User login
Calcipotriene–Betamethasone Dipropionate Topical Suspension in the Management of Psoriasis: A Status Report on Available Data With an Overview of Practical Clinical Application
Psoriasis is a common inflammatory skin disorder that appears to be induced by multifactorial pathophysiologic processes associated with immunologic dysregulation.1 It can affect patients of any age, gender, and ethnicity, and it presents clinically with a variety of visible manifestations. The disease course and severity of psoriasis varies among affected patients.1 Chronic plaque psoriasis (PP), also referred to as psoriasis vulgaris, is the most common clinical presentation.1,2 Although many patients are affected by psoriasis that is widespread and in some cases severe, the majority of affected patients exhibit localized involvement that usually affects less than 2% to 5% of the body surface area. Although the skin at any anatomic location can be affected, commonly involved sites are described by the mnemonic term SNAKES (scalp, nails, anogenital region, knees, elbows, sacral region).2,3
Because the majority of patients with PP present with localized disease, topical therapy is the foundation of treatment in most cases. Topical corticosteroids (TCs) are the most commonly utilized agents, supported by a long track record of favorable efficacy and safety over approximately 6 decades.4,5 However, optimal management of PP with TCs requires use of a formulation that is of adequate potency, is adaptable for application to the affected body sites, and is properly monitored and adjusted to avoid potential TC-induced adverse effects.4-6 Nonsteroidal topical therapies such as vitamin D analogues (eg, calcipotriene) and retinoids (eg, tazarotene) are commonly integrated into topical regimens to reduce the application frequency and duration of TC use as well as to sustain efficacy.5,7,8 Plaque psoriasis is characteristically a chronic disease associated with periods of persistence and episodes of flaring; therefore, intermittent use of TC therapy along with concurrent or sequential use of a nonsteroidal topical agent are commonly employed to achieve and sustain control of the disorder.7-9
In the last decade, several advances have revolutionized the management of psoriasis, especially for PP patients with extensive involvement who require systemic therapy and/or phototherapy as well as for those with psoriatic arthritis.10,11 The availability of biologic agents such as tumor necrosis factor a inhibitors and certain interleukin inhibitors (eg, IL-12/IL-23) have been at the forefront of major advances in PP treatment, with some agents also blocking the progression of joint destruction associated with psoriatic arthritis.10-12 However, even when patients with PP respond favorably to biologic therapy, it is not uncommon for them to still be affected by some persistent PP. In these cases, although much of the chronic PP may clear with use of the biologic agent, persistence of psoriatic plaques may involve the lower extremities, scalp, and/or trunk, with topical therapy often added to augment the therapeutic response.13-15
This article provides a review of a patented topical suspension combination formulation that contains calcipotriene hydrate 0.005%, a vitamin D analogue, and betamethasone dipropio-nate (Bd) 0.064%, a high-potency TC. In 2008, the US Food and Drug Administration approved the once-daily application of calcipotriene 0.005%–Bd 0.064% topical suspension (C/Bd-TS) for the treatment of PP; this formulation is approved for use on the scalp and body in patients 18 years of age and older. According to the product insert, the recommended maximum duration of treatment with C/Bd-TS once daily is 8 weeks, and patients may not exceed a maximum weekly dose of 100 g.16 It is important to note that the terms calcipotriene and calcipotriol refer to the same molecule and are used interchangeably in the literature. Formulation characteristics of C/Bd-TS, perspectives on modes of action, outcomes from pivotal trials, and efficacy and safety data reported from additional studies are discussed in this article.
What are the formulation characteristics of C/Bd-TS?
Each gram of C/Bd-TS contains 52.18 mg of calcipotriene hydrate (equivalent to 50 µg of calcipotriene) and 0.643 µg of Bd (equivalent to 0.5 mg of betamethasone), formulated together in a viscous, nearly odorless, almost clear to slightly off-white suspension. The excipients are hydrogenated castor oil, polypropylene glycol 11 stearyl ether, α-tocopherol, butylhydroxytoluene, and mineral oil, collectively producing a gel base in which both active ingredients are suspended.16 Although the viscous quality of the suspension warrants some additional effort for removal during hair washing, the tenacious gel-like viscosity assists in removing scale on psoriatic plaques, which is often adherent, especially on the scalp. Additionally, it is important that C/Bd-TS be shaken well before use.16 Initially, C/Bd-TS was studied and marketed in the United States for treatment of scalp psoriasis; however, the indication was expanded to include treatment of PP on the rest of the body, supported by evidence from randomized controlled trials (RCTs).16-23
Vitamin D analogues (eg, calcipotriene/calcitriol) have been shown to be photolabile when exposed to UV light, especially UVA. They also have been shown to be chemically incompatible and less stable when admixed with a variety of other active ingredients and/or vehicles used to treat PP, including hydrocortisone valerate ointment 0.2%, ammonium lactate lotion 12%, and salicylic acid compound ointment 6%.24-26 As a result, it is important for clinicians to consider avoidance of concomitant topical calcipotriene application with use of a TC unless the stability of the active ingredients has been tested when the formulations are combined. Calcipotriene 0.005%/Bd 0.064% topical suspension utilizes vehicle technology that maintains the stability and activity of both calcipotriene and Bd within the suspension formulation.16,26
What is the rationale behind combining calcipotriene and Bd in a single formulation for the treatment of PP?
The potential advantages of C/Bd-TS include the combined modes of action of 2 different active ingredients used for treatment of PP, complementary immunomodulatory effects as compared to use of a TC or vitamin D analogue alone, ease of use with a single product applied once daily, adaptability of the vehicle for use on scalp and/or body skin, and improvement in quality-of-life (QOL) measures.27-34
Combined Modes of Action
Calcipotriene 0.005%–Bd 0.064% topical suspension combines the modes of action of a high-potency topical suspension and a vitamin D analogue for the treatment of PP in a single stable gel formulation that is approved in the United States for treatment of PP in adults.16 The multiple anti-inflammatory properties of corticosteroids as well as the efficacy and safety of TC therapy for psoriasis have been well described.4,6,7,9,27 The antiproliferative and anti-inflammatory properties of vitamin D analogues that appear to correlate with therapeutic effects in the treatment of PP also have been discussed in the literature.28
Complementary Immunomodulatory Effects
More recent studies using various research assays have provided further evidence supporting relevant immunomodulatory properties of calcipotriene alone and in combination with Bd that favorably modify immune dysregulation pathways described more recently in the pathogenesis of PP.1,29,30 Treatment of psoriatic plaques with calcipotriene has been shown to suppress the increased production of peptide alarmins (psoriasin and koebnerisin) in psoriatic skin and their TH17-mediated regulation in epidermal ke-ratinocytes, thus interfering with the S100 amplification loop that appears to produce inflammation in psoriasis.29 In T-lymphocyte cultures evaluating exposure to calcipotriene and Bd both alone and as a combined therapy, calcipotriene inhibited IFN-g, IL-8, IL-17, and IL-22 expression, and it reversed the corticosteroid-induced suppression of IL-4, IL-5, IL-10, and IL-13; Bd inhibited both IL-6 and tumor necrosis factor α expression. The outcomes demonstrated that the combination of calcipotriene and Bd inhibited the endogenous release of TH1- and TH17-associated cytokines that are associated with psoriatic inflammation and together induced a more favorable anti-inflammatory cytokine profile.30 Although the broad range of anti-inflammatory effects provided by a TC of adequate potency, such as Bd, can clear or markedly improve PP, the concurrent use of calcipotriene was shown to provide additional immunomodulatory effects that suppressed the key TH17/TH1 pathophysiologic mediators of psoriatic inflammation and simultaneously induced a TH2/T regulatory response that is believed to provide therapeutic benefit.29,30
Ease of Use and Vehicle Adaptability
A once-daily regimen and a vehicle formulation adaptable for use on both the scalp and body are advantageous in enhancing the potential for greater patient adherence.31,32 The adaptability of the C/Bd-TS for use on the scalp and/or body is supported by several studies encompassing a large number of actively treated subjects. Calcipotriene 0.005%–Bd 0.064% topical suspension has been extensively studied in patients with PP on the scalp and/or body as evidenced by a pooled analysis of 9 eight-week RCTs (scalp, n=6; body, n=3) that encompassed 2777 total subjects treated once daily for PP (scalp, n=1953; body, n=824).23 Additionally, C/Bd-TS applied once daily was evaluated in an open-label, single-arm, 8-week, phase 2 study of adolescents (N=78; age range, 12–17 years [mean age, 14.6 years]) with scalp psoriasis (mean affected scalp area, 43.7%). The investigator global assessment of treatment success (clear or almost clear) and the patient global assessment of treatment success (clear or very mild) were essentially identical among participants and investigators with 85% and 87% reported after 8 weeks, respectively; approximately 50% of participants achieved treatment success after 2 weeks based on both the investigator global assessment and patient global assessment.33
Improvement in QOL Measures
Quality-of-life measures were compared in an 8-week RCT of participants with at least moderate scalp psoriasis treated with C/Bd-TS once daily (n=207) or calcipotriene solution twice daily (n=107). Significantly greater improvement in QOL scores compared to baseline were noted at all time points using the Skindex-16 questionnaire in participants treated with C/Bd-TS compared to calcipotriene solution (total score, P<.001 at weeks 2 and 4 and P=.008 at week 8; symptoms score, P<.001 at weeks 2 and 4 and P=.004 at week 8; emotions score, P<.001 at weeks 2 and 4 and P=.005 at week 8).34 A 4-week, open-label, noninterventional cohort, postmarketing (“real life”) study of 721 patients treated at 333 dermatology centers with C/Bd-TS showed a 69.5% improvement in the scalp life quality index score compared to baseline (P<.0001), with 89.5% and 90.4% of participants reporting that C/Bd-TS was better/much better than previously used therapies for scalp psoriasis and easy/very easy to use, respectively.35 An 8-week RCT trial evaluated C/Bd-TS once daily compared to calcipotriene alone, betamethasone dipropionate alone, and vehicle in 1152 participants with mild to moderate PP involving the trunk and extremities. Participants treated with C/Bd-TS (n=442) demonstrated superior reductions in QOL scores using the dermatology life quality index at weeks 4 and 8 compared to those treated with Bd alone (n=418) or vehicle (n=77) but not compared to calcipotriene alone (n=80).19
What data are available on the efficacy and safety of C/Bd-TS?
Several clinical studies have evaluated the efficacy, tolerability, and safety of C/Bd-TS applied once daily for PP of the scalp and body (ie, trunk, extremities). Most studies were completed over a duration of 8 weeks in adults16-23; however, studies also have been performed in adolescents,33 in adults treated for up to 52 weeks,36 and in a subgroup of Hispanic/Latino and black/African American patients with scalp psoriasis.37 The Table provides a detailed summary of primary efficacy data along with important tolerability and safety considerations based on study outcomes.
What practical recommendations can be made regarding the use of C/Bd-TS for PP?
Calcipotriene 0.005%–Bd 0.064% topical suspension applied once daily provides a formulation that allows for treatment of PP involving both the scalp and body using a single product, which provides an element of convenience and is likely to enhance compliance and reduce costs compared with the use of 2 separate products. The efficacy and safety of C/Bd-TS has been well established in several studies,16-23,37 including a 52-week trial in patients with scalp psoriasis.36 The combination of calcipotriene and Bd appears to favorably address the pathophysiologic pathways involved in psoriasis.29,30 Calcipotriene 0.005%–Bd 0.064% topical suspension is a rational option for the treatment of PP in patients with localized disease or in patients treated systemically or with phototherapy for more extensive disease who exhibit persistence or recurrence of scattered areas of PP.6-9,14,15 Appropriate use of C/Bd-TS is likely to achieve favorable efficacy with a low risk of tolerability reactions and a very low risk of major adverse drug reactions.16-23,36-38
1. Guttman-Yassky E, Krueger JG. Psoriasis: evolution of pathogenic concepts and new therapies through phases of translational research. Br J Dermatol. 2007;157:1103-1115.
2. Menter MA. An overview of psoriasis. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:1-21.
3. Sandoval LF, Feldman SR. General approach to psoriasis treatment. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:3-8.
4. Zeichner JA, Lebwohl MG, Menter A, et al. Optimizing topical therapies for treating psoriasis: a consensus conference. Cutis. 2010;(3 suppl):5-31.
5. American Academy of Dermatology Work Group, Menter A, Korman NJ, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions [published online ahead of print February 8, 2011]. J Am Acad Dermatol. 2011;65:137-174.
6. Del Rosso J, Friedlander SF. Corticosteroids: options in the era of steroid-sparing therapy. J Am Acad Dermatol. 2005;53(1, suppl 1):S50-S58.
7. Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies [published online ahead of print February 13, 2009]. J Am Acad Dermatol. 2009;60:643-659.
8. Koo J. New developments in topical sequential therapy for psoriasis. Skin Therapy Lett. 2005;10:1-4.
9. Mason AR, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis. Cochrane Database Syst Rev. 2009;2:CD005028.
10. Belge K, Brück J, Ghoreschi K. Advances in treating psoriasis. F1000Prime Rep. 2014;6:4.
11. Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-441.
12. Boehncke WH, Qureshi A, Merola JF, et al. Diagnosing and treating psoriatic arthritis: an update. Br J Dermatol. 2014;170:772-786.
13. Feldman SR. Effectiveness of clobetasol propionate spray 0.05% added to other stable treatments: add-on therapy in the COBRA trial. Cutis. 2007;80(suppl 5):20-28.
14. Feldman SR, Gelfand JM, Stein Gold L, et al. The role of topical therapy for patients with extensive psoriasis. Cutis. 2007;79(suppl 1[ii]):18-31.
15. Kircik L. Topical calcipotriene 0.005% and betamethasone dipropionate 0.064% maintains efficacy of etanercept after step-down dose in patients with moderate-to-severe plaque psoriasis: results of an open label trial. J Drugs Dermatol. 2011;10:878-882.
16. Taclonex [product insert]. Parsippany, NJ: LEO Pharma Inc; 2014.
17. Buckley C, Hoffmann V, Shapiro J, et al. Calcipotriol plus betamethasone dipropionate scalp formulation is effective and well tolerated in the treatment of scalp psoriasis: a phase II study. Dermatology. 2008;217:107-113.
18. Fleming C, Ganslandt C, Guenther L, et al. Calcipotriol plus betamethasone dipropionate gel compared with its active components in the same vehicle and the vehicle alone in the treatment of psoriasis vulgaris: a randomized, parallel group, double-blind, exploratory study. Eur J Dermatol. 2010;20:465-471.
19. Menter A, Stein Gold L, Bukhalo M, et al. Calcipotriene plus betamethasone dipropionate topical suspension for the treatment of mild to moderate psoriasis vulgaris on the body: a randomized, double-blind, vehicle-controlled trial. J Drugs Dermatol. 2013;12:92-98.
20. Jemec GBE, Ganslandt C, Ortonne JP, et al. A new scalp formulation of calcipotriene plus betamethasone compared with its active ingredients and the vehicle in the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. J Am Acad Dermatol. 2008;59:455-463.
21. van de Kerkhof PC, Hoffmann V, Anstey A, et al. A new scalp formulation of calcipotriol plus betamethasone dipropionate compared with each of its active ingredients in the same vehicle for the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. Br J Dermatol. 2009;160:170-176.
22. Langley RG, Gupta A, Papp K, et al. Calcipotriol plus betamethasone dipropionate gel compared with tacalcitol ointment and the gel vehicle alone in patients with psoriasis vulgaris: a randomized, controlled clinical trial. Dermatology. 2011;222:148-156.
23. Kragballe K, van de Kerkhof P. Pooled safety analysis of calcipotriol plus betamethasone dipropionate gel for the treatment of psoriasis on the body and scalp. J Eur Acad Dermatol Venereol. 2014;28:10-21.
24. Lebwohl MG, Corvari L. Compatibility of topical therapies for psoriasis: challenges and innovations. Cutis. 2007;79(suppl 1[ii]):5-10.
25. Patel B, Siskin S, Krazmien R, et al. Compatibility of calcipotriene with other topical medications. J Am Acad Dermatol. 1998;38(6, pt 1):1010-1011.
26. Traulsen J. Bioavailability of betamethasone dipropionate when combined with calcipotriol. Int J Dermatol. 2004;43:611-617.
27. Sandoval LF, Feldman SR. Topical corticosteroids. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:21-36.
28. deShazo R, Krueger GG, Duffin KC. Topical agents. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:41-65.
29. Hegyi Z, Zwicker S, Bureik D, et al. Vitamin D analog calcipotriol suppresses the Th17 cytokine-induced proinflammatory S100 “alarmins” psoriasin (S100A7) and koebnerisin (S100A15) in psoriasis. J Invest Dermatol. 2012;132:1416-1424.
30. Lovato P, Norsgaard H, Ropke M. Key immunomodulatory effects exerted by calcipotriol in combination with corticosteroid on human cells. Poster presented at: 21st European Academy of Dermatology and Venereology Congress; September 27-30, 2012; Prague, Czech Republic.
31. Renton C. Diagnosis and treatment of adults with scalp psoriasis. Nurs Stand. 2014;28:35-39.
32. Feldman SR, Housman TS. Patients’ vehicle preference for corticosteroid treatments of scalp psoriasis. Am J Clin Dermatol. 2003;4:221-224.
33. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriene plus betamethasone dipropionate topical suspension in adolescents with scalp psoriasis: an open, non-controlled, 8-week trial. Poster presented at: American Academy of Dermatology 72nd Annual Meeting; March 21-25, 2014; Denver, CO.
34. Ortonne JP, Tan J, Nordin P, et al. Quality of life of patients with scalp psoriasis treated with calcipotriene plus betamethasone dipropionate gel compared to calcipotriene solution. J Am Academy Dermatol. 2008;58(2, suppl 2):AB134.
35. Mrowietz U, Macheleidt O, Eicke C. Effective treatment and improvement of quality of life in patients with scalp psoriasis by topical use of calcipotriol/betamethasone (Xamiol®-gel): results [in German]. J Dtsch Dermatol Ges. 2011;9:825-831.
36. Luger TA, Cambazard F, Larsen FG, et al. A study of the safety and efficacy of calcipotriol and betamethasone dipropionate scalp formulation in the long-term management of scalp psoriasis. Dermatology. 2008;217:321-328.
37. Tyring S, Mendoza N, Appell M, et al. A calcipotriene/betamethasone dipropionate two-compound scalp formulation in the treatment of scalp psoriasis in Hispanic/Latino and Black/African American patients: results of the randomized, 8-week, double-blind phase of a clinical trial. Int J Dermatol. 2010;49:1328-1333.
38. Silver S, Tuppal R, Gupta AK, et al. Effect of calcipotriene plus betamethasone dipropionate topical suspension on the hypothalamic-pituitary-adrenal axis and calcium homeostasis in subjects with extensive psoriasis vulgaris: an open, non-controlled, 8-week trial. J Drugs Dermatol. 2013;12:882-888.
Psoriasis is a common inflammatory skin disorder that appears to be induced by multifactorial pathophysiologic processes associated with immunologic dysregulation.1 It can affect patients of any age, gender, and ethnicity, and it presents clinically with a variety of visible manifestations. The disease course and severity of psoriasis varies among affected patients.1 Chronic plaque psoriasis (PP), also referred to as psoriasis vulgaris, is the most common clinical presentation.1,2 Although many patients are affected by psoriasis that is widespread and in some cases severe, the majority of affected patients exhibit localized involvement that usually affects less than 2% to 5% of the body surface area. Although the skin at any anatomic location can be affected, commonly involved sites are described by the mnemonic term SNAKES (scalp, nails, anogenital region, knees, elbows, sacral region).2,3
Because the majority of patients with PP present with localized disease, topical therapy is the foundation of treatment in most cases. Topical corticosteroids (TCs) are the most commonly utilized agents, supported by a long track record of favorable efficacy and safety over approximately 6 decades.4,5 However, optimal management of PP with TCs requires use of a formulation that is of adequate potency, is adaptable for application to the affected body sites, and is properly monitored and adjusted to avoid potential TC-induced adverse effects.4-6 Nonsteroidal topical therapies such as vitamin D analogues (eg, calcipotriene) and retinoids (eg, tazarotene) are commonly integrated into topical regimens to reduce the application frequency and duration of TC use as well as to sustain efficacy.5,7,8 Plaque psoriasis is characteristically a chronic disease associated with periods of persistence and episodes of flaring; therefore, intermittent use of TC therapy along with concurrent or sequential use of a nonsteroidal topical agent are commonly employed to achieve and sustain control of the disorder.7-9
In the last decade, several advances have revolutionized the management of psoriasis, especially for PP patients with extensive involvement who require systemic therapy and/or phototherapy as well as for those with psoriatic arthritis.10,11 The availability of biologic agents such as tumor necrosis factor a inhibitors and certain interleukin inhibitors (eg, IL-12/IL-23) have been at the forefront of major advances in PP treatment, with some agents also blocking the progression of joint destruction associated with psoriatic arthritis.10-12 However, even when patients with PP respond favorably to biologic therapy, it is not uncommon for them to still be affected by some persistent PP. In these cases, although much of the chronic PP may clear with use of the biologic agent, persistence of psoriatic plaques may involve the lower extremities, scalp, and/or trunk, with topical therapy often added to augment the therapeutic response.13-15
This article provides a review of a patented topical suspension combination formulation that contains calcipotriene hydrate 0.005%, a vitamin D analogue, and betamethasone dipropio-nate (Bd) 0.064%, a high-potency TC. In 2008, the US Food and Drug Administration approved the once-daily application of calcipotriene 0.005%–Bd 0.064% topical suspension (C/Bd-TS) for the treatment of PP; this formulation is approved for use on the scalp and body in patients 18 years of age and older. According to the product insert, the recommended maximum duration of treatment with C/Bd-TS once daily is 8 weeks, and patients may not exceed a maximum weekly dose of 100 g.16 It is important to note that the terms calcipotriene and calcipotriol refer to the same molecule and are used interchangeably in the literature. Formulation characteristics of C/Bd-TS, perspectives on modes of action, outcomes from pivotal trials, and efficacy and safety data reported from additional studies are discussed in this article.
What are the formulation characteristics of C/Bd-TS?
Each gram of C/Bd-TS contains 52.18 mg of calcipotriene hydrate (equivalent to 50 µg of calcipotriene) and 0.643 µg of Bd (equivalent to 0.5 mg of betamethasone), formulated together in a viscous, nearly odorless, almost clear to slightly off-white suspension. The excipients are hydrogenated castor oil, polypropylene glycol 11 stearyl ether, α-tocopherol, butylhydroxytoluene, and mineral oil, collectively producing a gel base in which both active ingredients are suspended.16 Although the viscous quality of the suspension warrants some additional effort for removal during hair washing, the tenacious gel-like viscosity assists in removing scale on psoriatic plaques, which is often adherent, especially on the scalp. Additionally, it is important that C/Bd-TS be shaken well before use.16 Initially, C/Bd-TS was studied and marketed in the United States for treatment of scalp psoriasis; however, the indication was expanded to include treatment of PP on the rest of the body, supported by evidence from randomized controlled trials (RCTs).16-23
Vitamin D analogues (eg, calcipotriene/calcitriol) have been shown to be photolabile when exposed to UV light, especially UVA. They also have been shown to be chemically incompatible and less stable when admixed with a variety of other active ingredients and/or vehicles used to treat PP, including hydrocortisone valerate ointment 0.2%, ammonium lactate lotion 12%, and salicylic acid compound ointment 6%.24-26 As a result, it is important for clinicians to consider avoidance of concomitant topical calcipotriene application with use of a TC unless the stability of the active ingredients has been tested when the formulations are combined. Calcipotriene 0.005%/Bd 0.064% topical suspension utilizes vehicle technology that maintains the stability and activity of both calcipotriene and Bd within the suspension formulation.16,26
What is the rationale behind combining calcipotriene and Bd in a single formulation for the treatment of PP?
The potential advantages of C/Bd-TS include the combined modes of action of 2 different active ingredients used for treatment of PP, complementary immunomodulatory effects as compared to use of a TC or vitamin D analogue alone, ease of use with a single product applied once daily, adaptability of the vehicle for use on scalp and/or body skin, and improvement in quality-of-life (QOL) measures.27-34
Combined Modes of Action
Calcipotriene 0.005%–Bd 0.064% topical suspension combines the modes of action of a high-potency topical suspension and a vitamin D analogue for the treatment of PP in a single stable gel formulation that is approved in the United States for treatment of PP in adults.16 The multiple anti-inflammatory properties of corticosteroids as well as the efficacy and safety of TC therapy for psoriasis have been well described.4,6,7,9,27 The antiproliferative and anti-inflammatory properties of vitamin D analogues that appear to correlate with therapeutic effects in the treatment of PP also have been discussed in the literature.28
Complementary Immunomodulatory Effects
More recent studies using various research assays have provided further evidence supporting relevant immunomodulatory properties of calcipotriene alone and in combination with Bd that favorably modify immune dysregulation pathways described more recently in the pathogenesis of PP.1,29,30 Treatment of psoriatic plaques with calcipotriene has been shown to suppress the increased production of peptide alarmins (psoriasin and koebnerisin) in psoriatic skin and their TH17-mediated regulation in epidermal ke-ratinocytes, thus interfering with the S100 amplification loop that appears to produce inflammation in psoriasis.29 In T-lymphocyte cultures evaluating exposure to calcipotriene and Bd both alone and as a combined therapy, calcipotriene inhibited IFN-g, IL-8, IL-17, and IL-22 expression, and it reversed the corticosteroid-induced suppression of IL-4, IL-5, IL-10, and IL-13; Bd inhibited both IL-6 and tumor necrosis factor α expression. The outcomes demonstrated that the combination of calcipotriene and Bd inhibited the endogenous release of TH1- and TH17-associated cytokines that are associated with psoriatic inflammation and together induced a more favorable anti-inflammatory cytokine profile.30 Although the broad range of anti-inflammatory effects provided by a TC of adequate potency, such as Bd, can clear or markedly improve PP, the concurrent use of calcipotriene was shown to provide additional immunomodulatory effects that suppressed the key TH17/TH1 pathophysiologic mediators of psoriatic inflammation and simultaneously induced a TH2/T regulatory response that is believed to provide therapeutic benefit.29,30
Ease of Use and Vehicle Adaptability
A once-daily regimen and a vehicle formulation adaptable for use on both the scalp and body are advantageous in enhancing the potential for greater patient adherence.31,32 The adaptability of the C/Bd-TS for use on the scalp and/or body is supported by several studies encompassing a large number of actively treated subjects. Calcipotriene 0.005%–Bd 0.064% topical suspension has been extensively studied in patients with PP on the scalp and/or body as evidenced by a pooled analysis of 9 eight-week RCTs (scalp, n=6; body, n=3) that encompassed 2777 total subjects treated once daily for PP (scalp, n=1953; body, n=824).23 Additionally, C/Bd-TS applied once daily was evaluated in an open-label, single-arm, 8-week, phase 2 study of adolescents (N=78; age range, 12–17 years [mean age, 14.6 years]) with scalp psoriasis (mean affected scalp area, 43.7%). The investigator global assessment of treatment success (clear or almost clear) and the patient global assessment of treatment success (clear or very mild) were essentially identical among participants and investigators with 85% and 87% reported after 8 weeks, respectively; approximately 50% of participants achieved treatment success after 2 weeks based on both the investigator global assessment and patient global assessment.33
Improvement in QOL Measures
Quality-of-life measures were compared in an 8-week RCT of participants with at least moderate scalp psoriasis treated with C/Bd-TS once daily (n=207) or calcipotriene solution twice daily (n=107). Significantly greater improvement in QOL scores compared to baseline were noted at all time points using the Skindex-16 questionnaire in participants treated with C/Bd-TS compared to calcipotriene solution (total score, P<.001 at weeks 2 and 4 and P=.008 at week 8; symptoms score, P<.001 at weeks 2 and 4 and P=.004 at week 8; emotions score, P<.001 at weeks 2 and 4 and P=.005 at week 8).34 A 4-week, open-label, noninterventional cohort, postmarketing (“real life”) study of 721 patients treated at 333 dermatology centers with C/Bd-TS showed a 69.5% improvement in the scalp life quality index score compared to baseline (P<.0001), with 89.5% and 90.4% of participants reporting that C/Bd-TS was better/much better than previously used therapies for scalp psoriasis and easy/very easy to use, respectively.35 An 8-week RCT trial evaluated C/Bd-TS once daily compared to calcipotriene alone, betamethasone dipropionate alone, and vehicle in 1152 participants with mild to moderate PP involving the trunk and extremities. Participants treated with C/Bd-TS (n=442) demonstrated superior reductions in QOL scores using the dermatology life quality index at weeks 4 and 8 compared to those treated with Bd alone (n=418) or vehicle (n=77) but not compared to calcipotriene alone (n=80).19
What data are available on the efficacy and safety of C/Bd-TS?
Several clinical studies have evaluated the efficacy, tolerability, and safety of C/Bd-TS applied once daily for PP of the scalp and body (ie, trunk, extremities). Most studies were completed over a duration of 8 weeks in adults16-23; however, studies also have been performed in adolescents,33 in adults treated for up to 52 weeks,36 and in a subgroup of Hispanic/Latino and black/African American patients with scalp psoriasis.37 The Table provides a detailed summary of primary efficacy data along with important tolerability and safety considerations based on study outcomes.
What practical recommendations can be made regarding the use of C/Bd-TS for PP?
Calcipotriene 0.005%–Bd 0.064% topical suspension applied once daily provides a formulation that allows for treatment of PP involving both the scalp and body using a single product, which provides an element of convenience and is likely to enhance compliance and reduce costs compared with the use of 2 separate products. The efficacy and safety of C/Bd-TS has been well established in several studies,16-23,37 including a 52-week trial in patients with scalp psoriasis.36 The combination of calcipotriene and Bd appears to favorably address the pathophysiologic pathways involved in psoriasis.29,30 Calcipotriene 0.005%–Bd 0.064% topical suspension is a rational option for the treatment of PP in patients with localized disease or in patients treated systemically or with phototherapy for more extensive disease who exhibit persistence or recurrence of scattered areas of PP.6-9,14,15 Appropriate use of C/Bd-TS is likely to achieve favorable efficacy with a low risk of tolerability reactions and a very low risk of major adverse drug reactions.16-23,36-38
Psoriasis is a common inflammatory skin disorder that appears to be induced by multifactorial pathophysiologic processes associated with immunologic dysregulation.1 It can affect patients of any age, gender, and ethnicity, and it presents clinically with a variety of visible manifestations. The disease course and severity of psoriasis varies among affected patients.1 Chronic plaque psoriasis (PP), also referred to as psoriasis vulgaris, is the most common clinical presentation.1,2 Although many patients are affected by psoriasis that is widespread and in some cases severe, the majority of affected patients exhibit localized involvement that usually affects less than 2% to 5% of the body surface area. Although the skin at any anatomic location can be affected, commonly involved sites are described by the mnemonic term SNAKES (scalp, nails, anogenital region, knees, elbows, sacral region).2,3
Because the majority of patients with PP present with localized disease, topical therapy is the foundation of treatment in most cases. Topical corticosteroids (TCs) are the most commonly utilized agents, supported by a long track record of favorable efficacy and safety over approximately 6 decades.4,5 However, optimal management of PP with TCs requires use of a formulation that is of adequate potency, is adaptable for application to the affected body sites, and is properly monitored and adjusted to avoid potential TC-induced adverse effects.4-6 Nonsteroidal topical therapies such as vitamin D analogues (eg, calcipotriene) and retinoids (eg, tazarotene) are commonly integrated into topical regimens to reduce the application frequency and duration of TC use as well as to sustain efficacy.5,7,8 Plaque psoriasis is characteristically a chronic disease associated with periods of persistence and episodes of flaring; therefore, intermittent use of TC therapy along with concurrent or sequential use of a nonsteroidal topical agent are commonly employed to achieve and sustain control of the disorder.7-9
In the last decade, several advances have revolutionized the management of psoriasis, especially for PP patients with extensive involvement who require systemic therapy and/or phototherapy as well as for those with psoriatic arthritis.10,11 The availability of biologic agents such as tumor necrosis factor a inhibitors and certain interleukin inhibitors (eg, IL-12/IL-23) have been at the forefront of major advances in PP treatment, with some agents also blocking the progression of joint destruction associated with psoriatic arthritis.10-12 However, even when patients with PP respond favorably to biologic therapy, it is not uncommon for them to still be affected by some persistent PP. In these cases, although much of the chronic PP may clear with use of the biologic agent, persistence of psoriatic plaques may involve the lower extremities, scalp, and/or trunk, with topical therapy often added to augment the therapeutic response.13-15
This article provides a review of a patented topical suspension combination formulation that contains calcipotriene hydrate 0.005%, a vitamin D analogue, and betamethasone dipropio-nate (Bd) 0.064%, a high-potency TC. In 2008, the US Food and Drug Administration approved the once-daily application of calcipotriene 0.005%–Bd 0.064% topical suspension (C/Bd-TS) for the treatment of PP; this formulation is approved for use on the scalp and body in patients 18 years of age and older. According to the product insert, the recommended maximum duration of treatment with C/Bd-TS once daily is 8 weeks, and patients may not exceed a maximum weekly dose of 100 g.16 It is important to note that the terms calcipotriene and calcipotriol refer to the same molecule and are used interchangeably in the literature. Formulation characteristics of C/Bd-TS, perspectives on modes of action, outcomes from pivotal trials, and efficacy and safety data reported from additional studies are discussed in this article.
What are the formulation characteristics of C/Bd-TS?
Each gram of C/Bd-TS contains 52.18 mg of calcipotriene hydrate (equivalent to 50 µg of calcipotriene) and 0.643 µg of Bd (equivalent to 0.5 mg of betamethasone), formulated together in a viscous, nearly odorless, almost clear to slightly off-white suspension. The excipients are hydrogenated castor oil, polypropylene glycol 11 stearyl ether, α-tocopherol, butylhydroxytoluene, and mineral oil, collectively producing a gel base in which both active ingredients are suspended.16 Although the viscous quality of the suspension warrants some additional effort for removal during hair washing, the tenacious gel-like viscosity assists in removing scale on psoriatic plaques, which is often adherent, especially on the scalp. Additionally, it is important that C/Bd-TS be shaken well before use.16 Initially, C/Bd-TS was studied and marketed in the United States for treatment of scalp psoriasis; however, the indication was expanded to include treatment of PP on the rest of the body, supported by evidence from randomized controlled trials (RCTs).16-23
Vitamin D analogues (eg, calcipotriene/calcitriol) have been shown to be photolabile when exposed to UV light, especially UVA. They also have been shown to be chemically incompatible and less stable when admixed with a variety of other active ingredients and/or vehicles used to treat PP, including hydrocortisone valerate ointment 0.2%, ammonium lactate lotion 12%, and salicylic acid compound ointment 6%.24-26 As a result, it is important for clinicians to consider avoidance of concomitant topical calcipotriene application with use of a TC unless the stability of the active ingredients has been tested when the formulations are combined. Calcipotriene 0.005%/Bd 0.064% topical suspension utilizes vehicle technology that maintains the stability and activity of both calcipotriene and Bd within the suspension formulation.16,26
What is the rationale behind combining calcipotriene and Bd in a single formulation for the treatment of PP?
The potential advantages of C/Bd-TS include the combined modes of action of 2 different active ingredients used for treatment of PP, complementary immunomodulatory effects as compared to use of a TC or vitamin D analogue alone, ease of use with a single product applied once daily, adaptability of the vehicle for use on scalp and/or body skin, and improvement in quality-of-life (QOL) measures.27-34
Combined Modes of Action
Calcipotriene 0.005%–Bd 0.064% topical suspension combines the modes of action of a high-potency topical suspension and a vitamin D analogue for the treatment of PP in a single stable gel formulation that is approved in the United States for treatment of PP in adults.16 The multiple anti-inflammatory properties of corticosteroids as well as the efficacy and safety of TC therapy for psoriasis have been well described.4,6,7,9,27 The antiproliferative and anti-inflammatory properties of vitamin D analogues that appear to correlate with therapeutic effects in the treatment of PP also have been discussed in the literature.28
Complementary Immunomodulatory Effects
More recent studies using various research assays have provided further evidence supporting relevant immunomodulatory properties of calcipotriene alone and in combination with Bd that favorably modify immune dysregulation pathways described more recently in the pathogenesis of PP.1,29,30 Treatment of psoriatic plaques with calcipotriene has been shown to suppress the increased production of peptide alarmins (psoriasin and koebnerisin) in psoriatic skin and their TH17-mediated regulation in epidermal ke-ratinocytes, thus interfering with the S100 amplification loop that appears to produce inflammation in psoriasis.29 In T-lymphocyte cultures evaluating exposure to calcipotriene and Bd both alone and as a combined therapy, calcipotriene inhibited IFN-g, IL-8, IL-17, and IL-22 expression, and it reversed the corticosteroid-induced suppression of IL-4, IL-5, IL-10, and IL-13; Bd inhibited both IL-6 and tumor necrosis factor α expression. The outcomes demonstrated that the combination of calcipotriene and Bd inhibited the endogenous release of TH1- and TH17-associated cytokines that are associated with psoriatic inflammation and together induced a more favorable anti-inflammatory cytokine profile.30 Although the broad range of anti-inflammatory effects provided by a TC of adequate potency, such as Bd, can clear or markedly improve PP, the concurrent use of calcipotriene was shown to provide additional immunomodulatory effects that suppressed the key TH17/TH1 pathophysiologic mediators of psoriatic inflammation and simultaneously induced a TH2/T regulatory response that is believed to provide therapeutic benefit.29,30
Ease of Use and Vehicle Adaptability
A once-daily regimen and a vehicle formulation adaptable for use on both the scalp and body are advantageous in enhancing the potential for greater patient adherence.31,32 The adaptability of the C/Bd-TS for use on the scalp and/or body is supported by several studies encompassing a large number of actively treated subjects. Calcipotriene 0.005%–Bd 0.064% topical suspension has been extensively studied in patients with PP on the scalp and/or body as evidenced by a pooled analysis of 9 eight-week RCTs (scalp, n=6; body, n=3) that encompassed 2777 total subjects treated once daily for PP (scalp, n=1953; body, n=824).23 Additionally, C/Bd-TS applied once daily was evaluated in an open-label, single-arm, 8-week, phase 2 study of adolescents (N=78; age range, 12–17 years [mean age, 14.6 years]) with scalp psoriasis (mean affected scalp area, 43.7%). The investigator global assessment of treatment success (clear or almost clear) and the patient global assessment of treatment success (clear or very mild) were essentially identical among participants and investigators with 85% and 87% reported after 8 weeks, respectively; approximately 50% of participants achieved treatment success after 2 weeks based on both the investigator global assessment and patient global assessment.33
Improvement in QOL Measures
Quality-of-life measures were compared in an 8-week RCT of participants with at least moderate scalp psoriasis treated with C/Bd-TS once daily (n=207) or calcipotriene solution twice daily (n=107). Significantly greater improvement in QOL scores compared to baseline were noted at all time points using the Skindex-16 questionnaire in participants treated with C/Bd-TS compared to calcipotriene solution (total score, P<.001 at weeks 2 and 4 and P=.008 at week 8; symptoms score, P<.001 at weeks 2 and 4 and P=.004 at week 8; emotions score, P<.001 at weeks 2 and 4 and P=.005 at week 8).34 A 4-week, open-label, noninterventional cohort, postmarketing (“real life”) study of 721 patients treated at 333 dermatology centers with C/Bd-TS showed a 69.5% improvement in the scalp life quality index score compared to baseline (P<.0001), with 89.5% and 90.4% of participants reporting that C/Bd-TS was better/much better than previously used therapies for scalp psoriasis and easy/very easy to use, respectively.35 An 8-week RCT trial evaluated C/Bd-TS once daily compared to calcipotriene alone, betamethasone dipropionate alone, and vehicle in 1152 participants with mild to moderate PP involving the trunk and extremities. Participants treated with C/Bd-TS (n=442) demonstrated superior reductions in QOL scores using the dermatology life quality index at weeks 4 and 8 compared to those treated with Bd alone (n=418) or vehicle (n=77) but not compared to calcipotriene alone (n=80).19
What data are available on the efficacy and safety of C/Bd-TS?
Several clinical studies have evaluated the efficacy, tolerability, and safety of C/Bd-TS applied once daily for PP of the scalp and body (ie, trunk, extremities). Most studies were completed over a duration of 8 weeks in adults16-23; however, studies also have been performed in adolescents,33 in adults treated for up to 52 weeks,36 and in a subgroup of Hispanic/Latino and black/African American patients with scalp psoriasis.37 The Table provides a detailed summary of primary efficacy data along with important tolerability and safety considerations based on study outcomes.
What practical recommendations can be made regarding the use of C/Bd-TS for PP?
Calcipotriene 0.005%–Bd 0.064% topical suspension applied once daily provides a formulation that allows for treatment of PP involving both the scalp and body using a single product, which provides an element of convenience and is likely to enhance compliance and reduce costs compared with the use of 2 separate products. The efficacy and safety of C/Bd-TS has been well established in several studies,16-23,37 including a 52-week trial in patients with scalp psoriasis.36 The combination of calcipotriene and Bd appears to favorably address the pathophysiologic pathways involved in psoriasis.29,30 Calcipotriene 0.005%–Bd 0.064% topical suspension is a rational option for the treatment of PP in patients with localized disease or in patients treated systemically or with phototherapy for more extensive disease who exhibit persistence or recurrence of scattered areas of PP.6-9,14,15 Appropriate use of C/Bd-TS is likely to achieve favorable efficacy with a low risk of tolerability reactions and a very low risk of major adverse drug reactions.16-23,36-38
1. Guttman-Yassky E, Krueger JG. Psoriasis: evolution of pathogenic concepts and new therapies through phases of translational research. Br J Dermatol. 2007;157:1103-1115.
2. Menter MA. An overview of psoriasis. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:1-21.
3. Sandoval LF, Feldman SR. General approach to psoriasis treatment. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:3-8.
4. Zeichner JA, Lebwohl MG, Menter A, et al. Optimizing topical therapies for treating psoriasis: a consensus conference. Cutis. 2010;(3 suppl):5-31.
5. American Academy of Dermatology Work Group, Menter A, Korman NJ, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions [published online ahead of print February 8, 2011]. J Am Acad Dermatol. 2011;65:137-174.
6. Del Rosso J, Friedlander SF. Corticosteroids: options in the era of steroid-sparing therapy. J Am Acad Dermatol. 2005;53(1, suppl 1):S50-S58.
7. Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies [published online ahead of print February 13, 2009]. J Am Acad Dermatol. 2009;60:643-659.
8. Koo J. New developments in topical sequential therapy for psoriasis. Skin Therapy Lett. 2005;10:1-4.
9. Mason AR, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis. Cochrane Database Syst Rev. 2009;2:CD005028.
10. Belge K, Brück J, Ghoreschi K. Advances in treating psoriasis. F1000Prime Rep. 2014;6:4.
11. Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-441.
12. Boehncke WH, Qureshi A, Merola JF, et al. Diagnosing and treating psoriatic arthritis: an update. Br J Dermatol. 2014;170:772-786.
13. Feldman SR. Effectiveness of clobetasol propionate spray 0.05% added to other stable treatments: add-on therapy in the COBRA trial. Cutis. 2007;80(suppl 5):20-28.
14. Feldman SR, Gelfand JM, Stein Gold L, et al. The role of topical therapy for patients with extensive psoriasis. Cutis. 2007;79(suppl 1[ii]):18-31.
15. Kircik L. Topical calcipotriene 0.005% and betamethasone dipropionate 0.064% maintains efficacy of etanercept after step-down dose in patients with moderate-to-severe plaque psoriasis: results of an open label trial. J Drugs Dermatol. 2011;10:878-882.
16. Taclonex [product insert]. Parsippany, NJ: LEO Pharma Inc; 2014.
17. Buckley C, Hoffmann V, Shapiro J, et al. Calcipotriol plus betamethasone dipropionate scalp formulation is effective and well tolerated in the treatment of scalp psoriasis: a phase II study. Dermatology. 2008;217:107-113.
18. Fleming C, Ganslandt C, Guenther L, et al. Calcipotriol plus betamethasone dipropionate gel compared with its active components in the same vehicle and the vehicle alone in the treatment of psoriasis vulgaris: a randomized, parallel group, double-blind, exploratory study. Eur J Dermatol. 2010;20:465-471.
19. Menter A, Stein Gold L, Bukhalo M, et al. Calcipotriene plus betamethasone dipropionate topical suspension for the treatment of mild to moderate psoriasis vulgaris on the body: a randomized, double-blind, vehicle-controlled trial. J Drugs Dermatol. 2013;12:92-98.
20. Jemec GBE, Ganslandt C, Ortonne JP, et al. A new scalp formulation of calcipotriene plus betamethasone compared with its active ingredients and the vehicle in the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. J Am Acad Dermatol. 2008;59:455-463.
21. van de Kerkhof PC, Hoffmann V, Anstey A, et al. A new scalp formulation of calcipotriol plus betamethasone dipropionate compared with each of its active ingredients in the same vehicle for the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. Br J Dermatol. 2009;160:170-176.
22. Langley RG, Gupta A, Papp K, et al. Calcipotriol plus betamethasone dipropionate gel compared with tacalcitol ointment and the gel vehicle alone in patients with psoriasis vulgaris: a randomized, controlled clinical trial. Dermatology. 2011;222:148-156.
23. Kragballe K, van de Kerkhof P. Pooled safety analysis of calcipotriol plus betamethasone dipropionate gel for the treatment of psoriasis on the body and scalp. J Eur Acad Dermatol Venereol. 2014;28:10-21.
24. Lebwohl MG, Corvari L. Compatibility of topical therapies for psoriasis: challenges and innovations. Cutis. 2007;79(suppl 1[ii]):5-10.
25. Patel B, Siskin S, Krazmien R, et al. Compatibility of calcipotriene with other topical medications. J Am Acad Dermatol. 1998;38(6, pt 1):1010-1011.
26. Traulsen J. Bioavailability of betamethasone dipropionate when combined with calcipotriol. Int J Dermatol. 2004;43:611-617.
27. Sandoval LF, Feldman SR. Topical corticosteroids. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:21-36.
28. deShazo R, Krueger GG, Duffin KC. Topical agents. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:41-65.
29. Hegyi Z, Zwicker S, Bureik D, et al. Vitamin D analog calcipotriol suppresses the Th17 cytokine-induced proinflammatory S100 “alarmins” psoriasin (S100A7) and koebnerisin (S100A15) in psoriasis. J Invest Dermatol. 2012;132:1416-1424.
30. Lovato P, Norsgaard H, Ropke M. Key immunomodulatory effects exerted by calcipotriol in combination with corticosteroid on human cells. Poster presented at: 21st European Academy of Dermatology and Venereology Congress; September 27-30, 2012; Prague, Czech Republic.
31. Renton C. Diagnosis and treatment of adults with scalp psoriasis. Nurs Stand. 2014;28:35-39.
32. Feldman SR, Housman TS. Patients’ vehicle preference for corticosteroid treatments of scalp psoriasis. Am J Clin Dermatol. 2003;4:221-224.
33. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriene plus betamethasone dipropionate topical suspension in adolescents with scalp psoriasis: an open, non-controlled, 8-week trial. Poster presented at: American Academy of Dermatology 72nd Annual Meeting; March 21-25, 2014; Denver, CO.
34. Ortonne JP, Tan J, Nordin P, et al. Quality of life of patients with scalp psoriasis treated with calcipotriene plus betamethasone dipropionate gel compared to calcipotriene solution. J Am Academy Dermatol. 2008;58(2, suppl 2):AB134.
35. Mrowietz U, Macheleidt O, Eicke C. Effective treatment and improvement of quality of life in patients with scalp psoriasis by topical use of calcipotriol/betamethasone (Xamiol®-gel): results [in German]. J Dtsch Dermatol Ges. 2011;9:825-831.
36. Luger TA, Cambazard F, Larsen FG, et al. A study of the safety and efficacy of calcipotriol and betamethasone dipropionate scalp formulation in the long-term management of scalp psoriasis. Dermatology. 2008;217:321-328.
37. Tyring S, Mendoza N, Appell M, et al. A calcipotriene/betamethasone dipropionate two-compound scalp formulation in the treatment of scalp psoriasis in Hispanic/Latino and Black/African American patients: results of the randomized, 8-week, double-blind phase of a clinical trial. Int J Dermatol. 2010;49:1328-1333.
38. Silver S, Tuppal R, Gupta AK, et al. Effect of calcipotriene plus betamethasone dipropionate topical suspension on the hypothalamic-pituitary-adrenal axis and calcium homeostasis in subjects with extensive psoriasis vulgaris: an open, non-controlled, 8-week trial. J Drugs Dermatol. 2013;12:882-888.
1. Guttman-Yassky E, Krueger JG. Psoriasis: evolution of pathogenic concepts and new therapies through phases of translational research. Br J Dermatol. 2007;157:1103-1115.
2. Menter MA. An overview of psoriasis. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:1-21.
3. Sandoval LF, Feldman SR. General approach to psoriasis treatment. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:3-8.
4. Zeichner JA, Lebwohl MG, Menter A, et al. Optimizing topical therapies for treating psoriasis: a consensus conference. Cutis. 2010;(3 suppl):5-31.
5. American Academy of Dermatology Work Group, Menter A, Korman NJ, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 6. guidelines of care for the treatment of psoriasis and psoriatic arthritis: case-based presentations and evidence-based conclusions [published online ahead of print February 8, 2011]. J Am Acad Dermatol. 2011;65:137-174.
6. Del Rosso J, Friedlander SF. Corticosteroids: options in the era of steroid-sparing therapy. J Am Acad Dermatol. 2005;53(1, suppl 1):S50-S58.
7. Menter A, Korman NJ, Elmets CA, et al; American Academy of Dermatology. Guidelines of care for the management of psoriasis and psoriatic arthritis. section 3. guidelines of care for the management and treatment of psoriasis with topical therapies [published online ahead of print February 13, 2009]. J Am Acad Dermatol. 2009;60:643-659.
8. Koo J. New developments in topical sequential therapy for psoriasis. Skin Therapy Lett. 2005;10:1-4.
9. Mason AR, Mason J, Cork M, et al. Topical treatments for chronic plaque psoriasis. Cochrane Database Syst Rev. 2009;2:CD005028.
10. Belge K, Brück J, Ghoreschi K. Advances in treating psoriasis. F1000Prime Rep. 2014;6:4.
11. Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-441.
12. Boehncke WH, Qureshi A, Merola JF, et al. Diagnosing and treating psoriatic arthritis: an update. Br J Dermatol. 2014;170:772-786.
13. Feldman SR. Effectiveness of clobetasol propionate spray 0.05% added to other stable treatments: add-on therapy in the COBRA trial. Cutis. 2007;80(suppl 5):20-28.
14. Feldman SR, Gelfand JM, Stein Gold L, et al. The role of topical therapy for patients with extensive psoriasis. Cutis. 2007;79(suppl 1[ii]):18-31.
15. Kircik L. Topical calcipotriene 0.005% and betamethasone dipropionate 0.064% maintains efficacy of etanercept after step-down dose in patients with moderate-to-severe plaque psoriasis: results of an open label trial. J Drugs Dermatol. 2011;10:878-882.
16. Taclonex [product insert]. Parsippany, NJ: LEO Pharma Inc; 2014.
17. Buckley C, Hoffmann V, Shapiro J, et al. Calcipotriol plus betamethasone dipropionate scalp formulation is effective and well tolerated in the treatment of scalp psoriasis: a phase II study. Dermatology. 2008;217:107-113.
18. Fleming C, Ganslandt C, Guenther L, et al. Calcipotriol plus betamethasone dipropionate gel compared with its active components in the same vehicle and the vehicle alone in the treatment of psoriasis vulgaris: a randomized, parallel group, double-blind, exploratory study. Eur J Dermatol. 2010;20:465-471.
19. Menter A, Stein Gold L, Bukhalo M, et al. Calcipotriene plus betamethasone dipropionate topical suspension for the treatment of mild to moderate psoriasis vulgaris on the body: a randomized, double-blind, vehicle-controlled trial. J Drugs Dermatol. 2013;12:92-98.
20. Jemec GBE, Ganslandt C, Ortonne JP, et al. A new scalp formulation of calcipotriene plus betamethasone compared with its active ingredients and the vehicle in the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. J Am Acad Dermatol. 2008;59:455-463.
21. van de Kerkhof PC, Hoffmann V, Anstey A, et al. A new scalp formulation of calcipotriol plus betamethasone dipropionate compared with each of its active ingredients in the same vehicle for the treatment of scalp psoriasis: a randomized, double-blind, controlled trial. Br J Dermatol. 2009;160:170-176.
22. Langley RG, Gupta A, Papp K, et al. Calcipotriol plus betamethasone dipropionate gel compared with tacalcitol ointment and the gel vehicle alone in patients with psoriasis vulgaris: a randomized, controlled clinical trial. Dermatology. 2011;222:148-156.
23. Kragballe K, van de Kerkhof P. Pooled safety analysis of calcipotriol plus betamethasone dipropionate gel for the treatment of psoriasis on the body and scalp. J Eur Acad Dermatol Venereol. 2014;28:10-21.
24. Lebwohl MG, Corvari L. Compatibility of topical therapies for psoriasis: challenges and innovations. Cutis. 2007;79(suppl 1[ii]):5-10.
25. Patel B, Siskin S, Krazmien R, et al. Compatibility of calcipotriene with other topical medications. J Am Acad Dermatol. 1998;38(6, pt 1):1010-1011.
26. Traulsen J. Bioavailability of betamethasone dipropionate when combined with calcipotriol. Int J Dermatol. 2004;43:611-617.
27. Sandoval LF, Feldman SR. Topical corticosteroids. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:21-36.
28. deShazo R, Krueger GG, Duffin KC. Topical agents. In: Koo JYM, Levin EC, Leon A, et al, eds. Moderate to Severe Psoriasis. 4th ed. Boca Raton, FL: CRC Press Taylor & Francis Group; 2014:41-65.
29. Hegyi Z, Zwicker S, Bureik D, et al. Vitamin D analog calcipotriol suppresses the Th17 cytokine-induced proinflammatory S100 “alarmins” psoriasin (S100A7) and koebnerisin (S100A15) in psoriasis. J Invest Dermatol. 2012;132:1416-1424.
30. Lovato P, Norsgaard H, Ropke M. Key immunomodulatory effects exerted by calcipotriol in combination with corticosteroid on human cells. Poster presented at: 21st European Academy of Dermatology and Venereology Congress; September 27-30, 2012; Prague, Czech Republic.
31. Renton C. Diagnosis and treatment of adults with scalp psoriasis. Nurs Stand. 2014;28:35-39.
32. Feldman SR, Housman TS. Patients’ vehicle preference for corticosteroid treatments of scalp psoriasis. Am J Clin Dermatol. 2003;4:221-224.
33. Gooderham M, Debarre JM, Keddy-Grant J, et al. Safety and efficacy of calcipotriene plus betamethasone dipropionate topical suspension in adolescents with scalp psoriasis: an open, non-controlled, 8-week trial. Poster presented at: American Academy of Dermatology 72nd Annual Meeting; March 21-25, 2014; Denver, CO.
34. Ortonne JP, Tan J, Nordin P, et al. Quality of life of patients with scalp psoriasis treated with calcipotriene plus betamethasone dipropionate gel compared to calcipotriene solution. J Am Academy Dermatol. 2008;58(2, suppl 2):AB134.
35. Mrowietz U, Macheleidt O, Eicke C. Effective treatment and improvement of quality of life in patients with scalp psoriasis by topical use of calcipotriol/betamethasone (Xamiol®-gel): results [in German]. J Dtsch Dermatol Ges. 2011;9:825-831.
36. Luger TA, Cambazard F, Larsen FG, et al. A study of the safety and efficacy of calcipotriol and betamethasone dipropionate scalp formulation in the long-term management of scalp psoriasis. Dermatology. 2008;217:321-328.
37. Tyring S, Mendoza N, Appell M, et al. A calcipotriene/betamethasone dipropionate two-compound scalp formulation in the treatment of scalp psoriasis in Hispanic/Latino and Black/African American patients: results of the randomized, 8-week, double-blind phase of a clinical trial. Int J Dermatol. 2010;49:1328-1333.
38. Silver S, Tuppal R, Gupta AK, et al. Effect of calcipotriene plus betamethasone dipropionate topical suspension on the hypothalamic-pituitary-adrenal axis and calcium homeostasis in subjects with extensive psoriasis vulgaris: an open, non-controlled, 8-week trial. J Drugs Dermatol. 2013;12:882-888.
Practice Points
- Calcipotriene 0.005%–betamethasone dipropionate 0.064% topical suspension (C/Bd-TS) applied once daily has been shown in multiple studies to be effective, well tolerated, and safe for the treatment of plaque psoriasis (PP) involving the scalp and/or other body sites such as the trunk and extremities. Studies have included all severities of PP, with both investigator and subject assessments shown to be favorable overall.
- Most studies were completed in adults over a duration of 8 weeks; however, clinical trials also have been performed with C/Bd-TS in adults treated for up to 52 weeks for scalp psoriasis, in a subgroup of Hispanic/Latino and black/African American adult patients with scalp psoriasis, and in adolescents with scalp psoriasis.
- Studies evaluating application of C/Bd-TS once daily for PP affecting nonscalp sites have primarily involved use on the trunk and extremities.
- The adaptability for scalp and body application allows for use in many cases of a single topical product without needing to prescribe a second leave-on medication specifically for use on the scalp.
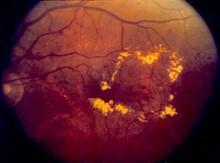
Fats may hold key to new malaria treatment
Credit: Stuart Hay
Scientists believe they have discovered a weak spot in the malaria life cycle that could be exploited to prevent the disease from spreading.
The team found that female malaria parasites take on fat differently than male parasites.
And the protein gABCG2, which controls the transport of fat molecules, plays a key role in malaria parasite survival.
Phuong Tran, PhD, of Australia National University in Canberra, and his colleagues recounted these findings in Nature Communications.
The researchers noted that ATP-binding cassette transporters are known to play key roles in drug resistance. And the genome of the Plasmodium falciparum parasite encodes multiple members of this family, including gABCG2, which is transcribed predominantly in the gametocyte stage.
So the team used gene deletion and tagging to investigate the expression, localization, and function of gABCG2. They found that gABCG2 was only present in female gametocytes—in a single, lipid-like structure.
“Female parasites build a deposit of fat in a localized spot, which is controlled by gABCG2,” said study author Alexander Maier, PhD, of Australia National University.
“However, malaria genetically modified to have no gABCG2 did not accumulate fat in the same way, and crucially, struggled to survive in the mosquito.”
Cell lines in which gABCG2 was knocked out produced more gametocytes of both sexes, but they showed a reduction in cholesteryl esters, diacylglycerols, and triacylglycerols.
The researchers therefore concluded that gABCG2 regulates gametocyte numbers and the accumulation of neutral lipids, which are likely important for parasite development in the insect stages of the parasite life cycle.
Dr Tran said this discovery could lead to new malaria drugs based on current drugs that influence fat digestion.
“If we can target the molecule gABCG2 and kill the females, then we can stop the fertilization, which will stop the development and transmission of the disease,” he said. “It may even lead to a vaccine for malaria.” ![]()
Credit: Stuart Hay
Scientists believe they have discovered a weak spot in the malaria life cycle that could be exploited to prevent the disease from spreading.
The team found that female malaria parasites take on fat differently than male parasites.
And the protein gABCG2, which controls the transport of fat molecules, plays a key role in malaria parasite survival.
Phuong Tran, PhD, of Australia National University in Canberra, and his colleagues recounted these findings in Nature Communications.
The researchers noted that ATP-binding cassette transporters are known to play key roles in drug resistance. And the genome of the Plasmodium falciparum parasite encodes multiple members of this family, including gABCG2, which is transcribed predominantly in the gametocyte stage.
So the team used gene deletion and tagging to investigate the expression, localization, and function of gABCG2. They found that gABCG2 was only present in female gametocytes—in a single, lipid-like structure.
“Female parasites build a deposit of fat in a localized spot, which is controlled by gABCG2,” said study author Alexander Maier, PhD, of Australia National University.
“However, malaria genetically modified to have no gABCG2 did not accumulate fat in the same way, and crucially, struggled to survive in the mosquito.”
Cell lines in which gABCG2 was knocked out produced more gametocytes of both sexes, but they showed a reduction in cholesteryl esters, diacylglycerols, and triacylglycerols.
The researchers therefore concluded that gABCG2 regulates gametocyte numbers and the accumulation of neutral lipids, which are likely important for parasite development in the insect stages of the parasite life cycle.
Dr Tran said this discovery could lead to new malaria drugs based on current drugs that influence fat digestion.
“If we can target the molecule gABCG2 and kill the females, then we can stop the fertilization, which will stop the development and transmission of the disease,” he said. “It may even lead to a vaccine for malaria.” ![]()
Credit: Stuart Hay
Scientists believe they have discovered a weak spot in the malaria life cycle that could be exploited to prevent the disease from spreading.
The team found that female malaria parasites take on fat differently than male parasites.
And the protein gABCG2, which controls the transport of fat molecules, plays a key role in malaria parasite survival.
Phuong Tran, PhD, of Australia National University in Canberra, and his colleagues recounted these findings in Nature Communications.
The researchers noted that ATP-binding cassette transporters are known to play key roles in drug resistance. And the genome of the Plasmodium falciparum parasite encodes multiple members of this family, including gABCG2, which is transcribed predominantly in the gametocyte stage.
So the team used gene deletion and tagging to investigate the expression, localization, and function of gABCG2. They found that gABCG2 was only present in female gametocytes—in a single, lipid-like structure.
“Female parasites build a deposit of fat in a localized spot, which is controlled by gABCG2,” said study author Alexander Maier, PhD, of Australia National University.
“However, malaria genetically modified to have no gABCG2 did not accumulate fat in the same way, and crucially, struggled to survive in the mosquito.”
Cell lines in which gABCG2 was knocked out produced more gametocytes of both sexes, but they showed a reduction in cholesteryl esters, diacylglycerols, and triacylglycerols.
The researchers therefore concluded that gABCG2 regulates gametocyte numbers and the accumulation of neutral lipids, which are likely important for parasite development in the insect stages of the parasite life cycle.
Dr Tran said this discovery could lead to new malaria drugs based on current drugs that influence fat digestion.
“If we can target the molecule gABCG2 and kill the females, then we can stop the fertilization, which will stop the development and transmission of the disease,” he said. “It may even lead to a vaccine for malaria.” ![]()
Re-analyses of RCTs may reveal different conclusions

Credit: Darren Baker
A new study suggests that as many as a third of randomized clinical trials (RCTs) could be re-analyzed in ways that modify their conclusions.
The study also indicates that such re-analyses are extremely rare, due to many researchers’ unwillingness to share data.
“There is a real need for researchers to provide access to their raw data for others to analyze,” said John Ioannidis, MD, DSc, of the Stanford Prevention Research Center in California.
“Without this access, and possibly incentives to perform this work, there is increasing lack of trust in whether the results of published, randomized trials are credible and can be taken at face value.”
Dr Ioannidis and his colleagues used the MEDLINE database to evaluate re-analyses of RCTs and detailed their findings in JAMA. A related editorial is also available in the journal.
The team searched for articles written in English describing the re-analysis of raw data used in previously published RCTs. Meta-analyses were excluded from the study, as were studies testing a different hypothesis than the original trial.
The researchers screened nearly 3000 articles of potential interest and read the full text of 226. Of these, 37 were ultimately included in the study. Thirty-two of them had an overlap of at least 1 author from the original paper.
New conclusions
Thirteen of the re-analyses (35% of the total) came to conclusions that differed from those of the original trial with regard to who could benefit from the tested medication or intervention.
Three concluded that the patient population to treat should be different from the one recommended by the original study. One concluded that fewer patients should be treated. And the remaining 9 indicated that more patients should be treated.
The differences between the original RCTs and the re-analyses often occurred because the researchers conducting the re-analyses used different statistical or analytical methods, ways of defining outcomes, or ways of handling missing data.
For example, an RCT on the treatment of bleeding esophageal varices concluded that sclerotherapy reduced mortality but didn’t prevent rebleeding.
The re-analysis, which used a different statistical model of risk, suggested the treatment did prevent rebleeding but didn’t reduce mortality. The new conclusion suggested the intervention would be most appropriate for patients with rebleeding, rather than those at the highest risk of death from the condition.
Another study investigated the best way to deliver an erythropoiesis-stimulating medication to anemia patients by comparing a fixed dose administered once every 3 weeks with weight-based weekly dosing. In the re-analysis, the conclusion changed when investigators used an updated hemoglobin threshold level to determine when therapy should be initiated.
“The high proportion of re-analyses reaching different conclusions than the original papers may be partly an artifact,” Dr Ioannidis said. “By that I mean that, in the current environment, re-analyses that reach exactly the same results as the original would have great difficulty getting published.”
“However, making the raw data of trials available for re-analyses is essential not only for re-evaluating whether the original claims were correct, but also for using these data to perform additional analyses of interest and combined analyses.”
In this way, existing raw data could be used to explore new clinical questions and might occasionally eliminate the need to conduct new trials. ![]()

Credit: Darren Baker
A new study suggests that as many as a third of randomized clinical trials (RCTs) could be re-analyzed in ways that modify their conclusions.
The study also indicates that such re-analyses are extremely rare, due to many researchers’ unwillingness to share data.
“There is a real need for researchers to provide access to their raw data for others to analyze,” said John Ioannidis, MD, DSc, of the Stanford Prevention Research Center in California.
“Without this access, and possibly incentives to perform this work, there is increasing lack of trust in whether the results of published, randomized trials are credible and can be taken at face value.”
Dr Ioannidis and his colleagues used the MEDLINE database to evaluate re-analyses of RCTs and detailed their findings in JAMA. A related editorial is also available in the journal.
The team searched for articles written in English describing the re-analysis of raw data used in previously published RCTs. Meta-analyses were excluded from the study, as were studies testing a different hypothesis than the original trial.
The researchers screened nearly 3000 articles of potential interest and read the full text of 226. Of these, 37 were ultimately included in the study. Thirty-two of them had an overlap of at least 1 author from the original paper.
New conclusions
Thirteen of the re-analyses (35% of the total) came to conclusions that differed from those of the original trial with regard to who could benefit from the tested medication or intervention.
Three concluded that the patient population to treat should be different from the one recommended by the original study. One concluded that fewer patients should be treated. And the remaining 9 indicated that more patients should be treated.
The differences between the original RCTs and the re-analyses often occurred because the researchers conducting the re-analyses used different statistical or analytical methods, ways of defining outcomes, or ways of handling missing data.
For example, an RCT on the treatment of bleeding esophageal varices concluded that sclerotherapy reduced mortality but didn’t prevent rebleeding.
The re-analysis, which used a different statistical model of risk, suggested the treatment did prevent rebleeding but didn’t reduce mortality. The new conclusion suggested the intervention would be most appropriate for patients with rebleeding, rather than those at the highest risk of death from the condition.
Another study investigated the best way to deliver an erythropoiesis-stimulating medication to anemia patients by comparing a fixed dose administered once every 3 weeks with weight-based weekly dosing. In the re-analysis, the conclusion changed when investigators used an updated hemoglobin threshold level to determine when therapy should be initiated.
“The high proportion of re-analyses reaching different conclusions than the original papers may be partly an artifact,” Dr Ioannidis said. “By that I mean that, in the current environment, re-analyses that reach exactly the same results as the original would have great difficulty getting published.”
“However, making the raw data of trials available for re-analyses is essential not only for re-evaluating whether the original claims were correct, but also for using these data to perform additional analyses of interest and combined analyses.”
In this way, existing raw data could be used to explore new clinical questions and might occasionally eliminate the need to conduct new trials. ![]()

Credit: Darren Baker
A new study suggests that as many as a third of randomized clinical trials (RCTs) could be re-analyzed in ways that modify their conclusions.
The study also indicates that such re-analyses are extremely rare, due to many researchers’ unwillingness to share data.
“There is a real need for researchers to provide access to their raw data for others to analyze,” said John Ioannidis, MD, DSc, of the Stanford Prevention Research Center in California.
“Without this access, and possibly incentives to perform this work, there is increasing lack of trust in whether the results of published, randomized trials are credible and can be taken at face value.”
Dr Ioannidis and his colleagues used the MEDLINE database to evaluate re-analyses of RCTs and detailed their findings in JAMA. A related editorial is also available in the journal.
The team searched for articles written in English describing the re-analysis of raw data used in previously published RCTs. Meta-analyses were excluded from the study, as were studies testing a different hypothesis than the original trial.
The researchers screened nearly 3000 articles of potential interest and read the full text of 226. Of these, 37 were ultimately included in the study. Thirty-two of them had an overlap of at least 1 author from the original paper.
New conclusions
Thirteen of the re-analyses (35% of the total) came to conclusions that differed from those of the original trial with regard to who could benefit from the tested medication or intervention.
Three concluded that the patient population to treat should be different from the one recommended by the original study. One concluded that fewer patients should be treated. And the remaining 9 indicated that more patients should be treated.
The differences between the original RCTs and the re-analyses often occurred because the researchers conducting the re-analyses used different statistical or analytical methods, ways of defining outcomes, or ways of handling missing data.
For example, an RCT on the treatment of bleeding esophageal varices concluded that sclerotherapy reduced mortality but didn’t prevent rebleeding.
The re-analysis, which used a different statistical model of risk, suggested the treatment did prevent rebleeding but didn’t reduce mortality. The new conclusion suggested the intervention would be most appropriate for patients with rebleeding, rather than those at the highest risk of death from the condition.
Another study investigated the best way to deliver an erythropoiesis-stimulating medication to anemia patients by comparing a fixed dose administered once every 3 weeks with weight-based weekly dosing. In the re-analysis, the conclusion changed when investigators used an updated hemoglobin threshold level to determine when therapy should be initiated.
“The high proportion of re-analyses reaching different conclusions than the original papers may be partly an artifact,” Dr Ioannidis said. “By that I mean that, in the current environment, re-analyses that reach exactly the same results as the original would have great difficulty getting published.”
“However, making the raw data of trials available for re-analyses is essential not only for re-evaluating whether the original claims were correct, but also for using these data to perform additional analyses of interest and combined analyses.”
In this way, existing raw data could be used to explore new clinical questions and might occasionally eliminate the need to conduct new trials. ![]()
NICE recommends eculizumab for aHUS despite cost

Credit: Globovision
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending eculizumab (Soliris) to treat atypical hemolytic uremic syndrome (aHUS), despite the drug’s high cost.
NICE estimates that eculizumab will cost the National Health Service (NHS) up to £58 million in the first year, rising to £82 million after 5 years.
The drug is currently funded by NHS England through interim specialized commissioning arrangements.
Eculizumab is ‘breakthrough’ for aHUS
aHUS is an extremely rare but life-threatening disease that causes inflammation of blood vessels and the formation of blood clots throughout the body. Patients with aHUS are at constant risk of sudden and progressive damage to, and failure of, vital organs.
Roughly 10% to 15% of patients die in the initial, acute phase of aHUS. The majority of patients—up to 70%—develop end-stage kidney failure requiring dialysis. And 1 in 5 patients has aHUS affecting organs other than the kidneys, most commonly the brain or heart.
Eculizumab inhibits the disease by blocking pro-thrombotic and pro-inflammatory processes, which can lead to cellular damage in small blood vessels throughout the body, renal failure, and damage to other organs.
“Eculizumab radically improves the quality of life of the small number of people with aHUS,” said NICE Chief Executive Sir Andrew Dillon.
“From the available evidence and from the testimony of clinicians and patients, families, and carers, it is clear that eculizumab is a significant breakthrough in the management of aHUS. The drug offers people with the disease the possibility of avoiding end-stage renal failure, dialysis, and kidney transplantation, as well as other organ damage.”
Breakthrough comes with considerable cost
Eculizumab costs £3150 per 30 mL vial (excluding value-added tax). The net budget impact of eculizumab based on the developer’s predicted rate of uptake over a 5-year period is confidential.
However, to allow consultees and commentators to properly engage in the consultation process, NICE has prepared an illustration of the possible budget impact of eculizumab for aHUS, using information available in the public domain.
This is based on a treatment cost of £340,200 per adult patient in the first year (based on the acquisition cost of the drug and the recommended dosing for an adult), and assumes a patient cohort of 170, as estimated by NHS England in its interim commissioning policy.
If all of these adult patients with aHUS are treated with eculizumab, the budget impact for the first year would be £57.8 million.
If an additional 20 new patients are treated the following year (based on a worldwide incidence of 0.4 per million), the budget impact will rise to £62.5 million in year 2. That assumes all new patients are treated, and all existing patients continue to be treated at the maintenance cost of £327,600 per year.
Using the same assumptions, the budget impact will rise to £69 million in year 3 (190 existing and 20 new patients), £75 million in year 4 (210 existing and 20 new patients), and £82 million in year 5 (230 existing and 20 new patients).
Conditions of the recommendation
The expert committee advising NICE on eculizumab believes the budget impact of recommending the drug for aHUS in relation to the benefits it offers would be lower if the potential for dose adjustment and treatment discontinuation was taken into account, according to Sir Dillon.
“Therefore, the draft guidance recommends that eculizumab is funded only if important conditions are met,” he said. “These include coordinating the use of eculizumab through an expert center and putting in place systems for monitoring how many people are diagnosed with aHUS, how many receive the drug, at what dose, and for how long.”
“The program also needs to develop protocols for starting and stopping treatment with eculizumab for clinical reasons and introduce a research program to collect data to evaluate when stopping treatment or adjusting the dose of the drug might occur.”
Given that the budget impact of eculizumab for treating aHUS will be considerable, the draft guidance also recommends that NHS England and the drug’s developer, Alexion, should consider what opportunities might exist to reduce the overall cost of eculizumab to the NHS.
NICE has not yet issued final guidance to the NHS. These decisions may change after consultation. The public can comment on the preliminary recommendations, which will be available until midday on September 25.
Comments received during this consultation period will be considered by the advisory committee at its meeting in October and, following this meeting, the next draft guidance will be issued. ![]()

Credit: Globovision
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending eculizumab (Soliris) to treat atypical hemolytic uremic syndrome (aHUS), despite the drug’s high cost.
NICE estimates that eculizumab will cost the National Health Service (NHS) up to £58 million in the first year, rising to £82 million after 5 years.
The drug is currently funded by NHS England through interim specialized commissioning arrangements.
Eculizumab is ‘breakthrough’ for aHUS
aHUS is an extremely rare but life-threatening disease that causes inflammation of blood vessels and the formation of blood clots throughout the body. Patients with aHUS are at constant risk of sudden and progressive damage to, and failure of, vital organs.
Roughly 10% to 15% of patients die in the initial, acute phase of aHUS. The majority of patients—up to 70%—develop end-stage kidney failure requiring dialysis. And 1 in 5 patients has aHUS affecting organs other than the kidneys, most commonly the brain or heart.
Eculizumab inhibits the disease by blocking pro-thrombotic and pro-inflammatory processes, which can lead to cellular damage in small blood vessels throughout the body, renal failure, and damage to other organs.
“Eculizumab radically improves the quality of life of the small number of people with aHUS,” said NICE Chief Executive Sir Andrew Dillon.
“From the available evidence and from the testimony of clinicians and patients, families, and carers, it is clear that eculizumab is a significant breakthrough in the management of aHUS. The drug offers people with the disease the possibility of avoiding end-stage renal failure, dialysis, and kidney transplantation, as well as other organ damage.”
Breakthrough comes with considerable cost
Eculizumab costs £3150 per 30 mL vial (excluding value-added tax). The net budget impact of eculizumab based on the developer’s predicted rate of uptake over a 5-year period is confidential.
However, to allow consultees and commentators to properly engage in the consultation process, NICE has prepared an illustration of the possible budget impact of eculizumab for aHUS, using information available in the public domain.
This is based on a treatment cost of £340,200 per adult patient in the first year (based on the acquisition cost of the drug and the recommended dosing for an adult), and assumes a patient cohort of 170, as estimated by NHS England in its interim commissioning policy.
If all of these adult patients with aHUS are treated with eculizumab, the budget impact for the first year would be £57.8 million.
If an additional 20 new patients are treated the following year (based on a worldwide incidence of 0.4 per million), the budget impact will rise to £62.5 million in year 2. That assumes all new patients are treated, and all existing patients continue to be treated at the maintenance cost of £327,600 per year.
Using the same assumptions, the budget impact will rise to £69 million in year 3 (190 existing and 20 new patients), £75 million in year 4 (210 existing and 20 new patients), and £82 million in year 5 (230 existing and 20 new patients).
Conditions of the recommendation
The expert committee advising NICE on eculizumab believes the budget impact of recommending the drug for aHUS in relation to the benefits it offers would be lower if the potential for dose adjustment and treatment discontinuation was taken into account, according to Sir Dillon.
“Therefore, the draft guidance recommends that eculizumab is funded only if important conditions are met,” he said. “These include coordinating the use of eculizumab through an expert center and putting in place systems for monitoring how many people are diagnosed with aHUS, how many receive the drug, at what dose, and for how long.”
“The program also needs to develop protocols for starting and stopping treatment with eculizumab for clinical reasons and introduce a research program to collect data to evaluate when stopping treatment or adjusting the dose of the drug might occur.”
Given that the budget impact of eculizumab for treating aHUS will be considerable, the draft guidance also recommends that NHS England and the drug’s developer, Alexion, should consider what opportunities might exist to reduce the overall cost of eculizumab to the NHS.
NICE has not yet issued final guidance to the NHS. These decisions may change after consultation. The public can comment on the preliminary recommendations, which will be available until midday on September 25.
Comments received during this consultation period will be considered by the advisory committee at its meeting in October and, following this meeting, the next draft guidance will be issued. ![]()

Credit: Globovision
The UK’s National Institute for Health and Care Excellence (NICE) has issued a draft guidance recommending eculizumab (Soliris) to treat atypical hemolytic uremic syndrome (aHUS), despite the drug’s high cost.
NICE estimates that eculizumab will cost the National Health Service (NHS) up to £58 million in the first year, rising to £82 million after 5 years.
The drug is currently funded by NHS England through interim specialized commissioning arrangements.
Eculizumab is ‘breakthrough’ for aHUS
aHUS is an extremely rare but life-threatening disease that causes inflammation of blood vessels and the formation of blood clots throughout the body. Patients with aHUS are at constant risk of sudden and progressive damage to, and failure of, vital organs.
Roughly 10% to 15% of patients die in the initial, acute phase of aHUS. The majority of patients—up to 70%—develop end-stage kidney failure requiring dialysis. And 1 in 5 patients has aHUS affecting organs other than the kidneys, most commonly the brain or heart.
Eculizumab inhibits the disease by blocking pro-thrombotic and pro-inflammatory processes, which can lead to cellular damage in small blood vessels throughout the body, renal failure, and damage to other organs.
“Eculizumab radically improves the quality of life of the small number of people with aHUS,” said NICE Chief Executive Sir Andrew Dillon.
“From the available evidence and from the testimony of clinicians and patients, families, and carers, it is clear that eculizumab is a significant breakthrough in the management of aHUS. The drug offers people with the disease the possibility of avoiding end-stage renal failure, dialysis, and kidney transplantation, as well as other organ damage.”
Breakthrough comes with considerable cost
Eculizumab costs £3150 per 30 mL vial (excluding value-added tax). The net budget impact of eculizumab based on the developer’s predicted rate of uptake over a 5-year period is confidential.
However, to allow consultees and commentators to properly engage in the consultation process, NICE has prepared an illustration of the possible budget impact of eculizumab for aHUS, using information available in the public domain.
This is based on a treatment cost of £340,200 per adult patient in the first year (based on the acquisition cost of the drug and the recommended dosing for an adult), and assumes a patient cohort of 170, as estimated by NHS England in its interim commissioning policy.
If all of these adult patients with aHUS are treated with eculizumab, the budget impact for the first year would be £57.8 million.
If an additional 20 new patients are treated the following year (based on a worldwide incidence of 0.4 per million), the budget impact will rise to £62.5 million in year 2. That assumes all new patients are treated, and all existing patients continue to be treated at the maintenance cost of £327,600 per year.
Using the same assumptions, the budget impact will rise to £69 million in year 3 (190 existing and 20 new patients), £75 million in year 4 (210 existing and 20 new patients), and £82 million in year 5 (230 existing and 20 new patients).
Conditions of the recommendation
The expert committee advising NICE on eculizumab believes the budget impact of recommending the drug for aHUS in relation to the benefits it offers would be lower if the potential for dose adjustment and treatment discontinuation was taken into account, according to Sir Dillon.
“Therefore, the draft guidance recommends that eculizumab is funded only if important conditions are met,” he said. “These include coordinating the use of eculizumab through an expert center and putting in place systems for monitoring how many people are diagnosed with aHUS, how many receive the drug, at what dose, and for how long.”
“The program also needs to develop protocols for starting and stopping treatment with eculizumab for clinical reasons and introduce a research program to collect data to evaluate when stopping treatment or adjusting the dose of the drug might occur.”
Given that the budget impact of eculizumab for treating aHUS will be considerable, the draft guidance also recommends that NHS England and the drug’s developer, Alexion, should consider what opportunities might exist to reduce the overall cost of eculizumab to the NHS.
NICE has not yet issued final guidance to the NHS. These decisions may change after consultation. The public can comment on the preliminary recommendations, which will be available until midday on September 25.
Comments received during this consultation period will be considered by the advisory committee at its meeting in October and, following this meeting, the next draft guidance will be issued. ![]()
Recommendations for managing SCD lack supporting evidence

Credit: St Jude Children’s
Research Hospital
A new set of guidelines includes some strong recommendations for managing patients with sickle cell disease (SCD) that are not supported by high-quality evidence, according to researchers.
The group reviewed the medical literature to examine the quality of evidence supporting each of the guideline’s recommendations.
And they discovered a lack of randomized controlled trials in SCD patients that have left “extensive” gaps in our knowledge of the disease.
So while the guidelines do provide some helpful advice for managing patients with SCD, they also leave healthcare professionals with some uncertainties, according to the researchers.
The National Heart, Lung, and Blood Institute convened an expert panel to develop the guidelines, which are now available on the institute’s website.
Barbara P. Yawn, MD, of the Olmsted Medical Center in Rochester, Minnesota, and her colleagues examined the quality of evidence supporting the guidelines and reported their results in JAMA alongside a related editorial. Several examples of guideline recommendations and supporting evidence follow.
Health management recommendations
The guidelines strongly recommend oral penicillin prophylaxis twice daily until age 5 years in all children with HbSS to prevent invasive pneumococcal infection. And this recommendation is supported by moderate-quality evidence.
But the guidelines also strongly recommend referral to an ophthalmologist for dilated eye examination to screen for retinopathy beginning at age 10 years, and the quality of evidence supporting this recommendation is poor.
Acute SCD complications
The guidelines strongly recommend rapid initiation of parenteral opioids in adults and children with a vaso-occlusive crisis associated with severe pain, a suggestion supported by high-quality evidence.
However, the guidelines also strongly recommend treating SCD patients with acute chest syndrome with an intravenous cephalosporin, an oral macrolide antibiotic, and supplemental oxygen (to maintain oxygen saturation of >95%), as well as closely monitoring patients for bronchospasm, acute anemia, and hypoxemia. And this is supported by low-quality evidence.
Chronic complications
A strong recommendation supported by high-quality evidence is to treat avascular necrosis with analgesics and consult physical therapy and orthopedic departments for assessment and follow-up.
A strong recommendation supported by low-quality evidence is to evaluate all children and adults with SCD and intermittent or chronic hip pain for avascular necrosis by history, physical examination, radiography, and magnetic resonance imaging, as needed.
Use of hydroxyurea
Dr Yawn and her colleagues found that strong recommendations for hydroxyurea are all supported by moderate- or high-quality evidence.
A strong recommendation supported by high-quality evidence is to initiate hydroxyurea in adults who have at least 3 moderate-to-severe pain crises associated with SCD during a 12-month period.
A strong recommendation supported by moderate-quality evidence is to initiate hydroxyurea in adults who have sickle cell-associated pain that interferes with daily activities and quality of life.
Transfusion therapy
For this category, the only strong recommendation supported by high-quality evidence is to transfuse a child with a transcranial Doppler reading greater than 200 cm/s.
The guidelines strongly recommend transfusing red blood cells in adults and children with SCD to bring the hemoglobin level to 10 g/dL prior to undergoing a surgical procedure involving general anesthesia, but this is supported by moderate-quality evidence.
A strong recommendation supported by low-quality evidence is to perform an exchange transfusion in a patient with symptomatic, severe acute chest syndrome (defined by an oxygen saturation less than 90% despite supplemental oxygen).
Conclusions
Dr Yawn and her colleagues said this investigation confirms that developing guidelines for managing SCD is challenging because high-quality evidence is limited in virtually every area related to SCD management.
Therefore, the guidelines leave healthcare professionals with some uncertainties about managing SCD patients. But the researchers hope their analysis will prompt new research that might provide more definitive guidance. ![]()

Credit: St Jude Children’s
Research Hospital
A new set of guidelines includes some strong recommendations for managing patients with sickle cell disease (SCD) that are not supported by high-quality evidence, according to researchers.
The group reviewed the medical literature to examine the quality of evidence supporting each of the guideline’s recommendations.
And they discovered a lack of randomized controlled trials in SCD patients that have left “extensive” gaps in our knowledge of the disease.
So while the guidelines do provide some helpful advice for managing patients with SCD, they also leave healthcare professionals with some uncertainties, according to the researchers.
The National Heart, Lung, and Blood Institute convened an expert panel to develop the guidelines, which are now available on the institute’s website.
Barbara P. Yawn, MD, of the Olmsted Medical Center in Rochester, Minnesota, and her colleagues examined the quality of evidence supporting the guidelines and reported their results in JAMA alongside a related editorial. Several examples of guideline recommendations and supporting evidence follow.
Health management recommendations
The guidelines strongly recommend oral penicillin prophylaxis twice daily until age 5 years in all children with HbSS to prevent invasive pneumococcal infection. And this recommendation is supported by moderate-quality evidence.
But the guidelines also strongly recommend referral to an ophthalmologist for dilated eye examination to screen for retinopathy beginning at age 10 years, and the quality of evidence supporting this recommendation is poor.
Acute SCD complications
The guidelines strongly recommend rapid initiation of parenteral opioids in adults and children with a vaso-occlusive crisis associated with severe pain, a suggestion supported by high-quality evidence.
However, the guidelines also strongly recommend treating SCD patients with acute chest syndrome with an intravenous cephalosporin, an oral macrolide antibiotic, and supplemental oxygen (to maintain oxygen saturation of >95%), as well as closely monitoring patients for bronchospasm, acute anemia, and hypoxemia. And this is supported by low-quality evidence.
Chronic complications
A strong recommendation supported by high-quality evidence is to treat avascular necrosis with analgesics and consult physical therapy and orthopedic departments for assessment and follow-up.
A strong recommendation supported by low-quality evidence is to evaluate all children and adults with SCD and intermittent or chronic hip pain for avascular necrosis by history, physical examination, radiography, and magnetic resonance imaging, as needed.
Use of hydroxyurea
Dr Yawn and her colleagues found that strong recommendations for hydroxyurea are all supported by moderate- or high-quality evidence.
A strong recommendation supported by high-quality evidence is to initiate hydroxyurea in adults who have at least 3 moderate-to-severe pain crises associated with SCD during a 12-month period.
A strong recommendation supported by moderate-quality evidence is to initiate hydroxyurea in adults who have sickle cell-associated pain that interferes with daily activities and quality of life.
Transfusion therapy
For this category, the only strong recommendation supported by high-quality evidence is to transfuse a child with a transcranial Doppler reading greater than 200 cm/s.
The guidelines strongly recommend transfusing red blood cells in adults and children with SCD to bring the hemoglobin level to 10 g/dL prior to undergoing a surgical procedure involving general anesthesia, but this is supported by moderate-quality evidence.
A strong recommendation supported by low-quality evidence is to perform an exchange transfusion in a patient with symptomatic, severe acute chest syndrome (defined by an oxygen saturation less than 90% despite supplemental oxygen).
Conclusions
Dr Yawn and her colleagues said this investigation confirms that developing guidelines for managing SCD is challenging because high-quality evidence is limited in virtually every area related to SCD management.
Therefore, the guidelines leave healthcare professionals with some uncertainties about managing SCD patients. But the researchers hope their analysis will prompt new research that might provide more definitive guidance. ![]()

Credit: St Jude Children’s
Research Hospital
A new set of guidelines includes some strong recommendations for managing patients with sickle cell disease (SCD) that are not supported by high-quality evidence, according to researchers.
The group reviewed the medical literature to examine the quality of evidence supporting each of the guideline’s recommendations.
And they discovered a lack of randomized controlled trials in SCD patients that have left “extensive” gaps in our knowledge of the disease.
So while the guidelines do provide some helpful advice for managing patients with SCD, they also leave healthcare professionals with some uncertainties, according to the researchers.
The National Heart, Lung, and Blood Institute convened an expert panel to develop the guidelines, which are now available on the institute’s website.
Barbara P. Yawn, MD, of the Olmsted Medical Center in Rochester, Minnesota, and her colleagues examined the quality of evidence supporting the guidelines and reported their results in JAMA alongside a related editorial. Several examples of guideline recommendations and supporting evidence follow.
Health management recommendations
The guidelines strongly recommend oral penicillin prophylaxis twice daily until age 5 years in all children with HbSS to prevent invasive pneumococcal infection. And this recommendation is supported by moderate-quality evidence.
But the guidelines also strongly recommend referral to an ophthalmologist for dilated eye examination to screen for retinopathy beginning at age 10 years, and the quality of evidence supporting this recommendation is poor.
Acute SCD complications
The guidelines strongly recommend rapid initiation of parenteral opioids in adults and children with a vaso-occlusive crisis associated with severe pain, a suggestion supported by high-quality evidence.
However, the guidelines also strongly recommend treating SCD patients with acute chest syndrome with an intravenous cephalosporin, an oral macrolide antibiotic, and supplemental oxygen (to maintain oxygen saturation of >95%), as well as closely monitoring patients for bronchospasm, acute anemia, and hypoxemia. And this is supported by low-quality evidence.
Chronic complications
A strong recommendation supported by high-quality evidence is to treat avascular necrosis with analgesics and consult physical therapy and orthopedic departments for assessment and follow-up.
A strong recommendation supported by low-quality evidence is to evaluate all children and adults with SCD and intermittent or chronic hip pain for avascular necrosis by history, physical examination, radiography, and magnetic resonance imaging, as needed.
Use of hydroxyurea
Dr Yawn and her colleagues found that strong recommendations for hydroxyurea are all supported by moderate- or high-quality evidence.
A strong recommendation supported by high-quality evidence is to initiate hydroxyurea in adults who have at least 3 moderate-to-severe pain crises associated with SCD during a 12-month period.
A strong recommendation supported by moderate-quality evidence is to initiate hydroxyurea in adults who have sickle cell-associated pain that interferes with daily activities and quality of life.
Transfusion therapy
For this category, the only strong recommendation supported by high-quality evidence is to transfuse a child with a transcranial Doppler reading greater than 200 cm/s.
The guidelines strongly recommend transfusing red blood cells in adults and children with SCD to bring the hemoglobin level to 10 g/dL prior to undergoing a surgical procedure involving general anesthesia, but this is supported by moderate-quality evidence.
A strong recommendation supported by low-quality evidence is to perform an exchange transfusion in a patient with symptomatic, severe acute chest syndrome (defined by an oxygen saturation less than 90% despite supplemental oxygen).
Conclusions
Dr Yawn and her colleagues said this investigation confirms that developing guidelines for managing SCD is challenging because high-quality evidence is limited in virtually every area related to SCD management.
Therefore, the guidelines leave healthcare professionals with some uncertainties about managing SCD patients. But the researchers hope their analysis will prompt new research that might provide more definitive guidance. ![]()
Statins do not worsen diabetes microvascular complications, may be protective
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Pharmacoepidemiological studies need cautious interpretation and can be regarded only as hypothesis generating; Dr. Nielsen and Dr. Nordestgaard are appropriately circumspect.
The study has many strengths, such as its size, the quality and coverage of the national registry, and external validity – i.e., statin use was associated with an increased risk of diabetes, an effect size similar to that reported in randomized trials of statins. However, important weaknesses of the study include the absence of data on important predictors of microvascular disease – e.g., hemoglobin A1c, urine albumin, and blood pressure. For now, any benefit of statins on microvascular complications remains unproven.
Dr. David Preiss, of the University of Glasgow (Scotland), is cochair of the Scottish Lipid Forum, whose annual meeting is supported by grants from pharmaceutical companies including MSD, AstraZeneca, and Sanofi. The remarks are taken from his accompanying commentary (Lancet Diabetes Endocrinol. 2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
Contrary to expectations, statin use before the development of type II diabetes did not worsen microvascular complications such as retinopathy, neuropathy, and gangrene of the foot.
In fact, despite concerns that statins have been seen to increase glucose levels and the risk of diabetes development, they may provide a protective effect from these conditions in newly developed diabetic patients, according to an analysis of data from more than 60,000 individuals in the Danish Patient Registry.
"The cumulative incidences of diabetic retinopathy, diabetic neuropathy, and gangrene were reduced in statin users compared with non–statin users, but [the] risk of diabetic nephropathy was similar for all patients with diabetes," stated Dr. Sune F. Nielsen, Ph.D., and Dr. Børge G. Nordestgaard of the Herlev Hospital, Copenhagen University Hospital. However, they did find that statin use, as previously seen, did significantly increase the risk of developing diabetes in the first place. Their study was published online Sept. 10 in the Lancet Diabetes & Endocrinology (2014 Sept. 10 [doi: 10.1016/S2213-8587(14)70173-1]).
The researchers performed a nested matched study of all men and women living in Denmark who were diagnosed with incident diabetes during 1996-2009 at age 40 years or older, and assessed their outcomes through use of the Danish Civil Registration System, the Danish Patient Registry, and the Danish Registry of Medicinal Product Statistics. After exclusions, 62,716 patients with diabetes were randomly selected for the study: 15,679 statin users and 47,037 non–statin users. The primary outcome was the incidence of diabetic retinopathy, diabetic neuropathy, diabetic nephropathy, and gangrene of the foot. The design "captured 100% of individuals in Denmark who had ever used a statin within the time frame of the study."
Follow-up was censored at date of death for 9,560 individuals. During 215,725 person-years of follow-up, diabetic retinopathy was recorded in 2,866 patients, diabetic neuropathy in 1,406, diabetic nephropathy in 1,248, and gangrene of the foot in 2,392.
Over a median follow-up of 2.7 years, statin users were significantly less likely to be diagnosed with diabetic neuropathy (hazard ratio, 0.66; 95% confidence interval, 0.57-0.75: P less than .0001) and diabetic retinopathy (HR, 0.60; 95% CI 0.54-0.66: P less than .0001) than were those who had not received statins. However, no difference was noted in the incidence of diabetic nephropathy (HR, 0.97; 95% CI, 0.85-1.10; P = .62).
In contrast, the researchers found that statin use significantly increased the risk of developing diabetes in people who did not have the disease when the study began. When they compared a random selection of 272,994 non–statin users with 90,998 statin users, the multivariable adjusted hazard ratio for the risk of developing diabetes was 1.17 (95% CI, 1.14-1.21). These results are similar to those seen in previous randomized studies of statin use.
"In conclusion, we found no evidence that statin use is associated with an increased risk of microvascular disease; this result is important and clinically reassuring on its own. Whether or not statins are protective against some forms of microvascular disease, a possibility raised by these data, and by which mechanism, will need to be addressed in studies similar to ours, or in Mendelian randomization studies," said Dr. Nielsen and Dr. Nordestgaard. "Ideally, however, this question should be addressed in the setting of a randomized controlled trial," they added.
Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
FROM THE LANCET DIABETES & ENDOCRINOLOGY
Key clinical point: Statins may protect against microvascular complications in diabetes patients.
Major finding: Statin users were significantly less likely to be diagnosed with diabetic neuropathy (HR, 0.66) and diabetic retinopathy (HR, 0.60) than non–statin users.
Data source: A registry study compared 62,716 patients with diabetes: 15,679 statin users and 47,037 non–statin users.
Disclosures: Dr. Nordestgaard has received consultancy fees or lecture honoraria from AstraZeneca, Pfizer, and Merck, and Dr. Nielsen declared no competing interests. The work was supported by Herlev Hospital, Copenhagen University Hospital.
NHLBI expert panel issues guideline on sickle cell disease
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
Yawn et al. have made a monumental effort to produce practical, evidence-based guidelines, but they were hampered at every turn by a pervasive lack of good quality evidence on which to base their recommendations. Still missing from this guideline are suggestions for how often and when to screen for kidney disease, how to screen for and treat the common clinical problem of asthma-like symptoms (when standard therapies are contraindicated in SCD), how to advocate for patients with the common sequelae of silent cerebral infarcts, or when to consider hematopoietic stem-cell transplantation.
The expert panel also failed to include representatives from the people most affected by SCD: patients and their families. Failure to listen to the perspective of the families, understand which of these recommendations are important to them, and deal with the obstacles families face in implementing the recommendations is a critically important omission.
Dr. Michael R. DeBaun is in the department of pediatrics at the Vanderbilt-Meharry Center of Excellence in Sickle Cell Disease, Nashville. He made his remarks in an editorial accompanying Dr. Yawn’s report (JAMA 2014:312;1004-5). Dr. DeBaun reported no financial conflicts of interest.
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
The "much anticipated" guideline to help primary care and emergency clinicians improve the management of sickle cell disease includes a consensus treatment protocol for implementing hydroxyurea therapy and more detailed guidance regarding long-term transfusion therapy, according to a summary report published online September 9 in Journal of the American Medical Association.
Sickle cell disease (SCD), a life-threatening genetically transmitted disorder affecting 70,000-100,000 Americans, is associated with a wide array of complex acute and chronic complications that require immediate medical attention. But high-quality data on which to base management decisions are sorely lacking, and clinicians get little in the way of guidance from existing recommendations. One result is that "the two most widely available disease-modifying therapies, hydroxyurea and long-term transfusions, are underused, and hematopoietic stem cell transplantation, the only curative approach, has been used in only a small proportion of affected individuals," said Dr. Barbara P. Yawn and her associates on the National Heart, Lung, and Blood Institute expert panel that issued the summary report.
Even this guideline is somewhat rudimentary due to the dearth of good data "in virtually every area related to SCD management," and cannot help but leave "many uncertainties for health professionals caring for individuals with SCD." But it is hoped that this guideline will furnish a critical foundation for future research and will now begin "to facilitate improved and more accessible care for all affected individuals," said Dr. Yawn, director of research at Olmsted Medical Center, Rochester, Minn., and her associates.
The guideline is based on an extensive literature review of more than 13,000 abstracts and articles, which was winnowed to 1,583 original studies regarding SCD. From this, a team of health care professionals in family medicine, internal medicine, pediatric and adult hematology, psychiatry and mental health, transfusion medicine, obstetrics and gynecology, maternal/fetal medicine, and emergency department nursing compiled the guideline as well as the summary, entitled Evidence-Based Management of Sickle Cell Disease: Expert Panel Report 2014 (JAMA 2014 September 9 [doi:10.1001/jama.2014.10517]).
In addition to establishing a protocol for implementing hydroxyurea therapy, the guideline addresses changes in pneumococcal vaccination recommendations for adults and children; annual transcranial Doppler screening coupled with long-term transfusion therapy when necessary to prevent stroke in children aged 2-16 years; rapid initiation of opioids for severe pain during vasoocclusive crises; analgesics and physical therapy for avascular necrosis; ACE inhibitor treatment for adults with microalbuminuria; referral to specialists for screening and treatment of proliferative retinopathy; echocardiography to assess signs of pulmonary hypertension; and monitoring for iron overload in patients receiving transfusion therapy.
Both the summary report and the full guideline are available at http://www.nhlbi.nih.gov/health-pro/guidelines/sickle-cell-disease-guidelines/.
FROM JAMA
Major finding: The two most widely available disease-modifying therapies for SCD, hydroxyurea and long-term transfusions, are underused, in large part because no evidence-based treatment protocols have been devised until now.
Data source: A review of the literature and compilation of management guidelines "to assist health care professionals in the management of common issues of sickle cell disease."
Disclosures: The National Heart, Lung, and Blood Institute sponsored the development of this guideline. All expert panel members served voluntarily. Many reported numerous ties to industry sources.
Facial Rejuvenation: Combining Cosmeceuticals With Cosmetic Procedures
Today’s cosmetic patient wants to look more youthful every day without spending a lot of money, feeling any pain, or having any postprocedure downtime. With continued technological improvements, dermatologists have been able to provide our patients with the more youthful appearance they desire; however, many of these procedures still are costly, painful, and may require some downtime. New cosmeceutical therapies can be used as adjuncts to these procedures, making antiaging regimens less painful for patients and requiring less postprocedure healing time. In this article, the use of cosmeceuticals in conjunction with chemical peels, lasers, and injectables will be discussed.
Chemical Peels
Chemical peels are used to create an injury of specific skin depth with a goal of stimulating new skin growth and improving surface texture and appearance. They generally are classified as superficial, medium, or deep according to the depth of action. Currently available agents for superficial chemical peels include α-hydroxy acids (AHAs)(eg, glycolic acid [GA]) and β-hydroxy acids (BHAs)(eg, salicylic acid). β-Lipohydroxy acid (up to 10%), a derivative of salicylic acid, is widely used in Europe. Trichloroacetic acid (TCA) can be used for superficial peels (10%–20%) and for medium-depth peels (35%). Combination peels such as Monheit combination (Jessner solution plus TCA), Brody combination (solid CO2 plus TCA), Coleman combination (GA 70% plus TCA), and Jessner solution with GA can be used as medium-depth peels. Deep peels typically are performed with phenol-based solutions, including the Baker-Gordon phenol peel and the Hetter peel (phenol or croton oil peel).
Specific agents for chemical peels should be selected based on the disorder being treated and should be administered using an appropriate peel depth determined by the histologic level or severity of skin pathology to maximize treatment success.1 However, other considerations, such as skin characteristics, area of skin to be treated, safety concerns, healing time, and patient adherence also should be taken into account to achieve the best overall results. Although many of the deeper peels recently have been replaced by laser-based ablative treatments, superficial to medium-depth peels still are commonly used in the treatment of fine lines, uneven texture, and dyspigmentation.2
Superficial peels are reasonably safe and well tolerated, usually with only mild discomfort (eg, transient burning, irritation, erythema). Scarring, postinflammatory hyperpigmentation (PIH), and infection are rare with superficial peels.1 Postinflammatory hyperpigmentation can be exacerbated by sun exposure, making it important for patients to be educated about sun protection and closely monitored during the recovery phase. In medium and deep peels, lines of demarcation related to the administration technique can occur. Feathering the chemical peel solution at junctions with nonpeeled skin can help to avoid this effect.1 Side effects associated with deeper chemical peels can include pigmentary changes, infections, allergic reactions, improper healing, hypersensitivity, and underlying disease exacerbation. The best way to prevent complications is to identify patients who are at risk and maintain an appropriate peel depth that balances efficacy with known adverse events.1
Many adjunctive agents (eg, AHAs, BHAs, retinoids, skin-bleaching preparations) can be used to enhance chemical peels and decrease the incidence of PIH. α-Hydroxy acids and BHAs can be beneficial when applied prior to chemical peels. Moisturizers containing AHAs and BHAs can be used for 2 to 3 weeks before superficial or medium-depth chemical peels.2 These agents cause thinning of the stratum corneum, thereby creating a more uniform cutaneous surface and allowing for deeper penetration of the chemical peeling agent. Retinoids also are superior prepeeling agents; however, retinoids also can increase the likelihood of irritation, which can be minimized by discontinuing retinoids for 1 week following chemical peels.2 A combination of chemical peels and topical bleaching agents has been shown to be effective in treating hyperpigmentation. The chemical peel causes superficial exfoliation, which allows the lightening agent to penetrate more deeply.2
Hydroquinone (HQ) is the gold standard for improvement of existing pigmentation.3 It is one of the most effective inhibitors of melanogenesis both in vitro and in vivo and is widely used for the treatment of melanosis and other hyperpigmentary disorders. It is widely accepted that the depigmentation activity of HQ may partly be related to its ability to act as an alternate substrate of tyrosinase, thereby competing for tyrosine oxidation in active melanocytes.3 Using HQ at a 4% concentration and combining it with retinoids is quite efficacious.2 Other commonly used depigmenting agents include kojic acid, ascorbic acid (vitamin C), and niacinamide, which often can be used as adjuncts with or maintenance therapy after HQ treatment.2,3
The risk for PIH is imminent for chemical peels and cosmetic laser treatments; therefore, it is crucial to educate patients about the importance of daily and aggressive sun protection. There are several methods of reducing or eliminating postprocedure melanin formation, such as inhibiting tyrosinase synthesis, using complex copper to inhibit tyrosinase function, eliminating oxidation reactions that lead to polymer formation, slowing down the transfer of melanosomes to keratinocytes, or acting upstream on the hormone that stimulates melanogenesis.3 Most of the depigmenting agents presently on the market act by inhibiting tyrosinase via one of these mechanisms.
Skin-lightening agents are primarily formulated as emulsions that have a higher aesthetic appeal. Many of the ingredients get better dispersions with emulsions, which is an added feature of these products. Recently, gel-based formulations also are being considered for their suitability in certain skin types. Efficacy studies for skin-lightening formulations are being carried out through clinical trials that utilize devices that measure skin color in addition to the dermatologist’s assessment.4 Other skin parameters (eg, moisturization, texture, barrier integrity, pH) also are being evaluated to give physicians a picture of skin health after the use of skin-lightening agents. With advances in technology and measurement techniques, it is becoming easier to identify the efficacy of these formulations in different skin types.4
Lasers
The ultimate goal of laser therapy often is to improve the canvas and color of the skin. Ablative laser resurfacing is reliably the most effective procedure for sun-damaged skin.2 This technique causes thermally induced full-thickness epidermal and dermal denudation, which in turn facilitates cytokine-led dermal collagen formation and reepithelialization. Various nonablative modalities also are used for treating photodamaged skin. The epidermis remains unaffected by these nonablative methods, thus decreasing the need for extensive wound care and downtime that is required with ablative treatments. Combining nonablative laser treatments with topical cosmeceuticals has been proven more effective than using either method alone.2 The use of topical retinoids prior to ablative laser resurfacing often results in remarkably faster postprocedure healing and reepithelialization (Figure). Retinoids are best applied nightly for at least 2 weeks and optimally for 3 months before ablative laser treatment. Application should be discontinued for 1 week immediately prior to the procedure.

|

|
| Before (A) and after (B) treatment with a fractional laser in combination with a pre- and postprocedure skin care regimen consisting of retinoids and sunscreen. |
Topical retinoids also are effective in reducing erythema and increasing dermal thickness after nonablative treatments. When used prior to laser treatments, retinoids have been shown to decrease the risk for postoperative milia and hyperpigmentation as well as to allow for better penetration of the laser beam secondary to a thinner stratum corneum.2 Following ablative resurfacing, retinoid use should be discontinued for several weeks to allow for reepithelialization and adequate healing.
Postprocedure Wound Healing
Most of the recommended products that help decrease postprocedural inflammation are cosmeceuticals containing both antioxidants and anti-inflammatories to help decrease redness and inflammation, including various barrier repair moisturizers. Restoring barrier integrity improves the overall appearance of the skin. The ingredients normally recommended in barrier repair moisturizers are epidermal lipids such as ceramides; hyaluronic acid (HA), which is a humectant; and occlusives for patients with very dry skin. Some of the ingredients in over-the-counter cosmeceuticals that can help decrease redness and inflammation include vitamin C, vitamin E, and vitamin B or niacinamide, which will help plump the barrier and also have anti-inflammatory properties. Additionally, polyphenolic flavonoids such as soy and green tea can help decrease inflammation, along with a number of other organic ingredients, such as caffeine, feverfew, and licorice.5 If topical vitamin C is being considered for postprocedure use, the non–ascorbic acid variant should be administered. The magnesium ascorbyl phosphate and ascorbyl palmitate forms of vitamin C have a neutral pH and tend to be better tolerated by patients.
In addition to current prescription and over-the-counter cosmeceuticals used for postprocedure irritation and inflammation, copper peptides and other well-tolerated and effective naturally occurring compounds are being investigated and tried. Copper is a biocide that regulates keratinocyte integrins for epithelization and extracellular matrix remodeling. The extracellular matrix consists of the structural fibrillar collagens and is remodeled or degraded by matrix metalloproteinases (MMPs) that facilitate epithelization. The predominant classes of MMPs include collagenases (ie, MMP-1) and gelatinases (ie, MMP-2, MMP-9) that degrade interstitial collagen and basement membrane proteins.6 The MMPs are endogenously inhibited by tissue inhibitors of metalloproteinases (TIMPs). Copper is a cofactor to lysyl oxidase, which cross-links collagen and stimulates expression of MMP-2 and collagen in a complex with a matrix-derived tripeptide (glycyl-histidyl-lysine or Gly-His-Lys [GHK]) in fibroblasts.6 Much attention has been focused on the tripeptides, such as GHK and Gly-Gly-His, and their copper complexes, which have high activity and good skin tolerance. These complexes have been shown to play a physiological role in the process of wound healing, tissue repair, and skin inflammation. Gly-Gly-His, GHK, copper chloride, and their copper complexes decrease tumor necrosis factor α–dependent IL-6 secretion in fibroblasts.7 IL-6 is crucial for normal wound healing, skin inflammation, and UVB-induced erythema. Because of their anti-inflammatory properties, these copper peptides could potentially be used in place of corticosteroids or nonsteroidal anti-inflammatory drugs, which have more side effects.
Botulinum Neurotoxin and Other Injectable Fillers
Acetyl Hexapeptide-3: A Topical Complement to Botulinum Neurotoxin
Acetyl hexapeptide-3 (Ac-Glu-Glu-Met-Gln-Arg-Arg-NH2) was discovered when looking for a less toxic variation of botulinum neurotoxin (BoNT) to treat aging skin.8 It is patterned from the N-terminal end of the synaptosome-associated protein of molecular weight 25 kDa (SNAP-25), which is essential for docking and fusion of synaptic vesicles to the presynaptic membrane for acetylcholine release.9 It prevents formation and stability of the soluble N-ethylmaleimide-sensitive factor attachment protein receptors (SNARE) complex, inhibiting vesicle docking and calcium-dependent catecholamine exocytosis.8 It also has been found to substantially inhibit the repetitive muscular contraction of facial expression similar to BoNT type A but with somewhat lower efficacy. Acetyl hexapeptide-3 was shown to inhibit 30% of total catecholamine exocytosis and had a remarkable capacity to permeate the skin.10 Thus this topical form of BoNT is a useful complement to intramuscular BoNT.
Studies showing the efficacy and safety of acetyl hexapeptide-3 have demonstrated reductions in wrinkle intensity, mainly in the lateral periorbital areas. In one early study, 10 women applied an emulsion containing 10% of the hexapeptide to one lateral periorbital region and the same emulsion without the hexapeptide to the contralateral side, both twice daily for 30 days.10 A 30% decrease in the depth of skin wrinkles was seen on the hexapeptide side compared with a 10% decrease in the depth of wrinkles on the side treated without hexapeptide. No irritation or toxicity was noted.10 In another trial, 10 women applied an acetyl hexapeptide-3 cream 5% twice daily to lateral periorbital rhytides, with a 27% improvement in wrinkle depth after a 30-day treatment period.9 A double-blind, placebo-controlled study of 60 women assessing the safety and efficacy of topical hexapeptide showed a total antiwrinkle efficacy of 48.9% on the side treated with an emulsion containing 10% of the hexapeptide compared with 0% efficacy on the placebo side.8 Similar to Blanes-Mira et al,10 no adverse events such as skin irritation or toxicity were seen.8 In all of these studies, wrinkle depth was measured by silicone replica analysis.
Topical acetyl hexapeptide-3 is effective in decreasing wrinkles, and its best use will likely be as an adjunct to intramuscular BoNT, as the intramuscular form likely has higher efficacy with the toxin injected directly into the target muscle; however, patients who want the effects of BoNT without the pain of injections may choose to use topical acetyl hexapeptide-3 alone. Patients who do use acetyl hexapeptide-3 as a complement to their intramuscular BoNT regimen may not need as many units of BoNT with each treatment or may not need certain areas injected as often, leading to fewer injections and less pain with each visit. Skin irritation was not seen as a side effect in these trials. Additionally, the topical form has insignificant acute toxicity (≥2000 mg/kg) compared to BoNT type A (20 ng/kg), and genotoxicity was not seen with testing, making it a safe complementary option to an injectable regimen.8
Topical Hyaluronic Acid: A Complement to Injectable Fillers
Hyaluronic acid (HA) is a glycosaminoglycan found in the extracellular matrix of the skin that greatly contributes to tissue hydration. Additionally, it plays a crucial role in the synthesis of extracellular matrix molecules and epidermal cell interaction with the environment.11 The water-binding capacity of HA approximates 1000 times its volume or 6 L of water per gram of HA; however, once an individual reaches adulthood, the amount of HA decreases to 5% of baseline levels, thus contributing to xerosis, loss of skin elasticity, and atrophy.11,12 Although photoaged skin can have increased glycosaminoglycans due to an increase in chondroitin sulfate proteoglycans, they are abnormally deposited on elastotic material in the superficial dermis rather than diffusely scattered, as seen in youthful skin.12
Many topical antiaging products contain HA, though evidence for efficacy in reducing wrinkles has been lacking, along with concerns that HA cannot penetrate the skin. This concern stems from the fact that the original molecule is 3000 nm in diameter and the intercellular space is only 15 to 50 nm. This space is only 6 to 10 nm at the hyaline membrane. Recently, scientists in Japan found a way to reduce the size of HA molecules to 5 nm (nano-HA) without changing its structure. A study of 33 women who applied the topical nano-HA twice daily for 8 weeks to one periorbital area while the contralateral side was left untreated showed improved hydration of the treated side that continued to increase when measured at 2, 4, and 8 weeks using corneometry.11 Roughness decreased and elasticity increased after week 2, which were maintained throughout the study. Additionally, erythema was measured using a chroma meter, which was found to have decreased at day 57 versus day 1.11 An earlier study by Pavicic et al12 evaluated the efficacy of topical hyalu-ronan 0.1% formulations of different molecular weights—50, 130, 300, 800, or 2000 kDa—in the periocular area. A randomized group of 76 women were treated twice daily for 2 months with HA cream on one side of the periocular area and placebo cream on the other. With regard to antiwrinkle properties, only the 50- and 130-kDa HA formulations showed marked effects compared with placebo after 2 months.12
Topical HA would be an effective addition to an antiwrinkle regimen, especially in patients who are averse to needles or are just starting to get wrinkles and are looking for a noninvasive therapy. Additionally, it would be beneficial for patients who have an injectable filler and BoNT regimen, as these patients will be able to target wrinkles simultaneously with both topical cosmeceuticals and injectables and likely will need fewer units of BoNT and/or filler and possibly fewer injections over time, which translates to decreased pain and adverse outcomes for patients.
Conclusion
The myriad of options dermatologists have to offer patients for cosmetic enhancement provides alternatives for patients who have contraindications to certain treatments, are needle averse, or have lifestyles that do not afford them a great deal of postprocedural healing time. Being knowledgeable about these options and how to combine them for improved outcomes is essential to any cosmetic practice.
1. Rendon MI, Berson DS, Cohen JL, et al. Evidence and considerations in the application of chemical peels in skin disorders and aesthetic resurfacing. J Clin Aesthet Dermatol. 2010;3:32-43.
2. Lupo MP, Jacob LG. Cosmeceuticals for enhancing cosmetic procedures. In: Farris PK, ed. Cosmeceuticals and Cosmetic Practice. Oxford, United Kingdom: Wiley-Blackwell; 2014:268-276.
3. Gruber JV, Holtz R. Examining the impact of skin lighteners in vitro [published online ahead of print April 28, 2013]. Oxid Med Cell Longev. 2013;2013:702120.
4. Antonio JR, Antonio CR, Cardeal ILS, et al. Nanotechnology in dermatology. An Bras Dermatol. 2014;89:126-136.
5. Ganceviciene R, Liakou AI, Theodoridis A, et al. Skin anti-aging strategies. Dermatoendocrinol. 2012;4:308-319.
6. Gruchlik A, Jurzak M, Chodurek, E, et al. Effect of GLY-GLY-HIS, GLY-HIS-LYS and their copper complexes on TNF-α-dependant IL-6 secretion in normal human dermal fibroblasts. Acta Pol Pharm. 2012;69:1303-1306.
7. Philips N, Hwang H, Chauhan S, et al. Stimulation of cell proliferation and expression of matrixmetalloproteinase-1 and interluekin-8 genes in dermal fibroblasts by copper. Connect Tissue Res. 2010;51:224-229.
8. Wang Y, Wang M, Xiao S, et al. The anti-wrinkle efficacy of Argireline, a synthetic hexapeptide, in Chinese subjects. Am J Clin Dermatol. 2013;14:147-153.
9. Lupo MP, Cole A. Cosmeceutical peptides. Dermatol Ther. 2007;20:343-349.
10. Blanes-Mira C, Clemente J, Jodas G, et al. A synthetic hexapeptide (Argireline) with antiwrinkle activity. Int J Cosmet Sci. 2002;24:303-310.
11. Jegasothy SM, Zabolotniaia V, Bielfeldt S. Efficacy of a new topical nano-hyaluronic acid in humans. J Clin Aesthet Dermatol. 2014;7:27-29.
12. Pavicic T, Gauglitz G, Lersch P, et al. Efficacy of cream-based novel formulations of hyaluronic acid of different molecular weights in anti-wrinkle treatment. J Drugs Dermatol. 2011;10:990-1000.
Today’s cosmetic patient wants to look more youthful every day without spending a lot of money, feeling any pain, or having any postprocedure downtime. With continued technological improvements, dermatologists have been able to provide our patients with the more youthful appearance they desire; however, many of these procedures still are costly, painful, and may require some downtime. New cosmeceutical therapies can be used as adjuncts to these procedures, making antiaging regimens less painful for patients and requiring less postprocedure healing time. In this article, the use of cosmeceuticals in conjunction with chemical peels, lasers, and injectables will be discussed.
Chemical Peels
Chemical peels are used to create an injury of specific skin depth with a goal of stimulating new skin growth and improving surface texture and appearance. They generally are classified as superficial, medium, or deep according to the depth of action. Currently available agents for superficial chemical peels include α-hydroxy acids (AHAs)(eg, glycolic acid [GA]) and β-hydroxy acids (BHAs)(eg, salicylic acid). β-Lipohydroxy acid (up to 10%), a derivative of salicylic acid, is widely used in Europe. Trichloroacetic acid (TCA) can be used for superficial peels (10%–20%) and for medium-depth peels (35%). Combination peels such as Monheit combination (Jessner solution plus TCA), Brody combination (solid CO2 plus TCA), Coleman combination (GA 70% plus TCA), and Jessner solution with GA can be used as medium-depth peels. Deep peels typically are performed with phenol-based solutions, including the Baker-Gordon phenol peel and the Hetter peel (phenol or croton oil peel).
Specific agents for chemical peels should be selected based on the disorder being treated and should be administered using an appropriate peel depth determined by the histologic level or severity of skin pathology to maximize treatment success.1 However, other considerations, such as skin characteristics, area of skin to be treated, safety concerns, healing time, and patient adherence also should be taken into account to achieve the best overall results. Although many of the deeper peels recently have been replaced by laser-based ablative treatments, superficial to medium-depth peels still are commonly used in the treatment of fine lines, uneven texture, and dyspigmentation.2
Superficial peels are reasonably safe and well tolerated, usually with only mild discomfort (eg, transient burning, irritation, erythema). Scarring, postinflammatory hyperpigmentation (PIH), and infection are rare with superficial peels.1 Postinflammatory hyperpigmentation can be exacerbated by sun exposure, making it important for patients to be educated about sun protection and closely monitored during the recovery phase. In medium and deep peels, lines of demarcation related to the administration technique can occur. Feathering the chemical peel solution at junctions with nonpeeled skin can help to avoid this effect.1 Side effects associated with deeper chemical peels can include pigmentary changes, infections, allergic reactions, improper healing, hypersensitivity, and underlying disease exacerbation. The best way to prevent complications is to identify patients who are at risk and maintain an appropriate peel depth that balances efficacy with known adverse events.1
Many adjunctive agents (eg, AHAs, BHAs, retinoids, skin-bleaching preparations) can be used to enhance chemical peels and decrease the incidence of PIH. α-Hydroxy acids and BHAs can be beneficial when applied prior to chemical peels. Moisturizers containing AHAs and BHAs can be used for 2 to 3 weeks before superficial or medium-depth chemical peels.2 These agents cause thinning of the stratum corneum, thereby creating a more uniform cutaneous surface and allowing for deeper penetration of the chemical peeling agent. Retinoids also are superior prepeeling agents; however, retinoids also can increase the likelihood of irritation, which can be minimized by discontinuing retinoids for 1 week following chemical peels.2 A combination of chemical peels and topical bleaching agents has been shown to be effective in treating hyperpigmentation. The chemical peel causes superficial exfoliation, which allows the lightening agent to penetrate more deeply.2
Hydroquinone (HQ) is the gold standard for improvement of existing pigmentation.3 It is one of the most effective inhibitors of melanogenesis both in vitro and in vivo and is widely used for the treatment of melanosis and other hyperpigmentary disorders. It is widely accepted that the depigmentation activity of HQ may partly be related to its ability to act as an alternate substrate of tyrosinase, thereby competing for tyrosine oxidation in active melanocytes.3 Using HQ at a 4% concentration and combining it with retinoids is quite efficacious.2 Other commonly used depigmenting agents include kojic acid, ascorbic acid (vitamin C), and niacinamide, which often can be used as adjuncts with or maintenance therapy after HQ treatment.2,3
The risk for PIH is imminent for chemical peels and cosmetic laser treatments; therefore, it is crucial to educate patients about the importance of daily and aggressive sun protection. There are several methods of reducing or eliminating postprocedure melanin formation, such as inhibiting tyrosinase synthesis, using complex copper to inhibit tyrosinase function, eliminating oxidation reactions that lead to polymer formation, slowing down the transfer of melanosomes to keratinocytes, or acting upstream on the hormone that stimulates melanogenesis.3 Most of the depigmenting agents presently on the market act by inhibiting tyrosinase via one of these mechanisms.
Skin-lightening agents are primarily formulated as emulsions that have a higher aesthetic appeal. Many of the ingredients get better dispersions with emulsions, which is an added feature of these products. Recently, gel-based formulations also are being considered for their suitability in certain skin types. Efficacy studies for skin-lightening formulations are being carried out through clinical trials that utilize devices that measure skin color in addition to the dermatologist’s assessment.4 Other skin parameters (eg, moisturization, texture, barrier integrity, pH) also are being evaluated to give physicians a picture of skin health after the use of skin-lightening agents. With advances in technology and measurement techniques, it is becoming easier to identify the efficacy of these formulations in different skin types.4
Lasers
The ultimate goal of laser therapy often is to improve the canvas and color of the skin. Ablative laser resurfacing is reliably the most effective procedure for sun-damaged skin.2 This technique causes thermally induced full-thickness epidermal and dermal denudation, which in turn facilitates cytokine-led dermal collagen formation and reepithelialization. Various nonablative modalities also are used for treating photodamaged skin. The epidermis remains unaffected by these nonablative methods, thus decreasing the need for extensive wound care and downtime that is required with ablative treatments. Combining nonablative laser treatments with topical cosmeceuticals has been proven more effective than using either method alone.2 The use of topical retinoids prior to ablative laser resurfacing often results in remarkably faster postprocedure healing and reepithelialization (Figure). Retinoids are best applied nightly for at least 2 weeks and optimally for 3 months before ablative laser treatment. Application should be discontinued for 1 week immediately prior to the procedure.

|

|
| Before (A) and after (B) treatment with a fractional laser in combination with a pre- and postprocedure skin care regimen consisting of retinoids and sunscreen. |
Topical retinoids also are effective in reducing erythema and increasing dermal thickness after nonablative treatments. When used prior to laser treatments, retinoids have been shown to decrease the risk for postoperative milia and hyperpigmentation as well as to allow for better penetration of the laser beam secondary to a thinner stratum corneum.2 Following ablative resurfacing, retinoid use should be discontinued for several weeks to allow for reepithelialization and adequate healing.
Postprocedure Wound Healing
Most of the recommended products that help decrease postprocedural inflammation are cosmeceuticals containing both antioxidants and anti-inflammatories to help decrease redness and inflammation, including various barrier repair moisturizers. Restoring barrier integrity improves the overall appearance of the skin. The ingredients normally recommended in barrier repair moisturizers are epidermal lipids such as ceramides; hyaluronic acid (HA), which is a humectant; and occlusives for patients with very dry skin. Some of the ingredients in over-the-counter cosmeceuticals that can help decrease redness and inflammation include vitamin C, vitamin E, and vitamin B or niacinamide, which will help plump the barrier and also have anti-inflammatory properties. Additionally, polyphenolic flavonoids such as soy and green tea can help decrease inflammation, along with a number of other organic ingredients, such as caffeine, feverfew, and licorice.5 If topical vitamin C is being considered for postprocedure use, the non–ascorbic acid variant should be administered. The magnesium ascorbyl phosphate and ascorbyl palmitate forms of vitamin C have a neutral pH and tend to be better tolerated by patients.
In addition to current prescription and over-the-counter cosmeceuticals used for postprocedure irritation and inflammation, copper peptides and other well-tolerated and effective naturally occurring compounds are being investigated and tried. Copper is a biocide that regulates keratinocyte integrins for epithelization and extracellular matrix remodeling. The extracellular matrix consists of the structural fibrillar collagens and is remodeled or degraded by matrix metalloproteinases (MMPs) that facilitate epithelization. The predominant classes of MMPs include collagenases (ie, MMP-1) and gelatinases (ie, MMP-2, MMP-9) that degrade interstitial collagen and basement membrane proteins.6 The MMPs are endogenously inhibited by tissue inhibitors of metalloproteinases (TIMPs). Copper is a cofactor to lysyl oxidase, which cross-links collagen and stimulates expression of MMP-2 and collagen in a complex with a matrix-derived tripeptide (glycyl-histidyl-lysine or Gly-His-Lys [GHK]) in fibroblasts.6 Much attention has been focused on the tripeptides, such as GHK and Gly-Gly-His, and their copper complexes, which have high activity and good skin tolerance. These complexes have been shown to play a physiological role in the process of wound healing, tissue repair, and skin inflammation. Gly-Gly-His, GHK, copper chloride, and their copper complexes decrease tumor necrosis factor α–dependent IL-6 secretion in fibroblasts.7 IL-6 is crucial for normal wound healing, skin inflammation, and UVB-induced erythema. Because of their anti-inflammatory properties, these copper peptides could potentially be used in place of corticosteroids or nonsteroidal anti-inflammatory drugs, which have more side effects.
Botulinum Neurotoxin and Other Injectable Fillers
Acetyl Hexapeptide-3: A Topical Complement to Botulinum Neurotoxin
Acetyl hexapeptide-3 (Ac-Glu-Glu-Met-Gln-Arg-Arg-NH2) was discovered when looking for a less toxic variation of botulinum neurotoxin (BoNT) to treat aging skin.8 It is patterned from the N-terminal end of the synaptosome-associated protein of molecular weight 25 kDa (SNAP-25), which is essential for docking and fusion of synaptic vesicles to the presynaptic membrane for acetylcholine release.9 It prevents formation and stability of the soluble N-ethylmaleimide-sensitive factor attachment protein receptors (SNARE) complex, inhibiting vesicle docking and calcium-dependent catecholamine exocytosis.8 It also has been found to substantially inhibit the repetitive muscular contraction of facial expression similar to BoNT type A but with somewhat lower efficacy. Acetyl hexapeptide-3 was shown to inhibit 30% of total catecholamine exocytosis and had a remarkable capacity to permeate the skin.10 Thus this topical form of BoNT is a useful complement to intramuscular BoNT.
Studies showing the efficacy and safety of acetyl hexapeptide-3 have demonstrated reductions in wrinkle intensity, mainly in the lateral periorbital areas. In one early study, 10 women applied an emulsion containing 10% of the hexapeptide to one lateral periorbital region and the same emulsion without the hexapeptide to the contralateral side, both twice daily for 30 days.10 A 30% decrease in the depth of skin wrinkles was seen on the hexapeptide side compared with a 10% decrease in the depth of wrinkles on the side treated without hexapeptide. No irritation or toxicity was noted.10 In another trial, 10 women applied an acetyl hexapeptide-3 cream 5% twice daily to lateral periorbital rhytides, with a 27% improvement in wrinkle depth after a 30-day treatment period.9 A double-blind, placebo-controlled study of 60 women assessing the safety and efficacy of topical hexapeptide showed a total antiwrinkle efficacy of 48.9% on the side treated with an emulsion containing 10% of the hexapeptide compared with 0% efficacy on the placebo side.8 Similar to Blanes-Mira et al,10 no adverse events such as skin irritation or toxicity were seen.8 In all of these studies, wrinkle depth was measured by silicone replica analysis.
Topical acetyl hexapeptide-3 is effective in decreasing wrinkles, and its best use will likely be as an adjunct to intramuscular BoNT, as the intramuscular form likely has higher efficacy with the toxin injected directly into the target muscle; however, patients who want the effects of BoNT without the pain of injections may choose to use topical acetyl hexapeptide-3 alone. Patients who do use acetyl hexapeptide-3 as a complement to their intramuscular BoNT regimen may not need as many units of BoNT with each treatment or may not need certain areas injected as often, leading to fewer injections and less pain with each visit. Skin irritation was not seen as a side effect in these trials. Additionally, the topical form has insignificant acute toxicity (≥2000 mg/kg) compared to BoNT type A (20 ng/kg), and genotoxicity was not seen with testing, making it a safe complementary option to an injectable regimen.8
Topical Hyaluronic Acid: A Complement to Injectable Fillers
Hyaluronic acid (HA) is a glycosaminoglycan found in the extracellular matrix of the skin that greatly contributes to tissue hydration. Additionally, it plays a crucial role in the synthesis of extracellular matrix molecules and epidermal cell interaction with the environment.11 The water-binding capacity of HA approximates 1000 times its volume or 6 L of water per gram of HA; however, once an individual reaches adulthood, the amount of HA decreases to 5% of baseline levels, thus contributing to xerosis, loss of skin elasticity, and atrophy.11,12 Although photoaged skin can have increased glycosaminoglycans due to an increase in chondroitin sulfate proteoglycans, they are abnormally deposited on elastotic material in the superficial dermis rather than diffusely scattered, as seen in youthful skin.12
Many topical antiaging products contain HA, though evidence for efficacy in reducing wrinkles has been lacking, along with concerns that HA cannot penetrate the skin. This concern stems from the fact that the original molecule is 3000 nm in diameter and the intercellular space is only 15 to 50 nm. This space is only 6 to 10 nm at the hyaline membrane. Recently, scientists in Japan found a way to reduce the size of HA molecules to 5 nm (nano-HA) without changing its structure. A study of 33 women who applied the topical nano-HA twice daily for 8 weeks to one periorbital area while the contralateral side was left untreated showed improved hydration of the treated side that continued to increase when measured at 2, 4, and 8 weeks using corneometry.11 Roughness decreased and elasticity increased after week 2, which were maintained throughout the study. Additionally, erythema was measured using a chroma meter, which was found to have decreased at day 57 versus day 1.11 An earlier study by Pavicic et al12 evaluated the efficacy of topical hyalu-ronan 0.1% formulations of different molecular weights—50, 130, 300, 800, or 2000 kDa—in the periocular area. A randomized group of 76 women were treated twice daily for 2 months with HA cream on one side of the periocular area and placebo cream on the other. With regard to antiwrinkle properties, only the 50- and 130-kDa HA formulations showed marked effects compared with placebo after 2 months.12
Topical HA would be an effective addition to an antiwrinkle regimen, especially in patients who are averse to needles or are just starting to get wrinkles and are looking for a noninvasive therapy. Additionally, it would be beneficial for patients who have an injectable filler and BoNT regimen, as these patients will be able to target wrinkles simultaneously with both topical cosmeceuticals and injectables and likely will need fewer units of BoNT and/or filler and possibly fewer injections over time, which translates to decreased pain and adverse outcomes for patients.
Conclusion
The myriad of options dermatologists have to offer patients for cosmetic enhancement provides alternatives for patients who have contraindications to certain treatments, are needle averse, or have lifestyles that do not afford them a great deal of postprocedural healing time. Being knowledgeable about these options and how to combine them for improved outcomes is essential to any cosmetic practice.
Today’s cosmetic patient wants to look more youthful every day without spending a lot of money, feeling any pain, or having any postprocedure downtime. With continued technological improvements, dermatologists have been able to provide our patients with the more youthful appearance they desire; however, many of these procedures still are costly, painful, and may require some downtime. New cosmeceutical therapies can be used as adjuncts to these procedures, making antiaging regimens less painful for patients and requiring less postprocedure healing time. In this article, the use of cosmeceuticals in conjunction with chemical peels, lasers, and injectables will be discussed.
Chemical Peels
Chemical peels are used to create an injury of specific skin depth with a goal of stimulating new skin growth and improving surface texture and appearance. They generally are classified as superficial, medium, or deep according to the depth of action. Currently available agents for superficial chemical peels include α-hydroxy acids (AHAs)(eg, glycolic acid [GA]) and β-hydroxy acids (BHAs)(eg, salicylic acid). β-Lipohydroxy acid (up to 10%), a derivative of salicylic acid, is widely used in Europe. Trichloroacetic acid (TCA) can be used for superficial peels (10%–20%) and for medium-depth peels (35%). Combination peels such as Monheit combination (Jessner solution plus TCA), Brody combination (solid CO2 plus TCA), Coleman combination (GA 70% plus TCA), and Jessner solution with GA can be used as medium-depth peels. Deep peels typically are performed with phenol-based solutions, including the Baker-Gordon phenol peel and the Hetter peel (phenol or croton oil peel).
Specific agents for chemical peels should be selected based on the disorder being treated and should be administered using an appropriate peel depth determined by the histologic level or severity of skin pathology to maximize treatment success.1 However, other considerations, such as skin characteristics, area of skin to be treated, safety concerns, healing time, and patient adherence also should be taken into account to achieve the best overall results. Although many of the deeper peels recently have been replaced by laser-based ablative treatments, superficial to medium-depth peels still are commonly used in the treatment of fine lines, uneven texture, and dyspigmentation.2
Superficial peels are reasonably safe and well tolerated, usually with only mild discomfort (eg, transient burning, irritation, erythema). Scarring, postinflammatory hyperpigmentation (PIH), and infection are rare with superficial peels.1 Postinflammatory hyperpigmentation can be exacerbated by sun exposure, making it important for patients to be educated about sun protection and closely monitored during the recovery phase. In medium and deep peels, lines of demarcation related to the administration technique can occur. Feathering the chemical peel solution at junctions with nonpeeled skin can help to avoid this effect.1 Side effects associated with deeper chemical peels can include pigmentary changes, infections, allergic reactions, improper healing, hypersensitivity, and underlying disease exacerbation. The best way to prevent complications is to identify patients who are at risk and maintain an appropriate peel depth that balances efficacy with known adverse events.1
Many adjunctive agents (eg, AHAs, BHAs, retinoids, skin-bleaching preparations) can be used to enhance chemical peels and decrease the incidence of PIH. α-Hydroxy acids and BHAs can be beneficial when applied prior to chemical peels. Moisturizers containing AHAs and BHAs can be used for 2 to 3 weeks before superficial or medium-depth chemical peels.2 These agents cause thinning of the stratum corneum, thereby creating a more uniform cutaneous surface and allowing for deeper penetration of the chemical peeling agent. Retinoids also are superior prepeeling agents; however, retinoids also can increase the likelihood of irritation, which can be minimized by discontinuing retinoids for 1 week following chemical peels.2 A combination of chemical peels and topical bleaching agents has been shown to be effective in treating hyperpigmentation. The chemical peel causes superficial exfoliation, which allows the lightening agent to penetrate more deeply.2
Hydroquinone (HQ) is the gold standard for improvement of existing pigmentation.3 It is one of the most effective inhibitors of melanogenesis both in vitro and in vivo and is widely used for the treatment of melanosis and other hyperpigmentary disorders. It is widely accepted that the depigmentation activity of HQ may partly be related to its ability to act as an alternate substrate of tyrosinase, thereby competing for tyrosine oxidation in active melanocytes.3 Using HQ at a 4% concentration and combining it with retinoids is quite efficacious.2 Other commonly used depigmenting agents include kojic acid, ascorbic acid (vitamin C), and niacinamide, which often can be used as adjuncts with or maintenance therapy after HQ treatment.2,3
The risk for PIH is imminent for chemical peels and cosmetic laser treatments; therefore, it is crucial to educate patients about the importance of daily and aggressive sun protection. There are several methods of reducing or eliminating postprocedure melanin formation, such as inhibiting tyrosinase synthesis, using complex copper to inhibit tyrosinase function, eliminating oxidation reactions that lead to polymer formation, slowing down the transfer of melanosomes to keratinocytes, or acting upstream on the hormone that stimulates melanogenesis.3 Most of the depigmenting agents presently on the market act by inhibiting tyrosinase via one of these mechanisms.
Skin-lightening agents are primarily formulated as emulsions that have a higher aesthetic appeal. Many of the ingredients get better dispersions with emulsions, which is an added feature of these products. Recently, gel-based formulations also are being considered for their suitability in certain skin types. Efficacy studies for skin-lightening formulations are being carried out through clinical trials that utilize devices that measure skin color in addition to the dermatologist’s assessment.4 Other skin parameters (eg, moisturization, texture, barrier integrity, pH) also are being evaluated to give physicians a picture of skin health after the use of skin-lightening agents. With advances in technology and measurement techniques, it is becoming easier to identify the efficacy of these formulations in different skin types.4
Lasers
The ultimate goal of laser therapy often is to improve the canvas and color of the skin. Ablative laser resurfacing is reliably the most effective procedure for sun-damaged skin.2 This technique causes thermally induced full-thickness epidermal and dermal denudation, which in turn facilitates cytokine-led dermal collagen formation and reepithelialization. Various nonablative modalities also are used for treating photodamaged skin. The epidermis remains unaffected by these nonablative methods, thus decreasing the need for extensive wound care and downtime that is required with ablative treatments. Combining nonablative laser treatments with topical cosmeceuticals has been proven more effective than using either method alone.2 The use of topical retinoids prior to ablative laser resurfacing often results in remarkably faster postprocedure healing and reepithelialization (Figure). Retinoids are best applied nightly for at least 2 weeks and optimally for 3 months before ablative laser treatment. Application should be discontinued for 1 week immediately prior to the procedure.

|

|
| Before (A) and after (B) treatment with a fractional laser in combination with a pre- and postprocedure skin care regimen consisting of retinoids and sunscreen. |
Topical retinoids also are effective in reducing erythema and increasing dermal thickness after nonablative treatments. When used prior to laser treatments, retinoids have been shown to decrease the risk for postoperative milia and hyperpigmentation as well as to allow for better penetration of the laser beam secondary to a thinner stratum corneum.2 Following ablative resurfacing, retinoid use should be discontinued for several weeks to allow for reepithelialization and adequate healing.
Postprocedure Wound Healing
Most of the recommended products that help decrease postprocedural inflammation are cosmeceuticals containing both antioxidants and anti-inflammatories to help decrease redness and inflammation, including various barrier repair moisturizers. Restoring barrier integrity improves the overall appearance of the skin. The ingredients normally recommended in barrier repair moisturizers are epidermal lipids such as ceramides; hyaluronic acid (HA), which is a humectant; and occlusives for patients with very dry skin. Some of the ingredients in over-the-counter cosmeceuticals that can help decrease redness and inflammation include vitamin C, vitamin E, and vitamin B or niacinamide, which will help plump the barrier and also have anti-inflammatory properties. Additionally, polyphenolic flavonoids such as soy and green tea can help decrease inflammation, along with a number of other organic ingredients, such as caffeine, feverfew, and licorice.5 If topical vitamin C is being considered for postprocedure use, the non–ascorbic acid variant should be administered. The magnesium ascorbyl phosphate and ascorbyl palmitate forms of vitamin C have a neutral pH and tend to be better tolerated by patients.
In addition to current prescription and over-the-counter cosmeceuticals used for postprocedure irritation and inflammation, copper peptides and other well-tolerated and effective naturally occurring compounds are being investigated and tried. Copper is a biocide that regulates keratinocyte integrins for epithelization and extracellular matrix remodeling. The extracellular matrix consists of the structural fibrillar collagens and is remodeled or degraded by matrix metalloproteinases (MMPs) that facilitate epithelization. The predominant classes of MMPs include collagenases (ie, MMP-1) and gelatinases (ie, MMP-2, MMP-9) that degrade interstitial collagen and basement membrane proteins.6 The MMPs are endogenously inhibited by tissue inhibitors of metalloproteinases (TIMPs). Copper is a cofactor to lysyl oxidase, which cross-links collagen and stimulates expression of MMP-2 and collagen in a complex with a matrix-derived tripeptide (glycyl-histidyl-lysine or Gly-His-Lys [GHK]) in fibroblasts.6 Much attention has been focused on the tripeptides, such as GHK and Gly-Gly-His, and their copper complexes, which have high activity and good skin tolerance. These complexes have been shown to play a physiological role in the process of wound healing, tissue repair, and skin inflammation. Gly-Gly-His, GHK, copper chloride, and their copper complexes decrease tumor necrosis factor α–dependent IL-6 secretion in fibroblasts.7 IL-6 is crucial for normal wound healing, skin inflammation, and UVB-induced erythema. Because of their anti-inflammatory properties, these copper peptides could potentially be used in place of corticosteroids or nonsteroidal anti-inflammatory drugs, which have more side effects.
Botulinum Neurotoxin and Other Injectable Fillers
Acetyl Hexapeptide-3: A Topical Complement to Botulinum Neurotoxin
Acetyl hexapeptide-3 (Ac-Glu-Glu-Met-Gln-Arg-Arg-NH2) was discovered when looking for a less toxic variation of botulinum neurotoxin (BoNT) to treat aging skin.8 It is patterned from the N-terminal end of the synaptosome-associated protein of molecular weight 25 kDa (SNAP-25), which is essential for docking and fusion of synaptic vesicles to the presynaptic membrane for acetylcholine release.9 It prevents formation and stability of the soluble N-ethylmaleimide-sensitive factor attachment protein receptors (SNARE) complex, inhibiting vesicle docking and calcium-dependent catecholamine exocytosis.8 It also has been found to substantially inhibit the repetitive muscular contraction of facial expression similar to BoNT type A but with somewhat lower efficacy. Acetyl hexapeptide-3 was shown to inhibit 30% of total catecholamine exocytosis and had a remarkable capacity to permeate the skin.10 Thus this topical form of BoNT is a useful complement to intramuscular BoNT.
Studies showing the efficacy and safety of acetyl hexapeptide-3 have demonstrated reductions in wrinkle intensity, mainly in the lateral periorbital areas. In one early study, 10 women applied an emulsion containing 10% of the hexapeptide to one lateral periorbital region and the same emulsion without the hexapeptide to the contralateral side, both twice daily for 30 days.10 A 30% decrease in the depth of skin wrinkles was seen on the hexapeptide side compared with a 10% decrease in the depth of wrinkles on the side treated without hexapeptide. No irritation or toxicity was noted.10 In another trial, 10 women applied an acetyl hexapeptide-3 cream 5% twice daily to lateral periorbital rhytides, with a 27% improvement in wrinkle depth after a 30-day treatment period.9 A double-blind, placebo-controlled study of 60 women assessing the safety and efficacy of topical hexapeptide showed a total antiwrinkle efficacy of 48.9% on the side treated with an emulsion containing 10% of the hexapeptide compared with 0% efficacy on the placebo side.8 Similar to Blanes-Mira et al,10 no adverse events such as skin irritation or toxicity were seen.8 In all of these studies, wrinkle depth was measured by silicone replica analysis.
Topical acetyl hexapeptide-3 is effective in decreasing wrinkles, and its best use will likely be as an adjunct to intramuscular BoNT, as the intramuscular form likely has higher efficacy with the toxin injected directly into the target muscle; however, patients who want the effects of BoNT without the pain of injections may choose to use topical acetyl hexapeptide-3 alone. Patients who do use acetyl hexapeptide-3 as a complement to their intramuscular BoNT regimen may not need as many units of BoNT with each treatment or may not need certain areas injected as often, leading to fewer injections and less pain with each visit. Skin irritation was not seen as a side effect in these trials. Additionally, the topical form has insignificant acute toxicity (≥2000 mg/kg) compared to BoNT type A (20 ng/kg), and genotoxicity was not seen with testing, making it a safe complementary option to an injectable regimen.8
Topical Hyaluronic Acid: A Complement to Injectable Fillers
Hyaluronic acid (HA) is a glycosaminoglycan found in the extracellular matrix of the skin that greatly contributes to tissue hydration. Additionally, it plays a crucial role in the synthesis of extracellular matrix molecules and epidermal cell interaction with the environment.11 The water-binding capacity of HA approximates 1000 times its volume or 6 L of water per gram of HA; however, once an individual reaches adulthood, the amount of HA decreases to 5% of baseline levels, thus contributing to xerosis, loss of skin elasticity, and atrophy.11,12 Although photoaged skin can have increased glycosaminoglycans due to an increase in chondroitin sulfate proteoglycans, they are abnormally deposited on elastotic material in the superficial dermis rather than diffusely scattered, as seen in youthful skin.12
Many topical antiaging products contain HA, though evidence for efficacy in reducing wrinkles has been lacking, along with concerns that HA cannot penetrate the skin. This concern stems from the fact that the original molecule is 3000 nm in diameter and the intercellular space is only 15 to 50 nm. This space is only 6 to 10 nm at the hyaline membrane. Recently, scientists in Japan found a way to reduce the size of HA molecules to 5 nm (nano-HA) without changing its structure. A study of 33 women who applied the topical nano-HA twice daily for 8 weeks to one periorbital area while the contralateral side was left untreated showed improved hydration of the treated side that continued to increase when measured at 2, 4, and 8 weeks using corneometry.11 Roughness decreased and elasticity increased after week 2, which were maintained throughout the study. Additionally, erythema was measured using a chroma meter, which was found to have decreased at day 57 versus day 1.11 An earlier study by Pavicic et al12 evaluated the efficacy of topical hyalu-ronan 0.1% formulations of different molecular weights—50, 130, 300, 800, or 2000 kDa—in the periocular area. A randomized group of 76 women were treated twice daily for 2 months with HA cream on one side of the periocular area and placebo cream on the other. With regard to antiwrinkle properties, only the 50- and 130-kDa HA formulations showed marked effects compared with placebo after 2 months.12
Topical HA would be an effective addition to an antiwrinkle regimen, especially in patients who are averse to needles or are just starting to get wrinkles and are looking for a noninvasive therapy. Additionally, it would be beneficial for patients who have an injectable filler and BoNT regimen, as these patients will be able to target wrinkles simultaneously with both topical cosmeceuticals and injectables and likely will need fewer units of BoNT and/or filler and possibly fewer injections over time, which translates to decreased pain and adverse outcomes for patients.
Conclusion
The myriad of options dermatologists have to offer patients for cosmetic enhancement provides alternatives for patients who have contraindications to certain treatments, are needle averse, or have lifestyles that do not afford them a great deal of postprocedural healing time. Being knowledgeable about these options and how to combine them for improved outcomes is essential to any cosmetic practice.
1. Rendon MI, Berson DS, Cohen JL, et al. Evidence and considerations in the application of chemical peels in skin disorders and aesthetic resurfacing. J Clin Aesthet Dermatol. 2010;3:32-43.
2. Lupo MP, Jacob LG. Cosmeceuticals for enhancing cosmetic procedures. In: Farris PK, ed. Cosmeceuticals and Cosmetic Practice. Oxford, United Kingdom: Wiley-Blackwell; 2014:268-276.
3. Gruber JV, Holtz R. Examining the impact of skin lighteners in vitro [published online ahead of print April 28, 2013]. Oxid Med Cell Longev. 2013;2013:702120.
4. Antonio JR, Antonio CR, Cardeal ILS, et al. Nanotechnology in dermatology. An Bras Dermatol. 2014;89:126-136.
5. Ganceviciene R, Liakou AI, Theodoridis A, et al. Skin anti-aging strategies. Dermatoendocrinol. 2012;4:308-319.
6. Gruchlik A, Jurzak M, Chodurek, E, et al. Effect of GLY-GLY-HIS, GLY-HIS-LYS and their copper complexes on TNF-α-dependant IL-6 secretion in normal human dermal fibroblasts. Acta Pol Pharm. 2012;69:1303-1306.
7. Philips N, Hwang H, Chauhan S, et al. Stimulation of cell proliferation and expression of matrixmetalloproteinase-1 and interluekin-8 genes in dermal fibroblasts by copper. Connect Tissue Res. 2010;51:224-229.
8. Wang Y, Wang M, Xiao S, et al. The anti-wrinkle efficacy of Argireline, a synthetic hexapeptide, in Chinese subjects. Am J Clin Dermatol. 2013;14:147-153.
9. Lupo MP, Cole A. Cosmeceutical peptides. Dermatol Ther. 2007;20:343-349.
10. Blanes-Mira C, Clemente J, Jodas G, et al. A synthetic hexapeptide (Argireline) with antiwrinkle activity. Int J Cosmet Sci. 2002;24:303-310.
11. Jegasothy SM, Zabolotniaia V, Bielfeldt S. Efficacy of a new topical nano-hyaluronic acid in humans. J Clin Aesthet Dermatol. 2014;7:27-29.
12. Pavicic T, Gauglitz G, Lersch P, et al. Efficacy of cream-based novel formulations of hyaluronic acid of different molecular weights in anti-wrinkle treatment. J Drugs Dermatol. 2011;10:990-1000.
1. Rendon MI, Berson DS, Cohen JL, et al. Evidence and considerations in the application of chemical peels in skin disorders and aesthetic resurfacing. J Clin Aesthet Dermatol. 2010;3:32-43.
2. Lupo MP, Jacob LG. Cosmeceuticals for enhancing cosmetic procedures. In: Farris PK, ed. Cosmeceuticals and Cosmetic Practice. Oxford, United Kingdom: Wiley-Blackwell; 2014:268-276.
3. Gruber JV, Holtz R. Examining the impact of skin lighteners in vitro [published online ahead of print April 28, 2013]. Oxid Med Cell Longev. 2013;2013:702120.
4. Antonio JR, Antonio CR, Cardeal ILS, et al. Nanotechnology in dermatology. An Bras Dermatol. 2014;89:126-136.
5. Ganceviciene R, Liakou AI, Theodoridis A, et al. Skin anti-aging strategies. Dermatoendocrinol. 2012;4:308-319.
6. Gruchlik A, Jurzak M, Chodurek, E, et al. Effect of GLY-GLY-HIS, GLY-HIS-LYS and their copper complexes on TNF-α-dependant IL-6 secretion in normal human dermal fibroblasts. Acta Pol Pharm. 2012;69:1303-1306.
7. Philips N, Hwang H, Chauhan S, et al. Stimulation of cell proliferation and expression of matrixmetalloproteinase-1 and interluekin-8 genes in dermal fibroblasts by copper. Connect Tissue Res. 2010;51:224-229.
8. Wang Y, Wang M, Xiao S, et al. The anti-wrinkle efficacy of Argireline, a synthetic hexapeptide, in Chinese subjects. Am J Clin Dermatol. 2013;14:147-153.
9. Lupo MP, Cole A. Cosmeceutical peptides. Dermatol Ther. 2007;20:343-349.
10. Blanes-Mira C, Clemente J, Jodas G, et al. A synthetic hexapeptide (Argireline) with antiwrinkle activity. Int J Cosmet Sci. 2002;24:303-310.
11. Jegasothy SM, Zabolotniaia V, Bielfeldt S. Efficacy of a new topical nano-hyaluronic acid in humans. J Clin Aesthet Dermatol. 2014;7:27-29.
12. Pavicic T, Gauglitz G, Lersch P, et al. Efficacy of cream-based novel formulations of hyaluronic acid of different molecular weights in anti-wrinkle treatment. J Drugs Dermatol. 2011;10:990-1000.
Practice Points
- Copper peptides could potentially be used in place of corticosteroids or nonsteroidal anti-inflammatory drugs for postprocedure irritation and inflammation.
- Acetyl hexapeptide-3 is a topical variation of botulinum toxin to be used on its own or adjunctively with the injectable form.
- Topical hyaluronic acid can be used on its own or adjunctively with injectable fillers.
Pulmonary vein isolation alone may be best ablative procedure for persistent atrial fibrillation
BARCELONA – More extensive catheter ablation procedures offered no benefit over pulmonary vein isolation alone for persistent atrial fibrillation in the largest-ever randomized trial examining outcomes of the three most popular ablation strategies.
"This study, the STAR AF 2 trial, will force a change in thinking both in the guidelines as well as in clinical practice," Dr. Atul Verma predicted, in presenting the study findings at the annual congress of the European Society of Cardiology.
Because of a widespread belief that catheter ablation success rates are probably lower in persistent AF than in paroxysmal AF, guidelines suggest "operators should consider more ablation based on linear lesions or complex fractionated electrograms," in addition to pulmonary vein isolation, in treating patients with persistent AF (Heart Rhythm 2012;9:632-96). The guidelines noted, however, that there is little evidence to support this recommendation.
The STAR AF 2 trial was conducted to learn if more complex ablation procedures really do provide greater efficacy than pulmonary vein isolation (PVI) alone. The study included 589 patients at 48 centers in 12 countries. All patients had persistent AF refractory to at least one antiarrhythmic drug and were about to undergo their first-ever catheter ablation.
Participants were randomized 1:4:4 to PVI alone with the procedural endpoint of entrance and exit block by circular mapping catheter, or PVI plus mapping and ablation of complex fractionated electrograms during AF identified using a validated 3-D mapping system, or PVI plus a left atrial roof line and another line along the mitral valve isthmus with the endpoint of bidirectional block confirmed by prespecified pacing maneuvers.
Patients remained blinded as to which of the three treatments they received. They were prospectively followed with 24-hour Holter monitoring at 3, 6, 9, 12, and 18 months along with weekly transtelephonic monitoring transmissions or at any time they felt symptoms.
Successful PVI was achieved in 97% of patients, complex fractionated electrograms were eliminated in 80% of patients assigned to that strategy, and both target lines were blocked in 74% of patients who underwent linear ablation.
The primary outcome was freedom from a documented episode of AF lasting more than 30 seconds after one procedure with or without antiarrhythmic medication through 18 months. The rates were 59% with PVI only, 48% with PVI plus complex fractionated electrograms, and 44% with PVI and linear ablation. These rates weren’t significantly different.
There were downsides to the two more elaborate ablation strategies. Procedural times were roughly 1 hour longer. Moreover, mean fluoroscopy time was 29 minutes in the PVI-only group, compared with 41 and 42 minutes with the more complex procedures. That translates to 44% more radiation exposure for both operators and patients, with absolutely no resultant added benefit over PVI alone, noted Dr. Verma, an electrophysiologist at Southlake Regional Health Center in Newmarket, Ont.
Complication rates across the board in STAR AF 2 were among the lowest ever reported in a multicenter clinical trial of catheter ablation. Of note, however, the sole fatal complication was the result of an atrial esophageal fistula in a patient assigned to PVI plus electrogram ablation.
Discussant Dr. Jagmeet P. Singh, director of the cardiac resynchronization therapy program at Massachusetts General Hospital, Boston, called STAR AF 2 "a fantastic trial."
"This study surely advocates that less ablation is more – and less works quite well," he said, noting that the roughly 50% success rate at 18 months with PVI alone is comparable to prior published success rates in paroxysmal AF.
Discussant Dr. Paulus Kirchhof said his own recent informal survey of high-volume catheter ablation centers in the United States and Europe indicated roughly one-third do PVI alone for patients with persistent AF, one-third do PVI plus ablation of complex fractionated electrograms, and one-third do PVI plus linear ablation.
"So I would say this was a question at equipoise," added Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham (England).
Zeroing in on the added fluoroscopy time associated with the more complex ablation procedures, he noted that observational data suggest lengthier fluoroscopy may be associated with silent, subclinical brain lesions. Based upon the STAR 2 AF results, therefore, a reasonable strategy now for persistent AF is to do PVI alone, then wait and see what happens before considering additional ablation procedures later, he said.
"More importantly, I think this study shows we have to go back to the drawing board. The time pattern of AF – its duration, whether it’s paroxysmal or persistent, the left atrial size – all these things we believe identify patients who need more therapy, they may not actually help us. We just have to accept that not all patients with AF are the same, and that the pattern of AF does not discriminate so well. I think what we can really learn from this trial moving forward is that we need a clinical classification of AF patients. We have to define the patient who would benefit before we continue to develop ever-more intensive interventional strategies," he commented.
Factors worthy of further study as potential tools for separating AF patients into subgroups for treatment purposes include markers of atrial fibrosis, whether by imaging, blood, or ECG patterns; markers of parasympathetic/sympathetic imbalance; clinical markers of abnormal calcium metabolism; or blood markers, Dr. Kirchhof added.
The STAR AF 2 trial was funded by St. Jude Medical. Dr. Verma, Dr. Singh, and Dr. Kirchhof reported receiving grant support from St. Jude Medical as well as other pharmaceutical and medical device companies. In addition, Dr. Verma and Dr. Singh have served on advisory boards for St. Jude.
BARCELONA – More extensive catheter ablation procedures offered no benefit over pulmonary vein isolation alone for persistent atrial fibrillation in the largest-ever randomized trial examining outcomes of the three most popular ablation strategies.
"This study, the STAR AF 2 trial, will force a change in thinking both in the guidelines as well as in clinical practice," Dr. Atul Verma predicted, in presenting the study findings at the annual congress of the European Society of Cardiology.
Because of a widespread belief that catheter ablation success rates are probably lower in persistent AF than in paroxysmal AF, guidelines suggest "operators should consider more ablation based on linear lesions or complex fractionated electrograms," in addition to pulmonary vein isolation, in treating patients with persistent AF (Heart Rhythm 2012;9:632-96). The guidelines noted, however, that there is little evidence to support this recommendation.
The STAR AF 2 trial was conducted to learn if more complex ablation procedures really do provide greater efficacy than pulmonary vein isolation (PVI) alone. The study included 589 patients at 48 centers in 12 countries. All patients had persistent AF refractory to at least one antiarrhythmic drug and were about to undergo their first-ever catheter ablation.
Participants were randomized 1:4:4 to PVI alone with the procedural endpoint of entrance and exit block by circular mapping catheter, or PVI plus mapping and ablation of complex fractionated electrograms during AF identified using a validated 3-D mapping system, or PVI plus a left atrial roof line and another line along the mitral valve isthmus with the endpoint of bidirectional block confirmed by prespecified pacing maneuvers.
Patients remained blinded as to which of the three treatments they received. They were prospectively followed with 24-hour Holter monitoring at 3, 6, 9, 12, and 18 months along with weekly transtelephonic monitoring transmissions or at any time they felt symptoms.
Successful PVI was achieved in 97% of patients, complex fractionated electrograms were eliminated in 80% of patients assigned to that strategy, and both target lines were blocked in 74% of patients who underwent linear ablation.
The primary outcome was freedom from a documented episode of AF lasting more than 30 seconds after one procedure with or without antiarrhythmic medication through 18 months. The rates were 59% with PVI only, 48% with PVI plus complex fractionated electrograms, and 44% with PVI and linear ablation. These rates weren’t significantly different.
There were downsides to the two more elaborate ablation strategies. Procedural times were roughly 1 hour longer. Moreover, mean fluoroscopy time was 29 minutes in the PVI-only group, compared with 41 and 42 minutes with the more complex procedures. That translates to 44% more radiation exposure for both operators and patients, with absolutely no resultant added benefit over PVI alone, noted Dr. Verma, an electrophysiologist at Southlake Regional Health Center in Newmarket, Ont.
Complication rates across the board in STAR AF 2 were among the lowest ever reported in a multicenter clinical trial of catheter ablation. Of note, however, the sole fatal complication was the result of an atrial esophageal fistula in a patient assigned to PVI plus electrogram ablation.
Discussant Dr. Jagmeet P. Singh, director of the cardiac resynchronization therapy program at Massachusetts General Hospital, Boston, called STAR AF 2 "a fantastic trial."
"This study surely advocates that less ablation is more – and less works quite well," he said, noting that the roughly 50% success rate at 18 months with PVI alone is comparable to prior published success rates in paroxysmal AF.
Discussant Dr. Paulus Kirchhof said his own recent informal survey of high-volume catheter ablation centers in the United States and Europe indicated roughly one-third do PVI alone for patients with persistent AF, one-third do PVI plus ablation of complex fractionated electrograms, and one-third do PVI plus linear ablation.
"So I would say this was a question at equipoise," added Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham (England).
Zeroing in on the added fluoroscopy time associated with the more complex ablation procedures, he noted that observational data suggest lengthier fluoroscopy may be associated with silent, subclinical brain lesions. Based upon the STAR 2 AF results, therefore, a reasonable strategy now for persistent AF is to do PVI alone, then wait and see what happens before considering additional ablation procedures later, he said.
"More importantly, I think this study shows we have to go back to the drawing board. The time pattern of AF – its duration, whether it’s paroxysmal or persistent, the left atrial size – all these things we believe identify patients who need more therapy, they may not actually help us. We just have to accept that not all patients with AF are the same, and that the pattern of AF does not discriminate so well. I think what we can really learn from this trial moving forward is that we need a clinical classification of AF patients. We have to define the patient who would benefit before we continue to develop ever-more intensive interventional strategies," he commented.
Factors worthy of further study as potential tools for separating AF patients into subgroups for treatment purposes include markers of atrial fibrosis, whether by imaging, blood, or ECG patterns; markers of parasympathetic/sympathetic imbalance; clinical markers of abnormal calcium metabolism; or blood markers, Dr. Kirchhof added.
The STAR AF 2 trial was funded by St. Jude Medical. Dr. Verma, Dr. Singh, and Dr. Kirchhof reported receiving grant support from St. Jude Medical as well as other pharmaceutical and medical device companies. In addition, Dr. Verma and Dr. Singh have served on advisory boards for St. Jude.
BARCELONA – More extensive catheter ablation procedures offered no benefit over pulmonary vein isolation alone for persistent atrial fibrillation in the largest-ever randomized trial examining outcomes of the three most popular ablation strategies.
"This study, the STAR AF 2 trial, will force a change in thinking both in the guidelines as well as in clinical practice," Dr. Atul Verma predicted, in presenting the study findings at the annual congress of the European Society of Cardiology.
Because of a widespread belief that catheter ablation success rates are probably lower in persistent AF than in paroxysmal AF, guidelines suggest "operators should consider more ablation based on linear lesions or complex fractionated electrograms," in addition to pulmonary vein isolation, in treating patients with persistent AF (Heart Rhythm 2012;9:632-96). The guidelines noted, however, that there is little evidence to support this recommendation.
The STAR AF 2 trial was conducted to learn if more complex ablation procedures really do provide greater efficacy than pulmonary vein isolation (PVI) alone. The study included 589 patients at 48 centers in 12 countries. All patients had persistent AF refractory to at least one antiarrhythmic drug and were about to undergo their first-ever catheter ablation.
Participants were randomized 1:4:4 to PVI alone with the procedural endpoint of entrance and exit block by circular mapping catheter, or PVI plus mapping and ablation of complex fractionated electrograms during AF identified using a validated 3-D mapping system, or PVI plus a left atrial roof line and another line along the mitral valve isthmus with the endpoint of bidirectional block confirmed by prespecified pacing maneuvers.
Patients remained blinded as to which of the three treatments they received. They were prospectively followed with 24-hour Holter monitoring at 3, 6, 9, 12, and 18 months along with weekly transtelephonic monitoring transmissions or at any time they felt symptoms.
Successful PVI was achieved in 97% of patients, complex fractionated electrograms were eliminated in 80% of patients assigned to that strategy, and both target lines were blocked in 74% of patients who underwent linear ablation.
The primary outcome was freedom from a documented episode of AF lasting more than 30 seconds after one procedure with or without antiarrhythmic medication through 18 months. The rates were 59% with PVI only, 48% with PVI plus complex fractionated electrograms, and 44% with PVI and linear ablation. These rates weren’t significantly different.
There were downsides to the two more elaborate ablation strategies. Procedural times were roughly 1 hour longer. Moreover, mean fluoroscopy time was 29 minutes in the PVI-only group, compared with 41 and 42 minutes with the more complex procedures. That translates to 44% more radiation exposure for both operators and patients, with absolutely no resultant added benefit over PVI alone, noted Dr. Verma, an electrophysiologist at Southlake Regional Health Center in Newmarket, Ont.
Complication rates across the board in STAR AF 2 were among the lowest ever reported in a multicenter clinical trial of catheter ablation. Of note, however, the sole fatal complication was the result of an atrial esophageal fistula in a patient assigned to PVI plus electrogram ablation.
Discussant Dr. Jagmeet P. Singh, director of the cardiac resynchronization therapy program at Massachusetts General Hospital, Boston, called STAR AF 2 "a fantastic trial."
"This study surely advocates that less ablation is more – and less works quite well," he said, noting that the roughly 50% success rate at 18 months with PVI alone is comparable to prior published success rates in paroxysmal AF.
Discussant Dr. Paulus Kirchhof said his own recent informal survey of high-volume catheter ablation centers in the United States and Europe indicated roughly one-third do PVI alone for patients with persistent AF, one-third do PVI plus ablation of complex fractionated electrograms, and one-third do PVI plus linear ablation.
"So I would say this was a question at equipoise," added Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham (England).
Zeroing in on the added fluoroscopy time associated with the more complex ablation procedures, he noted that observational data suggest lengthier fluoroscopy may be associated with silent, subclinical brain lesions. Based upon the STAR 2 AF results, therefore, a reasonable strategy now for persistent AF is to do PVI alone, then wait and see what happens before considering additional ablation procedures later, he said.
"More importantly, I think this study shows we have to go back to the drawing board. The time pattern of AF – its duration, whether it’s paroxysmal or persistent, the left atrial size – all these things we believe identify patients who need more therapy, they may not actually help us. We just have to accept that not all patients with AF are the same, and that the pattern of AF does not discriminate so well. I think what we can really learn from this trial moving forward is that we need a clinical classification of AF patients. We have to define the patient who would benefit before we continue to develop ever-more intensive interventional strategies," he commented.
Factors worthy of further study as potential tools for separating AF patients into subgroups for treatment purposes include markers of atrial fibrosis, whether by imaging, blood, or ECG patterns; markers of parasympathetic/sympathetic imbalance; clinical markers of abnormal calcium metabolism; or blood markers, Dr. Kirchhof added.
The STAR AF 2 trial was funded by St. Jude Medical. Dr. Verma, Dr. Singh, and Dr. Kirchhof reported receiving grant support from St. Jude Medical as well as other pharmaceutical and medical device companies. In addition, Dr. Verma and Dr. Singh have served on advisory boards for St. Jude.
AT THE ESC CONGRESS 2014
Key clinical point: Pulmonary vein isolation alone may offer advantages over more elaborate procedures for persistent atrial fibrillation.
Major finding: The rates of freedom from a documented episode of AF lasting more than 30 seconds were 59% with pulmonary vein isolation only, 48% with PVI plus complex fractionated electrograms, and 44% with PVI and linear ablation.
Data source: The STAR AF 2 trial was a randomized, multicenter prospective study in which 589 patients with persistent AF were randomized to one of three popular catheter ablation strategies.
Disclosures: The study was funded by St. Jude Medical. The presenter has received research grants from and served on advisory boards for St. Jude and other medical device and pharmaceutical companies.
High-dose statins don’t prevent postop AF
BARCELONA – Intensive perioperative statin therapy in patients undergoing CABG surgery doesn’t protect against postop atrial fibrillation or myocardial injury, according to a large randomized clinical trial hailed as the "definitive" study addressing this issue.
"There are many reasons why these patients should be put on statin treatment, but the prevention of postop complications is not one of them," Dr. Barbara Casadei said in presenting the findings of the Statin Therapy in Cardiac Surgery (STICS) trial at the annual congress of the European Society of Cardiology.

The STICS results are at odds with conventional wisdom. ESC guidelines give a favorable class IIa, level of evidence B recommendation that "statins should be considered for prevention of new-onset atrial fibrillation after coronary artery bypass grafting, either isolated or in combination with valvular interventions."
"STICS was a very carefully conducted, large scale, robust study that I think has definitely closed the door on this issue," commented Dr. Keith A.A. Fox, professor of cardiology at the University of Edinburgh and chair of the scientific and clinical program committee at ESC Congress 2014.
STICS was a double-blind prospective trial in which 1,922 patients scheduled for elective CABG were randomized to 20 mg per day of rosuvastatin (Crestor) or placebo starting up to 8 days prior to surgery and continued for 5 days postop. All participants were in sinus rhythm preoperatively, with no history of AF, said Dr. Casadei, professor of cardiovascular medicine at the University of Oxford, England.
The two coprimary endpoints in STICS were the incidence of new-onset AF during 5 days of postop Holter monitoring, and evidence of postop myocardial injury as demonstrated in serial troponin I assays.
Postop AF occurred in 21% of those given high-intensity therapy with rosuvastatin and 20% of placebo-treated controls. There was no subgroup where rosuvastatin was protective (see graphic).
Troponin I measurements obtained 6, 24, 48, and 120 hours postop showed areas under the curve that were superimposable in the two study groups, meaning perioperative high-dose statin therapy provided absolutely no protection against postop cardiac muscle injury.
Mean hospital length of stay and ICU time didn’t differ between the two groups, either.
The impetus for conducting STICS was recognition that the guidelines’ endorsement of perioperative high-dose statin therapy in conjunction with cardiac surgery was based upon a series of small randomized trials with serious limitations. Although the results of a meta-analysis of the 14 prior trials looked impressive at first glance – a 17% incidence of postop AF in statin-treated patients, compared with 30% in controls, for a near-halving of the risk of this important complication – these 14 studies totaled 1,300 patients, and there were many methodologic shortcomings.
The STICS researchers hypothesized that a large, well-designed trial – bigger than all previous studies combined – would shore up the previously shaky supporting evidence and perhaps provide grounds for statins to win a new indication from regulatory agencies. Post-CABG AF is associated with a doubled risk of stroke and mortality, and excess hospital costs of $8,000-$18,000 dollars per patient.
Discussant Dr. Paulus Kirchhof, a member of the task force that developed the current ESC guidelines (Europace 2010;12:1360-420), said those guidelines now clearly need to be revisited. Beyond that, he added, STICS provides important new contributions in understanding the pathophysiology of AF.
"We know that AF is caused by several vicious circles, and we believe that inflammation could influence those and cause AF. And we also thought that postop AF was the condition where inflammation plays the biggest role. Based upon the negative results with this anti-inflammatory intervention, I think we have to question this concept a bit," said Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham, England.
Dr. Casadei countered that she’s not ready to write off postop inflammation entirely as a major trigger of new-onset AF following CABG.
"The inflammation is there. We know from experimental work in animals that there is a strong association between inflammation and postop atrial fibrillation, but whether the association is causal, I think, is still debated. However, it may be that the anti-inflammatory effect of statins is not sufficiently strong to actually prevent this complication," she said.
Discussant Dr. Steven Nissen praised STICS as "an outstanding trial."
"I also think there’s a terribly important lesson here, which is the power of self-delusion in medicine. When we base our guidelines on small, poorly controlled trials, we are often making mistakes. This is one of countless examples where when someone finally does a careful, thoughtful trial, we find out that something that people believe just isn’t true. We can’t cut corners with evidence. We need good randomized trials," declared Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic.
The STICS trial was funded primarily by the British Heart Foundation, the Oxford Biomedical Research Center, and the UK Medical Research Council. In addition, Dr. Casadei reported receiving an unrestricted grant from AstraZeneca in conjunction with the trial.

|
| Dr. Hiren Shah |
There are two key lessons from the results of the STICS trial. First, extrapolation of results from biochemical pathways and measured cellular markers does not always translate into meaningful clinical outcomes. Thus, it has long been known from several large trials that statin therapy effectively and rapidly lowers CRP levels both in hyper- and normocholesterolemic patients and that statins are effective in decreasing systemic inflammation. It has also been known that inflammation contributes to the development and maintenance of AF, so it was postulated that by improving endothelial nitric oxide availability, reducing inflammation, and decreasing oxidative stress, and through neurohormonal activation, statins would reduce the incidence of post-op AF. This link was so strong that clinical guidelines adopted limited data from small trials to make treatment recommendations.
This leads us to consider the second key lesson from this study. Trials with small sample size, even when combined across many other trials (1,300 patients were involved across 14 trials in this case), do not always yield reliable results, especially when they have significant limitations, notably not always being blind and having been performed in statin-naive patients only. The large, randomized, and well-designed STICS trial puts to rest an important issue, given the high prevalence of AF after cardiac surgery, which is associated with a longer length of stay, an increased risk of stroke, higher mortality, and greater costs, and should prompt us to consider further evaluation of different strategies to reduce this significant complication.
Dr. Hiren Shah is medical director of the medicine and cardiac telemetry hospitalist unit at Northwestern Memorial Hospital in Chicago and an adviser to Hospitalist News. He is the national chair of the Clinician Committee for ACP’s Initiative on Stroke Prevention and Atrial Fibrillation and is the lead physician for the Society of Hospital Medicine’s National Atrial Fibrillation Initiative.

|
| Dr. Hiren Shah |
There are two key lessons from the results of the STICS trial. First, extrapolation of results from biochemical pathways and measured cellular markers does not always translate into meaningful clinical outcomes. Thus, it has long been known from several large trials that statin therapy effectively and rapidly lowers CRP levels both in hyper- and normocholesterolemic patients and that statins are effective in decreasing systemic inflammation. It has also been known that inflammation contributes to the development and maintenance of AF, so it was postulated that by improving endothelial nitric oxide availability, reducing inflammation, and decreasing oxidative stress, and through neurohormonal activation, statins would reduce the incidence of post-op AF. This link was so strong that clinical guidelines adopted limited data from small trials to make treatment recommendations.
This leads us to consider the second key lesson from this study. Trials with small sample size, even when combined across many other trials (1,300 patients were involved across 14 trials in this case), do not always yield reliable results, especially when they have significant limitations, notably not always being blind and having been performed in statin-naive patients only. The large, randomized, and well-designed STICS trial puts to rest an important issue, given the high prevalence of AF after cardiac surgery, which is associated with a longer length of stay, an increased risk of stroke, higher mortality, and greater costs, and should prompt us to consider further evaluation of different strategies to reduce this significant complication.
Dr. Hiren Shah is medical director of the medicine and cardiac telemetry hospitalist unit at Northwestern Memorial Hospital in Chicago and an adviser to Hospitalist News. He is the national chair of the Clinician Committee for ACP’s Initiative on Stroke Prevention and Atrial Fibrillation and is the lead physician for the Society of Hospital Medicine’s National Atrial Fibrillation Initiative.

|
| Dr. Hiren Shah |
There are two key lessons from the results of the STICS trial. First, extrapolation of results from biochemical pathways and measured cellular markers does not always translate into meaningful clinical outcomes. Thus, it has long been known from several large trials that statin therapy effectively and rapidly lowers CRP levels both in hyper- and normocholesterolemic patients and that statins are effective in decreasing systemic inflammation. It has also been known that inflammation contributes to the development and maintenance of AF, so it was postulated that by improving endothelial nitric oxide availability, reducing inflammation, and decreasing oxidative stress, and through neurohormonal activation, statins would reduce the incidence of post-op AF. This link was so strong that clinical guidelines adopted limited data from small trials to make treatment recommendations.
This leads us to consider the second key lesson from this study. Trials with small sample size, even when combined across many other trials (1,300 patients were involved across 14 trials in this case), do not always yield reliable results, especially when they have significant limitations, notably not always being blind and having been performed in statin-naive patients only. The large, randomized, and well-designed STICS trial puts to rest an important issue, given the high prevalence of AF after cardiac surgery, which is associated with a longer length of stay, an increased risk of stroke, higher mortality, and greater costs, and should prompt us to consider further evaluation of different strategies to reduce this significant complication.
Dr. Hiren Shah is medical director of the medicine and cardiac telemetry hospitalist unit at Northwestern Memorial Hospital in Chicago and an adviser to Hospitalist News. He is the national chair of the Clinician Committee for ACP’s Initiative on Stroke Prevention and Atrial Fibrillation and is the lead physician for the Society of Hospital Medicine’s National Atrial Fibrillation Initiative.
BARCELONA – Intensive perioperative statin therapy in patients undergoing CABG surgery doesn’t protect against postop atrial fibrillation or myocardial injury, according to a large randomized clinical trial hailed as the "definitive" study addressing this issue.
"There are many reasons why these patients should be put on statin treatment, but the prevention of postop complications is not one of them," Dr. Barbara Casadei said in presenting the findings of the Statin Therapy in Cardiac Surgery (STICS) trial at the annual congress of the European Society of Cardiology.

The STICS results are at odds with conventional wisdom. ESC guidelines give a favorable class IIa, level of evidence B recommendation that "statins should be considered for prevention of new-onset atrial fibrillation after coronary artery bypass grafting, either isolated or in combination with valvular interventions."
"STICS was a very carefully conducted, large scale, robust study that I think has definitely closed the door on this issue," commented Dr. Keith A.A. Fox, professor of cardiology at the University of Edinburgh and chair of the scientific and clinical program committee at ESC Congress 2014.
STICS was a double-blind prospective trial in which 1,922 patients scheduled for elective CABG were randomized to 20 mg per day of rosuvastatin (Crestor) or placebo starting up to 8 days prior to surgery and continued for 5 days postop. All participants were in sinus rhythm preoperatively, with no history of AF, said Dr. Casadei, professor of cardiovascular medicine at the University of Oxford, England.
The two coprimary endpoints in STICS were the incidence of new-onset AF during 5 days of postop Holter monitoring, and evidence of postop myocardial injury as demonstrated in serial troponin I assays.
Postop AF occurred in 21% of those given high-intensity therapy with rosuvastatin and 20% of placebo-treated controls. There was no subgroup where rosuvastatin was protective (see graphic).
Troponin I measurements obtained 6, 24, 48, and 120 hours postop showed areas under the curve that were superimposable in the two study groups, meaning perioperative high-dose statin therapy provided absolutely no protection against postop cardiac muscle injury.
Mean hospital length of stay and ICU time didn’t differ between the two groups, either.
The impetus for conducting STICS was recognition that the guidelines’ endorsement of perioperative high-dose statin therapy in conjunction with cardiac surgery was based upon a series of small randomized trials with serious limitations. Although the results of a meta-analysis of the 14 prior trials looked impressive at first glance – a 17% incidence of postop AF in statin-treated patients, compared with 30% in controls, for a near-halving of the risk of this important complication – these 14 studies totaled 1,300 patients, and there were many methodologic shortcomings.
The STICS researchers hypothesized that a large, well-designed trial – bigger than all previous studies combined – would shore up the previously shaky supporting evidence and perhaps provide grounds for statins to win a new indication from regulatory agencies. Post-CABG AF is associated with a doubled risk of stroke and mortality, and excess hospital costs of $8,000-$18,000 dollars per patient.
Discussant Dr. Paulus Kirchhof, a member of the task force that developed the current ESC guidelines (Europace 2010;12:1360-420), said those guidelines now clearly need to be revisited. Beyond that, he added, STICS provides important new contributions in understanding the pathophysiology of AF.
"We know that AF is caused by several vicious circles, and we believe that inflammation could influence those and cause AF. And we also thought that postop AF was the condition where inflammation plays the biggest role. Based upon the negative results with this anti-inflammatory intervention, I think we have to question this concept a bit," said Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham, England.
Dr. Casadei countered that she’s not ready to write off postop inflammation entirely as a major trigger of new-onset AF following CABG.
"The inflammation is there. We know from experimental work in animals that there is a strong association between inflammation and postop atrial fibrillation, but whether the association is causal, I think, is still debated. However, it may be that the anti-inflammatory effect of statins is not sufficiently strong to actually prevent this complication," she said.
Discussant Dr. Steven Nissen praised STICS as "an outstanding trial."
"I also think there’s a terribly important lesson here, which is the power of self-delusion in medicine. When we base our guidelines on small, poorly controlled trials, we are often making mistakes. This is one of countless examples where when someone finally does a careful, thoughtful trial, we find out that something that people believe just isn’t true. We can’t cut corners with evidence. We need good randomized trials," declared Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic.
The STICS trial was funded primarily by the British Heart Foundation, the Oxford Biomedical Research Center, and the UK Medical Research Council. In addition, Dr. Casadei reported receiving an unrestricted grant from AstraZeneca in conjunction with the trial.
BARCELONA – Intensive perioperative statin therapy in patients undergoing CABG surgery doesn’t protect against postop atrial fibrillation or myocardial injury, according to a large randomized clinical trial hailed as the "definitive" study addressing this issue.
"There are many reasons why these patients should be put on statin treatment, but the prevention of postop complications is not one of them," Dr. Barbara Casadei said in presenting the findings of the Statin Therapy in Cardiac Surgery (STICS) trial at the annual congress of the European Society of Cardiology.

The STICS results are at odds with conventional wisdom. ESC guidelines give a favorable class IIa, level of evidence B recommendation that "statins should be considered for prevention of new-onset atrial fibrillation after coronary artery bypass grafting, either isolated or in combination with valvular interventions."
"STICS was a very carefully conducted, large scale, robust study that I think has definitely closed the door on this issue," commented Dr. Keith A.A. Fox, professor of cardiology at the University of Edinburgh and chair of the scientific and clinical program committee at ESC Congress 2014.
STICS was a double-blind prospective trial in which 1,922 patients scheduled for elective CABG were randomized to 20 mg per day of rosuvastatin (Crestor) or placebo starting up to 8 days prior to surgery and continued for 5 days postop. All participants were in sinus rhythm preoperatively, with no history of AF, said Dr. Casadei, professor of cardiovascular medicine at the University of Oxford, England.
The two coprimary endpoints in STICS were the incidence of new-onset AF during 5 days of postop Holter monitoring, and evidence of postop myocardial injury as demonstrated in serial troponin I assays.
Postop AF occurred in 21% of those given high-intensity therapy with rosuvastatin and 20% of placebo-treated controls. There was no subgroup where rosuvastatin was protective (see graphic).
Troponin I measurements obtained 6, 24, 48, and 120 hours postop showed areas under the curve that were superimposable in the two study groups, meaning perioperative high-dose statin therapy provided absolutely no protection against postop cardiac muscle injury.
Mean hospital length of stay and ICU time didn’t differ between the two groups, either.
The impetus for conducting STICS was recognition that the guidelines’ endorsement of perioperative high-dose statin therapy in conjunction with cardiac surgery was based upon a series of small randomized trials with serious limitations. Although the results of a meta-analysis of the 14 prior trials looked impressive at first glance – a 17% incidence of postop AF in statin-treated patients, compared with 30% in controls, for a near-halving of the risk of this important complication – these 14 studies totaled 1,300 patients, and there were many methodologic shortcomings.
The STICS researchers hypothesized that a large, well-designed trial – bigger than all previous studies combined – would shore up the previously shaky supporting evidence and perhaps provide grounds for statins to win a new indication from regulatory agencies. Post-CABG AF is associated with a doubled risk of stroke and mortality, and excess hospital costs of $8,000-$18,000 dollars per patient.
Discussant Dr. Paulus Kirchhof, a member of the task force that developed the current ESC guidelines (Europace 2010;12:1360-420), said those guidelines now clearly need to be revisited. Beyond that, he added, STICS provides important new contributions in understanding the pathophysiology of AF.
"We know that AF is caused by several vicious circles, and we believe that inflammation could influence those and cause AF. And we also thought that postop AF was the condition where inflammation plays the biggest role. Based upon the negative results with this anti-inflammatory intervention, I think we have to question this concept a bit," said Dr. Kirchhof, professor of cardiovascular sciences at the University of Birmingham, England.
Dr. Casadei countered that she’s not ready to write off postop inflammation entirely as a major trigger of new-onset AF following CABG.
"The inflammation is there. We know from experimental work in animals that there is a strong association between inflammation and postop atrial fibrillation, but whether the association is causal, I think, is still debated. However, it may be that the anti-inflammatory effect of statins is not sufficiently strong to actually prevent this complication," she said.
Discussant Dr. Steven Nissen praised STICS as "an outstanding trial."
"I also think there’s a terribly important lesson here, which is the power of self-delusion in medicine. When we base our guidelines on small, poorly controlled trials, we are often making mistakes. This is one of countless examples where when someone finally does a careful, thoughtful trial, we find out that something that people believe just isn’t true. We can’t cut corners with evidence. We need good randomized trials," declared Dr. Nissen, chair of the department of cardiovascular medicine at the Cleveland Clinic.
The STICS trial was funded primarily by the British Heart Foundation, the Oxford Biomedical Research Center, and the UK Medical Research Council. In addition, Dr. Casadei reported receiving an unrestricted grant from AstraZeneca in conjunction with the trial.
AT THE ESC CONGRESS 2014
Key clinical point: Perioperative statin therapy in patients undergoing CABG failed to protect against new-onset postop atrial fibrillation.
Major finding: The incidence of postop atrial fibrillation within 5 days post-CABG was 21% in patients randomized to 20 mg/day of rosuvastatin and 20% in placebo-treated controls.
Data source: The multicenter STICS trial included 1,922 randomized patients scheduled for elective CABG.
Disclosures: STICS was funded by the British Heart Foundation, the Oxford Biomedical Research Center, and the UK Medical Research Council. The presenter reported having received a research grant from AstraZeneca.