User login
Siblings of patients with bipolar disorder at increased risk
The siblings of patients with bipolar disorder not only face a significantly increased lifetime risk of that affective disorder, but a whole panoply of other psychiatric disorders, according to a new Danish longitudinal national registry study.
“Our data show the healthy siblings of patients with bipolar disorder are themselves at increased risk of developing any kind of psychiatric disorder. Mainly bipolar disorder, but all other kinds as well,” Lars Vedel Kessing, MD, DMSc, said in presenting the results of the soon-to-be-published Danish study at the virtual congress of the European College of Neuropsychopharmacology.
Moreover, the long-term Danish study also demonstrated that several major psychiatric disorders follow a previously unappreciated bimodal distribution of age of onset in the siblings of patients with bipolar disorder. For example, the incidence of new-onset bipolar disorder and unipolar depression in the siblings was markedly increased during youth and early adulthood, compared with controls drawn from the general Danish population. Then, incidence rates dropped off and plateaued at a lower level in midlife before surging after age 60 years. The same was true for somatoform disorders as well as alcohol and substance use disorders.
“Strategies to prevent onset of psychiatric illness in individuals with a first-generation family history of bipolar disorder should not be limited to adolescence and early adulthood but should be lifelong, likely with differentiated age-specific approaches. And this is not now the case.
“Generally, most researchers and clinicians are focusing more on the early part of life and not the later part of life from age 60 and up, even though this is indeed also a risk period for any kind of psychiatric illness as well as bipolar disorder,” according to Dr. Kessing, professor of psychiatry at the University of Copenhagen.
Dr. Kessing, a past recipient of the Brain and Behavior Research Foundation’s Outstanding Achievement in Mood Disorders Research Award, also described his research group’s successful innovative efforts to prevent first recurrences after a single manic episode or bipolar disorder.
Danish national sibling study
The longitudinal registry study included all 19,995 Danish patients with a primary diagnosis of bipolar disorder during 1995-2017, along with 13,923 of their siblings and 278,460 age- and gender-matched controls drawn from the general population.
The cumulative incidence of any psychiatric disorder was 66% greater in siblings than controls. Leading the way was a 374% increased risk of bipolar disorder.
Strategies to prevent a first relapse of bipolar disorder
Dr. Kessing and coinvestigators demonstrated in a meta-analysis that, with current standard therapies, the risk of recurrence among patients after a single manic or mixed episode is high in both adult and pediatric patients. In three studies of adults, the risk of recurrence was 35% during the first year after recovery from the index episode and 59% at 2 years. In three studies of children and adolescents, the risk of recurrence within 1 year after recovery was 40% in children and 52% in adolescents. This makes a compelling case for starting maintenance therapy following onset of a single manic or mixed episode, according to the investigators.
More than half a decade ago, Dr. Kessing and colleagues demonstrated in a study of 4,714 Danish patients with bipolar disorder who were prescribed lithium while in a psychiatric hospital that those who started the drug for prophylaxis early – that is, following their first psychiatric contact – had a significantly higher response to lithium monotherapy than those who started it only after repeated contacts. Indeed, their risk of nonresponse to lithium prophylaxis as evidenced by repeat hospital admission after a 6-month lithium stabilization period was 13% lower than in those starting the drug later.
Early intervention aiming to stop clinical progression of bipolar disorder intuitively seems appealing, so Dr. Kessing and colleagues created a specialized outpatient mood disorders clinic combining optimized pharmacotherapy and evidence-based group psychoeducation. They then put it to the test in a clinical trial in which 158 patients discharged from an initial psychiatric hospital admission for bipolar disorder were randomized to the specialized outpatient mood disorders clinic or standard care.
The rate of psychiatric hospital readmission within the next 6 years was 40% lower in the group assigned to the specialized early intervention clinic. Their rate of adherence to medication – mostly lithium and antipsychotics – was significantly higher. So were their treatment satisfaction scores. And the clincher: The total net direct cost of treatment in the specialized mood disorders clinic averaged 3,194 euro less per patient, an 11% reduction relative to the cost of standard care, a striking economic benefit achieved mainly through avoided hospitalizations.
In a subsequent subgroup analysis of the randomized trial data, Dr. Kessing and coinvestigators demonstrated that young adults with bipolar disorder not only benefited from participation in the specialized outpatient clinic, but they appeared to have derived greater benefit than the older patients. The rehospitalization rate was 67% lower in 18- to 25-year-old patients randomized to the specialized outpatient mood disorder clinic than in standard-care controls, compared with a 32% relative risk reduction in outpatient clinic patients aged 26 years or older).
“There are now several centers around the world which also use this model involving early intervention,” Dr. Kessing said. “It is so important that, when the diagnosis is made for the first time, the patient gets sufficient evidence-based treatment comprised of mood maintenance medication as well as group-based psychoeducation, which is the psychotherapeutic intervention for which there is the strongest evidence of an effect.”
The sibling study was funded free of commercial support. Dr. Kessing reported serving as a consultant to Lundbeck.
SOURCE: Kessing LV. ECNP 2020, Session S.25.
The siblings of patients with bipolar disorder not only face a significantly increased lifetime risk of that affective disorder, but a whole panoply of other psychiatric disorders, according to a new Danish longitudinal national registry study.
“Our data show the healthy siblings of patients with bipolar disorder are themselves at increased risk of developing any kind of psychiatric disorder. Mainly bipolar disorder, but all other kinds as well,” Lars Vedel Kessing, MD, DMSc, said in presenting the results of the soon-to-be-published Danish study at the virtual congress of the European College of Neuropsychopharmacology.
Moreover, the long-term Danish study also demonstrated that several major psychiatric disorders follow a previously unappreciated bimodal distribution of age of onset in the siblings of patients with bipolar disorder. For example, the incidence of new-onset bipolar disorder and unipolar depression in the siblings was markedly increased during youth and early adulthood, compared with controls drawn from the general Danish population. Then, incidence rates dropped off and plateaued at a lower level in midlife before surging after age 60 years. The same was true for somatoform disorders as well as alcohol and substance use disorders.
“Strategies to prevent onset of psychiatric illness in individuals with a first-generation family history of bipolar disorder should not be limited to adolescence and early adulthood but should be lifelong, likely with differentiated age-specific approaches. And this is not now the case.
“Generally, most researchers and clinicians are focusing more on the early part of life and not the later part of life from age 60 and up, even though this is indeed also a risk period for any kind of psychiatric illness as well as bipolar disorder,” according to Dr. Kessing, professor of psychiatry at the University of Copenhagen.
Dr. Kessing, a past recipient of the Brain and Behavior Research Foundation’s Outstanding Achievement in Mood Disorders Research Award, also described his research group’s successful innovative efforts to prevent first recurrences after a single manic episode or bipolar disorder.
Danish national sibling study
The longitudinal registry study included all 19,995 Danish patients with a primary diagnosis of bipolar disorder during 1995-2017, along with 13,923 of their siblings and 278,460 age- and gender-matched controls drawn from the general population.
The cumulative incidence of any psychiatric disorder was 66% greater in siblings than controls. Leading the way was a 374% increased risk of bipolar disorder.
Strategies to prevent a first relapse of bipolar disorder
Dr. Kessing and coinvestigators demonstrated in a meta-analysis that, with current standard therapies, the risk of recurrence among patients after a single manic or mixed episode is high in both adult and pediatric patients. In three studies of adults, the risk of recurrence was 35% during the first year after recovery from the index episode and 59% at 2 years. In three studies of children and adolescents, the risk of recurrence within 1 year after recovery was 40% in children and 52% in adolescents. This makes a compelling case for starting maintenance therapy following onset of a single manic or mixed episode, according to the investigators.
More than half a decade ago, Dr. Kessing and colleagues demonstrated in a study of 4,714 Danish patients with bipolar disorder who were prescribed lithium while in a psychiatric hospital that those who started the drug for prophylaxis early – that is, following their first psychiatric contact – had a significantly higher response to lithium monotherapy than those who started it only after repeated contacts. Indeed, their risk of nonresponse to lithium prophylaxis as evidenced by repeat hospital admission after a 6-month lithium stabilization period was 13% lower than in those starting the drug later.
Early intervention aiming to stop clinical progression of bipolar disorder intuitively seems appealing, so Dr. Kessing and colleagues created a specialized outpatient mood disorders clinic combining optimized pharmacotherapy and evidence-based group psychoeducation. They then put it to the test in a clinical trial in which 158 patients discharged from an initial psychiatric hospital admission for bipolar disorder were randomized to the specialized outpatient mood disorders clinic or standard care.
The rate of psychiatric hospital readmission within the next 6 years was 40% lower in the group assigned to the specialized early intervention clinic. Their rate of adherence to medication – mostly lithium and antipsychotics – was significantly higher. So were their treatment satisfaction scores. And the clincher: The total net direct cost of treatment in the specialized mood disorders clinic averaged 3,194 euro less per patient, an 11% reduction relative to the cost of standard care, a striking economic benefit achieved mainly through avoided hospitalizations.
In a subsequent subgroup analysis of the randomized trial data, Dr. Kessing and coinvestigators demonstrated that young adults with bipolar disorder not only benefited from participation in the specialized outpatient clinic, but they appeared to have derived greater benefit than the older patients. The rehospitalization rate was 67% lower in 18- to 25-year-old patients randomized to the specialized outpatient mood disorder clinic than in standard-care controls, compared with a 32% relative risk reduction in outpatient clinic patients aged 26 years or older).
“There are now several centers around the world which also use this model involving early intervention,” Dr. Kessing said. “It is so important that, when the diagnosis is made for the first time, the patient gets sufficient evidence-based treatment comprised of mood maintenance medication as well as group-based psychoeducation, which is the psychotherapeutic intervention for which there is the strongest evidence of an effect.”
The sibling study was funded free of commercial support. Dr. Kessing reported serving as a consultant to Lundbeck.
SOURCE: Kessing LV. ECNP 2020, Session S.25.
The siblings of patients with bipolar disorder not only face a significantly increased lifetime risk of that affective disorder, but a whole panoply of other psychiatric disorders, according to a new Danish longitudinal national registry study.
“Our data show the healthy siblings of patients with bipolar disorder are themselves at increased risk of developing any kind of psychiatric disorder. Mainly bipolar disorder, but all other kinds as well,” Lars Vedel Kessing, MD, DMSc, said in presenting the results of the soon-to-be-published Danish study at the virtual congress of the European College of Neuropsychopharmacology.
Moreover, the long-term Danish study also demonstrated that several major psychiatric disorders follow a previously unappreciated bimodal distribution of age of onset in the siblings of patients with bipolar disorder. For example, the incidence of new-onset bipolar disorder and unipolar depression in the siblings was markedly increased during youth and early adulthood, compared with controls drawn from the general Danish population. Then, incidence rates dropped off and plateaued at a lower level in midlife before surging after age 60 years. The same was true for somatoform disorders as well as alcohol and substance use disorders.
“Strategies to prevent onset of psychiatric illness in individuals with a first-generation family history of bipolar disorder should not be limited to adolescence and early adulthood but should be lifelong, likely with differentiated age-specific approaches. And this is not now the case.
“Generally, most researchers and clinicians are focusing more on the early part of life and not the later part of life from age 60 and up, even though this is indeed also a risk period for any kind of psychiatric illness as well as bipolar disorder,” according to Dr. Kessing, professor of psychiatry at the University of Copenhagen.
Dr. Kessing, a past recipient of the Brain and Behavior Research Foundation’s Outstanding Achievement in Mood Disorders Research Award, also described his research group’s successful innovative efforts to prevent first recurrences after a single manic episode or bipolar disorder.
Danish national sibling study
The longitudinal registry study included all 19,995 Danish patients with a primary diagnosis of bipolar disorder during 1995-2017, along with 13,923 of their siblings and 278,460 age- and gender-matched controls drawn from the general population.
The cumulative incidence of any psychiatric disorder was 66% greater in siblings than controls. Leading the way was a 374% increased risk of bipolar disorder.
Strategies to prevent a first relapse of bipolar disorder
Dr. Kessing and coinvestigators demonstrated in a meta-analysis that, with current standard therapies, the risk of recurrence among patients after a single manic or mixed episode is high in both adult and pediatric patients. In three studies of adults, the risk of recurrence was 35% during the first year after recovery from the index episode and 59% at 2 years. In three studies of children and adolescents, the risk of recurrence within 1 year after recovery was 40% in children and 52% in adolescents. This makes a compelling case for starting maintenance therapy following onset of a single manic or mixed episode, according to the investigators.
More than half a decade ago, Dr. Kessing and colleagues demonstrated in a study of 4,714 Danish patients with bipolar disorder who were prescribed lithium while in a psychiatric hospital that those who started the drug for prophylaxis early – that is, following their first psychiatric contact – had a significantly higher response to lithium monotherapy than those who started it only after repeated contacts. Indeed, their risk of nonresponse to lithium prophylaxis as evidenced by repeat hospital admission after a 6-month lithium stabilization period was 13% lower than in those starting the drug later.
Early intervention aiming to stop clinical progression of bipolar disorder intuitively seems appealing, so Dr. Kessing and colleagues created a specialized outpatient mood disorders clinic combining optimized pharmacotherapy and evidence-based group psychoeducation. They then put it to the test in a clinical trial in which 158 patients discharged from an initial psychiatric hospital admission for bipolar disorder were randomized to the specialized outpatient mood disorders clinic or standard care.
The rate of psychiatric hospital readmission within the next 6 years was 40% lower in the group assigned to the specialized early intervention clinic. Their rate of adherence to medication – mostly lithium and antipsychotics – was significantly higher. So were their treatment satisfaction scores. And the clincher: The total net direct cost of treatment in the specialized mood disorders clinic averaged 3,194 euro less per patient, an 11% reduction relative to the cost of standard care, a striking economic benefit achieved mainly through avoided hospitalizations.
In a subsequent subgroup analysis of the randomized trial data, Dr. Kessing and coinvestigators demonstrated that young adults with bipolar disorder not only benefited from participation in the specialized outpatient clinic, but they appeared to have derived greater benefit than the older patients. The rehospitalization rate was 67% lower in 18- to 25-year-old patients randomized to the specialized outpatient mood disorder clinic than in standard-care controls, compared with a 32% relative risk reduction in outpatient clinic patients aged 26 years or older).
“There are now several centers around the world which also use this model involving early intervention,” Dr. Kessing said. “It is so important that, when the diagnosis is made for the first time, the patient gets sufficient evidence-based treatment comprised of mood maintenance medication as well as group-based psychoeducation, which is the psychotherapeutic intervention for which there is the strongest evidence of an effect.”
The sibling study was funded free of commercial support. Dr. Kessing reported serving as a consultant to Lundbeck.
SOURCE: Kessing LV. ECNP 2020, Session S.25.
FROM ECNP 2020
Clinical pearls for administering cognitive exams during the pandemic
Patients have often been labeled as “poor historians” if they are not able to recollect their own medical history, whether through illness or difficulties in communication. But Fred Ovsiew, MD, speaking at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sees that label as an excuse on the part of the clinician.
“I strongly advise you to drop that phrase from your vocabulary if you do use it, because the patient is not the historian. The doctor, the clinician is the historian,” Dr. Ovsiew said at the meeting, presented by Global Academy for Medical Education. “It is the clinician’s job to put the story together using the account by the patient as one source, but [also] interviewing a collateral informant and/or reviewing records, which is necessary in almost every case of a neuropsychiatric illness.”
Rather, clinicians taking history at the bedside should focus on why the patients cannot give a narrative account of their illness. Patients can have narrative incapacity on a psychogenic basis, such as in patients with conversion or somatoform disorder, he explained. “I think this is a result of the narrative incapacity that develops in people who have had trauma or adverse experiences in childhood and insecure attachment. This is shown on the adult attachment interview as a disorganized account of their childhoods.”
Other patients might not be able to recount their medical history because they are amnestic, which leaves their account vague because of a lack of access to information. “It may be frozen in time in the sense that, up to a certain point in their life, they can recount the history,” Dr. Ovsiew said. “But in recent years, their account becomes vague.”
Patients with right hemisphere lesions might not know that their account has incongruity and is implausible, while patients with dorsolateral prefrontal lesions might be aspontaneous, use few words to describe their situation, and have poor insight. Those with ventromedial prefrontal lesions can be impulsive and have poor insight, not considering alternative possibilities, Dr. Ovsiew noted.
Asking open-ended questions of the patient is the first step to identifying any potential narrative incapacity, followed by a detailed medical history by the clinician. When taking a medical history, try avoiding what Dr. Ovsiew calls the “anything like that?” problem, where a clinician asks a question about a cluster of symptoms that would make sense to a doctor, but not a patient. For example, a doctor might ask whether a patient is experiencing “chest pain or leg swelling – anything like that?” because he or she knows what those symptoms have in common, but the patient might not know the relationship between those symptoms. “You can’t count on the patient to tell you all the relevant information,” he said. “You have to know what to ask about.”
“Patients with brain disease have subtle personality changes, sometimes more obvious personality changes. These need to be inquired about,” Dr. Ovsiew said. “The patient with apathy has reduced negative as well as positive emotions. The patient with depression has reduced positive emotions, but often tells you very clearly about the negative emotions of sadness, guilt. The patient with depression has diurnal variation in mood, a very telling symptom, especially when it’s disclosed spontaneously,” Dr. Ovsiew explained. “The point is, you need to know to ask about it.”
When taking a sleep history, clinicians should be aware of sleep disturbances apart from insomnia and early waking. REM sleep behavior disorder is a condition that should be inquired about. Obstructive sleep apnea is a condition that might not be immediately apparent to the patient, but a bed partner can identify whether a patient has problems breathing throughout the night.
“This is an important condition to uncover for the neuropsychiatrist because it contributes to treatment resistance and depression, and it contributes to cognitive impairment,” Dr. Ovsiew said. “These patients commonly have mild difficulties with attention and concentration.”
Always ask about head injury in every history, which can be relevant to later onset depression, PTSD, and cognitive impairment. Every head injury follows a trajectory of retrograde amnesia and altered state of consciousness (including coma), followed by a period of posttraumatic amnesia. Duration of these states can be used to assess the severity of brain injury, but the 15-point Glasgow Coma Scale is another way to assess injury severity, Dr. Ovsiew explained.
However, the two do not always overlap, he noted. “Someone may have a Glasgow Coma Scale score that is 9-12, predicting moderate brain injury, but they may have a short duration of amnesia. These don’t always follow the same path. There are many different ways of classifying how severe the brain injury is.”
Keep probes brief, straightforward
Cognitive exams of patients with suspected psychiatric disorders should be simple, easy to administer and focused on a single domain of cognition. “Probes should be brief. They should not require specialized equipment. The Purdue Pegboard Test might be a great neuropsychological instrument, but very few of us carry a pegboard around in our medical bags,” Dr. Ovsiew said.
The probe administered should also be accessible to the patient. The serial sevens clinical test, where a patient is asked to repeatedly subtract 7 from 100, is only effective at testing concentration if the patient is capable of completing the test. “There are going to be patients who can’t do the task, but it’s not because of concentration failure, it’s because of subtraction failure,” he said.
When assessing attention, effective tasks include having the patient perform the digit span test forward and backward, count backward from 20 to 1, listing the months of the year in reverse, and performing the Mental Alternation Test. However, Dr. Ovsiew explained there may be some barriers for patients in completing these tasks. “The person may be aphasic and not know the alphabet. The person may have English as a second language and not be skilled at giving the alphabet in English. In some cases, you may want to check and not assume that the patient can count and does know the alphabet.”
In assessing language, listen for aphasic abnormalities. “The patient, of course, is speaking throughout the interview, but you need to take a moment to listen for prosody, to listen to rate of speech, to listen for paraphasic errors or word-finding problems,” Dr. Ovsiew said. Any abnormalities should be probed further through confrontation naming tasks, which can be done in person and with some success through video, but not by phone. Naming to definition (“What do you call the part of a shirt that covers the arm?”) is one way of administering the test over the phone.
Visuospatial function can be assessed by clock drawing but also carries problems. Patients who do not plan their clock before beginning to draw, for example, may have an executive function problem instead of a visuospatial problem, Dr. Ovsiew noted. Patients in whom a clinician suspects hemineglect should be given a visual search task or line by section task. “I like doing clock drawing. It’s a nice screening test. It’s becoming, I think, less useful as people count on digital clocks and have trouble even imagining what an analog clock looks like.”
An approach that is better suited to in-person assessment, but also works by video, is the Poppelreuter figure visual perceptual function test, which is a prompt for the patient that involves common household items overlaying one another “in atypical positions and atypical configurations” where the patient is instructed to describe the items they see on the card. Another approach that works over video is the interlocking finger test, where the patient is asked to copy the hand positions made by the clinician.
Dr. Ovsiew admitted that visuospatial function is nearly impossible to assess over the phone. Asking topographical questions (“If you’re driving from Chicago to Los Angeles, is the Pacific Ocean in front of you, behind you, to your left, or to your right?”) may help judge visuospatial function, but this relies on the patient having the topographic knowledge to answer the questions. Some patients who are topographically disoriented can’t do them at all,” Dr. Ovsiew said.
Bedside neuropsychiatry assesses encoding of a memory, its retention and its retrieval as well as verbal and visual cues. Each one of these aspects of memory can be impaired on its own and should be explored separately, Dr. Ovsiew explained. “Neuropsychiatric clinicians have a rough-and-ready, seat-of-the-pants way of approaching this that wouldn’t pass muster if you’re a psychologist, but is the best we can do at the bedside.”
To test retrieval and retention, the Three Words–Three Shapes test works well in person, with some difficulty by video, and is not possible to administer over the phone. In lieu of that test, giving the patient a simple word list and asking them to repeat the list in order. Using the word list, “these different stages of memory function can be parsed out pretty well at the bedside or chairside, and even by the phone. Figuring out where the memory failure is diagnostically important,” Dr. Ovsiew said.
Executive function, which involves activation, planning, sequencing, maintaining, self-monitoring, and flexible employment of action and attention, is “complicated to evaluate because there are multiple aspects of executive function, multiple deficits that can be seen with executive dysfunction, and they don’t all correlate with each other.”
Within executive function evaluation, the Mental Alternation Test can assess working memory, motor sequencing can be assessed through the ring/fist, fist/edge/palm, alternating fist, and rampart tests. The Go/No-Go test can be used to assess response inhibition. For effortful retrieval evaluation, spontaneous word-list generation – such as thinking of all the items one can buy at a supermarket– can test category fluency, while a task to name all the words starting with a certain letter can assess letter stimulus.
Executive function “is of crucial importance in the neuropsychiatric evaluation because it’s strongly correlated with how well the person functions outside the office,” Dr. Ovsiew said.
Global Academy and this news organization are owned by the same parent company. Dr. Ovsiew reported relationships with Wolters Kluwer Health in the form of consulting, receiving royalty payments, and related activities.
Patients have often been labeled as “poor historians” if they are not able to recollect their own medical history, whether through illness or difficulties in communication. But Fred Ovsiew, MD, speaking at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sees that label as an excuse on the part of the clinician.
“I strongly advise you to drop that phrase from your vocabulary if you do use it, because the patient is not the historian. The doctor, the clinician is the historian,” Dr. Ovsiew said at the meeting, presented by Global Academy for Medical Education. “It is the clinician’s job to put the story together using the account by the patient as one source, but [also] interviewing a collateral informant and/or reviewing records, which is necessary in almost every case of a neuropsychiatric illness.”
Rather, clinicians taking history at the bedside should focus on why the patients cannot give a narrative account of their illness. Patients can have narrative incapacity on a psychogenic basis, such as in patients with conversion or somatoform disorder, he explained. “I think this is a result of the narrative incapacity that develops in people who have had trauma or adverse experiences in childhood and insecure attachment. This is shown on the adult attachment interview as a disorganized account of their childhoods.”
Other patients might not be able to recount their medical history because they are amnestic, which leaves their account vague because of a lack of access to information. “It may be frozen in time in the sense that, up to a certain point in their life, they can recount the history,” Dr. Ovsiew said. “But in recent years, their account becomes vague.”
Patients with right hemisphere lesions might not know that their account has incongruity and is implausible, while patients with dorsolateral prefrontal lesions might be aspontaneous, use few words to describe their situation, and have poor insight. Those with ventromedial prefrontal lesions can be impulsive and have poor insight, not considering alternative possibilities, Dr. Ovsiew noted.
Asking open-ended questions of the patient is the first step to identifying any potential narrative incapacity, followed by a detailed medical history by the clinician. When taking a medical history, try avoiding what Dr. Ovsiew calls the “anything like that?” problem, where a clinician asks a question about a cluster of symptoms that would make sense to a doctor, but not a patient. For example, a doctor might ask whether a patient is experiencing “chest pain or leg swelling – anything like that?” because he or she knows what those symptoms have in common, but the patient might not know the relationship between those symptoms. “You can’t count on the patient to tell you all the relevant information,” he said. “You have to know what to ask about.”
“Patients with brain disease have subtle personality changes, sometimes more obvious personality changes. These need to be inquired about,” Dr. Ovsiew said. “The patient with apathy has reduced negative as well as positive emotions. The patient with depression has reduced positive emotions, but often tells you very clearly about the negative emotions of sadness, guilt. The patient with depression has diurnal variation in mood, a very telling symptom, especially when it’s disclosed spontaneously,” Dr. Ovsiew explained. “The point is, you need to know to ask about it.”
When taking a sleep history, clinicians should be aware of sleep disturbances apart from insomnia and early waking. REM sleep behavior disorder is a condition that should be inquired about. Obstructive sleep apnea is a condition that might not be immediately apparent to the patient, but a bed partner can identify whether a patient has problems breathing throughout the night.
“This is an important condition to uncover for the neuropsychiatrist because it contributes to treatment resistance and depression, and it contributes to cognitive impairment,” Dr. Ovsiew said. “These patients commonly have mild difficulties with attention and concentration.”
Always ask about head injury in every history, which can be relevant to later onset depression, PTSD, and cognitive impairment. Every head injury follows a trajectory of retrograde amnesia and altered state of consciousness (including coma), followed by a period of posttraumatic amnesia. Duration of these states can be used to assess the severity of brain injury, but the 15-point Glasgow Coma Scale is another way to assess injury severity, Dr. Ovsiew explained.
However, the two do not always overlap, he noted. “Someone may have a Glasgow Coma Scale score that is 9-12, predicting moderate brain injury, but they may have a short duration of amnesia. These don’t always follow the same path. There are many different ways of classifying how severe the brain injury is.”
Keep probes brief, straightforward
Cognitive exams of patients with suspected psychiatric disorders should be simple, easy to administer and focused on a single domain of cognition. “Probes should be brief. They should not require specialized equipment. The Purdue Pegboard Test might be a great neuropsychological instrument, but very few of us carry a pegboard around in our medical bags,” Dr. Ovsiew said.
The probe administered should also be accessible to the patient. The serial sevens clinical test, where a patient is asked to repeatedly subtract 7 from 100, is only effective at testing concentration if the patient is capable of completing the test. “There are going to be patients who can’t do the task, but it’s not because of concentration failure, it’s because of subtraction failure,” he said.
When assessing attention, effective tasks include having the patient perform the digit span test forward and backward, count backward from 20 to 1, listing the months of the year in reverse, and performing the Mental Alternation Test. However, Dr. Ovsiew explained there may be some barriers for patients in completing these tasks. “The person may be aphasic and not know the alphabet. The person may have English as a second language and not be skilled at giving the alphabet in English. In some cases, you may want to check and not assume that the patient can count and does know the alphabet.”
In assessing language, listen for aphasic abnormalities. “The patient, of course, is speaking throughout the interview, but you need to take a moment to listen for prosody, to listen to rate of speech, to listen for paraphasic errors or word-finding problems,” Dr. Ovsiew said. Any abnormalities should be probed further through confrontation naming tasks, which can be done in person and with some success through video, but not by phone. Naming to definition (“What do you call the part of a shirt that covers the arm?”) is one way of administering the test over the phone.
Visuospatial function can be assessed by clock drawing but also carries problems. Patients who do not plan their clock before beginning to draw, for example, may have an executive function problem instead of a visuospatial problem, Dr. Ovsiew noted. Patients in whom a clinician suspects hemineglect should be given a visual search task or line by section task. “I like doing clock drawing. It’s a nice screening test. It’s becoming, I think, less useful as people count on digital clocks and have trouble even imagining what an analog clock looks like.”
An approach that is better suited to in-person assessment, but also works by video, is the Poppelreuter figure visual perceptual function test, which is a prompt for the patient that involves common household items overlaying one another “in atypical positions and atypical configurations” where the patient is instructed to describe the items they see on the card. Another approach that works over video is the interlocking finger test, where the patient is asked to copy the hand positions made by the clinician.
Dr. Ovsiew admitted that visuospatial function is nearly impossible to assess over the phone. Asking topographical questions (“If you’re driving from Chicago to Los Angeles, is the Pacific Ocean in front of you, behind you, to your left, or to your right?”) may help judge visuospatial function, but this relies on the patient having the topographic knowledge to answer the questions. Some patients who are topographically disoriented can’t do them at all,” Dr. Ovsiew said.
Bedside neuropsychiatry assesses encoding of a memory, its retention and its retrieval as well as verbal and visual cues. Each one of these aspects of memory can be impaired on its own and should be explored separately, Dr. Ovsiew explained. “Neuropsychiatric clinicians have a rough-and-ready, seat-of-the-pants way of approaching this that wouldn’t pass muster if you’re a psychologist, but is the best we can do at the bedside.”
To test retrieval and retention, the Three Words–Three Shapes test works well in person, with some difficulty by video, and is not possible to administer over the phone. In lieu of that test, giving the patient a simple word list and asking them to repeat the list in order. Using the word list, “these different stages of memory function can be parsed out pretty well at the bedside or chairside, and even by the phone. Figuring out where the memory failure is diagnostically important,” Dr. Ovsiew said.
Executive function, which involves activation, planning, sequencing, maintaining, self-monitoring, and flexible employment of action and attention, is “complicated to evaluate because there are multiple aspects of executive function, multiple deficits that can be seen with executive dysfunction, and they don’t all correlate with each other.”
Within executive function evaluation, the Mental Alternation Test can assess working memory, motor sequencing can be assessed through the ring/fist, fist/edge/palm, alternating fist, and rampart tests. The Go/No-Go test can be used to assess response inhibition. For effortful retrieval evaluation, spontaneous word-list generation – such as thinking of all the items one can buy at a supermarket– can test category fluency, while a task to name all the words starting with a certain letter can assess letter stimulus.
Executive function “is of crucial importance in the neuropsychiatric evaluation because it’s strongly correlated with how well the person functions outside the office,” Dr. Ovsiew said.
Global Academy and this news organization are owned by the same parent company. Dr. Ovsiew reported relationships with Wolters Kluwer Health in the form of consulting, receiving royalty payments, and related activities.
Patients have often been labeled as “poor historians” if they are not able to recollect their own medical history, whether through illness or difficulties in communication. But Fred Ovsiew, MD, speaking at Focus on Neuropsychiatry presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sees that label as an excuse on the part of the clinician.
“I strongly advise you to drop that phrase from your vocabulary if you do use it, because the patient is not the historian. The doctor, the clinician is the historian,” Dr. Ovsiew said at the meeting, presented by Global Academy for Medical Education. “It is the clinician’s job to put the story together using the account by the patient as one source, but [also] interviewing a collateral informant and/or reviewing records, which is necessary in almost every case of a neuropsychiatric illness.”
Rather, clinicians taking history at the bedside should focus on why the patients cannot give a narrative account of their illness. Patients can have narrative incapacity on a psychogenic basis, such as in patients with conversion or somatoform disorder, he explained. “I think this is a result of the narrative incapacity that develops in people who have had trauma or adverse experiences in childhood and insecure attachment. This is shown on the adult attachment interview as a disorganized account of their childhoods.”
Other patients might not be able to recount their medical history because they are amnestic, which leaves their account vague because of a lack of access to information. “It may be frozen in time in the sense that, up to a certain point in their life, they can recount the history,” Dr. Ovsiew said. “But in recent years, their account becomes vague.”
Patients with right hemisphere lesions might not know that their account has incongruity and is implausible, while patients with dorsolateral prefrontal lesions might be aspontaneous, use few words to describe their situation, and have poor insight. Those with ventromedial prefrontal lesions can be impulsive and have poor insight, not considering alternative possibilities, Dr. Ovsiew noted.
Asking open-ended questions of the patient is the first step to identifying any potential narrative incapacity, followed by a detailed medical history by the clinician. When taking a medical history, try avoiding what Dr. Ovsiew calls the “anything like that?” problem, where a clinician asks a question about a cluster of symptoms that would make sense to a doctor, but not a patient. For example, a doctor might ask whether a patient is experiencing “chest pain or leg swelling – anything like that?” because he or she knows what those symptoms have in common, but the patient might not know the relationship between those symptoms. “You can’t count on the patient to tell you all the relevant information,” he said. “You have to know what to ask about.”
“Patients with brain disease have subtle personality changes, sometimes more obvious personality changes. These need to be inquired about,” Dr. Ovsiew said. “The patient with apathy has reduced negative as well as positive emotions. The patient with depression has reduced positive emotions, but often tells you very clearly about the negative emotions of sadness, guilt. The patient with depression has diurnal variation in mood, a very telling symptom, especially when it’s disclosed spontaneously,” Dr. Ovsiew explained. “The point is, you need to know to ask about it.”
When taking a sleep history, clinicians should be aware of sleep disturbances apart from insomnia and early waking. REM sleep behavior disorder is a condition that should be inquired about. Obstructive sleep apnea is a condition that might not be immediately apparent to the patient, but a bed partner can identify whether a patient has problems breathing throughout the night.
“This is an important condition to uncover for the neuropsychiatrist because it contributes to treatment resistance and depression, and it contributes to cognitive impairment,” Dr. Ovsiew said. “These patients commonly have mild difficulties with attention and concentration.”
Always ask about head injury in every history, which can be relevant to later onset depression, PTSD, and cognitive impairment. Every head injury follows a trajectory of retrograde amnesia and altered state of consciousness (including coma), followed by a period of posttraumatic amnesia. Duration of these states can be used to assess the severity of brain injury, but the 15-point Glasgow Coma Scale is another way to assess injury severity, Dr. Ovsiew explained.
However, the two do not always overlap, he noted. “Someone may have a Glasgow Coma Scale score that is 9-12, predicting moderate brain injury, but they may have a short duration of amnesia. These don’t always follow the same path. There are many different ways of classifying how severe the brain injury is.”
Keep probes brief, straightforward
Cognitive exams of patients with suspected psychiatric disorders should be simple, easy to administer and focused on a single domain of cognition. “Probes should be brief. They should not require specialized equipment. The Purdue Pegboard Test might be a great neuropsychological instrument, but very few of us carry a pegboard around in our medical bags,” Dr. Ovsiew said.
The probe administered should also be accessible to the patient. The serial sevens clinical test, where a patient is asked to repeatedly subtract 7 from 100, is only effective at testing concentration if the patient is capable of completing the test. “There are going to be patients who can’t do the task, but it’s not because of concentration failure, it’s because of subtraction failure,” he said.
When assessing attention, effective tasks include having the patient perform the digit span test forward and backward, count backward from 20 to 1, listing the months of the year in reverse, and performing the Mental Alternation Test. However, Dr. Ovsiew explained there may be some barriers for patients in completing these tasks. “The person may be aphasic and not know the alphabet. The person may have English as a second language and not be skilled at giving the alphabet in English. In some cases, you may want to check and not assume that the patient can count and does know the alphabet.”
In assessing language, listen for aphasic abnormalities. “The patient, of course, is speaking throughout the interview, but you need to take a moment to listen for prosody, to listen to rate of speech, to listen for paraphasic errors or word-finding problems,” Dr. Ovsiew said. Any abnormalities should be probed further through confrontation naming tasks, which can be done in person and with some success through video, but not by phone. Naming to definition (“What do you call the part of a shirt that covers the arm?”) is one way of administering the test over the phone.
Visuospatial function can be assessed by clock drawing but also carries problems. Patients who do not plan their clock before beginning to draw, for example, may have an executive function problem instead of a visuospatial problem, Dr. Ovsiew noted. Patients in whom a clinician suspects hemineglect should be given a visual search task or line by section task. “I like doing clock drawing. It’s a nice screening test. It’s becoming, I think, less useful as people count on digital clocks and have trouble even imagining what an analog clock looks like.”
An approach that is better suited to in-person assessment, but also works by video, is the Poppelreuter figure visual perceptual function test, which is a prompt for the patient that involves common household items overlaying one another “in atypical positions and atypical configurations” where the patient is instructed to describe the items they see on the card. Another approach that works over video is the interlocking finger test, where the patient is asked to copy the hand positions made by the clinician.
Dr. Ovsiew admitted that visuospatial function is nearly impossible to assess over the phone. Asking topographical questions (“If you’re driving from Chicago to Los Angeles, is the Pacific Ocean in front of you, behind you, to your left, or to your right?”) may help judge visuospatial function, but this relies on the patient having the topographic knowledge to answer the questions. Some patients who are topographically disoriented can’t do them at all,” Dr. Ovsiew said.
Bedside neuropsychiatry assesses encoding of a memory, its retention and its retrieval as well as verbal and visual cues. Each one of these aspects of memory can be impaired on its own and should be explored separately, Dr. Ovsiew explained. “Neuropsychiatric clinicians have a rough-and-ready, seat-of-the-pants way of approaching this that wouldn’t pass muster if you’re a psychologist, but is the best we can do at the bedside.”
To test retrieval and retention, the Three Words–Three Shapes test works well in person, with some difficulty by video, and is not possible to administer over the phone. In lieu of that test, giving the patient a simple word list and asking them to repeat the list in order. Using the word list, “these different stages of memory function can be parsed out pretty well at the bedside or chairside, and even by the phone. Figuring out where the memory failure is diagnostically important,” Dr. Ovsiew said.
Executive function, which involves activation, planning, sequencing, maintaining, self-monitoring, and flexible employment of action and attention, is “complicated to evaluate because there are multiple aspects of executive function, multiple deficits that can be seen with executive dysfunction, and they don’t all correlate with each other.”
Within executive function evaluation, the Mental Alternation Test can assess working memory, motor sequencing can be assessed through the ring/fist, fist/edge/palm, alternating fist, and rampart tests. The Go/No-Go test can be used to assess response inhibition. For effortful retrieval evaluation, spontaneous word-list generation – such as thinking of all the items one can buy at a supermarket– can test category fluency, while a task to name all the words starting with a certain letter can assess letter stimulus.
Executive function “is of crucial importance in the neuropsychiatric evaluation because it’s strongly correlated with how well the person functions outside the office,” Dr. Ovsiew said.
Global Academy and this news organization are owned by the same parent company. Dr. Ovsiew reported relationships with Wolters Kluwer Health in the form of consulting, receiving royalty payments, and related activities.
FROM FOCUS ON NEUROPSYCHIATRY 2020
PANS may be more prevalent than thought
Pediatric acute-onset neuropsychiatric syndrome (PANS), a rare acute onset of psychiatric symptoms, might be more common than initially thought, according to Kiki D. Chang, MD.
PANS is characterized by the National Center for Advancing Translational Sciences Genetic and Rare Diseases Information Center as a “sudden onset of obsessive-compulsive symptoms and/or severe eating restrictions, along with at least two other cognitive, behavioral, or neurological symptoms.” These symptoms can include anxiety, depression, oppositional behavior, difficulty concentrating, abnormalities in motor and sensory skills, and other somatic symptoms. The condition develops as a result of an infection that causes an autoimmune or inflammatory response in the brain, and patients tend to respond well to treatment from antibiotics, anti-inflammatory medication, and immunomodulatory therapy.
Both PANS and a subtype condition, pediatric autoimmune neuropsychiatric disorders associated with Streptococcus infections (PANDAS), are underrecognized, Dr. Chang said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. It is often misdiagnosed as Tourette syndrome or obsessive-compulsive disorder (OCD) because tics are present in about half of cases, he said, but more severe associated symptoms, such as psychosis, can be misdiagnosed as psychotic disorders or mood disorders. Currently, neither PANS nor PANDAS are officially recognized by the American Academy of Pediatrics or the DSM-5.
“We’re hoping that it is soon because it clearly exists,” Dr. Chang said at the meeting, presented by Global Academy for Medical Education. “If you’ve ever treated a child with PANS or PANDAS and you have seen antibiotics totally reverse OCD and tic-like behavior, if you’ve seen prednisone actually treat symptoms of mania or even psychosis and actually make those things better rather than worse, it’s really eye-opening and it makes a believer out of you.”
Anxiety is the most common psychiatric symptom in youth, and anxiety disorders are also common, said Dr. Chang. According to the National Comorbidity Survey: Adolescent Supplement, 2001-2004, 31.9% adolescents overall reported an anxiety disorder, and 8.3% said their anxiety disorder caused severe impairment. The COVID-19 pandemic has increased the level of anxiety for children and adolescents, which can lead to other disorders, such as separation anxiety disorder, panic disorder, specific phobia, social anxiety disorder, acute stress disorder, generalized anxiety disorder, OCD, or posttraumatic stress disorder. Psychiatrists should be suspicious of any sudden onset of symptoms that overlap with PANS, said Dr. Chang, who is now in private practice in Palo Alto, Calif.
“Anxiety disorders are incredibly common. Remember that you’ve got to carefully screen for other anxiety disorders, because they’re highly comorbid,” Dr. Chang said. “You’ve got to do a full workup. If there are other things going on, you’ve got to think PANS. If it’s acute onset, you’ve really got to think [PANS], and you should do that workup or refer to someone who does.”
The prevalence of PANS and PANDAS is not known, but it may be more common than psychiatrists realize, Dr. Chang said. “I’ve been doing this for about 10 years now in the PANS and PANDAS field, and it’s very clear to me that this is something that is prevalent,” he said.
Together with Jennifer Frankovich, MD, Dr. Chang founded a clinic at the Lucile Packard Children’s Hospital Stanford, and also helped to develop treatment guidelines for youth with PANS. At the clinic, patients are approximately 7.7 years old when developing the first symptoms, and are 10.7 years old when presenting for treatment. Most patients at the clinic are male (78%), and 40% are acute onset cases. Nearly all patients have symptoms of anxiety (92%), mood disorder (88%), OCD (86%), sensory/motor abnormalities (88%), irritability/aggression (82%), somatic symptoms, deterioration in school (76%), and behavioral regression (59%). More than one-third present with suicidal ideation (38%) and violence to themselves (29%), others (38%), or objects. About one-fourth have symptoms of psychosis (24%).
“These can be really sick kids,” Dr. Chang said. not able to eat because they’re afraid of things, not able to take care of their body or daily living. These were sometimes highly functional people beforehand, sometimes they weren’t, but it was still an acute change.”
Treatment for PANS
Treatment guidelines released by the PANS/PANDAS Consortium in 2017 recommend a first course of antistreptococcal treatment for new PANS cases. Psychiatrists should look for evidence of strep or other infection and use antibiotics to eradicate any underlying acute or residual infection.
“Very commonly, we’ll use things like azithromycin, or Augmentin, or amoxicillin, and you’ll see suddenly the OCD go away or at least diminish, the sleep return to normal, the mood come back down,” Dr. Chang said. “It’s pretty amazing when you see it.”
In other cases, ongoing treatment is needed for longer than the normal 5-day or 10-day course of antibiotics. “We’re not exactly sure how long: sometimes it’s 3 weeks, sometimes it’s 4 weeks, but you have to give it more than a week. Sometimes it’s the anti-inflammatory properties that are helping.” While concerns about haphazardly prescribing antibiotics are valid, “if you can cure this stuff on antibiotics, it’s low-hanging fruit,” Dr. Chang said.
There is evidence in the literature that prescribing antibiotics for PANS is beneficial. A randomized controlled trial published in 2017 showed that patients with PANS prescribed azithromycin for 4 weeks had greater reductions in severity of OCD, compared with placebo.
“We need more studies, but clearly, antibiotics do have the potential to help with certain kids. And certainly, in my practice, I see sometimes a slam-dunk response,” Dr. Chang said. “Unfortunately, sometimes you don’t see a slam-dunk response or you can’t find an infection. That’s when it might be more of an inflammation from some other reason. It could be a leftover infection, or it could be an anti-inflammatory situation.”
Immunomodulatory treatment for PANS includes use of NSAIDs, such as ibuprofen or naproxen sodium; steroids, such as prednisone or intravenous corticosteroids; intravenous immunoglobulin; or plasma exchange. Other therapies to consider are rituximab, mycophenolate mofetil, and cyclophosphamide.
Some psychiatric treatments may help patients with PANS. While there is no empirical evidence that psychotropics are effective in treating PANS, some SSRIs might help if patients are able to handle any adverse events. Psychotherapy and education of the family are also important for patients with PANS and their caregivers.
“Basically, [PANS] has as high a caregiver burden as having someone in the household with Alzheimer’s disease or cancer. It’s a huge burden, it’s very stressful, and the family needs support for this,” Dr. Chang said.
Global Academy and this news organization are owned by the same parent company. Dr. Chang reports he is a consultant for Allergan, Impel NeuroPharma, and Sunovion. He is also on the speaker’s bureau for Sunovion.
Pediatric acute-onset neuropsychiatric syndrome (PANS), a rare acute onset of psychiatric symptoms, might be more common than initially thought, according to Kiki D. Chang, MD.
PANS is characterized by the National Center for Advancing Translational Sciences Genetic and Rare Diseases Information Center as a “sudden onset of obsessive-compulsive symptoms and/or severe eating restrictions, along with at least two other cognitive, behavioral, or neurological symptoms.” These symptoms can include anxiety, depression, oppositional behavior, difficulty concentrating, abnormalities in motor and sensory skills, and other somatic symptoms. The condition develops as a result of an infection that causes an autoimmune or inflammatory response in the brain, and patients tend to respond well to treatment from antibiotics, anti-inflammatory medication, and immunomodulatory therapy.
Both PANS and a subtype condition, pediatric autoimmune neuropsychiatric disorders associated with Streptococcus infections (PANDAS), are underrecognized, Dr. Chang said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. It is often misdiagnosed as Tourette syndrome or obsessive-compulsive disorder (OCD) because tics are present in about half of cases, he said, but more severe associated symptoms, such as psychosis, can be misdiagnosed as psychotic disorders or mood disorders. Currently, neither PANS nor PANDAS are officially recognized by the American Academy of Pediatrics or the DSM-5.
“We’re hoping that it is soon because it clearly exists,” Dr. Chang said at the meeting, presented by Global Academy for Medical Education. “If you’ve ever treated a child with PANS or PANDAS and you have seen antibiotics totally reverse OCD and tic-like behavior, if you’ve seen prednisone actually treat symptoms of mania or even psychosis and actually make those things better rather than worse, it’s really eye-opening and it makes a believer out of you.”
Anxiety is the most common psychiatric symptom in youth, and anxiety disorders are also common, said Dr. Chang. According to the National Comorbidity Survey: Adolescent Supplement, 2001-2004, 31.9% adolescents overall reported an anxiety disorder, and 8.3% said their anxiety disorder caused severe impairment. The COVID-19 pandemic has increased the level of anxiety for children and adolescents, which can lead to other disorders, such as separation anxiety disorder, panic disorder, specific phobia, social anxiety disorder, acute stress disorder, generalized anxiety disorder, OCD, or posttraumatic stress disorder. Psychiatrists should be suspicious of any sudden onset of symptoms that overlap with PANS, said Dr. Chang, who is now in private practice in Palo Alto, Calif.
“Anxiety disorders are incredibly common. Remember that you’ve got to carefully screen for other anxiety disorders, because they’re highly comorbid,” Dr. Chang said. “You’ve got to do a full workup. If there are other things going on, you’ve got to think PANS. If it’s acute onset, you’ve really got to think [PANS], and you should do that workup or refer to someone who does.”
The prevalence of PANS and PANDAS is not known, but it may be more common than psychiatrists realize, Dr. Chang said. “I’ve been doing this for about 10 years now in the PANS and PANDAS field, and it’s very clear to me that this is something that is prevalent,” he said.
Together with Jennifer Frankovich, MD, Dr. Chang founded a clinic at the Lucile Packard Children’s Hospital Stanford, and also helped to develop treatment guidelines for youth with PANS. At the clinic, patients are approximately 7.7 years old when developing the first symptoms, and are 10.7 years old when presenting for treatment. Most patients at the clinic are male (78%), and 40% are acute onset cases. Nearly all patients have symptoms of anxiety (92%), mood disorder (88%), OCD (86%), sensory/motor abnormalities (88%), irritability/aggression (82%), somatic symptoms, deterioration in school (76%), and behavioral regression (59%). More than one-third present with suicidal ideation (38%) and violence to themselves (29%), others (38%), or objects. About one-fourth have symptoms of psychosis (24%).
“These can be really sick kids,” Dr. Chang said. not able to eat because they’re afraid of things, not able to take care of their body or daily living. These were sometimes highly functional people beforehand, sometimes they weren’t, but it was still an acute change.”
Treatment for PANS
Treatment guidelines released by the PANS/PANDAS Consortium in 2017 recommend a first course of antistreptococcal treatment for new PANS cases. Psychiatrists should look for evidence of strep or other infection and use antibiotics to eradicate any underlying acute or residual infection.
“Very commonly, we’ll use things like azithromycin, or Augmentin, or amoxicillin, and you’ll see suddenly the OCD go away or at least diminish, the sleep return to normal, the mood come back down,” Dr. Chang said. “It’s pretty amazing when you see it.”
In other cases, ongoing treatment is needed for longer than the normal 5-day or 10-day course of antibiotics. “We’re not exactly sure how long: sometimes it’s 3 weeks, sometimes it’s 4 weeks, but you have to give it more than a week. Sometimes it’s the anti-inflammatory properties that are helping.” While concerns about haphazardly prescribing antibiotics are valid, “if you can cure this stuff on antibiotics, it’s low-hanging fruit,” Dr. Chang said.
There is evidence in the literature that prescribing antibiotics for PANS is beneficial. A randomized controlled trial published in 2017 showed that patients with PANS prescribed azithromycin for 4 weeks had greater reductions in severity of OCD, compared with placebo.
“We need more studies, but clearly, antibiotics do have the potential to help with certain kids. And certainly, in my practice, I see sometimes a slam-dunk response,” Dr. Chang said. “Unfortunately, sometimes you don’t see a slam-dunk response or you can’t find an infection. That’s when it might be more of an inflammation from some other reason. It could be a leftover infection, or it could be an anti-inflammatory situation.”
Immunomodulatory treatment for PANS includes use of NSAIDs, such as ibuprofen or naproxen sodium; steroids, such as prednisone or intravenous corticosteroids; intravenous immunoglobulin; or plasma exchange. Other therapies to consider are rituximab, mycophenolate mofetil, and cyclophosphamide.
Some psychiatric treatments may help patients with PANS. While there is no empirical evidence that psychotropics are effective in treating PANS, some SSRIs might help if patients are able to handle any adverse events. Psychotherapy and education of the family are also important for patients with PANS and their caregivers.
“Basically, [PANS] has as high a caregiver burden as having someone in the household with Alzheimer’s disease or cancer. It’s a huge burden, it’s very stressful, and the family needs support for this,” Dr. Chang said.
Global Academy and this news organization are owned by the same parent company. Dr. Chang reports he is a consultant for Allergan, Impel NeuroPharma, and Sunovion. He is also on the speaker’s bureau for Sunovion.
Pediatric acute-onset neuropsychiatric syndrome (PANS), a rare acute onset of psychiatric symptoms, might be more common than initially thought, according to Kiki D. Chang, MD.
PANS is characterized by the National Center for Advancing Translational Sciences Genetic and Rare Diseases Information Center as a “sudden onset of obsessive-compulsive symptoms and/or severe eating restrictions, along with at least two other cognitive, behavioral, or neurological symptoms.” These symptoms can include anxiety, depression, oppositional behavior, difficulty concentrating, abnormalities in motor and sensory skills, and other somatic symptoms. The condition develops as a result of an infection that causes an autoimmune or inflammatory response in the brain, and patients tend to respond well to treatment from antibiotics, anti-inflammatory medication, and immunomodulatory therapy.
Both PANS and a subtype condition, pediatric autoimmune neuropsychiatric disorders associated with Streptococcus infections (PANDAS), are underrecognized, Dr. Chang said in a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. It is often misdiagnosed as Tourette syndrome or obsessive-compulsive disorder (OCD) because tics are present in about half of cases, he said, but more severe associated symptoms, such as psychosis, can be misdiagnosed as psychotic disorders or mood disorders. Currently, neither PANS nor PANDAS are officially recognized by the American Academy of Pediatrics or the DSM-5.
“We’re hoping that it is soon because it clearly exists,” Dr. Chang said at the meeting, presented by Global Academy for Medical Education. “If you’ve ever treated a child with PANS or PANDAS and you have seen antibiotics totally reverse OCD and tic-like behavior, if you’ve seen prednisone actually treat symptoms of mania or even psychosis and actually make those things better rather than worse, it’s really eye-opening and it makes a believer out of you.”
Anxiety is the most common psychiatric symptom in youth, and anxiety disorders are also common, said Dr. Chang. According to the National Comorbidity Survey: Adolescent Supplement, 2001-2004, 31.9% adolescents overall reported an anxiety disorder, and 8.3% said their anxiety disorder caused severe impairment. The COVID-19 pandemic has increased the level of anxiety for children and adolescents, which can lead to other disorders, such as separation anxiety disorder, panic disorder, specific phobia, social anxiety disorder, acute stress disorder, generalized anxiety disorder, OCD, or posttraumatic stress disorder. Psychiatrists should be suspicious of any sudden onset of symptoms that overlap with PANS, said Dr. Chang, who is now in private practice in Palo Alto, Calif.
“Anxiety disorders are incredibly common. Remember that you’ve got to carefully screen for other anxiety disorders, because they’re highly comorbid,” Dr. Chang said. “You’ve got to do a full workup. If there are other things going on, you’ve got to think PANS. If it’s acute onset, you’ve really got to think [PANS], and you should do that workup or refer to someone who does.”
The prevalence of PANS and PANDAS is not known, but it may be more common than psychiatrists realize, Dr. Chang said. “I’ve been doing this for about 10 years now in the PANS and PANDAS field, and it’s very clear to me that this is something that is prevalent,” he said.
Together with Jennifer Frankovich, MD, Dr. Chang founded a clinic at the Lucile Packard Children’s Hospital Stanford, and also helped to develop treatment guidelines for youth with PANS. At the clinic, patients are approximately 7.7 years old when developing the first symptoms, and are 10.7 years old when presenting for treatment. Most patients at the clinic are male (78%), and 40% are acute onset cases. Nearly all patients have symptoms of anxiety (92%), mood disorder (88%), OCD (86%), sensory/motor abnormalities (88%), irritability/aggression (82%), somatic symptoms, deterioration in school (76%), and behavioral regression (59%). More than one-third present with suicidal ideation (38%) and violence to themselves (29%), others (38%), or objects. About one-fourth have symptoms of psychosis (24%).
“These can be really sick kids,” Dr. Chang said. not able to eat because they’re afraid of things, not able to take care of their body or daily living. These were sometimes highly functional people beforehand, sometimes they weren’t, but it was still an acute change.”
Treatment for PANS
Treatment guidelines released by the PANS/PANDAS Consortium in 2017 recommend a first course of antistreptococcal treatment for new PANS cases. Psychiatrists should look for evidence of strep or other infection and use antibiotics to eradicate any underlying acute or residual infection.
“Very commonly, we’ll use things like azithromycin, or Augmentin, or amoxicillin, and you’ll see suddenly the OCD go away or at least diminish, the sleep return to normal, the mood come back down,” Dr. Chang said. “It’s pretty amazing when you see it.”
In other cases, ongoing treatment is needed for longer than the normal 5-day or 10-day course of antibiotics. “We’re not exactly sure how long: sometimes it’s 3 weeks, sometimes it’s 4 weeks, but you have to give it more than a week. Sometimes it’s the anti-inflammatory properties that are helping.” While concerns about haphazardly prescribing antibiotics are valid, “if you can cure this stuff on antibiotics, it’s low-hanging fruit,” Dr. Chang said.
There is evidence in the literature that prescribing antibiotics for PANS is beneficial. A randomized controlled trial published in 2017 showed that patients with PANS prescribed azithromycin for 4 weeks had greater reductions in severity of OCD, compared with placebo.
“We need more studies, but clearly, antibiotics do have the potential to help with certain kids. And certainly, in my practice, I see sometimes a slam-dunk response,” Dr. Chang said. “Unfortunately, sometimes you don’t see a slam-dunk response or you can’t find an infection. That’s when it might be more of an inflammation from some other reason. It could be a leftover infection, or it could be an anti-inflammatory situation.”
Immunomodulatory treatment for PANS includes use of NSAIDs, such as ibuprofen or naproxen sodium; steroids, such as prednisone or intravenous corticosteroids; intravenous immunoglobulin; or plasma exchange. Other therapies to consider are rituximab, mycophenolate mofetil, and cyclophosphamide.
Some psychiatric treatments may help patients with PANS. While there is no empirical evidence that psychotropics are effective in treating PANS, some SSRIs might help if patients are able to handle any adverse events. Psychotherapy and education of the family are also important for patients with PANS and their caregivers.
“Basically, [PANS] has as high a caregiver burden as having someone in the household with Alzheimer’s disease or cancer. It’s a huge burden, it’s very stressful, and the family needs support for this,” Dr. Chang said.
Global Academy and this news organization are owned by the same parent company. Dr. Chang reports he is a consultant for Allergan, Impel NeuroPharma, and Sunovion. He is also on the speaker’s bureau for Sunovion.
FROM CP/AACP PSYCHIATRY UPDATE
When the worry is worse than the actual illness
CASE Distraught over a medical illness
Ms. S, age 16, presents to the emergency department (ED) accompanied by her mother with superficial lacerations on her arm. Ms. S states, “I cut my arm because I was afraid I was going to do something serious if I didn’t get to go to the ED.” She says that 6 months earlier, she was diagnosed with superior mesenteric artery syndrome (SMAS), a rare, potentially life-threatening condition that occurs when the duodenum is compressed between the aorta and the superior mesenteric artery, causing a partial or complete blockage of the duodenum. Since receiving this diagnosis, Ms. S reports feeling anxious, depressed, and overwhelmed by both the pain she is experiencing from her illness and uncertainty about her prognosis.
HISTORY In pain and isolated
Since being diagnosed with SMAS, Ms. S has had approximately 30 medical and 7 ED visits for SMAS-related pain. Ms. S was referred to the outpatient clinic for ongoing support and treatment for SMAS.
Because of her pain and anxiety, Ms. S, a junior in high school, no longer attends school but has been working with a tutor. Ms. S says that some of her loneliness and hopelessness are due to the social isolation of being tutored at home. She states that she has been “out of sight and out of mind” from her friends. She also reports feeling different from them due to the pain brought on by SMAS.
Ms. S and her mother live in public housing. Ms. S says that overall, she has a good relationship with her mother, but that in certain situations, her mother’s anxiety causes her significant frustration and anxiety.
EVALUATION Transient suicidal thoughts
A physical examination reveals superficial lacerations to Ms. S’s left arm. Although she appears thin, her current body mass index (BMI) is 20.4 kg/m2, which is within normal range. She says she sees herself as “underweight” and “not fat at all.” Ms. S reports that she likes food and enjoyed eating until it became too painful following her SMAS diagnosis. Ms. S denies a history of binging or purging. Results from her laboratory workup and all values are within normal limits.
During the initial interview, Ms. S’s mother says they came to the ED because Ms. S urgently needs a psychiatric evaluation so she can be cleared for gastrointestinal (GI) surgery and placement of a nasogastric tube. Her mother says a surgeon from a different hospital told them that her insurance company required a psychiatric evaluation to rule out anorexia nervosa before they would authorize the GI surgery. When asked why psychiatry at this hospital was not consulted, Ms. S’s mother does not answer.
When asked about the symptoms she has been experiencing, Ms. S says that her sleep has been poor because of increased pain and excessive worrying about her health. She has limited her food intake. Ms. S reports that after eating, she lays on her left side to alleviate pain and help the food move through her body.
Continue to: Ms. S says...
Ms. S says she feels anxious and depressed due to her SMAS diagnosis, her mother’s online research and oversharing of poor prognoses, and being isolated from her friends. Most of her time outside the home is spent attending medical appointments with specialists. Several months ago, Ms. S had seen a psychotherapist, but her mother was unhappy with the treatment recommendations, which included seeking care from a nutritionist and joining group therapy. Ms. S’s mother says she ended her daughter’s psychotherapy because she was unable to obtain a signature ruling out anorexia nervosa within the first few appointments.
Ms. S also says she has had passive suicidal thoughts during the past month, usually twice a week. She reports that these thoughts lasted as long as several hours and were difficult to control, but she has no specific plan or intent. Ms. S denies current suicidal thoughts or ideation, and works with the treatment team to complete a safety plan, which she signs. Other than her recent visit to the ED, Ms. S denies any other thoughts or behaviors of self-injury or suicide.
[polldaddy:10586905]
The authors’ observations
The treatment team considered the following conditions as part of Ms. S’s differential diagnosis:
Major depressive disorder. The team was able to rule out MDD because Ms. S’s depression was attributed to SMAS. Ms. S reported that all depressive symptoms were manageable or nonexistent before the onset of pain from SMAS. There was no direct pathophysiological consequence of another medical condition. Ms. S was clear that her symptoms of anxiety and depression began after she was isolated from her friends and began having difficulty understanding her diagnosis and prognosis.
Anorexia nervosa also was ruled out. According to the DSM-5, a diagnosis of anorexia nervosa requires the following 3 criteria1:
- restriction of food intake resulting in significantly low body weight (defined as weight that is less than “minimally normal”) relative to age, gender, or development
- intense fear of gaining weight, or persistent behaviors that interfere with weight gain
- disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or lack of insight with regard to seriousness of current low body weight.
Continue to: Although Ms. S appeared...
Although Ms. S appeared thin, her BMI was within normal range. She added that she likes food and enjoyed eating, but that her medical condition made it too painful. Lastly, Ms. S denied a history of binging or purging.
Somatic symptom disorder.

Factitious disorder imposed on self. An individual with FDIS chronically stimulates, induces, or aggravates illnesses to gain the status of being a patient.
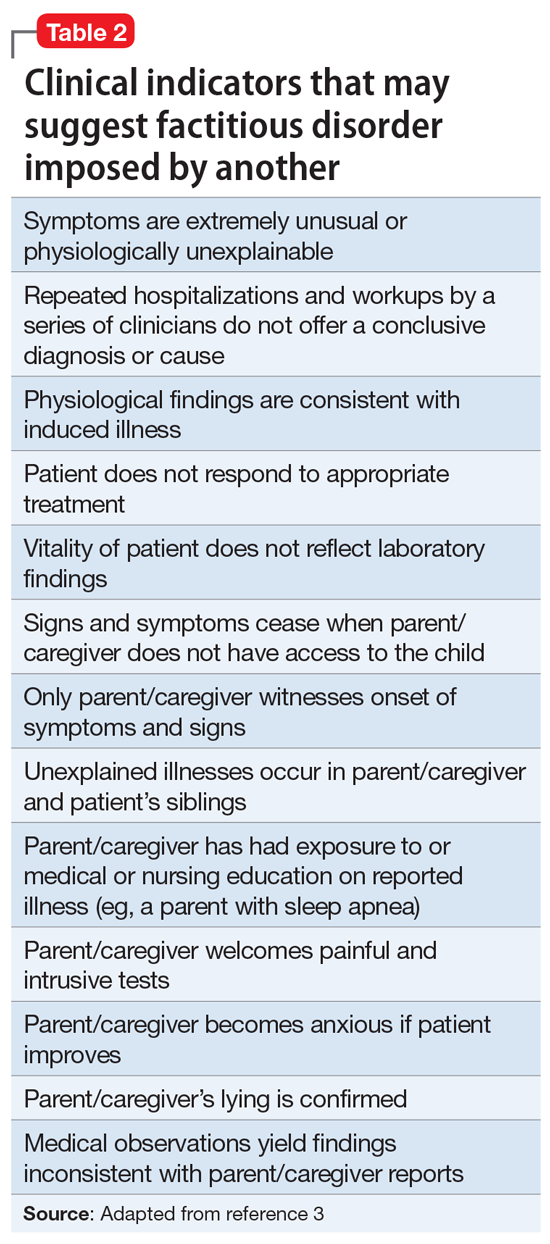
Factitious disorder imposed on another is the deliberate feigning or production of symptoms in another individual who is under the perpetrator’s supervision.1 Table 23 lists clinical indicators that raise suspicion for FDIA.
Before a diagnosis of somatic symptom disorder, FDIS, or FDIA could be established or ruled out, it was imperative to gather collateral information from other clinicians involved in Ms. S’s care. Ms. S and her mother had sought out help from a pediatric surgeon, a pediatric gastroenterologist, a pediatrician, and a psychotherapist.
Continue to: EVALUATION Collateral information
EVALUATION Collateral information
After Ms. S’s mother signs consent forms for exchange of information, the treatment team reaches out to the other clinicians. The therapist confirms that Ms. S’s mother had ended her daughter’s treatment after she was unable to quickly obtain documentation to rule out anorexia nervosa.
Both the pediatric surgeon and gastroenterologist report concerns of FDIA, which is why both clinicians had referred Ms. S and her mother to psychiatry. The pediatric surgeon states that on one occasion when he interviewed Ms. S separately from her mother, she seemed to be going down a checklist of symptoms. The surgeon reports that there was a partial occlusion of the superior mesenteric artery, confirming the diagnosis of SMAS, but he believed it was not severe enough to explain the symptoms Ms. S reported. The surgeon had scheduled another imaging appointment for 1 month later.
The pediatric gastroenterologist reports that Ms. S’s mother had demanded surgery and nasogastric tube placement for her daughter, which raised suspicion of FDIA. The gastroenterologist had convinced Ms. S and her mother to start low-dose doxepin, 20 mg twice a day, for anxiety, sleep, and abdominal pain.
Lastly, the pediatrician reports that she had not seen Ms. S for several months but stated that Ms. S always has been in the low normal BMI range. The pediatrician also reports that 6 months ago, the patient and her mother were frantically visiting EDs and scheduling doctor’s appointments.
[polldaddy:10586906]
The authors’ observations
The treatment team decided that Ms. S was not in imminent danger, and felt it was important to keep her in treatment without raising her mother’s suspicion. The team agreed to raise these concerns to the police, child protective services, and risk management if Ms. S’s health suddenly deteriorated or if her mother decided to remove Ms. S from our care.
Continue to: The treatment team...
The treatment team at the outpatient psychiatry clinic agreed that Ms. S did not currently meet criteria for anorexia nervosa, MDD, FDIS, or FDIA. However, Ms. S reported worries particular to persistent abdominal pain that was exacerbated by either eating or going to bed at night, which indicated that somatic symptom disorder was her likely diagnosis. Further, she endorsed a high level of anxiety and depression with regard to this somatic complaint that interfered with her daily activities and consumed an excessive amount of time, which also pointed to somatic symptom disorder. As a result of this diagnosis, the treatment team helped Ms. S manage her somatic symptoms and monitored for any other changes in her symptoms
Generally, cognitive-behavioral therapy (CBT) and mindfulness-based therapy may help relieve symptoms associated with somatic symptom disorder.4
TREATMENT Therapy sessions and medication management
At the psychiatric clinic, Ms. S is scheduled for biweekly therapy sessions with a social worker and biweekly appointments with a senior psychiatry resident for medication management. At each visit, Ms. S’s vital signs, height, and weight are measured. In the therapy sessions, she is taught mindfulness skills as well as CBT. The senior psychiatry resident maintains regular communication with the other clinicians involved in Ms. S’s care.
After the first month of treatment, Ms. S undergoes repeat imaging at the gastroenterologist’s office that indicates her SMAS is no longer occluded. Ms. S continues to report somatic symptoms, but with mild improvement.
Over the course of approximately 4 months, Ms. S begins to show signs of improvement in her pain, anxiety, and depression. Ms. S begins to feel well enough to get a summer job at a nursing home and expresses enthusiasm when her weight begins to increase. Her mother also became enthused and verbalized her appreciation that her daughter appeared to be improving.
Continue to: In the fall...
In the fall, Ms. S returns to high school for her senior year but has difficulty getting back into the routine and relating to her old friends. Ms. S continues to perseverate on thoughts of getting sick and her physical symptoms become overwhelming once again. She continues to be focused on any new symptoms she experiences, and to limit the types of foods she eats due to fear of the abdominal pain returning.
After several more months of psychiatric treatment, Ms. S reports significant relief from her abdominal pain, and no longer seeks corrective surgery for her SMAS. Although she occasionally struggles with perseverating thoughts and anxiety about her somatic symptoms such as abdominal pain and worrying about the types of foods she eats and becoming ill, she continues to work through symptoms of her somatic symptom disorder.
The authors’ observations
The main challenge of somatic symptom disorder is the patient’s “abnormal illness behavior.”2,5,6 For pediatric patients, there may an association between a parent’s psychological status and the patient’s somatic symptoms. Abdominal symptoms in a pediatric patient have a strong association with a parent who presents with depression, anxiety, or somatization. The effects of the parent’s psychological status could also manifest in the form of modeling catastrophic thinking or through reinforcement. Parents with certain traits, such as disproportionate worry about pain, may pay more attention to their child’s symptoms, and hence, reward the child when he/she reports somatic symptoms.7,8 In the case of Ms. S, her mother did not participate in therapy and the mother’s psychiatric history was never obtained.
OUTCOMES Making personal strides
Ms. S continues to use mindfulness skills as well as CBT to manage her symptoms of somatic symptom disorder. She continues to celebrate her weight gains, denies any thoughts of suicide or self-harm behaviors, and prepares for college by scheduling campus visits and completing admissions applications.
Bottom Line
Patients with somatic symptom disorder tend to have very high levels of worry about illness. Somatic symptoms in such patients may or may not have a medical explanation. Accurate diagnosis and careful management are necessary to reduce patient distress. Cognitive-behavioral therapy and mindfulness-based therapy may help relieve symptoms associated with this disorder.
Related Resources
- Henningsen P. Management of somatic symptom disorder. Dialogues Clin Neurosci. 2018;20(1):23-91.
- Rosic T, Kalra S, Samaan Z. Somatic symptom disorder, a new DSM-5 diagnosis of an old clinical challenge. BMJ Case Rep. 2016: bcr2015212553. doi: 10.1136/bcr-2015-212553.
Drug Brand Name
Doxepin • Silenor
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Stern T, Freudenreich O, Smith F, et al. Massachusetts General Hospital Handbook of General Hospital Psychiatry, 7th ed. New York, NY: Elsevier; 2017.
3. Feldman MD, Eisendrath SJ. The spectrum of factitious disorders. Washington, DC: American Psychiatric Association; 1997.
4. Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry, 11th ed. Philadelphia, PA: Wolters Kluwer; 2014:470.
5. Pilowsky I. The concept of abnormal illness behavior. Psychosomatics. 1990;31(2):207-213.
6. Kirmayer LJ, Looper KJ. Abnormal illness behavior: physiological, psychological and social dimensions of coping with stress. Curr Opin Psychiatry. 2006;19(1):54-60.
7. Walker LS, Garber J, Greene JW. Somatic complaints in pediatric patients: a prospective study of the role of negative life events, child social and academic competence, and parental somatic symptoms. J Consult Clin Psychology. 1994;62(6):1213-1221.
8. Van Oudenhove L, Levy RL, Crowell MD, et al. Biopsychosocial aspects of functional gastrointestinal disorders: how central and environmental processes contribute to the development and expression of functional gastrointestinal disorders. Gastroenterology. 2016;150(6):1355-1367.
CASE Distraught over a medical illness
Ms. S, age 16, presents to the emergency department (ED) accompanied by her mother with superficial lacerations on her arm. Ms. S states, “I cut my arm because I was afraid I was going to do something serious if I didn’t get to go to the ED.” She says that 6 months earlier, she was diagnosed with superior mesenteric artery syndrome (SMAS), a rare, potentially life-threatening condition that occurs when the duodenum is compressed between the aorta and the superior mesenteric artery, causing a partial or complete blockage of the duodenum. Since receiving this diagnosis, Ms. S reports feeling anxious, depressed, and overwhelmed by both the pain she is experiencing from her illness and uncertainty about her prognosis.
HISTORY In pain and isolated
Since being diagnosed with SMAS, Ms. S has had approximately 30 medical and 7 ED visits for SMAS-related pain. Ms. S was referred to the outpatient clinic for ongoing support and treatment for SMAS.
Because of her pain and anxiety, Ms. S, a junior in high school, no longer attends school but has been working with a tutor. Ms. S says that some of her loneliness and hopelessness are due to the social isolation of being tutored at home. She states that she has been “out of sight and out of mind” from her friends. She also reports feeling different from them due to the pain brought on by SMAS.
Ms. S and her mother live in public housing. Ms. S says that overall, she has a good relationship with her mother, but that in certain situations, her mother’s anxiety causes her significant frustration and anxiety.
EVALUATION Transient suicidal thoughts
A physical examination reveals superficial lacerations to Ms. S’s left arm. Although she appears thin, her current body mass index (BMI) is 20.4 kg/m2, which is within normal range. She says she sees herself as “underweight” and “not fat at all.” Ms. S reports that she likes food and enjoyed eating until it became too painful following her SMAS diagnosis. Ms. S denies a history of binging or purging. Results from her laboratory workup and all values are within normal limits.
During the initial interview, Ms. S’s mother says they came to the ED because Ms. S urgently needs a psychiatric evaluation so she can be cleared for gastrointestinal (GI) surgery and placement of a nasogastric tube. Her mother says a surgeon from a different hospital told them that her insurance company required a psychiatric evaluation to rule out anorexia nervosa before they would authorize the GI surgery. When asked why psychiatry at this hospital was not consulted, Ms. S’s mother does not answer.
When asked about the symptoms she has been experiencing, Ms. S says that her sleep has been poor because of increased pain and excessive worrying about her health. She has limited her food intake. Ms. S reports that after eating, she lays on her left side to alleviate pain and help the food move through her body.
Continue to: Ms. S says...
Ms. S says she feels anxious and depressed due to her SMAS diagnosis, her mother’s online research and oversharing of poor prognoses, and being isolated from her friends. Most of her time outside the home is spent attending medical appointments with specialists. Several months ago, Ms. S had seen a psychotherapist, but her mother was unhappy with the treatment recommendations, which included seeking care from a nutritionist and joining group therapy. Ms. S’s mother says she ended her daughter’s psychotherapy because she was unable to obtain a signature ruling out anorexia nervosa within the first few appointments.
Ms. S also says she has had passive suicidal thoughts during the past month, usually twice a week. She reports that these thoughts lasted as long as several hours and were difficult to control, but she has no specific plan or intent. Ms. S denies current suicidal thoughts or ideation, and works with the treatment team to complete a safety plan, which she signs. Other than her recent visit to the ED, Ms. S denies any other thoughts or behaviors of self-injury or suicide.
[polldaddy:10586905]
The authors’ observations
The treatment team considered the following conditions as part of Ms. S’s differential diagnosis:
Major depressive disorder. The team was able to rule out MDD because Ms. S’s depression was attributed to SMAS. Ms. S reported that all depressive symptoms were manageable or nonexistent before the onset of pain from SMAS. There was no direct pathophysiological consequence of another medical condition. Ms. S was clear that her symptoms of anxiety and depression began after she was isolated from her friends and began having difficulty understanding her diagnosis and prognosis.
Anorexia nervosa also was ruled out. According to the DSM-5, a diagnosis of anorexia nervosa requires the following 3 criteria1:
- restriction of food intake resulting in significantly low body weight (defined as weight that is less than “minimally normal”) relative to age, gender, or development
- intense fear of gaining weight, or persistent behaviors that interfere with weight gain
- disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or lack of insight with regard to seriousness of current low body weight.
Continue to: Although Ms. S appeared...
Although Ms. S appeared thin, her BMI was within normal range. She added that she likes food and enjoyed eating, but that her medical condition made it too painful. Lastly, Ms. S denied a history of binging or purging.
Somatic symptom disorder.

Factitious disorder imposed on self. An individual with FDIS chronically stimulates, induces, or aggravates illnesses to gain the status of being a patient.
Factitious disorder imposed on another is the deliberate feigning or production of symptoms in another individual who is under the perpetrator’s supervision.1 Table 23 lists clinical indicators that raise suspicion for FDIA.
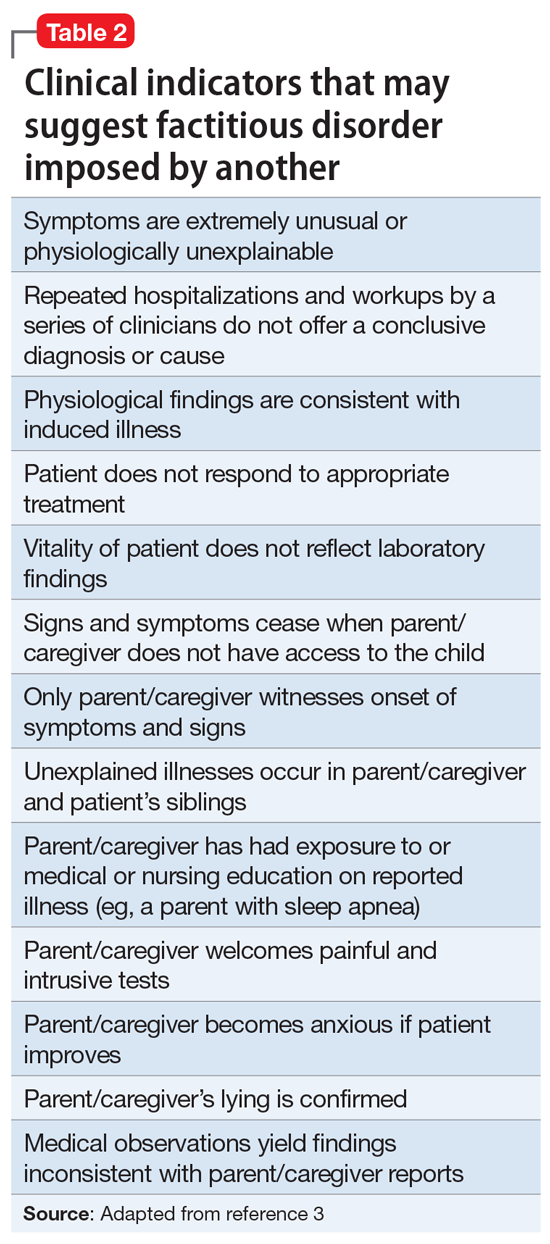
Before a diagnosis of somatic symptom disorder, FDIS, or FDIA could be established or ruled out, it was imperative to gather collateral information from other clinicians involved in Ms. S’s care. Ms. S and her mother had sought out help from a pediatric surgeon, a pediatric gastroenterologist, a pediatrician, and a psychotherapist.
Continue to: EVALUATION Collateral information
EVALUATION Collateral information
After Ms. S’s mother signs consent forms for exchange of information, the treatment team reaches out to the other clinicians. The therapist confirms that Ms. S’s mother had ended her daughter’s treatment after she was unable to quickly obtain documentation to rule out anorexia nervosa.
Both the pediatric surgeon and gastroenterologist report concerns of FDIA, which is why both clinicians had referred Ms. S and her mother to psychiatry. The pediatric surgeon states that on one occasion when he interviewed Ms. S separately from her mother, she seemed to be going down a checklist of symptoms. The surgeon reports that there was a partial occlusion of the superior mesenteric artery, confirming the diagnosis of SMAS, but he believed it was not severe enough to explain the symptoms Ms. S reported. The surgeon had scheduled another imaging appointment for 1 month later.
The pediatric gastroenterologist reports that Ms. S’s mother had demanded surgery and nasogastric tube placement for her daughter, which raised suspicion of FDIA. The gastroenterologist had convinced Ms. S and her mother to start low-dose doxepin, 20 mg twice a day, for anxiety, sleep, and abdominal pain.
Lastly, the pediatrician reports that she had not seen Ms. S for several months but stated that Ms. S always has been in the low normal BMI range. The pediatrician also reports that 6 months ago, the patient and her mother were frantically visiting EDs and scheduling doctor’s appointments.
[polldaddy:10586906]
The authors’ observations
The treatment team decided that Ms. S was not in imminent danger, and felt it was important to keep her in treatment without raising her mother’s suspicion. The team agreed to raise these concerns to the police, child protective services, and risk management if Ms. S’s health suddenly deteriorated or if her mother decided to remove Ms. S from our care.
Continue to: The treatment team...
The treatment team at the outpatient psychiatry clinic agreed that Ms. S did not currently meet criteria for anorexia nervosa, MDD, FDIS, or FDIA. However, Ms. S reported worries particular to persistent abdominal pain that was exacerbated by either eating or going to bed at night, which indicated that somatic symptom disorder was her likely diagnosis. Further, she endorsed a high level of anxiety and depression with regard to this somatic complaint that interfered with her daily activities and consumed an excessive amount of time, which also pointed to somatic symptom disorder. As a result of this diagnosis, the treatment team helped Ms. S manage her somatic symptoms and monitored for any other changes in her symptoms
Generally, cognitive-behavioral therapy (CBT) and mindfulness-based therapy may help relieve symptoms associated with somatic symptom disorder.4
TREATMENT Therapy sessions and medication management
At the psychiatric clinic, Ms. S is scheduled for biweekly therapy sessions with a social worker and biweekly appointments with a senior psychiatry resident for medication management. At each visit, Ms. S’s vital signs, height, and weight are measured. In the therapy sessions, she is taught mindfulness skills as well as CBT. The senior psychiatry resident maintains regular communication with the other clinicians involved in Ms. S’s care.
After the first month of treatment, Ms. S undergoes repeat imaging at the gastroenterologist’s office that indicates her SMAS is no longer occluded. Ms. S continues to report somatic symptoms, but with mild improvement.
Over the course of approximately 4 months, Ms. S begins to show signs of improvement in her pain, anxiety, and depression. Ms. S begins to feel well enough to get a summer job at a nursing home and expresses enthusiasm when her weight begins to increase. Her mother also became enthused and verbalized her appreciation that her daughter appeared to be improving.
Continue to: In the fall...
In the fall, Ms. S returns to high school for her senior year but has difficulty getting back into the routine and relating to her old friends. Ms. S continues to perseverate on thoughts of getting sick and her physical symptoms become overwhelming once again. She continues to be focused on any new symptoms she experiences, and to limit the types of foods she eats due to fear of the abdominal pain returning.
After several more months of psychiatric treatment, Ms. S reports significant relief from her abdominal pain, and no longer seeks corrective surgery for her SMAS. Although she occasionally struggles with perseverating thoughts and anxiety about her somatic symptoms such as abdominal pain and worrying about the types of foods she eats and becoming ill, she continues to work through symptoms of her somatic symptom disorder.
The authors’ observations
The main challenge of somatic symptom disorder is the patient’s “abnormal illness behavior.”2,5,6 For pediatric patients, there may an association between a parent’s psychological status and the patient’s somatic symptoms. Abdominal symptoms in a pediatric patient have a strong association with a parent who presents with depression, anxiety, or somatization. The effects of the parent’s psychological status could also manifest in the form of modeling catastrophic thinking or through reinforcement. Parents with certain traits, such as disproportionate worry about pain, may pay more attention to their child’s symptoms, and hence, reward the child when he/she reports somatic symptoms.7,8 In the case of Ms. S, her mother did not participate in therapy and the mother’s psychiatric history was never obtained.
OUTCOMES Making personal strides
Ms. S continues to use mindfulness skills as well as CBT to manage her symptoms of somatic symptom disorder. She continues to celebrate her weight gains, denies any thoughts of suicide or self-harm behaviors, and prepares for college by scheduling campus visits and completing admissions applications.
Bottom Line
Patients with somatic symptom disorder tend to have very high levels of worry about illness. Somatic symptoms in such patients may or may not have a medical explanation. Accurate diagnosis and careful management are necessary to reduce patient distress. Cognitive-behavioral therapy and mindfulness-based therapy may help relieve symptoms associated with this disorder.
Related Resources
- Henningsen P. Management of somatic symptom disorder. Dialogues Clin Neurosci. 2018;20(1):23-91.
- Rosic T, Kalra S, Samaan Z. Somatic symptom disorder, a new DSM-5 diagnosis of an old clinical challenge. BMJ Case Rep. 2016: bcr2015212553. doi: 10.1136/bcr-2015-212553.
Drug Brand Name
Doxepin • Silenor
CASE Distraught over a medical illness
Ms. S, age 16, presents to the emergency department (ED) accompanied by her mother with superficial lacerations on her arm. Ms. S states, “I cut my arm because I was afraid I was going to do something serious if I didn’t get to go to the ED.” She says that 6 months earlier, she was diagnosed with superior mesenteric artery syndrome (SMAS), a rare, potentially life-threatening condition that occurs when the duodenum is compressed between the aorta and the superior mesenteric artery, causing a partial or complete blockage of the duodenum. Since receiving this diagnosis, Ms. S reports feeling anxious, depressed, and overwhelmed by both the pain she is experiencing from her illness and uncertainty about her prognosis.
HISTORY In pain and isolated
Since being diagnosed with SMAS, Ms. S has had approximately 30 medical and 7 ED visits for SMAS-related pain. Ms. S was referred to the outpatient clinic for ongoing support and treatment for SMAS.
Because of her pain and anxiety, Ms. S, a junior in high school, no longer attends school but has been working with a tutor. Ms. S says that some of her loneliness and hopelessness are due to the social isolation of being tutored at home. She states that she has been “out of sight and out of mind” from her friends. She also reports feeling different from them due to the pain brought on by SMAS.
Ms. S and her mother live in public housing. Ms. S says that overall, she has a good relationship with her mother, but that in certain situations, her mother’s anxiety causes her significant frustration and anxiety.
EVALUATION Transient suicidal thoughts
A physical examination reveals superficial lacerations to Ms. S’s left arm. Although she appears thin, her current body mass index (BMI) is 20.4 kg/m2, which is within normal range. She says she sees herself as “underweight” and “not fat at all.” Ms. S reports that she likes food and enjoyed eating until it became too painful following her SMAS diagnosis. Ms. S denies a history of binging or purging. Results from her laboratory workup and all values are within normal limits.
During the initial interview, Ms. S’s mother says they came to the ED because Ms. S urgently needs a psychiatric evaluation so she can be cleared for gastrointestinal (GI) surgery and placement of a nasogastric tube. Her mother says a surgeon from a different hospital told them that her insurance company required a psychiatric evaluation to rule out anorexia nervosa before they would authorize the GI surgery. When asked why psychiatry at this hospital was not consulted, Ms. S’s mother does not answer.
When asked about the symptoms she has been experiencing, Ms. S says that her sleep has been poor because of increased pain and excessive worrying about her health. She has limited her food intake. Ms. S reports that after eating, she lays on her left side to alleviate pain and help the food move through her body.
Continue to: Ms. S says...
Ms. S says she feels anxious and depressed due to her SMAS diagnosis, her mother’s online research and oversharing of poor prognoses, and being isolated from her friends. Most of her time outside the home is spent attending medical appointments with specialists. Several months ago, Ms. S had seen a psychotherapist, but her mother was unhappy with the treatment recommendations, which included seeking care from a nutritionist and joining group therapy. Ms. S’s mother says she ended her daughter’s psychotherapy because she was unable to obtain a signature ruling out anorexia nervosa within the first few appointments.
Ms. S also says she has had passive suicidal thoughts during the past month, usually twice a week. She reports that these thoughts lasted as long as several hours and were difficult to control, but she has no specific plan or intent. Ms. S denies current suicidal thoughts or ideation, and works with the treatment team to complete a safety plan, which she signs. Other than her recent visit to the ED, Ms. S denies any other thoughts or behaviors of self-injury or suicide.
[polldaddy:10586905]
The authors’ observations
The treatment team considered the following conditions as part of Ms. S’s differential diagnosis:
Major depressive disorder. The team was able to rule out MDD because Ms. S’s depression was attributed to SMAS. Ms. S reported that all depressive symptoms were manageable or nonexistent before the onset of pain from SMAS. There was no direct pathophysiological consequence of another medical condition. Ms. S was clear that her symptoms of anxiety and depression began after she was isolated from her friends and began having difficulty understanding her diagnosis and prognosis.
Anorexia nervosa also was ruled out. According to the DSM-5, a diagnosis of anorexia nervosa requires the following 3 criteria1:
- restriction of food intake resulting in significantly low body weight (defined as weight that is less than “minimally normal”) relative to age, gender, or development
- intense fear of gaining weight, or persistent behaviors that interfere with weight gain
- disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or lack of insight with regard to seriousness of current low body weight.
Continue to: Although Ms. S appeared...
Although Ms. S appeared thin, her BMI was within normal range. She added that she likes food and enjoyed eating, but that her medical condition made it too painful. Lastly, Ms. S denied a history of binging or purging.
Somatic symptom disorder.

Factitious disorder imposed on self. An individual with FDIS chronically stimulates, induces, or aggravates illnesses to gain the status of being a patient.
Factitious disorder imposed on another is the deliberate feigning or production of symptoms in another individual who is under the perpetrator’s supervision.1 Table 23 lists clinical indicators that raise suspicion for FDIA.
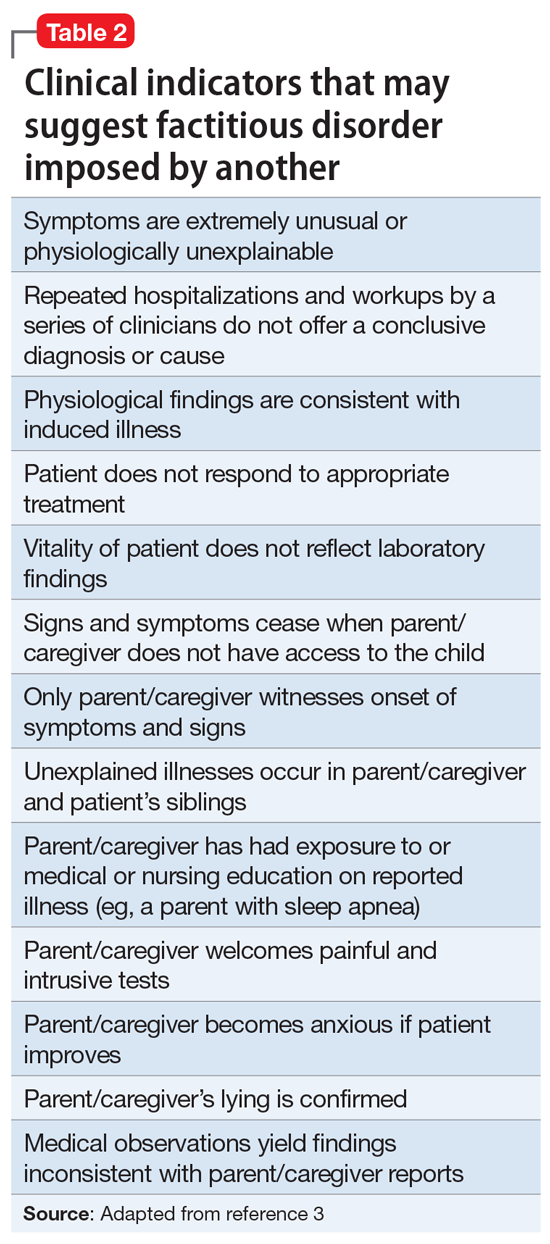
Before a diagnosis of somatic symptom disorder, FDIS, or FDIA could be established or ruled out, it was imperative to gather collateral information from other clinicians involved in Ms. S’s care. Ms. S and her mother had sought out help from a pediatric surgeon, a pediatric gastroenterologist, a pediatrician, and a psychotherapist.
Continue to: EVALUATION Collateral information
EVALUATION Collateral information
After Ms. S’s mother signs consent forms for exchange of information, the treatment team reaches out to the other clinicians. The therapist confirms that Ms. S’s mother had ended her daughter’s treatment after she was unable to quickly obtain documentation to rule out anorexia nervosa.
Both the pediatric surgeon and gastroenterologist report concerns of FDIA, which is why both clinicians had referred Ms. S and her mother to psychiatry. The pediatric surgeon states that on one occasion when he interviewed Ms. S separately from her mother, she seemed to be going down a checklist of symptoms. The surgeon reports that there was a partial occlusion of the superior mesenteric artery, confirming the diagnosis of SMAS, but he believed it was not severe enough to explain the symptoms Ms. S reported. The surgeon had scheduled another imaging appointment for 1 month later.
The pediatric gastroenterologist reports that Ms. S’s mother had demanded surgery and nasogastric tube placement for her daughter, which raised suspicion of FDIA. The gastroenterologist had convinced Ms. S and her mother to start low-dose doxepin, 20 mg twice a day, for anxiety, sleep, and abdominal pain.
Lastly, the pediatrician reports that she had not seen Ms. S for several months but stated that Ms. S always has been in the low normal BMI range. The pediatrician also reports that 6 months ago, the patient and her mother were frantically visiting EDs and scheduling doctor’s appointments.
[polldaddy:10586906]
The authors’ observations
The treatment team decided that Ms. S was not in imminent danger, and felt it was important to keep her in treatment without raising her mother’s suspicion. The team agreed to raise these concerns to the police, child protective services, and risk management if Ms. S’s health suddenly deteriorated or if her mother decided to remove Ms. S from our care.
Continue to: The treatment team...
The treatment team at the outpatient psychiatry clinic agreed that Ms. S did not currently meet criteria for anorexia nervosa, MDD, FDIS, or FDIA. However, Ms. S reported worries particular to persistent abdominal pain that was exacerbated by either eating or going to bed at night, which indicated that somatic symptom disorder was her likely diagnosis. Further, she endorsed a high level of anxiety and depression with regard to this somatic complaint that interfered with her daily activities and consumed an excessive amount of time, which also pointed to somatic symptom disorder. As a result of this diagnosis, the treatment team helped Ms. S manage her somatic symptoms and monitored for any other changes in her symptoms
Generally, cognitive-behavioral therapy (CBT) and mindfulness-based therapy may help relieve symptoms associated with somatic symptom disorder.4
TREATMENT Therapy sessions and medication management
At the psychiatric clinic, Ms. S is scheduled for biweekly therapy sessions with a social worker and biweekly appointments with a senior psychiatry resident for medication management. At each visit, Ms. S’s vital signs, height, and weight are measured. In the therapy sessions, she is taught mindfulness skills as well as CBT. The senior psychiatry resident maintains regular communication with the other clinicians involved in Ms. S’s care.
After the first month of treatment, Ms. S undergoes repeat imaging at the gastroenterologist’s office that indicates her SMAS is no longer occluded. Ms. S continues to report somatic symptoms, but with mild improvement.
Over the course of approximately 4 months, Ms. S begins to show signs of improvement in her pain, anxiety, and depression. Ms. S begins to feel well enough to get a summer job at a nursing home and expresses enthusiasm when her weight begins to increase. Her mother also became enthused and verbalized her appreciation that her daughter appeared to be improving.
Continue to: In the fall...
In the fall, Ms. S returns to high school for her senior year but has difficulty getting back into the routine and relating to her old friends. Ms. S continues to perseverate on thoughts of getting sick and her physical symptoms become overwhelming once again. She continues to be focused on any new symptoms she experiences, and to limit the types of foods she eats due to fear of the abdominal pain returning.
After several more months of psychiatric treatment, Ms. S reports significant relief from her abdominal pain, and no longer seeks corrective surgery for her SMAS. Although she occasionally struggles with perseverating thoughts and anxiety about her somatic symptoms such as abdominal pain and worrying about the types of foods she eats and becoming ill, she continues to work through symptoms of her somatic symptom disorder.
The authors’ observations
The main challenge of somatic symptom disorder is the patient’s “abnormal illness behavior.”2,5,6 For pediatric patients, there may an association between a parent’s psychological status and the patient’s somatic symptoms. Abdominal symptoms in a pediatric patient have a strong association with a parent who presents with depression, anxiety, or somatization. The effects of the parent’s psychological status could also manifest in the form of modeling catastrophic thinking or through reinforcement. Parents with certain traits, such as disproportionate worry about pain, may pay more attention to their child’s symptoms, and hence, reward the child when he/she reports somatic symptoms.7,8 In the case of Ms. S, her mother did not participate in therapy and the mother’s psychiatric history was never obtained.
OUTCOMES Making personal strides
Ms. S continues to use mindfulness skills as well as CBT to manage her symptoms of somatic symptom disorder. She continues to celebrate her weight gains, denies any thoughts of suicide or self-harm behaviors, and prepares for college by scheduling campus visits and completing admissions applications.
Bottom Line
Patients with somatic symptom disorder tend to have very high levels of worry about illness. Somatic symptoms in such patients may or may not have a medical explanation. Accurate diagnosis and careful management are necessary to reduce patient distress. Cognitive-behavioral therapy and mindfulness-based therapy may help relieve symptoms associated with this disorder.
Related Resources
- Henningsen P. Management of somatic symptom disorder. Dialogues Clin Neurosci. 2018;20(1):23-91.
- Rosic T, Kalra S, Samaan Z. Somatic symptom disorder, a new DSM-5 diagnosis of an old clinical challenge. BMJ Case Rep. 2016: bcr2015212553. doi: 10.1136/bcr-2015-212553.
Drug Brand Name
Doxepin • Silenor
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Stern T, Freudenreich O, Smith F, et al. Massachusetts General Hospital Handbook of General Hospital Psychiatry, 7th ed. New York, NY: Elsevier; 2017.
3. Feldman MD, Eisendrath SJ. The spectrum of factitious disorders. Washington, DC: American Psychiatric Association; 1997.
4. Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry, 11th ed. Philadelphia, PA: Wolters Kluwer; 2014:470.
5. Pilowsky I. The concept of abnormal illness behavior. Psychosomatics. 1990;31(2):207-213.
6. Kirmayer LJ, Looper KJ. Abnormal illness behavior: physiological, psychological and social dimensions of coping with stress. Curr Opin Psychiatry. 2006;19(1):54-60.
7. Walker LS, Garber J, Greene JW. Somatic complaints in pediatric patients: a prospective study of the role of negative life events, child social and academic competence, and parental somatic symptoms. J Consult Clin Psychology. 1994;62(6):1213-1221.
8. Van Oudenhove L, Levy RL, Crowell MD, et al. Biopsychosocial aspects of functional gastrointestinal disorders: how central and environmental processes contribute to the development and expression of functional gastrointestinal disorders. Gastroenterology. 2016;150(6):1355-1367.
1. Diagnostic and statistical manual of mental disorders, 5th ed. Washington, DC: American Psychiatric Association; 2013.
2. Stern T, Freudenreich O, Smith F, et al. Massachusetts General Hospital Handbook of General Hospital Psychiatry, 7th ed. New York, NY: Elsevier; 2017.
3. Feldman MD, Eisendrath SJ. The spectrum of factitious disorders. Washington, DC: American Psychiatric Association; 1997.
4. Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s synopsis of psychiatry: behavioral sciences/clinical psychiatry, 11th ed. Philadelphia, PA: Wolters Kluwer; 2014:470.
5. Pilowsky I. The concept of abnormal illness behavior. Psychosomatics. 1990;31(2):207-213.
6. Kirmayer LJ, Looper KJ. Abnormal illness behavior: physiological, psychological and social dimensions of coping with stress. Curr Opin Psychiatry. 2006;19(1):54-60.
7. Walker LS, Garber J, Greene JW. Somatic complaints in pediatric patients: a prospective study of the role of negative life events, child social and academic competence, and parental somatic symptoms. J Consult Clin Psychology. 1994;62(6):1213-1221.
8. Van Oudenhove L, Levy RL, Crowell MD, et al. Biopsychosocial aspects of functional gastrointestinal disorders: how central and environmental processes contribute to the development and expression of functional gastrointestinal disorders. Gastroenterology. 2016;150(6):1355-1367.
Pandemic-related stress causing health issues in many Americans
Over the last 2 months, more than half of Americans have experienced some sort of adverse effect caused by stress related to the COVID-19 pandemic, according to a survey from the Kaiser Family Foundation (KFF).
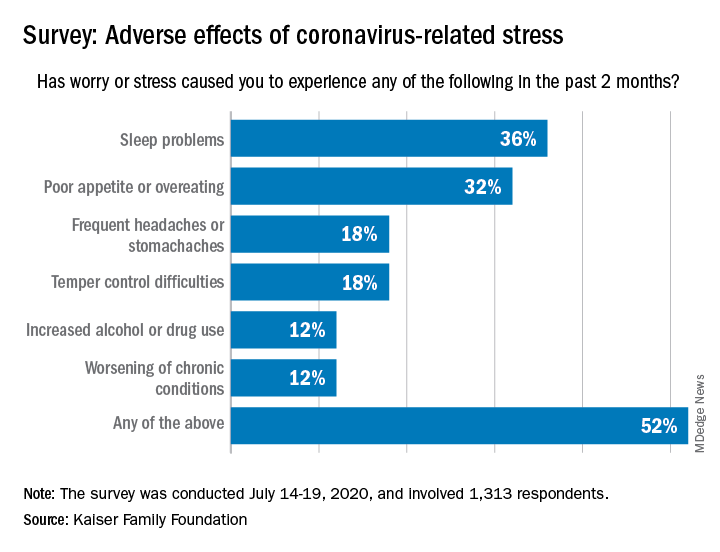
More than a third (36%) of the 1,313 respondents said they either had difficulty sleeping, falling asleep, or sleeping too much, KFF said in its latest Health Tracking Poll, conducted July 14-19, 2020. That was followed by poor appetite or overeating, which was mentioned by 32% of those surveyed.
Other adverse effects included frequent headaches or stomachaches (18%), temper-control issues (18%), increased drug or alcohol use (12%), and worsening of chronic conditions such as diabetes or hypertension (12%). Altogether, 52% of Americans have had at least one of these issues in the past 2 months, Liz Hamel and associates at KFF reported.
breaking down to 26% reporting a major impact and 28% reporting a minor impact (figures have been rounded), they said.
“As life with the coronavirus pandemic wears on, Americans increasingly say it is taking a negative toll on their mental health,” the investigators wrote. Earlier polls showed that pandemic-related stress was having an impact on mental health for 39% of respondents in May, compared with 45% in early April and 32% in March.
In the July poll, Black adults were much more likely to report a negative mental health impact (68%) than were Hispanics or Whites, who were both at 51%. Age was also a factor: The youngest group of respondents (ages 18-29 years) had the highest negative-impact rate (62%), and the oldest group (65 years and older) had the lowest (47%), they said.
When it came to reporting the adverse effects of stress or worry, however, the situation was somewhat different. Hispanics had the highest rate of such effects at 63%, while Blacks had a rate of 57% and 47% of Whites reported issues with sleep, eating, temper, and other problems, Ms. Hamel and associates reported.
Over the last 2 months, more than half of Americans have experienced some sort of adverse effect caused by stress related to the COVID-19 pandemic, according to a survey from the Kaiser Family Foundation (KFF).
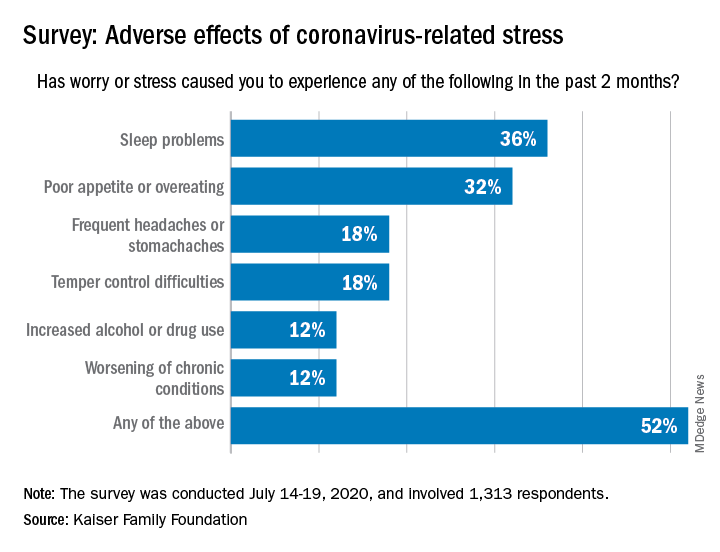
More than a third (36%) of the 1,313 respondents said they either had difficulty sleeping, falling asleep, or sleeping too much, KFF said in its latest Health Tracking Poll, conducted July 14-19, 2020. That was followed by poor appetite or overeating, which was mentioned by 32% of those surveyed.
Other adverse effects included frequent headaches or stomachaches (18%), temper-control issues (18%), increased drug or alcohol use (12%), and worsening of chronic conditions such as diabetes or hypertension (12%). Altogether, 52% of Americans have had at least one of these issues in the past 2 months, Liz Hamel and associates at KFF reported.
breaking down to 26% reporting a major impact and 28% reporting a minor impact (figures have been rounded), they said.
“As life with the coronavirus pandemic wears on, Americans increasingly say it is taking a negative toll on their mental health,” the investigators wrote. Earlier polls showed that pandemic-related stress was having an impact on mental health for 39% of respondents in May, compared with 45% in early April and 32% in March.
In the July poll, Black adults were much more likely to report a negative mental health impact (68%) than were Hispanics or Whites, who were both at 51%. Age was also a factor: The youngest group of respondents (ages 18-29 years) had the highest negative-impact rate (62%), and the oldest group (65 years and older) had the lowest (47%), they said.
When it came to reporting the adverse effects of stress or worry, however, the situation was somewhat different. Hispanics had the highest rate of such effects at 63%, while Blacks had a rate of 57% and 47% of Whites reported issues with sleep, eating, temper, and other problems, Ms. Hamel and associates reported.
Over the last 2 months, more than half of Americans have experienced some sort of adverse effect caused by stress related to the COVID-19 pandemic, according to a survey from the Kaiser Family Foundation (KFF).
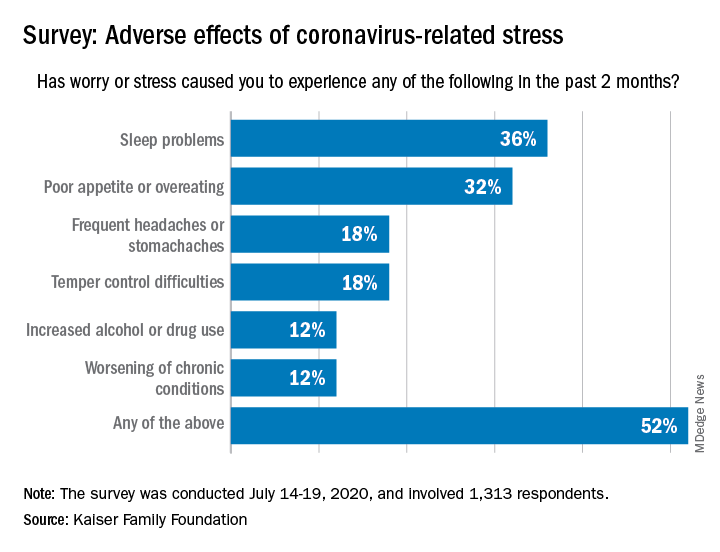
More than a third (36%) of the 1,313 respondents said they either had difficulty sleeping, falling asleep, or sleeping too much, KFF said in its latest Health Tracking Poll, conducted July 14-19, 2020. That was followed by poor appetite or overeating, which was mentioned by 32% of those surveyed.
Other adverse effects included frequent headaches or stomachaches (18%), temper-control issues (18%), increased drug or alcohol use (12%), and worsening of chronic conditions such as diabetes or hypertension (12%). Altogether, 52% of Americans have had at least one of these issues in the past 2 months, Liz Hamel and associates at KFF reported.
breaking down to 26% reporting a major impact and 28% reporting a minor impact (figures have been rounded), they said.
“As life with the coronavirus pandemic wears on, Americans increasingly say it is taking a negative toll on their mental health,” the investigators wrote. Earlier polls showed that pandemic-related stress was having an impact on mental health for 39% of respondents in May, compared with 45% in early April and 32% in March.
In the July poll, Black adults were much more likely to report a negative mental health impact (68%) than were Hispanics or Whites, who were both at 51%. Age was also a factor: The youngest group of respondents (ages 18-29 years) had the highest negative-impact rate (62%), and the oldest group (65 years and older) had the lowest (47%), they said.
When it came to reporting the adverse effects of stress or worry, however, the situation was somewhat different. Hispanics had the highest rate of such effects at 63%, while Blacks had a rate of 57% and 47% of Whites reported issues with sleep, eating, temper, and other problems, Ms. Hamel and associates reported.
Psychiatry trainees drive COVID-19 palliative care in New York
As SARS-CoV-2 cases surged in New York this past spring, one hospital system met the growing demand for palliative care in COVID-19 patients in acute care and emergency settings by training and redeploying psychiatry trainees, producing 100 consultations during a crisis period. Developers of this program wrote about their experience in the Journal of Pain and Symptom Management.
Research shows that psychiatrists can play an important, complementary role in palliative care, but not many models have explored this in practice. Over a 45-day period in March and April, New York Presbyterian/Columbia University Irving Medical Center saw an influx of 7,600 COVID-19 patients. Many were critically ill, and palliative care needs skyrocketed. Initial efforts to install a palliative care team at the emergency department and a proactive consultation model in the step-down units failed to meet demand for consults.
COVID-19 patients present unique challenges. Their clinical trajectory is less clear than those with cancer or other illnesses, Daniel Shalev, MD, a fellow in hospice and palliative medicine at Columbia University/New York State Psychiatric Institute, New York, and the study’s first author, said in an interview. “Ethical and systems issues around distribution of scarce resources may inflect patients’ and physicians’ responses,” Dr. Shalev said. “And families may not be able to be at the bedside with patients.”
To rapidly expand the palliative care workforce and meet patient needs, Dr. Shalev and colleagues recruited 16 psychiatry trainees from NYP, Columbia University Irving Medical Center, and Weill Cornell Medicine to work at NYP/Columbia University Irving Medical Center’s section of adult palliative medicine. Senior general psychiatry residents, child and adolescent psychiatry fellows, addiction psychiatry fellows, and postresidency T32 research fellows became part of a psychiatry-palliative care liaison team, offering psychosocial support and care goal strategies to patients and families.
Already well-versed in serious illness communication and psychosocial aspects of medical illness, the residents and fellows received additional training and education about SARS-CoV-2 and goals-of-care conversations. Child and adolescent psychiatry fellows participated in a communication workshop about the virus at Weill Cornell Medicine.
Working closely with the medical center’s palliative care service, the liaison team did consults around the clock at the ED under the supervision of a consultation-liaison (C-L) psychiatrist specializing in primary palliative care skills. The team managed 16 cases a day during the peak of New York’s COVID-19 outbreak, operating on a rotating schedule of one to three shifts weekly. Some shifts took place remotely to reduce exposure to the virus.
“We were fortunate that New York Presbyterian was early and aggressive in ensuring all clinical staff had personal protective equipment” in the treatment of COVID-19 patients, Dr. Shalev said.
The C-L psychiatry coordinator served as a traffic controller of sorts, overseeing daily staffing changes, maintaining a psychiatry–palliative care liaison team–shared patient list, and ensuring follow-up and continuity on patient care. The rotating schedule freed up time for trainees to meet other research and outpatient obligations.
The liaison team held a meeting each morning and accompanied the adult palliative care service on its daily virtual rounds to help streamline case management and care coordination among the various palliative care channels. Modifications in personnel took place as cases started to recede. Overall, the team participated in 100 consultations.
The findings show that there is significant overlap in psychiatry and palliative care skill sets, Dr. Shalev said. “Furthermore, many patients benefiting from palliative care services have mental health needs. But there are gaps between psychiatry and palliative care, including a lack of collaboration and cross-training. Our model showed how easily our disciplines can work together to improve the care available to all patients,” he added.
Some things could have gone more smoothly. Working under the duress of a pandemic, project leaders didn’t have enough time to train and supervise the team about advanced symptom management. Psychiatry staff members also weren’t as comfortable with nonpsychiatric symptom management as serious illness communication and psychiatric symptom management. Dr. Shalev expects these growth areas to improve over time.
The model could easily translate to other facilities, he believes. As of this writing, the liaison team was transitioning to a longer-term assignment involving patients on mechanical ventilation and their families.
The program increased access to care during a time of limited resources,and successfully combined psychiatric and palliative services – two specialties that, at times, can have conflicting recommendations, noted Maria I. Lapid, MD, a professor of psychiatry at the Mayo Clinic in Rochester, Minn., and a faculty member of the Mayo Clinic Center for Palliative Medicine, who was not part of the study. As urgent training for psychiatric trainees proved useful in the current crisis, long-term psychiatric programs will need to explore and consider how to integrate palliative care training into the psychiatric curriculum.
“Not only is this relevant in the current pandemic, but this will continue to be relevant in the context of the rapidly aging population” in the United States, said Dr. Lapid.
Dr. Shalev and colleagues declared no conflicts of interest in their study. Their research received no funds or grants from public, commercial, or nonprofit agencies.
SOURCE: Shalev D et al. J Pain Symptom Manage. 2020 Jun 13. doi.org/10.1016/j.jpainsymman.2020.06.009.
As SARS-CoV-2 cases surged in New York this past spring, one hospital system met the growing demand for palliative care in COVID-19 patients in acute care and emergency settings by training and redeploying psychiatry trainees, producing 100 consultations during a crisis period. Developers of this program wrote about their experience in the Journal of Pain and Symptom Management.
Research shows that psychiatrists can play an important, complementary role in palliative care, but not many models have explored this in practice. Over a 45-day period in March and April, New York Presbyterian/Columbia University Irving Medical Center saw an influx of 7,600 COVID-19 patients. Many were critically ill, and palliative care needs skyrocketed. Initial efforts to install a palliative care team at the emergency department and a proactive consultation model in the step-down units failed to meet demand for consults.
COVID-19 patients present unique challenges. Their clinical trajectory is less clear than those with cancer or other illnesses, Daniel Shalev, MD, a fellow in hospice and palliative medicine at Columbia University/New York State Psychiatric Institute, New York, and the study’s first author, said in an interview. “Ethical and systems issues around distribution of scarce resources may inflect patients’ and physicians’ responses,” Dr. Shalev said. “And families may not be able to be at the bedside with patients.”
To rapidly expand the palliative care workforce and meet patient needs, Dr. Shalev and colleagues recruited 16 psychiatry trainees from NYP, Columbia University Irving Medical Center, and Weill Cornell Medicine to work at NYP/Columbia University Irving Medical Center’s section of adult palliative medicine. Senior general psychiatry residents, child and adolescent psychiatry fellows, addiction psychiatry fellows, and postresidency T32 research fellows became part of a psychiatry-palliative care liaison team, offering psychosocial support and care goal strategies to patients and families.
Already well-versed in serious illness communication and psychosocial aspects of medical illness, the residents and fellows received additional training and education about SARS-CoV-2 and goals-of-care conversations. Child and adolescent psychiatry fellows participated in a communication workshop about the virus at Weill Cornell Medicine.
Working closely with the medical center’s palliative care service, the liaison team did consults around the clock at the ED under the supervision of a consultation-liaison (C-L) psychiatrist specializing in primary palliative care skills. The team managed 16 cases a day during the peak of New York’s COVID-19 outbreak, operating on a rotating schedule of one to three shifts weekly. Some shifts took place remotely to reduce exposure to the virus.
“We were fortunate that New York Presbyterian was early and aggressive in ensuring all clinical staff had personal protective equipment” in the treatment of COVID-19 patients, Dr. Shalev said.
The C-L psychiatry coordinator served as a traffic controller of sorts, overseeing daily staffing changes, maintaining a psychiatry–palliative care liaison team–shared patient list, and ensuring follow-up and continuity on patient care. The rotating schedule freed up time for trainees to meet other research and outpatient obligations.
The liaison team held a meeting each morning and accompanied the adult palliative care service on its daily virtual rounds to help streamline case management and care coordination among the various palliative care channels. Modifications in personnel took place as cases started to recede. Overall, the team participated in 100 consultations.
The findings show that there is significant overlap in psychiatry and palliative care skill sets, Dr. Shalev said. “Furthermore, many patients benefiting from palliative care services have mental health needs. But there are gaps between psychiatry and palliative care, including a lack of collaboration and cross-training. Our model showed how easily our disciplines can work together to improve the care available to all patients,” he added.
Some things could have gone more smoothly. Working under the duress of a pandemic, project leaders didn’t have enough time to train and supervise the team about advanced symptom management. Psychiatry staff members also weren’t as comfortable with nonpsychiatric symptom management as serious illness communication and psychiatric symptom management. Dr. Shalev expects these growth areas to improve over time.
The model could easily translate to other facilities, he believes. As of this writing, the liaison team was transitioning to a longer-term assignment involving patients on mechanical ventilation and their families.
The program increased access to care during a time of limited resources,and successfully combined psychiatric and palliative services – two specialties that, at times, can have conflicting recommendations, noted Maria I. Lapid, MD, a professor of psychiatry at the Mayo Clinic in Rochester, Minn., and a faculty member of the Mayo Clinic Center for Palliative Medicine, who was not part of the study. As urgent training for psychiatric trainees proved useful in the current crisis, long-term psychiatric programs will need to explore and consider how to integrate palliative care training into the psychiatric curriculum.
“Not only is this relevant in the current pandemic, but this will continue to be relevant in the context of the rapidly aging population” in the United States, said Dr. Lapid.
Dr. Shalev and colleagues declared no conflicts of interest in their study. Their research received no funds or grants from public, commercial, or nonprofit agencies.
SOURCE: Shalev D et al. J Pain Symptom Manage. 2020 Jun 13. doi.org/10.1016/j.jpainsymman.2020.06.009.
As SARS-CoV-2 cases surged in New York this past spring, one hospital system met the growing demand for palliative care in COVID-19 patients in acute care and emergency settings by training and redeploying psychiatry trainees, producing 100 consultations during a crisis period. Developers of this program wrote about their experience in the Journal of Pain and Symptom Management.
Research shows that psychiatrists can play an important, complementary role in palliative care, but not many models have explored this in practice. Over a 45-day period in March and April, New York Presbyterian/Columbia University Irving Medical Center saw an influx of 7,600 COVID-19 patients. Many were critically ill, and palliative care needs skyrocketed. Initial efforts to install a palliative care team at the emergency department and a proactive consultation model in the step-down units failed to meet demand for consults.
COVID-19 patients present unique challenges. Their clinical trajectory is less clear than those with cancer or other illnesses, Daniel Shalev, MD, a fellow in hospice and palliative medicine at Columbia University/New York State Psychiatric Institute, New York, and the study’s first author, said in an interview. “Ethical and systems issues around distribution of scarce resources may inflect patients’ and physicians’ responses,” Dr. Shalev said. “And families may not be able to be at the bedside with patients.”
To rapidly expand the palliative care workforce and meet patient needs, Dr. Shalev and colleagues recruited 16 psychiatry trainees from NYP, Columbia University Irving Medical Center, and Weill Cornell Medicine to work at NYP/Columbia University Irving Medical Center’s section of adult palliative medicine. Senior general psychiatry residents, child and adolescent psychiatry fellows, addiction psychiatry fellows, and postresidency T32 research fellows became part of a psychiatry-palliative care liaison team, offering psychosocial support and care goal strategies to patients and families.
Already well-versed in serious illness communication and psychosocial aspects of medical illness, the residents and fellows received additional training and education about SARS-CoV-2 and goals-of-care conversations. Child and adolescent psychiatry fellows participated in a communication workshop about the virus at Weill Cornell Medicine.
Working closely with the medical center’s palliative care service, the liaison team did consults around the clock at the ED under the supervision of a consultation-liaison (C-L) psychiatrist specializing in primary palliative care skills. The team managed 16 cases a day during the peak of New York’s COVID-19 outbreak, operating on a rotating schedule of one to three shifts weekly. Some shifts took place remotely to reduce exposure to the virus.
“We were fortunate that New York Presbyterian was early and aggressive in ensuring all clinical staff had personal protective equipment” in the treatment of COVID-19 patients, Dr. Shalev said.
The C-L psychiatry coordinator served as a traffic controller of sorts, overseeing daily staffing changes, maintaining a psychiatry–palliative care liaison team–shared patient list, and ensuring follow-up and continuity on patient care. The rotating schedule freed up time for trainees to meet other research and outpatient obligations.
The liaison team held a meeting each morning and accompanied the adult palliative care service on its daily virtual rounds to help streamline case management and care coordination among the various palliative care channels. Modifications in personnel took place as cases started to recede. Overall, the team participated in 100 consultations.
The findings show that there is significant overlap in psychiatry and palliative care skill sets, Dr. Shalev said. “Furthermore, many patients benefiting from palliative care services have mental health needs. But there are gaps between psychiatry and palliative care, including a lack of collaboration and cross-training. Our model showed how easily our disciplines can work together to improve the care available to all patients,” he added.
Some things could have gone more smoothly. Working under the duress of a pandemic, project leaders didn’t have enough time to train and supervise the team about advanced symptom management. Psychiatry staff members also weren’t as comfortable with nonpsychiatric symptom management as serious illness communication and psychiatric symptom management. Dr. Shalev expects these growth areas to improve over time.
The model could easily translate to other facilities, he believes. As of this writing, the liaison team was transitioning to a longer-term assignment involving patients on mechanical ventilation and their families.
The program increased access to care during a time of limited resources,and successfully combined psychiatric and palliative services – two specialties that, at times, can have conflicting recommendations, noted Maria I. Lapid, MD, a professor of psychiatry at the Mayo Clinic in Rochester, Minn., and a faculty member of the Mayo Clinic Center for Palliative Medicine, who was not part of the study. As urgent training for psychiatric trainees proved useful in the current crisis, long-term psychiatric programs will need to explore and consider how to integrate palliative care training into the psychiatric curriculum.
“Not only is this relevant in the current pandemic, but this will continue to be relevant in the context of the rapidly aging population” in the United States, said Dr. Lapid.
Dr. Shalev and colleagues declared no conflicts of interest in their study. Their research received no funds or grants from public, commercial, or nonprofit agencies.
SOURCE: Shalev D et al. J Pain Symptom Manage. 2020 Jun 13. doi.org/10.1016/j.jpainsymman.2020.06.009.
Helping families understand internalized racism
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at [email protected].
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at [email protected].
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Ms. Jones brings her 15-year-old daughter, Angela, to the resident clinic. Angela is becoming increasingly anxious, withdrawn, and difficult to manage. As part of the initial interview, the resident, Dr. Sota, asks about the sociocultural background of the family. Ms. Jones is African American and recently began a relationship with a white man. Her daughter, Angela, is biracial; her biological father is white and has moved out of state with little ongoing contact with Angela and her mother.
At interview, Angela expresses a lot of anger at her mother, her biological father, and her new “stepfather.” Ms. Jones says: “I do not want Angela growing up as an ‘angry black woman.’ ” When asked for an explanation, she stated that she doesn’t want her daughter to be stereotyped, to be perceived as an angry black person. “She needs to fit in with our new life. She has lots of opportunities if only she would take them.”
Dr. Sota recognizes that Angela’s struggle, and perhaps also the struggle of Ms. Jones, has a component of internalized racism. How should Dr. Sota proceed? Dr. Sota puts herself in Angela’s shoes: How does Angela see herself? Angela has light brown skin, and
The term internalized racism (IR) first appeared in the 1980s. IR was compared to the oppression of black people in the 1800s: “The slavery that captures the mind and incarcerates the motivation, perception, aspiration, and identity in a web of anti-self images, generating a personal and collective self destruction, is more cruel than the shackles on the wrists and ankles.”1 According to Susanne Lipsky,2 IR “in African Americans manifests as internalizing stereotypes, mistrusting the self and other Blacks, and narrows one’s view of authentic Black culture.”
IR refers to the internalization and acceptance of the dominant white culture’s actions and beliefs, while rejecting one’s own cultural background. There is a long history of negative cultural representations of African Americans in popular American culture, and IR has a detrimental impact on the emotional well-being of African Americans.3
IR is associated with poorer metabolic health4 and psychological distress, depression and anxiety,5-8 and decreased self-esteem.9 However, protective processes can reduce one’s response to risk and can be developed through the psychotherapeutic relationship.
Interventions at an individual, family, or community levels
Angela: Tell me about yourself: What type of person are you? How do you identify? How do you feel about yourself/your appearance/your language?
Tell me about your friends/family? What interests do you have?
“Tell me more” questions can reveal conflicted feelings, etc., even if Angela does not answer. A good therapist can talk about IR; even if Angela does not bring it up, it is important for the therapist to find language suitable for the age of the patient.
Dr. Sota has some luck with Angela, who nods her head but says little. Dr. Sota then turns to Ms. Jones and asks whether she can answer these questions, too, and rephrases the questions for an adult. Interviewing parents in the presence of their children gives Dr. Sota and Angela an idea of what is permitted to talk about in the family.
A therapist can also note other permissions in the family: How do Angela and her mother use language? Do they claim or reject words and phrases such as “angry black woman” and choose, instead, to use language to “fit in” with the dominant white culture?
Dr. Sota notices that Ms. Jones presents herself as keen to fit in with her new future husband’s life. She wants Angela to do likewise. Dr. Sota notices that Angela vacillates between wanting to claim her black identity and having to navigate what that means in this family (not a good thing) – and wanting to assimilate into white culture. Her peers fall into two separate groups: a set of black friends and a set of white friends. Her mother prefers that she see her white friends, mistrusting her black friends.
Dr. Sota’s supervisor suggests that she introduce IR more forcefully because this seems to be a major course of conflict for Angela and encourage a frank discussion between mother and daughter. Dr. Sota starts the next session in the following way: “I noticed last week that the way you each identify yourselves is quite different. Ms. Jones, you want Angela to ‘fit in’ and perhaps just embrace white culture, whereas Angela, perhaps you vacillate between a white identity and a black identity?”
The following questions can help Dr. Sota elicit IR:
- What information about yourself would you like others to know – about your heritage, country of origin, family, class background, and so on?
- What makes you proud about being a member of this group, and what do you love about other members of this group?
- What has been hard about being a member of this group, and what don’t you like about others in this group?
- What were your early life experiences with people in this group? How were you treated? How did you feel about others in your group when you were young?
At a community level, family workshops support positive cultural identities that strengthen family functioning and reducing behavioral health risks. In a study of 575 urban American Indian (AI) families from diverse tribal backgrounds, the AI families who participated in such a workshop had significant increases in their ethnic identity, improved sense of spirituality, and a more positive cultural identification. The workshops provided culturally adaptive parenting interventions.10
IR is a serious determinant of both physical and mental health. Assessment of IR can be done using rating scales, such as the Nadanolitization Scale11 or the Internalized Racial Oppression Scale.12 IR also can also be assessed using a more formalized interview guide, such as the DSM-5 Cultural Formulation Interview (CFI).13 This 16-question interview guide helps behavioral health providers better understand the way service users and their social networks (e.g., families, friends) understand what is happening to them and why, as well as the barriers they experience, such as racism, discrimination, stigma, and financial stressors.
Individuals’ cultures and experiences have a profound impact on their understanding of their symptoms and their engagement in care. The American Psychiatric Association considers it to be part of mental health providers’ duty of care to engage all individuals in culturally relevant conversations about their past experiences and care expectations. More relevant, I submit that you cannot treat someone without having made this inquiry. A cultural assessment improves understanding but also shifts power relationships between providers and patients. The DSM-5 CFI and training guides are widely available and provide additional information for those who want to improve their cultural literacy.
Conclusion
Internalized racism is the component of racism that is the most difficult to discern. Psychiatrists and mental health professionals are uniquely poised to address IR, and any subsequent internal conflict and identity difficulties. Each program, office, and clinic can easily find the resources to do this through the APA. If you would like help providing education, contact me at [email protected].
References
1. Akbar N. J Black Studies. 1984. doi: 10.11771002193478401400401.
2. Lipsky S. Internalized Racism. Seattle: Rational Island Publishers, 1987.
3. Williams DR and Mohammed SA. Am Behav Sci. 2013 May 8. doi: 10.1177/00027642134873340.
4. DeLilly CR and Flaskerud JH. Issues Ment Health Nurs. 2012 Nov;33(11):804-11.
5. Molina KM and James D. Group Process Intergroup Relat. 2016 Jul;19(4):439-61.
6. Szymanski D and Obiri O. Couns Psychologist. 2011;39(3):438-62.
7. Carter RT et al. J Multicul Couns Dev. 2017 Oct 5;45(4):232-59.
8. Mouzon DM and McLean JS. Ethn Health. 2017 Feb;22(1):36-48.
9. Szymanski DM and Gupta A. J Couns Psychol. 2009;56(1):110-18.
10. Kulis SS et al. Cultural Diversity and Ethnic Minority Psychol. 2019. doi: 10.1037/cpd000315.
11. Taylor J and Grundy C. “Measuring black internalization of white stereotypes about African Americans: The Nadanolization Scale.” In: Jones RL, ed. Handbook of Tests and Measurements of Black Populations. Hampton, Va.: Cobb & Henry, 1996.
12. Bailey T-K M et al. J Couns Psychol. 2011 Oct;58(4):481-93.
13. American Psychiatric Association. Cultural Formulation Interview. DSM-5. American Psychiatric Association Publishing: Arlington, Va. 2013.
Various aspects about the case described above have been changed to protect the clinician’s and patients’ identities. Thanks to the following individuals for their contributions to this article: Suzanne Huberty, MD, and Shiona Heru, JD.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest to disclose.
Human sitters in the COVID era
Data collection needed for care of suicidal hospitalized patients
I am writing this commentary to bring to readers’ attention a medical and ethical complexity related to human sitters for presumably suicidal, COVID-19–positive hospitalized patients.
To shape and bundle the ethics issues addressed here into a single question, I offer the following: Should policies and practices requiring that patients in presumed need of a sitter because of assessed suicidality change when the patient is COVID-19–positive? Although the analysis might be similar when a sitter is monitoring a Patient Under Investigation (PUI), here I focus only on COVID-19–positive patients. Similarly, there are other reasons for sitters, of course, such as to prevent elopement, or, if a patient is in restraints, to prevent the patient from pulling out lines or tubes. Again, discussion of some of these ethical complications is beyond the scope of this piece. Just considering the matter of potential suicidality and sitters is complex enough. And so, to start, I sought out existing sources for guidance.
In looking for such sources, I first turned to the Centers for Medicare and Medicaid Services before COVID-19. CMS has required that there be a sitter for a patient who is suicidal and that the sitter remain in the room so that the sitter can intervene expeditiously if the patient tries to hurt himself or herself. There has been no change in this guidance since the COVID-19 pandemic in the United States. To the best of my knowledge, there is no substantive guidance for protecting sitters from contagion other than PPE. Given this, it begs the question:
In my hospital, I already have begun discussing the potential risks of harm and potential benefits to our suicidal patients of having a sitter directly outside the patient’s room. I also have considered whether to have one sitter watching several room cameras at once, commonly referred to as “telehealth strategies.”
To be sure, sitting for hours in the room of a COVID-19–positive patient is onerous. The sitter is required to be in full PPE (N-95 mask, gown, and gloves), which is hot and uncomfortable. Current practice is resource intensive in other ways. It requires changing out the sitter every 2 hours, which uses substantial amounts of PPE and multiple sitters.
Regardless, however, there are really no data upon which to base any sound ethics judgment about what should or should not be tried. We just have no information on how to attempt to balance potential risks and prospects for the benefit of whom and when. And, given that good clinical ethics always begin with the facts, I write this piece to see whether readers have thought about these issues before – and whether any of clinicians have started collecting the valuable data needed to begin making sound ethical judgments about how to care for our presumably suicidal COVID-19–positive patients and the sitters who watch over them.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
This column is an outcome of a discussion that occurred during Psych/Ethics rounds on June 5, and does not represent any official statements of Medstar Washington Hospital Center or any entity of the MedStar Corp. Dr. Ritchie would like to thank Evan G. DeRenzo, PhD, of the John J. Lynch Center for Ethics, for her thoughtful review of a previous draft of this commentary.
Data collection needed for care of suicidal hospitalized patients
Data collection needed for care of suicidal hospitalized patients
I am writing this commentary to bring to readers’ attention a medical and ethical complexity related to human sitters for presumably suicidal, COVID-19–positive hospitalized patients.
To shape and bundle the ethics issues addressed here into a single question, I offer the following: Should policies and practices requiring that patients in presumed need of a sitter because of assessed suicidality change when the patient is COVID-19–positive? Although the analysis might be similar when a sitter is monitoring a Patient Under Investigation (PUI), here I focus only on COVID-19–positive patients. Similarly, there are other reasons for sitters, of course, such as to prevent elopement, or, if a patient is in restraints, to prevent the patient from pulling out lines or tubes. Again, discussion of some of these ethical complications is beyond the scope of this piece. Just considering the matter of potential suicidality and sitters is complex enough. And so, to start, I sought out existing sources for guidance.
In looking for such sources, I first turned to the Centers for Medicare and Medicaid Services before COVID-19. CMS has required that there be a sitter for a patient who is suicidal and that the sitter remain in the room so that the sitter can intervene expeditiously if the patient tries to hurt himself or herself. There has been no change in this guidance since the COVID-19 pandemic in the United States. To the best of my knowledge, there is no substantive guidance for protecting sitters from contagion other than PPE. Given this, it begs the question:
In my hospital, I already have begun discussing the potential risks of harm and potential benefits to our suicidal patients of having a sitter directly outside the patient’s room. I also have considered whether to have one sitter watching several room cameras at once, commonly referred to as “telehealth strategies.”
To be sure, sitting for hours in the room of a COVID-19–positive patient is onerous. The sitter is required to be in full PPE (N-95 mask, gown, and gloves), which is hot and uncomfortable. Current practice is resource intensive in other ways. It requires changing out the sitter every 2 hours, which uses substantial amounts of PPE and multiple sitters.
Regardless, however, there are really no data upon which to base any sound ethics judgment about what should or should not be tried. We just have no information on how to attempt to balance potential risks and prospects for the benefit of whom and when. And, given that good clinical ethics always begin with the facts, I write this piece to see whether readers have thought about these issues before – and whether any of clinicians have started collecting the valuable data needed to begin making sound ethical judgments about how to care for our presumably suicidal COVID-19–positive patients and the sitters who watch over them.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
This column is an outcome of a discussion that occurred during Psych/Ethics rounds on June 5, and does not represent any official statements of Medstar Washington Hospital Center or any entity of the MedStar Corp. Dr. Ritchie would like to thank Evan G. DeRenzo, PhD, of the John J. Lynch Center for Ethics, for her thoughtful review of a previous draft of this commentary.
I am writing this commentary to bring to readers’ attention a medical and ethical complexity related to human sitters for presumably suicidal, COVID-19–positive hospitalized patients.
To shape and bundle the ethics issues addressed here into a single question, I offer the following: Should policies and practices requiring that patients in presumed need of a sitter because of assessed suicidality change when the patient is COVID-19–positive? Although the analysis might be similar when a sitter is monitoring a Patient Under Investigation (PUI), here I focus only on COVID-19–positive patients. Similarly, there are other reasons for sitters, of course, such as to prevent elopement, or, if a patient is in restraints, to prevent the patient from pulling out lines or tubes. Again, discussion of some of these ethical complications is beyond the scope of this piece. Just considering the matter of potential suicidality and sitters is complex enough. And so, to start, I sought out existing sources for guidance.
In looking for such sources, I first turned to the Centers for Medicare and Medicaid Services before COVID-19. CMS has required that there be a sitter for a patient who is suicidal and that the sitter remain in the room so that the sitter can intervene expeditiously if the patient tries to hurt himself or herself. There has been no change in this guidance since the COVID-19 pandemic in the United States. To the best of my knowledge, there is no substantive guidance for protecting sitters from contagion other than PPE. Given this, it begs the question:
In my hospital, I already have begun discussing the potential risks of harm and potential benefits to our suicidal patients of having a sitter directly outside the patient’s room. I also have considered whether to have one sitter watching several room cameras at once, commonly referred to as “telehealth strategies.”
To be sure, sitting for hours in the room of a COVID-19–positive patient is onerous. The sitter is required to be in full PPE (N-95 mask, gown, and gloves), which is hot and uncomfortable. Current practice is resource intensive in other ways. It requires changing out the sitter every 2 hours, which uses substantial amounts of PPE and multiple sitters.
Regardless, however, there are really no data upon which to base any sound ethics judgment about what should or should not be tried. We just have no information on how to attempt to balance potential risks and prospects for the benefit of whom and when. And, given that good clinical ethics always begin with the facts, I write this piece to see whether readers have thought about these issues before – and whether any of clinicians have started collecting the valuable data needed to begin making sound ethical judgments about how to care for our presumably suicidal COVID-19–positive patients and the sitters who watch over them.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
This column is an outcome of a discussion that occurred during Psych/Ethics rounds on June 5, and does not represent any official statements of Medstar Washington Hospital Center or any entity of the MedStar Corp. Dr. Ritchie would like to thank Evan G. DeRenzo, PhD, of the John J. Lynch Center for Ethics, for her thoughtful review of a previous draft of this commentary.
New ‘atlas’ maps links between mental disorders, physical illnesses
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
Mental illnesses are associated with a significantly increased risk of subsequent physical diseases, new research shows.
An international team of researchers has created an “atlas” that maps the relationship between specific mental disorders and the risk of subsequent physical illnesses.
The researchers found that, following the diagnosis of a mental disorder, psychiatric patients are significantly more likely than the general population to develop potentially life-threatening conditions, including heart disease and stroke.
These findings, the investigators noted, highlight the need for better medical care in this vulnerable population. They have created a website with detailed information about the risks of specific physical ailments and the link to particular mental disorders.
“We found that women with anxiety disorders have a 50% increased risk of developing a heart condition or stroke – over 15 years, one in three women with anxiety disorders will develop these medical disorders,” lead investigator John McGrath, MD, PhD, University of Queensland’s Brain Institute, Brisbane, Australia, and Aarhus (Denmark) University, said in a statement.
“We also looked at men with substance use disorders such as alcohol-related disorders and found they have a 400% increased risk of gut or liver disorders, while over 15 years, one in five of them will develop gut or liver conditions,” he added.
The study was published in the New England Journal of Medicine.
New ‘atlas’
It’s well known that patients with mental disorders have decreased quality of life, increased health care utilization, and a shorter life expectancy than individuals in the general population – about 10 years for men and 7 years for women.
However, the investigators noted, previous research examining the relationship between mental disorders and medical conditions only focused on “particular pairs or a small set of mental disorders and medical conditions.”
“We needed a comprehensive study to map the links between different types of mental disorders versus different types of general medical conditions. Our study has provided this atlas,” Dr. McGrath said in an interview.
The clinical utility of such a map could provide comprehensive data on relative and absolute risks of various medical conditions after a diagnosis of a mental disorder. This information, the researchers noted, would “help clinicians and health care planners identify the primary prevention needs of their patients.”
The study included 5.9 million people born in Denmark between 1900 and 2015 and followed them from 2000 to 2016, a total of 83.9 million person-years. The researchers followed patients for up to 17 years (2000-2016) for medical diagnoses and up to 48 years (1969-2016) for diagnoses of mental disorders.
The study’s large sample size allowed investigators to assess 10 broad types of mental disorders and 9 broad categories of medical conditions that encompassed 31 specific conditions.
Categories of medical conditions included circulatory, endocrine, pulmonary, gastrointestinal, urogenital, musculoskeletal, hematologic, neurologic, and cancer. Mental disorder categories included organic disorders such as Alzheimer’s, substance abuse disorders, schizophrenia, mood disorders, neurotic disorders, eating disorders, personality disorders, developmental disorders, behavioral/emotional disorders, and intellectual disabilities.
The researchers estimated associations between 90 pairs of mental disorders and broad-category medical conditions, as well as 310 pairs of mental disorders and specific medical conditions.
‘Curious’ finding
Individuals with mental disorders showed a higher risk of medical conditions in 76 out of 90 specific mental disorder–medical condition pairs.
After adjusting for sex, age, calendar time, and previous coexisting mental disorders, the median hazard ratio for a subsequent medical condition was 1.37 in patients with a mental disorder.
The lowest HR was 0.82 for organic mental disorders and the broad category of cancer (95% confidence interval, 0.80-0.84), and the highest was 3.62 for eating disorders and urogenital conditions (95% CI, 3.11-4.22). On the other hand, schizophrenia was associated with a reduced risk of developing musculoskeletal conditions (HR, 0.87; 95% CI, 0.84-0.91).
Dr. McGrath described this finding as “curious” and speculated it “may be related to underlying genetic risk factors.”
compared with the matched reference group without a mood disorder (40.9% vs. 32.6%, respectively).
The risk of developing subsequent medical conditions after a mental disorder diagnosis did not remain steady over time. For instance, although mood disorders were associated with an increased risk of developing circulatory problems (HR, 1.32; 95% CI, 1.31-1.34), the highest risk occurred during the first 6 months following diagnosis and gradually decreased over the next 15 years (HR, 2.39; 95% CI, 2.29-2.48 and HR, 1.18; 95% CI, 1.17-1.20, respectively).
“Many people with mental disorders have unhealthy lifestyle, including low exercise, poor diet, smoking, and alcohol, which may account for the increased risk of physical illness, and also they may not seek and/or may not get quick treatment for their health conditions,” said Dr. McGrath.
Additionally, “perhaps some genetic and early life exposures, such as trauma, may increase the risk of both medical conditions and mental disorders,” he added. “We need better treatments for mental disorders, so that they do not slip into unemployment or poverty.”
A strong case
In a comment, Roger McIntyre, MD, professor of psychiatry and pharmacology at the University of Toronto and head of the mood disorders psychopharmacology unit, University Health Network, said that the research “really makes a strong case for the fact that persons who have mental disorders are at higher risk of chronic diseases, and it’s the chronic diseases that decrease their lifespan.”
Dr. McIntyre, who is also director of the Depression and Bipolar Support Alliance, said that the “takeaway message is that mental disorders are not just brain disorders but are multisystem disorders.”
For this reason, “the most appropriate way to provide care would be to provide a holistic approach to treat and prevent the chronic diseases that lead to increase in mortality,” recommended Dr. McIntyre, who was not involved with the current study.
The study was supported by grants from the Danish National Research Foundation, the National Health and Medical Research Council, the Novo Nordisk Foundation , the European Union’s Horizon 2020 Research and Innovation Program, the Aarhus University Research Foundation, the Lundbeck Foundation, the National Institutes of Health, the European Commission, Helsefonden, the Danish Council for Independent Research, the Independent Research Fund Denmark, the National Health and Medical Research Council of Australia, and the National Institute on Drug Abuse.
Dr. McGrath has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Dr. McIntyre reports receiving grants from Stanley Medical Research Institute; the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/Chinese National Natural Research Foundation; and receiving speaking/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
A version of this article originally appeared on Medscape.com.
Expert says progress in gut-brain research requires an open mind
A growing body of research links the gut with the brain and behavior, but compartmentalization within the medical community may be slowing investigation of the gut-brain axis, according to a leading expert.
Studies have shown that the microbiome may influence a diverse range of behavioral and neurological processes, from acute and chronic stress responses to development of Parkinson’s and Alzheimer’s disease, reported John F. Cryan, PhD, of University College Cork, Ireland.
Dr. Cryan began his presentation at the annual Gut Microbiota for Health World Summit by citing Hippocrates, who is thought to have stated that all diseases begin in the gut.
“That can be quite strange when I talk to my neurology or psychiatry colleagues,” Dr. Cryan said. “They sometimes look at me like I have two heads. Because in medicine we compartmentalize, and if you are studying neurology or psychiatry or [you are] in clinical practice, you are focusing on everything from the neck upwards.”
For more than a decade, Dr. Cryan and colleagues have been investigating the gut-brain axis, predominantly in mouse models, but also across animal species and in humans.
At the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Cryan reviewed a variety of representative studies.
For instance, in both mice and humans, research has shown that C-section, which is associated with poorer microbiome diversity than vaginal delivery, has also been linked with social deficits and elevated stress responses. And in the case of mice, coprophagia, in which cesarean-delivered mice eat the feces of vaginally born mice, has been shown to ameliorate these psychiatric effects.
Dr. Cryan likened this process to an “artificial fecal transplant.”
“You know, co-housing and eating each other’s poo is not the translational approach that we were advocating by any means,” Dr. Cryan said. “But at least it tells us – in a proof-of-concept way – that if we change the microbiome, then we can reverse what’s going on.”
While the mechanisms behind the gut-brain axis remain incompletely understood, Dr. Cryan noted that the vagus nerve, which travels from the gut to the brain, plays a central role, and that transecting this nerve in mice stops the microbiome from affecting the brain.
“What happens in vagus doesn’t just stay in vagus, but will actually affect our emotions in different ways,” Dr. Cryan said.
He emphasized that communication travels both ways along the gut-brain axis, and went on to describe how this phenomenon has been demonstrated across a wide array of animals.
“From insects all the way through to primates, if you start to interfere with social behavior, you change the microbiome,” Dr. Cryan said. “But the opposite is also true; if you start to change the microbiome you can start to have widespread effects on social behavior.”
In humans, manipulating the microbiome could open up new psychiatric frontiers, Dr. Cryan said.
“[In the past 30 years], there really have been no real advances in how we manage mental health,” he said. “That’s very sobering when we are having such a mental health problem across all ages right now. And so perhaps it’s time for what we’ve coined the ‘psychobiotic revolution’ – time for a new way of thinking about mental health.”
According to Dr. Cryan, psychobiotics are interventions that target the microbiome for mental health purposes, including fermented foods, probiotics, prebiotics, synbiotics, parabiotics, and postbiotics.
Among these, probiotics have been a focal point of interventional research. Although results have been mixed, Dr. Cryan suggested that negative probiotic studies are more likely due to bacterial strain than a failure of the concept as a whole.
“Most strains of bacteria will do absolutely nothing,” Dr. Cryan said. “Strain is really important.”
In demonstration of this concept, he recounted a 2017 study conducted at University College Cork in which 22 healthy volunteers were given Bifidobacterium longum 1714, and then subjected to a social stress test. The results, published in Translational Psychiatry, showed that the probiotic, compared with placebo, was associated with attenuated stress responses, reduced daily stress, and enhanced visuospatial memory.
In contrast, a similar study by Dr. Cryan and colleagues, which tested Lactobacillus rhamnosus (JB-1), fell short.
“You [could not have gotten] more negative data into one paper if you tried,” Dr. Cryan said, referring to the study. “It did absolutely nothing.”
To find out which psychobiotics may have an impact, and how, Dr. Cryan called for more research.
“It’s still early days,” he said. “We probably have more meta-analyses and systematic reviews of the field than we have primary research papers.
Dr. Cryan concluded his presentation on an optimistic note.
“Neurology is waking up ... to understand that the microbiome could be playing a key role in many, many other disorders. ... Overall, what we’re beginning to see is that our state of gut markedly affects our state of mind.”
Dr. Cryan disclosed relationships with Abbott Nutrition, Roche Pharma, Nutricia, and others.
A growing body of research links the gut with the brain and behavior, but compartmentalization within the medical community may be slowing investigation of the gut-brain axis, according to a leading expert.
Studies have shown that the microbiome may influence a diverse range of behavioral and neurological processes, from acute and chronic stress responses to development of Parkinson’s and Alzheimer’s disease, reported John F. Cryan, PhD, of University College Cork, Ireland.
Dr. Cryan began his presentation at the annual Gut Microbiota for Health World Summit by citing Hippocrates, who is thought to have stated that all diseases begin in the gut.
“That can be quite strange when I talk to my neurology or psychiatry colleagues,” Dr. Cryan said. “They sometimes look at me like I have two heads. Because in medicine we compartmentalize, and if you are studying neurology or psychiatry or [you are] in clinical practice, you are focusing on everything from the neck upwards.”
For more than a decade, Dr. Cryan and colleagues have been investigating the gut-brain axis, predominantly in mouse models, but also across animal species and in humans.
At the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Cryan reviewed a variety of representative studies.
For instance, in both mice and humans, research has shown that C-section, which is associated with poorer microbiome diversity than vaginal delivery, has also been linked with social deficits and elevated stress responses. And in the case of mice, coprophagia, in which cesarean-delivered mice eat the feces of vaginally born mice, has been shown to ameliorate these psychiatric effects.
Dr. Cryan likened this process to an “artificial fecal transplant.”
“You know, co-housing and eating each other’s poo is not the translational approach that we were advocating by any means,” Dr. Cryan said. “But at least it tells us – in a proof-of-concept way – that if we change the microbiome, then we can reverse what’s going on.”
While the mechanisms behind the gut-brain axis remain incompletely understood, Dr. Cryan noted that the vagus nerve, which travels from the gut to the brain, plays a central role, and that transecting this nerve in mice stops the microbiome from affecting the brain.
“What happens in vagus doesn’t just stay in vagus, but will actually affect our emotions in different ways,” Dr. Cryan said.
He emphasized that communication travels both ways along the gut-brain axis, and went on to describe how this phenomenon has been demonstrated across a wide array of animals.
“From insects all the way through to primates, if you start to interfere with social behavior, you change the microbiome,” Dr. Cryan said. “But the opposite is also true; if you start to change the microbiome you can start to have widespread effects on social behavior.”
In humans, manipulating the microbiome could open up new psychiatric frontiers, Dr. Cryan said.
“[In the past 30 years], there really have been no real advances in how we manage mental health,” he said. “That’s very sobering when we are having such a mental health problem across all ages right now. And so perhaps it’s time for what we’ve coined the ‘psychobiotic revolution’ – time for a new way of thinking about mental health.”
According to Dr. Cryan, psychobiotics are interventions that target the microbiome for mental health purposes, including fermented foods, probiotics, prebiotics, synbiotics, parabiotics, and postbiotics.
Among these, probiotics have been a focal point of interventional research. Although results have been mixed, Dr. Cryan suggested that negative probiotic studies are more likely due to bacterial strain than a failure of the concept as a whole.
“Most strains of bacteria will do absolutely nothing,” Dr. Cryan said. “Strain is really important.”
In demonstration of this concept, he recounted a 2017 study conducted at University College Cork in which 22 healthy volunteers were given Bifidobacterium longum 1714, and then subjected to a social stress test. The results, published in Translational Psychiatry, showed that the probiotic, compared with placebo, was associated with attenuated stress responses, reduced daily stress, and enhanced visuospatial memory.
In contrast, a similar study by Dr. Cryan and colleagues, which tested Lactobacillus rhamnosus (JB-1), fell short.
“You [could not have gotten] more negative data into one paper if you tried,” Dr. Cryan said, referring to the study. “It did absolutely nothing.”
To find out which psychobiotics may have an impact, and how, Dr. Cryan called for more research.
“It’s still early days,” he said. “We probably have more meta-analyses and systematic reviews of the field than we have primary research papers.
Dr. Cryan concluded his presentation on an optimistic note.
“Neurology is waking up ... to understand that the microbiome could be playing a key role in many, many other disorders. ... Overall, what we’re beginning to see is that our state of gut markedly affects our state of mind.”
Dr. Cryan disclosed relationships with Abbott Nutrition, Roche Pharma, Nutricia, and others.
A growing body of research links the gut with the brain and behavior, but compartmentalization within the medical community may be slowing investigation of the gut-brain axis, according to a leading expert.
Studies have shown that the microbiome may influence a diverse range of behavioral and neurological processes, from acute and chronic stress responses to development of Parkinson’s and Alzheimer’s disease, reported John F. Cryan, PhD, of University College Cork, Ireland.
Dr. Cryan began his presentation at the annual Gut Microbiota for Health World Summit by citing Hippocrates, who is thought to have stated that all diseases begin in the gut.
“That can be quite strange when I talk to my neurology or psychiatry colleagues,” Dr. Cryan said. “They sometimes look at me like I have two heads. Because in medicine we compartmentalize, and if you are studying neurology or psychiatry or [you are] in clinical practice, you are focusing on everything from the neck upwards.”
For more than a decade, Dr. Cryan and colleagues have been investigating the gut-brain axis, predominantly in mouse models, but also across animal species and in humans.
At the meeting, sponsored by the American Gastroenterological Association and the European Society for Neurogastroenterology and Motility, Dr. Cryan reviewed a variety of representative studies.
For instance, in both mice and humans, research has shown that C-section, which is associated with poorer microbiome diversity than vaginal delivery, has also been linked with social deficits and elevated stress responses. And in the case of mice, coprophagia, in which cesarean-delivered mice eat the feces of vaginally born mice, has been shown to ameliorate these psychiatric effects.
Dr. Cryan likened this process to an “artificial fecal transplant.”
“You know, co-housing and eating each other’s poo is not the translational approach that we were advocating by any means,” Dr. Cryan said. “But at least it tells us – in a proof-of-concept way – that if we change the microbiome, then we can reverse what’s going on.”
While the mechanisms behind the gut-brain axis remain incompletely understood, Dr. Cryan noted that the vagus nerve, which travels from the gut to the brain, plays a central role, and that transecting this nerve in mice stops the microbiome from affecting the brain.
“What happens in vagus doesn’t just stay in vagus, but will actually affect our emotions in different ways,” Dr. Cryan said.
He emphasized that communication travels both ways along the gut-brain axis, and went on to describe how this phenomenon has been demonstrated across a wide array of animals.
“From insects all the way through to primates, if you start to interfere with social behavior, you change the microbiome,” Dr. Cryan said. “But the opposite is also true; if you start to change the microbiome you can start to have widespread effects on social behavior.”
In humans, manipulating the microbiome could open up new psychiatric frontiers, Dr. Cryan said.
“[In the past 30 years], there really have been no real advances in how we manage mental health,” he said. “That’s very sobering when we are having such a mental health problem across all ages right now. And so perhaps it’s time for what we’ve coined the ‘psychobiotic revolution’ – time for a new way of thinking about mental health.”
According to Dr. Cryan, psychobiotics are interventions that target the microbiome for mental health purposes, including fermented foods, probiotics, prebiotics, synbiotics, parabiotics, and postbiotics.
Among these, probiotics have been a focal point of interventional research. Although results have been mixed, Dr. Cryan suggested that negative probiotic studies are more likely due to bacterial strain than a failure of the concept as a whole.
“Most strains of bacteria will do absolutely nothing,” Dr. Cryan said. “Strain is really important.”
In demonstration of this concept, he recounted a 2017 study conducted at University College Cork in which 22 healthy volunteers were given Bifidobacterium longum 1714, and then subjected to a social stress test. The results, published in Translational Psychiatry, showed that the probiotic, compared with placebo, was associated with attenuated stress responses, reduced daily stress, and enhanced visuospatial memory.
In contrast, a similar study by Dr. Cryan and colleagues, which tested Lactobacillus rhamnosus (JB-1), fell short.
“You [could not have gotten] more negative data into one paper if you tried,” Dr. Cryan said, referring to the study. “It did absolutely nothing.”
To find out which psychobiotics may have an impact, and how, Dr. Cryan called for more research.
“It’s still early days,” he said. “We probably have more meta-analyses and systematic reviews of the field than we have primary research papers.
Dr. Cryan concluded his presentation on an optimistic note.
“Neurology is waking up ... to understand that the microbiome could be playing a key role in many, many other disorders. ... Overall, what we’re beginning to see is that our state of gut markedly affects our state of mind.”
Dr. Cryan disclosed relationships with Abbott Nutrition, Roche Pharma, Nutricia, and others.
FROM GMFH 2020