User login
Paranoia and slowed cognition
CASE: Behavioral changes
Mr. K, age 45, is brought to the emergency department (ED) by his wife for severe paranoia, combative behavior, confusion, and slowed cognition. Mr. K tells the ED staff that a chemical abrasion he sustained a few weeks earlier has spread to his penis, and insists that his penis is retracting into his body. He has tied a string around his penis to keep it from disappearing into his body. According to Mr. K’s wife, he went to an urgent care clinic 2 weeks ago after he sustained chemical abrasions from exposure to cleaning solution at home. The provider at the urgent care clinic started Mr. K on an unknown dose of oral prednisone.
Mr. K’s wife reports that her husband had a dysphoric episode approximately 6 months ago when his business was struggling but his mood improved without psychiatric care. Mr. K’s medical history includes episodic sarcoidosis of the eyes, skin, and lungs. In the past these symptoms remitted after he received oral prednisone.
ED clinicians consider neurosarcoidosis and substance-induced delirium in the differential diagnosis (Table).1 A CT scan of the head fails to show lesions suggestive of neurosarcoidosis. Chest radiography does not reveal lesions suggestive of lung sarcoids and Mr. K has no skin lesions.
Table
DSM-IV-TR criteria for substance-induced delirium
|
| Source: Reference 1 |
Mr. K is admitted to the psychiatric inpatient unit for acute stabilization, where he remains aggressive and combative. He throws chairs at his peers and staff on the unit and is placed in physical restraints. He requires several doses of IM haloperidol, 5 mg, lorazepam, 2 mg, and diphenhydramine, 50 mg, for severe agitation. Mr. K is guarded, perseverative, and selectively mute. He avoids eye contact and has poor grooming. He has slow thought processing and displays concrete thought process. Prednisone is discontinued and olanzapine, titrated to 30 mg/d, and mirtazapine, titrated to 30 mg/d, are started for psychosis and depression.
Mr. K’s mood and behavior eventually return to baseline but slowed cognition persists. He is discharged from our facility.
The authors’ observations
Cortisone was first used to treat rheumatoid arthritis in 1948 and corticosteroids have been linked to multiple neuropsychiatric complications that have been broadly defined as steroid psychosis. This syndrome includes reversible behavioral manifestations such as hypomania, irritability, mood reactivity, anxiety, and insomnia in addition to more severe symptoms such as depression, mania, and psychosis.2 Although mild cognitive deficits have been noted in patients taking corticosteroids, most published cases have focused on steroid-induced psychosis.
In 1984, Varney et al3 noted a phenomenon they called “steroid dementia” in 6 patients treated with corticosteroids. On first evaluation, these patients presented with symptoms similar to early Alzheimer’s dementia—impaired memory, attention, and concentration. Three patients initially were diagnosed first with Alzheimer’s dementia until their symptoms spontaneously improved when steroids were reduced or discontinued. Although their presentation resembled Alzheimer’s dementia, patients with steroid dementia had a specific cognitive presentation associated with corticosteroid use. Symptoms included impaired verbal memory and spatial thinking but normal procedural memory. These patients showed intact immediate recall but impaired delayed recall with difficulty tracking conversations and word finding. Overall, patients with steroid dementia showed a predominance of verbal declarative memory deficits out of proportion to other cognitive symptoms. These symptoms and recent corticosteroid exposure differentiated steroid dementia from other forms of dementia.
In a later article, Varney reviewed electroencephalography (EEG) and CT findings associated with steroid dementia, noting bilateral EEG abnormalities and acute cortical atrophy on CT.4 Steroid dementia largely was reversible, resolving 3 to 11 months after corticosteroid discontinuation. Additionally, Varney noted that patients who had psychosis and dementia had more severe and longer-lasting dementia.
TREATMENT: Progressive decline
Mr. K is college educated, has been married for 15 years, has 2 children, age 9 and 11, and owns a successful basketball coaching business. He has no history of substance abuse, legal issues, or violence. He reports a good childhood with normal developmental milestones and no history of trauma.
In the 6 months after his initial psychiatric admission, Mr. K sees various outpatient providers, who change his psychotropics multiple times. He also receives 4 courses of prednisone for ocular sarcoidosis. He is admitted twice to other psychiatric facilities. After he has paranoid interactions with colleagues and families of the youth he coaches, his business fails.
After his third psychiatric inpatient hospitalization, Mr. K becomes severely paranoid, believing his wife is having an affair. He becomes physically abusive to his wife, who obtains a restraining order and leaves with their children. Mr. K barely leaves his house and stops grooming. A friend notes that Mr. K’s home has become uninhabitable, and it goes into foreclosure. After Mr. K’s neighbors report combative behavior and paranoia, police bring him in on an involuntary hold for a fourth psychiatric hospitalization (the second in our facility).
During this hospitalization—6 months after the initial ED presentation—the neurology team conducts a repeat medical workup. EEG shows generalized slowing. Head CT and MRI show diffuse cortical atrophy that was not seen in previous imaging. Mr. K has ocular lesions characteristic of ocular sarcoidosis. His mental status examination is similar to his first presentation except that the psychosis and thought disorganization are considerably worse. His cognitive functioning also shows significant decline. Cognitive screening reveals intact remote memory with impaired recent memory. His thinking is concrete and his verbal memory is markedly impaired. His Mini-Mental State Examination score is 27/30, indicating functional capacity that is better than his clinical presentation. Because of difficulty with concentration and verbal processing, Mr. K is unable to complete the Minnesota Multiphasic Personality Inventory despite substantial assistance. On most days he cannot recall recent conversations with his wife, staff, or physicians. He is taking no medications at this time.
Mr. K is restarted on olanzapine, titrated to 30 mg/d, to control his psychosis; this medication was effective during his last stay in our facility. Oral prednisone is discontinued and methotrexate, 10 mg/week, is initiated for ocular sarcoidosis. Based on recommendations from a case series report,5 we start Mr. K on lithium, titrated to 600 mg twice a day, for steroid-induced mood symptoms, Mr. K’s psychosis and mood improve dramatically once he reaches a therapeutic lithium level; however, his cognition remains slowed and he is unable to care for his basic needs.
The authors’ observations
Steroid dementia may be the result of effects in the medial temporal lobe, specifically dorsolateral prefrontal cortex, which impairs working memory, and the parahippocampal gyrus.6,7 The cognitive presentation of steroid dementia Varney et al3 described has been replicated in healthy volunteers who received corticosteroids.3 Patients with Cushing’s syndrome also have been noted to have diminished hippocampal volume and similar cognitive deficits. Cognitive impairment experienced by patients treated with corticosteroids may be caused by neuronal death in the hippocampus and dorsolateral prefrontal cortex. The etiology of cell death is multifactorial and includes glutamate-mediated excitotoxicity, activation of proinflammatory pathways, inhibited utilization of glucose in the hippocampus, telomere shortening, and diminished cell repair by brain-derived neurotrophic factor. The net result is significant, widespread damage that in some cases is irreversible.8
Because of the severity of Mr. K’s psychosis and personality change from baseline, his cognitive symptoms were largely overlooked during his first psychiatric hospitalization. The affective flattening, delayed verbal response, and markedly concrete thought process were considered within the spectrum of resolving psychosis. After further hospitalizations and abnormal results on cognitive testing, Mr. K’s cognitive impairment was fully noted. His symptoms match those of previously documented cases of steroid dementia, including verbal deficits out of proportion to other impairment, acute cerebral atrophy on CT after corticosteroid treatment, and gradual improvement of symptoms when corticosteroids were discontinued.
Management recommendations
Educate patients taking steroids about possible side effects of mood changes, psychosis, and cognitive deficits. Close monitoring of patients on corticosteroids is paramount. If psychiatric or cognitive symptoms develop, gradually discontinue the corticosteroid and seek other treatments.
Randomized, placebo-controlled trials of lamotrigine and memantine have shown these medications are cognitively protective for patients taking prednisone.9
OUTCOME: Long-term deficits
After a 33-day stay in our adult inpatient psychiatric facility, the county places Mr. K in a permanent conservatorship for severe grave disability. He is discharged to a long-term psychiatric care locked facility for ongoing management. Mr. K spends 20 months in the long-term care facility while his family remains hopeful for his recovery and return home. He is admitted to our facility for acute stabilization of psychotic symptoms after he is released from the locked facility. Although no imaging studies are conducted, he remains significantly forgetful. Additionally, his paranoia persists.
Mr. K is poorly compliant with his psychotropics, which include divalproex, 1,000 mg/d, and olanzapine, 30 mg/d. Although he is discharged home with his family, his functional capacity is less than expected and he requires continuous support. Insisting that Mr. K abstain from steroids after the first psychiatric hospitalization might have prevented this seemingly irreversible dementia.
Related Resources
- Sacks O, Shulman M. Steroid dementia: an overlooked diagnosis? Neurology. 2005;64(4):707-709.
- Cipriani G, Picchi L, Vedovello M, et al. Reversible dementia from corticosteroid therapy. Clinical Geriatrics. 2012;20(7):38-41.
Drug Brand Names
- Diphenhydramine • Benadryl
- Divalproex • Depakote
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Memantine • Namenda
- Methotrexate • Rheumatrex, Trexall
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Prednisone • Deltasone, Meticorten, others
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Arlington VA: American Psychiatric Association; 2000.
2. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367.
3. Varney NR, Alexander B, MacIndoe JH. Reversible steroid dementia in patients without steroid psychosis. Am J Psychiatry. 1984;141(3):369-372.
4. Varney NR. A case of reversible steroid dementia. Arch Clin Neuropsychol. 1997;12(2):167-171.
5. Sirois F. Steroid psychosis: a review. Gen Hosp Psychiatry. 2003;25(1):27-33.
6. Wolkowitz OM, Burke H, Epel ES, et al. Glucocorticoids: mood, memory, and mechanisms. Ann N Y Acad Sci. 2009;1179:19-40.
7. Lupien SJ, McEwen BS. The acute effects of corticosteroids on cognition: integration of animal and human model studies. Brain Res Brain Res Rev. 1997;24(1):1-27.
8. Sapolsky RM. The physiological relevance of glucocorticoid endangerment of the hippocampus. Ann NY Acad Sci. 1994;746:294-304.
9. Brown ES. Effects of glucocorticoids on mood memory and the hippocampus. Treatment and preventative therapy. Ann N Y Acad Sci. 2009;1179:41-55.
CASE: Behavioral changes
Mr. K, age 45, is brought to the emergency department (ED) by his wife for severe paranoia, combative behavior, confusion, and slowed cognition. Mr. K tells the ED staff that a chemical abrasion he sustained a few weeks earlier has spread to his penis, and insists that his penis is retracting into his body. He has tied a string around his penis to keep it from disappearing into his body. According to Mr. K’s wife, he went to an urgent care clinic 2 weeks ago after he sustained chemical abrasions from exposure to cleaning solution at home. The provider at the urgent care clinic started Mr. K on an unknown dose of oral prednisone.
Mr. K’s wife reports that her husband had a dysphoric episode approximately 6 months ago when his business was struggling but his mood improved without psychiatric care. Mr. K’s medical history includes episodic sarcoidosis of the eyes, skin, and lungs. In the past these symptoms remitted after he received oral prednisone.
ED clinicians consider neurosarcoidosis and substance-induced delirium in the differential diagnosis (Table).1 A CT scan of the head fails to show lesions suggestive of neurosarcoidosis. Chest radiography does not reveal lesions suggestive of lung sarcoids and Mr. K has no skin lesions.
Table
DSM-IV-TR criteria for substance-induced delirium
|
| Source: Reference 1 |
Mr. K is admitted to the psychiatric inpatient unit for acute stabilization, where he remains aggressive and combative. He throws chairs at his peers and staff on the unit and is placed in physical restraints. He requires several doses of IM haloperidol, 5 mg, lorazepam, 2 mg, and diphenhydramine, 50 mg, for severe agitation. Mr. K is guarded, perseverative, and selectively mute. He avoids eye contact and has poor grooming. He has slow thought processing and displays concrete thought process. Prednisone is discontinued and olanzapine, titrated to 30 mg/d, and mirtazapine, titrated to 30 mg/d, are started for psychosis and depression.
Mr. K’s mood and behavior eventually return to baseline but slowed cognition persists. He is discharged from our facility.
The authors’ observations
Cortisone was first used to treat rheumatoid arthritis in 1948 and corticosteroids have been linked to multiple neuropsychiatric complications that have been broadly defined as steroid psychosis. This syndrome includes reversible behavioral manifestations such as hypomania, irritability, mood reactivity, anxiety, and insomnia in addition to more severe symptoms such as depression, mania, and psychosis.2 Although mild cognitive deficits have been noted in patients taking corticosteroids, most published cases have focused on steroid-induced psychosis.
In 1984, Varney et al3 noted a phenomenon they called “steroid dementia” in 6 patients treated with corticosteroids. On first evaluation, these patients presented with symptoms similar to early Alzheimer’s dementia—impaired memory, attention, and concentration. Three patients initially were diagnosed first with Alzheimer’s dementia until their symptoms spontaneously improved when steroids were reduced or discontinued. Although their presentation resembled Alzheimer’s dementia, patients with steroid dementia had a specific cognitive presentation associated with corticosteroid use. Symptoms included impaired verbal memory and spatial thinking but normal procedural memory. These patients showed intact immediate recall but impaired delayed recall with difficulty tracking conversations and word finding. Overall, patients with steroid dementia showed a predominance of verbal declarative memory deficits out of proportion to other cognitive symptoms. These symptoms and recent corticosteroid exposure differentiated steroid dementia from other forms of dementia.
In a later article, Varney reviewed electroencephalography (EEG) and CT findings associated with steroid dementia, noting bilateral EEG abnormalities and acute cortical atrophy on CT.4 Steroid dementia largely was reversible, resolving 3 to 11 months after corticosteroid discontinuation. Additionally, Varney noted that patients who had psychosis and dementia had more severe and longer-lasting dementia.
TREATMENT: Progressive decline
Mr. K is college educated, has been married for 15 years, has 2 children, age 9 and 11, and owns a successful basketball coaching business. He has no history of substance abuse, legal issues, or violence. He reports a good childhood with normal developmental milestones and no history of trauma.
In the 6 months after his initial psychiatric admission, Mr. K sees various outpatient providers, who change his psychotropics multiple times. He also receives 4 courses of prednisone for ocular sarcoidosis. He is admitted twice to other psychiatric facilities. After he has paranoid interactions with colleagues and families of the youth he coaches, his business fails.
After his third psychiatric inpatient hospitalization, Mr. K becomes severely paranoid, believing his wife is having an affair. He becomes physically abusive to his wife, who obtains a restraining order and leaves with their children. Mr. K barely leaves his house and stops grooming. A friend notes that Mr. K’s home has become uninhabitable, and it goes into foreclosure. After Mr. K’s neighbors report combative behavior and paranoia, police bring him in on an involuntary hold for a fourth psychiatric hospitalization (the second in our facility).
During this hospitalization—6 months after the initial ED presentation—the neurology team conducts a repeat medical workup. EEG shows generalized slowing. Head CT and MRI show diffuse cortical atrophy that was not seen in previous imaging. Mr. K has ocular lesions characteristic of ocular sarcoidosis. His mental status examination is similar to his first presentation except that the psychosis and thought disorganization are considerably worse. His cognitive functioning also shows significant decline. Cognitive screening reveals intact remote memory with impaired recent memory. His thinking is concrete and his verbal memory is markedly impaired. His Mini-Mental State Examination score is 27/30, indicating functional capacity that is better than his clinical presentation. Because of difficulty with concentration and verbal processing, Mr. K is unable to complete the Minnesota Multiphasic Personality Inventory despite substantial assistance. On most days he cannot recall recent conversations with his wife, staff, or physicians. He is taking no medications at this time.
Mr. K is restarted on olanzapine, titrated to 30 mg/d, to control his psychosis; this medication was effective during his last stay in our facility. Oral prednisone is discontinued and methotrexate, 10 mg/week, is initiated for ocular sarcoidosis. Based on recommendations from a case series report,5 we start Mr. K on lithium, titrated to 600 mg twice a day, for steroid-induced mood symptoms, Mr. K’s psychosis and mood improve dramatically once he reaches a therapeutic lithium level; however, his cognition remains slowed and he is unable to care for his basic needs.
The authors’ observations
Steroid dementia may be the result of effects in the medial temporal lobe, specifically dorsolateral prefrontal cortex, which impairs working memory, and the parahippocampal gyrus.6,7 The cognitive presentation of steroid dementia Varney et al3 described has been replicated in healthy volunteers who received corticosteroids.3 Patients with Cushing’s syndrome also have been noted to have diminished hippocampal volume and similar cognitive deficits. Cognitive impairment experienced by patients treated with corticosteroids may be caused by neuronal death in the hippocampus and dorsolateral prefrontal cortex. The etiology of cell death is multifactorial and includes glutamate-mediated excitotoxicity, activation of proinflammatory pathways, inhibited utilization of glucose in the hippocampus, telomere shortening, and diminished cell repair by brain-derived neurotrophic factor. The net result is significant, widespread damage that in some cases is irreversible.8
Because of the severity of Mr. K’s psychosis and personality change from baseline, his cognitive symptoms were largely overlooked during his first psychiatric hospitalization. The affective flattening, delayed verbal response, and markedly concrete thought process were considered within the spectrum of resolving psychosis. After further hospitalizations and abnormal results on cognitive testing, Mr. K’s cognitive impairment was fully noted. His symptoms match those of previously documented cases of steroid dementia, including verbal deficits out of proportion to other impairment, acute cerebral atrophy on CT after corticosteroid treatment, and gradual improvement of symptoms when corticosteroids were discontinued.
Management recommendations
Educate patients taking steroids about possible side effects of mood changes, psychosis, and cognitive deficits. Close monitoring of patients on corticosteroids is paramount. If psychiatric or cognitive symptoms develop, gradually discontinue the corticosteroid and seek other treatments.
Randomized, placebo-controlled trials of lamotrigine and memantine have shown these medications are cognitively protective for patients taking prednisone.9
OUTCOME: Long-term deficits
After a 33-day stay in our adult inpatient psychiatric facility, the county places Mr. K in a permanent conservatorship for severe grave disability. He is discharged to a long-term psychiatric care locked facility for ongoing management. Mr. K spends 20 months in the long-term care facility while his family remains hopeful for his recovery and return home. He is admitted to our facility for acute stabilization of psychotic symptoms after he is released from the locked facility. Although no imaging studies are conducted, he remains significantly forgetful. Additionally, his paranoia persists.
Mr. K is poorly compliant with his psychotropics, which include divalproex, 1,000 mg/d, and olanzapine, 30 mg/d. Although he is discharged home with his family, his functional capacity is less than expected and he requires continuous support. Insisting that Mr. K abstain from steroids after the first psychiatric hospitalization might have prevented this seemingly irreversible dementia.
Related Resources
- Sacks O, Shulman M. Steroid dementia: an overlooked diagnosis? Neurology. 2005;64(4):707-709.
- Cipriani G, Picchi L, Vedovello M, et al. Reversible dementia from corticosteroid therapy. Clinical Geriatrics. 2012;20(7):38-41.
Drug Brand Names
- Diphenhydramine • Benadryl
- Divalproex • Depakote
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Memantine • Namenda
- Methotrexate • Rheumatrex, Trexall
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Prednisone • Deltasone, Meticorten, others
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
CASE: Behavioral changes
Mr. K, age 45, is brought to the emergency department (ED) by his wife for severe paranoia, combative behavior, confusion, and slowed cognition. Mr. K tells the ED staff that a chemical abrasion he sustained a few weeks earlier has spread to his penis, and insists that his penis is retracting into his body. He has tied a string around his penis to keep it from disappearing into his body. According to Mr. K’s wife, he went to an urgent care clinic 2 weeks ago after he sustained chemical abrasions from exposure to cleaning solution at home. The provider at the urgent care clinic started Mr. K on an unknown dose of oral prednisone.
Mr. K’s wife reports that her husband had a dysphoric episode approximately 6 months ago when his business was struggling but his mood improved without psychiatric care. Mr. K’s medical history includes episodic sarcoidosis of the eyes, skin, and lungs. In the past these symptoms remitted after he received oral prednisone.
ED clinicians consider neurosarcoidosis and substance-induced delirium in the differential diagnosis (Table).1 A CT scan of the head fails to show lesions suggestive of neurosarcoidosis. Chest radiography does not reveal lesions suggestive of lung sarcoids and Mr. K has no skin lesions.
Table
DSM-IV-TR criteria for substance-induced delirium
|
| Source: Reference 1 |
Mr. K is admitted to the psychiatric inpatient unit for acute stabilization, where he remains aggressive and combative. He throws chairs at his peers and staff on the unit and is placed in physical restraints. He requires several doses of IM haloperidol, 5 mg, lorazepam, 2 mg, and diphenhydramine, 50 mg, for severe agitation. Mr. K is guarded, perseverative, and selectively mute. He avoids eye contact and has poor grooming. He has slow thought processing and displays concrete thought process. Prednisone is discontinued and olanzapine, titrated to 30 mg/d, and mirtazapine, titrated to 30 mg/d, are started for psychosis and depression.
Mr. K’s mood and behavior eventually return to baseline but slowed cognition persists. He is discharged from our facility.
The authors’ observations
Cortisone was first used to treat rheumatoid arthritis in 1948 and corticosteroids have been linked to multiple neuropsychiatric complications that have been broadly defined as steroid psychosis. This syndrome includes reversible behavioral manifestations such as hypomania, irritability, mood reactivity, anxiety, and insomnia in addition to more severe symptoms such as depression, mania, and psychosis.2 Although mild cognitive deficits have been noted in patients taking corticosteroids, most published cases have focused on steroid-induced psychosis.
In 1984, Varney et al3 noted a phenomenon they called “steroid dementia” in 6 patients treated with corticosteroids. On first evaluation, these patients presented with symptoms similar to early Alzheimer’s dementia—impaired memory, attention, and concentration. Three patients initially were diagnosed first with Alzheimer’s dementia until their symptoms spontaneously improved when steroids were reduced or discontinued. Although their presentation resembled Alzheimer’s dementia, patients with steroid dementia had a specific cognitive presentation associated with corticosteroid use. Symptoms included impaired verbal memory and spatial thinking but normal procedural memory. These patients showed intact immediate recall but impaired delayed recall with difficulty tracking conversations and word finding. Overall, patients with steroid dementia showed a predominance of verbal declarative memory deficits out of proportion to other cognitive symptoms. These symptoms and recent corticosteroid exposure differentiated steroid dementia from other forms of dementia.
In a later article, Varney reviewed electroencephalography (EEG) and CT findings associated with steroid dementia, noting bilateral EEG abnormalities and acute cortical atrophy on CT.4 Steroid dementia largely was reversible, resolving 3 to 11 months after corticosteroid discontinuation. Additionally, Varney noted that patients who had psychosis and dementia had more severe and longer-lasting dementia.
TREATMENT: Progressive decline
Mr. K is college educated, has been married for 15 years, has 2 children, age 9 and 11, and owns a successful basketball coaching business. He has no history of substance abuse, legal issues, or violence. He reports a good childhood with normal developmental milestones and no history of trauma.
In the 6 months after his initial psychiatric admission, Mr. K sees various outpatient providers, who change his psychotropics multiple times. He also receives 4 courses of prednisone for ocular sarcoidosis. He is admitted twice to other psychiatric facilities. After he has paranoid interactions with colleagues and families of the youth he coaches, his business fails.
After his third psychiatric inpatient hospitalization, Mr. K becomes severely paranoid, believing his wife is having an affair. He becomes physically abusive to his wife, who obtains a restraining order and leaves with their children. Mr. K barely leaves his house and stops grooming. A friend notes that Mr. K’s home has become uninhabitable, and it goes into foreclosure. After Mr. K’s neighbors report combative behavior and paranoia, police bring him in on an involuntary hold for a fourth psychiatric hospitalization (the second in our facility).
During this hospitalization—6 months after the initial ED presentation—the neurology team conducts a repeat medical workup. EEG shows generalized slowing. Head CT and MRI show diffuse cortical atrophy that was not seen in previous imaging. Mr. K has ocular lesions characteristic of ocular sarcoidosis. His mental status examination is similar to his first presentation except that the psychosis and thought disorganization are considerably worse. His cognitive functioning also shows significant decline. Cognitive screening reveals intact remote memory with impaired recent memory. His thinking is concrete and his verbal memory is markedly impaired. His Mini-Mental State Examination score is 27/30, indicating functional capacity that is better than his clinical presentation. Because of difficulty with concentration and verbal processing, Mr. K is unable to complete the Minnesota Multiphasic Personality Inventory despite substantial assistance. On most days he cannot recall recent conversations with his wife, staff, or physicians. He is taking no medications at this time.
Mr. K is restarted on olanzapine, titrated to 30 mg/d, to control his psychosis; this medication was effective during his last stay in our facility. Oral prednisone is discontinued and methotrexate, 10 mg/week, is initiated for ocular sarcoidosis. Based on recommendations from a case series report,5 we start Mr. K on lithium, titrated to 600 mg twice a day, for steroid-induced mood symptoms, Mr. K’s psychosis and mood improve dramatically once he reaches a therapeutic lithium level; however, his cognition remains slowed and he is unable to care for his basic needs.
The authors’ observations
Steroid dementia may be the result of effects in the medial temporal lobe, specifically dorsolateral prefrontal cortex, which impairs working memory, and the parahippocampal gyrus.6,7 The cognitive presentation of steroid dementia Varney et al3 described has been replicated in healthy volunteers who received corticosteroids.3 Patients with Cushing’s syndrome also have been noted to have diminished hippocampal volume and similar cognitive deficits. Cognitive impairment experienced by patients treated with corticosteroids may be caused by neuronal death in the hippocampus and dorsolateral prefrontal cortex. The etiology of cell death is multifactorial and includes glutamate-mediated excitotoxicity, activation of proinflammatory pathways, inhibited utilization of glucose in the hippocampus, telomere shortening, and diminished cell repair by brain-derived neurotrophic factor. The net result is significant, widespread damage that in some cases is irreversible.8
Because of the severity of Mr. K’s psychosis and personality change from baseline, his cognitive symptoms were largely overlooked during his first psychiatric hospitalization. The affective flattening, delayed verbal response, and markedly concrete thought process were considered within the spectrum of resolving psychosis. After further hospitalizations and abnormal results on cognitive testing, Mr. K’s cognitive impairment was fully noted. His symptoms match those of previously documented cases of steroid dementia, including verbal deficits out of proportion to other impairment, acute cerebral atrophy on CT after corticosteroid treatment, and gradual improvement of symptoms when corticosteroids were discontinued.
Management recommendations
Educate patients taking steroids about possible side effects of mood changes, psychosis, and cognitive deficits. Close monitoring of patients on corticosteroids is paramount. If psychiatric or cognitive symptoms develop, gradually discontinue the corticosteroid and seek other treatments.
Randomized, placebo-controlled trials of lamotrigine and memantine have shown these medications are cognitively protective for patients taking prednisone.9
OUTCOME: Long-term deficits
After a 33-day stay in our adult inpatient psychiatric facility, the county places Mr. K in a permanent conservatorship for severe grave disability. He is discharged to a long-term psychiatric care locked facility for ongoing management. Mr. K spends 20 months in the long-term care facility while his family remains hopeful for his recovery and return home. He is admitted to our facility for acute stabilization of psychotic symptoms after he is released from the locked facility. Although no imaging studies are conducted, he remains significantly forgetful. Additionally, his paranoia persists.
Mr. K is poorly compliant with his psychotropics, which include divalproex, 1,000 mg/d, and olanzapine, 30 mg/d. Although he is discharged home with his family, his functional capacity is less than expected and he requires continuous support. Insisting that Mr. K abstain from steroids after the first psychiatric hospitalization might have prevented this seemingly irreversible dementia.
Related Resources
- Sacks O, Shulman M. Steroid dementia: an overlooked diagnosis? Neurology. 2005;64(4):707-709.
- Cipriani G, Picchi L, Vedovello M, et al. Reversible dementia from corticosteroid therapy. Clinical Geriatrics. 2012;20(7):38-41.
Drug Brand Names
- Diphenhydramine • Benadryl
- Divalproex • Depakote
- Haloperidol • Haldol
- Lamotrigine • Lamictal
- Lithium • Eskalith, Lithobid
- Lorazepam • Ativan
- Memantine • Namenda
- Methotrexate • Rheumatrex, Trexall
- Mirtazapine • Remeron
- Olanzapine • Zyprexa
- Prednisone • Deltasone, Meticorten, others
Disclosure
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Arlington VA: American Psychiatric Association; 2000.
2. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367.
3. Varney NR, Alexander B, MacIndoe JH. Reversible steroid dementia in patients without steroid psychosis. Am J Psychiatry. 1984;141(3):369-372.
4. Varney NR. A case of reversible steroid dementia. Arch Clin Neuropsychol. 1997;12(2):167-171.
5. Sirois F. Steroid psychosis: a review. Gen Hosp Psychiatry. 2003;25(1):27-33.
6. Wolkowitz OM, Burke H, Epel ES, et al. Glucocorticoids: mood, memory, and mechanisms. Ann N Y Acad Sci. 2009;1179:19-40.
7. Lupien SJ, McEwen BS. The acute effects of corticosteroids on cognition: integration of animal and human model studies. Brain Res Brain Res Rev. 1997;24(1):1-27.
8. Sapolsky RM. The physiological relevance of glucocorticoid endangerment of the hippocampus. Ann NY Acad Sci. 1994;746:294-304.
9. Brown ES. Effects of glucocorticoids on mood memory and the hippocampus. Treatment and preventative therapy. Ann N Y Acad Sci. 2009;1179:41-55.
1. Diagnostic and statistical manual of mental disorders 4th ed, text rev. Arlington VA: American Psychiatric Association; 2000.
2. Warrington TP, Bostwick JM. Psychiatric adverse effects of corticosteroids. Mayo Clin Proc. 2006;81(10):1361-1367.
3. Varney NR, Alexander B, MacIndoe JH. Reversible steroid dementia in patients without steroid psychosis. Am J Psychiatry. 1984;141(3):369-372.
4. Varney NR. A case of reversible steroid dementia. Arch Clin Neuropsychol. 1997;12(2):167-171.
5. Sirois F. Steroid psychosis: a review. Gen Hosp Psychiatry. 2003;25(1):27-33.
6. Wolkowitz OM, Burke H, Epel ES, et al. Glucocorticoids: mood, memory, and mechanisms. Ann N Y Acad Sci. 2009;1179:19-40.
7. Lupien SJ, McEwen BS. The acute effects of corticosteroids on cognition: integration of animal and human model studies. Brain Res Brain Res Rev. 1997;24(1):1-27.
8. Sapolsky RM. The physiological relevance of glucocorticoid endangerment of the hippocampus. Ann NY Acad Sci. 1994;746:294-304.
9. Brown ES. Effects of glucocorticoids on mood memory and the hippocampus. Treatment and preventative therapy. Ann N Y Acad Sci. 2009;1179:41-55.
Erythematous penile lesion
A 63-YEAR-OLD MAN came to our clinic complaining of a rash on his penis. He indicated that the rash had been there for almost 2 years and that he’d seen 2 other doctors about it, but they’d been unable to make a diagnosis.
The patient said the rash was mildly painful and tender. He denied pain on urination, discharge, fever, malaise, or arthralgias. He also denied any sexual contact outside of his marriage and indicated that he had not been able to have intimate contact with his wife because of the problem.
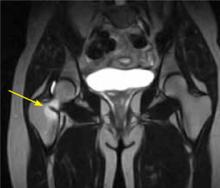
The patient was uncircumcised and when the foreskin was retracted, a bright red erythematous nonscaly circumferential plaque was visible on the glans penis, spreading to the foreskin (FIGURE 1).
FIGURE 1
A nonscaly, circumferential plaque on the glans penis
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Zoon’s balanitis
We ordered a biopsy because we suspected that the cause of the rash was either erythroplasia of Queyrat (a premalignant condition also known as Bowen’s disease of the glans penis) or Zoon’s balanitis (plasma cell balanitis or balanitis circumscripta plasmacellularis). The biopsy report confirmed the diagnosis of Zoon’s balanitis and showed no signs of malignancy. The features of Zoon’s balanitis include epidermal atrophy, loss of rete ridges, spongiosis, and subepidermal plasma cell infiltrate without evidence of malignancy (FIGURE 2).
FIGURE 2
Dense plasmacytic infiltration underlying the mucosal epidermis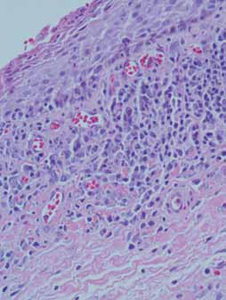
Condition affects older, uncircumcised men
Zoon’s balanitis is thought to be a benign condition that typically affects uncircumcised middle-aged to elderly men.1,2 Worldwide prevalence among uncircumcised men is approximately 3%.2 The etiology is unknown; it’s thought that this condition may be caused by friction, trauma, heat, lack of hygiene, exogenous or infectious agents, an IgE hypersensitivity, or a chronic infection with Mycobacterium smegmatis.1,2
Typically, the appearance of the lesion precedes diagnosis by about one to 2 years.1 The patient usually complains of mild pruritus and tenderness. Undergarments may be bloodstained.
The differential for penile lesions is extensive, and includes psoriasis, nummular eczema, candidiasis, herpes simplex, scabies, lichen sclerosus et atrophicus or lichen planus, syphilis, balanitis, and erythroplasia of Queyrat.
The lesion associated with Zoon’s balanitis is a solitary, glistening, shiny, red-to-orange plaque of the glans penis or prepuce of an uncircumcised male. Pinpoint erythematous spots or “cayenne pepper spots” may also be associated with this condition.
Patients with erythroplasia of Queyrat have either a solitary or multiple nonhealing erythematous plaques on the glans penis. These lesions may also affect the adjacent mucosal epithelium. As is true with Zoon’s balanitis, the typical patient is uncircumcised and middle-aged to elderly.1,2
Presentations may be similar, but treatment differs
Because the treatments for Zoon’s balanitis and erythroplasia of Queyrat are different, a biopsy is imperative. Erythroplasia of Queyrat is a premalignant condition that is treated with topical fluorouracil or surgical excision.3 Treatment for Zoon’s balanitis consists of a topical corticosteroid with or without topical anticandidal agents and circumcision after the acute inflammation resolves.1,2 (If a skin biopsy cannot be obtained in the clinic, the foreskin [if affected] can be sent for biopsy after the circumcision.)
If resolution is not seen with topical steroid treatment, other treatments have demonstrated efficacy. These include topical tacrolimus, as well as YAG and carbon dioxide laser treatments.4-6
Although information is limited on rates of recurrence, circumcision is considered the treatment of choice and is usually curative.1
Ointment does the trick for our patient
Our patient was treated with a single combined topical ointment consisting of nystatin and triamcinolone cream with zinc oxide. The lesion resolved completely after 10 days. We requested a urology consult so that a circumcision could be performed.
CORRESPONDENCE Matthew R. Noss, DO, MSEd, Fort Belvoir Community Hospital Family Medicine Clinic, 1st Floor, Eagle Pavilion, 9300 Dewitt Loop, Ft. Belvoir, VA 22060; [email protected]
1. Scheinfeld NS, Keough GC, Lehman DS. Balanitis circumscripta plasmacellularis. Medscape. June 8, 2012. Available at: emedicine.medscape.com/article/1122283. Accessed October 26, 2012.
2. Barrisford GW. Balanitis and balanoposthitis in adults. UpToDate. December 19, 2011. Available at: www.uptodate.com/contents/balanitis-and-balanoposthitis-in-adults. Accessed October 26, 2012.
3. Egan KM, Maino KL. Erythroplasia of Queyrat (Bowen disease of the glans penis). Medscape. May 31, 2012. Available at: emedicine.medscape.com/article/1100317. Accessed October 26, 2012.
4. Santos-Juanes J, Sanchez del Rio J, Galache C, et al. Topical tacrolimus: an effective therapy for Zoon balanitis. Arch Dermatol. 2004;140:1538-1539.
5. Wollina U. Ablative erbium: YAG laser treatment of idiopathic chronic inflammatory non-cicatricial balanoposthitis (Zoon’s disease)—a series of 20 patients with long-term outcome. J Cosmet Laser Ther. 2010;12:120-123.
6. Retamar RA, Kien MC, Couela EN. Zoon’s balanitis: presentation of 15 patients, five treated with a carbon dioxide laser. Int J Dermatol. 2003;42:305-307.
A 63-YEAR-OLD MAN came to our clinic complaining of a rash on his penis. He indicated that the rash had been there for almost 2 years and that he’d seen 2 other doctors about it, but they’d been unable to make a diagnosis.
The patient said the rash was mildly painful and tender. He denied pain on urination, discharge, fever, malaise, or arthralgias. He also denied any sexual contact outside of his marriage and indicated that he had not been able to have intimate contact with his wife because of the problem.
The patient was uncircumcised and when the foreskin was retracted, a bright red erythematous nonscaly circumferential plaque was visible on the glans penis, spreading to the foreskin (FIGURE 1).
FIGURE 1
A nonscaly, circumferential plaque on the glans penis
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Zoon’s balanitis
We ordered a biopsy because we suspected that the cause of the rash was either erythroplasia of Queyrat (a premalignant condition also known as Bowen’s disease of the glans penis) or Zoon’s balanitis (plasma cell balanitis or balanitis circumscripta plasmacellularis). The biopsy report confirmed the diagnosis of Zoon’s balanitis and showed no signs of malignancy. The features of Zoon’s balanitis include epidermal atrophy, loss of rete ridges, spongiosis, and subepidermal plasma cell infiltrate without evidence of malignancy (FIGURE 2).
FIGURE 2
Dense plasmacytic infiltration underlying the mucosal epidermis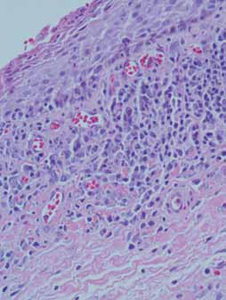
Condition affects older, uncircumcised men
Zoon’s balanitis is thought to be a benign condition that typically affects uncircumcised middle-aged to elderly men.1,2 Worldwide prevalence among uncircumcised men is approximately 3%.2 The etiology is unknown; it’s thought that this condition may be caused by friction, trauma, heat, lack of hygiene, exogenous or infectious agents, an IgE hypersensitivity, or a chronic infection with Mycobacterium smegmatis.1,2
Typically, the appearance of the lesion precedes diagnosis by about one to 2 years.1 The patient usually complains of mild pruritus and tenderness. Undergarments may be bloodstained.
The differential for penile lesions is extensive, and includes psoriasis, nummular eczema, candidiasis, herpes simplex, scabies, lichen sclerosus et atrophicus or lichen planus, syphilis, balanitis, and erythroplasia of Queyrat.
The lesion associated with Zoon’s balanitis is a solitary, glistening, shiny, red-to-orange plaque of the glans penis or prepuce of an uncircumcised male. Pinpoint erythematous spots or “cayenne pepper spots” may also be associated with this condition.
Patients with erythroplasia of Queyrat have either a solitary or multiple nonhealing erythematous plaques on the glans penis. These lesions may also affect the adjacent mucosal epithelium. As is true with Zoon’s balanitis, the typical patient is uncircumcised and middle-aged to elderly.1,2
Presentations may be similar, but treatment differs
Because the treatments for Zoon’s balanitis and erythroplasia of Queyrat are different, a biopsy is imperative. Erythroplasia of Queyrat is a premalignant condition that is treated with topical fluorouracil or surgical excision.3 Treatment for Zoon’s balanitis consists of a topical corticosteroid with or without topical anticandidal agents and circumcision after the acute inflammation resolves.1,2 (If a skin biopsy cannot be obtained in the clinic, the foreskin [if affected] can be sent for biopsy after the circumcision.)
If resolution is not seen with topical steroid treatment, other treatments have demonstrated efficacy. These include topical tacrolimus, as well as YAG and carbon dioxide laser treatments.4-6
Although information is limited on rates of recurrence, circumcision is considered the treatment of choice and is usually curative.1
Ointment does the trick for our patient
Our patient was treated with a single combined topical ointment consisting of nystatin and triamcinolone cream with zinc oxide. The lesion resolved completely after 10 days. We requested a urology consult so that a circumcision could be performed.
CORRESPONDENCE Matthew R. Noss, DO, MSEd, Fort Belvoir Community Hospital Family Medicine Clinic, 1st Floor, Eagle Pavilion, 9300 Dewitt Loop, Ft. Belvoir, VA 22060; [email protected]
A 63-YEAR-OLD MAN came to our clinic complaining of a rash on his penis. He indicated that the rash had been there for almost 2 years and that he’d seen 2 other doctors about it, but they’d been unable to make a diagnosis.
The patient said the rash was mildly painful and tender. He denied pain on urination, discharge, fever, malaise, or arthralgias. He also denied any sexual contact outside of his marriage and indicated that he had not been able to have intimate contact with his wife because of the problem.
The patient was uncircumcised and when the foreskin was retracted, a bright red erythematous nonscaly circumferential plaque was visible on the glans penis, spreading to the foreskin (FIGURE 1).
FIGURE 1
A nonscaly, circumferential plaque on the glans penis
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Zoon’s balanitis
We ordered a biopsy because we suspected that the cause of the rash was either erythroplasia of Queyrat (a premalignant condition also known as Bowen’s disease of the glans penis) or Zoon’s balanitis (plasma cell balanitis or balanitis circumscripta plasmacellularis). The biopsy report confirmed the diagnosis of Zoon’s balanitis and showed no signs of malignancy. The features of Zoon’s balanitis include epidermal atrophy, loss of rete ridges, spongiosis, and subepidermal plasma cell infiltrate without evidence of malignancy (FIGURE 2).
FIGURE 2
Dense plasmacytic infiltration underlying the mucosal epidermis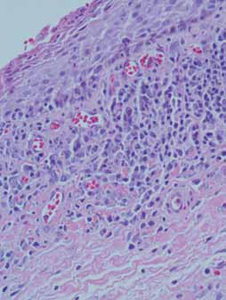
Condition affects older, uncircumcised men
Zoon’s balanitis is thought to be a benign condition that typically affects uncircumcised middle-aged to elderly men.1,2 Worldwide prevalence among uncircumcised men is approximately 3%.2 The etiology is unknown; it’s thought that this condition may be caused by friction, trauma, heat, lack of hygiene, exogenous or infectious agents, an IgE hypersensitivity, or a chronic infection with Mycobacterium smegmatis.1,2
Typically, the appearance of the lesion precedes diagnosis by about one to 2 years.1 The patient usually complains of mild pruritus and tenderness. Undergarments may be bloodstained.
The differential for penile lesions is extensive, and includes psoriasis, nummular eczema, candidiasis, herpes simplex, scabies, lichen sclerosus et atrophicus or lichen planus, syphilis, balanitis, and erythroplasia of Queyrat.
The lesion associated with Zoon’s balanitis is a solitary, glistening, shiny, red-to-orange plaque of the glans penis or prepuce of an uncircumcised male. Pinpoint erythematous spots or “cayenne pepper spots” may also be associated with this condition.
Patients with erythroplasia of Queyrat have either a solitary or multiple nonhealing erythematous plaques on the glans penis. These lesions may also affect the adjacent mucosal epithelium. As is true with Zoon’s balanitis, the typical patient is uncircumcised and middle-aged to elderly.1,2
Presentations may be similar, but treatment differs
Because the treatments for Zoon’s balanitis and erythroplasia of Queyrat are different, a biopsy is imperative. Erythroplasia of Queyrat is a premalignant condition that is treated with topical fluorouracil or surgical excision.3 Treatment for Zoon’s balanitis consists of a topical corticosteroid with or without topical anticandidal agents and circumcision after the acute inflammation resolves.1,2 (If a skin biopsy cannot be obtained in the clinic, the foreskin [if affected] can be sent for biopsy after the circumcision.)
If resolution is not seen with topical steroid treatment, other treatments have demonstrated efficacy. These include topical tacrolimus, as well as YAG and carbon dioxide laser treatments.4-6
Although information is limited on rates of recurrence, circumcision is considered the treatment of choice and is usually curative.1
Ointment does the trick for our patient
Our patient was treated with a single combined topical ointment consisting of nystatin and triamcinolone cream with zinc oxide. The lesion resolved completely after 10 days. We requested a urology consult so that a circumcision could be performed.
CORRESPONDENCE Matthew R. Noss, DO, MSEd, Fort Belvoir Community Hospital Family Medicine Clinic, 1st Floor, Eagle Pavilion, 9300 Dewitt Loop, Ft. Belvoir, VA 22060; [email protected]
1. Scheinfeld NS, Keough GC, Lehman DS. Balanitis circumscripta plasmacellularis. Medscape. June 8, 2012. Available at: emedicine.medscape.com/article/1122283. Accessed October 26, 2012.
2. Barrisford GW. Balanitis and balanoposthitis in adults. UpToDate. December 19, 2011. Available at: www.uptodate.com/contents/balanitis-and-balanoposthitis-in-adults. Accessed October 26, 2012.
3. Egan KM, Maino KL. Erythroplasia of Queyrat (Bowen disease of the glans penis). Medscape. May 31, 2012. Available at: emedicine.medscape.com/article/1100317. Accessed October 26, 2012.
4. Santos-Juanes J, Sanchez del Rio J, Galache C, et al. Topical tacrolimus: an effective therapy for Zoon balanitis. Arch Dermatol. 2004;140:1538-1539.
5. Wollina U. Ablative erbium: YAG laser treatment of idiopathic chronic inflammatory non-cicatricial balanoposthitis (Zoon’s disease)—a series of 20 patients with long-term outcome. J Cosmet Laser Ther. 2010;12:120-123.
6. Retamar RA, Kien MC, Couela EN. Zoon’s balanitis: presentation of 15 patients, five treated with a carbon dioxide laser. Int J Dermatol. 2003;42:305-307.
1. Scheinfeld NS, Keough GC, Lehman DS. Balanitis circumscripta plasmacellularis. Medscape. June 8, 2012. Available at: emedicine.medscape.com/article/1122283. Accessed October 26, 2012.
2. Barrisford GW. Balanitis and balanoposthitis in adults. UpToDate. December 19, 2011. Available at: www.uptodate.com/contents/balanitis-and-balanoposthitis-in-adults. Accessed October 26, 2012.
3. Egan KM, Maino KL. Erythroplasia of Queyrat (Bowen disease of the glans penis). Medscape. May 31, 2012. Available at: emedicine.medscape.com/article/1100317. Accessed October 26, 2012.
4. Santos-Juanes J, Sanchez del Rio J, Galache C, et al. Topical tacrolimus: an effective therapy for Zoon balanitis. Arch Dermatol. 2004;140:1538-1539.
5. Wollina U. Ablative erbium: YAG laser treatment of idiopathic chronic inflammatory non-cicatricial balanoposthitis (Zoon’s disease)—a series of 20 patients with long-term outcome. J Cosmet Laser Ther. 2010;12:120-123.
6. Retamar RA, Kien MC, Couela EN. Zoon’s balanitis: presentation of 15 patients, five treated with a carbon dioxide laser. Int J Dermatol. 2003;42:305-307.
Death follows a normal EKG ...Kidney failure after multiple meds
Death follows a normal EKG
MID-CHEST DISCOMFORT, A COUGH, AND SWEATING brought a 59-year-old man to his primary care physician. The patient had normal vital signs and reported that belching relieved the chest discomfort. He had a history of severe coronary artery disease and had undergone angioplasty and stenting several years earlier.
The primary care physician performed an electrocardiogram (EKG), which was normal and unchanged from one done the year before. The doctor suspected bronchitis, but prescribed omeprazole because the patient had previously been diagnosed with gastroesophageal reflux disease. He ordered a chemical stress test to be performed within a month and a chest radiograph to be done if the patient’s symptoms didn’t improve.
Two hours after returning home, the patient called an ambulance. He told paramedics that he’d been having chest pain for an hour. While they were putting the patient into the ambulance, he went into cardiac arrest. Four defibrillation attempts en route to the hospital and additional resuscitation attempts in the ED failed; he was pronounced dead 3½ hours after leaving his physician’s office.
No autopsy was performed. The patient’s widow found the omeprazole bottle, with one pill missing, and fast-food hamburger wrappers on the kitchen table.
PLAINTIFF’S CLAIM The primary care physician should have sent the patient to the ED to determine whether the chest pain had a cardiac cause; the patient was suffering from acute cardiac syndrome when the doctor saw him.
THE DEFENSE The patient’s normal EKG and vital signs and the fact that belching relieved his chest symptoms indicated that the complaints did not arise from cardiac causes or require emergency assessment. The patient didn’t report chest pain at the office visit; the later cardiac arrest probably resulted from a sudden plaque rupture unrelated to the earlier chest discomfort.
VERDICT $1.5 million Illinois verdict.
COMMENT I hope most doctors won’t have to learn this lesson from their own experience. A normal EKG does not rule out acute ischemia in a high-risk patient with chest pain and sweating. Admit such patients immediately to a cardiac observation unit.
Kidney failure after multiple meds
A MAN WAS TAKING MULTIPLE MEDICATIONS: 3 blood pressure drugs prescribed by his primary care physician, an NSAID prescribed by another doctor, and sizable doses of BC Powder, an over-the-counter analgesic containing aspirin, salicylamide, and caffeine. After 4 years on this medication regimen, the patient’s kidneys failed.
PLAINTIFF’S CLAIM The primary care physician failed to properly monitor kidney function with blood and urine tests while his patient was taking the medications. Proper testing would have resulted in a diagnosis of kidney disease before the patient’s kidneys failed completely. In addition, the primary care physician failed to explain the risks and side effects of the medications to the patient.
THE DEFENSE The patient refused kidney function testing and did not follow medical advice. He consumed excessive amounts of alcohol against medical advice, did not tell the primary care physician about other drugs he was taking, and had allowed his supply of blood pressure medication to run out.
VERDICT $2 million gross verdict in Georgia, with a finding of 47% comparative negligence.
COMMENT This case offers several lessons: First, each BC Powder packet contains the equivalent of 2 aspirin. Second, chronic, high-dose NSAIDs can cause renal failure, especially in patients whose renal function is compromised by hypertension. Third, all patients with hypertension should undergo periodic monitoring of renal function.
Death follows a normal EKG
MID-CHEST DISCOMFORT, A COUGH, AND SWEATING brought a 59-year-old man to his primary care physician. The patient had normal vital signs and reported that belching relieved the chest discomfort. He had a history of severe coronary artery disease and had undergone angioplasty and stenting several years earlier.
The primary care physician performed an electrocardiogram (EKG), which was normal and unchanged from one done the year before. The doctor suspected bronchitis, but prescribed omeprazole because the patient had previously been diagnosed with gastroesophageal reflux disease. He ordered a chemical stress test to be performed within a month and a chest radiograph to be done if the patient’s symptoms didn’t improve.
Two hours after returning home, the patient called an ambulance. He told paramedics that he’d been having chest pain for an hour. While they were putting the patient into the ambulance, he went into cardiac arrest. Four defibrillation attempts en route to the hospital and additional resuscitation attempts in the ED failed; he was pronounced dead 3½ hours after leaving his physician’s office.
No autopsy was performed. The patient’s widow found the omeprazole bottle, with one pill missing, and fast-food hamburger wrappers on the kitchen table.
PLAINTIFF’S CLAIM The primary care physician should have sent the patient to the ED to determine whether the chest pain had a cardiac cause; the patient was suffering from acute cardiac syndrome when the doctor saw him.
THE DEFENSE The patient’s normal EKG and vital signs and the fact that belching relieved his chest symptoms indicated that the complaints did not arise from cardiac causes or require emergency assessment. The patient didn’t report chest pain at the office visit; the later cardiac arrest probably resulted from a sudden plaque rupture unrelated to the earlier chest discomfort.
VERDICT $1.5 million Illinois verdict.
COMMENT I hope most doctors won’t have to learn this lesson from their own experience. A normal EKG does not rule out acute ischemia in a high-risk patient with chest pain and sweating. Admit such patients immediately to a cardiac observation unit.
Kidney failure after multiple meds
A MAN WAS TAKING MULTIPLE MEDICATIONS: 3 blood pressure drugs prescribed by his primary care physician, an NSAID prescribed by another doctor, and sizable doses of BC Powder, an over-the-counter analgesic containing aspirin, salicylamide, and caffeine. After 4 years on this medication regimen, the patient’s kidneys failed.
PLAINTIFF’S CLAIM The primary care physician failed to properly monitor kidney function with blood and urine tests while his patient was taking the medications. Proper testing would have resulted in a diagnosis of kidney disease before the patient’s kidneys failed completely. In addition, the primary care physician failed to explain the risks and side effects of the medications to the patient.
THE DEFENSE The patient refused kidney function testing and did not follow medical advice. He consumed excessive amounts of alcohol against medical advice, did not tell the primary care physician about other drugs he was taking, and had allowed his supply of blood pressure medication to run out.
VERDICT $2 million gross verdict in Georgia, with a finding of 47% comparative negligence.
COMMENT This case offers several lessons: First, each BC Powder packet contains the equivalent of 2 aspirin. Second, chronic, high-dose NSAIDs can cause renal failure, especially in patients whose renal function is compromised by hypertension. Third, all patients with hypertension should undergo periodic monitoring of renal function.
Death follows a normal EKG
MID-CHEST DISCOMFORT, A COUGH, AND SWEATING brought a 59-year-old man to his primary care physician. The patient had normal vital signs and reported that belching relieved the chest discomfort. He had a history of severe coronary artery disease and had undergone angioplasty and stenting several years earlier.
The primary care physician performed an electrocardiogram (EKG), which was normal and unchanged from one done the year before. The doctor suspected bronchitis, but prescribed omeprazole because the patient had previously been diagnosed with gastroesophageal reflux disease. He ordered a chemical stress test to be performed within a month and a chest radiograph to be done if the patient’s symptoms didn’t improve.
Two hours after returning home, the patient called an ambulance. He told paramedics that he’d been having chest pain for an hour. While they were putting the patient into the ambulance, he went into cardiac arrest. Four defibrillation attempts en route to the hospital and additional resuscitation attempts in the ED failed; he was pronounced dead 3½ hours after leaving his physician’s office.
No autopsy was performed. The patient’s widow found the omeprazole bottle, with one pill missing, and fast-food hamburger wrappers on the kitchen table.
PLAINTIFF’S CLAIM The primary care physician should have sent the patient to the ED to determine whether the chest pain had a cardiac cause; the patient was suffering from acute cardiac syndrome when the doctor saw him.
THE DEFENSE The patient’s normal EKG and vital signs and the fact that belching relieved his chest symptoms indicated that the complaints did not arise from cardiac causes or require emergency assessment. The patient didn’t report chest pain at the office visit; the later cardiac arrest probably resulted from a sudden plaque rupture unrelated to the earlier chest discomfort.
VERDICT $1.5 million Illinois verdict.
COMMENT I hope most doctors won’t have to learn this lesson from their own experience. A normal EKG does not rule out acute ischemia in a high-risk patient with chest pain and sweating. Admit such patients immediately to a cardiac observation unit.
Kidney failure after multiple meds
A MAN WAS TAKING MULTIPLE MEDICATIONS: 3 blood pressure drugs prescribed by his primary care physician, an NSAID prescribed by another doctor, and sizable doses of BC Powder, an over-the-counter analgesic containing aspirin, salicylamide, and caffeine. After 4 years on this medication regimen, the patient’s kidneys failed.
PLAINTIFF’S CLAIM The primary care physician failed to properly monitor kidney function with blood and urine tests while his patient was taking the medications. Proper testing would have resulted in a diagnosis of kidney disease before the patient’s kidneys failed completely. In addition, the primary care physician failed to explain the risks and side effects of the medications to the patient.
THE DEFENSE The patient refused kidney function testing and did not follow medical advice. He consumed excessive amounts of alcohol against medical advice, did not tell the primary care physician about other drugs he was taking, and had allowed his supply of blood pressure medication to run out.
VERDICT $2 million gross verdict in Georgia, with a finding of 47% comparative negligence.
COMMENT This case offers several lessons: First, each BC Powder packet contains the equivalent of 2 aspirin. Second, chronic, high-dose NSAIDs can cause renal failure, especially in patients whose renal function is compromised by hypertension. Third, all patients with hypertension should undergo periodic monitoring of renal function.
Hepatitis C: New CDC screening recommendations
The Centers for Disease Control and Prevention (CDC) recently released new recommendations for screening for hepatitis C virus (HCV) infection that include a one-time screening for everyone in the United States born between 1945 and 1965, regardless of risk.1 These new recommendations are an enhancement of, but not a replacement for, the recommendations for HCV screening made in 1998, which called for screening those at high risk.2
HCV causes considerable morbidity and mortality in this country. Approximately 17,000 new infections occurred in 2010.1 Between 2.7 and 3.9 million Americans (1%-1.5% of the population) are living with chronic HCV infection, and many do not know they are infected.1 This lack of awareness appears to be due to a failure of both health care providers to offer testing to those at known risk and patients to either acknowledge or recall past high-risk behaviors.
Those at highest risk for HCV infection are current or past users of illegal injected drugs and recipients of a blood transfusion before 1992 (when HCV screening of the blood supply was instituted). Other risk factors are listed in TABLE 1.1 Many of those with HCV infection do not report injection drug use or having received a transfusion prior to 1992, and they are not detected by current risk-based testing.
TABLE 1
Risk factors for HCV infection1
| Most common risks |
|
| Less common risks |
|
| HCV, hepatitis C virus |
Approximately three-fourths of those who acquire HCV are unable to clear the virus and become chronically infected.1 Twenty percent of these individuals will develop cirrhosis and 5% will die from an HCV-related liver disease, such as decompensated cirrhosis or hepatocellular carcinoma (HCC).3
New treatments. In 2011, 2 protease inhibitor drugs, telaprevir and boceprevir, were approved for the treatment of HCV geno-type 1. These are the first generation of a class of drugs called direct-acting antiviral agents (DAAs). When a DAA is added to the standard therapy of ribavirin and pegylated interferon, the rate of viral clearance increases (from 44% to 75% for telaprevir and from 38% to 63% for boceprevir).1 However, the adverse reactions caused by these new drugs can lead to a 34% rise in the rate at which patients stop treatment.1 Twenty potential new HCV antivirals are in clinical trials, and it is expected that treatment recommendations will change rapidly as some of these are approved.
Does treatment improve long-term outcomes?
Clinical guidelines recommend antiviral treatment for anyone with HCV infection and biopsy evidence of bridging fibrosis, septal fibrosis, or cirrhosis.4
A look at Tx and all-cause mortality. Studies looking at patient-oriented outcomes such as all-cause mortality and incidence of HCC have been conducted with pegylated interferon and ribavirin, without the newer DAAs. The most commonly cited study assessed all-cause mortality in a large sample of veterans with multiple comorbidities.
Those who achieved a sustained virological response after treatment exhibited a reduction in all-cause mortality >50% compared with nonresponders. This endpoint included substantially lower rates of liver-related deaths and cirrhosis complicated by ascites, variceal bleeding, or encephalopathy.5 However, in such a nonrandom clinical trial, an improved outcome for responders could be due to their relatively good health, with fewer comorbid conditions, and other undetected biases. While this study attempted to control for such biases, it didn’t provide evidence that treating infection detected by screening a low-risk population would improve intermediate or long-term outcomes.
Observational studies look at carcinoma incidence. Twelve observational studies have addressed treatment effects on HCC incidence. They showed a 75% reduction in HCC rates in those who achieved viral clearance compared with those who did not.1 Again, these studies did not compare treated and untreated patients in a controlled clinical trial; they looked only at treated individuals and compared the outcomes of responders and nonresponders.
HCV transmission research is lacking. The CDC found no studies in its evidence review that addressed the issue of HCV transmission. Nevertheless, the new recommendations state that HCV transmission was a critical factor in determining the strength of the recommendation for age cohort screening. It is expected that those who have a sustained viral response will be less likely to transmit the virus to others.
Why the 1945-1965 birth cohort?
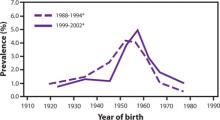
The prevalence of HCV infection in those born between 1945 and 1965 is 3.25%, and three-fourths of all those with HCV infection in the United States are in this cohort. The FIGURE depicts the large difference in prevalence between this age group and others. Within 3 cohorts defined by date of birth (1945-1965, 1950-1970, and 1945-1970), the prevalence of HCV infection is twice as high in men than in women, and in black non-Hispanics than in white non-Hispanics and Mexican Americans. However, extending the birth cohort to those born through 1970 yields only a marginal difference in prevalence figures. The CDC justifies restricting the new universal screening recommendation to the 1945-1965 age group mainly on the results of focus groups in which the public identified this cohort as “baby boomers” who would likely adopt the recommendation.
FIGURE
Prevalence of hepatitis C virus antibody by year of birth1
*National Health and Nutrition Examination Survey, United States, 1988–1994 and 1999–2002.
Two-step screening process
Screen individuals using a test for antibodies to HCV (anti-HCV). If the anti-HCV test result is positive, order a test for HCV nucleic acid that gives either a quantitative measure of viral load or a qualitative assessment of presence or absence of virus. If the confirmatory nucleic acid test result is negative, the individual does not have chronic HCV infection and is among the approximately 25% who clear the virus on their own. They do not need further testing or treatment.
What to tell infected patients
If the confirmatory test result is positive, presume the patient has HCV infection and offer the advice contained in TABLE 2.1 Patients should undergo further assessment for possible chronic liver disease and, with the counsel of their physician, decide whether to initiate treatment. They should also take measures to protect the liver from further damage, such as reducing alcohol consumption, avoiding medication and herbal products that can damage the liver, maintaining an optimal weight, and receiving vaccines against hepatitis A and B, if still susceptible to these viruses. Finally, encourage patients to take steps to avoid transmission of HCV to others.
TABLE 2
Advice for your patients with HCV infection1
Consult a health care provider (either a primary care physician or specialist [eg, in hepatology, gastroenterology, or infectious disease]) for:
|
Protect the liver from further harm by:
|
Maintain optimal weight by:
|
Minimize the risk of infecting others by:
|
| BMI, body mass index; HCV, hepatitis C virus; HIV, human immunodeficiency virus. |
The decision on whether to begin treatment immediately is complicated by the large number of new antivirals in development, which will be available in the near future and may be more effective with fewer adverse effects.
Lingering controversies
Given the lack of evidence of improved outcomes with HCV screening in the general population, it will be interesting to see how widely accepted the new CDC recommendations will be. The US Preventive Services Task Force is in the process of revising its HCV screening recommendations. Given the Task Force’s evidence-based methodology and the lack of evidence on the benefits and harms of screening those with no reported risks, there may be some differences with the new CDC recommendations.
If the CDC’s assumption proves correct—ie, that the benefits of treating high-risk populations will also occur with treating detected infection in the general population—and if the age cohort screening recommendation is fully implemented, 47,000 cases of HCC and 15,000 liver transplants will be prevented.1
1. CDC. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Morb Mortal Wkly Rep. 2012;61:1-18.Available at: http://www.cdc.gov/mmwr/pdf/rr/rr6104.pdf. Accessed October 5, 2012.
2. CDC. Recommendations for prevention and control of hepatitis C virus infection and HCV-related chronic disease. MMWR Morb Mortal Wkly Rep. 1998;47(RR-19):1-54.
3. Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis. 2000;20:17-35.
4. Ghany MG, Strader DB, Thomas DL, et al. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-1374.
5. Backus LI, Boothroyd DB, Phillips BR, et al. A sustained virological response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.
The Centers for Disease Control and Prevention (CDC) recently released new recommendations for screening for hepatitis C virus (HCV) infection that include a one-time screening for everyone in the United States born between 1945 and 1965, regardless of risk.1 These new recommendations are an enhancement of, but not a replacement for, the recommendations for HCV screening made in 1998, which called for screening those at high risk.2
HCV causes considerable morbidity and mortality in this country. Approximately 17,000 new infections occurred in 2010.1 Between 2.7 and 3.9 million Americans (1%-1.5% of the population) are living with chronic HCV infection, and many do not know they are infected.1 This lack of awareness appears to be due to a failure of both health care providers to offer testing to those at known risk and patients to either acknowledge or recall past high-risk behaviors.
Those at highest risk for HCV infection are current or past users of illegal injected drugs and recipients of a blood transfusion before 1992 (when HCV screening of the blood supply was instituted). Other risk factors are listed in TABLE 1.1 Many of those with HCV infection do not report injection drug use or having received a transfusion prior to 1992, and they are not detected by current risk-based testing.
TABLE 1
Risk factors for HCV infection1
| Most common risks |
|
| Less common risks |
|
| HCV, hepatitis C virus |
Approximately three-fourths of those who acquire HCV are unable to clear the virus and become chronically infected.1 Twenty percent of these individuals will develop cirrhosis and 5% will die from an HCV-related liver disease, such as decompensated cirrhosis or hepatocellular carcinoma (HCC).3
New treatments. In 2011, 2 protease inhibitor drugs, telaprevir and boceprevir, were approved for the treatment of HCV geno-type 1. These are the first generation of a class of drugs called direct-acting antiviral agents (DAAs). When a DAA is added to the standard therapy of ribavirin and pegylated interferon, the rate of viral clearance increases (from 44% to 75% for telaprevir and from 38% to 63% for boceprevir).1 However, the adverse reactions caused by these new drugs can lead to a 34% rise in the rate at which patients stop treatment.1 Twenty potential new HCV antivirals are in clinical trials, and it is expected that treatment recommendations will change rapidly as some of these are approved.
Does treatment improve long-term outcomes?
Clinical guidelines recommend antiviral treatment for anyone with HCV infection and biopsy evidence of bridging fibrosis, septal fibrosis, or cirrhosis.4
A look at Tx and all-cause mortality. Studies looking at patient-oriented outcomes such as all-cause mortality and incidence of HCC have been conducted with pegylated interferon and ribavirin, without the newer DAAs. The most commonly cited study assessed all-cause mortality in a large sample of veterans with multiple comorbidities.
Those who achieved a sustained virological response after treatment exhibited a reduction in all-cause mortality >50% compared with nonresponders. This endpoint included substantially lower rates of liver-related deaths and cirrhosis complicated by ascites, variceal bleeding, or encephalopathy.5 However, in such a nonrandom clinical trial, an improved outcome for responders could be due to their relatively good health, with fewer comorbid conditions, and other undetected biases. While this study attempted to control for such biases, it didn’t provide evidence that treating infection detected by screening a low-risk population would improve intermediate or long-term outcomes.
Observational studies look at carcinoma incidence. Twelve observational studies have addressed treatment effects on HCC incidence. They showed a 75% reduction in HCC rates in those who achieved viral clearance compared with those who did not.1 Again, these studies did not compare treated and untreated patients in a controlled clinical trial; they looked only at treated individuals and compared the outcomes of responders and nonresponders.
HCV transmission research is lacking. The CDC found no studies in its evidence review that addressed the issue of HCV transmission. Nevertheless, the new recommendations state that HCV transmission was a critical factor in determining the strength of the recommendation for age cohort screening. It is expected that those who have a sustained viral response will be less likely to transmit the virus to others.
Why the 1945-1965 birth cohort?
The prevalence of HCV infection in those born between 1945 and 1965 is 3.25%, and three-fourths of all those with HCV infection in the United States are in this cohort. The FIGURE depicts the large difference in prevalence between this age group and others. Within 3 cohorts defined by date of birth (1945-1965, 1950-1970, and 1945-1970), the prevalence of HCV infection is twice as high in men than in women, and in black non-Hispanics than in white non-Hispanics and Mexican Americans. However, extending the birth cohort to those born through 1970 yields only a marginal difference in prevalence figures. The CDC justifies restricting the new universal screening recommendation to the 1945-1965 age group mainly on the results of focus groups in which the public identified this cohort as “baby boomers” who would likely adopt the recommendation.
FIGURE
Prevalence of hepatitis C virus antibody by year of birth1
*National Health and Nutrition Examination Survey, United States, 1988–1994 and 1999–2002.
Two-step screening process
Screen individuals using a test for antibodies to HCV (anti-HCV). If the anti-HCV test result is positive, order a test for HCV nucleic acid that gives either a quantitative measure of viral load or a qualitative assessment of presence or absence of virus. If the confirmatory nucleic acid test result is negative, the individual does not have chronic HCV infection and is among the approximately 25% who clear the virus on their own. They do not need further testing or treatment.
What to tell infected patients
If the confirmatory test result is positive, presume the patient has HCV infection and offer the advice contained in TABLE 2.1 Patients should undergo further assessment for possible chronic liver disease and, with the counsel of their physician, decide whether to initiate treatment. They should also take measures to protect the liver from further damage, such as reducing alcohol consumption, avoiding medication and herbal products that can damage the liver, maintaining an optimal weight, and receiving vaccines against hepatitis A and B, if still susceptible to these viruses. Finally, encourage patients to take steps to avoid transmission of HCV to others.
TABLE 2
Advice for your patients with HCV infection1
Consult a health care provider (either a primary care physician or specialist [eg, in hepatology, gastroenterology, or infectious disease]) for:
|
Protect the liver from further harm by:
|
Maintain optimal weight by:
|
Minimize the risk of infecting others by:
|
| BMI, body mass index; HCV, hepatitis C virus; HIV, human immunodeficiency virus. |
The decision on whether to begin treatment immediately is complicated by the large number of new antivirals in development, which will be available in the near future and may be more effective with fewer adverse effects.
Lingering controversies
Given the lack of evidence of improved outcomes with HCV screening in the general population, it will be interesting to see how widely accepted the new CDC recommendations will be. The US Preventive Services Task Force is in the process of revising its HCV screening recommendations. Given the Task Force’s evidence-based methodology and the lack of evidence on the benefits and harms of screening those with no reported risks, there may be some differences with the new CDC recommendations.
If the CDC’s assumption proves correct—ie, that the benefits of treating high-risk populations will also occur with treating detected infection in the general population—and if the age cohort screening recommendation is fully implemented, 47,000 cases of HCC and 15,000 liver transplants will be prevented.1
The Centers for Disease Control and Prevention (CDC) recently released new recommendations for screening for hepatitis C virus (HCV) infection that include a one-time screening for everyone in the United States born between 1945 and 1965, regardless of risk.1 These new recommendations are an enhancement of, but not a replacement for, the recommendations for HCV screening made in 1998, which called for screening those at high risk.2
HCV causes considerable morbidity and mortality in this country. Approximately 17,000 new infections occurred in 2010.1 Between 2.7 and 3.9 million Americans (1%-1.5% of the population) are living with chronic HCV infection, and many do not know they are infected.1 This lack of awareness appears to be due to a failure of both health care providers to offer testing to those at known risk and patients to either acknowledge or recall past high-risk behaviors.
Those at highest risk for HCV infection are current or past users of illegal injected drugs and recipients of a blood transfusion before 1992 (when HCV screening of the blood supply was instituted). Other risk factors are listed in TABLE 1.1 Many of those with HCV infection do not report injection drug use or having received a transfusion prior to 1992, and they are not detected by current risk-based testing.
TABLE 1
Risk factors for HCV infection1
| Most common risks |
|
| Less common risks |
|
| HCV, hepatitis C virus |
Approximately three-fourths of those who acquire HCV are unable to clear the virus and become chronically infected.1 Twenty percent of these individuals will develop cirrhosis and 5% will die from an HCV-related liver disease, such as decompensated cirrhosis or hepatocellular carcinoma (HCC).3
New treatments. In 2011, 2 protease inhibitor drugs, telaprevir and boceprevir, were approved for the treatment of HCV geno-type 1. These are the first generation of a class of drugs called direct-acting antiviral agents (DAAs). When a DAA is added to the standard therapy of ribavirin and pegylated interferon, the rate of viral clearance increases (from 44% to 75% for telaprevir and from 38% to 63% for boceprevir).1 However, the adverse reactions caused by these new drugs can lead to a 34% rise in the rate at which patients stop treatment.1 Twenty potential new HCV antivirals are in clinical trials, and it is expected that treatment recommendations will change rapidly as some of these are approved.
Does treatment improve long-term outcomes?
Clinical guidelines recommend antiviral treatment for anyone with HCV infection and biopsy evidence of bridging fibrosis, septal fibrosis, or cirrhosis.4
A look at Tx and all-cause mortality. Studies looking at patient-oriented outcomes such as all-cause mortality and incidence of HCC have been conducted with pegylated interferon and ribavirin, without the newer DAAs. The most commonly cited study assessed all-cause mortality in a large sample of veterans with multiple comorbidities.
Those who achieved a sustained virological response after treatment exhibited a reduction in all-cause mortality >50% compared with nonresponders. This endpoint included substantially lower rates of liver-related deaths and cirrhosis complicated by ascites, variceal bleeding, or encephalopathy.5 However, in such a nonrandom clinical trial, an improved outcome for responders could be due to their relatively good health, with fewer comorbid conditions, and other undetected biases. While this study attempted to control for such biases, it didn’t provide evidence that treating infection detected by screening a low-risk population would improve intermediate or long-term outcomes.
Observational studies look at carcinoma incidence. Twelve observational studies have addressed treatment effects on HCC incidence. They showed a 75% reduction in HCC rates in those who achieved viral clearance compared with those who did not.1 Again, these studies did not compare treated and untreated patients in a controlled clinical trial; they looked only at treated individuals and compared the outcomes of responders and nonresponders.
HCV transmission research is lacking. The CDC found no studies in its evidence review that addressed the issue of HCV transmission. Nevertheless, the new recommendations state that HCV transmission was a critical factor in determining the strength of the recommendation for age cohort screening. It is expected that those who have a sustained viral response will be less likely to transmit the virus to others.
Why the 1945-1965 birth cohort?
The prevalence of HCV infection in those born between 1945 and 1965 is 3.25%, and three-fourths of all those with HCV infection in the United States are in this cohort. The FIGURE depicts the large difference in prevalence between this age group and others. Within 3 cohorts defined by date of birth (1945-1965, 1950-1970, and 1945-1970), the prevalence of HCV infection is twice as high in men than in women, and in black non-Hispanics than in white non-Hispanics and Mexican Americans. However, extending the birth cohort to those born through 1970 yields only a marginal difference in prevalence figures. The CDC justifies restricting the new universal screening recommendation to the 1945-1965 age group mainly on the results of focus groups in which the public identified this cohort as “baby boomers” who would likely adopt the recommendation.
FIGURE
Prevalence of hepatitis C virus antibody by year of birth1
*National Health and Nutrition Examination Survey, United States, 1988–1994 and 1999–2002.
Two-step screening process
Screen individuals using a test for antibodies to HCV (anti-HCV). If the anti-HCV test result is positive, order a test for HCV nucleic acid that gives either a quantitative measure of viral load or a qualitative assessment of presence or absence of virus. If the confirmatory nucleic acid test result is negative, the individual does not have chronic HCV infection and is among the approximately 25% who clear the virus on their own. They do not need further testing or treatment.
What to tell infected patients
If the confirmatory test result is positive, presume the patient has HCV infection and offer the advice contained in TABLE 2.1 Patients should undergo further assessment for possible chronic liver disease and, with the counsel of their physician, decide whether to initiate treatment. They should also take measures to protect the liver from further damage, such as reducing alcohol consumption, avoiding medication and herbal products that can damage the liver, maintaining an optimal weight, and receiving vaccines against hepatitis A and B, if still susceptible to these viruses. Finally, encourage patients to take steps to avoid transmission of HCV to others.
TABLE 2
Advice for your patients with HCV infection1
Consult a health care provider (either a primary care physician or specialist [eg, in hepatology, gastroenterology, or infectious disease]) for:
|
Protect the liver from further harm by:
|
Maintain optimal weight by:
|
Minimize the risk of infecting others by:
|
| BMI, body mass index; HCV, hepatitis C virus; HIV, human immunodeficiency virus. |
The decision on whether to begin treatment immediately is complicated by the large number of new antivirals in development, which will be available in the near future and may be more effective with fewer adverse effects.
Lingering controversies
Given the lack of evidence of improved outcomes with HCV screening in the general population, it will be interesting to see how widely accepted the new CDC recommendations will be. The US Preventive Services Task Force is in the process of revising its HCV screening recommendations. Given the Task Force’s evidence-based methodology and the lack of evidence on the benefits and harms of screening those with no reported risks, there may be some differences with the new CDC recommendations.
If the CDC’s assumption proves correct—ie, that the benefits of treating high-risk populations will also occur with treating detected infection in the general population—and if the age cohort screening recommendation is fully implemented, 47,000 cases of HCC and 15,000 liver transplants will be prevented.1
1. CDC. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Morb Mortal Wkly Rep. 2012;61:1-18.Available at: http://www.cdc.gov/mmwr/pdf/rr/rr6104.pdf. Accessed October 5, 2012.
2. CDC. Recommendations for prevention and control of hepatitis C virus infection and HCV-related chronic disease. MMWR Morb Mortal Wkly Rep. 1998;47(RR-19):1-54.
3. Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis. 2000;20:17-35.
4. Ghany MG, Strader DB, Thomas DL, et al. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-1374.
5. Backus LI, Boothroyd DB, Phillips BR, et al. A sustained virological response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.
1. CDC. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Morb Mortal Wkly Rep. 2012;61:1-18.Available at: http://www.cdc.gov/mmwr/pdf/rr/rr6104.pdf. Accessed October 5, 2012.
2. CDC. Recommendations for prevention and control of hepatitis C virus infection and HCV-related chronic disease. MMWR Morb Mortal Wkly Rep. 1998;47(RR-19):1-54.
3. Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis. 2000;20:17-35.
4. Ghany MG, Strader DB, Thomas DL, et al. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-1374.
5. Backus LI, Boothroyd DB, Phillips BR, et al. A sustained virological response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.
Hip pain in active patients: What you may be missing
• Consider both musculoskeletal and nonmusculoskeletal causes in patients with vague complaints of hip and groin pain. B
• Use imaging studies to confirm a hip pain diagnosis. B
• Refer patients who fail to respond to nonsurgical treatment to a sports medicine specialist or an orthopedic surgeon. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Hip pain is a common complaint, and commonly misunderstood. Although the pain can be associated with a broad spectrum of conditions, the presentation is often vague and nonspecific.
Thus, hip pain and injury are frequently attributed, often incorrectly, to a “hip pointer”—a contusion of soft tissues against the iliac crest. It’s not unusual for patients who receive this diagnosis to be treated conservatively for prolonged periods, leading some previously active individuals to abandon their favorite sport or self-impose limits on the activities they engage in.1
But it doesn’t have to be this way.
Minimally invasive hip arthroscopy and advances in imaging, instrumentation, and devices have made it easier to identify and address underlying pathology associated with hip pain, helping patients return to their previous level of activity more rapidly.2,3 And, while many conditions associated with hip pain can be treated conservatively, family physicians—whom patients often go to first—should not hesitate to provide a referral when more aggressive treatment or diagnostic confirmation is needed.
We created this guide with family physicians in mind. Our focus here is primarily on anterior hip pain—the most common presentation—in active, or athletic, patients.
When did the pain begin? Where does it hurt?
Before performing a physical examination, find out as much as possible about the onset of pain and when and under what circumstances it occurs. (A review of hip anatomy is provided here.) Did it begin suddenly, after an acute injury or a particular physical maneuver? Or is the pain insidious, as was the case with one of our patients?
Osseous morphology of the hip includes the anterior superior iliac spine, the origin of the sartorius muscle and the ilioinguinal ligament. The anterior inferior iliac spine attaches to the rectus femoris, a major hip flexor and knee extender. The adductors of the hip originate in the anterior pelvic region.
The inguinal canal contains the ilioinguinal nerve, which is responsible for radiation of pain to the anterior hip. The hip joint itself is a spheroid comprising the femoral head and acetabulum, with most of the articular hip innervated by the femoral or obturator nerves.
Most intra-articular conditions radiate to the anterior groin or hip, although there are cases in which the pain is referred to either the lateral aspect of the hip or the buttocks. The iliopsoas muscle is the major hip flexor, and crosses under the ilioinguinal ligament to insert on the lesser tuberosity after crossing over the anterior capsule of the hip. A large bursa surrounds it, helping the tendon glide smoothly over the hip.
CASE Mack Q, a 27-year-old man with an 8-month history of right hip pain, sought care at our medical center for an achy pain in his right groin; he also described an occasional “clicking and popping sensation” in his groin but denied any trauma. The pain worsened with prolonged sitting and certain activities, such as squatting, twisting, and putting on shoes and socks. Our patient had stopped playing soccer because it hurt too much. He had tried physical therapy, oral anti-inflammatories, and a corticosteroid injection, with little relief.
Start with a gait assessment
The physical examination should begin with a gait assessment. Consider the patient’s ability to bear weight and his or her foot angle.
An individual with a stress fracture will have difficulty bearing weight on the affected side, resulting in a limp, or antalgic gait. A patient with femoral acetabular impingement (FAI) will often exhibit greater external rotation of the foot on the affected side compared with the other foot. And a patient with weakened abductor muscles, typically because of severe osteoarthritis, will exhibit the Trendelenburg sign—a pelvic tilt when the weight is shifted to the affected extremity.
Although most individuals with hip pain will not have an obvious gait abnormality, any patient who walks with a limp or needs crutches requires an immediate referral to an orthopedic surgeon.
Include these elements in the physical exam
Examine the hip with the patient sitting on the side of the exam table. Assess range of motion (ROM), comparing the range of flexion, extension, and internal/external rotation on the affected and unaffected sides. Include the following maneuvers:
Impingement testing. In patients with FAI and osteoarthritis, impingement testing—encompassing Flexion, ADDuction, and Internal Rotation (FADDIR)—will elicit pain. The maneuver can be tested starting at 45° of hip flexion, increasing to approximately 120°. Pain with <45° of hip flexion indicates that the impingement is severe.
Such testing can also reveal labral tears, which may be caused by FAI or other structural abnormalities. In a patient with anterior labral tears, FADDIR will produce groin pain; posterior labral tears will produce pain when the patient is sitting with legs hanging off the exam table and the contralateral leg is brought to the chest and the affected limb fully extended.
In patients with hip pain and bursitis, applying downward pressure will elicit a snapping sound as the iliopsoas snaps over the iliopectineal eminence or femoral head. Flexion, ABduction, and External Rotation (FABER) can also be used to diagnose iliopsoas tendonitis: The test is positive if it elicits pain in the affected extremity or in the sacroiliac joint on the opposite side.
Log roll. A painful response to this test, which involves internally and externally rotating the affected hip while it is relaxed and the knee fully extended, is an indication of synovitis of the hip caused by intra-articular pathology. To test hip stability, externally rotate the leg while it is extended. If the hip is stable, the leg will return to a neutral position; microinstability of the hip is likely if the leg remains in the rotated position.
Muscular strength testing. To assess for tendinopathy in the hip area, the patient should be in a seated position and contract the internal and external rotators and the adductor muscles while you apply resistance. To test abductor strength, have the patient assume a lateral position and hold and abduct the leg on the affected side while you apply resistance.
Hip flexion strength should be tested with the patient in both supine and seated positions. A patient with quadriceps tendonitis will have much greater pain with resisted hip flexion in the supine position vs the seated position; the opposite is true for a patient with iliopsoas tendonitis. (See “Did you know…? Hip pain facts and findings” on for additional diagnostic tips.)
- A patient with quadriceps tendonitis will have much greater pain with resisted hip flexion in a supine position vs a seated position. The opposite is true for a patient with iliopsoas tendonitis.
- Patients with femoral neck stress fractures typically present with activity-related anterior groin pain that is relieved by rest. Initially, they may be only mildly affected, but the condition worsens in those who continue to “work through the pain.”
- Plain radiography can confirm a diagnosis of osteonecrosis in patients with advanced disease, but magnetic resonance imaging is useful for evaluating earlier clinical presentations.
- Patients with labral tears often exhibit what has been called the “c-sign”—so named for the shape patients make with their hand as they grip their hip just above the greater trochanter to indicate where it hurts.
- Athletes who experience adductor strains often play sports in which kicking or frequent changes in direction are required, such as football, hockey, and soccer, and are generally able to tell you exactly what they were doing when the injury occurred.
- Unlike other hernias, a sports hernia (athletic pubalgia) does not involve a bulge of tissue protruding through one part of the body into another. Instead, it occurs when the oblique abdominal muscles strain or completely tear away from the pubis.
Perform a neurologic evaluation to rule out a back condition that might radiate pain into the anterior hip; ask the patient to do a sit-up while you apply resistance to test for abdominal wall pathology, as well.
Hip palpation. This aspect of the physical exam is important regardless of the cause of the pain but especially crucial for pediatric and adolescent patients, whose anterior hip pain may be related to apophyseal injury. Palpate the superior iliac spine (and over the inferior iliac spine in thin patients) to determine if the sartorius or rectus femoris has been injured. The area just lateral to the symphysis will be tender to palpation in patients with osteitis pubis.
Refer or treat? Here’s what to consider
While the history and physical should provide ample information for a differential diagnosis, imaging studies are generally required for confirmation. Clinical assessment— including physical exam, imaging, and intra-articular injection—of patients with hip pain is up to 98% accurate in identifying hip abnormalities, with arthroscopy as the gold standard.4
CASE On physical examination, Mr. Q had right hip extension to 0°, flexion to 110°, external rotation to 50°, and internal rotation to neutral; he also had positive impingement and subspine impingement tests, a painful arc of motion from 12 to 4 o’clock, tenderness over the hip adductor, and pain with resisted hip adduction. He did not walk with a limp.
Diagnostic studies included plain radiographs, which demonstrated that the joint space was well preserved. We identified subtle anatomical abnormalities on the femoral head-neck junction, known as a cam deformity. Magnetic resonance imaging (MRI) revealed an anterior superior labral tear with cartilage delamination.
Stress fractures affect runners, military recruits
In addition to long-distance runners who have recently increased the frequency, duration, or intensity of training,5,6 military recruits have a higher incidence of stress fractures due to the rapid onset of intensive training. Stress fractures can also occur in patients who do not have a history of intense activity but have metabolically weakened bone, in some cases as a result of an eating disorder.7
Patients with femoral neck stress fractures typically present with activity-related anterior groin pain that is relieved by rest; initially, they may be only mildly affected, but the condition worsens in those who continue to “work through the pain.” By the time such individuals seek treatment, they almost always have pain with weight bearing and an antalgic gait.
Symptoms consistent with a femoral neck stress fracture can be further evaluated with plain radiographs. However, x-rays are often negative for up to 4 weeks after the onset of pain.8 In cases in which radiographs are negative but the physical exam is suggestive of a stress fracture, MRI—which can detect an abnormality within a day or 2 of injury8,9—should be used to confirm the diagnosis (FIGURE 1).
FIGURE 1
MRI reveals a femoral neck stress fracture
Treatment. A complete femoral neck fracture portends impending displacement and requires emergent evaluation by an orthopedist, and superior neck changes, also known as tension-sided stress fractures, require urgent treatment with percutaneous screw fixation.9 However, compression-sided, or inferior, stress fractures can be treated with restricted weight bearing and activity modification. Gradual resumption of activity is allowed only after the patient has been asymptomatic for 6 weeks; recurrent pain indicates residual stress reaction, and signals that activities should be abated.
Osteonecrosis has many causes
Necrosis of the femoral head is a debilitating and progressive condition primarily affecting patients between the ages of 20 and 50 years.10 It has multiple (and diverse) causes, including trauma, steroids, alcohol, smoking, lupus, sickle cell anemia, and coagulopathies, as well as scuba diving. But about 20% of cases have no apparent cause.11,12
Patients with osteonecrosis of the hip typically present with groin pain, often described as a deep, intermittent ache that interferes with activities of daily living. Exam findings depend on the stage of presentation. Early on, pain will occur only with extreme ROM; in advanced cases, ROM is restricted and pain occurs even with limited motion.
Femoral head collapse due to loss of the structural integrity of the subchondral bone—which occurs in 80% of cases12—is thought to be caused by decreased blood flow. Plain radiography can confirm a diagnosis of osteonecrosis in patients with advanced disease, but MRI is useful for evaluating patients with earlier clinical presentations.
Treatment of osteonecrosis is dictated by the stage of the disease, but remains controversial because no intervention has been shown to prevent progression in all cases.12 All patients should be referred to a specialist. Those without collapse or cartilage damage can be treated surgically with core decompression, possibly with additional vascularized bone grafting,13,14 while those with more advanced disease typically require a total hip replacement at a relatively young age. Results for total hip replacement in patients with osteonecrosis are thought to be inferior to hip replacement in patients with osteoarthritis, although comparison is difficult because of the differences in age and activity levels in these 2 groups.15,16
Femoral acetabular impingement can occur on the cam or pincer side
FAI pathology can exist on either the femoral (cam) or acetabular (pincer) side,17 or both.18 In pure cam impingement, the anterior femoral neck loses its normal concave anatomy and develops a “bump,” which impinges on the anterosuperior labrum during hip flexion, causing labral tears and delamination of the adjacent cartilage.
Pure pincer impingement arises from a prominent acetabular rim, causing overcoverage of the femoral head. Acetabular labral tears result from the repetitive impaction with flexion and internal rotation.
Patients report an insidious onset of groin pain that is exacerbated by flexion-type sports, such as hockey, football, and golf,19 as well as activities of daily living. In patients with cartilage damage, even walking can be painful. Physical examination of patients with FAI reveals findings that are similar to those of patients with acetabular labral tears. Abnormally large cam lesions or acetabular overcoverage will result in restriction of hip ROM, especially internal rotation and flexion due to a mechanical block.
Radiographs (FIGURE 2) are essential to diagnose FAI and to distinguish this condition from an isolated labral tear.20 Cam impingement will be best demonstrated on a cross-table lateral radiograph, which shows an asphericity of the femoral head/neck junction anteriorly, while pincer impingement will show overcoverage of the femoral head on an AP radiograph. MRI or magnetic resonance arthrography (MRA) is frequently obtained to see whether any cartilage deterioration has occurred. Computed tomography, which can provide a 3-dimensional reproduction of the hip morphology, is often used for preoperative planning when surgical intervention is required.
FIGURE 2
Femoral acetabular impingement with a prominent pincer lesion
Treatment. Surgical intervention is often needed to correct or remove the abnormal anatomy, and both arthroscopic and open surgery are recommended.20 Both methods include osteoplasty at the femoral head/neck junction and/or the acetabular rim to allow the proximal femur to articulate with the acetabulum without injury to the labrum with flexion and internal rotation.21
Results of both open and arthroscopic osteoplasty of the femur and acetabulum are still preliminary, with only a few studies reporting mid-term results. Open surgery typically has longer recovery and rehabilitation, but advocates emphasize the improved ability to contour the femur or acetabulum. Both open and arthroscopic procedures have about an 8% to 13% rate of revision in short-term follow-up.17
Labral tears occur with trauma and certain sports
In addition to FAI, causes of labral tears include dysplasia, instability, trauma, and degeneration, as well as sports that require repetitive hip flexion and/or pivoting, such as hockey, soccer, and football.22,23
Patients with labral tears typically present with anterior hip pain radiating to the groin, worsening with twisting motions, running, walking, and sitting for prolonged periods. Clicking or catching may occur, as well. Patients may exhibit what one researcher called the “c-sign”—so named for the shape patients make with their hand as they grip their hip just above the greater trochanter to indicate where it hurts.4 The work-up for labral tears includes radiographs and, often, MRA, which is nearly 100% specific.24
Treatment. Conservative treatment, which may include activity modification or rest and ice, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy, is often effective for labral tears; when such measures fail, surgical intervention is indicated. A systematic review found a 67% satisfaction rate after 3.5 years in patients who had undergone labral debridement, and complete resolution of mechanical symptoms in nearly 50%.25 Another study showed similar results for hip arthroscopy, with symptom relief continuing for 4.8 years after surgery, on average, and 84% of patients able to return to their previous level of activity.26
The long-term results of labral debridement are unknown, however, and the possibility of an association between this procedure and the development of arthritis remains. Most specialists prefer anatomic repair to restore normal hip kinematics and, potentially, long-term hip function,27,28 but structural abnormalities must also be addressed to prevent failure of the repair or recurrent tears.
Iliopsoas tendonitis: You know the snap
Often referred to as internal snapping of the hip or internal coxa saltans, iliopsoas tendonitis/bursitis can be a recalcitrant cause of anterior hip pain. Snapping of the iliopsoas leading to bursitis or tendonitis can occur at the iliopectineal eminence, the femoral head, or the lesser trochanter.29 Runners and ballet dancers are often affected.30,31
Snapping in itself is not an indication of pathology, but chronicity of symptoms is. Patients with relatively acute symptoms typically have only bursitis, while a longer duration of symptoms leads to tendonitis or tendinopathy.32
Treatment. First-line therapy is nonoperative, and includes activity modification, rest, ice, NSAIDs, and physical therapy. Advise patients to refrain from activities causing pain, and to apply ice to the affected every 20 minutes (with a 20- to 30-minute off period) for one to 2 hours. Physical therapy focuses on stretching the iliopsoas and rectus femoris muscles and strengthening the hamstring muscles to relieve the stress on the anterior pelvis. If such treatment is unsuccessful, ultrasound can be used to guide a therapeutic injection of cortisone.33 If this fails to bring relief, fractional lengthening of the iliopsoas tendon can be performed to eliminate snapping and relieve pain.34
Muscular strains/avulsion fractures: Sports and age play a role
Although strains can affect any of the anterior muscles around the hip, in active individuals the adductors are most commonly affected. Skeletally immature patients are an exception: apophyseal fractures at the origin of the sartorius and rectus femoris muscles are more common than muscular strains in this patient population.
Athletes who experience adductor strains often play sports in which kicking or frequent changes in direction are required—eg, football, hockey, and soccer35—and generally are able to tell you exactly what they were doing when the injury occurred. Physical examination can reveal focal findings, with swelling and tenderness confined to the anteromedial aspect of the hip along the adductor muscle group. MRI can help differentiate the site of true pathology.36
Treatment of adductor strains is nonoperative, with rest, ice, and activity modification until the tendon heals. In the rare case in which complete tendon avulsion is found, surgical reattachment is needed.
Apophyseal fracture in skeletally immature patients typically occurs during participation in a sport that requires rapid acceleration and deceleration with the hip in an extended position. In such patients, stretching the affected muscle should reproduce the pain. Radiographs are diagnostic and will often show minimal displacement of the apophysis. Treatment is almost always nonoperative. Surgical intervention is rarely needed, and only indicated with displacement >2 cm.37
Athletic pubalgia: A challenging Dx
Also referred to as sports hernia, athletic pubalgia is an enigmatic cause of anterior hip pain in athletes. Diagnosis can be especially challenging, and patients may have lingering symptoms for years before the cause is discovered.38 A sports hernia, unlike other hernias, does not involve a bulge of tissue protruding through one body part into another. In contrast, a sports hernia occurs when the oblique abdominal muscles strain or completely tear away from the pubis. A recent systematic review found that the underlying etiology involves posterior inguinal wall weakening, which can be a result of poorly balanced hip adductor and abdominal muscle activation.39
Patients with sports hernia will often present with anterior hip and/or groin pain, especially with hip extension, twisting, and turning. In addition, patients can have pain in the lower abdomen and, in males, in the testicles. Physical examination will usually show pubic point tenderness, which is exacerbated by resisted hip adduction.40 MRI and ultrasound are extremely helpful in diagnosing and forming a treatment plan.39
The initial treatment of choice for sports hernias is nonoperative, and the first step is always activity modification or temporary avoidance of symptom-producing activities. Additional modalities include NSAIDs, ice, and physical therapy to strengthen the surrounding muscles. Surgical intervention, if needed, may be done laparoscopically or via an open approach with direct repair.40,41
Less common causes to consider
While the conditions detailed here account for most anterior hip etiologies, there are other less common causes to consider. One such cause is osteitis pubis, an umbrella term for conditions that affect the area surrounding the symphysis pubis. Patients with osteitis pubis present with pain over the anterior aspect of the pelvis that is worse with sit-ups, rising from a chair, or any activity where contraction of the rectus muscles occurs.29 Tenderness is found directly over and just lateral to the pubic symphysis. Radiographs are frequently negative, but occasionally chronic degenerative changes at the symphysis are present in addition to symphyseal narrowing. Additional imaging is often necessary for diagnosis.
Neuropathies. When history, physical examination, and imaging studies have ruled out other causes, neuropathies (ilioinguinal, genitofemoral, and obturator) should be considered, particularly in patients with vague, radiating anterior hip and/or groin pain.42 In pediatric patients, Legg-Calve-Perthes disease and slipped capital femoral epiphysis are possibilities, as well.
Getting patients back on track
Rehabilitation after hip injury resulting in anterior hip pain will be determined by the site, type, and mechanism of injury, as well as the severity. Restrictions in weight bearing and the use of an assistive device may be needed to prevent excessive stress on bone and supporting soft-tissue structures in the early stages of healing. Physical therapy, as needed, should initially focus on early controlled ROM of the hip joint to prevent both intra- and extra-articular adhesions and excessive scar tissue formation.2
For patients who undergo surgery, much of the focus will be on strengthening the supporting musculature—the hip abductor group, anterior and posterior thigh musculature, and core stabilizing muscles. Neuromuscular training may be needed to promote normal biomechanics and minimize compensatory movement patterns. For athletes, cardiovascular training and a return-to-play program should be implemented, as well.2,43,44
CASE Mr. Q was diagnosed with right hip pain due to a labral tear secondary to a cam femoral acetabular impingement. Given that he had failed nonoperative treatment and had long-standing pain, we recommended surgery for this patient. He underwent right hip arthroscopic labral repair, acetabular rim trimming, acetabular microfracture, femoral osteochondroplasty with capsular plication. At 12-month follow-up, he was doing well, with resolution of the presurgical pain and return to all athletic activities.
CORRESPONDENCE Rachel M. Frank, MD, Department of Orthopedic Surgery, Rush University Medical Center, 1611 West Harrison Street, Suite 300, Chicago, IL 60612; [email protected]
1. Margo K, Drezner J, Motzkin D. Evaluation and management of hip pain: an algorithmic approach. J Fam Pract. 2003;52:607-617.
2. Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616-622.
3. Enseki KR, Martin RL, Draovitch P, et al. The hip joint: arthroscopic procedures and postoperative rehabilitation J Orthop Sports Phys Ther. 2006;36:516-525.
4. Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668-1674.
5. Fredericson M, Jennings F, Beaulieu C, et al. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17:309-325.
6. Matheson GO, Clement DB, McKenzie DC, et al. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15:46-58.
7. Stanitski CL, McMaster JH, Scranton PE. On the nature of stress fractures. Am J Sports Med. 1978;6:391-396.
8. Sofka CM. Imaging of stress fractures. Clin Sports Med. 2006;25:53-62, viii.
9. Shin AY, Gillingham BL. Fatigue fractures of the femoral neck in athletes. J Am Acad Orthop Surg. 1997;5:293-302.
10. Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459-474.
11. Lavernia CJ, Sierra RJ, Gomez-Marin O. Smoking and joint replacement: resource consumption and short-term outcome. Clin Orthop Relat Res. 1999;(367):172-180.
12. Lavernia CJ, Sierra RJ, Grieco FR. Osteonecrosis of the femoral head. J Am Acad Orthop Surg. 1999;7:250-261.
13. Smith SW, Fehring TK, Griffin WL, Beaver WB. Core decompression of the osteonecrotic femoral head. J Bone Joint Surg Am. 1995;77:674-680.
14. Fairbank AC, Bhatia D, Jinnah RH, et al. Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br. 1995;77:42-49.
15. Chandler HP, Reineck FT, Wixson RL, et al. Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426-1434.
16. Wei SY, Klimkiewicz JJ, Lai M, et al. Revision total hip arthroplasty in patients with avascular necrosis. Orthopedics. 1999;22:747-757.
17. Bedi A, Chen N, Robertson W, et al. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24:1135-1145.
18. Guanche CA, Bare AA. Arthroscopic treatment of femoroacetabular impingement. Arthroscopy. 2006;22:95-106.
19. Philippon M, Schenker M, Briggs K, et al. Femoroacetabular impingement in 45 professional athletes: Knee Surg Sports Traumatol Arthrosc. 2007;15:908-914.
20. Sierra RJ, Trousdale RT, Ganz R, et al. Hip disease in the young, active patient: evaluation and nonarthroplasty surgical options. J Am Acad Orthop Surg. 2008;16:689-703.
21. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res. 2009;468:741-746.
22. Burnett RS, Della Rocca GJ, Prather H, et al. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448-1457.
23. Bare AA, Guanche CA. Hip impingement: the role of arthroscopy. Orthopedics. 2005;28:266-273.
24. Toomayan GA, Holman WR, Major NM, et al. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006;186:449-453.
25. Robertson WJ, Kadrmas WR, Kelly BT. Arthroscopic management of labral tears in the hip: a systematic review of the literature. Clin Orthop Relat Res. 2007;455:88-92.
26. Kamath AF, Componovo R, Baldwin K, et al. Hip arthroscopy for labral tears: review of clinical outcomes with 4.8-year mean follow-up. Am J Sports Med. 2009;37:1721-1727.
27. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369-376.
28. Larson CM, Guanche CA, Kelly BT, et al. Advanced techniques in hip arthroscopy. Instr Course Lect. 2009;58:423-436.
29. Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24:1407-1421.
30. Holmich P. Long-standing groin pain in sportspeople falls into three primary patterns, a “clinical entity” approach: a prospective study of 207 patients. Br J Sports Med. 2007;41:247-252.
31. Winston P, Awan R, Cassidy JD, et al. Clinical examination and ultrasound of self-reported snapping hip syndrome in elite ballet dancers. Am J Sports Med. 2007;35:118-126.
32. Blankenbaker DG, De Smet AA, Keene JS. Sonography of the iliopsoas tendon and injection of the iliopsoas bursa for diagnosis and management of the painful snapping hip. Skeletal Radiol. 2006;35:565-571.
33. Adler RS, Buly R, Ambrose R, et al. Diagnostic and therapeutic use of sonography-guided iliopsoas peritendinous injections. AJR Am J Roentgenol. 2005;185:940-943.
34. Anderson SA, Keene JS. Results of arthroscopic iliopsoas tendon release in competitive and recreational athletes. Am J Sports Med. 2008;36:2363-2371.
35. Maffey L, Emery C. What are the risk factors for groin strain injury in sport? Sports Med. 2007;37:881-894.
36. Verrall GM, Slavotinek JP, Fon GT, et al. Outcome of conservative management of athletic chronic groin injury diagnosed as pubic bone stress injury. Am J Sports Med. 2007;35:467-474.
37. Pointinger H, Munk P, Poeschl GP. Avulsion fracture of the anterior superior iliac spine following apophysitis. Br J Sports Med. 2003;37:361-362.
38. Unverzagt CA, Schuemann T, Mathisen J. Differential diagnosis of a sports hernia in a high-school athlete. J Orthop Sports Phys Ther. 2008;38:63-70.
39. Caudill P, Nyland J, Smith C, et al. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42:954-964.
40. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55:393-396.
41. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533.
42. Petchprapa CN, Rosenberg ZS, Sconfienza LM, et al. MR imaging of entrapment neuropathies of the lower extremity. Part I. Radiographs. 2010;30:983-1000.
43. Voight M, Robinson K, Gill L, et al. Postoperative guidelines for hip arthroscopy in the active population. Sports Health. 2010;2:222-230.
44. Stalzer S, Wahoff M, Scanlan M. Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25:337-357.
• Consider both musculoskeletal and nonmusculoskeletal causes in patients with vague complaints of hip and groin pain. B
• Use imaging studies to confirm a hip pain diagnosis. B
• Refer patients who fail to respond to nonsurgical treatment to a sports medicine specialist or an orthopedic surgeon. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Hip pain is a common complaint, and commonly misunderstood. Although the pain can be associated with a broad spectrum of conditions, the presentation is often vague and nonspecific.
Thus, hip pain and injury are frequently attributed, often incorrectly, to a “hip pointer”—a contusion of soft tissues against the iliac crest. It’s not unusual for patients who receive this diagnosis to be treated conservatively for prolonged periods, leading some previously active individuals to abandon their favorite sport or self-impose limits on the activities they engage in.1
But it doesn’t have to be this way.
Minimally invasive hip arthroscopy and advances in imaging, instrumentation, and devices have made it easier to identify and address underlying pathology associated with hip pain, helping patients return to their previous level of activity more rapidly.2,3 And, while many conditions associated with hip pain can be treated conservatively, family physicians—whom patients often go to first—should not hesitate to provide a referral when more aggressive treatment or diagnostic confirmation is needed.
We created this guide with family physicians in mind. Our focus here is primarily on anterior hip pain—the most common presentation—in active, or athletic, patients.
When did the pain begin? Where does it hurt?
Before performing a physical examination, find out as much as possible about the onset of pain and when and under what circumstances it occurs. (A review of hip anatomy is provided here.) Did it begin suddenly, after an acute injury or a particular physical maneuver? Or is the pain insidious, as was the case with one of our patients?
Osseous morphology of the hip includes the anterior superior iliac spine, the origin of the sartorius muscle and the ilioinguinal ligament. The anterior inferior iliac spine attaches to the rectus femoris, a major hip flexor and knee extender. The adductors of the hip originate in the anterior pelvic region.
The inguinal canal contains the ilioinguinal nerve, which is responsible for radiation of pain to the anterior hip. The hip joint itself is a spheroid comprising the femoral head and acetabulum, with most of the articular hip innervated by the femoral or obturator nerves.
Most intra-articular conditions radiate to the anterior groin or hip, although there are cases in which the pain is referred to either the lateral aspect of the hip or the buttocks. The iliopsoas muscle is the major hip flexor, and crosses under the ilioinguinal ligament to insert on the lesser tuberosity after crossing over the anterior capsule of the hip. A large bursa surrounds it, helping the tendon glide smoothly over the hip.
CASE Mack Q, a 27-year-old man with an 8-month history of right hip pain, sought care at our medical center for an achy pain in his right groin; he also described an occasional “clicking and popping sensation” in his groin but denied any trauma. The pain worsened with prolonged sitting and certain activities, such as squatting, twisting, and putting on shoes and socks. Our patient had stopped playing soccer because it hurt too much. He had tried physical therapy, oral anti-inflammatories, and a corticosteroid injection, with little relief.
Start with a gait assessment
The physical examination should begin with a gait assessment. Consider the patient’s ability to bear weight and his or her foot angle.
An individual with a stress fracture will have difficulty bearing weight on the affected side, resulting in a limp, or antalgic gait. A patient with femoral acetabular impingement (FAI) will often exhibit greater external rotation of the foot on the affected side compared with the other foot. And a patient with weakened abductor muscles, typically because of severe osteoarthritis, will exhibit the Trendelenburg sign—a pelvic tilt when the weight is shifted to the affected extremity.
Although most individuals with hip pain will not have an obvious gait abnormality, any patient who walks with a limp or needs crutches requires an immediate referral to an orthopedic surgeon.
Include these elements in the physical exam
Examine the hip with the patient sitting on the side of the exam table. Assess range of motion (ROM), comparing the range of flexion, extension, and internal/external rotation on the affected and unaffected sides. Include the following maneuvers:
Impingement testing. In patients with FAI and osteoarthritis, impingement testing—encompassing Flexion, ADDuction, and Internal Rotation (FADDIR)—will elicit pain. The maneuver can be tested starting at 45° of hip flexion, increasing to approximately 120°. Pain with <45° of hip flexion indicates that the impingement is severe.
Such testing can also reveal labral tears, which may be caused by FAI or other structural abnormalities. In a patient with anterior labral tears, FADDIR will produce groin pain; posterior labral tears will produce pain when the patient is sitting with legs hanging off the exam table and the contralateral leg is brought to the chest and the affected limb fully extended.
In patients with hip pain and bursitis, applying downward pressure will elicit a snapping sound as the iliopsoas snaps over the iliopectineal eminence or femoral head. Flexion, ABduction, and External Rotation (FABER) can also be used to diagnose iliopsoas tendonitis: The test is positive if it elicits pain in the affected extremity or in the sacroiliac joint on the opposite side.
Log roll. A painful response to this test, which involves internally and externally rotating the affected hip while it is relaxed and the knee fully extended, is an indication of synovitis of the hip caused by intra-articular pathology. To test hip stability, externally rotate the leg while it is extended. If the hip is stable, the leg will return to a neutral position; microinstability of the hip is likely if the leg remains in the rotated position.
Muscular strength testing. To assess for tendinopathy in the hip area, the patient should be in a seated position and contract the internal and external rotators and the adductor muscles while you apply resistance. To test abductor strength, have the patient assume a lateral position and hold and abduct the leg on the affected side while you apply resistance.
Hip flexion strength should be tested with the patient in both supine and seated positions. A patient with quadriceps tendonitis will have much greater pain with resisted hip flexion in the supine position vs the seated position; the opposite is true for a patient with iliopsoas tendonitis. (See “Did you know…? Hip pain facts and findings” on for additional diagnostic tips.)
- A patient with quadriceps tendonitis will have much greater pain with resisted hip flexion in a supine position vs a seated position. The opposite is true for a patient with iliopsoas tendonitis.
- Patients with femoral neck stress fractures typically present with activity-related anterior groin pain that is relieved by rest. Initially, they may be only mildly affected, but the condition worsens in those who continue to “work through the pain.”
- Plain radiography can confirm a diagnosis of osteonecrosis in patients with advanced disease, but magnetic resonance imaging is useful for evaluating earlier clinical presentations.
- Patients with labral tears often exhibit what has been called the “c-sign”—so named for the shape patients make with their hand as they grip their hip just above the greater trochanter to indicate where it hurts.
- Athletes who experience adductor strains often play sports in which kicking or frequent changes in direction are required, such as football, hockey, and soccer, and are generally able to tell you exactly what they were doing when the injury occurred.
- Unlike other hernias, a sports hernia (athletic pubalgia) does not involve a bulge of tissue protruding through one part of the body into another. Instead, it occurs when the oblique abdominal muscles strain or completely tear away from the pubis.
Perform a neurologic evaluation to rule out a back condition that might radiate pain into the anterior hip; ask the patient to do a sit-up while you apply resistance to test for abdominal wall pathology, as well.
Hip palpation. This aspect of the physical exam is important regardless of the cause of the pain but especially crucial for pediatric and adolescent patients, whose anterior hip pain may be related to apophyseal injury. Palpate the superior iliac spine (and over the inferior iliac spine in thin patients) to determine if the sartorius or rectus femoris has been injured. The area just lateral to the symphysis will be tender to palpation in patients with osteitis pubis.
Refer or treat? Here’s what to consider
While the history and physical should provide ample information for a differential diagnosis, imaging studies are generally required for confirmation. Clinical assessment— including physical exam, imaging, and intra-articular injection—of patients with hip pain is up to 98% accurate in identifying hip abnormalities, with arthroscopy as the gold standard.4
CASE On physical examination, Mr. Q had right hip extension to 0°, flexion to 110°, external rotation to 50°, and internal rotation to neutral; he also had positive impingement and subspine impingement tests, a painful arc of motion from 12 to 4 o’clock, tenderness over the hip adductor, and pain with resisted hip adduction. He did not walk with a limp.
Diagnostic studies included plain radiographs, which demonstrated that the joint space was well preserved. We identified subtle anatomical abnormalities on the femoral head-neck junction, known as a cam deformity. Magnetic resonance imaging (MRI) revealed an anterior superior labral tear with cartilage delamination.
Stress fractures affect runners, military recruits
In addition to long-distance runners who have recently increased the frequency, duration, or intensity of training,5,6 military recruits have a higher incidence of stress fractures due to the rapid onset of intensive training. Stress fractures can also occur in patients who do not have a history of intense activity but have metabolically weakened bone, in some cases as a result of an eating disorder.7
Patients with femoral neck stress fractures typically present with activity-related anterior groin pain that is relieved by rest; initially, they may be only mildly affected, but the condition worsens in those who continue to “work through the pain.” By the time such individuals seek treatment, they almost always have pain with weight bearing and an antalgic gait.
Symptoms consistent with a femoral neck stress fracture can be further evaluated with plain radiographs. However, x-rays are often negative for up to 4 weeks after the onset of pain.8 In cases in which radiographs are negative but the physical exam is suggestive of a stress fracture, MRI—which can detect an abnormality within a day or 2 of injury8,9—should be used to confirm the diagnosis (FIGURE 1).
FIGURE 1
MRI reveals a femoral neck stress fracture
Treatment. A complete femoral neck fracture portends impending displacement and requires emergent evaluation by an orthopedist, and superior neck changes, also known as tension-sided stress fractures, require urgent treatment with percutaneous screw fixation.9 However, compression-sided, or inferior, stress fractures can be treated with restricted weight bearing and activity modification. Gradual resumption of activity is allowed only after the patient has been asymptomatic for 6 weeks; recurrent pain indicates residual stress reaction, and signals that activities should be abated.
Osteonecrosis has many causes
Necrosis of the femoral head is a debilitating and progressive condition primarily affecting patients between the ages of 20 and 50 years.10 It has multiple (and diverse) causes, including trauma, steroids, alcohol, smoking, lupus, sickle cell anemia, and coagulopathies, as well as scuba diving. But about 20% of cases have no apparent cause.11,12
Patients with osteonecrosis of the hip typically present with groin pain, often described as a deep, intermittent ache that interferes with activities of daily living. Exam findings depend on the stage of presentation. Early on, pain will occur only with extreme ROM; in advanced cases, ROM is restricted and pain occurs even with limited motion.
Femoral head collapse due to loss of the structural integrity of the subchondral bone—which occurs in 80% of cases12—is thought to be caused by decreased blood flow. Plain radiography can confirm a diagnosis of osteonecrosis in patients with advanced disease, but MRI is useful for evaluating patients with earlier clinical presentations.
Treatment of osteonecrosis is dictated by the stage of the disease, but remains controversial because no intervention has been shown to prevent progression in all cases.12 All patients should be referred to a specialist. Those without collapse or cartilage damage can be treated surgically with core decompression, possibly with additional vascularized bone grafting,13,14 while those with more advanced disease typically require a total hip replacement at a relatively young age. Results for total hip replacement in patients with osteonecrosis are thought to be inferior to hip replacement in patients with osteoarthritis, although comparison is difficult because of the differences in age and activity levels in these 2 groups.15,16
Femoral acetabular impingement can occur on the cam or pincer side
FAI pathology can exist on either the femoral (cam) or acetabular (pincer) side,17 or both.18 In pure cam impingement, the anterior femoral neck loses its normal concave anatomy and develops a “bump,” which impinges on the anterosuperior labrum during hip flexion, causing labral tears and delamination of the adjacent cartilage.
Pure pincer impingement arises from a prominent acetabular rim, causing overcoverage of the femoral head. Acetabular labral tears result from the repetitive impaction with flexion and internal rotation.
Patients report an insidious onset of groin pain that is exacerbated by flexion-type sports, such as hockey, football, and golf,19 as well as activities of daily living. In patients with cartilage damage, even walking can be painful. Physical examination of patients with FAI reveals findings that are similar to those of patients with acetabular labral tears. Abnormally large cam lesions or acetabular overcoverage will result in restriction of hip ROM, especially internal rotation and flexion due to a mechanical block.
Radiographs (FIGURE 2) are essential to diagnose FAI and to distinguish this condition from an isolated labral tear.20 Cam impingement will be best demonstrated on a cross-table lateral radiograph, which shows an asphericity of the femoral head/neck junction anteriorly, while pincer impingement will show overcoverage of the femoral head on an AP radiograph. MRI or magnetic resonance arthrography (MRA) is frequently obtained to see whether any cartilage deterioration has occurred. Computed tomography, which can provide a 3-dimensional reproduction of the hip morphology, is often used for preoperative planning when surgical intervention is required.
FIGURE 2
Femoral acetabular impingement with a prominent pincer lesion
Treatment. Surgical intervention is often needed to correct or remove the abnormal anatomy, and both arthroscopic and open surgery are recommended.20 Both methods include osteoplasty at the femoral head/neck junction and/or the acetabular rim to allow the proximal femur to articulate with the acetabulum without injury to the labrum with flexion and internal rotation.21
Results of both open and arthroscopic osteoplasty of the femur and acetabulum are still preliminary, with only a few studies reporting mid-term results. Open surgery typically has longer recovery and rehabilitation, but advocates emphasize the improved ability to contour the femur or acetabulum. Both open and arthroscopic procedures have about an 8% to 13% rate of revision in short-term follow-up.17
Labral tears occur with trauma and certain sports
In addition to FAI, causes of labral tears include dysplasia, instability, trauma, and degeneration, as well as sports that require repetitive hip flexion and/or pivoting, such as hockey, soccer, and football.22,23
Patients with labral tears typically present with anterior hip pain radiating to the groin, worsening with twisting motions, running, walking, and sitting for prolonged periods. Clicking or catching may occur, as well. Patients may exhibit what one researcher called the “c-sign”—so named for the shape patients make with their hand as they grip their hip just above the greater trochanter to indicate where it hurts.4 The work-up for labral tears includes radiographs and, often, MRA, which is nearly 100% specific.24
Treatment. Conservative treatment, which may include activity modification or rest and ice, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy, is often effective for labral tears; when such measures fail, surgical intervention is indicated. A systematic review found a 67% satisfaction rate after 3.5 years in patients who had undergone labral debridement, and complete resolution of mechanical symptoms in nearly 50%.25 Another study showed similar results for hip arthroscopy, with symptom relief continuing for 4.8 years after surgery, on average, and 84% of patients able to return to their previous level of activity.26
The long-term results of labral debridement are unknown, however, and the possibility of an association between this procedure and the development of arthritis remains. Most specialists prefer anatomic repair to restore normal hip kinematics and, potentially, long-term hip function,27,28 but structural abnormalities must also be addressed to prevent failure of the repair or recurrent tears.
Iliopsoas tendonitis: You know the snap
Often referred to as internal snapping of the hip or internal coxa saltans, iliopsoas tendonitis/bursitis can be a recalcitrant cause of anterior hip pain. Snapping of the iliopsoas leading to bursitis or tendonitis can occur at the iliopectineal eminence, the femoral head, or the lesser trochanter.29 Runners and ballet dancers are often affected.30,31
Snapping in itself is not an indication of pathology, but chronicity of symptoms is. Patients with relatively acute symptoms typically have only bursitis, while a longer duration of symptoms leads to tendonitis or tendinopathy.32
Treatment. First-line therapy is nonoperative, and includes activity modification, rest, ice, NSAIDs, and physical therapy. Advise patients to refrain from activities causing pain, and to apply ice to the affected every 20 minutes (with a 20- to 30-minute off period) for one to 2 hours. Physical therapy focuses on stretching the iliopsoas and rectus femoris muscles and strengthening the hamstring muscles to relieve the stress on the anterior pelvis. If such treatment is unsuccessful, ultrasound can be used to guide a therapeutic injection of cortisone.33 If this fails to bring relief, fractional lengthening of the iliopsoas tendon can be performed to eliminate snapping and relieve pain.34
Muscular strains/avulsion fractures: Sports and age play a role
Although strains can affect any of the anterior muscles around the hip, in active individuals the adductors are most commonly affected. Skeletally immature patients are an exception: apophyseal fractures at the origin of the sartorius and rectus femoris muscles are more common than muscular strains in this patient population.
Athletes who experience adductor strains often play sports in which kicking or frequent changes in direction are required—eg, football, hockey, and soccer35—and generally are able to tell you exactly what they were doing when the injury occurred. Physical examination can reveal focal findings, with swelling and tenderness confined to the anteromedial aspect of the hip along the adductor muscle group. MRI can help differentiate the site of true pathology.36
Treatment of adductor strains is nonoperative, with rest, ice, and activity modification until the tendon heals. In the rare case in which complete tendon avulsion is found, surgical reattachment is needed.
Apophyseal fracture in skeletally immature patients typically occurs during participation in a sport that requires rapid acceleration and deceleration with the hip in an extended position. In such patients, stretching the affected muscle should reproduce the pain. Radiographs are diagnostic and will often show minimal displacement of the apophysis. Treatment is almost always nonoperative. Surgical intervention is rarely needed, and only indicated with displacement >2 cm.37
Athletic pubalgia: A challenging Dx
Also referred to as sports hernia, athletic pubalgia is an enigmatic cause of anterior hip pain in athletes. Diagnosis can be especially challenging, and patients may have lingering symptoms for years before the cause is discovered.38 A sports hernia, unlike other hernias, does not involve a bulge of tissue protruding through one body part into another. In contrast, a sports hernia occurs when the oblique abdominal muscles strain or completely tear away from the pubis. A recent systematic review found that the underlying etiology involves posterior inguinal wall weakening, which can be a result of poorly balanced hip adductor and abdominal muscle activation.39
Patients with sports hernia will often present with anterior hip and/or groin pain, especially with hip extension, twisting, and turning. In addition, patients can have pain in the lower abdomen and, in males, in the testicles. Physical examination will usually show pubic point tenderness, which is exacerbated by resisted hip adduction.40 MRI and ultrasound are extremely helpful in diagnosing and forming a treatment plan.39
The initial treatment of choice for sports hernias is nonoperative, and the first step is always activity modification or temporary avoidance of symptom-producing activities. Additional modalities include NSAIDs, ice, and physical therapy to strengthen the surrounding muscles. Surgical intervention, if needed, may be done laparoscopically or via an open approach with direct repair.40,41
Less common causes to consider
While the conditions detailed here account for most anterior hip etiologies, there are other less common causes to consider. One such cause is osteitis pubis, an umbrella term for conditions that affect the area surrounding the symphysis pubis. Patients with osteitis pubis present with pain over the anterior aspect of the pelvis that is worse with sit-ups, rising from a chair, or any activity where contraction of the rectus muscles occurs.29 Tenderness is found directly over and just lateral to the pubic symphysis. Radiographs are frequently negative, but occasionally chronic degenerative changes at the symphysis are present in addition to symphyseal narrowing. Additional imaging is often necessary for diagnosis.
Neuropathies. When history, physical examination, and imaging studies have ruled out other causes, neuropathies (ilioinguinal, genitofemoral, and obturator) should be considered, particularly in patients with vague, radiating anterior hip and/or groin pain.42 In pediatric patients, Legg-Calve-Perthes disease and slipped capital femoral epiphysis are possibilities, as well.
Getting patients back on track
Rehabilitation after hip injury resulting in anterior hip pain will be determined by the site, type, and mechanism of injury, as well as the severity. Restrictions in weight bearing and the use of an assistive device may be needed to prevent excessive stress on bone and supporting soft-tissue structures in the early stages of healing. Physical therapy, as needed, should initially focus on early controlled ROM of the hip joint to prevent both intra- and extra-articular adhesions and excessive scar tissue formation.2
For patients who undergo surgery, much of the focus will be on strengthening the supporting musculature—the hip abductor group, anterior and posterior thigh musculature, and core stabilizing muscles. Neuromuscular training may be needed to promote normal biomechanics and minimize compensatory movement patterns. For athletes, cardiovascular training and a return-to-play program should be implemented, as well.2,43,44
CASE Mr. Q was diagnosed with right hip pain due to a labral tear secondary to a cam femoral acetabular impingement. Given that he had failed nonoperative treatment and had long-standing pain, we recommended surgery for this patient. He underwent right hip arthroscopic labral repair, acetabular rim trimming, acetabular microfracture, femoral osteochondroplasty with capsular plication. At 12-month follow-up, he was doing well, with resolution of the presurgical pain and return to all athletic activities.
CORRESPONDENCE Rachel M. Frank, MD, Department of Orthopedic Surgery, Rush University Medical Center, 1611 West Harrison Street, Suite 300, Chicago, IL 60612; [email protected]
• Consider both musculoskeletal and nonmusculoskeletal causes in patients with vague complaints of hip and groin pain. B
• Use imaging studies to confirm a hip pain diagnosis. B
• Refer patients who fail to respond to nonsurgical treatment to a sports medicine specialist or an orthopedic surgeon. B
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Hip pain is a common complaint, and commonly misunderstood. Although the pain can be associated with a broad spectrum of conditions, the presentation is often vague and nonspecific.
Thus, hip pain and injury are frequently attributed, often incorrectly, to a “hip pointer”—a contusion of soft tissues against the iliac crest. It’s not unusual for patients who receive this diagnosis to be treated conservatively for prolonged periods, leading some previously active individuals to abandon their favorite sport or self-impose limits on the activities they engage in.1
But it doesn’t have to be this way.
Minimally invasive hip arthroscopy and advances in imaging, instrumentation, and devices have made it easier to identify and address underlying pathology associated with hip pain, helping patients return to their previous level of activity more rapidly.2,3 And, while many conditions associated with hip pain can be treated conservatively, family physicians—whom patients often go to first—should not hesitate to provide a referral when more aggressive treatment or diagnostic confirmation is needed.
We created this guide with family physicians in mind. Our focus here is primarily on anterior hip pain—the most common presentation—in active, or athletic, patients.
When did the pain begin? Where does it hurt?
Before performing a physical examination, find out as much as possible about the onset of pain and when and under what circumstances it occurs. (A review of hip anatomy is provided here.) Did it begin suddenly, after an acute injury or a particular physical maneuver? Or is the pain insidious, as was the case with one of our patients?
Osseous morphology of the hip includes the anterior superior iliac spine, the origin of the sartorius muscle and the ilioinguinal ligament. The anterior inferior iliac spine attaches to the rectus femoris, a major hip flexor and knee extender. The adductors of the hip originate in the anterior pelvic region.
The inguinal canal contains the ilioinguinal nerve, which is responsible for radiation of pain to the anterior hip. The hip joint itself is a spheroid comprising the femoral head and acetabulum, with most of the articular hip innervated by the femoral or obturator nerves.
Most intra-articular conditions radiate to the anterior groin or hip, although there are cases in which the pain is referred to either the lateral aspect of the hip or the buttocks. The iliopsoas muscle is the major hip flexor, and crosses under the ilioinguinal ligament to insert on the lesser tuberosity after crossing over the anterior capsule of the hip. A large bursa surrounds it, helping the tendon glide smoothly over the hip.
CASE Mack Q, a 27-year-old man with an 8-month history of right hip pain, sought care at our medical center for an achy pain in his right groin; he also described an occasional “clicking and popping sensation” in his groin but denied any trauma. The pain worsened with prolonged sitting and certain activities, such as squatting, twisting, and putting on shoes and socks. Our patient had stopped playing soccer because it hurt too much. He had tried physical therapy, oral anti-inflammatories, and a corticosteroid injection, with little relief.
Start with a gait assessment
The physical examination should begin with a gait assessment. Consider the patient’s ability to bear weight and his or her foot angle.
An individual with a stress fracture will have difficulty bearing weight on the affected side, resulting in a limp, or antalgic gait. A patient with femoral acetabular impingement (FAI) will often exhibit greater external rotation of the foot on the affected side compared with the other foot. And a patient with weakened abductor muscles, typically because of severe osteoarthritis, will exhibit the Trendelenburg sign—a pelvic tilt when the weight is shifted to the affected extremity.
Although most individuals with hip pain will not have an obvious gait abnormality, any patient who walks with a limp or needs crutches requires an immediate referral to an orthopedic surgeon.
Include these elements in the physical exam
Examine the hip with the patient sitting on the side of the exam table. Assess range of motion (ROM), comparing the range of flexion, extension, and internal/external rotation on the affected and unaffected sides. Include the following maneuvers:
Impingement testing. In patients with FAI and osteoarthritis, impingement testing—encompassing Flexion, ADDuction, and Internal Rotation (FADDIR)—will elicit pain. The maneuver can be tested starting at 45° of hip flexion, increasing to approximately 120°. Pain with <45° of hip flexion indicates that the impingement is severe.
Such testing can also reveal labral tears, which may be caused by FAI or other structural abnormalities. In a patient with anterior labral tears, FADDIR will produce groin pain; posterior labral tears will produce pain when the patient is sitting with legs hanging off the exam table and the contralateral leg is brought to the chest and the affected limb fully extended.
In patients with hip pain and bursitis, applying downward pressure will elicit a snapping sound as the iliopsoas snaps over the iliopectineal eminence or femoral head. Flexion, ABduction, and External Rotation (FABER) can also be used to diagnose iliopsoas tendonitis: The test is positive if it elicits pain in the affected extremity or in the sacroiliac joint on the opposite side.
Log roll. A painful response to this test, which involves internally and externally rotating the affected hip while it is relaxed and the knee fully extended, is an indication of synovitis of the hip caused by intra-articular pathology. To test hip stability, externally rotate the leg while it is extended. If the hip is stable, the leg will return to a neutral position; microinstability of the hip is likely if the leg remains in the rotated position.
Muscular strength testing. To assess for tendinopathy in the hip area, the patient should be in a seated position and contract the internal and external rotators and the adductor muscles while you apply resistance. To test abductor strength, have the patient assume a lateral position and hold and abduct the leg on the affected side while you apply resistance.
Hip flexion strength should be tested with the patient in both supine and seated positions. A patient with quadriceps tendonitis will have much greater pain with resisted hip flexion in the supine position vs the seated position; the opposite is true for a patient with iliopsoas tendonitis. (See “Did you know…? Hip pain facts and findings” on for additional diagnostic tips.)
- A patient with quadriceps tendonitis will have much greater pain with resisted hip flexion in a supine position vs a seated position. The opposite is true for a patient with iliopsoas tendonitis.
- Patients with femoral neck stress fractures typically present with activity-related anterior groin pain that is relieved by rest. Initially, they may be only mildly affected, but the condition worsens in those who continue to “work through the pain.”
- Plain radiography can confirm a diagnosis of osteonecrosis in patients with advanced disease, but magnetic resonance imaging is useful for evaluating earlier clinical presentations.
- Patients with labral tears often exhibit what has been called the “c-sign”—so named for the shape patients make with their hand as they grip their hip just above the greater trochanter to indicate where it hurts.
- Athletes who experience adductor strains often play sports in which kicking or frequent changes in direction are required, such as football, hockey, and soccer, and are generally able to tell you exactly what they were doing when the injury occurred.
- Unlike other hernias, a sports hernia (athletic pubalgia) does not involve a bulge of tissue protruding through one part of the body into another. Instead, it occurs when the oblique abdominal muscles strain or completely tear away from the pubis.
Perform a neurologic evaluation to rule out a back condition that might radiate pain into the anterior hip; ask the patient to do a sit-up while you apply resistance to test for abdominal wall pathology, as well.
Hip palpation. This aspect of the physical exam is important regardless of the cause of the pain but especially crucial for pediatric and adolescent patients, whose anterior hip pain may be related to apophyseal injury. Palpate the superior iliac spine (and over the inferior iliac spine in thin patients) to determine if the sartorius or rectus femoris has been injured. The area just lateral to the symphysis will be tender to palpation in patients with osteitis pubis.
Refer or treat? Here’s what to consider
While the history and physical should provide ample information for a differential diagnosis, imaging studies are generally required for confirmation. Clinical assessment— including physical exam, imaging, and intra-articular injection—of patients with hip pain is up to 98% accurate in identifying hip abnormalities, with arthroscopy as the gold standard.4
CASE On physical examination, Mr. Q had right hip extension to 0°, flexion to 110°, external rotation to 50°, and internal rotation to neutral; he also had positive impingement and subspine impingement tests, a painful arc of motion from 12 to 4 o’clock, tenderness over the hip adductor, and pain with resisted hip adduction. He did not walk with a limp.
Diagnostic studies included plain radiographs, which demonstrated that the joint space was well preserved. We identified subtle anatomical abnormalities on the femoral head-neck junction, known as a cam deformity. Magnetic resonance imaging (MRI) revealed an anterior superior labral tear with cartilage delamination.
Stress fractures affect runners, military recruits
In addition to long-distance runners who have recently increased the frequency, duration, or intensity of training,5,6 military recruits have a higher incidence of stress fractures due to the rapid onset of intensive training. Stress fractures can also occur in patients who do not have a history of intense activity but have metabolically weakened bone, in some cases as a result of an eating disorder.7
Patients with femoral neck stress fractures typically present with activity-related anterior groin pain that is relieved by rest; initially, they may be only mildly affected, but the condition worsens in those who continue to “work through the pain.” By the time such individuals seek treatment, they almost always have pain with weight bearing and an antalgic gait.
Symptoms consistent with a femoral neck stress fracture can be further evaluated with plain radiographs. However, x-rays are often negative for up to 4 weeks after the onset of pain.8 In cases in which radiographs are negative but the physical exam is suggestive of a stress fracture, MRI—which can detect an abnormality within a day or 2 of injury8,9—should be used to confirm the diagnosis (FIGURE 1).
FIGURE 1
MRI reveals a femoral neck stress fracture
Treatment. A complete femoral neck fracture portends impending displacement and requires emergent evaluation by an orthopedist, and superior neck changes, also known as tension-sided stress fractures, require urgent treatment with percutaneous screw fixation.9 However, compression-sided, or inferior, stress fractures can be treated with restricted weight bearing and activity modification. Gradual resumption of activity is allowed only after the patient has been asymptomatic for 6 weeks; recurrent pain indicates residual stress reaction, and signals that activities should be abated.
Osteonecrosis has many causes
Necrosis of the femoral head is a debilitating and progressive condition primarily affecting patients between the ages of 20 and 50 years.10 It has multiple (and diverse) causes, including trauma, steroids, alcohol, smoking, lupus, sickle cell anemia, and coagulopathies, as well as scuba diving. But about 20% of cases have no apparent cause.11,12
Patients with osteonecrosis of the hip typically present with groin pain, often described as a deep, intermittent ache that interferes with activities of daily living. Exam findings depend on the stage of presentation. Early on, pain will occur only with extreme ROM; in advanced cases, ROM is restricted and pain occurs even with limited motion.
Femoral head collapse due to loss of the structural integrity of the subchondral bone—which occurs in 80% of cases12—is thought to be caused by decreased blood flow. Plain radiography can confirm a diagnosis of osteonecrosis in patients with advanced disease, but MRI is useful for evaluating patients with earlier clinical presentations.
Treatment of osteonecrosis is dictated by the stage of the disease, but remains controversial because no intervention has been shown to prevent progression in all cases.12 All patients should be referred to a specialist. Those without collapse or cartilage damage can be treated surgically with core decompression, possibly with additional vascularized bone grafting,13,14 while those with more advanced disease typically require a total hip replacement at a relatively young age. Results for total hip replacement in patients with osteonecrosis are thought to be inferior to hip replacement in patients with osteoarthritis, although comparison is difficult because of the differences in age and activity levels in these 2 groups.15,16
Femoral acetabular impingement can occur on the cam or pincer side
FAI pathology can exist on either the femoral (cam) or acetabular (pincer) side,17 or both.18 In pure cam impingement, the anterior femoral neck loses its normal concave anatomy and develops a “bump,” which impinges on the anterosuperior labrum during hip flexion, causing labral tears and delamination of the adjacent cartilage.
Pure pincer impingement arises from a prominent acetabular rim, causing overcoverage of the femoral head. Acetabular labral tears result from the repetitive impaction with flexion and internal rotation.
Patients report an insidious onset of groin pain that is exacerbated by flexion-type sports, such as hockey, football, and golf,19 as well as activities of daily living. In patients with cartilage damage, even walking can be painful. Physical examination of patients with FAI reveals findings that are similar to those of patients with acetabular labral tears. Abnormally large cam lesions or acetabular overcoverage will result in restriction of hip ROM, especially internal rotation and flexion due to a mechanical block.
Radiographs (FIGURE 2) are essential to diagnose FAI and to distinguish this condition from an isolated labral tear.20 Cam impingement will be best demonstrated on a cross-table lateral radiograph, which shows an asphericity of the femoral head/neck junction anteriorly, while pincer impingement will show overcoverage of the femoral head on an AP radiograph. MRI or magnetic resonance arthrography (MRA) is frequently obtained to see whether any cartilage deterioration has occurred. Computed tomography, which can provide a 3-dimensional reproduction of the hip morphology, is often used for preoperative planning when surgical intervention is required.
FIGURE 2
Femoral acetabular impingement with a prominent pincer lesion
Treatment. Surgical intervention is often needed to correct or remove the abnormal anatomy, and both arthroscopic and open surgery are recommended.20 Both methods include osteoplasty at the femoral head/neck junction and/or the acetabular rim to allow the proximal femur to articulate with the acetabulum without injury to the labrum with flexion and internal rotation.21
Results of both open and arthroscopic osteoplasty of the femur and acetabulum are still preliminary, with only a few studies reporting mid-term results. Open surgery typically has longer recovery and rehabilitation, but advocates emphasize the improved ability to contour the femur or acetabulum. Both open and arthroscopic procedures have about an 8% to 13% rate of revision in short-term follow-up.17
Labral tears occur with trauma and certain sports
In addition to FAI, causes of labral tears include dysplasia, instability, trauma, and degeneration, as well as sports that require repetitive hip flexion and/or pivoting, such as hockey, soccer, and football.22,23
Patients with labral tears typically present with anterior hip pain radiating to the groin, worsening with twisting motions, running, walking, and sitting for prolonged periods. Clicking or catching may occur, as well. Patients may exhibit what one researcher called the “c-sign”—so named for the shape patients make with their hand as they grip their hip just above the greater trochanter to indicate where it hurts.4 The work-up for labral tears includes radiographs and, often, MRA, which is nearly 100% specific.24
Treatment. Conservative treatment, which may include activity modification or rest and ice, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy, is often effective for labral tears; when such measures fail, surgical intervention is indicated. A systematic review found a 67% satisfaction rate after 3.5 years in patients who had undergone labral debridement, and complete resolution of mechanical symptoms in nearly 50%.25 Another study showed similar results for hip arthroscopy, with symptom relief continuing for 4.8 years after surgery, on average, and 84% of patients able to return to their previous level of activity.26
The long-term results of labral debridement are unknown, however, and the possibility of an association between this procedure and the development of arthritis remains. Most specialists prefer anatomic repair to restore normal hip kinematics and, potentially, long-term hip function,27,28 but structural abnormalities must also be addressed to prevent failure of the repair or recurrent tears.
Iliopsoas tendonitis: You know the snap
Often referred to as internal snapping of the hip or internal coxa saltans, iliopsoas tendonitis/bursitis can be a recalcitrant cause of anterior hip pain. Snapping of the iliopsoas leading to bursitis or tendonitis can occur at the iliopectineal eminence, the femoral head, or the lesser trochanter.29 Runners and ballet dancers are often affected.30,31
Snapping in itself is not an indication of pathology, but chronicity of symptoms is. Patients with relatively acute symptoms typically have only bursitis, while a longer duration of symptoms leads to tendonitis or tendinopathy.32
Treatment. First-line therapy is nonoperative, and includes activity modification, rest, ice, NSAIDs, and physical therapy. Advise patients to refrain from activities causing pain, and to apply ice to the affected every 20 minutes (with a 20- to 30-minute off period) for one to 2 hours. Physical therapy focuses on stretching the iliopsoas and rectus femoris muscles and strengthening the hamstring muscles to relieve the stress on the anterior pelvis. If such treatment is unsuccessful, ultrasound can be used to guide a therapeutic injection of cortisone.33 If this fails to bring relief, fractional lengthening of the iliopsoas tendon can be performed to eliminate snapping and relieve pain.34
Muscular strains/avulsion fractures: Sports and age play a role
Although strains can affect any of the anterior muscles around the hip, in active individuals the adductors are most commonly affected. Skeletally immature patients are an exception: apophyseal fractures at the origin of the sartorius and rectus femoris muscles are more common than muscular strains in this patient population.
Athletes who experience adductor strains often play sports in which kicking or frequent changes in direction are required—eg, football, hockey, and soccer35—and generally are able to tell you exactly what they were doing when the injury occurred. Physical examination can reveal focal findings, with swelling and tenderness confined to the anteromedial aspect of the hip along the adductor muscle group. MRI can help differentiate the site of true pathology.36
Treatment of adductor strains is nonoperative, with rest, ice, and activity modification until the tendon heals. In the rare case in which complete tendon avulsion is found, surgical reattachment is needed.
Apophyseal fracture in skeletally immature patients typically occurs during participation in a sport that requires rapid acceleration and deceleration with the hip in an extended position. In such patients, stretching the affected muscle should reproduce the pain. Radiographs are diagnostic and will often show minimal displacement of the apophysis. Treatment is almost always nonoperative. Surgical intervention is rarely needed, and only indicated with displacement >2 cm.37
Athletic pubalgia: A challenging Dx
Also referred to as sports hernia, athletic pubalgia is an enigmatic cause of anterior hip pain in athletes. Diagnosis can be especially challenging, and patients may have lingering symptoms for years before the cause is discovered.38 A sports hernia, unlike other hernias, does not involve a bulge of tissue protruding through one body part into another. In contrast, a sports hernia occurs when the oblique abdominal muscles strain or completely tear away from the pubis. A recent systematic review found that the underlying etiology involves posterior inguinal wall weakening, which can be a result of poorly balanced hip adductor and abdominal muscle activation.39
Patients with sports hernia will often present with anterior hip and/or groin pain, especially with hip extension, twisting, and turning. In addition, patients can have pain in the lower abdomen and, in males, in the testicles. Physical examination will usually show pubic point tenderness, which is exacerbated by resisted hip adduction.40 MRI and ultrasound are extremely helpful in diagnosing and forming a treatment plan.39
The initial treatment of choice for sports hernias is nonoperative, and the first step is always activity modification or temporary avoidance of symptom-producing activities. Additional modalities include NSAIDs, ice, and physical therapy to strengthen the surrounding muscles. Surgical intervention, if needed, may be done laparoscopically or via an open approach with direct repair.40,41
Less common causes to consider
While the conditions detailed here account for most anterior hip etiologies, there are other less common causes to consider. One such cause is osteitis pubis, an umbrella term for conditions that affect the area surrounding the symphysis pubis. Patients with osteitis pubis present with pain over the anterior aspect of the pelvis that is worse with sit-ups, rising from a chair, or any activity where contraction of the rectus muscles occurs.29 Tenderness is found directly over and just lateral to the pubic symphysis. Radiographs are frequently negative, but occasionally chronic degenerative changes at the symphysis are present in addition to symphyseal narrowing. Additional imaging is often necessary for diagnosis.
Neuropathies. When history, physical examination, and imaging studies have ruled out other causes, neuropathies (ilioinguinal, genitofemoral, and obturator) should be considered, particularly in patients with vague, radiating anterior hip and/or groin pain.42 In pediatric patients, Legg-Calve-Perthes disease and slipped capital femoral epiphysis are possibilities, as well.
Getting patients back on track
Rehabilitation after hip injury resulting in anterior hip pain will be determined by the site, type, and mechanism of injury, as well as the severity. Restrictions in weight bearing and the use of an assistive device may be needed to prevent excessive stress on bone and supporting soft-tissue structures in the early stages of healing. Physical therapy, as needed, should initially focus on early controlled ROM of the hip joint to prevent both intra- and extra-articular adhesions and excessive scar tissue formation.2
For patients who undergo surgery, much of the focus will be on strengthening the supporting musculature—the hip abductor group, anterior and posterior thigh musculature, and core stabilizing muscles. Neuromuscular training may be needed to promote normal biomechanics and minimize compensatory movement patterns. For athletes, cardiovascular training and a return-to-play program should be implemented, as well.2,43,44
CASE Mr. Q was diagnosed with right hip pain due to a labral tear secondary to a cam femoral acetabular impingement. Given that he had failed nonoperative treatment and had long-standing pain, we recommended surgery for this patient. He underwent right hip arthroscopic labral repair, acetabular rim trimming, acetabular microfracture, femoral osteochondroplasty with capsular plication. At 12-month follow-up, he was doing well, with resolution of the presurgical pain and return to all athletic activities.
CORRESPONDENCE Rachel M. Frank, MD, Department of Orthopedic Surgery, Rush University Medical Center, 1611 West Harrison Street, Suite 300, Chicago, IL 60612; [email protected]
1. Margo K, Drezner J, Motzkin D. Evaluation and management of hip pain: an algorithmic approach. J Fam Pract. 2003;52:607-617.
2. Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616-622.
3. Enseki KR, Martin RL, Draovitch P, et al. The hip joint: arthroscopic procedures and postoperative rehabilitation J Orthop Sports Phys Ther. 2006;36:516-525.
4. Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668-1674.
5. Fredericson M, Jennings F, Beaulieu C, et al. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17:309-325.
6. Matheson GO, Clement DB, McKenzie DC, et al. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15:46-58.
7. Stanitski CL, McMaster JH, Scranton PE. On the nature of stress fractures. Am J Sports Med. 1978;6:391-396.
8. Sofka CM. Imaging of stress fractures. Clin Sports Med. 2006;25:53-62, viii.
9. Shin AY, Gillingham BL. Fatigue fractures of the femoral neck in athletes. J Am Acad Orthop Surg. 1997;5:293-302.
10. Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459-474.
11. Lavernia CJ, Sierra RJ, Gomez-Marin O. Smoking and joint replacement: resource consumption and short-term outcome. Clin Orthop Relat Res. 1999;(367):172-180.
12. Lavernia CJ, Sierra RJ, Grieco FR. Osteonecrosis of the femoral head. J Am Acad Orthop Surg. 1999;7:250-261.
13. Smith SW, Fehring TK, Griffin WL, Beaver WB. Core decompression of the osteonecrotic femoral head. J Bone Joint Surg Am. 1995;77:674-680.
14. Fairbank AC, Bhatia D, Jinnah RH, et al. Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br. 1995;77:42-49.
15. Chandler HP, Reineck FT, Wixson RL, et al. Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426-1434.
16. Wei SY, Klimkiewicz JJ, Lai M, et al. Revision total hip arthroplasty in patients with avascular necrosis. Orthopedics. 1999;22:747-757.
17. Bedi A, Chen N, Robertson W, et al. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24:1135-1145.
18. Guanche CA, Bare AA. Arthroscopic treatment of femoroacetabular impingement. Arthroscopy. 2006;22:95-106.
19. Philippon M, Schenker M, Briggs K, et al. Femoroacetabular impingement in 45 professional athletes: Knee Surg Sports Traumatol Arthrosc. 2007;15:908-914.
20. Sierra RJ, Trousdale RT, Ganz R, et al. Hip disease in the young, active patient: evaluation and nonarthroplasty surgical options. J Am Acad Orthop Surg. 2008;16:689-703.
21. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res. 2009;468:741-746.
22. Burnett RS, Della Rocca GJ, Prather H, et al. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448-1457.
23. Bare AA, Guanche CA. Hip impingement: the role of arthroscopy. Orthopedics. 2005;28:266-273.
24. Toomayan GA, Holman WR, Major NM, et al. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006;186:449-453.
25. Robertson WJ, Kadrmas WR, Kelly BT. Arthroscopic management of labral tears in the hip: a systematic review of the literature. Clin Orthop Relat Res. 2007;455:88-92.
26. Kamath AF, Componovo R, Baldwin K, et al. Hip arthroscopy for labral tears: review of clinical outcomes with 4.8-year mean follow-up. Am J Sports Med. 2009;37:1721-1727.
27. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369-376.
28. Larson CM, Guanche CA, Kelly BT, et al. Advanced techniques in hip arthroscopy. Instr Course Lect. 2009;58:423-436.
29. Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24:1407-1421.
30. Holmich P. Long-standing groin pain in sportspeople falls into three primary patterns, a “clinical entity” approach: a prospective study of 207 patients. Br J Sports Med. 2007;41:247-252.
31. Winston P, Awan R, Cassidy JD, et al. Clinical examination and ultrasound of self-reported snapping hip syndrome in elite ballet dancers. Am J Sports Med. 2007;35:118-126.
32. Blankenbaker DG, De Smet AA, Keene JS. Sonography of the iliopsoas tendon and injection of the iliopsoas bursa for diagnosis and management of the painful snapping hip. Skeletal Radiol. 2006;35:565-571.
33. Adler RS, Buly R, Ambrose R, et al. Diagnostic and therapeutic use of sonography-guided iliopsoas peritendinous injections. AJR Am J Roentgenol. 2005;185:940-943.
34. Anderson SA, Keene JS. Results of arthroscopic iliopsoas tendon release in competitive and recreational athletes. Am J Sports Med. 2008;36:2363-2371.
35. Maffey L, Emery C. What are the risk factors for groin strain injury in sport? Sports Med. 2007;37:881-894.
36. Verrall GM, Slavotinek JP, Fon GT, et al. Outcome of conservative management of athletic chronic groin injury diagnosed as pubic bone stress injury. Am J Sports Med. 2007;35:467-474.
37. Pointinger H, Munk P, Poeschl GP. Avulsion fracture of the anterior superior iliac spine following apophysitis. Br J Sports Med. 2003;37:361-362.
38. Unverzagt CA, Schuemann T, Mathisen J. Differential diagnosis of a sports hernia in a high-school athlete. J Orthop Sports Phys Ther. 2008;38:63-70.
39. Caudill P, Nyland J, Smith C, et al. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42:954-964.
40. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55:393-396.
41. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533.
42. Petchprapa CN, Rosenberg ZS, Sconfienza LM, et al. MR imaging of entrapment neuropathies of the lower extremity. Part I. Radiographs. 2010;30:983-1000.
43. Voight M, Robinson K, Gill L, et al. Postoperative guidelines for hip arthroscopy in the active population. Sports Health. 2010;2:222-230.
44. Stalzer S, Wahoff M, Scanlan M. Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25:337-357.
1. Margo K, Drezner J, Motzkin D. Evaluation and management of hip pain: an algorithmic approach. J Fam Pract. 2003;52:607-617.
2. Leunig M, Beaule PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616-622.
3. Enseki KR, Martin RL, Draovitch P, et al. The hip joint: arthroscopic procedures and postoperative rehabilitation J Orthop Sports Phys Ther. 2006;36:516-525.
4. Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668-1674.
5. Fredericson M, Jennings F, Beaulieu C, et al. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17:309-325.
6. Matheson GO, Clement DB, McKenzie DC, et al. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15:46-58.
7. Stanitski CL, McMaster JH, Scranton PE. On the nature of stress fractures. Am J Sports Med. 1978;6:391-396.
8. Sofka CM. Imaging of stress fractures. Clin Sports Med. 2006;25:53-62, viii.
9. Shin AY, Gillingham BL. Fatigue fractures of the femoral neck in athletes. J Am Acad Orthop Surg. 1997;5:293-302.
10. Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459-474.
11. Lavernia CJ, Sierra RJ, Gomez-Marin O. Smoking and joint replacement: resource consumption and short-term outcome. Clin Orthop Relat Res. 1999;(367):172-180.
12. Lavernia CJ, Sierra RJ, Grieco FR. Osteonecrosis of the femoral head. J Am Acad Orthop Surg. 1999;7:250-261.
13. Smith SW, Fehring TK, Griffin WL, Beaver WB. Core decompression of the osteonecrotic femoral head. J Bone Joint Surg Am. 1995;77:674-680.
14. Fairbank AC, Bhatia D, Jinnah RH, et al. Long-term results of core decompression for ischaemic necrosis of the femoral head. J Bone Joint Surg Br. 1995;77:42-49.
15. Chandler HP, Reineck FT, Wixson RL, et al. Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426-1434.
16. Wei SY, Klimkiewicz JJ, Lai M, et al. Revision total hip arthroplasty in patients with avascular necrosis. Orthopedics. 1999;22:747-757.
17. Bedi A, Chen N, Robertson W, et al. The management of labral tears and femoroacetabular impingement of the hip in the young, active patient. Arthroscopy. 2008;24:1135-1145.
18. Guanche CA, Bare AA. Arthroscopic treatment of femoroacetabular impingement. Arthroscopy. 2006;22:95-106.
19. Philippon M, Schenker M, Briggs K, et al. Femoroacetabular impingement in 45 professional athletes: Knee Surg Sports Traumatol Arthrosc. 2007;15:908-914.
20. Sierra RJ, Trousdale RT, Ganz R, et al. Hip disease in the young, active patient: evaluation and nonarthroplasty surgical options. J Am Acad Orthop Surg. 2008;16:689-703.
21. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 10-year followup. Clin Orthop Relat Res. 2009;468:741-746.
22. Burnett RS, Della Rocca GJ, Prather H, et al. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448-1457.
23. Bare AA, Guanche CA. Hip impingement: the role of arthroscopy. Orthopedics. 2005;28:266-273.
24. Toomayan GA, Holman WR, Major NM, et al. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006;186:449-453.
25. Robertson WJ, Kadrmas WR, Kelly BT. Arthroscopic management of labral tears in the hip: a systematic review of the literature. Clin Orthop Relat Res. 2007;455:88-92.
26. Kamath AF, Componovo R, Baldwin K, et al. Hip arthroscopy for labral tears: review of clinical outcomes with 4.8-year mean follow-up. Am J Sports Med. 2009;37:1721-1727.
27. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369-376.
28. Larson CM, Guanche CA, Kelly BT, et al. Advanced techniques in hip arthroscopy. Instr Course Lect. 2009;58:423-436.
29. Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24:1407-1421.
30. Holmich P. Long-standing groin pain in sportspeople falls into three primary patterns, a “clinical entity” approach: a prospective study of 207 patients. Br J Sports Med. 2007;41:247-252.
31. Winston P, Awan R, Cassidy JD, et al. Clinical examination and ultrasound of self-reported snapping hip syndrome in elite ballet dancers. Am J Sports Med. 2007;35:118-126.
32. Blankenbaker DG, De Smet AA, Keene JS. Sonography of the iliopsoas tendon and injection of the iliopsoas bursa for diagnosis and management of the painful snapping hip. Skeletal Radiol. 2006;35:565-571.
33. Adler RS, Buly R, Ambrose R, et al. Diagnostic and therapeutic use of sonography-guided iliopsoas peritendinous injections. AJR Am J Roentgenol. 2005;185:940-943.
34. Anderson SA, Keene JS. Results of arthroscopic iliopsoas tendon release in competitive and recreational athletes. Am J Sports Med. 2008;36:2363-2371.
35. Maffey L, Emery C. What are the risk factors for groin strain injury in sport? Sports Med. 2007;37:881-894.
36. Verrall GM, Slavotinek JP, Fon GT, et al. Outcome of conservative management of athletic chronic groin injury diagnosed as pubic bone stress injury. Am J Sports Med. 2007;35:467-474.
37. Pointinger H, Munk P, Poeschl GP. Avulsion fracture of the anterior superior iliac spine following apophysitis. Br J Sports Med. 2003;37:361-362.
38. Unverzagt CA, Schuemann T, Mathisen J. Differential diagnosis of a sports hernia in a high-school athlete. J Orthop Sports Phys Ther. 2008;38:63-70.
39. Caudill P, Nyland J, Smith C, et al. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42:954-964.
40. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55:393-396.
41. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533.
42. Petchprapa CN, Rosenberg ZS, Sconfienza LM, et al. MR imaging of entrapment neuropathies of the lower extremity. Part I. Radiographs. 2010;30:983-1000.
43. Voight M, Robinson K, Gill L, et al. Postoperative guidelines for hip arthroscopy in the active population. Sports Health. 2010;2:222-230.
44. Stalzer S, Wahoff M, Scanlan M. Rehabilitation following hip arthroscopy. Clin Sports Med. 2006;25:337-357.
Carpal tunnel syndrome—try these diagnostic maneuvers
• Before considering surgery, offer patients with mild-to-moderate carpal tunnel syndrome (CTS) a trial of conservative therapy such as splinting or corticosteroids. A
• Order electrodiagnostic studies (EDS) as needed, to rule out other conditions with a similar presentation, confirm an uncertain diagnosis, and gauge the severity of CTS C, or when surgery is being considered. B
• Recommend carpal tunnel release for patients who have severe CTS or have failed to respond to nonsurgical t0reatment. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Jane K, 52, comes to see you because of discomfort in her right wrist and tingling in her hand. The symptoms began 3 months ago, but have been getting progressively worse, and have started to interfere with her sleep. Ms. K often awakens with “pins and needles” in her hand, and says that she often has the urge to “shake it out.” Her sister has carpal tunnel syndrome (CTS), and Ms. K suspects that she does, too. On exam, you find that Ms. K has a positive Phalen’s and Durkan’s compression test, but normal Tinel’s test. She has normal strength and sensation in her hands. Her neck and upper extremity exam is otherwise unremarkable. You note that her hypothyroidism is well controlled, with a recent thyroid-stimulating hormone level of 1.2 mIU/L.
The patient has tried acetaminophen and ibuprofen, with little relief. She has researched CTS on the Internet and read about cold laser therapy, and wants to know whether you think it will work. What should you tell her?
Carpal tunnel syndrome is one of the most common disorders of the upper extremities and the most prevalent compression neuropathy.1 About 3% of US adults are affected, typically those between the ages of 40 and 60 years.2 Women are almost 3 times more likely than men to develop CTS.1
Other risk factors include diabetes, hypothyroidism, rheumatoid arthritis, pregnancy, obesity, family history, and trauma. A history of hand-related repetitive motions also increases the risk.3-5 Evidence does not support a definite link between keyboard or mouse use and CTS; however, occupations that require use of hand-operated vibratory tools or repeated and forceful movements of the hand/wrist (such as assembly work and food processing or packaging) are associated with CTS.6
The optimal diagnostic approach incorporates history and physical exam findings, including the results of a number of provocative maneuvers, as well as electrodiagnostic studies (EDS) in some cases.7 While surgery is the definitive treatment for CTS, numerous nonsurgical options exist, including splinting, corticosteroids, and a variety of alternative therapies, some of which (eg, chiropractic and cold laser therapy) have little evidence to support them.
Because family physicians are often the first to see patients with symptoms associated with CTS, you need to know what to look for, when to test, and whether to provide treatment or a referral. Here’s what to keep in mind.
Clinical presentation of CTS
Increased pressure in the carpal tunnel compresses the median nerve, leading to numbness, tingling, or pain in the palmar aspect of the first 3 fingers and the radial half of the fourth (FIGURE). Symptoms vary widely, with pain or numbness localized to the hand or wrist in some cases and pain radiating into the forearm or shoulder in others.
Figure
Compressed median nerve leads to numbness and tingling
Early in the course of CTS, symptoms are often most bothersome at night. In a scenario like that reported by Ms. K, patients are often awakened by numbness or tingling and the desire to shake out the affected hand—a phenomenon known as the flick sign.8 Pain and numbness may occur intermittently at first, especially with repetitive wrist motion. Activities such as driving or holding a telephone often aggravate symptoms.
As CTS progresses, the intensity and duration of symptoms increase. Patients may complain of weakness in the hand and report that they often drop things. Paradoxically, patients with more severe CTS sometimes have less pain, rather than more, because of increasing sensory loss.9
Late in the course of CTS, physical exam findings typically include decreased sensation in the fingers innervated by the median nerve, sparing the thenar eminence. (A loss of sensation in the thenar eminence suggests the presence of a lesion proximal to the carpal tunnel, rather than CTS itself.10) In advanced cases, weakness of thumb abduction and opposition may occur, as well as atrophy of the thenar eminence.11
Sudden onset of severe symptoms with minimal trauma to the wrist should raise suspicion of a hematoma in the carpal tunnel—a particular risk for patients who have a clotting disorder or are being treated with newer anticoagulants such as dabigatran. Prompt surgical decompression is required to prevent permanent median nerve damage in such cases.12
Include these maneuvers in the physical exam
A thorough evaluation of the neck, shoulder, elbow, and wrist is crucial for all patients with signs and symptoms associated with CTS. Provocative maneuvers (TABLE 1)7,13 are also important as an aid to diagnosis. The results of the following tests should be viewed with caution, however, as studies have found wide variations in their sensitivity and specificity:
TABLE 1
Diagnosing carpal tunnel syndrome, using physical maneuvers7,13
| Test | Technique | Positive test | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| Phalen’s | Patient holds wrist flexed 90° with elbow in full extension | Pain or paresthesia ≤60 sec | 68 | 73 |
| Tinel’s | Clinician repetitively taps wrist over transverse carpal ligament | Pain or paresthesia | 50 | 77 |
| Median nerve compression* (MNC) | Clinician applies direct pressure over the transverse carpal ligament | Pain or paresthesia ≤30 sec | 64 | 83 |
| MNC + Phalen’s | Same as above | Same as above | 80 | 92 |
| *also known as Durkan’s test. | ||||
Phalen’s maneuver. The patient flexes his or her wrist with the elbow in full extension to increase pressure on the median nerve, and holds the position for 60 seconds. The onset of pain or paresthesia is a positive test. A meta-analysis found the sensitivity and specificity of a positive Phalen’s sign to be 68% and 73%, respectively.7
Tinel’s test. Tap the volar surface of the patient’s wrist just proximal to, or on top of, the carpal tunnel. Pain or paresthesia in the fingers innervated by the median nerve as a result of the percussion constitutes a positive result. Tinel’s test is less sensitive than the Phalen’s maneuver, but has a similar specificity.13
The median nerve (Durkan’s) compression test. Apply pressure over the transverse carpal ligament; the test is positive if pain or paresthesia develops within 30 seconds.7
The hand elevation test. The patient raises both hands overhead for 60 seconds; here, too, pain or paresthesia is a positive result.14
Combining results of provocative maneuvers may increase sensitivity and specificity. Positive results in both the Phalen’s and median nerve compression tests, for example, have a collective sensitivity and specificity of 80% and 92%, respectively.13
When (or whether) to order electrodiagnostic studies
While some clinicians consider EDS to be the gold standard in CTS diagnosis,6 evidence is limited. One issue is the lack of universally accepted reference standards; another is that most studies have been affected by “spectrum bias.”15 What’s more, EDS—which include nerve conduction studies (NCS) and electromyography (EMG)—do not always correlate directly with symptoms, and 16% to 34% of mild cases can be missed.16
EDS are useful in many instances, however. EMG can rule out other causes of CTS symptoms (TABLE 2 details the differential diagnosis),7,11 while NCS can aid in diagnosing CTS, gauging its severity, and arriving at a prognosis. Specifically, NCS can detect delayed distal latencies and slowed conduction velocities that can occur when the myelin sheath is damaged by prolonged compression of the median nerve.17 With more severe compression, axonal damage occurs, as evidenced by reduced action potential amplitudes on NCS. Results of the nerve conduction tests are compared to age-dependent normal values and to results from other nerves on either the same or the contralateral hand. In a 2002 systemic review, the sensitivity of NCS for CTS was 56% to 85% and the specificity was 94% to 99%.18
TABLE 2
Differential diagnosis for CTS7,11
| Condition | Characteristics |
|---|---|
| Carpometacarpal arthritis of thumb | Thumb is painful when in motion; radiographic findings |
| Cervical radiculopathy | Neck pain, nerve root distribution (eg, C6), positive Spurling’s test |
| DeQuervain’s tenosynovitis | Painful resisted thumb dorsiflexion, tender at base of thumb |
| Hypothyroidism | Fatigue, cold intolerance, dry skin, hair loss, abnormal thyroid function tests |
| Peripheral neuropathy | History of DM, lower extremity involvement |
| Pronator syndrome (median nerve compression at the elbow) | Tenderness at proximal forearm |
| Ulnar compressive neuropathy | Compression and positive Tinel’s sign: ulnar nerve at elbow or wrist produces pain or paresthesias in 4th and 5th fingers |
| Vibration white finger | History of use of power drill or other hand-held vibratory tool; symptoms of Raynaud’s syndrome |
| Wrist arthritis | Painful wrist ROM, radiographic findings |
| CTS, carpal tunnel syndrome; DM, diabetes mellitus; ROM, range of motion. | |
Before and after surgery. The American Academy of Orthopedic Surgeons (AAOS) recommends EDS when CTS surgery is being considered. 7 EDS may also be used after surgery, to verify neurologic improvement.
Ultrasound. In patients with CTS, ultrasound reveals an increased cross-sectional area of the median nerve, a finding that has prompted studies of this modality as a diagnostic tool.19 Although evidence suggests that ultrasound’s sensitivity and specificity for CTS would be similar to that of EDS, the optimal cutoff for an abnormal test has not been defined,19 and ultrasound does not provide information on prognosis or alternate causes.
Thus, AAOS does not currently recommend ultrasound for CTS diagnosis.7 Magnetic resonance imaging is inappropriate for routine CTS diagnosis, as well.7
Treatment: Start conservatively
Multiple nonsurgical options are available, but the best evidence supports splinting, steroid injection, and oral steroids. Splinting or steroids alone may bring long-term relief for patients with mild to moderate cases;20 in fact, about a third of mild cases improve spontaneously.21
Conservative therapy can also provide relief for those who wish to avoid or delay surgery and for cases of transient CTS (pediatric patients, for example, or those whose condition is associated with pregnancy or hypothyroidism).18 A successful response to therapy can also help to confirm a CTS diagnosis.
Most conservative treatments begin providing relief within 2 to 6 weeks and reach the maximal benefit at 3 months.22 If there is no response after 6 weeks, it’s time to consider another approach.
In initiating splinting or corticosteroids, here’s a look at what to keep in mind:
Splinting. A splint can be used to maintain the wrist in a position with the least intracanal pressure, thereby limiting pressure on the median nerve. Splinting is equally effective whether used continually or only at night.23
Splinting can relieve symptoms and improve functional status within 2 weeks and the effects can last for 3 to 6 months, eliminating the need for surgery for some patients with mild CTS.19,20 Nerve gliding exercises, (see image at left), have been evaluated in combination with splinting. While evidence is limited, an at-home program involving these simple exercises may be a beneficial adjunctive treatment with minimal cost or harm.24,25
Local corticosteroid injection. A Cochrane meta-analysis found significant improvement in symptoms and function at one month among patients with CTS who were treated with steroid injection.26 In many cases, the effects last for many months.
A recent trial found that nearly half of patients with mild to moderate CTS who were treated with steroid injections had improved symptoms and EDS results at the 12-month follow-up.20 However, while patients with severe CTS experienced improvement at 4 weeks postinjection, most eventually required surgery.20
Evidence does not support one particular steroid dose or formulation over another, or one particular injection site.22 Injecting 4 cm proximal to the wrist flexion crease is as effective as a more distal injection.26,27
Caution is required, however, as risks associated with local injections include tendon rupture and median nerve injury. If a patient experiences intense pain or paresthesia in the median nerve distribution when the needle is inserted, redirect the needle away from the median nerve immediately. For patients who respond well to this treatment, one additional injection can be given after 6 months if symptoms recur.
Oral corticosteroids. Oral prednisone at a dose of 20 mg/d for 2 weeks improves symptoms and function in patients with CTS, but is less effective than steroid injections.28 Treatment for 2 weeks is as effective as treatment for 4 weeks; the effects tend to wane after 8 weeks in both cases.29 Nonsteroidal anti-inflammatory drugs, diuretics, and vitamin B6 have not been found to be effective.30
CASE Ms. K also asks about “those needle tests”—a reference to EDS—which her sister had to diagnose her CTS. You explain that these studies are not necessary at this time because her symptoms are mild and there is no need for other causes to be ruled out.
Instead, you offer her a neutral wrist splint for night-time use and recommend home-based nerve glide exercises. There is no evidence that cold laser therapy is effective, you explain to Ms. K, and it is expensive. She agrees to try the splint and the exercises, and you schedule a follow-up visit in 6 weeks.
A look at alternative therapies
There are many nontraditional treatments for CTS, with yoga, carpal bone mobilization, ergonomic keyboards, and ultrasound therapy among them. Some have limited evidence to suggest that they may have a therapeutic effect;30 others have little or no evidence to support them.
Yoga. Stretching and improved joint posture with specific yoga exercises may lead to decreased compression within the carpal tunnel and increased blood flow to the median nerve. One small study found that yoga was more effective than nocturnal wrist splinting for pain relief, and had similar improvement for nocturnal symptoms and grip strength.31
Carpal bone mobilization. One small study found this physical therapy technique, which involves movement of the bones in the wrist, to improve symptoms such as numbness and tingling after 3 weeks of therapy. Yet carpal bone mobilization did not relieve pain or help restore function.32
Ergonomic keyboard. Patients who use computers at work may find that an ergonomic keyboard helps to relieve pain associated with CTS, compared with a standard keyboard.33
Therapeutic ultrasound. A recent meta-analysis found that there is only poor-quality evidence for ultrasound as an effective treatment for CTS—a process in which a round-headed instrument applied to the skin delivers sound waves that are absorbed by underlying tissues in the carpal tunnel. And there is insufficient evidence for one type of ultrasound over another, or to suggest that ultrasound is more effective than other nonsurgical treatments.34 Notably, ultrasound takes several weeks to provide a therapeutic benefit.
What about acupuncture? A recent trial found that acupuncture was no more effective than sham acupuncture in relieving symptoms of CTS in patients wearing wrist splints.35 Magnet therapy, chiropractic, and cold laser therapy are not supported by evidence either.28
Is the patient a candidate for surgery?
Carpal tunnel release provides good long-term outcomes for 70% to 90% of patients and is a cost-effective treatment.36,37 Evidence supports a trial of conservative therapy, however, before considering surgery for patients with mild-to-moderate CTS.22 Future studies are needed to identify prognostic characteristics of patients most likely to respond to each type of intervention, and the optimal timing for surgical release.
Patients with severe CTS—with findings such as thenar atrophy, diminished hand function, and median nerve denervation—should be referred for surgery without delay. This recommendation is based on expert opinion, however, as most clinical trials comparing surgical vs nonsurgical treatment exclude those with severe CTS.38
3 surgical techniques, and a novel approach
Surgical techniques include open, endoscopic, and minimal incision carpal tunnel release, with benefits and drawbacks for each. Compared with open release, for example, patients who undergo endoscopic release have less postoperative pain at 12 weeks, quicker return to work, and fewer wound complications, but are more likely to require surgical revision. And minimal incision release is associated with improved symptoms and function compared with open release.38 However, there is no long-term evidence that any one of these 3 surgical approaches is more effective than another.39
Percutaneous carpal tunnel release is a novel approach that may be offered in outpatient settings, with local anesthesia and ultrasound guidance to avoid median nerve damage.40 Because studies of the safety and efficacy of percutaneous carpal tunnel release are limited, however, this approach is considered experimental.41 Percutaneous release is not a treatment recommended by the AAOS.38
What to tell patients about postop care
Regardless of the method used for carpal tunnel release, most complications are minor—eg, a painful or hypertrophic scar, stiffness, swelling, and pain or tenderness on either side of the incision—and resolve within a few months.42 Advise patients not to continue to wear a wrist splint after surgery; doing so can cause stiffness or adhesions and may compromise surgical outcomes.41 Postoperatively, patients should be instructed to do nerve gliding exercises and to massage their scars, both of which they can safely do at home.43
Patients can expect significant symptomatic improvement within 1 week of surgery, and most will be able to return to normal activities in 2 weeks.44 Those with severe CTS should be warned, however, that it could take up to a year to determine the extent of recovery.22 Evidence suggests that from 3% to 19% of patients may have persistent or recurrent symptoms even after carpal tunnel release, with up to 12% requiring surgical revision.45
CASE When Ms. K returns, she reports that while there has been some improvement, some activities—such as driving long distances and talking on the phone—still cause numbness and tingling. And, if she doesn’t wear the splint at night, she awakens with tingling in her hands. You discuss 2 options—continued conservative treatment with a local steroid injection, or EDS and surgical referral. The patient opts for the injection and continued use of the nocturnal wrist splint and exercises. When she returns in another 6 weeks, Ms. K reports significant improvement. You agree to stop the wrist splint and exercises and advise her to follow-up on an as-needed basis if the symptoms return.
CORRESPONDENCE Jennifer Wipperman, MD, MPH, Via Christi Family Medicine, 1121 S. Clifton, Wichita, KS 67218; [email protected]
1. Atroshi I, Gummesson C, Johnsson, et al. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153-158.
2. Luckhaupt SE, Dahlhamer JM, Ward BW, et al. Prevalence and work-relatedness of carpal tunnel syndrome in the working population, United States, 2010 national health interview survey. Am J Ind Med. 2012 April 12. [Epub ahead of print.]
3. van Dijk MA, Reitsma JB, Fischer JC, et al. Indications for requesting laboratory tests for concurrent diseases in patients with carpal tunnel syndrome: a systematic review. Clin Chem. 2003;49:1437-1444.
4. Padua L, Di Pasquale A, Pazzaglia C, et al. Systematic review of pregnancy-related carpal tunnel syndrome. Muscle Nerve. 2010;42:697-702.
5. Bland JD. The relationship of obesity, age, and carpal tunnel syndrome: more complex than was thought? Muscle Nerve. 2005;32:527-532.
6. Prime MS, Palmer J, Khan WS, et al. Is there light at the end of the tunnel? Controversies in the diagnosis and management of carpal tunnel syndrome. Hand. 2010;5:354-360.
7. Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2009;91:2478-2479.
8. Hansen PA, Micklesen P, Robinson LR. Clinical utility of the flick maneuver in diagnosing carpal tunnel syndrome. Am J Phys Med Rehabil. 2004;83:363-367.
9. Padua L, Padua R, Aprile I, et al. Carpal tunnel syndrome: relationship between clinical and patient-oriented assessment. Clin Orthop Relat Res. 2002;395:128-134.
10. Bland JD. Carpal tunnel syndrome. BMJ. 2007;335:343-346.
11. Wright PE. Carpal tunnel syndrome. In: Canale ST, Beaty JH, eds. Campbell’s Operative Orthopaedics. 11th ed. Philadelphia, Pa: Mosby, Inc; 2008:4285–4291.
12. Sibley PA, Mandel RJ. Atraumatic acute carpal tunnel syndrome in a patient taking dabigatran. Orthopedics. 2012;35:e1286-e1289.
13. MacDermid JC, Wessel J. Clinical diagnosis of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17:309-319.
14. Ahn DS. Hand elevation: a new test for carpal tunnel syndrome. Ann Plastic Surg. 2001;46:120-124.
15. Boyer K, Wies J, Turkelson CM. Effects of bias on the results of diagnostic studies of carpal tunnel syndrome. J Hand Surg. 2009;34:1006-1013.
16. Witt JC, Hentz JG, Stevens JC. Carpal tunnel syndrome with normal nerve conduction studies. Muscle Nerve. 2004;29:515-522.
17. Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg. 2008;90:2587-2593.
18. Jablecki CK, Andary MT, Floeter MK, et al. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2002;58:1589-1592.
19. Descatha A, Huard L, Aubert F, et al. Meta-analysis on the performance of sonography for the diagnosis of carpal tunnel syndrome. Semin Arthritis Rheum. 2012;41:914-922.
20. Visser LH, Ngo Q, Groeneweg SJ, et al. Long term effect of local corticosteroid injection for carpal tunnel syndrome: a relation with electrodiagnostic severity. Clin Neurophysiol. 2012;123:838-841.
21. Padua L, Padua R, Aprile I, et al. Multiperspective follow-up of untreated carpal tunnel syndrome: a multicenter study. Neurology. 2001;56:1459-1466.
22. Shi Q, MacDermid JC. Is surgical intervention more effective than non-surgical treatment for carpal tunnel syndrome? A systematic review. J Orthop Surg Res. 2011;6:17.-
23. Walker WC, Metzler M, Cifu DX, et al. Neutral wrist splinting in carpal tunnel syndrome: a comparison of night-only versus full-time wear instructions. Arch Phys Med Rehabil. 2000;81:424-429.
24. Brininger TL, Rogers JC, Holm MB, et al. Efficacy of a fabricated customized splint and tendon and nerve gliding exercises for the treatment of carpal tunnel syndrome: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88:1429-1435.
25. Schmid AB, Elliott JM, Strudwick MW, et al. Effect of splinting and exercise on intraneural edema of the median nerve in carpal tunnel syndrome-an MRI study to reveal therapeutic mechanisms. J Orthop Res. 2012;30:1343-1350.
26. Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(2):CD001554.-
27. Kamanli A, Bezgincan M, Kaya A. Comparison of local steroid injection into carpal tunnel via proximal and distal approach in patients with carpal tunnel syndrome. Bratislavske Lek Listy. 2011;112:337-341.
28. Huisstede BM, Hoogvliet P, Randsdorp MS, et al. Carpal tunnel syndrome. Part I: effectiveness of nonsurgical treatments—a systematic review. Arch Phys Med Rehabil. 2010;91:981-1004.
29. Chang MH, Ger LP, Hsieh PF, et al. A randomised clinical trial of oral steroids in the treatment of carpal tunnel syndrome: a long term follow up. J Neurol Neurosurg Psychiatry. 2002;73:710-714.
30. O’Connor D, Marshall S, Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003;(1):CD003219.-
31. Garfinkel MS, Singhal A, Katz WA, et al. Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280:1601-1603.
32. Tal-Akabi A, Rushton A. An investigation to compare the effectiveness of carpal bone mobilisation and neurodynamic mobilisation as methods of treatment for carpal tunnel syndrome. Man Ther. 2000;5:214-222.
33. O’Connor D, Page MJ, Marshall SC, et al. Ergonomic positioning or equipment for treating carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;(1):CD009600.-
34. Page MJ, O’Connor D, Pitt V, et al. Therapeutic ultrasound for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;(1):CD009601.-
35. Yao E, Gerritz PK, Henricson E, et al. Randomized controlled trial comparing acupuncture with placebo acupuncture for the treatment of carpal tunnel syndrome. PMR. 2012;4:367-373.
36. Pomerance J, Zurakowski D, Fine I. The cost-effectiveness of nonsurgical versus surgical treatment for carpal tunnel syndrome. J Hand Surg. 2009;34:1193-1200.
37. Turner A, Kimble F, Gulyas K, et al. Can the outcome of open carpal tunnel release be predicted? A review of the literature. ANZ J Surg. 2010;80:50-54.
38. Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of carpal tunnel syndrome. J Bone Joint Surg. 2010;92:218-219.
39. Scholten RJ, Mink van der Molen A, Uitdehaag BM, et al. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(4):CD003905.-
40. Nakamichi K, Tachibana S, Yamamoto S, et al. Percutaneous carpal tunnel release compared with mini-open release using ultrasonographic guidance for both techniques. J Hand Surg Am. 2010;35:437-445.
41. Huisstede BM, Randsdorp MS, Coert JH, et al. Carpal tunnel syndrome. Part II: effectiveness of surgical treatments—a systematic review. Arch Phys Med Rehabil. 2010;91:1005-1024.
42. Ludlow KS, Merla JL, Cox JA, et al. Pillar pain as a postoperative complication of carpal tunnel release: a review of the literature. J Hand Ther. 1997;10:277-282.
43. Pomerance J, Fine I. Outcomes of carpal tunnel surgery with and without supervised postoperative therapy. J Hand Surg. 2007;32:1159-1163.
44. Acharya AD, Auchincloss JM. Return to functional hand use and work following open carpal tunnel surgery. J Hand Surg Br. 2005;30:607-610.
45. Dahlin LB, Salo M, Thomsen N, et al. Carpal tunnel syndrome and treatment of recurrent symptoms. Scand J Plast Reconstr Surg Hand Surg. 2010;44:4-11.
• Before considering surgery, offer patients with mild-to-moderate carpal tunnel syndrome (CTS) a trial of conservative therapy such as splinting or corticosteroids. A
• Order electrodiagnostic studies (EDS) as needed, to rule out other conditions with a similar presentation, confirm an uncertain diagnosis, and gauge the severity of CTS C, or when surgery is being considered. B
• Recommend carpal tunnel release for patients who have severe CTS or have failed to respond to nonsurgical t0reatment. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Jane K, 52, comes to see you because of discomfort in her right wrist and tingling in her hand. The symptoms began 3 months ago, but have been getting progressively worse, and have started to interfere with her sleep. Ms. K often awakens with “pins and needles” in her hand, and says that she often has the urge to “shake it out.” Her sister has carpal tunnel syndrome (CTS), and Ms. K suspects that she does, too. On exam, you find that Ms. K has a positive Phalen’s and Durkan’s compression test, but normal Tinel’s test. She has normal strength and sensation in her hands. Her neck and upper extremity exam is otherwise unremarkable. You note that her hypothyroidism is well controlled, with a recent thyroid-stimulating hormone level of 1.2 mIU/L.
The patient has tried acetaminophen and ibuprofen, with little relief. She has researched CTS on the Internet and read about cold laser therapy, and wants to know whether you think it will work. What should you tell her?
Carpal tunnel syndrome is one of the most common disorders of the upper extremities and the most prevalent compression neuropathy.1 About 3% of US adults are affected, typically those between the ages of 40 and 60 years.2 Women are almost 3 times more likely than men to develop CTS.1
Other risk factors include diabetes, hypothyroidism, rheumatoid arthritis, pregnancy, obesity, family history, and trauma. A history of hand-related repetitive motions also increases the risk.3-5 Evidence does not support a definite link between keyboard or mouse use and CTS; however, occupations that require use of hand-operated vibratory tools or repeated and forceful movements of the hand/wrist (such as assembly work and food processing or packaging) are associated with CTS.6
The optimal diagnostic approach incorporates history and physical exam findings, including the results of a number of provocative maneuvers, as well as electrodiagnostic studies (EDS) in some cases.7 While surgery is the definitive treatment for CTS, numerous nonsurgical options exist, including splinting, corticosteroids, and a variety of alternative therapies, some of which (eg, chiropractic and cold laser therapy) have little evidence to support them.
Because family physicians are often the first to see patients with symptoms associated with CTS, you need to know what to look for, when to test, and whether to provide treatment or a referral. Here’s what to keep in mind.
Clinical presentation of CTS
Increased pressure in the carpal tunnel compresses the median nerve, leading to numbness, tingling, or pain in the palmar aspect of the first 3 fingers and the radial half of the fourth (FIGURE). Symptoms vary widely, with pain or numbness localized to the hand or wrist in some cases and pain radiating into the forearm or shoulder in others.
Figure
Compressed median nerve leads to numbness and tingling
Early in the course of CTS, symptoms are often most bothersome at night. In a scenario like that reported by Ms. K, patients are often awakened by numbness or tingling and the desire to shake out the affected hand—a phenomenon known as the flick sign.8 Pain and numbness may occur intermittently at first, especially with repetitive wrist motion. Activities such as driving or holding a telephone often aggravate symptoms.
As CTS progresses, the intensity and duration of symptoms increase. Patients may complain of weakness in the hand and report that they often drop things. Paradoxically, patients with more severe CTS sometimes have less pain, rather than more, because of increasing sensory loss.9
Late in the course of CTS, physical exam findings typically include decreased sensation in the fingers innervated by the median nerve, sparing the thenar eminence. (A loss of sensation in the thenar eminence suggests the presence of a lesion proximal to the carpal tunnel, rather than CTS itself.10) In advanced cases, weakness of thumb abduction and opposition may occur, as well as atrophy of the thenar eminence.11
Sudden onset of severe symptoms with minimal trauma to the wrist should raise suspicion of a hematoma in the carpal tunnel—a particular risk for patients who have a clotting disorder or are being treated with newer anticoagulants such as dabigatran. Prompt surgical decompression is required to prevent permanent median nerve damage in such cases.12
Include these maneuvers in the physical exam
A thorough evaluation of the neck, shoulder, elbow, and wrist is crucial for all patients with signs and symptoms associated with CTS. Provocative maneuvers (TABLE 1)7,13 are also important as an aid to diagnosis. The results of the following tests should be viewed with caution, however, as studies have found wide variations in their sensitivity and specificity:
TABLE 1
Diagnosing carpal tunnel syndrome, using physical maneuvers7,13
| Test | Technique | Positive test | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| Phalen’s | Patient holds wrist flexed 90° with elbow in full extension | Pain or paresthesia ≤60 sec | 68 | 73 |
| Tinel’s | Clinician repetitively taps wrist over transverse carpal ligament | Pain or paresthesia | 50 | 77 |
| Median nerve compression* (MNC) | Clinician applies direct pressure over the transverse carpal ligament | Pain or paresthesia ≤30 sec | 64 | 83 |
| MNC + Phalen’s | Same as above | Same as above | 80 | 92 |
| *also known as Durkan’s test. | ||||
Phalen’s maneuver. The patient flexes his or her wrist with the elbow in full extension to increase pressure on the median nerve, and holds the position for 60 seconds. The onset of pain or paresthesia is a positive test. A meta-analysis found the sensitivity and specificity of a positive Phalen’s sign to be 68% and 73%, respectively.7
Tinel’s test. Tap the volar surface of the patient’s wrist just proximal to, or on top of, the carpal tunnel. Pain or paresthesia in the fingers innervated by the median nerve as a result of the percussion constitutes a positive result. Tinel’s test is less sensitive than the Phalen’s maneuver, but has a similar specificity.13
The median nerve (Durkan’s) compression test. Apply pressure over the transverse carpal ligament; the test is positive if pain or paresthesia develops within 30 seconds.7
The hand elevation test. The patient raises both hands overhead for 60 seconds; here, too, pain or paresthesia is a positive result.14
Combining results of provocative maneuvers may increase sensitivity and specificity. Positive results in both the Phalen’s and median nerve compression tests, for example, have a collective sensitivity and specificity of 80% and 92%, respectively.13
When (or whether) to order electrodiagnostic studies
While some clinicians consider EDS to be the gold standard in CTS diagnosis,6 evidence is limited. One issue is the lack of universally accepted reference standards; another is that most studies have been affected by “spectrum bias.”15 What’s more, EDS—which include nerve conduction studies (NCS) and electromyography (EMG)—do not always correlate directly with symptoms, and 16% to 34% of mild cases can be missed.16
EDS are useful in many instances, however. EMG can rule out other causes of CTS symptoms (TABLE 2 details the differential diagnosis),7,11 while NCS can aid in diagnosing CTS, gauging its severity, and arriving at a prognosis. Specifically, NCS can detect delayed distal latencies and slowed conduction velocities that can occur when the myelin sheath is damaged by prolonged compression of the median nerve.17 With more severe compression, axonal damage occurs, as evidenced by reduced action potential amplitudes on NCS. Results of the nerve conduction tests are compared to age-dependent normal values and to results from other nerves on either the same or the contralateral hand. In a 2002 systemic review, the sensitivity of NCS for CTS was 56% to 85% and the specificity was 94% to 99%.18
TABLE 2
Differential diagnosis for CTS7,11
| Condition | Characteristics |
|---|---|
| Carpometacarpal arthritis of thumb | Thumb is painful when in motion; radiographic findings |
| Cervical radiculopathy | Neck pain, nerve root distribution (eg, C6), positive Spurling’s test |
| DeQuervain’s tenosynovitis | Painful resisted thumb dorsiflexion, tender at base of thumb |
| Hypothyroidism | Fatigue, cold intolerance, dry skin, hair loss, abnormal thyroid function tests |
| Peripheral neuropathy | History of DM, lower extremity involvement |
| Pronator syndrome (median nerve compression at the elbow) | Tenderness at proximal forearm |
| Ulnar compressive neuropathy | Compression and positive Tinel’s sign: ulnar nerve at elbow or wrist produces pain or paresthesias in 4th and 5th fingers |
| Vibration white finger | History of use of power drill or other hand-held vibratory tool; symptoms of Raynaud’s syndrome |
| Wrist arthritis | Painful wrist ROM, radiographic findings |
| CTS, carpal tunnel syndrome; DM, diabetes mellitus; ROM, range of motion. | |
Before and after surgery. The American Academy of Orthopedic Surgeons (AAOS) recommends EDS when CTS surgery is being considered. 7 EDS may also be used after surgery, to verify neurologic improvement.
Ultrasound. In patients with CTS, ultrasound reveals an increased cross-sectional area of the median nerve, a finding that has prompted studies of this modality as a diagnostic tool.19 Although evidence suggests that ultrasound’s sensitivity and specificity for CTS would be similar to that of EDS, the optimal cutoff for an abnormal test has not been defined,19 and ultrasound does not provide information on prognosis or alternate causes.
Thus, AAOS does not currently recommend ultrasound for CTS diagnosis.7 Magnetic resonance imaging is inappropriate for routine CTS diagnosis, as well.7
Treatment: Start conservatively
Multiple nonsurgical options are available, but the best evidence supports splinting, steroid injection, and oral steroids. Splinting or steroids alone may bring long-term relief for patients with mild to moderate cases;20 in fact, about a third of mild cases improve spontaneously.21
Conservative therapy can also provide relief for those who wish to avoid or delay surgery and for cases of transient CTS (pediatric patients, for example, or those whose condition is associated with pregnancy or hypothyroidism).18 A successful response to therapy can also help to confirm a CTS diagnosis.
Most conservative treatments begin providing relief within 2 to 6 weeks and reach the maximal benefit at 3 months.22 If there is no response after 6 weeks, it’s time to consider another approach.
In initiating splinting or corticosteroids, here’s a look at what to keep in mind:
Splinting. A splint can be used to maintain the wrist in a position with the least intracanal pressure, thereby limiting pressure on the median nerve. Splinting is equally effective whether used continually or only at night.23
Splinting can relieve symptoms and improve functional status within 2 weeks and the effects can last for 3 to 6 months, eliminating the need for surgery for some patients with mild CTS.19,20 Nerve gliding exercises, (see image at left), have been evaluated in combination with splinting. While evidence is limited, an at-home program involving these simple exercises may be a beneficial adjunctive treatment with minimal cost or harm.24,25
Local corticosteroid injection. A Cochrane meta-analysis found significant improvement in symptoms and function at one month among patients with CTS who were treated with steroid injection.26 In many cases, the effects last for many months.
A recent trial found that nearly half of patients with mild to moderate CTS who were treated with steroid injections had improved symptoms and EDS results at the 12-month follow-up.20 However, while patients with severe CTS experienced improvement at 4 weeks postinjection, most eventually required surgery.20
Evidence does not support one particular steroid dose or formulation over another, or one particular injection site.22 Injecting 4 cm proximal to the wrist flexion crease is as effective as a more distal injection.26,27
Caution is required, however, as risks associated with local injections include tendon rupture and median nerve injury. If a patient experiences intense pain or paresthesia in the median nerve distribution when the needle is inserted, redirect the needle away from the median nerve immediately. For patients who respond well to this treatment, one additional injection can be given after 6 months if symptoms recur.
Oral corticosteroids. Oral prednisone at a dose of 20 mg/d for 2 weeks improves symptoms and function in patients with CTS, but is less effective than steroid injections.28 Treatment for 2 weeks is as effective as treatment for 4 weeks; the effects tend to wane after 8 weeks in both cases.29 Nonsteroidal anti-inflammatory drugs, diuretics, and vitamin B6 have not been found to be effective.30
CASE Ms. K also asks about “those needle tests”—a reference to EDS—which her sister had to diagnose her CTS. You explain that these studies are not necessary at this time because her symptoms are mild and there is no need for other causes to be ruled out.
Instead, you offer her a neutral wrist splint for night-time use and recommend home-based nerve glide exercises. There is no evidence that cold laser therapy is effective, you explain to Ms. K, and it is expensive. She agrees to try the splint and the exercises, and you schedule a follow-up visit in 6 weeks.
A look at alternative therapies
There are many nontraditional treatments for CTS, with yoga, carpal bone mobilization, ergonomic keyboards, and ultrasound therapy among them. Some have limited evidence to suggest that they may have a therapeutic effect;30 others have little or no evidence to support them.
Yoga. Stretching and improved joint posture with specific yoga exercises may lead to decreased compression within the carpal tunnel and increased blood flow to the median nerve. One small study found that yoga was more effective than nocturnal wrist splinting for pain relief, and had similar improvement for nocturnal symptoms and grip strength.31
Carpal bone mobilization. One small study found this physical therapy technique, which involves movement of the bones in the wrist, to improve symptoms such as numbness and tingling after 3 weeks of therapy. Yet carpal bone mobilization did not relieve pain or help restore function.32
Ergonomic keyboard. Patients who use computers at work may find that an ergonomic keyboard helps to relieve pain associated with CTS, compared with a standard keyboard.33
Therapeutic ultrasound. A recent meta-analysis found that there is only poor-quality evidence for ultrasound as an effective treatment for CTS—a process in which a round-headed instrument applied to the skin delivers sound waves that are absorbed by underlying tissues in the carpal tunnel. And there is insufficient evidence for one type of ultrasound over another, or to suggest that ultrasound is more effective than other nonsurgical treatments.34 Notably, ultrasound takes several weeks to provide a therapeutic benefit.
What about acupuncture? A recent trial found that acupuncture was no more effective than sham acupuncture in relieving symptoms of CTS in patients wearing wrist splints.35 Magnet therapy, chiropractic, and cold laser therapy are not supported by evidence either.28
Is the patient a candidate for surgery?
Carpal tunnel release provides good long-term outcomes for 70% to 90% of patients and is a cost-effective treatment.36,37 Evidence supports a trial of conservative therapy, however, before considering surgery for patients with mild-to-moderate CTS.22 Future studies are needed to identify prognostic characteristics of patients most likely to respond to each type of intervention, and the optimal timing for surgical release.
Patients with severe CTS—with findings such as thenar atrophy, diminished hand function, and median nerve denervation—should be referred for surgery without delay. This recommendation is based on expert opinion, however, as most clinical trials comparing surgical vs nonsurgical treatment exclude those with severe CTS.38
3 surgical techniques, and a novel approach
Surgical techniques include open, endoscopic, and minimal incision carpal tunnel release, with benefits and drawbacks for each. Compared with open release, for example, patients who undergo endoscopic release have less postoperative pain at 12 weeks, quicker return to work, and fewer wound complications, but are more likely to require surgical revision. And minimal incision release is associated with improved symptoms and function compared with open release.38 However, there is no long-term evidence that any one of these 3 surgical approaches is more effective than another.39
Percutaneous carpal tunnel release is a novel approach that may be offered in outpatient settings, with local anesthesia and ultrasound guidance to avoid median nerve damage.40 Because studies of the safety and efficacy of percutaneous carpal tunnel release are limited, however, this approach is considered experimental.41 Percutaneous release is not a treatment recommended by the AAOS.38
What to tell patients about postop care
Regardless of the method used for carpal tunnel release, most complications are minor—eg, a painful or hypertrophic scar, stiffness, swelling, and pain or tenderness on either side of the incision—and resolve within a few months.42 Advise patients not to continue to wear a wrist splint after surgery; doing so can cause stiffness or adhesions and may compromise surgical outcomes.41 Postoperatively, patients should be instructed to do nerve gliding exercises and to massage their scars, both of which they can safely do at home.43
Patients can expect significant symptomatic improvement within 1 week of surgery, and most will be able to return to normal activities in 2 weeks.44 Those with severe CTS should be warned, however, that it could take up to a year to determine the extent of recovery.22 Evidence suggests that from 3% to 19% of patients may have persistent or recurrent symptoms even after carpal tunnel release, with up to 12% requiring surgical revision.45
CASE When Ms. K returns, she reports that while there has been some improvement, some activities—such as driving long distances and talking on the phone—still cause numbness and tingling. And, if she doesn’t wear the splint at night, she awakens with tingling in her hands. You discuss 2 options—continued conservative treatment with a local steroid injection, or EDS and surgical referral. The patient opts for the injection and continued use of the nocturnal wrist splint and exercises. When she returns in another 6 weeks, Ms. K reports significant improvement. You agree to stop the wrist splint and exercises and advise her to follow-up on an as-needed basis if the symptoms return.
CORRESPONDENCE Jennifer Wipperman, MD, MPH, Via Christi Family Medicine, 1121 S. Clifton, Wichita, KS 67218; [email protected]
• Before considering surgery, offer patients with mild-to-moderate carpal tunnel syndrome (CTS) a trial of conservative therapy such as splinting or corticosteroids. A
• Order electrodiagnostic studies (EDS) as needed, to rule out other conditions with a similar presentation, confirm an uncertain diagnosis, and gauge the severity of CTS C, or when surgery is being considered. B
• Recommend carpal tunnel release for patients who have severe CTS or have failed to respond to nonsurgical t0reatment. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Jane K, 52, comes to see you because of discomfort in her right wrist and tingling in her hand. The symptoms began 3 months ago, but have been getting progressively worse, and have started to interfere with her sleep. Ms. K often awakens with “pins and needles” in her hand, and says that she often has the urge to “shake it out.” Her sister has carpal tunnel syndrome (CTS), and Ms. K suspects that she does, too. On exam, you find that Ms. K has a positive Phalen’s and Durkan’s compression test, but normal Tinel’s test. She has normal strength and sensation in her hands. Her neck and upper extremity exam is otherwise unremarkable. You note that her hypothyroidism is well controlled, with a recent thyroid-stimulating hormone level of 1.2 mIU/L.
The patient has tried acetaminophen and ibuprofen, with little relief. She has researched CTS on the Internet and read about cold laser therapy, and wants to know whether you think it will work. What should you tell her?
Carpal tunnel syndrome is one of the most common disorders of the upper extremities and the most prevalent compression neuropathy.1 About 3% of US adults are affected, typically those between the ages of 40 and 60 years.2 Women are almost 3 times more likely than men to develop CTS.1
Other risk factors include diabetes, hypothyroidism, rheumatoid arthritis, pregnancy, obesity, family history, and trauma. A history of hand-related repetitive motions also increases the risk.3-5 Evidence does not support a definite link between keyboard or mouse use and CTS; however, occupations that require use of hand-operated vibratory tools or repeated and forceful movements of the hand/wrist (such as assembly work and food processing or packaging) are associated with CTS.6
The optimal diagnostic approach incorporates history and physical exam findings, including the results of a number of provocative maneuvers, as well as electrodiagnostic studies (EDS) in some cases.7 While surgery is the definitive treatment for CTS, numerous nonsurgical options exist, including splinting, corticosteroids, and a variety of alternative therapies, some of which (eg, chiropractic and cold laser therapy) have little evidence to support them.
Because family physicians are often the first to see patients with symptoms associated with CTS, you need to know what to look for, when to test, and whether to provide treatment or a referral. Here’s what to keep in mind.
Clinical presentation of CTS
Increased pressure in the carpal tunnel compresses the median nerve, leading to numbness, tingling, or pain in the palmar aspect of the first 3 fingers and the radial half of the fourth (FIGURE). Symptoms vary widely, with pain or numbness localized to the hand or wrist in some cases and pain radiating into the forearm or shoulder in others.
Figure
Compressed median nerve leads to numbness and tingling
Early in the course of CTS, symptoms are often most bothersome at night. In a scenario like that reported by Ms. K, patients are often awakened by numbness or tingling and the desire to shake out the affected hand—a phenomenon known as the flick sign.8 Pain and numbness may occur intermittently at first, especially with repetitive wrist motion. Activities such as driving or holding a telephone often aggravate symptoms.
As CTS progresses, the intensity and duration of symptoms increase. Patients may complain of weakness in the hand and report that they often drop things. Paradoxically, patients with more severe CTS sometimes have less pain, rather than more, because of increasing sensory loss.9
Late in the course of CTS, physical exam findings typically include decreased sensation in the fingers innervated by the median nerve, sparing the thenar eminence. (A loss of sensation in the thenar eminence suggests the presence of a lesion proximal to the carpal tunnel, rather than CTS itself.10) In advanced cases, weakness of thumb abduction and opposition may occur, as well as atrophy of the thenar eminence.11
Sudden onset of severe symptoms with minimal trauma to the wrist should raise suspicion of a hematoma in the carpal tunnel—a particular risk for patients who have a clotting disorder or are being treated with newer anticoagulants such as dabigatran. Prompt surgical decompression is required to prevent permanent median nerve damage in such cases.12
Include these maneuvers in the physical exam
A thorough evaluation of the neck, shoulder, elbow, and wrist is crucial for all patients with signs and symptoms associated with CTS. Provocative maneuvers (TABLE 1)7,13 are also important as an aid to diagnosis. The results of the following tests should be viewed with caution, however, as studies have found wide variations in their sensitivity and specificity:
TABLE 1
Diagnosing carpal tunnel syndrome, using physical maneuvers7,13
| Test | Technique | Positive test | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|
| Phalen’s | Patient holds wrist flexed 90° with elbow in full extension | Pain or paresthesia ≤60 sec | 68 | 73 |
| Tinel’s | Clinician repetitively taps wrist over transverse carpal ligament | Pain or paresthesia | 50 | 77 |
| Median nerve compression* (MNC) | Clinician applies direct pressure over the transverse carpal ligament | Pain or paresthesia ≤30 sec | 64 | 83 |
| MNC + Phalen’s | Same as above | Same as above | 80 | 92 |
| *also known as Durkan’s test. | ||||
Phalen’s maneuver. The patient flexes his or her wrist with the elbow in full extension to increase pressure on the median nerve, and holds the position for 60 seconds. The onset of pain or paresthesia is a positive test. A meta-analysis found the sensitivity and specificity of a positive Phalen’s sign to be 68% and 73%, respectively.7
Tinel’s test. Tap the volar surface of the patient’s wrist just proximal to, or on top of, the carpal tunnel. Pain or paresthesia in the fingers innervated by the median nerve as a result of the percussion constitutes a positive result. Tinel’s test is less sensitive than the Phalen’s maneuver, but has a similar specificity.13
The median nerve (Durkan’s) compression test. Apply pressure over the transverse carpal ligament; the test is positive if pain or paresthesia develops within 30 seconds.7
The hand elevation test. The patient raises both hands overhead for 60 seconds; here, too, pain or paresthesia is a positive result.14
Combining results of provocative maneuvers may increase sensitivity and specificity. Positive results in both the Phalen’s and median nerve compression tests, for example, have a collective sensitivity and specificity of 80% and 92%, respectively.13
When (or whether) to order electrodiagnostic studies
While some clinicians consider EDS to be the gold standard in CTS diagnosis,6 evidence is limited. One issue is the lack of universally accepted reference standards; another is that most studies have been affected by “spectrum bias.”15 What’s more, EDS—which include nerve conduction studies (NCS) and electromyography (EMG)—do not always correlate directly with symptoms, and 16% to 34% of mild cases can be missed.16
EDS are useful in many instances, however. EMG can rule out other causes of CTS symptoms (TABLE 2 details the differential diagnosis),7,11 while NCS can aid in diagnosing CTS, gauging its severity, and arriving at a prognosis. Specifically, NCS can detect delayed distal latencies and slowed conduction velocities that can occur when the myelin sheath is damaged by prolonged compression of the median nerve.17 With more severe compression, axonal damage occurs, as evidenced by reduced action potential amplitudes on NCS. Results of the nerve conduction tests are compared to age-dependent normal values and to results from other nerves on either the same or the contralateral hand. In a 2002 systemic review, the sensitivity of NCS for CTS was 56% to 85% and the specificity was 94% to 99%.18
TABLE 2
Differential diagnosis for CTS7,11
| Condition | Characteristics |
|---|---|
| Carpometacarpal arthritis of thumb | Thumb is painful when in motion; radiographic findings |
| Cervical radiculopathy | Neck pain, nerve root distribution (eg, C6), positive Spurling’s test |
| DeQuervain’s tenosynovitis | Painful resisted thumb dorsiflexion, tender at base of thumb |
| Hypothyroidism | Fatigue, cold intolerance, dry skin, hair loss, abnormal thyroid function tests |
| Peripheral neuropathy | History of DM, lower extremity involvement |
| Pronator syndrome (median nerve compression at the elbow) | Tenderness at proximal forearm |
| Ulnar compressive neuropathy | Compression and positive Tinel’s sign: ulnar nerve at elbow or wrist produces pain or paresthesias in 4th and 5th fingers |
| Vibration white finger | History of use of power drill or other hand-held vibratory tool; symptoms of Raynaud’s syndrome |
| Wrist arthritis | Painful wrist ROM, radiographic findings |
| CTS, carpal tunnel syndrome; DM, diabetes mellitus; ROM, range of motion. | |
Before and after surgery. The American Academy of Orthopedic Surgeons (AAOS) recommends EDS when CTS surgery is being considered. 7 EDS may also be used after surgery, to verify neurologic improvement.
Ultrasound. In patients with CTS, ultrasound reveals an increased cross-sectional area of the median nerve, a finding that has prompted studies of this modality as a diagnostic tool.19 Although evidence suggests that ultrasound’s sensitivity and specificity for CTS would be similar to that of EDS, the optimal cutoff for an abnormal test has not been defined,19 and ultrasound does not provide information on prognosis or alternate causes.
Thus, AAOS does not currently recommend ultrasound for CTS diagnosis.7 Magnetic resonance imaging is inappropriate for routine CTS diagnosis, as well.7
Treatment: Start conservatively
Multiple nonsurgical options are available, but the best evidence supports splinting, steroid injection, and oral steroids. Splinting or steroids alone may bring long-term relief for patients with mild to moderate cases;20 in fact, about a third of mild cases improve spontaneously.21
Conservative therapy can also provide relief for those who wish to avoid or delay surgery and for cases of transient CTS (pediatric patients, for example, or those whose condition is associated with pregnancy or hypothyroidism).18 A successful response to therapy can also help to confirm a CTS diagnosis.
Most conservative treatments begin providing relief within 2 to 6 weeks and reach the maximal benefit at 3 months.22 If there is no response after 6 weeks, it’s time to consider another approach.
In initiating splinting or corticosteroids, here’s a look at what to keep in mind:
Splinting. A splint can be used to maintain the wrist in a position with the least intracanal pressure, thereby limiting pressure on the median nerve. Splinting is equally effective whether used continually or only at night.23
Splinting can relieve symptoms and improve functional status within 2 weeks and the effects can last for 3 to 6 months, eliminating the need for surgery for some patients with mild CTS.19,20 Nerve gliding exercises, (see image at left), have been evaluated in combination with splinting. While evidence is limited, an at-home program involving these simple exercises may be a beneficial adjunctive treatment with minimal cost or harm.24,25
Local corticosteroid injection. A Cochrane meta-analysis found significant improvement in symptoms and function at one month among patients with CTS who were treated with steroid injection.26 In many cases, the effects last for many months.
A recent trial found that nearly half of patients with mild to moderate CTS who were treated with steroid injections had improved symptoms and EDS results at the 12-month follow-up.20 However, while patients with severe CTS experienced improvement at 4 weeks postinjection, most eventually required surgery.20
Evidence does not support one particular steroid dose or formulation over another, or one particular injection site.22 Injecting 4 cm proximal to the wrist flexion crease is as effective as a more distal injection.26,27
Caution is required, however, as risks associated with local injections include tendon rupture and median nerve injury. If a patient experiences intense pain or paresthesia in the median nerve distribution when the needle is inserted, redirect the needle away from the median nerve immediately. For patients who respond well to this treatment, one additional injection can be given after 6 months if symptoms recur.
Oral corticosteroids. Oral prednisone at a dose of 20 mg/d for 2 weeks improves symptoms and function in patients with CTS, but is less effective than steroid injections.28 Treatment for 2 weeks is as effective as treatment for 4 weeks; the effects tend to wane after 8 weeks in both cases.29 Nonsteroidal anti-inflammatory drugs, diuretics, and vitamin B6 have not been found to be effective.30
CASE Ms. K also asks about “those needle tests”—a reference to EDS—which her sister had to diagnose her CTS. You explain that these studies are not necessary at this time because her symptoms are mild and there is no need for other causes to be ruled out.
Instead, you offer her a neutral wrist splint for night-time use and recommend home-based nerve glide exercises. There is no evidence that cold laser therapy is effective, you explain to Ms. K, and it is expensive. She agrees to try the splint and the exercises, and you schedule a follow-up visit in 6 weeks.
A look at alternative therapies
There are many nontraditional treatments for CTS, with yoga, carpal bone mobilization, ergonomic keyboards, and ultrasound therapy among them. Some have limited evidence to suggest that they may have a therapeutic effect;30 others have little or no evidence to support them.
Yoga. Stretching and improved joint posture with specific yoga exercises may lead to decreased compression within the carpal tunnel and increased blood flow to the median nerve. One small study found that yoga was more effective than nocturnal wrist splinting for pain relief, and had similar improvement for nocturnal symptoms and grip strength.31
Carpal bone mobilization. One small study found this physical therapy technique, which involves movement of the bones in the wrist, to improve symptoms such as numbness and tingling after 3 weeks of therapy. Yet carpal bone mobilization did not relieve pain or help restore function.32
Ergonomic keyboard. Patients who use computers at work may find that an ergonomic keyboard helps to relieve pain associated with CTS, compared with a standard keyboard.33
Therapeutic ultrasound. A recent meta-analysis found that there is only poor-quality evidence for ultrasound as an effective treatment for CTS—a process in which a round-headed instrument applied to the skin delivers sound waves that are absorbed by underlying tissues in the carpal tunnel. And there is insufficient evidence for one type of ultrasound over another, or to suggest that ultrasound is more effective than other nonsurgical treatments.34 Notably, ultrasound takes several weeks to provide a therapeutic benefit.
What about acupuncture? A recent trial found that acupuncture was no more effective than sham acupuncture in relieving symptoms of CTS in patients wearing wrist splints.35 Magnet therapy, chiropractic, and cold laser therapy are not supported by evidence either.28
Is the patient a candidate for surgery?
Carpal tunnel release provides good long-term outcomes for 70% to 90% of patients and is a cost-effective treatment.36,37 Evidence supports a trial of conservative therapy, however, before considering surgery for patients with mild-to-moderate CTS.22 Future studies are needed to identify prognostic characteristics of patients most likely to respond to each type of intervention, and the optimal timing for surgical release.
Patients with severe CTS—with findings such as thenar atrophy, diminished hand function, and median nerve denervation—should be referred for surgery without delay. This recommendation is based on expert opinion, however, as most clinical trials comparing surgical vs nonsurgical treatment exclude those with severe CTS.38
3 surgical techniques, and a novel approach
Surgical techniques include open, endoscopic, and minimal incision carpal tunnel release, with benefits and drawbacks for each. Compared with open release, for example, patients who undergo endoscopic release have less postoperative pain at 12 weeks, quicker return to work, and fewer wound complications, but are more likely to require surgical revision. And minimal incision release is associated with improved symptoms and function compared with open release.38 However, there is no long-term evidence that any one of these 3 surgical approaches is more effective than another.39
Percutaneous carpal tunnel release is a novel approach that may be offered in outpatient settings, with local anesthesia and ultrasound guidance to avoid median nerve damage.40 Because studies of the safety and efficacy of percutaneous carpal tunnel release are limited, however, this approach is considered experimental.41 Percutaneous release is not a treatment recommended by the AAOS.38
What to tell patients about postop care
Regardless of the method used for carpal tunnel release, most complications are minor—eg, a painful or hypertrophic scar, stiffness, swelling, and pain or tenderness on either side of the incision—and resolve within a few months.42 Advise patients not to continue to wear a wrist splint after surgery; doing so can cause stiffness or adhesions and may compromise surgical outcomes.41 Postoperatively, patients should be instructed to do nerve gliding exercises and to massage their scars, both of which they can safely do at home.43
Patients can expect significant symptomatic improvement within 1 week of surgery, and most will be able to return to normal activities in 2 weeks.44 Those with severe CTS should be warned, however, that it could take up to a year to determine the extent of recovery.22 Evidence suggests that from 3% to 19% of patients may have persistent or recurrent symptoms even after carpal tunnel release, with up to 12% requiring surgical revision.45
CASE When Ms. K returns, she reports that while there has been some improvement, some activities—such as driving long distances and talking on the phone—still cause numbness and tingling. And, if she doesn’t wear the splint at night, she awakens with tingling in her hands. You discuss 2 options—continued conservative treatment with a local steroid injection, or EDS and surgical referral. The patient opts for the injection and continued use of the nocturnal wrist splint and exercises. When she returns in another 6 weeks, Ms. K reports significant improvement. You agree to stop the wrist splint and exercises and advise her to follow-up on an as-needed basis if the symptoms return.
CORRESPONDENCE Jennifer Wipperman, MD, MPH, Via Christi Family Medicine, 1121 S. Clifton, Wichita, KS 67218; [email protected]
1. Atroshi I, Gummesson C, Johnsson, et al. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153-158.
2. Luckhaupt SE, Dahlhamer JM, Ward BW, et al. Prevalence and work-relatedness of carpal tunnel syndrome in the working population, United States, 2010 national health interview survey. Am J Ind Med. 2012 April 12. [Epub ahead of print.]
3. van Dijk MA, Reitsma JB, Fischer JC, et al. Indications for requesting laboratory tests for concurrent diseases in patients with carpal tunnel syndrome: a systematic review. Clin Chem. 2003;49:1437-1444.
4. Padua L, Di Pasquale A, Pazzaglia C, et al. Systematic review of pregnancy-related carpal tunnel syndrome. Muscle Nerve. 2010;42:697-702.
5. Bland JD. The relationship of obesity, age, and carpal tunnel syndrome: more complex than was thought? Muscle Nerve. 2005;32:527-532.
6. Prime MS, Palmer J, Khan WS, et al. Is there light at the end of the tunnel? Controversies in the diagnosis and management of carpal tunnel syndrome. Hand. 2010;5:354-360.
7. Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2009;91:2478-2479.
8. Hansen PA, Micklesen P, Robinson LR. Clinical utility of the flick maneuver in diagnosing carpal tunnel syndrome. Am J Phys Med Rehabil. 2004;83:363-367.
9. Padua L, Padua R, Aprile I, et al. Carpal tunnel syndrome: relationship between clinical and patient-oriented assessment. Clin Orthop Relat Res. 2002;395:128-134.
10. Bland JD. Carpal tunnel syndrome. BMJ. 2007;335:343-346.
11. Wright PE. Carpal tunnel syndrome. In: Canale ST, Beaty JH, eds. Campbell’s Operative Orthopaedics. 11th ed. Philadelphia, Pa: Mosby, Inc; 2008:4285–4291.
12. Sibley PA, Mandel RJ. Atraumatic acute carpal tunnel syndrome in a patient taking dabigatran. Orthopedics. 2012;35:e1286-e1289.
13. MacDermid JC, Wessel J. Clinical diagnosis of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17:309-319.
14. Ahn DS. Hand elevation: a new test for carpal tunnel syndrome. Ann Plastic Surg. 2001;46:120-124.
15. Boyer K, Wies J, Turkelson CM. Effects of bias on the results of diagnostic studies of carpal tunnel syndrome. J Hand Surg. 2009;34:1006-1013.
16. Witt JC, Hentz JG, Stevens JC. Carpal tunnel syndrome with normal nerve conduction studies. Muscle Nerve. 2004;29:515-522.
17. Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg. 2008;90:2587-2593.
18. Jablecki CK, Andary MT, Floeter MK, et al. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2002;58:1589-1592.
19. Descatha A, Huard L, Aubert F, et al. Meta-analysis on the performance of sonography for the diagnosis of carpal tunnel syndrome. Semin Arthritis Rheum. 2012;41:914-922.
20. Visser LH, Ngo Q, Groeneweg SJ, et al. Long term effect of local corticosteroid injection for carpal tunnel syndrome: a relation with electrodiagnostic severity. Clin Neurophysiol. 2012;123:838-841.
21. Padua L, Padua R, Aprile I, et al. Multiperspective follow-up of untreated carpal tunnel syndrome: a multicenter study. Neurology. 2001;56:1459-1466.
22. Shi Q, MacDermid JC. Is surgical intervention more effective than non-surgical treatment for carpal tunnel syndrome? A systematic review. J Orthop Surg Res. 2011;6:17.-
23. Walker WC, Metzler M, Cifu DX, et al. Neutral wrist splinting in carpal tunnel syndrome: a comparison of night-only versus full-time wear instructions. Arch Phys Med Rehabil. 2000;81:424-429.
24. Brininger TL, Rogers JC, Holm MB, et al. Efficacy of a fabricated customized splint and tendon and nerve gliding exercises for the treatment of carpal tunnel syndrome: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88:1429-1435.
25. Schmid AB, Elliott JM, Strudwick MW, et al. Effect of splinting and exercise on intraneural edema of the median nerve in carpal tunnel syndrome-an MRI study to reveal therapeutic mechanisms. J Orthop Res. 2012;30:1343-1350.
26. Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(2):CD001554.-
27. Kamanli A, Bezgincan M, Kaya A. Comparison of local steroid injection into carpal tunnel via proximal and distal approach in patients with carpal tunnel syndrome. Bratislavske Lek Listy. 2011;112:337-341.
28. Huisstede BM, Hoogvliet P, Randsdorp MS, et al. Carpal tunnel syndrome. Part I: effectiveness of nonsurgical treatments—a systematic review. Arch Phys Med Rehabil. 2010;91:981-1004.
29. Chang MH, Ger LP, Hsieh PF, et al. A randomised clinical trial of oral steroids in the treatment of carpal tunnel syndrome: a long term follow up. J Neurol Neurosurg Psychiatry. 2002;73:710-714.
30. O’Connor D, Marshall S, Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003;(1):CD003219.-
31. Garfinkel MS, Singhal A, Katz WA, et al. Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280:1601-1603.
32. Tal-Akabi A, Rushton A. An investigation to compare the effectiveness of carpal bone mobilisation and neurodynamic mobilisation as methods of treatment for carpal tunnel syndrome. Man Ther. 2000;5:214-222.
33. O’Connor D, Page MJ, Marshall SC, et al. Ergonomic positioning or equipment for treating carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;(1):CD009600.-
34. Page MJ, O’Connor D, Pitt V, et al. Therapeutic ultrasound for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;(1):CD009601.-
35. Yao E, Gerritz PK, Henricson E, et al. Randomized controlled trial comparing acupuncture with placebo acupuncture for the treatment of carpal tunnel syndrome. PMR. 2012;4:367-373.
36. Pomerance J, Zurakowski D, Fine I. The cost-effectiveness of nonsurgical versus surgical treatment for carpal tunnel syndrome. J Hand Surg. 2009;34:1193-1200.
37. Turner A, Kimble F, Gulyas K, et al. Can the outcome of open carpal tunnel release be predicted? A review of the literature. ANZ J Surg. 2010;80:50-54.
38. Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of carpal tunnel syndrome. J Bone Joint Surg. 2010;92:218-219.
39. Scholten RJ, Mink van der Molen A, Uitdehaag BM, et al. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(4):CD003905.-
40. Nakamichi K, Tachibana S, Yamamoto S, et al. Percutaneous carpal tunnel release compared with mini-open release using ultrasonographic guidance for both techniques. J Hand Surg Am. 2010;35:437-445.
41. Huisstede BM, Randsdorp MS, Coert JH, et al. Carpal tunnel syndrome. Part II: effectiveness of surgical treatments—a systematic review. Arch Phys Med Rehabil. 2010;91:1005-1024.
42. Ludlow KS, Merla JL, Cox JA, et al. Pillar pain as a postoperative complication of carpal tunnel release: a review of the literature. J Hand Ther. 1997;10:277-282.
43. Pomerance J, Fine I. Outcomes of carpal tunnel surgery with and without supervised postoperative therapy. J Hand Surg. 2007;32:1159-1163.
44. Acharya AD, Auchincloss JM. Return to functional hand use and work following open carpal tunnel surgery. J Hand Surg Br. 2005;30:607-610.
45. Dahlin LB, Salo M, Thomsen N, et al. Carpal tunnel syndrome and treatment of recurrent symptoms. Scand J Plast Reconstr Surg Hand Surg. 2010;44:4-11.
1. Atroshi I, Gummesson C, Johnsson, et al. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153-158.
2. Luckhaupt SE, Dahlhamer JM, Ward BW, et al. Prevalence and work-relatedness of carpal tunnel syndrome in the working population, United States, 2010 national health interview survey. Am J Ind Med. 2012 April 12. [Epub ahead of print.]
3. van Dijk MA, Reitsma JB, Fischer JC, et al. Indications for requesting laboratory tests for concurrent diseases in patients with carpal tunnel syndrome: a systematic review. Clin Chem. 2003;49:1437-1444.
4. Padua L, Di Pasquale A, Pazzaglia C, et al. Systematic review of pregnancy-related carpal tunnel syndrome. Muscle Nerve. 2010;42:697-702.
5. Bland JD. The relationship of obesity, age, and carpal tunnel syndrome: more complex than was thought? Muscle Nerve. 2005;32:527-532.
6. Prime MS, Palmer J, Khan WS, et al. Is there light at the end of the tunnel? Controversies in the diagnosis and management of carpal tunnel syndrome. Hand. 2010;5:354-360.
7. Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons Clinical Practice Guideline on diagnosis of carpal tunnel syndrome. J Bone Joint Surg Am. 2009;91:2478-2479.
8. Hansen PA, Micklesen P, Robinson LR. Clinical utility of the flick maneuver in diagnosing carpal tunnel syndrome. Am J Phys Med Rehabil. 2004;83:363-367.
9. Padua L, Padua R, Aprile I, et al. Carpal tunnel syndrome: relationship between clinical and patient-oriented assessment. Clin Orthop Relat Res. 2002;395:128-134.
10. Bland JD. Carpal tunnel syndrome. BMJ. 2007;335:343-346.
11. Wright PE. Carpal tunnel syndrome. In: Canale ST, Beaty JH, eds. Campbell’s Operative Orthopaedics. 11th ed. Philadelphia, Pa: Mosby, Inc; 2008:4285–4291.
12. Sibley PA, Mandel RJ. Atraumatic acute carpal tunnel syndrome in a patient taking dabigatran. Orthopedics. 2012;35:e1286-e1289.
13. MacDermid JC, Wessel J. Clinical diagnosis of carpal tunnel syndrome: a systematic review. J Hand Ther. 2004;17:309-319.
14. Ahn DS. Hand elevation: a new test for carpal tunnel syndrome. Ann Plastic Surg. 2001;46:120-124.
15. Boyer K, Wies J, Turkelson CM. Effects of bias on the results of diagnostic studies of carpal tunnel syndrome. J Hand Surg. 2009;34:1006-1013.
16. Witt JC, Hentz JG, Stevens JC. Carpal tunnel syndrome with normal nerve conduction studies. Muscle Nerve. 2004;29:515-522.
17. Graham B. The value added by electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Bone Joint Surg. 2008;90:2587-2593.
18. Jablecki CK, Andary MT, Floeter MK, et al. Practice parameter: electrodiagnostic studies in carpal tunnel syndrome. Report of the American Association of Electrodiagnostic Medicine, American Academy of Neurology, and the American Academy of Physical Medicine and Rehabilitation. Neurology. 2002;58:1589-1592.
19. Descatha A, Huard L, Aubert F, et al. Meta-analysis on the performance of sonography for the diagnosis of carpal tunnel syndrome. Semin Arthritis Rheum. 2012;41:914-922.
20. Visser LH, Ngo Q, Groeneweg SJ, et al. Long term effect of local corticosteroid injection for carpal tunnel syndrome: a relation with electrodiagnostic severity. Clin Neurophysiol. 2012;123:838-841.
21. Padua L, Padua R, Aprile I, et al. Multiperspective follow-up of untreated carpal tunnel syndrome: a multicenter study. Neurology. 2001;56:1459-1466.
22. Shi Q, MacDermid JC. Is surgical intervention more effective than non-surgical treatment for carpal tunnel syndrome? A systematic review. J Orthop Surg Res. 2011;6:17.-
23. Walker WC, Metzler M, Cifu DX, et al. Neutral wrist splinting in carpal tunnel syndrome: a comparison of night-only versus full-time wear instructions. Arch Phys Med Rehabil. 2000;81:424-429.
24. Brininger TL, Rogers JC, Holm MB, et al. Efficacy of a fabricated customized splint and tendon and nerve gliding exercises for the treatment of carpal tunnel syndrome: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88:1429-1435.
25. Schmid AB, Elliott JM, Strudwick MW, et al. Effect of splinting and exercise on intraneural edema of the median nerve in carpal tunnel syndrome-an MRI study to reveal therapeutic mechanisms. J Orthop Res. 2012;30:1343-1350.
26. Marshall S, Tardif G, Ashworth N. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(2):CD001554.-
27. Kamanli A, Bezgincan M, Kaya A. Comparison of local steroid injection into carpal tunnel via proximal and distal approach in patients with carpal tunnel syndrome. Bratislavske Lek Listy. 2011;112:337-341.
28. Huisstede BM, Hoogvliet P, Randsdorp MS, et al. Carpal tunnel syndrome. Part I: effectiveness of nonsurgical treatments—a systematic review. Arch Phys Med Rehabil. 2010;91:981-1004.
29. Chang MH, Ger LP, Hsieh PF, et al. A randomised clinical trial of oral steroids in the treatment of carpal tunnel syndrome: a long term follow up. J Neurol Neurosurg Psychiatry. 2002;73:710-714.
30. O’Connor D, Marshall S, Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003;(1):CD003219.-
31. Garfinkel MS, Singhal A, Katz WA, et al. Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998;280:1601-1603.
32. Tal-Akabi A, Rushton A. An investigation to compare the effectiveness of carpal bone mobilisation and neurodynamic mobilisation as methods of treatment for carpal tunnel syndrome. Man Ther. 2000;5:214-222.
33. O’Connor D, Page MJ, Marshall SC, et al. Ergonomic positioning or equipment for treating carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;(1):CD009600.-
34. Page MJ, O’Connor D, Pitt V, et al. Therapeutic ultrasound for carpal tunnel syndrome. Cochrane Database Syst Rev. 2012;(1):CD009601.-
35. Yao E, Gerritz PK, Henricson E, et al. Randomized controlled trial comparing acupuncture with placebo acupuncture for the treatment of carpal tunnel syndrome. PMR. 2012;4:367-373.
36. Pomerance J, Zurakowski D, Fine I. The cost-effectiveness of nonsurgical versus surgical treatment for carpal tunnel syndrome. J Hand Surg. 2009;34:1193-1200.
37. Turner A, Kimble F, Gulyas K, et al. Can the outcome of open carpal tunnel release be predicted? A review of the literature. ANZ J Surg. 2010;80:50-54.
38. Keith MW, Masear V, Chung KC, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on the treatment of carpal tunnel syndrome. J Bone Joint Surg. 2010;92:218-219.
39. Scholten RJ, Mink van der Molen A, Uitdehaag BM, et al. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(4):CD003905.-
40. Nakamichi K, Tachibana S, Yamamoto S, et al. Percutaneous carpal tunnel release compared with mini-open release using ultrasonographic guidance for both techniques. J Hand Surg Am. 2010;35:437-445.
41. Huisstede BM, Randsdorp MS, Coert JH, et al. Carpal tunnel syndrome. Part II: effectiveness of surgical treatments—a systematic review. Arch Phys Med Rehabil. 2010;91:1005-1024.
42. Ludlow KS, Merla JL, Cox JA, et al. Pillar pain as a postoperative complication of carpal tunnel release: a review of the literature. J Hand Ther. 1997;10:277-282.
43. Pomerance J, Fine I. Outcomes of carpal tunnel surgery with and without supervised postoperative therapy. J Hand Surg. 2007;32:1159-1163.
44. Acharya AD, Auchincloss JM. Return to functional hand use and work following open carpal tunnel surgery. J Hand Surg Br. 2005;30:607-610.
45. Dahlin LB, Salo M, Thomsen N, et al. Carpal tunnel syndrome and treatment of recurrent symptoms. Scand J Plast Reconstr Surg Hand Surg. 2010;44:4-11.
Gynecomastia: When is treatment indicated?
• Examine enlarged male breasts to differentiate between true gynecomastia and pseudogynecomastia (seen with obesity) or a mass suggestive of tumor activity. C
• Ask patients about the use of medications associated with gynecomastia, such as some antihypertensives, antibiotics, psychotropic agents, or hormones. C
• Order renal function tests and measure levels of liver enzymes, testosterone, and other hormones when initial history and examination findings are insufficient for a diagnosis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Harry J is a 57-year-old man who came to us for evaluation and management of hypertension. He also complained of chronic headaches. Our initial examination revealed a body mass index (BMI) of 29 kg/m2 and blood pressure (BP) of 150/100 mm Hg. The hypertension responded well to a combination of valsartan and hydrochlorothiazide. A few months later, he developed left breast soreness, as well as decreased libido. Examination revealed a round movable subareolar nodule 2 cm in diameter, with no associated skin changes or lymphadenopathy. Laboratory results were: total testosterone, 106 ng/dL (normal, 241-827); free testosterone, 23 pg/mL (47-244); thyroid-stimulating hormone (TSH), 2.222 mIU/mL (0.350-5.500); and prolactin, 102.7 ng/mL (2.1-17.7). Magnetic resonance imaging (MRI) of the brain revealed a nodular density <10 mm in the pituitary gland with minimal displacement of the stalk, consistent with a microadenoma.
Enlargement of the male breasts—gynecomastia—is caused by a benign proliferation of the ductal epithelium, due to a relative increase in the ratio of free estrogen to androgen locally in the breast. Gynecomastia of recent onset is often associated with pain and tenderness, as was the case with our patient.
Often self-limiting, age-related influences. Gynecomastia is common in newborns, during adolescence, and in old age.1 In both male and female newborns, maternal and placental estrogens induce bilateral proliferation of breast tissue. This resolves within a few weeks after birth. During the early stages of male puberty, there is a relative increase in estrogens derived mostly from peripheral aromatization of testicular and adrenal androgens. If gynecomastia results, it usually regresses spontaneously as testicular testosterone production increases in late puberty.2 Gynecomastia is also common in elderly men due to a decrease in testosterone production and an increase in sex hormone binding globulin (SHBG) that lowers free testosterone levels.
Deleterious contributing factors. Several other potential causes of gynecomastia exist (TABLE 1),3,4 and these can usually be identified with a systematic approach using a careful history, physical examination, and selected laboratory studies. Many medications are associated with gynecomastia (TABLE 2),5 one of the most common being spironolactone due to its antiandrogenic activity at the receptor level.5 Some drugs, although associated with gynecomastia, cannot be linked to a direct cause-and-effect mechanism. These factors are compounded in elderly, obese men who take medications such as spironolactone, known to cause gynecomastia.
TABLE 1
Causes of gynecomastia3,4
| Physiologic |
| Neonatal Adolescent Aging-related |
| Drug induced |
| Antiandrogens Antibiotics Antihypertensive agents GI agents Hormones Illicit drugs Psychiatric drugs |
| Decreased androgen production |
| Primary (testicular) hypogonadism Secondary (central) hypogonadism |
| Decreased androgen effect or synthesis |
| Androgen insensitivity syndrome 5α-Reductase deficiency 17-β-Hydroxysteroid dehydrogenase deficiency |
| Increased estrogen production |
| Adrenal tumor Testicular tumor hCG-secreting tumor Familial aromatase excess syndrome |
| Other |
| Liver disease Thyrotoxicosis Obesity Renal disease Malnutrition |
| GI, gastrointestinal; hCG, human chorionic gonadotropin. |
TABLE 2
Drugs associated with gynecomastia5
| Antiandrogens | Bicalutamide, flutamide, finasteride, spironolactone |
| Antibiotics | Isoniazid, ketoconazole, metronidazole |
| Antihypertensive agents | Amlodipine, diltiazem, nifedipine, verapamil, captopril, enalapril |
| GI agents | Cimetidine, ranitidine, omeprazole |
| Hormones | Anabolic steroids, estrogens, hCG, growth hormone, GnRH agonists |
| Illicit drugs, alcohol | Marijuana, methadone |
| Psychiatric drugs | Psychotropic agents, tricyclic antidepressants |
| Other | Antiretroviral agents, digitalis, fibrates, methotrexate, statins |
| GI, gastrointestinal; GnRH, gonadotropin-releasing hormone; hCG, human chorionic gonadotropin. | |
A patient’s medical history may reveal chronic conditions associated with gynecomastia. Such disorders include cirrhosis, hyperthyroidism, malnutrition, and chronic kidney disease. Rarely, gynecomastia can be a manifestation of a testicular, adrenal, or other neoplasm.
Despite a thorough evaluation, no detectable abnormality is found initially in 25% of gynecomastia cases.6 Close observation and monitoring is necessary in such instances, to ensure the earliest possible identification of the underlying cause and initiation of appropriate medical or surgical therapy.
First steps in the clinical evaluation
In cases of male breast enlargement, first determine whether you are dealing with true gynecomastia or “pseudogynecomastia,” which involves increased fat deposits typically seen in obese individuals.3 In cases of pseudogynecomastia, the tissue is uniformly enlarged and soft, with the same consistency as adipose tissue.
In about half of the cases of gynecomastia, the condition is bilateral.3 It is characteristically a rubbery or firm mass concentric with the nipple-areolar complex.
Clues to look for in the history. When examination suggests true gynecomastia, conduct a focused history to determine if medications or other substances might be causing the problem. (See “A case where drug therapy was to blame”) Some plant-derived oils used as skin care products have also been associated with gynecomastia due to weak estrogenic or anti-androgenic activity.7
Jed G is a 61-year-old man who reported decreased libido and erectile dysfunction. Examination revealed normal male external genitalia and prostate. Gynecomastia was not present. Laboratory results were: total testosterone, 159 ng/dL (normal, 241-827); free testosterone, 40 pg/mL (47-244); follicle-stimulating hormone (FSH), 9.1 mIU/mL (1.4-18.1); luteinizing hormone (LH), 3.4 mIU/mL (1.5-9.3); prolactin, 2.8 ng/mL (2.1-17.7); and normal values for ferritin and iron. His prostate-specific antigen (PSA) level was 0.8 ng/mL (normal, 0.00-4.00 ng/mL).
Mr. G was started on testosterone 1% gel at 5 g/d. The repeat total testosterone measurement was 215 ng/dL, and free testosterone was 82 pg/mL. The patient discontinued the testosterone gel a few months later due to the medication’s high cost.
Several years later, his total testosterone level had fallen to 110 ng/dL, and he continued to complain of fatigue, decreased libido, and erectile dysfunction. We initiated testosterone enanthate 100 mg IM every 3 weeks, which increased his testosterone level to 285 mg/dL. However, hemoglobin increased to 18.3 g/dL, and he noted bilateral nipple tenderness since the start of the injections. Small bilateral gynecomastia about 1 cm in diameter was noted. Testosterone injections were discontinued due to the erythrocytosis. The breast tenderness and gynecomastia resolved 4 months later.
Mr. G had idiopathic hypogonadism. The breast tenderness and gynecomastia he developed were most likely a result of peripheral aromatization of testosterone. This is similar to gynecomastia commonly observed during early puberty and would likely have regressed with continued therapy. However, as noted above, the testosterone injections had to be stopped due to significant erythrocytosis.
The history may also uncover significant weight gain, because obesity is associated with increased aromatase activity resulting in a relative increase in estrogens systemically and locally in the breast. When obesity is the cause of gynecomastia, the breast examination reveals firm, rubbery tissue (unlike the findings in pseudogynecomastia, where there is a soft enlargement of the breast). Alternatively, a history of weight loss is important because it can lead to hypothalamic dysfunction and a decrease in gonadotropin (follicle-stimulating hormone [FSH], luteinizing hormone [LH]) secretion, resulting in decreased testosterone levels.8
Also inquire about prior diagnoses of liver cirrhosis or thyrotoxicosis or the presence of symptoms suggestive of these disorders, such as fatigue, jaundice, bloating, heat intolerance, or heart palpitations. These conditions can alter the metabolism of sex steroids and their binding proteins. A history of decreased libido and erectile dysfunction is suggestive of low testosterone levels, also known as hypogonadism. Headaches, visual disturbances, and behavioral abnormalities suggest a hypothalamic or pituitary disorder resulting in decreased FSH and LH levels and secondary hypogonadism. A family history of gynecomastia is elicited in half the patients with persistent pubertal gynecomastia.9
Physical examination. For all patients (except newborns), calculate the BMI and measure arm span and upper and lower body segments. A eunuchoid proportion—arm span 2 cm or greater than height—is associated with early-onset hypogonadism that precedes fusion of the epiphyses.3 Thus, you’ll need to consider congenital disorders of the testes, such as Klinefelter syndrome, as well as hypothalamic or pituitary disease, such as Kallmann syndrome, resulting in deficient FSH and LH production.
As noted earlier, you’ll need to examine the breasts to determine if true gynecomastia exists, as opposed to increased adipose tissue or the presence of a suspicious mass. A hard or irregular mass outside the areola, especially if associated with skin changes such as dimpling or retraction, should raise the possibility of breast carcinoma. Promptly arrange for diagnostic mammography and possible biopsy in this setting.
Carefully examine the secondary sexual characteristics, including body hair distribution and muscle mass. Inspect the external genitalia, penile development, and position of the urethral meatus. Note testicular size and consistency. Small, firm testes are suggestive of dysgenetic gonads found in patients with Klinefelter syndrome (47 XXY), whereas small, soft testes suggest secondary hypogonadism. A unilateral testicular mass raises suspicion of a neoplasm. Palpate the prostate in older men, especially if contemplating androgen therapy, which could exacerbate a preexisting focal prostate cancer.
Look for signs of hyperthyroidism, such as goiter, exophthalmos, tachycardia, and hyper-reflexia. Examine the abdomen for masses, hepato- or splenomegaly, and signs of cirrhosis, such as ascites and venous congestion. The examination should also include visual fields, cranial nerves, and fundoscopy for possible pituitary (or other) central nervous system lesions. Look for spider angiomas and palmar erythema (as occur in cirrhosis); warm, moist skin and myxedema (as in Graves’ disease); and mucocutaneous lentigines (as in Peutz-Jeghers syndrome).10
When laboratory and radiologic testing may help
Most adolescents with gynecomastia are best managed by reassurance and observation11 (ALGORITHM),3 and no laboratory or radiographic studies are recommended in most cases. Exceptions would be gynecomastia that develops before the onset of puberty; evidence of undervirilization on physical examination; a testicular mass; or persistence of gynecomastia beyond the usual observation period of 12 to 18 months.11
ALGORITHM
Evaluating gynecomastia3
CT, computed tomography; hCG, human chorionic gonadotropin; LH, luteinizing hormone; MRI, magnetic resonance imaging; TSH, thyroid-stimulating hormone.
↑ = elevated; ↓ = lowered; ↔ = normal.
If findings on physical examination are consistent with a breast neoplasm, arrange for mammography immediately. The sensitivity and specificity of mammography for benign and malignant conditions exceed 90%.12 A biopsy may be necessary if uncertainty remains after imaging.
No specific tests are necessary when gynecomastia is clearly associated with intake of a medication known to be associated with the condition, especially if the history and examination are otherwise negative. A prompt regression of gynecomastia after discontinuation of the offending drug will confirm the diagnosis.
If the condition persists in an adolescent or adult and the cause is still unclear, perform renal function tests and measure levels of liver enzymes, early-morning serum human chorionic gonadotropin (hCG), LH, total testosterone, estradiol, TSH, and prolactin.
What lab results may mean. If the total testosterone level is borderline or low-normal (200-350 ng/dL), repeat the test and measure the free testosterone level.
If an elevated hCG level is found, repeat the testicular examination carefully and order ultrasonography. In the absence of a testicular tumor, consider an MRI of the brain and computed tomography (CT) of the abdomen and chest to help identify an extragonadal hCG-secreting tumor.
An elevated LH level and low testosterone level are diagnostic of primary testicular hypogonadism. A karyotype may be necessary in some individuals to diagnose Klinefelter syndrome. Elevated LH and testosterone levels are seen in patients with androgen insensitivity syndromes. These conditions are caused by abnormalities in the androgen receptor with a wide range of possible phenotypes, including ambiguous genitalia.
A low testosterone level with a low or normal LH level indicates secondary hypogonadism of hypothalamic or pituitary origin. An elevated prolactin level in such cases (as was seen in Mr. J.’s case) is usually due to a prolactin secreting pituitary adenoma.
Hereditary hemochromatosis is an important and often overlooked cause of hypogonadism. Obtain iron studies and ferritin levels in this setting.13 Unrecognized hemochromatosis may result in fibrosis and multiple organ failure.
Patients with secondary hypogonadism are best managed by a referral to an endocrinologist, as the potential list of causes is extensive.4,14,15
A low TSH level is consistent with thyrotoxicosis, which may result in increased levels of SHBG and altered metabolism of estrogens and androgens.16 Thus, about 10% of men with thyrotoxicosis present with gynecomastia and erectile dysfunction.16 If the estradiol level is elevated, a testicular ultrasound as well as an adrenal CT scan will help identify a neoplasm.
In a significant number of patients, the diagnostic tests are normal, leading to a diagnosis of idiopathic gynecomastia. In these cases, the alteration in androgen and estrogen levels can be subtle and intermittent.17 Continue surveillance and periodically reevaluate the patient.
Management of gynecomastia
Gynecomastia often results from transient hormonal imbalance and regresses spontaneously. Therefore, no specific treatment is necessary for neonatal, pubertal, or drug-induced gynecomastia. In other situations, prompt diagnosis and treatment are important to maximize the likelihood of successful medical therapy. It has been shown that fibrosis develops 6 to 12 months after the onset of gynecomastia, making it unlikely that medical treatments beyond that stage will result in significant regression of the breast enlargement.18 In such long-standing cases, surgical intervention with subcutaneous mastectomy or liposuction can be considered for patients who have significant psychological problems or esthetic issues. Indications for surgery also include continued growth and tenderness of breast tissue or malignancy.
Available medications include those aimed at decreasing estrogen production or estrogen effect on target breast tissue. Aromatase inhibitors such as testolactone, anastrozole, and letrozole can decrease the synthesis of estrogen by inhibiting aromatization of androgens. Although theoretically promising, results of the few controlled trials with aromatase inhibitors have been generally disappointing.19
Selective estrogen receptor modulators that alter the effect of estrogen on breast tissue are tamoxifen and raloxifene. Tamoxifen is not yet approved for treatment of gynecomastia, but has proven effective in randomized trials.20 At a dose of 20 mg/d for 3 or more months, tamoxifen resulted in complete regression of gynecomastia in 60% of patients and partial regression in 20% of patients.20 Tamoxifen also prevents gynecomastia after medial prostatectomy and treatment with the antiandrogen, bicalutamide.
CASE Mr. J had a pituitary prolactin-secreting microadenoma causing secondary hypogonadism and gynecomastia. He was started on cabergoline (a dopamine agonist) 0.5 mg orally once a week. Four months later, his total testosterone level was 291 ng/dL, and prolactin was 9.3 ng/mL. His headaches and gynecomastia had significantly decreased. He continued to do well on the same regimen and, 6 years later, his prolactin level was 1.4 ng/mL, indicating that treatment had been effective.
CORRESPONDENCE
Roy N. Morcos, MD, Department of Family Medicine, St. Elizabeth Health Center, 1044 Belmont Avenue, Youngstown, OH 44501; [email protected]
1. Haynes B, Mookadem F. Male gynecomastia. Mayo Clin Proc. 2009;84:672.-
2. Nordt C, Divanta A. Gynecomastia in adolescents. Curr Opin Pediatr. 2008;20:375-382.
3. Braunstein G. Gynecomastia. N Engl J Med. 2007;357:1229-1237.
4. Bhasin SI. Testicular disorders. In: Kronenberg HM, Melmed S, Polonsky KS, et al, eds. Williams Textbook of Endocrinology. 11th ed. Philadelphia, Pa: Saunders-Elsevier; 2008:569–671.
5. Eckman A, Dobs A. Drug-induced gynecomastia. Expert Opin Drug Saf. 2008;7:691-702.
6. Derkacz M, Chmiel-Perzyriska I, Nowakowski A. Gynecomastia – a difficult diagnostic problem. Endokrynol Pol. 2011;62:190-202.
7. Henley D, Lipson N, Kovach K, et al. Pubertal gynecomastia linked to lavender and tea tree oils. N Engl J Med. 2007;356:479-485.
8. Ma N, Geffnes M. Gynecomastia in prepubertal and pubertal boys. Curr Opin Pediatr. 2008;20:465-470.
9. Eberle AJ, Sparrow JT, Keenan BS. Treatment of persistent pubertal gynecomastia with dihydrotestosterone heptanoate. J Pediatr. 1986;109:144-149.
10. Kapoor S. Cutaneous manifestations of systemic condition associated with gynecomastia. Skinmed. 2010;8:87-92.
11. Johnson RE, Murad MH. Gynecomastia: pathophysiology, evaluation, and management. Mayo Clin Proc. 2009;84:1010-1015.
12. Evans GF, Anthony T, Turnage RH, et al. The diagnostic accuracy of mammography in the evaluation of male breast disease. Am J Surg. 2001;181:96-102.
13. Allen KJ, Gurrin LC, Constantine CC, et al. Iron-overload related disease in HFE hereditary hemochromatosis. N Engl J Med. 2008;358:221-230.
14. Sedlmeyer IL, Palmert MR. Delayed puberty: analysis of a large case series from an academic center. J Clin Endocrinol Metab. 2002;87:1613-1620.
15. Bhasin SI, Jameson JL. Disorders of the testes and male reproductive system. In: Longo D, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: McGraw-Hill; 2012:3019–3020.
16. Meikle AW. The interrelationships between thyroid dysfunction and hypogonadism in men and boys. Thyroid. 2004;14(suppl 1):S17-S25.
17. Wu FCW, Tajar A, Beynon JM, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363:123-135.
18. Di Lorenzo G, Autorino R, Perdona S, et al. Management of gynaecomastia in patients with prostate cancer: a systematic review. Lancet Oncol. 2005;6:972-979.
19. Mauras N, Bishop K, Merinbaum D, et al. Pharmacokinetics and pharmacodynamics of anastrozole in pubertal boys with recent onset gynecomastia. J Clin Endocrinol Metab. 2009;94:2975-2978.
20. Derman O, Kanbur N, Kilic I, et al. Long-term follow-up of tamoxifen treatment in adolescents with gynecomastia. J Pediatr Endocrinol Metab. 2008;21:449-453.
• Examine enlarged male breasts to differentiate between true gynecomastia and pseudogynecomastia (seen with obesity) or a mass suggestive of tumor activity. C
• Ask patients about the use of medications associated with gynecomastia, such as some antihypertensives, antibiotics, psychotropic agents, or hormones. C
• Order renal function tests and measure levels of liver enzymes, testosterone, and other hormones when initial history and examination findings are insufficient for a diagnosis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Harry J is a 57-year-old man who came to us for evaluation and management of hypertension. He also complained of chronic headaches. Our initial examination revealed a body mass index (BMI) of 29 kg/m2 and blood pressure (BP) of 150/100 mm Hg. The hypertension responded well to a combination of valsartan and hydrochlorothiazide. A few months later, he developed left breast soreness, as well as decreased libido. Examination revealed a round movable subareolar nodule 2 cm in diameter, with no associated skin changes or lymphadenopathy. Laboratory results were: total testosterone, 106 ng/dL (normal, 241-827); free testosterone, 23 pg/mL (47-244); thyroid-stimulating hormone (TSH), 2.222 mIU/mL (0.350-5.500); and prolactin, 102.7 ng/mL (2.1-17.7). Magnetic resonance imaging (MRI) of the brain revealed a nodular density <10 mm in the pituitary gland with minimal displacement of the stalk, consistent with a microadenoma.
Enlargement of the male breasts—gynecomastia—is caused by a benign proliferation of the ductal epithelium, due to a relative increase in the ratio of free estrogen to androgen locally in the breast. Gynecomastia of recent onset is often associated with pain and tenderness, as was the case with our patient.
Often self-limiting, age-related influences. Gynecomastia is common in newborns, during adolescence, and in old age.1 In both male and female newborns, maternal and placental estrogens induce bilateral proliferation of breast tissue. This resolves within a few weeks after birth. During the early stages of male puberty, there is a relative increase in estrogens derived mostly from peripheral aromatization of testicular and adrenal androgens. If gynecomastia results, it usually regresses spontaneously as testicular testosterone production increases in late puberty.2 Gynecomastia is also common in elderly men due to a decrease in testosterone production and an increase in sex hormone binding globulin (SHBG) that lowers free testosterone levels.
Deleterious contributing factors. Several other potential causes of gynecomastia exist (TABLE 1),3,4 and these can usually be identified with a systematic approach using a careful history, physical examination, and selected laboratory studies. Many medications are associated with gynecomastia (TABLE 2),5 one of the most common being spironolactone due to its antiandrogenic activity at the receptor level.5 Some drugs, although associated with gynecomastia, cannot be linked to a direct cause-and-effect mechanism. These factors are compounded in elderly, obese men who take medications such as spironolactone, known to cause gynecomastia.
TABLE 1
Causes of gynecomastia3,4
| Physiologic |
| Neonatal Adolescent Aging-related |
| Drug induced |
| Antiandrogens Antibiotics Antihypertensive agents GI agents Hormones Illicit drugs Psychiatric drugs |
| Decreased androgen production |
| Primary (testicular) hypogonadism Secondary (central) hypogonadism |
| Decreased androgen effect or synthesis |
| Androgen insensitivity syndrome 5α-Reductase deficiency 17-β-Hydroxysteroid dehydrogenase deficiency |
| Increased estrogen production |
| Adrenal tumor Testicular tumor hCG-secreting tumor Familial aromatase excess syndrome |
| Other |
| Liver disease Thyrotoxicosis Obesity Renal disease Malnutrition |
| GI, gastrointestinal; hCG, human chorionic gonadotropin. |
TABLE 2
Drugs associated with gynecomastia5
| Antiandrogens | Bicalutamide, flutamide, finasteride, spironolactone |
| Antibiotics | Isoniazid, ketoconazole, metronidazole |
| Antihypertensive agents | Amlodipine, diltiazem, nifedipine, verapamil, captopril, enalapril |
| GI agents | Cimetidine, ranitidine, omeprazole |
| Hormones | Anabolic steroids, estrogens, hCG, growth hormone, GnRH agonists |
| Illicit drugs, alcohol | Marijuana, methadone |
| Psychiatric drugs | Psychotropic agents, tricyclic antidepressants |
| Other | Antiretroviral agents, digitalis, fibrates, methotrexate, statins |
| GI, gastrointestinal; GnRH, gonadotropin-releasing hormone; hCG, human chorionic gonadotropin. | |
A patient’s medical history may reveal chronic conditions associated with gynecomastia. Such disorders include cirrhosis, hyperthyroidism, malnutrition, and chronic kidney disease. Rarely, gynecomastia can be a manifestation of a testicular, adrenal, or other neoplasm.
Despite a thorough evaluation, no detectable abnormality is found initially in 25% of gynecomastia cases.6 Close observation and monitoring is necessary in such instances, to ensure the earliest possible identification of the underlying cause and initiation of appropriate medical or surgical therapy.
First steps in the clinical evaluation
In cases of male breast enlargement, first determine whether you are dealing with true gynecomastia or “pseudogynecomastia,” which involves increased fat deposits typically seen in obese individuals.3 In cases of pseudogynecomastia, the tissue is uniformly enlarged and soft, with the same consistency as adipose tissue.
In about half of the cases of gynecomastia, the condition is bilateral.3 It is characteristically a rubbery or firm mass concentric with the nipple-areolar complex.
Clues to look for in the history. When examination suggests true gynecomastia, conduct a focused history to determine if medications or other substances might be causing the problem. (See “A case where drug therapy was to blame”) Some plant-derived oils used as skin care products have also been associated with gynecomastia due to weak estrogenic or anti-androgenic activity.7
Jed G is a 61-year-old man who reported decreased libido and erectile dysfunction. Examination revealed normal male external genitalia and prostate. Gynecomastia was not present. Laboratory results were: total testosterone, 159 ng/dL (normal, 241-827); free testosterone, 40 pg/mL (47-244); follicle-stimulating hormone (FSH), 9.1 mIU/mL (1.4-18.1); luteinizing hormone (LH), 3.4 mIU/mL (1.5-9.3); prolactin, 2.8 ng/mL (2.1-17.7); and normal values for ferritin and iron. His prostate-specific antigen (PSA) level was 0.8 ng/mL (normal, 0.00-4.00 ng/mL).
Mr. G was started on testosterone 1% gel at 5 g/d. The repeat total testosterone measurement was 215 ng/dL, and free testosterone was 82 pg/mL. The patient discontinued the testosterone gel a few months later due to the medication’s high cost.
Several years later, his total testosterone level had fallen to 110 ng/dL, and he continued to complain of fatigue, decreased libido, and erectile dysfunction. We initiated testosterone enanthate 100 mg IM every 3 weeks, which increased his testosterone level to 285 mg/dL. However, hemoglobin increased to 18.3 g/dL, and he noted bilateral nipple tenderness since the start of the injections. Small bilateral gynecomastia about 1 cm in diameter was noted. Testosterone injections were discontinued due to the erythrocytosis. The breast tenderness and gynecomastia resolved 4 months later.
Mr. G had idiopathic hypogonadism. The breast tenderness and gynecomastia he developed were most likely a result of peripheral aromatization of testosterone. This is similar to gynecomastia commonly observed during early puberty and would likely have regressed with continued therapy. However, as noted above, the testosterone injections had to be stopped due to significant erythrocytosis.
The history may also uncover significant weight gain, because obesity is associated with increased aromatase activity resulting in a relative increase in estrogens systemically and locally in the breast. When obesity is the cause of gynecomastia, the breast examination reveals firm, rubbery tissue (unlike the findings in pseudogynecomastia, where there is a soft enlargement of the breast). Alternatively, a history of weight loss is important because it can lead to hypothalamic dysfunction and a decrease in gonadotropin (follicle-stimulating hormone [FSH], luteinizing hormone [LH]) secretion, resulting in decreased testosterone levels.8
Also inquire about prior diagnoses of liver cirrhosis or thyrotoxicosis or the presence of symptoms suggestive of these disorders, such as fatigue, jaundice, bloating, heat intolerance, or heart palpitations. These conditions can alter the metabolism of sex steroids and their binding proteins. A history of decreased libido and erectile dysfunction is suggestive of low testosterone levels, also known as hypogonadism. Headaches, visual disturbances, and behavioral abnormalities suggest a hypothalamic or pituitary disorder resulting in decreased FSH and LH levels and secondary hypogonadism. A family history of gynecomastia is elicited in half the patients with persistent pubertal gynecomastia.9
Physical examination. For all patients (except newborns), calculate the BMI and measure arm span and upper and lower body segments. A eunuchoid proportion—arm span 2 cm or greater than height—is associated with early-onset hypogonadism that precedes fusion of the epiphyses.3 Thus, you’ll need to consider congenital disorders of the testes, such as Klinefelter syndrome, as well as hypothalamic or pituitary disease, such as Kallmann syndrome, resulting in deficient FSH and LH production.
As noted earlier, you’ll need to examine the breasts to determine if true gynecomastia exists, as opposed to increased adipose tissue or the presence of a suspicious mass. A hard or irregular mass outside the areola, especially if associated with skin changes such as dimpling or retraction, should raise the possibility of breast carcinoma. Promptly arrange for diagnostic mammography and possible biopsy in this setting.
Carefully examine the secondary sexual characteristics, including body hair distribution and muscle mass. Inspect the external genitalia, penile development, and position of the urethral meatus. Note testicular size and consistency. Small, firm testes are suggestive of dysgenetic gonads found in patients with Klinefelter syndrome (47 XXY), whereas small, soft testes suggest secondary hypogonadism. A unilateral testicular mass raises suspicion of a neoplasm. Palpate the prostate in older men, especially if contemplating androgen therapy, which could exacerbate a preexisting focal prostate cancer.
Look for signs of hyperthyroidism, such as goiter, exophthalmos, tachycardia, and hyper-reflexia. Examine the abdomen for masses, hepato- or splenomegaly, and signs of cirrhosis, such as ascites and venous congestion. The examination should also include visual fields, cranial nerves, and fundoscopy for possible pituitary (or other) central nervous system lesions. Look for spider angiomas and palmar erythema (as occur in cirrhosis); warm, moist skin and myxedema (as in Graves’ disease); and mucocutaneous lentigines (as in Peutz-Jeghers syndrome).10
When laboratory and radiologic testing may help
Most adolescents with gynecomastia are best managed by reassurance and observation11 (ALGORITHM),3 and no laboratory or radiographic studies are recommended in most cases. Exceptions would be gynecomastia that develops before the onset of puberty; evidence of undervirilization on physical examination; a testicular mass; or persistence of gynecomastia beyond the usual observation period of 12 to 18 months.11
ALGORITHM
Evaluating gynecomastia3
CT, computed tomography; hCG, human chorionic gonadotropin; LH, luteinizing hormone; MRI, magnetic resonance imaging; TSH, thyroid-stimulating hormone.
↑ = elevated; ↓ = lowered; ↔ = normal.
If findings on physical examination are consistent with a breast neoplasm, arrange for mammography immediately. The sensitivity and specificity of mammography for benign and malignant conditions exceed 90%.12 A biopsy may be necessary if uncertainty remains after imaging.
No specific tests are necessary when gynecomastia is clearly associated with intake of a medication known to be associated with the condition, especially if the history and examination are otherwise negative. A prompt regression of gynecomastia after discontinuation of the offending drug will confirm the diagnosis.
If the condition persists in an adolescent or adult and the cause is still unclear, perform renal function tests and measure levels of liver enzymes, early-morning serum human chorionic gonadotropin (hCG), LH, total testosterone, estradiol, TSH, and prolactin.
What lab results may mean. If the total testosterone level is borderline or low-normal (200-350 ng/dL), repeat the test and measure the free testosterone level.
If an elevated hCG level is found, repeat the testicular examination carefully and order ultrasonography. In the absence of a testicular tumor, consider an MRI of the brain and computed tomography (CT) of the abdomen and chest to help identify an extragonadal hCG-secreting tumor.
An elevated LH level and low testosterone level are diagnostic of primary testicular hypogonadism. A karyotype may be necessary in some individuals to diagnose Klinefelter syndrome. Elevated LH and testosterone levels are seen in patients with androgen insensitivity syndromes. These conditions are caused by abnormalities in the androgen receptor with a wide range of possible phenotypes, including ambiguous genitalia.
A low testosterone level with a low or normal LH level indicates secondary hypogonadism of hypothalamic or pituitary origin. An elevated prolactin level in such cases (as was seen in Mr. J.’s case) is usually due to a prolactin secreting pituitary adenoma.
Hereditary hemochromatosis is an important and often overlooked cause of hypogonadism. Obtain iron studies and ferritin levels in this setting.13 Unrecognized hemochromatosis may result in fibrosis and multiple organ failure.
Patients with secondary hypogonadism are best managed by a referral to an endocrinologist, as the potential list of causes is extensive.4,14,15
A low TSH level is consistent with thyrotoxicosis, which may result in increased levels of SHBG and altered metabolism of estrogens and androgens.16 Thus, about 10% of men with thyrotoxicosis present with gynecomastia and erectile dysfunction.16 If the estradiol level is elevated, a testicular ultrasound as well as an adrenal CT scan will help identify a neoplasm.
In a significant number of patients, the diagnostic tests are normal, leading to a diagnosis of idiopathic gynecomastia. In these cases, the alteration in androgen and estrogen levels can be subtle and intermittent.17 Continue surveillance and periodically reevaluate the patient.
Management of gynecomastia
Gynecomastia often results from transient hormonal imbalance and regresses spontaneously. Therefore, no specific treatment is necessary for neonatal, pubertal, or drug-induced gynecomastia. In other situations, prompt diagnosis and treatment are important to maximize the likelihood of successful medical therapy. It has been shown that fibrosis develops 6 to 12 months after the onset of gynecomastia, making it unlikely that medical treatments beyond that stage will result in significant regression of the breast enlargement.18 In such long-standing cases, surgical intervention with subcutaneous mastectomy or liposuction can be considered for patients who have significant psychological problems or esthetic issues. Indications for surgery also include continued growth and tenderness of breast tissue or malignancy.
Available medications include those aimed at decreasing estrogen production or estrogen effect on target breast tissue. Aromatase inhibitors such as testolactone, anastrozole, and letrozole can decrease the synthesis of estrogen by inhibiting aromatization of androgens. Although theoretically promising, results of the few controlled trials with aromatase inhibitors have been generally disappointing.19
Selective estrogen receptor modulators that alter the effect of estrogen on breast tissue are tamoxifen and raloxifene. Tamoxifen is not yet approved for treatment of gynecomastia, but has proven effective in randomized trials.20 At a dose of 20 mg/d for 3 or more months, tamoxifen resulted in complete regression of gynecomastia in 60% of patients and partial regression in 20% of patients.20 Tamoxifen also prevents gynecomastia after medial prostatectomy and treatment with the antiandrogen, bicalutamide.
CASE Mr. J had a pituitary prolactin-secreting microadenoma causing secondary hypogonadism and gynecomastia. He was started on cabergoline (a dopamine agonist) 0.5 mg orally once a week. Four months later, his total testosterone level was 291 ng/dL, and prolactin was 9.3 ng/mL. His headaches and gynecomastia had significantly decreased. He continued to do well on the same regimen and, 6 years later, his prolactin level was 1.4 ng/mL, indicating that treatment had been effective.
CORRESPONDENCE
Roy N. Morcos, MD, Department of Family Medicine, St. Elizabeth Health Center, 1044 Belmont Avenue, Youngstown, OH 44501; [email protected]
• Examine enlarged male breasts to differentiate between true gynecomastia and pseudogynecomastia (seen with obesity) or a mass suggestive of tumor activity. C
• Ask patients about the use of medications associated with gynecomastia, such as some antihypertensives, antibiotics, psychotropic agents, or hormones. C
• Order renal function tests and measure levels of liver enzymes, testosterone, and other hormones when initial history and examination findings are insufficient for a diagnosis. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
CASE Harry J is a 57-year-old man who came to us for evaluation and management of hypertension. He also complained of chronic headaches. Our initial examination revealed a body mass index (BMI) of 29 kg/m2 and blood pressure (BP) of 150/100 mm Hg. The hypertension responded well to a combination of valsartan and hydrochlorothiazide. A few months later, he developed left breast soreness, as well as decreased libido. Examination revealed a round movable subareolar nodule 2 cm in diameter, with no associated skin changes or lymphadenopathy. Laboratory results were: total testosterone, 106 ng/dL (normal, 241-827); free testosterone, 23 pg/mL (47-244); thyroid-stimulating hormone (TSH), 2.222 mIU/mL (0.350-5.500); and prolactin, 102.7 ng/mL (2.1-17.7). Magnetic resonance imaging (MRI) of the brain revealed a nodular density <10 mm in the pituitary gland with minimal displacement of the stalk, consistent with a microadenoma.
Enlargement of the male breasts—gynecomastia—is caused by a benign proliferation of the ductal epithelium, due to a relative increase in the ratio of free estrogen to androgen locally in the breast. Gynecomastia of recent onset is often associated with pain and tenderness, as was the case with our patient.
Often self-limiting, age-related influences. Gynecomastia is common in newborns, during adolescence, and in old age.1 In both male and female newborns, maternal and placental estrogens induce bilateral proliferation of breast tissue. This resolves within a few weeks after birth. During the early stages of male puberty, there is a relative increase in estrogens derived mostly from peripheral aromatization of testicular and adrenal androgens. If gynecomastia results, it usually regresses spontaneously as testicular testosterone production increases in late puberty.2 Gynecomastia is also common in elderly men due to a decrease in testosterone production and an increase in sex hormone binding globulin (SHBG) that lowers free testosterone levels.
Deleterious contributing factors. Several other potential causes of gynecomastia exist (TABLE 1),3,4 and these can usually be identified with a systematic approach using a careful history, physical examination, and selected laboratory studies. Many medications are associated with gynecomastia (TABLE 2),5 one of the most common being spironolactone due to its antiandrogenic activity at the receptor level.5 Some drugs, although associated with gynecomastia, cannot be linked to a direct cause-and-effect mechanism. These factors are compounded in elderly, obese men who take medications such as spironolactone, known to cause gynecomastia.
TABLE 1
Causes of gynecomastia3,4
| Physiologic |
| Neonatal Adolescent Aging-related |
| Drug induced |
| Antiandrogens Antibiotics Antihypertensive agents GI agents Hormones Illicit drugs Psychiatric drugs |
| Decreased androgen production |
| Primary (testicular) hypogonadism Secondary (central) hypogonadism |
| Decreased androgen effect or synthesis |
| Androgen insensitivity syndrome 5α-Reductase deficiency 17-β-Hydroxysteroid dehydrogenase deficiency |
| Increased estrogen production |
| Adrenal tumor Testicular tumor hCG-secreting tumor Familial aromatase excess syndrome |
| Other |
| Liver disease Thyrotoxicosis Obesity Renal disease Malnutrition |
| GI, gastrointestinal; hCG, human chorionic gonadotropin. |
TABLE 2
Drugs associated with gynecomastia5
| Antiandrogens | Bicalutamide, flutamide, finasteride, spironolactone |
| Antibiotics | Isoniazid, ketoconazole, metronidazole |
| Antihypertensive agents | Amlodipine, diltiazem, nifedipine, verapamil, captopril, enalapril |
| GI agents | Cimetidine, ranitidine, omeprazole |
| Hormones | Anabolic steroids, estrogens, hCG, growth hormone, GnRH agonists |
| Illicit drugs, alcohol | Marijuana, methadone |
| Psychiatric drugs | Psychotropic agents, tricyclic antidepressants |
| Other | Antiretroviral agents, digitalis, fibrates, methotrexate, statins |
| GI, gastrointestinal; GnRH, gonadotropin-releasing hormone; hCG, human chorionic gonadotropin. | |
A patient’s medical history may reveal chronic conditions associated with gynecomastia. Such disorders include cirrhosis, hyperthyroidism, malnutrition, and chronic kidney disease. Rarely, gynecomastia can be a manifestation of a testicular, adrenal, or other neoplasm.
Despite a thorough evaluation, no detectable abnormality is found initially in 25% of gynecomastia cases.6 Close observation and monitoring is necessary in such instances, to ensure the earliest possible identification of the underlying cause and initiation of appropriate medical or surgical therapy.
First steps in the clinical evaluation
In cases of male breast enlargement, first determine whether you are dealing with true gynecomastia or “pseudogynecomastia,” which involves increased fat deposits typically seen in obese individuals.3 In cases of pseudogynecomastia, the tissue is uniformly enlarged and soft, with the same consistency as adipose tissue.
In about half of the cases of gynecomastia, the condition is bilateral.3 It is characteristically a rubbery or firm mass concentric with the nipple-areolar complex.
Clues to look for in the history. When examination suggests true gynecomastia, conduct a focused history to determine if medications or other substances might be causing the problem. (See “A case where drug therapy was to blame”) Some plant-derived oils used as skin care products have also been associated with gynecomastia due to weak estrogenic or anti-androgenic activity.7
Jed G is a 61-year-old man who reported decreased libido and erectile dysfunction. Examination revealed normal male external genitalia and prostate. Gynecomastia was not present. Laboratory results were: total testosterone, 159 ng/dL (normal, 241-827); free testosterone, 40 pg/mL (47-244); follicle-stimulating hormone (FSH), 9.1 mIU/mL (1.4-18.1); luteinizing hormone (LH), 3.4 mIU/mL (1.5-9.3); prolactin, 2.8 ng/mL (2.1-17.7); and normal values for ferritin and iron. His prostate-specific antigen (PSA) level was 0.8 ng/mL (normal, 0.00-4.00 ng/mL).
Mr. G was started on testosterone 1% gel at 5 g/d. The repeat total testosterone measurement was 215 ng/dL, and free testosterone was 82 pg/mL. The patient discontinued the testosterone gel a few months later due to the medication’s high cost.
Several years later, his total testosterone level had fallen to 110 ng/dL, and he continued to complain of fatigue, decreased libido, and erectile dysfunction. We initiated testosterone enanthate 100 mg IM every 3 weeks, which increased his testosterone level to 285 mg/dL. However, hemoglobin increased to 18.3 g/dL, and he noted bilateral nipple tenderness since the start of the injections. Small bilateral gynecomastia about 1 cm in diameter was noted. Testosterone injections were discontinued due to the erythrocytosis. The breast tenderness and gynecomastia resolved 4 months later.
Mr. G had idiopathic hypogonadism. The breast tenderness and gynecomastia he developed were most likely a result of peripheral aromatization of testosterone. This is similar to gynecomastia commonly observed during early puberty and would likely have regressed with continued therapy. However, as noted above, the testosterone injections had to be stopped due to significant erythrocytosis.
The history may also uncover significant weight gain, because obesity is associated with increased aromatase activity resulting in a relative increase in estrogens systemically and locally in the breast. When obesity is the cause of gynecomastia, the breast examination reveals firm, rubbery tissue (unlike the findings in pseudogynecomastia, where there is a soft enlargement of the breast). Alternatively, a history of weight loss is important because it can lead to hypothalamic dysfunction and a decrease in gonadotropin (follicle-stimulating hormone [FSH], luteinizing hormone [LH]) secretion, resulting in decreased testosterone levels.8
Also inquire about prior diagnoses of liver cirrhosis or thyrotoxicosis or the presence of symptoms suggestive of these disorders, such as fatigue, jaundice, bloating, heat intolerance, or heart palpitations. These conditions can alter the metabolism of sex steroids and their binding proteins. A history of decreased libido and erectile dysfunction is suggestive of low testosterone levels, also known as hypogonadism. Headaches, visual disturbances, and behavioral abnormalities suggest a hypothalamic or pituitary disorder resulting in decreased FSH and LH levels and secondary hypogonadism. A family history of gynecomastia is elicited in half the patients with persistent pubertal gynecomastia.9
Physical examination. For all patients (except newborns), calculate the BMI and measure arm span and upper and lower body segments. A eunuchoid proportion—arm span 2 cm or greater than height—is associated with early-onset hypogonadism that precedes fusion of the epiphyses.3 Thus, you’ll need to consider congenital disorders of the testes, such as Klinefelter syndrome, as well as hypothalamic or pituitary disease, such as Kallmann syndrome, resulting in deficient FSH and LH production.
As noted earlier, you’ll need to examine the breasts to determine if true gynecomastia exists, as opposed to increased adipose tissue or the presence of a suspicious mass. A hard or irregular mass outside the areola, especially if associated with skin changes such as dimpling or retraction, should raise the possibility of breast carcinoma. Promptly arrange for diagnostic mammography and possible biopsy in this setting.
Carefully examine the secondary sexual characteristics, including body hair distribution and muscle mass. Inspect the external genitalia, penile development, and position of the urethral meatus. Note testicular size and consistency. Small, firm testes are suggestive of dysgenetic gonads found in patients with Klinefelter syndrome (47 XXY), whereas small, soft testes suggest secondary hypogonadism. A unilateral testicular mass raises suspicion of a neoplasm. Palpate the prostate in older men, especially if contemplating androgen therapy, which could exacerbate a preexisting focal prostate cancer.
Look for signs of hyperthyroidism, such as goiter, exophthalmos, tachycardia, and hyper-reflexia. Examine the abdomen for masses, hepato- or splenomegaly, and signs of cirrhosis, such as ascites and venous congestion. The examination should also include visual fields, cranial nerves, and fundoscopy for possible pituitary (or other) central nervous system lesions. Look for spider angiomas and palmar erythema (as occur in cirrhosis); warm, moist skin and myxedema (as in Graves’ disease); and mucocutaneous lentigines (as in Peutz-Jeghers syndrome).10
When laboratory and radiologic testing may help
Most adolescents with gynecomastia are best managed by reassurance and observation11 (ALGORITHM),3 and no laboratory or radiographic studies are recommended in most cases. Exceptions would be gynecomastia that develops before the onset of puberty; evidence of undervirilization on physical examination; a testicular mass; or persistence of gynecomastia beyond the usual observation period of 12 to 18 months.11
ALGORITHM
Evaluating gynecomastia3
CT, computed tomography; hCG, human chorionic gonadotropin; LH, luteinizing hormone; MRI, magnetic resonance imaging; TSH, thyroid-stimulating hormone.
↑ = elevated; ↓ = lowered; ↔ = normal.
If findings on physical examination are consistent with a breast neoplasm, arrange for mammography immediately. The sensitivity and specificity of mammography for benign and malignant conditions exceed 90%.12 A biopsy may be necessary if uncertainty remains after imaging.
No specific tests are necessary when gynecomastia is clearly associated with intake of a medication known to be associated with the condition, especially if the history and examination are otherwise negative. A prompt regression of gynecomastia after discontinuation of the offending drug will confirm the diagnosis.
If the condition persists in an adolescent or adult and the cause is still unclear, perform renal function tests and measure levels of liver enzymes, early-morning serum human chorionic gonadotropin (hCG), LH, total testosterone, estradiol, TSH, and prolactin.
What lab results may mean. If the total testosterone level is borderline or low-normal (200-350 ng/dL), repeat the test and measure the free testosterone level.
If an elevated hCG level is found, repeat the testicular examination carefully and order ultrasonography. In the absence of a testicular tumor, consider an MRI of the brain and computed tomography (CT) of the abdomen and chest to help identify an extragonadal hCG-secreting tumor.
An elevated LH level and low testosterone level are diagnostic of primary testicular hypogonadism. A karyotype may be necessary in some individuals to diagnose Klinefelter syndrome. Elevated LH and testosterone levels are seen in patients with androgen insensitivity syndromes. These conditions are caused by abnormalities in the androgen receptor with a wide range of possible phenotypes, including ambiguous genitalia.
A low testosterone level with a low or normal LH level indicates secondary hypogonadism of hypothalamic or pituitary origin. An elevated prolactin level in such cases (as was seen in Mr. J.’s case) is usually due to a prolactin secreting pituitary adenoma.
Hereditary hemochromatosis is an important and often overlooked cause of hypogonadism. Obtain iron studies and ferritin levels in this setting.13 Unrecognized hemochromatosis may result in fibrosis and multiple organ failure.
Patients with secondary hypogonadism are best managed by a referral to an endocrinologist, as the potential list of causes is extensive.4,14,15
A low TSH level is consistent with thyrotoxicosis, which may result in increased levels of SHBG and altered metabolism of estrogens and androgens.16 Thus, about 10% of men with thyrotoxicosis present with gynecomastia and erectile dysfunction.16 If the estradiol level is elevated, a testicular ultrasound as well as an adrenal CT scan will help identify a neoplasm.
In a significant number of patients, the diagnostic tests are normal, leading to a diagnosis of idiopathic gynecomastia. In these cases, the alteration in androgen and estrogen levels can be subtle and intermittent.17 Continue surveillance and periodically reevaluate the patient.
Management of gynecomastia
Gynecomastia often results from transient hormonal imbalance and regresses spontaneously. Therefore, no specific treatment is necessary for neonatal, pubertal, or drug-induced gynecomastia. In other situations, prompt diagnosis and treatment are important to maximize the likelihood of successful medical therapy. It has been shown that fibrosis develops 6 to 12 months after the onset of gynecomastia, making it unlikely that medical treatments beyond that stage will result in significant regression of the breast enlargement.18 In such long-standing cases, surgical intervention with subcutaneous mastectomy or liposuction can be considered for patients who have significant psychological problems or esthetic issues. Indications for surgery also include continued growth and tenderness of breast tissue or malignancy.
Available medications include those aimed at decreasing estrogen production or estrogen effect on target breast tissue. Aromatase inhibitors such as testolactone, anastrozole, and letrozole can decrease the synthesis of estrogen by inhibiting aromatization of androgens. Although theoretically promising, results of the few controlled trials with aromatase inhibitors have been generally disappointing.19
Selective estrogen receptor modulators that alter the effect of estrogen on breast tissue are tamoxifen and raloxifene. Tamoxifen is not yet approved for treatment of gynecomastia, but has proven effective in randomized trials.20 At a dose of 20 mg/d for 3 or more months, tamoxifen resulted in complete regression of gynecomastia in 60% of patients and partial regression in 20% of patients.20 Tamoxifen also prevents gynecomastia after medial prostatectomy and treatment with the antiandrogen, bicalutamide.
CASE Mr. J had a pituitary prolactin-secreting microadenoma causing secondary hypogonadism and gynecomastia. He was started on cabergoline (a dopamine agonist) 0.5 mg orally once a week. Four months later, his total testosterone level was 291 ng/dL, and prolactin was 9.3 ng/mL. His headaches and gynecomastia had significantly decreased. He continued to do well on the same regimen and, 6 years later, his prolactin level was 1.4 ng/mL, indicating that treatment had been effective.
CORRESPONDENCE
Roy N. Morcos, MD, Department of Family Medicine, St. Elizabeth Health Center, 1044 Belmont Avenue, Youngstown, OH 44501; [email protected]
1. Haynes B, Mookadem F. Male gynecomastia. Mayo Clin Proc. 2009;84:672.-
2. Nordt C, Divanta A. Gynecomastia in adolescents. Curr Opin Pediatr. 2008;20:375-382.
3. Braunstein G. Gynecomastia. N Engl J Med. 2007;357:1229-1237.
4. Bhasin SI. Testicular disorders. In: Kronenberg HM, Melmed S, Polonsky KS, et al, eds. Williams Textbook of Endocrinology. 11th ed. Philadelphia, Pa: Saunders-Elsevier; 2008:569–671.
5. Eckman A, Dobs A. Drug-induced gynecomastia. Expert Opin Drug Saf. 2008;7:691-702.
6. Derkacz M, Chmiel-Perzyriska I, Nowakowski A. Gynecomastia – a difficult diagnostic problem. Endokrynol Pol. 2011;62:190-202.
7. Henley D, Lipson N, Kovach K, et al. Pubertal gynecomastia linked to lavender and tea tree oils. N Engl J Med. 2007;356:479-485.
8. Ma N, Geffnes M. Gynecomastia in prepubertal and pubertal boys. Curr Opin Pediatr. 2008;20:465-470.
9. Eberle AJ, Sparrow JT, Keenan BS. Treatment of persistent pubertal gynecomastia with dihydrotestosterone heptanoate. J Pediatr. 1986;109:144-149.
10. Kapoor S. Cutaneous manifestations of systemic condition associated with gynecomastia. Skinmed. 2010;8:87-92.
11. Johnson RE, Murad MH. Gynecomastia: pathophysiology, evaluation, and management. Mayo Clin Proc. 2009;84:1010-1015.
12. Evans GF, Anthony T, Turnage RH, et al. The diagnostic accuracy of mammography in the evaluation of male breast disease. Am J Surg. 2001;181:96-102.
13. Allen KJ, Gurrin LC, Constantine CC, et al. Iron-overload related disease in HFE hereditary hemochromatosis. N Engl J Med. 2008;358:221-230.
14. Sedlmeyer IL, Palmert MR. Delayed puberty: analysis of a large case series from an academic center. J Clin Endocrinol Metab. 2002;87:1613-1620.
15. Bhasin SI, Jameson JL. Disorders of the testes and male reproductive system. In: Longo D, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: McGraw-Hill; 2012:3019–3020.
16. Meikle AW. The interrelationships between thyroid dysfunction and hypogonadism in men and boys. Thyroid. 2004;14(suppl 1):S17-S25.
17. Wu FCW, Tajar A, Beynon JM, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363:123-135.
18. Di Lorenzo G, Autorino R, Perdona S, et al. Management of gynaecomastia in patients with prostate cancer: a systematic review. Lancet Oncol. 2005;6:972-979.
19. Mauras N, Bishop K, Merinbaum D, et al. Pharmacokinetics and pharmacodynamics of anastrozole in pubertal boys with recent onset gynecomastia. J Clin Endocrinol Metab. 2009;94:2975-2978.
20. Derman O, Kanbur N, Kilic I, et al. Long-term follow-up of tamoxifen treatment in adolescents with gynecomastia. J Pediatr Endocrinol Metab. 2008;21:449-453.
1. Haynes B, Mookadem F. Male gynecomastia. Mayo Clin Proc. 2009;84:672.-
2. Nordt C, Divanta A. Gynecomastia in adolescents. Curr Opin Pediatr. 2008;20:375-382.
3. Braunstein G. Gynecomastia. N Engl J Med. 2007;357:1229-1237.
4. Bhasin SI. Testicular disorders. In: Kronenberg HM, Melmed S, Polonsky KS, et al, eds. Williams Textbook of Endocrinology. 11th ed. Philadelphia, Pa: Saunders-Elsevier; 2008:569–671.
5. Eckman A, Dobs A. Drug-induced gynecomastia. Expert Opin Drug Saf. 2008;7:691-702.
6. Derkacz M, Chmiel-Perzyriska I, Nowakowski A. Gynecomastia – a difficult diagnostic problem. Endokrynol Pol. 2011;62:190-202.
7. Henley D, Lipson N, Kovach K, et al. Pubertal gynecomastia linked to lavender and tea tree oils. N Engl J Med. 2007;356:479-485.
8. Ma N, Geffnes M. Gynecomastia in prepubertal and pubertal boys. Curr Opin Pediatr. 2008;20:465-470.
9. Eberle AJ, Sparrow JT, Keenan BS. Treatment of persistent pubertal gynecomastia with dihydrotestosterone heptanoate. J Pediatr. 1986;109:144-149.
10. Kapoor S. Cutaneous manifestations of systemic condition associated with gynecomastia. Skinmed. 2010;8:87-92.
11. Johnson RE, Murad MH. Gynecomastia: pathophysiology, evaluation, and management. Mayo Clin Proc. 2009;84:1010-1015.
12. Evans GF, Anthony T, Turnage RH, et al. The diagnostic accuracy of mammography in the evaluation of male breast disease. Am J Surg. 2001;181:96-102.
13. Allen KJ, Gurrin LC, Constantine CC, et al. Iron-overload related disease in HFE hereditary hemochromatosis. N Engl J Med. 2008;358:221-230.
14. Sedlmeyer IL, Palmert MR. Delayed puberty: analysis of a large case series from an academic center. J Clin Endocrinol Metab. 2002;87:1613-1620.
15. Bhasin SI, Jameson JL. Disorders of the testes and male reproductive system. In: Longo D, Fauci AS, Kasper DL, et al, eds. Harrison’s Principles of Internal Medicine. 18th ed. New York, NY: McGraw-Hill; 2012:3019–3020.
16. Meikle AW. The interrelationships between thyroid dysfunction and hypogonadism in men and boys. Thyroid. 2004;14(suppl 1):S17-S25.
17. Wu FCW, Tajar A, Beynon JM, et al. Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med. 2010;363:123-135.
18. Di Lorenzo G, Autorino R, Perdona S, et al. Management of gynaecomastia in patients with prostate cancer: a systematic review. Lancet Oncol. 2005;6:972-979.
19. Mauras N, Bishop K, Merinbaum D, et al. Pharmacokinetics and pharmacodynamics of anastrozole in pubertal boys with recent onset gynecomastia. J Clin Endocrinol Metab. 2009;94:2975-2978.
20. Derman O, Kanbur N, Kilic I, et al. Long-term follow-up of tamoxifen treatment in adolescents with gynecomastia. J Pediatr Endocrinol Metab. 2008;21:449-453.
When your patients disclose ‘insider information’
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient is an officer in a large corporation. During therapy, he sometimes talks about how the company is doing. Would I risk malpractice liability if I used this information in managing my retirement investments?
Submitted by “Dr. B”
As most physicians find out within a short time of finishing medical school, doctors learn all kinds of useful things from their patients, including information that can help them manage personal matters outside their practices. But are you allowed to use nonpublic business information to make investment decisions?
As this article explains, legal rules and case law suggest that if psychiatrists or therapists act on potentially profitable business information incidentally mentioned by a patient during treatment, they may be subject to serious legal problems. To explain why, we’ll begin with a brief overview of business terms, including “securities” and “insider trading.” Then, to answer Dr. B’s question, we’ll look at what kind of legal consequences may result if mental health professionals are found guilty of “misappropriating” confidential business information.
Securities and security rules
Approximately one-half to two-thirds of Americans have money invested in the stock market—either through their retirement plans, by owning mutual funds, or by holding stocks of individual companies.1 Stocks are a type of financial instrument, or security, that companies issue to raise capital. Companies also raise money by issuing debt, typically in the form of bonds that pay interest to the holder, who in buying the bond has in effect loaned money to the company. Derivatives refer to securities that have prices that move up or down depending on the value of some underlying asset, such as stock prices.2
Stock prices fluctuate in reaction to general economic developments—changes in the unemployment rate, in the cost of basic materials (eg, oil or metals used in manufacturing), or in government policies that influence consumers’ purchasing decisions. But the key factor in determining the price of a company’s stock is investors’ beliefs about the company’s future earnings.3 Because investors usually have to make educated guesses about a company’s future, actually knowing something about a company before the general public finds out would give an investor a huge—but possibly unfair—advantage over other investors.
Making markets fair for all investors is the key purpose of U.S. laws on trading securities. In the 1930s, Congress created the Securities and Exchange Commission (SEC), a federal agency charged with ensuring that companies report the truth about their financial situation and that potential investors receive full, fair disclosure of available public information.4 Among the many ways that the SEC does this is by enforcing regulations concerning “insider trading.”
‘Insider trading’
Corporate “insiders” (eg, directors or employees) often know a lot about how their businesses are doing, and they buy or sell stock in their own companies. Such trading is legal if the insiders follow federal regulations about the timing of their investments and report them publicly.
Insider trading is illegal, however, if an individual acquires material, nonpublic information about a corporation through a relationship that involves trust and confidence and then uses that information when buying or selling a security. The SEC has prosecuted corporate employees who traded securities after learning of confidential developments in their companies, friends and family members of corporate officers who bought or sold securities after getting such information, and employees of law firms who misused information they received while providing services to corporations whose securities they traded.5
To be guilty of insider trading, a person must:
- buy or sell a security based on information that the person realizes is material and nonpublic,6 and
- have received the confidential information under circumstances that create a duty of trust or confidence.7
If both of these conditions are met, the person has wrongfully used confidential information with which he was entrusted, or “misappropriated” that information for personal gain.8
Physicians sometimes gain information that, if used for investment decisions, might lead to accusations of insider trading. Stock prices of pharmaceutical companies rise before public announcements of clinical drug trials, which suggests that information about those results leaks out in advance.9 Recently, physicians have gotten into well-publicized legal trouble by making investment decisions based on information they obtained while participating on an institution’s board10 and from learning early results of clinical drug trials.11
But would it be wrong for a psychiatrist to make a potentially profitable investment based on information obtained incidentally during a treatment encounter? After all, it’s not as though the psychiatrist would be a corporate insider or would have acquired the information improperly. Yet courts have ruled that a psychiatrist’s trading on such information might constitute malpractice and could be grounds for even more serious legal consequences.
Potential malpractice issues
The federal court ruling in United States v Willis12 describes how a psychiatrist learned during treatment that a patient’s husband was seeking to become CEO of a large bank. Realizing that this development might make the bank more valuable, the psychiatrist told his broker what he had learned and purchased 13,000 shares of the bank’s stock for himself and his children. When the husband’s efforts were announced publicly a few weeks later, the psychiatrist sold the shares at a big profit.
Quoting the vow of confidentiality contained in the Hippocratic Oath (Box),13 the court held that the psychiatrist had an obligation to the patient not to disclose information learned during her treatment without her permission. The court said the patient “had an economic interest in preserving the confidentiality of the information disclosed,” and the psychiatrist’s actions “might have jeopardized her husband’s advancement” and financial benefits the wife would have gained. Also, the psychiatrist’s “disclosures jeopardized the psychiatrist-patient relationship,” which might negate the wife’s financial investment in her care, require her to find a new psychiatrist, or require additional treatment to deal with how the psychiatrist’s behavior had affected her.12
And about whatever I may see or hear in treatment, or even without treatment, in the life of human beings—things that should not ever be blurted out outside—I will remain silent, holding such things to be unutterable.
Source: Reference 13
More legal consequences
Dr. Willis had legal problems more serious than just a malpractice lawsuit. He faced criminal prosecution for insider trading and mail fraud, and the court refused to dismiss these charges. The court reasoned that the psychiatrist received the information while in a position of trust and confidence, and breached that trust when he used that confidential information for his personal benefit—behavior that meets the legal definition of “misappropriation.” Because the psychiatrist received stock trade confirmations through the U.S. mail, he also could face federal charges of mail fraud. Ultimately, Dr. Willis pled guilty and paid $137,000 in fines and penalties. Although Dr. Willis retained his New Jersey medical license and avoided a prison sentence, the district court sentenced him to 5 years of probation and required that he perform 3,000 hours of community service.14,15
In a second case,16 a licensed clinical social worker made investments through a broker based on information learned during a therapy session about upcoming business developments (the 1994 Lockheed-Martin Marietta merger). The social worker pled guilty to insider trading, forfeited the illegal gains, and paid a large fine.
Related Resources
- Insider trading versus medical professionalism. Lancet. 2005;366(9488):781.
- Nijm LM. The online message board controversy. Physicians hit with claims of libel and insider trading by their employers. J Leg Med. 2000;21(2):223-239.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Jacobe D. In U.S., 54% have stock market investments, lowest since 1999. Gallup Economy. http://www.gallup.com/poll/147206/stock-market-investments-lowest-1999.aspx. Published April 20, 2011. Accessed October 9, 2012.
2. Roman S. Introduction to the mathematics of finance: from risk management to options pricing. New York NY: Springer-Verlag; 2004.
3. Elton EJ, Gruber MJ, Brown SJ, et al. Modern portfolio theory and investment analysis. Hoboken, NJ: John Wiley & Sons; 2010.
4. Keller E, Gehlmann GA. Introductory comment: a historical introduction to the Securities Act of 1933 and the Securities Exchange Act of 1934. Ohio State Law Journal. 1988;49:329-352.
5. U.S. Securities and Exchange Commission. Insider trading. http://www.sec.gov/answers/insider.htm. Published April 19, 2001. Accessed October 9, 2012.
6. 17 CFR 240. 10b5-1.
7. 17 CFR 240. 10b5-2.
8. United States v O’Hagan, 521 U.S. 642 (1997).
9. Rothenstein JM, Tomlinson G, Tannock IF, et al. Company stock prices before and after public announcements related to oncology drugs. J Natl Cancer Inst. 2011;103(20):1507-1512.
10. U.S. Securities and Exchange Commission. SEC charges five physicians with insider trading in stock of medical professional liability insurer. http://www.sec.gov/news/press/2012/2012-132.htm. Published July 10, 2012. Accessed October 9, 2012.
11. Two more are sentenced in insider trading cases. New York Times. December 21 2011:B9. http://www.nytimes.com/2011/12/22/business/in-crackdown-on-insider-trading-two-more-are-sentenced.html?_r=0. Accessed October 9, 2012.
12. United States v Willis, 737 F Supp 269 (SD NY 1990).
13. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
14. 24 Sec Reg & L Rep (BNA) 7 (1992).
15. Psychiatrist is sentenced. New York Times. January 8 1992. http://www.nytimes.com/1992/01/08/business/credit-markets-psychiatrist-is-sentenced.html. Accessed November 5, 2012.
16. SEC v Cooper, Litigation Rel. No. 14754, 60 S.E.C. Docket 2430 (1995).
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient is an officer in a large corporation. During therapy, he sometimes talks about how the company is doing. Would I risk malpractice liability if I used this information in managing my retirement investments?
Submitted by “Dr. B”
As most physicians find out within a short time of finishing medical school, doctors learn all kinds of useful things from their patients, including information that can help them manage personal matters outside their practices. But are you allowed to use nonpublic business information to make investment decisions?
As this article explains, legal rules and case law suggest that if psychiatrists or therapists act on potentially profitable business information incidentally mentioned by a patient during treatment, they may be subject to serious legal problems. To explain why, we’ll begin with a brief overview of business terms, including “securities” and “insider trading.” Then, to answer Dr. B’s question, we’ll look at what kind of legal consequences may result if mental health professionals are found guilty of “misappropriating” confidential business information.
Securities and security rules
Approximately one-half to two-thirds of Americans have money invested in the stock market—either through their retirement plans, by owning mutual funds, or by holding stocks of individual companies.1 Stocks are a type of financial instrument, or security, that companies issue to raise capital. Companies also raise money by issuing debt, typically in the form of bonds that pay interest to the holder, who in buying the bond has in effect loaned money to the company. Derivatives refer to securities that have prices that move up or down depending on the value of some underlying asset, such as stock prices.2
Stock prices fluctuate in reaction to general economic developments—changes in the unemployment rate, in the cost of basic materials (eg, oil or metals used in manufacturing), or in government policies that influence consumers’ purchasing decisions. But the key factor in determining the price of a company’s stock is investors’ beliefs about the company’s future earnings.3 Because investors usually have to make educated guesses about a company’s future, actually knowing something about a company before the general public finds out would give an investor a huge—but possibly unfair—advantage over other investors.
Making markets fair for all investors is the key purpose of U.S. laws on trading securities. In the 1930s, Congress created the Securities and Exchange Commission (SEC), a federal agency charged with ensuring that companies report the truth about their financial situation and that potential investors receive full, fair disclosure of available public information.4 Among the many ways that the SEC does this is by enforcing regulations concerning “insider trading.”
‘Insider trading’
Corporate “insiders” (eg, directors or employees) often know a lot about how their businesses are doing, and they buy or sell stock in their own companies. Such trading is legal if the insiders follow federal regulations about the timing of their investments and report them publicly.
Insider trading is illegal, however, if an individual acquires material, nonpublic information about a corporation through a relationship that involves trust and confidence and then uses that information when buying or selling a security. The SEC has prosecuted corporate employees who traded securities after learning of confidential developments in their companies, friends and family members of corporate officers who bought or sold securities after getting such information, and employees of law firms who misused information they received while providing services to corporations whose securities they traded.5
To be guilty of insider trading, a person must:
- buy or sell a security based on information that the person realizes is material and nonpublic,6 and
- have received the confidential information under circumstances that create a duty of trust or confidence.7
If both of these conditions are met, the person has wrongfully used confidential information with which he was entrusted, or “misappropriated” that information for personal gain.8
Physicians sometimes gain information that, if used for investment decisions, might lead to accusations of insider trading. Stock prices of pharmaceutical companies rise before public announcements of clinical drug trials, which suggests that information about those results leaks out in advance.9 Recently, physicians have gotten into well-publicized legal trouble by making investment decisions based on information they obtained while participating on an institution’s board10 and from learning early results of clinical drug trials.11
But would it be wrong for a psychiatrist to make a potentially profitable investment based on information obtained incidentally during a treatment encounter? After all, it’s not as though the psychiatrist would be a corporate insider or would have acquired the information improperly. Yet courts have ruled that a psychiatrist’s trading on such information might constitute malpractice and could be grounds for even more serious legal consequences.
Potential malpractice issues
The federal court ruling in United States v Willis12 describes how a psychiatrist learned during treatment that a patient’s husband was seeking to become CEO of a large bank. Realizing that this development might make the bank more valuable, the psychiatrist told his broker what he had learned and purchased 13,000 shares of the bank’s stock for himself and his children. When the husband’s efforts were announced publicly a few weeks later, the psychiatrist sold the shares at a big profit.
Quoting the vow of confidentiality contained in the Hippocratic Oath (Box),13 the court held that the psychiatrist had an obligation to the patient not to disclose information learned during her treatment without her permission. The court said the patient “had an economic interest in preserving the confidentiality of the information disclosed,” and the psychiatrist’s actions “might have jeopardized her husband’s advancement” and financial benefits the wife would have gained. Also, the psychiatrist’s “disclosures jeopardized the psychiatrist-patient relationship,” which might negate the wife’s financial investment in her care, require her to find a new psychiatrist, or require additional treatment to deal with how the psychiatrist’s behavior had affected her.12
And about whatever I may see or hear in treatment, or even without treatment, in the life of human beings—things that should not ever be blurted out outside—I will remain silent, holding such things to be unutterable.
Source: Reference 13
More legal consequences
Dr. Willis had legal problems more serious than just a malpractice lawsuit. He faced criminal prosecution for insider trading and mail fraud, and the court refused to dismiss these charges. The court reasoned that the psychiatrist received the information while in a position of trust and confidence, and breached that trust when he used that confidential information for his personal benefit—behavior that meets the legal definition of “misappropriation.” Because the psychiatrist received stock trade confirmations through the U.S. mail, he also could face federal charges of mail fraud. Ultimately, Dr. Willis pled guilty and paid $137,000 in fines and penalties. Although Dr. Willis retained his New Jersey medical license and avoided a prison sentence, the district court sentenced him to 5 years of probation and required that he perform 3,000 hours of community service.14,15
In a second case,16 a licensed clinical social worker made investments through a broker based on information learned during a therapy session about upcoming business developments (the 1994 Lockheed-Martin Marietta merger). The social worker pled guilty to insider trading, forfeited the illegal gains, and paid a large fine.
Related Resources
- Insider trading versus medical professionalism. Lancet. 2005;366(9488):781.
- Nijm LM. The online message board controversy. Physicians hit with claims of libel and insider trading by their employers. J Leg Med. 2000;21(2):223-239.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Discuss this article at www.facebook.com/CurrentPsychiatry
Dear Dr. Mossman:
My patient is an officer in a large corporation. During therapy, he sometimes talks about how the company is doing. Would I risk malpractice liability if I used this information in managing my retirement investments?
Submitted by “Dr. B”
As most physicians find out within a short time of finishing medical school, doctors learn all kinds of useful things from their patients, including information that can help them manage personal matters outside their practices. But are you allowed to use nonpublic business information to make investment decisions?
As this article explains, legal rules and case law suggest that if psychiatrists or therapists act on potentially profitable business information incidentally mentioned by a patient during treatment, they may be subject to serious legal problems. To explain why, we’ll begin with a brief overview of business terms, including “securities” and “insider trading.” Then, to answer Dr. B’s question, we’ll look at what kind of legal consequences may result if mental health professionals are found guilty of “misappropriating” confidential business information.
Securities and security rules
Approximately one-half to two-thirds of Americans have money invested in the stock market—either through their retirement plans, by owning mutual funds, or by holding stocks of individual companies.1 Stocks are a type of financial instrument, or security, that companies issue to raise capital. Companies also raise money by issuing debt, typically in the form of bonds that pay interest to the holder, who in buying the bond has in effect loaned money to the company. Derivatives refer to securities that have prices that move up or down depending on the value of some underlying asset, such as stock prices.2
Stock prices fluctuate in reaction to general economic developments—changes in the unemployment rate, in the cost of basic materials (eg, oil or metals used in manufacturing), or in government policies that influence consumers’ purchasing decisions. But the key factor in determining the price of a company’s stock is investors’ beliefs about the company’s future earnings.3 Because investors usually have to make educated guesses about a company’s future, actually knowing something about a company before the general public finds out would give an investor a huge—but possibly unfair—advantage over other investors.
Making markets fair for all investors is the key purpose of U.S. laws on trading securities. In the 1930s, Congress created the Securities and Exchange Commission (SEC), a federal agency charged with ensuring that companies report the truth about their financial situation and that potential investors receive full, fair disclosure of available public information.4 Among the many ways that the SEC does this is by enforcing regulations concerning “insider trading.”
‘Insider trading’
Corporate “insiders” (eg, directors or employees) often know a lot about how their businesses are doing, and they buy or sell stock in their own companies. Such trading is legal if the insiders follow federal regulations about the timing of their investments and report them publicly.
Insider trading is illegal, however, if an individual acquires material, nonpublic information about a corporation through a relationship that involves trust and confidence and then uses that information when buying or selling a security. The SEC has prosecuted corporate employees who traded securities after learning of confidential developments in their companies, friends and family members of corporate officers who bought or sold securities after getting such information, and employees of law firms who misused information they received while providing services to corporations whose securities they traded.5
To be guilty of insider trading, a person must:
- buy or sell a security based on information that the person realizes is material and nonpublic,6 and
- have received the confidential information under circumstances that create a duty of trust or confidence.7
If both of these conditions are met, the person has wrongfully used confidential information with which he was entrusted, or “misappropriated” that information for personal gain.8
Physicians sometimes gain information that, if used for investment decisions, might lead to accusations of insider trading. Stock prices of pharmaceutical companies rise before public announcements of clinical drug trials, which suggests that information about those results leaks out in advance.9 Recently, physicians have gotten into well-publicized legal trouble by making investment decisions based on information they obtained while participating on an institution’s board10 and from learning early results of clinical drug trials.11
But would it be wrong for a psychiatrist to make a potentially profitable investment based on information obtained incidentally during a treatment encounter? After all, it’s not as though the psychiatrist would be a corporate insider or would have acquired the information improperly. Yet courts have ruled that a psychiatrist’s trading on such information might constitute malpractice and could be grounds for even more serious legal consequences.
Potential malpractice issues
The federal court ruling in United States v Willis12 describes how a psychiatrist learned during treatment that a patient’s husband was seeking to become CEO of a large bank. Realizing that this development might make the bank more valuable, the psychiatrist told his broker what he had learned and purchased 13,000 shares of the bank’s stock for himself and his children. When the husband’s efforts were announced publicly a few weeks later, the psychiatrist sold the shares at a big profit.
Quoting the vow of confidentiality contained in the Hippocratic Oath (Box),13 the court held that the psychiatrist had an obligation to the patient not to disclose information learned during her treatment without her permission. The court said the patient “had an economic interest in preserving the confidentiality of the information disclosed,” and the psychiatrist’s actions “might have jeopardized her husband’s advancement” and financial benefits the wife would have gained. Also, the psychiatrist’s “disclosures jeopardized the psychiatrist-patient relationship,” which might negate the wife’s financial investment in her care, require her to find a new psychiatrist, or require additional treatment to deal with how the psychiatrist’s behavior had affected her.12
And about whatever I may see or hear in treatment, or even without treatment, in the life of human beings—things that should not ever be blurted out outside—I will remain silent, holding such things to be unutterable.
Source: Reference 13
More legal consequences
Dr. Willis had legal problems more serious than just a malpractice lawsuit. He faced criminal prosecution for insider trading and mail fraud, and the court refused to dismiss these charges. The court reasoned that the psychiatrist received the information while in a position of trust and confidence, and breached that trust when he used that confidential information for his personal benefit—behavior that meets the legal definition of “misappropriation.” Because the psychiatrist received stock trade confirmations through the U.S. mail, he also could face federal charges of mail fraud. Ultimately, Dr. Willis pled guilty and paid $137,000 in fines and penalties. Although Dr. Willis retained his New Jersey medical license and avoided a prison sentence, the district court sentenced him to 5 years of probation and required that he perform 3,000 hours of community service.14,15
In a second case,16 a licensed clinical social worker made investments through a broker based on information learned during a therapy session about upcoming business developments (the 1994 Lockheed-Martin Marietta merger). The social worker pled guilty to insider trading, forfeited the illegal gains, and paid a large fine.
Related Resources
- Insider trading versus medical professionalism. Lancet. 2005;366(9488):781.
- Nijm LM. The online message board controversy. Physicians hit with claims of libel and insider trading by their employers. J Leg Med. 2000;21(2):223-239.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Jacobe D. In U.S., 54% have stock market investments, lowest since 1999. Gallup Economy. http://www.gallup.com/poll/147206/stock-market-investments-lowest-1999.aspx. Published April 20, 2011. Accessed October 9, 2012.
2. Roman S. Introduction to the mathematics of finance: from risk management to options pricing. New York NY: Springer-Verlag; 2004.
3. Elton EJ, Gruber MJ, Brown SJ, et al. Modern portfolio theory and investment analysis. Hoboken, NJ: John Wiley & Sons; 2010.
4. Keller E, Gehlmann GA. Introductory comment: a historical introduction to the Securities Act of 1933 and the Securities Exchange Act of 1934. Ohio State Law Journal. 1988;49:329-352.
5. U.S. Securities and Exchange Commission. Insider trading. http://www.sec.gov/answers/insider.htm. Published April 19, 2001. Accessed October 9, 2012.
6. 17 CFR 240. 10b5-1.
7. 17 CFR 240. 10b5-2.
8. United States v O’Hagan, 521 U.S. 642 (1997).
9. Rothenstein JM, Tomlinson G, Tannock IF, et al. Company stock prices before and after public announcements related to oncology drugs. J Natl Cancer Inst. 2011;103(20):1507-1512.
10. U.S. Securities and Exchange Commission. SEC charges five physicians with insider trading in stock of medical professional liability insurer. http://www.sec.gov/news/press/2012/2012-132.htm. Published July 10, 2012. Accessed October 9, 2012.
11. Two more are sentenced in insider trading cases. New York Times. December 21 2011:B9. http://www.nytimes.com/2011/12/22/business/in-crackdown-on-insider-trading-two-more-are-sentenced.html?_r=0. Accessed October 9, 2012.
12. United States v Willis, 737 F Supp 269 (SD NY 1990).
13. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
14. 24 Sec Reg & L Rep (BNA) 7 (1992).
15. Psychiatrist is sentenced. New York Times. January 8 1992. http://www.nytimes.com/1992/01/08/business/credit-markets-psychiatrist-is-sentenced.html. Accessed November 5, 2012.
16. SEC v Cooper, Litigation Rel. No. 14754, 60 S.E.C. Docket 2430 (1995).
1. Jacobe D. In U.S., 54% have stock market investments, lowest since 1999. Gallup Economy. http://www.gallup.com/poll/147206/stock-market-investments-lowest-1999.aspx. Published April 20, 2011. Accessed October 9, 2012.
2. Roman S. Introduction to the mathematics of finance: from risk management to options pricing. New York NY: Springer-Verlag; 2004.
3. Elton EJ, Gruber MJ, Brown SJ, et al. Modern portfolio theory and investment analysis. Hoboken, NJ: John Wiley & Sons; 2010.
4. Keller E, Gehlmann GA. Introductory comment: a historical introduction to the Securities Act of 1933 and the Securities Exchange Act of 1934. Ohio State Law Journal. 1988;49:329-352.
5. U.S. Securities and Exchange Commission. Insider trading. http://www.sec.gov/answers/insider.htm. Published April 19, 2001. Accessed October 9, 2012.
6. 17 CFR 240. 10b5-1.
7. 17 CFR 240. 10b5-2.
8. United States v O’Hagan, 521 U.S. 642 (1997).
9. Rothenstein JM, Tomlinson G, Tannock IF, et al. Company stock prices before and after public announcements related to oncology drugs. J Natl Cancer Inst. 2011;103(20):1507-1512.
10. U.S. Securities and Exchange Commission. SEC charges five physicians with insider trading in stock of medical professional liability insurer. http://www.sec.gov/news/press/2012/2012-132.htm. Published July 10, 2012. Accessed October 9, 2012.
11. Two more are sentenced in insider trading cases. New York Times. December 21 2011:B9. http://www.nytimes.com/2011/12/22/business/in-crackdown-on-insider-trading-two-more-are-sentenced.html?_r=0. Accessed October 9, 2012.
12. United States v Willis, 737 F Supp 269 (SD NY 1990).
13. von Staden H. “In a pure and holy way”: personal and professional conduct in the Hippocratic Oath? J Hist Med Allied Sci. 1996;51(4):404-437.
14. 24 Sec Reg & L Rep (BNA) 7 (1992).
15. Psychiatrist is sentenced. New York Times. January 8 1992. http://www.nytimes.com/1992/01/08/business/credit-markets-psychiatrist-is-sentenced.html. Accessed November 5, 2012.
16. SEC v Cooper, Litigation Rel. No. 14754, 60 S.E.C. Docket 2430 (1995).
BRCA1/2 testing and cancer risk management in underserved women at a public hospital
Background and objective Genetic test uptake and cancer risk management have been understudied in medically underserved populations. Study aims were to quantify rates of BRCA1/2 genetic testing and evidence-based cancer risk management (ie, prophylactic surgeries and surveillance practices) in women who were seen for breast and ovarian cancer genetic counseling in a public, safety net health system.
Methods We conducted a retrospective medical record abstraction of 195 women who presented for breast or ovarian genetic counseling within a 2-year period (2008-2009) at Parkland Health & Hospital System in Dallas, Texas.
Results The identified women represented a racially and ethnically diverse population: 48% Hispanic, 37% non-Hispanic black, 12% non-Hispanic white, and 3% Asian. Among the 158 women who were medically eligible for genetic testing, 134 (84.8%) received BRCA1/2 results, with most tests funded through a financial assistance program. In all, 29 women (22%) tested positive for BRCA1/2 mutations. Financial and funding barriers were identified for 20 of the untested women. Among the identified high-risk women (mutation carriers, selected variants, and noncarriers with pretest BRCAPRO scores 30 or more), 26% had prophylactic breast surgeries and 33% had prophylactic ovarian surgeries within the follow-up period averaging 35 months. Of those who opted for surveillance, 71% had at least 1 mammogram or MRI and 38% had CA-125 tests. Trends indicated lower rates of all risk management behaviors, except for mammogram or MRI, among non-Hispanic black women.
Conclusions Within this racially and ethnically diverse sample, BRCA1/2 test uptake was high, but financial barriers were identified for nontested women. The rates of breast cancer risk management were generally comparable with other studies, but risk management for ovarian cancer was limited, especially among non-Hispanic black women. The reasons for these apparen disparities should be further explored.
Click on the PDF icon at the top of this introduction to read the full article.
Background and objective Genetic test uptake and cancer risk management have been understudied in medically underserved populations. Study aims were to quantify rates of BRCA1/2 genetic testing and evidence-based cancer risk management (ie, prophylactic surgeries and surveillance practices) in women who were seen for breast and ovarian cancer genetic counseling in a public, safety net health system.
Methods We conducted a retrospective medical record abstraction of 195 women who presented for breast or ovarian genetic counseling within a 2-year period (2008-2009) at Parkland Health & Hospital System in Dallas, Texas.
Results The identified women represented a racially and ethnically diverse population: 48% Hispanic, 37% non-Hispanic black, 12% non-Hispanic white, and 3% Asian. Among the 158 women who were medically eligible for genetic testing, 134 (84.8%) received BRCA1/2 results, with most tests funded through a financial assistance program. In all, 29 women (22%) tested positive for BRCA1/2 mutations. Financial and funding barriers were identified for 20 of the untested women. Among the identified high-risk women (mutation carriers, selected variants, and noncarriers with pretest BRCAPRO scores 30 or more), 26% had prophylactic breast surgeries and 33% had prophylactic ovarian surgeries within the follow-up period averaging 35 months. Of those who opted for surveillance, 71% had at least 1 mammogram or MRI and 38% had CA-125 tests. Trends indicated lower rates of all risk management behaviors, except for mammogram or MRI, among non-Hispanic black women.
Conclusions Within this racially and ethnically diverse sample, BRCA1/2 test uptake was high, but financial barriers were identified for nontested women. The rates of breast cancer risk management were generally comparable with other studies, but risk management for ovarian cancer was limited, especially among non-Hispanic black women. The reasons for these apparen disparities should be further explored.
Click on the PDF icon at the top of this introduction to read the full article.
Background and objective Genetic test uptake and cancer risk management have been understudied in medically underserved populations. Study aims were to quantify rates of BRCA1/2 genetic testing and evidence-based cancer risk management (ie, prophylactic surgeries and surveillance practices) in women who were seen for breast and ovarian cancer genetic counseling in a public, safety net health system.
Methods We conducted a retrospective medical record abstraction of 195 women who presented for breast or ovarian genetic counseling within a 2-year period (2008-2009) at Parkland Health & Hospital System in Dallas, Texas.
Results The identified women represented a racially and ethnically diverse population: 48% Hispanic, 37% non-Hispanic black, 12% non-Hispanic white, and 3% Asian. Among the 158 women who were medically eligible for genetic testing, 134 (84.8%) received BRCA1/2 results, with most tests funded through a financial assistance program. In all, 29 women (22%) tested positive for BRCA1/2 mutations. Financial and funding barriers were identified for 20 of the untested women. Among the identified high-risk women (mutation carriers, selected variants, and noncarriers with pretest BRCAPRO scores 30 or more), 26% had prophylactic breast surgeries and 33% had prophylactic ovarian surgeries within the follow-up period averaging 35 months. Of those who opted for surveillance, 71% had at least 1 mammogram or MRI and 38% had CA-125 tests. Trends indicated lower rates of all risk management behaviors, except for mammogram or MRI, among non-Hispanic black women.
Conclusions Within this racially and ethnically diverse sample, BRCA1/2 test uptake was high, but financial barriers were identified for nontested women. The rates of breast cancer risk management were generally comparable with other studies, but risk management for ovarian cancer was limited, especially among non-Hispanic black women. The reasons for these apparen disparities should be further explored.
Click on the PDF icon at the top of this introduction to read the full article.
Community Oncology Podcast - Pazopanib in soft tissue sarcoma
Dr. David Henry's podcast covers highlights of the November issue including pazopanib in soft tissue sarcoma and dasatinib in first-line treatment of chronic myeloid leukemia.
Dr. David Henry's podcast covers highlights of the November issue including pazopanib in soft tissue sarcoma and dasatinib in first-line treatment of chronic myeloid leukemia.
Dr. David Henry's podcast covers highlights of the November issue including pazopanib in soft tissue sarcoma and dasatinib in first-line treatment of chronic myeloid leukemia.