User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
White Spots on the Extremities
The Diagnosis: Hypopigmented Mycosis Fungoides
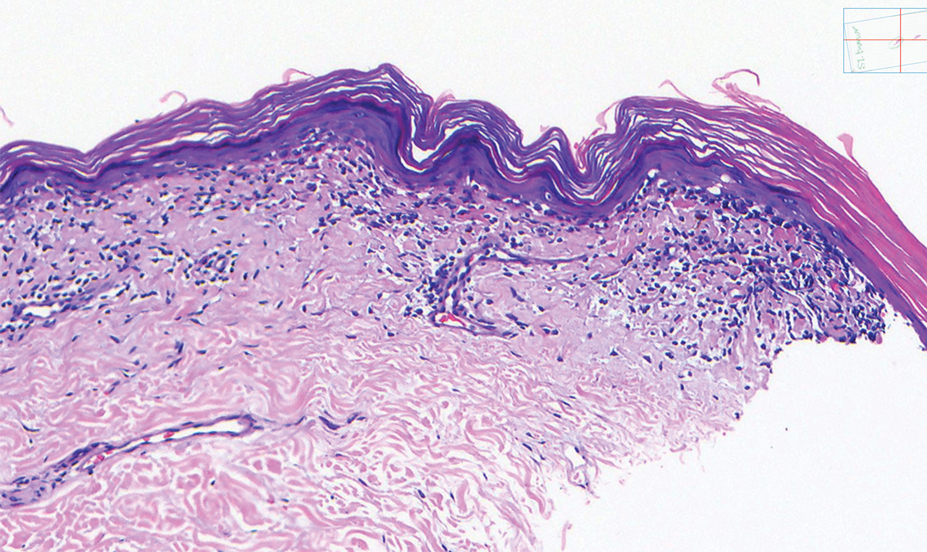
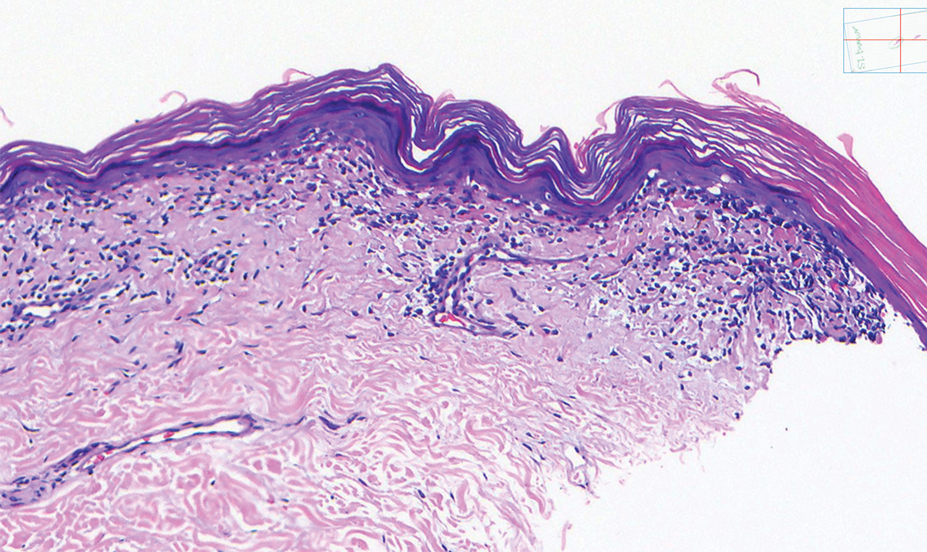
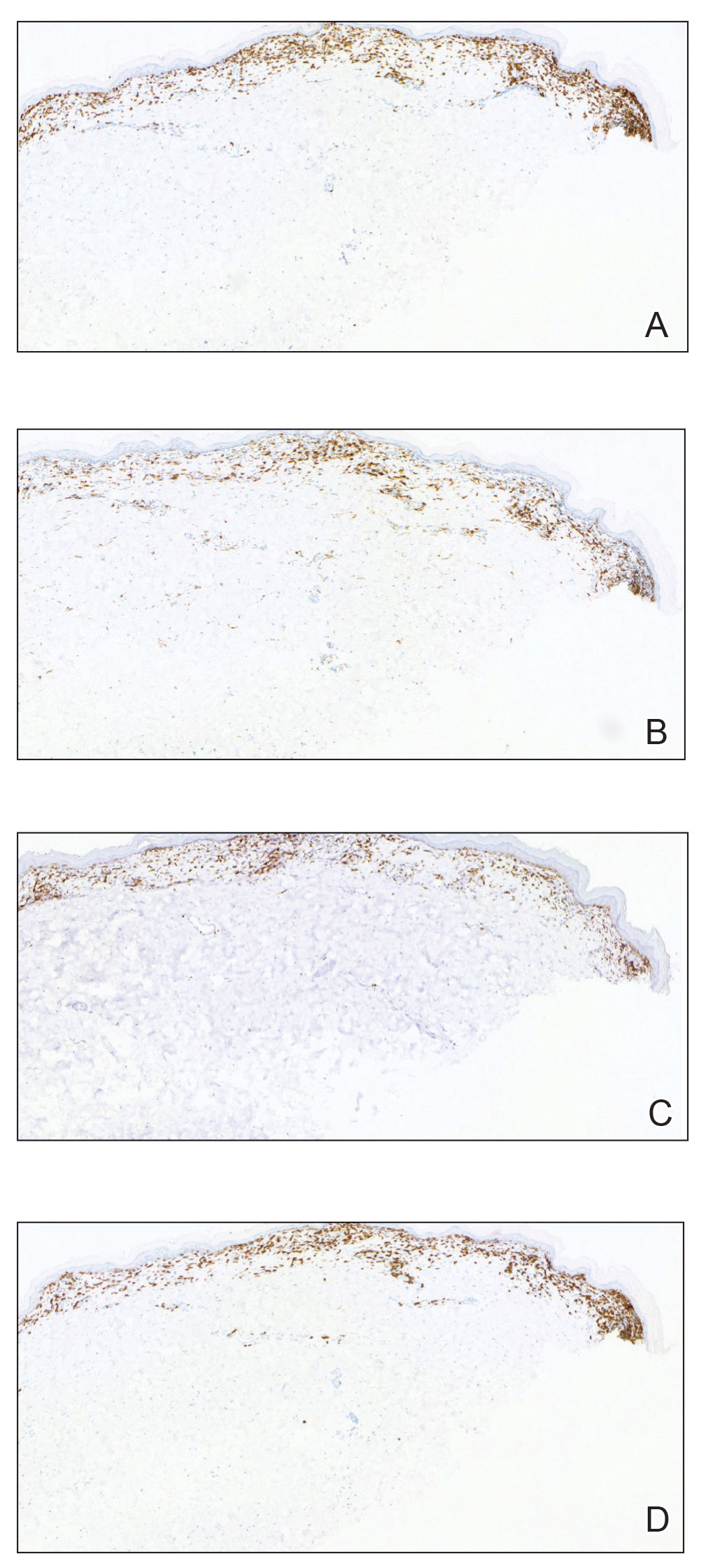
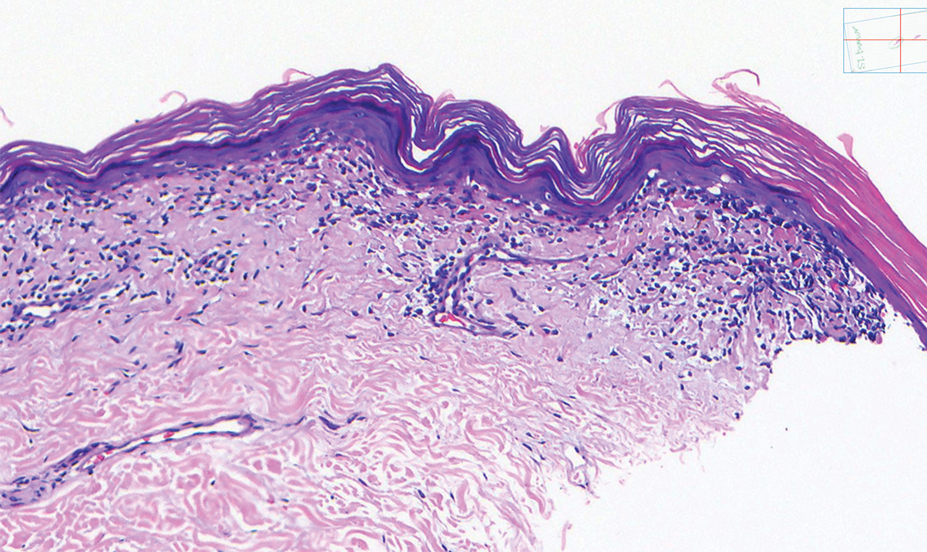
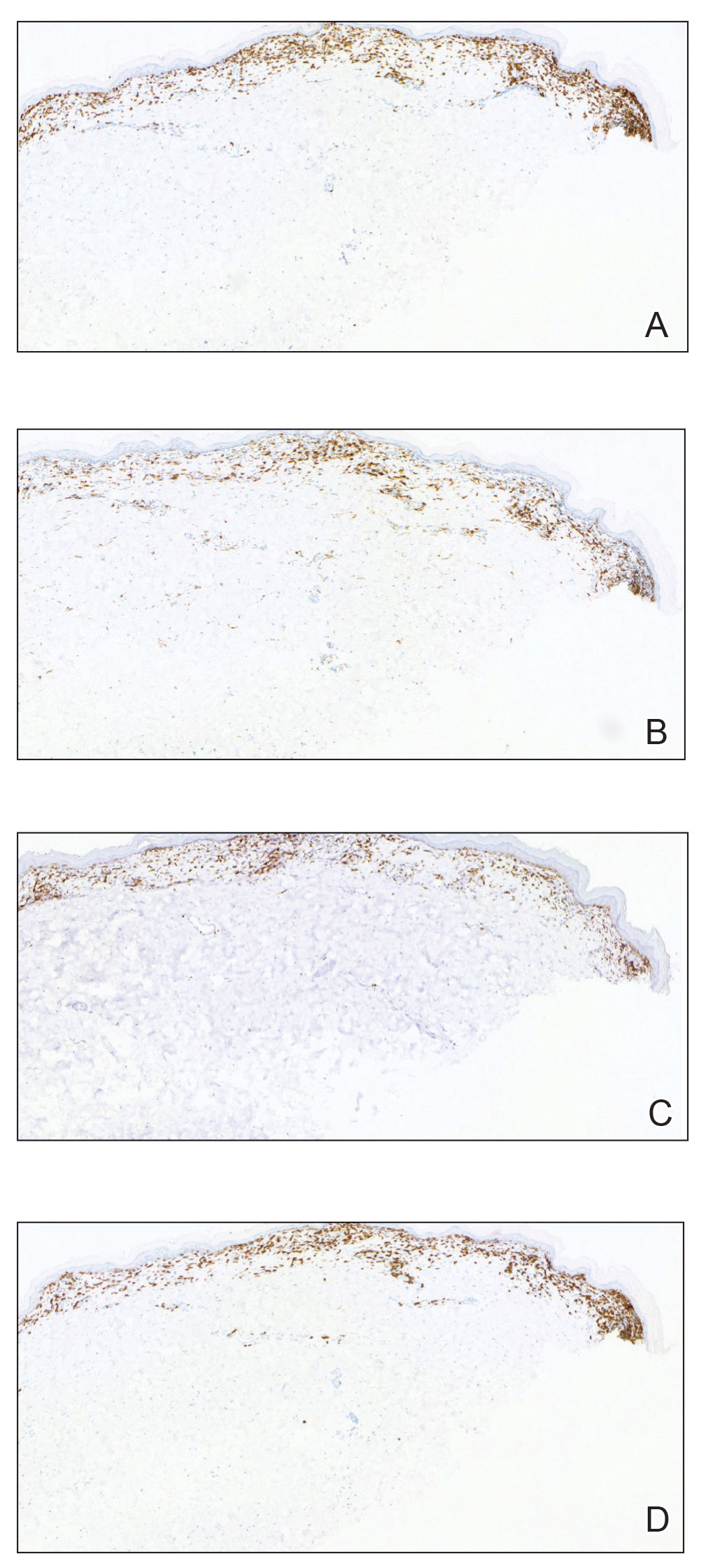
Histopathology showed an atypical lymphoid infiltrate with expanded cytoplasm and hyperchromatic nuclei of irregular contours in the dermoepidermal junction (Figure 1). Immunohistochemical stains of atypical lymphocytes demonstrated the presence of CD3, CD8, and CD5, as well as the absence of CD7 and CD4 lymphocytes (Figure 2). The T-cell γ rearrangement showed polyclonal lymphocytes with 5% tumor cells. The histologic and clinical findings along with our patient’s medical history led to a diagnosis of stage IA (<10% body surface area involvement) hypopigmented mycosis fungoides (hMF).1 Our patient was treated with triamcinolone cream 0.1%; she noted an improvement in her symptoms at 2-month follow-up.
Hypopigmented MF is an uncommon manifestation of MF with unknown prevalence and incidence rates. Mycosis fungoides is considered the most common subtype of cutaneous T-cell lymphoma that classically presents as a chronic, indolent, hypopigmented or depigmented macule or patch, commonly with scaling, in sunprotected areas such as the trunk and proximal arms and legs. It predominantly affects younger adults with darker skin tones and may be present in the pediatric population within the first decade of life.1 Classically, MF affects White patients aged 55 to 60 years. Disease progression is slow, with an incidence rate of 10% of tumor or extracutaneous involvement in the early stages of disease. A lack of specificity on the clinical and histopathologic findings in the initial stage often contributes to the diagnostic delay of hMF. As seen in our patient, this disease can be misdiagnosed as tinea versicolor, postinflammatory hypopigmentation, vitiligo, pityriasis alba, subcutaneous lupus erythematosus, or Hansen disease due to prolonged hypopigmented lesions.2 The clinical findings and histopathologic results including immunohistochemistry confirmed the diagnosis of hMF and ruled out pityriasis alba, postinflammatory hypopigmentation, subcutaneous lupus erythematosus, and vitiligo.
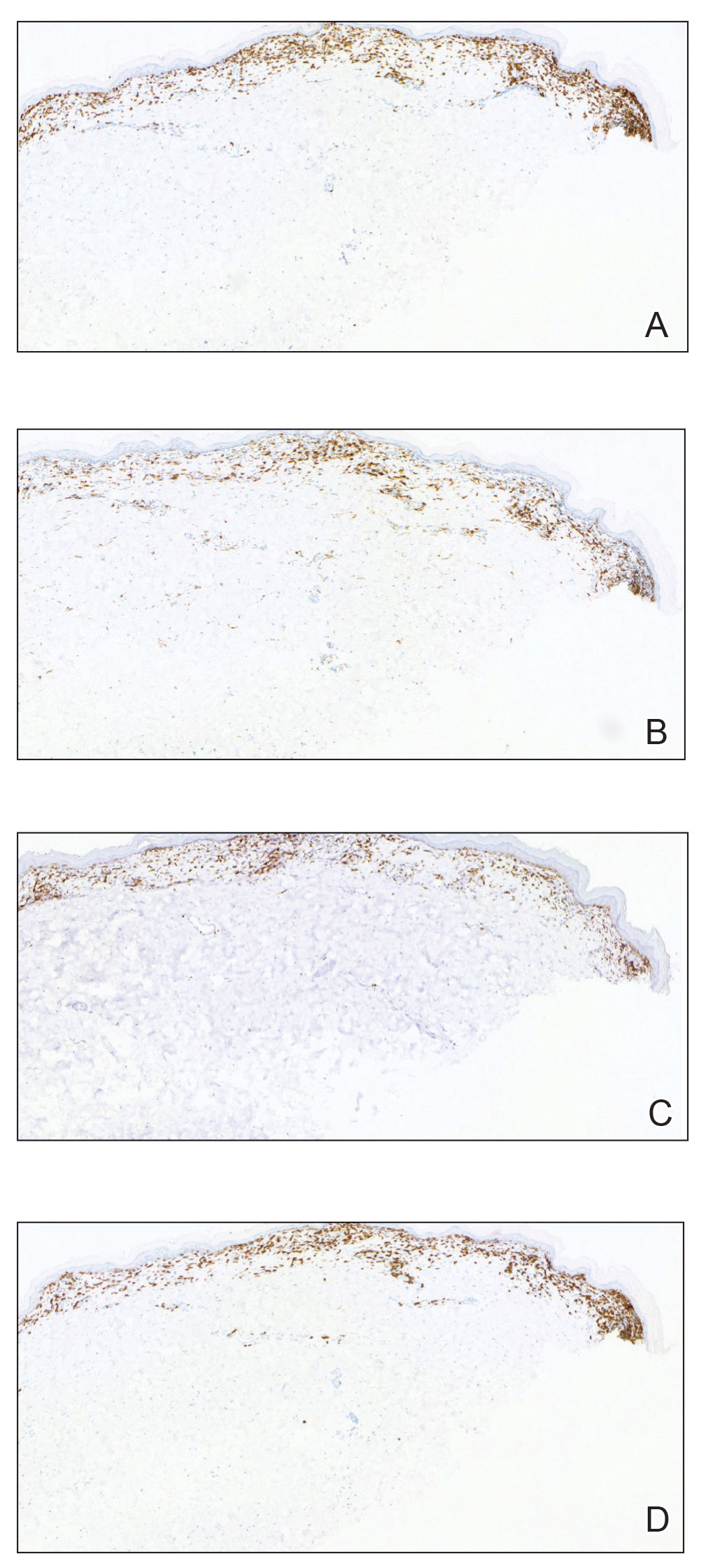
The etiology and pathophysiology of hMF are not fully understood; however, it is hypothesized that melanocyte degeneration, abnormal melanogenesis, and disturbance of melanosome transfer result from the clonal expansion of T helper memory cells. T-cell dyscrasia has been reported to evolve into hMF during etanercept therapy.3 Clinically, hMF presents as hypopigmented papulosquamous, eczematous, or erythrodermic patches, plaques, and tumors with poorly defined atrophied borders. Multiple biopsies of steroid-naive lesions are needed for the diagnosis, as the initial hMF histologic finding cannot be specific for diagnostic confirmation. Common histopathologic findings include a bandlike lymphocytic infiltrate with epidermotropism, intraepidermal nests of atypical cells, or cerebriform nuclei lymphocytes on hematoxylin and eosin staining. In comparison to classical MF epidermotropism, CD4− and CD8+ atypical cells aid in the diagnosis of hMF. Although hMF carries a good prognosis and a benign clinical course,4 full-body computed tomography or positron emission tomography/computed tomography as well as laboratory analysis for lactate dehydrogenase should be pursued if lymphadenopathy, systemic symptoms, or advancedstage hMF are present.
Treatment of hMF depends on the disease stage. Psoralen plus UVA and narrowband UVB can be utilized for the initial stages with a relatively fast response and remission of lesions as early as the first 2 months of treatment. In addition to phototherapy, stage IA to IIA mycosis fungoides with localized skin lesions can benefit from topical steroids, topical retinoids, imiquimod, nitrogen mustard, and carmustine. For advanced stages of mycosis fungoides, combination therapy consisting of psoralen plus UVA with an oral retinoid, interferon alfa, and systemic chemotherapy commonly are prescribed. Maintenance therapy is used for prolonging remission; however, long-term phototherapy is not recommended due to the risk for skin cancer. Unfortunately, hMF requires long-term treatment due to its waxing and waning course, and recurrence may occur after complete resolution.5
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Lambroza E, Cohen SR, Lebwohl M, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- Chuang GS, Wasserman DI, Byers HR, et al. Hypopigmented T-cell dyscrasia evolving to hypopigmented mycosis fungoides during etanercept therapy. J Am Acad Dermatol. 2008;59(5 suppl):S121-S122.
- Agar NS, Wedgeworth E, Crichton S, et al. Survival outcomes and prognostic factors in mycosis fungoides/Sézary syndrome: validation of the revised International Society for Cutaneous Lymphomas/ European Organisation for Research and Treatment of Cancer staging proposal. J Clin Oncol. 2010;28:4730-4739.
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part II. prognosis, management, and future directions. J Am Acad Dermatol. 2014; 70:223.e1-17; quiz 240-242.
The Diagnosis: Hypopigmented Mycosis Fungoides
Histopathology showed an atypical lymphoid infiltrate with expanded cytoplasm and hyperchromatic nuclei of irregular contours in the dermoepidermal junction (Figure 1). Immunohistochemical stains of atypical lymphocytes demonstrated the presence of CD3, CD8, and CD5, as well as the absence of CD7 and CD4 lymphocytes (Figure 2). The T-cell γ rearrangement showed polyclonal lymphocytes with 5% tumor cells. The histologic and clinical findings along with our patient’s medical history led to a diagnosis of stage IA (<10% body surface area involvement) hypopigmented mycosis fungoides (hMF).1 Our patient was treated with triamcinolone cream 0.1%; she noted an improvement in her symptoms at 2-month follow-up.
Hypopigmented MF is an uncommon manifestation of MF with unknown prevalence and incidence rates. Mycosis fungoides is considered the most common subtype of cutaneous T-cell lymphoma that classically presents as a chronic, indolent, hypopigmented or depigmented macule or patch, commonly with scaling, in sunprotected areas such as the trunk and proximal arms and legs. It predominantly affects younger adults with darker skin tones and may be present in the pediatric population within the first decade of life.1 Classically, MF affects White patients aged 55 to 60 years. Disease progression is slow, with an incidence rate of 10% of tumor or extracutaneous involvement in the early stages of disease. A lack of specificity on the clinical and histopathologic findings in the initial stage often contributes to the diagnostic delay of hMF. As seen in our patient, this disease can be misdiagnosed as tinea versicolor, postinflammatory hypopigmentation, vitiligo, pityriasis alba, subcutaneous lupus erythematosus, or Hansen disease due to prolonged hypopigmented lesions.2 The clinical findings and histopathologic results including immunohistochemistry confirmed the diagnosis of hMF and ruled out pityriasis alba, postinflammatory hypopigmentation, subcutaneous lupus erythematosus, and vitiligo.
The etiology and pathophysiology of hMF are not fully understood; however, it is hypothesized that melanocyte degeneration, abnormal melanogenesis, and disturbance of melanosome transfer result from the clonal expansion of T helper memory cells. T-cell dyscrasia has been reported to evolve into hMF during etanercept therapy.3 Clinically, hMF presents as hypopigmented papulosquamous, eczematous, or erythrodermic patches, plaques, and tumors with poorly defined atrophied borders. Multiple biopsies of steroid-naive lesions are needed for the diagnosis, as the initial hMF histologic finding cannot be specific for diagnostic confirmation. Common histopathologic findings include a bandlike lymphocytic infiltrate with epidermotropism, intraepidermal nests of atypical cells, or cerebriform nuclei lymphocytes on hematoxylin and eosin staining. In comparison to classical MF epidermotropism, CD4− and CD8+ atypical cells aid in the diagnosis of hMF. Although hMF carries a good prognosis and a benign clinical course,4 full-body computed tomography or positron emission tomography/computed tomography as well as laboratory analysis for lactate dehydrogenase should be pursued if lymphadenopathy, systemic symptoms, or advancedstage hMF are present.
Treatment of hMF depends on the disease stage. Psoralen plus UVA and narrowband UVB can be utilized for the initial stages with a relatively fast response and remission of lesions as early as the first 2 months of treatment. In addition to phototherapy, stage IA to IIA mycosis fungoides with localized skin lesions can benefit from topical steroids, topical retinoids, imiquimod, nitrogen mustard, and carmustine. For advanced stages of mycosis fungoides, combination therapy consisting of psoralen plus UVA with an oral retinoid, interferon alfa, and systemic chemotherapy commonly are prescribed. Maintenance therapy is used for prolonging remission; however, long-term phototherapy is not recommended due to the risk for skin cancer. Unfortunately, hMF requires long-term treatment due to its waxing and waning course, and recurrence may occur after complete resolution.5
The Diagnosis: Hypopigmented Mycosis Fungoides
Histopathology showed an atypical lymphoid infiltrate with expanded cytoplasm and hyperchromatic nuclei of irregular contours in the dermoepidermal junction (Figure 1). Immunohistochemical stains of atypical lymphocytes demonstrated the presence of CD3, CD8, and CD5, as well as the absence of CD7 and CD4 lymphocytes (Figure 2). The T-cell γ rearrangement showed polyclonal lymphocytes with 5% tumor cells. The histologic and clinical findings along with our patient’s medical history led to a diagnosis of stage IA (<10% body surface area involvement) hypopigmented mycosis fungoides (hMF).1 Our patient was treated with triamcinolone cream 0.1%; she noted an improvement in her symptoms at 2-month follow-up.
Hypopigmented MF is an uncommon manifestation of MF with unknown prevalence and incidence rates. Mycosis fungoides is considered the most common subtype of cutaneous T-cell lymphoma that classically presents as a chronic, indolent, hypopigmented or depigmented macule or patch, commonly with scaling, in sunprotected areas such as the trunk and proximal arms and legs. It predominantly affects younger adults with darker skin tones and may be present in the pediatric population within the first decade of life.1 Classically, MF affects White patients aged 55 to 60 years. Disease progression is slow, with an incidence rate of 10% of tumor or extracutaneous involvement in the early stages of disease. A lack of specificity on the clinical and histopathologic findings in the initial stage often contributes to the diagnostic delay of hMF. As seen in our patient, this disease can be misdiagnosed as tinea versicolor, postinflammatory hypopigmentation, vitiligo, pityriasis alba, subcutaneous lupus erythematosus, or Hansen disease due to prolonged hypopigmented lesions.2 The clinical findings and histopathologic results including immunohistochemistry confirmed the diagnosis of hMF and ruled out pityriasis alba, postinflammatory hypopigmentation, subcutaneous lupus erythematosus, and vitiligo.
The etiology and pathophysiology of hMF are not fully understood; however, it is hypothesized that melanocyte degeneration, abnormal melanogenesis, and disturbance of melanosome transfer result from the clonal expansion of T helper memory cells. T-cell dyscrasia has been reported to evolve into hMF during etanercept therapy.3 Clinically, hMF presents as hypopigmented papulosquamous, eczematous, or erythrodermic patches, plaques, and tumors with poorly defined atrophied borders. Multiple biopsies of steroid-naive lesions are needed for the diagnosis, as the initial hMF histologic finding cannot be specific for diagnostic confirmation. Common histopathologic findings include a bandlike lymphocytic infiltrate with epidermotropism, intraepidermal nests of atypical cells, or cerebriform nuclei lymphocytes on hematoxylin and eosin staining. In comparison to classical MF epidermotropism, CD4− and CD8+ atypical cells aid in the diagnosis of hMF. Although hMF carries a good prognosis and a benign clinical course,4 full-body computed tomography or positron emission tomography/computed tomography as well as laboratory analysis for lactate dehydrogenase should be pursued if lymphadenopathy, systemic symptoms, or advancedstage hMF are present.
Treatment of hMF depends on the disease stage. Psoralen plus UVA and narrowband UVB can be utilized for the initial stages with a relatively fast response and remission of lesions as early as the first 2 months of treatment. In addition to phototherapy, stage IA to IIA mycosis fungoides with localized skin lesions can benefit from topical steroids, topical retinoids, imiquimod, nitrogen mustard, and carmustine. For advanced stages of mycosis fungoides, combination therapy consisting of psoralen plus UVA with an oral retinoid, interferon alfa, and systemic chemotherapy commonly are prescribed. Maintenance therapy is used for prolonging remission; however, long-term phototherapy is not recommended due to the risk for skin cancer. Unfortunately, hMF requires long-term treatment due to its waxing and waning course, and recurrence may occur after complete resolution.5
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Lambroza E, Cohen SR, Lebwohl M, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- Chuang GS, Wasserman DI, Byers HR, et al. Hypopigmented T-cell dyscrasia evolving to hypopigmented mycosis fungoides during etanercept therapy. J Am Acad Dermatol. 2008;59(5 suppl):S121-S122.
- Agar NS, Wedgeworth E, Crichton S, et al. Survival outcomes and prognostic factors in mycosis fungoides/Sézary syndrome: validation of the revised International Society for Cutaneous Lymphomas/ European Organisation for Research and Treatment of Cancer staging proposal. J Clin Oncol. 2010;28:4730-4739.
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part II. prognosis, management, and future directions. J Am Acad Dermatol. 2014; 70:223.e1-17; quiz 240-242.
- Furlan FC, Sanches JA. Hypopigmented mycosis fungoides: a review of its clinical features and pathophysiology. An Bras Dermatol. 2013;88:954-960.
- Lambroza E, Cohen SR, Lebwohl M, et al. Hypopigmented variant of mycosis fungoides: demography, histopathology, and treatment of seven cases. J Am Acad Dermatol. 1995;32:987-993.
- Chuang GS, Wasserman DI, Byers HR, et al. Hypopigmented T-cell dyscrasia evolving to hypopigmented mycosis fungoides during etanercept therapy. J Am Acad Dermatol. 2008;59(5 suppl):S121-S122.
- Agar NS, Wedgeworth E, Crichton S, et al. Survival outcomes and prognostic factors in mycosis fungoides/Sézary syndrome: validation of the revised International Society for Cutaneous Lymphomas/ European Organisation for Research and Treatment of Cancer staging proposal. J Clin Oncol. 2010;28:4730-4739.
- Jawed SI, Myskowski PL, Horwitz S, et al. Primary cutaneous T-cell lymphoma (mycosis fungoides and Sézary syndrome): part II. prognosis, management, and future directions. J Am Acad Dermatol. 2014; 70:223.e1-17; quiz 240-242.
A 52-year-old Black woman presented with self-described whitened spots on the arms and legs of 2 years’ duration. She experienced no improvement with ketoconazole cream and topical calcineurin inhibitors prescribed during a prior dermatology visit at an outside institution. She denied pain or pruritus. A review of systems as well as the patient’s medical history were noncontributory. A prior biopsy at an outside institution revealed an interface dermatitis suggestive of cutaneous lupus erythematosus. The patient noted social drinking and denied tobacco use. She had no known allergies to medications and currently was on tamoxifen for breast cancer following a right mastectomy. Physical examination showed hypopigmented macules and patches on the left upper arm and right proximal leg. The center of the lesions was not erythematous or scaly. Palpation did not reveal enlarged lymph nodes, and laboratory analyses ruled out low levels of red blood cells, white blood cells, or platelets. Punch biopsies from the left arm and right thigh were performed.

New law allows international medical graduates to bypass U.S. residency
Pediatric nephrologist Bryan Carmody, MD, recalls working alongside an extremely experienced neonatologist during his residency. She had managed a neonatal intensive care unit in her home country of Lithuania, but because she wanted to practice in the United States, it took years of repeat training before she was eligible for a medical license.
“She was very accomplished, and she was wonderful to have as a coresident at the time,” Dr. Carmody said in an interview.
The neonatologist now practices at a U.S. academic medical center, but to obtain that position, she had to complete 3 years of pediatric residency and 3 years of fellowship in the United States, Dr. Carmody said.
Such training for international medical graduates (IMGs) is a routine part of obtaining a U.S. medical license, but
The American Medical Association took similar measures at its recent annual meeting, making it easier for IMGs to gain licensure. Because the pandemic and Russia’s invasion of Ukraine disrupted the process by which some IMGs had their licenses verified, the AMA is now encouraging state licensing boards and other credentialing institutions to accept certification from the Educational Commission for Foreign Medical Graduates as verification, rather than requiring documents directly from international medical schools.
When it comes to Tennessee’s new law, signed by Gov. Bill Lee in April, experienced IMGs who have received medical training abroad can skip U.S. residency requirements and obtain a temporary license to practice medicine in Tennessee if they meet certain qualifications.
The international doctors must demonstrate competency, as determined by the state medical board. In addition, they must have completed a 3-year postgraduate training program in the graduate’s licensing country or otherwise have practiced as a medical professional in which they performed the duties of a physician for at least 3 of the past 5 years outside the United States, according to the new law.
To be approved, IMGs must also have received an employment offer from a Tennessee health care provider that has a residency program accredited by the Accreditation Council for Graduate Medical Education.
If physicians remain in good standing for 2 years, the board will grant them a full and unrestricted license to practice in Tennessee.
“The new legislation opens up a lot of doors for international medical graduates and is also a lifeline for a lot of underserved areas in Tennessee,” said Asim Ansari, MD, a Canadian who attended medical school in the Caribbean and is an advocate for IMGs.
Dr. Ansari is participating in a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City, until he can apply for the sixth time to a residency program. “This could possibly be a model that other states may want to implement in a few years.”
What’s behind the law?
A predicted physician shortage in Tennessee drove the legislation, said Rep. Sabi “Doc” Kumar, MD, vice chair for the Tennessee House Health Committee and a cosponsor of the legislation. Legislators hope the law will mitigate that shortage and boost the number of physicians practicing in underserved areas of the state.
“Considering that one in four physicians in the U.S. are international medical gradates, it was important for us to be able to attract those physicians to Tennessee,” he said.
The Tennessee Board of Medical Examiners will develop administrative rules for the law, which may take up to a year, Rep. Kumar said. He expects the program to be available to IMGs beginning in mid-2024.
Upon completion of the program, IMGs will be able to practice general medicine in Tennessee, not a specialty. Requirements for specialty certification would have to be met through the specialties’ respective boards.
Dr. Carmody, who blogs about medical education, including the new legislation, said in an interview the law will greatly benefit experienced IMGs, who often are bypassed as residency candidates because they graduated years ago. Hospitals also win because they can fill positions that otherwise might sit vacant, he said.
Family physician Sahil Bawa, MD, an IMG from India who recently matched into his specialty, said the Tennessee legislation will help fellow IMGs find U.S. medical jobs.
“It’s very difficult for IMGs to get into residency in the U.S.,” he said. “I’ve seen people with medical degrees from other countries drive Uber or do odd jobs to sustain themselves here. I’ve known a few people who have left and gone back to their home country because they were not accepted into a residency.”
Who benefits most?
Dr. Bawa noted that the legislation would not have helped him, as he needed a visa to practice in the United States and the law does not include the sponsoring of visas. The legislation requires IMGs to show evidence of citizenship or evidence that they are legally entitled to live or work in the United States.
U.S. citizen IMGs who haven’t completed residency or who practiced in another country also are left out of the law, Dr. Carmody said.
“This law is designed to take the most accomplished cream of the crop international medical graduates with the most experience and the most sophisticated skill set and send them to Tennessee. I think that’s the intent,” he said. “But many international medical graduates are U.S. citizens who don’t have the opportunity to practice in countries other than United States or do residencies. A lot of these people are sitting on the sidelines, unable to secure residency positions. I’m sure they would be desperate for a program like this.”
Questions remain
“Just because the doctor can get a [temporary] license without the training doesn’t mean employers are going to be interested in sponsoring those doctors,” said Adam Cohen, an immigration attorney who practices in Memphis. “What is the inclination of these employers to hire these physicians who have undergone training outside the U.S.? And will there be skepticism on the part of employers about the competence of these doctors?”
“Hospital systems will be able to hire experienced practitioners for a very low cost,” Dr. Ansari said. “So now you have these additional bodies who can do the work of a physician, but you don’t have to pay them as much as a physician for 2 years. And because some are desperate to work, they will take lower pay as long as they have a pathway to full licensure in Tennessee. What are the protections for these physicians? Who will cover their insurance? Who will be responsible for them, the attendees? And will the attendees be willing to put their license on the line for them?”
In addition, Dr. Carmody questions what, if anything, will encourage IMGs to work in underserved areas in Tennessee after their 2 years are up and whether there will be any incentives to guide them. He wonders, too, whether the physicians will be stuck practicing in Tennessee following completion of the program.
“Will these physicians only be able to work in Tennessee?” he asked. “I think that’s probably going to be the case, because they’ll be licensed in Tennessee, but to go to another state, they would be missing the required residency training. So it might be these folks are stuck in Tennessee unless other states develop reciprocal arrangements.”
Other states would have to decide whether to recognize the Tennessee license acquired through this pathway, Rep. Kumar said.
He explained that the sponsoring sites would be responsible for providing work-hour restrictions and liability protections. There are currently no incentives in the legislation for IMGs to practice in rural, underserved areas, but the hospitals and communities there generally offer incentives when recruiting, Rep. Kumar said.
“The law definitely has the potential to be helpful,” Mr. Cohen said, “because there’s an ability to place providers in the state without having to go through the bottleneck of limited residency slots. If other states see a positive effect on Tennessee or are exploring ways to alleviate their own shortages, it’s possible [they] might follow suit.”
Rep. Kumar agreed that other states will be watching Tennessee to weigh the law’s success.
“I think the law will have to prove itself and show that Tennessee has benefited from it and that the results have been good,” he said. “We are providing a pioneering way for attracting medical graduates and making it easier for them to obtain a license. I would think other states would want to do that.”
A version of this article first appeared on Medscape.com.
Pediatric nephrologist Bryan Carmody, MD, recalls working alongside an extremely experienced neonatologist during his residency. She had managed a neonatal intensive care unit in her home country of Lithuania, but because she wanted to practice in the United States, it took years of repeat training before she was eligible for a medical license.
“She was very accomplished, and she was wonderful to have as a coresident at the time,” Dr. Carmody said in an interview.
The neonatologist now practices at a U.S. academic medical center, but to obtain that position, she had to complete 3 years of pediatric residency and 3 years of fellowship in the United States, Dr. Carmody said.
Such training for international medical graduates (IMGs) is a routine part of obtaining a U.S. medical license, but
The American Medical Association took similar measures at its recent annual meeting, making it easier for IMGs to gain licensure. Because the pandemic and Russia’s invasion of Ukraine disrupted the process by which some IMGs had their licenses verified, the AMA is now encouraging state licensing boards and other credentialing institutions to accept certification from the Educational Commission for Foreign Medical Graduates as verification, rather than requiring documents directly from international medical schools.
When it comes to Tennessee’s new law, signed by Gov. Bill Lee in April, experienced IMGs who have received medical training abroad can skip U.S. residency requirements and obtain a temporary license to practice medicine in Tennessee if they meet certain qualifications.
The international doctors must demonstrate competency, as determined by the state medical board. In addition, they must have completed a 3-year postgraduate training program in the graduate’s licensing country or otherwise have practiced as a medical professional in which they performed the duties of a physician for at least 3 of the past 5 years outside the United States, according to the new law.
To be approved, IMGs must also have received an employment offer from a Tennessee health care provider that has a residency program accredited by the Accreditation Council for Graduate Medical Education.
If physicians remain in good standing for 2 years, the board will grant them a full and unrestricted license to practice in Tennessee.
“The new legislation opens up a lot of doors for international medical graduates and is also a lifeline for a lot of underserved areas in Tennessee,” said Asim Ansari, MD, a Canadian who attended medical school in the Caribbean and is an advocate for IMGs.
Dr. Ansari is participating in a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City, until he can apply for the sixth time to a residency program. “This could possibly be a model that other states may want to implement in a few years.”
What’s behind the law?
A predicted physician shortage in Tennessee drove the legislation, said Rep. Sabi “Doc” Kumar, MD, vice chair for the Tennessee House Health Committee and a cosponsor of the legislation. Legislators hope the law will mitigate that shortage and boost the number of physicians practicing in underserved areas of the state.
“Considering that one in four physicians in the U.S. are international medical gradates, it was important for us to be able to attract those physicians to Tennessee,” he said.
The Tennessee Board of Medical Examiners will develop administrative rules for the law, which may take up to a year, Rep. Kumar said. He expects the program to be available to IMGs beginning in mid-2024.
Upon completion of the program, IMGs will be able to practice general medicine in Tennessee, not a specialty. Requirements for specialty certification would have to be met through the specialties’ respective boards.
Dr. Carmody, who blogs about medical education, including the new legislation, said in an interview the law will greatly benefit experienced IMGs, who often are bypassed as residency candidates because they graduated years ago. Hospitals also win because they can fill positions that otherwise might sit vacant, he said.
Family physician Sahil Bawa, MD, an IMG from India who recently matched into his specialty, said the Tennessee legislation will help fellow IMGs find U.S. medical jobs.
“It’s very difficult for IMGs to get into residency in the U.S.,” he said. “I’ve seen people with medical degrees from other countries drive Uber or do odd jobs to sustain themselves here. I’ve known a few people who have left and gone back to their home country because they were not accepted into a residency.”
Who benefits most?
Dr. Bawa noted that the legislation would not have helped him, as he needed a visa to practice in the United States and the law does not include the sponsoring of visas. The legislation requires IMGs to show evidence of citizenship or evidence that they are legally entitled to live or work in the United States.
U.S. citizen IMGs who haven’t completed residency or who practiced in another country also are left out of the law, Dr. Carmody said.
“This law is designed to take the most accomplished cream of the crop international medical graduates with the most experience and the most sophisticated skill set and send them to Tennessee. I think that’s the intent,” he said. “But many international medical graduates are U.S. citizens who don’t have the opportunity to practice in countries other than United States or do residencies. A lot of these people are sitting on the sidelines, unable to secure residency positions. I’m sure they would be desperate for a program like this.”
Questions remain
“Just because the doctor can get a [temporary] license without the training doesn’t mean employers are going to be interested in sponsoring those doctors,” said Adam Cohen, an immigration attorney who practices in Memphis. “What is the inclination of these employers to hire these physicians who have undergone training outside the U.S.? And will there be skepticism on the part of employers about the competence of these doctors?”
“Hospital systems will be able to hire experienced practitioners for a very low cost,” Dr. Ansari said. “So now you have these additional bodies who can do the work of a physician, but you don’t have to pay them as much as a physician for 2 years. And because some are desperate to work, they will take lower pay as long as they have a pathway to full licensure in Tennessee. What are the protections for these physicians? Who will cover their insurance? Who will be responsible for them, the attendees? And will the attendees be willing to put their license on the line for them?”
In addition, Dr. Carmody questions what, if anything, will encourage IMGs to work in underserved areas in Tennessee after their 2 years are up and whether there will be any incentives to guide them. He wonders, too, whether the physicians will be stuck practicing in Tennessee following completion of the program.
“Will these physicians only be able to work in Tennessee?” he asked. “I think that’s probably going to be the case, because they’ll be licensed in Tennessee, but to go to another state, they would be missing the required residency training. So it might be these folks are stuck in Tennessee unless other states develop reciprocal arrangements.”
Other states would have to decide whether to recognize the Tennessee license acquired through this pathway, Rep. Kumar said.
He explained that the sponsoring sites would be responsible for providing work-hour restrictions and liability protections. There are currently no incentives in the legislation for IMGs to practice in rural, underserved areas, but the hospitals and communities there generally offer incentives when recruiting, Rep. Kumar said.
“The law definitely has the potential to be helpful,” Mr. Cohen said, “because there’s an ability to place providers in the state without having to go through the bottleneck of limited residency slots. If other states see a positive effect on Tennessee or are exploring ways to alleviate their own shortages, it’s possible [they] might follow suit.”
Rep. Kumar agreed that other states will be watching Tennessee to weigh the law’s success.
“I think the law will have to prove itself and show that Tennessee has benefited from it and that the results have been good,” he said. “We are providing a pioneering way for attracting medical graduates and making it easier for them to obtain a license. I would think other states would want to do that.”
A version of this article first appeared on Medscape.com.
Pediatric nephrologist Bryan Carmody, MD, recalls working alongside an extremely experienced neonatologist during his residency. She had managed a neonatal intensive care unit in her home country of Lithuania, but because she wanted to practice in the United States, it took years of repeat training before she was eligible for a medical license.
“She was very accomplished, and she was wonderful to have as a coresident at the time,” Dr. Carmody said in an interview.
The neonatologist now practices at a U.S. academic medical center, but to obtain that position, she had to complete 3 years of pediatric residency and 3 years of fellowship in the United States, Dr. Carmody said.
Such training for international medical graduates (IMGs) is a routine part of obtaining a U.S. medical license, but
The American Medical Association took similar measures at its recent annual meeting, making it easier for IMGs to gain licensure. Because the pandemic and Russia’s invasion of Ukraine disrupted the process by which some IMGs had their licenses verified, the AMA is now encouraging state licensing boards and other credentialing institutions to accept certification from the Educational Commission for Foreign Medical Graduates as verification, rather than requiring documents directly from international medical schools.
When it comes to Tennessee’s new law, signed by Gov. Bill Lee in April, experienced IMGs who have received medical training abroad can skip U.S. residency requirements and obtain a temporary license to practice medicine in Tennessee if they meet certain qualifications.
The international doctors must demonstrate competency, as determined by the state medical board. In addition, they must have completed a 3-year postgraduate training program in the graduate’s licensing country or otherwise have practiced as a medical professional in which they performed the duties of a physician for at least 3 of the past 5 years outside the United States, according to the new law.
To be approved, IMGs must also have received an employment offer from a Tennessee health care provider that has a residency program accredited by the Accreditation Council for Graduate Medical Education.
If physicians remain in good standing for 2 years, the board will grant them a full and unrestricted license to practice in Tennessee.
“The new legislation opens up a lot of doors for international medical graduates and is also a lifeline for a lot of underserved areas in Tennessee,” said Asim Ansari, MD, a Canadian who attended medical school in the Caribbean and is an advocate for IMGs.
Dr. Ansari is participating in a child and adolescent psychiatry fellowship at the University of Kansas Medical Center, Kansas City, until he can apply for the sixth time to a residency program. “This could possibly be a model that other states may want to implement in a few years.”
What’s behind the law?
A predicted physician shortage in Tennessee drove the legislation, said Rep. Sabi “Doc” Kumar, MD, vice chair for the Tennessee House Health Committee and a cosponsor of the legislation. Legislators hope the law will mitigate that shortage and boost the number of physicians practicing in underserved areas of the state.
“Considering that one in four physicians in the U.S. are international medical gradates, it was important for us to be able to attract those physicians to Tennessee,” he said.
The Tennessee Board of Medical Examiners will develop administrative rules for the law, which may take up to a year, Rep. Kumar said. He expects the program to be available to IMGs beginning in mid-2024.
Upon completion of the program, IMGs will be able to practice general medicine in Tennessee, not a specialty. Requirements for specialty certification would have to be met through the specialties’ respective boards.
Dr. Carmody, who blogs about medical education, including the new legislation, said in an interview the law will greatly benefit experienced IMGs, who often are bypassed as residency candidates because they graduated years ago. Hospitals also win because they can fill positions that otherwise might sit vacant, he said.
Family physician Sahil Bawa, MD, an IMG from India who recently matched into his specialty, said the Tennessee legislation will help fellow IMGs find U.S. medical jobs.
“It’s very difficult for IMGs to get into residency in the U.S.,” he said. “I’ve seen people with medical degrees from other countries drive Uber or do odd jobs to sustain themselves here. I’ve known a few people who have left and gone back to their home country because they were not accepted into a residency.”
Who benefits most?
Dr. Bawa noted that the legislation would not have helped him, as he needed a visa to practice in the United States and the law does not include the sponsoring of visas. The legislation requires IMGs to show evidence of citizenship or evidence that they are legally entitled to live or work in the United States.
U.S. citizen IMGs who haven’t completed residency or who practiced in another country also are left out of the law, Dr. Carmody said.
“This law is designed to take the most accomplished cream of the crop international medical graduates with the most experience and the most sophisticated skill set and send them to Tennessee. I think that’s the intent,” he said. “But many international medical graduates are U.S. citizens who don’t have the opportunity to practice in countries other than United States or do residencies. A lot of these people are sitting on the sidelines, unable to secure residency positions. I’m sure they would be desperate for a program like this.”
Questions remain
“Just because the doctor can get a [temporary] license without the training doesn’t mean employers are going to be interested in sponsoring those doctors,” said Adam Cohen, an immigration attorney who practices in Memphis. “What is the inclination of these employers to hire these physicians who have undergone training outside the U.S.? And will there be skepticism on the part of employers about the competence of these doctors?”
“Hospital systems will be able to hire experienced practitioners for a very low cost,” Dr. Ansari said. “So now you have these additional bodies who can do the work of a physician, but you don’t have to pay them as much as a physician for 2 years. And because some are desperate to work, they will take lower pay as long as they have a pathway to full licensure in Tennessee. What are the protections for these physicians? Who will cover their insurance? Who will be responsible for them, the attendees? And will the attendees be willing to put their license on the line for them?”
In addition, Dr. Carmody questions what, if anything, will encourage IMGs to work in underserved areas in Tennessee after their 2 years are up and whether there will be any incentives to guide them. He wonders, too, whether the physicians will be stuck practicing in Tennessee following completion of the program.
“Will these physicians only be able to work in Tennessee?” he asked. “I think that’s probably going to be the case, because they’ll be licensed in Tennessee, but to go to another state, they would be missing the required residency training. So it might be these folks are stuck in Tennessee unless other states develop reciprocal arrangements.”
Other states would have to decide whether to recognize the Tennessee license acquired through this pathway, Rep. Kumar said.
He explained that the sponsoring sites would be responsible for providing work-hour restrictions and liability protections. There are currently no incentives in the legislation for IMGs to practice in rural, underserved areas, but the hospitals and communities there generally offer incentives when recruiting, Rep. Kumar said.
“The law definitely has the potential to be helpful,” Mr. Cohen said, “because there’s an ability to place providers in the state without having to go through the bottleneck of limited residency slots. If other states see a positive effect on Tennessee or are exploring ways to alleviate their own shortages, it’s possible [they] might follow suit.”
Rep. Kumar agreed that other states will be watching Tennessee to weigh the law’s success.
“I think the law will have to prove itself and show that Tennessee has benefited from it and that the results have been good,” he said. “We are providing a pioneering way for attracting medical graduates and making it easier for them to obtain a license. I would think other states would want to do that.”
A version of this article first appeared on Medscape.com.
Imaging techniques will revolutionize cancer detection, expert predicts
PHOENIX –
In a lecture during a multispecialty roundup of cutting-edge energy-based device applications at the annual conference of the American Society for Laser Medicine and Surgery, Dr. Barton, a biomedical engineer who directs the BIO5 Institute at the University of Arizona, Tucson, said that while no current modality exists to enable physicians in dermatology and other specialties to view internal structures throughout the entire body with cellular resolution, refining existing technologies is a good way to start.
In 2011, renowned cancer researchers Douglas Hanahan, PhD, and Robert A. Weinberg, PhD, proposed six hallmarks of cancer, which include sustaining proliferative signaling, evading growth suppressors, resisting cell death, enabling replicative immortality, inducing angiogenesis, and activating invasion and metastasis. Each hallmark poses unique imaging challenges. For example, enabling replicative immortality “means that the cell nuclei change size and shape; they change their position,” said Dr. Barton, who is also professor of biomedical engineering and optical sciences at the university. “If we want to see that, we’re going to need an imaging modality that’s subcellular in resolution.”
Similarly, if clinicians want to view how proliferative signaling is changing, “that means being able to visualize the cell surface receptors; those are even smaller to actually visualize,” she said. “But we have technologies where we can target those receptors with fluorophores. And then we can look at large areas very quickly.” Meanwhile, the ability of cancer cells to resist cell death and evade growth suppressors often results in thickening of epithelium throughout the body. “So, if we can measure the thickness of the epithelium, we can see that there’s something wrong with that tissue,” she said.
As for cancer’s propensity for invasion and metastasis, “here, we’re looking at how the collagen structure [between the cells] has changed and whether there’s layer breakdown or not. Optical imaging can detect cancer. However, high resolution optical techniques can only image about 1 mm deep, so unless you’re looking at the skin or the eye, you’re going to have to develop an endoscope to be able to view these hallmarks.”
OCT images the tissue microstructure, generally in a resolution of 2-20 microns, at a depth of 1-2 mm, and it measures reflected light. When possible, Dr. Barton combines OCT with laser-induced fluorescence for enhanced accuracy of detection of cancer. Induced fluorescence senses molecular information with the natural fluorophores in the body or with targeted exogenous agents. Then there’s multiphoton microscopy, an advanced imaging technique that enables clinicians to view cellular and subcellular events within living tissue. Early models of this technology “took up entire benches” in physics labs, Dr. Barton said, but she and other investigators are designing smaller devices for use in clinics. “This is exciting, because not only do we [view] subcellular structure with this modality, but it can also be highly sensitive to collagen structure,” she said.
Ovarian cancer model
In a model of ovarian cancer, she and colleagues externalized the ovaries of a mouse, imaged the organs, put them back in, and reassessed them at 8 weeks. “This model develops cancer very quickly,” said Dr. Barton, who once worked for McDonnell Douglas on the Space Station program. At 8 weeks, using fluorescence and targeted agents with a tabletop multiphoton microscopy system, they observed that the proliferation signals of cancer had begun. “So, with an agent targeted to the folate receptor or to other receptors that are implicated in cancer development, we can see that ovaries and fallopian tubes are lighting up,” she said.
With proof of concept established with the mouse study, she and other researchers are drawing from technological advances to create tiny laser systems for use in the clinic to image a variety of structures in the human body. Optics advances include bulk optics and all-fiber designs where engineers can create an imaging probe that’s only 125 microns in diameter, “or maybe even as small as 70 microns in diameter,” she said. “We can do fabrications on the tips of endoscopes to redirect the light and focus it. We can also do 3-D printing and spiral scanning to create miniature devices to make new advances. That means that instead of just white light imaging of the colon or the lung like we have had in the past, we can start moving into smaller structures, such as the eustachian tube, the fallopian tube, the bile ducts, or making miniature devices for brain biopsies, lung biopsies, and maybe being able to get into bronchioles and arterioles.”
According to Dr. Barton, prior research has demonstrated that cerebral vasculature can be imaged with a catheter 400 microns in diameter, the spaces in the lungs can be imaged with a needle that is 310 microns in diameter, and the inner structures of the eustachian tube can be viewed with an endoscope 1 mm in diameter.
She and her colleagues are developing an OCT/fluorescence imaging falloposcope that is 0.8 mm in diameter, flexible, and steerable, as a tool for early detection of ovarian cancer in humans. “It’s now known that most ovarian cancer starts in the fallopian tubes,” Dr. Barton said. “It’s metastatic disease when those cells break off from the fallopian tubes and go to the ovaries. We wanted to create an imaging system where we created a fiber bundle that we could navigate with white light and with fluorescence so that we can see these early stages of cancer [and] how they fluoresce differently. We also wanted to have an OCT system so that we could image through the wall of the fallopian tube and look for that layer thickening and other precursors to ovarian cancer.”
To date, in vivo testing in healthy women has demonstrated that the miniature endoscope is able to reach the fallopian tubes through the natural orifice of the vagina and uterus. “That is pretty exciting,” she said. “The images may not be of the highest quality, but we are advancing.”
Dr. Barton reported having no relevant financial disclosures.
PHOENIX –
In a lecture during a multispecialty roundup of cutting-edge energy-based device applications at the annual conference of the American Society for Laser Medicine and Surgery, Dr. Barton, a biomedical engineer who directs the BIO5 Institute at the University of Arizona, Tucson, said that while no current modality exists to enable physicians in dermatology and other specialties to view internal structures throughout the entire body with cellular resolution, refining existing technologies is a good way to start.
In 2011, renowned cancer researchers Douglas Hanahan, PhD, and Robert A. Weinberg, PhD, proposed six hallmarks of cancer, which include sustaining proliferative signaling, evading growth suppressors, resisting cell death, enabling replicative immortality, inducing angiogenesis, and activating invasion and metastasis. Each hallmark poses unique imaging challenges. For example, enabling replicative immortality “means that the cell nuclei change size and shape; they change their position,” said Dr. Barton, who is also professor of biomedical engineering and optical sciences at the university. “If we want to see that, we’re going to need an imaging modality that’s subcellular in resolution.”
Similarly, if clinicians want to view how proliferative signaling is changing, “that means being able to visualize the cell surface receptors; those are even smaller to actually visualize,” she said. “But we have technologies where we can target those receptors with fluorophores. And then we can look at large areas very quickly.” Meanwhile, the ability of cancer cells to resist cell death and evade growth suppressors often results in thickening of epithelium throughout the body. “So, if we can measure the thickness of the epithelium, we can see that there’s something wrong with that tissue,” she said.
As for cancer’s propensity for invasion and metastasis, “here, we’re looking at how the collagen structure [between the cells] has changed and whether there’s layer breakdown or not. Optical imaging can detect cancer. However, high resolution optical techniques can only image about 1 mm deep, so unless you’re looking at the skin or the eye, you’re going to have to develop an endoscope to be able to view these hallmarks.”
OCT images the tissue microstructure, generally in a resolution of 2-20 microns, at a depth of 1-2 mm, and it measures reflected light. When possible, Dr. Barton combines OCT with laser-induced fluorescence for enhanced accuracy of detection of cancer. Induced fluorescence senses molecular information with the natural fluorophores in the body or with targeted exogenous agents. Then there’s multiphoton microscopy, an advanced imaging technique that enables clinicians to view cellular and subcellular events within living tissue. Early models of this technology “took up entire benches” in physics labs, Dr. Barton said, but she and other investigators are designing smaller devices for use in clinics. “This is exciting, because not only do we [view] subcellular structure with this modality, but it can also be highly sensitive to collagen structure,” she said.
Ovarian cancer model
In a model of ovarian cancer, she and colleagues externalized the ovaries of a mouse, imaged the organs, put them back in, and reassessed them at 8 weeks. “This model develops cancer very quickly,” said Dr. Barton, who once worked for McDonnell Douglas on the Space Station program. At 8 weeks, using fluorescence and targeted agents with a tabletop multiphoton microscopy system, they observed that the proliferation signals of cancer had begun. “So, with an agent targeted to the folate receptor or to other receptors that are implicated in cancer development, we can see that ovaries and fallopian tubes are lighting up,” she said.
With proof of concept established with the mouse study, she and other researchers are drawing from technological advances to create tiny laser systems for use in the clinic to image a variety of structures in the human body. Optics advances include bulk optics and all-fiber designs where engineers can create an imaging probe that’s only 125 microns in diameter, “or maybe even as small as 70 microns in diameter,” she said. “We can do fabrications on the tips of endoscopes to redirect the light and focus it. We can also do 3-D printing and spiral scanning to create miniature devices to make new advances. That means that instead of just white light imaging of the colon or the lung like we have had in the past, we can start moving into smaller structures, such as the eustachian tube, the fallopian tube, the bile ducts, or making miniature devices for brain biopsies, lung biopsies, and maybe being able to get into bronchioles and arterioles.”
According to Dr. Barton, prior research has demonstrated that cerebral vasculature can be imaged with a catheter 400 microns in diameter, the spaces in the lungs can be imaged with a needle that is 310 microns in diameter, and the inner structures of the eustachian tube can be viewed with an endoscope 1 mm in diameter.
She and her colleagues are developing an OCT/fluorescence imaging falloposcope that is 0.8 mm in diameter, flexible, and steerable, as a tool for early detection of ovarian cancer in humans. “It’s now known that most ovarian cancer starts in the fallopian tubes,” Dr. Barton said. “It’s metastatic disease when those cells break off from the fallopian tubes and go to the ovaries. We wanted to create an imaging system where we created a fiber bundle that we could navigate with white light and with fluorescence so that we can see these early stages of cancer [and] how they fluoresce differently. We also wanted to have an OCT system so that we could image through the wall of the fallopian tube and look for that layer thickening and other precursors to ovarian cancer.”
To date, in vivo testing in healthy women has demonstrated that the miniature endoscope is able to reach the fallopian tubes through the natural orifice of the vagina and uterus. “That is pretty exciting,” she said. “The images may not be of the highest quality, but we are advancing.”
Dr. Barton reported having no relevant financial disclosures.
PHOENIX –
In a lecture during a multispecialty roundup of cutting-edge energy-based device applications at the annual conference of the American Society for Laser Medicine and Surgery, Dr. Barton, a biomedical engineer who directs the BIO5 Institute at the University of Arizona, Tucson, said that while no current modality exists to enable physicians in dermatology and other specialties to view internal structures throughout the entire body with cellular resolution, refining existing technologies is a good way to start.
In 2011, renowned cancer researchers Douglas Hanahan, PhD, and Robert A. Weinberg, PhD, proposed six hallmarks of cancer, which include sustaining proliferative signaling, evading growth suppressors, resisting cell death, enabling replicative immortality, inducing angiogenesis, and activating invasion and metastasis. Each hallmark poses unique imaging challenges. For example, enabling replicative immortality “means that the cell nuclei change size and shape; they change their position,” said Dr. Barton, who is also professor of biomedical engineering and optical sciences at the university. “If we want to see that, we’re going to need an imaging modality that’s subcellular in resolution.”
Similarly, if clinicians want to view how proliferative signaling is changing, “that means being able to visualize the cell surface receptors; those are even smaller to actually visualize,” she said. “But we have technologies where we can target those receptors with fluorophores. And then we can look at large areas very quickly.” Meanwhile, the ability of cancer cells to resist cell death and evade growth suppressors often results in thickening of epithelium throughout the body. “So, if we can measure the thickness of the epithelium, we can see that there’s something wrong with that tissue,” she said.
As for cancer’s propensity for invasion and metastasis, “here, we’re looking at how the collagen structure [between the cells] has changed and whether there’s layer breakdown or not. Optical imaging can detect cancer. However, high resolution optical techniques can only image about 1 mm deep, so unless you’re looking at the skin or the eye, you’re going to have to develop an endoscope to be able to view these hallmarks.”
OCT images the tissue microstructure, generally in a resolution of 2-20 microns, at a depth of 1-2 mm, and it measures reflected light. When possible, Dr. Barton combines OCT with laser-induced fluorescence for enhanced accuracy of detection of cancer. Induced fluorescence senses molecular information with the natural fluorophores in the body or with targeted exogenous agents. Then there’s multiphoton microscopy, an advanced imaging technique that enables clinicians to view cellular and subcellular events within living tissue. Early models of this technology “took up entire benches” in physics labs, Dr. Barton said, but she and other investigators are designing smaller devices for use in clinics. “This is exciting, because not only do we [view] subcellular structure with this modality, but it can also be highly sensitive to collagen structure,” she said.
Ovarian cancer model
In a model of ovarian cancer, she and colleagues externalized the ovaries of a mouse, imaged the organs, put them back in, and reassessed them at 8 weeks. “This model develops cancer very quickly,” said Dr. Barton, who once worked for McDonnell Douglas on the Space Station program. At 8 weeks, using fluorescence and targeted agents with a tabletop multiphoton microscopy system, they observed that the proliferation signals of cancer had begun. “So, with an agent targeted to the folate receptor or to other receptors that are implicated in cancer development, we can see that ovaries and fallopian tubes are lighting up,” she said.
With proof of concept established with the mouse study, she and other researchers are drawing from technological advances to create tiny laser systems for use in the clinic to image a variety of structures in the human body. Optics advances include bulk optics and all-fiber designs where engineers can create an imaging probe that’s only 125 microns in diameter, “or maybe even as small as 70 microns in diameter,” she said. “We can do fabrications on the tips of endoscopes to redirect the light and focus it. We can also do 3-D printing and spiral scanning to create miniature devices to make new advances. That means that instead of just white light imaging of the colon or the lung like we have had in the past, we can start moving into smaller structures, such as the eustachian tube, the fallopian tube, the bile ducts, or making miniature devices for brain biopsies, lung biopsies, and maybe being able to get into bronchioles and arterioles.”
According to Dr. Barton, prior research has demonstrated that cerebral vasculature can be imaged with a catheter 400 microns in diameter, the spaces in the lungs can be imaged with a needle that is 310 microns in diameter, and the inner structures of the eustachian tube can be viewed with an endoscope 1 mm in diameter.
She and her colleagues are developing an OCT/fluorescence imaging falloposcope that is 0.8 mm in diameter, flexible, and steerable, as a tool for early detection of ovarian cancer in humans. “It’s now known that most ovarian cancer starts in the fallopian tubes,” Dr. Barton said. “It’s metastatic disease when those cells break off from the fallopian tubes and go to the ovaries. We wanted to create an imaging system where we created a fiber bundle that we could navigate with white light and with fluorescence so that we can see these early stages of cancer [and] how they fluoresce differently. We also wanted to have an OCT system so that we could image through the wall of the fallopian tube and look for that layer thickening and other precursors to ovarian cancer.”
To date, in vivo testing in healthy women has demonstrated that the miniature endoscope is able to reach the fallopian tubes through the natural orifice of the vagina and uterus. “That is pretty exciting,” she said. “The images may not be of the highest quality, but we are advancing.”
Dr. Barton reported having no relevant financial disclosures.
AT ASLMS 2023
The metaverse is the dermatologist’s ally
MADRID – There are endless possibilities within the dermoverse (a term coined by joining “dermatology” and “metaverse”), from a robot office assistant to the brand new world it offers for virtual training and simulation.
A group of dermatologists expert in new technologies came together at the 50th National Congress of the Spanish Academy for Dermatology and Venereology to discuss the metaverse: that sum of all virtual spaces that bridges physical and digital reality, where users interact through their avatars and where these experts are discovering new opportunities for treating their patients. The metaverse and AI offer a massive opportunity for improving telehealth visits, immersive surgical planning, or virtual training using 3-D skin models. These are just a few examples of what this technology may eventually provide.
“The possibilities offered by the metaverse in the field of dermatology could be endless,” explained Miriam Fernández-Parrado, MD, dermatologist at Navarre Hospital, Pamplona, Spain. To her, “the metaverse could mean a step forward in teledermatology, which has come of age as a result of the pandemic.” These past few years have shown that it’s possible to perform some screenings online. This, in turn, has produced significant time and cost savings, along with greater efficacy in initial screening and early detection of serious diseases.
The overall percentage of cases that are potentially treatable in absentia is estimated to exceed 70%. “This isn’t a matter of replacing in-person visits but of finding a quality alternative that, far from dehumanizing the doctor-patient relationship, helps to satisfy the growing need for this relationship,” said Dr. Fernández-Parrado.
Always on duty
Julián Conejo-Mir, MD, PhD, professor and head of dermatology at the Virgen del Rocío Hospital in Seville, Spain, told this news organization that AI will help with day-to-day interactions with patients. It’s already a reality. “But to say that with a simple photo, we can address 70% of dermatology cases without being physically present with our patients – I don’t think that will become a reality in the next 20 years.”
Currently, algorithms can identify tumors with high success rates (80%-90%) using photographs and dermoscopic images; rates increase significantly when both kinds of images are available. These high success rates are possible because tumor morphology is stationary. “However, for inflammatory conditions, accurate diagnosis generally doesn’t exceed 60%, since these are conditions in which morphology can change a lot from one day to the next and can vary significantly, depending on their anatomic location or the patient’s age.”
Maybe once metaclinics, with 3-D virtual reality, have been established and clinicians can see the patient in real time from their offices, the rate of accurate diagnosis will reach 70%, especially with patients who have limited mobility or who live at a distance from the hospital. “But that’s still 10-15 years away, since more powerful computers are needed, most likely quantum computers,” cautioned Dr. Conejo-Mir.
The patient’s ally
In clinical practice, facilitating access to the dermoverse may help reduce pain and divert the patient’s attention, especially during in-person visits that require bothersome or uncomfortable interventions. “This is especially effective in pediatric dermatology, since settings of immersive virtual reality may contribute to relaxation among children,” explained Dr. Fernández-Parrado. She also sees potential applications among patients who need surgery. The metaverse would allow them to preview a simulation of their operation before undergoing it, thus reducing their anxiety and allaying their fears about these procedures.
Two lines are being pursued: automated diagnosis for telehealth consultations, which are primarily for tumors, and robotic office assistants.
“We have been using the first one in clinical practice, and we can achieve a success rate of 85%-90%.” The second one is much more complex, “and we’re having a hard time moving it forward within our research team, since it doesn’t involve only one algorithm. Instead, it requires five algorithms working together simultaneously (chatbot, automatic writing, image analysis, selecting the most appropriate treatment, ability to make recommendations, and even an additional one involving feelings),” explained Dr. Conejo-Mir.
A wise consultant
Dr. Conejo-Mir offered examples of how this might work in the near future. “In under 5 years, you’ll be able to sit in front of a computer or your smartphone, talk to an avatar that we’re able to select (sex, appearance, age, kind/serious), show the avatar your lesions, and it will tell us a basic diagnostic impression and even the treatment.”
With virtual learning, physicians can also gather knowledge or take refresher courses, using skin models in augmented reality with tumors and other skin lesions, or using immersive simulation courses that aid learning. Digital models that replicate the anatomy and elasticity of the skin or other characteristics unique to the patient can be used to reach decisions regarding surgeries and to practice interventions before entering the operating room, explained Dr. Fernández-Parrado.
Optimal virtual training
Virtual reality and simulation will doubtless play a major role in this promising field of using these devices for training purposes. “There will be virtual dermatology clinics or metaclinics, where you can do everything with virtual simulated patients, from gaining experience in interviews or health histories (even with patients who are difficult to deal with), to taking biopsies and performing interventions,” said Dr. Conejo-Mir.
A recent study titled “How the World Sees the Metaverse and Extended Reality” gathered data from 29 countries regarding the next 10 years. One of the greatest benefits of this technology is expected in health resources (59%), even more than in the trading of digital assets. While it is difficult to predict when the dermoverse will be in operation, Dr. Fernández-Parrado says she’s a techno-optimist. Together with Dr. Héctor Perandones, MD, a dermatologist at the University Healthcare Complex in León, Spain, and coauthor with Dr. Fernández-Parrado of the article, “A New Universe in Dermatology: From Metaverse to Dermoverse,” she’s convinced that “if we can imagine it, we can create it.”
A differential diagnostician
Over the past 10 years, AI has become a major ally of dermatology, providing new techniques that simplify the diagnosis and treatment of patients. There are many applications for which it adds tremendous value in dermatology: establishing precise differential diagnoses for common diseases, such as psoriasis, atopic dermatitis, or acne; eveloping personalized therapeutic protocols; and predicting medium- and long-term outcomes.
Furthermore, in onco-dermatology, AI has helped to automate the diagnosis of skin tumors by making it possible to differentiate between melanocytic and nonmelanocytic lesions. This distinction promotes early diagnosis and helps produce screening systems that are capable of prioritizing cases on the basis of their seriousness.
When asked whether any group has published any promising tools with good preliminary results, Dr. Conejo-Mir stated that his group has produced three articles that have been published in top-ranking journals. In these articles, “we explain our experience with artificial intelligence in Mohs surgery, in automated diagnosis, and for calculating the thickness of melanomas.” The eight-person research team, which comprises dermatologists and software engineers, has been working together in this area for the past 4 years.
Aesthetic dermatology
Unlike other specialists, dermatologists have 4-D vision when it comes to aesthetics, since they are also skin experts. AI plays a major role in aesthetic dermatology. It supports this specialty by providing a greater analytic capacity and by evaluating the procedure and technique to be used. “It’s going to help us think and make decisions. It has taken great strides in aesthetic dermatology, especially when it comes to techniques and products. There have been products like collagen, hyaluronic acid, then thread lifts ... Also, different techniques have been developed, like Botox, for example. Before, Botox was given following one method. Now, there are other methods,” explained Dr. Conejo-Mir.
He explained, “We have analyzed the facial image to detect wrinkles, spots, enlarged pores, et cetera, to see whether there are any lesions, and, depending on what the machine says you have, it provides you with a personalized treatment. It tells you the pattern of care that the patient should follow. It also tells you what you’re going to do, whether or not there is any problem, depending on the location and on what the person is like, et cetera. Then, for follow-up, you’re given an AI program that tells you if you’re doing well or not. Lastly, it gives you product recommendations.
“We are among the specialties that are going through the most change,” said Dr. Conejo-Mir.
An intrusive technology?
AI will be a tremendous help in decision-making, to the point where “in 4 or 5 years, it will become indispensable, just like the loupe in years past, and then the dermatoscope.” However, the machine will have to depend on human beings. “They won’t replace us, but they will become unavoidable assistants in our day-to-day medical practice.”
Questions have arisen regarding the potential dangers of these new technologies, like that of reducing the number of dermatologists within the population, and whether they might encourage intrusiveness. Dr. Conejo-Mir made no bones about it. “AI will never cut back the number of specialists. That is false. When AI supports us in teledermatology, even currently on our team, it spits out information, but the one making the decision is the practitioner, not the machine.”
AI is a tool but is not in itself something that treats patients. It is akin to the dermatoscope. Dermatologists use these tools every day, and they help arrive at diagnoses in difficult cases, but they are not a replacement for humans. “At least for the next 50 years, then we’ll see. In 2050 is when they say AI will surpass humans in its intelligence and reasoning capacity,” said Dr. Conejo-Mir.
Dr. Conejo-Mir has disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version of this article appeared on Medscape.com.
MADRID – There are endless possibilities within the dermoverse (a term coined by joining “dermatology” and “metaverse”), from a robot office assistant to the brand new world it offers for virtual training and simulation.
A group of dermatologists expert in new technologies came together at the 50th National Congress of the Spanish Academy for Dermatology and Venereology to discuss the metaverse: that sum of all virtual spaces that bridges physical and digital reality, where users interact through their avatars and where these experts are discovering new opportunities for treating their patients. The metaverse and AI offer a massive opportunity for improving telehealth visits, immersive surgical planning, or virtual training using 3-D skin models. These are just a few examples of what this technology may eventually provide.
“The possibilities offered by the metaverse in the field of dermatology could be endless,” explained Miriam Fernández-Parrado, MD, dermatologist at Navarre Hospital, Pamplona, Spain. To her, “the metaverse could mean a step forward in teledermatology, which has come of age as a result of the pandemic.” These past few years have shown that it’s possible to perform some screenings online. This, in turn, has produced significant time and cost savings, along with greater efficacy in initial screening and early detection of serious diseases.
The overall percentage of cases that are potentially treatable in absentia is estimated to exceed 70%. “This isn’t a matter of replacing in-person visits but of finding a quality alternative that, far from dehumanizing the doctor-patient relationship, helps to satisfy the growing need for this relationship,” said Dr. Fernández-Parrado.
Always on duty
Julián Conejo-Mir, MD, PhD, professor and head of dermatology at the Virgen del Rocío Hospital in Seville, Spain, told this news organization that AI will help with day-to-day interactions with patients. It’s already a reality. “But to say that with a simple photo, we can address 70% of dermatology cases without being physically present with our patients – I don’t think that will become a reality in the next 20 years.”
Currently, algorithms can identify tumors with high success rates (80%-90%) using photographs and dermoscopic images; rates increase significantly when both kinds of images are available. These high success rates are possible because tumor morphology is stationary. “However, for inflammatory conditions, accurate diagnosis generally doesn’t exceed 60%, since these are conditions in which morphology can change a lot from one day to the next and can vary significantly, depending on their anatomic location or the patient’s age.”
Maybe once metaclinics, with 3-D virtual reality, have been established and clinicians can see the patient in real time from their offices, the rate of accurate diagnosis will reach 70%, especially with patients who have limited mobility or who live at a distance from the hospital. “But that’s still 10-15 years away, since more powerful computers are needed, most likely quantum computers,” cautioned Dr. Conejo-Mir.
The patient’s ally
In clinical practice, facilitating access to the dermoverse may help reduce pain and divert the patient’s attention, especially during in-person visits that require bothersome or uncomfortable interventions. “This is especially effective in pediatric dermatology, since settings of immersive virtual reality may contribute to relaxation among children,” explained Dr. Fernández-Parrado. She also sees potential applications among patients who need surgery. The metaverse would allow them to preview a simulation of their operation before undergoing it, thus reducing their anxiety and allaying their fears about these procedures.
Two lines are being pursued: automated diagnosis for telehealth consultations, which are primarily for tumors, and robotic office assistants.
“We have been using the first one in clinical practice, and we can achieve a success rate of 85%-90%.” The second one is much more complex, “and we’re having a hard time moving it forward within our research team, since it doesn’t involve only one algorithm. Instead, it requires five algorithms working together simultaneously (chatbot, automatic writing, image analysis, selecting the most appropriate treatment, ability to make recommendations, and even an additional one involving feelings),” explained Dr. Conejo-Mir.
A wise consultant
Dr. Conejo-Mir offered examples of how this might work in the near future. “In under 5 years, you’ll be able to sit in front of a computer or your smartphone, talk to an avatar that we’re able to select (sex, appearance, age, kind/serious), show the avatar your lesions, and it will tell us a basic diagnostic impression and even the treatment.”
With virtual learning, physicians can also gather knowledge or take refresher courses, using skin models in augmented reality with tumors and other skin lesions, or using immersive simulation courses that aid learning. Digital models that replicate the anatomy and elasticity of the skin or other characteristics unique to the patient can be used to reach decisions regarding surgeries and to practice interventions before entering the operating room, explained Dr. Fernández-Parrado.
Optimal virtual training
Virtual reality and simulation will doubtless play a major role in this promising field of using these devices for training purposes. “There will be virtual dermatology clinics or metaclinics, where you can do everything with virtual simulated patients, from gaining experience in interviews or health histories (even with patients who are difficult to deal with), to taking biopsies and performing interventions,” said Dr. Conejo-Mir.
A recent study titled “How the World Sees the Metaverse and Extended Reality” gathered data from 29 countries regarding the next 10 years. One of the greatest benefits of this technology is expected in health resources (59%), even more than in the trading of digital assets. While it is difficult to predict when the dermoverse will be in operation, Dr. Fernández-Parrado says she’s a techno-optimist. Together with Dr. Héctor Perandones, MD, a dermatologist at the University Healthcare Complex in León, Spain, and coauthor with Dr. Fernández-Parrado of the article, “A New Universe in Dermatology: From Metaverse to Dermoverse,” she’s convinced that “if we can imagine it, we can create it.”
A differential diagnostician
Over the past 10 years, AI has become a major ally of dermatology, providing new techniques that simplify the diagnosis and treatment of patients. There are many applications for which it adds tremendous value in dermatology: establishing precise differential diagnoses for common diseases, such as psoriasis, atopic dermatitis, or acne; eveloping personalized therapeutic protocols; and predicting medium- and long-term outcomes.
Furthermore, in onco-dermatology, AI has helped to automate the diagnosis of skin tumors by making it possible to differentiate between melanocytic and nonmelanocytic lesions. This distinction promotes early diagnosis and helps produce screening systems that are capable of prioritizing cases on the basis of their seriousness.
When asked whether any group has published any promising tools with good preliminary results, Dr. Conejo-Mir stated that his group has produced three articles that have been published in top-ranking journals. In these articles, “we explain our experience with artificial intelligence in Mohs surgery, in automated diagnosis, and for calculating the thickness of melanomas.” The eight-person research team, which comprises dermatologists and software engineers, has been working together in this area for the past 4 years.
Aesthetic dermatology
Unlike other specialists, dermatologists have 4-D vision when it comes to aesthetics, since they are also skin experts. AI plays a major role in aesthetic dermatology. It supports this specialty by providing a greater analytic capacity and by evaluating the procedure and technique to be used. “It’s going to help us think and make decisions. It has taken great strides in aesthetic dermatology, especially when it comes to techniques and products. There have been products like collagen, hyaluronic acid, then thread lifts ... Also, different techniques have been developed, like Botox, for example. Before, Botox was given following one method. Now, there are other methods,” explained Dr. Conejo-Mir.
He explained, “We have analyzed the facial image to detect wrinkles, spots, enlarged pores, et cetera, to see whether there are any lesions, and, depending on what the machine says you have, it provides you with a personalized treatment. It tells you the pattern of care that the patient should follow. It also tells you what you’re going to do, whether or not there is any problem, depending on the location and on what the person is like, et cetera. Then, for follow-up, you’re given an AI program that tells you if you’re doing well or not. Lastly, it gives you product recommendations.
“We are among the specialties that are going through the most change,” said Dr. Conejo-Mir.
An intrusive technology?
AI will be a tremendous help in decision-making, to the point where “in 4 or 5 years, it will become indispensable, just like the loupe in years past, and then the dermatoscope.” However, the machine will have to depend on human beings. “They won’t replace us, but they will become unavoidable assistants in our day-to-day medical practice.”
Questions have arisen regarding the potential dangers of these new technologies, like that of reducing the number of dermatologists within the population, and whether they might encourage intrusiveness. Dr. Conejo-Mir made no bones about it. “AI will never cut back the number of specialists. That is false. When AI supports us in teledermatology, even currently on our team, it spits out information, but the one making the decision is the practitioner, not the machine.”
AI is a tool but is not in itself something that treats patients. It is akin to the dermatoscope. Dermatologists use these tools every day, and they help arrive at diagnoses in difficult cases, but they are not a replacement for humans. “At least for the next 50 years, then we’ll see. In 2050 is when they say AI will surpass humans in its intelligence and reasoning capacity,” said Dr. Conejo-Mir.
Dr. Conejo-Mir has disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version of this article appeared on Medscape.com.
MADRID – There are endless possibilities within the dermoverse (a term coined by joining “dermatology” and “metaverse”), from a robot office assistant to the brand new world it offers for virtual training and simulation.
A group of dermatologists expert in new technologies came together at the 50th National Congress of the Spanish Academy for Dermatology and Venereology to discuss the metaverse: that sum of all virtual spaces that bridges physical and digital reality, where users interact through their avatars and where these experts are discovering new opportunities for treating their patients. The metaverse and AI offer a massive opportunity for improving telehealth visits, immersive surgical planning, or virtual training using 3-D skin models. These are just a few examples of what this technology may eventually provide.
“The possibilities offered by the metaverse in the field of dermatology could be endless,” explained Miriam Fernández-Parrado, MD, dermatologist at Navarre Hospital, Pamplona, Spain. To her, “the metaverse could mean a step forward in teledermatology, which has come of age as a result of the pandemic.” These past few years have shown that it’s possible to perform some screenings online. This, in turn, has produced significant time and cost savings, along with greater efficacy in initial screening and early detection of serious diseases.
The overall percentage of cases that are potentially treatable in absentia is estimated to exceed 70%. “This isn’t a matter of replacing in-person visits but of finding a quality alternative that, far from dehumanizing the doctor-patient relationship, helps to satisfy the growing need for this relationship,” said Dr. Fernández-Parrado.
Always on duty
Julián Conejo-Mir, MD, PhD, professor and head of dermatology at the Virgen del Rocío Hospital in Seville, Spain, told this news organization that AI will help with day-to-day interactions with patients. It’s already a reality. “But to say that with a simple photo, we can address 70% of dermatology cases without being physically present with our patients – I don’t think that will become a reality in the next 20 years.”
Currently, algorithms can identify tumors with high success rates (80%-90%) using photographs and dermoscopic images; rates increase significantly when both kinds of images are available. These high success rates are possible because tumor morphology is stationary. “However, for inflammatory conditions, accurate diagnosis generally doesn’t exceed 60%, since these are conditions in which morphology can change a lot from one day to the next and can vary significantly, depending on their anatomic location or the patient’s age.”
Maybe once metaclinics, with 3-D virtual reality, have been established and clinicians can see the patient in real time from their offices, the rate of accurate diagnosis will reach 70%, especially with patients who have limited mobility or who live at a distance from the hospital. “But that’s still 10-15 years away, since more powerful computers are needed, most likely quantum computers,” cautioned Dr. Conejo-Mir.
The patient’s ally
In clinical practice, facilitating access to the dermoverse may help reduce pain and divert the patient’s attention, especially during in-person visits that require bothersome or uncomfortable interventions. “This is especially effective in pediatric dermatology, since settings of immersive virtual reality may contribute to relaxation among children,” explained Dr. Fernández-Parrado. She also sees potential applications among patients who need surgery. The metaverse would allow them to preview a simulation of their operation before undergoing it, thus reducing their anxiety and allaying their fears about these procedures.
Two lines are being pursued: automated diagnosis for telehealth consultations, which are primarily for tumors, and robotic office assistants.
“We have been using the first one in clinical practice, and we can achieve a success rate of 85%-90%.” The second one is much more complex, “and we’re having a hard time moving it forward within our research team, since it doesn’t involve only one algorithm. Instead, it requires five algorithms working together simultaneously (chatbot, automatic writing, image analysis, selecting the most appropriate treatment, ability to make recommendations, and even an additional one involving feelings),” explained Dr. Conejo-Mir.
A wise consultant
Dr. Conejo-Mir offered examples of how this might work in the near future. “In under 5 years, you’ll be able to sit in front of a computer or your smartphone, talk to an avatar that we’re able to select (sex, appearance, age, kind/serious), show the avatar your lesions, and it will tell us a basic diagnostic impression and even the treatment.”
With virtual learning, physicians can also gather knowledge or take refresher courses, using skin models in augmented reality with tumors and other skin lesions, or using immersive simulation courses that aid learning. Digital models that replicate the anatomy and elasticity of the skin or other characteristics unique to the patient can be used to reach decisions regarding surgeries and to practice interventions before entering the operating room, explained Dr. Fernández-Parrado.
Optimal virtual training
Virtual reality and simulation will doubtless play a major role in this promising field of using these devices for training purposes. “There will be virtual dermatology clinics or metaclinics, where you can do everything with virtual simulated patients, from gaining experience in interviews or health histories (even with patients who are difficult to deal with), to taking biopsies and performing interventions,” said Dr. Conejo-Mir.
A recent study titled “How the World Sees the Metaverse and Extended Reality” gathered data from 29 countries regarding the next 10 years. One of the greatest benefits of this technology is expected in health resources (59%), even more than in the trading of digital assets. While it is difficult to predict when the dermoverse will be in operation, Dr. Fernández-Parrado says she’s a techno-optimist. Together with Dr. Héctor Perandones, MD, a dermatologist at the University Healthcare Complex in León, Spain, and coauthor with Dr. Fernández-Parrado of the article, “A New Universe in Dermatology: From Metaverse to Dermoverse,” she’s convinced that “if we can imagine it, we can create it.”
A differential diagnostician
Over the past 10 years, AI has become a major ally of dermatology, providing new techniques that simplify the diagnosis and treatment of patients. There are many applications for which it adds tremendous value in dermatology: establishing precise differential diagnoses for common diseases, such as psoriasis, atopic dermatitis, or acne; eveloping personalized therapeutic protocols; and predicting medium- and long-term outcomes.
Furthermore, in onco-dermatology, AI has helped to automate the diagnosis of skin tumors by making it possible to differentiate between melanocytic and nonmelanocytic lesions. This distinction promotes early diagnosis and helps produce screening systems that are capable of prioritizing cases on the basis of their seriousness.
When asked whether any group has published any promising tools with good preliminary results, Dr. Conejo-Mir stated that his group has produced three articles that have been published in top-ranking journals. In these articles, “we explain our experience with artificial intelligence in Mohs surgery, in automated diagnosis, and for calculating the thickness of melanomas.” The eight-person research team, which comprises dermatologists and software engineers, has been working together in this area for the past 4 years.
Aesthetic dermatology
Unlike other specialists, dermatologists have 4-D vision when it comes to aesthetics, since they are also skin experts. AI plays a major role in aesthetic dermatology. It supports this specialty by providing a greater analytic capacity and by evaluating the procedure and technique to be used. “It’s going to help us think and make decisions. It has taken great strides in aesthetic dermatology, especially when it comes to techniques and products. There have been products like collagen, hyaluronic acid, then thread lifts ... Also, different techniques have been developed, like Botox, for example. Before, Botox was given following one method. Now, there are other methods,” explained Dr. Conejo-Mir.
He explained, “We have analyzed the facial image to detect wrinkles, spots, enlarged pores, et cetera, to see whether there are any lesions, and, depending on what the machine says you have, it provides you with a personalized treatment. It tells you the pattern of care that the patient should follow. It also tells you what you’re going to do, whether or not there is any problem, depending on the location and on what the person is like, et cetera. Then, for follow-up, you’re given an AI program that tells you if you’re doing well or not. Lastly, it gives you product recommendations.
“We are among the specialties that are going through the most change,” said Dr. Conejo-Mir.
An intrusive technology?
AI will be a tremendous help in decision-making, to the point where “in 4 or 5 years, it will become indispensable, just like the loupe in years past, and then the dermatoscope.” However, the machine will have to depend on human beings. “They won’t replace us, but they will become unavoidable assistants in our day-to-day medical practice.”
Questions have arisen regarding the potential dangers of these new technologies, like that of reducing the number of dermatologists within the population, and whether they might encourage intrusiveness. Dr. Conejo-Mir made no bones about it. “AI will never cut back the number of specialists. That is false. When AI supports us in teledermatology, even currently on our team, it spits out information, but the one making the decision is the practitioner, not the machine.”
AI is a tool but is not in itself something that treats patients. It is akin to the dermatoscope. Dermatologists use these tools every day, and they help arrive at diagnoses in difficult cases, but they are not a replacement for humans. “At least for the next 50 years, then we’ll see. In 2050 is when they say AI will surpass humans in its intelligence and reasoning capacity,” said Dr. Conejo-Mir.
Dr. Conejo-Mir has disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition. A version of this article appeared on Medscape.com.
FDA approves ritlecitinib for ages 12 and up for alopecia areata
Taken as a once-daily pill, ritlecitinib is a dual inhibitor of the TEC family of tyrosine kinases and of Janus kinase 3 (JAK3). The recommended dose of ritlecitinib, which will be marketed as Litfulo, is 50 mg once a day, according to the statement announcing the approval from Pfizer.
It is the second JAK inhibitor approved for treating alopecia areata, following approval of baricitinib (Olumiant) in June 2022 for AA in adults. Ritlecitinib is the first JAK inhibitor approved for children ages 12 and older with AA.
The European Medicines Agency has also accepted the Marketing Authorization Application for ritlecitinib in the same population and a decision is expected in the fourth quarter of this year.
Approval based on ALLEGRO trials
Approval was based on previously announced results from trials, including the phase 2b/3 ALLEGRO study of ritlecitinib in 718 patients aged 12 years and older with alopecia areata, with 50% of more scalp hair loss, as measured by the Severity of Alopecia Tool (SALT), including patients with alopecia totalis (complete scalp hair loss) and alopecia universalis (complete scalp, face, and body hair loss).
Patients in the trial were experiencing a current episode of alopecia areata that had lasted between 6 months and 10 years. They were randomized to receive once-daily ritlecitinib at doses of 30 mg or 50 mg (with or without 1 month of initial treatment with once-daily ritlecitinib 200 mg), ritlecitinib 10 mg, or placebo.
Statistically significantly higher proportions of patients treated with ritlecitinib 30 mg and 50 mg (with or without the loading dose) had 80% or more scalp hair coverage, as measured by a SALT score of 20 or less after 6 months of treatment versus placebo. After 6 months of treatment, among those on the 50-mg dose, 23% had achieved a SALT score of 20 or less, compared with 2% of those on placebo. The results were published in The Lancet.
According to the company release, efficacy and safety of ritlecitinib was consistent between those ages 12-17 and adults, and the most common adverse events reported in the study, in at least 4% of patients treated with ritlecitinib, were headache (10.8%), diarrhea (10%), acne (6.2%), rash (5.4%), and urticaria (4.6%).
Ritlecitinib labeling includes the boxed warning about the risk for serious infections, mortality, malignancy, major adverse cardiovascular events, and thrombosis, which is included in the labels for other JAK inhibitors.
Ritlecitinib evaluated for other diseases
In addition to alopecia areata, ritlecitinib has shown efficacy and acceptable safety in treating ulcerative colitis and is being evaluated for treating vitiligo, Crohn’s disease, and rheumatoid arthritis.
In the statement, the company says that ritlecitinib will be available “in the coming weeks.” The manufacturer says it also has completed regulatory submissions for ritlecitinib in the United Kingdom, China, and Japan, and expects decisions this year.
Alopecia areata affects about 6.8 million people in the United States and 147 million globally.
In a statement, Nicole Friedland, president and CEO of the National Alopecia Areata Foundation, said that NAAF “is thrilled to have a second FDA-approved treatment for alopecia areata, which is the first approved for adolescents.”
A version of this article first appeared on Medscape.com.
Taken as a once-daily pill, ritlecitinib is a dual inhibitor of the TEC family of tyrosine kinases and of Janus kinase 3 (JAK3). The recommended dose of ritlecitinib, which will be marketed as Litfulo, is 50 mg once a day, according to the statement announcing the approval from Pfizer.
It is the second JAK inhibitor approved for treating alopecia areata, following approval of baricitinib (Olumiant) in June 2022 for AA in adults. Ritlecitinib is the first JAK inhibitor approved for children ages 12 and older with AA.
The European Medicines Agency has also accepted the Marketing Authorization Application for ritlecitinib in the same population and a decision is expected in the fourth quarter of this year.
Approval based on ALLEGRO trials
Approval was based on previously announced results from trials, including the phase 2b/3 ALLEGRO study of ritlecitinib in 718 patients aged 12 years and older with alopecia areata, with 50% of more scalp hair loss, as measured by the Severity of Alopecia Tool (SALT), including patients with alopecia totalis (complete scalp hair loss) and alopecia universalis (complete scalp, face, and body hair loss).
Patients in the trial were experiencing a current episode of alopecia areata that had lasted between 6 months and 10 years. They were randomized to receive once-daily ritlecitinib at doses of 30 mg or 50 mg (with or without 1 month of initial treatment with once-daily ritlecitinib 200 mg), ritlecitinib 10 mg, or placebo.
Statistically significantly higher proportions of patients treated with ritlecitinib 30 mg and 50 mg (with or without the loading dose) had 80% or more scalp hair coverage, as measured by a SALT score of 20 or less after 6 months of treatment versus placebo. After 6 months of treatment, among those on the 50-mg dose, 23% had achieved a SALT score of 20 or less, compared with 2% of those on placebo. The results were published in The Lancet.
According to the company release, efficacy and safety of ritlecitinib was consistent between those ages 12-17 and adults, and the most common adverse events reported in the study, in at least 4% of patients treated with ritlecitinib, were headache (10.8%), diarrhea (10%), acne (6.2%), rash (5.4%), and urticaria (4.6%).
Ritlecitinib labeling includes the boxed warning about the risk for serious infections, mortality, malignancy, major adverse cardiovascular events, and thrombosis, which is included in the labels for other JAK inhibitors.
Ritlecitinib evaluated for other diseases
In addition to alopecia areata, ritlecitinib has shown efficacy and acceptable safety in treating ulcerative colitis and is being evaluated for treating vitiligo, Crohn’s disease, and rheumatoid arthritis.
In the statement, the company says that ritlecitinib will be available “in the coming weeks.” The manufacturer says it also has completed regulatory submissions for ritlecitinib in the United Kingdom, China, and Japan, and expects decisions this year.
Alopecia areata affects about 6.8 million people in the United States and 147 million globally.
In a statement, Nicole Friedland, president and CEO of the National Alopecia Areata Foundation, said that NAAF “is thrilled to have a second FDA-approved treatment for alopecia areata, which is the first approved for adolescents.”
A version of this article first appeared on Medscape.com.
Taken as a once-daily pill, ritlecitinib is a dual inhibitor of the TEC family of tyrosine kinases and of Janus kinase 3 (JAK3). The recommended dose of ritlecitinib, which will be marketed as Litfulo, is 50 mg once a day, according to the statement announcing the approval from Pfizer.
It is the second JAK inhibitor approved for treating alopecia areata, following approval of baricitinib (Olumiant) in June 2022 for AA in adults. Ritlecitinib is the first JAK inhibitor approved for children ages 12 and older with AA.
The European Medicines Agency has also accepted the Marketing Authorization Application for ritlecitinib in the same population and a decision is expected in the fourth quarter of this year.
Approval based on ALLEGRO trials
Approval was based on previously announced results from trials, including the phase 2b/3 ALLEGRO study of ritlecitinib in 718 patients aged 12 years and older with alopecia areata, with 50% of more scalp hair loss, as measured by the Severity of Alopecia Tool (SALT), including patients with alopecia totalis (complete scalp hair loss) and alopecia universalis (complete scalp, face, and body hair loss).
Patients in the trial were experiencing a current episode of alopecia areata that had lasted between 6 months and 10 years. They were randomized to receive once-daily ritlecitinib at doses of 30 mg or 50 mg (with or without 1 month of initial treatment with once-daily ritlecitinib 200 mg), ritlecitinib 10 mg, or placebo.
Statistically significantly higher proportions of patients treated with ritlecitinib 30 mg and 50 mg (with or without the loading dose) had 80% or more scalp hair coverage, as measured by a SALT score of 20 or less after 6 months of treatment versus placebo. After 6 months of treatment, among those on the 50-mg dose, 23% had achieved a SALT score of 20 or less, compared with 2% of those on placebo. The results were published in The Lancet.
According to the company release, efficacy and safety of ritlecitinib was consistent between those ages 12-17 and adults, and the most common adverse events reported in the study, in at least 4% of patients treated with ritlecitinib, were headache (10.8%), diarrhea (10%), acne (6.2%), rash (5.4%), and urticaria (4.6%).
Ritlecitinib labeling includes the boxed warning about the risk for serious infections, mortality, malignancy, major adverse cardiovascular events, and thrombosis, which is included in the labels for other JAK inhibitors.
Ritlecitinib evaluated for other diseases
In addition to alopecia areata, ritlecitinib has shown efficacy and acceptable safety in treating ulcerative colitis and is being evaluated for treating vitiligo, Crohn’s disease, and rheumatoid arthritis.
In the statement, the company says that ritlecitinib will be available “in the coming weeks.” The manufacturer says it also has completed regulatory submissions for ritlecitinib in the United Kingdom, China, and Japan, and expects decisions this year.
Alopecia areata affects about 6.8 million people in the United States and 147 million globally.
In a statement, Nicole Friedland, president and CEO of the National Alopecia Areata Foundation, said that NAAF “is thrilled to have a second FDA-approved treatment for alopecia areata, which is the first approved for adolescents.”
A version of this article first appeared on Medscape.com.
Study supports new NCCN classification for cutaneous squamous cell carcinoma
, according to new findings.
In addition, regardless of the NCCN risk group, the study found that Mohs surgery or peripheral and deep en face margin assessment (PDEMA) conferred a lower risk of developing LR, DM, and disease-related death.
“Although the NCCN included this new high-risk group in the last iteration of the guidelines, there were no studies that identified whether the high-risk group achieved the goal of identifying riskier tumors,” said senior author Emily Ruiz, MD, MPH, associate physician at the Mohs and Dermatologic Surgery Center at Brigham and Women’s Faulkner Hospital, Boston. “Based on the data in our study, the risk groups did risk stratify tumors and so clinicians can utilize the high-risk group risk factors to identify which tumors may require additional surveillance or treatment.”
The study was published online in JAMA Dermatology.
Most patients with CSCC are successfully treated with Mohs micrographic surgery or wide local excision (WLE) alone, but a subset will experience more severe and aggressive disease. While useful for prognostication, current staging systems do not incorporate patient factors or other high-risk tumor features that influence outcomes, which led to the NCCN reclassifying CSCC into low-, high-, and very high-risk groups. The NCCN guidelines also made a new recommendation that Mohs or PDEMA be the preferred method for tissue processing for high- and very-high-risk tumors, based on this new stratification.
However, these changes to the NCCN guidelines have not been validated. The goal of this study was to compare outcomes in very-high-, high-, and low-risk NCCN groups as well as comparing outcomes of CSCCs stratified by Mohs and WLE.
Dr. Ruiz and colleagues conducted a retrospective cohort study using patient data from two tertiary care academic medical centers. Their analysis included 10,196 tumors from 8,727 patients that were then stratified into low-risk (3,054 tumors [30.0%]), high-risk (6,269 tumors [61.5%]), and very-high-risk (873 tumors [8.6%]) groups.
Tumors in the very-high-risk group were more likely to have high-risk tumor and histologic features, such as large-caliber perineural invasion, large diameter, invasion beyond the subcutaneous fat or bone, poor differentiation, and lymphovascular invasion.
The authors found that, compared with the low-risk group, the high- and very-high-risk groups demonstrated a greater risk of LR (high-risk subhazard ratio, 1.99; P = .007; very-high-risk SHR, 12.66; P < .001); NM (high-risk SHR, 4.26; P = .02; very-high-risk SHR, 62.98; P < .001); DM (high-risk SHR, 2.2 × 107; P < .001; very-high-risk SHR, 6.3 × 108; P < .001); and DSD (high-risk SHR, 4.02; P = .03; very-high-risk SHR, 93.87; P < .001).
Adjusted 5-year cumulative incidence was also significantly higher in very-high- vs. high- and low-risk groups for all endpoints.
They next compared the procedures used to treat the tumors. Compared with WLE, patients treated with Mohs or PDEMA had a lower risk of LR (SHR, 0.65; P = .009), DM (SHR, 0.38; P = .02), and DSD (SHR, 0.55; P = .006).
Mohs and PDEMA have already became preferred surgical modalities for high- and very-high-risk tumors, and Dr. Ruiz pointed out that their analysis was for the entire cohort.
“We did not stratify this by risk group,” she said. “So our results do not change anything clinically at this time, but support prior studies that have found Mohs/PDEMA to have improved outcomes, compared to WLE. Further studies are needed evaluating surgical approach by risk-group.”
However, she emphasized, “our studies further validate prior evidence showing Mohs/PDEMA to have the lowest rates of recurrence and in this study, even disease-related death.”
Approached for an independent comment, Jeffrey M. Farma, MD, codirector of the melanoma and skin cancer program, and interim chair, department of surgical oncology, Fox Chase Cancer Center, Philadelphia, noted that this study supports the new reclassification of CSCC tumors by the NCCN, and confirms that the high-risk and very-high-risk tumors surely have a higher propensity for worse outcomes overall.
“That being said, the notion for type of resection and margin assessment is still an area of controversy in the dermatology, surgical oncology, and pathology community,” said Dr. Farma, who is also on the NCCN panel. “I believe we need further studies to truly understand the role of the type of resection and the pathologic evaluation play in this disease process.”
He also pointed out that it is unclear in this dataset if patients initially had any imaging to evaluate for local or regional metastatic disease. “It would be helpful to have a further understanding of which type of provider was performing the excisions, the type of excision decided upon, and if there was a standardized approach to [decide] which patients had MOHS or PDEMA and what was the surveillance for these patients both with imaging and physical examinations,” said Dr. Farma. “This data also evaluated patients over a long time period where practice patterns have evolved.”
Finally, he noted that the number of local and metastatic events subjectively seems low in this cohort. “We also do not know any information about the initial workup of the patients, patterns of recurrence, and adjuvant or palliative treatment after recurrence,” he added. “It is unclear from this manuscript how the type of resection or pathologic evaluation of margins leads to improved outcomes and further prospective studies are warranted.”
Dr. Ruiz reports reported serving as a coinvestigator and principal investigator for Regeneron Pharmaceuticals and as a coinvestigator for Merck and consulting for Checkpoint Therapeutics, BDO, and Genentech outside the submitted work. Dr. Farma has no disclosures other than the NCCN panel. The study was supported by Harvard Catalyst and the Harvard University Clinical and Translational Science Center and by Harvard University and its affiliated academic health care centers and partially supported by the Melvin Markey Discovery Fund at Cleveland Clinic Foundation.
, according to new findings.
In addition, regardless of the NCCN risk group, the study found that Mohs surgery or peripheral and deep en face margin assessment (PDEMA) conferred a lower risk of developing LR, DM, and disease-related death.
“Although the NCCN included this new high-risk group in the last iteration of the guidelines, there were no studies that identified whether the high-risk group achieved the goal of identifying riskier tumors,” said senior author Emily Ruiz, MD, MPH, associate physician at the Mohs and Dermatologic Surgery Center at Brigham and Women’s Faulkner Hospital, Boston. “Based on the data in our study, the risk groups did risk stratify tumors and so clinicians can utilize the high-risk group risk factors to identify which tumors may require additional surveillance or treatment.”
The study was published online in JAMA Dermatology.
Most patients with CSCC are successfully treated with Mohs micrographic surgery or wide local excision (WLE) alone, but a subset will experience more severe and aggressive disease. While useful for prognostication, current staging systems do not incorporate patient factors or other high-risk tumor features that influence outcomes, which led to the NCCN reclassifying CSCC into low-, high-, and very high-risk groups. The NCCN guidelines also made a new recommendation that Mohs or PDEMA be the preferred method for tissue processing for high- and very-high-risk tumors, based on this new stratification.
However, these changes to the NCCN guidelines have not been validated. The goal of this study was to compare outcomes in very-high-, high-, and low-risk NCCN groups as well as comparing outcomes of CSCCs stratified by Mohs and WLE.
Dr. Ruiz and colleagues conducted a retrospective cohort study using patient data from two tertiary care academic medical centers. Their analysis included 10,196 tumors from 8,727 patients that were then stratified into low-risk (3,054 tumors [30.0%]), high-risk (6,269 tumors [61.5%]), and very-high-risk (873 tumors [8.6%]) groups.
Tumors in the very-high-risk group were more likely to have high-risk tumor and histologic features, such as large-caliber perineural invasion, large diameter, invasion beyond the subcutaneous fat or bone, poor differentiation, and lymphovascular invasion.
The authors found that, compared with the low-risk group, the high- and very-high-risk groups demonstrated a greater risk of LR (high-risk subhazard ratio, 1.99; P = .007; very-high-risk SHR, 12.66; P < .001); NM (high-risk SHR, 4.26; P = .02; very-high-risk SHR, 62.98; P < .001); DM (high-risk SHR, 2.2 × 107; P < .001; very-high-risk SHR, 6.3 × 108; P < .001); and DSD (high-risk SHR, 4.02; P = .03; very-high-risk SHR, 93.87; P < .001).
Adjusted 5-year cumulative incidence was also significantly higher in very-high- vs. high- and low-risk groups for all endpoints.
They next compared the procedures used to treat the tumors. Compared with WLE, patients treated with Mohs or PDEMA had a lower risk of LR (SHR, 0.65; P = .009), DM (SHR, 0.38; P = .02), and DSD (SHR, 0.55; P = .006).
Mohs and PDEMA have already became preferred surgical modalities for high- and very-high-risk tumors, and Dr. Ruiz pointed out that their analysis was for the entire cohort.
“We did not stratify this by risk group,” she said. “So our results do not change anything clinically at this time, but support prior studies that have found Mohs/PDEMA to have improved outcomes, compared to WLE. Further studies are needed evaluating surgical approach by risk-group.”
However, she emphasized, “our studies further validate prior evidence showing Mohs/PDEMA to have the lowest rates of recurrence and in this study, even disease-related death.”
Approached for an independent comment, Jeffrey M. Farma, MD, codirector of the melanoma and skin cancer program, and interim chair, department of surgical oncology, Fox Chase Cancer Center, Philadelphia, noted that this study supports the new reclassification of CSCC tumors by the NCCN, and confirms that the high-risk and very-high-risk tumors surely have a higher propensity for worse outcomes overall.
“That being said, the notion for type of resection and margin assessment is still an area of controversy in the dermatology, surgical oncology, and pathology community,” said Dr. Farma, who is also on the NCCN panel. “I believe we need further studies to truly understand the role of the type of resection and the pathologic evaluation play in this disease process.”
He also pointed out that it is unclear in this dataset if patients initially had any imaging to evaluate for local or regional metastatic disease. “It would be helpful to have a further understanding of which type of provider was performing the excisions, the type of excision decided upon, and if there was a standardized approach to [decide] which patients had MOHS or PDEMA and what was the surveillance for these patients both with imaging and physical examinations,” said Dr. Farma. “This data also evaluated patients over a long time period where practice patterns have evolved.”
Finally, he noted that the number of local and metastatic events subjectively seems low in this cohort. “We also do not know any information about the initial workup of the patients, patterns of recurrence, and adjuvant or palliative treatment after recurrence,” he added. “It is unclear from this manuscript how the type of resection or pathologic evaluation of margins leads to improved outcomes and further prospective studies are warranted.”
Dr. Ruiz reports reported serving as a coinvestigator and principal investigator for Regeneron Pharmaceuticals and as a coinvestigator for Merck and consulting for Checkpoint Therapeutics, BDO, and Genentech outside the submitted work. Dr. Farma has no disclosures other than the NCCN panel. The study was supported by Harvard Catalyst and the Harvard University Clinical and Translational Science Center and by Harvard University and its affiliated academic health care centers and partially supported by the Melvin Markey Discovery Fund at Cleveland Clinic Foundation.
, according to new findings.
In addition, regardless of the NCCN risk group, the study found that Mohs surgery or peripheral and deep en face margin assessment (PDEMA) conferred a lower risk of developing LR, DM, and disease-related death.
“Although the NCCN included this new high-risk group in the last iteration of the guidelines, there were no studies that identified whether the high-risk group achieved the goal of identifying riskier tumors,” said senior author Emily Ruiz, MD, MPH, associate physician at the Mohs and Dermatologic Surgery Center at Brigham and Women’s Faulkner Hospital, Boston. “Based on the data in our study, the risk groups did risk stratify tumors and so clinicians can utilize the high-risk group risk factors to identify which tumors may require additional surveillance or treatment.”
The study was published online in JAMA Dermatology.
Most patients with CSCC are successfully treated with Mohs micrographic surgery or wide local excision (WLE) alone, but a subset will experience more severe and aggressive disease. While useful for prognostication, current staging systems do not incorporate patient factors or other high-risk tumor features that influence outcomes, which led to the NCCN reclassifying CSCC into low-, high-, and very high-risk groups. The NCCN guidelines also made a new recommendation that Mohs or PDEMA be the preferred method for tissue processing for high- and very-high-risk tumors, based on this new stratification.
However, these changes to the NCCN guidelines have not been validated. The goal of this study was to compare outcomes in very-high-, high-, and low-risk NCCN groups as well as comparing outcomes of CSCCs stratified by Mohs and WLE.
Dr. Ruiz and colleagues conducted a retrospective cohort study using patient data from two tertiary care academic medical centers. Their analysis included 10,196 tumors from 8,727 patients that were then stratified into low-risk (3,054 tumors [30.0%]), high-risk (6,269 tumors [61.5%]), and very-high-risk (873 tumors [8.6%]) groups.
Tumors in the very-high-risk group were more likely to have high-risk tumor and histologic features, such as large-caliber perineural invasion, large diameter, invasion beyond the subcutaneous fat or bone, poor differentiation, and lymphovascular invasion.
The authors found that, compared with the low-risk group, the high- and very-high-risk groups demonstrated a greater risk of LR (high-risk subhazard ratio, 1.99; P = .007; very-high-risk SHR, 12.66; P < .001); NM (high-risk SHR, 4.26; P = .02; very-high-risk SHR, 62.98; P < .001); DM (high-risk SHR, 2.2 × 107; P < .001; very-high-risk SHR, 6.3 × 108; P < .001); and DSD (high-risk SHR, 4.02; P = .03; very-high-risk SHR, 93.87; P < .001).
Adjusted 5-year cumulative incidence was also significantly higher in very-high- vs. high- and low-risk groups for all endpoints.
They next compared the procedures used to treat the tumors. Compared with WLE, patients treated with Mohs or PDEMA had a lower risk of LR (SHR, 0.65; P = .009), DM (SHR, 0.38; P = .02), and DSD (SHR, 0.55; P = .006).
Mohs and PDEMA have already became preferred surgical modalities for high- and very-high-risk tumors, and Dr. Ruiz pointed out that their analysis was for the entire cohort.
“We did not stratify this by risk group,” she said. “So our results do not change anything clinically at this time, but support prior studies that have found Mohs/PDEMA to have improved outcomes, compared to WLE. Further studies are needed evaluating surgical approach by risk-group.”
However, she emphasized, “our studies further validate prior evidence showing Mohs/PDEMA to have the lowest rates of recurrence and in this study, even disease-related death.”
Approached for an independent comment, Jeffrey M. Farma, MD, codirector of the melanoma and skin cancer program, and interim chair, department of surgical oncology, Fox Chase Cancer Center, Philadelphia, noted that this study supports the new reclassification of CSCC tumors by the NCCN, and confirms that the high-risk and very-high-risk tumors surely have a higher propensity for worse outcomes overall.
“That being said, the notion for type of resection and margin assessment is still an area of controversy in the dermatology, surgical oncology, and pathology community,” said Dr. Farma, who is also on the NCCN panel. “I believe we need further studies to truly understand the role of the type of resection and the pathologic evaluation play in this disease process.”
He also pointed out that it is unclear in this dataset if patients initially had any imaging to evaluate for local or regional metastatic disease. “It would be helpful to have a further understanding of which type of provider was performing the excisions, the type of excision decided upon, and if there was a standardized approach to [decide] which patients had MOHS or PDEMA and what was the surveillance for these patients both with imaging and physical examinations,” said Dr. Farma. “This data also evaluated patients over a long time period where practice patterns have evolved.”
Finally, he noted that the number of local and metastatic events subjectively seems low in this cohort. “We also do not know any information about the initial workup of the patients, patterns of recurrence, and adjuvant or palliative treatment after recurrence,” he added. “It is unclear from this manuscript how the type of resection or pathologic evaluation of margins leads to improved outcomes and further prospective studies are warranted.”
Dr. Ruiz reports reported serving as a coinvestigator and principal investigator for Regeneron Pharmaceuticals and as a coinvestigator for Merck and consulting for Checkpoint Therapeutics, BDO, and Genentech outside the submitted work. Dr. Farma has no disclosures other than the NCCN panel. The study was supported by Harvard Catalyst and the Harvard University Clinical and Translational Science Center and by Harvard University and its affiliated academic health care centers and partially supported by the Melvin Markey Discovery Fund at Cleveland Clinic Foundation.
FROM JAMA DERMATOLOGY
Drugmakers are abandoning cheap generics, and now U.S. cancer patients can’t get meds
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
On Nov. 22, three Food and Drug Administration inspectors arrived at the sprawling Intas Pharmaceuticals plant south of Ahmedabad, India, and found hundreds of trash bags full of shredded documents tossed into a garbage truck. Over the next 10 days, the inspectors assessed what looked like a systematic effort to conceal quality problems at the plant, which provided more than half of the U.S. supply of generic cisplatin and carboplatin, two cheap drugs used to treat as many as 500,000 new cancer cases every year.
Their decisions are likely to result in preventable deaths.
Cisplatin and carboplatin are among scores of drugs in shortage, including 12 other cancer drugs, ADHD pills, blood thinners, and antibiotics. COVID-hangover supply chain issues and limited FDA oversight are part of the problem, but the main cause, experts agree, is the underlying weakness of the generic drug industry. Made mostly overseas, these old but crucial drugs are often sold at a loss or for little profit. Domestic manufacturers have little interest in making them, setting their sights instead on high-priced drugs with plump profit margins.
The problem isn’t new, and that’s particularly infuriating to many clinicians. President Joe Biden, whose son Beau died of an aggressive brain cancer, has focused his Cancer Moonshot on discovering cures – undoubtedly expensive ones. Indeed, existing brand-name cancer drugs often cost tens of thousands of dollars a year.
But what about the thousands of patients today who can’t get a drug like cisplatin, approved by the FDA in 1978 and costing as little as $6 a dose?
“It’s just insane,” said Mark Ratain, MD, a cancer doctor and pharmacologist at the University of Chicago. “Your roof is caving in, but you want to build a basketball court in the backyard because your wife is pregnant with twin boys and you want them to be NBA stars when they grow up?”
“It’s just a travesty that this is the level of health care in the United States of America right now,” said Stephen Divers, MD, an oncologist in Hot Springs, Ark., who in recent weeks has had to delay or change treatment for numerous bladder, breast, and ovarian cancer patients because his clinic cannot find enough cisplatin and carboplatin. Results from a survey of academic cancer centers released June 7 found 93% couldn’t find enough carboplatin and 70% had cisplatin shortages.
“All day, in between patients, we hold staff meetings trying to figure this out,” said Bonny Moore, MD, an oncologist in Fredericksburg, Virginia. “It’s the most nauseous I’ve ever felt. Our office stayed open during COVID; we never had to stop treating patients. We got them vaccinated, kept them safe, and now I can’t get them a $10 drug.”
The cancer clinicians KFF Health News interviewed for this story said that, given current shortages, they prioritize patients who can be cured over later-stage patients, in whom the drugs generally can only slow the disease, and for whom alternatives – though sometimes less effective and often with more side effects – are available. But some doctors are even rationing doses intended to cure.
Isabella McDonald, then a junior at Utah Valley University, was diagnosed in April with a rare, often fatal bone cancer, whose sole treatment for young adults includes the drug methotrexate. When Isabella’s second cycle of treatment began June 5, clinicians advised that she would be getting less than the full dose because of a methotrexate shortage, said her father, Brent.
“They don’t think it will have a negative impact on her treatment, but as far as I am aware, there isn’t any scientific basis to make that conclusion,” he said. “As you can imagine, when they gave us such low odds of her beating this cancer, it feels like we want to give it everything we can and not something short of the standard.”
Mr. McDonald stressed that he didn’t blame the staffers at Intermountain Health who take care of Isabella. The family – his other daughter, Cate, made a TikTok video about her sister’s plight – were simply stunned at such a basic flaw in the health care system.
At Dr. Moore’s practice, in Virginia, clinicians gave 60% of the optimal dose of carboplatin to some uterine cancer patients during the week of May 16, then shifted to 80% after a small shipment came in the following week. The doctors had to omit carboplatin from normal combination treatments for patients with recurrent disease, she said.
On June 2, Dr. Moore and colleagues were glued to their drug distributor’s website, anxious as teenagers waiting for Taylor Swift tickets to go on sale – only with mortal consequences at stake.
She later emailed KFF Health News: “Carboplatin did NOT come back in stock today. Neither did cisplatin.”
Doses remained at 80%, she said. Things hadn’t changed 10 days later.
Generics manufacturers are pulling out
The causes of shortages are well established. Everyone wants to pay less, and the middlemen who procure and distribute generics keep driving down wholesale prices. The average net price of generic drugs fell by more than half between 2016 and 2022, according to research by Anthony Sardella, a business professor at Washington University in St. Louis.
As generics manufacturers compete to win sales contracts with the big negotiators of such purchases, such as Vizient and Premier, their profits sink. Some are going out of business. Akorn, which made 75 common generics, went bankrupt and closed in February. Israeli generics giant Teva, which has a portfolio of 3,600 medicines, announced May 18 it was shifting to brand-name drugs and “high-value generics.” Lannett, with about 120 generics, announced a Chapter 11 reorganization amid declining revenue. Other companies are in trouble too, said David Gaugh, interim CEO of the Association for Accessible Medicines, the leading generics trade group.
The generics industry used to lose money on about a third of the drugs it produced, but now it’s more like half, Mr. Gaugh said. So when a company stops making a drug, others do not necessarily step up, he said. Officials at Fresenius Kabi and Pfizer said they have increased their carboplatin production since March, but not enough to end the shortage. On June 2, FDA Commissioner Robert Califf announced the agency had given emergency authorization for Chinese-made cisplatin to enter the U.S. market, but the impact of the move wasn’t immediately clear.
Cisplatin and carboplatin are made in special production lines under sterile conditions, and expanding or changing the lines requires FDA approval. Bargain-basement prices have pushed production overseas, where it’s harder for the FDA to track quality standards. The Intas plant inspection was a relative rarity in India, where the FDA in 2022 reportedly inspected only 3% of sites that make drugs for the U.S. market. Mr. Sardella testified in May that a quarter of all U.S. drug prescriptions are filled by companies that received FDA warning letters in the past 26 months. And pharmaceutical industry product recalls are at their highest level in 18 years, reflecting fragile supply conditions.
The FDA listed 137 drugs in shortage as of June 13, including many essential medicines made by few companies.
Intas voluntarily shut down its Ahmedabad plant after the FDA inspection, and the agency posted its shocking inspection report in January. Accord Healthcare, the U.S. subsidiary of Intas, said in mid-June it had no date for restarting production.
Asked why it waited 2 months after its inspection to announce the cisplatin shortage, given that Intas supplied more than half the U.S. market for the drug, the FDA said via email that it doesn’t list a drug in shortage until it has “confirmed that overall market demand is not being met.”
Prices for carboplatin, cisplatin, and other drugs have skyrocketed on the so-called gray market, where speculators sell medicines they snapped up in anticipation of shortages. A 600-mg bottle of carboplatin, normally available for $30, was going for $185 in early May and $345 a week later, said Richard Scanlon, the pharmacist at dr. Moore’s clinic.
“It’s hard to have these conversations with patients – ‘I have your dose for this cycle, but not sure about next cycle,’” said Mark Einstein, MD, chair of the department of obstetrics, gynecology and reproductive health at New Jersey Medical School, Newark.
Should government step in?
Despite a drug shortage task force and numerous congressional hearings, progress has been slow at best. The 2020 CARES Act gave the FDA the power to require companies to have contingency plans enabling them to respond to shortages, but the agency has not yet implemented guidance to enforce the provisions.
As a result, neither Accord nor other cisplatin makers had a response plan in place when Intas’ plant was shut down, said Soumi Saha, senior vice president of government affairs for Premier, which arranges wholesale drug purchases for more than 4,400 hospitals and health systems.
Premier understood in December that the shutdown endangered the U.S. supply of cisplatin and carboplatin, but it also didn’t issue an immediate alarm. “It’s a fine balance,” she said. “You don’t want to create panic-buying or hoarding.”
More lasting solutions are under discussion. Mr. Sardella and others have proposed government subsidies to get U.S. generics plants running full time. Their capacity is now half-idle. If federal agencies like the Centers for Medicare & Medicaid Services paid more for more safely and efficiently produced drugs, it would promote a more stable supply chain, he said.
“At a certain point the system needs to recognize there’s a high cost to low-cost drugs,” said Allan Coukell, senior vice president for public policy at Civica Rx, a nonprofit funded by health systems, foundations, and the federal government that provides about 80 drugs to hospitals in its network. Civica is building a $140 million factory near Petersburg, Va., that will produce dozens more, Mr. Coukell said.
Dr. Ratain and his University of Chicago colleague Satyajit Kosuri, MD, recently called for the creation of a strategic inventory buffer for generic medications, something like the Strategic Petroleum Reserve, set up in 1975 in response to the OPEC oil crisis.
In fact, Dr. Ratain reckons, selling a quarter-million barrels of oil would probably generate enough cash to make and store 2 years’ worth of carboplatin and cisplatin.
“It would almost literally be a drop in the bucket.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF – an independent source of health policy research, polling, and journalism. Learn more about KFF.
Commentary: Topical treatments, dupilumab, and long-term treatment of AD, July 2023
Silverberg and colleagues described a very well-designed, vehicle-controlled, randomized 8-week study of a topical formulation of a purified strain of Nitrosomonas eutropha, an ammonia-oxidizing bacterium. In theory, this bacterium may reduce Staphylococcus aureus. The study compared two concentrations of the bacterium vs vehicle delivered as a spray twice per day. Study participants were adults with AD affecting 10%-40% of body surface area.
The study found "meaningful" improvements in itch and objective signs of disease, with clear separation between both doses of the bacterial spray compared with vehicle. At week 4, about 23% of participants treated with the bacterium were clear or almost clear (with a 2-point improvement) compared with 12% in the vehicle group (for comparison, in a phase 2 study comparing topical ruxolitinib with 0.1% triamcinolone cream, there was a 25% clear or almost clear rate [with 2-point improvement] in the triamcinolone-treated individuals).
Though an "all-natural" bacterial approach to managing AD may be appealing to some, it sounded like magic to me. But this well-done study makes it seem like the bacterial approach could be more promising than I had thought. This study also reported about twice as many adverse events (including gastrointestinal issues) with the bacterium-treated participants compared with those who received vehicle, adding to my belief that the bacterial product has efficacy. Whether any other topical will be more effective and safer than is topical triamcinolone remains to be seen. I'm still pessimistic about topicals because of patients' poor adherence to topical treatment, but perhaps an easy-to-use spray that isn't associated with patients' fear of "steroids" will be helpful.
Chen and colleagues. They analyzed data on hundreds of thousands of patients with and without AD. Adults with AD had a "significantly increased risk" of developing venous thromboembolism compared with adults without AD. The huge sample size of their study seems compelling. That huge sample size allows detection of effects so small that they may be clinically insignificant.
They report that patients with AD had a venous thromboembolism at a rate of 1.05/1000 patients-years; the rate was 0.82 for patients without AD. From that, we can calculate that there would be an additional 23 patients with venous thromboembolism for every 100,000 patient-years or about one more venous thromboembolism in the AD group in every 4000 patient-years. Though the finding was statistically significant, I don't think it is clinically meaningful.
The authors correctly conclude that "vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients with AD who present with relevant symptoms (eg, unexplained dyspnea, chest tightness, and limb swelling)." But it is probably also true that vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients without AD who present with those symptoms. I think the authors might have been on solid ground if they had concluded that there was a statistically significant but clinically insignificant increased risk for venous thromboembolism in patients with AD.
Eichenfeld and colleagues examined the use of topical crisaborole once per day as a maintenance treatment for patients with mild to moderate AD. The study compared patients given topical crisaborole with those randomly assigned to vehicle. The active treatment was effective because topical crisaborole treated patients had longer times to the first flare following treatment and fewer flares over the 1 year of treatment. The differences were not huge, but I think they were clinically meaningful. I'm guessing that the topical crisaborole maintenance treatment would have been even more effective had it been used regularly. The study did not, as far as I could tell, assess how well the treatment was used.
An interesting aspect of this study is that it began with nearly 500 participants who started on twice daily topical crisaborole. The 270 patients who responded to the treatment (achieving clear or almost clear with at least a 2-point improvement) were enrolled in the 1-year maintenance phase. Thus, the participants in the maintenance phase were preselected for patients who respond to topical crisaborole. We don't know why they were responders (I, of course, expect it is because they selected for patients who are better than others are at using a topical treatment), but it may be best not to try to generalize these results and assume this form of maintenance treatment would work equally well in a population who achieve initial success with an oral therapy regimen (for example, a quick course of oral prednisone).
Dupilumab was a revolutionary treatment for AD. I didn't think that I'd ever see a more effective treatment. It's so safe too! It has been a first-line treatment for AD since its introduction. Now, we also have oral Janus kinase inhibitor options. Blauvelt and colleagues examined what happens when patients who have been on dupilumab are switched to a high dose (30 mg/d) of upadacitinib (the standard starting dose of upadacitinib is 15 mg/d). Though dupilumab is very effective, upadacitinib is more so. After 4 weeks of switching to upadacitinib, nearly half the patients were completely clear of AD compared with only 16.0% after 24 weeks of dupilumab! The authors point out, optimistically, that "No new safety risks were observed." Though there were no cancers, gastrointestinal perforations, major adverse cardiovascular events, or venous thromboembolic events, there were cases of eczema herpeticum and zoster in patients treated with upadacitinib. Having upadacitinib available for patients who fail dupilumab is a clear benefit; the role of upadacitinib before dupilumab seems less clear.
Patients doing great on dupilumab for AD may be wondering: Do I still need to take it every 2 weeks? Spekhorst and colleagues may have the answer. They describe the response to tapering dupilumab in patients who had been on the drug for at least 1 year with well-controlled disease for at least 6 months. Patients in the study then continued dupilumab with the longest possible dosing interval while maintaining control of their AD.
Generally, patients maintained good control of their AD, with only a small increase in mean disease severity and in concomitant use of topical steroids. For the patients who attempted prolongation, 83% successfully continued dupilumab treatment with a prolonged interval. Not at all surprisingly, the authors calculated that prolonging the interval between dosing led to large savings in cost.
One of the nice features of dupilumab treatment is that loss of response over time seems unusual. Perhaps there is a low propensity for forming antidrug antibodies when dupilumab is used in the standard every 2-week dosing regimen. I don't know whether antidrug antibodies would be more likely with the intermittent dosing regimen. But now that we have other good systemic treatment options for AD, losing dupilumab efficacy would not be as critical a problem as it used to be. I also want to point out that patients' adherence to injection treatment, though better than adherence to topicals, is far from perfect. It's likely that many patients have already been prolonging the interval between taking their treatments. If you want to know, just ask them. The way I like to phrase the question is: "Are you keeping the extra injectors you've accumulated refrigerated like you are supposed to?"
Silverberg and colleagues described a very well-designed, vehicle-controlled, randomized 8-week study of a topical formulation of a purified strain of Nitrosomonas eutropha, an ammonia-oxidizing bacterium. In theory, this bacterium may reduce Staphylococcus aureus. The study compared two concentrations of the bacterium vs vehicle delivered as a spray twice per day. Study participants were adults with AD affecting 10%-40% of body surface area.
The study found "meaningful" improvements in itch and objective signs of disease, with clear separation between both doses of the bacterial spray compared with vehicle. At week 4, about 23% of participants treated with the bacterium were clear or almost clear (with a 2-point improvement) compared with 12% in the vehicle group (for comparison, in a phase 2 study comparing topical ruxolitinib with 0.1% triamcinolone cream, there was a 25% clear or almost clear rate [with 2-point improvement] in the triamcinolone-treated individuals).
Though an "all-natural" bacterial approach to managing AD may be appealing to some, it sounded like magic to me. But this well-done study makes it seem like the bacterial approach could be more promising than I had thought. This study also reported about twice as many adverse events (including gastrointestinal issues) with the bacterium-treated participants compared with those who received vehicle, adding to my belief that the bacterial product has efficacy. Whether any other topical will be more effective and safer than is topical triamcinolone remains to be seen. I'm still pessimistic about topicals because of patients' poor adherence to topical treatment, but perhaps an easy-to-use spray that isn't associated with patients' fear of "steroids" will be helpful.
Chen and colleagues. They analyzed data on hundreds of thousands of patients with and without AD. Adults with AD had a "significantly increased risk" of developing venous thromboembolism compared with adults without AD. The huge sample size of their study seems compelling. That huge sample size allows detection of effects so small that they may be clinically insignificant.
They report that patients with AD had a venous thromboembolism at a rate of 1.05/1000 patients-years; the rate was 0.82 for patients without AD. From that, we can calculate that there would be an additional 23 patients with venous thromboembolism for every 100,000 patient-years or about one more venous thromboembolism in the AD group in every 4000 patient-years. Though the finding was statistically significant, I don't think it is clinically meaningful.
The authors correctly conclude that "vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients with AD who present with relevant symptoms (eg, unexplained dyspnea, chest tightness, and limb swelling)." But it is probably also true that vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients without AD who present with those symptoms. I think the authors might have been on solid ground if they had concluded that there was a statistically significant but clinically insignificant increased risk for venous thromboembolism in patients with AD.
Eichenfeld and colleagues examined the use of topical crisaborole once per day as a maintenance treatment for patients with mild to moderate AD. The study compared patients given topical crisaborole with those randomly assigned to vehicle. The active treatment was effective because topical crisaborole treated patients had longer times to the first flare following treatment and fewer flares over the 1 year of treatment. The differences were not huge, but I think they were clinically meaningful. I'm guessing that the topical crisaborole maintenance treatment would have been even more effective had it been used regularly. The study did not, as far as I could tell, assess how well the treatment was used.
An interesting aspect of this study is that it began with nearly 500 participants who started on twice daily topical crisaborole. The 270 patients who responded to the treatment (achieving clear or almost clear with at least a 2-point improvement) were enrolled in the 1-year maintenance phase. Thus, the participants in the maintenance phase were preselected for patients who respond to topical crisaborole. We don't know why they were responders (I, of course, expect it is because they selected for patients who are better than others are at using a topical treatment), but it may be best not to try to generalize these results and assume this form of maintenance treatment would work equally well in a population who achieve initial success with an oral therapy regimen (for example, a quick course of oral prednisone).
Dupilumab was a revolutionary treatment for AD. I didn't think that I'd ever see a more effective treatment. It's so safe too! It has been a first-line treatment for AD since its introduction. Now, we also have oral Janus kinase inhibitor options. Blauvelt and colleagues examined what happens when patients who have been on dupilumab are switched to a high dose (30 mg/d) of upadacitinib (the standard starting dose of upadacitinib is 15 mg/d). Though dupilumab is very effective, upadacitinib is more so. After 4 weeks of switching to upadacitinib, nearly half the patients were completely clear of AD compared with only 16.0% after 24 weeks of dupilumab! The authors point out, optimistically, that "No new safety risks were observed." Though there were no cancers, gastrointestinal perforations, major adverse cardiovascular events, or venous thromboembolic events, there were cases of eczema herpeticum and zoster in patients treated with upadacitinib. Having upadacitinib available for patients who fail dupilumab is a clear benefit; the role of upadacitinib before dupilumab seems less clear.
Patients doing great on dupilumab for AD may be wondering: Do I still need to take it every 2 weeks? Spekhorst and colleagues may have the answer. They describe the response to tapering dupilumab in patients who had been on the drug for at least 1 year with well-controlled disease for at least 6 months. Patients in the study then continued dupilumab with the longest possible dosing interval while maintaining control of their AD.
Generally, patients maintained good control of their AD, with only a small increase in mean disease severity and in concomitant use of topical steroids. For the patients who attempted prolongation, 83% successfully continued dupilumab treatment with a prolonged interval. Not at all surprisingly, the authors calculated that prolonging the interval between dosing led to large savings in cost.
One of the nice features of dupilumab treatment is that loss of response over time seems unusual. Perhaps there is a low propensity for forming antidrug antibodies when dupilumab is used in the standard every 2-week dosing regimen. I don't know whether antidrug antibodies would be more likely with the intermittent dosing regimen. But now that we have other good systemic treatment options for AD, losing dupilumab efficacy would not be as critical a problem as it used to be. I also want to point out that patients' adherence to injection treatment, though better than adherence to topicals, is far from perfect. It's likely that many patients have already been prolonging the interval between taking their treatments. If you want to know, just ask them. The way I like to phrase the question is: "Are you keeping the extra injectors you've accumulated refrigerated like you are supposed to?"
Silverberg and colleagues described a very well-designed, vehicle-controlled, randomized 8-week study of a topical formulation of a purified strain of Nitrosomonas eutropha, an ammonia-oxidizing bacterium. In theory, this bacterium may reduce Staphylococcus aureus. The study compared two concentrations of the bacterium vs vehicle delivered as a spray twice per day. Study participants were adults with AD affecting 10%-40% of body surface area.
The study found "meaningful" improvements in itch and objective signs of disease, with clear separation between both doses of the bacterial spray compared with vehicle. At week 4, about 23% of participants treated with the bacterium were clear or almost clear (with a 2-point improvement) compared with 12% in the vehicle group (for comparison, in a phase 2 study comparing topical ruxolitinib with 0.1% triamcinolone cream, there was a 25% clear or almost clear rate [with 2-point improvement] in the triamcinolone-treated individuals).
Though an "all-natural" bacterial approach to managing AD may be appealing to some, it sounded like magic to me. But this well-done study makes it seem like the bacterial approach could be more promising than I had thought. This study also reported about twice as many adverse events (including gastrointestinal issues) with the bacterium-treated participants compared with those who received vehicle, adding to my belief that the bacterial product has efficacy. Whether any other topical will be more effective and safer than is topical triamcinolone remains to be seen. I'm still pessimistic about topicals because of patients' poor adherence to topical treatment, but perhaps an easy-to-use spray that isn't associated with patients' fear of "steroids" will be helpful.
Chen and colleagues. They analyzed data on hundreds of thousands of patients with and without AD. Adults with AD had a "significantly increased risk" of developing venous thromboembolism compared with adults without AD. The huge sample size of their study seems compelling. That huge sample size allows detection of effects so small that they may be clinically insignificant.
They report that patients with AD had a venous thromboembolism at a rate of 1.05/1000 patients-years; the rate was 0.82 for patients without AD. From that, we can calculate that there would be an additional 23 patients with venous thromboembolism for every 100,000 patient-years or about one more venous thromboembolism in the AD group in every 4000 patient-years. Though the finding was statistically significant, I don't think it is clinically meaningful.
The authors correctly conclude that "vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients with AD who present with relevant symptoms (eg, unexplained dyspnea, chest tightness, and limb swelling)." But it is probably also true that vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients without AD who present with those symptoms. I think the authors might have been on solid ground if they had concluded that there was a statistically significant but clinically insignificant increased risk for venous thromboembolism in patients with AD.
Eichenfeld and colleagues examined the use of topical crisaborole once per day as a maintenance treatment for patients with mild to moderate AD. The study compared patients given topical crisaborole with those randomly assigned to vehicle. The active treatment was effective because topical crisaborole treated patients had longer times to the first flare following treatment and fewer flares over the 1 year of treatment. The differences were not huge, but I think they were clinically meaningful. I'm guessing that the topical crisaborole maintenance treatment would have been even more effective had it been used regularly. The study did not, as far as I could tell, assess how well the treatment was used.
An interesting aspect of this study is that it began with nearly 500 participants who started on twice daily topical crisaborole. The 270 patients who responded to the treatment (achieving clear or almost clear with at least a 2-point improvement) were enrolled in the 1-year maintenance phase. Thus, the participants in the maintenance phase were preselected for patients who respond to topical crisaborole. We don't know why they were responders (I, of course, expect it is because they selected for patients who are better than others are at using a topical treatment), but it may be best not to try to generalize these results and assume this form of maintenance treatment would work equally well in a population who achieve initial success with an oral therapy regimen (for example, a quick course of oral prednisone).
Dupilumab was a revolutionary treatment for AD. I didn't think that I'd ever see a more effective treatment. It's so safe too! It has been a first-line treatment for AD since its introduction. Now, we also have oral Janus kinase inhibitor options. Blauvelt and colleagues examined what happens when patients who have been on dupilumab are switched to a high dose (30 mg/d) of upadacitinib (the standard starting dose of upadacitinib is 15 mg/d). Though dupilumab is very effective, upadacitinib is more so. After 4 weeks of switching to upadacitinib, nearly half the patients were completely clear of AD compared with only 16.0% after 24 weeks of dupilumab! The authors point out, optimistically, that "No new safety risks were observed." Though there were no cancers, gastrointestinal perforations, major adverse cardiovascular events, or venous thromboembolic events, there were cases of eczema herpeticum and zoster in patients treated with upadacitinib. Having upadacitinib available for patients who fail dupilumab is a clear benefit; the role of upadacitinib before dupilumab seems less clear.
Patients doing great on dupilumab for AD may be wondering: Do I still need to take it every 2 weeks? Spekhorst and colleagues may have the answer. They describe the response to tapering dupilumab in patients who had been on the drug for at least 1 year with well-controlled disease for at least 6 months. Patients in the study then continued dupilumab with the longest possible dosing interval while maintaining control of their AD.
Generally, patients maintained good control of their AD, with only a small increase in mean disease severity and in concomitant use of topical steroids. For the patients who attempted prolongation, 83% successfully continued dupilumab treatment with a prolonged interval. Not at all surprisingly, the authors calculated that prolonging the interval between dosing led to large savings in cost.
One of the nice features of dupilumab treatment is that loss of response over time seems unusual. Perhaps there is a low propensity for forming antidrug antibodies when dupilumab is used in the standard every 2-week dosing regimen. I don't know whether antidrug antibodies would be more likely with the intermittent dosing regimen. But now that we have other good systemic treatment options for AD, losing dupilumab efficacy would not be as critical a problem as it used to be. I also want to point out that patients' adherence to injection treatment, though better than adherence to topicals, is far from perfect. It's likely that many patients have already been prolonging the interval between taking their treatments. If you want to know, just ask them. The way I like to phrase the question is: "Are you keeping the extra injectors you've accumulated refrigerated like you are supposed to?"
Commentary: Topical treatments, dupilumab, and long-term treatment of AD, July 2023
There is a tremendous amount of atopic dermatitis (AD) research underway. This month, we have several interesting articles to present.
Silverberg and colleagues described a very well-designed, vehicle-controlled, randomized 8-week study of a topical formulation of a purified strain of Nitrosomonas eutropha, an ammonia-oxidizing bacterium. In theory, this bacterium may reduce Staphylococcus aureus. The study compared two concentrations of the bacterium vs vehicle delivered as a spray twice per day. Study participants were adults with AD affecting 10%-40% of body surface area.
The study found "meaningful" improvements in itch and objective signs of disease, with clear separation between both doses of the bacterial spray compared with vehicle. At week 4, about 23% of participants treated with the bacterium were clear or almost clear (with a 2-point improvement) compared with 12% in the vehicle group (for comparison, in a phase 2 study comparing topical ruxolitinib with 0.1% triamcinolone cream, there was a 25% clear or almost clear rate [with 2-point improvement] in the triamcinolone-treated individuals).
Though an "all-natural" bacterial approach to managing AD may be appealing to some, it sounded like magic to me. But this well-done study makes it seem like the bacterial approach could be more promising than I had thought. This study also reported about twice as many adverse events (including gastrointestinal issues) with the bacterium-treated participants compared with those who received vehicle, adding to my belief that the bacterial product has efficacy. Whether any other topical will be more effective and safer than is topical triamcinolone remains to be seen. I'm still pessimistic about topicals because of patients' poor adherence to topical treatment, but perhaps an easy-to-use spray that isn't associated with patients' fear of "steroids" will be helpful.
I love articles like this one from Chen and colleagues. They analyzed data on hundreds of thousands of patients with and without AD. Adults with AD had a "significantly increased risk" of developing venous thromboembolism compared with adults without AD. The huge sample size of their study seems compelling. That huge sample size allows detection of effects so small that they may be clinically insignificant.
They report that patients with AD had a venous thromboembolism at a rate of 1.05/1000 patients-years; the rate was 0.82 for patients without AD. From that, we can calculate that there would be an additional 23 patients with venous thromboembolism for every 100,000 patient-years or about one more venous thromboembolism in the AD group in every 4000 patient-years. Though the finding was statistically significant, I don't think it is clinically meaningful.
The authors correctly conclude that "vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients with AD who present with relevant symptoms (eg, unexplained dyspnea, chest tightness, and limb swelling)." But it is probably also true that vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients without AD who present with those symptoms. I think the authors might have been on solid ground if they had concluded that there was a statistically significant but clinically insignificant increased risk for venous thromboembolism in patients with AD.
Eichenfeld and colleagues examined the use of topical crisaborole once per day as a maintenance treatment for patients with mild to moderate AD. The study compared patients given topical crisaborole with those randomly assigned to vehicle. The active treatment was effective because topical crisaborole treated patients had longer times to the first flare following treatment and fewer flares over the 1 year of treatment. The differences were not huge, but I think they were clinically meaningful. I'm guessing that the topical crisaborole maintenance treatment would have been even more effective had it been used regularly. The study did not, as far as I could tell, assess how well the treatment was used.
An interesting aspect of this study is that it began with nearly 500 participants who started on twice daily topical crisaborole. The 270 patients who responded to the treatment (achieving clear or almost clear with at least a 2-point improvement) were enrolled in the 1-year maintenance phase. Thus, the participants in the maintenance phase were preselected for patients who respond to topical crisaborole. We don't know why they were responders (I, of course, expect it is because they selected for patients who are better than others are at using a topical treatment), but it may be best not to try to generalize these results and assume this form of maintenance treatment would work equally well in a population who achieve initial success with an oral therapy regimen (for example, a quick course of oral prednisone).
Dupilumab was a revolutionary treatment for AD. I didn't think that I'd ever see a more effective treatment. It's so safe too! It has been a first-line treatment for AD since its introduction. Now, we also have oral Janus kinase inhibitor options. Blauvelt and colleagues examined what happens when patients who have been on dupilumab are switched to a high dose (30 mg/d) of upadacitinib (the standard starting dose of upadacitinib is 15 mg/d). Though dupilumab is very effective, upadacitinib is more so. After 4 weeks of switching to upadacitinib, nearly half the patients were completely clear of AD compared with only 16.0% after 24 weeks of dupilumab! The authors point out, optimistically, that "No new safety risks were observed." Though there were no cancers, gastrointestinal perforations, major adverse cardiovascular events, or venous thromboembolic events, there were cases of eczema herpeticum and zoster in patients treated with upadacitinib. Having upadacitinib available for patients who fail dupilumab is a clear benefit; the role of upadacitinib before dupilumab seems less clear.
Patients doing great on dupilumab for AD may be wondering: Do I still need to take it every 2 weeks? Spekhorst and colleagues may have the answer. They describe the response to tapering dupilumab in patients who had been on the drug for at least 1 year with well-controlled disease for at least 6 months. Patients in the study then continued dupilumab with the longest possible dosing interval while maintaining control of their AD.
Generally, patients maintained good control of their AD, with only a small increase in mean disease severity and in concomitant use of topical steroids. For the patients who attempted prolongation, 83% successfully continued dupilumab treatment with a prolonged interval. Not at all surprisingly, the authors calculated that prolonging the interval between dosing led to large savings in cost.
One of the nice features of dupilumab treatment is that loss of response over time seems unusual. Perhaps there is a low propensity for forming antidrug antibodies when dupilumab is used in the standard every 2-week dosing regimen. I don't know whether antidrug antibodies would be more likely with the intermittent dosing regimen. But now that we have other good systemic treatment options for AD, losing dupilumab efficacy would not be as critical a problem as it used to be. I also want to point out that patients' adherence to injection treatment, though better than adherence to topicals, is far from perfect. It's likely that many patients have already been prolonging the interval between taking their treatments. If you want to know, just ask them. The way I like to phrase the question is: "Are you keeping the extra injectors you've accumulated refrigerated like you are supposed to?"
There is a tremendous amount of atopic dermatitis (AD) research underway. This month, we have several interesting articles to present.
Silverberg and colleagues described a very well-designed, vehicle-controlled, randomized 8-week study of a topical formulation of a purified strain of Nitrosomonas eutropha, an ammonia-oxidizing bacterium. In theory, this bacterium may reduce Staphylococcus aureus. The study compared two concentrations of the bacterium vs vehicle delivered as a spray twice per day. Study participants were adults with AD affecting 10%-40% of body surface area.
The study found "meaningful" improvements in itch and objective signs of disease, with clear separation between both doses of the bacterial spray compared with vehicle. At week 4, about 23% of participants treated with the bacterium were clear or almost clear (with a 2-point improvement) compared with 12% in the vehicle group (for comparison, in a phase 2 study comparing topical ruxolitinib with 0.1% triamcinolone cream, there was a 25% clear or almost clear rate [with 2-point improvement] in the triamcinolone-treated individuals).
Though an "all-natural" bacterial approach to managing AD may be appealing to some, it sounded like magic to me. But this well-done study makes it seem like the bacterial approach could be more promising than I had thought. This study also reported about twice as many adverse events (including gastrointestinal issues) with the bacterium-treated participants compared with those who received vehicle, adding to my belief that the bacterial product has efficacy. Whether any other topical will be more effective and safer than is topical triamcinolone remains to be seen. I'm still pessimistic about topicals because of patients' poor adherence to topical treatment, but perhaps an easy-to-use spray that isn't associated with patients' fear of "steroids" will be helpful.
I love articles like this one from Chen and colleagues. They analyzed data on hundreds of thousands of patients with and without AD. Adults with AD had a "significantly increased risk" of developing venous thromboembolism compared with adults without AD. The huge sample size of their study seems compelling. That huge sample size allows detection of effects so small that they may be clinically insignificant.
They report that patients with AD had a venous thromboembolism at a rate of 1.05/1000 patients-years; the rate was 0.82 for patients without AD. From that, we can calculate that there would be an additional 23 patients with venous thromboembolism for every 100,000 patient-years or about one more venous thromboembolism in the AD group in every 4000 patient-years. Though the finding was statistically significant, I don't think it is clinically meaningful.
The authors correctly conclude that "vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients with AD who present with relevant symptoms (eg, unexplained dyspnea, chest tightness, and limb swelling)." But it is probably also true that vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients without AD who present with those symptoms. I think the authors might have been on solid ground if they had concluded that there was a statistically significant but clinically insignificant increased risk for venous thromboembolism in patients with AD.
Eichenfeld and colleagues examined the use of topical crisaborole once per day as a maintenance treatment for patients with mild to moderate AD. The study compared patients given topical crisaborole with those randomly assigned to vehicle. The active treatment was effective because topical crisaborole treated patients had longer times to the first flare following treatment and fewer flares over the 1 year of treatment. The differences were not huge, but I think they were clinically meaningful. I'm guessing that the topical crisaborole maintenance treatment would have been even more effective had it been used regularly. The study did not, as far as I could tell, assess how well the treatment was used.
An interesting aspect of this study is that it began with nearly 500 participants who started on twice daily topical crisaborole. The 270 patients who responded to the treatment (achieving clear or almost clear with at least a 2-point improvement) were enrolled in the 1-year maintenance phase. Thus, the participants in the maintenance phase were preselected for patients who respond to topical crisaborole. We don't know why they were responders (I, of course, expect it is because they selected for patients who are better than others are at using a topical treatment), but it may be best not to try to generalize these results and assume this form of maintenance treatment would work equally well in a population who achieve initial success with an oral therapy regimen (for example, a quick course of oral prednisone).
Dupilumab was a revolutionary treatment for AD. I didn't think that I'd ever see a more effective treatment. It's so safe too! It has been a first-line treatment for AD since its introduction. Now, we also have oral Janus kinase inhibitor options. Blauvelt and colleagues examined what happens when patients who have been on dupilumab are switched to a high dose (30 mg/d) of upadacitinib (the standard starting dose of upadacitinib is 15 mg/d). Though dupilumab is very effective, upadacitinib is more so. After 4 weeks of switching to upadacitinib, nearly half the patients were completely clear of AD compared with only 16.0% after 24 weeks of dupilumab! The authors point out, optimistically, that "No new safety risks were observed." Though there were no cancers, gastrointestinal perforations, major adverse cardiovascular events, or venous thromboembolic events, there were cases of eczema herpeticum and zoster in patients treated with upadacitinib. Having upadacitinib available for patients who fail dupilumab is a clear benefit; the role of upadacitinib before dupilumab seems less clear.
Patients doing great on dupilumab for AD may be wondering: Do I still need to take it every 2 weeks? Spekhorst and colleagues may have the answer. They describe the response to tapering dupilumab in patients who had been on the drug for at least 1 year with well-controlled disease for at least 6 months. Patients in the study then continued dupilumab with the longest possible dosing interval while maintaining control of their AD.
Generally, patients maintained good control of their AD, with only a small increase in mean disease severity and in concomitant use of topical steroids. For the patients who attempted prolongation, 83% successfully continued dupilumab treatment with a prolonged interval. Not at all surprisingly, the authors calculated that prolonging the interval between dosing led to large savings in cost.
One of the nice features of dupilumab treatment is that loss of response over time seems unusual. Perhaps there is a low propensity for forming antidrug antibodies when dupilumab is used in the standard every 2-week dosing regimen. I don't know whether antidrug antibodies would be more likely with the intermittent dosing regimen. But now that we have other good systemic treatment options for AD, losing dupilumab efficacy would not be as critical a problem as it used to be. I also want to point out that patients' adherence to injection treatment, though better than adherence to topicals, is far from perfect. It's likely that many patients have already been prolonging the interval between taking their treatments. If you want to know, just ask them. The way I like to phrase the question is: "Are you keeping the extra injectors you've accumulated refrigerated like you are supposed to?"
There is a tremendous amount of atopic dermatitis (AD) research underway. This month, we have several interesting articles to present.
Silverberg and colleagues described a very well-designed, vehicle-controlled, randomized 8-week study of a topical formulation of a purified strain of Nitrosomonas eutropha, an ammonia-oxidizing bacterium. In theory, this bacterium may reduce Staphylococcus aureus. The study compared two concentrations of the bacterium vs vehicle delivered as a spray twice per day. Study participants were adults with AD affecting 10%-40% of body surface area.
The study found "meaningful" improvements in itch and objective signs of disease, with clear separation between both doses of the bacterial spray compared with vehicle. At week 4, about 23% of participants treated with the bacterium were clear or almost clear (with a 2-point improvement) compared with 12% in the vehicle group (for comparison, in a phase 2 study comparing topical ruxolitinib with 0.1% triamcinolone cream, there was a 25% clear or almost clear rate [with 2-point improvement] in the triamcinolone-treated individuals).
Though an "all-natural" bacterial approach to managing AD may be appealing to some, it sounded like magic to me. But this well-done study makes it seem like the bacterial approach could be more promising than I had thought. This study also reported about twice as many adverse events (including gastrointestinal issues) with the bacterium-treated participants compared with those who received vehicle, adding to my belief that the bacterial product has efficacy. Whether any other topical will be more effective and safer than is topical triamcinolone remains to be seen. I'm still pessimistic about topicals because of patients' poor adherence to topical treatment, but perhaps an easy-to-use spray that isn't associated with patients' fear of "steroids" will be helpful.
I love articles like this one from Chen and colleagues. They analyzed data on hundreds of thousands of patients with and without AD. Adults with AD had a "significantly increased risk" of developing venous thromboembolism compared with adults without AD. The huge sample size of their study seems compelling. That huge sample size allows detection of effects so small that they may be clinically insignificant.
They report that patients with AD had a venous thromboembolism at a rate of 1.05/1000 patients-years; the rate was 0.82 for patients without AD. From that, we can calculate that there would be an additional 23 patients with venous thromboembolism for every 100,000 patient-years or about one more venous thromboembolism in the AD group in every 4000 patient-years. Though the finding was statistically significant, I don't think it is clinically meaningful.
The authors correctly conclude that "vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients with AD who present with relevant symptoms (eg, unexplained dyspnea, chest tightness, and limb swelling)." But it is probably also true that vascular examination and consultation with the emergency department, cardiologists, or pulmonologists are indicated for patients without AD who present with those symptoms. I think the authors might have been on solid ground if they had concluded that there was a statistically significant but clinically insignificant increased risk for venous thromboembolism in patients with AD.
Eichenfeld and colleagues examined the use of topical crisaborole once per day as a maintenance treatment for patients with mild to moderate AD. The study compared patients given topical crisaborole with those randomly assigned to vehicle. The active treatment was effective because topical crisaborole treated patients had longer times to the first flare following treatment and fewer flares over the 1 year of treatment. The differences were not huge, but I think they were clinically meaningful. I'm guessing that the topical crisaborole maintenance treatment would have been even more effective had it been used regularly. The study did not, as far as I could tell, assess how well the treatment was used.
An interesting aspect of this study is that it began with nearly 500 participants who started on twice daily topical crisaborole. The 270 patients who responded to the treatment (achieving clear or almost clear with at least a 2-point improvement) were enrolled in the 1-year maintenance phase. Thus, the participants in the maintenance phase were preselected for patients who respond to topical crisaborole. We don't know why they were responders (I, of course, expect it is because they selected for patients who are better than others are at using a topical treatment), but it may be best not to try to generalize these results and assume this form of maintenance treatment would work equally well in a population who achieve initial success with an oral therapy regimen (for example, a quick course of oral prednisone).
Dupilumab was a revolutionary treatment for AD. I didn't think that I'd ever see a more effective treatment. It's so safe too! It has been a first-line treatment for AD since its introduction. Now, we also have oral Janus kinase inhibitor options. Blauvelt and colleagues examined what happens when patients who have been on dupilumab are switched to a high dose (30 mg/d) of upadacitinib (the standard starting dose of upadacitinib is 15 mg/d). Though dupilumab is very effective, upadacitinib is more so. After 4 weeks of switching to upadacitinib, nearly half the patients were completely clear of AD compared with only 16.0% after 24 weeks of dupilumab! The authors point out, optimistically, that "No new safety risks were observed." Though there were no cancers, gastrointestinal perforations, major adverse cardiovascular events, or venous thromboembolic events, there were cases of eczema herpeticum and zoster in patients treated with upadacitinib. Having upadacitinib available for patients who fail dupilumab is a clear benefit; the role of upadacitinib before dupilumab seems less clear.
Patients doing great on dupilumab for AD may be wondering: Do I still need to take it every 2 weeks? Spekhorst and colleagues may have the answer. They describe the response to tapering dupilumab in patients who had been on the drug for at least 1 year with well-controlled disease for at least 6 months. Patients in the study then continued dupilumab with the longest possible dosing interval while maintaining control of their AD.
Generally, patients maintained good control of their AD, with only a small increase in mean disease severity and in concomitant use of topical steroids. For the patients who attempted prolongation, 83% successfully continued dupilumab treatment with a prolonged interval. Not at all surprisingly, the authors calculated that prolonging the interval between dosing led to large savings in cost.
One of the nice features of dupilumab treatment is that loss of response over time seems unusual. Perhaps there is a low propensity for forming antidrug antibodies when dupilumab is used in the standard every 2-week dosing regimen. I don't know whether antidrug antibodies would be more likely with the intermittent dosing regimen. But now that we have other good systemic treatment options for AD, losing dupilumab efficacy would not be as critical a problem as it used to be. I also want to point out that patients' adherence to injection treatment, though better than adherence to topicals, is far from perfect. It's likely that many patients have already been prolonging the interval between taking their treatments. If you want to know, just ask them. The way I like to phrase the question is: "Are you keeping the extra injectors you've accumulated refrigerated like you are supposed to?"
Should you dismiss a difficult patient?
Some patients continually cancel their appointments, ignore your medical directions, treat your staff rudely, or send you harassing emails.
Do you have to tolerate their behavior?
No, these are all appropriate reasons to terminate patients, attorneys say. Patients also can be dismissed for misleading doctors about their past medical history, chronic drug-seeking, displaying threatening or seductive behavior toward staff members or physicians, or any criminal behavior in the office, experts say.
But even if a reason seems legitimate, that doesn’t make it legal. Doctors should consider whether the reason is legal, said Chicago-area attorney Ericka Adler, JD, a partner at Roetzel & Andress, who advises doctors about terminating patients.
Ms. Adler said.
Terminating patients for an “illegal” reason such as discrimination based on race or gender or sexual orientation – even if couched as a legitimate patient issue – could open the practice to a lawsuit, Ms. Adler said.
Doctors also want to avoid patient abandonment claims by talking to the patient about problems and documenting them as they arise. If they can’t be resolved, doctors should ensure that there’s continuity of care when patients change physicians, said Ms. Adler.
About 90% of physicians have dismissed at least one patient during their career, according to a study of nearly 800 primary care practices. The most common reasons were legitimate: a patient was “extremely disruptive and/or behaved inappropriately toward clinicians or staff”; a patient had “violated chronic pain and controlled substance policies”; and a patient had “repeatedly missed appointments.”
Jacqui O’Kane, DO, a family physician at South Georgia Medical Center in rural Nashville, said she has dismissed about 15 of 3,000 patients she has seen in the past 3 years at the clinic. Before she dismisses a patient, she looks at whether there has been a pattern of behavior and tries to talk to them about the problem first to find out if there are other reasons for it.
She also gives patients a warning: If the unacceptable behavior continues, it will lead to their dismissal.
When patients cross a line
Dr. O’Kane warned an elderly man who used the N-word with her that she wouldn’t tolerate that language in her office. Then, when he later called her front office employee the N-word, she decided to dismiss him.
“I said, ‘That’s it, you can’t say that to someone in this office. I already told you once, and you did it again. I’m sorry, you have to find another doctor,’ ” said Dr. O’Kane.
Another patient crossed a line when she missed four appointments, refused to come in, and kept sending Dr. O’Kane long messages on MyChart demanding medications and advice. One message was fairly obtrusive: “If you don’t give me something stronger for my nerves TODAY, I am going to LOSE MY MIND!!!” Dr. O’Kane said the patient wrote.
“I then told her that’s not how I run my practice and that she needed to find someone else.”
Another common reason doctors dismiss patients is for nonpayment, says Ms. Adler.
Recently, however, some patients have also begun demanding their money back from doctors for services already received and billed because they were unhappy about something that occurred at the doctor’s office, said Ms. Adler.
“I advise doctors to respond: ‘We disagree that you didn’t get the service, but we will give you your money back, and we’re also terminating you from our practice.’ At that point, the doctor-patient relationship has become impossible,” said Ms. Adler.
How to dismiss difficult patients ethically and legally
According to the AMA’s Council on Ethical and Judicial Affairs, a physician may not discontinue treatment of a patient if further treatment is medically indicated without giving the patient reasonable notice and sufficient opportunity to make alternative arrangements for care.
Terminating a patient abruptly without transferring their care could lead to a claim of patient abandonment and the physician being called before a licensing board for potentially violating the state’s Medical Practice Act, said Ms. Adler.
Doctors can take these six steps to set the stage for dismissal and avoid a claim of patient abandonment.
1. Create written policies. Medical practices can describe the rules and behavior they expect from patients in these policies, which can cover, for example, payment, treating staff with courtesy, and medications. “When the rules are in writing and patients sign off on them, that gives doctors a certain comfort level in being able to refer to them and say that the patient hasn’t been compliant,” said Ms. Adler.
She also recommends that your practice create a policy that doctors should let the patient know about their concerns and meet with them to discuss the problem before receiving a termination letter.
2. Document any consistent problems you’re having with a patient. When you start having problems with a patient, you should document when the problem occurred, how often it occurred, any discussions with the patient about the problem, warnings you gave the patient, and if and when you decided to terminate the patient.
3. Meet with the patient to discuss the problem. “Talking and meeting with a patient also allows the physician to assess whether there’s another issue. For example, is there a mental health concern? Is there a financial reason for nonpayment or no-shows? There are multiple benefits to finding out what the problem is,” said Ms. Adler.
Once you’ve decided to terminate a patient, here’s what you should do:
4. Allow enough time for the patient to find alternative care. Ms. Adler recommends giving patients 30 days’ notice and that physicians offer to provide emergency care during that time. However, if the patient is undergoing treatment or has other challenges, more time may be needed to transfer care.
“It’s important to consider the patient’s context – if the patient is receiving cancer treatment, or is in a late stage of pregnancy, or lives in a rural area where few specialists are available, you may want to treat them longer – at least until they finish their treatment,” said Ms. Adler. Also, states may have their own requirements about minimum notice periods, she said.
5. Provide patients with written notice that you intend to terminate their care. Ms. Adler recommends that each letter be tailored to the patient’s specific circumstances. “You could spell out a patient’s history of noncompliance or nonpayment or inappropriate conduct because it’s been documented and the patient is already aware of it from a previous discussion,” she said.
Ms. Adler also recommends that doctors consult with legal counsel when in doubt or if contacted by the patient’s lawyer. Some lawyers will draft the termination letters, she said.
6. Include the following information in the written letter: The date that they will no longer receive care, how they can obtain copies of their medical records, and how they can find a new physician by providing contact information for a state medical association or similar organization, which often maintains a database of clinicians by specialty and location.
The letter should also state that the doctor will provide emergency care during the 30 days. Ms. Adler also recommends sending the notice by certified mail.
Dr. O’Kane said she may be more likely to give patients a second chance because she practices in a rural underserved area, and she understands that her patients don’t have many other options for health care. She also has developed a reputation for being willing to take on difficult patients that other physicians didn’t want to deal with, she said.
She encourages physicians to talk to patients to find out why, for example, they may not be compliant with medications.
“The patient may say, ‘I had to choose between paying for medications and putting food on the table,’ ” said Dr. O’Kane.
A version of this article first appeared on Medscape.com.
Some patients continually cancel their appointments, ignore your medical directions, treat your staff rudely, or send you harassing emails.
Do you have to tolerate their behavior?
No, these are all appropriate reasons to terminate patients, attorneys say. Patients also can be dismissed for misleading doctors about their past medical history, chronic drug-seeking, displaying threatening or seductive behavior toward staff members or physicians, or any criminal behavior in the office, experts say.
But even if a reason seems legitimate, that doesn’t make it legal. Doctors should consider whether the reason is legal, said Chicago-area attorney Ericka Adler, JD, a partner at Roetzel & Andress, who advises doctors about terminating patients.
Ms. Adler said.
Terminating patients for an “illegal” reason such as discrimination based on race or gender or sexual orientation – even if couched as a legitimate patient issue – could open the practice to a lawsuit, Ms. Adler said.
Doctors also want to avoid patient abandonment claims by talking to the patient about problems and documenting them as they arise. If they can’t be resolved, doctors should ensure that there’s continuity of care when patients change physicians, said Ms. Adler.
About 90% of physicians have dismissed at least one patient during their career, according to a study of nearly 800 primary care practices. The most common reasons were legitimate: a patient was “extremely disruptive and/or behaved inappropriately toward clinicians or staff”; a patient had “violated chronic pain and controlled substance policies”; and a patient had “repeatedly missed appointments.”
Jacqui O’Kane, DO, a family physician at South Georgia Medical Center in rural Nashville, said she has dismissed about 15 of 3,000 patients she has seen in the past 3 years at the clinic. Before she dismisses a patient, she looks at whether there has been a pattern of behavior and tries to talk to them about the problem first to find out if there are other reasons for it.
She also gives patients a warning: If the unacceptable behavior continues, it will lead to their dismissal.
When patients cross a line
Dr. O’Kane warned an elderly man who used the N-word with her that she wouldn’t tolerate that language in her office. Then, when he later called her front office employee the N-word, she decided to dismiss him.
“I said, ‘That’s it, you can’t say that to someone in this office. I already told you once, and you did it again. I’m sorry, you have to find another doctor,’ ” said Dr. O’Kane.
Another patient crossed a line when she missed four appointments, refused to come in, and kept sending Dr. O’Kane long messages on MyChart demanding medications and advice. One message was fairly obtrusive: “If you don’t give me something stronger for my nerves TODAY, I am going to LOSE MY MIND!!!” Dr. O’Kane said the patient wrote.
“I then told her that’s not how I run my practice and that she needed to find someone else.”
Another common reason doctors dismiss patients is for nonpayment, says Ms. Adler.
Recently, however, some patients have also begun demanding their money back from doctors for services already received and billed because they were unhappy about something that occurred at the doctor’s office, said Ms. Adler.
“I advise doctors to respond: ‘We disagree that you didn’t get the service, but we will give you your money back, and we’re also terminating you from our practice.’ At that point, the doctor-patient relationship has become impossible,” said Ms. Adler.
How to dismiss difficult patients ethically and legally
According to the AMA’s Council on Ethical and Judicial Affairs, a physician may not discontinue treatment of a patient if further treatment is medically indicated without giving the patient reasonable notice and sufficient opportunity to make alternative arrangements for care.
Terminating a patient abruptly without transferring their care could lead to a claim of patient abandonment and the physician being called before a licensing board for potentially violating the state’s Medical Practice Act, said Ms. Adler.
Doctors can take these six steps to set the stage for dismissal and avoid a claim of patient abandonment.
1. Create written policies. Medical practices can describe the rules and behavior they expect from patients in these policies, which can cover, for example, payment, treating staff with courtesy, and medications. “When the rules are in writing and patients sign off on them, that gives doctors a certain comfort level in being able to refer to them and say that the patient hasn’t been compliant,” said Ms. Adler.
She also recommends that your practice create a policy that doctors should let the patient know about their concerns and meet with them to discuss the problem before receiving a termination letter.
2. Document any consistent problems you’re having with a patient. When you start having problems with a patient, you should document when the problem occurred, how often it occurred, any discussions with the patient about the problem, warnings you gave the patient, and if and when you decided to terminate the patient.
3. Meet with the patient to discuss the problem. “Talking and meeting with a patient also allows the physician to assess whether there’s another issue. For example, is there a mental health concern? Is there a financial reason for nonpayment or no-shows? There are multiple benefits to finding out what the problem is,” said Ms. Adler.
Once you’ve decided to terminate a patient, here’s what you should do:
4. Allow enough time for the patient to find alternative care. Ms. Adler recommends giving patients 30 days’ notice and that physicians offer to provide emergency care during that time. However, if the patient is undergoing treatment or has other challenges, more time may be needed to transfer care.
“It’s important to consider the patient’s context – if the patient is receiving cancer treatment, or is in a late stage of pregnancy, or lives in a rural area where few specialists are available, you may want to treat them longer – at least until they finish their treatment,” said Ms. Adler. Also, states may have their own requirements about minimum notice periods, she said.
5. Provide patients with written notice that you intend to terminate their care. Ms. Adler recommends that each letter be tailored to the patient’s specific circumstances. “You could spell out a patient’s history of noncompliance or nonpayment or inappropriate conduct because it’s been documented and the patient is already aware of it from a previous discussion,” she said.
Ms. Adler also recommends that doctors consult with legal counsel when in doubt or if contacted by the patient’s lawyer. Some lawyers will draft the termination letters, she said.
6. Include the following information in the written letter: The date that they will no longer receive care, how they can obtain copies of their medical records, and how they can find a new physician by providing contact information for a state medical association or similar organization, which often maintains a database of clinicians by specialty and location.
The letter should also state that the doctor will provide emergency care during the 30 days. Ms. Adler also recommends sending the notice by certified mail.
Dr. O’Kane said she may be more likely to give patients a second chance because she practices in a rural underserved area, and she understands that her patients don’t have many other options for health care. She also has developed a reputation for being willing to take on difficult patients that other physicians didn’t want to deal with, she said.
She encourages physicians to talk to patients to find out why, for example, they may not be compliant with medications.
“The patient may say, ‘I had to choose between paying for medications and putting food on the table,’ ” said Dr. O’Kane.
A version of this article first appeared on Medscape.com.
Some patients continually cancel their appointments, ignore your medical directions, treat your staff rudely, or send you harassing emails.
Do you have to tolerate their behavior?
No, these are all appropriate reasons to terminate patients, attorneys say. Patients also can be dismissed for misleading doctors about their past medical history, chronic drug-seeking, displaying threatening or seductive behavior toward staff members or physicians, or any criminal behavior in the office, experts say.
But even if a reason seems legitimate, that doesn’t make it legal. Doctors should consider whether the reason is legal, said Chicago-area attorney Ericka Adler, JD, a partner at Roetzel & Andress, who advises doctors about terminating patients.
Ms. Adler said.
Terminating patients for an “illegal” reason such as discrimination based on race or gender or sexual orientation – even if couched as a legitimate patient issue – could open the practice to a lawsuit, Ms. Adler said.
Doctors also want to avoid patient abandonment claims by talking to the patient about problems and documenting them as they arise. If they can’t be resolved, doctors should ensure that there’s continuity of care when patients change physicians, said Ms. Adler.
About 90% of physicians have dismissed at least one patient during their career, according to a study of nearly 800 primary care practices. The most common reasons were legitimate: a patient was “extremely disruptive and/or behaved inappropriately toward clinicians or staff”; a patient had “violated chronic pain and controlled substance policies”; and a patient had “repeatedly missed appointments.”
Jacqui O’Kane, DO, a family physician at South Georgia Medical Center in rural Nashville, said she has dismissed about 15 of 3,000 patients she has seen in the past 3 years at the clinic. Before she dismisses a patient, she looks at whether there has been a pattern of behavior and tries to talk to them about the problem first to find out if there are other reasons for it.
She also gives patients a warning: If the unacceptable behavior continues, it will lead to their dismissal.
When patients cross a line
Dr. O’Kane warned an elderly man who used the N-word with her that she wouldn’t tolerate that language in her office. Then, when he later called her front office employee the N-word, she decided to dismiss him.
“I said, ‘That’s it, you can’t say that to someone in this office. I already told you once, and you did it again. I’m sorry, you have to find another doctor,’ ” said Dr. O’Kane.
Another patient crossed a line when she missed four appointments, refused to come in, and kept sending Dr. O’Kane long messages on MyChart demanding medications and advice. One message was fairly obtrusive: “If you don’t give me something stronger for my nerves TODAY, I am going to LOSE MY MIND!!!” Dr. O’Kane said the patient wrote.
“I then told her that’s not how I run my practice and that she needed to find someone else.”
Another common reason doctors dismiss patients is for nonpayment, says Ms. Adler.
Recently, however, some patients have also begun demanding their money back from doctors for services already received and billed because they were unhappy about something that occurred at the doctor’s office, said Ms. Adler.
“I advise doctors to respond: ‘We disagree that you didn’t get the service, but we will give you your money back, and we’re also terminating you from our practice.’ At that point, the doctor-patient relationship has become impossible,” said Ms. Adler.
How to dismiss difficult patients ethically and legally
According to the AMA’s Council on Ethical and Judicial Affairs, a physician may not discontinue treatment of a patient if further treatment is medically indicated without giving the patient reasonable notice and sufficient opportunity to make alternative arrangements for care.
Terminating a patient abruptly without transferring their care could lead to a claim of patient abandonment and the physician being called before a licensing board for potentially violating the state’s Medical Practice Act, said Ms. Adler.
Doctors can take these six steps to set the stage for dismissal and avoid a claim of patient abandonment.
1. Create written policies. Medical practices can describe the rules and behavior they expect from patients in these policies, which can cover, for example, payment, treating staff with courtesy, and medications. “When the rules are in writing and patients sign off on them, that gives doctors a certain comfort level in being able to refer to them and say that the patient hasn’t been compliant,” said Ms. Adler.
She also recommends that your practice create a policy that doctors should let the patient know about their concerns and meet with them to discuss the problem before receiving a termination letter.
2. Document any consistent problems you’re having with a patient. When you start having problems with a patient, you should document when the problem occurred, how often it occurred, any discussions with the patient about the problem, warnings you gave the patient, and if and when you decided to terminate the patient.
3. Meet with the patient to discuss the problem. “Talking and meeting with a patient also allows the physician to assess whether there’s another issue. For example, is there a mental health concern? Is there a financial reason for nonpayment or no-shows? There are multiple benefits to finding out what the problem is,” said Ms. Adler.
Once you’ve decided to terminate a patient, here’s what you should do:
4. Allow enough time for the patient to find alternative care. Ms. Adler recommends giving patients 30 days’ notice and that physicians offer to provide emergency care during that time. However, if the patient is undergoing treatment or has other challenges, more time may be needed to transfer care.
“It’s important to consider the patient’s context – if the patient is receiving cancer treatment, or is in a late stage of pregnancy, or lives in a rural area where few specialists are available, you may want to treat them longer – at least until they finish their treatment,” said Ms. Adler. Also, states may have their own requirements about minimum notice periods, she said.
5. Provide patients with written notice that you intend to terminate their care. Ms. Adler recommends that each letter be tailored to the patient’s specific circumstances. “You could spell out a patient’s history of noncompliance or nonpayment or inappropriate conduct because it’s been documented and the patient is already aware of it from a previous discussion,” she said.
Ms. Adler also recommends that doctors consult with legal counsel when in doubt or if contacted by the patient’s lawyer. Some lawyers will draft the termination letters, she said.
6. Include the following information in the written letter: The date that they will no longer receive care, how they can obtain copies of their medical records, and how they can find a new physician by providing contact information for a state medical association or similar organization, which often maintains a database of clinicians by specialty and location.
The letter should also state that the doctor will provide emergency care during the 30 days. Ms. Adler also recommends sending the notice by certified mail.
Dr. O’Kane said she may be more likely to give patients a second chance because she practices in a rural underserved area, and she understands that her patients don’t have many other options for health care. She also has developed a reputation for being willing to take on difficult patients that other physicians didn’t want to deal with, she said.
She encourages physicians to talk to patients to find out why, for example, they may not be compliant with medications.
“The patient may say, ‘I had to choose between paying for medications and putting food on the table,’ ” said Dr. O’Kane.
A version of this article first appeared on Medscape.com.