User login
Storybooks Can Help Children Deal with Skin Conditions
TORONTO —
So far, “the study demonstrates that these books have value to patients and families,” one of the study authors, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital Kansas City, Kansas City, Missouri, said in an interview.
“There are tools to help kids cope with their skin conditions, but we’re underutilizing them,” she added. “And part of the reason we’re underutilizing storybooks is that we just don’t know what’s out there.” For the study, the researchers received funding to purchase 18 “creative and thoughtful” storybooks related to pediatric skin conditions, reviewed by at least two pediatric dermatologists before being selected, which are just a sample of related books that are available.
The study results were presented as a poster at the annual meeting of the Society for Pediatric Dermatology.
Children with visible skin conditions, which can include port-wine stains, capillary malformations, and congenital moles, may be subjected to teasing or bullying at school, and the conditions can also affect their quality of life.
Beauty and the Birthmark
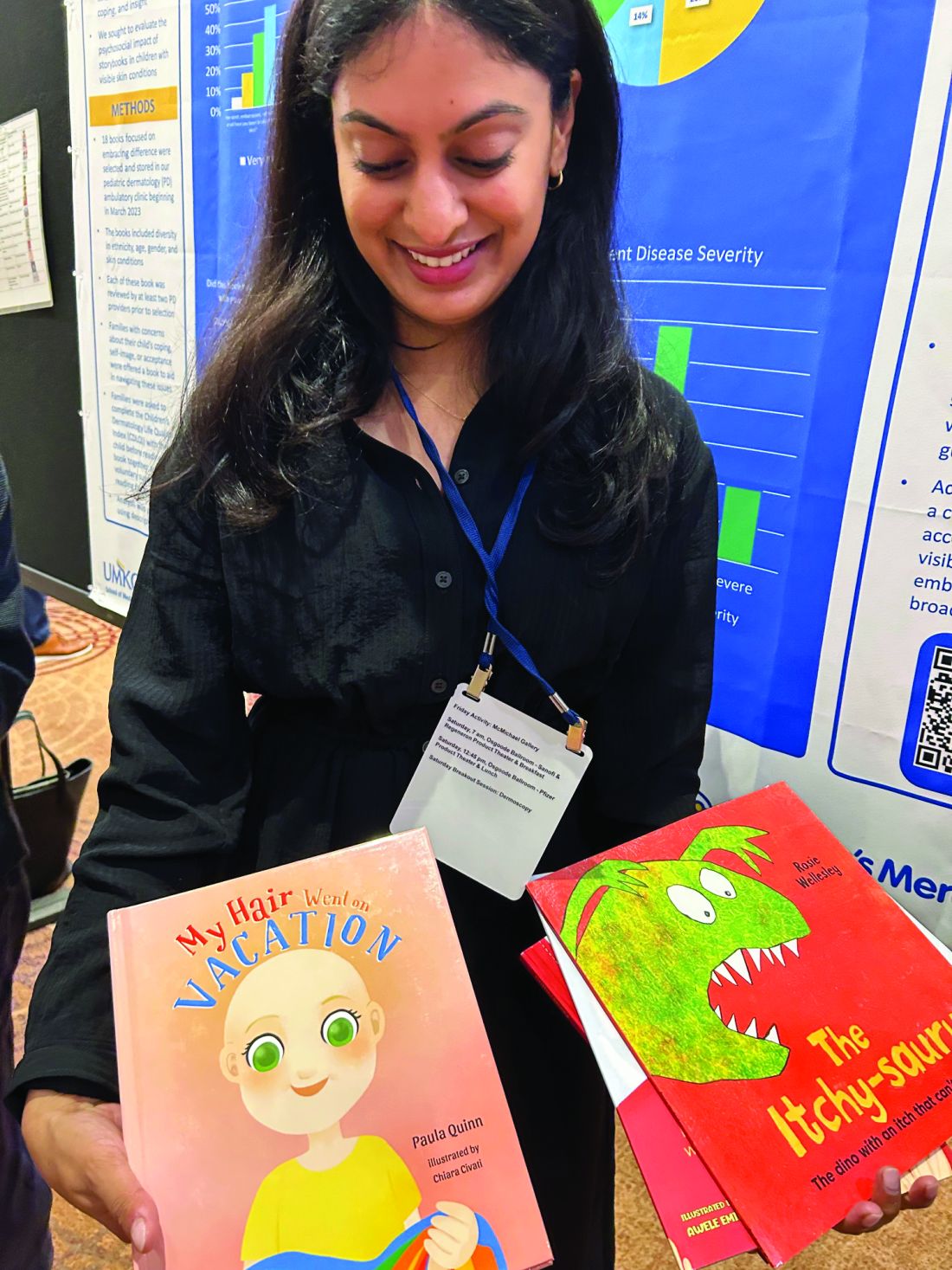
The books include one titled “Beauty with a Birthmark” and another, “My Hair Went on Vacation.” An illustrated book, “Just Ask: Be Different, Be Brave, Be You,” by US Supreme Court Justice Sonia Sotomayor, offers tips on how to answer common questions about someone’s appearance.
Dr. Havele said that Justice Sotomayor’s book “empowers kids, their siblings, their classmates ... to ask questions, and it teaches patients not to be afraid of those questions, and to really lean into educating their peers, and their family members.”
“Kids are really just curious,” she added. “They’ll make comments like: ‘Hey, what’s that spot on your face?’ Or, they’ll ask about vitiligo because they’ve never seen somebody with it before.”
To evaluate the psychosocial impact of these types of books for children with visible skin conditions, Dr. Havele and colleagues designed a study that includes patients aged 2-12 years dealing with issues related to self-esteem, acceptance, coping, or bullying. Parents are provided with a relevant storybook to read at home with their child in a “safe and comfortable space” and “at their own pace and their own time,” said Dr. Havele.
Inside the book is a QR code to access the validated Children’s Dermatology Life Quality Index (CDLQI). Families complete the survey at baseline and provide feedback after reading the book. Researchers collect information about demographics, age, gender, and skin conditions, which included atopic dermatitis, alopecia areata, vitiligo, hemangioma, and port-wine stain.
The response rate so far is 34%, and close to 80 parents have completed the survey with their child, Dr. Havele said.
At baseline, many of the children were either moderately or severely affected in terms of their quality of life (45% scored ≥ 6 on the CDLQI).
After reading the book, about 80% of parents reported it had a positive impact, and about 20% said it had a somewhat positive impact on their child’s self-image or confidence. Almost 80% agreed, and the remainder somewhat agreed it encouraged their child to embrace differences.
Most respondents also said the book helped the parent and child cope with the child’s condition. “So really, it was overall a positive response,” said Dr. Havele. “We are able to demonstrate that these books have value in a more scientific or objective way.”
This may not be surprising. Dr. Havele referred to more formal bibliotherapy (book therapy), which has been studied in other pediatric populations, including patients with cancer and those who have experienced trauma.
Awesome Space
Pediatric dermatologists are perfectly positioned to play a role in improving the lives of their patients with skin issues. “We see the impact of visible skin disease on children all the time,” said Dr. Havele. “The dermatology visit is an awesome space and opportunity to introduce these books to families and potentially help them talk about the skin condition with their child.”
In addition to prescribing therapies, “we’re also with these kids through an emotional journey, and I think giving them tools for that emotional journey is very helpful,” she added.
Such books would have been a great help to Dr. Havele herself. Growing up, she had severe atopic dermatitis covering much of her body. “Having such a resource would have helped me better cope with my reality of being different than everyone else.”
She hopes a database will be established to house these resources so other providers can refer patients to the list of books. Other books include “The Itchy-saurus: The Dino with an itch that can’t be scratched,” “Hair in My Brush,” and “I am Unique!”
Dr. Havele had no relevant disclosures.
A version of this article first appeared on Medscape.com.
TORONTO —
So far, “the study demonstrates that these books have value to patients and families,” one of the study authors, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital Kansas City, Kansas City, Missouri, said in an interview.
“There are tools to help kids cope with their skin conditions, but we’re underutilizing them,” she added. “And part of the reason we’re underutilizing storybooks is that we just don’t know what’s out there.” For the study, the researchers received funding to purchase 18 “creative and thoughtful” storybooks related to pediatric skin conditions, reviewed by at least two pediatric dermatologists before being selected, which are just a sample of related books that are available.
The study results were presented as a poster at the annual meeting of the Society for Pediatric Dermatology.
Children with visible skin conditions, which can include port-wine stains, capillary malformations, and congenital moles, may be subjected to teasing or bullying at school, and the conditions can also affect their quality of life.
Beauty and the Birthmark
The books include one titled “Beauty with a Birthmark” and another, “My Hair Went on Vacation.” An illustrated book, “Just Ask: Be Different, Be Brave, Be You,” by US Supreme Court Justice Sonia Sotomayor, offers tips on how to answer common questions about someone’s appearance.
Dr. Havele said that Justice Sotomayor’s book “empowers kids, their siblings, their classmates ... to ask questions, and it teaches patients not to be afraid of those questions, and to really lean into educating their peers, and their family members.”
“Kids are really just curious,” she added. “They’ll make comments like: ‘Hey, what’s that spot on your face?’ Or, they’ll ask about vitiligo because they’ve never seen somebody with it before.”
To evaluate the psychosocial impact of these types of books for children with visible skin conditions, Dr. Havele and colleagues designed a study that includes patients aged 2-12 years dealing with issues related to self-esteem, acceptance, coping, or bullying. Parents are provided with a relevant storybook to read at home with their child in a “safe and comfortable space” and “at their own pace and their own time,” said Dr. Havele.
Inside the book is a QR code to access the validated Children’s Dermatology Life Quality Index (CDLQI). Families complete the survey at baseline and provide feedback after reading the book. Researchers collect information about demographics, age, gender, and skin conditions, which included atopic dermatitis, alopecia areata, vitiligo, hemangioma, and port-wine stain.
The response rate so far is 34%, and close to 80 parents have completed the survey with their child, Dr. Havele said.
At baseline, many of the children were either moderately or severely affected in terms of their quality of life (45% scored ≥ 6 on the CDLQI).
After reading the book, about 80% of parents reported it had a positive impact, and about 20% said it had a somewhat positive impact on their child’s self-image or confidence. Almost 80% agreed, and the remainder somewhat agreed it encouraged their child to embrace differences.
Most respondents also said the book helped the parent and child cope with the child’s condition. “So really, it was overall a positive response,” said Dr. Havele. “We are able to demonstrate that these books have value in a more scientific or objective way.”
This may not be surprising. Dr. Havele referred to more formal bibliotherapy (book therapy), which has been studied in other pediatric populations, including patients with cancer and those who have experienced trauma.
Awesome Space
Pediatric dermatologists are perfectly positioned to play a role in improving the lives of their patients with skin issues. “We see the impact of visible skin disease on children all the time,” said Dr. Havele. “The dermatology visit is an awesome space and opportunity to introduce these books to families and potentially help them talk about the skin condition with their child.”
In addition to prescribing therapies, “we’re also with these kids through an emotional journey, and I think giving them tools for that emotional journey is very helpful,” she added.
Such books would have been a great help to Dr. Havele herself. Growing up, she had severe atopic dermatitis covering much of her body. “Having such a resource would have helped me better cope with my reality of being different than everyone else.”
She hopes a database will be established to house these resources so other providers can refer patients to the list of books. Other books include “The Itchy-saurus: The Dino with an itch that can’t be scratched,” “Hair in My Brush,” and “I am Unique!”
Dr. Havele had no relevant disclosures.
A version of this article first appeared on Medscape.com.
TORONTO —
So far, “the study demonstrates that these books have value to patients and families,” one of the study authors, Sonia Havele, MD, a pediatrician and dermatology resident at Children’s Mercy Hospital Kansas City, Kansas City, Missouri, said in an interview.
“There are tools to help kids cope with their skin conditions, but we’re underutilizing them,” she added. “And part of the reason we’re underutilizing storybooks is that we just don’t know what’s out there.” For the study, the researchers received funding to purchase 18 “creative and thoughtful” storybooks related to pediatric skin conditions, reviewed by at least two pediatric dermatologists before being selected, which are just a sample of related books that are available.
The study results were presented as a poster at the annual meeting of the Society for Pediatric Dermatology.
Children with visible skin conditions, which can include port-wine stains, capillary malformations, and congenital moles, may be subjected to teasing or bullying at school, and the conditions can also affect their quality of life.
Beauty and the Birthmark
The books include one titled “Beauty with a Birthmark” and another, “My Hair Went on Vacation.” An illustrated book, “Just Ask: Be Different, Be Brave, Be You,” by US Supreme Court Justice Sonia Sotomayor, offers tips on how to answer common questions about someone’s appearance.
Dr. Havele said that Justice Sotomayor’s book “empowers kids, their siblings, their classmates ... to ask questions, and it teaches patients not to be afraid of those questions, and to really lean into educating their peers, and their family members.”
“Kids are really just curious,” she added. “They’ll make comments like: ‘Hey, what’s that spot on your face?’ Or, they’ll ask about vitiligo because they’ve never seen somebody with it before.”
To evaluate the psychosocial impact of these types of books for children with visible skin conditions, Dr. Havele and colleagues designed a study that includes patients aged 2-12 years dealing with issues related to self-esteem, acceptance, coping, or bullying. Parents are provided with a relevant storybook to read at home with their child in a “safe and comfortable space” and “at their own pace and their own time,” said Dr. Havele.
Inside the book is a QR code to access the validated Children’s Dermatology Life Quality Index (CDLQI). Families complete the survey at baseline and provide feedback after reading the book. Researchers collect information about demographics, age, gender, and skin conditions, which included atopic dermatitis, alopecia areata, vitiligo, hemangioma, and port-wine stain.
The response rate so far is 34%, and close to 80 parents have completed the survey with their child, Dr. Havele said.
At baseline, many of the children were either moderately or severely affected in terms of their quality of life (45% scored ≥ 6 on the CDLQI).
After reading the book, about 80% of parents reported it had a positive impact, and about 20% said it had a somewhat positive impact on their child’s self-image or confidence. Almost 80% agreed, and the remainder somewhat agreed it encouraged their child to embrace differences.
Most respondents also said the book helped the parent and child cope with the child’s condition. “So really, it was overall a positive response,” said Dr. Havele. “We are able to demonstrate that these books have value in a more scientific or objective way.”
This may not be surprising. Dr. Havele referred to more formal bibliotherapy (book therapy), which has been studied in other pediatric populations, including patients with cancer and those who have experienced trauma.
Awesome Space
Pediatric dermatologists are perfectly positioned to play a role in improving the lives of their patients with skin issues. “We see the impact of visible skin disease on children all the time,” said Dr. Havele. “The dermatology visit is an awesome space and opportunity to introduce these books to families and potentially help them talk about the skin condition with their child.”
In addition to prescribing therapies, “we’re also with these kids through an emotional journey, and I think giving them tools for that emotional journey is very helpful,” she added.
Such books would have been a great help to Dr. Havele herself. Growing up, she had severe atopic dermatitis covering much of her body. “Having such a resource would have helped me better cope with my reality of being different than everyone else.”
She hopes a database will be established to house these resources so other providers can refer patients to the list of books. Other books include “The Itchy-saurus: The Dino with an itch that can’t be scratched,” “Hair in My Brush,” and “I am Unique!”
Dr. Havele had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024
Predicting RSV’s Role in the Upcoming Winter Respiratory Season
For children younger than 5 years old, RSV is the main drive — approximately 2,000,000 outpatient/ED visits and about 75,000 hospitalizations annually. RSV disease ranges from upper respiratory tract infections, eg, in older children and healthy adults, to more severe lower tract disease in young children and the elderly. Premature infants and high-risk groups are particularly prone to severe disease.1 Up to 300 pediatric RSV deaths occur yearly. “Normal” RSV seasons start in mid-November, peak in late December-January, and end after April. Note: More drawn out seasons occur in southern latitudes, eg Texas or Florida. But lately RSV seasons have been anything but normal.
2015-2016 to 2022-2023
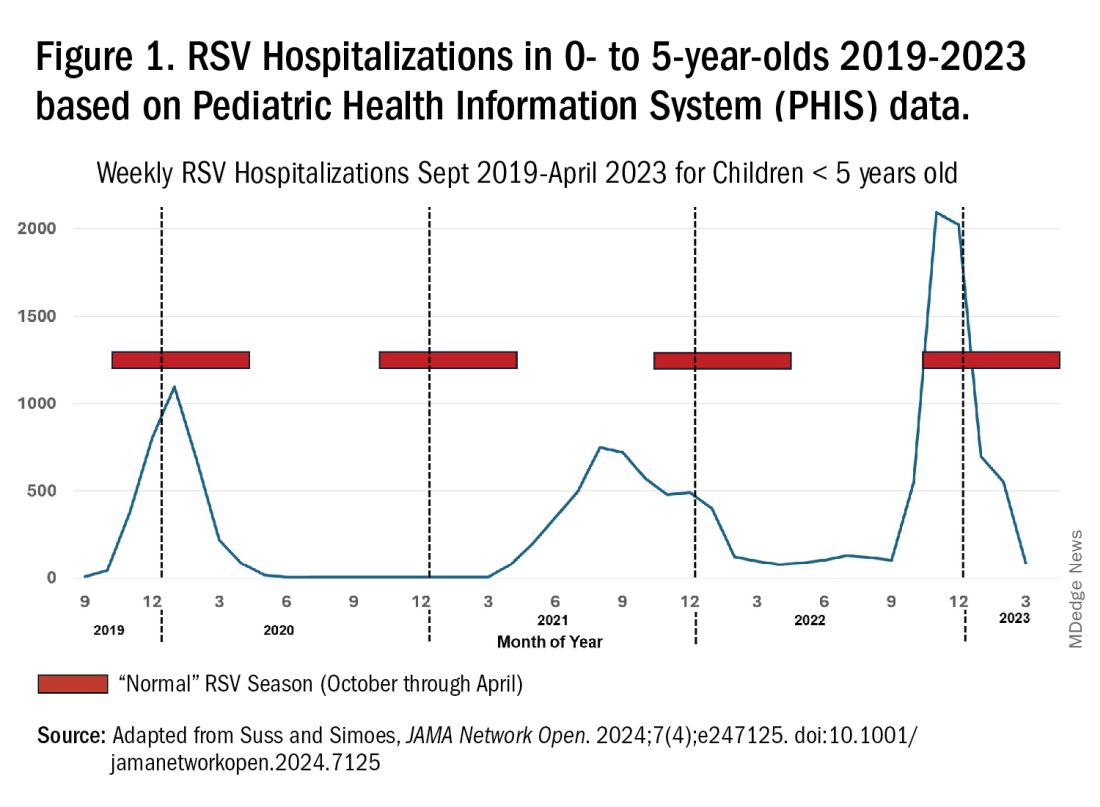
RSV data from the Pediatric Health Information System (PHIS), collected at over 49 US children’s hospitals during 2015 to early 2023, show how crazy RSV seasons have been lately.2 The involved months, intensity, and duration of four prepandemic seasons were pretty “normal” (Figure 1). The 2019-2020 season started normally, peaked in January 2020, and was slowing as expected by February. But when SARS-Cov-2 restrictions kicked in during mid-March, RSV detections tanked to almost nothing (ditto other respiratory viruses). A near 14-month RSV hiatus meant that the 2020-2021 RSV season never materialized. However, RSV was not done with us in 2021. It rebounded in May with weekly hospitalizations peaking in late July; this “rebound season” lasted 9 months, not dropping to baseline until February 2022 (Figure 1).
I guess we should have expected a post-pandemic “disturbance in the Force,” as Yoda once said; but I sure didn’t see a prolonged summer/fall/early winter RSV season coming. It was like two “normal” seasons mashed up into one late-but-long season. Not to be outdone, the 2022-2023 RSV season started early (September) and hospitalizations skyrocketed to peak in November at over twice the peak number from any year since 2015, overloading hospitals (influenza and SARS-Cov-2 seasons were co-circulating). The season terminated early though (March 2023).
Okay, so RSV seasonality/intensity were weird post pandemic, but was anything else different? Some 2021-2023 data suggest more RSV disease in older children, rather than the usual younger than 18 month-olds going through their first winter.3 More medically attended RSV in older ages (2-4 years of life) may have been due to the pandemic year without RSV circulation distorting herd immunity, ie older children remained RSV naive. Other data suggest the apparent increase was really just more frequent multiplex viral testing in older children triggered by SARS-CoV-2 co-circulation.4 More data are needed to decide.
CDC 2023-2024 RESP-NET data
The 2023-2024 winter surge (Figure 2), as measured by RESP-NET’s cumulative RSV, influenza and SARS-CoV-2 hospitalization rates for 0- to 5-year-olds,5 shows that all three viruses’ seasonal months were normal-ish: late October 2023 start, late December-early January peak, and mid-May 2024 return to baseline. RSV season was approximately 22% less severe by area-under-the-curve calculations compared with 2022-2023, but still worse than prepandemic years.6 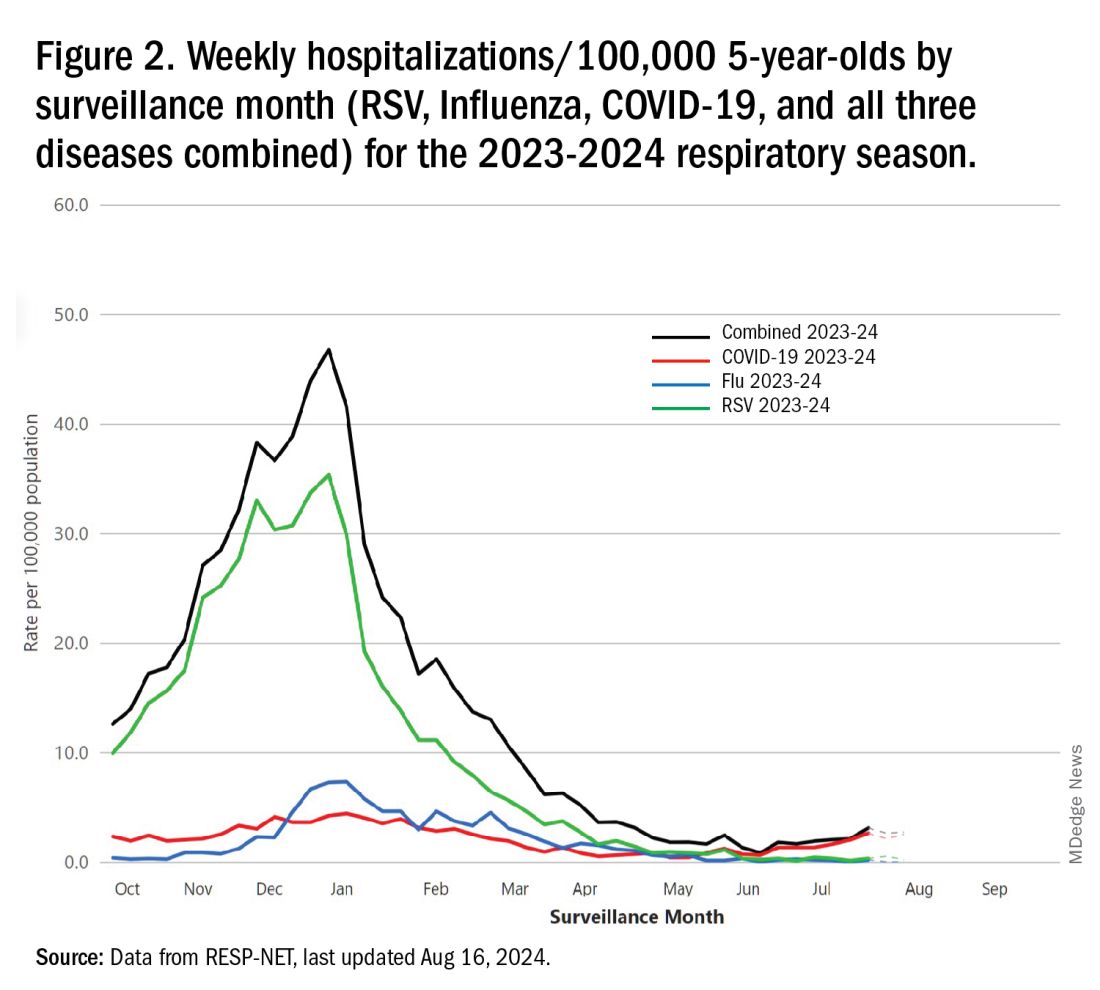
One wonders if the 2022-2023 RSV season might have been worse but for use of the limited supply of nirsevimab.7
Viral Parade
Now we ready ourselves for the 2024-2025 respiratory surge, wondering what nature has in store for us. Will the usual “respiratory virus parade” occur? Will rhinovirus and parainfluenza prevalence bump after a few weeks of schools being in session, adding to the now-usual summer/fall SARS-CoV-2 surge? Note: Twenty-seven states as of Aug. 16 had high SARS-CoV-2 detection in wastewater. Will RSV and influenza start sometime in October/November, peak in January (along with rising SARS-CoV2 activity), followed by a second parainfluenza bump as SARS-CoV-2, influenza, and RSV drop off in April/May? Further, will RSV and influenza seasons be more or less severe than the last 2 years?
Prediction
The overall 2024-2025 respiratory season will be less severe than the past 2 years and hopefully than recent prepandemic years. What is the blueprint for a milder season? First, herd immunity to non-RSV and non-influenza viruses (parainfluenza, rhinovirus, metapneumovirus, adenovirus) in older children should be normalized after 2 years back to usual social activity. So, I expect no mega-seasons from them. The emerging SARS-CoV-2 virus (LB.1) is immunologically close to its recent still-circulating ancestors (KP.2, KP.2.3, KP.3 and KP.3.1.1), so existing SARS-CoV2 herd immunity along with recommended booster vaccine uptake should keep the lid on SARS-CoV2.
Influenza Could Be the Bad News
Which type will dominate? Will a drift/shift occur or vaccine-mismatch reduce vaccine effectiveness? Can we get at least half the population influenza vaccinated, given the vaccine fatigue permeating the US population? The influenza season now underway in the Southern Hemisphere usually helps us predict our season. The Australian May-August 2024 experience (still on an upward trajectory for severity in mid-August) saw no drift/shift or vaccine mismatch. However, this 2024 season has been as severe as 2022 (their worst in a decade). That said, more than 95% has been type A (mostly H1N1 but H3N2 increased in July). So, if our overall 2024-2025 respiratory season is not milder, influenza is the most likely culprit. To reduce chances of influenza being the fly-in-the-ointment, we need to be particularly proactive with seasonal influenza vaccine which is back to the traditional trivalent formulation (one H1N1, one H3N2, and one B type).8 All of this could go out the window if avian influenza becomes more transmissible, but that seems unlikely at present.
Mild RSV Season?
RSV season should be blunted because of the increased use of both the remarkably effective CDC-recommended maternal RSV vaccine9 (one dose during pregnancy weeks 32 through 36, administered September through January) and of nirsevimab (up to 90% reduction in hospitalizations and ED visits).10 (See Figure 3.) 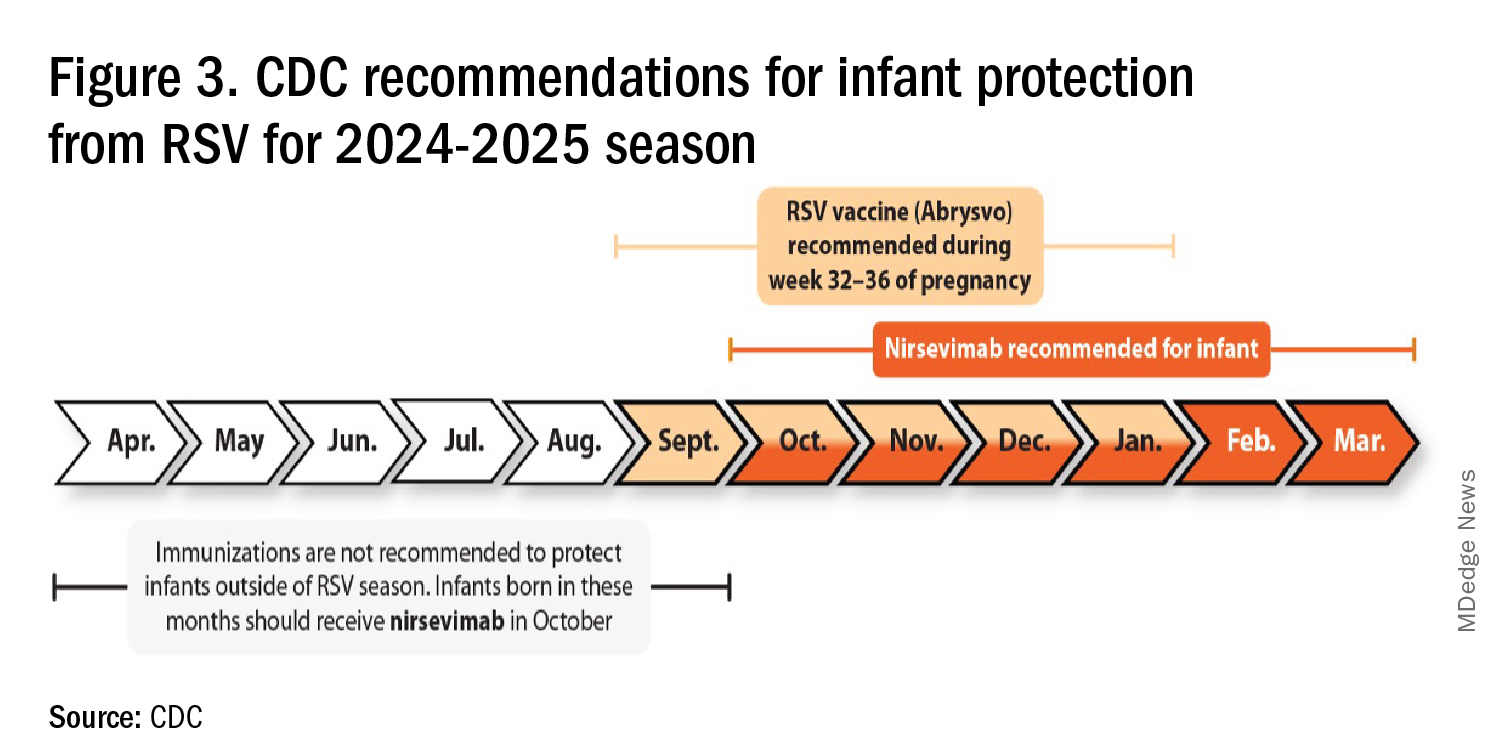
I also expect residual disease to occur mostly in younger than 18 month-olds (the “normal” aged population experiencing their first winter), who received no passive immunity (mother RSV unvaccinated and child did not receive nirsevimab). Some disease will still occur in high-risk infants/children. However, unlike active vaccination strategies, a competent immune system is not required to benefit from passive antibody, whether transplacental or directly administered.
Deep Thought
What if the traditional RSV seasonal hospitalization surge fails to materialize this season? It could happen. If we could get high acceptance/uptake of maternal vaccine and infant nirsevimab, RSV season could resemble the dramatic drop in rotavirus disease the second year after rotavirus vaccine introduction. We could be asking ourselves — “What happened to RSV?”
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Missouri. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. CDC. RSV in Infants and Young Children. Respiratory Syncytial Virus Infection (RSV). June 18, 2024. https://www.cdc.gov/rsv/infants-young-children/index.html.
2. Suss RJ and Simões EAF. Respiratory Syncytial Virus Hospital-Based Burden of Disease in Children Younger Than 5 Respiratory Syncytial Virus Hospital-Based Burden of Disease in Children Younger Than 5 Years, 2015-2022. JAMA Netw Open. 2024;7(4):e247125. doi:10.1001/jamanetworkopen.2024.7125.
3. Winthrop ZA et al. Pediatric Respiratory Syncytial Virus Hospitalizations and Respiratory Support After the COVID-19 Pandemic. JAMA Netw Open. 2024;7(6):e2416852. doi:10.1001/jamanetworkopen.2024.16852.
4. Petros BA et al. Increased Pediatric RSV Case Counts Following the Emergence of SARS-CoV-2 Are Attributable to Increased Testing. medRxiv [Preprint]. 2024 Feb 12:2024.02.06.24302387. doi: 10.1101/2024.02.06.24302387.
5. Rates of Laboratory-Confirmed RSV, COVID-19, and Flu Hospitalizations from the RESP-NET Surveillance Systems. Centers for Disease Control and Prevention. https://data.cdc.gov/Public-Health-Surveillance/Rates-of-Laboratory-Confirmed-RSV-COVID-19-and-Flu/kvib-3txy/about_data.
6. CDC. Evaluating the 2023-2024 Respiratory Disease Season Outlook. CFA: Qualitative Assessments. August 14, 2024. https://www.cdc.gov/cfa-qualitative-assessments/php/data-research/2023-2024-season-outlook-retro.html.
7. Health Alert Network (HAN). Limited Availability of Nirsevimab in the United States—Interim CDC Recommendations to Protect Infants from Respiratory Syncytial Virus (RSV) during the 2023–2024 Respiratory Virus Season. October 23, 2023. https://emergency.cdc.gov/han/2023/han00499.asp.
8. CDC. Information for the 2024-2025 Flu Season. Centers for Disease Control and Prevention. March 14, 2024. https://www.cdc.gov/flu/season/faq-flu-season-2024-2025.htm.
9. Kampmann B et al. Bivalent Prefusion F Vaccine in Pregnancy to Prevent RSV Illness in Infants. N Engl J Med. 2023 Apr 20;388(16):1451-1464. doi: 10.1056/NEJMoa2216480.
10. Moline HL. Early Estimate of Nirsevimab Effectiveness for Prevention of Respiratory Syncytial Virus–Associated Hospitalization Among Infants Entering Their First Respiratory Syncytial Virus Season — New Vaccine Surveillance Network, October 2023–February 2024. MMWR Morb Mortal Wkly Rep. 2024;73. doi: 10.15585/mmwr.mm7309a4.
For children younger than 5 years old, RSV is the main drive — approximately 2,000,000 outpatient/ED visits and about 75,000 hospitalizations annually. RSV disease ranges from upper respiratory tract infections, eg, in older children and healthy adults, to more severe lower tract disease in young children and the elderly. Premature infants and high-risk groups are particularly prone to severe disease.1 Up to 300 pediatric RSV deaths occur yearly. “Normal” RSV seasons start in mid-November, peak in late December-January, and end after April. Note: More drawn out seasons occur in southern latitudes, eg Texas or Florida. But lately RSV seasons have been anything but normal.
2015-2016 to 2022-2023
RSV data from the Pediatric Health Information System (PHIS), collected at over 49 US children’s hospitals during 2015 to early 2023, show how crazy RSV seasons have been lately.2 The involved months, intensity, and duration of four prepandemic seasons were pretty “normal” (Figure 1). The 2019-2020 season started normally, peaked in January 2020, and was slowing as expected by February. But when SARS-Cov-2 restrictions kicked in during mid-March, RSV detections tanked to almost nothing (ditto other respiratory viruses). A near 14-month RSV hiatus meant that the 2020-2021 RSV season never materialized. However, RSV was not done with us in 2021. It rebounded in May with weekly hospitalizations peaking in late July; this “rebound season” lasted 9 months, not dropping to baseline until February 2022 (Figure 1).
I guess we should have expected a post-pandemic “disturbance in the Force,” as Yoda once said; but I sure didn’t see a prolonged summer/fall/early winter RSV season coming. It was like two “normal” seasons mashed up into one late-but-long season. Not to be outdone, the 2022-2023 RSV season started early (September) and hospitalizations skyrocketed to peak in November at over twice the peak number from any year since 2015, overloading hospitals (influenza and SARS-Cov-2 seasons were co-circulating). The season terminated early though (March 2023).
Okay, so RSV seasonality/intensity were weird post pandemic, but was anything else different? Some 2021-2023 data suggest more RSV disease in older children, rather than the usual younger than 18 month-olds going through their first winter.3 More medically attended RSV in older ages (2-4 years of life) may have been due to the pandemic year without RSV circulation distorting herd immunity, ie older children remained RSV naive. Other data suggest the apparent increase was really just more frequent multiplex viral testing in older children triggered by SARS-CoV-2 co-circulation.4 More data are needed to decide.
CDC 2023-2024 RESP-NET data
The 2023-2024 winter surge (Figure 2), as measured by RESP-NET’s cumulative RSV, influenza and SARS-CoV-2 hospitalization rates for 0- to 5-year-olds,5 shows that all three viruses’ seasonal months were normal-ish: late October 2023 start, late December-early January peak, and mid-May 2024 return to baseline. RSV season was approximately 22% less severe by area-under-the-curve calculations compared with 2022-2023, but still worse than prepandemic years.6 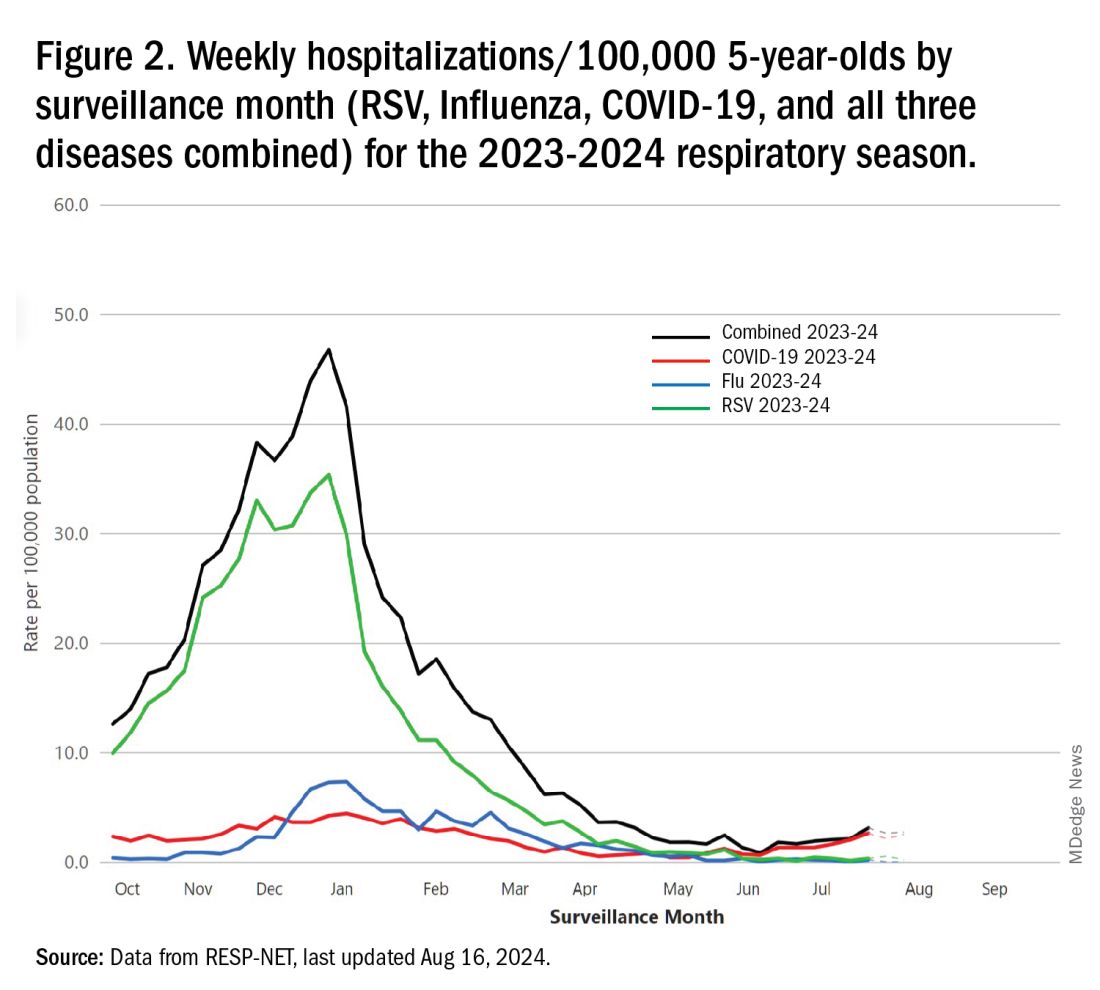
One wonders if the 2022-2023 RSV season might have been worse but for use of the limited supply of nirsevimab.7
Viral Parade
Now we ready ourselves for the 2024-2025 respiratory surge, wondering what nature has in store for us. Will the usual “respiratory virus parade” occur? Will rhinovirus and parainfluenza prevalence bump after a few weeks of schools being in session, adding to the now-usual summer/fall SARS-CoV-2 surge? Note: Twenty-seven states as of Aug. 16 had high SARS-CoV-2 detection in wastewater. Will RSV and influenza start sometime in October/November, peak in January (along with rising SARS-CoV2 activity), followed by a second parainfluenza bump as SARS-CoV-2, influenza, and RSV drop off in April/May? Further, will RSV and influenza seasons be more or less severe than the last 2 years?
Prediction
The overall 2024-2025 respiratory season will be less severe than the past 2 years and hopefully than recent prepandemic years. What is the blueprint for a milder season? First, herd immunity to non-RSV and non-influenza viruses (parainfluenza, rhinovirus, metapneumovirus, adenovirus) in older children should be normalized after 2 years back to usual social activity. So, I expect no mega-seasons from them. The emerging SARS-CoV-2 virus (LB.1) is immunologically close to its recent still-circulating ancestors (KP.2, KP.2.3, KP.3 and KP.3.1.1), so existing SARS-CoV2 herd immunity along with recommended booster vaccine uptake should keep the lid on SARS-CoV2.
Influenza Could Be the Bad News
Which type will dominate? Will a drift/shift occur or vaccine-mismatch reduce vaccine effectiveness? Can we get at least half the population influenza vaccinated, given the vaccine fatigue permeating the US population? The influenza season now underway in the Southern Hemisphere usually helps us predict our season. The Australian May-August 2024 experience (still on an upward trajectory for severity in mid-August) saw no drift/shift or vaccine mismatch. However, this 2024 season has been as severe as 2022 (their worst in a decade). That said, more than 95% has been type A (mostly H1N1 but H3N2 increased in July). So, if our overall 2024-2025 respiratory season is not milder, influenza is the most likely culprit. To reduce chances of influenza being the fly-in-the-ointment, we need to be particularly proactive with seasonal influenza vaccine which is back to the traditional trivalent formulation (one H1N1, one H3N2, and one B type).8 All of this could go out the window if avian influenza becomes more transmissible, but that seems unlikely at present.
Mild RSV Season?
RSV season should be blunted because of the increased use of both the remarkably effective CDC-recommended maternal RSV vaccine9 (one dose during pregnancy weeks 32 through 36, administered September through January) and of nirsevimab (up to 90% reduction in hospitalizations and ED visits).10 (See Figure 3.) 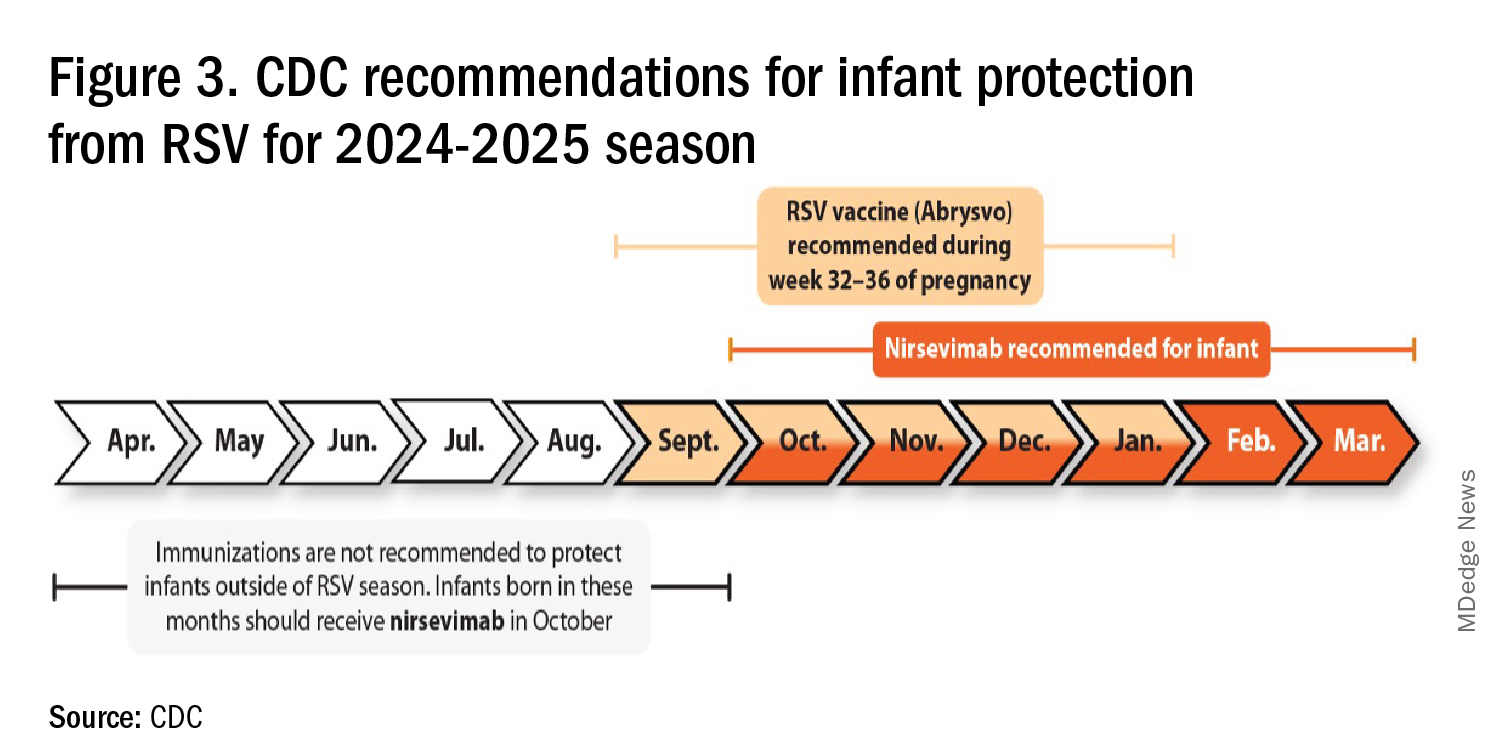
I also expect residual disease to occur mostly in younger than 18 month-olds (the “normal” aged population experiencing their first winter), who received no passive immunity (mother RSV unvaccinated and child did not receive nirsevimab). Some disease will still occur in high-risk infants/children. However, unlike active vaccination strategies, a competent immune system is not required to benefit from passive antibody, whether transplacental or directly administered.
Deep Thought
What if the traditional RSV seasonal hospitalization surge fails to materialize this season? It could happen. If we could get high acceptance/uptake of maternal vaccine and infant nirsevimab, RSV season could resemble the dramatic drop in rotavirus disease the second year after rotavirus vaccine introduction. We could be asking ourselves — “What happened to RSV?”
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Missouri. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. CDC. RSV in Infants and Young Children. Respiratory Syncytial Virus Infection (RSV). June 18, 2024. https://www.cdc.gov/rsv/infants-young-children/index.html.
2. Suss RJ and Simões EAF. Respiratory Syncytial Virus Hospital-Based Burden of Disease in Children Younger Than 5 Respiratory Syncytial Virus Hospital-Based Burden of Disease in Children Younger Than 5 Years, 2015-2022. JAMA Netw Open. 2024;7(4):e247125. doi:10.1001/jamanetworkopen.2024.7125.
3. Winthrop ZA et al. Pediatric Respiratory Syncytial Virus Hospitalizations and Respiratory Support After the COVID-19 Pandemic. JAMA Netw Open. 2024;7(6):e2416852. doi:10.1001/jamanetworkopen.2024.16852.
4. Petros BA et al. Increased Pediatric RSV Case Counts Following the Emergence of SARS-CoV-2 Are Attributable to Increased Testing. medRxiv [Preprint]. 2024 Feb 12:2024.02.06.24302387. doi: 10.1101/2024.02.06.24302387.
5. Rates of Laboratory-Confirmed RSV, COVID-19, and Flu Hospitalizations from the RESP-NET Surveillance Systems. Centers for Disease Control and Prevention. https://data.cdc.gov/Public-Health-Surveillance/Rates-of-Laboratory-Confirmed-RSV-COVID-19-and-Flu/kvib-3txy/about_data.
6. CDC. Evaluating the 2023-2024 Respiratory Disease Season Outlook. CFA: Qualitative Assessments. August 14, 2024. https://www.cdc.gov/cfa-qualitative-assessments/php/data-research/2023-2024-season-outlook-retro.html.
7. Health Alert Network (HAN). Limited Availability of Nirsevimab in the United States—Interim CDC Recommendations to Protect Infants from Respiratory Syncytial Virus (RSV) during the 2023–2024 Respiratory Virus Season. October 23, 2023. https://emergency.cdc.gov/han/2023/han00499.asp.
8. CDC. Information for the 2024-2025 Flu Season. Centers for Disease Control and Prevention. March 14, 2024. https://www.cdc.gov/flu/season/faq-flu-season-2024-2025.htm.
9. Kampmann B et al. Bivalent Prefusion F Vaccine in Pregnancy to Prevent RSV Illness in Infants. N Engl J Med. 2023 Apr 20;388(16):1451-1464. doi: 10.1056/NEJMoa2216480.
10. Moline HL. Early Estimate of Nirsevimab Effectiveness for Prevention of Respiratory Syncytial Virus–Associated Hospitalization Among Infants Entering Their First Respiratory Syncytial Virus Season — New Vaccine Surveillance Network, October 2023–February 2024. MMWR Morb Mortal Wkly Rep. 2024;73. doi: 10.15585/mmwr.mm7309a4.
For children younger than 5 years old, RSV is the main drive — approximately 2,000,000 outpatient/ED visits and about 75,000 hospitalizations annually. RSV disease ranges from upper respiratory tract infections, eg, in older children and healthy adults, to more severe lower tract disease in young children and the elderly. Premature infants and high-risk groups are particularly prone to severe disease.1 Up to 300 pediatric RSV deaths occur yearly. “Normal” RSV seasons start in mid-November, peak in late December-January, and end after April. Note: More drawn out seasons occur in southern latitudes, eg Texas or Florida. But lately RSV seasons have been anything but normal.
2015-2016 to 2022-2023
RSV data from the Pediatric Health Information System (PHIS), collected at over 49 US children’s hospitals during 2015 to early 2023, show how crazy RSV seasons have been lately.2 The involved months, intensity, and duration of four prepandemic seasons were pretty “normal” (Figure 1). The 2019-2020 season started normally, peaked in January 2020, and was slowing as expected by February. But when SARS-Cov-2 restrictions kicked in during mid-March, RSV detections tanked to almost nothing (ditto other respiratory viruses). A near 14-month RSV hiatus meant that the 2020-2021 RSV season never materialized. However, RSV was not done with us in 2021. It rebounded in May with weekly hospitalizations peaking in late July; this “rebound season” lasted 9 months, not dropping to baseline until February 2022 (Figure 1).
I guess we should have expected a post-pandemic “disturbance in the Force,” as Yoda once said; but I sure didn’t see a prolonged summer/fall/early winter RSV season coming. It was like two “normal” seasons mashed up into one late-but-long season. Not to be outdone, the 2022-2023 RSV season started early (September) and hospitalizations skyrocketed to peak in November at over twice the peak number from any year since 2015, overloading hospitals (influenza and SARS-Cov-2 seasons were co-circulating). The season terminated early though (March 2023).
Okay, so RSV seasonality/intensity were weird post pandemic, but was anything else different? Some 2021-2023 data suggest more RSV disease in older children, rather than the usual younger than 18 month-olds going through their first winter.3 More medically attended RSV in older ages (2-4 years of life) may have been due to the pandemic year without RSV circulation distorting herd immunity, ie older children remained RSV naive. Other data suggest the apparent increase was really just more frequent multiplex viral testing in older children triggered by SARS-CoV-2 co-circulation.4 More data are needed to decide.
CDC 2023-2024 RESP-NET data
The 2023-2024 winter surge (Figure 2), as measured by RESP-NET’s cumulative RSV, influenza and SARS-CoV-2 hospitalization rates for 0- to 5-year-olds,5 shows that all three viruses’ seasonal months were normal-ish: late October 2023 start, late December-early January peak, and mid-May 2024 return to baseline. RSV season was approximately 22% less severe by area-under-the-curve calculations compared with 2022-2023, but still worse than prepandemic years.6 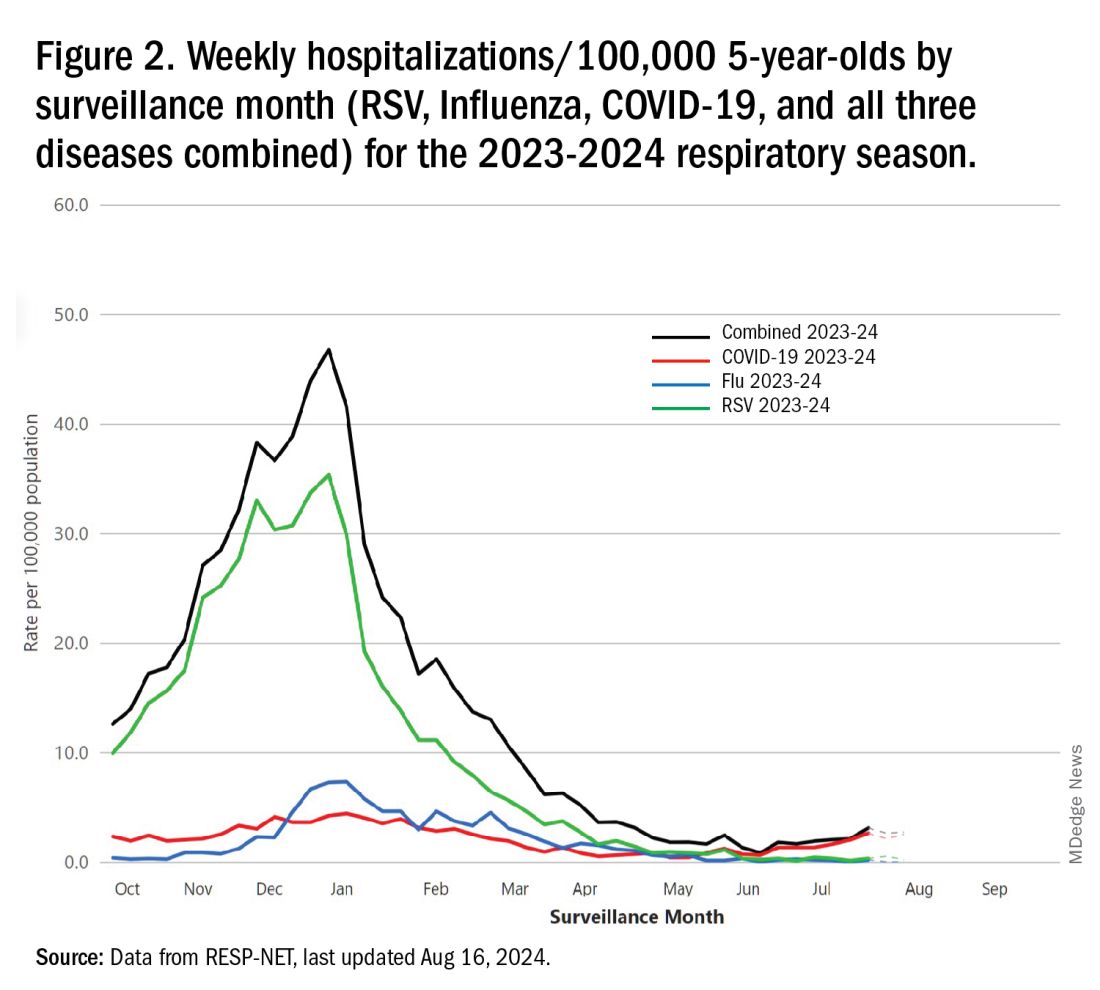
One wonders if the 2022-2023 RSV season might have been worse but for use of the limited supply of nirsevimab.7
Viral Parade
Now we ready ourselves for the 2024-2025 respiratory surge, wondering what nature has in store for us. Will the usual “respiratory virus parade” occur? Will rhinovirus and parainfluenza prevalence bump after a few weeks of schools being in session, adding to the now-usual summer/fall SARS-CoV-2 surge? Note: Twenty-seven states as of Aug. 16 had high SARS-CoV-2 detection in wastewater. Will RSV and influenza start sometime in October/November, peak in January (along with rising SARS-CoV2 activity), followed by a second parainfluenza bump as SARS-CoV-2, influenza, and RSV drop off in April/May? Further, will RSV and influenza seasons be more or less severe than the last 2 years?
Prediction
The overall 2024-2025 respiratory season will be less severe than the past 2 years and hopefully than recent prepandemic years. What is the blueprint for a milder season? First, herd immunity to non-RSV and non-influenza viruses (parainfluenza, rhinovirus, metapneumovirus, adenovirus) in older children should be normalized after 2 years back to usual social activity. So, I expect no mega-seasons from them. The emerging SARS-CoV-2 virus (LB.1) is immunologically close to its recent still-circulating ancestors (KP.2, KP.2.3, KP.3 and KP.3.1.1), so existing SARS-CoV2 herd immunity along with recommended booster vaccine uptake should keep the lid on SARS-CoV2.
Influenza Could Be the Bad News
Which type will dominate? Will a drift/shift occur or vaccine-mismatch reduce vaccine effectiveness? Can we get at least half the population influenza vaccinated, given the vaccine fatigue permeating the US population? The influenza season now underway in the Southern Hemisphere usually helps us predict our season. The Australian May-August 2024 experience (still on an upward trajectory for severity in mid-August) saw no drift/shift or vaccine mismatch. However, this 2024 season has been as severe as 2022 (their worst in a decade). That said, more than 95% has been type A (mostly H1N1 but H3N2 increased in July). So, if our overall 2024-2025 respiratory season is not milder, influenza is the most likely culprit. To reduce chances of influenza being the fly-in-the-ointment, we need to be particularly proactive with seasonal influenza vaccine which is back to the traditional trivalent formulation (one H1N1, one H3N2, and one B type).8 All of this could go out the window if avian influenza becomes more transmissible, but that seems unlikely at present.
Mild RSV Season?
RSV season should be blunted because of the increased use of both the remarkably effective CDC-recommended maternal RSV vaccine9 (one dose during pregnancy weeks 32 through 36, administered September through January) and of nirsevimab (up to 90% reduction in hospitalizations and ED visits).10 (See Figure 3.) 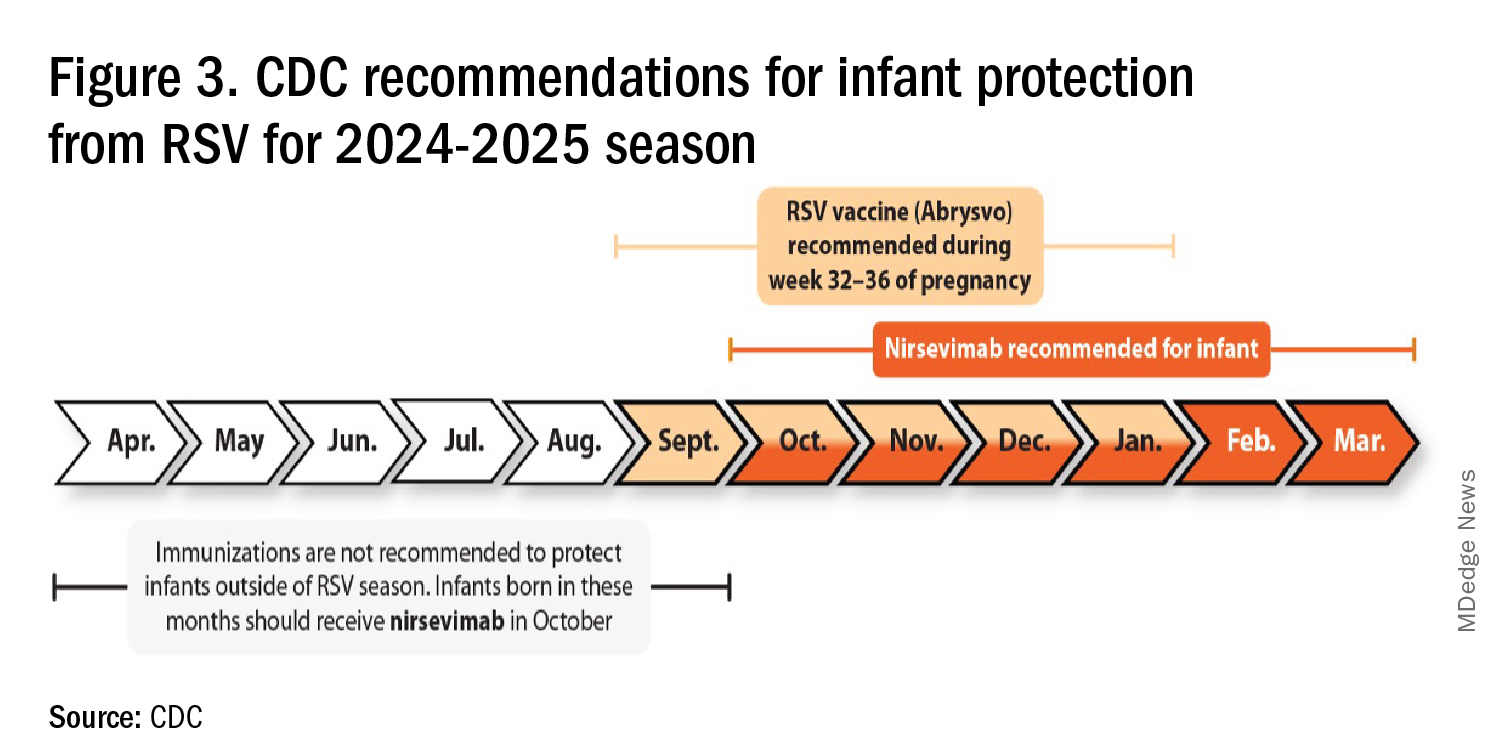
I also expect residual disease to occur mostly in younger than 18 month-olds (the “normal” aged population experiencing their first winter), who received no passive immunity (mother RSV unvaccinated and child did not receive nirsevimab). Some disease will still occur in high-risk infants/children. However, unlike active vaccination strategies, a competent immune system is not required to benefit from passive antibody, whether transplacental or directly administered.
Deep Thought
What if the traditional RSV seasonal hospitalization surge fails to materialize this season? It could happen. If we could get high acceptance/uptake of maternal vaccine and infant nirsevimab, RSV season could resemble the dramatic drop in rotavirus disease the second year after rotavirus vaccine introduction. We could be asking ourselves — “What happened to RSV?”
Dr. Harrison is professor of pediatrics and pediatric infectious diseases at Children’s Mercy Hospitals and Clinics, Kansas City, Missouri. He said he had no relevant financial disclosures. Email him at [email protected].
References
1. CDC. RSV in Infants and Young Children. Respiratory Syncytial Virus Infection (RSV). June 18, 2024. https://www.cdc.gov/rsv/infants-young-children/index.html.
2. Suss RJ and Simões EAF. Respiratory Syncytial Virus Hospital-Based Burden of Disease in Children Younger Than 5 Respiratory Syncytial Virus Hospital-Based Burden of Disease in Children Younger Than 5 Years, 2015-2022. JAMA Netw Open. 2024;7(4):e247125. doi:10.1001/jamanetworkopen.2024.7125.
3. Winthrop ZA et al. Pediatric Respiratory Syncytial Virus Hospitalizations and Respiratory Support After the COVID-19 Pandemic. JAMA Netw Open. 2024;7(6):e2416852. doi:10.1001/jamanetworkopen.2024.16852.
4. Petros BA et al. Increased Pediatric RSV Case Counts Following the Emergence of SARS-CoV-2 Are Attributable to Increased Testing. medRxiv [Preprint]. 2024 Feb 12:2024.02.06.24302387. doi: 10.1101/2024.02.06.24302387.
5. Rates of Laboratory-Confirmed RSV, COVID-19, and Flu Hospitalizations from the RESP-NET Surveillance Systems. Centers for Disease Control and Prevention. https://data.cdc.gov/Public-Health-Surveillance/Rates-of-Laboratory-Confirmed-RSV-COVID-19-and-Flu/kvib-3txy/about_data.
6. CDC. Evaluating the 2023-2024 Respiratory Disease Season Outlook. CFA: Qualitative Assessments. August 14, 2024. https://www.cdc.gov/cfa-qualitative-assessments/php/data-research/2023-2024-season-outlook-retro.html.
7. Health Alert Network (HAN). Limited Availability of Nirsevimab in the United States—Interim CDC Recommendations to Protect Infants from Respiratory Syncytial Virus (RSV) during the 2023–2024 Respiratory Virus Season. October 23, 2023. https://emergency.cdc.gov/han/2023/han00499.asp.
8. CDC. Information for the 2024-2025 Flu Season. Centers for Disease Control and Prevention. March 14, 2024. https://www.cdc.gov/flu/season/faq-flu-season-2024-2025.htm.
9. Kampmann B et al. Bivalent Prefusion F Vaccine in Pregnancy to Prevent RSV Illness in Infants. N Engl J Med. 2023 Apr 20;388(16):1451-1464. doi: 10.1056/NEJMoa2216480.
10. Moline HL. Early Estimate of Nirsevimab Effectiveness for Prevention of Respiratory Syncytial Virus–Associated Hospitalization Among Infants Entering Their First Respiratory Syncytial Virus Season — New Vaccine Surveillance Network, October 2023–February 2024. MMWR Morb Mortal Wkly Rep. 2024;73. doi: 10.15585/mmwr.mm7309a4.
A 7-Month-Old Female Presented With Nail Changes
Given the clinical presentation and the absence of other systemic or dermatological findings, the diagnosis of chevron nails was made.
Discussion
The condition is characterized by transverse ridges on the nails that converge towards the center, forming a V or chevron shape. This condition was first described by Perry et al. and later by Shuster et al., who explained that the condition might result from axial growth of the nail with synchronous growth occurring from a chevron-shaped growing edge of the nail root. Alternatively, Shuster suggested that sequential growth, with localized variation in the nail production rate, could propagate a wave from the center of the nail to the edge.
The etiology of chevron nails is not well understood, but it is believed to result from temporary disruptions in the nail matrix, possibly related to minor illness or physiological stress during infancy.
In the case of our 7-month-old patient, the history of mild upper respiratory infections might have contributed to the development of chevron nails. However, the lack of other significant illness, skin involvement, or systemic findings supports the benign and self-limiting nature of this condition. Parents were reassured that chevron nails typically resolve on their own as the child grows and that no specific treatment is necessary.
Differential Diagnosis
The differential diagnosis of transverse nail changes in children includes other conditions such as trachyonychia, lichen planus, Darier disease, and pachyonychia congenita.
Trachyonychia, also known as “sandpaper nails,” trachyonychia is characterized by the roughening of the nail surface, giving it a dull and ridged appearance. The condition may affect all 20 nails and is often associated with underlying dermatological conditions such as lichen planus or alopecia areata. Unlike chevron nails, trachyonychia presents with more diffuse nail changes and does not typically feature the distinct V-shaped ridging seen in this patient.
Lichen planus is an inflammatory condition that can affect the skin, mucous membranes, and nails. Nail involvement in lichen planus can lead to longitudinal ridging, thinning, and sometimes even complete nail loss. The absence of other characteristic features of lichen planus, such as violaceous papules on the skin or white lacy patterns on mucous membranes (Wickham striae), makes this diagnosis less likely in our patient.
Darier disease, also known as keratosis follicularis, is a genetic disorder characterized by greasy, warty papules primarily on seborrheic areas of the skin, nail abnormalities, and sometimes mucosal involvement. Nail changes in Darier disease include longitudinal red and white streaks, V-shaped notching at the free edge of the nails, and subungual hyperkeratosis. These nail changes are more severe and distinct than the simple transverse ridging seen in chevron nails. The absence of other clinical signs of Darier disease, such as skin papules or characteristic nail notching, makes this diagnosis unlikely in our patient.
Pachyonychia congenita is a rare genetic disorder characterized by thickened nails (pachyonychia), painful plantar keratoderma, and sometimes oral leukokeratosis. The condition typically presents with significant nail thickening and other systemic findings, which were absent in our patient. The distinct pattern of V-shaped ridging observed in chevron nails does not align with the typical presentation of pachyonychia congenita.
Next Steps
No specific treatment is required for chevron nails. The condition is typically self-resolving, and the nails usually return to a normal appearance as the child continues to grow. Parents were advised to monitor the nails for any changes or new symptoms and were reassured about the benign nature of the findings. Follow-up was scheduled to ensure the resolution of the condition as the child develops.
Conclusion
Chevron nails are an important consideration in the differential diagnosis of transverse nail ridging in infants and young children. While the condition is benign and self-limiting, it is crucial to differentiate it from other nail dystrophies, such as trachyonychia, lichen planus, Darier disease, and pachyonychia congenita, which may require further investigation or intervention. Awareness of chevron nails can help prevent unnecessary worry and provide reassurance to parents and caregivers.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
Suggested Reading
Delano S, Belazarian L. Chevron nails: A normal variant in the pediatric population. Pediatr Dermatol. 2014 Jan-Feb;31(1):e24-5. doi: 10.1111/pde.12193.
John JM et al. Chevron nail — An under-recognised normal variant of nail development. Arch Dis Child. 2024 Jul 18;109(8):648. doi: 10.1136/archdischild-2024-326975.
Shuster S. The significance of chevron nails. Br J Dermatol. 1996;135:151–152. doi: 10.1046/j.1365-2133.1996.d01-961.x.
Starace M et al. Nail disorders in children. Skin Appendage Disord. 2018 Oct;4(4):217-229. doi: 10.1159/000486020.
Given the clinical presentation and the absence of other systemic or dermatological findings, the diagnosis of chevron nails was made.
Discussion
The condition is characterized by transverse ridges on the nails that converge towards the center, forming a V or chevron shape. This condition was first described by Perry et al. and later by Shuster et al., who explained that the condition might result from axial growth of the nail with synchronous growth occurring from a chevron-shaped growing edge of the nail root. Alternatively, Shuster suggested that sequential growth, with localized variation in the nail production rate, could propagate a wave from the center of the nail to the edge.
The etiology of chevron nails is not well understood, but it is believed to result from temporary disruptions in the nail matrix, possibly related to minor illness or physiological stress during infancy.
In the case of our 7-month-old patient, the history of mild upper respiratory infections might have contributed to the development of chevron nails. However, the lack of other significant illness, skin involvement, or systemic findings supports the benign and self-limiting nature of this condition. Parents were reassured that chevron nails typically resolve on their own as the child grows and that no specific treatment is necessary.
Differential Diagnosis
The differential diagnosis of transverse nail changes in children includes other conditions such as trachyonychia, lichen planus, Darier disease, and pachyonychia congenita.
Trachyonychia, also known as “sandpaper nails,” trachyonychia is characterized by the roughening of the nail surface, giving it a dull and ridged appearance. The condition may affect all 20 nails and is often associated with underlying dermatological conditions such as lichen planus or alopecia areata. Unlike chevron nails, trachyonychia presents with more diffuse nail changes and does not typically feature the distinct V-shaped ridging seen in this patient.
Lichen planus is an inflammatory condition that can affect the skin, mucous membranes, and nails. Nail involvement in lichen planus can lead to longitudinal ridging, thinning, and sometimes even complete nail loss. The absence of other characteristic features of lichen planus, such as violaceous papules on the skin or white lacy patterns on mucous membranes (Wickham striae), makes this diagnosis less likely in our patient.
Darier disease, also known as keratosis follicularis, is a genetic disorder characterized by greasy, warty papules primarily on seborrheic areas of the skin, nail abnormalities, and sometimes mucosal involvement. Nail changes in Darier disease include longitudinal red and white streaks, V-shaped notching at the free edge of the nails, and subungual hyperkeratosis. These nail changes are more severe and distinct than the simple transverse ridging seen in chevron nails. The absence of other clinical signs of Darier disease, such as skin papules or characteristic nail notching, makes this diagnosis unlikely in our patient.
Pachyonychia congenita is a rare genetic disorder characterized by thickened nails (pachyonychia), painful plantar keratoderma, and sometimes oral leukokeratosis. The condition typically presents with significant nail thickening and other systemic findings, which were absent in our patient. The distinct pattern of V-shaped ridging observed in chevron nails does not align with the typical presentation of pachyonychia congenita.
Next Steps
No specific treatment is required for chevron nails. The condition is typically self-resolving, and the nails usually return to a normal appearance as the child continues to grow. Parents were advised to monitor the nails for any changes or new symptoms and were reassured about the benign nature of the findings. Follow-up was scheduled to ensure the resolution of the condition as the child develops.
Conclusion
Chevron nails are an important consideration in the differential diagnosis of transverse nail ridging in infants and young children. While the condition is benign and self-limiting, it is crucial to differentiate it from other nail dystrophies, such as trachyonychia, lichen planus, Darier disease, and pachyonychia congenita, which may require further investigation or intervention. Awareness of chevron nails can help prevent unnecessary worry and provide reassurance to parents and caregivers.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
Suggested Reading
Delano S, Belazarian L. Chevron nails: A normal variant in the pediatric population. Pediatr Dermatol. 2014 Jan-Feb;31(1):e24-5. doi: 10.1111/pde.12193.
John JM et al. Chevron nail — An under-recognised normal variant of nail development. Arch Dis Child. 2024 Jul 18;109(8):648. doi: 10.1136/archdischild-2024-326975.
Shuster S. The significance of chevron nails. Br J Dermatol. 1996;135:151–152. doi: 10.1046/j.1365-2133.1996.d01-961.x.
Starace M et al. Nail disorders in children. Skin Appendage Disord. 2018 Oct;4(4):217-229. doi: 10.1159/000486020.
Given the clinical presentation and the absence of other systemic or dermatological findings, the diagnosis of chevron nails was made.
Discussion
The condition is characterized by transverse ridges on the nails that converge towards the center, forming a V or chevron shape. This condition was first described by Perry et al. and later by Shuster et al., who explained that the condition might result from axial growth of the nail with synchronous growth occurring from a chevron-shaped growing edge of the nail root. Alternatively, Shuster suggested that sequential growth, with localized variation in the nail production rate, could propagate a wave from the center of the nail to the edge.
The etiology of chevron nails is not well understood, but it is believed to result from temporary disruptions in the nail matrix, possibly related to minor illness or physiological stress during infancy.
In the case of our 7-month-old patient, the history of mild upper respiratory infections might have contributed to the development of chevron nails. However, the lack of other significant illness, skin involvement, or systemic findings supports the benign and self-limiting nature of this condition. Parents were reassured that chevron nails typically resolve on their own as the child grows and that no specific treatment is necessary.
Differential Diagnosis
The differential diagnosis of transverse nail changes in children includes other conditions such as trachyonychia, lichen planus, Darier disease, and pachyonychia congenita.
Trachyonychia, also known as “sandpaper nails,” trachyonychia is characterized by the roughening of the nail surface, giving it a dull and ridged appearance. The condition may affect all 20 nails and is often associated with underlying dermatological conditions such as lichen planus or alopecia areata. Unlike chevron nails, trachyonychia presents with more diffuse nail changes and does not typically feature the distinct V-shaped ridging seen in this patient.
Lichen planus is an inflammatory condition that can affect the skin, mucous membranes, and nails. Nail involvement in lichen planus can lead to longitudinal ridging, thinning, and sometimes even complete nail loss. The absence of other characteristic features of lichen planus, such as violaceous papules on the skin or white lacy patterns on mucous membranes (Wickham striae), makes this diagnosis less likely in our patient.
Darier disease, also known as keratosis follicularis, is a genetic disorder characterized by greasy, warty papules primarily on seborrheic areas of the skin, nail abnormalities, and sometimes mucosal involvement. Nail changes in Darier disease include longitudinal red and white streaks, V-shaped notching at the free edge of the nails, and subungual hyperkeratosis. These nail changes are more severe and distinct than the simple transverse ridging seen in chevron nails. The absence of other clinical signs of Darier disease, such as skin papules or characteristic nail notching, makes this diagnosis unlikely in our patient.
Pachyonychia congenita is a rare genetic disorder characterized by thickened nails (pachyonychia), painful plantar keratoderma, and sometimes oral leukokeratosis. The condition typically presents with significant nail thickening and other systemic findings, which were absent in our patient. The distinct pattern of V-shaped ridging observed in chevron nails does not align with the typical presentation of pachyonychia congenita.
Next Steps
No specific treatment is required for chevron nails. The condition is typically self-resolving, and the nails usually return to a normal appearance as the child continues to grow. Parents were advised to monitor the nails for any changes or new symptoms and were reassured about the benign nature of the findings. Follow-up was scheduled to ensure the resolution of the condition as the child develops.
Conclusion
Chevron nails are an important consideration in the differential diagnosis of transverse nail ridging in infants and young children. While the condition is benign and self-limiting, it is crucial to differentiate it from other nail dystrophies, such as trachyonychia, lichen planus, Darier disease, and pachyonychia congenita, which may require further investigation or intervention. Awareness of chevron nails can help prevent unnecessary worry and provide reassurance to parents and caregivers.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
Suggested Reading
Delano S, Belazarian L. Chevron nails: A normal variant in the pediatric population. Pediatr Dermatol. 2014 Jan-Feb;31(1):e24-5. doi: 10.1111/pde.12193.
John JM et al. Chevron nail — An under-recognised normal variant of nail development. Arch Dis Child. 2024 Jul 18;109(8):648. doi: 10.1136/archdischild-2024-326975.
Shuster S. The significance of chevron nails. Br J Dermatol. 1996;135:151–152. doi: 10.1046/j.1365-2133.1996.d01-961.x.
Starace M et al. Nail disorders in children. Skin Appendage Disord. 2018 Oct;4(4):217-229. doi: 10.1159/000486020.
There was no family history of similar nail findings and no relatives had a history of chronic skin conditions or congenital nail disorders.
On physical examination, several of the child’s fingernails exhibited distinct longitudinal ridges, with a characteristic pattern where the ridges converged at the center of the nail, forming a V-shape. There were no other concerning dermatologic findings, such as rashes, plaques, or erosions, and the skin and hair appeared otherwise normal. The rest of the physical exam was unremarkable.
New Biological Pathway May Explain BPA Exposure, Autism Link
BPA is a potent endocrine disruptor found in polycarbonate plastics and epoxy resins and has been banned by the Food and Drug Administration for use in baby bottles, sippy cups, and infant formula packaging.
“Exposure to BPA has already been shown in some studies to be associated with subsequent autism in offspring,” lead researcher Anne-Louise Ponsonby, PhD, The Florey Institute, Heidelberg, Australia, said in a statement.
“Our work is important because it demonstrates one of the biological mechanisms potentially involved. BPA can disrupt hormone-controlled male fetal brain development in several ways, including silencing a key enzyme, aromatase, that controls neurohormones and is especially important in fetal male brain development. This appears to be part of the autism puzzle,” she said.
Brain aromatase, encoded by CYP19A1, converts neural androgens to neural estrogens and has been implicated in ASD. Postmortem analyses of men with ASD also show markedly reduced aromatase activity.
The findings were published online in Nature Communications.
New Biological Mechanism
For the study, the researchers analyzed data from the Barwon Infant Study in 1067 infants in Australia. At age 7-11 years, 43 children had a confirmed ASD diagnosis, and 249 infants with Child Behavior Checklist (CBCL) data at age 2 years had an autism spectrum problem score above the median.
The researchers developed a CYP19A1 genetic score for aromatase activity based on five single nucleotide polymorphisms associated with lower estrogen levels. Among 595 children with prenatal BPA and CBCL, those with three or more variants were classified as “low aromatase activity” and the remaining were classified as “high.”
In regression analyses, boys with low aromatase activity and high prenatal BPA exposure (top quartile > 2.18 µg/L) were 3.5 times more likely to have autism symptoms at age 2 years (odds ratio [OR], 3.56; 95% CI, 1.13-11.22).
The odds of a confirmed ASD diagnosis were six times higher at age 9 years only in men with low aromatase activity (OR, 6.24; 95% CI, 1.02-38.26).
The researchers also found that higher BPA levels predicted higher methylation in cord blood across the CYP19A1 brain promoter PI.f region (P = .009).
To replicate the findings, data were used from the Columbia Centre for Children’s Health Study–Mothers and Newborns cohort in the United States. Once again, the BPA level was associated with hypermethylation of the aromatase brain promoter PI.f (P = .0089).
In both cohorts, there was evidence that the effect of increased BPA on brain-derived neurotrophic factor hypermethylation was mediated partly through higher aromatase gene methylation (P = .001).
To validate the findings, the researchers examined human neuroblastoma SH-SY5Y cell lines and found aromatase protein levels were more than halved in the presence of BPA 50 µg/L (P = .01).
Additionally, mouse studies showed that male mice exposed to BPA 50 µg/L mid-gestation and male aromatase knockout mice — but not female mice — had social behavior deficits, such as interacting with a strange mouse, as well as structural and functional brain changes.
“We found that BPA suppresses the aromatase enzyme and is associated with anatomical, neurologic, and behavioral changes in the male mice that may be consistent with autism spectrum disorder,” Wah Chin Boon, PhD, co–lead researcher and research fellow, also with The Florey Institute, said in a statement.
“This is the first time a biological pathway has been identified that might help explain the connection between autism and BPA,” she said.
“In this study, not only were the levels of BPA higher than most people would be exposed to, but in at least one of the experiments the mice were injected with BPA directly, whereas humans would be exposed via food and drink,” observed Oliver Jones, PhD, MSc, professor of chemistry, RMIT University, Melbourne, Australia. “If you ingest the food, it undergoes metabolism before it gets to the bloodstream, which reduces the effective dose.”
Dr. Jones said further studies with larger numbers of participants measuring BPA throughout pregnancy and other chemicals the mother and child were exposed to are needed to be sure of any such link. “Just because there is a possible mechanism in place does not automatically mean that it is activated,” he said.
Dr. Ponsonby pointed out that BPA and other endocrine-disrupting chemicals are “almost impossible for individuals to avoid” and can enter the body through plastic food and drink packaging, home renovation fumes, and sources such as cosmetics.
Fatty Acid Helpful?
Building on earlier observations that 10-hydroxy-2-decenoic acid (10HDA) may have estrogenic modulating activities, the researchers conducted additional studies suggesting that 10HDA may be effective as a competitive ligand that could counteract the effects of BPA on estrogen signaling within cells.
Further, among 3-week-old mice pups prenatally exposed to BPA, daily injections of 10HDA for 3 weeks showed striking and significant improvements in social interaction. Stopping 10HDA resulted in a deficit in social interaction that was again ameliorated by subsequent 10HDA treatment.
“10-hydroxy-2-decenoic acid shows early indications of potential in activating opposing biological pathways to improve autism-like characteristics when administered to animals that have been prenatally exposed to BPA,” Dr. Boon said. “It warrants further studies to see whether this potential treatment could be realized in humans.”
Reached for comment, Dr. Jones said “the human studies are not strong at all,” in large part because BPA levels were tested only once at 36 weeks in the BIS cohort.
“I would argue that if BPA is in the urine, it has been excreted and is no longer in the bloodstream, thus not able to affect the child,” he said. “I’d also argue that a single measurement at 36 weeks cannot give you any idea of the mother’s exposure to BPA over the rest of the pregnancy or what the child was exposed to after birth.”
The study was funded by the Minderoo Foundation, the National Health and Medical Research Council of Australia, the Australian Research Council, and numerous other sponsors. Dr. Boon is a coinventor on “Methods of treating neurodevelopmental diseases and disorders” and is a board member of Meizon Innovation Holdings. Dr. Ponsonby is a scientific adviser to Meizon Innovation Holdings. The remaining authors declared no competing interests.
A version of this article first appeared on Medscape.com.
BPA is a potent endocrine disruptor found in polycarbonate plastics and epoxy resins and has been banned by the Food and Drug Administration for use in baby bottles, sippy cups, and infant formula packaging.
“Exposure to BPA has already been shown in some studies to be associated with subsequent autism in offspring,” lead researcher Anne-Louise Ponsonby, PhD, The Florey Institute, Heidelberg, Australia, said in a statement.
“Our work is important because it demonstrates one of the biological mechanisms potentially involved. BPA can disrupt hormone-controlled male fetal brain development in several ways, including silencing a key enzyme, aromatase, that controls neurohormones and is especially important in fetal male brain development. This appears to be part of the autism puzzle,” she said.
Brain aromatase, encoded by CYP19A1, converts neural androgens to neural estrogens and has been implicated in ASD. Postmortem analyses of men with ASD also show markedly reduced aromatase activity.
The findings were published online in Nature Communications.
New Biological Mechanism
For the study, the researchers analyzed data from the Barwon Infant Study in 1067 infants in Australia. At age 7-11 years, 43 children had a confirmed ASD diagnosis, and 249 infants with Child Behavior Checklist (CBCL) data at age 2 years had an autism spectrum problem score above the median.
The researchers developed a CYP19A1 genetic score for aromatase activity based on five single nucleotide polymorphisms associated with lower estrogen levels. Among 595 children with prenatal BPA and CBCL, those with three or more variants were classified as “low aromatase activity” and the remaining were classified as “high.”
In regression analyses, boys with low aromatase activity and high prenatal BPA exposure (top quartile > 2.18 µg/L) were 3.5 times more likely to have autism symptoms at age 2 years (odds ratio [OR], 3.56; 95% CI, 1.13-11.22).
The odds of a confirmed ASD diagnosis were six times higher at age 9 years only in men with low aromatase activity (OR, 6.24; 95% CI, 1.02-38.26).
The researchers also found that higher BPA levels predicted higher methylation in cord blood across the CYP19A1 brain promoter PI.f region (P = .009).
To replicate the findings, data were used from the Columbia Centre for Children’s Health Study–Mothers and Newborns cohort in the United States. Once again, the BPA level was associated with hypermethylation of the aromatase brain promoter PI.f (P = .0089).
In both cohorts, there was evidence that the effect of increased BPA on brain-derived neurotrophic factor hypermethylation was mediated partly through higher aromatase gene methylation (P = .001).
To validate the findings, the researchers examined human neuroblastoma SH-SY5Y cell lines and found aromatase protein levels were more than halved in the presence of BPA 50 µg/L (P = .01).
Additionally, mouse studies showed that male mice exposed to BPA 50 µg/L mid-gestation and male aromatase knockout mice — but not female mice — had social behavior deficits, such as interacting with a strange mouse, as well as structural and functional brain changes.
“We found that BPA suppresses the aromatase enzyme and is associated with anatomical, neurologic, and behavioral changes in the male mice that may be consistent with autism spectrum disorder,” Wah Chin Boon, PhD, co–lead researcher and research fellow, also with The Florey Institute, said in a statement.
“This is the first time a biological pathway has been identified that might help explain the connection between autism and BPA,” she said.
“In this study, not only were the levels of BPA higher than most people would be exposed to, but in at least one of the experiments the mice were injected with BPA directly, whereas humans would be exposed via food and drink,” observed Oliver Jones, PhD, MSc, professor of chemistry, RMIT University, Melbourne, Australia. “If you ingest the food, it undergoes metabolism before it gets to the bloodstream, which reduces the effective dose.”
Dr. Jones said further studies with larger numbers of participants measuring BPA throughout pregnancy and other chemicals the mother and child were exposed to are needed to be sure of any such link. “Just because there is a possible mechanism in place does not automatically mean that it is activated,” he said.
Dr. Ponsonby pointed out that BPA and other endocrine-disrupting chemicals are “almost impossible for individuals to avoid” and can enter the body through plastic food and drink packaging, home renovation fumes, and sources such as cosmetics.
Fatty Acid Helpful?
Building on earlier observations that 10-hydroxy-2-decenoic acid (10HDA) may have estrogenic modulating activities, the researchers conducted additional studies suggesting that 10HDA may be effective as a competitive ligand that could counteract the effects of BPA on estrogen signaling within cells.
Further, among 3-week-old mice pups prenatally exposed to BPA, daily injections of 10HDA for 3 weeks showed striking and significant improvements in social interaction. Stopping 10HDA resulted in a deficit in social interaction that was again ameliorated by subsequent 10HDA treatment.
“10-hydroxy-2-decenoic acid shows early indications of potential in activating opposing biological pathways to improve autism-like characteristics when administered to animals that have been prenatally exposed to BPA,” Dr. Boon said. “It warrants further studies to see whether this potential treatment could be realized in humans.”
Reached for comment, Dr. Jones said “the human studies are not strong at all,” in large part because BPA levels were tested only once at 36 weeks in the BIS cohort.
“I would argue that if BPA is in the urine, it has been excreted and is no longer in the bloodstream, thus not able to affect the child,” he said. “I’d also argue that a single measurement at 36 weeks cannot give you any idea of the mother’s exposure to BPA over the rest of the pregnancy or what the child was exposed to after birth.”
The study was funded by the Minderoo Foundation, the National Health and Medical Research Council of Australia, the Australian Research Council, and numerous other sponsors. Dr. Boon is a coinventor on “Methods of treating neurodevelopmental diseases and disorders” and is a board member of Meizon Innovation Holdings. Dr. Ponsonby is a scientific adviser to Meizon Innovation Holdings. The remaining authors declared no competing interests.
A version of this article first appeared on Medscape.com.
BPA is a potent endocrine disruptor found in polycarbonate plastics and epoxy resins and has been banned by the Food and Drug Administration for use in baby bottles, sippy cups, and infant formula packaging.
“Exposure to BPA has already been shown in some studies to be associated with subsequent autism in offspring,” lead researcher Anne-Louise Ponsonby, PhD, The Florey Institute, Heidelberg, Australia, said in a statement.
“Our work is important because it demonstrates one of the biological mechanisms potentially involved. BPA can disrupt hormone-controlled male fetal brain development in several ways, including silencing a key enzyme, aromatase, that controls neurohormones and is especially important in fetal male brain development. This appears to be part of the autism puzzle,” she said.
Brain aromatase, encoded by CYP19A1, converts neural androgens to neural estrogens and has been implicated in ASD. Postmortem analyses of men with ASD also show markedly reduced aromatase activity.
The findings were published online in Nature Communications.
New Biological Mechanism
For the study, the researchers analyzed data from the Barwon Infant Study in 1067 infants in Australia. At age 7-11 years, 43 children had a confirmed ASD diagnosis, and 249 infants with Child Behavior Checklist (CBCL) data at age 2 years had an autism spectrum problem score above the median.
The researchers developed a CYP19A1 genetic score for aromatase activity based on five single nucleotide polymorphisms associated with lower estrogen levels. Among 595 children with prenatal BPA and CBCL, those with three or more variants were classified as “low aromatase activity” and the remaining were classified as “high.”
In regression analyses, boys with low aromatase activity and high prenatal BPA exposure (top quartile > 2.18 µg/L) were 3.5 times more likely to have autism symptoms at age 2 years (odds ratio [OR], 3.56; 95% CI, 1.13-11.22).
The odds of a confirmed ASD diagnosis were six times higher at age 9 years only in men with low aromatase activity (OR, 6.24; 95% CI, 1.02-38.26).
The researchers also found that higher BPA levels predicted higher methylation in cord blood across the CYP19A1 brain promoter PI.f region (P = .009).
To replicate the findings, data were used from the Columbia Centre for Children’s Health Study–Mothers and Newborns cohort in the United States. Once again, the BPA level was associated with hypermethylation of the aromatase brain promoter PI.f (P = .0089).
In both cohorts, there was evidence that the effect of increased BPA on brain-derived neurotrophic factor hypermethylation was mediated partly through higher aromatase gene methylation (P = .001).
To validate the findings, the researchers examined human neuroblastoma SH-SY5Y cell lines and found aromatase protein levels were more than halved in the presence of BPA 50 µg/L (P = .01).
Additionally, mouse studies showed that male mice exposed to BPA 50 µg/L mid-gestation and male aromatase knockout mice — but not female mice — had social behavior deficits, such as interacting with a strange mouse, as well as structural and functional brain changes.
“We found that BPA suppresses the aromatase enzyme and is associated with anatomical, neurologic, and behavioral changes in the male mice that may be consistent with autism spectrum disorder,” Wah Chin Boon, PhD, co–lead researcher and research fellow, also with The Florey Institute, said in a statement.
“This is the first time a biological pathway has been identified that might help explain the connection between autism and BPA,” she said.
“In this study, not only were the levels of BPA higher than most people would be exposed to, but in at least one of the experiments the mice were injected with BPA directly, whereas humans would be exposed via food and drink,” observed Oliver Jones, PhD, MSc, professor of chemistry, RMIT University, Melbourne, Australia. “If you ingest the food, it undergoes metabolism before it gets to the bloodstream, which reduces the effective dose.”
Dr. Jones said further studies with larger numbers of participants measuring BPA throughout pregnancy and other chemicals the mother and child were exposed to are needed to be sure of any such link. “Just because there is a possible mechanism in place does not automatically mean that it is activated,” he said.
Dr. Ponsonby pointed out that BPA and other endocrine-disrupting chemicals are “almost impossible for individuals to avoid” and can enter the body through plastic food and drink packaging, home renovation fumes, and sources such as cosmetics.
Fatty Acid Helpful?
Building on earlier observations that 10-hydroxy-2-decenoic acid (10HDA) may have estrogenic modulating activities, the researchers conducted additional studies suggesting that 10HDA may be effective as a competitive ligand that could counteract the effects of BPA on estrogen signaling within cells.
Further, among 3-week-old mice pups prenatally exposed to BPA, daily injections of 10HDA for 3 weeks showed striking and significant improvements in social interaction. Stopping 10HDA resulted in a deficit in social interaction that was again ameliorated by subsequent 10HDA treatment.
“10-hydroxy-2-decenoic acid shows early indications of potential in activating opposing biological pathways to improve autism-like characteristics when administered to animals that have been prenatally exposed to BPA,” Dr. Boon said. “It warrants further studies to see whether this potential treatment could be realized in humans.”
Reached for comment, Dr. Jones said “the human studies are not strong at all,” in large part because BPA levels were tested only once at 36 weeks in the BIS cohort.
“I would argue that if BPA is in the urine, it has been excreted and is no longer in the bloodstream, thus not able to affect the child,” he said. “I’d also argue that a single measurement at 36 weeks cannot give you any idea of the mother’s exposure to BPA over the rest of the pregnancy or what the child was exposed to after birth.”
The study was funded by the Minderoo Foundation, the National Health and Medical Research Council of Australia, the Australian Research Council, and numerous other sponsors. Dr. Boon is a coinventor on “Methods of treating neurodevelopmental diseases and disorders” and is a board member of Meizon Innovation Holdings. Dr. Ponsonby is a scientific adviser to Meizon Innovation Holdings. The remaining authors declared no competing interests.
A version of this article first appeared on Medscape.com.
FROM NATURE COMMUNICATIONS
How Common Is Pediatric Emergency Mistriage?
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
, according to a multicenter retrospective study published in JAMA Pediatrics. Researchers also identified gender, age, race, ethnicity, and comorbidity disparities in those who were undertriaged.
The researchers found that only 34.1% of visits were correctly triaged while 58.5% were overtriaged and 7.4% were undertriaged. The findings were based on analysis of more than 1 million pediatric emergency visits over a 5-year period that used the Emergency Severity Index (ESI) version 4 for triage.
“The ESI had poor sensitivity in identifying a critically ill pediatric patient, and undertriage occurred in 1 in 14 children,” wrote Dana R. Sax, MD, a senior emergency physician at The Permanente Medical Group in northern California, and her colleagues.

“More than 90% of pediatric visits were assigned a mid to low triage acuity category, and actual resource use and care intensity frequently did not align with ESI predictions,” the authors wrote. “Our findings highlight an opportunity to improve triage for pediatric patients to mitigate critical undertriage, optimize resource decisions, standardize processes across time and setting, and promote more equitable care.”
The authors added that the study findings are currently being used by the Permanente system “to develop standardized triage education across centers to improve early identification of high-risk patients.”
Disparities in Emergency Care
The results underscore the need for more work to address disparities in emergency care, wrote Warren D. Frankenberger, PhD, RN, a nurse scientist at Children’s Hospital of Philadelphia, and two colleagues in an accompanying editorial.
“Decisions in triage can have significant downstream effects on subsequent care during the ED visit,” they wrote in their editorial. “Given that the triage process in most instances is fully executed by nurses, nurse researchers are in a key position to evaluate these and other covariates to influence further improvements in triage.” They suggested that use of clinical decision support tools and artificial intelligence (AI) may improve the triage process, albeit with the caveat that AI often relies on models with pre-existing historical bias that may perpetuate structural inequalities.
Study Methodology
The researchers analyzed 1,016,816 pediatric visits at 21 emergency departments in Kaiser Permanente Northern California between January 2016 and December 2020. The patients were an average 7 years old, and 47% were female. The researchers excluded visits that lacked ESI data or had incomplete ED time variables as well as those with patients who left against medical advice, were not seen, or were transferred from another ED.
The study relied on novel definitions of ESI undertriage and overtriage developed through a modified Delphi process by a team of four emergency physicians, one pediatric emergency physician, two emergency nurses, and one pediatric ICU physician. The definition involved comparing ESI levels to the clinical outcomes and resource use.
Resources included laboratory analysis, electrocardiography, radiography, CT, MRI, diagnostic ultrasonography (not point of care), angiography, IV fluids, and IV, intramuscular, or nebulized medications. Resources did not include “oral medications, tetanus immunizations, point-of-care testing, history and physical examination, saline or heparin lock, prescription refills, simple wound care, crutches, splints, and slings.”
Level 1 events were those requiring time-sensitive, critical intervention, including high-risk sepsis. Level 2 events included most level 1 events that occurred after the first hour (except operating room admission or hospital transfer) as well as respiratory therapy, toxicology consult, lumbar puncture, suicidality as chief concern, at least 2 doses of albuterol or continuous albuterol nebulization, a skeletal survey x-ray order, and medical social work consult with an ED length of stay of at least 2 hours. Level 3 events included IV mediation order, any CT order, OR admission or hospital transfer after one hour, or any pediatric hospitalist consult.
Analyzing the ED Visits
Overtriaged cases were ESI level 1 or 2 cases in which fewer than 2 resources were used; level 3 cases where fewer than 2 resources were used and no level 1 or 2 events occurred; and level 4 cases where no resources were used.
Undertriaged cases were defined as the following:
- ESI level 5 cases where any resource was used and any level 1, 2, or 3 events occurred.
- Level 4 cases where more than 1 resource was used and any level 1, 2, or 3 events occurred.
- Level 3 cases where any level 1 event occurred, more than one level 2 event occurred, or any level 2 event occurred and more than one additional ED resource type was used.
- Level 2 cases where any level 1 event occurred.
About half the visits (51%) were assigned ESI 3, which was the category with the highest proportion of mistriage. After adjusting for study facility and triage vital signs, the researchers found that children age 6 and older were more likely to be undertriaged than those younger than 6, particularly those age 15 and older (relative risk [RR], 1.36).
Undertriage was also modestly more likely with male patients (female patients’ RR, 0.93), patients with comorbidities (RR, 1.11-1.2), patients who arrived by ambulance (RR, 1.04), and patients who were Asian (RR, 1.10), Black (RR, 1.05), or Hispanic (RR, 1.04). Undertriage became gradually less likely with each additional year in the study period, with an RR of 0.89 in 2019 and 2020.
Among the study’s limitations were use of ESI version 4, instead of the currently used 5, and the omission of common procedures from the outcome definition that “may systematically bias the analysis toward overtriage,” the editorial noted. The authors also did not include pain as a variable in the analysis, which can often indicate patient acuity.
Further, this study was unable to include covariates identified in other research that may influence clinical decision-making, such as “the presenting illness or injury, children with complex medical needs, and language proficiency,” Dr. Frankenberger and colleagues wrote. “Furthermore, environmental stressors, such as ED volume and crowding, can influence how a nurse prioritizes care and may increase bias in decision-making and/or increase practice variability.”
The study was funded by the Kaiser Permanente Northern California (KPNC) Community Health program. One author had consulting payments from CSL Behring and Abbott Point-of-Care, and six of the authors have received grant funding from the KPNC Community Health program. The editorial authors reported no conflicts of interest.
FROM JAMA PEDIATRICS
E-Bikes: The Good ... and the Ugly
Bicycles have been woven into my life since I first straddled a hand-me-down with a fan belt drive when I was 3. At age 12 my friend Ricky and I took a 250 mile–plus 2-night adventure on our 3-speed “English” style bikes. We still marvel that our parents let us do it when neither cell phones nor GPS existed.
I have always bike commuted to work, including the years when that involved a perilous navigation into Boston from the suburbs. In our mid-50s my wife and I biked from Washington state back here to Maine with another couple unsupported. We continue to do at least one self-guided cycle tour out of the country each year.
Not surprisingly, I keep a close eye on what’s happening in the bicycle market. For decades the trends have shifted back and forth between sleek road models and beefier off-roaders. There have been boom years here and there for the dealers and manufacturers, but nothing like what the bike industry is experiencing now with the arrival of e-bikes on the market. Driven primarily by electrification, micromobility ridership (which includes conventional bikes and scooters) has grown more than 50-fold over the last 10 years. Projections suggest the market’s value will be $300 billion by 2030.
It doesn’t take an MBA with a major in marketing to understand the broad appeal of electrification. Most adults have ridden a bicycle as children, but several decades of gap years has left many of them with a level of fitness that makes pedaling against the wind or up any incline difficult and unappealing. An e-bike can put even the least fitness conscious back in the saddle and open the options for outdoor recreation they haven’t dreamed of since childhood.
In large part the people flocking to e-bikes are retiree’s who thought they were “over the hill.” They are having so much fun they don’t care if the Lycra-clad “serious” cyclists notice the battery bulge in the frame on their e-bikes. Another group of e-bike adopters are motivated by the “greenness” of a fossil-fuel–free electric powered transportation which, with minimal compromise, can be used as they would a car around town and for longer commutes than they would have considered on a purely pedal-powered bicycle.
Unfortunately, there is a growing group of younger e-bike riders who are motivated and uninhibited by the potential that the power boost of a small electric motor can provide. And here is where the ugliness begins to intrude on what was otherwise a beautiful and expanding landscape. However, it is the young who are, not surprisingly, drawn to the speed, and with any vehicle – motorized or conventional – as speed increases so does the frequency and seriousness of accidents.
The term e-bike covers a broad range of vehicles, from those designated class 1, which require pedaling and are limited to 20 miles per hour, to class 3, which may have a throttle and unmodified can hit 28 mph. Class 2 bikes have a throttle that will allow the rider to reach 20 mph without pedaling. Modifying any class of e-bike can substantially increase its speed, but this is more common in classes 2 and 3. As an example, some very fast micromobiles are considered unclassified e-bikes and avoid being labeled motorcycles simply because they have pedals.
One has to give some credit to the e-bike industry for eventually adopting this classification system. But, we must give the rest of us, including parents and public safety officials, a failing grade for doing a poor job of translating these scores into enforceable regulations to protect both riders and pedestrians from serious injury.
On the governmental side only a little more than half of US states have used the three category classification to craft their regulations. Many jurisdictions have failed to differentiate between streets, sidewalks, and trails. Regulations vary from state to state, and many states leave it up to local communities. From my experience chairing our town’s Bicycle and Pedestrian Advisory Committee, I can tell you that even “progressive” communities are struggling to decide who can ride what where. The result has been that people of all ages, but mostly adolescents, are traveling on busy streets and sidewalks at speeds that put themselves and pedestrians at risk.
On the parental side of the problem are families that have either allowed or enabled their children to ride class 2 and 3 e-bikes without proper safety equipment or consideration for the safety of the rest of the community. Currently, this is not much of a problem here in Maine thanks to the weather and the high price of e-bikes. However, I frequently visit an affluent community in the San Francisco Bay Area, where it is not uncommon to see middle school children speeding along well in excess of 20 mph.
Unfortunately this is another example, like television and cell phone, in which our society has been unable to keep up with technology by molding the behavior of our children and/or creating enforceable rules that allow us to reap the benefits of new discoveries while minimizing the collateral damage that can accompany them.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Bicycles have been woven into my life since I first straddled a hand-me-down with a fan belt drive when I was 3. At age 12 my friend Ricky and I took a 250 mile–plus 2-night adventure on our 3-speed “English” style bikes. We still marvel that our parents let us do it when neither cell phones nor GPS existed.
I have always bike commuted to work, including the years when that involved a perilous navigation into Boston from the suburbs. In our mid-50s my wife and I biked from Washington state back here to Maine with another couple unsupported. We continue to do at least one self-guided cycle tour out of the country each year.
Not surprisingly, I keep a close eye on what’s happening in the bicycle market. For decades the trends have shifted back and forth between sleek road models and beefier off-roaders. There have been boom years here and there for the dealers and manufacturers, but nothing like what the bike industry is experiencing now with the arrival of e-bikes on the market. Driven primarily by electrification, micromobility ridership (which includes conventional bikes and scooters) has grown more than 50-fold over the last 10 years. Projections suggest the market’s value will be $300 billion by 2030.
It doesn’t take an MBA with a major in marketing to understand the broad appeal of electrification. Most adults have ridden a bicycle as children, but several decades of gap years has left many of them with a level of fitness that makes pedaling against the wind or up any incline difficult and unappealing. An e-bike can put even the least fitness conscious back in the saddle and open the options for outdoor recreation they haven’t dreamed of since childhood.
In large part the people flocking to e-bikes are retiree’s who thought they were “over the hill.” They are having so much fun they don’t care if the Lycra-clad “serious” cyclists notice the battery bulge in the frame on their e-bikes. Another group of e-bike adopters are motivated by the “greenness” of a fossil-fuel–free electric powered transportation which, with minimal compromise, can be used as they would a car around town and for longer commutes than they would have considered on a purely pedal-powered bicycle.
Unfortunately, there is a growing group of younger e-bike riders who are motivated and uninhibited by the potential that the power boost of a small electric motor can provide. And here is where the ugliness begins to intrude on what was otherwise a beautiful and expanding landscape. However, it is the young who are, not surprisingly, drawn to the speed, and with any vehicle – motorized or conventional – as speed increases so does the frequency and seriousness of accidents.
The term e-bike covers a broad range of vehicles, from those designated class 1, which require pedaling and are limited to 20 miles per hour, to class 3, which may have a throttle and unmodified can hit 28 mph. Class 2 bikes have a throttle that will allow the rider to reach 20 mph without pedaling. Modifying any class of e-bike can substantially increase its speed, but this is more common in classes 2 and 3. As an example, some very fast micromobiles are considered unclassified e-bikes and avoid being labeled motorcycles simply because they have pedals.
One has to give some credit to the e-bike industry for eventually adopting this classification system. But, we must give the rest of us, including parents and public safety officials, a failing grade for doing a poor job of translating these scores into enforceable regulations to protect both riders and pedestrians from serious injury.
On the governmental side only a little more than half of US states have used the three category classification to craft their regulations. Many jurisdictions have failed to differentiate between streets, sidewalks, and trails. Regulations vary from state to state, and many states leave it up to local communities. From my experience chairing our town’s Bicycle and Pedestrian Advisory Committee, I can tell you that even “progressive” communities are struggling to decide who can ride what where. The result has been that people of all ages, but mostly adolescents, are traveling on busy streets and sidewalks at speeds that put themselves and pedestrians at risk.
On the parental side of the problem are families that have either allowed or enabled their children to ride class 2 and 3 e-bikes without proper safety equipment or consideration for the safety of the rest of the community. Currently, this is not much of a problem here in Maine thanks to the weather and the high price of e-bikes. However, I frequently visit an affluent community in the San Francisco Bay Area, where it is not uncommon to see middle school children speeding along well in excess of 20 mph.
Unfortunately this is another example, like television and cell phone, in which our society has been unable to keep up with technology by molding the behavior of our children and/or creating enforceable rules that allow us to reap the benefits of new discoveries while minimizing the collateral damage that can accompany them.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Bicycles have been woven into my life since I first straddled a hand-me-down with a fan belt drive when I was 3. At age 12 my friend Ricky and I took a 250 mile–plus 2-night adventure on our 3-speed “English” style bikes. We still marvel that our parents let us do it when neither cell phones nor GPS existed.
I have always bike commuted to work, including the years when that involved a perilous navigation into Boston from the suburbs. In our mid-50s my wife and I biked from Washington state back here to Maine with another couple unsupported. We continue to do at least one self-guided cycle tour out of the country each year.
Not surprisingly, I keep a close eye on what’s happening in the bicycle market. For decades the trends have shifted back and forth between sleek road models and beefier off-roaders. There have been boom years here and there for the dealers and manufacturers, but nothing like what the bike industry is experiencing now with the arrival of e-bikes on the market. Driven primarily by electrification, micromobility ridership (which includes conventional bikes and scooters) has grown more than 50-fold over the last 10 years. Projections suggest the market’s value will be $300 billion by 2030.
It doesn’t take an MBA with a major in marketing to understand the broad appeal of electrification. Most adults have ridden a bicycle as children, but several decades of gap years has left many of them with a level of fitness that makes pedaling against the wind or up any incline difficult and unappealing. An e-bike can put even the least fitness conscious back in the saddle and open the options for outdoor recreation they haven’t dreamed of since childhood.
In large part the people flocking to e-bikes are retiree’s who thought they were “over the hill.” They are having so much fun they don’t care if the Lycra-clad “serious” cyclists notice the battery bulge in the frame on their e-bikes. Another group of e-bike adopters are motivated by the “greenness” of a fossil-fuel–free electric powered transportation which, with minimal compromise, can be used as they would a car around town and for longer commutes than they would have considered on a purely pedal-powered bicycle.
Unfortunately, there is a growing group of younger e-bike riders who are motivated and uninhibited by the potential that the power boost of a small electric motor can provide. And here is where the ugliness begins to intrude on what was otherwise a beautiful and expanding landscape. However, it is the young who are, not surprisingly, drawn to the speed, and with any vehicle – motorized or conventional – as speed increases so does the frequency and seriousness of accidents.
The term e-bike covers a broad range of vehicles, from those designated class 1, which require pedaling and are limited to 20 miles per hour, to class 3, which may have a throttle and unmodified can hit 28 mph. Class 2 bikes have a throttle that will allow the rider to reach 20 mph without pedaling. Modifying any class of e-bike can substantially increase its speed, but this is more common in classes 2 and 3. As an example, some very fast micromobiles are considered unclassified e-bikes and avoid being labeled motorcycles simply because they have pedals.
One has to give some credit to the e-bike industry for eventually adopting this classification system. But, we must give the rest of us, including parents and public safety officials, a failing grade for doing a poor job of translating these scores into enforceable regulations to protect both riders and pedestrians from serious injury.
On the governmental side only a little more than half of US states have used the three category classification to craft their regulations. Many jurisdictions have failed to differentiate between streets, sidewalks, and trails. Regulations vary from state to state, and many states leave it up to local communities. From my experience chairing our town’s Bicycle and Pedestrian Advisory Committee, I can tell you that even “progressive” communities are struggling to decide who can ride what where. The result has been that people of all ages, but mostly adolescents, are traveling on busy streets and sidewalks at speeds that put themselves and pedestrians at risk.
On the parental side of the problem are families that have either allowed or enabled their children to ride class 2 and 3 e-bikes without proper safety equipment or consideration for the safety of the rest of the community. Currently, this is not much of a problem here in Maine thanks to the weather and the high price of e-bikes. However, I frequently visit an affluent community in the San Francisco Bay Area, where it is not uncommon to see middle school children speeding along well in excess of 20 mph.
Unfortunately this is another example, like television and cell phone, in which our society has been unable to keep up with technology by molding the behavior of our children and/or creating enforceable rules that allow us to reap the benefits of new discoveries while minimizing the collateral damage that can accompany them.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Doctor I-Don’t-Know
Many, many years ago there was a Thanksgiving when as I was just beginning to earn a reputation in my wife’s family. There were no place cards on the table and the usual hovering and jockeying seats was well underway. From behind me I heard one of my young nieces pipe up: “I want to sit next to Doctor I-don’t-know.”
After a few words of negotiation we were all settled in our places and ready to enjoy our meal. It took only a few seconds of introspection for me to grasp how I had received that moniker, which some physicians might consider disrespectful.
I was the only physician within several generations of that family and, as such, my in-laws thought it only appropriate to ask me medical questions. They courteously seemed to avoid personal questions about their own health and were particularly careful not to roll up their sleeves or unbutton their shirts to show me a lesion or a recently acquired surgical scar. No, my wife’s family members were curious. They wanted answers to deeper questions, the hard science so to speak. “How does aspirin work?” was a typical and painful example. Maybe pharmacologists today have better answers but 40 years ago I’m not so sure; I certainly didn’t know back then and would reply, “I don’t know.” Probably for the third or fourth time that day.
Usually I genuinely didn’t know the answer. However, sometimes my answer was going to be so different from the beliefs and biases of my inquisitor that, in the interest of expediency, “I don’t know” seemed the most appropriate response.
If you were reading Letters from Maine 25 years ago, that scenario might sound familiar. I have chosen to pull it out of the archives as a jumping-off point for a consideration of the unfortunate example some of us set when the COVID pandemic threw a tsunami of unknowns at us. Too many physician-“experts” were afraid to say, “I don’t know.” Instead, and maybe because, they themselves were afraid that the patients couldn’t handle the truth that none of us in the profession knew the correct answers. When so many initial pronouncements proved incorrect, it was too late to undo the damage that had been done to the community’s trust in the rest of us.
It turns out that my in-laws were not the only folks who thought of me as Doctor I-don’t-know. One of the perks of remaining in the same community after one retires is that encounters with former patients and their parents happen frequently. On more than one occasion a parent has thanked me for admitting my ignorance. Some have even claimed that my candid approach was what they remembered most fondly. And, that quality increased their trust when I finally provided an answer.
There is an art to delivering “I don’t know.” Thirty years ago I would excuse myself and tell the family I was going to my office to pull a book off the shelf or call a previous mentor. Now one only needs to ask Dr. Google. No need to leave the room. If appropriate, the provider can swing the computer screen so that the patient can share in the search for the answer.
That strategy only works when the provider merely needs to update or expand his/her knowledge. However, there are those difficult situations when no one could know the answer given the current parameters of the patient’s situation. More lab work might be needed. It may be too early in the trajectory of the patient’s illness for the illnesses signs and symptoms to declare themselves.
In these situations “I don’t know” must be followed by a “but.” It is what comes after that “but” and how it is delivered that can convert the provider’s admission of ignorance into a demonstration of his or her character. Is he/she a caring person trying to understand the patient’s concerns? Willing to enter into a cooperative relationship as together they search for the cause and hopefully for a cure for the patient’s currently mysterious illness?
I recently read about a physician who is encouraging medical educators to incorporate more discussions of “humility” and its role in patient care into the medical school and postgraduate training curricula. He feels, as do I, that
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Many, many years ago there was a Thanksgiving when as I was just beginning to earn a reputation in my wife’s family. There were no place cards on the table and the usual hovering and jockeying seats was well underway. From behind me I heard one of my young nieces pipe up: “I want to sit next to Doctor I-don’t-know.”
After a few words of negotiation we were all settled in our places and ready to enjoy our meal. It took only a few seconds of introspection for me to grasp how I had received that moniker, which some physicians might consider disrespectful.
I was the only physician within several generations of that family and, as such, my in-laws thought it only appropriate to ask me medical questions. They courteously seemed to avoid personal questions about their own health and were particularly careful not to roll up their sleeves or unbutton their shirts to show me a lesion or a recently acquired surgical scar. No, my wife’s family members were curious. They wanted answers to deeper questions, the hard science so to speak. “How does aspirin work?” was a typical and painful example. Maybe pharmacologists today have better answers but 40 years ago I’m not so sure; I certainly didn’t know back then and would reply, “I don’t know.” Probably for the third or fourth time that day.
Usually I genuinely didn’t know the answer. However, sometimes my answer was going to be so different from the beliefs and biases of my inquisitor that, in the interest of expediency, “I don’t know” seemed the most appropriate response.
If you were reading Letters from Maine 25 years ago, that scenario might sound familiar. I have chosen to pull it out of the archives as a jumping-off point for a consideration of the unfortunate example some of us set when the COVID pandemic threw a tsunami of unknowns at us. Too many physician-“experts” were afraid to say, “I don’t know.” Instead, and maybe because, they themselves were afraid that the patients couldn’t handle the truth that none of us in the profession knew the correct answers. When so many initial pronouncements proved incorrect, it was too late to undo the damage that had been done to the community’s trust in the rest of us.
It turns out that my in-laws were not the only folks who thought of me as Doctor I-don’t-know. One of the perks of remaining in the same community after one retires is that encounters with former patients and their parents happen frequently. On more than one occasion a parent has thanked me for admitting my ignorance. Some have even claimed that my candid approach was what they remembered most fondly. And, that quality increased their trust when I finally provided an answer.
There is an art to delivering “I don’t know.” Thirty years ago I would excuse myself and tell the family I was going to my office to pull a book off the shelf or call a previous mentor. Now one only needs to ask Dr. Google. No need to leave the room. If appropriate, the provider can swing the computer screen so that the patient can share in the search for the answer.
That strategy only works when the provider merely needs to update or expand his/her knowledge. However, there are those difficult situations when no one could know the answer given the current parameters of the patient’s situation. More lab work might be needed. It may be too early in the trajectory of the patient’s illness for the illnesses signs and symptoms to declare themselves.
In these situations “I don’t know” must be followed by a “but.” It is what comes after that “but” and how it is delivered that can convert the provider’s admission of ignorance into a demonstration of his or her character. Is he/she a caring person trying to understand the patient’s concerns? Willing to enter into a cooperative relationship as together they search for the cause and hopefully for a cure for the patient’s currently mysterious illness?
I recently read about a physician who is encouraging medical educators to incorporate more discussions of “humility” and its role in patient care into the medical school and postgraduate training curricula. He feels, as do I, that
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Many, many years ago there was a Thanksgiving when as I was just beginning to earn a reputation in my wife’s family. There were no place cards on the table and the usual hovering and jockeying seats was well underway. From behind me I heard one of my young nieces pipe up: “I want to sit next to Doctor I-don’t-know.”
After a few words of negotiation we were all settled in our places and ready to enjoy our meal. It took only a few seconds of introspection for me to grasp how I had received that moniker, which some physicians might consider disrespectful.
I was the only physician within several generations of that family and, as such, my in-laws thought it only appropriate to ask me medical questions. They courteously seemed to avoid personal questions about their own health and were particularly careful not to roll up their sleeves or unbutton their shirts to show me a lesion or a recently acquired surgical scar. No, my wife’s family members were curious. They wanted answers to deeper questions, the hard science so to speak. “How does aspirin work?” was a typical and painful example. Maybe pharmacologists today have better answers but 40 years ago I’m not so sure; I certainly didn’t know back then and would reply, “I don’t know.” Probably for the third or fourth time that day.
Usually I genuinely didn’t know the answer. However, sometimes my answer was going to be so different from the beliefs and biases of my inquisitor that, in the interest of expediency, “I don’t know” seemed the most appropriate response.
If you were reading Letters from Maine 25 years ago, that scenario might sound familiar. I have chosen to pull it out of the archives as a jumping-off point for a consideration of the unfortunate example some of us set when the COVID pandemic threw a tsunami of unknowns at us. Too many physician-“experts” were afraid to say, “I don’t know.” Instead, and maybe because, they themselves were afraid that the patients couldn’t handle the truth that none of us in the profession knew the correct answers. When so many initial pronouncements proved incorrect, it was too late to undo the damage that had been done to the community’s trust in the rest of us.
It turns out that my in-laws were not the only folks who thought of me as Doctor I-don’t-know. One of the perks of remaining in the same community after one retires is that encounters with former patients and their parents happen frequently. On more than one occasion a parent has thanked me for admitting my ignorance. Some have even claimed that my candid approach was what they remembered most fondly. And, that quality increased their trust when I finally provided an answer.
There is an art to delivering “I don’t know.” Thirty years ago I would excuse myself and tell the family I was going to my office to pull a book off the shelf or call a previous mentor. Now one only needs to ask Dr. Google. No need to leave the room. If appropriate, the provider can swing the computer screen so that the patient can share in the search for the answer.
That strategy only works when the provider merely needs to update or expand his/her knowledge. However, there are those difficult situations when no one could know the answer given the current parameters of the patient’s situation. More lab work might be needed. It may be too early in the trajectory of the patient’s illness for the illnesses signs and symptoms to declare themselves.
In these situations “I don’t know” must be followed by a “but.” It is what comes after that “but” and how it is delivered that can convert the provider’s admission of ignorance into a demonstration of his or her character. Is he/she a caring person trying to understand the patient’s concerns? Willing to enter into a cooperative relationship as together they search for the cause and hopefully for a cure for the patient’s currently mysterious illness?
I recently read about a physician who is encouraging medical educators to incorporate more discussions of “humility” and its role in patient care into the medical school and postgraduate training curricula. He feels, as do I, that
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
US Experience With Infliximab Biosimilars Suggests Need for More Development Incentives
TOPLINE:
Uptake of infliximab biosimilars rose slowly across private insurance, Medicaid, and Medicare when two were available in the United States during 2016-2020 but increased significantly through 2022 after the third biosimilar became available in July 2020. However, prescriptions in Medicare still lagged behind those in private insurance and Medicaid.
METHODOLOGY:
- Researchers analyzed electronic health records from over 1100 US rheumatologists who participated in a national registry, the Rheumatology Informatics System for Effectiveness (RISE), for all infliximab administrations (bio-originator or biosimilar) to patients older than 18 years from April 2016 to September 2022.
- They conducted an interrupted time series to account for autocorrelation and model the effect of each infliximab biosimilar release (infliximab-dyyb in November 2016, infliximab-abda in July 2017, and infliximab-axxq in July 2020) on uptake across Medicare, Medicaid, and private insurers.
TAKEAWAY:
- The researchers identified 659,988 infliximab administrations for 37,560 unique patients, with 52% on Medicare, 4.8% on Medicaid, and 43% on private insurance.
- Biosimilar uptake rose slowly with average annual increases < 5% from 2016 to June 2020 (Medicare, 3.2%; Medicaid, 5.2%; private insurance, 1.8%).
- After the third biosimilar release in July 2020, the average annual increase reached 13% for Medicaid and 16.4% for private insurance but remained low for Medicare (5.6%).
- By September 2022, biosimilar uptake was higher for Medicaid (43.8%) and private insurance (38.5%) than for Medicare (24%).
IN PRACTICE:
“Our results suggest policymakers may need to do more to allow biosimilars to get a foothold in the market by incentivizing the development and entry of multiple biosimilars, address anticompetitive pricing strategies, and may need to amend Medicare policy to [incentivize] uptake in order to ensure a competitive and sustainable biosimilar market that gradually reduces total drug expenditures and out-of-pocket costs over time,” wrote the authors of the study.
SOURCE:
The study was led by Eric T. Roberts, PhD, University of California, San Francisco. It was published online on July 30, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
First, while the biosimilar introductions are likely catalysts for many changes in the market, some changes in slopes may also be attributable to the natural growth of the market over time. Second, this study may neither be generalizable to academic medical centers, which are underrepresented in RISE, nor be generalizable to infliximab prescriptions from other specialties. Third, uptake among privately insured patients changed shortly after November-December 2020, raising the possibility that the delay reflected negotiations between insurance companies and relevant entities regarding formulary coverage.
DISCLOSURES:
This study was funded by grants from the Agency for Healthcare Research and Quality and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One author disclosed receiving consulting fees from Pfizer, AstraZeneca, and Bristol-Myers Squibb and grant funding from AstraZeneca, the Bristol-Myers Squibb Foundation, and Aurinia.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Uptake of infliximab biosimilars rose slowly across private insurance, Medicaid, and Medicare when two were available in the United States during 2016-2020 but increased significantly through 2022 after the third biosimilar became available in July 2020. However, prescriptions in Medicare still lagged behind those in private insurance and Medicaid.
METHODOLOGY:
- Researchers analyzed electronic health records from over 1100 US rheumatologists who participated in a national registry, the Rheumatology Informatics System for Effectiveness (RISE), for all infliximab administrations (bio-originator or biosimilar) to patients older than 18 years from April 2016 to September 2022.
- They conducted an interrupted time series to account for autocorrelation and model the effect of each infliximab biosimilar release (infliximab-dyyb in November 2016, infliximab-abda in July 2017, and infliximab-axxq in July 2020) on uptake across Medicare, Medicaid, and private insurers.
TAKEAWAY:
- The researchers identified 659,988 infliximab administrations for 37,560 unique patients, with 52% on Medicare, 4.8% on Medicaid, and 43% on private insurance.
- Biosimilar uptake rose slowly with average annual increases < 5% from 2016 to June 2020 (Medicare, 3.2%; Medicaid, 5.2%; private insurance, 1.8%).
- After the third biosimilar release in July 2020, the average annual increase reached 13% for Medicaid and 16.4% for private insurance but remained low for Medicare (5.6%).
- By September 2022, biosimilar uptake was higher for Medicaid (43.8%) and private insurance (38.5%) than for Medicare (24%).
IN PRACTICE:
“Our results suggest policymakers may need to do more to allow biosimilars to get a foothold in the market by incentivizing the development and entry of multiple biosimilars, address anticompetitive pricing strategies, and may need to amend Medicare policy to [incentivize] uptake in order to ensure a competitive and sustainable biosimilar market that gradually reduces total drug expenditures and out-of-pocket costs over time,” wrote the authors of the study.
SOURCE:
The study was led by Eric T. Roberts, PhD, University of California, San Francisco. It was published online on July 30, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
First, while the biosimilar introductions are likely catalysts for many changes in the market, some changes in slopes may also be attributable to the natural growth of the market over time. Second, this study may neither be generalizable to academic medical centers, which are underrepresented in RISE, nor be generalizable to infliximab prescriptions from other specialties. Third, uptake among privately insured patients changed shortly after November-December 2020, raising the possibility that the delay reflected negotiations between insurance companies and relevant entities regarding formulary coverage.
DISCLOSURES:
This study was funded by grants from the Agency for Healthcare Research and Quality and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One author disclosed receiving consulting fees from Pfizer, AstraZeneca, and Bristol-Myers Squibb and grant funding from AstraZeneca, the Bristol-Myers Squibb Foundation, and Aurinia.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Uptake of infliximab biosimilars rose slowly across private insurance, Medicaid, and Medicare when two were available in the United States during 2016-2020 but increased significantly through 2022 after the third biosimilar became available in July 2020. However, prescriptions in Medicare still lagged behind those in private insurance and Medicaid.
METHODOLOGY:
- Researchers analyzed electronic health records from over 1100 US rheumatologists who participated in a national registry, the Rheumatology Informatics System for Effectiveness (RISE), for all infliximab administrations (bio-originator or biosimilar) to patients older than 18 years from April 2016 to September 2022.
- They conducted an interrupted time series to account for autocorrelation and model the effect of each infliximab biosimilar release (infliximab-dyyb in November 2016, infliximab-abda in July 2017, and infliximab-axxq in July 2020) on uptake across Medicare, Medicaid, and private insurers.
TAKEAWAY:
- The researchers identified 659,988 infliximab administrations for 37,560 unique patients, with 52% on Medicare, 4.8% on Medicaid, and 43% on private insurance.
- Biosimilar uptake rose slowly with average annual increases < 5% from 2016 to June 2020 (Medicare, 3.2%; Medicaid, 5.2%; private insurance, 1.8%).
- After the third biosimilar release in July 2020, the average annual increase reached 13% for Medicaid and 16.4% for private insurance but remained low for Medicare (5.6%).
- By September 2022, biosimilar uptake was higher for Medicaid (43.8%) and private insurance (38.5%) than for Medicare (24%).
IN PRACTICE:
“Our results suggest policymakers may need to do more to allow biosimilars to get a foothold in the market by incentivizing the development and entry of multiple biosimilars, address anticompetitive pricing strategies, and may need to amend Medicare policy to [incentivize] uptake in order to ensure a competitive and sustainable biosimilar market that gradually reduces total drug expenditures and out-of-pocket costs over time,” wrote the authors of the study.
SOURCE:
The study was led by Eric T. Roberts, PhD, University of California, San Francisco. It was published online on July 30, 2024, in Arthritis & Rheumatology.
LIMITATIONS:
First, while the biosimilar introductions are likely catalysts for many changes in the market, some changes in slopes may also be attributable to the natural growth of the market over time. Second, this study may neither be generalizable to academic medical centers, which are underrepresented in RISE, nor be generalizable to infliximab prescriptions from other specialties. Third, uptake among privately insured patients changed shortly after November-December 2020, raising the possibility that the delay reflected negotiations between insurance companies and relevant entities regarding formulary coverage.
DISCLOSURES:
This study was funded by grants from the Agency for Healthcare Research and Quality and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. One author disclosed receiving consulting fees from Pfizer, AstraZeneca, and Bristol-Myers Squibb and grant funding from AstraZeneca, the Bristol-Myers Squibb Foundation, and Aurinia.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Nemolizumab Benefits Seen in Adults, Teens With Atopic Dermatitis
TOPLINE:
(AD).
METHODOLOGY:
- The researchers conducted two 48-week randomized, double-blind, placebo-controlled phase 3 trials, ARCADIA 1 (n = 941; 47% women) and ARCADIA 2 (n = 787; 52% women), involving patients aged 12 and older with moderate to severe AD.
- Participants were randomly assigned in a 2:1 ratio to receive either 30 mg nemolizumab (with a 60-mg loading dose) or placebo, along with background topical corticosteroids with or without topical calcineurin inhibitors. The mean age range was 33.3-35.2 years.
- The coprimary endpoints were Investigator’s Global Assessment (IGA) success (score of 0 or 1 with at least a two-point improvement from baseline) and at least a 75% improvement in the Eczema Area and Severity Index (EASI-75) at week 16.
TAKEAWAY:
- At week 16, significantly more patients receiving nemolizumab vs placebo achieved IGA success in both the ARCADIA 1 (36% vs 25%; P = .0003) and ARCADIA 2 (38% vs 26%; P = .0006) trials.
- EASI-75 response rates were also significantly higher in the nemolizumab group than in the placebo group in both trials: ARCADIA 1 (44% vs 29%; P < .0001) and 2 (42% vs 30%; P = .0006).
- Significant improvements in pruritus were observed as early as week 1, with a greater proportion of participants in the nemolizumab vs placebo group achieving at least a four-point reduction in the Peak Pruritus Numerical Rating Scale score in both trials.
- Rates of adverse events were similar between the nemolizumab and placebo groups, with severe treatment-emergent adverse events occurring in 2%-4% of patients.
IN PRACTICE:
“Nemolizumab showed statistically and clinically significant improvements in inflammation and pruritus in adults and adolescents with moderate to severe atopic dermatitis and a rapid effect in reducing pruritus, as one of the primary complaints of patients. As such, nemolizumab might offer a valuable extension of the therapeutic armament if approved,” the authors concluded.
SOURCE:
The study was led by Jonathan Silverberg, MD, PhD, from the Department of Dermatology, George Washington University, Washington, DC. It was published online in The Lancet.
LIMITATIONS:
The study’s limitations included the absence of longer-term safety data. Additionally, the predominantly White population of the trials may limit the generalizability of the findings to other racial and ethnic groups. The use of concomitant topical therapy might have influenced the placebo response.
DISCLOSURES:
This study was funded by Galderma. Dr. Silverberg received honoraria from pharmaceutical companies, including Galderma, and his institution also received grants from Galderma, Incyte, and Pfizer. Four authors were employees of Galderma. Other authors also declared having ties with pharmaceutical companies, including Galderma, outside this work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
(AD).
METHODOLOGY:
- The researchers conducted two 48-week randomized, double-blind, placebo-controlled phase 3 trials, ARCADIA 1 (n = 941; 47% women) and ARCADIA 2 (n = 787; 52% women), involving patients aged 12 and older with moderate to severe AD.
- Participants were randomly assigned in a 2:1 ratio to receive either 30 mg nemolizumab (with a 60-mg loading dose) or placebo, along with background topical corticosteroids with or without topical calcineurin inhibitors. The mean age range was 33.3-35.2 years.
- The coprimary endpoints were Investigator’s Global Assessment (IGA) success (score of 0 or 1 with at least a two-point improvement from baseline) and at least a 75% improvement in the Eczema Area and Severity Index (EASI-75) at week 16.
TAKEAWAY:
- At week 16, significantly more patients receiving nemolizumab vs placebo achieved IGA success in both the ARCADIA 1 (36% vs 25%; P = .0003) and ARCADIA 2 (38% vs 26%; P = .0006) trials.
- EASI-75 response rates were also significantly higher in the nemolizumab group than in the placebo group in both trials: ARCADIA 1 (44% vs 29%; P < .0001) and 2 (42% vs 30%; P = .0006).
- Significant improvements in pruritus were observed as early as week 1, with a greater proportion of participants in the nemolizumab vs placebo group achieving at least a four-point reduction in the Peak Pruritus Numerical Rating Scale score in both trials.
- Rates of adverse events were similar between the nemolizumab and placebo groups, with severe treatment-emergent adverse events occurring in 2%-4% of patients.
IN PRACTICE:
“Nemolizumab showed statistically and clinically significant improvements in inflammation and pruritus in adults and adolescents with moderate to severe atopic dermatitis and a rapid effect in reducing pruritus, as one of the primary complaints of patients. As such, nemolizumab might offer a valuable extension of the therapeutic armament if approved,” the authors concluded.
SOURCE:
The study was led by Jonathan Silverberg, MD, PhD, from the Department of Dermatology, George Washington University, Washington, DC. It was published online in The Lancet.
LIMITATIONS:
The study’s limitations included the absence of longer-term safety data. Additionally, the predominantly White population of the trials may limit the generalizability of the findings to other racial and ethnic groups. The use of concomitant topical therapy might have influenced the placebo response.
DISCLOSURES:
This study was funded by Galderma. Dr. Silverberg received honoraria from pharmaceutical companies, including Galderma, and his institution also received grants from Galderma, Incyte, and Pfizer. Four authors were employees of Galderma. Other authors also declared having ties with pharmaceutical companies, including Galderma, outside this work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
(AD).
METHODOLOGY:
- The researchers conducted two 48-week randomized, double-blind, placebo-controlled phase 3 trials, ARCADIA 1 (n = 941; 47% women) and ARCADIA 2 (n = 787; 52% women), involving patients aged 12 and older with moderate to severe AD.
- Participants were randomly assigned in a 2:1 ratio to receive either 30 mg nemolizumab (with a 60-mg loading dose) or placebo, along with background topical corticosteroids with or without topical calcineurin inhibitors. The mean age range was 33.3-35.2 years.
- The coprimary endpoints were Investigator’s Global Assessment (IGA) success (score of 0 or 1 with at least a two-point improvement from baseline) and at least a 75% improvement in the Eczema Area and Severity Index (EASI-75) at week 16.
TAKEAWAY:
- At week 16, significantly more patients receiving nemolizumab vs placebo achieved IGA success in both the ARCADIA 1 (36% vs 25%; P = .0003) and ARCADIA 2 (38% vs 26%; P = .0006) trials.
- EASI-75 response rates were also significantly higher in the nemolizumab group than in the placebo group in both trials: ARCADIA 1 (44% vs 29%; P < .0001) and 2 (42% vs 30%; P = .0006).
- Significant improvements in pruritus were observed as early as week 1, with a greater proportion of participants in the nemolizumab vs placebo group achieving at least a four-point reduction in the Peak Pruritus Numerical Rating Scale score in both trials.
- Rates of adverse events were similar between the nemolizumab and placebo groups, with severe treatment-emergent adverse events occurring in 2%-4% of patients.
IN PRACTICE:
“Nemolizumab showed statistically and clinically significant improvements in inflammation and pruritus in adults and adolescents with moderate to severe atopic dermatitis and a rapid effect in reducing pruritus, as one of the primary complaints of patients. As such, nemolizumab might offer a valuable extension of the therapeutic armament if approved,” the authors concluded.
SOURCE:
The study was led by Jonathan Silverberg, MD, PhD, from the Department of Dermatology, George Washington University, Washington, DC. It was published online in The Lancet.
LIMITATIONS:
The study’s limitations included the absence of longer-term safety data. Additionally, the predominantly White population of the trials may limit the generalizability of the findings to other racial and ethnic groups. The use of concomitant topical therapy might have influenced the placebo response.
DISCLOSURES:
This study was funded by Galderma. Dr. Silverberg received honoraria from pharmaceutical companies, including Galderma, and his institution also received grants from Galderma, Incyte, and Pfizer. Four authors were employees of Galderma. Other authors also declared having ties with pharmaceutical companies, including Galderma, outside this work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Recommendations From a Pediatric Dermatologist on Using AI in Daily Practice
TORONTO — with the various AI models.
He reminds doctors that many of their colleagues and patients and their families are already using these systems, “and you don’t want to be left behind.”
In an interview following his presentation on AI at the annual meeting of the Society for Pediatric Dermatology (SPD), Dr. Yan discussed his tips for using AI.
Changing Fast
From the outset, most generative AI systems have been very good at processing language — for example, generating letters of medical necessity and summarizing disease processes into lay terms. But now they’re becoming “truly multimodal,” said Dr. Yan. “You can enter images; you could have it process audio; you can even start to have it refine video.”
To get started, he recommends signing up for a free account with ChatGPT, Gemini, Perplexity, Claude, and/or Microsoft Copilot. “To make the best choice, you have to try them out yourself because they each have their own kind of flavor and strengths and weaknesses,” said Dr. Yan.
Personally, he finds that ChatGPT is the most versatile, Gemini perhaps a little better in terms of image generation, and Perplexity probably the best at references because it was designed as an online library.
Once you figure out which platforms you prefer, consider signing up for a premium subscription, which is typically month to month and can be canceled at any time, Dr. Yan said. “This will allow you to get the most out of the AI model.”
As these AI systems are based on large language models, they are excellent at text, Dr. Yan noted. He suggests asking one to generate a letter or patient instruction sheet. “If you have a premium model, give it a PDF to summarize an article or take a photo of something that you want its opinion on.”
Privacy Critical
Always pay attention to privacy issues and avoid entering any private health information that would violate the Health Insurance Portability and Accountability Act (HIPAA), he said.
“We have to be very careful about how we interact with AI,” said Dr. Yan. “We can’t be posting private patient health information into these systems, no matter how useful these systems are.” Many academic institutions are creating “walled gardens” — private areas of AI access that don’t allow patient information to “leak out,” he said. “These AI models may have HIPAA protections in place and come with specific guidelines of use.”
The AI “scribe,” which helps with electronic health record documentation, is one of the most useful tools for clinicians, he said. He referred to a recent study showing that an AI scribe saved users an average of 1 hour at the keyboard every day, and a small patient survey showing 71% reported that it led to spending more time with their physician.
When entering requests into a prompt line with an AI system, Dr. Yan stressed that these prompts need to be clear and concise. For a complicated calculation or multistep problem, try adding the words “let’s do this step by step,” he said. “This is a technique invoking a ‘chain of thought’ that allows the system to enhance its accuracy when solving problems.”
If the response is not satisfactory, try being more detailed in the request, he advised, and consider giving the system examples of what you’re looking for and telling it what you don’t want in the output.
“For instance, if you’re asking for a differential diagnosis of rashes that affect the hands and feet, you can stipulate that you only want rashes that are vesicular or that arise in neonates, so you can get a more focused answer,” said Dr. Yan.
If there are “long-winded verbose” responses, add the phrase “be concise,” and it will shorten the response by about 50%, he added.
AI Hallucinations
Dr. Yan broached an issue that occasionally comes up, AI hallucinations, which refer to inaccurate or misleading responses on the basis of incomplete training or intrinsic biases within the model. He pointed to the case of a doctor discussing issues related to a patient’s hands, feet, and mouth, which the AI-generated model summarized as “the patient being diagnosed with hand, foot, and mouth disease.”
Another example he provided was a request to generate a letter of medical necessity for using ustekinumab (Stelara) for treating hidradenitis suppurative in a child that included references for its effectiveness and safety in children. The AI system generated “false references that sounded like they should be real because the authors are often people who have written in that field or on that subject,” said Dr. Yan.
When pressed, the system did acknowledge the references were hypothetical but were meant to illustrate the types of studies that would typically support the use of this drug in pediatric patients with HS. “ It’s well meaning, in the sense that it’s trying to help you achieve your goals using this training system,” said Dr. Yan.
“If you’re skeptical about a response, double-check the answer with a Google search or run the response through another AI [tool] asking it to check if the response is accurate,” he added.
While AI systems won’t replace the clinician, they are continuing to improve and becoming more sophisticated. Dr. Yan advises keeping up with emerging developments and engaging and adapting the most appropriate AI tool for an individual clinician’s work.
Asked to comment on the presentation at the SPD meeting, Sheilagh Maguiness, MD, director of the Division of Pediatric Dermatology at the University of Minnesota, Minneapolis, who, like other doctors, is increasingly testing AI, said she foresees a time when AI scribes fully replace humans for completing tasks during patient interactions.
“The hope is that if the AI scribes get good enough, we can just open our phone, have them translate the interaction, and create the notes for us.”
While she likes the idea of using ChatGPT to help with tasks like letters of recommendation for medications, Dr. Yan’s comments reiterated the importance of “checking and double-checking ChatGPT because it’s not correct all the time.” She particularly welcomed the advice “that we can just go back and ask it again to clarify, and that may improve its answers.”
Dr. Yan’s disclosures included an investment portfolio that includes companies working in the AI space, including Google, Apple, Nvidia, Amazon, Microsoft, and Arm. Dr. Maguiness had no relevant disclosures.
A version of this article first appeared on Medscape.com.
TORONTO — with the various AI models.
He reminds doctors that many of their colleagues and patients and their families are already using these systems, “and you don’t want to be left behind.”
In an interview following his presentation on AI at the annual meeting of the Society for Pediatric Dermatology (SPD), Dr. Yan discussed his tips for using AI.
Changing Fast
From the outset, most generative AI systems have been very good at processing language — for example, generating letters of medical necessity and summarizing disease processes into lay terms. But now they’re becoming “truly multimodal,” said Dr. Yan. “You can enter images; you could have it process audio; you can even start to have it refine video.”
To get started, he recommends signing up for a free account with ChatGPT, Gemini, Perplexity, Claude, and/or Microsoft Copilot. “To make the best choice, you have to try them out yourself because they each have their own kind of flavor and strengths and weaknesses,” said Dr. Yan.
Personally, he finds that ChatGPT is the most versatile, Gemini perhaps a little better in terms of image generation, and Perplexity probably the best at references because it was designed as an online library.
Once you figure out which platforms you prefer, consider signing up for a premium subscription, which is typically month to month and can be canceled at any time, Dr. Yan said. “This will allow you to get the most out of the AI model.”
As these AI systems are based on large language models, they are excellent at text, Dr. Yan noted. He suggests asking one to generate a letter or patient instruction sheet. “If you have a premium model, give it a PDF to summarize an article or take a photo of something that you want its opinion on.”
Privacy Critical
Always pay attention to privacy issues and avoid entering any private health information that would violate the Health Insurance Portability and Accountability Act (HIPAA), he said.
“We have to be very careful about how we interact with AI,” said Dr. Yan. “We can’t be posting private patient health information into these systems, no matter how useful these systems are.” Many academic institutions are creating “walled gardens” — private areas of AI access that don’t allow patient information to “leak out,” he said. “These AI models may have HIPAA protections in place and come with specific guidelines of use.”
The AI “scribe,” which helps with electronic health record documentation, is one of the most useful tools for clinicians, he said. He referred to a recent study showing that an AI scribe saved users an average of 1 hour at the keyboard every day, and a small patient survey showing 71% reported that it led to spending more time with their physician.
When entering requests into a prompt line with an AI system, Dr. Yan stressed that these prompts need to be clear and concise. For a complicated calculation or multistep problem, try adding the words “let’s do this step by step,” he said. “This is a technique invoking a ‘chain of thought’ that allows the system to enhance its accuracy when solving problems.”
If the response is not satisfactory, try being more detailed in the request, he advised, and consider giving the system examples of what you’re looking for and telling it what you don’t want in the output.
“For instance, if you’re asking for a differential diagnosis of rashes that affect the hands and feet, you can stipulate that you only want rashes that are vesicular or that arise in neonates, so you can get a more focused answer,” said Dr. Yan.
If there are “long-winded verbose” responses, add the phrase “be concise,” and it will shorten the response by about 50%, he added.
AI Hallucinations
Dr. Yan broached an issue that occasionally comes up, AI hallucinations, which refer to inaccurate or misleading responses on the basis of incomplete training or intrinsic biases within the model. He pointed to the case of a doctor discussing issues related to a patient’s hands, feet, and mouth, which the AI-generated model summarized as “the patient being diagnosed with hand, foot, and mouth disease.”
Another example he provided was a request to generate a letter of medical necessity for using ustekinumab (Stelara) for treating hidradenitis suppurative in a child that included references for its effectiveness and safety in children. The AI system generated “false references that sounded like they should be real because the authors are often people who have written in that field or on that subject,” said Dr. Yan.
When pressed, the system did acknowledge the references were hypothetical but were meant to illustrate the types of studies that would typically support the use of this drug in pediatric patients with HS. “ It’s well meaning, in the sense that it’s trying to help you achieve your goals using this training system,” said Dr. Yan.
“If you’re skeptical about a response, double-check the answer with a Google search or run the response through another AI [tool] asking it to check if the response is accurate,” he added.
While AI systems won’t replace the clinician, they are continuing to improve and becoming more sophisticated. Dr. Yan advises keeping up with emerging developments and engaging and adapting the most appropriate AI tool for an individual clinician’s work.
Asked to comment on the presentation at the SPD meeting, Sheilagh Maguiness, MD, director of the Division of Pediatric Dermatology at the University of Minnesota, Minneapolis, who, like other doctors, is increasingly testing AI, said she foresees a time when AI scribes fully replace humans for completing tasks during patient interactions.
“The hope is that if the AI scribes get good enough, we can just open our phone, have them translate the interaction, and create the notes for us.”
While she likes the idea of using ChatGPT to help with tasks like letters of recommendation for medications, Dr. Yan’s comments reiterated the importance of “checking and double-checking ChatGPT because it’s not correct all the time.” She particularly welcomed the advice “that we can just go back and ask it again to clarify, and that may improve its answers.”
Dr. Yan’s disclosures included an investment portfolio that includes companies working in the AI space, including Google, Apple, Nvidia, Amazon, Microsoft, and Arm. Dr. Maguiness had no relevant disclosures.
A version of this article first appeared on Medscape.com.
TORONTO — with the various AI models.
He reminds doctors that many of their colleagues and patients and their families are already using these systems, “and you don’t want to be left behind.”
In an interview following his presentation on AI at the annual meeting of the Society for Pediatric Dermatology (SPD), Dr. Yan discussed his tips for using AI.
Changing Fast
From the outset, most generative AI systems have been very good at processing language — for example, generating letters of medical necessity and summarizing disease processes into lay terms. But now they’re becoming “truly multimodal,” said Dr. Yan. “You can enter images; you could have it process audio; you can even start to have it refine video.”
To get started, he recommends signing up for a free account with ChatGPT, Gemini, Perplexity, Claude, and/or Microsoft Copilot. “To make the best choice, you have to try them out yourself because they each have their own kind of flavor and strengths and weaknesses,” said Dr. Yan.
Personally, he finds that ChatGPT is the most versatile, Gemini perhaps a little better in terms of image generation, and Perplexity probably the best at references because it was designed as an online library.
Once you figure out which platforms you prefer, consider signing up for a premium subscription, which is typically month to month and can be canceled at any time, Dr. Yan said. “This will allow you to get the most out of the AI model.”
As these AI systems are based on large language models, they are excellent at text, Dr. Yan noted. He suggests asking one to generate a letter or patient instruction sheet. “If you have a premium model, give it a PDF to summarize an article or take a photo of something that you want its opinion on.”
Privacy Critical
Always pay attention to privacy issues and avoid entering any private health information that would violate the Health Insurance Portability and Accountability Act (HIPAA), he said.
“We have to be very careful about how we interact with AI,” said Dr. Yan. “We can’t be posting private patient health information into these systems, no matter how useful these systems are.” Many academic institutions are creating “walled gardens” — private areas of AI access that don’t allow patient information to “leak out,” he said. “These AI models may have HIPAA protections in place and come with specific guidelines of use.”
The AI “scribe,” which helps with electronic health record documentation, is one of the most useful tools for clinicians, he said. He referred to a recent study showing that an AI scribe saved users an average of 1 hour at the keyboard every day, and a small patient survey showing 71% reported that it led to spending more time with their physician.
When entering requests into a prompt line with an AI system, Dr. Yan stressed that these prompts need to be clear and concise. For a complicated calculation or multistep problem, try adding the words “let’s do this step by step,” he said. “This is a technique invoking a ‘chain of thought’ that allows the system to enhance its accuracy when solving problems.”
If the response is not satisfactory, try being more detailed in the request, he advised, and consider giving the system examples of what you’re looking for and telling it what you don’t want in the output.
“For instance, if you’re asking for a differential diagnosis of rashes that affect the hands and feet, you can stipulate that you only want rashes that are vesicular or that arise in neonates, so you can get a more focused answer,” said Dr. Yan.
If there are “long-winded verbose” responses, add the phrase “be concise,” and it will shorten the response by about 50%, he added.
AI Hallucinations
Dr. Yan broached an issue that occasionally comes up, AI hallucinations, which refer to inaccurate or misleading responses on the basis of incomplete training or intrinsic biases within the model. He pointed to the case of a doctor discussing issues related to a patient’s hands, feet, and mouth, which the AI-generated model summarized as “the patient being diagnosed with hand, foot, and mouth disease.”
Another example he provided was a request to generate a letter of medical necessity for using ustekinumab (Stelara) for treating hidradenitis suppurative in a child that included references for its effectiveness and safety in children. The AI system generated “false references that sounded like they should be real because the authors are often people who have written in that field or on that subject,” said Dr. Yan.
When pressed, the system did acknowledge the references were hypothetical but were meant to illustrate the types of studies that would typically support the use of this drug in pediatric patients with HS. “ It’s well meaning, in the sense that it’s trying to help you achieve your goals using this training system,” said Dr. Yan.
“If you’re skeptical about a response, double-check the answer with a Google search or run the response through another AI [tool] asking it to check if the response is accurate,” he added.
While AI systems won’t replace the clinician, they are continuing to improve and becoming more sophisticated. Dr. Yan advises keeping up with emerging developments and engaging and adapting the most appropriate AI tool for an individual clinician’s work.
Asked to comment on the presentation at the SPD meeting, Sheilagh Maguiness, MD, director of the Division of Pediatric Dermatology at the University of Minnesota, Minneapolis, who, like other doctors, is increasingly testing AI, said she foresees a time when AI scribes fully replace humans for completing tasks during patient interactions.
“The hope is that if the AI scribes get good enough, we can just open our phone, have them translate the interaction, and create the notes for us.”
While she likes the idea of using ChatGPT to help with tasks like letters of recommendation for medications, Dr. Yan’s comments reiterated the importance of “checking and double-checking ChatGPT because it’s not correct all the time.” She particularly welcomed the advice “that we can just go back and ask it again to clarify, and that may improve its answers.”
Dr. Yan’s disclosures included an investment portfolio that includes companies working in the AI space, including Google, Apple, Nvidia, Amazon, Microsoft, and Arm. Dr. Maguiness had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM SPD 2024