User login
The older we are, the more unique we become
I was rounding at the nursing home and my day began as it often did. I reviewed the doctor communication book at the nursing station to see which patients I needed to visit and checked in with the floor nurse for any important updates.
A mother waiting for her son to visit
The first patient on my list was Rose. She had become increasingly withdrawn and less mobile. She used to walk the corridors asking when her son, Billy, would visit. We would all remind her that Billy visited her two or three times a week, but she never remembered the visits and blamed him for moving her out of her comfortable home in New Jersey where she’d lived with her husband before his death several years earlier.
Rose was declining, and we were trying to optimize her function and quality of life. She fell frequently while trying to get up at night to use the bathroom. None of our fall-reduction strategies had worked, and she had broken her hip a year prior. She’d fully recovered, but the combination of mental and physical frailty was becoming obvious to everyone, including her son. She had lost another five pounds and was approaching the end of her life.
“Good morning, Rose.” (She had demanded that I use her first name.) “How are you doing today?”
“I am doing okay, doctor. Have you seen Billy? When is he going to visit me?”
“I really can’t say when he’ll visit next, but I saw in a note that he was here yesterday.”
“No, he didn’t come to see me,” she said. “He doesn’t care about me. He spends more time with his wife and family than with his own mother.”
“Well, is there anything special that I can do for you?”
“Yes. Please tell Billy to visit his mother,” she said.
I completed her evaluation and made my way down the hall.
A wife ready to rejoin her husband
Next on my list was a widow named Violet. She reminded me of Whistler’s mother. As was her custom, she was sitting up in her chair reading her Bible when I came in. Her husband had been a minister, and she enjoyed reading the Bible or meditating for several hours each morning. Her bedside table had the most recent devotional and a picture of her husband in his vestments.
Violet was quiet and direct, and she had steely blue eyes that could communicate with your soul. Her nun-like quality was not overpowering; her manner was warm and welcoming.
“Good morning!” I said. “I hope I’m not bothering you.”
“Good morning, doctor. It’s always nice to see you.”
“I haven’t been by in a while, and I wanted to check your heart and lungs and make sure everything is going okay for you.”
“Of course; help yourself,” she said. “I feel fine. And as you know, I am ready to join my husband whenever the Lord calls me. I have lived a blessed life and do not wish to prolong it unless it is God’s will.”
“You certainly have made your wishes clear to me, and you are still in excellent health,” I said.
She really was in good health, and I made a quick note to call her daughter – who lived on the other side of the country – with an update.
A beauty queen ready for her close-up
Gabby was next on my list. She was a former beauty queen who had competed in local and state beauty contests. Her looks were the cornerstone of her identity, and she had done a truly remarkable job of maintaining her physical appearance.
Gabby had three attentive daughters who lived locally and supplied her with the latest makeup, beauty creams, and anti-aging nostrums. She always managed to look natural (and not like a caricature) with her face made up and her blond wig in place. Over the years, she’d made good use of the services offered by the local plastic surgeons and dermatologists. And to her credit – and theirs – she looked 30 years younger than her chronological age. In fairness, she had also taken good care of her overall health.
Gabby’s nickname was appropriate as she was chatty, to the extreme. She enjoyed being the center of attention.
When I entered her room, she was putting on her makeup. She was seated near her bedside table, which looked like it belonged in the backstage dressing room of a Broadway star. Lined up on the table were various bottles, brushes, and a mirror surrounded by lights.
“Oh, doctor, you can’t come in now. I’m a dreadful mess,” she said. “Please come back in 10 minutes. I am so embarrassed that you are seeing me this way. I just have a few things to fix, and then I will be presentable. My daughters are taking me out for lunch at the club, and I do not want to look like an old lady.”
“Gabby,” I said, “I have seen you before without your makeup. Do you remember last year when you developed pneumonia? You were really sick, and frankly, we were not sure you were going to pull through. One of the clues that you were getting ill was your smeared mascara and lipstick.”
I pressed on, and she let me examine her while she continued to apply her eyeliner.
“Everything sounds good. And I like your fresh pedicure,” I said. “Is there anything I can do for you?”
“No, thank you. Have a nice day, doctor!”
A mother devoted to her daughter’s care
Unlike my other patients, Mabel shared a room with a family member – her daughter, Hope. Mabel’s daughter had a congenital illness with significant physical, functional, and cognitive deficits. Mabel had considerable guilt regarding her daughter’s condition. Mabel’s husband had divorced her decades earlier, and she had devoted her life to caring for Hope. When Mabel’s health began to decline and she realized she could no longer care for Hope alone, the two moved into the facility together. Mabel told me that she simply couldn’t die before her daughter, because no one could oversee her care like she could.
Mabel was frail physically but sharp and vigilant mentally. Hope had had numerous hospitalizations, and Mabel had been with her through each experience. Hope could not communicate with others, but Mabel could express Hope’s concerns.
“How are you doing today?” I asked.
“Not well. I am concerned about Hope. She has not had a bowel movement in two days and does not want to eat breakfast.”
I checked out Hope, and her examination was reassuring. She looked up at me with her distorted features and managed a broad smile. I went back over to Mabel.
“She likes you, doctor. She thinks you smell good.”
I turned to Hope and thanked her for the compliment.
“I will check with the nurse and see if we can give you something simple to help your bowels.”
“Warm prune juice often works,” said Mabel. “Please come by again tomorrow to check on her. I don’t want this to progress. She is miserable.”
“I will be back tomorrow, and I will make a special trip to see you both.”
Upon reflection ...
When I sat down to write my clinical notes for the day, I realized that Rose, Violet, Gabby, and Mabel were each over 100 years old. I had seen four centenarians in a single day! Each of them manifested a fundamental principle of geriatrics: The older we are, the more unique and differentiated we become. A one-size approach to geriatric care does not fit all. Our care must be personalized to the unique individual in front of us.
Patients’ names and some details have been changed to protect their privacy. Dr. Williams is the Emeritus Ward K. Ensminger Distinguished Professor of Geriatric Medicine, University of Virginia, Charlottesville and attending physician, internal medicine and geriatrics, New Hanover Regional Medical Center, Wilmington, N.C. He disclosed no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
I was rounding at the nursing home and my day began as it often did. I reviewed the doctor communication book at the nursing station to see which patients I needed to visit and checked in with the floor nurse for any important updates.
A mother waiting for her son to visit
The first patient on my list was Rose. She had become increasingly withdrawn and less mobile. She used to walk the corridors asking when her son, Billy, would visit. We would all remind her that Billy visited her two or three times a week, but she never remembered the visits and blamed him for moving her out of her comfortable home in New Jersey where she’d lived with her husband before his death several years earlier.
Rose was declining, and we were trying to optimize her function and quality of life. She fell frequently while trying to get up at night to use the bathroom. None of our fall-reduction strategies had worked, and she had broken her hip a year prior. She’d fully recovered, but the combination of mental and physical frailty was becoming obvious to everyone, including her son. She had lost another five pounds and was approaching the end of her life.
“Good morning, Rose.” (She had demanded that I use her first name.) “How are you doing today?”
“I am doing okay, doctor. Have you seen Billy? When is he going to visit me?”
“I really can’t say when he’ll visit next, but I saw in a note that he was here yesterday.”
“No, he didn’t come to see me,” she said. “He doesn’t care about me. He spends more time with his wife and family than with his own mother.”
“Well, is there anything special that I can do for you?”
“Yes. Please tell Billy to visit his mother,” she said.
I completed her evaluation and made my way down the hall.
A wife ready to rejoin her husband
Next on my list was a widow named Violet. She reminded me of Whistler’s mother. As was her custom, she was sitting up in her chair reading her Bible when I came in. Her husband had been a minister, and she enjoyed reading the Bible or meditating for several hours each morning. Her bedside table had the most recent devotional and a picture of her husband in his vestments.
Violet was quiet and direct, and she had steely blue eyes that could communicate with your soul. Her nun-like quality was not overpowering; her manner was warm and welcoming.
“Good morning!” I said. “I hope I’m not bothering you.”
“Good morning, doctor. It’s always nice to see you.”
“I haven’t been by in a while, and I wanted to check your heart and lungs and make sure everything is going okay for you.”
“Of course; help yourself,” she said. “I feel fine. And as you know, I am ready to join my husband whenever the Lord calls me. I have lived a blessed life and do not wish to prolong it unless it is God’s will.”
“You certainly have made your wishes clear to me, and you are still in excellent health,” I said.
She really was in good health, and I made a quick note to call her daughter – who lived on the other side of the country – with an update.
A beauty queen ready for her close-up
Gabby was next on my list. She was a former beauty queen who had competed in local and state beauty contests. Her looks were the cornerstone of her identity, and she had done a truly remarkable job of maintaining her physical appearance.
Gabby had three attentive daughters who lived locally and supplied her with the latest makeup, beauty creams, and anti-aging nostrums. She always managed to look natural (and not like a caricature) with her face made up and her blond wig in place. Over the years, she’d made good use of the services offered by the local plastic surgeons and dermatologists. And to her credit – and theirs – she looked 30 years younger than her chronological age. In fairness, she had also taken good care of her overall health.
Gabby’s nickname was appropriate as she was chatty, to the extreme. She enjoyed being the center of attention.
When I entered her room, she was putting on her makeup. She was seated near her bedside table, which looked like it belonged in the backstage dressing room of a Broadway star. Lined up on the table were various bottles, brushes, and a mirror surrounded by lights.
“Oh, doctor, you can’t come in now. I’m a dreadful mess,” she said. “Please come back in 10 minutes. I am so embarrassed that you are seeing me this way. I just have a few things to fix, and then I will be presentable. My daughters are taking me out for lunch at the club, and I do not want to look like an old lady.”
“Gabby,” I said, “I have seen you before without your makeup. Do you remember last year when you developed pneumonia? You were really sick, and frankly, we were not sure you were going to pull through. One of the clues that you were getting ill was your smeared mascara and lipstick.”
I pressed on, and she let me examine her while she continued to apply her eyeliner.
“Everything sounds good. And I like your fresh pedicure,” I said. “Is there anything I can do for you?”
“No, thank you. Have a nice day, doctor!”
A mother devoted to her daughter’s care
Unlike my other patients, Mabel shared a room with a family member – her daughter, Hope. Mabel’s daughter had a congenital illness with significant physical, functional, and cognitive deficits. Mabel had considerable guilt regarding her daughter’s condition. Mabel’s husband had divorced her decades earlier, and she had devoted her life to caring for Hope. When Mabel’s health began to decline and she realized she could no longer care for Hope alone, the two moved into the facility together. Mabel told me that she simply couldn’t die before her daughter, because no one could oversee her care like she could.
Mabel was frail physically but sharp and vigilant mentally. Hope had had numerous hospitalizations, and Mabel had been with her through each experience. Hope could not communicate with others, but Mabel could express Hope’s concerns.
“How are you doing today?” I asked.
“Not well. I am concerned about Hope. She has not had a bowel movement in two days and does not want to eat breakfast.”
I checked out Hope, and her examination was reassuring. She looked up at me with her distorted features and managed a broad smile. I went back over to Mabel.
“She likes you, doctor. She thinks you smell good.”
I turned to Hope and thanked her for the compliment.
“I will check with the nurse and see if we can give you something simple to help your bowels.”
“Warm prune juice often works,” said Mabel. “Please come by again tomorrow to check on her. I don’t want this to progress. She is miserable.”
“I will be back tomorrow, and I will make a special trip to see you both.”
Upon reflection ...
When I sat down to write my clinical notes for the day, I realized that Rose, Violet, Gabby, and Mabel were each over 100 years old. I had seen four centenarians in a single day! Each of them manifested a fundamental principle of geriatrics: The older we are, the more unique and differentiated we become. A one-size approach to geriatric care does not fit all. Our care must be personalized to the unique individual in front of us.
Patients’ names and some details have been changed to protect their privacy. Dr. Williams is the Emeritus Ward K. Ensminger Distinguished Professor of Geriatric Medicine, University of Virginia, Charlottesville and attending physician, internal medicine and geriatrics, New Hanover Regional Medical Center, Wilmington, N.C. He disclosed no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
I was rounding at the nursing home and my day began as it often did. I reviewed the doctor communication book at the nursing station to see which patients I needed to visit and checked in with the floor nurse for any important updates.
A mother waiting for her son to visit
The first patient on my list was Rose. She had become increasingly withdrawn and less mobile. She used to walk the corridors asking when her son, Billy, would visit. We would all remind her that Billy visited her two or three times a week, but she never remembered the visits and blamed him for moving her out of her comfortable home in New Jersey where she’d lived with her husband before his death several years earlier.
Rose was declining, and we were trying to optimize her function and quality of life. She fell frequently while trying to get up at night to use the bathroom. None of our fall-reduction strategies had worked, and she had broken her hip a year prior. She’d fully recovered, but the combination of mental and physical frailty was becoming obvious to everyone, including her son. She had lost another five pounds and was approaching the end of her life.
“Good morning, Rose.” (She had demanded that I use her first name.) “How are you doing today?”
“I am doing okay, doctor. Have you seen Billy? When is he going to visit me?”
“I really can’t say when he’ll visit next, but I saw in a note that he was here yesterday.”
“No, he didn’t come to see me,” she said. “He doesn’t care about me. He spends more time with his wife and family than with his own mother.”
“Well, is there anything special that I can do for you?”
“Yes. Please tell Billy to visit his mother,” she said.
I completed her evaluation and made my way down the hall.
A wife ready to rejoin her husband
Next on my list was a widow named Violet. She reminded me of Whistler’s mother. As was her custom, she was sitting up in her chair reading her Bible when I came in. Her husband had been a minister, and she enjoyed reading the Bible or meditating for several hours each morning. Her bedside table had the most recent devotional and a picture of her husband in his vestments.
Violet was quiet and direct, and she had steely blue eyes that could communicate with your soul. Her nun-like quality was not overpowering; her manner was warm and welcoming.
“Good morning!” I said. “I hope I’m not bothering you.”
“Good morning, doctor. It’s always nice to see you.”
“I haven’t been by in a while, and I wanted to check your heart and lungs and make sure everything is going okay for you.”
“Of course; help yourself,” she said. “I feel fine. And as you know, I am ready to join my husband whenever the Lord calls me. I have lived a blessed life and do not wish to prolong it unless it is God’s will.”
“You certainly have made your wishes clear to me, and you are still in excellent health,” I said.
She really was in good health, and I made a quick note to call her daughter – who lived on the other side of the country – with an update.
A beauty queen ready for her close-up
Gabby was next on my list. She was a former beauty queen who had competed in local and state beauty contests. Her looks were the cornerstone of her identity, and she had done a truly remarkable job of maintaining her physical appearance.
Gabby had three attentive daughters who lived locally and supplied her with the latest makeup, beauty creams, and anti-aging nostrums. She always managed to look natural (and not like a caricature) with her face made up and her blond wig in place. Over the years, she’d made good use of the services offered by the local plastic surgeons and dermatologists. And to her credit – and theirs – she looked 30 years younger than her chronological age. In fairness, she had also taken good care of her overall health.
Gabby’s nickname was appropriate as she was chatty, to the extreme. She enjoyed being the center of attention.
When I entered her room, she was putting on her makeup. She was seated near her bedside table, which looked like it belonged in the backstage dressing room of a Broadway star. Lined up on the table were various bottles, brushes, and a mirror surrounded by lights.
“Oh, doctor, you can’t come in now. I’m a dreadful mess,” she said. “Please come back in 10 minutes. I am so embarrassed that you are seeing me this way. I just have a few things to fix, and then I will be presentable. My daughters are taking me out for lunch at the club, and I do not want to look like an old lady.”
“Gabby,” I said, “I have seen you before without your makeup. Do you remember last year when you developed pneumonia? You were really sick, and frankly, we were not sure you were going to pull through. One of the clues that you were getting ill was your smeared mascara and lipstick.”
I pressed on, and she let me examine her while she continued to apply her eyeliner.
“Everything sounds good. And I like your fresh pedicure,” I said. “Is there anything I can do for you?”
“No, thank you. Have a nice day, doctor!”
A mother devoted to her daughter’s care
Unlike my other patients, Mabel shared a room with a family member – her daughter, Hope. Mabel’s daughter had a congenital illness with significant physical, functional, and cognitive deficits. Mabel had considerable guilt regarding her daughter’s condition. Mabel’s husband had divorced her decades earlier, and she had devoted her life to caring for Hope. When Mabel’s health began to decline and she realized she could no longer care for Hope alone, the two moved into the facility together. Mabel told me that she simply couldn’t die before her daughter, because no one could oversee her care like she could.
Mabel was frail physically but sharp and vigilant mentally. Hope had had numerous hospitalizations, and Mabel had been with her through each experience. Hope could not communicate with others, but Mabel could express Hope’s concerns.
“How are you doing today?” I asked.
“Not well. I am concerned about Hope. She has not had a bowel movement in two days and does not want to eat breakfast.”
I checked out Hope, and her examination was reassuring. She looked up at me with her distorted features and managed a broad smile. I went back over to Mabel.
“She likes you, doctor. She thinks you smell good.”
I turned to Hope and thanked her for the compliment.
“I will check with the nurse and see if we can give you something simple to help your bowels.”
“Warm prune juice often works,” said Mabel. “Please come by again tomorrow to check on her. I don’t want this to progress. She is miserable.”
“I will be back tomorrow, and I will make a special trip to see you both.”
Upon reflection ...
When I sat down to write my clinical notes for the day, I realized that Rose, Violet, Gabby, and Mabel were each over 100 years old. I had seen four centenarians in a single day! Each of them manifested a fundamental principle of geriatrics: The older we are, the more unique and differentiated we become. A one-size approach to geriatric care does not fit all. Our care must be personalized to the unique individual in front of us.
Patients’ names and some details have been changed to protect their privacy. Dr. Williams is the Emeritus Ward K. Ensminger Distinguished Professor of Geriatric Medicine, University of Virginia, Charlottesville and attending physician, internal medicine and geriatrics, New Hanover Regional Medical Center, Wilmington, N.C. He disclosed no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Low depression scores may miss seniors with suicidal intent
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
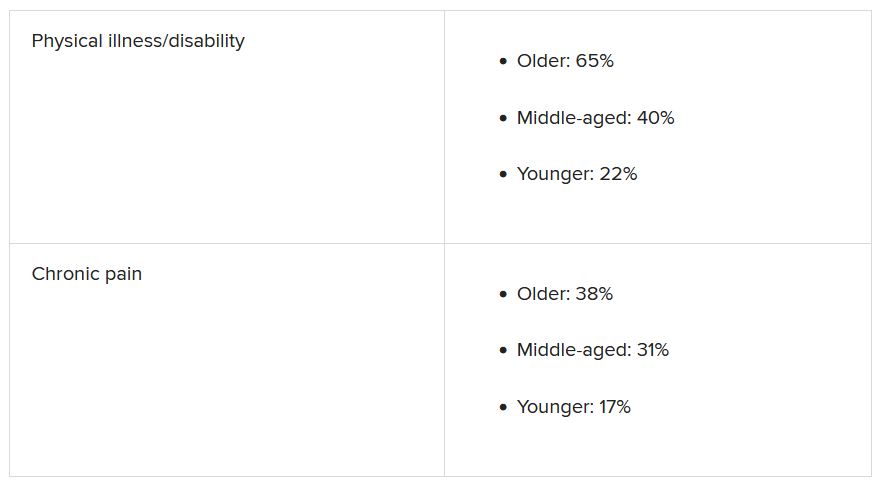
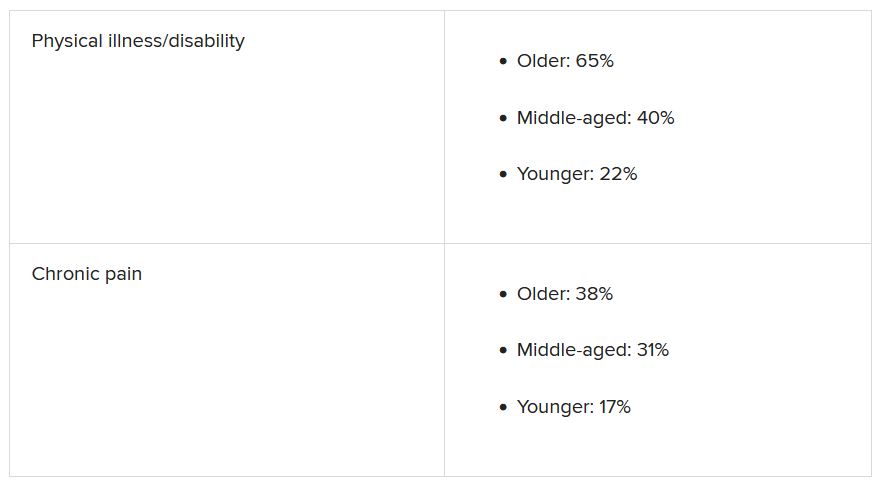
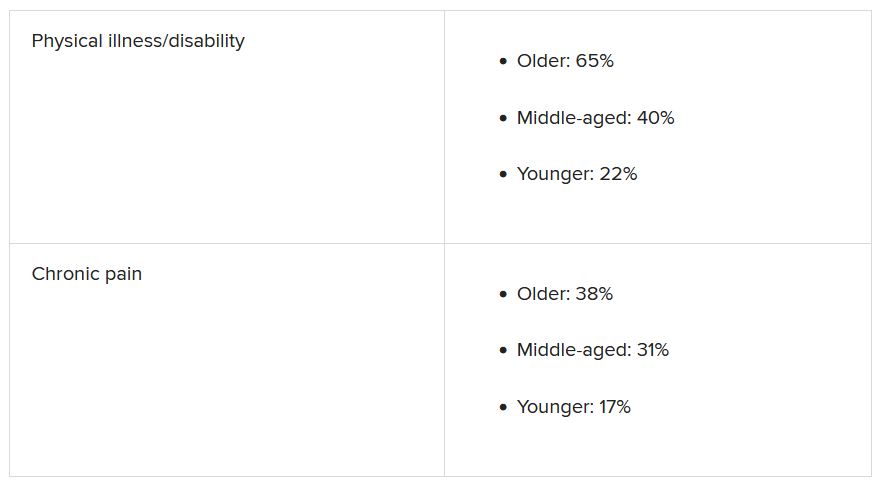
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Managing sleep in the elderly
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
FROM FOCUS ON NEUROPSYCHIATRY 2021
Diet, exercise in older adults with knee OA have long-term payoff
Older patients with knee osteoarthritis (OA) who underwent lengthy diet and exercise interventions reported less pain and maintained some weight loss years after the program ended, according to a new study published in Arthritis Care & Research.
“These data imply that clinicians who treat people with knee osteoarthritis have a variety of nonpharmacologic options that preserve clinically important effects 3.5 years after the treatments end,” wrote lead author Stephen P. Messier, PhD, professor and director of the J.B. Snow Biomechanics Laboratory at Wake Forest University, Winston-Salem, N.C.
The study involved patients with overweight or obesity aged 55 years or older who were previously enrolled in the 1.5-year Intensive Diet and Exercise for Arthritis (IDEA) trial.
“You have to remember, this is 3.5 years after the IDEA trial ended,” Dr. Messier said in an interview. “There was no contact with them for that entire time; you’d expect, based on the literature, that they’d revert back to where they were before they entered the trial. And certainly, there was some regression, there was some weight regain, but the important part of the study is that, even after 3.5 years, and even with some weight regain, there were some clinically important effects that lasted.”
“What we feel now is that if we can somehow prepare people better for that time after they finish a weight loss intervention, from a psychological standpoint, it will make a real difference,” he added. “We are very good at helping people have the confidence to lose weight. But having the confidence to lose weight is totally different than having confidence to maintain weight loss. If we can give folks an intervention that has a psychological component, hopefully we can increase their confidence to maintain the weight loss that they attained.”
Study details
Of the 184 participants who were contacted for a follow-up visit, 94 consented to participate, 67% of whom were females and 88% of whom were White. A total of 27 participants had completed the diet and exercise intervention, and another 35 completed the diet-only and 32 exercise-only interventions.
In the 3.5-year period between the IDEA trial’s end and follow-up, body weight increased by 5.9 kg in the diet and exercise group (P < .0001) and by 3.1 kg in the diet-only group (P = .0006) but decreased in the exercise-only group by 1.0 kg (P = .25). However, from baseline to 5-year follow-up, all groups saw a reduction in body weight. Mean weight loss was –3.7 kg for the diet and exercise group (P = .0007), –5.8 kg for the diet group (P < .0001), and –2.9 kg for the exercise group (P = .003). Body mass index also decreased in all groups: by –1.2 kg/m2 in the diet and exercise group (P = .001), by –2.0 kg/m2 in the diet group (P < .0001), and by –1.0 kg/m2 in the exercise group (P = .004).
Pain – as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score – was reduced in all groups across 5-year follow-up: –1.2 (P = .03) for the diet and exercise group, –1.5 (P = .001) for the diet-only group, and –1.6 (P = .0008) for the exercise-only group. WOMAC function also significantly improved relative to baseline by 6.2 (P = .0001) in the diet and exercise group, by 6.1 (P < .0001) in the diet group, and by 3.7 (P = .01) in the exercise-only group.
Finding time to advise on weight loss, exercise
“If exercise and weight loss were easy, this country wouldn’t be in the state we’re in,” Tuhina Neogi, MD, PhD, of Boston University said in an interview. “Shared decision-making and personalized medicine are important; unfortunately, for the majority of physicians – particularly primary care physicians, where a good deal of OA management is undertaken – they don’t have a lot of time in their 20 minutes with a patient who has OA to counsel individuals toward a healthy weight and physical activity program when they’re also addressing common comorbidities seen in OA such as diabetes and heart disease.
“But as we know,” she added, “when you do address weight loss and physical activity, it has wide-ranging health benefits. This study provides support for utilizing formal diet and exercise programs to achieve important and durable benefits for people with OA.”
Dr. Neogi did note one of the study’s acknowledged limitations: Only slightly more than half of the contacted participants returned for follow-up. Though the authors stated that the individuals who returned were representative of both the pool of potential participants and the IDEA cohort as a whole, “we don’t want to make too many inferences when you don’t have the whole study population available,” she said. “The people who have agreed to come back 3.5 years later for follow-up testing, maybe they are a little more health conscious, more resilient. Those people might be systematically different than the people who [did not return], even though most of the factors were not statistically different between the groups.
“Whatever positive attributes they may have, though, we need to understand more about them,” she added. “We need to know how they maintained the benefits they had 3.5 years prior. That kind of understanding is important to inform long-term strategies in OA management.”
Dr. Messier highlighted a related, ongoing study he’s leading in which more than 800 overweight patients in North Carolina who suffer from knee pain are being led through diet and exercise interventions in a community setting. The goal is to replicate the IDEA results outside of a clinical trial setting and show skeptical physicians that diet and exercise can be enacted and maintained in this subset of patients.
“I think we know how effective weight loss is, especially when combined with exercise, in reducing pain, improving function, improving quality of life in these patients,” he said. “The next step is to allow them to maintain those benefits for a long period of time after the intervention ends.”
The study was supported by grants from the National Institutes of Health and by General Nutrition Centers. Its authors reported no potential conflicts of interest.
Older patients with knee osteoarthritis (OA) who underwent lengthy diet and exercise interventions reported less pain and maintained some weight loss years after the program ended, according to a new study published in Arthritis Care & Research.
“These data imply that clinicians who treat people with knee osteoarthritis have a variety of nonpharmacologic options that preserve clinically important effects 3.5 years after the treatments end,” wrote lead author Stephen P. Messier, PhD, professor and director of the J.B. Snow Biomechanics Laboratory at Wake Forest University, Winston-Salem, N.C.
The study involved patients with overweight or obesity aged 55 years or older who were previously enrolled in the 1.5-year Intensive Diet and Exercise for Arthritis (IDEA) trial.
“You have to remember, this is 3.5 years after the IDEA trial ended,” Dr. Messier said in an interview. “There was no contact with them for that entire time; you’d expect, based on the literature, that they’d revert back to where they were before they entered the trial. And certainly, there was some regression, there was some weight regain, but the important part of the study is that, even after 3.5 years, and even with some weight regain, there were some clinically important effects that lasted.”
“What we feel now is that if we can somehow prepare people better for that time after they finish a weight loss intervention, from a psychological standpoint, it will make a real difference,” he added. “We are very good at helping people have the confidence to lose weight. But having the confidence to lose weight is totally different than having confidence to maintain weight loss. If we can give folks an intervention that has a psychological component, hopefully we can increase their confidence to maintain the weight loss that they attained.”
Study details
Of the 184 participants who were contacted for a follow-up visit, 94 consented to participate, 67% of whom were females and 88% of whom were White. A total of 27 participants had completed the diet and exercise intervention, and another 35 completed the diet-only and 32 exercise-only interventions.
In the 3.5-year period between the IDEA trial’s end and follow-up, body weight increased by 5.9 kg in the diet and exercise group (P < .0001) and by 3.1 kg in the diet-only group (P = .0006) but decreased in the exercise-only group by 1.0 kg (P = .25). However, from baseline to 5-year follow-up, all groups saw a reduction in body weight. Mean weight loss was –3.7 kg for the diet and exercise group (P = .0007), –5.8 kg for the diet group (P < .0001), and –2.9 kg for the exercise group (P = .003). Body mass index also decreased in all groups: by –1.2 kg/m2 in the diet and exercise group (P = .001), by –2.0 kg/m2 in the diet group (P < .0001), and by –1.0 kg/m2 in the exercise group (P = .004).
Pain – as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score – was reduced in all groups across 5-year follow-up: –1.2 (P = .03) for the diet and exercise group, –1.5 (P = .001) for the diet-only group, and –1.6 (P = .0008) for the exercise-only group. WOMAC function also significantly improved relative to baseline by 6.2 (P = .0001) in the diet and exercise group, by 6.1 (P < .0001) in the diet group, and by 3.7 (P = .01) in the exercise-only group.
Finding time to advise on weight loss, exercise
“If exercise and weight loss were easy, this country wouldn’t be in the state we’re in,” Tuhina Neogi, MD, PhD, of Boston University said in an interview. “Shared decision-making and personalized medicine are important; unfortunately, for the majority of physicians – particularly primary care physicians, where a good deal of OA management is undertaken – they don’t have a lot of time in their 20 minutes with a patient who has OA to counsel individuals toward a healthy weight and physical activity program when they’re also addressing common comorbidities seen in OA such as diabetes and heart disease.
“But as we know,” she added, “when you do address weight loss and physical activity, it has wide-ranging health benefits. This study provides support for utilizing formal diet and exercise programs to achieve important and durable benefits for people with OA.”
Dr. Neogi did note one of the study’s acknowledged limitations: Only slightly more than half of the contacted participants returned for follow-up. Though the authors stated that the individuals who returned were representative of both the pool of potential participants and the IDEA cohort as a whole, “we don’t want to make too many inferences when you don’t have the whole study population available,” she said. “The people who have agreed to come back 3.5 years later for follow-up testing, maybe they are a little more health conscious, more resilient. Those people might be systematically different than the people who [did not return], even though most of the factors were not statistically different between the groups.
“Whatever positive attributes they may have, though, we need to understand more about them,” she added. “We need to know how they maintained the benefits they had 3.5 years prior. That kind of understanding is important to inform long-term strategies in OA management.”
Dr. Messier highlighted a related, ongoing study he’s leading in which more than 800 overweight patients in North Carolina who suffer from knee pain are being led through diet and exercise interventions in a community setting. The goal is to replicate the IDEA results outside of a clinical trial setting and show skeptical physicians that diet and exercise can be enacted and maintained in this subset of patients.
“I think we know how effective weight loss is, especially when combined with exercise, in reducing pain, improving function, improving quality of life in these patients,” he said. “The next step is to allow them to maintain those benefits for a long period of time after the intervention ends.”
The study was supported by grants from the National Institutes of Health and by General Nutrition Centers. Its authors reported no potential conflicts of interest.
Older patients with knee osteoarthritis (OA) who underwent lengthy diet and exercise interventions reported less pain and maintained some weight loss years after the program ended, according to a new study published in Arthritis Care & Research.
“These data imply that clinicians who treat people with knee osteoarthritis have a variety of nonpharmacologic options that preserve clinically important effects 3.5 years after the treatments end,” wrote lead author Stephen P. Messier, PhD, professor and director of the J.B. Snow Biomechanics Laboratory at Wake Forest University, Winston-Salem, N.C.
The study involved patients with overweight or obesity aged 55 years or older who were previously enrolled in the 1.5-year Intensive Diet and Exercise for Arthritis (IDEA) trial.
“You have to remember, this is 3.5 years after the IDEA trial ended,” Dr. Messier said in an interview. “There was no contact with them for that entire time; you’d expect, based on the literature, that they’d revert back to where they were before they entered the trial. And certainly, there was some regression, there was some weight regain, but the important part of the study is that, even after 3.5 years, and even with some weight regain, there were some clinically important effects that lasted.”
“What we feel now is that if we can somehow prepare people better for that time after they finish a weight loss intervention, from a psychological standpoint, it will make a real difference,” he added. “We are very good at helping people have the confidence to lose weight. But having the confidence to lose weight is totally different than having confidence to maintain weight loss. If we can give folks an intervention that has a psychological component, hopefully we can increase their confidence to maintain the weight loss that they attained.”
Study details
Of the 184 participants who were contacted for a follow-up visit, 94 consented to participate, 67% of whom were females and 88% of whom were White. A total of 27 participants had completed the diet and exercise intervention, and another 35 completed the diet-only and 32 exercise-only interventions.
In the 3.5-year period between the IDEA trial’s end and follow-up, body weight increased by 5.9 kg in the diet and exercise group (P < .0001) and by 3.1 kg in the diet-only group (P = .0006) but decreased in the exercise-only group by 1.0 kg (P = .25). However, from baseline to 5-year follow-up, all groups saw a reduction in body weight. Mean weight loss was –3.7 kg for the diet and exercise group (P = .0007), –5.8 kg for the diet group (P < .0001), and –2.9 kg for the exercise group (P = .003). Body mass index also decreased in all groups: by –1.2 kg/m2 in the diet and exercise group (P = .001), by –2.0 kg/m2 in the diet group (P < .0001), and by –1.0 kg/m2 in the exercise group (P = .004).
Pain – as measured by the Western Ontario and McMaster Universities Arthritis Index (WOMAC) score – was reduced in all groups across 5-year follow-up: –1.2 (P = .03) for the diet and exercise group, –1.5 (P = .001) for the diet-only group, and –1.6 (P = .0008) for the exercise-only group. WOMAC function also significantly improved relative to baseline by 6.2 (P = .0001) in the diet and exercise group, by 6.1 (P < .0001) in the diet group, and by 3.7 (P = .01) in the exercise-only group.
Finding time to advise on weight loss, exercise
“If exercise and weight loss were easy, this country wouldn’t be in the state we’re in,” Tuhina Neogi, MD, PhD, of Boston University said in an interview. “Shared decision-making and personalized medicine are important; unfortunately, for the majority of physicians – particularly primary care physicians, where a good deal of OA management is undertaken – they don’t have a lot of time in their 20 minutes with a patient who has OA to counsel individuals toward a healthy weight and physical activity program when they’re also addressing common comorbidities seen in OA such as diabetes and heart disease.
“But as we know,” she added, “when you do address weight loss and physical activity, it has wide-ranging health benefits. This study provides support for utilizing formal diet and exercise programs to achieve important and durable benefits for people with OA.”
Dr. Neogi did note one of the study’s acknowledged limitations: Only slightly more than half of the contacted participants returned for follow-up. Though the authors stated that the individuals who returned were representative of both the pool of potential participants and the IDEA cohort as a whole, “we don’t want to make too many inferences when you don’t have the whole study population available,” she said. “The people who have agreed to come back 3.5 years later for follow-up testing, maybe they are a little more health conscious, more resilient. Those people might be systematically different than the people who [did not return], even though most of the factors were not statistically different between the groups.
“Whatever positive attributes they may have, though, we need to understand more about them,” she added. “We need to know how they maintained the benefits they had 3.5 years prior. That kind of understanding is important to inform long-term strategies in OA management.”
Dr. Messier highlighted a related, ongoing study he’s leading in which more than 800 overweight patients in North Carolina who suffer from knee pain are being led through diet and exercise interventions in a community setting. The goal is to replicate the IDEA results outside of a clinical trial setting and show skeptical physicians that diet and exercise can be enacted and maintained in this subset of patients.
“I think we know how effective weight loss is, especially when combined with exercise, in reducing pain, improving function, improving quality of life in these patients,” he said. “The next step is to allow them to maintain those benefits for a long period of time after the intervention ends.”
The study was supported by grants from the National Institutes of Health and by General Nutrition Centers. Its authors reported no potential conflicts of interest.
FROM ARTHRITIS CARE & RESEARCH
Wisdom may counter loneliness, burnout in older adults
Wisdom increases with age, and although this personality trait is regarded as nebulous by many, there is evidence that it has biological and neuropsychiatric underpinnings. It could even hold the key to reducing loneliness and burnout among older people.
Those were some of the key messages delivered by Tanya T. Nguyen, PhD, of the department of psychiatry at the University of California, San Diego, who spoke at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“To many people, wisdom remains a fuzzy concept that’s difficult to operationalize and measure. It’s analogous to the concepts of consciousness, emotions, and cognitions, which at one point were considered nonscientific, but today we accept them as biological and scientific entities,” Dr. Nguyen said during her talk at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Interest in quantifying and studying wisdom has picked up in recent years, and Dr. Nguyen gave a definition with six elements that includes prosocial behaviors such as empathy and compassion, as well as emotional regulation, self-reflection, decisiveness, and social decision-making. She also included a spirituality component, though she conceded that this is controversial.
She noted that there are cultural variations in the definition of wisdom, but it has changed little over time, suggesting that it may be biological rather than cultural in nature, and therefore may have a neuropsychiatric underpinning.
Loss of some or all characteristics of wisdom occurs in some behaviors and disorders, including most markedly in the neurodegenerative disorder frontotemporal dementia (FTD), which is characterized by damage only in the prefrontal cortex and anterior temporal lobes. It usually occurs before age 60, and patients exhibit poor social awareness, impulsivity, antisocial behavior, and a lack of insight and empathy.
This and other lines of evidence have led to the suggestion that wisdom may be governed by processes in the prefrontal cortex and the limbic striatum. The prefrontal cortex controls executive functions such as planning, predicting, and anticipating events, as well as managing emotional reactions and impulses. “Thus, wisdom involves parts of the brain that balance cold, hard analytical reasoning with primitive desires and drives, which ultimately leads to self-regulation, social insight, theory of mind, and empathy,” said Dr. Nguyen.
Wisdom has long been associated with age, but age is also linked to cognitive decline. A recent discovery that the brain does not stop evolving at older age may help explain this contradiction. Brains develop in a back to front order, so that the prefrontal cortex is the last to mature. As we age, neural activity shifts from the occipital lobes to the prefrontal cortex and its executive decision-making power.
“The brain may recruit higher-order networks to the prefrontal cortex that are associated with wisdom development,” said Dr. Nguyen. She also pointed out that asymmetry between the left and right hemisphere is reduced with age, as tasks that relied on circuits from one hemisphere or another more often call upon both. “In order to make up for lost synapses and neurons with aging, active older adults use more neuronal networks from both hemispheres to perform the same mental activity,” Dr. Nguyen said.
Some interventions can improve scores in traits associated with wisdom in older adults, and could be an important contributor to improvements in health and longevity, said Dr. Nguyen. Randomized, controlled trials have demonstrated that psychosocial or behavioral interventions can improve elements of wisdom such as prosocial behaviors and emotional regulation, both in people with mental illness and in the general population, with moderate to large effect sizes. But such studies don’t prove an effect on overall wisdom.
The intervention achieved positive results in 89 participants in senior housing communities, though the effect sizes were small, possibly because of high baseline resilience. A subanalysis suggested that reduction in loneliness was mediated by an increase in compassion.
“One of the most striking findings from our research on wisdom is this consistent and very strongly negative correlation between wisdom and loneliness,” Dr. Nguyen said. She highlighted other U.S. nationwide and cross-cultural studies that showed inverse relationships between loneliness and wisdom.
Loneliness is an important topic because it can contribute to burnout and suicide rates.
“Loneliness has a profound effect on how we show up in the workplace, in school, and in our communities. And that leads to anxiety, depression, depersonalization, and emotional fatigue. All are key features of burnout. And together loneliness and burnout have contributed to increased rates of suicide by 30%, and opioid-related deaths almost sixfold since the late 1990s,” Dr. Nguyen said.
Loneliness also is associated with worse physical health, and it may be linked to wisdom. “Loneliness can be conceptualized as being caused and maintained by objective circumstances, such as physical or social distancing, and by thoughts, behaviors, and feelings surrounding those experiences, including biased perceptions of social relations, and a negative assessment of one’s social skills, which then results in a discrepancy between one’s desired and perceived social relationships, which then can contribute to social withdrawal,” Dr. Nguyen said.
Dr. Nguyen highlighted the AARP Foundation’s Experience Corps program, which recruits older adults to act as mentors and tutors for children in kindergarten through third grade. It involves 15 hours per week over an entire school year, with a focus on child literacy, development, and behavioral management skills. A study revealed a significant impact. “It showed improvements in children’s grades and happiness, as well as seniors’ mental and physical health,” Dr. Nguyen said.
Dr. Nguyen concluded that wisdom “may be a vaccine against compassion fatigue and burnout that drive today’s behavioral epidemics of loneliness, opioid abuse, and suicide. It’s a tool for our times. It’s nuanced, flexible, pragmatic, compassionate, and it presents a reasonable framework for getting along in the often messy world that we all share.”
Implications for psychiatrists
Henry A. Nasrallah, MD, who organized the conference, suggested that the benefits of wisdom may not be limited to patients. He pointed out that surgeons often retire at age 60 or 65 because of declining physical skills, while psychiatrists continue to practice.
“We develop more wisdom and better skills, and we can practice into our 60s and 70s. I know psychiatrists who practice sometimes into their 80s. It’s really a wonderful thing to know that what you do in life develops or enhances the neuroplasticity of certain brain regions. In our case, in psychiatry, it is the brain regions involved in wisdom,” commented Dr. Nasrallah, who is a professor of psychiatry, neurology, and neuroscience at the University of Cincinnati.
Dr. Nguyen has no financial disclosures. Dr. Nasrallah has received grants from Abbott, AstraZeneca, Forest, Janssen, Lilly, Pfizer, and Shire, and advises Abbott, AstraZeneca, and Shire.
Wisdom increases with age, and although this personality trait is regarded as nebulous by many, there is evidence that it has biological and neuropsychiatric underpinnings. It could even hold the key to reducing loneliness and burnout among older people.
Those were some of the key messages delivered by Tanya T. Nguyen, PhD, of the department of psychiatry at the University of California, San Diego, who spoke at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“To many people, wisdom remains a fuzzy concept that’s difficult to operationalize and measure. It’s analogous to the concepts of consciousness, emotions, and cognitions, which at one point were considered nonscientific, but today we accept them as biological and scientific entities,” Dr. Nguyen said during her talk at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Interest in quantifying and studying wisdom has picked up in recent years, and Dr. Nguyen gave a definition with six elements that includes prosocial behaviors such as empathy and compassion, as well as emotional regulation, self-reflection, decisiveness, and social decision-making. She also included a spirituality component, though she conceded that this is controversial.
She noted that there are cultural variations in the definition of wisdom, but it has changed little over time, suggesting that it may be biological rather than cultural in nature, and therefore may have a neuropsychiatric underpinning.
Loss of some or all characteristics of wisdom occurs in some behaviors and disorders, including most markedly in the neurodegenerative disorder frontotemporal dementia (FTD), which is characterized by damage only in the prefrontal cortex and anterior temporal lobes. It usually occurs before age 60, and patients exhibit poor social awareness, impulsivity, antisocial behavior, and a lack of insight and empathy.
This and other lines of evidence have led to the suggestion that wisdom may be governed by processes in the prefrontal cortex and the limbic striatum. The prefrontal cortex controls executive functions such as planning, predicting, and anticipating events, as well as managing emotional reactions and impulses. “Thus, wisdom involves parts of the brain that balance cold, hard analytical reasoning with primitive desires and drives, which ultimately leads to self-regulation, social insight, theory of mind, and empathy,” said Dr. Nguyen.
Wisdom has long been associated with age, but age is also linked to cognitive decline. A recent discovery that the brain does not stop evolving at older age may help explain this contradiction. Brains develop in a back to front order, so that the prefrontal cortex is the last to mature. As we age, neural activity shifts from the occipital lobes to the prefrontal cortex and its executive decision-making power.
“The brain may recruit higher-order networks to the prefrontal cortex that are associated with wisdom development,” said Dr. Nguyen. She also pointed out that asymmetry between the left and right hemisphere is reduced with age, as tasks that relied on circuits from one hemisphere or another more often call upon both. “In order to make up for lost synapses and neurons with aging, active older adults use more neuronal networks from both hemispheres to perform the same mental activity,” Dr. Nguyen said.
Some interventions can improve scores in traits associated with wisdom in older adults, and could be an important contributor to improvements in health and longevity, said Dr. Nguyen. Randomized, controlled trials have demonstrated that psychosocial or behavioral interventions can improve elements of wisdom such as prosocial behaviors and emotional regulation, both in people with mental illness and in the general population, with moderate to large effect sizes. But such studies don’t prove an effect on overall wisdom.
The intervention achieved positive results in 89 participants in senior housing communities, though the effect sizes were small, possibly because of high baseline resilience. A subanalysis suggested that reduction in loneliness was mediated by an increase in compassion.
“One of the most striking findings from our research on wisdom is this consistent and very strongly negative correlation between wisdom and loneliness,” Dr. Nguyen said. She highlighted other U.S. nationwide and cross-cultural studies that showed inverse relationships between loneliness and wisdom.
Loneliness is an important topic because it can contribute to burnout and suicide rates.
“Loneliness has a profound effect on how we show up in the workplace, in school, and in our communities. And that leads to anxiety, depression, depersonalization, and emotional fatigue. All are key features of burnout. And together loneliness and burnout have contributed to increased rates of suicide by 30%, and opioid-related deaths almost sixfold since the late 1990s,” Dr. Nguyen said.
Loneliness also is associated with worse physical health, and it may be linked to wisdom. “Loneliness can be conceptualized as being caused and maintained by objective circumstances, such as physical or social distancing, and by thoughts, behaviors, and feelings surrounding those experiences, including biased perceptions of social relations, and a negative assessment of one’s social skills, which then results in a discrepancy between one’s desired and perceived social relationships, which then can contribute to social withdrawal,” Dr. Nguyen said.
Dr. Nguyen highlighted the AARP Foundation’s Experience Corps program, which recruits older adults to act as mentors and tutors for children in kindergarten through third grade. It involves 15 hours per week over an entire school year, with a focus on child literacy, development, and behavioral management skills. A study revealed a significant impact. “It showed improvements in children’s grades and happiness, as well as seniors’ mental and physical health,” Dr. Nguyen said.
Dr. Nguyen concluded that wisdom “may be a vaccine against compassion fatigue and burnout that drive today’s behavioral epidemics of loneliness, opioid abuse, and suicide. It’s a tool for our times. It’s nuanced, flexible, pragmatic, compassionate, and it presents a reasonable framework for getting along in the often messy world that we all share.”
Implications for psychiatrists
Henry A. Nasrallah, MD, who organized the conference, suggested that the benefits of wisdom may not be limited to patients. He pointed out that surgeons often retire at age 60 or 65 because of declining physical skills, while psychiatrists continue to practice.
“We develop more wisdom and better skills, and we can practice into our 60s and 70s. I know psychiatrists who practice sometimes into their 80s. It’s really a wonderful thing to know that what you do in life develops or enhances the neuroplasticity of certain brain regions. In our case, in psychiatry, it is the brain regions involved in wisdom,” commented Dr. Nasrallah, who is a professor of psychiatry, neurology, and neuroscience at the University of Cincinnati.
Dr. Nguyen has no financial disclosures. Dr. Nasrallah has received grants from Abbott, AstraZeneca, Forest, Janssen, Lilly, Pfizer, and Shire, and advises Abbott, AstraZeneca, and Shire.
Wisdom increases with age, and although this personality trait is regarded as nebulous by many, there is evidence that it has biological and neuropsychiatric underpinnings. It could even hold the key to reducing loneliness and burnout among older people.
Those were some of the key messages delivered by Tanya T. Nguyen, PhD, of the department of psychiatry at the University of California, San Diego, who spoke at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists.
“To many people, wisdom remains a fuzzy concept that’s difficult to operationalize and measure. It’s analogous to the concepts of consciousness, emotions, and cognitions, which at one point were considered nonscientific, but today we accept them as biological and scientific entities,” Dr. Nguyen said during her talk at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Interest in quantifying and studying wisdom has picked up in recent years, and Dr. Nguyen gave a definition with six elements that includes prosocial behaviors such as empathy and compassion, as well as emotional regulation, self-reflection, decisiveness, and social decision-making. She also included a spirituality component, though she conceded that this is controversial.
She noted that there are cultural variations in the definition of wisdom, but it has changed little over time, suggesting that it may be biological rather than cultural in nature, and therefore may have a neuropsychiatric underpinning.
Loss of some or all characteristics of wisdom occurs in some behaviors and disorders, including most markedly in the neurodegenerative disorder frontotemporal dementia (FTD), which is characterized by damage only in the prefrontal cortex and anterior temporal lobes. It usually occurs before age 60, and patients exhibit poor social awareness, impulsivity, antisocial behavior, and a lack of insight and empathy.
This and other lines of evidence have led to the suggestion that wisdom may be governed by processes in the prefrontal cortex and the limbic striatum. The prefrontal cortex controls executive functions such as planning, predicting, and anticipating events, as well as managing emotional reactions and impulses. “Thus, wisdom involves parts of the brain that balance cold, hard analytical reasoning with primitive desires and drives, which ultimately leads to self-regulation, social insight, theory of mind, and empathy,” said Dr. Nguyen.
Wisdom has long been associated with age, but age is also linked to cognitive decline. A recent discovery that the brain does not stop evolving at older age may help explain this contradiction. Brains develop in a back to front order, so that the prefrontal cortex is the last to mature. As we age, neural activity shifts from the occipital lobes to the prefrontal cortex and its executive decision-making power.
“The brain may recruit higher-order networks to the prefrontal cortex that are associated with wisdom development,” said Dr. Nguyen. She also pointed out that asymmetry between the left and right hemisphere is reduced with age, as tasks that relied on circuits from one hemisphere or another more often call upon both. “In order to make up for lost synapses and neurons with aging, active older adults use more neuronal networks from both hemispheres to perform the same mental activity,” Dr. Nguyen said.
Some interventions can improve scores in traits associated with wisdom in older adults, and could be an important contributor to improvements in health and longevity, said Dr. Nguyen. Randomized, controlled trials have demonstrated that psychosocial or behavioral interventions can improve elements of wisdom such as prosocial behaviors and emotional regulation, both in people with mental illness and in the general population, with moderate to large effect sizes. But such studies don’t prove an effect on overall wisdom.
The intervention achieved positive results in 89 participants in senior housing communities, though the effect sizes were small, possibly because of high baseline resilience. A subanalysis suggested that reduction in loneliness was mediated by an increase in compassion.
“One of the most striking findings from our research on wisdom is this consistent and very strongly negative correlation between wisdom and loneliness,” Dr. Nguyen said. She highlighted other U.S. nationwide and cross-cultural studies that showed inverse relationships between loneliness and wisdom.
Loneliness is an important topic because it can contribute to burnout and suicide rates.
“Loneliness has a profound effect on how we show up in the workplace, in school, and in our communities. And that leads to anxiety, depression, depersonalization, and emotional fatigue. All are key features of burnout. And together loneliness and burnout have contributed to increased rates of suicide by 30%, and opioid-related deaths almost sixfold since the late 1990s,” Dr. Nguyen said.
Loneliness also is associated with worse physical health, and it may be linked to wisdom. “Loneliness can be conceptualized as being caused and maintained by objective circumstances, such as physical or social distancing, and by thoughts, behaviors, and feelings surrounding those experiences, including biased perceptions of social relations, and a negative assessment of one’s social skills, which then results in a discrepancy between one’s desired and perceived social relationships, which then can contribute to social withdrawal,” Dr. Nguyen said.
Dr. Nguyen highlighted the AARP Foundation’s Experience Corps program, which recruits older adults to act as mentors and tutors for children in kindergarten through third grade. It involves 15 hours per week over an entire school year, with a focus on child literacy, development, and behavioral management skills. A study revealed a significant impact. “It showed improvements in children’s grades and happiness, as well as seniors’ mental and physical health,” Dr. Nguyen said.
Dr. Nguyen concluded that wisdom “may be a vaccine against compassion fatigue and burnout that drive today’s behavioral epidemics of loneliness, opioid abuse, and suicide. It’s a tool for our times. It’s nuanced, flexible, pragmatic, compassionate, and it presents a reasonable framework for getting along in the often messy world that we all share.”
Implications for psychiatrists
Henry A. Nasrallah, MD, who organized the conference, suggested that the benefits of wisdom may not be limited to patients. He pointed out that surgeons often retire at age 60 or 65 because of declining physical skills, while psychiatrists continue to practice.
“We develop more wisdom and better skills, and we can practice into our 60s and 70s. I know psychiatrists who practice sometimes into their 80s. It’s really a wonderful thing to know that what you do in life develops or enhances the neuroplasticity of certain brain regions. In our case, in psychiatry, it is the brain regions involved in wisdom,” commented Dr. Nasrallah, who is a professor of psychiatry, neurology, and neuroscience at the University of Cincinnati.
Dr. Nguyen has no financial disclosures. Dr. Nasrallah has received grants from Abbott, AstraZeneca, Forest, Janssen, Lilly, Pfizer, and Shire, and advises Abbott, AstraZeneca, and Shire.
REPORTING FROM FOCUS ON NEUROPSYCHIATRY 2021
How forgone heart failure care drives up costs
Elderly carry disproportionate cost burden
About one in six patients with heart failure in the United States are skipping doctors’ appointments, not taking their medications as directed, or forgoing some other type of care, and their recalcitrance actually ends up costing the health care system 20%-30% more per patient.
That’s according to a cross-sectional study using data from a large public database reported in JACC: Heart Failure on Aug. 11.
The investigators pooled data on 2,050 patients with HF enrolled in the Medical Expenditure Panel Survey, a public database sponsored by the Agency for Healthcare Research and Quality, from 2004 to 2015. Some 339 of those HF patients were classified in the forgone or delayed (F/D) care group. This is the first study to describe the cost impact of missed care in heart failure, lead author Alexander Thomas, MD, and colleagues wrote.
“I think we make a pretty strong case linking forgone care to higher cost,” Dr. Thomas said in an interview. “Obviously this is a prospective study, so causality is not made based on this study, but there’s a strong association, it appears.” He acknowledged that prospective studies would need to confirm these findings, but added, “I think even this is enough to give us cause to look at the somewhat granular reasons as to why patients are forgoing care.”
Average annual total costs for adults who skipped care were $8,027 higher than for those heart failure patients who kept up with their regimen (P = .02). However, for people 65 and older, the cost differential was even higher: $10,581 (P = .02), which translates into a 50% premium over average costs for compliant elderly patients, noted Dr. Thomas, a cardiovascular medicine fellow at Yale University, New Haven, Conn.
In the nonelderly F/D group, average per-patient costs were $27,000 annually; in the elderly, it was a little over $30,000.
However, nonelderly patients were more likely to forgo care. While 16% of all patients in the study were considered F/D, 27% of nonelderly patients were classified as such vs. 10% of the elderly.
Elderly forgoing care drives cost
But, Dr. Thomas said, elderly patients forgoing care drive higher costs because they’re more fragile, have more comorbidities and more advanced heart failure, and tend to decompensate more quickly. “For them, missing one appointment or missing some medications is not nearly as well tolerated as it is in the younger population,” he said. In these elderly patients, inpatient costs accounted for 75% of the increased expense, Dr. Thomas added.
Reasons for forgoing care range from the obvious, such as cost or insurance issues – 191 individuals cited the former, 69 the latter – to more granular reasons, such as transportation issues or lack of time.
The study also found a number of demographic features that were associated with forgone or delayed care: non-Hispanic Black race; lack of insurance; low-income; and worse cardiovascular risk factor profiles.
The study’s call to action is for further research and policy changes aimed at better understanding barriers to care and improving access. “It’s a really great driver for policy interventions to attack this problem and to have the financial backing also to put money and resources into fixing this problem – which is probably not only going to decrease costs and allow more cost-effective care, but lead to better outcomes in this population as well,” Dr. Thomas said.
The sentiment for policy changes was echoed in an accompanying editorial by Khadijah Breathett, MD, MS, a heart failure/transplant cardiologist at the Sarver Heart Center, University of Arizona, Tucson. But she also noted the study exposed insufficiencies with Medicare. In an interview, she expanded on that.
“Our system is failing this population,” she said of the elderly with heart failure who have forgone care. “I think that’s because of the complexity of our system: One person’s Medicare is different from another’s. There are multiple parts to Medicare that provide different forms of care – hospital care, prescription care, and so forth – and everyone does not necessarily have the same parts.” Also, many Medicare beneficiaries are still working, and “they’re still trying to figure out how to make ends meet,” Dr. Breathett added.
The study also showed that the pre-Medicare population requires the attention of policymakers. “How do we help the younger population so that they don’t develop the comorbidities that worsen their quality of life and contribute to rising hospital costs?” Dr. Breathett said.
Dr. Thomas had no financial relationships to disclose. Dr. Breathett has received grants from the National Heart, Lung, and Blood Institute.
Elderly carry disproportionate cost burden
Elderly carry disproportionate cost burden
About one in six patients with heart failure in the United States are skipping doctors’ appointments, not taking their medications as directed, or forgoing some other type of care, and their recalcitrance actually ends up costing the health care system 20%-30% more per patient.
That’s according to a cross-sectional study using data from a large public database reported in JACC: Heart Failure on Aug. 11.
The investigators pooled data on 2,050 patients with HF enrolled in the Medical Expenditure Panel Survey, a public database sponsored by the Agency for Healthcare Research and Quality, from 2004 to 2015. Some 339 of those HF patients were classified in the forgone or delayed (F/D) care group. This is the first study to describe the cost impact of missed care in heart failure, lead author Alexander Thomas, MD, and colleagues wrote.
“I think we make a pretty strong case linking forgone care to higher cost,” Dr. Thomas said in an interview. “Obviously this is a prospective study, so causality is not made based on this study, but there’s a strong association, it appears.” He acknowledged that prospective studies would need to confirm these findings, but added, “I think even this is enough to give us cause to look at the somewhat granular reasons as to why patients are forgoing care.”
Average annual total costs for adults who skipped care were $8,027 higher than for those heart failure patients who kept up with their regimen (P = .02). However, for people 65 and older, the cost differential was even higher: $10,581 (P = .02), which translates into a 50% premium over average costs for compliant elderly patients, noted Dr. Thomas, a cardiovascular medicine fellow at Yale University, New Haven, Conn.
In the nonelderly F/D group, average per-patient costs were $27,000 annually; in the elderly, it was a little over $30,000.
However, nonelderly patients were more likely to forgo care. While 16% of all patients in the study were considered F/D, 27% of nonelderly patients were classified as such vs. 10% of the elderly.
Elderly forgoing care drives cost
But, Dr. Thomas said, elderly patients forgoing care drive higher costs because they’re more fragile, have more comorbidities and more advanced heart failure, and tend to decompensate more quickly. “For them, missing one appointment or missing some medications is not nearly as well tolerated as it is in the younger population,” he said. In these elderly patients, inpatient costs accounted for 75% of the increased expense, Dr. Thomas added.
Reasons for forgoing care range from the obvious, such as cost or insurance issues – 191 individuals cited the former, 69 the latter – to more granular reasons, such as transportation issues or lack of time.
The study also found a number of demographic features that were associated with forgone or delayed care: non-Hispanic Black race; lack of insurance; low-income; and worse cardiovascular risk factor profiles.
The study’s call to action is for further research and policy changes aimed at better understanding barriers to care and improving access. “It’s a really great driver for policy interventions to attack this problem and to have the financial backing also to put money and resources into fixing this problem – which is probably not only going to decrease costs and allow more cost-effective care, but lead to better outcomes in this population as well,” Dr. Thomas said.
The sentiment for policy changes was echoed in an accompanying editorial by Khadijah Breathett, MD, MS, a heart failure/transplant cardiologist at the Sarver Heart Center, University of Arizona, Tucson. But she also noted the study exposed insufficiencies with Medicare. In an interview, she expanded on that.
“Our system is failing this population,” she said of the elderly with heart failure who have forgone care. “I think that’s because of the complexity of our system: One person’s Medicare is different from another’s. There are multiple parts to Medicare that provide different forms of care – hospital care, prescription care, and so forth – and everyone does not necessarily have the same parts.” Also, many Medicare beneficiaries are still working, and “they’re still trying to figure out how to make ends meet,” Dr. Breathett added.
The study also showed that the pre-Medicare population requires the attention of policymakers. “How do we help the younger population so that they don’t develop the comorbidities that worsen their quality of life and contribute to rising hospital costs?” Dr. Breathett said.
Dr. Thomas had no financial relationships to disclose. Dr. Breathett has received grants from the National Heart, Lung, and Blood Institute.
About one in six patients with heart failure in the United States are skipping doctors’ appointments, not taking their medications as directed, or forgoing some other type of care, and their recalcitrance actually ends up costing the health care system 20%-30% more per patient.
That’s according to a cross-sectional study using data from a large public database reported in JACC: Heart Failure on Aug. 11.
The investigators pooled data on 2,050 patients with HF enrolled in the Medical Expenditure Panel Survey, a public database sponsored by the Agency for Healthcare Research and Quality, from 2004 to 2015. Some 339 of those HF patients were classified in the forgone or delayed (F/D) care group. This is the first study to describe the cost impact of missed care in heart failure, lead author Alexander Thomas, MD, and colleagues wrote.
“I think we make a pretty strong case linking forgone care to higher cost,” Dr. Thomas said in an interview. “Obviously this is a prospective study, so causality is not made based on this study, but there’s a strong association, it appears.” He acknowledged that prospective studies would need to confirm these findings, but added, “I think even this is enough to give us cause to look at the somewhat granular reasons as to why patients are forgoing care.”
Average annual total costs for adults who skipped care were $8,027 higher than for those heart failure patients who kept up with their regimen (P = .02). However, for people 65 and older, the cost differential was even higher: $10,581 (P = .02), which translates into a 50% premium over average costs for compliant elderly patients, noted Dr. Thomas, a cardiovascular medicine fellow at Yale University, New Haven, Conn.
In the nonelderly F/D group, average per-patient costs were $27,000 annually; in the elderly, it was a little over $30,000.
However, nonelderly patients were more likely to forgo care. While 16% of all patients in the study were considered F/D, 27% of nonelderly patients were classified as such vs. 10% of the elderly.
Elderly forgoing care drives cost
But, Dr. Thomas said, elderly patients forgoing care drive higher costs because they’re more fragile, have more comorbidities and more advanced heart failure, and tend to decompensate more quickly. “For them, missing one appointment or missing some medications is not nearly as well tolerated as it is in the younger population,” he said. In these elderly patients, inpatient costs accounted for 75% of the increased expense, Dr. Thomas added.
Reasons for forgoing care range from the obvious, such as cost or insurance issues – 191 individuals cited the former, 69 the latter – to more granular reasons, such as transportation issues or lack of time.
The study also found a number of demographic features that were associated with forgone or delayed care: non-Hispanic Black race; lack of insurance; low-income; and worse cardiovascular risk factor profiles.
The study’s call to action is for further research and policy changes aimed at better understanding barriers to care and improving access. “It’s a really great driver for policy interventions to attack this problem and to have the financial backing also to put money and resources into fixing this problem – which is probably not only going to decrease costs and allow more cost-effective care, but lead to better outcomes in this population as well,” Dr. Thomas said.
The sentiment for policy changes was echoed in an accompanying editorial by Khadijah Breathett, MD, MS, a heart failure/transplant cardiologist at the Sarver Heart Center, University of Arizona, Tucson. But she also noted the study exposed insufficiencies with Medicare. In an interview, she expanded on that.
“Our system is failing this population,” she said of the elderly with heart failure who have forgone care. “I think that’s because of the complexity of our system: One person’s Medicare is different from another’s. There are multiple parts to Medicare that provide different forms of care – hospital care, prescription care, and so forth – and everyone does not necessarily have the same parts.” Also, many Medicare beneficiaries are still working, and “they’re still trying to figure out how to make ends meet,” Dr. Breathett added.
The study also showed that the pre-Medicare population requires the attention of policymakers. “How do we help the younger population so that they don’t develop the comorbidities that worsen their quality of life and contribute to rising hospital costs?” Dr. Breathett said.
Dr. Thomas had no financial relationships to disclose. Dr. Breathett has received grants from the National Heart, Lung, and Blood Institute.
FROM JACC: HEART FAILURE
Recent Trends in Diabetes Treatment and Control in US Adults: A Geriatrician’s Point of View
Study Overview
Objective. To update national trends in the treatment and risk factor control of diabetic patients from 1999 through 2018 in the US using data from the National Health and Nutrition Examination Survey (NHANES) with the goal of identifying population subgroups with the highest probability of having untreated risk factors.
Design. The authors conducted a cross-sectional analysis of data from NHANES focusing on adults with diabetes. They examined patient characteristics and medication use over time and estimated the prevalence of risk factor control and medication use. To minimize the effects of a small sample size, the survey years were pooled into 4-year intervals. The variables studied included glycated hemoglobin (HbA1c), blood pressure, serum cholesterol, medication use, sociodemographic characteristics, and weight status. For statistical analysis, logistic and multinomial logistic regression models were used to examine factors associated with treatment in participants who did not achieve targets for glycemic, blood pressure, and lipid control. Temporal trends were estimated using 2-piece linear spline models with 1 knot at inflection points.
Setting and participants. The NHANES program began in the early 1960s to monitor the health of the US population. In 1999, the survey became a continuous program combining interviews and physical examinations. The survey examines a nationally representative sample of about 5000 persons each year. This study included 6653 participants who were nonpregnant, aged older than 20 years, reported a diagnosis of diabetes from a physician, and participated in NHANES from 1999 through 2018.
Main outcome measures. The main outcome measures were temporal trends in risk factor control (glycemic, blood pressure, or lipid levels) and medication use (glucose lowering, blood pressure lowering, or lipid lowering medications), and number as well as class of drug used, from 1999 through 2018 in diabetic adults from the US participating in NHANES.
Results. Sociodemographic characteristics of the studied diabetes population—The age and racial or ethnic distribution of participants with diabetes were stable from 1999 through 2018, whereas participants with a college degree, higher income, health insurance, obesity, or long-standing diabetes increased during the same period.
Trends in diabetes risk factor control—The trends for glycemic, blood pressure, and lipid control were nonlinear, with an inflection point around 2010. Glycemic control was defined as HbA1c less than 7%, blood pressure was considered controlled if less than 140/90 mmHg, and lipid was controlled if non-HDL cholesterol level was less than 130 mg/dL. Although these chosen targets were based on the most recent clinical guidelines, the authors declared that they observed similar trends when alternative targets were used. The level of risk factor control improved in all diabetic patients from 1999 through 2010. However, the percentage of adult diabetic participants for whom glycemic control was achieved declined from 57.4% (95% CI, 52.9-61.8) in 2007-2010 to 50.5% (95% CI, 45.8-55.3) in 2015-2018. Blood pressure control was achieved in 74.2% of participants (95% CI, 70.7-77.4) in 2011-2014 but declined to 70.4% (95% CI, 66.7-73.8) in 2015-2018. Control in lipid levels improved during the entire study period; however, the rate of improvement heavily declined after 2007 with lipid target levels attained in 52.3% of participants (95% CI, 49.2-55.3) in 2007-2014 and 55.7% (95% CI, 50.8-60.5) in 2015-2018. Finally, the percentage of participants in whom targets for all 3 risk factors were simultaneously achieved plateaued after 2010 and was 22.2% (95% CI, 17.9-27.3) in 2015-2018.
Trends in diabetes treatment—The use of glucose lowering drugs increased from 74.1% in 1999-2002 to 82.7% in 2007-2010 and then stabilized. A shift toward a safer glucose lowering treatment choice was observed with a decline in the use of older glucose lowering medications such as sulfonylureas, which increases the risk of hypoglycemia, and an increase in the use of metformin, insulin, and newer agents such as sodium-glucose cotransporter 2 inhibitors.
Similarly, blood pressure lowering medication use rose from 1999-2002 to 2007-2010 and then stabilized, with increased use of first-line recommended treatments including angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers. Likewise, statin use rose from 28.4% in 1999-2002 to 56% in 2011-2014 and then stabilized. The total number of drugs used culminated in 2011-2014 with 60% of participants using more than 5 drugs and then leveled off to 57.2% in 2015-2018. Lastly, health insurance status and race or ethnicity impacted the likelihood of receiving monotherapy or combination drug therapy when targets for glycemic, blood pressure, or lipid control were not achieved.
Conclusion. Despite great progress in the control of diabetes and its associated risk factors between 1999 and 2010, this trend declined for glycemic and blood pressure control and leveled off for lipid control in adult NHANES participants with diabetes after 2010. First-line treatments for diabetes and associated risk factors remain underused, and treatment intensification may not be sufficiently considered in patients with uncontrolled risk factors despite clinical guideline recommendations. The findings of this study may portend a possible population-level increase in diabetes-related illnesses in the years to come.
Commentary
The thorough understanding of trends in management of diseases is critical to inform public health policies and planning. Well designed clinical studies heavily influence the development of public health policies and clinical guidelines, which in turn drive real-world clinical practice. In a recent analysis utilizing data from NHANES, Fang et al1 showed evidence of a general shift toward less intensive treatment of diabetes, hypertension, and hypercholesterolemia in adults living in the US during the last decade.
Similarly, in a separate study using NHANES data collected between 1999 and 2018 published in JAMA just 2 weeks after the current report, Wang et al2 confirms this declining trend in diabetes management with only 21.2% of diabetic adults simultaneously attaining glycemic, blood pressure, and lipid level targets during the same period. What led to the decline in more stringent risk factor and diabetes management since 2010 observed in these studies? One possible explanation, as suggested by Fang et al, is that major clinical trials from the late 2000s—including Action to Control Cardiovascular Risk in Diabetes, UK Prospective Diabetes Study, Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation, and Veterans Affairs Diabetes Trial—that assessed the effects of intensive glycemic control (with target HbA1c < 6.5%) found that intensive treatment of diabetes compared to standard care had no cardiovascular benefit albeit increasing the risk of hypoglycemia. Thus, these trial findings may have translated into suboptimal diabetes treatment observed in some NHANES participants. Wang et al propose that effective tailored approaches are needed to improve risk factor control in diabetic patients, such as enhance and maintain adherence to medications and healthy lifestyle behaviors, as well as better access to health care and therapeutic education.
The changes in recent trends in diabetes management have immense clinical implications. The authors of this study suggest a link between the recent relaxation of glycemic targets, as well as risk factor control, and a resurgence of diabetic complications such as lower limb amputation or stroke. Indeed, several recent studies indicate an upward trend or plateau in diabetic complications which had been decreasing in prevalence prior to 2010.3 For example, lower extremity amputation has surged by more than 25% between 2010 and 2015, especially in young and middle-aged adults.4 Among the arguments brought forward that this recent resurgence in amputations is directly linked to worsening glycemic control is the fact that between 2007 and 2010, when glucose levels were best controlled within the previous 30-year period, amputations were also at the lowest levels. Moreover, data from the Centers for Disease Control and Prevention also show a 55% increase in mortality (from 15.7 to 24.2 per 1000) among diabetic patients between 2010 and 2015.14 On the other hand, a growing number of studies show that an increase of inappropriate treatment intensification—reaching HbA1c levels that are way below the recommended targets—is associated with adverse consequences in diabetic patients particularly in those aged more than 65 years.5-7 These seemingly contradictory findings highlight the importance of a personalized and thoughtful approach to the management of diabetes and its risk factors. As an example, an increase in the use of newer and safer glucose lowering drugs (eg, sodium-glucose cotransporter 2 inhibitors, glucagon-like peptide 1 receptor agonists, and dipeptidyl peptidase 4 inhibitors) can help achieve better HbA1c goals with a reduced risk of hypoglycemic episodes as recently shown by a Danish study.8 In this study, the authors concluded that the reduction of the rate of hypoglycemic episodes leading to hospitalization in Denmark was directly linked to the use of these safer and newer glucose lowering drugs.
A discussion on the specifics of trends in diabetes treatment and control must include considerations in older adults aged more than 65 years who constitute more than 40% of the diabetic population. Despite the high prevalence of diabetes in this vulnerable population, such data are still insufficient in the literature and are critically needed to inform public health policies and clinical guidelines. In epidemiological studies focusing on diabetic complications from the last 10 years, concerning increases have been observed in younger9 and middle-aged adults while remaining stable in older adults. However, the risk of hypoglycemia or severe hypoglycemia remains high in older adults living in nursing facilities, even in those with an elevated HbA1c of greater than 8%.7 Moreover, in light of more relaxed HbA1c treatment goals for older frail adults as recommended by international guidelines since 2010,10,11 recent findings from the French GERODIAB cohort show an increased mortality (hazard ratio, 1.76) in type 2 diabetics aged 70 years and older with HbA1c greater than or equal to 8.6%.12 Similarly, a 5-year retrospective British study from 2018 which included patients aged 70 years and older, shows an increased overall mortality in those with HbA1c greater than 8.5%.13 Taken together, further age-stratified analysis utilizing data from large cohort studies including NHANES may help to clarify national trends in diabetes treatment and risk factor control as well as diabetic complications specific to the geriatric population. By being better informed of such trends, clinicians could then develop treatment strategies that minimize complications (eg, hypoglycemia, falls) while achieving favorable outcomes (eg, reduce hyperglycemic emergencies, improve survival) in frail older patients.
Applications for Clinical Practice
The understanding of population-wide trends in diabetes control is critical to planning public health approaches for the prevention and treatment of this disease and its complications. In older adults, the high risk of hypoglycemic events and insufficient epidemiological data on trends of diabetes control hinder diabetes management. Personalized treatment targets taking into account geriatric syndromes and general health status, as well as multidisciplinary management involving endocrinologists, geriatricians, and clinical pharmacists, are necessary to optimize care in older adults with diabetes.
1. Fang M, Wang D, Coresh J, Selvin E. Trends in Diabetes Treatment and Control in U.S. Adults, 1999-2018. N Engl J Med. 2021;384(23):2219-28. doi:10.1056/NEJMsa2032271
2. Wang L, Li X, Wang Z, et al. Trends in Prevalence of Diabetes and Control of Risk Factors in Diabetes Among US Adults, 1999-2018. JAMA. 2021. doi:10.1001/jama.2021.9883
3. Gregg EW, Hora I, Benoit SR. Resurgence in Diabetes-Related Complications. JAMA. 2019;321(19):1867-8. doi:10.1001/jama.2019.3471
4. Caruso P, Scappaticcio L, Maiorino MI, et al. Up and down waves of glycemic control and lower-extremity amputation in diabetes. Cardiovasc Diabetol. 2021;20(1):135. doi:10.1186/s12933-021-01325-3
5. Bongaerts B, Arnold SV, Charbonnel BH, et al. Inappropriate intensification of glucose-lowering treatment in older patients with type 2 diabetes: the global DISCOVER study. BMJ Open Diabetes Res Care. 2021;9(1)e001585. doi:10.1136/bmjdrc-2020-001585
6. Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116-1124. doi: 10.1001/jamainternmed.2014.1824
7. Bouillet B, Tscherter P, Vaillard L, et al. Frequent and severe hypoglycaemia detected with continuous glucose monitoring in older institutionalised patients with diabetes. Age Ageing. 2021;afab128. doi: 10.1093/ageing/afab128
8. Jensen MH, Hejlesen O, Vestergaard P. Epidemiology of hypoglycaemic episodes leading to hospitalisations in Denmark in 1998-2018. Diabetologia. 2021. doi: 10.1007/s00125-021-05507-2
9. TODAY Study Group, Bjornstad P, Drews KL, et al. Long-Term Complications in Youth-Onset Type 2 Diabetes. N Engl J Med. 2021;385(5):416-426. doi: 10.1056/NEJMoa2100165
10. Sinclair AJ, Paolisso G, Castro M, et al. European Diabetes Working Party for Older People 2011 clinical guidelines for type 2 diabetes mellitus. Executive summary. Diabetes Metab. 2011;37 Suppl 3:S27-S38. doi:10.1016/S1262-3636(11)70962-4
11. Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care. 2012;35(12):2650-2664. doi: 10.2337/dc12-1801
12. Doucet J, Verny C, Balkau B, et al. Haemoglobin A1c and 5-year all-cause mortality in French type 2 diabetic patients aged 70 years and older: The GERODIAB observational cohort. Diabetes Metab. 2018;44(6):465-472. doi: 10.1016/j.diabet.2018.05.003
13. Forbes A, Murrells T, Mulnier H, Sinclair AJ. Mean HbA1c, HbA1c variability, and mortality in people with diabetes aged 70 years and older: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6(6):476-486. doi: 10.1016/S2213-8587(18)30048-2
14. US Centers for Disease Control and Prevention. US diabetes surveillance system and diabetes atlas, 2019. https://www.cdc.gov/diabetes/data
Study Overview
Objective. To update national trends in the treatment and risk factor control of diabetic patients from 1999 through 2018 in the US using data from the National Health and Nutrition Examination Survey (NHANES) with the goal of identifying population subgroups with the highest probability of having untreated risk factors.
Design. The authors conducted a cross-sectional analysis of data from NHANES focusing on adults with diabetes. They examined patient characteristics and medication use over time and estimated the prevalence of risk factor control and medication use. To minimize the effects of a small sample size, the survey years were pooled into 4-year intervals. The variables studied included glycated hemoglobin (HbA1c), blood pressure, serum cholesterol, medication use, sociodemographic characteristics, and weight status. For statistical analysis, logistic and multinomial logistic regression models were used to examine factors associated with treatment in participants who did not achieve targets for glycemic, blood pressure, and lipid control. Temporal trends were estimated using 2-piece linear spline models with 1 knot at inflection points.
Setting and participants. The NHANES program began in the early 1960s to monitor the health of the US population. In 1999, the survey became a continuous program combining interviews and physical examinations. The survey examines a nationally representative sample of about 5000 persons each year. This study included 6653 participants who were nonpregnant, aged older than 20 years, reported a diagnosis of diabetes from a physician, and participated in NHANES from 1999 through 2018.
Main outcome measures. The main outcome measures were temporal trends in risk factor control (glycemic, blood pressure, or lipid levels) and medication use (glucose lowering, blood pressure lowering, or lipid lowering medications), and number as well as class of drug used, from 1999 through 2018 in diabetic adults from the US participating in NHANES.
Results. Sociodemographic characteristics of the studied diabetes population—The age and racial or ethnic distribution of participants with diabetes were stable from 1999 through 2018, whereas participants with a college degree, higher income, health insurance, obesity, or long-standing diabetes increased during the same period.
Trends in diabetes risk factor control—The trends for glycemic, blood pressure, and lipid control were nonlinear, with an inflection point around 2010. Glycemic control was defined as HbA1c less than 7%, blood pressure was considered controlled if less than 140/90 mmHg, and lipid was controlled if non-HDL cholesterol level was less than 130 mg/dL. Although these chosen targets were based on the most recent clinical guidelines, the authors declared that they observed similar trends when alternative targets were used. The level of risk factor control improved in all diabetic patients from 1999 through 2010. However, the percentage of adult diabetic participants for whom glycemic control was achieved declined from 57.4% (95% CI, 52.9-61.8) in 2007-2010 to 50.5% (95% CI, 45.8-55.3) in 2015-2018. Blood pressure control was achieved in 74.2% of participants (95% CI, 70.7-77.4) in 2011-2014 but declined to 70.4% (95% CI, 66.7-73.8) in 2015-2018. Control in lipid levels improved during the entire study period; however, the rate of improvement heavily declined after 2007 with lipid target levels attained in 52.3% of participants (95% CI, 49.2-55.3) in 2007-2014 and 55.7% (95% CI, 50.8-60.5) in 2015-2018. Finally, the percentage of participants in whom targets for all 3 risk factors were simultaneously achieved plateaued after 2010 and was 22.2% (95% CI, 17.9-27.3) in 2015-2018.
Trends in diabetes treatment—The use of glucose lowering drugs increased from 74.1% in 1999-2002 to 82.7% in 2007-2010 and then stabilized. A shift toward a safer glucose lowering treatment choice was observed with a decline in the use of older glucose lowering medications such as sulfonylureas, which increases the risk of hypoglycemia, and an increase in the use of metformin, insulin, and newer agents such as sodium-glucose cotransporter 2 inhibitors.
Similarly, blood pressure lowering medication use rose from 1999-2002 to 2007-2010 and then stabilized, with increased use of first-line recommended treatments including angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers. Likewise, statin use rose from 28.4% in 1999-2002 to 56% in 2011-2014 and then stabilized. The total number of drugs used culminated in 2011-2014 with 60% of participants using more than 5 drugs and then leveled off to 57.2% in 2015-2018. Lastly, health insurance status and race or ethnicity impacted the likelihood of receiving monotherapy or combination drug therapy when targets for glycemic, blood pressure, or lipid control were not achieved.
Conclusion. Despite great progress in the control of diabetes and its associated risk factors between 1999 and 2010, this trend declined for glycemic and blood pressure control and leveled off for lipid control in adult NHANES participants with diabetes after 2010. First-line treatments for diabetes and associated risk factors remain underused, and treatment intensification may not be sufficiently considered in patients with uncontrolled risk factors despite clinical guideline recommendations. The findings of this study may portend a possible population-level increase in diabetes-related illnesses in the years to come.
Commentary
The thorough understanding of trends in management of diseases is critical to inform public health policies and planning. Well designed clinical studies heavily influence the development of public health policies and clinical guidelines, which in turn drive real-world clinical practice. In a recent analysis utilizing data from NHANES, Fang et al1 showed evidence of a general shift toward less intensive treatment of diabetes, hypertension, and hypercholesterolemia in adults living in the US during the last decade.
Similarly, in a separate study using NHANES data collected between 1999 and 2018 published in JAMA just 2 weeks after the current report, Wang et al2 confirms this declining trend in diabetes management with only 21.2% of diabetic adults simultaneously attaining glycemic, blood pressure, and lipid level targets during the same period. What led to the decline in more stringent risk factor and diabetes management since 2010 observed in these studies? One possible explanation, as suggested by Fang et al, is that major clinical trials from the late 2000s—including Action to Control Cardiovascular Risk in Diabetes, UK Prospective Diabetes Study, Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation, and Veterans Affairs Diabetes Trial—that assessed the effects of intensive glycemic control (with target HbA1c < 6.5%) found that intensive treatment of diabetes compared to standard care had no cardiovascular benefit albeit increasing the risk of hypoglycemia. Thus, these trial findings may have translated into suboptimal diabetes treatment observed in some NHANES participants. Wang et al propose that effective tailored approaches are needed to improve risk factor control in diabetic patients, such as enhance and maintain adherence to medications and healthy lifestyle behaviors, as well as better access to health care and therapeutic education.
The changes in recent trends in diabetes management have immense clinical implications. The authors of this study suggest a link between the recent relaxation of glycemic targets, as well as risk factor control, and a resurgence of diabetic complications such as lower limb amputation or stroke. Indeed, several recent studies indicate an upward trend or plateau in diabetic complications which had been decreasing in prevalence prior to 2010.3 For example, lower extremity amputation has surged by more than 25% between 2010 and 2015, especially in young and middle-aged adults.4 Among the arguments brought forward that this recent resurgence in amputations is directly linked to worsening glycemic control is the fact that between 2007 and 2010, when glucose levels were best controlled within the previous 30-year period, amputations were also at the lowest levels. Moreover, data from the Centers for Disease Control and Prevention also show a 55% increase in mortality (from 15.7 to 24.2 per 1000) among diabetic patients between 2010 and 2015.14 On the other hand, a growing number of studies show that an increase of inappropriate treatment intensification—reaching HbA1c levels that are way below the recommended targets—is associated with adverse consequences in diabetic patients particularly in those aged more than 65 years.5-7 These seemingly contradictory findings highlight the importance of a personalized and thoughtful approach to the management of diabetes and its risk factors. As an example, an increase in the use of newer and safer glucose lowering drugs (eg, sodium-glucose cotransporter 2 inhibitors, glucagon-like peptide 1 receptor agonists, and dipeptidyl peptidase 4 inhibitors) can help achieve better HbA1c goals with a reduced risk of hypoglycemic episodes as recently shown by a Danish study.8 In this study, the authors concluded that the reduction of the rate of hypoglycemic episodes leading to hospitalization in Denmark was directly linked to the use of these safer and newer glucose lowering drugs.
A discussion on the specifics of trends in diabetes treatment and control must include considerations in older adults aged more than 65 years who constitute more than 40% of the diabetic population. Despite the high prevalence of diabetes in this vulnerable population, such data are still insufficient in the literature and are critically needed to inform public health policies and clinical guidelines. In epidemiological studies focusing on diabetic complications from the last 10 years, concerning increases have been observed in younger9 and middle-aged adults while remaining stable in older adults. However, the risk of hypoglycemia or severe hypoglycemia remains high in older adults living in nursing facilities, even in those with an elevated HbA1c of greater than 8%.7 Moreover, in light of more relaxed HbA1c treatment goals for older frail adults as recommended by international guidelines since 2010,10,11 recent findings from the French GERODIAB cohort show an increased mortality (hazard ratio, 1.76) in type 2 diabetics aged 70 years and older with HbA1c greater than or equal to 8.6%.12 Similarly, a 5-year retrospective British study from 2018 which included patients aged 70 years and older, shows an increased overall mortality in those with HbA1c greater than 8.5%.13 Taken together, further age-stratified analysis utilizing data from large cohort studies including NHANES may help to clarify national trends in diabetes treatment and risk factor control as well as diabetic complications specific to the geriatric population. By being better informed of such trends, clinicians could then develop treatment strategies that minimize complications (eg, hypoglycemia, falls) while achieving favorable outcomes (eg, reduce hyperglycemic emergencies, improve survival) in frail older patients.
Applications for Clinical Practice
The understanding of population-wide trends in diabetes control is critical to planning public health approaches for the prevention and treatment of this disease and its complications. In older adults, the high risk of hypoglycemic events and insufficient epidemiological data on trends of diabetes control hinder diabetes management. Personalized treatment targets taking into account geriatric syndromes and general health status, as well as multidisciplinary management involving endocrinologists, geriatricians, and clinical pharmacists, are necessary to optimize care in older adults with diabetes.
Study Overview
Objective. To update national trends in the treatment and risk factor control of diabetic patients from 1999 through 2018 in the US using data from the National Health and Nutrition Examination Survey (NHANES) with the goal of identifying population subgroups with the highest probability of having untreated risk factors.
Design. The authors conducted a cross-sectional analysis of data from NHANES focusing on adults with diabetes. They examined patient characteristics and medication use over time and estimated the prevalence of risk factor control and medication use. To minimize the effects of a small sample size, the survey years were pooled into 4-year intervals. The variables studied included glycated hemoglobin (HbA1c), blood pressure, serum cholesterol, medication use, sociodemographic characteristics, and weight status. For statistical analysis, logistic and multinomial logistic regression models were used to examine factors associated with treatment in participants who did not achieve targets for glycemic, blood pressure, and lipid control. Temporal trends were estimated using 2-piece linear spline models with 1 knot at inflection points.
Setting and participants. The NHANES program began in the early 1960s to monitor the health of the US population. In 1999, the survey became a continuous program combining interviews and physical examinations. The survey examines a nationally representative sample of about 5000 persons each year. This study included 6653 participants who were nonpregnant, aged older than 20 years, reported a diagnosis of diabetes from a physician, and participated in NHANES from 1999 through 2018.
Main outcome measures. The main outcome measures were temporal trends in risk factor control (glycemic, blood pressure, or lipid levels) and medication use (glucose lowering, blood pressure lowering, or lipid lowering medications), and number as well as class of drug used, from 1999 through 2018 in diabetic adults from the US participating in NHANES.
Results. Sociodemographic characteristics of the studied diabetes population—The age and racial or ethnic distribution of participants with diabetes were stable from 1999 through 2018, whereas participants with a college degree, higher income, health insurance, obesity, or long-standing diabetes increased during the same period.
Trends in diabetes risk factor control—The trends for glycemic, blood pressure, and lipid control were nonlinear, with an inflection point around 2010. Glycemic control was defined as HbA1c less than 7%, blood pressure was considered controlled if less than 140/90 mmHg, and lipid was controlled if non-HDL cholesterol level was less than 130 mg/dL. Although these chosen targets were based on the most recent clinical guidelines, the authors declared that they observed similar trends when alternative targets were used. The level of risk factor control improved in all diabetic patients from 1999 through 2010. However, the percentage of adult diabetic participants for whom glycemic control was achieved declined from 57.4% (95% CI, 52.9-61.8) in 2007-2010 to 50.5% (95% CI, 45.8-55.3) in 2015-2018. Blood pressure control was achieved in 74.2% of participants (95% CI, 70.7-77.4) in 2011-2014 but declined to 70.4% (95% CI, 66.7-73.8) in 2015-2018. Control in lipid levels improved during the entire study period; however, the rate of improvement heavily declined after 2007 with lipid target levels attained in 52.3% of participants (95% CI, 49.2-55.3) in 2007-2014 and 55.7% (95% CI, 50.8-60.5) in 2015-2018. Finally, the percentage of participants in whom targets for all 3 risk factors were simultaneously achieved plateaued after 2010 and was 22.2% (95% CI, 17.9-27.3) in 2015-2018.
Trends in diabetes treatment—The use of glucose lowering drugs increased from 74.1% in 1999-2002 to 82.7% in 2007-2010 and then stabilized. A shift toward a safer glucose lowering treatment choice was observed with a decline in the use of older glucose lowering medications such as sulfonylureas, which increases the risk of hypoglycemia, and an increase in the use of metformin, insulin, and newer agents such as sodium-glucose cotransporter 2 inhibitors.
Similarly, blood pressure lowering medication use rose from 1999-2002 to 2007-2010 and then stabilized, with increased use of first-line recommended treatments including angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers. Likewise, statin use rose from 28.4% in 1999-2002 to 56% in 2011-2014 and then stabilized. The total number of drugs used culminated in 2011-2014 with 60% of participants using more than 5 drugs and then leveled off to 57.2% in 2015-2018. Lastly, health insurance status and race or ethnicity impacted the likelihood of receiving monotherapy or combination drug therapy when targets for glycemic, blood pressure, or lipid control were not achieved.
Conclusion. Despite great progress in the control of diabetes and its associated risk factors between 1999 and 2010, this trend declined for glycemic and blood pressure control and leveled off for lipid control in adult NHANES participants with diabetes after 2010. First-line treatments for diabetes and associated risk factors remain underused, and treatment intensification may not be sufficiently considered in patients with uncontrolled risk factors despite clinical guideline recommendations. The findings of this study may portend a possible population-level increase in diabetes-related illnesses in the years to come.
Commentary
The thorough understanding of trends in management of diseases is critical to inform public health policies and planning. Well designed clinical studies heavily influence the development of public health policies and clinical guidelines, which in turn drive real-world clinical practice. In a recent analysis utilizing data from NHANES, Fang et al1 showed evidence of a general shift toward less intensive treatment of diabetes, hypertension, and hypercholesterolemia in adults living in the US during the last decade.
Similarly, in a separate study using NHANES data collected between 1999 and 2018 published in JAMA just 2 weeks after the current report, Wang et al2 confirms this declining trend in diabetes management with only 21.2% of diabetic adults simultaneously attaining glycemic, blood pressure, and lipid level targets during the same period. What led to the decline in more stringent risk factor and diabetes management since 2010 observed in these studies? One possible explanation, as suggested by Fang et al, is that major clinical trials from the late 2000s—including Action to Control Cardiovascular Risk in Diabetes, UK Prospective Diabetes Study, Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation, and Veterans Affairs Diabetes Trial—that assessed the effects of intensive glycemic control (with target HbA1c < 6.5%) found that intensive treatment of diabetes compared to standard care had no cardiovascular benefit albeit increasing the risk of hypoglycemia. Thus, these trial findings may have translated into suboptimal diabetes treatment observed in some NHANES participants. Wang et al propose that effective tailored approaches are needed to improve risk factor control in diabetic patients, such as enhance and maintain adherence to medications and healthy lifestyle behaviors, as well as better access to health care and therapeutic education.
The changes in recent trends in diabetes management have immense clinical implications. The authors of this study suggest a link between the recent relaxation of glycemic targets, as well as risk factor control, and a resurgence of diabetic complications such as lower limb amputation or stroke. Indeed, several recent studies indicate an upward trend or plateau in diabetic complications which had been decreasing in prevalence prior to 2010.3 For example, lower extremity amputation has surged by more than 25% between 2010 and 2015, especially in young and middle-aged adults.4 Among the arguments brought forward that this recent resurgence in amputations is directly linked to worsening glycemic control is the fact that between 2007 and 2010, when glucose levels were best controlled within the previous 30-year period, amputations were also at the lowest levels. Moreover, data from the Centers for Disease Control and Prevention also show a 55% increase in mortality (from 15.7 to 24.2 per 1000) among diabetic patients between 2010 and 2015.14 On the other hand, a growing number of studies show that an increase of inappropriate treatment intensification—reaching HbA1c levels that are way below the recommended targets—is associated with adverse consequences in diabetic patients particularly in those aged more than 65 years.5-7 These seemingly contradictory findings highlight the importance of a personalized and thoughtful approach to the management of diabetes and its risk factors. As an example, an increase in the use of newer and safer glucose lowering drugs (eg, sodium-glucose cotransporter 2 inhibitors, glucagon-like peptide 1 receptor agonists, and dipeptidyl peptidase 4 inhibitors) can help achieve better HbA1c goals with a reduced risk of hypoglycemic episodes as recently shown by a Danish study.8 In this study, the authors concluded that the reduction of the rate of hypoglycemic episodes leading to hospitalization in Denmark was directly linked to the use of these safer and newer glucose lowering drugs.
A discussion on the specifics of trends in diabetes treatment and control must include considerations in older adults aged more than 65 years who constitute more than 40% of the diabetic population. Despite the high prevalence of diabetes in this vulnerable population, such data are still insufficient in the literature and are critically needed to inform public health policies and clinical guidelines. In epidemiological studies focusing on diabetic complications from the last 10 years, concerning increases have been observed in younger9 and middle-aged adults while remaining stable in older adults. However, the risk of hypoglycemia or severe hypoglycemia remains high in older adults living in nursing facilities, even in those with an elevated HbA1c of greater than 8%.7 Moreover, in light of more relaxed HbA1c treatment goals for older frail adults as recommended by international guidelines since 2010,10,11 recent findings from the French GERODIAB cohort show an increased mortality (hazard ratio, 1.76) in type 2 diabetics aged 70 years and older with HbA1c greater than or equal to 8.6%.12 Similarly, a 5-year retrospective British study from 2018 which included patients aged 70 years and older, shows an increased overall mortality in those with HbA1c greater than 8.5%.13 Taken together, further age-stratified analysis utilizing data from large cohort studies including NHANES may help to clarify national trends in diabetes treatment and risk factor control as well as diabetic complications specific to the geriatric population. By being better informed of such trends, clinicians could then develop treatment strategies that minimize complications (eg, hypoglycemia, falls) while achieving favorable outcomes (eg, reduce hyperglycemic emergencies, improve survival) in frail older patients.
Applications for Clinical Practice
The understanding of population-wide trends in diabetes control is critical to planning public health approaches for the prevention and treatment of this disease and its complications. In older adults, the high risk of hypoglycemic events and insufficient epidemiological data on trends of diabetes control hinder diabetes management. Personalized treatment targets taking into account geriatric syndromes and general health status, as well as multidisciplinary management involving endocrinologists, geriatricians, and clinical pharmacists, are necessary to optimize care in older adults with diabetes.
1. Fang M, Wang D, Coresh J, Selvin E. Trends in Diabetes Treatment and Control in U.S. Adults, 1999-2018. N Engl J Med. 2021;384(23):2219-28. doi:10.1056/NEJMsa2032271
2. Wang L, Li X, Wang Z, et al. Trends in Prevalence of Diabetes and Control of Risk Factors in Diabetes Among US Adults, 1999-2018. JAMA. 2021. doi:10.1001/jama.2021.9883
3. Gregg EW, Hora I, Benoit SR. Resurgence in Diabetes-Related Complications. JAMA. 2019;321(19):1867-8. doi:10.1001/jama.2019.3471
4. Caruso P, Scappaticcio L, Maiorino MI, et al. Up and down waves of glycemic control and lower-extremity amputation in diabetes. Cardiovasc Diabetol. 2021;20(1):135. doi:10.1186/s12933-021-01325-3
5. Bongaerts B, Arnold SV, Charbonnel BH, et al. Inappropriate intensification of glucose-lowering treatment in older patients with type 2 diabetes: the global DISCOVER study. BMJ Open Diabetes Res Care. 2021;9(1)e001585. doi:10.1136/bmjdrc-2020-001585
6. Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116-1124. doi: 10.1001/jamainternmed.2014.1824
7. Bouillet B, Tscherter P, Vaillard L, et al. Frequent and severe hypoglycaemia detected with continuous glucose monitoring in older institutionalised patients with diabetes. Age Ageing. 2021;afab128. doi: 10.1093/ageing/afab128
8. Jensen MH, Hejlesen O, Vestergaard P. Epidemiology of hypoglycaemic episodes leading to hospitalisations in Denmark in 1998-2018. Diabetologia. 2021. doi: 10.1007/s00125-021-05507-2
9. TODAY Study Group, Bjornstad P, Drews KL, et al. Long-Term Complications in Youth-Onset Type 2 Diabetes. N Engl J Med. 2021;385(5):416-426. doi: 10.1056/NEJMoa2100165
10. Sinclair AJ, Paolisso G, Castro M, et al. European Diabetes Working Party for Older People 2011 clinical guidelines for type 2 diabetes mellitus. Executive summary. Diabetes Metab. 2011;37 Suppl 3:S27-S38. doi:10.1016/S1262-3636(11)70962-4
11. Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care. 2012;35(12):2650-2664. doi: 10.2337/dc12-1801
12. Doucet J, Verny C, Balkau B, et al. Haemoglobin A1c and 5-year all-cause mortality in French type 2 diabetic patients aged 70 years and older: The GERODIAB observational cohort. Diabetes Metab. 2018;44(6):465-472. doi: 10.1016/j.diabet.2018.05.003
13. Forbes A, Murrells T, Mulnier H, Sinclair AJ. Mean HbA1c, HbA1c variability, and mortality in people with diabetes aged 70 years and older: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6(6):476-486. doi: 10.1016/S2213-8587(18)30048-2
14. US Centers for Disease Control and Prevention. US diabetes surveillance system and diabetes atlas, 2019. https://www.cdc.gov/diabetes/data
1. Fang M, Wang D, Coresh J, Selvin E. Trends in Diabetes Treatment and Control in U.S. Adults, 1999-2018. N Engl J Med. 2021;384(23):2219-28. doi:10.1056/NEJMsa2032271
2. Wang L, Li X, Wang Z, et al. Trends in Prevalence of Diabetes and Control of Risk Factors in Diabetes Among US Adults, 1999-2018. JAMA. 2021. doi:10.1001/jama.2021.9883
3. Gregg EW, Hora I, Benoit SR. Resurgence in Diabetes-Related Complications. JAMA. 2019;321(19):1867-8. doi:10.1001/jama.2019.3471
4. Caruso P, Scappaticcio L, Maiorino MI, et al. Up and down waves of glycemic control and lower-extremity amputation in diabetes. Cardiovasc Diabetol. 2021;20(1):135. doi:10.1186/s12933-021-01325-3
5. Bongaerts B, Arnold SV, Charbonnel BH, et al. Inappropriate intensification of glucose-lowering treatment in older patients with type 2 diabetes: the global DISCOVER study. BMJ Open Diabetes Res Care. 2021;9(1)e001585. doi:10.1136/bmjdrc-2020-001585
6. Lipska KJ, Ross JS, Wang Y, et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med. 2014;174(7):1116-1124. doi: 10.1001/jamainternmed.2014.1824
7. Bouillet B, Tscherter P, Vaillard L, et al. Frequent and severe hypoglycaemia detected with continuous glucose monitoring in older institutionalised patients with diabetes. Age Ageing. 2021;afab128. doi: 10.1093/ageing/afab128
8. Jensen MH, Hejlesen O, Vestergaard P. Epidemiology of hypoglycaemic episodes leading to hospitalisations in Denmark in 1998-2018. Diabetologia. 2021. doi: 10.1007/s00125-021-05507-2
9. TODAY Study Group, Bjornstad P, Drews KL, et al. Long-Term Complications in Youth-Onset Type 2 Diabetes. N Engl J Med. 2021;385(5):416-426. doi: 10.1056/NEJMoa2100165
10. Sinclair AJ, Paolisso G, Castro M, et al. European Diabetes Working Party for Older People 2011 clinical guidelines for type 2 diabetes mellitus. Executive summary. Diabetes Metab. 2011;37 Suppl 3:S27-S38. doi:10.1016/S1262-3636(11)70962-4
11. Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care. 2012;35(12):2650-2664. doi: 10.2337/dc12-1801
12. Doucet J, Verny C, Balkau B, et al. Haemoglobin A1c and 5-year all-cause mortality in French type 2 diabetic patients aged 70 years and older: The GERODIAB observational cohort. Diabetes Metab. 2018;44(6):465-472. doi: 10.1016/j.diabet.2018.05.003
13. Forbes A, Murrells T, Mulnier H, Sinclair AJ. Mean HbA1c, HbA1c variability, and mortality in people with diabetes aged 70 years and older: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018;6(6):476-486. doi: 10.1016/S2213-8587(18)30048-2
14. US Centers for Disease Control and Prevention. US diabetes surveillance system and diabetes atlas, 2019. https://www.cdc.gov/diabetes/data
Modest calorie reduction plus exercise linked with improved vascular health
Finding applies to seniors with obesity, who were part of a new study
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
Finding applies to seniors with obesity, who were part of a new study
Finding applies to seniors with obesity, who were part of a new study
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
The authors of the paper, published in Circulation, found a link between greater vascular benefits and exercise with modest – rather than intense – calorie restriction (CR) in elderly individuals with obesity.
“The finding that higher-intensity calorie restriction may not be necessary or advised has important implications for weight loss recommendations,” noted Tina E. Brinkley, Ph.D., lead author of the study and associate professor of gerontology and geriatric medicine at the Sticht Center for Healthy Aging and Alzheimer’s Prevention at Wake Forest University in Winston-Salem, N.C.
It’s “not entirely clear” why greater calorie restriction did not translate to greater vascular benefit, but it “could be related in part to potentially adverse effects of severe CR on vascular function,” she noted. “These findings have important implications for reducing cardiovascular risk with nonpharmacological interventions in high-risk populations.”
Methods and findings
The study included 160 men and women aged 65-79 years, with a body mass index (BMI) of 30 to 45 kg/m2. The subjects were randomized to one of three groups for 20 weeks of aerobic exercise only, aerobic exercise plus moderate CR, or aerobic exercise plus more intensive CR. Their exercise regimen involved 30 minutes of supervised treadmill walking for 4 days per week at 65%-70% of heart rate reserve.
Subjects in the moderate CR group decreased caloric intake by 250 kcals a day, while the intense calorie reduction group cut 600 kcals per day. Their meals contained less than 30% of calories from fat and at least 0.8 g of protein per kg of ideal body weight. They were also provided with supplemental calcium (1,200 mg/day) and vitamin D (800 IU/day).
Cardiovascular magnetic resonance imaging was used to assess various aspects of aortic structure and function, including aortic arch pulse wave velocity, aortic distensibility and dimensions, and periaortic fat.
Weight loss was greater among subjects with CR plus exercise, compared with that of patients in the exercise-only group. The degree of weight loss was not significantly different between those with moderate versus intense CR ( 8.02 kg vs. 8.98 kg).
Among the exercise-only group, researchers observed no changes in aortic stiffness. However, adding moderate CR significantly improved this measure, while intense CR did not.
Specifically, subjects in the moderate-CR group had a “robust” 21% increase in distensibility in the descending aorta (DA), and an 8% decrease in aortic arch pulse wave velocity, whereas there were no significant vascular changes in the intense-CR group.
Bests results seen in exercise plus modest CR group
“Collectively, these data suggest that combining exercise with modest CR (as opposed to more intensive CR or no CR) provides the greatest benefit for proximal aortic stiffness, while also optimizing weight loss and improvements in body composition and body fat distribution,” noted the authors in their paper.
“Our data support the growing number of studies indicating that intentional weight loss can be safe for older adults with obesity and extend our previous findings, suggesting that obesity may blunt the beneficial effects of exercise for not only cardiorespiratory fitness, but likely vascular health as well.”
William E. Kraus, MD, professor in the Department of Medicine, Division of Cardiology at Duke University Medical Center, in Durham, NC, described the study as important and interesting for several reasons.
“First, it demonstrates one can change aortic vascular function with a combined diet and exercise program, even in older, obese Americans. This implies it is never too late to make meaningful lifestyle changes that will benefit cardiovascular health,” he said. “Second, it is among an increasing number of studies demonstrating that more is not always better than less in exercise and diet lifestyle changes - and in fact the converse is true.”
“This gives hope that more people can benefit from modest lifestyle changes - in this case following guidelines for physical activity and only a modest reduction of 250 kilocalories per day resulted in benefit,” Dr. Kraus added.
The authors of the paper and Dr. Kraus disclosed no conflicts of interest.
FROM CIRCULATION
‘Staggering’ increase in global dementia cases predicted by 2050
, new global prevalence data show. “These extreme increases are due largely to demographic trends, including population growth and aging,” said study investigator Emma Nichols, MPH, a researcher at the Institute for Health Metrics and Evaluation at the University of Washington in Seattle.
“Our estimates of expected increases can and should inform policy and planning efforts that will be needed to address the needs of the growing number of individuals with dementia in the future,” Ms. Nichols said.
The latest global prevalence data were reported at the 2021 Alzheimer’s Association International Conference.
“The numbers are staggering: Nearly 153 million cases of dementia are predicted worldwide by the year 2050. To put that in context, that number is equal to approximately half of the U.S. population in 2020,” Heather M. Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said in a statement.
Prevalence by country
To more accurately forecast global dementia prevalence and produce country-level estimates, the investigators leveraged data from 1999 to 2019 from the Global Burden of Disease study, a comprehensive set of estimates of worldwide health trends.
These data suggest global dementia cases will increase from 57.4 million (50.4 to 65.1) in 2019 to 152.8 million (130.8 to 175.9) in 2050.
Regions that will experience the worst of the increase are eastern Sub-Saharan Africa, North Africa, and the Middle East.
The researchers also factored into the forecasts expected trends in obesity, diabetes, smoking, and educational attainment.
Increases in better education around the world are projected to decrease dementia prevalence by 6.2 million cases worldwide by 2050. However, anticipated trends in smoking, high body mass index, and diabetes will offset this gain, increasing global dementia cases by 6.8 million cases.
“A reversal of these expected trends in cardiovascular risks would be necessary to alter the anticipated trends,” Ms. Nichols said. “Interventions targeted at modifiable risk factors for dementia represent a viable strategy to help address the anticipated trends in dementia burden,” she added.
Need for effective prevention, treatment
Commenting on the research, Rebecca M. Edelmayer, PhD, senior director of scientific engagement at the Alzheimer’s Association, said the global increase in dementia cases is something the association has been following for many years. “We know that if we do not find effective treatments that are going to stop, slow, or prevent Alzheimer’s disease, this number will continue to grow and it will continue to impact people globally,” Dr. Edelmayer said.
She noted that although there are some positive trends, including the fact that increased education may drive down dementia risk, other factors, such as smoking, high body mass index, and high blood sugar level, are predicted to increase in prevalence.
“Some of these factors are actually counterbalancing each other, and in the end, if we don’t continue to develop culturally tailored interventions or even risk reduction strategies for individuals across the globe, we will continue to see those numbers rise overall,” Dr. Edelmayer said.
A version of this article first appeared on Medscape.com.
, new global prevalence data show. “These extreme increases are due largely to demographic trends, including population growth and aging,” said study investigator Emma Nichols, MPH, a researcher at the Institute for Health Metrics and Evaluation at the University of Washington in Seattle.
“Our estimates of expected increases can and should inform policy and planning efforts that will be needed to address the needs of the growing number of individuals with dementia in the future,” Ms. Nichols said.
The latest global prevalence data were reported at the 2021 Alzheimer’s Association International Conference.
“The numbers are staggering: Nearly 153 million cases of dementia are predicted worldwide by the year 2050. To put that in context, that number is equal to approximately half of the U.S. population in 2020,” Heather M. Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said in a statement.
Prevalence by country
To more accurately forecast global dementia prevalence and produce country-level estimates, the investigators leveraged data from 1999 to 2019 from the Global Burden of Disease study, a comprehensive set of estimates of worldwide health trends.
These data suggest global dementia cases will increase from 57.4 million (50.4 to 65.1) in 2019 to 152.8 million (130.8 to 175.9) in 2050.
Regions that will experience the worst of the increase are eastern Sub-Saharan Africa, North Africa, and the Middle East.
The researchers also factored into the forecasts expected trends in obesity, diabetes, smoking, and educational attainment.
Increases in better education around the world are projected to decrease dementia prevalence by 6.2 million cases worldwide by 2050. However, anticipated trends in smoking, high body mass index, and diabetes will offset this gain, increasing global dementia cases by 6.8 million cases.
“A reversal of these expected trends in cardiovascular risks would be necessary to alter the anticipated trends,” Ms. Nichols said. “Interventions targeted at modifiable risk factors for dementia represent a viable strategy to help address the anticipated trends in dementia burden,” she added.
Need for effective prevention, treatment
Commenting on the research, Rebecca M. Edelmayer, PhD, senior director of scientific engagement at the Alzheimer’s Association, said the global increase in dementia cases is something the association has been following for many years. “We know that if we do not find effective treatments that are going to stop, slow, or prevent Alzheimer’s disease, this number will continue to grow and it will continue to impact people globally,” Dr. Edelmayer said.
She noted that although there are some positive trends, including the fact that increased education may drive down dementia risk, other factors, such as smoking, high body mass index, and high blood sugar level, are predicted to increase in prevalence.
“Some of these factors are actually counterbalancing each other, and in the end, if we don’t continue to develop culturally tailored interventions or even risk reduction strategies for individuals across the globe, we will continue to see those numbers rise overall,” Dr. Edelmayer said.
A version of this article first appeared on Medscape.com.
, new global prevalence data show. “These extreme increases are due largely to demographic trends, including population growth and aging,” said study investigator Emma Nichols, MPH, a researcher at the Institute for Health Metrics and Evaluation at the University of Washington in Seattle.
“Our estimates of expected increases can and should inform policy and planning efforts that will be needed to address the needs of the growing number of individuals with dementia in the future,” Ms. Nichols said.
The latest global prevalence data were reported at the 2021 Alzheimer’s Association International Conference.
“The numbers are staggering: Nearly 153 million cases of dementia are predicted worldwide by the year 2050. To put that in context, that number is equal to approximately half of the U.S. population in 2020,” Heather M. Snyder, PhD, vice president of medical and scientific relations for the Alzheimer’s Association, said in a statement.
Prevalence by country
To more accurately forecast global dementia prevalence and produce country-level estimates, the investigators leveraged data from 1999 to 2019 from the Global Burden of Disease study, a comprehensive set of estimates of worldwide health trends.
These data suggest global dementia cases will increase from 57.4 million (50.4 to 65.1) in 2019 to 152.8 million (130.8 to 175.9) in 2050.
Regions that will experience the worst of the increase are eastern Sub-Saharan Africa, North Africa, and the Middle East.
The researchers also factored into the forecasts expected trends in obesity, diabetes, smoking, and educational attainment.
Increases in better education around the world are projected to decrease dementia prevalence by 6.2 million cases worldwide by 2050. However, anticipated trends in smoking, high body mass index, and diabetes will offset this gain, increasing global dementia cases by 6.8 million cases.
“A reversal of these expected trends in cardiovascular risks would be necessary to alter the anticipated trends,” Ms. Nichols said. “Interventions targeted at modifiable risk factors for dementia represent a viable strategy to help address the anticipated trends in dementia burden,” she added.
Need for effective prevention, treatment
Commenting on the research, Rebecca M. Edelmayer, PhD, senior director of scientific engagement at the Alzheimer’s Association, said the global increase in dementia cases is something the association has been following for many years. “We know that if we do not find effective treatments that are going to stop, slow, or prevent Alzheimer’s disease, this number will continue to grow and it will continue to impact people globally,” Dr. Edelmayer said.
She noted that although there are some positive trends, including the fact that increased education may drive down dementia risk, other factors, such as smoking, high body mass index, and high blood sugar level, are predicted to increase in prevalence.
“Some of these factors are actually counterbalancing each other, and in the end, if we don’t continue to develop culturally tailored interventions or even risk reduction strategies for individuals across the globe, we will continue to see those numbers rise overall,” Dr. Edelmayer said.
A version of this article first appeared on Medscape.com.
From AAIC 2021
Mt. Sinai leads nation in geriatric hospital services
The Cleveland Clinic in Ohio, and the Mayo Clinic in Rochester, Minn., followed.
Rounding out the top 10 hospitals in caring for patients older than age 75 were (4) UCLA Medical Center, Los Angeles; (5) NYU Langone Hospitals in New York; (6) Johns Hopkins Hospital in Baltimore; (7) New York–Presbyterian Hospital–Columbia and Cornell, New York; (8) Northwestern Memorial Hospital, Chicago; (9) UCSF Medical Center, San Francisco; and (10) Cedars-Sinai Medical Center, Los Angeles.
Those were followed by (11) Keck Medical Center of USC, Los Angeles; (12) University of Michigan Hospitals–Michigan Medicine, Ann Arbor; (13) UC San Diego Health–Jacobs Medical Center, San Diego; (14) Massachusetts General Hospital, Boston; (15) Stanford Health Care–Stanford Hospital, Palo Alto, Calif.; (16) Rush University Medical Center, Chicago; (17) Hospitals of the University of Pennsylvania–Penn Presbyterian, Philadelphia; (18) Brigham and Women’s Hospital, Boston; (19) Barnes-Jewish Hospital, St. Louis, Mo.; (tied for 19) UPMC Presbyterian Shadyside, Pittsburgh.
Data for the 2021-2022 edition of the “Best Hospitals” were not affected by the COVID-19 pandemic, which began after the end of the data collection period.
U.S. News also investigated racial disparities in health care and debuted health equity measures alongside each hospital’s rankings. Among other aspects of health equity, the new measures examine whether the patients each hospital treated reflect the racial and ethnic diversity of its community.
Ben Harder, managing editor and chief of health analysis, said in a statement, “At roughly four out of five hospitals, we found that the community’s minority residents were underrepresented among patients receiving services such as joint replacement, cancer surgery, and common heart procedures. Against this backdrop, however, we found important exceptions – hospitals that provide care to a disproportionate share of their community’s minority residents.”
U.S. News compared more than 4,750 medical centers nationwide in 15 specialties. Of those, 531 were recognized as Best Regional Hospitals on the basis of their strong performance in multiple areas of care.
The top 20 hospitals overall were also named to the Honor Roll.
Mayo Clinic was again No. 1 on the honor roll, a ranking it has held for 6 years in a row, according to a press release. The Cleveland Clinic ranked No. 2, followed by UCLA Medical Center at No. 3.
In other top specialties, the University of Texas MD Anderson Cancer Center in Houston ranked No. 1 in cancer; the Cleveland Clinic is No. 1 in cardiology and heart surgery; and the Hospital for Special Surgery in New York is No. 1 in orthopedics.
A full list of rankings is available on the website.
In 12 of the 15 specialty areas, including geriatrics, rankings are derived from data sources such as Medicare. In the other three specialties – ophthalmology, psychiatry, and rheumatology – ranking is determined by expert opinion based on responses from 3 years of surveys of physician specialists who were asked to name the hospitals to which they would likely refer their sickest patients.
This year’s analysis adds seven new procedures and conditions: Heart attack, stroke, pneumonia, diabetes, kidney failure, hip fracture, and back surgery (spinal fusion).
The expanded list will help patients, in consultation with their physicians, choose their hospital on the basis of the specific type of care they need with consideration of distance to a facility and insurance coverage.
A version of this article first appeared on Medscape.com.
The Cleveland Clinic in Ohio, and the Mayo Clinic in Rochester, Minn., followed.
Rounding out the top 10 hospitals in caring for patients older than age 75 were (4) UCLA Medical Center, Los Angeles; (5) NYU Langone Hospitals in New York; (6) Johns Hopkins Hospital in Baltimore; (7) New York–Presbyterian Hospital–Columbia and Cornell, New York; (8) Northwestern Memorial Hospital, Chicago; (9) UCSF Medical Center, San Francisco; and (10) Cedars-Sinai Medical Center, Los Angeles.
Those were followed by (11) Keck Medical Center of USC, Los Angeles; (12) University of Michigan Hospitals–Michigan Medicine, Ann Arbor; (13) UC San Diego Health–Jacobs Medical Center, San Diego; (14) Massachusetts General Hospital, Boston; (15) Stanford Health Care–Stanford Hospital, Palo Alto, Calif.; (16) Rush University Medical Center, Chicago; (17) Hospitals of the University of Pennsylvania–Penn Presbyterian, Philadelphia; (18) Brigham and Women’s Hospital, Boston; (19) Barnes-Jewish Hospital, St. Louis, Mo.; (tied for 19) UPMC Presbyterian Shadyside, Pittsburgh.
Data for the 2021-2022 edition of the “Best Hospitals” were not affected by the COVID-19 pandemic, which began after the end of the data collection period.
U.S. News also investigated racial disparities in health care and debuted health equity measures alongside each hospital’s rankings. Among other aspects of health equity, the new measures examine whether the patients each hospital treated reflect the racial and ethnic diversity of its community.
Ben Harder, managing editor and chief of health analysis, said in a statement, “At roughly four out of five hospitals, we found that the community’s minority residents were underrepresented among patients receiving services such as joint replacement, cancer surgery, and common heart procedures. Against this backdrop, however, we found important exceptions – hospitals that provide care to a disproportionate share of their community’s minority residents.”
U.S. News compared more than 4,750 medical centers nationwide in 15 specialties. Of those, 531 were recognized as Best Regional Hospitals on the basis of their strong performance in multiple areas of care.
The top 20 hospitals overall were also named to the Honor Roll.
Mayo Clinic was again No. 1 on the honor roll, a ranking it has held for 6 years in a row, according to a press release. The Cleveland Clinic ranked No. 2, followed by UCLA Medical Center at No. 3.
In other top specialties, the University of Texas MD Anderson Cancer Center in Houston ranked No. 1 in cancer; the Cleveland Clinic is No. 1 in cardiology and heart surgery; and the Hospital for Special Surgery in New York is No. 1 in orthopedics.
A full list of rankings is available on the website.
In 12 of the 15 specialty areas, including geriatrics, rankings are derived from data sources such as Medicare. In the other three specialties – ophthalmology, psychiatry, and rheumatology – ranking is determined by expert opinion based on responses from 3 years of surveys of physician specialists who were asked to name the hospitals to which they would likely refer their sickest patients.
This year’s analysis adds seven new procedures and conditions: Heart attack, stroke, pneumonia, diabetes, kidney failure, hip fracture, and back surgery (spinal fusion).
The expanded list will help patients, in consultation with their physicians, choose their hospital on the basis of the specific type of care they need with consideration of distance to a facility and insurance coverage.
A version of this article first appeared on Medscape.com.
The Cleveland Clinic in Ohio, and the Mayo Clinic in Rochester, Minn., followed.
Rounding out the top 10 hospitals in caring for patients older than age 75 were (4) UCLA Medical Center, Los Angeles; (5) NYU Langone Hospitals in New York; (6) Johns Hopkins Hospital in Baltimore; (7) New York–Presbyterian Hospital–Columbia and Cornell, New York; (8) Northwestern Memorial Hospital, Chicago; (9) UCSF Medical Center, San Francisco; and (10) Cedars-Sinai Medical Center, Los Angeles.
Those were followed by (11) Keck Medical Center of USC, Los Angeles; (12) University of Michigan Hospitals–Michigan Medicine, Ann Arbor; (13) UC San Diego Health–Jacobs Medical Center, San Diego; (14) Massachusetts General Hospital, Boston; (15) Stanford Health Care–Stanford Hospital, Palo Alto, Calif.; (16) Rush University Medical Center, Chicago; (17) Hospitals of the University of Pennsylvania–Penn Presbyterian, Philadelphia; (18) Brigham and Women’s Hospital, Boston; (19) Barnes-Jewish Hospital, St. Louis, Mo.; (tied for 19) UPMC Presbyterian Shadyside, Pittsburgh.
Data for the 2021-2022 edition of the “Best Hospitals” were not affected by the COVID-19 pandemic, which began after the end of the data collection period.
U.S. News also investigated racial disparities in health care and debuted health equity measures alongside each hospital’s rankings. Among other aspects of health equity, the new measures examine whether the patients each hospital treated reflect the racial and ethnic diversity of its community.
Ben Harder, managing editor and chief of health analysis, said in a statement, “At roughly four out of five hospitals, we found that the community’s minority residents were underrepresented among patients receiving services such as joint replacement, cancer surgery, and common heart procedures. Against this backdrop, however, we found important exceptions – hospitals that provide care to a disproportionate share of their community’s minority residents.”
U.S. News compared more than 4,750 medical centers nationwide in 15 specialties. Of those, 531 were recognized as Best Regional Hospitals on the basis of their strong performance in multiple areas of care.
The top 20 hospitals overall were also named to the Honor Roll.
Mayo Clinic was again No. 1 on the honor roll, a ranking it has held for 6 years in a row, according to a press release. The Cleveland Clinic ranked No. 2, followed by UCLA Medical Center at No. 3.
In other top specialties, the University of Texas MD Anderson Cancer Center in Houston ranked No. 1 in cancer; the Cleveland Clinic is No. 1 in cardiology and heart surgery; and the Hospital for Special Surgery in New York is No. 1 in orthopedics.
A full list of rankings is available on the website.
In 12 of the 15 specialty areas, including geriatrics, rankings are derived from data sources such as Medicare. In the other three specialties – ophthalmology, psychiatry, and rheumatology – ranking is determined by expert opinion based on responses from 3 years of surveys of physician specialists who were asked to name the hospitals to which they would likely refer their sickest patients.
This year’s analysis adds seven new procedures and conditions: Heart attack, stroke, pneumonia, diabetes, kidney failure, hip fracture, and back surgery (spinal fusion).
The expanded list will help patients, in consultation with their physicians, choose their hospital on the basis of the specific type of care they need with consideration of distance to a facility and insurance coverage.
A version of this article first appeared on Medscape.com.