User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'main-prefix')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
New data on traumatic brain injury show it’s chronic, evolving
The data show that patients with TBI may continue to improve or decline during a period of up to 7 years after injury, making it more of a chronic condition, the investigators report.
“Our results dispute the notion that TBI is a discrete, isolated medical event with a finite, static functional outcome following a relatively short period of upward recovery (typically up to 1 year),” Benjamin Brett, PhD, assistant professor, departments of neurosurgery and neurology, Medical College of Wisconsin, Milwaukee, told this news organization.
“Rather, individuals continue to exhibit improvement and decline across a range of domains, including psychiatric, cognitive, and functional outcomes, even 2-7 years after their injury,” Dr. Brett said.
“Ultimately, our findings support conceptualizing TBI as a chronic condition for many patients, which requires routine follow-up, medical monitoring, responsive care, and support, adapting to their evolving needs many years following injury,” he said.
Results of the TRACK TBI LONG (Transforming Research and Clinical Knowledge in TBI Longitudinal study) were published online in Neurology.
Chronic and evolving
The results are based on 1,264 adults (mean age at injury, 41 years) from the initial TRACK TBI study, including 917 with mild TBI (mTBI) and 193 with moderate/severe TBI (msTBI), who were matched to 154 control patients who had experienced orthopedic trauma without evidence of head injury (OTC).
The participants were followed annually for up to 7 years after injury using the Glasgow Outcome Scale–Extended (GOSE), Brief Symptom Inventory–18 (BSI), and the Brief Test of Adult Cognition by Telephone (BTACT), as well as a self-reported perception of function. The researchers calculated rates of change (classified as stable, improved, or declined) for individual outcomes at each long-term follow-up.
In general, “stable” was the most frequent change outcome for the individual measures from postinjury baseline assessment to 7 years post injury.
However, a substantial proportion of patients with TBI (regardless of severity) experienced changes in psychiatric status, cognition, and functional outcomes over the years.
When the GOSE, BSI, and BTACT were considered collectively, rates of decline were 21% for mTBI, 26% for msTBI, and 15% for OTC.
The highest rates of decline were in functional outcomes (GOSE scores). On average, over the course of 2-7 years post injury, 29% of patients with mTBI and 23% of those with msTBI experienced a decline in the ability to function with daily activities.
A pattern of improvement on the GOSE was noted in 36% of patients with msTBI and 22% patients with mTBI.
Notably, said Dr. Brett, patients who experienced greater difficulties near the time of injury showed improvement for a period of 2-7 years post injury. Patient factors, such as older age at the time of the injury, were associated with greater risk of long-term decline.
“Our findings highlight the need to embrace conceptualization of TBI as a chronic condition in order to establish systems of care that provide continued follow-up with treatment and supports that adapt to evolving patient needs, regardless of the directions of change,” Dr. Brett told this news organization.
Important and novel work
In a linked editorial, Robynne Braun, MD, PhD, with the department of neurology, University of Maryland, Baltimore, notes that there have been “few prospective studies examining postinjury outcomes on this longer timescale, especially in mild TBI, making this an important and novel body of work.”
The study “effectively demonstrates that changes in function across multiple domains continue to occur well beyond the conventionally tracked 6- to 12-month period of injury recovery,” Dr. Braun writes.
The observation that over the 7-year follow-up, a substantial proportion of patients with mTBI and msTBI exhibited a pattern of decline on the GOSE suggests that they “may have needed more ongoing medical monitoring, rehabilitation, or supportive services to prevent worsening,” Dr. Braun adds.
At the same time, the improvement pattern on the GOSE suggests “opportunities for recovery that further rehabilitative or medical services might have enhanced.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the National Football League Scientific Advisory Board, and the U.S. Department of Defense. Dr. Brett and Dr. Braun have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The data show that patients with TBI may continue to improve or decline during a period of up to 7 years after injury, making it more of a chronic condition, the investigators report.
“Our results dispute the notion that TBI is a discrete, isolated medical event with a finite, static functional outcome following a relatively short period of upward recovery (typically up to 1 year),” Benjamin Brett, PhD, assistant professor, departments of neurosurgery and neurology, Medical College of Wisconsin, Milwaukee, told this news organization.
“Rather, individuals continue to exhibit improvement and decline across a range of domains, including psychiatric, cognitive, and functional outcomes, even 2-7 years after their injury,” Dr. Brett said.
“Ultimately, our findings support conceptualizing TBI as a chronic condition for many patients, which requires routine follow-up, medical monitoring, responsive care, and support, adapting to their evolving needs many years following injury,” he said.
Results of the TRACK TBI LONG (Transforming Research and Clinical Knowledge in TBI Longitudinal study) were published online in Neurology.
Chronic and evolving
The results are based on 1,264 adults (mean age at injury, 41 years) from the initial TRACK TBI study, including 917 with mild TBI (mTBI) and 193 with moderate/severe TBI (msTBI), who were matched to 154 control patients who had experienced orthopedic trauma without evidence of head injury (OTC).
The participants were followed annually for up to 7 years after injury using the Glasgow Outcome Scale–Extended (GOSE), Brief Symptom Inventory–18 (BSI), and the Brief Test of Adult Cognition by Telephone (BTACT), as well as a self-reported perception of function. The researchers calculated rates of change (classified as stable, improved, or declined) for individual outcomes at each long-term follow-up.
In general, “stable” was the most frequent change outcome for the individual measures from postinjury baseline assessment to 7 years post injury.
However, a substantial proportion of patients with TBI (regardless of severity) experienced changes in psychiatric status, cognition, and functional outcomes over the years.
When the GOSE, BSI, and BTACT were considered collectively, rates of decline were 21% for mTBI, 26% for msTBI, and 15% for OTC.
The highest rates of decline were in functional outcomes (GOSE scores). On average, over the course of 2-7 years post injury, 29% of patients with mTBI and 23% of those with msTBI experienced a decline in the ability to function with daily activities.
A pattern of improvement on the GOSE was noted in 36% of patients with msTBI and 22% patients with mTBI.
Notably, said Dr. Brett, patients who experienced greater difficulties near the time of injury showed improvement for a period of 2-7 years post injury. Patient factors, such as older age at the time of the injury, were associated with greater risk of long-term decline.
“Our findings highlight the need to embrace conceptualization of TBI as a chronic condition in order to establish systems of care that provide continued follow-up with treatment and supports that adapt to evolving patient needs, regardless of the directions of change,” Dr. Brett told this news organization.
Important and novel work
In a linked editorial, Robynne Braun, MD, PhD, with the department of neurology, University of Maryland, Baltimore, notes that there have been “few prospective studies examining postinjury outcomes on this longer timescale, especially in mild TBI, making this an important and novel body of work.”
The study “effectively demonstrates that changes in function across multiple domains continue to occur well beyond the conventionally tracked 6- to 12-month period of injury recovery,” Dr. Braun writes.
The observation that over the 7-year follow-up, a substantial proportion of patients with mTBI and msTBI exhibited a pattern of decline on the GOSE suggests that they “may have needed more ongoing medical monitoring, rehabilitation, or supportive services to prevent worsening,” Dr. Braun adds.
At the same time, the improvement pattern on the GOSE suggests “opportunities for recovery that further rehabilitative or medical services might have enhanced.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the National Football League Scientific Advisory Board, and the U.S. Department of Defense. Dr. Brett and Dr. Braun have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The data show that patients with TBI may continue to improve or decline during a period of up to 7 years after injury, making it more of a chronic condition, the investigators report.
“Our results dispute the notion that TBI is a discrete, isolated medical event with a finite, static functional outcome following a relatively short period of upward recovery (typically up to 1 year),” Benjamin Brett, PhD, assistant professor, departments of neurosurgery and neurology, Medical College of Wisconsin, Milwaukee, told this news organization.
“Rather, individuals continue to exhibit improvement and decline across a range of domains, including psychiatric, cognitive, and functional outcomes, even 2-7 years after their injury,” Dr. Brett said.
“Ultimately, our findings support conceptualizing TBI as a chronic condition for many patients, which requires routine follow-up, medical monitoring, responsive care, and support, adapting to their evolving needs many years following injury,” he said.
Results of the TRACK TBI LONG (Transforming Research and Clinical Knowledge in TBI Longitudinal study) were published online in Neurology.
Chronic and evolving
The results are based on 1,264 adults (mean age at injury, 41 years) from the initial TRACK TBI study, including 917 with mild TBI (mTBI) and 193 with moderate/severe TBI (msTBI), who were matched to 154 control patients who had experienced orthopedic trauma without evidence of head injury (OTC).
The participants were followed annually for up to 7 years after injury using the Glasgow Outcome Scale–Extended (GOSE), Brief Symptom Inventory–18 (BSI), and the Brief Test of Adult Cognition by Telephone (BTACT), as well as a self-reported perception of function. The researchers calculated rates of change (classified as stable, improved, or declined) for individual outcomes at each long-term follow-up.
In general, “stable” was the most frequent change outcome for the individual measures from postinjury baseline assessment to 7 years post injury.
However, a substantial proportion of patients with TBI (regardless of severity) experienced changes in psychiatric status, cognition, and functional outcomes over the years.
When the GOSE, BSI, and BTACT were considered collectively, rates of decline were 21% for mTBI, 26% for msTBI, and 15% for OTC.
The highest rates of decline were in functional outcomes (GOSE scores). On average, over the course of 2-7 years post injury, 29% of patients with mTBI and 23% of those with msTBI experienced a decline in the ability to function with daily activities.
A pattern of improvement on the GOSE was noted in 36% of patients with msTBI and 22% patients with mTBI.
Notably, said Dr. Brett, patients who experienced greater difficulties near the time of injury showed improvement for a period of 2-7 years post injury. Patient factors, such as older age at the time of the injury, were associated with greater risk of long-term decline.
“Our findings highlight the need to embrace conceptualization of TBI as a chronic condition in order to establish systems of care that provide continued follow-up with treatment and supports that adapt to evolving patient needs, regardless of the directions of change,” Dr. Brett told this news organization.
Important and novel work
In a linked editorial, Robynne Braun, MD, PhD, with the department of neurology, University of Maryland, Baltimore, notes that there have been “few prospective studies examining postinjury outcomes on this longer timescale, especially in mild TBI, making this an important and novel body of work.”
The study “effectively demonstrates that changes in function across multiple domains continue to occur well beyond the conventionally tracked 6- to 12-month period of injury recovery,” Dr. Braun writes.
The observation that over the 7-year follow-up, a substantial proportion of patients with mTBI and msTBI exhibited a pattern of decline on the GOSE suggests that they “may have needed more ongoing medical monitoring, rehabilitation, or supportive services to prevent worsening,” Dr. Braun adds.
At the same time, the improvement pattern on the GOSE suggests “opportunities for recovery that further rehabilitative or medical services might have enhanced.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institute on Aging, the National Football League Scientific Advisory Board, and the U.S. Department of Defense. Dr. Brett and Dr. Braun have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM NEUROLOGY
More than 30 experts question validity of serotonin/depression study
The authors of the article, however, stand by their conclusion.
“The methodology doesn’t conform to a conventional umbrella review,” said the commentary’s lead author, Sameer Jauhar, MD, PhD, first author of the commentary criticizing the review, which was published online in Molecular Psychiatry.
In addition, preeminent psychiatrist David J. Nutt, MD, PhD, Edmond J. Safra Professor of Neuropsychopharmacology, Imperial College London, is calling for the review to be retracted. In an interview with The Daily Mail, he said the article is “full of flaws and it should never have been published in the first place. Yet it has been frequently cited and people believe it is true. It’s essentially misinformation. That’s why I’m calling on the journal to retract it.” Dr. Nutt is one of the authors of the published commentary.
‘No convincing evidence’
Led by Joanna Moncrieff, MD, professor of clinical and social psychiatry, University College London, the authors analyzed systematic reviews and meta-analyses to determine whether low serotonin levels are, in fact, associated with depression.
Of 361 potential studies, 17 were selected for the review, including meta-analyses, systematic reviews, and a genetic association study.
The review included examinations of 5-HT and its metabolite 5-hydroxyindoleacetic acid (5-HIAA) in “body fluids,” 5HT1A receptor and serotonin transporter protein (SERT) availability in imaging and postmortem studies, investigations of SERT gene polymorphisms, interactions between SERT and stress in depression, and effects of tryptophan depletion on mood.
The tryptophan hypothesis suggests depression occurs through tryptophan depletion, which lowers available serotonin. According to the review, two crossover studies of patients with depression who were currently receiving or had recently received antidepressant treatment did not show substantial effects of depletion, and data from studies involving volunteers largely showed no effect.
Ultimately, Dr. Moncrieff and colleagues concluded that “there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity.”
‘Unconventional, odd’ methodology
However, Dr. Jauhar and the commentary’s coauthors disagree with the study’s conclusion. The researchers claim that “we don’t see depression symptoms in healthy volunteers when given tryptophan depletion; everyone knows that and agrees with that; it’s only in people vulnerable to depression who will have it.”
Furthermore, he said, the study’s conclusion does not consider that experimental medicine studies of tryptophan depletion are difficult to conduct. “You’re not going to have huge sample sizes as you would in a genetic study or big epidemiological studies.
Dr. Jauhar said he found it “unconventional” and “odd” that the review included individual tryptophan depletion studies that were not in the prespecified protocol.
For studies involving molecular imaging, Dr. Jauhar said the review’s inferences were “simplistic” and the review authors are “basically shaping the argument” to fit their desired narrative.
He also noted factual errors in the review. “They make a mistake when they talk about serotonin transporter imaging; they say there are no consistent findings across studies when, in fact, there are.”
With both tryptophan depletion and molecular imaging studies, the review “glosses over findings” from the original studies, said Dr. Jauhar.
For tryptophan depletion, “a more accurate, constructive conclusion would be that acute tryptophan depletion and decreased plasma tryptophan in depression indicate a role for 5-HT in those vulnerable to or suffering from depression, and that molecular imaging suggests the system is perturbed,” the commentators wrote.
“The proven efficacy of SSRIs in a proportion of people with depression lends credibility to this position,” they added.
Dr. Jauhar also took issue with criteria for certainty of finding of these and other studies used in the review. “If you’re setting the criteria yourself, it’s arbitrary.”
No new data
An umbrella review is supposed to be of the highest quality and should entail “taking out the studies and analysing them yourself,” but here, “all they have done is put a synthesis forward of other people’s reviews, so essentially there’s no new data there,” said Dr. Jauhar.
And sometimes the review’s findings differ from the original research. “When you have people who haven’t conducted original research themselves quoting someone else’s work and ignoring what those people say, we’re all in trouble,” said Dr. Jauhar.
In an additional commentary also published in Molecular Psychiatry, Jacob Pade Ramsøe Jacobsen, Evecxia Therapeutics, Durham, N.C., also criticized the review by Dr. Moncrieff and colleagues.
Its authors appear unfamiliar with serotonin biology and pharmacology, Dr. Jacobsen wrote.
“The review contains factual errors, makes conclusions serotonin neurobiology may not support, and quotes the cited literature in a selective manner,” he added.
“Most troubling, they misinterpret some data reviewed and intimate that serotonin reuptake inhibitor antidepressants, e.g., SSRIs, may decrease, rather than increase, serotonin function.”
If accepted by general practitioners and the public, the review’s conclusions “could lead to reduced use of antidepressants among patients in need and increased morbidity related to depression.”
Dr. Moncrieff pushes back
Responding to the torrent of criticism of her study, Dr. Moncrieff told this news organization via email that they stand by the review, adding that Dr. Jauhar and others “don’t want to let the cat out of the bag” that there’s no good evidence to support the hypothesis that low serotonin causes depression because it challenges antidepressant use.
“The idea that antidepressants work by correcting an underlying chemical imbalance or serotonin abnormality has led research up a blind alley and meant scientists have not taken the harmful effects of these drugs seriously enough.”
These critics, she added, “want business as usual – which means people will continue to be misinformed and exposed to harmful effects of drugs that have minimal and uncertain benefits.”
In a letter to the editor of Molecular Psychiatry, Dr. Moncrieff and her fellow authors maintain that they used approved and well-accepted methods for the umbrella review, including preregistering the protocol and using recommended search methods and quality assessments, and that they did not miss certain studies, as has been claimed.
In her blog, Dr. Moncrieff wrote that the “marginal differences between antidepressants and placebo that are apparent in clinical trials are likely to be produced by alternative, more plausible mechanisms like the emotional blunting effects of the drugs or by amplified placebo effects, rather than by targeting underlying biological mechanisms (since these have not been demonstrated).”
It also highlights “how we don’t know what antidepressants do to the brain exactly, which is a cause for concern,” she adds.
Dr. Jauhar has received honoraria for nonpromotional educational talks on antipsychotics from Janssen, Sunovion, and Lundbeck and on causes of schizophrenia for Boehringer-Ingelheim. He has also received honoraria for consulting on antipsychotics for LB Pharmaceuticals. He sits on Council for the British Association for Psychopharmacology and was a recent panel member for the Wellcome Trust.
A version of this article originally appeared on Medscape.com.
The authors of the article, however, stand by their conclusion.
“The methodology doesn’t conform to a conventional umbrella review,” said the commentary’s lead author, Sameer Jauhar, MD, PhD, first author of the commentary criticizing the review, which was published online in Molecular Psychiatry.
In addition, preeminent psychiatrist David J. Nutt, MD, PhD, Edmond J. Safra Professor of Neuropsychopharmacology, Imperial College London, is calling for the review to be retracted. In an interview with The Daily Mail, he said the article is “full of flaws and it should never have been published in the first place. Yet it has been frequently cited and people believe it is true. It’s essentially misinformation. That’s why I’m calling on the journal to retract it.” Dr. Nutt is one of the authors of the published commentary.
‘No convincing evidence’
Led by Joanna Moncrieff, MD, professor of clinical and social psychiatry, University College London, the authors analyzed systematic reviews and meta-analyses to determine whether low serotonin levels are, in fact, associated with depression.
Of 361 potential studies, 17 were selected for the review, including meta-analyses, systematic reviews, and a genetic association study.
The review included examinations of 5-HT and its metabolite 5-hydroxyindoleacetic acid (5-HIAA) in “body fluids,” 5HT1A receptor and serotonin transporter protein (SERT) availability in imaging and postmortem studies, investigations of SERT gene polymorphisms, interactions between SERT and stress in depression, and effects of tryptophan depletion on mood.
The tryptophan hypothesis suggests depression occurs through tryptophan depletion, which lowers available serotonin. According to the review, two crossover studies of patients with depression who were currently receiving or had recently received antidepressant treatment did not show substantial effects of depletion, and data from studies involving volunteers largely showed no effect.
Ultimately, Dr. Moncrieff and colleagues concluded that “there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity.”
‘Unconventional, odd’ methodology
However, Dr. Jauhar and the commentary’s coauthors disagree with the study’s conclusion. The researchers claim that “we don’t see depression symptoms in healthy volunteers when given tryptophan depletion; everyone knows that and agrees with that; it’s only in people vulnerable to depression who will have it.”
Furthermore, he said, the study’s conclusion does not consider that experimental medicine studies of tryptophan depletion are difficult to conduct. “You’re not going to have huge sample sizes as you would in a genetic study or big epidemiological studies.
Dr. Jauhar said he found it “unconventional” and “odd” that the review included individual tryptophan depletion studies that were not in the prespecified protocol.
For studies involving molecular imaging, Dr. Jauhar said the review’s inferences were “simplistic” and the review authors are “basically shaping the argument” to fit their desired narrative.
He also noted factual errors in the review. “They make a mistake when they talk about serotonin transporter imaging; they say there are no consistent findings across studies when, in fact, there are.”
With both tryptophan depletion and molecular imaging studies, the review “glosses over findings” from the original studies, said Dr. Jauhar.
For tryptophan depletion, “a more accurate, constructive conclusion would be that acute tryptophan depletion and decreased plasma tryptophan in depression indicate a role for 5-HT in those vulnerable to or suffering from depression, and that molecular imaging suggests the system is perturbed,” the commentators wrote.
“The proven efficacy of SSRIs in a proportion of people with depression lends credibility to this position,” they added.
Dr. Jauhar also took issue with criteria for certainty of finding of these and other studies used in the review. “If you’re setting the criteria yourself, it’s arbitrary.”
No new data
An umbrella review is supposed to be of the highest quality and should entail “taking out the studies and analysing them yourself,” but here, “all they have done is put a synthesis forward of other people’s reviews, so essentially there’s no new data there,” said Dr. Jauhar.
And sometimes the review’s findings differ from the original research. “When you have people who haven’t conducted original research themselves quoting someone else’s work and ignoring what those people say, we’re all in trouble,” said Dr. Jauhar.
In an additional commentary also published in Molecular Psychiatry, Jacob Pade Ramsøe Jacobsen, Evecxia Therapeutics, Durham, N.C., also criticized the review by Dr. Moncrieff and colleagues.
Its authors appear unfamiliar with serotonin biology and pharmacology, Dr. Jacobsen wrote.
“The review contains factual errors, makes conclusions serotonin neurobiology may not support, and quotes the cited literature in a selective manner,” he added.
“Most troubling, they misinterpret some data reviewed and intimate that serotonin reuptake inhibitor antidepressants, e.g., SSRIs, may decrease, rather than increase, serotonin function.”
If accepted by general practitioners and the public, the review’s conclusions “could lead to reduced use of antidepressants among patients in need and increased morbidity related to depression.”
Dr. Moncrieff pushes back
Responding to the torrent of criticism of her study, Dr. Moncrieff told this news organization via email that they stand by the review, adding that Dr. Jauhar and others “don’t want to let the cat out of the bag” that there’s no good evidence to support the hypothesis that low serotonin causes depression because it challenges antidepressant use.
“The idea that antidepressants work by correcting an underlying chemical imbalance or serotonin abnormality has led research up a blind alley and meant scientists have not taken the harmful effects of these drugs seriously enough.”
These critics, she added, “want business as usual – which means people will continue to be misinformed and exposed to harmful effects of drugs that have minimal and uncertain benefits.”
In a letter to the editor of Molecular Psychiatry, Dr. Moncrieff and her fellow authors maintain that they used approved and well-accepted methods for the umbrella review, including preregistering the protocol and using recommended search methods and quality assessments, and that they did not miss certain studies, as has been claimed.
In her blog, Dr. Moncrieff wrote that the “marginal differences between antidepressants and placebo that are apparent in clinical trials are likely to be produced by alternative, more plausible mechanisms like the emotional blunting effects of the drugs or by amplified placebo effects, rather than by targeting underlying biological mechanisms (since these have not been demonstrated).”
It also highlights “how we don’t know what antidepressants do to the brain exactly, which is a cause for concern,” she adds.
Dr. Jauhar has received honoraria for nonpromotional educational talks on antipsychotics from Janssen, Sunovion, and Lundbeck and on causes of schizophrenia for Boehringer-Ingelheim. He has also received honoraria for consulting on antipsychotics for LB Pharmaceuticals. He sits on Council for the British Association for Psychopharmacology and was a recent panel member for the Wellcome Trust.
A version of this article originally appeared on Medscape.com.
The authors of the article, however, stand by their conclusion.
“The methodology doesn’t conform to a conventional umbrella review,” said the commentary’s lead author, Sameer Jauhar, MD, PhD, first author of the commentary criticizing the review, which was published online in Molecular Psychiatry.
In addition, preeminent psychiatrist David J. Nutt, MD, PhD, Edmond J. Safra Professor of Neuropsychopharmacology, Imperial College London, is calling for the review to be retracted. In an interview with The Daily Mail, he said the article is “full of flaws and it should never have been published in the first place. Yet it has been frequently cited and people believe it is true. It’s essentially misinformation. That’s why I’m calling on the journal to retract it.” Dr. Nutt is one of the authors of the published commentary.
‘No convincing evidence’
Led by Joanna Moncrieff, MD, professor of clinical and social psychiatry, University College London, the authors analyzed systematic reviews and meta-analyses to determine whether low serotonin levels are, in fact, associated with depression.
Of 361 potential studies, 17 were selected for the review, including meta-analyses, systematic reviews, and a genetic association study.
The review included examinations of 5-HT and its metabolite 5-hydroxyindoleacetic acid (5-HIAA) in “body fluids,” 5HT1A receptor and serotonin transporter protein (SERT) availability in imaging and postmortem studies, investigations of SERT gene polymorphisms, interactions between SERT and stress in depression, and effects of tryptophan depletion on mood.
The tryptophan hypothesis suggests depression occurs through tryptophan depletion, which lowers available serotonin. According to the review, two crossover studies of patients with depression who were currently receiving or had recently received antidepressant treatment did not show substantial effects of depletion, and data from studies involving volunteers largely showed no effect.
Ultimately, Dr. Moncrieff and colleagues concluded that “there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity.”
‘Unconventional, odd’ methodology
However, Dr. Jauhar and the commentary’s coauthors disagree with the study’s conclusion. The researchers claim that “we don’t see depression symptoms in healthy volunteers when given tryptophan depletion; everyone knows that and agrees with that; it’s only in people vulnerable to depression who will have it.”
Furthermore, he said, the study’s conclusion does not consider that experimental medicine studies of tryptophan depletion are difficult to conduct. “You’re not going to have huge sample sizes as you would in a genetic study or big epidemiological studies.
Dr. Jauhar said he found it “unconventional” and “odd” that the review included individual tryptophan depletion studies that were not in the prespecified protocol.
For studies involving molecular imaging, Dr. Jauhar said the review’s inferences were “simplistic” and the review authors are “basically shaping the argument” to fit their desired narrative.
He also noted factual errors in the review. “They make a mistake when they talk about serotonin transporter imaging; they say there are no consistent findings across studies when, in fact, there are.”
With both tryptophan depletion and molecular imaging studies, the review “glosses over findings” from the original studies, said Dr. Jauhar.
For tryptophan depletion, “a more accurate, constructive conclusion would be that acute tryptophan depletion and decreased plasma tryptophan in depression indicate a role for 5-HT in those vulnerable to or suffering from depression, and that molecular imaging suggests the system is perturbed,” the commentators wrote.
“The proven efficacy of SSRIs in a proportion of people with depression lends credibility to this position,” they added.
Dr. Jauhar also took issue with criteria for certainty of finding of these and other studies used in the review. “If you’re setting the criteria yourself, it’s arbitrary.”
No new data
An umbrella review is supposed to be of the highest quality and should entail “taking out the studies and analysing them yourself,” but here, “all they have done is put a synthesis forward of other people’s reviews, so essentially there’s no new data there,” said Dr. Jauhar.
And sometimes the review’s findings differ from the original research. “When you have people who haven’t conducted original research themselves quoting someone else’s work and ignoring what those people say, we’re all in trouble,” said Dr. Jauhar.
In an additional commentary also published in Molecular Psychiatry, Jacob Pade Ramsøe Jacobsen, Evecxia Therapeutics, Durham, N.C., also criticized the review by Dr. Moncrieff and colleagues.
Its authors appear unfamiliar with serotonin biology and pharmacology, Dr. Jacobsen wrote.
“The review contains factual errors, makes conclusions serotonin neurobiology may not support, and quotes the cited literature in a selective manner,” he added.
“Most troubling, they misinterpret some data reviewed and intimate that serotonin reuptake inhibitor antidepressants, e.g., SSRIs, may decrease, rather than increase, serotonin function.”
If accepted by general practitioners and the public, the review’s conclusions “could lead to reduced use of antidepressants among patients in need and increased morbidity related to depression.”
Dr. Moncrieff pushes back
Responding to the torrent of criticism of her study, Dr. Moncrieff told this news organization via email that they stand by the review, adding that Dr. Jauhar and others “don’t want to let the cat out of the bag” that there’s no good evidence to support the hypothesis that low serotonin causes depression because it challenges antidepressant use.
“The idea that antidepressants work by correcting an underlying chemical imbalance or serotonin abnormality has led research up a blind alley and meant scientists have not taken the harmful effects of these drugs seriously enough.”
These critics, she added, “want business as usual – which means people will continue to be misinformed and exposed to harmful effects of drugs that have minimal and uncertain benefits.”
In a letter to the editor of Molecular Psychiatry, Dr. Moncrieff and her fellow authors maintain that they used approved and well-accepted methods for the umbrella review, including preregistering the protocol and using recommended search methods and quality assessments, and that they did not miss certain studies, as has been claimed.
In her blog, Dr. Moncrieff wrote that the “marginal differences between antidepressants and placebo that are apparent in clinical trials are likely to be produced by alternative, more plausible mechanisms like the emotional blunting effects of the drugs or by amplified placebo effects, rather than by targeting underlying biological mechanisms (since these have not been demonstrated).”
It also highlights “how we don’t know what antidepressants do to the brain exactly, which is a cause for concern,” she adds.
Dr. Jauhar has received honoraria for nonpromotional educational talks on antipsychotics from Janssen, Sunovion, and Lundbeck and on causes of schizophrenia for Boehringer-Ingelheim. He has also received honoraria for consulting on antipsychotics for LB Pharmaceuticals. He sits on Council for the British Association for Psychopharmacology and was a recent panel member for the Wellcome Trust.
A version of this article originally appeared on Medscape.com.
Limiting social media use in youths brings challenges, benefits
Amelia Kennedy, 19, of Royersford, Pa., a point guard on the Catholic University of America, Washington, basketball team who will begin her sophomore year in the fall, uses TikTok, Snapchat, Instagram, and YouTube regularly.
How regularly? She estimates 7 hours a day and about 9 on weekends. She’s aware of the time-wasting potential. “If my mom says, ‘Do dishes,’ and I say, ‘5 more minutes,’ it can be longer,’’ she said.
Now imagine the challenge of cutting that 7 or 9 hours a day of social media use down to 30 minutes.
A very tall order, considering a 2022 Pew Research Center survey of more than 1,300 teens found 35% are “nearly constantly” on at least one of the top five social media platforms: YouTube, TikTok, Instagram, Snapchat, and Facebook.
Researchers from Iowa State University, Ames, recently took on that daunting challenge, limiting a group of students to only 30 minutes of social media a day to see what happens. Two weeks into the study, the students reported improvement in psychological well-being and other important measures, including sleep quality, compared with a control group assigned to continue using social media as usual.
And the dreaded FOMO, or fear of missing out, didn’t happen, the researchers said. At the end, the students were rethinking their social media use and feeling positive about it.
As social media becomes more common and youth mental health more endangered, experts are sounding the alarm. In late May, U.S. Surgeon General Vivek Murthy, MD, issued an advisory on social media and youth mental health, calling for tech companies to do better, policymakers to strengthen safety, and researchers to get more information, among other actions.
After that, the Biden administration took actions including the launch of a task force on kids’ online health and safety. The American Psychological Association has issued recommendations on social media use in youths. And the Social Media Victims Law Center in Seattle has sued numerous social media companies for online activity resulting in death and other tragedies.
While experts acknowledge that much more research is needed to sort out how to balance social media’s risks and benefits to preserve youth mental health and prevent such disasters, the new Iowa State study, as well as other recent research, suggests that
Goal: 30 minutes a day
In the Iowa State study, 230 undergraduate students were assigned to one of two groups, with 99 in the 30-minute-a-day social media use group and 131 in the “usual” or control group, which made no changes. For those in the intervention group, “we sent a daily reminder email,” said Ella Faulhaber, a PhD candidate at Iowa State and the study’s lead author. It simply reminded them to limit social medial use to the 30-minute maximum.
At the study start and end, all participants provided a screenshot of their weekly social media usage time. The researchers gave both groups a battery of tests to assess anxiety, depression, loneliness, fear of missing out, and negative and positive feelings.
“By limiting their social media time, that resulted in less anxiety, less depression, less FOMO, fewer negative emotions, and greater positive emotions,” said Douglas Gentile, PhD, a distinguished professor of psychology at Iowa State and a study coauthor. “We know that it is the limiting [of] the social media that is causing that.”
Ms. Faulhaber recalled one participant who mentioned having trouble at first adjusting to the 30-minute time frame, but once sleep improved, it was easier to stick to that guidance. Another who gave up phone use at bedtime found: “Instead of looking at my phone, it was much easier to go straight to bed.”
Sleep improvements, of course, affect many parts of physical and mental health, Dr. Gentile said. And the study also showed that even with reduced screen time, “we can still get the benefit of being connected.” Those who didn’t make the 30-minute mark, but cut back, got benefits, too, the researchers said.
‘Youth are aware’
Self-monitoring works, agreed Jane Harness, DO, an adjunct clinical assistant professor of psychiatry at the University of Michigan, Ann Arbor, because “having that insight is often the first step.”
In a study she conducted, Dr. Harness aimed to gather youths’ insights about how their social media use affected them. With her colleagues, she asked more than 1,100 youths, aged 14-24, what advice they would give to those new to social media, if they ever felt they needed to change social media habits, and if they have deleted or considered deleting social media accounts.
From the 871 responses, Harness found that youths were especially concerned about safety online, that most had thought about deleting a social media app and some had, and that youths were more likely to say they wanted to change the amount of time spent on social media, compared with the content they view.
“Users responded with great advice for each other,” she said. “Safety was brought up,” with users reminding others to keep accounts private and to be aware of location tracking links and content that seems to promote eating disorders, suicide, and other harms.
In the study report, Dr. Harness concluded: “Youth are aware of ways in which social media could be negatively impacting them and they have employed methods to modulate their use because of this awareness.”
Less FOMO, less anxiety
In an earlier study, University of Pennsylvania, Philadelphia, researchers had 143 college students self-monitor social media for a week, then randomly assigned them either to a group told to limit Facebook, Instagram, and Snapchat use to 10 minutes per platform, per day, or to a group told to use social media as usual for 3 weeks.
At the end of the study, the researchers evaluated both groups and found “significant reductions in loneliness and depression over 3 weeks’’ in the limited-use group, compared with the usual-use group, according to study researcher Melissa G. Hunt, PhD, associate director of clinical training at the University of Pennsylvania.
And both groups showed declines in anxiety and fear of missing out, suggesting a benefit tied to self-monitoring itself, she said.
While Dr. Hunt’s study focused on 30 minutes a day, she said “about an hour a day seems to be the sweet spot for maximizing the positive effects of connecting, but limiting the negative effects of social media use.”
She also suggested that smartphones have no place in middle or high school classrooms. Instead, they should be on lockdown during classes.
“Parents need to set real limits of cellphone use during meals and in bedrooms,” Dr. Hunt said. At mealtime, for instance, all phones should be absent from the table. And after 10 p.m., “all family phones remain in the kitchen.”
Be ‘more mindful’
These recent study findings about self-monitoring and limiting social media time may not work the same for everyone, especially among those who aren’t as motivated, said psychiatrist Elizabeth Ortiz-Schwartz, MD, team lead for the adolescent inpatient unit at Silver Hill Hospital in New Canaan, Conn.
But “the bigger take-home piece is that being intentional and attempting to decrease the use in these individuals, even if they were not always successful, was clearly beneficial,” she said.
As we await clearer guidelines about what is the “right” amount of use in terms of social media content and time, Dr. Ortiz-Schwartz said, “becoming more mindful and aware of the risks and benefits can hopefully help individuals become more mindful and deliberate about its use.”
Real-world strategies
Max Schwandt, 23, is an outlier, but a happy one. He works as a sales clerk at a Los Angeles–area recreational gear shop, and he uses no social media. Why not? “It takes up too much time,” he explained. As simple as that.
But for many other teens and young adults, the struggle to stay off social media is real.
Amelia Kennedy, the Catholic University of America student, is trying to reduce her screen time. One way is to track it on her phone. These days, her summer job at a restaurant serving breakfast gets her up early. “If I have to work, I still go on my phone, but not that long.” And once at work, she only has time for quick checks between work responsibilities. “I definitely am more productive,” she said about days when she has work.
Last December, Lauren Young, 25, whose father was a researcher on the Iowa State study, was finishing law school at Georgetown University, Washington, and decided to take a break from social media for the entire month. “I can’t say I was always successful in avoiding it,” she said. But cutting down greatly “made me a lot more present in my day-to-day life, and it was easier to concentrate.”
She could even get through a meal, out with friends, without her phone, keeping it in her purse. That was a definite change from the norm. “I noticed I would go out to dinner and the standard for people my age is having the phone on the table. If you are being polite, you turn it over.”
During her social media “blackout,” Ms. Young had deleted TikTok, Instagram, and Facebook apps. Then, when she graduated, she had to reinstall to post a picture. But now, she is back to minimal social media use.
“I’m studying for the bar, so it’s kind of necessary, but it always makes me happier.” She figures she can always text family and friends if necessary, instead of posting. “I felt for a while I was missing out on things, but not now,” she said.
Others, including Sarah Goldstein, 22, of Chatsworth, Calif., a supermarket courtesy clerk who is thinking of returning to college, said she has developed a healthier attitude toward social media as she has gotten older.
“In middle and early high school, I would see parties, things I wasn’t invited to, on Snapchat and Instagram.” While she realized there could be legitimate reasons for not being included, she said it was easy to internalize those feelings of being left out.
These days, she said she doesn’t let it affect her mental health that way. She enjoys social media – especially TikTok and Instagram – for its benefits. “It kills time, gives you something to watch, can make you laugh and feel like you have a connection with other people.”
A version of this article first appeared on WebMD.com.
Amelia Kennedy, 19, of Royersford, Pa., a point guard on the Catholic University of America, Washington, basketball team who will begin her sophomore year in the fall, uses TikTok, Snapchat, Instagram, and YouTube regularly.
How regularly? She estimates 7 hours a day and about 9 on weekends. She’s aware of the time-wasting potential. “If my mom says, ‘Do dishes,’ and I say, ‘5 more minutes,’ it can be longer,’’ she said.
Now imagine the challenge of cutting that 7 or 9 hours a day of social media use down to 30 minutes.
A very tall order, considering a 2022 Pew Research Center survey of more than 1,300 teens found 35% are “nearly constantly” on at least one of the top five social media platforms: YouTube, TikTok, Instagram, Snapchat, and Facebook.
Researchers from Iowa State University, Ames, recently took on that daunting challenge, limiting a group of students to only 30 minutes of social media a day to see what happens. Two weeks into the study, the students reported improvement in psychological well-being and other important measures, including sleep quality, compared with a control group assigned to continue using social media as usual.
And the dreaded FOMO, or fear of missing out, didn’t happen, the researchers said. At the end, the students were rethinking their social media use and feeling positive about it.
As social media becomes more common and youth mental health more endangered, experts are sounding the alarm. In late May, U.S. Surgeon General Vivek Murthy, MD, issued an advisory on social media and youth mental health, calling for tech companies to do better, policymakers to strengthen safety, and researchers to get more information, among other actions.
After that, the Biden administration took actions including the launch of a task force on kids’ online health and safety. The American Psychological Association has issued recommendations on social media use in youths. And the Social Media Victims Law Center in Seattle has sued numerous social media companies for online activity resulting in death and other tragedies.
While experts acknowledge that much more research is needed to sort out how to balance social media’s risks and benefits to preserve youth mental health and prevent such disasters, the new Iowa State study, as well as other recent research, suggests that
Goal: 30 minutes a day
In the Iowa State study, 230 undergraduate students were assigned to one of two groups, with 99 in the 30-minute-a-day social media use group and 131 in the “usual” or control group, which made no changes. For those in the intervention group, “we sent a daily reminder email,” said Ella Faulhaber, a PhD candidate at Iowa State and the study’s lead author. It simply reminded them to limit social medial use to the 30-minute maximum.
At the study start and end, all participants provided a screenshot of their weekly social media usage time. The researchers gave both groups a battery of tests to assess anxiety, depression, loneliness, fear of missing out, and negative and positive feelings.
“By limiting their social media time, that resulted in less anxiety, less depression, less FOMO, fewer negative emotions, and greater positive emotions,” said Douglas Gentile, PhD, a distinguished professor of psychology at Iowa State and a study coauthor. “We know that it is the limiting [of] the social media that is causing that.”
Ms. Faulhaber recalled one participant who mentioned having trouble at first adjusting to the 30-minute time frame, but once sleep improved, it was easier to stick to that guidance. Another who gave up phone use at bedtime found: “Instead of looking at my phone, it was much easier to go straight to bed.”
Sleep improvements, of course, affect many parts of physical and mental health, Dr. Gentile said. And the study also showed that even with reduced screen time, “we can still get the benefit of being connected.” Those who didn’t make the 30-minute mark, but cut back, got benefits, too, the researchers said.
‘Youth are aware’
Self-monitoring works, agreed Jane Harness, DO, an adjunct clinical assistant professor of psychiatry at the University of Michigan, Ann Arbor, because “having that insight is often the first step.”
In a study she conducted, Dr. Harness aimed to gather youths’ insights about how their social media use affected them. With her colleagues, she asked more than 1,100 youths, aged 14-24, what advice they would give to those new to social media, if they ever felt they needed to change social media habits, and if they have deleted or considered deleting social media accounts.
From the 871 responses, Harness found that youths were especially concerned about safety online, that most had thought about deleting a social media app and some had, and that youths were more likely to say they wanted to change the amount of time spent on social media, compared with the content they view.
“Users responded with great advice for each other,” she said. “Safety was brought up,” with users reminding others to keep accounts private and to be aware of location tracking links and content that seems to promote eating disorders, suicide, and other harms.
In the study report, Dr. Harness concluded: “Youth are aware of ways in which social media could be negatively impacting them and they have employed methods to modulate their use because of this awareness.”
Less FOMO, less anxiety
In an earlier study, University of Pennsylvania, Philadelphia, researchers had 143 college students self-monitor social media for a week, then randomly assigned them either to a group told to limit Facebook, Instagram, and Snapchat use to 10 minutes per platform, per day, or to a group told to use social media as usual for 3 weeks.
At the end of the study, the researchers evaluated both groups and found “significant reductions in loneliness and depression over 3 weeks’’ in the limited-use group, compared with the usual-use group, according to study researcher Melissa G. Hunt, PhD, associate director of clinical training at the University of Pennsylvania.
And both groups showed declines in anxiety and fear of missing out, suggesting a benefit tied to self-monitoring itself, she said.
While Dr. Hunt’s study focused on 30 minutes a day, she said “about an hour a day seems to be the sweet spot for maximizing the positive effects of connecting, but limiting the negative effects of social media use.”
She also suggested that smartphones have no place in middle or high school classrooms. Instead, they should be on lockdown during classes.
“Parents need to set real limits of cellphone use during meals and in bedrooms,” Dr. Hunt said. At mealtime, for instance, all phones should be absent from the table. And after 10 p.m., “all family phones remain in the kitchen.”
Be ‘more mindful’
These recent study findings about self-monitoring and limiting social media time may not work the same for everyone, especially among those who aren’t as motivated, said psychiatrist Elizabeth Ortiz-Schwartz, MD, team lead for the adolescent inpatient unit at Silver Hill Hospital in New Canaan, Conn.
But “the bigger take-home piece is that being intentional and attempting to decrease the use in these individuals, even if they were not always successful, was clearly beneficial,” she said.
As we await clearer guidelines about what is the “right” amount of use in terms of social media content and time, Dr. Ortiz-Schwartz said, “becoming more mindful and aware of the risks and benefits can hopefully help individuals become more mindful and deliberate about its use.”
Real-world strategies
Max Schwandt, 23, is an outlier, but a happy one. He works as a sales clerk at a Los Angeles–area recreational gear shop, and he uses no social media. Why not? “It takes up too much time,” he explained. As simple as that.
But for many other teens and young adults, the struggle to stay off social media is real.
Amelia Kennedy, the Catholic University of America student, is trying to reduce her screen time. One way is to track it on her phone. These days, her summer job at a restaurant serving breakfast gets her up early. “If I have to work, I still go on my phone, but not that long.” And once at work, she only has time for quick checks between work responsibilities. “I definitely am more productive,” she said about days when she has work.
Last December, Lauren Young, 25, whose father was a researcher on the Iowa State study, was finishing law school at Georgetown University, Washington, and decided to take a break from social media for the entire month. “I can’t say I was always successful in avoiding it,” she said. But cutting down greatly “made me a lot more present in my day-to-day life, and it was easier to concentrate.”
She could even get through a meal, out with friends, without her phone, keeping it in her purse. That was a definite change from the norm. “I noticed I would go out to dinner and the standard for people my age is having the phone on the table. If you are being polite, you turn it over.”
During her social media “blackout,” Ms. Young had deleted TikTok, Instagram, and Facebook apps. Then, when she graduated, she had to reinstall to post a picture. But now, she is back to minimal social media use.
“I’m studying for the bar, so it’s kind of necessary, but it always makes me happier.” She figures she can always text family and friends if necessary, instead of posting. “I felt for a while I was missing out on things, but not now,” she said.
Others, including Sarah Goldstein, 22, of Chatsworth, Calif., a supermarket courtesy clerk who is thinking of returning to college, said she has developed a healthier attitude toward social media as she has gotten older.
“In middle and early high school, I would see parties, things I wasn’t invited to, on Snapchat and Instagram.” While she realized there could be legitimate reasons for not being included, she said it was easy to internalize those feelings of being left out.
These days, she said she doesn’t let it affect her mental health that way. She enjoys social media – especially TikTok and Instagram – for its benefits. “It kills time, gives you something to watch, can make you laugh and feel like you have a connection with other people.”
A version of this article first appeared on WebMD.com.
Amelia Kennedy, 19, of Royersford, Pa., a point guard on the Catholic University of America, Washington, basketball team who will begin her sophomore year in the fall, uses TikTok, Snapchat, Instagram, and YouTube regularly.
How regularly? She estimates 7 hours a day and about 9 on weekends. She’s aware of the time-wasting potential. “If my mom says, ‘Do dishes,’ and I say, ‘5 more minutes,’ it can be longer,’’ she said.
Now imagine the challenge of cutting that 7 or 9 hours a day of social media use down to 30 minutes.
A very tall order, considering a 2022 Pew Research Center survey of more than 1,300 teens found 35% are “nearly constantly” on at least one of the top five social media platforms: YouTube, TikTok, Instagram, Snapchat, and Facebook.
Researchers from Iowa State University, Ames, recently took on that daunting challenge, limiting a group of students to only 30 minutes of social media a day to see what happens. Two weeks into the study, the students reported improvement in psychological well-being and other important measures, including sleep quality, compared with a control group assigned to continue using social media as usual.
And the dreaded FOMO, or fear of missing out, didn’t happen, the researchers said. At the end, the students were rethinking their social media use and feeling positive about it.
As social media becomes more common and youth mental health more endangered, experts are sounding the alarm. In late May, U.S. Surgeon General Vivek Murthy, MD, issued an advisory on social media and youth mental health, calling for tech companies to do better, policymakers to strengthen safety, and researchers to get more information, among other actions.
After that, the Biden administration took actions including the launch of a task force on kids’ online health and safety. The American Psychological Association has issued recommendations on social media use in youths. And the Social Media Victims Law Center in Seattle has sued numerous social media companies for online activity resulting in death and other tragedies.
While experts acknowledge that much more research is needed to sort out how to balance social media’s risks and benefits to preserve youth mental health and prevent such disasters, the new Iowa State study, as well as other recent research, suggests that
Goal: 30 minutes a day
In the Iowa State study, 230 undergraduate students were assigned to one of two groups, with 99 in the 30-minute-a-day social media use group and 131 in the “usual” or control group, which made no changes. For those in the intervention group, “we sent a daily reminder email,” said Ella Faulhaber, a PhD candidate at Iowa State and the study’s lead author. It simply reminded them to limit social medial use to the 30-minute maximum.
At the study start and end, all participants provided a screenshot of their weekly social media usage time. The researchers gave both groups a battery of tests to assess anxiety, depression, loneliness, fear of missing out, and negative and positive feelings.
“By limiting their social media time, that resulted in less anxiety, less depression, less FOMO, fewer negative emotions, and greater positive emotions,” said Douglas Gentile, PhD, a distinguished professor of psychology at Iowa State and a study coauthor. “We know that it is the limiting [of] the social media that is causing that.”
Ms. Faulhaber recalled one participant who mentioned having trouble at first adjusting to the 30-minute time frame, but once sleep improved, it was easier to stick to that guidance. Another who gave up phone use at bedtime found: “Instead of looking at my phone, it was much easier to go straight to bed.”
Sleep improvements, of course, affect many parts of physical and mental health, Dr. Gentile said. And the study also showed that even with reduced screen time, “we can still get the benefit of being connected.” Those who didn’t make the 30-minute mark, but cut back, got benefits, too, the researchers said.
‘Youth are aware’
Self-monitoring works, agreed Jane Harness, DO, an adjunct clinical assistant professor of psychiatry at the University of Michigan, Ann Arbor, because “having that insight is often the first step.”
In a study she conducted, Dr. Harness aimed to gather youths’ insights about how their social media use affected them. With her colleagues, she asked more than 1,100 youths, aged 14-24, what advice they would give to those new to social media, if they ever felt they needed to change social media habits, and if they have deleted or considered deleting social media accounts.
From the 871 responses, Harness found that youths were especially concerned about safety online, that most had thought about deleting a social media app and some had, and that youths were more likely to say they wanted to change the amount of time spent on social media, compared with the content they view.
“Users responded with great advice for each other,” she said. “Safety was brought up,” with users reminding others to keep accounts private and to be aware of location tracking links and content that seems to promote eating disorders, suicide, and other harms.
In the study report, Dr. Harness concluded: “Youth are aware of ways in which social media could be negatively impacting them and they have employed methods to modulate their use because of this awareness.”
Less FOMO, less anxiety
In an earlier study, University of Pennsylvania, Philadelphia, researchers had 143 college students self-monitor social media for a week, then randomly assigned them either to a group told to limit Facebook, Instagram, and Snapchat use to 10 minutes per platform, per day, or to a group told to use social media as usual for 3 weeks.
At the end of the study, the researchers evaluated both groups and found “significant reductions in loneliness and depression over 3 weeks’’ in the limited-use group, compared with the usual-use group, according to study researcher Melissa G. Hunt, PhD, associate director of clinical training at the University of Pennsylvania.
And both groups showed declines in anxiety and fear of missing out, suggesting a benefit tied to self-monitoring itself, she said.
While Dr. Hunt’s study focused on 30 minutes a day, she said “about an hour a day seems to be the sweet spot for maximizing the positive effects of connecting, but limiting the negative effects of social media use.”
She also suggested that smartphones have no place in middle or high school classrooms. Instead, they should be on lockdown during classes.
“Parents need to set real limits of cellphone use during meals and in bedrooms,” Dr. Hunt said. At mealtime, for instance, all phones should be absent from the table. And after 10 p.m., “all family phones remain in the kitchen.”
Be ‘more mindful’
These recent study findings about self-monitoring and limiting social media time may not work the same for everyone, especially among those who aren’t as motivated, said psychiatrist Elizabeth Ortiz-Schwartz, MD, team lead for the adolescent inpatient unit at Silver Hill Hospital in New Canaan, Conn.
But “the bigger take-home piece is that being intentional and attempting to decrease the use in these individuals, even if they were not always successful, was clearly beneficial,” she said.
As we await clearer guidelines about what is the “right” amount of use in terms of social media content and time, Dr. Ortiz-Schwartz said, “becoming more mindful and aware of the risks and benefits can hopefully help individuals become more mindful and deliberate about its use.”
Real-world strategies
Max Schwandt, 23, is an outlier, but a happy one. He works as a sales clerk at a Los Angeles–area recreational gear shop, and he uses no social media. Why not? “It takes up too much time,” he explained. As simple as that.
But for many other teens and young adults, the struggle to stay off social media is real.
Amelia Kennedy, the Catholic University of America student, is trying to reduce her screen time. One way is to track it on her phone. These days, her summer job at a restaurant serving breakfast gets her up early. “If I have to work, I still go on my phone, but not that long.” And once at work, she only has time for quick checks between work responsibilities. “I definitely am more productive,” she said about days when she has work.
Last December, Lauren Young, 25, whose father was a researcher on the Iowa State study, was finishing law school at Georgetown University, Washington, and decided to take a break from social media for the entire month. “I can’t say I was always successful in avoiding it,” she said. But cutting down greatly “made me a lot more present in my day-to-day life, and it was easier to concentrate.”
She could even get through a meal, out with friends, without her phone, keeping it in her purse. That was a definite change from the norm. “I noticed I would go out to dinner and the standard for people my age is having the phone on the table. If you are being polite, you turn it over.”
During her social media “blackout,” Ms. Young had deleted TikTok, Instagram, and Facebook apps. Then, when she graduated, she had to reinstall to post a picture. But now, she is back to minimal social media use.
“I’m studying for the bar, so it’s kind of necessary, but it always makes me happier.” She figures she can always text family and friends if necessary, instead of posting. “I felt for a while I was missing out on things, but not now,” she said.
Others, including Sarah Goldstein, 22, of Chatsworth, Calif., a supermarket courtesy clerk who is thinking of returning to college, said she has developed a healthier attitude toward social media as she has gotten older.
“In middle and early high school, I would see parties, things I wasn’t invited to, on Snapchat and Instagram.” While she realized there could be legitimate reasons for not being included, she said it was easy to internalize those feelings of being left out.
These days, she said she doesn’t let it affect her mental health that way. She enjoys social media – especially TikTok and Instagram – for its benefits. “It kills time, gives you something to watch, can make you laugh and feel like you have a connection with other people.”
A version of this article first appeared on WebMD.com.
Agency issues advisory on mental health symptoms of long COVID
The nine mental health symptoms highlighted in the advisory are fatigue; cognitive impairment, including brain fog; anxiety; depression; obsessive-compulsive disorder; sleep disorders; PTSD; psychotic disorder; and start of a substance use disorder.
The advisory noted that social factors can contribute to the mental health problems for racial and ethnic minorities; people with limited access to health care; people who already have behavioral health conditions and physical disabilities; and people who are lesbian, gay, bisexual, transgender, queer, or intersex.
“Long COVID has a range of burdensome physical symptoms and can take a toll on a person’s mental health. It can be very challenging for a person, whether they are impacted themselves, or they are a caregiver for someone who is affected,” Health and Human Services Secretary Xavier Becerra said in a statement. “This advisory helps to raise awareness, especially among primary care practitioners and clinicians who are often the ones treating patients with long COVID.”
The department says about 10% of people infected with COVID have at least one long COVID symptom. Physical symptoms include dizziness, stomach upset, heart palpitations, issues with sexual desire or capacity, loss of smell or taste, thirst, chronic coughing, chest pain, and abnormal movements.
“We know that people living with long COVID need help today, and providers need help understanding what long COVID is and how to treat it,” Admiral Rachel Levine, MD, assistant secretary for health, said in the statement. “This advisory helps bridge that gap for the behavioral health impacts of long COVID.”
A version of this article first appeared on WebMD.com.
The nine mental health symptoms highlighted in the advisory are fatigue; cognitive impairment, including brain fog; anxiety; depression; obsessive-compulsive disorder; sleep disorders; PTSD; psychotic disorder; and start of a substance use disorder.
The advisory noted that social factors can contribute to the mental health problems for racial and ethnic minorities; people with limited access to health care; people who already have behavioral health conditions and physical disabilities; and people who are lesbian, gay, bisexual, transgender, queer, or intersex.
“Long COVID has a range of burdensome physical symptoms and can take a toll on a person’s mental health. It can be very challenging for a person, whether they are impacted themselves, or they are a caregiver for someone who is affected,” Health and Human Services Secretary Xavier Becerra said in a statement. “This advisory helps to raise awareness, especially among primary care practitioners and clinicians who are often the ones treating patients with long COVID.”
The department says about 10% of people infected with COVID have at least one long COVID symptom. Physical symptoms include dizziness, stomach upset, heart palpitations, issues with sexual desire or capacity, loss of smell or taste, thirst, chronic coughing, chest pain, and abnormal movements.
“We know that people living with long COVID need help today, and providers need help understanding what long COVID is and how to treat it,” Admiral Rachel Levine, MD, assistant secretary for health, said in the statement. “This advisory helps bridge that gap for the behavioral health impacts of long COVID.”
A version of this article first appeared on WebMD.com.
The nine mental health symptoms highlighted in the advisory are fatigue; cognitive impairment, including brain fog; anxiety; depression; obsessive-compulsive disorder; sleep disorders; PTSD; psychotic disorder; and start of a substance use disorder.
The advisory noted that social factors can contribute to the mental health problems for racial and ethnic minorities; people with limited access to health care; people who already have behavioral health conditions and physical disabilities; and people who are lesbian, gay, bisexual, transgender, queer, or intersex.
“Long COVID has a range of burdensome physical symptoms and can take a toll on a person’s mental health. It can be very challenging for a person, whether they are impacted themselves, or they are a caregiver for someone who is affected,” Health and Human Services Secretary Xavier Becerra said in a statement. “This advisory helps to raise awareness, especially among primary care practitioners and clinicians who are often the ones treating patients with long COVID.”
The department says about 10% of people infected with COVID have at least one long COVID symptom. Physical symptoms include dizziness, stomach upset, heart palpitations, issues with sexual desire or capacity, loss of smell or taste, thirst, chronic coughing, chest pain, and abnormal movements.
“We know that people living with long COVID need help today, and providers need help understanding what long COVID is and how to treat it,” Admiral Rachel Levine, MD, assistant secretary for health, said in the statement. “This advisory helps bridge that gap for the behavioral health impacts of long COVID.”
A version of this article first appeared on WebMD.com.
New DEA CME mandate affects 2 million prescribers
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.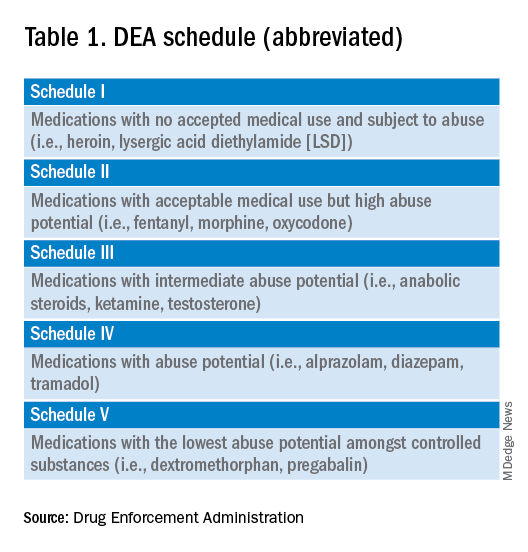
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 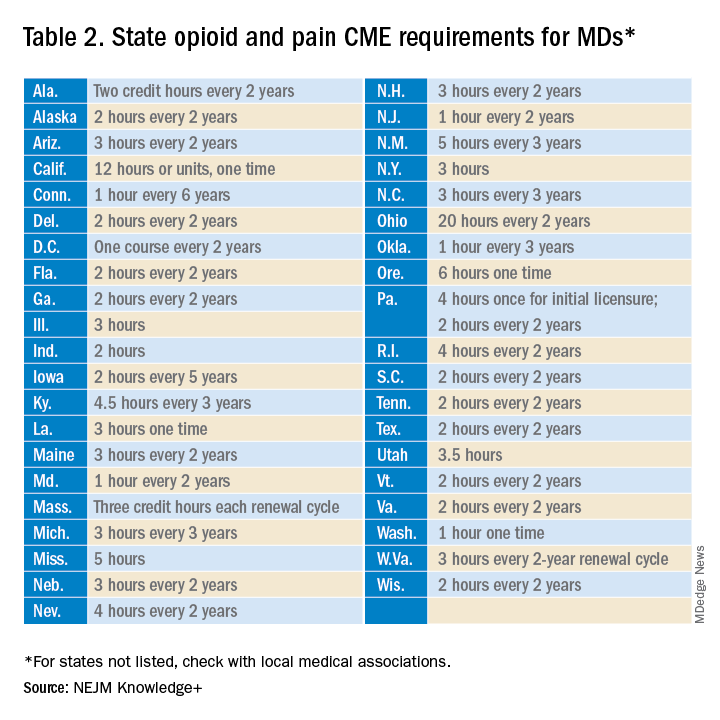
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
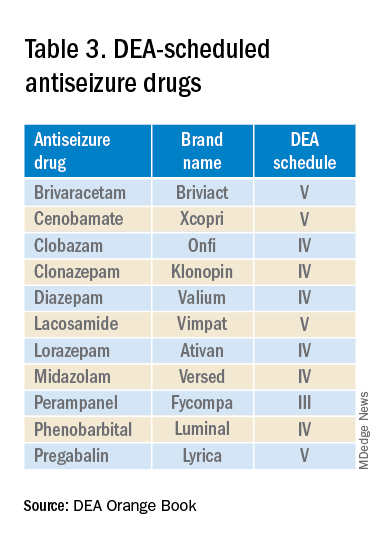
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 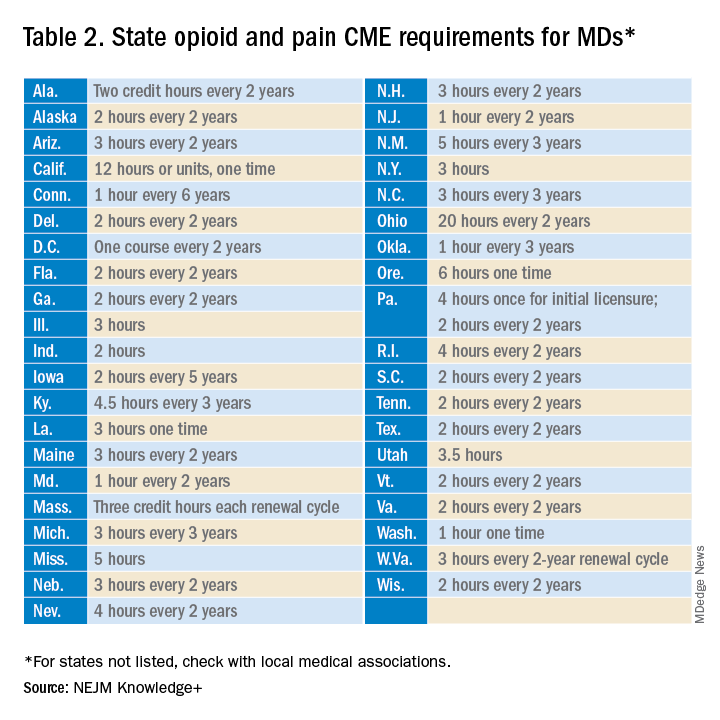
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
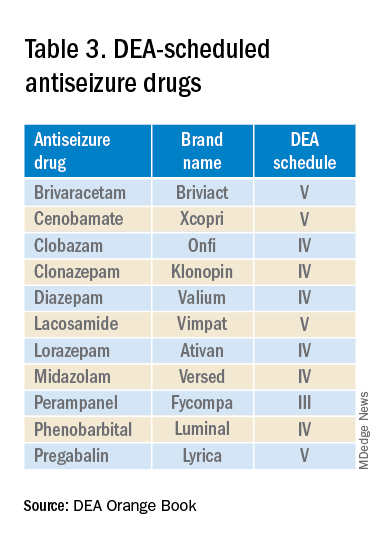
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
The Consolidated Appropriations Act of 2023 mandates that all Drug Enforcement Administration–registered physicians and health care providers complete a one-time, 8-hour CME training on managing and treating opioid and other substance abuse disorders. This requirement goes into effect on June 27, 2023. New DEA registrants must also comply. Veterinarians are exempt.
A DEA registration is required to prescribe any controlled substance. The DEA categorizes these as Schedule I-V, with V being the least likely to be abused (Table 1). For example, opioids like fentanyl, oxycodone, and morphine are Schedule II. Medications without abuse potential are not scheduled.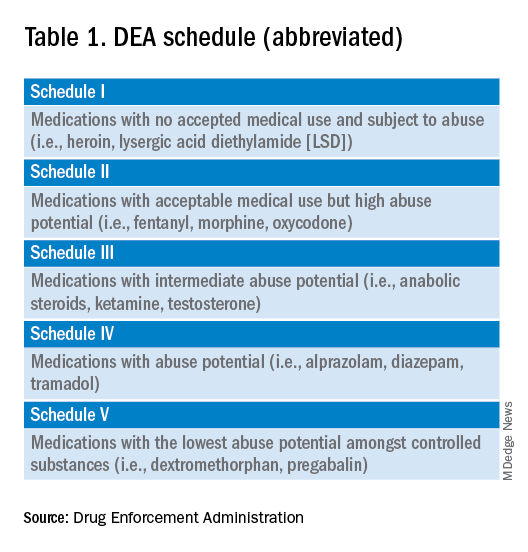
Will 16 million hours of opioid education save lives?
One should not underestimate the sweeping scope of this new federal requirement. DEA registrants include physicians and other health care providers such as nurse practitioners, physician assistants, and dentists. That is 8 hours per provider x 2 million providers: 16 million hours of CME!
Many states already require 1 or more hours of opioid training and pain management as part of their relicensure requirements (Table 2). To avoid redundancy, the DEA-mandated 8-hour training satisfies the various states’ requirements. 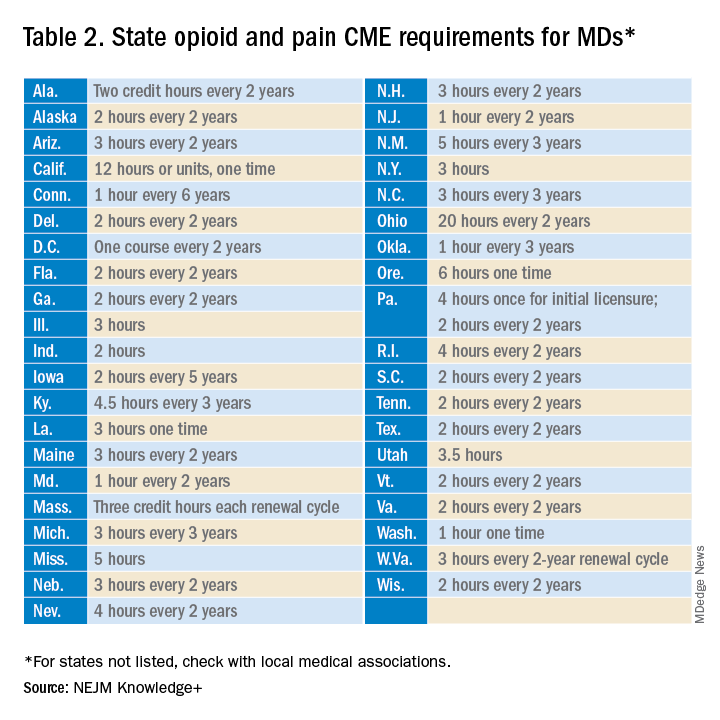
An uncompensated mandate
Physicians are no strangers to lifelong learning and most eagerly pursue educational opportunities. Though some physicians may have CME time and stipends allocated by their employers, many others, such as the approximately 50,000 locum tenens doctors, do not. However, as enthusiastic as these physicians may be about this new CME course, they will likely lose a day of seeing patients (and income) to comply with this new obligation.
Not just pain doctors
The mandate’s broad brush includes many health care providers who hold DEA certificates but do not prescribe opioids. For example, as a general neurologist and epileptologist, I do not treat patients with chronic pain and cannot remember the last time I wrote an opioid prescription. However, I frequently prescribe lacosamide, a Schedule V drug. A surprisingly large number of antiseizure drugs are Schedule III, IV, or V drugs (Table 3).
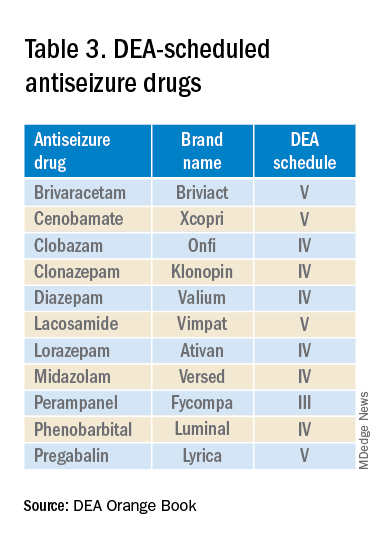
Real-world abuse?
How often scheduled antiseizure drugs are diverted or abused in an epilepsy population is unknown but appears to be infrequent. For example, perampanel abuse has not been reported despite its classification as a Schedule III drug. Anecdotally, in more than 40 years of clinical practice, I have never known a patient with epilepsy to abuse their antiseizure medications.
Take the course
Many organizations are happy to charge for the new 8-hour course. For example, the Tennessee Medical Association offers the training for $299 online or $400 in person. Materials from Elite Learning satisfy the 8-hour requirement for $80. However, NEJM Knowledge+ provides a complimentary 10-hour DEA-compliant course.
I recently completed the NEJM course. The information was thorough and took the whole 10 hours to finish. As excellent as it was, the content was only tangentially relevant to my clinical practice.
Conclusions
To obtain or renew a DEA certificate, neurologists, epilepsy specialists, and many other health care providers must comply with the new 8-hour CME opioid training mandate. Because the course requires 1 day to complete, health care providers would be prudent to obtain their CME well before their DEA certificate expires.
Though efforts to control the morbidity and mortality of the opioid epidemic are laudatory, perhaps the training should be more targeted to physicians who actually prescribe opioids rather than every DEA registrant. In the meantime, whether 16 million CME hours will save lives remains to be seen.
Dr. Wilner is professor of neurology at the University of Tennessee Health Science Center, Memphis. He reported a conflict of interest with Accordant Health Services.
A version of this article first appeared on Medscape.com.
Pharmacotherapy underprescribed for alcohol use disorder
Health care providers are missing opportunities to give medical treatment to high-risk individuals hospitalized for alcohol use disorder (AUD), a national analysis of Medicare beneficiaries reported.
Increasing such patients’ access to psychiatric care and addiction medicine, as well as encouraging medication prescribing by generalists and nonaddiction specialists, are remedial strategies recommended by lead author Eden Y. Bernstein, MD, of the division of general internal medicine at Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues.
“Hospitalizations for alcohol use disorder are common,” Dr. Bernstein said in an interview. “Our work shows they represent an underutilized opportunity to engage patients with appropriate treatment, including initiation of medications for alcohol use disorder.”
There is a pressing need for such treatment strategies since 29 million U.S. adults have AUD, and alcohol contributes to more than 140,000 deaths annually, the authors noted.
Rarely initiated either at hospital discharge or during follow-up care, medical therapy for AUD was more likely to be provided to younger patients and those involved with psychiatric care or addiction medicine, Dr. Bernstein’s group reported in Annals of Internal Medicine.Hospital admissions, they argued, give patients more access to clinicians and social workers and the vulnerability experienced during hospitalization may motivate behavioral change.
National study
The cohort included 28,601 AUD hospitalizations for 20,401 unique Medicare patients from 2015 to 2017. About 30% of admissions were for women and about 72% for non-Hispanic Blacks. Discharge initiation of medication for AUD was defined as a pharmacy claim for naltrexone, acamprosate, or disulfiram from the day before discharge to 2 days after.
Overall, just 206 patients (0.7%) initiated medication for AUD within 2 days of discharge and 364 (1.3%) started it within 30 days. Among those discharged with a primary diagnosis of AUD, only 70 (2.3%) started medical therapy within 2 days.
The most predictive demographic factor for discharge medication for AUD was younger age: 18-39 years versus 75 years and older (adjusted odds ratio, 3.87; 95% confidence interval, 1.34-11.16).
Initiation of medication for AUD should involve a long-term treatment plan, according to Dr. Bernstein’s group, and if that is not feasible during hospitalization, patients should be referred for outpatient treatment.
An accompanying editorial agrees that the results offer strong evidence of a missed opportunity to address AUD at a potential flexion point. “Hospitalization is a critical touch point for identifying and treating AUD,” wrote Michael F. Mayo-Smith, MD, MPH, of White River Junction (Vt.) VA Medical Center, and Geisel School of Medicine at Dartmouth, Hanover, N.H., and David Lawrence, MD, of the VA Greater Los Angeles Healthcare System and the University of California, Los Angeles.
An intentional discharge protocol can be effective, they noted, as evidenced by a 2014 report in which this approach increased medication-assisted treatment from 0% to 64% in tandem with a decrease in all-cause, 30-day readmission rates.
“There is also growing interest in inpatient addiction consultation services, which have shown [medication] for AUD treatment initiation rates of up to 70% as well as improved engagement in posthospital treatment,” Dr. Mayo-Smith and Dr. Lawrence wrote.
Minority populations need particular attention, they added. “Unfortunately, the availability of evidence-based treatments for AUD does not by itself lead to improved care. We need strategies for widespread adoption so that patients can realize the benefits of these treatments.”
Dr. Bernstein reported funding support from a National Research Service Award and the Massachusetts General Hospital division of general internal medicine; he disclosed fees from Alosa Health. One coauthor was supported by the Agency for Healthcare Research and Quality. Another was supported by the National Institute on Aging and reported relationships with the American College of Cardiology, Boston OIAC Pepper Center, American Heart Association, and US Deprescribing Research Network. Dr. Mayo-Smith disclosed no competing interests. Dr. Lawrence reported fees related to presentations at DDW 2023 and the California Society of Addiction Medicine 2022.
Health care providers are missing opportunities to give medical treatment to high-risk individuals hospitalized for alcohol use disorder (AUD), a national analysis of Medicare beneficiaries reported.
Increasing such patients’ access to psychiatric care and addiction medicine, as well as encouraging medication prescribing by generalists and nonaddiction specialists, are remedial strategies recommended by lead author Eden Y. Bernstein, MD, of the division of general internal medicine at Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues.
“Hospitalizations for alcohol use disorder are common,” Dr. Bernstein said in an interview. “Our work shows they represent an underutilized opportunity to engage patients with appropriate treatment, including initiation of medications for alcohol use disorder.”
There is a pressing need for such treatment strategies since 29 million U.S. adults have AUD, and alcohol contributes to more than 140,000 deaths annually, the authors noted.
Rarely initiated either at hospital discharge or during follow-up care, medical therapy for AUD was more likely to be provided to younger patients and those involved with psychiatric care or addiction medicine, Dr. Bernstein’s group reported in Annals of Internal Medicine.Hospital admissions, they argued, give patients more access to clinicians and social workers and the vulnerability experienced during hospitalization may motivate behavioral change.
National study
The cohort included 28,601 AUD hospitalizations for 20,401 unique Medicare patients from 2015 to 2017. About 30% of admissions were for women and about 72% for non-Hispanic Blacks. Discharge initiation of medication for AUD was defined as a pharmacy claim for naltrexone, acamprosate, or disulfiram from the day before discharge to 2 days after.
Overall, just 206 patients (0.7%) initiated medication for AUD within 2 days of discharge and 364 (1.3%) started it within 30 days. Among those discharged with a primary diagnosis of AUD, only 70 (2.3%) started medical therapy within 2 days.
The most predictive demographic factor for discharge medication for AUD was younger age: 18-39 years versus 75 years and older (adjusted odds ratio, 3.87; 95% confidence interval, 1.34-11.16).
Initiation of medication for AUD should involve a long-term treatment plan, according to Dr. Bernstein’s group, and if that is not feasible during hospitalization, patients should be referred for outpatient treatment.
An accompanying editorial agrees that the results offer strong evidence of a missed opportunity to address AUD at a potential flexion point. “Hospitalization is a critical touch point for identifying and treating AUD,” wrote Michael F. Mayo-Smith, MD, MPH, of White River Junction (Vt.) VA Medical Center, and Geisel School of Medicine at Dartmouth, Hanover, N.H., and David Lawrence, MD, of the VA Greater Los Angeles Healthcare System and the University of California, Los Angeles.
An intentional discharge protocol can be effective, they noted, as evidenced by a 2014 report in which this approach increased medication-assisted treatment from 0% to 64% in tandem with a decrease in all-cause, 30-day readmission rates.
“There is also growing interest in inpatient addiction consultation services, which have shown [medication] for AUD treatment initiation rates of up to 70% as well as improved engagement in posthospital treatment,” Dr. Mayo-Smith and Dr. Lawrence wrote.
Minority populations need particular attention, they added. “Unfortunately, the availability of evidence-based treatments for AUD does not by itself lead to improved care. We need strategies for widespread adoption so that patients can realize the benefits of these treatments.”
Dr. Bernstein reported funding support from a National Research Service Award and the Massachusetts General Hospital division of general internal medicine; he disclosed fees from Alosa Health. One coauthor was supported by the Agency for Healthcare Research and Quality. Another was supported by the National Institute on Aging and reported relationships with the American College of Cardiology, Boston OIAC Pepper Center, American Heart Association, and US Deprescribing Research Network. Dr. Mayo-Smith disclosed no competing interests. Dr. Lawrence reported fees related to presentations at DDW 2023 and the California Society of Addiction Medicine 2022.
Health care providers are missing opportunities to give medical treatment to high-risk individuals hospitalized for alcohol use disorder (AUD), a national analysis of Medicare beneficiaries reported.
Increasing such patients’ access to psychiatric care and addiction medicine, as well as encouraging medication prescribing by generalists and nonaddiction specialists, are remedial strategies recommended by lead author Eden Y. Bernstein, MD, of the division of general internal medicine at Massachusetts General Hospital and Harvard Medical School, both in Boston, and colleagues.
“Hospitalizations for alcohol use disorder are common,” Dr. Bernstein said in an interview. “Our work shows they represent an underutilized opportunity to engage patients with appropriate treatment, including initiation of medications for alcohol use disorder.”
There is a pressing need for such treatment strategies since 29 million U.S. adults have AUD, and alcohol contributes to more than 140,000 deaths annually, the authors noted.
Rarely initiated either at hospital discharge or during follow-up care, medical therapy for AUD was more likely to be provided to younger patients and those involved with psychiatric care or addiction medicine, Dr. Bernstein’s group reported in Annals of Internal Medicine.Hospital admissions, they argued, give patients more access to clinicians and social workers and the vulnerability experienced during hospitalization may motivate behavioral change.
National study
The cohort included 28,601 AUD hospitalizations for 20,401 unique Medicare patients from 2015 to 2017. About 30% of admissions were for women and about 72% for non-Hispanic Blacks. Discharge initiation of medication for AUD was defined as a pharmacy claim for naltrexone, acamprosate, or disulfiram from the day before discharge to 2 days after.
Overall, just 206 patients (0.7%) initiated medication for AUD within 2 days of discharge and 364 (1.3%) started it within 30 days. Among those discharged with a primary diagnosis of AUD, only 70 (2.3%) started medical therapy within 2 days.
The most predictive demographic factor for discharge medication for AUD was younger age: 18-39 years versus 75 years and older (adjusted odds ratio, 3.87; 95% confidence interval, 1.34-11.16).
Initiation of medication for AUD should involve a long-term treatment plan, according to Dr. Bernstein’s group, and if that is not feasible during hospitalization, patients should be referred for outpatient treatment.
An accompanying editorial agrees that the results offer strong evidence of a missed opportunity to address AUD at a potential flexion point. “Hospitalization is a critical touch point for identifying and treating AUD,” wrote Michael F. Mayo-Smith, MD, MPH, of White River Junction (Vt.) VA Medical Center, and Geisel School of Medicine at Dartmouth, Hanover, N.H., and David Lawrence, MD, of the VA Greater Los Angeles Healthcare System and the University of California, Los Angeles.
An intentional discharge protocol can be effective, they noted, as evidenced by a 2014 report in which this approach increased medication-assisted treatment from 0% to 64% in tandem with a decrease in all-cause, 30-day readmission rates.
“There is also growing interest in inpatient addiction consultation services, which have shown [medication] for AUD treatment initiation rates of up to 70% as well as improved engagement in posthospital treatment,” Dr. Mayo-Smith and Dr. Lawrence wrote.
Minority populations need particular attention, they added. “Unfortunately, the availability of evidence-based treatments for AUD does not by itself lead to improved care. We need strategies for widespread adoption so that patients can realize the benefits of these treatments.”
Dr. Bernstein reported funding support from a National Research Service Award and the Massachusetts General Hospital division of general internal medicine; he disclosed fees from Alosa Health. One coauthor was supported by the Agency for Healthcare Research and Quality. Another was supported by the National Institute on Aging and reported relationships with the American College of Cardiology, Boston OIAC Pepper Center, American Heart Association, and US Deprescribing Research Network. Dr. Mayo-Smith disclosed no competing interests. Dr. Lawrence reported fees related to presentations at DDW 2023 and the California Society of Addiction Medicine 2022.
FROM ANNALS OF INTERNAL MEDICINE
New law allows international medical graduates to bypass U.S. residency
Pediatric nephrologist Bryan Carmody, MD, recalls working alongside an extremely experienced neonatologist during his residency. She had managed a neonatal intensive care unit in her home country of Lithuania, but because she wanted to practice in the United States, it took years of repeat training before she was eligible for a medical license.
“She was very accomplished, and she was wonderful to have as a coresident at the time,” Dr. Carmody said in an interview.
The neonatologist now practices at a U.S. academic medical center, but to obtain that position, she had to complete 3 years of pediatric residency and 3 years of fellowship in the United States, Dr. Carmody said.
Such training for international medical graduates (IMGs) is a routine part of obtaining a U.S. medical license, but
The American Medical Association took similar measures at its recent annual meeting, making it easier for IMGs to gain licensure. Because the pandemic and Russia’s invasion of Ukraine disrupted the process by which some IMGs had their licenses verified, the AMA is now encouraging state licensing boards and other credentialing institutions to accept certification from the Educational Commission for Foreign Medical Graduates as verification, rather than requiring documents directly from international medical schools.
When it comes to Tennessee’s new law, signed by Gov. Bill Lee in April, experienced IMGs who have received medical training abroad can skip U.S. residency requirements and obtain a temporary license to practice medicine in Tennessee if they meet certain qualifications.
The international doctors must demonstrate competency, as determined by the state medical board. In addition, they must have completed a 3-year postgraduate training program in the graduate’s licensing country or otherwise have practiced as a medical professional in which they performed the duties of a physician for at least 3 of the past 5 years outside the United States, according to the new law.
To be approved, IMGs must also have received an employment offer from a Tennessee health care provider that has a residency program accredited by the Accreditation Council for Graduate Medical Education.
If physicians remain in good standing for 2 years, the board will grant them a full and unrestricted license to practice in Tennessee.
“The new legislation opens up a lot of doors for international medical graduates and is also a lifeline for a lot of underserved areas in Tennessee,” said Asim Ansari, MD, a Canadian who attended medical school in the Caribbean and is an advocate for IMGs.
Dr. Ansari is participating in a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City, until he can apply for the sixth time to a residency program. “This could possibly be a model that other states may want to implement in a few years.”
What’s behind the law?
A predicted physician shortage in Tennessee drove the legislation, said Rep. Sabi “Doc” Kumar, MD, vice chair for the Tennessee House Health Committee and a cosponsor of the legislation. Legislators hope the law will mitigate that shortage and boost the number of physicians practicing in underserved areas of the state.
“Considering that one in four physicians in the U.S. are international medical gradates, it was important for us to be able to attract those physicians to Tennessee,” he said.
The Tennessee Board of Medical Examiners will develop administrative rules for the law, which may take up to a year, Rep. Kumar said. He expects the program to be available to IMGs beginning in mid-2024.
Upon completion of the program, IMGs will be able to practice general medicine in Tennessee, not a specialty. Requirements for specialty certification would have to be met through the specialties’ respective boards.
Dr. Carmody, who blogs about medical education, including the new legislation, said in an interview the law will greatly benefit experienced IMGs, who often are bypassed as residency candidates because they graduated years ago. Hospitals also win because they can fill positions that otherwise might sit vacant, he said.
Family physician Sahil Bawa, MD, an IMG from India who recently matched into his specialty, said the Tennessee legislation will help fellow IMGs find U.S. medical jobs.
“It’s very difficult for IMGs to get into residency in the U.S.,” he said. “I’ve seen people with medical degrees from other countries drive Uber or do odd jobs to sustain themselves here. I’ve known a few people who have left and gone back to their home country because they were not accepted into a residency.”
Who benefits most?
Dr. Bawa noted that the legislation would not have helped him, as he needed a visa to practice in the United States and the law does not include the sponsoring of visas. The legislation requires IMGs to show evidence of citizenship or evidence that they are legally entitled to live or work in the United States.
U.S. citizen IMGs who haven’t completed residency or who practiced in another country also are left out of the law, Dr. Carmody said.
“This law is designed to take the most accomplished cream of the crop international medical graduates with the most experience and the most sophisticated skill set and send them to Tennessee. I think that’s the intent,” he said. “But many international medical graduates are U.S. citizens who don’t have the opportunity to practice in countries other than United States or do residencies. A lot of these people are sitting on the sidelines, unable to secure residency positions. I’m sure they would be desperate for a program like this.”
Questions remain
“Just because the doctor can get a [temporary] license without the training doesn’t mean employers are going to be interested in sponsoring those doctors,” said Adam Cohen, an immigration attorney who practices in Memphis. “What is the inclination of these employers to hire these physicians who have undergone training outside the U.S.? And will there be skepticism on the part of employers about the competence of these doctors?”
“Hospital systems will be able to hire experienced practitioners for a very low cost,” Dr. Ansari said. “So now you have these additional bodies who can do the work of a physician, but you don’t have to pay them as much as a physician for 2 years. And because some are desperate to work, they will take lower pay as long as they have a pathway to full licensure in Tennessee. What are the protections for these physicians? Who will cover their insurance? Who will be responsible for them, the attendees? And will the attendees be willing to put their license on the line for them?”
In addition, Dr. Carmody questions what, if anything, will encourage IMGs to work in underserved areas in Tennessee after their 2 years are up and whether there will be any incentives to guide them. He wonders, too, whether the physicians will be stuck practicing in Tennessee following completion of the program.
“Will these physicians only be able to work in Tennessee?” he asked. “I think that’s probably going to be the case, because they’ll be licensed in Tennessee, but to go to another state, they would be missing the required residency training. So it might be these folks are stuck in Tennessee unless other states develop reciprocal arrangements.”
Other states would have to decide whether to recognize the Tennessee license acquired through this pathway, Rep. Kumar said.
He explained that the sponsoring sites would be responsible for providing work-hour restrictions and liability protections. There are currently no incentives in the legislation for IMGs to practice in rural, underserved areas, but the hospitals and communities there generally offer incentives when recruiting, Rep. Kumar said.
“The law definitely has the potential to be helpful,” Mr. Cohen said, “because there’s an ability to place providers in the state without having to go through the bottleneck of limited residency slots. If other states see a positive effect on Tennessee or are exploring ways to alleviate their own shortages, it’s possible [they] might follow suit.”
Rep. Kumar agreed that other states will be watching Tennessee to weigh the law’s success.
“I think the law will have to prove itself and show that Tennessee has benefited from it and that the results have been good,” he said. “We are providing a pioneering way for attracting medical graduates and making it easier for them to obtain a license. I would think other states would want to do that.”
A version of this article first appeared on Medscape.com.
Pediatric nephrologist Bryan Carmody, MD, recalls working alongside an extremely experienced neonatologist during his residency. She had managed a neonatal intensive care unit in her home country of Lithuania, but because she wanted to practice in the United States, it took years of repeat training before she was eligible for a medical license.
“She was very accomplished, and she was wonderful to have as a coresident at the time,” Dr. Carmody said in an interview.
The neonatologist now practices at a U.S. academic medical center, but to obtain that position, she had to complete 3 years of pediatric residency and 3 years of fellowship in the United States, Dr. Carmody said.
Such training for international medical graduates (IMGs) is a routine part of obtaining a U.S. medical license, but
The American Medical Association took similar measures at its recent annual meeting, making it easier for IMGs to gain licensure. Because the pandemic and Russia’s invasion of Ukraine disrupted the process by which some IMGs had their licenses verified, the AMA is now encouraging state licensing boards and other credentialing institutions to accept certification from the Educational Commission for Foreign Medical Graduates as verification, rather than requiring documents directly from international medical schools.
When it comes to Tennessee’s new law, signed by Gov. Bill Lee in April, experienced IMGs who have received medical training abroad can skip U.S. residency requirements and obtain a temporary license to practice medicine in Tennessee if they meet certain qualifications.
The international doctors must demonstrate competency, as determined by the state medical board. In addition, they must have completed a 3-year postgraduate training program in the graduate’s licensing country or otherwise have practiced as a medical professional in which they performed the duties of a physician for at least 3 of the past 5 years outside the United States, according to the new law.
To be approved, IMGs must also have received an employment offer from a Tennessee health care provider that has a residency program accredited by the Accreditation Council for Graduate Medical Education.
If physicians remain in good standing for 2 years, the board will grant them a full and unrestricted license to practice in Tennessee.
“The new legislation opens up a lot of doors for international medical graduates and is also a lifeline for a lot of underserved areas in Tennessee,” said Asim Ansari, MD, a Canadian who attended medical school in the Caribbean and is an advocate for IMGs.
Dr. Ansari is participating in a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City, until he can apply for the sixth time to a residency program. “This could possibly be a model that other states may want to implement in a few years.”
What’s behind the law?
A predicted physician shortage in Tennessee drove the legislation, said Rep. Sabi “Doc” Kumar, MD, vice chair for the Tennessee House Health Committee and a cosponsor of the legislation. Legislators hope the law will mitigate that shortage and boost the number of physicians practicing in underserved areas of the state.
“Considering that one in four physicians in the U.S. are international medical gradates, it was important for us to be able to attract those physicians to Tennessee,” he said.
The Tennessee Board of Medical Examiners will develop administrative rules for the law, which may take up to a year, Rep. Kumar said. He expects the program to be available to IMGs beginning in mid-2024.
Upon completion of the program, IMGs will be able to practice general medicine in Tennessee, not a specialty. Requirements for specialty certification would have to be met through the specialties’ respective boards.
Dr. Carmody, who blogs about medical education, including the new legislation, said in an interview the law will greatly benefit experienced IMGs, who often are bypassed as residency candidates because they graduated years ago. Hospitals also win because they can fill positions that otherwise might sit vacant, he said.
Family physician Sahil Bawa, MD, an IMG from India who recently matched into his specialty, said the Tennessee legislation will help fellow IMGs find U.S. medical jobs.
“It’s very difficult for IMGs to get into residency in the U.S.,” he said. “I’ve seen people with medical degrees from other countries drive Uber or do odd jobs to sustain themselves here. I’ve known a few people who have left and gone back to their home country because they were not accepted into a residency.”
Who benefits most?
Dr. Bawa noted that the legislation would not have helped him, as he needed a visa to practice in the United States and the law does not include the sponsoring of visas. The legislation requires IMGs to show evidence of citizenship or evidence that they are legally entitled to live or work in the United States.
U.S. citizen IMGs who haven’t completed residency or who practiced in another country also are left out of the law, Dr. Carmody said.
“This law is designed to take the most accomplished cream of the crop international medical graduates with the most experience and the most sophisticated skill set and send them to Tennessee. I think that’s the intent,” he said. “But many international medical graduates are U.S. citizens who don’t have the opportunity to practice in countries other than United States or do residencies. A lot of these people are sitting on the sidelines, unable to secure residency positions. I’m sure they would be desperate for a program like this.”
Questions remain
“Just because the doctor can get a [temporary] license without the training doesn’t mean employers are going to be interested in sponsoring those doctors,” said Adam Cohen, an immigration attorney who practices in Memphis. “What is the inclination of these employers to hire these physicians who have undergone training outside the U.S.? And will there be skepticism on the part of employers about the competence of these doctors?”
“Hospital systems will be able to hire experienced practitioners for a very low cost,” Dr. Ansari said. “So now you have these additional bodies who can do the work of a physician, but you don’t have to pay them as much as a physician for 2 years. And because some are desperate to work, they will take lower pay as long as they have a pathway to full licensure in Tennessee. What are the protections for these physicians? Who will cover their insurance? Who will be responsible for them, the attendees? And will the attendees be willing to put their license on the line for them?”
In addition, Dr. Carmody questions what, if anything, will encourage IMGs to work in underserved areas in Tennessee after their 2 years are up and whether there will be any incentives to guide them. He wonders, too, whether the physicians will be stuck practicing in Tennessee following completion of the program.
“Will these physicians only be able to work in Tennessee?” he asked. “I think that’s probably going to be the case, because they’ll be licensed in Tennessee, but to go to another state, they would be missing the required residency training. So it might be these folks are stuck in Tennessee unless other states develop reciprocal arrangements.”
Other states would have to decide whether to recognize the Tennessee license acquired through this pathway, Rep. Kumar said.
He explained that the sponsoring sites would be responsible for providing work-hour restrictions and liability protections. There are currently no incentives in the legislation for IMGs to practice in rural, underserved areas, but the hospitals and communities there generally offer incentives when recruiting, Rep. Kumar said.
“The law definitely has the potential to be helpful,” Mr. Cohen said, “because there’s an ability to place providers in the state without having to go through the bottleneck of limited residency slots. If other states see a positive effect on Tennessee or are exploring ways to alleviate their own shortages, it’s possible [they] might follow suit.”
Rep. Kumar agreed that other states will be watching Tennessee to weigh the law’s success.
“I think the law will have to prove itself and show that Tennessee has benefited from it and that the results have been good,” he said. “We are providing a pioneering way for attracting medical graduates and making it easier for them to obtain a license. I would think other states would want to do that.”
A version of this article first appeared on Medscape.com.
Pediatric nephrologist Bryan Carmody, MD, recalls working alongside an extremely experienced neonatologist during his residency. She had managed a neonatal intensive care unit in her home country of Lithuania, but because she wanted to practice in the United States, it took years of repeat training before she was eligible for a medical license.
“She was very accomplished, and she was wonderful to have as a coresident at the time,” Dr. Carmody said in an interview.
The neonatologist now practices at a U.S. academic medical center, but to obtain that position, she had to complete 3 years of pediatric residency and 3 years of fellowship in the United States, Dr. Carmody said.
Such training for international medical graduates (IMGs) is a routine part of obtaining a U.S. medical license, but
The American Medical Association took similar measures at its recent annual meeting, making it easier for IMGs to gain licensure. Because the pandemic and Russia’s invasion of Ukraine disrupted the process by which some IMGs had their licenses verified, the AMA is now encouraging state licensing boards and other credentialing institutions to accept certification from the Educational Commission for Foreign Medical Graduates as verification, rather than requiring documents directly from international medical schools.
When it comes to Tennessee’s new law, signed by Gov. Bill Lee in April, experienced IMGs who have received medical training abroad can skip U.S. residency requirements and obtain a temporary license to practice medicine in Tennessee if they meet certain qualifications.
The international doctors must demonstrate competency, as determined by the state medical board. In addition, they must have completed a 3-year postgraduate training program in the graduate’s licensing country or otherwise have practiced as a medical professional in which they performed the duties of a physician for at least 3 of the past 5 years outside the United States, according to the new law.
To be approved, IMGs must also have received an employment offer from a Tennessee health care provider that has a residency program accredited by the Accreditation Council for Graduate Medical Education.
If physicians remain in good standing for 2 years, the board will grant them a full and unrestricted license to practice in Tennessee.
“The new legislation opens up a lot of doors for international medical graduates and is also a lifeline for a lot of underserved areas in Tennessee,” said Asim Ansari, MD, a Canadian who attended medical school in the Caribbean and is an advocate for IMGs.
Dr. Ansari is participating in a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City, until he can apply for the sixth time to a residency program. “This could possibly be a model that other states may want to implement in a few years.”
What’s behind the law?
A predicted physician shortage in Tennessee drove the legislation, said Rep. Sabi “Doc” Kumar, MD, vice chair for the Tennessee House Health Committee and a cosponsor of the legislation. Legislators hope the law will mitigate that shortage and boost the number of physicians practicing in underserved areas of the state.
“Considering that one in four physicians in the U.S. are international medical gradates, it was important for us to be able to attract those physicians to Tennessee,” he said.
The Tennessee Board of Medical Examiners will develop administrative rules for the law, which may take up to a year, Rep. Kumar said. He expects the program to be available to IMGs beginning in mid-2024.
Upon completion of the program, IMGs will be able to practice general medicine in Tennessee, not a specialty. Requirements for specialty certification would have to be met through the specialties’ respective boards.
Dr. Carmody, who blogs about medical education, including the new legislation, said in an interview the law will greatly benefit experienced IMGs, who often are bypassed as residency candidates because they graduated years ago. Hospitals also win because they can fill positions that otherwise might sit vacant, he said.
Family physician Sahil Bawa, MD, an IMG from India who recently matched into his specialty, said the Tennessee legislation will help fellow IMGs find U.S. medical jobs.
“It’s very difficult for IMGs to get into residency in the U.S.,” he said. “I’ve seen people with medical degrees from other countries drive Uber or do odd jobs to sustain themselves here. I’ve known a few people who have left and gone back to their home country because they were not accepted into a residency.”
Who benefits most?
Dr. Bawa noted that the legislation would not have helped him, as he needed a visa to practice in the United States and the law does not include the sponsoring of visas. The legislation requires IMGs to show evidence of citizenship or evidence that they are legally entitled to live or work in the United States.
U.S. citizen IMGs who haven’t completed residency or who practiced in another country also are left out of the law, Dr. Carmody said.
“This law is designed to take the most accomplished cream of the crop international medical graduates with the most experience and the most sophisticated skill set and send them to Tennessee. I think that’s the intent,” he said. “But many international medical graduates are U.S. citizens who don’t have the opportunity to practice in countries other than United States or do residencies. A lot of these people are sitting on the sidelines, unable to secure residency positions. I’m sure they would be desperate for a program like this.”
Questions remain
“Just because the doctor can get a [temporary] license without the training doesn’t mean employers are going to be interested in sponsoring those doctors,” said Adam Cohen, an immigration attorney who practices in Memphis. “What is the inclination of these employers to hire these physicians who have undergone training outside the U.S.? And will there be skepticism on the part of employers about the competence of these doctors?”
“Hospital systems will be able to hire experienced practitioners for a very low cost,” Dr. Ansari said. “So now you have these additional bodies who can do the work of a physician, but you don’t have to pay them as much as a physician for 2 years. And because some are desperate to work, they will take lower pay as long as they have a pathway to full licensure in Tennessee. What are the protections for these physicians? Who will cover their insurance? Who will be responsible for them, the attendees? And will the attendees be willing to put their license on the line for them?”
In addition, Dr. Carmody questions what, if anything, will encourage IMGs to work in underserved areas in Tennessee after their 2 years are up and whether there will be any incentives to guide them. He wonders, too, whether the physicians will be stuck practicing in Tennessee following completion of the program.
“Will these physicians only be able to work in Tennessee?” he asked. “I think that’s probably going to be the case, because they’ll be licensed in Tennessee, but to go to another state, they would be missing the required residency training. So it might be these folks are stuck in Tennessee unless other states develop reciprocal arrangements.”
Other states would have to decide whether to recognize the Tennessee license acquired through this pathway, Rep. Kumar said.
He explained that the sponsoring sites would be responsible for providing work-hour restrictions and liability protections. There are currently no incentives in the legislation for IMGs to practice in rural, underserved areas, but the hospitals and communities there generally offer incentives when recruiting, Rep. Kumar said.
“The law definitely has the potential to be helpful,” Mr. Cohen said, “because there’s an ability to place providers in the state without having to go through the bottleneck of limited residency slots. If other states see a positive effect on Tennessee or are exploring ways to alleviate their own shortages, it’s possible [they] might follow suit.”
Rep. Kumar agreed that other states will be watching Tennessee to weigh the law’s success.
“I think the law will have to prove itself and show that Tennessee has benefited from it and that the results have been good,” he said. “We are providing a pioneering way for attracting medical graduates and making it easier for them to obtain a license. I would think other states would want to do that.”
A version of this article first appeared on Medscape.com.
CBSM phone app eases anxiety, depression in cancer patients
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
CHICAGO – One-third of patients with cancer also experience anxiety or depression, and an estimated 70% of the 18 million patients with cancer and cancer survivors in the US experience emotional symptoms, including fear of recurrence.
Despite many having these symptoms, few patients with cancer have access to psycho-oncologic support.
A digital cognitive-behavioral stress management (CBSM) application may help to ease some of the burden, reported Allison Ramiller, MPH, of Blue Note Therapeutics in San Francisco, which developed the app version of the program.
In addition, patients assigned to the CBSM app were twice as likely as control persons to report that their symptoms were “much” or “very much” improved after using the app for 12 weeks, Ms. Ramiller reported at an oral abstract session at the annual meeting of the American Society of Clinical Oncology (ASCO).
However, the investigators did not report baseline characteristics of patients in each of the study arms, which might have helped to clarify the depth of the effects they saw.
The CBSM program was developed by Michael H. Antoni, PhD, and colleagues in the University of Miami Health System. It is based on cognitive-behavioral therapy but also includes stress management and relaxation techniques to help patients cope with cancer-specific stress.
“”It has been clinically validated and shown to benefit patients with cancer,” Ms. Ramiller said. “However, access is a problem,” she said.
“There aren’t enough qualified, trained providers for the need, and patients with cancer encounter barriers to in-person participation, including things like transportation or financial barriers. So to overcome this, we developed a digitized version of CBSM,” she explained.
Impressive and elegant
“Everything about [the study] I thought was very impressive, very elegant, very nicely done,” said invited discussant Raymond U. Osarogiagbon, MBBS, FACP, chief scientist at Baptist Memorial Health Care Corp in Memphis, Tenn.
“They showed efficacy, they showed safety – very nice – user friendliness – very good. Certainly they look like they’re trying to address a highly important, unmet need in a very elegant way. Certainly, they pointed out it needs longer follow-up to see sustainability. We need to see will this work in other settings. Will this be cost-effective? You’ve gotta believe it probably will be,” he said.
CBSM has previously been shown to help patients with cancer reduce stress, improve general and cancer-specific quality of life at various stages of treatment, reduce symptom burden, and improve coping skills, Ms. Ramiller said.
To see whether these benefits could be conveyed digitally rather than in face-to-face encounters, Ms. Ramiller and colleagues worked with Dr. Antoni to develop the CBSM app.
Patients using the app received therapeutic content over 10 sessions with audio, video, and interactive tools that mimicked the sessions they would have received during in-person interventions.
They then compared the app against the control educational app in the randomized, decentralized RESTORE study.
High-quality control
Ms. Ramiller said that the control app set “a high bar.”
“The control also offered 10 interactive self-guided sessions. Both treatment apps were professionally designed and visually similar in styling, and they were presented as digital therapeutic-specific for cancer patients. And they were also in a match condition, meaning they received the same attention from study staff and cadence of reminders, but importantly, only the intervention app was based on CBSM,” she explained.
A total of 449 patients with cancers of stage I–III who were undergoing active systemic treatment or were planning to undergo such treatment within 6 months were randomly assigned to the CBSM app or the control app.
The CBSM app was superior to the control app for the primary outcome of anxiety reduction over baseline, as measured at 4, 8 and 12 weeks by the Patient-Reported Outcomes Measurement Information System Anxiety Scale (PROMIS-A) (beta = -.03; P = .019).
CBSM was also significantly better than the control app for the secondary endpoints of reducing symptoms of depression, as measured by the PROMIS-D scale (beta = -.02, P = .042), and also at increasing the percentage of patients who reported improvement in anxiety and depression symptoms on the Patient Global Impression of Change instrument (P < .001)
An extension study of the durability of the effects at 3 and 6 months is underway.
The investigators noted that the incremental cost of management of anxiety or depression is greater than $17,000 per patient per year.
“One of the big promises of a digital therapeutic like this is that it could potentially reduce costs,” Ms. Ramiller told the audience, but she acknowledged, “More work is really needed, however, to directly test the potential savings.”
The RESTORE study is funded by Blue Note Therapeutics. Dr. Osarogiagbon owns stock in Gilead, Lilly, and Pfizer, has received honoraria from Biodesix and Medscape, and has a consulting or advisory role for the American Cancer Society AstraZeneca, Genentech/Roche, LUNGevity, National Cancer Institute, and Triptych Health Partners.
A version of this article originally appeared on Medscape.com.
AT ASCO 2023
Regular napping linked to greater brain volume
Investigators at University College London, and the University of the Republic of Uruguay, Montevideo, found individuals genetically predisposed to regular napping had larger total brain volume, a surrogate of better cognitive health.
“Our results suggest that napping may improve brain health,” first author Valentina Paz, MSc, a PhD candidate at the University of the Republic of Uruguay said in an interview. “Specifically, our work revealed a 15.8 cubic cm increase in total brain volume with more frequent daytime napping,” she said.
The findings were published online in Sleep Health.
Higher brain volume
Previous studies examining the potential link between napping and cognition in older adults have yielded conflicting results.
To clarify this association, Ms. Paz and colleagues used Mendelian randomization to study DNA samples, cognitive outcomes, and functional magnetic resonance imaging data in participants from the ongoing UK Biobank Study.
Starting with data from 378,932 study participants (mean age 57), investigators compared measures of brain health and cognition of those who are more genetically programmed to nap with people who did not have these genetic variations.
More specifically, the investigators examined 97 sections of genetic code previously linked to the likelihood of regular napping and correlated these results with fMRI and cognitive outcomes between those genetically predisposed to take regular naps and those who weren’t.
Study outcomes included total brain volume, hippocampal volume, reaction time, and visual memory.
The final study sample included 35,080 with neuroimaging, cognitive assessment, and genotype data.
The researchers estimated that the average difference in brain volume between individuals genetically programmed to be habitual nappers and those who were not was equivalent to 15.8 cubic cm, or 2.6-6.5 years of aging.
However, there was no difference in the other three outcomes – hippocampal volume, reaction time, and visual processing – between the two study groups.
Since investigators did not have information on the length of time participants napped, Ms. Paz suggested that “taking a short nap in the early afternoon may help cognition in those needing it.”
However, she added, the study’s findings need to be replicated before any firm conclusions can be made.
“More work is needed to examine the associations between napping and cognition, and the replication of these findings using other datasets and methods,” she said.
The investigators note that the study’s findings augment the knowledge of the “impact of habitual daytime napping on brain health, which is essential to understanding cognitive impairment in the aging population. The lack of evidence for an association between napping and hippocampal volume and cognitive outcomes (for example, alertness) may be affected by habitual daytime napping and should be studied in the future.”
Strengths, limitations
Tara Spires-Jones, PhD, president of the British Neuroscience Association and group leader at the UK Dementia Research Institute, said, “the study shows a small but significant increase in brain volume in people who have a genetic signature associated with taking daytime naps.”
Dr. Spires-Jones, who was not involved in the research, noted that while the study is well-conducted, it has limitations. Because Mendelian randomization uses a genetic signature, she noted, outcomes depend on the accuracy of the signature.
“The napping habits of UK Biobank participants were self-reported, which might not be entirely accurate, and the ‘napping’ signature overlapped substantially with the signature for cognitive outcomes in the study, which makes the causal link weaker,” she said.
“Even with those limitations, this study is interesting because it adds to the data indicating that sleep is important for brain health,” said Dr. Spires-Jones.
The study was supported by Diabetes UK, the British Heart Foundation, and the Diabetes Research and Wellness Foundation. In Uruguay, it was supported by Programa de Desarrollo de las Ciencias Básicas, Agencia Nacional de Investigación e Innovación, Comisión Sectorial de Investigación Científica, and Comisión Académica de Posgrado. In the United States it was supported by the National Heart, Lung, and Blood Institute. There were no disclosures reported.
A version of this article first appeared on Medscape.com.
Investigators at University College London, and the University of the Republic of Uruguay, Montevideo, found individuals genetically predisposed to regular napping had larger total brain volume, a surrogate of better cognitive health.
“Our results suggest that napping may improve brain health,” first author Valentina Paz, MSc, a PhD candidate at the University of the Republic of Uruguay said in an interview. “Specifically, our work revealed a 15.8 cubic cm increase in total brain volume with more frequent daytime napping,” she said.
The findings were published online in Sleep Health.
Higher brain volume
Previous studies examining the potential link between napping and cognition in older adults have yielded conflicting results.
To clarify this association, Ms. Paz and colleagues used Mendelian randomization to study DNA samples, cognitive outcomes, and functional magnetic resonance imaging data in participants from the ongoing UK Biobank Study.
Starting with data from 378,932 study participants (mean age 57), investigators compared measures of brain health and cognition of those who are more genetically programmed to nap with people who did not have these genetic variations.
More specifically, the investigators examined 97 sections of genetic code previously linked to the likelihood of regular napping and correlated these results with fMRI and cognitive outcomes between those genetically predisposed to take regular naps and those who weren’t.
Study outcomes included total brain volume, hippocampal volume, reaction time, and visual memory.
The final study sample included 35,080 with neuroimaging, cognitive assessment, and genotype data.
The researchers estimated that the average difference in brain volume between individuals genetically programmed to be habitual nappers and those who were not was equivalent to 15.8 cubic cm, or 2.6-6.5 years of aging.
However, there was no difference in the other three outcomes – hippocampal volume, reaction time, and visual processing – between the two study groups.
Since investigators did not have information on the length of time participants napped, Ms. Paz suggested that “taking a short nap in the early afternoon may help cognition in those needing it.”
However, she added, the study’s findings need to be replicated before any firm conclusions can be made.
“More work is needed to examine the associations between napping and cognition, and the replication of these findings using other datasets and methods,” she said.
The investigators note that the study’s findings augment the knowledge of the “impact of habitual daytime napping on brain health, which is essential to understanding cognitive impairment in the aging population. The lack of evidence for an association between napping and hippocampal volume and cognitive outcomes (for example, alertness) may be affected by habitual daytime napping and should be studied in the future.”
Strengths, limitations
Tara Spires-Jones, PhD, president of the British Neuroscience Association and group leader at the UK Dementia Research Institute, said, “the study shows a small but significant increase in brain volume in people who have a genetic signature associated with taking daytime naps.”
Dr. Spires-Jones, who was not involved in the research, noted that while the study is well-conducted, it has limitations. Because Mendelian randomization uses a genetic signature, she noted, outcomes depend on the accuracy of the signature.
“The napping habits of UK Biobank participants were self-reported, which might not be entirely accurate, and the ‘napping’ signature overlapped substantially with the signature for cognitive outcomes in the study, which makes the causal link weaker,” she said.
“Even with those limitations, this study is interesting because it adds to the data indicating that sleep is important for brain health,” said Dr. Spires-Jones.
The study was supported by Diabetes UK, the British Heart Foundation, and the Diabetes Research and Wellness Foundation. In Uruguay, it was supported by Programa de Desarrollo de las Ciencias Básicas, Agencia Nacional de Investigación e Innovación, Comisión Sectorial de Investigación Científica, and Comisión Académica de Posgrado. In the United States it was supported by the National Heart, Lung, and Blood Institute. There were no disclosures reported.
A version of this article first appeared on Medscape.com.
Investigators at University College London, and the University of the Republic of Uruguay, Montevideo, found individuals genetically predisposed to regular napping had larger total brain volume, a surrogate of better cognitive health.
“Our results suggest that napping may improve brain health,” first author Valentina Paz, MSc, a PhD candidate at the University of the Republic of Uruguay said in an interview. “Specifically, our work revealed a 15.8 cubic cm increase in total brain volume with more frequent daytime napping,” she said.
The findings were published online in Sleep Health.
Higher brain volume
Previous studies examining the potential link between napping and cognition in older adults have yielded conflicting results.
To clarify this association, Ms. Paz and colleagues used Mendelian randomization to study DNA samples, cognitive outcomes, and functional magnetic resonance imaging data in participants from the ongoing UK Biobank Study.
Starting with data from 378,932 study participants (mean age 57), investigators compared measures of brain health and cognition of those who are more genetically programmed to nap with people who did not have these genetic variations.
More specifically, the investigators examined 97 sections of genetic code previously linked to the likelihood of regular napping and correlated these results with fMRI and cognitive outcomes between those genetically predisposed to take regular naps and those who weren’t.
Study outcomes included total brain volume, hippocampal volume, reaction time, and visual memory.
The final study sample included 35,080 with neuroimaging, cognitive assessment, and genotype data.
The researchers estimated that the average difference in brain volume between individuals genetically programmed to be habitual nappers and those who were not was equivalent to 15.8 cubic cm, or 2.6-6.5 years of aging.
However, there was no difference in the other three outcomes – hippocampal volume, reaction time, and visual processing – between the two study groups.
Since investigators did not have information on the length of time participants napped, Ms. Paz suggested that “taking a short nap in the early afternoon may help cognition in those needing it.”
However, she added, the study’s findings need to be replicated before any firm conclusions can be made.
“More work is needed to examine the associations between napping and cognition, and the replication of these findings using other datasets and methods,” she said.
The investigators note that the study’s findings augment the knowledge of the “impact of habitual daytime napping on brain health, which is essential to understanding cognitive impairment in the aging population. The lack of evidence for an association between napping and hippocampal volume and cognitive outcomes (for example, alertness) may be affected by habitual daytime napping and should be studied in the future.”
Strengths, limitations
Tara Spires-Jones, PhD, president of the British Neuroscience Association and group leader at the UK Dementia Research Institute, said, “the study shows a small but significant increase in brain volume in people who have a genetic signature associated with taking daytime naps.”
Dr. Spires-Jones, who was not involved in the research, noted that while the study is well-conducted, it has limitations. Because Mendelian randomization uses a genetic signature, she noted, outcomes depend on the accuracy of the signature.
“The napping habits of UK Biobank participants were self-reported, which might not be entirely accurate, and the ‘napping’ signature overlapped substantially with the signature for cognitive outcomes in the study, which makes the causal link weaker,” she said.
“Even with those limitations, this study is interesting because it adds to the data indicating that sleep is important for brain health,” said Dr. Spires-Jones.
The study was supported by Diabetes UK, the British Heart Foundation, and the Diabetes Research and Wellness Foundation. In Uruguay, it was supported by Programa de Desarrollo de las Ciencias Básicas, Agencia Nacional de Investigación e Innovación, Comisión Sectorial de Investigación Científica, and Comisión Académica de Posgrado. In the United States it was supported by the National Heart, Lung, and Blood Institute. There were no disclosures reported.
A version of this article first appeared on Medscape.com.
FROM SLEEP HEALTH
New cannabis laws, higher binge drinking rates linked
TOPLINE:
METHODOLOGY:
Among adolescents, binge drinking, defined as having five or more drinks for men and four or more drinks for women at one time, is associated with poor academic performance, sexual risk, and injury in the short term, as well as the development of alcohol use disorder and academic disengagement in the long term.
Current evidence regarding the association between recreational cannabis laws (RCLs) and binge drinking is limited.
States in which RCLs have been implemented include Colorado, Washington, Alaska, Oregon, Nevada, California, Massachusetts, and Vermont, as well as the District of Columbia.
The study included 817,359 people aged 12 and older who participated in the 2008-2019 National Survey on Drug Use and Health (NSDUH), a nationally representative survey of the U.S. population.
TAKEAWAY:
Overall, states that have not enacted cannabis laws showed consistently lower rates of binge drinking over time among all age groups.
In all states, there were substantial declines in reporting of past-month binge drinking in some age groups – from 17.5% (95% confidence interval, 16.9-18.2) in 2008 to 11.1% (10.4-11.8) in 2019 among those aged 12-20 and a drop from 43.7% (42.4-44.9) to 40.2% (39.1-41.1) among those aged 21-30.
There were overall increases in binge drinking in all states regardless of cannabis laws among individuals aged 31 and older. The most extensive increases were among people aged 31-40 (from 28.1% [95% CI, 26.6-29.6] to 33.3% [32.1-34.6]), followed by participants aged 51 and over (from 13.3% [95% CI, 12.2-14.4] to 16.8% [15.8-17.7]).
IN PRACTICE:
“Our findings support calls to reinforce health care providers’ discussions about alcohol use with older adults,” particularly in RCL states, the researchers write.
STUDY DETAILS:
The study was conducted out by Priscila Dib Gonçalves, PhD, department of epidemiology, Columbia University School of Public Health, New York, and colleagues. It was published in the International Journal of Drug Policy.
LIMITATIONS:
Alcohol-related measures, including binge drinking, were self-reported, which may introduce recall bias and underreporting. NSDUH binge drinking measures were not adjusted for sex differences from 2008 to 2014, which may result in underreporting of binge drinking in females before 2015. The researchers did not examine cannabis policy provisions, such as cultivation restrictions, pricing control, the tax imposed, and consumption restrictions.
DISCLOSURES:
The study received support from the National Institutes of Health, the National Institute on Drug Abuse, the National Center for Injury Prevention and Control, and the Centers for Disease Control and Prevention. The authors report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
Among adolescents, binge drinking, defined as having five or more drinks for men and four or more drinks for women at one time, is associated with poor academic performance, sexual risk, and injury in the short term, as well as the development of alcohol use disorder and academic disengagement in the long term.
Current evidence regarding the association between recreational cannabis laws (RCLs) and binge drinking is limited.
States in which RCLs have been implemented include Colorado, Washington, Alaska, Oregon, Nevada, California, Massachusetts, and Vermont, as well as the District of Columbia.
The study included 817,359 people aged 12 and older who participated in the 2008-2019 National Survey on Drug Use and Health (NSDUH), a nationally representative survey of the U.S. population.
TAKEAWAY:
Overall, states that have not enacted cannabis laws showed consistently lower rates of binge drinking over time among all age groups.
In all states, there were substantial declines in reporting of past-month binge drinking in some age groups – from 17.5% (95% confidence interval, 16.9-18.2) in 2008 to 11.1% (10.4-11.8) in 2019 among those aged 12-20 and a drop from 43.7% (42.4-44.9) to 40.2% (39.1-41.1) among those aged 21-30.
There were overall increases in binge drinking in all states regardless of cannabis laws among individuals aged 31 and older. The most extensive increases were among people aged 31-40 (from 28.1% [95% CI, 26.6-29.6] to 33.3% [32.1-34.6]), followed by participants aged 51 and over (from 13.3% [95% CI, 12.2-14.4] to 16.8% [15.8-17.7]).
IN PRACTICE:
“Our findings support calls to reinforce health care providers’ discussions about alcohol use with older adults,” particularly in RCL states, the researchers write.
STUDY DETAILS:
The study was conducted out by Priscila Dib Gonçalves, PhD, department of epidemiology, Columbia University School of Public Health, New York, and colleagues. It was published in the International Journal of Drug Policy.
LIMITATIONS:
Alcohol-related measures, including binge drinking, were self-reported, which may introduce recall bias and underreporting. NSDUH binge drinking measures were not adjusted for sex differences from 2008 to 2014, which may result in underreporting of binge drinking in females before 2015. The researchers did not examine cannabis policy provisions, such as cultivation restrictions, pricing control, the tax imposed, and consumption restrictions.
DISCLOSURES:
The study received support from the National Institutes of Health, the National Institute on Drug Abuse, the National Center for Injury Prevention and Control, and the Centers for Disease Control and Prevention. The authors report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
Among adolescents, binge drinking, defined as having five or more drinks for men and four or more drinks for women at one time, is associated with poor academic performance, sexual risk, and injury in the short term, as well as the development of alcohol use disorder and academic disengagement in the long term.
Current evidence regarding the association between recreational cannabis laws (RCLs) and binge drinking is limited.
States in which RCLs have been implemented include Colorado, Washington, Alaska, Oregon, Nevada, California, Massachusetts, and Vermont, as well as the District of Columbia.
The study included 817,359 people aged 12 and older who participated in the 2008-2019 National Survey on Drug Use and Health (NSDUH), a nationally representative survey of the U.S. population.
TAKEAWAY:
Overall, states that have not enacted cannabis laws showed consistently lower rates of binge drinking over time among all age groups.
In all states, there were substantial declines in reporting of past-month binge drinking in some age groups – from 17.5% (95% confidence interval, 16.9-18.2) in 2008 to 11.1% (10.4-11.8) in 2019 among those aged 12-20 and a drop from 43.7% (42.4-44.9) to 40.2% (39.1-41.1) among those aged 21-30.
There were overall increases in binge drinking in all states regardless of cannabis laws among individuals aged 31 and older. The most extensive increases were among people aged 31-40 (from 28.1% [95% CI, 26.6-29.6] to 33.3% [32.1-34.6]), followed by participants aged 51 and over (from 13.3% [95% CI, 12.2-14.4] to 16.8% [15.8-17.7]).
IN PRACTICE:
“Our findings support calls to reinforce health care providers’ discussions about alcohol use with older adults,” particularly in RCL states, the researchers write.
STUDY DETAILS:
The study was conducted out by Priscila Dib Gonçalves, PhD, department of epidemiology, Columbia University School of Public Health, New York, and colleagues. It was published in the International Journal of Drug Policy.
LIMITATIONS:
Alcohol-related measures, including binge drinking, were self-reported, which may introduce recall bias and underreporting. NSDUH binge drinking measures were not adjusted for sex differences from 2008 to 2014, which may result in underreporting of binge drinking in females before 2015. The researchers did not examine cannabis policy provisions, such as cultivation restrictions, pricing control, the tax imposed, and consumption restrictions.
DISCLOSURES:
The study received support from the National Institutes of Health, the National Institute on Drug Abuse, the National Center for Injury Prevention and Control, and the Centers for Disease Control and Prevention. The authors report no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.