User login
Psychosocial Burden of Hidradenitis Suppurativa
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that typically presents as inflamed nodules, abscesses, and sinus tracts in the apocrine gland–bearing regions.
Chronic pain, fatigue, and social isolation put patients with HS at risk for psychiatric comorbidities, with the prevalence of depression estimated to be as high as 43%. Work productivity and sexual relationships may also be affected.
Early treatment of the condition, as well as screening for depression, may help alleviate the psychosocial burden of HS.
In this ReCAP, Dr Jennifer Hsiao from Keck School of Medicine, University of Southern California, Los Angeles, outlines mental health screening tools that dermatologists can use to help recognize at-risk patients and potentially refer them to mental health experts.
--
Jennifer Hsiao, MD, Associate Professor, Department of Dermatology, Keck School of Medicine, University of Southern California, Los Angeles, California
Jennifer Hsiao, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AbbVie; Boehringer Ingelheim; Novartis; UCB
Serve(d) as a speaker or a member of a speakers bureau for: AbbVie
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that typically presents as inflamed nodules, abscesses, and sinus tracts in the apocrine gland–bearing regions.
Chronic pain, fatigue, and social isolation put patients with HS at risk for psychiatric comorbidities, with the prevalence of depression estimated to be as high as 43%. Work productivity and sexual relationships may also be affected.
Early treatment of the condition, as well as screening for depression, may help alleviate the psychosocial burden of HS.
In this ReCAP, Dr Jennifer Hsiao from Keck School of Medicine, University of Southern California, Los Angeles, outlines mental health screening tools that dermatologists can use to help recognize at-risk patients and potentially refer them to mental health experts.
--
Jennifer Hsiao, MD, Associate Professor, Department of Dermatology, Keck School of Medicine, University of Southern California, Los Angeles, California
Jennifer Hsiao, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AbbVie; Boehringer Ingelheim; Novartis; UCB
Serve(d) as a speaker or a member of a speakers bureau for: AbbVie
Hidradenitis suppurativa (HS) is a chronic inflammatory skin disease that typically presents as inflamed nodules, abscesses, and sinus tracts in the apocrine gland–bearing regions.
Chronic pain, fatigue, and social isolation put patients with HS at risk for psychiatric comorbidities, with the prevalence of depression estimated to be as high as 43%. Work productivity and sexual relationships may also be affected.
Early treatment of the condition, as well as screening for depression, may help alleviate the psychosocial burden of HS.
In this ReCAP, Dr Jennifer Hsiao from Keck School of Medicine, University of Southern California, Los Angeles, outlines mental health screening tools that dermatologists can use to help recognize at-risk patients and potentially refer them to mental health experts.
--
Jennifer Hsiao, MD, Associate Professor, Department of Dermatology, Keck School of Medicine, University of Southern California, Los Angeles, California
Jennifer Hsiao, MD, has disclosed the following relevant financial relationships:
Serve(d) as a director, officer, partner, employee, advisor, consultant, or trustee for: AbbVie; Boehringer Ingelheim; Novartis; UCB
Serve(d) as a speaker or a member of a speakers bureau for: AbbVie

Pfizer COVID vaccine effective in young children, study shows
A new study shows the Pfizer vaccine is safe and highly effective against COVID-19 in children as young as 6 months old.
A three-dose series of the Pfizer COVID-19 vaccine was 73% effective at preventing symptomatic COVID-19 in children aged 6 months to 4 years, the researchers found. They also found that an examination of reactions and safety results “did not suggest any concerns.”
The study, published in the New England Journal of Medicine, included 1,776 children aged 6 months to 2 years old, and 2,750 children aged 2-4 years. Children were randomly assigned to receive either the three-shot series of the Pfizer vaccine or placebo shots. Participants received the first dose of the vaccine by March 31, 2022, and lived in Brazil, Finland, Poland, Spain, or the United States.
The authors wrote that having safe and effective COVID vaccines for young children is important to protect them from hospitalization or death and because young children play a role in spreading highly transmissible variants of the virus. COVID hospitalizations for children under 5 years old peaked at a rate of 14.5 per 100,000 in January 2022, the authors wrote, noting that the Omicron virus variant appeared to affect young children more severely than the previous variant, Delta.
When the researchers evaluated vaccine effectiveness by age group, they found that it prevented symptomatic COVID in 75.8% of children aged 6 months to 2 years, and in 71.8% of children aged 2-4 years.
Less than 0.5% of participants reported severe reactions to the vaccine. The most common reactions reported were tenderness or pain. Reactions typically appeared within the first couple days following vaccine administration and resolved within 2 days. No cases of inflammation of the heart muscle or its lining were reported among participants.
Uptake of COVID vaccines for young children has been lower than other age groups in the United States. The Centers for Disease Control and Prevention says 10% of children younger than 5 have received at least one dose of a COVID-19 vaccine, and 5% have completed a primary vaccine series.
A version of this article originally appeared on WebMD.com.
A new study shows the Pfizer vaccine is safe and highly effective against COVID-19 in children as young as 6 months old.
A three-dose series of the Pfizer COVID-19 vaccine was 73% effective at preventing symptomatic COVID-19 in children aged 6 months to 4 years, the researchers found. They also found that an examination of reactions and safety results “did not suggest any concerns.”
The study, published in the New England Journal of Medicine, included 1,776 children aged 6 months to 2 years old, and 2,750 children aged 2-4 years. Children were randomly assigned to receive either the three-shot series of the Pfizer vaccine or placebo shots. Participants received the first dose of the vaccine by March 31, 2022, and lived in Brazil, Finland, Poland, Spain, or the United States.
The authors wrote that having safe and effective COVID vaccines for young children is important to protect them from hospitalization or death and because young children play a role in spreading highly transmissible variants of the virus. COVID hospitalizations for children under 5 years old peaked at a rate of 14.5 per 100,000 in January 2022, the authors wrote, noting that the Omicron virus variant appeared to affect young children more severely than the previous variant, Delta.
When the researchers evaluated vaccine effectiveness by age group, they found that it prevented symptomatic COVID in 75.8% of children aged 6 months to 2 years, and in 71.8% of children aged 2-4 years.
Less than 0.5% of participants reported severe reactions to the vaccine. The most common reactions reported were tenderness or pain. Reactions typically appeared within the first couple days following vaccine administration and resolved within 2 days. No cases of inflammation of the heart muscle or its lining were reported among participants.
Uptake of COVID vaccines for young children has been lower than other age groups in the United States. The Centers for Disease Control and Prevention says 10% of children younger than 5 have received at least one dose of a COVID-19 vaccine, and 5% have completed a primary vaccine series.
A version of this article originally appeared on WebMD.com.
A new study shows the Pfizer vaccine is safe and highly effective against COVID-19 in children as young as 6 months old.
A three-dose series of the Pfizer COVID-19 vaccine was 73% effective at preventing symptomatic COVID-19 in children aged 6 months to 4 years, the researchers found. They also found that an examination of reactions and safety results “did not suggest any concerns.”
The study, published in the New England Journal of Medicine, included 1,776 children aged 6 months to 2 years old, and 2,750 children aged 2-4 years. Children were randomly assigned to receive either the three-shot series of the Pfizer vaccine or placebo shots. Participants received the first dose of the vaccine by March 31, 2022, and lived in Brazil, Finland, Poland, Spain, or the United States.
The authors wrote that having safe and effective COVID vaccines for young children is important to protect them from hospitalization or death and because young children play a role in spreading highly transmissible variants of the virus. COVID hospitalizations for children under 5 years old peaked at a rate of 14.5 per 100,000 in January 2022, the authors wrote, noting that the Omicron virus variant appeared to affect young children more severely than the previous variant, Delta.
When the researchers evaluated vaccine effectiveness by age group, they found that it prevented symptomatic COVID in 75.8% of children aged 6 months to 2 years, and in 71.8% of children aged 2-4 years.
Less than 0.5% of participants reported severe reactions to the vaccine. The most common reactions reported were tenderness or pain. Reactions typically appeared within the first couple days following vaccine administration and resolved within 2 days. No cases of inflammation of the heart muscle or its lining were reported among participants.
Uptake of COVID vaccines for young children has been lower than other age groups in the United States. The Centers for Disease Control and Prevention says 10% of children younger than 5 have received at least one dose of a COVID-19 vaccine, and 5% have completed a primary vaccine series.
A version of this article originally appeared on WebMD.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Obesity Workup
Are ‘Momi Pods’ the future of postnatal care?
Mindi Rosen met Seuli Brill, MD, at just the right time.
Ms. Rosen’s firstborn son was in the neointensive natal unit at The Ohio State University Wexner Medical Center in Columbus, and she didn’t have a pediatrician picked out yet for the baby. Nor did she have a primary care physician who could help her manage the gestational diabetes she developed during her pregnancy.
Dr. Brill, a clinical associate professor of internal medicine and pediatrics at Ohio State, suggested Ms. Rosen visit her at the new clinic she was piloting in Columbus. There, she provided pediatric care for newborns and primary care for mothers who had developed gestational diabetes.
“I looked at my husband, my husband looked at me, and I said: ‘Why not?’ “ Ms. Rosen, 38, recalled of that 2019 meeting. “I’m so glad she walked in at that moment.”
The mother of two is still part of the rapidly growing program at the medical facility that provides care for more than 200 mothers and babies.
Launched in 2018, the clinic – called the Multi-Modal Maternal Infant Perinatal Outpatient Delivery System, or “Momi Pods,” started with a focus on helping women with gestational diabetes, which occurs in up to 10% of pregnancies.
The program allows moms to book regular checkups for their baby, and then a follow-up appointment immediately after for themselves. Women are seen for the first 1,000 days (just under 3 years) after giving birth.
The idea was simple. Dr. Brill wanted to develop a more formalized program for the work she was already doing as a primary care physician and pediatrician. At the time, she was fielding referrals from specialists for young women who didn’t have a physician. She’d often develop a relationship with the patient over the years, go on to help oversee their care during pregnancy, then new mothers would select her as their newborn’s pediatrician.
“I would have a relationship with the mom when they did have the newborn, and then I would see the baby because I’m a pediatrician,” Dr. Brill said.
Dr. Brill was serving on the Ohio Gestational Diabetes Mellitus Collaborative, a state-backed program that aims to raise awareness about the condition and encourage more preventative care for patients. She presented her proposal to launch the program to the Ohio Department of Medicaid, which helped to fund the pilot.
The idea, she hoped, would improve postpartum follow-up care for mothers diagnosed with the condition.
Follow-up care is especially important for women who develop gestational diabetes because the condition raises their lifetime risk of developing type 2 diabetes up to 10-fold.
Yet most of those mothers don’t get the appropriate follow-up care during the crucial postpartum period, said Maya Subbalakshmi Venkataramani, MD, MPH, an assistant professor of medicine at Johns Hopkins University in Baltimore, who has researched parental care.
“Things get very busy after you have a child. There’s just the general logistics of a mom having to take care of a newborn and thinking about themselves,” Dr. Venkataramani, a primary care clinician and pediatrician, said. “A lot of parents in general may not put a lot of emphasis on their own health.”
Seeking care may be especially difficult for low-income mothers who might not have consistent health care coverage, she added.
In fact, only half of women who developed gestational diabetes received primary follow-up care, according to a study published in JAMA Network Open. The study, which examined more than 280,000 insurance claims between 2015 and 2018, found only 36% of women with gestational diabetes received the recommended blood glucose testing in the first 12 weeks of the postpartum period.
In the Momi Pods program, Dr. Brill checked in on Ms. Rosen’s gestational diabetes regularly during pediatric office visits for her newborn’s care. Ms. Rosen said whenever she brought her baby in for a visit during the postpartum period, Dr. Brill measured her blood sugar.
Dr. Brill and her team also asked how Ms. Rosen was doing physically and mentally during each visit. The screenings helped to catch a bout of postpartum depression Ms. Rosen experienced after the birth of her first son.
“I thought it was great, because honestly as a new mom I wouldn’t have followed up with myself so much,” Ms. Rosen said. “Every time you went into the doctor appointments, they’d ask you how you are doing. As a new mom, it’s so much easier to do it at the same time.”
Those who participate in the program are also more likely to complete postpartum visits with their ob.gyn. (95% vs. 58%, respectively; P < .001) than those who don’t participate, according to research Dr. Brill and colleagues published.
Dr. Brill began expanding the program’s reach nearly 2 years after its launch, targeting the services for women who are at risk for poor postpartum outcomes, including those with a history of depression, preterm labor, diabetes and congenital heart disease. Ob.gyns. in Ohio State’s network can refer their patients to the program, which now has 43 doctors trained to provide primary and pediatric care through Momi Pods. Soon-to-be moms can be referred to the program as early as the second trimester, Dr. Brill said.
Many of the mothers referred to the program don’t have a primary care clinician when they talk to Paola Beamon, RN, at Ohio State. Ms. Beamon reaches out to each referred patient over voicemail, a MyChart message, and even regular mail in hopes of helping them navigate the postpartum period. She also provides education on what a primary care clinician can offer new moms.
“Really, we’re pursuing these moms and doing everything we can so there’s less of a burden for them,” Ms. Beamon said. “A lot of them don’t even know what a primary care office does.”
One of the biggest perks to the program for new moms is that they don’t have to spend time and money traveling to a different doctor’s office, take time off work, or secure childcare in order to schedule a separate appointment for themselves, she said.
The program, which receives funding from the university and the state, even helps women get bus passes to a doctor’s appointment if needed.
Dyad programs targeting women with substance abuse disorders or mental health conditions have existed for many years. But catering to women with gestational diabetes or other medical conditions appears to be new. In part, Dr. Venkataramani said, because scheduling and space can be big hurdles to launch such a program, as well as finding doctors who can care for both baby and mother.
“There are logistical challenges to even doing this that makes it less common,” she said.
Dr. Brill said she is not aware of any other programs that are structured like the tandem care clinic at Ohio State. She hopes, however, that the program can be a model for other hospital systems to consider, and she is working to expand the program regionally. Her team is collecting data – including on the best way to schedule patients – to help other clinics develop something similar.
“We really want to leverage that expertise to make it easier for moms to get care with their infants and remove barriers to care,” she said.
A version of this article first appeared on Medscape.com.
Mindi Rosen met Seuli Brill, MD, at just the right time.
Ms. Rosen’s firstborn son was in the neointensive natal unit at The Ohio State University Wexner Medical Center in Columbus, and she didn’t have a pediatrician picked out yet for the baby. Nor did she have a primary care physician who could help her manage the gestational diabetes she developed during her pregnancy.
Dr. Brill, a clinical associate professor of internal medicine and pediatrics at Ohio State, suggested Ms. Rosen visit her at the new clinic she was piloting in Columbus. There, she provided pediatric care for newborns and primary care for mothers who had developed gestational diabetes.
“I looked at my husband, my husband looked at me, and I said: ‘Why not?’ “ Ms. Rosen, 38, recalled of that 2019 meeting. “I’m so glad she walked in at that moment.”
The mother of two is still part of the rapidly growing program at the medical facility that provides care for more than 200 mothers and babies.
Launched in 2018, the clinic – called the Multi-Modal Maternal Infant Perinatal Outpatient Delivery System, or “Momi Pods,” started with a focus on helping women with gestational diabetes, which occurs in up to 10% of pregnancies.
The program allows moms to book regular checkups for their baby, and then a follow-up appointment immediately after for themselves. Women are seen for the first 1,000 days (just under 3 years) after giving birth.
The idea was simple. Dr. Brill wanted to develop a more formalized program for the work she was already doing as a primary care physician and pediatrician. At the time, she was fielding referrals from specialists for young women who didn’t have a physician. She’d often develop a relationship with the patient over the years, go on to help oversee their care during pregnancy, then new mothers would select her as their newborn’s pediatrician.
“I would have a relationship with the mom when they did have the newborn, and then I would see the baby because I’m a pediatrician,” Dr. Brill said.
Dr. Brill was serving on the Ohio Gestational Diabetes Mellitus Collaborative, a state-backed program that aims to raise awareness about the condition and encourage more preventative care for patients. She presented her proposal to launch the program to the Ohio Department of Medicaid, which helped to fund the pilot.
The idea, she hoped, would improve postpartum follow-up care for mothers diagnosed with the condition.
Follow-up care is especially important for women who develop gestational diabetes because the condition raises their lifetime risk of developing type 2 diabetes up to 10-fold.
Yet most of those mothers don’t get the appropriate follow-up care during the crucial postpartum period, said Maya Subbalakshmi Venkataramani, MD, MPH, an assistant professor of medicine at Johns Hopkins University in Baltimore, who has researched parental care.
“Things get very busy after you have a child. There’s just the general logistics of a mom having to take care of a newborn and thinking about themselves,” Dr. Venkataramani, a primary care clinician and pediatrician, said. “A lot of parents in general may not put a lot of emphasis on their own health.”
Seeking care may be especially difficult for low-income mothers who might not have consistent health care coverage, she added.
In fact, only half of women who developed gestational diabetes received primary follow-up care, according to a study published in JAMA Network Open. The study, which examined more than 280,000 insurance claims between 2015 and 2018, found only 36% of women with gestational diabetes received the recommended blood glucose testing in the first 12 weeks of the postpartum period.
In the Momi Pods program, Dr. Brill checked in on Ms. Rosen’s gestational diabetes regularly during pediatric office visits for her newborn’s care. Ms. Rosen said whenever she brought her baby in for a visit during the postpartum period, Dr. Brill measured her blood sugar.
Dr. Brill and her team also asked how Ms. Rosen was doing physically and mentally during each visit. The screenings helped to catch a bout of postpartum depression Ms. Rosen experienced after the birth of her first son.
“I thought it was great, because honestly as a new mom I wouldn’t have followed up with myself so much,” Ms. Rosen said. “Every time you went into the doctor appointments, they’d ask you how you are doing. As a new mom, it’s so much easier to do it at the same time.”
Those who participate in the program are also more likely to complete postpartum visits with their ob.gyn. (95% vs. 58%, respectively; P < .001) than those who don’t participate, according to research Dr. Brill and colleagues published.
Dr. Brill began expanding the program’s reach nearly 2 years after its launch, targeting the services for women who are at risk for poor postpartum outcomes, including those with a history of depression, preterm labor, diabetes and congenital heart disease. Ob.gyns. in Ohio State’s network can refer their patients to the program, which now has 43 doctors trained to provide primary and pediatric care through Momi Pods. Soon-to-be moms can be referred to the program as early as the second trimester, Dr. Brill said.
Many of the mothers referred to the program don’t have a primary care clinician when they talk to Paola Beamon, RN, at Ohio State. Ms. Beamon reaches out to each referred patient over voicemail, a MyChart message, and even regular mail in hopes of helping them navigate the postpartum period. She also provides education on what a primary care clinician can offer new moms.
“Really, we’re pursuing these moms and doing everything we can so there’s less of a burden for them,” Ms. Beamon said. “A lot of them don’t even know what a primary care office does.”
One of the biggest perks to the program for new moms is that they don’t have to spend time and money traveling to a different doctor’s office, take time off work, or secure childcare in order to schedule a separate appointment for themselves, she said.
The program, which receives funding from the university and the state, even helps women get bus passes to a doctor’s appointment if needed.
Dyad programs targeting women with substance abuse disorders or mental health conditions have existed for many years. But catering to women with gestational diabetes or other medical conditions appears to be new. In part, Dr. Venkataramani said, because scheduling and space can be big hurdles to launch such a program, as well as finding doctors who can care for both baby and mother.
“There are logistical challenges to even doing this that makes it less common,” she said.
Dr. Brill said she is not aware of any other programs that are structured like the tandem care clinic at Ohio State. She hopes, however, that the program can be a model for other hospital systems to consider, and she is working to expand the program regionally. Her team is collecting data – including on the best way to schedule patients – to help other clinics develop something similar.
“We really want to leverage that expertise to make it easier for moms to get care with their infants and remove barriers to care,” she said.
A version of this article first appeared on Medscape.com.
Mindi Rosen met Seuli Brill, MD, at just the right time.
Ms. Rosen’s firstborn son was in the neointensive natal unit at The Ohio State University Wexner Medical Center in Columbus, and she didn’t have a pediatrician picked out yet for the baby. Nor did she have a primary care physician who could help her manage the gestational diabetes she developed during her pregnancy.
Dr. Brill, a clinical associate professor of internal medicine and pediatrics at Ohio State, suggested Ms. Rosen visit her at the new clinic she was piloting in Columbus. There, she provided pediatric care for newborns and primary care for mothers who had developed gestational diabetes.
“I looked at my husband, my husband looked at me, and I said: ‘Why not?’ “ Ms. Rosen, 38, recalled of that 2019 meeting. “I’m so glad she walked in at that moment.”
The mother of two is still part of the rapidly growing program at the medical facility that provides care for more than 200 mothers and babies.
Launched in 2018, the clinic – called the Multi-Modal Maternal Infant Perinatal Outpatient Delivery System, or “Momi Pods,” started with a focus on helping women with gestational diabetes, which occurs in up to 10% of pregnancies.
The program allows moms to book regular checkups for their baby, and then a follow-up appointment immediately after for themselves. Women are seen for the first 1,000 days (just under 3 years) after giving birth.
The idea was simple. Dr. Brill wanted to develop a more formalized program for the work she was already doing as a primary care physician and pediatrician. At the time, she was fielding referrals from specialists for young women who didn’t have a physician. She’d often develop a relationship with the patient over the years, go on to help oversee their care during pregnancy, then new mothers would select her as their newborn’s pediatrician.
“I would have a relationship with the mom when they did have the newborn, and then I would see the baby because I’m a pediatrician,” Dr. Brill said.
Dr. Brill was serving on the Ohio Gestational Diabetes Mellitus Collaborative, a state-backed program that aims to raise awareness about the condition and encourage more preventative care for patients. She presented her proposal to launch the program to the Ohio Department of Medicaid, which helped to fund the pilot.
The idea, she hoped, would improve postpartum follow-up care for mothers diagnosed with the condition.
Follow-up care is especially important for women who develop gestational diabetes because the condition raises their lifetime risk of developing type 2 diabetes up to 10-fold.
Yet most of those mothers don’t get the appropriate follow-up care during the crucial postpartum period, said Maya Subbalakshmi Venkataramani, MD, MPH, an assistant professor of medicine at Johns Hopkins University in Baltimore, who has researched parental care.
“Things get very busy after you have a child. There’s just the general logistics of a mom having to take care of a newborn and thinking about themselves,” Dr. Venkataramani, a primary care clinician and pediatrician, said. “A lot of parents in general may not put a lot of emphasis on their own health.”
Seeking care may be especially difficult for low-income mothers who might not have consistent health care coverage, she added.
In fact, only half of women who developed gestational diabetes received primary follow-up care, according to a study published in JAMA Network Open. The study, which examined more than 280,000 insurance claims between 2015 and 2018, found only 36% of women with gestational diabetes received the recommended blood glucose testing in the first 12 weeks of the postpartum period.
In the Momi Pods program, Dr. Brill checked in on Ms. Rosen’s gestational diabetes regularly during pediatric office visits for her newborn’s care. Ms. Rosen said whenever she brought her baby in for a visit during the postpartum period, Dr. Brill measured her blood sugar.
Dr. Brill and her team also asked how Ms. Rosen was doing physically and mentally during each visit. The screenings helped to catch a bout of postpartum depression Ms. Rosen experienced after the birth of her first son.
“I thought it was great, because honestly as a new mom I wouldn’t have followed up with myself so much,” Ms. Rosen said. “Every time you went into the doctor appointments, they’d ask you how you are doing. As a new mom, it’s so much easier to do it at the same time.”
Those who participate in the program are also more likely to complete postpartum visits with their ob.gyn. (95% vs. 58%, respectively; P < .001) than those who don’t participate, according to research Dr. Brill and colleagues published.
Dr. Brill began expanding the program’s reach nearly 2 years after its launch, targeting the services for women who are at risk for poor postpartum outcomes, including those with a history of depression, preterm labor, diabetes and congenital heart disease. Ob.gyns. in Ohio State’s network can refer their patients to the program, which now has 43 doctors trained to provide primary and pediatric care through Momi Pods. Soon-to-be moms can be referred to the program as early as the second trimester, Dr. Brill said.
Many of the mothers referred to the program don’t have a primary care clinician when they talk to Paola Beamon, RN, at Ohio State. Ms. Beamon reaches out to each referred patient over voicemail, a MyChart message, and even regular mail in hopes of helping them navigate the postpartum period. She also provides education on what a primary care clinician can offer new moms.
“Really, we’re pursuing these moms and doing everything we can so there’s less of a burden for them,” Ms. Beamon said. “A lot of them don’t even know what a primary care office does.”
One of the biggest perks to the program for new moms is that they don’t have to spend time and money traveling to a different doctor’s office, take time off work, or secure childcare in order to schedule a separate appointment for themselves, she said.
The program, which receives funding from the university and the state, even helps women get bus passes to a doctor’s appointment if needed.
Dyad programs targeting women with substance abuse disorders or mental health conditions have existed for many years. But catering to women with gestational diabetes or other medical conditions appears to be new. In part, Dr. Venkataramani said, because scheduling and space can be big hurdles to launch such a program, as well as finding doctors who can care for both baby and mother.
“There are logistical challenges to even doing this that makes it less common,” she said.
Dr. Brill said she is not aware of any other programs that are structured like the tandem care clinic at Ohio State. She hopes, however, that the program can be a model for other hospital systems to consider, and she is working to expand the program regionally. Her team is collecting data – including on the best way to schedule patients – to help other clinics develop something similar.
“We really want to leverage that expertise to make it easier for moms to get care with their infants and remove barriers to care,” she said.
A version of this article first appeared on Medscape.com.
Maternal infection in pregnancy ups risk for childhood leukemia?
Children born to mothers who had urinary or genital tract infections during pregnancy appear to have an increased risk for childhood leukemia, said researchers reporting a Danish registry analysis that may point to preventive strategies for the disease.
The research was published online in JAMA Network Open.
The team studied more than 2.2 million children born in Denmark over more than 3 decades, linking their records across multiple national registries to examine both later cancer risk and maternal infection rates.
They found that, overall, at least one maternal infection during pregnancy was associated with a 35% increased risk for leukemia in the children, rising to 65% for urinary tract infections, and 142% for genital infections.
“The findings of this large population-based cohort study suggest that maternal urinary and genital tract infections during pregnancy are associated with a higher risk of childhood leukemia in offspring,” said lead author Jian-Rong He, DPhil, division of birth cohort study, Guangzhou (China) Women and Children’s Medical Center.
However, he added, “the associated absolute risk remained small given the rarity” of the disease. In absolute terms, the risk difference between exposed and unexposed children was 1.8 cases per 100,000 person-years for any infection, 3.4 cases per 100,000 person-years for urinary traction infection, and 7.1 cases per 100,000 person-years for genital tract infection.
Maternal infections during pregnancy may be associated with chromosomal and immunologic alterations in the fetus, the authors speculated.
“Given that little is known about the etiology of childhood leukemia,” these results “suggest an important direction for research on the etiology of childhood leukemia as well as development of potential preventive measures,” they wrote.
In many countries, pregnant women are tested for urinary tract infection and bacterial vaginosis, and treated with antibiotics in antenatal care, as these infections are linked to adverse perinatal outcomes, they pointed out.
Study details
The team conducted a large population-based study that included all live births in Denmark between 1978 and 2015.
After exclusions, they gathered information on 2,222,797 children, linking data from several national registries, including the Danish Medical Birth Register, the Danish National Patient Registry, and the Danish National Cancer Registry, to identify cases of childhood cancers and maternal infection during pregnancy.
The results were then validated by comparing them with those in 2.6 million live births in Sweden between 1988 and 2014, for whom similar data were available through linkage with several Swedish registries.
The Danish cohort was followed up for a mean of 12 years per person, yielding a total of 27 million person-years. Just over half (51.3%) were boys.
Cancer was diagnosed in 4,362 children before 15 years of age, of whom 1,307 had leukemia (1,050 had acute lymphocytic leukemia), 1,267 had a brain tumor, 224 had lymphoma, and 1,564 had other cancers.
At least one infection during pregnancy was diagnosed in 81,717 mothers (3.7%). Urinary tract infections were the most common (in 1.7% of women), followed by genital tract infection (in 0.7%), digestive system infection (in 0.5%), and respiratory tract infection (in 0.3%).
Women with any infection during pregnancy were more likely to be younger and primiparous than were women who did not have infections, and they were also more likely to have fewer years of education, higher prepregnancy BMI, diabetes, and to smoke during early pregnancy.
Preterm delivery and low-birth-weight infants were also more common in women with infections during pregnancy.
Cox proportional hazards regression models revealed that, after adjustment for confounders, any maternal infection was associated with a hazard ratio of childhood leukemia of 1.35.
Further analysis revealed that the association was driven by genital tract infection, at a hazard ratio for childhood leukemia of 2.42, and urinary tract infection, at a hazard ratio 1.65.
Moreover, children born to women who had a sexually transmitted infection during pregnancy had a hazard ratio for developing leukemia of 3.13 compared with unexposed children.
There were no associations between other maternal infections and childhood leukemia.
The patterns of association between maternal infections and childhood leukemia were similar when looking at disease subtypes, as well as in the Swedish validation cohort, they added.
When interpreting the results, the researchers caution that, as data on maternal infection were drawn from hospital data, “milder infections and those not diagnosed or treated in specialized health care facilities were not captured.”
“Also, some infections could be captured because the mother sought care for other, more serious conditions, which might bias the association of maternal infections and childhood leukemia.”
The study was supported by grants from the China Scholarship Council–University of Oxford; National Natural Science Foundation of China; Danish Council for Independent Research; Nordic Cancer Union; Novo Nordisk Fonden; and the Swedish Council for Working Life and Social Research. Dr He reported receiving a PhD scholarship from the China Scholarship Council during the conduct of the study. Several other coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
Children born to mothers who had urinary or genital tract infections during pregnancy appear to have an increased risk for childhood leukemia, said researchers reporting a Danish registry analysis that may point to preventive strategies for the disease.
The research was published online in JAMA Network Open.
The team studied more than 2.2 million children born in Denmark over more than 3 decades, linking their records across multiple national registries to examine both later cancer risk and maternal infection rates.
They found that, overall, at least one maternal infection during pregnancy was associated with a 35% increased risk for leukemia in the children, rising to 65% for urinary tract infections, and 142% for genital infections.
“The findings of this large population-based cohort study suggest that maternal urinary and genital tract infections during pregnancy are associated with a higher risk of childhood leukemia in offspring,” said lead author Jian-Rong He, DPhil, division of birth cohort study, Guangzhou (China) Women and Children’s Medical Center.
However, he added, “the associated absolute risk remained small given the rarity” of the disease. In absolute terms, the risk difference between exposed and unexposed children was 1.8 cases per 100,000 person-years for any infection, 3.4 cases per 100,000 person-years for urinary traction infection, and 7.1 cases per 100,000 person-years for genital tract infection.
Maternal infections during pregnancy may be associated with chromosomal and immunologic alterations in the fetus, the authors speculated.
“Given that little is known about the etiology of childhood leukemia,” these results “suggest an important direction for research on the etiology of childhood leukemia as well as development of potential preventive measures,” they wrote.
In many countries, pregnant women are tested for urinary tract infection and bacterial vaginosis, and treated with antibiotics in antenatal care, as these infections are linked to adverse perinatal outcomes, they pointed out.
Study details
The team conducted a large population-based study that included all live births in Denmark between 1978 and 2015.
After exclusions, they gathered information on 2,222,797 children, linking data from several national registries, including the Danish Medical Birth Register, the Danish National Patient Registry, and the Danish National Cancer Registry, to identify cases of childhood cancers and maternal infection during pregnancy.
The results were then validated by comparing them with those in 2.6 million live births in Sweden between 1988 and 2014, for whom similar data were available through linkage with several Swedish registries.
The Danish cohort was followed up for a mean of 12 years per person, yielding a total of 27 million person-years. Just over half (51.3%) were boys.
Cancer was diagnosed in 4,362 children before 15 years of age, of whom 1,307 had leukemia (1,050 had acute lymphocytic leukemia), 1,267 had a brain tumor, 224 had lymphoma, and 1,564 had other cancers.
At least one infection during pregnancy was diagnosed in 81,717 mothers (3.7%). Urinary tract infections were the most common (in 1.7% of women), followed by genital tract infection (in 0.7%), digestive system infection (in 0.5%), and respiratory tract infection (in 0.3%).
Women with any infection during pregnancy were more likely to be younger and primiparous than were women who did not have infections, and they were also more likely to have fewer years of education, higher prepregnancy BMI, diabetes, and to smoke during early pregnancy.
Preterm delivery and low-birth-weight infants were also more common in women with infections during pregnancy.
Cox proportional hazards regression models revealed that, after adjustment for confounders, any maternal infection was associated with a hazard ratio of childhood leukemia of 1.35.
Further analysis revealed that the association was driven by genital tract infection, at a hazard ratio for childhood leukemia of 2.42, and urinary tract infection, at a hazard ratio 1.65.
Moreover, children born to women who had a sexually transmitted infection during pregnancy had a hazard ratio for developing leukemia of 3.13 compared with unexposed children.
There were no associations between other maternal infections and childhood leukemia.
The patterns of association between maternal infections and childhood leukemia were similar when looking at disease subtypes, as well as in the Swedish validation cohort, they added.
When interpreting the results, the researchers caution that, as data on maternal infection were drawn from hospital data, “milder infections and those not diagnosed or treated in specialized health care facilities were not captured.”
“Also, some infections could be captured because the mother sought care for other, more serious conditions, which might bias the association of maternal infections and childhood leukemia.”
The study was supported by grants from the China Scholarship Council–University of Oxford; National Natural Science Foundation of China; Danish Council for Independent Research; Nordic Cancer Union; Novo Nordisk Fonden; and the Swedish Council for Working Life and Social Research. Dr He reported receiving a PhD scholarship from the China Scholarship Council during the conduct of the study. Several other coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
Children born to mothers who had urinary or genital tract infections during pregnancy appear to have an increased risk for childhood leukemia, said researchers reporting a Danish registry analysis that may point to preventive strategies for the disease.
The research was published online in JAMA Network Open.
The team studied more than 2.2 million children born in Denmark over more than 3 decades, linking their records across multiple national registries to examine both later cancer risk and maternal infection rates.
They found that, overall, at least one maternal infection during pregnancy was associated with a 35% increased risk for leukemia in the children, rising to 65% for urinary tract infections, and 142% for genital infections.
“The findings of this large population-based cohort study suggest that maternal urinary and genital tract infections during pregnancy are associated with a higher risk of childhood leukemia in offspring,” said lead author Jian-Rong He, DPhil, division of birth cohort study, Guangzhou (China) Women and Children’s Medical Center.
However, he added, “the associated absolute risk remained small given the rarity” of the disease. In absolute terms, the risk difference between exposed and unexposed children was 1.8 cases per 100,000 person-years for any infection, 3.4 cases per 100,000 person-years for urinary traction infection, and 7.1 cases per 100,000 person-years for genital tract infection.
Maternal infections during pregnancy may be associated with chromosomal and immunologic alterations in the fetus, the authors speculated.
“Given that little is known about the etiology of childhood leukemia,” these results “suggest an important direction for research on the etiology of childhood leukemia as well as development of potential preventive measures,” they wrote.
In many countries, pregnant women are tested for urinary tract infection and bacterial vaginosis, and treated with antibiotics in antenatal care, as these infections are linked to adverse perinatal outcomes, they pointed out.
Study details
The team conducted a large population-based study that included all live births in Denmark between 1978 and 2015.
After exclusions, they gathered information on 2,222,797 children, linking data from several national registries, including the Danish Medical Birth Register, the Danish National Patient Registry, and the Danish National Cancer Registry, to identify cases of childhood cancers and maternal infection during pregnancy.
The results were then validated by comparing them with those in 2.6 million live births in Sweden between 1988 and 2014, for whom similar data were available through linkage with several Swedish registries.
The Danish cohort was followed up for a mean of 12 years per person, yielding a total of 27 million person-years. Just over half (51.3%) were boys.
Cancer was diagnosed in 4,362 children before 15 years of age, of whom 1,307 had leukemia (1,050 had acute lymphocytic leukemia), 1,267 had a brain tumor, 224 had lymphoma, and 1,564 had other cancers.
At least one infection during pregnancy was diagnosed in 81,717 mothers (3.7%). Urinary tract infections were the most common (in 1.7% of women), followed by genital tract infection (in 0.7%), digestive system infection (in 0.5%), and respiratory tract infection (in 0.3%).
Women with any infection during pregnancy were more likely to be younger and primiparous than were women who did not have infections, and they were also more likely to have fewer years of education, higher prepregnancy BMI, diabetes, and to smoke during early pregnancy.
Preterm delivery and low-birth-weight infants were also more common in women with infections during pregnancy.
Cox proportional hazards regression models revealed that, after adjustment for confounders, any maternal infection was associated with a hazard ratio of childhood leukemia of 1.35.
Further analysis revealed that the association was driven by genital tract infection, at a hazard ratio for childhood leukemia of 2.42, and urinary tract infection, at a hazard ratio 1.65.
Moreover, children born to women who had a sexually transmitted infection during pregnancy had a hazard ratio for developing leukemia of 3.13 compared with unexposed children.
There were no associations between other maternal infections and childhood leukemia.
The patterns of association between maternal infections and childhood leukemia were similar when looking at disease subtypes, as well as in the Swedish validation cohort, they added.
When interpreting the results, the researchers caution that, as data on maternal infection were drawn from hospital data, “milder infections and those not diagnosed or treated in specialized health care facilities were not captured.”
“Also, some infections could be captured because the mother sought care for other, more serious conditions, which might bias the association of maternal infections and childhood leukemia.”
The study was supported by grants from the China Scholarship Council–University of Oxford; National Natural Science Foundation of China; Danish Council for Independent Research; Nordic Cancer Union; Novo Nordisk Fonden; and the Swedish Council for Working Life and Social Research. Dr He reported receiving a PhD scholarship from the China Scholarship Council during the conduct of the study. Several other coauthors have disclosures; the full list can be found with the original article.
A version of this article originally appeared on Medscape.com.
New influx of Humira biosimilars may not drive immediate change
Gastroenterologists in 2023 will have more tools in their arsenal to treat patients with Crohn’s disease or ulcerative colitis. As many as 8-10 adalimumab biosimilars are anticipated to come on the market this year, giving mainstay drug Humira some vigorous competition.
Three scenarios will drive adalimumab biosimilar initiation: Insurance preference for the initial treatment of a newly diagnosed condition, a change in a patient’s insurance plan, or an insurance-mandated switch, said Edward C. Oldfield IV, MD, assistant professor at Eastern Virginia Medical School’s division of gastroenterology in Norfolk.
“Outside of these scenarios, I would encourage patients to remain on their current biologic so long as cost and accessibility remain stable,” said Dr. Oldfield.
Many factors will contribute to the success of biosimilars. Will physicians be prescribing them? How are biosimilars placed on formularies and will they be given preferred status? How will manufacturers price their biosimilars? “We have to wait and see to get the answers to these questions,” said Steven Newmark, JD, MPA, chief legal officer and director of policy, Global Healthy Living Foundation/CreakyJoints, a nonprofit advocacy organization based in New York.
Prescribing biosimilars is no different than prescribing originator biologics, so providers should know how to use them, said Mr. Newmark. “Most important will be the availability of patient-friendly resources that providers can share with their patients to provide education about and confidence in using biosimilars,” he added.
Overall, biosimilars are a good thing, said Dr. Oldfield. “In the long run they should bring down costs and increase access to medications for our patients.”
Others are skeptical that the adalimumab biosimilars will save patients much money.
Biosimilar laws were created to lower costs. However, if a patient with insurance pays only $5 a month out of pocket for Humira – a drug that normally costs $7,000 without coverage – it’s unlikely they would want to switch unless there’s comparable savings from the biosimilar, said Stephen B. Hanauer, MD, medical director of the Digestive Health Center and professor of medicine at Northwestern Medicine, Northwestern University, Evanston, Ill.
Like generics, Humira biosimilars may face some initial backlash, said Dr. Hanauer.
2023 broadens scope of adalimumab treatments
The American Gastroenterological Association describes a biosimilar as something that’s “highly similar to, but not an exact copy of, a biologic reference product already approved” by the Food and Drug Administration. Congress under the 2010 Affordable Care Act created a special, abbreviated pathway to approval for biosimilars.
AbbVie’s Humira, the global revenue for which exceeded $20 billion in 2021, has long dominated the U.S. market on injectable treatments for autoimmune diseases. The popular drug faces some competition in 2023, however, following a series of legal settlements that allowed AbbVie competitors to release their own adalimumab biosimilars.
“So far, we haven’t seen biosimilars live up to their potential in the U.S. in the inflammatory space,” said Mr. Newmark. This may change, however. Previously, biosimilars have required infusion, which demanded more time, commitment, and travel from patients. “The new set of forthcoming Humira biosimilars are injectables, an administration method preferred by patients,” he said.
The FDA will approve a biosimilar if it determines that the biological product is highly similar to the reference product, and that there are no clinically meaningful differences between the biological and reference product in terms of the safety, purity, and potency of the product.
The agency to date has approved 8 adalimumab biosimilars. These include: Idacio (adalimumab-aacf, Fresenius Kabi); Amjevita (adalimumab-atto, Amgen); Hadlima (adalimumab-bwwd, Organon); Cyltezo (adalimumab-adbm, Boehringer Ingelheim); Yusimry (adalimumab-aqvh from Coherus BioSciences); Hulio (adalimumab-fkjp; Mylan/Fujifilm Kyowa Kirin Biologics); Hyrimoz (adalimumab-adaz, Sandoz), and Abrilada (adalimumab-afzb, Pfizer).
“While FDA doesn’t formally track when products come to market, we know based on published reports that application holders for many of the currently FDA-approved biosimilars plan to market this year, starting with Amjevita being the first adalimumab biosimilar launched” in January, said Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars at the agency.
At press time, two other companies (Celltrion and Alvotech/Teva) were awaiting FDA approval for their adalimumab biosimilar drugs.
Among the eight approved drugs, Cyltezo is the only one that has a designation for interchangeability with Humira.
An interchangeable biosimilar may be substituted at the pharmacy without the intervention of the prescriber – much like generics are substituted, depending on state laws, said Dr. Yim. “However, in terms of safety and effectiveness, FDA’s standards for approval mean that biosimilar or interchangeable biosimilar products can be used in place of the reference product they were compared to.”
FDA-approved biosimilars undergo a rigorous evaluation for safety, effectiveness, and quality for their approved conditions of use, she continued. “Therefore, patients and health care providers can rely on a biosimilar to be as safe and effective for its approved uses as the original biological product.”
Remicade as a yardstick
Gastroenterologists dealt with this situation once before, when Remicade (infliximab) biosimilars came on the market in 2016, noted Miguel Regueiro, MD, chair of the Digestive Disease and Surgery Institute at the Cleveland Clinic.
Remicade and Humira are both tumor necrosis factor inhibitors with the same mechanism of action and many of the same indications. “We already had that experience with Remicade and biosimilar switch 2 or 3 years ago. Now we’re talking about Humira,” said Dr. Regueiro.
Most GI doctors have prescribed one of the more common infliximab biosimilars (Inflectra or Renflexis), noted Dr. Oldfield.
Cardinal Health, which recently surveyed 300 gastroenterologists, rheumatologists, and dermatologists about adalimumab biosimilars, found that gastroenterologists had the highest comfort level in prescribing them. Their top concern, however, was changing a patient from adalimumab to an adalimumab biosimilar.
For most patients, Dr. Oldfield sees the Humira reference biologic and biosimilar as equivalent.
However, he said he would change a patient’s drug only if there were a good reason or if his hand was forced by insurance. He would not make the change for a patient who recently began induction with the reference biologic or a patient with highly active clinical disease.
“While there is limited data to support this, I would also have some qualms about changing a patient from reference biologic to a biosimilar if they previously had immune-mediated pharmacokinetic failure due to antibody development with a biologic and were currently doing well on their new biologic,” he said.
Those with a new ulcerative colitis or Crohn’s diagnosis who are initiating a biologic for the first time might consider a biosimilar. If a patient is transitioning from a reference biologic to a biosimilar, “I would want to make that change during a time of stable remission and with the recognition that the switch is not a temporary switch, but a long-term switch,” he continued.
A paper that reviewed 23 observational studies of adalimumab and other biosimilars found that switching biosimilars was safe and effective. But if possible, patients should minimize the number of switches until more robust long-term data are available, added Dr. Oldfield.
If a patient is apprehensive about switching to a new therapy, “one may need to be cognizant of the ‘nocebo’ effect in which there is an unexplained or unfavorable therapeutic effect after switching,” he said.
Other gastroenterologists voiced similar reservations about switching. “I won’t use an adalimumab biosimilar unless the patient requests it, the insurance requires it, or there is a cost advantage for the patient such that they prefer it,” said Doug Wolf, MD, an Atlanta gastroenterologist.
“There is no medical treatment advantage to a biosimilar, especially if switching from Humira,” added Dr. Wolf.
Insurance will guide treatment
Once a drug is approved for use by the FDA, that drug will be available in all 50 states. “Different private insurance formularies, as well as state Medicaid formularies, might affect the actual ability of patients to receive such drugs,” said Mr. Newmark.
Patients should consult with their providers and insurance companies to see what therapies are available, he advised.
Dr. Hanauer anticipates some headaches arising for patients and doctors alike when negotiating for a specific drug.
Cyltezo may be the only biosimilar interchangeable with Humira, but the third-party pharmacy benefit manager (PBM) could negotiate for one of the noninterchangeable ones. “On a yearly basis they could switch their preference,” said Dr. Hanauer.
In the Cardinal Health survey, more than 60% of respondents said they would feel comfortable prescribing an adalimumab biosimilar only with an interchangeability designation.
A PBM may offer a patient Cyltezo if it’s cheaper than Humira. If the patient insists on staying on Humira, then they’ll have to pay more for that drug on their payer’s formulary, said Dr. Hanauer. In a worst-case scenario, a physician may have to appeal on a patient’s behalf to get Humira if the insurer offers only the biosimilar.
Taking that step to appeal is a major hassle for the physician, and leads to extra back door costs as well, said Dr. Hanauer.
Humira manufacturer AbbVie, in turn, may offer discounts and rebates to the PBMs to put Humira on their formulary. “That’s the AbbVie negotiating power. It’s not that the cost is going to be that much different. It’s going to be that there are rebates and discounts that are going to make the cost different,” he added.
As a community physician, Dr. Oldfield has specific concerns about accessibility.
The ever-increasing burden of insurance documentation and prior authorization means it can take weeks or months to get these medications approved. “The addition of new biosimilars is a welcome entrance if it can get patients the medications they need when they need it,” he said.
When it comes to prescribing biologics, many physicians rely on ancillary staff for assistance. It’s a team effort to sift through all the paperwork, observed Dr. Oldfield.
“While many community GI practices have specialized staff to deal with prior authorizations, they are still a far cry from the IBD [inflammatory bowel disease] academic centers where there are often pharmacists, nursing specialists, and home-monitoring programs to check in on patients,” he explained.
Landscape on cost is uncertain
At present, little is known about the cost of the biosimilars and impact on future drug pricing, said Dr. Oldfield.
At least for Medicare, Humira biosimilars will be considered Medicare Part D drugs if used for a medically accepted indication, said a spokesperson for the Centers for Medicare and Medicaid Services.
Part D sponsors (pharmacy and therapeutic committees) “will make the determination as to whether Amjevita and other products will be added to their formularies,” said the spokesperson.
Patients never saw a significant cost savings with Remicade biosimilars. “I imagine the same would be true with biosimilars for Humira,” said Dr. Regueiro. Patients may see greater access to these drugs, however, because the insurance plan or the pharmacy plan will make them more readily available, he added.
The hope is that, as biosimilars are introduced, the price of the originator biologic will go down, said Mr. Newmark. “Therefore, we can expect Humira to be offered at a lower price as it faces competition. Where it will sit in comparison to the forthcoming biosimilars will depend on how much biosimilar companies drop their price and how much pressure will be on PBMs and insurers to cover the lowest list price drug,” he said.
AbbVie did not respond to several requests for comment.
Charitable patient assistance programs for biosimilars or biologics can help offset the price of copayments, Mr. Newmark offered.
Ideally, insurers will offer designated biosimilars at a reduced or even no out-of-pocket expense on their formularies. This should lead to a decreased administrative burden for approval with streamlined (or even removal) of prior authorizations for certain medications, said Dr. Oldfield.
Without insurance or medication assistance programs, the cost of biosimilars is prohibitively expensive, he added.
“Biosimilars have higher research, development, and manufacturing costs than what people conventionally think of [for] a generic medication.”
Educating, advising patients
Dr. Oldfield advised that gastroenterologists refer to biologics by the generic name rather than branded name when initiating therapy unless there is a very specific reason not to. “This approach should make the process more streamlined and less subjected to quick denials for brand-only requests as biosimilars start to assume a larger market share,” he said.
Uptake of the Humira biosimilars also will depend on proper education of physicians and patients and their comfort level with the biosimilars, said Dr. Regueiro. Cleveland Clinic uses a team approach to educate on this topic, relying on pharmacists, clinicians, and nurses to explain that there’s no real difference between the reference drug and its biosimilars, based on efficacy and safety data.
Physicians can also direct patients to patient-friendly resources, said Mr. Newmark. “By starting the conversation early, it ensures that when/if the time comes that your patient is switched to or chooses a biosimilar they will feel more confident because they have the knowledge to make decisions about their care.”
The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars , is a free resource for patients, he added.
It’s important that doctors also understand these products so they can explain to their patients what to expect, said the FDA’s Dr. Yim. The FDA provides educational materials on its website, including a comprehensive curriculum toolkit.
Dr. Hanauer has served as a consultant for AbbVie, Amgen, American College of Gastroenterology, GlaxoSmithKline, American Gastroenterological Association, Pfizer, and a host of other companies . Dr. Regueiro has served on advisory boards and as a consultant for Abbvie, Janssen, UCB, Takeda, Pfizer, BMS, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET Pharma Solutions,Trellis, and Boehringer Ingelheim Pharmaceuticals. Dr. Wolf, Dr. Yim, Dr. Oldfield, and Mr. Newmark have no financial conflicts of interest.
Help your patients understand biologics and biosimilars by using AGA resources for providers and patients available at gastro.org/biosimilars .
Gastroenterologists in 2023 will have more tools in their arsenal to treat patients with Crohn’s disease or ulcerative colitis. As many as 8-10 adalimumab biosimilars are anticipated to come on the market this year, giving mainstay drug Humira some vigorous competition.
Three scenarios will drive adalimumab biosimilar initiation: Insurance preference for the initial treatment of a newly diagnosed condition, a change in a patient’s insurance plan, or an insurance-mandated switch, said Edward C. Oldfield IV, MD, assistant professor at Eastern Virginia Medical School’s division of gastroenterology in Norfolk.
“Outside of these scenarios, I would encourage patients to remain on their current biologic so long as cost and accessibility remain stable,” said Dr. Oldfield.
Many factors will contribute to the success of biosimilars. Will physicians be prescribing them? How are biosimilars placed on formularies and will they be given preferred status? How will manufacturers price their biosimilars? “We have to wait and see to get the answers to these questions,” said Steven Newmark, JD, MPA, chief legal officer and director of policy, Global Healthy Living Foundation/CreakyJoints, a nonprofit advocacy organization based in New York.
Prescribing biosimilars is no different than prescribing originator biologics, so providers should know how to use them, said Mr. Newmark. “Most important will be the availability of patient-friendly resources that providers can share with their patients to provide education about and confidence in using biosimilars,” he added.
Overall, biosimilars are a good thing, said Dr. Oldfield. “In the long run they should bring down costs and increase access to medications for our patients.”
Others are skeptical that the adalimumab biosimilars will save patients much money.
Biosimilar laws were created to lower costs. However, if a patient with insurance pays only $5 a month out of pocket for Humira – a drug that normally costs $7,000 without coverage – it’s unlikely they would want to switch unless there’s comparable savings from the biosimilar, said Stephen B. Hanauer, MD, medical director of the Digestive Health Center and professor of medicine at Northwestern Medicine, Northwestern University, Evanston, Ill.
Like generics, Humira biosimilars may face some initial backlash, said Dr. Hanauer.
2023 broadens scope of adalimumab treatments
The American Gastroenterological Association describes a biosimilar as something that’s “highly similar to, but not an exact copy of, a biologic reference product already approved” by the Food and Drug Administration. Congress under the 2010 Affordable Care Act created a special, abbreviated pathway to approval for biosimilars.
AbbVie’s Humira, the global revenue for which exceeded $20 billion in 2021, has long dominated the U.S. market on injectable treatments for autoimmune diseases. The popular drug faces some competition in 2023, however, following a series of legal settlements that allowed AbbVie competitors to release their own adalimumab biosimilars.
“So far, we haven’t seen biosimilars live up to their potential in the U.S. in the inflammatory space,” said Mr. Newmark. This may change, however. Previously, biosimilars have required infusion, which demanded more time, commitment, and travel from patients. “The new set of forthcoming Humira biosimilars are injectables, an administration method preferred by patients,” he said.
The FDA will approve a biosimilar if it determines that the biological product is highly similar to the reference product, and that there are no clinically meaningful differences between the biological and reference product in terms of the safety, purity, and potency of the product.
The agency to date has approved 8 adalimumab biosimilars. These include: Idacio (adalimumab-aacf, Fresenius Kabi); Amjevita (adalimumab-atto, Amgen); Hadlima (adalimumab-bwwd, Organon); Cyltezo (adalimumab-adbm, Boehringer Ingelheim); Yusimry (adalimumab-aqvh from Coherus BioSciences); Hulio (adalimumab-fkjp; Mylan/Fujifilm Kyowa Kirin Biologics); Hyrimoz (adalimumab-adaz, Sandoz), and Abrilada (adalimumab-afzb, Pfizer).
“While FDA doesn’t formally track when products come to market, we know based on published reports that application holders for many of the currently FDA-approved biosimilars plan to market this year, starting with Amjevita being the first adalimumab biosimilar launched” in January, said Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars at the agency.
At press time, two other companies (Celltrion and Alvotech/Teva) were awaiting FDA approval for their adalimumab biosimilar drugs.
Among the eight approved drugs, Cyltezo is the only one that has a designation for interchangeability with Humira.
An interchangeable biosimilar may be substituted at the pharmacy without the intervention of the prescriber – much like generics are substituted, depending on state laws, said Dr. Yim. “However, in terms of safety and effectiveness, FDA’s standards for approval mean that biosimilar or interchangeable biosimilar products can be used in place of the reference product they were compared to.”
FDA-approved biosimilars undergo a rigorous evaluation for safety, effectiveness, and quality for their approved conditions of use, she continued. “Therefore, patients and health care providers can rely on a biosimilar to be as safe and effective for its approved uses as the original biological product.”
Remicade as a yardstick
Gastroenterologists dealt with this situation once before, when Remicade (infliximab) biosimilars came on the market in 2016, noted Miguel Regueiro, MD, chair of the Digestive Disease and Surgery Institute at the Cleveland Clinic.
Remicade and Humira are both tumor necrosis factor inhibitors with the same mechanism of action and many of the same indications. “We already had that experience with Remicade and biosimilar switch 2 or 3 years ago. Now we’re talking about Humira,” said Dr. Regueiro.
Most GI doctors have prescribed one of the more common infliximab biosimilars (Inflectra or Renflexis), noted Dr. Oldfield.
Cardinal Health, which recently surveyed 300 gastroenterologists, rheumatologists, and dermatologists about adalimumab biosimilars, found that gastroenterologists had the highest comfort level in prescribing them. Their top concern, however, was changing a patient from adalimumab to an adalimumab biosimilar.
For most patients, Dr. Oldfield sees the Humira reference biologic and biosimilar as equivalent.
However, he said he would change a patient’s drug only if there were a good reason or if his hand was forced by insurance. He would not make the change for a patient who recently began induction with the reference biologic or a patient with highly active clinical disease.
“While there is limited data to support this, I would also have some qualms about changing a patient from reference biologic to a biosimilar if they previously had immune-mediated pharmacokinetic failure due to antibody development with a biologic and were currently doing well on their new biologic,” he said.
Those with a new ulcerative colitis or Crohn’s diagnosis who are initiating a biologic for the first time might consider a biosimilar. If a patient is transitioning from a reference biologic to a biosimilar, “I would want to make that change during a time of stable remission and with the recognition that the switch is not a temporary switch, but a long-term switch,” he continued.
A paper that reviewed 23 observational studies of adalimumab and other biosimilars found that switching biosimilars was safe and effective. But if possible, patients should minimize the number of switches until more robust long-term data are available, added Dr. Oldfield.
If a patient is apprehensive about switching to a new therapy, “one may need to be cognizant of the ‘nocebo’ effect in which there is an unexplained or unfavorable therapeutic effect after switching,” he said.
Other gastroenterologists voiced similar reservations about switching. “I won’t use an adalimumab biosimilar unless the patient requests it, the insurance requires it, or there is a cost advantage for the patient such that they prefer it,” said Doug Wolf, MD, an Atlanta gastroenterologist.
“There is no medical treatment advantage to a biosimilar, especially if switching from Humira,” added Dr. Wolf.
Insurance will guide treatment
Once a drug is approved for use by the FDA, that drug will be available in all 50 states. “Different private insurance formularies, as well as state Medicaid formularies, might affect the actual ability of patients to receive such drugs,” said Mr. Newmark.
Patients should consult with their providers and insurance companies to see what therapies are available, he advised.
Dr. Hanauer anticipates some headaches arising for patients and doctors alike when negotiating for a specific drug.
Cyltezo may be the only biosimilar interchangeable with Humira, but the third-party pharmacy benefit manager (PBM) could negotiate for one of the noninterchangeable ones. “On a yearly basis they could switch their preference,” said Dr. Hanauer.
In the Cardinal Health survey, more than 60% of respondents said they would feel comfortable prescribing an adalimumab biosimilar only with an interchangeability designation.
A PBM may offer a patient Cyltezo if it’s cheaper than Humira. If the patient insists on staying on Humira, then they’ll have to pay more for that drug on their payer’s formulary, said Dr. Hanauer. In a worst-case scenario, a physician may have to appeal on a patient’s behalf to get Humira if the insurer offers only the biosimilar.
Taking that step to appeal is a major hassle for the physician, and leads to extra back door costs as well, said Dr. Hanauer.
Humira manufacturer AbbVie, in turn, may offer discounts and rebates to the PBMs to put Humira on their formulary. “That’s the AbbVie negotiating power. It’s not that the cost is going to be that much different. It’s going to be that there are rebates and discounts that are going to make the cost different,” he added.
As a community physician, Dr. Oldfield has specific concerns about accessibility.
The ever-increasing burden of insurance documentation and prior authorization means it can take weeks or months to get these medications approved. “The addition of new biosimilars is a welcome entrance if it can get patients the medications they need when they need it,” he said.
When it comes to prescribing biologics, many physicians rely on ancillary staff for assistance. It’s a team effort to sift through all the paperwork, observed Dr. Oldfield.
“While many community GI practices have specialized staff to deal with prior authorizations, they are still a far cry from the IBD [inflammatory bowel disease] academic centers where there are often pharmacists, nursing specialists, and home-monitoring programs to check in on patients,” he explained.
Landscape on cost is uncertain
At present, little is known about the cost of the biosimilars and impact on future drug pricing, said Dr. Oldfield.
At least for Medicare, Humira biosimilars will be considered Medicare Part D drugs if used for a medically accepted indication, said a spokesperson for the Centers for Medicare and Medicaid Services.
Part D sponsors (pharmacy and therapeutic committees) “will make the determination as to whether Amjevita and other products will be added to their formularies,” said the spokesperson.
Patients never saw a significant cost savings with Remicade biosimilars. “I imagine the same would be true with biosimilars for Humira,” said Dr. Regueiro. Patients may see greater access to these drugs, however, because the insurance plan or the pharmacy plan will make them more readily available, he added.
The hope is that, as biosimilars are introduced, the price of the originator biologic will go down, said Mr. Newmark. “Therefore, we can expect Humira to be offered at a lower price as it faces competition. Where it will sit in comparison to the forthcoming biosimilars will depend on how much biosimilar companies drop their price and how much pressure will be on PBMs and insurers to cover the lowest list price drug,” he said.
AbbVie did not respond to several requests for comment.
Charitable patient assistance programs for biosimilars or biologics can help offset the price of copayments, Mr. Newmark offered.
Ideally, insurers will offer designated biosimilars at a reduced or even no out-of-pocket expense on their formularies. This should lead to a decreased administrative burden for approval with streamlined (or even removal) of prior authorizations for certain medications, said Dr. Oldfield.
Without insurance or medication assistance programs, the cost of biosimilars is prohibitively expensive, he added.
“Biosimilars have higher research, development, and manufacturing costs than what people conventionally think of [for] a generic medication.”
Educating, advising patients
Dr. Oldfield advised that gastroenterologists refer to biologics by the generic name rather than branded name when initiating therapy unless there is a very specific reason not to. “This approach should make the process more streamlined and less subjected to quick denials for brand-only requests as biosimilars start to assume a larger market share,” he said.
Uptake of the Humira biosimilars also will depend on proper education of physicians and patients and their comfort level with the biosimilars, said Dr. Regueiro. Cleveland Clinic uses a team approach to educate on this topic, relying on pharmacists, clinicians, and nurses to explain that there’s no real difference between the reference drug and its biosimilars, based on efficacy and safety data.
Physicians can also direct patients to patient-friendly resources, said Mr. Newmark. “By starting the conversation early, it ensures that when/if the time comes that your patient is switched to or chooses a biosimilar they will feel more confident because they have the knowledge to make decisions about their care.”
The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars , is a free resource for patients, he added.
It’s important that doctors also understand these products so they can explain to their patients what to expect, said the FDA’s Dr. Yim. The FDA provides educational materials on its website, including a comprehensive curriculum toolkit.
Dr. Hanauer has served as a consultant for AbbVie, Amgen, American College of Gastroenterology, GlaxoSmithKline, American Gastroenterological Association, Pfizer, and a host of other companies . Dr. Regueiro has served on advisory boards and as a consultant for Abbvie, Janssen, UCB, Takeda, Pfizer, BMS, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET Pharma Solutions,Trellis, and Boehringer Ingelheim Pharmaceuticals. Dr. Wolf, Dr. Yim, Dr. Oldfield, and Mr. Newmark have no financial conflicts of interest.
Help your patients understand biologics and biosimilars by using AGA resources for providers and patients available at gastro.org/biosimilars .
Gastroenterologists in 2023 will have more tools in their arsenal to treat patients with Crohn’s disease or ulcerative colitis. As many as 8-10 adalimumab biosimilars are anticipated to come on the market this year, giving mainstay drug Humira some vigorous competition.
Three scenarios will drive adalimumab biosimilar initiation: Insurance preference for the initial treatment of a newly diagnosed condition, a change in a patient’s insurance plan, or an insurance-mandated switch, said Edward C. Oldfield IV, MD, assistant professor at Eastern Virginia Medical School’s division of gastroenterology in Norfolk.
“Outside of these scenarios, I would encourage patients to remain on their current biologic so long as cost and accessibility remain stable,” said Dr. Oldfield.
Many factors will contribute to the success of biosimilars. Will physicians be prescribing them? How are biosimilars placed on formularies and will they be given preferred status? How will manufacturers price their biosimilars? “We have to wait and see to get the answers to these questions,” said Steven Newmark, JD, MPA, chief legal officer and director of policy, Global Healthy Living Foundation/CreakyJoints, a nonprofit advocacy organization based in New York.
Prescribing biosimilars is no different than prescribing originator biologics, so providers should know how to use them, said Mr. Newmark. “Most important will be the availability of patient-friendly resources that providers can share with their patients to provide education about and confidence in using biosimilars,” he added.
Overall, biosimilars are a good thing, said Dr. Oldfield. “In the long run they should bring down costs and increase access to medications for our patients.”
Others are skeptical that the adalimumab biosimilars will save patients much money.
Biosimilar laws were created to lower costs. However, if a patient with insurance pays only $5 a month out of pocket for Humira – a drug that normally costs $7,000 without coverage – it’s unlikely they would want to switch unless there’s comparable savings from the biosimilar, said Stephen B. Hanauer, MD, medical director of the Digestive Health Center and professor of medicine at Northwestern Medicine, Northwestern University, Evanston, Ill.
Like generics, Humira biosimilars may face some initial backlash, said Dr. Hanauer.
2023 broadens scope of adalimumab treatments
The American Gastroenterological Association describes a biosimilar as something that’s “highly similar to, but not an exact copy of, a biologic reference product already approved” by the Food and Drug Administration. Congress under the 2010 Affordable Care Act created a special, abbreviated pathway to approval for biosimilars.
AbbVie’s Humira, the global revenue for which exceeded $20 billion in 2021, has long dominated the U.S. market on injectable treatments for autoimmune diseases. The popular drug faces some competition in 2023, however, following a series of legal settlements that allowed AbbVie competitors to release their own adalimumab biosimilars.
“So far, we haven’t seen biosimilars live up to their potential in the U.S. in the inflammatory space,” said Mr. Newmark. This may change, however. Previously, biosimilars have required infusion, which demanded more time, commitment, and travel from patients. “The new set of forthcoming Humira biosimilars are injectables, an administration method preferred by patients,” he said.
The FDA will approve a biosimilar if it determines that the biological product is highly similar to the reference product, and that there are no clinically meaningful differences between the biological and reference product in terms of the safety, purity, and potency of the product.
The agency to date has approved 8 adalimumab biosimilars. These include: Idacio (adalimumab-aacf, Fresenius Kabi); Amjevita (adalimumab-atto, Amgen); Hadlima (adalimumab-bwwd, Organon); Cyltezo (adalimumab-adbm, Boehringer Ingelheim); Yusimry (adalimumab-aqvh from Coherus BioSciences); Hulio (adalimumab-fkjp; Mylan/Fujifilm Kyowa Kirin Biologics); Hyrimoz (adalimumab-adaz, Sandoz), and Abrilada (adalimumab-afzb, Pfizer).
“While FDA doesn’t formally track when products come to market, we know based on published reports that application holders for many of the currently FDA-approved biosimilars plan to market this year, starting with Amjevita being the first adalimumab biosimilar launched” in January, said Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars at the agency.
At press time, two other companies (Celltrion and Alvotech/Teva) were awaiting FDA approval for their adalimumab biosimilar drugs.
Among the eight approved drugs, Cyltezo is the only one that has a designation for interchangeability with Humira.
An interchangeable biosimilar may be substituted at the pharmacy without the intervention of the prescriber – much like generics are substituted, depending on state laws, said Dr. Yim. “However, in terms of safety and effectiveness, FDA’s standards for approval mean that biosimilar or interchangeable biosimilar products can be used in place of the reference product they were compared to.”
FDA-approved biosimilars undergo a rigorous evaluation for safety, effectiveness, and quality for their approved conditions of use, she continued. “Therefore, patients and health care providers can rely on a biosimilar to be as safe and effective for its approved uses as the original biological product.”
Remicade as a yardstick
Gastroenterologists dealt with this situation once before, when Remicade (infliximab) biosimilars came on the market in 2016, noted Miguel Regueiro, MD, chair of the Digestive Disease and Surgery Institute at the Cleveland Clinic.
Remicade and Humira are both tumor necrosis factor inhibitors with the same mechanism of action and many of the same indications. “We already had that experience with Remicade and biosimilar switch 2 or 3 years ago. Now we’re talking about Humira,” said Dr. Regueiro.
Most GI doctors have prescribed one of the more common infliximab biosimilars (Inflectra or Renflexis), noted Dr. Oldfield.
Cardinal Health, which recently surveyed 300 gastroenterologists, rheumatologists, and dermatologists about adalimumab biosimilars, found that gastroenterologists had the highest comfort level in prescribing them. Their top concern, however, was changing a patient from adalimumab to an adalimumab biosimilar.
For most patients, Dr. Oldfield sees the Humira reference biologic and biosimilar as equivalent.
However, he said he would change a patient’s drug only if there were a good reason or if his hand was forced by insurance. He would not make the change for a patient who recently began induction with the reference biologic or a patient with highly active clinical disease.
“While there is limited data to support this, I would also have some qualms about changing a patient from reference biologic to a biosimilar if they previously had immune-mediated pharmacokinetic failure due to antibody development with a biologic and were currently doing well on their new biologic,” he said.
Those with a new ulcerative colitis or Crohn’s diagnosis who are initiating a biologic for the first time might consider a biosimilar. If a patient is transitioning from a reference biologic to a biosimilar, “I would want to make that change during a time of stable remission and with the recognition that the switch is not a temporary switch, but a long-term switch,” he continued.
A paper that reviewed 23 observational studies of adalimumab and other biosimilars found that switching biosimilars was safe and effective. But if possible, patients should minimize the number of switches until more robust long-term data are available, added Dr. Oldfield.
If a patient is apprehensive about switching to a new therapy, “one may need to be cognizant of the ‘nocebo’ effect in which there is an unexplained or unfavorable therapeutic effect after switching,” he said.
Other gastroenterologists voiced similar reservations about switching. “I won’t use an adalimumab biosimilar unless the patient requests it, the insurance requires it, or there is a cost advantage for the patient such that they prefer it,” said Doug Wolf, MD, an Atlanta gastroenterologist.
“There is no medical treatment advantage to a biosimilar, especially if switching from Humira,” added Dr. Wolf.
Insurance will guide treatment
Once a drug is approved for use by the FDA, that drug will be available in all 50 states. “Different private insurance formularies, as well as state Medicaid formularies, might affect the actual ability of patients to receive such drugs,” said Mr. Newmark.
Patients should consult with their providers and insurance companies to see what therapies are available, he advised.
Dr. Hanauer anticipates some headaches arising for patients and doctors alike when negotiating for a specific drug.
Cyltezo may be the only biosimilar interchangeable with Humira, but the third-party pharmacy benefit manager (PBM) could negotiate for one of the noninterchangeable ones. “On a yearly basis they could switch their preference,” said Dr. Hanauer.
In the Cardinal Health survey, more than 60% of respondents said they would feel comfortable prescribing an adalimumab biosimilar only with an interchangeability designation.
A PBM may offer a patient Cyltezo if it’s cheaper than Humira. If the patient insists on staying on Humira, then they’ll have to pay more for that drug on their payer’s formulary, said Dr. Hanauer. In a worst-case scenario, a physician may have to appeal on a patient’s behalf to get Humira if the insurer offers only the biosimilar.
Taking that step to appeal is a major hassle for the physician, and leads to extra back door costs as well, said Dr. Hanauer.
Humira manufacturer AbbVie, in turn, may offer discounts and rebates to the PBMs to put Humira on their formulary. “That’s the AbbVie negotiating power. It’s not that the cost is going to be that much different. It’s going to be that there are rebates and discounts that are going to make the cost different,” he added.
As a community physician, Dr. Oldfield has specific concerns about accessibility.
The ever-increasing burden of insurance documentation and prior authorization means it can take weeks or months to get these medications approved. “The addition of new biosimilars is a welcome entrance if it can get patients the medications they need when they need it,” he said.
When it comes to prescribing biologics, many physicians rely on ancillary staff for assistance. It’s a team effort to sift through all the paperwork, observed Dr. Oldfield.
“While many community GI practices have specialized staff to deal with prior authorizations, they are still a far cry from the IBD [inflammatory bowel disease] academic centers where there are often pharmacists, nursing specialists, and home-monitoring programs to check in on patients,” he explained.
Landscape on cost is uncertain
At present, little is known about the cost of the biosimilars and impact on future drug pricing, said Dr. Oldfield.
At least for Medicare, Humira biosimilars will be considered Medicare Part D drugs if used for a medically accepted indication, said a spokesperson for the Centers for Medicare and Medicaid Services.
Part D sponsors (pharmacy and therapeutic committees) “will make the determination as to whether Amjevita and other products will be added to their formularies,” said the spokesperson.
Patients never saw a significant cost savings with Remicade biosimilars. “I imagine the same would be true with biosimilars for Humira,” said Dr. Regueiro. Patients may see greater access to these drugs, however, because the insurance plan or the pharmacy plan will make them more readily available, he added.
The hope is that, as biosimilars are introduced, the price of the originator biologic will go down, said Mr. Newmark. “Therefore, we can expect Humira to be offered at a lower price as it faces competition. Where it will sit in comparison to the forthcoming biosimilars will depend on how much biosimilar companies drop their price and how much pressure will be on PBMs and insurers to cover the lowest list price drug,” he said.
AbbVie did not respond to several requests for comment.
Charitable patient assistance programs for biosimilars or biologics can help offset the price of copayments, Mr. Newmark offered.
Ideally, insurers will offer designated biosimilars at a reduced or even no out-of-pocket expense on their formularies. This should lead to a decreased administrative burden for approval with streamlined (or even removal) of prior authorizations for certain medications, said Dr. Oldfield.
Without insurance or medication assistance programs, the cost of biosimilars is prohibitively expensive, he added.
“Biosimilars have higher research, development, and manufacturing costs than what people conventionally think of [for] a generic medication.”
Educating, advising patients
Dr. Oldfield advised that gastroenterologists refer to biologics by the generic name rather than branded name when initiating therapy unless there is a very specific reason not to. “This approach should make the process more streamlined and less subjected to quick denials for brand-only requests as biosimilars start to assume a larger market share,” he said.
Uptake of the Humira biosimilars also will depend on proper education of physicians and patients and their comfort level with the biosimilars, said Dr. Regueiro. Cleveland Clinic uses a team approach to educate on this topic, relying on pharmacists, clinicians, and nurses to explain that there’s no real difference between the reference drug and its biosimilars, based on efficacy and safety data.
Physicians can also direct patients to patient-friendly resources, said Mr. Newmark. “By starting the conversation early, it ensures that when/if the time comes that your patient is switched to or chooses a biosimilar they will feel more confident because they have the knowledge to make decisions about their care.”
The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars , is a free resource for patients, he added.
It’s important that doctors also understand these products so they can explain to their patients what to expect, said the FDA’s Dr. Yim. The FDA provides educational materials on its website, including a comprehensive curriculum toolkit.
Dr. Hanauer has served as a consultant for AbbVie, Amgen, American College of Gastroenterology, GlaxoSmithKline, American Gastroenterological Association, Pfizer, and a host of other companies . Dr. Regueiro has served on advisory boards and as a consultant for Abbvie, Janssen, UCB, Takeda, Pfizer, BMS, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET Pharma Solutions,Trellis, and Boehringer Ingelheim Pharmaceuticals. Dr. Wolf, Dr. Yim, Dr. Oldfield, and Mr. Newmark have no financial conflicts of interest.
Help your patients understand biologics and biosimilars by using AGA resources for providers and patients available at gastro.org/biosimilars .
New influx of Humira biosimilars may not drive immediate change
Gastroenterologists in 2023 will have more tools in their arsenal to treat patients with Crohn’s disease or ulcerative colitis. As many as 8-10 adalimumab biosimilars are anticipated to come on the market this year, giving mainstay drug Humira some vigorous competition.
Three scenarios will drive adalimumab biosimilar initiation: Insurance preference for the initial treatment of a newly diagnosed condition, a change in a patient’s insurance plan, or an insurance-mandated switch, said Edward C. Oldfield IV, MD, assistant professor at Eastern Virginia Medical School’s division of gastroenterology in Norfolk.
“Outside of these scenarios, I would encourage patients to remain on their current biologic so long as cost and accessibility remain stable,” said Dr. Oldfield.
Many factors will contribute to the success of biosimilars. Will physicians be prescribing them? How are biosimilars placed on formularies and will they be given preferred status? How will manufacturers price their biosimilars? “We have to wait and see to get the answers to these questions,” said Steven Newmark, JD, MPA, chief legal officer and director of policy, Global Healthy Living Foundation/CreakyJoints, a nonprofit advocacy organization based in New York.
Prescribing biosimilars is no different than prescribing originator biologics, so providers should know how to use them, said Mr. Newmark. “Most important will be the availability of patient-friendly resources that providers can share with their patients to provide education about and confidence in using biosimilars,” he added.
Overall, biosimilars are a good thing, said Dr. Oldfield. “In the long run they should bring down costs and increase access to medications for our patients.”
Others are skeptical that the adalimumab biosimilars will save patients much money.
Biosimilar laws were created to lower costs. However, if a patient with insurance pays only $5 a month out of pocket for Humira – a drug that normally costs $7,000 without coverage – it’s unlikely they would want to switch unless there’s comparable savings from the biosimilar, said Stephen B. Hanauer, MD, medical director of the Digestive Health Center and professor of medicine at Northwestern Medicine, Northwestern University, Evanston, Ill.
Like generics, Humira biosimilars may face some initial backlash, said Dr. Hanauer.
2023 broadens scope of adalimumab treatments
The American Gastroenterological Association describes a biosimilar as something that’s “highly similar to, but not an exact copy of, a biologic reference product already approved” by the Food and Drug Administration. Congress under the 2010 Affordable Care Act created a special, abbreviated pathway to approval for biosimilars.
AbbVie’s Humira, the global revenue for which exceeded $20 billion in 2021, has long dominated the U.S. market on injectable treatments for autoimmune diseases. The popular drug faces some competition in 2023, however, following a series of legal settlements that allowed AbbVie competitors to release their own adalimumab biosimilars.
“So far, we haven’t seen biosimilars live up to their potential in the U.S. in the inflammatory space,” said Mr. Newmark. This may change, however. Previously, biosimilars have required infusion, which demanded more time, commitment, and travel from patients. “The new set of forthcoming Humira biosimilars are injectables, an administration method preferred by patients,” he said.
The FDA will approve a biosimilar if it determines that the biological product is highly similar to the reference product, and that there are no clinically meaningful differences between the biological and reference product in terms of the safety, purity, and potency of the product.
The agency to date has approved 8 adalimumab biosimilars. These include: Idacio (adalimumab-aacf, Fresenius Kabi); Amjevita (adalimumab-atto, Amgen); Hadlima (adalimumab-bwwd, Organon); Cyltezo (adalimumab-adbm, Boehringer Ingelheim); Yusimry (adalimumab-aqvh from Coherus BioSciences); Hulio (adalimumab-fkjp; Mylan/Fujifilm Kyowa Kirin Biologics); Hyrimoz (adalimumab-adaz, Sandoz), and Abrilada (adalimumab-afzb, Pfizer).
“While FDA doesn’t formally track when products come to market, we know based on published reports that application holders for many of the currently FDA-approved biosimilars plan to market this year, starting with Amjevita being the first adalimumab biosimilar launched” in January, said Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars at the agency.
At press time, two other companies (Celltrion and Alvotech/Teva) were awaiting FDA approval for their adalimumab biosimilar drugs.
Among the eight approved drugs, Cyltezo is the only one that has a designation for interchangeability with Humira.
An interchangeable biosimilar may be substituted at the pharmacy without the intervention of the prescriber – much like generics are substituted, depending on state laws, said Dr. Yim. “However, in terms of safety and effectiveness, FDA’s standards for approval mean that biosimilar or interchangeable biosimilar products can be used in place of the reference product they were compared to.”
FDA-approved biosimilars undergo a rigorous evaluation for safety, effectiveness, and quality for their approved conditions of use, she continued. “Therefore, patients and health care providers can rely on a biosimilar to be as safe and effective for its approved uses as the original biological product.”
Remicade as a yard stick
Gastroenterologists dealt with this situation once before, when Remicade (infliximab) biosimilars came on the market in 2016, noted Miguel Regueiro, MD, chair of the Digestive Disease and Surgery Institute at the Cleveland Clinic.
Remicade and Humira are both tumor necrosis factor inhibitors with the same mechanism of action and many of the same indications. “We already had that experience with Remicade and biosimilar switch 2 or 3 years ago. Now we’re talking about Humira,” said Dr. Regueiro.
Most GI doctors have prescribed one of the more common infliximab biosimilars (Inflectra or Renflexis), noted Dr. Oldfield.
Cardinal Health, which recently surveyed 300 gastroenterologists, rheumatologists, and dermatologists about adalimumab biosimilars, found that gastroenterologists had the highest comfort level in prescribing them. Their top concern, however, was changing a patient from adalimumab to an adalimumab biosimilar.
For most patients, Dr. Oldfield sees the Humira reference biologic and biosimilar as equivalent.
However, he said he would change a patient’s drug only if there were a good reason or if his hand was forced by insurance. He would not make the change for a patient who recently began induction with the reference biologic or a patient with highly active clinical disease.
“While there is limited data to support this, I would also have some qualms about changing a patient from reference biologic to a biosimilar if they previously had immune-mediated pharmacokinetic failure due to antibody development with a biologic and were currently doing well on their new biologic,” he said.
Those with a new ulcerative colitis or Crohn’s diagnosis who are initiating a biologic for the first time might consider a biosimilar. If a patient is transitioning from a reference biologic to a biosimilar, “I would want to make that change during a time of stable remission and with the recognition that the switch is not a temporary switch, but a long-term switch,” he continued.
A paper that reviewed 23 observational studies of adalimumab and other biosimilars found that switching biosimilars was safe and effective. But if possible, patients should minimize the number of switches until more robust long-term data are available, added Dr. Oldfield.
If a patient is apprehensive about switching to a new therapy, “one may need to be cognizant of the ‘nocebo’ effect in which there is an unexplained or unfavorable therapeutic effect after switching,” he said.
Other gastroenterologists voiced similar reservations about switching. “I won’t use an adalimumab biosimilar unless the patient requests it, the insurance requires it, or there is a cost advantage for the patient such that they prefer it,” said Doug Wolf, MD, an Atlanta gastroenterologist.
“There is no medical treatment advantage to a biosimilar, especially if switching from Humira,” added Dr. Wolf.
Insurance will guide treatment
Once a drug is approved for use by the FDA, that drug will be available in all 50 states. “Different private insurance formularies, as well as state Medicaid formularies, might affect the actual ability of patients to receive such drugs,” said Mr. Newmark.
Patients should consult with their providers and insurance companies to see what therapies are available, he advised.
Dr. Hanauer anticipates some headaches arising for patients and doctors alike when negotiating for a specific drug.
Cyltezo may be the only biosimilar interchangeable with Humira, but the third-party pharmacy benefit manager (PBM) could negotiate for one of the noninterchangeable ones. “On a yearly basis they could switch their preference,” said Dr. Hanauer.
In the Cardinal Health survey, more than 60% of respondents said they would feel comfortable prescribing an adalimumab biosimilar only with an interchangeability designation.
A PBM may offer a patient Cyltezo if it’s cheaper than Humira. If the patient insists on staying on Humira, then they’ll have to pay more for that drug on their payer’s formulary, said Dr. Hanauer. In a worst-case scenario, a physician may have to appeal on a patient’s behalf to get Humira if the insurer offers only the biosimilar.
Taking that step to appeal is a major hassle for the physician, and leads to extra back door costs as well, said Dr. Hanauer.
Humira manufacturer AbbVie, in turn, may offer discounts and rebates to the PBMs to put Humira on their formulary. “That’s the AbbVie negotiating power. It’s not that the cost is going to be that much different. It’s going to be that there are rebates and discounts that are going to make the cost different,” he added.
As a community physician, Dr. Oldfield has specific concerns about accessibility.
The ever-increasing burden of insurance documentation and prior authorization means it can take weeks or months to get these medications approved. “The addition of new biosimilars is a welcome entrance if it can get patients the medications they need when they need it,” he said.
When it comes to prescribing biologics, many physicians rely on ancillary staff for assistance. It’s a team effort to sift through all the paperwork, observed Dr. Oldfield.
“While many community GI practices have specialized staff to deal with prior authorizations, they are still a far cry from the IBD [inflammatory bowel disease] academic centers where there are often pharmacists, nursing specialists, and home-monitoring programs to check in on patients,” he explained.
Landscape on cost is uncertain
At present, little is known about the cost of the biosimilars and impact on future drug pricing, said Dr. Oldfield.
At least for Medicare, Humira biosimilars will be considered Medicare Part D drugs if used for a medically accepted indication, said a spokesperson for the Centers for Medicare and Medicaid Services.
Part D sponsors (pharmacy and therapeutic committees) “will make the determination as to whether Amjevita and other products will be added to their formularies,” said the spokesperson.
Patients never saw a significant cost savings with Remicade biosimilars. “I imagine the same would be true with biosimilars for Humira,” said Dr. Regueiro. Patients may see greater access to these drugs, however, because the insurance plan or the pharmacy plan will make them more readily available, he added.
The hope is that, as biosimilars are introduced, the price of the originator biologic will go down, said Mr. Newmark. “Therefore, we can expect Humira to be offered at a lower price as it faces competition. Where it will sit in comparison to the forthcoming biosimilars will depend on how much biosimilar companies drop their price and how much pressure will be on PBMs and insurers to cover the lowest list price drug,” he said.
AbbVie did not respond to several requests for comment.
Charitable patient assistance programs for biosimilars or biologics can help offset the price of copayments, Mr. Newmark offered.
Ideally, insurers will offer designated biosimilars at a reduced or even no out-of-pocket expense on their formularies. This should lead to a decreased administrative burden for approval with streamlined (or even removal) of prior authorizations for certain medications, said Dr. Oldfield.
Without insurance or medication assistance programs, the cost of biosimilars is prohibitively expensive, he added.
“Biosimilars have higher research, development, and manufacturing costs than what people conventionally think of [for] a generic medication.”
Educating, advising patients
Dr. Oldfield advised that gastroenterologists refer to biologics by the generic name rather than branded name when initiating therapy unless there is a very specific reason not to. “This approach should make the process more streamlined and less subjected to quick denials for brand-only requests as biosimilars start to assume a larger market share,” he said.
Uptake of the Humira biosimilars also will depend on proper education of physicians and patients and their comfort level with the biosimilars, said Dr. Regueiro. Cleveland Clinic uses a team approach to educate on this topic, relying on pharmacists, clinicians, and nurses to explain that there’s no real difference between the reference drug and its biosimilars, based on efficacy and safety data.
Physicians can also direct patients to patient-friendly resources, said Mr. Newmark. “By starting the conversation early, it ensures that when/if the time comes that your patient is switched to or chooses a biosimilar they will feel more confident because they have the knowledge to make decisions about their care.”
The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars , is a free resource for patients, he added.
It’s important that doctors also understand these products so they can explain to their patients what to expect, said the FDA’s Dr. Yim. The FDA provides educational materials on its website, including a comprehensive curriculum toolkit.
Dr. Hanauer has served as a consultant for AbbVie, Amgen, American College of Gastroenterology, GlaxoSmithKline, American Gastroenterological Association, Pfizer, and a host of other companies . Dr. Regueiro has served on advisory boards and as a consultant for Abbvie, Janssen, UCB, Takeda, Pfizer, BMS, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET Pharma Solutions,Trellis, and Boehringer Ingelheim Pharmaceuticals. Dr. Wolf, Dr. Yim, Dr. Oldfield, and Mr. Newmark have no financial conflicts of interest.
Gastroenterologists in 2023 will have more tools in their arsenal to treat patients with Crohn’s disease or ulcerative colitis. As many as 8-10 adalimumab biosimilars are anticipated to come on the market this year, giving mainstay drug Humira some vigorous competition.
Three scenarios will drive adalimumab biosimilar initiation: Insurance preference for the initial treatment of a newly diagnosed condition, a change in a patient’s insurance plan, or an insurance-mandated switch, said Edward C. Oldfield IV, MD, assistant professor at Eastern Virginia Medical School’s division of gastroenterology in Norfolk.
“Outside of these scenarios, I would encourage patients to remain on their current biologic so long as cost and accessibility remain stable,” said Dr. Oldfield.
Many factors will contribute to the success of biosimilars. Will physicians be prescribing them? How are biosimilars placed on formularies and will they be given preferred status? How will manufacturers price their biosimilars? “We have to wait and see to get the answers to these questions,” said Steven Newmark, JD, MPA, chief legal officer and director of policy, Global Healthy Living Foundation/CreakyJoints, a nonprofit advocacy organization based in New York.
Prescribing biosimilars is no different than prescribing originator biologics, so providers should know how to use them, said Mr. Newmark. “Most important will be the availability of patient-friendly resources that providers can share with their patients to provide education about and confidence in using biosimilars,” he added.
Overall, biosimilars are a good thing, said Dr. Oldfield. “In the long run they should bring down costs and increase access to medications for our patients.”
Others are skeptical that the adalimumab biosimilars will save patients much money.
Biosimilar laws were created to lower costs. However, if a patient with insurance pays only $5 a month out of pocket for Humira – a drug that normally costs $7,000 without coverage – it’s unlikely they would want to switch unless there’s comparable savings from the biosimilar, said Stephen B. Hanauer, MD, medical director of the Digestive Health Center and professor of medicine at Northwestern Medicine, Northwestern University, Evanston, Ill.
Like generics, Humira biosimilars may face some initial backlash, said Dr. Hanauer.
2023 broadens scope of adalimumab treatments
The American Gastroenterological Association describes a biosimilar as something that’s “highly similar to, but not an exact copy of, a biologic reference product already approved” by the Food and Drug Administration. Congress under the 2010 Affordable Care Act created a special, abbreviated pathway to approval for biosimilars.
AbbVie’s Humira, the global revenue for which exceeded $20 billion in 2021, has long dominated the U.S. market on injectable treatments for autoimmune diseases. The popular drug faces some competition in 2023, however, following a series of legal settlements that allowed AbbVie competitors to release their own adalimumab biosimilars.
“So far, we haven’t seen biosimilars live up to their potential in the U.S. in the inflammatory space,” said Mr. Newmark. This may change, however. Previously, biosimilars have required infusion, which demanded more time, commitment, and travel from patients. “The new set of forthcoming Humira biosimilars are injectables, an administration method preferred by patients,” he said.
The FDA will approve a biosimilar if it determines that the biological product is highly similar to the reference product, and that there are no clinically meaningful differences between the biological and reference product in terms of the safety, purity, and potency of the product.
The agency to date has approved 8 adalimumab biosimilars. These include: Idacio (adalimumab-aacf, Fresenius Kabi); Amjevita (adalimumab-atto, Amgen); Hadlima (adalimumab-bwwd, Organon); Cyltezo (adalimumab-adbm, Boehringer Ingelheim); Yusimry (adalimumab-aqvh from Coherus BioSciences); Hulio (adalimumab-fkjp; Mylan/Fujifilm Kyowa Kirin Biologics); Hyrimoz (adalimumab-adaz, Sandoz), and Abrilada (adalimumab-afzb, Pfizer).
“While FDA doesn’t formally track when products come to market, we know based on published reports that application holders for many of the currently FDA-approved biosimilars plan to market this year, starting with Amjevita being the first adalimumab biosimilar launched” in January, said Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars at the agency.
At press time, two other companies (Celltrion and Alvotech/Teva) were awaiting FDA approval for their adalimumab biosimilar drugs.
Among the eight approved drugs, Cyltezo is the only one that has a designation for interchangeability with Humira.
An interchangeable biosimilar may be substituted at the pharmacy without the intervention of the prescriber – much like generics are substituted, depending on state laws, said Dr. Yim. “However, in terms of safety and effectiveness, FDA’s standards for approval mean that biosimilar or interchangeable biosimilar products can be used in place of the reference product they were compared to.”
FDA-approved biosimilars undergo a rigorous evaluation for safety, effectiveness, and quality for their approved conditions of use, she continued. “Therefore, patients and health care providers can rely on a biosimilar to be as safe and effective for its approved uses as the original biological product.”
Remicade as a yard stick
Gastroenterologists dealt with this situation once before, when Remicade (infliximab) biosimilars came on the market in 2016, noted Miguel Regueiro, MD, chair of the Digestive Disease and Surgery Institute at the Cleveland Clinic.
Remicade and Humira are both tumor necrosis factor inhibitors with the same mechanism of action and many of the same indications. “We already had that experience with Remicade and biosimilar switch 2 or 3 years ago. Now we’re talking about Humira,” said Dr. Regueiro.
Most GI doctors have prescribed one of the more common infliximab biosimilars (Inflectra or Renflexis), noted Dr. Oldfield.
Cardinal Health, which recently surveyed 300 gastroenterologists, rheumatologists, and dermatologists about adalimumab biosimilars, found that gastroenterologists had the highest comfort level in prescribing them. Their top concern, however, was changing a patient from adalimumab to an adalimumab biosimilar.
For most patients, Dr. Oldfield sees the Humira reference biologic and biosimilar as equivalent.
However, he said he would change a patient’s drug only if there were a good reason or if his hand was forced by insurance. He would not make the change for a patient who recently began induction with the reference biologic or a patient with highly active clinical disease.
“While there is limited data to support this, I would also have some qualms about changing a patient from reference biologic to a biosimilar if they previously had immune-mediated pharmacokinetic failure due to antibody development with a biologic and were currently doing well on their new biologic,” he said.
Those with a new ulcerative colitis or Crohn’s diagnosis who are initiating a biologic for the first time might consider a biosimilar. If a patient is transitioning from a reference biologic to a biosimilar, “I would want to make that change during a time of stable remission and with the recognition that the switch is not a temporary switch, but a long-term switch,” he continued.
A paper that reviewed 23 observational studies of adalimumab and other biosimilars found that switching biosimilars was safe and effective. But if possible, patients should minimize the number of switches until more robust long-term data are available, added Dr. Oldfield.
If a patient is apprehensive about switching to a new therapy, “one may need to be cognizant of the ‘nocebo’ effect in which there is an unexplained or unfavorable therapeutic effect after switching,” he said.
Other gastroenterologists voiced similar reservations about switching. “I won’t use an adalimumab biosimilar unless the patient requests it, the insurance requires it, or there is a cost advantage for the patient such that they prefer it,” said Doug Wolf, MD, an Atlanta gastroenterologist.
“There is no medical treatment advantage to a biosimilar, especially if switching from Humira,” added Dr. Wolf.
Insurance will guide treatment
Once a drug is approved for use by the FDA, that drug will be available in all 50 states. “Different private insurance formularies, as well as state Medicaid formularies, might affect the actual ability of patients to receive such drugs,” said Mr. Newmark.
Patients should consult with their providers and insurance companies to see what therapies are available, he advised.
Dr. Hanauer anticipates some headaches arising for patients and doctors alike when negotiating for a specific drug.
Cyltezo may be the only biosimilar interchangeable with Humira, but the third-party pharmacy benefit manager (PBM) could negotiate for one of the noninterchangeable ones. “On a yearly basis they could switch their preference,” said Dr. Hanauer.
In the Cardinal Health survey, more than 60% of respondents said they would feel comfortable prescribing an adalimumab biosimilar only with an interchangeability designation.
A PBM may offer a patient Cyltezo if it’s cheaper than Humira. If the patient insists on staying on Humira, then they’ll have to pay more for that drug on their payer’s formulary, said Dr. Hanauer. In a worst-case scenario, a physician may have to appeal on a patient’s behalf to get Humira if the insurer offers only the biosimilar.
Taking that step to appeal is a major hassle for the physician, and leads to extra back door costs as well, said Dr. Hanauer.
Humira manufacturer AbbVie, in turn, may offer discounts and rebates to the PBMs to put Humira on their formulary. “That’s the AbbVie negotiating power. It’s not that the cost is going to be that much different. It’s going to be that there are rebates and discounts that are going to make the cost different,” he added.
As a community physician, Dr. Oldfield has specific concerns about accessibility.
The ever-increasing burden of insurance documentation and prior authorization means it can take weeks or months to get these medications approved. “The addition of new biosimilars is a welcome entrance if it can get patients the medications they need when they need it,” he said.
When it comes to prescribing biologics, many physicians rely on ancillary staff for assistance. It’s a team effort to sift through all the paperwork, observed Dr. Oldfield.
“While many community GI practices have specialized staff to deal with prior authorizations, they are still a far cry from the IBD [inflammatory bowel disease] academic centers where there are often pharmacists, nursing specialists, and home-monitoring programs to check in on patients,” he explained.
Landscape on cost is uncertain
At present, little is known about the cost of the biosimilars and impact on future drug pricing, said Dr. Oldfield.
At least for Medicare, Humira biosimilars will be considered Medicare Part D drugs if used for a medically accepted indication, said a spokesperson for the Centers for Medicare and Medicaid Services.
Part D sponsors (pharmacy and therapeutic committees) “will make the determination as to whether Amjevita and other products will be added to their formularies,” said the spokesperson.
Patients never saw a significant cost savings with Remicade biosimilars. “I imagine the same would be true with biosimilars for Humira,” said Dr. Regueiro. Patients may see greater access to these drugs, however, because the insurance plan or the pharmacy plan will make them more readily available, he added.
The hope is that, as biosimilars are introduced, the price of the originator biologic will go down, said Mr. Newmark. “Therefore, we can expect Humira to be offered at a lower price as it faces competition. Where it will sit in comparison to the forthcoming biosimilars will depend on how much biosimilar companies drop their price and how much pressure will be on PBMs and insurers to cover the lowest list price drug,” he said.
AbbVie did not respond to several requests for comment.
Charitable patient assistance programs for biosimilars or biologics can help offset the price of copayments, Mr. Newmark offered.
Ideally, insurers will offer designated biosimilars at a reduced or even no out-of-pocket expense on their formularies. This should lead to a decreased administrative burden for approval with streamlined (or even removal) of prior authorizations for certain medications, said Dr. Oldfield.
Without insurance or medication assistance programs, the cost of biosimilars is prohibitively expensive, he added.
“Biosimilars have higher research, development, and manufacturing costs than what people conventionally think of [for] a generic medication.”
Educating, advising patients
Dr. Oldfield advised that gastroenterologists refer to biologics by the generic name rather than branded name when initiating therapy unless there is a very specific reason not to. “This approach should make the process more streamlined and less subjected to quick denials for brand-only requests as biosimilars start to assume a larger market share,” he said.
Uptake of the Humira biosimilars also will depend on proper education of physicians and patients and their comfort level with the biosimilars, said Dr. Regueiro. Cleveland Clinic uses a team approach to educate on this topic, relying on pharmacists, clinicians, and nurses to explain that there’s no real difference between the reference drug and its biosimilars, based on efficacy and safety data.
Physicians can also direct patients to patient-friendly resources, said Mr. Newmark. “By starting the conversation early, it ensures that when/if the time comes that your patient is switched to or chooses a biosimilar they will feel more confident because they have the knowledge to make decisions about their care.”
The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars , is a free resource for patients, he added.
It’s important that doctors also understand these products so they can explain to their patients what to expect, said the FDA’s Dr. Yim. The FDA provides educational materials on its website, including a comprehensive curriculum toolkit.
Dr. Hanauer has served as a consultant for AbbVie, Amgen, American College of Gastroenterology, GlaxoSmithKline, American Gastroenterological Association, Pfizer, and a host of other companies . Dr. Regueiro has served on advisory boards and as a consultant for Abbvie, Janssen, UCB, Takeda, Pfizer, BMS, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET Pharma Solutions,Trellis, and Boehringer Ingelheim Pharmaceuticals. Dr. Wolf, Dr. Yim, Dr. Oldfield, and Mr. Newmark have no financial conflicts of interest.
Gastroenterologists in 2023 will have more tools in their arsenal to treat patients with Crohn’s disease or ulcerative colitis. As many as 8-10 adalimumab biosimilars are anticipated to come on the market this year, giving mainstay drug Humira some vigorous competition.
Three scenarios will drive adalimumab biosimilar initiation: Insurance preference for the initial treatment of a newly diagnosed condition, a change in a patient’s insurance plan, or an insurance-mandated switch, said Edward C. Oldfield IV, MD, assistant professor at Eastern Virginia Medical School’s division of gastroenterology in Norfolk.
“Outside of these scenarios, I would encourage patients to remain on their current biologic so long as cost and accessibility remain stable,” said Dr. Oldfield.
Many factors will contribute to the success of biosimilars. Will physicians be prescribing them? How are biosimilars placed on formularies and will they be given preferred status? How will manufacturers price their biosimilars? “We have to wait and see to get the answers to these questions,” said Steven Newmark, JD, MPA, chief legal officer and director of policy, Global Healthy Living Foundation/CreakyJoints, a nonprofit advocacy organization based in New York.
Prescribing biosimilars is no different than prescribing originator biologics, so providers should know how to use them, said Mr. Newmark. “Most important will be the availability of patient-friendly resources that providers can share with their patients to provide education about and confidence in using biosimilars,” he added.
Overall, biosimilars are a good thing, said Dr. Oldfield. “In the long run they should bring down costs and increase access to medications for our patients.”
Others are skeptical that the adalimumab biosimilars will save patients much money.
Biosimilar laws were created to lower costs. However, if a patient with insurance pays only $5 a month out of pocket for Humira – a drug that normally costs $7,000 without coverage – it’s unlikely they would want to switch unless there’s comparable savings from the biosimilar, said Stephen B. Hanauer, MD, medical director of the Digestive Health Center and professor of medicine at Northwestern Medicine, Northwestern University, Evanston, Ill.
Like generics, Humira biosimilars may face some initial backlash, said Dr. Hanauer.
2023 broadens scope of adalimumab treatments
The American Gastroenterological Association describes a biosimilar as something that’s “highly similar to, but not an exact copy of, a biologic reference product already approved” by the Food and Drug Administration. Congress under the 2010 Affordable Care Act created a special, abbreviated pathway to approval for biosimilars.
AbbVie’s Humira, the global revenue for which exceeded $20 billion in 2021, has long dominated the U.S. market on injectable treatments for autoimmune diseases. The popular drug faces some competition in 2023, however, following a series of legal settlements that allowed AbbVie competitors to release their own adalimumab biosimilars.
“So far, we haven’t seen biosimilars live up to their potential in the U.S. in the inflammatory space,” said Mr. Newmark. This may change, however. Previously, biosimilars have required infusion, which demanded more time, commitment, and travel from patients. “The new set of forthcoming Humira biosimilars are injectables, an administration method preferred by patients,” he said.
The FDA will approve a biosimilar if it determines that the biological product is highly similar to the reference product, and that there are no clinically meaningful differences between the biological and reference product in terms of the safety, purity, and potency of the product.
The agency to date has approved 8 adalimumab biosimilars. These include: Idacio (adalimumab-aacf, Fresenius Kabi); Amjevita (adalimumab-atto, Amgen); Hadlima (adalimumab-bwwd, Organon); Cyltezo (adalimumab-adbm, Boehringer Ingelheim); Yusimry (adalimumab-aqvh from Coherus BioSciences); Hulio (adalimumab-fkjp; Mylan/Fujifilm Kyowa Kirin Biologics); Hyrimoz (adalimumab-adaz, Sandoz), and Abrilada (adalimumab-afzb, Pfizer).
“While FDA doesn’t formally track when products come to market, we know based on published reports that application holders for many of the currently FDA-approved biosimilars plan to market this year, starting with Amjevita being the first adalimumab biosimilar launched” in January, said Sarah Yim, MD, director of the Office of Therapeutic Biologics and Biosimilars at the agency.
At press time, two other companies (Celltrion and Alvotech/Teva) were awaiting FDA approval for their adalimumab biosimilar drugs.
Among the eight approved drugs, Cyltezo is the only one that has a designation for interchangeability with Humira.
An interchangeable biosimilar may be substituted at the pharmacy without the intervention of the prescriber – much like generics are substituted, depending on state laws, said Dr. Yim. “However, in terms of safety and effectiveness, FDA’s standards for approval mean that biosimilar or interchangeable biosimilar products can be used in place of the reference product they were compared to.”
FDA-approved biosimilars undergo a rigorous evaluation for safety, effectiveness, and quality for their approved conditions of use, she continued. “Therefore, patients and health care providers can rely on a biosimilar to be as safe and effective for its approved uses as the original biological product.”
Remicade as a yard stick
Gastroenterologists dealt with this situation once before, when Remicade (infliximab) biosimilars came on the market in 2016, noted Miguel Regueiro, MD, chair of the Digestive Disease and Surgery Institute at the Cleveland Clinic.
Remicade and Humira are both tumor necrosis factor inhibitors with the same mechanism of action and many of the same indications. “We already had that experience with Remicade and biosimilar switch 2 or 3 years ago. Now we’re talking about Humira,” said Dr. Regueiro.
Most GI doctors have prescribed one of the more common infliximab biosimilars (Inflectra or Renflexis), noted Dr. Oldfield.
Cardinal Health, which recently surveyed 300 gastroenterologists, rheumatologists, and dermatologists about adalimumab biosimilars, found that gastroenterologists had the highest comfort level in prescribing them. Their top concern, however, was changing a patient from adalimumab to an adalimumab biosimilar.
For most patients, Dr. Oldfield sees the Humira reference biologic and biosimilar as equivalent.
However, he said he would change a patient’s drug only if there were a good reason or if his hand was forced by insurance. He would not make the change for a patient who recently began induction with the reference biologic or a patient with highly active clinical disease.
“While there is limited data to support this, I would also have some qualms about changing a patient from reference biologic to a biosimilar if they previously had immune-mediated pharmacokinetic failure due to antibody development with a biologic and were currently doing well on their new biologic,” he said.
Those with a new ulcerative colitis or Crohn’s diagnosis who are initiating a biologic for the first time might consider a biosimilar. If a patient is transitioning from a reference biologic to a biosimilar, “I would want to make that change during a time of stable remission and with the recognition that the switch is not a temporary switch, but a long-term switch,” he continued.
A paper that reviewed 23 observational studies of adalimumab and other biosimilars found that switching biosimilars was safe and effective. But if possible, patients should minimize the number of switches until more robust long-term data are available, added Dr. Oldfield.
If a patient is apprehensive about switching to a new therapy, “one may need to be cognizant of the ‘nocebo’ effect in which there is an unexplained or unfavorable therapeutic effect after switching,” he said.
Other gastroenterologists voiced similar reservations about switching. “I won’t use an adalimumab biosimilar unless the patient requests it, the insurance requires it, or there is a cost advantage for the patient such that they prefer it,” said Doug Wolf, MD, an Atlanta gastroenterologist.
“There is no medical treatment advantage to a biosimilar, especially if switching from Humira,” added Dr. Wolf.
Insurance will guide treatment
Once a drug is approved for use by the FDA, that drug will be available in all 50 states. “Different private insurance formularies, as well as state Medicaid formularies, might affect the actual ability of patients to receive such drugs,” said Mr. Newmark.
Patients should consult with their providers and insurance companies to see what therapies are available, he advised.
Dr. Hanauer anticipates some headaches arising for patients and doctors alike when negotiating for a specific drug.
Cyltezo may be the only biosimilar interchangeable with Humira, but the third-party pharmacy benefit manager (PBM) could negotiate for one of the noninterchangeable ones. “On a yearly basis they could switch their preference,” said Dr. Hanauer.
In the Cardinal Health survey, more than 60% of respondents said they would feel comfortable prescribing an adalimumab biosimilar only with an interchangeability designation.
A PBM may offer a patient Cyltezo if it’s cheaper than Humira. If the patient insists on staying on Humira, then they’ll have to pay more for that drug on their payer’s formulary, said Dr. Hanauer. In a worst-case scenario, a physician may have to appeal on a patient’s behalf to get Humira if the insurer offers only the biosimilar.
Taking that step to appeal is a major hassle for the physician, and leads to extra back door costs as well, said Dr. Hanauer.
Humira manufacturer AbbVie, in turn, may offer discounts and rebates to the PBMs to put Humira on their formulary. “That’s the AbbVie negotiating power. It’s not that the cost is going to be that much different. It’s going to be that there are rebates and discounts that are going to make the cost different,” he added.
As a community physician, Dr. Oldfield has specific concerns about accessibility.
The ever-increasing burden of insurance documentation and prior authorization means it can take weeks or months to get these medications approved. “The addition of new biosimilars is a welcome entrance if it can get patients the medications they need when they need it,” he said.
When it comes to prescribing biologics, many physicians rely on ancillary staff for assistance. It’s a team effort to sift through all the paperwork, observed Dr. Oldfield.
“While many community GI practices have specialized staff to deal with prior authorizations, they are still a far cry from the IBD [inflammatory bowel disease] academic centers where there are often pharmacists, nursing specialists, and home-monitoring programs to check in on patients,” he explained.
Landscape on cost is uncertain
At present, little is known about the cost of the biosimilars and impact on future drug pricing, said Dr. Oldfield.
At least for Medicare, Humira biosimilars will be considered Medicare Part D drugs if used for a medically accepted indication, said a spokesperson for the Centers for Medicare and Medicaid Services.
Part D sponsors (pharmacy and therapeutic committees) “will make the determination as to whether Amjevita and other products will be added to their formularies,” said the spokesperson.
Patients never saw a significant cost savings with Remicade biosimilars. “I imagine the same would be true with biosimilars for Humira,” said Dr. Regueiro. Patients may see greater access to these drugs, however, because the insurance plan or the pharmacy plan will make them more readily available, he added.
The hope is that, as biosimilars are introduced, the price of the originator biologic will go down, said Mr. Newmark. “Therefore, we can expect Humira to be offered at a lower price as it faces competition. Where it will sit in comparison to the forthcoming biosimilars will depend on how much biosimilar companies drop their price and how much pressure will be on PBMs and insurers to cover the lowest list price drug,” he said.
AbbVie did not respond to several requests for comment.
Charitable patient assistance programs for biosimilars or biologics can help offset the price of copayments, Mr. Newmark offered.
Ideally, insurers will offer designated biosimilars at a reduced or even no out-of-pocket expense on their formularies. This should lead to a decreased administrative burden for approval with streamlined (or even removal) of prior authorizations for certain medications, said Dr. Oldfield.
Without insurance or medication assistance programs, the cost of biosimilars is prohibitively expensive, he added.
“Biosimilars have higher research, development, and manufacturing costs than what people conventionally think of [for] a generic medication.”
Educating, advising patients
Dr. Oldfield advised that gastroenterologists refer to biologics by the generic name rather than branded name when initiating therapy unless there is a very specific reason not to. “This approach should make the process more streamlined and less subjected to quick denials for brand-only requests as biosimilars start to assume a larger market share,” he said.
Uptake of the Humira biosimilars also will depend on proper education of physicians and patients and their comfort level with the biosimilars, said Dr. Regueiro. Cleveland Clinic uses a team approach to educate on this topic, relying on pharmacists, clinicians, and nurses to explain that there’s no real difference between the reference drug and its biosimilars, based on efficacy and safety data.
Physicians can also direct patients to patient-friendly resources, said Mr. Newmark. “By starting the conversation early, it ensures that when/if the time comes that your patient is switched to or chooses a biosimilar they will feel more confident because they have the knowledge to make decisions about their care.”
The Global Healthy Living Foundation’s podcast, Breaking Down Biosimilars , is a free resource for patients, he added.
It’s important that doctors also understand these products so they can explain to their patients what to expect, said the FDA’s Dr. Yim. The FDA provides educational materials on its website, including a comprehensive curriculum toolkit.
Dr. Hanauer has served as a consultant for AbbVie, Amgen, American College of Gastroenterology, GlaxoSmithKline, American Gastroenterological Association, Pfizer, and a host of other companies . Dr. Regueiro has served on advisory boards and as a consultant for Abbvie, Janssen, UCB, Takeda, Pfizer, BMS, Organon, Amgen, Genentech, Gilead, Salix, Prometheus, Lilly, Celgene, TARGET Pharma Solutions,Trellis, and Boehringer Ingelheim Pharmaceuticals. Dr. Wolf, Dr. Yim, Dr. Oldfield, and Mr. Newmark have no financial conflicts of interest.
Are there long-term benefits to infants born to patients after bariatric surgery?
Rives-Lange C, Poghosyan T, Phan A, et al. Risk-benefit balance associated with obstetric, neonatal, and child outcomes after metabolic and bariatric surgery. JAMA Surg. 2023;158:36-44. doi:10.1001/jamasurg.2022.5450.
EXPERT COMMENTARY
Prepregnancy obesity continues to rise, with approximately 40% of reproductive-aged patients having a body mass index greater than 30 kg/m2.1 Several adverse perinatal outcomes are more common in pregnant patients with obesity.2 In addition, their infants have a higher risk of obesity, insulin resistance, hypertension, and neurodevelopmental disorders in the long term.
Bariatric surgery is an effective procedure for weight loss and has been shown to lower adverse pregnancy outcomes, such as hypertensive disorders of pregnancy and gestational diabetes.5,6 Benefits to newborns, however, have been debated.5 In addition, long-term benefits to infants were unknown until a recent study evaluated neonatal and child outcomes up to 2 years after pregnancy among patients who had undergone bariatric surgery.
Details of the study
Using the French nationwide database, Rives-Lange and colleagues performed a population-based study that included patients who had at least 1 pregnancy before and 1 pregnancy after bariatric surgery. Their objective was to compare pregnancy, neonatal, and child outcomes between pregnancies pre- and post-bariatric surgery.
Results. Among 3,686 patients who had at least 1 pregnancy before and after bariatric surgery, the authors found that pregnancies after bariatric surgery had lower rates of several adverse pregnancy outcomes, including preeclampsia (OR, 0.19), gestational hypertension (OR, 0.16), and gestational diabetes (OR, 0.39), compared with pregnancies before bariatric surgery. Regarding neonatal and child outcomes up to 2 years after pregnancy, there were lower rates of birth injuries (OR, 0.27), convulsions (OR, 0.43), newborn carbohydrate metabolism disorders (OR, 0.54),and viral intestinal infections (OR, 0.56) in pregnancies after bariatric surgery compared with those before surgery.
Notably, respiratory failure rates associated with bronchiolitis increased in pregnancies after bariatric surgery (OR, 2.42). This finding remained associated after adjusting for prematurity and small for gestational age as well as including 2 successive pregnancies before bariatric surgery (OR, 1.37).
Study strengths and limitations
A limitation of this study is the use of an administrative database, which may be biased and missing relevant variables. However, the study’s major strength was the large sample of patients serving as their own control to compare outcomes from pre-bariatric surgery with those of post-bariatric surgery. In addition, to account for confounders such as age and parity, the authors also evaluated for associations between 2 consecutive pregnancies among patients before bariatric surgery. They did not consider diagnoses found to be associated with bariatric surgery if they were also significant in the analysis between 2 consecutive pregnancies before bariatric surgery.
The finding of increased risk of respiratory failure from bronchiolitis after bariatric surgery is surprising given that obesity is a risk factor for the severity of bronchiolitis.7 Although this risk remained significant after including the analysis that used 2 consecutive pregnancies pre-bariatric surgery, the risk was lower (from an OR of 2.42 to an OR of 1.37). Thus, more data are required to confirm this potential risk. Despite this concerning finding, the overwhelming pregnancy, neonatal, and child benefits found and confirmed in this large, well-designed study support the continued practice of counseling on the benefits of bariatric surgery to our obese patients. ●
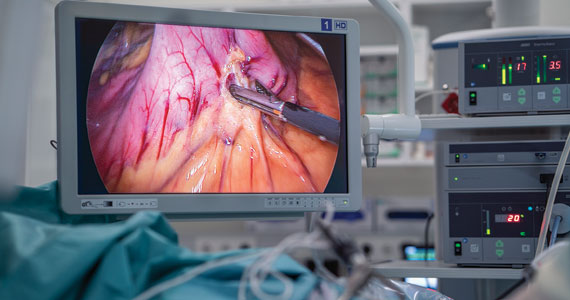
Bariatric surgery remains an effective procedure for weight loss, and it lowers the risks of several important perinatal, neonatal, and child outcomes, including hypertensive disorders, birth injuries, convulsions, and viral intestinal infections. Clinicians should include the benefits of neonatal and child outcomes in their counseling of bariatric surgery for their obese patients who are planning pregnancy.
RODNEY A. MCLAREN JR, MD
- Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8.
- Sagi-Dain L. Obesity in pregnancy: ACOG practice bulletin, number 230. Obstet Gynecol. 2021;138:489. doi:10.1097 /AOG.0000000000004527.
- O’Reilly JR, Reynolds RM. The risk of maternal obesity to the long-term health of the offspring. Clin Endocrinol (Oxf). 2013;78:9-16. doi:10.1111/cen.12055.
- Edlow AG. Maternal obesity and neurodevelopmental and psychiatric disorders in offspring. Prenat Diagn. 2017;37:95-110. doi:10.1002/pd.4932.
- Johansson K, Cnattinguius S, Näslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814-824. doi:10.1056/NEJMoa1405789.
- Getahun D, Fassett MJ, Jacobsen SJ, et al. Perinatal outcomes after bariatric surgery. Am J Obstet Gynecol. 2022;226:121.e1-121.e16. doi:10.1016/j.ajog.2021.06.087.
- James T, Samakar K, Martin MJ. Special delivery—metabolic bariatric surgery as a key component of maternal-fetal health care. JAMA Surg. 2023;158:44-45. doi:10.1001 /jamasurg.2022.5458.
Rives-Lange C, Poghosyan T, Phan A, et al. Risk-benefit balance associated with obstetric, neonatal, and child outcomes after metabolic and bariatric surgery. JAMA Surg. 2023;158:36-44. doi:10.1001/jamasurg.2022.5450.
EXPERT COMMENTARY
Prepregnancy obesity continues to rise, with approximately 40% of reproductive-aged patients having a body mass index greater than 30 kg/m2.1 Several adverse perinatal outcomes are more common in pregnant patients with obesity.2 In addition, their infants have a higher risk of obesity, insulin resistance, hypertension, and neurodevelopmental disorders in the long term.
Bariatric surgery is an effective procedure for weight loss and has been shown to lower adverse pregnancy outcomes, such as hypertensive disorders of pregnancy and gestational diabetes.5,6 Benefits to newborns, however, have been debated.5 In addition, long-term benefits to infants were unknown until a recent study evaluated neonatal and child outcomes up to 2 years after pregnancy among patients who had undergone bariatric surgery.
Details of the study
Using the French nationwide database, Rives-Lange and colleagues performed a population-based study that included patients who had at least 1 pregnancy before and 1 pregnancy after bariatric surgery. Their objective was to compare pregnancy, neonatal, and child outcomes between pregnancies pre- and post-bariatric surgery.
Results. Among 3,686 patients who had at least 1 pregnancy before and after bariatric surgery, the authors found that pregnancies after bariatric surgery had lower rates of several adverse pregnancy outcomes, including preeclampsia (OR, 0.19), gestational hypertension (OR, 0.16), and gestational diabetes (OR, 0.39), compared with pregnancies before bariatric surgery. Regarding neonatal and child outcomes up to 2 years after pregnancy, there were lower rates of birth injuries (OR, 0.27), convulsions (OR, 0.43), newborn carbohydrate metabolism disorders (OR, 0.54),and viral intestinal infections (OR, 0.56) in pregnancies after bariatric surgery compared with those before surgery.
Notably, respiratory failure rates associated with bronchiolitis increased in pregnancies after bariatric surgery (OR, 2.42). This finding remained associated after adjusting for prematurity and small for gestational age as well as including 2 successive pregnancies before bariatric surgery (OR, 1.37).
Study strengths and limitations
A limitation of this study is the use of an administrative database, which may be biased and missing relevant variables. However, the study’s major strength was the large sample of patients serving as their own control to compare outcomes from pre-bariatric surgery with those of post-bariatric surgery. In addition, to account for confounders such as age and parity, the authors also evaluated for associations between 2 consecutive pregnancies among patients before bariatric surgery. They did not consider diagnoses found to be associated with bariatric surgery if they were also significant in the analysis between 2 consecutive pregnancies before bariatric surgery.
The finding of increased risk of respiratory failure from bronchiolitis after bariatric surgery is surprising given that obesity is a risk factor for the severity of bronchiolitis.7 Although this risk remained significant after including the analysis that used 2 consecutive pregnancies pre-bariatric surgery, the risk was lower (from an OR of 2.42 to an OR of 1.37). Thus, more data are required to confirm this potential risk. Despite this concerning finding, the overwhelming pregnancy, neonatal, and child benefits found and confirmed in this large, well-designed study support the continued practice of counseling on the benefits of bariatric surgery to our obese patients. ●
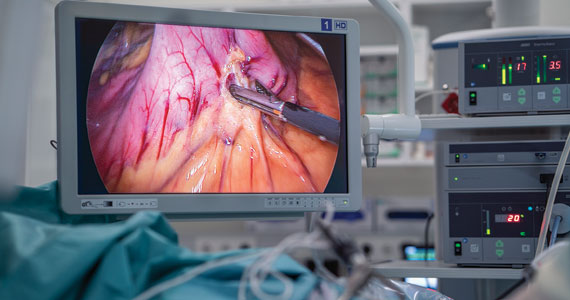
Bariatric surgery remains an effective procedure for weight loss, and it lowers the risks of several important perinatal, neonatal, and child outcomes, including hypertensive disorders, birth injuries, convulsions, and viral intestinal infections. Clinicians should include the benefits of neonatal and child outcomes in their counseling of bariatric surgery for their obese patients who are planning pregnancy.
RODNEY A. MCLAREN JR, MD
Rives-Lange C, Poghosyan T, Phan A, et al. Risk-benefit balance associated with obstetric, neonatal, and child outcomes after metabolic and bariatric surgery. JAMA Surg. 2023;158:36-44. doi:10.1001/jamasurg.2022.5450.
EXPERT COMMENTARY
Prepregnancy obesity continues to rise, with approximately 40% of reproductive-aged patients having a body mass index greater than 30 kg/m2.1 Several adverse perinatal outcomes are more common in pregnant patients with obesity.2 In addition, their infants have a higher risk of obesity, insulin resistance, hypertension, and neurodevelopmental disorders in the long term.
Bariatric surgery is an effective procedure for weight loss and has been shown to lower adverse pregnancy outcomes, such as hypertensive disorders of pregnancy and gestational diabetes.5,6 Benefits to newborns, however, have been debated.5 In addition, long-term benefits to infants were unknown until a recent study evaluated neonatal and child outcomes up to 2 years after pregnancy among patients who had undergone bariatric surgery.
Details of the study
Using the French nationwide database, Rives-Lange and colleagues performed a population-based study that included patients who had at least 1 pregnancy before and 1 pregnancy after bariatric surgery. Their objective was to compare pregnancy, neonatal, and child outcomes between pregnancies pre- and post-bariatric surgery.
Results. Among 3,686 patients who had at least 1 pregnancy before and after bariatric surgery, the authors found that pregnancies after bariatric surgery had lower rates of several adverse pregnancy outcomes, including preeclampsia (OR, 0.19), gestational hypertension (OR, 0.16), and gestational diabetes (OR, 0.39), compared with pregnancies before bariatric surgery. Regarding neonatal and child outcomes up to 2 years after pregnancy, there were lower rates of birth injuries (OR, 0.27), convulsions (OR, 0.43), newborn carbohydrate metabolism disorders (OR, 0.54),and viral intestinal infections (OR, 0.56) in pregnancies after bariatric surgery compared with those before surgery.
Notably, respiratory failure rates associated with bronchiolitis increased in pregnancies after bariatric surgery (OR, 2.42). This finding remained associated after adjusting for prematurity and small for gestational age as well as including 2 successive pregnancies before bariatric surgery (OR, 1.37).
Study strengths and limitations
A limitation of this study is the use of an administrative database, which may be biased and missing relevant variables. However, the study’s major strength was the large sample of patients serving as their own control to compare outcomes from pre-bariatric surgery with those of post-bariatric surgery. In addition, to account for confounders such as age and parity, the authors also evaluated for associations between 2 consecutive pregnancies among patients before bariatric surgery. They did not consider diagnoses found to be associated with bariatric surgery if they were also significant in the analysis between 2 consecutive pregnancies before bariatric surgery.
The finding of increased risk of respiratory failure from bronchiolitis after bariatric surgery is surprising given that obesity is a risk factor for the severity of bronchiolitis.7 Although this risk remained significant after including the analysis that used 2 consecutive pregnancies pre-bariatric surgery, the risk was lower (from an OR of 2.42 to an OR of 1.37). Thus, more data are required to confirm this potential risk. Despite this concerning finding, the overwhelming pregnancy, neonatal, and child benefits found and confirmed in this large, well-designed study support the continued practice of counseling on the benefits of bariatric surgery to our obese patients. ●
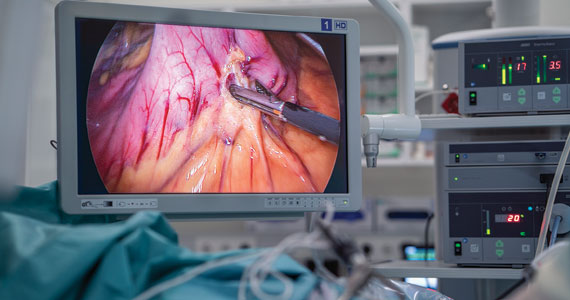
Bariatric surgery remains an effective procedure for weight loss, and it lowers the risks of several important perinatal, neonatal, and child outcomes, including hypertensive disorders, birth injuries, convulsions, and viral intestinal infections. Clinicians should include the benefits of neonatal and child outcomes in their counseling of bariatric surgery for their obese patients who are planning pregnancy.
RODNEY A. MCLAREN JR, MD
- Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8.
- Sagi-Dain L. Obesity in pregnancy: ACOG practice bulletin, number 230. Obstet Gynecol. 2021;138:489. doi:10.1097 /AOG.0000000000004527.
- O’Reilly JR, Reynolds RM. The risk of maternal obesity to the long-term health of the offspring. Clin Endocrinol (Oxf). 2013;78:9-16. doi:10.1111/cen.12055.
- Edlow AG. Maternal obesity and neurodevelopmental and psychiatric disorders in offspring. Prenat Diagn. 2017;37:95-110. doi:10.1002/pd.4932.
- Johansson K, Cnattinguius S, Näslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814-824. doi:10.1056/NEJMoa1405789.
- Getahun D, Fassett MJ, Jacobsen SJ, et al. Perinatal outcomes after bariatric surgery. Am J Obstet Gynecol. 2022;226:121.e1-121.e16. doi:10.1016/j.ajog.2021.06.087.
- James T, Samakar K, Martin MJ. Special delivery—metabolic bariatric surgery as a key component of maternal-fetal health care. JAMA Surg. 2023;158:44-45. doi:10.1001 /jamasurg.2022.5458.
- Hales CM, Carroll MD, Fryar CD, et al. Prevalence of obesity and severe obesity among adults: United States, 2017-2018. NCHS Data Brief. 2020;(360):1-8.
- Sagi-Dain L. Obesity in pregnancy: ACOG practice bulletin, number 230. Obstet Gynecol. 2021;138:489. doi:10.1097 /AOG.0000000000004527.
- O’Reilly JR, Reynolds RM. The risk of maternal obesity to the long-term health of the offspring. Clin Endocrinol (Oxf). 2013;78:9-16. doi:10.1111/cen.12055.
- Edlow AG. Maternal obesity and neurodevelopmental and psychiatric disorders in offspring. Prenat Diagn. 2017;37:95-110. doi:10.1002/pd.4932.
- Johansson K, Cnattinguius S, Näslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814-824. doi:10.1056/NEJMoa1405789.
- Getahun D, Fassett MJ, Jacobsen SJ, et al. Perinatal outcomes after bariatric surgery. Am J Obstet Gynecol. 2022;226:121.e1-121.e16. doi:10.1016/j.ajog.2021.06.087.
- James T, Samakar K, Martin MJ. Special delivery—metabolic bariatric surgery as a key component of maternal-fetal health care. JAMA Surg. 2023;158:44-45. doi:10.1001 /jamasurg.2022.5458.
CML: Preventing chemo-induced vascular toxicity
PARIS –
Cardiologist Gabrielle Sarlon, MD, PhD, a professor at Marseille (France) University Hospital, offered her recommendations at the European Days of the French Society of Cardiology Conference 2023.
In the literature, we find many hypotheses that seek to explain why these drugs bring about the formation of atheromatous plaque. The findings of one French study led Dr. Sarlon to state, “I firmly believe that, in some patients, these treatments make LDL cholesterol go up.” This would be the main cause of the coronary and peripheral arterial diseases that are being seen.
Therefore, “LDL-C should start being monitored when the therapy starts, and a statin may have to be prescribed,” she said.
Arterial diseases
By bringing about a marked improvement in patients’ chances of survival, TKIs “have revolutionized the management of chronic myeloid leukemia,” Dr. Sarlon added. But these treatments have side effects. The most common is high blood pressure, “an effect that attests to the efficacy of targeted therapies and that must be quickly treated” with antihypertensives.
It is well known that the targeted therapies cause the rise in blood pressure. What was unexpected, though, was the vascular toxicity seen with the latest generation of TKIs. “This is a real toxicity that we need to know about, detect, and manage,” said Dr. Sarlon.
The prevalence of arterial diseases induced by nilotinib, a second-generation TKI, can be as high as 10%. Single-center studies have indicated much higher numbers. In a small study that Dr. Sarlon and her team conducted at Marseille University Hospital, atherosclerotic-type arterial injuries were observed in more than 30% of patients treated with nilotinib.
Dr. Sarlon noted that the signs of arterial toxicity occurring with this treatment have not appeared in clinical trials. Observations of the real-life use of nilotinib led French and German teams to sound the alarm. They noticed that some patients treated for CML had developed claudication and progression to critical limb ischemia of the lower extremities.
Risk factors uncovered
The first retrospective analysis to explore this risk was carried out by a German team. They included 179 patients who received nilotinib and found that 11 (6.2%) developed severe and previously unrecognized lower-extremity peripheral arterial disease (PAD) that required invasive therapy. The mean time from initiation of nilotinib to the first PAD event was 105.1 weeks (range = 16-212 weeks).
The following have emerged as major risk factors for nilotinib-induced PAD: the presence of cardiovascular risk factors, age older than 60 years, and long duration of exposure to nilotinib. Some of these factors were confirmed in the more recent study conducted at Marseille University Hospital involving patients treated with nilotinib. According to other research, there seems to be a correlation between this risk and the dose administered.
In the case of ponatinib, the side effects are even more common – so much so that, a few months after this third-generation TKI was authorized, a warning was issued about its use. A long-term follow-up study reported a 28% prevalence of cardiovascular events, while arterial diseases were observed in 20% of cases after 1-2 years on the treatment.
In terms of pathophysiology, the Marseilles University Hospital study found that arterial injuries were associated with stenosis greater than 50% in almost half of cases. “The atheromatous plaques were found where they typically are,” with the carotid bulb being the most involved territory, according to the researchers. But they’re also found in other arteries – femoral, vertebral, even renal – “sometimes in patients without cardiovascular risk factors.”
One distinctive characteristic to keep in mind is that “lipid-rich atheromatous plaques appear very dark on imaging” and thus can go unnoticed during a Doppler ultrasound. And, Dr. Sarlon added, “surprisingly, the thickening can extend to the external carotid artery.”
Ankle-brachial index
Published last year, the first European Society of Cardiology Guidelines on Cardio-Oncology present specific baseline risk-assessment and monitoring recommendations regarding patients treated with nilotinib and ponatinib. One suggests that a cardiovascular risk assessment be done every 3 months during the first year and every 6-12 months thereafter. This assessment would include such items as ECGs, blood pressure measurements, and lipid profile tests.
In addition, it is advised that every 6 months an ankle-brachial index test be performed to check for PAD. At Marseille University Hospital, a Doppler ultrasound is also done at each follow-up appointment to look for arterial plaques, “even for patients at low risk for cardiovascular disease,” said Dr. Sarlon. “It seems, above all, absolutely necessary that hematologists order an LDL-C test and, if needed, consider statin therapy,” all the while keeping in mind that “the target LDL-C level is 1 gram per liter.”
This article was translated from the Medscape French edition. A version of this article first appeared on Medscape.com.
PARIS –
Cardiologist Gabrielle Sarlon, MD, PhD, a professor at Marseille (France) University Hospital, offered her recommendations at the European Days of the French Society of Cardiology Conference 2023.
In the literature, we find many hypotheses that seek to explain why these drugs bring about the formation of atheromatous plaque. The findings of one French study led Dr. Sarlon to state, “I firmly believe that, in some patients, these treatments make LDL cholesterol go up.” This would be the main cause of the coronary and peripheral arterial diseases that are being seen.
Therefore, “LDL-C should start being monitored when the therapy starts, and a statin may have to be prescribed,” she said.
Arterial diseases
By bringing about a marked improvement in patients’ chances of survival, TKIs “have revolutionized the management of chronic myeloid leukemia,” Dr. Sarlon added. But these treatments have side effects. The most common is high blood pressure, “an effect that attests to the efficacy of targeted therapies and that must be quickly treated” with antihypertensives.
It is well known that the targeted therapies cause the rise in blood pressure. What was unexpected, though, was the vascular toxicity seen with the latest generation of TKIs. “This is a real toxicity that we need to know about, detect, and manage,” said Dr. Sarlon.
The prevalence of arterial diseases induced by nilotinib, a second-generation TKI, can be as high as 10%. Single-center studies have indicated much higher numbers. In a small study that Dr. Sarlon and her team conducted at Marseille University Hospital, atherosclerotic-type arterial injuries were observed in more than 30% of patients treated with nilotinib.
Dr. Sarlon noted that the signs of arterial toxicity occurring with this treatment have not appeared in clinical trials. Observations of the real-life use of nilotinib led French and German teams to sound the alarm. They noticed that some patients treated for CML had developed claudication and progression to critical limb ischemia of the lower extremities.
Risk factors uncovered
The first retrospective analysis to explore this risk was carried out by a German team. They included 179 patients who received nilotinib and found that 11 (6.2%) developed severe and previously unrecognized lower-extremity peripheral arterial disease (PAD) that required invasive therapy. The mean time from initiation of nilotinib to the first PAD event was 105.1 weeks (range = 16-212 weeks).
The following have emerged as major risk factors for nilotinib-induced PAD: the presence of cardiovascular risk factors, age older than 60 years, and long duration of exposure to nilotinib. Some of these factors were confirmed in the more recent study conducted at Marseille University Hospital involving patients treated with nilotinib. According to other research, there seems to be a correlation between this risk and the dose administered.
In the case of ponatinib, the side effects are even more common – so much so that, a few months after this third-generation TKI was authorized, a warning was issued about its use. A long-term follow-up study reported a 28% prevalence of cardiovascular events, while arterial diseases were observed in 20% of cases after 1-2 years on the treatment.
In terms of pathophysiology, the Marseilles University Hospital study found that arterial injuries were associated with stenosis greater than 50% in almost half of cases. “The atheromatous plaques were found where they typically are,” with the carotid bulb being the most involved territory, according to the researchers. But they’re also found in other arteries – femoral, vertebral, even renal – “sometimes in patients without cardiovascular risk factors.”
One distinctive characteristic to keep in mind is that “lipid-rich atheromatous plaques appear very dark on imaging” and thus can go unnoticed during a Doppler ultrasound. And, Dr. Sarlon added, “surprisingly, the thickening can extend to the external carotid artery.”
Ankle-brachial index
Published last year, the first European Society of Cardiology Guidelines on Cardio-Oncology present specific baseline risk-assessment and monitoring recommendations regarding patients treated with nilotinib and ponatinib. One suggests that a cardiovascular risk assessment be done every 3 months during the first year and every 6-12 months thereafter. This assessment would include such items as ECGs, blood pressure measurements, and lipid profile tests.
In addition, it is advised that every 6 months an ankle-brachial index test be performed to check for PAD. At Marseille University Hospital, a Doppler ultrasound is also done at each follow-up appointment to look for arterial plaques, “even for patients at low risk for cardiovascular disease,” said Dr. Sarlon. “It seems, above all, absolutely necessary that hematologists order an LDL-C test and, if needed, consider statin therapy,” all the while keeping in mind that “the target LDL-C level is 1 gram per liter.”
This article was translated from the Medscape French edition. A version of this article first appeared on Medscape.com.
PARIS –
Cardiologist Gabrielle Sarlon, MD, PhD, a professor at Marseille (France) University Hospital, offered her recommendations at the European Days of the French Society of Cardiology Conference 2023.
In the literature, we find many hypotheses that seek to explain why these drugs bring about the formation of atheromatous plaque. The findings of one French study led Dr. Sarlon to state, “I firmly believe that, in some patients, these treatments make LDL cholesterol go up.” This would be the main cause of the coronary and peripheral arterial diseases that are being seen.
Therefore, “LDL-C should start being monitored when the therapy starts, and a statin may have to be prescribed,” she said.
Arterial diseases
By bringing about a marked improvement in patients’ chances of survival, TKIs “have revolutionized the management of chronic myeloid leukemia,” Dr. Sarlon added. But these treatments have side effects. The most common is high blood pressure, “an effect that attests to the efficacy of targeted therapies and that must be quickly treated” with antihypertensives.
It is well known that the targeted therapies cause the rise in blood pressure. What was unexpected, though, was the vascular toxicity seen with the latest generation of TKIs. “This is a real toxicity that we need to know about, detect, and manage,” said Dr. Sarlon.
The prevalence of arterial diseases induced by nilotinib, a second-generation TKI, can be as high as 10%. Single-center studies have indicated much higher numbers. In a small study that Dr. Sarlon and her team conducted at Marseille University Hospital, atherosclerotic-type arterial injuries were observed in more than 30% of patients treated with nilotinib.
Dr. Sarlon noted that the signs of arterial toxicity occurring with this treatment have not appeared in clinical trials. Observations of the real-life use of nilotinib led French and German teams to sound the alarm. They noticed that some patients treated for CML had developed claudication and progression to critical limb ischemia of the lower extremities.
Risk factors uncovered
The first retrospective analysis to explore this risk was carried out by a German team. They included 179 patients who received nilotinib and found that 11 (6.2%) developed severe and previously unrecognized lower-extremity peripheral arterial disease (PAD) that required invasive therapy. The mean time from initiation of nilotinib to the first PAD event was 105.1 weeks (range = 16-212 weeks).
The following have emerged as major risk factors for nilotinib-induced PAD: the presence of cardiovascular risk factors, age older than 60 years, and long duration of exposure to nilotinib. Some of these factors were confirmed in the more recent study conducted at Marseille University Hospital involving patients treated with nilotinib. According to other research, there seems to be a correlation between this risk and the dose administered.
In the case of ponatinib, the side effects are even more common – so much so that, a few months after this third-generation TKI was authorized, a warning was issued about its use. A long-term follow-up study reported a 28% prevalence of cardiovascular events, while arterial diseases were observed in 20% of cases after 1-2 years on the treatment.
In terms of pathophysiology, the Marseilles University Hospital study found that arterial injuries were associated with stenosis greater than 50% in almost half of cases. “The atheromatous plaques were found where they typically are,” with the carotid bulb being the most involved territory, according to the researchers. But they’re also found in other arteries – femoral, vertebral, even renal – “sometimes in patients without cardiovascular risk factors.”
One distinctive characteristic to keep in mind is that “lipid-rich atheromatous plaques appear very dark on imaging” and thus can go unnoticed during a Doppler ultrasound. And, Dr. Sarlon added, “surprisingly, the thickening can extend to the external carotid artery.”
Ankle-brachial index
Published last year, the first European Society of Cardiology Guidelines on Cardio-Oncology present specific baseline risk-assessment and monitoring recommendations regarding patients treated with nilotinib and ponatinib. One suggests that a cardiovascular risk assessment be done every 3 months during the first year and every 6-12 months thereafter. This assessment would include such items as ECGs, blood pressure measurements, and lipid profile tests.
In addition, it is advised that every 6 months an ankle-brachial index test be performed to check for PAD. At Marseille University Hospital, a Doppler ultrasound is also done at each follow-up appointment to look for arterial plaques, “even for patients at low risk for cardiovascular disease,” said Dr. Sarlon. “It seems, above all, absolutely necessary that hematologists order an LDL-C test and, if needed, consider statin therapy,” all the while keeping in mind that “the target LDL-C level is 1 gram per liter.”
This article was translated from the Medscape French edition. A version of this article first appeared on Medscape.com.
New cancer screen, same issues: Physicians confront Galleri test
In January 2022, Anthony Arenz, a 51-year-old living in Mesa, Ariz., breathed a small sigh of relief.
The Galleri blood test, which screens for 50 types of cancer, hadn’t detected any positive signs.
It would be welcome news to anyone but especially to a firefighter with a 9% greater risk of developing cancer and a 14% greater risk of dying from it than the average person. The Mesa unit had lost two servicemen to cancer in the past 3 years. Both were more than a decade younger than Mr. Arenz.
When the city of Mesa offered additional free screening – including a full-body MRI – to firefighters over 50, Mr. Arenz initially shrugged it off. With a negative Galleri test in hand, he didn’t want to spend more time dwelling on it.
Still, he began to feel a creeping guilt for skipping a test that many of his fallen colleagues hadn’t been offered. He tried to soothe his anxiety with research. A look through the company’s website didn’t set him at ease. According to Grail Bio, a test result of “no cancer signal detected” does not rule out cancer.
Mr. Arenz booked his free MRI.
The results left him heavy: stage I kidney cancer. The Galleri test had missed it.
Mr. Arenz received his free Galleri test through a cancer screening program funded by the city of Mesa. The program is housed at Vincere Cancer Center in Scottsdale, Ariz. Under the leadership of radiation oncologist and Vincere co-owner Vershalee Shukla, MD, the program currently screens first responders in more than 10 Arizona cities at no cost to them.
Vincere began using Galleri shortly after the test launched for consumers in June 2021. Since then, the first responder program has become the largest commercial user of the test in North America.
The Galleri test, which has not yet been approved by the Food and Drug Administration, is so new that few know what incorrect results look like in practice and how often they might occur.
After running the test on about 2,000 servicemen and servicewomen, Dr. Shukla can offer some insight about the test’s real-world value in a high-risk population.
“Cancer screening is a very complicated issue,” Dr. Shukla said in an interview. “Being honest, the tests are good but are not ready yet [for wider use].”
Mr. Arenz was not the only firefighter who got a surprise after taking a Galleri test.
In nearby Phoenix, 51-year-old firefighter Mike Curtis knew his risk for cancer was high, but he wasn’t that worried. Mr. Curtis had been running into fires since he was 17. His dad, also a firefighter, had died of cancer at age 58.
Mr. Curtis had taken the Vincere Cancer Center up on every free screening service since the program began in late 2018 – well before Dr. Shukla started using Galleri in 2021. His most recent lung CT was clear. But he underwent the Galleri test just to stay vigilant.
His result was a shock. The test detected signs of cancer.
Mr. Curtis decided to tell no one, not even his wife. He’d bear the bad news alone until he was certain.
Dr. Shukla, however, immediately doubted the blood test result. She expedited several follow-up tests. One week, a PET, and CT of the abdomen and pelvis later, her hunch was confirmed. The Galleri test result was wrong, Mr. Curtis did not have cancer.
The price of his peace of mind: an extensive workup with a $4,000 price tag. Fortunately, the bill was covered by the screening program.
Overall, in just over 18 months of using the blood test, Dr. Shukla has only encountered 1 other false positive out of about 2,000 Galleri results.
She also discovered two positive signals for cancer using Galleri that were confirmed with follow-up tests. One was a chordoma, a rare type of bone cancer, and the other was a squamous cell carcinoma of the head and neck. The Galleri test caught both remarkably early, in time for treatment.
For Dr. Shukla, however, false negatives were particularly “horrible.” Mr. Arenz’s was just 1 of 28 cancers that the blood test missed. And because 500 negative tests are yet to be validated, the 28 false negatives may be an underestimate.
In her experience, the binary test result – a simple positive or negative cancer signal – is an oversimplification of risk, she said. It “gives a false perception that you have cancer or you don’t,” although the test itself is not definitive.
Grail senior medical director Whitney Jones, MD, agreed that the test is not meant to be a stand-alone screening test for cancer. The purpose of the Galleri test is to “complement other screenings, not replace them,” Dr. Jones told this news organization.
According to an analysis of Galleri data and Dr. Shukla’s experience, the test’s specificity was over 99%. That means the test successfully minimizes false positives.
But the test’s sensitivity was much lower. From data from first responders, Dr. Shukla determined the sensitivity to be 6.7%. That means the test misses about 93 of every 100 cancers. According to Grail’s latest data from more than 6,300 people older than 50, the test’s sensitivity was 29%.
Specificity and sensitivity are metrics used to credential a test and establish confidence in its ability to detect the target disease. A test with high specificity can correctly identify patients who do not have the condition in question, while a test with high sensitivity can correctly identify patients who do have the disease. But there are trade-offs between sensitivity and specificity. One value is increased at the expense of the other.
It’s normal for a cancer screening test to prioritize specificity, according to Aparna Parikh, MD, an oncologist at Mass General Cancer Center in Boston. In a test like Galleri, which is meant to be an adjunct to other screening modalities, “at least we are seeing a good specificity, which is important, because we don’t want false positives, where the downstream impact on the patient can be high.”
Overall, Dr. Jones said, Grail Bio’s aim is to build a test that’s sensitive enough to catch the most dangerous cancers without inundating the healthcare system with false positives. In addition, Dr. Jones explained, sensitivity varies by cancer type. It tends to be lower for cancers for which other screening modalities are available, as well as for earlier-stage disease.
However, the Galleri sensitivity values are “a little bit scary,” said Ji-Hyun Lee, DrPH, professor of biostatistics at the University of Florida and director of the division of quantitative sciences at the University of Florida Health Cancer Center, both in Gainesville. Dr. Lee, who is not affiliated with Grail, reviewed the company’s publicly available data as well as Dr. Shukla’s data at the request of this news organization.
While there’s no definitive threshold for sensitivity, miss rates as high as 93% and 71% “provide little confidence in the [accuracy of the] test,” Dr. Lee said.
Positive and negative predictive values, however, are more clinically relevant measures of a screening test. These numbers indicate how likely it is that a patient’s results are true and therefore how worried they should be about a positive result and how much they should trust a negative result.
Galleri’s data in the over-50 population and Dr. Shukla’s in first responders suggest the test’s negative predictive value is very high – 98.6% and 98.1%, respectively – which means most people can trust a negative test result.
The positive predictive value, however, was less straightforward. In first responders, Dr. Shukla found that only half of positive Galleri tests were confirmed cases of cancer. And an analysis of Grail’s data found that only 38% of positive Galleri tests – 35 of 92 tests – represented a validated cancer diagnosis.
“In a clinical setting, positive predictive value is more usable for decision-making for the patient,” said Dr. Lee. “Positive predictive value isn’t always high, because everything doesn’t always transfer perfectly to the clinic.” But in the general population, if only 38% of patients with positive Galleri results truly have cancer, the test is “not quite useful to make a decision for the patient or the providers.”
Galleri may also be a costly prospect for patients, no matter the result, cautioned Electra Paskett, PhD, an epidemiologist and cancer screening expert at Ohio State University, Columbus. A positive Galleri test leads to a cascade of follow-up diagnostic tests, which payers may not cover. For a negative result, Galleri recommends that the patient undergo screening again in a year, at an annual cost of $950 plus the cost of any follow-up testing when Galleri does pick something up.
“If a provider wants to offer the Galleri test, all those things need to be made abundantly clear, in my opinion,” Dr. Paskett said.
Following the negative Galleri test, Mr. Arenz’s cancer didn’t slip through the cracks because he received other advanced imaging free of charge. But whether all doctors will go to such lengths to back up Galleri results, even for patients with negative results, is unknown.
A negative result can give patients “a huge false sense of security,” said Dr. Shukla. And if a test is positive, the workup isn’t simple. Chasing cancer, especially one that’s not really there, can be nerve-wracking and expensive.
The question, then, is why perform the Galleri test at all if results require so much validation?
Dr. Parikh explained that a high-risk group such as firefighters represents an ideal-use case for Galleri and other liquid biopsy tests. But she noted that she would be “wary of the ability of the system to manage this test en masse” were the test to be used more widely in the general population.
Dr. Shukla said it’s less about the results she’s getting today and more about making the test more effective for her patients in the future. First responders need a test such as this that can quickly identify multiple cancers. However, to improve the test, Grail needs more data from this high-risk population. That’s what she’s after.
Mr. Curtis doesn’t regret taking the Galleri test. The emotional toll of thinking he had cancer for a few days wasn’t too high a price, in his opinion. It’s part of cancer screening. But he acknowledged that it would have been a much more burdensome experience had he’d been financially responsible for the workup or if he hadn’t had Dr. Shukla to manage his case from start to finish.
Because it was free, Mr. Arenz doesn’t regret undergoing the Galleri test either. But he tells his coworkers to check the site, do their research, and get more screening.
“Any medical center that’s just doing this one test, you just have to be careful,” Dr. Shukla said. “It’s not that easy.”
A version of this article first appeared on Medscape.com.
In January 2022, Anthony Arenz, a 51-year-old living in Mesa, Ariz., breathed a small sigh of relief.
The Galleri blood test, which screens for 50 types of cancer, hadn’t detected any positive signs.
It would be welcome news to anyone but especially to a firefighter with a 9% greater risk of developing cancer and a 14% greater risk of dying from it than the average person. The Mesa unit had lost two servicemen to cancer in the past 3 years. Both were more than a decade younger than Mr. Arenz.
When the city of Mesa offered additional free screening – including a full-body MRI – to firefighters over 50, Mr. Arenz initially shrugged it off. With a negative Galleri test in hand, he didn’t want to spend more time dwelling on it.
Still, he began to feel a creeping guilt for skipping a test that many of his fallen colleagues hadn’t been offered. He tried to soothe his anxiety with research. A look through the company’s website didn’t set him at ease. According to Grail Bio, a test result of “no cancer signal detected” does not rule out cancer.
Mr. Arenz booked his free MRI.
The results left him heavy: stage I kidney cancer. The Galleri test had missed it.
Mr. Arenz received his free Galleri test through a cancer screening program funded by the city of Mesa. The program is housed at Vincere Cancer Center in Scottsdale, Ariz. Under the leadership of radiation oncologist and Vincere co-owner Vershalee Shukla, MD, the program currently screens first responders in more than 10 Arizona cities at no cost to them.
Vincere began using Galleri shortly after the test launched for consumers in June 2021. Since then, the first responder program has become the largest commercial user of the test in North America.
The Galleri test, which has not yet been approved by the Food and Drug Administration, is so new that few know what incorrect results look like in practice and how often they might occur.
After running the test on about 2,000 servicemen and servicewomen, Dr. Shukla can offer some insight about the test’s real-world value in a high-risk population.
“Cancer screening is a very complicated issue,” Dr. Shukla said in an interview. “Being honest, the tests are good but are not ready yet [for wider use].”
Mr. Arenz was not the only firefighter who got a surprise after taking a Galleri test.
In nearby Phoenix, 51-year-old firefighter Mike Curtis knew his risk for cancer was high, but he wasn’t that worried. Mr. Curtis had been running into fires since he was 17. His dad, also a firefighter, had died of cancer at age 58.
Mr. Curtis had taken the Vincere Cancer Center up on every free screening service since the program began in late 2018 – well before Dr. Shukla started using Galleri in 2021. His most recent lung CT was clear. But he underwent the Galleri test just to stay vigilant.
His result was a shock. The test detected signs of cancer.
Mr. Curtis decided to tell no one, not even his wife. He’d bear the bad news alone until he was certain.
Dr. Shukla, however, immediately doubted the blood test result. She expedited several follow-up tests. One week, a PET, and CT of the abdomen and pelvis later, her hunch was confirmed. The Galleri test result was wrong, Mr. Curtis did not have cancer.
The price of his peace of mind: an extensive workup with a $4,000 price tag. Fortunately, the bill was covered by the screening program.
Overall, in just over 18 months of using the blood test, Dr. Shukla has only encountered 1 other false positive out of about 2,000 Galleri results.
She also discovered two positive signals for cancer using Galleri that were confirmed with follow-up tests. One was a chordoma, a rare type of bone cancer, and the other was a squamous cell carcinoma of the head and neck. The Galleri test caught both remarkably early, in time for treatment.
For Dr. Shukla, however, false negatives were particularly “horrible.” Mr. Arenz’s was just 1 of 28 cancers that the blood test missed. And because 500 negative tests are yet to be validated, the 28 false negatives may be an underestimate.
In her experience, the binary test result – a simple positive or negative cancer signal – is an oversimplification of risk, she said. It “gives a false perception that you have cancer or you don’t,” although the test itself is not definitive.
Grail senior medical director Whitney Jones, MD, agreed that the test is not meant to be a stand-alone screening test for cancer. The purpose of the Galleri test is to “complement other screenings, not replace them,” Dr. Jones told this news organization.
According to an analysis of Galleri data and Dr. Shukla’s experience, the test’s specificity was over 99%. That means the test successfully minimizes false positives.
But the test’s sensitivity was much lower. From data from first responders, Dr. Shukla determined the sensitivity to be 6.7%. That means the test misses about 93 of every 100 cancers. According to Grail’s latest data from more than 6,300 people older than 50, the test’s sensitivity was 29%.
Specificity and sensitivity are metrics used to credential a test and establish confidence in its ability to detect the target disease. A test with high specificity can correctly identify patients who do not have the condition in question, while a test with high sensitivity can correctly identify patients who do have the disease. But there are trade-offs between sensitivity and specificity. One value is increased at the expense of the other.
It’s normal for a cancer screening test to prioritize specificity, according to Aparna Parikh, MD, an oncologist at Mass General Cancer Center in Boston. In a test like Galleri, which is meant to be an adjunct to other screening modalities, “at least we are seeing a good specificity, which is important, because we don’t want false positives, where the downstream impact on the patient can be high.”
Overall, Dr. Jones said, Grail Bio’s aim is to build a test that’s sensitive enough to catch the most dangerous cancers without inundating the healthcare system with false positives. In addition, Dr. Jones explained, sensitivity varies by cancer type. It tends to be lower for cancers for which other screening modalities are available, as well as for earlier-stage disease.
However, the Galleri sensitivity values are “a little bit scary,” said Ji-Hyun Lee, DrPH, professor of biostatistics at the University of Florida and director of the division of quantitative sciences at the University of Florida Health Cancer Center, both in Gainesville. Dr. Lee, who is not affiliated with Grail, reviewed the company’s publicly available data as well as Dr. Shukla’s data at the request of this news organization.
While there’s no definitive threshold for sensitivity, miss rates as high as 93% and 71% “provide little confidence in the [accuracy of the] test,” Dr. Lee said.
Positive and negative predictive values, however, are more clinically relevant measures of a screening test. These numbers indicate how likely it is that a patient’s results are true and therefore how worried they should be about a positive result and how much they should trust a negative result.
Galleri’s data in the over-50 population and Dr. Shukla’s in first responders suggest the test’s negative predictive value is very high – 98.6% and 98.1%, respectively – which means most people can trust a negative test result.
The positive predictive value, however, was less straightforward. In first responders, Dr. Shukla found that only half of positive Galleri tests were confirmed cases of cancer. And an analysis of Grail’s data found that only 38% of positive Galleri tests – 35 of 92 tests – represented a validated cancer diagnosis.
“In a clinical setting, positive predictive value is more usable for decision-making for the patient,” said Dr. Lee. “Positive predictive value isn’t always high, because everything doesn’t always transfer perfectly to the clinic.” But in the general population, if only 38% of patients with positive Galleri results truly have cancer, the test is “not quite useful to make a decision for the patient or the providers.”
Galleri may also be a costly prospect for patients, no matter the result, cautioned Electra Paskett, PhD, an epidemiologist and cancer screening expert at Ohio State University, Columbus. A positive Galleri test leads to a cascade of follow-up diagnostic tests, which payers may not cover. For a negative result, Galleri recommends that the patient undergo screening again in a year, at an annual cost of $950 plus the cost of any follow-up testing when Galleri does pick something up.
“If a provider wants to offer the Galleri test, all those things need to be made abundantly clear, in my opinion,” Dr. Paskett said.
Following the negative Galleri test, Mr. Arenz’s cancer didn’t slip through the cracks because he received other advanced imaging free of charge. But whether all doctors will go to such lengths to back up Galleri results, even for patients with negative results, is unknown.
A negative result can give patients “a huge false sense of security,” said Dr. Shukla. And if a test is positive, the workup isn’t simple. Chasing cancer, especially one that’s not really there, can be nerve-wracking and expensive.
The question, then, is why perform the Galleri test at all if results require so much validation?
Dr. Parikh explained that a high-risk group such as firefighters represents an ideal-use case for Galleri and other liquid biopsy tests. But she noted that she would be “wary of the ability of the system to manage this test en masse” were the test to be used more widely in the general population.
Dr. Shukla said it’s less about the results she’s getting today and more about making the test more effective for her patients in the future. First responders need a test such as this that can quickly identify multiple cancers. However, to improve the test, Grail needs more data from this high-risk population. That’s what she’s after.
Mr. Curtis doesn’t regret taking the Galleri test. The emotional toll of thinking he had cancer for a few days wasn’t too high a price, in his opinion. It’s part of cancer screening. But he acknowledged that it would have been a much more burdensome experience had he’d been financially responsible for the workup or if he hadn’t had Dr. Shukla to manage his case from start to finish.
Because it was free, Mr. Arenz doesn’t regret undergoing the Galleri test either. But he tells his coworkers to check the site, do their research, and get more screening.
“Any medical center that’s just doing this one test, you just have to be careful,” Dr. Shukla said. “It’s not that easy.”
A version of this article first appeared on Medscape.com.
In January 2022, Anthony Arenz, a 51-year-old living in Mesa, Ariz., breathed a small sigh of relief.
The Galleri blood test, which screens for 50 types of cancer, hadn’t detected any positive signs.
It would be welcome news to anyone but especially to a firefighter with a 9% greater risk of developing cancer and a 14% greater risk of dying from it than the average person. The Mesa unit had lost two servicemen to cancer in the past 3 years. Both were more than a decade younger than Mr. Arenz.
When the city of Mesa offered additional free screening – including a full-body MRI – to firefighters over 50, Mr. Arenz initially shrugged it off. With a negative Galleri test in hand, he didn’t want to spend more time dwelling on it.
Still, he began to feel a creeping guilt for skipping a test that many of his fallen colleagues hadn’t been offered. He tried to soothe his anxiety with research. A look through the company’s website didn’t set him at ease. According to Grail Bio, a test result of “no cancer signal detected” does not rule out cancer.
Mr. Arenz booked his free MRI.
The results left him heavy: stage I kidney cancer. The Galleri test had missed it.
Mr. Arenz received his free Galleri test through a cancer screening program funded by the city of Mesa. The program is housed at Vincere Cancer Center in Scottsdale, Ariz. Under the leadership of radiation oncologist and Vincere co-owner Vershalee Shukla, MD, the program currently screens first responders in more than 10 Arizona cities at no cost to them.
Vincere began using Galleri shortly after the test launched for consumers in June 2021. Since then, the first responder program has become the largest commercial user of the test in North America.
The Galleri test, which has not yet been approved by the Food and Drug Administration, is so new that few know what incorrect results look like in practice and how often they might occur.
After running the test on about 2,000 servicemen and servicewomen, Dr. Shukla can offer some insight about the test’s real-world value in a high-risk population.
“Cancer screening is a very complicated issue,” Dr. Shukla said in an interview. “Being honest, the tests are good but are not ready yet [for wider use].”
Mr. Arenz was not the only firefighter who got a surprise after taking a Galleri test.
In nearby Phoenix, 51-year-old firefighter Mike Curtis knew his risk for cancer was high, but he wasn’t that worried. Mr. Curtis had been running into fires since he was 17. His dad, also a firefighter, had died of cancer at age 58.
Mr. Curtis had taken the Vincere Cancer Center up on every free screening service since the program began in late 2018 – well before Dr. Shukla started using Galleri in 2021. His most recent lung CT was clear. But he underwent the Galleri test just to stay vigilant.
His result was a shock. The test detected signs of cancer.
Mr. Curtis decided to tell no one, not even his wife. He’d bear the bad news alone until he was certain.
Dr. Shukla, however, immediately doubted the blood test result. She expedited several follow-up tests. One week, a PET, and CT of the abdomen and pelvis later, her hunch was confirmed. The Galleri test result was wrong, Mr. Curtis did not have cancer.
The price of his peace of mind: an extensive workup with a $4,000 price tag. Fortunately, the bill was covered by the screening program.
Overall, in just over 18 months of using the blood test, Dr. Shukla has only encountered 1 other false positive out of about 2,000 Galleri results.
She also discovered two positive signals for cancer using Galleri that were confirmed with follow-up tests. One was a chordoma, a rare type of bone cancer, and the other was a squamous cell carcinoma of the head and neck. The Galleri test caught both remarkably early, in time for treatment.
For Dr. Shukla, however, false negatives were particularly “horrible.” Mr. Arenz’s was just 1 of 28 cancers that the blood test missed. And because 500 negative tests are yet to be validated, the 28 false negatives may be an underestimate.
In her experience, the binary test result – a simple positive or negative cancer signal – is an oversimplification of risk, she said. It “gives a false perception that you have cancer or you don’t,” although the test itself is not definitive.
Grail senior medical director Whitney Jones, MD, agreed that the test is not meant to be a stand-alone screening test for cancer. The purpose of the Galleri test is to “complement other screenings, not replace them,” Dr. Jones told this news organization.
According to an analysis of Galleri data and Dr. Shukla’s experience, the test’s specificity was over 99%. That means the test successfully minimizes false positives.
But the test’s sensitivity was much lower. From data from first responders, Dr. Shukla determined the sensitivity to be 6.7%. That means the test misses about 93 of every 100 cancers. According to Grail’s latest data from more than 6,300 people older than 50, the test’s sensitivity was 29%.
Specificity and sensitivity are metrics used to credential a test and establish confidence in its ability to detect the target disease. A test with high specificity can correctly identify patients who do not have the condition in question, while a test with high sensitivity can correctly identify patients who do have the disease. But there are trade-offs between sensitivity and specificity. One value is increased at the expense of the other.
It’s normal for a cancer screening test to prioritize specificity, according to Aparna Parikh, MD, an oncologist at Mass General Cancer Center in Boston. In a test like Galleri, which is meant to be an adjunct to other screening modalities, “at least we are seeing a good specificity, which is important, because we don’t want false positives, where the downstream impact on the patient can be high.”
Overall, Dr. Jones said, Grail Bio’s aim is to build a test that’s sensitive enough to catch the most dangerous cancers without inundating the healthcare system with false positives. In addition, Dr. Jones explained, sensitivity varies by cancer type. It tends to be lower for cancers for which other screening modalities are available, as well as for earlier-stage disease.
However, the Galleri sensitivity values are “a little bit scary,” said Ji-Hyun Lee, DrPH, professor of biostatistics at the University of Florida and director of the division of quantitative sciences at the University of Florida Health Cancer Center, both in Gainesville. Dr. Lee, who is not affiliated with Grail, reviewed the company’s publicly available data as well as Dr. Shukla’s data at the request of this news organization.
While there’s no definitive threshold for sensitivity, miss rates as high as 93% and 71% “provide little confidence in the [accuracy of the] test,” Dr. Lee said.
Positive and negative predictive values, however, are more clinically relevant measures of a screening test. These numbers indicate how likely it is that a patient’s results are true and therefore how worried they should be about a positive result and how much they should trust a negative result.
Galleri’s data in the over-50 population and Dr. Shukla’s in first responders suggest the test’s negative predictive value is very high – 98.6% and 98.1%, respectively – which means most people can trust a negative test result.
The positive predictive value, however, was less straightforward. In first responders, Dr. Shukla found that only half of positive Galleri tests were confirmed cases of cancer. And an analysis of Grail’s data found that only 38% of positive Galleri tests – 35 of 92 tests – represented a validated cancer diagnosis.
“In a clinical setting, positive predictive value is more usable for decision-making for the patient,” said Dr. Lee. “Positive predictive value isn’t always high, because everything doesn’t always transfer perfectly to the clinic.” But in the general population, if only 38% of patients with positive Galleri results truly have cancer, the test is “not quite useful to make a decision for the patient or the providers.”
Galleri may also be a costly prospect for patients, no matter the result, cautioned Electra Paskett, PhD, an epidemiologist and cancer screening expert at Ohio State University, Columbus. A positive Galleri test leads to a cascade of follow-up diagnostic tests, which payers may not cover. For a negative result, Galleri recommends that the patient undergo screening again in a year, at an annual cost of $950 plus the cost of any follow-up testing when Galleri does pick something up.
“If a provider wants to offer the Galleri test, all those things need to be made abundantly clear, in my opinion,” Dr. Paskett said.
Following the negative Galleri test, Mr. Arenz’s cancer didn’t slip through the cracks because he received other advanced imaging free of charge. But whether all doctors will go to such lengths to back up Galleri results, even for patients with negative results, is unknown.
A negative result can give patients “a huge false sense of security,” said Dr. Shukla. And if a test is positive, the workup isn’t simple. Chasing cancer, especially one that’s not really there, can be nerve-wracking and expensive.
The question, then, is why perform the Galleri test at all if results require so much validation?
Dr. Parikh explained that a high-risk group such as firefighters represents an ideal-use case for Galleri and other liquid biopsy tests. But she noted that she would be “wary of the ability of the system to manage this test en masse” were the test to be used more widely in the general population.
Dr. Shukla said it’s less about the results she’s getting today and more about making the test more effective for her patients in the future. First responders need a test such as this that can quickly identify multiple cancers. However, to improve the test, Grail needs more data from this high-risk population. That’s what she’s after.
Mr. Curtis doesn’t regret taking the Galleri test. The emotional toll of thinking he had cancer for a few days wasn’t too high a price, in his opinion. It’s part of cancer screening. But he acknowledged that it would have been a much more burdensome experience had he’d been financially responsible for the workup or if he hadn’t had Dr. Shukla to manage his case from start to finish.
Because it was free, Mr. Arenz doesn’t regret undergoing the Galleri test either. But he tells his coworkers to check the site, do their research, and get more screening.
“Any medical center that’s just doing this one test, you just have to be careful,” Dr. Shukla said. “It’s not that easy.”
A version of this article first appeared on Medscape.com.



