User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
The ADA and hearing-impaired patients
A recent claim against a New Jersey physician attracted considerable attention in both the medical and legal communities, not only because it resulted in a substantial jury award, but because that award was not covered by malpractice insurance.
It is a good reminder for the rest of us: This case involved a charge of discrimination against a hearing-impaired patient – which meant the physician not only had to fund his own defense, but was personally responsible for the $400,000 award against him.
The Americans with Disabilities Act (ADA) was designed to protect individuals with various disabilities against discrimination in various public situations – including, specifically, “the professional office of a health care professional.”
When the disability is impaired hearing, the law requires physicians to provide any “auxiliary aids and services” that might be necessary to insure clear communication between doctor and patient. In the vast majority of such situations, a pad and pencil will satisfy that requirement. But occasionally it does not, particularly when complex medical concepts are involved; and in such cases, as the New Jersey trial demonstrated, failure to make the necessary extra effort can be very expensive.
The claim involved a hearing-impaired patient with lupus erythematosus under treatment by a rheumatologist. For almost 2 years the patient’s partner and her daughter provided translation; but that arrangement was inadequate, she testified, because her partner and daughter were unfamiliar with medical terminology and she was “unable to understand and participate in her care,” which left her “unaware of risks and available alternatives.”
She repeatedly requested that the rheumatologist provide an American Sign Language interpreter for her office visits. He refused on grounds that the cost of an interpreter would exceed the payment he would receive for the visits, which made it an “undue financial burden,” and therefore exempt from ADA requirements.
But the undue-burden exemption is not automatic; it must be demonstrated in court. And the jury decided the rheumatologist’s annual income of $425,000 rendered the cost of an interpreter quite affordable.
The lessons are clear: Physicians must take antidiscrimination laws seriously, particularly when uninsurable issues are involved; and we must be constantly aware of the needs of disabled patients, to be sure their care is not substantially different from that of any other patient.
In the case of hearing-impaired or deaf patients, it is important to remember that forms of communication that are quite adequate for most are not appropriate for some. Lip reading, written notes, and the use of family members as interpreters may be perfectly acceptable to one patient and unsuitable for another.
If the patient agrees to written notes and lip reading, as most do, you need to remember to speak slowly, and to write down critical information to avoid any miscommunications. And as always, it is crucial to document all communication, as well as the methods used for that communication – specifically including the fact that the patient agreed to those forms of communication. Documentation, as I’ve often said, is like garlic: There is no such thing as too much of it.
Should a patient not agree that written notes are sufficient, other alternatives can be offered: computer transcription, assistive listening devices, videotext displays (often available in hospitals), and telecommunication devices such as TTY and TDD. But if the patient rejects all of those options and continues to insist on a professional interpreter, the precedent set by the New Jersey case suggests that you need to acquiesce, even if the interpreter’s fee exceeds the visit reimbursement – and the ADA prohibits you from passing your cost along to the patient. But any such cost will be far less than a noninsured judgment against you.
If you must go that route, make sure the interpreter you hire is familiar with medical terminology, and is not acquainted or related to the patient (for HIPAA reasons). Your state may have an online registry of available interpreters, or your hospital may have a sign language interpreter on its staff that they might allow you to “borrow.”
The good news is several states have responded to this issue by introducing legislation that would require health insurance carriers to pay for the cost of interpreters, although none, as of this writing, have yet become law.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
A recent claim against a New Jersey physician attracted considerable attention in both the medical and legal communities, not only because it resulted in a substantial jury award, but because that award was not covered by malpractice insurance.
It is a good reminder for the rest of us: This case involved a charge of discrimination against a hearing-impaired patient – which meant the physician not only had to fund his own defense, but was personally responsible for the $400,000 award against him.
The Americans with Disabilities Act (ADA) was designed to protect individuals with various disabilities against discrimination in various public situations – including, specifically, “the professional office of a health care professional.”
When the disability is impaired hearing, the law requires physicians to provide any “auxiliary aids and services” that might be necessary to insure clear communication between doctor and patient. In the vast majority of such situations, a pad and pencil will satisfy that requirement. But occasionally it does not, particularly when complex medical concepts are involved; and in such cases, as the New Jersey trial demonstrated, failure to make the necessary extra effort can be very expensive.
The claim involved a hearing-impaired patient with lupus erythematosus under treatment by a rheumatologist. For almost 2 years the patient’s partner and her daughter provided translation; but that arrangement was inadequate, she testified, because her partner and daughter were unfamiliar with medical terminology and she was “unable to understand and participate in her care,” which left her “unaware of risks and available alternatives.”
She repeatedly requested that the rheumatologist provide an American Sign Language interpreter for her office visits. He refused on grounds that the cost of an interpreter would exceed the payment he would receive for the visits, which made it an “undue financial burden,” and therefore exempt from ADA requirements.
But the undue-burden exemption is not automatic; it must be demonstrated in court. And the jury decided the rheumatologist’s annual income of $425,000 rendered the cost of an interpreter quite affordable.
The lessons are clear: Physicians must take antidiscrimination laws seriously, particularly when uninsurable issues are involved; and we must be constantly aware of the needs of disabled patients, to be sure their care is not substantially different from that of any other patient.
In the case of hearing-impaired or deaf patients, it is important to remember that forms of communication that are quite adequate for most are not appropriate for some. Lip reading, written notes, and the use of family members as interpreters may be perfectly acceptable to one patient and unsuitable for another.
If the patient agrees to written notes and lip reading, as most do, you need to remember to speak slowly, and to write down critical information to avoid any miscommunications. And as always, it is crucial to document all communication, as well as the methods used for that communication – specifically including the fact that the patient agreed to those forms of communication. Documentation, as I’ve often said, is like garlic: There is no such thing as too much of it.
Should a patient not agree that written notes are sufficient, other alternatives can be offered: computer transcription, assistive listening devices, videotext displays (often available in hospitals), and telecommunication devices such as TTY and TDD. But if the patient rejects all of those options and continues to insist on a professional interpreter, the precedent set by the New Jersey case suggests that you need to acquiesce, even if the interpreter’s fee exceeds the visit reimbursement – and the ADA prohibits you from passing your cost along to the patient. But any such cost will be far less than a noninsured judgment against you.
If you must go that route, make sure the interpreter you hire is familiar with medical terminology, and is not acquainted or related to the patient (for HIPAA reasons). Your state may have an online registry of available interpreters, or your hospital may have a sign language interpreter on its staff that they might allow you to “borrow.”
The good news is several states have responded to this issue by introducing legislation that would require health insurance carriers to pay for the cost of interpreters, although none, as of this writing, have yet become law.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
A recent claim against a New Jersey physician attracted considerable attention in both the medical and legal communities, not only because it resulted in a substantial jury award, but because that award was not covered by malpractice insurance.
It is a good reminder for the rest of us: This case involved a charge of discrimination against a hearing-impaired patient – which meant the physician not only had to fund his own defense, but was personally responsible for the $400,000 award against him.
The Americans with Disabilities Act (ADA) was designed to protect individuals with various disabilities against discrimination in various public situations – including, specifically, “the professional office of a health care professional.”
When the disability is impaired hearing, the law requires physicians to provide any “auxiliary aids and services” that might be necessary to insure clear communication between doctor and patient. In the vast majority of such situations, a pad and pencil will satisfy that requirement. But occasionally it does not, particularly when complex medical concepts are involved; and in such cases, as the New Jersey trial demonstrated, failure to make the necessary extra effort can be very expensive.
The claim involved a hearing-impaired patient with lupus erythematosus under treatment by a rheumatologist. For almost 2 years the patient’s partner and her daughter provided translation; but that arrangement was inadequate, she testified, because her partner and daughter were unfamiliar with medical terminology and she was “unable to understand and participate in her care,” which left her “unaware of risks and available alternatives.”
She repeatedly requested that the rheumatologist provide an American Sign Language interpreter for her office visits. He refused on grounds that the cost of an interpreter would exceed the payment he would receive for the visits, which made it an “undue financial burden,” and therefore exempt from ADA requirements.
But the undue-burden exemption is not automatic; it must be demonstrated in court. And the jury decided the rheumatologist’s annual income of $425,000 rendered the cost of an interpreter quite affordable.
The lessons are clear: Physicians must take antidiscrimination laws seriously, particularly when uninsurable issues are involved; and we must be constantly aware of the needs of disabled patients, to be sure their care is not substantially different from that of any other patient.
In the case of hearing-impaired or deaf patients, it is important to remember that forms of communication that are quite adequate for most are not appropriate for some. Lip reading, written notes, and the use of family members as interpreters may be perfectly acceptable to one patient and unsuitable for another.
If the patient agrees to written notes and lip reading, as most do, you need to remember to speak slowly, and to write down critical information to avoid any miscommunications. And as always, it is crucial to document all communication, as well as the methods used for that communication – specifically including the fact that the patient agreed to those forms of communication. Documentation, as I’ve often said, is like garlic: There is no such thing as too much of it.
Should a patient not agree that written notes are sufficient, other alternatives can be offered: computer transcription, assistive listening devices, videotext displays (often available in hospitals), and telecommunication devices such as TTY and TDD. But if the patient rejects all of those options and continues to insist on a professional interpreter, the precedent set by the New Jersey case suggests that you need to acquiesce, even if the interpreter’s fee exceeds the visit reimbursement – and the ADA prohibits you from passing your cost along to the patient. But any such cost will be far less than a noninsured judgment against you.
If you must go that route, make sure the interpreter you hire is familiar with medical terminology, and is not acquainted or related to the patient (for HIPAA reasons). Your state may have an online registry of available interpreters, or your hospital may have a sign language interpreter on its staff that they might allow you to “borrow.”
The good news is several states have responded to this issue by introducing legislation that would require health insurance carriers to pay for the cost of interpreters, although none, as of this writing, have yet become law.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Does early delivery for FGR affect school outcomes?
Iatrogenic delivery for suspected fetal growth restriction (FGR) may be associated with an increased likelihood of poorer school outcomes among infants born severely small for gestational age, a study of children in Australia suggests.
researchers reported in JAMA.
“It raises the question: in our efforts to improve outcomes in babies that are small, are we potentially doing more harm than good?” said Robert M. Silver, MD, of the department of obstetrics and gynecology at the University of Utah, Salt Lake City, who was not involved in the study. “I think that is a very important question to ask.”
However, “we can’t make that conclusion based on this one study,” he said in an interview. It could be that, in cases where severely small infants were delivered early, there may have been testing that indicated acute risks, and these infants may have tended to be sicker overall. “It may have been that if those babies weren’t delivered, they would have suffered a stillbirth or major brain injury,” Dr. Silver said. “It is really important that we acknowledge that we shouldn’t change our clinical practice” based on this one study.”
At the same time, the study underscores questions and challenges that surround the definition, identification, and management of suspected FGR, Dr. Silver said.
The study authors described their research as exploratory. In a related editorial Dr. Silver and Nathan R. Blue, MD said the findings should be considered hypothesis generating.
For the study, Roshan John Selvaratnam, BMedSc(Hons), a researcher affiliated with Monash University, Melbourne, and colleagues analyzed data from 181,902 children with developmental outcomes and 425,717 children with educational outcomes in Australia. They included children born at 32 weeks’ or more gestation between 2003 and 2013.
Severely small infants delivered early for suspected FGR had an average gestation of 37.9 weeks, whereas those not suspected of having FGR had an average gestation of 39.4 weeks.
Among infants who were severely small for gestational age, those delivered early for suspected FGR were more likely to be in the bottom 10th percentile on at least two developmental domains when they started school, compared with those not suspected of having FGR (16.2% vs. 12.7%; adjusted odds ratio, 1.36). They also were more likely to have low test scores in subsequent years. In grade 7, for example, the adjusted odds ratio for scoring below the national minimum standard on at least two educational domains was 1.33 (13.4% vs. 10.5%).
The researchers defined severely small for gestational age as birth weight below the third percentile. Among infants with normal growth, defined as birth weight at the 10th percentile or greater, school outcomes did not significantly differ between those with early delivery for suspected FGR and those not suspected of having FGR. Approximately 8% of the infants with normal growth had poor developmental outcomes.
The study authors described the dilemma that clinicians face with suspected FGR: “Either intervene early to prevent a small risk of stillbirth but potentially cause immediate and lifelong harm to the child or accept the increasing risk of stillbirth associated with prolonging the pregnancy to avoid more common neonatal and longer-term morbidities.”
It could be that severely small infants with suspected FGR in the study were “more compromised than those not suspected of having FGR,” which might explain the outcomes, Mr. Selvaratnam and coauthors wrote.
Another more plausible explanation is that “iatrogenic prematurity was harmful,” they said.
The researchers were unable to adjust for many factors that may influence academic success, including smoking and alcohol use during pregnancy, maternal body mass index, and breastfeeding, they noted. They also lacked information about the etiology for FGR and whether children had genetic abnormalities.
The study also does not take into account neonatal, infant, and childhood complications, Dr. Silver and Dr. Blue wrote in their editorial. “Nonetheless, these data are a welcome contribution given the knowledge gaps with regard to the optimal obstetric management of FGR.”
The establishment of a diagnostic standard for FGR is needed to properly investigate ways to improve risk stratification, diagnosis, and management, Dr. Silver and Dr. Blue added.
“What we have to do is get better at predicting which babies are at very high risk for continuing the pregnancy and which babies are at low risk for continuing the pregnancy so that we can better decide which babies would benefit from slightly early delivery,” Dr. Silver said.
Improved detection and management of FGR may be on the horizon. “Our ability to image the placental function has gotten a lot better, and I think that is really going to help us,” Dr. Silver said. Studies that aim to further improve the ability to assess whether babies are getting adequate blood flow during pregnancy are ongoing, which could further help doctors evaluate risks.
The study investigators and Dr. Silver had no conflict of interest disclosures. Dr. Blue disclosed grants from Samsung Medison and personal fees from Elsevier. The study was supported by a grant from the Australian government’s National Health and Medical Research Council Program, and Mr. Selvaratnam is supported by scholarships from an Australian government research training program and the National Centre of Research Excellence in Stillbirth.
Iatrogenic delivery for suspected fetal growth restriction (FGR) may be associated with an increased likelihood of poorer school outcomes among infants born severely small for gestational age, a study of children in Australia suggests.
researchers reported in JAMA.
“It raises the question: in our efforts to improve outcomes in babies that are small, are we potentially doing more harm than good?” said Robert M. Silver, MD, of the department of obstetrics and gynecology at the University of Utah, Salt Lake City, who was not involved in the study. “I think that is a very important question to ask.”
However, “we can’t make that conclusion based on this one study,” he said in an interview. It could be that, in cases where severely small infants were delivered early, there may have been testing that indicated acute risks, and these infants may have tended to be sicker overall. “It may have been that if those babies weren’t delivered, they would have suffered a stillbirth or major brain injury,” Dr. Silver said. “It is really important that we acknowledge that we shouldn’t change our clinical practice” based on this one study.”
At the same time, the study underscores questions and challenges that surround the definition, identification, and management of suspected FGR, Dr. Silver said.
The study authors described their research as exploratory. In a related editorial Dr. Silver and Nathan R. Blue, MD said the findings should be considered hypothesis generating.
For the study, Roshan John Selvaratnam, BMedSc(Hons), a researcher affiliated with Monash University, Melbourne, and colleagues analyzed data from 181,902 children with developmental outcomes and 425,717 children with educational outcomes in Australia. They included children born at 32 weeks’ or more gestation between 2003 and 2013.
Severely small infants delivered early for suspected FGR had an average gestation of 37.9 weeks, whereas those not suspected of having FGR had an average gestation of 39.4 weeks.
Among infants who were severely small for gestational age, those delivered early for suspected FGR were more likely to be in the bottom 10th percentile on at least two developmental domains when they started school, compared with those not suspected of having FGR (16.2% vs. 12.7%; adjusted odds ratio, 1.36). They also were more likely to have low test scores in subsequent years. In grade 7, for example, the adjusted odds ratio for scoring below the national minimum standard on at least two educational domains was 1.33 (13.4% vs. 10.5%).
The researchers defined severely small for gestational age as birth weight below the third percentile. Among infants with normal growth, defined as birth weight at the 10th percentile or greater, school outcomes did not significantly differ between those with early delivery for suspected FGR and those not suspected of having FGR. Approximately 8% of the infants with normal growth had poor developmental outcomes.
The study authors described the dilemma that clinicians face with suspected FGR: “Either intervene early to prevent a small risk of stillbirth but potentially cause immediate and lifelong harm to the child or accept the increasing risk of stillbirth associated with prolonging the pregnancy to avoid more common neonatal and longer-term morbidities.”
It could be that severely small infants with suspected FGR in the study were “more compromised than those not suspected of having FGR,” which might explain the outcomes, Mr. Selvaratnam and coauthors wrote.
Another more plausible explanation is that “iatrogenic prematurity was harmful,” they said.
The researchers were unable to adjust for many factors that may influence academic success, including smoking and alcohol use during pregnancy, maternal body mass index, and breastfeeding, they noted. They also lacked information about the etiology for FGR and whether children had genetic abnormalities.
The study also does not take into account neonatal, infant, and childhood complications, Dr. Silver and Dr. Blue wrote in their editorial. “Nonetheless, these data are a welcome contribution given the knowledge gaps with regard to the optimal obstetric management of FGR.”
The establishment of a diagnostic standard for FGR is needed to properly investigate ways to improve risk stratification, diagnosis, and management, Dr. Silver and Dr. Blue added.
“What we have to do is get better at predicting which babies are at very high risk for continuing the pregnancy and which babies are at low risk for continuing the pregnancy so that we can better decide which babies would benefit from slightly early delivery,” Dr. Silver said.
Improved detection and management of FGR may be on the horizon. “Our ability to image the placental function has gotten a lot better, and I think that is really going to help us,” Dr. Silver said. Studies that aim to further improve the ability to assess whether babies are getting adequate blood flow during pregnancy are ongoing, which could further help doctors evaluate risks.
The study investigators and Dr. Silver had no conflict of interest disclosures. Dr. Blue disclosed grants from Samsung Medison and personal fees from Elsevier. The study was supported by a grant from the Australian government’s National Health and Medical Research Council Program, and Mr. Selvaratnam is supported by scholarships from an Australian government research training program and the National Centre of Research Excellence in Stillbirth.
Iatrogenic delivery for suspected fetal growth restriction (FGR) may be associated with an increased likelihood of poorer school outcomes among infants born severely small for gestational age, a study of children in Australia suggests.
researchers reported in JAMA.
“It raises the question: in our efforts to improve outcomes in babies that are small, are we potentially doing more harm than good?” said Robert M. Silver, MD, of the department of obstetrics and gynecology at the University of Utah, Salt Lake City, who was not involved in the study. “I think that is a very important question to ask.”
However, “we can’t make that conclusion based on this one study,” he said in an interview. It could be that, in cases where severely small infants were delivered early, there may have been testing that indicated acute risks, and these infants may have tended to be sicker overall. “It may have been that if those babies weren’t delivered, they would have suffered a stillbirth or major brain injury,” Dr. Silver said. “It is really important that we acknowledge that we shouldn’t change our clinical practice” based on this one study.”
At the same time, the study underscores questions and challenges that surround the definition, identification, and management of suspected FGR, Dr. Silver said.
The study authors described their research as exploratory. In a related editorial Dr. Silver and Nathan R. Blue, MD said the findings should be considered hypothesis generating.
For the study, Roshan John Selvaratnam, BMedSc(Hons), a researcher affiliated with Monash University, Melbourne, and colleagues analyzed data from 181,902 children with developmental outcomes and 425,717 children with educational outcomes in Australia. They included children born at 32 weeks’ or more gestation between 2003 and 2013.
Severely small infants delivered early for suspected FGR had an average gestation of 37.9 weeks, whereas those not suspected of having FGR had an average gestation of 39.4 weeks.
Among infants who were severely small for gestational age, those delivered early for suspected FGR were more likely to be in the bottom 10th percentile on at least two developmental domains when they started school, compared with those not suspected of having FGR (16.2% vs. 12.7%; adjusted odds ratio, 1.36). They also were more likely to have low test scores in subsequent years. In grade 7, for example, the adjusted odds ratio for scoring below the national minimum standard on at least two educational domains was 1.33 (13.4% vs. 10.5%).
The researchers defined severely small for gestational age as birth weight below the third percentile. Among infants with normal growth, defined as birth weight at the 10th percentile or greater, school outcomes did not significantly differ between those with early delivery for suspected FGR and those not suspected of having FGR. Approximately 8% of the infants with normal growth had poor developmental outcomes.
The study authors described the dilemma that clinicians face with suspected FGR: “Either intervene early to prevent a small risk of stillbirth but potentially cause immediate and lifelong harm to the child or accept the increasing risk of stillbirth associated with prolonging the pregnancy to avoid more common neonatal and longer-term morbidities.”
It could be that severely small infants with suspected FGR in the study were “more compromised than those not suspected of having FGR,” which might explain the outcomes, Mr. Selvaratnam and coauthors wrote.
Another more plausible explanation is that “iatrogenic prematurity was harmful,” they said.
The researchers were unable to adjust for many factors that may influence academic success, including smoking and alcohol use during pregnancy, maternal body mass index, and breastfeeding, they noted. They also lacked information about the etiology for FGR and whether children had genetic abnormalities.
The study also does not take into account neonatal, infant, and childhood complications, Dr. Silver and Dr. Blue wrote in their editorial. “Nonetheless, these data are a welcome contribution given the knowledge gaps with regard to the optimal obstetric management of FGR.”
The establishment of a diagnostic standard for FGR is needed to properly investigate ways to improve risk stratification, diagnosis, and management, Dr. Silver and Dr. Blue added.
“What we have to do is get better at predicting which babies are at very high risk for continuing the pregnancy and which babies are at low risk for continuing the pregnancy so that we can better decide which babies would benefit from slightly early delivery,” Dr. Silver said.
Improved detection and management of FGR may be on the horizon. “Our ability to image the placental function has gotten a lot better, and I think that is really going to help us,” Dr. Silver said. Studies that aim to further improve the ability to assess whether babies are getting adequate blood flow during pregnancy are ongoing, which could further help doctors evaluate risks.
The study investigators and Dr. Silver had no conflict of interest disclosures. Dr. Blue disclosed grants from Samsung Medison and personal fees from Elsevier. The study was supported by a grant from the Australian government’s National Health and Medical Research Council Program, and Mr. Selvaratnam is supported by scholarships from an Australian government research training program and the National Centre of Research Excellence in Stillbirth.
FROM JAMA
When patients demand vaccinated health care providers
Should a hospital or medical practice fulfill a patient’s request to be treated or cared for only by vaccinated health care providers?The answer is yes, in a perfect world. Patients should feel assured that their health care providers – clinicians and caregivers – are not exposing them to infectious diseases.But issues are being raised – subquestions that need to be answered to understand the current situation and assist health care employers in their decision-making:
- Must health care employers ensure that their employees are vaccinated?
- Can health care employers require that their employees be vaccinated?
- Do employees have any rights to refuse vaccination or to refuse to supply their employer with their vaccination status?
- Can a health care employer terminate an employee who refuses vaccination?
- Does a patient have a legal right to a vaccinated health care provider?
At present, federal policy says that employers may, but are not required to, insist that employees be vaccinated. The currently prevailing state case law says that hospitals and other employers can require staff to be vaccinated and can terminate employees who refuse vaccination. In June, a Texas court dismissed a case in which 117 employees sued a hospital for requiring that employees be vaccinated. More cases are pending in other states, and there may be differing decisions in other states and on appeal.
State laws enacted years ago also weigh in on employer obligations. In at least one state, Oregon, employers of health care providers may not require vaccination, even though other employers may. Other states have laws about what an employer may or may not require of an employee regarding vaccination, and some have introduced laws which are pending.
So, in most states, health care employers may, not must, require that employees be vaccinated. In most states, hospitals and medical practices may terminate employees who refuse vaccination. However, employers should research the laws of their own states before requiring vaccinations and before terminating employees who are not vaccinated.
The issue of employer mandates is complicated further by the practicality that, in some areas of the country, health care providers are in scarce supply. Employers don’t want to lose the providers they have.
And there are additional questions about how certain federal laws affect the situation. Federal law that may apply includes:
- U.S. Food and Drug Administration regulation on approval of vaccines
- The Americans With Disabilities Act (ADA)
- The Health Insurance Portability and Accountability Act of 1996, which protects sensitive patient health information from being disclosed without the patient’s consent
- Civil rights laws
- Patients’ rights
FDA. Some health care providers who refuse vaccination argue that employers have no legal right to require a vaccine that is not fully approved by the FDA. COVID-19 vaccinations have emergency use authorization – something less than full approval. Courts have not yet ruled on this issue.
ADA. Some attorneys believe that honoring a patient’s request to be attended only by a vaccinated health care provider can implicate the ADA. However, the ADA doesn’t protect healthy individuals who don’t want to be vaccinated. The ADA protects the person who, because of their disability, shouldn’t get the vaccination. If an employer mandates vaccination, the employer must, under the ADA, consider requests for exemptions from disabled individuals. However, even when an employee has a disability that may qualify the employee for an exemption to the vaccination requirement, an employer may argue that giving an exemption would be a direct threat to the safety of others; in that case, the ADA may require that the disabled employee and hospital work something out. A compromise might be that the unvaccinated disabled individual would not provide direct patient care or would wear a mask and maintain physical distance.
HIPAA. Some argue that federal privacy law enters into the discussion, maintaining that health care employers can’t disclose employees’ vaccination status under HIPAA. That is not true. Employers are not “covered entities” under HIPAA. It is health care providers who are precluded under HIPAA from disclosing a patient’s personal information. So, if an employer were to ask an employee’s health care provider about the employee’s vaccination status, the health care provider could disclose that status only if the employee consented to the disclosure. An employer may ask an employee for the employee’s proof of vaccination card. However, employers must not ask for unnecessary details that might reveal disability information protected by the ADA.
Civil rights law. Civil rights laws may protect certain individuals from employment consequences of refusing vaccination. Specifically, individuals with sincerely held religious convictions against vaccinations are protected from retaliation by employers for refusing vaccination, under the Constitutional right of freedom of religion. The individual without sincerely held religious convictions against vaccinations and without a relevant disability doesn’t have legal remedies under civil rights laws.
Civil rights laws may apply if employers don’t apply their vaccination requirements to all employees equally. That is, employers can’t require vaccinations of some employees but not others.
Patients’ rights. Legal protections for patients who want a vaccinated health care provider are nowhere to be seen, at this time. It is unlikely that a single patient will be able to convince a hospital or medical practice to require that its staff be vaccinated. However, if a patient becomes infected with COVID-19 and can prove that the illness is causally related to interacting with an unvaccinated health care worker, the patient may have a case against the employer. The legal theory would be malpractice or negligence under informed consent law: That is, the patient did not consent to be treated by an unvaccinated person.
Employer options
So, what can health care employers do? They have three options:
- Require vaccination of all employees, independent contractors, and other providers who have privileges to see patients. Then, as long as the employer enforces the vaccination mandate, the employer can tell patients that all providers are vaccinated.
- Not require that employees and others with access to patients be vaccinated, and if a patient requests to be seen only by vaccinated providers, provide that patient with a vaccinated provider. It is especially important that health care employers take care with patients who are unvaccinated and who have been advised not to be vaccinated because of a medical condition. Both the patient and the health care employer would be protected best by avoiding having two unvaccinated individuals interact. Masks and physical distancing may decrease the risk.
- Not require that employees be vaccinated and refuse to guarantee that providers are vaccinated. To avoid risk for future lawsuits, employers should inform patients that there is no assurance that providers are vaccinated. That leaves it to each patient to ask individual providers about the provider’s vaccination status. If a patient doesn’t like a provider’s answer, then the patient has the right to leave. It’s not clear that the patient has a legal right to stay and demand a vaccinated provider.
Option three is problematic for a number of reasons. Patients aren’t always in a position to query each provider who enters the room about vaccination status. Patients may be sedated or too ill to exert that effort. And it puts supervisors in the position of having to mediate situations where a patient wants to leave against medical advice but the option of staying may also be dangerous.
Health care employers should discuss the options with their legal counsel before deciding which option to adopt.
A version of this article first appeared on Medscape.com.
Should a hospital or medical practice fulfill a patient’s request to be treated or cared for only by vaccinated health care providers?The answer is yes, in a perfect world. Patients should feel assured that their health care providers – clinicians and caregivers – are not exposing them to infectious diseases.But issues are being raised – subquestions that need to be answered to understand the current situation and assist health care employers in their decision-making:
- Must health care employers ensure that their employees are vaccinated?
- Can health care employers require that their employees be vaccinated?
- Do employees have any rights to refuse vaccination or to refuse to supply their employer with their vaccination status?
- Can a health care employer terminate an employee who refuses vaccination?
- Does a patient have a legal right to a vaccinated health care provider?
At present, federal policy says that employers may, but are not required to, insist that employees be vaccinated. The currently prevailing state case law says that hospitals and other employers can require staff to be vaccinated and can terminate employees who refuse vaccination. In June, a Texas court dismissed a case in which 117 employees sued a hospital for requiring that employees be vaccinated. More cases are pending in other states, and there may be differing decisions in other states and on appeal.
State laws enacted years ago also weigh in on employer obligations. In at least one state, Oregon, employers of health care providers may not require vaccination, even though other employers may. Other states have laws about what an employer may or may not require of an employee regarding vaccination, and some have introduced laws which are pending.
So, in most states, health care employers may, not must, require that employees be vaccinated. In most states, hospitals and medical practices may terminate employees who refuse vaccination. However, employers should research the laws of their own states before requiring vaccinations and before terminating employees who are not vaccinated.
The issue of employer mandates is complicated further by the practicality that, in some areas of the country, health care providers are in scarce supply. Employers don’t want to lose the providers they have.
And there are additional questions about how certain federal laws affect the situation. Federal law that may apply includes:
- U.S. Food and Drug Administration regulation on approval of vaccines
- The Americans With Disabilities Act (ADA)
- The Health Insurance Portability and Accountability Act of 1996, which protects sensitive patient health information from being disclosed without the patient’s consent
- Civil rights laws
- Patients’ rights
FDA. Some health care providers who refuse vaccination argue that employers have no legal right to require a vaccine that is not fully approved by the FDA. COVID-19 vaccinations have emergency use authorization – something less than full approval. Courts have not yet ruled on this issue.
ADA. Some attorneys believe that honoring a patient’s request to be attended only by a vaccinated health care provider can implicate the ADA. However, the ADA doesn’t protect healthy individuals who don’t want to be vaccinated. The ADA protects the person who, because of their disability, shouldn’t get the vaccination. If an employer mandates vaccination, the employer must, under the ADA, consider requests for exemptions from disabled individuals. However, even when an employee has a disability that may qualify the employee for an exemption to the vaccination requirement, an employer may argue that giving an exemption would be a direct threat to the safety of others; in that case, the ADA may require that the disabled employee and hospital work something out. A compromise might be that the unvaccinated disabled individual would not provide direct patient care or would wear a mask and maintain physical distance.
HIPAA. Some argue that federal privacy law enters into the discussion, maintaining that health care employers can’t disclose employees’ vaccination status under HIPAA. That is not true. Employers are not “covered entities” under HIPAA. It is health care providers who are precluded under HIPAA from disclosing a patient’s personal information. So, if an employer were to ask an employee’s health care provider about the employee’s vaccination status, the health care provider could disclose that status only if the employee consented to the disclosure. An employer may ask an employee for the employee’s proof of vaccination card. However, employers must not ask for unnecessary details that might reveal disability information protected by the ADA.
Civil rights law. Civil rights laws may protect certain individuals from employment consequences of refusing vaccination. Specifically, individuals with sincerely held religious convictions against vaccinations are protected from retaliation by employers for refusing vaccination, under the Constitutional right of freedom of religion. The individual without sincerely held religious convictions against vaccinations and without a relevant disability doesn’t have legal remedies under civil rights laws.
Civil rights laws may apply if employers don’t apply their vaccination requirements to all employees equally. That is, employers can’t require vaccinations of some employees but not others.
Patients’ rights. Legal protections for patients who want a vaccinated health care provider are nowhere to be seen, at this time. It is unlikely that a single patient will be able to convince a hospital or medical practice to require that its staff be vaccinated. However, if a patient becomes infected with COVID-19 and can prove that the illness is causally related to interacting with an unvaccinated health care worker, the patient may have a case against the employer. The legal theory would be malpractice or negligence under informed consent law: That is, the patient did not consent to be treated by an unvaccinated person.
Employer options
So, what can health care employers do? They have three options:
- Require vaccination of all employees, independent contractors, and other providers who have privileges to see patients. Then, as long as the employer enforces the vaccination mandate, the employer can tell patients that all providers are vaccinated.
- Not require that employees and others with access to patients be vaccinated, and if a patient requests to be seen only by vaccinated providers, provide that patient with a vaccinated provider. It is especially important that health care employers take care with patients who are unvaccinated and who have been advised not to be vaccinated because of a medical condition. Both the patient and the health care employer would be protected best by avoiding having two unvaccinated individuals interact. Masks and physical distancing may decrease the risk.
- Not require that employees be vaccinated and refuse to guarantee that providers are vaccinated. To avoid risk for future lawsuits, employers should inform patients that there is no assurance that providers are vaccinated. That leaves it to each patient to ask individual providers about the provider’s vaccination status. If a patient doesn’t like a provider’s answer, then the patient has the right to leave. It’s not clear that the patient has a legal right to stay and demand a vaccinated provider.
Option three is problematic for a number of reasons. Patients aren’t always in a position to query each provider who enters the room about vaccination status. Patients may be sedated or too ill to exert that effort. And it puts supervisors in the position of having to mediate situations where a patient wants to leave against medical advice but the option of staying may also be dangerous.
Health care employers should discuss the options with their legal counsel before deciding which option to adopt.
A version of this article first appeared on Medscape.com.
Should a hospital or medical practice fulfill a patient’s request to be treated or cared for only by vaccinated health care providers?The answer is yes, in a perfect world. Patients should feel assured that their health care providers – clinicians and caregivers – are not exposing them to infectious diseases.But issues are being raised – subquestions that need to be answered to understand the current situation and assist health care employers in their decision-making:
- Must health care employers ensure that their employees are vaccinated?
- Can health care employers require that their employees be vaccinated?
- Do employees have any rights to refuse vaccination or to refuse to supply their employer with their vaccination status?
- Can a health care employer terminate an employee who refuses vaccination?
- Does a patient have a legal right to a vaccinated health care provider?
At present, federal policy says that employers may, but are not required to, insist that employees be vaccinated. The currently prevailing state case law says that hospitals and other employers can require staff to be vaccinated and can terminate employees who refuse vaccination. In June, a Texas court dismissed a case in which 117 employees sued a hospital for requiring that employees be vaccinated. More cases are pending in other states, and there may be differing decisions in other states and on appeal.
State laws enacted years ago also weigh in on employer obligations. In at least one state, Oregon, employers of health care providers may not require vaccination, even though other employers may. Other states have laws about what an employer may or may not require of an employee regarding vaccination, and some have introduced laws which are pending.
So, in most states, health care employers may, not must, require that employees be vaccinated. In most states, hospitals and medical practices may terminate employees who refuse vaccination. However, employers should research the laws of their own states before requiring vaccinations and before terminating employees who are not vaccinated.
The issue of employer mandates is complicated further by the practicality that, in some areas of the country, health care providers are in scarce supply. Employers don’t want to lose the providers they have.
And there are additional questions about how certain federal laws affect the situation. Federal law that may apply includes:
- U.S. Food and Drug Administration regulation on approval of vaccines
- The Americans With Disabilities Act (ADA)
- The Health Insurance Portability and Accountability Act of 1996, which protects sensitive patient health information from being disclosed without the patient’s consent
- Civil rights laws
- Patients’ rights
FDA. Some health care providers who refuse vaccination argue that employers have no legal right to require a vaccine that is not fully approved by the FDA. COVID-19 vaccinations have emergency use authorization – something less than full approval. Courts have not yet ruled on this issue.
ADA. Some attorneys believe that honoring a patient’s request to be attended only by a vaccinated health care provider can implicate the ADA. However, the ADA doesn’t protect healthy individuals who don’t want to be vaccinated. The ADA protects the person who, because of their disability, shouldn’t get the vaccination. If an employer mandates vaccination, the employer must, under the ADA, consider requests for exemptions from disabled individuals. However, even when an employee has a disability that may qualify the employee for an exemption to the vaccination requirement, an employer may argue that giving an exemption would be a direct threat to the safety of others; in that case, the ADA may require that the disabled employee and hospital work something out. A compromise might be that the unvaccinated disabled individual would not provide direct patient care or would wear a mask and maintain physical distance.
HIPAA. Some argue that federal privacy law enters into the discussion, maintaining that health care employers can’t disclose employees’ vaccination status under HIPAA. That is not true. Employers are not “covered entities” under HIPAA. It is health care providers who are precluded under HIPAA from disclosing a patient’s personal information. So, if an employer were to ask an employee’s health care provider about the employee’s vaccination status, the health care provider could disclose that status only if the employee consented to the disclosure. An employer may ask an employee for the employee’s proof of vaccination card. However, employers must not ask for unnecessary details that might reveal disability information protected by the ADA.
Civil rights law. Civil rights laws may protect certain individuals from employment consequences of refusing vaccination. Specifically, individuals with sincerely held religious convictions against vaccinations are protected from retaliation by employers for refusing vaccination, under the Constitutional right of freedom of religion. The individual without sincerely held religious convictions against vaccinations and without a relevant disability doesn’t have legal remedies under civil rights laws.
Civil rights laws may apply if employers don’t apply their vaccination requirements to all employees equally. That is, employers can’t require vaccinations of some employees but not others.
Patients’ rights. Legal protections for patients who want a vaccinated health care provider are nowhere to be seen, at this time. It is unlikely that a single patient will be able to convince a hospital or medical practice to require that its staff be vaccinated. However, if a patient becomes infected with COVID-19 and can prove that the illness is causally related to interacting with an unvaccinated health care worker, the patient may have a case against the employer. The legal theory would be malpractice or negligence under informed consent law: That is, the patient did not consent to be treated by an unvaccinated person.
Employer options
So, what can health care employers do? They have three options:
- Require vaccination of all employees, independent contractors, and other providers who have privileges to see patients. Then, as long as the employer enforces the vaccination mandate, the employer can tell patients that all providers are vaccinated.
- Not require that employees and others with access to patients be vaccinated, and if a patient requests to be seen only by vaccinated providers, provide that patient with a vaccinated provider. It is especially important that health care employers take care with patients who are unvaccinated and who have been advised not to be vaccinated because of a medical condition. Both the patient and the health care employer would be protected best by avoiding having two unvaccinated individuals interact. Masks and physical distancing may decrease the risk.
- Not require that employees be vaccinated and refuse to guarantee that providers are vaccinated. To avoid risk for future lawsuits, employers should inform patients that there is no assurance that providers are vaccinated. That leaves it to each patient to ask individual providers about the provider’s vaccination status. If a patient doesn’t like a provider’s answer, then the patient has the right to leave. It’s not clear that the patient has a legal right to stay and demand a vaccinated provider.
Option three is problematic for a number of reasons. Patients aren’t always in a position to query each provider who enters the room about vaccination status. Patients may be sedated or too ill to exert that effort. And it puts supervisors in the position of having to mediate situations where a patient wants to leave against medical advice but the option of staying may also be dangerous.
Health care employers should discuss the options with their legal counsel before deciding which option to adopt.
A version of this article first appeared on Medscape.com.
‘Gold cards’ allow Texas docs to skip prior authorizations
The law was passed in June and will take effect in September. It excuses physicians from having to obtain prior authorization if, during the previous 6 months, 90% of their treatments met medical necessity criteria by the health insurer. Through this law, doctors in the state will spend less time getting approvals for treatments for their patients.
Automatic approval of authorizations for treatments – or what the Texas Medical Association (TMA) calls a “gold card” – “allows patients to get the care they need in a more timely fashion,” says Debra Patt, MD, an Austin, Tex.–based oncologist and former chair of the council on legislation for the TMA.
Eighty-seven percent of Texas physicians reported a “drastic increase over the past five years in the burden of prior authorization on their patients and their practices,” per a 2020 survey by the TMA. Nearly half (48%) of Texas physicians have hired staff whose work focuses on processing requests for prior authorization, according to the survey.
Jack Resneck Jr., MD, a San Francisco–based dermatologist and president-elect of the American Medical Association (AMA), said other states have investigated ways to ease the impact of prior authorizations on physicians, but no other state has passed such a law.
Administrative burdens plague physicians around the country. The Medscape Physician Compensation Report 2021 found that physicians spend on average 15.6 hours per week on paperwork and administrative duties.
Better outcomes, less anxiety for patients
Dr. Patt, who testified in support of the law’s passage in the Texas legislature, says automatic approval of authorizations “is better for patients because it reduces their anxiety about whether they’re able to get the treatments they need now, and they will have better outcomes if they’re able to receive more timely care.”
Recently, a chemotherapy treatment Dr. Patt prescribed for one of her patients was not authorized by an insurer. The result is “a lot of anxiety and potentially health problems” for the patient, said Dr. Patt.
She expects that automatic approval for treatments will be based on prescribing patterns during the preceding 6 months. “It means that when I order a test today, the [health insurer] looks back at my record 6 months previously,” she said. Still, Dr. Patt awaits guidance from the Texas Department of Insurance, which regulates health insurers in the state, regarding the law.
Dr. Resneck said the pharmacy counter is where most patients encounter prior authorization delays. “That’s when the pharmacist looks at them and says, ‘Actually, this isn’t covered by your health insurer’s formulary,’ or it isn’t covered fully on their formulary.”
One of Dr. Resneck’s patients had a life-altering case of eczema that lasted many years. Because of the condition, the patient couldn’t work or maintain meaningful bonds with family members. A biologic treatment transformed his patient’s life. The patient was able to return to work and to re-engage with family, said Dr. Resneck. But a year after his patient started the treatment, the health insurer wouldn’t authorize the treatment because the patient wasn’t experiencing the same symptoms.
The patient didn’t have the same symptoms because the biologic treatment worked, said Dr. Resneck.
Kristine Grow, a spokesperson for America’s Health Insurance Plans, a national association for health insurers, said, “The use of prior authorization is relatively small – typically, less than 15% – and can help ensure safer opioid prescribing, help prevent dangerous drug interactions, and help protect patients from unnecessary exposure to potentially harmful radiation for inappropriate diagnostic imaging. Numerous studies show that Americans frequently receive inappropriate care, and 25% of unnecessary treatments are associated with complications or adverse events.”
Medical management tools, such as prior authorization, are an “an important way” to deliver “safe, high-quality care” to patients, she added.
State and federal efforts to curb prior authorization
In addition to efforts to curb prior authorization in other states, the AMA supports the Improving Seniors’ Timely Access to Care Act (HR 3173). The act includes a provision related to “gold-carding,” said Robert Mills, an AMA spokesperson.
The bill establishes requirements and standards for prior authorization processes related to Medicare Advantage (MA) plans. The requirements and standards for MA plans include the following:
- Establishing an electronic prior authorization program that meets specific standards, such as the ability to provide real-time decisions in response to requests for items and services that are routinely approved.
- Publishing on an annual basis specific prior authorization information, including the percentage of requests approved and the average response time.
- Meeting standards set by the Centers for Medicare & Medicaid Services related to the quality and timeliness of prior authorization determinations.
The act was introduced to the U.S. House of Representatives in May, after which it was referred to two committees for consideration.
A version of this article first appeared on Medscape.com.
The law was passed in June and will take effect in September. It excuses physicians from having to obtain prior authorization if, during the previous 6 months, 90% of their treatments met medical necessity criteria by the health insurer. Through this law, doctors in the state will spend less time getting approvals for treatments for their patients.
Automatic approval of authorizations for treatments – or what the Texas Medical Association (TMA) calls a “gold card” – “allows patients to get the care they need in a more timely fashion,” says Debra Patt, MD, an Austin, Tex.–based oncologist and former chair of the council on legislation for the TMA.
Eighty-seven percent of Texas physicians reported a “drastic increase over the past five years in the burden of prior authorization on their patients and their practices,” per a 2020 survey by the TMA. Nearly half (48%) of Texas physicians have hired staff whose work focuses on processing requests for prior authorization, according to the survey.
Jack Resneck Jr., MD, a San Francisco–based dermatologist and president-elect of the American Medical Association (AMA), said other states have investigated ways to ease the impact of prior authorizations on physicians, but no other state has passed such a law.
Administrative burdens plague physicians around the country. The Medscape Physician Compensation Report 2021 found that physicians spend on average 15.6 hours per week on paperwork and administrative duties.
Better outcomes, less anxiety for patients
Dr. Patt, who testified in support of the law’s passage in the Texas legislature, says automatic approval of authorizations “is better for patients because it reduces their anxiety about whether they’re able to get the treatments they need now, and they will have better outcomes if they’re able to receive more timely care.”
Recently, a chemotherapy treatment Dr. Patt prescribed for one of her patients was not authorized by an insurer. The result is “a lot of anxiety and potentially health problems” for the patient, said Dr. Patt.
She expects that automatic approval for treatments will be based on prescribing patterns during the preceding 6 months. “It means that when I order a test today, the [health insurer] looks back at my record 6 months previously,” she said. Still, Dr. Patt awaits guidance from the Texas Department of Insurance, which regulates health insurers in the state, regarding the law.
Dr. Resneck said the pharmacy counter is where most patients encounter prior authorization delays. “That’s when the pharmacist looks at them and says, ‘Actually, this isn’t covered by your health insurer’s formulary,’ or it isn’t covered fully on their formulary.”
One of Dr. Resneck’s patients had a life-altering case of eczema that lasted many years. Because of the condition, the patient couldn’t work or maintain meaningful bonds with family members. A biologic treatment transformed his patient’s life. The patient was able to return to work and to re-engage with family, said Dr. Resneck. But a year after his patient started the treatment, the health insurer wouldn’t authorize the treatment because the patient wasn’t experiencing the same symptoms.
The patient didn’t have the same symptoms because the biologic treatment worked, said Dr. Resneck.
Kristine Grow, a spokesperson for America’s Health Insurance Plans, a national association for health insurers, said, “The use of prior authorization is relatively small – typically, less than 15% – and can help ensure safer opioid prescribing, help prevent dangerous drug interactions, and help protect patients from unnecessary exposure to potentially harmful radiation for inappropriate diagnostic imaging. Numerous studies show that Americans frequently receive inappropriate care, and 25% of unnecessary treatments are associated with complications or adverse events.”
Medical management tools, such as prior authorization, are an “an important way” to deliver “safe, high-quality care” to patients, she added.
State and federal efforts to curb prior authorization
In addition to efforts to curb prior authorization in other states, the AMA supports the Improving Seniors’ Timely Access to Care Act (HR 3173). The act includes a provision related to “gold-carding,” said Robert Mills, an AMA spokesperson.
The bill establishes requirements and standards for prior authorization processes related to Medicare Advantage (MA) plans. The requirements and standards for MA plans include the following:
- Establishing an electronic prior authorization program that meets specific standards, such as the ability to provide real-time decisions in response to requests for items and services that are routinely approved.
- Publishing on an annual basis specific prior authorization information, including the percentage of requests approved and the average response time.
- Meeting standards set by the Centers for Medicare & Medicaid Services related to the quality and timeliness of prior authorization determinations.
The act was introduced to the U.S. House of Representatives in May, after which it was referred to two committees for consideration.
A version of this article first appeared on Medscape.com.
The law was passed in June and will take effect in September. It excuses physicians from having to obtain prior authorization if, during the previous 6 months, 90% of their treatments met medical necessity criteria by the health insurer. Through this law, doctors in the state will spend less time getting approvals for treatments for their patients.
Automatic approval of authorizations for treatments – or what the Texas Medical Association (TMA) calls a “gold card” – “allows patients to get the care they need in a more timely fashion,” says Debra Patt, MD, an Austin, Tex.–based oncologist and former chair of the council on legislation for the TMA.
Eighty-seven percent of Texas physicians reported a “drastic increase over the past five years in the burden of prior authorization on their patients and their practices,” per a 2020 survey by the TMA. Nearly half (48%) of Texas physicians have hired staff whose work focuses on processing requests for prior authorization, according to the survey.
Jack Resneck Jr., MD, a San Francisco–based dermatologist and president-elect of the American Medical Association (AMA), said other states have investigated ways to ease the impact of prior authorizations on physicians, but no other state has passed such a law.
Administrative burdens plague physicians around the country. The Medscape Physician Compensation Report 2021 found that physicians spend on average 15.6 hours per week on paperwork and administrative duties.
Better outcomes, less anxiety for patients
Dr. Patt, who testified in support of the law’s passage in the Texas legislature, says automatic approval of authorizations “is better for patients because it reduces their anxiety about whether they’re able to get the treatments they need now, and they will have better outcomes if they’re able to receive more timely care.”
Recently, a chemotherapy treatment Dr. Patt prescribed for one of her patients was not authorized by an insurer. The result is “a lot of anxiety and potentially health problems” for the patient, said Dr. Patt.
She expects that automatic approval for treatments will be based on prescribing patterns during the preceding 6 months. “It means that when I order a test today, the [health insurer] looks back at my record 6 months previously,” she said. Still, Dr. Patt awaits guidance from the Texas Department of Insurance, which regulates health insurers in the state, regarding the law.
Dr. Resneck said the pharmacy counter is where most patients encounter prior authorization delays. “That’s when the pharmacist looks at them and says, ‘Actually, this isn’t covered by your health insurer’s formulary,’ or it isn’t covered fully on their formulary.”
One of Dr. Resneck’s patients had a life-altering case of eczema that lasted many years. Because of the condition, the patient couldn’t work or maintain meaningful bonds with family members. A biologic treatment transformed his patient’s life. The patient was able to return to work and to re-engage with family, said Dr. Resneck. But a year after his patient started the treatment, the health insurer wouldn’t authorize the treatment because the patient wasn’t experiencing the same symptoms.
The patient didn’t have the same symptoms because the biologic treatment worked, said Dr. Resneck.
Kristine Grow, a spokesperson for America’s Health Insurance Plans, a national association for health insurers, said, “The use of prior authorization is relatively small – typically, less than 15% – and can help ensure safer opioid prescribing, help prevent dangerous drug interactions, and help protect patients from unnecessary exposure to potentially harmful radiation for inappropriate diagnostic imaging. Numerous studies show that Americans frequently receive inappropriate care, and 25% of unnecessary treatments are associated with complications or adverse events.”
Medical management tools, such as prior authorization, are an “an important way” to deliver “safe, high-quality care” to patients, she added.
State and federal efforts to curb prior authorization
In addition to efforts to curb prior authorization in other states, the AMA supports the Improving Seniors’ Timely Access to Care Act (HR 3173). The act includes a provision related to “gold-carding,” said Robert Mills, an AMA spokesperson.
The bill establishes requirements and standards for prior authorization processes related to Medicare Advantage (MA) plans. The requirements and standards for MA plans include the following:
- Establishing an electronic prior authorization program that meets specific standards, such as the ability to provide real-time decisions in response to requests for items and services that are routinely approved.
- Publishing on an annual basis specific prior authorization information, including the percentage of requests approved and the average response time.
- Meeting standards set by the Centers for Medicare & Medicaid Services related to the quality and timeliness of prior authorization determinations.
The act was introduced to the U.S. House of Representatives in May, after which it was referred to two committees for consideration.
A version of this article first appeared on Medscape.com.
Stop using Neutrogena and Aveeno spray sunscreen, J&J warns
Benzene is not an ingredient of sunscreen, and should not be present in these products. The levels detected were low and would not be expected to have an adverse effect on health, but the company says it is recalling the products anyway “out of an abundance of caution.”
The sunscreen products that have been recalled are:
- NEUTROGENA® Beach Defense® aerosol sunscreen.
- NEUTROGENA® Cool Dry Sport aerosol sunscreen.
- NEUTROGENA® Invisible Daily™ defense aerosol sunscreen.
- NEUTROGENA® Ultra Sheer® aerosol sunscreen.
- AVEENO® Protect + Refresh aerosol sunscreen.
These products were distributed nationwide through a variety of retail stores. Consumers should stop using these products and throw them away, the company said.
At the same time, it emphasized the importance of using alternative sunscreen products to protect the skin from excessive sun exposure, which can lead to skin cancer including melanoma.
Johnson & Johnson has launched an investigation into how benzene got into these products.
One of the company’s other spray sunscreen products, Neutrogena Wet Skin, was not included in the recall.
Recently, benzene was found in 78 widely-used sunscreen products in tests conducted by the online pharmacy and laboratory Valisure. Most of the products were aerosol sprays, and the company called on the Food and Drug Administration to recall them all.
That petition suggested that the finding of benzene was the result of contamination somewhere in the manufacturing process.
“This isn’t a sunscreen issue, it’s a manufacturing issue,” said Adam Friedman, MD, professor and chief of dermatology at George Washington University. “We don’t want those things to be blurred.”
There is a risk that people take away the wrong message from these findings.
“People already have ambivalence about sunscreen, and this is just going to make that worse,” Dr. Friedman said in an interview.
He pointed out that benzene is present in car exhaust, second-hand smoke, and elsewhere. Inhalation exposure has been the primary focus of toxicology investigations, as has exposure from things such as contaminated drinking water – not via topical application. “We don’t know how effectively [benzene] gets through the skin, if it gets absorbed systemically, and how that then behaves downstream,” he noted.
On the other hand, ultraviolet radiation is a well-established carcinogen. Avoiding an effective preventive measure such as sunscreen could prove more harmful than exposure to trace amounts of benzene, he said.
A version of this article first appeared on WebMD.com.
Benzene is not an ingredient of sunscreen, and should not be present in these products. The levels detected were low and would not be expected to have an adverse effect on health, but the company says it is recalling the products anyway “out of an abundance of caution.”
The sunscreen products that have been recalled are:
- NEUTROGENA® Beach Defense® aerosol sunscreen.
- NEUTROGENA® Cool Dry Sport aerosol sunscreen.
- NEUTROGENA® Invisible Daily™ defense aerosol sunscreen.
- NEUTROGENA® Ultra Sheer® aerosol sunscreen.
- AVEENO® Protect + Refresh aerosol sunscreen.
These products were distributed nationwide through a variety of retail stores. Consumers should stop using these products and throw them away, the company said.
At the same time, it emphasized the importance of using alternative sunscreen products to protect the skin from excessive sun exposure, which can lead to skin cancer including melanoma.
Johnson & Johnson has launched an investigation into how benzene got into these products.
One of the company’s other spray sunscreen products, Neutrogena Wet Skin, was not included in the recall.
Recently, benzene was found in 78 widely-used sunscreen products in tests conducted by the online pharmacy and laboratory Valisure. Most of the products were aerosol sprays, and the company called on the Food and Drug Administration to recall them all.
That petition suggested that the finding of benzene was the result of contamination somewhere in the manufacturing process.
“This isn’t a sunscreen issue, it’s a manufacturing issue,” said Adam Friedman, MD, professor and chief of dermatology at George Washington University. “We don’t want those things to be blurred.”
There is a risk that people take away the wrong message from these findings.
“People already have ambivalence about sunscreen, and this is just going to make that worse,” Dr. Friedman said in an interview.
He pointed out that benzene is present in car exhaust, second-hand smoke, and elsewhere. Inhalation exposure has been the primary focus of toxicology investigations, as has exposure from things such as contaminated drinking water – not via topical application. “We don’t know how effectively [benzene] gets through the skin, if it gets absorbed systemically, and how that then behaves downstream,” he noted.
On the other hand, ultraviolet radiation is a well-established carcinogen. Avoiding an effective preventive measure such as sunscreen could prove more harmful than exposure to trace amounts of benzene, he said.
A version of this article first appeared on WebMD.com.
Benzene is not an ingredient of sunscreen, and should not be present in these products. The levels detected were low and would not be expected to have an adverse effect on health, but the company says it is recalling the products anyway “out of an abundance of caution.”
The sunscreen products that have been recalled are:
- NEUTROGENA® Beach Defense® aerosol sunscreen.
- NEUTROGENA® Cool Dry Sport aerosol sunscreen.
- NEUTROGENA® Invisible Daily™ defense aerosol sunscreen.
- NEUTROGENA® Ultra Sheer® aerosol sunscreen.
- AVEENO® Protect + Refresh aerosol sunscreen.
These products were distributed nationwide through a variety of retail stores. Consumers should stop using these products and throw them away, the company said.
At the same time, it emphasized the importance of using alternative sunscreen products to protect the skin from excessive sun exposure, which can lead to skin cancer including melanoma.
Johnson & Johnson has launched an investigation into how benzene got into these products.
One of the company’s other spray sunscreen products, Neutrogena Wet Skin, was not included in the recall.
Recently, benzene was found in 78 widely-used sunscreen products in tests conducted by the online pharmacy and laboratory Valisure. Most of the products were aerosol sprays, and the company called on the Food and Drug Administration to recall them all.
That petition suggested that the finding of benzene was the result of contamination somewhere in the manufacturing process.
“This isn’t a sunscreen issue, it’s a manufacturing issue,” said Adam Friedman, MD, professor and chief of dermatology at George Washington University. “We don’t want those things to be blurred.”
There is a risk that people take away the wrong message from these findings.
“People already have ambivalence about sunscreen, and this is just going to make that worse,” Dr. Friedman said in an interview.
He pointed out that benzene is present in car exhaust, second-hand smoke, and elsewhere. Inhalation exposure has been the primary focus of toxicology investigations, as has exposure from things such as contaminated drinking water – not via topical application. “We don’t know how effectively [benzene] gets through the skin, if it gets absorbed systemically, and how that then behaves downstream,” he noted.
On the other hand, ultraviolet radiation is a well-established carcinogen. Avoiding an effective preventive measure such as sunscreen could prove more harmful than exposure to trace amounts of benzene, he said.
A version of this article first appeared on WebMD.com.
Closing the racial gap in minimally invasive gyn hysterectomy and myomectomy
The historical mistreatment of Black bodies in gynecologic care has bled into present day inequities—from surgeries performed on enslaved Black women and sterilization of low-income Black women under federally funded programs, to higher rates of adverse health-related outcomes among Black women compared with their non-Black counterparts.1-3 Not only is the foundation of gynecology imperfect, so too is its current-day structure.
It is not enough to identify and describe racial inequities in health care; action plans to provide equitable care are called for. In this report, we aim to 1) contextualize the data on disparities in minimally invasive gynecologic surgery, specifically hysterectomy and myomectomy candidates and postsurgical outcomes, and 2) provide recommendations to close racial gaps in gynecologic treatment for more equitable experiences for minority women.
Black women and uterine fibroids
Uterine leiomyomas, or fibroids, are not only the most common benign pelvic tumor but they also cause a significant medical and financial burden in the United States, with estimated direct costs of $4.1 ̶ 9.4 billion.4 Fibroids can affect fertility and cause pain, bulk symptoms, heavy bleeding, anemia requiring blood transfusion, and poor pregnancy outcomes. The burden of disease for uterine fibroids is greatest for Black women.
The incidence of fibroids is 2 to 3 times higher in Black women compared with White women.5 According to ultrasound-based studies, the prevalence of fibroids among women aged 18 to 30 years was 26% among Black and 7% among White asymptomatic women.6 Earlier onset and more severe symptoms mean that there is a larger potential for impact on fertility for Black women. This coupled with the historical context of mistreatment of Black bodies makes the need for personalized medicine and culturally sensitive care critical.
Inequitable management of uterine fibroids
Although tumor size, location, and patient risk factors are used to determine the best treatment approach, the American College of Obstetricians and Gynecologists (ACOG) guidelines suggest that the use of alternative treatments to surgery should be first-line management instead of hysterectomy for most benign conditions.9 Conservative management will often help alleviate symptoms, slow the growth of fibroid(s), or bridge women to menopause, and treatment options include hormonal contraception, gonadotropin-releasing hormone agonists, hysteroscopic resection, uterine artery embolization, magnetic resonance-guided focused ultrasound, and myomectomy.
The rate of conservative management prior to hysterectomy varies by setting, reflecting potential bias in treatment decisions. Some medical settings have reported a 29% alternative management rate prior to hysterectomy, while others report much higher rates.10 A study using patient data from Kaiser Permanente Northern California (KPNC) showed that, within a large, diverse, and integrated health care system, more than 80% of patients received alternative treatments before undergoing hysterectomy; for those with symptomatic leiomyomas, 74.1% used alternative treatments prior to hysterectomy, and in logistic regression there was not a difference by race.11 Nationally, Black women are more likely to have hysterectomy or myomectomy compared with a nonsurgical uterine-sparing therapy.12,13
With about 600,000 cases per year within the United States, the hysterectomy is the most frequently performed benign gynecologic surgery.14 The most common indication is for “symptomatic fibroid uterus.” The approach to decision making for route of hysterectomy involves multiple patient and surgeon factors, including history of vaginal delivery, body mass index, history of previous surgery, uterine size, informed patient preference, and surgeon volume.15-17 ACOG recommends a minimally invasive hysterectomy (MIH) whenever feasible given its benefits in postoperative pain, recovery time, and blood loss. Myomectomy, particularly among women in their reproductive years desiring management of leiomyomas, is a uterine-sparing procedure versus hysterectomy. Minimally invasive myomectomy (MIM), compared with an open abdominal route, provides for lower drop in hemoglobin levels, shorter hospital stay, less adhesion formation, and decreased postoperative pain.18
Racial variations in hysterectomy rates persist overall and according to hysterectomy type. Black women are 2 to 3 times more likely to undergo hysterectomy for leiomyomas than other racial groups.19 These differences in rates have been shown to persist even when burden of disease is the same. One study found that Black women had increased odds of hysterectomy compared with their White counterparts even when there was no difference in mean fibroid volume by race,20 calling into question provider bias. Even in a universal insurance setting, Black patients have been found to have higher rates of open hysterectomies.21 Previous studies found that, despite growing frequency of laparoscopic and robotic-assisted hysterectomies, patients of a minority race had decreased odds of undergoing a MIH compared with their White counterparts.22
While little data exist on route of myomectomy by race, a recent study found minority women were more likely to undergo abdominal myomectomy compared with White women; Black women were twice as likely to undergo abdominal myomectomy (adjusted odds ratio [aOR], 1.9; 95% confidence interval [CI], 1.7–2.0), Asian American women were more than twice as likely (aOR, 2.3; 95% CI, 1.8–2.8), and Hispanic American women were 50% more likely to undergo abdominal myomectomy (aOR, 1.5; 95% CI, 1.2–1.9) when compared with White women.23 These differences remained after controlling for potential confounders, and there appeared to be an interaction between race and fibroid weight such that racial bias alone may not explain the differences.
Finally, Black women have higher perioperative complication rates compared with non-Black women. Postoperative complications including blood transfusion after myomectomy have been shown to be twice as high among Black women compared with White women. However, once uterine size, comorbidities, and fibroid number were controlled, race was not associated with higher complications. Black women, compared with White women, have been found to have 50% increased odds of morbidity after an abdominal myomectomy.24
Continue to: How to ensure that BIPOC women get the best management...
How to ensure that BIPOC women get the best management
Eliminating disparities and providing equitable and patient-centered care for Black, Indigenous, and people of color (BIPOC) women will require research, education, training, and targeted quality improvement initiatives.
Research into fibroids and comparative treatment outcomes
Uterine fibroids, despite their major public health impact, remain understudied. With Black women carrying the highest fibroid prevalence and severity burden, especially in their childbearing years, it is imperative that research efforts be focused on outcomes by race and ethnicity. Given the significant economic impact of fibroids, more efforts should be directed toward primary prevention of fibroid formation as well as secondary prevention and limitation of fibroid growth by affordable, effective, and safe means. For example, Bratka and colleagues researched the role of vitamin D in inhibiting growth of leiomyoma cells in animal models.25 Other innovative forms of management under investigation include aromatase inhibitors, green tea, cabergoline, elagolix, paricalcitol, and epigallocatechin gallate.26 Considerations such as stress, diet, and environmental risk factors have yet to be investigated in large studies.
Research contributing to evidence-based guidelines that address the needs of different patient populations affected by uterine fibroids is critical.8 Additionally, research conducted by Black women about Black women should be prioritized. In March 2021, the Stephanie Tubbs Jones Uterine Fibroid Research and Education Act of 2021 was introduced to fund $150 million in research supported by the National Institutes of Health (NIH). This is an opportunity to develop a research database to inform evidence-based culturally informed care regarding fertility counseling, medical management, and optimal surgical approach, as well as to award funding to minority researchers. There are disparities in distribution of funds from the NIH to minority researchers. Under-represented minorities are awarded fewer NIH grants compared with their counterparts despite initiatives to increase funding. Furthermore, in 2011, Black applicants for NIH funding were two-thirds as likely as White applicants to receive grants from 2000 ̶ 2006, even when accounting for publication record and training.27 Funding BIPOC researchers fuels diversity-driven investigation and can be useful in the charge to increase fibroid research.
Education and training: Changing the work force
Achieving equity requires change in provider work force. In a study of trends across multiple specialties including obstetrics and gynecology, Blacks and Latinx are more under-represented in 2016 than in 1990 across all specialties except for Black women in obstetrics and gynecology.28 It is well documented that under-represented minorities are more likely to engage in practice, research, service, and mentorship activities aligned with their identity.29 As a higher proportion of under-represented minority obstetricians and gynecologists practice in medically underserved areas,30 this presents a unique opportunity for gynecologists to improve care for and increase research involvement among BIPOC women.
Increasing BIPOC representation in medical and health care institutions and practices is not enough, however, to achieve health equity. Data from the Association of American Medical Colleges demonstrate that between 1978 and 2017 the total number of full-time obstetrics and gynecology faculty rose nearly fourfold from 1,688 to 6,347; however, the greatest rise in proportion of faculty who were nontenured was among women who were under-represented minorities.31 Additionally, there are disparities in wage by race even after controlling for hours worked and state of residence.32 Medical and academic centers and health care institutions and practices should proactively and systematically engage in the recruitment and retention of under-represented minority physicians and people in leadership roles. This will involve creating safe and inclusive work environments, with equal pay and promotion structures.
Quality initiatives to address provider bias
Provider bias should be addressed in clinical decision making and counseling of patients. Studies focused on ultrasonography have shown an estimated cumulative incidence of fibroids by age 50 of greater than 80% for Black women and nearly 70% for White women.5 Due to the prevalence and burden of fibroids among Black women there may be a provider bias in approach to management. Addressing this bias requires quality improvement efforts and investigation into patient and provider factors in management of fibroids. Black women have been a vulnerable population in medicine due to instances of mistreatment, and often times mistrust can play a role in how a patient views his or her care decisions. A patient-centered strategy allows patient factors such as age, uterine size, and cultural background to be considered such that a provider can tailor an approach that is best for the patient. Previous minority women focus groups have demonstrated that women have a strong desire for elective treatment;33 therefore, providers should listen openly to patients about their values and their perspectives on how fibroids affect their lives. Provider bias toward surgical volume, incentive for surgery, and implicit bias need to be addressed at every institution to work toward equitable and cost-effective care.
Integrated health care systems like Southern and Northern California Permanente Medical Group, using quality initiatives, have increased their minimally invasive surgery rates. Southern California Permanente Medical Group reached a 78% rate of MIH in a system of more than 350 surgeons performing benign indication hysterectomies as reported in 2011.34 Similarly, a study within KPNC, an institution with an MIH rate greater than 95%,35 found that racial disparities in route of MIH were eliminated through a quality improvement initiative described in detail in 2018 (FIGURE and TABLE).36
Conclusions
There are recognized successes in the gynecology field’s efforts to address racial disparities. Prior studies provide insight into opportunities to improve care in medical management of leiomyomas, minimally invasive route of hysterectomy and myomectomy, postsurgical outcomes, and institutional leadership. Particularly, when systemwide approaches are taken in the delivery of health care it is possible to significantly diminish racial disparities in gynecology.35 Much work remains to be done for our health care systems to provide equitable care.
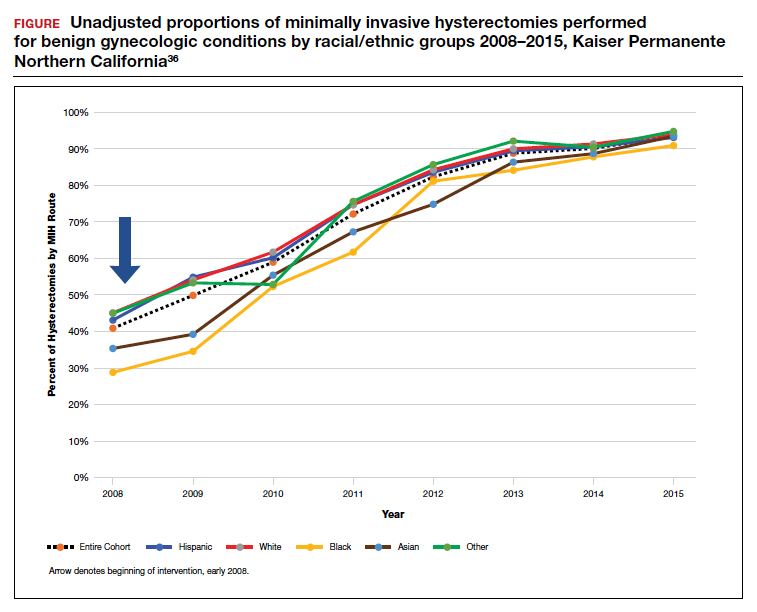
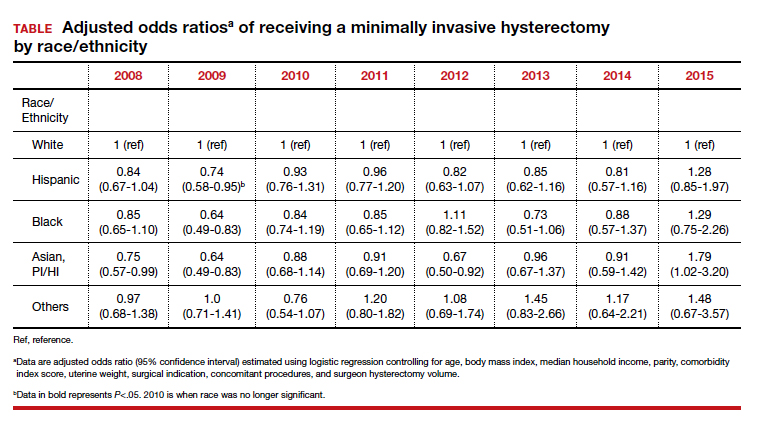
- Ojanuga D. The medical ethics of the ‘father of gynaecology,’ Dr J Marion Sims. J Med Ethics. 1993;19:28-31. doi: 10.1136/jme.19.1.28.
- Borrero S, Zite N, Creinin MD. Federally funded sterilization: time to rethink policy? Am J Public Health. 2012;102:1822-1825.
- Eaglehouse YL, Georg MW, Shriver CD, et al. Racial differences in time to breast cancer surgery and overall survival in the US Military Health System. JAMA Surg. 2019;154:e185113. doi: 10.1001/jamasurg.2018.5113.
- Soliman AM, Yang H, Du EX, et al. The direct and indirect costs of uterine fibroid tumors: a systematic review of the literature between 2000 and 2013. Am J Obstet Gynecol. 2015;213:141-160.
- Baird DD, Dunson DB, Hill MC, et al. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100-107.
- Marshall LM, Spiegelman D, Barbieri RL, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol. 1997;90:967-973. doi: 10.1016/s0029-7844(97)00534-6.
- Styer AK, Rueda BR. The epidemiology and genetics of uterine leiomyoma. Best Pract Res Clin Obstet Gynaecol. 2016;34:3-12. doi: 10.1016/j.bpobgyn.2015.11.018.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med. 2017;35:473-480. doi: 10.1055/s-0037-1607264.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol. 2008;112(2 pt 1):387-400.
- Corona LE, Swenson CW, Sheetz KH, et al. Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative. Am J Obstet Gynecol. 2015;212:304.e1-e7. doi: 10.1016/j.ajog.2014.11.031.
- Nguyen NT, Merchant M, Ritterman Weintraub ML, et al. Alternative treatment utilization before hysterectomy for benign gynecologic conditions at a large integrated health system. J Minim Invasive Gynecol. 2019;26:847-855. doi: 10.1016/j.jmig.2018.08.013.
- Laughlin-Tommaso SK, Jacoby VL, Myers ER. Disparities in fibroid incidence, prognosis, and management. Obstet Gynecol Clin North Am. 2017;44:81-94. doi: 10.1016/j.ogc.2016.11.007.
- Borah BJ, Laughlin-Tommaso SK, Myers ER, et al. Association between patient characteristics and treatment procedure among patients with uterine leiomyomas. Obstet Gynecol. 2016;127:67-77.
- Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hysterectomy surveillance in the United States, 2000-2004. Am J Obstet Gynecol. 2008;198:34.e1-e7. doi:10.1016/j.ajog.2007.05.039.
- Bardens D, Solomayer E, Baum S, et al. The impact of the body mass index (BMI) on laparoscopic hysterectomy for benign disease. Arch Gynecol Obstet. 2014;289:803-807. doi: 10.1007/s00404-013-3050-2.
- Seracchioli R, Venturoli S, Vianello F, et al. Total laparoscopic hysterectomy compared with abdominal hysterectomy in the presence of a large uterus. J Am Assoc Gynecol Laparosc. 2002;9:333-338. doi: 10.1016/s1074-3804(05)60413.
- Boyd LR, Novetsky AP, Curtin JP. Effect of surgical volume on route of hysterectomy and short-term morbidity. Obstet Gynecol. 2010;116:909-915. doi: 10.1097/AOG.0b013e3181f395d9.
- Jin C, Hu Y, Chen XC, et al. Laparoscopic versus open myomectomy—a meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2009;145:14-21. doi: 10.1016/j.ejogrb.2009.03.009.
- Wechter ME, Stewart EA, Myers ER, et al. Leiomyoma-related hospitalization and surgery: prevalence and predicted growth based on population trends. Am J Obstet Gynecol. 2011;205:492.e1-e5. doi: 10.1016/j.ajog.2011.07.008.
- Bower JK, Schreiner PJ, Sternfeld B, et al. Black-White differences in hysterectomy prevalence: the CARDIA study. Am J Public Health. 2009;99:300-307. doi: 10.2105/AJPH.2008.133702.
- Ranjit A, Sharma M, Romano A, et al. Does universal insurance mitigate racial differences in minimally invasive hysterectomy? J Minim Invasive Gynecol. 2017;24. doi:10.1016/j.jmig.2017.03.016.
- Pollack LM, Olsen MA, Gehlert SJ, et al. Racial/ethnic disparities/differences in hysterectomy route in women likely eligible for minimally invasive surgery. J Minim Invasive Gynecol. 2020;27:1167-1177.e2. doi:10.1016/j.jmig.2019.09.003.
- Stentz NC, Cooney LG, Sammel MD, et al. Association of patient race with surgical practice and perioperative morbidity after myomectomy. Obstet Gynecol. 2018;132:291-297. doi: 10.1097/AOG.0000000000002738.
- Roth TM, Gustilo-Ashby T, Barber MD, et al. Effects of race and clinical factors on short-term outcomes of abdominal myomectomy. Obstet Gynecol. 2003;101(5 pt 1):881-884. doi: 10.1016/s0029-7844(03)00015-2.
- Bratka S, Diamond JS, Al-Hendy A, et al. The role of vitamin D in uterine fibroid biology. Fertil Steril. 2015;104:698-706. doi: 10.1016/j.fertnstert.2015.05.031.
- Ciebiera M, Łukaszuk K, Męczekalski B, et al. Alternative oral agents in prophylaxis and therapy of uterine fibroids—an up-to-date review. Int J Mol Sci. 2017;18:2586. doi:10.3390/ijms18122586.
- Hayden EC. Racial bias haunts NIH funding. Nature. 2015;527:145.
- Lett LA, Orji WU, Sebro R. Declining racial and ethnic representation in clinical academic medicine: a longitudinal study of 16 US medical specialties. PLoS One. 2018;13:e0207274. doi: 10.1371/journal.pone.0207274.
- Sánchez JP, Poll-Hunter N, Stern N, et al. Balancing two cultures: American Indian/Alaska Native medical students’ perceptions of academic medicine careers. J Community Health. 2016;41:871-880.
- Rayburn WF, Xierali IM, Castillo-Page L, et al. Racial and ethnic differences between obstetrician-gynecologists and other adult medical specialists. Obstet Gynecol. 2016;127:148-152. doi: 10.1097/AOG.0000000000001184.
- Esters D, Xierali IM, Nivet MA, et al. The rise of nontenured faculty in obstetrics and gynecology by sex and underrepresented in medicine status. Obstet Gynecol. 2019;134 suppl 1:34S-39S. doi: 10.1097/AOG.0000000000003484.
- Ly DP, Seabury SA, Jena AB. Differences in incomes of physicians in the United States by race and sex: observational study. BMJ. 2016;I2923. doi:10.1136/bmj.i2923.
- Groff JY, Mullen PD, Byrd T, et al. Decision making, beliefs, and attitudes toward hysterectomy: a focus group study with medically underserved women in Texas. J Womens Health Gend Based Med. 2000;9 suppl 2:S39-50. doi: 10.1089/152460900318759.
- Andryjowicz E, Wray T. Regional expansion of minimally invasive surgery for hysterectomy: implementation and methodology in a large multispecialty group. Perm J. 2011;15:42-46.
- Zaritsky E, Ojo A, Tucker LY, et al. Racial disparities in route of hysterectomy for benign indications within an integrated health care system. JAMA Netw Open. 2019;2:e1917004. doi: 10.1001/jamanetworkopen.2019.17004.
- Abel MK, Kho KA, Walter A, et al. Measuring quality in minimally invasive gynecologic surgery: what, how, and why? J Minim Invasive Gynecol. 2019;26:321-326. doi: 10.1016/j.jmig.2018.11.013.
The historical mistreatment of Black bodies in gynecologic care has bled into present day inequities—from surgeries performed on enslaved Black women and sterilization of low-income Black women under federally funded programs, to higher rates of adverse health-related outcomes among Black women compared with their non-Black counterparts.1-3 Not only is the foundation of gynecology imperfect, so too is its current-day structure.
It is not enough to identify and describe racial inequities in health care; action plans to provide equitable care are called for. In this report, we aim to 1) contextualize the data on disparities in minimally invasive gynecologic surgery, specifically hysterectomy and myomectomy candidates and postsurgical outcomes, and 2) provide recommendations to close racial gaps in gynecologic treatment for more equitable experiences for minority women.
Black women and uterine fibroids
Uterine leiomyomas, or fibroids, are not only the most common benign pelvic tumor but they also cause a significant medical and financial burden in the United States, with estimated direct costs of $4.1 ̶ 9.4 billion.4 Fibroids can affect fertility and cause pain, bulk symptoms, heavy bleeding, anemia requiring blood transfusion, and poor pregnancy outcomes. The burden of disease for uterine fibroids is greatest for Black women.
The incidence of fibroids is 2 to 3 times higher in Black women compared with White women.5 According to ultrasound-based studies, the prevalence of fibroids among women aged 18 to 30 years was 26% among Black and 7% among White asymptomatic women.6 Earlier onset and more severe symptoms mean that there is a larger potential for impact on fertility for Black women. This coupled with the historical context of mistreatment of Black bodies makes the need for personalized medicine and culturally sensitive care critical.
Inequitable management of uterine fibroids
Although tumor size, location, and patient risk factors are used to determine the best treatment approach, the American College of Obstetricians and Gynecologists (ACOG) guidelines suggest that the use of alternative treatments to surgery should be first-line management instead of hysterectomy for most benign conditions.9 Conservative management will often help alleviate symptoms, slow the growth of fibroid(s), or bridge women to menopause, and treatment options include hormonal contraception, gonadotropin-releasing hormone agonists, hysteroscopic resection, uterine artery embolization, magnetic resonance-guided focused ultrasound, and myomectomy.
The rate of conservative management prior to hysterectomy varies by setting, reflecting potential bias in treatment decisions. Some medical settings have reported a 29% alternative management rate prior to hysterectomy, while others report much higher rates.10 A study using patient data from Kaiser Permanente Northern California (KPNC) showed that, within a large, diverse, and integrated health care system, more than 80% of patients received alternative treatments before undergoing hysterectomy; for those with symptomatic leiomyomas, 74.1% used alternative treatments prior to hysterectomy, and in logistic regression there was not a difference by race.11 Nationally, Black women are more likely to have hysterectomy or myomectomy compared with a nonsurgical uterine-sparing therapy.12,13
With about 600,000 cases per year within the United States, the hysterectomy is the most frequently performed benign gynecologic surgery.14 The most common indication is for “symptomatic fibroid uterus.” The approach to decision making for route of hysterectomy involves multiple patient and surgeon factors, including history of vaginal delivery, body mass index, history of previous surgery, uterine size, informed patient preference, and surgeon volume.15-17 ACOG recommends a minimally invasive hysterectomy (MIH) whenever feasible given its benefits in postoperative pain, recovery time, and blood loss. Myomectomy, particularly among women in their reproductive years desiring management of leiomyomas, is a uterine-sparing procedure versus hysterectomy. Minimally invasive myomectomy (MIM), compared with an open abdominal route, provides for lower drop in hemoglobin levels, shorter hospital stay, less adhesion formation, and decreased postoperative pain.18
Racial variations in hysterectomy rates persist overall and according to hysterectomy type. Black women are 2 to 3 times more likely to undergo hysterectomy for leiomyomas than other racial groups.19 These differences in rates have been shown to persist even when burden of disease is the same. One study found that Black women had increased odds of hysterectomy compared with their White counterparts even when there was no difference in mean fibroid volume by race,20 calling into question provider bias. Even in a universal insurance setting, Black patients have been found to have higher rates of open hysterectomies.21 Previous studies found that, despite growing frequency of laparoscopic and robotic-assisted hysterectomies, patients of a minority race had decreased odds of undergoing a MIH compared with their White counterparts.22
While little data exist on route of myomectomy by race, a recent study found minority women were more likely to undergo abdominal myomectomy compared with White women; Black women were twice as likely to undergo abdominal myomectomy (adjusted odds ratio [aOR], 1.9; 95% confidence interval [CI], 1.7–2.0), Asian American women were more than twice as likely (aOR, 2.3; 95% CI, 1.8–2.8), and Hispanic American women were 50% more likely to undergo abdominal myomectomy (aOR, 1.5; 95% CI, 1.2–1.9) when compared with White women.23 These differences remained after controlling for potential confounders, and there appeared to be an interaction between race and fibroid weight such that racial bias alone may not explain the differences.
Finally, Black women have higher perioperative complication rates compared with non-Black women. Postoperative complications including blood transfusion after myomectomy have been shown to be twice as high among Black women compared with White women. However, once uterine size, comorbidities, and fibroid number were controlled, race was not associated with higher complications. Black women, compared with White women, have been found to have 50% increased odds of morbidity after an abdominal myomectomy.24
Continue to: How to ensure that BIPOC women get the best management...
How to ensure that BIPOC women get the best management
Eliminating disparities and providing equitable and patient-centered care for Black, Indigenous, and people of color (BIPOC) women will require research, education, training, and targeted quality improvement initiatives.
Research into fibroids and comparative treatment outcomes
Uterine fibroids, despite their major public health impact, remain understudied. With Black women carrying the highest fibroid prevalence and severity burden, especially in their childbearing years, it is imperative that research efforts be focused on outcomes by race and ethnicity. Given the significant economic impact of fibroids, more efforts should be directed toward primary prevention of fibroid formation as well as secondary prevention and limitation of fibroid growth by affordable, effective, and safe means. For example, Bratka and colleagues researched the role of vitamin D in inhibiting growth of leiomyoma cells in animal models.25 Other innovative forms of management under investigation include aromatase inhibitors, green tea, cabergoline, elagolix, paricalcitol, and epigallocatechin gallate.26 Considerations such as stress, diet, and environmental risk factors have yet to be investigated in large studies.
Research contributing to evidence-based guidelines that address the needs of different patient populations affected by uterine fibroids is critical.8 Additionally, research conducted by Black women about Black women should be prioritized. In March 2021, the Stephanie Tubbs Jones Uterine Fibroid Research and Education Act of 2021 was introduced to fund $150 million in research supported by the National Institutes of Health (NIH). This is an opportunity to develop a research database to inform evidence-based culturally informed care regarding fertility counseling, medical management, and optimal surgical approach, as well as to award funding to minority researchers. There are disparities in distribution of funds from the NIH to minority researchers. Under-represented minorities are awarded fewer NIH grants compared with their counterparts despite initiatives to increase funding. Furthermore, in 2011, Black applicants for NIH funding were two-thirds as likely as White applicants to receive grants from 2000 ̶ 2006, even when accounting for publication record and training.27 Funding BIPOC researchers fuels diversity-driven investigation and can be useful in the charge to increase fibroid research.
Education and training: Changing the work force
Achieving equity requires change in provider work force. In a study of trends across multiple specialties including obstetrics and gynecology, Blacks and Latinx are more under-represented in 2016 than in 1990 across all specialties except for Black women in obstetrics and gynecology.28 It is well documented that under-represented minorities are more likely to engage in practice, research, service, and mentorship activities aligned with their identity.29 As a higher proportion of under-represented minority obstetricians and gynecologists practice in medically underserved areas,30 this presents a unique opportunity for gynecologists to improve care for and increase research involvement among BIPOC women.
Increasing BIPOC representation in medical and health care institutions and practices is not enough, however, to achieve health equity. Data from the Association of American Medical Colleges demonstrate that between 1978 and 2017 the total number of full-time obstetrics and gynecology faculty rose nearly fourfold from 1,688 to 6,347; however, the greatest rise in proportion of faculty who were nontenured was among women who were under-represented minorities.31 Additionally, there are disparities in wage by race even after controlling for hours worked and state of residence.32 Medical and academic centers and health care institutions and practices should proactively and systematically engage in the recruitment and retention of under-represented minority physicians and people in leadership roles. This will involve creating safe and inclusive work environments, with equal pay and promotion structures.
Quality initiatives to address provider bias
Provider bias should be addressed in clinical decision making and counseling of patients. Studies focused on ultrasonography have shown an estimated cumulative incidence of fibroids by age 50 of greater than 80% for Black women and nearly 70% for White women.5 Due to the prevalence and burden of fibroids among Black women there may be a provider bias in approach to management. Addressing this bias requires quality improvement efforts and investigation into patient and provider factors in management of fibroids. Black women have been a vulnerable population in medicine due to instances of mistreatment, and often times mistrust can play a role in how a patient views his or her care decisions. A patient-centered strategy allows patient factors such as age, uterine size, and cultural background to be considered such that a provider can tailor an approach that is best for the patient. Previous minority women focus groups have demonstrated that women have a strong desire for elective treatment;33 therefore, providers should listen openly to patients about their values and their perspectives on how fibroids affect their lives. Provider bias toward surgical volume, incentive for surgery, and implicit bias need to be addressed at every institution to work toward equitable and cost-effective care.
Integrated health care systems like Southern and Northern California Permanente Medical Group, using quality initiatives, have increased their minimally invasive surgery rates. Southern California Permanente Medical Group reached a 78% rate of MIH in a system of more than 350 surgeons performing benign indication hysterectomies as reported in 2011.34 Similarly, a study within KPNC, an institution with an MIH rate greater than 95%,35 found that racial disparities in route of MIH were eliminated through a quality improvement initiative described in detail in 2018 (FIGURE and TABLE).36
Conclusions
There are recognized successes in the gynecology field’s efforts to address racial disparities. Prior studies provide insight into opportunities to improve care in medical management of leiomyomas, minimally invasive route of hysterectomy and myomectomy, postsurgical outcomes, and institutional leadership. Particularly, when systemwide approaches are taken in the delivery of health care it is possible to significantly diminish racial disparities in gynecology.35 Much work remains to be done for our health care systems to provide equitable care.
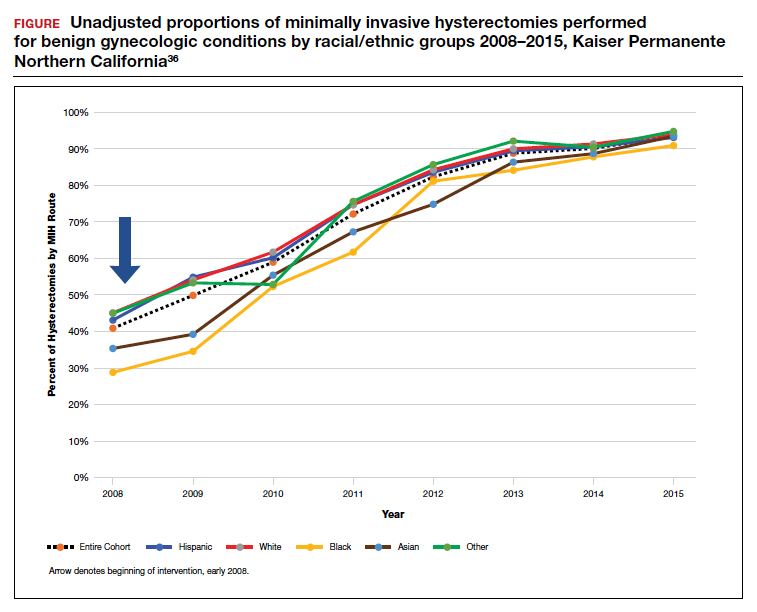
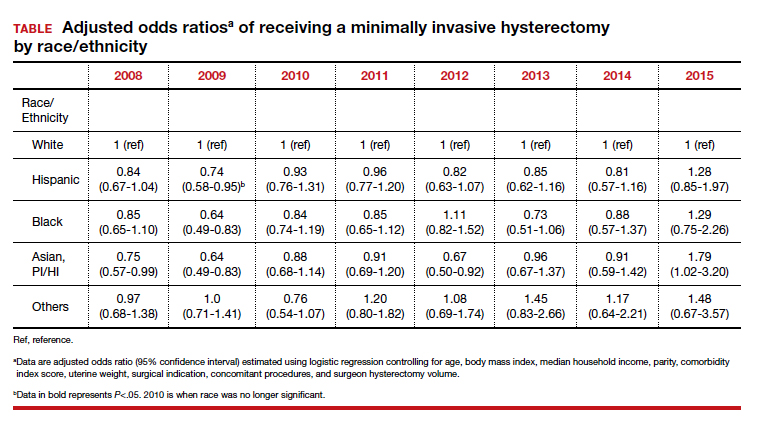
The historical mistreatment of Black bodies in gynecologic care has bled into present day inequities—from surgeries performed on enslaved Black women and sterilization of low-income Black women under federally funded programs, to higher rates of adverse health-related outcomes among Black women compared with their non-Black counterparts.1-3 Not only is the foundation of gynecology imperfect, so too is its current-day structure.
It is not enough to identify and describe racial inequities in health care; action plans to provide equitable care are called for. In this report, we aim to 1) contextualize the data on disparities in minimally invasive gynecologic surgery, specifically hysterectomy and myomectomy candidates and postsurgical outcomes, and 2) provide recommendations to close racial gaps in gynecologic treatment for more equitable experiences for minority women.
Black women and uterine fibroids
Uterine leiomyomas, or fibroids, are not only the most common benign pelvic tumor but they also cause a significant medical and financial burden in the United States, with estimated direct costs of $4.1 ̶ 9.4 billion.4 Fibroids can affect fertility and cause pain, bulk symptoms, heavy bleeding, anemia requiring blood transfusion, and poor pregnancy outcomes. The burden of disease for uterine fibroids is greatest for Black women.
The incidence of fibroids is 2 to 3 times higher in Black women compared with White women.5 According to ultrasound-based studies, the prevalence of fibroids among women aged 18 to 30 years was 26% among Black and 7% among White asymptomatic women.6 Earlier onset and more severe symptoms mean that there is a larger potential for impact on fertility for Black women. This coupled with the historical context of mistreatment of Black bodies makes the need for personalized medicine and culturally sensitive care critical.
Inequitable management of uterine fibroids
Although tumor size, location, and patient risk factors are used to determine the best treatment approach, the American College of Obstetricians and Gynecologists (ACOG) guidelines suggest that the use of alternative treatments to surgery should be first-line management instead of hysterectomy for most benign conditions.9 Conservative management will often help alleviate symptoms, slow the growth of fibroid(s), or bridge women to menopause, and treatment options include hormonal contraception, gonadotropin-releasing hormone agonists, hysteroscopic resection, uterine artery embolization, magnetic resonance-guided focused ultrasound, and myomectomy.
The rate of conservative management prior to hysterectomy varies by setting, reflecting potential bias in treatment decisions. Some medical settings have reported a 29% alternative management rate prior to hysterectomy, while others report much higher rates.10 A study using patient data from Kaiser Permanente Northern California (KPNC) showed that, within a large, diverse, and integrated health care system, more than 80% of patients received alternative treatments before undergoing hysterectomy; for those with symptomatic leiomyomas, 74.1% used alternative treatments prior to hysterectomy, and in logistic regression there was not a difference by race.11 Nationally, Black women are more likely to have hysterectomy or myomectomy compared with a nonsurgical uterine-sparing therapy.12,13
With about 600,000 cases per year within the United States, the hysterectomy is the most frequently performed benign gynecologic surgery.14 The most common indication is for “symptomatic fibroid uterus.” The approach to decision making for route of hysterectomy involves multiple patient and surgeon factors, including history of vaginal delivery, body mass index, history of previous surgery, uterine size, informed patient preference, and surgeon volume.15-17 ACOG recommends a minimally invasive hysterectomy (MIH) whenever feasible given its benefits in postoperative pain, recovery time, and blood loss. Myomectomy, particularly among women in their reproductive years desiring management of leiomyomas, is a uterine-sparing procedure versus hysterectomy. Minimally invasive myomectomy (MIM), compared with an open abdominal route, provides for lower drop in hemoglobin levels, shorter hospital stay, less adhesion formation, and decreased postoperative pain.18
Racial variations in hysterectomy rates persist overall and according to hysterectomy type. Black women are 2 to 3 times more likely to undergo hysterectomy for leiomyomas than other racial groups.19 These differences in rates have been shown to persist even when burden of disease is the same. One study found that Black women had increased odds of hysterectomy compared with their White counterparts even when there was no difference in mean fibroid volume by race,20 calling into question provider bias. Even in a universal insurance setting, Black patients have been found to have higher rates of open hysterectomies.21 Previous studies found that, despite growing frequency of laparoscopic and robotic-assisted hysterectomies, patients of a minority race had decreased odds of undergoing a MIH compared with their White counterparts.22
While little data exist on route of myomectomy by race, a recent study found minority women were more likely to undergo abdominal myomectomy compared with White women; Black women were twice as likely to undergo abdominal myomectomy (adjusted odds ratio [aOR], 1.9; 95% confidence interval [CI], 1.7–2.0), Asian American women were more than twice as likely (aOR, 2.3; 95% CI, 1.8–2.8), and Hispanic American women were 50% more likely to undergo abdominal myomectomy (aOR, 1.5; 95% CI, 1.2–1.9) when compared with White women.23 These differences remained after controlling for potential confounders, and there appeared to be an interaction between race and fibroid weight such that racial bias alone may not explain the differences.
Finally, Black women have higher perioperative complication rates compared with non-Black women. Postoperative complications including blood transfusion after myomectomy have been shown to be twice as high among Black women compared with White women. However, once uterine size, comorbidities, and fibroid number were controlled, race was not associated with higher complications. Black women, compared with White women, have been found to have 50% increased odds of morbidity after an abdominal myomectomy.24
Continue to: How to ensure that BIPOC women get the best management...
How to ensure that BIPOC women get the best management
Eliminating disparities and providing equitable and patient-centered care for Black, Indigenous, and people of color (BIPOC) women will require research, education, training, and targeted quality improvement initiatives.
Research into fibroids and comparative treatment outcomes
Uterine fibroids, despite their major public health impact, remain understudied. With Black women carrying the highest fibroid prevalence and severity burden, especially in their childbearing years, it is imperative that research efforts be focused on outcomes by race and ethnicity. Given the significant economic impact of fibroids, more efforts should be directed toward primary prevention of fibroid formation as well as secondary prevention and limitation of fibroid growth by affordable, effective, and safe means. For example, Bratka and colleagues researched the role of vitamin D in inhibiting growth of leiomyoma cells in animal models.25 Other innovative forms of management under investigation include aromatase inhibitors, green tea, cabergoline, elagolix, paricalcitol, and epigallocatechin gallate.26 Considerations such as stress, diet, and environmental risk factors have yet to be investigated in large studies.
Research contributing to evidence-based guidelines that address the needs of different patient populations affected by uterine fibroids is critical.8 Additionally, research conducted by Black women about Black women should be prioritized. In March 2021, the Stephanie Tubbs Jones Uterine Fibroid Research and Education Act of 2021 was introduced to fund $150 million in research supported by the National Institutes of Health (NIH). This is an opportunity to develop a research database to inform evidence-based culturally informed care regarding fertility counseling, medical management, and optimal surgical approach, as well as to award funding to minority researchers. There are disparities in distribution of funds from the NIH to minority researchers. Under-represented minorities are awarded fewer NIH grants compared with their counterparts despite initiatives to increase funding. Furthermore, in 2011, Black applicants for NIH funding were two-thirds as likely as White applicants to receive grants from 2000 ̶ 2006, even when accounting for publication record and training.27 Funding BIPOC researchers fuels diversity-driven investigation and can be useful in the charge to increase fibroid research.
Education and training: Changing the work force
Achieving equity requires change in provider work force. In a study of trends across multiple specialties including obstetrics and gynecology, Blacks and Latinx are more under-represented in 2016 than in 1990 across all specialties except for Black women in obstetrics and gynecology.28 It is well documented that under-represented minorities are more likely to engage in practice, research, service, and mentorship activities aligned with their identity.29 As a higher proportion of under-represented minority obstetricians and gynecologists practice in medically underserved areas,30 this presents a unique opportunity for gynecologists to improve care for and increase research involvement among BIPOC women.
Increasing BIPOC representation in medical and health care institutions and practices is not enough, however, to achieve health equity. Data from the Association of American Medical Colleges demonstrate that between 1978 and 2017 the total number of full-time obstetrics and gynecology faculty rose nearly fourfold from 1,688 to 6,347; however, the greatest rise in proportion of faculty who were nontenured was among women who were under-represented minorities.31 Additionally, there are disparities in wage by race even after controlling for hours worked and state of residence.32 Medical and academic centers and health care institutions and practices should proactively and systematically engage in the recruitment and retention of under-represented minority physicians and people in leadership roles. This will involve creating safe and inclusive work environments, with equal pay and promotion structures.
Quality initiatives to address provider bias
Provider bias should be addressed in clinical decision making and counseling of patients. Studies focused on ultrasonography have shown an estimated cumulative incidence of fibroids by age 50 of greater than 80% for Black women and nearly 70% for White women.5 Due to the prevalence and burden of fibroids among Black women there may be a provider bias in approach to management. Addressing this bias requires quality improvement efforts and investigation into patient and provider factors in management of fibroids. Black women have been a vulnerable population in medicine due to instances of mistreatment, and often times mistrust can play a role in how a patient views his or her care decisions. A patient-centered strategy allows patient factors such as age, uterine size, and cultural background to be considered such that a provider can tailor an approach that is best for the patient. Previous minority women focus groups have demonstrated that women have a strong desire for elective treatment;33 therefore, providers should listen openly to patients about their values and their perspectives on how fibroids affect their lives. Provider bias toward surgical volume, incentive for surgery, and implicit bias need to be addressed at every institution to work toward equitable and cost-effective care.
Integrated health care systems like Southern and Northern California Permanente Medical Group, using quality initiatives, have increased their minimally invasive surgery rates. Southern California Permanente Medical Group reached a 78% rate of MIH in a system of more than 350 surgeons performing benign indication hysterectomies as reported in 2011.34 Similarly, a study within KPNC, an institution with an MIH rate greater than 95%,35 found that racial disparities in route of MIH were eliminated through a quality improvement initiative described in detail in 2018 (FIGURE and TABLE).36
Conclusions
There are recognized successes in the gynecology field’s efforts to address racial disparities. Prior studies provide insight into opportunities to improve care in medical management of leiomyomas, minimally invasive route of hysterectomy and myomectomy, postsurgical outcomes, and institutional leadership. Particularly, when systemwide approaches are taken in the delivery of health care it is possible to significantly diminish racial disparities in gynecology.35 Much work remains to be done for our health care systems to provide equitable care.
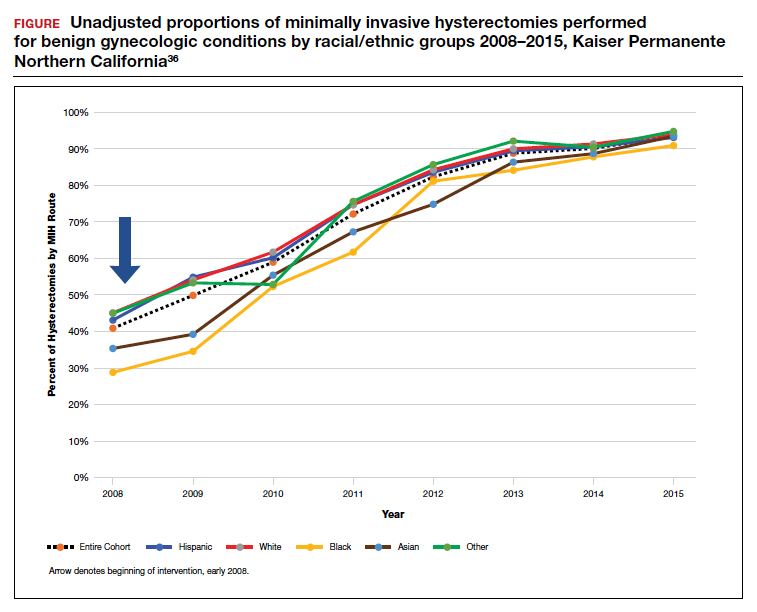
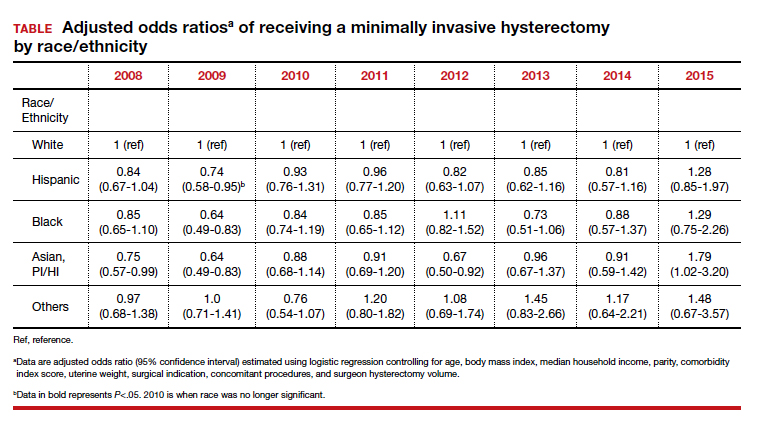
- Ojanuga D. The medical ethics of the ‘father of gynaecology,’ Dr J Marion Sims. J Med Ethics. 1993;19:28-31. doi: 10.1136/jme.19.1.28.
- Borrero S, Zite N, Creinin MD. Federally funded sterilization: time to rethink policy? Am J Public Health. 2012;102:1822-1825.
- Eaglehouse YL, Georg MW, Shriver CD, et al. Racial differences in time to breast cancer surgery and overall survival in the US Military Health System. JAMA Surg. 2019;154:e185113. doi: 10.1001/jamasurg.2018.5113.
- Soliman AM, Yang H, Du EX, et al. The direct and indirect costs of uterine fibroid tumors: a systematic review of the literature between 2000 and 2013. Am J Obstet Gynecol. 2015;213:141-160.
- Baird DD, Dunson DB, Hill MC, et al. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100-107.
- Marshall LM, Spiegelman D, Barbieri RL, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol. 1997;90:967-973. doi: 10.1016/s0029-7844(97)00534-6.
- Styer AK, Rueda BR. The epidemiology and genetics of uterine leiomyoma. Best Pract Res Clin Obstet Gynaecol. 2016;34:3-12. doi: 10.1016/j.bpobgyn.2015.11.018.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med. 2017;35:473-480. doi: 10.1055/s-0037-1607264.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol. 2008;112(2 pt 1):387-400.
- Corona LE, Swenson CW, Sheetz KH, et al. Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative. Am J Obstet Gynecol. 2015;212:304.e1-e7. doi: 10.1016/j.ajog.2014.11.031.
- Nguyen NT, Merchant M, Ritterman Weintraub ML, et al. Alternative treatment utilization before hysterectomy for benign gynecologic conditions at a large integrated health system. J Minim Invasive Gynecol. 2019;26:847-855. doi: 10.1016/j.jmig.2018.08.013.
- Laughlin-Tommaso SK, Jacoby VL, Myers ER. Disparities in fibroid incidence, prognosis, and management. Obstet Gynecol Clin North Am. 2017;44:81-94. doi: 10.1016/j.ogc.2016.11.007.
- Borah BJ, Laughlin-Tommaso SK, Myers ER, et al. Association between patient characteristics and treatment procedure among patients with uterine leiomyomas. Obstet Gynecol. 2016;127:67-77.
- Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hysterectomy surveillance in the United States, 2000-2004. Am J Obstet Gynecol. 2008;198:34.e1-e7. doi:10.1016/j.ajog.2007.05.039.
- Bardens D, Solomayer E, Baum S, et al. The impact of the body mass index (BMI) on laparoscopic hysterectomy for benign disease. Arch Gynecol Obstet. 2014;289:803-807. doi: 10.1007/s00404-013-3050-2.
- Seracchioli R, Venturoli S, Vianello F, et al. Total laparoscopic hysterectomy compared with abdominal hysterectomy in the presence of a large uterus. J Am Assoc Gynecol Laparosc. 2002;9:333-338. doi: 10.1016/s1074-3804(05)60413.
- Boyd LR, Novetsky AP, Curtin JP. Effect of surgical volume on route of hysterectomy and short-term morbidity. Obstet Gynecol. 2010;116:909-915. doi: 10.1097/AOG.0b013e3181f395d9.
- Jin C, Hu Y, Chen XC, et al. Laparoscopic versus open myomectomy—a meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2009;145:14-21. doi: 10.1016/j.ejogrb.2009.03.009.
- Wechter ME, Stewart EA, Myers ER, et al. Leiomyoma-related hospitalization and surgery: prevalence and predicted growth based on population trends. Am J Obstet Gynecol. 2011;205:492.e1-e5. doi: 10.1016/j.ajog.2011.07.008.
- Bower JK, Schreiner PJ, Sternfeld B, et al. Black-White differences in hysterectomy prevalence: the CARDIA study. Am J Public Health. 2009;99:300-307. doi: 10.2105/AJPH.2008.133702.
- Ranjit A, Sharma M, Romano A, et al. Does universal insurance mitigate racial differences in minimally invasive hysterectomy? J Minim Invasive Gynecol. 2017;24. doi:10.1016/j.jmig.2017.03.016.
- Pollack LM, Olsen MA, Gehlert SJ, et al. Racial/ethnic disparities/differences in hysterectomy route in women likely eligible for minimally invasive surgery. J Minim Invasive Gynecol. 2020;27:1167-1177.e2. doi:10.1016/j.jmig.2019.09.003.
- Stentz NC, Cooney LG, Sammel MD, et al. Association of patient race with surgical practice and perioperative morbidity after myomectomy. Obstet Gynecol. 2018;132:291-297. doi: 10.1097/AOG.0000000000002738.
- Roth TM, Gustilo-Ashby T, Barber MD, et al. Effects of race and clinical factors on short-term outcomes of abdominal myomectomy. Obstet Gynecol. 2003;101(5 pt 1):881-884. doi: 10.1016/s0029-7844(03)00015-2.
- Bratka S, Diamond JS, Al-Hendy A, et al. The role of vitamin D in uterine fibroid biology. Fertil Steril. 2015;104:698-706. doi: 10.1016/j.fertnstert.2015.05.031.
- Ciebiera M, Łukaszuk K, Męczekalski B, et al. Alternative oral agents in prophylaxis and therapy of uterine fibroids—an up-to-date review. Int J Mol Sci. 2017;18:2586. doi:10.3390/ijms18122586.
- Hayden EC. Racial bias haunts NIH funding. Nature. 2015;527:145.
- Lett LA, Orji WU, Sebro R. Declining racial and ethnic representation in clinical academic medicine: a longitudinal study of 16 US medical specialties. PLoS One. 2018;13:e0207274. doi: 10.1371/journal.pone.0207274.
- Sánchez JP, Poll-Hunter N, Stern N, et al. Balancing two cultures: American Indian/Alaska Native medical students’ perceptions of academic medicine careers. J Community Health. 2016;41:871-880.
- Rayburn WF, Xierali IM, Castillo-Page L, et al. Racial and ethnic differences between obstetrician-gynecologists and other adult medical specialists. Obstet Gynecol. 2016;127:148-152. doi: 10.1097/AOG.0000000000001184.
- Esters D, Xierali IM, Nivet MA, et al. The rise of nontenured faculty in obstetrics and gynecology by sex and underrepresented in medicine status. Obstet Gynecol. 2019;134 suppl 1:34S-39S. doi: 10.1097/AOG.0000000000003484.
- Ly DP, Seabury SA, Jena AB. Differences in incomes of physicians in the United States by race and sex: observational study. BMJ. 2016;I2923. doi:10.1136/bmj.i2923.
- Groff JY, Mullen PD, Byrd T, et al. Decision making, beliefs, and attitudes toward hysterectomy: a focus group study with medically underserved women in Texas. J Womens Health Gend Based Med. 2000;9 suppl 2:S39-50. doi: 10.1089/152460900318759.
- Andryjowicz E, Wray T. Regional expansion of minimally invasive surgery for hysterectomy: implementation and methodology in a large multispecialty group. Perm J. 2011;15:42-46.
- Zaritsky E, Ojo A, Tucker LY, et al. Racial disparities in route of hysterectomy for benign indications within an integrated health care system. JAMA Netw Open. 2019;2:e1917004. doi: 10.1001/jamanetworkopen.2019.17004.
- Abel MK, Kho KA, Walter A, et al. Measuring quality in minimally invasive gynecologic surgery: what, how, and why? J Minim Invasive Gynecol. 2019;26:321-326. doi: 10.1016/j.jmig.2018.11.013.
- Ojanuga D. The medical ethics of the ‘father of gynaecology,’ Dr J Marion Sims. J Med Ethics. 1993;19:28-31. doi: 10.1136/jme.19.1.28.
- Borrero S, Zite N, Creinin MD. Federally funded sterilization: time to rethink policy? Am J Public Health. 2012;102:1822-1825.
- Eaglehouse YL, Georg MW, Shriver CD, et al. Racial differences in time to breast cancer surgery and overall survival in the US Military Health System. JAMA Surg. 2019;154:e185113. doi: 10.1001/jamasurg.2018.5113.
- Soliman AM, Yang H, Du EX, et al. The direct and indirect costs of uterine fibroid tumors: a systematic review of the literature between 2000 and 2013. Am J Obstet Gynecol. 2015;213:141-160.
- Baird DD, Dunson DB, Hill MC, et al. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100-107.
- Marshall LM, Spiegelman D, Barbieri RL, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and race. Obstet Gynecol. 1997;90:967-973. doi: 10.1016/s0029-7844(97)00534-6.
- Styer AK, Rueda BR. The epidemiology and genetics of uterine leiomyoma. Best Pract Res Clin Obstet Gynaecol. 2016;34:3-12. doi: 10.1016/j.bpobgyn.2015.11.018.
- Al-Hendy A, Myers ER, Stewart E. Uterine fibroids: burden and unmet medical need. Semin Reprod Med. 2017;35:473-480. doi: 10.1055/s-0037-1607264.
- American College of Obstetricians and Gynecologists. ACOG practice bulletin. Alternatives to hysterectomy in the management of leiomyomas. Obstet Gynecol. 2008;112(2 pt 1):387-400.
- Corona LE, Swenson CW, Sheetz KH, et al. Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative. Am J Obstet Gynecol. 2015;212:304.e1-e7. doi: 10.1016/j.ajog.2014.11.031.
- Nguyen NT, Merchant M, Ritterman Weintraub ML, et al. Alternative treatment utilization before hysterectomy for benign gynecologic conditions at a large integrated health system. J Minim Invasive Gynecol. 2019;26:847-855. doi: 10.1016/j.jmig.2018.08.013.
- Laughlin-Tommaso SK, Jacoby VL, Myers ER. Disparities in fibroid incidence, prognosis, and management. Obstet Gynecol Clin North Am. 2017;44:81-94. doi: 10.1016/j.ogc.2016.11.007.
- Borah BJ, Laughlin-Tommaso SK, Myers ER, et al. Association between patient characteristics and treatment procedure among patients with uterine leiomyomas. Obstet Gynecol. 2016;127:67-77.
- Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hysterectomy surveillance in the United States, 2000-2004. Am J Obstet Gynecol. 2008;198:34.e1-e7. doi:10.1016/j.ajog.2007.05.039.
- Bardens D, Solomayer E, Baum S, et al. The impact of the body mass index (BMI) on laparoscopic hysterectomy for benign disease. Arch Gynecol Obstet. 2014;289:803-807. doi: 10.1007/s00404-013-3050-2.
- Seracchioli R, Venturoli S, Vianello F, et al. Total laparoscopic hysterectomy compared with abdominal hysterectomy in the presence of a large uterus. J Am Assoc Gynecol Laparosc. 2002;9:333-338. doi: 10.1016/s1074-3804(05)60413.
- Boyd LR, Novetsky AP, Curtin JP. Effect of surgical volume on route of hysterectomy and short-term morbidity. Obstet Gynecol. 2010;116:909-915. doi: 10.1097/AOG.0b013e3181f395d9.
- Jin C, Hu Y, Chen XC, et al. Laparoscopic versus open myomectomy—a meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2009;145:14-21. doi: 10.1016/j.ejogrb.2009.03.009.
- Wechter ME, Stewart EA, Myers ER, et al. Leiomyoma-related hospitalization and surgery: prevalence and predicted growth based on population trends. Am J Obstet Gynecol. 2011;205:492.e1-e5. doi: 10.1016/j.ajog.2011.07.008.
- Bower JK, Schreiner PJ, Sternfeld B, et al. Black-White differences in hysterectomy prevalence: the CARDIA study. Am J Public Health. 2009;99:300-307. doi: 10.2105/AJPH.2008.133702.
- Ranjit A, Sharma M, Romano A, et al. Does universal insurance mitigate racial differences in minimally invasive hysterectomy? J Minim Invasive Gynecol. 2017;24. doi:10.1016/j.jmig.2017.03.016.
- Pollack LM, Olsen MA, Gehlert SJ, et al. Racial/ethnic disparities/differences in hysterectomy route in women likely eligible for minimally invasive surgery. J Minim Invasive Gynecol. 2020;27:1167-1177.e2. doi:10.1016/j.jmig.2019.09.003.
- Stentz NC, Cooney LG, Sammel MD, et al. Association of patient race with surgical practice and perioperative morbidity after myomectomy. Obstet Gynecol. 2018;132:291-297. doi: 10.1097/AOG.0000000000002738.
- Roth TM, Gustilo-Ashby T, Barber MD, et al. Effects of race and clinical factors on short-term outcomes of abdominal myomectomy. Obstet Gynecol. 2003;101(5 pt 1):881-884. doi: 10.1016/s0029-7844(03)00015-2.
- Bratka S, Diamond JS, Al-Hendy A, et al. The role of vitamin D in uterine fibroid biology. Fertil Steril. 2015;104:698-706. doi: 10.1016/j.fertnstert.2015.05.031.
- Ciebiera M, Łukaszuk K, Męczekalski B, et al. Alternative oral agents in prophylaxis and therapy of uterine fibroids—an up-to-date review. Int J Mol Sci. 2017;18:2586. doi:10.3390/ijms18122586.
- Hayden EC. Racial bias haunts NIH funding. Nature. 2015;527:145.
- Lett LA, Orji WU, Sebro R. Declining racial and ethnic representation in clinical academic medicine: a longitudinal study of 16 US medical specialties. PLoS One. 2018;13:e0207274. doi: 10.1371/journal.pone.0207274.
- Sánchez JP, Poll-Hunter N, Stern N, et al. Balancing two cultures: American Indian/Alaska Native medical students’ perceptions of academic medicine careers. J Community Health. 2016;41:871-880.
- Rayburn WF, Xierali IM, Castillo-Page L, et al. Racial and ethnic differences between obstetrician-gynecologists and other adult medical specialists. Obstet Gynecol. 2016;127:148-152. doi: 10.1097/AOG.0000000000001184.
- Esters D, Xierali IM, Nivet MA, et al. The rise of nontenured faculty in obstetrics and gynecology by sex and underrepresented in medicine status. Obstet Gynecol. 2019;134 suppl 1:34S-39S. doi: 10.1097/AOG.0000000000003484.
- Ly DP, Seabury SA, Jena AB. Differences in incomes of physicians in the United States by race and sex: observational study. BMJ. 2016;I2923. doi:10.1136/bmj.i2923.
- Groff JY, Mullen PD, Byrd T, et al. Decision making, beliefs, and attitudes toward hysterectomy: a focus group study with medically underserved women in Texas. J Womens Health Gend Based Med. 2000;9 suppl 2:S39-50. doi: 10.1089/152460900318759.
- Andryjowicz E, Wray T. Regional expansion of minimally invasive surgery for hysterectomy: implementation and methodology in a large multispecialty group. Perm J. 2011;15:42-46.
- Zaritsky E, Ojo A, Tucker LY, et al. Racial disparities in route of hysterectomy for benign indications within an integrated health care system. JAMA Netw Open. 2019;2:e1917004. doi: 10.1001/jamanetworkopen.2019.17004.
- Abel MK, Kho KA, Walter A, et al. Measuring quality in minimally invasive gynecologic surgery: what, how, and why? J Minim Invasive Gynecol. 2019;26:321-326. doi: 10.1016/j.jmig.2018.11.013.
Tennessee fires top vaccine official as COVID cases increase
Tennessee officials have fired the state’s top vaccination manager, who faced recent criticism from Republican lawmakers about her efforts to vaccinate teens against COVID-19.
Michelle Fiscus, MD, the medical director for vaccine-preventable diseases and immunization programs at the Tennessee Department of Health, was terminated on July 12. The termination letter doesn’t explain the reason for her dismissal, according to the newspaper, which received a copy of the letter.
“It was my job to provide evidence-based education and vaccine access so that Tennesseans could protect themselves against COVID-19,” Dr. Fiscus told the Tennessean. “I have now been terminated for doing exactly that.”
In May, Dr. Fiscus sent a memo to medical providers that described the state’s “Mature Minor Doctrine,” a legal mechanism established in 1987 that allows some minors between the ages if 14 and 17 years to receive medical care without parental consent. Tennessee is one of five states that allows health care providers to decide if a minor has the capacity to consent to care, according to CNN.
Dr. Fiscus said she sent the letter in response to providers’ questions and that it contained no new information. She also said the wording was approved by the health department’s attorney and the governor’s office, the newspaper reported.
At a June 16 hearing of the state’s Joint Government Operations Committee, however, Republican officials criticized the memo and Dr. Fiscus, saying that the state misinterpreted its legal authority. During the meeting, some lawmakers discussed dissolving the state health department to stop it from promoting vaccines to teens, the newspaper reported.
Since then, the health department has backed down from promoting vaccines to teens by deleting social media posts that recommended vaccines to anyone over age 12. Internal emails, which were obtained by the Tennessean, showed that department leaders ordered county-level employees to avoid holding vaccine events targeted toward adolescents.
Dr. Fiscus’s firing comes as vaccination efforts lag in the state. About 38% of residents have been fully vaccinated. At the current pace, Tennessee won’t pass the 50% mark until next March, according to an internal report obtained by the newspaper.
COVID-19 cases are beginning to climb again, particularly with the Delta variant circulating among unvaccinated residents. After months of a decline in cases, the average of daily cases has more than doubled since the end of June. The state’s test positivity rate has increased from 2% to 4.5% during that time as well.
In a long written statement, Dr. Fiscus said she was the 25th of 64 state and territorial immunization program directors to leave their positions during the pandemic, whether through resignation or termination. With a loss of institutional knowledge and leadership, COVID-19 vaccine efforts will fall behind.
“Each of us should be waking up every morning with one question on our minds: ‘What can I do protect the people of Tennessee against COVID-19?’ ” she wrote. “Instead, our leaders are putting barriers in place to ensure the people of Tennessee remain at risk, even with the Delta variant bearing down upon us.”
A version of this article first appeared on WebMD.com.
Tennessee officials have fired the state’s top vaccination manager, who faced recent criticism from Republican lawmakers about her efforts to vaccinate teens against COVID-19.
Michelle Fiscus, MD, the medical director for vaccine-preventable diseases and immunization programs at the Tennessee Department of Health, was terminated on July 12. The termination letter doesn’t explain the reason for her dismissal, according to the newspaper, which received a copy of the letter.
“It was my job to provide evidence-based education and vaccine access so that Tennesseans could protect themselves against COVID-19,” Dr. Fiscus told the Tennessean. “I have now been terminated for doing exactly that.”
In May, Dr. Fiscus sent a memo to medical providers that described the state’s “Mature Minor Doctrine,” a legal mechanism established in 1987 that allows some minors between the ages if 14 and 17 years to receive medical care without parental consent. Tennessee is one of five states that allows health care providers to decide if a minor has the capacity to consent to care, according to CNN.
Dr. Fiscus said she sent the letter in response to providers’ questions and that it contained no new information. She also said the wording was approved by the health department’s attorney and the governor’s office, the newspaper reported.
At a June 16 hearing of the state’s Joint Government Operations Committee, however, Republican officials criticized the memo and Dr. Fiscus, saying that the state misinterpreted its legal authority. During the meeting, some lawmakers discussed dissolving the state health department to stop it from promoting vaccines to teens, the newspaper reported.
Since then, the health department has backed down from promoting vaccines to teens by deleting social media posts that recommended vaccines to anyone over age 12. Internal emails, which were obtained by the Tennessean, showed that department leaders ordered county-level employees to avoid holding vaccine events targeted toward adolescents.
Dr. Fiscus’s firing comes as vaccination efforts lag in the state. About 38% of residents have been fully vaccinated. At the current pace, Tennessee won’t pass the 50% mark until next March, according to an internal report obtained by the newspaper.
COVID-19 cases are beginning to climb again, particularly with the Delta variant circulating among unvaccinated residents. After months of a decline in cases, the average of daily cases has more than doubled since the end of June. The state’s test positivity rate has increased from 2% to 4.5% during that time as well.
In a long written statement, Dr. Fiscus said she was the 25th of 64 state and territorial immunization program directors to leave their positions during the pandemic, whether through resignation or termination. With a loss of institutional knowledge and leadership, COVID-19 vaccine efforts will fall behind.
“Each of us should be waking up every morning with one question on our minds: ‘What can I do protect the people of Tennessee against COVID-19?’ ” she wrote. “Instead, our leaders are putting barriers in place to ensure the people of Tennessee remain at risk, even with the Delta variant bearing down upon us.”
A version of this article first appeared on WebMD.com.
Tennessee officials have fired the state’s top vaccination manager, who faced recent criticism from Republican lawmakers about her efforts to vaccinate teens against COVID-19.
Michelle Fiscus, MD, the medical director for vaccine-preventable diseases and immunization programs at the Tennessee Department of Health, was terminated on July 12. The termination letter doesn’t explain the reason for her dismissal, according to the newspaper, which received a copy of the letter.
“It was my job to provide evidence-based education and vaccine access so that Tennesseans could protect themselves against COVID-19,” Dr. Fiscus told the Tennessean. “I have now been terminated for doing exactly that.”
In May, Dr. Fiscus sent a memo to medical providers that described the state’s “Mature Minor Doctrine,” a legal mechanism established in 1987 that allows some minors between the ages if 14 and 17 years to receive medical care without parental consent. Tennessee is one of five states that allows health care providers to decide if a minor has the capacity to consent to care, according to CNN.
Dr. Fiscus said she sent the letter in response to providers’ questions and that it contained no new information. She also said the wording was approved by the health department’s attorney and the governor’s office, the newspaper reported.
At a June 16 hearing of the state’s Joint Government Operations Committee, however, Republican officials criticized the memo and Dr. Fiscus, saying that the state misinterpreted its legal authority. During the meeting, some lawmakers discussed dissolving the state health department to stop it from promoting vaccines to teens, the newspaper reported.
Since then, the health department has backed down from promoting vaccines to teens by deleting social media posts that recommended vaccines to anyone over age 12. Internal emails, which were obtained by the Tennessean, showed that department leaders ordered county-level employees to avoid holding vaccine events targeted toward adolescents.
Dr. Fiscus’s firing comes as vaccination efforts lag in the state. About 38% of residents have been fully vaccinated. At the current pace, Tennessee won’t pass the 50% mark until next March, according to an internal report obtained by the newspaper.
COVID-19 cases are beginning to climb again, particularly with the Delta variant circulating among unvaccinated residents. After months of a decline in cases, the average of daily cases has more than doubled since the end of June. The state’s test positivity rate has increased from 2% to 4.5% during that time as well.
In a long written statement, Dr. Fiscus said she was the 25th of 64 state and territorial immunization program directors to leave their positions during the pandemic, whether through resignation or termination. With a loss of institutional knowledge and leadership, COVID-19 vaccine efforts will fall behind.
“Each of us should be waking up every morning with one question on our minds: ‘What can I do protect the people of Tennessee against COVID-19?’ ” she wrote. “Instead, our leaders are putting barriers in place to ensure the people of Tennessee remain at risk, even with the Delta variant bearing down upon us.”
A version of this article first appeared on WebMD.com.
Obstetric units place twice as many wrong-patient orders as medical-surgical units
Clinicians in obstetric units place nearly twice as many wrong-patient orders as their medical-surgical counterparts, based on a retrospective look at more than 1.3 million orders.
These findings suggest that obstetric patients are at particular risk for this type of medical error, and that steps are needed to address obstetric clinical culture, work flow, and electronic medical record interfaces, reported lead author Adina R. Kern-Goldberger, MD, of the department of obstetrics and gynecology at the University of Pennsylvania, Philadelphia, and colleagues.
The root of the issue may come from the very nature of obstetrics, and the homogeneity of the patient population, they wrote in Obstetrics & Gynecology.
“Obstetrics is a unique clinical environment because all patients are admitted with a common diagnosis – pregnancy – and have much more overlap in demographic characteristics than a typical inpatient unit given that they are all females of reproductive age,” the investigators wrote. “The labor and delivery environment also is distinct in the hospital given its dynamic tempo and unpredictable work flow. There also is the added risk of neonates typically being registered in the hospital record under the mother’s name after birth. This generates abundant opportunity for errors in order placement, both between obstetric patients and between postpartum patients and their newborns.”
To determine the relative magnitude of this risk, Dr. Kern-Goldberger and colleagues analyzed EMRs from 45,436 obstetric patients and 12,915 medical-surgical patients at “a large, urban, integrated health system in New York City,” including 1,329,463 order sessions placed between 2016 and 2018.
The primary outcome was near-miss wrong-patient orders, which were identified by the Wrong-Patient Retract-and-Reorder measure.
“The measure uses an electronic query to detect retract-and-reorder events, defined as one or more orders placed for patient A, canceled by the same clinician within 10 minutes, and reordered by the same clinician for patient B within the next 10 minutes,” the investigators wrote.In obstetric units, 79.5 wrong-patient orders were placed per 100,000 order sessions, which was 98% higher than the rate of 42.3 wrong-patient orders per 100,000 order sessions in medical-surgical units (odds ratio, 1.98; 95% confidence interval, 1.64-2.39), a disparity that was observed across clinician types and times of day.Advanced practice clinicians in obstetrics placed 47.3 wrong-patient orders per 100,000 order sessions, which was significantly lower than that of their colleagues: attending physicians (127.0 per 100,000) and house staff (119.9 per 100,000).
Wrong-patient orders in obstetrics most often involved medication (73.2 per 100,000), particularly nifedipine, antibiotics, tocolytics, and nonoxytocin uterotonics. The “other” category, including but not limited to lab studies and nursing orders, was associated with 51.0 wrong-patient orders per 100,000 order sessions, while errors in diagnostic imaging orders followed distantly behind, at a rate of 5.7 per 1000,000.
“Although the obstetric clinical environment – particularly labor and delivery – is vibrant and frequently chaotic, it is critical to establish a calm, orderly, and safe culture around order entry,” the investigators wrote. “This, combined with efforts to improve house staff work flow and to optimize EMR interfaces, is likely to help mitigate the threat of wrong order errors to patient care and ultimately improve maternal health and safety.”
According to Catherine D. Cansino, MD, associate clinical professor of obstetrics and gynecology at UC Davis (Calif.) Health, the findings highlight the value of medical informatics while revealing a need to improve EMR interfaces.
“Medical informatics is a growing field and expertise among ob.gyns. is very important,” Dr. Cansino said in an interview. “This study by Kern-Goldberger and colleagues highlights the vulnerability of our EMR systems (and our patients, indirectly) when medical informatics systems are not optimized. The investigators present a study that advocates for greater emphasis on optimizing such systems in obstetrics units, especially in the context of high acuity settings such as obstetrics, compared to medical-surgical units. Appropriately, the study highlights the avoided harm when correcting medical errors for obstetric patients since such errors potentially affect both the delivering patient and the newborn.”
The study was funded by AHRQ. One coauthor disclosed funding from the Icahn School of Medicine at Mount Sinai, Georgetown University, the National Institutes of Health – Office of Scientific Review, and the Social Science Research Council. Another reported funding from Roche.
Clinicians in obstetric units place nearly twice as many wrong-patient orders as their medical-surgical counterparts, based on a retrospective look at more than 1.3 million orders.
These findings suggest that obstetric patients are at particular risk for this type of medical error, and that steps are needed to address obstetric clinical culture, work flow, and electronic medical record interfaces, reported lead author Adina R. Kern-Goldberger, MD, of the department of obstetrics and gynecology at the University of Pennsylvania, Philadelphia, and colleagues.
The root of the issue may come from the very nature of obstetrics, and the homogeneity of the patient population, they wrote in Obstetrics & Gynecology.
“Obstetrics is a unique clinical environment because all patients are admitted with a common diagnosis – pregnancy – and have much more overlap in demographic characteristics than a typical inpatient unit given that they are all females of reproductive age,” the investigators wrote. “The labor and delivery environment also is distinct in the hospital given its dynamic tempo and unpredictable work flow. There also is the added risk of neonates typically being registered in the hospital record under the mother’s name after birth. This generates abundant opportunity for errors in order placement, both between obstetric patients and between postpartum patients and their newborns.”
To determine the relative magnitude of this risk, Dr. Kern-Goldberger and colleagues analyzed EMRs from 45,436 obstetric patients and 12,915 medical-surgical patients at “a large, urban, integrated health system in New York City,” including 1,329,463 order sessions placed between 2016 and 2018.
The primary outcome was near-miss wrong-patient orders, which were identified by the Wrong-Patient Retract-and-Reorder measure.
“The measure uses an electronic query to detect retract-and-reorder events, defined as one or more orders placed for patient A, canceled by the same clinician within 10 minutes, and reordered by the same clinician for patient B within the next 10 minutes,” the investigators wrote.In obstetric units, 79.5 wrong-patient orders were placed per 100,000 order sessions, which was 98% higher than the rate of 42.3 wrong-patient orders per 100,000 order sessions in medical-surgical units (odds ratio, 1.98; 95% confidence interval, 1.64-2.39), a disparity that was observed across clinician types and times of day.Advanced practice clinicians in obstetrics placed 47.3 wrong-patient orders per 100,000 order sessions, which was significantly lower than that of their colleagues: attending physicians (127.0 per 100,000) and house staff (119.9 per 100,000).
Wrong-patient orders in obstetrics most often involved medication (73.2 per 100,000), particularly nifedipine, antibiotics, tocolytics, and nonoxytocin uterotonics. The “other” category, including but not limited to lab studies and nursing orders, was associated with 51.0 wrong-patient orders per 100,000 order sessions, while errors in diagnostic imaging orders followed distantly behind, at a rate of 5.7 per 1000,000.
“Although the obstetric clinical environment – particularly labor and delivery – is vibrant and frequently chaotic, it is critical to establish a calm, orderly, and safe culture around order entry,” the investigators wrote. “This, combined with efforts to improve house staff work flow and to optimize EMR interfaces, is likely to help mitigate the threat of wrong order errors to patient care and ultimately improve maternal health and safety.”
According to Catherine D. Cansino, MD, associate clinical professor of obstetrics and gynecology at UC Davis (Calif.) Health, the findings highlight the value of medical informatics while revealing a need to improve EMR interfaces.
“Medical informatics is a growing field and expertise among ob.gyns. is very important,” Dr. Cansino said in an interview. “This study by Kern-Goldberger and colleagues highlights the vulnerability of our EMR systems (and our patients, indirectly) when medical informatics systems are not optimized. The investigators present a study that advocates for greater emphasis on optimizing such systems in obstetrics units, especially in the context of high acuity settings such as obstetrics, compared to medical-surgical units. Appropriately, the study highlights the avoided harm when correcting medical errors for obstetric patients since such errors potentially affect both the delivering patient and the newborn.”
The study was funded by AHRQ. One coauthor disclosed funding from the Icahn School of Medicine at Mount Sinai, Georgetown University, the National Institutes of Health – Office of Scientific Review, and the Social Science Research Council. Another reported funding from Roche.
Clinicians in obstetric units place nearly twice as many wrong-patient orders as their medical-surgical counterparts, based on a retrospective look at more than 1.3 million orders.
These findings suggest that obstetric patients are at particular risk for this type of medical error, and that steps are needed to address obstetric clinical culture, work flow, and electronic medical record interfaces, reported lead author Adina R. Kern-Goldberger, MD, of the department of obstetrics and gynecology at the University of Pennsylvania, Philadelphia, and colleagues.
The root of the issue may come from the very nature of obstetrics, and the homogeneity of the patient population, they wrote in Obstetrics & Gynecology.
“Obstetrics is a unique clinical environment because all patients are admitted with a common diagnosis – pregnancy – and have much more overlap in demographic characteristics than a typical inpatient unit given that they are all females of reproductive age,” the investigators wrote. “The labor and delivery environment also is distinct in the hospital given its dynamic tempo and unpredictable work flow. There also is the added risk of neonates typically being registered in the hospital record under the mother’s name after birth. This generates abundant opportunity for errors in order placement, both between obstetric patients and between postpartum patients and their newborns.”
To determine the relative magnitude of this risk, Dr. Kern-Goldberger and colleagues analyzed EMRs from 45,436 obstetric patients and 12,915 medical-surgical patients at “a large, urban, integrated health system in New York City,” including 1,329,463 order sessions placed between 2016 and 2018.
The primary outcome was near-miss wrong-patient orders, which were identified by the Wrong-Patient Retract-and-Reorder measure.
“The measure uses an electronic query to detect retract-and-reorder events, defined as one or more orders placed for patient A, canceled by the same clinician within 10 minutes, and reordered by the same clinician for patient B within the next 10 minutes,” the investigators wrote.In obstetric units, 79.5 wrong-patient orders were placed per 100,000 order sessions, which was 98% higher than the rate of 42.3 wrong-patient orders per 100,000 order sessions in medical-surgical units (odds ratio, 1.98; 95% confidence interval, 1.64-2.39), a disparity that was observed across clinician types and times of day.Advanced practice clinicians in obstetrics placed 47.3 wrong-patient orders per 100,000 order sessions, which was significantly lower than that of their colleagues: attending physicians (127.0 per 100,000) and house staff (119.9 per 100,000).
Wrong-patient orders in obstetrics most often involved medication (73.2 per 100,000), particularly nifedipine, antibiotics, tocolytics, and nonoxytocin uterotonics. The “other” category, including but not limited to lab studies and nursing orders, was associated with 51.0 wrong-patient orders per 100,000 order sessions, while errors in diagnostic imaging orders followed distantly behind, at a rate of 5.7 per 1000,000.
“Although the obstetric clinical environment – particularly labor and delivery – is vibrant and frequently chaotic, it is critical to establish a calm, orderly, and safe culture around order entry,” the investigators wrote. “This, combined with efforts to improve house staff work flow and to optimize EMR interfaces, is likely to help mitigate the threat of wrong order errors to patient care and ultimately improve maternal health and safety.”
According to Catherine D. Cansino, MD, associate clinical professor of obstetrics and gynecology at UC Davis (Calif.) Health, the findings highlight the value of medical informatics while revealing a need to improve EMR interfaces.
“Medical informatics is a growing field and expertise among ob.gyns. is very important,” Dr. Cansino said in an interview. “This study by Kern-Goldberger and colleagues highlights the vulnerability of our EMR systems (and our patients, indirectly) when medical informatics systems are not optimized. The investigators present a study that advocates for greater emphasis on optimizing such systems in obstetrics units, especially in the context of high acuity settings such as obstetrics, compared to medical-surgical units. Appropriately, the study highlights the avoided harm when correcting medical errors for obstetric patients since such errors potentially affect both the delivering patient and the newborn.”
The study was funded by AHRQ. One coauthor disclosed funding from the Icahn School of Medicine at Mount Sinai, Georgetown University, the National Institutes of Health – Office of Scientific Review, and the Social Science Research Council. Another reported funding from Roche.
FROM OBSTETRICS & GYNECOLOGY
Bullying in academic medicine rife, underreported
Bullying in academic medicine, especially among women, is rife, underreported, and remains largely unaddressed, new research suggests.
Investigators reviewed close to 70 studies, encompassing over 82,000 medical consultants or trainees in academic medical settings, and found that men were identified as the most common perpetrators – close to 70% of respondents – whereas women were the most common victims (56%).
Collectively, respondents in all of the studies identified the most common bullies to be consultants (54%), followed by residents (22%), and nurses (15%).
Disturbingly, less than one-third of victims overall reported that they were bullied, and close to 60% who formally reported the abuse said they did not have a positive outcome.
“We found that bullies are commonly men and senior consultants, while more than half of their victims are women,” senior author Harriette G.C. Van Spall, MD, MPH, associate professor of medicine and director of e-health and virtual care, Division of Cardiology, McMaster University, Hamilton, Ont., said in an interview.
“The greatest barriers to addressing academic bullying are the fear of reprisal, lack of impact of reporting, and non-enforcement of anti-bullying policies,” she added.
The study was published online July 12 in BMJ Open.
Personal experience
“Some behaviors were excruciating to deal with, protesting against them would bring more on, and every day was filled with dread. It took sheer will to show up at work to care for patients, to complete research I was leading, and to have hope, and my academic output, income, and personal well-being dropped during those years,” she added.
Dr. Van Spall thought the subject “merited research because our performance as clinicians, researchers, and educators relies on our work environment.”
To investigate, the researchers reviewed 68 studies (n = 82,349 respondents) conducted between 1999 and 2021 in academic medical settings, in which victims were either consultants or trainees. Many of the studies (31) were conducted in the U.S.
Other countries included the United Kingdom, Canada, Australia, Pakistan, Egypt, Iran, Turkey, New Zealand, Lithuania, Greece, India, Germany, Nigeria, Oman, and Finland.
Studies were required to describe the method and impact of bullying; characteristics of the perpetrators and victims; or interventions that were used to address the bullying.
“Bullying” was defined as “the abuse of authority by a perpetrator who targets the victim in an academic setting through punishing behaviors that include overwork, destabilization, and isolation in order to impede the education or career of the target.”
Systemic sexism
Bullying behaviors, reported in 28 studies (n = 35,779 respondents), were grouped into destabilization, threats to professional status, overwork, and isolation, with overwork found to be the most common form of bullying.
The most common impact of being bullied was psychological distress, reported by 39.1% of respondents in 14 studies, followed by considerations of quitting (35.9%; 7 studies), and worsening of clinical performance (34.6%, 8 studies).
“Among demographic groups, men were identified as the most common perpetrators (67.2% of 4,722 respondents in 5 studies) and women the most common victims (56.2% of 15,246 respondents in 27 studies),” the authors report.
“Academic medicine in many institutions is encumbered by systemic sexism that is evident in processes around remuneration, recognition, opportunities for advancement, and leadership positions,” said Dr. Van Spall.
“There are fewer women at decision-making tables in academic medicine, the climb is uphill at the best of times, and women are likely easier targets for bullies, as their voices are easier to drown out,” she added.
She noted that many men do “exhibit wonderful attributes of professionalism and decency,” but “some in positions of power are given impunity by virtue of other accomplishments.”
Multiple deterrents
Thirty-one studies (n = 15,868) described characteristics of the bullies and showed the most common to be consultants (53.6% [30 studies]), residents (22% [22 studies]), and nurses (14.9% [21 studies]).
Only a minority of victims (28.9% of 9,410 victims [10 studies]) formally reported the bullying. The researchers identified multiple deterrents to reporting.
When a formal complaint was submitted (n = 1,139 respondents), it most frequently had no perceived effect (35.6%); more than one-fifth (21.9%) experienced worsening of the bullying, and only 13.7% reported improvement.
The common institutional facilitators of bullying, described in 25 studies, included lack of enforcement of anti-bullying policies (13 studies), the hierarchical structure of medicine (7 studies), and normalization of bullying (10 studies).
Forty-nine studies looked at strategies to address academic bullying, including anti-bullying policies, mandatory workshops on mistreatment, establishing an anti-bullying oversight committee, and institutional support for victims. However, the studies testing the effectiveness of these interventions “had a high risk of bias.”
Support available
Commenting on the research for this news organization, Roberta Gebhard, DO, past president of the American Medical Women’s Association (AMWA) and a member of the advisory board for Physician Just Equity, called it a “good study, large, international, and well-written.”
Dr. Gebhard, a member of the Governing Council for the American Medical Association Women Physician Section, was not associated with this study but said she is currently researching women who left medical school and residency.
“A common reason for leaving is being bullied. Bullying is often not reported and if reported, often not addressed. Or, if addressed, the person who reports it is often retaliated against, which is a common experience, especially in women.”
She advised female physicians who are bullied to get support from other female physicians – for example, by joining the AMWA, which has an online women’s leadership group.
“Having other women physicians throughout the country you can call for advice and support can be helpful,” said Dr. Gebhard, a family practice physician based in Grand Island, New York.
Dr. Van Spall receives support from the Canadian Institutes of Health Research, the Heart and Stroke Foundation, the Women As One Escalator Award, and McMaster Department of Medicine. The study authors and Dr. Gebhard have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bullying in academic medicine, especially among women, is rife, underreported, and remains largely unaddressed, new research suggests.
Investigators reviewed close to 70 studies, encompassing over 82,000 medical consultants or trainees in academic medical settings, and found that men were identified as the most common perpetrators – close to 70% of respondents – whereas women were the most common victims (56%).
Collectively, respondents in all of the studies identified the most common bullies to be consultants (54%), followed by residents (22%), and nurses (15%).
Disturbingly, less than one-third of victims overall reported that they were bullied, and close to 60% who formally reported the abuse said they did not have a positive outcome.
“We found that bullies are commonly men and senior consultants, while more than half of their victims are women,” senior author Harriette G.C. Van Spall, MD, MPH, associate professor of medicine and director of e-health and virtual care, Division of Cardiology, McMaster University, Hamilton, Ont., said in an interview.
“The greatest barriers to addressing academic bullying are the fear of reprisal, lack of impact of reporting, and non-enforcement of anti-bullying policies,” she added.
The study was published online July 12 in BMJ Open.
Personal experience
“Some behaviors were excruciating to deal with, protesting against them would bring more on, and every day was filled with dread. It took sheer will to show up at work to care for patients, to complete research I was leading, and to have hope, and my academic output, income, and personal well-being dropped during those years,” she added.
Dr. Van Spall thought the subject “merited research because our performance as clinicians, researchers, and educators relies on our work environment.”
To investigate, the researchers reviewed 68 studies (n = 82,349 respondents) conducted between 1999 and 2021 in academic medical settings, in which victims were either consultants or trainees. Many of the studies (31) were conducted in the U.S.
Other countries included the United Kingdom, Canada, Australia, Pakistan, Egypt, Iran, Turkey, New Zealand, Lithuania, Greece, India, Germany, Nigeria, Oman, and Finland.
Studies were required to describe the method and impact of bullying; characteristics of the perpetrators and victims; or interventions that were used to address the bullying.
“Bullying” was defined as “the abuse of authority by a perpetrator who targets the victim in an academic setting through punishing behaviors that include overwork, destabilization, and isolation in order to impede the education or career of the target.”
Systemic sexism
Bullying behaviors, reported in 28 studies (n = 35,779 respondents), were grouped into destabilization, threats to professional status, overwork, and isolation, with overwork found to be the most common form of bullying.
The most common impact of being bullied was psychological distress, reported by 39.1% of respondents in 14 studies, followed by considerations of quitting (35.9%; 7 studies), and worsening of clinical performance (34.6%, 8 studies).
“Among demographic groups, men were identified as the most common perpetrators (67.2% of 4,722 respondents in 5 studies) and women the most common victims (56.2% of 15,246 respondents in 27 studies),” the authors report.
“Academic medicine in many institutions is encumbered by systemic sexism that is evident in processes around remuneration, recognition, opportunities for advancement, and leadership positions,” said Dr. Van Spall.
“There are fewer women at decision-making tables in academic medicine, the climb is uphill at the best of times, and women are likely easier targets for bullies, as their voices are easier to drown out,” she added.
She noted that many men do “exhibit wonderful attributes of professionalism and decency,” but “some in positions of power are given impunity by virtue of other accomplishments.”
Multiple deterrents
Thirty-one studies (n = 15,868) described characteristics of the bullies and showed the most common to be consultants (53.6% [30 studies]), residents (22% [22 studies]), and nurses (14.9% [21 studies]).
Only a minority of victims (28.9% of 9,410 victims [10 studies]) formally reported the bullying. The researchers identified multiple deterrents to reporting.
When a formal complaint was submitted (n = 1,139 respondents), it most frequently had no perceived effect (35.6%); more than one-fifth (21.9%) experienced worsening of the bullying, and only 13.7% reported improvement.
The common institutional facilitators of bullying, described in 25 studies, included lack of enforcement of anti-bullying policies (13 studies), the hierarchical structure of medicine (7 studies), and normalization of bullying (10 studies).
Forty-nine studies looked at strategies to address academic bullying, including anti-bullying policies, mandatory workshops on mistreatment, establishing an anti-bullying oversight committee, and institutional support for victims. However, the studies testing the effectiveness of these interventions “had a high risk of bias.”
Support available
Commenting on the research for this news organization, Roberta Gebhard, DO, past president of the American Medical Women’s Association (AMWA) and a member of the advisory board for Physician Just Equity, called it a “good study, large, international, and well-written.”
Dr. Gebhard, a member of the Governing Council for the American Medical Association Women Physician Section, was not associated with this study but said she is currently researching women who left medical school and residency.
“A common reason for leaving is being bullied. Bullying is often not reported and if reported, often not addressed. Or, if addressed, the person who reports it is often retaliated against, which is a common experience, especially in women.”
She advised female physicians who are bullied to get support from other female physicians – for example, by joining the AMWA, which has an online women’s leadership group.
“Having other women physicians throughout the country you can call for advice and support can be helpful,” said Dr. Gebhard, a family practice physician based in Grand Island, New York.
Dr. Van Spall receives support from the Canadian Institutes of Health Research, the Heart and Stroke Foundation, the Women As One Escalator Award, and McMaster Department of Medicine. The study authors and Dr. Gebhard have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Bullying in academic medicine, especially among women, is rife, underreported, and remains largely unaddressed, new research suggests.
Investigators reviewed close to 70 studies, encompassing over 82,000 medical consultants or trainees in academic medical settings, and found that men were identified as the most common perpetrators – close to 70% of respondents – whereas women were the most common victims (56%).
Collectively, respondents in all of the studies identified the most common bullies to be consultants (54%), followed by residents (22%), and nurses (15%).
Disturbingly, less than one-third of victims overall reported that they were bullied, and close to 60% who formally reported the abuse said they did not have a positive outcome.
“We found that bullies are commonly men and senior consultants, while more than half of their victims are women,” senior author Harriette G.C. Van Spall, MD, MPH, associate professor of medicine and director of e-health and virtual care, Division of Cardiology, McMaster University, Hamilton, Ont., said in an interview.
“The greatest barriers to addressing academic bullying are the fear of reprisal, lack of impact of reporting, and non-enforcement of anti-bullying policies,” she added.
The study was published online July 12 in BMJ Open.
Personal experience
“Some behaviors were excruciating to deal with, protesting against them would bring more on, and every day was filled with dread. It took sheer will to show up at work to care for patients, to complete research I was leading, and to have hope, and my academic output, income, and personal well-being dropped during those years,” she added.
Dr. Van Spall thought the subject “merited research because our performance as clinicians, researchers, and educators relies on our work environment.”
To investigate, the researchers reviewed 68 studies (n = 82,349 respondents) conducted between 1999 and 2021 in academic medical settings, in which victims were either consultants or trainees. Many of the studies (31) were conducted in the U.S.
Other countries included the United Kingdom, Canada, Australia, Pakistan, Egypt, Iran, Turkey, New Zealand, Lithuania, Greece, India, Germany, Nigeria, Oman, and Finland.
Studies were required to describe the method and impact of bullying; characteristics of the perpetrators and victims; or interventions that were used to address the bullying.
“Bullying” was defined as “the abuse of authority by a perpetrator who targets the victim in an academic setting through punishing behaviors that include overwork, destabilization, and isolation in order to impede the education or career of the target.”
Systemic sexism
Bullying behaviors, reported in 28 studies (n = 35,779 respondents), were grouped into destabilization, threats to professional status, overwork, and isolation, with overwork found to be the most common form of bullying.
The most common impact of being bullied was psychological distress, reported by 39.1% of respondents in 14 studies, followed by considerations of quitting (35.9%; 7 studies), and worsening of clinical performance (34.6%, 8 studies).
“Among demographic groups, men were identified as the most common perpetrators (67.2% of 4,722 respondents in 5 studies) and women the most common victims (56.2% of 15,246 respondents in 27 studies),” the authors report.
“Academic medicine in many institutions is encumbered by systemic sexism that is evident in processes around remuneration, recognition, opportunities for advancement, and leadership positions,” said Dr. Van Spall.
“There are fewer women at decision-making tables in academic medicine, the climb is uphill at the best of times, and women are likely easier targets for bullies, as their voices are easier to drown out,” she added.
She noted that many men do “exhibit wonderful attributes of professionalism and decency,” but “some in positions of power are given impunity by virtue of other accomplishments.”
Multiple deterrents
Thirty-one studies (n = 15,868) described characteristics of the bullies and showed the most common to be consultants (53.6% [30 studies]), residents (22% [22 studies]), and nurses (14.9% [21 studies]).
Only a minority of victims (28.9% of 9,410 victims [10 studies]) formally reported the bullying. The researchers identified multiple deterrents to reporting.
When a formal complaint was submitted (n = 1,139 respondents), it most frequently had no perceived effect (35.6%); more than one-fifth (21.9%) experienced worsening of the bullying, and only 13.7% reported improvement.
The common institutional facilitators of bullying, described in 25 studies, included lack of enforcement of anti-bullying policies (13 studies), the hierarchical structure of medicine (7 studies), and normalization of bullying (10 studies).
Forty-nine studies looked at strategies to address academic bullying, including anti-bullying policies, mandatory workshops on mistreatment, establishing an anti-bullying oversight committee, and institutional support for victims. However, the studies testing the effectiveness of these interventions “had a high risk of bias.”
Support available
Commenting on the research for this news organization, Roberta Gebhard, DO, past president of the American Medical Women’s Association (AMWA) and a member of the advisory board for Physician Just Equity, called it a “good study, large, international, and well-written.”
Dr. Gebhard, a member of the Governing Council for the American Medical Association Women Physician Section, was not associated with this study but said she is currently researching women who left medical school and residency.
“A common reason for leaving is being bullied. Bullying is often not reported and if reported, often not addressed. Or, if addressed, the person who reports it is often retaliated against, which is a common experience, especially in women.”
She advised female physicians who are bullied to get support from other female physicians – for example, by joining the AMWA, which has an online women’s leadership group.
“Having other women physicians throughout the country you can call for advice and support can be helpful,” said Dr. Gebhard, a family practice physician based in Grand Island, New York.
Dr. Van Spall receives support from the Canadian Institutes of Health Research, the Heart and Stroke Foundation, the Women As One Escalator Award, and McMaster Department of Medicine. The study authors and Dr. Gebhard have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Dogs know their humans, but humans don’t know expiration dates
An extreme price to pay for immortality
We know that men don’t live as long as women, but the reasons aren’t entirely clear. However, some New Zealand scientists have a thought on the subject, thanks to a sheep called Shrek.
The researchers were inspired by a famous old sheep who escaped captivity, but was captured 6 years later at the age of 10. The sheep then lived 6 more years, far beyond the lifespan of a normal sheep, capturing the hearts and minds of Kiwis everywhere. Look, it’s New Zealand, sheep are life, so it’s only natural the country got attached. Scientists from the University of Otago suspected that Shrek lived such a long life because he was castrated.
So they undertook a study of sheep, and lo and behold, sheep that were castrated lived significantly longer than their uncastrated kin, thanks to a slowing of their epigenetic clocks – the DNA aged noticeably slower in the castrated sheep.
Although the research can most immediately be applied to the improvement of the New Zealand sheep industry, the implication for humanity is also apparent. Want to live longer? Get rid of the testosterone. An extreme solution to be sure. As previously reported in this column, researchers wanted to torture our mouths to get us to lose weight, and now they want to castrate people for longer life. What exactly is going on down there in New Zealand?
Man’s best mind reader
There are a lot of reasons why dogs are sometimes called “man’s best friend,” but the root of it may actually have something to do with how easily we communicate with each other. Researchers dug deeper and fetched something that Fido is born with, but his wild wolf cousin isn’t.
That something is known as the “theory of mind” ability. Have you noticed that when you point and tell dogs to grab a leash or toy, they react as if they understood the language you spoke? Researchers from Duke University wondered if this ability is a canine thing or just a domesticated dog thing.
They compared 44 canine puppies and 37 wolf pups between 5 and 18 weeks old. The wolf pups were taken into human homes and raised with a great amount of human interaction, while the dog pups were left with their mothers and raised with less human interaction.
All the puppies were then put through multiple tests. In one test, they were given clues to find a treat under a bowl. In another test, a block of wood was placed next to the treat as a physical marker. During yet another test, researchers pointed to the food directly.
The researchers discovered that the dog puppies knew where the treat was every time, while their wild relatives didn’t.
“This study really solidifies the evidence that the social genius of dogs is a product of domestication,” senior author Brian Hare said in a separate statement.
The domestication hypothesis theorizes that dogs picked up the human social cues through thousands of years of interaction. The more friendly and cooperative a wolf was with humans, the more likely it was to survive and pass on those same traits and practices. Even within the study, the dog puppies were 30 times more likely to approach a stranger than were the wolf pups.
You may think your dog understands everything you say, but it’s actually body language that Fido is most fluent in.
I’m not a dentist, but I play one on TikTok
In last week’s column, it was garlic cloves up the nose to treat a cold. This week, TikTok brings us a new way to whiten teeth.
Familiar with the Mr. Clean Magic Eraser? If not, we’ll save you the trouble of Googling it: Check it out here and here.
Have you heard anything about using it to clean your teeth? No, neither did we, and we did a lot of Googling. Proctor & Gamble, which makes the Magic Eraser, goes so far as to say on the package: “Do not use on skin or other parts of the body. Using on skin will likely cause abrasions.” (The warning is actually in all caps, but we are stylistically forbidden by our editorial overlords to do that.)
But it’s magic, right? How can you not use it on your teeth? Enter TikTok. Heather Dunn posted a video in which she rubbed a bit of a Magic Eraser on her teeth – being careful to avoid her gums, because you can never be too careful – “as the product squeaked back and forth,” the Miami Herald reported. The video has almost 256,000 likes so far.
“Yeah, your teeth are white because you scrubbed all the enamel off them. So don’t do this,” Dr. Benjamin Winters, aka the Bentist, said in a YouTube video that has 105,000 likes.
In this race for common sense, common sense is losing. Please help the Bentist restore sanity to the dental world by liking his video. It would make Mr. Clean happy.
Don’t let an expiration date boss you around
Surely you’ve been there: It’s Taco Tuesday and you’re rummaging through the refrigerator to find that shredded cheese you’re sure you have. Jackpot! You find it, but realize it’s probably been in the refrigerator for a while. You open the bag, it smells and looks fine, but the expiration date was 2 days ago. Now you have a decision to make. Maybe you’ll be fine, or maybe you’ll risk food poisoning right before your brother’s wedding.
But here’s the truth: Americans throw away perfectly good food every day. The average American family throws out $1,365 to $2,275 worth of food a year, according to a 2013 study.
Truthfully, expiration dates are not for buyers, rather they’re for stores to have an idea of their stock’s freshness. Emily Broad Leib, director of the Harvard Law School Food and Policy Clinic and lead author of the 2013 study, told Vox that manufacturers use the dates as a way of “protecting the brand” to keep consumers from eating food that’s just a little past its peak.
With approximately 40 million people in the United States concerned about where their next meal is coming from, the Vox article noted, we need to reevaluate our system. Our national misunderstanding of expiration labels is hurting both suppliers and consumers because perfectly good food is wasted.
Sure, there is always that chance that something might be a little funky after a certain amount of time, but all in all, food probably stays fresh a lot longer than we think. Don’t always judge the shredded cheese by its expiration date.
An extreme price to pay for immortality
We know that men don’t live as long as women, but the reasons aren’t entirely clear. However, some New Zealand scientists have a thought on the subject, thanks to a sheep called Shrek.
The researchers were inspired by a famous old sheep who escaped captivity, but was captured 6 years later at the age of 10. The sheep then lived 6 more years, far beyond the lifespan of a normal sheep, capturing the hearts and minds of Kiwis everywhere. Look, it’s New Zealand, sheep are life, so it’s only natural the country got attached. Scientists from the University of Otago suspected that Shrek lived such a long life because he was castrated.
So they undertook a study of sheep, and lo and behold, sheep that were castrated lived significantly longer than their uncastrated kin, thanks to a slowing of their epigenetic clocks – the DNA aged noticeably slower in the castrated sheep.
Although the research can most immediately be applied to the improvement of the New Zealand sheep industry, the implication for humanity is also apparent. Want to live longer? Get rid of the testosterone. An extreme solution to be sure. As previously reported in this column, researchers wanted to torture our mouths to get us to lose weight, and now they want to castrate people for longer life. What exactly is going on down there in New Zealand?
Man’s best mind reader
There are a lot of reasons why dogs are sometimes called “man’s best friend,” but the root of it may actually have something to do with how easily we communicate with each other. Researchers dug deeper and fetched something that Fido is born with, but his wild wolf cousin isn’t.
That something is known as the “theory of mind” ability. Have you noticed that when you point and tell dogs to grab a leash or toy, they react as if they understood the language you spoke? Researchers from Duke University wondered if this ability is a canine thing or just a domesticated dog thing.
They compared 44 canine puppies and 37 wolf pups between 5 and 18 weeks old. The wolf pups were taken into human homes and raised with a great amount of human interaction, while the dog pups were left with their mothers and raised with less human interaction.
All the puppies were then put through multiple tests. In one test, they were given clues to find a treat under a bowl. In another test, a block of wood was placed next to the treat as a physical marker. During yet another test, researchers pointed to the food directly.
The researchers discovered that the dog puppies knew where the treat was every time, while their wild relatives didn’t.
“This study really solidifies the evidence that the social genius of dogs is a product of domestication,” senior author Brian Hare said in a separate statement.
The domestication hypothesis theorizes that dogs picked up the human social cues through thousands of years of interaction. The more friendly and cooperative a wolf was with humans, the more likely it was to survive and pass on those same traits and practices. Even within the study, the dog puppies were 30 times more likely to approach a stranger than were the wolf pups.
You may think your dog understands everything you say, but it’s actually body language that Fido is most fluent in.
I’m not a dentist, but I play one on TikTok
In last week’s column, it was garlic cloves up the nose to treat a cold. This week, TikTok brings us a new way to whiten teeth.
Familiar with the Mr. Clean Magic Eraser? If not, we’ll save you the trouble of Googling it: Check it out here and here.
Have you heard anything about using it to clean your teeth? No, neither did we, and we did a lot of Googling. Proctor & Gamble, which makes the Magic Eraser, goes so far as to say on the package: “Do not use on skin or other parts of the body. Using on skin will likely cause abrasions.” (The warning is actually in all caps, but we are stylistically forbidden by our editorial overlords to do that.)
But it’s magic, right? How can you not use it on your teeth? Enter TikTok. Heather Dunn posted a video in which she rubbed a bit of a Magic Eraser on her teeth – being careful to avoid her gums, because you can never be too careful – “as the product squeaked back and forth,” the Miami Herald reported. The video has almost 256,000 likes so far.
“Yeah, your teeth are white because you scrubbed all the enamel off them. So don’t do this,” Dr. Benjamin Winters, aka the Bentist, said in a YouTube video that has 105,000 likes.
In this race for common sense, common sense is losing. Please help the Bentist restore sanity to the dental world by liking his video. It would make Mr. Clean happy.
Don’t let an expiration date boss you around
Surely you’ve been there: It’s Taco Tuesday and you’re rummaging through the refrigerator to find that shredded cheese you’re sure you have. Jackpot! You find it, but realize it’s probably been in the refrigerator for a while. You open the bag, it smells and looks fine, but the expiration date was 2 days ago. Now you have a decision to make. Maybe you’ll be fine, or maybe you’ll risk food poisoning right before your brother’s wedding.
But here’s the truth: Americans throw away perfectly good food every day. The average American family throws out $1,365 to $2,275 worth of food a year, according to a 2013 study.
Truthfully, expiration dates are not for buyers, rather they’re for stores to have an idea of their stock’s freshness. Emily Broad Leib, director of the Harvard Law School Food and Policy Clinic and lead author of the 2013 study, told Vox that manufacturers use the dates as a way of “protecting the brand” to keep consumers from eating food that’s just a little past its peak.
With approximately 40 million people in the United States concerned about where their next meal is coming from, the Vox article noted, we need to reevaluate our system. Our national misunderstanding of expiration labels is hurting both suppliers and consumers because perfectly good food is wasted.
Sure, there is always that chance that something might be a little funky after a certain amount of time, but all in all, food probably stays fresh a lot longer than we think. Don’t always judge the shredded cheese by its expiration date.
An extreme price to pay for immortality
We know that men don’t live as long as women, but the reasons aren’t entirely clear. However, some New Zealand scientists have a thought on the subject, thanks to a sheep called Shrek.
The researchers were inspired by a famous old sheep who escaped captivity, but was captured 6 years later at the age of 10. The sheep then lived 6 more years, far beyond the lifespan of a normal sheep, capturing the hearts and minds of Kiwis everywhere. Look, it’s New Zealand, sheep are life, so it’s only natural the country got attached. Scientists from the University of Otago suspected that Shrek lived such a long life because he was castrated.
So they undertook a study of sheep, and lo and behold, sheep that were castrated lived significantly longer than their uncastrated kin, thanks to a slowing of their epigenetic clocks – the DNA aged noticeably slower in the castrated sheep.
Although the research can most immediately be applied to the improvement of the New Zealand sheep industry, the implication for humanity is also apparent. Want to live longer? Get rid of the testosterone. An extreme solution to be sure. As previously reported in this column, researchers wanted to torture our mouths to get us to lose weight, and now they want to castrate people for longer life. What exactly is going on down there in New Zealand?
Man’s best mind reader
There are a lot of reasons why dogs are sometimes called “man’s best friend,” but the root of it may actually have something to do with how easily we communicate with each other. Researchers dug deeper and fetched something that Fido is born with, but his wild wolf cousin isn’t.
That something is known as the “theory of mind” ability. Have you noticed that when you point and tell dogs to grab a leash or toy, they react as if they understood the language you spoke? Researchers from Duke University wondered if this ability is a canine thing or just a domesticated dog thing.
They compared 44 canine puppies and 37 wolf pups between 5 and 18 weeks old. The wolf pups were taken into human homes and raised with a great amount of human interaction, while the dog pups were left with their mothers and raised with less human interaction.
All the puppies were then put through multiple tests. In one test, they were given clues to find a treat under a bowl. In another test, a block of wood was placed next to the treat as a physical marker. During yet another test, researchers pointed to the food directly.
The researchers discovered that the dog puppies knew where the treat was every time, while their wild relatives didn’t.
“This study really solidifies the evidence that the social genius of dogs is a product of domestication,” senior author Brian Hare said in a separate statement.
The domestication hypothesis theorizes that dogs picked up the human social cues through thousands of years of interaction. The more friendly and cooperative a wolf was with humans, the more likely it was to survive and pass on those same traits and practices. Even within the study, the dog puppies were 30 times more likely to approach a stranger than were the wolf pups.
You may think your dog understands everything you say, but it’s actually body language that Fido is most fluent in.
I’m not a dentist, but I play one on TikTok
In last week’s column, it was garlic cloves up the nose to treat a cold. This week, TikTok brings us a new way to whiten teeth.
Familiar with the Mr. Clean Magic Eraser? If not, we’ll save you the trouble of Googling it: Check it out here and here.
Have you heard anything about using it to clean your teeth? No, neither did we, and we did a lot of Googling. Proctor & Gamble, which makes the Magic Eraser, goes so far as to say on the package: “Do not use on skin or other parts of the body. Using on skin will likely cause abrasions.” (The warning is actually in all caps, but we are stylistically forbidden by our editorial overlords to do that.)
But it’s magic, right? How can you not use it on your teeth? Enter TikTok. Heather Dunn posted a video in which she rubbed a bit of a Magic Eraser on her teeth – being careful to avoid her gums, because you can never be too careful – “as the product squeaked back and forth,” the Miami Herald reported. The video has almost 256,000 likes so far.
“Yeah, your teeth are white because you scrubbed all the enamel off them. So don’t do this,” Dr. Benjamin Winters, aka the Bentist, said in a YouTube video that has 105,000 likes.
In this race for common sense, common sense is losing. Please help the Bentist restore sanity to the dental world by liking his video. It would make Mr. Clean happy.
Don’t let an expiration date boss you around
Surely you’ve been there: It’s Taco Tuesday and you’re rummaging through the refrigerator to find that shredded cheese you’re sure you have. Jackpot! You find it, but realize it’s probably been in the refrigerator for a while. You open the bag, it smells and looks fine, but the expiration date was 2 days ago. Now you have a decision to make. Maybe you’ll be fine, or maybe you’ll risk food poisoning right before your brother’s wedding.
But here’s the truth: Americans throw away perfectly good food every day. The average American family throws out $1,365 to $2,275 worth of food a year, according to a 2013 study.
Truthfully, expiration dates are not for buyers, rather they’re for stores to have an idea of their stock’s freshness. Emily Broad Leib, director of the Harvard Law School Food and Policy Clinic and lead author of the 2013 study, told Vox that manufacturers use the dates as a way of “protecting the brand” to keep consumers from eating food that’s just a little past its peak.
With approximately 40 million people in the United States concerned about where their next meal is coming from, the Vox article noted, we need to reevaluate our system. Our national misunderstanding of expiration labels is hurting both suppliers and consumers because perfectly good food is wasted.
Sure, there is always that chance that something might be a little funky after a certain amount of time, but all in all, food probably stays fresh a lot longer than we think. Don’t always judge the shredded cheese by its expiration date.