failure, anemia, or chronic obstructive pulmonary disease). In patients with true lower extremity weakness it is prudent to assess for a myelopathy with a focused history and exam that includes assessment of bowel or bladder impairment and anal reflex. The presence of pain along with weakness might suggest disease of the muscle itself. A myopathy may arise from an infectious (eg, influenza), inflammatory (eg, polymyositis), endocrine (eg, hypothyroidism), or drug‐related (eg, statin) process.
The patient described 1 month of generalized weakness and pain in his lower extremities, which had worsened progressively to the point where ambulation was difficult. He was able to rise from a seated position using his arms for assistance, but had difficulty balancing in a standing position without assistance. The pain also involved both of his knees and increased with weight bearing. He also complained of bilateral lower extremity numbness and paresthesias, which had been migrating proximally from his toes over several months. He denied any recent trauma to his legs or back.
These symmetrical, distal sensory deficits favor a peripheral neuropathy over a myopathy, with neuropathic pain and arthralgia causing his impaired ability to ambulate or remain standing. In polyneuropathy, the type of nerve involvement (sensory vs motor) and pathology (axonal vs demyelinating) helps prioritize the differential. In developed countries, the most common causes of polyneuropathy are diabetes mellitus and alcohol. However, the tempo of his disease broadens the possibilities to include acute inflammatory demyelinating polyneuropathy, paraneoplastic syndrome (eg, monoclonal gammopathy), an autoimmune process (eg, rheumatoid arthritis, vasculitis), and heavy metal toxicity such as lead poisoning.
He had no history of chronic medical illness or hospitalizations and took no medications. His social history was notable for a history of alcohol abuse. For the past several years, he had only been drinking 1 to 2 beers daily due to cost, but had a history of more significant alcohol abuse in the distant past. He smoked 1 pack of tobacco per day, and denied illicit drug use. He denied any sexual activity or recent travel. He lived in a van, and had been homeless for over 10 years.
His socioeconomic status adds a layer of complexity to the case. Human immunodeficiency virus and hepatitis C virus (HCV) are more prevalent in the homeless and are associated with polyneuropathy. His lack of funds may drive him to drink illegally distilled alcohol, which can cause polyneuropathy through lead or arsenic toxicity. Excessive smoking could be linked to a peripheral neuropathy through a paraneoplastic syndrome (eg, small cell lung cancer).
Alcohol causes polyneuropathy through toxic effects on nerves and may be playing a role in his polyneuropathy, but the rapid pace and severity suggests an additional process. Alcoholism can be associated with deficiency of various B vitamins, such as thiamine, pyridoxine, and cobalamin, which can cause polyneuropathy. In alcoholics who are hospitalized, thiamine should be administered prior to glucose to decrease risk of Wernicke encephalopathy.
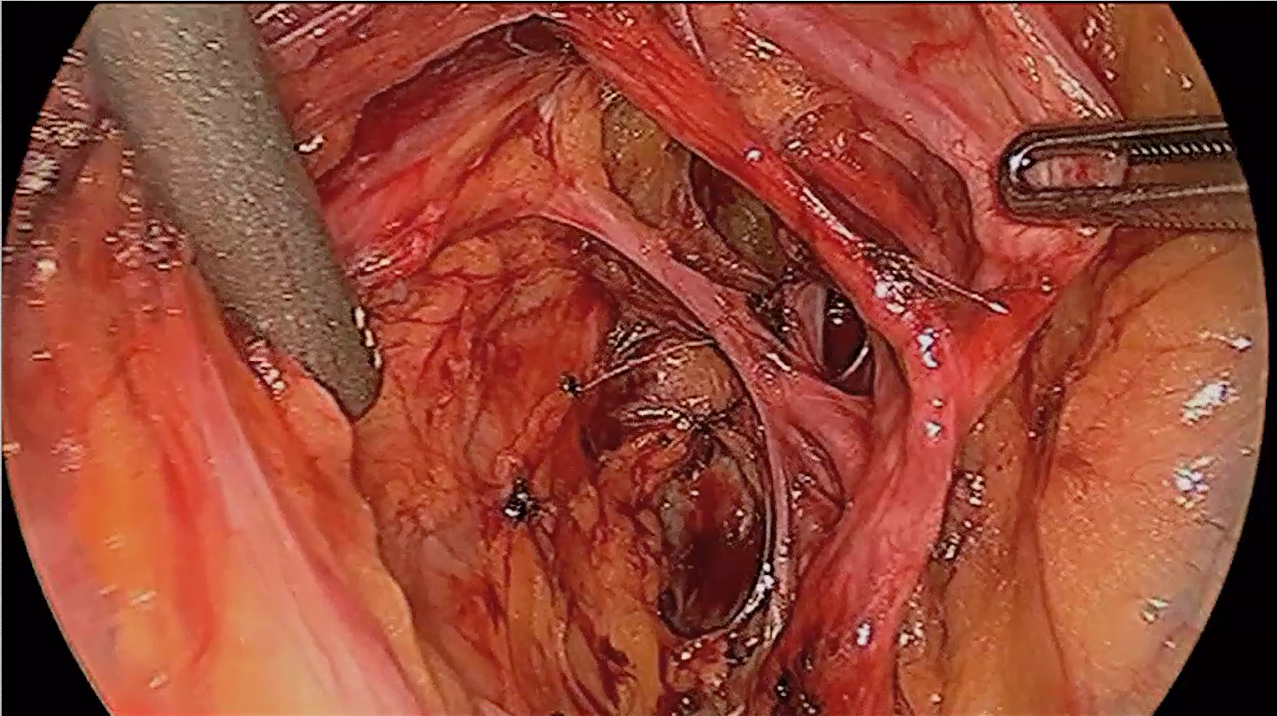
His temperature was 38.0C, heart rate 93 beats/min, blood pressure 121/60 mm Hg, respiratory rate 14/min, with an oxygen saturation of 97% on ambient air. He appeared cachectic and disheveled. He had moist mucous membranes, poor dentition with missing teeth, and no mucosal bleeding or oropharyngeal erythema. His cardiac exam revealed no murmurs, rubs, or gallops. His lungs were clear. His abdominal exam was benign, without masses or tenderness. His skin exam (Figure 1) was notable for nonpalpable petechiae on his anterior shins and thighs up to his buttocks. His extremity exam was significant for diffuse tenderness to light palpation on both lower extremities, a large indurated tender ecchymosis 15 15 cm behind the right knee, and another ecchymosis 6 8 cm behind the left knee. His dorsalis pedis and anterior tibialis pulses were appreciated by Doppler but not by palpation. He had decreased sensation to light touch of his bilateral feet to his ankles. Strength exam was challenging to assess secondary to posterior leg pain, but he demonstrated 4/5 strength of his hip flexors, quadriceps, and plantar flexors of the foot. His upper extremity strength and sensory exam were normal. Examination of the cranial nerves was normal. He had 2+ patellar and Achilles reflexes. Gait could not be adequately assessed.

Petechiae manifest as a nonblanchable rash caused by extravasated red blood cells. Common etiologies include quantitative or qualitative platelet defects, disseminated intravascular coagulopathy, trauma, and vasculitis. Cirrhosis from alcohol leading to thrombocytopenia and petechial rash is unlikely given no other stigmata of liver disease such as jaundice, spider angiomata, caput medusae, or palmar erythema. Less common causes include nutritional deficiency and light chain (AL) amyloidosis, which could explain both the neuropathy and rash.
The constellation of fever and petechial rash can represent a life‐threatening systemic process. Infectious agents that require immediate consideration with fever and petechiae include Neisseria meningitidis (meningococcemia), Rickettsia rickettsii (Rocky Mountain spotted fever), Staphylococcus, and Streptococcus. However, his normal blood pressure, dependent distribution of rash, and neuropathy make a severe bacterial infection less likely. Thrombotic thrombocytopenic purpura is possible and should prompt assessment of platelets, peripheral blood smear, and lactate dehydrogenase. Among vasculitides, the polyneuropathy, fever, and dependent distribution of petechial rash prioritize a small‐to‐medium vessel vasculitis, where the pathophysiology involves inflammation of dermal vessels and vasa nervorum (blood supply of nerves). Examples include HCV‐related cryoglobulinemic vasculitis, polyarteritis nodosa (PAN), and antineutrophilic cytoplasmic antibody (ANCA)associated vasculitis. However, ANCA‐associated vasculitis is less likely without upper or lower respiratory symptoms. Henoch‐Schonlein purpura may explain the rash but is more common in children and is not associated with neuropathy.
Posterior knee ecchymosis, in absence of trauma, raises suspicion for a ruptured Baker's cyst. However, the bilateral involvement and lack of calf manifestations makes this unlikely. The location raises concern for hemarthrosis, so a more likely explanation would be coagulopathy (eg, an acquired factor inhibitor) or a collagen defect. In developed countries, a commonly overlooked category of diseasenutritional deficiencywarrants serious consideration in alcoholics. Vitamin C deficiency (scurvy) may cause a petechial rash and ecchymosis from perifollicular hemorrhage and impaired collagen synthesis, respectively. Scurvy can masquerade as small vessel vasculitis because of its associated petechial rash. The neuropathy might be explained by concomitant thiamine or cobalamin deficiency. It is important to obtain a thorough dietary history and assess vibration and proprioception, which may be impaired from pathology of the dorsal column in cobalamin deficiency. The low‐grade fever may be a red herring, but if it becomes significant would be difficult to explain with nutritional deficiency.
In summary, a judicious evaluation for infection is mandatory, but the leading diagnoses are a small‐to‐medium vessel vasculitis (PAN or HCV‐related cryoglobulinemia), deficiency of multiple vitamins, and AL amyloidosis.
Initial labs showed white blood cell count 7800/L, hematocrit 39.2%, and platelet count of 251,000/L. Serum chemistry demonstrated a sodium of 131 mEq/L, potassium 4.7 mEq/L, chloride 93 mEq/L, bicarbonate 23 mEq/L, blood urea nitrogen 8 mg/dL, and creatinine 0.8 mg/dL. His aminotransferases, albumin, alkaline phosphatase, and coagulation studies were within normal limits. Urinalysis was remarkable for 2+ urobilinogen, 1+ ketones, and a bland sediment. Urine toxicology screen was negative.
His white blood cell count is normal, so with a heart rate of 93 beats/minute, he barely meets a single criterion of systemic inflammatory response syndrome (SIRS). The lack of SIRS and normal platelet, albumin, white blood cell, and red blood cell counts significantly reduces the likelihood of an infectious or inflammatory process. Without any clinical or biochemical evidence of HCV infection, HCV‐associated cryoglobulinemia is less likely. A normal creatinine might overestimate renal function in setting of decreased protein intake and muscle mass; nevertheless, the bland urine sediment further lowers probability of PAN and ANCA‐associated vasculitides. The normal platelet count and coagulation studies suggest either a qualitative platelet defect (eg, acquired von Willebrand disease) or impaired vessel integrity (eg, collagen defect) to explain the petechial rash. The urine ketones likely represent alcohol and/or starvation‐related ketosis. These data reduce the probability of infection and vasculitis, and prioritize vitamin deficiency and AL amyloidosis. Antibiotic therapy is not appropriate, given the absence of SIRS and subacute course. His presentation likely prompted a wide variety of tests, but most relevant would be a dietary history, cobalamin and vitamin C levels, serum free light chains, and skin biopsy. Biopsy of the rash would allow assessment for vasculitis and AL amyloidosis. The former is marked by inflammatory infiltrate of vessels, and the latter by perivascular invasion with amyloid fibrils. If the dietary history was consistent with ascorbic acid deficiency (scurvy), in addition to thiamine, he should be empirically treated with vitamin C. Patients with scurvy demonstrate rapid clinical improvement with treatment.
C‐reactive protein (CRP) was 47.9 mg/L and erythrocyte sedimentation rate (ESR) was 44 mm/hr. Human immunodeficiency antibody screen was negative. Anti‐nuclear antibodies and anti‐nuclear cytoplasmic antibody panel were negative. Computed tomography angiogram (CTA) of the lower extremities demonstrated severe stenosis of the left superficial femoral artery and severe stenosis of the right posterior tibial artery. Ankle‐brachial indices were 0.83 on the right side and 0.72 on the left, indicating mild to moderate arterial disease.
ESR and CRP are nonspecific markers of inflammation. Their elevation does not prioritize malignancy, autoimmunity, or infection. ANCA might be negative in commonly ANCA‐associated vasculitides such as eosinophilic granulomatosis with polyangiitis, microscopic polyangiitis, and granulomatosis with polyangiitis. However, the lack of respiratory and renal involvement in addition to the negative ANCA panel make such diagnoses unlikely. CTA of the patient's legs showed significant peripheral artery disease (PAD). This is unlikely to be the cause of his presentation; PAD should not cause petechiae, and his pain is disproportionate to the severity of the vascular disease reported. The additional information leaves the differential unchanged.
A dermatologist was consulted. She described and photographed a perifollicular distribution of the lower extremity petechiae with associated perifollicular hyperkeratosis and retained curled hairs (Figure 2).

The described rash is specific for scurvy. His homelessness and alcohol intake likely made him vulnerable to ascorbic acid deficiency from lack of access to fruits and vegetables. Measurement of vitamin C level is unnecessary as the pretest probability for scurvy is very high. More relevant than a vitamin C level or skin biopsy is empiric treatment with ascorbic acid; as mentioned, patients with scurvy respond rapidly to vitamin C therapy. Given the neuropathy, he should be assessed for concomitant thiamine and/or cobalamin deficiency. His peripheral arterial disease is unlikely to be related.
His ascorbic acid level was 0.0 mg/dL (reference range, 0.22.0 mg/dL). Further history was obtained, and the patient reported exclusively eating frozen hamburgers and burritos for almost 1 year. He believed he had not had a fruit or vegetable in over 10 years. He was started on 1000 mg daily of ascorbic acid. By hospital day 2, his rash had mostly resolved and he was able to stand with some support. The patient was seen by his primary care physician 3 weeks after diagnosis, with his exercise tolerance nearly back to baseline. His rash had entirely resolved.
DISCUSSION
Unlike other mammals, humans do not have the ability to convert glucose to vitamin C and thus require an exogenous source, such as fruits and vegetables. The oft‐cited observation of scurvy in sailors during long journeys in the 18th century is a classic example of clinical disease due to vitamin C deficiency.[1] Once replete, body stores of vitamin C are usually sufficient to last over 6 months of deprivation. In some patients, symptoms of deficiency may appear within 3 months.[2] The patient in this report likely suffered years of vitamin C deficiency, resulting in the significant manifestations of scurvy reported here.
Vitamin C is a water‐soluble vitamin necessary for the biosynthesis of collagen, L‐carnitine, and neurotransmitters.[3] With deficiency, the resulting impairment in the formation of collagen affects blood vessel integrity and results in perivascular edema and erythrocyte extravasation. Clinically, this leads to hemorrhagic manifestations (eg, periosteal hemorrhage and perifollicular petechiae) and poor wound healing. Corkscrew hairs result because of vitamin C's role in disulfide bonding during hair formation. Woody edema and dyspnea are thought to be a consequence of leaky capillaries.[4]
Scurvy is still a significant cause of morbidity in at‐risk populations in the United States. Several populations have been identified as high risk for vitamin C deficiency, including the elderly, persons who live alone, alcoholics, smokers, individuals of low socioeconomic status, patients on hemodialysis, and those with psychiatric disease.[5] Specifically, the high oxidative stress associated with smoking, the history of alcohol abuse, and homelessness put this patient at an especially high risk.[6] Those with oxidative stressors have been postulated to require up to 125 mg/d of vitamin C compared to 60 to 90 mg/d of those without the same risks.[7] In a national health and nutrition survey in the United States in 2004, the prevalence of vitamin C deficiency as defined by a serum level 0.2 mg/dL was noted in 7.1% of those surveyed.[8] This study also noted a significantly higher prevalence of deficiency in smokers and individuals with low socioeconomic status.
Scurvy is a clinical diagnosis based on clinical features and dietary history. Severe manifestations of scurvy may happen quickly after the initial presentation, making early diagnosis especially important.[2] These include anemia, bone pain, ocular hemorrhage, cerebral hemorrhage, and hemopericardium.[2, 4] If needed, laboratory diagnosis can be made by demonstrating a serum ascorbic acid level 0.2 mg/dL. However, the level may be normal if the patient has had recent intake of vitamin C. In that scenario, the leukocyte vitamin C concentration may be a more accurate measure of the body stores as leukocyte levels change more slowly.[4] Biopsy of skin lesions is not necessary for the diagnosis and typically show a dilated hair follicle with keratin plugging and perifollicular hemorrhage.[9] Given the lack of adverse effects, treatment with vitamin C supplementation should begin immediately, even with low suspicion of scurvy, and response can serve as further clinical evidence and render laboratory testing unnecessary.
In this patient, the diagnosis was challenging for several reasons. The presentation was concerning for vasculitis given the dependent petechiae and elevated inflammatory markers. However, in scurvy, the petechiae are perifollicular and associated with hyperkeratosis, as opposed to the palpable purpura often described in vasculitis. Further, marked elevations in ESR and CRP have also been reported in scurvy.[10] The initial concern for vasculitis and clinician discomfort with a diagnosis based solely on a rash delayed the diagnosis. The complaint of polyneuropathy also seemed inconsistent with scurvy. Very rarely, scurvy may cause a neuropathy by hemorrhage into the nerve sheath, as seen in a case of bilateral femoral neuropathy.[11] Most likely, this patient had an underlying vitamin B deficiency explaining his polyneuropathy. Unfortunately, the patient was lost to follow‐up after his postdischarge visit with his primary physician and was not tested for other concomitant vitamin deficiencies.
Scurvy is very responsive to even small doses of vitamin C supplementation. For rapid recovery, doses ranging from 100 mg 3 times daily to 1000 mg daily of oral vitamin C are recommended for at least 1 month. Resolution of symptoms will begin within 24 hours, and complete recovery should occur by 3 months.[4] Scurvy is a classic example of how nutritional deficiencies can have a myriad of presentations and may mimic other systemic diseases. Clinicians who recall these manifestations and carefully assess patients for nutritional risks may be able to quickly identify the missing element (or elements) in a patient's diet, and initiate treatment that is often rapidly effective.
KEY TEACHING POINTS
- Vitamin C deficiency initially presents with classic dermatological findings of perifollicular petechiae with associated hyperkeratosis and corkscrew hairs.
- Scurvy is a clinical diagnosis based on history and presentation. Vitamin C serum level may not accurately reflect body stores, and a leukocyte vitamin C level may be obtained. The diagnosis may also be confirmed with observed response to vitamin C supplementation.
- Scurvy should be suspected in high‐risk populations, especially the marginally housed, the elderly, alcoholics, and smokers.
- Clinicians should screen patients with scurvy for other nutritional deficiencies including thiamine, folate, B12, and vitamin D levels.
Disclosures: Nothing to report.
- . The discovery of vitamin C. Ann Nutr Metab. 2012;61(3):259–264.
- , , , , . Clinical manifestations of ascorbic acid deficiency in man. Am J Clin Nutr. 1971;24(4):432–443.
- . New concepts in the biology and biochemistry of ascorbic acid. N Engl J Med. 1986;314(14):892–902.
- , . Adult scurvy. J Am Acad Dermatol. 1999;41(6):895–910.
- , . Be vigilant for scurvy in high‐risk groups. Practitioner. 2012;256(1755):23–5, 3.
- . Estimating ascorbic acid requirements for cigarette smokers. Ann N Y Acad Sci. 1993;686:335–346.
- , , . Vitamin C deficiency and depletion in the United States: the Third National Health and Nutrition Examination Survey, 1988 to 1994. Am J Public Health. 2004;94(5):870–875.
- , , , . Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES). Am J Clin Nutr. 2009;90(5):1252–1263.
- , , . Scurvy: a cutaneous clinical diagnosis. Australas J Dermatol. 2003;44(1):48–51.
- , . Rheumatic manifestations of scurvy: a report of three recent cases in a major urban center and a review. Semin Arthritis Rheum. 2011;41(2):286–290.
- . Femoral neuropathy in scurvy. N Engl J Med. 1969;281(23):1292–1293.
A 57‐year‐old man presented to an emergency department with 1 month of progressive, bilateral lower extremity pain and weakness.
The first step in evaluating weakness is to determine whether it is objective (ie, decreased muscle strength due to pathology along the neuromuscular axis) or subjective. The sensation of weakness without loss of muscle strength may result from a debilitating chronic disease (eg, congestive heart failure, anemia, or chronic obstructive pulmonary disease). In patients with true lower extremity weakness it is prudent to assess for a myelopathy with a focused history and exam that includes assessment of bowel or bladder impairment and anal reflex. The presence of pain along with weakness might suggest disease of the muscle itself. A myopathy may arise from an infectious (eg, influenza), inflammatory (eg, polymyositis), endocrine (eg, hypothyroidism), or drug‐related (eg, statin) process.
The patient described 1 month of generalized weakness and pain in his lower extremities, which had worsened progressively to the point where ambulation was difficult. He was able to rise from a seated position using his arms for assistance, but had difficulty balancing in a standing position without assistance. The pain also involved both of his knees and increased with weight bearing. He also complained of bilateral lower extremity numbness and paresthesias, which had been migrating proximally from his toes over several months. He denied any recent trauma to his legs or back.
These symmetrical, distal sensory deficits favor a peripheral neuropathy over a myopathy, with neuropathic pain and arthralgia causing his impaired ability to ambulate or remain standing. In polyneuropathy, the type of nerve involvement (sensory vs motor) and pathology (axonal vs demyelinating) helps prioritize the differential. In developed countries, the most common causes of polyneuropathy are diabetes mellitus and alcohol. However, the tempo of his disease broadens the possibilities to include acute inflammatory demyelinating polyneuropathy, paraneoplastic syndrome (eg, monoclonal gammopathy), an autoimmune process (eg, rheumatoid arthritis, vasculitis), and heavy metal toxicity such as lead poisoning.
He had no history of chronic medical illness or hospitalizations and took no medications. His social history was notable for a history of alcohol abuse. For the past several years, he had only been drinking 1 to 2 beers daily due to cost, but had a history of more significant alcohol abuse in the distant past. He smoked 1 pack of tobacco per day, and denied illicit drug use. He denied any sexual activity or recent travel. He lived in a van, and had been homeless for over 10 years.
His socioeconomic status adds a layer of complexity to the case. Human immunodeficiency virus and hepatitis C virus (HCV) are more prevalent in the homeless and are associated with polyneuropathy. His lack of funds may drive him to drink illegally distilled alcohol, which can cause polyneuropathy through lead or arsenic toxicity. Excessive smoking could be linked to a peripheral neuropathy through a paraneoplastic syndrome (eg, small cell lung cancer).
Alcohol causes polyneuropathy through toxic effects on nerves and may be playing a role in his polyneuropathy, but the rapid pace and severity suggests an additional process. Alcoholism can be associated with deficiency of various B vitamins, such as thiamine, pyridoxine, and cobalamin, which can cause polyneuropathy. In alcoholics who are hospitalized, thiamine should be administered prior to glucose to decrease risk of Wernicke encephalopathy.
His temperature was 38.0C, heart rate 93 beats/min, blood pressure 121/60 mm Hg, respiratory rate 14/min, with an oxygen saturation of 97% on ambient air. He appeared cachectic and disheveled. He had moist mucous membranes, poor dentition with missing teeth, and no mucosal bleeding or oropharyngeal erythema. His cardiac exam revealed no murmurs, rubs, or gallops. His lungs were clear. His abdominal exam was benign, without masses or tenderness. His skin exam (Figure 1) was notable for nonpalpable petechiae on his anterior shins and thighs up to his buttocks. His extremity exam was significant for diffuse tenderness to light palpation on both lower extremities, a large indurated tender ecchymosis 15 15 cm behind the right knee, and another ecchymosis 6 8 cm behind the left knee. His dorsalis pedis and anterior tibialis pulses were appreciated by Doppler but not by palpation. He had decreased sensation to light touch of his bilateral feet to his ankles. Strength exam was challenging to assess secondary to posterior leg pain, but he demonstrated 4/5 strength of his hip flexors, quadriceps, and plantar flexors of the foot. His upper extremity strength and sensory exam were normal. Examination of the cranial nerves was normal. He had 2+ patellar and Achilles reflexes. Gait could not be adequately assessed.

Petechiae manifest as a nonblanchable rash caused by extravasated red blood cells. Common etiologies include quantitative or qualitative platelet defects, disseminated intravascular coagulopathy, trauma, and vasculitis. Cirrhosis from alcohol leading to thrombocytopenia and petechial rash is unlikely given no other stigmata of liver disease such as jaundice, spider angiomata, caput medusae, or palmar erythema. Less common causes include nutritional deficiency and light chain (AL) amyloidosis, which could explain both the neuropathy and rash.
The constellation of fever and petechial rash can represent a life‐threatening systemic process. Infectious agents that require immediate consideration with fever and petechiae include Neisseria meningitidis (meningococcemia), Rickettsia rickettsii (Rocky Mountain spotted fever), Staphylococcus, and Streptococcus. However, his normal blood pressure, dependent distribution of rash, and neuropathy make a severe bacterial infection less likely. Thrombotic thrombocytopenic purpura is possible and should prompt assessment of platelets, peripheral blood smear, and lactate dehydrogenase. Among vasculitides, the polyneuropathy, fever, and dependent distribution of petechial rash prioritize a small‐to‐medium vessel vasculitis, where the pathophysiology involves inflammation of dermal vessels and vasa nervorum (blood supply of nerves). Examples include HCV‐related cryoglobulinemic vasculitis, polyarteritis nodosa (PAN), and antineutrophilic cytoplasmic antibody (ANCA)associated vasculitis. However, ANCA‐associated vasculitis is less likely without upper or lower respiratory symptoms. Henoch‐Schonlein purpura may explain the rash but is more common in children and is not associated with neuropathy.
Posterior knee ecchymosis, in absence of trauma, raises suspicion for a ruptured Baker's cyst. However, the bilateral involvement and lack of calf manifestations makes this unlikely. The location raises concern for hemarthrosis, so a more likely explanation would be coagulopathy (eg, an acquired factor inhibitor) or a collagen defect. In developed countries, a commonly overlooked category of diseasenutritional deficiencywarrants serious consideration in alcoholics. Vitamin C deficiency (scurvy) may cause a petechial rash and ecchymosis from perifollicular hemorrhage and impaired collagen synthesis, respectively. Scurvy can masquerade as small vessel vasculitis because of its associated petechial rash. The neuropathy might be explained by concomitant thiamine or cobalamin deficiency. It is important to obtain a thorough dietary history and assess vibration and proprioception, which may be impaired from pathology of the dorsal column in cobalamin deficiency. The low‐grade fever may be a red herring, but if it becomes significant would be difficult to explain with nutritional deficiency.
In summary, a judicious evaluation for infection is mandatory, but the leading diagnoses are a small‐to‐medium vessel vasculitis (PAN or HCV‐related cryoglobulinemia), deficiency of multiple vitamins, and AL amyloidosis.
Initial labs showed white blood cell count 7800/L, hematocrit 39.2%, and platelet count of 251,000/L. Serum chemistry demonstrated a sodium of 131 mEq/L, potassium 4.7 mEq/L, chloride 93 mEq/L, bicarbonate 23 mEq/L, blood urea nitrogen 8 mg/dL, and creatinine 0.8 mg/dL. His aminotransferases, albumin, alkaline phosphatase, and coagulation studies were within normal limits. Urinalysis was remarkable for 2+ urobilinogen, 1+ ketones, and a bland sediment. Urine toxicology screen was negative.
His white blood cell count is normal, so with a heart rate of 93 beats/minute, he barely meets a single criterion of systemic inflammatory response syndrome (SIRS). The lack of SIRS and normal platelet, albumin, white blood cell, and red blood cell counts significantly reduces the likelihood of an infectious or inflammatory process. Without any clinical or biochemical evidence of HCV infection, HCV‐associated cryoglobulinemia is less likely. A normal creatinine might overestimate renal function in setting of decreased protein intake and muscle mass; nevertheless, the bland urine sediment further lowers probability of PAN and ANCA‐associated vasculitides. The normal platelet count and coagulation studies suggest either a qualitative platelet defect (eg, acquired von Willebrand disease) or impaired vessel integrity (eg, collagen defect) to explain the petechial rash. The urine ketones likely represent alcohol and/or starvation‐related ketosis. These data reduce the probability of infection and vasculitis, and prioritize vitamin deficiency and AL amyloidosis. Antibiotic therapy is not appropriate, given the absence of SIRS and subacute course. His presentation likely prompted a wide variety of tests, but most relevant would be a dietary history, cobalamin and vitamin C levels, serum free light chains, and skin biopsy. Biopsy of the rash would allow assessment for vasculitis and AL amyloidosis. The former is marked by inflammatory infiltrate of vessels, and the latter by perivascular invasion with amyloid fibrils. If the dietary history was consistent with ascorbic acid deficiency (scurvy), in addition to thiamine, he should be empirically treated with vitamin C. Patients with scurvy demonstrate rapid clinical improvement with treatment.
C‐reactive protein (CRP) was 47.9 mg/L and erythrocyte sedimentation rate (ESR) was 44 mm/hr. Human immunodeficiency antibody screen was negative. Anti‐nuclear antibodies and anti‐nuclear cytoplasmic antibody panel were negative. Computed tomography angiogram (CTA) of the lower extremities demonstrated severe stenosis of the left superficial femoral artery and severe stenosis of the right posterior tibial artery. Ankle‐brachial indices were 0.83 on the right side and 0.72 on the left, indicating mild to moderate arterial disease.
ESR and CRP are nonspecific markers of inflammation. Their elevation does not prioritize malignancy, autoimmunity, or infection. ANCA might be negative in commonly ANCA‐associated vasculitides such as eosinophilic granulomatosis with polyangiitis, microscopic polyangiitis, and granulomatosis with polyangiitis. However, the lack of respiratory and renal involvement in addition to the negative ANCA panel make such diagnoses unlikely. CTA of the patient's legs showed significant peripheral artery disease (PAD). This is unlikely to be the cause of his presentation; PAD should not cause petechiae, and his pain is disproportionate to the severity of the vascular disease reported. The additional information leaves the differential unchanged.
A dermatologist was consulted. She described and photographed a perifollicular distribution of the lower extremity petechiae with associated perifollicular hyperkeratosis and retained curled hairs (Figure 2).

The described rash is specific for scurvy. His homelessness and alcohol intake likely made him vulnerable to ascorbic acid deficiency from lack of access to fruits and vegetables. Measurement of vitamin C level is unnecessary as the pretest probability for scurvy is very high. More relevant than a vitamin C level or skin biopsy is empiric treatment with ascorbic acid; as mentioned, patients with scurvy respond rapidly to vitamin C therapy. Given the neuropathy, he should be assessed for concomitant thiamine and/or cobalamin deficiency. His peripheral arterial disease is unlikely to be related.
His ascorbic acid level was 0.0 mg/dL (reference range, 0.22.0 mg/dL). Further history was obtained, and the patient reported exclusively eating frozen hamburgers and burritos for almost 1 year. He believed he had not had a fruit or vegetable in over 10 years. He was started on 1000 mg daily of ascorbic acid. By hospital day 2, his rash had mostly resolved and he was able to stand with some support. The patient was seen by his primary care physician 3 weeks after diagnosis, with his exercise tolerance nearly back to baseline. His rash had entirely resolved.
DISCUSSION
Unlike other mammals, humans do not have the ability to convert glucose to vitamin C and thus require an exogenous source, such as fruits and vegetables. The oft‐cited observation of scurvy in sailors during long journeys in the 18th century is a classic example of clinical disease due to vitamin C deficiency.[1] Once replete, body stores of vitamin C are usually sufficient to last over 6 months of deprivation. In some patients, symptoms of deficiency may appear within 3 months.[2] The patient in this report likely suffered years of vitamin C deficiency, resulting in the significant manifestations of scurvy reported here.
Vitamin C is a water‐soluble vitamin necessary for the biosynthesis of collagen, L‐carnitine, and neurotransmitters.[3] With deficiency, the resulting impairment in the formation of collagen affects blood vessel integrity and results in perivascular edema and erythrocyte extravasation. Clinically, this leads to hemorrhagic manifestations (eg, periosteal hemorrhage and perifollicular petechiae) and poor wound healing. Corkscrew hairs result because of vitamin C's role in disulfide bonding during hair formation. Woody edema and dyspnea are thought to be a consequence of leaky capillaries.[4]
Scurvy is still a significant cause of morbidity in at‐risk populations in the United States. Several populations have been identified as high risk for vitamin C deficiency, including the elderly, persons who live alone, alcoholics, smokers, individuals of low socioeconomic status, patients on hemodialysis, and those with psychiatric disease.[5] Specifically, the high oxidative stress associated with smoking, the history of alcohol abuse, and homelessness put this patient at an especially high risk.[6] Those with oxidative stressors have been postulated to require up to 125 mg/d of vitamin C compared to 60 to 90 mg/d of those without the same risks.[7] In a national health and nutrition survey in the United States in 2004, the prevalence of vitamin C deficiency as defined by a serum level 0.2 mg/dL was noted in 7.1% of those surveyed.[8] This study also noted a significantly higher prevalence of deficiency in smokers and individuals with low socioeconomic status.
Scurvy is a clinical diagnosis based on clinical features and dietary history. Severe manifestations of scurvy may happen quickly after the initial presentation, making early diagnosis especially important.[2] These include anemia, bone pain, ocular hemorrhage, cerebral hemorrhage, and hemopericardium.[2, 4] If needed, laboratory diagnosis can be made by demonstrating a serum ascorbic acid level 0.2 mg/dL. However, the level may be normal if the patient has had recent intake of vitamin C. In that scenario, the leukocyte vitamin C concentration may be a more accurate measure of the body stores as leukocyte levels change more slowly.[4] Biopsy of skin lesions is not necessary for the diagnosis and typically show a dilated hair follicle with keratin plugging and perifollicular hemorrhage.[9] Given the lack of adverse effects, treatment with vitamin C supplementation should begin immediately, even with low suspicion of scurvy, and response can serve as further clinical evidence and render laboratory testing unnecessary.
In this patient, the diagnosis was challenging for several reasons. The presentation was concerning for vasculitis given the dependent petechiae and elevated inflammatory markers. However, in scurvy, the petechiae are perifollicular and associated with hyperkeratosis, as opposed to the palpable purpura often described in vasculitis. Further, marked elevations in ESR and CRP have also been reported in scurvy.[10] The initial concern for vasculitis and clinician discomfort with a diagnosis based solely on a rash delayed the diagnosis. The complaint of polyneuropathy also seemed inconsistent with scurvy. Very rarely, scurvy may cause a neuropathy by hemorrhage into the nerve sheath, as seen in a case of bilateral femoral neuropathy.[11] Most likely, this patient had an underlying vitamin B deficiency explaining his polyneuropathy. Unfortunately, the patient was lost to follow‐up after his postdischarge visit with his primary physician and was not tested for other concomitant vitamin deficiencies.
Scurvy is very responsive to even small doses of vitamin C supplementation. For rapid recovery, doses ranging from 100 mg 3 times daily to 1000 mg daily of oral vitamin C are recommended for at least 1 month. Resolution of symptoms will begin within 24 hours, and complete recovery should occur by 3 months.[4] Scurvy is a classic example of how nutritional deficiencies can have a myriad of presentations and may mimic other systemic diseases. Clinicians who recall these manifestations and carefully assess patients for nutritional risks may be able to quickly identify the missing element (or elements) in a patient's diet, and initiate treatment that is often rapidly effective.
KEY TEACHING POINTS
- Vitamin C deficiency initially presents with classic dermatological findings of perifollicular petechiae with associated hyperkeratosis and corkscrew hairs.
- Scurvy is a clinical diagnosis based on history and presentation. Vitamin C serum level may not accurately reflect body stores, and a leukocyte vitamin C level may be obtained. The diagnosis may also be confirmed with observed response to vitamin C supplementation.
- Scurvy should be suspected in high‐risk populations, especially the marginally housed, the elderly, alcoholics, and smokers.
- Clinicians should screen patients with scurvy for other nutritional deficiencies including thiamine, folate, B12, and vitamin D levels.
Disclosures: Nothing to report.
A 57‐year‐old man presented to an emergency department with 1 month of progressive, bilateral lower extremity pain and weakness.
The first step in evaluating weakness is to determine whether it is objective (ie, decreased muscle strength due to pathology along the neuromuscular axis) or subjective. The sensation of weakness without loss of muscle strength may result from a debilitating chronic disease (eg, congestive heart failure, anemia, or chronic obstructive pulmonary disease). In patients with true lower extremity weakness it is prudent to assess for a myelopathy with a focused history and exam that includes assessment of bowel or bladder impairment and anal reflex. The presence of pain along with weakness might suggest disease of the muscle itself. A myopathy may arise from an infectious (eg, influenza), inflammatory (eg, polymyositis), endocrine (eg, hypothyroidism), or drug‐related (eg, statin) process.
The patient described 1 month of generalized weakness and pain in his lower extremities, which had worsened progressively to the point where ambulation was difficult. He was able to rise from a seated position using his arms for assistance, but had difficulty balancing in a standing position without assistance. The pain also involved both of his knees and increased with weight bearing. He also complained of bilateral lower extremity numbness and paresthesias, which had been migrating proximally from his toes over several months. He denied any recent trauma to his legs or back.
These symmetrical, distal sensory deficits favor a peripheral neuropathy over a myopathy, with neuropathic pain and arthralgia causing his impaired ability to ambulate or remain standing. In polyneuropathy, the type of nerve involvement (sensory vs motor) and pathology (axonal vs demyelinating) helps prioritize the differential. In developed countries, the most common causes of polyneuropathy are diabetes mellitus and alcohol. However, the tempo of his disease broadens the possibilities to include acute inflammatory demyelinating polyneuropathy, paraneoplastic syndrome (eg, monoclonal gammopathy), an autoimmune process (eg, rheumatoid arthritis, vasculitis), and heavy metal toxicity such as lead poisoning.
He had no history of chronic medical illness or hospitalizations and took no medications. His social history was notable for a history of alcohol abuse. For the past several years, he had only been drinking 1 to 2 beers daily due to cost, but had a history of more significant alcohol abuse in the distant past. He smoked 1 pack of tobacco per day, and denied illicit drug use. He denied any sexual activity or recent travel. He lived in a van, and had been homeless for over 10 years.
His socioeconomic status adds a layer of complexity to the case. Human immunodeficiency virus and hepatitis C virus (HCV) are more prevalent in the homeless and are associated with polyneuropathy. His lack of funds may drive him to drink illegally distilled alcohol, which can cause polyneuropathy through lead or arsenic toxicity. Excessive smoking could be linked to a peripheral neuropathy through a paraneoplastic syndrome (eg, small cell lung cancer).
Alcohol causes polyneuropathy through toxic effects on nerves and may be playing a role in his polyneuropathy, but the rapid pace and severity suggests an additional process. Alcoholism can be associated with deficiency of various B vitamins, such as thiamine, pyridoxine, and cobalamin, which can cause polyneuropathy. In alcoholics who are hospitalized, thiamine should be administered prior to glucose to decrease risk of Wernicke encephalopathy.
His temperature was 38.0C, heart rate 93 beats/min, blood pressure 121/60 mm Hg, respiratory rate 14/min, with an oxygen saturation of 97% on ambient air. He appeared cachectic and disheveled. He had moist mucous membranes, poor dentition with missing teeth, and no mucosal bleeding or oropharyngeal erythema. His cardiac exam revealed no murmurs, rubs, or gallops. His lungs were clear. His abdominal exam was benign, without masses or tenderness. His skin exam (Figure 1) was notable for nonpalpable petechiae on his anterior shins and thighs up to his buttocks. His extremity exam was significant for diffuse tenderness to light palpation on both lower extremities, a large indurated tender ecchymosis 15 15 cm behind the right knee, and another ecchymosis 6 8 cm behind the left knee. His dorsalis pedis and anterior tibialis pulses were appreciated by Doppler but not by palpation. He had decreased sensation to light touch of his bilateral feet to his ankles. Strength exam was challenging to assess secondary to posterior leg pain, but he demonstrated 4/5 strength of his hip flexors, quadriceps, and plantar flexors of the foot. His upper extremity strength and sensory exam were normal. Examination of the cranial nerves was normal. He had 2+ patellar and Achilles reflexes. Gait could not be adequately assessed.

Petechiae manifest as a nonblanchable rash caused by extravasated red blood cells. Common etiologies include quantitative or qualitative platelet defects, disseminated intravascular coagulopathy, trauma, and vasculitis. Cirrhosis from alcohol leading to thrombocytopenia and petechial rash is unlikely given no other stigmata of liver disease such as jaundice, spider angiomata, caput medusae, or palmar erythema. Less common causes include nutritional deficiency and light chain (AL) amyloidosis, which could explain both the neuropathy and rash.
The constellation of fever and petechial rash can represent a life‐threatening systemic process. Infectious agents that require immediate consideration with fever and petechiae include Neisseria meningitidis (meningococcemia), Rickettsia rickettsii (Rocky Mountain spotted fever), Staphylococcus, and Streptococcus. However, his normal blood pressure, dependent distribution of rash, and neuropathy make a severe bacterial infection less likely. Thrombotic thrombocytopenic purpura is possible and should prompt assessment of platelets, peripheral blood smear, and lactate dehydrogenase. Among vasculitides, the polyneuropathy, fever, and dependent distribution of petechial rash prioritize a small‐to‐medium vessel vasculitis, where the pathophysiology involves inflammation of dermal vessels and vasa nervorum (blood supply of nerves). Examples include HCV‐related cryoglobulinemic vasculitis, polyarteritis nodosa (PAN), and antineutrophilic cytoplasmic antibody (ANCA)associated vasculitis. However, ANCA‐associated vasculitis is less likely without upper or lower respiratory symptoms. Henoch‐Schonlein purpura may explain the rash but is more common in children and is not associated with neuropathy.
Posterior knee ecchymosis, in absence of trauma, raises suspicion for a ruptured Baker's cyst. However, the bilateral involvement and lack of calf manifestations makes this unlikely. The location raises concern for hemarthrosis, so a more likely explanation would be coagulopathy (eg, an acquired factor inhibitor) or a collagen defect. In developed countries, a commonly overlooked category of diseasenutritional deficiencywarrants serious consideration in alcoholics. Vitamin C deficiency (scurvy) may cause a petechial rash and ecchymosis from perifollicular hemorrhage and impaired collagen synthesis, respectively. Scurvy can masquerade as small vessel vasculitis because of its associated petechial rash. The neuropathy might be explained by concomitant thiamine or cobalamin deficiency. It is important to obtain a thorough dietary history and assess vibration and proprioception, which may be impaired from pathology of the dorsal column in cobalamin deficiency. The low‐grade fever may be a red herring, but if it becomes significant would be difficult to explain with nutritional deficiency.
In summary, a judicious evaluation for infection is mandatory, but the leading diagnoses are a small‐to‐medium vessel vasculitis (PAN or HCV‐related cryoglobulinemia), deficiency of multiple vitamins, and AL amyloidosis.
Initial labs showed white blood cell count 7800/L, hematocrit 39.2%, and platelet count of 251,000/L. Serum chemistry demonstrated a sodium of 131 mEq/L, potassium 4.7 mEq/L, chloride 93 mEq/L, bicarbonate 23 mEq/L, blood urea nitrogen 8 mg/dL, and creatinine 0.8 mg/dL. His aminotransferases, albumin, alkaline phosphatase, and coagulation studies were within normal limits. Urinalysis was remarkable for 2+ urobilinogen, 1+ ketones, and a bland sediment. Urine toxicology screen was negative.
His white blood cell count is normal, so with a heart rate of 93 beats/minute, he barely meets a single criterion of systemic inflammatory response syndrome (SIRS). The lack of SIRS and normal platelet, albumin, white blood cell, and red blood cell counts significantly reduces the likelihood of an infectious or inflammatory process. Without any clinical or biochemical evidence of HCV infection, HCV‐associated cryoglobulinemia is less likely. A normal creatinine might overestimate renal function in setting of decreased protein intake and muscle mass; nevertheless, the bland urine sediment further lowers probability of PAN and ANCA‐associated vasculitides. The normal platelet count and coagulation studies suggest either a qualitative platelet defect (eg, acquired von Willebrand disease) or impaired vessel integrity (eg, collagen defect) to explain the petechial rash. The urine ketones likely represent alcohol and/or starvation‐related ketosis. These data reduce the probability of infection and vasculitis, and prioritize vitamin deficiency and AL amyloidosis. Antibiotic therapy is not appropriate, given the absence of SIRS and subacute course. His presentation likely prompted a wide variety of tests, but most relevant would be a dietary history, cobalamin and vitamin C levels, serum free light chains, and skin biopsy. Biopsy of the rash would allow assessment for vasculitis and AL amyloidosis. The former is marked by inflammatory infiltrate of vessels, and the latter by perivascular invasion with amyloid fibrils. If the dietary history was consistent with ascorbic acid deficiency (scurvy), in addition to thiamine, he should be empirically treated with vitamin C. Patients with scurvy demonstrate rapid clinical improvement with treatment.
C‐reactive protein (CRP) was 47.9 mg/L and erythrocyte sedimentation rate (ESR) was 44 mm/hr. Human immunodeficiency antibody screen was negative. Anti‐nuclear antibodies and anti‐nuclear cytoplasmic antibody panel were negative. Computed tomography angiogram (CTA) of the lower extremities demonstrated severe stenosis of the left superficial femoral artery and severe stenosis of the right posterior tibial artery. Ankle‐brachial indices were 0.83 on the right side and 0.72 on the left, indicating mild to moderate arterial disease.
ESR and CRP are nonspecific markers of inflammation. Their elevation does not prioritize malignancy, autoimmunity, or infection. ANCA might be negative in commonly ANCA‐associated vasculitides such as eosinophilic granulomatosis with polyangiitis, microscopic polyangiitis, and granulomatosis with polyangiitis. However, the lack of respiratory and renal involvement in addition to the negative ANCA panel make such diagnoses unlikely. CTA of the patient's legs showed significant peripheral artery disease (PAD). This is unlikely to be the cause of his presentation; PAD should not cause petechiae, and his pain is disproportionate to the severity of the vascular disease reported. The additional information leaves the differential unchanged.
A dermatologist was consulted. She described and photographed a perifollicular distribution of the lower extremity petechiae with associated perifollicular hyperkeratosis and retained curled hairs (Figure 2).

The described rash is specific for scurvy. His homelessness and alcohol intake likely made him vulnerable to ascorbic acid deficiency from lack of access to fruits and vegetables. Measurement of vitamin C level is unnecessary as the pretest probability for scurvy is very high. More relevant than a vitamin C level or skin biopsy is empiric treatment with ascorbic acid; as mentioned, patients with scurvy respond rapidly to vitamin C therapy. Given the neuropathy, he should be assessed for concomitant thiamine and/or cobalamin deficiency. His peripheral arterial disease is unlikely to be related.
His ascorbic acid level was 0.0 mg/dL (reference range, 0.22.0 mg/dL). Further history was obtained, and the patient reported exclusively eating frozen hamburgers and burritos for almost 1 year. He believed he had not had a fruit or vegetable in over 10 years. He was started on 1000 mg daily of ascorbic acid. By hospital day 2, his rash had mostly resolved and he was able to stand with some support. The patient was seen by his primary care physician 3 weeks after diagnosis, with his exercise tolerance nearly back to baseline. His rash had entirely resolved.
DISCUSSION
Unlike other mammals, humans do not have the ability to convert glucose to vitamin C and thus require an exogenous source, such as fruits and vegetables. The oft‐cited observation of scurvy in sailors during long journeys in the 18th century is a classic example of clinical disease due to vitamin C deficiency.[1] Once replete, body stores of vitamin C are usually sufficient to last over 6 months of deprivation. In some patients, symptoms of deficiency may appear within 3 months.[2] The patient in this report likely suffered years of vitamin C deficiency, resulting in the significant manifestations of scurvy reported here.
Vitamin C is a water‐soluble vitamin necessary for the biosynthesis of collagen, L‐carnitine, and neurotransmitters.[3] With deficiency, the resulting impairment in the formation of collagen affects blood vessel integrity and results in perivascular edema and erythrocyte extravasation. Clinically, this leads to hemorrhagic manifestations (eg, periosteal hemorrhage and perifollicular petechiae) and poor wound healing. Corkscrew hairs result because of vitamin C's role in disulfide bonding during hair formation. Woody edema and dyspnea are thought to be a consequence of leaky capillaries.[4]
Scurvy is still a significant cause of morbidity in at‐risk populations in the United States. Several populations have been identified as high risk for vitamin C deficiency, including the elderly, persons who live alone, alcoholics, smokers, individuals of low socioeconomic status, patients on hemodialysis, and those with psychiatric disease.[5] Specifically, the high oxidative stress associated with smoking, the history of alcohol abuse, and homelessness put this patient at an especially high risk.[6] Those with oxidative stressors have been postulated to require up to 125 mg/d of vitamin C compared to 60 to 90 mg/d of those without the same risks.[7] In a national health and nutrition survey in the United States in 2004, the prevalence of vitamin C deficiency as defined by a serum level 0.2 mg/dL was noted in 7.1% of those surveyed.[8] This study also noted a significantly higher prevalence of deficiency in smokers and individuals with low socioeconomic status.
Scurvy is a clinical diagnosis based on clinical features and dietary history. Severe manifestations of scurvy may happen quickly after the initial presentation, making early diagnosis especially important.[2] These include anemia, bone pain, ocular hemorrhage, cerebral hemorrhage, and hemopericardium.[2, 4] If needed, laboratory diagnosis can be made by demonstrating a serum ascorbic acid level 0.2 mg/dL. However, the level may be normal if the patient has had recent intake of vitamin C. In that scenario, the leukocyte vitamin C concentration may be a more accurate measure of the body stores as leukocyte levels change more slowly.[4] Biopsy of skin lesions is not necessary for the diagnosis and typically show a dilated hair follicle with keratin plugging and perifollicular hemorrhage.[9] Given the lack of adverse effects, treatment with vitamin C supplementation should begin immediately, even with low suspicion of scurvy, and response can serve as further clinical evidence and render laboratory testing unnecessary.
In this patient, the diagnosis was challenging for several reasons. The presentation was concerning for vasculitis given the dependent petechiae and elevated inflammatory markers. However, in scurvy, the petechiae are perifollicular and associated with hyperkeratosis, as opposed to the palpable purpura often described in vasculitis. Further, marked elevations in ESR and CRP have also been reported in scurvy.[10] The initial concern for vasculitis and clinician discomfort with a diagnosis based solely on a rash delayed the diagnosis. The complaint of polyneuropathy also seemed inconsistent with scurvy. Very rarely, scurvy may cause a neuropathy by hemorrhage into the nerve sheath, as seen in a case of bilateral femoral neuropathy.[11] Most likely, this patient had an underlying vitamin B deficiency explaining his polyneuropathy. Unfortunately, the patient was lost to follow‐up after his postdischarge visit with his primary physician and was not tested for other concomitant vitamin deficiencies.
Scurvy is very responsive to even small doses of vitamin C supplementation. For rapid recovery, doses ranging from 100 mg 3 times daily to 1000 mg daily of oral vitamin C are recommended for at least 1 month. Resolution of symptoms will begin within 24 hours, and complete recovery should occur by 3 months.[4] Scurvy is a classic example of how nutritional deficiencies can have a myriad of presentations and may mimic other systemic diseases. Clinicians who recall these manifestations and carefully assess patients for nutritional risks may be able to quickly identify the missing element (or elements) in a patient's diet, and initiate treatment that is often rapidly effective.
KEY TEACHING POINTS
- Vitamin C deficiency initially presents with classic dermatological findings of perifollicular petechiae with associated hyperkeratosis and corkscrew hairs.
- Scurvy is a clinical diagnosis based on history and presentation. Vitamin C serum level may not accurately reflect body stores, and a leukocyte vitamin C level may be obtained. The diagnosis may also be confirmed with observed response to vitamin C supplementation.
- Scurvy should be suspected in high‐risk populations, especially the marginally housed, the elderly, alcoholics, and smokers.
- Clinicians should screen patients with scurvy for other nutritional deficiencies including thiamine, folate, B12, and vitamin D levels.
Disclosures: Nothing to report.
- . The discovery of vitamin C. Ann Nutr Metab. 2012;61(3):259–264.
- , , , , . Clinical manifestations of ascorbic acid deficiency in man. Am J Clin Nutr. 1971;24(4):432–443.
- . New concepts in the biology and biochemistry of ascorbic acid. N Engl J Med. 1986;314(14):892–902.
- , . Adult scurvy. J Am Acad Dermatol. 1999;41(6):895–910.
- , . Be vigilant for scurvy in high‐risk groups. Practitioner. 2012;256(1755):23–5, 3.
- . Estimating ascorbic acid requirements for cigarette smokers. Ann N Y Acad Sci. 1993;686:335–346.
- , , . Vitamin C deficiency and depletion in the United States: the Third National Health and Nutrition Examination Survey, 1988 to 1994. Am J Public Health. 2004;94(5):870–875.
- , , , . Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES). Am J Clin Nutr. 2009;90(5):1252–1263.
- , , . Scurvy: a cutaneous clinical diagnosis. Australas J Dermatol. 2003;44(1):48–51.
- , . Rheumatic manifestations of scurvy: a report of three recent cases in a major urban center and a review. Semin Arthritis Rheum. 2011;41(2):286–290.
- . Femoral neuropathy in scurvy. N Engl J Med. 1969;281(23):1292–1293.
- . The discovery of vitamin C. Ann Nutr Metab. 2012;61(3):259–264.
- , , , , . Clinical manifestations of ascorbic acid deficiency in man. Am J Clin Nutr. 1971;24(4):432–443.
- . New concepts in the biology and biochemistry of ascorbic acid. N Engl J Med. 1986;314(14):892–902.
- , . Adult scurvy. J Am Acad Dermatol. 1999;41(6):895–910.
- , . Be vigilant for scurvy in high‐risk groups. Practitioner. 2012;256(1755):23–5, 3.
- . Estimating ascorbic acid requirements for cigarette smokers. Ann N Y Acad Sci. 1993;686:335–346.
- , , . Vitamin C deficiency and depletion in the United States: the Third National Health and Nutrition Examination Survey, 1988 to 1994. Am J Public Health. 2004;94(5):870–875.
- , , , . Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES). Am J Clin Nutr. 2009;90(5):1252–1263.
- , , . Scurvy: a cutaneous clinical diagnosis. Australas J Dermatol. 2003;44(1):48–51.
- , . Rheumatic manifestations of scurvy: a report of three recent cases in a major urban center and a review. Semin Arthritis Rheum. 2011;41(2):286–290.
- . Femoral neuropathy in scurvy. N Engl J Med. 1969;281(23):1292–1293.
Uterine artery ligation: Advanced techniques and considerations for the difficult laparoscopic hysterectomy

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
- A novel approach to overcoming cervical stenosis and false passages

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
- A novel approach to overcoming cervical stenosis and false passages

For more videos from the Society of Gynecologic Surgeons, click here
Visit the Society of Gynecologic Surgeons online: sgsonline.org
Related articles:
- Cervical injection of methylene blue for identification of sentinel lymph nodes in cervical cancer
- Misplaced hysteroscopic sterilization micro-insert in the peritoneal cavity: A corpus alienum
- Laparoscopic cystectomy for large, bilateral ovarian dermoids
- Small bowel surgery for the benign gynecologist
- A novel approach to overcoming cervical stenosis and false passages
This video is brought to you by ![]()
Gallstone disease boosts heart disease risk
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Key clinical point: Gallstone disease is associated with an increased risk for coronary heart disease; preventing the former can help mitigate chances of developing the latter.
Major finding: A meta-analysis revealed a 23% increased chance of CHD in gallstone disease patients.
Data source: A meta-analysis of seven studies involving 842,553 subjects, and a prospective cohort study of 269,142 participants in three separate studies that took place from 1980 to 2011.
Disclosures: Funding provided by NIH, Boston Obesity Nutrition Research Center, and United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Pertussis often goes undiagnosed, especially in adults
A majority of pertussis cases in the United States may go undetected in people under the age of 50, particularly in adults, results of a retrospective database cohort study suggest.
“The incidence of pertussis in adolescents and adults is very difficult to quantify,” wrote Chi-Chang Chen, MD, of IMS Health, Plymouth Meeting, Pa., and associates. Symptoms may be misdiagnosed as other respiratory illnesses, infected individuals may not seek treatment, and pertussis may not be considered as a possible diagnosis in adults, they noted.
To project the possible range of pertussis incidence in this population, the investigator used three different models to analyze information from private insurance and laboratory databases as well as data from the Centers for Disease Control and Prevention for a 6-year period. The first method, which used medical claims for ICD-9 diagnosed pertussis, found an annual incidence rate of 9/100,000 population. The second used a proxy pertussis model that was based on symptoms that could indicate undiagnosed pertussis, showing an incidence rate of 21/100,000. The third method used pathogen data to estimate the fraction of cough illness statistically attributable to pertussis, resulting in an incidence rate of 649/100,000 population, which is 58-93 times higher than the ICD-9 estimated incidence.
These estimates “highlight the need for improved preventive measures – such as increased vaccination – against pertussis,” the investigators said, noting that immunization recommendations for additional age groups and research involving strategies to reduce waning immunity after vaccination should be considered.
The study was funded by GlaxoSmithKline Vaccines.
Read the full study in Human Vaccines & Immunotherapeutics (2016 May. doi: 10.1080/21645515.2016.1186313).
A majority of pertussis cases in the United States may go undetected in people under the age of 50, particularly in adults, results of a retrospective database cohort study suggest.
“The incidence of pertussis in adolescents and adults is very difficult to quantify,” wrote Chi-Chang Chen, MD, of IMS Health, Plymouth Meeting, Pa., and associates. Symptoms may be misdiagnosed as other respiratory illnesses, infected individuals may not seek treatment, and pertussis may not be considered as a possible diagnosis in adults, they noted.
To project the possible range of pertussis incidence in this population, the investigator used three different models to analyze information from private insurance and laboratory databases as well as data from the Centers for Disease Control and Prevention for a 6-year period. The first method, which used medical claims for ICD-9 diagnosed pertussis, found an annual incidence rate of 9/100,000 population. The second used a proxy pertussis model that was based on symptoms that could indicate undiagnosed pertussis, showing an incidence rate of 21/100,000. The third method used pathogen data to estimate the fraction of cough illness statistically attributable to pertussis, resulting in an incidence rate of 649/100,000 population, which is 58-93 times higher than the ICD-9 estimated incidence.
These estimates “highlight the need for improved preventive measures – such as increased vaccination – against pertussis,” the investigators said, noting that immunization recommendations for additional age groups and research involving strategies to reduce waning immunity after vaccination should be considered.
The study was funded by GlaxoSmithKline Vaccines.
Read the full study in Human Vaccines & Immunotherapeutics (2016 May. doi: 10.1080/21645515.2016.1186313).
A majority of pertussis cases in the United States may go undetected in people under the age of 50, particularly in adults, results of a retrospective database cohort study suggest.
“The incidence of pertussis in adolescents and adults is very difficult to quantify,” wrote Chi-Chang Chen, MD, of IMS Health, Plymouth Meeting, Pa., and associates. Symptoms may be misdiagnosed as other respiratory illnesses, infected individuals may not seek treatment, and pertussis may not be considered as a possible diagnosis in adults, they noted.
To project the possible range of pertussis incidence in this population, the investigator used three different models to analyze information from private insurance and laboratory databases as well as data from the Centers for Disease Control and Prevention for a 6-year period. The first method, which used medical claims for ICD-9 diagnosed pertussis, found an annual incidence rate of 9/100,000 population. The second used a proxy pertussis model that was based on symptoms that could indicate undiagnosed pertussis, showing an incidence rate of 21/100,000. The third method used pathogen data to estimate the fraction of cough illness statistically attributable to pertussis, resulting in an incidence rate of 649/100,000 population, which is 58-93 times higher than the ICD-9 estimated incidence.
These estimates “highlight the need for improved preventive measures – such as increased vaccination – against pertussis,” the investigators said, noting that immunization recommendations for additional age groups and research involving strategies to reduce waning immunity after vaccination should be considered.
The study was funded by GlaxoSmithKline Vaccines.
Read the full study in Human Vaccines & Immunotherapeutics (2016 May. doi: 10.1080/21645515.2016.1186313).
FROM HUMAN VACCINES & IMMUNOTHERAPEUTICS
A new model for gout: pharmacy-based care
Something new is being tried to improve gout outcomes in the United States: Pharmacists are being recruited to help manage patients.
People with too-high serum urate levels who agree to extra help are being referred to pharmacists empowered to order blood tests and allopurinol. Pharmacists contact patients by mail or phone, at first, and then maybe automated messages or emails, and educate them about why they need to lower their urate and how to do it. Pharmacists monitor lab results and titrate allopurinol as needed to hit serum urate levels of 6 mg/dL or less. The tune-up usually takes a year, at which point physicians resume ongoing management. The referring doctor is in the background to make sure everything goes okay.
It’s a simple, inexpensive approach that seems to help patients with a serious but notoriously undertreated condition. “It gives them the extra personal attention they might need. They appreciate the extra nudge most of the time,” said Kimberly Low, PharmD, the ambulatory pharmacist in an ongoing study of the approach at Kaiser Permanente Southern California in Pasadena (Contemp Clin Trials. 2016 Jul 20;50:106-15. doi: 10.1016/j.cct.2016.07.019).
“We need to deliver gout care in a more efficient way that doesn’t put it all on primary care,” where almost all gout is managed. “Pharmacy is a possible way to do that,” said Ted Mikuls, MD, a rheumatology professor at the University of Nebraska in Omaha, and senior investigator on the project. Results will be published soon.
The only randomized trial so far was published recently by Kaiser Permanente Northern California. The chance of hitting the 6-mg/dL mark at 6 months almost tripled when a pharmacist was involved. “The next step is to try to get a large-scale program funded using this model” at Kaiser, said lead investigator Robert Goldfien, MD, chair of the Chiefs of Rheumatology for the Permanente Medical Group in Richmond, Calif (Perm J. 2016 Jul 1;20[3]. doi: 10.7812/TPP/15-234).
Other places are turning to pharmacists, too, even when there isn’t a study involved. One of them is the San Diego Veterans Affairs Medical Center. It’s a “huge help; otherwise our clinic would be flooded with gout patients,” said rheumatologist Robert Terkeltaub, MD, who oversees the program.
Patients there are happy to have fewer flares and not to have to drive to the San Diego VA for blood draws; they go to a nearby clinic instead, and “we mail them their medications. We’ve had tremendous success” with pharmacists, and their “charges are affordable. We have treated hundreds of patients this way,” Dr. Terkeltaub said.
There doesn’t seem to be a downside. The only issue is how reimbursements will work. That’s not much of a problem when everyone is in the same health system and on the same electronic health record, with paychecks coming from the same place. Perhaps not surprisingly, large health systems are where the model is taking hold. How it could work with smaller practices and community pharmacists is unclear.
An obvious need
It’s no secret that gout care isn’t very good in the United States, or, really, anywhere else. Gout is a curable or at least imminently manageable condition with the right drugs for flares and lowering urate, but emergency department visits are up; hospitalizations for gout attacks have surpassed rheumatoid arthritis; and allopurinol dosing is routinely too low, if it’s prescribed at all.
Meanwhile, hyperuricemia has been linked to cardiovascular disease and other problems. Some now consider it part of the metabolic syndrome.
There are a lot of reasons why gout care is subpar, but one of them is that primary care providers are just too busy managing diabetes, hypertension, and other problems that seem more important in 10-minute office visits; that’s where pharmacists come in.
“They understand medications, drug-drug, and drug-herb interactions in a way that I don’t,” and also “have access, hopefully, to a more accurate picture of what patients take. I am all thumbs up for any involvement with pharmacists,” said Reid Blackwelder, MD, a recent president of the American Academy of Family Physicians and a family practice professor at East Tennessee State University in Mountain Home, where pharmacists are embedded in primary care.
Gout is a natural fit for pharmacy. Although the pharmacy-gout literature is thin, there have been plenty of reports about pharmacists improving outcomes, saving money, and increasing patient satisfaction when they help family practice and other doctors manage chronic problems. That’s one of the reasons why pharmacists are part of the primary care team in Mountain Home and other places that can afford them. Pharmacist-managed Coumadin clinics are the precedent.
“I think pharmacy is really excited about providing these types of services. Pharmacists managing gout patients is perfectly in line with what is going on now” in the field. “I can’t imagine how” outcomes “are not going to be positive,” said pharmacist Jan Hirsch, PhD, a professor of clinical pharmacy at the University of California, San Diego, where pharmacists are also on primary care teams.
Who’s going to pay?
No one wants a zero-sum game; physicians and pharmacists both need to be paid fairly for their services. The goal is collaborative care, not stealing patients.
Even so, the issue for a lot of primary care providers “will be who pays for this, and who doesn’t get paid when other people do this,” Dr. Blackwelder said.
One option outside of large health systems is for primary care practices to contract with a trusted local pharmacist to come in every few weeks to help with gout and other chronic problems.
Since they would be in the same office as the physician, family doctors could bill under their own name and split the payment with the pharmacist. “I would just contract with [pharmacists] personally,” Dr. Blackwelder said. “That way you don’t have to worry if the pharmacist” is considered “a provider or not” under Medicare Part B.
Meanwhile, Medicare Part D and some commercial plans reimburse for medication management, which is another option for pharmacist payments.
Additional options are likely to emerge, as well. “Payment models are evolving for pharmacists,” Dr. Hirsch said.
Dr. Mikuls disclosed pending research funding from AstraZeneca. Dr. Terkeltaub is a consultant for AstraZeneca, CymaBay, Revive, Relburn, and other companies.
Something new is being tried to improve gout outcomes in the United States: Pharmacists are being recruited to help manage patients.
People with too-high serum urate levels who agree to extra help are being referred to pharmacists empowered to order blood tests and allopurinol. Pharmacists contact patients by mail or phone, at first, and then maybe automated messages or emails, and educate them about why they need to lower their urate and how to do it. Pharmacists monitor lab results and titrate allopurinol as needed to hit serum urate levels of 6 mg/dL or less. The tune-up usually takes a year, at which point physicians resume ongoing management. The referring doctor is in the background to make sure everything goes okay.
It’s a simple, inexpensive approach that seems to help patients with a serious but notoriously undertreated condition. “It gives them the extra personal attention they might need. They appreciate the extra nudge most of the time,” said Kimberly Low, PharmD, the ambulatory pharmacist in an ongoing study of the approach at Kaiser Permanente Southern California in Pasadena (Contemp Clin Trials. 2016 Jul 20;50:106-15. doi: 10.1016/j.cct.2016.07.019).
“We need to deliver gout care in a more efficient way that doesn’t put it all on primary care,” where almost all gout is managed. “Pharmacy is a possible way to do that,” said Ted Mikuls, MD, a rheumatology professor at the University of Nebraska in Omaha, and senior investigator on the project. Results will be published soon.
The only randomized trial so far was published recently by Kaiser Permanente Northern California. The chance of hitting the 6-mg/dL mark at 6 months almost tripled when a pharmacist was involved. “The next step is to try to get a large-scale program funded using this model” at Kaiser, said lead investigator Robert Goldfien, MD, chair of the Chiefs of Rheumatology for the Permanente Medical Group in Richmond, Calif (Perm J. 2016 Jul 1;20[3]. doi: 10.7812/TPP/15-234).
Other places are turning to pharmacists, too, even when there isn’t a study involved. One of them is the San Diego Veterans Affairs Medical Center. It’s a “huge help; otherwise our clinic would be flooded with gout patients,” said rheumatologist Robert Terkeltaub, MD, who oversees the program.
Patients there are happy to have fewer flares and not to have to drive to the San Diego VA for blood draws; they go to a nearby clinic instead, and “we mail them their medications. We’ve had tremendous success” with pharmacists, and their “charges are affordable. We have treated hundreds of patients this way,” Dr. Terkeltaub said.
There doesn’t seem to be a downside. The only issue is how reimbursements will work. That’s not much of a problem when everyone is in the same health system and on the same electronic health record, with paychecks coming from the same place. Perhaps not surprisingly, large health systems are where the model is taking hold. How it could work with smaller practices and community pharmacists is unclear.
An obvious need
It’s no secret that gout care isn’t very good in the United States, or, really, anywhere else. Gout is a curable or at least imminently manageable condition with the right drugs for flares and lowering urate, but emergency department visits are up; hospitalizations for gout attacks have surpassed rheumatoid arthritis; and allopurinol dosing is routinely too low, if it’s prescribed at all.
Meanwhile, hyperuricemia has been linked to cardiovascular disease and other problems. Some now consider it part of the metabolic syndrome.
There are a lot of reasons why gout care is subpar, but one of them is that primary care providers are just too busy managing diabetes, hypertension, and other problems that seem more important in 10-minute office visits; that’s where pharmacists come in.
“They understand medications, drug-drug, and drug-herb interactions in a way that I don’t,” and also “have access, hopefully, to a more accurate picture of what patients take. I am all thumbs up for any involvement with pharmacists,” said Reid Blackwelder, MD, a recent president of the American Academy of Family Physicians and a family practice professor at East Tennessee State University in Mountain Home, where pharmacists are embedded in primary care.
Gout is a natural fit for pharmacy. Although the pharmacy-gout literature is thin, there have been plenty of reports about pharmacists improving outcomes, saving money, and increasing patient satisfaction when they help family practice and other doctors manage chronic problems. That’s one of the reasons why pharmacists are part of the primary care team in Mountain Home and other places that can afford them. Pharmacist-managed Coumadin clinics are the precedent.
“I think pharmacy is really excited about providing these types of services. Pharmacists managing gout patients is perfectly in line with what is going on now” in the field. “I can’t imagine how” outcomes “are not going to be positive,” said pharmacist Jan Hirsch, PhD, a professor of clinical pharmacy at the University of California, San Diego, where pharmacists are also on primary care teams.
Who’s going to pay?
No one wants a zero-sum game; physicians and pharmacists both need to be paid fairly for their services. The goal is collaborative care, not stealing patients.
Even so, the issue for a lot of primary care providers “will be who pays for this, and who doesn’t get paid when other people do this,” Dr. Blackwelder said.
One option outside of large health systems is for primary care practices to contract with a trusted local pharmacist to come in every few weeks to help with gout and other chronic problems.
Since they would be in the same office as the physician, family doctors could bill under their own name and split the payment with the pharmacist. “I would just contract with [pharmacists] personally,” Dr. Blackwelder said. “That way you don’t have to worry if the pharmacist” is considered “a provider or not” under Medicare Part B.
Meanwhile, Medicare Part D and some commercial plans reimburse for medication management, which is another option for pharmacist payments.
Additional options are likely to emerge, as well. “Payment models are evolving for pharmacists,” Dr. Hirsch said.
Dr. Mikuls disclosed pending research funding from AstraZeneca. Dr. Terkeltaub is a consultant for AstraZeneca, CymaBay, Revive, Relburn, and other companies.
Something new is being tried to improve gout outcomes in the United States: Pharmacists are being recruited to help manage patients.
People with too-high serum urate levels who agree to extra help are being referred to pharmacists empowered to order blood tests and allopurinol. Pharmacists contact patients by mail or phone, at first, and then maybe automated messages or emails, and educate them about why they need to lower their urate and how to do it. Pharmacists monitor lab results and titrate allopurinol as needed to hit serum urate levels of 6 mg/dL or less. The tune-up usually takes a year, at which point physicians resume ongoing management. The referring doctor is in the background to make sure everything goes okay.
It’s a simple, inexpensive approach that seems to help patients with a serious but notoriously undertreated condition. “It gives them the extra personal attention they might need. They appreciate the extra nudge most of the time,” said Kimberly Low, PharmD, the ambulatory pharmacist in an ongoing study of the approach at Kaiser Permanente Southern California in Pasadena (Contemp Clin Trials. 2016 Jul 20;50:106-15. doi: 10.1016/j.cct.2016.07.019).
“We need to deliver gout care in a more efficient way that doesn’t put it all on primary care,” where almost all gout is managed. “Pharmacy is a possible way to do that,” said Ted Mikuls, MD, a rheumatology professor at the University of Nebraska in Omaha, and senior investigator on the project. Results will be published soon.
The only randomized trial so far was published recently by Kaiser Permanente Northern California. The chance of hitting the 6-mg/dL mark at 6 months almost tripled when a pharmacist was involved. “The next step is to try to get a large-scale program funded using this model” at Kaiser, said lead investigator Robert Goldfien, MD, chair of the Chiefs of Rheumatology for the Permanente Medical Group in Richmond, Calif (Perm J. 2016 Jul 1;20[3]. doi: 10.7812/TPP/15-234).
Other places are turning to pharmacists, too, even when there isn’t a study involved. One of them is the San Diego Veterans Affairs Medical Center. It’s a “huge help; otherwise our clinic would be flooded with gout patients,” said rheumatologist Robert Terkeltaub, MD, who oversees the program.
Patients there are happy to have fewer flares and not to have to drive to the San Diego VA for blood draws; they go to a nearby clinic instead, and “we mail them their medications. We’ve had tremendous success” with pharmacists, and their “charges are affordable. We have treated hundreds of patients this way,” Dr. Terkeltaub said.
There doesn’t seem to be a downside. The only issue is how reimbursements will work. That’s not much of a problem when everyone is in the same health system and on the same electronic health record, with paychecks coming from the same place. Perhaps not surprisingly, large health systems are where the model is taking hold. How it could work with smaller practices and community pharmacists is unclear.
An obvious need
It’s no secret that gout care isn’t very good in the United States, or, really, anywhere else. Gout is a curable or at least imminently manageable condition with the right drugs for flares and lowering urate, but emergency department visits are up; hospitalizations for gout attacks have surpassed rheumatoid arthritis; and allopurinol dosing is routinely too low, if it’s prescribed at all.
Meanwhile, hyperuricemia has been linked to cardiovascular disease and other problems. Some now consider it part of the metabolic syndrome.
There are a lot of reasons why gout care is subpar, but one of them is that primary care providers are just too busy managing diabetes, hypertension, and other problems that seem more important in 10-minute office visits; that’s where pharmacists come in.
“They understand medications, drug-drug, and drug-herb interactions in a way that I don’t,” and also “have access, hopefully, to a more accurate picture of what patients take. I am all thumbs up for any involvement with pharmacists,” said Reid Blackwelder, MD, a recent president of the American Academy of Family Physicians and a family practice professor at East Tennessee State University in Mountain Home, where pharmacists are embedded in primary care.
Gout is a natural fit for pharmacy. Although the pharmacy-gout literature is thin, there have been plenty of reports about pharmacists improving outcomes, saving money, and increasing patient satisfaction when they help family practice and other doctors manage chronic problems. That’s one of the reasons why pharmacists are part of the primary care team in Mountain Home and other places that can afford them. Pharmacist-managed Coumadin clinics are the precedent.
“I think pharmacy is really excited about providing these types of services. Pharmacists managing gout patients is perfectly in line with what is going on now” in the field. “I can’t imagine how” outcomes “are not going to be positive,” said pharmacist Jan Hirsch, PhD, a professor of clinical pharmacy at the University of California, San Diego, where pharmacists are also on primary care teams.
Who’s going to pay?
No one wants a zero-sum game; physicians and pharmacists both need to be paid fairly for their services. The goal is collaborative care, not stealing patients.
Even so, the issue for a lot of primary care providers “will be who pays for this, and who doesn’t get paid when other people do this,” Dr. Blackwelder said.
One option outside of large health systems is for primary care practices to contract with a trusted local pharmacist to come in every few weeks to help with gout and other chronic problems.
Since they would be in the same office as the physician, family doctors could bill under their own name and split the payment with the pharmacist. “I would just contract with [pharmacists] personally,” Dr. Blackwelder said. “That way you don’t have to worry if the pharmacist” is considered “a provider or not” under Medicare Part B.
Meanwhile, Medicare Part D and some commercial plans reimburse for medication management, which is another option for pharmacist payments.
Additional options are likely to emerge, as well. “Payment models are evolving for pharmacists,” Dr. Hirsch said.
Dr. Mikuls disclosed pending research funding from AstraZeneca. Dr. Terkeltaub is a consultant for AstraZeneca, CymaBay, Revive, Relburn, and other companies.
When to consider an interventional approach to pain management
DEET and picaridin safely protect against insect bites
BOSTON – Insect repellents containing DEET or picaridin are safe when used properly, and are important for bite protection in children, according to Mercedes E. Gonzalez, MD.
Insect bite reactions are common in children aged 2-10 years, and the emergence of Zika virus raises new concerns about the dangers of mosquito bites, in particular; the World Health Organization has declared Zika-related effects – namely microcephaly and Guillain-Barré syndrome – to be a “public health emergency of international concern.”
In children, illness associated with Zika virus is generally mild, but can include fever, rash, conjunctivitis, and/or arthralgia, Dr. Gonzalez said at the American Academy of Dermatology summer meeting.
DEET, used since 1957, is effective against mosquitoes, black flies, ticks, mites, and land leeches. It works by forming a vapor barrier that deters insects from coming into contact with the skin. The barrier extends about 4 cm from the skin. DEET can also be used on clothing but may cause damage to spandex, rayon, acetate, and leather, and can dissolve plastic and vinyl.
Although it is available in concentrations of 5%-100%, concentrations of 10%-35% provide adequate protection in most situations, said Dr. Gonzalez of the University of Miami.
Animal studies using large doses have shown that DEET is not a specific neurotoxin, and while there have been case reports of central nervous system toxicity in humans, there is no link to DEET dose or mechanistic pathway. Reported deaths have involved intentional ingestion and overuse or incorrect use of products, she said.
In fact, safety concerns are so minimal that the Environmental Protection Agency removed labels indicating caution in children, and the American Academy of Pediatrics recommends the use of DEET for preventing insect bites in children older than age 2 months, and in pregnant and lactating women.
One DEET safety concern, however, is flammability. Both DEET and the aerosol vehicle used in some DEET-containing products, are flammable, so caution is warranted, she said. Occlusion following use of DEET should also be avoided as it can increase absorption, and the product should be washed off after use.
Picaridin is another insect repellent that, like DEET, forms a vapor barrier to deter insects from getting close to the skin and biting, and can be used on both the skin and clothing, but it does not damage plastics or fabrics.
It has similar efficacy as DEET, and has a number of advantages over DEET in that it is odorless and does not feel sticky or greasy when applied. It has not been reported to cause any serious toxicity or mutagenesis.
Picaridin – which is effective against mosquitoes, dog and deer ticks, chiggers, and flies – has been used in Australia since 1998, and in the United States since 2005. That year, the Centers for Disease Control and Prevention recommended that it be used to protect against West Nile virus, and the World Health Organization said it was the best agent for preventing malaria, Dr. Gonzalez noted.
“So when [patients] ask about the best insect repellent, for most situations I do recommend DEET or picaridin, at 10%-25% for DEET, or 7%-15% for picaridin,” she said. She encourages people to read labels, noting that the EPA is encouraging the use of “repellency awareness” labels on insect repellents to inform the consumer whether it prevents against mosquitoes and/or ticks, and for how long.
It helps to provide specific recommendations, providing pictures and circling those that are recommended. Selling the products in the office is also a good idea to make sure patients “leave with the right product,” she said.
Also, advise patients about what to avoid, such as products that contain blends of natural plant oils, which have been shown to be ineffective, providing less than an hour of protection, she said.
Dr. Gonzalez also advises against the use of combination insect repellent/sunscreen products. One reason is that sunscreen needs frequent reapplication, while insect repellent does not. Further, studies have demonstrated that using sunscreen over insect repellent dramatically increases the percutaneous absorption of DEET, and reduces the SPF of the sunscreen. If both are needed, sunscreen should be applied first to reduce transdermal penetration of the active insect repellent ingredient, and should be reapplied every 2 hours, she said.
“Proper insect repellent use is just one part of protection,” she added.
Other measures that should be encouraged include the use of protective clothing, such as light cotton long sleeves and pants; avoidance of clothing with bright colors or flowery prints; avoidance of scented soaps, perfumes, or hair spray; removal of mosquito habitats by eliminating any standing water, covering gaps in doors, using screens and nets; and, if possible, staying indoors at sunrise, sunset, and early evening when mosquitoes are most active.
Dr. Gonzalez noted that many free resources are available online, including a tool at the epa.gov site that helps in selection of an appropriate product for one’s specific needs.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
BOSTON – Insect repellents containing DEET or picaridin are safe when used properly, and are important for bite protection in children, according to Mercedes E. Gonzalez, MD.
Insect bite reactions are common in children aged 2-10 years, and the emergence of Zika virus raises new concerns about the dangers of mosquito bites, in particular; the World Health Organization has declared Zika-related effects – namely microcephaly and Guillain-Barré syndrome – to be a “public health emergency of international concern.”
In children, illness associated with Zika virus is generally mild, but can include fever, rash, conjunctivitis, and/or arthralgia, Dr. Gonzalez said at the American Academy of Dermatology summer meeting.
DEET, used since 1957, is effective against mosquitoes, black flies, ticks, mites, and land leeches. It works by forming a vapor barrier that deters insects from coming into contact with the skin. The barrier extends about 4 cm from the skin. DEET can also be used on clothing but may cause damage to spandex, rayon, acetate, and leather, and can dissolve plastic and vinyl.
Although it is available in concentrations of 5%-100%, concentrations of 10%-35% provide adequate protection in most situations, said Dr. Gonzalez of the University of Miami.
Animal studies using large doses have shown that DEET is not a specific neurotoxin, and while there have been case reports of central nervous system toxicity in humans, there is no link to DEET dose or mechanistic pathway. Reported deaths have involved intentional ingestion and overuse or incorrect use of products, she said.
In fact, safety concerns are so minimal that the Environmental Protection Agency removed labels indicating caution in children, and the American Academy of Pediatrics recommends the use of DEET for preventing insect bites in children older than age 2 months, and in pregnant and lactating women.
One DEET safety concern, however, is flammability. Both DEET and the aerosol vehicle used in some DEET-containing products, are flammable, so caution is warranted, she said. Occlusion following use of DEET should also be avoided as it can increase absorption, and the product should be washed off after use.
Picaridin is another insect repellent that, like DEET, forms a vapor barrier to deter insects from getting close to the skin and biting, and can be used on both the skin and clothing, but it does not damage plastics or fabrics.
It has similar efficacy as DEET, and has a number of advantages over DEET in that it is odorless and does not feel sticky or greasy when applied. It has not been reported to cause any serious toxicity or mutagenesis.
Picaridin – which is effective against mosquitoes, dog and deer ticks, chiggers, and flies – has been used in Australia since 1998, and in the United States since 2005. That year, the Centers for Disease Control and Prevention recommended that it be used to protect against West Nile virus, and the World Health Organization said it was the best agent for preventing malaria, Dr. Gonzalez noted.
“So when [patients] ask about the best insect repellent, for most situations I do recommend DEET or picaridin, at 10%-25% for DEET, or 7%-15% for picaridin,” she said. She encourages people to read labels, noting that the EPA is encouraging the use of “repellency awareness” labels on insect repellents to inform the consumer whether it prevents against mosquitoes and/or ticks, and for how long.
It helps to provide specific recommendations, providing pictures and circling those that are recommended. Selling the products in the office is also a good idea to make sure patients “leave with the right product,” she said.
Also, advise patients about what to avoid, such as products that contain blends of natural plant oils, which have been shown to be ineffective, providing less than an hour of protection, she said.
Dr. Gonzalez also advises against the use of combination insect repellent/sunscreen products. One reason is that sunscreen needs frequent reapplication, while insect repellent does not. Further, studies have demonstrated that using sunscreen over insect repellent dramatically increases the percutaneous absorption of DEET, and reduces the SPF of the sunscreen. If both are needed, sunscreen should be applied first to reduce transdermal penetration of the active insect repellent ingredient, and should be reapplied every 2 hours, she said.
“Proper insect repellent use is just one part of protection,” she added.
Other measures that should be encouraged include the use of protective clothing, such as light cotton long sleeves and pants; avoidance of clothing with bright colors or flowery prints; avoidance of scented soaps, perfumes, or hair spray; removal of mosquito habitats by eliminating any standing water, covering gaps in doors, using screens and nets; and, if possible, staying indoors at sunrise, sunset, and early evening when mosquitoes are most active.
Dr. Gonzalez noted that many free resources are available online, including a tool at the epa.gov site that helps in selection of an appropriate product for one’s specific needs.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
BOSTON – Insect repellents containing DEET or picaridin are safe when used properly, and are important for bite protection in children, according to Mercedes E. Gonzalez, MD.
Insect bite reactions are common in children aged 2-10 years, and the emergence of Zika virus raises new concerns about the dangers of mosquito bites, in particular; the World Health Organization has declared Zika-related effects – namely microcephaly and Guillain-Barré syndrome – to be a “public health emergency of international concern.”
In children, illness associated with Zika virus is generally mild, but can include fever, rash, conjunctivitis, and/or arthralgia, Dr. Gonzalez said at the American Academy of Dermatology summer meeting.
DEET, used since 1957, is effective against mosquitoes, black flies, ticks, mites, and land leeches. It works by forming a vapor barrier that deters insects from coming into contact with the skin. The barrier extends about 4 cm from the skin. DEET can also be used on clothing but may cause damage to spandex, rayon, acetate, and leather, and can dissolve plastic and vinyl.
Although it is available in concentrations of 5%-100%, concentrations of 10%-35% provide adequate protection in most situations, said Dr. Gonzalez of the University of Miami.
Animal studies using large doses have shown that DEET is not a specific neurotoxin, and while there have been case reports of central nervous system toxicity in humans, there is no link to DEET dose or mechanistic pathway. Reported deaths have involved intentional ingestion and overuse or incorrect use of products, she said.
In fact, safety concerns are so minimal that the Environmental Protection Agency removed labels indicating caution in children, and the American Academy of Pediatrics recommends the use of DEET for preventing insect bites in children older than age 2 months, and in pregnant and lactating women.
One DEET safety concern, however, is flammability. Both DEET and the aerosol vehicle used in some DEET-containing products, are flammable, so caution is warranted, she said. Occlusion following use of DEET should also be avoided as it can increase absorption, and the product should be washed off after use.
Picaridin is another insect repellent that, like DEET, forms a vapor barrier to deter insects from getting close to the skin and biting, and can be used on both the skin and clothing, but it does not damage plastics or fabrics.
It has similar efficacy as DEET, and has a number of advantages over DEET in that it is odorless and does not feel sticky or greasy when applied. It has not been reported to cause any serious toxicity or mutagenesis.
Picaridin – which is effective against mosquitoes, dog and deer ticks, chiggers, and flies – has been used in Australia since 1998, and in the United States since 2005. That year, the Centers for Disease Control and Prevention recommended that it be used to protect against West Nile virus, and the World Health Organization said it was the best agent for preventing malaria, Dr. Gonzalez noted.
“So when [patients] ask about the best insect repellent, for most situations I do recommend DEET or picaridin, at 10%-25% for DEET, or 7%-15% for picaridin,” she said. She encourages people to read labels, noting that the EPA is encouraging the use of “repellency awareness” labels on insect repellents to inform the consumer whether it prevents against mosquitoes and/or ticks, and for how long.
It helps to provide specific recommendations, providing pictures and circling those that are recommended. Selling the products in the office is also a good idea to make sure patients “leave with the right product,” she said.
Also, advise patients about what to avoid, such as products that contain blends of natural plant oils, which have been shown to be ineffective, providing less than an hour of protection, she said.
Dr. Gonzalez also advises against the use of combination insect repellent/sunscreen products. One reason is that sunscreen needs frequent reapplication, while insect repellent does not. Further, studies have demonstrated that using sunscreen over insect repellent dramatically increases the percutaneous absorption of DEET, and reduces the SPF of the sunscreen. If both are needed, sunscreen should be applied first to reduce transdermal penetration of the active insect repellent ingredient, and should be reapplied every 2 hours, she said.
“Proper insect repellent use is just one part of protection,” she added.
Other measures that should be encouraged include the use of protective clothing, such as light cotton long sleeves and pants; avoidance of clothing with bright colors or flowery prints; avoidance of scented soaps, perfumes, or hair spray; removal of mosquito habitats by eliminating any standing water, covering gaps in doors, using screens and nets; and, if possible, staying indoors at sunrise, sunset, and early evening when mosquitoes are most active.
Dr. Gonzalez noted that many free resources are available online, including a tool at the epa.gov site that helps in selection of an appropriate product for one’s specific needs.
Dr. Gonzalez reported serving as a speaker and/or advisory board member and receiving honoraria from Pierre Fabre Dermatologie, Anacor Pharmaceuticals, Encore Dermatology, and PuraCap Pharmaceutical.
EXPERT ANALYSIS FROM AAD SUMMER ACADEMY 2016