User login
Psychedelic drugs ‘truly have potential’ in headache care
DENVER – Psychedelics such as psilocybin “truly have the potential to transform how we treat a number of neuropsychiatric diseases, including headaches,” a neuropharmacologist told colleagues at the annual meeting of the American Headache Society.
However, Bryan Roth, MD, PhD, professor of pharmacology at the University of North Carolina at Chapel Hill, also offered a major cautionary note: There have been no randomized, phase 3 trials of psychedelics, and he bluntly said that “I do not recommend the use of psychedelics for any medical condition.”
The potential disease-altering powers of psychedelics have received a tremendous amount of research and media attention over the past several years. A landmark randomized, double-blind study released in 2016 triggered much of the interest, Dr. Roth said, when it suggested that high-dose psilocybin significantly lowered levels of depressed mood/anxiety in patients with life-threatening cancer. At 6 months, 80% of patients who took the dose reported moderate or greater improvement in well-being/life satisfaction.
“You have the potential – unprecedented in psychiatry – that a single dose of a therapeutic agent may induce a rapid, robust, and sustained antidepressant action,” he said. Also of note: The “vast majority” of subjects say their encounter with a psychedelic was “one of the most meaningful experiences of their lives.”
Dr. Roth said his own research suggests that psychedelics cause a “huge increase” in the asynchronous firing of neurons. “Noise is being injected into the system and is interpreted by the brain or the mind, which always likes to make a story about what’s going on. The story it makes up is idiosyncratic to every person and memorable for reasons that are not understood.”
Now, Dr. Roth said, he and colleagues are working to “create drugs that have this potential remarkable therapeutic efficacy in psychiatric and neurologic disorders without the psychedelic effects.” A $27 million grant from the Defense Advanced Research Projects Agency is providing support for their efforts, he said.
For the moment, he said, there’s no way to know if “the psychedelic experience is essential to the therapeutic action of these drugs. But it’s a testable hypothesis.”
As he noted, a tiny 2010 study of 2-bromo-lysergic acid diethylamide (LSD), which doesn’t cause hallucinations, showed promise as a treatment for cluster headaches.
For now, Dr. Roth said, his lab is synthesizing and testing new compounds that interact with the crucial 5-HT2A receptor.
Additional research
In another presentation at the AHS annual meeting, neurologist Emmanuelle A. D. Schindler, MD, PhD, of Yale School of Medicine, highlighted her 2021 study of an exploratory double-blind, placebo-controlled, cross-over study of psilocybin versus placebo for migraine headache. A single oral dose of the drug, the researchers found, reduced headache frequency and pain over 2 weeks. The study is small, with just 10 subjects, and multiple exclusion criteria.
She also revealed preliminary findings from an ongoing randomized, double-blind, placebo-controlled study of psilocybin versus placebo in cluster headaches. In 14 subjects, a psilocybin pulse was linked to fewer cluster attacks over 3 weeks, although the effect wasn’t statistically significant. However, there was a statistically significant reduction over 8 weeks in patients with chronic headache.
Dr. Schindler noted that “with these early studies, we only looked out to 2 weeks for migraine, and we only looked out to 2 months for cluster.” There are multiple other limitations, she acknowledged. “We have to do a lot more research and consider safety as well.”
However, “there is a really unique capacity for lasting effects after limited dosing,” she added, and the studies do show reductions in headache burden “that do not correlate with acute psychedelic effects.”
Moving forward, Dr. Roth cautioned that while U.S. states are allowing the use of psychedelics for medical purposes, “we don’t know if they ultimately are therapeutic. And we have strong reason to believe that microdosing or chronic dosing of these compounds is ultimately going to be deleterious to the health of our patients.”
Dr. Roth did not provide disclosure information. Dr. Schindler discloses research funding (Ceruvia Lifesciences, Wallace Research Foundation, Clusterbusters, Department of Veterans Affairs), serves on advisory boards (Ceruvia Lifesciences, Clusterbusters), and has a patent.
DENVER – Psychedelics such as psilocybin “truly have the potential to transform how we treat a number of neuropsychiatric diseases, including headaches,” a neuropharmacologist told colleagues at the annual meeting of the American Headache Society.
However, Bryan Roth, MD, PhD, professor of pharmacology at the University of North Carolina at Chapel Hill, also offered a major cautionary note: There have been no randomized, phase 3 trials of psychedelics, and he bluntly said that “I do not recommend the use of psychedelics for any medical condition.”
The potential disease-altering powers of psychedelics have received a tremendous amount of research and media attention over the past several years. A landmark randomized, double-blind study released in 2016 triggered much of the interest, Dr. Roth said, when it suggested that high-dose psilocybin significantly lowered levels of depressed mood/anxiety in patients with life-threatening cancer. At 6 months, 80% of patients who took the dose reported moderate or greater improvement in well-being/life satisfaction.
“You have the potential – unprecedented in psychiatry – that a single dose of a therapeutic agent may induce a rapid, robust, and sustained antidepressant action,” he said. Also of note: The “vast majority” of subjects say their encounter with a psychedelic was “one of the most meaningful experiences of their lives.”
Dr. Roth said his own research suggests that psychedelics cause a “huge increase” in the asynchronous firing of neurons. “Noise is being injected into the system and is interpreted by the brain or the mind, which always likes to make a story about what’s going on. The story it makes up is idiosyncratic to every person and memorable for reasons that are not understood.”
Now, Dr. Roth said, he and colleagues are working to “create drugs that have this potential remarkable therapeutic efficacy in psychiatric and neurologic disorders without the psychedelic effects.” A $27 million grant from the Defense Advanced Research Projects Agency is providing support for their efforts, he said.
For the moment, he said, there’s no way to know if “the psychedelic experience is essential to the therapeutic action of these drugs. But it’s a testable hypothesis.”
As he noted, a tiny 2010 study of 2-bromo-lysergic acid diethylamide (LSD), which doesn’t cause hallucinations, showed promise as a treatment for cluster headaches.
For now, Dr. Roth said, his lab is synthesizing and testing new compounds that interact with the crucial 5-HT2A receptor.
Additional research
In another presentation at the AHS annual meeting, neurologist Emmanuelle A. D. Schindler, MD, PhD, of Yale School of Medicine, highlighted her 2021 study of an exploratory double-blind, placebo-controlled, cross-over study of psilocybin versus placebo for migraine headache. A single oral dose of the drug, the researchers found, reduced headache frequency and pain over 2 weeks. The study is small, with just 10 subjects, and multiple exclusion criteria.
She also revealed preliminary findings from an ongoing randomized, double-blind, placebo-controlled study of psilocybin versus placebo in cluster headaches. In 14 subjects, a psilocybin pulse was linked to fewer cluster attacks over 3 weeks, although the effect wasn’t statistically significant. However, there was a statistically significant reduction over 8 weeks in patients with chronic headache.
Dr. Schindler noted that “with these early studies, we only looked out to 2 weeks for migraine, and we only looked out to 2 months for cluster.” There are multiple other limitations, she acknowledged. “We have to do a lot more research and consider safety as well.”
However, “there is a really unique capacity for lasting effects after limited dosing,” she added, and the studies do show reductions in headache burden “that do not correlate with acute psychedelic effects.”
Moving forward, Dr. Roth cautioned that while U.S. states are allowing the use of psychedelics for medical purposes, “we don’t know if they ultimately are therapeutic. And we have strong reason to believe that microdosing or chronic dosing of these compounds is ultimately going to be deleterious to the health of our patients.”
Dr. Roth did not provide disclosure information. Dr. Schindler discloses research funding (Ceruvia Lifesciences, Wallace Research Foundation, Clusterbusters, Department of Veterans Affairs), serves on advisory boards (Ceruvia Lifesciences, Clusterbusters), and has a patent.
DENVER – Psychedelics such as psilocybin “truly have the potential to transform how we treat a number of neuropsychiatric diseases, including headaches,” a neuropharmacologist told colleagues at the annual meeting of the American Headache Society.
However, Bryan Roth, MD, PhD, professor of pharmacology at the University of North Carolina at Chapel Hill, also offered a major cautionary note: There have been no randomized, phase 3 trials of psychedelics, and he bluntly said that “I do not recommend the use of psychedelics for any medical condition.”
The potential disease-altering powers of psychedelics have received a tremendous amount of research and media attention over the past several years. A landmark randomized, double-blind study released in 2016 triggered much of the interest, Dr. Roth said, when it suggested that high-dose psilocybin significantly lowered levels of depressed mood/anxiety in patients with life-threatening cancer. At 6 months, 80% of patients who took the dose reported moderate or greater improvement in well-being/life satisfaction.
“You have the potential – unprecedented in psychiatry – that a single dose of a therapeutic agent may induce a rapid, robust, and sustained antidepressant action,” he said. Also of note: The “vast majority” of subjects say their encounter with a psychedelic was “one of the most meaningful experiences of their lives.”
Dr. Roth said his own research suggests that psychedelics cause a “huge increase” in the asynchronous firing of neurons. “Noise is being injected into the system and is interpreted by the brain or the mind, which always likes to make a story about what’s going on. The story it makes up is idiosyncratic to every person and memorable for reasons that are not understood.”
Now, Dr. Roth said, he and colleagues are working to “create drugs that have this potential remarkable therapeutic efficacy in psychiatric and neurologic disorders without the psychedelic effects.” A $27 million grant from the Defense Advanced Research Projects Agency is providing support for their efforts, he said.
For the moment, he said, there’s no way to know if “the psychedelic experience is essential to the therapeutic action of these drugs. But it’s a testable hypothesis.”
As he noted, a tiny 2010 study of 2-bromo-lysergic acid diethylamide (LSD), which doesn’t cause hallucinations, showed promise as a treatment for cluster headaches.
For now, Dr. Roth said, his lab is synthesizing and testing new compounds that interact with the crucial 5-HT2A receptor.
Additional research
In another presentation at the AHS annual meeting, neurologist Emmanuelle A. D. Schindler, MD, PhD, of Yale School of Medicine, highlighted her 2021 study of an exploratory double-blind, placebo-controlled, cross-over study of psilocybin versus placebo for migraine headache. A single oral dose of the drug, the researchers found, reduced headache frequency and pain over 2 weeks. The study is small, with just 10 subjects, and multiple exclusion criteria.
She also revealed preliminary findings from an ongoing randomized, double-blind, placebo-controlled study of psilocybin versus placebo in cluster headaches. In 14 subjects, a psilocybin pulse was linked to fewer cluster attacks over 3 weeks, although the effect wasn’t statistically significant. However, there was a statistically significant reduction over 8 weeks in patients with chronic headache.
Dr. Schindler noted that “with these early studies, we only looked out to 2 weeks for migraine, and we only looked out to 2 months for cluster.” There are multiple other limitations, she acknowledged. “We have to do a lot more research and consider safety as well.”
However, “there is a really unique capacity for lasting effects after limited dosing,” she added, and the studies do show reductions in headache burden “that do not correlate with acute psychedelic effects.”
Moving forward, Dr. Roth cautioned that while U.S. states are allowing the use of psychedelics for medical purposes, “we don’t know if they ultimately are therapeutic. And we have strong reason to believe that microdosing or chronic dosing of these compounds is ultimately going to be deleterious to the health of our patients.”
Dr. Roth did not provide disclosure information. Dr. Schindler discloses research funding (Ceruvia Lifesciences, Wallace Research Foundation, Clusterbusters, Department of Veterans Affairs), serves on advisory boards (Ceruvia Lifesciences, Clusterbusters), and has a patent.
FROM AHS 2022
Adolescent female with rash on the arms and posterior legs
Erythema annulare centrifugum
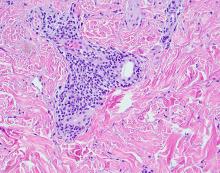
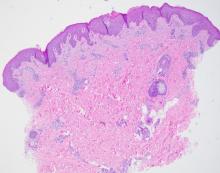
A thorough body examination failed to reveal any other rashes or lesions suggestive of a fungal infection. A blood count and urinalysis were within normal limits. She had no lymphadenopathy or hepatosplenomegaly. A potassium hydroxide analysis of skin scrapings was negative for fungal elements. Punch biopsy of the skin on the left arm revealed focal intermittent parakeratosis, mildly acanthotic and spongiotic epidermis, and a tight superficial perivascular chronic dermatitis consisting of lymphocytes and histiocytes (Figures). Given these findings, a diagnosis of erythema annulare centrifugum (EAC) was rendered.
EAC is a rare, reactive skin rash characterized by redness (erythema) and ring-shaped lesions (annulare) that slowly spread from the center (centrifugum). The lesions present with a characteristic trailing scale on the inner border of the erythematous ring. Lesions may be asymptomatic or mildly pruritic and commonly involve the trunk, buttocks, hips, and upper legs. It is important to note that its duration is highly variable, ranging from weeks to decades, with most cases persisting for 9 months. EAC typically affects young or middle-aged adults but can occur at any age.
Although the etiology of EAC is unknown, it is believed to be a hypersensitivity reaction to a foreign antigen. Cutaneous fungal infections are commonly reported as triggers as well as other viral infections, medications, malignancy, underlying systemic disease, and certain foods. Treatment depends on the underlying condition and removing the implicated agent. However, most cases of EAC are idiopathic and self-limiting. It is possible that our patient’s prior history of tinea capitis could have triggered the skin lesions suggestive of EAC, but interestingly, these lesions did not go away after the fungal infection was cleared and have continued to recur. For patients with refractory lesions or treatment of patients without an identifiable cause, the use of oral antimicrobials has been proposed. Medications such as azithromycin, erythromycin, fluconazole, and metronidazole have been reported to be helpful in some patients with refractory EAC. Our patient wanted to continue topical treatment with betamethasone as needed and may consider antimicrobial therapy if the lesions continue to recur.
Tinea corporis refers to a superficial fungal infection of the skin. It may present as one or more asymmetrical, annular, pruritic plaques with a raised scaly leading edge rather than the trailing scale seen with EAC. Diagnosis is made by KOH examination of skin scrapings. Common risk factors include close contact with an infected person or animal, warm, moist environments, sharing personal items, and prolonged use of systemic corticosteroids. Our patient’s KOH analysis of skin scrapings was negative for fungal elements.
Erythema marginatum is a rare skin rash commonly seen with acute rheumatic fever secondary to streptococcal infection. It presents as annular erythematous lesions on the trunk and proximal extremities that are exacerbated by heat. It is often associated with active carditis related to rheumatic fever. This self-limited rash usually resolves in 2-3 days. Our patient was asymptomatic without involvement of other organs.
Like EAC, granuloma annulare is a benign chronic skin condition that presents with ring-shaped lesions. Its etiology is unknown, and lesions may be asymptomatic or mildly pruritic. Localized granuloma annulare typically presents as reddish-brown papules or plaques on the fingers, hands, elbows, dorsal feet, or ankles. The distinguishing feature of granuloma annulare from other annular lesions is its absence of scale.
Urticaria multiforme is an allergic hypersensitivity reaction commonly linked to viral infections, medications, and immunizations. Clinical features include blanchable annular/polycyclic lesions with a central purplish or dusky hue. Diagnostic pearls include the presence of pruritus, dermatographism, and individual lesions that resolve within 24 hours, all of which were not found in our patient’s case.
Ms. Laborada is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital. Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Ms. Laborada and Dr. Matiz have no relevant financial disclosures.
References
1. Paller A and Mancini AJ. Hurwitz Clinical Pediatric Dermatology: A Textbook of Skin Disorders of Childhood and Adolescence. 4th ed. Philadelphia: Elsevier Saunders, 2011.
2. McDaniel B and Cook C. “Erythema annulare centrifugum” 2021 Aug 27. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing, 2022 Jan. PMID: 29494101.
3. Leung AK e al. Drugs Context. 2020 Jul 20;9:5-6.
4. Majmundar VD and Nagalli S. “Erythema marginatum” 2022 May 8. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing, 2022 Jan.
5. Piette EW and Rosenbach M. J Am Acad Dermatol. 2016 Sep;75(3):467-79.
6. Barros M et al. BMJ Case Rep. 2021 Jan 28;14(1):e241011.
Erythema annulare centrifugum
A thorough body examination failed to reveal any other rashes or lesions suggestive of a fungal infection. A blood count and urinalysis were within normal limits. She had no lymphadenopathy or hepatosplenomegaly. A potassium hydroxide analysis of skin scrapings was negative for fungal elements. Punch biopsy of the skin on the left arm revealed focal intermittent parakeratosis, mildly acanthotic and spongiotic epidermis, and a tight superficial perivascular chronic dermatitis consisting of lymphocytes and histiocytes (Figures). Given these findings, a diagnosis of erythema annulare centrifugum (EAC) was rendered.
EAC is a rare, reactive skin rash characterized by redness (erythema) and ring-shaped lesions (annulare) that slowly spread from the center (centrifugum). The lesions present with a characteristic trailing scale on the inner border of the erythematous ring. Lesions may be asymptomatic or mildly pruritic and commonly involve the trunk, buttocks, hips, and upper legs. It is important to note that its duration is highly variable, ranging from weeks to decades, with most cases persisting for 9 months. EAC typically affects young or middle-aged adults but can occur at any age.
Although the etiology of EAC is unknown, it is believed to be a hypersensitivity reaction to a foreign antigen. Cutaneous fungal infections are commonly reported as triggers as well as other viral infections, medications, malignancy, underlying systemic disease, and certain foods. Treatment depends on the underlying condition and removing the implicated agent. However, most cases of EAC are idiopathic and self-limiting. It is possible that our patient’s prior history of tinea capitis could have triggered the skin lesions suggestive of EAC, but interestingly, these lesions did not go away after the fungal infection was cleared and have continued to recur. For patients with refractory lesions or treatment of patients without an identifiable cause, the use of oral antimicrobials has been proposed. Medications such as azithromycin, erythromycin, fluconazole, and metronidazole have been reported to be helpful in some patients with refractory EAC. Our patient wanted to continue topical treatment with betamethasone as needed and may consider antimicrobial therapy if the lesions continue to recur.
Tinea corporis refers to a superficial fungal infection of the skin. It may present as one or more asymmetrical, annular, pruritic plaques with a raised scaly leading edge rather than the trailing scale seen with EAC. Diagnosis is made by KOH examination of skin scrapings. Common risk factors include close contact with an infected person or animal, warm, moist environments, sharing personal items, and prolonged use of systemic corticosteroids. Our patient’s KOH analysis of skin scrapings was negative for fungal elements.
Erythema marginatum is a rare skin rash commonly seen with acute rheumatic fever secondary to streptococcal infection. It presents as annular erythematous lesions on the trunk and proximal extremities that are exacerbated by heat. It is often associated with active carditis related to rheumatic fever. This self-limited rash usually resolves in 2-3 days. Our patient was asymptomatic without involvement of other organs.
Like EAC, granuloma annulare is a benign chronic skin condition that presents with ring-shaped lesions. Its etiology is unknown, and lesions may be asymptomatic or mildly pruritic. Localized granuloma annulare typically presents as reddish-brown papules or plaques on the fingers, hands, elbows, dorsal feet, or ankles. The distinguishing feature of granuloma annulare from other annular lesions is its absence of scale.
Urticaria multiforme is an allergic hypersensitivity reaction commonly linked to viral infections, medications, and immunizations. Clinical features include blanchable annular/polycyclic lesions with a central purplish or dusky hue. Diagnostic pearls include the presence of pruritus, dermatographism, and individual lesions that resolve within 24 hours, all of which were not found in our patient’s case.
Ms. Laborada is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital. Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Ms. Laborada and Dr. Matiz have no relevant financial disclosures.
References
1. Paller A and Mancini AJ. Hurwitz Clinical Pediatric Dermatology: A Textbook of Skin Disorders of Childhood and Adolescence. 4th ed. Philadelphia: Elsevier Saunders, 2011.
2. McDaniel B and Cook C. “Erythema annulare centrifugum” 2021 Aug 27. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing, 2022 Jan. PMID: 29494101.
3. Leung AK e al. Drugs Context. 2020 Jul 20;9:5-6.
4. Majmundar VD and Nagalli S. “Erythema marginatum” 2022 May 8. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing, 2022 Jan.
5. Piette EW and Rosenbach M. J Am Acad Dermatol. 2016 Sep;75(3):467-79.
6. Barros M et al. BMJ Case Rep. 2021 Jan 28;14(1):e241011.
Erythema annulare centrifugum
A thorough body examination failed to reveal any other rashes or lesions suggestive of a fungal infection. A blood count and urinalysis were within normal limits. She had no lymphadenopathy or hepatosplenomegaly. A potassium hydroxide analysis of skin scrapings was negative for fungal elements. Punch biopsy of the skin on the left arm revealed focal intermittent parakeratosis, mildly acanthotic and spongiotic epidermis, and a tight superficial perivascular chronic dermatitis consisting of lymphocytes and histiocytes (Figures). Given these findings, a diagnosis of erythema annulare centrifugum (EAC) was rendered.
EAC is a rare, reactive skin rash characterized by redness (erythema) and ring-shaped lesions (annulare) that slowly spread from the center (centrifugum). The lesions present with a characteristic trailing scale on the inner border of the erythematous ring. Lesions may be asymptomatic or mildly pruritic and commonly involve the trunk, buttocks, hips, and upper legs. It is important to note that its duration is highly variable, ranging from weeks to decades, with most cases persisting for 9 months. EAC typically affects young or middle-aged adults but can occur at any age.
Although the etiology of EAC is unknown, it is believed to be a hypersensitivity reaction to a foreign antigen. Cutaneous fungal infections are commonly reported as triggers as well as other viral infections, medications, malignancy, underlying systemic disease, and certain foods. Treatment depends on the underlying condition and removing the implicated agent. However, most cases of EAC are idiopathic and self-limiting. It is possible that our patient’s prior history of tinea capitis could have triggered the skin lesions suggestive of EAC, but interestingly, these lesions did not go away after the fungal infection was cleared and have continued to recur. For patients with refractory lesions or treatment of patients without an identifiable cause, the use of oral antimicrobials has been proposed. Medications such as azithromycin, erythromycin, fluconazole, and metronidazole have been reported to be helpful in some patients with refractory EAC. Our patient wanted to continue topical treatment with betamethasone as needed and may consider antimicrobial therapy if the lesions continue to recur.
Tinea corporis refers to a superficial fungal infection of the skin. It may present as one or more asymmetrical, annular, pruritic plaques with a raised scaly leading edge rather than the trailing scale seen with EAC. Diagnosis is made by KOH examination of skin scrapings. Common risk factors include close contact with an infected person or animal, warm, moist environments, sharing personal items, and prolonged use of systemic corticosteroids. Our patient’s KOH analysis of skin scrapings was negative for fungal elements.
Erythema marginatum is a rare skin rash commonly seen with acute rheumatic fever secondary to streptococcal infection. It presents as annular erythematous lesions on the trunk and proximal extremities that are exacerbated by heat. It is often associated with active carditis related to rheumatic fever. This self-limited rash usually resolves in 2-3 days. Our patient was asymptomatic without involvement of other organs.
Like EAC, granuloma annulare is a benign chronic skin condition that presents with ring-shaped lesions. Its etiology is unknown, and lesions may be asymptomatic or mildly pruritic. Localized granuloma annulare typically presents as reddish-brown papules or plaques on the fingers, hands, elbows, dorsal feet, or ankles. The distinguishing feature of granuloma annulare from other annular lesions is its absence of scale.
Urticaria multiforme is an allergic hypersensitivity reaction commonly linked to viral infections, medications, and immunizations. Clinical features include blanchable annular/polycyclic lesions with a central purplish or dusky hue. Diagnostic pearls include the presence of pruritus, dermatographism, and individual lesions that resolve within 24 hours, all of which were not found in our patient’s case.
Ms. Laborada is a pediatric dermatology research associate in the division of pediatric and adolescent dermatology at the University of California, San Diego, and Rady Children’s Hospital. Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Ms. Laborada and Dr. Matiz have no relevant financial disclosures.
References
1. Paller A and Mancini AJ. Hurwitz Clinical Pediatric Dermatology: A Textbook of Skin Disorders of Childhood and Adolescence. 4th ed. Philadelphia: Elsevier Saunders, 2011.
2. McDaniel B and Cook C. “Erythema annulare centrifugum” 2021 Aug 27. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing, 2022 Jan. PMID: 29494101.
3. Leung AK e al. Drugs Context. 2020 Jul 20;9:5-6.
4. Majmundar VD and Nagalli S. “Erythema marginatum” 2022 May 8. In: StatPearls [Internet]. Treasure Island, Fla.: StatPearls Publishing, 2022 Jan.
5. Piette EW and Rosenbach M. J Am Acad Dermatol. 2016 Sep;75(3):467-79.
6. Barros M et al. BMJ Case Rep. 2021 Jan 28;14(1):e241011.
A review of systems was noncontributory. She was not taking any other medications or vitamin supplements. There were no pets at home and no other affected family members. Physical exam was notable for scattered, pink, annular plaques with central clearing, faint brownish pigmentation, and fine scale.
Employment and buyout agreements
. The most common question was, “Do I really need to go to the trouble and expense of negotiating them?” If you have more than one physician in your group, you absolutely do need written contracts for a variety of reasons, but mostly to avoid conflicts later on. The proverbial “handshake agreement” is worthless in a major business dispute; everyone loses in such situations except the lawyers and accountants.
Mergers and buy-ins were covered at some length in my two previous columns. If the arrangement is to be one of employer and employees rather than a merger of equal partners, you will need an employment agreement to cover duties, requirements, expectations, and benefits. They define how each practitioner/employee will be paid, along with paid time off, health insurance, expense allowances, and malpractice coverage, among other basics. The more that is spelled out in the employment agreement, the fewer disagreements you are likely to have down the road.
Many employment contracts include a “termination without cause” clause, which benefits both the practice and the practitioners. It allows a practice to terminate a new associate if it feels a mistake has been made, even if he or she has done nothing wrong. On the other hand, the newcomer has the option to terminate if a better offer arises, their spouse hates the area, or for any other reason.
Buyouts should be addressed in advance as well. Several recent correspondents told me they didn’t see the necessity of writing a buyout agreement, because they plan to eventually sell their practice, rendering any buyout conditions moot. But what happens if an associate dies, becomes permanently disabled, or abruptly decides to leave the practice? If you haven’t prepared for such eventualities, you could find yourself receiving a demand from your ex-partner (or surviving spouse) for immediate payment of that partner’s portion of the practice’s value. And your valuation of the practice is likely to be severely at odds with the other party’s. Meanwhile, remaining partners must cover all the practice’s expenses and deal with an increased patient load.
A buyout agreement avoids these problems by planning for such eventualities in advance. You must agree on how a buyout amount will be valued. As I’ve said in previous columns, I strongly advise using a formula, not a fixed amount. If a buyout is based on 15- or 20-year-old reimbursements, the buyout will have no relationship to what the partners are currently being paid. Likewise, any buyout calculated at “appraised value” is a problem, because the buyout amount remains a mystery until an appraisal is performed. If the appraised value ends up being too high, the remaining owners may refuse to pay it. Have an actuary create a formula, so that a buyout figure can be calculated at any time. This area, especially, is where you need experienced, competent legal advice.
To avoid surprises, any buyout should require ample notice (6-12 months is common) to allow time to rearrange finances and recruit a new provider. Vesting schedules, similar to those used in retirement plans, are also popular. If a partner leaves before a prescribed time period has elapsed – say, 20 years – the buyout is proportionally reduced.
Buyouts can also be useful when dealing with noncompete agreements, which are notoriously difficult (and expensive) to enforce. One solution is a buyout penalty; a departing partner can compete with his or her former practice, but at the cost of a substantially reduced buyout. This permits competition, but discourages it, and compensates the targeted practice.
Buyouts are also a potential solution to some buy-in issues. A new associate entering an established practice may not be able to contribute assets equal to existing partners’ stakes and may lack the cash necessary to make up the difference. One alternative is to agree that any inequalities will be compensated at the other end in buyout value. Those partners contributing more assets will receive larger buyouts than those contributing less.
As I’ve said many times, these are not negotiations to undertake on your own. Enlist the aid of a consultant or attorney (or both) with ample medical practice experience.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
. The most common question was, “Do I really need to go to the trouble and expense of negotiating them?” If you have more than one physician in your group, you absolutely do need written contracts for a variety of reasons, but mostly to avoid conflicts later on. The proverbial “handshake agreement” is worthless in a major business dispute; everyone loses in such situations except the lawyers and accountants.
Mergers and buy-ins were covered at some length in my two previous columns. If the arrangement is to be one of employer and employees rather than a merger of equal partners, you will need an employment agreement to cover duties, requirements, expectations, and benefits. They define how each practitioner/employee will be paid, along with paid time off, health insurance, expense allowances, and malpractice coverage, among other basics. The more that is spelled out in the employment agreement, the fewer disagreements you are likely to have down the road.
Many employment contracts include a “termination without cause” clause, which benefits both the practice and the practitioners. It allows a practice to terminate a new associate if it feels a mistake has been made, even if he or she has done nothing wrong. On the other hand, the newcomer has the option to terminate if a better offer arises, their spouse hates the area, or for any other reason.
Buyouts should be addressed in advance as well. Several recent correspondents told me they didn’t see the necessity of writing a buyout agreement, because they plan to eventually sell their practice, rendering any buyout conditions moot. But what happens if an associate dies, becomes permanently disabled, or abruptly decides to leave the practice? If you haven’t prepared for such eventualities, you could find yourself receiving a demand from your ex-partner (or surviving spouse) for immediate payment of that partner’s portion of the practice’s value. And your valuation of the practice is likely to be severely at odds with the other party’s. Meanwhile, remaining partners must cover all the practice’s expenses and deal with an increased patient load.
A buyout agreement avoids these problems by planning for such eventualities in advance. You must agree on how a buyout amount will be valued. As I’ve said in previous columns, I strongly advise using a formula, not a fixed amount. If a buyout is based on 15- or 20-year-old reimbursements, the buyout will have no relationship to what the partners are currently being paid. Likewise, any buyout calculated at “appraised value” is a problem, because the buyout amount remains a mystery until an appraisal is performed. If the appraised value ends up being too high, the remaining owners may refuse to pay it. Have an actuary create a formula, so that a buyout figure can be calculated at any time. This area, especially, is where you need experienced, competent legal advice.
To avoid surprises, any buyout should require ample notice (6-12 months is common) to allow time to rearrange finances and recruit a new provider. Vesting schedules, similar to those used in retirement plans, are also popular. If a partner leaves before a prescribed time period has elapsed – say, 20 years – the buyout is proportionally reduced.
Buyouts can also be useful when dealing with noncompete agreements, which are notoriously difficult (and expensive) to enforce. One solution is a buyout penalty; a departing partner can compete with his or her former practice, but at the cost of a substantially reduced buyout. This permits competition, but discourages it, and compensates the targeted practice.
Buyouts are also a potential solution to some buy-in issues. A new associate entering an established practice may not be able to contribute assets equal to existing partners’ stakes and may lack the cash necessary to make up the difference. One alternative is to agree that any inequalities will be compensated at the other end in buyout value. Those partners contributing more assets will receive larger buyouts than those contributing less.
As I’ve said many times, these are not negotiations to undertake on your own. Enlist the aid of a consultant or attorney (or both) with ample medical practice experience.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
. The most common question was, “Do I really need to go to the trouble and expense of negotiating them?” If you have more than one physician in your group, you absolutely do need written contracts for a variety of reasons, but mostly to avoid conflicts later on. The proverbial “handshake agreement” is worthless in a major business dispute; everyone loses in such situations except the lawyers and accountants.
Mergers and buy-ins were covered at some length in my two previous columns. If the arrangement is to be one of employer and employees rather than a merger of equal partners, you will need an employment agreement to cover duties, requirements, expectations, and benefits. They define how each practitioner/employee will be paid, along with paid time off, health insurance, expense allowances, and malpractice coverage, among other basics. The more that is spelled out in the employment agreement, the fewer disagreements you are likely to have down the road.
Many employment contracts include a “termination without cause” clause, which benefits both the practice and the practitioners. It allows a practice to terminate a new associate if it feels a mistake has been made, even if he or she has done nothing wrong. On the other hand, the newcomer has the option to terminate if a better offer arises, their spouse hates the area, or for any other reason.
Buyouts should be addressed in advance as well. Several recent correspondents told me they didn’t see the necessity of writing a buyout agreement, because they plan to eventually sell their practice, rendering any buyout conditions moot. But what happens if an associate dies, becomes permanently disabled, or abruptly decides to leave the practice? If you haven’t prepared for such eventualities, you could find yourself receiving a demand from your ex-partner (or surviving spouse) for immediate payment of that partner’s portion of the practice’s value. And your valuation of the practice is likely to be severely at odds with the other party’s. Meanwhile, remaining partners must cover all the practice’s expenses and deal with an increased patient load.
A buyout agreement avoids these problems by planning for such eventualities in advance. You must agree on how a buyout amount will be valued. As I’ve said in previous columns, I strongly advise using a formula, not a fixed amount. If a buyout is based on 15- or 20-year-old reimbursements, the buyout will have no relationship to what the partners are currently being paid. Likewise, any buyout calculated at “appraised value” is a problem, because the buyout amount remains a mystery until an appraisal is performed. If the appraised value ends up being too high, the remaining owners may refuse to pay it. Have an actuary create a formula, so that a buyout figure can be calculated at any time. This area, especially, is where you need experienced, competent legal advice.
To avoid surprises, any buyout should require ample notice (6-12 months is common) to allow time to rearrange finances and recruit a new provider. Vesting schedules, similar to those used in retirement plans, are also popular. If a partner leaves before a prescribed time period has elapsed – say, 20 years – the buyout is proportionally reduced.
Buyouts can also be useful when dealing with noncompete agreements, which are notoriously difficult (and expensive) to enforce. One solution is a buyout penalty; a departing partner can compete with his or her former practice, but at the cost of a substantially reduced buyout. This permits competition, but discourages it, and compensates the targeted practice.
Buyouts are also a potential solution to some buy-in issues. A new associate entering an established practice may not be able to contribute assets equal to existing partners’ stakes and may lack the cash necessary to make up the difference. One alternative is to agree that any inequalities will be compensated at the other end in buyout value. Those partners contributing more assets will receive larger buyouts than those contributing less.
As I’ve said many times, these are not negotiations to undertake on your own. Enlist the aid of a consultant or attorney (or both) with ample medical practice experience.
Dr. Eastern practices dermatology and dermatologic surgery in Belleville, N.J. He is the author of numerous articles and textbook chapters, and is a longtime monthly columnist for Dermatology News. Write to him at [email protected].
COVID-19 Cycle Threshold/Cycle Number Testing at a Community Living Center
COVID-19, caused by SARS-CoV-2, is more severe in individuals with underlying illnesses. Because complete social distancing might be more difficult in nursing homes and community living centers (CLCs), public health leaders and clinicians have been concerned about the epidemiology and disease course in nursing homes even before the COVID-19 pandemic.1-7 A report of a COVID-19 outbreak in a nursing home facility in King County, Washington, documented a 33.7% overall fatality rate for residents and 52.4% among the most critically ill.4,5 The experience at King County, Washington, shows that proactive steps to identify, monitor, and apply preventive control measures is important for future outbreaks.5
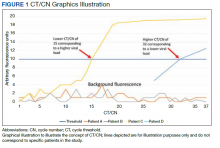
Reverse transcriptase polymerase chain reaction (RT-PCR) testing produces a cycle threshold (CT) or cycle number (CN) that correlates with viral load and infectiousness. 8-14 CT/CN represents the number of RT-PCR cycles required for the fluorescent signal to cross the detection threshold (exceed background level) and is inversely proportional to the viral load. Effectively, the higher the viral load, the lower the CT/ CN value (Figure 1). Tracking CT/CN values was not documented in the Washington nursing home outbreak. Reports of COVID- 19 testing in CLCs during outbreaks are sparse, and CT/CN values and demographic distribution of these veterans has not been reported.15 The CLC veteran population, with known higher vulnerability to infection and chronic diseases, is epidemiologically different from the general nursing home population.15-18 To address these literature gaps, we present the first report of COVID- 19 testing with CT/CN value correlations in the high-risk veteran CLC population.
Methods
A retrospective review of all COVID-19 CT/CN testing at the Corporal Michael J. Crescenz Veterans Affairs Medical Center (VAMC) CLC in Philadelphia, Pennsylvania, from March 28, 2020, to April 24, 2020, was performed with a US Department of Veterans Affairs (VA) Veterans Health Information System Architecture VistA/FileMan search. Only veteran residents were included in this review. Data collected included initial and serial test results, CT/CN on positive test results, test dates, testing platform used, demographic information (age, self-reported ethnicity, and sex), and clinical follow-up information. Health records were reviewed retrospectively to identify death, the first day after diagnosis with no documented symptoms, or hospitalization status.
RT-PCR testing was performed with the Abbott RealTime SARS-CoV-2 assay on the Abbott m2000 platform and the Xpert Xpress SARS-CoV-2 assay on the Cepheid Infinity platform. The Xpert Xpress assay gave 2 CT values for the E and N2 targets on positive samples.19 For this assay to indicate a positive specimen, amplification by RT-PCR of the N2 target or both the N2 and E target is required. The Xpert Xpress assay results as presumptive positive if only the E target amplified. This assay counts a maximum of 45 cycles. The Abbott RealTime SARS-CoV-2 assay gave 1 CN derived from the RNA-dependent RNA polymerase and N targets on positive samples.20 The Abbott assay on the m2000 counts a maximum of 37 cycles. The CT/CN value is the number of cycles required by RT-PCR for the fluorescence signal to cross a threshold value exceeding background level.19,20
Samples that are negative for COVID-19 by RT-PCR do not produce a CT/CN value. Although both instruments were used for RT-PCR, the precise CT/CN values are not interchangeable and CT/CN observations over time between the 2 instruments during the disease course would be based on CT/CN value movement (general upward or downward trend) rather than absolute CT/CN differences. Both assays have been approved by emergency use authorization as qualitative tests for the presence/absence of COVID-19. Although the CT/CN value is available to laboratory staff after test completion, the CT/CN value is not reported routinely in the patient health record. All veteran patients identified on the initial review from March 28, 2020, to April 24, 2020, had all serial COVID-19 testing recorded until November 10, 2020. The CN values at the limit of detection (LOD) for the Abbott m2000 platform from the initial validation study were reviewed for reference.21
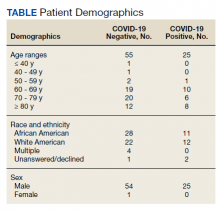
Results
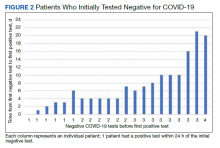
Of 80 patients, 25 (31%) were COVID-19 positive over the course of testing. The study population had a mean age of 73.5 years; 92% were aged > 60 years. The group was predominantly male (79 male vs 1 female). Among the 77 patients with a stated ethnicity, 39 (51%) were African American. In comparison, 43% of residents in Philadelphia County are African American (Table).22,23 Additionally, a previously published total COVID-19 tested population by ethnicity at the same regional VAMC revealed 46.8% of tested veteran patients were African American. 24 Three patients had no stated ethnicity. Among those who tested positive, 11 were African American patients, 12 were White patients, and 2 had no stated ethnicity. Four patients tested positive on their first test. The other 21 patients were positive on repeat testing. Interestingly, 6 patients had 1 initial negative test before a positive test, 6 patients had 2, 8 patients had 3, and 1 patient had 4 initial negative tests before a positive test result. Among the 25 positive patients, 22 were either positive within 10 days of the initial negative test result or initially positive (Figure 2). Three patients who tested positive after 10 days did so at 16, 20, and 21 days after the initial negative test result. Among the 25 positive patients, 23 had initial and serial testing from both the Abbott and Xpert Xpress assays. The remaining 2 positive patients had initial and serial testing from the Abbott assay exclusively.
Only positive COVID-19 results by RTPCR produced a CT/CN value. After disease resolution with a negative test, no CT/CN value was produced with the negative test result on either testing platform. Because repeat testing after the initial positive result took place no sooner than 10 days, we observed that the CT/CN value increased after the initial positive result until the disease resolved, and a negative result was obtained (eAppendix 1, available online at doi:10.12788/fp.0276). A t test comparing the initial CT/CN value to the value more than 10 days after the initial positive showed the CT/CN was statistically significantly higher (P < .05).
Prompt repeat testing after the initial test can show a decrease in the CT/CN value because of increasing viral load before the expected increase until disease resolution if the initial test caught the infection early. Twelve patients had a negative test result between 2 serial positive results. These negative test results occurred later, near the end of the disease course. Among the 12 patients with this positive-negativepositive CT/CN pattern, 7 were symptomatic and no longer had documented symptoms or hospitalization around the time of this positive-negative-positive pattern. Four of these individuals were asymptomatic during the entire infection course. One of the 12 patients with this pattern expired with the negative result occurring on day 27 of the disease in the context of rising CT/CN. One of these 12 patients only had a presumptive positive test result on the Cepheid because it detected only the E target with a CT value of 38.7. In 1 of the 12 patients, the negative test result occurred between 2 positive test results with CT/CN values < 20 (12.05 and 19.05 for the positive tests before and after the negative result, respectively). When the initial CT/CN values was separated based on ethnicity, the average CT/CN value for African Americans (23.3) was higher than for other ethnicities (19.9), although it did not reach statistical significance (P = .35).
Ten of the 25 patients testing positive were admitted to the hospital, including 1 admitted 15 days before diagnosis (patient 20) and 1 admitted 80 days after diagnosis (patient 7). Among these 10 patients, 6 were admitted to the intensive care unit, including patient 7. None of the patients were intubated. Three of the 10 admitted patients died (patients 7, 20, and 24). Patient 7 was a 79-year-old male with a history of dementia, cerebrovascular accident, hypertension, hyperlipidemia, and chronic kidney disease with symptoms of lethargy and refusal of oral intake when he was diagnosed with COVID-19. He was admitted 80 days after diagnosis for hyponatremia and acute renal failure, with death on day 87 recorded as complications from the earlier COVID-19 infection. Patient 20, an 89-year-old male with a history of dementia, chronic kidney disease, and hyperlipidemia, had been admitted with fever, cough, and leukocytosis 17 days before COVID-19 diagnosis. He continued to be symptomatic after diagnosis with development of hypotension, dehydration, and refusal of oral intake while on comfort measures/endof- life care and died 15 days after COVID- 19 infection diagnosis. Patient 24 was a 96-year-old male with history of heart failure, hypertension, coronary artery disease, prostate carcinoma, and dementia who developed a cough at the time of diagnosis; because of his underlying condition, he remained in the CLC on comfort care. His symptoms, including hypoxia, worsened until he died 7 days after diagnosis.
Among the 25 patients, 17 were symptomatic at the time of diagnosis; the 14 initially symptomatic patients who survived improved clinically and returned to baseline. Eight of the 25 patients were asymptomatic initially and 3 developed symptoms 2 to 5 days after diagnosis. Only 1 patient who remained asymptomatic was admitted for inability to adhere to quarantine at the CLC. Review of the health records of all surviving symptomatic patients showed symptom resolution with return to baseline that corresponds to an increasing CT/CN value. A 1-tailed t test comparing the initial CT/ CN at the time of diagnosis to the last CT/CN value for symptomatic patients who recovered revealed a statistically significant increase (P < .05). For the symptomatic, symptom resolution and hospital discharge took (if required) a mean 20 days (range, 7-46). Among those who were not hospitalized, symptoms resolved in 7 to 36 days (18 days). Among those requiring hospitalization at any time (excluding patients who died or were asymptomatic), symptom and hospitalization resolution took a mean 22 days (range, 10-46). Asymptomatic patients (patients 8, 10, 15, 16, and 25) also showed increasing CT/CN value during the infection course, although there was no correlation with the continued lack of symptoms.
During the initial validation of the Abbott m2000 instrument, an LOD study included concentrations of 1000, 500, 250, 100, 70, 60, and 50 virus copies/mL (eAppendix 2, available online at doi:10.12788/fp.0276).21 The average CN at 100 virus copies/mL—the manufacturer provided LOD in the instructions for use—was 25.74.20 At a concentration of one-half that (50 virus copies/mL), the average CN was 28.39.
Discussion
This is the first study in the English literature to track CT/CN values as part of serial testing of a veteran CLC. Widescale testing and repeat screening in the absence of symptoms of nursing home residents would identify those who are infected and allow providers to track viral load clearance.9-14 CT/CN values, when serially tracked during the infection course, appear to increase with illness resolution, consistent with earlier reports that CT/CN correlates with viral load.8-14 Serial CT/CN values that are high (> 25) and continue to increase with each test suggest progression toward disease resolution or viral RNA clearance.8-14 After symptom resolution, patients can have a persistent low level of viral shedding (corresponding to a high CT/CN value).10-14,25 Near the end of disease resolution, a negative serial RT-PCR sample test before a subsequent positive might be a promising clinical sign of near disease recovery. Once the viral load is low with a CT/CN significantly higher than 25, some specimens might result as negative but turn up positive on subsequent sampling with a high CT/CN value. This pattern, with attendant high CT/CN values for the positive results, are consistent with the known effect of viral load (ie, a low viral load correlates to a high CT/CN) and adequacy of specimen collection on CT/CN values.25 If the patient’s viral load is low, the sample collected might have a viral load at or near the testing platform’s LOD.
For Abbott m2000, the manufacturer provided LOD is 100 virus copies/mL, although the instrument was able to detect virus concentrations below that level during the initial validation.20 The actual LOD of the instrument at our institution is < 100 virus copies/mL. For the Cepheid Xpert Xpress SARS-CoV-2 assay, the manufacturer-provided LOD is 250 virus copies/mL.19 An LOD study including samples below the manufacturer-provided LOD was not part of the initial validation study for the Xpert Xpress assay. Nonetheless, the virus concentration of samples with very high CT values at or near the maximum CT value of 45 is expected to be at or near the platform’s actual LOD.
If the samples collected near the end of the patient’s disease course have viral loads near these low concentrations, the encouraging positive-negative-positive pattern with high CT/CN values might be a promising sign for viral clearance. On the other hand, a positive-negative-positive pattern in the setting of low CT/CN values before and after the negative test might indicate poor sampling for the negative specimen. The back-and-forth or positive-negative-positive pattern generally appears to indicate near resolution of the infection course, although clinical correlation is necessary to rule out inadequate sampling earlier in the disease course or prolonged viral RNA shedding.9-14 In all of the surviving symptomatic patients who showed the positive-negative-positive pattern, this sign occurred around or after symptom resolution. It also is important to consider that in some patients, SARS-CoV-2 RNA might remain detectable with increasing CT/CN after symptom resolution, and samples from these patients might not result positive. Therefore, CT/CN values cannot be interpreted without considering the clinical picture.25
Studies on infectiousness and virus culture from COVID-19 samples with CT/ CN correlation have shown that patients with high CT/CN at the end of their disease course might not be as infectious.9-14,25 Because 1 patient had a presumptive positive result after the negative result, this study shows that this positive-negative-positive pattern could include presumptive positive results. Also, in the setting of a recent positive result on the same testing platform, a patient with this pattern is presumed to be positive for COVID-19 RNA because of scant viral material.
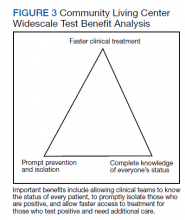
Taiwan’s public health response to the outbreak illustrates the ability to mitigate an outbreak throughout a society.26 These actions could help blunt an outbreak within a civilian nursing home population.5 Mitigation within a veteran CLC population has been documented, but the study, which focused on mitigation, did not consider CT/CN values, demographic distribution, testing access of the studied population, or laboratory findings related to disease pathophysiology.15 A key ingredient in widescale, serial testing is the availability of a rapid turnaround from testing in-house that allowed identification within 24 hours instead of several days at a reference laboratory. 15 Rapid widescale testing would allow clinical teams to optimize the Triangle of Benefit of Widescale Timely Tests for CLC (Figure 3).15 Timely laboratory testing remains pivotal for CLC veteran residents to aid successful clinical triage and management. Reporting serial CT/CN values can provide additional information to clinicians about the disease course because CT/ CN correlates with viral load, which varies based on where the patient is in the disease course.9-14 CT/CN values carry significant prognostic value, particularly with respect to intubation and mortality.8
Limitations
Important limitations to our study include the use of 2 separate RT-PCR platforms. Using different RT-PCR platforms is common in clinical laboratories trying to take advantage of the unique characteristics of different platforms—for example, turnaround time vs high throughput— to manage COVID-19 testing workflow.25 However, the exact CT/CN values obtained from each platform might not translate to the other, and the general trend (CT/CN values are rising or falling across serial tests) rather than a single value could be useful for clinical correlation. Even when the same platform is used for the serial testing, CT/CN values can be affected by adequacy of specimen collection; therefore, clinical correlation and considering the trend in CT/CN values is necessary for interpretation.10-14,25 Because of the known trend in viral dynamics, a positive specimen collected with a high CT/CN followed by a subsequent (within 2 days) positive specimen collected with a low CT/CN might be compatible with early detection of COVID- 19 infection in the appropriate clinical context. 10-14 However, detection late in the infection course or even after the symptomatic disease resolved with prolonged viral shedding might show serial positive samples with increasing CT/CN values.10-14
Patients with prolonged viral shedding might not be infectious.27 Because of the clinical correlation required for interpretation and the other factors that might affect CT/CN values, recommendations advise against using CT/CN values in clinical practice at this time, although these recommendations could change with future research.25 Serial CT/CN values have the potential, if appropriately correlated with the clinical picture, to provide useful information, such as whether the viral load of the sample is relatively high or low and increasing or decreasing.
Veterans, as a population, are more susceptible to poor health outcomes and morbidity compared with similar civilian counterparts.2,14-16 Veteran CLC patients likely would experience worse outcomes with COVID-19, including more infections, expiration, and morbidity compared with similar general population nursing homes. Similar to what had been reported for the civilian population, a trend (high CT/CN values early in the disease course with repeat testing needed to detect all positives followed by lower CT/CN value to correlate with increased viral load and then increased CT/CN value as the infection resolved) also was observed in this veteran population.
It has been extensively documented that minority groups experience decreased health care access and worse health outcomes. 28-30 Considering the critical medical supply shortages, including personal protective equipment, ventilators, and even testing supplies, there is the potential for a resource access disparity by ethnicity.28-31 Because the VA does not depend on measures of wealth and privilege such as health insurance, there was no disparity noted in access to testing by race or ethnicity at the VAMC CLC. When considering the health outcome of viral load from the measured CT/CN value, the viral loads of African American patients and those of other ethnicities was not significantly different in this study.
Conclusions
This is the first study to bring up critical points including serial CT/CN value correlation in RT-PCR tests, demographic distributions demonstrating easy and equal access in a veteran nursing home to COVID-19 testing, and clinical laboratory signs related to disease pathophysiology. Unlike other populations who have undergone serial CT/CN monitoring, nursing homes represent a particularly vulnerable population who require measures to prevent the spread and mitigate outbreaks of COVID-19.2,4,5 Test measurements obtained such as the CT/CN value during routine clinical care can provide useful information for public health, epidemiologic, or clinical purposes with appropriate correlation to clinical and other laboratory parameters. This study demonstrates early intervention of serial testing of an outbreak in a veterans nursing home with CT/CN value correlation.
1. Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi:10.1136/bmj.m1091
2. Tsan L, Davis C, Langberg R, et al. Prevalence of nursing home-associated infections in the Department of Veterans Affairs nursing home care units. Am J Infect Control. 2008;36(3):173-179. doi:10.1016/j.ajic.2007.06.008
3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi:10.1016/S0140-6736(20)30566-3
4. Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323(16):1612-1614. doi:10.1001/jama.2020.4326
5. McMichael TM, Currie DW, Clark S, et al. Public Health–Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005-2011. doi:10.1056/NEJMoa2005412
6. Childs A, Zullo AR, Joyce NR, et al. The burden of respiratory infections among older adults in long-term care: a systematic review. BMC Geriatr. 2019;19(1):210. doi:10.1186/s12877-019-1236-6
7. Eriksen HM, Iversen BG, Aavitsland PJ. Prevalence of nosocomial infections and use of antibiotics in long-term care facilities in Norway, 2002 and 2003. Hosp Infect. 2004;57(4):316-320. doi:10.1016/j.jhin.2004.03.028
8. Magleby R, Westblade LF, Trzebucki A, et al. Impact Severe acute respiratory syndrome coronavirus 2 viral load on risk of intubation and mortality among hospitalized patients with coronavirus disease 2019. Clin Infect Dis. 2021;73(11):e4197-e4205. doi:10.1093/cid/ciaa851
9. Buchan B, Hoff J, Gmehlin C, et al. Distribution of SARSCoV- 2 PCR cycle threshold values provide practical insight into overall and target-specific sensitivity among symptomatic patients. Am Clin Pathol. 2020;154:479-485. doi:10.1093/ajcp/aqaa133
10. He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26(5):672-675. doi:10.1038/s41591-020-0869-5
11. Zou L, Ruan F, Huang M, et al. SARS-CoV-2 Viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177-1179. doi:10.1056/NEJMc2001737
12. Singanayagam A, Patel M, Charlett A, et al. Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Euro Surveill. 2020;25(32):2001483. doi:10.2807/1560-7917.ES.2020.25.32.2001483
13. Salvatore P, Dawson P, Wadhwa A, et al. Epidemiological correlates of PCR cycles threshold values in the detection of SARS-CoV-2. Clin Infect Dis. 2021;72(11):e761-e767. doi:10.1093/cid/ciaa1469
14. Kissler S, Fauver J, Mack C, et al. Viral dynamics of SARS-CoV-2 infection and the predictive value of repeat testing. medRxiv. 2020;10.21.20217042. doi:10.1101/2020.10.21.20217042 1
5. Escobar DJ, Lanzi M, Saberi P, et al. Mitigation of a COVID-19 outbreak in a nursing home through serial testing of residents and staff. Clin Infect Dis. 2021;72(9):e394- e396. doi:10.1093/cid/ciaa1021
16. Eibner C, Krull H, Brown KM, et al. Current and projected characteristics and unique health care needs of the patient population served by the Department of Veterans Affairs. Rand Health Q. 2016;5(4):13.
17. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
18. Morgan RO, Teal CR, Reddy SG, Ford ME, Ashton CM. Measurement in Veterans Affairs Health Services Research: veterans as a special population. Health Serv Res. 2005;40(5 Pt 2):1573-1583. doi:10.1111/j.1475-6773.2005.00448.x 1
9. Xpert Xpress SARS-CoV-2. Instructions for use. Cepheid. 302-2562, Rev. C April 2020. Accessed January 7, 2021. https://www.fda.gov/media/136314/download
20. Abbott RealTime SARS-CoV-2. Instructions for use Abbott. 09N77-95. July 2020. Accessed January 7, 2021. https:// www.fda.gov/media/136258/download
21. Petersen JM, Dalal S, Jhala D. Successful implementation of SARS-CoV-2 testing in midst of pandemic with emphasis on all phases of testing. J Clin Pathol. 2021;74:273- 278. doi:10.1136/jclinpath-2020-207175
22. United States Census Bureau. Quick Facts: Philadelphia County, Pennsylvania. Accessed April 16, 2020. https://www .census.gov/quickfacts/philadelphiacountypennsylvania
23. Centers for Disease Control and Prevention. United States COVID-19 cases, deaths, and laboratory testing (NAATS) by state, territory, and jurisdiction. Accessed April 26, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases -updates/cases-in-us.html 2
4. Petersen J, Jhala D. Ethnicity, comorbid medical conditions, and SARS-CoV-2 test cycle thresholds in the veteran population [published online ahead of print, 2021 Jul 28]. J Racial Ethn Health Disparities. 2021;1-8. doi:10.1007/s40615-021-01114-4
25. Infectious Diseases Society of America, Association for Molecular Pathology. IDSA and AMP joint statement on the use of SARS-CoV-2 PCR cycle threshold (Ct) values for clinical decision-making. Accessed August 28, 2021. https://www.idsociety.org/globalassets/idsa/public-health /covid-19/idsa-amp-statement.pdf
26. Wang J, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analysis, new technology, and proactive testing. JAMA. 2020;323(14):1341-1342. doi:10.1001/jama.2020.3151
27. Centers for Disease Control and Prevention. Overview of testing for SARS-CoV-2, the virus that causes COVID- 19. Accessed July 28, 2021. https://www.cdc.gov /coronavirus/2019-ncov/hcp/testing-overview.html
28. Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996-1999. Health Aff. 2003;22(2):139-153. doi:10.1377/hlthaff.22.2.139
29. Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med. 2006;21(6):667-669. doi:10.1111/j.1525-1497.2006.0512.x
30. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, Nelson AR, eds. Unequal treatment: confronting racial and ethnic disparities in health care. National Academies Press; 2003. doi:10.17226/12875
31. Ranney ML, Griffeth V, Jha AK. Critical supply shortages – the need for ventilators and personal protective equipment during the Covid-19 Pandemic. N Engl J Med. 2020;382(18):e41. doi:10.1056/NEJMp2006141
COVID-19, caused by SARS-CoV-2, is more severe in individuals with underlying illnesses. Because complete social distancing might be more difficult in nursing homes and community living centers (CLCs), public health leaders and clinicians have been concerned about the epidemiology and disease course in nursing homes even before the COVID-19 pandemic.1-7 A report of a COVID-19 outbreak in a nursing home facility in King County, Washington, documented a 33.7% overall fatality rate for residents and 52.4% among the most critically ill.4,5 The experience at King County, Washington, shows that proactive steps to identify, monitor, and apply preventive control measures is important for future outbreaks.5
Reverse transcriptase polymerase chain reaction (RT-PCR) testing produces a cycle threshold (CT) or cycle number (CN) that correlates with viral load and infectiousness. 8-14 CT/CN represents the number of RT-PCR cycles required for the fluorescent signal to cross the detection threshold (exceed background level) and is inversely proportional to the viral load. Effectively, the higher the viral load, the lower the CT/ CN value (Figure 1). Tracking CT/CN values was not documented in the Washington nursing home outbreak. Reports of COVID- 19 testing in CLCs during outbreaks are sparse, and CT/CN values and demographic distribution of these veterans has not been reported.15 The CLC veteran population, with known higher vulnerability to infection and chronic diseases, is epidemiologically different from the general nursing home population.15-18 To address these literature gaps, we present the first report of COVID- 19 testing with CT/CN value correlations in the high-risk veteran CLC population.
Methods
A retrospective review of all COVID-19 CT/CN testing at the Corporal Michael J. Crescenz Veterans Affairs Medical Center (VAMC) CLC in Philadelphia, Pennsylvania, from March 28, 2020, to April 24, 2020, was performed with a US Department of Veterans Affairs (VA) Veterans Health Information System Architecture VistA/FileMan search. Only veteran residents were included in this review. Data collected included initial and serial test results, CT/CN on positive test results, test dates, testing platform used, demographic information (age, self-reported ethnicity, and sex), and clinical follow-up information. Health records were reviewed retrospectively to identify death, the first day after diagnosis with no documented symptoms, or hospitalization status.
RT-PCR testing was performed with the Abbott RealTime SARS-CoV-2 assay on the Abbott m2000 platform and the Xpert Xpress SARS-CoV-2 assay on the Cepheid Infinity platform. The Xpert Xpress assay gave 2 CT values for the E and N2 targets on positive samples.19 For this assay to indicate a positive specimen, amplification by RT-PCR of the N2 target or both the N2 and E target is required. The Xpert Xpress assay results as presumptive positive if only the E target amplified. This assay counts a maximum of 45 cycles. The Abbott RealTime SARS-CoV-2 assay gave 1 CN derived from the RNA-dependent RNA polymerase and N targets on positive samples.20 The Abbott assay on the m2000 counts a maximum of 37 cycles. The CT/CN value is the number of cycles required by RT-PCR for the fluorescence signal to cross a threshold value exceeding background level.19,20
Samples that are negative for COVID-19 by RT-PCR do not produce a CT/CN value. Although both instruments were used for RT-PCR, the precise CT/CN values are not interchangeable and CT/CN observations over time between the 2 instruments during the disease course would be based on CT/CN value movement (general upward or downward trend) rather than absolute CT/CN differences. Both assays have been approved by emergency use authorization as qualitative tests for the presence/absence of COVID-19. Although the CT/CN value is available to laboratory staff after test completion, the CT/CN value is not reported routinely in the patient health record. All veteran patients identified on the initial review from March 28, 2020, to April 24, 2020, had all serial COVID-19 testing recorded until November 10, 2020. The CN values at the limit of detection (LOD) for the Abbott m2000 platform from the initial validation study were reviewed for reference.21
Results
Of 80 patients, 25 (31%) were COVID-19 positive over the course of testing. The study population had a mean age of 73.5 years; 92% were aged > 60 years. The group was predominantly male (79 male vs 1 female). Among the 77 patients with a stated ethnicity, 39 (51%) were African American. In comparison, 43% of residents in Philadelphia County are African American (Table).22,23 Additionally, a previously published total COVID-19 tested population by ethnicity at the same regional VAMC revealed 46.8% of tested veteran patients were African American. 24 Three patients had no stated ethnicity. Among those who tested positive, 11 were African American patients, 12 were White patients, and 2 had no stated ethnicity. Four patients tested positive on their first test. The other 21 patients were positive on repeat testing. Interestingly, 6 patients had 1 initial negative test before a positive test, 6 patients had 2, 8 patients had 3, and 1 patient had 4 initial negative tests before a positive test result. Among the 25 positive patients, 22 were either positive within 10 days of the initial negative test result or initially positive (Figure 2). Three patients who tested positive after 10 days did so at 16, 20, and 21 days after the initial negative test result. Among the 25 positive patients, 23 had initial and serial testing from both the Abbott and Xpert Xpress assays. The remaining 2 positive patients had initial and serial testing from the Abbott assay exclusively.
Only positive COVID-19 results by RTPCR produced a CT/CN value. After disease resolution with a negative test, no CT/CN value was produced with the negative test result on either testing platform. Because repeat testing after the initial positive result took place no sooner than 10 days, we observed that the CT/CN value increased after the initial positive result until the disease resolved, and a negative result was obtained (eAppendix 1, available online at doi:10.12788/fp.0276). A t test comparing the initial CT/CN value to the value more than 10 days after the initial positive showed the CT/CN was statistically significantly higher (P < .05).
Prompt repeat testing after the initial test can show a decrease in the CT/CN value because of increasing viral load before the expected increase until disease resolution if the initial test caught the infection early. Twelve patients had a negative test result between 2 serial positive results. These negative test results occurred later, near the end of the disease course. Among the 12 patients with this positive-negativepositive CT/CN pattern, 7 were symptomatic and no longer had documented symptoms or hospitalization around the time of this positive-negative-positive pattern. Four of these individuals were asymptomatic during the entire infection course. One of the 12 patients with this pattern expired with the negative result occurring on day 27 of the disease in the context of rising CT/CN. One of these 12 patients only had a presumptive positive test result on the Cepheid because it detected only the E target with a CT value of 38.7. In 1 of the 12 patients, the negative test result occurred between 2 positive test results with CT/CN values < 20 (12.05 and 19.05 for the positive tests before and after the negative result, respectively). When the initial CT/CN values was separated based on ethnicity, the average CT/CN value for African Americans (23.3) was higher than for other ethnicities (19.9), although it did not reach statistical significance (P = .35).
Ten of the 25 patients testing positive were admitted to the hospital, including 1 admitted 15 days before diagnosis (patient 20) and 1 admitted 80 days after diagnosis (patient 7). Among these 10 patients, 6 were admitted to the intensive care unit, including patient 7. None of the patients were intubated. Three of the 10 admitted patients died (patients 7, 20, and 24). Patient 7 was a 79-year-old male with a history of dementia, cerebrovascular accident, hypertension, hyperlipidemia, and chronic kidney disease with symptoms of lethargy and refusal of oral intake when he was diagnosed with COVID-19. He was admitted 80 days after diagnosis for hyponatremia and acute renal failure, with death on day 87 recorded as complications from the earlier COVID-19 infection. Patient 20, an 89-year-old male with a history of dementia, chronic kidney disease, and hyperlipidemia, had been admitted with fever, cough, and leukocytosis 17 days before COVID-19 diagnosis. He continued to be symptomatic after diagnosis with development of hypotension, dehydration, and refusal of oral intake while on comfort measures/endof- life care and died 15 days after COVID- 19 infection diagnosis. Patient 24 was a 96-year-old male with history of heart failure, hypertension, coronary artery disease, prostate carcinoma, and dementia who developed a cough at the time of diagnosis; because of his underlying condition, he remained in the CLC on comfort care. His symptoms, including hypoxia, worsened until he died 7 days after diagnosis.
Among the 25 patients, 17 were symptomatic at the time of diagnosis; the 14 initially symptomatic patients who survived improved clinically and returned to baseline. Eight of the 25 patients were asymptomatic initially and 3 developed symptoms 2 to 5 days after diagnosis. Only 1 patient who remained asymptomatic was admitted for inability to adhere to quarantine at the CLC. Review of the health records of all surviving symptomatic patients showed symptom resolution with return to baseline that corresponds to an increasing CT/CN value. A 1-tailed t test comparing the initial CT/ CN at the time of diagnosis to the last CT/CN value for symptomatic patients who recovered revealed a statistically significant increase (P < .05). For the symptomatic, symptom resolution and hospital discharge took (if required) a mean 20 days (range, 7-46). Among those who were not hospitalized, symptoms resolved in 7 to 36 days (18 days). Among those requiring hospitalization at any time (excluding patients who died or were asymptomatic), symptom and hospitalization resolution took a mean 22 days (range, 10-46). Asymptomatic patients (patients 8, 10, 15, 16, and 25) also showed increasing CT/CN value during the infection course, although there was no correlation with the continued lack of symptoms.
During the initial validation of the Abbott m2000 instrument, an LOD study included concentrations of 1000, 500, 250, 100, 70, 60, and 50 virus copies/mL (eAppendix 2, available online at doi:10.12788/fp.0276).21 The average CN at 100 virus copies/mL—the manufacturer provided LOD in the instructions for use—was 25.74.20 At a concentration of one-half that (50 virus copies/mL), the average CN was 28.39.
Discussion
This is the first study in the English literature to track CT/CN values as part of serial testing of a veteran CLC. Widescale testing and repeat screening in the absence of symptoms of nursing home residents would identify those who are infected and allow providers to track viral load clearance.9-14 CT/CN values, when serially tracked during the infection course, appear to increase with illness resolution, consistent with earlier reports that CT/CN correlates with viral load.8-14 Serial CT/CN values that are high (> 25) and continue to increase with each test suggest progression toward disease resolution or viral RNA clearance.8-14 After symptom resolution, patients can have a persistent low level of viral shedding (corresponding to a high CT/CN value).10-14,25 Near the end of disease resolution, a negative serial RT-PCR sample test before a subsequent positive might be a promising clinical sign of near disease recovery. Once the viral load is low with a CT/CN significantly higher than 25, some specimens might result as negative but turn up positive on subsequent sampling with a high CT/CN value. This pattern, with attendant high CT/CN values for the positive results, are consistent with the known effect of viral load (ie, a low viral load correlates to a high CT/CN) and adequacy of specimen collection on CT/CN values.25 If the patient’s viral load is low, the sample collected might have a viral load at or near the testing platform’s LOD.
For Abbott m2000, the manufacturer provided LOD is 100 virus copies/mL, although the instrument was able to detect virus concentrations below that level during the initial validation.20 The actual LOD of the instrument at our institution is < 100 virus copies/mL. For the Cepheid Xpert Xpress SARS-CoV-2 assay, the manufacturer-provided LOD is 250 virus copies/mL.19 An LOD study including samples below the manufacturer-provided LOD was not part of the initial validation study for the Xpert Xpress assay. Nonetheless, the virus concentration of samples with very high CT values at or near the maximum CT value of 45 is expected to be at or near the platform’s actual LOD.
If the samples collected near the end of the patient’s disease course have viral loads near these low concentrations, the encouraging positive-negative-positive pattern with high CT/CN values might be a promising sign for viral clearance. On the other hand, a positive-negative-positive pattern in the setting of low CT/CN values before and after the negative test might indicate poor sampling for the negative specimen. The back-and-forth or positive-negative-positive pattern generally appears to indicate near resolution of the infection course, although clinical correlation is necessary to rule out inadequate sampling earlier in the disease course or prolonged viral RNA shedding.9-14 In all of the surviving symptomatic patients who showed the positive-negative-positive pattern, this sign occurred around or after symptom resolution. It also is important to consider that in some patients, SARS-CoV-2 RNA might remain detectable with increasing CT/CN after symptom resolution, and samples from these patients might not result positive. Therefore, CT/CN values cannot be interpreted without considering the clinical picture.25
Studies on infectiousness and virus culture from COVID-19 samples with CT/ CN correlation have shown that patients with high CT/CN at the end of their disease course might not be as infectious.9-14,25 Because 1 patient had a presumptive positive result after the negative result, this study shows that this positive-negative-positive pattern could include presumptive positive results. Also, in the setting of a recent positive result on the same testing platform, a patient with this pattern is presumed to be positive for COVID-19 RNA because of scant viral material.
Taiwan’s public health response to the outbreak illustrates the ability to mitigate an outbreak throughout a society.26 These actions could help blunt an outbreak within a civilian nursing home population.5 Mitigation within a veteran CLC population has been documented, but the study, which focused on mitigation, did not consider CT/CN values, demographic distribution, testing access of the studied population, or laboratory findings related to disease pathophysiology.15 A key ingredient in widescale, serial testing is the availability of a rapid turnaround from testing in-house that allowed identification within 24 hours instead of several days at a reference laboratory. 15 Rapid widescale testing would allow clinical teams to optimize the Triangle of Benefit of Widescale Timely Tests for CLC (Figure 3).15 Timely laboratory testing remains pivotal for CLC veteran residents to aid successful clinical triage and management. Reporting serial CT/CN values can provide additional information to clinicians about the disease course because CT/ CN correlates with viral load, which varies based on where the patient is in the disease course.9-14 CT/CN values carry significant prognostic value, particularly with respect to intubation and mortality.8
Limitations
Important limitations to our study include the use of 2 separate RT-PCR platforms. Using different RT-PCR platforms is common in clinical laboratories trying to take advantage of the unique characteristics of different platforms—for example, turnaround time vs high throughput— to manage COVID-19 testing workflow.25 However, the exact CT/CN values obtained from each platform might not translate to the other, and the general trend (CT/CN values are rising or falling across serial tests) rather than a single value could be useful for clinical correlation. Even when the same platform is used for the serial testing, CT/CN values can be affected by adequacy of specimen collection; therefore, clinical correlation and considering the trend in CT/CN values is necessary for interpretation.10-14,25 Because of the known trend in viral dynamics, a positive specimen collected with a high CT/CN followed by a subsequent (within 2 days) positive specimen collected with a low CT/CN might be compatible with early detection of COVID- 19 infection in the appropriate clinical context. 10-14 However, detection late in the infection course or even after the symptomatic disease resolved with prolonged viral shedding might show serial positive samples with increasing CT/CN values.10-14
Patients with prolonged viral shedding might not be infectious.27 Because of the clinical correlation required for interpretation and the other factors that might affect CT/CN values, recommendations advise against using CT/CN values in clinical practice at this time, although these recommendations could change with future research.25 Serial CT/CN values have the potential, if appropriately correlated with the clinical picture, to provide useful information, such as whether the viral load of the sample is relatively high or low and increasing or decreasing.
Veterans, as a population, are more susceptible to poor health outcomes and morbidity compared with similar civilian counterparts.2,14-16 Veteran CLC patients likely would experience worse outcomes with COVID-19, including more infections, expiration, and morbidity compared with similar general population nursing homes. Similar to what had been reported for the civilian population, a trend (high CT/CN values early in the disease course with repeat testing needed to detect all positives followed by lower CT/CN value to correlate with increased viral load and then increased CT/CN value as the infection resolved) also was observed in this veteran population.
It has been extensively documented that minority groups experience decreased health care access and worse health outcomes. 28-30 Considering the critical medical supply shortages, including personal protective equipment, ventilators, and even testing supplies, there is the potential for a resource access disparity by ethnicity.28-31 Because the VA does not depend on measures of wealth and privilege such as health insurance, there was no disparity noted in access to testing by race or ethnicity at the VAMC CLC. When considering the health outcome of viral load from the measured CT/CN value, the viral loads of African American patients and those of other ethnicities was not significantly different in this study.
Conclusions
This is the first study to bring up critical points including serial CT/CN value correlation in RT-PCR tests, demographic distributions demonstrating easy and equal access in a veteran nursing home to COVID-19 testing, and clinical laboratory signs related to disease pathophysiology. Unlike other populations who have undergone serial CT/CN monitoring, nursing homes represent a particularly vulnerable population who require measures to prevent the spread and mitigate outbreaks of COVID-19.2,4,5 Test measurements obtained such as the CT/CN value during routine clinical care can provide useful information for public health, epidemiologic, or clinical purposes with appropriate correlation to clinical and other laboratory parameters. This study demonstrates early intervention of serial testing of an outbreak in a veterans nursing home with CT/CN value correlation.
COVID-19, caused by SARS-CoV-2, is more severe in individuals with underlying illnesses. Because complete social distancing might be more difficult in nursing homes and community living centers (CLCs), public health leaders and clinicians have been concerned about the epidemiology and disease course in nursing homes even before the COVID-19 pandemic.1-7 A report of a COVID-19 outbreak in a nursing home facility in King County, Washington, documented a 33.7% overall fatality rate for residents and 52.4% among the most critically ill.4,5 The experience at King County, Washington, shows that proactive steps to identify, monitor, and apply preventive control measures is important for future outbreaks.5
Reverse transcriptase polymerase chain reaction (RT-PCR) testing produces a cycle threshold (CT) or cycle number (CN) that correlates with viral load and infectiousness. 8-14 CT/CN represents the number of RT-PCR cycles required for the fluorescent signal to cross the detection threshold (exceed background level) and is inversely proportional to the viral load. Effectively, the higher the viral load, the lower the CT/ CN value (Figure 1). Tracking CT/CN values was not documented in the Washington nursing home outbreak. Reports of COVID- 19 testing in CLCs during outbreaks are sparse, and CT/CN values and demographic distribution of these veterans has not been reported.15 The CLC veteran population, with known higher vulnerability to infection and chronic diseases, is epidemiologically different from the general nursing home population.15-18 To address these literature gaps, we present the first report of COVID- 19 testing with CT/CN value correlations in the high-risk veteran CLC population.
Methods
A retrospective review of all COVID-19 CT/CN testing at the Corporal Michael J. Crescenz Veterans Affairs Medical Center (VAMC) CLC in Philadelphia, Pennsylvania, from March 28, 2020, to April 24, 2020, was performed with a US Department of Veterans Affairs (VA) Veterans Health Information System Architecture VistA/FileMan search. Only veteran residents were included in this review. Data collected included initial and serial test results, CT/CN on positive test results, test dates, testing platform used, demographic information (age, self-reported ethnicity, and sex), and clinical follow-up information. Health records were reviewed retrospectively to identify death, the first day after diagnosis with no documented symptoms, or hospitalization status.
RT-PCR testing was performed with the Abbott RealTime SARS-CoV-2 assay on the Abbott m2000 platform and the Xpert Xpress SARS-CoV-2 assay on the Cepheid Infinity platform. The Xpert Xpress assay gave 2 CT values for the E and N2 targets on positive samples.19 For this assay to indicate a positive specimen, amplification by RT-PCR of the N2 target or both the N2 and E target is required. The Xpert Xpress assay results as presumptive positive if only the E target amplified. This assay counts a maximum of 45 cycles. The Abbott RealTime SARS-CoV-2 assay gave 1 CN derived from the RNA-dependent RNA polymerase and N targets on positive samples.20 The Abbott assay on the m2000 counts a maximum of 37 cycles. The CT/CN value is the number of cycles required by RT-PCR for the fluorescence signal to cross a threshold value exceeding background level.19,20
Samples that are negative for COVID-19 by RT-PCR do not produce a CT/CN value. Although both instruments were used for RT-PCR, the precise CT/CN values are not interchangeable and CT/CN observations over time between the 2 instruments during the disease course would be based on CT/CN value movement (general upward or downward trend) rather than absolute CT/CN differences. Both assays have been approved by emergency use authorization as qualitative tests for the presence/absence of COVID-19. Although the CT/CN value is available to laboratory staff after test completion, the CT/CN value is not reported routinely in the patient health record. All veteran patients identified on the initial review from March 28, 2020, to April 24, 2020, had all serial COVID-19 testing recorded until November 10, 2020. The CN values at the limit of detection (LOD) for the Abbott m2000 platform from the initial validation study were reviewed for reference.21
Results
Of 80 patients, 25 (31%) were COVID-19 positive over the course of testing. The study population had a mean age of 73.5 years; 92% were aged > 60 years. The group was predominantly male (79 male vs 1 female). Among the 77 patients with a stated ethnicity, 39 (51%) were African American. In comparison, 43% of residents in Philadelphia County are African American (Table).22,23 Additionally, a previously published total COVID-19 tested population by ethnicity at the same regional VAMC revealed 46.8% of tested veteran patients were African American. 24 Three patients had no stated ethnicity. Among those who tested positive, 11 were African American patients, 12 were White patients, and 2 had no stated ethnicity. Four patients tested positive on their first test. The other 21 patients were positive on repeat testing. Interestingly, 6 patients had 1 initial negative test before a positive test, 6 patients had 2, 8 patients had 3, and 1 patient had 4 initial negative tests before a positive test result. Among the 25 positive patients, 22 were either positive within 10 days of the initial negative test result or initially positive (Figure 2). Three patients who tested positive after 10 days did so at 16, 20, and 21 days after the initial negative test result. Among the 25 positive patients, 23 had initial and serial testing from both the Abbott and Xpert Xpress assays. The remaining 2 positive patients had initial and serial testing from the Abbott assay exclusively.
Only positive COVID-19 results by RTPCR produced a CT/CN value. After disease resolution with a negative test, no CT/CN value was produced with the negative test result on either testing platform. Because repeat testing after the initial positive result took place no sooner than 10 days, we observed that the CT/CN value increased after the initial positive result until the disease resolved, and a negative result was obtained (eAppendix 1, available online at doi:10.12788/fp.0276). A t test comparing the initial CT/CN value to the value more than 10 days after the initial positive showed the CT/CN was statistically significantly higher (P < .05).
Prompt repeat testing after the initial test can show a decrease in the CT/CN value because of increasing viral load before the expected increase until disease resolution if the initial test caught the infection early. Twelve patients had a negative test result between 2 serial positive results. These negative test results occurred later, near the end of the disease course. Among the 12 patients with this positive-negativepositive CT/CN pattern, 7 were symptomatic and no longer had documented symptoms or hospitalization around the time of this positive-negative-positive pattern. Four of these individuals were asymptomatic during the entire infection course. One of the 12 patients with this pattern expired with the negative result occurring on day 27 of the disease in the context of rising CT/CN. One of these 12 patients only had a presumptive positive test result on the Cepheid because it detected only the E target with a CT value of 38.7. In 1 of the 12 patients, the negative test result occurred between 2 positive test results with CT/CN values < 20 (12.05 and 19.05 for the positive tests before and after the negative result, respectively). When the initial CT/CN values was separated based on ethnicity, the average CT/CN value for African Americans (23.3) was higher than for other ethnicities (19.9), although it did not reach statistical significance (P = .35).
Ten of the 25 patients testing positive were admitted to the hospital, including 1 admitted 15 days before diagnosis (patient 20) and 1 admitted 80 days after diagnosis (patient 7). Among these 10 patients, 6 were admitted to the intensive care unit, including patient 7. None of the patients were intubated. Three of the 10 admitted patients died (patients 7, 20, and 24). Patient 7 was a 79-year-old male with a history of dementia, cerebrovascular accident, hypertension, hyperlipidemia, and chronic kidney disease with symptoms of lethargy and refusal of oral intake when he was diagnosed with COVID-19. He was admitted 80 days after diagnosis for hyponatremia and acute renal failure, with death on day 87 recorded as complications from the earlier COVID-19 infection. Patient 20, an 89-year-old male with a history of dementia, chronic kidney disease, and hyperlipidemia, had been admitted with fever, cough, and leukocytosis 17 days before COVID-19 diagnosis. He continued to be symptomatic after diagnosis with development of hypotension, dehydration, and refusal of oral intake while on comfort measures/endof- life care and died 15 days after COVID- 19 infection diagnosis. Patient 24 was a 96-year-old male with history of heart failure, hypertension, coronary artery disease, prostate carcinoma, and dementia who developed a cough at the time of diagnosis; because of his underlying condition, he remained in the CLC on comfort care. His symptoms, including hypoxia, worsened until he died 7 days after diagnosis.
Among the 25 patients, 17 were symptomatic at the time of diagnosis; the 14 initially symptomatic patients who survived improved clinically and returned to baseline. Eight of the 25 patients were asymptomatic initially and 3 developed symptoms 2 to 5 days after diagnosis. Only 1 patient who remained asymptomatic was admitted for inability to adhere to quarantine at the CLC. Review of the health records of all surviving symptomatic patients showed symptom resolution with return to baseline that corresponds to an increasing CT/CN value. A 1-tailed t test comparing the initial CT/ CN at the time of diagnosis to the last CT/CN value for symptomatic patients who recovered revealed a statistically significant increase (P < .05). For the symptomatic, symptom resolution and hospital discharge took (if required) a mean 20 days (range, 7-46). Among those who were not hospitalized, symptoms resolved in 7 to 36 days (18 days). Among those requiring hospitalization at any time (excluding patients who died or were asymptomatic), symptom and hospitalization resolution took a mean 22 days (range, 10-46). Asymptomatic patients (patients 8, 10, 15, 16, and 25) also showed increasing CT/CN value during the infection course, although there was no correlation with the continued lack of symptoms.
During the initial validation of the Abbott m2000 instrument, an LOD study included concentrations of 1000, 500, 250, 100, 70, 60, and 50 virus copies/mL (eAppendix 2, available online at doi:10.12788/fp.0276).21 The average CN at 100 virus copies/mL—the manufacturer provided LOD in the instructions for use—was 25.74.20 At a concentration of one-half that (50 virus copies/mL), the average CN was 28.39.
Discussion
This is the first study in the English literature to track CT/CN values as part of serial testing of a veteran CLC. Widescale testing and repeat screening in the absence of symptoms of nursing home residents would identify those who are infected and allow providers to track viral load clearance.9-14 CT/CN values, when serially tracked during the infection course, appear to increase with illness resolution, consistent with earlier reports that CT/CN correlates with viral load.8-14 Serial CT/CN values that are high (> 25) and continue to increase with each test suggest progression toward disease resolution or viral RNA clearance.8-14 After symptom resolution, patients can have a persistent low level of viral shedding (corresponding to a high CT/CN value).10-14,25 Near the end of disease resolution, a negative serial RT-PCR sample test before a subsequent positive might be a promising clinical sign of near disease recovery. Once the viral load is low with a CT/CN significantly higher than 25, some specimens might result as negative but turn up positive on subsequent sampling with a high CT/CN value. This pattern, with attendant high CT/CN values for the positive results, are consistent with the known effect of viral load (ie, a low viral load correlates to a high CT/CN) and adequacy of specimen collection on CT/CN values.25 If the patient’s viral load is low, the sample collected might have a viral load at or near the testing platform’s LOD.
For Abbott m2000, the manufacturer provided LOD is 100 virus copies/mL, although the instrument was able to detect virus concentrations below that level during the initial validation.20 The actual LOD of the instrument at our institution is < 100 virus copies/mL. For the Cepheid Xpert Xpress SARS-CoV-2 assay, the manufacturer-provided LOD is 250 virus copies/mL.19 An LOD study including samples below the manufacturer-provided LOD was not part of the initial validation study for the Xpert Xpress assay. Nonetheless, the virus concentration of samples with very high CT values at or near the maximum CT value of 45 is expected to be at or near the platform’s actual LOD.
If the samples collected near the end of the patient’s disease course have viral loads near these low concentrations, the encouraging positive-negative-positive pattern with high CT/CN values might be a promising sign for viral clearance. On the other hand, a positive-negative-positive pattern in the setting of low CT/CN values before and after the negative test might indicate poor sampling for the negative specimen. The back-and-forth or positive-negative-positive pattern generally appears to indicate near resolution of the infection course, although clinical correlation is necessary to rule out inadequate sampling earlier in the disease course or prolonged viral RNA shedding.9-14 In all of the surviving symptomatic patients who showed the positive-negative-positive pattern, this sign occurred around or after symptom resolution. It also is important to consider that in some patients, SARS-CoV-2 RNA might remain detectable with increasing CT/CN after symptom resolution, and samples from these patients might not result positive. Therefore, CT/CN values cannot be interpreted without considering the clinical picture.25
Studies on infectiousness and virus culture from COVID-19 samples with CT/ CN correlation have shown that patients with high CT/CN at the end of their disease course might not be as infectious.9-14,25 Because 1 patient had a presumptive positive result after the negative result, this study shows that this positive-negative-positive pattern could include presumptive positive results. Also, in the setting of a recent positive result on the same testing platform, a patient with this pattern is presumed to be positive for COVID-19 RNA because of scant viral material.
Taiwan’s public health response to the outbreak illustrates the ability to mitigate an outbreak throughout a society.26 These actions could help blunt an outbreak within a civilian nursing home population.5 Mitigation within a veteran CLC population has been documented, but the study, which focused on mitigation, did not consider CT/CN values, demographic distribution, testing access of the studied population, or laboratory findings related to disease pathophysiology.15 A key ingredient in widescale, serial testing is the availability of a rapid turnaround from testing in-house that allowed identification within 24 hours instead of several days at a reference laboratory. 15 Rapid widescale testing would allow clinical teams to optimize the Triangle of Benefit of Widescale Timely Tests for CLC (Figure 3).15 Timely laboratory testing remains pivotal for CLC veteran residents to aid successful clinical triage and management. Reporting serial CT/CN values can provide additional information to clinicians about the disease course because CT/ CN correlates with viral load, which varies based on where the patient is in the disease course.9-14 CT/CN values carry significant prognostic value, particularly with respect to intubation and mortality.8
Limitations
Important limitations to our study include the use of 2 separate RT-PCR platforms. Using different RT-PCR platforms is common in clinical laboratories trying to take advantage of the unique characteristics of different platforms—for example, turnaround time vs high throughput— to manage COVID-19 testing workflow.25 However, the exact CT/CN values obtained from each platform might not translate to the other, and the general trend (CT/CN values are rising or falling across serial tests) rather than a single value could be useful for clinical correlation. Even when the same platform is used for the serial testing, CT/CN values can be affected by adequacy of specimen collection; therefore, clinical correlation and considering the trend in CT/CN values is necessary for interpretation.10-14,25 Because of the known trend in viral dynamics, a positive specimen collected with a high CT/CN followed by a subsequent (within 2 days) positive specimen collected with a low CT/CN might be compatible with early detection of COVID- 19 infection in the appropriate clinical context. 10-14 However, detection late in the infection course or even after the symptomatic disease resolved with prolonged viral shedding might show serial positive samples with increasing CT/CN values.10-14
Patients with prolonged viral shedding might not be infectious.27 Because of the clinical correlation required for interpretation and the other factors that might affect CT/CN values, recommendations advise against using CT/CN values in clinical practice at this time, although these recommendations could change with future research.25 Serial CT/CN values have the potential, if appropriately correlated with the clinical picture, to provide useful information, such as whether the viral load of the sample is relatively high or low and increasing or decreasing.
Veterans, as a population, are more susceptible to poor health outcomes and morbidity compared with similar civilian counterparts.2,14-16 Veteran CLC patients likely would experience worse outcomes with COVID-19, including more infections, expiration, and morbidity compared with similar general population nursing homes. Similar to what had been reported for the civilian population, a trend (high CT/CN values early in the disease course with repeat testing needed to detect all positives followed by lower CT/CN value to correlate with increased viral load and then increased CT/CN value as the infection resolved) also was observed in this veteran population.
It has been extensively documented that minority groups experience decreased health care access and worse health outcomes. 28-30 Considering the critical medical supply shortages, including personal protective equipment, ventilators, and even testing supplies, there is the potential for a resource access disparity by ethnicity.28-31 Because the VA does not depend on measures of wealth and privilege such as health insurance, there was no disparity noted in access to testing by race or ethnicity at the VAMC CLC. When considering the health outcome of viral load from the measured CT/CN value, the viral loads of African American patients and those of other ethnicities was not significantly different in this study.
Conclusions
This is the first study to bring up critical points including serial CT/CN value correlation in RT-PCR tests, demographic distributions demonstrating easy and equal access in a veteran nursing home to COVID-19 testing, and clinical laboratory signs related to disease pathophysiology. Unlike other populations who have undergone serial CT/CN monitoring, nursing homes represent a particularly vulnerable population who require measures to prevent the spread and mitigate outbreaks of COVID-19.2,4,5 Test measurements obtained such as the CT/CN value during routine clinical care can provide useful information for public health, epidemiologic, or clinical purposes with appropriate correlation to clinical and other laboratory parameters. This study demonstrates early intervention of serial testing of an outbreak in a veterans nursing home with CT/CN value correlation.
1. Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi:10.1136/bmj.m1091
2. Tsan L, Davis C, Langberg R, et al. Prevalence of nursing home-associated infections in the Department of Veterans Affairs nursing home care units. Am J Infect Control. 2008;36(3):173-179. doi:10.1016/j.ajic.2007.06.008
3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi:10.1016/S0140-6736(20)30566-3
4. Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323(16):1612-1614. doi:10.1001/jama.2020.4326
5. McMichael TM, Currie DW, Clark S, et al. Public Health–Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005-2011. doi:10.1056/NEJMoa2005412
6. Childs A, Zullo AR, Joyce NR, et al. The burden of respiratory infections among older adults in long-term care: a systematic review. BMC Geriatr. 2019;19(1):210. doi:10.1186/s12877-019-1236-6
7. Eriksen HM, Iversen BG, Aavitsland PJ. Prevalence of nosocomial infections and use of antibiotics in long-term care facilities in Norway, 2002 and 2003. Hosp Infect. 2004;57(4):316-320. doi:10.1016/j.jhin.2004.03.028
8. Magleby R, Westblade LF, Trzebucki A, et al. Impact Severe acute respiratory syndrome coronavirus 2 viral load on risk of intubation and mortality among hospitalized patients with coronavirus disease 2019. Clin Infect Dis. 2021;73(11):e4197-e4205. doi:10.1093/cid/ciaa851
9. Buchan B, Hoff J, Gmehlin C, et al. Distribution of SARSCoV- 2 PCR cycle threshold values provide practical insight into overall and target-specific sensitivity among symptomatic patients. Am Clin Pathol. 2020;154:479-485. doi:10.1093/ajcp/aqaa133
10. He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26(5):672-675. doi:10.1038/s41591-020-0869-5
11. Zou L, Ruan F, Huang M, et al. SARS-CoV-2 Viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177-1179. doi:10.1056/NEJMc2001737
12. Singanayagam A, Patel M, Charlett A, et al. Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Euro Surveill. 2020;25(32):2001483. doi:10.2807/1560-7917.ES.2020.25.32.2001483
13. Salvatore P, Dawson P, Wadhwa A, et al. Epidemiological correlates of PCR cycles threshold values in the detection of SARS-CoV-2. Clin Infect Dis. 2021;72(11):e761-e767. doi:10.1093/cid/ciaa1469
14. Kissler S, Fauver J, Mack C, et al. Viral dynamics of SARS-CoV-2 infection and the predictive value of repeat testing. medRxiv. 2020;10.21.20217042. doi:10.1101/2020.10.21.20217042 1
5. Escobar DJ, Lanzi M, Saberi P, et al. Mitigation of a COVID-19 outbreak in a nursing home through serial testing of residents and staff. Clin Infect Dis. 2021;72(9):e394- e396. doi:10.1093/cid/ciaa1021
16. Eibner C, Krull H, Brown KM, et al. Current and projected characteristics and unique health care needs of the patient population served by the Department of Veterans Affairs. Rand Health Q. 2016;5(4):13.
17. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
18. Morgan RO, Teal CR, Reddy SG, Ford ME, Ashton CM. Measurement in Veterans Affairs Health Services Research: veterans as a special population. Health Serv Res. 2005;40(5 Pt 2):1573-1583. doi:10.1111/j.1475-6773.2005.00448.x 1
9. Xpert Xpress SARS-CoV-2. Instructions for use. Cepheid. 302-2562, Rev. C April 2020. Accessed January 7, 2021. https://www.fda.gov/media/136314/download
20. Abbott RealTime SARS-CoV-2. Instructions for use Abbott. 09N77-95. July 2020. Accessed January 7, 2021. https:// www.fda.gov/media/136258/download
21. Petersen JM, Dalal S, Jhala D. Successful implementation of SARS-CoV-2 testing in midst of pandemic with emphasis on all phases of testing. J Clin Pathol. 2021;74:273- 278. doi:10.1136/jclinpath-2020-207175
22. United States Census Bureau. Quick Facts: Philadelphia County, Pennsylvania. Accessed April 16, 2020. https://www .census.gov/quickfacts/philadelphiacountypennsylvania
23. Centers for Disease Control and Prevention. United States COVID-19 cases, deaths, and laboratory testing (NAATS) by state, territory, and jurisdiction. Accessed April 26, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases -updates/cases-in-us.html 2
4. Petersen J, Jhala D. Ethnicity, comorbid medical conditions, and SARS-CoV-2 test cycle thresholds in the veteran population [published online ahead of print, 2021 Jul 28]. J Racial Ethn Health Disparities. 2021;1-8. doi:10.1007/s40615-021-01114-4
25. Infectious Diseases Society of America, Association for Molecular Pathology. IDSA and AMP joint statement on the use of SARS-CoV-2 PCR cycle threshold (Ct) values for clinical decision-making. Accessed August 28, 2021. https://www.idsociety.org/globalassets/idsa/public-health /covid-19/idsa-amp-statement.pdf
26. Wang J, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analysis, new technology, and proactive testing. JAMA. 2020;323(14):1341-1342. doi:10.1001/jama.2020.3151
27. Centers for Disease Control and Prevention. Overview of testing for SARS-CoV-2, the virus that causes COVID- 19. Accessed July 28, 2021. https://www.cdc.gov /coronavirus/2019-ncov/hcp/testing-overview.html
28. Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996-1999. Health Aff. 2003;22(2):139-153. doi:10.1377/hlthaff.22.2.139
29. Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med. 2006;21(6):667-669. doi:10.1111/j.1525-1497.2006.0512.x
30. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, Nelson AR, eds. Unequal treatment: confronting racial and ethnic disparities in health care. National Academies Press; 2003. doi:10.17226/12875
31. Ranney ML, Griffeth V, Jha AK. Critical supply shortages – the need for ventilators and personal protective equipment during the Covid-19 Pandemic. N Engl J Med. 2020;382(18):e41. doi:10.1056/NEJMp2006141
1. Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. doi:10.1136/bmj.m1091
2. Tsan L, Davis C, Langberg R, et al. Prevalence of nursing home-associated infections in the Department of Veterans Affairs nursing home care units. Am J Infect Control. 2008;36(3):173-179. doi:10.1016/j.ajic.2007.06.008
3. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062. doi:10.1016/S0140-6736(20)30566-3
4. Arentz M, Yim E, Klaff L, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323(16):1612-1614. doi:10.1001/jama.2020.4326
5. McMichael TM, Currie DW, Clark S, et al. Public Health–Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med. 2020;382(21):2005-2011. doi:10.1056/NEJMoa2005412
6. Childs A, Zullo AR, Joyce NR, et al. The burden of respiratory infections among older adults in long-term care: a systematic review. BMC Geriatr. 2019;19(1):210. doi:10.1186/s12877-019-1236-6
7. Eriksen HM, Iversen BG, Aavitsland PJ. Prevalence of nosocomial infections and use of antibiotics in long-term care facilities in Norway, 2002 and 2003. Hosp Infect. 2004;57(4):316-320. doi:10.1016/j.jhin.2004.03.028
8. Magleby R, Westblade LF, Trzebucki A, et al. Impact Severe acute respiratory syndrome coronavirus 2 viral load on risk of intubation and mortality among hospitalized patients with coronavirus disease 2019. Clin Infect Dis. 2021;73(11):e4197-e4205. doi:10.1093/cid/ciaa851
9. Buchan B, Hoff J, Gmehlin C, et al. Distribution of SARSCoV- 2 PCR cycle threshold values provide practical insight into overall and target-specific sensitivity among symptomatic patients. Am Clin Pathol. 2020;154:479-485. doi:10.1093/ajcp/aqaa133
10. He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26(5):672-675. doi:10.1038/s41591-020-0869-5
11. Zou L, Ruan F, Huang M, et al. SARS-CoV-2 Viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177-1179. doi:10.1056/NEJMc2001737
12. Singanayagam A, Patel M, Charlett A, et al. Duration of infectiousness and correlation with RT-PCR cycle threshold values in cases of COVID-19, England, January to May 2020. Euro Surveill. 2020;25(32):2001483. doi:10.2807/1560-7917.ES.2020.25.32.2001483
13. Salvatore P, Dawson P, Wadhwa A, et al. Epidemiological correlates of PCR cycles threshold values in the detection of SARS-CoV-2. Clin Infect Dis. 2021;72(11):e761-e767. doi:10.1093/cid/ciaa1469
14. Kissler S, Fauver J, Mack C, et al. Viral dynamics of SARS-CoV-2 infection and the predictive value of repeat testing. medRxiv. 2020;10.21.20217042. doi:10.1101/2020.10.21.20217042 1
5. Escobar DJ, Lanzi M, Saberi P, et al. Mitigation of a COVID-19 outbreak in a nursing home through serial testing of residents and staff. Clin Infect Dis. 2021;72(9):e394- e396. doi:10.1093/cid/ciaa1021
16. Eibner C, Krull H, Brown KM, et al. Current and projected characteristics and unique health care needs of the patient population served by the Department of Veterans Affairs. Rand Health Q. 2016;5(4):13.
17. Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Arch Intern Med. 2000;160(21):3252-3257. doi:10.1001/archinte.160.21.3252
18. Morgan RO, Teal CR, Reddy SG, Ford ME, Ashton CM. Measurement in Veterans Affairs Health Services Research: veterans as a special population. Health Serv Res. 2005;40(5 Pt 2):1573-1583. doi:10.1111/j.1475-6773.2005.00448.x 1
9. Xpert Xpress SARS-CoV-2. Instructions for use. Cepheid. 302-2562, Rev. C April 2020. Accessed January 7, 2021. https://www.fda.gov/media/136314/download
20. Abbott RealTime SARS-CoV-2. Instructions for use Abbott. 09N77-95. July 2020. Accessed January 7, 2021. https:// www.fda.gov/media/136258/download
21. Petersen JM, Dalal S, Jhala D. Successful implementation of SARS-CoV-2 testing in midst of pandemic with emphasis on all phases of testing. J Clin Pathol. 2021;74:273- 278. doi:10.1136/jclinpath-2020-207175
22. United States Census Bureau. Quick Facts: Philadelphia County, Pennsylvania. Accessed April 16, 2020. https://www .census.gov/quickfacts/philadelphiacountypennsylvania
23. Centers for Disease Control and Prevention. United States COVID-19 cases, deaths, and laboratory testing (NAATS) by state, territory, and jurisdiction. Accessed April 26, 2020. https://www.cdc.gov/coronavirus/2019-ncov/cases -updates/cases-in-us.html 2
4. Petersen J, Jhala D. Ethnicity, comorbid medical conditions, and SARS-CoV-2 test cycle thresholds in the veteran population [published online ahead of print, 2021 Jul 28]. J Racial Ethn Health Disparities. 2021;1-8. doi:10.1007/s40615-021-01114-4
25. Infectious Diseases Society of America, Association for Molecular Pathology. IDSA and AMP joint statement on the use of SARS-CoV-2 PCR cycle threshold (Ct) values for clinical decision-making. Accessed August 28, 2021. https://www.idsociety.org/globalassets/idsa/public-health /covid-19/idsa-amp-statement.pdf
26. Wang J, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analysis, new technology, and proactive testing. JAMA. 2020;323(14):1341-1342. doi:10.1001/jama.2020.3151
27. Centers for Disease Control and Prevention. Overview of testing for SARS-CoV-2, the virus that causes COVID- 19. Accessed July 28, 2021. https://www.cdc.gov /coronavirus/2019-ncov/hcp/testing-overview.html
28. Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996-1999. Health Aff. 2003;22(2):139-153. doi:10.1377/hlthaff.22.2.139
29. Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med. 2006;21(6):667-669. doi:10.1111/j.1525-1497.2006.0512.x
30. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Smedley BD, Stith AY, Nelson AR, eds. Unequal treatment: confronting racial and ethnic disparities in health care. National Academies Press; 2003. doi:10.17226/12875
31. Ranney ML, Griffeth V, Jha AK. Critical supply shortages – the need for ventilators and personal protective equipment during the Covid-19 Pandemic. N Engl J Med. 2020;382(18):e41. doi:10.1056/NEJMp2006141
New treatment reduces risk of anal cancer in people with HIV
It all began with the question, “Has your butt been getting enough attention?”
Though that may seem unorthodox, it led researchers to discovering a treatment that may help prevent anal cancer in people with HIV/AIDS. It’s still featured on their study’s website, with this further explanation: “You get your viral load checked, your T-cell count checked, but what about your anus? Did you know that half of HIV+ men have cell changes in their anus caused by HPV?”
The Anal Cancer/HSIL Outcomes Research (ANCHOR) study, led by Joel Palefsky, MD, was published in The New England Journal of Medicine. Dr. Palefsky, an infectious disease expert at the University of California, San Francisco, and his team set out to determine whether a treatment that prevents cervical cancer in people with human papillomavirus (HPV) would benefit people with HIV/AIDS. The new treatment reduced the likelihood of anal cancer by more than 50%.
The team worked over 7 years, during which time they tested 4,459 men, women, transgender, and nonbinary individuals at 25 sites across the United States. The participants were sorted into two groups: Some received treatment for high-grade squamous intraepithelial lesions (HSILs), and some did not but were monitored for signs of disease. These included individuals over 35 who were living with HIV/AIDS and who were found to have patches of abnormal cells in their rectal lining.
HSILs are the cells gynecologists look for in performing a pap smear. They are precancerous cells commonly found in the cervix of persons with HPV. Finding HSILs during a gynecologic examination alerts clinicians to potential problems.
HSILs can also be found in the anal tract of men and women with HIV. Dr. Palefsky therefore hypothesized that, as with HPV and cervical cancer, these anal HSILs may be a precursor of anal cancer.
The scientists decided to treat these cells the same way they would treat them if found in the cervix and to see whether that reduced the risk of cancer. Doctors used lidocaine to numb the area, then removed the HSILs with an electric probe. The team then assessed whether the treatment prevented people from getting cancer.
It turns out that in many cases, it did. The study concluded after 30 of the participants developed anal cancer. Of those, 21 patients had not received HSIL treatment, compared with nine who did receive the treatment. The treatment resulted in a 57% reduction in the rate of anal cancer among patients who received treatment for their HSILs.
These results are encouraging, said Aasma Shaukat, MD, director of outcomes research in the Division of Gastroenterology and Hepatology at NYU Langone Health. Dr. Shaukat was not involved with the study. She believes it’s going to cause ripples across the field.
“The study is likely to change guidelines in favor of active and early treatment for HSIL and away from watchful waiting in individuals living with HIV to reduce the risk of developing anal squamous cell carcinoma, akin to removing polyps during colonoscopy to progression to and incidence of colorectal cancer,” she said in an email interview.
Treatments for this group of patients are more important now than ever. Since the beginning of the AIDS epidemic in the 1980s, the number of people with HIV has increased, Dr. Palefsky detailed in a press conference announcing the ANCHOR results. That’s partially because of new transmissions and partially owing to the fact that new treatments make it possible for people with HIV to live long, healthy lives. So as more people with HIV move into their sunset years, there are more people at risk for developing cancer, which is a disease associated with aging. Anal cancer sits at the intersection of risk for aging people who have HIV.
Any defense we have against the risk of cancer in this growing demographic is a good thing, says Hanna K. Sanoff, MD, a gastrointestinal oncologist at the Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, who was also not involved in the study. Although it’s not ready to be applied in doctors’ offices now, it could be a tool in the future. “Anything we can do to try and decrease the chance of precancerous lesions progressing to a real invasive cancer is of great importance. This kind of prevention work is critical to helping minimize the burden of cancer on our communities,” Dr. Sanoff said in an interview.
The study was funded by the National Cancer Institute of the National Institutes of Health and was conducted through the NCI-supported AIDS Malignancy Consortium. Dr. Shaukat and Dr. Sanoff report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It all began with the question, “Has your butt been getting enough attention?”
Though that may seem unorthodox, it led researchers to discovering a treatment that may help prevent anal cancer in people with HIV/AIDS. It’s still featured on their study’s website, with this further explanation: “You get your viral load checked, your T-cell count checked, but what about your anus? Did you know that half of HIV+ men have cell changes in their anus caused by HPV?”
The Anal Cancer/HSIL Outcomes Research (ANCHOR) study, led by Joel Palefsky, MD, was published in The New England Journal of Medicine. Dr. Palefsky, an infectious disease expert at the University of California, San Francisco, and his team set out to determine whether a treatment that prevents cervical cancer in people with human papillomavirus (HPV) would benefit people with HIV/AIDS. The new treatment reduced the likelihood of anal cancer by more than 50%.
The team worked over 7 years, during which time they tested 4,459 men, women, transgender, and nonbinary individuals at 25 sites across the United States. The participants were sorted into two groups: Some received treatment for high-grade squamous intraepithelial lesions (HSILs), and some did not but were monitored for signs of disease. These included individuals over 35 who were living with HIV/AIDS and who were found to have patches of abnormal cells in their rectal lining.
HSILs are the cells gynecologists look for in performing a pap smear. They are precancerous cells commonly found in the cervix of persons with HPV. Finding HSILs during a gynecologic examination alerts clinicians to potential problems.
HSILs can also be found in the anal tract of men and women with HIV. Dr. Palefsky therefore hypothesized that, as with HPV and cervical cancer, these anal HSILs may be a precursor of anal cancer.
The scientists decided to treat these cells the same way they would treat them if found in the cervix and to see whether that reduced the risk of cancer. Doctors used lidocaine to numb the area, then removed the HSILs with an electric probe. The team then assessed whether the treatment prevented people from getting cancer.
It turns out that in many cases, it did. The study concluded after 30 of the participants developed anal cancer. Of those, 21 patients had not received HSIL treatment, compared with nine who did receive the treatment. The treatment resulted in a 57% reduction in the rate of anal cancer among patients who received treatment for their HSILs.
These results are encouraging, said Aasma Shaukat, MD, director of outcomes research in the Division of Gastroenterology and Hepatology at NYU Langone Health. Dr. Shaukat was not involved with the study. She believes it’s going to cause ripples across the field.
“The study is likely to change guidelines in favor of active and early treatment for HSIL and away from watchful waiting in individuals living with HIV to reduce the risk of developing anal squamous cell carcinoma, akin to removing polyps during colonoscopy to progression to and incidence of colorectal cancer,” she said in an email interview.
Treatments for this group of patients are more important now than ever. Since the beginning of the AIDS epidemic in the 1980s, the number of people with HIV has increased, Dr. Palefsky detailed in a press conference announcing the ANCHOR results. That’s partially because of new transmissions and partially owing to the fact that new treatments make it possible for people with HIV to live long, healthy lives. So as more people with HIV move into their sunset years, there are more people at risk for developing cancer, which is a disease associated with aging. Anal cancer sits at the intersection of risk for aging people who have HIV.
Any defense we have against the risk of cancer in this growing demographic is a good thing, says Hanna K. Sanoff, MD, a gastrointestinal oncologist at the Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, who was also not involved in the study. Although it’s not ready to be applied in doctors’ offices now, it could be a tool in the future. “Anything we can do to try and decrease the chance of precancerous lesions progressing to a real invasive cancer is of great importance. This kind of prevention work is critical to helping minimize the burden of cancer on our communities,” Dr. Sanoff said in an interview.
The study was funded by the National Cancer Institute of the National Institutes of Health and was conducted through the NCI-supported AIDS Malignancy Consortium. Dr. Shaukat and Dr. Sanoff report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It all began with the question, “Has your butt been getting enough attention?”
Though that may seem unorthodox, it led researchers to discovering a treatment that may help prevent anal cancer in people with HIV/AIDS. It’s still featured on their study’s website, with this further explanation: “You get your viral load checked, your T-cell count checked, but what about your anus? Did you know that half of HIV+ men have cell changes in their anus caused by HPV?”
The Anal Cancer/HSIL Outcomes Research (ANCHOR) study, led by Joel Palefsky, MD, was published in The New England Journal of Medicine. Dr. Palefsky, an infectious disease expert at the University of California, San Francisco, and his team set out to determine whether a treatment that prevents cervical cancer in people with human papillomavirus (HPV) would benefit people with HIV/AIDS. The new treatment reduced the likelihood of anal cancer by more than 50%.
The team worked over 7 years, during which time they tested 4,459 men, women, transgender, and nonbinary individuals at 25 sites across the United States. The participants were sorted into two groups: Some received treatment for high-grade squamous intraepithelial lesions (HSILs), and some did not but were monitored for signs of disease. These included individuals over 35 who were living with HIV/AIDS and who were found to have patches of abnormal cells in their rectal lining.
HSILs are the cells gynecologists look for in performing a pap smear. They are precancerous cells commonly found in the cervix of persons with HPV. Finding HSILs during a gynecologic examination alerts clinicians to potential problems.
HSILs can also be found in the anal tract of men and women with HIV. Dr. Palefsky therefore hypothesized that, as with HPV and cervical cancer, these anal HSILs may be a precursor of anal cancer.
The scientists decided to treat these cells the same way they would treat them if found in the cervix and to see whether that reduced the risk of cancer. Doctors used lidocaine to numb the area, then removed the HSILs with an electric probe. The team then assessed whether the treatment prevented people from getting cancer.
It turns out that in many cases, it did. The study concluded after 30 of the participants developed anal cancer. Of those, 21 patients had not received HSIL treatment, compared with nine who did receive the treatment. The treatment resulted in a 57% reduction in the rate of anal cancer among patients who received treatment for their HSILs.
These results are encouraging, said Aasma Shaukat, MD, director of outcomes research in the Division of Gastroenterology and Hepatology at NYU Langone Health. Dr. Shaukat was not involved with the study. She believes it’s going to cause ripples across the field.
“The study is likely to change guidelines in favor of active and early treatment for HSIL and away from watchful waiting in individuals living with HIV to reduce the risk of developing anal squamous cell carcinoma, akin to removing polyps during colonoscopy to progression to and incidence of colorectal cancer,” she said in an email interview.
Treatments for this group of patients are more important now than ever. Since the beginning of the AIDS epidemic in the 1980s, the number of people with HIV has increased, Dr. Palefsky detailed in a press conference announcing the ANCHOR results. That’s partially because of new transmissions and partially owing to the fact that new treatments make it possible for people with HIV to live long, healthy lives. So as more people with HIV move into their sunset years, there are more people at risk for developing cancer, which is a disease associated with aging. Anal cancer sits at the intersection of risk for aging people who have HIV.
Any defense we have against the risk of cancer in this growing demographic is a good thing, says Hanna K. Sanoff, MD, a gastrointestinal oncologist at the Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, who was also not involved in the study. Although it’s not ready to be applied in doctors’ offices now, it could be a tool in the future. “Anything we can do to try and decrease the chance of precancerous lesions progressing to a real invasive cancer is of great importance. This kind of prevention work is critical to helping minimize the burden of cancer on our communities,” Dr. Sanoff said in an interview.
The study was funded by the National Cancer Institute of the National Institutes of Health and was conducted through the NCI-supported AIDS Malignancy Consortium. Dr. Shaukat and Dr. Sanoff report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Disturbed sleep drives poor PrEP adherence in young Black sexual-minority men
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.
Disappointing results for investigational Alzheimer’s drug
, new research suggests.
Top-line results for a phase 2 trial showed the novel drug, a monoclonal antibody designed to neutralize neurotoxic oligomers (a form of beta-amyloid), was not statistically superior to placebo in terms of cognitive ability or episodic memory function among cognitively unimpaired individuals with a genetic mutation for early-onset AD.
Genentech announced the negative results on June 16 together with Banner Alzheimer’s Institute, Phoenix.
During a press briefing, company representatives and researchers expressed disappointment with the initial results – but stressed numerous ongoing analyses have yet to be completed.
“This is the beginning of the story, but by no means the end of it,” Pierre N. Tariot, MD, director, Banner Alzheimer’s Institute, and one of the study leaders, said at the briefing.
API ADAD trial
The prospective, double-blind parallel-group Alzheimer’s Prevention Initiative (API) Autosomal Dominant Alzheimer’s Disease (ADAD) phase 2 trial enrolled 252 members of the world’s largest extended family with ADAD in Colombia. A total of 94% of the participants completed the study.
Two-thirds of participants carried the Presenilin 1 (PSEN1) E280A mutation, which virtually guarantees that carriers will develop AD at an average age of 44 years and dementia at an average age of 49 years.
Study participants were randomly assigned to receive crenezumab or placebo over a period of 5-8 years. The dose of crenezumab was increased at different time points during the trial as knowledge about potential treatment approaches for AD evolved.
Dr. Tariot noted the maximum dose was not provided for the entire treatment period. “The longest people received the highest dose was about 2 years,” he added.
Coprimary endpoints were rate of change in cognitive abilities, as measured by the API ADAD composite cognitive score, or episodic memory function, measured by the Free and Cued Selective Reminding Test Cueing Index.
Results showed these outcomes were not statistically significant for those receiving the active medication.
In addition to a range of cognitive measures, researchers also assessed amyloid PET and, later in the study, tau PET. MRI and cerebrospinal fluid (CSF) measures were also examined.
The investigators did find small numerical differences favoring crenezumab across the coprimary and multiple secondary and exploratory endpoints, but these were also not statistically significant.
Finally, no new safety issues were identified with crenezumab during the study.
Further analyses of data are ongoing and additional brain imaging and CSF biomarker results will be presented at the Alzheimer’s Association International Conference on Aug. 2.
While the study was not positive, it demonstrated that prevention trials are possible, even in less-than-ideal circumstances and generated a wealth of useful data, the investigators note.
“There were some differences between the treated and untreated patients, and we still need to understand which patients were most likely to experience those differences,” Rachelle Doody, MD, PhD, global head of neurodegeneration at Roche and Genentech, told briefing attendees.
“We need to understand the biomarkers involved and what [they’re] telling us about the disease and the timing of the intervention,” Dr. Doody said.
Prevention “needs to be one of our targeted therapeutic approaches but probably not our only one,” she added.
Beyond amyloid?
Commenting on the negative results, Howard Fillit, MD, cofounder and chief science officer of the Alzheimer’s Drug Discovery Foundation, said they demonstrate the need to focus beyond amyloid and more on the biology of aging.
“This broader approach coupled with advances in novel biomarkers is bringing us closer to the day when physicians will be able to zero in on the root causes of each patient’s Alzheimer’s – and tailor combinations of drug therapies to provide precision medicine,” Dr. Fillit, who was not involved with the research, said in statement.
Genentech is also evaluating the potential of gantenerumab for ADAD and for the prevention of sporadic AD and treatment of early Alzheimer’s in late-stage clinical trials. Results from the phase 3 GRADUATE studies of gantenerumab in early AD are expected by the end of the year.
The study was supported by the National Institute on Aging, contributions to Banner Alzheimer’s Foundation, and Genentech.
A version of this article first appeared on Medscape.com.
, new research suggests.
Top-line results for a phase 2 trial showed the novel drug, a monoclonal antibody designed to neutralize neurotoxic oligomers (a form of beta-amyloid), was not statistically superior to placebo in terms of cognitive ability or episodic memory function among cognitively unimpaired individuals with a genetic mutation for early-onset AD.
Genentech announced the negative results on June 16 together with Banner Alzheimer’s Institute, Phoenix.
During a press briefing, company representatives and researchers expressed disappointment with the initial results – but stressed numerous ongoing analyses have yet to be completed.
“This is the beginning of the story, but by no means the end of it,” Pierre N. Tariot, MD, director, Banner Alzheimer’s Institute, and one of the study leaders, said at the briefing.
API ADAD trial
The prospective, double-blind parallel-group Alzheimer’s Prevention Initiative (API) Autosomal Dominant Alzheimer’s Disease (ADAD) phase 2 trial enrolled 252 members of the world’s largest extended family with ADAD in Colombia. A total of 94% of the participants completed the study.
Two-thirds of participants carried the Presenilin 1 (PSEN1) E280A mutation, which virtually guarantees that carriers will develop AD at an average age of 44 years and dementia at an average age of 49 years.
Study participants were randomly assigned to receive crenezumab or placebo over a period of 5-8 years. The dose of crenezumab was increased at different time points during the trial as knowledge about potential treatment approaches for AD evolved.
Dr. Tariot noted the maximum dose was not provided for the entire treatment period. “The longest people received the highest dose was about 2 years,” he added.
Coprimary endpoints were rate of change in cognitive abilities, as measured by the API ADAD composite cognitive score, or episodic memory function, measured by the Free and Cued Selective Reminding Test Cueing Index.
Results showed these outcomes were not statistically significant for those receiving the active medication.
In addition to a range of cognitive measures, researchers also assessed amyloid PET and, later in the study, tau PET. MRI and cerebrospinal fluid (CSF) measures were also examined.
The investigators did find small numerical differences favoring crenezumab across the coprimary and multiple secondary and exploratory endpoints, but these were also not statistically significant.
Finally, no new safety issues were identified with crenezumab during the study.
Further analyses of data are ongoing and additional brain imaging and CSF biomarker results will be presented at the Alzheimer’s Association International Conference on Aug. 2.
While the study was not positive, it demonstrated that prevention trials are possible, even in less-than-ideal circumstances and generated a wealth of useful data, the investigators note.
“There were some differences between the treated and untreated patients, and we still need to understand which patients were most likely to experience those differences,” Rachelle Doody, MD, PhD, global head of neurodegeneration at Roche and Genentech, told briefing attendees.
“We need to understand the biomarkers involved and what [they’re] telling us about the disease and the timing of the intervention,” Dr. Doody said.
Prevention “needs to be one of our targeted therapeutic approaches but probably not our only one,” she added.
Beyond amyloid?
Commenting on the negative results, Howard Fillit, MD, cofounder and chief science officer of the Alzheimer’s Drug Discovery Foundation, said they demonstrate the need to focus beyond amyloid and more on the biology of aging.
“This broader approach coupled with advances in novel biomarkers is bringing us closer to the day when physicians will be able to zero in on the root causes of each patient’s Alzheimer’s – and tailor combinations of drug therapies to provide precision medicine,” Dr. Fillit, who was not involved with the research, said in statement.
Genentech is also evaluating the potential of gantenerumab for ADAD and for the prevention of sporadic AD and treatment of early Alzheimer’s in late-stage clinical trials. Results from the phase 3 GRADUATE studies of gantenerumab in early AD are expected by the end of the year.
The study was supported by the National Institute on Aging, contributions to Banner Alzheimer’s Foundation, and Genentech.
A version of this article first appeared on Medscape.com.
, new research suggests.
Top-line results for a phase 2 trial showed the novel drug, a monoclonal antibody designed to neutralize neurotoxic oligomers (a form of beta-amyloid), was not statistically superior to placebo in terms of cognitive ability or episodic memory function among cognitively unimpaired individuals with a genetic mutation for early-onset AD.
Genentech announced the negative results on June 16 together with Banner Alzheimer’s Institute, Phoenix.
During a press briefing, company representatives and researchers expressed disappointment with the initial results – but stressed numerous ongoing analyses have yet to be completed.
“This is the beginning of the story, but by no means the end of it,” Pierre N. Tariot, MD, director, Banner Alzheimer’s Institute, and one of the study leaders, said at the briefing.
API ADAD trial
The prospective, double-blind parallel-group Alzheimer’s Prevention Initiative (API) Autosomal Dominant Alzheimer’s Disease (ADAD) phase 2 trial enrolled 252 members of the world’s largest extended family with ADAD in Colombia. A total of 94% of the participants completed the study.
Two-thirds of participants carried the Presenilin 1 (PSEN1) E280A mutation, which virtually guarantees that carriers will develop AD at an average age of 44 years and dementia at an average age of 49 years.
Study participants were randomly assigned to receive crenezumab or placebo over a period of 5-8 years. The dose of crenezumab was increased at different time points during the trial as knowledge about potential treatment approaches for AD evolved.
Dr. Tariot noted the maximum dose was not provided for the entire treatment period. “The longest people received the highest dose was about 2 years,” he added.
Coprimary endpoints were rate of change in cognitive abilities, as measured by the API ADAD composite cognitive score, or episodic memory function, measured by the Free and Cued Selective Reminding Test Cueing Index.
Results showed these outcomes were not statistically significant for those receiving the active medication.
In addition to a range of cognitive measures, researchers also assessed amyloid PET and, later in the study, tau PET. MRI and cerebrospinal fluid (CSF) measures were also examined.
The investigators did find small numerical differences favoring crenezumab across the coprimary and multiple secondary and exploratory endpoints, but these were also not statistically significant.
Finally, no new safety issues were identified with crenezumab during the study.
Further analyses of data are ongoing and additional brain imaging and CSF biomarker results will be presented at the Alzheimer’s Association International Conference on Aug. 2.
While the study was not positive, it demonstrated that prevention trials are possible, even in less-than-ideal circumstances and generated a wealth of useful data, the investigators note.
“There were some differences between the treated and untreated patients, and we still need to understand which patients were most likely to experience those differences,” Rachelle Doody, MD, PhD, global head of neurodegeneration at Roche and Genentech, told briefing attendees.
“We need to understand the biomarkers involved and what [they’re] telling us about the disease and the timing of the intervention,” Dr. Doody said.
Prevention “needs to be one of our targeted therapeutic approaches but probably not our only one,” she added.
Beyond amyloid?
Commenting on the negative results, Howard Fillit, MD, cofounder and chief science officer of the Alzheimer’s Drug Discovery Foundation, said they demonstrate the need to focus beyond amyloid and more on the biology of aging.
“This broader approach coupled with advances in novel biomarkers is bringing us closer to the day when physicians will be able to zero in on the root causes of each patient’s Alzheimer’s – and tailor combinations of drug therapies to provide precision medicine,” Dr. Fillit, who was not involved with the research, said in statement.
Genentech is also evaluating the potential of gantenerumab for ADAD and for the prevention of sporadic AD and treatment of early Alzheimer’s in late-stage clinical trials. Results from the phase 3 GRADUATE studies of gantenerumab in early AD are expected by the end of the year.
The study was supported by the National Institute on Aging, contributions to Banner Alzheimer’s Foundation, and Genentech.
A version of this article first appeared on Medscape.com.
FDA approves risankizumab (Skyrizi) for Crohn’s disease
The U.S. Food and Drug Administration – making it the first specific anti–interleukin-23 monoclonal antibody indicated for Crohn’s disease.
The safety and efficacy of risankizumab in Crohn’s disease is supported by data from two induction clinical trials (ADVANCE and MOTIVATE) and one maintenance clinical trial (FORTIFY).
Results of the three studies were presented at the annual scientific meeting of the American College of Gastroenterology in 2021.
“In both the induction and maintenance clinical trials, a significantly greater number of adult patients saw few or no symptoms and a meaningful reduction of visible signs of intestinal inflammation, compared to placebo,” Marla Dubinsky, MD, gastroenterologist with the Mount Sinai Health System and codirector of the IBD Center at Mount Sinai, New York, said in a news release from AbbVie.
“This approval provides health care professionals with a greatly needed additional option for treating the disruptive symptoms of Crohn’s disease,” Dr. Dubinsky said.
For the treatment of Crohn’s disease, risankizumab is dosed at 600 mg administered by intravenous infusion over at least 1 hour at week 0, 4, and 8, followed by 360 mg self-administered by subcutaneous injection at week 12, and every 8 weeks thereafter.
Risankizumab is already approved in the United States for the treatment of adults with active psoriatic arthritis and moderate to severe plaque psoriasis.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration – making it the first specific anti–interleukin-23 monoclonal antibody indicated for Crohn’s disease.
The safety and efficacy of risankizumab in Crohn’s disease is supported by data from two induction clinical trials (ADVANCE and MOTIVATE) and one maintenance clinical trial (FORTIFY).
Results of the three studies were presented at the annual scientific meeting of the American College of Gastroenterology in 2021.
“In both the induction and maintenance clinical trials, a significantly greater number of adult patients saw few or no symptoms and a meaningful reduction of visible signs of intestinal inflammation, compared to placebo,” Marla Dubinsky, MD, gastroenterologist with the Mount Sinai Health System and codirector of the IBD Center at Mount Sinai, New York, said in a news release from AbbVie.
“This approval provides health care professionals with a greatly needed additional option for treating the disruptive symptoms of Crohn’s disease,” Dr. Dubinsky said.
For the treatment of Crohn’s disease, risankizumab is dosed at 600 mg administered by intravenous infusion over at least 1 hour at week 0, 4, and 8, followed by 360 mg self-administered by subcutaneous injection at week 12, and every 8 weeks thereafter.
Risankizumab is already approved in the United States for the treatment of adults with active psoriatic arthritis and moderate to severe plaque psoriasis.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration – making it the first specific anti–interleukin-23 monoclonal antibody indicated for Crohn’s disease.
The safety and efficacy of risankizumab in Crohn’s disease is supported by data from two induction clinical trials (ADVANCE and MOTIVATE) and one maintenance clinical trial (FORTIFY).
Results of the three studies were presented at the annual scientific meeting of the American College of Gastroenterology in 2021.
“In both the induction and maintenance clinical trials, a significantly greater number of adult patients saw few or no symptoms and a meaningful reduction of visible signs of intestinal inflammation, compared to placebo,” Marla Dubinsky, MD, gastroenterologist with the Mount Sinai Health System and codirector of the IBD Center at Mount Sinai, New York, said in a news release from AbbVie.
“This approval provides health care professionals with a greatly needed additional option for treating the disruptive symptoms of Crohn’s disease,” Dr. Dubinsky said.
For the treatment of Crohn’s disease, risankizumab is dosed at 600 mg administered by intravenous infusion over at least 1 hour at week 0, 4, and 8, followed by 360 mg self-administered by subcutaneous injection at week 12, and every 8 weeks thereafter.
Risankizumab is already approved in the United States for the treatment of adults with active psoriatic arthritis and moderate to severe plaque psoriasis.
A version of this article first appeared on Medscape.com.
Ultra-processed: Doctors debate whether putting this label on foods is useful
The NOVA system divides foods into “fresh or minimally processed,” such as strawberries or steel-cut oats; “processed culinary ingredients,” such as olive oil; “processed foods,” such as cheeses; and “ultra-processed foods.” UPFs are defined as “industrial formulations made by deconstructing natural food into its chemical constituents, modifying them and recombining them with additives into products liable to displace all other NOVA food groups.”
According to doctors who presented during the meeting, ultra-processed foods are drawing increased attention, because researchers have been examining them in National Institutes of Health–funded studies and journalists have been writing about them.
During the debate session at the meeting, some experts said that, with obesity and poor health skyrocketing, increased awareness and labeling of UPFs can only be a good thing. In contrast others noted at the meeting that the classification system that has come to be used for identifying UPFs – the NOVA Food Classification system – is too mushy, confusing, and, ultimately unhelpful.
Carlos Monteiro, MD, PhD, professor of nutrition and public health at the University of Sao Paolo, was part of the group favoring the NOVA system’s classifying certain foods as UPFs, during the debate. He drew attention to the extent to which the world’s population is getting its calories from UPFs.
Mexico and France get about 30% of calories from these foods. In Canada, it’s 48%. And in the United States, it’s 57%, Dr. Monteiro said.
Studies have found that UPFs, many of which are designed to be exceedingly flavorful and intended to replace consumption of unprocessed whole foods, lead to more overall energy intake, more added sugar in the diet, and less fiber and protein intake, he said.
To further support his arguments, Dr. Monteiro pointed to studies suggesting that it is not just the resulting change in the nutritional intake that is unhealthy, but the UPF manufacturing process itself. When adjusting for fat, sugar, and sodium intake, for example, health outcomes associated with UPFs remain poor, he explained.
“I’m sorry,” he said in the debate. “If you don’t reduce this, you don’t reduce your obesity, your diabetes prevalence.”
A study presented by Jacqueline Vernarelli, PhD, during a different session at the meeting suggested there may be other downsides to consuming UPFs. This research, which was based on the U.S. National Youth Fitness Survey, found that poorer locomotor skills among children aged 3-5 and poorer cardiovascular fitness among those aged 12-15 were associated with getting more calories from UPFs.
Those with lower cardiovascular fitness consumed 1,234 calories a day from UPFs, and those with higher cardiovascular fitness consumed 1,007 calories a day from UPFs (P = .002), according to the new research.
“It’s notable here that, although these differences are significant, both groups are consuming a pretty high proportion of their diet from ultra-processed foods,” said Dr. Vernarelli, associate professor of public health at Sacred Heart University, Fairfield, Conn., during her presentation.
In the debate session, Arne Astrup, MD, PhD, senior project director at the Healthy Weight Center at the Novo Nordisk Foundation, Hellerup, Denmark, presented an opposing view.
He said the definition of UPFs makes it too difficult to categorize many foods, pointing to a study from this year in which about 150 nutrition experts, doctors, and dietitians classified 120 foods. Only three marketed foods and one generic food were classified the same by all the evaluators.
Referring to the study Dr. Astrup cited, Dr. Monteiro said it was a mere “exercise,” and the experts involved in it had conflicts of interest.
Dr. Astrup touted this study’s size and its appearance in the peer-reviewed journal the European Journal of Clinical Nutrition.
Defending his point of view, Dr. Astrup said, “The definition and classification is so ambiguous, and the risk of misclassification is so extremely high, I think we really miss the basic requirement of science, namely that we know what we are talking about,” he said.
If you take an unprocessed food, and insert a “little additive … suddenly it’s an ultra-processed food,” he added.
UPF definition doesn’t flag some unhealthy foods
Susan Roberts, PhD, professor of nutrition at Tufts University, Boston, was a discussant at the debate and touched on the merits of both sides. She noted that the UPF definition doesn’t flag some “clearly unhealthy foods,” such as table sugar, but does flag some healthy ones, such as plant-based burgers – to which Dr. Monteiro said that the system was not a system meant to divide foods into healthy and unhealthy groups, during the debate session.
The inclusion of both healthy and unhealthy foods in NOVA’s definition of a UPF is a serious problem, Dr. Roberts said.
“It’s almost like it’s an emotional classification designed to get at the food industry rather than focusing on health – and I think that’s asking for trouble because it’s just going to be such a mess to tell consumers, ‘Well, this ultra-processed food is healthy and this one isn’t,’ ” she said. What’s happening is the term ultra-processed is being used interchangeably with unhealthy.
The discussion that the UPF classification has generated is useful, Dr. Roberts continued. “This definition grew out of that recognition that we’re engaged in an unprecedented experiment of how unhealthy can you make the world without having a major catastrophe.”
She added that the UPF concept deserves a more formalized and rigorous evaluation.
“This is an important topic for the future of public health, and I think it needs big committees to address it seriously,” she said. “I think we should not be dealing with this individually in different labs.”
Doctor’s take on usefulness of discussing UPF concept with patients
Mark Corkins, MD, who did not participate in the debate at the meeting, said he talks to parents and children about nutrition at every office visit in which he sees a child with an unhealthy weight.
“Persistence wears down resistance,” said the chair of the American Academy of Pediatrics nutrition committee, in an interview.“A consistent message – you say the same thing and you say it multiple times.”
The idea of “ultra-processed foods” plays a role in those conversations, but largely in the background. It’s a topic that’s important for pediatric health, Dr. Corkins said – but he doesn’t make it the focal point.
“It’s not a direct attack on ultra-processed foods that usually I take as my direction,” said Dr. Corkins, who is also chief of pediatric gastroenterology at Le Bonheur Children’s Hospital in Memphis, Tenn.. “What I try to focus on, and what I think the American Academy of Pediatrics would focus on, is that we need to focus on making the diet better.”
He added, “Parents are aware – they don’t call it ultra-processed food, they call it junk food.”
Dr. Corkins continued that he is reluctant to directly challenge parents on feeding their children unhealthy foods – ultra-processed or not – lest he shame them and harm the relationship.
“Guilt as a motivator isn’t really highly successful,” he said, in an interview.
Dr. Astrup reported advisory committee or board member involvement with Green Leaf Medical and RNPC, France. Dr. Roberts reported advisory committee or board member involvement with Danone, and an ownership interest in Instinct Health Science. Dr. Monteiro and Dr. Corkins reported no relevant disclosures.
The NOVA system divides foods into “fresh or minimally processed,” such as strawberries or steel-cut oats; “processed culinary ingredients,” such as olive oil; “processed foods,” such as cheeses; and “ultra-processed foods.” UPFs are defined as “industrial formulations made by deconstructing natural food into its chemical constituents, modifying them and recombining them with additives into products liable to displace all other NOVA food groups.”
According to doctors who presented during the meeting, ultra-processed foods are drawing increased attention, because researchers have been examining them in National Institutes of Health–funded studies and journalists have been writing about them.
During the debate session at the meeting, some experts said that, with obesity and poor health skyrocketing, increased awareness and labeling of UPFs can only be a good thing. In contrast others noted at the meeting that the classification system that has come to be used for identifying UPFs – the NOVA Food Classification system – is too mushy, confusing, and, ultimately unhelpful.
Carlos Monteiro, MD, PhD, professor of nutrition and public health at the University of Sao Paolo, was part of the group favoring the NOVA system’s classifying certain foods as UPFs, during the debate. He drew attention to the extent to which the world’s population is getting its calories from UPFs.
Mexico and France get about 30% of calories from these foods. In Canada, it’s 48%. And in the United States, it’s 57%, Dr. Monteiro said.
Studies have found that UPFs, many of which are designed to be exceedingly flavorful and intended to replace consumption of unprocessed whole foods, lead to more overall energy intake, more added sugar in the diet, and less fiber and protein intake, he said.
To further support his arguments, Dr. Monteiro pointed to studies suggesting that it is not just the resulting change in the nutritional intake that is unhealthy, but the UPF manufacturing process itself. When adjusting for fat, sugar, and sodium intake, for example, health outcomes associated with UPFs remain poor, he explained.
“I’m sorry,” he said in the debate. “If you don’t reduce this, you don’t reduce your obesity, your diabetes prevalence.”
A study presented by Jacqueline Vernarelli, PhD, during a different session at the meeting suggested there may be other downsides to consuming UPFs. This research, which was based on the U.S. National Youth Fitness Survey, found that poorer locomotor skills among children aged 3-5 and poorer cardiovascular fitness among those aged 12-15 were associated with getting more calories from UPFs.
Those with lower cardiovascular fitness consumed 1,234 calories a day from UPFs, and those with higher cardiovascular fitness consumed 1,007 calories a day from UPFs (P = .002), according to the new research.
“It’s notable here that, although these differences are significant, both groups are consuming a pretty high proportion of their diet from ultra-processed foods,” said Dr. Vernarelli, associate professor of public health at Sacred Heart University, Fairfield, Conn., during her presentation.
In the debate session, Arne Astrup, MD, PhD, senior project director at the Healthy Weight Center at the Novo Nordisk Foundation, Hellerup, Denmark, presented an opposing view.
He said the definition of UPFs makes it too difficult to categorize many foods, pointing to a study from this year in which about 150 nutrition experts, doctors, and dietitians classified 120 foods. Only three marketed foods and one generic food were classified the same by all the evaluators.
Referring to the study Dr. Astrup cited, Dr. Monteiro said it was a mere “exercise,” and the experts involved in it had conflicts of interest.
Dr. Astrup touted this study’s size and its appearance in the peer-reviewed journal the European Journal of Clinical Nutrition.
Defending his point of view, Dr. Astrup said, “The definition and classification is so ambiguous, and the risk of misclassification is so extremely high, I think we really miss the basic requirement of science, namely that we know what we are talking about,” he said.
If you take an unprocessed food, and insert a “little additive … suddenly it’s an ultra-processed food,” he added.
UPF definition doesn’t flag some unhealthy foods
Susan Roberts, PhD, professor of nutrition at Tufts University, Boston, was a discussant at the debate and touched on the merits of both sides. She noted that the UPF definition doesn’t flag some “clearly unhealthy foods,” such as table sugar, but does flag some healthy ones, such as plant-based burgers – to which Dr. Monteiro said that the system was not a system meant to divide foods into healthy and unhealthy groups, during the debate session.
The inclusion of both healthy and unhealthy foods in NOVA’s definition of a UPF is a serious problem, Dr. Roberts said.
“It’s almost like it’s an emotional classification designed to get at the food industry rather than focusing on health – and I think that’s asking for trouble because it’s just going to be such a mess to tell consumers, ‘Well, this ultra-processed food is healthy and this one isn’t,’ ” she said. What’s happening is the term ultra-processed is being used interchangeably with unhealthy.
The discussion that the UPF classification has generated is useful, Dr. Roberts continued. “This definition grew out of that recognition that we’re engaged in an unprecedented experiment of how unhealthy can you make the world without having a major catastrophe.”
She added that the UPF concept deserves a more formalized and rigorous evaluation.
“This is an important topic for the future of public health, and I think it needs big committees to address it seriously,” she said. “I think we should not be dealing with this individually in different labs.”
Doctor’s take on usefulness of discussing UPF concept with patients
Mark Corkins, MD, who did not participate in the debate at the meeting, said he talks to parents and children about nutrition at every office visit in which he sees a child with an unhealthy weight.
“Persistence wears down resistance,” said the chair of the American Academy of Pediatrics nutrition committee, in an interview.“A consistent message – you say the same thing and you say it multiple times.”
The idea of “ultra-processed foods” plays a role in those conversations, but largely in the background. It’s a topic that’s important for pediatric health, Dr. Corkins said – but he doesn’t make it the focal point.
“It’s not a direct attack on ultra-processed foods that usually I take as my direction,” said Dr. Corkins, who is also chief of pediatric gastroenterology at Le Bonheur Children’s Hospital in Memphis, Tenn.. “What I try to focus on, and what I think the American Academy of Pediatrics would focus on, is that we need to focus on making the diet better.”
He added, “Parents are aware – they don’t call it ultra-processed food, they call it junk food.”
Dr. Corkins continued that he is reluctant to directly challenge parents on feeding their children unhealthy foods – ultra-processed or not – lest he shame them and harm the relationship.
“Guilt as a motivator isn’t really highly successful,” he said, in an interview.
Dr. Astrup reported advisory committee or board member involvement with Green Leaf Medical and RNPC, France. Dr. Roberts reported advisory committee or board member involvement with Danone, and an ownership interest in Instinct Health Science. Dr. Monteiro and Dr. Corkins reported no relevant disclosures.
The NOVA system divides foods into “fresh or minimally processed,” such as strawberries or steel-cut oats; “processed culinary ingredients,” such as olive oil; “processed foods,” such as cheeses; and “ultra-processed foods.” UPFs are defined as “industrial formulations made by deconstructing natural food into its chemical constituents, modifying them and recombining them with additives into products liable to displace all other NOVA food groups.”
According to doctors who presented during the meeting, ultra-processed foods are drawing increased attention, because researchers have been examining them in National Institutes of Health–funded studies and journalists have been writing about them.
During the debate session at the meeting, some experts said that, with obesity and poor health skyrocketing, increased awareness and labeling of UPFs can only be a good thing. In contrast others noted at the meeting that the classification system that has come to be used for identifying UPFs – the NOVA Food Classification system – is too mushy, confusing, and, ultimately unhelpful.
Carlos Monteiro, MD, PhD, professor of nutrition and public health at the University of Sao Paolo, was part of the group favoring the NOVA system’s classifying certain foods as UPFs, during the debate. He drew attention to the extent to which the world’s population is getting its calories from UPFs.
Mexico and France get about 30% of calories from these foods. In Canada, it’s 48%. And in the United States, it’s 57%, Dr. Monteiro said.
Studies have found that UPFs, many of which are designed to be exceedingly flavorful and intended to replace consumption of unprocessed whole foods, lead to more overall energy intake, more added sugar in the diet, and less fiber and protein intake, he said.
To further support his arguments, Dr. Monteiro pointed to studies suggesting that it is not just the resulting change in the nutritional intake that is unhealthy, but the UPF manufacturing process itself. When adjusting for fat, sugar, and sodium intake, for example, health outcomes associated with UPFs remain poor, he explained.
“I’m sorry,” he said in the debate. “If you don’t reduce this, you don’t reduce your obesity, your diabetes prevalence.”
A study presented by Jacqueline Vernarelli, PhD, during a different session at the meeting suggested there may be other downsides to consuming UPFs. This research, which was based on the U.S. National Youth Fitness Survey, found that poorer locomotor skills among children aged 3-5 and poorer cardiovascular fitness among those aged 12-15 were associated with getting more calories from UPFs.
Those with lower cardiovascular fitness consumed 1,234 calories a day from UPFs, and those with higher cardiovascular fitness consumed 1,007 calories a day from UPFs (P = .002), according to the new research.
“It’s notable here that, although these differences are significant, both groups are consuming a pretty high proportion of their diet from ultra-processed foods,” said Dr. Vernarelli, associate professor of public health at Sacred Heart University, Fairfield, Conn., during her presentation.
In the debate session, Arne Astrup, MD, PhD, senior project director at the Healthy Weight Center at the Novo Nordisk Foundation, Hellerup, Denmark, presented an opposing view.
He said the definition of UPFs makes it too difficult to categorize many foods, pointing to a study from this year in which about 150 nutrition experts, doctors, and dietitians classified 120 foods. Only three marketed foods and one generic food were classified the same by all the evaluators.
Referring to the study Dr. Astrup cited, Dr. Monteiro said it was a mere “exercise,” and the experts involved in it had conflicts of interest.
Dr. Astrup touted this study’s size and its appearance in the peer-reviewed journal the European Journal of Clinical Nutrition.
Defending his point of view, Dr. Astrup said, “The definition and classification is so ambiguous, and the risk of misclassification is so extremely high, I think we really miss the basic requirement of science, namely that we know what we are talking about,” he said.
If you take an unprocessed food, and insert a “little additive … suddenly it’s an ultra-processed food,” he added.
UPF definition doesn’t flag some unhealthy foods
Susan Roberts, PhD, professor of nutrition at Tufts University, Boston, was a discussant at the debate and touched on the merits of both sides. She noted that the UPF definition doesn’t flag some “clearly unhealthy foods,” such as table sugar, but does flag some healthy ones, such as plant-based burgers – to which Dr. Monteiro said that the system was not a system meant to divide foods into healthy and unhealthy groups, during the debate session.
The inclusion of both healthy and unhealthy foods in NOVA’s definition of a UPF is a serious problem, Dr. Roberts said.
“It’s almost like it’s an emotional classification designed to get at the food industry rather than focusing on health – and I think that’s asking for trouble because it’s just going to be such a mess to tell consumers, ‘Well, this ultra-processed food is healthy and this one isn’t,’ ” she said. What’s happening is the term ultra-processed is being used interchangeably with unhealthy.
The discussion that the UPF classification has generated is useful, Dr. Roberts continued. “This definition grew out of that recognition that we’re engaged in an unprecedented experiment of how unhealthy can you make the world without having a major catastrophe.”
She added that the UPF concept deserves a more formalized and rigorous evaluation.
“This is an important topic for the future of public health, and I think it needs big committees to address it seriously,” she said. “I think we should not be dealing with this individually in different labs.”
Doctor’s take on usefulness of discussing UPF concept with patients
Mark Corkins, MD, who did not participate in the debate at the meeting, said he talks to parents and children about nutrition at every office visit in which he sees a child with an unhealthy weight.
“Persistence wears down resistance,” said the chair of the American Academy of Pediatrics nutrition committee, in an interview.“A consistent message – you say the same thing and you say it multiple times.”
The idea of “ultra-processed foods” plays a role in those conversations, but largely in the background. It’s a topic that’s important for pediatric health, Dr. Corkins said – but he doesn’t make it the focal point.
“It’s not a direct attack on ultra-processed foods that usually I take as my direction,” said Dr. Corkins, who is also chief of pediatric gastroenterology at Le Bonheur Children’s Hospital in Memphis, Tenn.. “What I try to focus on, and what I think the American Academy of Pediatrics would focus on, is that we need to focus on making the diet better.”
He added, “Parents are aware – they don’t call it ultra-processed food, they call it junk food.”
Dr. Corkins continued that he is reluctant to directly challenge parents on feeding their children unhealthy foods – ultra-processed or not – lest he shame them and harm the relationship.
“Guilt as a motivator isn’t really highly successful,” he said, in an interview.
Dr. Astrup reported advisory committee or board member involvement with Green Leaf Medical and RNPC, France. Dr. Roberts reported advisory committee or board member involvement with Danone, and an ownership interest in Instinct Health Science. Dr. Monteiro and Dr. Corkins reported no relevant disclosures.
FROM NUTRITION 2022
Ready to make a difference, dermatologist takes the helm as AMA president
Jack S. Resneck Jr., MD, is not usually the loudest voice in the room, but when he speaks, his words carry a heft and an appeal that is straightforward and undeniable.
That was on full display as.
He did not mince words when it came to describing the current landscape. “I doubt you imagined a divided country such as this, where physicians and public health officials often face antiscience aggression and threats of violence simply for doing our jobs,” he said. “You probably didn’t plan on insurers questioning every prescription and every procedure you asked for. Or government criminalizing routine and vital health care, enshrining discrimination against our LGBTQ patients or attacking a woman’s right to control health care decisions that should only be between her and her doctor,” said Dr. Resneck.
But, he added, all was not lost. “While it would be easy to get overwhelmed by despair as I begin this new role, I’ve never been prouder of my physician colleagues,” he said.
Dr. Resneck is the first dermatologist to lead the 175-year-old organization since 1925. Colleagues in the field speak of pride in having one of their own at the top, and they are even more complimentary about his depth of health policy knowledge, his communications skills, and his ability to find common ground.
“He loves looking at both sides,” said Marta J. Van Beek, MD, clinical professor of dermatology at the University of Iowa, Iowa City. “That’s how he builds consensus,” said Dr. Van Beek, who has known Dr. Resneck for more than 20 years, since they were chief dermatology residents – she at Iowa and he at UCSF.
Dr. Van Beek and Dr. Resneck have a deep interest in health policy and have long worked side by side on committees at both the American Academy of Dermatology (AAD) and the AMA. She looks back to the lead-up period before the 2010 passage of the Affordable Care Act as one of Dr. Resneck’s shining moments. “Those were contentious times in medicine,” Dr. Van Beek told this news organization. Dr. Resneck, as chair of the AAD’s Council on Government Affairs and Health Policy from 2008 to 2012, rallied the board to agree on a set of health care reform principles, she noted.
Dr. Resneck is “really very unifying,” agreed Bruce A. Brod, MD, clinical professor of dermatology at the University of Pennsylvania, Philadelphia. Dr. Brod has worked with Dr. Resneck for 2 decades on various committees at the AAD. They’ve also known each other through the AMA House of Delegates.
Now Dr. Brod is following in Dr. Resneck’s footsteps as chair of the AAD’s Council on Government Affairs and Health Policy. “Big shoes to fill there,” said Dr. Brod. He said he’s been inspired by Dr. Resneck’s always-positive approach, punctuated by his ever-constant belief that “there’s a lot more common ground than meets the eye here.”
“I really think he’s the perfect leader at this time,” he said.
Outgoing AMA President Gerald E. Harmon, MD, said that Dr. Resneck’s long experience as a teacher and a mentor, and what he describes as a “good, active listening talent,” have been integral to his success as a leader. He expects those qualities to make Dr. Resneck an effective advocate for all of medicine. “He identifies the problem, he identifies the gap, and then he establishes a workable, executable plan to close that gap,” Dr. Harmon told this news organization, adding that he’s seen this at work in AMA board meetings.
“He was a good teacher for me,” said Dr. Harmon, who had known Dr. Resneck through the House of Delegates and various AMA councils for at least a decade before they both joined the AMA board. “He can be such a mentor to all age groups, including senior physicians like myself,” said Dr. Harmon.
Dr. Resneck is excited, but also measured. “This has been a tumultuous couple of years in the country with the pandemic and with the fractured politics,” he said in an interview. Thinking about taking on the AMA presidency, he said, “I’ve had some moments of trepidation. I wanted to be sure that I was going to be able to make a difference.”
Long interest in health policy
Growing up in Shreveport, La., as the son of a dermatologist, Dr. Resneck said, “at first, I swore I was going to do something other than medicine.” It was not out of rebellion. He got along fine with his father. He wanted to pursue his own journey.
Dr. Resneck began his long love affair with health policy at Brown University, graduating magna cum laude with honors in public policy. A 1991 U.S. Department of Health & Human Services internship between his junior and senior years helped inform his honors thesis on health care financing policy.
Ultimately, Dr. Resneck did not stray far from his father’s career path. While still at Brown, he decided to go to medical school, entering UCSF in the fall of 1993. “At the end of the day, there was this undeniable influence that he loved his job,” Dr. Resneck said in the interview. His father was energized by the work and helping patients. “If burnout was in his vocabulary, I never heard it,” said Dr. Resneck.
Initially, he did a 1-year internal medicine residency at UCSF, but then switched to dermatology and became chief resident in 2000.
He was quickly pegged as a leader and an inspirational speaker. The AAD gave him its Young Physician Leadership Development Award in 2001, and the AMA gave Dr. Resneck its Excellence in Medicine National Award for Young Physician Leadership in 2004. He began giving talks at national meetings in 2002 and has been busy ever since, addressing the AMA, the AAD, state medical and dermatology societies, subspecialty groups such as the American College of Mohs Surgery and the Association of Professors of Dermatology, and other organizations such as the American Telemedicine Association.
He’s a sought-after speaker in part because of his ability to simply communicate health policy, said Dr. Brod. “He can connect the real-world issues really well to the policy needs and communicate it very well, and come in at just the right level,” he said.
Dr. Resneck has been immersed in policy and practice issues since the start of his career, serving on AAD and AMA committees addressing quality measures, data collection, access to care, workforce issues, and telemedicine. He started writing about dermatology workforce challenges in 2001 and has revisited that topic with regularity.
He has published often on the difficulties of patient access, looking at wait times for appointments, among other issues. In 2018, he expressed concern in a commentary in JAMA Dermatology that private equity purchases of dermatology practices might lead to an improper focus on profits over patients and that it could reduce the diversity of practice models.
At heart, Dr. Resneck is an institutionalist, someone who believes that the “collaborative, collective voice can make change,” said Dr. Brod. Dr. Resneck said as much in his inaugural speech. “I believe those who show up can use levers of power to confront our system’s flaws,” he said. “This is the nerdy policy part of my life, which my friends will force me to admit is most of my life,” said Dr. Resneck.
Prior authorization, telemedicine, equity
Beneath the reserved exterior lies an intense yearning to act on his passions, both at work and at play.
Dr. Resneck notes almost in passing that he likes to ski when he’s not practicing medicine or serving on a committee. Dr. Van Beek – whose family has vacationed with Dr. Resneck, his wife, Ellen Hufbauer, MD, a family medicine physician in Concord, Calif., and their two teenaged children Zachary and Amelia – said he’s “a very good skier.”
She noted that he and his children share the same enthusiasm for researching every aspect of wherever they travel, including the best places to eat. “He embraces work and life with an incredible amount of intellectual curiosity,” Dr. Van Beek said.
That curiosity – and the passion to make a difference – has driven his deep dives into what he sees as the corrosive practice of prior authorization and the promise of telemedicine, which he has explained and supported in testimony on Capitol Hill.
Dr. Brod said that Dr. Resneck was among those who helped convince the federal government to expand coverage for telemedicine during the COVID-19 pandemic. “He brought together his patient experience in dermatology and his policy experience,” and was able to deftly explain how it could increase access during the shutdown, said Dr. Brod.
Prior authorization gets him fired up. “We’ve reached a point where there’s almost not anything I will write a prescription for that doesn’t oftentimes require all of these hoops that we have to jump through,” he told this news organization. Prescriptions for generic topical cortisones that have been around for 50 years “now all of the sudden require a week of arguing,” said Dr. Resneck. In the meantime, patients aren’t getting treatment, he said.
Dr. Resneck’s passion for health equity is borne in part out of the racism witnessed by him and his family, including an uncle who started an antisegregationist newspaper and was kicked out of medical school for his views in the 1950s. Dr. Resneck said he had a rudimentary understanding of racism as a youngster. But he told the AMA delegates, “I knew enough at age 16 to write an op-ed in our city’s newspaper about the need to remove Confederate monuments from our courthouse lawn.” Added Dr. Resneck, “You can imagine how that went over in 1987.”
The pandemic shined a bright light on inequities and heightened awareness of “the institutionalized systems that have perpetuated racism and gender discrimination in medicine for as far back as we want to look,” Dr. Resneck said during his inaugural speech. Pointedly, he told his colleagues that “the AMA has not always been on the right side of history,” adding, “Each of us must do our part to eliminate health inequities by engaging in antiracist and antisexist work.”
That kind of talk is signature Resneck, said Dr. Brod. “He’s not afraid to exhibit very brave leadership,” especially “when there are issues that jeopardize the needs of patient access or patient safety,” he said.
“He’ll be a tremendous AMA president,” said Dr. Van Beek. “He’s present, he’s devoted, and he’s typically the expert in the room.”
Dr. Harmon said that Dr. Resneck is “cut from the same cloth that I am. He believes that if you get an opportunity to make things better, you take it.”
His advice to Dr. Resneck: “Rarely turn an opportunity down.” Dr. Harmon has little doubt that Dr. Resneck is up to the job but said, “I’m going to encourage him to keep that energy and enthusiasm up.”
Dr. Resneck told physician colleagues not to worry: “I will keep relentlessly showing up.”
A version of this article first appeared on Medscape.com.
Jack S. Resneck Jr., MD, is not usually the loudest voice in the room, but when he speaks, his words carry a heft and an appeal that is straightforward and undeniable.
That was on full display as.
He did not mince words when it came to describing the current landscape. “I doubt you imagined a divided country such as this, where physicians and public health officials often face antiscience aggression and threats of violence simply for doing our jobs,” he said. “You probably didn’t plan on insurers questioning every prescription and every procedure you asked for. Or government criminalizing routine and vital health care, enshrining discrimination against our LGBTQ patients or attacking a woman’s right to control health care decisions that should only be between her and her doctor,” said Dr. Resneck.
But, he added, all was not lost. “While it would be easy to get overwhelmed by despair as I begin this new role, I’ve never been prouder of my physician colleagues,” he said.
Dr. Resneck is the first dermatologist to lead the 175-year-old organization since 1925. Colleagues in the field speak of pride in having one of their own at the top, and they are even more complimentary about his depth of health policy knowledge, his communications skills, and his ability to find common ground.
“He loves looking at both sides,” said Marta J. Van Beek, MD, clinical professor of dermatology at the University of Iowa, Iowa City. “That’s how he builds consensus,” said Dr. Van Beek, who has known Dr. Resneck for more than 20 years, since they were chief dermatology residents – she at Iowa and he at UCSF.
Dr. Van Beek and Dr. Resneck have a deep interest in health policy and have long worked side by side on committees at both the American Academy of Dermatology (AAD) and the AMA. She looks back to the lead-up period before the 2010 passage of the Affordable Care Act as one of Dr. Resneck’s shining moments. “Those were contentious times in medicine,” Dr. Van Beek told this news organization. Dr. Resneck, as chair of the AAD’s Council on Government Affairs and Health Policy from 2008 to 2012, rallied the board to agree on a set of health care reform principles, she noted.
Dr. Resneck is “really very unifying,” agreed Bruce A. Brod, MD, clinical professor of dermatology at the University of Pennsylvania, Philadelphia. Dr. Brod has worked with Dr. Resneck for 2 decades on various committees at the AAD. They’ve also known each other through the AMA House of Delegates.
Now Dr. Brod is following in Dr. Resneck’s footsteps as chair of the AAD’s Council on Government Affairs and Health Policy. “Big shoes to fill there,” said Dr. Brod. He said he’s been inspired by Dr. Resneck’s always-positive approach, punctuated by his ever-constant belief that “there’s a lot more common ground than meets the eye here.”
“I really think he’s the perfect leader at this time,” he said.
Outgoing AMA President Gerald E. Harmon, MD, said that Dr. Resneck’s long experience as a teacher and a mentor, and what he describes as a “good, active listening talent,” have been integral to his success as a leader. He expects those qualities to make Dr. Resneck an effective advocate for all of medicine. “He identifies the problem, he identifies the gap, and then he establishes a workable, executable plan to close that gap,” Dr. Harmon told this news organization, adding that he’s seen this at work in AMA board meetings.
“He was a good teacher for me,” said Dr. Harmon, who had known Dr. Resneck through the House of Delegates and various AMA councils for at least a decade before they both joined the AMA board. “He can be such a mentor to all age groups, including senior physicians like myself,” said Dr. Harmon.
Dr. Resneck is excited, but also measured. “This has been a tumultuous couple of years in the country with the pandemic and with the fractured politics,” he said in an interview. Thinking about taking on the AMA presidency, he said, “I’ve had some moments of trepidation. I wanted to be sure that I was going to be able to make a difference.”
Long interest in health policy
Growing up in Shreveport, La., as the son of a dermatologist, Dr. Resneck said, “at first, I swore I was going to do something other than medicine.” It was not out of rebellion. He got along fine with his father. He wanted to pursue his own journey.
Dr. Resneck began his long love affair with health policy at Brown University, graduating magna cum laude with honors in public policy. A 1991 U.S. Department of Health & Human Services internship between his junior and senior years helped inform his honors thesis on health care financing policy.
Ultimately, Dr. Resneck did not stray far from his father’s career path. While still at Brown, he decided to go to medical school, entering UCSF in the fall of 1993. “At the end of the day, there was this undeniable influence that he loved his job,” Dr. Resneck said in the interview. His father was energized by the work and helping patients. “If burnout was in his vocabulary, I never heard it,” said Dr. Resneck.
Initially, he did a 1-year internal medicine residency at UCSF, but then switched to dermatology and became chief resident in 2000.
He was quickly pegged as a leader and an inspirational speaker. The AAD gave him its Young Physician Leadership Development Award in 2001, and the AMA gave Dr. Resneck its Excellence in Medicine National Award for Young Physician Leadership in 2004. He began giving talks at national meetings in 2002 and has been busy ever since, addressing the AMA, the AAD, state medical and dermatology societies, subspecialty groups such as the American College of Mohs Surgery and the Association of Professors of Dermatology, and other organizations such as the American Telemedicine Association.
He’s a sought-after speaker in part because of his ability to simply communicate health policy, said Dr. Brod. “He can connect the real-world issues really well to the policy needs and communicate it very well, and come in at just the right level,” he said.
Dr. Resneck has been immersed in policy and practice issues since the start of his career, serving on AAD and AMA committees addressing quality measures, data collection, access to care, workforce issues, and telemedicine. He started writing about dermatology workforce challenges in 2001 and has revisited that topic with regularity.
He has published often on the difficulties of patient access, looking at wait times for appointments, among other issues. In 2018, he expressed concern in a commentary in JAMA Dermatology that private equity purchases of dermatology practices might lead to an improper focus on profits over patients and that it could reduce the diversity of practice models.
At heart, Dr. Resneck is an institutionalist, someone who believes that the “collaborative, collective voice can make change,” said Dr. Brod. Dr. Resneck said as much in his inaugural speech. “I believe those who show up can use levers of power to confront our system’s flaws,” he said. “This is the nerdy policy part of my life, which my friends will force me to admit is most of my life,” said Dr. Resneck.
Prior authorization, telemedicine, equity
Beneath the reserved exterior lies an intense yearning to act on his passions, both at work and at play.
Dr. Resneck notes almost in passing that he likes to ski when he’s not practicing medicine or serving on a committee. Dr. Van Beek – whose family has vacationed with Dr. Resneck, his wife, Ellen Hufbauer, MD, a family medicine physician in Concord, Calif., and their two teenaged children Zachary and Amelia – said he’s “a very good skier.”
She noted that he and his children share the same enthusiasm for researching every aspect of wherever they travel, including the best places to eat. “He embraces work and life with an incredible amount of intellectual curiosity,” Dr. Van Beek said.
That curiosity – and the passion to make a difference – has driven his deep dives into what he sees as the corrosive practice of prior authorization and the promise of telemedicine, which he has explained and supported in testimony on Capitol Hill.
Dr. Brod said that Dr. Resneck was among those who helped convince the federal government to expand coverage for telemedicine during the COVID-19 pandemic. “He brought together his patient experience in dermatology and his policy experience,” and was able to deftly explain how it could increase access during the shutdown, said Dr. Brod.
Prior authorization gets him fired up. “We’ve reached a point where there’s almost not anything I will write a prescription for that doesn’t oftentimes require all of these hoops that we have to jump through,” he told this news organization. Prescriptions for generic topical cortisones that have been around for 50 years “now all of the sudden require a week of arguing,” said Dr. Resneck. In the meantime, patients aren’t getting treatment, he said.
Dr. Resneck’s passion for health equity is borne in part out of the racism witnessed by him and his family, including an uncle who started an antisegregationist newspaper and was kicked out of medical school for his views in the 1950s. Dr. Resneck said he had a rudimentary understanding of racism as a youngster. But he told the AMA delegates, “I knew enough at age 16 to write an op-ed in our city’s newspaper about the need to remove Confederate monuments from our courthouse lawn.” Added Dr. Resneck, “You can imagine how that went over in 1987.”
The pandemic shined a bright light on inequities and heightened awareness of “the institutionalized systems that have perpetuated racism and gender discrimination in medicine for as far back as we want to look,” Dr. Resneck said during his inaugural speech. Pointedly, he told his colleagues that “the AMA has not always been on the right side of history,” adding, “Each of us must do our part to eliminate health inequities by engaging in antiracist and antisexist work.”
That kind of talk is signature Resneck, said Dr. Brod. “He’s not afraid to exhibit very brave leadership,” especially “when there are issues that jeopardize the needs of patient access or patient safety,” he said.
“He’ll be a tremendous AMA president,” said Dr. Van Beek. “He’s present, he’s devoted, and he’s typically the expert in the room.”
Dr. Harmon said that Dr. Resneck is “cut from the same cloth that I am. He believes that if you get an opportunity to make things better, you take it.”
His advice to Dr. Resneck: “Rarely turn an opportunity down.” Dr. Harmon has little doubt that Dr. Resneck is up to the job but said, “I’m going to encourage him to keep that energy and enthusiasm up.”
Dr. Resneck told physician colleagues not to worry: “I will keep relentlessly showing up.”
A version of this article first appeared on Medscape.com.
Jack S. Resneck Jr., MD, is not usually the loudest voice in the room, but when he speaks, his words carry a heft and an appeal that is straightforward and undeniable.
That was on full display as.
He did not mince words when it came to describing the current landscape. “I doubt you imagined a divided country such as this, where physicians and public health officials often face antiscience aggression and threats of violence simply for doing our jobs,” he said. “You probably didn’t plan on insurers questioning every prescription and every procedure you asked for. Or government criminalizing routine and vital health care, enshrining discrimination against our LGBTQ patients or attacking a woman’s right to control health care decisions that should only be between her and her doctor,” said Dr. Resneck.
But, he added, all was not lost. “While it would be easy to get overwhelmed by despair as I begin this new role, I’ve never been prouder of my physician colleagues,” he said.
Dr. Resneck is the first dermatologist to lead the 175-year-old organization since 1925. Colleagues in the field speak of pride in having one of their own at the top, and they are even more complimentary about his depth of health policy knowledge, his communications skills, and his ability to find common ground.
“He loves looking at both sides,” said Marta J. Van Beek, MD, clinical professor of dermatology at the University of Iowa, Iowa City. “That’s how he builds consensus,” said Dr. Van Beek, who has known Dr. Resneck for more than 20 years, since they were chief dermatology residents – she at Iowa and he at UCSF.
Dr. Van Beek and Dr. Resneck have a deep interest in health policy and have long worked side by side on committees at both the American Academy of Dermatology (AAD) and the AMA. She looks back to the lead-up period before the 2010 passage of the Affordable Care Act as one of Dr. Resneck’s shining moments. “Those were contentious times in medicine,” Dr. Van Beek told this news organization. Dr. Resneck, as chair of the AAD’s Council on Government Affairs and Health Policy from 2008 to 2012, rallied the board to agree on a set of health care reform principles, she noted.
Dr. Resneck is “really very unifying,” agreed Bruce A. Brod, MD, clinical professor of dermatology at the University of Pennsylvania, Philadelphia. Dr. Brod has worked with Dr. Resneck for 2 decades on various committees at the AAD. They’ve also known each other through the AMA House of Delegates.
Now Dr. Brod is following in Dr. Resneck’s footsteps as chair of the AAD’s Council on Government Affairs and Health Policy. “Big shoes to fill there,” said Dr. Brod. He said he’s been inspired by Dr. Resneck’s always-positive approach, punctuated by his ever-constant belief that “there’s a lot more common ground than meets the eye here.”
“I really think he’s the perfect leader at this time,” he said.
Outgoing AMA President Gerald E. Harmon, MD, said that Dr. Resneck’s long experience as a teacher and a mentor, and what he describes as a “good, active listening talent,” have been integral to his success as a leader. He expects those qualities to make Dr. Resneck an effective advocate for all of medicine. “He identifies the problem, he identifies the gap, and then he establishes a workable, executable plan to close that gap,” Dr. Harmon told this news organization, adding that he’s seen this at work in AMA board meetings.
“He was a good teacher for me,” said Dr. Harmon, who had known Dr. Resneck through the House of Delegates and various AMA councils for at least a decade before they both joined the AMA board. “He can be such a mentor to all age groups, including senior physicians like myself,” said Dr. Harmon.
Dr. Resneck is excited, but also measured. “This has been a tumultuous couple of years in the country with the pandemic and with the fractured politics,” he said in an interview. Thinking about taking on the AMA presidency, he said, “I’ve had some moments of trepidation. I wanted to be sure that I was going to be able to make a difference.”
Long interest in health policy
Growing up in Shreveport, La., as the son of a dermatologist, Dr. Resneck said, “at first, I swore I was going to do something other than medicine.” It was not out of rebellion. He got along fine with his father. He wanted to pursue his own journey.
Dr. Resneck began his long love affair with health policy at Brown University, graduating magna cum laude with honors in public policy. A 1991 U.S. Department of Health & Human Services internship between his junior and senior years helped inform his honors thesis on health care financing policy.
Ultimately, Dr. Resneck did not stray far from his father’s career path. While still at Brown, he decided to go to medical school, entering UCSF in the fall of 1993. “At the end of the day, there was this undeniable influence that he loved his job,” Dr. Resneck said in the interview. His father was energized by the work and helping patients. “If burnout was in his vocabulary, I never heard it,” said Dr. Resneck.
Initially, he did a 1-year internal medicine residency at UCSF, but then switched to dermatology and became chief resident in 2000.
He was quickly pegged as a leader and an inspirational speaker. The AAD gave him its Young Physician Leadership Development Award in 2001, and the AMA gave Dr. Resneck its Excellence in Medicine National Award for Young Physician Leadership in 2004. He began giving talks at national meetings in 2002 and has been busy ever since, addressing the AMA, the AAD, state medical and dermatology societies, subspecialty groups such as the American College of Mohs Surgery and the Association of Professors of Dermatology, and other organizations such as the American Telemedicine Association.
He’s a sought-after speaker in part because of his ability to simply communicate health policy, said Dr. Brod. “He can connect the real-world issues really well to the policy needs and communicate it very well, and come in at just the right level,” he said.
Dr. Resneck has been immersed in policy and practice issues since the start of his career, serving on AAD and AMA committees addressing quality measures, data collection, access to care, workforce issues, and telemedicine. He started writing about dermatology workforce challenges in 2001 and has revisited that topic with regularity.
He has published often on the difficulties of patient access, looking at wait times for appointments, among other issues. In 2018, he expressed concern in a commentary in JAMA Dermatology that private equity purchases of dermatology practices might lead to an improper focus on profits over patients and that it could reduce the diversity of practice models.
At heart, Dr. Resneck is an institutionalist, someone who believes that the “collaborative, collective voice can make change,” said Dr. Brod. Dr. Resneck said as much in his inaugural speech. “I believe those who show up can use levers of power to confront our system’s flaws,” he said. “This is the nerdy policy part of my life, which my friends will force me to admit is most of my life,” said Dr. Resneck.
Prior authorization, telemedicine, equity
Beneath the reserved exterior lies an intense yearning to act on his passions, both at work and at play.
Dr. Resneck notes almost in passing that he likes to ski when he’s not practicing medicine or serving on a committee. Dr. Van Beek – whose family has vacationed with Dr. Resneck, his wife, Ellen Hufbauer, MD, a family medicine physician in Concord, Calif., and their two teenaged children Zachary and Amelia – said he’s “a very good skier.”
She noted that he and his children share the same enthusiasm for researching every aspect of wherever they travel, including the best places to eat. “He embraces work and life with an incredible amount of intellectual curiosity,” Dr. Van Beek said.
That curiosity – and the passion to make a difference – has driven his deep dives into what he sees as the corrosive practice of prior authorization and the promise of telemedicine, which he has explained and supported in testimony on Capitol Hill.
Dr. Brod said that Dr. Resneck was among those who helped convince the federal government to expand coverage for telemedicine during the COVID-19 pandemic. “He brought together his patient experience in dermatology and his policy experience,” and was able to deftly explain how it could increase access during the shutdown, said Dr. Brod.
Prior authorization gets him fired up. “We’ve reached a point where there’s almost not anything I will write a prescription for that doesn’t oftentimes require all of these hoops that we have to jump through,” he told this news organization. Prescriptions for generic topical cortisones that have been around for 50 years “now all of the sudden require a week of arguing,” said Dr. Resneck. In the meantime, patients aren’t getting treatment, he said.
Dr. Resneck’s passion for health equity is borne in part out of the racism witnessed by him and his family, including an uncle who started an antisegregationist newspaper and was kicked out of medical school for his views in the 1950s. Dr. Resneck said he had a rudimentary understanding of racism as a youngster. But he told the AMA delegates, “I knew enough at age 16 to write an op-ed in our city’s newspaper about the need to remove Confederate monuments from our courthouse lawn.” Added Dr. Resneck, “You can imagine how that went over in 1987.”
The pandemic shined a bright light on inequities and heightened awareness of “the institutionalized systems that have perpetuated racism and gender discrimination in medicine for as far back as we want to look,” Dr. Resneck said during his inaugural speech. Pointedly, he told his colleagues that “the AMA has not always been on the right side of history,” adding, “Each of us must do our part to eliminate health inequities by engaging in antiracist and antisexist work.”
That kind of talk is signature Resneck, said Dr. Brod. “He’s not afraid to exhibit very brave leadership,” especially “when there are issues that jeopardize the needs of patient access or patient safety,” he said.
“He’ll be a tremendous AMA president,” said Dr. Van Beek. “He’s present, he’s devoted, and he’s typically the expert in the room.”
Dr. Harmon said that Dr. Resneck is “cut from the same cloth that I am. He believes that if you get an opportunity to make things better, you take it.”
His advice to Dr. Resneck: “Rarely turn an opportunity down.” Dr. Harmon has little doubt that Dr. Resneck is up to the job but said, “I’m going to encourage him to keep that energy and enthusiasm up.”
Dr. Resneck told physician colleagues not to worry: “I will keep relentlessly showing up.”
A version of this article first appeared on Medscape.com.