User login
Economic Burden and Quality of Life of Patients With Moderate to Severe Atopic Dermatitis in a Tertiary Care Hospital in Helsinki, Finland: A Survey-Based Study
Atopic dermatitis (AD) is a common inflammatory skin disease that may severely decrease quality of life (QOL) and lead to psychiatric comorbidities.1-3 Prior studies have indicated that AD causes a substantial economic burden, and disease severity has been proportionally linked to medical costs.4,5 Results of a multicenter cost-of-illness study from Germany estimated that a relapse of AD costs approximately €123 (US $136). The authors calculated the average annual cost of AD per patient to be €1425 (US $1580), whereas it is €956 (US $1060) in moderate disease and €2068 (US $2293) in severe disease (direct and indirect medical costs included).6 An observational cohort study from the Netherlands found that total direct cost per patient-year (PPY) was €4401 (US $4879) for patients with controlled AD vs €6993 (US $7756) for patients with uncontrolled AD.7
In a retrospective survey-based study, it was estimated that the annual cost of AD in Canada was approximately CAD $1.4 billion. The cost per patient varied from CAD $282 to CAD $1242 depending on disease severity.8 In another retrospective cohort study from the Netherlands, the average direct medical cost per patient with AD seeing a general practitioner was US $71 during follow-up in primary care. If the patient needed specialist consultation, the cost increased to an average of US $186.9
We aimed to assess the direct and indirect medical costs in adult patients with moderate to severe AD who attended a tertiary health care center in Finland. In addition, we evaluated the impact of AD on QOL in this patient cohort.
Methods
Study Design—Patients with AD who were treated at the Department of Dermatology and Allergology, Helsinki University Hospital, Finland, between February 2018 and December 2019 were randomly selected to participate in our survey study. All participants provided written informed consent. In Finland, patients with mild AD generally are treated in primary health care centers, and only patients with moderate to severe AD are referred to specialists and tertiary care centers. Patients were excluded if they were younger than 18 years, had AD confined to the hands, or reported the presence of other concomitant skin diseases that were being treated with topical or systemic therapies. The protocol for the study was approved by the local ethics committee of the University of Helsinki.
Questionnaire and Analysis of Disease Severity—The survey included the medical history, signs of atopy, former treatment(s) for AD, skin infections, visits to dermatologists or general practitioners, questions on mental health and hospitalization, and absence from work due to AD in the last 12 months. Disease severity was evaluated using the patient-oriented Rajka & Langeland eczema severity score and Patient Oriented Eczema Measure (POEM).10,11 The impact on QOL was evaluated by the Dermatology Life Quality Index (DLQI).12
Medication Costs—The cost of prescription drugs was based on data from the Finnish national electronic prescription center. In Finland, all prescriptions are made electronically in the database. We analyzed all topical medications (eg, topical corticosteroids [TCSs], topical calcineurin inhibitors [TCIs], and emollients) and systemic medicaments (eg, antibiotics, antihistamines, cyclosporine, methotrexate, and corticosteroids) prescribed for the treatment of AD. In Finland, dupilumab was introduced for the treatment of severe AD in early 2019, and patients receiving dupilumab were excluded from the study. Over-the-counter medications were not included. The costs for laboratory testing were estimations based on the standard monitoring protocols of the Helsinki University Hospital. All costs were based on the Finnish price level standard for the year 2019.
Inpatient/Outpatient Visits and Sick Leave Due to AD—The number of inpatient and outpatient visits due to AD in the last 12 months was evaluated. Outpatient specialist consultations or nurse appointments at Helsinki University Hospital were verified from electronic patient records. In addition, inpatient treatment and phototherapy sessions were calculated from the database.
We assessed the number of sick leave days from work or educational activities during the last year. All costs of transportation for doctors’ appointments, laboratory monitoring, and phototherapy treatments were summed together to estimate the total transportation cost. Visits to nurse and inpatient visits were not included in the total transportation cost because patients often were hospitalized directly after consultation visits, and nurse appointments often were combined with inpatient and outpatient visits. To calculate the total transportation cost, we used a rate of €0.43 per kilometer measured from the patients’ home addresses, which was the official compensation rate of the Finnish Tax Administration for 2019.13
Statistical Analysis—Statistical analyses were performed using SPSS Statistics 25 (IBM). Descriptive analyses were used to describe baseline characteristics and to evaluate the mean costs of AD. The patients were divided into 2 groups according to POEM: (1) controlled AD (patients with clear skin or only mild AD; POEM score 0–7) and (2) uncontrolled AD (patients with moderate to very severe AD; POEM score 8–28). The Mann-Whitney U statistic was used to evaluate differences between the study groups.
Results
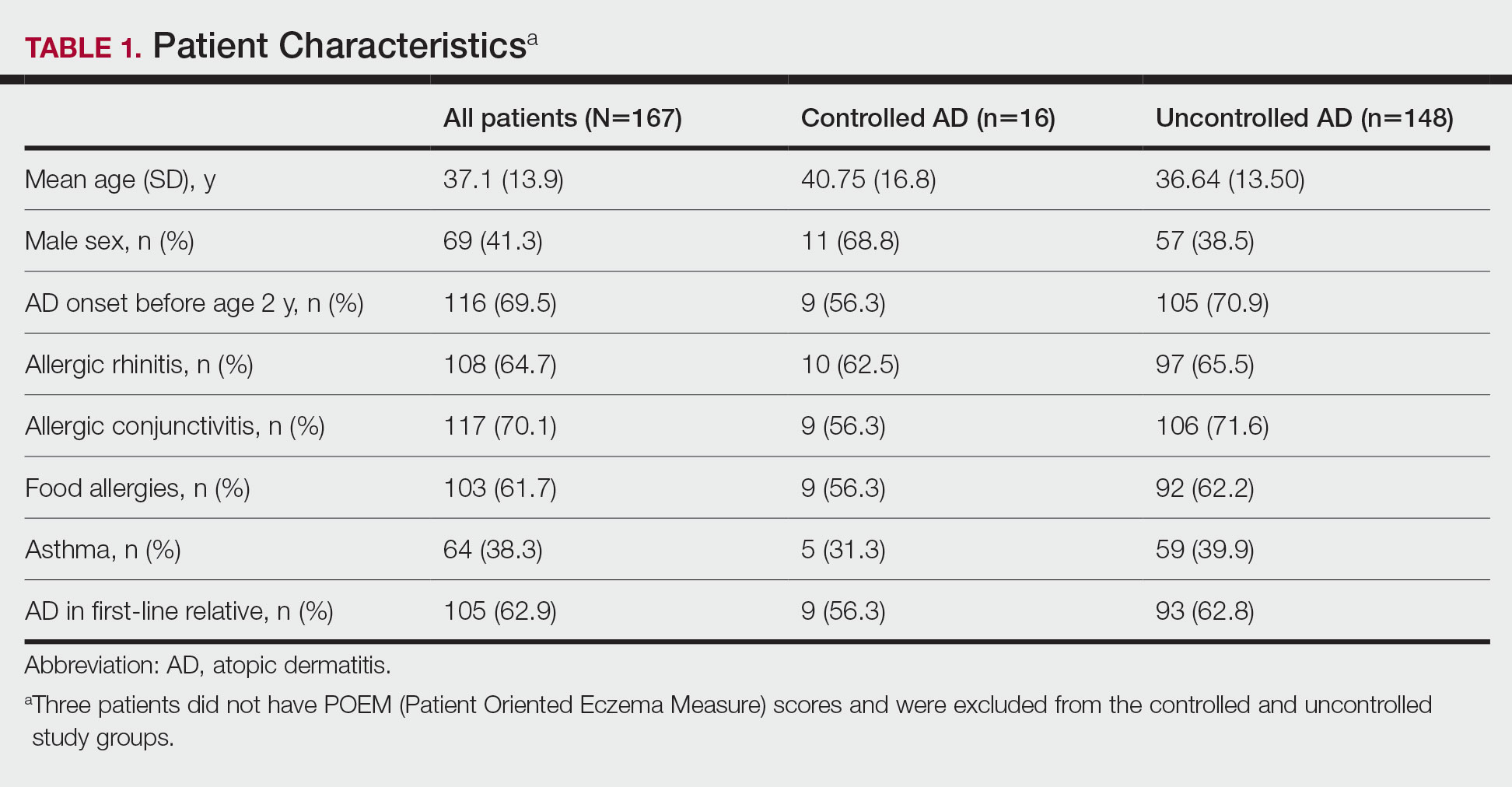
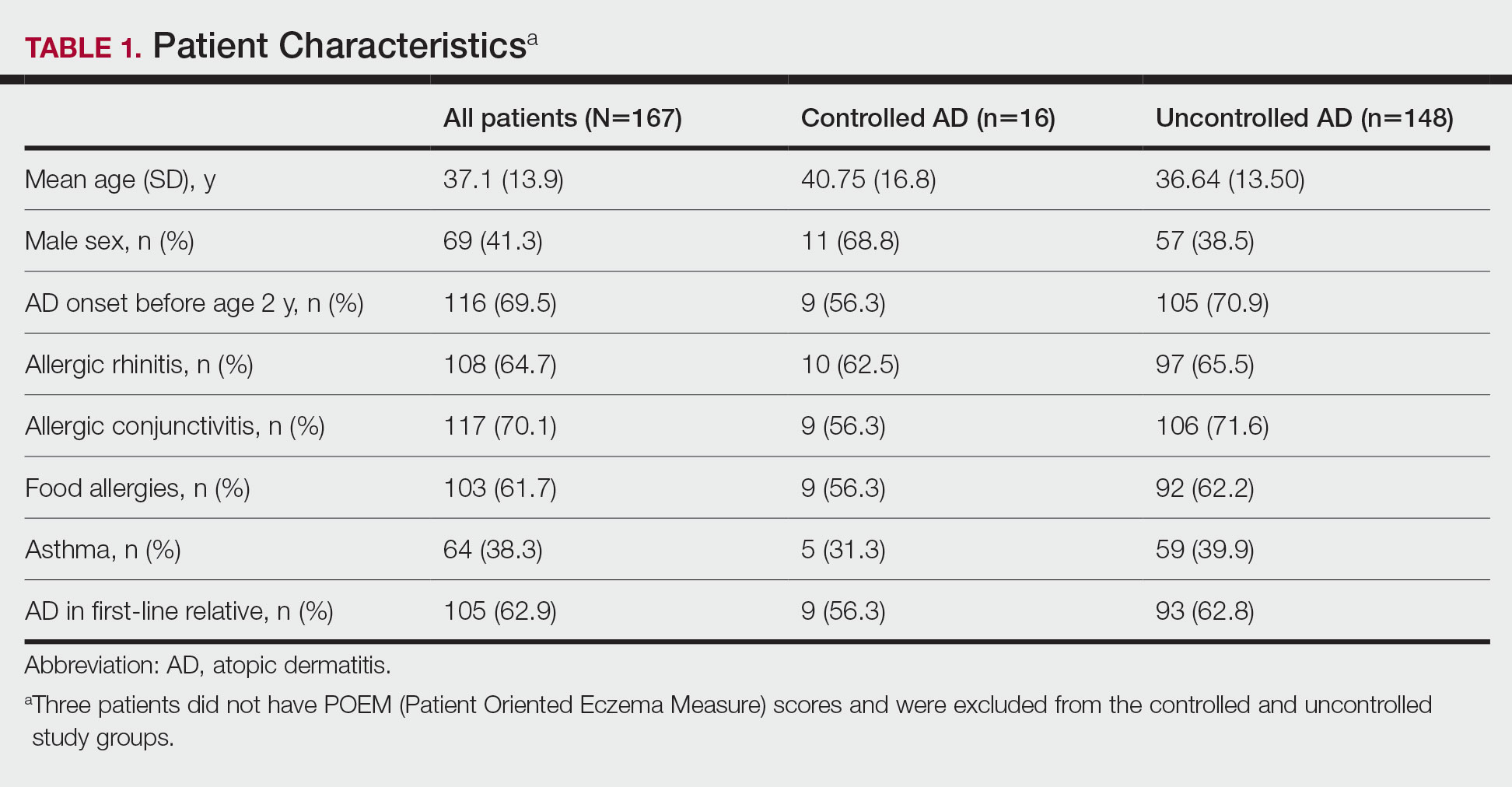
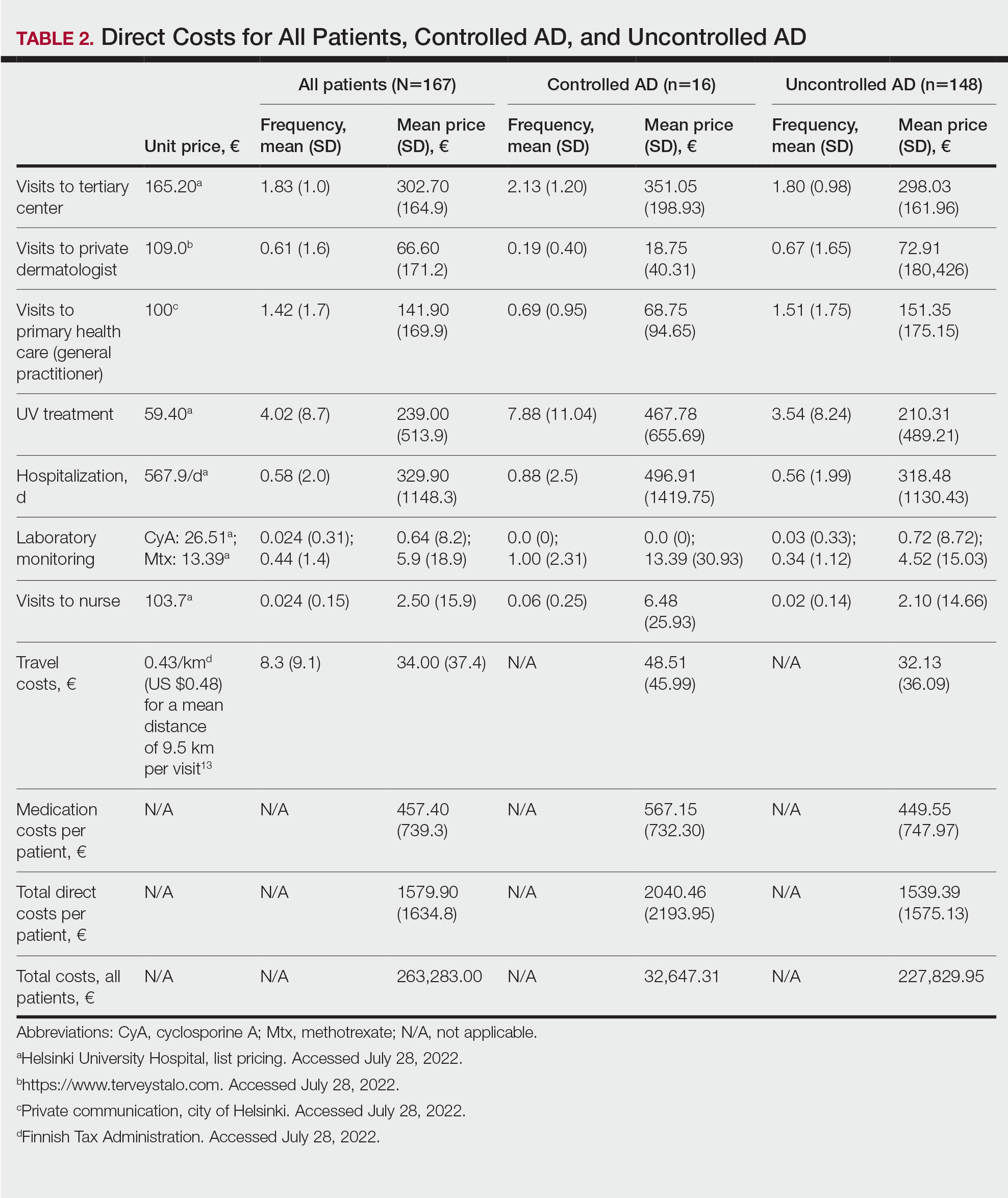
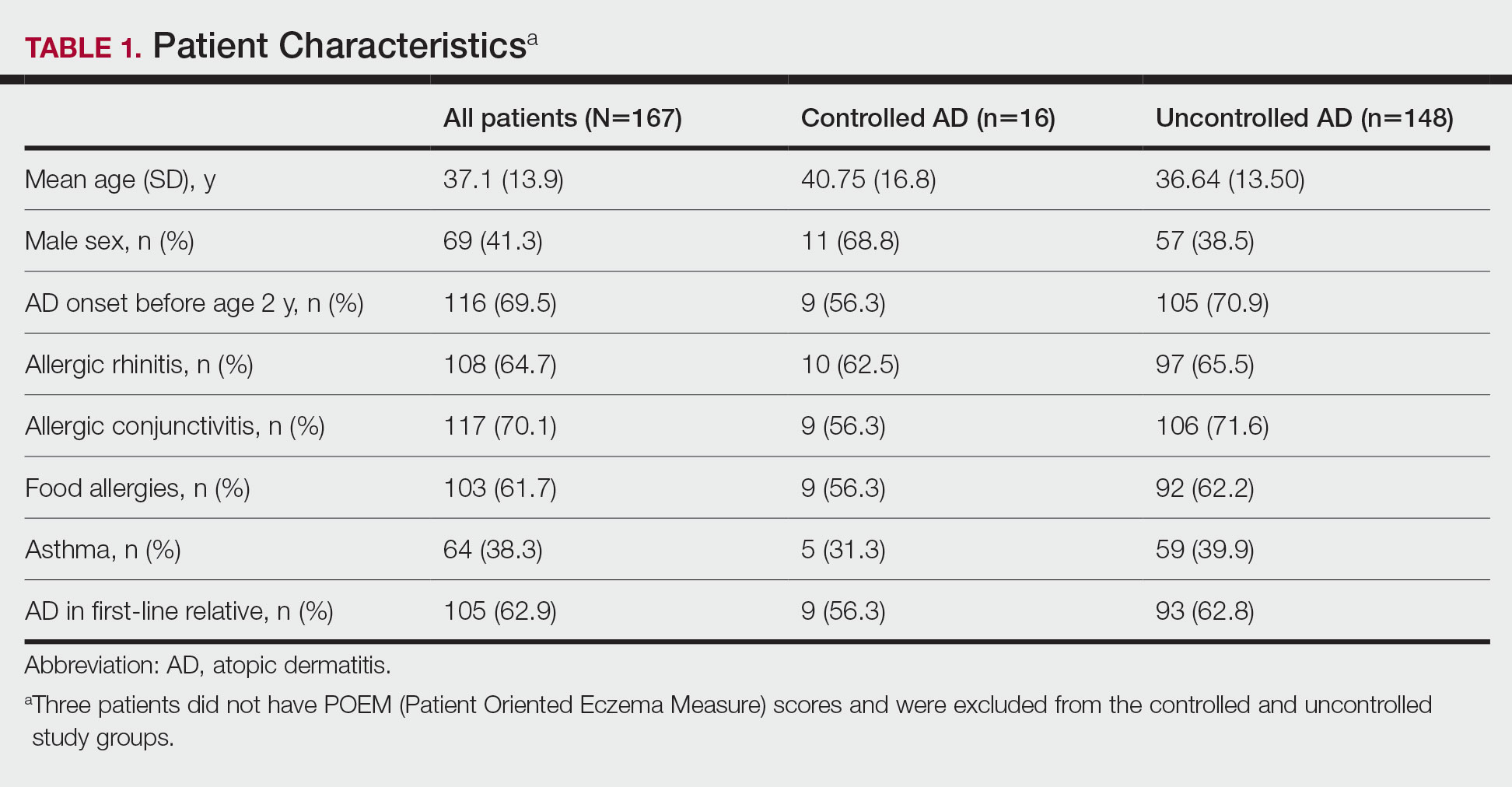
Patient Characteristics—One hundred sixty-seven patients answered the survey, of which 69 (41.3%) were males and 98 (58.7%) were females. There were 16 patients with controlled AD and 148 patients with uncontrolled AD. Three patients did not answer to POEM and were excluded. The baseline characteristics are presented in Table 1 and include self-reported symptoms related to atopy.
The most-used topical treatments were TCSs (n=155; 92.8%) and emollients (n=166; 99.4%). One hundred sixteen (69.5%) patients had used TCIs. The median amount of TCSs used was 300 g/y vs 30 g/y for TCIs (range, 0-5160 g/y) and 1200 g/y for emollients.
Fifteen (9.0%) patients had been hospitalized for AD in the last year. The mean (SD) length of hospitalization was 6.5 (2.8) days. Thirty-four (20.4%) patients received UVB phototherapy. Thirty-four (20.4%) patients were treated with at least 1 antibiotic course for secondary AD infection. Thirty-six (21.6%) patients needed at least 1 oral corticosteroid course for the treatment of an AD flare.
Fifteen (9.0%) patients reported a diagnosed psychiatric illness, and 17 (10.2%) patients were using prescription drugs for psychiatric illness. Forty-nine (29.3%) patients reported anxiety or depression often or very often, 54 (32.3%) patients reported sometimes, 33 (19.8%) patients reported rarely, and only 30 (18.0%) patients reported none.
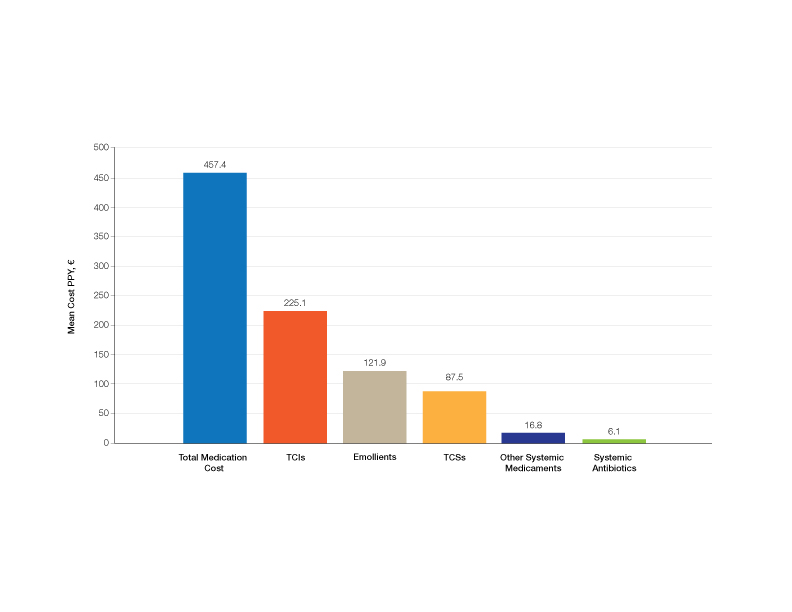
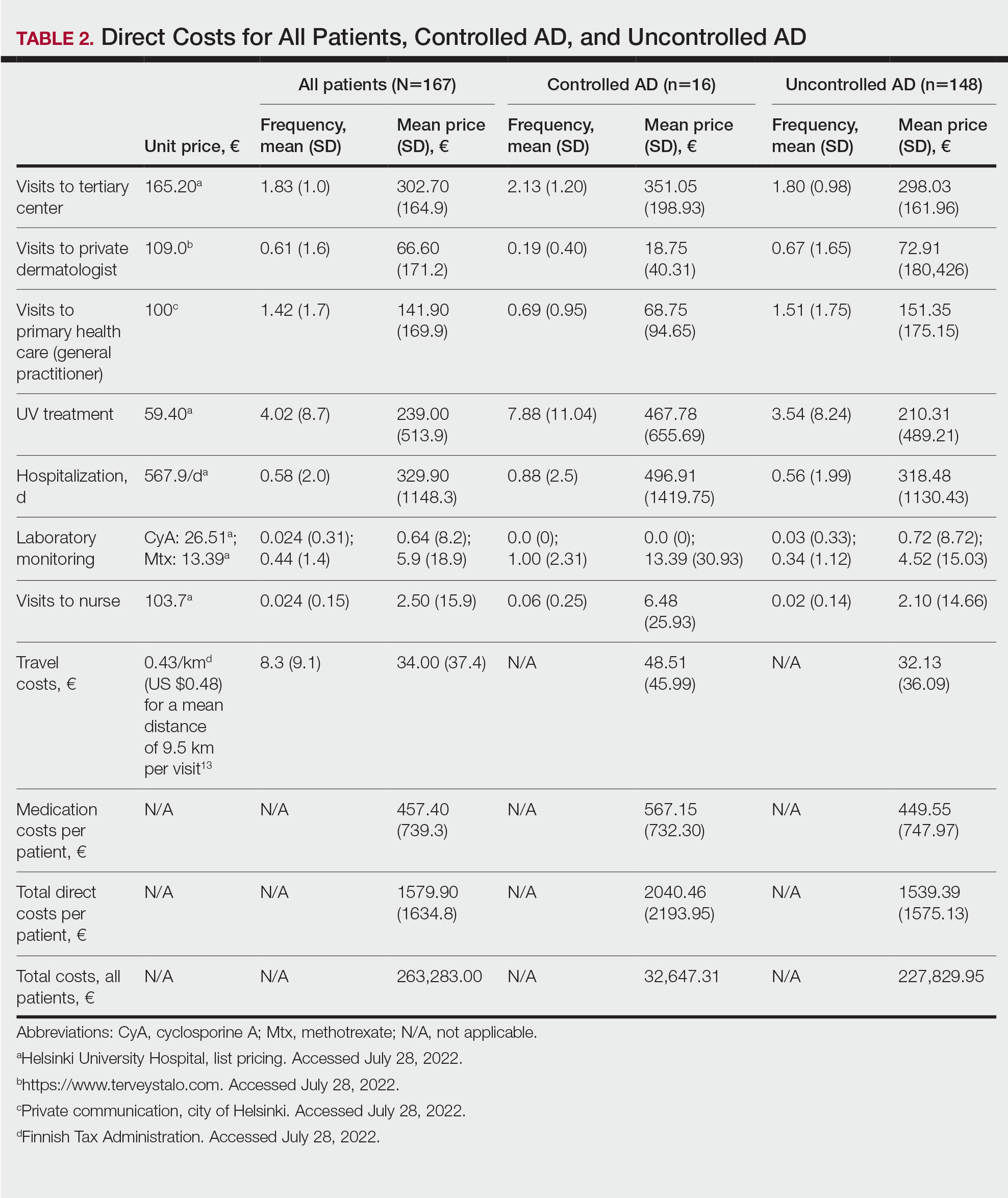
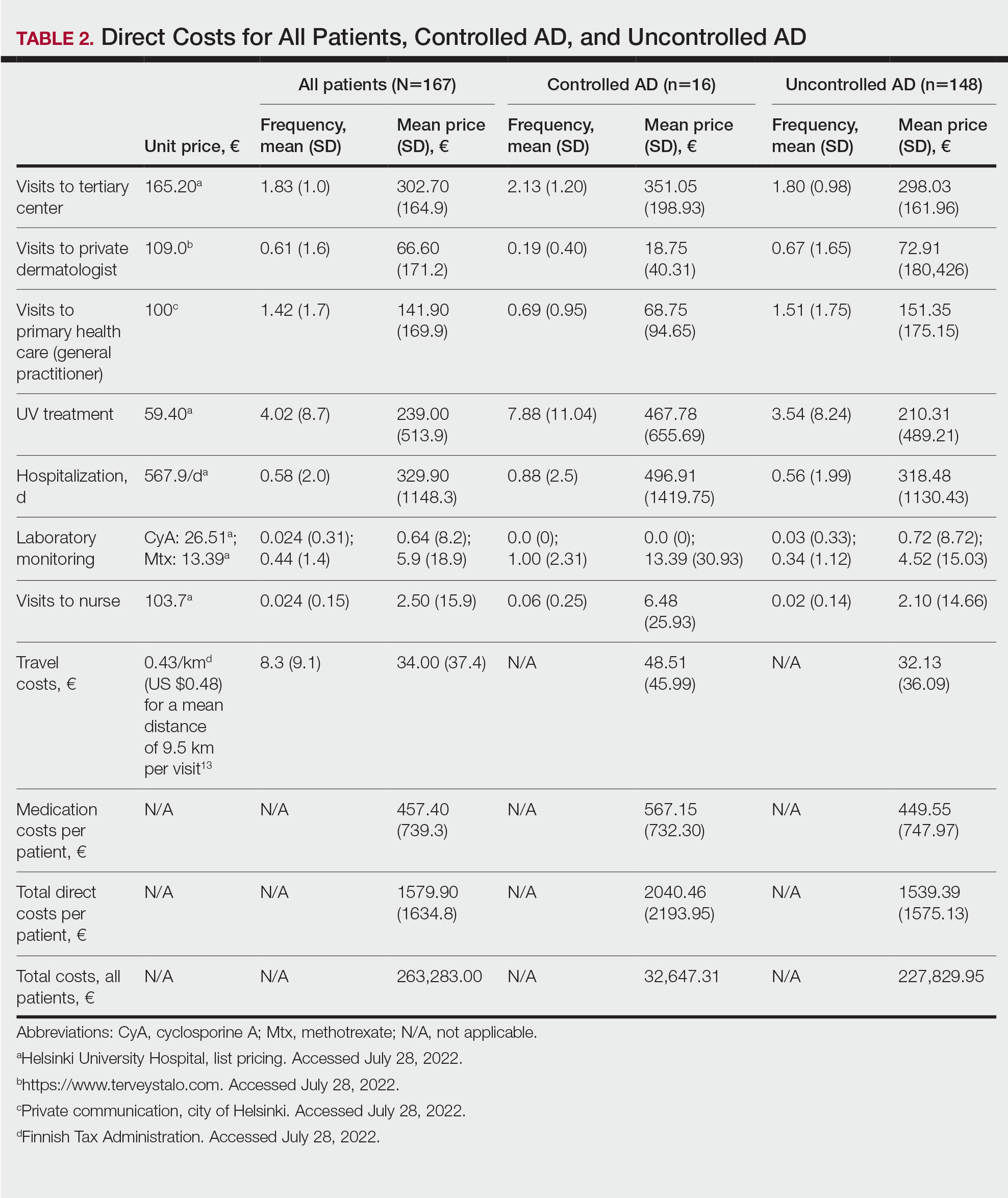
Medication Costs—Mean medication cost PPY was €457.40 (US $507.34)(Figure 1 and Table 2). On average, one patient spent €87.50 (US $97.05) for TCSs, €121.90 (US $135.21) for emollients, and €225.10 (US $249.68) for TCIs. The average cost PPY for antibiotics was €6.10 (US $6.77). Other systemic treatments, including (US $18.65). Seventeen patients (10.2%) were on methotrexate therapy for AD in the last year, and 1 patient also used cyclosporine. The costs for laboratory monitoring in these patients were included in the direct cost calculations. The mean cost PPY of laboratory monitoring in the whole study cohort was €6.60 (US $7.32). In patients with systemic immunosuppressive therapy, the mean cost PPY for laboratory monitoring was €65.00 (US $72.09). Five patients had been tested for contact dermatitis; the costs of patch tests or other diagnostic tests were not included.
Visits to Health Care Providers—In the last year, patients had an average of 1.83 dermatologist consultations in the tertiary center (Table 2). In addition, the mean number of visits to private dermatologists was 0.61 and 1.42 visits to general practitioners. The mean cost of physician visits was €302.70 (US $335.75) in the tertiary center, €66.60 (US $73.87) in the private sector, and €141.90 (US $157.39) in primary health care. In total, the average cost of doctors’ appointments PPY was €506.30 (US $561.57). The mean estimated distance traveled per visit was 9.5 km.
The mean cost PPY of inpatient treatments was €329.90 (US $365.92) and €239.00 (US $265.09) for UV phototherapy. Only 4 patients had visited a nurse in the last year, with an average cost PPY of €2.50 (US $2.78).
In total, the cost PPY for health care provider visits was €1084.20, which included specialist consultations in a tertiary center and private sector, visits in primary health care, inpatient treatments, UV phototherapy sessions, nurse appointments in a tertiary center, and laboratory monitoring. The average transportation cost PPY was €34.00 (US $37.71). The mean number of visits to health care providers was 8.3 per year. Altogether, the direct cost PPY in the study cohort was €1580.60 (US $1752.39)(Table 2 and Figure 2).

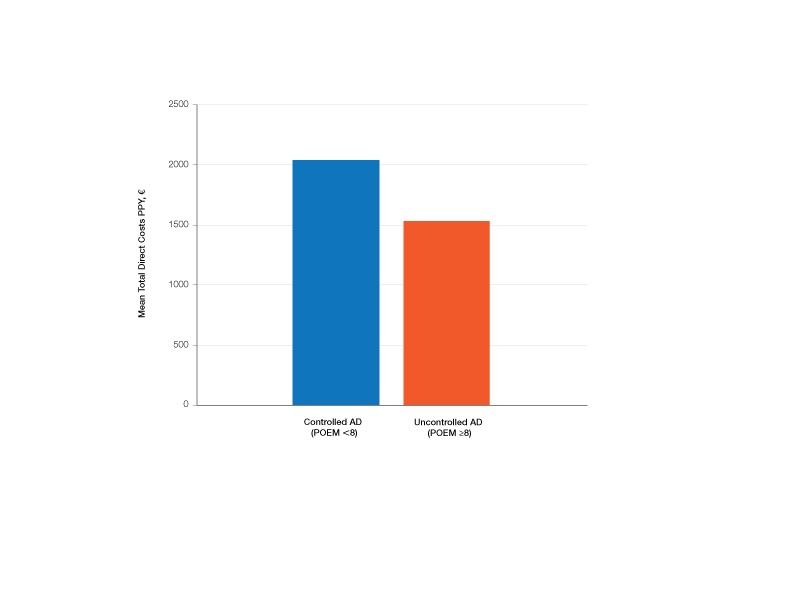
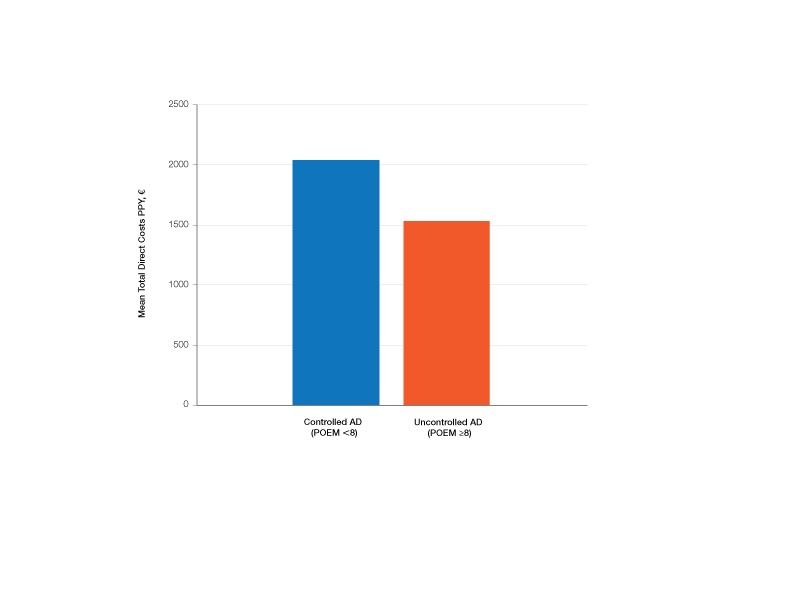
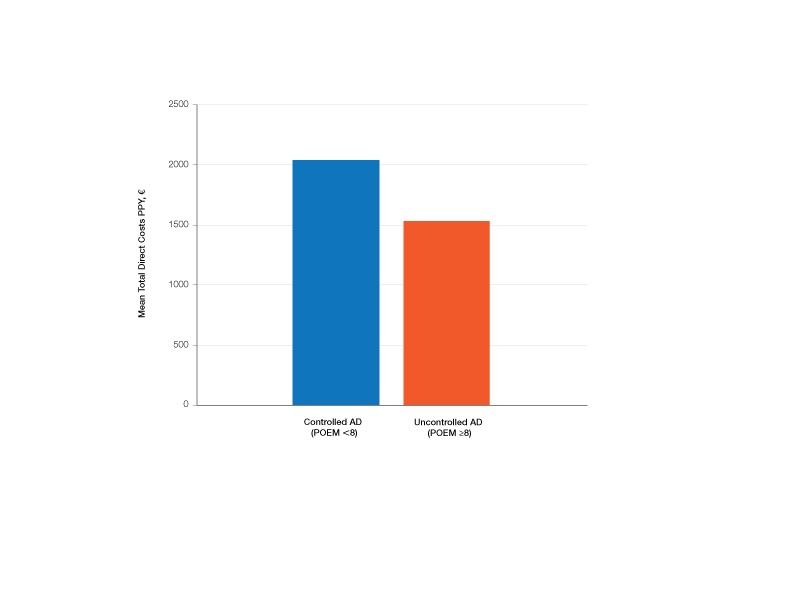
Comparison of Medical Costs in Controlled vs Uncontrolled AD—In the controlled AD group (POEM score <8), the mean medication cost PPY was €567.15 (US $629.13), and the mean total direct cost PPY was €2040.46 (US $2263.24). In the uncontrolled AD group (POEM score ≥8), the mean medication cost PPY was €449.55 (US $498.63), and the mean total direct cost PPY was €1539.39 (US $1707.36)(Table 2). The comparisons of the study groups—controlled vs uncontrolled AD—showed no significant differences regarding medication costs PPY (P=.305, Mann-Whitney U statistic) and total direct costs PPY (P=.361, Mann-Whitney U statistic)(Figure 3). Thus, the distribution of medical costs was similar across all categories of the POEM score.
AD Severity and QOL—The mean (SD) POEM score in the study cohort was 17.9 (6.9). Sixteen (9.6%) patients had clear to almost clear skin or mild AD (POEM score 0–7). Forty-two (25.1%) patients had moderate AD (POEM score 8–16). Most of the patients (106; 63.5%) had severe or very severe AD (POEM score 17–28). According to the Rajka & Langeland score, 5 (3.0%) patients had mild disease (score 34), 81 (48.5%) patients had moderate disease (score 5–7), and 81 (48.5%) patients had severe disease (score 8–9). Eighty-one (48.5%) patients answered that AD affects their lives greatly, and 58 (34.7%) patients answered that it affects their lives extremely. Twenty-five (15.0%) patients answered that AD affects their everyday life to some extent, and only 2 (1.2%) patients answered that AD had little or no effect.
The mean (SD) DLQI was 13 (7.2). Based on the DLQI, 31 (18.6%) patients answered that AD had no effect or only a small effect on QOL (DLQI 0–5). In 36 (21.6%) patients, AD had a moderate effect on QOL (DLQI 6–10). The QOL impact was large (DLQI 11–20) and very large (DLQI 21–30) in 67 (40.1%) and 33 (19.8%) patients, respectively.
There was no significant difference in the impact of disease severity (POEM score) on the decrease of QOL (severe or very severe disease; P=.305, Mann-Whitney U statistic).
Absence From Work or Studies—At the study inclusion, 12 (7.2%) patients were not working or studying. Of the remaining 155 patients, 73 (47.1%) reported absence from work or educational activities due to AD in the last 12 months. The mean (SD) length of absence was 11.6 (10.2) days.
Comment
In this survey-based study of Finnish patients with moderate to severe AD, we observed that AD creates a substantial economic burden14 and negative impact on everyday life and QOL. According to DLQI, AD had a large or very large effect on most of the patients’ (59.9%) lives, and 90.2% of the included patients had self-reported moderate to very severe symptoms (POEM score 8–28). Our observations can partly be explained by characteristics of the Finnish health care system, in which patients with moderate to severe AD mainly are referred to specialist consultation. In the investigated cohort, many patients had used antibiotics (20.4%) and/or oral corticosteroids (21.6%) in the last year for the treatment of AD, which might indicate inadequate treatment of AD in the Finnish health care system.
Motivating patients to remain compliant is one of the main challenges in AD therapy.15 Fear of adverse effects from TCSs is common among patients and may cause poor treatment adherence.16 In a prospective study from the United Kingdom, the use of emollients in moderate to severe AD was considerably lower than AD guidelines recommend—approximately 10 g/d on average in adult patients. The median use of TCSs was between 35 and 38 g/mo.17 In our Finnish patient cohort, the amount of topical treatments was even lower, with a median use of emollients of 3.3 g/d and median use of TCSs of 25 g/mo. In another study from Denmark (N=322), 31% of patients with AD did not redeem their topical prescription medicaments, indicating poor adherence to topical treatment.18
It has been demonstrated that most of the patients’ habituation (tachyphylaxis) to TCSs is due to poor adherence instead of physiologic changes in tissue corticosteroid receptors.19,20 Treatment adherence may be increased by scheduling early follow-up visits and providing adequate therapeutic patient education,21 which requires major efforts by the health care system and a financial investment.
Inadequate treatment will lead to more frequent disease flares and subsequently increase the medical costs for the patients and the health care system.22 In our Finnish patient cohort, a large part of direct treatment costs was due to inpatient treatment (Figure 2) even though only a small proportion of patients had been hospitalized. The patients were frequently young and otherwise in good general health, and they did not necessarily need continuous inpatient treatment and monitoring. In Finland, it will be necessary to develop more cost-effective treatment regimens for patients with AD with severe and frequent flares. Many patients would benefit from subsequent and regular sessions of topical treatment in an outpatient setting. In addition, the prevention of flares in moderate to severe AD will decrease medical costs.23
The mean medication cost PPY was €457.40 (US $507.34), and mean total direct cost PPY was €1579.90 (US $1752.40), which indicates that AD causes a major economic burden to Finnish patients and to the Finnish health care system (Figures 1 and 2).24 We did not observe significant differences between controlled and uncontrolled AD medical costs in our patient cohort (Figure 3), which may have been due to the relatively small sample size of only 16 patients in the controlled AD group. All patients attending the tertiary care hospital had moderate to severe AD, so it is likely that the patients with lower POEM scores had better-controlled disease. The POEM score estimates the grade of AD in the last 7 days, but based on the relapsing course of the disease, the grading score may differ substantially during the year in the same patient depending on the timing.25,26
Topical calcineurin inhibitors comprised almost half of the medication costs (Figure 1), which may be caused by their higher prices compared with TCSs in Finland. In the beginning of 2019, a 50% less expensive biosimilar of tacrolimus ointment 0.1% was introduced to the Finnish market, which might decrease future treatment costs of TCIs. However, availability problems in both topical tacrolimus products were seen throughout 2019, which also may have affected the results in our study cohort. The median use of TCIs was unexpectedly low (only 30 g/y), which may be explained by different application habits. The use of large TCI amounts in some patients may have elevated mean costs.27
In the Finnish public health care system, 40% of the cost for prescription medication and emollients is reimbursed after an initial deductible of €50. Emollients are reimbursed up to an amount of 1500 g/mo. Therefore, patients mostly acquired emollients as prescription medicine and not over-the-counter. Nonprescription medicaments were not included in our study, so the actual costs of topical treatment may have been higher.28
In our cohort, 61.7% of the patients reported food allergies, and 70.1% reported allergic conjunctivitis. However, the study included only questionnaire-based data, and many of these patients probably had symptoms not associated with IgE-mediated allergies. The high prevalence indicates a substantial concomitant burden of more than skin symptoms in patients with AD.29 Nine percent of patients reported a diagnosed psychiatric disorder, and 29.3% had self-reported anxiety or depression often or very often in the last year. Based on these findings, there may be high percentages of undiagnosed psychiatric comorbidities such as depression and anxiety disorders in patients with moderate to severe AD in Finland.30 An important limitation of our study was that the patient data were based on a voluntary and anonymous survey and that depression and anxiety were addressed solely by a single question. In addition, the response rate cannot be analyzed correctly, and the demographics of the survey responders likely will differ substantially from all patients with AD at the university hospital.
Atopic dermatitis had a substantial effect on QOL in our patient cohort. Inadequate treatment of AD is known to negatively affect patient QOL and may lead to hospitalization or frequent oral corticosteroid courses.31,32 In most cases, structured patient education and early follow-up visits may improve patient adherence to treatment and should be considered as an integral part of AD treatment.33 In the investigated Finnish tertiary care hospital, a structured patient education system unfortunately was still lacking, though it has been proven effective elsewhere.34 In addition, patient-centred educational programs are recommended in European guidelines for the treatment of AD.35
Medical costs of AD may increase in the future as new treatments with higher direct costs, such as dupilumab, are introduced. Eichenfeld et al36 analyzed electronic health plan claims in patients with AD with newly introduced systemic therapies and phototherapies after the availability of dupilumab in the United States (March 2017). Mean annualized total cost in all patients was $20,722; the highest in the dupilumab group with $36,505. Compared to our data, the total costs are much higher, but these are likely to rise in Finland in the future if a substantial amount (eg, 1%–5%) of patients will be on advanced therapies, including dupilumab. If advanced therapies will be introduced more broadly in Finland (eg, in the treatment of moderate AD [10%–20% of patients]), they will represent a major direct cost to the health care system. Zimmermann et al37 showed in a cost-utility analysis that dupilumab improves health outcomes but with additional direct costs, and it is likely more cost-effective in patients with severe AD. Conversely, more efficient treatments may improve severe AD, reduce the need for hospitalization and recurrent doctors’ appointments as well as absence from work, and improve patient QOL,38 consequently decreasing indirect medical costs and disease burden. Ariëns et al39 showed in a recent registry-based study that dupilumab treatment induces a notable rise in work productivity and reduction of associated costs in patients with difficult-to-treat AD.
Conclusion
We aimed to analyze the economic burden of AD in Finland before the introduction of dupilumab. It will be interesting to see what the introduction of dupilumab and other novel systemic therapies have on total economic burden and medical costs. Most patients with AD in Finland can achieve disease control with topical treatments, but it is important to efficiently manage the patients who require additional supportive measures and specialist consultations, which may be challenging in the primary health care system because of the relapsing and remitting nature of the disease.
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015;66(suppl 1):8-16.
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351.
- Yang EJ, Beck KM, Sekhon S, et al. The impact of pediatric atopic dermatitis on families: a review. Pediatr Dermatol. 2019;36:66-71.
- Eckert L, Gupta S, Amand C, et al. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: an analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77:274-279.
- Drucker AM, Wang AR, Li WQ, et al. The burden of atopic dermatitis: summary of a report for the National Eczema Association. J Invest Dermatol. 2017;137:26-30.
- Ehlken B, Möhrenschlager M, Kugland B, et al. Cost-of-illness study in patients suffering from atopic eczema in Germany. Der Hautarzt. 2006;56:1144-1151.
- Ariëns LFM, van Nimwegen KJM, Shams M, et al. Economic burden of adult patients with moderate to severe atopic dermatitis indicated for systemic treatment. Acta Derm Venereol. 2019;99:762-768.
- Barbeau M, Bpharm HL. Burden of atopic dermatitis in Canada. Int J Dermatol. 2006;45:31-36.
- Verboom P, Hakkaart‐Van Roijen L, Sturkenboom M, et al. The cost of atopic dermatitis in the Netherlands: an international comparison. Br J Dermatol. 2002;147:716-724.
- Gånemo A, Svensson Å, Svedman C, et al. Usefulness of Rajka & Langeland eczema severity score in clinical practice. Acta Derm Venereol. 2016;96:521-524.
- Charman CR, Venn AJ, Williams HC. The Patient-Oriented Eczema Measure: development and initial validation of a new tool for measuring atopic eczema severity from the patients’ perspective. Arch Dermatol. 2004;140:1513-1519.
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI): a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
- Rehunen A, Reissell E, Honkatukia J, et al. Social and health services: regional changes in need, use and production and future options. Accessed July 20, 2023. http://urn.fi/URN:ISBN:978-952-287-294-4
- Reed B, Blaiss MS. The burden of atopic dermatitis. Allergy Asthma Proc. 2018;39:406-410.
- Koszorú K, Borza J, Gulácsi L, et al. Quality of life in patients with atopic dermatitis. Cutis. 2019;104:174-177.
- Li AW, Yin ES, Antaya RJ. Topical corticosteroid phobia in atopic dermatitis: a systematic review. JAMA Dermatol. 2017;153:1036-1042.
- Choi J, Dawe R, Ibbotson S, et al. Quantitative analysis of topical treatments in atopic dermatitis: unexpectedly low use of emollients and strong correlation of topical corticosteroid use both with depression and concurrent asthma. Br J Dermatol. 2020;182:1017-1025.
- Storm A, Andersen SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
- Okwundu N, Cardwell LA, Cline A, et al. Topical corticosteroids for treatment-resistant atopic dermatitis. Cutis. 2018;102:205-209.
- Eicher L, Knop M, Aszodi N, et al. A systematic review of factors influencing treatment adherence in chronic inflammatory skin disease—strategies for optimizing treatment outcome. J Eur Acad Dermatol Venereol. 2019;33:2253-2263.
- Heratizadeh A, Werfel T, Wollenberg A, et al; Arbeitsgemeinschaft Neurodermitisschulung für Erwachsene (ARNE) Study Group. Effects of structured patient education in adults with atopic dermatitis: multicenter randomized controlled trial. J Allergy Clin Immunol. 2017;140:845-853.
- Dierick BJH, van der Molen T, Flokstra-de Blok BMJ, et al. Burden and socioeconomics of asthma, allergic rhinitis, atopic dermatitis and food allergy. Expert Rev Pharmacoecon Outcomes Res. 2020;20:437-453.
- Olsson M, Bajpai R, Yew YW, et al. Associations between health-related quality of life and health care costs among children with atopic dermatitis and their caregivers: a cross-sectional study. Pediatr Dermatol. 2020;37:284-293.
- Bruin-Weller M, Pink AE, Patrizi A, et al. Disease burden and treatment history among adults with atopic dermatitis receiving systemic therapy: baseline characteristics of participants on the EUROSTAD prospective observational study. J Dermatolog Treat. 2021;32:164-173.
- Silverberg JI, Lei D, Yousaf M, et al. Comparison of Patient-Oriented Eczema Measure and Patient-Oriented Scoring Atopic Dermatitis vs Eczema Area and Severity Index and other measures of atopic dermatitis: a validation study. Ann Allergy Asthma Immunol. 2020;125:78-83.
- Kido-Nakahara M, Nakahara T, Yasukochi Y, et al. Patient-oriented eczema measure score: a useful tool for web-based surveys in patients with atopic dermatitis. Acta Derm Venereol. 2020;47:924-925.
- Komura Y, Kogure T, Kawahara K, et al. Economic assessment of actual prescription of drugs for treatment of atopic dermatitis: differences between dermatology and pediatrics in large-scale receipt data. J Dermatol. 2018;45:165-174.
- Thompson AM, Chan A, Torabi M, et al. Eczema moisturizers: allergenic potential, marketing claims, and costs. Dermatol Ther. 2020;33:E14228.
- Egeberg A, Andersen YM, Gislason GH, et al. Prevalence of comorbidity and associated risk factors in adults with atopic dermatitis. Allergy. 2017;72:783-791.
- Kauppi S, Jokelainen J, Timonen M, et al. Adult patients with atopic eczema have a high burden of psychiatric disease: a Finnish nationwide registry study. Acta Derm Venereol. 2019;99:647-651.
- Ali F, Vyas J, Finlay AY. Counting the burden: atopic dermatitis and health-related quality of life. Acta Derm Venereol. 2020;100:adv00161.
- Birdi G, Cooke R, Knibb RC. Impact of atopic dermatitis on quality of life in adults: a systematic review and meta-analysis. Int J Dermatol. 2020;59:E75-E91.
- Gabes M, Tischer C, Apfelbacher C; quality of life working group of the Harmonising Outcome Measures for Eczema (HOME) initiative. Measurement properties of quality-of-life outcome measures for children and adults with eczema: an updated systematic review. Pediatr Allergy Immunol. 2020;31:66-77.
- Staab D, Diepgen TL, Fartasch M, et al. Age related, structured educational programmes for the management of atopic dermatitis in children and adolescents: multicentre, randomised controlled trial. BMJ. 2006;332:933-938.
- Wollenberg A, Barbarot S, Bieber T, et al; European Dermatology Forum (EDF), the European Academy of Dermatology and Venereology (EADV), the European Academy of Allergy and Clinical Immunology (EAACI), the European Task Force on Atopic Dermatitis (ETFAD), European Federation of Allergy and Airways Diseases Patients’ Associations (EFA), the European Society for Dermatology and Psychiatry (ESDaP), the European Society of Pediatric Dermatology (ESPD), Global Allergy and Asthma European Network (GA2LEN) and the European Union of Medical Specialists (UEMS). Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part II. J Eur Acad Dermatol Venereol. 2018;32:850-878.
- Eichenfield LF, DiBonaventura M, Xenakis J, et al. Costs and treatment patterns among patients with atopic dermatitis using advanced therapies in the United States: analysis of a retrospective claims database. Dermatol Ther (Heidelb). 2020;10:791-806.
- Zimmermann M, Rind D, Chapman R, et al. Economic evaluation of dupilumab for moderate-to-severe atopic dermatitis: a cost-utility analysis. J Drugs Dermatol. 2018;17:750-756.
- Mata E, Loh TY, Ludwig C, et al. Pharmacy costs of systemic and topical medications for atopic dermatitis. J Dermatolog Treat. 2019;12:1-3.
- Ariëns LFM, Bakker DS, Spekhorst LS, et al. Rapid and sustained effect of dupilumab on work productivity in patients with difficult-to-treat atopic dermatitis: results from the Dutch BioDay Registry. Acta Derm Venereol. 2021;19;101:adv00573.
Atopic dermatitis (AD) is a common inflammatory skin disease that may severely decrease quality of life (QOL) and lead to psychiatric comorbidities.1-3 Prior studies have indicated that AD causes a substantial economic burden, and disease severity has been proportionally linked to medical costs.4,5 Results of a multicenter cost-of-illness study from Germany estimated that a relapse of AD costs approximately €123 (US $136). The authors calculated the average annual cost of AD per patient to be €1425 (US $1580), whereas it is €956 (US $1060) in moderate disease and €2068 (US $2293) in severe disease (direct and indirect medical costs included).6 An observational cohort study from the Netherlands found that total direct cost per patient-year (PPY) was €4401 (US $4879) for patients with controlled AD vs €6993 (US $7756) for patients with uncontrolled AD.7
In a retrospective survey-based study, it was estimated that the annual cost of AD in Canada was approximately CAD $1.4 billion. The cost per patient varied from CAD $282 to CAD $1242 depending on disease severity.8 In another retrospective cohort study from the Netherlands, the average direct medical cost per patient with AD seeing a general practitioner was US $71 during follow-up in primary care. If the patient needed specialist consultation, the cost increased to an average of US $186.9
We aimed to assess the direct and indirect medical costs in adult patients with moderate to severe AD who attended a tertiary health care center in Finland. In addition, we evaluated the impact of AD on QOL in this patient cohort.
Methods
Study Design—Patients with AD who were treated at the Department of Dermatology and Allergology, Helsinki University Hospital, Finland, between February 2018 and December 2019 were randomly selected to participate in our survey study. All participants provided written informed consent. In Finland, patients with mild AD generally are treated in primary health care centers, and only patients with moderate to severe AD are referred to specialists and tertiary care centers. Patients were excluded if they were younger than 18 years, had AD confined to the hands, or reported the presence of other concomitant skin diseases that were being treated with topical or systemic therapies. The protocol for the study was approved by the local ethics committee of the University of Helsinki.
Questionnaire and Analysis of Disease Severity—The survey included the medical history, signs of atopy, former treatment(s) for AD, skin infections, visits to dermatologists or general practitioners, questions on mental health and hospitalization, and absence from work due to AD in the last 12 months. Disease severity was evaluated using the patient-oriented Rajka & Langeland eczema severity score and Patient Oriented Eczema Measure (POEM).10,11 The impact on QOL was evaluated by the Dermatology Life Quality Index (DLQI).12
Medication Costs—The cost of prescription drugs was based on data from the Finnish national electronic prescription center. In Finland, all prescriptions are made electronically in the database. We analyzed all topical medications (eg, topical corticosteroids [TCSs], topical calcineurin inhibitors [TCIs], and emollients) and systemic medicaments (eg, antibiotics, antihistamines, cyclosporine, methotrexate, and corticosteroids) prescribed for the treatment of AD. In Finland, dupilumab was introduced for the treatment of severe AD in early 2019, and patients receiving dupilumab were excluded from the study. Over-the-counter medications were not included. The costs for laboratory testing were estimations based on the standard monitoring protocols of the Helsinki University Hospital. All costs were based on the Finnish price level standard for the year 2019.
Inpatient/Outpatient Visits and Sick Leave Due to AD—The number of inpatient and outpatient visits due to AD in the last 12 months was evaluated. Outpatient specialist consultations or nurse appointments at Helsinki University Hospital were verified from electronic patient records. In addition, inpatient treatment and phototherapy sessions were calculated from the database.
We assessed the number of sick leave days from work or educational activities during the last year. All costs of transportation for doctors’ appointments, laboratory monitoring, and phototherapy treatments were summed together to estimate the total transportation cost. Visits to nurse and inpatient visits were not included in the total transportation cost because patients often were hospitalized directly after consultation visits, and nurse appointments often were combined with inpatient and outpatient visits. To calculate the total transportation cost, we used a rate of €0.43 per kilometer measured from the patients’ home addresses, which was the official compensation rate of the Finnish Tax Administration for 2019.13
Statistical Analysis—Statistical analyses were performed using SPSS Statistics 25 (IBM). Descriptive analyses were used to describe baseline characteristics and to evaluate the mean costs of AD. The patients were divided into 2 groups according to POEM: (1) controlled AD (patients with clear skin or only mild AD; POEM score 0–7) and (2) uncontrolled AD (patients with moderate to very severe AD; POEM score 8–28). The Mann-Whitney U statistic was used to evaluate differences between the study groups.
Results
Patient Characteristics—One hundred sixty-seven patients answered the survey, of which 69 (41.3%) were males and 98 (58.7%) were females. There were 16 patients with controlled AD and 148 patients with uncontrolled AD. Three patients did not answer to POEM and were excluded. The baseline characteristics are presented in Table 1 and include self-reported symptoms related to atopy.
The most-used topical treatments were TCSs (n=155; 92.8%) and emollients (n=166; 99.4%). One hundred sixteen (69.5%) patients had used TCIs. The median amount of TCSs used was 300 g/y vs 30 g/y for TCIs (range, 0-5160 g/y) and 1200 g/y for emollients.
Fifteen (9.0%) patients had been hospitalized for AD in the last year. The mean (SD) length of hospitalization was 6.5 (2.8) days. Thirty-four (20.4%) patients received UVB phototherapy. Thirty-four (20.4%) patients were treated with at least 1 antibiotic course for secondary AD infection. Thirty-six (21.6%) patients needed at least 1 oral corticosteroid course for the treatment of an AD flare.
Fifteen (9.0%) patients reported a diagnosed psychiatric illness, and 17 (10.2%) patients were using prescription drugs for psychiatric illness. Forty-nine (29.3%) patients reported anxiety or depression often or very often, 54 (32.3%) patients reported sometimes, 33 (19.8%) patients reported rarely, and only 30 (18.0%) patients reported none.
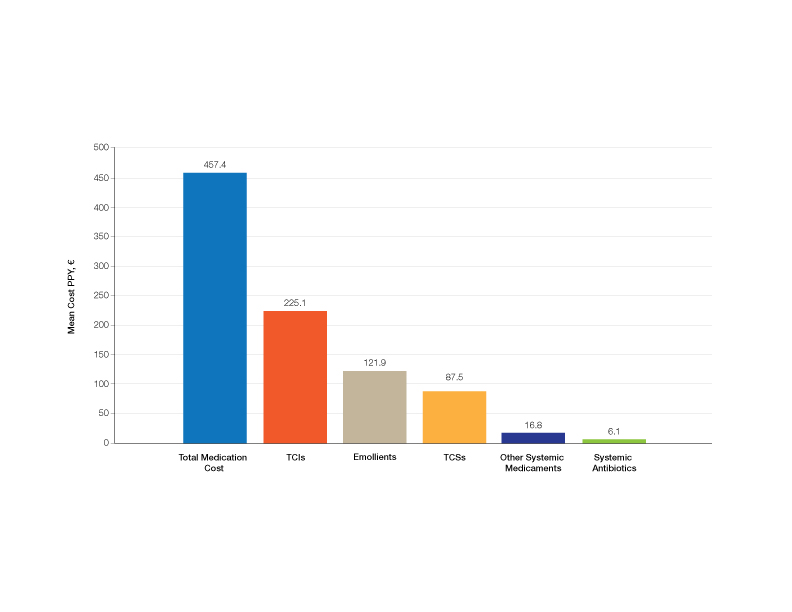
Medication Costs—Mean medication cost PPY was €457.40 (US $507.34)(Figure 1 and Table 2). On average, one patient spent €87.50 (US $97.05) for TCSs, €121.90 (US $135.21) for emollients, and €225.10 (US $249.68) for TCIs. The average cost PPY for antibiotics was €6.10 (US $6.77). Other systemic treatments, including (US $18.65). Seventeen patients (10.2%) were on methotrexate therapy for AD in the last year, and 1 patient also used cyclosporine. The costs for laboratory monitoring in these patients were included in the direct cost calculations. The mean cost PPY of laboratory monitoring in the whole study cohort was €6.60 (US $7.32). In patients with systemic immunosuppressive therapy, the mean cost PPY for laboratory monitoring was €65.00 (US $72.09). Five patients had been tested for contact dermatitis; the costs of patch tests or other diagnostic tests were not included.
Visits to Health Care Providers—In the last year, patients had an average of 1.83 dermatologist consultations in the tertiary center (Table 2). In addition, the mean number of visits to private dermatologists was 0.61 and 1.42 visits to general practitioners. The mean cost of physician visits was €302.70 (US $335.75) in the tertiary center, €66.60 (US $73.87) in the private sector, and €141.90 (US $157.39) in primary health care. In total, the average cost of doctors’ appointments PPY was €506.30 (US $561.57). The mean estimated distance traveled per visit was 9.5 km.
The mean cost PPY of inpatient treatments was €329.90 (US $365.92) and €239.00 (US $265.09) for UV phototherapy. Only 4 patients had visited a nurse in the last year, with an average cost PPY of €2.50 (US $2.78).
In total, the cost PPY for health care provider visits was €1084.20, which included specialist consultations in a tertiary center and private sector, visits in primary health care, inpatient treatments, UV phototherapy sessions, nurse appointments in a tertiary center, and laboratory monitoring. The average transportation cost PPY was €34.00 (US $37.71). The mean number of visits to health care providers was 8.3 per year. Altogether, the direct cost PPY in the study cohort was €1580.60 (US $1752.39)(Table 2 and Figure 2).

Comparison of Medical Costs in Controlled vs Uncontrolled AD—In the controlled AD group (POEM score <8), the mean medication cost PPY was €567.15 (US $629.13), and the mean total direct cost PPY was €2040.46 (US $2263.24). In the uncontrolled AD group (POEM score ≥8), the mean medication cost PPY was €449.55 (US $498.63), and the mean total direct cost PPY was €1539.39 (US $1707.36)(Table 2). The comparisons of the study groups—controlled vs uncontrolled AD—showed no significant differences regarding medication costs PPY (P=.305, Mann-Whitney U statistic) and total direct costs PPY (P=.361, Mann-Whitney U statistic)(Figure 3). Thus, the distribution of medical costs was similar across all categories of the POEM score.
AD Severity and QOL—The mean (SD) POEM score in the study cohort was 17.9 (6.9). Sixteen (9.6%) patients had clear to almost clear skin or mild AD (POEM score 0–7). Forty-two (25.1%) patients had moderate AD (POEM score 8–16). Most of the patients (106; 63.5%) had severe or very severe AD (POEM score 17–28). According to the Rajka & Langeland score, 5 (3.0%) patients had mild disease (score 34), 81 (48.5%) patients had moderate disease (score 5–7), and 81 (48.5%) patients had severe disease (score 8–9). Eighty-one (48.5%) patients answered that AD affects their lives greatly, and 58 (34.7%) patients answered that it affects their lives extremely. Twenty-five (15.0%) patients answered that AD affects their everyday life to some extent, and only 2 (1.2%) patients answered that AD had little or no effect.
The mean (SD) DLQI was 13 (7.2). Based on the DLQI, 31 (18.6%) patients answered that AD had no effect or only a small effect on QOL (DLQI 0–5). In 36 (21.6%) patients, AD had a moderate effect on QOL (DLQI 6–10). The QOL impact was large (DLQI 11–20) and very large (DLQI 21–30) in 67 (40.1%) and 33 (19.8%) patients, respectively.
There was no significant difference in the impact of disease severity (POEM score) on the decrease of QOL (severe or very severe disease; P=.305, Mann-Whitney U statistic).
Absence From Work or Studies—At the study inclusion, 12 (7.2%) patients were not working or studying. Of the remaining 155 patients, 73 (47.1%) reported absence from work or educational activities due to AD in the last 12 months. The mean (SD) length of absence was 11.6 (10.2) days.
Comment
In this survey-based study of Finnish patients with moderate to severe AD, we observed that AD creates a substantial economic burden14 and negative impact on everyday life and QOL. According to DLQI, AD had a large or very large effect on most of the patients’ (59.9%) lives, and 90.2% of the included patients had self-reported moderate to very severe symptoms (POEM score 8–28). Our observations can partly be explained by characteristics of the Finnish health care system, in which patients with moderate to severe AD mainly are referred to specialist consultation. In the investigated cohort, many patients had used antibiotics (20.4%) and/or oral corticosteroids (21.6%) in the last year for the treatment of AD, which might indicate inadequate treatment of AD in the Finnish health care system.
Motivating patients to remain compliant is one of the main challenges in AD therapy.15 Fear of adverse effects from TCSs is common among patients and may cause poor treatment adherence.16 In a prospective study from the United Kingdom, the use of emollients in moderate to severe AD was considerably lower than AD guidelines recommend—approximately 10 g/d on average in adult patients. The median use of TCSs was between 35 and 38 g/mo.17 In our Finnish patient cohort, the amount of topical treatments was even lower, with a median use of emollients of 3.3 g/d and median use of TCSs of 25 g/mo. In another study from Denmark (N=322), 31% of patients with AD did not redeem their topical prescription medicaments, indicating poor adherence to topical treatment.18
It has been demonstrated that most of the patients’ habituation (tachyphylaxis) to TCSs is due to poor adherence instead of physiologic changes in tissue corticosteroid receptors.19,20 Treatment adherence may be increased by scheduling early follow-up visits and providing adequate therapeutic patient education,21 which requires major efforts by the health care system and a financial investment.
Inadequate treatment will lead to more frequent disease flares and subsequently increase the medical costs for the patients and the health care system.22 In our Finnish patient cohort, a large part of direct treatment costs was due to inpatient treatment (Figure 2) even though only a small proportion of patients had been hospitalized. The patients were frequently young and otherwise in good general health, and they did not necessarily need continuous inpatient treatment and monitoring. In Finland, it will be necessary to develop more cost-effective treatment regimens for patients with AD with severe and frequent flares. Many patients would benefit from subsequent and regular sessions of topical treatment in an outpatient setting. In addition, the prevention of flares in moderate to severe AD will decrease medical costs.23
The mean medication cost PPY was €457.40 (US $507.34), and mean total direct cost PPY was €1579.90 (US $1752.40), which indicates that AD causes a major economic burden to Finnish patients and to the Finnish health care system (Figures 1 and 2).24 We did not observe significant differences between controlled and uncontrolled AD medical costs in our patient cohort (Figure 3), which may have been due to the relatively small sample size of only 16 patients in the controlled AD group. All patients attending the tertiary care hospital had moderate to severe AD, so it is likely that the patients with lower POEM scores had better-controlled disease. The POEM score estimates the grade of AD in the last 7 days, but based on the relapsing course of the disease, the grading score may differ substantially during the year in the same patient depending on the timing.25,26
Topical calcineurin inhibitors comprised almost half of the medication costs (Figure 1), which may be caused by their higher prices compared with TCSs in Finland. In the beginning of 2019, a 50% less expensive biosimilar of tacrolimus ointment 0.1% was introduced to the Finnish market, which might decrease future treatment costs of TCIs. However, availability problems in both topical tacrolimus products were seen throughout 2019, which also may have affected the results in our study cohort. The median use of TCIs was unexpectedly low (only 30 g/y), which may be explained by different application habits. The use of large TCI amounts in some patients may have elevated mean costs.27
In the Finnish public health care system, 40% of the cost for prescription medication and emollients is reimbursed after an initial deductible of €50. Emollients are reimbursed up to an amount of 1500 g/mo. Therefore, patients mostly acquired emollients as prescription medicine and not over-the-counter. Nonprescription medicaments were not included in our study, so the actual costs of topical treatment may have been higher.28
In our cohort, 61.7% of the patients reported food allergies, and 70.1% reported allergic conjunctivitis. However, the study included only questionnaire-based data, and many of these patients probably had symptoms not associated with IgE-mediated allergies. The high prevalence indicates a substantial concomitant burden of more than skin symptoms in patients with AD.29 Nine percent of patients reported a diagnosed psychiatric disorder, and 29.3% had self-reported anxiety or depression often or very often in the last year. Based on these findings, there may be high percentages of undiagnosed psychiatric comorbidities such as depression and anxiety disorders in patients with moderate to severe AD in Finland.30 An important limitation of our study was that the patient data were based on a voluntary and anonymous survey and that depression and anxiety were addressed solely by a single question. In addition, the response rate cannot be analyzed correctly, and the demographics of the survey responders likely will differ substantially from all patients with AD at the university hospital.
Atopic dermatitis had a substantial effect on QOL in our patient cohort. Inadequate treatment of AD is known to negatively affect patient QOL and may lead to hospitalization or frequent oral corticosteroid courses.31,32 In most cases, structured patient education and early follow-up visits may improve patient adherence to treatment and should be considered as an integral part of AD treatment.33 In the investigated Finnish tertiary care hospital, a structured patient education system unfortunately was still lacking, though it has been proven effective elsewhere.34 In addition, patient-centred educational programs are recommended in European guidelines for the treatment of AD.35
Medical costs of AD may increase in the future as new treatments with higher direct costs, such as dupilumab, are introduced. Eichenfeld et al36 analyzed electronic health plan claims in patients with AD with newly introduced systemic therapies and phototherapies after the availability of dupilumab in the United States (March 2017). Mean annualized total cost in all patients was $20,722; the highest in the dupilumab group with $36,505. Compared to our data, the total costs are much higher, but these are likely to rise in Finland in the future if a substantial amount (eg, 1%–5%) of patients will be on advanced therapies, including dupilumab. If advanced therapies will be introduced more broadly in Finland (eg, in the treatment of moderate AD [10%–20% of patients]), they will represent a major direct cost to the health care system. Zimmermann et al37 showed in a cost-utility analysis that dupilumab improves health outcomes but with additional direct costs, and it is likely more cost-effective in patients with severe AD. Conversely, more efficient treatments may improve severe AD, reduce the need for hospitalization and recurrent doctors’ appointments as well as absence from work, and improve patient QOL,38 consequently decreasing indirect medical costs and disease burden. Ariëns et al39 showed in a recent registry-based study that dupilumab treatment induces a notable rise in work productivity and reduction of associated costs in patients with difficult-to-treat AD.
Conclusion
We aimed to analyze the economic burden of AD in Finland before the introduction of dupilumab. It will be interesting to see what the introduction of dupilumab and other novel systemic therapies have on total economic burden and medical costs. Most patients with AD in Finland can achieve disease control with topical treatments, but it is important to efficiently manage the patients who require additional supportive measures and specialist consultations, which may be challenging in the primary health care system because of the relapsing and remitting nature of the disease.
Atopic dermatitis (AD) is a common inflammatory skin disease that may severely decrease quality of life (QOL) and lead to psychiatric comorbidities.1-3 Prior studies have indicated that AD causes a substantial economic burden, and disease severity has been proportionally linked to medical costs.4,5 Results of a multicenter cost-of-illness study from Germany estimated that a relapse of AD costs approximately €123 (US $136). The authors calculated the average annual cost of AD per patient to be €1425 (US $1580), whereas it is €956 (US $1060) in moderate disease and €2068 (US $2293) in severe disease (direct and indirect medical costs included).6 An observational cohort study from the Netherlands found that total direct cost per patient-year (PPY) was €4401 (US $4879) for patients with controlled AD vs €6993 (US $7756) for patients with uncontrolled AD.7
In a retrospective survey-based study, it was estimated that the annual cost of AD in Canada was approximately CAD $1.4 billion. The cost per patient varied from CAD $282 to CAD $1242 depending on disease severity.8 In another retrospective cohort study from the Netherlands, the average direct medical cost per patient with AD seeing a general practitioner was US $71 during follow-up in primary care. If the patient needed specialist consultation, the cost increased to an average of US $186.9
We aimed to assess the direct and indirect medical costs in adult patients with moderate to severe AD who attended a tertiary health care center in Finland. In addition, we evaluated the impact of AD on QOL in this patient cohort.
Methods
Study Design—Patients with AD who were treated at the Department of Dermatology and Allergology, Helsinki University Hospital, Finland, between February 2018 and December 2019 were randomly selected to participate in our survey study. All participants provided written informed consent. In Finland, patients with mild AD generally are treated in primary health care centers, and only patients with moderate to severe AD are referred to specialists and tertiary care centers. Patients were excluded if they were younger than 18 years, had AD confined to the hands, or reported the presence of other concomitant skin diseases that were being treated with topical or systemic therapies. The protocol for the study was approved by the local ethics committee of the University of Helsinki.
Questionnaire and Analysis of Disease Severity—The survey included the medical history, signs of atopy, former treatment(s) for AD, skin infections, visits to dermatologists or general practitioners, questions on mental health and hospitalization, and absence from work due to AD in the last 12 months. Disease severity was evaluated using the patient-oriented Rajka & Langeland eczema severity score and Patient Oriented Eczema Measure (POEM).10,11 The impact on QOL was evaluated by the Dermatology Life Quality Index (DLQI).12
Medication Costs—The cost of prescription drugs was based on data from the Finnish national electronic prescription center. In Finland, all prescriptions are made electronically in the database. We analyzed all topical medications (eg, topical corticosteroids [TCSs], topical calcineurin inhibitors [TCIs], and emollients) and systemic medicaments (eg, antibiotics, antihistamines, cyclosporine, methotrexate, and corticosteroids) prescribed for the treatment of AD. In Finland, dupilumab was introduced for the treatment of severe AD in early 2019, and patients receiving dupilumab were excluded from the study. Over-the-counter medications were not included. The costs for laboratory testing were estimations based on the standard monitoring protocols of the Helsinki University Hospital. All costs were based on the Finnish price level standard for the year 2019.
Inpatient/Outpatient Visits and Sick Leave Due to AD—The number of inpatient and outpatient visits due to AD in the last 12 months was evaluated. Outpatient specialist consultations or nurse appointments at Helsinki University Hospital were verified from electronic patient records. In addition, inpatient treatment and phototherapy sessions were calculated from the database.
We assessed the number of sick leave days from work or educational activities during the last year. All costs of transportation for doctors’ appointments, laboratory monitoring, and phototherapy treatments were summed together to estimate the total transportation cost. Visits to nurse and inpatient visits were not included in the total transportation cost because patients often were hospitalized directly after consultation visits, and nurse appointments often were combined with inpatient and outpatient visits. To calculate the total transportation cost, we used a rate of €0.43 per kilometer measured from the patients’ home addresses, which was the official compensation rate of the Finnish Tax Administration for 2019.13
Statistical Analysis—Statistical analyses were performed using SPSS Statistics 25 (IBM). Descriptive analyses were used to describe baseline characteristics and to evaluate the mean costs of AD. The patients were divided into 2 groups according to POEM: (1) controlled AD (patients with clear skin or only mild AD; POEM score 0–7) and (2) uncontrolled AD (patients with moderate to very severe AD; POEM score 8–28). The Mann-Whitney U statistic was used to evaluate differences between the study groups.
Results
Patient Characteristics—One hundred sixty-seven patients answered the survey, of which 69 (41.3%) were males and 98 (58.7%) were females. There were 16 patients with controlled AD and 148 patients with uncontrolled AD. Three patients did not answer to POEM and were excluded. The baseline characteristics are presented in Table 1 and include self-reported symptoms related to atopy.
The most-used topical treatments were TCSs (n=155; 92.8%) and emollients (n=166; 99.4%). One hundred sixteen (69.5%) patients had used TCIs. The median amount of TCSs used was 300 g/y vs 30 g/y for TCIs (range, 0-5160 g/y) and 1200 g/y for emollients.
Fifteen (9.0%) patients had been hospitalized for AD in the last year. The mean (SD) length of hospitalization was 6.5 (2.8) days. Thirty-four (20.4%) patients received UVB phototherapy. Thirty-four (20.4%) patients were treated with at least 1 antibiotic course for secondary AD infection. Thirty-six (21.6%) patients needed at least 1 oral corticosteroid course for the treatment of an AD flare.
Fifteen (9.0%) patients reported a diagnosed psychiatric illness, and 17 (10.2%) patients were using prescription drugs for psychiatric illness. Forty-nine (29.3%) patients reported anxiety or depression often or very often, 54 (32.3%) patients reported sometimes, 33 (19.8%) patients reported rarely, and only 30 (18.0%) patients reported none.
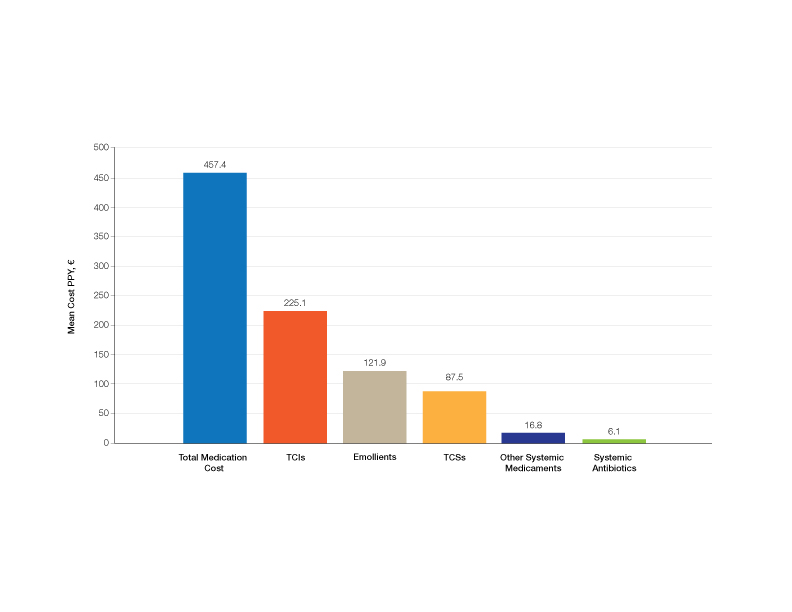
Medication Costs—Mean medication cost PPY was €457.40 (US $507.34)(Figure 1 and Table 2). On average, one patient spent €87.50 (US $97.05) for TCSs, €121.90 (US $135.21) for emollients, and €225.10 (US $249.68) for TCIs. The average cost PPY for antibiotics was €6.10 (US $6.77). Other systemic treatments, including (US $18.65). Seventeen patients (10.2%) were on methotrexate therapy for AD in the last year, and 1 patient also used cyclosporine. The costs for laboratory monitoring in these patients were included in the direct cost calculations. The mean cost PPY of laboratory monitoring in the whole study cohort was €6.60 (US $7.32). In patients with systemic immunosuppressive therapy, the mean cost PPY for laboratory monitoring was €65.00 (US $72.09). Five patients had been tested for contact dermatitis; the costs of patch tests or other diagnostic tests were not included.
Visits to Health Care Providers—In the last year, patients had an average of 1.83 dermatologist consultations in the tertiary center (Table 2). In addition, the mean number of visits to private dermatologists was 0.61 and 1.42 visits to general practitioners. The mean cost of physician visits was €302.70 (US $335.75) in the tertiary center, €66.60 (US $73.87) in the private sector, and €141.90 (US $157.39) in primary health care. In total, the average cost of doctors’ appointments PPY was €506.30 (US $561.57). The mean estimated distance traveled per visit was 9.5 km.
The mean cost PPY of inpatient treatments was €329.90 (US $365.92) and €239.00 (US $265.09) for UV phototherapy. Only 4 patients had visited a nurse in the last year, with an average cost PPY of €2.50 (US $2.78).
In total, the cost PPY for health care provider visits was €1084.20, which included specialist consultations in a tertiary center and private sector, visits in primary health care, inpatient treatments, UV phototherapy sessions, nurse appointments in a tertiary center, and laboratory monitoring. The average transportation cost PPY was €34.00 (US $37.71). The mean number of visits to health care providers was 8.3 per year. Altogether, the direct cost PPY in the study cohort was €1580.60 (US $1752.39)(Table 2 and Figure 2).

Comparison of Medical Costs in Controlled vs Uncontrolled AD—In the controlled AD group (POEM score <8), the mean medication cost PPY was €567.15 (US $629.13), and the mean total direct cost PPY was €2040.46 (US $2263.24). In the uncontrolled AD group (POEM score ≥8), the mean medication cost PPY was €449.55 (US $498.63), and the mean total direct cost PPY was €1539.39 (US $1707.36)(Table 2). The comparisons of the study groups—controlled vs uncontrolled AD—showed no significant differences regarding medication costs PPY (P=.305, Mann-Whitney U statistic) and total direct costs PPY (P=.361, Mann-Whitney U statistic)(Figure 3). Thus, the distribution of medical costs was similar across all categories of the POEM score.
AD Severity and QOL—The mean (SD) POEM score in the study cohort was 17.9 (6.9). Sixteen (9.6%) patients had clear to almost clear skin or mild AD (POEM score 0–7). Forty-two (25.1%) patients had moderate AD (POEM score 8–16). Most of the patients (106; 63.5%) had severe or very severe AD (POEM score 17–28). According to the Rajka & Langeland score, 5 (3.0%) patients had mild disease (score 34), 81 (48.5%) patients had moderate disease (score 5–7), and 81 (48.5%) patients had severe disease (score 8–9). Eighty-one (48.5%) patients answered that AD affects their lives greatly, and 58 (34.7%) patients answered that it affects their lives extremely. Twenty-five (15.0%) patients answered that AD affects their everyday life to some extent, and only 2 (1.2%) patients answered that AD had little or no effect.
The mean (SD) DLQI was 13 (7.2). Based on the DLQI, 31 (18.6%) patients answered that AD had no effect or only a small effect on QOL (DLQI 0–5). In 36 (21.6%) patients, AD had a moderate effect on QOL (DLQI 6–10). The QOL impact was large (DLQI 11–20) and very large (DLQI 21–30) in 67 (40.1%) and 33 (19.8%) patients, respectively.
There was no significant difference in the impact of disease severity (POEM score) on the decrease of QOL (severe or very severe disease; P=.305, Mann-Whitney U statistic).
Absence From Work or Studies—At the study inclusion, 12 (7.2%) patients were not working or studying. Of the remaining 155 patients, 73 (47.1%) reported absence from work or educational activities due to AD in the last 12 months. The mean (SD) length of absence was 11.6 (10.2) days.
Comment
In this survey-based study of Finnish patients with moderate to severe AD, we observed that AD creates a substantial economic burden14 and negative impact on everyday life and QOL. According to DLQI, AD had a large or very large effect on most of the patients’ (59.9%) lives, and 90.2% of the included patients had self-reported moderate to very severe symptoms (POEM score 8–28). Our observations can partly be explained by characteristics of the Finnish health care system, in which patients with moderate to severe AD mainly are referred to specialist consultation. In the investigated cohort, many patients had used antibiotics (20.4%) and/or oral corticosteroids (21.6%) in the last year for the treatment of AD, which might indicate inadequate treatment of AD in the Finnish health care system.
Motivating patients to remain compliant is one of the main challenges in AD therapy.15 Fear of adverse effects from TCSs is common among patients and may cause poor treatment adherence.16 In a prospective study from the United Kingdom, the use of emollients in moderate to severe AD was considerably lower than AD guidelines recommend—approximately 10 g/d on average in adult patients. The median use of TCSs was between 35 and 38 g/mo.17 In our Finnish patient cohort, the amount of topical treatments was even lower, with a median use of emollients of 3.3 g/d and median use of TCSs of 25 g/mo. In another study from Denmark (N=322), 31% of patients with AD did not redeem their topical prescription medicaments, indicating poor adherence to topical treatment.18
It has been demonstrated that most of the patients’ habituation (tachyphylaxis) to TCSs is due to poor adherence instead of physiologic changes in tissue corticosteroid receptors.19,20 Treatment adherence may be increased by scheduling early follow-up visits and providing adequate therapeutic patient education,21 which requires major efforts by the health care system and a financial investment.
Inadequate treatment will lead to more frequent disease flares and subsequently increase the medical costs for the patients and the health care system.22 In our Finnish patient cohort, a large part of direct treatment costs was due to inpatient treatment (Figure 2) even though only a small proportion of patients had been hospitalized. The patients were frequently young and otherwise in good general health, and they did not necessarily need continuous inpatient treatment and monitoring. In Finland, it will be necessary to develop more cost-effective treatment regimens for patients with AD with severe and frequent flares. Many patients would benefit from subsequent and regular sessions of topical treatment in an outpatient setting. In addition, the prevention of flares in moderate to severe AD will decrease medical costs.23
The mean medication cost PPY was €457.40 (US $507.34), and mean total direct cost PPY was €1579.90 (US $1752.40), which indicates that AD causes a major economic burden to Finnish patients and to the Finnish health care system (Figures 1 and 2).24 We did not observe significant differences between controlled and uncontrolled AD medical costs in our patient cohort (Figure 3), which may have been due to the relatively small sample size of only 16 patients in the controlled AD group. All patients attending the tertiary care hospital had moderate to severe AD, so it is likely that the patients with lower POEM scores had better-controlled disease. The POEM score estimates the grade of AD in the last 7 days, but based on the relapsing course of the disease, the grading score may differ substantially during the year in the same patient depending on the timing.25,26
Topical calcineurin inhibitors comprised almost half of the medication costs (Figure 1), which may be caused by their higher prices compared with TCSs in Finland. In the beginning of 2019, a 50% less expensive biosimilar of tacrolimus ointment 0.1% was introduced to the Finnish market, which might decrease future treatment costs of TCIs. However, availability problems in both topical tacrolimus products were seen throughout 2019, which also may have affected the results in our study cohort. The median use of TCIs was unexpectedly low (only 30 g/y), which may be explained by different application habits. The use of large TCI amounts in some patients may have elevated mean costs.27
In the Finnish public health care system, 40% of the cost for prescription medication and emollients is reimbursed after an initial deductible of €50. Emollients are reimbursed up to an amount of 1500 g/mo. Therefore, patients mostly acquired emollients as prescription medicine and not over-the-counter. Nonprescription medicaments were not included in our study, so the actual costs of topical treatment may have been higher.28
In our cohort, 61.7% of the patients reported food allergies, and 70.1% reported allergic conjunctivitis. However, the study included only questionnaire-based data, and many of these patients probably had symptoms not associated with IgE-mediated allergies. The high prevalence indicates a substantial concomitant burden of more than skin symptoms in patients with AD.29 Nine percent of patients reported a diagnosed psychiatric disorder, and 29.3% had self-reported anxiety or depression often or very often in the last year. Based on these findings, there may be high percentages of undiagnosed psychiatric comorbidities such as depression and anxiety disorders in patients with moderate to severe AD in Finland.30 An important limitation of our study was that the patient data were based on a voluntary and anonymous survey and that depression and anxiety were addressed solely by a single question. In addition, the response rate cannot be analyzed correctly, and the demographics of the survey responders likely will differ substantially from all patients with AD at the university hospital.
Atopic dermatitis had a substantial effect on QOL in our patient cohort. Inadequate treatment of AD is known to negatively affect patient QOL and may lead to hospitalization or frequent oral corticosteroid courses.31,32 In most cases, structured patient education and early follow-up visits may improve patient adherence to treatment and should be considered as an integral part of AD treatment.33 In the investigated Finnish tertiary care hospital, a structured patient education system unfortunately was still lacking, though it has been proven effective elsewhere.34 In addition, patient-centred educational programs are recommended in European guidelines for the treatment of AD.35
Medical costs of AD may increase in the future as new treatments with higher direct costs, such as dupilumab, are introduced. Eichenfeld et al36 analyzed electronic health plan claims in patients with AD with newly introduced systemic therapies and phototherapies after the availability of dupilumab in the United States (March 2017). Mean annualized total cost in all patients was $20,722; the highest in the dupilumab group with $36,505. Compared to our data, the total costs are much higher, but these are likely to rise in Finland in the future if a substantial amount (eg, 1%–5%) of patients will be on advanced therapies, including dupilumab. If advanced therapies will be introduced more broadly in Finland (eg, in the treatment of moderate AD [10%–20% of patients]), they will represent a major direct cost to the health care system. Zimmermann et al37 showed in a cost-utility analysis that dupilumab improves health outcomes but with additional direct costs, and it is likely more cost-effective in patients with severe AD. Conversely, more efficient treatments may improve severe AD, reduce the need for hospitalization and recurrent doctors’ appointments as well as absence from work, and improve patient QOL,38 consequently decreasing indirect medical costs and disease burden. Ariëns et al39 showed in a recent registry-based study that dupilumab treatment induces a notable rise in work productivity and reduction of associated costs in patients with difficult-to-treat AD.
Conclusion
We aimed to analyze the economic burden of AD in Finland before the introduction of dupilumab. It will be interesting to see what the introduction of dupilumab and other novel systemic therapies have on total economic burden and medical costs. Most patients with AD in Finland can achieve disease control with topical treatments, but it is important to efficiently manage the patients who require additional supportive measures and specialist consultations, which may be challenging in the primary health care system because of the relapsing and remitting nature of the disease.
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015;66(suppl 1):8-16.
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351.
- Yang EJ, Beck KM, Sekhon S, et al. The impact of pediatric atopic dermatitis on families: a review. Pediatr Dermatol. 2019;36:66-71.
- Eckert L, Gupta S, Amand C, et al. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: an analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77:274-279.
- Drucker AM, Wang AR, Li WQ, et al. The burden of atopic dermatitis: summary of a report for the National Eczema Association. J Invest Dermatol. 2017;137:26-30.
- Ehlken B, Möhrenschlager M, Kugland B, et al. Cost-of-illness study in patients suffering from atopic eczema in Germany. Der Hautarzt. 2006;56:1144-1151.
- Ariëns LFM, van Nimwegen KJM, Shams M, et al. Economic burden of adult patients with moderate to severe atopic dermatitis indicated for systemic treatment. Acta Derm Venereol. 2019;99:762-768.
- Barbeau M, Bpharm HL. Burden of atopic dermatitis in Canada. Int J Dermatol. 2006;45:31-36.
- Verboom P, Hakkaart‐Van Roijen L, Sturkenboom M, et al. The cost of atopic dermatitis in the Netherlands: an international comparison. Br J Dermatol. 2002;147:716-724.
- Gånemo A, Svensson Å, Svedman C, et al. Usefulness of Rajka & Langeland eczema severity score in clinical practice. Acta Derm Venereol. 2016;96:521-524.
- Charman CR, Venn AJ, Williams HC. The Patient-Oriented Eczema Measure: development and initial validation of a new tool for measuring atopic eczema severity from the patients’ perspective. Arch Dermatol. 2004;140:1513-1519.
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI): a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
- Rehunen A, Reissell E, Honkatukia J, et al. Social and health services: regional changes in need, use and production and future options. Accessed July 20, 2023. http://urn.fi/URN:ISBN:978-952-287-294-4
- Reed B, Blaiss MS. The burden of atopic dermatitis. Allergy Asthma Proc. 2018;39:406-410.
- Koszorú K, Borza J, Gulácsi L, et al. Quality of life in patients with atopic dermatitis. Cutis. 2019;104:174-177.
- Li AW, Yin ES, Antaya RJ. Topical corticosteroid phobia in atopic dermatitis: a systematic review. JAMA Dermatol. 2017;153:1036-1042.
- Choi J, Dawe R, Ibbotson S, et al. Quantitative analysis of topical treatments in atopic dermatitis: unexpectedly low use of emollients and strong correlation of topical corticosteroid use both with depression and concurrent asthma. Br J Dermatol. 2020;182:1017-1025.
- Storm A, Andersen SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
- Okwundu N, Cardwell LA, Cline A, et al. Topical corticosteroids for treatment-resistant atopic dermatitis. Cutis. 2018;102:205-209.
- Eicher L, Knop M, Aszodi N, et al. A systematic review of factors influencing treatment adherence in chronic inflammatory skin disease—strategies for optimizing treatment outcome. J Eur Acad Dermatol Venereol. 2019;33:2253-2263.
- Heratizadeh A, Werfel T, Wollenberg A, et al; Arbeitsgemeinschaft Neurodermitisschulung für Erwachsene (ARNE) Study Group. Effects of structured patient education in adults with atopic dermatitis: multicenter randomized controlled trial. J Allergy Clin Immunol. 2017;140:845-853.
- Dierick BJH, van der Molen T, Flokstra-de Blok BMJ, et al. Burden and socioeconomics of asthma, allergic rhinitis, atopic dermatitis and food allergy. Expert Rev Pharmacoecon Outcomes Res. 2020;20:437-453.
- Olsson M, Bajpai R, Yew YW, et al. Associations between health-related quality of life and health care costs among children with atopic dermatitis and their caregivers: a cross-sectional study. Pediatr Dermatol. 2020;37:284-293.
- Bruin-Weller M, Pink AE, Patrizi A, et al. Disease burden and treatment history among adults with atopic dermatitis receiving systemic therapy: baseline characteristics of participants on the EUROSTAD prospective observational study. J Dermatolog Treat. 2021;32:164-173.
- Silverberg JI, Lei D, Yousaf M, et al. Comparison of Patient-Oriented Eczema Measure and Patient-Oriented Scoring Atopic Dermatitis vs Eczema Area and Severity Index and other measures of atopic dermatitis: a validation study. Ann Allergy Asthma Immunol. 2020;125:78-83.
- Kido-Nakahara M, Nakahara T, Yasukochi Y, et al. Patient-oriented eczema measure score: a useful tool for web-based surveys in patients with atopic dermatitis. Acta Derm Venereol. 2020;47:924-925.
- Komura Y, Kogure T, Kawahara K, et al. Economic assessment of actual prescription of drugs for treatment of atopic dermatitis: differences between dermatology and pediatrics in large-scale receipt data. J Dermatol. 2018;45:165-174.
- Thompson AM, Chan A, Torabi M, et al. Eczema moisturizers: allergenic potential, marketing claims, and costs. Dermatol Ther. 2020;33:E14228.
- Egeberg A, Andersen YM, Gislason GH, et al. Prevalence of comorbidity and associated risk factors in adults with atopic dermatitis. Allergy. 2017;72:783-791.
- Kauppi S, Jokelainen J, Timonen M, et al. Adult patients with atopic eczema have a high burden of psychiatric disease: a Finnish nationwide registry study. Acta Derm Venereol. 2019;99:647-651.
- Ali F, Vyas J, Finlay AY. Counting the burden: atopic dermatitis and health-related quality of life. Acta Derm Venereol. 2020;100:adv00161.
- Birdi G, Cooke R, Knibb RC. Impact of atopic dermatitis on quality of life in adults: a systematic review and meta-analysis. Int J Dermatol. 2020;59:E75-E91.
- Gabes M, Tischer C, Apfelbacher C; quality of life working group of the Harmonising Outcome Measures for Eczema (HOME) initiative. Measurement properties of quality-of-life outcome measures for children and adults with eczema: an updated systematic review. Pediatr Allergy Immunol. 2020;31:66-77.
- Staab D, Diepgen TL, Fartasch M, et al. Age related, structured educational programmes for the management of atopic dermatitis in children and adolescents: multicentre, randomised controlled trial. BMJ. 2006;332:933-938.
- Wollenberg A, Barbarot S, Bieber T, et al; European Dermatology Forum (EDF), the European Academy of Dermatology and Venereology (EADV), the European Academy of Allergy and Clinical Immunology (EAACI), the European Task Force on Atopic Dermatitis (ETFAD), European Federation of Allergy and Airways Diseases Patients’ Associations (EFA), the European Society for Dermatology and Psychiatry (ESDaP), the European Society of Pediatric Dermatology (ESPD), Global Allergy and Asthma European Network (GA2LEN) and the European Union of Medical Specialists (UEMS). Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part II. J Eur Acad Dermatol Venereol. 2018;32:850-878.
- Eichenfield LF, DiBonaventura M, Xenakis J, et al. Costs and treatment patterns among patients with atopic dermatitis using advanced therapies in the United States: analysis of a retrospective claims database. Dermatol Ther (Heidelb). 2020;10:791-806.
- Zimmermann M, Rind D, Chapman R, et al. Economic evaluation of dupilumab for moderate-to-severe atopic dermatitis: a cost-utility analysis. J Drugs Dermatol. 2018;17:750-756.
- Mata E, Loh TY, Ludwig C, et al. Pharmacy costs of systemic and topical medications for atopic dermatitis. J Dermatolog Treat. 2019;12:1-3.
- Ariëns LFM, Bakker DS, Spekhorst LS, et al. Rapid and sustained effect of dupilumab on work productivity in patients with difficult-to-treat atopic dermatitis: results from the Dutch BioDay Registry. Acta Derm Venereol. 2021;19;101:adv00573.
- Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015;66(suppl 1):8-16.
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70:338-351.
- Yang EJ, Beck KM, Sekhon S, et al. The impact of pediatric atopic dermatitis on families: a review. Pediatr Dermatol. 2019;36:66-71.
- Eckert L, Gupta S, Amand C, et al. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: an analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77:274-279.
- Drucker AM, Wang AR, Li WQ, et al. The burden of atopic dermatitis: summary of a report for the National Eczema Association. J Invest Dermatol. 2017;137:26-30.
- Ehlken B, Möhrenschlager M, Kugland B, et al. Cost-of-illness study in patients suffering from atopic eczema in Germany. Der Hautarzt. 2006;56:1144-1151.
- Ariëns LFM, van Nimwegen KJM, Shams M, et al. Economic burden of adult patients with moderate to severe atopic dermatitis indicated for systemic treatment. Acta Derm Venereol. 2019;99:762-768.
- Barbeau M, Bpharm HL. Burden of atopic dermatitis in Canada. Int J Dermatol. 2006;45:31-36.
- Verboom P, Hakkaart‐Van Roijen L, Sturkenboom M, et al. The cost of atopic dermatitis in the Netherlands: an international comparison. Br J Dermatol. 2002;147:716-724.
- Gånemo A, Svensson Å, Svedman C, et al. Usefulness of Rajka & Langeland eczema severity score in clinical practice. Acta Derm Venereol. 2016;96:521-524.
- Charman CR, Venn AJ, Williams HC. The Patient-Oriented Eczema Measure: development and initial validation of a new tool for measuring atopic eczema severity from the patients’ perspective. Arch Dermatol. 2004;140:1513-1519.
- Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI): a simple practical measure for routine clinical use. Clin Exp Dermatol. 1994;19:210-216.
- Rehunen A, Reissell E, Honkatukia J, et al. Social and health services: regional changes in need, use and production and future options. Accessed July 20, 2023. http://urn.fi/URN:ISBN:978-952-287-294-4
- Reed B, Blaiss MS. The burden of atopic dermatitis. Allergy Asthma Proc. 2018;39:406-410.
- Koszorú K, Borza J, Gulácsi L, et al. Quality of life in patients with atopic dermatitis. Cutis. 2019;104:174-177.
- Li AW, Yin ES, Antaya RJ. Topical corticosteroid phobia in atopic dermatitis: a systematic review. JAMA Dermatol. 2017;153:1036-1042.
- Choi J, Dawe R, Ibbotson S, et al. Quantitative analysis of topical treatments in atopic dermatitis: unexpectedly low use of emollients and strong correlation of topical corticosteroid use both with depression and concurrent asthma. Br J Dermatol. 2020;182:1017-1025.
- Storm A, Andersen SE, Benfeldt E, et al. One in 3 prescriptions are never redeemed: primary nonadherence in an outpatient clinic. J Am Acad Dermatol. 2008;59:27-33.
- Okwundu N, Cardwell LA, Cline A, et al. Topical corticosteroids for treatment-resistant atopic dermatitis. Cutis. 2018;102:205-209.
- Eicher L, Knop M, Aszodi N, et al. A systematic review of factors influencing treatment adherence in chronic inflammatory skin disease—strategies for optimizing treatment outcome. J Eur Acad Dermatol Venereol. 2019;33:2253-2263.
- Heratizadeh A, Werfel T, Wollenberg A, et al; Arbeitsgemeinschaft Neurodermitisschulung für Erwachsene (ARNE) Study Group. Effects of structured patient education in adults with atopic dermatitis: multicenter randomized controlled trial. J Allergy Clin Immunol. 2017;140:845-853.
- Dierick BJH, van der Molen T, Flokstra-de Blok BMJ, et al. Burden and socioeconomics of asthma, allergic rhinitis, atopic dermatitis and food allergy. Expert Rev Pharmacoecon Outcomes Res. 2020;20:437-453.
- Olsson M, Bajpai R, Yew YW, et al. Associations between health-related quality of life and health care costs among children with atopic dermatitis and their caregivers: a cross-sectional study. Pediatr Dermatol. 2020;37:284-293.
- Bruin-Weller M, Pink AE, Patrizi A, et al. Disease burden and treatment history among adults with atopic dermatitis receiving systemic therapy: baseline characteristics of participants on the EUROSTAD prospective observational study. J Dermatolog Treat. 2021;32:164-173.
- Silverberg JI, Lei D, Yousaf M, et al. Comparison of Patient-Oriented Eczema Measure and Patient-Oriented Scoring Atopic Dermatitis vs Eczema Area and Severity Index and other measures of atopic dermatitis: a validation study. Ann Allergy Asthma Immunol. 2020;125:78-83.
- Kido-Nakahara M, Nakahara T, Yasukochi Y, et al. Patient-oriented eczema measure score: a useful tool for web-based surveys in patients with atopic dermatitis. Acta Derm Venereol. 2020;47:924-925.
- Komura Y, Kogure T, Kawahara K, et al. Economic assessment of actual prescription of drugs for treatment of atopic dermatitis: differences between dermatology and pediatrics in large-scale receipt data. J Dermatol. 2018;45:165-174.
- Thompson AM, Chan A, Torabi M, et al. Eczema moisturizers: allergenic potential, marketing claims, and costs. Dermatol Ther. 2020;33:E14228.
- Egeberg A, Andersen YM, Gislason GH, et al. Prevalence of comorbidity and associated risk factors in adults with atopic dermatitis. Allergy. 2017;72:783-791.
- Kauppi S, Jokelainen J, Timonen M, et al. Adult patients with atopic eczema have a high burden of psychiatric disease: a Finnish nationwide registry study. Acta Derm Venereol. 2019;99:647-651.
- Ali F, Vyas J, Finlay AY. Counting the burden: atopic dermatitis and health-related quality of life. Acta Derm Venereol. 2020;100:adv00161.
- Birdi G, Cooke R, Knibb RC. Impact of atopic dermatitis on quality of life in adults: a systematic review and meta-analysis. Int J Dermatol. 2020;59:E75-E91.
- Gabes M, Tischer C, Apfelbacher C; quality of life working group of the Harmonising Outcome Measures for Eczema (HOME) initiative. Measurement properties of quality-of-life outcome measures for children and adults with eczema: an updated systematic review. Pediatr Allergy Immunol. 2020;31:66-77.
- Staab D, Diepgen TL, Fartasch M, et al. Age related, structured educational programmes for the management of atopic dermatitis in children and adolescents: multicentre, randomised controlled trial. BMJ. 2006;332:933-938.
- Wollenberg A, Barbarot S, Bieber T, et al; European Dermatology Forum (EDF), the European Academy of Dermatology and Venereology (EADV), the European Academy of Allergy and Clinical Immunology (EAACI), the European Task Force on Atopic Dermatitis (ETFAD), European Federation of Allergy and Airways Diseases Patients’ Associations (EFA), the European Society for Dermatology and Psychiatry (ESDaP), the European Society of Pediatric Dermatology (ESPD), Global Allergy and Asthma European Network (GA2LEN) and the European Union of Medical Specialists (UEMS). Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: part II. J Eur Acad Dermatol Venereol. 2018;32:850-878.
- Eichenfield LF, DiBonaventura M, Xenakis J, et al. Costs and treatment patterns among patients with atopic dermatitis using advanced therapies in the United States: analysis of a retrospective claims database. Dermatol Ther (Heidelb). 2020;10:791-806.
- Zimmermann M, Rind D, Chapman R, et al. Economic evaluation of dupilumab for moderate-to-severe atopic dermatitis: a cost-utility analysis. J Drugs Dermatol. 2018;17:750-756.
- Mata E, Loh TY, Ludwig C, et al. Pharmacy costs of systemic and topical medications for atopic dermatitis. J Dermatolog Treat. 2019;12:1-3.
- Ariëns LFM, Bakker DS, Spekhorst LS, et al. Rapid and sustained effect of dupilumab on work productivity in patients with difficult-to-treat atopic dermatitis: results from the Dutch BioDay Registry. Acta Derm Venereol. 2021;19;101:adv00573.
Practice Points
- Atopic dermatitis (AD) causes a substantial economic burden.
- Atopic dermatitis profoundly affects quality of life and is associated with psychiatric comorbidities. With effective treatments, AD-associated comorbidities may be decreased and the economic burden for the patient and health care system reduced.
Imaging Tools for Noninvasive Hair Assessment
New imaging tools along with adaptations to existing technologies have been emerging in recent years, with the potential to improve hair diagnostics and treatment monitoring. We provide an overview of 4 noninvasive hair imaging technologies: global photography, trichoscopy, reflectance confocal microscopy (RCM), and optical coherence tomography (OCT). For each instrument, we discuss current and future applications in clinical practice and research along with advantages and disadvantages.
Global Photography
Global photography allows for the analysis of hair growth, volume, distribution, and density through serial standardized photographs.1 Global photography was first introduced for hair growth studies in 1987 and soon after was used for hair and scalp assessments in finasteride clinical trials.2
Hair Assessment—Washed, dried, and combed hair, without hair product, are required for accurate imaging; wet conditions increase reflection and promote hair clumping, thus revealing more scalp and depicting the patient as having less hair.1 Headshots are taken from short distances and use stereotactic positioning devices to create 4 global views: vertex, midline, frontal, and temporal.3 Stereotactic positioning involves fixing the patient’s chin and forehead as well as mounting the camera and flash device to ensure proper magnification. These adjustments ensure lighting remains consistent throughout consecutive study visits.4 Various grading scales are available for use in hair growth clinical studies to increase objectivity in the analysis of serial global photographs. A blinded evaluator should assess the before and after photographs to limit experimenter bias. Global photography often is combined with quantitative software analysis for improved detection of hair changes.1
Advancements—Growing interest in improving global photography has resulted in various application-based, artificial intelligence (AI)–mediated tools to simplify photograph collection and analysis. For instance, new hair analysis software utilizes AI algorithms to account for facial features in determining the optimal angle for capturing global photographs (Figure 1), which simplifies the generation of global photography images through smartphone applications and obviates the need for additional stereotactic positioning equipment.5,6

Limitations—Clinicians should be aware of global photography’s requirements for consistency in lighting, camera settings, film, and image processing, which can limit the accuracy of hair assessment over time if not replicated correctly.7,8 Emerging global photography software has helped to overcome some of these limitations.
Global photography is less precise when a patient’s hair loss is less than 50%, as it is difficult to discern subtle hair changes. Thus, global photography provides limited utility in assessing minimal to moderate hair loss.9 Currently, global photography largely functions as an adjunct tool for other hair analysis methods rather than as a stand-alone tool.
Trichoscopy
Trichoscopy (also known as dermoscopy of the hair and scalp) may be performed with a manual dermoscope (with 10× magnification) or a digital videodermatoscope (up to 1000× magnification).10-12 Unlike global photography, trichoscopy provides a detailed structural analysis of hair shafts, follicular openings, and perifollicular and interfollicular areas.13 Kinoshita-Ise and Sachdeva13 provided an in-depth, updated review of trichoscopy terminology with their definitions and associated conditions (with prevalence), which should be referenced when performing trichoscopic examination.
Hair Assessment—Trichoscopic assessment begins with inspection of follicular openings (also referred to as “dots”), which vary in color depending on the material filling them—degrading keratinocytes, keratin, sebaceous debris, melanin, or fractured hairs.13 The structure of hair shafts also is examined, showing broken hairs, short vellus hairs, and comma hairs, among others. Perifollicular areas are examined for scale, erythema, blue-gray dots, and whitish halos. Interfollicular areas are examined for pigment pattern as well as vascularization, which often presents in a looping configuration under dermoscopy. A combination of dot colorization, hair shaft structure, and perifollicular and interfollicular findings inform diagnostic algorithms of hair and scalp conditions. For example, central centrifugal cicatricial alopecia, the most common alopecia seen in Black women, has been associated with a combination of honeycomb pigment pattern, perifollicular whitish halo, pinpoint white dots, white patches, and perifollicular erythema.13
Advantages—Perhaps the most useful feature of trichoscopy is its ability to translate visualized features into simple diagnostic algorithms. For instance, if the clinician has diagnosed the patient with noncicatricial alopecia, they would next focus on dot colors. With black dots, the next step would be to determine whether the hairs are tapered or coiled, and so on. This systematic approach enables the clinician to narrow possible diagnoses.2 An additional advantage of trichoscopy is that it examines large surface areas noninvasively as compared to hair-pull tests and scalp biopsy.14,15 Trichoscopy allows temporal comparisons of the same area for disease and treatment monitoring with more diagnostic detail than global photography.16 Trichoscopy also is useful in selecting biopsy locations by discerning and avoiding areas of scar tissue.17
Limitations—Diagnosis via the trichoscopy algorithm is limiting because it is not comprehensive of all hair and scalp disease.18 Additionally, many pathologies exhibit overlapping follicular and interfollicular patterning. For example, almost all subtypes of scarring alopecia present with hair loss and scarred follicles once they have progressed to advanced stages. Further studies should identify more specific patterns of hair and scalp pathologies, which could then be incorporated into a diagnostic algorithm.13
Advancements—The advent of hair analysis software has expanded the role of videodermoscopy by rapidly quantifying hair growth parameters such as hair count, follicular density, and follicular diameter, as well as interfollicular distances (Figure 2).14,17 Vellus and terminal hairs are differentiated according to their thickness and length.17 Moreover, the software can analyze the same area of the scalp over time by either virtual tattoos, semipermanent markings, or precise location measurements, increasing intra- and interclass correlation. The rate of hair growth, hair shedding, and parameters of anagen and telogen hairs can be studied by a method termed phototrichogram whereby a transitional area of hair loss and normal hair growth is identified and trimmed to less than 1 mm from the skin surface.19 A baseline photograph is taken using videodermoscopy. After approximately 3 days, the identical region is photographed and compared with the initial image to observe changes in the hair. Software programs can distinguish the growing hair as anagen and nongrowing hair as telogen, calculating the anagen-to-telogen ratio as well as hair growth rate, which are essential measurements in hair research and clinical studies. Software programs have replaced laborious and time-consuming manual hair counts and have rapidly grown in popularity in evaluating patterned hair loss.
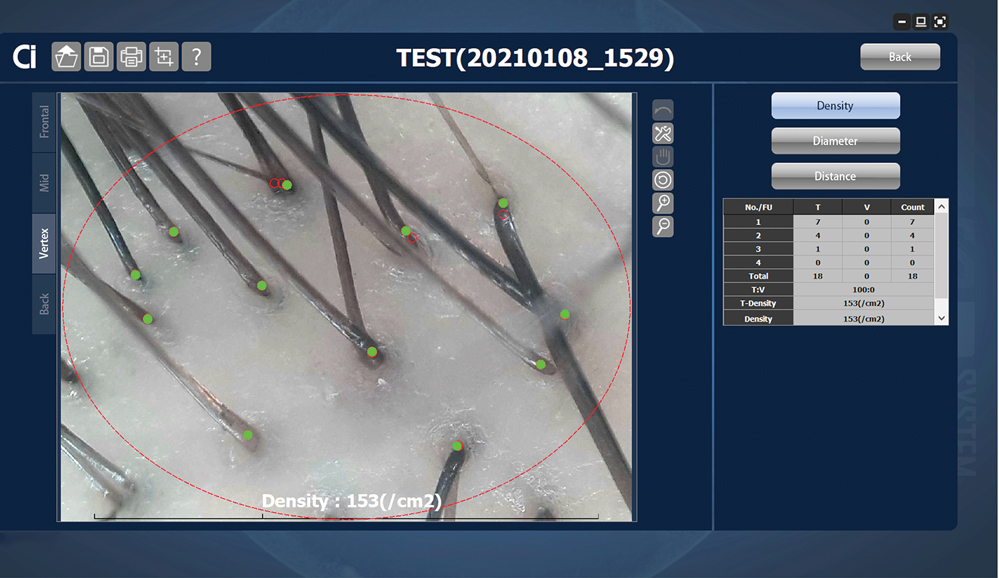
Reflectance Confocal Microscopy
Reflectance confocal microscopy is a noninvasive imaging tool that visualizes skin and its appendages at near-histologic resolution (lateral resolution of 0.5–1 μm). It produces grayscale horizontal images that can be taken at levels ranging from the stratum corneum to the superficial papillary dermis, corresponding to a depth of approximately 100 to 150 µm. Thus, a hair follicle can be imaged starting from the follicular ostia down to the reachable papillary dermis (Figure 3).20 Image contrast is provided by differences in the size and refractive indices of cellular organelles.21,22 There are 2 commercially available RCM devices: VivaScope 1500 and VivaScope 3000 (Caliber Imaging & Diagnostics, Inc).
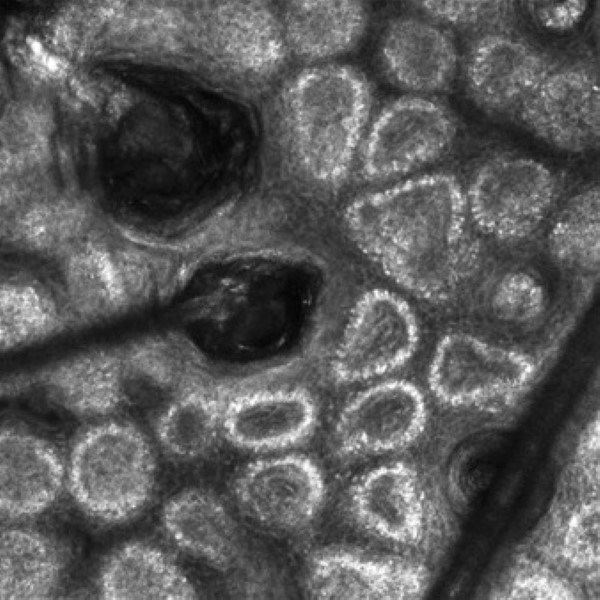
VivaScope 1500, a wide-probe microscope, requires the attachment of a plastic window to the desired imaging area. The plastic window is lined with medical adhesive tape to prevent movement during imaging. The adhesive tape can pull on hair upon removal, which is not ideal for patients with existing hair loss. Additionally, the image quality of VivaSope 1500 is best in flat areas and areas where hair is shaved.20,23,24 Despite these disadvantages, VivaScope 1500 has successfully shown utility in research studies, which suggests that these obstacles can be overcome by experienced users. The handheld VivaScope 3000 is ergonomically designed and suitable for curved surfaces such as the scalp, with the advantage of not requiring any adhesive. However, the images acquired from the VivaScope 3000 cover a smaller surface area.
Structures Visualized—Structures distinguished with RCM include keratinocytes, melanocytes, inflammatory cells, hair follicles, hair shafts, adnexal infundibular epithelium, blood vessels, fibroblasts, and collagen.23 Real-time visualization of blood flow also can be seen.
Applications of RCM—Reflectance confocal microscopy has been used to study scalp discoid lupus, lichen planopilaris, frontal fibrosing alopecia, folliculitis decalvans, chemotherapy-induced alopecia (CIA), alopecia areata, and androgenetic alopecia. Diagnostic RCM criteria for such alopecias have been developed based on their correspondence to histopathology. An RCM study of classic lichen planopilaris and frontal fibrosing alopecia identified features of epidermal disarray, infundibular hyperkeratosis, inflammatory cells, pigment incontinence, perifollicular fibrosis, bandlike scarring, melanophages in the dermis, dilated blood vessels, basal layer vacuolar degeneration, and necrotic keratinocytes.25 Pigment incontinence in the superficial epidermis, perifollicular lichenoid inflammation, and hyperkeratosis were characteristic RCM features of early-stage lichen planopilaris, while perifollicular fibrosis and dilated blood vessels were characteristic RCM features of late-stage disease. The ability of RCM features to distinguish different stages of lichen planopilaris shows its potential in treating early disease and preventing irreversible hair loss.
Differentiating between scarring and nonscarring alopecia also is possible through RCM. The presence of periadnexal, epidermal, and dermal inflammatory cells, in addition to periadnexal sclerosis, are defining RCM features of scarring alopecia.26 These features are absent in nonscarring alopecias. Reflectance confocal microscopy additionally has been shown to be useful in the treatment monitoring of lichen planopilaris and discoid lupus erythematosus.20 Independent reviewers, blinded to the patients’ identities, were able to characterize and follow features of these scarring alopecias by RCM. The assessed RCM features were comparable to those observed by histopathologic evaluation: epidermal disarray, spongiosis, exocytosis of inflammatory cells in the epidermis, interface dermatitis, peri- and intra-adnexal infiltration of inflammatory cells, dilated vessels in the dermis, dermal infiltration of inflammatory cells and melanophages, and dermal sclerosis. A reduction in inflammatory cells across multiple skin layers and at the level of the adnexal epithelium correlated with clinical response to treatment. Reflectance confocal microscopy also was able to detect recurrence of inflammation in cases where treatment had been interrupted before clinical signs of disease recurrence were evident. The authors thus concluded that RCM’s sensitivity can guide timing of treatment and avoid delays in starting or restarting treatment.20
Reflectance confocal microscopy also has served as a learning tool for new subclinical understandings of alopecia. In a study of CIA, the disease was found to be a dynamic process that could be categorized into 4 distinct phases distinguishable by combined confocal and dermoscopic features. This study also identified a new feature observable on RCM images—a CIA dot—defined as a dilated follicular infundibulum containing mashed, malted, nonhomogeneous material and normal or fragmented hair. This dot is thought to represent the initial microscopic sign of direct toxicity of chemotherapy on the hair follicle. Chemotherapy-induced alopecia dots persist throughout chemotherapy and subsequently disappear after chemotherapy ends.27
Limitations and Advantages—Currently, subtypes of cicatricial alopecias cannot be characterized on RCM because inflammatory cell types are not distinguished from each other (eg, eosinophils vs neutrophils). Another limitation of RCM is the loss of resolution below the superficial papillary dermis (a depth of approximately 150 µm); thus, deeper structures, such as the hair bulb, cannot be visualized.
Unlike global photography and trichoscopy, which are low-cost methods, RCM is much more costly, ranging upwards of several thousand dollars, and it may require additional technical support fees, making it less accessible for clinical practice. However, RCM imaging continues to be recommended as an intermediate step between trichoscopy and histology for the diagnosis and management of hair disease.26 If a biopsy is required, RCM can aid in the selection of a biopsy site, as areas with active inflammation are more informative than atrophic and fibrosed areas.23 The role of RCM in trichoscopy can be expanded by designing a more cost-effective and ergonomically suited scope for hair and scalp assessment.
Optical Coherence Tomography
Optical coherence tomography is a noninvasive handheld device that emits low-power infrared light to visualize the skin and adnexal structures. Optical coherence tomography relies on the principle of interferometry to detect phase differences in optical backscattering at varying tissue depths.28,29 It allows visualization up to 2 mm, which is 2 to 5 times deeper than RCM.36 Unlike RCM, which has cellular resolution, OCT has an axial resolution of 3 to 15 μm, which allows only for the detection of structural boundaries.30 There are various OCT modalities that differ in lateral and axial resolutions and maximum depth. Commercial software is available that measures changes in vascular density by depth, epidermal thickness, skin surface texture, and optical attenuation—the latter being an indirect measurement of collagen density and skin hydration.
Structures Visualized—Hair follicles can be well distinguished on OCT images, and as such, OCT is recognized as a diagnostic tool in trichology (Figure 4).31 Follicular openings, interfollicular collagen, and outlines of the hair shafts are visible; however, detailed components of the follicular unit cannot be visualized by OCT. Keratin hyperrefractivity identifies the hair shaft. Additionally, the hair matrix is denoted by a slightly granular texture in the dermis. Dynamic OCT produces colorized images that visualize blood flow within vessels.
Applications of OCT—Optical coherence tomography is utilized in investigative trichology because it provides highly reproducible measurements of hair shaft diameters, cross-sectional surface areas, and form factor, which is a surrogate parameter for hair shape. The cross-section of hair shafts provides insight into local metabolism and perifollicular inflammation. Cross-sections of hair shafts in areas of alopecia areata were found to be smaller than cross-sections in the unaffected scalp within the same individual.32 Follicular density can be manually quantified on OCT images, but there also is promise for automated quantification. A recent study by Urban et al33 described training a convolutional neural network to automatically count hair as well as hair-bearing and non–hair-bearing follicles in OCT scans. These investigators also were able to color-code hair according to height, resulting in the creation of a “height” map.
Optical coherence tomography has furthered our understanding of the pathophysiology of cicatricial and nonscarring alopecias. Vazquez-Herrera et al34 assessed the inflammatory and cicatricial stages of frontal fibrosing alopecia by OCT imaging. Inflammatory hairlines, which are seen in the early stages of frontal fibrosing alopecia, exhibited a thickened dermis, irregular distribution of collagen, and increased vascularity in both the superficial and deep dermal layers compared to cicatricial and healthy scalp. Conversely, late-stage cicatricial areas exhibited a thin dermis and collagen that appeared in a hyperreflective, concentric, onion-shaped pattern around remnant follicular openings. Vascular flow was reduced in the superficial dermis of a cicatricial scalp but increased in the deep dermal layers compared with a healthy scalp. The attenuation coefficients of these disease stages also were assessed. The attenuation coefficient of the inflammatory hairline was higher compared with normal skin, likely as a reflection of inflammatory infiltrate and edema, whereas the attenuation coefficient of cicatricial scalp was lower compared with normal skin, likely reflecting the reduced water content of atrophic skin.34 This differentiation of early- and late-stage cicatricial alopecias has implications for early treatment and improved prognosis. Additionally, there is potential for OCT to assist in the differentiation of alopecia subtypes, as it can measure the epidermal thickness and follicular density and was previously used to compare scarring and nonscarring alopecia.35
Advantages and Limitations—Similar to RCM, OCT may be cost prohibitive for some clinicians. In addition, OCT cannot visualize the follicular unit in cellular detail. However, the extent of OCT’s capabilities may not be fully realized. Dynamic OCT is a new angiographic type of OCT that shows potential in monitoring early subclinical responses to novel alopecia therapies, such as platelet-rich plasminogen, which is hypothesized to stimulate hair growth through angiogenesis. Additionally, OCT may improve outcomes of hair transplantation procedures by allowing for visualization of the subcutaneous angle of hair follicles. Blind extraction of hair follicles in follicular unit extraction procedures can result in inadvertent transection and damage to the hair follicle; OCT could help identify good candidates for follicular unit extraction, such as patients with hair follicles in parallel arrangement, who are predicted to have better results.36
Conclusion
The field of trichology will continue to evolve with the emergence of noninvasive imaging technologies that diagnose hair disease in early stages and enable treatment monitoring with quantification of hair parameters. As discussed in this review, global photography, trichoscopy, RCM, and OCT have furthered our understanding of alopecia pathophysiology and provided objective methods of treatment evaluation. The capabilities of these tools will continue to expand with advancements in add-on software and AI algorithms.
- Canfield D. Photographic documentation of hair growth in androgenetic alopecia. Dermatol Clin. 1996;14:713-721.
- Peytavi U, Hillmann K, Guarrera M. Hair growth assessment techniques. In: Peytavi U, Hillmann K, Guarrera M, eds. Hair Growth and Disorders. 4th ed. Springer; 2008:140-144.
- Chamberlain AJ, Dawber RP. Methods of evaluating hair growth. Australas J Dermatol. 2003;44:10-18.
- Dhurat R, Saraogi P. Hair evaluation methods: merits and demerits. Int J Trichology. 2009;1:108-119.
- Kaufman KD, Olsen EA, Whiting D, et al. Finasteride in the treatment of men with androgenetic alopecia. J Am Acad Dermatol. 1998;39:578-579.
- Capily Institute. Artificial intelligence (A.I.) powered hair growth tracking. Accessed July 31, 2023. https://tss-aesthetics.com/capily-hair-tracking-syst
- Dinh Q, Sinclair R. Female pattern hair loss: current treatment concepts. Clin Interv Aging. 2007;2:189-199.
- Dhurat R, Saraogi P. Hair evaluation methods: merits and demerits. Int J Trichology. 2009;1:108-119.
- Wikramanayake TC, Mauro LM, Tabas IA, et al. Cross-section trichometry: a clinical tool for assessing the progression and treatment response of alopecia. Int J Trichology. 2012;4:259-264.
- Alessandrini A, Bruni F, Piraccini BM, et al. Common causes of hair loss—clinical manifestations, trichoscopy and therapy. J Eur Acad Dermatol Venereol. 2021;35:629-640.
- Ashique K, Kaliyadan F. Clinical photography for trichology practice: tips and tricks. Int J Trichology. 2011;3:7-13.
- Rudnicka L, Olszewska M, Rakowska A, et al. Trichoscopy: a new method for diagnosing hair loss. J Drugs Dermatol. 2008;7:651-654.
- Kinoshita-Ise M, Sachdeva M. Update on trichoscopy: integration of the terminology by systematic approach and a proposal of a diagnostic flowchart. J Dermatol. 2022;49:4-18. doi:10.1111/1346-8138.16233
- Van Neste D, Trüeb RM. Critical study of hair growth analysis with computer-assisted methods. J Eur Acad Dermatol Venereol. 2006;20:578-583.
- Romero J, Grimalt R. Trichoscopy: essentials for the dermatologist. World J Dermatol. 2015;4:63-68.
- Trichoscopy: a new frontier for the diagnosis of hair diseases. Exp Rev Dermatol. 2012;7:429-437.
- Lee B, Chan J, Monselise A, et al. Assessment of hair density and caliber in Caucasian and Asian female subjects with female pattern hair loss by using the Folliscope. J Am Acad Dermatol. 2012;66:166-167.
- Inui S. Trichoscopy for common hair loss diseases: algorithmic method for diagnosis. J Dermatol. 2010;38:71-75.
- Dhurat R. Phototrichogram. Indian J Dermatol Venereol Leprol. 2006;72:242-244.
- Agozzino M, Tosti A, Barbieri L, et al. Confocal microscopic features of scarring alopecia: preliminary report. Br J Dermatol. 2011;165:534-540.
- Kuck M, Schanzer S, Ulrich M, et al. Analysis of the efficiency of hair removal by different optical methods: comparison of Trichoscan, reflectance confocal microscopy, and optical coherence tomography. J Biomed Opt. 2012;17:101504.
- Levine A, Markowitz O. Introduction to reflectance confocal microscopy and its use in clinical practice. JAAD Case Rep. 2018;4:1014-1023.
- Agozzino M, Ardigò M. Scalp confocal microscopy. In: Humbert P, Maibach H, Fanian F, et al, eds. Agache’s Measuring the Skin: Non-invasive Investigations, Physiology, Normal Constants. 2nd ed. Springer International Publishing; 2016:311-326.
- Rudnicka L, Olszewska M, Rakowska A. In vivo reflectance confocal microscopy: usefulness for diagnosing hair diseases. J Dermatol Case Rep. 2008;2:55-59.
- Kurzeja M, Czuwara J, Walecka I, et al. Features of classic lichen planopilaris and frontal fibrosing alopecia in reflectance confocal microscopy: a preliminary study. Skin Res Technol. 2021;27:266-271.
- Ardigò M, Agozzino M, Franceschini C, et al. Reflectance confocal microscopy for scarring and non-scarring alopecia real-time assessment. Arch Dermatol Res. 2016;308:309-318.
- Franceschini C, Garelli V, Persechino F, et al. Dermoscopy and confocal microscopy for different chemotherapy-induced alopecia (CIA) phases characterization: preliminary study. Skin Res Technol. 2020;26:269-276.
- Martinez-Velasco MA, Perper M, Maddy AJ, et al. In vitro determination of Mexican Mestizo hair shaft diameter using optical coherence tomography. Skin Res Technol. 2018;24;274-277.
- Srivastava R, Manfredini M, Rao BK. Noninvasive imaging tools in dermatology. Cutis. 2019;104:108-113.
- Wan B, Ganier C, Du-Harpur X, et al. Applications and future directions for optical coherence tomography in dermatology. Br J Dermatol. 2021;184:1014-1022.
- Blume-Peytavi U, Vieten J, Knuttel A et al. Optical coherent tomography (OCT): a new method for online-measurement of hair shaft thickness. J Dtsch Dermatol Ges. 2004;2:546.
- Garcia Bartels N, Jahnke I, Patzelt A, et al. Hair shaft abnormalities in alopecia areata evaluated by optical coherence tomography. Skin Res Technol. 2011;17:201-205.
- Urban G, Feil N, Csuka E, et al. Combining deep learning with optical coherence tomography imaging to determine scalp hair and follicle counts. Lasers Surg Med. 2021;53:171-178.
- Vazquez-Herrera NE, Eber AE, Martinez-Velasco MA, et al. Optical coherence tomography for the investigation of frontal fibrosing alopecia. J Eur Acad Dermatol Venereol. 2018;32:318-322.
- Ekelem C, Feil N, Csuka E, et al. Optical coherence tomography in the evaluation of the scalp and hair: common features and clinical utility. Lasers Surg Med. 2021;53:129-140.
- Schicho K, Seemann R, Binder M, et al. Optical coherence tomography for planning of follicular unit extraction. Dermatol Surg. 2015;41:358-363.
New imaging tools along with adaptations to existing technologies have been emerging in recent years, with the potential to improve hair diagnostics and treatment monitoring. We provide an overview of 4 noninvasive hair imaging technologies: global photography, trichoscopy, reflectance confocal microscopy (RCM), and optical coherence tomography (OCT). For each instrument, we discuss current and future applications in clinical practice and research along with advantages and disadvantages.
Global Photography
Global photography allows for the analysis of hair growth, volume, distribution, and density through serial standardized photographs.1 Global photography was first introduced for hair growth studies in 1987 and soon after was used for hair and scalp assessments in finasteride clinical trials.2
Hair Assessment—Washed, dried, and combed hair, without hair product, are required for accurate imaging; wet conditions increase reflection and promote hair clumping, thus revealing more scalp and depicting the patient as having less hair.1 Headshots are taken from short distances and use stereotactic positioning devices to create 4 global views: vertex, midline, frontal, and temporal.3 Stereotactic positioning involves fixing the patient’s chin and forehead as well as mounting the camera and flash device to ensure proper magnification. These adjustments ensure lighting remains consistent throughout consecutive study visits.4 Various grading scales are available for use in hair growth clinical studies to increase objectivity in the analysis of serial global photographs. A blinded evaluator should assess the before and after photographs to limit experimenter bias. Global photography often is combined with quantitative software analysis for improved detection of hair changes.1
Advancements—Growing interest in improving global photography has resulted in various application-based, artificial intelligence (AI)–mediated tools to simplify photograph collection and analysis. For instance, new hair analysis software utilizes AI algorithms to account for facial features in determining the optimal angle for capturing global photographs (Figure 1), which simplifies the generation of global photography images through smartphone applications and obviates the need for additional stereotactic positioning equipment.5,6

Limitations—Clinicians should be aware of global photography’s requirements for consistency in lighting, camera settings, film, and image processing, which can limit the accuracy of hair assessment over time if not replicated correctly.7,8 Emerging global photography software has helped to overcome some of these limitations.
Global photography is less precise when a patient’s hair loss is less than 50%, as it is difficult to discern subtle hair changes. Thus, global photography provides limited utility in assessing minimal to moderate hair loss.9 Currently, global photography largely functions as an adjunct tool for other hair analysis methods rather than as a stand-alone tool.
Trichoscopy
Trichoscopy (also known as dermoscopy of the hair and scalp) may be performed with a manual dermoscope (with 10× magnification) or a digital videodermatoscope (up to 1000× magnification).10-12 Unlike global photography, trichoscopy provides a detailed structural analysis of hair shafts, follicular openings, and perifollicular and interfollicular areas.13 Kinoshita-Ise and Sachdeva13 provided an in-depth, updated review of trichoscopy terminology with their definitions and associated conditions (with prevalence), which should be referenced when performing trichoscopic examination.
Hair Assessment—Trichoscopic assessment begins with inspection of follicular openings (also referred to as “dots”), which vary in color depending on the material filling them—degrading keratinocytes, keratin, sebaceous debris, melanin, or fractured hairs.13 The structure of hair shafts also is examined, showing broken hairs, short vellus hairs, and comma hairs, among others. Perifollicular areas are examined for scale, erythema, blue-gray dots, and whitish halos. Interfollicular areas are examined for pigment pattern as well as vascularization, which often presents in a looping configuration under dermoscopy. A combination of dot colorization, hair shaft structure, and perifollicular and interfollicular findings inform diagnostic algorithms of hair and scalp conditions. For example, central centrifugal cicatricial alopecia, the most common alopecia seen in Black women, has been associated with a combination of honeycomb pigment pattern, perifollicular whitish halo, pinpoint white dots, white patches, and perifollicular erythema.13
Advantages—Perhaps the most useful feature of trichoscopy is its ability to translate visualized features into simple diagnostic algorithms. For instance, if the clinician has diagnosed the patient with noncicatricial alopecia, they would next focus on dot colors. With black dots, the next step would be to determine whether the hairs are tapered or coiled, and so on. This systematic approach enables the clinician to narrow possible diagnoses.2 An additional advantage of trichoscopy is that it examines large surface areas noninvasively as compared to hair-pull tests and scalp biopsy.14,15 Trichoscopy allows temporal comparisons of the same area for disease and treatment monitoring with more diagnostic detail than global photography.16 Trichoscopy also is useful in selecting biopsy locations by discerning and avoiding areas of scar tissue.17
Limitations—Diagnosis via the trichoscopy algorithm is limiting because it is not comprehensive of all hair and scalp disease.18 Additionally, many pathologies exhibit overlapping follicular and interfollicular patterning. For example, almost all subtypes of scarring alopecia present with hair loss and scarred follicles once they have progressed to advanced stages. Further studies should identify more specific patterns of hair and scalp pathologies, which could then be incorporated into a diagnostic algorithm.13
Advancements—The advent of hair analysis software has expanded the role of videodermoscopy by rapidly quantifying hair growth parameters such as hair count, follicular density, and follicular diameter, as well as interfollicular distances (Figure 2).14,17 Vellus and terminal hairs are differentiated according to their thickness and length.17 Moreover, the software can analyze the same area of the scalp over time by either virtual tattoos, semipermanent markings, or precise location measurements, increasing intra- and interclass correlation. The rate of hair growth, hair shedding, and parameters of anagen and telogen hairs can be studied by a method termed phototrichogram whereby a transitional area of hair loss and normal hair growth is identified and trimmed to less than 1 mm from the skin surface.19 A baseline photograph is taken using videodermoscopy. After approximately 3 days, the identical region is photographed and compared with the initial image to observe changes in the hair. Software programs can distinguish the growing hair as anagen and nongrowing hair as telogen, calculating the anagen-to-telogen ratio as well as hair growth rate, which are essential measurements in hair research and clinical studies. Software programs have replaced laborious and time-consuming manual hair counts and have rapidly grown in popularity in evaluating patterned hair loss.
Reflectance Confocal Microscopy
Reflectance confocal microscopy is a noninvasive imaging tool that visualizes skin and its appendages at near-histologic resolution (lateral resolution of 0.5–1 μm). It produces grayscale horizontal images that can be taken at levels ranging from the stratum corneum to the superficial papillary dermis, corresponding to a depth of approximately 100 to 150 µm. Thus, a hair follicle can be imaged starting from the follicular ostia down to the reachable papillary dermis (Figure 3).20 Image contrast is provided by differences in the size and refractive indices of cellular organelles.21,22 There are 2 commercially available RCM devices: VivaScope 1500 and VivaScope 3000 (Caliber Imaging & Diagnostics, Inc).
VivaScope 1500, a wide-probe microscope, requires the attachment of a plastic window to the desired imaging area. The plastic window is lined with medical adhesive tape to prevent movement during imaging. The adhesive tape can pull on hair upon removal, which is not ideal for patients with existing hair loss. Additionally, the image quality of VivaSope 1500 is best in flat areas and areas where hair is shaved.20,23,24 Despite these disadvantages, VivaScope 1500 has successfully shown utility in research studies, which suggests that these obstacles can be overcome by experienced users. The handheld VivaScope 3000 is ergonomically designed and suitable for curved surfaces such as the scalp, with the advantage of not requiring any adhesive. However, the images acquired from the VivaScope 3000 cover a smaller surface area.
Structures Visualized—Structures distinguished with RCM include keratinocytes, melanocytes, inflammatory cells, hair follicles, hair shafts, adnexal infundibular epithelium, blood vessels, fibroblasts, and collagen.23 Real-time visualization of blood flow also can be seen.
Applications of RCM—Reflectance confocal microscopy has been used to study scalp discoid lupus, lichen planopilaris, frontal fibrosing alopecia, folliculitis decalvans, chemotherapy-induced alopecia (CIA), alopecia areata, and androgenetic alopecia. Diagnostic RCM criteria for such alopecias have been developed based on their correspondence to histopathology. An RCM study of classic lichen planopilaris and frontal fibrosing alopecia identified features of epidermal disarray, infundibular hyperkeratosis, inflammatory cells, pigment incontinence, perifollicular fibrosis, bandlike scarring, melanophages in the dermis, dilated blood vessels, basal layer vacuolar degeneration, and necrotic keratinocytes.25 Pigment incontinence in the superficial epidermis, perifollicular lichenoid inflammation, and hyperkeratosis were characteristic RCM features of early-stage lichen planopilaris, while perifollicular fibrosis and dilated blood vessels were characteristic RCM features of late-stage disease. The ability of RCM features to distinguish different stages of lichen planopilaris shows its potential in treating early disease and preventing irreversible hair loss.
Differentiating between scarring and nonscarring alopecia also is possible through RCM. The presence of periadnexal, epidermal, and dermal inflammatory cells, in addition to periadnexal sclerosis, are defining RCM features of scarring alopecia.26 These features are absent in nonscarring alopecias. Reflectance confocal microscopy additionally has been shown to be useful in the treatment monitoring of lichen planopilaris and discoid lupus erythematosus.20 Independent reviewers, blinded to the patients’ identities, were able to characterize and follow features of these scarring alopecias by RCM. The assessed RCM features were comparable to those observed by histopathologic evaluation: epidermal disarray, spongiosis, exocytosis of inflammatory cells in the epidermis, interface dermatitis, peri- and intra-adnexal infiltration of inflammatory cells, dilated vessels in the dermis, dermal infiltration of inflammatory cells and melanophages, and dermal sclerosis. A reduction in inflammatory cells across multiple skin layers and at the level of the adnexal epithelium correlated with clinical response to treatment. Reflectance confocal microscopy also was able to detect recurrence of inflammation in cases where treatment had been interrupted before clinical signs of disease recurrence were evident. The authors thus concluded that RCM’s sensitivity can guide timing of treatment and avoid delays in starting or restarting treatment.20
Reflectance confocal microscopy also has served as a learning tool for new subclinical understandings of alopecia. In a study of CIA, the disease was found to be a dynamic process that could be categorized into 4 distinct phases distinguishable by combined confocal and dermoscopic features. This study also identified a new feature observable on RCM images—a CIA dot—defined as a dilated follicular infundibulum containing mashed, malted, nonhomogeneous material and normal or fragmented hair. This dot is thought to represent the initial microscopic sign of direct toxicity of chemotherapy on the hair follicle. Chemotherapy-induced alopecia dots persist throughout chemotherapy and subsequently disappear after chemotherapy ends.27
Limitations and Advantages—Currently, subtypes of cicatricial alopecias cannot be characterized on RCM because inflammatory cell types are not distinguished from each other (eg, eosinophils vs neutrophils). Another limitation of RCM is the loss of resolution below the superficial papillary dermis (a depth of approximately 150 µm); thus, deeper structures, such as the hair bulb, cannot be visualized.
Unlike global photography and trichoscopy, which are low-cost methods, RCM is much more costly, ranging upwards of several thousand dollars, and it may require additional technical support fees, making it less accessible for clinical practice. However, RCM imaging continues to be recommended as an intermediate step between trichoscopy and histology for the diagnosis and management of hair disease.26 If a biopsy is required, RCM can aid in the selection of a biopsy site, as areas with active inflammation are more informative than atrophic and fibrosed areas.23 The role of RCM in trichoscopy can be expanded by designing a more cost-effective and ergonomically suited scope for hair and scalp assessment.
Optical Coherence Tomography
Optical coherence tomography is a noninvasive handheld device that emits low-power infrared light to visualize the skin and adnexal structures. Optical coherence tomography relies on the principle of interferometry to detect phase differences in optical backscattering at varying tissue depths.28,29 It allows visualization up to 2 mm, which is 2 to 5 times deeper than RCM.36 Unlike RCM, which has cellular resolution, OCT has an axial resolution of 3 to 15 μm, which allows only for the detection of structural boundaries.30 There are various OCT modalities that differ in lateral and axial resolutions and maximum depth. Commercial software is available that measures changes in vascular density by depth, epidermal thickness, skin surface texture, and optical attenuation—the latter being an indirect measurement of collagen density and skin hydration.
Structures Visualized—Hair follicles can be well distinguished on OCT images, and as such, OCT is recognized as a diagnostic tool in trichology (Figure 4).31 Follicular openings, interfollicular collagen, and outlines of the hair shafts are visible; however, detailed components of the follicular unit cannot be visualized by OCT. Keratin hyperrefractivity identifies the hair shaft. Additionally, the hair matrix is denoted by a slightly granular texture in the dermis. Dynamic OCT produces colorized images that visualize blood flow within vessels.
Applications of OCT—Optical coherence tomography is utilized in investigative trichology because it provides highly reproducible measurements of hair shaft diameters, cross-sectional surface areas, and form factor, which is a surrogate parameter for hair shape. The cross-section of hair shafts provides insight into local metabolism and perifollicular inflammation. Cross-sections of hair shafts in areas of alopecia areata were found to be smaller than cross-sections in the unaffected scalp within the same individual.32 Follicular density can be manually quantified on OCT images, but there also is promise for automated quantification. A recent study by Urban et al33 described training a convolutional neural network to automatically count hair as well as hair-bearing and non–hair-bearing follicles in OCT scans. These investigators also were able to color-code hair according to height, resulting in the creation of a “height” map.
Optical coherence tomography has furthered our understanding of the pathophysiology of cicatricial and nonscarring alopecias. Vazquez-Herrera et al34 assessed the inflammatory and cicatricial stages of frontal fibrosing alopecia by OCT imaging. Inflammatory hairlines, which are seen in the early stages of frontal fibrosing alopecia, exhibited a thickened dermis, irregular distribution of collagen, and increased vascularity in both the superficial and deep dermal layers compared to cicatricial and healthy scalp. Conversely, late-stage cicatricial areas exhibited a thin dermis and collagen that appeared in a hyperreflective, concentric, onion-shaped pattern around remnant follicular openings. Vascular flow was reduced in the superficial dermis of a cicatricial scalp but increased in the deep dermal layers compared with a healthy scalp. The attenuation coefficients of these disease stages also were assessed. The attenuation coefficient of the inflammatory hairline was higher compared with normal skin, likely as a reflection of inflammatory infiltrate and edema, whereas the attenuation coefficient of cicatricial scalp was lower compared with normal skin, likely reflecting the reduced water content of atrophic skin.34 This differentiation of early- and late-stage cicatricial alopecias has implications for early treatment and improved prognosis. Additionally, there is potential for OCT to assist in the differentiation of alopecia subtypes, as it can measure the epidermal thickness and follicular density and was previously used to compare scarring and nonscarring alopecia.35
Advantages and Limitations—Similar to RCM, OCT may be cost prohibitive for some clinicians. In addition, OCT cannot visualize the follicular unit in cellular detail. However, the extent of OCT’s capabilities may not be fully realized. Dynamic OCT is a new angiographic type of OCT that shows potential in monitoring early subclinical responses to novel alopecia therapies, such as platelet-rich plasminogen, which is hypothesized to stimulate hair growth through angiogenesis. Additionally, OCT may improve outcomes of hair transplantation procedures by allowing for visualization of the subcutaneous angle of hair follicles. Blind extraction of hair follicles in follicular unit extraction procedures can result in inadvertent transection and damage to the hair follicle; OCT could help identify good candidates for follicular unit extraction, such as patients with hair follicles in parallel arrangement, who are predicted to have better results.36
Conclusion
The field of trichology will continue to evolve with the emergence of noninvasive imaging technologies that diagnose hair disease in early stages and enable treatment monitoring with quantification of hair parameters. As discussed in this review, global photography, trichoscopy, RCM, and OCT have furthered our understanding of alopecia pathophysiology and provided objective methods of treatment evaluation. The capabilities of these tools will continue to expand with advancements in add-on software and AI algorithms.
New imaging tools along with adaptations to existing technologies have been emerging in recent years, with the potential to improve hair diagnostics and treatment monitoring. We provide an overview of 4 noninvasive hair imaging technologies: global photography, trichoscopy, reflectance confocal microscopy (RCM), and optical coherence tomography (OCT). For each instrument, we discuss current and future applications in clinical practice and research along with advantages and disadvantages.
Global Photography
Global photography allows for the analysis of hair growth, volume, distribution, and density through serial standardized photographs.1 Global photography was first introduced for hair growth studies in 1987 and soon after was used for hair and scalp assessments in finasteride clinical trials.2
Hair Assessment—Washed, dried, and combed hair, without hair product, are required for accurate imaging; wet conditions increase reflection and promote hair clumping, thus revealing more scalp and depicting the patient as having less hair.1 Headshots are taken from short distances and use stereotactic positioning devices to create 4 global views: vertex, midline, frontal, and temporal.3 Stereotactic positioning involves fixing the patient’s chin and forehead as well as mounting the camera and flash device to ensure proper magnification. These adjustments ensure lighting remains consistent throughout consecutive study visits.4 Various grading scales are available for use in hair growth clinical studies to increase objectivity in the analysis of serial global photographs. A blinded evaluator should assess the before and after photographs to limit experimenter bias. Global photography often is combined with quantitative software analysis for improved detection of hair changes.1
Advancements—Growing interest in improving global photography has resulted in various application-based, artificial intelligence (AI)–mediated tools to simplify photograph collection and analysis. For instance, new hair analysis software utilizes AI algorithms to account for facial features in determining the optimal angle for capturing global photographs (Figure 1), which simplifies the generation of global photography images through smartphone applications and obviates the need for additional stereotactic positioning equipment.5,6

Limitations—Clinicians should be aware of global photography’s requirements for consistency in lighting, camera settings, film, and image processing, which can limit the accuracy of hair assessment over time if not replicated correctly.7,8 Emerging global photography software has helped to overcome some of these limitations.
Global photography is less precise when a patient’s hair loss is less than 50%, as it is difficult to discern subtle hair changes. Thus, global photography provides limited utility in assessing minimal to moderate hair loss.9 Currently, global photography largely functions as an adjunct tool for other hair analysis methods rather than as a stand-alone tool.
Trichoscopy
Trichoscopy (also known as dermoscopy of the hair and scalp) may be performed with a manual dermoscope (with 10× magnification) or a digital videodermatoscope (up to 1000× magnification).10-12 Unlike global photography, trichoscopy provides a detailed structural analysis of hair shafts, follicular openings, and perifollicular and interfollicular areas.13 Kinoshita-Ise and Sachdeva13 provided an in-depth, updated review of trichoscopy terminology with their definitions and associated conditions (with prevalence), which should be referenced when performing trichoscopic examination.
Hair Assessment—Trichoscopic assessment begins with inspection of follicular openings (also referred to as “dots”), which vary in color depending on the material filling them—degrading keratinocytes, keratin, sebaceous debris, melanin, or fractured hairs.13 The structure of hair shafts also is examined, showing broken hairs, short vellus hairs, and comma hairs, among others. Perifollicular areas are examined for scale, erythema, blue-gray dots, and whitish halos. Interfollicular areas are examined for pigment pattern as well as vascularization, which often presents in a looping configuration under dermoscopy. A combination of dot colorization, hair shaft structure, and perifollicular and interfollicular findings inform diagnostic algorithms of hair and scalp conditions. For example, central centrifugal cicatricial alopecia, the most common alopecia seen in Black women, has been associated with a combination of honeycomb pigment pattern, perifollicular whitish halo, pinpoint white dots, white patches, and perifollicular erythema.13
Advantages—Perhaps the most useful feature of trichoscopy is its ability to translate visualized features into simple diagnostic algorithms. For instance, if the clinician has diagnosed the patient with noncicatricial alopecia, they would next focus on dot colors. With black dots, the next step would be to determine whether the hairs are tapered or coiled, and so on. This systematic approach enables the clinician to narrow possible diagnoses.2 An additional advantage of trichoscopy is that it examines large surface areas noninvasively as compared to hair-pull tests and scalp biopsy.14,15 Trichoscopy allows temporal comparisons of the same area for disease and treatment monitoring with more diagnostic detail than global photography.16 Trichoscopy also is useful in selecting biopsy locations by discerning and avoiding areas of scar tissue.17
Limitations—Diagnosis via the trichoscopy algorithm is limiting because it is not comprehensive of all hair and scalp disease.18 Additionally, many pathologies exhibit overlapping follicular and interfollicular patterning. For example, almost all subtypes of scarring alopecia present with hair loss and scarred follicles once they have progressed to advanced stages. Further studies should identify more specific patterns of hair and scalp pathologies, which could then be incorporated into a diagnostic algorithm.13
Advancements—The advent of hair analysis software has expanded the role of videodermoscopy by rapidly quantifying hair growth parameters such as hair count, follicular density, and follicular diameter, as well as interfollicular distances (Figure 2).14,17 Vellus and terminal hairs are differentiated according to their thickness and length.17 Moreover, the software can analyze the same area of the scalp over time by either virtual tattoos, semipermanent markings, or precise location measurements, increasing intra- and interclass correlation. The rate of hair growth, hair shedding, and parameters of anagen and telogen hairs can be studied by a method termed phototrichogram whereby a transitional area of hair loss and normal hair growth is identified and trimmed to less than 1 mm from the skin surface.19 A baseline photograph is taken using videodermoscopy. After approximately 3 days, the identical region is photographed and compared with the initial image to observe changes in the hair. Software programs can distinguish the growing hair as anagen and nongrowing hair as telogen, calculating the anagen-to-telogen ratio as well as hair growth rate, which are essential measurements in hair research and clinical studies. Software programs have replaced laborious and time-consuming manual hair counts and have rapidly grown in popularity in evaluating patterned hair loss.
Reflectance Confocal Microscopy
Reflectance confocal microscopy is a noninvasive imaging tool that visualizes skin and its appendages at near-histologic resolution (lateral resolution of 0.5–1 μm). It produces grayscale horizontal images that can be taken at levels ranging from the stratum corneum to the superficial papillary dermis, corresponding to a depth of approximately 100 to 150 µm. Thus, a hair follicle can be imaged starting from the follicular ostia down to the reachable papillary dermis (Figure 3).20 Image contrast is provided by differences in the size and refractive indices of cellular organelles.21,22 There are 2 commercially available RCM devices: VivaScope 1500 and VivaScope 3000 (Caliber Imaging & Diagnostics, Inc).
VivaScope 1500, a wide-probe microscope, requires the attachment of a plastic window to the desired imaging area. The plastic window is lined with medical adhesive tape to prevent movement during imaging. The adhesive tape can pull on hair upon removal, which is not ideal for patients with existing hair loss. Additionally, the image quality of VivaSope 1500 is best in flat areas and areas where hair is shaved.20,23,24 Despite these disadvantages, VivaScope 1500 has successfully shown utility in research studies, which suggests that these obstacles can be overcome by experienced users. The handheld VivaScope 3000 is ergonomically designed and suitable for curved surfaces such as the scalp, with the advantage of not requiring any adhesive. However, the images acquired from the VivaScope 3000 cover a smaller surface area.
Structures Visualized—Structures distinguished with RCM include keratinocytes, melanocytes, inflammatory cells, hair follicles, hair shafts, adnexal infundibular epithelium, blood vessels, fibroblasts, and collagen.23 Real-time visualization of blood flow also can be seen.
Applications of RCM—Reflectance confocal microscopy has been used to study scalp discoid lupus, lichen planopilaris, frontal fibrosing alopecia, folliculitis decalvans, chemotherapy-induced alopecia (CIA), alopecia areata, and androgenetic alopecia. Diagnostic RCM criteria for such alopecias have been developed based on their correspondence to histopathology. An RCM study of classic lichen planopilaris and frontal fibrosing alopecia identified features of epidermal disarray, infundibular hyperkeratosis, inflammatory cells, pigment incontinence, perifollicular fibrosis, bandlike scarring, melanophages in the dermis, dilated blood vessels, basal layer vacuolar degeneration, and necrotic keratinocytes.25 Pigment incontinence in the superficial epidermis, perifollicular lichenoid inflammation, and hyperkeratosis were characteristic RCM features of early-stage lichen planopilaris, while perifollicular fibrosis and dilated blood vessels were characteristic RCM features of late-stage disease. The ability of RCM features to distinguish different stages of lichen planopilaris shows its potential in treating early disease and preventing irreversible hair loss.
Differentiating between scarring and nonscarring alopecia also is possible through RCM. The presence of periadnexal, epidermal, and dermal inflammatory cells, in addition to periadnexal sclerosis, are defining RCM features of scarring alopecia.26 These features are absent in nonscarring alopecias. Reflectance confocal microscopy additionally has been shown to be useful in the treatment monitoring of lichen planopilaris and discoid lupus erythematosus.20 Independent reviewers, blinded to the patients’ identities, were able to characterize and follow features of these scarring alopecias by RCM. The assessed RCM features were comparable to those observed by histopathologic evaluation: epidermal disarray, spongiosis, exocytosis of inflammatory cells in the epidermis, interface dermatitis, peri- and intra-adnexal infiltration of inflammatory cells, dilated vessels in the dermis, dermal infiltration of inflammatory cells and melanophages, and dermal sclerosis. A reduction in inflammatory cells across multiple skin layers and at the level of the adnexal epithelium correlated with clinical response to treatment. Reflectance confocal microscopy also was able to detect recurrence of inflammation in cases where treatment had been interrupted before clinical signs of disease recurrence were evident. The authors thus concluded that RCM’s sensitivity can guide timing of treatment and avoid delays in starting or restarting treatment.20
Reflectance confocal microscopy also has served as a learning tool for new subclinical understandings of alopecia. In a study of CIA, the disease was found to be a dynamic process that could be categorized into 4 distinct phases distinguishable by combined confocal and dermoscopic features. This study also identified a new feature observable on RCM images—a CIA dot—defined as a dilated follicular infundibulum containing mashed, malted, nonhomogeneous material and normal or fragmented hair. This dot is thought to represent the initial microscopic sign of direct toxicity of chemotherapy on the hair follicle. Chemotherapy-induced alopecia dots persist throughout chemotherapy and subsequently disappear after chemotherapy ends.27
Limitations and Advantages—Currently, subtypes of cicatricial alopecias cannot be characterized on RCM because inflammatory cell types are not distinguished from each other (eg, eosinophils vs neutrophils). Another limitation of RCM is the loss of resolution below the superficial papillary dermis (a depth of approximately 150 µm); thus, deeper structures, such as the hair bulb, cannot be visualized.
Unlike global photography and trichoscopy, which are low-cost methods, RCM is much more costly, ranging upwards of several thousand dollars, and it may require additional technical support fees, making it less accessible for clinical practice. However, RCM imaging continues to be recommended as an intermediate step between trichoscopy and histology for the diagnosis and management of hair disease.26 If a biopsy is required, RCM can aid in the selection of a biopsy site, as areas with active inflammation are more informative than atrophic and fibrosed areas.23 The role of RCM in trichoscopy can be expanded by designing a more cost-effective and ergonomically suited scope for hair and scalp assessment.
Optical Coherence Tomography
Optical coherence tomography is a noninvasive handheld device that emits low-power infrared light to visualize the skin and adnexal structures. Optical coherence tomography relies on the principle of interferometry to detect phase differences in optical backscattering at varying tissue depths.28,29 It allows visualization up to 2 mm, which is 2 to 5 times deeper than RCM.36 Unlike RCM, which has cellular resolution, OCT has an axial resolution of 3 to 15 μm, which allows only for the detection of structural boundaries.30 There are various OCT modalities that differ in lateral and axial resolutions and maximum depth. Commercial software is available that measures changes in vascular density by depth, epidermal thickness, skin surface texture, and optical attenuation—the latter being an indirect measurement of collagen density and skin hydration.
Structures Visualized—Hair follicles can be well distinguished on OCT images, and as such, OCT is recognized as a diagnostic tool in trichology (Figure 4).31 Follicular openings, interfollicular collagen, and outlines of the hair shafts are visible; however, detailed components of the follicular unit cannot be visualized by OCT. Keratin hyperrefractivity identifies the hair shaft. Additionally, the hair matrix is denoted by a slightly granular texture in the dermis. Dynamic OCT produces colorized images that visualize blood flow within vessels.
Applications of OCT—Optical coherence tomography is utilized in investigative trichology because it provides highly reproducible measurements of hair shaft diameters, cross-sectional surface areas, and form factor, which is a surrogate parameter for hair shape. The cross-section of hair shafts provides insight into local metabolism and perifollicular inflammation. Cross-sections of hair shafts in areas of alopecia areata were found to be smaller than cross-sections in the unaffected scalp within the same individual.32 Follicular density can be manually quantified on OCT images, but there also is promise for automated quantification. A recent study by Urban et al33 described training a convolutional neural network to automatically count hair as well as hair-bearing and non–hair-bearing follicles in OCT scans. These investigators also were able to color-code hair according to height, resulting in the creation of a “height” map.
Optical coherence tomography has furthered our understanding of the pathophysiology of cicatricial and nonscarring alopecias. Vazquez-Herrera et al34 assessed the inflammatory and cicatricial stages of frontal fibrosing alopecia by OCT imaging. Inflammatory hairlines, which are seen in the early stages of frontal fibrosing alopecia, exhibited a thickened dermis, irregular distribution of collagen, and increased vascularity in both the superficial and deep dermal layers compared to cicatricial and healthy scalp. Conversely, late-stage cicatricial areas exhibited a thin dermis and collagen that appeared in a hyperreflective, concentric, onion-shaped pattern around remnant follicular openings. Vascular flow was reduced in the superficial dermis of a cicatricial scalp but increased in the deep dermal layers compared with a healthy scalp. The attenuation coefficients of these disease stages also were assessed. The attenuation coefficient of the inflammatory hairline was higher compared with normal skin, likely as a reflection of inflammatory infiltrate and edema, whereas the attenuation coefficient of cicatricial scalp was lower compared with normal skin, likely reflecting the reduced water content of atrophic skin.34 This differentiation of early- and late-stage cicatricial alopecias has implications for early treatment and improved prognosis. Additionally, there is potential for OCT to assist in the differentiation of alopecia subtypes, as it can measure the epidermal thickness and follicular density and was previously used to compare scarring and nonscarring alopecia.35
Advantages and Limitations—Similar to RCM, OCT may be cost prohibitive for some clinicians. In addition, OCT cannot visualize the follicular unit in cellular detail. However, the extent of OCT’s capabilities may not be fully realized. Dynamic OCT is a new angiographic type of OCT that shows potential in monitoring early subclinical responses to novel alopecia therapies, such as platelet-rich plasminogen, which is hypothesized to stimulate hair growth through angiogenesis. Additionally, OCT may improve outcomes of hair transplantation procedures by allowing for visualization of the subcutaneous angle of hair follicles. Blind extraction of hair follicles in follicular unit extraction procedures can result in inadvertent transection and damage to the hair follicle; OCT could help identify good candidates for follicular unit extraction, such as patients with hair follicles in parallel arrangement, who are predicted to have better results.36
Conclusion
The field of trichology will continue to evolve with the emergence of noninvasive imaging technologies that diagnose hair disease in early stages and enable treatment monitoring with quantification of hair parameters. As discussed in this review, global photography, trichoscopy, RCM, and OCT have furthered our understanding of alopecia pathophysiology and provided objective methods of treatment evaluation. The capabilities of these tools will continue to expand with advancements in add-on software and AI algorithms.
- Canfield D. Photographic documentation of hair growth in androgenetic alopecia. Dermatol Clin. 1996;14:713-721.
- Peytavi U, Hillmann K, Guarrera M. Hair growth assessment techniques. In: Peytavi U, Hillmann K, Guarrera M, eds. Hair Growth and Disorders. 4th ed. Springer; 2008:140-144.
- Chamberlain AJ, Dawber RP. Methods of evaluating hair growth. Australas J Dermatol. 2003;44:10-18.
- Dhurat R, Saraogi P. Hair evaluation methods: merits and demerits. Int J Trichology. 2009;1:108-119.
- Kaufman KD, Olsen EA, Whiting D, et al. Finasteride in the treatment of men with androgenetic alopecia. J Am Acad Dermatol. 1998;39:578-579.
- Capily Institute. Artificial intelligence (A.I.) powered hair growth tracking. Accessed July 31, 2023. https://tss-aesthetics.com/capily-hair-tracking-syst
- Dinh Q, Sinclair R. Female pattern hair loss: current treatment concepts. Clin Interv Aging. 2007;2:189-199.
- Dhurat R, Saraogi P. Hair evaluation methods: merits and demerits. Int J Trichology. 2009;1:108-119.
- Wikramanayake TC, Mauro LM, Tabas IA, et al. Cross-section trichometry: a clinical tool for assessing the progression and treatment response of alopecia. Int J Trichology. 2012;4:259-264.
- Alessandrini A, Bruni F, Piraccini BM, et al. Common causes of hair loss—clinical manifestations, trichoscopy and therapy. J Eur Acad Dermatol Venereol. 2021;35:629-640.
- Ashique K, Kaliyadan F. Clinical photography for trichology practice: tips and tricks. Int J Trichology. 2011;3:7-13.
- Rudnicka L, Olszewska M, Rakowska A, et al. Trichoscopy: a new method for diagnosing hair loss. J Drugs Dermatol. 2008;7:651-654.
- Kinoshita-Ise M, Sachdeva M. Update on trichoscopy: integration of the terminology by systematic approach and a proposal of a diagnostic flowchart. J Dermatol. 2022;49:4-18. doi:10.1111/1346-8138.16233
- Van Neste D, Trüeb RM. Critical study of hair growth analysis with computer-assisted methods. J Eur Acad Dermatol Venereol. 2006;20:578-583.
- Romero J, Grimalt R. Trichoscopy: essentials for the dermatologist. World J Dermatol. 2015;4:63-68.
- Trichoscopy: a new frontier for the diagnosis of hair diseases. Exp Rev Dermatol. 2012;7:429-437.
- Lee B, Chan J, Monselise A, et al. Assessment of hair density and caliber in Caucasian and Asian female subjects with female pattern hair loss by using the Folliscope. J Am Acad Dermatol. 2012;66:166-167.
- Inui S. Trichoscopy for common hair loss diseases: algorithmic method for diagnosis. J Dermatol. 2010;38:71-75.
- Dhurat R. Phototrichogram. Indian J Dermatol Venereol Leprol. 2006;72:242-244.
- Agozzino M, Tosti A, Barbieri L, et al. Confocal microscopic features of scarring alopecia: preliminary report. Br J Dermatol. 2011;165:534-540.
- Kuck M, Schanzer S, Ulrich M, et al. Analysis of the efficiency of hair removal by different optical methods: comparison of Trichoscan, reflectance confocal microscopy, and optical coherence tomography. J Biomed Opt. 2012;17:101504.
- Levine A, Markowitz O. Introduction to reflectance confocal microscopy and its use in clinical practice. JAAD Case Rep. 2018;4:1014-1023.
- Agozzino M, Ardigò M. Scalp confocal microscopy. In: Humbert P, Maibach H, Fanian F, et al, eds. Agache’s Measuring the Skin: Non-invasive Investigations, Physiology, Normal Constants. 2nd ed. Springer International Publishing; 2016:311-326.
- Rudnicka L, Olszewska M, Rakowska A. In vivo reflectance confocal microscopy: usefulness for diagnosing hair diseases. J Dermatol Case Rep. 2008;2:55-59.
- Kurzeja M, Czuwara J, Walecka I, et al. Features of classic lichen planopilaris and frontal fibrosing alopecia in reflectance confocal microscopy: a preliminary study. Skin Res Technol. 2021;27:266-271.
- Ardigò M, Agozzino M, Franceschini C, et al. Reflectance confocal microscopy for scarring and non-scarring alopecia real-time assessment. Arch Dermatol Res. 2016;308:309-318.
- Franceschini C, Garelli V, Persechino F, et al. Dermoscopy and confocal microscopy for different chemotherapy-induced alopecia (CIA) phases characterization: preliminary study. Skin Res Technol. 2020;26:269-276.
- Martinez-Velasco MA, Perper M, Maddy AJ, et al. In vitro determination of Mexican Mestizo hair shaft diameter using optical coherence tomography. Skin Res Technol. 2018;24;274-277.
- Srivastava R, Manfredini M, Rao BK. Noninvasive imaging tools in dermatology. Cutis. 2019;104:108-113.
- Wan B, Ganier C, Du-Harpur X, et al. Applications and future directions for optical coherence tomography in dermatology. Br J Dermatol. 2021;184:1014-1022.
- Blume-Peytavi U, Vieten J, Knuttel A et al. Optical coherent tomography (OCT): a new method for online-measurement of hair shaft thickness. J Dtsch Dermatol Ges. 2004;2:546.
- Garcia Bartels N, Jahnke I, Patzelt A, et al. Hair shaft abnormalities in alopecia areata evaluated by optical coherence tomography. Skin Res Technol. 2011;17:201-205.
- Urban G, Feil N, Csuka E, et al. Combining deep learning with optical coherence tomography imaging to determine scalp hair and follicle counts. Lasers Surg Med. 2021;53:171-178.
- Vazquez-Herrera NE, Eber AE, Martinez-Velasco MA, et al. Optical coherence tomography for the investigation of frontal fibrosing alopecia. J Eur Acad Dermatol Venereol. 2018;32:318-322.
- Ekelem C, Feil N, Csuka E, et al. Optical coherence tomography in the evaluation of the scalp and hair: common features and clinical utility. Lasers Surg Med. 2021;53:129-140.
- Schicho K, Seemann R, Binder M, et al. Optical coherence tomography for planning of follicular unit extraction. Dermatol Surg. 2015;41:358-363.
- Canfield D. Photographic documentation of hair growth in androgenetic alopecia. Dermatol Clin. 1996;14:713-721.
- Peytavi U, Hillmann K, Guarrera M. Hair growth assessment techniques. In: Peytavi U, Hillmann K, Guarrera M, eds. Hair Growth and Disorders. 4th ed. Springer; 2008:140-144.
- Chamberlain AJ, Dawber RP. Methods of evaluating hair growth. Australas J Dermatol. 2003;44:10-18.
- Dhurat R, Saraogi P. Hair evaluation methods: merits and demerits. Int J Trichology. 2009;1:108-119.
- Kaufman KD, Olsen EA, Whiting D, et al. Finasteride in the treatment of men with androgenetic alopecia. J Am Acad Dermatol. 1998;39:578-579.
- Capily Institute. Artificial intelligence (A.I.) powered hair growth tracking. Accessed July 31, 2023. https://tss-aesthetics.com/capily-hair-tracking-syst
- Dinh Q, Sinclair R. Female pattern hair loss: current treatment concepts. Clin Interv Aging. 2007;2:189-199.
- Dhurat R, Saraogi P. Hair evaluation methods: merits and demerits. Int J Trichology. 2009;1:108-119.
- Wikramanayake TC, Mauro LM, Tabas IA, et al. Cross-section trichometry: a clinical tool for assessing the progression and treatment response of alopecia. Int J Trichology. 2012;4:259-264.
- Alessandrini A, Bruni F, Piraccini BM, et al. Common causes of hair loss—clinical manifestations, trichoscopy and therapy. J Eur Acad Dermatol Venereol. 2021;35:629-640.
- Ashique K, Kaliyadan F. Clinical photography for trichology practice: tips and tricks. Int J Trichology. 2011;3:7-13.
- Rudnicka L, Olszewska M, Rakowska A, et al. Trichoscopy: a new method for diagnosing hair loss. J Drugs Dermatol. 2008;7:651-654.
- Kinoshita-Ise M, Sachdeva M. Update on trichoscopy: integration of the terminology by systematic approach and a proposal of a diagnostic flowchart. J Dermatol. 2022;49:4-18. doi:10.1111/1346-8138.16233
- Van Neste D, Trüeb RM. Critical study of hair growth analysis with computer-assisted methods. J Eur Acad Dermatol Venereol. 2006;20:578-583.
- Romero J, Grimalt R. Trichoscopy: essentials for the dermatologist. World J Dermatol. 2015;4:63-68.
- Trichoscopy: a new frontier for the diagnosis of hair diseases. Exp Rev Dermatol. 2012;7:429-437.
- Lee B, Chan J, Monselise A, et al. Assessment of hair density and caliber in Caucasian and Asian female subjects with female pattern hair loss by using the Folliscope. J Am Acad Dermatol. 2012;66:166-167.
- Inui S. Trichoscopy for common hair loss diseases: algorithmic method for diagnosis. J Dermatol. 2010;38:71-75.
- Dhurat R. Phototrichogram. Indian J Dermatol Venereol Leprol. 2006;72:242-244.
- Agozzino M, Tosti A, Barbieri L, et al. Confocal microscopic features of scarring alopecia: preliminary report. Br J Dermatol. 2011;165:534-540.
- Kuck M, Schanzer S, Ulrich M, et al. Analysis of the efficiency of hair removal by different optical methods: comparison of Trichoscan, reflectance confocal microscopy, and optical coherence tomography. J Biomed Opt. 2012;17:101504.
- Levine A, Markowitz O. Introduction to reflectance confocal microscopy and its use in clinical practice. JAAD Case Rep. 2018;4:1014-1023.
- Agozzino M, Ardigò M. Scalp confocal microscopy. In: Humbert P, Maibach H, Fanian F, et al, eds. Agache’s Measuring the Skin: Non-invasive Investigations, Physiology, Normal Constants. 2nd ed. Springer International Publishing; 2016:311-326.
- Rudnicka L, Olszewska M, Rakowska A. In vivo reflectance confocal microscopy: usefulness for diagnosing hair diseases. J Dermatol Case Rep. 2008;2:55-59.
- Kurzeja M, Czuwara J, Walecka I, et al. Features of classic lichen planopilaris and frontal fibrosing alopecia in reflectance confocal microscopy: a preliminary study. Skin Res Technol. 2021;27:266-271.
- Ardigò M, Agozzino M, Franceschini C, et al. Reflectance confocal microscopy for scarring and non-scarring alopecia real-time assessment. Arch Dermatol Res. 2016;308:309-318.
- Franceschini C, Garelli V, Persechino F, et al. Dermoscopy and confocal microscopy for different chemotherapy-induced alopecia (CIA) phases characterization: preliminary study. Skin Res Technol. 2020;26:269-276.
- Martinez-Velasco MA, Perper M, Maddy AJ, et al. In vitro determination of Mexican Mestizo hair shaft diameter using optical coherence tomography. Skin Res Technol. 2018;24;274-277.
- Srivastava R, Manfredini M, Rao BK. Noninvasive imaging tools in dermatology. Cutis. 2019;104:108-113.
- Wan B, Ganier C, Du-Harpur X, et al. Applications and future directions for optical coherence tomography in dermatology. Br J Dermatol. 2021;184:1014-1022.
- Blume-Peytavi U, Vieten J, Knuttel A et al. Optical coherent tomography (OCT): a new method for online-measurement of hair shaft thickness. J Dtsch Dermatol Ges. 2004;2:546.
- Garcia Bartels N, Jahnke I, Patzelt A, et al. Hair shaft abnormalities in alopecia areata evaluated by optical coherence tomography. Skin Res Technol. 2011;17:201-205.
- Urban G, Feil N, Csuka E, et al. Combining deep learning with optical coherence tomography imaging to determine scalp hair and follicle counts. Lasers Surg Med. 2021;53:171-178.
- Vazquez-Herrera NE, Eber AE, Martinez-Velasco MA, et al. Optical coherence tomography for the investigation of frontal fibrosing alopecia. J Eur Acad Dermatol Venereol. 2018;32:318-322.
- Ekelem C, Feil N, Csuka E, et al. Optical coherence tomography in the evaluation of the scalp and hair: common features and clinical utility. Lasers Surg Med. 2021;53:129-140.
- Schicho K, Seemann R, Binder M, et al. Optical coherence tomography for planning of follicular unit extraction. Dermatol Surg. 2015;41:358-363.
Practice Points
- Reflectance confocal microscopy (RCM) imaging can be taken at levels from the stratum corneum to the papillary dermis and can be used to study scalp discoid lupus, lichen planopilaris, frontal fibrosing alopecia, alopecia areata, and androgenetic alopecia.
- Because of its ability to distinguish different stages of disease, RCM can be recommended as an intermediate step between trichoscopy and histology for the diagnosis and management of hair disease.
- Optical coherence tomography has the potential to monitor early subclinical responses to alopecia therapies while also improving hair transplantation outcomes by allowing for visualization of the subcutaneous angle of hair follicles.
- Software development paired with trichoscopy has the ability to quantify hair growth parameters such as hair count, density, and diameter.
A new and completely different pain medicine
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
When you stub your toe or get a paper cut on your finger, you feel the pain in that part of your body. It feels like the pain is coming from that place. But, of course, that’s not really what is happening. Pain doesn’t really happen in your toe or your finger. It happens in your brain.
It’s a game of telephone, really. The afferent nerve fiber detects the noxious stimulus, passing that signal to the second-order neuron in the dorsal root ganglia of the spinal cord, which runs it up to the thalamus to be passed to the third-order neuron which brings it to the cortex for localization and conscious perception. It’s not even a very good game of telephone. It takes about 100 ms for a pain signal to get from the hand to the brain – longer from the feet, given the greater distance. You see your foot hit the corner of the coffee table and have just enough time to think: “Oh no!” before the pain hits.
Given the Rube Goldberg nature of the process, it would seem like there are any number of places we could stop pain sensation. And sure, local anesthetics at the site of injury, or even spinal anesthetics, are powerful – if temporary and hard to administer – solutions to acute pain.
But in our everyday armamentarium, let’s be honest – we essentially have three options: opiates and opioids, which activate the mu-receptors in the brain to dull pain (and cause a host of other nasty side effects); NSAIDs, which block prostaglandin synthesis and thus limit the ability for pain-conducting neurons to get excited; and acetaminophen, which, despite being used for a century, is poorly understood.
But
If you were to zoom in on the connection between that first afferent pain fiber and the secondary nerve in the spinal cord dorsal root ganglion, you would see a receptor called Nav1.8, a voltage-gated sodium channel.
This receptor is a key part of the apparatus that passes information from nerve 1 to nerve 2, but only for fibers that transmit pain signals. In fact, humans with mutations in this receptor that leave it always in the “open” state have a severe pain syndrome. Blocking the receptor, therefore, might reduce pain.
In preclinical work, researchers identified VX-548, which doesn’t have a brand name yet, as a potent blocker of that channel even in nanomolar concentrations. Importantly, the compound was highly selective for that particular channel – about 30,000 times more selective than it was for the other sodium channels in that family.
Of course, a highly selective and specific drug does not a blockbuster analgesic make. To determine how this drug would work on humans in pain, they turned to two populations: 303 individuals undergoing abdominoplasty and 274 undergoing bunionectomy, as reported in a new paper in the New England Journal of Medicine.
I know this seems a bit random, but abdominoplasty is quite painful and a good model for soft-tissue pain. Bunionectomy is also quite a painful procedure and a useful model of bone pain. After the surgeries, patients were randomized to several different doses of VX-548, hydrocodone plus acetaminophen, or placebo for 48 hours.
At 19 time points over that 48-hour period, participants were asked to rate their pain on a scale from 0 to 10. The primary outcome was the cumulative pain experienced over the 48 hours. So, higher pain would be worse here, but longer duration of pain would also be worse.
The story of the study is really told in this chart.
Yes, those assigned to the highest dose of VX-548 had a statistically significant lower cumulative amount of pain in the 48 hours after surgery. But the picture is really worth more than the stats here. You can see that the onset of pain relief was fairly quick, and that pain relief was sustained over time. You can also see that this is not a miracle drug. Pain scores were a bit better 48 hours out, but only by about a point and a half.
Placebo isn’t really the fair comparison here; few of us treat our postabdominoplasty patients with placebo, after all. The authors do not formally compare the effect of VX-548 with that of the opioid hydrocodone, for instance. But that doesn’t stop us.
This graph, which I put together from data in the paper, shows pain control across the four randomization categories, with higher numbers indicating more (cumulative) control. While all the active agents do a bit better than placebo, VX-548 at the higher dose appears to do the best. But I should note that 5 mg of hydrocodone may not be an adequate dose for most people.
Yes, I would really have killed for an NSAID arm in this trial. Its absence, given that NSAIDs are a staple of postoperative care, is ... well, let’s just say, notable.
Although not a pain-destroying machine, VX-548 has some other things to recommend it. The receptor is really not found in the brain at all, which suggests that the drug should not carry much risk for dependency, though that has not been formally studied.
The side effects were generally mild – headache was the most common – and less prevalent than what you see even in the placebo arm.
Perhaps most notable is the fact that the rate of discontinuation of the study drug was lowest in the VX-548 arm. Patients could stop taking the pill they were assigned for any reason, ranging from perceived lack of efficacy to side effects. A low discontinuation rate indicates to me a sort of “voting with your feet” that suggests this might be a well-tolerated and reasonably effective drug.
VX-548 isn’t on the market yet; phase 3 trials are ongoing. But whether it is this particular drug or another in this class, I’m happy to see researchers trying to find new ways to target that most primeval form of suffering: pain.
Dr. Wilson is an associate professor of medicine and public health and director of Yale’s Clinical and Translational Research Accelerator, New Haven, Conn. He disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Pandemic blamed for failed trial of inhaled antibiotic
NEW YORK – When data were combined from two parallel phase 3 bronchiectasis treatment trials, inhaled colistimethate sodium failed to significantly reduce the rate of exacerbations associated with Pseudomonas aeruginosa infection, but the disparity in the findings from the two trials, presented at the 6th World Bronchiectasis & NTM Conference (WBC) 2023, strongly suggests that this therapy is effective after all.
“The totality of the evidence supports a consistent and clinically meaningful benefit [of this therapy] outside of pandemic conditions,” reported Charles Haworth, MD, director, Cambridge Centre for Lung Infection, Royal Papworth Hospital, Cambridge, England.
The key phrase is “outside of pandemic conditions.” PROMIS I, which was fully enrolled before the COVID-19 pandemic descended, associated the inhaled therapy with highly significant benefits. PROMIS II, which was initiated later and enrolled 40% of its participants during the pandemic, did not.
The difference between these two trials, which were essentially identical, was the timing, according to Dr. Haworth. By starting later, PROMIS II caught the onset of the pandemic, which he believes introduced numerous problems that defeated the opportunity to show an advantage for the inhaled antibiotic.
Injectable colistimethate sodium, a decades-old formulation of colistin, is already approved in the United States for gram-negative infections and is considered helpful even in challenging diseases, such as cystic fibrosis. Positive results from a phase 2 trial with inhaled colistimethate sodium in bronchiectasis patients with P. aeruginosa infection provided the rationale for the phase 3 PROMIS program.
The key entry criterion of PROMIS I and PROMIS II, each with nearly 90 participating study sites, was a history of bronchiectasis and ≥ two P. aeruginosa infections requiring oral therapy or ≥ 1 infection requiring intravenous therapy in the prior 12 months. Patients were randomly assigned to receive colistimethate sodium delivered in the proprietary I-neb nebulizer (CMS I-neb) or a matching placebo.
On the primary endpoint of annualized rate of exacerbations, the figures per year were 0.58 for CMS I-neb and 0.95 for placebo in the PROMIS I trial. This produced a rate ratio of 0.65, signaling a significant 35% (P = .00101) reduction in risk. In PROMIS II, the annualized rates of exacerbation were essentially identical in the experimental and control arms (0.089 vs. 0.088; P = .97).
With “no signal of benefit” in the PROMIS II trial, the numerical advantage of CMS I-neb for the combined data did not reach statistical significance, Dr. Haworth reported.
Other endpoints told the same story. For example, the time to first exacerbation was reduced by 41% in PROMIS I (HR, 0.59; P = .0074) but was not reduced significantly (P = .603) in PROMIS II. In PROMIS I, there was a nearly 60% reduction in the risk of severe exacerbations associated with CMS I-neb, but the risk ratio of severe infections was slightly but not significantly higher on CMS I-neb in PROMIS II.
There were signals of benefit in PROMIS II. For example, the reductions in P. aeruginosa density were similar in the two studies (P < .00001 in both), and assessment with the Severe Exacerbations and Quality of Life (SQOL) tool associated CMS I-neb with end-of-study improvement in QOL for the experimental arm in both studies.
While Dr. Haworth acknowledged that he recognizes the “issues of post hoc analysis with any data,” obscuring a benefit that would have been otherwise shown.
Besides the dramatic reduction in rates of hospitalization during the pandemic, an obstacle for showing differences in exacerbations, and other COVID-related factors with the potential to skew results, Dr. Haworth also provided several sets of objective data to make his point.
Most importantly, Dr. Haworth and his coinvestigators conducted a meta-analysis that combined data from the phase 2 trial, data from PROMIS I, and data from the patients enrolled in PROMIS II prior to the COVID pandemic. In this analysis the rate ratio for annualized exacerbations was a “pretty impressive” 0.65 favoring CMS I-neb. Moreover, in contrast to data from the PROMIS II patients enrolled during the COVID pandemic, the other three sets of data were “remarkably consistent.”
If PROMIS II data collected from patients enrolled during COVID are compared with the other sets of data, they are “the clear outlier,” he asserted.
Many guidelines in Europe, including those from the European Respiratory Society and the British Thoracic Society, already recommend inhaled colistin in patients with bronchiectasis for the treatment of P. aeruginosa. Although Dr. Haworth believes that the preponderance of controlled data now argue that CMS I-neb is effective as well as safe (adverse events in the experimental and placebo arms of PROMIS I and II were similar), he is not sure what steps will be taken to confirm a benefit to regulatory authorities. According to Dr. Haworth, there are no approved inhaled antibiotics in the United States.
Referring to Zambon, which funded the trials and is developing CMS I-neb, Dr. Haworth said, “This will be a company decision. There are some logistical hurdles to doing another trial.”
Not least of these hurdles is that clinicians and patients already consider inhalational antibiotics in general and inhaled colistin specifically to be effective for several types of infections, including P. aeruginosa, according to Eva Polverino, MD, PhD, a pulmonologist associated with the Hospital Clinic of Barcelona. She said that these drugs are already a standard of care in her own country as well as in many other countries in Europe.
“There has been a loss of equipoise needed to conduct a randomized placebo-controlled trial,” Dr. Polverino said. In her opinion, the U.S. FDA “should start thinking of other pathways to approval.” She thinks that enrollment in a placebo-controlled trial is no longer appropriate.
Dr. Haworth and Dr. Polverino have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW YORK – When data were combined from two parallel phase 3 bronchiectasis treatment trials, inhaled colistimethate sodium failed to significantly reduce the rate of exacerbations associated with Pseudomonas aeruginosa infection, but the disparity in the findings from the two trials, presented at the 6th World Bronchiectasis & NTM Conference (WBC) 2023, strongly suggests that this therapy is effective after all.
“The totality of the evidence supports a consistent and clinically meaningful benefit [of this therapy] outside of pandemic conditions,” reported Charles Haworth, MD, director, Cambridge Centre for Lung Infection, Royal Papworth Hospital, Cambridge, England.
The key phrase is “outside of pandemic conditions.” PROMIS I, which was fully enrolled before the COVID-19 pandemic descended, associated the inhaled therapy with highly significant benefits. PROMIS II, which was initiated later and enrolled 40% of its participants during the pandemic, did not.
The difference between these two trials, which were essentially identical, was the timing, according to Dr. Haworth. By starting later, PROMIS II caught the onset of the pandemic, which he believes introduced numerous problems that defeated the opportunity to show an advantage for the inhaled antibiotic.
Injectable colistimethate sodium, a decades-old formulation of colistin, is already approved in the United States for gram-negative infections and is considered helpful even in challenging diseases, such as cystic fibrosis. Positive results from a phase 2 trial with inhaled colistimethate sodium in bronchiectasis patients with P. aeruginosa infection provided the rationale for the phase 3 PROMIS program.
The key entry criterion of PROMIS I and PROMIS II, each with nearly 90 participating study sites, was a history of bronchiectasis and ≥ two P. aeruginosa infections requiring oral therapy or ≥ 1 infection requiring intravenous therapy in the prior 12 months. Patients were randomly assigned to receive colistimethate sodium delivered in the proprietary I-neb nebulizer (CMS I-neb) or a matching placebo.
On the primary endpoint of annualized rate of exacerbations, the figures per year were 0.58 for CMS I-neb and 0.95 for placebo in the PROMIS I trial. This produced a rate ratio of 0.65, signaling a significant 35% (P = .00101) reduction in risk. In PROMIS II, the annualized rates of exacerbation were essentially identical in the experimental and control arms (0.089 vs. 0.088; P = .97).
With “no signal of benefit” in the PROMIS II trial, the numerical advantage of CMS I-neb for the combined data did not reach statistical significance, Dr. Haworth reported.
Other endpoints told the same story. For example, the time to first exacerbation was reduced by 41% in PROMIS I (HR, 0.59; P = .0074) but was not reduced significantly (P = .603) in PROMIS II. In PROMIS I, there was a nearly 60% reduction in the risk of severe exacerbations associated with CMS I-neb, but the risk ratio of severe infections was slightly but not significantly higher on CMS I-neb in PROMIS II.
There were signals of benefit in PROMIS II. For example, the reductions in P. aeruginosa density were similar in the two studies (P < .00001 in both), and assessment with the Severe Exacerbations and Quality of Life (SQOL) tool associated CMS I-neb with end-of-study improvement in QOL for the experimental arm in both studies.
While Dr. Haworth acknowledged that he recognizes the “issues of post hoc analysis with any data,” obscuring a benefit that would have been otherwise shown.
Besides the dramatic reduction in rates of hospitalization during the pandemic, an obstacle for showing differences in exacerbations, and other COVID-related factors with the potential to skew results, Dr. Haworth also provided several sets of objective data to make his point.
Most importantly, Dr. Haworth and his coinvestigators conducted a meta-analysis that combined data from the phase 2 trial, data from PROMIS I, and data from the patients enrolled in PROMIS II prior to the COVID pandemic. In this analysis the rate ratio for annualized exacerbations was a “pretty impressive” 0.65 favoring CMS I-neb. Moreover, in contrast to data from the PROMIS II patients enrolled during the COVID pandemic, the other three sets of data were “remarkably consistent.”
If PROMIS II data collected from patients enrolled during COVID are compared with the other sets of data, they are “the clear outlier,” he asserted.
Many guidelines in Europe, including those from the European Respiratory Society and the British Thoracic Society, already recommend inhaled colistin in patients with bronchiectasis for the treatment of P. aeruginosa. Although Dr. Haworth believes that the preponderance of controlled data now argue that CMS I-neb is effective as well as safe (adverse events in the experimental and placebo arms of PROMIS I and II were similar), he is not sure what steps will be taken to confirm a benefit to regulatory authorities. According to Dr. Haworth, there are no approved inhaled antibiotics in the United States.
Referring to Zambon, which funded the trials and is developing CMS I-neb, Dr. Haworth said, “This will be a company decision. There are some logistical hurdles to doing another trial.”
Not least of these hurdles is that clinicians and patients already consider inhalational antibiotics in general and inhaled colistin specifically to be effective for several types of infections, including P. aeruginosa, according to Eva Polverino, MD, PhD, a pulmonologist associated with the Hospital Clinic of Barcelona. She said that these drugs are already a standard of care in her own country as well as in many other countries in Europe.
“There has been a loss of equipoise needed to conduct a randomized placebo-controlled trial,” Dr. Polverino said. In her opinion, the U.S. FDA “should start thinking of other pathways to approval.” She thinks that enrollment in a placebo-controlled trial is no longer appropriate.
Dr. Haworth and Dr. Polverino have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
NEW YORK – When data were combined from two parallel phase 3 bronchiectasis treatment trials, inhaled colistimethate sodium failed to significantly reduce the rate of exacerbations associated with Pseudomonas aeruginosa infection, but the disparity in the findings from the two trials, presented at the 6th World Bronchiectasis & NTM Conference (WBC) 2023, strongly suggests that this therapy is effective after all.
“The totality of the evidence supports a consistent and clinically meaningful benefit [of this therapy] outside of pandemic conditions,” reported Charles Haworth, MD, director, Cambridge Centre for Lung Infection, Royal Papworth Hospital, Cambridge, England.
The key phrase is “outside of pandemic conditions.” PROMIS I, which was fully enrolled before the COVID-19 pandemic descended, associated the inhaled therapy with highly significant benefits. PROMIS II, which was initiated later and enrolled 40% of its participants during the pandemic, did not.
The difference between these two trials, which were essentially identical, was the timing, according to Dr. Haworth. By starting later, PROMIS II caught the onset of the pandemic, which he believes introduced numerous problems that defeated the opportunity to show an advantage for the inhaled antibiotic.
Injectable colistimethate sodium, a decades-old formulation of colistin, is already approved in the United States for gram-negative infections and is considered helpful even in challenging diseases, such as cystic fibrosis. Positive results from a phase 2 trial with inhaled colistimethate sodium in bronchiectasis patients with P. aeruginosa infection provided the rationale for the phase 3 PROMIS program.
The key entry criterion of PROMIS I and PROMIS II, each with nearly 90 participating study sites, was a history of bronchiectasis and ≥ two P. aeruginosa infections requiring oral therapy or ≥ 1 infection requiring intravenous therapy in the prior 12 months. Patients were randomly assigned to receive colistimethate sodium delivered in the proprietary I-neb nebulizer (CMS I-neb) or a matching placebo.
On the primary endpoint of annualized rate of exacerbations, the figures per year were 0.58 for CMS I-neb and 0.95 for placebo in the PROMIS I trial. This produced a rate ratio of 0.65, signaling a significant 35% (P = .00101) reduction in risk. In PROMIS II, the annualized rates of exacerbation were essentially identical in the experimental and control arms (0.089 vs. 0.088; P = .97).
With “no signal of benefit” in the PROMIS II trial, the numerical advantage of CMS I-neb for the combined data did not reach statistical significance, Dr. Haworth reported.
Other endpoints told the same story. For example, the time to first exacerbation was reduced by 41% in PROMIS I (HR, 0.59; P = .0074) but was not reduced significantly (P = .603) in PROMIS II. In PROMIS I, there was a nearly 60% reduction in the risk of severe exacerbations associated with CMS I-neb, but the risk ratio of severe infections was slightly but not significantly higher on CMS I-neb in PROMIS II.
There were signals of benefit in PROMIS II. For example, the reductions in P. aeruginosa density were similar in the two studies (P < .00001 in both), and assessment with the Severe Exacerbations and Quality of Life (SQOL) tool associated CMS I-neb with end-of-study improvement in QOL for the experimental arm in both studies.
While Dr. Haworth acknowledged that he recognizes the “issues of post hoc analysis with any data,” obscuring a benefit that would have been otherwise shown.
Besides the dramatic reduction in rates of hospitalization during the pandemic, an obstacle for showing differences in exacerbations, and other COVID-related factors with the potential to skew results, Dr. Haworth also provided several sets of objective data to make his point.
Most importantly, Dr. Haworth and his coinvestigators conducted a meta-analysis that combined data from the phase 2 trial, data from PROMIS I, and data from the patients enrolled in PROMIS II prior to the COVID pandemic. In this analysis the rate ratio for annualized exacerbations was a “pretty impressive” 0.65 favoring CMS I-neb. Moreover, in contrast to data from the PROMIS II patients enrolled during the COVID pandemic, the other three sets of data were “remarkably consistent.”
If PROMIS II data collected from patients enrolled during COVID are compared with the other sets of data, they are “the clear outlier,” he asserted.
Many guidelines in Europe, including those from the European Respiratory Society and the British Thoracic Society, already recommend inhaled colistin in patients with bronchiectasis for the treatment of P. aeruginosa. Although Dr. Haworth believes that the preponderance of controlled data now argue that CMS I-neb is effective as well as safe (adverse events in the experimental and placebo arms of PROMIS I and II were similar), he is not sure what steps will be taken to confirm a benefit to regulatory authorities. According to Dr. Haworth, there are no approved inhaled antibiotics in the United States.
Referring to Zambon, which funded the trials and is developing CMS I-neb, Dr. Haworth said, “This will be a company decision. There are some logistical hurdles to doing another trial.”
Not least of these hurdles is that clinicians and patients already consider inhalational antibiotics in general and inhaled colistin specifically to be effective for several types of infections, including P. aeruginosa, according to Eva Polverino, MD, PhD, a pulmonologist associated with the Hospital Clinic of Barcelona. She said that these drugs are already a standard of care in her own country as well as in many other countries in Europe.
“There has been a loss of equipoise needed to conduct a randomized placebo-controlled trial,” Dr. Polverino said. In her opinion, the U.S. FDA “should start thinking of other pathways to approval.” She thinks that enrollment in a placebo-controlled trial is no longer appropriate.
Dr. Haworth and Dr. Polverino have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM WBC 2023
Vasopressin may promote lower mortality in septic shock
according to a review of three recent studies.
“Patients with septic shock require vasoactive agents to restore adequate tissue perfusion,” writes Gretchen L. Sacha, PharmD, of the Cleveland Clinic and colleagues.
Vasopressin is an attractive alternative to norepinephrine because it avoids the adverse effects associated with catecholamines, the researchers say. Although vasopressin is the recommended second-line adjunct after norepinephrine for patients with septic shock, findings to guide its use are inconsistent and data on the timing are limited, they note.
In a review published in the journal CHEST, the researchers summarize the three large, randomized trials to date examining the use of norepinephrine and vasopressin in patients with septic shock.
In the Vasopressin in Septic Shock Trial (VASST), 382 patients with septic shock were randomized to open-label norepinephrine with blinded norepinephrine, and 382 were randomized to open-label norepinephrine with blinded adjunctive vasopressin.
After initiation of the study drug, patients randomized to vasopressin had significantly lower requirements for open-label norepinephrine (P < .001). Although no differences occurred in the primary outcome of 28-day mortality, 90-day mortality was lower in the vasopressin group.
In the Vasopressin vs Norepinephrine as Initial Therapy in Septic Shock (VANISH) trial, 204 patients with septic shock were randomized to norepinephrine and 204 to vasopressin as an initial vasoactive agent. Although no differences appeared between the groups for the two primary outcomes of 28-day mortality and days free of kidney failure, the vasopressin group had a lower frequency of the use of kidney replacement therapy (absolute difference –9.9% vs. –0.6%).
The VANISH study was limited by the fact that 85% of the patients were receiving norepinephrine when they were randomized; “therefore, this study is best described as evaluating catecholamine-adjunctive vasopressin,” the researchers say.
The third clinical trial, published only as an abstract, randomized 387 patients with septic shock who were already receiving low doses of norepinephrine to either norepinephrine with adjunctive vasopressin or norepinephrine alone. Rates of 28-day mortality were significantly lower in the vasopressin group (34.0% vs. 42.3%; P = .03).
Several meta-analyses involving multiple vasopressin receptor agonists have shown an association between reduced mortality and their use. In addition, recent observational studies have shown an association between lower mortality and the initiation of vasopressors at a lower norepinephrine-equivalent dose or lower lactate concentration.
As for clinical implications, the 2021 version of the Surviving Sepsis Campaign (SSC) guidelines included a meta-analysis of 10 randomized, controlled trials that showed improved mortality associated with vasopressin use. This version of the guidelines was the first to address the timing of vasopressin initiation.
Because of insufficient evidence, the guidance was worded as “in our practice, vasopressin is usually started when the dose of norepinephrine is in the range of 0.25-0.5 mcg/kg/min,” the researchers write. “Although this is not a recommendation by the SSC for a specific threshold of catecholamine dose where vasopressin should be initiated, this statement represents clinician interest and the need for further research on the topic,” they note.
“Future studies of vasopressin should focus on the timing of its initiation at various clinical thresholds and patient selection for receipt of vasopressin,” they conclude.
The study was supported by the National Institutes of Health, National Institute of General Medical Sciences. Dr. Sacha has disclosed consulting for Wolters Kluwer.
A version of this article first appeared on Medscape.com.
according to a review of three recent studies.
“Patients with septic shock require vasoactive agents to restore adequate tissue perfusion,” writes Gretchen L. Sacha, PharmD, of the Cleveland Clinic and colleagues.
Vasopressin is an attractive alternative to norepinephrine because it avoids the adverse effects associated with catecholamines, the researchers say. Although vasopressin is the recommended second-line adjunct after norepinephrine for patients with septic shock, findings to guide its use are inconsistent and data on the timing are limited, they note.
In a review published in the journal CHEST, the researchers summarize the three large, randomized trials to date examining the use of norepinephrine and vasopressin in patients with septic shock.
In the Vasopressin in Septic Shock Trial (VASST), 382 patients with septic shock were randomized to open-label norepinephrine with blinded norepinephrine, and 382 were randomized to open-label norepinephrine with blinded adjunctive vasopressin.
After initiation of the study drug, patients randomized to vasopressin had significantly lower requirements for open-label norepinephrine (P < .001). Although no differences occurred in the primary outcome of 28-day mortality, 90-day mortality was lower in the vasopressin group.
In the Vasopressin vs Norepinephrine as Initial Therapy in Septic Shock (VANISH) trial, 204 patients with septic shock were randomized to norepinephrine and 204 to vasopressin as an initial vasoactive agent. Although no differences appeared between the groups for the two primary outcomes of 28-day mortality and days free of kidney failure, the vasopressin group had a lower frequency of the use of kidney replacement therapy (absolute difference –9.9% vs. –0.6%).
The VANISH study was limited by the fact that 85% of the patients were receiving norepinephrine when they were randomized; “therefore, this study is best described as evaluating catecholamine-adjunctive vasopressin,” the researchers say.
The third clinical trial, published only as an abstract, randomized 387 patients with septic shock who were already receiving low doses of norepinephrine to either norepinephrine with adjunctive vasopressin or norepinephrine alone. Rates of 28-day mortality were significantly lower in the vasopressin group (34.0% vs. 42.3%; P = .03).
Several meta-analyses involving multiple vasopressin receptor agonists have shown an association between reduced mortality and their use. In addition, recent observational studies have shown an association between lower mortality and the initiation of vasopressors at a lower norepinephrine-equivalent dose or lower lactate concentration.
As for clinical implications, the 2021 version of the Surviving Sepsis Campaign (SSC) guidelines included a meta-analysis of 10 randomized, controlled trials that showed improved mortality associated with vasopressin use. This version of the guidelines was the first to address the timing of vasopressin initiation.
Because of insufficient evidence, the guidance was worded as “in our practice, vasopressin is usually started when the dose of norepinephrine is in the range of 0.25-0.5 mcg/kg/min,” the researchers write. “Although this is not a recommendation by the SSC for a specific threshold of catecholamine dose where vasopressin should be initiated, this statement represents clinician interest and the need for further research on the topic,” they note.
“Future studies of vasopressin should focus on the timing of its initiation at various clinical thresholds and patient selection for receipt of vasopressin,” they conclude.
The study was supported by the National Institutes of Health, National Institute of General Medical Sciences. Dr. Sacha has disclosed consulting for Wolters Kluwer.
A version of this article first appeared on Medscape.com.
according to a review of three recent studies.
“Patients with septic shock require vasoactive agents to restore adequate tissue perfusion,” writes Gretchen L. Sacha, PharmD, of the Cleveland Clinic and colleagues.
Vasopressin is an attractive alternative to norepinephrine because it avoids the adverse effects associated with catecholamines, the researchers say. Although vasopressin is the recommended second-line adjunct after norepinephrine for patients with septic shock, findings to guide its use are inconsistent and data on the timing are limited, they note.
In a review published in the journal CHEST, the researchers summarize the three large, randomized trials to date examining the use of norepinephrine and vasopressin in patients with septic shock.
In the Vasopressin in Septic Shock Trial (VASST), 382 patients with septic shock were randomized to open-label norepinephrine with blinded norepinephrine, and 382 were randomized to open-label norepinephrine with blinded adjunctive vasopressin.
After initiation of the study drug, patients randomized to vasopressin had significantly lower requirements for open-label norepinephrine (P < .001). Although no differences occurred in the primary outcome of 28-day mortality, 90-day mortality was lower in the vasopressin group.
In the Vasopressin vs Norepinephrine as Initial Therapy in Septic Shock (VANISH) trial, 204 patients with septic shock were randomized to norepinephrine and 204 to vasopressin as an initial vasoactive agent. Although no differences appeared between the groups for the two primary outcomes of 28-day mortality and days free of kidney failure, the vasopressin group had a lower frequency of the use of kidney replacement therapy (absolute difference –9.9% vs. –0.6%).
The VANISH study was limited by the fact that 85% of the patients were receiving norepinephrine when they were randomized; “therefore, this study is best described as evaluating catecholamine-adjunctive vasopressin,” the researchers say.
The third clinical trial, published only as an abstract, randomized 387 patients with septic shock who were already receiving low doses of norepinephrine to either norepinephrine with adjunctive vasopressin or norepinephrine alone. Rates of 28-day mortality were significantly lower in the vasopressin group (34.0% vs. 42.3%; P = .03).
Several meta-analyses involving multiple vasopressin receptor agonists have shown an association between reduced mortality and their use. In addition, recent observational studies have shown an association between lower mortality and the initiation of vasopressors at a lower norepinephrine-equivalent dose or lower lactate concentration.
As for clinical implications, the 2021 version of the Surviving Sepsis Campaign (SSC) guidelines included a meta-analysis of 10 randomized, controlled trials that showed improved mortality associated with vasopressin use. This version of the guidelines was the first to address the timing of vasopressin initiation.
Because of insufficient evidence, the guidance was worded as “in our practice, vasopressin is usually started when the dose of norepinephrine is in the range of 0.25-0.5 mcg/kg/min,” the researchers write. “Although this is not a recommendation by the SSC for a specific threshold of catecholamine dose where vasopressin should be initiated, this statement represents clinician interest and the need for further research on the topic,” they note.
“Future studies of vasopressin should focus on the timing of its initiation at various clinical thresholds and patient selection for receipt of vasopressin,” they conclude.
The study was supported by the National Institutes of Health, National Institute of General Medical Sciences. Dr. Sacha has disclosed consulting for Wolters Kluwer.
A version of this article first appeared on Medscape.com.
FROM CHEST
Neutropenia affects clinical presentation of pulmonary mucormycosis
, based on data from 114 individuals.
Diagnosis of pulmonary mucormycosis (PM), an invasive and potentially life-threatening fungal infection, is often delayed because of its variable presentation, wrote Anne Coste, MD, of La Cavale Blanche Hospital and Brest (France) University Hospital, and colleagues.
Improved diagnostic tools including molecular identification and image-guided lung biopsies are now available in many centers, but relations between underlying conditions, clinical presentations, and diagnostic methods have not been described, they said.
In a study published in the journal Chest, the researchers reviewed data from all cases of PM seen at six hospitals in France between 2008 and 2019. PM cases were based on European Organization for Research and Treatment of Cancer and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) criteria. Diabetes and trauma were included as additional host factors, and positive serum or tissue PCR (serum qPCR) were included as mycological evidence. Participants also underwent thoracic computed tomography (CT) scans.
The most common underlying conditions among the 114 patients were hematological malignancy (49%), allogeneic hematopoietic stem-cell transplantation (21%), and solid organ transplantation (17%).
Among the 40% of the cases that involved dissemination, the most common sites were the liver (48%), spleen (48%), brain (44%), and kidneys (37%).
A review of radiology findings showed consolidation in a majority of patients (58%), as well as pleural effusion (52%). Other findings included reversed halo sign (RHS, 26%), halo sign (24%), vascular abnormalities (26%), and cavity (23%).
Bronchoalveolar lavage (BAL) was present in 46 of 96 patients (50%), and transthoracic lung biopsy was used for diagnosis in 8 of 11 (73%) patients with previous negative BALs.
Seventy patients had neutropenia. Overall, patients with neutropenia were significantly more likely than were those without neutropenia to show an angioinvasive presentation that included both RHS and disease dissemination (P < .05).
In addition, serum qPCR was positive in 42 of 53 patients for whom data were available (79%). Serum qPCR was significantly more likely to be positive in neutropenic patients (91% vs. 62%, P = .02). Positive qPCR was associated with an early diagnosis (P = .03) and treatment onset (P = .01).
Possible reasons for the high rate of disseminated PM in the current study may be the large number of patients with pulmonary involvement, use of body CT data, and availability of autopsy results (for 11% of cases), the researchers wrote in their discussion.
Neutropenia and radiological findings influence disease presentation and contribution of diagnostic tools during PM. Serum qPCR is more contributive in neutropenic patients and BAL examination in nonneutropenic patients. Lung biopsies are highly contributive in case of non-contributive BAL.
The findings were limited by several factors including the retrospective design, the inability to calculate sensitivity and specificity of diagnostic methods, and lack of data on patients with COVID-19, the researchers noted. However, the results provide real-life information for clinicians in centers with current mycological platforms, they concluded.
The study received no outside funding. Dr. Coste had no financial conflicts to disclose.
, based on data from 114 individuals.
Diagnosis of pulmonary mucormycosis (PM), an invasive and potentially life-threatening fungal infection, is often delayed because of its variable presentation, wrote Anne Coste, MD, of La Cavale Blanche Hospital and Brest (France) University Hospital, and colleagues.
Improved diagnostic tools including molecular identification and image-guided lung biopsies are now available in many centers, but relations between underlying conditions, clinical presentations, and diagnostic methods have not been described, they said.
In a study published in the journal Chest, the researchers reviewed data from all cases of PM seen at six hospitals in France between 2008 and 2019. PM cases were based on European Organization for Research and Treatment of Cancer and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) criteria. Diabetes and trauma were included as additional host factors, and positive serum or tissue PCR (serum qPCR) were included as mycological evidence. Participants also underwent thoracic computed tomography (CT) scans.
The most common underlying conditions among the 114 patients were hematological malignancy (49%), allogeneic hematopoietic stem-cell transplantation (21%), and solid organ transplantation (17%).
Among the 40% of the cases that involved dissemination, the most common sites were the liver (48%), spleen (48%), brain (44%), and kidneys (37%).
A review of radiology findings showed consolidation in a majority of patients (58%), as well as pleural effusion (52%). Other findings included reversed halo sign (RHS, 26%), halo sign (24%), vascular abnormalities (26%), and cavity (23%).
Bronchoalveolar lavage (BAL) was present in 46 of 96 patients (50%), and transthoracic lung biopsy was used for diagnosis in 8 of 11 (73%) patients with previous negative BALs.
Seventy patients had neutropenia. Overall, patients with neutropenia were significantly more likely than were those without neutropenia to show an angioinvasive presentation that included both RHS and disease dissemination (P < .05).
In addition, serum qPCR was positive in 42 of 53 patients for whom data were available (79%). Serum qPCR was significantly more likely to be positive in neutropenic patients (91% vs. 62%, P = .02). Positive qPCR was associated with an early diagnosis (P = .03) and treatment onset (P = .01).
Possible reasons for the high rate of disseminated PM in the current study may be the large number of patients with pulmonary involvement, use of body CT data, and availability of autopsy results (for 11% of cases), the researchers wrote in their discussion.
Neutropenia and radiological findings influence disease presentation and contribution of diagnostic tools during PM. Serum qPCR is more contributive in neutropenic patients and BAL examination in nonneutropenic patients. Lung biopsies are highly contributive in case of non-contributive BAL.
The findings were limited by several factors including the retrospective design, the inability to calculate sensitivity and specificity of diagnostic methods, and lack of data on patients with COVID-19, the researchers noted. However, the results provide real-life information for clinicians in centers with current mycological platforms, they concluded.
The study received no outside funding. Dr. Coste had no financial conflicts to disclose.
, based on data from 114 individuals.
Diagnosis of pulmonary mucormycosis (PM), an invasive and potentially life-threatening fungal infection, is often delayed because of its variable presentation, wrote Anne Coste, MD, of La Cavale Blanche Hospital and Brest (France) University Hospital, and colleagues.
Improved diagnostic tools including molecular identification and image-guided lung biopsies are now available in many centers, but relations between underlying conditions, clinical presentations, and diagnostic methods have not been described, they said.
In a study published in the journal Chest, the researchers reviewed data from all cases of PM seen at six hospitals in France between 2008 and 2019. PM cases were based on European Organization for Research and Treatment of Cancer and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) criteria. Diabetes and trauma were included as additional host factors, and positive serum or tissue PCR (serum qPCR) were included as mycological evidence. Participants also underwent thoracic computed tomography (CT) scans.
The most common underlying conditions among the 114 patients were hematological malignancy (49%), allogeneic hematopoietic stem-cell transplantation (21%), and solid organ transplantation (17%).
Among the 40% of the cases that involved dissemination, the most common sites were the liver (48%), spleen (48%), brain (44%), and kidneys (37%).
A review of radiology findings showed consolidation in a majority of patients (58%), as well as pleural effusion (52%). Other findings included reversed halo sign (RHS, 26%), halo sign (24%), vascular abnormalities (26%), and cavity (23%).
Bronchoalveolar lavage (BAL) was present in 46 of 96 patients (50%), and transthoracic lung biopsy was used for diagnosis in 8 of 11 (73%) patients with previous negative BALs.
Seventy patients had neutropenia. Overall, patients with neutropenia were significantly more likely than were those without neutropenia to show an angioinvasive presentation that included both RHS and disease dissemination (P < .05).
In addition, serum qPCR was positive in 42 of 53 patients for whom data were available (79%). Serum qPCR was significantly more likely to be positive in neutropenic patients (91% vs. 62%, P = .02). Positive qPCR was associated with an early diagnosis (P = .03) and treatment onset (P = .01).
Possible reasons for the high rate of disseminated PM in the current study may be the large number of patients with pulmonary involvement, use of body CT data, and availability of autopsy results (for 11% of cases), the researchers wrote in their discussion.
Neutropenia and radiological findings influence disease presentation and contribution of diagnostic tools during PM. Serum qPCR is more contributive in neutropenic patients and BAL examination in nonneutropenic patients. Lung biopsies are highly contributive in case of non-contributive BAL.
The findings were limited by several factors including the retrospective design, the inability to calculate sensitivity and specificity of diagnostic methods, and lack of data on patients with COVID-19, the researchers noted. However, the results provide real-life information for clinicians in centers with current mycological platforms, they concluded.
The study received no outside funding. Dr. Coste had no financial conflicts to disclose.
FROM THE JOURNAL CHEST
In 133-vehicle pileup, bleeding paramedic helps while hurt
It seemed like a typical kind of day. I was out the door by 6:00 a.m., heading into work for a shift on I-35 West, my daily commute. It was still dark out. A little bit colder that morning, but nothing us Texans aren’t used to.
I was cruising down the tollway, which is separated from the main highway by a barrier. That stretch has a slight hill and turns to the left. You can’t see anything beyond the hill when you’re at the bottom.
As I made my way up, I spotted brake lights about 400 yards ahead. I eased on my brake, and next thing I knew, I was sliding.
I realized, I’m on black ice.
I was driving a 2011 Toyota FJ Cruiser and I had it all beefed up – lift tires, winch bumpers front and back. I had never had any sort of issue like that.
My ABS brakes kicked in. I slowed, but not fast enough. I saw a wall of crashed cars in front of me.
I was in the left-hand lane, so I turned my steering wheel into the center median. I could hear the whole side of my vehicle scraping against it. I managed to slow down enough to just tap the vehicle in front of me.
I looked in my passenger side-view mirror and saw headlights coming in the right lane. But this car couldn’t slow down. It crashed into the wreckage to my right.
That’s when it sunk in: There was going to be a car coming in my lane, and it might not be able to stop.
I looked in my rear-view mirror and saw headlights. Sparks flying off that center median.
I didn’t know at the time, but it was a fully loaded semi-truck traveling about 60 miles an hour.
I had a split second to think: This is it. This is how it ends. I closed my eyes.
It was the most violent impact I’ve ever experienced in my life.
I had no idea until afterward, but I had slammed into the vehicle in front of me and my SUV did a kind of 360° barrel roll over the median into the northbound lanes, landing wheels down on top of my sheared off roof rack.
Everything stopped. I opened my eyes. All my airbags had deployed. I gently tried moving my arms and legs, and they worked. I couldn’t move my left foot. It was wedged underneath the brake pedal. But I wasn’t in any pain, just very confused and disoriented. I knew I needed to get out of the vehicle.
My door was wedged shut, so I crawled out of the broken window, slipping on the black ice. I realized I had hit a Fort Worth police cruiser, now all smashed up. The driver couldn’t open his door. So, I helped him force it open, got him out of the vehicle, and checked on him. He was fine.
I had no idea how many vehicles and people were involved. I was in so much shock that the only thing I could do was immediately revert back to my training. I was the only first responder there.
I was helping people with lacerations, back and neck issues from the violent impacts. When you’re involved in a mass casualty incident like that, you have to assess which patients will be the most viable and need the most immediate attention. You have greens, yellows, reds, and then blacks – the deceased. Someone who doesn’t have a pulse and isn’t breathing, you can’t necessarily do CPR because you don’t have enough resources. You have to use your best judgment.
Meanwhile, the crashes kept coming. I found out later I was roughly vehicle No. 50 in the pileup; 83 more would follow. I heard them over and over – a crash and then screams from people in their vehicles. Each time a car hit, the entire pileup would move a couple of inches, getting more and more compacted. With that going on, I couldn’t go in there to pull people out. That scene was absolutely unsafe.
It felt like forever, but about 10 minutes later, an ambulance showed up, and I walked over to them. Because I was in my work uniform, they thought I was there on a call.
A couple fire crews came, and a firefighter yelled, “Hey, we need a backboard!” So, I grabbed a backboard from their unit and helped load up a patient. Then I heard somebody screaming, “This patient needs a stretcher!” A woman was having lumbar pain that seemed excruciating. I helped move her from the wreckage and carry her over to the stretcher. I started trying to get as many people as I could out of their cars.
Around this time, one of my supervisors showed up. He thought I was there working. But then he asked me, “Why is your face bleeding? Why do you have blood coming from your nose?” I pointed to my vehicle, and his jaw just dropped. He said, “Okay, you’re done. Go sit in my vehicle over there.”
He put a stop to my helping out, which was probably for the best. Because I actually had a concussion, a bone contusion in my foot, and a severely sprained ankle. The next day, I felt like I had gotten hit by a truck. (I had!) But when you have so much adrenaline pumping, you don’t feel pain or emotion. You don’t really feel anything.
While I was sitting in that vehicle, I called my mom to let her know I was okay. My parents were watching the news, and there was an aerial view of the accident. It was massive – a giant pile of metal stretching 200 or 300 yards. Six people had perished, more than 60 were hurt.
That night, our public information officer reached out to me about doing an interview with NBC. So, I told my story about what happened. Because of the concussion, a lot of it was a blur.
A day later, I got a call on my cell phone and someone said, “This is Tyler from Toyota. We saw the NBC interview. We wanted to let you know, don’t worry about getting a new vehicle. Just tell us what color 4Runner you want.”
My first thought was: Okay, this can’t be real. This doesn’t happen to people like me. But it turned out that it was, and they put me in a brand new vehicle.
Toyota started sending me to events like NASCAR races, putting me up in VIP suites. It was a cool experience. But it’s just surface stuff – it’s never going to erase what happened. The experience left a mark. It took me 6 months to a year to get rid of that feeling of the impact. Every time I tried to fall asleep, the whole scenario would replay in my head.
In EMS, we have a saying: “Every patient is practice for the next one.” That pileup – you can’t train for something like that. We all learned from it, so we can better prepare if anything like that happens again.
Since then, I’ve seen people die in motor vehicle collisions from a lot less than what happened to me. I’m not religious or spiritual, but I believe there must be a reason why I’m still here.
Now I see patients in traffic accidents who are very distraught even though they’re going to be okay. I tell them, “I’m sorry this happened to you. But remember, this is not the end. You are alive. And I’m going to do everything I can to make sure that doesn’t change while you’re with me.”
Trey McDaniel is a paramedic with MedStar Mobile Healthcare in Fort Worth, Tex.
A version of this article first appeared on Medscape.com.
It seemed like a typical kind of day. I was out the door by 6:00 a.m., heading into work for a shift on I-35 West, my daily commute. It was still dark out. A little bit colder that morning, but nothing us Texans aren’t used to.
I was cruising down the tollway, which is separated from the main highway by a barrier. That stretch has a slight hill and turns to the left. You can’t see anything beyond the hill when you’re at the bottom.
As I made my way up, I spotted brake lights about 400 yards ahead. I eased on my brake, and next thing I knew, I was sliding.
I realized, I’m on black ice.
I was driving a 2011 Toyota FJ Cruiser and I had it all beefed up – lift tires, winch bumpers front and back. I had never had any sort of issue like that.
My ABS brakes kicked in. I slowed, but not fast enough. I saw a wall of crashed cars in front of me.
I was in the left-hand lane, so I turned my steering wheel into the center median. I could hear the whole side of my vehicle scraping against it. I managed to slow down enough to just tap the vehicle in front of me.
I looked in my passenger side-view mirror and saw headlights coming in the right lane. But this car couldn’t slow down. It crashed into the wreckage to my right.
That’s when it sunk in: There was going to be a car coming in my lane, and it might not be able to stop.
I looked in my rear-view mirror and saw headlights. Sparks flying off that center median.
I didn’t know at the time, but it was a fully loaded semi-truck traveling about 60 miles an hour.
I had a split second to think: This is it. This is how it ends. I closed my eyes.
It was the most violent impact I’ve ever experienced in my life.
I had no idea until afterward, but I had slammed into the vehicle in front of me and my SUV did a kind of 360° barrel roll over the median into the northbound lanes, landing wheels down on top of my sheared off roof rack.
Everything stopped. I opened my eyes. All my airbags had deployed. I gently tried moving my arms and legs, and they worked. I couldn’t move my left foot. It was wedged underneath the brake pedal. But I wasn’t in any pain, just very confused and disoriented. I knew I needed to get out of the vehicle.
My door was wedged shut, so I crawled out of the broken window, slipping on the black ice. I realized I had hit a Fort Worth police cruiser, now all smashed up. The driver couldn’t open his door. So, I helped him force it open, got him out of the vehicle, and checked on him. He was fine.
I had no idea how many vehicles and people were involved. I was in so much shock that the only thing I could do was immediately revert back to my training. I was the only first responder there.
I was helping people with lacerations, back and neck issues from the violent impacts. When you’re involved in a mass casualty incident like that, you have to assess which patients will be the most viable and need the most immediate attention. You have greens, yellows, reds, and then blacks – the deceased. Someone who doesn’t have a pulse and isn’t breathing, you can’t necessarily do CPR because you don’t have enough resources. You have to use your best judgment.
Meanwhile, the crashes kept coming. I found out later I was roughly vehicle No. 50 in the pileup; 83 more would follow. I heard them over and over – a crash and then screams from people in their vehicles. Each time a car hit, the entire pileup would move a couple of inches, getting more and more compacted. With that going on, I couldn’t go in there to pull people out. That scene was absolutely unsafe.
It felt like forever, but about 10 minutes later, an ambulance showed up, and I walked over to them. Because I was in my work uniform, they thought I was there on a call.
A couple fire crews came, and a firefighter yelled, “Hey, we need a backboard!” So, I grabbed a backboard from their unit and helped load up a patient. Then I heard somebody screaming, “This patient needs a stretcher!” A woman was having lumbar pain that seemed excruciating. I helped move her from the wreckage and carry her over to the stretcher. I started trying to get as many people as I could out of their cars.
Around this time, one of my supervisors showed up. He thought I was there working. But then he asked me, “Why is your face bleeding? Why do you have blood coming from your nose?” I pointed to my vehicle, and his jaw just dropped. He said, “Okay, you’re done. Go sit in my vehicle over there.”
He put a stop to my helping out, which was probably for the best. Because I actually had a concussion, a bone contusion in my foot, and a severely sprained ankle. The next day, I felt like I had gotten hit by a truck. (I had!) But when you have so much adrenaline pumping, you don’t feel pain or emotion. You don’t really feel anything.
While I was sitting in that vehicle, I called my mom to let her know I was okay. My parents were watching the news, and there was an aerial view of the accident. It was massive – a giant pile of metal stretching 200 or 300 yards. Six people had perished, more than 60 were hurt.
That night, our public information officer reached out to me about doing an interview with NBC. So, I told my story about what happened. Because of the concussion, a lot of it was a blur.
A day later, I got a call on my cell phone and someone said, “This is Tyler from Toyota. We saw the NBC interview. We wanted to let you know, don’t worry about getting a new vehicle. Just tell us what color 4Runner you want.”
My first thought was: Okay, this can’t be real. This doesn’t happen to people like me. But it turned out that it was, and they put me in a brand new vehicle.
Toyota started sending me to events like NASCAR races, putting me up in VIP suites. It was a cool experience. But it’s just surface stuff – it’s never going to erase what happened. The experience left a mark. It took me 6 months to a year to get rid of that feeling of the impact. Every time I tried to fall asleep, the whole scenario would replay in my head.
In EMS, we have a saying: “Every patient is practice for the next one.” That pileup – you can’t train for something like that. We all learned from it, so we can better prepare if anything like that happens again.
Since then, I’ve seen people die in motor vehicle collisions from a lot less than what happened to me. I’m not religious or spiritual, but I believe there must be a reason why I’m still here.
Now I see patients in traffic accidents who are very distraught even though they’re going to be okay. I tell them, “I’m sorry this happened to you. But remember, this is not the end. You are alive. And I’m going to do everything I can to make sure that doesn’t change while you’re with me.”
Trey McDaniel is a paramedic with MedStar Mobile Healthcare in Fort Worth, Tex.
A version of this article first appeared on Medscape.com.
It seemed like a typical kind of day. I was out the door by 6:00 a.m., heading into work for a shift on I-35 West, my daily commute. It was still dark out. A little bit colder that morning, but nothing us Texans aren’t used to.
I was cruising down the tollway, which is separated from the main highway by a barrier. That stretch has a slight hill and turns to the left. You can’t see anything beyond the hill when you’re at the bottom.
As I made my way up, I spotted brake lights about 400 yards ahead. I eased on my brake, and next thing I knew, I was sliding.
I realized, I’m on black ice.
I was driving a 2011 Toyota FJ Cruiser and I had it all beefed up – lift tires, winch bumpers front and back. I had never had any sort of issue like that.
My ABS brakes kicked in. I slowed, but not fast enough. I saw a wall of crashed cars in front of me.
I was in the left-hand lane, so I turned my steering wheel into the center median. I could hear the whole side of my vehicle scraping against it. I managed to slow down enough to just tap the vehicle in front of me.
I looked in my passenger side-view mirror and saw headlights coming in the right lane. But this car couldn’t slow down. It crashed into the wreckage to my right.
That’s when it sunk in: There was going to be a car coming in my lane, and it might not be able to stop.
I looked in my rear-view mirror and saw headlights. Sparks flying off that center median.
I didn’t know at the time, but it was a fully loaded semi-truck traveling about 60 miles an hour.
I had a split second to think: This is it. This is how it ends. I closed my eyes.
It was the most violent impact I’ve ever experienced in my life.
I had no idea until afterward, but I had slammed into the vehicle in front of me and my SUV did a kind of 360° barrel roll over the median into the northbound lanes, landing wheels down on top of my sheared off roof rack.
Everything stopped. I opened my eyes. All my airbags had deployed. I gently tried moving my arms and legs, and they worked. I couldn’t move my left foot. It was wedged underneath the brake pedal. But I wasn’t in any pain, just very confused and disoriented. I knew I needed to get out of the vehicle.
My door was wedged shut, so I crawled out of the broken window, slipping on the black ice. I realized I had hit a Fort Worth police cruiser, now all smashed up. The driver couldn’t open his door. So, I helped him force it open, got him out of the vehicle, and checked on him. He was fine.
I had no idea how many vehicles and people were involved. I was in so much shock that the only thing I could do was immediately revert back to my training. I was the only first responder there.
I was helping people with lacerations, back and neck issues from the violent impacts. When you’re involved in a mass casualty incident like that, you have to assess which patients will be the most viable and need the most immediate attention. You have greens, yellows, reds, and then blacks – the deceased. Someone who doesn’t have a pulse and isn’t breathing, you can’t necessarily do CPR because you don’t have enough resources. You have to use your best judgment.
Meanwhile, the crashes kept coming. I found out later I was roughly vehicle No. 50 in the pileup; 83 more would follow. I heard them over and over – a crash and then screams from people in their vehicles. Each time a car hit, the entire pileup would move a couple of inches, getting more and more compacted. With that going on, I couldn’t go in there to pull people out. That scene was absolutely unsafe.
It felt like forever, but about 10 minutes later, an ambulance showed up, and I walked over to them. Because I was in my work uniform, they thought I was there on a call.
A couple fire crews came, and a firefighter yelled, “Hey, we need a backboard!” So, I grabbed a backboard from their unit and helped load up a patient. Then I heard somebody screaming, “This patient needs a stretcher!” A woman was having lumbar pain that seemed excruciating. I helped move her from the wreckage and carry her over to the stretcher. I started trying to get as many people as I could out of their cars.
Around this time, one of my supervisors showed up. He thought I was there working. But then he asked me, “Why is your face bleeding? Why do you have blood coming from your nose?” I pointed to my vehicle, and his jaw just dropped. He said, “Okay, you’re done. Go sit in my vehicle over there.”
He put a stop to my helping out, which was probably for the best. Because I actually had a concussion, a bone contusion in my foot, and a severely sprained ankle. The next day, I felt like I had gotten hit by a truck. (I had!) But when you have so much adrenaline pumping, you don’t feel pain or emotion. You don’t really feel anything.
While I was sitting in that vehicle, I called my mom to let her know I was okay. My parents were watching the news, and there was an aerial view of the accident. It was massive – a giant pile of metal stretching 200 or 300 yards. Six people had perished, more than 60 were hurt.
That night, our public information officer reached out to me about doing an interview with NBC. So, I told my story about what happened. Because of the concussion, a lot of it was a blur.
A day later, I got a call on my cell phone and someone said, “This is Tyler from Toyota. We saw the NBC interview. We wanted to let you know, don’t worry about getting a new vehicle. Just tell us what color 4Runner you want.”
My first thought was: Okay, this can’t be real. This doesn’t happen to people like me. But it turned out that it was, and they put me in a brand new vehicle.
Toyota started sending me to events like NASCAR races, putting me up in VIP suites. It was a cool experience. But it’s just surface stuff – it’s never going to erase what happened. The experience left a mark. It took me 6 months to a year to get rid of that feeling of the impact. Every time I tried to fall asleep, the whole scenario would replay in my head.
In EMS, we have a saying: “Every patient is practice for the next one.” That pileup – you can’t train for something like that. We all learned from it, so we can better prepare if anything like that happens again.
Since then, I’ve seen people die in motor vehicle collisions from a lot less than what happened to me. I’m not religious or spiritual, but I believe there must be a reason why I’m still here.
Now I see patients in traffic accidents who are very distraught even though they’re going to be okay. I tell them, “I’m sorry this happened to you. But remember, this is not the end. You are alive. And I’m going to do everything I can to make sure that doesn’t change while you’re with me.”
Trey McDaniel is a paramedic with MedStar Mobile Healthcare in Fort Worth, Tex.
A version of this article first appeared on Medscape.com.
Using Ozempic for ‘minor’ weight loss: Fair or foul?
Ashley Raibick is familiar with the weight loss yo-yo. She’s bounced through the big names: Weight Watchers, Jenny Craig, and so on. She drops 10 pounds and then slides off the plan only to see her weight pop back up.
But a day at her local med spa – where she gets facials, Botox, and fillers – changed all that for the 28-year-old hairstylist who just wanted to lose 18 pounds.
During one of her visits, she noticed that the spa’s owner was thinner. When Ms. Raibick asked her how she did it, the owner explained that she was on semaglutide and talked Ms. Raibick through the process. Ms. Raibick was convinced. That same day, she got a prescription from a doctor at the spa and got her first shot.
“Are people going to think I’m crazy for doing this?” she recalls thinking.
At 5 foot 4, her starting weight before the drug was 158, which would put her in the overweight, but not obese, category based on body mass index (BMI). And she really just wanted to get down to 140 and stop there.
Ozempic is part of an ever-growing group of GLP-1 receptor agonists that contain a peptide called semaglutide as its main ingredient. Although first meant to treat type 2 diabetes, the reputation of Ozempic and its siblings picked up when already-thin celebrities were suspected of using the injectable drugs to become even slimmer.
The FDA approved Ozempic’s cousin, Wegovy, for “weight management” in patients with obesity a few years ago, whereas Ozempic is currently approved only for diabetes treatment. Curious patients who don’t fit the criteria can – and do – get off-label prescriptions if they can afford to pay out of pocket, often to the tune of more than $1,400 a month.
For many – mainly those who have been on the drug for a couple of months and have lost weight as a result – taking Ozempic has not only helped them shed stubborn weight, but has also freed them from the constant internal chatter around eating, commonly called “food noise.” But experts do not all agree that semaglutide is the right path for those who aren’t technically obese – especially in the long term.
After her first 9 weeks on semaglutide, Ms. Raibick had already lost 18 pounds. That’s when she decided to post about it on TikTok, and her videos on GLP-1s were viewed hundreds of thousands of times.
For the time being, there is no data on how many semaglutide takers are using the drug for diabetes and/or obesity, and how many are using it off-label for weight loss alone. But the company that makes Ozempic, Novo Nordisk, has reported sharp increases in sales and projects more profits down the road.
Ms. Raibick knows of others like her, who sought out the drug for more minor weight loss but aren’t as candid about their journeys. Some feel a stigma about having to resort to a weight-loss drug intended to treat obesity, rather than achieving their goals with diet and lifestyle change alone.
Another reason for the secrecy is the guilt some who take Ozempic feel about using their financial privilege to get a drug that had serious shortages, which made it harder for some patients who need the drug for diabetes or obesity treatment to get their doses.
That’s what Diana Thiara, MD, the medical director of the University of California, San Francisco’s weight management program, has been seeing on the ground.
“It’s one of the most depressing things I’ve experienced as a physician,” she said. In her practice, she has seen patients who have finally been able to access GLP-1s and have started to lose weight, only for them to regain the weight in the time it takes to find another prescription under their insurance coverage.
“It’s just horrible, there are patients spending all day calling dozens of pharmacies. I’ve never had a situation like this in my career,” said Dr. Thiara.
Ann, 48, a mom who works from home full-time, has been taking Ozempic since the end of January. (Ann is not her real name; she asked that we use a pseudonym in order to feel comfortable speaking publicly about her use of Ozempic). Like Ms. Raibick, she has been paying out of pocket for her shots. At first, she was going to have to pay $1,400 a month, but she found a pharmacy in Canada that offers the medication for $350. It’s sourced globally, she said, so sometimes her Ozempic boxes will be in Czech or another foreign language.
Unlike a lot of women, Ann never had any qualms with her weight or the way her body looked. She was never big on exercise, but it wasn’t until the pandemic that she started to gain weight. She noticed the changes in her body once places started opening back up, and her clothes didn’t fit anymore.
She tried moving more and eating healthier. She tried former Real Housewives of Beverly Hills cast member Teddi Mellencamp’s controversial weight-loss program, infamous for its incredibly restrictive dietary plan and excessive cardio recommendations. Nothing worked until another mom at her daughter’s school mentioned that she was on Ozempic.
Ann also started to get hot flashes and missed periods. The doctor who prescribed her Ozempic confirmed that she was perimenopausal and that, for women in this stage of life, losing weight can be harder than ever.
Ann, who is 5 foot 7, started out at 176 pounds (considered overweight) and now weighs in at 151, which is considered a normal weight by BMI measurements. She’s still on Ozempic but continues to struggle with the shame around the idea she’s potentially taking the drug away from someone else who might desperately need it. And she doesn’t know how long she’ll have to stay on Ozempic to maintain her weight loss.
Ann has reason for concern. A 2022 study found that most people regain the weight they lost within a year of stopping Ozempic.
Once Ms. Raibick hit her initial goal weight, she felt that she could keep going and lose a little more. It wasn’t until she got into the 120-pound range that she decided it was time to wean off the dose of semaglutide she had been taking.
“I got to the point where my mom was like, ‘All right, you’re a little too thin.’ But I’m just so happy where I’m at. I’m not mentally stressed out about fitting into clothes or getting into a bathing suit,” said Ms. Raibick, who has now lost around 30 pounds in total since she started the shots.
At one point, she stopped taking the drug altogether, and all of the hunger cravings and food noise semaglutide had suppressed came back to the surface. She didn’t gain any weight that month, she said, but the internal chatter around food was enough to make her start back on a lower dose, geared toward weight maintenance.
There’s also the issue of side effects. Ms. Raibick says she never had the overwhelming nausea and digestive problems that so many on the drug – including Ann – have reported. But Dr. Thiara said that even beyond these more common side effects, there are a number of other concerns – like the long-lasting effects on thyroid and reproductive health, especially for women – that we still don’t know enough about. And just recently, CNN reported that some Ozempic users have developed stomach paralysis due to the drug’s ability to slow down the passage of food through the digestive tract.
For Ms. Raibick, the out-of-pocket cost for the drug is around $600 a month. It’s an expense she’s willing to keep paying for, even just for the peace of mind the drug provides. She doesn’t have any plans to stop her semaglutide shots soon.
“There is nothing stopping me from – a year from now, when I’ve put a little weight back on – looking back at photos from this time and thinking I was way too skinny.”
Dan Azagury, MD, a bariatric surgeon and associate professor of surgery at Stanford (Calif.) University, tries GLP-1s for patients with obesity before considering bariatric surgery. For his patient population, it’s possible that drugs like Ozempic will be part of their lifelong treatment plans.
“We’re not doing it for the cosmetic part of it, we’re doing it for health,” he said. “What I tell my patients is, if you’re planning to start on this medication, you should be OK with the idea of staying on it forever.”
For doctors like Dr. Thiara who specialize in weight management, using Ozempic long-term for patients in a healthy weight range is the wrong approach.
“It’s not about the way people look, it’s about health. If you’re a normal weight or even in an overweight category, but not showing signs of risk of having elevated cardiometabolic disease ... You don’t need to be taking medications for weight loss,” she said. “This idea of using medications for aesthetic reasons is really more related to societal ills around how we value fitness above anything else. That’s not the goal, and it’s not safe.”
A version of this article first appeared on WebMD.com.
Ashley Raibick is familiar with the weight loss yo-yo. She’s bounced through the big names: Weight Watchers, Jenny Craig, and so on. She drops 10 pounds and then slides off the plan only to see her weight pop back up.
But a day at her local med spa – where she gets facials, Botox, and fillers – changed all that for the 28-year-old hairstylist who just wanted to lose 18 pounds.
During one of her visits, she noticed that the spa’s owner was thinner. When Ms. Raibick asked her how she did it, the owner explained that she was on semaglutide and talked Ms. Raibick through the process. Ms. Raibick was convinced. That same day, she got a prescription from a doctor at the spa and got her first shot.
“Are people going to think I’m crazy for doing this?” she recalls thinking.
At 5 foot 4, her starting weight before the drug was 158, which would put her in the overweight, but not obese, category based on body mass index (BMI). And she really just wanted to get down to 140 and stop there.
Ozempic is part of an ever-growing group of GLP-1 receptor agonists that contain a peptide called semaglutide as its main ingredient. Although first meant to treat type 2 diabetes, the reputation of Ozempic and its siblings picked up when already-thin celebrities were suspected of using the injectable drugs to become even slimmer.
The FDA approved Ozempic’s cousin, Wegovy, for “weight management” in patients with obesity a few years ago, whereas Ozempic is currently approved only for diabetes treatment. Curious patients who don’t fit the criteria can – and do – get off-label prescriptions if they can afford to pay out of pocket, often to the tune of more than $1,400 a month.
For many – mainly those who have been on the drug for a couple of months and have lost weight as a result – taking Ozempic has not only helped them shed stubborn weight, but has also freed them from the constant internal chatter around eating, commonly called “food noise.” But experts do not all agree that semaglutide is the right path for those who aren’t technically obese – especially in the long term.
After her first 9 weeks on semaglutide, Ms. Raibick had already lost 18 pounds. That’s when she decided to post about it on TikTok, and her videos on GLP-1s were viewed hundreds of thousands of times.
For the time being, there is no data on how many semaglutide takers are using the drug for diabetes and/or obesity, and how many are using it off-label for weight loss alone. But the company that makes Ozempic, Novo Nordisk, has reported sharp increases in sales and projects more profits down the road.
Ms. Raibick knows of others like her, who sought out the drug for more minor weight loss but aren’t as candid about their journeys. Some feel a stigma about having to resort to a weight-loss drug intended to treat obesity, rather than achieving their goals with diet and lifestyle change alone.
Another reason for the secrecy is the guilt some who take Ozempic feel about using their financial privilege to get a drug that had serious shortages, which made it harder for some patients who need the drug for diabetes or obesity treatment to get their doses.
That’s what Diana Thiara, MD, the medical director of the University of California, San Francisco’s weight management program, has been seeing on the ground.
“It’s one of the most depressing things I’ve experienced as a physician,” she said. In her practice, she has seen patients who have finally been able to access GLP-1s and have started to lose weight, only for them to regain the weight in the time it takes to find another prescription under their insurance coverage.
“It’s just horrible, there are patients spending all day calling dozens of pharmacies. I’ve never had a situation like this in my career,” said Dr. Thiara.
Ann, 48, a mom who works from home full-time, has been taking Ozempic since the end of January. (Ann is not her real name; she asked that we use a pseudonym in order to feel comfortable speaking publicly about her use of Ozempic). Like Ms. Raibick, she has been paying out of pocket for her shots. At first, she was going to have to pay $1,400 a month, but she found a pharmacy in Canada that offers the medication for $350. It’s sourced globally, she said, so sometimes her Ozempic boxes will be in Czech or another foreign language.
Unlike a lot of women, Ann never had any qualms with her weight or the way her body looked. She was never big on exercise, but it wasn’t until the pandemic that she started to gain weight. She noticed the changes in her body once places started opening back up, and her clothes didn’t fit anymore.
She tried moving more and eating healthier. She tried former Real Housewives of Beverly Hills cast member Teddi Mellencamp’s controversial weight-loss program, infamous for its incredibly restrictive dietary plan and excessive cardio recommendations. Nothing worked until another mom at her daughter’s school mentioned that she was on Ozempic.
Ann also started to get hot flashes and missed periods. The doctor who prescribed her Ozempic confirmed that she was perimenopausal and that, for women in this stage of life, losing weight can be harder than ever.
Ann, who is 5 foot 7, started out at 176 pounds (considered overweight) and now weighs in at 151, which is considered a normal weight by BMI measurements. She’s still on Ozempic but continues to struggle with the shame around the idea she’s potentially taking the drug away from someone else who might desperately need it. And she doesn’t know how long she’ll have to stay on Ozempic to maintain her weight loss.
Ann has reason for concern. A 2022 study found that most people regain the weight they lost within a year of stopping Ozempic.
Once Ms. Raibick hit her initial goal weight, she felt that she could keep going and lose a little more. It wasn’t until she got into the 120-pound range that she decided it was time to wean off the dose of semaglutide she had been taking.
“I got to the point where my mom was like, ‘All right, you’re a little too thin.’ But I’m just so happy where I’m at. I’m not mentally stressed out about fitting into clothes or getting into a bathing suit,” said Ms. Raibick, who has now lost around 30 pounds in total since she started the shots.
At one point, she stopped taking the drug altogether, and all of the hunger cravings and food noise semaglutide had suppressed came back to the surface. She didn’t gain any weight that month, she said, but the internal chatter around food was enough to make her start back on a lower dose, geared toward weight maintenance.
There’s also the issue of side effects. Ms. Raibick says she never had the overwhelming nausea and digestive problems that so many on the drug – including Ann – have reported. But Dr. Thiara said that even beyond these more common side effects, there are a number of other concerns – like the long-lasting effects on thyroid and reproductive health, especially for women – that we still don’t know enough about. And just recently, CNN reported that some Ozempic users have developed stomach paralysis due to the drug’s ability to slow down the passage of food through the digestive tract.
For Ms. Raibick, the out-of-pocket cost for the drug is around $600 a month. It’s an expense she’s willing to keep paying for, even just for the peace of mind the drug provides. She doesn’t have any plans to stop her semaglutide shots soon.
“There is nothing stopping me from – a year from now, when I’ve put a little weight back on – looking back at photos from this time and thinking I was way too skinny.”
Dan Azagury, MD, a bariatric surgeon and associate professor of surgery at Stanford (Calif.) University, tries GLP-1s for patients with obesity before considering bariatric surgery. For his patient population, it’s possible that drugs like Ozempic will be part of their lifelong treatment plans.
“We’re not doing it for the cosmetic part of it, we’re doing it for health,” he said. “What I tell my patients is, if you’re planning to start on this medication, you should be OK with the idea of staying on it forever.”
For doctors like Dr. Thiara who specialize in weight management, using Ozempic long-term for patients in a healthy weight range is the wrong approach.
“It’s not about the way people look, it’s about health. If you’re a normal weight or even in an overweight category, but not showing signs of risk of having elevated cardiometabolic disease ... You don’t need to be taking medications for weight loss,” she said. “This idea of using medications for aesthetic reasons is really more related to societal ills around how we value fitness above anything else. That’s not the goal, and it’s not safe.”
A version of this article first appeared on WebMD.com.
Ashley Raibick is familiar with the weight loss yo-yo. She’s bounced through the big names: Weight Watchers, Jenny Craig, and so on. She drops 10 pounds and then slides off the plan only to see her weight pop back up.
But a day at her local med spa – where she gets facials, Botox, and fillers – changed all that for the 28-year-old hairstylist who just wanted to lose 18 pounds.
During one of her visits, she noticed that the spa’s owner was thinner. When Ms. Raibick asked her how she did it, the owner explained that she was on semaglutide and talked Ms. Raibick through the process. Ms. Raibick was convinced. That same day, she got a prescription from a doctor at the spa and got her first shot.
“Are people going to think I’m crazy for doing this?” she recalls thinking.
At 5 foot 4, her starting weight before the drug was 158, which would put her in the overweight, but not obese, category based on body mass index (BMI). And she really just wanted to get down to 140 and stop there.
Ozempic is part of an ever-growing group of GLP-1 receptor agonists that contain a peptide called semaglutide as its main ingredient. Although first meant to treat type 2 diabetes, the reputation of Ozempic and its siblings picked up when already-thin celebrities were suspected of using the injectable drugs to become even slimmer.
The FDA approved Ozempic’s cousin, Wegovy, for “weight management” in patients with obesity a few years ago, whereas Ozempic is currently approved only for diabetes treatment. Curious patients who don’t fit the criteria can – and do – get off-label prescriptions if they can afford to pay out of pocket, often to the tune of more than $1,400 a month.
For many – mainly those who have been on the drug for a couple of months and have lost weight as a result – taking Ozempic has not only helped them shed stubborn weight, but has also freed them from the constant internal chatter around eating, commonly called “food noise.” But experts do not all agree that semaglutide is the right path for those who aren’t technically obese – especially in the long term.
After her first 9 weeks on semaglutide, Ms. Raibick had already lost 18 pounds. That’s when she decided to post about it on TikTok, and her videos on GLP-1s were viewed hundreds of thousands of times.
For the time being, there is no data on how many semaglutide takers are using the drug for diabetes and/or obesity, and how many are using it off-label for weight loss alone. But the company that makes Ozempic, Novo Nordisk, has reported sharp increases in sales and projects more profits down the road.
Ms. Raibick knows of others like her, who sought out the drug for more minor weight loss but aren’t as candid about their journeys. Some feel a stigma about having to resort to a weight-loss drug intended to treat obesity, rather than achieving their goals with diet and lifestyle change alone.
Another reason for the secrecy is the guilt some who take Ozempic feel about using their financial privilege to get a drug that had serious shortages, which made it harder for some patients who need the drug for diabetes or obesity treatment to get their doses.
That’s what Diana Thiara, MD, the medical director of the University of California, San Francisco’s weight management program, has been seeing on the ground.
“It’s one of the most depressing things I’ve experienced as a physician,” she said. In her practice, she has seen patients who have finally been able to access GLP-1s and have started to lose weight, only for them to regain the weight in the time it takes to find another prescription under their insurance coverage.
“It’s just horrible, there are patients spending all day calling dozens of pharmacies. I’ve never had a situation like this in my career,” said Dr. Thiara.
Ann, 48, a mom who works from home full-time, has been taking Ozempic since the end of January. (Ann is not her real name; she asked that we use a pseudonym in order to feel comfortable speaking publicly about her use of Ozempic). Like Ms. Raibick, she has been paying out of pocket for her shots. At first, she was going to have to pay $1,400 a month, but she found a pharmacy in Canada that offers the medication for $350. It’s sourced globally, she said, so sometimes her Ozempic boxes will be in Czech or another foreign language.
Unlike a lot of women, Ann never had any qualms with her weight or the way her body looked. She was never big on exercise, but it wasn’t until the pandemic that she started to gain weight. She noticed the changes in her body once places started opening back up, and her clothes didn’t fit anymore.
She tried moving more and eating healthier. She tried former Real Housewives of Beverly Hills cast member Teddi Mellencamp’s controversial weight-loss program, infamous for its incredibly restrictive dietary plan and excessive cardio recommendations. Nothing worked until another mom at her daughter’s school mentioned that she was on Ozempic.
Ann also started to get hot flashes and missed periods. The doctor who prescribed her Ozempic confirmed that she was perimenopausal and that, for women in this stage of life, losing weight can be harder than ever.
Ann, who is 5 foot 7, started out at 176 pounds (considered overweight) and now weighs in at 151, which is considered a normal weight by BMI measurements. She’s still on Ozempic but continues to struggle with the shame around the idea she’s potentially taking the drug away from someone else who might desperately need it. And she doesn’t know how long she’ll have to stay on Ozempic to maintain her weight loss.
Ann has reason for concern. A 2022 study found that most people regain the weight they lost within a year of stopping Ozempic.
Once Ms. Raibick hit her initial goal weight, she felt that she could keep going and lose a little more. It wasn’t until she got into the 120-pound range that she decided it was time to wean off the dose of semaglutide she had been taking.
“I got to the point where my mom was like, ‘All right, you’re a little too thin.’ But I’m just so happy where I’m at. I’m not mentally stressed out about fitting into clothes or getting into a bathing suit,” said Ms. Raibick, who has now lost around 30 pounds in total since she started the shots.
At one point, she stopped taking the drug altogether, and all of the hunger cravings and food noise semaglutide had suppressed came back to the surface. She didn’t gain any weight that month, she said, but the internal chatter around food was enough to make her start back on a lower dose, geared toward weight maintenance.
There’s also the issue of side effects. Ms. Raibick says she never had the overwhelming nausea and digestive problems that so many on the drug – including Ann – have reported. But Dr. Thiara said that even beyond these more common side effects, there are a number of other concerns – like the long-lasting effects on thyroid and reproductive health, especially for women – that we still don’t know enough about. And just recently, CNN reported that some Ozempic users have developed stomach paralysis due to the drug’s ability to slow down the passage of food through the digestive tract.
For Ms. Raibick, the out-of-pocket cost for the drug is around $600 a month. It’s an expense she’s willing to keep paying for, even just for the peace of mind the drug provides. She doesn’t have any plans to stop her semaglutide shots soon.
“There is nothing stopping me from – a year from now, when I’ve put a little weight back on – looking back at photos from this time and thinking I was way too skinny.”
Dan Azagury, MD, a bariatric surgeon and associate professor of surgery at Stanford (Calif.) University, tries GLP-1s for patients with obesity before considering bariatric surgery. For his patient population, it’s possible that drugs like Ozempic will be part of their lifelong treatment plans.
“We’re not doing it for the cosmetic part of it, we’re doing it for health,” he said. “What I tell my patients is, if you’re planning to start on this medication, you should be OK with the idea of staying on it forever.”
For doctors like Dr. Thiara who specialize in weight management, using Ozempic long-term for patients in a healthy weight range is the wrong approach.
“It’s not about the way people look, it’s about health. If you’re a normal weight or even in an overweight category, but not showing signs of risk of having elevated cardiometabolic disease ... You don’t need to be taking medications for weight loss,” she said. “This idea of using medications for aesthetic reasons is really more related to societal ills around how we value fitness above anything else. That’s not the goal, and it’s not safe.”
A version of this article first appeared on WebMD.com.
New tech promises better blood oxygen readings on dark skin
A recent study adds weight to earlier findings that their device works.
“It is a new, first-in-class technology,” said Sanjay Gokhale, MD, the bioengineer who is leading this research at the University of Texas at Arlington. “The team conducted extensive preclinical work and carried out phase 1 studies in human volunteers, demonstrating sensitivity and accuracy.”
It’s one of several projects underway to update pulse oximetry, a technology based on research in lighter-skinned people that has not changed much in 50 years.
The pulse oximeter, or “pulse ox,” measures the saturation of oxygen in your hemoglobin (a protein in red blood cells). But it tends to overestimate the oxygen saturation in patients with darker skin by about 2%-3%. That may not sound like a lot, but it’s enough to delay major treatment for respiratory issues like COVID-19.
“Falsely elevated readings from commercial oximeters have delayed treatment of Black COVID-19 patients for hours in some cases,” said Divya Chander, MD, PhD, an anesthesiologist in Oakland, Calif., and chair of neuroscience at The Singularity Group. (Dr. Chander was not involved in the UT Arlington research.)
Early research happening separately at Brown University and Tufts University aims to redesign the pulse oximeter to get accurate readings in patients of all skin tones. University of California, San Diego, researchers are looking into a method that measures blood oxygen using sound in combination with light. Other solutions try to correct for skin tone with algorithms.
The device from UT Arlington uses an algorithm too, but its main innovation is that it replaces red light with green light.
Red light, green light
Traditional oximetry devices, which typically clip on to the patient’s fingertip, use LEDs to beam light through the skin at two wavelengths: one in the red part of the spectrum, the other in the infrared. The light transmits from one side of the clip to the other, passing through arterial blood as it pulses.
The device calculates a patient’s oxygenation based on how much light of each wavelength is absorbed by hemoglobin in the blood. Oxygenated hemoglobin absorbs the light differently than deoxygenated hemoglobin, so oxygenation can be represented as a percentage; 100% means all hemoglobin is completely oxygenated. But the melanin in skin can interfere with the absorption of light and affect the results.
The green light strategy measures not absorption but reflectance – how much of the light bounces back. As with traditional oximetry, the green-light method uses two wavelengths. Each is a different shade of green, and the two forms of hemoglobin reflect them differently.
Using an algorithm developed by the researchers, the device can capture readings in patients of all skin tones, the researchers say. And because it works on the wrist rather than a finger, the device also eliminates issues with cold fingers and dark nail polish – both known to reduce accuracy in traditional oximetry.
In the latest experiments, the researchers tested the technology on synthetic skin samples with varying amounts of melanin, Dr. Gokhale said. The device picked up changes in blood oxygen saturation even in samples with high melanin levels.
In a study published last year, the technology was tested in 16 people against an invasive handheld blood analyzer and a noninvasive commercial pulse oximeter, and found to be comparable to the invasive method.
A drawback
The green light approach could be “game changing,” Dr. Chander said. But there is a drawback.
Since green light doesn’t penetrate as deeply, this approach measures blood oxygen saturation in capillary beds (small blood vessels very close to the skin surface). By contrast, traditional oximetry measures oxygen saturation in an artery as it pulses – thus the name pulse oximetry.
Valuable information can be obtained from an arterial pulse.
Changes in arterial pulse, known as the waveforms, “can tell us about a patient’s hydration status [for instance],” Dr. Chander said. “In a mechanically ventilated patient, this variation with a patient’s respiratory cycle can give us feedback about how responsive the patient will be to fluid resuscitation if their blood pressure is too low.”
Given such considerations, the green light method may be useful as an adjunct, not a full replacement, to a standard pulse ox, Dr. Chander noted.
A version of this article appeared on WebMD.com.
A recent study adds weight to earlier findings that their device works.
“It is a new, first-in-class technology,” said Sanjay Gokhale, MD, the bioengineer who is leading this research at the University of Texas at Arlington. “The team conducted extensive preclinical work and carried out phase 1 studies in human volunteers, demonstrating sensitivity and accuracy.”
It’s one of several projects underway to update pulse oximetry, a technology based on research in lighter-skinned people that has not changed much in 50 years.
The pulse oximeter, or “pulse ox,” measures the saturation of oxygen in your hemoglobin (a protein in red blood cells). But it tends to overestimate the oxygen saturation in patients with darker skin by about 2%-3%. That may not sound like a lot, but it’s enough to delay major treatment for respiratory issues like COVID-19.
“Falsely elevated readings from commercial oximeters have delayed treatment of Black COVID-19 patients for hours in some cases,” said Divya Chander, MD, PhD, an anesthesiologist in Oakland, Calif., and chair of neuroscience at The Singularity Group. (Dr. Chander was not involved in the UT Arlington research.)
Early research happening separately at Brown University and Tufts University aims to redesign the pulse oximeter to get accurate readings in patients of all skin tones. University of California, San Diego, researchers are looking into a method that measures blood oxygen using sound in combination with light. Other solutions try to correct for skin tone with algorithms.
The device from UT Arlington uses an algorithm too, but its main innovation is that it replaces red light with green light.
Red light, green light
Traditional oximetry devices, which typically clip on to the patient’s fingertip, use LEDs to beam light through the skin at two wavelengths: one in the red part of the spectrum, the other in the infrared. The light transmits from one side of the clip to the other, passing through arterial blood as it pulses.
The device calculates a patient’s oxygenation based on how much light of each wavelength is absorbed by hemoglobin in the blood. Oxygenated hemoglobin absorbs the light differently than deoxygenated hemoglobin, so oxygenation can be represented as a percentage; 100% means all hemoglobin is completely oxygenated. But the melanin in skin can interfere with the absorption of light and affect the results.
The green light strategy measures not absorption but reflectance – how much of the light bounces back. As with traditional oximetry, the green-light method uses two wavelengths. Each is a different shade of green, and the two forms of hemoglobin reflect them differently.
Using an algorithm developed by the researchers, the device can capture readings in patients of all skin tones, the researchers say. And because it works on the wrist rather than a finger, the device also eliminates issues with cold fingers and dark nail polish – both known to reduce accuracy in traditional oximetry.
In the latest experiments, the researchers tested the technology on synthetic skin samples with varying amounts of melanin, Dr. Gokhale said. The device picked up changes in blood oxygen saturation even in samples with high melanin levels.
In a study published last year, the technology was tested in 16 people against an invasive handheld blood analyzer and a noninvasive commercial pulse oximeter, and found to be comparable to the invasive method.
A drawback
The green light approach could be “game changing,” Dr. Chander said. But there is a drawback.
Since green light doesn’t penetrate as deeply, this approach measures blood oxygen saturation in capillary beds (small blood vessels very close to the skin surface). By contrast, traditional oximetry measures oxygen saturation in an artery as it pulses – thus the name pulse oximetry.
Valuable information can be obtained from an arterial pulse.
Changes in arterial pulse, known as the waveforms, “can tell us about a patient’s hydration status [for instance],” Dr. Chander said. “In a mechanically ventilated patient, this variation with a patient’s respiratory cycle can give us feedback about how responsive the patient will be to fluid resuscitation if their blood pressure is too low.”
Given such considerations, the green light method may be useful as an adjunct, not a full replacement, to a standard pulse ox, Dr. Chander noted.
A version of this article appeared on WebMD.com.
A recent study adds weight to earlier findings that their device works.
“It is a new, first-in-class technology,” said Sanjay Gokhale, MD, the bioengineer who is leading this research at the University of Texas at Arlington. “The team conducted extensive preclinical work and carried out phase 1 studies in human volunteers, demonstrating sensitivity and accuracy.”
It’s one of several projects underway to update pulse oximetry, a technology based on research in lighter-skinned people that has not changed much in 50 years.
The pulse oximeter, or “pulse ox,” measures the saturation of oxygen in your hemoglobin (a protein in red blood cells). But it tends to overestimate the oxygen saturation in patients with darker skin by about 2%-3%. That may not sound like a lot, but it’s enough to delay major treatment for respiratory issues like COVID-19.
“Falsely elevated readings from commercial oximeters have delayed treatment of Black COVID-19 patients for hours in some cases,” said Divya Chander, MD, PhD, an anesthesiologist in Oakland, Calif., and chair of neuroscience at The Singularity Group. (Dr. Chander was not involved in the UT Arlington research.)
Early research happening separately at Brown University and Tufts University aims to redesign the pulse oximeter to get accurate readings in patients of all skin tones. University of California, San Diego, researchers are looking into a method that measures blood oxygen using sound in combination with light. Other solutions try to correct for skin tone with algorithms.
The device from UT Arlington uses an algorithm too, but its main innovation is that it replaces red light with green light.
Red light, green light
Traditional oximetry devices, which typically clip on to the patient’s fingertip, use LEDs to beam light through the skin at two wavelengths: one in the red part of the spectrum, the other in the infrared. The light transmits from one side of the clip to the other, passing through arterial blood as it pulses.
The device calculates a patient’s oxygenation based on how much light of each wavelength is absorbed by hemoglobin in the blood. Oxygenated hemoglobin absorbs the light differently than deoxygenated hemoglobin, so oxygenation can be represented as a percentage; 100% means all hemoglobin is completely oxygenated. But the melanin in skin can interfere with the absorption of light and affect the results.
The green light strategy measures not absorption but reflectance – how much of the light bounces back. As with traditional oximetry, the green-light method uses two wavelengths. Each is a different shade of green, and the two forms of hemoglobin reflect them differently.
Using an algorithm developed by the researchers, the device can capture readings in patients of all skin tones, the researchers say. And because it works on the wrist rather than a finger, the device also eliminates issues with cold fingers and dark nail polish – both known to reduce accuracy in traditional oximetry.
In the latest experiments, the researchers tested the technology on synthetic skin samples with varying amounts of melanin, Dr. Gokhale said. The device picked up changes in blood oxygen saturation even in samples with high melanin levels.
In a study published last year, the technology was tested in 16 people against an invasive handheld blood analyzer and a noninvasive commercial pulse oximeter, and found to be comparable to the invasive method.
A drawback
The green light approach could be “game changing,” Dr. Chander said. But there is a drawback.
Since green light doesn’t penetrate as deeply, this approach measures blood oxygen saturation in capillary beds (small blood vessels very close to the skin surface). By contrast, traditional oximetry measures oxygen saturation in an artery as it pulses – thus the name pulse oximetry.
Valuable information can be obtained from an arterial pulse.
Changes in arterial pulse, known as the waveforms, “can tell us about a patient’s hydration status [for instance],” Dr. Chander said. “In a mechanically ventilated patient, this variation with a patient’s respiratory cycle can give us feedback about how responsive the patient will be to fluid resuscitation if their blood pressure is too low.”
Given such considerations, the green light method may be useful as an adjunct, not a full replacement, to a standard pulse ox, Dr. Chander noted.
A version of this article appeared on WebMD.com.
Long COVID disability court battles just ‘tip of iceberg’
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.
At least 30 lawsuits have been filed seeking legal resolution of disability insurance claims, according to searches of court records. In addition, the Social Security Administration said it has received about 52,000 disability claims tied to SARS-CoV-2 infections, which represents 1% of all applications.
But legal experts say those cases may not reflect the total number of cases that have gone to court. They note many claims are initially dismissed and are not appealed by claimants.
“With this system, they deny two-thirds of initial applications, then people who appeal get denied almost 90% of the time, and then they can appeal before a judge,” said Kevin LaPorte, a Social Security disability attorney at LaPorte Law Firm in Oakland, Calif. “What happens next doesn’t have a lot of precedent because long COVID is a mass disabling event, and we haven’t seen that many of these cases get all the way through the legal system yet.”
As a result, the exact number of long COVID disability claims and the number of these cases going to court isn’t clear, he said.
“It can take a year or more for cases to get to court, and even longer to reach resolution,” Mr. LaPorte added. “I suspect the few cases we’ve heard about at this point are going to be the tip of the iceberg.”
The process is convoluted and can drag on for months with multiple denials and appeals along the way. Many disabled workers find their only recourse is to take insurers to court.
Long COVID patients typically apply for disability benefits through private insurance or Social Security. But the process can drag on for months, so many find their only recourse is to take insurers to court, according to legal experts.
But even in the courts, many encounter delays and hurdles to resolution.
In one of the first federal lawsuits involving long COVID disability benefits, William Abrams, a trial and appellate attorney and active marathon runner, sued Unum Life Insurance seeking long-term disability income. Symptoms included extreme fatigue, brain fog, decreased attention and concentration, and nearly daily fevers, causing him to stop working in April 2020.
His diagnosis wasn’t definitive. Three doctors said he had long COVID, and four said he had chronic fatigue syndrome. Unum cited this inconsistency as a rationale for rejecting his claim. But the court sided with Mr. Abrams, granting him disability income. The court concluded: “Unum may be correct that [the plaintiff] has not been correctly diagnosed. But that does not mean he is not sick. If [the plaintiff’s] complaints, and [the doctor’s] assessments, are to be believed, [the plaintiff] cannot focus for more than a few minutes at a time, making it impossible for [the plaintiff] to perform the varied and complex tasks his job requires.”
Unum said in an emailed statement that the company doesn’t comment on specific claims as a matter of policy, adding that its total payouts for disability claims from March 2020 to February 2022 were 35% higher than prepandemic levels. “In general, disability and leave claims connected to COVID-19 have been primarily short-term events with the majority of claimants recovering prior to completing the normal qualification period for long-term disability insurance,” Unum said.
Mr. Abrams prevailed in part because he had detailed documentation of the numerous impairments that eventually required him to stop work, said Michelle Roberts of Roberts Disability Law in Oakland, Calif.
He submitted videos of himself taking his temperature to prove he had almost daily fevers, according to court records. He underwent neuropsychological testing, which found learning deficiencies and memory deficits.
Mr. Abrams also submitted statements from a colleague who worked with him on a complex technology patent case involving radiofrequency identification. Before he got COVID, Mr. Abrams “had the analytical ability, legal acumen, and mental energy to attack that learning curve and get up to speed very rapidly,” according to court records.
“The court focused on credulity.” Ms. Roberts said. “There was all this work to be done to show this person was high functioning and ran marathons and worked in an intense, high-pressure occupation but then couldn’t do anything after long COVID.”
Documentation was also crucial in another early federal long COVID disability lawsuit that was filed in 2022 on behalf of Wendy Haut, an educational software sales representative in California who turned to the courts seeking disability income through her company’s employee benefits plan.
Several of Ms. Haut’s doctors documented a detailed list of long COVID symptoms, including “profound fatigue and extreme cognitive difficulties,” that they said prevented her from working as a sales representative or doing any other type of job. A settlement agreement in June 2022 required Reliance Standard Life Insurance to pay Ms. Haut long-term disability benefits, including previously unpaid benefits, according to a report by the advocacy group Pandemic Patients.
Representatives of Reliance Standard didn’t respond to a request for comment.
The growing number of workers being sidelined by long COVID makes more claims and more court cases likely. Right now, an estimated 16 million working-age Americans aged 18-65 years have long COVID, and as many as 4 million of them can’t work, according to a July 2023 Census Bureau report.
Uncertainty about the volume of claims in the pipeline is part of what’s driving some insurers to fight long COVID claims, Ms. Roberts said. Another factor is the lack of clarity around how many years people with long COVID may be out of work, particularly if they’re in their 30s or 40s and might be seeking disability income until they reach retirement age.
“Doctors are not always saying that this person will be permanently disabled,” Ms. Roberts said. “If this person doesn’t get better and they’re disabled until retirement age, this could be a payout in the high six or seven figures if a person is very young and was a very high earner.”
Insurance companies routinely deny claims that can’t be backed up with objective measures, such as specific lab test results or clear findings from a physical exam. But there are steps that can increase the odds of a successful claim for long COVID disability benefits, according to New York–based law firm Hiller.
For starters, patients can document COVID test results, and if testing wasn’t conducted, patients can detail the specific symptoms that led to this diagnosis, Hiller advises. Then patients can keep a daily symptom log at home that run lists all of the specific symptoms that occur at different times during the day and night to help establish a pattern of disability. These logs should provide specific details about every job duty patients have and exactly how specific symptoms of long COVID interfere with these duties.
Even though objective testing is hard to come by for long COVID, people should undergo all the tests they can that may help document the frequency or severity of specific symptoms that make it impossible to carry on with business as usual at work, Hiller advises. This may include neuropsychological testing to document brain fog, a cardiopulmonary exercise test to demonstrate chronic fatigue and the inability to exercise, or a tilt table test to measure dizziness.
Seeking a doctor’s diagnosis can be key to collecting disability payments, in or out of court.
All of this puts a lot of pressure on doctors and patients to build strong cases, said Jonathan Whiteson, MD, codirector of the NYU Langone Health post-COVID care program in New York. “Many physicians are not familiar with the disability benefit paperwork, and so this is a challenge for the doctors to know how to complete and to build the time into their highly scheduled days to take the time needed to complete.
“It’s also challenging because most of the disability benefit forms are ‘generic’ and do not ask specific questions about COVID disability,” Dr. Whiteson added. “It can be like trying to drive a square peg into a round hole.”
Still, when it comes to long COVID, completing disability paperwork is increasingly becoming part of standard care, along with managing medication, rehabilitation therapies, and lifestyle changes to navigate daily life with this illness, Dr. Whiteson noted.
Monica Verduzco-Gutierrez, MD, chair of rehabilitation medicine and director of the Post-COVID-19 Recovery Clinic at the University of Texas Health Science Center, San Antonio, agreed with this assessment.
“I have done letter upon letter of appeal to disability insurance companies,” she said.
Some doctors, however, are reluctant to step up in such cases, in part because no standard diagnostic guidelines exist for long COVID and because it can be frustrating.
“This is the work that is not paid and causes burnout in physicians,” Dr. Verduzco-Gutierrez said. “The paperwork, the fighting with insurance companies, the resubmission of forms for disability all to get what your patient needs – and then it gets denied.
“We will keep doing this because our patients need this disability income in order to live their lives and to afford what they need for recovery,” said Dr. Verduzco-Gutierrez. “But at some point something has to change because this isn’t sustainable.”
A version of this article appeared on Medscape.com.