User login
ID Practitioner is an independent news source that provides infectious disease specialists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the infectious disease specialist’s practice. Specialty focus topics include antimicrobial resistance, emerging infections, global ID, hepatitis, HIV, hospital-acquired infections, immunizations and vaccines, influenza, mycoses, pediatric infections, and STIs. Infectious Diseases News is owned by Frontline Medical Communications.
sofosbuvir
ritonavir with dasabuvir
discount
support path
program
ritonavir
greedy
ledipasvir
assistance
viekira pak
vpak
advocacy
needy
protest
abbvie
paritaprevir
ombitasvir
direct-acting antivirals
dasabuvir
gilead
fake-ovir
support
v pak
oasis
harvoni
section[contains(@class, 'footer-nav-section-wrapper')]
div[contains(@class, 'pane-pub-article-idp')]
div[contains(@class, 'pane-medstat-latest-articles-articles-section')]
div[contains(@class, 'pane-pub-home-idp')]
div[contains(@class, 'pane-pub-topic-idp')]
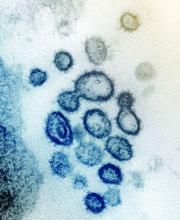
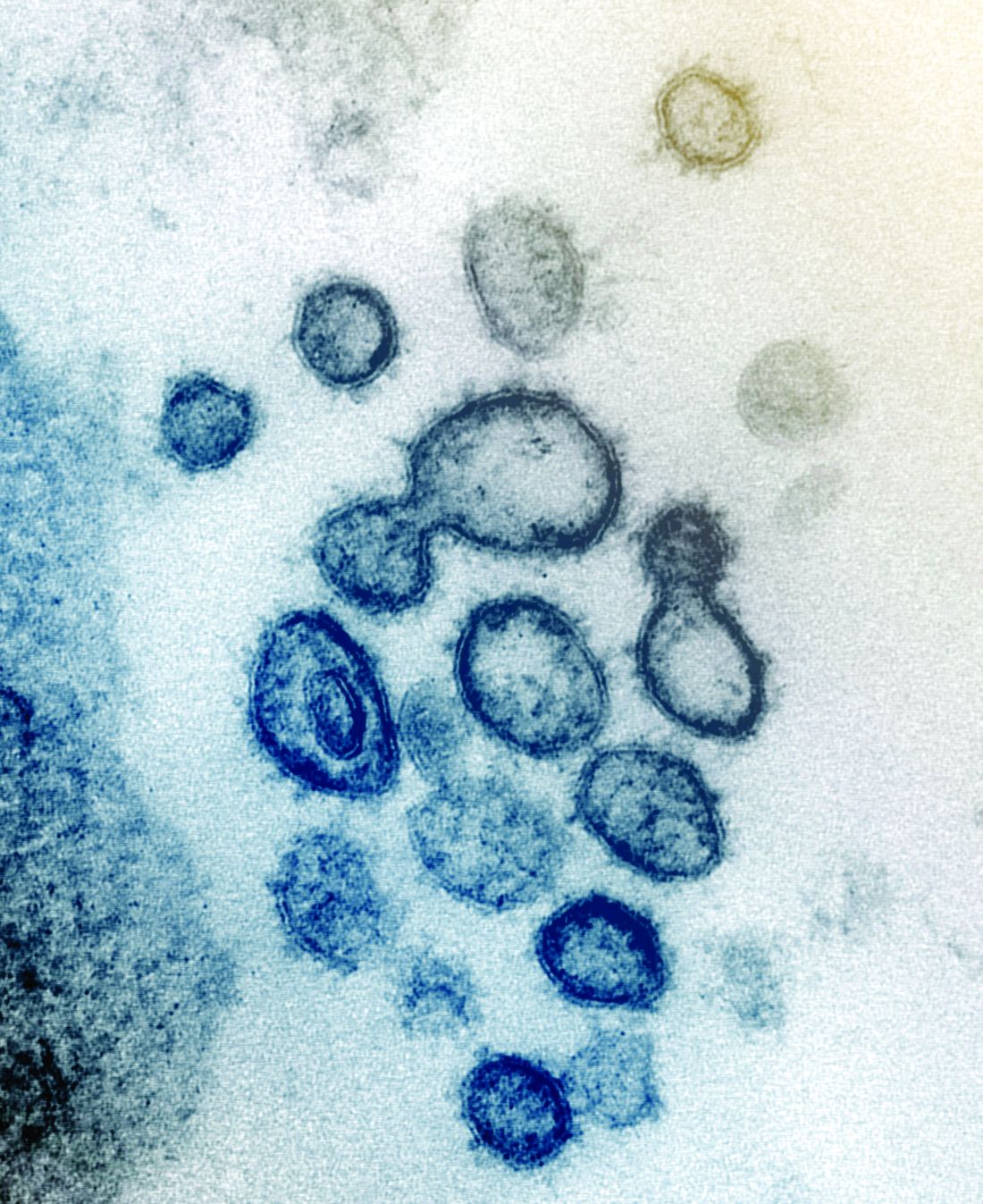
First presumptive case of encephalitis linked to COVID-19 reported
“As the number of patients with COVID-19 increases worldwide, clinicians and radiologists should be watching for this presentation among patients presenting with COVID-19 and altered mental status,” the clinicians advise in a report published online March 31 in Radiology.
“This is significant for all providers to be aware of and looking out for in [COVID-19] patients who present with an altered level of consciousness. This complication is as devastating as severe lung disease,” Elissa Fory, MD, a neurologist with Henry Ford who was part of the team of medical experts that made the diagnosis, said in a statement.
“We need to be thinking of how we’re going to incorporate patients with severe neurological disease into our treatment paradigm,” Fory added.
Brent Griffith, MD, radiologist with Henry Ford and senior author of the case report, said the case shows “the important role that imaging can play in COVID-19 cases.”
Diagnosed via neuroimaging
The 58-year-old woman presented with a 3-day history of fever, cough, and muscle aches ― symptoms consistent with COVID-19. She was transported by ambulance to the emergency department and showed signs of confusion, lethargy, and disorientation.
The woman tested negative for influenza, but a rapid COVID-19 test confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. She was later diagnosed with acute hemorrhagic necrotizing encephalopathy.
“The team had suspected encephalitis at the outset, but then back-to-back CT and MRI scans made the diagnosis,” Fory said in the statement.
Noncontrast head CT revealed “symmetric hypoattenuation within the bilateral medial thalami with a normal CT angiogram and CT venogram,” the team reports in their article. Brain MRI showed “hemorrhagic rim enhancing lesions within the bilateral thalami, medial temporal lobes, and subinsular regions.”
The patient was started on intravenous immunoglobulin but not high-dose steroids, because of concern for respiratory compromise. As of April 1, the patient was hospitalized in serious condition. Henry Ford Hospital has not provided an update.
Acute necrotizing encephalopathy (ANE) is a rare complication of viral infections, but until now, it has not been known to have occurred as a result of COVID-19 infection. ANE has been associated with intracranial “cytokine storms,” and a recent report in the Lancet suggested that a subgroup of patients with severe COVID-19 might develop a cytokine storm syndrome.
Commenting for Medscape Medical News, Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University in St. Louis, Missouri, said, “Since this is just one report of one patient, the findings are the most preliminary we can conceive, and more research is needed to determine the extent to which COVID-19 may affect the central nervous system.”
Fory, Griffith, and Raji have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
“As the number of patients with COVID-19 increases worldwide, clinicians and radiologists should be watching for this presentation among patients presenting with COVID-19 and altered mental status,” the clinicians advise in a report published online March 31 in Radiology.
“This is significant for all providers to be aware of and looking out for in [COVID-19] patients who present with an altered level of consciousness. This complication is as devastating as severe lung disease,” Elissa Fory, MD, a neurologist with Henry Ford who was part of the team of medical experts that made the diagnosis, said in a statement.
“We need to be thinking of how we’re going to incorporate patients with severe neurological disease into our treatment paradigm,” Fory added.
Brent Griffith, MD, radiologist with Henry Ford and senior author of the case report, said the case shows “the important role that imaging can play in COVID-19 cases.”
Diagnosed via neuroimaging
The 58-year-old woman presented with a 3-day history of fever, cough, and muscle aches ― symptoms consistent with COVID-19. She was transported by ambulance to the emergency department and showed signs of confusion, lethargy, and disorientation.
The woman tested negative for influenza, but a rapid COVID-19 test confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. She was later diagnosed with acute hemorrhagic necrotizing encephalopathy.
“The team had suspected encephalitis at the outset, but then back-to-back CT and MRI scans made the diagnosis,” Fory said in the statement.
Noncontrast head CT revealed “symmetric hypoattenuation within the bilateral medial thalami with a normal CT angiogram and CT venogram,” the team reports in their article. Brain MRI showed “hemorrhagic rim enhancing lesions within the bilateral thalami, medial temporal lobes, and subinsular regions.”
The patient was started on intravenous immunoglobulin but not high-dose steroids, because of concern for respiratory compromise. As of April 1, the patient was hospitalized in serious condition. Henry Ford Hospital has not provided an update.
Acute necrotizing encephalopathy (ANE) is a rare complication of viral infections, but until now, it has not been known to have occurred as a result of COVID-19 infection. ANE has been associated with intracranial “cytokine storms,” and a recent report in the Lancet suggested that a subgroup of patients with severe COVID-19 might develop a cytokine storm syndrome.
Commenting for Medscape Medical News, Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University in St. Louis, Missouri, said, “Since this is just one report of one patient, the findings are the most preliminary we can conceive, and more research is needed to determine the extent to which COVID-19 may affect the central nervous system.”
Fory, Griffith, and Raji have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
“As the number of patients with COVID-19 increases worldwide, clinicians and radiologists should be watching for this presentation among patients presenting with COVID-19 and altered mental status,” the clinicians advise in a report published online March 31 in Radiology.
“This is significant for all providers to be aware of and looking out for in [COVID-19] patients who present with an altered level of consciousness. This complication is as devastating as severe lung disease,” Elissa Fory, MD, a neurologist with Henry Ford who was part of the team of medical experts that made the diagnosis, said in a statement.
“We need to be thinking of how we’re going to incorporate patients with severe neurological disease into our treatment paradigm,” Fory added.
Brent Griffith, MD, radiologist with Henry Ford and senior author of the case report, said the case shows “the important role that imaging can play in COVID-19 cases.”
Diagnosed via neuroimaging
The 58-year-old woman presented with a 3-day history of fever, cough, and muscle aches ― symptoms consistent with COVID-19. She was transported by ambulance to the emergency department and showed signs of confusion, lethargy, and disorientation.
The woman tested negative for influenza, but a rapid COVID-19 test confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. She was later diagnosed with acute hemorrhagic necrotizing encephalopathy.
“The team had suspected encephalitis at the outset, but then back-to-back CT and MRI scans made the diagnosis,” Fory said in the statement.
Noncontrast head CT revealed “symmetric hypoattenuation within the bilateral medial thalami with a normal CT angiogram and CT venogram,” the team reports in their article. Brain MRI showed “hemorrhagic rim enhancing lesions within the bilateral thalami, medial temporal lobes, and subinsular regions.”
The patient was started on intravenous immunoglobulin but not high-dose steroids, because of concern for respiratory compromise. As of April 1, the patient was hospitalized in serious condition. Henry Ford Hospital has not provided an update.
Acute necrotizing encephalopathy (ANE) is a rare complication of viral infections, but until now, it has not been known to have occurred as a result of COVID-19 infection. ANE has been associated with intracranial “cytokine storms,” and a recent report in the Lancet suggested that a subgroup of patients with severe COVID-19 might develop a cytokine storm syndrome.
Commenting for Medscape Medical News, Cyrus A. Raji, MD, PhD, assistant professor of radiology and neurology, Washington University in St. Louis, Missouri, said, “Since this is just one report of one patient, the findings are the most preliminary we can conceive, and more research is needed to determine the extent to which COVID-19 may affect the central nervous system.”
Fory, Griffith, and Raji have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Survey shows just how dire PPE shortages are at many hospitals
As the COVID-19 pandemic spreads over the country, nearly half (48%) of US healthcare facilities — of various types and sizes — are already or almost out of respirators for treating patients, according to the results of a national online survey of infection prevention professionals.
Conducted during March 23-25 by the Association for Professionals in Infection Control and Epidemiology (APIC), the survey asked APIC’s 11,922 US-based infection preventionist members to rank their facilities’ supply of personal protective equipment (PPE) and key items, such as hand sanitizer and cleaning products, on a 5-point scale from having “plenty” to “none.”
Overall, 1,140 (9.6%) infection preventionists responded. Almost 70% of respondents represented a healthcare system rather than a single facility, and facilities ranged from hospitals (42.7%) to ambulatory care (17.4%) and dialysis (2.7%). The centers, from all 50 states and Washington, D.C., ranged in size from those with 1 to 50 beds to those with more than 300 beds.
and 317 (27.8%) said they were almost out of the devices, which are needed to protect healthcare workers managing patients with COVID-19 and different infectious diseases.
The survey was posted Friday on the APIC website.
Other findings from the survey include:
- Nearly half of respondents (49.2%) said their centers lack sufficient enough face shields, with 36.5% reporting being almost out and 12.6% reporting being completely out.
- Approximately one third (31.7%) of respondents reported being completely or nearly out of face masks.
- Even simple hand sanitizer is in short supply at more than 1 in 4 facilities surveyed; 25.6% of respondents said they are almost out and 2.6% are completely out.
- Nearly 30% of respondents reported accessing supplemental PPE through state or local resources, while 24.6% said they accepted private donations of supplies.
- Fewer than one-third (31.5%) said they had sufficient gowns.
- About 28% said they were almost out of protective respirators, while 20.5% said they have none.
- Only 12.3% said they have received supplies from federal resources, including the Strategic National Stockpile, which is controlled by the Department of Health and Human Services.
- 17.2% of respondents reported resorting to DIY measures such as sewing their own masks.
In terms of staffing resources, 67% of respondents said their center has only one (or fewer) full-time–equivalent infection preventionist on staff to develop protocols for managing COVID-19. That is not surprising given the general underresourcing of infection control programs, the survey compilers said.
“Hospitals and health facilities with fewer than one full-time person on staff to direct infection prevention activities may have been disadvantaged even before the COVID-19 pandemic,” said APIC president Connie Steed, MSN, RN, in a related news release.
On a more positive note, about two thirds of facilities said they have sufficient supplies of gloves (63.4%) and hand washing soap (67.1%).
“I am concerned that many facilities will not be able to protect healthcare workers and patients from not only COVID-19, but also MRSA, C diff., and other antibiotic-resistant infections,” Steed said.
At some centers, however, the situation is not so grim — yet. The large Harris Health System in Houston has enough PPE on hand to support all infection prevention protocols in place, according to Bryan McLeod, director of corporate communications. “The PPE inventory varies from a few weeks to well over a month depending on the specific item,” McLeod told Medscape Medical News. “But everything is dependent on the utilization rate, which can vary with patient volume. Our concern is long-term resupply while demand is peaking around the world, and we continue to pursue all avenues to secure resupply.”
Above all, Steed emphasizes healthcare workers’ need for clarity. “They need to know when exactly they can expect desperately needed supplies to arrive so they don’t have to turn to unproven crisis methods for PPE,” she said. “There have been grim reports from health officials about the supply shortage for weeks and we’re not getting any answers. This is unacceptable.”
APIC is urging the federal government for immediate activation of the Cold War–era Defense Production Act and any other available means to quickly manufacture vital supplies to protect healthcare workers treating the escalating numbers of COVID-19 patients.
In the meantime, frontline healthcare workers are scouring the Internet for suppliers and begging online for donations of masks.
APIC notes that the COVID-19 pandemic is compounded by this year’s particularly severe influenza season, which had already led overcrowded healthcare facilities.
This article first appeared on Medscape.com.
As the COVID-19 pandemic spreads over the country, nearly half (48%) of US healthcare facilities — of various types and sizes — are already or almost out of respirators for treating patients, according to the results of a national online survey of infection prevention professionals.
Conducted during March 23-25 by the Association for Professionals in Infection Control and Epidemiology (APIC), the survey asked APIC’s 11,922 US-based infection preventionist members to rank their facilities’ supply of personal protective equipment (PPE) and key items, such as hand sanitizer and cleaning products, on a 5-point scale from having “plenty” to “none.”
Overall, 1,140 (9.6%) infection preventionists responded. Almost 70% of respondents represented a healthcare system rather than a single facility, and facilities ranged from hospitals (42.7%) to ambulatory care (17.4%) and dialysis (2.7%). The centers, from all 50 states and Washington, D.C., ranged in size from those with 1 to 50 beds to those with more than 300 beds.
and 317 (27.8%) said they were almost out of the devices, which are needed to protect healthcare workers managing patients with COVID-19 and different infectious diseases.
The survey was posted Friday on the APIC website.
Other findings from the survey include:
- Nearly half of respondents (49.2%) said their centers lack sufficient enough face shields, with 36.5% reporting being almost out and 12.6% reporting being completely out.
- Approximately one third (31.7%) of respondents reported being completely or nearly out of face masks.
- Even simple hand sanitizer is in short supply at more than 1 in 4 facilities surveyed; 25.6% of respondents said they are almost out and 2.6% are completely out.
- Nearly 30% of respondents reported accessing supplemental PPE through state or local resources, while 24.6% said they accepted private donations of supplies.
- Fewer than one-third (31.5%) said they had sufficient gowns.
- About 28% said they were almost out of protective respirators, while 20.5% said they have none.
- Only 12.3% said they have received supplies from federal resources, including the Strategic National Stockpile, which is controlled by the Department of Health and Human Services.
- 17.2% of respondents reported resorting to DIY measures such as sewing their own masks.
In terms of staffing resources, 67% of respondents said their center has only one (or fewer) full-time–equivalent infection preventionist on staff to develop protocols for managing COVID-19. That is not surprising given the general underresourcing of infection control programs, the survey compilers said.
“Hospitals and health facilities with fewer than one full-time person on staff to direct infection prevention activities may have been disadvantaged even before the COVID-19 pandemic,” said APIC president Connie Steed, MSN, RN, in a related news release.
On a more positive note, about two thirds of facilities said they have sufficient supplies of gloves (63.4%) and hand washing soap (67.1%).
“I am concerned that many facilities will not be able to protect healthcare workers and patients from not only COVID-19, but also MRSA, C diff., and other antibiotic-resistant infections,” Steed said.
At some centers, however, the situation is not so grim — yet. The large Harris Health System in Houston has enough PPE on hand to support all infection prevention protocols in place, according to Bryan McLeod, director of corporate communications. “The PPE inventory varies from a few weeks to well over a month depending on the specific item,” McLeod told Medscape Medical News. “But everything is dependent on the utilization rate, which can vary with patient volume. Our concern is long-term resupply while demand is peaking around the world, and we continue to pursue all avenues to secure resupply.”
Above all, Steed emphasizes healthcare workers’ need for clarity. “They need to know when exactly they can expect desperately needed supplies to arrive so they don’t have to turn to unproven crisis methods for PPE,” she said. “There have been grim reports from health officials about the supply shortage for weeks and we’re not getting any answers. This is unacceptable.”
APIC is urging the federal government for immediate activation of the Cold War–era Defense Production Act and any other available means to quickly manufacture vital supplies to protect healthcare workers treating the escalating numbers of COVID-19 patients.
In the meantime, frontline healthcare workers are scouring the Internet for suppliers and begging online for donations of masks.
APIC notes that the COVID-19 pandemic is compounded by this year’s particularly severe influenza season, which had already led overcrowded healthcare facilities.
This article first appeared on Medscape.com.
As the COVID-19 pandemic spreads over the country, nearly half (48%) of US healthcare facilities — of various types and sizes — are already or almost out of respirators for treating patients, according to the results of a national online survey of infection prevention professionals.
Conducted during March 23-25 by the Association for Professionals in Infection Control and Epidemiology (APIC), the survey asked APIC’s 11,922 US-based infection preventionist members to rank their facilities’ supply of personal protective equipment (PPE) and key items, such as hand sanitizer and cleaning products, on a 5-point scale from having “plenty” to “none.”
Overall, 1,140 (9.6%) infection preventionists responded. Almost 70% of respondents represented a healthcare system rather than a single facility, and facilities ranged from hospitals (42.7%) to ambulatory care (17.4%) and dialysis (2.7%). The centers, from all 50 states and Washington, D.C., ranged in size from those with 1 to 50 beds to those with more than 300 beds.
and 317 (27.8%) said they were almost out of the devices, which are needed to protect healthcare workers managing patients with COVID-19 and different infectious diseases.
The survey was posted Friday on the APIC website.
Other findings from the survey include:
- Nearly half of respondents (49.2%) said their centers lack sufficient enough face shields, with 36.5% reporting being almost out and 12.6% reporting being completely out.
- Approximately one third (31.7%) of respondents reported being completely or nearly out of face masks.
- Even simple hand sanitizer is in short supply at more than 1 in 4 facilities surveyed; 25.6% of respondents said they are almost out and 2.6% are completely out.
- Nearly 30% of respondents reported accessing supplemental PPE through state or local resources, while 24.6% said they accepted private donations of supplies.
- Fewer than one-third (31.5%) said they had sufficient gowns.
- About 28% said they were almost out of protective respirators, while 20.5% said they have none.
- Only 12.3% said they have received supplies from federal resources, including the Strategic National Stockpile, which is controlled by the Department of Health and Human Services.
- 17.2% of respondents reported resorting to DIY measures such as sewing their own masks.
In terms of staffing resources, 67% of respondents said their center has only one (or fewer) full-time–equivalent infection preventionist on staff to develop protocols for managing COVID-19. That is not surprising given the general underresourcing of infection control programs, the survey compilers said.
“Hospitals and health facilities with fewer than one full-time person on staff to direct infection prevention activities may have been disadvantaged even before the COVID-19 pandemic,” said APIC president Connie Steed, MSN, RN, in a related news release.
On a more positive note, about two thirds of facilities said they have sufficient supplies of gloves (63.4%) and hand washing soap (67.1%).
“I am concerned that many facilities will not be able to protect healthcare workers and patients from not only COVID-19, but also MRSA, C diff., and other antibiotic-resistant infections,” Steed said.
At some centers, however, the situation is not so grim — yet. The large Harris Health System in Houston has enough PPE on hand to support all infection prevention protocols in place, according to Bryan McLeod, director of corporate communications. “The PPE inventory varies from a few weeks to well over a month depending on the specific item,” McLeod told Medscape Medical News. “But everything is dependent on the utilization rate, which can vary with patient volume. Our concern is long-term resupply while demand is peaking around the world, and we continue to pursue all avenues to secure resupply.”
Above all, Steed emphasizes healthcare workers’ need for clarity. “They need to know when exactly they can expect desperately needed supplies to arrive so they don’t have to turn to unproven crisis methods for PPE,” she said. “There have been grim reports from health officials about the supply shortage for weeks and we’re not getting any answers. This is unacceptable.”
APIC is urging the federal government for immediate activation of the Cold War–era Defense Production Act and any other available means to quickly manufacture vital supplies to protect healthcare workers treating the escalating numbers of COVID-19 patients.
In the meantime, frontline healthcare workers are scouring the Internet for suppliers and begging online for donations of masks.
APIC notes that the COVID-19 pandemic is compounded by this year’s particularly severe influenza season, which had already led overcrowded healthcare facilities.
This article first appeared on Medscape.com.
iPLEDGE allows at-home pregnancy tests during pandemic
tests to comply with the requirements of the iPLEDGE program during the COVID-19 pandemic, according to an update program posted on the iPLEDGE website.
The program’s other requirements – the prescription window and two forms of birth control – remain unchanged.
The change follows recent guidance from the Department of Health & Human Services and the Food and Drug Administration regarding accommodations for medical care and drugs subject to Risk Evaluation and Mitigation Strategies (REMS) in the midst of a public health emergency that requires most people to remain in their homes except for essential services.
Allowing females to take at-home pregnancy tests and communicate the results to physician according to their preference is “a game changer for the middle of a pandemic, obviously,” Neil Goldberg, MD, a dermatologist in Westchester County, New York, said in an interview. “These are patients who don’t need to spend time outside just to get pregnancy tests done. It makes it a lot easier.”
Dr. Goldberg is frustrated, however, that the accommodations have not been more widely publicized; he discovered the change incidentally when speaking to an iPLEDGE program representative to request a waiver for a patient who had taken her pregnancy test too early. The program had denied a similar request for a 15-year-old patient of his the previous week, despite the patient being abstinent and having been in shelter-in-place for several weeks.
“The size of your notice [on the website] should be proportionate to how important it is,” Dr. Goldberg said, and the small red box on the site is easy to miss. By contrast, asking anyone to leave their homes to go to a lab for a pregnancy test in the midst of a global pandemic so they can continue their medication would be putting patients at risk, he added.
The iPLEDGE program is designed in part to ensure unplanned pregnancies do not occur in females while taking the teratogenic acne drug. But the rules are onerous and difficult even during normal times, pointed out Hilary Baldwin, MD, medical director of the Acne Treatment and Research Center in New York City and past president of the American Acne and Rosacea Society.
Male patients taking isotretinoin must visit their physician every month to get a new no-refills prescription, but females must get a pregnancy test at a Clinical Laboratory Improvement Amendments–certified lab, which must then provide physical results to the prescribing physician. The doctor enters the negative pregnancy test and the two forms of birth control the patient is taking in the iPLEDGE program site.
Then the patient must take an online test at home to acknowledge they understand what it means to not get pregnant and enter the two forms of birth control they are using – which must match what the doctor enters – before the pharmacy can dispense the drug. The entire process must occur within 7 days or else the patient has to wait 19 days before starting the process over.
“We run a very tight schedule for girls. And every month, we would worry that something would interfere, a snow storm or something else, and that they wouldn’t be able to complete their objectives within the 7-day period,” Dr Baldwin said in an interview. “It was always difficult, and now with us not being able to see the patient and the patient not wanting to go to the lab, this became completely impossible.”
Until this change, some patients may not have been able to get their prescription for severe nodulocystic acne, which can cause physical and psychological scarring, and “postponing treatment increases the likelihood of scarring,” Dr. Baldwin pointed out.
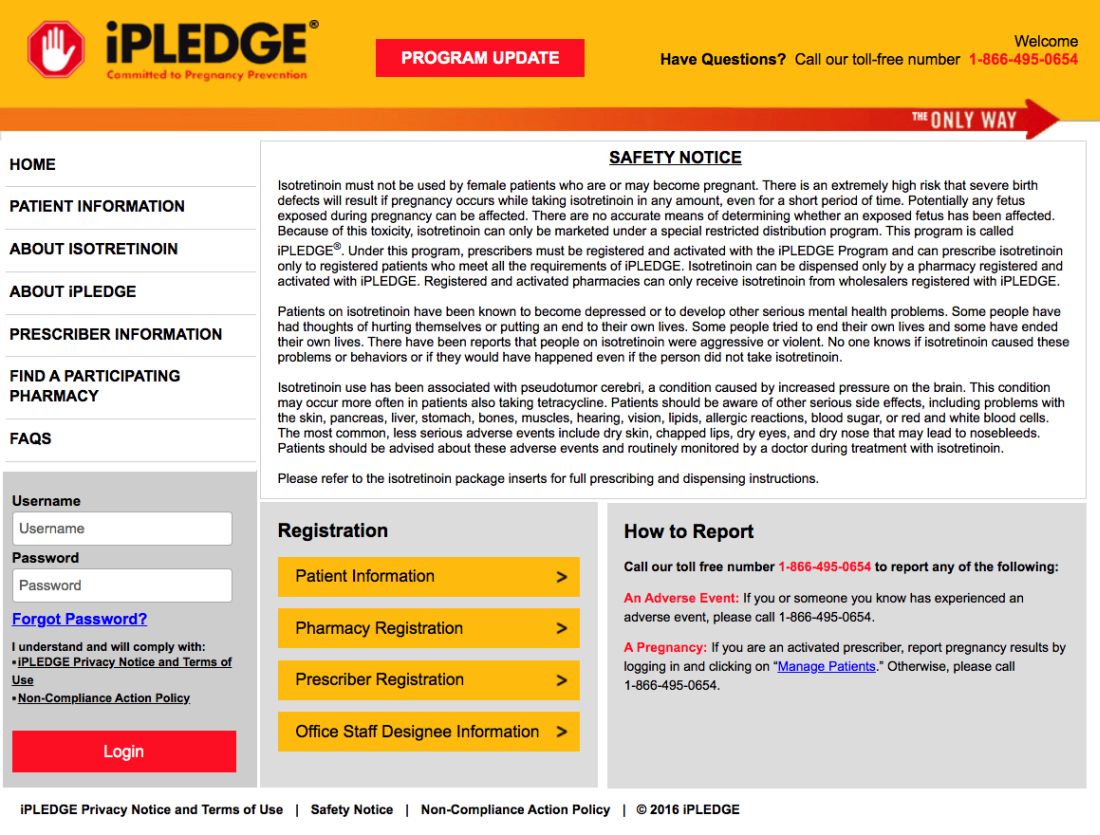
Dr. Goldberg’s patients now take a pregnancy test at home and send him a photo of the negative test that he then inserts into their EMR.
According to a March 17 statement from HHS, potential penalties for HIPAA violations are waived for good-faith use of “everyday communication technologies,” such as Skype or FaceTime, for telehealth treatment or diagnostics. The change was intended to allow telehealth services to continue healthcare for practices that had not previously had secure telehealth technology established.
Despite the changes for at-home pregnancy tests for females and in-person visits for all patients, the program has not altered the 7-day prescription window or the requirement to have two forms of birth control.
With reports of a global condom shortage, Dr Baldwin said she has more concerns about her adult patients being able to find a required barrier method of birth control than about her adolescent patients.
“This is a unique opportunity for us to trust our teenage patients because they can’t leave the house,” Dr. Baldwin said. “I’m actually more worried about my adult women on the drug who are bored and cooped up in a house with their significant other.”
Dr. Baldwin and Dr. Goldberg had no relevant disclosures. Dr. Goldberg is a Dermatology News board member.
tests to comply with the requirements of the iPLEDGE program during the COVID-19 pandemic, according to an update program posted on the iPLEDGE website.
The program’s other requirements – the prescription window and two forms of birth control – remain unchanged.
The change follows recent guidance from the Department of Health & Human Services and the Food and Drug Administration regarding accommodations for medical care and drugs subject to Risk Evaluation and Mitigation Strategies (REMS) in the midst of a public health emergency that requires most people to remain in their homes except for essential services.
Allowing females to take at-home pregnancy tests and communicate the results to physician according to their preference is “a game changer for the middle of a pandemic, obviously,” Neil Goldberg, MD, a dermatologist in Westchester County, New York, said in an interview. “These are patients who don’t need to spend time outside just to get pregnancy tests done. It makes it a lot easier.”
Dr. Goldberg is frustrated, however, that the accommodations have not been more widely publicized; he discovered the change incidentally when speaking to an iPLEDGE program representative to request a waiver for a patient who had taken her pregnancy test too early. The program had denied a similar request for a 15-year-old patient of his the previous week, despite the patient being abstinent and having been in shelter-in-place for several weeks.
“The size of your notice [on the website] should be proportionate to how important it is,” Dr. Goldberg said, and the small red box on the site is easy to miss. By contrast, asking anyone to leave their homes to go to a lab for a pregnancy test in the midst of a global pandemic so they can continue their medication would be putting patients at risk, he added.
The iPLEDGE program is designed in part to ensure unplanned pregnancies do not occur in females while taking the teratogenic acne drug. But the rules are onerous and difficult even during normal times, pointed out Hilary Baldwin, MD, medical director of the Acne Treatment and Research Center in New York City and past president of the American Acne and Rosacea Society.
Male patients taking isotretinoin must visit their physician every month to get a new no-refills prescription, but females must get a pregnancy test at a Clinical Laboratory Improvement Amendments–certified lab, which must then provide physical results to the prescribing physician. The doctor enters the negative pregnancy test and the two forms of birth control the patient is taking in the iPLEDGE program site.
Then the patient must take an online test at home to acknowledge they understand what it means to not get pregnant and enter the two forms of birth control they are using – which must match what the doctor enters – before the pharmacy can dispense the drug. The entire process must occur within 7 days or else the patient has to wait 19 days before starting the process over.
“We run a very tight schedule for girls. And every month, we would worry that something would interfere, a snow storm or something else, and that they wouldn’t be able to complete their objectives within the 7-day period,” Dr Baldwin said in an interview. “It was always difficult, and now with us not being able to see the patient and the patient not wanting to go to the lab, this became completely impossible.”
Until this change, some patients may not have been able to get their prescription for severe nodulocystic acne, which can cause physical and psychological scarring, and “postponing treatment increases the likelihood of scarring,” Dr. Baldwin pointed out.
Dr. Goldberg’s patients now take a pregnancy test at home and send him a photo of the negative test that he then inserts into their EMR.
According to a March 17 statement from HHS, potential penalties for HIPAA violations are waived for good-faith use of “everyday communication technologies,” such as Skype or FaceTime, for telehealth treatment or diagnostics. The change was intended to allow telehealth services to continue healthcare for practices that had not previously had secure telehealth technology established.
Despite the changes for at-home pregnancy tests for females and in-person visits for all patients, the program has not altered the 7-day prescription window or the requirement to have two forms of birth control.
With reports of a global condom shortage, Dr Baldwin said she has more concerns about her adult patients being able to find a required barrier method of birth control than about her adolescent patients.
“This is a unique opportunity for us to trust our teenage patients because they can’t leave the house,” Dr. Baldwin said. “I’m actually more worried about my adult women on the drug who are bored and cooped up in a house with their significant other.”
Dr. Baldwin and Dr. Goldberg had no relevant disclosures. Dr. Goldberg is a Dermatology News board member.
tests to comply with the requirements of the iPLEDGE program during the COVID-19 pandemic, according to an update program posted on the iPLEDGE website.
The program’s other requirements – the prescription window and two forms of birth control – remain unchanged.
The change follows recent guidance from the Department of Health & Human Services and the Food and Drug Administration regarding accommodations for medical care and drugs subject to Risk Evaluation and Mitigation Strategies (REMS) in the midst of a public health emergency that requires most people to remain in their homes except for essential services.
Allowing females to take at-home pregnancy tests and communicate the results to physician according to their preference is “a game changer for the middle of a pandemic, obviously,” Neil Goldberg, MD, a dermatologist in Westchester County, New York, said in an interview. “These are patients who don’t need to spend time outside just to get pregnancy tests done. It makes it a lot easier.”
Dr. Goldberg is frustrated, however, that the accommodations have not been more widely publicized; he discovered the change incidentally when speaking to an iPLEDGE program representative to request a waiver for a patient who had taken her pregnancy test too early. The program had denied a similar request for a 15-year-old patient of his the previous week, despite the patient being abstinent and having been in shelter-in-place for several weeks.
“The size of your notice [on the website] should be proportionate to how important it is,” Dr. Goldberg said, and the small red box on the site is easy to miss. By contrast, asking anyone to leave their homes to go to a lab for a pregnancy test in the midst of a global pandemic so they can continue their medication would be putting patients at risk, he added.
The iPLEDGE program is designed in part to ensure unplanned pregnancies do not occur in females while taking the teratogenic acne drug. But the rules are onerous and difficult even during normal times, pointed out Hilary Baldwin, MD, medical director of the Acne Treatment and Research Center in New York City and past president of the American Acne and Rosacea Society.
Male patients taking isotretinoin must visit their physician every month to get a new no-refills prescription, but females must get a pregnancy test at a Clinical Laboratory Improvement Amendments–certified lab, which must then provide physical results to the prescribing physician. The doctor enters the negative pregnancy test and the two forms of birth control the patient is taking in the iPLEDGE program site.
Then the patient must take an online test at home to acknowledge they understand what it means to not get pregnant and enter the two forms of birth control they are using – which must match what the doctor enters – before the pharmacy can dispense the drug. The entire process must occur within 7 days or else the patient has to wait 19 days before starting the process over.
“We run a very tight schedule for girls. And every month, we would worry that something would interfere, a snow storm or something else, and that they wouldn’t be able to complete their objectives within the 7-day period,” Dr Baldwin said in an interview. “It was always difficult, and now with us not being able to see the patient and the patient not wanting to go to the lab, this became completely impossible.”
Until this change, some patients may not have been able to get their prescription for severe nodulocystic acne, which can cause physical and psychological scarring, and “postponing treatment increases the likelihood of scarring,” Dr. Baldwin pointed out.
Dr. Goldberg’s patients now take a pregnancy test at home and send him a photo of the negative test that he then inserts into their EMR.
According to a March 17 statement from HHS, potential penalties for HIPAA violations are waived for good-faith use of “everyday communication technologies,” such as Skype or FaceTime, for telehealth treatment or diagnostics. The change was intended to allow telehealth services to continue healthcare for practices that had not previously had secure telehealth technology established.
Despite the changes for at-home pregnancy tests for females and in-person visits for all patients, the program has not altered the 7-day prescription window or the requirement to have two forms of birth control.
With reports of a global condom shortage, Dr Baldwin said she has more concerns about her adult patients being able to find a required barrier method of birth control than about her adolescent patients.
“This is a unique opportunity for us to trust our teenage patients because they can’t leave the house,” Dr. Baldwin said. “I’m actually more worried about my adult women on the drug who are bored and cooped up in a house with their significant other.”
Dr. Baldwin and Dr. Goldberg had no relevant disclosures. Dr. Goldberg is a Dermatology News board member.
Case study shows CLL may mask COVID-19 infection
Characteristics of patients with chronic lymphocytic leukemia can mask COVID-19 infection, creating a risk for patients, practitioners, and the community, according to a case study published in the Lancet Haematology.
A 39-year-old man with a history of non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL) presented at a clinic in Wenzhou, China, with symptoms of fever, sore throat, productive cough, and dyspnea, according to the authors. COVID-19 infection was not initially suspected, as his whole blood cell and lymphocyte counts were high, the CLL masked a potential infection, and the patient claimed he had no suspect recent travel history.
However, a CT chest scan showed bilateral ground-glass opacities and a small amount of fluid in the patient’s left pleural cavity, leading the attending physician to suspect COVID-19. Testing was ordered and the real-time reverse-transcription polymerase chain reaction assay result was positive. The patient was immediately transferred to the isolation ward for management and confirmed COVID-19 infection.
Subsequently, the patient admitted travel to the COVID-19 epicenter in Wuhan province, although it was 25 days prior, indicating a longer period of incubation than generally believed, according to the authors. The patient survived treatment and was eventually discharged.
“Clinical and biochemical data of COVID-19 might be partly masked by coexisting chronic lymphocytic leukemia; better diagnostic strategies (i.e., superior CT differential techniques such as radiomics) could be used for diagnosis,” the researchers concluded, speculating that the apparently longer-than-normal COVID-19 incubation period might be the result of the patient’s compromised immune system.
The authors reported that they had no conflicts of interest.
SOURCE: Jin X-H et al. Lancet Haematol. 2020;7(4):E351-2.
Characteristics of patients with chronic lymphocytic leukemia can mask COVID-19 infection, creating a risk for patients, practitioners, and the community, according to a case study published in the Lancet Haematology.
A 39-year-old man with a history of non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL) presented at a clinic in Wenzhou, China, with symptoms of fever, sore throat, productive cough, and dyspnea, according to the authors. COVID-19 infection was not initially suspected, as his whole blood cell and lymphocyte counts were high, the CLL masked a potential infection, and the patient claimed he had no suspect recent travel history.
However, a CT chest scan showed bilateral ground-glass opacities and a small amount of fluid in the patient’s left pleural cavity, leading the attending physician to suspect COVID-19. Testing was ordered and the real-time reverse-transcription polymerase chain reaction assay result was positive. The patient was immediately transferred to the isolation ward for management and confirmed COVID-19 infection.
Subsequently, the patient admitted travel to the COVID-19 epicenter in Wuhan province, although it was 25 days prior, indicating a longer period of incubation than generally believed, according to the authors. The patient survived treatment and was eventually discharged.
“Clinical and biochemical data of COVID-19 might be partly masked by coexisting chronic lymphocytic leukemia; better diagnostic strategies (i.e., superior CT differential techniques such as radiomics) could be used for diagnosis,” the researchers concluded, speculating that the apparently longer-than-normal COVID-19 incubation period might be the result of the patient’s compromised immune system.
The authors reported that they had no conflicts of interest.
SOURCE: Jin X-H et al. Lancet Haematol. 2020;7(4):E351-2.
Characteristics of patients with chronic lymphocytic leukemia can mask COVID-19 infection, creating a risk for patients, practitioners, and the community, according to a case study published in the Lancet Haematology.
A 39-year-old man with a history of non-Hodgkin lymphoma and chronic lymphocytic leukemia (CLL) presented at a clinic in Wenzhou, China, with symptoms of fever, sore throat, productive cough, and dyspnea, according to the authors. COVID-19 infection was not initially suspected, as his whole blood cell and lymphocyte counts were high, the CLL masked a potential infection, and the patient claimed he had no suspect recent travel history.
However, a CT chest scan showed bilateral ground-glass opacities and a small amount of fluid in the patient’s left pleural cavity, leading the attending physician to suspect COVID-19. Testing was ordered and the real-time reverse-transcription polymerase chain reaction assay result was positive. The patient was immediately transferred to the isolation ward for management and confirmed COVID-19 infection.
Subsequently, the patient admitted travel to the COVID-19 epicenter in Wuhan province, although it was 25 days prior, indicating a longer period of incubation than generally believed, according to the authors. The patient survived treatment and was eventually discharged.
“Clinical and biochemical data of COVID-19 might be partly masked by coexisting chronic lymphocytic leukemia; better diagnostic strategies (i.e., superior CT differential techniques such as radiomics) could be used for diagnosis,” the researchers concluded, speculating that the apparently longer-than-normal COVID-19 incubation period might be the result of the patient’s compromised immune system.
The authors reported that they had no conflicts of interest.
SOURCE: Jin X-H et al. Lancet Haematol. 2020;7(4):E351-2.
FROM THE LANCET HAEMATOLOGY
Skin manifestations are emerging in the coronavirus pandemic
Dermatologists there were pulled from their usual duty to help with the pandemic and looked at what was going on with the skin in 148 COVID-19 inpatients. They excluded 60 who had started new drugs within 15 days to rule out acute drug reactions, then reported what they saw (J Eur Acad Dermatol Venereol. 2020 Mar 26. doi: 10.1111/jdv.16387).
Of the 88 COVID-19 patients, 20.5% developed skin manifestations. Eight of the 18 (44%) had skin eruptions at symptom onset, and the rest after hospitalization. Fourteen (78%) had red rashes, three had widespread urticaria, and one had chickenpox-like vesicles. The most commonly affected area was the trunk. Itching was mild or absent, and lesions usually healed up in a few days. Most importantly, skin manifestations did not correlate with disease severity.
These skin manifestations “are similar to cutaneous involvement occurring during common viral infections,” said the author of the report, Sebastiano Recalcati, MD, a dermatologist at Alessandro Manzoni Hospital.
COVID-19 skin manifestations can cloud the diagnosis, according to the authors of another report from Thailand, where the first case of COVID-19 outside of China was reported.
They described a case of a COVID-19 infection in a Bangkok hospital that masqueraded as dengue fever. A person there presented with only a skin rash, petechiae, and a low platelet count, and was diagnosed with Dengue because that’s exactly what it looked like, the authors wrote (J Am Acad Dermatol. 2020 Mar 22. pii: S0190-9622[20]30454-0. doi: 10.1016/j.jaad.2020.03.036).
The correct diagnosis, COVID-19, was made at a tertiary care center after the patient was admitted with respiratory problems.
“There is a possibility that a COVID-19 patient might initially present with a skin rash that can be misdiagnosed as another common disease. ... The practitioner should recognize the possibility that the patient might have only a skin rash” at first, said the lead author of that report, Beuy Joob, PhD, of the Sanitation1 Medical Academic Center, Bangkok, and a coauthor.
There are similar reports in the United States, too. “Many have wondered if COVID-19 presents with any particular skin changes. The answer is yes,” said Randy Jacobs, MD, an assistant clinical professor of dermatology at the University of California, Riverside, who also has a private practice in southern California.
“COVID-19 can feature signs of small blood vessel occlusion. These can be petechiae or tiny bruises, and transient livedoid eruptions,” he said in an interview.
Dr. Jacobs had a 67-year-old patient who presented with a low fever, nasal congestion, postnasal drip, and a wet cough but no shortness of breath. It looked like a common cold. But a week later, the man had a nonpruritic blanching livedoid vascular eruption on his right anterior thigh, and blood in his urine, and he felt weak. The vascular eruption and bloody urine resolved in 24 hours, but the COVID-19 test came back positive and his cough became dry and hacking, and the weakness persisted. He’s in a hospital now and on oxygen, but not ventilated so far.
“Another dermatologist friend of mine also reported a similar transient COVID-19 unilateral livedoid eruption,” Dr. Jacobs said.
It suggests vaso-occlusion. Whether it’s neurogenic, microthrombotic, or immune complex mediated is unknown, but it’s “a skin finding that can help clinicians as they work up their patients with COVID-19 symptoms,” he noted.
Dr. Jacobs and the authors of the studies had no disclosures.
Dermatologists there were pulled from their usual duty to help with the pandemic and looked at what was going on with the skin in 148 COVID-19 inpatients. They excluded 60 who had started new drugs within 15 days to rule out acute drug reactions, then reported what they saw (J Eur Acad Dermatol Venereol. 2020 Mar 26. doi: 10.1111/jdv.16387).
Of the 88 COVID-19 patients, 20.5% developed skin manifestations. Eight of the 18 (44%) had skin eruptions at symptom onset, and the rest after hospitalization. Fourteen (78%) had red rashes, three had widespread urticaria, and one had chickenpox-like vesicles. The most commonly affected area was the trunk. Itching was mild or absent, and lesions usually healed up in a few days. Most importantly, skin manifestations did not correlate with disease severity.
These skin manifestations “are similar to cutaneous involvement occurring during common viral infections,” said the author of the report, Sebastiano Recalcati, MD, a dermatologist at Alessandro Manzoni Hospital.
COVID-19 skin manifestations can cloud the diagnosis, according to the authors of another report from Thailand, where the first case of COVID-19 outside of China was reported.
They described a case of a COVID-19 infection in a Bangkok hospital that masqueraded as dengue fever. A person there presented with only a skin rash, petechiae, and a low platelet count, and was diagnosed with Dengue because that’s exactly what it looked like, the authors wrote (J Am Acad Dermatol. 2020 Mar 22. pii: S0190-9622[20]30454-0. doi: 10.1016/j.jaad.2020.03.036).
The correct diagnosis, COVID-19, was made at a tertiary care center after the patient was admitted with respiratory problems.
“There is a possibility that a COVID-19 patient might initially present with a skin rash that can be misdiagnosed as another common disease. ... The practitioner should recognize the possibility that the patient might have only a skin rash” at first, said the lead author of that report, Beuy Joob, PhD, of the Sanitation1 Medical Academic Center, Bangkok, and a coauthor.
There are similar reports in the United States, too. “Many have wondered if COVID-19 presents with any particular skin changes. The answer is yes,” said Randy Jacobs, MD, an assistant clinical professor of dermatology at the University of California, Riverside, who also has a private practice in southern California.
“COVID-19 can feature signs of small blood vessel occlusion. These can be petechiae or tiny bruises, and transient livedoid eruptions,” he said in an interview.
Dr. Jacobs had a 67-year-old patient who presented with a low fever, nasal congestion, postnasal drip, and a wet cough but no shortness of breath. It looked like a common cold. But a week later, the man had a nonpruritic blanching livedoid vascular eruption on his right anterior thigh, and blood in his urine, and he felt weak. The vascular eruption and bloody urine resolved in 24 hours, but the COVID-19 test came back positive and his cough became dry and hacking, and the weakness persisted. He’s in a hospital now and on oxygen, but not ventilated so far.
“Another dermatologist friend of mine also reported a similar transient COVID-19 unilateral livedoid eruption,” Dr. Jacobs said.
It suggests vaso-occlusion. Whether it’s neurogenic, microthrombotic, or immune complex mediated is unknown, but it’s “a skin finding that can help clinicians as they work up their patients with COVID-19 symptoms,” he noted.
Dr. Jacobs and the authors of the studies had no disclosures.
Dermatologists there were pulled from their usual duty to help with the pandemic and looked at what was going on with the skin in 148 COVID-19 inpatients. They excluded 60 who had started new drugs within 15 days to rule out acute drug reactions, then reported what they saw (J Eur Acad Dermatol Venereol. 2020 Mar 26. doi: 10.1111/jdv.16387).
Of the 88 COVID-19 patients, 20.5% developed skin manifestations. Eight of the 18 (44%) had skin eruptions at symptom onset, and the rest after hospitalization. Fourteen (78%) had red rashes, three had widespread urticaria, and one had chickenpox-like vesicles. The most commonly affected area was the trunk. Itching was mild or absent, and lesions usually healed up in a few days. Most importantly, skin manifestations did not correlate with disease severity.
These skin manifestations “are similar to cutaneous involvement occurring during common viral infections,” said the author of the report, Sebastiano Recalcati, MD, a dermatologist at Alessandro Manzoni Hospital.
COVID-19 skin manifestations can cloud the diagnosis, according to the authors of another report from Thailand, where the first case of COVID-19 outside of China was reported.
They described a case of a COVID-19 infection in a Bangkok hospital that masqueraded as dengue fever. A person there presented with only a skin rash, petechiae, and a low platelet count, and was diagnosed with Dengue because that’s exactly what it looked like, the authors wrote (J Am Acad Dermatol. 2020 Mar 22. pii: S0190-9622[20]30454-0. doi: 10.1016/j.jaad.2020.03.036).
The correct diagnosis, COVID-19, was made at a tertiary care center after the patient was admitted with respiratory problems.
“There is a possibility that a COVID-19 patient might initially present with a skin rash that can be misdiagnosed as another common disease. ... The practitioner should recognize the possibility that the patient might have only a skin rash” at first, said the lead author of that report, Beuy Joob, PhD, of the Sanitation1 Medical Academic Center, Bangkok, and a coauthor.
There are similar reports in the United States, too. “Many have wondered if COVID-19 presents with any particular skin changes. The answer is yes,” said Randy Jacobs, MD, an assistant clinical professor of dermatology at the University of California, Riverside, who also has a private practice in southern California.
“COVID-19 can feature signs of small blood vessel occlusion. These can be petechiae or tiny bruises, and transient livedoid eruptions,” he said in an interview.
Dr. Jacobs had a 67-year-old patient who presented with a low fever, nasal congestion, postnasal drip, and a wet cough but no shortness of breath. It looked like a common cold. But a week later, the man had a nonpruritic blanching livedoid vascular eruption on his right anterior thigh, and blood in his urine, and he felt weak. The vascular eruption and bloody urine resolved in 24 hours, but the COVID-19 test came back positive and his cough became dry and hacking, and the weakness persisted. He’s in a hospital now and on oxygen, but not ventilated so far.
“Another dermatologist friend of mine also reported a similar transient COVID-19 unilateral livedoid eruption,” Dr. Jacobs said.
It suggests vaso-occlusion. Whether it’s neurogenic, microthrombotic, or immune complex mediated is unknown, but it’s “a skin finding that can help clinicians as they work up their patients with COVID-19 symptoms,” he noted.
Dr. Jacobs and the authors of the studies had no disclosures.
COVID-19: Mental health pros come to the aid of frontline comrades
Frontline COVID-19 healthcare workers across North America are dealing with unprecedented stress, but mental health therapists in both Canada and the US are doing their part to ensure the psychological well-being of their colleagues on the frontlines of the pandemic.
Over the past few weeks, thousands of licensed psychologists, psychotherapists, and social workers have signed up to offer free therapy sessions to healthcare professionals who find themselves psychologically overwhelmed by the pandemic’s economic, social, and financial fallout.
In Canada, the movement was started by Toronto psychotherapist Karen Dougherty, MA, who saw a social media post from someone in New York asking mental health workers to volunteer their time.
Inspired by this, Dougherty reached out to some of her close colleagues with a social media post of her own. A few days later, 450 people had signed up to volunteer and Ontario COVID-19 Therapists was born.
The sessions are provided by licensed Canadian psychotherapists and are free of charge to healthcare workers providing frontline COVID-19 care. After signing up online, users can choose from one of three therapists who will provide up to five free phone sessions.
In New York state, a similar initiative — which is not limited to healthcare workers — has gained incredible momentum. On March 21, Gov. Andrew Cuomo announced the creation of a statewide hotline [844-863-9314] to provide free mental health services to individuals sheltering at home who may be experiencing stress and anxiety as a result of COVID-19.
The governor called on mental-health professionals to volunteer their time and provide telephone and/or telehealth counseling. The New York State Psychiatric Association quickly got on board and encouraged its members to participate.
Just four days later, more than 6,000 mental health workers had volunteered their services, making New York the first state to address the mental health consequences of the pandemic in this way.
Self-care is vital for healthcare workers during the COVID-19 pandemic, particularly as stress mounts and workdays become longer and grimmer. Dougherty recommended that frontline workers manage overwhelming thoughts by limiting their intake of information about the virus.
Self-Care a “Selfless Act”
Clinicians need to balance the need to stay informed with the potential for information overload, which can contribute to anxiety, she said.
She also recommended that individuals continue to connect with loved ones while practicing social distancing. Equally important is talking to someone about the struggles people may be facing at work.
For Amin Azzam MD, MA, the benefits of these initiatives are obvious.
“There is always value in providing additional mental health services and tending to psychological well-being,” Azzam, adjunct professor of psychiatry, University of California, San Francisco and UC Berkeley, told Medscape Medical News.
“If there ever were a time when we can use all the emotional support possible, then it would be during a global pandemic,” added Azzam, who is also director of Open Learning Initiatives at Osmosis, a nonprofit health education company.
Azzam urged healthcare professionals to avail themselves of such resources as often as necessary.
“Taking care of ourselves is not a selfish act. When the oxygen masks come down on airplanes we are always instructed to put our own masks on first before helping those in need. It’s a sign of strength, not weakness, to seek emotional support,” he said.
However, it isn’t always easy. The longstanding stigma associated with seeking help for mental health issues has not stopped for COVID-19. Even workers who are in close daily contact with people infected with the virus are finding they’re not immune to the stigma associated with seeking mental health treatment, Azzam added.
“Nevertheless, the burden these frontline workers are facing is real…and often crushing. Some Ontario doctors have reported pretraumatic stress disorder, which they attribute to having watched the virus wreak havoc in other countries, and knowing that similar difficulties are headed their way,” he said.
A Growing Movement
Doris Grinspun, PhD, MSN, the CEO of Registered Nurses’ Association of Ontario (RNAO), said the province’s nurses are under intense pressure at work, then fear infecting family members once they come home. Some are even staying at hotels to ensure they don’t infect others, as reported by CBC News.
However, she added, most recognize the important role that psychotherapy can play, especially since many frontline healthcare workers find it difficult to speak with their families about the issues they face at work, for fear of adding stress to their family life as well.
“None of us are superhuman and immune to stress. When healthcare workers are facing workplace challenges never before seen in their lifetimes, they need opportunities to decompress to maintain their own health and well-being. This will help them pace themselves for the marathon — not sprint — to continue doing the important work of helping others,” said Azzam.
Given the attention it has garnered in such a short time, Azzam is hopeful that the free therapy movement will spread.
In Canada, mental health professionals in other provinces have already reached out to Dougherty, lending credence to the notion of a pan-Canadian network of therapists offering free services to healthcare workers during the outbreak.
In the US, other local initiatives are already underway.
“The one that I’m personally aware of is at my home institution at the University of California, San Francisco,” Azzam said. “We have a Care for the Caregiver program that is being greatly expanded at this time. As part of that initiative, the institution’s psychiatry department has solicited licensed mental health care providers to volunteer their time to provide those additional services.”
Azzam has also worked with colleagues developing a series of mental health tools that Osmosis has made available free of charge.
These include a central site with educational material about COVID-19, a video about supporting educators’ mental health during high-stress periods; a video about managing students’ mental health during public health emergencies; a summary of recommended resources for psychological health in distressing times; and a YouTube Live event he held regarding tips for maximizing psychological health during stressful times.
This article first appeared on Medscape.com.
Frontline COVID-19 healthcare workers across North America are dealing with unprecedented stress, but mental health therapists in both Canada and the US are doing their part to ensure the psychological well-being of their colleagues on the frontlines of the pandemic.
Over the past few weeks, thousands of licensed psychologists, psychotherapists, and social workers have signed up to offer free therapy sessions to healthcare professionals who find themselves psychologically overwhelmed by the pandemic’s economic, social, and financial fallout.
In Canada, the movement was started by Toronto psychotherapist Karen Dougherty, MA, who saw a social media post from someone in New York asking mental health workers to volunteer their time.
Inspired by this, Dougherty reached out to some of her close colleagues with a social media post of her own. A few days later, 450 people had signed up to volunteer and Ontario COVID-19 Therapists was born.
The sessions are provided by licensed Canadian psychotherapists and are free of charge to healthcare workers providing frontline COVID-19 care. After signing up online, users can choose from one of three therapists who will provide up to five free phone sessions.
In New York state, a similar initiative — which is not limited to healthcare workers — has gained incredible momentum. On March 21, Gov. Andrew Cuomo announced the creation of a statewide hotline [844-863-9314] to provide free mental health services to individuals sheltering at home who may be experiencing stress and anxiety as a result of COVID-19.
The governor called on mental-health professionals to volunteer their time and provide telephone and/or telehealth counseling. The New York State Psychiatric Association quickly got on board and encouraged its members to participate.
Just four days later, more than 6,000 mental health workers had volunteered their services, making New York the first state to address the mental health consequences of the pandemic in this way.
Self-care is vital for healthcare workers during the COVID-19 pandemic, particularly as stress mounts and workdays become longer and grimmer. Dougherty recommended that frontline workers manage overwhelming thoughts by limiting their intake of information about the virus.
Self-Care a “Selfless Act”
Clinicians need to balance the need to stay informed with the potential for information overload, which can contribute to anxiety, she said.
She also recommended that individuals continue to connect with loved ones while practicing social distancing. Equally important is talking to someone about the struggles people may be facing at work.
For Amin Azzam MD, MA, the benefits of these initiatives are obvious.
“There is always value in providing additional mental health services and tending to psychological well-being,” Azzam, adjunct professor of psychiatry, University of California, San Francisco and UC Berkeley, told Medscape Medical News.
“If there ever were a time when we can use all the emotional support possible, then it would be during a global pandemic,” added Azzam, who is also director of Open Learning Initiatives at Osmosis, a nonprofit health education company.
Azzam urged healthcare professionals to avail themselves of such resources as often as necessary.
“Taking care of ourselves is not a selfish act. When the oxygen masks come down on airplanes we are always instructed to put our own masks on first before helping those in need. It’s a sign of strength, not weakness, to seek emotional support,” he said.
However, it isn’t always easy. The longstanding stigma associated with seeking help for mental health issues has not stopped for COVID-19. Even workers who are in close daily contact with people infected with the virus are finding they’re not immune to the stigma associated with seeking mental health treatment, Azzam added.
“Nevertheless, the burden these frontline workers are facing is real…and often crushing. Some Ontario doctors have reported pretraumatic stress disorder, which they attribute to having watched the virus wreak havoc in other countries, and knowing that similar difficulties are headed their way,” he said.
A Growing Movement
Doris Grinspun, PhD, MSN, the CEO of Registered Nurses’ Association of Ontario (RNAO), said the province’s nurses are under intense pressure at work, then fear infecting family members once they come home. Some are even staying at hotels to ensure they don’t infect others, as reported by CBC News.
However, she added, most recognize the important role that psychotherapy can play, especially since many frontline healthcare workers find it difficult to speak with their families about the issues they face at work, for fear of adding stress to their family life as well.
“None of us are superhuman and immune to stress. When healthcare workers are facing workplace challenges never before seen in their lifetimes, they need opportunities to decompress to maintain their own health and well-being. This will help them pace themselves for the marathon — not sprint — to continue doing the important work of helping others,” said Azzam.
Given the attention it has garnered in such a short time, Azzam is hopeful that the free therapy movement will spread.
In Canada, mental health professionals in other provinces have already reached out to Dougherty, lending credence to the notion of a pan-Canadian network of therapists offering free services to healthcare workers during the outbreak.
In the US, other local initiatives are already underway.
“The one that I’m personally aware of is at my home institution at the University of California, San Francisco,” Azzam said. “We have a Care for the Caregiver program that is being greatly expanded at this time. As part of that initiative, the institution’s psychiatry department has solicited licensed mental health care providers to volunteer their time to provide those additional services.”
Azzam has also worked with colleagues developing a series of mental health tools that Osmosis has made available free of charge.
These include a central site with educational material about COVID-19, a video about supporting educators’ mental health during high-stress periods; a video about managing students’ mental health during public health emergencies; a summary of recommended resources for psychological health in distressing times; and a YouTube Live event he held regarding tips for maximizing psychological health during stressful times.
This article first appeared on Medscape.com.
Frontline COVID-19 healthcare workers across North America are dealing with unprecedented stress, but mental health therapists in both Canada and the US are doing their part to ensure the psychological well-being of their colleagues on the frontlines of the pandemic.
Over the past few weeks, thousands of licensed psychologists, psychotherapists, and social workers have signed up to offer free therapy sessions to healthcare professionals who find themselves psychologically overwhelmed by the pandemic’s economic, social, and financial fallout.
In Canada, the movement was started by Toronto psychotherapist Karen Dougherty, MA, who saw a social media post from someone in New York asking mental health workers to volunteer their time.
Inspired by this, Dougherty reached out to some of her close colleagues with a social media post of her own. A few days later, 450 people had signed up to volunteer and Ontario COVID-19 Therapists was born.
The sessions are provided by licensed Canadian psychotherapists and are free of charge to healthcare workers providing frontline COVID-19 care. After signing up online, users can choose from one of three therapists who will provide up to five free phone sessions.
In New York state, a similar initiative — which is not limited to healthcare workers — has gained incredible momentum. On March 21, Gov. Andrew Cuomo announced the creation of a statewide hotline [844-863-9314] to provide free mental health services to individuals sheltering at home who may be experiencing stress and anxiety as a result of COVID-19.
The governor called on mental-health professionals to volunteer their time and provide telephone and/or telehealth counseling. The New York State Psychiatric Association quickly got on board and encouraged its members to participate.
Just four days later, more than 6,000 mental health workers had volunteered their services, making New York the first state to address the mental health consequences of the pandemic in this way.
Self-care is vital for healthcare workers during the COVID-19 pandemic, particularly as stress mounts and workdays become longer and grimmer. Dougherty recommended that frontline workers manage overwhelming thoughts by limiting their intake of information about the virus.
Self-Care a “Selfless Act”
Clinicians need to balance the need to stay informed with the potential for information overload, which can contribute to anxiety, she said.
She also recommended that individuals continue to connect with loved ones while practicing social distancing. Equally important is talking to someone about the struggles people may be facing at work.
For Amin Azzam MD, MA, the benefits of these initiatives are obvious.
“There is always value in providing additional mental health services and tending to psychological well-being,” Azzam, adjunct professor of psychiatry, University of California, San Francisco and UC Berkeley, told Medscape Medical News.
“If there ever were a time when we can use all the emotional support possible, then it would be during a global pandemic,” added Azzam, who is also director of Open Learning Initiatives at Osmosis, a nonprofit health education company.
Azzam urged healthcare professionals to avail themselves of such resources as often as necessary.
“Taking care of ourselves is not a selfish act. When the oxygen masks come down on airplanes we are always instructed to put our own masks on first before helping those in need. It’s a sign of strength, not weakness, to seek emotional support,” he said.
However, it isn’t always easy. The longstanding stigma associated with seeking help for mental health issues has not stopped for COVID-19. Even workers who are in close daily contact with people infected with the virus are finding they’re not immune to the stigma associated with seeking mental health treatment, Azzam added.
“Nevertheless, the burden these frontline workers are facing is real…and often crushing. Some Ontario doctors have reported pretraumatic stress disorder, which they attribute to having watched the virus wreak havoc in other countries, and knowing that similar difficulties are headed their way,” he said.
A Growing Movement
Doris Grinspun, PhD, MSN, the CEO of Registered Nurses’ Association of Ontario (RNAO), said the province’s nurses are under intense pressure at work, then fear infecting family members once they come home. Some are even staying at hotels to ensure they don’t infect others, as reported by CBC News.
However, she added, most recognize the important role that psychotherapy can play, especially since many frontline healthcare workers find it difficult to speak with their families about the issues they face at work, for fear of adding stress to their family life as well.
“None of us are superhuman and immune to stress. When healthcare workers are facing workplace challenges never before seen in their lifetimes, they need opportunities to decompress to maintain their own health and well-being. This will help them pace themselves for the marathon — not sprint — to continue doing the important work of helping others,” said Azzam.
Given the attention it has garnered in such a short time, Azzam is hopeful that the free therapy movement will spread.
In Canada, mental health professionals in other provinces have already reached out to Dougherty, lending credence to the notion of a pan-Canadian network of therapists offering free services to healthcare workers during the outbreak.
In the US, other local initiatives are already underway.
“The one that I’m personally aware of is at my home institution at the University of California, San Francisco,” Azzam said. “We have a Care for the Caregiver program that is being greatly expanded at this time. As part of that initiative, the institution’s psychiatry department has solicited licensed mental health care providers to volunteer their time to provide those additional services.”
Azzam has also worked with colleagues developing a series of mental health tools that Osmosis has made available free of charge.
These include a central site with educational material about COVID-19, a video about supporting educators’ mental health during high-stress periods; a video about managing students’ mental health during public health emergencies; a summary of recommended resources for psychological health in distressing times; and a YouTube Live event he held regarding tips for maximizing psychological health during stressful times.
This article first appeared on Medscape.com.
COVID-19 transmission can occur before symptom onset
based on clinical and epidemiologic data for all cases reported in the country by March 16.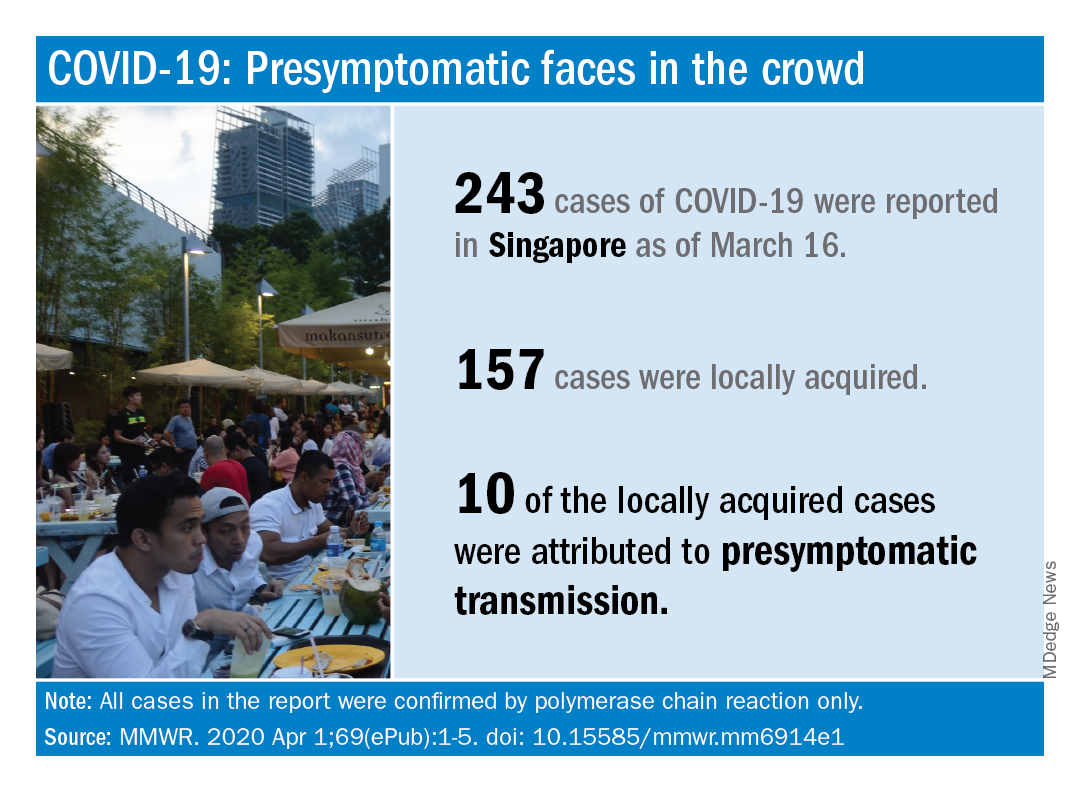
As of that date, there had been 243 cases of COVID-19, of which 157 were locally acquired. Among those 157 were 10 cases (6.4%) that involved probable presymptomatic transmission, Wycliffe E. Wei, MPH, and associates said April 1 in the Morbidity and Mortality Weekly Report.
They defined presymptomatic transmission “as the transmission of SARS-CoV-2 from an infected person (source patient) to a secondary patient before the source patient developed symptoms, as ascertained by exposure and symptom onset dates, with no evidence that the secondary patient had been exposed to anyone else with COVID-19.”
Investigation of all 243 cases in Singapore identified seven clusters, each involving two to five patients, as sources of presymptomatic transmission. In four of the clusters, the “exposure occurred 1-3 days before the source patient developed symptoms,” said Mr. Wei of the Singapore Ministry of Health and associates.
These findings, along with evidence from Chinese studies – one of which reported presymptomatic transmission in 12.6% of cases – support “the likelihood that viral shedding can occur in the absence of symptoms and before symptom onset,” they said.
SOURCE: Wei WE et al. MMWR. 2020 Apr 1;69(ePub):1-5. doi: 10.15585/mmwr.mm6914e1.
based on clinical and epidemiologic data for all cases reported in the country by March 16.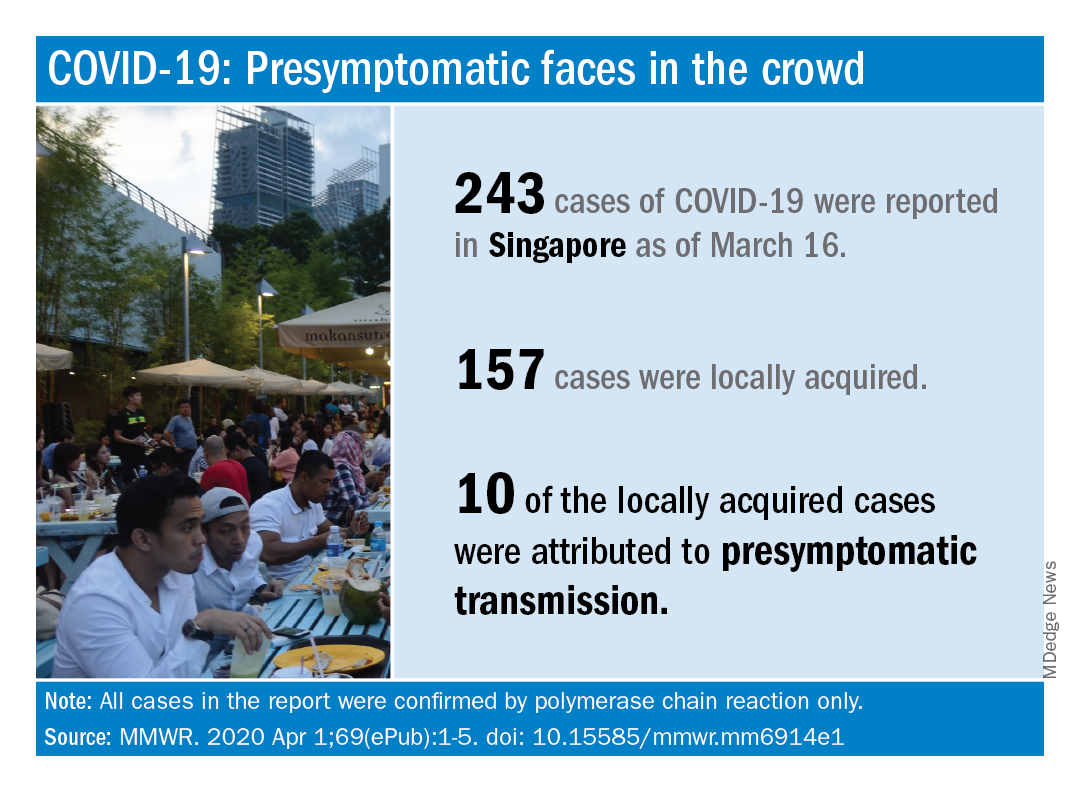
As of that date, there had been 243 cases of COVID-19, of which 157 were locally acquired. Among those 157 were 10 cases (6.4%) that involved probable presymptomatic transmission, Wycliffe E. Wei, MPH, and associates said April 1 in the Morbidity and Mortality Weekly Report.
They defined presymptomatic transmission “as the transmission of SARS-CoV-2 from an infected person (source patient) to a secondary patient before the source patient developed symptoms, as ascertained by exposure and symptom onset dates, with no evidence that the secondary patient had been exposed to anyone else with COVID-19.”
Investigation of all 243 cases in Singapore identified seven clusters, each involving two to five patients, as sources of presymptomatic transmission. In four of the clusters, the “exposure occurred 1-3 days before the source patient developed symptoms,” said Mr. Wei of the Singapore Ministry of Health and associates.
These findings, along with evidence from Chinese studies – one of which reported presymptomatic transmission in 12.6% of cases – support “the likelihood that viral shedding can occur in the absence of symptoms and before symptom onset,” they said.
SOURCE: Wei WE et al. MMWR. 2020 Apr 1;69(ePub):1-5. doi: 10.15585/mmwr.mm6914e1.
based on clinical and epidemiologic data for all cases reported in the country by March 16.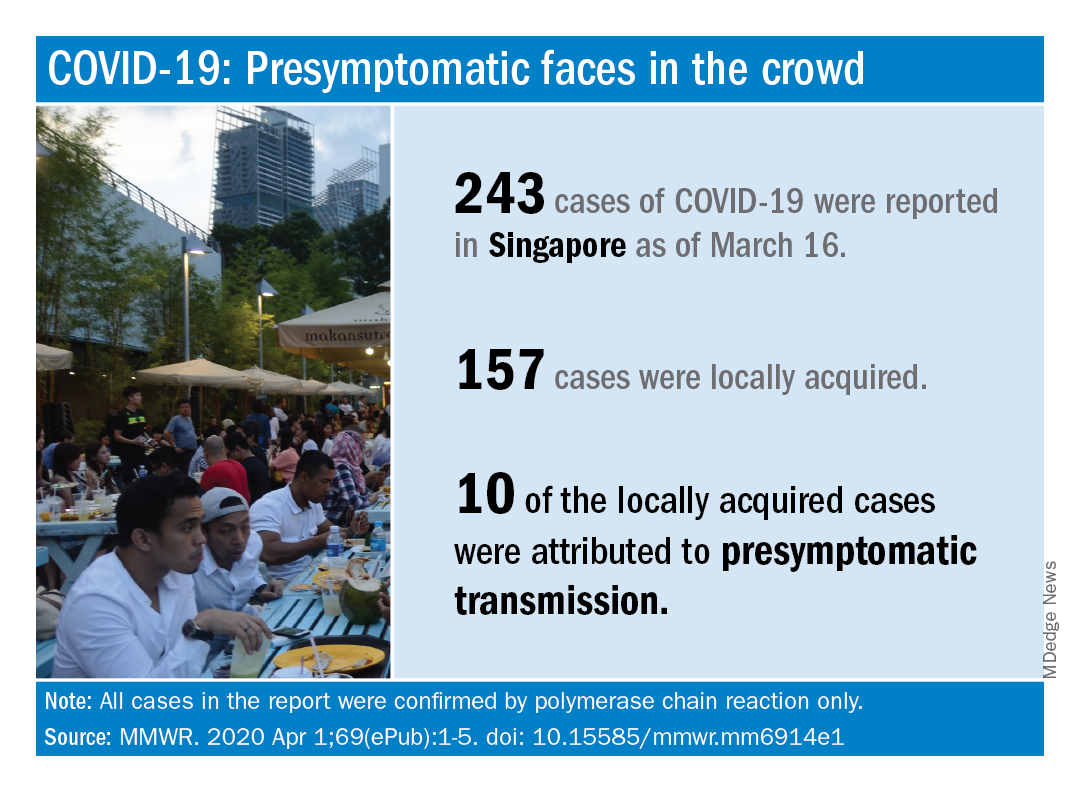
As of that date, there had been 243 cases of COVID-19, of which 157 were locally acquired. Among those 157 were 10 cases (6.4%) that involved probable presymptomatic transmission, Wycliffe E. Wei, MPH, and associates said April 1 in the Morbidity and Mortality Weekly Report.
They defined presymptomatic transmission “as the transmission of SARS-CoV-2 from an infected person (source patient) to a secondary patient before the source patient developed symptoms, as ascertained by exposure and symptom onset dates, with no evidence that the secondary patient had been exposed to anyone else with COVID-19.”
Investigation of all 243 cases in Singapore identified seven clusters, each involving two to five patients, as sources of presymptomatic transmission. In four of the clusters, the “exposure occurred 1-3 days before the source patient developed symptoms,” said Mr. Wei of the Singapore Ministry of Health and associates.
These findings, along with evidence from Chinese studies – one of which reported presymptomatic transmission in 12.6% of cases – support “the likelihood that viral shedding can occur in the absence of symptoms and before symptom onset,” they said.
SOURCE: Wei WE et al. MMWR. 2020 Apr 1;69(ePub):1-5. doi: 10.15585/mmwr.mm6914e1.
FROM MMWR
Advice from the front lines: How cancer centers can cope with COVID-19
according to the medical director of a cancer care alliance in the first U.S. epicenter of the coronavirus outbreak.
Jennie R. Crews, MD, the medical director of the Seattle Cancer Care Alliance (SCCA), discussed the SCCA experience and offered advice for other cancer centers in a webinar hosted by the Association of Community Cancer Centers.
Dr. Crews highlighted the SCCA’s use of algorithms to predict which patients can be managed via telehealth and which require face-to-face visits, human resource issues that arose at SCCA, screening and testing procedures, and the importance of communication with patients, caregivers, and staff.
Communication
Dr. Crews stressed the value of clear, regular, and internally consistent staff communication in a variety of formats. SCCA sends daily email blasts to their personnel regarding policies and procedures, which are archived on the SCCA intranet site.
SCCA also holds weekly town hall meetings at which leaders respond to staff questions regarding practical matters they have encountered and future plans. Providers’ up-to-the-minute familiarity with policies and procedures enables all team members to uniformly and clearly communicate to patients and caregivers.
Dr. Crews emphasized the value of consistency and “over-communication” in projecting confidence and preparedness to patients and caregivers during an unsettling time. SCCA has developed fact sheets, posted current information on the SCCA website, and provided education during doorway screenings.
Screening and testing
All SCCA staff members are screened daily at the practice entrance so they have personal experience with the process utilized for patients. Because symptoms associated with coronavirus infection may overlap with cancer treatment–related complaints, SCCA clinicians have expanded the typical coronavirus screening questionnaire for patients on cancer treatment.
Patients with ambiguous symptoms are masked, taken to a physically separate area of the SCCA clinics, and screened further by an advanced practice provider. The patients are then triaged to either the clinic for treatment or to the emergency department for further triage and care.
Although testing processes and procedures have been modified, Dr. Crews advised codifying those policies and procedures, including notification of results and follow-up for both patients and staff. Dr. Crews also stressed the importance of clearly articulated return-to-work policies for staff who have potential exposure and/or positive test results.
At the University of Washington’s virology laboratory, they have a test turnaround time of less than 12 hours.
Planning ahead
Dr. Crews highlighted the importance of community-based surge planning, utilizing predictive models to assess inpatient capacity requirements and potential repurposing of providers.
The SCCA is prepared to close selected community sites and shift personnel to other locations if personnel needs cannot be met because of illness or quarantine. Contingency plans include specialized pharmacy services for patients requiring chemotherapy.
The SCCA has not yet experienced shortages of personal protective equipment (PPE). However, Dr. Crews said staff require detailed education regarding the use of PPE in order to safeguard the supply while providing maximal staff protection.
Helping the helpers
During the pandemic, SCCA has dealt with a variety of challenging human resource issues, including:
- Extending sick time beyond what was previously “stored” in staff members’ earned time off.
- Childcare during an extended hiatus in school and daycare schedules.
- Programs to maintain and/or restore employee wellness (including staff-centered support services, spiritual care, mindfulness exercises, and town halls).
Dr. Crews also discussed recruitment of community resources to provide meals for staff from local restaurants with restricted hours and transportation resources for staff and patients, as visitors are restricted (currently one per patient).
Managing care
Dr. Crews noted that the University of Washington had a foundational structure for a telehealth program prior to the pandemic. Their telehealth committee enabled SCCA to scale up the service quickly with their academic partners, including training modules for and certification of providers, outfitting off-site personnel with dedicated lines and hardware, and provision of personal Zoom accounts.
SCCA also devised algorithms for determining when face-to-face visits, remote management, or deferred visits are appropriate in various scenarios. The algorithms were developed by disease-specialized teams.
As a general rule, routine chemotherapy and radiation are administered on schedule. On-treatment and follow-up office visits are conducted via telehealth if possible. In some cases, initiation of chemotherapy and radiation has been delayed, and screening services have been suspended.
In response to questions about palliative care during the pandemic, Dr. Crews said SCCA has encouraged their patients to complete, review, or update their advance directives. The SCCA has not had the need to resuscitate a coronavirus-infected outpatient but has instituted policies for utilizing full PPE on any patient requiring resuscitation.
In her closing remarks, Dr. Crews stressed that the response to COVID-19 in Washington state has required an intense collaboration among colleagues, the community, and government leaders, as the actions required extended far beyond medical decision makers alone.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
according to the medical director of a cancer care alliance in the first U.S. epicenter of the coronavirus outbreak.
Jennie R. Crews, MD, the medical director of the Seattle Cancer Care Alliance (SCCA), discussed the SCCA experience and offered advice for other cancer centers in a webinar hosted by the Association of Community Cancer Centers.
Dr. Crews highlighted the SCCA’s use of algorithms to predict which patients can be managed via telehealth and which require face-to-face visits, human resource issues that arose at SCCA, screening and testing procedures, and the importance of communication with patients, caregivers, and staff.
Communication
Dr. Crews stressed the value of clear, regular, and internally consistent staff communication in a variety of formats. SCCA sends daily email blasts to their personnel regarding policies and procedures, which are archived on the SCCA intranet site.
SCCA also holds weekly town hall meetings at which leaders respond to staff questions regarding practical matters they have encountered and future plans. Providers’ up-to-the-minute familiarity with policies and procedures enables all team members to uniformly and clearly communicate to patients and caregivers.
Dr. Crews emphasized the value of consistency and “over-communication” in projecting confidence and preparedness to patients and caregivers during an unsettling time. SCCA has developed fact sheets, posted current information on the SCCA website, and provided education during doorway screenings.
Screening and testing
All SCCA staff members are screened daily at the practice entrance so they have personal experience with the process utilized for patients. Because symptoms associated with coronavirus infection may overlap with cancer treatment–related complaints, SCCA clinicians have expanded the typical coronavirus screening questionnaire for patients on cancer treatment.
Patients with ambiguous symptoms are masked, taken to a physically separate area of the SCCA clinics, and screened further by an advanced practice provider. The patients are then triaged to either the clinic for treatment or to the emergency department for further triage and care.
Although testing processes and procedures have been modified, Dr. Crews advised codifying those policies and procedures, including notification of results and follow-up for both patients and staff. Dr. Crews also stressed the importance of clearly articulated return-to-work policies for staff who have potential exposure and/or positive test results.
At the University of Washington’s virology laboratory, they have a test turnaround time of less than 12 hours.
Planning ahead
Dr. Crews highlighted the importance of community-based surge planning, utilizing predictive models to assess inpatient capacity requirements and potential repurposing of providers.
The SCCA is prepared to close selected community sites and shift personnel to other locations if personnel needs cannot be met because of illness or quarantine. Contingency plans include specialized pharmacy services for patients requiring chemotherapy.
The SCCA has not yet experienced shortages of personal protective equipment (PPE). However, Dr. Crews said staff require detailed education regarding the use of PPE in order to safeguard the supply while providing maximal staff protection.
Helping the helpers
During the pandemic, SCCA has dealt with a variety of challenging human resource issues, including:
- Extending sick time beyond what was previously “stored” in staff members’ earned time off.
- Childcare during an extended hiatus in school and daycare schedules.
- Programs to maintain and/or restore employee wellness (including staff-centered support services, spiritual care, mindfulness exercises, and town halls).
Dr. Crews also discussed recruitment of community resources to provide meals for staff from local restaurants with restricted hours and transportation resources for staff and patients, as visitors are restricted (currently one per patient).
Managing care
Dr. Crews noted that the University of Washington had a foundational structure for a telehealth program prior to the pandemic. Their telehealth committee enabled SCCA to scale up the service quickly with their academic partners, including training modules for and certification of providers, outfitting off-site personnel with dedicated lines and hardware, and provision of personal Zoom accounts.
SCCA also devised algorithms for determining when face-to-face visits, remote management, or deferred visits are appropriate in various scenarios. The algorithms were developed by disease-specialized teams.
As a general rule, routine chemotherapy and radiation are administered on schedule. On-treatment and follow-up office visits are conducted via telehealth if possible. In some cases, initiation of chemotherapy and radiation has been delayed, and screening services have been suspended.
In response to questions about palliative care during the pandemic, Dr. Crews said SCCA has encouraged their patients to complete, review, or update their advance directives. The SCCA has not had the need to resuscitate a coronavirus-infected outpatient but has instituted policies for utilizing full PPE on any patient requiring resuscitation.
In her closing remarks, Dr. Crews stressed that the response to COVID-19 in Washington state has required an intense collaboration among colleagues, the community, and government leaders, as the actions required extended far beyond medical decision makers alone.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
according to the medical director of a cancer care alliance in the first U.S. epicenter of the coronavirus outbreak.
Jennie R. Crews, MD, the medical director of the Seattle Cancer Care Alliance (SCCA), discussed the SCCA experience and offered advice for other cancer centers in a webinar hosted by the Association of Community Cancer Centers.
Dr. Crews highlighted the SCCA’s use of algorithms to predict which patients can be managed via telehealth and which require face-to-face visits, human resource issues that arose at SCCA, screening and testing procedures, and the importance of communication with patients, caregivers, and staff.
Communication
Dr. Crews stressed the value of clear, regular, and internally consistent staff communication in a variety of formats. SCCA sends daily email blasts to their personnel regarding policies and procedures, which are archived on the SCCA intranet site.
SCCA also holds weekly town hall meetings at which leaders respond to staff questions regarding practical matters they have encountered and future plans. Providers’ up-to-the-minute familiarity with policies and procedures enables all team members to uniformly and clearly communicate to patients and caregivers.
Dr. Crews emphasized the value of consistency and “over-communication” in projecting confidence and preparedness to patients and caregivers during an unsettling time. SCCA has developed fact sheets, posted current information on the SCCA website, and provided education during doorway screenings.
Screening and testing
All SCCA staff members are screened daily at the practice entrance so they have personal experience with the process utilized for patients. Because symptoms associated with coronavirus infection may overlap with cancer treatment–related complaints, SCCA clinicians have expanded the typical coronavirus screening questionnaire for patients on cancer treatment.
Patients with ambiguous symptoms are masked, taken to a physically separate area of the SCCA clinics, and screened further by an advanced practice provider. The patients are then triaged to either the clinic for treatment or to the emergency department for further triage and care.
Although testing processes and procedures have been modified, Dr. Crews advised codifying those policies and procedures, including notification of results and follow-up for both patients and staff. Dr. Crews also stressed the importance of clearly articulated return-to-work policies for staff who have potential exposure and/or positive test results.
At the University of Washington’s virology laboratory, they have a test turnaround time of less than 12 hours.
Planning ahead
Dr. Crews highlighted the importance of community-based surge planning, utilizing predictive models to assess inpatient capacity requirements and potential repurposing of providers.
The SCCA is prepared to close selected community sites and shift personnel to other locations if personnel needs cannot be met because of illness or quarantine. Contingency plans include specialized pharmacy services for patients requiring chemotherapy.
The SCCA has not yet experienced shortages of personal protective equipment (PPE). However, Dr. Crews said staff require detailed education regarding the use of PPE in order to safeguard the supply while providing maximal staff protection.
Helping the helpers
During the pandemic, SCCA has dealt with a variety of challenging human resource issues, including:
- Extending sick time beyond what was previously “stored” in staff members’ earned time off.
- Childcare during an extended hiatus in school and daycare schedules.
- Programs to maintain and/or restore employee wellness (including staff-centered support services, spiritual care, mindfulness exercises, and town halls).
Dr. Crews also discussed recruitment of community resources to provide meals for staff from local restaurants with restricted hours and transportation resources for staff and patients, as visitors are restricted (currently one per patient).
Managing care
Dr. Crews noted that the University of Washington had a foundational structure for a telehealth program prior to the pandemic. Their telehealth committee enabled SCCA to scale up the service quickly with their academic partners, including training modules for and certification of providers, outfitting off-site personnel with dedicated lines and hardware, and provision of personal Zoom accounts.
SCCA also devised algorithms for determining when face-to-face visits, remote management, or deferred visits are appropriate in various scenarios. The algorithms were developed by disease-specialized teams.
As a general rule, routine chemotherapy and radiation are administered on schedule. On-treatment and follow-up office visits are conducted via telehealth if possible. In some cases, initiation of chemotherapy and radiation has been delayed, and screening services have been suspended.
In response to questions about palliative care during the pandemic, Dr. Crews said SCCA has encouraged their patients to complete, review, or update their advance directives. The SCCA has not had the need to resuscitate a coronavirus-infected outpatient but has instituted policies for utilizing full PPE on any patient requiring resuscitation.
In her closing remarks, Dr. Crews stressed that the response to COVID-19 in Washington state has required an intense collaboration among colleagues, the community, and government leaders, as the actions required extended far beyond medical decision makers alone.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
NYU med student joins COVID fight: ‘Time to step up’
On the evening of March 24, I got the email. When the bolded letters “We ask for your help” flashed across my screen, I knew exactly what was being asked of me: to graduate early and join the fight against COVID-19.
For the 120 fourth-year medical students in my class at NYU Grossman School of Medicine, the arrival of that email was always more a question of when than if. Similar moves had already been made in Italy as well as the United Kingdom, where the surge in patients with COVID-19 has devastated hospitals and left healthcare workers dead or drained. The New York hospitals where I’ve trained, places I have grown to love over the past 4 years, are now experiencing similar horrors. Residents and attending doctors – mentors and teachers – are burned out and exhausted. They need help.
Like most medical students, I chose to pursue medicine out of a desire to help. On both my medical school and residency applications, I spoke about my resolve to bear witness to and provide support to those suffering. Yet, being recruited to the front lines of a global pandemic felt deeply unsettling. Is this how I want to finally enter the world of medicine? The scope of what is actually being asked of me was immense.
Given the onslaught of bad news coming in on every device I had cozied up to during my social distancing, how could I want to do this? I’ve seen the death toll climb in Italy, with dozens of doctors dead. I’ve seen the photos of faces marred by masks worn for 12-16 hours at a time. I’ve been repeatedly reminded that we are just behind Italy. Things are certainly going to get worse.
It sounds selfish and petty, but I feel like COVID-19 has already robbed me of so much. Yet that was my first thought when I received the email. The end of fourth year in medical school is supposed to be a joyous, celebratory time. We have worked years for this moment. So many of us have fought burnout to reach this time, a brief moment of rest between being a medical student and becoming a full-fledged physician.
I matched into residency just 4 days before being asked to join the front lines of the pandemic. I found out my match results without the usual fanfare, sitting on a bench in Madison Square Park, FaceTiming my dad and safely social-distanced from my mom. They both cried tears of joy. Like so many people around the world right now, I couldn’t even embrace my parents. Would they want me to volunteer?
I reached out to my classmates. I thought that some of them would certainly share my worries. I thought they also had to be carrying this uncomfortable kind of grief, a heavy and acidic feeling of dreams collapsing into a moral duty. I received a unanimous reply: “We are needed. It’s our time to step up.” No matter how many “what ifs” I voiced, they wouldn’t crack or waver. Still, even if they never admitted it to me, I wondered whether they privately shared some of my concerns and fears.
Everyone knows information is shared instantly in our Twitter-centric world, but I was still shocked and unprepared for how quickly I was at the center of a major news story. Within an hour of that email, I was contacted by an old acquaintance from elementary school, now a journalist. He had found me through Facebook and asked, “Will you be one of the NYU students graduating early? Would love to get a comment.” Another friend texted me a photo of the leaked email, quipping, “Are you going to save us from the pandemic, Dr. Gabe?!” “It’s not a small decision!” I snapped back.
I went through something like the seven stages of grief in rapid succession. I found that with each excuse I made why I shouldn’t volunteer, I somehow became increasingly more anxious. To my surprise, when I decided I would join 50 of my peers at NYU, graduate early, and volunteer, my mind settled. The more I thought about it, the more I was overtaken by the selfless beauty of the profession I’m entering. This is what it means to be a doctor. I recalled a key part of the Hippocratic Oath: “I will remember that I remain a member of society, with special obligations to all my fellow human beings, those sound of mind and body as well as the infirm.”
I am going to fulfill my special obligations.
The fear is still there. I’m scared of COVID. I’m scared to infect others. I’m scared of winding up paralyzed and intubated. But I have also realized that all we have is each other. Healthcare workers supporting healthcare workers. New Yorkers supporting New Yorkers. Citizens of the world supporting citizens of the world. This is my time to be there for others, unwaveringly.
Logistical details continue to roll in, although they feel trivial in relation to the decision I have already made. The paperwork tells me that I will be onboarded to NYU’s internal medicine residency program. I will be compensated and protected under a similar contract to what current NYU residents sign. I have been promised that I will remain insured until I start my official residency program in July. My student loans won’t begin accruing interest until my normally planned graduation date. I am told that I will have personal protective equipment in line with the Centers for Disease Control and Prevention recommendations.
Questions still linger. Is it safe for me and my newly minted physician peers to continue living with our spouses, children, and friends? How long will I need to quarantine after my contract ends? Will there be a virtual graduation ceremony for my parents and loved ones to enjoy? In these challenging times, each day gives me a little more clarity about what exactly I am signing up for, but there are still so many uncertainties.
Am I naive to say that I do feel prepared? Or at least as prepared as anyone can be. With respect to my training, I have completed the requirements to graduate, which is why I am being permitted to graduate early in the first place. Our faculty points to our professionalism as the most promising indicator of our preparedness. They are heartened that we have embraced this truest test: our duty to others.
There is an eerie calm to New York City that contradicts what is shown on the news. With stores closed and streets quiet, it almost feels like Christmas morning here. Yet, inside the hospital, a fire rages. All the metaphors being used right now speak about violence, devastation, and immeasurable human suffering. “A war is being fought.” Or so I have heard. I guess I am about to find out.
Gabriel Redel-Traub is a fourth-year medical student at NYU Grossman School of Medicine. He will be starting residency in internal medicine at Columbia Presbyterian this summer. He is the former editor-in-chief of Dartmouth College’s Mouth Magazine, an editor of NYU’s LitMed Database, and has published most recently in the Hasting’s Center Magazine. Gabriel Redel-Traub has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
On the evening of March 24, I got the email. When the bolded letters “We ask for your help” flashed across my screen, I knew exactly what was being asked of me: to graduate early and join the fight against COVID-19.
For the 120 fourth-year medical students in my class at NYU Grossman School of Medicine, the arrival of that email was always more a question of when than if. Similar moves had already been made in Italy as well as the United Kingdom, where the surge in patients with COVID-19 has devastated hospitals and left healthcare workers dead or drained. The New York hospitals where I’ve trained, places I have grown to love over the past 4 years, are now experiencing similar horrors. Residents and attending doctors – mentors and teachers – are burned out and exhausted. They need help.
Like most medical students, I chose to pursue medicine out of a desire to help. On both my medical school and residency applications, I spoke about my resolve to bear witness to and provide support to those suffering. Yet, being recruited to the front lines of a global pandemic felt deeply unsettling. Is this how I want to finally enter the world of medicine? The scope of what is actually being asked of me was immense.
Given the onslaught of bad news coming in on every device I had cozied up to during my social distancing, how could I want to do this? I’ve seen the death toll climb in Italy, with dozens of doctors dead. I’ve seen the photos of faces marred by masks worn for 12-16 hours at a time. I’ve been repeatedly reminded that we are just behind Italy. Things are certainly going to get worse.
It sounds selfish and petty, but I feel like COVID-19 has already robbed me of so much. Yet that was my first thought when I received the email. The end of fourth year in medical school is supposed to be a joyous, celebratory time. We have worked years for this moment. So many of us have fought burnout to reach this time, a brief moment of rest between being a medical student and becoming a full-fledged physician.
I matched into residency just 4 days before being asked to join the front lines of the pandemic. I found out my match results without the usual fanfare, sitting on a bench in Madison Square Park, FaceTiming my dad and safely social-distanced from my mom. They both cried tears of joy. Like so many people around the world right now, I couldn’t even embrace my parents. Would they want me to volunteer?
I reached out to my classmates. I thought that some of them would certainly share my worries. I thought they also had to be carrying this uncomfortable kind of grief, a heavy and acidic feeling of dreams collapsing into a moral duty. I received a unanimous reply: “We are needed. It’s our time to step up.” No matter how many “what ifs” I voiced, they wouldn’t crack or waver. Still, even if they never admitted it to me, I wondered whether they privately shared some of my concerns and fears.
Everyone knows information is shared instantly in our Twitter-centric world, but I was still shocked and unprepared for how quickly I was at the center of a major news story. Within an hour of that email, I was contacted by an old acquaintance from elementary school, now a journalist. He had found me through Facebook and asked, “Will you be one of the NYU students graduating early? Would love to get a comment.” Another friend texted me a photo of the leaked email, quipping, “Are you going to save us from the pandemic, Dr. Gabe?!” “It’s not a small decision!” I snapped back.
I went through something like the seven stages of grief in rapid succession. I found that with each excuse I made why I shouldn’t volunteer, I somehow became increasingly more anxious. To my surprise, when I decided I would join 50 of my peers at NYU, graduate early, and volunteer, my mind settled. The more I thought about it, the more I was overtaken by the selfless beauty of the profession I’m entering. This is what it means to be a doctor. I recalled a key part of the Hippocratic Oath: “I will remember that I remain a member of society, with special obligations to all my fellow human beings, those sound of mind and body as well as the infirm.”
I am going to fulfill my special obligations.
The fear is still there. I’m scared of COVID. I’m scared to infect others. I’m scared of winding up paralyzed and intubated. But I have also realized that all we have is each other. Healthcare workers supporting healthcare workers. New Yorkers supporting New Yorkers. Citizens of the world supporting citizens of the world. This is my time to be there for others, unwaveringly.
Logistical details continue to roll in, although they feel trivial in relation to the decision I have already made. The paperwork tells me that I will be onboarded to NYU’s internal medicine residency program. I will be compensated and protected under a similar contract to what current NYU residents sign. I have been promised that I will remain insured until I start my official residency program in July. My student loans won’t begin accruing interest until my normally planned graduation date. I am told that I will have personal protective equipment in line with the Centers for Disease Control and Prevention recommendations.
Questions still linger. Is it safe for me and my newly minted physician peers to continue living with our spouses, children, and friends? How long will I need to quarantine after my contract ends? Will there be a virtual graduation ceremony for my parents and loved ones to enjoy? In these challenging times, each day gives me a little more clarity about what exactly I am signing up for, but there are still so many uncertainties.
Am I naive to say that I do feel prepared? Or at least as prepared as anyone can be. With respect to my training, I have completed the requirements to graduate, which is why I am being permitted to graduate early in the first place. Our faculty points to our professionalism as the most promising indicator of our preparedness. They are heartened that we have embraced this truest test: our duty to others.
There is an eerie calm to New York City that contradicts what is shown on the news. With stores closed and streets quiet, it almost feels like Christmas morning here. Yet, inside the hospital, a fire rages. All the metaphors being used right now speak about violence, devastation, and immeasurable human suffering. “A war is being fought.” Or so I have heard. I guess I am about to find out.
Gabriel Redel-Traub is a fourth-year medical student at NYU Grossman School of Medicine. He will be starting residency in internal medicine at Columbia Presbyterian this summer. He is the former editor-in-chief of Dartmouth College’s Mouth Magazine, an editor of NYU’s LitMed Database, and has published most recently in the Hasting’s Center Magazine. Gabriel Redel-Traub has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
On the evening of March 24, I got the email. When the bolded letters “We ask for your help” flashed across my screen, I knew exactly what was being asked of me: to graduate early and join the fight against COVID-19.
For the 120 fourth-year medical students in my class at NYU Grossman School of Medicine, the arrival of that email was always more a question of when than if. Similar moves had already been made in Italy as well as the United Kingdom, where the surge in patients with COVID-19 has devastated hospitals and left healthcare workers dead or drained. The New York hospitals where I’ve trained, places I have grown to love over the past 4 years, are now experiencing similar horrors. Residents and attending doctors – mentors and teachers – are burned out and exhausted. They need help.
Like most medical students, I chose to pursue medicine out of a desire to help. On both my medical school and residency applications, I spoke about my resolve to bear witness to and provide support to those suffering. Yet, being recruited to the front lines of a global pandemic felt deeply unsettling. Is this how I want to finally enter the world of medicine? The scope of what is actually being asked of me was immense.
Given the onslaught of bad news coming in on every device I had cozied up to during my social distancing, how could I want to do this? I’ve seen the death toll climb in Italy, with dozens of doctors dead. I’ve seen the photos of faces marred by masks worn for 12-16 hours at a time. I’ve been repeatedly reminded that we are just behind Italy. Things are certainly going to get worse.
It sounds selfish and petty, but I feel like COVID-19 has already robbed me of so much. Yet that was my first thought when I received the email. The end of fourth year in medical school is supposed to be a joyous, celebratory time. We have worked years for this moment. So many of us have fought burnout to reach this time, a brief moment of rest between being a medical student and becoming a full-fledged physician.
I matched into residency just 4 days before being asked to join the front lines of the pandemic. I found out my match results without the usual fanfare, sitting on a bench in Madison Square Park, FaceTiming my dad and safely social-distanced from my mom. They both cried tears of joy. Like so many people around the world right now, I couldn’t even embrace my parents. Would they want me to volunteer?
I reached out to my classmates. I thought that some of them would certainly share my worries. I thought they also had to be carrying this uncomfortable kind of grief, a heavy and acidic feeling of dreams collapsing into a moral duty. I received a unanimous reply: “We are needed. It’s our time to step up.” No matter how many “what ifs” I voiced, they wouldn’t crack or waver. Still, even if they never admitted it to me, I wondered whether they privately shared some of my concerns and fears.
Everyone knows information is shared instantly in our Twitter-centric world, but I was still shocked and unprepared for how quickly I was at the center of a major news story. Within an hour of that email, I was contacted by an old acquaintance from elementary school, now a journalist. He had found me through Facebook and asked, “Will you be one of the NYU students graduating early? Would love to get a comment.” Another friend texted me a photo of the leaked email, quipping, “Are you going to save us from the pandemic, Dr. Gabe?!” “It’s not a small decision!” I snapped back.
I went through something like the seven stages of grief in rapid succession. I found that with each excuse I made why I shouldn’t volunteer, I somehow became increasingly more anxious. To my surprise, when I decided I would join 50 of my peers at NYU, graduate early, and volunteer, my mind settled. The more I thought about it, the more I was overtaken by the selfless beauty of the profession I’m entering. This is what it means to be a doctor. I recalled a key part of the Hippocratic Oath: “I will remember that I remain a member of society, with special obligations to all my fellow human beings, those sound of mind and body as well as the infirm.”
I am going to fulfill my special obligations.
The fear is still there. I’m scared of COVID. I’m scared to infect others. I’m scared of winding up paralyzed and intubated. But I have also realized that all we have is each other. Healthcare workers supporting healthcare workers. New Yorkers supporting New Yorkers. Citizens of the world supporting citizens of the world. This is my time to be there for others, unwaveringly.
Logistical details continue to roll in, although they feel trivial in relation to the decision I have already made. The paperwork tells me that I will be onboarded to NYU’s internal medicine residency program. I will be compensated and protected under a similar contract to what current NYU residents sign. I have been promised that I will remain insured until I start my official residency program in July. My student loans won’t begin accruing interest until my normally planned graduation date. I am told that I will have personal protective equipment in line with the Centers for Disease Control and Prevention recommendations.
Questions still linger. Is it safe for me and my newly minted physician peers to continue living with our spouses, children, and friends? How long will I need to quarantine after my contract ends? Will there be a virtual graduation ceremony for my parents and loved ones to enjoy? In these challenging times, each day gives me a little more clarity about what exactly I am signing up for, but there are still so many uncertainties.
Am I naive to say that I do feel prepared? Or at least as prepared as anyone can be. With respect to my training, I have completed the requirements to graduate, which is why I am being permitted to graduate early in the first place. Our faculty points to our professionalism as the most promising indicator of our preparedness. They are heartened that we have embraced this truest test: our duty to others.
There is an eerie calm to New York City that contradicts what is shown on the news. With stores closed and streets quiet, it almost feels like Christmas morning here. Yet, inside the hospital, a fire rages. All the metaphors being used right now speak about violence, devastation, and immeasurable human suffering. “A war is being fought.” Or so I have heard. I guess I am about to find out.
Gabriel Redel-Traub is a fourth-year medical student at NYU Grossman School of Medicine. He will be starting residency in internal medicine at Columbia Presbyterian this summer. He is the former editor-in-chief of Dartmouth College’s Mouth Magazine, an editor of NYU’s LitMed Database, and has published most recently in the Hasting’s Center Magazine. Gabriel Redel-Traub has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Neurologists navigate unknown territory during COVID-19 pandemic
Neurologic disorders are among the “underlying medical conditions that may increase the risk of serious COVID-19 for individuals of any age,” according to the Centers for Disease Control and Prevention.
Potentially relevant drug interactions, how immunosuppressive medications may influence the risk of COVID-19, and neurologic diseases that may be associated with greater risk are among the questions that experts and groups have addressed.
According to the CDC, neurologic conditions that may heighten the risk of severe COVID-19 include “disorders of the brain, spinal cord, peripheral nerve, and muscle such as cerebral palsy, epilepsy (seizure disorders), stroke, intellectual disability, moderate to severe developmental delay, muscular dystrophy, or spinal cord injury.” Many patients, however, may not have substantially increased risks, neurologists suggest.
“Patients with conditions that do not affect their swallowing or breathing muscles and in whom the immune system is working normally are not considered to be at increased risk from COVID-19,” according to March 26 guidance from the Association of British Neurologists (ABN). “Milder or moderate forms of many of the commoner neurological disorders, such as Parkinson’s disease, multiple sclerosis, epilepsy, are not currently considered to confer increased risk, so long as the breathing and swallowing muscles are functioning well.”
Neurologists should tailor treatment decisions to individual patients, according to the ABN. “Although some neurological conditions or treatments increase the risk of complicated COVID-19, most patients in these groups will overcome the infection,” the association noted.
Interactions with potential COVID-19 treatments
Standard drugs in neurology may interact with potential COVID-19 treatments. For example, “preliminary experience suggests that there is a possible benefit from hydroxychloroquine and azithromycin treatment in COVID-19 infection,” but either of those drugs “may lead to a deterioration in myasthenia gravis,” the ABN notes. “Doctors will have to balance the risks from myasthenia and COVID-19 on a case-by-case basis.” The Liverpool Drug Interactions Group has published tables that describe interactions between potential COVID-19 treatments and anticonvulsants, analgesics, immunosuppressants, and other medication classes.
Many muscle diseases and neuromuscular junction diseases may entail higher risks of complicated COVID-19, the ABN suggested. For patients on immunotherapy, the medication may be a more important consideration for COVID-19 than the underlying disease. Other comorbidities such as hypertension, renal impairment, neutropenia, lymphopenia, liver disease, diabetes mellitus, ischemic heart disease, and lung disease may be important factors, according to the association.
Seizures may not worsen
After the CDC added epilepsy to its list of conditions that entail higher risk of severe COVID-19, M. Scott Perry, MD, medical director of neurology at Cook Children’s Medical Center in Fort Worth, Tex., commented on Twitter that “most healthy people with controlled epilepsy [are] probably at no more risk than others.”
“Those treated with steroids or other immunosuppressive drugs are likely higher risk,” Dr. Perry said. “Likewise, patients with other medical comorbidities such as muscle weakness, swallowing or breathing problems, and other complex cases of epilepsy are likely higher risk. Regardless: be responsible, avoid crowds, wash your hands, avoid sick contacts.”
Doctors in Italy, based on small numbers of cases, have found that seizures are not worse in patients with epilepsy and COVID-19, said Dr. Perry. A few children, including several patients with Dravet syndrome, “had uncomplicated illness and seizures were no worse,” he said. “That is reassuring.”
“Until now, there is no evidence of a direct effect of COVID-19 on seizures or epilepsy,” according to the International League Against Epilepsy (ILAE). “However, patients may experience worsening of seizures due to systemic illnesses, drug interactions, decreased access to antiseizure medications, and increased stress.”
“In younger children, the fever that accompanies COVID-19 may exacerbate seizures, as might any febrile illness,” according to an American Epilepsy Society (AES) resource for epilepsy clinicians. “The main known elevated risk factors related to COVID-19 are age, respiratory disease, and other chronic medical conditions not related to epilepsy. As for all, people with epilepsy should adhere to the CDC recommendations for reducing risk of infection.” Neurologists should review with patients the importance of treatment adherence, update plans for managing breakthrough seizures, and ensure necessary medications are on hand, according to the AES.
The Epilepsy Foundation created a page with information about COVID-19 for patients with epilepsy and recorded a discussion with epilepsy specialists. DEE-P (Developmental Epileptic Encephalopathy–Project) Connections recorded a webinar about protecting medically complex or immune-suppressed children with epilepsy from COVID-19.
MS DMTs and the coronavirus
The National Multiple Sclerosis (MS) Society has provided guidance on the use of disease-modifying therapies (DMTs) during the COVID-19 pandemic. “There are numerous recommendations circulating that attempt to provide clarity and guidance, however, differences among the recommendations have created confusion,” the society says. “DMT decision making varies significantly from country to country, ranging from highly provider-directed to a collaborative decision-making model. ... DMT decisions should be individualized and made collaboratively between the person with MS and his/her healthcare provider.”
Patients with MS and their physicians should weigh risks and benefits before starting cell-depleting DMTs such as alemtuzumab, cladribine, ocrelizumab, or rituximab, according the National MS Society. They also should consider the risks and benefits of DMTs that carry warnings of a potentially severe increase in disability after stopping therapy, such as fingolimod and natalizumab. “We endorse the global advice provided by the MS International Federation (MSIF) – but emphasize that DMT decision making must be individualized and based upon multiple factors,” the National MS Society said.
Neurologists currently lack evidence about how COVID-19 affects patients with MS, according to the MSIF, which based its DMT guidance on advice from MS neurologists and research experts from member organizations. Many DMTs suppress or modify the immune system, and “some MS medications might increase the likelihood of developing complications from a COVID-19 infection but this risk needs to be balanced with the risks of stopping treatment,” according to the federation.
Patients currently taking DMTs should continue treatment, and those who develop symptoms of COVID-19 or test positive for the infection should discuss their DMT with a health care professional familiar with their care, the MSIF recommends. Decisions about starting a DMT should take into account a patient’s disease course, disease activity, and regional COVID-19 risks, according to the federation. For patients due to start DMT, treatments that do not reduce lymphocytes, such as interferons, glatiramer acetate, or natalizumab, should be considered.
Fingolimod, dimethyl fumarate, teriflunomide, and siponimod “may reduce the ability of the immune system to respond to an infection,” and “people should carefully consider the risks and benefits of initiating these treatments during the COVID-19 pandemic,” according to the federation. “People with MS who are currently taking alemtuzumab, cladribine, ocrelizumab, rituximab, fingolimod, dimethyl fumarate, teriflunomide or siponimod and are living in a community with a COVID-19 outbreak should isolate as much as possible to reduce their risk of infection.”
Extended isolation during the COVID-19 outbreak may be warranted for patients with MS who have recently undergone autologous hematopoietic stem cell treatment, which entails intensive chemotherapy, the guidance says. In addition, postponement of this procedure should be considered.
Child neurology, migraine, movement disorders, and stroke
The Child Neurology Foundation (CNF) and Child Neurology Society (CNS) published a joint statement about COVID-19. “Most children who contract COVID-19 appear to exhibit only mild symptoms,” said Scott Pomeroy, MD, president of CNF’s board of directors and chair of the department of neurology at Boston Children’s Hospital, in the statement. “However, if your child is taking a medication such as steroids that can lower their immune system response, there could be an increased risk for more significant symptoms. In addition, children with lung disease, such as asthma, may also be at higher risk. Therefore, it is important to practice preventative precautions. We hope that this information will help to reduce some of the fears that families in our community may be experiencing.”
The American Migraine Foundation shared COVID-19 considerations for patients with migraine from Mia Minen, MD, associate professor of neurology and population health at NYU Langone in New York. Patients with migraine who are otherwise in good health are not expected to be at increased risk of severe COVID-19, according to Dr. Minen. Best practices include having an adequate supply of medicine, considering alternatives to in-person doctor visits, and being “mindful of routine and diet to reduce migraine triggers,” the foundation suggests. In addition, patients should try to limit stress and seek out “alternative methods of social interaction.”
“The relationship between COVID-19 and Parkinson’s disease or other movement disorders remains unknown,” the International Parkinson and Movement Disorder Society said. “In general, we recommend that our movement disorder patients do not assume they are at extreme risks, which for the time being are uncertain. Nevertheless, we strongly recommend following the standard measures strictly to avoid exposures to the virus.”
The American Heart Association (AHA) cautions that older patients with coronary heart disease or hypertension “may be more likely than others to be infected by the coronavirus that causes COVID-19 and to develop more severe symptoms.” In addition, people with a history of stroke “may face a higher risk of complications,” according to the AHA. “As a result, people who have heart disease or another underlying condition should stay home to limit their risk of contracting the virus.”
Several groups emphasized the importance of telemedicine as an option for patients with neurologic conditions during the pandemic. The American Headache Society has hosted discussions on conducting neurologic exams via telemedicine. The American Academy of Neurology also conducted a webinar on telemedicine and COVID-19 and created a page with COVID-19 resources. The journal Neurology is publishing invited commentaries about neurologic aspects of the COVID-19 pandemic.
Neurologic disorders are among the “underlying medical conditions that may increase the risk of serious COVID-19 for individuals of any age,” according to the Centers for Disease Control and Prevention.
Potentially relevant drug interactions, how immunosuppressive medications may influence the risk of COVID-19, and neurologic diseases that may be associated with greater risk are among the questions that experts and groups have addressed.
According to the CDC, neurologic conditions that may heighten the risk of severe COVID-19 include “disorders of the brain, spinal cord, peripheral nerve, and muscle such as cerebral palsy, epilepsy (seizure disorders), stroke, intellectual disability, moderate to severe developmental delay, muscular dystrophy, or spinal cord injury.” Many patients, however, may not have substantially increased risks, neurologists suggest.
“Patients with conditions that do not affect their swallowing or breathing muscles and in whom the immune system is working normally are not considered to be at increased risk from COVID-19,” according to March 26 guidance from the Association of British Neurologists (ABN). “Milder or moderate forms of many of the commoner neurological disorders, such as Parkinson’s disease, multiple sclerosis, epilepsy, are not currently considered to confer increased risk, so long as the breathing and swallowing muscles are functioning well.”
Neurologists should tailor treatment decisions to individual patients, according to the ABN. “Although some neurological conditions or treatments increase the risk of complicated COVID-19, most patients in these groups will overcome the infection,” the association noted.
Interactions with potential COVID-19 treatments
Standard drugs in neurology may interact with potential COVID-19 treatments. For example, “preliminary experience suggests that there is a possible benefit from hydroxychloroquine and azithromycin treatment in COVID-19 infection,” but either of those drugs “may lead to a deterioration in myasthenia gravis,” the ABN notes. “Doctors will have to balance the risks from myasthenia and COVID-19 on a case-by-case basis.” The Liverpool Drug Interactions Group has published tables that describe interactions between potential COVID-19 treatments and anticonvulsants, analgesics, immunosuppressants, and other medication classes.
Many muscle diseases and neuromuscular junction diseases may entail higher risks of complicated COVID-19, the ABN suggested. For patients on immunotherapy, the medication may be a more important consideration for COVID-19 than the underlying disease. Other comorbidities such as hypertension, renal impairment, neutropenia, lymphopenia, liver disease, diabetes mellitus, ischemic heart disease, and lung disease may be important factors, according to the association.
Seizures may not worsen
After the CDC added epilepsy to its list of conditions that entail higher risk of severe COVID-19, M. Scott Perry, MD, medical director of neurology at Cook Children’s Medical Center in Fort Worth, Tex., commented on Twitter that “most healthy people with controlled epilepsy [are] probably at no more risk than others.”
“Those treated with steroids or other immunosuppressive drugs are likely higher risk,” Dr. Perry said. “Likewise, patients with other medical comorbidities such as muscle weakness, swallowing or breathing problems, and other complex cases of epilepsy are likely higher risk. Regardless: be responsible, avoid crowds, wash your hands, avoid sick contacts.”
Doctors in Italy, based on small numbers of cases, have found that seizures are not worse in patients with epilepsy and COVID-19, said Dr. Perry. A few children, including several patients with Dravet syndrome, “had uncomplicated illness and seizures were no worse,” he said. “That is reassuring.”
“Until now, there is no evidence of a direct effect of COVID-19 on seizures or epilepsy,” according to the International League Against Epilepsy (ILAE). “However, patients may experience worsening of seizures due to systemic illnesses, drug interactions, decreased access to antiseizure medications, and increased stress.”
“In younger children, the fever that accompanies COVID-19 may exacerbate seizures, as might any febrile illness,” according to an American Epilepsy Society (AES) resource for epilepsy clinicians. “The main known elevated risk factors related to COVID-19 are age, respiratory disease, and other chronic medical conditions not related to epilepsy. As for all, people with epilepsy should adhere to the CDC recommendations for reducing risk of infection.” Neurologists should review with patients the importance of treatment adherence, update plans for managing breakthrough seizures, and ensure necessary medications are on hand, according to the AES.
The Epilepsy Foundation created a page with information about COVID-19 for patients with epilepsy and recorded a discussion with epilepsy specialists. DEE-P (Developmental Epileptic Encephalopathy–Project) Connections recorded a webinar about protecting medically complex or immune-suppressed children with epilepsy from COVID-19.
MS DMTs and the coronavirus
The National Multiple Sclerosis (MS) Society has provided guidance on the use of disease-modifying therapies (DMTs) during the COVID-19 pandemic. “There are numerous recommendations circulating that attempt to provide clarity and guidance, however, differences among the recommendations have created confusion,” the society says. “DMT decision making varies significantly from country to country, ranging from highly provider-directed to a collaborative decision-making model. ... DMT decisions should be individualized and made collaboratively between the person with MS and his/her healthcare provider.”
Patients with MS and their physicians should weigh risks and benefits before starting cell-depleting DMTs such as alemtuzumab, cladribine, ocrelizumab, or rituximab, according the National MS Society. They also should consider the risks and benefits of DMTs that carry warnings of a potentially severe increase in disability after stopping therapy, such as fingolimod and natalizumab. “We endorse the global advice provided by the MS International Federation (MSIF) – but emphasize that DMT decision making must be individualized and based upon multiple factors,” the National MS Society said.
Neurologists currently lack evidence about how COVID-19 affects patients with MS, according to the MSIF, which based its DMT guidance on advice from MS neurologists and research experts from member organizations. Many DMTs suppress or modify the immune system, and “some MS medications might increase the likelihood of developing complications from a COVID-19 infection but this risk needs to be balanced with the risks of stopping treatment,” according to the federation.
Patients currently taking DMTs should continue treatment, and those who develop symptoms of COVID-19 or test positive for the infection should discuss their DMT with a health care professional familiar with their care, the MSIF recommends. Decisions about starting a DMT should take into account a patient’s disease course, disease activity, and regional COVID-19 risks, according to the federation. For patients due to start DMT, treatments that do not reduce lymphocytes, such as interferons, glatiramer acetate, or natalizumab, should be considered.
Fingolimod, dimethyl fumarate, teriflunomide, and siponimod “may reduce the ability of the immune system to respond to an infection,” and “people should carefully consider the risks and benefits of initiating these treatments during the COVID-19 pandemic,” according to the federation. “People with MS who are currently taking alemtuzumab, cladribine, ocrelizumab, rituximab, fingolimod, dimethyl fumarate, teriflunomide or siponimod and are living in a community with a COVID-19 outbreak should isolate as much as possible to reduce their risk of infection.”
Extended isolation during the COVID-19 outbreak may be warranted for patients with MS who have recently undergone autologous hematopoietic stem cell treatment, which entails intensive chemotherapy, the guidance says. In addition, postponement of this procedure should be considered.
Child neurology, migraine, movement disorders, and stroke
The Child Neurology Foundation (CNF) and Child Neurology Society (CNS) published a joint statement about COVID-19. “Most children who contract COVID-19 appear to exhibit only mild symptoms,” said Scott Pomeroy, MD, president of CNF’s board of directors and chair of the department of neurology at Boston Children’s Hospital, in the statement. “However, if your child is taking a medication such as steroids that can lower their immune system response, there could be an increased risk for more significant symptoms. In addition, children with lung disease, such as asthma, may also be at higher risk. Therefore, it is important to practice preventative precautions. We hope that this information will help to reduce some of the fears that families in our community may be experiencing.”
The American Migraine Foundation shared COVID-19 considerations for patients with migraine from Mia Minen, MD, associate professor of neurology and population health at NYU Langone in New York. Patients with migraine who are otherwise in good health are not expected to be at increased risk of severe COVID-19, according to Dr. Minen. Best practices include having an adequate supply of medicine, considering alternatives to in-person doctor visits, and being “mindful of routine and diet to reduce migraine triggers,” the foundation suggests. In addition, patients should try to limit stress and seek out “alternative methods of social interaction.”
“The relationship between COVID-19 and Parkinson’s disease or other movement disorders remains unknown,” the International Parkinson and Movement Disorder Society said. “In general, we recommend that our movement disorder patients do not assume they are at extreme risks, which for the time being are uncertain. Nevertheless, we strongly recommend following the standard measures strictly to avoid exposures to the virus.”
The American Heart Association (AHA) cautions that older patients with coronary heart disease or hypertension “may be more likely than others to be infected by the coronavirus that causes COVID-19 and to develop more severe symptoms.” In addition, people with a history of stroke “may face a higher risk of complications,” according to the AHA. “As a result, people who have heart disease or another underlying condition should stay home to limit their risk of contracting the virus.”
Several groups emphasized the importance of telemedicine as an option for patients with neurologic conditions during the pandemic. The American Headache Society has hosted discussions on conducting neurologic exams via telemedicine. The American Academy of Neurology also conducted a webinar on telemedicine and COVID-19 and created a page with COVID-19 resources. The journal Neurology is publishing invited commentaries about neurologic aspects of the COVID-19 pandemic.
Neurologic disorders are among the “underlying medical conditions that may increase the risk of serious COVID-19 for individuals of any age,” according to the Centers for Disease Control and Prevention.
Potentially relevant drug interactions, how immunosuppressive medications may influence the risk of COVID-19, and neurologic diseases that may be associated with greater risk are among the questions that experts and groups have addressed.
According to the CDC, neurologic conditions that may heighten the risk of severe COVID-19 include “disorders of the brain, spinal cord, peripheral nerve, and muscle such as cerebral palsy, epilepsy (seizure disorders), stroke, intellectual disability, moderate to severe developmental delay, muscular dystrophy, or spinal cord injury.” Many patients, however, may not have substantially increased risks, neurologists suggest.
“Patients with conditions that do not affect their swallowing or breathing muscles and in whom the immune system is working normally are not considered to be at increased risk from COVID-19,” according to March 26 guidance from the Association of British Neurologists (ABN). “Milder or moderate forms of many of the commoner neurological disorders, such as Parkinson’s disease, multiple sclerosis, epilepsy, are not currently considered to confer increased risk, so long as the breathing and swallowing muscles are functioning well.”
Neurologists should tailor treatment decisions to individual patients, according to the ABN. “Although some neurological conditions or treatments increase the risk of complicated COVID-19, most patients in these groups will overcome the infection,” the association noted.
Interactions with potential COVID-19 treatments
Standard drugs in neurology may interact with potential COVID-19 treatments. For example, “preliminary experience suggests that there is a possible benefit from hydroxychloroquine and azithromycin treatment in COVID-19 infection,” but either of those drugs “may lead to a deterioration in myasthenia gravis,” the ABN notes. “Doctors will have to balance the risks from myasthenia and COVID-19 on a case-by-case basis.” The Liverpool Drug Interactions Group has published tables that describe interactions between potential COVID-19 treatments and anticonvulsants, analgesics, immunosuppressants, and other medication classes.
Many muscle diseases and neuromuscular junction diseases may entail higher risks of complicated COVID-19, the ABN suggested. For patients on immunotherapy, the medication may be a more important consideration for COVID-19 than the underlying disease. Other comorbidities such as hypertension, renal impairment, neutropenia, lymphopenia, liver disease, diabetes mellitus, ischemic heart disease, and lung disease may be important factors, according to the association.
Seizures may not worsen
After the CDC added epilepsy to its list of conditions that entail higher risk of severe COVID-19, M. Scott Perry, MD, medical director of neurology at Cook Children’s Medical Center in Fort Worth, Tex., commented on Twitter that “most healthy people with controlled epilepsy [are] probably at no more risk than others.”
“Those treated with steroids or other immunosuppressive drugs are likely higher risk,” Dr. Perry said. “Likewise, patients with other medical comorbidities such as muscle weakness, swallowing or breathing problems, and other complex cases of epilepsy are likely higher risk. Regardless: be responsible, avoid crowds, wash your hands, avoid sick contacts.”
Doctors in Italy, based on small numbers of cases, have found that seizures are not worse in patients with epilepsy and COVID-19, said Dr. Perry. A few children, including several patients with Dravet syndrome, “had uncomplicated illness and seizures were no worse,” he said. “That is reassuring.”
“Until now, there is no evidence of a direct effect of COVID-19 on seizures or epilepsy,” according to the International League Against Epilepsy (ILAE). “However, patients may experience worsening of seizures due to systemic illnesses, drug interactions, decreased access to antiseizure medications, and increased stress.”
“In younger children, the fever that accompanies COVID-19 may exacerbate seizures, as might any febrile illness,” according to an American Epilepsy Society (AES) resource for epilepsy clinicians. “The main known elevated risk factors related to COVID-19 are age, respiratory disease, and other chronic medical conditions not related to epilepsy. As for all, people with epilepsy should adhere to the CDC recommendations for reducing risk of infection.” Neurologists should review with patients the importance of treatment adherence, update plans for managing breakthrough seizures, and ensure necessary medications are on hand, according to the AES.
The Epilepsy Foundation created a page with information about COVID-19 for patients with epilepsy and recorded a discussion with epilepsy specialists. DEE-P (Developmental Epileptic Encephalopathy–Project) Connections recorded a webinar about protecting medically complex or immune-suppressed children with epilepsy from COVID-19.
MS DMTs and the coronavirus
The National Multiple Sclerosis (MS) Society has provided guidance on the use of disease-modifying therapies (DMTs) during the COVID-19 pandemic. “There are numerous recommendations circulating that attempt to provide clarity and guidance, however, differences among the recommendations have created confusion,” the society says. “DMT decision making varies significantly from country to country, ranging from highly provider-directed to a collaborative decision-making model. ... DMT decisions should be individualized and made collaboratively between the person with MS and his/her healthcare provider.”
Patients with MS and their physicians should weigh risks and benefits before starting cell-depleting DMTs such as alemtuzumab, cladribine, ocrelizumab, or rituximab, according the National MS Society. They also should consider the risks and benefits of DMTs that carry warnings of a potentially severe increase in disability after stopping therapy, such as fingolimod and natalizumab. “We endorse the global advice provided by the MS International Federation (MSIF) – but emphasize that DMT decision making must be individualized and based upon multiple factors,” the National MS Society said.
Neurologists currently lack evidence about how COVID-19 affects patients with MS, according to the MSIF, which based its DMT guidance on advice from MS neurologists and research experts from member organizations. Many DMTs suppress or modify the immune system, and “some MS medications might increase the likelihood of developing complications from a COVID-19 infection but this risk needs to be balanced with the risks of stopping treatment,” according to the federation.
Patients currently taking DMTs should continue treatment, and those who develop symptoms of COVID-19 or test positive for the infection should discuss their DMT with a health care professional familiar with their care, the MSIF recommends. Decisions about starting a DMT should take into account a patient’s disease course, disease activity, and regional COVID-19 risks, according to the federation. For patients due to start DMT, treatments that do not reduce lymphocytes, such as interferons, glatiramer acetate, or natalizumab, should be considered.
Fingolimod, dimethyl fumarate, teriflunomide, and siponimod “may reduce the ability of the immune system to respond to an infection,” and “people should carefully consider the risks and benefits of initiating these treatments during the COVID-19 pandemic,” according to the federation. “People with MS who are currently taking alemtuzumab, cladribine, ocrelizumab, rituximab, fingolimod, dimethyl fumarate, teriflunomide or siponimod and are living in a community with a COVID-19 outbreak should isolate as much as possible to reduce their risk of infection.”
Extended isolation during the COVID-19 outbreak may be warranted for patients with MS who have recently undergone autologous hematopoietic stem cell treatment, which entails intensive chemotherapy, the guidance says. In addition, postponement of this procedure should be considered.
Child neurology, migraine, movement disorders, and stroke
The Child Neurology Foundation (CNF) and Child Neurology Society (CNS) published a joint statement about COVID-19. “Most children who contract COVID-19 appear to exhibit only mild symptoms,” said Scott Pomeroy, MD, president of CNF’s board of directors and chair of the department of neurology at Boston Children’s Hospital, in the statement. “However, if your child is taking a medication such as steroids that can lower their immune system response, there could be an increased risk for more significant symptoms. In addition, children with lung disease, such as asthma, may also be at higher risk. Therefore, it is important to practice preventative precautions. We hope that this information will help to reduce some of the fears that families in our community may be experiencing.”
The American Migraine Foundation shared COVID-19 considerations for patients with migraine from Mia Minen, MD, associate professor of neurology and population health at NYU Langone in New York. Patients with migraine who are otherwise in good health are not expected to be at increased risk of severe COVID-19, according to Dr. Minen. Best practices include having an adequate supply of medicine, considering alternatives to in-person doctor visits, and being “mindful of routine and diet to reduce migraine triggers,” the foundation suggests. In addition, patients should try to limit stress and seek out “alternative methods of social interaction.”
“The relationship between COVID-19 and Parkinson’s disease or other movement disorders remains unknown,” the International Parkinson and Movement Disorder Society said. “In general, we recommend that our movement disorder patients do not assume they are at extreme risks, which for the time being are uncertain. Nevertheless, we strongly recommend following the standard measures strictly to avoid exposures to the virus.”
The American Heart Association (AHA) cautions that older patients with coronary heart disease or hypertension “may be more likely than others to be infected by the coronavirus that causes COVID-19 and to develop more severe symptoms.” In addition, people with a history of stroke “may face a higher risk of complications,” according to the AHA. “As a result, people who have heart disease or another underlying condition should stay home to limit their risk of contracting the virus.”
Several groups emphasized the importance of telemedicine as an option for patients with neurologic conditions during the pandemic. The American Headache Society has hosted discussions on conducting neurologic exams via telemedicine. The American Academy of Neurology also conducted a webinar on telemedicine and COVID-19 and created a page with COVID-19 resources. The journal Neurology is publishing invited commentaries about neurologic aspects of the COVID-19 pandemic.