User login
Out-of-hospital cardiac arrests soar during COVID-19 in Italy
Out-of-hospital cardiac arrests increased 58% during the peak of the COVID-19 outbreak in the hard-hit region of Lombardy, Italy, compared with the same period last year, a new analysis shows.
During the first 40 days of the outbreak beginning Feb. 21, four provinces in northern Italy reported 362 cases of out-of-hospital cardiac arrest compared with 229 during the same period in 2019.
The increases in these provinces varied in magnitude from 18% in Mantua, where there were 1,688 confirmed COVID-19 cases, to 187% in Lodi, which had 2,116 COVID-19 cases. The Cremona province, which had the highest number of COVID-19 cases at 3,869, saw a 143% increase in out-of-hospital cardiac arrests.
The mortality rate in the field was 14.9 percentage points higher in 2020 than in 2019 among patients in whom resuscitation was attempted by emergency medical services (EMS), Enrico Baldi, MD, University of Pavia, Italy, and colleagues reported in a letter April 29 in the New England Journal of Medicine.
“The sex and age of the patients were similar in the 2020 and 2019 periods, but in 2020, the incidence of out-of-hospital cardiac arrest due to a medical cause was 6.5 percentage points higher, the incidence of out-of-hospital cardiac arrest at home was 7.3 percentage points higher, and the incidence of unwitnessed cardiac arrest was 11.3 percentage points higher,” the authors wrote.
Patients were also less likely to receive cardiopulmonary resuscitation from bystanders in 2020 vs 2019 (–15.6 percentage points) and were more likely to die before reaching the hospital when resuscitation was attempted by EMS (+14.9 percentage points).
Among all patients, the death rate in the field increased 11.4 percentage points during the outbreak, from 77.3% in 2019 to 88.7% in 2020.
The cumulative incidence of out-of-hospital cardiac arrest in 2020 was “strongly associated” with the cumulative incidence of COVID-19 (Spearman rank correlation coefficient, 0.87; 95% confidence interval, 0.83-0.91) and the spike in cases “followed the time course of the COVID-19 outbreak,” the researchers noted.
A total of 103 patients, who arrested out of hospital and were diagnosed with or suspected of having COVID-19, “account for 77.4% of the increase in cases of out-of-hospital cardiac arrest observed in these provinces in 2020,” the investigators noted.
As the pandemic has taken hold, hospitals and physicians across the United States are also voicing concerns about the drop in the number of patients presenting with myocardial infarction (MI) or stroke.
Nearly one-third of Americans (29%) report having delayed or avoided medical care because of concerns of catching COVID-19, according to a new poll released April 28 from the American College of Emergency Physicians (ACEP) and Morning Consult, a global data research firm.
Despite many emergency departments reporting a decline in patient volume, 74% of respondents said they were worried about hospital wait times and overcrowding. Another 59% expressed concerns about being turned away from the hospital or doctor’s office.
At the same time, the survey found strong support for emergency physicians and 73% of respondents said they were concerned about overstressing the health care system.
The drop-off in Americans seeking care for MI and strokes nationally prompted eight professional societies – including ACEP, the American Heart Association, and the Association of Black Cardiologists – to issue a joint statement urging those experiencing symptoms to call 911 and seek care for these life-threatening events.
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Out-of-hospital cardiac arrests increased 58% during the peak of the COVID-19 outbreak in the hard-hit region of Lombardy, Italy, compared with the same period last year, a new analysis shows.
During the first 40 days of the outbreak beginning Feb. 21, four provinces in northern Italy reported 362 cases of out-of-hospital cardiac arrest compared with 229 during the same period in 2019.
The increases in these provinces varied in magnitude from 18% in Mantua, where there were 1,688 confirmed COVID-19 cases, to 187% in Lodi, which had 2,116 COVID-19 cases. The Cremona province, which had the highest number of COVID-19 cases at 3,869, saw a 143% increase in out-of-hospital cardiac arrests.
The mortality rate in the field was 14.9 percentage points higher in 2020 than in 2019 among patients in whom resuscitation was attempted by emergency medical services (EMS), Enrico Baldi, MD, University of Pavia, Italy, and colleagues reported in a letter April 29 in the New England Journal of Medicine.
“The sex and age of the patients were similar in the 2020 and 2019 periods, but in 2020, the incidence of out-of-hospital cardiac arrest due to a medical cause was 6.5 percentage points higher, the incidence of out-of-hospital cardiac arrest at home was 7.3 percentage points higher, and the incidence of unwitnessed cardiac arrest was 11.3 percentage points higher,” the authors wrote.
Patients were also less likely to receive cardiopulmonary resuscitation from bystanders in 2020 vs 2019 (–15.6 percentage points) and were more likely to die before reaching the hospital when resuscitation was attempted by EMS (+14.9 percentage points).
Among all patients, the death rate in the field increased 11.4 percentage points during the outbreak, from 77.3% in 2019 to 88.7% in 2020.
The cumulative incidence of out-of-hospital cardiac arrest in 2020 was “strongly associated” with the cumulative incidence of COVID-19 (Spearman rank correlation coefficient, 0.87; 95% confidence interval, 0.83-0.91) and the spike in cases “followed the time course of the COVID-19 outbreak,” the researchers noted.
A total of 103 patients, who arrested out of hospital and were diagnosed with or suspected of having COVID-19, “account for 77.4% of the increase in cases of out-of-hospital cardiac arrest observed in these provinces in 2020,” the investigators noted.
As the pandemic has taken hold, hospitals and physicians across the United States are also voicing concerns about the drop in the number of patients presenting with myocardial infarction (MI) or stroke.
Nearly one-third of Americans (29%) report having delayed or avoided medical care because of concerns of catching COVID-19, according to a new poll released April 28 from the American College of Emergency Physicians (ACEP) and Morning Consult, a global data research firm.
Despite many emergency departments reporting a decline in patient volume, 74% of respondents said they were worried about hospital wait times and overcrowding. Another 59% expressed concerns about being turned away from the hospital or doctor’s office.
At the same time, the survey found strong support for emergency physicians and 73% of respondents said they were concerned about overstressing the health care system.
The drop-off in Americans seeking care for MI and strokes nationally prompted eight professional societies – including ACEP, the American Heart Association, and the Association of Black Cardiologists – to issue a joint statement urging those experiencing symptoms to call 911 and seek care for these life-threatening events.
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Out-of-hospital cardiac arrests increased 58% during the peak of the COVID-19 outbreak in the hard-hit region of Lombardy, Italy, compared with the same period last year, a new analysis shows.
During the first 40 days of the outbreak beginning Feb. 21, four provinces in northern Italy reported 362 cases of out-of-hospital cardiac arrest compared with 229 during the same period in 2019.
The increases in these provinces varied in magnitude from 18% in Mantua, where there were 1,688 confirmed COVID-19 cases, to 187% in Lodi, which had 2,116 COVID-19 cases. The Cremona province, which had the highest number of COVID-19 cases at 3,869, saw a 143% increase in out-of-hospital cardiac arrests.
The mortality rate in the field was 14.9 percentage points higher in 2020 than in 2019 among patients in whom resuscitation was attempted by emergency medical services (EMS), Enrico Baldi, MD, University of Pavia, Italy, and colleagues reported in a letter April 29 in the New England Journal of Medicine.
“The sex and age of the patients were similar in the 2020 and 2019 periods, but in 2020, the incidence of out-of-hospital cardiac arrest due to a medical cause was 6.5 percentage points higher, the incidence of out-of-hospital cardiac arrest at home was 7.3 percentage points higher, and the incidence of unwitnessed cardiac arrest was 11.3 percentage points higher,” the authors wrote.
Patients were also less likely to receive cardiopulmonary resuscitation from bystanders in 2020 vs 2019 (–15.6 percentage points) and were more likely to die before reaching the hospital when resuscitation was attempted by EMS (+14.9 percentage points).
Among all patients, the death rate in the field increased 11.4 percentage points during the outbreak, from 77.3% in 2019 to 88.7% in 2020.
The cumulative incidence of out-of-hospital cardiac arrest in 2020 was “strongly associated” with the cumulative incidence of COVID-19 (Spearman rank correlation coefficient, 0.87; 95% confidence interval, 0.83-0.91) and the spike in cases “followed the time course of the COVID-19 outbreak,” the researchers noted.
A total of 103 patients, who arrested out of hospital and were diagnosed with or suspected of having COVID-19, “account for 77.4% of the increase in cases of out-of-hospital cardiac arrest observed in these provinces in 2020,” the investigators noted.
As the pandemic has taken hold, hospitals and physicians across the United States are also voicing concerns about the drop in the number of patients presenting with myocardial infarction (MI) or stroke.
Nearly one-third of Americans (29%) report having delayed or avoided medical care because of concerns of catching COVID-19, according to a new poll released April 28 from the American College of Emergency Physicians (ACEP) and Morning Consult, a global data research firm.
Despite many emergency departments reporting a decline in patient volume, 74% of respondents said they were worried about hospital wait times and overcrowding. Another 59% expressed concerns about being turned away from the hospital or doctor’s office.
At the same time, the survey found strong support for emergency physicians and 73% of respondents said they were concerned about overstressing the health care system.
The drop-off in Americans seeking care for MI and strokes nationally prompted eight professional societies – including ACEP, the American Heart Association, and the Association of Black Cardiologists – to issue a joint statement urging those experiencing symptoms to call 911 and seek care for these life-threatening events.
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19: Addressing the mental health needs of clinicians
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
Continuity rules
Simple operational adjustments your team can make
Although there are many benefits to the hospital medicine model of inpatient care, there is perhaps no greater Achilles heel than the discontinuity inherent to the care model. The trust and familiarity garnered from longitudinal patient-provider relationships is sacrificed for the benefits of focused practice, efficiency, and enhanced availability.
Any system involves competing priorities, and some degree of discontinuity is inevitable. Would it make sense for a hospitalist to stay on service until every panel patient is discharged? For obvious economic, lifestyle, and other reasons, of course not. Our charge then is not to make the perfect the enemy of the good, but to ensure thoughtful and consistent continuity for the good of the patient, the provider, and the hospital. The following tips should help your team achieve the best possible balance.
Avoid orphan rounding shifts
An “orphan” rounding shift refers to a single shift untethered to a stretch. For admitting or administrative duties, this generally poses no problem, but for a rounding shift it is undesirable. No matter how talented or industrious the provider, it is very difficult for them to effectively provide seamless care for a single day; such care is often disconcerting for patients, families, case managers, and consultants. In situations such as significant census spikes, this may be a necessary evil, but avoid this if you can.
Orphan shift duties
If you can’t avoid an orphan rounding shift, be creative regarding which patients get assigned. Can that provider cover observation or simple short stay patients who may be discharged, or consult follow ups that may be signed off? Can they see stable long-stay patients where the plan isn’t changing and the patient isn’t going anywhere? (Think guardianships, chronic ventilated patients awaiting a facility, stable patients with a history of intravenous drug abuse who may not be safely discharged with a line, etc.) Can they do lab, culture, or path report follow-up calls? Getting creative in responsibilities for an orphan shift can benefit all involved.
Rounding shifts following admitting shifts
Dedicated admitting and rounding shifts are the norm these days. But rather than a pure stretch of one or the other, consider a few days admitting followed by the rest of the stretch rounding. Particularly in a small- to mid-sized hospital, multiple admits done over a few days (and especially if also cross-covering floor calls) will mean many familiar cases when rounding thereafter.
Standard sign-out that travels with patients
The hospital is a dynamic environment. Patients, providers and staff move around a lot. Given this reality, the importance of a complete standardized and accessible sign-out is paramount.
Imagine a rounder starting their last day with 15 patients. By the end of the shift, some have been discharged, transferred to telemetry or the ICU, or left against medical advice, leaving seven patients to sign out. By the next day, there are eight new faces, including fresh admits or consults from the prior day, swing, and night providers as well as existing patients transferred from telemetry/ICU to the general medical ward. A practical solution incorporates an asynchronous sign-out that travels with the patient regardless of geographic location or which provider(s) are following them. Billing software or census reports can typically achieve this. Of course, allow for additional verbal communication as necessary and appropriate.
Geographic rounds, with exceptions
Geographic rounds make a lot of sense most of the time. Less transit time and phone tag and more frequent interactions with the care team make for a more efficient day. But sometimes it’s best to bend this rule.
A patient that you’ve seen for 5 days and was transferred off your telemetry floor to go home tomorrow might best be served by you trekking up a flight of stairs to do the discharge. Similarly, complicated medical, psychosocial, or other circumstances may argue for keeping the patient on your list despite a change in location.
The above rules are foundational elements for good continuity. Two bonus considerations include:
Wind up, wind down
It’s difficult to walk into a full panel of patients especially when many have been in house for a while. Consider overlapping providers coming onto and going off a shared service.
In a buddy arrangement the oncoming provider starting would take new patients from the outgoing provider finishing. The provider finishing discharges patients with long length of stays and continues to round on more-complicated patients with whom they are familiar. Opportunities for face-to-face verbal handover, and even bedside introduction to the provider starting, can improve care coordination and safety and enhance the patient experience.
Reconsider split rounding and admitting
Most physicians would attest that the second time seeing a patient is much easier than the first, the third easier than the second, and so on. This holds true even more so when the first encounter is the history and physical, and the provider subsequently rounds on the patient for the duration of the hospitalization.
You know what the plan is because you made it; you are confident that the patient’s leg with cellulitis looks better or the patient with congested lungs sounds clearer because the baseline against which you’re comparing is your own. It can be a challenge to interrupt a busy day of clinical rounds, discharges, and interdisciplinary meetings to admit a patient. But the upstream investment pays rich downstream dividends and is well worth consideration.
Hospital medicine outcomes as measured by cost, quality, and patient and provider experience are often hampered by suboptimal continuity of care. With recognition of the problem and some simple operational adjustments as outlined above, your team can minimize negative impacts.
Dr. Krisa is a former regional medical director for a national hospitalist group and currently serves as a physician advisor for St. Peter’s Health Partners, a large integrated health system in Albany, N.Y. You can contact him at [email protected].
Simple operational adjustments your team can make
Simple operational adjustments your team can make
Although there are many benefits to the hospital medicine model of inpatient care, there is perhaps no greater Achilles heel than the discontinuity inherent to the care model. The trust and familiarity garnered from longitudinal patient-provider relationships is sacrificed for the benefits of focused practice, efficiency, and enhanced availability.
Any system involves competing priorities, and some degree of discontinuity is inevitable. Would it make sense for a hospitalist to stay on service until every panel patient is discharged? For obvious economic, lifestyle, and other reasons, of course not. Our charge then is not to make the perfect the enemy of the good, but to ensure thoughtful and consistent continuity for the good of the patient, the provider, and the hospital. The following tips should help your team achieve the best possible balance.
Avoid orphan rounding shifts
An “orphan” rounding shift refers to a single shift untethered to a stretch. For admitting or administrative duties, this generally poses no problem, but for a rounding shift it is undesirable. No matter how talented or industrious the provider, it is very difficult for them to effectively provide seamless care for a single day; such care is often disconcerting for patients, families, case managers, and consultants. In situations such as significant census spikes, this may be a necessary evil, but avoid this if you can.
Orphan shift duties
If you can’t avoid an orphan rounding shift, be creative regarding which patients get assigned. Can that provider cover observation or simple short stay patients who may be discharged, or consult follow ups that may be signed off? Can they see stable long-stay patients where the plan isn’t changing and the patient isn’t going anywhere? (Think guardianships, chronic ventilated patients awaiting a facility, stable patients with a history of intravenous drug abuse who may not be safely discharged with a line, etc.) Can they do lab, culture, or path report follow-up calls? Getting creative in responsibilities for an orphan shift can benefit all involved.
Rounding shifts following admitting shifts
Dedicated admitting and rounding shifts are the norm these days. But rather than a pure stretch of one or the other, consider a few days admitting followed by the rest of the stretch rounding. Particularly in a small- to mid-sized hospital, multiple admits done over a few days (and especially if also cross-covering floor calls) will mean many familiar cases when rounding thereafter.
Standard sign-out that travels with patients
The hospital is a dynamic environment. Patients, providers and staff move around a lot. Given this reality, the importance of a complete standardized and accessible sign-out is paramount.
Imagine a rounder starting their last day with 15 patients. By the end of the shift, some have been discharged, transferred to telemetry or the ICU, or left against medical advice, leaving seven patients to sign out. By the next day, there are eight new faces, including fresh admits or consults from the prior day, swing, and night providers as well as existing patients transferred from telemetry/ICU to the general medical ward. A practical solution incorporates an asynchronous sign-out that travels with the patient regardless of geographic location or which provider(s) are following them. Billing software or census reports can typically achieve this. Of course, allow for additional verbal communication as necessary and appropriate.
Geographic rounds, with exceptions
Geographic rounds make a lot of sense most of the time. Less transit time and phone tag and more frequent interactions with the care team make for a more efficient day. But sometimes it’s best to bend this rule.
A patient that you’ve seen for 5 days and was transferred off your telemetry floor to go home tomorrow might best be served by you trekking up a flight of stairs to do the discharge. Similarly, complicated medical, psychosocial, or other circumstances may argue for keeping the patient on your list despite a change in location.
The above rules are foundational elements for good continuity. Two bonus considerations include:
Wind up, wind down
It’s difficult to walk into a full panel of patients especially when many have been in house for a while. Consider overlapping providers coming onto and going off a shared service.
In a buddy arrangement the oncoming provider starting would take new patients from the outgoing provider finishing. The provider finishing discharges patients with long length of stays and continues to round on more-complicated patients with whom they are familiar. Opportunities for face-to-face verbal handover, and even bedside introduction to the provider starting, can improve care coordination and safety and enhance the patient experience.
Reconsider split rounding and admitting
Most physicians would attest that the second time seeing a patient is much easier than the first, the third easier than the second, and so on. This holds true even more so when the first encounter is the history and physical, and the provider subsequently rounds on the patient for the duration of the hospitalization.
You know what the plan is because you made it; you are confident that the patient’s leg with cellulitis looks better or the patient with congested lungs sounds clearer because the baseline against which you’re comparing is your own. It can be a challenge to interrupt a busy day of clinical rounds, discharges, and interdisciplinary meetings to admit a patient. But the upstream investment pays rich downstream dividends and is well worth consideration.
Hospital medicine outcomes as measured by cost, quality, and patient and provider experience are often hampered by suboptimal continuity of care. With recognition of the problem and some simple operational adjustments as outlined above, your team can minimize negative impacts.
Dr. Krisa is a former regional medical director for a national hospitalist group and currently serves as a physician advisor for St. Peter’s Health Partners, a large integrated health system in Albany, N.Y. You can contact him at [email protected].
Although there are many benefits to the hospital medicine model of inpatient care, there is perhaps no greater Achilles heel than the discontinuity inherent to the care model. The trust and familiarity garnered from longitudinal patient-provider relationships is sacrificed for the benefits of focused practice, efficiency, and enhanced availability.
Any system involves competing priorities, and some degree of discontinuity is inevitable. Would it make sense for a hospitalist to stay on service until every panel patient is discharged? For obvious economic, lifestyle, and other reasons, of course not. Our charge then is not to make the perfect the enemy of the good, but to ensure thoughtful and consistent continuity for the good of the patient, the provider, and the hospital. The following tips should help your team achieve the best possible balance.
Avoid orphan rounding shifts
An “orphan” rounding shift refers to a single shift untethered to a stretch. For admitting or administrative duties, this generally poses no problem, but for a rounding shift it is undesirable. No matter how talented or industrious the provider, it is very difficult for them to effectively provide seamless care for a single day; such care is often disconcerting for patients, families, case managers, and consultants. In situations such as significant census spikes, this may be a necessary evil, but avoid this if you can.
Orphan shift duties
If you can’t avoid an orphan rounding shift, be creative regarding which patients get assigned. Can that provider cover observation or simple short stay patients who may be discharged, or consult follow ups that may be signed off? Can they see stable long-stay patients where the plan isn’t changing and the patient isn’t going anywhere? (Think guardianships, chronic ventilated patients awaiting a facility, stable patients with a history of intravenous drug abuse who may not be safely discharged with a line, etc.) Can they do lab, culture, or path report follow-up calls? Getting creative in responsibilities for an orphan shift can benefit all involved.
Rounding shifts following admitting shifts
Dedicated admitting and rounding shifts are the norm these days. But rather than a pure stretch of one or the other, consider a few days admitting followed by the rest of the stretch rounding. Particularly in a small- to mid-sized hospital, multiple admits done over a few days (and especially if also cross-covering floor calls) will mean many familiar cases when rounding thereafter.
Standard sign-out that travels with patients
The hospital is a dynamic environment. Patients, providers and staff move around a lot. Given this reality, the importance of a complete standardized and accessible sign-out is paramount.
Imagine a rounder starting their last day with 15 patients. By the end of the shift, some have been discharged, transferred to telemetry or the ICU, or left against medical advice, leaving seven patients to sign out. By the next day, there are eight new faces, including fresh admits or consults from the prior day, swing, and night providers as well as existing patients transferred from telemetry/ICU to the general medical ward. A practical solution incorporates an asynchronous sign-out that travels with the patient regardless of geographic location or which provider(s) are following them. Billing software or census reports can typically achieve this. Of course, allow for additional verbal communication as necessary and appropriate.
Geographic rounds, with exceptions
Geographic rounds make a lot of sense most of the time. Less transit time and phone tag and more frequent interactions with the care team make for a more efficient day. But sometimes it’s best to bend this rule.
A patient that you’ve seen for 5 days and was transferred off your telemetry floor to go home tomorrow might best be served by you trekking up a flight of stairs to do the discharge. Similarly, complicated medical, psychosocial, or other circumstances may argue for keeping the patient on your list despite a change in location.
The above rules are foundational elements for good continuity. Two bonus considerations include:
Wind up, wind down
It’s difficult to walk into a full panel of patients especially when many have been in house for a while. Consider overlapping providers coming onto and going off a shared service.
In a buddy arrangement the oncoming provider starting would take new patients from the outgoing provider finishing. The provider finishing discharges patients with long length of stays and continues to round on more-complicated patients with whom they are familiar. Opportunities for face-to-face verbal handover, and even bedside introduction to the provider starting, can improve care coordination and safety and enhance the patient experience.
Reconsider split rounding and admitting
Most physicians would attest that the second time seeing a patient is much easier than the first, the third easier than the second, and so on. This holds true even more so when the first encounter is the history and physical, and the provider subsequently rounds on the patient for the duration of the hospitalization.
You know what the plan is because you made it; you are confident that the patient’s leg with cellulitis looks better or the patient with congested lungs sounds clearer because the baseline against which you’re comparing is your own. It can be a challenge to interrupt a busy day of clinical rounds, discharges, and interdisciplinary meetings to admit a patient. But the upstream investment pays rich downstream dividends and is well worth consideration.
Hospital medicine outcomes as measured by cost, quality, and patient and provider experience are often hampered by suboptimal continuity of care. With recognition of the problem and some simple operational adjustments as outlined above, your team can minimize negative impacts.
Dr. Krisa is a former regional medical director for a national hospitalist group and currently serves as a physician advisor for St. Peter’s Health Partners, a large integrated health system in Albany, N.Y. You can contact him at [email protected].
Excess cancer deaths predicted as care is disrupted by COVID-19
The majority of patients who have cancer or are suspected of having cancer are not accessing healthcare services in the United Kingdom or the United States because of the COVID-19 pandemic, the first report of its kind estimates.
As a result, there will be an excess of deaths among patients who have cancer and multiple comorbidities in both countries during the current coronavirus emergency, the report warns.
The authors calculate that there will be 6,270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients in the United States. (In the United States, the estimated excess number of deaths applies only to patients older than 40 years, they note.)
“The recorded underlying cause of these excess deaths may be cancer, COVID-19, or comorbidity (such as myocardial infarction),” Alvina Lai, PhD, University College London, United Kingdom, and colleagues observe.
“Our data have highlighted how cancer patients with multimorbidity are a particularly at-risk group during the current pandemic,” they emphasize.
The study was published on ResearchGate as a preprint and has not undergone peer review.
Commenting on the study on the UK Science Media Center, several experts emphasized the lack of peer review, noting that interpretation of these data needs to be further refined on the basis of that input. One expert suggested that there are “substantial uncertainties that this paper does not adequately communicate.” But others argued that this topic was important enough to warrant early release of the data.
Chris Bunce, PhD, University of Birmingham, United Kingdom, said this study represents “a highly valuable contribution.”
“It is universally accepted that early diagnosis and treatment and adherence to treatment regimens saves lives,” he pointed out.
“Therefore, these COVID-19-related impacts will cost lives,” Bunce said.
“And if this information is to influence cancer care and guide policy during the COVID-19 crisis, then it is important that the findings are disseminated and discussed immediately, warranting their release ahead of peer view,” he added.
In a Medscape UK commentary, oncologist Karol Sikora, MD, PhD, argues that “restarting cancer services can’t come soon enough.”
“Resonably Argued Numerical Estimate”
“It’s well known that there have been considerable changes in the provision of health care for many conditions, including cancers, as a result of all the measures to deal with the COVID-19 crisis,” said Kevin McConway, PhD, professor emeritus of applied statistics, the Open University, Milton Keynes, United Kingdom.
“It seems inevitable that there will be increased deaths in cancer patients if they are infected with the virus or because of changes in the health services available to them, and quite possibly also from socio-economic effects of the responses to the crisis,” he continued.
“This study is the first that I have seen that produces a reasonably argued numerical estimate of the number of excess deaths of people with cancer arising from these factors in the UK and the USA,” he added.
Declines in Urgent Referrals and Chemo Attendance
For the study, the team used DATA-CAN, the UK National Health Data Research Hub for Cancer, to assess weekly returns for urgent cancer referrals for early diagnosis and also chemotherapy attendances for hospitals in Leeds, London, and Northern Ireland going back to 2018.
The data revealed that there have been major declines in chemotherapy attendances. There has been, on average, a 60% decrease from prepandemic levels in eight hospitals in the three regions that were assessed.
Urgent cancer referrals have dropped by an average of 76% compared to prepandemic levels in the three regions.
On the conservative assumption that the COVID-19 pandemic will only affect patients with newly diagnosed cancer (incident cases), the researchers estimate that the proportion of the population affected by the emergency (PAE) is 40% and that the relative impact of the emergency (RIE) is 1.5.
PAE is a summary measure of exposure to the adverse health consequences of the emergency; RIE is a summary measure of the combined impact on mortality of infection, health service change, physical distancing, and economic downturn, the authors explain.
Comorbidities Common
“Comorbidities were common in people with cancer,” the study authors note. For example, more than one quarter of the study population had at least one comorbidity; more than 14% had two.
For incident cancers, the number of excess deaths steadily increased in conjunction with an increase in the number of comorbidities, such that more than 80% of deaths occurred in patients with one or more comorbidities.
“When considering both prevalent and incident cancers together with a COVID-19 PAE of 40%, we estimated 17,991 excess deaths at a RIE of 1.5; 78.1% of these deaths occur in patients with ≥1 comorbidities,” the authors report.
“The excess risk of death in people living with cancer during the COVID-19 emergency may be due not only to COVID-19 infection, but also to the unintended health consequences of changes in health service provision, the physical or psychological effects of social distancing, and economic upheaval,” they state.
“This is the first study demonstrating profound recent changes in cancer care delivery in multiple centers,” the authors observe.
Lai has disclosed no relevant financial relationships. Several coauthors have various relationships with industry, as listed in their article. The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The majority of patients who have cancer or are suspected of having cancer are not accessing healthcare services in the United Kingdom or the United States because of the COVID-19 pandemic, the first report of its kind estimates.
As a result, there will be an excess of deaths among patients who have cancer and multiple comorbidities in both countries during the current coronavirus emergency, the report warns.
The authors calculate that there will be 6,270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients in the United States. (In the United States, the estimated excess number of deaths applies only to patients older than 40 years, they note.)
“The recorded underlying cause of these excess deaths may be cancer, COVID-19, or comorbidity (such as myocardial infarction),” Alvina Lai, PhD, University College London, United Kingdom, and colleagues observe.
“Our data have highlighted how cancer patients with multimorbidity are a particularly at-risk group during the current pandemic,” they emphasize.
The study was published on ResearchGate as a preprint and has not undergone peer review.
Commenting on the study on the UK Science Media Center, several experts emphasized the lack of peer review, noting that interpretation of these data needs to be further refined on the basis of that input. One expert suggested that there are “substantial uncertainties that this paper does not adequately communicate.” But others argued that this topic was important enough to warrant early release of the data.
Chris Bunce, PhD, University of Birmingham, United Kingdom, said this study represents “a highly valuable contribution.”
“It is universally accepted that early diagnosis and treatment and adherence to treatment regimens saves lives,” he pointed out.
“Therefore, these COVID-19-related impacts will cost lives,” Bunce said.
“And if this information is to influence cancer care and guide policy during the COVID-19 crisis, then it is important that the findings are disseminated and discussed immediately, warranting their release ahead of peer view,” he added.
In a Medscape UK commentary, oncologist Karol Sikora, MD, PhD, argues that “restarting cancer services can’t come soon enough.”
“Resonably Argued Numerical Estimate”
“It’s well known that there have been considerable changes in the provision of health care for many conditions, including cancers, as a result of all the measures to deal with the COVID-19 crisis,” said Kevin McConway, PhD, professor emeritus of applied statistics, the Open University, Milton Keynes, United Kingdom.
“It seems inevitable that there will be increased deaths in cancer patients if they are infected with the virus or because of changes in the health services available to them, and quite possibly also from socio-economic effects of the responses to the crisis,” he continued.
“This study is the first that I have seen that produces a reasonably argued numerical estimate of the number of excess deaths of people with cancer arising from these factors in the UK and the USA,” he added.
Declines in Urgent Referrals and Chemo Attendance
For the study, the team used DATA-CAN, the UK National Health Data Research Hub for Cancer, to assess weekly returns for urgent cancer referrals for early diagnosis and also chemotherapy attendances for hospitals in Leeds, London, and Northern Ireland going back to 2018.
The data revealed that there have been major declines in chemotherapy attendances. There has been, on average, a 60% decrease from prepandemic levels in eight hospitals in the three regions that were assessed.
Urgent cancer referrals have dropped by an average of 76% compared to prepandemic levels in the three regions.
On the conservative assumption that the COVID-19 pandemic will only affect patients with newly diagnosed cancer (incident cases), the researchers estimate that the proportion of the population affected by the emergency (PAE) is 40% and that the relative impact of the emergency (RIE) is 1.5.
PAE is a summary measure of exposure to the adverse health consequences of the emergency; RIE is a summary measure of the combined impact on mortality of infection, health service change, physical distancing, and economic downturn, the authors explain.
Comorbidities Common
“Comorbidities were common in people with cancer,” the study authors note. For example, more than one quarter of the study population had at least one comorbidity; more than 14% had two.
For incident cancers, the number of excess deaths steadily increased in conjunction with an increase in the number of comorbidities, such that more than 80% of deaths occurred in patients with one or more comorbidities.
“When considering both prevalent and incident cancers together with a COVID-19 PAE of 40%, we estimated 17,991 excess deaths at a RIE of 1.5; 78.1% of these deaths occur in patients with ≥1 comorbidities,” the authors report.
“The excess risk of death in people living with cancer during the COVID-19 emergency may be due not only to COVID-19 infection, but also to the unintended health consequences of changes in health service provision, the physical or psychological effects of social distancing, and economic upheaval,” they state.
“This is the first study demonstrating profound recent changes in cancer care delivery in multiple centers,” the authors observe.
Lai has disclosed no relevant financial relationships. Several coauthors have various relationships with industry, as listed in their article. The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The majority of patients who have cancer or are suspected of having cancer are not accessing healthcare services in the United Kingdom or the United States because of the COVID-19 pandemic, the first report of its kind estimates.
As a result, there will be an excess of deaths among patients who have cancer and multiple comorbidities in both countries during the current coronavirus emergency, the report warns.
The authors calculate that there will be 6,270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients in the United States. (In the United States, the estimated excess number of deaths applies only to patients older than 40 years, they note.)
“The recorded underlying cause of these excess deaths may be cancer, COVID-19, or comorbidity (such as myocardial infarction),” Alvina Lai, PhD, University College London, United Kingdom, and colleagues observe.
“Our data have highlighted how cancer patients with multimorbidity are a particularly at-risk group during the current pandemic,” they emphasize.
The study was published on ResearchGate as a preprint and has not undergone peer review.
Commenting on the study on the UK Science Media Center, several experts emphasized the lack of peer review, noting that interpretation of these data needs to be further refined on the basis of that input. One expert suggested that there are “substantial uncertainties that this paper does not adequately communicate.” But others argued that this topic was important enough to warrant early release of the data.
Chris Bunce, PhD, University of Birmingham, United Kingdom, said this study represents “a highly valuable contribution.”
“It is universally accepted that early diagnosis and treatment and adherence to treatment regimens saves lives,” he pointed out.
“Therefore, these COVID-19-related impacts will cost lives,” Bunce said.
“And if this information is to influence cancer care and guide policy during the COVID-19 crisis, then it is important that the findings are disseminated and discussed immediately, warranting their release ahead of peer view,” he added.
In a Medscape UK commentary, oncologist Karol Sikora, MD, PhD, argues that “restarting cancer services can’t come soon enough.”
“Resonably Argued Numerical Estimate”
“It’s well known that there have been considerable changes in the provision of health care for many conditions, including cancers, as a result of all the measures to deal with the COVID-19 crisis,” said Kevin McConway, PhD, professor emeritus of applied statistics, the Open University, Milton Keynes, United Kingdom.
“It seems inevitable that there will be increased deaths in cancer patients if they are infected with the virus or because of changes in the health services available to them, and quite possibly also from socio-economic effects of the responses to the crisis,” he continued.
“This study is the first that I have seen that produces a reasonably argued numerical estimate of the number of excess deaths of people with cancer arising from these factors in the UK and the USA,” he added.
Declines in Urgent Referrals and Chemo Attendance
For the study, the team used DATA-CAN, the UK National Health Data Research Hub for Cancer, to assess weekly returns for urgent cancer referrals for early diagnosis and also chemotherapy attendances for hospitals in Leeds, London, and Northern Ireland going back to 2018.
The data revealed that there have been major declines in chemotherapy attendances. There has been, on average, a 60% decrease from prepandemic levels in eight hospitals in the three regions that were assessed.
Urgent cancer referrals have dropped by an average of 76% compared to prepandemic levels in the three regions.
On the conservative assumption that the COVID-19 pandemic will only affect patients with newly diagnosed cancer (incident cases), the researchers estimate that the proportion of the population affected by the emergency (PAE) is 40% and that the relative impact of the emergency (RIE) is 1.5.
PAE is a summary measure of exposure to the adverse health consequences of the emergency; RIE is a summary measure of the combined impact on mortality of infection, health service change, physical distancing, and economic downturn, the authors explain.
Comorbidities Common
“Comorbidities were common in people with cancer,” the study authors note. For example, more than one quarter of the study population had at least one comorbidity; more than 14% had two.
For incident cancers, the number of excess deaths steadily increased in conjunction with an increase in the number of comorbidities, such that more than 80% of deaths occurred in patients with one or more comorbidities.
“When considering both prevalent and incident cancers together with a COVID-19 PAE of 40%, we estimated 17,991 excess deaths at a RIE of 1.5; 78.1% of these deaths occur in patients with ≥1 comorbidities,” the authors report.
“The excess risk of death in people living with cancer during the COVID-19 emergency may be due not only to COVID-19 infection, but also to the unintended health consequences of changes in health service provision, the physical or psychological effects of social distancing, and economic upheaval,” they state.
“This is the first study demonstrating profound recent changes in cancer care delivery in multiple centers,” the authors observe.
Lai has disclosed no relevant financial relationships. Several coauthors have various relationships with industry, as listed in their article. The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
New tetracycline antibiotic effective in acute bacterial skin and skin-structure infections
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
COVID-19: A ‘marathon, not a sprint’ for psychiatry
The tragic death by suicide of an emergency department physician who had been caring for COVID-19 patients in New York City underscores the huge psychological impact of the pandemic – which will linger long after the virus is gone, experts say.
“For frontline responders, the trauma of witnessing so much illness and death will have lasting effects for many,” Bruce Schwartz, MD, president of the American Psychiatric Association (APA), said during the opening session of the annual meeting of the American Psychiatric Association, which was held as a virtual live event, replacing the organization’s canceled annual meeting.
“We will need the full workforce to cope with the psychiatric effects” of the pandemic, added Dr. Schwartz, deputy chairman and professor, department of psychiatry and behavioral sciences, Montefiore Medical Center and Albert Einstein College of Medicine, New York.
Joshua Morganstein, MD, chair of the APA’s Committee on the Psychiatric Dimensions of Disaster, led an afternoon session at the virtual meeting on “healthcare worker and organizational sustainment during COVID-19.”
The crisis is shaping up to be “a marathon, not a sprint; and self-care will remain a critical and ongoing issue. We are in this together,” he said.
Once the pandemic passes, Dr. Morganstein added.
Psychological first aid
It is important to realize that the psychological and behavioral effects of disasters are experienced by “more people, over a greater geography, across a much longer period of time than all other medical effects combined. This is important for disaster resource planning,” Dr. Morganstein told meeting attendees.
At times of crisis, many people will experience distress reactions and engage in behaviors that put their health at risk. Insomnia, increased alcohol and substance use, and family conflict are common and have a negative impact on functioning, he said.
In addition, pandemics result in unique responses. Protracted fear and uncertainty, elements of isolation, anger, misinformation, and faltering confidence in government/institutions may alter perceptions of risk.
“It’s the perception of risk, not the actual risk, that will ultimately determine how people behave,” Dr. Morganstein said.
“The ability to influence risk perception will alter the degree to which any group, community, or population ultimately chooses to engage in or reject recommended health behaviors,” he added.
In times of crisis, it’s also helpful to keep in mind and act upon the five essential elements of “psychological first aid,” he noted. These are safety, calming, self/community efficacy, social connectedness, and hope/optimism.
Psychological first aid is an evidence-based framework of supporting resilience in individuals, communities, and organizations, Dr. Morganstein said.
Individuals have a wide range of needs during times of crisis, and support should be tailored accordingly, he noted. As with many crises, instrumental support needs are significant and may be the primary need for many people. These include the need for food, clothing, rent/mortgage, financial relief, and child care.
Providing emotional support – empathy, validation, self-actualization, encouragement, and insight – will help individuals engage with instrumental supports.
“The reality is that it’s often difficult to talk about being sad when you feel hungry or worried you can’t pay the rent,” said Dr. Morganstein.
He also emphasized the importance of appropriate messaging and language during a crisis. These can have a profound impact on community well-being and the willingness of the public to engage in recommended health behaviors.
“As psychiatrists, we understand [that] the words we choose when we discuss this pandemic will have power. Communication is not only a means by which we deliver interventions, but it is, in and of itself, a behavioral health intervention. Good communication can serve to normalize experiences and function as an antidote to distress during times of uncertainty,” Dr. Morganstein said.
Importantly, “we need to remind people that eventually this will end and the vast majority of people, including those who have difficulties along the way, will ultimately be okay.”
The APA has provided a COVID-19 resource page on its website.
Dr. Morganstein and Dr. Schwartz have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The tragic death by suicide of an emergency department physician who had been caring for COVID-19 patients in New York City underscores the huge psychological impact of the pandemic – which will linger long after the virus is gone, experts say.
“For frontline responders, the trauma of witnessing so much illness and death will have lasting effects for many,” Bruce Schwartz, MD, president of the American Psychiatric Association (APA), said during the opening session of the annual meeting of the American Psychiatric Association, which was held as a virtual live event, replacing the organization’s canceled annual meeting.
“We will need the full workforce to cope with the psychiatric effects” of the pandemic, added Dr. Schwartz, deputy chairman and professor, department of psychiatry and behavioral sciences, Montefiore Medical Center and Albert Einstein College of Medicine, New York.
Joshua Morganstein, MD, chair of the APA’s Committee on the Psychiatric Dimensions of Disaster, led an afternoon session at the virtual meeting on “healthcare worker and organizational sustainment during COVID-19.”
The crisis is shaping up to be “a marathon, not a sprint; and self-care will remain a critical and ongoing issue. We are in this together,” he said.
Once the pandemic passes, Dr. Morganstein added.
Psychological first aid
It is important to realize that the psychological and behavioral effects of disasters are experienced by “more people, over a greater geography, across a much longer period of time than all other medical effects combined. This is important for disaster resource planning,” Dr. Morganstein told meeting attendees.
At times of crisis, many people will experience distress reactions and engage in behaviors that put their health at risk. Insomnia, increased alcohol and substance use, and family conflict are common and have a negative impact on functioning, he said.
In addition, pandemics result in unique responses. Protracted fear and uncertainty, elements of isolation, anger, misinformation, and faltering confidence in government/institutions may alter perceptions of risk.
“It’s the perception of risk, not the actual risk, that will ultimately determine how people behave,” Dr. Morganstein said.
“The ability to influence risk perception will alter the degree to which any group, community, or population ultimately chooses to engage in or reject recommended health behaviors,” he added.
In times of crisis, it’s also helpful to keep in mind and act upon the five essential elements of “psychological first aid,” he noted. These are safety, calming, self/community efficacy, social connectedness, and hope/optimism.
Psychological first aid is an evidence-based framework of supporting resilience in individuals, communities, and organizations, Dr. Morganstein said.
Individuals have a wide range of needs during times of crisis, and support should be tailored accordingly, he noted. As with many crises, instrumental support needs are significant and may be the primary need for many people. These include the need for food, clothing, rent/mortgage, financial relief, and child care.
Providing emotional support – empathy, validation, self-actualization, encouragement, and insight – will help individuals engage with instrumental supports.
“The reality is that it’s often difficult to talk about being sad when you feel hungry or worried you can’t pay the rent,” said Dr. Morganstein.
He also emphasized the importance of appropriate messaging and language during a crisis. These can have a profound impact on community well-being and the willingness of the public to engage in recommended health behaviors.
“As psychiatrists, we understand [that] the words we choose when we discuss this pandemic will have power. Communication is not only a means by which we deliver interventions, but it is, in and of itself, a behavioral health intervention. Good communication can serve to normalize experiences and function as an antidote to distress during times of uncertainty,” Dr. Morganstein said.
Importantly, “we need to remind people that eventually this will end and the vast majority of people, including those who have difficulties along the way, will ultimately be okay.”
The APA has provided a COVID-19 resource page on its website.
Dr. Morganstein and Dr. Schwartz have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The tragic death by suicide of an emergency department physician who had been caring for COVID-19 patients in New York City underscores the huge psychological impact of the pandemic – which will linger long after the virus is gone, experts say.
“For frontline responders, the trauma of witnessing so much illness and death will have lasting effects for many,” Bruce Schwartz, MD, president of the American Psychiatric Association (APA), said during the opening session of the annual meeting of the American Psychiatric Association, which was held as a virtual live event, replacing the organization’s canceled annual meeting.
“We will need the full workforce to cope with the psychiatric effects” of the pandemic, added Dr. Schwartz, deputy chairman and professor, department of psychiatry and behavioral sciences, Montefiore Medical Center and Albert Einstein College of Medicine, New York.
Joshua Morganstein, MD, chair of the APA’s Committee on the Psychiatric Dimensions of Disaster, led an afternoon session at the virtual meeting on “healthcare worker and organizational sustainment during COVID-19.”
The crisis is shaping up to be “a marathon, not a sprint; and self-care will remain a critical and ongoing issue. We are in this together,” he said.
Once the pandemic passes, Dr. Morganstein added.
Psychological first aid
It is important to realize that the psychological and behavioral effects of disasters are experienced by “more people, over a greater geography, across a much longer period of time than all other medical effects combined. This is important for disaster resource planning,” Dr. Morganstein told meeting attendees.
At times of crisis, many people will experience distress reactions and engage in behaviors that put their health at risk. Insomnia, increased alcohol and substance use, and family conflict are common and have a negative impact on functioning, he said.
In addition, pandemics result in unique responses. Protracted fear and uncertainty, elements of isolation, anger, misinformation, and faltering confidence in government/institutions may alter perceptions of risk.
“It’s the perception of risk, not the actual risk, that will ultimately determine how people behave,” Dr. Morganstein said.
“The ability to influence risk perception will alter the degree to which any group, community, or population ultimately chooses to engage in or reject recommended health behaviors,” he added.
In times of crisis, it’s also helpful to keep in mind and act upon the five essential elements of “psychological first aid,” he noted. These are safety, calming, self/community efficacy, social connectedness, and hope/optimism.
Psychological first aid is an evidence-based framework of supporting resilience in individuals, communities, and organizations, Dr. Morganstein said.
Individuals have a wide range of needs during times of crisis, and support should be tailored accordingly, he noted. As with many crises, instrumental support needs are significant and may be the primary need for many people. These include the need for food, clothing, rent/mortgage, financial relief, and child care.
Providing emotional support – empathy, validation, self-actualization, encouragement, and insight – will help individuals engage with instrumental supports.
“The reality is that it’s often difficult to talk about being sad when you feel hungry or worried you can’t pay the rent,” said Dr. Morganstein.
He also emphasized the importance of appropriate messaging and language during a crisis. These can have a profound impact on community well-being and the willingness of the public to engage in recommended health behaviors.
“As psychiatrists, we understand [that] the words we choose when we discuss this pandemic will have power. Communication is not only a means by which we deliver interventions, but it is, in and of itself, a behavioral health intervention. Good communication can serve to normalize experiences and function as an antidote to distress during times of uncertainty,” Dr. Morganstein said.
Importantly, “we need to remind people that eventually this will end and the vast majority of people, including those who have difficulties along the way, will ultimately be okay.”
The APA has provided a COVID-19 resource page on its website.
Dr. Morganstein and Dr. Schwartz have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM APA 2020
New study of diabetes drug for COVID-19 raises eyebrows
A just-launched study of the type 2 diabetes agent dapagliflozin (Farxiga, AstraZeneca) in patients with mild to moderate COVID-19 is raising eyebrows, given that several expert groups have advised that drugs in this class – the sodium-glucose cotransporter 2 (SGLT2) inhibitors – be stopped in all patients hospitalized with COVID-19 because of the increased risk for diabetic ketoacidosis (DKA).
The randomized, double-blind, placebo-controlled, phase 3 Dapagliflozin in Respiratory Failure in Patients With COVID-19 (DARE-19) study is sponsored by AstraZeneca and Saint Luke’s Mid America Heart Institute.
The trial will assess whether dapagliflozin reduces the risks of disease progression, clinical complications, and death because of COVID-19 in patients with type 2 diabetes, cardiovascular disease, and/or mild to moderate chronic kidney disease (CKD).
“Dapagliflozin has demonstrated cardio- and renal-protective benefits and improved outcomes in high-risk patients with type 2 diabetes, heart failure with reduced ejection fraction, and CKD,” said the principal investigator of DARE-19, Mikhail N. Kosiborod, MD, a cardiologist at Saint Luke’s Mid America Heart Institute, Kansas City, Mo.
And “patients with COVID-19 and underlying cardiometabolic disease appear to be at the highest risk of morbid complications,” he explained in an AstraZeneca statement.
“Through DARE-19, we hope to decrease the severity of illness, and prevent cardiovascular, respiratory, and kidney decompensation, which are common in patients with COVID-19,” Dr. Kosiborod continued.
However, advice to stop SGLT2 inhibitors in patients hospitalized with COVID-19 because of its associated DKA risk has come from several channels.
These include initial guidance from Diabetes UK; experts who spoke during an American Diabetes Association webinar; and most recently, an international panel of diabetes experts.
Some clinicians went so far as to say that they view the trial as potentially dangerous, while others said they could see some logic to it, as long as it is carefully managed.
“A dangerous proposition – a DARE I would not take”
Partha Kar, MD, of Portsmouth Hospitals NHS Trust and national clinical director of diabetes at NHS England, said in an interview: “It’s interesting to see [AstraZeneca] embark on a study with a particular class of drug whereby ... [in] the UK we have said that if you get sent to hospital with COVID-19 you should stop [SGLT2 inhibitors] immediately.”
It “sounds like a risky proposition to go ahead with, [and it] definitely made me raise an eyebrow,” he added.
Nephrologist Bruce R. Leslie, MD, of Seventh Doctor Consulting in Princeton, N.J., agreed with Dr. Kar.
“Giving SGLT2 inhibitors to patients in the DARE-19 study is a dangerous proposition because these drugs can induce ketoacidosis during the stress of acute illness such as COVID-19. ... Moreover, ketoacidosis is associated with hypercoagulability which could be especially dangerous in COVID-19, given that it has been causing thrombophilia with large-vessel occlusive strokes in young patients,” he said in an interview.
“One wonders how these risks were assessed by the authorities that approved the DARE-19 study,” said Dr. Leslie, who formerly worked for Bristol-Myers Squibb.
“How does the sponsor intend to secure informed consent given the risks? This is a DARE I would not take,” he said.
Asked to address these concerns, Dr. Kosiborod said in an interview that “the DARE-19 trial will assess both the efficacy and the safety of dapagliflozin in this patient population in a closely monitored environment of a rigorously designed randomized clinical trial. The trial protocol excludes patients with type 1 diabetes or at high risk for DKA.
“Furthermore, the protocol includes detailed specific instructions to ensure careful monitoring for DKA, including frequent assessments of acid-base status in the hospital setting. The safety data will be closely monitored by an independent data-monitoring committee,” he continued.
Dr. Kosiborod also pointed out that there is “no systematically collected information on the use of dapagliflozin or any other SGLT2 inhibitor in patients being treated for COVID-19, including the associated potential benefits, possible risks such as DKA, and the balance of these potential benefits and risks.”
DARE-19 design: Several outcomes will be examined
The DARE-19 trial is designed to enroll 900 adults with confirmed SARS-CoV-2 infection and oxygen saturation of 94% or greater.
Inclusion criteria include a medical history of hypertension, type 2 diabetes, atherosclerotic cardiovascular disease, heart failure, and/or stage 3-4 CKD. Exclusion criteria include current SGLT2 inhibitor treatment, type 1 diabetes, severe CKD, and severe COVID-19.
Dapagliflozin is approved in the EU for use in some patients with type 1 diabetes; this is not the case in the United States, although SGLT2 inhibitors in general are sometimes used off label in these patients.
Patients in DARE-19 will be randomized to 10 mg/day dapagliflozin or placebo for 30 days, in addition to standard care, in participating hospital. Primary outcomes are time to first occurrence of either death or new or worsened organ dysfunction, including respiratory decompensation, new or worsening heart failure, requirement for vasopressor therapy, ventricular tachycardia, and renal failure.
Secondary outcomes include a composite of time to death from any cause, time to new/worsened organ dysfunction, clinical status at day 30, and time to hospital discharge.
Rationale for the study
Irl B. Hirsch, MD, professor and diabetes treatment and teaching chair at the University of Washington, Seattle, said in an interview that he does see some logic to the trial.
Admitting that he doesn’t know much about “COVID-19 cardiomyopathy” – which would be one of the targets of dapagliflozin – other than it is quite common, he said that this, along with the potential renal benefits of dapagliflozin in the setting of COVID-19, make the study “intriguing.”
“Perhaps there is some rationale to it,” he said. However, “my concern is these sick COVID-19 patients are often acidemic, and besides the very complex acid-base challenges we see with intubated patients, these patients likely have combination lactic and ketoacidemia, the latter at least some from starvation.
“Still, if enough dextrose and insulin are provided to prevent ketoacid accumulation, my guess is it would do at least as well as hydroxychloroquine,” he said.
And Simon Heller, MD, professor of clinical diabetes at the University of Sheffield (England), said in an interview: “I think it is quite a brave study, mainly because of the increased risk of DKA.
“However, on the basis that these patients will be carefully monitored, the risk of DKA shouldn’t be great. I think it is important that patients with type 2 diabetes can participate whenever possible in such trials,” he said.
The estimated completion date for DARE-19 is December 2020.
Dr. Kosiborod has reported receiving grant support, honoraria, and/or research support from AstraZeneca, Boehringer Ingelheim, Sanofi, Amgen, Novo Nordisk, Merck, Eisai, Janssen, Bayer, GlaxoSmithKline, Glytec, Intarcia Therapeutics, Novartis, Applied Therapeutics, Amarin, and Eli Lilly. Dr. Leslie has reported owning stock in Bristol-Myers Squibb, Pfizer, and Lilly. Dr. Hirsch has reported consulting for Abbott Diabetes Care, Roche, and Bigfoot Biomedical, conducting research for Medtronic, and is a diabetes editor for UpToDate. Dr. Heller has received advisory or consultation fees from Lilly, Novo Nordisk, Takeda, MSD, and Becton Dickinson; has served as a speaker for AstraZeneca, Lilly, Novo Nordisk, Boehringer Ingelheim, and Takeda; and has received research support from Medtronic UK. He is on the advisory board for Medscape. Dr. Kar has reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A just-launched study of the type 2 diabetes agent dapagliflozin (Farxiga, AstraZeneca) in patients with mild to moderate COVID-19 is raising eyebrows, given that several expert groups have advised that drugs in this class – the sodium-glucose cotransporter 2 (SGLT2) inhibitors – be stopped in all patients hospitalized with COVID-19 because of the increased risk for diabetic ketoacidosis (DKA).
The randomized, double-blind, placebo-controlled, phase 3 Dapagliflozin in Respiratory Failure in Patients With COVID-19 (DARE-19) study is sponsored by AstraZeneca and Saint Luke’s Mid America Heart Institute.
The trial will assess whether dapagliflozin reduces the risks of disease progression, clinical complications, and death because of COVID-19 in patients with type 2 diabetes, cardiovascular disease, and/or mild to moderate chronic kidney disease (CKD).
“Dapagliflozin has demonstrated cardio- and renal-protective benefits and improved outcomes in high-risk patients with type 2 diabetes, heart failure with reduced ejection fraction, and CKD,” said the principal investigator of DARE-19, Mikhail N. Kosiborod, MD, a cardiologist at Saint Luke’s Mid America Heart Institute, Kansas City, Mo.
And “patients with COVID-19 and underlying cardiometabolic disease appear to be at the highest risk of morbid complications,” he explained in an AstraZeneca statement.
“Through DARE-19, we hope to decrease the severity of illness, and prevent cardiovascular, respiratory, and kidney decompensation, which are common in patients with COVID-19,” Dr. Kosiborod continued.
However, advice to stop SGLT2 inhibitors in patients hospitalized with COVID-19 because of its associated DKA risk has come from several channels.
These include initial guidance from Diabetes UK; experts who spoke during an American Diabetes Association webinar; and most recently, an international panel of diabetes experts.
Some clinicians went so far as to say that they view the trial as potentially dangerous, while others said they could see some logic to it, as long as it is carefully managed.
“A dangerous proposition – a DARE I would not take”
Partha Kar, MD, of Portsmouth Hospitals NHS Trust and national clinical director of diabetes at NHS England, said in an interview: “It’s interesting to see [AstraZeneca] embark on a study with a particular class of drug whereby ... [in] the UK we have said that if you get sent to hospital with COVID-19 you should stop [SGLT2 inhibitors] immediately.”
It “sounds like a risky proposition to go ahead with, [and it] definitely made me raise an eyebrow,” he added.
Nephrologist Bruce R. Leslie, MD, of Seventh Doctor Consulting in Princeton, N.J., agreed with Dr. Kar.
“Giving SGLT2 inhibitors to patients in the DARE-19 study is a dangerous proposition because these drugs can induce ketoacidosis during the stress of acute illness such as COVID-19. ... Moreover, ketoacidosis is associated with hypercoagulability which could be especially dangerous in COVID-19, given that it has been causing thrombophilia with large-vessel occlusive strokes in young patients,” he said in an interview.
“One wonders how these risks were assessed by the authorities that approved the DARE-19 study,” said Dr. Leslie, who formerly worked for Bristol-Myers Squibb.
“How does the sponsor intend to secure informed consent given the risks? This is a DARE I would not take,” he said.
Asked to address these concerns, Dr. Kosiborod said in an interview that “the DARE-19 trial will assess both the efficacy and the safety of dapagliflozin in this patient population in a closely monitored environment of a rigorously designed randomized clinical trial. The trial protocol excludes patients with type 1 diabetes or at high risk for DKA.
“Furthermore, the protocol includes detailed specific instructions to ensure careful monitoring for DKA, including frequent assessments of acid-base status in the hospital setting. The safety data will be closely monitored by an independent data-monitoring committee,” he continued.
Dr. Kosiborod also pointed out that there is “no systematically collected information on the use of dapagliflozin or any other SGLT2 inhibitor in patients being treated for COVID-19, including the associated potential benefits, possible risks such as DKA, and the balance of these potential benefits and risks.”
DARE-19 design: Several outcomes will be examined
The DARE-19 trial is designed to enroll 900 adults with confirmed SARS-CoV-2 infection and oxygen saturation of 94% or greater.
Inclusion criteria include a medical history of hypertension, type 2 diabetes, atherosclerotic cardiovascular disease, heart failure, and/or stage 3-4 CKD. Exclusion criteria include current SGLT2 inhibitor treatment, type 1 diabetes, severe CKD, and severe COVID-19.
Dapagliflozin is approved in the EU for use in some patients with type 1 diabetes; this is not the case in the United States, although SGLT2 inhibitors in general are sometimes used off label in these patients.
Patients in DARE-19 will be randomized to 10 mg/day dapagliflozin or placebo for 30 days, in addition to standard care, in participating hospital. Primary outcomes are time to first occurrence of either death or new or worsened organ dysfunction, including respiratory decompensation, new or worsening heart failure, requirement for vasopressor therapy, ventricular tachycardia, and renal failure.
Secondary outcomes include a composite of time to death from any cause, time to new/worsened organ dysfunction, clinical status at day 30, and time to hospital discharge.
Rationale for the study
Irl B. Hirsch, MD, professor and diabetes treatment and teaching chair at the University of Washington, Seattle, said in an interview that he does see some logic to the trial.
Admitting that he doesn’t know much about “COVID-19 cardiomyopathy” – which would be one of the targets of dapagliflozin – other than it is quite common, he said that this, along with the potential renal benefits of dapagliflozin in the setting of COVID-19, make the study “intriguing.”
“Perhaps there is some rationale to it,” he said. However, “my concern is these sick COVID-19 patients are often acidemic, and besides the very complex acid-base challenges we see with intubated patients, these patients likely have combination lactic and ketoacidemia, the latter at least some from starvation.
“Still, if enough dextrose and insulin are provided to prevent ketoacid accumulation, my guess is it would do at least as well as hydroxychloroquine,” he said.
And Simon Heller, MD, professor of clinical diabetes at the University of Sheffield (England), said in an interview: “I think it is quite a brave study, mainly because of the increased risk of DKA.
“However, on the basis that these patients will be carefully monitored, the risk of DKA shouldn’t be great. I think it is important that patients with type 2 diabetes can participate whenever possible in such trials,” he said.
The estimated completion date for DARE-19 is December 2020.
Dr. Kosiborod has reported receiving grant support, honoraria, and/or research support from AstraZeneca, Boehringer Ingelheim, Sanofi, Amgen, Novo Nordisk, Merck, Eisai, Janssen, Bayer, GlaxoSmithKline, Glytec, Intarcia Therapeutics, Novartis, Applied Therapeutics, Amarin, and Eli Lilly. Dr. Leslie has reported owning stock in Bristol-Myers Squibb, Pfizer, and Lilly. Dr. Hirsch has reported consulting for Abbott Diabetes Care, Roche, and Bigfoot Biomedical, conducting research for Medtronic, and is a diabetes editor for UpToDate. Dr. Heller has received advisory or consultation fees from Lilly, Novo Nordisk, Takeda, MSD, and Becton Dickinson; has served as a speaker for AstraZeneca, Lilly, Novo Nordisk, Boehringer Ingelheim, and Takeda; and has received research support from Medtronic UK. He is on the advisory board for Medscape. Dr. Kar has reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A just-launched study of the type 2 diabetes agent dapagliflozin (Farxiga, AstraZeneca) in patients with mild to moderate COVID-19 is raising eyebrows, given that several expert groups have advised that drugs in this class – the sodium-glucose cotransporter 2 (SGLT2) inhibitors – be stopped in all patients hospitalized with COVID-19 because of the increased risk for diabetic ketoacidosis (DKA).
The randomized, double-blind, placebo-controlled, phase 3 Dapagliflozin in Respiratory Failure in Patients With COVID-19 (DARE-19) study is sponsored by AstraZeneca and Saint Luke’s Mid America Heart Institute.
The trial will assess whether dapagliflozin reduces the risks of disease progression, clinical complications, and death because of COVID-19 in patients with type 2 diabetes, cardiovascular disease, and/or mild to moderate chronic kidney disease (CKD).
“Dapagliflozin has demonstrated cardio- and renal-protective benefits and improved outcomes in high-risk patients with type 2 diabetes, heart failure with reduced ejection fraction, and CKD,” said the principal investigator of DARE-19, Mikhail N. Kosiborod, MD, a cardiologist at Saint Luke’s Mid America Heart Institute, Kansas City, Mo.
And “patients with COVID-19 and underlying cardiometabolic disease appear to be at the highest risk of morbid complications,” he explained in an AstraZeneca statement.
“Through DARE-19, we hope to decrease the severity of illness, and prevent cardiovascular, respiratory, and kidney decompensation, which are common in patients with COVID-19,” Dr. Kosiborod continued.
However, advice to stop SGLT2 inhibitors in patients hospitalized with COVID-19 because of its associated DKA risk has come from several channels.
These include initial guidance from Diabetes UK; experts who spoke during an American Diabetes Association webinar; and most recently, an international panel of diabetes experts.
Some clinicians went so far as to say that they view the trial as potentially dangerous, while others said they could see some logic to it, as long as it is carefully managed.
“A dangerous proposition – a DARE I would not take”
Partha Kar, MD, of Portsmouth Hospitals NHS Trust and national clinical director of diabetes at NHS England, said in an interview: “It’s interesting to see [AstraZeneca] embark on a study with a particular class of drug whereby ... [in] the UK we have said that if you get sent to hospital with COVID-19 you should stop [SGLT2 inhibitors] immediately.”
It “sounds like a risky proposition to go ahead with, [and it] definitely made me raise an eyebrow,” he added.
Nephrologist Bruce R. Leslie, MD, of Seventh Doctor Consulting in Princeton, N.J., agreed with Dr. Kar.
“Giving SGLT2 inhibitors to patients in the DARE-19 study is a dangerous proposition because these drugs can induce ketoacidosis during the stress of acute illness such as COVID-19. ... Moreover, ketoacidosis is associated with hypercoagulability which could be especially dangerous in COVID-19, given that it has been causing thrombophilia with large-vessel occlusive strokes in young patients,” he said in an interview.
“One wonders how these risks were assessed by the authorities that approved the DARE-19 study,” said Dr. Leslie, who formerly worked for Bristol-Myers Squibb.
“How does the sponsor intend to secure informed consent given the risks? This is a DARE I would not take,” he said.
Asked to address these concerns, Dr. Kosiborod said in an interview that “the DARE-19 trial will assess both the efficacy and the safety of dapagliflozin in this patient population in a closely monitored environment of a rigorously designed randomized clinical trial. The trial protocol excludes patients with type 1 diabetes or at high risk for DKA.
“Furthermore, the protocol includes detailed specific instructions to ensure careful monitoring for DKA, including frequent assessments of acid-base status in the hospital setting. The safety data will be closely monitored by an independent data-monitoring committee,” he continued.
Dr. Kosiborod also pointed out that there is “no systematically collected information on the use of dapagliflozin or any other SGLT2 inhibitor in patients being treated for COVID-19, including the associated potential benefits, possible risks such as DKA, and the balance of these potential benefits and risks.”
DARE-19 design: Several outcomes will be examined
The DARE-19 trial is designed to enroll 900 adults with confirmed SARS-CoV-2 infection and oxygen saturation of 94% or greater.
Inclusion criteria include a medical history of hypertension, type 2 diabetes, atherosclerotic cardiovascular disease, heart failure, and/or stage 3-4 CKD. Exclusion criteria include current SGLT2 inhibitor treatment, type 1 diabetes, severe CKD, and severe COVID-19.
Dapagliflozin is approved in the EU for use in some patients with type 1 diabetes; this is not the case in the United States, although SGLT2 inhibitors in general are sometimes used off label in these patients.
Patients in DARE-19 will be randomized to 10 mg/day dapagliflozin or placebo for 30 days, in addition to standard care, in participating hospital. Primary outcomes are time to first occurrence of either death or new or worsened organ dysfunction, including respiratory decompensation, new or worsening heart failure, requirement for vasopressor therapy, ventricular tachycardia, and renal failure.
Secondary outcomes include a composite of time to death from any cause, time to new/worsened organ dysfunction, clinical status at day 30, and time to hospital discharge.
Rationale for the study
Irl B. Hirsch, MD, professor and diabetes treatment and teaching chair at the University of Washington, Seattle, said in an interview that he does see some logic to the trial.
Admitting that he doesn’t know much about “COVID-19 cardiomyopathy” – which would be one of the targets of dapagliflozin – other than it is quite common, he said that this, along with the potential renal benefits of dapagliflozin in the setting of COVID-19, make the study “intriguing.”
“Perhaps there is some rationale to it,” he said. However, “my concern is these sick COVID-19 patients are often acidemic, and besides the very complex acid-base challenges we see with intubated patients, these patients likely have combination lactic and ketoacidemia, the latter at least some from starvation.
“Still, if enough dextrose and insulin are provided to prevent ketoacid accumulation, my guess is it would do at least as well as hydroxychloroquine,” he said.
And Simon Heller, MD, professor of clinical diabetes at the University of Sheffield (England), said in an interview: “I think it is quite a brave study, mainly because of the increased risk of DKA.
“However, on the basis that these patients will be carefully monitored, the risk of DKA shouldn’t be great. I think it is important that patients with type 2 diabetes can participate whenever possible in such trials,” he said.
The estimated completion date for DARE-19 is December 2020.
Dr. Kosiborod has reported receiving grant support, honoraria, and/or research support from AstraZeneca, Boehringer Ingelheim, Sanofi, Amgen, Novo Nordisk, Merck, Eisai, Janssen, Bayer, GlaxoSmithKline, Glytec, Intarcia Therapeutics, Novartis, Applied Therapeutics, Amarin, and Eli Lilly. Dr. Leslie has reported owning stock in Bristol-Myers Squibb, Pfizer, and Lilly. Dr. Hirsch has reported consulting for Abbott Diabetes Care, Roche, and Bigfoot Biomedical, conducting research for Medtronic, and is a diabetes editor for UpToDate. Dr. Heller has received advisory or consultation fees from Lilly, Novo Nordisk, Takeda, MSD, and Becton Dickinson; has served as a speaker for AstraZeneca, Lilly, Novo Nordisk, Boehringer Ingelheim, and Takeda; and has received research support from Medtronic UK. He is on the advisory board for Medscape. Dr. Kar has reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Case series suggests biologics, JAK inhibitors safe during pandemic
Use of biologics and Janus kinase (JAK) inhibitors was not associated with worse outcomes in 86 people with inflammatory diseases who contracted COVID-19, according to a case series from New York University Langone Health.
“We are not seeing worse outcomes with overall use of either. It’s reassuring” that the data support continued use during the pandemic, said rheumatologist and senior investigator Jose Scher, MD, an associate professor at New York University.
There have been concerns among rheumatologists, gastroenterologists, and dermatologists that underlying inflammatory diseases and the agents used to treat them would impact outcomes in COVID-19.
Dr. Scher and colleagues, including lead author and rheumatologist Rebecca Haberman, MD, wanted to address the issue, so they reviewed the experience in their own health system of patients with inflammatory diseases – most commonly psoriatic arthritis, RA, and Crohn’s disease – who were assessed for COVID-19 from March 3 to April 3.
Fever, cough, and shortness of breath were the most common symptoms. The infection was confirmed by polymerase chain reaction in 59 (69%) and highly suspected in 27.
A total of 62 patients (72%) were on JAK inhibitors or biologics at baseline, including 38 (44%) on tumor necrosis factor inhibitors.
Overall, 14 patients (16%) were hospitalized with COVID-19, which is consistent the 26% hospitalization rate among the general population in New York City.
Baseline biologic and JAK inhibitor use was actually lower among hospitalized patients than among those who weren’t hospitalized (50% vs. 76%), and the hospitalization rate was only 11% among 62 subjects who had been on the agents long term, more than a year among most.
Hospitalized patients tended to be slightly older (mean, 50 vs. 46 years) with a higher prevalence of hypertension, diabetes, and chronic obstructive pulmonary disease. They also had a higher prevalence of RA (43% vs. 19%), methotrexate use (43% vs. 15%), and use of hydroxychloroquine (21% vs. 7%) and oral glucocorticoids (29% vs. 6%).
It’s unknown what to make of those findings for now, Dr. Scher said. The study didn’t address differences in the severity of the underlying inflammatory illness, but a new and significantly larger case series is in the works that will analyze that and other potential confounders.
Dr. Scher noted that he’s particularly interested in drilling down further on the higher prevalence of RA and methotrexate in hospitalized patients. “We want to understand those signals better. All of this needs further validation,” he said.
Of the 14 hospitalized patients, 11 (79%) were discharged after a mean of 5.6 days. One died in the ED, and two remained hospitalized as of April 3, including one in the ICU.
The investigators are contributing to COVID-19 registries for inflammatory disease patients. The registries are tending to report higher hospitalization rates, but Dr. Scher noted they might be biased towards more severe cases, among other issues.
As for the current situation in New York City, he said that the “last week in March and first 3 in April were indescribable in terms of admissions, intubations, and deaths. Over the last week or so, it has calmed down significantly.”
There was no external funding. Dr. Haberman reported ties to Janssen, and Dr. Scher reported ties to Janssen, Novartis, Pfizer, and other companies.
SOURCE: Haberman R et al. N Engl J Med. 2020 Apr 29. doi: 10.1056/NEJMc2009567.
Use of biologics and Janus kinase (JAK) inhibitors was not associated with worse outcomes in 86 people with inflammatory diseases who contracted COVID-19, according to a case series from New York University Langone Health.
“We are not seeing worse outcomes with overall use of either. It’s reassuring” that the data support continued use during the pandemic, said rheumatologist and senior investigator Jose Scher, MD, an associate professor at New York University.
There have been concerns among rheumatologists, gastroenterologists, and dermatologists that underlying inflammatory diseases and the agents used to treat them would impact outcomes in COVID-19.
Dr. Scher and colleagues, including lead author and rheumatologist Rebecca Haberman, MD, wanted to address the issue, so they reviewed the experience in their own health system of patients with inflammatory diseases – most commonly psoriatic arthritis, RA, and Crohn’s disease – who were assessed for COVID-19 from March 3 to April 3.
Fever, cough, and shortness of breath were the most common symptoms. The infection was confirmed by polymerase chain reaction in 59 (69%) and highly suspected in 27.
A total of 62 patients (72%) were on JAK inhibitors or biologics at baseline, including 38 (44%) on tumor necrosis factor inhibitors.
Overall, 14 patients (16%) were hospitalized with COVID-19, which is consistent the 26% hospitalization rate among the general population in New York City.
Baseline biologic and JAK inhibitor use was actually lower among hospitalized patients than among those who weren’t hospitalized (50% vs. 76%), and the hospitalization rate was only 11% among 62 subjects who had been on the agents long term, more than a year among most.
Hospitalized patients tended to be slightly older (mean, 50 vs. 46 years) with a higher prevalence of hypertension, diabetes, and chronic obstructive pulmonary disease. They also had a higher prevalence of RA (43% vs. 19%), methotrexate use (43% vs. 15%), and use of hydroxychloroquine (21% vs. 7%) and oral glucocorticoids (29% vs. 6%).
It’s unknown what to make of those findings for now, Dr. Scher said. The study didn’t address differences in the severity of the underlying inflammatory illness, but a new and significantly larger case series is in the works that will analyze that and other potential confounders.
Dr. Scher noted that he’s particularly interested in drilling down further on the higher prevalence of RA and methotrexate in hospitalized patients. “We want to understand those signals better. All of this needs further validation,” he said.
Of the 14 hospitalized patients, 11 (79%) were discharged after a mean of 5.6 days. One died in the ED, and two remained hospitalized as of April 3, including one in the ICU.
The investigators are contributing to COVID-19 registries for inflammatory disease patients. The registries are tending to report higher hospitalization rates, but Dr. Scher noted they might be biased towards more severe cases, among other issues.
As for the current situation in New York City, he said that the “last week in March and first 3 in April were indescribable in terms of admissions, intubations, and deaths. Over the last week or so, it has calmed down significantly.”
There was no external funding. Dr. Haberman reported ties to Janssen, and Dr. Scher reported ties to Janssen, Novartis, Pfizer, and other companies.
SOURCE: Haberman R et al. N Engl J Med. 2020 Apr 29. doi: 10.1056/NEJMc2009567.
Use of biologics and Janus kinase (JAK) inhibitors was not associated with worse outcomes in 86 people with inflammatory diseases who contracted COVID-19, according to a case series from New York University Langone Health.
“We are not seeing worse outcomes with overall use of either. It’s reassuring” that the data support continued use during the pandemic, said rheumatologist and senior investigator Jose Scher, MD, an associate professor at New York University.
There have been concerns among rheumatologists, gastroenterologists, and dermatologists that underlying inflammatory diseases and the agents used to treat them would impact outcomes in COVID-19.
Dr. Scher and colleagues, including lead author and rheumatologist Rebecca Haberman, MD, wanted to address the issue, so they reviewed the experience in their own health system of patients with inflammatory diseases – most commonly psoriatic arthritis, RA, and Crohn’s disease – who were assessed for COVID-19 from March 3 to April 3.
Fever, cough, and shortness of breath were the most common symptoms. The infection was confirmed by polymerase chain reaction in 59 (69%) and highly suspected in 27.
A total of 62 patients (72%) were on JAK inhibitors or biologics at baseline, including 38 (44%) on tumor necrosis factor inhibitors.
Overall, 14 patients (16%) were hospitalized with COVID-19, which is consistent the 26% hospitalization rate among the general population in New York City.
Baseline biologic and JAK inhibitor use was actually lower among hospitalized patients than among those who weren’t hospitalized (50% vs. 76%), and the hospitalization rate was only 11% among 62 subjects who had been on the agents long term, more than a year among most.
Hospitalized patients tended to be slightly older (mean, 50 vs. 46 years) with a higher prevalence of hypertension, diabetes, and chronic obstructive pulmonary disease. They also had a higher prevalence of RA (43% vs. 19%), methotrexate use (43% vs. 15%), and use of hydroxychloroquine (21% vs. 7%) and oral glucocorticoids (29% vs. 6%).
It’s unknown what to make of those findings for now, Dr. Scher said. The study didn’t address differences in the severity of the underlying inflammatory illness, but a new and significantly larger case series is in the works that will analyze that and other potential confounders.
Dr. Scher noted that he’s particularly interested in drilling down further on the higher prevalence of RA and methotrexate in hospitalized patients. “We want to understand those signals better. All of this needs further validation,” he said.
Of the 14 hospitalized patients, 11 (79%) were discharged after a mean of 5.6 days. One died in the ED, and two remained hospitalized as of April 3, including one in the ICU.
The investigators are contributing to COVID-19 registries for inflammatory disease patients. The registries are tending to report higher hospitalization rates, but Dr. Scher noted they might be biased towards more severe cases, among other issues.
As for the current situation in New York City, he said that the “last week in March and first 3 in April were indescribable in terms of admissions, intubations, and deaths. Over the last week or so, it has calmed down significantly.”
There was no external funding. Dr. Haberman reported ties to Janssen, and Dr. Scher reported ties to Janssen, Novartis, Pfizer, and other companies.
SOURCE: Haberman R et al. N Engl J Med. 2020 Apr 29. doi: 10.1056/NEJMc2009567.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Antitumor treatment may increase risk of severe events in COVID-19 patients
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
FROM AACR 2020
Yale’s COVID-19 inpatient protocol: Hydroxychloroquine plus/minus tocilizumab
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
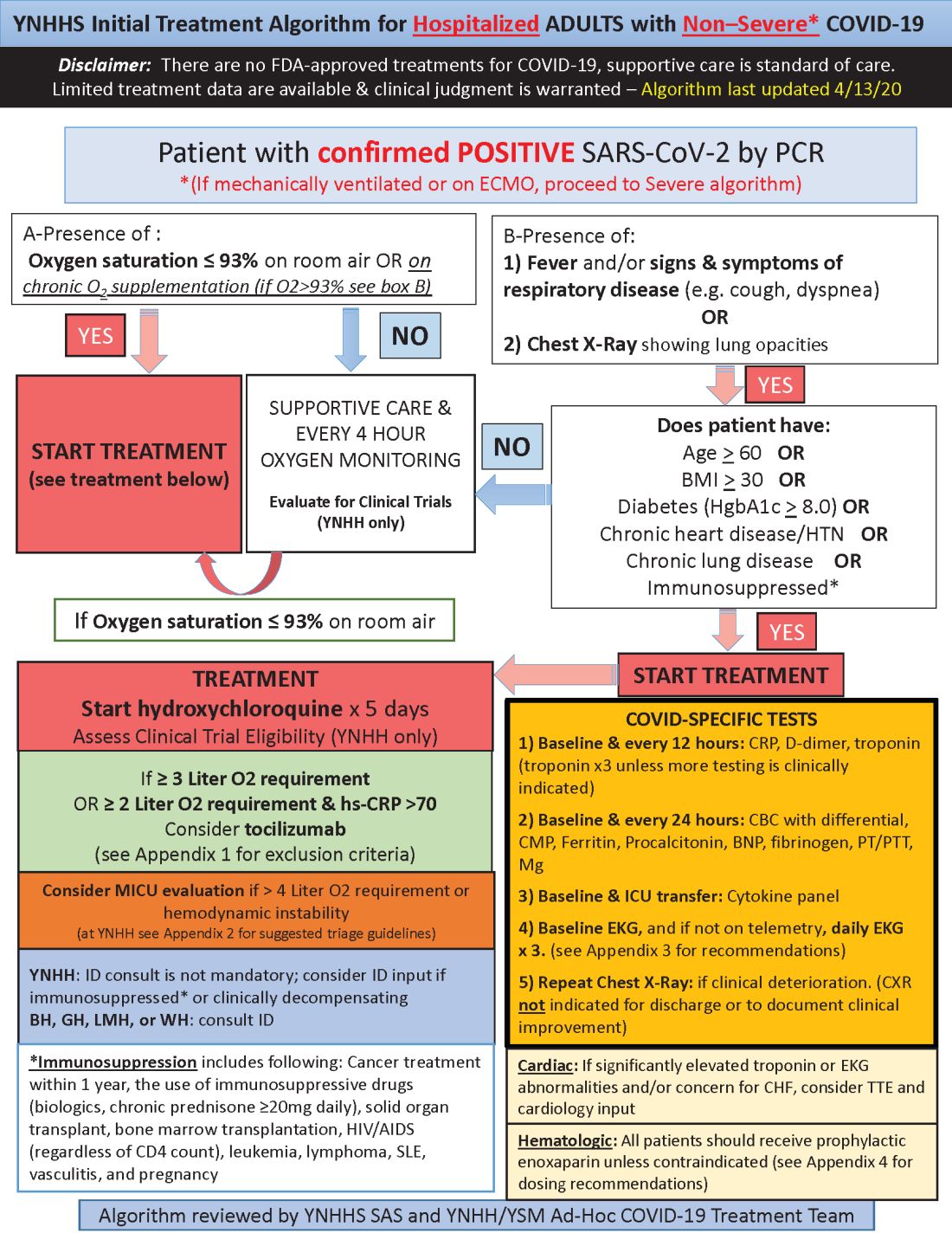
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
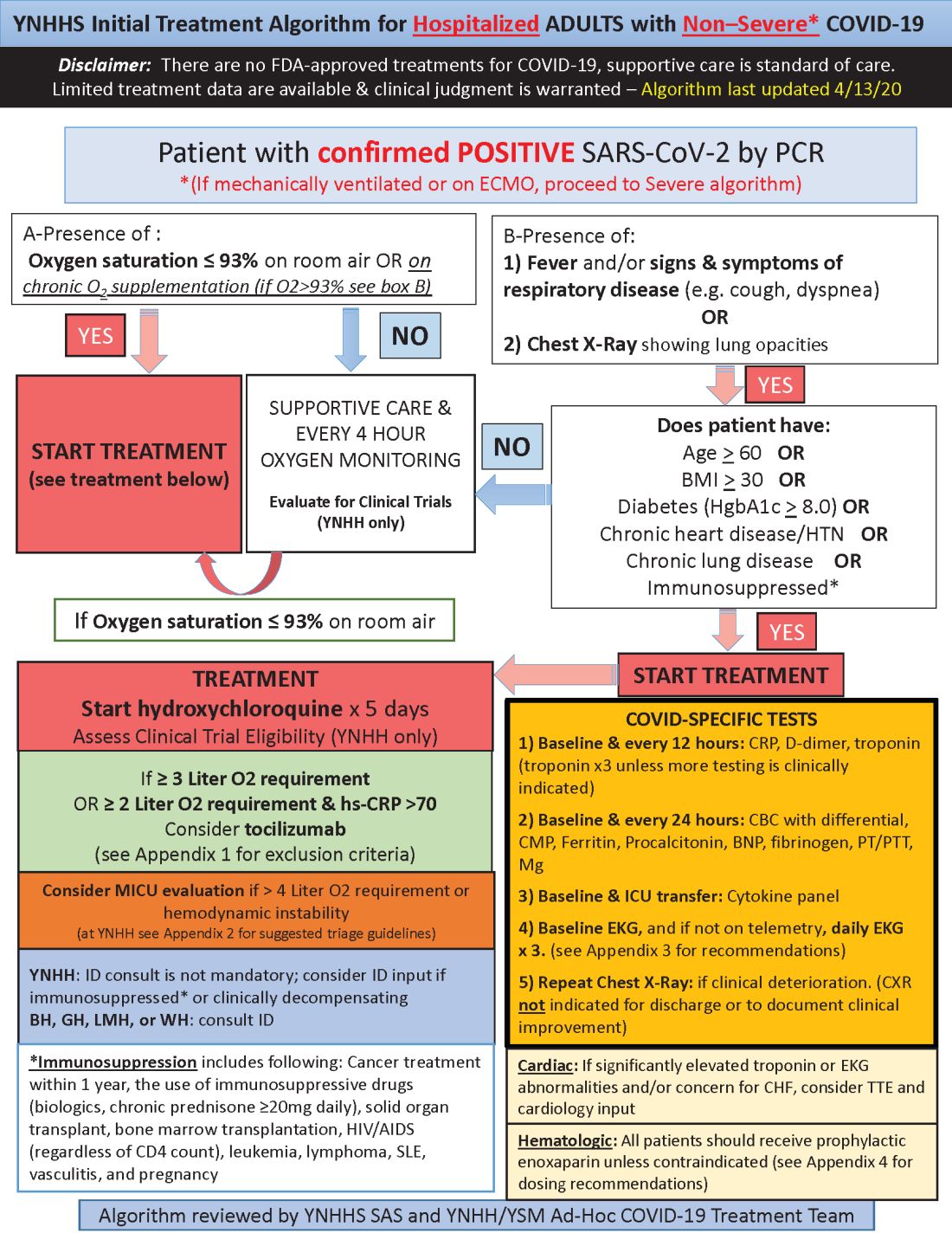
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
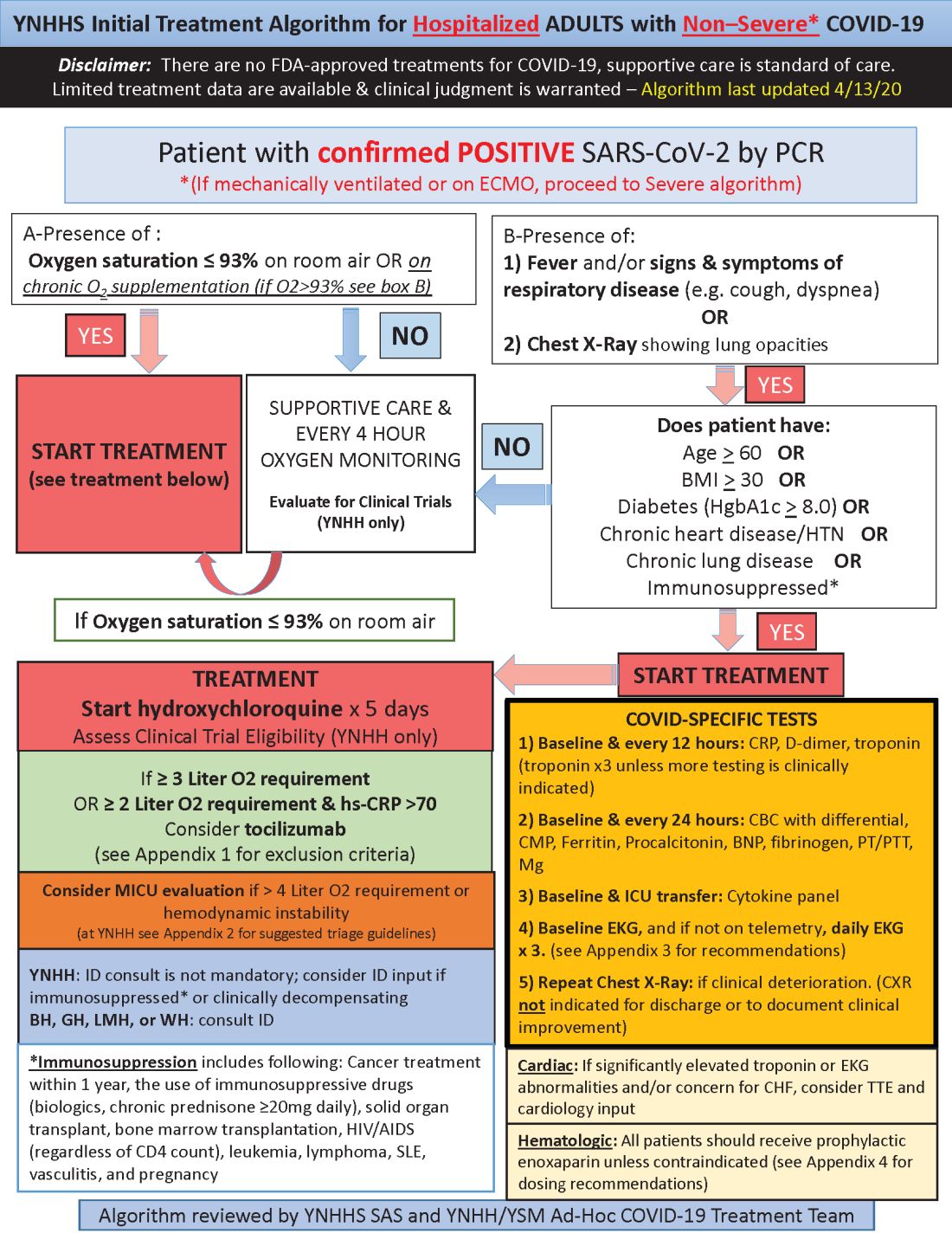
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.














