User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Can Atopic Dermatitis and Allergic Contact Dermatitis Coexist?
Atopic dermatitis (AD) and allergic contact dermatitis (ACD) are 2 common inflammatory skin conditions that may have similar clinical presentations. Historically, it was thought that these conditions could not be diagnosed simultaneously due to their differing immune mechanisms; however, this belief has been challenged by recent evidence suggesting a more nuanced relationship between the 2 disease processes. In this review, we examine the complex interplay between AD and ACD and explain how shifts in conventional understanding of the 2 conditions shaped our evolving recognition of their ability to coexist.
Epidemiology of AD and ACD
Atopic dermatitis is the most common inflammatory skin disease in children and adolescents, with an estimated prevalence reaching 21%.1 In 60% of cases, onset of AD will occur within the first year of life, and 90% of cases begin within the first 5 years.2 Resolution may occur by adulthood; however, AD may continue to impact up to 8% to 9% of adults, with an increased prevalence in those older than 75 years.1 This may represent an underestimation of the burden of adult AD; one systematic review of 17 studies found that the pooled proportion of adult-onset AD was greater than 25%.3
In contrast, ACD previously was assumed to be a disease that more commonly impacted adults and only rarely children, primarily due to an early misconception that children were not frequently exposed to contact allergens and their immune systems were too immature to react to them even if exposed.4,5 However, it is now known that children do have risk factors for development of ACD, including a thinner stratum corneum and potentially a more absorbent skin surface.4 In addition, a 2022 study by the North American Contact Dermatitis Group (NACDG) found similar rates of ACD in children (n=1871) and adults (n=41,699) referred for patch testing (55.2% and 57.3%, respectively) as well as similar rates of having at least 1 relevant positive patch test (49.2% and 52.2%).6
In opposition to traditional beliefs, these findings highlight that AD and ACD can occur across age groups.
Immune Mechanism
The pathogenesis of AD represents a multifactorial process involving the immune system, cutaneous flora, genetic predisposition, and surrounding environment. Immunologically, acute AD is driven by a predominantly TH2 helper T-cell response with high levels of IL-4, IL-5, and IL-137; TH22, TH17, and TH1 also have been implicated.8 Notably, TH17 is found in high levels during the acute eczema phase, while TH1 and TH22are associated with the chronic phase.7
The pathophysiology of ACD is not completely understood. The classic paradigm involves 2 phases: sensitization and elicitation. Sensitization involves antigen-presenting cells that take up allergens absorbed by the skin to present them in regional lymph nodes where antigen-specific T lymphocytes are generated. Elicitation occurs upon re-exposure to the allergen, at which time the primed T lymphocytes are recruited to the skin, causing inflammation.9 Allergic contact dermatitis initially was thought to be driven by TH1 cytokines and IL-17 but now is understood to be more complex.10 Studies have revealed immune polarization of contact allergens, demonstrating that nickel primarily induces a TH1/TH17 response, whereas fragrance and rubber accelerators skew to TH2; TH9 and TH22 also may be involved depending on the causative allergen.11,12
Of note, the immunologic differences between AD and ACD led early investigators to believe that patients with AD were relatively protected from ACD.13 However, as previously described, there are several overlapping cytokines between AD and ACD. Furthermore, research has revealed that risk of contact sensitization might be increased in the chronic eczema phase due to the shared TH1 pathway.14 Barrier-disrupted skin (such as that in AD) also may increase the cytokine response and the density of antigen-presenting cells, leading to a proallergic state.15 This suggests that the immunologic pathways of AD and ACD are more intertwined than was previously understood.
Underlying Risk Factors
Skin barrier dysfunction is a key step in the pathogenesis of AD. Patients with AD commonly have loss-of-function mutations in the filaggrin gene, a protein that is key to the function of the stratum corneum. Loss of this protein may not only impact the immune response as previously noted but also may lead to increased transepidermal water loss and bacterial colonization.16 Interestingly, a 2014 review examined how this mutation could lead to an increased risk of sensitization to bivalent metal ions via an impaired chelating ability of the skin.17 Furthermore, a 2016 study conducted in Dutch construction workers revealed an increased risk for contact dermatitis (irritant and allergic) for those with a loss-of-function filaggrin mutation.18
Importantly, this same mutation may explain why patients with AD tend to have increased skin colonization by Staphylococcus aureus. The abundance of S aureus and the relative decrease in the diversity of other microorganisms on the skin may be associated with increased AD severity.19 Likewise, S aureus may play a role in the pathogenesis of ACD via production of its exotoxin directed at the T-cell receptor V beta 17 region. In particular, this receptor has been associated with nickel sensitization.17
Another risk factor to consider is increased exposure to contact sensitizers when treating AD. For instance, management often includes use of over-the-counter emollients, natural or botanical remedies with purported benefits for AD, cleansers, and detergents. However, these products can contain some of the most prevalent contact allergens seen in those with AD, including methyl-isothiazolinone, formaldehyde releasers, and fragrance.20 Topical corticosteroids also are frequently used, and ACD to steroid molecules can occur, particularly to tixocortol-21-pivalate (a marker for class A corticosteroids) and budesonide (a marker for class B corticosteroids).21 Other allergens (eg, benzyl alcohol, propylene glycol) also may be found as inactive ingredients of topical corticosteroids.22 These exposures may place AD patients at risk for ACD.
The Coexistence of AD and ACD
Given the overlapping epidemiology, immunology, and potentially increased risk for the development of ACD in patients with AD, it would be reasonable to assume that the 2 diagnoses could coexist; however, is there clinical data to support this idea? Based on recent database reviews, the answer appears to be yes.20,23-26 An analysis from the Pediatric Contact Dermatitis Registry revealed that 30% of 1142 pediatric patch test cases analyzed were diagnosed as AD and ACD simultaneously.24 The NACDG found similar results in its 2021 review, as 29.5% of children (n=1648) and 20.7% of adults (n=36,834) had a concurrent diagnosis of AD and ACD.20 Notably, older results from these databases also demonstrated an association between the 2 conditions.23,25,26
It remains unclear whether the prevalence of ACD is higher in those with or without AD. A comprehensive systematic review conducted in 2017 examined this topic through analysis of 74 studies. The results demonstrated a similar prevalence of contact sensitization in individuals with and without AD.27 Another systematic review of 31 studies conducted in 2017 found a higher prevalence for ACD in children without AD; however, the authors noted that the included studies were too variable (eg, size, design, allergens tested) to draw definitive conclusions.28
Even though there is no clear overall increased risk for ACD in patients with AD, research has suggested that certain allergens may be more prevalent in the setting of AD. An NACDG study found that adults with AD had increased odds of reacting to 10 of the top 25 NACDG screening allergens compared to those without AD.20 Other studies have found that AD patients may be more likely to become sensitized to certain allergens, such as fragrance and lanolin.14
Considerations for Management
Diagnosis of ACD in patients with AD can be challenging because these conditions may present similarly with chronic, pruritic, inflammatory patches and plaques. Chronic ACD may be misdiagnosed as AD if patch testing is not performed.29 Given the prevalence of ACD in the setting of AD, there should be a low threshold to pursue patch testing, especially when dermatitis is recalcitrant to standard therapies or presents in an atypical distribution (ie, perioral, predominantly head/neck, hand and foot, isolated eyelid involvement, buttocks).4,30 Various allergen series are available for patch testing adults and children including the NACDG Standard Series, American Contact Dermatitis Society Core Allergen Series, or the Pediatric Baseline Series.31-33
If potentially relevant allergens are uncovered by patch testing, patients should be counseled on avoidance strategies. However, allergen avoidance may not always lead to complete symptom resolution, especially if AD is present concomitantly with ACD. Therefore, use of topical or systemic therapies still may be required. Topical corticosteroids can be used when dermatitis is acute and localized. Systemic corticosteroids are utilized for both diagnoses when cases are more severe or extensive, but their adverse-effect profile limits long-term use. Other systemic treatments, including conventional agents (ie, azathioprine, cyclosporine, methotrexate, mycophenolate mofetil), biologics, and small molecule inhibitors also may be considered for severe cases.34,35 Dupilumab, a monoclonal antibody targeting IL-4/IL-13, is approved for use in moderate to severe AD in patients 6 months and older. Recent evidence has suggested that dupilumab also may be an effective off-label treatment choice for ACD when allergen avoidance alone is insufficient.36 Studies have been conducted on secukinumab, a monoclonal antibody against IL-17; however, it has not been shown to be effective in either AD or ACD.37,38 This indicates that targeted biologics may not always be successful in treating these diagnoses, likely due to their complex immune pathways. Finally, there is an emerging role for JAK inhibitors. Three are approved for AD: topical ruxolitinib, oral abrocitinib, and oral upadacitinib.39 Further investigation is needed to determine the efficacy of JAK inhibitors in ACD.
Final Interpretation
Evolving evidence shows that AD and ACD can occur at the same time despite the historical perspective that their immune pathways were too polarized for this to happen. Atopic dermatitis may be an important risk factor for subsequent development of ACD. Management should include a low threshold to perform patch testing, while pharmacotherapies utilized in the treatment of both conditions should be considered.
- Chan LN, Magyari A, Ye M, et al. The epidemiology of atopic dermatitis in older adults: a population-based study in the United Kingdom. PLoS One. 2021;16:E0258219. doi:10.1371/journal.pone.0258219
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis [published online November 27, 2013]. J Am Acad Dermatol. 2014;70:338-351. doi:10.1016/j.jaad.2013.10.010
- Lee HH, Patel KR, Singam V, et al. A systematic review and meta-analysis of the prevalence and phenotype of adult-onset atopic dermatitis [published online June 2, 2018]. J Am Acad Dermatol. 2019;80:1526-1532.e7. doi:10.1016/j.jaad.2018.05.1241
- Borok J, Matiz C, Goldenberg A, et al. Contact dermatitis in atopic dermatitis children—past, present, and future. Clin Rev Allergy Immunol. 2019;56:86-98. doi:10.1007/s12016-018-8711-2
- Goldenberg A, Silverberg N, Silverberg JI, et al. Pediatric allergic contact dermatitis: lessons for better care. J Allergy Clin Immunol Pract. 2015;3:661-667; quiz 668. doi:10.1016/j.jaip.2015.02.007
- Silverberg JI, Hou A, Warshaw EM, et al. Age-related differences in patch testing results among children: analysis of North American Contact Dermatitis Group data, 2001-2018 [published online July 24, 2021]. J Am Acad Dermatol. 2022;86:818-826. doi:10.1016/j.jaad.2021.07.030
- Tokura Y, Phadungsaksawasdi P, Ito T. Atopic dermatitis as Th2 disease revisited. J Cutan Immunol Allergy. 2018;1:158-164. doi:10.1002/cia2.12033
- Brunner PM, Guttman-Yassky E, Leung DY. The immunology of atopic dermatitis and its reversibility with broad-spectrum and targeted therapies. J Allergy Clin Immunol. 2017;139(suppl 4):S65-S76. doi:10.1016/j.jaci.2017.01.011
- Murphy PB, Atwater AR, Mueller M. Allergic Contact Dermatitis. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK532866/
- He D, Wu L, Kim HK, et al. IL-17 and IFN-gamma mediate the elicitation of contact hypersensitivity responses by different mechanisms and both are required for optimal responses [published online June 24, 2009]. J Immunol. 2009;183:1463-1470. doi:10.4049/jimmunol.0804108.
- Dhingra N, Shemer A, Correa da Rosa J, et al. Molecular profiling of contact dermatitis skin identifies allergen-dependent differences in immune response [published April 25, 2014]. J Allergy Clin Immunol. 2014;134:362-372. doi:10.1016/j.jaci.2014.03.009
- Owen JL, Vakharia PP, Silverberg JI. The role and diagnosis of allergic contact dermatitis in patients with atopic dermatitis. Am J Clin Dermatol. 2018;19:293-302. doi:10.1007/s40257-017-0340-7
- Uehara M, Sawai T. A longitudinal study of contact sensitivity in patients with atopic dermatitis. Arch Dermatol. 1989;125:366-368.
- Yüksel YT, Nørreslet LB, Thyssen JP. Allergic contact dermatitis in patients with atopic dermatitis. Curr Derm Rep. 2021;10:67-76.
- Gittler JK, Krueger JG, Guttman-Yassky E. Atopic dermatitis results in intrinsic barrier and immune abnormalities: implications for contact dermatitis [published online August 28, 2012]. J Allergy Clin Immunol. 2013;131:300-313. doi:10.1016/j.jaci.2012.06.048
- Drislane C, Irvine AD. The role of filaggrin in atopic dermatitis and allergic disease [published online October 14, 2019]. Ann Allergy Asthma Immunol. 2020;124:36-43. doi:10.1016/j.anai.2019.10.008
- Thyssen JP, McFadden JP, Kimber I. The multiple factors affectingthe association between atopic dermatitis and contact sensitization [published online December 26, 2013]. Allergy. 2014;69:28-36. doi:10.1111/all.12358
- Timmerman JG, Heederik D, Spee T, et al. Contact dermatitis in the construction industry: the role of filaggrin loss-of-function mutations [published online December 12, 2015]. Br J Dermatol. 2016;174:348-355. doi:10.1111/bjd.14215
- Edslev SM, Agner T, Andersen PS. Skin microbiome in atopic dermatitis. Acta Derm Venereol. 2020;100:adv00164. doi:
10.2340/00015555-3514 - Silverberg JI, Hou A, Warshaw EM, et al. Prevalence and trend of allergen sensitization in adults and children with atopic dermatitis referred for patch testing, North American Contact Dermatitis Group data, 2001-2016 [published online March 27, 2021]. J Allergy Clin Immunol Pract. 2021;9:2853-2866.e14. doi:10.1016/j.jaip.2021.03.028
- Pratt MD, Mufti A, Lipson J, et al. Patch test reactions to corticosteroids: retrospective analysis from the North American Contact Dermatitis Group 2007-2014. Dermatitis. 2017;28:58-63. doi:10.1097/DER.0000000000000251
- Xiong M, Peterson MY, Hylwa S. Allergic contact dermatitis from benzyl alcohol in hydrocortisone cream [published online January 14, 2022]. Contact Dermatitis. 2022;86:424-425. doi:10.1111/cod.14042
- Goldenberg A, Mousdicas N, Silverberg N, et al. Pediatric Contact Dermatitis Registry inaugural case data. Dermatitis. 2016;27:293-302. doi:10.1097/DER.0000000000000214
- Jacob SE, McGowan M, Silverberg NB, et al. Pediatric Contact Dermatitis Registry data on contact allergy in children with atopic dermatitis. JAMA Dermatol. 2017;153:765-770. doi:10.1001/jamadermatol.2016.6136
- Zug KA, McGinley-Smith D, Warshaw EM, et al. Contact allergy in children referred for patch testing: North American Contact Dermatitis Group data, 2001-2004. Arch Dermatol. 2008;144:1329-1336. doi:10.1001/archderm.144.10.1329
- Zug KA, Pham AK, Belsito DV, et al. Patch testing in children from 2005 to 2012: results from the North American contact dermatitis group. Dermatitis. 2014;25:345-355. doi:10.1097/DER.0000000000000083
- Hamann CR, Hamann D, Egeberg A, et al. Association between atopic dermatitis and contact sensitization: a systematic review and meta-analysis [published online April 6, 2017]. J Am Acad Dermatol. 2017;77:70-78. doi:10.1016/j.jaad.2017.02.001
- Simonsen AB, Johansen JD, Deleuran M, et al. Contact allergy in children with atopic dermatitis: a systematic review [published online June 12, 2017]. Br J Dermatol. 2017;177:395-405. doi:10.1111/bjd.15628
- Chen R, Raffi J, Murase JE. Tocopherol allergic dermatitis masquerading as lifelong atopic dermatitis. Dermatitis. 2020;31:E3-E4. doi:10.1097/DER.0000000000000543
- Tam I, Yu J. Pediatric contact dermatitis: what’s new. Curr Opin Pediatr. 2020;32:524-530. doi:10.1097/MOP.0000000000000919
- Cohen DE, Rao S, Brancaccio RR. Use of the North American Contact Dermatitis Group Standard 65-allergen series alone in the evaluation of allergic contact dermatitis: a series of 794 patients. Dermatitis. 2008;19:137-141.
- Schalock PC, Dunnick CA, Nedorost S, et al. American Contact Dermatitis Society Core Allergen Series: 2020 update. Dermatitis. 2020;31:279-282. doi:10.1097/DER.0000000000000621
- Yu J, Atwater AR, Brod B, et al. Pediatric baseline patch test series: Pediatric Contact Dermatitis Workgroup. Dermatitis. 2018;29:206-212. doi:10.1097/DER.0000000000000385
- Bußmann C, Novak N. Systemic therapy of atopic dermatitis. Allergol Select. 2017;1:1-8. doi:10.5414/ALX01285E
- Sung CT, McGowan MA, Machler BC, et al. Systemic treatments for allergic contact dermatitis. Dermatitis. 2019;30:46-53. doi:10.1097/DER.0000000000000435
- Johnson H, Adler BL, Yu J. Dupilumab for allergic contact dermatitis: an overview of its use and impact on patch testing. Cutis. 2022;109:265-267, E4-E5. doi:10.12788/cutis.0519
- Todberg T, Zachariae C, Krustrup D, et al. The effect of treatment with anti-interleukin-17 in patients with allergic contact dermatitis. Contact Dermatitis. 2018;78:431-432. doi:10.1111/cod.12988
- Ungar B, Pavel AB, Li R, et al. Phase 2 randomized, double-blind study of IL-17 targeting with secukinumab in atopic dermatitis [published online May 16, 2020]. J Allergy Clin Immunol. 2021;147:394-397. doi:10.1016/j.jaci.2020.04.055
- Perche PO, Cook MK, Feldman SR. Abrocitinib: a new FDA-approved drug for moderate-to-severe atopic dermatitis [published online May 19, 2022]. Ann Pharmacother. doi:10.1177/10600280221096713
Atopic dermatitis (AD) and allergic contact dermatitis (ACD) are 2 common inflammatory skin conditions that may have similar clinical presentations. Historically, it was thought that these conditions could not be diagnosed simultaneously due to their differing immune mechanisms; however, this belief has been challenged by recent evidence suggesting a more nuanced relationship between the 2 disease processes. In this review, we examine the complex interplay between AD and ACD and explain how shifts in conventional understanding of the 2 conditions shaped our evolving recognition of their ability to coexist.
Epidemiology of AD and ACD
Atopic dermatitis is the most common inflammatory skin disease in children and adolescents, with an estimated prevalence reaching 21%.1 In 60% of cases, onset of AD will occur within the first year of life, and 90% of cases begin within the first 5 years.2 Resolution may occur by adulthood; however, AD may continue to impact up to 8% to 9% of adults, with an increased prevalence in those older than 75 years.1 This may represent an underestimation of the burden of adult AD; one systematic review of 17 studies found that the pooled proportion of adult-onset AD was greater than 25%.3
In contrast, ACD previously was assumed to be a disease that more commonly impacted adults and only rarely children, primarily due to an early misconception that children were not frequently exposed to contact allergens and their immune systems were too immature to react to them even if exposed.4,5 However, it is now known that children do have risk factors for development of ACD, including a thinner stratum corneum and potentially a more absorbent skin surface.4 In addition, a 2022 study by the North American Contact Dermatitis Group (NACDG) found similar rates of ACD in children (n=1871) and adults (n=41,699) referred for patch testing (55.2% and 57.3%, respectively) as well as similar rates of having at least 1 relevant positive patch test (49.2% and 52.2%).6
In opposition to traditional beliefs, these findings highlight that AD and ACD can occur across age groups.
Immune Mechanism
The pathogenesis of AD represents a multifactorial process involving the immune system, cutaneous flora, genetic predisposition, and surrounding environment. Immunologically, acute AD is driven by a predominantly TH2 helper T-cell response with high levels of IL-4, IL-5, and IL-137; TH22, TH17, and TH1 also have been implicated.8 Notably, TH17 is found in high levels during the acute eczema phase, while TH1 and TH22are associated with the chronic phase.7
The pathophysiology of ACD is not completely understood. The classic paradigm involves 2 phases: sensitization and elicitation. Sensitization involves antigen-presenting cells that take up allergens absorbed by the skin to present them in regional lymph nodes where antigen-specific T lymphocytes are generated. Elicitation occurs upon re-exposure to the allergen, at which time the primed T lymphocytes are recruited to the skin, causing inflammation.9 Allergic contact dermatitis initially was thought to be driven by TH1 cytokines and IL-17 but now is understood to be more complex.10 Studies have revealed immune polarization of contact allergens, demonstrating that nickel primarily induces a TH1/TH17 response, whereas fragrance and rubber accelerators skew to TH2; TH9 and TH22 also may be involved depending on the causative allergen.11,12
Of note, the immunologic differences between AD and ACD led early investigators to believe that patients with AD were relatively protected from ACD.13 However, as previously described, there are several overlapping cytokines between AD and ACD. Furthermore, research has revealed that risk of contact sensitization might be increased in the chronic eczema phase due to the shared TH1 pathway.14 Barrier-disrupted skin (such as that in AD) also may increase the cytokine response and the density of antigen-presenting cells, leading to a proallergic state.15 This suggests that the immunologic pathways of AD and ACD are more intertwined than was previously understood.
Underlying Risk Factors
Skin barrier dysfunction is a key step in the pathogenesis of AD. Patients with AD commonly have loss-of-function mutations in the filaggrin gene, a protein that is key to the function of the stratum corneum. Loss of this protein may not only impact the immune response as previously noted but also may lead to increased transepidermal water loss and bacterial colonization.16 Interestingly, a 2014 review examined how this mutation could lead to an increased risk of sensitization to bivalent metal ions via an impaired chelating ability of the skin.17 Furthermore, a 2016 study conducted in Dutch construction workers revealed an increased risk for contact dermatitis (irritant and allergic) for those with a loss-of-function filaggrin mutation.18
Importantly, this same mutation may explain why patients with AD tend to have increased skin colonization by Staphylococcus aureus. The abundance of S aureus and the relative decrease in the diversity of other microorganisms on the skin may be associated with increased AD severity.19 Likewise, S aureus may play a role in the pathogenesis of ACD via production of its exotoxin directed at the T-cell receptor V beta 17 region. In particular, this receptor has been associated with nickel sensitization.17
Another risk factor to consider is increased exposure to contact sensitizers when treating AD. For instance, management often includes use of over-the-counter emollients, natural or botanical remedies with purported benefits for AD, cleansers, and detergents. However, these products can contain some of the most prevalent contact allergens seen in those with AD, including methyl-isothiazolinone, formaldehyde releasers, and fragrance.20 Topical corticosteroids also are frequently used, and ACD to steroid molecules can occur, particularly to tixocortol-21-pivalate (a marker for class A corticosteroids) and budesonide (a marker for class B corticosteroids).21 Other allergens (eg, benzyl alcohol, propylene glycol) also may be found as inactive ingredients of topical corticosteroids.22 These exposures may place AD patients at risk for ACD.
The Coexistence of AD and ACD
Given the overlapping epidemiology, immunology, and potentially increased risk for the development of ACD in patients with AD, it would be reasonable to assume that the 2 diagnoses could coexist; however, is there clinical data to support this idea? Based on recent database reviews, the answer appears to be yes.20,23-26 An analysis from the Pediatric Contact Dermatitis Registry revealed that 30% of 1142 pediatric patch test cases analyzed were diagnosed as AD and ACD simultaneously.24 The NACDG found similar results in its 2021 review, as 29.5% of children (n=1648) and 20.7% of adults (n=36,834) had a concurrent diagnosis of AD and ACD.20 Notably, older results from these databases also demonstrated an association between the 2 conditions.23,25,26
It remains unclear whether the prevalence of ACD is higher in those with or without AD. A comprehensive systematic review conducted in 2017 examined this topic through analysis of 74 studies. The results demonstrated a similar prevalence of contact sensitization in individuals with and without AD.27 Another systematic review of 31 studies conducted in 2017 found a higher prevalence for ACD in children without AD; however, the authors noted that the included studies were too variable (eg, size, design, allergens tested) to draw definitive conclusions.28
Even though there is no clear overall increased risk for ACD in patients with AD, research has suggested that certain allergens may be more prevalent in the setting of AD. An NACDG study found that adults with AD had increased odds of reacting to 10 of the top 25 NACDG screening allergens compared to those without AD.20 Other studies have found that AD patients may be more likely to become sensitized to certain allergens, such as fragrance and lanolin.14
Considerations for Management
Diagnosis of ACD in patients with AD can be challenging because these conditions may present similarly with chronic, pruritic, inflammatory patches and plaques. Chronic ACD may be misdiagnosed as AD if patch testing is not performed.29 Given the prevalence of ACD in the setting of AD, there should be a low threshold to pursue patch testing, especially when dermatitis is recalcitrant to standard therapies or presents in an atypical distribution (ie, perioral, predominantly head/neck, hand and foot, isolated eyelid involvement, buttocks).4,30 Various allergen series are available for patch testing adults and children including the NACDG Standard Series, American Contact Dermatitis Society Core Allergen Series, or the Pediatric Baseline Series.31-33
If potentially relevant allergens are uncovered by patch testing, patients should be counseled on avoidance strategies. However, allergen avoidance may not always lead to complete symptom resolution, especially if AD is present concomitantly with ACD. Therefore, use of topical or systemic therapies still may be required. Topical corticosteroids can be used when dermatitis is acute and localized. Systemic corticosteroids are utilized for both diagnoses when cases are more severe or extensive, but their adverse-effect profile limits long-term use. Other systemic treatments, including conventional agents (ie, azathioprine, cyclosporine, methotrexate, mycophenolate mofetil), biologics, and small molecule inhibitors also may be considered for severe cases.34,35 Dupilumab, a monoclonal antibody targeting IL-4/IL-13, is approved for use in moderate to severe AD in patients 6 months and older. Recent evidence has suggested that dupilumab also may be an effective off-label treatment choice for ACD when allergen avoidance alone is insufficient.36 Studies have been conducted on secukinumab, a monoclonal antibody against IL-17; however, it has not been shown to be effective in either AD or ACD.37,38 This indicates that targeted biologics may not always be successful in treating these diagnoses, likely due to their complex immune pathways. Finally, there is an emerging role for JAK inhibitors. Three are approved for AD: topical ruxolitinib, oral abrocitinib, and oral upadacitinib.39 Further investigation is needed to determine the efficacy of JAK inhibitors in ACD.
Final Interpretation
Evolving evidence shows that AD and ACD can occur at the same time despite the historical perspective that their immune pathways were too polarized for this to happen. Atopic dermatitis may be an important risk factor for subsequent development of ACD. Management should include a low threshold to perform patch testing, while pharmacotherapies utilized in the treatment of both conditions should be considered.
Atopic dermatitis (AD) and allergic contact dermatitis (ACD) are 2 common inflammatory skin conditions that may have similar clinical presentations. Historically, it was thought that these conditions could not be diagnosed simultaneously due to their differing immune mechanisms; however, this belief has been challenged by recent evidence suggesting a more nuanced relationship between the 2 disease processes. In this review, we examine the complex interplay between AD and ACD and explain how shifts in conventional understanding of the 2 conditions shaped our evolving recognition of their ability to coexist.
Epidemiology of AD and ACD
Atopic dermatitis is the most common inflammatory skin disease in children and adolescents, with an estimated prevalence reaching 21%.1 In 60% of cases, onset of AD will occur within the first year of life, and 90% of cases begin within the first 5 years.2 Resolution may occur by adulthood; however, AD may continue to impact up to 8% to 9% of adults, with an increased prevalence in those older than 75 years.1 This may represent an underestimation of the burden of adult AD; one systematic review of 17 studies found that the pooled proportion of adult-onset AD was greater than 25%.3
In contrast, ACD previously was assumed to be a disease that more commonly impacted adults and only rarely children, primarily due to an early misconception that children were not frequently exposed to contact allergens and their immune systems were too immature to react to them even if exposed.4,5 However, it is now known that children do have risk factors for development of ACD, including a thinner stratum corneum and potentially a more absorbent skin surface.4 In addition, a 2022 study by the North American Contact Dermatitis Group (NACDG) found similar rates of ACD in children (n=1871) and adults (n=41,699) referred for patch testing (55.2% and 57.3%, respectively) as well as similar rates of having at least 1 relevant positive patch test (49.2% and 52.2%).6
In opposition to traditional beliefs, these findings highlight that AD and ACD can occur across age groups.
Immune Mechanism
The pathogenesis of AD represents a multifactorial process involving the immune system, cutaneous flora, genetic predisposition, and surrounding environment. Immunologically, acute AD is driven by a predominantly TH2 helper T-cell response with high levels of IL-4, IL-5, and IL-137; TH22, TH17, and TH1 also have been implicated.8 Notably, TH17 is found in high levels during the acute eczema phase, while TH1 and TH22are associated with the chronic phase.7
The pathophysiology of ACD is not completely understood. The classic paradigm involves 2 phases: sensitization and elicitation. Sensitization involves antigen-presenting cells that take up allergens absorbed by the skin to present them in regional lymph nodes where antigen-specific T lymphocytes are generated. Elicitation occurs upon re-exposure to the allergen, at which time the primed T lymphocytes are recruited to the skin, causing inflammation.9 Allergic contact dermatitis initially was thought to be driven by TH1 cytokines and IL-17 but now is understood to be more complex.10 Studies have revealed immune polarization of contact allergens, demonstrating that nickel primarily induces a TH1/TH17 response, whereas fragrance and rubber accelerators skew to TH2; TH9 and TH22 also may be involved depending on the causative allergen.11,12
Of note, the immunologic differences between AD and ACD led early investigators to believe that patients with AD were relatively protected from ACD.13 However, as previously described, there are several overlapping cytokines between AD and ACD. Furthermore, research has revealed that risk of contact sensitization might be increased in the chronic eczema phase due to the shared TH1 pathway.14 Barrier-disrupted skin (such as that in AD) also may increase the cytokine response and the density of antigen-presenting cells, leading to a proallergic state.15 This suggests that the immunologic pathways of AD and ACD are more intertwined than was previously understood.
Underlying Risk Factors
Skin barrier dysfunction is a key step in the pathogenesis of AD. Patients with AD commonly have loss-of-function mutations in the filaggrin gene, a protein that is key to the function of the stratum corneum. Loss of this protein may not only impact the immune response as previously noted but also may lead to increased transepidermal water loss and bacterial colonization.16 Interestingly, a 2014 review examined how this mutation could lead to an increased risk of sensitization to bivalent metal ions via an impaired chelating ability of the skin.17 Furthermore, a 2016 study conducted in Dutch construction workers revealed an increased risk for contact dermatitis (irritant and allergic) for those with a loss-of-function filaggrin mutation.18
Importantly, this same mutation may explain why patients with AD tend to have increased skin colonization by Staphylococcus aureus. The abundance of S aureus and the relative decrease in the diversity of other microorganisms on the skin may be associated with increased AD severity.19 Likewise, S aureus may play a role in the pathogenesis of ACD via production of its exotoxin directed at the T-cell receptor V beta 17 region. In particular, this receptor has been associated with nickel sensitization.17
Another risk factor to consider is increased exposure to contact sensitizers when treating AD. For instance, management often includes use of over-the-counter emollients, natural or botanical remedies with purported benefits for AD, cleansers, and detergents. However, these products can contain some of the most prevalent contact allergens seen in those with AD, including methyl-isothiazolinone, formaldehyde releasers, and fragrance.20 Topical corticosteroids also are frequently used, and ACD to steroid molecules can occur, particularly to tixocortol-21-pivalate (a marker for class A corticosteroids) and budesonide (a marker for class B corticosteroids).21 Other allergens (eg, benzyl alcohol, propylene glycol) also may be found as inactive ingredients of topical corticosteroids.22 These exposures may place AD patients at risk for ACD.
The Coexistence of AD and ACD
Given the overlapping epidemiology, immunology, and potentially increased risk for the development of ACD in patients with AD, it would be reasonable to assume that the 2 diagnoses could coexist; however, is there clinical data to support this idea? Based on recent database reviews, the answer appears to be yes.20,23-26 An analysis from the Pediatric Contact Dermatitis Registry revealed that 30% of 1142 pediatric patch test cases analyzed were diagnosed as AD and ACD simultaneously.24 The NACDG found similar results in its 2021 review, as 29.5% of children (n=1648) and 20.7% of adults (n=36,834) had a concurrent diagnosis of AD and ACD.20 Notably, older results from these databases also demonstrated an association between the 2 conditions.23,25,26
It remains unclear whether the prevalence of ACD is higher in those with or without AD. A comprehensive systematic review conducted in 2017 examined this topic through analysis of 74 studies. The results demonstrated a similar prevalence of contact sensitization in individuals with and without AD.27 Another systematic review of 31 studies conducted in 2017 found a higher prevalence for ACD in children without AD; however, the authors noted that the included studies were too variable (eg, size, design, allergens tested) to draw definitive conclusions.28
Even though there is no clear overall increased risk for ACD in patients with AD, research has suggested that certain allergens may be more prevalent in the setting of AD. An NACDG study found that adults with AD had increased odds of reacting to 10 of the top 25 NACDG screening allergens compared to those without AD.20 Other studies have found that AD patients may be more likely to become sensitized to certain allergens, such as fragrance and lanolin.14
Considerations for Management
Diagnosis of ACD in patients with AD can be challenging because these conditions may present similarly with chronic, pruritic, inflammatory patches and plaques. Chronic ACD may be misdiagnosed as AD if patch testing is not performed.29 Given the prevalence of ACD in the setting of AD, there should be a low threshold to pursue patch testing, especially when dermatitis is recalcitrant to standard therapies or presents in an atypical distribution (ie, perioral, predominantly head/neck, hand and foot, isolated eyelid involvement, buttocks).4,30 Various allergen series are available for patch testing adults and children including the NACDG Standard Series, American Contact Dermatitis Society Core Allergen Series, or the Pediatric Baseline Series.31-33
If potentially relevant allergens are uncovered by patch testing, patients should be counseled on avoidance strategies. However, allergen avoidance may not always lead to complete symptom resolution, especially if AD is present concomitantly with ACD. Therefore, use of topical or systemic therapies still may be required. Topical corticosteroids can be used when dermatitis is acute and localized. Systemic corticosteroids are utilized for both diagnoses when cases are more severe or extensive, but their adverse-effect profile limits long-term use. Other systemic treatments, including conventional agents (ie, azathioprine, cyclosporine, methotrexate, mycophenolate mofetil), biologics, and small molecule inhibitors also may be considered for severe cases.34,35 Dupilumab, a monoclonal antibody targeting IL-4/IL-13, is approved for use in moderate to severe AD in patients 6 months and older. Recent evidence has suggested that dupilumab also may be an effective off-label treatment choice for ACD when allergen avoidance alone is insufficient.36 Studies have been conducted on secukinumab, a monoclonal antibody against IL-17; however, it has not been shown to be effective in either AD or ACD.37,38 This indicates that targeted biologics may not always be successful in treating these diagnoses, likely due to their complex immune pathways. Finally, there is an emerging role for JAK inhibitors. Three are approved for AD: topical ruxolitinib, oral abrocitinib, and oral upadacitinib.39 Further investigation is needed to determine the efficacy of JAK inhibitors in ACD.
Final Interpretation
Evolving evidence shows that AD and ACD can occur at the same time despite the historical perspective that their immune pathways were too polarized for this to happen. Atopic dermatitis may be an important risk factor for subsequent development of ACD. Management should include a low threshold to perform patch testing, while pharmacotherapies utilized in the treatment of both conditions should be considered.
- Chan LN, Magyari A, Ye M, et al. The epidemiology of atopic dermatitis in older adults: a population-based study in the United Kingdom. PLoS One. 2021;16:E0258219. doi:10.1371/journal.pone.0258219
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis [published online November 27, 2013]. J Am Acad Dermatol. 2014;70:338-351. doi:10.1016/j.jaad.2013.10.010
- Lee HH, Patel KR, Singam V, et al. A systematic review and meta-analysis of the prevalence and phenotype of adult-onset atopic dermatitis [published online June 2, 2018]. J Am Acad Dermatol. 2019;80:1526-1532.e7. doi:10.1016/j.jaad.2018.05.1241
- Borok J, Matiz C, Goldenberg A, et al. Contact dermatitis in atopic dermatitis children—past, present, and future. Clin Rev Allergy Immunol. 2019;56:86-98. doi:10.1007/s12016-018-8711-2
- Goldenberg A, Silverberg N, Silverberg JI, et al. Pediatric allergic contact dermatitis: lessons for better care. J Allergy Clin Immunol Pract. 2015;3:661-667; quiz 668. doi:10.1016/j.jaip.2015.02.007
- Silverberg JI, Hou A, Warshaw EM, et al. Age-related differences in patch testing results among children: analysis of North American Contact Dermatitis Group data, 2001-2018 [published online July 24, 2021]. J Am Acad Dermatol. 2022;86:818-826. doi:10.1016/j.jaad.2021.07.030
- Tokura Y, Phadungsaksawasdi P, Ito T. Atopic dermatitis as Th2 disease revisited. J Cutan Immunol Allergy. 2018;1:158-164. doi:10.1002/cia2.12033
- Brunner PM, Guttman-Yassky E, Leung DY. The immunology of atopic dermatitis and its reversibility with broad-spectrum and targeted therapies. J Allergy Clin Immunol. 2017;139(suppl 4):S65-S76. doi:10.1016/j.jaci.2017.01.011
- Murphy PB, Atwater AR, Mueller M. Allergic Contact Dermatitis. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK532866/
- He D, Wu L, Kim HK, et al. IL-17 and IFN-gamma mediate the elicitation of contact hypersensitivity responses by different mechanisms and both are required for optimal responses [published online June 24, 2009]. J Immunol. 2009;183:1463-1470. doi:10.4049/jimmunol.0804108.
- Dhingra N, Shemer A, Correa da Rosa J, et al. Molecular profiling of contact dermatitis skin identifies allergen-dependent differences in immune response [published April 25, 2014]. J Allergy Clin Immunol. 2014;134:362-372. doi:10.1016/j.jaci.2014.03.009
- Owen JL, Vakharia PP, Silverberg JI. The role and diagnosis of allergic contact dermatitis in patients with atopic dermatitis. Am J Clin Dermatol. 2018;19:293-302. doi:10.1007/s40257-017-0340-7
- Uehara M, Sawai T. A longitudinal study of contact sensitivity in patients with atopic dermatitis. Arch Dermatol. 1989;125:366-368.
- Yüksel YT, Nørreslet LB, Thyssen JP. Allergic contact dermatitis in patients with atopic dermatitis. Curr Derm Rep. 2021;10:67-76.
- Gittler JK, Krueger JG, Guttman-Yassky E. Atopic dermatitis results in intrinsic barrier and immune abnormalities: implications for contact dermatitis [published online August 28, 2012]. J Allergy Clin Immunol. 2013;131:300-313. doi:10.1016/j.jaci.2012.06.048
- Drislane C, Irvine AD. The role of filaggrin in atopic dermatitis and allergic disease [published online October 14, 2019]. Ann Allergy Asthma Immunol. 2020;124:36-43. doi:10.1016/j.anai.2019.10.008
- Thyssen JP, McFadden JP, Kimber I. The multiple factors affectingthe association between atopic dermatitis and contact sensitization [published online December 26, 2013]. Allergy. 2014;69:28-36. doi:10.1111/all.12358
- Timmerman JG, Heederik D, Spee T, et al. Contact dermatitis in the construction industry: the role of filaggrin loss-of-function mutations [published online December 12, 2015]. Br J Dermatol. 2016;174:348-355. doi:10.1111/bjd.14215
- Edslev SM, Agner T, Andersen PS. Skin microbiome in atopic dermatitis. Acta Derm Venereol. 2020;100:adv00164. doi:
10.2340/00015555-3514 - Silverberg JI, Hou A, Warshaw EM, et al. Prevalence and trend of allergen sensitization in adults and children with atopic dermatitis referred for patch testing, North American Contact Dermatitis Group data, 2001-2016 [published online March 27, 2021]. J Allergy Clin Immunol Pract. 2021;9:2853-2866.e14. doi:10.1016/j.jaip.2021.03.028
- Pratt MD, Mufti A, Lipson J, et al. Patch test reactions to corticosteroids: retrospective analysis from the North American Contact Dermatitis Group 2007-2014. Dermatitis. 2017;28:58-63. doi:10.1097/DER.0000000000000251
- Xiong M, Peterson MY, Hylwa S. Allergic contact dermatitis from benzyl alcohol in hydrocortisone cream [published online January 14, 2022]. Contact Dermatitis. 2022;86:424-425. doi:10.1111/cod.14042
- Goldenberg A, Mousdicas N, Silverberg N, et al. Pediatric Contact Dermatitis Registry inaugural case data. Dermatitis. 2016;27:293-302. doi:10.1097/DER.0000000000000214
- Jacob SE, McGowan M, Silverberg NB, et al. Pediatric Contact Dermatitis Registry data on contact allergy in children with atopic dermatitis. JAMA Dermatol. 2017;153:765-770. doi:10.1001/jamadermatol.2016.6136
- Zug KA, McGinley-Smith D, Warshaw EM, et al. Contact allergy in children referred for patch testing: North American Contact Dermatitis Group data, 2001-2004. Arch Dermatol. 2008;144:1329-1336. doi:10.1001/archderm.144.10.1329
- Zug KA, Pham AK, Belsito DV, et al. Patch testing in children from 2005 to 2012: results from the North American contact dermatitis group. Dermatitis. 2014;25:345-355. doi:10.1097/DER.0000000000000083
- Hamann CR, Hamann D, Egeberg A, et al. Association between atopic dermatitis and contact sensitization: a systematic review and meta-analysis [published online April 6, 2017]. J Am Acad Dermatol. 2017;77:70-78. doi:10.1016/j.jaad.2017.02.001
- Simonsen AB, Johansen JD, Deleuran M, et al. Contact allergy in children with atopic dermatitis: a systematic review [published online June 12, 2017]. Br J Dermatol. 2017;177:395-405. doi:10.1111/bjd.15628
- Chen R, Raffi J, Murase JE. Tocopherol allergic dermatitis masquerading as lifelong atopic dermatitis. Dermatitis. 2020;31:E3-E4. doi:10.1097/DER.0000000000000543
- Tam I, Yu J. Pediatric contact dermatitis: what’s new. Curr Opin Pediatr. 2020;32:524-530. doi:10.1097/MOP.0000000000000919
- Cohen DE, Rao S, Brancaccio RR. Use of the North American Contact Dermatitis Group Standard 65-allergen series alone in the evaluation of allergic contact dermatitis: a series of 794 patients. Dermatitis. 2008;19:137-141.
- Schalock PC, Dunnick CA, Nedorost S, et al. American Contact Dermatitis Society Core Allergen Series: 2020 update. Dermatitis. 2020;31:279-282. doi:10.1097/DER.0000000000000621
- Yu J, Atwater AR, Brod B, et al. Pediatric baseline patch test series: Pediatric Contact Dermatitis Workgroup. Dermatitis. 2018;29:206-212. doi:10.1097/DER.0000000000000385
- Bußmann C, Novak N. Systemic therapy of atopic dermatitis. Allergol Select. 2017;1:1-8. doi:10.5414/ALX01285E
- Sung CT, McGowan MA, Machler BC, et al. Systemic treatments for allergic contact dermatitis. Dermatitis. 2019;30:46-53. doi:10.1097/DER.0000000000000435
- Johnson H, Adler BL, Yu J. Dupilumab for allergic contact dermatitis: an overview of its use and impact on patch testing. Cutis. 2022;109:265-267, E4-E5. doi:10.12788/cutis.0519
- Todberg T, Zachariae C, Krustrup D, et al. The effect of treatment with anti-interleukin-17 in patients with allergic contact dermatitis. Contact Dermatitis. 2018;78:431-432. doi:10.1111/cod.12988
- Ungar B, Pavel AB, Li R, et al. Phase 2 randomized, double-blind study of IL-17 targeting with secukinumab in atopic dermatitis [published online May 16, 2020]. J Allergy Clin Immunol. 2021;147:394-397. doi:10.1016/j.jaci.2020.04.055
- Perche PO, Cook MK, Feldman SR. Abrocitinib: a new FDA-approved drug for moderate-to-severe atopic dermatitis [published online May 19, 2022]. Ann Pharmacother. doi:10.1177/10600280221096713
- Chan LN, Magyari A, Ye M, et al. The epidemiology of atopic dermatitis in older adults: a population-based study in the United Kingdom. PLoS One. 2021;16:E0258219. doi:10.1371/journal.pone.0258219
- Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. diagnosis and assessment of atopic dermatitis [published online November 27, 2013]. J Am Acad Dermatol. 2014;70:338-351. doi:10.1016/j.jaad.2013.10.010
- Lee HH, Patel KR, Singam V, et al. A systematic review and meta-analysis of the prevalence and phenotype of adult-onset atopic dermatitis [published online June 2, 2018]. J Am Acad Dermatol. 2019;80:1526-1532.e7. doi:10.1016/j.jaad.2018.05.1241
- Borok J, Matiz C, Goldenberg A, et al. Contact dermatitis in atopic dermatitis children—past, present, and future. Clin Rev Allergy Immunol. 2019;56:86-98. doi:10.1007/s12016-018-8711-2
- Goldenberg A, Silverberg N, Silverberg JI, et al. Pediatric allergic contact dermatitis: lessons for better care. J Allergy Clin Immunol Pract. 2015;3:661-667; quiz 668. doi:10.1016/j.jaip.2015.02.007
- Silverberg JI, Hou A, Warshaw EM, et al. Age-related differences in patch testing results among children: analysis of North American Contact Dermatitis Group data, 2001-2018 [published online July 24, 2021]. J Am Acad Dermatol. 2022;86:818-826. doi:10.1016/j.jaad.2021.07.030
- Tokura Y, Phadungsaksawasdi P, Ito T. Atopic dermatitis as Th2 disease revisited. J Cutan Immunol Allergy. 2018;1:158-164. doi:10.1002/cia2.12033
- Brunner PM, Guttman-Yassky E, Leung DY. The immunology of atopic dermatitis and its reversibility with broad-spectrum and targeted therapies. J Allergy Clin Immunol. 2017;139(suppl 4):S65-S76. doi:10.1016/j.jaci.2017.01.011
- Murphy PB, Atwater AR, Mueller M. Allergic Contact Dermatitis. StatPearls Publishing; 2021. https://www.ncbi.nlm.nih.gov/books/NBK532866/
- He D, Wu L, Kim HK, et al. IL-17 and IFN-gamma mediate the elicitation of contact hypersensitivity responses by different mechanisms and both are required for optimal responses [published online June 24, 2009]. J Immunol. 2009;183:1463-1470. doi:10.4049/jimmunol.0804108.
- Dhingra N, Shemer A, Correa da Rosa J, et al. Molecular profiling of contact dermatitis skin identifies allergen-dependent differences in immune response [published April 25, 2014]. J Allergy Clin Immunol. 2014;134:362-372. doi:10.1016/j.jaci.2014.03.009
- Owen JL, Vakharia PP, Silverberg JI. The role and diagnosis of allergic contact dermatitis in patients with atopic dermatitis. Am J Clin Dermatol. 2018;19:293-302. doi:10.1007/s40257-017-0340-7
- Uehara M, Sawai T. A longitudinal study of contact sensitivity in patients with atopic dermatitis. Arch Dermatol. 1989;125:366-368.
- Yüksel YT, Nørreslet LB, Thyssen JP. Allergic contact dermatitis in patients with atopic dermatitis. Curr Derm Rep. 2021;10:67-76.
- Gittler JK, Krueger JG, Guttman-Yassky E. Atopic dermatitis results in intrinsic barrier and immune abnormalities: implications for contact dermatitis [published online August 28, 2012]. J Allergy Clin Immunol. 2013;131:300-313. doi:10.1016/j.jaci.2012.06.048
- Drislane C, Irvine AD. The role of filaggrin in atopic dermatitis and allergic disease [published online October 14, 2019]. Ann Allergy Asthma Immunol. 2020;124:36-43. doi:10.1016/j.anai.2019.10.008
- Thyssen JP, McFadden JP, Kimber I. The multiple factors affectingthe association between atopic dermatitis and contact sensitization [published online December 26, 2013]. Allergy. 2014;69:28-36. doi:10.1111/all.12358
- Timmerman JG, Heederik D, Spee T, et al. Contact dermatitis in the construction industry: the role of filaggrin loss-of-function mutations [published online December 12, 2015]. Br J Dermatol. 2016;174:348-355. doi:10.1111/bjd.14215
- Edslev SM, Agner T, Andersen PS. Skin microbiome in atopic dermatitis. Acta Derm Venereol. 2020;100:adv00164. doi:
10.2340/00015555-3514 - Silverberg JI, Hou A, Warshaw EM, et al. Prevalence and trend of allergen sensitization in adults and children with atopic dermatitis referred for patch testing, North American Contact Dermatitis Group data, 2001-2016 [published online March 27, 2021]. J Allergy Clin Immunol Pract. 2021;9:2853-2866.e14. doi:10.1016/j.jaip.2021.03.028
- Pratt MD, Mufti A, Lipson J, et al. Patch test reactions to corticosteroids: retrospective analysis from the North American Contact Dermatitis Group 2007-2014. Dermatitis. 2017;28:58-63. doi:10.1097/DER.0000000000000251
- Xiong M, Peterson MY, Hylwa S. Allergic contact dermatitis from benzyl alcohol in hydrocortisone cream [published online January 14, 2022]. Contact Dermatitis. 2022;86:424-425. doi:10.1111/cod.14042
- Goldenberg A, Mousdicas N, Silverberg N, et al. Pediatric Contact Dermatitis Registry inaugural case data. Dermatitis. 2016;27:293-302. doi:10.1097/DER.0000000000000214
- Jacob SE, McGowan M, Silverberg NB, et al. Pediatric Contact Dermatitis Registry data on contact allergy in children with atopic dermatitis. JAMA Dermatol. 2017;153:765-770. doi:10.1001/jamadermatol.2016.6136
- Zug KA, McGinley-Smith D, Warshaw EM, et al. Contact allergy in children referred for patch testing: North American Contact Dermatitis Group data, 2001-2004. Arch Dermatol. 2008;144:1329-1336. doi:10.1001/archderm.144.10.1329
- Zug KA, Pham AK, Belsito DV, et al. Patch testing in children from 2005 to 2012: results from the North American contact dermatitis group. Dermatitis. 2014;25:345-355. doi:10.1097/DER.0000000000000083
- Hamann CR, Hamann D, Egeberg A, et al. Association between atopic dermatitis and contact sensitization: a systematic review and meta-analysis [published online April 6, 2017]. J Am Acad Dermatol. 2017;77:70-78. doi:10.1016/j.jaad.2017.02.001
- Simonsen AB, Johansen JD, Deleuran M, et al. Contact allergy in children with atopic dermatitis: a systematic review [published online June 12, 2017]. Br J Dermatol. 2017;177:395-405. doi:10.1111/bjd.15628
- Chen R, Raffi J, Murase JE. Tocopherol allergic dermatitis masquerading as lifelong atopic dermatitis. Dermatitis. 2020;31:E3-E4. doi:10.1097/DER.0000000000000543
- Tam I, Yu J. Pediatric contact dermatitis: what’s new. Curr Opin Pediatr. 2020;32:524-530. doi:10.1097/MOP.0000000000000919
- Cohen DE, Rao S, Brancaccio RR. Use of the North American Contact Dermatitis Group Standard 65-allergen series alone in the evaluation of allergic contact dermatitis: a series of 794 patients. Dermatitis. 2008;19:137-141.
- Schalock PC, Dunnick CA, Nedorost S, et al. American Contact Dermatitis Society Core Allergen Series: 2020 update. Dermatitis. 2020;31:279-282. doi:10.1097/DER.0000000000000621
- Yu J, Atwater AR, Brod B, et al. Pediatric baseline patch test series: Pediatric Contact Dermatitis Workgroup. Dermatitis. 2018;29:206-212. doi:10.1097/DER.0000000000000385
- Bußmann C, Novak N. Systemic therapy of atopic dermatitis. Allergol Select. 2017;1:1-8. doi:10.5414/ALX01285E
- Sung CT, McGowan MA, Machler BC, et al. Systemic treatments for allergic contact dermatitis. Dermatitis. 2019;30:46-53. doi:10.1097/DER.0000000000000435
- Johnson H, Adler BL, Yu J. Dupilumab for allergic contact dermatitis: an overview of its use and impact on patch testing. Cutis. 2022;109:265-267, E4-E5. doi:10.12788/cutis.0519
- Todberg T, Zachariae C, Krustrup D, et al. The effect of treatment with anti-interleukin-17 in patients with allergic contact dermatitis. Contact Dermatitis. 2018;78:431-432. doi:10.1111/cod.12988
- Ungar B, Pavel AB, Li R, et al. Phase 2 randomized, double-blind study of IL-17 targeting with secukinumab in atopic dermatitis [published online May 16, 2020]. J Allergy Clin Immunol. 2021;147:394-397. doi:10.1016/j.jaci.2020.04.055
- Perche PO, Cook MK, Feldman SR. Abrocitinib: a new FDA-approved drug for moderate-to-severe atopic dermatitis [published online May 19, 2022]. Ann Pharmacother. doi:10.1177/10600280221096713
Practice Points
- Although it previously was thought that atopic dermatitis (AD) and allergic contact dermatitis (ACD) could not coexist due to their polarized immune pathways, current evidence suggests otherwise.
- When both diagnoses are suspected, patch testing should be considered as well as therapeutic strategies that can treat both AD and ACD simultaneously.
Vismodegib for Basal Cell Carcinoma and Beyond: What Dermatologists Need to Know
Basal cell carcinomas (BCCs) are considered the most common cutaneous cancers. Approximately 80% of nonmelanoma skin cancers are BCCs.1,2 Surgical management is the gold standard for early-stage and localized BCCs; it may include simple excision vs Mohs micrographic surgery.3,4 However, if left untreated, these lesions can progress to an advanced stage (locally advanced BCC) or infrequently may spread to distant sites (metastatic BCC). In the advanced stage, the lesions are no longer manageable by surgery or radiation therapy.5,6 Recently, inhibitors targeting the hedgehog (Hh) pathway have shown great promise for these patients. The first drug approved by the US Food and Drug Administration (FDA) for locally advanced and metastatic BCC is vismodegib.7 In this article, we provide a clinical review of vismodegib for the management of BCC, including a discussion of the Hh pathway in BCC, adverse effects of vismodegib, use of vismodegib in adnexal skin tumors, recommended doses for vismodegib therapy in BCC, and management of the side effects of treatment.
Hh Pathway in BCC
In embryonic development, the Hh signaling pathway is crucial across a broad spectrum of species, including humans. Various members of the Hh family have been recognized, all working as secreted regulatory proteins.8 The name of the Hh signaling pathway is derived from a polypeptide ligand called hedgehog found in some fruit flies. Mutations in the gene led to fruit fly larvae that had a spiky hairy pattern of denticles similar to hedgehogs, leading to the name of this molecule.9 The transmembrane protein smoothened (SMO) is the main component of the Hh signaling pathway and initiates a signaling cascade that in turn leads to an increased expression of target genes, such as GLI1. Patched (PTCH), also a transmembrane protein and a cell-surface receptor for the secreted Hh ligand, suppresses the signaling capacity of SMO. Upon binding of the Hh ligand to the PTCH receptor, the suppression of SMO is relieved and a signal is propagated, evoking a cellular response.10 Molecular and genetic studies have reported that genetic alterations in the Hh signaling pathway are almost universally present in all BCCs, leading to an aberrant activation of the pathway and an uncontrolled proliferation of the basal cells. Frequently, these alterations have been shown to cause loss of function of PTCH homologue 1, which usually acts to inhibit the SMO homologue signaling activity.11,12
Because of the potential importance of Hh signaling in other solid malignancies and the failure of topical inhibition of SMO,13 subsequent studies on the development of Hh pathway inhibitors have mostly focused on the systemic approach. A multitude of Hh pathway inhibitors have been developed thus far, such as SANT1-SANT4, GDC-0449, IPI-926, BMS-833923 (XL139), HhAntag-691, and MK-4101.14 Many of these inhibitors have been clinically investigated.13,15,16
Systemic SMO Inhibitor: Vismodegib
Vismodegib was the earliest systemic SMO inhibitor to fulfill early clinical evaluation15,16 and the first drug to receive FDA approval for the management of advanced or metastatic BCC. Vismodegib is a small-molecule SMO inhibitor used for the management of selected locally advanced BCC and metastatic BCC in adults.3,17 Although there is a possibility of recurrence following drug withdrawal, vismodegib constitutes a new therapeutic strategy presenting positive benefits to patients. It may provide superior improvement over sunitinib, which has shown efficacy in a few patients; however, the efficacy and tolerance of sunitinib have been shown to be limited.18,19
Adverse Effects of Vismodegib Therapy
Adverse events with vismodegib use have been reported in 98% of patients (N=491); most of these were mild to moderate.20 However, the frequency of adverse events could prove to be a therapeutic challenge for patients requiring extended treatment. The most frequently reported reversible side effects were muscle spasms (64%), alopecia (62%), weight loss (33%), fatigue (28%), decreased appetite (25%), diarrhea (17%), nausea (16%), dysgeusia (54%), and ageusia (22%).20 In clinical trials, amenorrhea was noticed in 30% (3/10) of females with reproductive potential.2 Apart from alopecia and possibly amenorrhea, these side effects are reversible.17 Alkeraye et al17 reported 3 clinical cases of persistent alopecia following the use of vismodegib. Amenorrhea is a possible side effect of unknown reversibility.7
Vismodegib is a pregnancy category D medication.4 Severe birth defects, including craniofacial abnormalities, retardations in normal growth, open perineum, and absence of digital fusion at a corresponding 20% of the recommended daily dose, were found in rat studies. Embryo-fetal death was noted when rats were exposedto concentrations comparable to the recommended human dose.4
Hepatic events with the use of vismodegib have been reported. The use of vismodegib in randomized controlled trials resulted in elevation of both alanine aminotransferase and aspartate aminotransferase levels compared with placebo.21 Moreover, severe hepatotoxicity with vismodegib has been reported.22-24 A study conducted by Edwards et al25 concluded that the use of vismodegib in patients with severe liver disease must include thorough risk-benefit assessment, with caution in using other concomitant hepatotoxic medications.
Rare adverse events also have been reported in the literature, including vismodegib-induced pancreatitis in a 79-year-old patient treated for locally advanced, recurrent BCC that was cleared following cessation of therapy.26 Additionally, atypical fibroxanthoma was observed in an 83-year-old patient after 30 days of treatment with vismodegib for multiple BCCs.27 The development of other secondary malignancies, such as squamous cell carcinoma, melanoma, keratoacanthomas, and pilomatricomas, during or after the long-term use of vismodegib also have been described.28-35
Use of Vismodegib for Adnexal Skin Tumors
The role of the sonic Hh–PTCH pathway in the pathogenesis of adnexal tumors varies in the literature. Some studies propose the involvement of this pathway in the formation of adnexal tumors such as trichoblastoma, trichoepithelioma, and cylindroma, as in BCC. Various lines of evidence support this involvement. Firstly, in mice, the spontaneous generation of numerous BCCs, trichoblastomas, trichoepitheliomas, and cylindromas has been observed following constitutive activation of the sonic Hh–PTCH pathway.36 Secondly, in trichoepitheliomas, there have been positive results in molecular research into the tumor suppressor gene PTCH homologue 1, PTCH1, whose mutations cause constitutive activation of the sonic Hh–PTCH pathway.37 Thirdly, GLI138 and SOX939 transcription factors associated with the signaling pathway of sonic Hh–PTCH appear to have increased levels in adnexal carcinomas.19 Lepesant et al19 reported a notable clinical response to vismodegib in trichoblastic carcinoma. Baur et al40 reported successful treatment of multiple familial trichoepitheliomas with vismodegib. Nonetheless, more studies are required to assess the efficacy and reliability of vismodegib in the management of adnexal tumors.
Recommended Dose of Vismodegib Therapy
The vismodegib dosage that is approved by the FDA is 150 mg/d until disease progression or the development of intolerable side effects.4 Higher dosing regimens were evaluated with 270 mg/d and 540 mg/d. No added therapeutic benefit was noted with the increase in the dose, and no dose-limiting toxic effects were observed.41
Management of Vismodegib Side Effects
Managing patient expectations is a crucial step in improving dysgeusia. The experience of dysgeusia varies among patients; thus, patients should be instructed to adjust their diets according to their level of dysgeusia, which can be achieved by changing ingredients or dressings used with their diet. This step has been proven to be effective in overcoming vismodegib-related dysgeusia. Also, fluid taste distortion may lead to dehydration and an increase in creatine level. Thus, patients should be encouraged to monitor fluid intake. Moreover, a treatment hiatus of 2 to 8 months results in near-complete improvement of taste distortion.
For muscle spasms, quinine, treatment break for 1 month, gentle exercise of affected areas, or muscle relaxants such as baclofen and temazepam all are effective methods. For vismodegib-related alopecia, managing patient expectations is key; patients should be aware that hair may take 6 to 12 months or even longer to regrow. In addition, shaving less frequently helps improve alopecia.
For gastrointestinal disorders, loperamide with or without codeine phosphate is effective in resolving diarrhea, and metoclopramide is mostly adequate in treating nausea. Another adverse event is weight loss; weight loss of 5% or more of total body weight prompts dietetic referral. If weight loss persists, a treatment break might be needed to regain weight.
Overall, treatment breaks are sufficient to resolve adverse events caused by vismodegib and do not compromise efficacy of treatment. The duration of a treatment break should be considered before initiation. In one clinical trial, a longer treatment break was associated with fewer adverse effects without affecting the efficacy of treatment.42
Conclusion
Vismodegib provides an effective alternative to surgical intervention in the management of BCC. However, patients must be monitored vigilantly, as adverse events are common (>90%).
- Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366:2171-2179.
- Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146:283-287.
- Von Hoff DD, LoRusso PM, Rudin CM, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164-1172.
- Cirrone F, Harris CS. Vismodegib and the hedgehog pathway: a new treatment for basal cell carcinoma. Clin Ther. 2012;34:2039-2050.
- Ruiz-Salas V, Alegre M, López-Ferrer A, et al. Vismodegib: a review [article in English, Spanish]. Actas Dermosifiliogr. 2014;105:744-751.
- Rubin AI, Chen EH, Ratner D. Basal-cell carcinoma. N Engl J Med. 2005;353:2262-2269.
- Cusack CA, Nijhawan R, Miller B, et al. Vismodegib for locally advanced basal cell carcinoma in a heart transplant patient. JAMA Dermatol. 2015;151:70-72.
- Aszterbaum M, Rothman A, Johnson RL, et al. Identification of mutations in the human PATCHED gene in sporadic basal cell carcinomas and in patients with the basal cell nevus syndrome. J Invest Dermatol. 1998;110:885-888.
- Abidi A. Hedgehog signaling pathway: a novel target for cancer therapy: vismodegib, a promising therapeutic option in treatment of basal cell carcinomas. Indian J Pharmacol. 2014;46:3-12.
- St-Jacques B, Dassule HR, Karavanova I, et al. Sonic hedgehog signaling is essential for hair development. Curr Biol. 1998;8:1058-1068.
- Gailani MR, Ståhle-Bäckdahl M, Leffell DJ, et al. The role of the human homologue of Drosophila patched in sporadic basal cell carcinomas. Nat Genet. 1996;14:78-81.
- Hall JM, Bell ML, Finger TE. Disruption of sonic hedgehog signaling alters growth and patterning of lingual taste papillae. Dev Biol. 2003;255:263-277.
- Bai CB, Stephen D, Joyner AL. All mouse ventral spinal cord patterning by hedgehog is Gli dependent and involves an activator function of Gli3. Dev Cell. 2004;6:103-115.
- Wang B, Fallon JF, Beachy PA. Hedgehog-regulated processing of Gli3 produces an anterior/posterior repressor gradient in the developing vertebrate limb. Cell. 2000;100:423-434.
- Sekulic A, Mangold AR, Northfelt DW, et al. Advanced basal cell carcinoma of the skin: targeting the hedgehog pathway. Curr Opin Oncol. 2013;25:218-223.
- Ingham PW, Placzek M. Orchestrating ontogenesis: variations on a theme by sonic hedgehog. Nature Rev Genet. 2006;7:841-850.
- Alkeraye S, Maire C, Desmedt E, et al. Persistent alopecia induced by vismodegib. Br J Dermatol. 2015;172:1671-1672.
- Battistella M, Mateus C, Lassau N, et al. Sunitinib efficacy in the treatment of metastatic skin adnexal carcinomas: report of two patients with hidradenocarcinoma and trichoblastic carcinoma. J Eur Acad Dermatol Venereol. 2010;24:199-203.
- Lepesant P, Crinquette M, Alkeraye S, et al. Vismodegib induces significant clinical response in locally advanced trichoblastic carcinoma. Br J Dermatol. 2015;173:1059-1062.
- Basset-Seguin N, Hauschild A, Grob JJ, et al. Vismodegib in patients with advanced basal cell carcinoma (STEVIE): a pre-plannedinterim analysis of an international, open-label trial. Lancet Oncol. 2015;16:729-736.
- Catenacci DV, Junttila MR, Karrison T, et al. Randomized phase Ib/II study of gemcitabine plus placebo or vismodegib, a hedgehog pathway inhibitor, in patients with metastatic pancreatic cancer. J Clin Oncol. 2015;33:4284-4292.
- Sanchez BE, Hajjafar L. Severe hepatotoxicity in a patient treated with hedgehog inhibitor: first case report. Gastroenterology. 2011;140:S974-S975.
- Ly P, Wolf K, Wilson J. A case of hepatotoxicity associated with vismodegib. JAAD Case Rep. 2018;5:57-59.
- Eiger-Moscovich M, Reich E, Tauber G, et al. Efficacy of vismodegib for the treatment of orbital and advanced periocular basal cell carcinoma. Am J Ophthalmol. 2019;207:62-70.
- Edwards BJ, Raisch DW, Saraykar SS, et al. Hepatotoxicity with vismodegib: an MD Anderson Cancer Center and Research on Adverse Drug Events and Reports Project. Drugs R D. 2017;17:211-218.
- Velter C, Blanc J, Robert C. Acute pancreatitis after vismodegib for basal cell carcinoma: a causal relation? Eur J Cancer. 2019;118:67-69.
- Giorgini C, Barbaccia V, Croci GA, et al. Rapid development of atypical fibroxanthoma during vismodegib treatment. Clin Exp Dermatol. 2019;44:86-88.
- Saintes C, Saint-Jean M, Brocard A, et al. Development of squamous cell carcinoma into basal cell carcinoma under treatment with vismodegib. J Eur Acad Dermatol Venereol. 2015;29:1006-1009.
- Zhu GA, Sundram U, Chang ALS. Two different scenarios of squamous cell carcinoma within advanced basal cell carcinomas: cases illustrating the importance of serial biopsy during vismodegib usage. JAMA Dermatol. 2014;150:970-973.
- Poulalhon N, Dalle S, Balme B, et al. Fast-growing cutaneous squamous cell carcinoma in a patient treated with vismodegib. Dermatology. 2015;230:101-104.
- Orouji A, Goerdt S, Utikal J, et al. Multiple highly and moderately differentiated squamous cell carcinomas of the skin during vismodegib treatment of inoperable basal cell carcinoma. Br J Dermatol. 2014;171:431-433.
- Iarrobino A, Messina JL, Kudchadkar R, et al. Emergence of a squamous cell carcinoma phenotype following treatment of metastatic basal cell carcinoma with vismodegib. J Am Acad Dermatol. 2013;69:E33-E34.
- Giuffrida R, Kashofer K, Dika E, et al. Fast growing melanoma following treatment with vismodegib for locally advanced basal cell carcinomas: report of two cases. Eur J Cancer. 2018;91:177-179.
- Aasi S, Silkiss R, Tang JY, et al. New onset of keratoacanthomas after vismodegib treatment for locally advanced basal cell carcinomas: a report of 2 cases. JAMA Dermatol. 2013;149:242-243.
- Magdaleno-Tapial J, Valenzuela-Oñate C, Ortiz-Salvador JM, et al. Pilomatricomas secondary to treatment with vismodegib. JAAD Case Rep. 2018;5:12-14.
- Nilsson M, Undèn AB, Krause D, et al. Induction of basal cell carcinomas and trichoepitheliomas in mice overexpressing GLI-1. Proc Natl Acad Sci U S A. 2000;97:3438-3443.
- Vorechovský I, Undén AB, Sandstedt B, et al. Trichoepitheliomas contain somatic mutations in the overexpressed PTCH gene: support for a gatekeeper mechanism in skin tumorigenesis. Cancer Res. 1997;57:4677-4681.
- Hatta N, Hirano T, Kimura T, et al. Molecular diagnosis of basal cell carcinoma and other basaloid cell neoplasms of the skin by the quantification of Gli1 transcript levels. J Cutan Pathol. 2005;32:131-136.
- Vidal VP, Ortonne N, Schedl A. SOX9 expression is a general marker of basal cell carcinoma and adnexal-related neoplasms. J Cutan Pathol. 2008;35:373-379.
- Baur V, Papadopoulos T, Kazakov DV, et al. A case of multiple familial trichoepitheliomas responding to treatment with the hedgehog signaling pathway inhibitor vismodegib. Virchows Arch. 2018;473:241-246.
- LoRusso PM, Rudin CM, Reddy JC, et al. Phase I trial of hedgehog pathway inhibitor vismodegib (GDC-0449) in patients with refractory, locally advanced or metastatic solid tumors. Clin Cancer Res. 2011;17:2502-2511.
- Fife K, Herd R, Lalondrelle S, et al. Managing adverse events associated with vismodegib in the treatment of basal cell carcinoma. Future Oncol. 2017;13:175-184.
Basal cell carcinomas (BCCs) are considered the most common cutaneous cancers. Approximately 80% of nonmelanoma skin cancers are BCCs.1,2 Surgical management is the gold standard for early-stage and localized BCCs; it may include simple excision vs Mohs micrographic surgery.3,4 However, if left untreated, these lesions can progress to an advanced stage (locally advanced BCC) or infrequently may spread to distant sites (metastatic BCC). In the advanced stage, the lesions are no longer manageable by surgery or radiation therapy.5,6 Recently, inhibitors targeting the hedgehog (Hh) pathway have shown great promise for these patients. The first drug approved by the US Food and Drug Administration (FDA) for locally advanced and metastatic BCC is vismodegib.7 In this article, we provide a clinical review of vismodegib for the management of BCC, including a discussion of the Hh pathway in BCC, adverse effects of vismodegib, use of vismodegib in adnexal skin tumors, recommended doses for vismodegib therapy in BCC, and management of the side effects of treatment.
Hh Pathway in BCC
In embryonic development, the Hh signaling pathway is crucial across a broad spectrum of species, including humans. Various members of the Hh family have been recognized, all working as secreted regulatory proteins.8 The name of the Hh signaling pathway is derived from a polypeptide ligand called hedgehog found in some fruit flies. Mutations in the gene led to fruit fly larvae that had a spiky hairy pattern of denticles similar to hedgehogs, leading to the name of this molecule.9 The transmembrane protein smoothened (SMO) is the main component of the Hh signaling pathway and initiates a signaling cascade that in turn leads to an increased expression of target genes, such as GLI1. Patched (PTCH), also a transmembrane protein and a cell-surface receptor for the secreted Hh ligand, suppresses the signaling capacity of SMO. Upon binding of the Hh ligand to the PTCH receptor, the suppression of SMO is relieved and a signal is propagated, evoking a cellular response.10 Molecular and genetic studies have reported that genetic alterations in the Hh signaling pathway are almost universally present in all BCCs, leading to an aberrant activation of the pathway and an uncontrolled proliferation of the basal cells. Frequently, these alterations have been shown to cause loss of function of PTCH homologue 1, which usually acts to inhibit the SMO homologue signaling activity.11,12
Because of the potential importance of Hh signaling in other solid malignancies and the failure of topical inhibition of SMO,13 subsequent studies on the development of Hh pathway inhibitors have mostly focused on the systemic approach. A multitude of Hh pathway inhibitors have been developed thus far, such as SANT1-SANT4, GDC-0449, IPI-926, BMS-833923 (XL139), HhAntag-691, and MK-4101.14 Many of these inhibitors have been clinically investigated.13,15,16
Systemic SMO Inhibitor: Vismodegib
Vismodegib was the earliest systemic SMO inhibitor to fulfill early clinical evaluation15,16 and the first drug to receive FDA approval for the management of advanced or metastatic BCC. Vismodegib is a small-molecule SMO inhibitor used for the management of selected locally advanced BCC and metastatic BCC in adults.3,17 Although there is a possibility of recurrence following drug withdrawal, vismodegib constitutes a new therapeutic strategy presenting positive benefits to patients. It may provide superior improvement over sunitinib, which has shown efficacy in a few patients; however, the efficacy and tolerance of sunitinib have been shown to be limited.18,19
Adverse Effects of Vismodegib Therapy
Adverse events with vismodegib use have been reported in 98% of patients (N=491); most of these were mild to moderate.20 However, the frequency of adverse events could prove to be a therapeutic challenge for patients requiring extended treatment. The most frequently reported reversible side effects were muscle spasms (64%), alopecia (62%), weight loss (33%), fatigue (28%), decreased appetite (25%), diarrhea (17%), nausea (16%), dysgeusia (54%), and ageusia (22%).20 In clinical trials, amenorrhea was noticed in 30% (3/10) of females with reproductive potential.2 Apart from alopecia and possibly amenorrhea, these side effects are reversible.17 Alkeraye et al17 reported 3 clinical cases of persistent alopecia following the use of vismodegib. Amenorrhea is a possible side effect of unknown reversibility.7
Vismodegib is a pregnancy category D medication.4 Severe birth defects, including craniofacial abnormalities, retardations in normal growth, open perineum, and absence of digital fusion at a corresponding 20% of the recommended daily dose, were found in rat studies. Embryo-fetal death was noted when rats were exposedto concentrations comparable to the recommended human dose.4
Hepatic events with the use of vismodegib have been reported. The use of vismodegib in randomized controlled trials resulted in elevation of both alanine aminotransferase and aspartate aminotransferase levels compared with placebo.21 Moreover, severe hepatotoxicity with vismodegib has been reported.22-24 A study conducted by Edwards et al25 concluded that the use of vismodegib in patients with severe liver disease must include thorough risk-benefit assessment, with caution in using other concomitant hepatotoxic medications.
Rare adverse events also have been reported in the literature, including vismodegib-induced pancreatitis in a 79-year-old patient treated for locally advanced, recurrent BCC that was cleared following cessation of therapy.26 Additionally, atypical fibroxanthoma was observed in an 83-year-old patient after 30 days of treatment with vismodegib for multiple BCCs.27 The development of other secondary malignancies, such as squamous cell carcinoma, melanoma, keratoacanthomas, and pilomatricomas, during or after the long-term use of vismodegib also have been described.28-35
Use of Vismodegib for Adnexal Skin Tumors
The role of the sonic Hh–PTCH pathway in the pathogenesis of adnexal tumors varies in the literature. Some studies propose the involvement of this pathway in the formation of adnexal tumors such as trichoblastoma, trichoepithelioma, and cylindroma, as in BCC. Various lines of evidence support this involvement. Firstly, in mice, the spontaneous generation of numerous BCCs, trichoblastomas, trichoepitheliomas, and cylindromas has been observed following constitutive activation of the sonic Hh–PTCH pathway.36 Secondly, in trichoepitheliomas, there have been positive results in molecular research into the tumor suppressor gene PTCH homologue 1, PTCH1, whose mutations cause constitutive activation of the sonic Hh–PTCH pathway.37 Thirdly, GLI138 and SOX939 transcription factors associated with the signaling pathway of sonic Hh–PTCH appear to have increased levels in adnexal carcinomas.19 Lepesant et al19 reported a notable clinical response to vismodegib in trichoblastic carcinoma. Baur et al40 reported successful treatment of multiple familial trichoepitheliomas with vismodegib. Nonetheless, more studies are required to assess the efficacy and reliability of vismodegib in the management of adnexal tumors.
Recommended Dose of Vismodegib Therapy
The vismodegib dosage that is approved by the FDA is 150 mg/d until disease progression or the development of intolerable side effects.4 Higher dosing regimens were evaluated with 270 mg/d and 540 mg/d. No added therapeutic benefit was noted with the increase in the dose, and no dose-limiting toxic effects were observed.41
Management of Vismodegib Side Effects
Managing patient expectations is a crucial step in improving dysgeusia. The experience of dysgeusia varies among patients; thus, patients should be instructed to adjust their diets according to their level of dysgeusia, which can be achieved by changing ingredients or dressings used with their diet. This step has been proven to be effective in overcoming vismodegib-related dysgeusia. Also, fluid taste distortion may lead to dehydration and an increase in creatine level. Thus, patients should be encouraged to monitor fluid intake. Moreover, a treatment hiatus of 2 to 8 months results in near-complete improvement of taste distortion.
For muscle spasms, quinine, treatment break for 1 month, gentle exercise of affected areas, or muscle relaxants such as baclofen and temazepam all are effective methods. For vismodegib-related alopecia, managing patient expectations is key; patients should be aware that hair may take 6 to 12 months or even longer to regrow. In addition, shaving less frequently helps improve alopecia.
For gastrointestinal disorders, loperamide with or without codeine phosphate is effective in resolving diarrhea, and metoclopramide is mostly adequate in treating nausea. Another adverse event is weight loss; weight loss of 5% or more of total body weight prompts dietetic referral. If weight loss persists, a treatment break might be needed to regain weight.
Overall, treatment breaks are sufficient to resolve adverse events caused by vismodegib and do not compromise efficacy of treatment. The duration of a treatment break should be considered before initiation. In one clinical trial, a longer treatment break was associated with fewer adverse effects without affecting the efficacy of treatment.42
Conclusion
Vismodegib provides an effective alternative to surgical intervention in the management of BCC. However, patients must be monitored vigilantly, as adverse events are common (>90%).
Basal cell carcinomas (BCCs) are considered the most common cutaneous cancers. Approximately 80% of nonmelanoma skin cancers are BCCs.1,2 Surgical management is the gold standard for early-stage and localized BCCs; it may include simple excision vs Mohs micrographic surgery.3,4 However, if left untreated, these lesions can progress to an advanced stage (locally advanced BCC) or infrequently may spread to distant sites (metastatic BCC). In the advanced stage, the lesions are no longer manageable by surgery or radiation therapy.5,6 Recently, inhibitors targeting the hedgehog (Hh) pathway have shown great promise for these patients. The first drug approved by the US Food and Drug Administration (FDA) for locally advanced and metastatic BCC is vismodegib.7 In this article, we provide a clinical review of vismodegib for the management of BCC, including a discussion of the Hh pathway in BCC, adverse effects of vismodegib, use of vismodegib in adnexal skin tumors, recommended doses for vismodegib therapy in BCC, and management of the side effects of treatment.
Hh Pathway in BCC
In embryonic development, the Hh signaling pathway is crucial across a broad spectrum of species, including humans. Various members of the Hh family have been recognized, all working as secreted regulatory proteins.8 The name of the Hh signaling pathway is derived from a polypeptide ligand called hedgehog found in some fruit flies. Mutations in the gene led to fruit fly larvae that had a spiky hairy pattern of denticles similar to hedgehogs, leading to the name of this molecule.9 The transmembrane protein smoothened (SMO) is the main component of the Hh signaling pathway and initiates a signaling cascade that in turn leads to an increased expression of target genes, such as GLI1. Patched (PTCH), also a transmembrane protein and a cell-surface receptor for the secreted Hh ligand, suppresses the signaling capacity of SMO. Upon binding of the Hh ligand to the PTCH receptor, the suppression of SMO is relieved and a signal is propagated, evoking a cellular response.10 Molecular and genetic studies have reported that genetic alterations in the Hh signaling pathway are almost universally present in all BCCs, leading to an aberrant activation of the pathway and an uncontrolled proliferation of the basal cells. Frequently, these alterations have been shown to cause loss of function of PTCH homologue 1, which usually acts to inhibit the SMO homologue signaling activity.11,12
Because of the potential importance of Hh signaling in other solid malignancies and the failure of topical inhibition of SMO,13 subsequent studies on the development of Hh pathway inhibitors have mostly focused on the systemic approach. A multitude of Hh pathway inhibitors have been developed thus far, such as SANT1-SANT4, GDC-0449, IPI-926, BMS-833923 (XL139), HhAntag-691, and MK-4101.14 Many of these inhibitors have been clinically investigated.13,15,16
Systemic SMO Inhibitor: Vismodegib
Vismodegib was the earliest systemic SMO inhibitor to fulfill early clinical evaluation15,16 and the first drug to receive FDA approval for the management of advanced or metastatic BCC. Vismodegib is a small-molecule SMO inhibitor used for the management of selected locally advanced BCC and metastatic BCC in adults.3,17 Although there is a possibility of recurrence following drug withdrawal, vismodegib constitutes a new therapeutic strategy presenting positive benefits to patients. It may provide superior improvement over sunitinib, which has shown efficacy in a few patients; however, the efficacy and tolerance of sunitinib have been shown to be limited.18,19
Adverse Effects of Vismodegib Therapy
Adverse events with vismodegib use have been reported in 98% of patients (N=491); most of these were mild to moderate.20 However, the frequency of adverse events could prove to be a therapeutic challenge for patients requiring extended treatment. The most frequently reported reversible side effects were muscle spasms (64%), alopecia (62%), weight loss (33%), fatigue (28%), decreased appetite (25%), diarrhea (17%), nausea (16%), dysgeusia (54%), and ageusia (22%).20 In clinical trials, amenorrhea was noticed in 30% (3/10) of females with reproductive potential.2 Apart from alopecia and possibly amenorrhea, these side effects are reversible.17 Alkeraye et al17 reported 3 clinical cases of persistent alopecia following the use of vismodegib. Amenorrhea is a possible side effect of unknown reversibility.7
Vismodegib is a pregnancy category D medication.4 Severe birth defects, including craniofacial abnormalities, retardations in normal growth, open perineum, and absence of digital fusion at a corresponding 20% of the recommended daily dose, were found in rat studies. Embryo-fetal death was noted when rats were exposedto concentrations comparable to the recommended human dose.4
Hepatic events with the use of vismodegib have been reported. The use of vismodegib in randomized controlled trials resulted in elevation of both alanine aminotransferase and aspartate aminotransferase levels compared with placebo.21 Moreover, severe hepatotoxicity with vismodegib has been reported.22-24 A study conducted by Edwards et al25 concluded that the use of vismodegib in patients with severe liver disease must include thorough risk-benefit assessment, with caution in using other concomitant hepatotoxic medications.
Rare adverse events also have been reported in the literature, including vismodegib-induced pancreatitis in a 79-year-old patient treated for locally advanced, recurrent BCC that was cleared following cessation of therapy.26 Additionally, atypical fibroxanthoma was observed in an 83-year-old patient after 30 days of treatment with vismodegib for multiple BCCs.27 The development of other secondary malignancies, such as squamous cell carcinoma, melanoma, keratoacanthomas, and pilomatricomas, during or after the long-term use of vismodegib also have been described.28-35
Use of Vismodegib for Adnexal Skin Tumors
The role of the sonic Hh–PTCH pathway in the pathogenesis of adnexal tumors varies in the literature. Some studies propose the involvement of this pathway in the formation of adnexal tumors such as trichoblastoma, trichoepithelioma, and cylindroma, as in BCC. Various lines of evidence support this involvement. Firstly, in mice, the spontaneous generation of numerous BCCs, trichoblastomas, trichoepitheliomas, and cylindromas has been observed following constitutive activation of the sonic Hh–PTCH pathway.36 Secondly, in trichoepitheliomas, there have been positive results in molecular research into the tumor suppressor gene PTCH homologue 1, PTCH1, whose mutations cause constitutive activation of the sonic Hh–PTCH pathway.37 Thirdly, GLI138 and SOX939 transcription factors associated with the signaling pathway of sonic Hh–PTCH appear to have increased levels in adnexal carcinomas.19 Lepesant et al19 reported a notable clinical response to vismodegib in trichoblastic carcinoma. Baur et al40 reported successful treatment of multiple familial trichoepitheliomas with vismodegib. Nonetheless, more studies are required to assess the efficacy and reliability of vismodegib in the management of adnexal tumors.
Recommended Dose of Vismodegib Therapy
The vismodegib dosage that is approved by the FDA is 150 mg/d until disease progression or the development of intolerable side effects.4 Higher dosing regimens were evaluated with 270 mg/d and 540 mg/d. No added therapeutic benefit was noted with the increase in the dose, and no dose-limiting toxic effects were observed.41
Management of Vismodegib Side Effects
Managing patient expectations is a crucial step in improving dysgeusia. The experience of dysgeusia varies among patients; thus, patients should be instructed to adjust their diets according to their level of dysgeusia, which can be achieved by changing ingredients or dressings used with their diet. This step has been proven to be effective in overcoming vismodegib-related dysgeusia. Also, fluid taste distortion may lead to dehydration and an increase in creatine level. Thus, patients should be encouraged to monitor fluid intake. Moreover, a treatment hiatus of 2 to 8 months results in near-complete improvement of taste distortion.
For muscle spasms, quinine, treatment break for 1 month, gentle exercise of affected areas, or muscle relaxants such as baclofen and temazepam all are effective methods. For vismodegib-related alopecia, managing patient expectations is key; patients should be aware that hair may take 6 to 12 months or even longer to regrow. In addition, shaving less frequently helps improve alopecia.
For gastrointestinal disorders, loperamide with or without codeine phosphate is effective in resolving diarrhea, and metoclopramide is mostly adequate in treating nausea. Another adverse event is weight loss; weight loss of 5% or more of total body weight prompts dietetic referral. If weight loss persists, a treatment break might be needed to regain weight.
Overall, treatment breaks are sufficient to resolve adverse events caused by vismodegib and do not compromise efficacy of treatment. The duration of a treatment break should be considered before initiation. In one clinical trial, a longer treatment break was associated with fewer adverse effects without affecting the efficacy of treatment.42
Conclusion
Vismodegib provides an effective alternative to surgical intervention in the management of BCC. However, patients must be monitored vigilantly, as adverse events are common (>90%).
- Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366:2171-2179.
- Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146:283-287.
- Von Hoff DD, LoRusso PM, Rudin CM, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164-1172.
- Cirrone F, Harris CS. Vismodegib and the hedgehog pathway: a new treatment for basal cell carcinoma. Clin Ther. 2012;34:2039-2050.
- Ruiz-Salas V, Alegre M, López-Ferrer A, et al. Vismodegib: a review [article in English, Spanish]. Actas Dermosifiliogr. 2014;105:744-751.
- Rubin AI, Chen EH, Ratner D. Basal-cell carcinoma. N Engl J Med. 2005;353:2262-2269.
- Cusack CA, Nijhawan R, Miller B, et al. Vismodegib for locally advanced basal cell carcinoma in a heart transplant patient. JAMA Dermatol. 2015;151:70-72.
- Aszterbaum M, Rothman A, Johnson RL, et al. Identification of mutations in the human PATCHED gene in sporadic basal cell carcinomas and in patients with the basal cell nevus syndrome. J Invest Dermatol. 1998;110:885-888.
- Abidi A. Hedgehog signaling pathway: a novel target for cancer therapy: vismodegib, a promising therapeutic option in treatment of basal cell carcinomas. Indian J Pharmacol. 2014;46:3-12.
- St-Jacques B, Dassule HR, Karavanova I, et al. Sonic hedgehog signaling is essential for hair development. Curr Biol. 1998;8:1058-1068.
- Gailani MR, Ståhle-Bäckdahl M, Leffell DJ, et al. The role of the human homologue of Drosophila patched in sporadic basal cell carcinomas. Nat Genet. 1996;14:78-81.
- Hall JM, Bell ML, Finger TE. Disruption of sonic hedgehog signaling alters growth and patterning of lingual taste papillae. Dev Biol. 2003;255:263-277.
- Bai CB, Stephen D, Joyner AL. All mouse ventral spinal cord patterning by hedgehog is Gli dependent and involves an activator function of Gli3. Dev Cell. 2004;6:103-115.
- Wang B, Fallon JF, Beachy PA. Hedgehog-regulated processing of Gli3 produces an anterior/posterior repressor gradient in the developing vertebrate limb. Cell. 2000;100:423-434.
- Sekulic A, Mangold AR, Northfelt DW, et al. Advanced basal cell carcinoma of the skin: targeting the hedgehog pathway. Curr Opin Oncol. 2013;25:218-223.
- Ingham PW, Placzek M. Orchestrating ontogenesis: variations on a theme by sonic hedgehog. Nature Rev Genet. 2006;7:841-850.
- Alkeraye S, Maire C, Desmedt E, et al. Persistent alopecia induced by vismodegib. Br J Dermatol. 2015;172:1671-1672.
- Battistella M, Mateus C, Lassau N, et al. Sunitinib efficacy in the treatment of metastatic skin adnexal carcinomas: report of two patients with hidradenocarcinoma and trichoblastic carcinoma. J Eur Acad Dermatol Venereol. 2010;24:199-203.
- Lepesant P, Crinquette M, Alkeraye S, et al. Vismodegib induces significant clinical response in locally advanced trichoblastic carcinoma. Br J Dermatol. 2015;173:1059-1062.
- Basset-Seguin N, Hauschild A, Grob JJ, et al. Vismodegib in patients with advanced basal cell carcinoma (STEVIE): a pre-plannedinterim analysis of an international, open-label trial. Lancet Oncol. 2015;16:729-736.
- Catenacci DV, Junttila MR, Karrison T, et al. Randomized phase Ib/II study of gemcitabine plus placebo or vismodegib, a hedgehog pathway inhibitor, in patients with metastatic pancreatic cancer. J Clin Oncol. 2015;33:4284-4292.
- Sanchez BE, Hajjafar L. Severe hepatotoxicity in a patient treated with hedgehog inhibitor: first case report. Gastroenterology. 2011;140:S974-S975.
- Ly P, Wolf K, Wilson J. A case of hepatotoxicity associated with vismodegib. JAAD Case Rep. 2018;5:57-59.
- Eiger-Moscovich M, Reich E, Tauber G, et al. Efficacy of vismodegib for the treatment of orbital and advanced periocular basal cell carcinoma. Am J Ophthalmol. 2019;207:62-70.
- Edwards BJ, Raisch DW, Saraykar SS, et al. Hepatotoxicity with vismodegib: an MD Anderson Cancer Center and Research on Adverse Drug Events and Reports Project. Drugs R D. 2017;17:211-218.
- Velter C, Blanc J, Robert C. Acute pancreatitis after vismodegib for basal cell carcinoma: a causal relation? Eur J Cancer. 2019;118:67-69.
- Giorgini C, Barbaccia V, Croci GA, et al. Rapid development of atypical fibroxanthoma during vismodegib treatment. Clin Exp Dermatol. 2019;44:86-88.
- Saintes C, Saint-Jean M, Brocard A, et al. Development of squamous cell carcinoma into basal cell carcinoma under treatment with vismodegib. J Eur Acad Dermatol Venereol. 2015;29:1006-1009.
- Zhu GA, Sundram U, Chang ALS. Two different scenarios of squamous cell carcinoma within advanced basal cell carcinomas: cases illustrating the importance of serial biopsy during vismodegib usage. JAMA Dermatol. 2014;150:970-973.
- Poulalhon N, Dalle S, Balme B, et al. Fast-growing cutaneous squamous cell carcinoma in a patient treated with vismodegib. Dermatology. 2015;230:101-104.
- Orouji A, Goerdt S, Utikal J, et al. Multiple highly and moderately differentiated squamous cell carcinomas of the skin during vismodegib treatment of inoperable basal cell carcinoma. Br J Dermatol. 2014;171:431-433.
- Iarrobino A, Messina JL, Kudchadkar R, et al. Emergence of a squamous cell carcinoma phenotype following treatment of metastatic basal cell carcinoma with vismodegib. J Am Acad Dermatol. 2013;69:E33-E34.
- Giuffrida R, Kashofer K, Dika E, et al. Fast growing melanoma following treatment with vismodegib for locally advanced basal cell carcinomas: report of two cases. Eur J Cancer. 2018;91:177-179.
- Aasi S, Silkiss R, Tang JY, et al. New onset of keratoacanthomas after vismodegib treatment for locally advanced basal cell carcinomas: a report of 2 cases. JAMA Dermatol. 2013;149:242-243.
- Magdaleno-Tapial J, Valenzuela-Oñate C, Ortiz-Salvador JM, et al. Pilomatricomas secondary to treatment with vismodegib. JAAD Case Rep. 2018;5:12-14.
- Nilsson M, Undèn AB, Krause D, et al. Induction of basal cell carcinomas and trichoepitheliomas in mice overexpressing GLI-1. Proc Natl Acad Sci U S A. 2000;97:3438-3443.
- Vorechovský I, Undén AB, Sandstedt B, et al. Trichoepitheliomas contain somatic mutations in the overexpressed PTCH gene: support for a gatekeeper mechanism in skin tumorigenesis. Cancer Res. 1997;57:4677-4681.
- Hatta N, Hirano T, Kimura T, et al. Molecular diagnosis of basal cell carcinoma and other basaloid cell neoplasms of the skin by the quantification of Gli1 transcript levels. J Cutan Pathol. 2005;32:131-136.
- Vidal VP, Ortonne N, Schedl A. SOX9 expression is a general marker of basal cell carcinoma and adnexal-related neoplasms. J Cutan Pathol. 2008;35:373-379.
- Baur V, Papadopoulos T, Kazakov DV, et al. A case of multiple familial trichoepitheliomas responding to treatment with the hedgehog signaling pathway inhibitor vismodegib. Virchows Arch. 2018;473:241-246.
- LoRusso PM, Rudin CM, Reddy JC, et al. Phase I trial of hedgehog pathway inhibitor vismodegib (GDC-0449) in patients with refractory, locally advanced or metastatic solid tumors. Clin Cancer Res. 2011;17:2502-2511.
- Fife K, Herd R, Lalondrelle S, et al. Managing adverse events associated with vismodegib in the treatment of basal cell carcinoma. Future Oncol. 2017;13:175-184.
- Sekulic A, Migden MR, Oro AE, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med. 2012;366:2171-2179.
- Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146:283-287.
- Von Hoff DD, LoRusso PM, Rudin CM, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med. 2009;361:1164-1172.
- Cirrone F, Harris CS. Vismodegib and the hedgehog pathway: a new treatment for basal cell carcinoma. Clin Ther. 2012;34:2039-2050.
- Ruiz-Salas V, Alegre M, López-Ferrer A, et al. Vismodegib: a review [article in English, Spanish]. Actas Dermosifiliogr. 2014;105:744-751.
- Rubin AI, Chen EH, Ratner D. Basal-cell carcinoma. N Engl J Med. 2005;353:2262-2269.
- Cusack CA, Nijhawan R, Miller B, et al. Vismodegib for locally advanced basal cell carcinoma in a heart transplant patient. JAMA Dermatol. 2015;151:70-72.
- Aszterbaum M, Rothman A, Johnson RL, et al. Identification of mutations in the human PATCHED gene in sporadic basal cell carcinomas and in patients with the basal cell nevus syndrome. J Invest Dermatol. 1998;110:885-888.
- Abidi A. Hedgehog signaling pathway: a novel target for cancer therapy: vismodegib, a promising therapeutic option in treatment of basal cell carcinomas. Indian J Pharmacol. 2014;46:3-12.
- St-Jacques B, Dassule HR, Karavanova I, et al. Sonic hedgehog signaling is essential for hair development. Curr Biol. 1998;8:1058-1068.
- Gailani MR, Ståhle-Bäckdahl M, Leffell DJ, et al. The role of the human homologue of Drosophila patched in sporadic basal cell carcinomas. Nat Genet. 1996;14:78-81.
- Hall JM, Bell ML, Finger TE. Disruption of sonic hedgehog signaling alters growth and patterning of lingual taste papillae. Dev Biol. 2003;255:263-277.
- Bai CB, Stephen D, Joyner AL. All mouse ventral spinal cord patterning by hedgehog is Gli dependent and involves an activator function of Gli3. Dev Cell. 2004;6:103-115.
- Wang B, Fallon JF, Beachy PA. Hedgehog-regulated processing of Gli3 produces an anterior/posterior repressor gradient in the developing vertebrate limb. Cell. 2000;100:423-434.
- Sekulic A, Mangold AR, Northfelt DW, et al. Advanced basal cell carcinoma of the skin: targeting the hedgehog pathway. Curr Opin Oncol. 2013;25:218-223.
- Ingham PW, Placzek M. Orchestrating ontogenesis: variations on a theme by sonic hedgehog. Nature Rev Genet. 2006;7:841-850.
- Alkeraye S, Maire C, Desmedt E, et al. Persistent alopecia induced by vismodegib. Br J Dermatol. 2015;172:1671-1672.
- Battistella M, Mateus C, Lassau N, et al. Sunitinib efficacy in the treatment of metastatic skin adnexal carcinomas: report of two patients with hidradenocarcinoma and trichoblastic carcinoma. J Eur Acad Dermatol Venereol. 2010;24:199-203.
- Lepesant P, Crinquette M, Alkeraye S, et al. Vismodegib induces significant clinical response in locally advanced trichoblastic carcinoma. Br J Dermatol. 2015;173:1059-1062.
- Basset-Seguin N, Hauschild A, Grob JJ, et al. Vismodegib in patients with advanced basal cell carcinoma (STEVIE): a pre-plannedinterim analysis of an international, open-label trial. Lancet Oncol. 2015;16:729-736.
- Catenacci DV, Junttila MR, Karrison T, et al. Randomized phase Ib/II study of gemcitabine plus placebo or vismodegib, a hedgehog pathway inhibitor, in patients with metastatic pancreatic cancer. J Clin Oncol. 2015;33:4284-4292.
- Sanchez BE, Hajjafar L. Severe hepatotoxicity in a patient treated with hedgehog inhibitor: first case report. Gastroenterology. 2011;140:S974-S975.
- Ly P, Wolf K, Wilson J. A case of hepatotoxicity associated with vismodegib. JAAD Case Rep. 2018;5:57-59.
- Eiger-Moscovich M, Reich E, Tauber G, et al. Efficacy of vismodegib for the treatment of orbital and advanced periocular basal cell carcinoma. Am J Ophthalmol. 2019;207:62-70.
- Edwards BJ, Raisch DW, Saraykar SS, et al. Hepatotoxicity with vismodegib: an MD Anderson Cancer Center and Research on Adverse Drug Events and Reports Project. Drugs R D. 2017;17:211-218.
- Velter C, Blanc J, Robert C. Acute pancreatitis after vismodegib for basal cell carcinoma: a causal relation? Eur J Cancer. 2019;118:67-69.
- Giorgini C, Barbaccia V, Croci GA, et al. Rapid development of atypical fibroxanthoma during vismodegib treatment. Clin Exp Dermatol. 2019;44:86-88.
- Saintes C, Saint-Jean M, Brocard A, et al. Development of squamous cell carcinoma into basal cell carcinoma under treatment with vismodegib. J Eur Acad Dermatol Venereol. 2015;29:1006-1009.
- Zhu GA, Sundram U, Chang ALS. Two different scenarios of squamous cell carcinoma within advanced basal cell carcinomas: cases illustrating the importance of serial biopsy during vismodegib usage. JAMA Dermatol. 2014;150:970-973.
- Poulalhon N, Dalle S, Balme B, et al. Fast-growing cutaneous squamous cell carcinoma in a patient treated with vismodegib. Dermatology. 2015;230:101-104.
- Orouji A, Goerdt S, Utikal J, et al. Multiple highly and moderately differentiated squamous cell carcinomas of the skin during vismodegib treatment of inoperable basal cell carcinoma. Br J Dermatol. 2014;171:431-433.
- Iarrobino A, Messina JL, Kudchadkar R, et al. Emergence of a squamous cell carcinoma phenotype following treatment of metastatic basal cell carcinoma with vismodegib. J Am Acad Dermatol. 2013;69:E33-E34.
- Giuffrida R, Kashofer K, Dika E, et al. Fast growing melanoma following treatment with vismodegib for locally advanced basal cell carcinomas: report of two cases. Eur J Cancer. 2018;91:177-179.
- Aasi S, Silkiss R, Tang JY, et al. New onset of keratoacanthomas after vismodegib treatment for locally advanced basal cell carcinomas: a report of 2 cases. JAMA Dermatol. 2013;149:242-243.
- Magdaleno-Tapial J, Valenzuela-Oñate C, Ortiz-Salvador JM, et al. Pilomatricomas secondary to treatment with vismodegib. JAAD Case Rep. 2018;5:12-14.
- Nilsson M, Undèn AB, Krause D, et al. Induction of basal cell carcinomas and trichoepitheliomas in mice overexpressing GLI-1. Proc Natl Acad Sci U S A. 2000;97:3438-3443.
- Vorechovský I, Undén AB, Sandstedt B, et al. Trichoepitheliomas contain somatic mutations in the overexpressed PTCH gene: support for a gatekeeper mechanism in skin tumorigenesis. Cancer Res. 1997;57:4677-4681.
- Hatta N, Hirano T, Kimura T, et al. Molecular diagnosis of basal cell carcinoma and other basaloid cell neoplasms of the skin by the quantification of Gli1 transcript levels. J Cutan Pathol. 2005;32:131-136.
- Vidal VP, Ortonne N, Schedl A. SOX9 expression is a general marker of basal cell carcinoma and adnexal-related neoplasms. J Cutan Pathol. 2008;35:373-379.
- Baur V, Papadopoulos T, Kazakov DV, et al. A case of multiple familial trichoepitheliomas responding to treatment with the hedgehog signaling pathway inhibitor vismodegib. Virchows Arch. 2018;473:241-246.
- LoRusso PM, Rudin CM, Reddy JC, et al. Phase I trial of hedgehog pathway inhibitor vismodegib (GDC-0449) in patients with refractory, locally advanced or metastatic solid tumors. Clin Cancer Res. 2011;17:2502-2511.
- Fife K, Herd R, Lalondrelle S, et al. Managing adverse events associated with vismodegib in the treatment of basal cell carcinoma. Future Oncol. 2017;13:175-184.
Practice Points
- The recommended dosage of vismodegib is 150 mg/d until unendurable side effects develop or disease progression occurs.
- The efficacy of vismodegib in the management of locally advanced basal cell carcinoma (BCC) and metastatic BCC is promising. Thus, it is now considered an effective substitute to surgical therapy.
- Patients using vismodegib must be closely monitored, as it is commonly associated with adverse events.
Surgical Deroofing for Hidradenitis Suppurativa
Practice Gap
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by inflammatory nodules, abscesses, sinus tracts, fistulae, and scarring, mainly in intertriginous areas. The extent of disease—classified using the Hurley staging system (stages I–III)—helps guide treatment, which includes medical management and surgical intervention in later stages.
First-line treatment of HS includes topical or systemic medications, or both. Surgical therapy typically is reserved for refractory HS in moderate to severe disease (Hurley stages II and III) and is combined with pharmacotherapy. Specifically, clinical management guidelines issued by an expert committee of the United States and Canadian Hidradenitis Suppurativa Foundations recommend excision or deroofing for recurrent nodules and tunnels.1
Surgical options for HS that are available to the outpatient dermatologist include incision and drainage, electrosurgery, CO2 laser evaporation, excision, and deroofing (also known as unroofing).2 Deroofing is a fairly novel therapy; many dermatologists are unfamiliar with the procedure. A PubMed search of articles indexed for MEDLINE related to HS prior to 2010 revealed only 1 article containing the word deroofing and only 4 articles containing unroofing.
The pathophysiology of HS has important implications for successful treatment. Inflammation of the follicular pilosebaceous unit along with follicular occlusion create challenges with treatment.3 It is postulated that a defect in the glassy membrane of the infra-infundibular wall predisposes the pilosebaceous follicle to lose its structural integrality as pressure builds from plugging of the duct,4 which can result in the clinical hallmarks of HS including tunneling tracts, bridging nodules, abscesses, and fistulae that form with lateral expansion of the plugged follicle.
Leaking of the contents of these plugged follicles into surrounding tissue produces an inflammatory response in characteristic HS lesions. Because debris within the lesions moves laterally instead of being able to burst to the surface, the lesions have difficulty fully healing. Unroofing the lesions and removing built-up debris allows them to heal more expediently and quiets the underlying immune response by removing the stimulus.4
Herein, we describe the benefits, risks, and surgical process of deroofing for HS.
Technique and Tools
Deroofing is performed under local anesthesia, stepwise as follows:
1. Identify sinus tracts and infiltrate the area with lidocaine (Figure, A).
2. Use a blunt probe to define the borders of the area to be unroofed and to evaluate for any communicating sinus tracts (Figure, B).
3. Remove the roof of underlying abscesses and tracts, using a probe as a guide (Figure, C).
4. Enter through the skin or sinus opening using electrocautery or with a scalpel or scissors; perform blunt dissection.
5. Reflect back the entirety of skin overlying the probed areas and remove the skin to expose the base of the lesion (Figure, D).
6. Explore the exposed base and walls of the lesion with the probe again to assess for hidden tracts; take care not to create false tracts.
7. Debride the surgical wound using curettage or rough gauze grattage to remove remaining inflammatory debris or biofilm. To achieve hemostasis, apply aluminum chloride or ferric chloride. Coat the wound with petroleum jelly and gauze and allow it to heal by secondary intention.
8. Educate the patient on wound care—once-daily gentle cleansing with soap and water, followed by application of a moist dressing—which is similar to wound healing by secondary intention from other causes.2,4

Practice Implications
A deroofing procedure has many benefits compared to other surgical modalities for the treatment of HS. Deroofing requires only a probe, curette, and electrocautery device, making the procedure more cost-effective than excision, which requires a full tray of equipment and sutures. Furthermore, margins do not need to be taken with deroofing, and no undermining or closure is needed, which saves time during the operation and minimizes the risk for complications, including dehiscence and formation of new sinus tracts.4 No specialized equipment, such as a CO2 laser, is required, which makes deroofing accessible to every clinical dermatologist in any demographic or geographic setting.
Evidence of Benefit—Saylor and colleagues5 found that deroofing carries a 12.5% complication rate, which includes postoperative bleeding, hypergranulation tissue, and rarely wound infection. This rate is significantly lower than the 26% complication rate associated with local excision, which includes wound dehiscence, infection, and contracture (P<.001). Deroofing also was found to have an HS recurrence rate of 14.5%, which is significantly less than the 30% recurrence rate seen with local excision (P=.015). Saylor et al5 also concluded that incision and drainage was recommended only for immediate relief of HS because of its 100% recurrence rate.
van der Zee2 reported on 88 lesions from 44 patients that were treated by surgical deroofing, resulting in an average defect of 3.0 cm in length and a mean healing time of 14 days. The typical outcome was cosmetically acceptable scarring; this finding was supported by a postoperative survey (>1 year), to which 37 of 44 patients responded and assigned an average satisfaction score of 8 (of a possible 10) and a recommendation rate of 90%.2
Procedural Coding—Specific Current Procedural Terminology codes (11450-11471) from the International Classification of Diseases, Tenth Revision, exist for HS deroofing procedures; the applicable code for a given case depends on the final length of the surgical defect. Documentation to support these codes is similar to the note for an excision procedure, taking care to include location, depth, and length of the excision; healing by secondary intention; and the diagnosis of HS.
Final Thoughts
Deroofing is a surgical option that can be beneficial to patients with HS. It is a relatively simple procedure available to any dermatologist, regardless of setting. We encourage dermatologists to consider deroofing, even in patients with Hurley stage II lesions, because it can yield cosmetically acceptable and definitive results, given the variety of therapies available for HS. Deroofing also can be superior to standard excision, especially because of the potential complications with standard excision and quicker operative time with deroofing. As more providers become familiar with the deroofing procedure for HS, further studies can be undertaken to add to the paucity of data about deroofing and how it compares to other surgical treatments.
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81:76-90. doi:10.1016/j.jaad.2019.02.067
- van der Zee HH, Prens EP, Boer J. Deroofing: a tissue-saving surgical technique for the treatment of mild to moderate hidradenitis suppurativa lesions. J Am Acad Dermatol. 2010;63:475-480. doi:10.1016/j.jaad.2009.12.018
- Napolitano M, Megna M, Timoshchuk EA, et al. Hidradenitis suppurativa: from pathogenesis to diagnosis and treatment. Clin Cosmet Investig Dermatol. 2017;10:105-115. doi:10.2147/CCID.S111019
- Danby FW. Commentary: unroofing for hidradenitis suppurativa, why and how. J Am Acad Dermatol. 2010;63:481.e1-481.e3. doi:10.1016/j.jaad.2010.01.033
- Saylor DK, Brownstone ND, Naik HB. Office-based surgical intervention for hidradenitis suppurativa (HS): a focused review for dermatologists. Dermatol Ther (Heidelb). 2020;10:529-549. doi:10.1007/s13555-020-00391-x
Practice Gap
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by inflammatory nodules, abscesses, sinus tracts, fistulae, and scarring, mainly in intertriginous areas. The extent of disease—classified using the Hurley staging system (stages I–III)—helps guide treatment, which includes medical management and surgical intervention in later stages.
First-line treatment of HS includes topical or systemic medications, or both. Surgical therapy typically is reserved for refractory HS in moderate to severe disease (Hurley stages II and III) and is combined with pharmacotherapy. Specifically, clinical management guidelines issued by an expert committee of the United States and Canadian Hidradenitis Suppurativa Foundations recommend excision or deroofing for recurrent nodules and tunnels.1
Surgical options for HS that are available to the outpatient dermatologist include incision and drainage, electrosurgery, CO2 laser evaporation, excision, and deroofing (also known as unroofing).2 Deroofing is a fairly novel therapy; many dermatologists are unfamiliar with the procedure. A PubMed search of articles indexed for MEDLINE related to HS prior to 2010 revealed only 1 article containing the word deroofing and only 4 articles containing unroofing.
The pathophysiology of HS has important implications for successful treatment. Inflammation of the follicular pilosebaceous unit along with follicular occlusion create challenges with treatment.3 It is postulated that a defect in the glassy membrane of the infra-infundibular wall predisposes the pilosebaceous follicle to lose its structural integrality as pressure builds from plugging of the duct,4 which can result in the clinical hallmarks of HS including tunneling tracts, bridging nodules, abscesses, and fistulae that form with lateral expansion of the plugged follicle.
Leaking of the contents of these plugged follicles into surrounding tissue produces an inflammatory response in characteristic HS lesions. Because debris within the lesions moves laterally instead of being able to burst to the surface, the lesions have difficulty fully healing. Unroofing the lesions and removing built-up debris allows them to heal more expediently and quiets the underlying immune response by removing the stimulus.4
Herein, we describe the benefits, risks, and surgical process of deroofing for HS.
Technique and Tools
Deroofing is performed under local anesthesia, stepwise as follows:
1. Identify sinus tracts and infiltrate the area with lidocaine (Figure, A).
2. Use a blunt probe to define the borders of the area to be unroofed and to evaluate for any communicating sinus tracts (Figure, B).
3. Remove the roof of underlying abscesses and tracts, using a probe as a guide (Figure, C).
4. Enter through the skin or sinus opening using electrocautery or with a scalpel or scissors; perform blunt dissection.
5. Reflect back the entirety of skin overlying the probed areas and remove the skin to expose the base of the lesion (Figure, D).
6. Explore the exposed base and walls of the lesion with the probe again to assess for hidden tracts; take care not to create false tracts.
7. Debride the surgical wound using curettage or rough gauze grattage to remove remaining inflammatory debris or biofilm. To achieve hemostasis, apply aluminum chloride or ferric chloride. Coat the wound with petroleum jelly and gauze and allow it to heal by secondary intention.
8. Educate the patient on wound care—once-daily gentle cleansing with soap and water, followed by application of a moist dressing—which is similar to wound healing by secondary intention from other causes.2,4

Practice Implications
A deroofing procedure has many benefits compared to other surgical modalities for the treatment of HS. Deroofing requires only a probe, curette, and electrocautery device, making the procedure more cost-effective than excision, which requires a full tray of equipment and sutures. Furthermore, margins do not need to be taken with deroofing, and no undermining or closure is needed, which saves time during the operation and minimizes the risk for complications, including dehiscence and formation of new sinus tracts.4 No specialized equipment, such as a CO2 laser, is required, which makes deroofing accessible to every clinical dermatologist in any demographic or geographic setting.
Evidence of Benefit—Saylor and colleagues5 found that deroofing carries a 12.5% complication rate, which includes postoperative bleeding, hypergranulation tissue, and rarely wound infection. This rate is significantly lower than the 26% complication rate associated with local excision, which includes wound dehiscence, infection, and contracture (P<.001). Deroofing also was found to have an HS recurrence rate of 14.5%, which is significantly less than the 30% recurrence rate seen with local excision (P=.015). Saylor et al5 also concluded that incision and drainage was recommended only for immediate relief of HS because of its 100% recurrence rate.
van der Zee2 reported on 88 lesions from 44 patients that were treated by surgical deroofing, resulting in an average defect of 3.0 cm in length and a mean healing time of 14 days. The typical outcome was cosmetically acceptable scarring; this finding was supported by a postoperative survey (>1 year), to which 37 of 44 patients responded and assigned an average satisfaction score of 8 (of a possible 10) and a recommendation rate of 90%.2
Procedural Coding—Specific Current Procedural Terminology codes (11450-11471) from the International Classification of Diseases, Tenth Revision, exist for HS deroofing procedures; the applicable code for a given case depends on the final length of the surgical defect. Documentation to support these codes is similar to the note for an excision procedure, taking care to include location, depth, and length of the excision; healing by secondary intention; and the diagnosis of HS.
Final Thoughts
Deroofing is a surgical option that can be beneficial to patients with HS. It is a relatively simple procedure available to any dermatologist, regardless of setting. We encourage dermatologists to consider deroofing, even in patients with Hurley stage II lesions, because it can yield cosmetically acceptable and definitive results, given the variety of therapies available for HS. Deroofing also can be superior to standard excision, especially because of the potential complications with standard excision and quicker operative time with deroofing. As more providers become familiar with the deroofing procedure for HS, further studies can be undertaken to add to the paucity of data about deroofing and how it compares to other surgical treatments.
Practice Gap
Hidradenitis suppurativa (HS) is a chronic inflammatory skin condition characterized by inflammatory nodules, abscesses, sinus tracts, fistulae, and scarring, mainly in intertriginous areas. The extent of disease—classified using the Hurley staging system (stages I–III)—helps guide treatment, which includes medical management and surgical intervention in later stages.
First-line treatment of HS includes topical or systemic medications, or both. Surgical therapy typically is reserved for refractory HS in moderate to severe disease (Hurley stages II and III) and is combined with pharmacotherapy. Specifically, clinical management guidelines issued by an expert committee of the United States and Canadian Hidradenitis Suppurativa Foundations recommend excision or deroofing for recurrent nodules and tunnels.1
Surgical options for HS that are available to the outpatient dermatologist include incision and drainage, electrosurgery, CO2 laser evaporation, excision, and deroofing (also known as unroofing).2 Deroofing is a fairly novel therapy; many dermatologists are unfamiliar with the procedure. A PubMed search of articles indexed for MEDLINE related to HS prior to 2010 revealed only 1 article containing the word deroofing and only 4 articles containing unroofing.
The pathophysiology of HS has important implications for successful treatment. Inflammation of the follicular pilosebaceous unit along with follicular occlusion create challenges with treatment.3 It is postulated that a defect in the glassy membrane of the infra-infundibular wall predisposes the pilosebaceous follicle to lose its structural integrality as pressure builds from plugging of the duct,4 which can result in the clinical hallmarks of HS including tunneling tracts, bridging nodules, abscesses, and fistulae that form with lateral expansion of the plugged follicle.
Leaking of the contents of these plugged follicles into surrounding tissue produces an inflammatory response in characteristic HS lesions. Because debris within the lesions moves laterally instead of being able to burst to the surface, the lesions have difficulty fully healing. Unroofing the lesions and removing built-up debris allows them to heal more expediently and quiets the underlying immune response by removing the stimulus.4
Herein, we describe the benefits, risks, and surgical process of deroofing for HS.
Technique and Tools
Deroofing is performed under local anesthesia, stepwise as follows:
1. Identify sinus tracts and infiltrate the area with lidocaine (Figure, A).
2. Use a blunt probe to define the borders of the area to be unroofed and to evaluate for any communicating sinus tracts (Figure, B).
3. Remove the roof of underlying abscesses and tracts, using a probe as a guide (Figure, C).
4. Enter through the skin or sinus opening using electrocautery or with a scalpel or scissors; perform blunt dissection.
5. Reflect back the entirety of skin overlying the probed areas and remove the skin to expose the base of the lesion (Figure, D).
6. Explore the exposed base and walls of the lesion with the probe again to assess for hidden tracts; take care not to create false tracts.
7. Debride the surgical wound using curettage or rough gauze grattage to remove remaining inflammatory debris or biofilm. To achieve hemostasis, apply aluminum chloride or ferric chloride. Coat the wound with petroleum jelly and gauze and allow it to heal by secondary intention.
8. Educate the patient on wound care—once-daily gentle cleansing with soap and water, followed by application of a moist dressing—which is similar to wound healing by secondary intention from other causes.2,4

Practice Implications
A deroofing procedure has many benefits compared to other surgical modalities for the treatment of HS. Deroofing requires only a probe, curette, and electrocautery device, making the procedure more cost-effective than excision, which requires a full tray of equipment and sutures. Furthermore, margins do not need to be taken with deroofing, and no undermining or closure is needed, which saves time during the operation and minimizes the risk for complications, including dehiscence and formation of new sinus tracts.4 No specialized equipment, such as a CO2 laser, is required, which makes deroofing accessible to every clinical dermatologist in any demographic or geographic setting.
Evidence of Benefit—Saylor and colleagues5 found that deroofing carries a 12.5% complication rate, which includes postoperative bleeding, hypergranulation tissue, and rarely wound infection. This rate is significantly lower than the 26% complication rate associated with local excision, which includes wound dehiscence, infection, and contracture (P<.001). Deroofing also was found to have an HS recurrence rate of 14.5%, which is significantly less than the 30% recurrence rate seen with local excision (P=.015). Saylor et al5 also concluded that incision and drainage was recommended only for immediate relief of HS because of its 100% recurrence rate.
van der Zee2 reported on 88 lesions from 44 patients that were treated by surgical deroofing, resulting in an average defect of 3.0 cm in length and a mean healing time of 14 days. The typical outcome was cosmetically acceptable scarring; this finding was supported by a postoperative survey (>1 year), to which 37 of 44 patients responded and assigned an average satisfaction score of 8 (of a possible 10) and a recommendation rate of 90%.2
Procedural Coding—Specific Current Procedural Terminology codes (11450-11471) from the International Classification of Diseases, Tenth Revision, exist for HS deroofing procedures; the applicable code for a given case depends on the final length of the surgical defect. Documentation to support these codes is similar to the note for an excision procedure, taking care to include location, depth, and length of the excision; healing by secondary intention; and the diagnosis of HS.
Final Thoughts
Deroofing is a surgical option that can be beneficial to patients with HS. It is a relatively simple procedure available to any dermatologist, regardless of setting. We encourage dermatologists to consider deroofing, even in patients with Hurley stage II lesions, because it can yield cosmetically acceptable and definitive results, given the variety of therapies available for HS. Deroofing also can be superior to standard excision, especially because of the potential complications with standard excision and quicker operative time with deroofing. As more providers become familiar with the deroofing procedure for HS, further studies can be undertaken to add to the paucity of data about deroofing and how it compares to other surgical treatments.
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81:76-90. doi:10.1016/j.jaad.2019.02.067
- van der Zee HH, Prens EP, Boer J. Deroofing: a tissue-saving surgical technique for the treatment of mild to moderate hidradenitis suppurativa lesions. J Am Acad Dermatol. 2010;63:475-480. doi:10.1016/j.jaad.2009.12.018
- Napolitano M, Megna M, Timoshchuk EA, et al. Hidradenitis suppurativa: from pathogenesis to diagnosis and treatment. Clin Cosmet Investig Dermatol. 2017;10:105-115. doi:10.2147/CCID.S111019
- Danby FW. Commentary: unroofing for hidradenitis suppurativa, why and how. J Am Acad Dermatol. 2010;63:481.e1-481.e3. doi:10.1016/j.jaad.2010.01.033
- Saylor DK, Brownstone ND, Naik HB. Office-based surgical intervention for hidradenitis suppurativa (HS): a focused review for dermatologists. Dermatol Ther (Heidelb). 2020;10:529-549. doi:10.1007/s13555-020-00391-x
- Alikhan A, Sayed C, Alavi A, et al. North American clinical management guidelines for hidradenitis suppurativa: a publication from the United States and Canadian Hidradenitis Suppurativa Foundations: part I: diagnosis, evaluation, and the use of complementary and procedural management. J Am Acad Dermatol. 2019;81:76-90. doi:10.1016/j.jaad.2019.02.067
- van der Zee HH, Prens EP, Boer J. Deroofing: a tissue-saving surgical technique for the treatment of mild to moderate hidradenitis suppurativa lesions. J Am Acad Dermatol. 2010;63:475-480. doi:10.1016/j.jaad.2009.12.018
- Napolitano M, Megna M, Timoshchuk EA, et al. Hidradenitis suppurativa: from pathogenesis to diagnosis and treatment. Clin Cosmet Investig Dermatol. 2017;10:105-115. doi:10.2147/CCID.S111019
- Danby FW. Commentary: unroofing for hidradenitis suppurativa, why and how. J Am Acad Dermatol. 2010;63:481.e1-481.e3. doi:10.1016/j.jaad.2010.01.033
- Saylor DK, Brownstone ND, Naik HB. Office-based surgical intervention for hidradenitis suppurativa (HS): a focused review for dermatologists. Dermatol Ther (Heidelb). 2020;10:529-549. doi:10.1007/s13555-020-00391-x
Polypodium leucotomos found to reverse AK skin damage
MILAN – Application of topical or both treated over 12 months, in a randomized, blinded study presented at the annual congress of the European Academy of Dermatology and Venereology.
At 12 months, the percentage of patients with a normal or almost normal honeycomb pattern when evaluated blindly with reflectance confocal microscopy (RCM) was about twice as great in either of the two groups that received PLE relative to those treated with topical photoprotection alone, according to Giovanni Pellacani, MD, PhD, chair of dermatology, University of Sapienza, Rome.
“In patients with severe actinic keratosis, the 12-month use of a PLE-based topical or oral photoprotection is associated with positive clinical and anatomical outcomes,” Dr. Pellacani said.
PLE, which is already commonly used in sun protection products, is derived from a South American species of fern and has been proposed for a broad array of dermatologic diseases. According to Dr. Pellacani, in vivo studies associating PLE with immune photoprotection make this agent particularly promising for severe AKs.
In this study involving two clinical research centers in Italy, 131 patients with photoaging and at least three AKs were randomized to one of three treatment arms. The control arm received topical photoprotection with an SPF of 100 or higher applied twice daily to all sun-exposed areas. The two treatment arms received the same topical photoprotection plus either a PLE-containing topical cream alone or a PLE-containing topical cream plus PLE in an oral form (240 mg) once daily
Patients were evaluated at 3 months, 6 months, and 1 year with several measures, including the Actinic Keratosis Area Score Index (AKASI) and the AK Field Assessment Scale Area (AK-FAS). They were also assessed with RCM. All clinical assessments and RCM evaluations, which assessed seven different parameters, such as honeycomb pattern, mottled pigmentation, and reticulated collagen, were performed by dermatologists blinded to the treatment assignment.
Complete data were available for 116 patients who completed all three evaluations over the 12 months of follow-up. On RCM, 50% of those receiving the oral and topical forms of PLE and 45% of those receiving topical PLE had normalization of the honeycomb pattern. These responses were significantly greater (P = .04 for both) than the 26% with normalization in the control group.
Although there were no significant differences in any of the other parameters evaluated by RCM, the improvement in the honeycomb pattern was accompanied by a 7% improvement in the AKASI score in patients taking PLE, either topically or orally and topically, while there was a 6% worsening (P < .001) among controls.
The AK-FAS score improved at 12 months by 26% in the group on oral/topical PLE and by 4% in the group on topical PLE. The score worsened by 13% among controls.
Over the course of the study, patients were permitted to take an appropriate therapy, such as imiquimod, cryotherapy, or 5-flourouracil if there was worsening of the AK-FAS score or if new lesions appeared.
On this measure, 38% of controls and 11% of those randomized to topical PLE had progressive disease versus only 2% of those randomized to take both topical and oral PLE, Dr. Pellacani reported.
The lower rate of new lesions or a start of a new drug over the course of the study in the group receiving both the topical and the oral formulations of PLE relative to those receiving topical PLE alone did not reach statistical significance, but Dr. Pellacani concluded that the addition of PLE to topical photoprotection without PLE seemed to provide a potentially clinically meaningful advantage.
Larger studies and longer term studies are needed, according to Dr. Pellacani, who noted that the substantial body of clinical studies associating PLE with benefit in a variety of dermatologic disorders has been weakened by the absence of well-designed studies that are adequately powered to guide clinical use.
Salvador González, MD, PhD, a dermatology specialist at Alcalá University, Madrid, also believes that PLE deserves further evaluation not just for photoprotection but for reinvigorating damaged skin due to its antioxidant and anti-inflammatory properties. He was the senior author of a 2020 paper in Photochemical and Photobiological Sciences that summarized the potential benefits of PLE in preventing damage related to sun exposure.
Among its mechanism, PLE generates reactive oxygen species (ROS) and prevents depletion of Langerhans cells induced by ultraviolet (UV) light, Dr. González explained in an interview. “At the cellular level, PLE activates tumor suppression p53, inhibits UV-induced COX-2 expression, reduces inflammation, and preventions immunosuppression,” he continued. In addition, he said PLE also prevents UV-A-induced common deletions related to mitochondrial damage and MMP1 expression induced by various UV wavelengths.
“These molecular and cellular effects may translate into long-term inhibition of carcinogenesis including actinic keratosis,” he said, noting that all of these findings “justify the work by Pellacani and collaborators.”
Dr. Pellacani reports no potential conflicts of interest. Dr. González has a financial relationship with Cantabria Laboratories.
MILAN – Application of topical or both treated over 12 months, in a randomized, blinded study presented at the annual congress of the European Academy of Dermatology and Venereology.
At 12 months, the percentage of patients with a normal or almost normal honeycomb pattern when evaluated blindly with reflectance confocal microscopy (RCM) was about twice as great in either of the two groups that received PLE relative to those treated with topical photoprotection alone, according to Giovanni Pellacani, MD, PhD, chair of dermatology, University of Sapienza, Rome.
“In patients with severe actinic keratosis, the 12-month use of a PLE-based topical or oral photoprotection is associated with positive clinical and anatomical outcomes,” Dr. Pellacani said.
PLE, which is already commonly used in sun protection products, is derived from a South American species of fern and has been proposed for a broad array of dermatologic diseases. According to Dr. Pellacani, in vivo studies associating PLE with immune photoprotection make this agent particularly promising for severe AKs.
In this study involving two clinical research centers in Italy, 131 patients with photoaging and at least three AKs were randomized to one of three treatment arms. The control arm received topical photoprotection with an SPF of 100 or higher applied twice daily to all sun-exposed areas. The two treatment arms received the same topical photoprotection plus either a PLE-containing topical cream alone or a PLE-containing topical cream plus PLE in an oral form (240 mg) once daily
Patients were evaluated at 3 months, 6 months, and 1 year with several measures, including the Actinic Keratosis Area Score Index (AKASI) and the AK Field Assessment Scale Area (AK-FAS). They were also assessed with RCM. All clinical assessments and RCM evaluations, which assessed seven different parameters, such as honeycomb pattern, mottled pigmentation, and reticulated collagen, were performed by dermatologists blinded to the treatment assignment.
Complete data were available for 116 patients who completed all three evaluations over the 12 months of follow-up. On RCM, 50% of those receiving the oral and topical forms of PLE and 45% of those receiving topical PLE had normalization of the honeycomb pattern. These responses were significantly greater (P = .04 for both) than the 26% with normalization in the control group.
Although there were no significant differences in any of the other parameters evaluated by RCM, the improvement in the honeycomb pattern was accompanied by a 7% improvement in the AKASI score in patients taking PLE, either topically or orally and topically, while there was a 6% worsening (P < .001) among controls.
The AK-FAS score improved at 12 months by 26% in the group on oral/topical PLE and by 4% in the group on topical PLE. The score worsened by 13% among controls.
Over the course of the study, patients were permitted to take an appropriate therapy, such as imiquimod, cryotherapy, or 5-flourouracil if there was worsening of the AK-FAS score or if new lesions appeared.
On this measure, 38% of controls and 11% of those randomized to topical PLE had progressive disease versus only 2% of those randomized to take both topical and oral PLE, Dr. Pellacani reported.
The lower rate of new lesions or a start of a new drug over the course of the study in the group receiving both the topical and the oral formulations of PLE relative to those receiving topical PLE alone did not reach statistical significance, but Dr. Pellacani concluded that the addition of PLE to topical photoprotection without PLE seemed to provide a potentially clinically meaningful advantage.
Larger studies and longer term studies are needed, according to Dr. Pellacani, who noted that the substantial body of clinical studies associating PLE with benefit in a variety of dermatologic disorders has been weakened by the absence of well-designed studies that are adequately powered to guide clinical use.
Salvador González, MD, PhD, a dermatology specialist at Alcalá University, Madrid, also believes that PLE deserves further evaluation not just for photoprotection but for reinvigorating damaged skin due to its antioxidant and anti-inflammatory properties. He was the senior author of a 2020 paper in Photochemical and Photobiological Sciences that summarized the potential benefits of PLE in preventing damage related to sun exposure.
Among its mechanism, PLE generates reactive oxygen species (ROS) and prevents depletion of Langerhans cells induced by ultraviolet (UV) light, Dr. González explained in an interview. “At the cellular level, PLE activates tumor suppression p53, inhibits UV-induced COX-2 expression, reduces inflammation, and preventions immunosuppression,” he continued. In addition, he said PLE also prevents UV-A-induced common deletions related to mitochondrial damage and MMP1 expression induced by various UV wavelengths.
“These molecular and cellular effects may translate into long-term inhibition of carcinogenesis including actinic keratosis,” he said, noting that all of these findings “justify the work by Pellacani and collaborators.”
Dr. Pellacani reports no potential conflicts of interest. Dr. González has a financial relationship with Cantabria Laboratories.
MILAN – Application of topical or both treated over 12 months, in a randomized, blinded study presented at the annual congress of the European Academy of Dermatology and Venereology.
At 12 months, the percentage of patients with a normal or almost normal honeycomb pattern when evaluated blindly with reflectance confocal microscopy (RCM) was about twice as great in either of the two groups that received PLE relative to those treated with topical photoprotection alone, according to Giovanni Pellacani, MD, PhD, chair of dermatology, University of Sapienza, Rome.
“In patients with severe actinic keratosis, the 12-month use of a PLE-based topical or oral photoprotection is associated with positive clinical and anatomical outcomes,” Dr. Pellacani said.
PLE, which is already commonly used in sun protection products, is derived from a South American species of fern and has been proposed for a broad array of dermatologic diseases. According to Dr. Pellacani, in vivo studies associating PLE with immune photoprotection make this agent particularly promising for severe AKs.
In this study involving two clinical research centers in Italy, 131 patients with photoaging and at least three AKs were randomized to one of three treatment arms. The control arm received topical photoprotection with an SPF of 100 or higher applied twice daily to all sun-exposed areas. The two treatment arms received the same topical photoprotection plus either a PLE-containing topical cream alone or a PLE-containing topical cream plus PLE in an oral form (240 mg) once daily
Patients were evaluated at 3 months, 6 months, and 1 year with several measures, including the Actinic Keratosis Area Score Index (AKASI) and the AK Field Assessment Scale Area (AK-FAS). They were also assessed with RCM. All clinical assessments and RCM evaluations, which assessed seven different parameters, such as honeycomb pattern, mottled pigmentation, and reticulated collagen, were performed by dermatologists blinded to the treatment assignment.
Complete data were available for 116 patients who completed all three evaluations over the 12 months of follow-up. On RCM, 50% of those receiving the oral and topical forms of PLE and 45% of those receiving topical PLE had normalization of the honeycomb pattern. These responses were significantly greater (P = .04 for both) than the 26% with normalization in the control group.
Although there were no significant differences in any of the other parameters evaluated by RCM, the improvement in the honeycomb pattern was accompanied by a 7% improvement in the AKASI score in patients taking PLE, either topically or orally and topically, while there was a 6% worsening (P < .001) among controls.
The AK-FAS score improved at 12 months by 26% in the group on oral/topical PLE and by 4% in the group on topical PLE. The score worsened by 13% among controls.
Over the course of the study, patients were permitted to take an appropriate therapy, such as imiquimod, cryotherapy, or 5-flourouracil if there was worsening of the AK-FAS score or if new lesions appeared.
On this measure, 38% of controls and 11% of those randomized to topical PLE had progressive disease versus only 2% of those randomized to take both topical and oral PLE, Dr. Pellacani reported.
The lower rate of new lesions or a start of a new drug over the course of the study in the group receiving both the topical and the oral formulations of PLE relative to those receiving topical PLE alone did not reach statistical significance, but Dr. Pellacani concluded that the addition of PLE to topical photoprotection without PLE seemed to provide a potentially clinically meaningful advantage.
Larger studies and longer term studies are needed, according to Dr. Pellacani, who noted that the substantial body of clinical studies associating PLE with benefit in a variety of dermatologic disorders has been weakened by the absence of well-designed studies that are adequately powered to guide clinical use.
Salvador González, MD, PhD, a dermatology specialist at Alcalá University, Madrid, also believes that PLE deserves further evaluation not just for photoprotection but for reinvigorating damaged skin due to its antioxidant and anti-inflammatory properties. He was the senior author of a 2020 paper in Photochemical and Photobiological Sciences that summarized the potential benefits of PLE in preventing damage related to sun exposure.
Among its mechanism, PLE generates reactive oxygen species (ROS) and prevents depletion of Langerhans cells induced by ultraviolet (UV) light, Dr. González explained in an interview. “At the cellular level, PLE activates tumor suppression p53, inhibits UV-induced COX-2 expression, reduces inflammation, and preventions immunosuppression,” he continued. In addition, he said PLE also prevents UV-A-induced common deletions related to mitochondrial damage and MMP1 expression induced by various UV wavelengths.
“These molecular and cellular effects may translate into long-term inhibition of carcinogenesis including actinic keratosis,” he said, noting that all of these findings “justify the work by Pellacani and collaborators.”
Dr. Pellacani reports no potential conflicts of interest. Dr. González has a financial relationship with Cantabria Laboratories.
AT THE EADV CONGRESS
Isotretinoin prescribers need better education on emergency contraception
, in a survey of 57 clinicians.
Pregnancies among patients on isotretinoin have declined since the iPLEDGE risk management program was introduced in 2005, but from 2011 to 2017, 210 to 310 pregnancies were reported to the Food and Drug Administration every year, wrote Catherine E. Smiley of Penn State University, Hershey, Pa., and coauthors Melissa Butt, DrPH, and Andrea L. Zaenglein, MD, of Penn State.
For patients on isotretinoin, EC “becomes critical when abstinence fails or contraception is not used properly,” but EC merits only a brief mention in iPLEDGE materials for patients and providers, they noted.
Patients on isotretinoin who choose abstinence as their form of birth control are the group at greatest risk for pregnancy, Dr. Zaenglein, professor of dermatology and pediatric dermatology, Penn State University, said in an interview. “However, the iPLEDGE program fails to educate patients adequately on emergency contraception,” she explained.
To assess pediatric dermatologists’ understanding of EC and their contraception counseling practices for isotretinoin patients, the researchers surveyed 57 pediatric dermatologists who prescribed isotretinoin as part of their practices. The findings were published in Pediatric Dermatology.Respondents included 53 practicing dermatologists, 2 residents, and 2 fellows. Approximately one-third (31.6%) had been in practice for 6-10 years, almost 23% had been in practice for 3-5 years, and almost 20% had been in practice for 21 or more years. Almost two-thirds practiced pediatric dermatology only.
Overall, 58% of the respondents strongly agreed that they provided contraception counseling to patients at their initial visit for isotretinoin, but only 7% and 3.5% reported providing EC counseling at initial and follow-up visits, respectively. More than half (58%) said they did not counsel patients on the side effects of EC.
As for provider education, 7.1% of respondents said they had received formal education on EC counseling, 25% reported receiving informal education on EC counseling, and 68% said they received no education on EC counseling.
A total of 32% of respondents said they were at least somewhat confident in how to obtain EC in their state.
EC is an effective form of contraception if used after unprotected intercourse, and discounts can reduce the price to as low as $9.69, the researchers wrote in their discussion. “Given that most providers in this study did not receive formal education on EC, and most do not provide EC counseling to their patients of reproductive potential on isotretinoin, EC education should be a core competency in dermatology residency education on isotretinoin prescribing,” the researchers noted. In addition, EC counseling in the iPLEDGE program should be improved by including more information in education materials and reminding patients that EC is an option, they said.
The study findings were limited by several factors including the small sample size and the multiple-choice format that prevented respondents to share rationales for their responses, the researchers noted.
However, the results highlight the need to improve EC education among pediatric dermatologists to better inform patients considering isotretinoin, especially those choosing abstinence as a method of birth control, they emphasized.
“This study is very important at this specific time for two reasons,” Dr. Zaenglein said in an interview. “The first is that with the recent disastrous rollout of the new iPLEDGE changes, there have been many calls to reform the REMS program. For the first time in the 22-year history of the program, the isotretinoin manufacturers, who manage the iPLEDGE program as an unidentified group (the IPMG), have been forced by the FDA to meet with the AAD iPLEDGE Task Force,” said Dr. Zaenglein, a member of the task force.
“The task force is currently advocating for common sense changes to iPLEDGE and I think enhancing education on emergency contraception is vital to the goal of the program, stated as ‘to manage the risk of isotretinoin’s teratogenicity and to minimize fetal exposure,’ ” she added. For many patients who previously became pregnant on isotretinoin, Plan B, an over-the-counter, FDA-approved form of contraception, might have prevented that pregnancy if the patients received adequate education on EC, she said.
The current study is especially relevant now, said Dr. Zaenglein. “With the reversal of Roe v. Wade, access to abortion is restricted or completely banned in many states, which makes educating our patients on how to prevent pregnancy even more important.”
Dr. Zaenglein said she was “somewhat surprised” by how many respondents were not educating their isotretinoin patients on EC. “However, these results follow a known trend among dermatologists. Only 50% of dermatologists prescribe oral contraceptives for acne, despite its being an FDA-approved treatment for the most common dermatologic condition we see in adolescents and young adults,” she noted.
“In general, dermatologists, and subsequently dermatology residents, are poorly educated on issues of reproductive health and how they are relevant to dermatologic care,” she added.
Dr. Zaenglein’s take home message: “Dermatologists should educate all patients of childbearing potential taking isotretinoin on how to acquire and use emergency contraception at every visit.” As for additional research, she said that since the study was conducted with pediatric dermatologists, “it would be very interesting to see if general dermatologists had the same lack of comfort in educating patients on emergency contraception and what their standard counseling practices are.”
The study received no outside funding. Dr. Zaenglein is a member of the AAD’s iPLEDGE Work Group and serves as an editor-in-chief of Pediatric Dermatology.
, in a survey of 57 clinicians.
Pregnancies among patients on isotretinoin have declined since the iPLEDGE risk management program was introduced in 2005, but from 2011 to 2017, 210 to 310 pregnancies were reported to the Food and Drug Administration every year, wrote Catherine E. Smiley of Penn State University, Hershey, Pa., and coauthors Melissa Butt, DrPH, and Andrea L. Zaenglein, MD, of Penn State.
For patients on isotretinoin, EC “becomes critical when abstinence fails or contraception is not used properly,” but EC merits only a brief mention in iPLEDGE materials for patients and providers, they noted.
Patients on isotretinoin who choose abstinence as their form of birth control are the group at greatest risk for pregnancy, Dr. Zaenglein, professor of dermatology and pediatric dermatology, Penn State University, said in an interview. “However, the iPLEDGE program fails to educate patients adequately on emergency contraception,” she explained.
To assess pediatric dermatologists’ understanding of EC and their contraception counseling practices for isotretinoin patients, the researchers surveyed 57 pediatric dermatologists who prescribed isotretinoin as part of their practices. The findings were published in Pediatric Dermatology.Respondents included 53 practicing dermatologists, 2 residents, and 2 fellows. Approximately one-third (31.6%) had been in practice for 6-10 years, almost 23% had been in practice for 3-5 years, and almost 20% had been in practice for 21 or more years. Almost two-thirds practiced pediatric dermatology only.
Overall, 58% of the respondents strongly agreed that they provided contraception counseling to patients at their initial visit for isotretinoin, but only 7% and 3.5% reported providing EC counseling at initial and follow-up visits, respectively. More than half (58%) said they did not counsel patients on the side effects of EC.
As for provider education, 7.1% of respondents said they had received formal education on EC counseling, 25% reported receiving informal education on EC counseling, and 68% said they received no education on EC counseling.
A total of 32% of respondents said they were at least somewhat confident in how to obtain EC in their state.
EC is an effective form of contraception if used after unprotected intercourse, and discounts can reduce the price to as low as $9.69, the researchers wrote in their discussion. “Given that most providers in this study did not receive formal education on EC, and most do not provide EC counseling to their patients of reproductive potential on isotretinoin, EC education should be a core competency in dermatology residency education on isotretinoin prescribing,” the researchers noted. In addition, EC counseling in the iPLEDGE program should be improved by including more information in education materials and reminding patients that EC is an option, they said.
The study findings were limited by several factors including the small sample size and the multiple-choice format that prevented respondents to share rationales for their responses, the researchers noted.
However, the results highlight the need to improve EC education among pediatric dermatologists to better inform patients considering isotretinoin, especially those choosing abstinence as a method of birth control, they emphasized.
“This study is very important at this specific time for two reasons,” Dr. Zaenglein said in an interview. “The first is that with the recent disastrous rollout of the new iPLEDGE changes, there have been many calls to reform the REMS program. For the first time in the 22-year history of the program, the isotretinoin manufacturers, who manage the iPLEDGE program as an unidentified group (the IPMG), have been forced by the FDA to meet with the AAD iPLEDGE Task Force,” said Dr. Zaenglein, a member of the task force.
“The task force is currently advocating for common sense changes to iPLEDGE and I think enhancing education on emergency contraception is vital to the goal of the program, stated as ‘to manage the risk of isotretinoin’s teratogenicity and to minimize fetal exposure,’ ” she added. For many patients who previously became pregnant on isotretinoin, Plan B, an over-the-counter, FDA-approved form of contraception, might have prevented that pregnancy if the patients received adequate education on EC, she said.
The current study is especially relevant now, said Dr. Zaenglein. “With the reversal of Roe v. Wade, access to abortion is restricted or completely banned in many states, which makes educating our patients on how to prevent pregnancy even more important.”
Dr. Zaenglein said she was “somewhat surprised” by how many respondents were not educating their isotretinoin patients on EC. “However, these results follow a known trend among dermatologists. Only 50% of dermatologists prescribe oral contraceptives for acne, despite its being an FDA-approved treatment for the most common dermatologic condition we see in adolescents and young adults,” she noted.
“In general, dermatologists, and subsequently dermatology residents, are poorly educated on issues of reproductive health and how they are relevant to dermatologic care,” she added.
Dr. Zaenglein’s take home message: “Dermatologists should educate all patients of childbearing potential taking isotretinoin on how to acquire and use emergency contraception at every visit.” As for additional research, she said that since the study was conducted with pediatric dermatologists, “it would be very interesting to see if general dermatologists had the same lack of comfort in educating patients on emergency contraception and what their standard counseling practices are.”
The study received no outside funding. Dr. Zaenglein is a member of the AAD’s iPLEDGE Work Group and serves as an editor-in-chief of Pediatric Dermatology.
, in a survey of 57 clinicians.
Pregnancies among patients on isotretinoin have declined since the iPLEDGE risk management program was introduced in 2005, but from 2011 to 2017, 210 to 310 pregnancies were reported to the Food and Drug Administration every year, wrote Catherine E. Smiley of Penn State University, Hershey, Pa., and coauthors Melissa Butt, DrPH, and Andrea L. Zaenglein, MD, of Penn State.
For patients on isotretinoin, EC “becomes critical when abstinence fails or contraception is not used properly,” but EC merits only a brief mention in iPLEDGE materials for patients and providers, they noted.
Patients on isotretinoin who choose abstinence as their form of birth control are the group at greatest risk for pregnancy, Dr. Zaenglein, professor of dermatology and pediatric dermatology, Penn State University, said in an interview. “However, the iPLEDGE program fails to educate patients adequately on emergency contraception,” she explained.
To assess pediatric dermatologists’ understanding of EC and their contraception counseling practices for isotretinoin patients, the researchers surveyed 57 pediatric dermatologists who prescribed isotretinoin as part of their practices. The findings were published in Pediatric Dermatology.Respondents included 53 practicing dermatologists, 2 residents, and 2 fellows. Approximately one-third (31.6%) had been in practice for 6-10 years, almost 23% had been in practice for 3-5 years, and almost 20% had been in practice for 21 or more years. Almost two-thirds practiced pediatric dermatology only.
Overall, 58% of the respondents strongly agreed that they provided contraception counseling to patients at their initial visit for isotretinoin, but only 7% and 3.5% reported providing EC counseling at initial and follow-up visits, respectively. More than half (58%) said they did not counsel patients on the side effects of EC.
As for provider education, 7.1% of respondents said they had received formal education on EC counseling, 25% reported receiving informal education on EC counseling, and 68% said they received no education on EC counseling.
A total of 32% of respondents said they were at least somewhat confident in how to obtain EC in their state.
EC is an effective form of contraception if used after unprotected intercourse, and discounts can reduce the price to as low as $9.69, the researchers wrote in their discussion. “Given that most providers in this study did not receive formal education on EC, and most do not provide EC counseling to their patients of reproductive potential on isotretinoin, EC education should be a core competency in dermatology residency education on isotretinoin prescribing,” the researchers noted. In addition, EC counseling in the iPLEDGE program should be improved by including more information in education materials and reminding patients that EC is an option, they said.
The study findings were limited by several factors including the small sample size and the multiple-choice format that prevented respondents to share rationales for their responses, the researchers noted.
However, the results highlight the need to improve EC education among pediatric dermatologists to better inform patients considering isotretinoin, especially those choosing abstinence as a method of birth control, they emphasized.
“This study is very important at this specific time for two reasons,” Dr. Zaenglein said in an interview. “The first is that with the recent disastrous rollout of the new iPLEDGE changes, there have been many calls to reform the REMS program. For the first time in the 22-year history of the program, the isotretinoin manufacturers, who manage the iPLEDGE program as an unidentified group (the IPMG), have been forced by the FDA to meet with the AAD iPLEDGE Task Force,” said Dr. Zaenglein, a member of the task force.
“The task force is currently advocating for common sense changes to iPLEDGE and I think enhancing education on emergency contraception is vital to the goal of the program, stated as ‘to manage the risk of isotretinoin’s teratogenicity and to minimize fetal exposure,’ ” she added. For many patients who previously became pregnant on isotretinoin, Plan B, an over-the-counter, FDA-approved form of contraception, might have prevented that pregnancy if the patients received adequate education on EC, she said.
The current study is especially relevant now, said Dr. Zaenglein. “With the reversal of Roe v. Wade, access to abortion is restricted or completely banned in many states, which makes educating our patients on how to prevent pregnancy even more important.”
Dr. Zaenglein said she was “somewhat surprised” by how many respondents were not educating their isotretinoin patients on EC. “However, these results follow a known trend among dermatologists. Only 50% of dermatologists prescribe oral contraceptives for acne, despite its being an FDA-approved treatment for the most common dermatologic condition we see in adolescents and young adults,” she noted.
“In general, dermatologists, and subsequently dermatology residents, are poorly educated on issues of reproductive health and how they are relevant to dermatologic care,” she added.
Dr. Zaenglein’s take home message: “Dermatologists should educate all patients of childbearing potential taking isotretinoin on how to acquire and use emergency contraception at every visit.” As for additional research, she said that since the study was conducted with pediatric dermatologists, “it would be very interesting to see if general dermatologists had the same lack of comfort in educating patients on emergency contraception and what their standard counseling practices are.”
The study received no outside funding. Dr. Zaenglein is a member of the AAD’s iPLEDGE Work Group and serves as an editor-in-chief of Pediatric Dermatology.
FROM PEDIATRIC DERMATOLOGY
FDA approves Botox challenger Daxxify for frown lines
The U.S. .
According to a company news release, Daxxify, an acetylcholine release inhibitor and neuromuscular blocking agent, is the first peptide-formulated, long-acting neuromodulator approved for this indication.
The approval of Daxxify, manufactured by Revance Therapeutics, was based on the data from the SAKURA phase 3 clinical trial program, which included more than 2,700 adults who received roughly 4,200 treatments, according to the company.
About three-quarters of participants achieved at least a two-grade improvement in glabellar lines at week 4 as judged by both investigator and patient, and 98% achieved “none or mild wrinkle severity” at week 4 per investigator assessment, the company said.
The median duration of treatment effect was 6 months, with some patients maintaining treatment results at 9 months, compared with a 3- to 4-month duration of treatment effect with conventional neuromodulators.
“Compelling data from the largest phase 3 clinical program ever conducted for glabellar lines demonstrated that Daxxify was well tolerated and achieved clinically significant improvement with long-lasting results and high patient satisfaction,” SAKURA investigator Jeffrey Dover, MD, co-director of SkinCare Physicians, Chestnut Hill, Mass., said in the news release.
“Notably,” said Dr. Dover, “Daxxify was able to demonstrate a long duration of effect while only utilizing 0.18 ng of core active ingredient in the 40-unit labeled indication for glabellar lines.”
Daxxify has a safety profile in line with other currently available neuromodulators in the aesthetics market, the company said, with no serious treatment-related adverse events reported in clinical trial participants.
The most common treatment-related adverse events in the pivotal studies were headache (6%), eyelid ptosis (2%) and facial paresis, including facial asymmetry (1%).
Daxxify is contraindicated in adults with hypersensitivity to any botulinum toxin preparation or any of the components in the formulation and infection at the injection sites.
Full prescribing information is available online.
A version of this article first appeared on Medscape.com.
The U.S. .
According to a company news release, Daxxify, an acetylcholine release inhibitor and neuromuscular blocking agent, is the first peptide-formulated, long-acting neuromodulator approved for this indication.
The approval of Daxxify, manufactured by Revance Therapeutics, was based on the data from the SAKURA phase 3 clinical trial program, which included more than 2,700 adults who received roughly 4,200 treatments, according to the company.
About three-quarters of participants achieved at least a two-grade improvement in glabellar lines at week 4 as judged by both investigator and patient, and 98% achieved “none or mild wrinkle severity” at week 4 per investigator assessment, the company said.
The median duration of treatment effect was 6 months, with some patients maintaining treatment results at 9 months, compared with a 3- to 4-month duration of treatment effect with conventional neuromodulators.
“Compelling data from the largest phase 3 clinical program ever conducted for glabellar lines demonstrated that Daxxify was well tolerated and achieved clinically significant improvement with long-lasting results and high patient satisfaction,” SAKURA investigator Jeffrey Dover, MD, co-director of SkinCare Physicians, Chestnut Hill, Mass., said in the news release.
“Notably,” said Dr. Dover, “Daxxify was able to demonstrate a long duration of effect while only utilizing 0.18 ng of core active ingredient in the 40-unit labeled indication for glabellar lines.”
Daxxify has a safety profile in line with other currently available neuromodulators in the aesthetics market, the company said, with no serious treatment-related adverse events reported in clinical trial participants.
The most common treatment-related adverse events in the pivotal studies were headache (6%), eyelid ptosis (2%) and facial paresis, including facial asymmetry (1%).
Daxxify is contraindicated in adults with hypersensitivity to any botulinum toxin preparation or any of the components in the formulation and infection at the injection sites.
Full prescribing information is available online.
A version of this article first appeared on Medscape.com.
The U.S. .
According to a company news release, Daxxify, an acetylcholine release inhibitor and neuromuscular blocking agent, is the first peptide-formulated, long-acting neuromodulator approved for this indication.
The approval of Daxxify, manufactured by Revance Therapeutics, was based on the data from the SAKURA phase 3 clinical trial program, which included more than 2,700 adults who received roughly 4,200 treatments, according to the company.
About three-quarters of participants achieved at least a two-grade improvement in glabellar lines at week 4 as judged by both investigator and patient, and 98% achieved “none or mild wrinkle severity” at week 4 per investigator assessment, the company said.
The median duration of treatment effect was 6 months, with some patients maintaining treatment results at 9 months, compared with a 3- to 4-month duration of treatment effect with conventional neuromodulators.
“Compelling data from the largest phase 3 clinical program ever conducted for glabellar lines demonstrated that Daxxify was well tolerated and achieved clinically significant improvement with long-lasting results and high patient satisfaction,” SAKURA investigator Jeffrey Dover, MD, co-director of SkinCare Physicians, Chestnut Hill, Mass., said in the news release.
“Notably,” said Dr. Dover, “Daxxify was able to demonstrate a long duration of effect while only utilizing 0.18 ng of core active ingredient in the 40-unit labeled indication for glabellar lines.”
Daxxify has a safety profile in line with other currently available neuromodulators in the aesthetics market, the company said, with no serious treatment-related adverse events reported in clinical trial participants.
The most common treatment-related adverse events in the pivotal studies were headache (6%), eyelid ptosis (2%) and facial paresis, including facial asymmetry (1%).
Daxxify is contraindicated in adults with hypersensitivity to any botulinum toxin preparation or any of the components in the formulation and infection at the injection sites.
Full prescribing information is available online.
A version of this article first appeared on Medscape.com.
Should patients with PsA or ankylosing spondylitis with axial disease be ‘lumped’ or ‘split’?
A new study provides evidence that two conditions that fall under the umbrella of spondyloarthritis – isolated axial disease in patients with psoriatic arthritis (PsA) and isolated axial disease in patients with ankylosing spondylitis (AS) accompanied by psoriasis – are different clinical entities and may need different treatments. These relatively rare rheumatologic conditions, defined by their back involvement, have considerable clinical overlap and are often lumped together under the label axial spondyloarthritis.
This is a hot topic and current matter of debate within the scientific community: Are axial PsA and axial AS two separate diseases or just two phenotypes under the spondyloarthritis umbrella? said Fabian Proft, MD, a rheumatologist and researcher at Charité Universitätsmedizin Berlin, commenting on the new study, which was published online in Annals of the Rheumatic Diseases.
Both conditions belong to the spectrum of spondyloarthritis, but with varying viewpoints on nomenclature. They have intersections and overlaps, but not all treatments are equally effective for both. “We need to better understand their differences and similarities,” Dr. Proft said, adding that the new study is noteworthy for the size of the population included, its long-term follow-up data, and the researchers’ depth of experience treating these patients.
The researchers are based at the University of Toronto, which has separate clinics dedicated to PsA and to AS, said Dafna D. Gladman, MD, professor of medicine at the university, codirector of the PsA clinic, and corresponding author for the new study. The two clinics follow the same standardized protocols, including clinical, radiographic, genetic, and laboratory assessments. Even though the patients present quite similarly, she credits referring physicians for recognizing the distinctions by their referrals to the PsA or AS clinic.
According to previous research, pure axial PsA, without peripheral involvement, is rare, affecting about 2%-5% of patients with PsA. For this study, an observational cohort of 1,576 patients from the PsA clinic included 31% (n = 495) with axial disease, 2% (n = 32) with isolated axial PsA, and 29% (n = 463) with both axial and peripheral involvement. A total of 25 of the patients with isolated axial PsA ultimately developed peripheral disease by their most recent clinic follow-up visit. In a second cohort of 1,688 patients with AS, nearly 5% (n = 68) had isolated axial disease with psoriasis.
“In our logistic regression analysis, isolated axial PsA was found to be a different clinical entity than isolated AS with psoriasis. They are not the same patients,” Dr. Gladman said. The patients with isolated axial PsA were older at diagnosis, more likely to have psoriatic nail lesions, and less likely to have inflammatory back pain than were patients with isolated axial AS and accompanying psoriasis.
When interviewed in early September, Dr. Gladman was preparing to fly to Ghent, Belgium, to participate in a debate at the International Congress on Spondyloarthritides, taking the pro position on the thesis: Is axial inflammation in PsA distinct from axial spondyloarthritis? Taking the con position was to be Robert Landewé, MD, PhD, of Amsterdam University Medical Center in the Netherlands.
“This is an old debate, splitters versus lumpers,” Dr. Gladman told this news organization. “My message is that when you place patients in more homogeneous groups, you can learn more and perhaps find better opportunities for treating their disease.” For example, even with the similarities, do these patients need to be treated with different medications? Medications for psoriasis, including those targeting the interleukin-23 cytokine, may not be effective for AS, but patients with axial PsA may not get them because of the association with axial AS.
“Now is the opportunity to really understand what – if any – are the differences between various components of this disease group. If you lump people together, you may miss the forest for the trees,” Dr. Gladman said. “If, at the end of the day, we find out these patients essentially are the same, I will lump. But until we have proved that there are no important differences, I will split.” She added that it is important for practicing rheumatologists to make the correct diagnosis so that they know to access certain drugs.
Dr. Proft credited Dr. Gladman and colleagues’ study for adding another piece of the puzzle to better understand differences and similarities for these two axial diseases. He noted, however, that the study did not include MRI scans for every participating patient, which could have given a deeper picture.
“International efforts are being made to recruit patients for a multinational, multicenter study of axial involvement in PsA,” which will include MRI data, Dr. Gladman said. She and Dr. Proft are both part of AXIS, the Axial Involvement in Psoriatic Arthritis cohort, now recruiting patients for such a study. AXIS is a joint project of the Assessment of SpondyloArthritis international Society and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“We don’t have final answers yet, although we have given evidence to support the differences.” The proof is in the pudding, she said, and that pudding will be the clinical trials.
The University of Toronto Psoriatic Arthritis Program is supported by a grant from the Krembil Foundation. The study authors declared no competing interests. Dr. Proft reported receiving research support from Novartis, Eli Lilly, and UCB, and fees for consulting and serving on speakers bureaus from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, Hexal, Janssen, Merck Sharp & Dohme, Novartis, Pfizer, Roche, and UCB.
A new study provides evidence that two conditions that fall under the umbrella of spondyloarthritis – isolated axial disease in patients with psoriatic arthritis (PsA) and isolated axial disease in patients with ankylosing spondylitis (AS) accompanied by psoriasis – are different clinical entities and may need different treatments. These relatively rare rheumatologic conditions, defined by their back involvement, have considerable clinical overlap and are often lumped together under the label axial spondyloarthritis.
This is a hot topic and current matter of debate within the scientific community: Are axial PsA and axial AS two separate diseases or just two phenotypes under the spondyloarthritis umbrella? said Fabian Proft, MD, a rheumatologist and researcher at Charité Universitätsmedizin Berlin, commenting on the new study, which was published online in Annals of the Rheumatic Diseases.
Both conditions belong to the spectrum of spondyloarthritis, but with varying viewpoints on nomenclature. They have intersections and overlaps, but not all treatments are equally effective for both. “We need to better understand their differences and similarities,” Dr. Proft said, adding that the new study is noteworthy for the size of the population included, its long-term follow-up data, and the researchers’ depth of experience treating these patients.
The researchers are based at the University of Toronto, which has separate clinics dedicated to PsA and to AS, said Dafna D. Gladman, MD, professor of medicine at the university, codirector of the PsA clinic, and corresponding author for the new study. The two clinics follow the same standardized protocols, including clinical, radiographic, genetic, and laboratory assessments. Even though the patients present quite similarly, she credits referring physicians for recognizing the distinctions by their referrals to the PsA or AS clinic.
According to previous research, pure axial PsA, without peripheral involvement, is rare, affecting about 2%-5% of patients with PsA. For this study, an observational cohort of 1,576 patients from the PsA clinic included 31% (n = 495) with axial disease, 2% (n = 32) with isolated axial PsA, and 29% (n = 463) with both axial and peripheral involvement. A total of 25 of the patients with isolated axial PsA ultimately developed peripheral disease by their most recent clinic follow-up visit. In a second cohort of 1,688 patients with AS, nearly 5% (n = 68) had isolated axial disease with psoriasis.
“In our logistic regression analysis, isolated axial PsA was found to be a different clinical entity than isolated AS with psoriasis. They are not the same patients,” Dr. Gladman said. The patients with isolated axial PsA were older at diagnosis, more likely to have psoriatic nail lesions, and less likely to have inflammatory back pain than were patients with isolated axial AS and accompanying psoriasis.
When interviewed in early September, Dr. Gladman was preparing to fly to Ghent, Belgium, to participate in a debate at the International Congress on Spondyloarthritides, taking the pro position on the thesis: Is axial inflammation in PsA distinct from axial spondyloarthritis? Taking the con position was to be Robert Landewé, MD, PhD, of Amsterdam University Medical Center in the Netherlands.
“This is an old debate, splitters versus lumpers,” Dr. Gladman told this news organization. “My message is that when you place patients in more homogeneous groups, you can learn more and perhaps find better opportunities for treating their disease.” For example, even with the similarities, do these patients need to be treated with different medications? Medications for psoriasis, including those targeting the interleukin-23 cytokine, may not be effective for AS, but patients with axial PsA may not get them because of the association with axial AS.
“Now is the opportunity to really understand what – if any – are the differences between various components of this disease group. If you lump people together, you may miss the forest for the trees,” Dr. Gladman said. “If, at the end of the day, we find out these patients essentially are the same, I will lump. But until we have proved that there are no important differences, I will split.” She added that it is important for practicing rheumatologists to make the correct diagnosis so that they know to access certain drugs.
Dr. Proft credited Dr. Gladman and colleagues’ study for adding another piece of the puzzle to better understand differences and similarities for these two axial diseases. He noted, however, that the study did not include MRI scans for every participating patient, which could have given a deeper picture.
“International efforts are being made to recruit patients for a multinational, multicenter study of axial involvement in PsA,” which will include MRI data, Dr. Gladman said. She and Dr. Proft are both part of AXIS, the Axial Involvement in Psoriatic Arthritis cohort, now recruiting patients for such a study. AXIS is a joint project of the Assessment of SpondyloArthritis international Society and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“We don’t have final answers yet, although we have given evidence to support the differences.” The proof is in the pudding, she said, and that pudding will be the clinical trials.
The University of Toronto Psoriatic Arthritis Program is supported by a grant from the Krembil Foundation. The study authors declared no competing interests. Dr. Proft reported receiving research support from Novartis, Eli Lilly, and UCB, and fees for consulting and serving on speakers bureaus from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, Hexal, Janssen, Merck Sharp & Dohme, Novartis, Pfizer, Roche, and UCB.
A new study provides evidence that two conditions that fall under the umbrella of spondyloarthritis – isolated axial disease in patients with psoriatic arthritis (PsA) and isolated axial disease in patients with ankylosing spondylitis (AS) accompanied by psoriasis – are different clinical entities and may need different treatments. These relatively rare rheumatologic conditions, defined by their back involvement, have considerable clinical overlap and are often lumped together under the label axial spondyloarthritis.
This is a hot topic and current matter of debate within the scientific community: Are axial PsA and axial AS two separate diseases or just two phenotypes under the spondyloarthritis umbrella? said Fabian Proft, MD, a rheumatologist and researcher at Charité Universitätsmedizin Berlin, commenting on the new study, which was published online in Annals of the Rheumatic Diseases.
Both conditions belong to the spectrum of spondyloarthritis, but with varying viewpoints on nomenclature. They have intersections and overlaps, but not all treatments are equally effective for both. “We need to better understand their differences and similarities,” Dr. Proft said, adding that the new study is noteworthy for the size of the population included, its long-term follow-up data, and the researchers’ depth of experience treating these patients.
The researchers are based at the University of Toronto, which has separate clinics dedicated to PsA and to AS, said Dafna D. Gladman, MD, professor of medicine at the university, codirector of the PsA clinic, and corresponding author for the new study. The two clinics follow the same standardized protocols, including clinical, radiographic, genetic, and laboratory assessments. Even though the patients present quite similarly, she credits referring physicians for recognizing the distinctions by their referrals to the PsA or AS clinic.
According to previous research, pure axial PsA, without peripheral involvement, is rare, affecting about 2%-5% of patients with PsA. For this study, an observational cohort of 1,576 patients from the PsA clinic included 31% (n = 495) with axial disease, 2% (n = 32) with isolated axial PsA, and 29% (n = 463) with both axial and peripheral involvement. A total of 25 of the patients with isolated axial PsA ultimately developed peripheral disease by their most recent clinic follow-up visit. In a second cohort of 1,688 patients with AS, nearly 5% (n = 68) had isolated axial disease with psoriasis.
“In our logistic regression analysis, isolated axial PsA was found to be a different clinical entity than isolated AS with psoriasis. They are not the same patients,” Dr. Gladman said. The patients with isolated axial PsA were older at diagnosis, more likely to have psoriatic nail lesions, and less likely to have inflammatory back pain than were patients with isolated axial AS and accompanying psoriasis.
When interviewed in early September, Dr. Gladman was preparing to fly to Ghent, Belgium, to participate in a debate at the International Congress on Spondyloarthritides, taking the pro position on the thesis: Is axial inflammation in PsA distinct from axial spondyloarthritis? Taking the con position was to be Robert Landewé, MD, PhD, of Amsterdam University Medical Center in the Netherlands.
“This is an old debate, splitters versus lumpers,” Dr. Gladman told this news organization. “My message is that when you place patients in more homogeneous groups, you can learn more and perhaps find better opportunities for treating their disease.” For example, even with the similarities, do these patients need to be treated with different medications? Medications for psoriasis, including those targeting the interleukin-23 cytokine, may not be effective for AS, but patients with axial PsA may not get them because of the association with axial AS.
“Now is the opportunity to really understand what – if any – are the differences between various components of this disease group. If you lump people together, you may miss the forest for the trees,” Dr. Gladman said. “If, at the end of the day, we find out these patients essentially are the same, I will lump. But until we have proved that there are no important differences, I will split.” She added that it is important for practicing rheumatologists to make the correct diagnosis so that they know to access certain drugs.
Dr. Proft credited Dr. Gladman and colleagues’ study for adding another piece of the puzzle to better understand differences and similarities for these two axial diseases. He noted, however, that the study did not include MRI scans for every participating patient, which could have given a deeper picture.
“International efforts are being made to recruit patients for a multinational, multicenter study of axial involvement in PsA,” which will include MRI data, Dr. Gladman said. She and Dr. Proft are both part of AXIS, the Axial Involvement in Psoriatic Arthritis cohort, now recruiting patients for such a study. AXIS is a joint project of the Assessment of SpondyloArthritis international Society and the Group for Research and Assessment of Psoriasis and Psoriatic Arthritis.
“We don’t have final answers yet, although we have given evidence to support the differences.” The proof is in the pudding, she said, and that pudding will be the clinical trials.
The University of Toronto Psoriatic Arthritis Program is supported by a grant from the Krembil Foundation. The study authors declared no competing interests. Dr. Proft reported receiving research support from Novartis, Eli Lilly, and UCB, and fees for consulting and serving on speakers bureaus from AbbVie, Amgen, Bristol-Myers Squibb, Celgene, Eli Lilly, Hexal, Janssen, Merck Sharp & Dohme, Novartis, Pfizer, Roche, and UCB.
FROM ANNALS OF THE RHEUMATIC DISEASES
One fish, two fish, are good fish for you ... fish
Good news for pregnant women; bad news for fish
As soon as women find out they’re pregnant, doctors recommend they give up smoking, drinking, and eating certain types of fish. That last item may need to be reconsidered, since a recent study supports the idea that it doesn’t matter what type of fish pregnant women are eating, as long as they’re eating it.
Researchers collected data from two different studies that reviewed the mercury levels of mothers from Bristol, England, and the Seychelles, a island chain off East Africa where “fish consumption is high and prenatal mercury levels are 10 times higher than in the [United States],” they said in NeuroToxicology.
Those data showed that the mercury levels had no adverse effects on child development as long as the mother ate fish. The nutrients and vitamins in the fish – vitamin D, long-chain fatty acids, selenium, and iodine – provide protection against mercury. There’s also the already-known benefits to eyesight and intellectual abilities that have been associated with fish consumption.
This analysis goes starkly against the grain of what is commonly recommended to expectant mothers, which is to cut out fish altogether. The researchers suggested that governments should review and change those recommendations to focus on the benefits instead.
As long as women follow the researchers’ recommendation to eat “at least two portions of fish a week, one of which should be oily,” they may not have to lay off on the sushi after all.
We’ll show our gut worms the world
Never let it be said that mankind is not a generous species. Sure, we could maybe be kinder to our fellow human beings, maybe declare a little less war on each other, but for the past 50,000 years, we’ve been giving a free ride to millions upon millions to one of mankind’s closest companions: the whipworm.
This revelation into human kindness comes from Denmark, where researchers from Copenhagen conducted a genetic analysis of ancient preserved whipworm eggs found in old Viking and Norse settlements, some of which date back over 2,000 years. In normal conditions genetic material wouldn’t last very long, but these were Viking whipworms eggs with tiny little horned helmets, so the DNA within has remained unchanged. Or it may be the tough chitinous exterior of the eggs protecting the DNA from degrading, combined with their preservation in moist soil.
Once they had their Viking whipworm DNA, the researchers compared it with whipworm DNA from all over the world, tracing its history as it followed mankind from Africa. And it’s been a while: We brought whipworms with us during our initial migration into Asia and Europe over 50,000 years ago. When the Bering land bridge opened up and humanity moved into the Americas, the worms came as well.
This is all possible because the whipworm goes about its parasitic business quietly and cleverly. It mostly sits harmlessly in our digestive systems, producing thousands of eggs a day that get expelled through poop and picked up by another host (human or otherwise); whipworms only cause disease in those with compromised immune systems.
The researchers noted that their study, the first complete genetic analysis of the whipworm, could help combat the parasite, which to this day infects hundred of millions who don’t have access to modern medicine or sanitary conditions. Hopefully, though, the days of free rides will soon be over for the whipworm. After all, if we have to pay hundreds or thousands of dollars to visit other countries, it’s only fair that our parasites do as well.
From zero to vasectomy in 6.7 seconds
There’s an old saying that you’ve probably heard: When life gives you lemons, make lemonade. It’s meant to encourage optimism in the face of adversity. Then there’s the new saying we just made up: When life gives you a power outage, plug your surgical instruments into an electric pickup.
That’s what Dr. Christopher Yang did, and now we’re making the urologist from Austin, Tex., famous by sharing his surgical/electrical adventure with all 17 of LOTME’s regular readers. That’s some serious lemonade.
Dr. Yang’s tale begins when the electricity went out at his clinic, seemingly forcing him to cancel or reschedule several surgical procedures. Not so fast. Dr. Yang happens to own a Rivian R1T, an electric pickup truck that has four power outlets. A staff member suggested plugging the surgical instruments into the truck and, surprisingly, one of the day’s patients agreed to go ahead with his vasectomy.
“We were fortunate that my normal parking spot is close enough to a patient room to run an extension cord,” Dr. Yang said on TheDrive.com. That extension cord was attached to an electrocautery device, with a handheld device available as backup, and “after we were done, I told his family. We all had a good laugh together too,” Dr. Yang told radio station WGLT in Normal, Ill.
To us, anyway, this opens up all sorts of alternative energy possibilities. Can a windmill power a liposuction? Is a gerbil running in a wheel enough to do a colonoscopy? How many potatoes do you need to keep an EHR going?
Learning through random acts of not-exactly noisiness
First things first. Transcranial random noise stimulation (tRNS) is not really noise in the auditory sense of the word. For some people with learning disabilities, though, it can actually be very helpful. The technology, which uses electrodes attached to the head so a weak current can pass through specific parts of the brain, may help those with learning disabilities, perhaps even those with brain injuries and visual deficits, learn, said Dr. Onno van der Groen of Edith Cowan University in Perth, Australia.
“When you add this type of stimulation during learning, you get better performance, faster learning and better attention afterwards as well,” he said in a statement from the university.
The researchers say that tRNS can allow the brain to form new connections and pathways, which in turn help a person learn more effectively. “If you do 10 sessions of a visual perception task with the tRNS and then come back and do it again without it, you’ll find you perform better than the control group who hasn’t used it,” Dr. van der Groen noted.
Can this also work for the average person? It’s possible, but tRNS didn’t seem to improve the math skills of a top-level mathematician who underwent the process, according to a case study that Dr. van der Groen mentioned.
This line of work is still pretty new, though, so researchers don’t have all the answers yet. As always, we’re rooting for you, science!
Good news for pregnant women; bad news for fish
As soon as women find out they’re pregnant, doctors recommend they give up smoking, drinking, and eating certain types of fish. That last item may need to be reconsidered, since a recent study supports the idea that it doesn’t matter what type of fish pregnant women are eating, as long as they’re eating it.
Researchers collected data from two different studies that reviewed the mercury levels of mothers from Bristol, England, and the Seychelles, a island chain off East Africa where “fish consumption is high and prenatal mercury levels are 10 times higher than in the [United States],” they said in NeuroToxicology.
Those data showed that the mercury levels had no adverse effects on child development as long as the mother ate fish. The nutrients and vitamins in the fish – vitamin D, long-chain fatty acids, selenium, and iodine – provide protection against mercury. There’s also the already-known benefits to eyesight and intellectual abilities that have been associated with fish consumption.
This analysis goes starkly against the grain of what is commonly recommended to expectant mothers, which is to cut out fish altogether. The researchers suggested that governments should review and change those recommendations to focus on the benefits instead.
As long as women follow the researchers’ recommendation to eat “at least two portions of fish a week, one of which should be oily,” they may not have to lay off on the sushi after all.
We’ll show our gut worms the world
Never let it be said that mankind is not a generous species. Sure, we could maybe be kinder to our fellow human beings, maybe declare a little less war on each other, but for the past 50,000 years, we’ve been giving a free ride to millions upon millions to one of mankind’s closest companions: the whipworm.
This revelation into human kindness comes from Denmark, where researchers from Copenhagen conducted a genetic analysis of ancient preserved whipworm eggs found in old Viking and Norse settlements, some of which date back over 2,000 years. In normal conditions genetic material wouldn’t last very long, but these were Viking whipworms eggs with tiny little horned helmets, so the DNA within has remained unchanged. Or it may be the tough chitinous exterior of the eggs protecting the DNA from degrading, combined with their preservation in moist soil.
Once they had their Viking whipworm DNA, the researchers compared it with whipworm DNA from all over the world, tracing its history as it followed mankind from Africa. And it’s been a while: We brought whipworms with us during our initial migration into Asia and Europe over 50,000 years ago. When the Bering land bridge opened up and humanity moved into the Americas, the worms came as well.
This is all possible because the whipworm goes about its parasitic business quietly and cleverly. It mostly sits harmlessly in our digestive systems, producing thousands of eggs a day that get expelled through poop and picked up by another host (human or otherwise); whipworms only cause disease in those with compromised immune systems.
The researchers noted that their study, the first complete genetic analysis of the whipworm, could help combat the parasite, which to this day infects hundred of millions who don’t have access to modern medicine or sanitary conditions. Hopefully, though, the days of free rides will soon be over for the whipworm. After all, if we have to pay hundreds or thousands of dollars to visit other countries, it’s only fair that our parasites do as well.
From zero to vasectomy in 6.7 seconds
There’s an old saying that you’ve probably heard: When life gives you lemons, make lemonade. It’s meant to encourage optimism in the face of adversity. Then there’s the new saying we just made up: When life gives you a power outage, plug your surgical instruments into an electric pickup.
That’s what Dr. Christopher Yang did, and now we’re making the urologist from Austin, Tex., famous by sharing his surgical/electrical adventure with all 17 of LOTME’s regular readers. That’s some serious lemonade.
Dr. Yang’s tale begins when the electricity went out at his clinic, seemingly forcing him to cancel or reschedule several surgical procedures. Not so fast. Dr. Yang happens to own a Rivian R1T, an electric pickup truck that has four power outlets. A staff member suggested plugging the surgical instruments into the truck and, surprisingly, one of the day’s patients agreed to go ahead with his vasectomy.
“We were fortunate that my normal parking spot is close enough to a patient room to run an extension cord,” Dr. Yang said on TheDrive.com. That extension cord was attached to an electrocautery device, with a handheld device available as backup, and “after we were done, I told his family. We all had a good laugh together too,” Dr. Yang told radio station WGLT in Normal, Ill.
To us, anyway, this opens up all sorts of alternative energy possibilities. Can a windmill power a liposuction? Is a gerbil running in a wheel enough to do a colonoscopy? How many potatoes do you need to keep an EHR going?
Learning through random acts of not-exactly noisiness
First things first. Transcranial random noise stimulation (tRNS) is not really noise in the auditory sense of the word. For some people with learning disabilities, though, it can actually be very helpful. The technology, which uses electrodes attached to the head so a weak current can pass through specific parts of the brain, may help those with learning disabilities, perhaps even those with brain injuries and visual deficits, learn, said Dr. Onno van der Groen of Edith Cowan University in Perth, Australia.
“When you add this type of stimulation during learning, you get better performance, faster learning and better attention afterwards as well,” he said in a statement from the university.
The researchers say that tRNS can allow the brain to form new connections and pathways, which in turn help a person learn more effectively. “If you do 10 sessions of a visual perception task with the tRNS and then come back and do it again without it, you’ll find you perform better than the control group who hasn’t used it,” Dr. van der Groen noted.
Can this also work for the average person? It’s possible, but tRNS didn’t seem to improve the math skills of a top-level mathematician who underwent the process, according to a case study that Dr. van der Groen mentioned.
This line of work is still pretty new, though, so researchers don’t have all the answers yet. As always, we’re rooting for you, science!
Good news for pregnant women; bad news for fish
As soon as women find out they’re pregnant, doctors recommend they give up smoking, drinking, and eating certain types of fish. That last item may need to be reconsidered, since a recent study supports the idea that it doesn’t matter what type of fish pregnant women are eating, as long as they’re eating it.
Researchers collected data from two different studies that reviewed the mercury levels of mothers from Bristol, England, and the Seychelles, a island chain off East Africa where “fish consumption is high and prenatal mercury levels are 10 times higher than in the [United States],” they said in NeuroToxicology.
Those data showed that the mercury levels had no adverse effects on child development as long as the mother ate fish. The nutrients and vitamins in the fish – vitamin D, long-chain fatty acids, selenium, and iodine – provide protection against mercury. There’s also the already-known benefits to eyesight and intellectual abilities that have been associated with fish consumption.
This analysis goes starkly against the grain of what is commonly recommended to expectant mothers, which is to cut out fish altogether. The researchers suggested that governments should review and change those recommendations to focus on the benefits instead.
As long as women follow the researchers’ recommendation to eat “at least two portions of fish a week, one of which should be oily,” they may not have to lay off on the sushi after all.
We’ll show our gut worms the world
Never let it be said that mankind is not a generous species. Sure, we could maybe be kinder to our fellow human beings, maybe declare a little less war on each other, but for the past 50,000 years, we’ve been giving a free ride to millions upon millions to one of mankind’s closest companions: the whipworm.
This revelation into human kindness comes from Denmark, where researchers from Copenhagen conducted a genetic analysis of ancient preserved whipworm eggs found in old Viking and Norse settlements, some of which date back over 2,000 years. In normal conditions genetic material wouldn’t last very long, but these were Viking whipworms eggs with tiny little horned helmets, so the DNA within has remained unchanged. Or it may be the tough chitinous exterior of the eggs protecting the DNA from degrading, combined with their preservation in moist soil.
Once they had their Viking whipworm DNA, the researchers compared it with whipworm DNA from all over the world, tracing its history as it followed mankind from Africa. And it’s been a while: We brought whipworms with us during our initial migration into Asia and Europe over 50,000 years ago. When the Bering land bridge opened up and humanity moved into the Americas, the worms came as well.
This is all possible because the whipworm goes about its parasitic business quietly and cleverly. It mostly sits harmlessly in our digestive systems, producing thousands of eggs a day that get expelled through poop and picked up by another host (human or otherwise); whipworms only cause disease in those with compromised immune systems.
The researchers noted that their study, the first complete genetic analysis of the whipworm, could help combat the parasite, which to this day infects hundred of millions who don’t have access to modern medicine or sanitary conditions. Hopefully, though, the days of free rides will soon be over for the whipworm. After all, if we have to pay hundreds or thousands of dollars to visit other countries, it’s only fair that our parasites do as well.
From zero to vasectomy in 6.7 seconds
There’s an old saying that you’ve probably heard: When life gives you lemons, make lemonade. It’s meant to encourage optimism in the face of adversity. Then there’s the new saying we just made up: When life gives you a power outage, plug your surgical instruments into an electric pickup.
That’s what Dr. Christopher Yang did, and now we’re making the urologist from Austin, Tex., famous by sharing his surgical/electrical adventure with all 17 of LOTME’s regular readers. That’s some serious lemonade.
Dr. Yang’s tale begins when the electricity went out at his clinic, seemingly forcing him to cancel or reschedule several surgical procedures. Not so fast. Dr. Yang happens to own a Rivian R1T, an electric pickup truck that has four power outlets. A staff member suggested plugging the surgical instruments into the truck and, surprisingly, one of the day’s patients agreed to go ahead with his vasectomy.
“We were fortunate that my normal parking spot is close enough to a patient room to run an extension cord,” Dr. Yang said on TheDrive.com. That extension cord was attached to an electrocautery device, with a handheld device available as backup, and “after we were done, I told his family. We all had a good laugh together too,” Dr. Yang told radio station WGLT in Normal, Ill.
To us, anyway, this opens up all sorts of alternative energy possibilities. Can a windmill power a liposuction? Is a gerbil running in a wheel enough to do a colonoscopy? How many potatoes do you need to keep an EHR going?
Learning through random acts of not-exactly noisiness
First things first. Transcranial random noise stimulation (tRNS) is not really noise in the auditory sense of the word. For some people with learning disabilities, though, it can actually be very helpful. The technology, which uses electrodes attached to the head so a weak current can pass through specific parts of the brain, may help those with learning disabilities, perhaps even those with brain injuries and visual deficits, learn, said Dr. Onno van der Groen of Edith Cowan University in Perth, Australia.
“When you add this type of stimulation during learning, you get better performance, faster learning and better attention afterwards as well,” he said in a statement from the university.
The researchers say that tRNS can allow the brain to form new connections and pathways, which in turn help a person learn more effectively. “If you do 10 sessions of a visual perception task with the tRNS and then come back and do it again without it, you’ll find you perform better than the control group who hasn’t used it,” Dr. van der Groen noted.
Can this also work for the average person? It’s possible, but tRNS didn’t seem to improve the math skills of a top-level mathematician who underwent the process, according to a case study that Dr. van der Groen mentioned.
This line of work is still pretty new, though, so researchers don’t have all the answers yet. As always, we’re rooting for you, science!
Punked By the Punctum: Domestically Acquired Cutaneous Myiasis
To the Editor:
Cutaneous myiasis is a skin infestation with dipterous larvae that feed on the host’s tissue and cause a wide range of manifestations depending on the location of infestation. Cutaneous myiasis, which includes furuncular, wound, and migratory types, is the most common clinical form of this condition.1 It is endemic to tropical and subtropical areas and is not common in the United States, thus it can pose a diagnostic challenge when presenting in nonendemic areas. We present the case of a woman from Michigan who acquired furuncular myiasis without travel history to a tropical or subtropical locale.
A 72-year-old woman presented to our clinic with a chief concern of a burning, pruritic, migratory skin lesion on the left arm of approximately 1 week’s duration. She had a medical history of squamous cell carcinoma, keratoacanthoma, and multiple tick bites. She reported that the lesion started on the distal aspect of the left arm as an eraser-sized, perfectly round, raised bruise with a dark pepperlike bump in the center. The lesion then spread proximally over the course of 1 week, creating 3 more identical lesions. As one lesion resolved, a new lesion appeared approximately 2 to 4 cm proximal to the preceding lesion. The patient had traveled to England, Scotland, and Ireland 2 months prior but otherwise denied leaving the state of Michigan. She reported frequent exposure to gardens, meadows, and wetlands in search of milkweed and monarch butterfly larvae that she raises in northeast Michigan. She denied any recent illness or associated systemic symptoms. Initial evaluation by a primary care physician resulted in a diagnosis of a furuncle or tick bite; she completed a 10-day course of amoxicillin and a methylprednisolone dose pack without improvement.
Physical examination revealed a 1-cm, firm, violaceous nodule with a small distinct central punctum and surrounding erythema on the proximal aspect of the left arm. Dermoscopy revealed a pulsating motion and expulsion of serosanguineous fluid from the central punctum (Figure 1). Further inspection of the patient’s left arm exposed several noninflammatory puncta distal to the primary lesion spaced at 2- to 4-cm intervals.

Gross examination of a 6-mm punch biopsy from the primary inflammatory nodule uncovered a small, motile, gray-white larval organism in the inferior portion of the specimen (Figure 2). Histopathology revealed superficial and deep eosinophil-rich inflammation, fibrosis, and hemorrhage. There was a complex wedge-shaped organism with extensive internal muscle bounded by a thin cuticle bearing rows of chitinous hooklets located at one side within the deep dermis (Figure 3). The findings were consistent with a diagnosis of cutaneous myiasis. No further treatment was required, as the organism was completely excised with the biopsy.

The most common causative agents of furuncular myiasis obtained from travelers returning from Mexico and Central and South America are Dermatobia hominis and Cordylobia anthropophaga. Cases of furuncular myiasis acquired in the United States without recent foreign travel are rare. Most of these cases are caused by larvae of the Cuterebra species (also known as the rabbit botfly or rodent botfly).2 In a 2003 literature review by Safdar et al3 on 56 cases of furuncular myiasis in the United States, the median age of patients was 14 years, 87% of cases occurred in August and September, and most involved exposure in rural or suburban settings; 53% of cases presented in the northeastern United States.
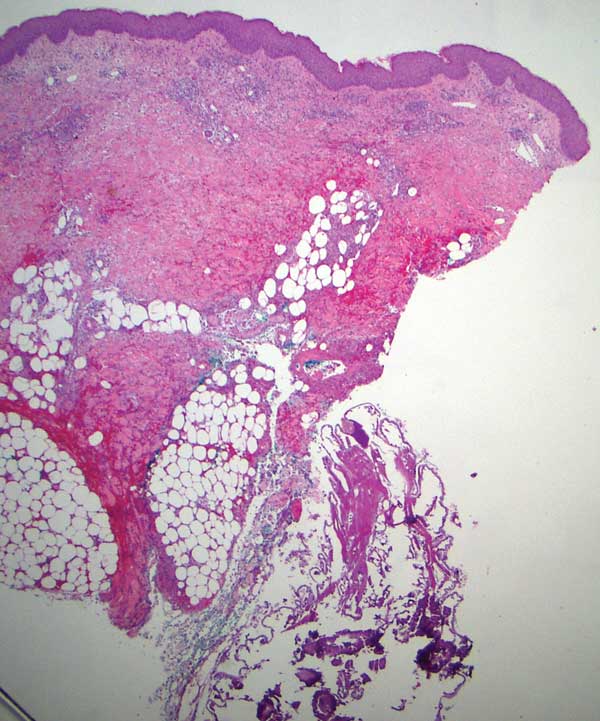
Furuncular myiasis occurs when the organism’s ova are deposited on the skin of a human host by the parent organism or a mosquito vector. The heat of the skin causes the eggs to hatch and the dipteran larvae must penetrate the skin within 20 days.1 Signs of infection typically are seen 6 to 10 days after infestation.3 The larvae then feed on human tissue and burrow deep in the dermis, forming an erythematous furunculoid nodule containing one or multiple maggots. After 5 to 10 weeks, the adult larvae drop to the ground, where they mature into adult organisms in the soil.1
The most reported symptoms of furuncular myiasis include pruritus, pain, and movement sensation, typically occurring suddenly at night.4 The most common presentation is a furunclelike lesion that exudes serosanguineous or purulent fluid,1 but there have been reports of vesicular, bullous, pustular, erosive, ecchymotic, and ulcerative lesions.5Dermatobia hominis usually presents on an exposed site, such as the scalp, face, and extremities. It may present with paroxysmal episodes of lancinating pain. Over time, the lesion usually heals without a scar, though hyperpigmentation and scarring can occur. The most reported complication is secondary bacterial infection.4 Local lymphadenopathy or systemic symptoms should raise concern for infection. Staphylococcus aureus and group B Streptococcus have been cultured from lesions.6,7
The differential diagnosis for myiasis should include furuncle, insect bite, insect prurigo, pyoderma, inflamed cyst, and tungiasis. Myiasis also can present similarly to severe soft tissue infections or cellulitis. If located on the breasts, it can be mistaken for periductal mastitis, a benign mass with microcalcification, or inflammatory carcinoma. Lastly, due to pain, erythema, pruritus, small vesicles, and crusting, it may be confused for herpes simplex virus.1
Furuncular myiasis typically is diagnosed based on clinical presentation, especially in endemic regions. In nonendemic areas, the patient’s history may reveal recent travel or predisposition to myiasis. In cases where there is uncertainty, dermoscopy may be used to identify the maggot in the lesion, or ultrasonography can be used to confirm myiasis through the detection of larval movement.8 Dermoscopy will reveal a furuncular lesion with a central opening surrounded by dilated blood vessels and a yellowish structure with black barblike spines.9 Within the dermis is a fibrous cystic sinus tract containing the dipteran larva. Laboratory studies typically are unremarkable. In chronic cases, a complete blood cell count and other laboratory tests may show systemic inflammation, peripheral eosinophilia, and elevated IgE.10 Biopsies of furuncular myiasis are not necessary for diagnosis. Histopathology reveals an ulcerated epidermis with or without hyperkeratosis and an inflammatory infiltrate composed of lymphocytes and neutrophils with eosinophils, fibroblasts, histiocytes, basophils, mast cells, plasma cells, and Langerhans cells within the dermis and subcutis.11
There are various approaches to treating furuncular myiasis, with the goal of complete removal of the larva and prevention of secondary infection. One treatment option is to apply a toxic substance to the larva, effectively killing it. Another approach is to force the larva to emerge via localized hypoxia, which can be done by occluding the punctum of the lesion for at least 24 hours. A complication of this method is suffocation of the larva without migration, leading to incomplete extraction and secondary infection.1 A third method is to surgically remove the larva, which allows for debridement of necrotic tissue surrounding the lesion if present.12 Ultrasonography also can be used therapeutically to aid in the removal of the larvae. The last method is to inject lidocaine into the base of the lesion, forcing the larva out of the punctum via fluid pressure.13 Oral treatments such as ivermectin are not recommended because they can result in the death of larvae within the lesion, leading to an inflammatory response.8
Furuncular myiasis is a form of cutaneous larvae infestation not commonly seen in individuals who do not live or travel in endemic, tropical, and subtropical regions. Diagnosis is based on clinical presentation, with imaging and laboratory studies available to supplement in unclear or atypical manifestations. Treatment involves complete removal of the larva, typically through forced evacuation via hypoxia or through surgical removal. Most cases resolve without notable scarring or other sequelae; however, in those who do have complications, the most common is secondary bacterial infection. Our patient’s absence of notable travel history and frequent environmental exposure in Michigan led us to believe the organism was from a domestic source. Our case underlines the importance of a thorough history and clinical examination of furuncular lesions including the use of dermoscopy to yield an appropriate diagnosis and treatment plan.
- Francesconi F, Lupi O. Myiasis. Clin Microbiol Rev. 2012;25:79-105. doi:10.1128/CMR.00010-11
- Schiff TA. Furuncular cutaneous myiasis caused by Cuterebra larva. J Am Acad Dermatol 1993;28:261-263.
- Safdar N, Young DK, Andes D. Autochthonous furuncular myiasis in the United States: case report and literature review. Clin Infect Dis. 2003;26:73-80.
- Mahal JJ, Sperling JD. Furuncular myiasis from Dermatobia hominus: a case of human botfly infestation. J Emerg Med. 2012;43:618-621.
- Francesconi F, Lupi O. Myiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. Elsevier; 2006:232-239.
- Gordon PM, Hepburn NC, Williams AE, et al. Cutaneous myiasis due to Dermatobia hominis: a report of six cases. Br J Dermatol. 1995;132:811-814.
- Hubler WR Jr, Rudolph AH, Dougherty EF. Dermal myiasis. Arch Dermatol. 1974;110:109-110.
- Quintanilla-Cedillo MR, León-Ureña H, Contreras-Ruiz J, et al. The value of Doppler ultrasound in diagnosis in 25 cases of furunculoid myiasis. Int J Dermatol. 2005;44:34-37.
- Bakos RM, Bakos L. Dermoscopic diagnosis of furuncular myiasis. Arch Dermatol. 2007;143:123-124.
- Varani S, Tassinari D, Elleri D, et al. A case of furuncular myiasis associated with systemic inflammation. Parasitol Int. 2007;56:330-333.
- Grogan TM, Payne CM, Spier C, et al. Cutaneous myiasis. immunohistologic and ultrastructural morphometric features of a human botfly lesion. Am J Dermatopathol. 1987;9:232-239.
- Krajewski A, Allen B, Hoss D, et al. Cutaneous myiasis. J Plast Reconstr Aesthet Surg. 2009;62:383-386.
- Lebwohl MG, Heymann WR, Berth-Jones J, et al. Myiasis: Treatment of Skin Diseases. Comprehensive Therapeutic Strategies. 2nd ed. Elsevier-Mosby; 2006.
To the Editor:
Cutaneous myiasis is a skin infestation with dipterous larvae that feed on the host’s tissue and cause a wide range of manifestations depending on the location of infestation. Cutaneous myiasis, which includes furuncular, wound, and migratory types, is the most common clinical form of this condition.1 It is endemic to tropical and subtropical areas and is not common in the United States, thus it can pose a diagnostic challenge when presenting in nonendemic areas. We present the case of a woman from Michigan who acquired furuncular myiasis without travel history to a tropical or subtropical locale.
A 72-year-old woman presented to our clinic with a chief concern of a burning, pruritic, migratory skin lesion on the left arm of approximately 1 week’s duration. She had a medical history of squamous cell carcinoma, keratoacanthoma, and multiple tick bites. She reported that the lesion started on the distal aspect of the left arm as an eraser-sized, perfectly round, raised bruise with a dark pepperlike bump in the center. The lesion then spread proximally over the course of 1 week, creating 3 more identical lesions. As one lesion resolved, a new lesion appeared approximately 2 to 4 cm proximal to the preceding lesion. The patient had traveled to England, Scotland, and Ireland 2 months prior but otherwise denied leaving the state of Michigan. She reported frequent exposure to gardens, meadows, and wetlands in search of milkweed and monarch butterfly larvae that she raises in northeast Michigan. She denied any recent illness or associated systemic symptoms. Initial evaluation by a primary care physician resulted in a diagnosis of a furuncle or tick bite; she completed a 10-day course of amoxicillin and a methylprednisolone dose pack without improvement.
Physical examination revealed a 1-cm, firm, violaceous nodule with a small distinct central punctum and surrounding erythema on the proximal aspect of the left arm. Dermoscopy revealed a pulsating motion and expulsion of serosanguineous fluid from the central punctum (Figure 1). Further inspection of the patient’s left arm exposed several noninflammatory puncta distal to the primary lesion spaced at 2- to 4-cm intervals.

Gross examination of a 6-mm punch biopsy from the primary inflammatory nodule uncovered a small, motile, gray-white larval organism in the inferior portion of the specimen (Figure 2). Histopathology revealed superficial and deep eosinophil-rich inflammation, fibrosis, and hemorrhage. There was a complex wedge-shaped organism with extensive internal muscle bounded by a thin cuticle bearing rows of chitinous hooklets located at one side within the deep dermis (Figure 3). The findings were consistent with a diagnosis of cutaneous myiasis. No further treatment was required, as the organism was completely excised with the biopsy.

The most common causative agents of furuncular myiasis obtained from travelers returning from Mexico and Central and South America are Dermatobia hominis and Cordylobia anthropophaga. Cases of furuncular myiasis acquired in the United States without recent foreign travel are rare. Most of these cases are caused by larvae of the Cuterebra species (also known as the rabbit botfly or rodent botfly).2 In a 2003 literature review by Safdar et al3 on 56 cases of furuncular myiasis in the United States, the median age of patients was 14 years, 87% of cases occurred in August and September, and most involved exposure in rural or suburban settings; 53% of cases presented in the northeastern United States.
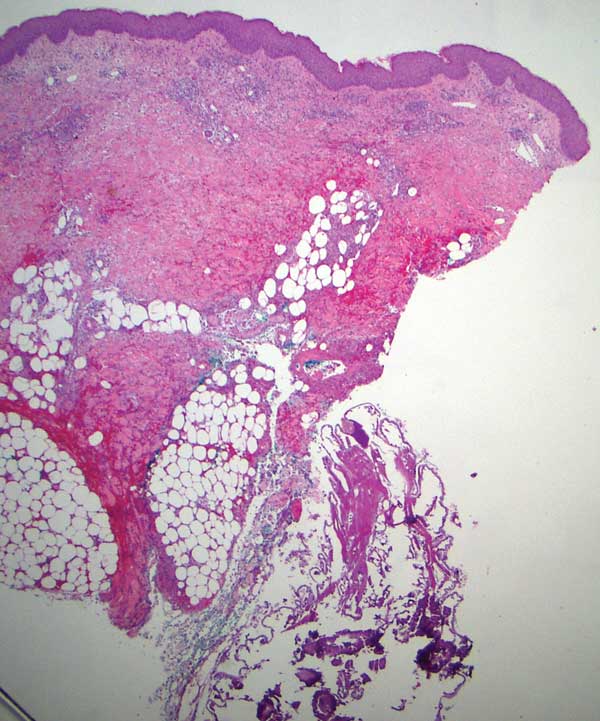
Furuncular myiasis occurs when the organism’s ova are deposited on the skin of a human host by the parent organism or a mosquito vector. The heat of the skin causes the eggs to hatch and the dipteran larvae must penetrate the skin within 20 days.1 Signs of infection typically are seen 6 to 10 days after infestation.3 The larvae then feed on human tissue and burrow deep in the dermis, forming an erythematous furunculoid nodule containing one or multiple maggots. After 5 to 10 weeks, the adult larvae drop to the ground, where they mature into adult organisms in the soil.1
The most reported symptoms of furuncular myiasis include pruritus, pain, and movement sensation, typically occurring suddenly at night.4 The most common presentation is a furunclelike lesion that exudes serosanguineous or purulent fluid,1 but there have been reports of vesicular, bullous, pustular, erosive, ecchymotic, and ulcerative lesions.5Dermatobia hominis usually presents on an exposed site, such as the scalp, face, and extremities. It may present with paroxysmal episodes of lancinating pain. Over time, the lesion usually heals without a scar, though hyperpigmentation and scarring can occur. The most reported complication is secondary bacterial infection.4 Local lymphadenopathy or systemic symptoms should raise concern for infection. Staphylococcus aureus and group B Streptococcus have been cultured from lesions.6,7
The differential diagnosis for myiasis should include furuncle, insect bite, insect prurigo, pyoderma, inflamed cyst, and tungiasis. Myiasis also can present similarly to severe soft tissue infections or cellulitis. If located on the breasts, it can be mistaken for periductal mastitis, a benign mass with microcalcification, or inflammatory carcinoma. Lastly, due to pain, erythema, pruritus, small vesicles, and crusting, it may be confused for herpes simplex virus.1
Furuncular myiasis typically is diagnosed based on clinical presentation, especially in endemic regions. In nonendemic areas, the patient’s history may reveal recent travel or predisposition to myiasis. In cases where there is uncertainty, dermoscopy may be used to identify the maggot in the lesion, or ultrasonography can be used to confirm myiasis through the detection of larval movement.8 Dermoscopy will reveal a furuncular lesion with a central opening surrounded by dilated blood vessels and a yellowish structure with black barblike spines.9 Within the dermis is a fibrous cystic sinus tract containing the dipteran larva. Laboratory studies typically are unremarkable. In chronic cases, a complete blood cell count and other laboratory tests may show systemic inflammation, peripheral eosinophilia, and elevated IgE.10 Biopsies of furuncular myiasis are not necessary for diagnosis. Histopathology reveals an ulcerated epidermis with or without hyperkeratosis and an inflammatory infiltrate composed of lymphocytes and neutrophils with eosinophils, fibroblasts, histiocytes, basophils, mast cells, plasma cells, and Langerhans cells within the dermis and subcutis.11
There are various approaches to treating furuncular myiasis, with the goal of complete removal of the larva and prevention of secondary infection. One treatment option is to apply a toxic substance to the larva, effectively killing it. Another approach is to force the larva to emerge via localized hypoxia, which can be done by occluding the punctum of the lesion for at least 24 hours. A complication of this method is suffocation of the larva without migration, leading to incomplete extraction and secondary infection.1 A third method is to surgically remove the larva, which allows for debridement of necrotic tissue surrounding the lesion if present.12 Ultrasonography also can be used therapeutically to aid in the removal of the larvae. The last method is to inject lidocaine into the base of the lesion, forcing the larva out of the punctum via fluid pressure.13 Oral treatments such as ivermectin are not recommended because they can result in the death of larvae within the lesion, leading to an inflammatory response.8
Furuncular myiasis is a form of cutaneous larvae infestation not commonly seen in individuals who do not live or travel in endemic, tropical, and subtropical regions. Diagnosis is based on clinical presentation, with imaging and laboratory studies available to supplement in unclear or atypical manifestations. Treatment involves complete removal of the larva, typically through forced evacuation via hypoxia or through surgical removal. Most cases resolve without notable scarring or other sequelae; however, in those who do have complications, the most common is secondary bacterial infection. Our patient’s absence of notable travel history and frequent environmental exposure in Michigan led us to believe the organism was from a domestic source. Our case underlines the importance of a thorough history and clinical examination of furuncular lesions including the use of dermoscopy to yield an appropriate diagnosis and treatment plan.
To the Editor:
Cutaneous myiasis is a skin infestation with dipterous larvae that feed on the host’s tissue and cause a wide range of manifestations depending on the location of infestation. Cutaneous myiasis, which includes furuncular, wound, and migratory types, is the most common clinical form of this condition.1 It is endemic to tropical and subtropical areas and is not common in the United States, thus it can pose a diagnostic challenge when presenting in nonendemic areas. We present the case of a woman from Michigan who acquired furuncular myiasis without travel history to a tropical or subtropical locale.
A 72-year-old woman presented to our clinic with a chief concern of a burning, pruritic, migratory skin lesion on the left arm of approximately 1 week’s duration. She had a medical history of squamous cell carcinoma, keratoacanthoma, and multiple tick bites. She reported that the lesion started on the distal aspect of the left arm as an eraser-sized, perfectly round, raised bruise with a dark pepperlike bump in the center. The lesion then spread proximally over the course of 1 week, creating 3 more identical lesions. As one lesion resolved, a new lesion appeared approximately 2 to 4 cm proximal to the preceding lesion. The patient had traveled to England, Scotland, and Ireland 2 months prior but otherwise denied leaving the state of Michigan. She reported frequent exposure to gardens, meadows, and wetlands in search of milkweed and monarch butterfly larvae that she raises in northeast Michigan. She denied any recent illness or associated systemic symptoms. Initial evaluation by a primary care physician resulted in a diagnosis of a furuncle or tick bite; she completed a 10-day course of amoxicillin and a methylprednisolone dose pack without improvement.
Physical examination revealed a 1-cm, firm, violaceous nodule with a small distinct central punctum and surrounding erythema on the proximal aspect of the left arm. Dermoscopy revealed a pulsating motion and expulsion of serosanguineous fluid from the central punctum (Figure 1). Further inspection of the patient’s left arm exposed several noninflammatory puncta distal to the primary lesion spaced at 2- to 4-cm intervals.

Gross examination of a 6-mm punch biopsy from the primary inflammatory nodule uncovered a small, motile, gray-white larval organism in the inferior portion of the specimen (Figure 2). Histopathology revealed superficial and deep eosinophil-rich inflammation, fibrosis, and hemorrhage. There was a complex wedge-shaped organism with extensive internal muscle bounded by a thin cuticle bearing rows of chitinous hooklets located at one side within the deep dermis (Figure 3). The findings were consistent with a diagnosis of cutaneous myiasis. No further treatment was required, as the organism was completely excised with the biopsy.

The most common causative agents of furuncular myiasis obtained from travelers returning from Mexico and Central and South America are Dermatobia hominis and Cordylobia anthropophaga. Cases of furuncular myiasis acquired in the United States without recent foreign travel are rare. Most of these cases are caused by larvae of the Cuterebra species (also known as the rabbit botfly or rodent botfly).2 In a 2003 literature review by Safdar et al3 on 56 cases of furuncular myiasis in the United States, the median age of patients was 14 years, 87% of cases occurred in August and September, and most involved exposure in rural or suburban settings; 53% of cases presented in the northeastern United States.
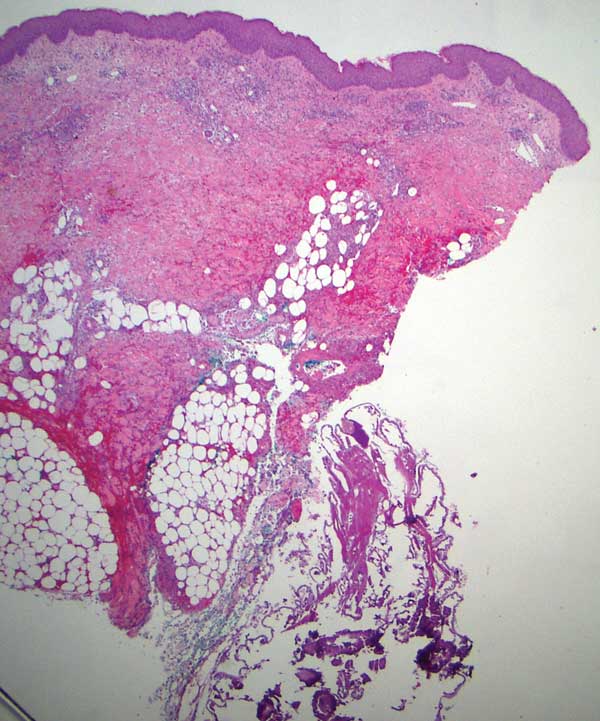
Furuncular myiasis occurs when the organism’s ova are deposited on the skin of a human host by the parent organism or a mosquito vector. The heat of the skin causes the eggs to hatch and the dipteran larvae must penetrate the skin within 20 days.1 Signs of infection typically are seen 6 to 10 days after infestation.3 The larvae then feed on human tissue and burrow deep in the dermis, forming an erythematous furunculoid nodule containing one or multiple maggots. After 5 to 10 weeks, the adult larvae drop to the ground, where they mature into adult organisms in the soil.1
The most reported symptoms of furuncular myiasis include pruritus, pain, and movement sensation, typically occurring suddenly at night.4 The most common presentation is a furunclelike lesion that exudes serosanguineous or purulent fluid,1 but there have been reports of vesicular, bullous, pustular, erosive, ecchymotic, and ulcerative lesions.5Dermatobia hominis usually presents on an exposed site, such as the scalp, face, and extremities. It may present with paroxysmal episodes of lancinating pain. Over time, the lesion usually heals without a scar, though hyperpigmentation and scarring can occur. The most reported complication is secondary bacterial infection.4 Local lymphadenopathy or systemic symptoms should raise concern for infection. Staphylococcus aureus and group B Streptococcus have been cultured from lesions.6,7
The differential diagnosis for myiasis should include furuncle, insect bite, insect prurigo, pyoderma, inflamed cyst, and tungiasis. Myiasis also can present similarly to severe soft tissue infections or cellulitis. If located on the breasts, it can be mistaken for periductal mastitis, a benign mass with microcalcification, or inflammatory carcinoma. Lastly, due to pain, erythema, pruritus, small vesicles, and crusting, it may be confused for herpes simplex virus.1
Furuncular myiasis typically is diagnosed based on clinical presentation, especially in endemic regions. In nonendemic areas, the patient’s history may reveal recent travel or predisposition to myiasis. In cases where there is uncertainty, dermoscopy may be used to identify the maggot in the lesion, or ultrasonography can be used to confirm myiasis through the detection of larval movement.8 Dermoscopy will reveal a furuncular lesion with a central opening surrounded by dilated blood vessels and a yellowish structure with black barblike spines.9 Within the dermis is a fibrous cystic sinus tract containing the dipteran larva. Laboratory studies typically are unremarkable. In chronic cases, a complete blood cell count and other laboratory tests may show systemic inflammation, peripheral eosinophilia, and elevated IgE.10 Biopsies of furuncular myiasis are not necessary for diagnosis. Histopathology reveals an ulcerated epidermis with or without hyperkeratosis and an inflammatory infiltrate composed of lymphocytes and neutrophils with eosinophils, fibroblasts, histiocytes, basophils, mast cells, plasma cells, and Langerhans cells within the dermis and subcutis.11
There are various approaches to treating furuncular myiasis, with the goal of complete removal of the larva and prevention of secondary infection. One treatment option is to apply a toxic substance to the larva, effectively killing it. Another approach is to force the larva to emerge via localized hypoxia, which can be done by occluding the punctum of the lesion for at least 24 hours. A complication of this method is suffocation of the larva without migration, leading to incomplete extraction and secondary infection.1 A third method is to surgically remove the larva, which allows for debridement of necrotic tissue surrounding the lesion if present.12 Ultrasonography also can be used therapeutically to aid in the removal of the larvae. The last method is to inject lidocaine into the base of the lesion, forcing the larva out of the punctum via fluid pressure.13 Oral treatments such as ivermectin are not recommended because they can result in the death of larvae within the lesion, leading to an inflammatory response.8
Furuncular myiasis is a form of cutaneous larvae infestation not commonly seen in individuals who do not live or travel in endemic, tropical, and subtropical regions. Diagnosis is based on clinical presentation, with imaging and laboratory studies available to supplement in unclear or atypical manifestations. Treatment involves complete removal of the larva, typically through forced evacuation via hypoxia or through surgical removal. Most cases resolve without notable scarring or other sequelae; however, in those who do have complications, the most common is secondary bacterial infection. Our patient’s absence of notable travel history and frequent environmental exposure in Michigan led us to believe the organism was from a domestic source. Our case underlines the importance of a thorough history and clinical examination of furuncular lesions including the use of dermoscopy to yield an appropriate diagnosis and treatment plan.
- Francesconi F, Lupi O. Myiasis. Clin Microbiol Rev. 2012;25:79-105. doi:10.1128/CMR.00010-11
- Schiff TA. Furuncular cutaneous myiasis caused by Cuterebra larva. J Am Acad Dermatol 1993;28:261-263.
- Safdar N, Young DK, Andes D. Autochthonous furuncular myiasis in the United States: case report and literature review. Clin Infect Dis. 2003;26:73-80.
- Mahal JJ, Sperling JD. Furuncular myiasis from Dermatobia hominus: a case of human botfly infestation. J Emerg Med. 2012;43:618-621.
- Francesconi F, Lupi O. Myiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. Elsevier; 2006:232-239.
- Gordon PM, Hepburn NC, Williams AE, et al. Cutaneous myiasis due to Dermatobia hominis: a report of six cases. Br J Dermatol. 1995;132:811-814.
- Hubler WR Jr, Rudolph AH, Dougherty EF. Dermal myiasis. Arch Dermatol. 1974;110:109-110.
- Quintanilla-Cedillo MR, León-Ureña H, Contreras-Ruiz J, et al. The value of Doppler ultrasound in diagnosis in 25 cases of furunculoid myiasis. Int J Dermatol. 2005;44:34-37.
- Bakos RM, Bakos L. Dermoscopic diagnosis of furuncular myiasis. Arch Dermatol. 2007;143:123-124.
- Varani S, Tassinari D, Elleri D, et al. A case of furuncular myiasis associated with systemic inflammation. Parasitol Int. 2007;56:330-333.
- Grogan TM, Payne CM, Spier C, et al. Cutaneous myiasis. immunohistologic and ultrastructural morphometric features of a human botfly lesion. Am J Dermatopathol. 1987;9:232-239.
- Krajewski A, Allen B, Hoss D, et al. Cutaneous myiasis. J Plast Reconstr Aesthet Surg. 2009;62:383-386.
- Lebwohl MG, Heymann WR, Berth-Jones J, et al. Myiasis: Treatment of Skin Diseases. Comprehensive Therapeutic Strategies. 2nd ed. Elsevier-Mosby; 2006.
- Francesconi F, Lupi O. Myiasis. Clin Microbiol Rev. 2012;25:79-105. doi:10.1128/CMR.00010-11
- Schiff TA. Furuncular cutaneous myiasis caused by Cuterebra larva. J Am Acad Dermatol 1993;28:261-263.
- Safdar N, Young DK, Andes D. Autochthonous furuncular myiasis in the United States: case report and literature review. Clin Infect Dis. 2003;26:73-80.
- Mahal JJ, Sperling JD. Furuncular myiasis from Dermatobia hominus: a case of human botfly infestation. J Emerg Med. 2012;43:618-621.
- Francesconi F, Lupi O. Myiasis. In: Tyring SK, Lupi O, Hengge UR, eds. Tropical Dermatology. Elsevier; 2006:232-239.
- Gordon PM, Hepburn NC, Williams AE, et al. Cutaneous myiasis due to Dermatobia hominis: a report of six cases. Br J Dermatol. 1995;132:811-814.
- Hubler WR Jr, Rudolph AH, Dougherty EF. Dermal myiasis. Arch Dermatol. 1974;110:109-110.
- Quintanilla-Cedillo MR, León-Ureña H, Contreras-Ruiz J, et al. The value of Doppler ultrasound in diagnosis in 25 cases of furunculoid myiasis. Int J Dermatol. 2005;44:34-37.
- Bakos RM, Bakos L. Dermoscopic diagnosis of furuncular myiasis. Arch Dermatol. 2007;143:123-124.
- Varani S, Tassinari D, Elleri D, et al. A case of furuncular myiasis associated with systemic inflammation. Parasitol Int. 2007;56:330-333.
- Grogan TM, Payne CM, Spier C, et al. Cutaneous myiasis. immunohistologic and ultrastructural morphometric features of a human botfly lesion. Am J Dermatopathol. 1987;9:232-239.
- Krajewski A, Allen B, Hoss D, et al. Cutaneous myiasis. J Plast Reconstr Aesthet Surg. 2009;62:383-386.
- Lebwohl MG, Heymann WR, Berth-Jones J, et al. Myiasis: Treatment of Skin Diseases. Comprehensive Therapeutic Strategies. 2nd ed. Elsevier-Mosby; 2006.
Practice Points
- Cutaneous myiasis is a skin infestation with dipterous larvae that feed on the host’s tissue and cause a wide range of manifestations depending on the location of infestation. It consists of 3 types: furuncular, wound, and migratory forms.
- It is uncommon in the United States and not typically seen in patients who have no history of recent travel to tropical or subtropical areas.
- The most common cause of African furuncular myiasis acquired in the United States is larvae of the Cuterebra species (also known as the rabbit botfly or rodent botfly).
Ultra-Late Cutaneous Melanoma Recurrence Following 49 Years of Quiescence
To the Editor:
Ultra-late melanoma recurrence represents a minority of cases in which the quiescent period lasts longer than 15 years, and epidemiologic studies have reported recurrence rates of 6% to 10% during the ultra-late period.1 Even more uncommon are cases that span many decades (eg, >30 years), but all are useful in understanding the cellular behavior leading to the reactivation of fully excised melanomas. Few cases have been reported in which recurrence occurs more than 35 years after the original diagnosis of melanoma. Unfortunately, mechanisms underlying this long stable quiescence and subsequent reactivation are poorly understood, which is why it is important to identify and document cases. We present a case of local recurrence of cutaneous melanoma on the patient’s lower back after a 49-year disease-free period.
A 78-year-old White woman presented to a private dermatology office for a full-body skin examination. She had a medical history of a cutaneous melanoma that had been removed on the lower back 49 years prior; Parkinson disease of 10 years’ duration; and an enlarged thyroid nodule with decreased thyrotropin and hyperthyroidism, atrial fibrillation, mitral valve prolapse, osteoarthritis in the knees, and actinic keratoses, all of which were chronic conditions lasting years to decades. She was taking several medications for these medical conditions. Her surgical history included a hysterectomy, hip replacement, hernia repair, cardioversion, and tonsillectomy in childhood. Her family medical history included breast cancer in her paternal grandmother and aunt; hypertension in her father; and sarcoma in her mother at 78 years of age, which initially was identified in the sacrum and metastasized to the lungs causing death. No family history of melanoma or other skin cancers was reported. Prior to the original diagnosis of melanoma at 29 years of age, she had no history of skin cancer or any other medical condition other than acne. The patient did report spending a great deal of time in the sun during high school.
The patient reported developing the original cutaneous melanoma during her second pregnancy at 29 years of age and recalled that it was excised with wide margins. There had been a mole on her back that was present for years but changed in size during pregnancy, prompting the original visit to the primary care physician for evaluation. Remarkably, the original pathology report was obtained from the patient and revealed a specimen consisting of a 3.7×1.7-cm skin
Physical examination at the current presentation 49 years later revealed an even-bordered 2-mm black macule that was located approximately 1 cm from the original melanoma excision scar line (Figure). A biopsy was performed and sent to a dermatopathologist. Microscopic evaluation revealed nests, islands, and sheets of atypical epithelioid melanocytes extending through the dermis between collagen bundles. The melanocytes varied in size and shape with moderate nuclear pleomorphism present. Scattered mitotic figures and necrotic melanocytes were present, which most likely represented cutaneous satellite metastases of melanoma. Subsequent chest radiography, full-body positron emission tomography, and standard laboratory blood tests were unremarkable except for an enlarged right thyroid gland and moderate cardiomegaly. The patient was sent to a surgical oncologist for excision with wide surgical margins, and she elected not to have a sentinel lymph node biopsy. At follow-up 3, 6, 12, and 24 months later, there were no signs of recurrence based on direct clinical examination. The patient subsequently was lost to follow-up.

Recurrence rates of melanoma vary by stage and age at diagnosis, but prior studies have reported a recurrence rate of approximately 6% after 10 or more years following the initial diagnosis.2 Ultra-late recurrences of approximately 4 decades or more are extremely rare. A PubMed search of articles indexed for MEDLINE using the terms melanoma and ultra-late recurrence revealed 4 reported cases with a quiescent period of 38 or more years.3-6 All cases were metastatic melanomas in women; spanned 38, 40, 41, and 45 years from the initial melanoma diagnosis to recurrence; and all of the recurrences except one were regional or distal metastatic lesions (eg, lymph node, brain). In one case, both the original and recurrent lesions occurred on the left elbow.6 The original lesions occurred on the legs, elbow, and back of the neck, and there were no notable concomitant medical conditions. The patients were aged 72, 73, 73, and 84 years at recurrence.3-6 However, generalizations from these cases are limited given the potential for selection bias (eg, men may be less likely to visit a clinic for follow-up and nevi examination) and the likelihood that many cases of ultra-late melanoma recurrence are unrecognized or unreported.
More recently, genomic analyses on melanoma lesions occurring 30 years apart confirmed that the second lesion was indeed a recurrence, although with numerous additional mutations.7 The specific mechanisms underlying the dormancy and subsequent reemergence of metastatic lesions are unclear, but
It also is worth highlighting the concomitant diagnosis of Parkinson disease in our patient. In recent years, Parkinson disease has been linked to melanoma in both epidemiologic and genetic studies. For example, one large-scale study found a 50% increased risk for developing Parkinson disease in patients with melanoma (and vice versa), and this finding has been replicated in other studies.10 Moreover, patients with Parkinson disease have a 2-fold increase in their risk for developing melanoma, demonstrating that it is a bidirectional pathway. Not surprisingly, associations between melanin and neuromelanin pathways have been identified as a potential link between these diseases, and scientists are in the process of understanding the genetic components of both.10 It is unknown if specific genetic mutations contributed to both diseases in our case, but follow-up genetic testing on the recurrent melanoma specimen currently is being pursued.
The 49-year quiescent period in our case of recurrent cutaneous malignant melanoma potentially represents the longest ultra-late recurrence of melanoma in the literature to date based on a review of indexed publications. Moreover, it is relatively unique compared to other similar cases in that the recurrence was within a centimeter of the original excisional scar. Most metastases occur in locoregional lymph nodes or the lungs3; therefore, it is unusual to find one so close to the original lesion, especially one that occurred decades later. Factors associated with ultra-late recurrences are unknown, primarily because of the rarity of these cases as well as the biases and other factors that limit existing studies. However, genetic sequencing may provide information regarding these factors and related processes. Genetic sequencing specifically points to a small cell group remaining after excision of the primary tumor, which mutates while proliferating. Low antigenicity and tolerance to immunity during the quiescent period may explain the long duration of dormancy.6 More recently, there have been efforts to identify immunohistochemical signatures that may predict late recurrences, though the data are preliminary in nature.11
Given the latency period and location of the recurrence, our case demonstrates that even fully excised melanomas may recur locally many decades later, hence patients should be aware of the importance of a lifetime of vigilance after being diagnosed with melanoma.
- Tsao H, Cosimi AB, Sober AJ. Ultra-late recurrence (15 years or longer) of cutaneous melanoma. Cancer. 1997;79:2361-2370.
- Faries MB, Steen S, Ye X, et al. Late recurrence in melanoma: clinical implications of lost dormancy. J Am Coll Surg. 2013;217:27-34.
- Mansour D, Kejariwal D. It is never too late: ultra-late recurrence of melanoma with distant metastases [published online March 8, 2012]. BMJ Case Rep. 2012:bcr0120125474. doi:10.1136/bcr.01.2012.5474
- Saleh D, Peach AHS. Ultra-late recurrence of malignant melanoma after 40 years of quiescent disease. J Surg Oncol. 2011;103:290-291.
- Goodenough J, Cozon CL, Liew SH. An incidental finding of a nodal recurrence of cutaneous malignant melanoma after a 45-year disease-free period [published online June 4, 2014]. BMJ Case Rep. 2014:bcr2014204289. doi:10.1136/bcr-2014-204289
- Nakamura M, Obayashi M, Yoshimitsu M, et al. Comparative whole-exome sequencing of an ultra-late recurrent malignant melanoma. Br J Dermatol. 2021;184:762-763.
- Miller JJ, Lofgren KA, Hughes SR, et al. Genomic analysis of melanoma evolution following a 30-year disease-free interval. J Cutan Pathol. 2017;44:805-808.
- North JP, Kageshita T, Pinkel D, et al. Distribution and significance of occult intraepidermal tumor cells surrounding primary melanoma. J Invest Dermatol. 2008;128:2024-2030.
- Massi G, LeBoit PE. Recurrent and persistent melanoma. In: Massi G, LeBoit PE, eds. Histological Diagnosis of Nevi and Melanoma. 2nd ed. Springer-Verlag; 2014:689-698.
- Bose A, Petsko GA, Eliezer D. Parkinson’s disease and melanoma: co-occurrence and mechanisms. J Parkinsons Dis. 2018;8:385-398.
- Reschke R, Dumann K, Ziemer M. Risk stratification and clinical characteristics of patients with late recurrence of melanoma (>10 years).J Clin Med. 2022;11:2026.
To the Editor:
Ultra-late melanoma recurrence represents a minority of cases in which the quiescent period lasts longer than 15 years, and epidemiologic studies have reported recurrence rates of 6% to 10% during the ultra-late period.1 Even more uncommon are cases that span many decades (eg, >30 years), but all are useful in understanding the cellular behavior leading to the reactivation of fully excised melanomas. Few cases have been reported in which recurrence occurs more than 35 years after the original diagnosis of melanoma. Unfortunately, mechanisms underlying this long stable quiescence and subsequent reactivation are poorly understood, which is why it is important to identify and document cases. We present a case of local recurrence of cutaneous melanoma on the patient’s lower back after a 49-year disease-free period.
A 78-year-old White woman presented to a private dermatology office for a full-body skin examination. She had a medical history of a cutaneous melanoma that had been removed on the lower back 49 years prior; Parkinson disease of 10 years’ duration; and an enlarged thyroid nodule with decreased thyrotropin and hyperthyroidism, atrial fibrillation, mitral valve prolapse, osteoarthritis in the knees, and actinic keratoses, all of which were chronic conditions lasting years to decades. She was taking several medications for these medical conditions. Her surgical history included a hysterectomy, hip replacement, hernia repair, cardioversion, and tonsillectomy in childhood. Her family medical history included breast cancer in her paternal grandmother and aunt; hypertension in her father; and sarcoma in her mother at 78 years of age, which initially was identified in the sacrum and metastasized to the lungs causing death. No family history of melanoma or other skin cancers was reported. Prior to the original diagnosis of melanoma at 29 years of age, she had no history of skin cancer or any other medical condition other than acne. The patient did report spending a great deal of time in the sun during high school.
The patient reported developing the original cutaneous melanoma during her second pregnancy at 29 years of age and recalled that it was excised with wide margins. There had been a mole on her back that was present for years but changed in size during pregnancy, prompting the original visit to the primary care physician for evaluation. Remarkably, the original pathology report was obtained from the patient and revealed a specimen consisting of a 3.7×1.7-cm skin
Physical examination at the current presentation 49 years later revealed an even-bordered 2-mm black macule that was located approximately 1 cm from the original melanoma excision scar line (Figure). A biopsy was performed and sent to a dermatopathologist. Microscopic evaluation revealed nests, islands, and sheets of atypical epithelioid melanocytes extending through the dermis between collagen bundles. The melanocytes varied in size and shape with moderate nuclear pleomorphism present. Scattered mitotic figures and necrotic melanocytes were present, which most likely represented cutaneous satellite metastases of melanoma. Subsequent chest radiography, full-body positron emission tomography, and standard laboratory blood tests were unremarkable except for an enlarged right thyroid gland and moderate cardiomegaly. The patient was sent to a surgical oncologist for excision with wide surgical margins, and she elected not to have a sentinel lymph node biopsy. At follow-up 3, 6, 12, and 24 months later, there were no signs of recurrence based on direct clinical examination. The patient subsequently was lost to follow-up.

Recurrence rates of melanoma vary by stage and age at diagnosis, but prior studies have reported a recurrence rate of approximately 6% after 10 or more years following the initial diagnosis.2 Ultra-late recurrences of approximately 4 decades or more are extremely rare. A PubMed search of articles indexed for MEDLINE using the terms melanoma and ultra-late recurrence revealed 4 reported cases with a quiescent period of 38 or more years.3-6 All cases were metastatic melanomas in women; spanned 38, 40, 41, and 45 years from the initial melanoma diagnosis to recurrence; and all of the recurrences except one were regional or distal metastatic lesions (eg, lymph node, brain). In one case, both the original and recurrent lesions occurred on the left elbow.6 The original lesions occurred on the legs, elbow, and back of the neck, and there were no notable concomitant medical conditions. The patients were aged 72, 73, 73, and 84 years at recurrence.3-6 However, generalizations from these cases are limited given the potential for selection bias (eg, men may be less likely to visit a clinic for follow-up and nevi examination) and the likelihood that many cases of ultra-late melanoma recurrence are unrecognized or unreported.
More recently, genomic analyses on melanoma lesions occurring 30 years apart confirmed that the second lesion was indeed a recurrence, although with numerous additional mutations.7 The specific mechanisms underlying the dormancy and subsequent reemergence of metastatic lesions are unclear, but
It also is worth highlighting the concomitant diagnosis of Parkinson disease in our patient. In recent years, Parkinson disease has been linked to melanoma in both epidemiologic and genetic studies. For example, one large-scale study found a 50% increased risk for developing Parkinson disease in patients with melanoma (and vice versa), and this finding has been replicated in other studies.10 Moreover, patients with Parkinson disease have a 2-fold increase in their risk for developing melanoma, demonstrating that it is a bidirectional pathway. Not surprisingly, associations between melanin and neuromelanin pathways have been identified as a potential link between these diseases, and scientists are in the process of understanding the genetic components of both.10 It is unknown if specific genetic mutations contributed to both diseases in our case, but follow-up genetic testing on the recurrent melanoma specimen currently is being pursued.
The 49-year quiescent period in our case of recurrent cutaneous malignant melanoma potentially represents the longest ultra-late recurrence of melanoma in the literature to date based on a review of indexed publications. Moreover, it is relatively unique compared to other similar cases in that the recurrence was within a centimeter of the original excisional scar. Most metastases occur in locoregional lymph nodes or the lungs3; therefore, it is unusual to find one so close to the original lesion, especially one that occurred decades later. Factors associated with ultra-late recurrences are unknown, primarily because of the rarity of these cases as well as the biases and other factors that limit existing studies. However, genetic sequencing may provide information regarding these factors and related processes. Genetic sequencing specifically points to a small cell group remaining after excision of the primary tumor, which mutates while proliferating. Low antigenicity and tolerance to immunity during the quiescent period may explain the long duration of dormancy.6 More recently, there have been efforts to identify immunohistochemical signatures that may predict late recurrences, though the data are preliminary in nature.11
Given the latency period and location of the recurrence, our case demonstrates that even fully excised melanomas may recur locally many decades later, hence patients should be aware of the importance of a lifetime of vigilance after being diagnosed with melanoma.
To the Editor:
Ultra-late melanoma recurrence represents a minority of cases in which the quiescent period lasts longer than 15 years, and epidemiologic studies have reported recurrence rates of 6% to 10% during the ultra-late period.1 Even more uncommon are cases that span many decades (eg, >30 years), but all are useful in understanding the cellular behavior leading to the reactivation of fully excised melanomas. Few cases have been reported in which recurrence occurs more than 35 years after the original diagnosis of melanoma. Unfortunately, mechanisms underlying this long stable quiescence and subsequent reactivation are poorly understood, which is why it is important to identify and document cases. We present a case of local recurrence of cutaneous melanoma on the patient’s lower back after a 49-year disease-free period.
A 78-year-old White woman presented to a private dermatology office for a full-body skin examination. She had a medical history of a cutaneous melanoma that had been removed on the lower back 49 years prior; Parkinson disease of 10 years’ duration; and an enlarged thyroid nodule with decreased thyrotropin and hyperthyroidism, atrial fibrillation, mitral valve prolapse, osteoarthritis in the knees, and actinic keratoses, all of which were chronic conditions lasting years to decades. She was taking several medications for these medical conditions. Her surgical history included a hysterectomy, hip replacement, hernia repair, cardioversion, and tonsillectomy in childhood. Her family medical history included breast cancer in her paternal grandmother and aunt; hypertension in her father; and sarcoma in her mother at 78 years of age, which initially was identified in the sacrum and metastasized to the lungs causing death. No family history of melanoma or other skin cancers was reported. Prior to the original diagnosis of melanoma at 29 years of age, she had no history of skin cancer or any other medical condition other than acne. The patient did report spending a great deal of time in the sun during high school.
The patient reported developing the original cutaneous melanoma during her second pregnancy at 29 years of age and recalled that it was excised with wide margins. There had been a mole on her back that was present for years but changed in size during pregnancy, prompting the original visit to the primary care physician for evaluation. Remarkably, the original pathology report was obtained from the patient and revealed a specimen consisting of a 3.7×1.7-cm skin
Physical examination at the current presentation 49 years later revealed an even-bordered 2-mm black macule that was located approximately 1 cm from the original melanoma excision scar line (Figure). A biopsy was performed and sent to a dermatopathologist. Microscopic evaluation revealed nests, islands, and sheets of atypical epithelioid melanocytes extending through the dermis between collagen bundles. The melanocytes varied in size and shape with moderate nuclear pleomorphism present. Scattered mitotic figures and necrotic melanocytes were present, which most likely represented cutaneous satellite metastases of melanoma. Subsequent chest radiography, full-body positron emission tomography, and standard laboratory blood tests were unremarkable except for an enlarged right thyroid gland and moderate cardiomegaly. The patient was sent to a surgical oncologist for excision with wide surgical margins, and she elected not to have a sentinel lymph node biopsy. At follow-up 3, 6, 12, and 24 months later, there were no signs of recurrence based on direct clinical examination. The patient subsequently was lost to follow-up.

Recurrence rates of melanoma vary by stage and age at diagnosis, but prior studies have reported a recurrence rate of approximately 6% after 10 or more years following the initial diagnosis.2 Ultra-late recurrences of approximately 4 decades or more are extremely rare. A PubMed search of articles indexed for MEDLINE using the terms melanoma and ultra-late recurrence revealed 4 reported cases with a quiescent period of 38 or more years.3-6 All cases were metastatic melanomas in women; spanned 38, 40, 41, and 45 years from the initial melanoma diagnosis to recurrence; and all of the recurrences except one were regional or distal metastatic lesions (eg, lymph node, brain). In one case, both the original and recurrent lesions occurred on the left elbow.6 The original lesions occurred on the legs, elbow, and back of the neck, and there were no notable concomitant medical conditions. The patients were aged 72, 73, 73, and 84 years at recurrence.3-6 However, generalizations from these cases are limited given the potential for selection bias (eg, men may be less likely to visit a clinic for follow-up and nevi examination) and the likelihood that many cases of ultra-late melanoma recurrence are unrecognized or unreported.
More recently, genomic analyses on melanoma lesions occurring 30 years apart confirmed that the second lesion was indeed a recurrence, although with numerous additional mutations.7 The specific mechanisms underlying the dormancy and subsequent reemergence of metastatic lesions are unclear, but
It also is worth highlighting the concomitant diagnosis of Parkinson disease in our patient. In recent years, Parkinson disease has been linked to melanoma in both epidemiologic and genetic studies. For example, one large-scale study found a 50% increased risk for developing Parkinson disease in patients with melanoma (and vice versa), and this finding has been replicated in other studies.10 Moreover, patients with Parkinson disease have a 2-fold increase in their risk for developing melanoma, demonstrating that it is a bidirectional pathway. Not surprisingly, associations between melanin and neuromelanin pathways have been identified as a potential link between these diseases, and scientists are in the process of understanding the genetic components of both.10 It is unknown if specific genetic mutations contributed to both diseases in our case, but follow-up genetic testing on the recurrent melanoma specimen currently is being pursued.
The 49-year quiescent period in our case of recurrent cutaneous malignant melanoma potentially represents the longest ultra-late recurrence of melanoma in the literature to date based on a review of indexed publications. Moreover, it is relatively unique compared to other similar cases in that the recurrence was within a centimeter of the original excisional scar. Most metastases occur in locoregional lymph nodes or the lungs3; therefore, it is unusual to find one so close to the original lesion, especially one that occurred decades later. Factors associated with ultra-late recurrences are unknown, primarily because of the rarity of these cases as well as the biases and other factors that limit existing studies. However, genetic sequencing may provide information regarding these factors and related processes. Genetic sequencing specifically points to a small cell group remaining after excision of the primary tumor, which mutates while proliferating. Low antigenicity and tolerance to immunity during the quiescent period may explain the long duration of dormancy.6 More recently, there have been efforts to identify immunohistochemical signatures that may predict late recurrences, though the data are preliminary in nature.11
Given the latency period and location of the recurrence, our case demonstrates that even fully excised melanomas may recur locally many decades later, hence patients should be aware of the importance of a lifetime of vigilance after being diagnosed with melanoma.
- Tsao H, Cosimi AB, Sober AJ. Ultra-late recurrence (15 years or longer) of cutaneous melanoma. Cancer. 1997;79:2361-2370.
- Faries MB, Steen S, Ye X, et al. Late recurrence in melanoma: clinical implications of lost dormancy. J Am Coll Surg. 2013;217:27-34.
- Mansour D, Kejariwal D. It is never too late: ultra-late recurrence of melanoma with distant metastases [published online March 8, 2012]. BMJ Case Rep. 2012:bcr0120125474. doi:10.1136/bcr.01.2012.5474
- Saleh D, Peach AHS. Ultra-late recurrence of malignant melanoma after 40 years of quiescent disease. J Surg Oncol. 2011;103:290-291.
- Goodenough J, Cozon CL, Liew SH. An incidental finding of a nodal recurrence of cutaneous malignant melanoma after a 45-year disease-free period [published online June 4, 2014]. BMJ Case Rep. 2014:bcr2014204289. doi:10.1136/bcr-2014-204289
- Nakamura M, Obayashi M, Yoshimitsu M, et al. Comparative whole-exome sequencing of an ultra-late recurrent malignant melanoma. Br J Dermatol. 2021;184:762-763.
- Miller JJ, Lofgren KA, Hughes SR, et al. Genomic analysis of melanoma evolution following a 30-year disease-free interval. J Cutan Pathol. 2017;44:805-808.
- North JP, Kageshita T, Pinkel D, et al. Distribution and significance of occult intraepidermal tumor cells surrounding primary melanoma. J Invest Dermatol. 2008;128:2024-2030.
- Massi G, LeBoit PE. Recurrent and persistent melanoma. In: Massi G, LeBoit PE, eds. Histological Diagnosis of Nevi and Melanoma. 2nd ed. Springer-Verlag; 2014:689-698.
- Bose A, Petsko GA, Eliezer D. Parkinson’s disease and melanoma: co-occurrence and mechanisms. J Parkinsons Dis. 2018;8:385-398.
- Reschke R, Dumann K, Ziemer M. Risk stratification and clinical characteristics of patients with late recurrence of melanoma (>10 years).J Clin Med. 2022;11:2026.
- Tsao H, Cosimi AB, Sober AJ. Ultra-late recurrence (15 years or longer) of cutaneous melanoma. Cancer. 1997;79:2361-2370.
- Faries MB, Steen S, Ye X, et al. Late recurrence in melanoma: clinical implications of lost dormancy. J Am Coll Surg. 2013;217:27-34.
- Mansour D, Kejariwal D. It is never too late: ultra-late recurrence of melanoma with distant metastases [published online March 8, 2012]. BMJ Case Rep. 2012:bcr0120125474. doi:10.1136/bcr.01.2012.5474
- Saleh D, Peach AHS. Ultra-late recurrence of malignant melanoma after 40 years of quiescent disease. J Surg Oncol. 2011;103:290-291.
- Goodenough J, Cozon CL, Liew SH. An incidental finding of a nodal recurrence of cutaneous malignant melanoma after a 45-year disease-free period [published online June 4, 2014]. BMJ Case Rep. 2014:bcr2014204289. doi:10.1136/bcr-2014-204289
- Nakamura M, Obayashi M, Yoshimitsu M, et al. Comparative whole-exome sequencing of an ultra-late recurrent malignant melanoma. Br J Dermatol. 2021;184:762-763.
- Miller JJ, Lofgren KA, Hughes SR, et al. Genomic analysis of melanoma evolution following a 30-year disease-free interval. J Cutan Pathol. 2017;44:805-808.
- North JP, Kageshita T, Pinkel D, et al. Distribution and significance of occult intraepidermal tumor cells surrounding primary melanoma. J Invest Dermatol. 2008;128:2024-2030.
- Massi G, LeBoit PE. Recurrent and persistent melanoma. In: Massi G, LeBoit PE, eds. Histological Diagnosis of Nevi and Melanoma. 2nd ed. Springer-Verlag; 2014:689-698.
- Bose A, Petsko GA, Eliezer D. Parkinson’s disease and melanoma: co-occurrence and mechanisms. J Parkinsons Dis. 2018;8:385-398.
- Reschke R, Dumann K, Ziemer M. Risk stratification and clinical characteristics of patients with late recurrence of melanoma (>10 years).J Clin Med. 2022;11:2026.
Practice Points
- In some cases of ultra-late malignant melanoma recurrence, the quiescent period can last more than 30 years.
- There does not appear to be specificity with location since ultra-late melanoma recurrences can occur locally, regionally, and distally, and original lesions appear to be randomly distributed in these cases.
- Mechanisms for ultra-late melanoma recurrence are poorly understood; histologically, unrecognizable aberrations in the skin beyond the histopathologic margins may represent an early phase of disease that lies dormant for many years before reemerging in response to external or immunologic changes.
- Patients with malignant melanoma are at a higher risk for developing Parkinson disease (and vice versa) given the link between melanin and neuromelanin pathways.












