User login
EC approves long-acting hemophilia B therapy

The European Commission (EC) has approved albutrepenonacog alfa (Idelvion) to treat and prevent bleeding in children and adults with hemophilia B.
Albutrepenonacog alfa is a long-acting albumin fusion protein linking recombinant coagulation factor IX with recombinant albumin.
The product is now approved for use as routine prophylaxis, for on-demand control of bleeding, and for the perioperative management of bleeding.
Appropriate patients age 12 and older can go up to 14 days between albutrepenonacog alfa infusions. This dosing interval has been achieved while maintaining high levels of factor IX activity—above 5% over 14 days at 75 IU/kg.
“Offering 14-day dosing, Idelvion helps patients maintain higher factor IX levels over a long period of time, providing them with greater freedom from frequent infusions,” said Elena Santagostino, MD, PhD, of the University of Milan/IRCCS Maggiore Hospital in Italy.
“This is an important attribute for my patients who require a prophylactic regimen but don’t want treatment to disrupt their active lives.”
Albutrepenonacog alfa is being developed by CSL Behring. The company said the product will be launched in European markets in the coming months, as market access and pricing are obtained.
Phase 3 trial
The EC approved albutrepenonacog alfa based on results of the PROLONG-9FP clinical development program. PROLONG-9FP includes phase 1, 2, and 3 studies evaluating the safety and efficacy of albutrepenonacog alfa in adults and children (ages 1 to 61) with hemophilia B.
Data from the phase 3 study were recently published in Blood. This study included 63 previously treated male patients with severe hemophilia B. They had a mean age of 33 (range, 12 to 61).
The patients were divided into 2 groups. Group 1 (n=40) received routine prophylaxis with albutrepenonacog alfa once every 7 days for 26 weeks,
followed by a 7-, 10-, or 14-day prophylaxis regimen for a mean of 50, 38, or 51 weeks, respectively.
Group 2 received on-demand treatment with albutrepenonacog alfa for bleeding episodes for 26 weeks (n=23) and then switched to a 7-day prophylaxis regimen for a mean of 45 weeks (n=19).
The median annualized bleeding rate (ABR) was 2.0 in the prophylaxis arm (group 1) and 23.5 in the on-demand treatment arm (group 2). The median spontaneous ABRs were 0.0 and 17.0, respectively.
For patients in group 2, there was a significant reduction in median ABRs when patients switched from on-demand treatment to prophylaxis—19.22 and 1.58, respectively (P<0.0001). And there was a significant reduction in median spontaneous ABRs—15.43 and 0.00, respectively (P<0.0001).
Overall, 98.6% of bleeding episodes were treated successfully, including 93.6% that were treated with a single injection of albutrepenonacog alfa.
None of the patients developed inhibitors or experienced thromboembolic events, anaphylaxis, or life-threatening adverse events (AEs).
There were 347 treatment-emergent AEs reported in 54 (85.7%) patients. The most common were nasopharyngitis (25.4%), headache (23.8%), arthralgia (4.3%), and influenza (11.1%).
Eleven mild/moderate AEs in 5 patients (7.9%) were considered possibly related to albutrepenonacog alfa. Two patients discontinued treatment due to AEs—1 with hypersensitivity and 1 with headache. ![]()

The European Commission (EC) has approved albutrepenonacog alfa (Idelvion) to treat and prevent bleeding in children and adults with hemophilia B.
Albutrepenonacog alfa is a long-acting albumin fusion protein linking recombinant coagulation factor IX with recombinant albumin.
The product is now approved for use as routine prophylaxis, for on-demand control of bleeding, and for the perioperative management of bleeding.
Appropriate patients age 12 and older can go up to 14 days between albutrepenonacog alfa infusions. This dosing interval has been achieved while maintaining high levels of factor IX activity—above 5% over 14 days at 75 IU/kg.
“Offering 14-day dosing, Idelvion helps patients maintain higher factor IX levels over a long period of time, providing them with greater freedom from frequent infusions,” said Elena Santagostino, MD, PhD, of the University of Milan/IRCCS Maggiore Hospital in Italy.
“This is an important attribute for my patients who require a prophylactic regimen but don’t want treatment to disrupt their active lives.”
Albutrepenonacog alfa is being developed by CSL Behring. The company said the product will be launched in European markets in the coming months, as market access and pricing are obtained.
Phase 3 trial
The EC approved albutrepenonacog alfa based on results of the PROLONG-9FP clinical development program. PROLONG-9FP includes phase 1, 2, and 3 studies evaluating the safety and efficacy of albutrepenonacog alfa in adults and children (ages 1 to 61) with hemophilia B.
Data from the phase 3 study were recently published in Blood. This study included 63 previously treated male patients with severe hemophilia B. They had a mean age of 33 (range, 12 to 61).
The patients were divided into 2 groups. Group 1 (n=40) received routine prophylaxis with albutrepenonacog alfa once every 7 days for 26 weeks,
followed by a 7-, 10-, or 14-day prophylaxis regimen for a mean of 50, 38, or 51 weeks, respectively.
Group 2 received on-demand treatment with albutrepenonacog alfa for bleeding episodes for 26 weeks (n=23) and then switched to a 7-day prophylaxis regimen for a mean of 45 weeks (n=19).
The median annualized bleeding rate (ABR) was 2.0 in the prophylaxis arm (group 1) and 23.5 in the on-demand treatment arm (group 2). The median spontaneous ABRs were 0.0 and 17.0, respectively.
For patients in group 2, there was a significant reduction in median ABRs when patients switched from on-demand treatment to prophylaxis—19.22 and 1.58, respectively (P<0.0001). And there was a significant reduction in median spontaneous ABRs—15.43 and 0.00, respectively (P<0.0001).
Overall, 98.6% of bleeding episodes were treated successfully, including 93.6% that were treated with a single injection of albutrepenonacog alfa.
None of the patients developed inhibitors or experienced thromboembolic events, anaphylaxis, or life-threatening adverse events (AEs).
There were 347 treatment-emergent AEs reported in 54 (85.7%) patients. The most common were nasopharyngitis (25.4%), headache (23.8%), arthralgia (4.3%), and influenza (11.1%).
Eleven mild/moderate AEs in 5 patients (7.9%) were considered possibly related to albutrepenonacog alfa. Two patients discontinued treatment due to AEs—1 with hypersensitivity and 1 with headache. ![]()

The European Commission (EC) has approved albutrepenonacog alfa (Idelvion) to treat and prevent bleeding in children and adults with hemophilia B.
Albutrepenonacog alfa is a long-acting albumin fusion protein linking recombinant coagulation factor IX with recombinant albumin.
The product is now approved for use as routine prophylaxis, for on-demand control of bleeding, and for the perioperative management of bleeding.
Appropriate patients age 12 and older can go up to 14 days between albutrepenonacog alfa infusions. This dosing interval has been achieved while maintaining high levels of factor IX activity—above 5% over 14 days at 75 IU/kg.
“Offering 14-day dosing, Idelvion helps patients maintain higher factor IX levels over a long period of time, providing them with greater freedom from frequent infusions,” said Elena Santagostino, MD, PhD, of the University of Milan/IRCCS Maggiore Hospital in Italy.
“This is an important attribute for my patients who require a prophylactic regimen but don’t want treatment to disrupt their active lives.”
Albutrepenonacog alfa is being developed by CSL Behring. The company said the product will be launched in European markets in the coming months, as market access and pricing are obtained.
Phase 3 trial
The EC approved albutrepenonacog alfa based on results of the PROLONG-9FP clinical development program. PROLONG-9FP includes phase 1, 2, and 3 studies evaluating the safety and efficacy of albutrepenonacog alfa in adults and children (ages 1 to 61) with hemophilia B.
Data from the phase 3 study were recently published in Blood. This study included 63 previously treated male patients with severe hemophilia B. They had a mean age of 33 (range, 12 to 61).
The patients were divided into 2 groups. Group 1 (n=40) received routine prophylaxis with albutrepenonacog alfa once every 7 days for 26 weeks,
followed by a 7-, 10-, or 14-day prophylaxis regimen for a mean of 50, 38, or 51 weeks, respectively.
Group 2 received on-demand treatment with albutrepenonacog alfa for bleeding episodes for 26 weeks (n=23) and then switched to a 7-day prophylaxis regimen for a mean of 45 weeks (n=19).
The median annualized bleeding rate (ABR) was 2.0 in the prophylaxis arm (group 1) and 23.5 in the on-demand treatment arm (group 2). The median spontaneous ABRs were 0.0 and 17.0, respectively.
For patients in group 2, there was a significant reduction in median ABRs when patients switched from on-demand treatment to prophylaxis—19.22 and 1.58, respectively (P<0.0001). And there was a significant reduction in median spontaneous ABRs—15.43 and 0.00, respectively (P<0.0001).
Overall, 98.6% of bleeding episodes were treated successfully, including 93.6% that were treated with a single injection of albutrepenonacog alfa.
None of the patients developed inhibitors or experienced thromboembolic events, anaphylaxis, or life-threatening adverse events (AEs).
There were 347 treatment-emergent AEs reported in 54 (85.7%) patients. The most common were nasopharyngitis (25.4%), headache (23.8%), arthralgia (4.3%), and influenza (11.1%).
Eleven mild/moderate AEs in 5 patients (7.9%) were considered possibly related to albutrepenonacog alfa. Two patients discontinued treatment due to AEs—1 with hypersensitivity and 1 with headache. ![]()
Clinical Trials Update
Are you a clinical trials investigator with unused capacity? Would you like to refer patients to participate in groundbreaking clinical trials?
The CHEST Clinical Trials Registry is a free service that connects physicians to information about clinical trials in respiratory disease conducted by participating pharmaceutical companies.
Ongoing groundbreaking research could have a measurable impact on patient care, but a lack of clinical trial participants is significantly slowing research and threatening the development of new treatments. Recruiting and retaining trial participants are the greatest challenges to developing the next generation of treatment options.
Participation in clinical trials provides an opportunity to advance and accelerate medical research and contribute to an improved health outlook for future generations. Use our registry to get immediate information on how you can be involved in a clinical trial.
Access to learn more: chestnet.org/Guidelines-and-Resources/Clinical-Trials/Clinical-Trials-Registry.
Are you a clinical trials investigator with unused capacity? Would you like to refer patients to participate in groundbreaking clinical trials?
The CHEST Clinical Trials Registry is a free service that connects physicians to information about clinical trials in respiratory disease conducted by participating pharmaceutical companies.
Ongoing groundbreaking research could have a measurable impact on patient care, but a lack of clinical trial participants is significantly slowing research and threatening the development of new treatments. Recruiting and retaining trial participants are the greatest challenges to developing the next generation of treatment options.
Participation in clinical trials provides an opportunity to advance and accelerate medical research and contribute to an improved health outlook for future generations. Use our registry to get immediate information on how you can be involved in a clinical trial.
Access to learn more: chestnet.org/Guidelines-and-Resources/Clinical-Trials/Clinical-Trials-Registry.
Are you a clinical trials investigator with unused capacity? Would you like to refer patients to participate in groundbreaking clinical trials?
The CHEST Clinical Trials Registry is a free service that connects physicians to information about clinical trials in respiratory disease conducted by participating pharmaceutical companies.
Ongoing groundbreaking research could have a measurable impact on patient care, but a lack of clinical trial participants is significantly slowing research and threatening the development of new treatments. Recruiting and retaining trial participants are the greatest challenges to developing the next generation of treatment options.
Participation in clinical trials provides an opportunity to advance and accelerate medical research and contribute to an improved health outlook for future generations. Use our registry to get immediate information on how you can be involved in a clinical trial.
Access to learn more: chestnet.org/Guidelines-and-Resources/Clinical-Trials/Clinical-Trials-Registry.
In Memoriam
Lawrence H. Cohn, MD, FCCP, a past president of the American College of Chest Physicians (1986-1987), pioneering cardiac surgeon and devoted educator, former chief of the Division of Cardiac Surgery at Brigham and Women’s Hospital, and the Virginia and James Hubbard Chair in Cardiac Surgery at Harvard Medical School, died Jan. 9, 2016. An internationally renowned surgeon, he was a pioneer in minimally invasive procedures to fix heart valves.
He aso performed more than 11,000 cardiac surgeries, including being part of the team for New England’s first heart transplant, which took place at the Brigham hospital. Dr. Cohn published more than 500 peer-reviewed publications, 105 book chapters, and 12 books, including four editions of “Cardiac Surgery in the Adult.” CHEST extends its heartfelt condolences to the entire Cohn family.
Lawrence H. Cohn, MD, FCCP, a past president of the American College of Chest Physicians (1986-1987), pioneering cardiac surgeon and devoted educator, former chief of the Division of Cardiac Surgery at Brigham and Women’s Hospital, and the Virginia and James Hubbard Chair in Cardiac Surgery at Harvard Medical School, died Jan. 9, 2016. An internationally renowned surgeon, he was a pioneer in minimally invasive procedures to fix heart valves.
He aso performed more than 11,000 cardiac surgeries, including being part of the team for New England’s first heart transplant, which took place at the Brigham hospital. Dr. Cohn published more than 500 peer-reviewed publications, 105 book chapters, and 12 books, including four editions of “Cardiac Surgery in the Adult.” CHEST extends its heartfelt condolences to the entire Cohn family.
Lawrence H. Cohn, MD, FCCP, a past president of the American College of Chest Physicians (1986-1987), pioneering cardiac surgeon and devoted educator, former chief of the Division of Cardiac Surgery at Brigham and Women’s Hospital, and the Virginia and James Hubbard Chair in Cardiac Surgery at Harvard Medical School, died Jan. 9, 2016. An internationally renowned surgeon, he was a pioneer in minimally invasive procedures to fix heart valves.
He aso performed more than 11,000 cardiac surgeries, including being part of the team for New England’s first heart transplant, which took place at the Brigham hospital. Dr. Cohn published more than 500 peer-reviewed publications, 105 book chapters, and 12 books, including four editions of “Cardiac Surgery in the Adult.” CHEST extends its heartfelt condolences to the entire Cohn family.
President’s Report Who’s Running the Show?
Dr. Barbara Phillips, MSPH, FCCP
CHEST President 2015-2016
Nancy MacRae
Senior Vice President, Governance and Operations
Jenny Nemkovich, CAE
Chief Strategy Officer, Executive Office
Ever wonder how decisions get made and work gets done at CHEST? It all starts with our strategic plan (www.chestnet.org/About/Overview/Strategic-Plan), which was developed by the Board of Regents and other key stakeholders. The development of the strategic plan was informed by our vision to be the global leader in advancing best patient outcomes through innovative chest medicine, education, clinical research, and team-based care, as well as our mission and values. As a result of our strategic planning, CHEST is all about clinical education, which is our “hedgehog,” in organization-speak (1), but we also have goals in guideline development, global impact, membership recruitment and retention, and (of course) fiscal health. We follow progress toward our goals with measurable, relevant key performance indicators (KPIs), and the board reviews progress toward KPIs and goals at nearly every meeting, making recommendations for adjustments, as needed.
But how do decisions get made? CHEST volunteer and staff leadership work together to initiate and execute projects consistent with our plan and respond to requests from others to explore collaborative opportunities to advance our goals.
An example of a process that was initiated by leadership was the development of our new membership model. The Community and Engagement Work Group, along with key staff and other stakeholders, reviewed environmental scans, their personal knowledge and situations, and data from surveys of CHEST members, as well as association trends. They then proposed a new membership model to the Board of Regents (BoR). The BoR reviewed the proposal, along with other important information, and expressed concerns about several key constituent groups, such as global members and members in training, along with several other issues. In fact, the BoR sent the proposal back to the Work Group. Twice. As with any new project, the BoR makes a concerted effort to focus on the strategic plan in these types of deliberations and was guided particularly by the strategy to “optimize new membership model to increase engagement of all clinicians on the health-care team.” The final proposal, implemented in May 2015, truly reflects input and concerns from the BoR, key staff, the Membership Committee, and those CHEST members who responded to the surveys.
An example of a request by another organization to sign on, endorse, cosponsor, or otherwise support a guideline or project is the Campaign for Tobacco-Free Kids contacting us asking us to sign on to a letter to all members of the United States Senate and House of Representatives supporting the tobacco control measure included in the Trans-Pacific Partnership (TPP) trade agreement. The provision will protect the rights of nations participating in the TPP to adopt public health measures that reduce tobacco use without fear of facing lengthy and expensive trade disputes under the TPP initiated by tobacco companies.
Our process in these situations is to gather as much input as possible from CHEST members and experts. Again, using our strategic plan as guidance, in this specific instance, we are expanding our global impact, using targeted strategic alliances, so the decision was made to support this initiative. The CHEST name and brand are valuable assets, and we take endorsement of any project or document very seriously.
Key to our organizational success is our outstanding volunteer/staff partnership that fosters teamwork in translating the strategic vision, mission, and goals of the organization, engaging in a deliberative process that considers organizational history, data, trends, and expert opinion – all to help inform leadership in its decision-making. This collaboration between our content experts and our association professionals is a huge asset to our organization and one that will continue to propel CHEST to achieve our goals.
1. Collins J. Good to Great and the Social Sectors: A Monograph to Accompany Good to Great. New York, NY: HarperCollins Publishers; 2005.
Dr. Barbara Phillips, MSPH, FCCP
CHEST President 2015-2016
Nancy MacRae
Senior Vice President, Governance and Operations
Jenny Nemkovich, CAE
Chief Strategy Officer, Executive Office
Ever wonder how decisions get made and work gets done at CHEST? It all starts with our strategic plan (www.chestnet.org/About/Overview/Strategic-Plan), which was developed by the Board of Regents and other key stakeholders. The development of the strategic plan was informed by our vision to be the global leader in advancing best patient outcomes through innovative chest medicine, education, clinical research, and team-based care, as well as our mission and values. As a result of our strategic planning, CHEST is all about clinical education, which is our “hedgehog,” in organization-speak (1), but we also have goals in guideline development, global impact, membership recruitment and retention, and (of course) fiscal health. We follow progress toward our goals with measurable, relevant key performance indicators (KPIs), and the board reviews progress toward KPIs and goals at nearly every meeting, making recommendations for adjustments, as needed.
But how do decisions get made? CHEST volunteer and staff leadership work together to initiate and execute projects consistent with our plan and respond to requests from others to explore collaborative opportunities to advance our goals.
An example of a process that was initiated by leadership was the development of our new membership model. The Community and Engagement Work Group, along with key staff and other stakeholders, reviewed environmental scans, their personal knowledge and situations, and data from surveys of CHEST members, as well as association trends. They then proposed a new membership model to the Board of Regents (BoR). The BoR reviewed the proposal, along with other important information, and expressed concerns about several key constituent groups, such as global members and members in training, along with several other issues. In fact, the BoR sent the proposal back to the Work Group. Twice. As with any new project, the BoR makes a concerted effort to focus on the strategic plan in these types of deliberations and was guided particularly by the strategy to “optimize new membership model to increase engagement of all clinicians on the health-care team.” The final proposal, implemented in May 2015, truly reflects input and concerns from the BoR, key staff, the Membership Committee, and those CHEST members who responded to the surveys.
An example of a request by another organization to sign on, endorse, cosponsor, or otherwise support a guideline or project is the Campaign for Tobacco-Free Kids contacting us asking us to sign on to a letter to all members of the United States Senate and House of Representatives supporting the tobacco control measure included in the Trans-Pacific Partnership (TPP) trade agreement. The provision will protect the rights of nations participating in the TPP to adopt public health measures that reduce tobacco use without fear of facing lengthy and expensive trade disputes under the TPP initiated by tobacco companies.
Our process in these situations is to gather as much input as possible from CHEST members and experts. Again, using our strategic plan as guidance, in this specific instance, we are expanding our global impact, using targeted strategic alliances, so the decision was made to support this initiative. The CHEST name and brand are valuable assets, and we take endorsement of any project or document very seriously.
Key to our organizational success is our outstanding volunteer/staff partnership that fosters teamwork in translating the strategic vision, mission, and goals of the organization, engaging in a deliberative process that considers organizational history, data, trends, and expert opinion – all to help inform leadership in its decision-making. This collaboration between our content experts and our association professionals is a huge asset to our organization and one that will continue to propel CHEST to achieve our goals.
1. Collins J. Good to Great and the Social Sectors: A Monograph to Accompany Good to Great. New York, NY: HarperCollins Publishers; 2005.
Dr. Barbara Phillips, MSPH, FCCP
CHEST President 2015-2016
Nancy MacRae
Senior Vice President, Governance and Operations
Jenny Nemkovich, CAE
Chief Strategy Officer, Executive Office
Ever wonder how decisions get made and work gets done at CHEST? It all starts with our strategic plan (www.chestnet.org/About/Overview/Strategic-Plan), which was developed by the Board of Regents and other key stakeholders. The development of the strategic plan was informed by our vision to be the global leader in advancing best patient outcomes through innovative chest medicine, education, clinical research, and team-based care, as well as our mission and values. As a result of our strategic planning, CHEST is all about clinical education, which is our “hedgehog,” in organization-speak (1), but we also have goals in guideline development, global impact, membership recruitment and retention, and (of course) fiscal health. We follow progress toward our goals with measurable, relevant key performance indicators (KPIs), and the board reviews progress toward KPIs and goals at nearly every meeting, making recommendations for adjustments, as needed.
But how do decisions get made? CHEST volunteer and staff leadership work together to initiate and execute projects consistent with our plan and respond to requests from others to explore collaborative opportunities to advance our goals.
An example of a process that was initiated by leadership was the development of our new membership model. The Community and Engagement Work Group, along with key staff and other stakeholders, reviewed environmental scans, their personal knowledge and situations, and data from surveys of CHEST members, as well as association trends. They then proposed a new membership model to the Board of Regents (BoR). The BoR reviewed the proposal, along with other important information, and expressed concerns about several key constituent groups, such as global members and members in training, along with several other issues. In fact, the BoR sent the proposal back to the Work Group. Twice. As with any new project, the BoR makes a concerted effort to focus on the strategic plan in these types of deliberations and was guided particularly by the strategy to “optimize new membership model to increase engagement of all clinicians on the health-care team.” The final proposal, implemented in May 2015, truly reflects input and concerns from the BoR, key staff, the Membership Committee, and those CHEST members who responded to the surveys.
An example of a request by another organization to sign on, endorse, cosponsor, or otherwise support a guideline or project is the Campaign for Tobacco-Free Kids contacting us asking us to sign on to a letter to all members of the United States Senate and House of Representatives supporting the tobacco control measure included in the Trans-Pacific Partnership (TPP) trade agreement. The provision will protect the rights of nations participating in the TPP to adopt public health measures that reduce tobacco use without fear of facing lengthy and expensive trade disputes under the TPP initiated by tobacco companies.
Our process in these situations is to gather as much input as possible from CHEST members and experts. Again, using our strategic plan as guidance, in this specific instance, we are expanding our global impact, using targeted strategic alliances, so the decision was made to support this initiative. The CHEST name and brand are valuable assets, and we take endorsement of any project or document very seriously.
Key to our organizational success is our outstanding volunteer/staff partnership that fosters teamwork in translating the strategic vision, mission, and goals of the organization, engaging in a deliberative process that considers organizational history, data, trends, and expert opinion – all to help inform leadership in its decision-making. This collaboration between our content experts and our association professionals is a huge asset to our organization and one that will continue to propel CHEST to achieve our goals.
1. Collins J. Good to Great and the Social Sectors: A Monograph to Accompany Good to Great. New York, NY: HarperCollins Publishers; 2005.
CHEST announces a historic collaboration
The American College of Chest Physicians (CHEST) and the Chinese Association of Chest Physicians (CACP), the respiratory arm of the Chinese Medical Doctor Association (CMDA), have signed an exclusive agreement to collaborate on expanding China’s first-ever fellowship training program, providing clinical education in pulmonary and critical care medicine (PCCM) for Chinese physicians.
This historic announcement came during the opening session of CHEST World Congress 2016 in Shanghai, where approximately 2,000 health care professionals gathered for a 3-day event aimed at connecting clinicians from the United States, China, and around the world for hands-on clinical education in pulmonary, critical care, and sleep medicine. Among those in attendance were fellows and faculty from the 12 institutions that participated in the inaugural offering of the China-CHEST PCCM program, which was developed and implemented over the past 4 years and is expected to grow to dozens of institutions over the next several years.
Since 2012, CHEST has worked with the Chinese Thoracic Society on the development of China’s first fellowship program, offering standardized training in PCCM for Chinese physicians. As a result of these collective efforts, PCCM has now officially earned recognition as a medical subspecialty by the Chinese Ministry of Health – the first subspecialty of its kind in a country where medical training typically ends after a physician completes residency training. Only a decade ago, physicians in China went directly into practice following medical school. The development of a PCCM subspecialty in China – made possible through the engagement of CHEST’s expert faculty and administration – parallels what has occurred over the past 3 decades in the United States, during which the fields of pulmonary and critical care medicine evolved into the combined subspecialty of PCCM.
Through their groundbreaking collaboration announced today, CHEST and the CACP have committed to working exclusively as partners in continuing to advance the PCCM subspecialty in China to improve patient care, expand in-depth clinical training for Chinese physicians, and develop a growing force of expert Chinese faculty. The goal of such training is to ensure that patients receive the best possible care from Chinese physicians who complete the China-CHEST PCCM fellowship program.
“Recognition by the Chinese Ministry of Health of PCCM as this country’s first-ever physician subspecialty is welcomed acknowledgment that we’re making tremendous headway in advancing physician fellowship training in China,” said Barbara Phillips, MD, MPH, FCCP, President of the American College of Chest Physicians. “We are proud to join collaborative partners like the CMDA in these cooperative efforts to prepare Chinese physicians in the PCCM subspecialty, partnering in this historic effort to drive immeasurable improvements in clinical training and the delivery of patient care.”
The American College of Chest Physicians (CHEST) and the Chinese Association of Chest Physicians (CACP), the respiratory arm of the Chinese Medical Doctor Association (CMDA), have signed an exclusive agreement to collaborate on expanding China’s first-ever fellowship training program, providing clinical education in pulmonary and critical care medicine (PCCM) for Chinese physicians.
This historic announcement came during the opening session of CHEST World Congress 2016 in Shanghai, where approximately 2,000 health care professionals gathered for a 3-day event aimed at connecting clinicians from the United States, China, and around the world for hands-on clinical education in pulmonary, critical care, and sleep medicine. Among those in attendance were fellows and faculty from the 12 institutions that participated in the inaugural offering of the China-CHEST PCCM program, which was developed and implemented over the past 4 years and is expected to grow to dozens of institutions over the next several years.
Since 2012, CHEST has worked with the Chinese Thoracic Society on the development of China’s first fellowship program, offering standardized training in PCCM for Chinese physicians. As a result of these collective efforts, PCCM has now officially earned recognition as a medical subspecialty by the Chinese Ministry of Health – the first subspecialty of its kind in a country where medical training typically ends after a physician completes residency training. Only a decade ago, physicians in China went directly into practice following medical school. The development of a PCCM subspecialty in China – made possible through the engagement of CHEST’s expert faculty and administration – parallels what has occurred over the past 3 decades in the United States, during which the fields of pulmonary and critical care medicine evolved into the combined subspecialty of PCCM.
Through their groundbreaking collaboration announced today, CHEST and the CACP have committed to working exclusively as partners in continuing to advance the PCCM subspecialty in China to improve patient care, expand in-depth clinical training for Chinese physicians, and develop a growing force of expert Chinese faculty. The goal of such training is to ensure that patients receive the best possible care from Chinese physicians who complete the China-CHEST PCCM fellowship program.
“Recognition by the Chinese Ministry of Health of PCCM as this country’s first-ever physician subspecialty is welcomed acknowledgment that we’re making tremendous headway in advancing physician fellowship training in China,” said Barbara Phillips, MD, MPH, FCCP, President of the American College of Chest Physicians. “We are proud to join collaborative partners like the CMDA in these cooperative efforts to prepare Chinese physicians in the PCCM subspecialty, partnering in this historic effort to drive immeasurable improvements in clinical training and the delivery of patient care.”
The American College of Chest Physicians (CHEST) and the Chinese Association of Chest Physicians (CACP), the respiratory arm of the Chinese Medical Doctor Association (CMDA), have signed an exclusive agreement to collaborate on expanding China’s first-ever fellowship training program, providing clinical education in pulmonary and critical care medicine (PCCM) for Chinese physicians.
This historic announcement came during the opening session of CHEST World Congress 2016 in Shanghai, where approximately 2,000 health care professionals gathered for a 3-day event aimed at connecting clinicians from the United States, China, and around the world for hands-on clinical education in pulmonary, critical care, and sleep medicine. Among those in attendance were fellows and faculty from the 12 institutions that participated in the inaugural offering of the China-CHEST PCCM program, which was developed and implemented over the past 4 years and is expected to grow to dozens of institutions over the next several years.
Since 2012, CHEST has worked with the Chinese Thoracic Society on the development of China’s first fellowship program, offering standardized training in PCCM for Chinese physicians. As a result of these collective efforts, PCCM has now officially earned recognition as a medical subspecialty by the Chinese Ministry of Health – the first subspecialty of its kind in a country where medical training typically ends after a physician completes residency training. Only a decade ago, physicians in China went directly into practice following medical school. The development of a PCCM subspecialty in China – made possible through the engagement of CHEST’s expert faculty and administration – parallels what has occurred over the past 3 decades in the United States, during which the fields of pulmonary and critical care medicine evolved into the combined subspecialty of PCCM.
Through their groundbreaking collaboration announced today, CHEST and the CACP have committed to working exclusively as partners in continuing to advance the PCCM subspecialty in China to improve patient care, expand in-depth clinical training for Chinese physicians, and develop a growing force of expert Chinese faculty. The goal of such training is to ensure that patients receive the best possible care from Chinese physicians who complete the China-CHEST PCCM fellowship program.
“Recognition by the Chinese Ministry of Health of PCCM as this country’s first-ever physician subspecialty is welcomed acknowledgment that we’re making tremendous headway in advancing physician fellowship training in China,” said Barbara Phillips, MD, MPH, FCCP, President of the American College of Chest Physicians. “We are proud to join collaborative partners like the CMDA in these cooperative efforts to prepare Chinese physicians in the PCCM subspecialty, partnering in this historic effort to drive immeasurable improvements in clinical training and the delivery of patient care.”
Recharge in Los Angeles
When you imagine Los Angeles, you probably envision images of glamorous Hollywood celebrities and ritzy beaches featured on television shows. While LA does, indeed, allure visitors with its high-end environment, there are also many opportunities to unwind and recharge in the Golden State. With mild temperatures and sunshine nearly 300 days a year, Los Angeles provides a haven for outdoor activities. While you’re attending CHEST 2016 from October 22 to 26, we encourage you to trade your stilettos for hiking boots or athletic shoes, and get outside during your free time.
The San Gabriel Mountains are about an hour’s drive from the Los Angeles Convention Center. Visitors can hike, picnic, and enjoy equestrian trails. Our favorite LA experts – CHEST members – have recommended renting a mountain bike and riding up to Mount Wilson. You can also hike the Eaton Canyon Trail and find the Eaton Canyon Waterfall, a 40-foot waterfall with a pool at its base. You can find more mountain ranges and hiking opportunities in the Santa Monica mountains, as well. Find more tips on trails and hiking at discoverlosangeles.com.
If you’re not interested in retreating from Los Angeles’s urban oasis, but you still want to enjoy some fresh air and exercise, you have a couple options closer to downtown. Runyon Canyon is about a 20-minute drive from the convention center. It features a gently paved path for beginners, a rugged outer path for a more intense workout, free yoga near the Fuller Avenue entrance, a great setting for watching the sunset, and strong possibilities of celebrity sightings. You can also rent a bike and cycle along the beaches. You can stop off for a bite to eat, some sand volleyball, or just to do some people watching.
And if you’re a golf enthusiast, there is a bevy of options for golfing in and around LA. The most iconic golf course is the Trump National Golf Club located on the Palos Verdes Peninsula, about a 40-minute drive from the convention center. You’ll experience uncompromising luxury overlooking the beautiful Pacific Ocean. If you’d like to stay close to the convention center but still get out to play 9 holes, you may want to check out Wilshire Country Club (20-minute drive) or Monterey Park Golf Club (12-minute drive).
While Los Angeles refreshes you with outdoor beauty and sunshine, CHEST 2016 will energize and recharge you with the latest information in chest medicine. You’ll connect with an international community of the best minds in pulmonary, critical care, and sleep medicine. Find everything you need to know to make the best clinical decisions and inspire your patient care. Learn more at chestmeeting.chestnet.org.
When you imagine Los Angeles, you probably envision images of glamorous Hollywood celebrities and ritzy beaches featured on television shows. While LA does, indeed, allure visitors with its high-end environment, there are also many opportunities to unwind and recharge in the Golden State. With mild temperatures and sunshine nearly 300 days a year, Los Angeles provides a haven for outdoor activities. While you’re attending CHEST 2016 from October 22 to 26, we encourage you to trade your stilettos for hiking boots or athletic shoes, and get outside during your free time.
The San Gabriel Mountains are about an hour’s drive from the Los Angeles Convention Center. Visitors can hike, picnic, and enjoy equestrian trails. Our favorite LA experts – CHEST members – have recommended renting a mountain bike and riding up to Mount Wilson. You can also hike the Eaton Canyon Trail and find the Eaton Canyon Waterfall, a 40-foot waterfall with a pool at its base. You can find more mountain ranges and hiking opportunities in the Santa Monica mountains, as well. Find more tips on trails and hiking at discoverlosangeles.com.
If you’re not interested in retreating from Los Angeles’s urban oasis, but you still want to enjoy some fresh air and exercise, you have a couple options closer to downtown. Runyon Canyon is about a 20-minute drive from the convention center. It features a gently paved path for beginners, a rugged outer path for a more intense workout, free yoga near the Fuller Avenue entrance, a great setting for watching the sunset, and strong possibilities of celebrity sightings. You can also rent a bike and cycle along the beaches. You can stop off for a bite to eat, some sand volleyball, or just to do some people watching.
And if you’re a golf enthusiast, there is a bevy of options for golfing in and around LA. The most iconic golf course is the Trump National Golf Club located on the Palos Verdes Peninsula, about a 40-minute drive from the convention center. You’ll experience uncompromising luxury overlooking the beautiful Pacific Ocean. If you’d like to stay close to the convention center but still get out to play 9 holes, you may want to check out Wilshire Country Club (20-minute drive) or Monterey Park Golf Club (12-minute drive).
While Los Angeles refreshes you with outdoor beauty and sunshine, CHEST 2016 will energize and recharge you with the latest information in chest medicine. You’ll connect with an international community of the best minds in pulmonary, critical care, and sleep medicine. Find everything you need to know to make the best clinical decisions and inspire your patient care. Learn more at chestmeeting.chestnet.org.
When you imagine Los Angeles, you probably envision images of glamorous Hollywood celebrities and ritzy beaches featured on television shows. While LA does, indeed, allure visitors with its high-end environment, there are also many opportunities to unwind and recharge in the Golden State. With mild temperatures and sunshine nearly 300 days a year, Los Angeles provides a haven for outdoor activities. While you’re attending CHEST 2016 from October 22 to 26, we encourage you to trade your stilettos for hiking boots or athletic shoes, and get outside during your free time.
The San Gabriel Mountains are about an hour’s drive from the Los Angeles Convention Center. Visitors can hike, picnic, and enjoy equestrian trails. Our favorite LA experts – CHEST members – have recommended renting a mountain bike and riding up to Mount Wilson. You can also hike the Eaton Canyon Trail and find the Eaton Canyon Waterfall, a 40-foot waterfall with a pool at its base. You can find more mountain ranges and hiking opportunities in the Santa Monica mountains, as well. Find more tips on trails and hiking at discoverlosangeles.com.
If you’re not interested in retreating from Los Angeles’s urban oasis, but you still want to enjoy some fresh air and exercise, you have a couple options closer to downtown. Runyon Canyon is about a 20-minute drive from the convention center. It features a gently paved path for beginners, a rugged outer path for a more intense workout, free yoga near the Fuller Avenue entrance, a great setting for watching the sunset, and strong possibilities of celebrity sightings. You can also rent a bike and cycle along the beaches. You can stop off for a bite to eat, some sand volleyball, or just to do some people watching.
And if you’re a golf enthusiast, there is a bevy of options for golfing in and around LA. The most iconic golf course is the Trump National Golf Club located on the Palos Verdes Peninsula, about a 40-minute drive from the convention center. You’ll experience uncompromising luxury overlooking the beautiful Pacific Ocean. If you’d like to stay close to the convention center but still get out to play 9 holes, you may want to check out Wilshire Country Club (20-minute drive) or Monterey Park Golf Club (12-minute drive).
While Los Angeles refreshes you with outdoor beauty and sunshine, CHEST 2016 will energize and recharge you with the latest information in chest medicine. You’ll connect with an international community of the best minds in pulmonary, critical care, and sleep medicine. Find everything you need to know to make the best clinical decisions and inspire your patient care. Learn more at chestmeeting.chestnet.org.
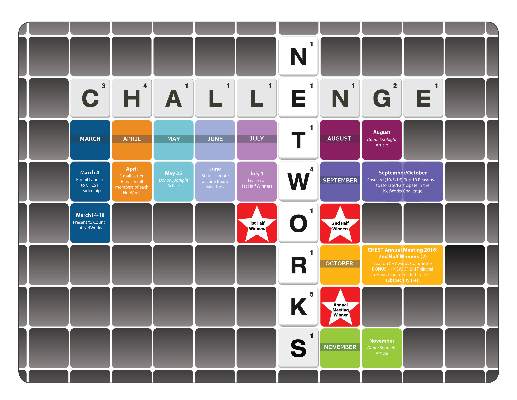
NETWORKS Pulmonary Physiology, Function, and Rehabilitation Disaster Response Pulmonary Vascular Disease Thoracic Oncology
Clinical utility of the acute bronchodilator response
Recently, numerous articles evaluating the acute bronchodilator (BD) response in various disease states have appeared in the literature (Chest. 2015;148[6]:1489; J Thorac Dis. 2016;8[1]:14; Int J Chron Obstruct Pulmon Dis. 2016;11:93; Respir Med. 2016;112:45). New algorithms have been proposed to improve quality control in BD (Eur Clin Respir J. 2015;30;2).
In our lab, requests for pre- and post-BD spirometry continue unabated. Undoubtedly, many labs comply with these requests without regard for pre-BD values. The number of these requests far exceeds the number needed to confirm asthma diagnosis, or to assure that post-BD FEV1/FVC ratio remains below 0.7 for COPD diagnosis, which are the only universally accepted indications for BD testing.
Acute BD testing technique, interpretation, and clinical application involve important issues that remain unresolved, even in COPD where this test has been studied more than any other disease state except asthma (Chest. 2011;140[4]:1055; Int J Chron Obstruct Pulmon Dis. 2015;10:407). There remains no clear consensus for a clinically relevant BD response. The ACCP definition proposed in 1974 (FEV1 improvement by greater than 15%) has not been updated, and the widely used ATS/ERS definition (FEV1 and/or FVC improvement by greater than 12% and 200 mL) is felt to be arbitrary and based more on expert opinion than scientific evidence (Respir Care. 2012;57[10]:1564). Literature review (excluding asthma) reveals no well-done, reproducible studies that demonstrate meaningful or widely applicable uses for the acute BD response.
Overcoming the many factors influencing acute bronchodilator testing, developing a unified definition for a positive test, and then showing a predictive significance to the acute-BD response is an extremely difficult task. Until this test is further studied in a rigorous manner, any meaning attached to a positive response outside of asthma is purely arbitrary.
Dr. Oleh Hnatiuk, FCCP
Steering Committee Member
Gun violence in the hospital
Thirty-one thousand fatal gunshot wounds (GSW) occur in the United States each year and are increasing; 55% are self-inflicted, mostly isolated incidents. However, mass shooting events (MSE = more than 3 victims) are rising with 355 events in 2015 (462 deaths and 1,314 injuries). The mortality of GSW has risen due to the use of high caliber automatic handguns. Health-care providers, facilities, and systems need to include preparation for primary prevention and secondary mitigation for violent acts of this nature.
MSE attacker demographics reveal a male predominance (90%) with ethnicity mirroring the US population (65% Caucasian, 16% black, and 9% Asian) and mainly occurring in urban settings. The psychosocial basis of these changes is complex and multifactorial. Two-thirds of mass shooters have a history of mental illness with paranoid schizophrenia predominating. Motives are shifting from self-destruction to grievance-related events. Targets and victims of GSW violence also seem to be changing, and health-care workers are potential targets for GSW violence.
A 12-year review of hospital shooting events (HSE) found 154 events with 235 victims. There is a rise in this type of violent act. Grievance motives are dominant in these events. Most HSE occur in the ED or at the entrance to the hospital or parking lot (77%). The case fatality rate in HSE averages 50%. The perpetrators are injured in 85% of cases. Nurses are the most common victims of HSE.
Prevention strategies such as metal detectors, camera surveillance, strengthened security staff, and emergency protocols are vital. However, in many hospitals, these strategies are inadequate or not considered. Secondary mitigation requires special education and training and some material preparation to be successful. Providers must consider themselves potential gun violence victims. We encourage all medical providers to engage in planning and preparation for HSE, as well as advocate for gun safety laws
Dr. Dennis Amundson, FCCP
NetWork Member
Critical violent injury in the United States: A review and call to action. Crit Care Med. 2015;43(11):2460-2466.
Hospital-based shooting in the United States: 2000-2011. Ann Emerg Med. 2012;60(6):790-798.
The epidemiology of trauma-related mortality in the United States From 2002-2012. J Trauma Acute Care Surg. 2014;76(4):913-920.
Balloon pulmonary angioplasty for CTEPH
The gold-standard treatment for chronic thromboembolic pulmonary hypertension (CTEPH) is pulmonary thromboendarterectomy (PTE). However, not every patient is a surgical candidate, including those who are deemed technically inoperable (after review by a multidisciplinary, experienced CTEPH team) or those whose goals of care are more palliative.
Such factors created an opportunity for an alternative procedure to manage CTEPH: catheter-based balloon pulmonary angioplasty (BPA). Despite the limited success with early BPA experience, with initial set-backs including high reperfusion edema rates and other procedure complications, BPA has become more refined over time. Initially led by the efforts of several groups based in Japan, modifications included greater precision in “right-sizing” balloons, staging the procedure (average two to five sessions/patient), and better vascular imaging techniques with advancing technical capabilities.
BPA has received attention due to the favorable hemodynamic and functional outcomes reported in select patients. Despite a lack of consensus regarding who might benefit most, these preliminary results have stimulated considerable interest for acquiring this technique worldwide.
Caution should be exercised when BPA is considered for CTEPH treatment. Critical to success is the selection of patients who might benefit, and adequate training and technical expertise is essential for BPA performance. For those with operable CTEPH who are otherwise surgical candidates, data do not yet exist to suggest BPA as a comparable alternative to PTE. Furthermore, the absence of head-to-head comparison between medical therapy and BPA for inoperable CTEPH further blurs the role BPA will have in this unique patient population. But, it holds promise, awaiting further trials data.
Dr. Wassim H. Fares, FCCP, NetWork Member
Dr. William R. Auger, FCCP, Steering Committee Member
Pulmonary nodules: Are you seeing spots?
Pulmonary nodules are increasingly being identified in clinical practice. A recent study estimated that 1.5 million nodules are identified annually in the United States (Gould et al. 2015; Am J Respir Crit Care Med. 192[10], 1208). This 10-fold increase in number over prior estimates reflects the steep escalation in utilization of CT scanning over the past several decades, and is likely to rise further as lung cancer screening is implemented. While the majority of nodules are benign, evaluation necessarily includes an assessment of the probability of malignancy, since this is a major driver of the decision as to whether no further intervention is required, or whether watchful surveillance or further noninvasive or invasive evaluation is appropriate (Gould et al., 2013). It is reassuring that experienced chest physicians perform well in the assessment of the probability of malignancy (Gould et al., 2013; Swensen et al., 1999), but also important to recognize that evidence-based guidelines for nodule evaluation as well as validated tools for assessing the likelihood of malignancy are readily available (Gould, Ananth, Barnett, & Veterans Affairs, 2007; Gould et al., 2013; McWilliams et al., 2013; Swensen, Silverstein, Ilstrup, Schleck, & Edell, 1997). It is important to engage our radiology colleagues in this discussion; guidelines from the Fleischner Society and the American College of Radiology for reporting on incidentally identified small solid nodules, incidentally identified subsolid nodules, and screening-detected nodules are individually distinct in definitions of abnormality as well as recommendations for follow up, and should be applied appropriately in the context of the individual patient as well as the situation for which the CT was performed (“Lung-RADS Version 1.0 Assessment Categories Release date: April 28, 2014,” 2014; MacMahon et al., 2005; Naidich et al., 2013). All of these potential sources of variation highlight the value of standardizing the approach to nodule evaluation, to ensure that appropriate evaluation will be done to maximize the likelihood of identifying nodules that are actually cancer, and minimize harm potentially incurred by unnecessary invasive and noninvasive testing of nodules that are actually benign.
Dr. Lynn Tanoue, FCCP
NetWork Chair
Gould MK, Ananth L, Barnett PG, and Veterans Affairs, S. C. S. G. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131(2):383-388.
Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143(5 suppl):e93S.
Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015; 192(10):1208-1214.
Lung-RADS Version 1.0 Assessment Categories Release date: April 28,2014. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/LungRADS/AssessmentCategories.pdf. Accessed Oct 31, 2014.
MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237(2):395-400.
McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910-919.
Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266(1):304-317.
Swensen SJ, Silverstein MD, Edell ES, et al. Solitary pulmonary nodules: clinical prediction model versus physicians. Mayo Clin Proc. 1999;74(4):319-329.
Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: Application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157(8): 849-855.
Clinical utility of the acute bronchodilator response
Recently, numerous articles evaluating the acute bronchodilator (BD) response in various disease states have appeared in the literature (Chest. 2015;148[6]:1489; J Thorac Dis. 2016;8[1]:14; Int J Chron Obstruct Pulmon Dis. 2016;11:93; Respir Med. 2016;112:45). New algorithms have been proposed to improve quality control in BD (Eur Clin Respir J. 2015;30;2).
In our lab, requests for pre- and post-BD spirometry continue unabated. Undoubtedly, many labs comply with these requests without regard for pre-BD values. The number of these requests far exceeds the number needed to confirm asthma diagnosis, or to assure that post-BD FEV1/FVC ratio remains below 0.7 for COPD diagnosis, which are the only universally accepted indications for BD testing.
Acute BD testing technique, interpretation, and clinical application involve important issues that remain unresolved, even in COPD where this test has been studied more than any other disease state except asthma (Chest. 2011;140[4]:1055; Int J Chron Obstruct Pulmon Dis. 2015;10:407). There remains no clear consensus for a clinically relevant BD response. The ACCP definition proposed in 1974 (FEV1 improvement by greater than 15%) has not been updated, and the widely used ATS/ERS definition (FEV1 and/or FVC improvement by greater than 12% and 200 mL) is felt to be arbitrary and based more on expert opinion than scientific evidence (Respir Care. 2012;57[10]:1564). Literature review (excluding asthma) reveals no well-done, reproducible studies that demonstrate meaningful or widely applicable uses for the acute BD response.
Overcoming the many factors influencing acute bronchodilator testing, developing a unified definition for a positive test, and then showing a predictive significance to the acute-BD response is an extremely difficult task. Until this test is further studied in a rigorous manner, any meaning attached to a positive response outside of asthma is purely arbitrary.
Dr. Oleh Hnatiuk, FCCP
Steering Committee Member
Gun violence in the hospital
Thirty-one thousand fatal gunshot wounds (GSW) occur in the United States each year and are increasing; 55% are self-inflicted, mostly isolated incidents. However, mass shooting events (MSE = more than 3 victims) are rising with 355 events in 2015 (462 deaths and 1,314 injuries). The mortality of GSW has risen due to the use of high caliber automatic handguns. Health-care providers, facilities, and systems need to include preparation for primary prevention and secondary mitigation for violent acts of this nature.
MSE attacker demographics reveal a male predominance (90%) with ethnicity mirroring the US population (65% Caucasian, 16% black, and 9% Asian) and mainly occurring in urban settings. The psychosocial basis of these changes is complex and multifactorial. Two-thirds of mass shooters have a history of mental illness with paranoid schizophrenia predominating. Motives are shifting from self-destruction to grievance-related events. Targets and victims of GSW violence also seem to be changing, and health-care workers are potential targets for GSW violence.
A 12-year review of hospital shooting events (HSE) found 154 events with 235 victims. There is a rise in this type of violent act. Grievance motives are dominant in these events. Most HSE occur in the ED or at the entrance to the hospital or parking lot (77%). The case fatality rate in HSE averages 50%. The perpetrators are injured in 85% of cases. Nurses are the most common victims of HSE.
Prevention strategies such as metal detectors, camera surveillance, strengthened security staff, and emergency protocols are vital. However, in many hospitals, these strategies are inadequate or not considered. Secondary mitigation requires special education and training and some material preparation to be successful. Providers must consider themselves potential gun violence victims. We encourage all medical providers to engage in planning and preparation for HSE, as well as advocate for gun safety laws
Dr. Dennis Amundson, FCCP
NetWork Member
Critical violent injury in the United States: A review and call to action. Crit Care Med. 2015;43(11):2460-2466.
Hospital-based shooting in the United States: 2000-2011. Ann Emerg Med. 2012;60(6):790-798.
The epidemiology of trauma-related mortality in the United States From 2002-2012. J Trauma Acute Care Surg. 2014;76(4):913-920.
Balloon pulmonary angioplasty for CTEPH
The gold-standard treatment for chronic thromboembolic pulmonary hypertension (CTEPH) is pulmonary thromboendarterectomy (PTE). However, not every patient is a surgical candidate, including those who are deemed technically inoperable (after review by a multidisciplinary, experienced CTEPH team) or those whose goals of care are more palliative.
Such factors created an opportunity for an alternative procedure to manage CTEPH: catheter-based balloon pulmonary angioplasty (BPA). Despite the limited success with early BPA experience, with initial set-backs including high reperfusion edema rates and other procedure complications, BPA has become more refined over time. Initially led by the efforts of several groups based in Japan, modifications included greater precision in “right-sizing” balloons, staging the procedure (average two to five sessions/patient), and better vascular imaging techniques with advancing technical capabilities.
BPA has received attention due to the favorable hemodynamic and functional outcomes reported in select patients. Despite a lack of consensus regarding who might benefit most, these preliminary results have stimulated considerable interest for acquiring this technique worldwide.
Caution should be exercised when BPA is considered for CTEPH treatment. Critical to success is the selection of patients who might benefit, and adequate training and technical expertise is essential for BPA performance. For those with operable CTEPH who are otherwise surgical candidates, data do not yet exist to suggest BPA as a comparable alternative to PTE. Furthermore, the absence of head-to-head comparison between medical therapy and BPA for inoperable CTEPH further blurs the role BPA will have in this unique patient population. But, it holds promise, awaiting further trials data.
Dr. Wassim H. Fares, FCCP, NetWork Member
Dr. William R. Auger, FCCP, Steering Committee Member
Pulmonary nodules: Are you seeing spots?
Pulmonary nodules are increasingly being identified in clinical practice. A recent study estimated that 1.5 million nodules are identified annually in the United States (Gould et al. 2015; Am J Respir Crit Care Med. 192[10], 1208). This 10-fold increase in number over prior estimates reflects the steep escalation in utilization of CT scanning over the past several decades, and is likely to rise further as lung cancer screening is implemented. While the majority of nodules are benign, evaluation necessarily includes an assessment of the probability of malignancy, since this is a major driver of the decision as to whether no further intervention is required, or whether watchful surveillance or further noninvasive or invasive evaluation is appropriate (Gould et al., 2013). It is reassuring that experienced chest physicians perform well in the assessment of the probability of malignancy (Gould et al., 2013; Swensen et al., 1999), but also important to recognize that evidence-based guidelines for nodule evaluation as well as validated tools for assessing the likelihood of malignancy are readily available (Gould, Ananth, Barnett, & Veterans Affairs, 2007; Gould et al., 2013; McWilliams et al., 2013; Swensen, Silverstein, Ilstrup, Schleck, & Edell, 1997). It is important to engage our radiology colleagues in this discussion; guidelines from the Fleischner Society and the American College of Radiology for reporting on incidentally identified small solid nodules, incidentally identified subsolid nodules, and screening-detected nodules are individually distinct in definitions of abnormality as well as recommendations for follow up, and should be applied appropriately in the context of the individual patient as well as the situation for which the CT was performed (“Lung-RADS Version 1.0 Assessment Categories Release date: April 28, 2014,” 2014; MacMahon et al., 2005; Naidich et al., 2013). All of these potential sources of variation highlight the value of standardizing the approach to nodule evaluation, to ensure that appropriate evaluation will be done to maximize the likelihood of identifying nodules that are actually cancer, and minimize harm potentially incurred by unnecessary invasive and noninvasive testing of nodules that are actually benign.
Dr. Lynn Tanoue, FCCP
NetWork Chair
Gould MK, Ananth L, Barnett PG, and Veterans Affairs, S. C. S. G. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131(2):383-388.
Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143(5 suppl):e93S.
Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015; 192(10):1208-1214.
Lung-RADS Version 1.0 Assessment Categories Release date: April 28,2014. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/LungRADS/AssessmentCategories.pdf. Accessed Oct 31, 2014.
MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237(2):395-400.
McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910-919.
Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266(1):304-317.
Swensen SJ, Silverstein MD, Edell ES, et al. Solitary pulmonary nodules: clinical prediction model versus physicians. Mayo Clin Proc. 1999;74(4):319-329.
Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: Application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157(8): 849-855.
Clinical utility of the acute bronchodilator response
Recently, numerous articles evaluating the acute bronchodilator (BD) response in various disease states have appeared in the literature (Chest. 2015;148[6]:1489; J Thorac Dis. 2016;8[1]:14; Int J Chron Obstruct Pulmon Dis. 2016;11:93; Respir Med. 2016;112:45). New algorithms have been proposed to improve quality control in BD (Eur Clin Respir J. 2015;30;2).
In our lab, requests for pre- and post-BD spirometry continue unabated. Undoubtedly, many labs comply with these requests without regard for pre-BD values. The number of these requests far exceeds the number needed to confirm asthma diagnosis, or to assure that post-BD FEV1/FVC ratio remains below 0.7 for COPD diagnosis, which are the only universally accepted indications for BD testing.
Acute BD testing technique, interpretation, and clinical application involve important issues that remain unresolved, even in COPD where this test has been studied more than any other disease state except asthma (Chest. 2011;140[4]:1055; Int J Chron Obstruct Pulmon Dis. 2015;10:407). There remains no clear consensus for a clinically relevant BD response. The ACCP definition proposed in 1974 (FEV1 improvement by greater than 15%) has not been updated, and the widely used ATS/ERS definition (FEV1 and/or FVC improvement by greater than 12% and 200 mL) is felt to be arbitrary and based more on expert opinion than scientific evidence (Respir Care. 2012;57[10]:1564). Literature review (excluding asthma) reveals no well-done, reproducible studies that demonstrate meaningful or widely applicable uses for the acute BD response.
Overcoming the many factors influencing acute bronchodilator testing, developing a unified definition for a positive test, and then showing a predictive significance to the acute-BD response is an extremely difficult task. Until this test is further studied in a rigorous manner, any meaning attached to a positive response outside of asthma is purely arbitrary.
Dr. Oleh Hnatiuk, FCCP
Steering Committee Member
Gun violence in the hospital
Thirty-one thousand fatal gunshot wounds (GSW) occur in the United States each year and are increasing; 55% are self-inflicted, mostly isolated incidents. However, mass shooting events (MSE = more than 3 victims) are rising with 355 events in 2015 (462 deaths and 1,314 injuries). The mortality of GSW has risen due to the use of high caliber automatic handguns. Health-care providers, facilities, and systems need to include preparation for primary prevention and secondary mitigation for violent acts of this nature.
MSE attacker demographics reveal a male predominance (90%) with ethnicity mirroring the US population (65% Caucasian, 16% black, and 9% Asian) and mainly occurring in urban settings. The psychosocial basis of these changes is complex and multifactorial. Two-thirds of mass shooters have a history of mental illness with paranoid schizophrenia predominating. Motives are shifting from self-destruction to grievance-related events. Targets and victims of GSW violence also seem to be changing, and health-care workers are potential targets for GSW violence.
A 12-year review of hospital shooting events (HSE) found 154 events with 235 victims. There is a rise in this type of violent act. Grievance motives are dominant in these events. Most HSE occur in the ED or at the entrance to the hospital or parking lot (77%). The case fatality rate in HSE averages 50%. The perpetrators are injured in 85% of cases. Nurses are the most common victims of HSE.
Prevention strategies such as metal detectors, camera surveillance, strengthened security staff, and emergency protocols are vital. However, in many hospitals, these strategies are inadequate or not considered. Secondary mitigation requires special education and training and some material preparation to be successful. Providers must consider themselves potential gun violence victims. We encourage all medical providers to engage in planning and preparation for HSE, as well as advocate for gun safety laws
Dr. Dennis Amundson, FCCP
NetWork Member
Critical violent injury in the United States: A review and call to action. Crit Care Med. 2015;43(11):2460-2466.
Hospital-based shooting in the United States: 2000-2011. Ann Emerg Med. 2012;60(6):790-798.
The epidemiology of trauma-related mortality in the United States From 2002-2012. J Trauma Acute Care Surg. 2014;76(4):913-920.
Balloon pulmonary angioplasty for CTEPH
The gold-standard treatment for chronic thromboembolic pulmonary hypertension (CTEPH) is pulmonary thromboendarterectomy (PTE). However, not every patient is a surgical candidate, including those who are deemed technically inoperable (after review by a multidisciplinary, experienced CTEPH team) or those whose goals of care are more palliative.
Such factors created an opportunity for an alternative procedure to manage CTEPH: catheter-based balloon pulmonary angioplasty (BPA). Despite the limited success with early BPA experience, with initial set-backs including high reperfusion edema rates and other procedure complications, BPA has become more refined over time. Initially led by the efforts of several groups based in Japan, modifications included greater precision in “right-sizing” balloons, staging the procedure (average two to five sessions/patient), and better vascular imaging techniques with advancing technical capabilities.
BPA has received attention due to the favorable hemodynamic and functional outcomes reported in select patients. Despite a lack of consensus regarding who might benefit most, these preliminary results have stimulated considerable interest for acquiring this technique worldwide.
Caution should be exercised when BPA is considered for CTEPH treatment. Critical to success is the selection of patients who might benefit, and adequate training and technical expertise is essential for BPA performance. For those with operable CTEPH who are otherwise surgical candidates, data do not yet exist to suggest BPA as a comparable alternative to PTE. Furthermore, the absence of head-to-head comparison between medical therapy and BPA for inoperable CTEPH further blurs the role BPA will have in this unique patient population. But, it holds promise, awaiting further trials data.
Dr. Wassim H. Fares, FCCP, NetWork Member
Dr. William R. Auger, FCCP, Steering Committee Member
Pulmonary nodules: Are you seeing spots?
Pulmonary nodules are increasingly being identified in clinical practice. A recent study estimated that 1.5 million nodules are identified annually in the United States (Gould et al. 2015; Am J Respir Crit Care Med. 192[10], 1208). This 10-fold increase in number over prior estimates reflects the steep escalation in utilization of CT scanning over the past several decades, and is likely to rise further as lung cancer screening is implemented. While the majority of nodules are benign, evaluation necessarily includes an assessment of the probability of malignancy, since this is a major driver of the decision as to whether no further intervention is required, or whether watchful surveillance or further noninvasive or invasive evaluation is appropriate (Gould et al., 2013). It is reassuring that experienced chest physicians perform well in the assessment of the probability of malignancy (Gould et al., 2013; Swensen et al., 1999), but also important to recognize that evidence-based guidelines for nodule evaluation as well as validated tools for assessing the likelihood of malignancy are readily available (Gould, Ananth, Barnett, & Veterans Affairs, 2007; Gould et al., 2013; McWilliams et al., 2013; Swensen, Silverstein, Ilstrup, Schleck, & Edell, 1997). It is important to engage our radiology colleagues in this discussion; guidelines from the Fleischner Society and the American College of Radiology for reporting on incidentally identified small solid nodules, incidentally identified subsolid nodules, and screening-detected nodules are individually distinct in definitions of abnormality as well as recommendations for follow up, and should be applied appropriately in the context of the individual patient as well as the situation for which the CT was performed (“Lung-RADS Version 1.0 Assessment Categories Release date: April 28, 2014,” 2014; MacMahon et al., 2005; Naidich et al., 2013). All of these potential sources of variation highlight the value of standardizing the approach to nodule evaluation, to ensure that appropriate evaluation will be done to maximize the likelihood of identifying nodules that are actually cancer, and minimize harm potentially incurred by unnecessary invasive and noninvasive testing of nodules that are actually benign.
Dr. Lynn Tanoue, FCCP
NetWork Chair
Gould MK, Ananth L, Barnett PG, and Veterans Affairs, S. C. S. G. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131(2):383-388.
Gould MK, Donington J, Lynch WR, et al. Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013; 143(5 suppl):e93S.
Gould MK, Tang T, Liu IL, et al. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015; 192(10):1208-1214.
Lung-RADS Version 1.0 Assessment Categories Release date: April 28,2014. http://www.acr.org/~/media/ACR/Documents/PDF/QualitySafety/Resources/LungRADS/AssessmentCategories.pdf. Accessed Oct 31, 2014.
MacMahon H, Austin JH, Gamsu G, et al. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237(2):395-400.
McWilliams A, Tammemagi MC, Mayo JR, et al. Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med. 2013;369(10):910-919.
Naidich DP, Bankier AA, MacMahon H, et al. Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology. 2013;266(1):304-317.
Swensen SJ, Silverstein MD, Edell ES, et al. Solitary pulmonary nodules: clinical prediction model versus physicians. Mayo Clin Proc. 1999;74(4):319-329.
Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: Application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157(8): 849-855.
This Month in CHEST: Editor’s Picks
Editorial
New Sepsis Criteria: A Change We Should Not Make.By Dr. S. Q. Simpson.
Giants in Chest Medicine
Arthur P. Wheeler, MD, FCCP. By Dr. G. R. Bernard.
Topics In Practice Management
Update on Exhaled Nitric Oxide in Clinical Practice.By Dr. S.R. Mummadi and Dr. P.Y. Hahn.
Original Research
Airway Surfactant Protein D Deficiency in Adults With Severe Asthma.By Dr. R.A. Mackay et al.
Outcomes of Nurse Practitioner–Delivered Critical Care: A Prospective Cohort Study.By Dr. J.S. Landsperger et al.
Editorial
New Sepsis Criteria: A Change We Should Not Make.By Dr. S. Q. Simpson.
Giants in Chest Medicine
Arthur P. Wheeler, MD, FCCP. By Dr. G. R. Bernard.
Topics In Practice Management
Update on Exhaled Nitric Oxide in Clinical Practice.By Dr. S.R. Mummadi and Dr. P.Y. Hahn.
Original Research
Airway Surfactant Protein D Deficiency in Adults With Severe Asthma.By Dr. R.A. Mackay et al.
Outcomes of Nurse Practitioner–Delivered Critical Care: A Prospective Cohort Study.By Dr. J.S. Landsperger et al.
Editorial
New Sepsis Criteria: A Change We Should Not Make.By Dr. S. Q. Simpson.
Giants in Chest Medicine
Arthur P. Wheeler, MD, FCCP. By Dr. G. R. Bernard.
Topics In Practice Management
Update on Exhaled Nitric Oxide in Clinical Practice.By Dr. S.R. Mummadi and Dr. P.Y. Hahn.
Original Research
Airway Surfactant Protein D Deficiency in Adults With Severe Asthma.By Dr. R.A. Mackay et al.
Outcomes of Nurse Practitioner–Delivered Critical Care: A Prospective Cohort Study.By Dr. J.S. Landsperger et al.
2016 NetWorks Challenge
In March, the foundation kicked off the 2016 NetWorks Challenge, and we’re delighted to see a very enthusiastic response from our NetWorks Steering Committee members. In fact, we are thrilled to announce that the first NetWorks Steering Committee to achieve 100% participation is the Women’s Health NetWork. Every member on the steering committee made a donation to the CHEST Foundation last month.
“Physicians are competitive by nature and always welcome a challenge; the CHEST Foundation challenge is no exception,” stated Ghada Bourjeily, MD, FCCP, and Chair of the Women’s Health NetWork. “The Women’s Health NetWork Steering Committee members jumped on the opportunity to donate as soon as they heard about this great opportunity and donated to the CHEST Foundation.”
This year, the prizes for winning the NetWorks Challenge are more enticing than ever before. In the first round, the highest percentage of participation by a NetWork Steering Committee will receive additional time for the NetWorks Featured Lecture at CHEST 2016. And, for the very first time, the CHEST Foundation is offering up to two travel grants to CHEST 2016. In the second round, the top two NetWorks Steering Committees that are able to contribute the highest total amount will receive a seat on the CHEST Foundation’s Awards Committee and a potential clinical research grant. Up to two travel grants to CHEST 2017 will also be awarded in the final round to the NetWork that has the highest percentage of participation among their membership.
David Schulman, MD, MPH, FCCP, Chair of the Council of NetWorks, recently commented on why it is critical to take part in the NetWorks Challenge. “Participating in the NetWorks Challenge will serve many great purposes. First, it’s an opportunity to give to a great organization that does fantastic work. Second, if you’re a member of a NetWork and you participate, it allows your NetWork to achieve greatness. How? Because you get extra time at the annual meeting to show off your wares to your members by letting your national leaders speak to your members. Third, you can get travel grants for your colleagues, which allow them to attend the annual Meeting at no cost. Fourth, you can participate in awarding grants to next year’s foundation awardees as a public member of the CHEST Foundation Awards Committee. In short, there is no reason not to give to the foundation as part of the NetWorks Challenge.”
In March, the foundation kicked off the 2016 NetWorks Challenge, and we’re delighted to see a very enthusiastic response from our NetWorks Steering Committee members. In fact, we are thrilled to announce that the first NetWorks Steering Committee to achieve 100% participation is the Women’s Health NetWork. Every member on the steering committee made a donation to the CHEST Foundation last month.
“Physicians are competitive by nature and always welcome a challenge; the CHEST Foundation challenge is no exception,” stated Ghada Bourjeily, MD, FCCP, and Chair of the Women’s Health NetWork. “The Women’s Health NetWork Steering Committee members jumped on the opportunity to donate as soon as they heard about this great opportunity and donated to the CHEST Foundation.”
This year, the prizes for winning the NetWorks Challenge are more enticing than ever before. In the first round, the highest percentage of participation by a NetWork Steering Committee will receive additional time for the NetWorks Featured Lecture at CHEST 2016. And, for the very first time, the CHEST Foundation is offering up to two travel grants to CHEST 2016. In the second round, the top two NetWorks Steering Committees that are able to contribute the highest total amount will receive a seat on the CHEST Foundation’s Awards Committee and a potential clinical research grant. Up to two travel grants to CHEST 2017 will also be awarded in the final round to the NetWork that has the highest percentage of participation among their membership.
David Schulman, MD, MPH, FCCP, Chair of the Council of NetWorks, recently commented on why it is critical to take part in the NetWorks Challenge. “Participating in the NetWorks Challenge will serve many great purposes. First, it’s an opportunity to give to a great organization that does fantastic work. Second, if you’re a member of a NetWork and you participate, it allows your NetWork to achieve greatness. How? Because you get extra time at the annual meeting to show off your wares to your members by letting your national leaders speak to your members. Third, you can get travel grants for your colleagues, which allow them to attend the annual Meeting at no cost. Fourth, you can participate in awarding grants to next year’s foundation awardees as a public member of the CHEST Foundation Awards Committee. In short, there is no reason not to give to the foundation as part of the NetWorks Challenge.”
In March, the foundation kicked off the 2016 NetWorks Challenge, and we’re delighted to see a very enthusiastic response from our NetWorks Steering Committee members. In fact, we are thrilled to announce that the first NetWorks Steering Committee to achieve 100% participation is the Women’s Health NetWork. Every member on the steering committee made a donation to the CHEST Foundation last month.
“Physicians are competitive by nature and always welcome a challenge; the CHEST Foundation challenge is no exception,” stated Ghada Bourjeily, MD, FCCP, and Chair of the Women’s Health NetWork. “The Women’s Health NetWork Steering Committee members jumped on the opportunity to donate as soon as they heard about this great opportunity and donated to the CHEST Foundation.”
This year, the prizes for winning the NetWorks Challenge are more enticing than ever before. In the first round, the highest percentage of participation by a NetWork Steering Committee will receive additional time for the NetWorks Featured Lecture at CHEST 2016. And, for the very first time, the CHEST Foundation is offering up to two travel grants to CHEST 2016. In the second round, the top two NetWorks Steering Committees that are able to contribute the highest total amount will receive a seat on the CHEST Foundation’s Awards Committee and a potential clinical research grant. Up to two travel grants to CHEST 2017 will also be awarded in the final round to the NetWork that has the highest percentage of participation among their membership.
David Schulman, MD, MPH, FCCP, Chair of the Council of NetWorks, recently commented on why it is critical to take part in the NetWorks Challenge. “Participating in the NetWorks Challenge will serve many great purposes. First, it’s an opportunity to give to a great organization that does fantastic work. Second, if you’re a member of a NetWork and you participate, it allows your NetWork to achieve greatness. How? Because you get extra time at the annual meeting to show off your wares to your members by letting your national leaders speak to your members. Third, you can get travel grants for your colleagues, which allow them to attend the annual Meeting at no cost. Fourth, you can participate in awarding grants to next year’s foundation awardees as a public member of the CHEST Foundation Awards Committee. In short, there is no reason not to give to the foundation as part of the NetWorks Challenge.”
The Changing Face of MOC More information
On April 8, 2106, CHEST joined 29 other medical specialty societies at the American Board of Internal Medicine’s (ABIM’s) biannual Liaison Committee on Certification and Recertification (LCCR) meeting in Philadelphia. The meeting focused on the changing face of Maintenance of Certification (MOC) and the vision ABIM has for the future of MOC.
President Richard J. Baron, MD, responded to a letter signed by several medical specialty societies, asking for clarification on ABIM’s vision and philosophy for MOC and the future changes ABIM is considering for the MOC program. Dr. Baron articulated the desire for MOC to be relevant to physicians’ practices in collaboration with the ABIM and the medical specialty societies, to produce, “a credential that speaks to whether physicians are staying current in knowledge and practice over the course of their career in their specialty.”
Dr. Richard G. Battaglia, ABIM Chief Medical Officer, and Eric McKeeby, ABIM Director of Community Engagement, reported the results of a membership survey and focus group discussions regarding ABIM’s Assessment 2020 Report, published in September 2015. They highlighted the challenges, opportunities, and future plans for the MOC program, in light of diplomates’ input through these mechanisms. In the feedback received, the majority of diplomates favored a move away from the secure 10-year MOC recertification examination. Several options were presented, including smaller, more frequent exams, secure exams taken from home or office, and the ability to “test out” of the 10-year exam by successfully completing smaller assessments along the way. Ultimately, participants favored a move away from assessment and toward learning and improvement through a mechanism that is relevant to their real-world practices. Dr. Baron noted the ABIM survey results in which 76.3% of diplomates said they wanted the MOC credential to mean “I am staying current in the knowledge I need to practice,” and he reiterated the Board’s commitment to developing assessment approaches that would result in a meaningful credential based on performance. The ABIM Board of Directors met in April, with the exam format being a priority for them.
Regarding the future of MOC, while the practice assessment requirement is on hold through 2018, ABIM recognizes the work in this area many physicians are currently doing. By early 2017, ABIM is planning on extending the partnership with ACCME to recognize practice assessment activities, along with current medical knowledge activities, for both CME and MOC. This expansion would include blended activities that meet both medical knowledge and practice assessment requirements.
In addition to ABIM staff’s perspectives, three medical societies, including CHEST, reported on their MOC efforts. Heather Dethloff, CHEST Education and Accreditation Specialist, participated in a panel discussion, along with the Endocrine Society and the American Academy of Hospice and Palliative Medicine regarding the ongoing efforts to incorporate MOC into educational activities within their organizations. Successes and challenges encountered through the ABIM MOC certification process were the topics for discussion. During this presentation, CHEST announced its plan to incorporate ABIM MOC into the entire CHEST Annual Meeting 2016; details will be communicated to CHEST members and meeting registrants in coming months.
Throughout these changes to the MOC program, CHEST has been, and will continue to be, in communication with ABIM, advocating for our members. Any questions or concerns about this process can be directed to Heather Dethloff, Education and Accreditation Specialist, at [email protected].
More information
New ABIM Survey Indicates Physician Interest in Potential Changes to MOC Assessment: www.abim.org/news/new-abim-survey-indicates-physician-interest-in-potential-changes-to-moc-assessment.aspx
On April 8, 2106, CHEST joined 29 other medical specialty societies at the American Board of Internal Medicine’s (ABIM’s) biannual Liaison Committee on Certification and Recertification (LCCR) meeting in Philadelphia. The meeting focused on the changing face of Maintenance of Certification (MOC) and the vision ABIM has for the future of MOC.
President Richard J. Baron, MD, responded to a letter signed by several medical specialty societies, asking for clarification on ABIM’s vision and philosophy for MOC and the future changes ABIM is considering for the MOC program. Dr. Baron articulated the desire for MOC to be relevant to physicians’ practices in collaboration with the ABIM and the medical specialty societies, to produce, “a credential that speaks to whether physicians are staying current in knowledge and practice over the course of their career in their specialty.”
Dr. Richard G. Battaglia, ABIM Chief Medical Officer, and Eric McKeeby, ABIM Director of Community Engagement, reported the results of a membership survey and focus group discussions regarding ABIM’s Assessment 2020 Report, published in September 2015. They highlighted the challenges, opportunities, and future plans for the MOC program, in light of diplomates’ input through these mechanisms. In the feedback received, the majority of diplomates favored a move away from the secure 10-year MOC recertification examination. Several options were presented, including smaller, more frequent exams, secure exams taken from home or office, and the ability to “test out” of the 10-year exam by successfully completing smaller assessments along the way. Ultimately, participants favored a move away from assessment and toward learning and improvement through a mechanism that is relevant to their real-world practices. Dr. Baron noted the ABIM survey results in which 76.3% of diplomates said they wanted the MOC credential to mean “I am staying current in the knowledge I need to practice,” and he reiterated the Board’s commitment to developing assessment approaches that would result in a meaningful credential based on performance. The ABIM Board of Directors met in April, with the exam format being a priority for them.
Regarding the future of MOC, while the practice assessment requirement is on hold through 2018, ABIM recognizes the work in this area many physicians are currently doing. By early 2017, ABIM is planning on extending the partnership with ACCME to recognize practice assessment activities, along with current medical knowledge activities, for both CME and MOC. This expansion would include blended activities that meet both medical knowledge and practice assessment requirements.
In addition to ABIM staff’s perspectives, three medical societies, including CHEST, reported on their MOC efforts. Heather Dethloff, CHEST Education and Accreditation Specialist, participated in a panel discussion, along with the Endocrine Society and the American Academy of Hospice and Palliative Medicine regarding the ongoing efforts to incorporate MOC into educational activities within their organizations. Successes and challenges encountered through the ABIM MOC certification process were the topics for discussion. During this presentation, CHEST announced its plan to incorporate ABIM MOC into the entire CHEST Annual Meeting 2016; details will be communicated to CHEST members and meeting registrants in coming months.
Throughout these changes to the MOC program, CHEST has been, and will continue to be, in communication with ABIM, advocating for our members. Any questions or concerns about this process can be directed to Heather Dethloff, Education and Accreditation Specialist, at [email protected].
More information
New ABIM Survey Indicates Physician Interest in Potential Changes to MOC Assessment: www.abim.org/news/new-abim-survey-indicates-physician-interest-in-potential-changes-to-moc-assessment.aspx
On April 8, 2106, CHEST joined 29 other medical specialty societies at the American Board of Internal Medicine’s (ABIM’s) biannual Liaison Committee on Certification and Recertification (LCCR) meeting in Philadelphia. The meeting focused on the changing face of Maintenance of Certification (MOC) and the vision ABIM has for the future of MOC.
President Richard J. Baron, MD, responded to a letter signed by several medical specialty societies, asking for clarification on ABIM’s vision and philosophy for MOC and the future changes ABIM is considering for the MOC program. Dr. Baron articulated the desire for MOC to be relevant to physicians’ practices in collaboration with the ABIM and the medical specialty societies, to produce, “a credential that speaks to whether physicians are staying current in knowledge and practice over the course of their career in their specialty.”
Dr. Richard G. Battaglia, ABIM Chief Medical Officer, and Eric McKeeby, ABIM Director of Community Engagement, reported the results of a membership survey and focus group discussions regarding ABIM’s Assessment 2020 Report, published in September 2015. They highlighted the challenges, opportunities, and future plans for the MOC program, in light of diplomates’ input through these mechanisms. In the feedback received, the majority of diplomates favored a move away from the secure 10-year MOC recertification examination. Several options were presented, including smaller, more frequent exams, secure exams taken from home or office, and the ability to “test out” of the 10-year exam by successfully completing smaller assessments along the way. Ultimately, participants favored a move away from assessment and toward learning and improvement through a mechanism that is relevant to their real-world practices. Dr. Baron noted the ABIM survey results in which 76.3% of diplomates said they wanted the MOC credential to mean “I am staying current in the knowledge I need to practice,” and he reiterated the Board’s commitment to developing assessment approaches that would result in a meaningful credential based on performance. The ABIM Board of Directors met in April, with the exam format being a priority for them.
Regarding the future of MOC, while the practice assessment requirement is on hold through 2018, ABIM recognizes the work in this area many physicians are currently doing. By early 2017, ABIM is planning on extending the partnership with ACCME to recognize practice assessment activities, along with current medical knowledge activities, for both CME and MOC. This expansion would include blended activities that meet both medical knowledge and practice assessment requirements.
In addition to ABIM staff’s perspectives, three medical societies, including CHEST, reported on their MOC efforts. Heather Dethloff, CHEST Education and Accreditation Specialist, participated in a panel discussion, along with the Endocrine Society and the American Academy of Hospice and Palliative Medicine regarding the ongoing efforts to incorporate MOC into educational activities within their organizations. Successes and challenges encountered through the ABIM MOC certification process were the topics for discussion. During this presentation, CHEST announced its plan to incorporate ABIM MOC into the entire CHEST Annual Meeting 2016; details will be communicated to CHEST members and meeting registrants in coming months.
Throughout these changes to the MOC program, CHEST has been, and will continue to be, in communication with ABIM, advocating for our members. Any questions or concerns about this process can be directed to Heather Dethloff, Education and Accreditation Specialist, at [email protected].
More information
New ABIM Survey Indicates Physician Interest in Potential Changes to MOC Assessment: www.abim.org/news/new-abim-survey-indicates-physician-interest-in-potential-changes-to-moc-assessment.aspx