User login
Inaccurate depictions of inpatient psychiatry foster stigma
When it comes to the portrayal of physicians in popular culture, psychiatrists are second only to surgeons.1 Far too often, these portrayals of psychiatry have misrepresented our specialty – and stigmatized our patients. Some of the content produced by entertainment giants Netflix and Marvel is a case in point.
That Netflix-Marvel collaboration has proven fruitful, resulting in six television series spanning seven seasons of entertainment to date. Last year alone saw the release of three Netflix-Marvel productions, including Marvel’s “Iron Fist” in March, “The Defenders” in August, and “The Punisher” in November. Given the popularity and ease of streaming Marvel’s Netflix productions, these series have the potential to entertain and inform a wide audience. Unfortunately, however, part of their influence might be to perpetuate stigma and fear surrounding inpatient psychiatric care. Take the inaccurate portrayal of psychiatry in “Iron Fist” compared with the reality of modern psychiatric care, for example.
While hospitalized, Danny is repeatedly shown in restraints, including four-point restraints, a belt, and a straitjacket. The use of restraints is sometimes portrayed as unprovoked, without evidence of aggression on the part of Danny. In addition, it appears that he is left in restraints for extended periods of time, as he is shown, for example, waking up in the night still restrained. While the use of restraints may be warranted in instances of extreme aggression or violence, the current culture of inpatient psychiatric care has shifted toward safely minimizing the use of restraints and seclusion.2 Straitjackets might be an icon of a bygone era of psychiatric care, but they no longer are a mainstream form of restraint used in the United States. Modern best practices would not result in a nonthreatening patient being placed in restraints and left in them for an extended period of time as shown in “Iron Fist.”
Danny is shown being forcibly administered medications, even in nonthreatening situations. These medications are given via parenteral injection as well as orally, with a psychiatric technician shown roughly inserting a tongue depressor deep in Danny’s mouth, pouring pills into his oral cavity, and manually holding his mouth shut to ensure ingestion. In truth, psychiatric patients are sometimes given intramuscular injections of calming agents when their level of agitation threatens to harm others or themselves. For patients to be given an involuntary injection when not acutely threatening, typically states require some form of legal application for forced medication (a process that does not appear to have been observed in “Iron Fist”). As we know, forced oral medications never should be undertaken given the significant risk to patient (possible choking) as well as staff (bitten fingers).
Staff supervision of patients at the fictional Birch Psychiatric Hospital is extremely poor. At one point, a fellow patient enters Danny’s room dressed in a white coat, pretending to be his doctor. As the conversation progresses, the patient grabs a fork from Danny’s food tray and holds it to his throat, threatening to kill him before being gruffly dragged off by hospital staff. At another point, Danny is shown in four-point restraints, and a patient simply walks into his room and removes the restraints for him. By contrast, in a real, modern inpatient psychiatric facility unit, staff would be routinely providing safety checks on patients throughout the day. If a patient is at risk for violence, sharp metal cutlery would not be included on accessible food trays. Patient attire would be subject to hospital inspection and approval, so it is unclear how or where a patient would have access to a physician’s coat to pull off such an impersonation. And finally, if a patient were sufficiently agitated to require the use of four-point restraints, he or she would be closely supervised and not left alone in an open area where other patients could remove the restraints.
The hospital stays described in “Iron Fist” are very long, and it is strongly implied that psychiatric diagnoses are invented to prolong inpatient care indefinitely. Referring to the duration of his initial involuntary hold, one patient tells Danny: “That what they tell you? Seventy-two hours? (laughs) Me, I had a little incident inside a pharmacy. Seventy-two hours later, I’m a bipolar with mixed affective episodes layered atop a substance abuse disorder. That was 2 years ago. Billy was living under a bridge. Seventy-two hours later, he’s a paranoid personality disorder. That was just over a year ago. And Jimmy was screaming at people in Times Square. Seventy-two hours later, he’s a schizoaffective disorder. He’s been here almost 15 years. Don’t think you’ll be any different.”
Most modern inpatient psychiatric care is designed around short-term hospitalization (days to weeks rather than months to years) with a goal of reintegrating patients back into the community with ongoing outpatient care as soon as they can safely make that transition. In addition, to insinuate that psychiatrists invent diagnoses to keep patients “locked up” insults the integrity of the many dedicated mental health workers who provide care for an ill and often overlooked population.
The most egregious examples of poor psychiatric care portrayed in “Iron Fist” involve illegal or criminal activities. Video cameras placed throughout the hospital transmit a live feed to a shadowy figure who has no role in patient care. A psychiatric technician escorts Danny to a room full of patients hired to kill him. These particular concerns are outlandish enough that perhaps they don’t even need to be directly addressed, but for the sake of completeness it is worth noting that psychiatric hospitals are subject to rigorous oversight from numerous regulatory bodies to ensure that patient care is delivered in a safe and respectable manner and that all protected health information is accessible only by those whose treatment role necessitates such access.
Marvel’s “Iron Fist” seeks to entertain its audience, but it does a poor job of showing viewers a realistic portrayal of inpatient psychiatric care. The show presents a psychiatric hospital as the setting for inappropriate use of restraints, unwarranted use of forced oral and injectable medications, a lack of supervision leading to violence between patients, and even attempted murder accommodated by a hospital employee. Also, the show strongly implies that psychiatric diagnoses are invented for the purpose of continuing inpatient care indefinitely.
In sum, the psychiatric hospital is seen as an inhumane form of imprisonment from which one can only hope to escape with the benefit of a glowing, magical fist. Although this is fiction, these kinds of narratives can have very real consequences in perpetuating stigma against psychiatric care. Ultimately, such storylines undermine the public’s confidence in clinicians seeking to provide caring and compassionate care.
Dr. Weber is psychiatry department chair at Logan (Utah) Regional Hospital with Intermountain Healthcare.
References
1 J Nat Med Assoc. 2002 Jul. 94[7]:635-58.
2 Aggress Violent Behav. 2017;34:139-46.
When it comes to the portrayal of physicians in popular culture, psychiatrists are second only to surgeons.1 Far too often, these portrayals of psychiatry have misrepresented our specialty – and stigmatized our patients. Some of the content produced by entertainment giants Netflix and Marvel is a case in point.
That Netflix-Marvel collaboration has proven fruitful, resulting in six television series spanning seven seasons of entertainment to date. Last year alone saw the release of three Netflix-Marvel productions, including Marvel’s “Iron Fist” in March, “The Defenders” in August, and “The Punisher” in November. Given the popularity and ease of streaming Marvel’s Netflix productions, these series have the potential to entertain and inform a wide audience. Unfortunately, however, part of their influence might be to perpetuate stigma and fear surrounding inpatient psychiatric care. Take the inaccurate portrayal of psychiatry in “Iron Fist” compared with the reality of modern psychiatric care, for example.
While hospitalized, Danny is repeatedly shown in restraints, including four-point restraints, a belt, and a straitjacket. The use of restraints is sometimes portrayed as unprovoked, without evidence of aggression on the part of Danny. In addition, it appears that he is left in restraints for extended periods of time, as he is shown, for example, waking up in the night still restrained. While the use of restraints may be warranted in instances of extreme aggression or violence, the current culture of inpatient psychiatric care has shifted toward safely minimizing the use of restraints and seclusion.2 Straitjackets might be an icon of a bygone era of psychiatric care, but they no longer are a mainstream form of restraint used in the United States. Modern best practices would not result in a nonthreatening patient being placed in restraints and left in them for an extended period of time as shown in “Iron Fist.”
Danny is shown being forcibly administered medications, even in nonthreatening situations. These medications are given via parenteral injection as well as orally, with a psychiatric technician shown roughly inserting a tongue depressor deep in Danny’s mouth, pouring pills into his oral cavity, and manually holding his mouth shut to ensure ingestion. In truth, psychiatric patients are sometimes given intramuscular injections of calming agents when their level of agitation threatens to harm others or themselves. For patients to be given an involuntary injection when not acutely threatening, typically states require some form of legal application for forced medication (a process that does not appear to have been observed in “Iron Fist”). As we know, forced oral medications never should be undertaken given the significant risk to patient (possible choking) as well as staff (bitten fingers).
Staff supervision of patients at the fictional Birch Psychiatric Hospital is extremely poor. At one point, a fellow patient enters Danny’s room dressed in a white coat, pretending to be his doctor. As the conversation progresses, the patient grabs a fork from Danny’s food tray and holds it to his throat, threatening to kill him before being gruffly dragged off by hospital staff. At another point, Danny is shown in four-point restraints, and a patient simply walks into his room and removes the restraints for him. By contrast, in a real, modern inpatient psychiatric facility unit, staff would be routinely providing safety checks on patients throughout the day. If a patient is at risk for violence, sharp metal cutlery would not be included on accessible food trays. Patient attire would be subject to hospital inspection and approval, so it is unclear how or where a patient would have access to a physician’s coat to pull off such an impersonation. And finally, if a patient were sufficiently agitated to require the use of four-point restraints, he or she would be closely supervised and not left alone in an open area where other patients could remove the restraints.
The hospital stays described in “Iron Fist” are very long, and it is strongly implied that psychiatric diagnoses are invented to prolong inpatient care indefinitely. Referring to the duration of his initial involuntary hold, one patient tells Danny: “That what they tell you? Seventy-two hours? (laughs) Me, I had a little incident inside a pharmacy. Seventy-two hours later, I’m a bipolar with mixed affective episodes layered atop a substance abuse disorder. That was 2 years ago. Billy was living under a bridge. Seventy-two hours later, he’s a paranoid personality disorder. That was just over a year ago. And Jimmy was screaming at people in Times Square. Seventy-two hours later, he’s a schizoaffective disorder. He’s been here almost 15 years. Don’t think you’ll be any different.”
Most modern inpatient psychiatric care is designed around short-term hospitalization (days to weeks rather than months to years) with a goal of reintegrating patients back into the community with ongoing outpatient care as soon as they can safely make that transition. In addition, to insinuate that psychiatrists invent diagnoses to keep patients “locked up” insults the integrity of the many dedicated mental health workers who provide care for an ill and often overlooked population.
The most egregious examples of poor psychiatric care portrayed in “Iron Fist” involve illegal or criminal activities. Video cameras placed throughout the hospital transmit a live feed to a shadowy figure who has no role in patient care. A psychiatric technician escorts Danny to a room full of patients hired to kill him. These particular concerns are outlandish enough that perhaps they don’t even need to be directly addressed, but for the sake of completeness it is worth noting that psychiatric hospitals are subject to rigorous oversight from numerous regulatory bodies to ensure that patient care is delivered in a safe and respectable manner and that all protected health information is accessible only by those whose treatment role necessitates such access.
Marvel’s “Iron Fist” seeks to entertain its audience, but it does a poor job of showing viewers a realistic portrayal of inpatient psychiatric care. The show presents a psychiatric hospital as the setting for inappropriate use of restraints, unwarranted use of forced oral and injectable medications, a lack of supervision leading to violence between patients, and even attempted murder accommodated by a hospital employee. Also, the show strongly implies that psychiatric diagnoses are invented for the purpose of continuing inpatient care indefinitely.
In sum, the psychiatric hospital is seen as an inhumane form of imprisonment from which one can only hope to escape with the benefit of a glowing, magical fist. Although this is fiction, these kinds of narratives can have very real consequences in perpetuating stigma against psychiatric care. Ultimately, such storylines undermine the public’s confidence in clinicians seeking to provide caring and compassionate care.
Dr. Weber is psychiatry department chair at Logan (Utah) Regional Hospital with Intermountain Healthcare.
References
1 J Nat Med Assoc. 2002 Jul. 94[7]:635-58.
2 Aggress Violent Behav. 2017;34:139-46.
When it comes to the portrayal of physicians in popular culture, psychiatrists are second only to surgeons.1 Far too often, these portrayals of psychiatry have misrepresented our specialty – and stigmatized our patients. Some of the content produced by entertainment giants Netflix and Marvel is a case in point.
That Netflix-Marvel collaboration has proven fruitful, resulting in six television series spanning seven seasons of entertainment to date. Last year alone saw the release of three Netflix-Marvel productions, including Marvel’s “Iron Fist” in March, “The Defenders” in August, and “The Punisher” in November. Given the popularity and ease of streaming Marvel’s Netflix productions, these series have the potential to entertain and inform a wide audience. Unfortunately, however, part of their influence might be to perpetuate stigma and fear surrounding inpatient psychiatric care. Take the inaccurate portrayal of psychiatry in “Iron Fist” compared with the reality of modern psychiatric care, for example.
While hospitalized, Danny is repeatedly shown in restraints, including four-point restraints, a belt, and a straitjacket. The use of restraints is sometimes portrayed as unprovoked, without evidence of aggression on the part of Danny. In addition, it appears that he is left in restraints for extended periods of time, as he is shown, for example, waking up in the night still restrained. While the use of restraints may be warranted in instances of extreme aggression or violence, the current culture of inpatient psychiatric care has shifted toward safely minimizing the use of restraints and seclusion.2 Straitjackets might be an icon of a bygone era of psychiatric care, but they no longer are a mainstream form of restraint used in the United States. Modern best practices would not result in a nonthreatening patient being placed in restraints and left in them for an extended period of time as shown in “Iron Fist.”
Danny is shown being forcibly administered medications, even in nonthreatening situations. These medications are given via parenteral injection as well as orally, with a psychiatric technician shown roughly inserting a tongue depressor deep in Danny’s mouth, pouring pills into his oral cavity, and manually holding his mouth shut to ensure ingestion. In truth, psychiatric patients are sometimes given intramuscular injections of calming agents when their level of agitation threatens to harm others or themselves. For patients to be given an involuntary injection when not acutely threatening, typically states require some form of legal application for forced medication (a process that does not appear to have been observed in “Iron Fist”). As we know, forced oral medications never should be undertaken given the significant risk to patient (possible choking) as well as staff (bitten fingers).
Staff supervision of patients at the fictional Birch Psychiatric Hospital is extremely poor. At one point, a fellow patient enters Danny’s room dressed in a white coat, pretending to be his doctor. As the conversation progresses, the patient grabs a fork from Danny’s food tray and holds it to his throat, threatening to kill him before being gruffly dragged off by hospital staff. At another point, Danny is shown in four-point restraints, and a patient simply walks into his room and removes the restraints for him. By contrast, in a real, modern inpatient psychiatric facility unit, staff would be routinely providing safety checks on patients throughout the day. If a patient is at risk for violence, sharp metal cutlery would not be included on accessible food trays. Patient attire would be subject to hospital inspection and approval, so it is unclear how or where a patient would have access to a physician’s coat to pull off such an impersonation. And finally, if a patient were sufficiently agitated to require the use of four-point restraints, he or she would be closely supervised and not left alone in an open area where other patients could remove the restraints.
The hospital stays described in “Iron Fist” are very long, and it is strongly implied that psychiatric diagnoses are invented to prolong inpatient care indefinitely. Referring to the duration of his initial involuntary hold, one patient tells Danny: “That what they tell you? Seventy-two hours? (laughs) Me, I had a little incident inside a pharmacy. Seventy-two hours later, I’m a bipolar with mixed affective episodes layered atop a substance abuse disorder. That was 2 years ago. Billy was living under a bridge. Seventy-two hours later, he’s a paranoid personality disorder. That was just over a year ago. And Jimmy was screaming at people in Times Square. Seventy-two hours later, he’s a schizoaffective disorder. He’s been here almost 15 years. Don’t think you’ll be any different.”
Most modern inpatient psychiatric care is designed around short-term hospitalization (days to weeks rather than months to years) with a goal of reintegrating patients back into the community with ongoing outpatient care as soon as they can safely make that transition. In addition, to insinuate that psychiatrists invent diagnoses to keep patients “locked up” insults the integrity of the many dedicated mental health workers who provide care for an ill and often overlooked population.
The most egregious examples of poor psychiatric care portrayed in “Iron Fist” involve illegal or criminal activities. Video cameras placed throughout the hospital transmit a live feed to a shadowy figure who has no role in patient care. A psychiatric technician escorts Danny to a room full of patients hired to kill him. These particular concerns are outlandish enough that perhaps they don’t even need to be directly addressed, but for the sake of completeness it is worth noting that psychiatric hospitals are subject to rigorous oversight from numerous regulatory bodies to ensure that patient care is delivered in a safe and respectable manner and that all protected health information is accessible only by those whose treatment role necessitates such access.
Marvel’s “Iron Fist” seeks to entertain its audience, but it does a poor job of showing viewers a realistic portrayal of inpatient psychiatric care. The show presents a psychiatric hospital as the setting for inappropriate use of restraints, unwarranted use of forced oral and injectable medications, a lack of supervision leading to violence between patients, and even attempted murder accommodated by a hospital employee. Also, the show strongly implies that psychiatric diagnoses are invented for the purpose of continuing inpatient care indefinitely.
In sum, the psychiatric hospital is seen as an inhumane form of imprisonment from which one can only hope to escape with the benefit of a glowing, magical fist. Although this is fiction, these kinds of narratives can have very real consequences in perpetuating stigma against psychiatric care. Ultimately, such storylines undermine the public’s confidence in clinicians seeking to provide caring and compassionate care.
Dr. Weber is psychiatry department chair at Logan (Utah) Regional Hospital with Intermountain Healthcare.
References
1 J Nat Med Assoc. 2002 Jul. 94[7]:635-58.
2 Aggress Violent Behav. 2017;34:139-46.
Action to address gun violence is long overdue
On Feb. 14 in Parkland, Florida, 17 students and teachers were murdered in yet another school shooting. Yet another mass killing. More than a dozen others were injured and some are fighting for their lives under the care of physicians and nurses.
The pervasiveness of gun violence and the weapons used in these crimes have changed the way we live. In movie theaters, places of worship, offices, restaurants, night clubs and schools, people today make clear note of escape routes. Schools, including the one attacked yesterday, regularly practice for active shooter situations.
And in emergency departments and trauma centers, we struggle with much more complicated, dangerous injuries inflicted by lethal ammunition fired by military-grade weapons.
At the 2016 AMA Annual Meeting, which began the day after the deadly shooting at the Pulse Nightclub in Orlando, physicians from across the country and at every stage in their career spoke about treating gunshot victims and the scale of violence we are experiencing today. Their stories resonate as much today as they did nearly two years ago.
The shooting at Marjory Stoneman Douglas High School was the 30th mass shooting – a shooting in which four or more people are killed or injured – of 2018. It was also the 17th time a gun has been fired on the grounds of an American school this year. The problem is getting worse – the regularity of, and death from, mass shootings is increasing. With the shooting in Parkland, three of the 10 deadliest mass shootings in modern U.S. history have come in the past five months.
Time to act
Gun violence in America today is a public health crisis, one that requires a comprehensive and far-reaching solution. And that is not just my own sentiment; that is the determination of the AMA House of Delegates. With more than 30,000 American men, women and children dying from gun violence and firearm-related accidents each year, the time to act is now.
Today, more than ever before, America’s physicians must lend their voice and their considerable political muscle to force lawmakers to examine this urgent health crisis – through federally funded research – and take appropriate steps to address it. Let me be very clear about this. We are not talking about Second Amendment rights or restricting your ability to own a firearm.
We are talking about a public health crisis that our Congress has failed to address. This must end.
In the wake of the Sandy Hook shooting in 2012 – a massacre that left 20 first-graders and six adults dead – the AMA wrote to President Obama and to the leaders in the House and Senate. We expressed our sense of grief and sadness and offered our expertise and experience in finding workable, commonsense solutions to reduce the epidemic of gun violence – indeed the overall culture of violence – in America.
We noted that the relatively easy access to the increased firepower of assault weapons, semiautomatic firearms, high-capacity magazines, and high-velocity ammunition heightens the risk of multiple gunshot wounds and severe penetrating trauma, resulting in more critical injuries and deaths. Even for those who manage to survive gun violence involving these weapons, the severity and lasting impact of their wounds, disabilities and treatment leads to devastating consequences for the families affected and for society as a whole, contributing to high medical costs for treatment and recovery.
We called for renewing and strengthening the assault weapons ban, including banning high-capacity magazines, as a step in the right direction. We also called for more resources for safety education programs that promote more responsible use and storage of firearms, and noted that part of ensuring firearms safety means that physicians need to be able to have frank discussions with their patients and parents of patients about firearm safety issues and risks to help them safeguard their families from accidents.
We also urged the nation to strengthen its commitment and resources to comprehensive access to mental health services, including screening, prevention and treatment. While the overwhelming majority of patients with mental illness are not violent, physicians and other health professionals must be trained to respond to those who have a mental illness that might make them more prone to commit violence.
On an average day, more than 100 Americans die from gun violence and firearm-related accidents. In communities like yours – regardless of where you live or how safe it feels – people are losing their lives to this scourge.
For many Americans, gun violence used to be a distant idea relegated mostly to the nightly news, movies and faraway places. But today, in communities such as Parkland, it is horrifyingly real. The victims are our friends, neighbors and, unfathomably, our children.
As physicians, we have dedicated our lives to public health. And at the AMA, our mission is improving the health of the nation. That mission today must include determining the root causes of this epidemic and turning the tide on gun violence.
We must do more than pray for families who lost loved ones. It is time to act to prevent future deaths and injuries.
Dr. Barbe is president of the American Medical Association. His commentary originally was published on AMA Wire.
On Feb. 14 in Parkland, Florida, 17 students and teachers were murdered in yet another school shooting. Yet another mass killing. More than a dozen others were injured and some are fighting for their lives under the care of physicians and nurses.
The pervasiveness of gun violence and the weapons used in these crimes have changed the way we live. In movie theaters, places of worship, offices, restaurants, night clubs and schools, people today make clear note of escape routes. Schools, including the one attacked yesterday, regularly practice for active shooter situations.
And in emergency departments and trauma centers, we struggle with much more complicated, dangerous injuries inflicted by lethal ammunition fired by military-grade weapons.
At the 2016 AMA Annual Meeting, which began the day after the deadly shooting at the Pulse Nightclub in Orlando, physicians from across the country and at every stage in their career spoke about treating gunshot victims and the scale of violence we are experiencing today. Their stories resonate as much today as they did nearly two years ago.
The shooting at Marjory Stoneman Douglas High School was the 30th mass shooting – a shooting in which four or more people are killed or injured – of 2018. It was also the 17th time a gun has been fired on the grounds of an American school this year. The problem is getting worse – the regularity of, and death from, mass shootings is increasing. With the shooting in Parkland, three of the 10 deadliest mass shootings in modern U.S. history have come in the past five months.
Time to act
Gun violence in America today is a public health crisis, one that requires a comprehensive and far-reaching solution. And that is not just my own sentiment; that is the determination of the AMA House of Delegates. With more than 30,000 American men, women and children dying from gun violence and firearm-related accidents each year, the time to act is now.
Today, more than ever before, America’s physicians must lend their voice and their considerable political muscle to force lawmakers to examine this urgent health crisis – through federally funded research – and take appropriate steps to address it. Let me be very clear about this. We are not talking about Second Amendment rights or restricting your ability to own a firearm.
We are talking about a public health crisis that our Congress has failed to address. This must end.
In the wake of the Sandy Hook shooting in 2012 – a massacre that left 20 first-graders and six adults dead – the AMA wrote to President Obama and to the leaders in the House and Senate. We expressed our sense of grief and sadness and offered our expertise and experience in finding workable, commonsense solutions to reduce the epidemic of gun violence – indeed the overall culture of violence – in America.
We noted that the relatively easy access to the increased firepower of assault weapons, semiautomatic firearms, high-capacity magazines, and high-velocity ammunition heightens the risk of multiple gunshot wounds and severe penetrating trauma, resulting in more critical injuries and deaths. Even for those who manage to survive gun violence involving these weapons, the severity and lasting impact of their wounds, disabilities and treatment leads to devastating consequences for the families affected and for society as a whole, contributing to high medical costs for treatment and recovery.
We called for renewing and strengthening the assault weapons ban, including banning high-capacity magazines, as a step in the right direction. We also called for more resources for safety education programs that promote more responsible use and storage of firearms, and noted that part of ensuring firearms safety means that physicians need to be able to have frank discussions with their patients and parents of patients about firearm safety issues and risks to help them safeguard their families from accidents.
We also urged the nation to strengthen its commitment and resources to comprehensive access to mental health services, including screening, prevention and treatment. While the overwhelming majority of patients with mental illness are not violent, physicians and other health professionals must be trained to respond to those who have a mental illness that might make them more prone to commit violence.
On an average day, more than 100 Americans die from gun violence and firearm-related accidents. In communities like yours – regardless of where you live or how safe it feels – people are losing their lives to this scourge.
For many Americans, gun violence used to be a distant idea relegated mostly to the nightly news, movies and faraway places. But today, in communities such as Parkland, it is horrifyingly real. The victims are our friends, neighbors and, unfathomably, our children.
As physicians, we have dedicated our lives to public health. And at the AMA, our mission is improving the health of the nation. That mission today must include determining the root causes of this epidemic and turning the tide on gun violence.
We must do more than pray for families who lost loved ones. It is time to act to prevent future deaths and injuries.
Dr. Barbe is president of the American Medical Association. His commentary originally was published on AMA Wire.
On Feb. 14 in Parkland, Florida, 17 students and teachers were murdered in yet another school shooting. Yet another mass killing. More than a dozen others were injured and some are fighting for their lives under the care of physicians and nurses.
The pervasiveness of gun violence and the weapons used in these crimes have changed the way we live. In movie theaters, places of worship, offices, restaurants, night clubs and schools, people today make clear note of escape routes. Schools, including the one attacked yesterday, regularly practice for active shooter situations.
And in emergency departments and trauma centers, we struggle with much more complicated, dangerous injuries inflicted by lethal ammunition fired by military-grade weapons.
At the 2016 AMA Annual Meeting, which began the day after the deadly shooting at the Pulse Nightclub in Orlando, physicians from across the country and at every stage in their career spoke about treating gunshot victims and the scale of violence we are experiencing today. Their stories resonate as much today as they did nearly two years ago.
The shooting at Marjory Stoneman Douglas High School was the 30th mass shooting – a shooting in which four or more people are killed or injured – of 2018. It was also the 17th time a gun has been fired on the grounds of an American school this year. The problem is getting worse – the regularity of, and death from, mass shootings is increasing. With the shooting in Parkland, three of the 10 deadliest mass shootings in modern U.S. history have come in the past five months.
Time to act
Gun violence in America today is a public health crisis, one that requires a comprehensive and far-reaching solution. And that is not just my own sentiment; that is the determination of the AMA House of Delegates. With more than 30,000 American men, women and children dying from gun violence and firearm-related accidents each year, the time to act is now.
Today, more than ever before, America’s physicians must lend their voice and their considerable political muscle to force lawmakers to examine this urgent health crisis – through federally funded research – and take appropriate steps to address it. Let me be very clear about this. We are not talking about Second Amendment rights or restricting your ability to own a firearm.
We are talking about a public health crisis that our Congress has failed to address. This must end.
In the wake of the Sandy Hook shooting in 2012 – a massacre that left 20 first-graders and six adults dead – the AMA wrote to President Obama and to the leaders in the House and Senate. We expressed our sense of grief and sadness and offered our expertise and experience in finding workable, commonsense solutions to reduce the epidemic of gun violence – indeed the overall culture of violence – in America.
We noted that the relatively easy access to the increased firepower of assault weapons, semiautomatic firearms, high-capacity magazines, and high-velocity ammunition heightens the risk of multiple gunshot wounds and severe penetrating trauma, resulting in more critical injuries and deaths. Even for those who manage to survive gun violence involving these weapons, the severity and lasting impact of their wounds, disabilities and treatment leads to devastating consequences for the families affected and for society as a whole, contributing to high medical costs for treatment and recovery.
We called for renewing and strengthening the assault weapons ban, including banning high-capacity magazines, as a step in the right direction. We also called for more resources for safety education programs that promote more responsible use and storage of firearms, and noted that part of ensuring firearms safety means that physicians need to be able to have frank discussions with their patients and parents of patients about firearm safety issues and risks to help them safeguard their families from accidents.
We also urged the nation to strengthen its commitment and resources to comprehensive access to mental health services, including screening, prevention and treatment. While the overwhelming majority of patients with mental illness are not violent, physicians and other health professionals must be trained to respond to those who have a mental illness that might make them more prone to commit violence.
On an average day, more than 100 Americans die from gun violence and firearm-related accidents. In communities like yours – regardless of where you live or how safe it feels – people are losing their lives to this scourge.
For many Americans, gun violence used to be a distant idea relegated mostly to the nightly news, movies and faraway places. But today, in communities such as Parkland, it is horrifyingly real. The victims are our friends, neighbors and, unfathomably, our children.
As physicians, we have dedicated our lives to public health. And at the AMA, our mission is improving the health of the nation. That mission today must include determining the root causes of this epidemic and turning the tide on gun violence.
We must do more than pray for families who lost loved ones. It is time to act to prevent future deaths and injuries.
Dr. Barbe is president of the American Medical Association. His commentary originally was published on AMA Wire.
Allscripts’ charges for sending, refilling prescriptions
How much is $9 worth? Not much. Probably less than most people spend on coffee in a given week.
And yet, that $9 is really irritating to me.
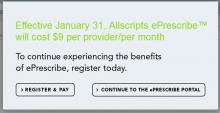
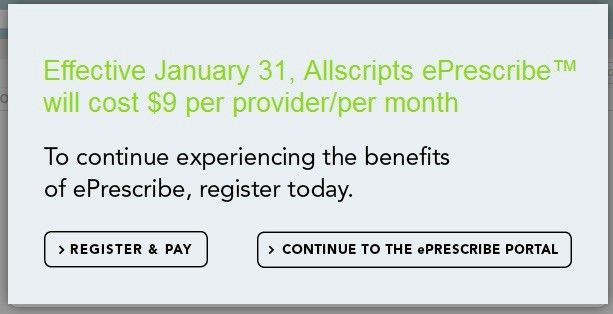
For the last few weeks, when signing into Allscripts to send and refill prescriptions, I’ve encountered this:
I know that $9 a month doesn’t seem like much: It’s $108 a year. But still, it’s irritating.
I understand Allscripts, and every other health care company, is here to make a living. Heck, so am I. Software development isn’t cheap. Neither are the servers hosting it or the security software needed, or the buildings to house them, and a million other things. I get that. None of these things are free.
But, at the same time, it’s part of a general trend of modern health care. Our landlords and vendors can arbitrarily raise prices to keep up with their costs, but we can’t do the same to keep up with ours.
The majority of doctors aren’t in a position to raise our prices to account for these things. We’re stuck with insurance companies and government agencies that tell us to accept a given amount or eat rocks.
There are, of course, concierge practices that can raise their prices, but they’re mostly boutique-level general care with wealthy patients who can afford them. Most small specialists aren’t in that position. We can’t afford to put Keurigs in the lobby.
The few revenue streams most of us have for which we can increase prices, such as legal work and cash patients, are typically not enough of the practice where it would make a difference to overcome it. In fact, the lien company I see patients for recently told me they were lowering their reimbursements to me to compensate for their own higher expenses.
Some people may see the $9 a month as a minor issue and move on. But to a small practice, it’s now another $108 in revenue that I have to bring in each year to cover. And, in a field in which, unlike every other product or service people pay for, I’m not allowed to control my own prices to make up for it.
That doesn’t seem fair, does it?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How much is $9 worth? Not much. Probably less than most people spend on coffee in a given week.
And yet, that $9 is really irritating to me.
For the last few weeks, when signing into Allscripts to send and refill prescriptions, I’ve encountered this:
I know that $9 a month doesn’t seem like much: It’s $108 a year. But still, it’s irritating.
I understand Allscripts, and every other health care company, is here to make a living. Heck, so am I. Software development isn’t cheap. Neither are the servers hosting it or the security software needed, or the buildings to house them, and a million other things. I get that. None of these things are free.
But, at the same time, it’s part of a general trend of modern health care. Our landlords and vendors can arbitrarily raise prices to keep up with their costs, but we can’t do the same to keep up with ours.
The majority of doctors aren’t in a position to raise our prices to account for these things. We’re stuck with insurance companies and government agencies that tell us to accept a given amount or eat rocks.
There are, of course, concierge practices that can raise their prices, but they’re mostly boutique-level general care with wealthy patients who can afford them. Most small specialists aren’t in that position. We can’t afford to put Keurigs in the lobby.
The few revenue streams most of us have for which we can increase prices, such as legal work and cash patients, are typically not enough of the practice where it would make a difference to overcome it. In fact, the lien company I see patients for recently told me they were lowering their reimbursements to me to compensate for their own higher expenses.
Some people may see the $9 a month as a minor issue and move on. But to a small practice, it’s now another $108 in revenue that I have to bring in each year to cover. And, in a field in which, unlike every other product or service people pay for, I’m not allowed to control my own prices to make up for it.
That doesn’t seem fair, does it?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
How much is $9 worth? Not much. Probably less than most people spend on coffee in a given week.
And yet, that $9 is really irritating to me.
For the last few weeks, when signing into Allscripts to send and refill prescriptions, I’ve encountered this:
I know that $9 a month doesn’t seem like much: It’s $108 a year. But still, it’s irritating.
I understand Allscripts, and every other health care company, is here to make a living. Heck, so am I. Software development isn’t cheap. Neither are the servers hosting it or the security software needed, or the buildings to house them, and a million other things. I get that. None of these things are free.
But, at the same time, it’s part of a general trend of modern health care. Our landlords and vendors can arbitrarily raise prices to keep up with their costs, but we can’t do the same to keep up with ours.
The majority of doctors aren’t in a position to raise our prices to account for these things. We’re stuck with insurance companies and government agencies that tell us to accept a given amount or eat rocks.
There are, of course, concierge practices that can raise their prices, but they’re mostly boutique-level general care with wealthy patients who can afford them. Most small specialists aren’t in that position. We can’t afford to put Keurigs in the lobby.
The few revenue streams most of us have for which we can increase prices, such as legal work and cash patients, are typically not enough of the practice where it would make a difference to overcome it. In fact, the lien company I see patients for recently told me they were lowering their reimbursements to me to compensate for their own higher expenses.
Some people may see the $9 a month as a minor issue and move on. But to a small practice, it’s now another $108 in revenue that I have to bring in each year to cover. And, in a field in which, unlike every other product or service people pay for, I’m not allowed to control my own prices to make up for it.
That doesn’t seem fair, does it?
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
From the ACS President: The joy and privilege of a surgical career
As a Fellow of the American College of Surgeons (ACS), only you can recall the personal sacrifices you have made to attain the skills and knowledge necessary to enjoy the privilege of being a surgeon – years of missed time with family and friends, sleepless nights, and endless formative hours of deep experiential learning in the hospital. Someone else could have been there instead; you could have made a different career choice. But, no – surgery chose you, and you dove in. Thank you, thank you.
I hope you never lose sight of the lives you touched during those “lost” times – injured people, previously unknown neighbors with deadly diseases, or simply patients needing a little “repair.” People with a surgical disease are experiencing a rare life event: an operation. Never forget that each of those individuals, each patient, came to you – you personally – to help them.
Challenges
Regrettably, however, at times the cherished bond between a surgeon and a patient can get lost in our busy, burdened lives. It can get lost in physical fatigue, regulatory hoops, frustrations of the electronic health record, contract negotiations, challenging reimbursement policies, and on and on.
Add to that list other challenges that will surely arise in the course of your career: You will face various forms of threatened obsolescence in knowledge, skills, and technology. You will age. You will suffer personal tragedy and loss. You will become ill. That you may stumble when facing such challenges is not a sign of weakness. It is life.
I believe there is a bit of light ahead as our health care industry begins to recognize that this thing we call burnout is not a personal failing, but rather a function of our flawed work environments – and a significant threat not only to the surgeon, but also to patient safety, quality of care, and institutional financial stability. An active voice and actions in these essential domains of our work environment are mission critical for our College, as are efforts that are pursued on many fronts by Fellows and professionals in the Division of Advocacy and Health Policy in Washington, DC, and the Divisions of Research and Optimal Patient Care, Education, and Member Services in Chicago, IL. Fostering an environment to optimally support the care of the surgical patient – and surgeons – is core business in all we do in the ACS.
Let’s tackle a few other challenges. First, consider your personal and society’s investment in surgical training. Getting you to this skilled and knowledgeable point reflects an investment of more than $1 million dollars in costs of medical school and graduate medical education, and inestimable time and effort.
Second, the dire anticipated shortage of surgeons of many disciplines – general surgeons, orthopedists, urologists – appears to be real. If we are to keep our surgical pipeline full, we need to offer careers that are attractive to men and women equally. The U.S. general surgery pathway has entering classes of 40% women; however, other high-demand disciplines, such as neurosurgery, orthopedics, and cardiothoracic surgery, have not yet attracted women to their ranks in sufficient numbers, despite the fact that 50% of our medical school graduates are women. We need to examine the pathways to those surgical disciplines to ensure that gender- and ethnicity-based barriers are receding. Efforts are underway to address these challenges by the leadership in these disciplines that our College can help with.
Although much has changed for women in surgery in recent years, there are still differences in the lives of many female surgeons compared to their male colleagues. They remain at risk for pay inequity, being in aggregate compensated 10-17% less than their male colleagues for equal work. Despite a mature gender pipeline in some surgical specialties, women are still less likely to rise to leadership roles in their group practices, hospital structures, professional organizations, and academic institutions. The ACS can serve as a professional home to develop strategies to highlight and remedy these imbalances.
Parenting, to engage as fully and successfully as one may wish, is a challenge for many who choose our careers, regardless of gender. However, for most female surgeons beginning a family, the first step often comes with pregnancy and infant care, conditions that we have yet to embrace and support as a societal good rather than an individual’s gauntlet to run. Given our long and arduous educational pathways, these women often find themselves starting a family, be it by pregnancy or adoption, at the same moment they are beginning their busy early years of practice. Policies and practices to support surgeons who choose parenthood in the workforce are sorely needed and will, in fact, benefit all in the long run.
Our College, with guidance from the Women in Surgery Committee and the Association of Women Surgeons, has advanced that goal, issuing a statement that acknowledges the need for appropriate pregnancy and parental leave and that clearly articulates that the choice to become a parent in no way diminishes a surgeon’s commitment to career. The next steps will be building the institutional, financial, and community infrastructure to foster success in both career and parenting for all.
Retooling reimagined
Let’s ponder another challenge: the need to add to your repertoire a new, potentially transformative skill. How do we safely retool?
Twenty years ago, in the flawed early adoption of laparoscopic surgery, the ACS Committee on Emerging Surgical Technology Education articulated the principles of new skill acquisition: didactic learning, coupled with simulation-based training, and then proctored early experience, leading to independent practice and assessment of outcomes.
Subsequently, the College took the visionary step of establishing the ACS Accredited Education Institutes (AEI) program to develop a network of centers that would leverage emerging simulation technologies to enhance surgical training. The 96 national and international AEIs now serve as both educational and research centers to teach technical and nontechnical skills to surgeons and other health care professionals. At Houston Methodist Hospital, for example, we have built MITIE (Methodist Institute for Technology Innovation and Education), a comprehensive center with a focus on retooling surgeons in practice. We have hosted more than 13,000 surgeons in practice for retooling hands-on courses, along with more than 30,000 other health care professionals.
To ensure our surgical workforce stays at the top of their performance over a 40-year career, our College has convened a group of stakeholders, including payers, consumers, liability carriers, surgical technology industries, hospital executives, and, of course, surgeons, to define the infrastructure – facilities, faculty, curricula, assessment tools, and finances – needed to incorporate retooling and retraining into our health care system. Work to do.
Shape your future
The retooling reimagined initiative is but one example of how we can shape our professional futures. Remember, the ACS was founded nearly 105 years ago by surgeons who sought to improve the care of the surgical patient. Since then, individual surgeons, banding together within our College, have created some of the most effective systems in the world to improve surgical care – including the formation of the Committee on Trauma and the Commission on Cancer, which have led initiatives that have vastly improved care for their respective patient populations.
The ACS National Surgical Quality Improvement Program, born of the vision of Shukri Khuri, MD, FACS, who, when tasked with resolving a perceived problem in surgical care in the Veterans Affairs Health Care System, launched a research study to measure quality. Soon thereafter, he led an army of surgeons to improve surgical care in their own hospitals, founding a nationwide movement that now flourishes in thousands of hospitals as the world’s most effective surgical quality measurement and improvement system.
We can go on and on. A surgeon identifies a gap and with a good idea, and coupled to abundant College focus and the engagement of our Fellows, a valuable new program is launched. These initiatives were not delivered from on high. They were created by regular surgeons, like you and me, who saw gaps in their professional worlds and took steps to effect meaningful change.
Caring for each other
I have one more request: I want you to be aware of your colleagues. I want you to watch them for signs of stress and disturbances in their forces. And if you see something, ask a supportive question or offer needed assistance. Be aware of help that is available in your institution; know how to move a concern up the chain with sensitivity, but also with efficacy, coupled with compassionate concern for your colleague.
These are not easy discussions and may prove fruitless, but they are worth the effort to try, for we surgeons are a high-risk group for depression, substance abuse, and suicide – and for failing to seek assistance. This situation must change, but doing so will require that we destigmatize these conditions in ourselves and our colleagues, and destigmatize seeking assistance.
But, for now, on a joyful or a challenging day in your surgical life, I hope you are proud of your Fellowship in the ACS and your FACS initials that signify your commitment to the values of our profession. I hope you will draw endless support and friendship from those around you and that you will contribute more than you receive. And I hope that you will forever treasure your opportunity to practice as a surgeon, an exceptional joy and privilege.
Dr. Bass is the John F. and Carolyn Bookout Presidential Endowed Chair, professor of surgery and chair, department of surgery, Houston Methodist Hospital, TX, and the President of the American College of Surgeons (ACS).
As a Fellow of the American College of Surgeons (ACS), only you can recall the personal sacrifices you have made to attain the skills and knowledge necessary to enjoy the privilege of being a surgeon – years of missed time with family and friends, sleepless nights, and endless formative hours of deep experiential learning in the hospital. Someone else could have been there instead; you could have made a different career choice. But, no – surgery chose you, and you dove in. Thank you, thank you.
I hope you never lose sight of the lives you touched during those “lost” times – injured people, previously unknown neighbors with deadly diseases, or simply patients needing a little “repair.” People with a surgical disease are experiencing a rare life event: an operation. Never forget that each of those individuals, each patient, came to you – you personally – to help them.
Challenges
Regrettably, however, at times the cherished bond between a surgeon and a patient can get lost in our busy, burdened lives. It can get lost in physical fatigue, regulatory hoops, frustrations of the electronic health record, contract negotiations, challenging reimbursement policies, and on and on.
Add to that list other challenges that will surely arise in the course of your career: You will face various forms of threatened obsolescence in knowledge, skills, and technology. You will age. You will suffer personal tragedy and loss. You will become ill. That you may stumble when facing such challenges is not a sign of weakness. It is life.
I believe there is a bit of light ahead as our health care industry begins to recognize that this thing we call burnout is not a personal failing, but rather a function of our flawed work environments – and a significant threat not only to the surgeon, but also to patient safety, quality of care, and institutional financial stability. An active voice and actions in these essential domains of our work environment are mission critical for our College, as are efforts that are pursued on many fronts by Fellows and professionals in the Division of Advocacy and Health Policy in Washington, DC, and the Divisions of Research and Optimal Patient Care, Education, and Member Services in Chicago, IL. Fostering an environment to optimally support the care of the surgical patient – and surgeons – is core business in all we do in the ACS.
Let’s tackle a few other challenges. First, consider your personal and society’s investment in surgical training. Getting you to this skilled and knowledgeable point reflects an investment of more than $1 million dollars in costs of medical school and graduate medical education, and inestimable time and effort.
Second, the dire anticipated shortage of surgeons of many disciplines – general surgeons, orthopedists, urologists – appears to be real. If we are to keep our surgical pipeline full, we need to offer careers that are attractive to men and women equally. The U.S. general surgery pathway has entering classes of 40% women; however, other high-demand disciplines, such as neurosurgery, orthopedics, and cardiothoracic surgery, have not yet attracted women to their ranks in sufficient numbers, despite the fact that 50% of our medical school graduates are women. We need to examine the pathways to those surgical disciplines to ensure that gender- and ethnicity-based barriers are receding. Efforts are underway to address these challenges by the leadership in these disciplines that our College can help with.
Although much has changed for women in surgery in recent years, there are still differences in the lives of many female surgeons compared to their male colleagues. They remain at risk for pay inequity, being in aggregate compensated 10-17% less than their male colleagues for equal work. Despite a mature gender pipeline in some surgical specialties, women are still less likely to rise to leadership roles in their group practices, hospital structures, professional organizations, and academic institutions. The ACS can serve as a professional home to develop strategies to highlight and remedy these imbalances.
Parenting, to engage as fully and successfully as one may wish, is a challenge for many who choose our careers, regardless of gender. However, for most female surgeons beginning a family, the first step often comes with pregnancy and infant care, conditions that we have yet to embrace and support as a societal good rather than an individual’s gauntlet to run. Given our long and arduous educational pathways, these women often find themselves starting a family, be it by pregnancy or adoption, at the same moment they are beginning their busy early years of practice. Policies and practices to support surgeons who choose parenthood in the workforce are sorely needed and will, in fact, benefit all in the long run.
Our College, with guidance from the Women in Surgery Committee and the Association of Women Surgeons, has advanced that goal, issuing a statement that acknowledges the need for appropriate pregnancy and parental leave and that clearly articulates that the choice to become a parent in no way diminishes a surgeon’s commitment to career. The next steps will be building the institutional, financial, and community infrastructure to foster success in both career and parenting for all.
Retooling reimagined
Let’s ponder another challenge: the need to add to your repertoire a new, potentially transformative skill. How do we safely retool?
Twenty years ago, in the flawed early adoption of laparoscopic surgery, the ACS Committee on Emerging Surgical Technology Education articulated the principles of new skill acquisition: didactic learning, coupled with simulation-based training, and then proctored early experience, leading to independent practice and assessment of outcomes.
Subsequently, the College took the visionary step of establishing the ACS Accredited Education Institutes (AEI) program to develop a network of centers that would leverage emerging simulation technologies to enhance surgical training. The 96 national and international AEIs now serve as both educational and research centers to teach technical and nontechnical skills to surgeons and other health care professionals. At Houston Methodist Hospital, for example, we have built MITIE (Methodist Institute for Technology Innovation and Education), a comprehensive center with a focus on retooling surgeons in practice. We have hosted more than 13,000 surgeons in practice for retooling hands-on courses, along with more than 30,000 other health care professionals.
To ensure our surgical workforce stays at the top of their performance over a 40-year career, our College has convened a group of stakeholders, including payers, consumers, liability carriers, surgical technology industries, hospital executives, and, of course, surgeons, to define the infrastructure – facilities, faculty, curricula, assessment tools, and finances – needed to incorporate retooling and retraining into our health care system. Work to do.
Shape your future
The retooling reimagined initiative is but one example of how we can shape our professional futures. Remember, the ACS was founded nearly 105 years ago by surgeons who sought to improve the care of the surgical patient. Since then, individual surgeons, banding together within our College, have created some of the most effective systems in the world to improve surgical care – including the formation of the Committee on Trauma and the Commission on Cancer, which have led initiatives that have vastly improved care for their respective patient populations.
The ACS National Surgical Quality Improvement Program, born of the vision of Shukri Khuri, MD, FACS, who, when tasked with resolving a perceived problem in surgical care in the Veterans Affairs Health Care System, launched a research study to measure quality. Soon thereafter, he led an army of surgeons to improve surgical care in their own hospitals, founding a nationwide movement that now flourishes in thousands of hospitals as the world’s most effective surgical quality measurement and improvement system.
We can go on and on. A surgeon identifies a gap and with a good idea, and coupled to abundant College focus and the engagement of our Fellows, a valuable new program is launched. These initiatives were not delivered from on high. They were created by regular surgeons, like you and me, who saw gaps in their professional worlds and took steps to effect meaningful change.
Caring for each other
I have one more request: I want you to be aware of your colleagues. I want you to watch them for signs of stress and disturbances in their forces. And if you see something, ask a supportive question or offer needed assistance. Be aware of help that is available in your institution; know how to move a concern up the chain with sensitivity, but also with efficacy, coupled with compassionate concern for your colleague.
These are not easy discussions and may prove fruitless, but they are worth the effort to try, for we surgeons are a high-risk group for depression, substance abuse, and suicide – and for failing to seek assistance. This situation must change, but doing so will require that we destigmatize these conditions in ourselves and our colleagues, and destigmatize seeking assistance.
But, for now, on a joyful or a challenging day in your surgical life, I hope you are proud of your Fellowship in the ACS and your FACS initials that signify your commitment to the values of our profession. I hope you will draw endless support and friendship from those around you and that you will contribute more than you receive. And I hope that you will forever treasure your opportunity to practice as a surgeon, an exceptional joy and privilege.
Dr. Bass is the John F. and Carolyn Bookout Presidential Endowed Chair, professor of surgery and chair, department of surgery, Houston Methodist Hospital, TX, and the President of the American College of Surgeons (ACS).
As a Fellow of the American College of Surgeons (ACS), only you can recall the personal sacrifices you have made to attain the skills and knowledge necessary to enjoy the privilege of being a surgeon – years of missed time with family and friends, sleepless nights, and endless formative hours of deep experiential learning in the hospital. Someone else could have been there instead; you could have made a different career choice. But, no – surgery chose you, and you dove in. Thank you, thank you.
I hope you never lose sight of the lives you touched during those “lost” times – injured people, previously unknown neighbors with deadly diseases, or simply patients needing a little “repair.” People with a surgical disease are experiencing a rare life event: an operation. Never forget that each of those individuals, each patient, came to you – you personally – to help them.
Challenges
Regrettably, however, at times the cherished bond between a surgeon and a patient can get lost in our busy, burdened lives. It can get lost in physical fatigue, regulatory hoops, frustrations of the electronic health record, contract negotiations, challenging reimbursement policies, and on and on.
Add to that list other challenges that will surely arise in the course of your career: You will face various forms of threatened obsolescence in knowledge, skills, and technology. You will age. You will suffer personal tragedy and loss. You will become ill. That you may stumble when facing such challenges is not a sign of weakness. It is life.
I believe there is a bit of light ahead as our health care industry begins to recognize that this thing we call burnout is not a personal failing, but rather a function of our flawed work environments – and a significant threat not only to the surgeon, but also to patient safety, quality of care, and institutional financial stability. An active voice and actions in these essential domains of our work environment are mission critical for our College, as are efforts that are pursued on many fronts by Fellows and professionals in the Division of Advocacy and Health Policy in Washington, DC, and the Divisions of Research and Optimal Patient Care, Education, and Member Services in Chicago, IL. Fostering an environment to optimally support the care of the surgical patient – and surgeons – is core business in all we do in the ACS.
Let’s tackle a few other challenges. First, consider your personal and society’s investment in surgical training. Getting you to this skilled and knowledgeable point reflects an investment of more than $1 million dollars in costs of medical school and graduate medical education, and inestimable time and effort.
Second, the dire anticipated shortage of surgeons of many disciplines – general surgeons, orthopedists, urologists – appears to be real. If we are to keep our surgical pipeline full, we need to offer careers that are attractive to men and women equally. The U.S. general surgery pathway has entering classes of 40% women; however, other high-demand disciplines, such as neurosurgery, orthopedics, and cardiothoracic surgery, have not yet attracted women to their ranks in sufficient numbers, despite the fact that 50% of our medical school graduates are women. We need to examine the pathways to those surgical disciplines to ensure that gender- and ethnicity-based barriers are receding. Efforts are underway to address these challenges by the leadership in these disciplines that our College can help with.
Although much has changed for women in surgery in recent years, there are still differences in the lives of many female surgeons compared to their male colleagues. They remain at risk for pay inequity, being in aggregate compensated 10-17% less than their male colleagues for equal work. Despite a mature gender pipeline in some surgical specialties, women are still less likely to rise to leadership roles in their group practices, hospital structures, professional organizations, and academic institutions. The ACS can serve as a professional home to develop strategies to highlight and remedy these imbalances.
Parenting, to engage as fully and successfully as one may wish, is a challenge for many who choose our careers, regardless of gender. However, for most female surgeons beginning a family, the first step often comes with pregnancy and infant care, conditions that we have yet to embrace and support as a societal good rather than an individual’s gauntlet to run. Given our long and arduous educational pathways, these women often find themselves starting a family, be it by pregnancy or adoption, at the same moment they are beginning their busy early years of practice. Policies and practices to support surgeons who choose parenthood in the workforce are sorely needed and will, in fact, benefit all in the long run.
Our College, with guidance from the Women in Surgery Committee and the Association of Women Surgeons, has advanced that goal, issuing a statement that acknowledges the need for appropriate pregnancy and parental leave and that clearly articulates that the choice to become a parent in no way diminishes a surgeon’s commitment to career. The next steps will be building the institutional, financial, and community infrastructure to foster success in both career and parenting for all.
Retooling reimagined
Let’s ponder another challenge: the need to add to your repertoire a new, potentially transformative skill. How do we safely retool?
Twenty years ago, in the flawed early adoption of laparoscopic surgery, the ACS Committee on Emerging Surgical Technology Education articulated the principles of new skill acquisition: didactic learning, coupled with simulation-based training, and then proctored early experience, leading to independent practice and assessment of outcomes.
Subsequently, the College took the visionary step of establishing the ACS Accredited Education Institutes (AEI) program to develop a network of centers that would leverage emerging simulation technologies to enhance surgical training. The 96 national and international AEIs now serve as both educational and research centers to teach technical and nontechnical skills to surgeons and other health care professionals. At Houston Methodist Hospital, for example, we have built MITIE (Methodist Institute for Technology Innovation and Education), a comprehensive center with a focus on retooling surgeons in practice. We have hosted more than 13,000 surgeons in practice for retooling hands-on courses, along with more than 30,000 other health care professionals.
To ensure our surgical workforce stays at the top of their performance over a 40-year career, our College has convened a group of stakeholders, including payers, consumers, liability carriers, surgical technology industries, hospital executives, and, of course, surgeons, to define the infrastructure – facilities, faculty, curricula, assessment tools, and finances – needed to incorporate retooling and retraining into our health care system. Work to do.
Shape your future
The retooling reimagined initiative is but one example of how we can shape our professional futures. Remember, the ACS was founded nearly 105 years ago by surgeons who sought to improve the care of the surgical patient. Since then, individual surgeons, banding together within our College, have created some of the most effective systems in the world to improve surgical care – including the formation of the Committee on Trauma and the Commission on Cancer, which have led initiatives that have vastly improved care for their respective patient populations.
The ACS National Surgical Quality Improvement Program, born of the vision of Shukri Khuri, MD, FACS, who, when tasked with resolving a perceived problem in surgical care in the Veterans Affairs Health Care System, launched a research study to measure quality. Soon thereafter, he led an army of surgeons to improve surgical care in their own hospitals, founding a nationwide movement that now flourishes in thousands of hospitals as the world’s most effective surgical quality measurement and improvement system.
We can go on and on. A surgeon identifies a gap and with a good idea, and coupled to abundant College focus and the engagement of our Fellows, a valuable new program is launched. These initiatives were not delivered from on high. They were created by regular surgeons, like you and me, who saw gaps in their professional worlds and took steps to effect meaningful change.
Caring for each other
I have one more request: I want you to be aware of your colleagues. I want you to watch them for signs of stress and disturbances in their forces. And if you see something, ask a supportive question or offer needed assistance. Be aware of help that is available in your institution; know how to move a concern up the chain with sensitivity, but also with efficacy, coupled with compassionate concern for your colleague.
These are not easy discussions and may prove fruitless, but they are worth the effort to try, for we surgeons are a high-risk group for depression, substance abuse, and suicide – and for failing to seek assistance. This situation must change, but doing so will require that we destigmatize these conditions in ourselves and our colleagues, and destigmatize seeking assistance.
But, for now, on a joyful or a challenging day in your surgical life, I hope you are proud of your Fellowship in the ACS and your FACS initials that signify your commitment to the values of our profession. I hope you will draw endless support and friendship from those around you and that you will contribute more than you receive. And I hope that you will forever treasure your opportunity to practice as a surgeon, an exceptional joy and privilege.
Dr. Bass is the John F. and Carolyn Bookout Presidential Endowed Chair, professor of surgery and chair, department of surgery, Houston Methodist Hospital, TX, and the President of the American College of Surgeons (ACS).
Consent and DNR orders
Question: Paramedics brought an unconscious 70-year-old man to a Florida hospital emergency department. The patient had the words “Do Not Resuscitate” tattooed onto his chest. No one accompanied him, and he had no identifications on his person. His blood alcohol level was elevated, and a few hours after his arrival, he lapsed into severe metabolic acidosis and hypotensive shock. The treating team decided to enter a DNR order, and the patient died shortly thereafter without benefit of cardiopulmonary resuscitation.
Which of the following is best?
A. An ethics consult may suggest honoring the patient’s DNR wishes, as it is reasonable to infer that the tattoo expressed an authentic preference.
B. It has been said, but remains debatable, that tattoos might represent “permanent reminders of regretted decisions made while the person was intoxicated.”
C. An earlier case report in the literature cautioned that the tattooed expression of a DNR request did not reflect that particular patient’s current wishes.
D. If this patient’s Florida Department of Health out-of-hospital DNR order confirms his DNR preference, then it is appropriate to withhold resuscitation.
E. All are correct.
ANSWER: E. The above hypothetical situation is modified from a recent case report in the correspondence section of the New England Journal of Medicine.1 It can be read as offering a sharp and dramatic focus on the issue of consent surrounding decisions to withhold CPR.
In 1983, the President’s Commission for the Study of Ethical Problems in Medicine supported DNR protocols (“no code”) based on three value considerations: self-determination, well-being, and equity.2
The physician is obligated to discuss with the patient or surrogate the procedure, risks, and benefits of CPR so that an informed choice can be made. DNR means that, in the event of a cardiac or respiratory arrest, no CPR efforts would be undertaken. DNR orders are not exclusive to the in-hospital setting, as some states, for example, Florida and Texas, have also enacted statutes that allow such orders to be valid outside the hospital.
Critics lament that problems – many surrounding the consent issue – continue to plague DNR orders.3 Discussions are often vague, and they may not meet the threshold of informed consent requirements, because they frequently omit risks and complications. A resident, rather than the attending physician, typically performs this important task. This is compounded by ill-timed discussions and wrong assumptions about patients’ preferences, which may in fact be ignored.4
Physicians sometimes extrapolate DNR orders to limit other treatments. Or, they perform CPR in contraindicated situations such as terminal illnesses, where death is expected, which amounts to “a positive violation of an individual’s right to die with dignity.” In some situations, physicians are known to override a patient’s DNR request.
Take the operating-room conundrum. There, the immediate availability of drugs, heightened skills, and in-place procedures significantly improve survival following a cardiopulmonary arrest. Studies show a 50% survival rate, versus 8%-14% elsewhere in the hospital. A Swedish study showed that 65% of the patients who had a cardiac arrest perioperatively were successfully resuscitated. When anesthesia caused the arrest, for example, esophageal intubation, disconnection from mechanical ventilation, or prolonged exposure to high concentrations of anesthetics, the recovery rate jumped to 92%.
Terminally ill patients typically disavow CPR when choosing a palliative course of action. However, surgery can be a part of palliation. In 1991, approximately 15% of patients with DNR orders had a surgical procedure, with most interventions targeting comfort and/or nursing care. When a terminally ill patient with a DNR order undergoes surgery, how should physicians deal with the patient’s no-code status, especially if an iatrogenic cardiac arrest should occur?
Because overriding a patient’s DNR wish violates the right of self-determination, a reasonable rule is to require the surgeon and/or anesthesiologist to discuss preoperatively the increased risk of a cardiac arrest during surgery, as well as the markedly improved chance of a successful resuscitation. The patient will then decide whether to retain his/her original DNR intent, or to suspend its execution in the perioperative period.5
What about iatrogenesis?
In 1999, David Casarett, MD, and Lainie F. Ross, MD, PhD, assessed whether physicians were more likely to override a DNR order if a hypothetical cardiac arrest was caused iatrogenically.6 Their survey revealed that 69% of physicians were very likely to do so. The authors suggested three explanations: 1) concern for malpractice litigation, 2) feelings of guilt or responsibility, and 3) the belief that patients do not consider the possibility of an iatrogenic cardiac arrest when they consent to a DNR order. Physicians may also believe a “properly negotiated DNR order does not apply to all foreseeable circumstances.”
However, some ethicists believe that an iatrogenic mishap does not make it permissible to override a patient’s prior refusal of treatment, because errors should not alter ethical obligations to respect a patient’s wishes to forgo treatment, including CPR.
Can a DNR order exist if it is against a patient’s wishes?7 In Gilgunn v. Massachusetts General Hospital, a 71-year-old diabetic woman with heart disease, breast cancer, and a hip fracture suffered two grand mal seizures and lapsed into a coma.8 Her daughter was the surrogate decision maker, and she made it clear that her mother always said she wanted everything done. After several weeks, the physicians decided that further treatment would be futile.
The chair of the ethics committee felt that the daughter’s opinion was not relevant because CPR was not a genuine therapeutic option and would be “medically contraindicated, inhumane, and unethical.” Accordingly, the attending physician entered a DNR order despite strong protest from the daughter. The patient died shortly thereafter without receiving CPR, and the daughter filed a negligence lawsuit against the hospital.
Still, there are state and federal statutes touching on DNR orders that warrant careful attention. For example, New York Public Health Law Section 2962, paragraph 1, states: “Every person admitted to a hospital shall be presumed to consent to the administration of cardiopulmonary resuscitation in the event of cardiac or respiratory arrest, unless there is consent to the issuance of an order not to resuscitate ...” This raises the question as to whether it is ever legally permissible in New York to enter a unilateral DNR order against the wishes of the patient.
And the federal “anti-dumping” law governing emergency treatment, widely known as EMTALA (Emergency Medical Treatment and Labor Act), requires all emergency departments to provide treatment necessary to prevent the material deterioration of the individual’s condition. This would always include the use of CPR unless specifically rejected by the patient or surrogate, as the law does not contain a “standard of care” or “futility” exception.9
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. N Engl J Med. 2017 Nov 30;377(22):2192-3.
2. President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to Forego Life-Sustaining Treatment. Washington, DC: Government Printing Office, 1983.
3. J Gen Intern Med. 2011 Jul;26(7):791-7.
4. JAMA. 1995 Nov 22-29;274(20):1591-8.
5. Hawaii Med J. 2001 Mar;60(3):64-7.
6. N Engl J Med. 1997 Jun 26;336(26):1908-10.
7. Tan SY. Futility and DNR Orders. Internal Medicine News, March 21, 2014.
8. Gilgunn v. Mass. General Hosp. No. 92-4820 (Mass. Super Ct. Apr. 21, 1995).
9. In re Baby K, 16 F.3d 590 (4th Cir. 1994).
Question: Paramedics brought an unconscious 70-year-old man to a Florida hospital emergency department. The patient had the words “Do Not Resuscitate” tattooed onto his chest. No one accompanied him, and he had no identifications on his person. His blood alcohol level was elevated, and a few hours after his arrival, he lapsed into severe metabolic acidosis and hypotensive shock. The treating team decided to enter a DNR order, and the patient died shortly thereafter without benefit of cardiopulmonary resuscitation.
Which of the following is best?
A. An ethics consult may suggest honoring the patient’s DNR wishes, as it is reasonable to infer that the tattoo expressed an authentic preference.
B. It has been said, but remains debatable, that tattoos might represent “permanent reminders of regretted decisions made while the person was intoxicated.”
C. An earlier case report in the literature cautioned that the tattooed expression of a DNR request did not reflect that particular patient’s current wishes.
D. If this patient’s Florida Department of Health out-of-hospital DNR order confirms his DNR preference, then it is appropriate to withhold resuscitation.
E. All are correct.
ANSWER: E. The above hypothetical situation is modified from a recent case report in the correspondence section of the New England Journal of Medicine.1 It can be read as offering a sharp and dramatic focus on the issue of consent surrounding decisions to withhold CPR.
In 1983, the President’s Commission for the Study of Ethical Problems in Medicine supported DNR protocols (“no code”) based on three value considerations: self-determination, well-being, and equity.2
The physician is obligated to discuss with the patient or surrogate the procedure, risks, and benefits of CPR so that an informed choice can be made. DNR means that, in the event of a cardiac or respiratory arrest, no CPR efforts would be undertaken. DNR orders are not exclusive to the in-hospital setting, as some states, for example, Florida and Texas, have also enacted statutes that allow such orders to be valid outside the hospital.
Critics lament that problems – many surrounding the consent issue – continue to plague DNR orders.3 Discussions are often vague, and they may not meet the threshold of informed consent requirements, because they frequently omit risks and complications. A resident, rather than the attending physician, typically performs this important task. This is compounded by ill-timed discussions and wrong assumptions about patients’ preferences, which may in fact be ignored.4
Physicians sometimes extrapolate DNR orders to limit other treatments. Or, they perform CPR in contraindicated situations such as terminal illnesses, where death is expected, which amounts to “a positive violation of an individual’s right to die with dignity.” In some situations, physicians are known to override a patient’s DNR request.
Take the operating-room conundrum. There, the immediate availability of drugs, heightened skills, and in-place procedures significantly improve survival following a cardiopulmonary arrest. Studies show a 50% survival rate, versus 8%-14% elsewhere in the hospital. A Swedish study showed that 65% of the patients who had a cardiac arrest perioperatively were successfully resuscitated. When anesthesia caused the arrest, for example, esophageal intubation, disconnection from mechanical ventilation, or prolonged exposure to high concentrations of anesthetics, the recovery rate jumped to 92%.
Terminally ill patients typically disavow CPR when choosing a palliative course of action. However, surgery can be a part of palliation. In 1991, approximately 15% of patients with DNR orders had a surgical procedure, with most interventions targeting comfort and/or nursing care. When a terminally ill patient with a DNR order undergoes surgery, how should physicians deal with the patient’s no-code status, especially if an iatrogenic cardiac arrest should occur?
Because overriding a patient’s DNR wish violates the right of self-determination, a reasonable rule is to require the surgeon and/or anesthesiologist to discuss preoperatively the increased risk of a cardiac arrest during surgery, as well as the markedly improved chance of a successful resuscitation. The patient will then decide whether to retain his/her original DNR intent, or to suspend its execution in the perioperative period.5
What about iatrogenesis?
In 1999, David Casarett, MD, and Lainie F. Ross, MD, PhD, assessed whether physicians were more likely to override a DNR order if a hypothetical cardiac arrest was caused iatrogenically.6 Their survey revealed that 69% of physicians were very likely to do so. The authors suggested three explanations: 1) concern for malpractice litigation, 2) feelings of guilt or responsibility, and 3) the belief that patients do not consider the possibility of an iatrogenic cardiac arrest when they consent to a DNR order. Physicians may also believe a “properly negotiated DNR order does not apply to all foreseeable circumstances.”
However, some ethicists believe that an iatrogenic mishap does not make it permissible to override a patient’s prior refusal of treatment, because errors should not alter ethical obligations to respect a patient’s wishes to forgo treatment, including CPR.
Can a DNR order exist if it is against a patient’s wishes?7 In Gilgunn v. Massachusetts General Hospital, a 71-year-old diabetic woman with heart disease, breast cancer, and a hip fracture suffered two grand mal seizures and lapsed into a coma.8 Her daughter was the surrogate decision maker, and she made it clear that her mother always said she wanted everything done. After several weeks, the physicians decided that further treatment would be futile.
The chair of the ethics committee felt that the daughter’s opinion was not relevant because CPR was not a genuine therapeutic option and would be “medically contraindicated, inhumane, and unethical.” Accordingly, the attending physician entered a DNR order despite strong protest from the daughter. The patient died shortly thereafter without receiving CPR, and the daughter filed a negligence lawsuit against the hospital.
Still, there are state and federal statutes touching on DNR orders that warrant careful attention. For example, New York Public Health Law Section 2962, paragraph 1, states: “Every person admitted to a hospital shall be presumed to consent to the administration of cardiopulmonary resuscitation in the event of cardiac or respiratory arrest, unless there is consent to the issuance of an order not to resuscitate ...” This raises the question as to whether it is ever legally permissible in New York to enter a unilateral DNR order against the wishes of the patient.
And the federal “anti-dumping” law governing emergency treatment, widely known as EMTALA (Emergency Medical Treatment and Labor Act), requires all emergency departments to provide treatment necessary to prevent the material deterioration of the individual’s condition. This would always include the use of CPR unless specifically rejected by the patient or surrogate, as the law does not contain a “standard of care” or “futility” exception.9
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. N Engl J Med. 2017 Nov 30;377(22):2192-3.
2. President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to Forego Life-Sustaining Treatment. Washington, DC: Government Printing Office, 1983.
3. J Gen Intern Med. 2011 Jul;26(7):791-7.
4. JAMA. 1995 Nov 22-29;274(20):1591-8.
5. Hawaii Med J. 2001 Mar;60(3):64-7.
6. N Engl J Med. 1997 Jun 26;336(26):1908-10.
7. Tan SY. Futility and DNR Orders. Internal Medicine News, March 21, 2014.
8. Gilgunn v. Mass. General Hosp. No. 92-4820 (Mass. Super Ct. Apr. 21, 1995).
9. In re Baby K, 16 F.3d 590 (4th Cir. 1994).
Question: Paramedics brought an unconscious 70-year-old man to a Florida hospital emergency department. The patient had the words “Do Not Resuscitate” tattooed onto his chest. No one accompanied him, and he had no identifications on his person. His blood alcohol level was elevated, and a few hours after his arrival, he lapsed into severe metabolic acidosis and hypotensive shock. The treating team decided to enter a DNR order, and the patient died shortly thereafter without benefit of cardiopulmonary resuscitation.
Which of the following is best?
A. An ethics consult may suggest honoring the patient’s DNR wishes, as it is reasonable to infer that the tattoo expressed an authentic preference.
B. It has been said, but remains debatable, that tattoos might represent “permanent reminders of regretted decisions made while the person was intoxicated.”
C. An earlier case report in the literature cautioned that the tattooed expression of a DNR request did not reflect that particular patient’s current wishes.
D. If this patient’s Florida Department of Health out-of-hospital DNR order confirms his DNR preference, then it is appropriate to withhold resuscitation.
E. All are correct.
ANSWER: E. The above hypothetical situation is modified from a recent case report in the correspondence section of the New England Journal of Medicine.1 It can be read as offering a sharp and dramatic focus on the issue of consent surrounding decisions to withhold CPR.
In 1983, the President’s Commission for the Study of Ethical Problems in Medicine supported DNR protocols (“no code”) based on three value considerations: self-determination, well-being, and equity.2
The physician is obligated to discuss with the patient or surrogate the procedure, risks, and benefits of CPR so that an informed choice can be made. DNR means that, in the event of a cardiac or respiratory arrest, no CPR efforts would be undertaken. DNR orders are not exclusive to the in-hospital setting, as some states, for example, Florida and Texas, have also enacted statutes that allow such orders to be valid outside the hospital.
Critics lament that problems – many surrounding the consent issue – continue to plague DNR orders.3 Discussions are often vague, and they may not meet the threshold of informed consent requirements, because they frequently omit risks and complications. A resident, rather than the attending physician, typically performs this important task. This is compounded by ill-timed discussions and wrong assumptions about patients’ preferences, which may in fact be ignored.4
Physicians sometimes extrapolate DNR orders to limit other treatments. Or, they perform CPR in contraindicated situations such as terminal illnesses, where death is expected, which amounts to “a positive violation of an individual’s right to die with dignity.” In some situations, physicians are known to override a patient’s DNR request.
Take the operating-room conundrum. There, the immediate availability of drugs, heightened skills, and in-place procedures significantly improve survival following a cardiopulmonary arrest. Studies show a 50% survival rate, versus 8%-14% elsewhere in the hospital. A Swedish study showed that 65% of the patients who had a cardiac arrest perioperatively were successfully resuscitated. When anesthesia caused the arrest, for example, esophageal intubation, disconnection from mechanical ventilation, or prolonged exposure to high concentrations of anesthetics, the recovery rate jumped to 92%.
Terminally ill patients typically disavow CPR when choosing a palliative course of action. However, surgery can be a part of palliation. In 1991, approximately 15% of patients with DNR orders had a surgical procedure, with most interventions targeting comfort and/or nursing care. When a terminally ill patient with a DNR order undergoes surgery, how should physicians deal with the patient’s no-code status, especially if an iatrogenic cardiac arrest should occur?
Because overriding a patient’s DNR wish violates the right of self-determination, a reasonable rule is to require the surgeon and/or anesthesiologist to discuss preoperatively the increased risk of a cardiac arrest during surgery, as well as the markedly improved chance of a successful resuscitation. The patient will then decide whether to retain his/her original DNR intent, or to suspend its execution in the perioperative period.5
What about iatrogenesis?
In 1999, David Casarett, MD, and Lainie F. Ross, MD, PhD, assessed whether physicians were more likely to override a DNR order if a hypothetical cardiac arrest was caused iatrogenically.6 Their survey revealed that 69% of physicians were very likely to do so. The authors suggested three explanations: 1) concern for malpractice litigation, 2) feelings of guilt or responsibility, and 3) the belief that patients do not consider the possibility of an iatrogenic cardiac arrest when they consent to a DNR order. Physicians may also believe a “properly negotiated DNR order does not apply to all foreseeable circumstances.”
However, some ethicists believe that an iatrogenic mishap does not make it permissible to override a patient’s prior refusal of treatment, because errors should not alter ethical obligations to respect a patient’s wishes to forgo treatment, including CPR.
Can a DNR order exist if it is against a patient’s wishes?7 In Gilgunn v. Massachusetts General Hospital, a 71-year-old diabetic woman with heart disease, breast cancer, and a hip fracture suffered two grand mal seizures and lapsed into a coma.8 Her daughter was the surrogate decision maker, and she made it clear that her mother always said she wanted everything done. After several weeks, the physicians decided that further treatment would be futile.
The chair of the ethics committee felt that the daughter’s opinion was not relevant because CPR was not a genuine therapeutic option and would be “medically contraindicated, inhumane, and unethical.” Accordingly, the attending physician entered a DNR order despite strong protest from the daughter. The patient died shortly thereafter without receiving CPR, and the daughter filed a negligence lawsuit against the hospital.
Still, there are state and federal statutes touching on DNR orders that warrant careful attention. For example, New York Public Health Law Section 2962, paragraph 1, states: “Every person admitted to a hospital shall be presumed to consent to the administration of cardiopulmonary resuscitation in the event of cardiac or respiratory arrest, unless there is consent to the issuance of an order not to resuscitate ...” This raises the question as to whether it is ever legally permissible in New York to enter a unilateral DNR order against the wishes of the patient.
And the federal “anti-dumping” law governing emergency treatment, widely known as EMTALA (Emergency Medical Treatment and Labor Act), requires all emergency departments to provide treatment necessary to prevent the material deterioration of the individual’s condition. This would always include the use of CPR unless specifically rejected by the patient or surrogate, as the law does not contain a “standard of care” or “futility” exception.9
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at [email protected].
References
1. N Engl J Med. 2017 Nov 30;377(22):2192-3.
2. President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Deciding to Forego Life-Sustaining Treatment. Washington, DC: Government Printing Office, 1983.
3. J Gen Intern Med. 2011 Jul;26(7):791-7.
4. JAMA. 1995 Nov 22-29;274(20):1591-8.
5. Hawaii Med J. 2001 Mar;60(3):64-7.
6. N Engl J Med. 1997 Jun 26;336(26):1908-10.
7. Tan SY. Futility and DNR Orders. Internal Medicine News, March 21, 2014.
8. Gilgunn v. Mass. General Hosp. No. 92-4820 (Mass. Super Ct. Apr. 21, 1995).
9. In re Baby K, 16 F.3d 590 (4th Cir. 1994).
Are you as frustrated with medical care as we are?
How did the experience of office visits get to be so frustrating for both patients and doctors? Let’s put it under the microscope and examine it.
To medicine’s credit, it realized the value of looking for diseases before symptoms occurred, such as using mammograms to detect breast cancer and controlling blood pressure and blood sugar to avert comorbidities.
Today, a doctor looks at the computer screen and checks off when a mammogram was done and whether blood pressure and blood sugar are controlled. “Authorities” believe that good health is achieved by performing positive checkoffs to questions like this. This definition of quality care is, in reality, “quantity care” and can be tied to physician compensation. Physicians who did not adequately meet Physician Quality Reporting System requirements have received letters informing them that their Medicare Part B payments for 2018 will be reduced by 3%.
Many seasoned clinicians recognize that practicing good medicine involves more than following a computer printout of tests and treatments based on the patient’s symptoms, more than plugging into the diagnostic and prescription mills that are part of today’s managed care system. Making the correct diagnosis requires a carefully taken history, listening to the patients’ stories of their journeys into and through illness, and using a bio-psychosocial-spiritual approach.
Getting to know the patient as a person requires that the doctor and patient take a journey together. In that journey, when the doctor empathizes with the patient and understands what makes the patient tick, the doctor can empower the patient – giving the patient a fuller understanding of their medical conditions, greater participation in the diagnostic work-up and in treatments, and hope for success – all leading to better outcomes.
Doctors are frustrated with the current medical assembly-line system. A study has shown that physicians spend 2 hours on electronic health records and clerical work for every hour they provide direct patient care (Ann Intern Med. 2016;165[11]:753-60). Nearly half of physicians now report that they are “burned out” by the demand to achieve the quantitative requirements on the one hand and their inability to minister to the needs of their patients on the other hand. Patients are also frustrated by the system as they cope with health insurance and costs, with the short time allocated for office visits, and with a fragmented and impersonal medical system. Patients feel that they are little more than a source of information for boxes to be checked off by the physician whose eyes are forced to be on the computer and the clock.
How can we begin to integrate these measures of quality into “quantity medicine” and make the experience of medical visits less frustrating for doctors and patients? How can we reward the skills that recognize that the course of an illness is influenced by patients’ emotions and thoughts related to their problems, their supportive or stressful relationships with others, and the context within which they conceptualize their lives – particularly their religious and spiritual beliefs about life’s purpose and challenges and attitudes toward death?
Caring for patients requires a more sophisticated approach than seeing patients as computer checkoffs. Office visits need to focus on the patient who has the symptoms, not just the symptoms the patient has.
Isn’t it time to make patient-centered care a reality and not just a slogan? If this speaks to you, then what should you do? Even though solutions may not be simple, we should not be deterred from finding patient-centered systems since patients and doctors are unhappy with today’s system. Why not have patients grade their office visits?
While this approach has its shortcomings, and isn’t the only solution, it does place the patient at the center of the process, answering questions about whether the doctor listened to them, heard their concerns, and presented a reasonable plan to help them get better.
In addition, all those involved with medical care should be involved in the process to replace today’s deficient system. The nation’s main organizations representing physicians should propose solutions to support patient-centered care. Individual physicians should become involved, speaking up and sending articles and letters to medical journals and the lay press.
Patients should be empowered to open up a public discussion – in print and broadcast media – on how they want to improve their own medical experiences and the quality of their health care.
It’s worth it. It’s our health.
Dr. Banner is a practicing internist in Philadelphia and chair emeritus of the Albert Einstein Medical Center Medical Ethics Committee. Dr. Benor is a psychiatric psychotherapist in the United States and a wholistic psychotherapist in Canada. Dr. Reiser is adjunct professor, University of Texas School of Public Health, Austin, and the UT Austin Plan II Honors Program, and teaches medical history, medical ethics, and public policy. The authors are indebted to Benjamin Sharfman, PhD, and Jane Brown, PhD, for their important roles in creating this article.
How did the experience of office visits get to be so frustrating for both patients and doctors? Let’s put it under the microscope and examine it.
To medicine’s credit, it realized the value of looking for diseases before symptoms occurred, such as using mammograms to detect breast cancer and controlling blood pressure and blood sugar to avert comorbidities.
Today, a doctor looks at the computer screen and checks off when a mammogram was done and whether blood pressure and blood sugar are controlled. “Authorities” believe that good health is achieved by performing positive checkoffs to questions like this. This definition of quality care is, in reality, “quantity care” and can be tied to physician compensation. Physicians who did not adequately meet Physician Quality Reporting System requirements have received letters informing them that their Medicare Part B payments for 2018 will be reduced by 3%.
Many seasoned clinicians recognize that practicing good medicine involves more than following a computer printout of tests and treatments based on the patient’s symptoms, more than plugging into the diagnostic and prescription mills that are part of today’s managed care system. Making the correct diagnosis requires a carefully taken history, listening to the patients’ stories of their journeys into and through illness, and using a bio-psychosocial-spiritual approach.
Getting to know the patient as a person requires that the doctor and patient take a journey together. In that journey, when the doctor empathizes with the patient and understands what makes the patient tick, the doctor can empower the patient – giving the patient a fuller understanding of their medical conditions, greater participation in the diagnostic work-up and in treatments, and hope for success – all leading to better outcomes.
Doctors are frustrated with the current medical assembly-line system. A study has shown that physicians spend 2 hours on electronic health records and clerical work for every hour they provide direct patient care (Ann Intern Med. 2016;165[11]:753-60). Nearly half of physicians now report that they are “burned out” by the demand to achieve the quantitative requirements on the one hand and their inability to minister to the needs of their patients on the other hand. Patients are also frustrated by the system as they cope with health insurance and costs, with the short time allocated for office visits, and with a fragmented and impersonal medical system. Patients feel that they are little more than a source of information for boxes to be checked off by the physician whose eyes are forced to be on the computer and the clock.
How can we begin to integrate these measures of quality into “quantity medicine” and make the experience of medical visits less frustrating for doctors and patients? How can we reward the skills that recognize that the course of an illness is influenced by patients’ emotions and thoughts related to their problems, their supportive or stressful relationships with others, and the context within which they conceptualize their lives – particularly their religious and spiritual beliefs about life’s purpose and challenges and attitudes toward death?
Caring for patients requires a more sophisticated approach than seeing patients as computer checkoffs. Office visits need to focus on the patient who has the symptoms, not just the symptoms the patient has.
Isn’t it time to make patient-centered care a reality and not just a slogan? If this speaks to you, then what should you do? Even though solutions may not be simple, we should not be deterred from finding patient-centered systems since patients and doctors are unhappy with today’s system. Why not have patients grade their office visits?
While this approach has its shortcomings, and isn’t the only solution, it does place the patient at the center of the process, answering questions about whether the doctor listened to them, heard their concerns, and presented a reasonable plan to help them get better.
In addition, all those involved with medical care should be involved in the process to replace today’s deficient system. The nation’s main organizations representing physicians should propose solutions to support patient-centered care. Individual physicians should become involved, speaking up and sending articles and letters to medical journals and the lay press.
Patients should be empowered to open up a public discussion – in print and broadcast media – on how they want to improve their own medical experiences and the quality of their health care.
It’s worth it. It’s our health.
Dr. Banner is a practicing internist in Philadelphia and chair emeritus of the Albert Einstein Medical Center Medical Ethics Committee. Dr. Benor is a psychiatric psychotherapist in the United States and a wholistic psychotherapist in Canada. Dr. Reiser is adjunct professor, University of Texas School of Public Health, Austin, and the UT Austin Plan II Honors Program, and teaches medical history, medical ethics, and public policy. The authors are indebted to Benjamin Sharfman, PhD, and Jane Brown, PhD, for their important roles in creating this article.
How did the experience of office visits get to be so frustrating for both patients and doctors? Let’s put it under the microscope and examine it.
To medicine’s credit, it realized the value of looking for diseases before symptoms occurred, such as using mammograms to detect breast cancer and controlling blood pressure and blood sugar to avert comorbidities.
Today, a doctor looks at the computer screen and checks off when a mammogram was done and whether blood pressure and blood sugar are controlled. “Authorities” believe that good health is achieved by performing positive checkoffs to questions like this. This definition of quality care is, in reality, “quantity care” and can be tied to physician compensation. Physicians who did not adequately meet Physician Quality Reporting System requirements have received letters informing them that their Medicare Part B payments for 2018 will be reduced by 3%.
Many seasoned clinicians recognize that practicing good medicine involves more than following a computer printout of tests and treatments based on the patient’s symptoms, more than plugging into the diagnostic and prescription mills that are part of today’s managed care system. Making the correct diagnosis requires a carefully taken history, listening to the patients’ stories of their journeys into and through illness, and using a bio-psychosocial-spiritual approach.
Getting to know the patient as a person requires that the doctor and patient take a journey together. In that journey, when the doctor empathizes with the patient and understands what makes the patient tick, the doctor can empower the patient – giving the patient a fuller understanding of their medical conditions, greater participation in the diagnostic work-up and in treatments, and hope for success – all leading to better outcomes.
Doctors are frustrated with the current medical assembly-line system. A study has shown that physicians spend 2 hours on electronic health records and clerical work for every hour they provide direct patient care (Ann Intern Med. 2016;165[11]:753-60). Nearly half of physicians now report that they are “burned out” by the demand to achieve the quantitative requirements on the one hand and their inability to minister to the needs of their patients on the other hand. Patients are also frustrated by the system as they cope with health insurance and costs, with the short time allocated for office visits, and with a fragmented and impersonal medical system. Patients feel that they are little more than a source of information for boxes to be checked off by the physician whose eyes are forced to be on the computer and the clock.
How can we begin to integrate these measures of quality into “quantity medicine” and make the experience of medical visits less frustrating for doctors and patients? How can we reward the skills that recognize that the course of an illness is influenced by patients’ emotions and thoughts related to their problems, their supportive or stressful relationships with others, and the context within which they conceptualize their lives – particularly their religious and spiritual beliefs about life’s purpose and challenges and attitudes toward death?
Caring for patients requires a more sophisticated approach than seeing patients as computer checkoffs. Office visits need to focus on the patient who has the symptoms, not just the symptoms the patient has.
Isn’t it time to make patient-centered care a reality and not just a slogan? If this speaks to you, then what should you do? Even though solutions may not be simple, we should not be deterred from finding patient-centered systems since patients and doctors are unhappy with today’s system. Why not have patients grade their office visits?
While this approach has its shortcomings, and isn’t the only solution, it does place the patient at the center of the process, answering questions about whether the doctor listened to them, heard their concerns, and presented a reasonable plan to help them get better.
In addition, all those involved with medical care should be involved in the process to replace today’s deficient system. The nation’s main organizations representing physicians should propose solutions to support patient-centered care. Individual physicians should become involved, speaking up and sending articles and letters to medical journals and the lay press.
Patients should be empowered to open up a public discussion – in print and broadcast media – on how they want to improve their own medical experiences and the quality of their health care.
It’s worth it. It’s our health.
Dr. Banner is a practicing internist in Philadelphia and chair emeritus of the Albert Einstein Medical Center Medical Ethics Committee. Dr. Benor is a psychiatric psychotherapist in the United States and a wholistic psychotherapist in Canada. Dr. Reiser is adjunct professor, University of Texas School of Public Health, Austin, and the UT Austin Plan II Honors Program, and teaches medical history, medical ethics, and public policy. The authors are indebted to Benjamin Sharfman, PhD, and Jane Brown, PhD, for their important roles in creating this article.
Impostor syndrome
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Why are you bothering to read this? What could I offer that could possibly be useful to you? In fact, I was invited to write this column simply because I happened to be at the right conference at the right time. Soon, if not already, you’ll discover I’m actually not that clever. I’m an impostor.
I’ve thought this while staring at the blank page that is to be my article for the month. Reflecting on it, I realize you’ve probably had the same feelings of fraud at one time or another. It often occurs at moments of transition, such as when you were accepted into medical school or matched into a competitive specialty. Looking at your peers, watching how your colleagues perform, you feel you just aren’t smart enough to be there; either someone made a mistake or you just got lucky.
There are potentially positive aspects of impostor syndrome: Humility can make us more effective over time and more tolerable to be around. It also, however, can be destructive. When we feel undeserving, we grow anxious and focus ever more tightly on ourselves. It can be paralyzing. When you think about how you are perceived, you fail to be present and attentive to others around you. Believing you lack innate ability, you can slip into a fixed mindset and fail to grow. Trying to keep your insecurities a secret from others, the foundation of impostor syndrome, is stressful and will stoke the fire of burnout which threatens us all. Fortunately, there is a cure.
The first step in escaping this maladaptive experience is to do what I’ve just done: Share it with others. Find colleagues or partners who care about you and who can speak frankly. By sharing how you feel with others, you banish any power that impostor syndrome might have over you. You can’t worry about being a fraud once you’ve just announced that you are a fraud; the gig is up! Choose your confidantes carefully, as not everyone is suitable to help. Avoid sharing such feelings with your patients; it can erode their confidence in you.
Reframe how you interpret situations when you feel like an impostor. Committing an error doesn’t mean you’re incompetent; moreover, you needn’t be supremely confident to be competent. Marveling at others’ abilities doesn’t mean you could not perform as well. Remember, you don’t know how much effort and time they’ve invested, and chances are you’re underestimating the work they’ve put forth.
Last, take the time to write about your success. Journaling can be a powerful tool to make your successes more salient and remind you that you are truly accomplished. Try writing in the third person, telling the story of your journey and the obstacles you’ve overcome to reach your current prestigious destination. If you still feel like a fake sometimes, there is good news. Having some self-doubt correlates with success, probably because it keeps you motivated to work hard.
Did this article resonate with you? It should. It took me lots of drafts before I got it right.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
Fetal alcohol syndrome: Context matters
Recently, there was a lot of hoopla in the popular press caused by the report by Philip A. May, PhD, and his team showing that the rates of fetal alcohol spectrum disorder (FASD) ran between 1.1 to 5.0% in first graders in four U.S. communities (JAMA. 2018;319[5]:474-82). This publication and the press it received made my heart sing because the findings made national news – meaning the issue would be in the public’s consciousness for a day or two. That is progress.
As psychiatrists, we should know that context is important. For example, I was at the Northeast Conference on Fetal Alcohol Spectrum Disorders in 2017 in Colby, Maine, and heard Larry Burd, PhD, a longstanding expert in the area of FASD, describe the drinking habits of the Native American women who had children with FASD. He described them as being alcoholics. I was floored, because engaged in social drinking during this time, but stopped cold when they realized that they were pregnant. I only saw two of 500 women that I would consider alcoholics, and one went on a 3-day binge with her girlfriends when she learned that she was pregnant. Clearly, context matters.
I continue to maintain that increasing choline in prenatal vitamins is a way out of this mess the United States is in with its hidden epidemic of FASD.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; a clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; a former president/CEO of Community Mental Health Council; and a former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
Recently, there was a lot of hoopla in the popular press caused by the report by Philip A. May, PhD, and his team showing that the rates of fetal alcohol spectrum disorder (FASD) ran between 1.1 to 5.0% in first graders in four U.S. communities (JAMA. 2018;319[5]:474-82). This publication and the press it received made my heart sing because the findings made national news – meaning the issue would be in the public’s consciousness for a day or two. That is progress.
As psychiatrists, we should know that context is important. For example, I was at the Northeast Conference on Fetal Alcohol Spectrum Disorders in 2017 in Colby, Maine, and heard Larry Burd, PhD, a longstanding expert in the area of FASD, describe the drinking habits of the Native American women who had children with FASD. He described them as being alcoholics. I was floored, because engaged in social drinking during this time, but stopped cold when they realized that they were pregnant. I only saw two of 500 women that I would consider alcoholics, and one went on a 3-day binge with her girlfriends when she learned that she was pregnant. Clearly, context matters.
I continue to maintain that increasing choline in prenatal vitamins is a way out of this mess the United States is in with its hidden epidemic of FASD.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; a clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; a former president/CEO of Community Mental Health Council; and a former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
Recently, there was a lot of hoopla in the popular press caused by the report by Philip A. May, PhD, and his team showing that the rates of fetal alcohol spectrum disorder (FASD) ran between 1.1 to 5.0% in first graders in four U.S. communities (JAMA. 2018;319[5]:474-82). This publication and the press it received made my heart sing because the findings made national news – meaning the issue would be in the public’s consciousness for a day or two. That is progress.
As psychiatrists, we should know that context is important. For example, I was at the Northeast Conference on Fetal Alcohol Spectrum Disorders in 2017 in Colby, Maine, and heard Larry Burd, PhD, a longstanding expert in the area of FASD, describe the drinking habits of the Native American women who had children with FASD. He described them as being alcoholics. I was floored, because engaged in social drinking during this time, but stopped cold when they realized that they were pregnant. I only saw two of 500 women that I would consider alcoholics, and one went on a 3-day binge with her girlfriends when she learned that she was pregnant. Clearly, context matters.
I continue to maintain that increasing choline in prenatal vitamins is a way out of this mess the United States is in with its hidden epidemic of FASD.
Dr. Bell is a staff psychiatrist at Jackson Park Hospital Family Medicine Clinic in Chicago; a clinical psychiatrist emeritus in the department of psychiatry at the University of Illinois at Chicago; a former president/CEO of Community Mental Health Council; and a former director of the Institute for Juvenile Research (birthplace of child psychiatry), also in Chicago.
Sharpening the saw
Few movies have universal appeal these days, but one that comes close is Bill Murray’s 1993 classic, “Groundhog Day,” in which Murray’s character is trapped in a time loop, living the same day over and over until he finally “gets it right.”
One reason that this film resonates with so many, I think, is that we are all, in essence, similarly trapped. Not in a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. Sooner or later, no matter how dedicated we are, the grind gets to all of us, leading to fatigue, irritability, and a progressive decline in motivation. And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well-being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of 1 a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lesson, or a long weekend away with my wife. And we take longer vacations, without fail, each year.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations. It all averages out in the end.
Besides, this is much more important than money: This is breaking the routine, clearing the cobwebs, living your life. And trust me, your practice will still be there when you return.
More than once I’ve recounted the story of K. Alexander Müller, PhD, and J. Georg Bednorz, PhD, the Swiss Nobel laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Dr. Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Dr. Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you. Any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Few movies have universal appeal these days, but one that comes close is Bill Murray’s 1993 classic, “Groundhog Day,” in which Murray’s character is trapped in a time loop, living the same day over and over until he finally “gets it right.”
One reason that this film resonates with so many, I think, is that we are all, in essence, similarly trapped. Not in a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. Sooner or later, no matter how dedicated we are, the grind gets to all of us, leading to fatigue, irritability, and a progressive decline in motivation. And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well-being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of 1 a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lesson, or a long weekend away with my wife. And we take longer vacations, without fail, each year.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations. It all averages out in the end.
Besides, this is much more important than money: This is breaking the routine, clearing the cobwebs, living your life. And trust me, your practice will still be there when you return.
More than once I’ve recounted the story of K. Alexander Müller, PhD, and J. Georg Bednorz, PhD, the Swiss Nobel laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Dr. Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Dr. Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you. Any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Few movies have universal appeal these days, but one that comes close is Bill Murray’s 1993 classic, “Groundhog Day,” in which Murray’s character is trapped in a time loop, living the same day over and over until he finally “gets it right.”
One reason that this film resonates with so many, I think, is that we are all, in essence, similarly trapped. Not in a same-day loop, of course; but each week seems eerily similar to the last, as does each month, each year – on and on, ad infinitum. That’s why it is so important, every so often, to step out of the “loop” and reassess the bigger picture.
I write this reminder every couple of years because it’s so easy to lose sight of the overall landscape among the pressures of our daily routines. Sooner or later, no matter how dedicated we are, the grind gets to all of us, leading to fatigue, irritability, and a progressive decline in motivation. And we are too busy to sit down and think about what we might do to break that vicious cycle. This is detrimental to our own well-being, as well as that of our patients.
There are many ways to maintain your intellectual and emotional health, but here’s how I do it: I take individual days off (average of 1 a month) to catch up on journals or taking a CME course; or to try something new – something I’ve been thinking about doing “someday, when there is time” – such as a guitar, bass, or sailing lesson, or a long weekend away with my wife. And we take longer vacations, without fail, each year.
I know how some of you feel about “wasting” a day – or, God forbid, a week. Patients might go elsewhere while you’re gone, and every day the office is idle you “lose money.” That whole paradigm is wrong. You bring in a given amount of revenue per year – more on some days, less on other days, none on weekends and vacations. It all averages out in the end.
Besides, this is much more important than money: This is breaking the routine, clearing the cobwebs, living your life. And trust me, your practice will still be there when you return.
More than once I’ve recounted the story of K. Alexander Müller, PhD, and J. Georg Bednorz, PhD, the Swiss Nobel laureates whose superconductivity research ground to a halt in 1986. The harder they pressed, the more elusive progress became. So Dr. Müller decided to take a break to read a new book on ceramics – a subject that had always interested him.
Nothing could have been less relevant to his work, of course; ceramics are among the poorest conductors known. But in that lower-pressure environment, Dr. Müller realized that a unique property of ceramics might apply to their project.
Back in the lab, the team created a ceramic compound that became the first successful “high-temperature” superconductor, which in turn triggered an explosion of research leading to breakthroughs in computing, electricity transmission, magnetically-elevated trains, and many applications yet to be realized.
Sharpening your saw may not change the world, but it will change you. Any nudge out of your comfort zone will give you fresh ideas and help you look at seemingly insoluble problems in completely new ways.
And to those who still can’t bear the thought of taking time off, remember the dying words that no one has spoken, ever: “I wish I had spent more time in my office!”
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
Singing Praises, Naming Names
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.
Being a peer-reviewed journal, Federal Practitioner relies on the dedicated efforts of a great number of unsung (and uncompensated) people, and we would like to recognize these efforts. This journal exists because of the large body of federal health care providers who devote their time and energy to sharing best practices, case studies, literature reviews, and original research. An even larger number of men and women review the many submissions, check the research, and provide essential feedback to our authors. By design, this army of reviewers remains anonymous, but that does not diminish their importance.
Although it would be impossible to adequately thank our reviewers, authors, and other contributors, sufficiently, we are trying. We are delighted to induct some of the most engaged members of the Federal Practitioner community to the Editorial Advisory Association (EAA). The EAA helps guide the journal to ensure it remains focused on the essential issues that confront federal health care providers. Federal Practitioner strives for continuous improvement and is focused on enhancing the breadth, depth, and quality of the online and print content. The EAA plays an important role in that process, and we thank all the current EAA and new members for their guidance.
New EAA Members
Susanne G. Barnett, PharmD, BCPS, has directed the Pharmacy Notes column for Federal Practitioner since 2015. Dr. Barnett is an associate professor at the University of Wisconsin-Madison School of Pharmacy and a clinical pharmacist at the William S. Middleton Memorial Veterans Hospital. She has focused on antimicrobial stewardship and infectious diseases.
Anthony Breu, MD, conceived and directs the VA Boston Medical Forum series
Maggie Chartier, PsyD, MPH, has authored multiple articles for Federal Practitioner and provided guidance and direction for the 2017 and (forthcoming) 2018 editions of the public pathogens/infectious diseases special issues. Dr. Chartier is the deputy director for the HIV, Hepatitis, and Related Conditions Program in the VHA Office of Specialty Care Services and an assistant clinical professor at the University of California, San Francisco.
Marcia Johnson, DNP, FNP-BC, has been a highly active author and peer reviewer. Dr. Johnson has been a nurse practitioner at the VA for 18 years, and currently provides primary care at the Clermont CBOC in Florida. She previously served as the hepatitis C research coordinator at Philadelphia VAMC and practiced at the Orlando VAMC spinal cord injury clinic.
William Rodríguez-Cintrón, MD, is another active peer reviewer and a prolific contributor. Dr. Rodríguez-Cintrón is chief of the pulmonary, critical care and sleep medicine departments at the VA Caribbean Healthcare System in Puerto Rico.
Col. (Ret) Mona Pearl Treyball, PhD, MS, RN, USAF, also has been a dedicated peer reviewer. Col. Treyball is professor and specialty director of the
Federal Practitioner would like to thank all of the current and new members of the EAA for their continued support. All of the journal’s successes are built on their dedication and commitment. Federal Practitioner encourages all the members of the federal health care community to become more involved, whether as a peer reviewer, author, or by responding to our content in print, online, or via social media. Your feedback and involvement makes this journal better.