User login
High CV risk factor burden in young adults a ‘smoldering’ crisis
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New data show a high and rising burden of most cardiovascular (CV) risk factors among young adults aged 20-44 years in the United States.
In this age group, over the past 10 years, there has been an increase in the prevalence of diabetes and obesity, no improvement in the prevalence of hypertension, and a decrease in the prevalence of hyperlipidemia.
Yet medical treatment rates for CV risk factors are “surprisingly” low among young adults, study investigator Rishi Wadhera, MD, with Beth Israel Deaconess Medical Center and Harvard Medical School, both in Boston, told this news organization.
The findings are “extremely concerning. We’re witnessing a smoldering public health crisis. The onset of these risk factors earlier in life is associated with a higher lifetime risk of heart disease and potentially life-threatening,” Dr. Wadhera added.
The study was presented March 5 at the joint scientific sessions of the American College of Cardiology and the World Heart Federation and was simultaneously published in JAMA.
The burden of CV risk factors among young adults is “unacceptably high and increasing,” write the co-authors of a JAMA editorial.
“The time is now for aggressive preventive measures in young adults. Without immediate action there will continue to be a rise in heart disease and the burden it places on patients, families, and communities,” say Norrina Allen, PhD, and John Wilkins, MD, with Northwestern University, Chicago.
Preventing a tsunami of heart disease
The findings stem from a cross-sectional study of 12,294 U.S. adults aged 20-44 years (mean age, 32; 51% women) who participated in National Health and Nutrition Examination Survey (NHANES) cycles for 2009-2010 to 2017-2020.
Overall, the prevalence of hypertension was 9.3% in 2009-2010 and increased to 11.5% in 2017-2020. The prevalence of diabetes rose from 3.0% to 4.1%, and the prevalence of obesity rose from 32.7% to 40.9%. The prevalence of hyperlipidemia decreased from 40.5% to 36.1%.
Black adults consistently had high rates of hypertension during the study period – 16.2% in 2009-2010 and 20.1% in 2017-2020 – and significant increases in hypertension occurred among Mexican American adults (from 6.5% to 9.5%) and other Hispanic adults (from 4.4% to 10.5%), while Mexican American adults had a significant uptick in diabetes (from 4.3% to 7.5%).
Equally concerning, said Dr. Wadhera, is the fact that only about 55% of young adults with hypertension were receiving antihypertensive medication, and just 1 in 2 young adults with diabetes were receiving treatment. “These low rates were driven, in part, by many young adults not being aware of their diagnosis,” he noted.
The NHANES data also show that the percentage of young adults who were treated for hypertension and who achieved blood pressure control did not change significantly over the study period (65.0% in 2009-2010 and 74.8% in 2017-2020). Blood sugar control among young adults being treated for diabetes remained suboptimal throughout the study period (45.5% in 2009-2010 and 56.6% in 2017-2020).
“The fact that blood pressure control and glycemic control are so poor is really worrisome,” Jeffrey Berger, MD, director of the Center for the Prevention of Cardiovascular Disease at NYU Langone Heart, who wasn’t involved in the study, told this news organization.
“Even in the lipid control, while it did get a little bit better, it’s still only around 30%-40%. So, I think we have ways to go as a society,” Dr. Berger noted.
Double down on screening
Dr. Wadhera said “we need to double down on efforts to screen for and treat cardiovascular risk factors like high blood pressure and diabetes in young adults. We need to intensify clinical and public health interventions focused on primordial and primary prevention in young adults now so that we can avoid a tsunami of cardiovascular disease in the long term.”
“It’s critically important that young adults speak with their health care provider about whether – and when – they should undergo screening for high blood pressure, diabetes, and high cholesterol,” Dr. Wadhera added.
Dr. Berger said one problem is that younger people often have a “superman or superwoman” view and don’t comprehend that they are at risk for some of these conditions. Studies such as this “reinforce the idea that it’s never too young to be checked out.”
As a cardiologist who specializes in cardiovascular prevention, Dr. Berger said he sometimes hears patients say things like, “I don’t ever want to need a cardiologist,” or “I hope I never need a cardiologist.”
“My response is, ‘There are many different types of cardiologists,’ and I think it would really be helpful for many people to see a prevention-focused cardiologist way before they have problems,” he said in an interview.
“As a system, medicine has become very good at treating patients with different diseases. I think we need to get better in terms of preventing some of these problems,” Dr. Berger added.
In their editorial, Dr. Allen and Dr. Wilkins say the “foundation of cardiovascular health begins early in life. These worsening trends in risk factors highlight the importance of focusing on prevention in adolescence and young adulthood in order to promote cardiovascular health across the lifetime.”
The study was funded by a grant from the National Heart, Lung, and Blood Institute. Dr. Wadhera has served as a consultant for Abbott and CVS Health. Dr. Wilkins has received personal fees from 3M. Dr. Berger has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACC 2023
COORDINATEd effort boosts optimal therapy in patients with T2D and ASCVD
NEW ORLEANS – Twenty cardiology clinics successfully intensified the medical care they gave patients with type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) after receiving a simple and scalable investigational intervention that gave the clinics’ staffs guidance on best prescribing practices and implementation and also provided quality-improvement feedback.
Within a year, these clinics quadrupled optimal medical management of these patients, compared with control clinics, in a randomized trial involving a total of 43 clinics and 1,049 patients.
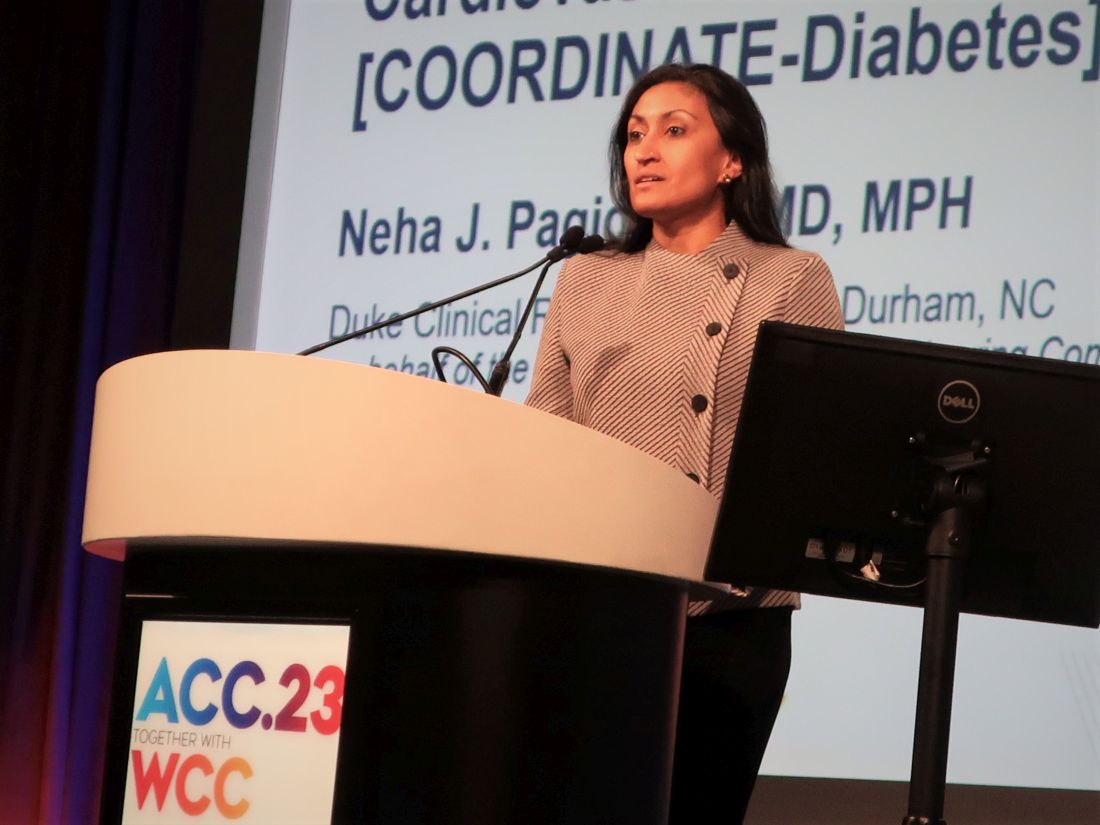
“This multifaceted intervention is effective in increasing the prescription of evidence-based therapies in adults with T2D and ASCVD,” Neha J. Pagidipati, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
“The next step is to scale this intervention across cardiology practices” interested in improving the quality of care they deliver to these patients, added Dr. Pagidipati, a cardiologist specializing in cardiometabolic disease prevention at Duke University in Durham, N.C.
The goal is getting patients on triple therapy
The primary outcome of the COORDINATE-Diabetes trial was the change in the number of patients with T2D and ASCVD who received prescriptions for agents from three recommended medication classes and at recommended dosages: a high-intensity statin, a renin-angiotensin system inhibitor (RASi), and at least one agent from either of two classes that have both cardiovascular-protective and antihyperglycemic effects: the sodium-glucose cotransporter 2 (SGLT2) inhibitors, or the glucagonlike peptide 1 (GLP-1)–receptor agonists.
Among the 457 patients treated at the 20 cardiology clinics who received the quality-improvement intervention, 37.9% were on the promoted triple therapy after 12 months, compared with 14.5% of the 588 patients treated at the 23 clinics that continued with their usual care approach. This 23.4–percentage point increase in triple-class prescribing at recommended dosages represented a significant 4.4-fold increase in the goal prescribing endpoint after adjustment for possible confounders, Dr. Pagidipati reported.
Simultaneously with her report, the findings also appeared online in JAMA.
At baseline, 41%-50% of the patients were on both a high-intensity statin and a RASi, with a total of about 58%-67% on a high-intensity statin and about 70%-75% on a RASi. Fewer than 1% of patients were on SGLT2 inhibitors or GLP-1–receptor agonists at baseline. By design, no patient could be on all three categories of medication at baseline.
At their last follow-up visit (after 12 months for 97% of patients, or after 6 months for the remainder) 71% of the patients at practices that received the intervention were on a high-intensity statin, 81% were taking a RASi, and 60% were on an SGLT2 inhibitor or GLP-1–receptor agonist. Among the control patients, 58% were on a high-intensity statin, 68% on a RASi, and 36% were on one of the antihyperglycemic agents.
Effective interventions and the need for a champion
The clinics randomized to the active arm received instruction from a three-member team, either from an in-person or virtual one-time visit, on an intervention comprising several initiatives:
- Analysis of the barriers to evidence-based care at each clinic.
- Development of local interdisciplinary care pathways to address the identified barriers.
- Facilitation of care coordination among clinicians – particularly among cardiology, endocrinology, and primary care clinicians.
- Education of the clinic staff, including provision of educational materials.
- Auditing of clinic performance using specified metrics and feedback on the findings.
Clinics in the usual care group were given current clinical practice guidelines.
The investigational intervention was, by design, “low-tech and designed to be scalable,” explained Dr. Pagidipati, and once the COVID pandemic started the intervention team shifted to a virtual consultation with participating practices that was mostly front-loaded, followed by monthly phone calls to give clinics feedback on their progress.
Among the most helpful aspects of the intervention was involving the entire clinic staff, including pharmacists, nurses, and advanced care practitioners; boosting familiarity with the relevant medications and their appropriate use; and advice on navigating insurance-coverage barriers such as prior authorizations.
“What was most critical was having a local champion who took on making this effort an important part” of what the clinic was trying to do, she explained. “All it takes is passion, and the tenacity of a bulldog,” Dr. Pagidipati said.
Research advances often don’t translate into management changes
“We don’t do a great job of translating findings from trials to patient care, so any method we can use to improve that will improve practice,” commented Kristen B. Campbell, PharmD, a clinical pharmacist at Duke who was not involved in the study.
“Although the trial was not powered to look at patient outcomes, we think that patients will benefit” because all the recommended medication uses have been proven to help patients in prior trials, Dr. Campbell noted.
“A particular strength of this study was its simple design. All the interventions are low-tech and scalable.”
The low level of use of guideline-directed medical therapy in American adults with type 2 diabetes and atherosclerotic cardiovascular disease is “incredible,” said Christopher B. Granger, MD, a senior investigator on the study and a cardiologist and professor at Duke.
The researchers who ran the study are now focused on evaluating which cardiology clinics and patients had the most success from the intervention and are using that information to further refine implementation. They are also planning to encourage cardiology practices as well as other relevant medical groups to incorporate the intervention and implementation model used in the trial. The intervention program is detailed and available at no charge on the COORDINATE-Diabetes website.
COORDINATE-Diabetes received funding from Boehringer Ingelheim and Eli Lilly. Dr. Pagidipati has received personal fees from Boehringer Ingelheim, Lilly, AstraZeneca, Novartis, Novo Nordisk, Merck, and CRISPR Therapeutics, and she has received research grants from Amgen, Novartis, Novo Nordisk, and Eggland’s Best. Dr. Campbell had no disclosures. Dr. Granger has received personal fees and research funding from numerous companies.
NEW ORLEANS – Twenty cardiology clinics successfully intensified the medical care they gave patients with type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) after receiving a simple and scalable investigational intervention that gave the clinics’ staffs guidance on best prescribing practices and implementation and also provided quality-improvement feedback.
Within a year, these clinics quadrupled optimal medical management of these patients, compared with control clinics, in a randomized trial involving a total of 43 clinics and 1,049 patients.
“This multifaceted intervention is effective in increasing the prescription of evidence-based therapies in adults with T2D and ASCVD,” Neha J. Pagidipati, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
“The next step is to scale this intervention across cardiology practices” interested in improving the quality of care they deliver to these patients, added Dr. Pagidipati, a cardiologist specializing in cardiometabolic disease prevention at Duke University in Durham, N.C.
The goal is getting patients on triple therapy
The primary outcome of the COORDINATE-Diabetes trial was the change in the number of patients with T2D and ASCVD who received prescriptions for agents from three recommended medication classes and at recommended dosages: a high-intensity statin, a renin-angiotensin system inhibitor (RASi), and at least one agent from either of two classes that have both cardiovascular-protective and antihyperglycemic effects: the sodium-glucose cotransporter 2 (SGLT2) inhibitors, or the glucagonlike peptide 1 (GLP-1)–receptor agonists.
Among the 457 patients treated at the 20 cardiology clinics who received the quality-improvement intervention, 37.9% were on the promoted triple therapy after 12 months, compared with 14.5% of the 588 patients treated at the 23 clinics that continued with their usual care approach. This 23.4–percentage point increase in triple-class prescribing at recommended dosages represented a significant 4.4-fold increase in the goal prescribing endpoint after adjustment for possible confounders, Dr. Pagidipati reported.
Simultaneously with her report, the findings also appeared online in JAMA.
At baseline, 41%-50% of the patients were on both a high-intensity statin and a RASi, with a total of about 58%-67% on a high-intensity statin and about 70%-75% on a RASi. Fewer than 1% of patients were on SGLT2 inhibitors or GLP-1–receptor agonists at baseline. By design, no patient could be on all three categories of medication at baseline.
At their last follow-up visit (after 12 months for 97% of patients, or after 6 months for the remainder) 71% of the patients at practices that received the intervention were on a high-intensity statin, 81% were taking a RASi, and 60% were on an SGLT2 inhibitor or GLP-1–receptor agonist. Among the control patients, 58% were on a high-intensity statin, 68% on a RASi, and 36% were on one of the antihyperglycemic agents.
Effective interventions and the need for a champion
The clinics randomized to the active arm received instruction from a three-member team, either from an in-person or virtual one-time visit, on an intervention comprising several initiatives:
- Analysis of the barriers to evidence-based care at each clinic.
- Development of local interdisciplinary care pathways to address the identified barriers.
- Facilitation of care coordination among clinicians – particularly among cardiology, endocrinology, and primary care clinicians.
- Education of the clinic staff, including provision of educational materials.
- Auditing of clinic performance using specified metrics and feedback on the findings.
Clinics in the usual care group were given current clinical practice guidelines.
The investigational intervention was, by design, “low-tech and designed to be scalable,” explained Dr. Pagidipati, and once the COVID pandemic started the intervention team shifted to a virtual consultation with participating practices that was mostly front-loaded, followed by monthly phone calls to give clinics feedback on their progress.
Among the most helpful aspects of the intervention was involving the entire clinic staff, including pharmacists, nurses, and advanced care practitioners; boosting familiarity with the relevant medications and their appropriate use; and advice on navigating insurance-coverage barriers such as prior authorizations.
“What was most critical was having a local champion who took on making this effort an important part” of what the clinic was trying to do, she explained. “All it takes is passion, and the tenacity of a bulldog,” Dr. Pagidipati said.
Research advances often don’t translate into management changes
“We don’t do a great job of translating findings from trials to patient care, so any method we can use to improve that will improve practice,” commented Kristen B. Campbell, PharmD, a clinical pharmacist at Duke who was not involved in the study.
“Although the trial was not powered to look at patient outcomes, we think that patients will benefit” because all the recommended medication uses have been proven to help patients in prior trials, Dr. Campbell noted.
“A particular strength of this study was its simple design. All the interventions are low-tech and scalable.”
The low level of use of guideline-directed medical therapy in American adults with type 2 diabetes and atherosclerotic cardiovascular disease is “incredible,” said Christopher B. Granger, MD, a senior investigator on the study and a cardiologist and professor at Duke.
The researchers who ran the study are now focused on evaluating which cardiology clinics and patients had the most success from the intervention and are using that information to further refine implementation. They are also planning to encourage cardiology practices as well as other relevant medical groups to incorporate the intervention and implementation model used in the trial. The intervention program is detailed and available at no charge on the COORDINATE-Diabetes website.
COORDINATE-Diabetes received funding from Boehringer Ingelheim and Eli Lilly. Dr. Pagidipati has received personal fees from Boehringer Ingelheim, Lilly, AstraZeneca, Novartis, Novo Nordisk, Merck, and CRISPR Therapeutics, and she has received research grants from Amgen, Novartis, Novo Nordisk, and Eggland’s Best. Dr. Campbell had no disclosures. Dr. Granger has received personal fees and research funding from numerous companies.
NEW ORLEANS – Twenty cardiology clinics successfully intensified the medical care they gave patients with type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) after receiving a simple and scalable investigational intervention that gave the clinics’ staffs guidance on best prescribing practices and implementation and also provided quality-improvement feedback.
Within a year, these clinics quadrupled optimal medical management of these patients, compared with control clinics, in a randomized trial involving a total of 43 clinics and 1,049 patients.
“This multifaceted intervention is effective in increasing the prescription of evidence-based therapies in adults with T2D and ASCVD,” Neha J. Pagidipati, MD, said at the joint scientific sessions of the American College of Cardiology and the World Heart Federation.
“The next step is to scale this intervention across cardiology practices” interested in improving the quality of care they deliver to these patients, added Dr. Pagidipati, a cardiologist specializing in cardiometabolic disease prevention at Duke University in Durham, N.C.
The goal is getting patients on triple therapy
The primary outcome of the COORDINATE-Diabetes trial was the change in the number of patients with T2D and ASCVD who received prescriptions for agents from three recommended medication classes and at recommended dosages: a high-intensity statin, a renin-angiotensin system inhibitor (RASi), and at least one agent from either of two classes that have both cardiovascular-protective and antihyperglycemic effects: the sodium-glucose cotransporter 2 (SGLT2) inhibitors, or the glucagonlike peptide 1 (GLP-1)–receptor agonists.
Among the 457 patients treated at the 20 cardiology clinics who received the quality-improvement intervention, 37.9% were on the promoted triple therapy after 12 months, compared with 14.5% of the 588 patients treated at the 23 clinics that continued with their usual care approach. This 23.4–percentage point increase in triple-class prescribing at recommended dosages represented a significant 4.4-fold increase in the goal prescribing endpoint after adjustment for possible confounders, Dr. Pagidipati reported.
Simultaneously with her report, the findings also appeared online in JAMA.
At baseline, 41%-50% of the patients were on both a high-intensity statin and a RASi, with a total of about 58%-67% on a high-intensity statin and about 70%-75% on a RASi. Fewer than 1% of patients were on SGLT2 inhibitors or GLP-1–receptor agonists at baseline. By design, no patient could be on all three categories of medication at baseline.
At their last follow-up visit (after 12 months for 97% of patients, or after 6 months for the remainder) 71% of the patients at practices that received the intervention were on a high-intensity statin, 81% were taking a RASi, and 60% were on an SGLT2 inhibitor or GLP-1–receptor agonist. Among the control patients, 58% were on a high-intensity statin, 68% on a RASi, and 36% were on one of the antihyperglycemic agents.
Effective interventions and the need for a champion
The clinics randomized to the active arm received instruction from a three-member team, either from an in-person or virtual one-time visit, on an intervention comprising several initiatives:
- Analysis of the barriers to evidence-based care at each clinic.
- Development of local interdisciplinary care pathways to address the identified barriers.
- Facilitation of care coordination among clinicians – particularly among cardiology, endocrinology, and primary care clinicians.
- Education of the clinic staff, including provision of educational materials.
- Auditing of clinic performance using specified metrics and feedback on the findings.
Clinics in the usual care group were given current clinical practice guidelines.
The investigational intervention was, by design, “low-tech and designed to be scalable,” explained Dr. Pagidipati, and once the COVID pandemic started the intervention team shifted to a virtual consultation with participating practices that was mostly front-loaded, followed by monthly phone calls to give clinics feedback on their progress.
Among the most helpful aspects of the intervention was involving the entire clinic staff, including pharmacists, nurses, and advanced care practitioners; boosting familiarity with the relevant medications and their appropriate use; and advice on navigating insurance-coverage barriers such as prior authorizations.
“What was most critical was having a local champion who took on making this effort an important part” of what the clinic was trying to do, she explained. “All it takes is passion, and the tenacity of a bulldog,” Dr. Pagidipati said.
Research advances often don’t translate into management changes
“We don’t do a great job of translating findings from trials to patient care, so any method we can use to improve that will improve practice,” commented Kristen B. Campbell, PharmD, a clinical pharmacist at Duke who was not involved in the study.
“Although the trial was not powered to look at patient outcomes, we think that patients will benefit” because all the recommended medication uses have been proven to help patients in prior trials, Dr. Campbell noted.
“A particular strength of this study was its simple design. All the interventions are low-tech and scalable.”
The low level of use of guideline-directed medical therapy in American adults with type 2 diabetes and atherosclerotic cardiovascular disease is “incredible,” said Christopher B. Granger, MD, a senior investigator on the study and a cardiologist and professor at Duke.
The researchers who ran the study are now focused on evaluating which cardiology clinics and patients had the most success from the intervention and are using that information to further refine implementation. They are also planning to encourage cardiology practices as well as other relevant medical groups to incorporate the intervention and implementation model used in the trial. The intervention program is detailed and available at no charge on the COORDINATE-Diabetes website.
COORDINATE-Diabetes received funding from Boehringer Ingelheim and Eli Lilly. Dr. Pagidipati has received personal fees from Boehringer Ingelheim, Lilly, AstraZeneca, Novartis, Novo Nordisk, Merck, and CRISPR Therapeutics, and she has received research grants from Amgen, Novartis, Novo Nordisk, and Eggland’s Best. Dr. Campbell had no disclosures. Dr. Granger has received personal fees and research funding from numerous companies.
AT ACC 2023
Biomarkers linked to elevated T2D MACE risk in DECLARE-TIMI 58
The researchers found that N-terminal pro-B-type natriuretic peptide (NT-proBNP) and high-sensitivity cardiac troponin T (hsTnT) levels helped identify a subset of T2D patients at higher risk of major adverse cardiovascular events who would benefit most from dapagliflozin.
“We’ve shown previously that these two biomarkers are very robust risk indicators for cardiovascular death and heart failure events,” senior study author David A. Morrow, MD, of Harvard University, Boston, said in an interview. “In this study, we now show that the two biomarkers also yield important prognostic information for MACE [major adverse cardiovascular events].”
Although NT-proBNP is typically measured to diagnose heart failure, and hsTnT to diagnose acute MI, Dr. Morrow pointed out that this analysis demonstrated the potential for using the two tests to evaluate risks in T2D patients.
Study results
The secondary analysis included 14,565 patients in the DECLARE-TIMI 58 trial. The patients had T2D and multiple risk factors for atherosclerotic cardiovascular disease (about 60%) or established ASCVD (about 40%). All patients had available blood samples and the data were collected from May 2013 to September 2018. The primary outcome was MACE, a composite of MI, ischemic stroke, and cardiovascular death. The results were reported online in JAMA Cardiology.
The analysis found that higher baseline concentrations of NT-proBNP increased MACE risks by 62% (95% confidence interval, 1.49-1.76) and hsTnT elevated those risks by 59% (95% CI, 1.46-1.74).
Among placebo patients, when divided into risk quartiles, those in the highest quartile had significantly higher risk with both elevated NT-proBNP and hsTnT, compared with those with low concentrations. For example, patients with established ASCVD had a 22.9% risk vs. 9.5% with elevated NT-proBNP (P < .001) and a 24.2% vs. 7.2% risk with elevated hsTnT (P < .001). The gap was similar for patients with multiple risk factors.
Dr. Morrow noted that the main DECLARE-TIMI 58 trial showed that dapagliflozin reduced the rates of cardiovascular death or hospitalization for heart failure in patients with T2D, when compared to placebo, but didn’t reach statistical significance for MACE (N Engl J Med. 2019;380:347-57).
“We have previously shown that among patients with T2D who have high risk indicators, such as prior MI or long-standing diabetes, dapagliflozin also appeared to reduce MACE,” Dr. Morrow said. “In this study, we find that these two widely available biomarkers also identify a high-risk group who may have even more potential benefits from treatment with an SGLT2i.”
Dr. Morrow noted that the study design – a nested prospective biomarker study within a randomized, double-blind, placebo-controlled clinical trial – “is a particular strength.”
Results clarify which patients will benefit
This secondary analysis of DECLARE-TIMI 58 brings more clarity to the types of T2D patients who will get the most cardiovascular benefits from dapagliflozin, said Matthew J. Budoff, MD, professor of medicine at University of California, Los Angeles, and Endowed Chair of Preventive Cardiology at the Lundquist Institute in Torrance, Calif.
“The big picture is, we’ve known for some time from epidemiologic studies that these biomarkers, when they’re elevated, mean that the patient is at higher risk of having a cardiovascular event,” he said, “but I think what it helps us with is in knowing in whom to use dapagliflozin for prevention of ASCVD. The effect in the DECLARE-TIMI 58 trial was quite modest, but if you can subgroup it, in these high-risk people there’s a more profound effect. It helps in risk stratification because the absolute benefit is larger.”
The specific biomarkers, NT-proBNP and hsTnT, “haven’t been explored very much in clinical trials,” Dr. Budoff said, “so I do think that it’s nice that in a randomized trial it plays out the way we might expect.”
He added that “for many clinicians this is novel, because I don’t think they were aware of the biomarker data, so I think that this does add some clinical benefit in that context.” The findings also strengthen the case to get T2D patients with higher ASCVD risk onto SGLT2 inhibitors if they’re not already, he said.
Dr. Morrow disclosed relationships with AstraZeneca, Roche Diagnostics, Abbott Laboratories, Anthos Therapeutics, ARCA Biopharma, Merck, Novartis, Pfizer, Regeneron, Siemens, and InCarda outside the reported work.
Dr. Budoff has no relevant disclosures.
The researchers found that N-terminal pro-B-type natriuretic peptide (NT-proBNP) and high-sensitivity cardiac troponin T (hsTnT) levels helped identify a subset of T2D patients at higher risk of major adverse cardiovascular events who would benefit most from dapagliflozin.
“We’ve shown previously that these two biomarkers are very robust risk indicators for cardiovascular death and heart failure events,” senior study author David A. Morrow, MD, of Harvard University, Boston, said in an interview. “In this study, we now show that the two biomarkers also yield important prognostic information for MACE [major adverse cardiovascular events].”
Although NT-proBNP is typically measured to diagnose heart failure, and hsTnT to diagnose acute MI, Dr. Morrow pointed out that this analysis demonstrated the potential for using the two tests to evaluate risks in T2D patients.
Study results
The secondary analysis included 14,565 patients in the DECLARE-TIMI 58 trial. The patients had T2D and multiple risk factors for atherosclerotic cardiovascular disease (about 60%) or established ASCVD (about 40%). All patients had available blood samples and the data were collected from May 2013 to September 2018. The primary outcome was MACE, a composite of MI, ischemic stroke, and cardiovascular death. The results were reported online in JAMA Cardiology.
The analysis found that higher baseline concentrations of NT-proBNP increased MACE risks by 62% (95% confidence interval, 1.49-1.76) and hsTnT elevated those risks by 59% (95% CI, 1.46-1.74).
Among placebo patients, when divided into risk quartiles, those in the highest quartile had significantly higher risk with both elevated NT-proBNP and hsTnT, compared with those with low concentrations. For example, patients with established ASCVD had a 22.9% risk vs. 9.5% with elevated NT-proBNP (P < .001) and a 24.2% vs. 7.2% risk with elevated hsTnT (P < .001). The gap was similar for patients with multiple risk factors.
Dr. Morrow noted that the main DECLARE-TIMI 58 trial showed that dapagliflozin reduced the rates of cardiovascular death or hospitalization for heart failure in patients with T2D, when compared to placebo, but didn’t reach statistical significance for MACE (N Engl J Med. 2019;380:347-57).
“We have previously shown that among patients with T2D who have high risk indicators, such as prior MI or long-standing diabetes, dapagliflozin also appeared to reduce MACE,” Dr. Morrow said. “In this study, we find that these two widely available biomarkers also identify a high-risk group who may have even more potential benefits from treatment with an SGLT2i.”
Dr. Morrow noted that the study design – a nested prospective biomarker study within a randomized, double-blind, placebo-controlled clinical trial – “is a particular strength.”
Results clarify which patients will benefit
This secondary analysis of DECLARE-TIMI 58 brings more clarity to the types of T2D patients who will get the most cardiovascular benefits from dapagliflozin, said Matthew J. Budoff, MD, professor of medicine at University of California, Los Angeles, and Endowed Chair of Preventive Cardiology at the Lundquist Institute in Torrance, Calif.
“The big picture is, we’ve known for some time from epidemiologic studies that these biomarkers, when they’re elevated, mean that the patient is at higher risk of having a cardiovascular event,” he said, “but I think what it helps us with is in knowing in whom to use dapagliflozin for prevention of ASCVD. The effect in the DECLARE-TIMI 58 trial was quite modest, but if you can subgroup it, in these high-risk people there’s a more profound effect. It helps in risk stratification because the absolute benefit is larger.”
The specific biomarkers, NT-proBNP and hsTnT, “haven’t been explored very much in clinical trials,” Dr. Budoff said, “so I do think that it’s nice that in a randomized trial it plays out the way we might expect.”
He added that “for many clinicians this is novel, because I don’t think they were aware of the biomarker data, so I think that this does add some clinical benefit in that context.” The findings also strengthen the case to get T2D patients with higher ASCVD risk onto SGLT2 inhibitors if they’re not already, he said.
Dr. Morrow disclosed relationships with AstraZeneca, Roche Diagnostics, Abbott Laboratories, Anthos Therapeutics, ARCA Biopharma, Merck, Novartis, Pfizer, Regeneron, Siemens, and InCarda outside the reported work.
Dr. Budoff has no relevant disclosures.
The researchers found that N-terminal pro-B-type natriuretic peptide (NT-proBNP) and high-sensitivity cardiac troponin T (hsTnT) levels helped identify a subset of T2D patients at higher risk of major adverse cardiovascular events who would benefit most from dapagliflozin.
“We’ve shown previously that these two biomarkers are very robust risk indicators for cardiovascular death and heart failure events,” senior study author David A. Morrow, MD, of Harvard University, Boston, said in an interview. “In this study, we now show that the two biomarkers also yield important prognostic information for MACE [major adverse cardiovascular events].”
Although NT-proBNP is typically measured to diagnose heart failure, and hsTnT to diagnose acute MI, Dr. Morrow pointed out that this analysis demonstrated the potential for using the two tests to evaluate risks in T2D patients.
Study results
The secondary analysis included 14,565 patients in the DECLARE-TIMI 58 trial. The patients had T2D and multiple risk factors for atherosclerotic cardiovascular disease (about 60%) or established ASCVD (about 40%). All patients had available blood samples and the data were collected from May 2013 to September 2018. The primary outcome was MACE, a composite of MI, ischemic stroke, and cardiovascular death. The results were reported online in JAMA Cardiology.
The analysis found that higher baseline concentrations of NT-proBNP increased MACE risks by 62% (95% confidence interval, 1.49-1.76) and hsTnT elevated those risks by 59% (95% CI, 1.46-1.74).
Among placebo patients, when divided into risk quartiles, those in the highest quartile had significantly higher risk with both elevated NT-proBNP and hsTnT, compared with those with low concentrations. For example, patients with established ASCVD had a 22.9% risk vs. 9.5% with elevated NT-proBNP (P < .001) and a 24.2% vs. 7.2% risk with elevated hsTnT (P < .001). The gap was similar for patients with multiple risk factors.
Dr. Morrow noted that the main DECLARE-TIMI 58 trial showed that dapagliflozin reduced the rates of cardiovascular death or hospitalization for heart failure in patients with T2D, when compared to placebo, but didn’t reach statistical significance for MACE (N Engl J Med. 2019;380:347-57).
“We have previously shown that among patients with T2D who have high risk indicators, such as prior MI or long-standing diabetes, dapagliflozin also appeared to reduce MACE,” Dr. Morrow said. “In this study, we find that these two widely available biomarkers also identify a high-risk group who may have even more potential benefits from treatment with an SGLT2i.”
Dr. Morrow noted that the study design – a nested prospective biomarker study within a randomized, double-blind, placebo-controlled clinical trial – “is a particular strength.”
Results clarify which patients will benefit
This secondary analysis of DECLARE-TIMI 58 brings more clarity to the types of T2D patients who will get the most cardiovascular benefits from dapagliflozin, said Matthew J. Budoff, MD, professor of medicine at University of California, Los Angeles, and Endowed Chair of Preventive Cardiology at the Lundquist Institute in Torrance, Calif.
“The big picture is, we’ve known for some time from epidemiologic studies that these biomarkers, when they’re elevated, mean that the patient is at higher risk of having a cardiovascular event,” he said, “but I think what it helps us with is in knowing in whom to use dapagliflozin for prevention of ASCVD. The effect in the DECLARE-TIMI 58 trial was quite modest, but if you can subgroup it, in these high-risk people there’s a more profound effect. It helps in risk stratification because the absolute benefit is larger.”
The specific biomarkers, NT-proBNP and hsTnT, “haven’t been explored very much in clinical trials,” Dr. Budoff said, “so I do think that it’s nice that in a randomized trial it plays out the way we might expect.”
He added that “for many clinicians this is novel, because I don’t think they were aware of the biomarker data, so I think that this does add some clinical benefit in that context.” The findings also strengthen the case to get T2D patients with higher ASCVD risk onto SGLT2 inhibitors if they’re not already, he said.
Dr. Morrow disclosed relationships with AstraZeneca, Roche Diagnostics, Abbott Laboratories, Anthos Therapeutics, ARCA Biopharma, Merck, Novartis, Pfizer, Regeneron, Siemens, and InCarda outside the reported work.
Dr. Budoff has no relevant disclosures.
FROM JAMA CARDIOLOGY
Lilly cuts insulin price by 70%, caps out-of-pocket cost
Eli Lilly will cut prices for most of its insulins in the United States by 70% and cap out-of-pocket costs for insulin at $35 per month, the company announced on March 1.
“Lilly is taking these actions to make it easier to access Lilly insulin and help Americans who may have difficulty navigating a complex healthcare system that may keep them from getting affordable insulin,” the company said in a statement.
The $35 price cap is effective immediately at participating retail pharmacies for people with commercial insurance. Those without insurance can go to InsulinAffordability.com and download the Lilly Insulin Value Program savings card to receive Lilly insulins for $35 per month.
The company says it will cut the list price of its nonbranded Insulin Lispro Injection 100 units/mL to $25 a vial, effective May 1, 2023. The list price of the branded Humalog (insulin lispro injection) 100 units/mL will be cut by 70%, effective in the fourth quarter of 2023.
Lilly is among the three main companies that manufacture insulin, along with Novo Nordisk and Sanofi, that have come under fire over the cost of insulin in the US. Studies have shown that up to 25% of people with type 1 diabetes ration insulin because of costs, putting their health and often their lives in jeopardy.
Prices in the United States are around 10 times higher than in other countries. California is the latest state to say it plans to sue these big three companies over the high price of insulin and has announced plans to make its own cheaper versions.
Asked at a telephone press briefing if the lawsuit prompted the company’s move, Lilly chair and CEO David A. Ricks said: “Of course there are complaints against the industry and the company. We see those as completely unfounded. However, we can probably all agree that patients should have a consistent and lower-cost experience at the pharmacy counter, and that’s what today’s announcement is about. We’re doing this completely voluntarily because it’s time and it’s the right thing to do.”
On hearing the company announcement, Laura Nally, MD, a pediatric endocrinologist living with type 1 diabetes, @drnallypants, tweeted: “YES. After years of advocacy, the list price of Lispro/Humalog is now similar to what it was in the late 1990s. Cheers to all the #pwd [people with diabetes] who have advocated through #insulin4all! But we still have work to do to improve access to other diabetes medications & supplies.”
#insulin4all is a worldwide campaign to ensure that people with type 1 diabetes have access to affordable insulin and other supplies needed to manage the condition, such as glucose strips. It is supported, among others, by the advocacy group T1International.
Also giving his reaction to the Lilly announcement, Chuck Henderson, CEO of the American Diabetes Association, said: “We applaud Eli Lilly for taking the important step to limit cost-sharing for its insulin, and we encourage other insulin manufacturers to do the same.
“While we have been able to help achieve significant progress on the issue of insulin affordability, including Medicare’s new out-of-pocket cost cap on insulin, state copay caps, and patient assistance developments from insulin manufacturers, we know that our work is not done,” he added.
“ADA will work to ensure that Eli Lilly’s patient assistance program is benefiting patients as intended and continue the fight so that everyone who needs insulin has access.”
And Endocrine Society chief medical officer Robert Lash, MD, said: “Lilly’s move to apply a $35/month cap for people with private insurance will be a significant improvement for adults and children with diabetes who use Lilly’s products.
“We encourage all insulin manufacturers to join in the effort to reduce out-of-pocket costs for people who need insulin.”
Lilly will also launch a new insulin biosimilar, Rezvoglar (insulin glargine-aglr) injection, which is similar to and interchangeable with insulin glargine (Lantus). The cost will by $92 for a five pack of KwikPens, a 78% discount, compared with the cost of Lantus, beginning April 1, 2023.
A version of this article first appeared on Medscape.com.
Eli Lilly will cut prices for most of its insulins in the United States by 70% and cap out-of-pocket costs for insulin at $35 per month, the company announced on March 1.
“Lilly is taking these actions to make it easier to access Lilly insulin and help Americans who may have difficulty navigating a complex healthcare system that may keep them from getting affordable insulin,” the company said in a statement.
The $35 price cap is effective immediately at participating retail pharmacies for people with commercial insurance. Those without insurance can go to InsulinAffordability.com and download the Lilly Insulin Value Program savings card to receive Lilly insulins for $35 per month.
The company says it will cut the list price of its nonbranded Insulin Lispro Injection 100 units/mL to $25 a vial, effective May 1, 2023. The list price of the branded Humalog (insulin lispro injection) 100 units/mL will be cut by 70%, effective in the fourth quarter of 2023.
Lilly is among the three main companies that manufacture insulin, along with Novo Nordisk and Sanofi, that have come under fire over the cost of insulin in the US. Studies have shown that up to 25% of people with type 1 diabetes ration insulin because of costs, putting their health and often their lives in jeopardy.
Prices in the United States are around 10 times higher than in other countries. California is the latest state to say it plans to sue these big three companies over the high price of insulin and has announced plans to make its own cheaper versions.
Asked at a telephone press briefing if the lawsuit prompted the company’s move, Lilly chair and CEO David A. Ricks said: “Of course there are complaints against the industry and the company. We see those as completely unfounded. However, we can probably all agree that patients should have a consistent and lower-cost experience at the pharmacy counter, and that’s what today’s announcement is about. We’re doing this completely voluntarily because it’s time and it’s the right thing to do.”
On hearing the company announcement, Laura Nally, MD, a pediatric endocrinologist living with type 1 diabetes, @drnallypants, tweeted: “YES. After years of advocacy, the list price of Lispro/Humalog is now similar to what it was in the late 1990s. Cheers to all the #pwd [people with diabetes] who have advocated through #insulin4all! But we still have work to do to improve access to other diabetes medications & supplies.”
#insulin4all is a worldwide campaign to ensure that people with type 1 diabetes have access to affordable insulin and other supplies needed to manage the condition, such as glucose strips. It is supported, among others, by the advocacy group T1International.
Also giving his reaction to the Lilly announcement, Chuck Henderson, CEO of the American Diabetes Association, said: “We applaud Eli Lilly for taking the important step to limit cost-sharing for its insulin, and we encourage other insulin manufacturers to do the same.
“While we have been able to help achieve significant progress on the issue of insulin affordability, including Medicare’s new out-of-pocket cost cap on insulin, state copay caps, and patient assistance developments from insulin manufacturers, we know that our work is not done,” he added.
“ADA will work to ensure that Eli Lilly’s patient assistance program is benefiting patients as intended and continue the fight so that everyone who needs insulin has access.”
And Endocrine Society chief medical officer Robert Lash, MD, said: “Lilly’s move to apply a $35/month cap for people with private insurance will be a significant improvement for adults and children with diabetes who use Lilly’s products.
“We encourage all insulin manufacturers to join in the effort to reduce out-of-pocket costs for people who need insulin.”
Lilly will also launch a new insulin biosimilar, Rezvoglar (insulin glargine-aglr) injection, which is similar to and interchangeable with insulin glargine (Lantus). The cost will by $92 for a five pack of KwikPens, a 78% discount, compared with the cost of Lantus, beginning April 1, 2023.
A version of this article first appeared on Medscape.com.
Eli Lilly will cut prices for most of its insulins in the United States by 70% and cap out-of-pocket costs for insulin at $35 per month, the company announced on March 1.
“Lilly is taking these actions to make it easier to access Lilly insulin and help Americans who may have difficulty navigating a complex healthcare system that may keep them from getting affordable insulin,” the company said in a statement.
The $35 price cap is effective immediately at participating retail pharmacies for people with commercial insurance. Those without insurance can go to InsulinAffordability.com and download the Lilly Insulin Value Program savings card to receive Lilly insulins for $35 per month.
The company says it will cut the list price of its nonbranded Insulin Lispro Injection 100 units/mL to $25 a vial, effective May 1, 2023. The list price of the branded Humalog (insulin lispro injection) 100 units/mL will be cut by 70%, effective in the fourth quarter of 2023.
Lilly is among the three main companies that manufacture insulin, along with Novo Nordisk and Sanofi, that have come under fire over the cost of insulin in the US. Studies have shown that up to 25% of people with type 1 diabetes ration insulin because of costs, putting their health and often their lives in jeopardy.
Prices in the United States are around 10 times higher than in other countries. California is the latest state to say it plans to sue these big three companies over the high price of insulin and has announced plans to make its own cheaper versions.
Asked at a telephone press briefing if the lawsuit prompted the company’s move, Lilly chair and CEO David A. Ricks said: “Of course there are complaints against the industry and the company. We see those as completely unfounded. However, we can probably all agree that patients should have a consistent and lower-cost experience at the pharmacy counter, and that’s what today’s announcement is about. We’re doing this completely voluntarily because it’s time and it’s the right thing to do.”
On hearing the company announcement, Laura Nally, MD, a pediatric endocrinologist living with type 1 diabetes, @drnallypants, tweeted: “YES. After years of advocacy, the list price of Lispro/Humalog is now similar to what it was in the late 1990s. Cheers to all the #pwd [people with diabetes] who have advocated through #insulin4all! But we still have work to do to improve access to other diabetes medications & supplies.”
#insulin4all is a worldwide campaign to ensure that people with type 1 diabetes have access to affordable insulin and other supplies needed to manage the condition, such as glucose strips. It is supported, among others, by the advocacy group T1International.
Also giving his reaction to the Lilly announcement, Chuck Henderson, CEO of the American Diabetes Association, said: “We applaud Eli Lilly for taking the important step to limit cost-sharing for its insulin, and we encourage other insulin manufacturers to do the same.
“While we have been able to help achieve significant progress on the issue of insulin affordability, including Medicare’s new out-of-pocket cost cap on insulin, state copay caps, and patient assistance developments from insulin manufacturers, we know that our work is not done,” he added.
“ADA will work to ensure that Eli Lilly’s patient assistance program is benefiting patients as intended and continue the fight so that everyone who needs insulin has access.”
And Endocrine Society chief medical officer Robert Lash, MD, said: “Lilly’s move to apply a $35/month cap for people with private insurance will be a significant improvement for adults and children with diabetes who use Lilly’s products.
“We encourage all insulin manufacturers to join in the effort to reduce out-of-pocket costs for people who need insulin.”
Lilly will also launch a new insulin biosimilar, Rezvoglar (insulin glargine-aglr) injection, which is similar to and interchangeable with insulin glargine (Lantus). The cost will by $92 for a five pack of KwikPens, a 78% discount, compared with the cost of Lantus, beginning April 1, 2023.
A version of this article first appeared on Medscape.com.
Fewer than 10% of eligible type 2 diabetes patients get new, pricey drugs
Fewer than 10% of American adults with type 2 diabetes who qualified for treatment with newer agents – such as an SGLT2 inhibitor or GLP-1 agonist – actually received treatment with at least one drug from drug class in 2017-2020, based on a new analysis of just over a thousand adults who participated in a representative, biannual survey and self-reported a diabetes diagnosis.
The cost of these agents, and their uncertain cost-effectiveness at current prices, is likely a key driver of the low usage rate, say the authors of a brief report published in Annals of Internal Medicine.
“Clinical studies have shown that both GLP-1 [glucagonlike peptide–1] receptor agonists and SGLT2 [sodium-glucose cotransporter 2] inhibitors yield additional clinical benefits, compared with older treatments in reducing body weight and progression of cardiovascular disease and chronic kidney disease,” write Shichao Tang, PhD, from the U.S. Centers for Disease Control and Prevention, Atlanta, and colleagues.
“However, these medications come at a substantially higher cost,” they stress.
Dr. Tang explained in an interview that the new study “points to prior studies about the high cost of these medications as a potential barrier to use, but more research is needed to understand cost-effectiveness and any potential barriers to use, including cost.”
The work “did not include research into cost-effectiveness or why the percentage of people already using these medications was low,” he emphasized.
Dr. Tang and colleagues used data collected by the U.S. National Health and Nutrition Examination Survey during two 2-year cycles between 2017 and 2020 that included 1,417 people who self-identified a diagnosis of diabetes.
Excluding those who likely had type 1 diabetes and those with incomplete data left 1,330 survey participants, including 1,133 (85%) who fit criteria for the treatment of type 2 diabetes with an agent from one of the two studied classes, as recommended in 2022 by a panel representing the American Diabetes Association and the European Association for the Study of Diabetes.
Among these 1,133 people – who represent more than 22 million American adults with type 2 diabetes who fit the 2022 criteria – a scant 3.7% were actually taking a GLP-1 agonist and 5.3% were taking an SGLT2 inhibitor.
“While it’s important to note that our data predate the 2022 recommendations, these drugs were offered as second-line therapy for patients with certain diabetes-related complications in 2017-2020” and hence provide potentially useful insights, noted Dr. Tang, a health economist with the CDC National Center for Chronic Disease Prevention and Health Promotion.
Based on retail prices listed on a United States–based website, a 30-day supply of an oral SGLT2 inhibitor can cost about $550-$600 per month, while common subcutaneously injected GLP-1 receptor agonists can run from a few hundred dollars for a daily injection or close to $1,000 for a formulation administered weekly.
“Cost-effectiveness was not formally considered in the current guideline, but an assessment of cost-effectiveness may assist better targeting of interventions to achieve the greatest effect at a sustainable cost,” the researchers conclude.
The study received no commercial funding. None of the authors had relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Fewer than 10% of American adults with type 2 diabetes who qualified for treatment with newer agents – such as an SGLT2 inhibitor or GLP-1 agonist – actually received treatment with at least one drug from drug class in 2017-2020, based on a new analysis of just over a thousand adults who participated in a representative, biannual survey and self-reported a diabetes diagnosis.
The cost of these agents, and their uncertain cost-effectiveness at current prices, is likely a key driver of the low usage rate, say the authors of a brief report published in Annals of Internal Medicine.
“Clinical studies have shown that both GLP-1 [glucagonlike peptide–1] receptor agonists and SGLT2 [sodium-glucose cotransporter 2] inhibitors yield additional clinical benefits, compared with older treatments in reducing body weight and progression of cardiovascular disease and chronic kidney disease,” write Shichao Tang, PhD, from the U.S. Centers for Disease Control and Prevention, Atlanta, and colleagues.
“However, these medications come at a substantially higher cost,” they stress.
Dr. Tang explained in an interview that the new study “points to prior studies about the high cost of these medications as a potential barrier to use, but more research is needed to understand cost-effectiveness and any potential barriers to use, including cost.”
The work “did not include research into cost-effectiveness or why the percentage of people already using these medications was low,” he emphasized.
Dr. Tang and colleagues used data collected by the U.S. National Health and Nutrition Examination Survey during two 2-year cycles between 2017 and 2020 that included 1,417 people who self-identified a diagnosis of diabetes.
Excluding those who likely had type 1 diabetes and those with incomplete data left 1,330 survey participants, including 1,133 (85%) who fit criteria for the treatment of type 2 diabetes with an agent from one of the two studied classes, as recommended in 2022 by a panel representing the American Diabetes Association and the European Association for the Study of Diabetes.
Among these 1,133 people – who represent more than 22 million American adults with type 2 diabetes who fit the 2022 criteria – a scant 3.7% were actually taking a GLP-1 agonist and 5.3% were taking an SGLT2 inhibitor.
“While it’s important to note that our data predate the 2022 recommendations, these drugs were offered as second-line therapy for patients with certain diabetes-related complications in 2017-2020” and hence provide potentially useful insights, noted Dr. Tang, a health economist with the CDC National Center for Chronic Disease Prevention and Health Promotion.
Based on retail prices listed on a United States–based website, a 30-day supply of an oral SGLT2 inhibitor can cost about $550-$600 per month, while common subcutaneously injected GLP-1 receptor agonists can run from a few hundred dollars for a daily injection or close to $1,000 for a formulation administered weekly.
“Cost-effectiveness was not formally considered in the current guideline, but an assessment of cost-effectiveness may assist better targeting of interventions to achieve the greatest effect at a sustainable cost,” the researchers conclude.
The study received no commercial funding. None of the authors had relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Fewer than 10% of American adults with type 2 diabetes who qualified for treatment with newer agents – such as an SGLT2 inhibitor or GLP-1 agonist – actually received treatment with at least one drug from drug class in 2017-2020, based on a new analysis of just over a thousand adults who participated in a representative, biannual survey and self-reported a diabetes diagnosis.
The cost of these agents, and their uncertain cost-effectiveness at current prices, is likely a key driver of the low usage rate, say the authors of a brief report published in Annals of Internal Medicine.
“Clinical studies have shown that both GLP-1 [glucagonlike peptide–1] receptor agonists and SGLT2 [sodium-glucose cotransporter 2] inhibitors yield additional clinical benefits, compared with older treatments in reducing body weight and progression of cardiovascular disease and chronic kidney disease,” write Shichao Tang, PhD, from the U.S. Centers for Disease Control and Prevention, Atlanta, and colleagues.
“However, these medications come at a substantially higher cost,” they stress.
Dr. Tang explained in an interview that the new study “points to prior studies about the high cost of these medications as a potential barrier to use, but more research is needed to understand cost-effectiveness and any potential barriers to use, including cost.”
The work “did not include research into cost-effectiveness or why the percentage of people already using these medications was low,” he emphasized.
Dr. Tang and colleagues used data collected by the U.S. National Health and Nutrition Examination Survey during two 2-year cycles between 2017 and 2020 that included 1,417 people who self-identified a diagnosis of diabetes.
Excluding those who likely had type 1 diabetes and those with incomplete data left 1,330 survey participants, including 1,133 (85%) who fit criteria for the treatment of type 2 diabetes with an agent from one of the two studied classes, as recommended in 2022 by a panel representing the American Diabetes Association and the European Association for the Study of Diabetes.
Among these 1,133 people – who represent more than 22 million American adults with type 2 diabetes who fit the 2022 criteria – a scant 3.7% were actually taking a GLP-1 agonist and 5.3% were taking an SGLT2 inhibitor.
“While it’s important to note that our data predate the 2022 recommendations, these drugs were offered as second-line therapy for patients with certain diabetes-related complications in 2017-2020” and hence provide potentially useful insights, noted Dr. Tang, a health economist with the CDC National Center for Chronic Disease Prevention and Health Promotion.
Based on retail prices listed on a United States–based website, a 30-day supply of an oral SGLT2 inhibitor can cost about $550-$600 per month, while common subcutaneously injected GLP-1 receptor agonists can run from a few hundred dollars for a daily injection or close to $1,000 for a formulation administered weekly.
“Cost-effectiveness was not formally considered in the current guideline, but an assessment of cost-effectiveness may assist better targeting of interventions to achieve the greatest effect at a sustainable cost,” the researchers conclude.
The study received no commercial funding. None of the authors had relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Toxic chemicals we consume without knowing it
Life expectancy is falling precipitously. Three-fourths of Americans are overweight or obese, half have diabetes or prediabetes, and a majority are metabolically unhealthy. Furthermore, the rates of allergic, inflammatory, and autoimmune diseases are rising at rates of 3%-9% per year in the West, far faster than the speed of genetic change in this population.
Of course, diet and lifestyle are major factors behind such trends, but a grossly underappreciated driver in what ails us is the role of environmental toxins and endocrine-disrupting chemicals. In years past, these factors have largely evaded the traditional Western medical establishment; however, mounting evidence now supports their significance in fertility, metabolic health, and cancer.
Although several industrial chemicals and toxins have been identified as carcinogens and have subsequently been regulated, many more remain persistent in the environment and continue to be freely used. It is therefore incumbent upon both the general public and clinicians to be knowledgeable about these exposures. Here, we review some of the most common exposures and the substantial health risks associated with them, along with some general guidance around best practices for how to minimize exposure.
Microplastics
“Microplastics” is a term used to describe small fragments or particles of plastic breakdown or microbeads from household or personal care products, measuring less than 5 mm in length.
Plastic waste is accumulating at alarming and devastating proportions – by 2050, it is estimated that by weight, there will be more plastic than fish in the oceans. That translates into hundreds of thousands of tons of microplastics and trillions of these particles in the seas. A recent study demonstrated that microplastics were present in the bloodstream in the majority of 22 otherwise healthy participants.
Since the 1950s, plastic exposure has been shown to promote tumorigenesis in animal studies, and in vitro studies have demonstrated the toxicity of microplastics at the cellular level. However, it is not well known whether the plastic itself is toxic or if it simply serves as a carrier for other environmental toxins to bioaccumulate.
According to Tasha Stoiber, a senior scientist at the Environmental Working Group, “Microplastics have been widely detected in fish and seafood, as well as other products like bottled water, beer, honey, and tap water.” The EWG states there are no formal advisories on fish consumption to avoid exposure to microplastics at the moment.
Pressure also is mounting for a ban on microbeads in personal care products.
Until such bans are put in place, it is advised to avoid single-use plastics, favor reusable tote bags for grocery shopping rather than plastic bags, and opt for loose leaf tea or paper tea bags rather than mesh-based alternatives.
Phthalates
Phthalates are chemicals used to make plastics soft and durable, as well as to bind fragrances. They are commonly found in household items such as vinyl (for example, flooring, shower curtains) and fragrances, air fresheners, and perfumes.
Phthalates are known hormone-disrupting chemicals, exposure to which has been associated with abnormal sexual and brain development in children, as well as lower levels of testosterone in men. Exposures are thought to occur via inhalation, ingestion, and skin contact; however, fasting studies demonstrate that a majority of exposure is probably food related.
To avoid phthalate exposures, recommendations include avoiding polyvinyl chloride plastics (particularly food containers, plastic wrap, and children’s toys), which are identifiable by the recycle code number 3, as well as air fresheners and fragranced products.
The EWG’s Skin Deep database provides an important resource on phthalate-free personal care products.
Despite pressure from consumer advocacy groups, the U.S. Food and Drug Administration has not yet banned phthalates in food packaging.
Bisphenol A (BPA)
BPA is a chemical additive used to make clear and hard polycarbonate plastics, as well as epoxy and thermal papers. BPA is one of the highest-volume chemicals, with roughly 6 billion pounds produced each year. BPA is traditionally found in many clear plastic bottles and sippy cups, as well as in the lining of canned foods.
Structurally, BPA acts as an estrogen mimetic and has been associated with cardiovascular disease, obesity, and male sexual dysfunction. Since 2012, BPA has been banned in sippy cups and baby bottles, but there is some debate as to whether its replacements (bisphenol S and bisphenol F) are any safer; they appear to have similar hormonal effects as BPA.
As with phthalates, the majority of ingestion is thought to be food related. BPA has been found in more than 90% of a representative study population in the United States.
Guidance advises avoiding polycarbonate plastics (identifiable with the recycling code number 7), as well as avoiding handling thermal papers such as tickets and receipts, if possible. Food and beverages should be stored in glass or stainless steel. If plastic must be used, opt for polycarbonate- and polyvinyl chloride–free plastics, and food and beverages should never be reheated in plastic containers or wrapping. Canned foods should ideally be avoided, particularly canned tunas and condensed soups. If canned products are bought, they should ideally be BPA free.
Dioxins and polychlorinated biphenyls (PCBs)
Dioxins are mainly the byproducts of industrial practices; they are released after incineration, trash burning, and fires. PCBs, which are somewhat structurally related to dioxins, were previously found in products such as flame retardants and coolants. Dioxins and PCBs are often grouped in the same category under the umbrella term “persistent organic pollutants” because they break down slowly and remain in the environment even after emissions have been curbed.
Tetrachlorodibenzodioxin, perhaps the best-known dioxin, is a known carcinogen. Dioxins also have been associated with a host of health implications in development, immunity, and reproductive and endocrine systems. Higher levels of PCB exposure have also been associated with an increased risk for mortality from cardiovascular disease.
Notably, dioxin emissions have been reduced by 90% since the 1980s, and the U.S. Environmental Protection Agency has banned the use of PCBs in industrial manufacturing since 1979. However, environmental dioxins and PCBs still enter the food chain and accumulate in fat.
The best ways to avoid exposures are through limiting meat, fish, and dairy consumption and trimming the skin and fat from meats. The level of dioxins and PCBs found in meat, eggs, fish, and dairy are approximately 5-10 times higher than they are in plant-based foods. Research has shown that farmed salmon is likely to be the most PCB-contaminated protein source in the U.S. diet; however, newer forms of land-based and sustainable aquaculture probably avoid this exposure.
Pesticides
The growth of modern monoculture agriculture in the United States over the past century has coincided with a dramatic surge in the use of industrial pesticides. In fact, over 90% of the U.S. population have pesticides in their urine and blood, regardless of where they live. Exposures are thought to be food related.
Approximately 1 billion pounds of pesticides are used annually in the United States, including nearly 300 million pounds of glyphosate, which has been identified as a probable carcinogen by European agencies. The EPA has not yet reached this conclusion, although the matter is currently being litigated.
A large European prospective cohort trial demonstrated a lower risk for cancer in those with a greater frequency of self-reported organic food consumption. In addition to cancer risk, relatively elevated blood levels of a pesticide known as beta-hexachlorocyclohexane (B-HCH) are associated with higher all-cause mortality. Also, exposure to DDE – a metabolite of DDT, a chlorinated pesticide heavily used in the 1940s-1960s that still persists in the environment today – has been shown to increase the risk for Alzheimer’s-type dementia as well as overall cognitive decline.
Because these chlorinated pesticides are often fat soluble, they seem to accumulate in animal products. Therefore, people consuming a vegetarian diet have been found to have lower levels of B-HCH. This has led to the recommendation that consumers of produce should favor organic over conventional, if possible. Here too, the EWG provides an important resource to consumers in the form of shopper guides regarding pesticides in produce.
Per- and polyfluoroalkyl substances (PFAS)
PFAS are a group of fluorinated compounds discovered in the 1930s. Their chemical composition includes a durable carbon-fluoride bond, giving them a persistence within the environment that has led to their being referred to as “forever chemicals.”
PFAS have been detected in the blood of 98% of Americans, and in the rainwater of locations as far afield as Tibet and Antarctica. Even low levels of exposure have been associated with an increased risk for cancer, liver disease, low birth weight, and hormonal disruption.
The properties of PFAS also make them both durable at very high heat and water repellent. Notoriously, the chemical was used by 3M to make Scotchgard for carpets and fabrics and by Dupont to make Teflon for nonstick coating of pots and pans. Although perfluorooctanoic acid (PFOA) was removed from nonstick cookware in 2013, PFAS – a family of thousands of synthetic compounds – remain common in fast-food packaging, water- and stain-repellent clothing, firefighting foam, and personal care products. PFAS are released into the environment during the breakdown of these consumer and industrial products, as well as from dumping from waste facilities.
Alarmingly, the EWG notes that up to 200 million Americans may be exposed to PFAS in their drinking water. In March 2021, the EPA announced that they will be regulating PFAS in drinking water; however, the regulations have not been finalized. Currently, it is up to individual states to test for its presence in the water. The EWG has compiled a map of all known PFAS contamination sites.
To avoid or prevent exposures from PFAS, recommendations include filtering tap water with either reverse osmosis or activated carbon filters, as well as avoiding fast food and carry-out food, if possible, and consumer products labeled as “water resistant,” “stain-resistant,” and “nonstick.”
In a testament to how harmful these chemicals are, the EPA recently revised their lifetime health advisories for PFAS, such as PFOA, to 0.004 parts per trillion, which is more than 10,000 times smaller than the previous limit of 70 parts per trillion. The EPA also has proposed formally designating certain PFAS chemicals as “hazardous substances.”
Dr. Goel, clinical assistant professor of medicine at Weill Cornell Medicine, New York, has disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
Life expectancy is falling precipitously. Three-fourths of Americans are overweight or obese, half have diabetes or prediabetes, and a majority are metabolically unhealthy. Furthermore, the rates of allergic, inflammatory, and autoimmune diseases are rising at rates of 3%-9% per year in the West, far faster than the speed of genetic change in this population.
Of course, diet and lifestyle are major factors behind such trends, but a grossly underappreciated driver in what ails us is the role of environmental toxins and endocrine-disrupting chemicals. In years past, these factors have largely evaded the traditional Western medical establishment; however, mounting evidence now supports their significance in fertility, metabolic health, and cancer.
Although several industrial chemicals and toxins have been identified as carcinogens and have subsequently been regulated, many more remain persistent in the environment and continue to be freely used. It is therefore incumbent upon both the general public and clinicians to be knowledgeable about these exposures. Here, we review some of the most common exposures and the substantial health risks associated with them, along with some general guidance around best practices for how to minimize exposure.
Microplastics
“Microplastics” is a term used to describe small fragments or particles of plastic breakdown or microbeads from household or personal care products, measuring less than 5 mm in length.
Plastic waste is accumulating at alarming and devastating proportions – by 2050, it is estimated that by weight, there will be more plastic than fish in the oceans. That translates into hundreds of thousands of tons of microplastics and trillions of these particles in the seas. A recent study demonstrated that microplastics were present in the bloodstream in the majority of 22 otherwise healthy participants.
Since the 1950s, plastic exposure has been shown to promote tumorigenesis in animal studies, and in vitro studies have demonstrated the toxicity of microplastics at the cellular level. However, it is not well known whether the plastic itself is toxic or if it simply serves as a carrier for other environmental toxins to bioaccumulate.
According to Tasha Stoiber, a senior scientist at the Environmental Working Group, “Microplastics have been widely detected in fish and seafood, as well as other products like bottled water, beer, honey, and tap water.” The EWG states there are no formal advisories on fish consumption to avoid exposure to microplastics at the moment.
Pressure also is mounting for a ban on microbeads in personal care products.
Until such bans are put in place, it is advised to avoid single-use plastics, favor reusable tote bags for grocery shopping rather than plastic bags, and opt for loose leaf tea or paper tea bags rather than mesh-based alternatives.
Phthalates
Phthalates are chemicals used to make plastics soft and durable, as well as to bind fragrances. They are commonly found in household items such as vinyl (for example, flooring, shower curtains) and fragrances, air fresheners, and perfumes.
Phthalates are known hormone-disrupting chemicals, exposure to which has been associated with abnormal sexual and brain development in children, as well as lower levels of testosterone in men. Exposures are thought to occur via inhalation, ingestion, and skin contact; however, fasting studies demonstrate that a majority of exposure is probably food related.
To avoid phthalate exposures, recommendations include avoiding polyvinyl chloride plastics (particularly food containers, plastic wrap, and children’s toys), which are identifiable by the recycle code number 3, as well as air fresheners and fragranced products.
The EWG’s Skin Deep database provides an important resource on phthalate-free personal care products.
Despite pressure from consumer advocacy groups, the U.S. Food and Drug Administration has not yet banned phthalates in food packaging.
Bisphenol A (BPA)
BPA is a chemical additive used to make clear and hard polycarbonate plastics, as well as epoxy and thermal papers. BPA is one of the highest-volume chemicals, with roughly 6 billion pounds produced each year. BPA is traditionally found in many clear plastic bottles and sippy cups, as well as in the lining of canned foods.
Structurally, BPA acts as an estrogen mimetic and has been associated with cardiovascular disease, obesity, and male sexual dysfunction. Since 2012, BPA has been banned in sippy cups and baby bottles, but there is some debate as to whether its replacements (bisphenol S and bisphenol F) are any safer; they appear to have similar hormonal effects as BPA.
As with phthalates, the majority of ingestion is thought to be food related. BPA has been found in more than 90% of a representative study population in the United States.
Guidance advises avoiding polycarbonate plastics (identifiable with the recycling code number 7), as well as avoiding handling thermal papers such as tickets and receipts, if possible. Food and beverages should be stored in glass or stainless steel. If plastic must be used, opt for polycarbonate- and polyvinyl chloride–free plastics, and food and beverages should never be reheated in plastic containers or wrapping. Canned foods should ideally be avoided, particularly canned tunas and condensed soups. If canned products are bought, they should ideally be BPA free.
Dioxins and polychlorinated biphenyls (PCBs)
Dioxins are mainly the byproducts of industrial practices; they are released after incineration, trash burning, and fires. PCBs, which are somewhat structurally related to dioxins, were previously found in products such as flame retardants and coolants. Dioxins and PCBs are often grouped in the same category under the umbrella term “persistent organic pollutants” because they break down slowly and remain in the environment even after emissions have been curbed.
Tetrachlorodibenzodioxin, perhaps the best-known dioxin, is a known carcinogen. Dioxins also have been associated with a host of health implications in development, immunity, and reproductive and endocrine systems. Higher levels of PCB exposure have also been associated with an increased risk for mortality from cardiovascular disease.
Notably, dioxin emissions have been reduced by 90% since the 1980s, and the U.S. Environmental Protection Agency has banned the use of PCBs in industrial manufacturing since 1979. However, environmental dioxins and PCBs still enter the food chain and accumulate in fat.
The best ways to avoid exposures are through limiting meat, fish, and dairy consumption and trimming the skin and fat from meats. The level of dioxins and PCBs found in meat, eggs, fish, and dairy are approximately 5-10 times higher than they are in plant-based foods. Research has shown that farmed salmon is likely to be the most PCB-contaminated protein source in the U.S. diet; however, newer forms of land-based and sustainable aquaculture probably avoid this exposure.
Pesticides
The growth of modern monoculture agriculture in the United States over the past century has coincided with a dramatic surge in the use of industrial pesticides. In fact, over 90% of the U.S. population have pesticides in their urine and blood, regardless of where they live. Exposures are thought to be food related.
Approximately 1 billion pounds of pesticides are used annually in the United States, including nearly 300 million pounds of glyphosate, which has been identified as a probable carcinogen by European agencies. The EPA has not yet reached this conclusion, although the matter is currently being litigated.
A large European prospective cohort trial demonstrated a lower risk for cancer in those with a greater frequency of self-reported organic food consumption. In addition to cancer risk, relatively elevated blood levels of a pesticide known as beta-hexachlorocyclohexane (B-HCH) are associated with higher all-cause mortality. Also, exposure to DDE – a metabolite of DDT, a chlorinated pesticide heavily used in the 1940s-1960s that still persists in the environment today – has been shown to increase the risk for Alzheimer’s-type dementia as well as overall cognitive decline.
Because these chlorinated pesticides are often fat soluble, they seem to accumulate in animal products. Therefore, people consuming a vegetarian diet have been found to have lower levels of B-HCH. This has led to the recommendation that consumers of produce should favor organic over conventional, if possible. Here too, the EWG provides an important resource to consumers in the form of shopper guides regarding pesticides in produce.
Per- and polyfluoroalkyl substances (PFAS)
PFAS are a group of fluorinated compounds discovered in the 1930s. Their chemical composition includes a durable carbon-fluoride bond, giving them a persistence within the environment that has led to their being referred to as “forever chemicals.”
PFAS have been detected in the blood of 98% of Americans, and in the rainwater of locations as far afield as Tibet and Antarctica. Even low levels of exposure have been associated with an increased risk for cancer, liver disease, low birth weight, and hormonal disruption.
The properties of PFAS also make them both durable at very high heat and water repellent. Notoriously, the chemical was used by 3M to make Scotchgard for carpets and fabrics and by Dupont to make Teflon for nonstick coating of pots and pans. Although perfluorooctanoic acid (PFOA) was removed from nonstick cookware in 2013, PFAS – a family of thousands of synthetic compounds – remain common in fast-food packaging, water- and stain-repellent clothing, firefighting foam, and personal care products. PFAS are released into the environment during the breakdown of these consumer and industrial products, as well as from dumping from waste facilities.
Alarmingly, the EWG notes that up to 200 million Americans may be exposed to PFAS in their drinking water. In March 2021, the EPA announced that they will be regulating PFAS in drinking water; however, the regulations have not been finalized. Currently, it is up to individual states to test for its presence in the water. The EWG has compiled a map of all known PFAS contamination sites.
To avoid or prevent exposures from PFAS, recommendations include filtering tap water with either reverse osmosis or activated carbon filters, as well as avoiding fast food and carry-out food, if possible, and consumer products labeled as “water resistant,” “stain-resistant,” and “nonstick.”
In a testament to how harmful these chemicals are, the EPA recently revised their lifetime health advisories for PFAS, such as PFOA, to 0.004 parts per trillion, which is more than 10,000 times smaller than the previous limit of 70 parts per trillion. The EPA also has proposed formally designating certain PFAS chemicals as “hazardous substances.”
Dr. Goel, clinical assistant professor of medicine at Weill Cornell Medicine, New York, has disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
Life expectancy is falling precipitously. Three-fourths of Americans are overweight or obese, half have diabetes or prediabetes, and a majority are metabolically unhealthy. Furthermore, the rates of allergic, inflammatory, and autoimmune diseases are rising at rates of 3%-9% per year in the West, far faster than the speed of genetic change in this population.
Of course, diet and lifestyle are major factors behind such trends, but a grossly underappreciated driver in what ails us is the role of environmental toxins and endocrine-disrupting chemicals. In years past, these factors have largely evaded the traditional Western medical establishment; however, mounting evidence now supports their significance in fertility, metabolic health, and cancer.
Although several industrial chemicals and toxins have been identified as carcinogens and have subsequently been regulated, many more remain persistent in the environment and continue to be freely used. It is therefore incumbent upon both the general public and clinicians to be knowledgeable about these exposures. Here, we review some of the most common exposures and the substantial health risks associated with them, along with some general guidance around best practices for how to minimize exposure.
Microplastics
“Microplastics” is a term used to describe small fragments or particles of plastic breakdown or microbeads from household or personal care products, measuring less than 5 mm in length.
Plastic waste is accumulating at alarming and devastating proportions – by 2050, it is estimated that by weight, there will be more plastic than fish in the oceans. That translates into hundreds of thousands of tons of microplastics and trillions of these particles in the seas. A recent study demonstrated that microplastics were present in the bloodstream in the majority of 22 otherwise healthy participants.
Since the 1950s, plastic exposure has been shown to promote tumorigenesis in animal studies, and in vitro studies have demonstrated the toxicity of microplastics at the cellular level. However, it is not well known whether the plastic itself is toxic or if it simply serves as a carrier for other environmental toxins to bioaccumulate.
According to Tasha Stoiber, a senior scientist at the Environmental Working Group, “Microplastics have been widely detected in fish and seafood, as well as other products like bottled water, beer, honey, and tap water.” The EWG states there are no formal advisories on fish consumption to avoid exposure to microplastics at the moment.
Pressure also is mounting for a ban on microbeads in personal care products.
Until such bans are put in place, it is advised to avoid single-use plastics, favor reusable tote bags for grocery shopping rather than plastic bags, and opt for loose leaf tea or paper tea bags rather than mesh-based alternatives.
Phthalates
Phthalates are chemicals used to make plastics soft and durable, as well as to bind fragrances. They are commonly found in household items such as vinyl (for example, flooring, shower curtains) and fragrances, air fresheners, and perfumes.
Phthalates are known hormone-disrupting chemicals, exposure to which has been associated with abnormal sexual and brain development in children, as well as lower levels of testosterone in men. Exposures are thought to occur via inhalation, ingestion, and skin contact; however, fasting studies demonstrate that a majority of exposure is probably food related.
To avoid phthalate exposures, recommendations include avoiding polyvinyl chloride plastics (particularly food containers, plastic wrap, and children’s toys), which are identifiable by the recycle code number 3, as well as air fresheners and fragranced products.
The EWG’s Skin Deep database provides an important resource on phthalate-free personal care products.
Despite pressure from consumer advocacy groups, the U.S. Food and Drug Administration has not yet banned phthalates in food packaging.
Bisphenol A (BPA)
BPA is a chemical additive used to make clear and hard polycarbonate plastics, as well as epoxy and thermal papers. BPA is one of the highest-volume chemicals, with roughly 6 billion pounds produced each year. BPA is traditionally found in many clear plastic bottles and sippy cups, as well as in the lining of canned foods.
Structurally, BPA acts as an estrogen mimetic and has been associated with cardiovascular disease, obesity, and male sexual dysfunction. Since 2012, BPA has been banned in sippy cups and baby bottles, but there is some debate as to whether its replacements (bisphenol S and bisphenol F) are any safer; they appear to have similar hormonal effects as BPA.
As with phthalates, the majority of ingestion is thought to be food related. BPA has been found in more than 90% of a representative study population in the United States.
Guidance advises avoiding polycarbonate plastics (identifiable with the recycling code number 7), as well as avoiding handling thermal papers such as tickets and receipts, if possible. Food and beverages should be stored in glass or stainless steel. If plastic must be used, opt for polycarbonate- and polyvinyl chloride–free plastics, and food and beverages should never be reheated in plastic containers or wrapping. Canned foods should ideally be avoided, particularly canned tunas and condensed soups. If canned products are bought, they should ideally be BPA free.
Dioxins and polychlorinated biphenyls (PCBs)
Dioxins are mainly the byproducts of industrial practices; they are released after incineration, trash burning, and fires. PCBs, which are somewhat structurally related to dioxins, were previously found in products such as flame retardants and coolants. Dioxins and PCBs are often grouped in the same category under the umbrella term “persistent organic pollutants” because they break down slowly and remain in the environment even after emissions have been curbed.
Tetrachlorodibenzodioxin, perhaps the best-known dioxin, is a known carcinogen. Dioxins also have been associated with a host of health implications in development, immunity, and reproductive and endocrine systems. Higher levels of PCB exposure have also been associated with an increased risk for mortality from cardiovascular disease.
Notably, dioxin emissions have been reduced by 90% since the 1980s, and the U.S. Environmental Protection Agency has banned the use of PCBs in industrial manufacturing since 1979. However, environmental dioxins and PCBs still enter the food chain and accumulate in fat.
The best ways to avoid exposures are through limiting meat, fish, and dairy consumption and trimming the skin and fat from meats. The level of dioxins and PCBs found in meat, eggs, fish, and dairy are approximately 5-10 times higher than they are in plant-based foods. Research has shown that farmed salmon is likely to be the most PCB-contaminated protein source in the U.S. diet; however, newer forms of land-based and sustainable aquaculture probably avoid this exposure.
Pesticides
The growth of modern monoculture agriculture in the United States over the past century has coincided with a dramatic surge in the use of industrial pesticides. In fact, over 90% of the U.S. population have pesticides in their urine and blood, regardless of where they live. Exposures are thought to be food related.
Approximately 1 billion pounds of pesticides are used annually in the United States, including nearly 300 million pounds of glyphosate, which has been identified as a probable carcinogen by European agencies. The EPA has not yet reached this conclusion, although the matter is currently being litigated.
A large European prospective cohort trial demonstrated a lower risk for cancer in those with a greater frequency of self-reported organic food consumption. In addition to cancer risk, relatively elevated blood levels of a pesticide known as beta-hexachlorocyclohexane (B-HCH) are associated with higher all-cause mortality. Also, exposure to DDE – a metabolite of DDT, a chlorinated pesticide heavily used in the 1940s-1960s that still persists in the environment today – has been shown to increase the risk for Alzheimer’s-type dementia as well as overall cognitive decline.
Because these chlorinated pesticides are often fat soluble, they seem to accumulate in animal products. Therefore, people consuming a vegetarian diet have been found to have lower levels of B-HCH. This has led to the recommendation that consumers of produce should favor organic over conventional, if possible. Here too, the EWG provides an important resource to consumers in the form of shopper guides regarding pesticides in produce.
Per- and polyfluoroalkyl substances (PFAS)
PFAS are a group of fluorinated compounds discovered in the 1930s. Their chemical composition includes a durable carbon-fluoride bond, giving them a persistence within the environment that has led to their being referred to as “forever chemicals.”
PFAS have been detected in the blood of 98% of Americans, and in the rainwater of locations as far afield as Tibet and Antarctica. Even low levels of exposure have been associated with an increased risk for cancer, liver disease, low birth weight, and hormonal disruption.
The properties of PFAS also make them both durable at very high heat and water repellent. Notoriously, the chemical was used by 3M to make Scotchgard for carpets and fabrics and by Dupont to make Teflon for nonstick coating of pots and pans. Although perfluorooctanoic acid (PFOA) was removed from nonstick cookware in 2013, PFAS – a family of thousands of synthetic compounds – remain common in fast-food packaging, water- and stain-repellent clothing, firefighting foam, and personal care products. PFAS are released into the environment during the breakdown of these consumer and industrial products, as well as from dumping from waste facilities.
Alarmingly, the EWG notes that up to 200 million Americans may be exposed to PFAS in their drinking water. In March 2021, the EPA announced that they will be regulating PFAS in drinking water; however, the regulations have not been finalized. Currently, it is up to individual states to test for its presence in the water. The EWG has compiled a map of all known PFAS contamination sites.
To avoid or prevent exposures from PFAS, recommendations include filtering tap water with either reverse osmosis or activated carbon filters, as well as avoiding fast food and carry-out food, if possible, and consumer products labeled as “water resistant,” “stain-resistant,” and “nonstick.”
In a testament to how harmful these chemicals are, the EPA recently revised their lifetime health advisories for PFAS, such as PFOA, to 0.004 parts per trillion, which is more than 10,000 times smaller than the previous limit of 70 parts per trillion. The EPA also has proposed formally designating certain PFAS chemicals as “hazardous substances.”
Dr. Goel, clinical assistant professor of medicine at Weill Cornell Medicine, New York, has disclosed no relevant financial relationships. A version of this article originally appeared on Medscape.com.
Irregular sleep tied to markers of atherosclerosis
a new report suggests.
In particular, variation in sleep duration of more than 2 hours per night in the same week was tied to higher rates of atherosclerosis.
“Poor sleep is linked with several cardiovascular conditions, including heart disease, hypertension, and type 2 diabetes,” lead author Kelsie M. Full, PhD, MPH, assistant professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
“Overall, we found that participants who slept varying amounts of hours throughout the week (meaning that one night they slept less, one night they slept more) were more likely to have atherosclerosis than participants who slept about the same amount of time each night,” she said.
The study was published online in the Journal of the American Heart Association.
Analyzing associations
Dr. Full and colleagues examined data from 2032 participants in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study, which included adults aged between 45 and 84 years in six U.S. communities who completed 7-day wrist actigraphy assessment and kept a sleep diary between 2010 and 2013.
For subclinical markers of cardiovascular disease, participants underwent assessments of coronary artery calcium, carotid plaque presence, carotid intima-media thickness, and ankle-brachial index.
The research team assessed sleep duration, or the total number of minutes of sleep in a night, and sleep timing regularity, which was determined on the basis of the time someone initially fell asleep each night. They adjusted for cardiovascular disease risk factors and sleep characteristics, such as obstructive sleep apnea, sleep duration, and sleep fragmentation.
The average age of the participants was 68.6 years, and 53.6% were women. About 37.9% identified as White, 27.6% as Black or African American, 23.4% as Hispanic American, and 11.1% as Chinese American.
During the 7-day period, about 38% of participants experienced a change in sleep duration of more than 90 minutes, and 18% experienced a sleep duration change of more than 120 minutes. Those who had irregular sleep were more likely to be non-White, current smokers, have lower average annual incomes, have work shift schedules or did not work, and have a higher average body mass index.
For the study, sleep duration irregularity was defined as a standard deviation of more than 120 minutes. Those participants who had a greater degree of sleep irregularity were more likely to have high coronary artery calcium burden than those whose sleep duration was more more regular, defined as an SD of 60 minutes or less (> 300; prevalence ratio, 1.33; 95% confidence interval, 1.03-1.71), as well as abnormal ankle-brachial index (< 0.9, prevalence ratio, 1.75;95% CI, 1.03-2.95).
Further, those with irregular sleep timing (SD > 90 minutes) were more likely to have a high coronary artery calcium burden (prevalence ratio, 1.39; 95% CI, 1.07-1.82) in comparison with those with more regular sleep timing (SD < 30 minutes).
“The biggest surprise to me was that 30% of the participants in the study had total sleep times that varied by more than 90 minutes over the course of the week,” Dr. Full said. “This is consistent with prior studies that suggest that a large proportion of the general public have irregular sleep patterns, not just shift workers.”
Investigating next steps
In additional analyses, Dr. Full and colleagues found that sleep duration regularity continued to be associated with high coronary artery calcium burden and abnormal ankle-brachial index when accounting for severe obstructive sleep apnea, average nightly sleep duration, and average sleep fragmentation.
Notably, when sleep duration was added, all participants with more irregular sleep durations (SD > 60 minutes) were more likely to have a high coronary artery calcium burden, compared with those with regular sleep durations (SD < 60 minutes). The results remained when participants who reported shift work, including night shift work, were excluded.
Additional studies are needed to understand the mechanisms, the study authors wrote. Night-to-night variability in sleep duration and sleep timing can cause desynchronization in the sleep-wake timing and circadian disruption.
“A key issue highlighted in this study is that sleep irregularity itself, independent of how much sleep people were getting, was related to heart health. Sleep is a naturally recurring phenomenon, and maintaining regularity helps provide stability and predictability to the body,” Michael Grandner, PhD, associate professor of psychiatry and director of the sleep and health research program at the University of Arizona, Tucson, said in an interview.
Dr. Grandner, who wasn’t involved with this study, has researched sleep irregularity and associations with cardiovascular disease, diabetes, obesity, and many other adverse outcomes.
“When people have very irregular sleep schedules, it may make it harder for the body to optimally make good use of the sleep it is getting, since it such a moving target,” he said. “The unique angle here is the ability to focus on regularity of sleep.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences of the National Institutes of Health. One author received grants and consulting fees from pharmaceutical companies unrelated to the research. The other authors and Dr. Grandner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
a new report suggests.
In particular, variation in sleep duration of more than 2 hours per night in the same week was tied to higher rates of atherosclerosis.
“Poor sleep is linked with several cardiovascular conditions, including heart disease, hypertension, and type 2 diabetes,” lead author Kelsie M. Full, PhD, MPH, assistant professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
“Overall, we found that participants who slept varying amounts of hours throughout the week (meaning that one night they slept less, one night they slept more) were more likely to have atherosclerosis than participants who slept about the same amount of time each night,” she said.
The study was published online in the Journal of the American Heart Association.
Analyzing associations
Dr. Full and colleagues examined data from 2032 participants in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study, which included adults aged between 45 and 84 years in six U.S. communities who completed 7-day wrist actigraphy assessment and kept a sleep diary between 2010 and 2013.
For subclinical markers of cardiovascular disease, participants underwent assessments of coronary artery calcium, carotid plaque presence, carotid intima-media thickness, and ankle-brachial index.
The research team assessed sleep duration, or the total number of minutes of sleep in a night, and sleep timing regularity, which was determined on the basis of the time someone initially fell asleep each night. They adjusted for cardiovascular disease risk factors and sleep characteristics, such as obstructive sleep apnea, sleep duration, and sleep fragmentation.
The average age of the participants was 68.6 years, and 53.6% were women. About 37.9% identified as White, 27.6% as Black or African American, 23.4% as Hispanic American, and 11.1% as Chinese American.
During the 7-day period, about 38% of participants experienced a change in sleep duration of more than 90 minutes, and 18% experienced a sleep duration change of more than 120 minutes. Those who had irregular sleep were more likely to be non-White, current smokers, have lower average annual incomes, have work shift schedules or did not work, and have a higher average body mass index.
For the study, sleep duration irregularity was defined as a standard deviation of more than 120 minutes. Those participants who had a greater degree of sleep irregularity were more likely to have high coronary artery calcium burden than those whose sleep duration was more more regular, defined as an SD of 60 minutes or less (> 300; prevalence ratio, 1.33; 95% confidence interval, 1.03-1.71), as well as abnormal ankle-brachial index (< 0.9, prevalence ratio, 1.75;95% CI, 1.03-2.95).
Further, those with irregular sleep timing (SD > 90 minutes) were more likely to have a high coronary artery calcium burden (prevalence ratio, 1.39; 95% CI, 1.07-1.82) in comparison with those with more regular sleep timing (SD < 30 minutes).
“The biggest surprise to me was that 30% of the participants in the study had total sleep times that varied by more than 90 minutes over the course of the week,” Dr. Full said. “This is consistent with prior studies that suggest that a large proportion of the general public have irregular sleep patterns, not just shift workers.”
Investigating next steps
In additional analyses, Dr. Full and colleagues found that sleep duration regularity continued to be associated with high coronary artery calcium burden and abnormal ankle-brachial index when accounting for severe obstructive sleep apnea, average nightly sleep duration, and average sleep fragmentation.
Notably, when sleep duration was added, all participants with more irregular sleep durations (SD > 60 minutes) were more likely to have a high coronary artery calcium burden, compared with those with regular sleep durations (SD < 60 minutes). The results remained when participants who reported shift work, including night shift work, were excluded.
Additional studies are needed to understand the mechanisms, the study authors wrote. Night-to-night variability in sleep duration and sleep timing can cause desynchronization in the sleep-wake timing and circadian disruption.
“A key issue highlighted in this study is that sleep irregularity itself, independent of how much sleep people were getting, was related to heart health. Sleep is a naturally recurring phenomenon, and maintaining regularity helps provide stability and predictability to the body,” Michael Grandner, PhD, associate professor of psychiatry and director of the sleep and health research program at the University of Arizona, Tucson, said in an interview.
Dr. Grandner, who wasn’t involved with this study, has researched sleep irregularity and associations with cardiovascular disease, diabetes, obesity, and many other adverse outcomes.
“When people have very irregular sleep schedules, it may make it harder for the body to optimally make good use of the sleep it is getting, since it such a moving target,” he said. “The unique angle here is the ability to focus on regularity of sleep.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences of the National Institutes of Health. One author received grants and consulting fees from pharmaceutical companies unrelated to the research. The other authors and Dr. Grandner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
a new report suggests.
In particular, variation in sleep duration of more than 2 hours per night in the same week was tied to higher rates of atherosclerosis.
“Poor sleep is linked with several cardiovascular conditions, including heart disease, hypertension, and type 2 diabetes,” lead author Kelsie M. Full, PhD, MPH, assistant professor of medicine at Vanderbilt University Medical Center, Nashville, Tenn., said in an interview.
“Overall, we found that participants who slept varying amounts of hours throughout the week (meaning that one night they slept less, one night they slept more) were more likely to have atherosclerosis than participants who slept about the same amount of time each night,” she said.
The study was published online in the Journal of the American Heart Association.
Analyzing associations
Dr. Full and colleagues examined data from 2032 participants in the Multi-Ethnic Study of Atherosclerosis Sleep Ancillary Study, which included adults aged between 45 and 84 years in six U.S. communities who completed 7-day wrist actigraphy assessment and kept a sleep diary between 2010 and 2013.
For subclinical markers of cardiovascular disease, participants underwent assessments of coronary artery calcium, carotid plaque presence, carotid intima-media thickness, and ankle-brachial index.
The research team assessed sleep duration, or the total number of minutes of sleep in a night, and sleep timing regularity, which was determined on the basis of the time someone initially fell asleep each night. They adjusted for cardiovascular disease risk factors and sleep characteristics, such as obstructive sleep apnea, sleep duration, and sleep fragmentation.
The average age of the participants was 68.6 years, and 53.6% were women. About 37.9% identified as White, 27.6% as Black or African American, 23.4% as Hispanic American, and 11.1% as Chinese American.
During the 7-day period, about 38% of participants experienced a change in sleep duration of more than 90 minutes, and 18% experienced a sleep duration change of more than 120 minutes. Those who had irregular sleep were more likely to be non-White, current smokers, have lower average annual incomes, have work shift schedules or did not work, and have a higher average body mass index.
For the study, sleep duration irregularity was defined as a standard deviation of more than 120 minutes. Those participants who had a greater degree of sleep irregularity were more likely to have high coronary artery calcium burden than those whose sleep duration was more more regular, defined as an SD of 60 minutes or less (> 300; prevalence ratio, 1.33; 95% confidence interval, 1.03-1.71), as well as abnormal ankle-brachial index (< 0.9, prevalence ratio, 1.75;95% CI, 1.03-2.95).
Further, those with irregular sleep timing (SD > 90 minutes) were more likely to have a high coronary artery calcium burden (prevalence ratio, 1.39; 95% CI, 1.07-1.82) in comparison with those with more regular sleep timing (SD < 30 minutes).
“The biggest surprise to me was that 30% of the participants in the study had total sleep times that varied by more than 90 minutes over the course of the week,” Dr. Full said. “This is consistent with prior studies that suggest that a large proportion of the general public have irregular sleep patterns, not just shift workers.”
Investigating next steps
In additional analyses, Dr. Full and colleagues found that sleep duration regularity continued to be associated with high coronary artery calcium burden and abnormal ankle-brachial index when accounting for severe obstructive sleep apnea, average nightly sleep duration, and average sleep fragmentation.
Notably, when sleep duration was added, all participants with more irregular sleep durations (SD > 60 minutes) were more likely to have a high coronary artery calcium burden, compared with those with regular sleep durations (SD < 60 minutes). The results remained when participants who reported shift work, including night shift work, were excluded.
Additional studies are needed to understand the mechanisms, the study authors wrote. Night-to-night variability in sleep duration and sleep timing can cause desynchronization in the sleep-wake timing and circadian disruption.
“A key issue highlighted in this study is that sleep irregularity itself, independent of how much sleep people were getting, was related to heart health. Sleep is a naturally recurring phenomenon, and maintaining regularity helps provide stability and predictability to the body,” Michael Grandner, PhD, associate professor of psychiatry and director of the sleep and health research program at the University of Arizona, Tucson, said in an interview.
Dr. Grandner, who wasn’t involved with this study, has researched sleep irregularity and associations with cardiovascular disease, diabetes, obesity, and many other adverse outcomes.
“When people have very irregular sleep schedules, it may make it harder for the body to optimally make good use of the sleep it is getting, since it such a moving target,” he said. “The unique angle here is the ability to focus on regularity of sleep.”
The study was supported by the National Heart, Lung, and Blood Institute and the National Center for Advancing Translational Sciences of the National Institutes of Health. One author received grants and consulting fees from pharmaceutical companies unrelated to the research. The other authors and Dr. Grandner disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Therapy app cut A1c, drug intensification in T2D
An investigational smartphone app that delivers cognitive behavioral therapy (CBT) to people with type 2 diabetes led to a significant 10 percentage point cut in the incidence of antihyperglycemic-drug intensification during 6 months’ follow-up, when compared with a control phone app, in the CBT app’s pivotal trial with 669 randomized patients.
Previously reported results from this trial, called BT-001, showed that people randomized to use the CBT app had a significant average 0.4 percentage point reduction in hemoglobin A1c, compared with controls, after 90 days for the trial’s primary endpoint, and a significant 0.29 percentage point reduction in A1c, compared with controls, after 180 days.
The new finding, that these incremental drops in A1c occurred while the control patients also received significantly more intensification of their antihyperglycemic medication, provides further evidence for the efficacy of the CBT app, said Marc P. Bonaca, MD, in a press conference organized by the American College of Cardiology in advance of its upcoming joint scientific sessions.
The CBT app “significantly reduced A1c despite less intensification of antihyperglycemic therapy,” noted Dr. Bonaca, a vascular medicine specialist and executive director of CPC Clinical Research, an academic research organization created by and affiliated with the University of Colorado at Denver, Aurora.
Based on positive safety and efficacy findings from the primary-endpoint phase of the BT-001 trial, reported in Diabetes Care, the company developing the CBT app, Better Therapeutics, said in a statement that the U.S. Food and Drug Administration accepted the company’s application for de novo classification and marketing approval of the app, also called BT-001. If the agency grants this classification and marketing approval, the company plans to sell the app on a prescription basis for use by people with type 2 diabetes.
CBT app gives patients problem-solving skills
CBT gives people with type 2 diabetes a way to better understand their unhelpful behaviors and motivations and teaches them problem-solving skills. Providing this counseling via an app addresses the challenge of making the intervention scalable to a broad range of patients, Dr. Bonaca explained.
“Clinicians are frustrated by trying to produce behavioral change” in patients. The BT-001 app “provides a new avenue to treatment,” an approach that clinicians have been “very receptive” to using “once they understand the mechanism,” Dr. Bonaca said during the press conference. “The effect at 90 days was very similar to what a drug would do. It’s not just drugs any more” for treating people with type 2 diabetes, he declared.
“CBT is an empirically supported psychotherapy for a variety of emotional disorders, and it has been adapted to target specific emotional distress in the context of chronic illness,” commented Amit Shapira, PhD, a clinical psychologist at the Joslin Diabetes Center in Boston who has not been involved in the BT-001 studies. A CBT protocol designed for diabetes, CBT for Adherence and Depression “has been shown to have a positive impact on depression symptoms and glycemic control in adults with type 2 diabetes,” Dr. Shapira noted in an interview.
“Once a physician explains this [CBT] app and patients understand how to use it, then patients will be happy to use it,” commented Julia Grapsa, MD, PhD, a cardiologist at St. Thomas Hospital in London, who moderated the press conference. “We may see an explosion of apps like this one, designed to help better control” other chronic disorders, such as elevated blood pressure or abnormal lipid levels, Dr. Grapsa predicted. “I’m very optimistic that these apps have a great future in health care.”
Forty percent relative cut in new antihyperglycemic drug use
The BT-001 study randomized 669 adults with smartphone access and type 2 diabetes at any of six U.S. sites. The enrolled patients had type 2 diabetes for an average of 11 years, and an A1c of 7%-10.9% with an average level of 8.2%. Participants had to be on a stable medication regimen for at least 3 months but not using prandial insulin, and their treatment regimens could undergo adjustment during the trial. At baseline, each subject was on an average of 2.1 antihyperglycemic medications, including 90% on metformin and 42% on a sulfonylurea.
The new results reported by Dr. Bonaca showed that, during follow-up, people using the app had a 14.4% rate of antihyperglycemic drug intensification compared with a 24.4% rate among the controls, a roughly 40% relative decrease in new antihyperglycemic medication use. In addition, among those using insulin at baseline, 3.8% of controls increased their insulin dose, compared with 1.5% of those using the CBT app, while insulin doses decreased in 0.9% of the control subjects and in 2.2% of those using the BT-001 app.
Further study findings, first reported by Dr. Bonaca at the American Heart Association scientific sessions in late 2022, also showed a clear dose-response pattern for the CBT app: the more CBT lessons a person completed, the greater their reduction in A1c over 180 days of app use. People who used the app fewer than 10 times had an average reduction from baseline in their A1c of less than 0.1 percentage points. Among those who used the app 10-20 times (a subgroup with roughly one-third of the people randomized to app use), average A1c reduction increased to about 0.4 percentage points, and among those who used the app more than 20 times (also about one-third of the intervention group), the average A1c reduction from baseline was about 0.6 percentage points.
“It would be interesting to learn more about the adults who engaged with the app” and had a higher use rate “to provide more targeted care” with the app to people who match the profiles of those who were more likely to use the app during the trial, said Dr. Shapira.
This “clear” dose-response relationship “was one of the most exciting findings. It helps validate the mechanism,” Dr. Bonaca said during the press conference. “We’re now modeling which patients were the most engaged” with using the app, and “looking at ways to increase app engagement.”
Better Therapeutics also announced, in December 2022, results from a separate, uncontrolled study of a similar CBT app in 19 people with nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. The findings showed that use of the tested app linked with an average 16% drop from baseline in liver fat content as measured by MRI, as well as other improvements in markers of hepatic function. The company said in a statement that based on these findings it planned to apply for breakthrough-device designation with the FDA for use of a liver-specific CBT app in people with nonalcoholic fatty liver disease and nonalcoholic steatohepatitis.
The BT-001 trial was sponsored by Better Therapeutics, the company developing the app. CPC Clinical Research receives research and consulting funding from numerous companies. Dr. Bonaca has been a consultant to Audentes, and is a stockholder of Medtronic and Pfizer. Dr. Shapira and Dr. Grapsa had no disclosures.
An investigational smartphone app that delivers cognitive behavioral therapy (CBT) to people with type 2 diabetes led to a significant 10 percentage point cut in the incidence of antihyperglycemic-drug intensification during 6 months’ follow-up, when compared with a control phone app, in the CBT app’s pivotal trial with 669 randomized patients.
Previously reported results from this trial, called BT-001, showed that people randomized to use the CBT app had a significant average 0.4 percentage point reduction in hemoglobin A1c, compared with controls, after 90 days for the trial’s primary endpoint, and a significant 0.29 percentage point reduction in A1c, compared with controls, after 180 days.
The new finding, that these incremental drops in A1c occurred while the control patients also received significantly more intensification of their antihyperglycemic medication, provides further evidence for the efficacy of the CBT app, said Marc P. Bonaca, MD, in a press conference organized by the American College of Cardiology in advance of its upcoming joint scientific sessions.
The CBT app “significantly reduced A1c despite less intensification of antihyperglycemic therapy,” noted Dr. Bonaca, a vascular medicine specialist and executive director of CPC Clinical Research, an academic research organization created by and affiliated with the University of Colorado at Denver, Aurora.
Based on positive safety and efficacy findings from the primary-endpoint phase of the BT-001 trial, reported in Diabetes Care, the company developing the CBT app, Better Therapeutics, said in a statement that the U.S. Food and Drug Administration accepted the company’s application for de novo classification and marketing approval of the app, also called BT-001. If the agency grants this classification and marketing approval, the company plans to sell the app on a prescription basis for use by people with type 2 diabetes.
CBT app gives patients problem-solving skills
CBT gives people with type 2 diabetes a way to better understand their unhelpful behaviors and motivations and teaches them problem-solving skills. Providing this counseling via an app addresses the challenge of making the intervention scalable to a broad range of patients, Dr. Bonaca explained.
“Clinicians are frustrated by trying to produce behavioral change” in patients. The BT-001 app “provides a new avenue to treatment,” an approach that clinicians have been “very receptive” to using “once they understand the mechanism,” Dr. Bonaca said during the press conference. “The effect at 90 days was very similar to what a drug would do. It’s not just drugs any more” for treating people with type 2 diabetes, he declared.
“CBT is an empirically supported psychotherapy for a variety of emotional disorders, and it has been adapted to target specific emotional distress in the context of chronic illness,” commented Amit Shapira, PhD, a clinical psychologist at the Joslin Diabetes Center in Boston who has not been involved in the BT-001 studies. A CBT protocol designed for diabetes, CBT for Adherence and Depression “has been shown to have a positive impact on depression symptoms and glycemic control in adults with type 2 diabetes,” Dr. Shapira noted in an interview.
“Once a physician explains this [CBT] app and patients understand how to use it, then patients will be happy to use it,” commented Julia Grapsa, MD, PhD, a cardiologist at St. Thomas Hospital in London, who moderated the press conference. “We may see an explosion of apps like this one, designed to help better control” other chronic disorders, such as elevated blood pressure or abnormal lipid levels, Dr. Grapsa predicted. “I’m very optimistic that these apps have a great future in health care.”
Forty percent relative cut in new antihyperglycemic drug use
The BT-001 study randomized 669 adults with smartphone access and type 2 diabetes at any of six U.S. sites. The enrolled patients had type 2 diabetes for an average of 11 years, and an A1c of 7%-10.9% with an average level of 8.2%. Participants had to be on a stable medication regimen for at least 3 months but not using prandial insulin, and their treatment regimens could undergo adjustment during the trial. At baseline, each subject was on an average of 2.1 antihyperglycemic medications, including 90% on metformin and 42% on a sulfonylurea.
The new results reported by Dr. Bonaca showed that, during follow-up, people using the app had a 14.4% rate of antihyperglycemic drug intensification compared with a 24.4% rate among the controls, a roughly 40% relative decrease in new antihyperglycemic medication use. In addition, among those using insulin at baseline, 3.8% of controls increased their insulin dose, compared with 1.5% of those using the CBT app, while insulin doses decreased in 0.9% of the control subjects and in 2.2% of those using the BT-001 app.
Further study findings, first reported by Dr. Bonaca at the American Heart Association scientific sessions in late 2022, also showed a clear dose-response pattern for the CBT app: the more CBT lessons a person completed, the greater their reduction in A1c over 180 days of app use. People who used the app fewer than 10 times had an average reduction from baseline in their A1c of less than 0.1 percentage points. Among those who used the app 10-20 times (a subgroup with roughly one-third of the people randomized to app use), average A1c reduction increased to about 0.4 percentage points, and among those who used the app more than 20 times (also about one-third of the intervention group), the average A1c reduction from baseline was about 0.6 percentage points.
“It would be interesting to learn more about the adults who engaged with the app” and had a higher use rate “to provide more targeted care” with the app to people who match the profiles of those who were more likely to use the app during the trial, said Dr. Shapira.
This “clear” dose-response relationship “was one of the most exciting findings. It helps validate the mechanism,” Dr. Bonaca said during the press conference. “We’re now modeling which patients were the most engaged” with using the app, and “looking at ways to increase app engagement.”
Better Therapeutics also announced, in December 2022, results from a separate, uncontrolled study of a similar CBT app in 19 people with nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. The findings showed that use of the tested app linked with an average 16% drop from baseline in liver fat content as measured by MRI, as well as other improvements in markers of hepatic function. The company said in a statement that based on these findings it planned to apply for breakthrough-device designation with the FDA for use of a liver-specific CBT app in people with nonalcoholic fatty liver disease and nonalcoholic steatohepatitis.
The BT-001 trial was sponsored by Better Therapeutics, the company developing the app. CPC Clinical Research receives research and consulting funding from numerous companies. Dr. Bonaca has been a consultant to Audentes, and is a stockholder of Medtronic and Pfizer. Dr. Shapira and Dr. Grapsa had no disclosures.
An investigational smartphone app that delivers cognitive behavioral therapy (CBT) to people with type 2 diabetes led to a significant 10 percentage point cut in the incidence of antihyperglycemic-drug intensification during 6 months’ follow-up, when compared with a control phone app, in the CBT app’s pivotal trial with 669 randomized patients.
Previously reported results from this trial, called BT-001, showed that people randomized to use the CBT app had a significant average 0.4 percentage point reduction in hemoglobin A1c, compared with controls, after 90 days for the trial’s primary endpoint, and a significant 0.29 percentage point reduction in A1c, compared with controls, after 180 days.
The new finding, that these incremental drops in A1c occurred while the control patients also received significantly more intensification of their antihyperglycemic medication, provides further evidence for the efficacy of the CBT app, said Marc P. Bonaca, MD, in a press conference organized by the American College of Cardiology in advance of its upcoming joint scientific sessions.
The CBT app “significantly reduced A1c despite less intensification of antihyperglycemic therapy,” noted Dr. Bonaca, a vascular medicine specialist and executive director of CPC Clinical Research, an academic research organization created by and affiliated with the University of Colorado at Denver, Aurora.
Based on positive safety and efficacy findings from the primary-endpoint phase of the BT-001 trial, reported in Diabetes Care, the company developing the CBT app, Better Therapeutics, said in a statement that the U.S. Food and Drug Administration accepted the company’s application for de novo classification and marketing approval of the app, also called BT-001. If the agency grants this classification and marketing approval, the company plans to sell the app on a prescription basis for use by people with type 2 diabetes.
CBT app gives patients problem-solving skills
CBT gives people with type 2 diabetes a way to better understand their unhelpful behaviors and motivations and teaches them problem-solving skills. Providing this counseling via an app addresses the challenge of making the intervention scalable to a broad range of patients, Dr. Bonaca explained.
“Clinicians are frustrated by trying to produce behavioral change” in patients. The BT-001 app “provides a new avenue to treatment,” an approach that clinicians have been “very receptive” to using “once they understand the mechanism,” Dr. Bonaca said during the press conference. “The effect at 90 days was very similar to what a drug would do. It’s not just drugs any more” for treating people with type 2 diabetes, he declared.
“CBT is an empirically supported psychotherapy for a variety of emotional disorders, and it has been adapted to target specific emotional distress in the context of chronic illness,” commented Amit Shapira, PhD, a clinical psychologist at the Joslin Diabetes Center in Boston who has not been involved in the BT-001 studies. A CBT protocol designed for diabetes, CBT for Adherence and Depression “has been shown to have a positive impact on depression symptoms and glycemic control in adults with type 2 diabetes,” Dr. Shapira noted in an interview.
“Once a physician explains this [CBT] app and patients understand how to use it, then patients will be happy to use it,” commented Julia Grapsa, MD, PhD, a cardiologist at St. Thomas Hospital in London, who moderated the press conference. “We may see an explosion of apps like this one, designed to help better control” other chronic disorders, such as elevated blood pressure or abnormal lipid levels, Dr. Grapsa predicted. “I’m very optimistic that these apps have a great future in health care.”
Forty percent relative cut in new antihyperglycemic drug use
The BT-001 study randomized 669 adults with smartphone access and type 2 diabetes at any of six U.S. sites. The enrolled patients had type 2 diabetes for an average of 11 years, and an A1c of 7%-10.9% with an average level of 8.2%. Participants had to be on a stable medication regimen for at least 3 months but not using prandial insulin, and their treatment regimens could undergo adjustment during the trial. At baseline, each subject was on an average of 2.1 antihyperglycemic medications, including 90% on metformin and 42% on a sulfonylurea.
The new results reported by Dr. Bonaca showed that, during follow-up, people using the app had a 14.4% rate of antihyperglycemic drug intensification compared with a 24.4% rate among the controls, a roughly 40% relative decrease in new antihyperglycemic medication use. In addition, among those using insulin at baseline, 3.8% of controls increased their insulin dose, compared with 1.5% of those using the CBT app, while insulin doses decreased in 0.9% of the control subjects and in 2.2% of those using the BT-001 app.
Further study findings, first reported by Dr. Bonaca at the American Heart Association scientific sessions in late 2022, also showed a clear dose-response pattern for the CBT app: the more CBT lessons a person completed, the greater their reduction in A1c over 180 days of app use. People who used the app fewer than 10 times had an average reduction from baseline in their A1c of less than 0.1 percentage points. Among those who used the app 10-20 times (a subgroup with roughly one-third of the people randomized to app use), average A1c reduction increased to about 0.4 percentage points, and among those who used the app more than 20 times (also about one-third of the intervention group), the average A1c reduction from baseline was about 0.6 percentage points.
“It would be interesting to learn more about the adults who engaged with the app” and had a higher use rate “to provide more targeted care” with the app to people who match the profiles of those who were more likely to use the app during the trial, said Dr. Shapira.
This “clear” dose-response relationship “was one of the most exciting findings. It helps validate the mechanism,” Dr. Bonaca said during the press conference. “We’re now modeling which patients were the most engaged” with using the app, and “looking at ways to increase app engagement.”
Better Therapeutics also announced, in December 2022, results from a separate, uncontrolled study of a similar CBT app in 19 people with nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. The findings showed that use of the tested app linked with an average 16% drop from baseline in liver fat content as measured by MRI, as well as other improvements in markers of hepatic function. The company said in a statement that based on these findings it planned to apply for breakthrough-device designation with the FDA for use of a liver-specific CBT app in people with nonalcoholic fatty liver disease and nonalcoholic steatohepatitis.
The BT-001 trial was sponsored by Better Therapeutics, the company developing the app. CPC Clinical Research receives research and consulting funding from numerous companies. Dr. Bonaca has been a consultant to Audentes, and is a stockholder of Medtronic and Pfizer. Dr. Shapira and Dr. Grapsa had no disclosures.
FROM ACC 2023
Prone positioning curbs need for intubation in nonintubated COVID-19 patients
as indicated by data from a new meta-analysis of more than 2,000 individuals.
The use of prone positioning for nonintubated patients (so-called “awake prone positioning”) has been common since the early days of the COVID-19 pandemic. Prone positioning is more comfortable for patients, and it entails no additional cost. Also, awake prone positioning is less labor intensive than prone positioning for intubated patients, said Jie Li, PhD, in a presentation at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
However, data on the specific benefits of prone positioning are lacking and contradictory, said Dr. Li, a respiratory care specialist at Rush University, Chicago.
Dr. Li and colleagues from a multinational research group found that outcomes were improved for patients who were treated with awake prone positioning – notably, fewer treatment failures at day 28 – but a pair of subsequent studies by other researchers showed contradictory outcomes.
For more definitive evidence, Dr. Li and colleagues conducted a systematic review and meta-analysis of 11 randomized, controlled trials and one unpublished study of awake prone positioning for patients with COVID-19. The studies were published between Jan. 1, 2020, and July 1, 2022, and included a total of 2,886 adult patients.
The primary outcome was the reported cumulative risk of intubation among nonintubated COVID-19 patients. Secondary outcomes included mortality, the need for escalating respiratory support, length of hospital length of stay, ICU admission, and adverse events.
Overall, awake prone positioning significantly reduced the intubation risk among nonintubated patients compared to standard care (risk ratio, 0.85).
A further subgroup analysis showed a significant reduction in risk for intubation among patients supported by high-flow nasal cannula or noninvasive ventilation (RR, 0.83).
However, no additional reduction in intubation risk occurred among patients who received conventional oxygen therapy (RR, 1.02).
Mortality rates were similar for patients who underwent awake prone positioning and those who underwent supine positioning (RR, 0.96), as was the need for additional respiratory support (RR, 1.03). The length of hospital stay, ICU admission, and adverse events were similar between the patients who underwent prone positioning and those who underwent supine positioning.
The findings were limited by several factors. There was a potential for confounding by disease severity, which may have increased the use of respiratory support devices, Li said in her presentation.
“Another factor we should not ignore is the daily duration of prone positioning,” said Dr. Li. More research is needed to identify which factors play the greatest roles in treatment success.
The current study was important in that it evaluated the current evidence of awake prone positioning, “particularly to identify the patients who benefit most from this treatment, in order to guide clinical practice,” Dr. Li said in an interview.
“Since early in the pandemic, awake prone positioning has been broadly utilized to treat patients with COVID-19,” she said. “In 2021, we published a multinational randomized controlled trial with over 1,100 patients enrolled and reported lower treatment failure. However, no significant differences of treatment failure were reported in several subsequent multicenter randomized, controlled trials published after our study.”
Dr. Li said she was not surprised by the findings, which reflect those of her team’s previously published meta-analysis. “The increased number of patients helps confirm our previous finding, even with the inclusion of several recently published randomized controlled trials,” she said.
For clinicians, “the current evidence supports the use of awake prone positioning for patients with COVID-19, particularly those who require advanced respiratory support from high-flow nasal cannula or noninvasive ventilation,” Dr. Li said.
The study received no outside funding. Dr. Li has relationships with AARC, Heyer, Aeorgen, the Rice Foundation, and Fisher & Paykel Healthcare.
A version of this article first appeared on Medscape.com.
as indicated by data from a new meta-analysis of more than 2,000 individuals.
The use of prone positioning for nonintubated patients (so-called “awake prone positioning”) has been common since the early days of the COVID-19 pandemic. Prone positioning is more comfortable for patients, and it entails no additional cost. Also, awake prone positioning is less labor intensive than prone positioning for intubated patients, said Jie Li, PhD, in a presentation at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
However, data on the specific benefits of prone positioning are lacking and contradictory, said Dr. Li, a respiratory care specialist at Rush University, Chicago.
Dr. Li and colleagues from a multinational research group found that outcomes were improved for patients who were treated with awake prone positioning – notably, fewer treatment failures at day 28 – but a pair of subsequent studies by other researchers showed contradictory outcomes.
For more definitive evidence, Dr. Li and colleagues conducted a systematic review and meta-analysis of 11 randomized, controlled trials and one unpublished study of awake prone positioning for patients with COVID-19. The studies were published between Jan. 1, 2020, and July 1, 2022, and included a total of 2,886 adult patients.
The primary outcome was the reported cumulative risk of intubation among nonintubated COVID-19 patients. Secondary outcomes included mortality, the need for escalating respiratory support, length of hospital length of stay, ICU admission, and adverse events.
Overall, awake prone positioning significantly reduced the intubation risk among nonintubated patients compared to standard care (risk ratio, 0.85).
A further subgroup analysis showed a significant reduction in risk for intubation among patients supported by high-flow nasal cannula or noninvasive ventilation (RR, 0.83).
However, no additional reduction in intubation risk occurred among patients who received conventional oxygen therapy (RR, 1.02).
Mortality rates were similar for patients who underwent awake prone positioning and those who underwent supine positioning (RR, 0.96), as was the need for additional respiratory support (RR, 1.03). The length of hospital stay, ICU admission, and adverse events were similar between the patients who underwent prone positioning and those who underwent supine positioning.
The findings were limited by several factors. There was a potential for confounding by disease severity, which may have increased the use of respiratory support devices, Li said in her presentation.
“Another factor we should not ignore is the daily duration of prone positioning,” said Dr. Li. More research is needed to identify which factors play the greatest roles in treatment success.
The current study was important in that it evaluated the current evidence of awake prone positioning, “particularly to identify the patients who benefit most from this treatment, in order to guide clinical practice,” Dr. Li said in an interview.
“Since early in the pandemic, awake prone positioning has been broadly utilized to treat patients with COVID-19,” she said. “In 2021, we published a multinational randomized controlled trial with over 1,100 patients enrolled and reported lower treatment failure. However, no significant differences of treatment failure were reported in several subsequent multicenter randomized, controlled trials published after our study.”
Dr. Li said she was not surprised by the findings, which reflect those of her team’s previously published meta-analysis. “The increased number of patients helps confirm our previous finding, even with the inclusion of several recently published randomized controlled trials,” she said.
For clinicians, “the current evidence supports the use of awake prone positioning for patients with COVID-19, particularly those who require advanced respiratory support from high-flow nasal cannula or noninvasive ventilation,” Dr. Li said.
The study received no outside funding. Dr. Li has relationships with AARC, Heyer, Aeorgen, the Rice Foundation, and Fisher & Paykel Healthcare.
A version of this article first appeared on Medscape.com.
as indicated by data from a new meta-analysis of more than 2,000 individuals.
The use of prone positioning for nonintubated patients (so-called “awake prone positioning”) has been common since the early days of the COVID-19 pandemic. Prone positioning is more comfortable for patients, and it entails no additional cost. Also, awake prone positioning is less labor intensive than prone positioning for intubated patients, said Jie Li, PhD, in a presentation at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
However, data on the specific benefits of prone positioning are lacking and contradictory, said Dr. Li, a respiratory care specialist at Rush University, Chicago.
Dr. Li and colleagues from a multinational research group found that outcomes were improved for patients who were treated with awake prone positioning – notably, fewer treatment failures at day 28 – but a pair of subsequent studies by other researchers showed contradictory outcomes.
For more definitive evidence, Dr. Li and colleagues conducted a systematic review and meta-analysis of 11 randomized, controlled trials and one unpublished study of awake prone positioning for patients with COVID-19. The studies were published between Jan. 1, 2020, and July 1, 2022, and included a total of 2,886 adult patients.
The primary outcome was the reported cumulative risk of intubation among nonintubated COVID-19 patients. Secondary outcomes included mortality, the need for escalating respiratory support, length of hospital length of stay, ICU admission, and adverse events.
Overall, awake prone positioning significantly reduced the intubation risk among nonintubated patients compared to standard care (risk ratio, 0.85).
A further subgroup analysis showed a significant reduction in risk for intubation among patients supported by high-flow nasal cannula or noninvasive ventilation (RR, 0.83).
However, no additional reduction in intubation risk occurred among patients who received conventional oxygen therapy (RR, 1.02).
Mortality rates were similar for patients who underwent awake prone positioning and those who underwent supine positioning (RR, 0.96), as was the need for additional respiratory support (RR, 1.03). The length of hospital stay, ICU admission, and adverse events were similar between the patients who underwent prone positioning and those who underwent supine positioning.
The findings were limited by several factors. There was a potential for confounding by disease severity, which may have increased the use of respiratory support devices, Li said in her presentation.
“Another factor we should not ignore is the daily duration of prone positioning,” said Dr. Li. More research is needed to identify which factors play the greatest roles in treatment success.
The current study was important in that it evaluated the current evidence of awake prone positioning, “particularly to identify the patients who benefit most from this treatment, in order to guide clinical practice,” Dr. Li said in an interview.
“Since early in the pandemic, awake prone positioning has been broadly utilized to treat patients with COVID-19,” she said. “In 2021, we published a multinational randomized controlled trial with over 1,100 patients enrolled and reported lower treatment failure. However, no significant differences of treatment failure were reported in several subsequent multicenter randomized, controlled trials published after our study.”
Dr. Li said she was not surprised by the findings, which reflect those of her team’s previously published meta-analysis. “The increased number of patients helps confirm our previous finding, even with the inclusion of several recently published randomized controlled trials,” she said.
For clinicians, “the current evidence supports the use of awake prone positioning for patients with COVID-19, particularly those who require advanced respiratory support from high-flow nasal cannula or noninvasive ventilation,” Dr. Li said.
The study received no outside funding. Dr. Li has relationships with AARC, Heyer, Aeorgen, the Rice Foundation, and Fisher & Paykel Healthcare.
A version of this article first appeared on Medscape.com.
FROM SCCM 2023
COVID vs. flu: Which is deadlier?
a new study shows.
People who were hospitalized with Omicron COVID-19 infections were 54% more likely to die, compared with people who were hospitalized with the flu, Swiss researchers found.
The results of the study continue to debunk an earlier belief from the start of the pandemic that the flu was the more dangerous of the two respiratory viruses. The researchers noted that the deadliness of COVID-19, compared with flu, persisted “despite virus evolution and improved management strategies.”
The study was published in JAMA Network Open and included 5,212 patients in Switzerland hospitalized with COVID-19 or the flu. All the COVID patients were infected with the Omicron variant and hospitalized between Jan. 15, 2022, and March 15, 2022. Flu data included cases from January 2018 to March 15, 2022.
Overall, 7% of COVID-19 patients died, compared with 4.4% of flu patients. Researchers noted that the death rate for hospitalized COVID patients had declined since their previous study, which was conducted during the first COVID wave in the first half of 2020. At that time, the death rate of hospitalized COVID patients was 12.8%.
Since then, 98% of the Swiss population has been vaccinated. “Vaccination still plays a significant role regarding the main outcome,” the authors concluded, since a secondary analysis in this most recent study showed that unvaccinated COVID patients were twice as likely to die, compared with flu patients.
“Our results demonstrate that COVID-19 still cannot simply be compared with influenza,” they wrote.
While the death rate among COVID patients was significantly higher, there was no difference in the rate that COVID or flu patients were admitted to the ICU, which was around 8%.
A limitation of the study was that all the COVID cases did not have laboratory testing to confirm the Omicron variant. However, the study authors noted that Omicron accounted for at least 95% of cases during the time the patients were hospitalized. The authors were confident that their results were not biased by the potential for other variants being included in the data.
Four coauthors reported receiving grants and personal fees from various sources.
A version of this article first appeared on WebMD.com.
a new study shows.
People who were hospitalized with Omicron COVID-19 infections were 54% more likely to die, compared with people who were hospitalized with the flu, Swiss researchers found.
The results of the study continue to debunk an earlier belief from the start of the pandemic that the flu was the more dangerous of the two respiratory viruses. The researchers noted that the deadliness of COVID-19, compared with flu, persisted “despite virus evolution and improved management strategies.”
The study was published in JAMA Network Open and included 5,212 patients in Switzerland hospitalized with COVID-19 or the flu. All the COVID patients were infected with the Omicron variant and hospitalized between Jan. 15, 2022, and March 15, 2022. Flu data included cases from January 2018 to March 15, 2022.
Overall, 7% of COVID-19 patients died, compared with 4.4% of flu patients. Researchers noted that the death rate for hospitalized COVID patients had declined since their previous study, which was conducted during the first COVID wave in the first half of 2020. At that time, the death rate of hospitalized COVID patients was 12.8%.
Since then, 98% of the Swiss population has been vaccinated. “Vaccination still plays a significant role regarding the main outcome,” the authors concluded, since a secondary analysis in this most recent study showed that unvaccinated COVID patients were twice as likely to die, compared with flu patients.
“Our results demonstrate that COVID-19 still cannot simply be compared with influenza,” they wrote.
While the death rate among COVID patients was significantly higher, there was no difference in the rate that COVID or flu patients were admitted to the ICU, which was around 8%.
A limitation of the study was that all the COVID cases did not have laboratory testing to confirm the Omicron variant. However, the study authors noted that Omicron accounted for at least 95% of cases during the time the patients were hospitalized. The authors were confident that their results were not biased by the potential for other variants being included in the data.
Four coauthors reported receiving grants and personal fees from various sources.
A version of this article first appeared on WebMD.com.
a new study shows.
People who were hospitalized with Omicron COVID-19 infections were 54% more likely to die, compared with people who were hospitalized with the flu, Swiss researchers found.
The results of the study continue to debunk an earlier belief from the start of the pandemic that the flu was the more dangerous of the two respiratory viruses. The researchers noted that the deadliness of COVID-19, compared with flu, persisted “despite virus evolution and improved management strategies.”
The study was published in JAMA Network Open and included 5,212 patients in Switzerland hospitalized with COVID-19 or the flu. All the COVID patients were infected with the Omicron variant and hospitalized between Jan. 15, 2022, and March 15, 2022. Flu data included cases from January 2018 to March 15, 2022.
Overall, 7% of COVID-19 patients died, compared with 4.4% of flu patients. Researchers noted that the death rate for hospitalized COVID patients had declined since their previous study, which was conducted during the first COVID wave in the first half of 2020. At that time, the death rate of hospitalized COVID patients was 12.8%.
Since then, 98% of the Swiss population has been vaccinated. “Vaccination still plays a significant role regarding the main outcome,” the authors concluded, since a secondary analysis in this most recent study showed that unvaccinated COVID patients were twice as likely to die, compared with flu patients.
“Our results demonstrate that COVID-19 still cannot simply be compared with influenza,” they wrote.
While the death rate among COVID patients was significantly higher, there was no difference in the rate that COVID or flu patients were admitted to the ICU, which was around 8%.
A limitation of the study was that all the COVID cases did not have laboratory testing to confirm the Omicron variant. However, the study authors noted that Omicron accounted for at least 95% of cases during the time the patients were hospitalized. The authors were confident that their results were not biased by the potential for other variants being included in the data.
Four coauthors reported receiving grants and personal fees from various sources.
A version of this article first appeared on WebMD.com.
FROM JAMA NETWORK OPEN